User login
Sugammadex OK’d to reverse neuromuscular blockade during surgery
The Food and Drug Administration approved on Dec. 15 Merck’s sugammadex (Bridion) injection to reverse the effects of neuromuscular blockade induced by rocuronium bromide and vecuronium bromide during surgery.
The safety and efficacy of sugammadex were evaluated in three phase III trials involving 456 participants; most recovered within 5 minutes. An FDA review of the drug found that there was less residual neuromuscular blockade with sugammadex compared to neostigmine, and a 4-minute time savings to extubation and operating room discharge.
“Bridion provides a new treatment option that may help patients recover sooner from medications used for intubation or ventilation during surgery. This drug enables medical personnel to reverse the effects of neuromuscular blocking drugs and restore spontaneous breathing after surgery,” Dr. Sharon Hertz, director of the FDA’s Division of Anesthesia, Analgesia, and Addiction Products, said in a statement.
Although approved in other countries, sugammadex has been in the FDA’s review process since 2007, previously rejected and held up by concerns over anaphylaxis and other issues.
Because of that, sugammadex was further evaluated in a randomized, double-blind, parallel-group, repeat-dose trial. Of the 299 participants treated with Bridion, one person had an anaphylactic reaction. “Clinicians should be aware of the possibility of a hypersensitivity reaction or anaphylaxis and should intervene as appropriate,” the agency said in its statement.
Cases of marked bradycardia, some of which have resulted in cardiac arrest, have also been observed within minutes after the administration of Bridion. Tachycardia and bradycardia have been associated with cases of anaphylaxis. “Patients should be closely monitored for hemodynamic changes during and after reversal of neuromuscular blockade, and treatment with anticholinergic agents, such as atropine, should be administered if clinically significant bradycardia is observed,” the agency said.
The most common side effects reported in trials were vomiting, hypotension, pain, headache, and nausea. “Doctors should also advise women using hormonal contraceptives that Bridion may temporarily reduce the contraceptive effect so they must use an alternate method of birth control for a period of time,” the agency said.
Rocuronium bromide and vecuronium bromide are used to paralyze the vocal cords for tracheal intubation, as well as to paralyze patients under general anesthesia and prevent spontaneous breathing during ventilation. Sugammadex is a new molecular entity of the gamma-cyclodextrin class, designed to bind rocuronium and vecuronium.
The Food and Drug Administration approved on Dec. 15 Merck’s sugammadex (Bridion) injection to reverse the effects of neuromuscular blockade induced by rocuronium bromide and vecuronium bromide during surgery.
The safety and efficacy of sugammadex were evaluated in three phase III trials involving 456 participants; most recovered within 5 minutes. An FDA review of the drug found that there was less residual neuromuscular blockade with sugammadex compared to neostigmine, and a 4-minute time savings to extubation and operating room discharge.
“Bridion provides a new treatment option that may help patients recover sooner from medications used for intubation or ventilation during surgery. This drug enables medical personnel to reverse the effects of neuromuscular blocking drugs and restore spontaneous breathing after surgery,” Dr. Sharon Hertz, director of the FDA’s Division of Anesthesia, Analgesia, and Addiction Products, said in a statement.
Although approved in other countries, sugammadex has been in the FDA’s review process since 2007, previously rejected and held up by concerns over anaphylaxis and other issues.
Because of that, sugammadex was further evaluated in a randomized, double-blind, parallel-group, repeat-dose trial. Of the 299 participants treated with Bridion, one person had an anaphylactic reaction. “Clinicians should be aware of the possibility of a hypersensitivity reaction or anaphylaxis and should intervene as appropriate,” the agency said in its statement.
Cases of marked bradycardia, some of which have resulted in cardiac arrest, have also been observed within minutes after the administration of Bridion. Tachycardia and bradycardia have been associated with cases of anaphylaxis. “Patients should be closely monitored for hemodynamic changes during and after reversal of neuromuscular blockade, and treatment with anticholinergic agents, such as atropine, should be administered if clinically significant bradycardia is observed,” the agency said.
The most common side effects reported in trials were vomiting, hypotension, pain, headache, and nausea. “Doctors should also advise women using hormonal contraceptives that Bridion may temporarily reduce the contraceptive effect so they must use an alternate method of birth control for a period of time,” the agency said.
Rocuronium bromide and vecuronium bromide are used to paralyze the vocal cords for tracheal intubation, as well as to paralyze patients under general anesthesia and prevent spontaneous breathing during ventilation. Sugammadex is a new molecular entity of the gamma-cyclodextrin class, designed to bind rocuronium and vecuronium.
The Food and Drug Administration approved on Dec. 15 Merck’s sugammadex (Bridion) injection to reverse the effects of neuromuscular blockade induced by rocuronium bromide and vecuronium bromide during surgery.
The safety and efficacy of sugammadex were evaluated in three phase III trials involving 456 participants; most recovered within 5 minutes. An FDA review of the drug found that there was less residual neuromuscular blockade with sugammadex compared to neostigmine, and a 4-minute time savings to extubation and operating room discharge.
“Bridion provides a new treatment option that may help patients recover sooner from medications used for intubation or ventilation during surgery. This drug enables medical personnel to reverse the effects of neuromuscular blocking drugs and restore spontaneous breathing after surgery,” Dr. Sharon Hertz, director of the FDA’s Division of Anesthesia, Analgesia, and Addiction Products, said in a statement.
Although approved in other countries, sugammadex has been in the FDA’s review process since 2007, previously rejected and held up by concerns over anaphylaxis and other issues.
Because of that, sugammadex was further evaluated in a randomized, double-blind, parallel-group, repeat-dose trial. Of the 299 participants treated with Bridion, one person had an anaphylactic reaction. “Clinicians should be aware of the possibility of a hypersensitivity reaction or anaphylaxis and should intervene as appropriate,” the agency said in its statement.
Cases of marked bradycardia, some of which have resulted in cardiac arrest, have also been observed within minutes after the administration of Bridion. Tachycardia and bradycardia have been associated with cases of anaphylaxis. “Patients should be closely monitored for hemodynamic changes during and after reversal of neuromuscular blockade, and treatment with anticholinergic agents, such as atropine, should be administered if clinically significant bradycardia is observed,” the agency said.
The most common side effects reported in trials were vomiting, hypotension, pain, headache, and nausea. “Doctors should also advise women using hormonal contraceptives that Bridion may temporarily reduce the contraceptive effect so they must use an alternate method of birth control for a period of time,” the agency said.
Rocuronium bromide and vecuronium bromide are used to paralyze the vocal cords for tracheal intubation, as well as to paralyze patients under general anesthesia and prevent spontaneous breathing during ventilation. Sugammadex is a new molecular entity of the gamma-cyclodextrin class, designed to bind rocuronium and vecuronium.
Functional dependence linked to risk of complications after spine surgery
SAN DIEGO – Functional dependence following elective cervical spine procedures was associated with a significantly increased risk of almost all 30-day complications analyzed, including mortality, a large retrospective analysis of national data demonstrated.
The findings suggest that physicians should “include the patient’s level of functional independence, in addition to more traditional medical comorbidities, in the risk-benefit analysis of surgical decision making,” Dr. Alpesh A. Patel said in an interview in advance of the annual meeting of the Cervical Spine Research Society. “Those individuals with dependence need to be counseled appropriately about their increased risk of complications including mortality.”
Dr. Patel, professor and director of orthopedic spine surgery at Northwestern University Feinberg School of Medicine, Chicago, and his associates retrospectively reviewed the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) data files from 2006 to 2013 and limited their analysis to patients undergoing elective anterior cervical fusions, posterior cervical fusions, cervical laminectomy, cervical laminotomy, cervical discectomy, or corpectomy. They divided patients into one of three groups based on the following preoperative functional status parameters: independent, comprising those not requiring assistance or any equipment for activities of daily living (ADLs); partially dependent, including those with equipment such as prosthetics, equipment, or devices and requiring some assistance from another person for ADLs; and totally dependent, in which patients require total assistance for all ADLs. The researchers used univariate analysis to compare patient demographics, comorbidities, and 30-day postoperative complications among the three groups, followed by multivariate logistic regression to analyze the independent association of functional dependence on 30-day complications when controlling for procedure and comorbidity variances.
Dr. Patel reported findings from 24,357 patients: 23,620 (97.0%) functionally independent, 664 (2.7%) partially dependent, and 73 (0.3%) totally dependent. Dependent patients were significantly older and had higher rates of all comorbidities (P less than .001), with the exception of obesity (P = .214). In addition, 30-day complication rates were higher for all complications (P less than .001) other than neurological (P =.060) and surgical site complications (P =.668). When the researchers controlled for type of procedure and for disparities in patient preoperative variables, multivariate analyses demonstrated that functional dependence was independently associated with sepsis (odds ratio 6.40; P less than .001), pulmonary (OR 4.13; P less than .001), venous thromboembolism (OR 4.27, P less than .001), renal (OR 3.32; P less than .001), and cardiac complications (OR 4.68; P =.001), along with mortality (OR 8.31; P less than .001).
“The very strong association between functional dependence and mortality was quite surprising,” Dr. Patel said. “It was, to the contrary, also surprising to see that, despite wide variance in medical comorbidities and functional status, surgical complications such as infection and neurological injury were similar in all groups.” He characterized the study as “the first large-scale assessment of functional status as a predictor of patient outcomes after cervical spine surgery. It fits in line with other studies utilizing large databases. Big data analysis of outcomes can be used to identify risk factors for complications including death after surgery. Identifying these factors is important if we are going to improve the care we provide. Accurately quantifying the impact of these risk factors is also critical when we risk stratify and compare hospitals and physicians.”
He acknowledged certain limitations of the study, including the fact that it is a retrospective study “with a heterogeneous population of patients, surgeons, hospitals, and procedures. This adds uncertainty to the analysis at the level of the individual patient but does provide generalizability to a broader patient population.”
Dr. Patel reported having no conflicts of interest.
SAN DIEGO – Functional dependence following elective cervical spine procedures was associated with a significantly increased risk of almost all 30-day complications analyzed, including mortality, a large retrospective analysis of national data demonstrated.
The findings suggest that physicians should “include the patient’s level of functional independence, in addition to more traditional medical comorbidities, in the risk-benefit analysis of surgical decision making,” Dr. Alpesh A. Patel said in an interview in advance of the annual meeting of the Cervical Spine Research Society. “Those individuals with dependence need to be counseled appropriately about their increased risk of complications including mortality.”
Dr. Patel, professor and director of orthopedic spine surgery at Northwestern University Feinberg School of Medicine, Chicago, and his associates retrospectively reviewed the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) data files from 2006 to 2013 and limited their analysis to patients undergoing elective anterior cervical fusions, posterior cervical fusions, cervical laminectomy, cervical laminotomy, cervical discectomy, or corpectomy. They divided patients into one of three groups based on the following preoperative functional status parameters: independent, comprising those not requiring assistance or any equipment for activities of daily living (ADLs); partially dependent, including those with equipment such as prosthetics, equipment, or devices and requiring some assistance from another person for ADLs; and totally dependent, in which patients require total assistance for all ADLs. The researchers used univariate analysis to compare patient demographics, comorbidities, and 30-day postoperative complications among the three groups, followed by multivariate logistic regression to analyze the independent association of functional dependence on 30-day complications when controlling for procedure and comorbidity variances.
Dr. Patel reported findings from 24,357 patients: 23,620 (97.0%) functionally independent, 664 (2.7%) partially dependent, and 73 (0.3%) totally dependent. Dependent patients were significantly older and had higher rates of all comorbidities (P less than .001), with the exception of obesity (P = .214). In addition, 30-day complication rates were higher for all complications (P less than .001) other than neurological (P =.060) and surgical site complications (P =.668). When the researchers controlled for type of procedure and for disparities in patient preoperative variables, multivariate analyses demonstrated that functional dependence was independently associated with sepsis (odds ratio 6.40; P less than .001), pulmonary (OR 4.13; P less than .001), venous thromboembolism (OR 4.27, P less than .001), renal (OR 3.32; P less than .001), and cardiac complications (OR 4.68; P =.001), along with mortality (OR 8.31; P less than .001).
“The very strong association between functional dependence and mortality was quite surprising,” Dr. Patel said. “It was, to the contrary, also surprising to see that, despite wide variance in medical comorbidities and functional status, surgical complications such as infection and neurological injury were similar in all groups.” He characterized the study as “the first large-scale assessment of functional status as a predictor of patient outcomes after cervical spine surgery. It fits in line with other studies utilizing large databases. Big data analysis of outcomes can be used to identify risk factors for complications including death after surgery. Identifying these factors is important if we are going to improve the care we provide. Accurately quantifying the impact of these risk factors is also critical when we risk stratify and compare hospitals and physicians.”
He acknowledged certain limitations of the study, including the fact that it is a retrospective study “with a heterogeneous population of patients, surgeons, hospitals, and procedures. This adds uncertainty to the analysis at the level of the individual patient but does provide generalizability to a broader patient population.”
Dr. Patel reported having no conflicts of interest.
SAN DIEGO – Functional dependence following elective cervical spine procedures was associated with a significantly increased risk of almost all 30-day complications analyzed, including mortality, a large retrospective analysis of national data demonstrated.
The findings suggest that physicians should “include the patient’s level of functional independence, in addition to more traditional medical comorbidities, in the risk-benefit analysis of surgical decision making,” Dr. Alpesh A. Patel said in an interview in advance of the annual meeting of the Cervical Spine Research Society. “Those individuals with dependence need to be counseled appropriately about their increased risk of complications including mortality.”
Dr. Patel, professor and director of orthopedic spine surgery at Northwestern University Feinberg School of Medicine, Chicago, and his associates retrospectively reviewed the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) data files from 2006 to 2013 and limited their analysis to patients undergoing elective anterior cervical fusions, posterior cervical fusions, cervical laminectomy, cervical laminotomy, cervical discectomy, or corpectomy. They divided patients into one of three groups based on the following preoperative functional status parameters: independent, comprising those not requiring assistance or any equipment for activities of daily living (ADLs); partially dependent, including those with equipment such as prosthetics, equipment, or devices and requiring some assistance from another person for ADLs; and totally dependent, in which patients require total assistance for all ADLs. The researchers used univariate analysis to compare patient demographics, comorbidities, and 30-day postoperative complications among the three groups, followed by multivariate logistic regression to analyze the independent association of functional dependence on 30-day complications when controlling for procedure and comorbidity variances.
Dr. Patel reported findings from 24,357 patients: 23,620 (97.0%) functionally independent, 664 (2.7%) partially dependent, and 73 (0.3%) totally dependent. Dependent patients were significantly older and had higher rates of all comorbidities (P less than .001), with the exception of obesity (P = .214). In addition, 30-day complication rates were higher for all complications (P less than .001) other than neurological (P =.060) and surgical site complications (P =.668). When the researchers controlled for type of procedure and for disparities in patient preoperative variables, multivariate analyses demonstrated that functional dependence was independently associated with sepsis (odds ratio 6.40; P less than .001), pulmonary (OR 4.13; P less than .001), venous thromboembolism (OR 4.27, P less than .001), renal (OR 3.32; P less than .001), and cardiac complications (OR 4.68; P =.001), along with mortality (OR 8.31; P less than .001).
“The very strong association between functional dependence and mortality was quite surprising,” Dr. Patel said. “It was, to the contrary, also surprising to see that, despite wide variance in medical comorbidities and functional status, surgical complications such as infection and neurological injury were similar in all groups.” He characterized the study as “the first large-scale assessment of functional status as a predictor of patient outcomes after cervical spine surgery. It fits in line with other studies utilizing large databases. Big data analysis of outcomes can be used to identify risk factors for complications including death after surgery. Identifying these factors is important if we are going to improve the care we provide. Accurately quantifying the impact of these risk factors is also critical when we risk stratify and compare hospitals and physicians.”
He acknowledged certain limitations of the study, including the fact that it is a retrospective study “with a heterogeneous population of patients, surgeons, hospitals, and procedures. This adds uncertainty to the analysis at the level of the individual patient but does provide generalizability to a broader patient population.”
Dr. Patel reported having no conflicts of interest.
AT CSRS 2015
Key clinical point: Preoperative functional status is predictive of morbidity and mortality following elective cervical spine surgery.
Major finding: Patients who were dependent from a functional standpoint were significantly older and had higher rates of all comorbidities, compared with their counterparts who were partially dependent or functionally independent (P less than .001).
Data source: A retrospective analysis of 24,357 patient files from the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP).
Disclosures: Dr. Patel reported having no conflicts of interest.
Perioperative statins for cardiac surgery didn’t reduce kidney injury
SAN DIEGO – High-dose perioperative atorvastatin treatment did not reduce acute kidney injury following elective cardiac surgery, and it may increase risk in patients with chronic kidney disease (CKD) who are naive to statin treatment, results from a large, randomized trial showed.
“Despite advances in patient management that have reduced mortality during cardiac surgery, acute kidney injury continues to complicate the postoperative course in 20%-30% of patients,” Dr. Frederic Tremaine Billings said during a press briefing at a meeting sponsored by the American Society of Nephrology.
“Its diagnosis is independently associated with a fivefold increase in mortality following the surgery,” Dr. Tremaine added. “Statins affect several mechanisms underlying postoperative acute kidney injury. Widely prescribed to reduce cholesterol synthesis, these drugs also reduce lipid modification of intracellular signaling molecules, which have been shown to improve perfusion and reduce oxidative stress – both mechanisms important in acute kidney injury following cardiac surgery.”
Dr. Billings of the department of anesthesiology and critical care medicine at Vanderbilt University Medical Center, Nashville, Tenn., and his associates tested the hypothesis that short-term, high-dose perioperative (preoperative, intraoperative, and postoperative) atorvastatin reduces acute kidney injury (AKI) following elective cardiac surgery.
The researchers randomly assigned preoperative statin-naive patients to 80 mg of atorvastatin on the morning before surgery, 40 mg on the morning of surgery, and 40 mg daily throughout hospitalization, or to a matching placebo regimen. In addition, they randomly assigned patients who were already using statins prior to surgery to 80 mg of atorvastatin the morning of surgery, and 40 mg on the morning after surgery, or to a matching placebo regimen.
“We felt it was important to not withhold statin treatment in patients already using statins prior to surgery, beyond what is typically done in clinical practice,” Dr. Billings explained. “For this reason, preoperative statin–using subjects continued their statin up until the day before surgery, and then resumed their statin use on postoperative day 2.”
The primary endpoint of the study was the incidence of AKI as determined by Acute Kidney Injury Network criteria (a 0.3 mg/dL increase in serum creatinine concentrations within 48 hours of surgery). Secondary endpoints included the maximum creatinine increase from baseline to 48 hours after surgery, ICU delirium diagnosed by the Confusion Assessment Method for the ICU, myocardial injury, and the incidence of atrial fibrillation, pneumonia, and stroke. Safety endpoints included liver toxicity, muscle toxicity, and adverse events.
The study was limited to adults having elective cardiac surgery and excluded those with statin intolerance, acute coronary syndrome, liver dysfunction, use of CYP3A4 inhibitors, kidney transplant recipients, those currently on dialysis, and those who were pregnant.
From November 2009 to October 2014, the researchers recruited 653 patients. But the trial was halted on recommendation of Vanderbilt’s data and safety monitoring board because of futility and an increased incidence of AKI among statin-naive patients with CKD randomized to atorvastatin.
Among all patients, AKI occurred in 20.8% of those randomized to atorvastatin, compared with 19.5% of those randomized to placebo, a difference that was neither clinically nor statistically significant (P = .75), Dr. Billings reported.
However, among the 199 patients who were statin naive, AKI occurred in 21.6% of those randomized to atorvastatin, compared with 13.4% of those randomized to placebo (P = .14). “An 8% difference in the incidence of AKI is of clinical importance, if true,” he said.
Among the 36 statin-naive patients with CKD, AKI occurred in 52.9% of those randomized to atorvastatin, compared with 15.8% of those randomized to placebo (P = .03). “While the number of patients in this subgroup is small, the magnitude of effect is striking,” Dr. Billings said.
Among the 416 patients who were using statins prior to surgery, AKI occurred in 20.4% of those randomized to atorvastatin, compared with 22.4% of those randomized to placebo (P = .63). Results were similar among the subset of those patients who had CKD (31.3% vs. 36.3%; P = .59).
Safety endpoints were similar between the two groups.
Strengths of the study, Dr. Billings said, include the fact that it’s the largest randomized, controlled trial to date to test this hypothesis, the pragmatic design of the protocol, and rigorous methodology.
Limitations include the “small number of patients in the statin-naive CKD subgroup,” he noted. “And the short duration of treatment among prestudy statin-using patients could limit the observation that short-term withdrawal is not harmful – although we felt it appropriate not to limit statins beyond what’s typical in clinical practice, based on prior reports that even short-term statin withdrawal may be harmful.”
The National Institutes of Health and the department of anesthesiology at Vanderbilt University supported the study. Dr. Billings reported having no financial disclosures.
SAN DIEGO – High-dose perioperative atorvastatin treatment did not reduce acute kidney injury following elective cardiac surgery, and it may increase risk in patients with chronic kidney disease (CKD) who are naive to statin treatment, results from a large, randomized trial showed.
“Despite advances in patient management that have reduced mortality during cardiac surgery, acute kidney injury continues to complicate the postoperative course in 20%-30% of patients,” Dr. Frederic Tremaine Billings said during a press briefing at a meeting sponsored by the American Society of Nephrology.
“Its diagnosis is independently associated with a fivefold increase in mortality following the surgery,” Dr. Tremaine added. “Statins affect several mechanisms underlying postoperative acute kidney injury. Widely prescribed to reduce cholesterol synthesis, these drugs also reduce lipid modification of intracellular signaling molecules, which have been shown to improve perfusion and reduce oxidative stress – both mechanisms important in acute kidney injury following cardiac surgery.”
Dr. Billings of the department of anesthesiology and critical care medicine at Vanderbilt University Medical Center, Nashville, Tenn., and his associates tested the hypothesis that short-term, high-dose perioperative (preoperative, intraoperative, and postoperative) atorvastatin reduces acute kidney injury (AKI) following elective cardiac surgery.
The researchers randomly assigned preoperative statin-naive patients to 80 mg of atorvastatin on the morning before surgery, 40 mg on the morning of surgery, and 40 mg daily throughout hospitalization, or to a matching placebo regimen. In addition, they randomly assigned patients who were already using statins prior to surgery to 80 mg of atorvastatin the morning of surgery, and 40 mg on the morning after surgery, or to a matching placebo regimen.
“We felt it was important to not withhold statin treatment in patients already using statins prior to surgery, beyond what is typically done in clinical practice,” Dr. Billings explained. “For this reason, preoperative statin–using subjects continued their statin up until the day before surgery, and then resumed their statin use on postoperative day 2.”
The primary endpoint of the study was the incidence of AKI as determined by Acute Kidney Injury Network criteria (a 0.3 mg/dL increase in serum creatinine concentrations within 48 hours of surgery). Secondary endpoints included the maximum creatinine increase from baseline to 48 hours after surgery, ICU delirium diagnosed by the Confusion Assessment Method for the ICU, myocardial injury, and the incidence of atrial fibrillation, pneumonia, and stroke. Safety endpoints included liver toxicity, muscle toxicity, and adverse events.
The study was limited to adults having elective cardiac surgery and excluded those with statin intolerance, acute coronary syndrome, liver dysfunction, use of CYP3A4 inhibitors, kidney transplant recipients, those currently on dialysis, and those who were pregnant.
From November 2009 to October 2014, the researchers recruited 653 patients. But the trial was halted on recommendation of Vanderbilt’s data and safety monitoring board because of futility and an increased incidence of AKI among statin-naive patients with CKD randomized to atorvastatin.
Among all patients, AKI occurred in 20.8% of those randomized to atorvastatin, compared with 19.5% of those randomized to placebo, a difference that was neither clinically nor statistically significant (P = .75), Dr. Billings reported.
However, among the 199 patients who were statin naive, AKI occurred in 21.6% of those randomized to atorvastatin, compared with 13.4% of those randomized to placebo (P = .14). “An 8% difference in the incidence of AKI is of clinical importance, if true,” he said.
Among the 36 statin-naive patients with CKD, AKI occurred in 52.9% of those randomized to atorvastatin, compared with 15.8% of those randomized to placebo (P = .03). “While the number of patients in this subgroup is small, the magnitude of effect is striking,” Dr. Billings said.
Among the 416 patients who were using statins prior to surgery, AKI occurred in 20.4% of those randomized to atorvastatin, compared with 22.4% of those randomized to placebo (P = .63). Results were similar among the subset of those patients who had CKD (31.3% vs. 36.3%; P = .59).
Safety endpoints were similar between the two groups.
Strengths of the study, Dr. Billings said, include the fact that it’s the largest randomized, controlled trial to date to test this hypothesis, the pragmatic design of the protocol, and rigorous methodology.
Limitations include the “small number of patients in the statin-naive CKD subgroup,” he noted. “And the short duration of treatment among prestudy statin-using patients could limit the observation that short-term withdrawal is not harmful – although we felt it appropriate not to limit statins beyond what’s typical in clinical practice, based on prior reports that even short-term statin withdrawal may be harmful.”
The National Institutes of Health and the department of anesthesiology at Vanderbilt University supported the study. Dr. Billings reported having no financial disclosures.
SAN DIEGO – High-dose perioperative atorvastatin treatment did not reduce acute kidney injury following elective cardiac surgery, and it may increase risk in patients with chronic kidney disease (CKD) who are naive to statin treatment, results from a large, randomized trial showed.
“Despite advances in patient management that have reduced mortality during cardiac surgery, acute kidney injury continues to complicate the postoperative course in 20%-30% of patients,” Dr. Frederic Tremaine Billings said during a press briefing at a meeting sponsored by the American Society of Nephrology.
“Its diagnosis is independently associated with a fivefold increase in mortality following the surgery,” Dr. Tremaine added. “Statins affect several mechanisms underlying postoperative acute kidney injury. Widely prescribed to reduce cholesterol synthesis, these drugs also reduce lipid modification of intracellular signaling molecules, which have been shown to improve perfusion and reduce oxidative stress – both mechanisms important in acute kidney injury following cardiac surgery.”
Dr. Billings of the department of anesthesiology and critical care medicine at Vanderbilt University Medical Center, Nashville, Tenn., and his associates tested the hypothesis that short-term, high-dose perioperative (preoperative, intraoperative, and postoperative) atorvastatin reduces acute kidney injury (AKI) following elective cardiac surgery.
The researchers randomly assigned preoperative statin-naive patients to 80 mg of atorvastatin on the morning before surgery, 40 mg on the morning of surgery, and 40 mg daily throughout hospitalization, or to a matching placebo regimen. In addition, they randomly assigned patients who were already using statins prior to surgery to 80 mg of atorvastatin the morning of surgery, and 40 mg on the morning after surgery, or to a matching placebo regimen.
“We felt it was important to not withhold statin treatment in patients already using statins prior to surgery, beyond what is typically done in clinical practice,” Dr. Billings explained. “For this reason, preoperative statin–using subjects continued their statin up until the day before surgery, and then resumed their statin use on postoperative day 2.”
The primary endpoint of the study was the incidence of AKI as determined by Acute Kidney Injury Network criteria (a 0.3 mg/dL increase in serum creatinine concentrations within 48 hours of surgery). Secondary endpoints included the maximum creatinine increase from baseline to 48 hours after surgery, ICU delirium diagnosed by the Confusion Assessment Method for the ICU, myocardial injury, and the incidence of atrial fibrillation, pneumonia, and stroke. Safety endpoints included liver toxicity, muscle toxicity, and adverse events.
The study was limited to adults having elective cardiac surgery and excluded those with statin intolerance, acute coronary syndrome, liver dysfunction, use of CYP3A4 inhibitors, kidney transplant recipients, those currently on dialysis, and those who were pregnant.
From November 2009 to October 2014, the researchers recruited 653 patients. But the trial was halted on recommendation of Vanderbilt’s data and safety monitoring board because of futility and an increased incidence of AKI among statin-naive patients with CKD randomized to atorvastatin.
Among all patients, AKI occurred in 20.8% of those randomized to atorvastatin, compared with 19.5% of those randomized to placebo, a difference that was neither clinically nor statistically significant (P = .75), Dr. Billings reported.
However, among the 199 patients who were statin naive, AKI occurred in 21.6% of those randomized to atorvastatin, compared with 13.4% of those randomized to placebo (P = .14). “An 8% difference in the incidence of AKI is of clinical importance, if true,” he said.
Among the 36 statin-naive patients with CKD, AKI occurred in 52.9% of those randomized to atorvastatin, compared with 15.8% of those randomized to placebo (P = .03). “While the number of patients in this subgroup is small, the magnitude of effect is striking,” Dr. Billings said.
Among the 416 patients who were using statins prior to surgery, AKI occurred in 20.4% of those randomized to atorvastatin, compared with 22.4% of those randomized to placebo (P = .63). Results were similar among the subset of those patients who had CKD (31.3% vs. 36.3%; P = .59).
Safety endpoints were similar between the two groups.
Strengths of the study, Dr. Billings said, include the fact that it’s the largest randomized, controlled trial to date to test this hypothesis, the pragmatic design of the protocol, and rigorous methodology.
Limitations include the “small number of patients in the statin-naive CKD subgroup,” he noted. “And the short duration of treatment among prestudy statin-using patients could limit the observation that short-term withdrawal is not harmful – although we felt it appropriate not to limit statins beyond what’s typical in clinical practice, based on prior reports that even short-term statin withdrawal may be harmful.”
The National Institutes of Health and the department of anesthesiology at Vanderbilt University supported the study. Dr. Billings reported having no financial disclosures.
AT KIDNEY WEEK 2015
Key clinical point: The use of high-dose perioperative atorvastatin did not reduce acute kidney injury in patients undergoing elective cardiac surgery.
Major finding: Among all patients, acute kidney injury occurred in 20.8% of those randomized to atorvastatin, compared with 19.5% of those randomized to placebo, a difference that is neither clinically nor statistically significant (P = .75).
Data source: A randomized, controlled trial of 653 patients to test the hypothesis that short-term, high-dose perioperative atorvastatin reduces acute kidney injury following elective cardiac surgery.
Disclosures: The National Institutes of Health and the department of anesthesiology at Vanderbilt University supported the study. Dr. Billings reported having no financial disclosures.
Self-reported poor functional status predicts perioperative morbidity
SAN DIEGO – Among patients with pulmonary hypertension presenting for elective surgery, self-reported poor functional status is associated with multiple comorbidities and is independently predictive of longer hospital length of stay, results from an ongoing single-center study suggest.
“Patients with pulmonary hypertension (PHTN) presenting for elective surgery are at significantly higher risk for adverse perioperative outcomes, including increased hospital length of stay, right ventricular failure, cardiac arrhythmia, persistent postoperative hypoxemia, coronary ischemia and death,” researchers led by Dr. Aalap C. Shah wrote in an abstract presented at the at the annual meeting of the American Society of Anesthesiologists. “The diagnosis of PHTN is based on costly echocardiographic examination and right heart catheterization and should be reserved for high-risk patients. No studies have assessed the role of self-reported functional classification on PHTN severity stratification, and few studies have achieved a sufficiently large patient sample size.”
In an effort to evaluate the predictive value of self-reported exercise tolerance on echocardiogram findings, outcomes, and length of stay (LOS) after noncardiac, nonobstetric surgery, the researchers queried the University of Washington database for all PHTN seen in preoperative anesthesia clinic for noncardiac, nonobstetric procedures from April 2007 through September 2013. Inclusion criteria required an echocardiogram less than 1 year prior to the procedure and available patient-reported functional status, which was defined as less than four metabolic equivalents (METS) in exercise testing or four METS or greater. Dr. Shah, formerly a resident in the University of Washington’s department of anesthesiology and pain medicine, and his associates used univariate analyses to compare functional status with echocardiographic findings, complication rates, and length of stay (LOS). At the meeting he presented results from 294 patients evaluated to date: 143 with normal functional status and 151 with poor functional status. Their mean age was 62 years, and 51% of patients were female.
Compared with their counterparts with normal functional status, patients with poor functional status trended toward a higher complication rate at hospital discharge (14.6% vs. 7%, respectively; P = .041) and had a higher cumulative rate of complications (33 vs. 15; P = .035). However, no association between functional status and complications was observed 30 days postoperatively.
Patients with poor functional status had a significantly longer average LOS, compared with patients with normal functional status (7.21 vs. 4.73 days; P = .047). Open surgical approach was also an independent predictor of increased LOS (odds ratio 2.39; P = .005). No significant independent predictors of complications were observed at discharge or 30 days postoperatively.
“Going forward, the goal is to use these data to create a risk stratification algorithm to figure out: Does a patient with good functional status and pulmonary hypertension undergoing toe surgery, for example, really need an echocardiogram before getting surgery?” said Dr. Shah said, who is now an anesthesiology fellow at Boston Children’s Hospital. “Hopefully we can show that using these risk stratification algorithms can decrease the costs and decrease the time to actually getting surgery.”
The researchers reported having no financial disclosures.
SAN DIEGO – Among patients with pulmonary hypertension presenting for elective surgery, self-reported poor functional status is associated with multiple comorbidities and is independently predictive of longer hospital length of stay, results from an ongoing single-center study suggest.
“Patients with pulmonary hypertension (PHTN) presenting for elective surgery are at significantly higher risk for adverse perioperative outcomes, including increased hospital length of stay, right ventricular failure, cardiac arrhythmia, persistent postoperative hypoxemia, coronary ischemia and death,” researchers led by Dr. Aalap C. Shah wrote in an abstract presented at the at the annual meeting of the American Society of Anesthesiologists. “The diagnosis of PHTN is based on costly echocardiographic examination and right heart catheterization and should be reserved for high-risk patients. No studies have assessed the role of self-reported functional classification on PHTN severity stratification, and few studies have achieved a sufficiently large patient sample size.”
In an effort to evaluate the predictive value of self-reported exercise tolerance on echocardiogram findings, outcomes, and length of stay (LOS) after noncardiac, nonobstetric surgery, the researchers queried the University of Washington database for all PHTN seen in preoperative anesthesia clinic for noncardiac, nonobstetric procedures from April 2007 through September 2013. Inclusion criteria required an echocardiogram less than 1 year prior to the procedure and available patient-reported functional status, which was defined as less than four metabolic equivalents (METS) in exercise testing or four METS or greater. Dr. Shah, formerly a resident in the University of Washington’s department of anesthesiology and pain medicine, and his associates used univariate analyses to compare functional status with echocardiographic findings, complication rates, and length of stay (LOS). At the meeting he presented results from 294 patients evaluated to date: 143 with normal functional status and 151 with poor functional status. Their mean age was 62 years, and 51% of patients were female.
Compared with their counterparts with normal functional status, patients with poor functional status trended toward a higher complication rate at hospital discharge (14.6% vs. 7%, respectively; P = .041) and had a higher cumulative rate of complications (33 vs. 15; P = .035). However, no association between functional status and complications was observed 30 days postoperatively.
Patients with poor functional status had a significantly longer average LOS, compared with patients with normal functional status (7.21 vs. 4.73 days; P = .047). Open surgical approach was also an independent predictor of increased LOS (odds ratio 2.39; P = .005). No significant independent predictors of complications were observed at discharge or 30 days postoperatively.
“Going forward, the goal is to use these data to create a risk stratification algorithm to figure out: Does a patient with good functional status and pulmonary hypertension undergoing toe surgery, for example, really need an echocardiogram before getting surgery?” said Dr. Shah said, who is now an anesthesiology fellow at Boston Children’s Hospital. “Hopefully we can show that using these risk stratification algorithms can decrease the costs and decrease the time to actually getting surgery.”
The researchers reported having no financial disclosures.
SAN DIEGO – Among patients with pulmonary hypertension presenting for elective surgery, self-reported poor functional status is associated with multiple comorbidities and is independently predictive of longer hospital length of stay, results from an ongoing single-center study suggest.
“Patients with pulmonary hypertension (PHTN) presenting for elective surgery are at significantly higher risk for adverse perioperative outcomes, including increased hospital length of stay, right ventricular failure, cardiac arrhythmia, persistent postoperative hypoxemia, coronary ischemia and death,” researchers led by Dr. Aalap C. Shah wrote in an abstract presented at the at the annual meeting of the American Society of Anesthesiologists. “The diagnosis of PHTN is based on costly echocardiographic examination and right heart catheterization and should be reserved for high-risk patients. No studies have assessed the role of self-reported functional classification on PHTN severity stratification, and few studies have achieved a sufficiently large patient sample size.”
In an effort to evaluate the predictive value of self-reported exercise tolerance on echocardiogram findings, outcomes, and length of stay (LOS) after noncardiac, nonobstetric surgery, the researchers queried the University of Washington database for all PHTN seen in preoperative anesthesia clinic for noncardiac, nonobstetric procedures from April 2007 through September 2013. Inclusion criteria required an echocardiogram less than 1 year prior to the procedure and available patient-reported functional status, which was defined as less than four metabolic equivalents (METS) in exercise testing or four METS or greater. Dr. Shah, formerly a resident in the University of Washington’s department of anesthesiology and pain medicine, and his associates used univariate analyses to compare functional status with echocardiographic findings, complication rates, and length of stay (LOS). At the meeting he presented results from 294 patients evaluated to date: 143 with normal functional status and 151 with poor functional status. Their mean age was 62 years, and 51% of patients were female.
Compared with their counterparts with normal functional status, patients with poor functional status trended toward a higher complication rate at hospital discharge (14.6% vs. 7%, respectively; P = .041) and had a higher cumulative rate of complications (33 vs. 15; P = .035). However, no association between functional status and complications was observed 30 days postoperatively.
Patients with poor functional status had a significantly longer average LOS, compared with patients with normal functional status (7.21 vs. 4.73 days; P = .047). Open surgical approach was also an independent predictor of increased LOS (odds ratio 2.39; P = .005). No significant independent predictors of complications were observed at discharge or 30 days postoperatively.
“Going forward, the goal is to use these data to create a risk stratification algorithm to figure out: Does a patient with good functional status and pulmonary hypertension undergoing toe surgery, for example, really need an echocardiogram before getting surgery?” said Dr. Shah said, who is now an anesthesiology fellow at Boston Children’s Hospital. “Hopefully we can show that using these risk stratification algorithms can decrease the costs and decrease the time to actually getting surgery.”
The researchers reported having no financial disclosures.
AT THE ASA ANNUAL MEETING
Key clinical point:Poor self-reported exercise tolerance by patients with pulmonary hypertension is associated with multiple comorbidities and increased hospital length of stay.
Major finding: Compared with their counterparts with normal functional status, patients with poor functional status trended toward a higher complication rate at hospital discharge (14.6% vs. 7%, respectively; P = .041) and had a higher cumulative rate of complications (33 vs. 15; P = .035).
Data source: A study 294 PHTN patients seen in preoperative anesthesia clinic at the University of Washington for non-cardiac, nonobstetric procedures from April 2007 through September 2013.
Disclosures: The researchers reported having no financial disclosures.
Endobronchial valves improve pulmonary function in emphysema
Endobronchial valves improved pulmonary function, exercise capacity, and quality of life in a prospective randomized controlled trial involving 68 adults with severe emphysema, according to a report published online Dec. 10 in the New England Journal of Medicine.
“The improvements we found were of greater magnitude than those noted with pharmacologic treatment in comparable patients and were similar to improvements with surgical lung-volume reduction, but with significantly less morbidity,” said Karin Klooster of the department of pulmonary diseases, University Medical Center Groningen (the Netherlands) and her associates.
Previous research suggested that bronchoscopic lung-volume reduction using one-way endobronchial valves to block inspiratory but not expiratory air flow would be most effective in patients who had a complete rather than an incomplete fissure between the targeted lobe and the adjacent lobe on high-resolution CT. “A complete fissure on HRCT [high-resolution computed tomography] is a surrogate finding for the absence of interlobar collateral ventilation; if there is collateral ventilation, an occluded lobe can be reinflated through its collaterals,” defeating the purpose of the procedure, the researchers wrote.
During a 3-year period, Ms. Klooster and her associates studied emphysema patients who were older than 35 years (mean age, 58-59) and had a postbronchodilator forced expiratory volume in 1 second (FEV1) less than 60% of predicted volume, a total lung capacity more than 100% of the predicted value, and residual volume more than 150% of predicted volume. On HRCT, all the study participants showed a complete or nearly complete fissure between the targeted lobe and the adjacent lobe. They were randomly assigned to receive endobronchial valves (34 patients) or usual care (34 control subjects) and followed for 6 months. At that time, control subjects were allowed to crossover and receive endobronchial valves as well.
The median procedure time was 18 minutes (range, 6-51 minutes), and the median number of valves placed in each patient was 4 (range, 2-7 valves). The median hospital stay was 1 day (range, 1-13 days).
Compared with the control subjects, patients who received endobronchial valves showed a reduction in target lobar volume of 1,366 mL. This was accompanied by improvements in FEV1 by 191 mL, in forced vital capacity by 442 mL, in residual lung volume, in longer 6-minute walk distance by 106 meters, in scores on the Clinical COPD Questionnaire measuring daily functioning, and in scores on the St. George’s Respiratory Questionnaire measuring quality of life. The results for the control subjects who crossed over to the active-treatment group were very similar, the investigators said (N Engl J Med. 2015 Dec 10;373:2325-35. doi:10.1056/NEJMoa1507807).
However, several adverse effects occurred, and close monitoring of this patient population is crucial. The most common complication was pneumothorax, which developed in 6 of the 34 patients (18%), usually within 1 day of undergoing the procedure. Pneumothorax resolved spontaneously in one patient but required chest-tube drainage in the other five; it resolved in one patient after temporary removal of the valves to promote healing, and in another after permanent removal of all valves.
Other adverse effects, some of which required repeat bronchoscopy, included torsion of the lower-lobe bronchus after upper-lobe treatment (two patients), pneumonia distal to the valves (one patient), increased dyspnea and sputum production (two patients), valve migration (two patients), valve dislocation because of granulation-tissue formation (one patient), and persistent cough (one patient). Despite these setbacks, “the overall outcome of treatment was positive,” Ms. Klooster and her associates said.
All patients who underwent valve removal recovered without any further adverse effects, indicating that this treatment “is fully reversible and doesn’t preclude further therapeutic options,” they added.
The study was supported by the Netherlands Organization for Health Research and Development and the University Medical Center Groningen. Ms. Klooster reported receiving fees, devices, travel support, and grant support from Pulmonx and PneumRx/BTG; her associates reported ties to numerous industry sponsors. Pulmonx commercially supplied the endobronchial valves for the study.
Endobronchial valves improved pulmonary function, exercise capacity, and quality of life in a prospective randomized controlled trial involving 68 adults with severe emphysema, according to a report published online Dec. 10 in the New England Journal of Medicine.
“The improvements we found were of greater magnitude than those noted with pharmacologic treatment in comparable patients and were similar to improvements with surgical lung-volume reduction, but with significantly less morbidity,” said Karin Klooster of the department of pulmonary diseases, University Medical Center Groningen (the Netherlands) and her associates.
Previous research suggested that bronchoscopic lung-volume reduction using one-way endobronchial valves to block inspiratory but not expiratory air flow would be most effective in patients who had a complete rather than an incomplete fissure between the targeted lobe and the adjacent lobe on high-resolution CT. “A complete fissure on HRCT [high-resolution computed tomography] is a surrogate finding for the absence of interlobar collateral ventilation; if there is collateral ventilation, an occluded lobe can be reinflated through its collaterals,” defeating the purpose of the procedure, the researchers wrote.
During a 3-year period, Ms. Klooster and her associates studied emphysema patients who were older than 35 years (mean age, 58-59) and had a postbronchodilator forced expiratory volume in 1 second (FEV1) less than 60% of predicted volume, a total lung capacity more than 100% of the predicted value, and residual volume more than 150% of predicted volume. On HRCT, all the study participants showed a complete or nearly complete fissure between the targeted lobe and the adjacent lobe. They were randomly assigned to receive endobronchial valves (34 patients) or usual care (34 control subjects) and followed for 6 months. At that time, control subjects were allowed to crossover and receive endobronchial valves as well.
The median procedure time was 18 minutes (range, 6-51 minutes), and the median number of valves placed in each patient was 4 (range, 2-7 valves). The median hospital stay was 1 day (range, 1-13 days).
Compared with the control subjects, patients who received endobronchial valves showed a reduction in target lobar volume of 1,366 mL. This was accompanied by improvements in FEV1 by 191 mL, in forced vital capacity by 442 mL, in residual lung volume, in longer 6-minute walk distance by 106 meters, in scores on the Clinical COPD Questionnaire measuring daily functioning, and in scores on the St. George’s Respiratory Questionnaire measuring quality of life. The results for the control subjects who crossed over to the active-treatment group were very similar, the investigators said (N Engl J Med. 2015 Dec 10;373:2325-35. doi:10.1056/NEJMoa1507807).
However, several adverse effects occurred, and close monitoring of this patient population is crucial. The most common complication was pneumothorax, which developed in 6 of the 34 patients (18%), usually within 1 day of undergoing the procedure. Pneumothorax resolved spontaneously in one patient but required chest-tube drainage in the other five; it resolved in one patient after temporary removal of the valves to promote healing, and in another after permanent removal of all valves.
Other adverse effects, some of which required repeat bronchoscopy, included torsion of the lower-lobe bronchus after upper-lobe treatment (two patients), pneumonia distal to the valves (one patient), increased dyspnea and sputum production (two patients), valve migration (two patients), valve dislocation because of granulation-tissue formation (one patient), and persistent cough (one patient). Despite these setbacks, “the overall outcome of treatment was positive,” Ms. Klooster and her associates said.
All patients who underwent valve removal recovered without any further adverse effects, indicating that this treatment “is fully reversible and doesn’t preclude further therapeutic options,” they added.
The study was supported by the Netherlands Organization for Health Research and Development and the University Medical Center Groningen. Ms. Klooster reported receiving fees, devices, travel support, and grant support from Pulmonx and PneumRx/BTG; her associates reported ties to numerous industry sponsors. Pulmonx commercially supplied the endobronchial valves for the study.
Endobronchial valves improved pulmonary function, exercise capacity, and quality of life in a prospective randomized controlled trial involving 68 adults with severe emphysema, according to a report published online Dec. 10 in the New England Journal of Medicine.
“The improvements we found were of greater magnitude than those noted with pharmacologic treatment in comparable patients and were similar to improvements with surgical lung-volume reduction, but with significantly less morbidity,” said Karin Klooster of the department of pulmonary diseases, University Medical Center Groningen (the Netherlands) and her associates.
Previous research suggested that bronchoscopic lung-volume reduction using one-way endobronchial valves to block inspiratory but not expiratory air flow would be most effective in patients who had a complete rather than an incomplete fissure between the targeted lobe and the adjacent lobe on high-resolution CT. “A complete fissure on HRCT [high-resolution computed tomography] is a surrogate finding for the absence of interlobar collateral ventilation; if there is collateral ventilation, an occluded lobe can be reinflated through its collaterals,” defeating the purpose of the procedure, the researchers wrote.
During a 3-year period, Ms. Klooster and her associates studied emphysema patients who were older than 35 years (mean age, 58-59) and had a postbronchodilator forced expiratory volume in 1 second (FEV1) less than 60% of predicted volume, a total lung capacity more than 100% of the predicted value, and residual volume more than 150% of predicted volume. On HRCT, all the study participants showed a complete or nearly complete fissure between the targeted lobe and the adjacent lobe. They were randomly assigned to receive endobronchial valves (34 patients) or usual care (34 control subjects) and followed for 6 months. At that time, control subjects were allowed to crossover and receive endobronchial valves as well.
The median procedure time was 18 minutes (range, 6-51 minutes), and the median number of valves placed in each patient was 4 (range, 2-7 valves). The median hospital stay was 1 day (range, 1-13 days).
Compared with the control subjects, patients who received endobronchial valves showed a reduction in target lobar volume of 1,366 mL. This was accompanied by improvements in FEV1 by 191 mL, in forced vital capacity by 442 mL, in residual lung volume, in longer 6-minute walk distance by 106 meters, in scores on the Clinical COPD Questionnaire measuring daily functioning, and in scores on the St. George’s Respiratory Questionnaire measuring quality of life. The results for the control subjects who crossed over to the active-treatment group were very similar, the investigators said (N Engl J Med. 2015 Dec 10;373:2325-35. doi:10.1056/NEJMoa1507807).
However, several adverse effects occurred, and close monitoring of this patient population is crucial. The most common complication was pneumothorax, which developed in 6 of the 34 patients (18%), usually within 1 day of undergoing the procedure. Pneumothorax resolved spontaneously in one patient but required chest-tube drainage in the other five; it resolved in one patient after temporary removal of the valves to promote healing, and in another after permanent removal of all valves.
Other adverse effects, some of which required repeat bronchoscopy, included torsion of the lower-lobe bronchus after upper-lobe treatment (two patients), pneumonia distal to the valves (one patient), increased dyspnea and sputum production (two patients), valve migration (two patients), valve dislocation because of granulation-tissue formation (one patient), and persistent cough (one patient). Despite these setbacks, “the overall outcome of treatment was positive,” Ms. Klooster and her associates said.
All patients who underwent valve removal recovered without any further adverse effects, indicating that this treatment “is fully reversible and doesn’t preclude further therapeutic options,” they added.
The study was supported by the Netherlands Organization for Health Research and Development and the University Medical Center Groningen. Ms. Klooster reported receiving fees, devices, travel support, and grant support from Pulmonx and PneumRx/BTG; her associates reported ties to numerous industry sponsors. Pulmonx commercially supplied the endobronchial valves for the study.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Endobronchial valves improved pulmonary function, exercise capacity, and QOL in severe emphysema.
Major finding: Patients who received endobronchial valves showed improved FEV1 by 191 mL, forced vital capacity by 442 mL, residual lung volume, 6-minute walk distance by 106 meters, and QOL scores.
Data source: A prospective randomized controlled trial involving 68 patients treated during a 3-year period at a single medical center.
Disclosures: The Netherlands Organization for Health Research and Development and the University Medical Center Groningen funded the study. Ms. Klooster reported receiving fees, devices, travel support, and grant support from Pulmonx and PneumRx/BTG; her associates reported ties to numerous industry sponsors. Pulmonx commercially supplied the endobronchial valves for this study.
Study: TKA patients recover faster with periarticular analgesia injection
Patients more often recovered faster from a total knee arthroplasty (TKA) when they received a periarticular injection of analgesic medication than when they received a femoral nerve block for the same surgery on the opposite knee in a study.
The study included 16 recipients of bilateral primary TKA, who received a femoral nerve block at their first TKA operation and a periarticular injection of an extended-release bupivacaine liposome mixture at the second operation. An average of 2.3 years passed between the two procedures, and the same surgeon performed all surgeries, which occurred between March 2009 and August 2013. Two patients were excluded from the study because of subacute rehabilitation admission delay and a third patient was left out of the study because of respiratory failure, resulting in admission to the ICU.
Following the TKA with a periarticular injection of analgesic medication, the average number of inpatient physical therapy sessions a patient completed was 2.3 (standard deviation: 1.0); the average number of inpatient physical therapy sessions a patient completed after having the TKA with femoral nerve block was 3.5 (SD: 1.3). The average number of hospital days following the TKA with periarticular injection was also a smaller number. The mean number of hospital days following the periarticular injection was 1.5 (SD: 0.6 days). compared with 1.9 days (SD: 0.6 days; P is less than .032) following the femoral nerve block.
“Our data demonstrate that periarticular injection of analgesia allowed patients to complete their inpatient physical therapy sessions and to be discharged sooner, compared with femoral nerve block. This finding suggests that patients who receive periarticular injection of analgesia are able to ambulate independently faster because it does not affect postoperative motor function,” according to Dr. Brandon J. Horn and his colleagues.
Read the full study in the Journal of the American Osteopathic Association (doi: 10.7556/jaoa.2015.146).
Patients more often recovered faster from a total knee arthroplasty (TKA) when they received a periarticular injection of analgesic medication than when they received a femoral nerve block for the same surgery on the opposite knee in a study.
The study included 16 recipients of bilateral primary TKA, who received a femoral nerve block at their first TKA operation and a periarticular injection of an extended-release bupivacaine liposome mixture at the second operation. An average of 2.3 years passed between the two procedures, and the same surgeon performed all surgeries, which occurred between March 2009 and August 2013. Two patients were excluded from the study because of subacute rehabilitation admission delay and a third patient was left out of the study because of respiratory failure, resulting in admission to the ICU.
Following the TKA with a periarticular injection of analgesic medication, the average number of inpatient physical therapy sessions a patient completed was 2.3 (standard deviation: 1.0); the average number of inpatient physical therapy sessions a patient completed after having the TKA with femoral nerve block was 3.5 (SD: 1.3). The average number of hospital days following the TKA with periarticular injection was also a smaller number. The mean number of hospital days following the periarticular injection was 1.5 (SD: 0.6 days). compared with 1.9 days (SD: 0.6 days; P is less than .032) following the femoral nerve block.
“Our data demonstrate that periarticular injection of analgesia allowed patients to complete their inpatient physical therapy sessions and to be discharged sooner, compared with femoral nerve block. This finding suggests that patients who receive periarticular injection of analgesia are able to ambulate independently faster because it does not affect postoperative motor function,” according to Dr. Brandon J. Horn and his colleagues.
Read the full study in the Journal of the American Osteopathic Association (doi: 10.7556/jaoa.2015.146).
Patients more often recovered faster from a total knee arthroplasty (TKA) when they received a periarticular injection of analgesic medication than when they received a femoral nerve block for the same surgery on the opposite knee in a study.
The study included 16 recipients of bilateral primary TKA, who received a femoral nerve block at their first TKA operation and a periarticular injection of an extended-release bupivacaine liposome mixture at the second operation. An average of 2.3 years passed between the two procedures, and the same surgeon performed all surgeries, which occurred between March 2009 and August 2013. Two patients were excluded from the study because of subacute rehabilitation admission delay and a third patient was left out of the study because of respiratory failure, resulting in admission to the ICU.
Following the TKA with a periarticular injection of analgesic medication, the average number of inpatient physical therapy sessions a patient completed was 2.3 (standard deviation: 1.0); the average number of inpatient physical therapy sessions a patient completed after having the TKA with femoral nerve block was 3.5 (SD: 1.3). The average number of hospital days following the TKA with periarticular injection was also a smaller number. The mean number of hospital days following the periarticular injection was 1.5 (SD: 0.6 days). compared with 1.9 days (SD: 0.6 days; P is less than .032) following the femoral nerve block.
“Our data demonstrate that periarticular injection of analgesia allowed patients to complete their inpatient physical therapy sessions and to be discharged sooner, compared with femoral nerve block. This finding suggests that patients who receive periarticular injection of analgesia are able to ambulate independently faster because it does not affect postoperative motor function,” according to Dr. Brandon J. Horn and his colleagues.
Read the full study in the Journal of the American Osteopathic Association (doi: 10.7556/jaoa.2015.146).
FROM THE JOURNAL OF THE AMERICAN OSTEOPATHIC ASSOCIATION
Postop C. diff infection associated with presurgical antibiotics
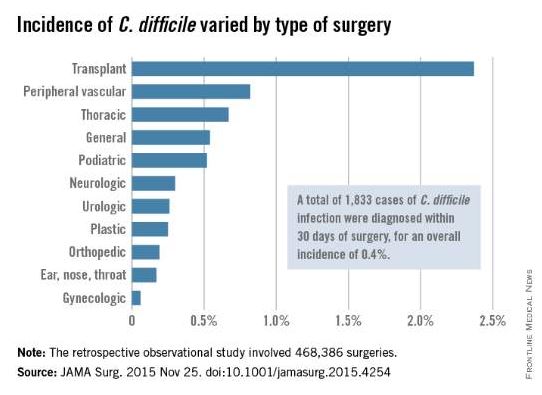
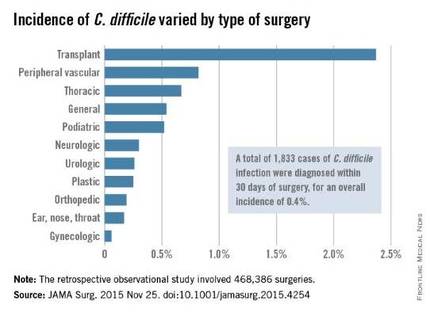
A hospital’s rate of postoperative Clostridium difficile infection is related to the number of preoperative antibiotics patients have taken, the complexity of their procedures, and the complexity of the hospital’s surgical program, in addition to known risk factors for the infection, according to a report published online in JAMA Surgery.
Several risk factors for postoperative C. difficile infection have already been identified, including advanced age and comorbidity. To examine known risk factors and identify possible new ones, researchers analyzed information from the Veterans Affairs Surgical Quality Improvement Program’s database, which documents all noncardiac operations at 134 VA medical centers each year.
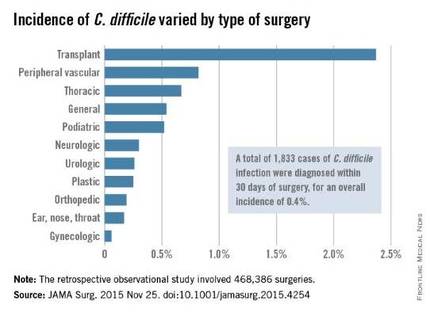
The investigators focused on 468,386 procedures performed during a 4-year period. A total of 1,833 cases of C. difficile infection were diagnosed within 30 days of surgery, for an overall incidence of 0.4% in this predominantly male, elderly population, said Xinli Li, Ph.D., of the Veterans Health Administration, Washington, and associates.
As expected, patients who developed postoperative C. difficile infection were significantly older than those who didn’t (mean age, 67.4 vs. 60.6 years) and were significantly more likely to have comorbidities such as impaired functional status, heart failure, chronic obstructive pulmonary disease, ascites, renal failure, bleeding disorders, wound infection, and recent weight loss.
Unexpectedly, the number of different antibiotics taken during the 60 days preceding surgery also was significantly associated with C. difficile infection. Patients who had taken three or more antibiotics from different classes were nearly six times more likely to develop C. difficile than patients who had taken only one or no antibiotics, the investigators reported (JAMA Surg. 2015 Nov 25. doi: 10.1001/jamasurg.2015.4263).In addition, patients who underwent more complex surgical procedures were at increased risk of this complication, as were patients at hospitals that frequently handled complex procedures. “These factors reflect the illness of patients, duration of operation, and hospital setting; each is an established risk factor for C. difficile infection,” Dr. Li and associates wrote.
Patients with C. difficile infection had higher rates of postoperative other morbidity (86.0% vs. 7.1%) and 30-day mortality (5.3% vs. 1.0%) and longer postoperative hospital stays (17.9 days vs. 3.6 days).
Contrary to previous studies, this study did not show a temporal increase in C. difficile infection. The overall incidence, as well as the incidences at individual hospitals, remained constant during the entire 4-year study period, the investigators added.
The incidence of C. difficile varied substantially among the 134 VA medical centers, from 0% to 1.35% of all surgical patients. “Surgical administrators and clinical teams may consider the results of this study to target interventions for specific patients undergoing high-risk procedures. Such interventions include selective antibiotic administration, early testing of at-risk patients, hand hygiene with nonalcohol agents, early contact precautions, and specific environmental cleaning protocols,” Dr. Li and associates wrote.
This study was supported by the Veterans Health Administration. Dr. Li and associates reported having no relevant financial disclosures.
The most important finding to highlight in the report by Li et al. is the 12-fold increase in morbidity and 5-fold increase in mortality among patients who developed postoperative C. difficile infection.
The study results underscore the importance of infection control and prevention efforts. They also show how important it is to develop prophylactic strategies, expeditious recognition of C. difficile, adequate supportive care, and improved therapies.
Dr. Paul K. Waltz and Dr. Brian S. Zuckerbraun are at the VA Pittsburgh Healthcare System and the University of Pennsylvania, Pittsburgh. They made these remarks in an invited commentary accompanying Dr. Li’s report (JAMA Surg. 2015 Nov 25. doi: 10.1001/jamasurg.2015.4254).
The most important finding to highlight in the report by Li et al. is the 12-fold increase in morbidity and 5-fold increase in mortality among patients who developed postoperative C. difficile infection.
The study results underscore the importance of infection control and prevention efforts. They also show how important it is to develop prophylactic strategies, expeditious recognition of C. difficile, adequate supportive care, and improved therapies.
Dr. Paul K. Waltz and Dr. Brian S. Zuckerbraun are at the VA Pittsburgh Healthcare System and the University of Pennsylvania, Pittsburgh. They made these remarks in an invited commentary accompanying Dr. Li’s report (JAMA Surg. 2015 Nov 25. doi: 10.1001/jamasurg.2015.4254).
The most important finding to highlight in the report by Li et al. is the 12-fold increase in morbidity and 5-fold increase in mortality among patients who developed postoperative C. difficile infection.
The study results underscore the importance of infection control and prevention efforts. They also show how important it is to develop prophylactic strategies, expeditious recognition of C. difficile, adequate supportive care, and improved therapies.
Dr. Paul K. Waltz and Dr. Brian S. Zuckerbraun are at the VA Pittsburgh Healthcare System and the University of Pennsylvania, Pittsburgh. They made these remarks in an invited commentary accompanying Dr. Li’s report (JAMA Surg. 2015 Nov 25. doi: 10.1001/jamasurg.2015.4254).
A hospital’s rate of postoperative Clostridium difficile infection is related to the number of preoperative antibiotics patients have taken, the complexity of their procedures, and the complexity of the hospital’s surgical program, in addition to known risk factors for the infection, according to a report published online in JAMA Surgery.
Several risk factors for postoperative C. difficile infection have already been identified, including advanced age and comorbidity. To examine known risk factors and identify possible new ones, researchers analyzed information from the Veterans Affairs Surgical Quality Improvement Program’s database, which documents all noncardiac operations at 134 VA medical centers each year.
The investigators focused on 468,386 procedures performed during a 4-year period. A total of 1,833 cases of C. difficile infection were diagnosed within 30 days of surgery, for an overall incidence of 0.4% in this predominantly male, elderly population, said Xinli Li, Ph.D., of the Veterans Health Administration, Washington, and associates.
As expected, patients who developed postoperative C. difficile infection were significantly older than those who didn’t (mean age, 67.4 vs. 60.6 years) and were significantly more likely to have comorbidities such as impaired functional status, heart failure, chronic obstructive pulmonary disease, ascites, renal failure, bleeding disorders, wound infection, and recent weight loss.
Unexpectedly, the number of different antibiotics taken during the 60 days preceding surgery also was significantly associated with C. difficile infection. Patients who had taken three or more antibiotics from different classes were nearly six times more likely to develop C. difficile than patients who had taken only one or no antibiotics, the investigators reported (JAMA Surg. 2015 Nov 25. doi: 10.1001/jamasurg.2015.4263).In addition, patients who underwent more complex surgical procedures were at increased risk of this complication, as were patients at hospitals that frequently handled complex procedures. “These factors reflect the illness of patients, duration of operation, and hospital setting; each is an established risk factor for C. difficile infection,” Dr. Li and associates wrote.
Patients with C. difficile infection had higher rates of postoperative other morbidity (86.0% vs. 7.1%) and 30-day mortality (5.3% vs. 1.0%) and longer postoperative hospital stays (17.9 days vs. 3.6 days).
Contrary to previous studies, this study did not show a temporal increase in C. difficile infection. The overall incidence, as well as the incidences at individual hospitals, remained constant during the entire 4-year study period, the investigators added.
The incidence of C. difficile varied substantially among the 134 VA medical centers, from 0% to 1.35% of all surgical patients. “Surgical administrators and clinical teams may consider the results of this study to target interventions for specific patients undergoing high-risk procedures. Such interventions include selective antibiotic administration, early testing of at-risk patients, hand hygiene with nonalcohol agents, early contact precautions, and specific environmental cleaning protocols,” Dr. Li and associates wrote.
This study was supported by the Veterans Health Administration. Dr. Li and associates reported having no relevant financial disclosures.
A hospital’s rate of postoperative Clostridium difficile infection is related to the number of preoperative antibiotics patients have taken, the complexity of their procedures, and the complexity of the hospital’s surgical program, in addition to known risk factors for the infection, according to a report published online in JAMA Surgery.
Several risk factors for postoperative C. difficile infection have already been identified, including advanced age and comorbidity. To examine known risk factors and identify possible new ones, researchers analyzed information from the Veterans Affairs Surgical Quality Improvement Program’s database, which documents all noncardiac operations at 134 VA medical centers each year.
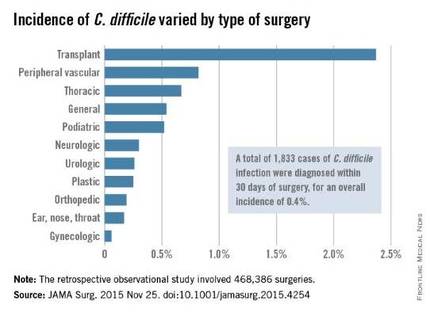
The investigators focused on 468,386 procedures performed during a 4-year period. A total of 1,833 cases of C. difficile infection were diagnosed within 30 days of surgery, for an overall incidence of 0.4% in this predominantly male, elderly population, said Xinli Li, Ph.D., of the Veterans Health Administration, Washington, and associates.
As expected, patients who developed postoperative C. difficile infection were significantly older than those who didn’t (mean age, 67.4 vs. 60.6 years) and were significantly more likely to have comorbidities such as impaired functional status, heart failure, chronic obstructive pulmonary disease, ascites, renal failure, bleeding disorders, wound infection, and recent weight loss.
Unexpectedly, the number of different antibiotics taken during the 60 days preceding surgery also was significantly associated with C. difficile infection. Patients who had taken three or more antibiotics from different classes were nearly six times more likely to develop C. difficile than patients who had taken only one or no antibiotics, the investigators reported (JAMA Surg. 2015 Nov 25. doi: 10.1001/jamasurg.2015.4263).In addition, patients who underwent more complex surgical procedures were at increased risk of this complication, as were patients at hospitals that frequently handled complex procedures. “These factors reflect the illness of patients, duration of operation, and hospital setting; each is an established risk factor for C. difficile infection,” Dr. Li and associates wrote.
Patients with C. difficile infection had higher rates of postoperative other morbidity (86.0% vs. 7.1%) and 30-day mortality (5.3% vs. 1.0%) and longer postoperative hospital stays (17.9 days vs. 3.6 days).
Contrary to previous studies, this study did not show a temporal increase in C. difficile infection. The overall incidence, as well as the incidences at individual hospitals, remained constant during the entire 4-year study period, the investigators added.
The incidence of C. difficile varied substantially among the 134 VA medical centers, from 0% to 1.35% of all surgical patients. “Surgical administrators and clinical teams may consider the results of this study to target interventions for specific patients undergoing high-risk procedures. Such interventions include selective antibiotic administration, early testing of at-risk patients, hand hygiene with nonalcohol agents, early contact precautions, and specific environmental cleaning protocols,” Dr. Li and associates wrote.
This study was supported by the Veterans Health Administration. Dr. Li and associates reported having no relevant financial disclosures.
FROM JAMA SURGERY
Key clinical point: A hospital’s rate of postoperative C. difficile infection is related to the number of preoperative antibiotics patients took and the complexity of their surgeries.
Major finding: Patients who had taken three or more preoperative antibiotics from different classes were nearly six times more likely to develop C. difficile than patients who had taken only one or no antibiotics.
Data source: A retrospective observational study involving 468,386 surgeries at 134 VA medical centers during a 4-year period.
Disclosures: This study was supported by the Veterans Health Administration. Dr. Li and associates reported having no relevant financial disclosures.
ASA: Pediatric clinicians over-dispensing opioids, study finds
SAN DIEGO – Pediatric clinicians are dispensing more medicine than needed to treat pain and may be contributing to the epidemic of nonmedical use of prescription opioids, results from a prospective cohort study suggest.
“On the one hand, we have an ethical and more responsibility to treat pain,” Dr. Myron Yaster said in an interview at the annual meeting of the American Society of Anesthesiologists. “I think we’re doing a pretty good job of that. But there’s also a societal issue in what happens to medicines that are left over. That leftover medicine is the most important element in drug addiction. What this study showed is that in the pediatric population, about 60% of what is prescribed is left over.”
As part of a larger ongoing project, Dr. Yaster, professor of pediatric anesthesiology, critical care medicine, and pain management at Johns Hopkins University Hospital, Baltimore, Md., and his associates recruited 433 English-speaking inpatients who were given opioids on discharge from the university’s pediatric hospital. All prescriptions were analyzed by the investigators following discharge for drug, formulation, and amount dispensed. Parents of the patients were interviewed within 2 days of discharge and again up to 2 weeks after discharge to determine if the prescription was filled, to determine pain control on a 4-point Likert scale, how long opioids were used, the amount of medication left at completion of therapy, if patients were given instructions about how to dispose of leftover drug, and if the remaining medications were discarded.
Of the 433 parents, 292 (67%) completed both sets of interviews. The average age of patients was 11 years and their average weight was 44 kg. The majority of patients (89%) were prescribed oxycodone, a liquid formulation 44% of the time. A minority (5%) did not fill their prescriptions, 25% misidentified or did not know the name of their prescription opioid, and patients took opioids for an average of 5 days. “We need to know more about what the prescribers are thinking when they prescribe,” Dr. Yaster said. “Do they actually believe that [patients are] going to take the medicine for 10 days?”
Nearly half of the time (47%), parents rated pain control as “excellent,” followed by “good” (34%), “fair” (10%), or poor (0%). The remaining 9% gave no response. At 2 weeks, an average of 36 opioid tablets and an average of 67 mL of opioid liquid medication remained unused. Overall, patients used only 42% of their prescribed amount.
The researchers also found that 82% of parents were not provided instructions as to what to do with leftover medicine, and only 6% actually did dispose of it. “That means that all that leftover medicine is in people’s medicine cabinets,” Dr. Yaster said. “The study also found that almost half of patients had a teenage sibling. That’s the target population of drug abuse.”
Dr. Yaster reported having no financial disclosures. One of the study authors was Aaron Hsu, a medical student at Johns Hopkins.
SAN DIEGO – Pediatric clinicians are dispensing more medicine than needed to treat pain and may be contributing to the epidemic of nonmedical use of prescription opioids, results from a prospective cohort study suggest.
“On the one hand, we have an ethical and more responsibility to treat pain,” Dr. Myron Yaster said in an interview at the annual meeting of the American Society of Anesthesiologists. “I think we’re doing a pretty good job of that. But there’s also a societal issue in what happens to medicines that are left over. That leftover medicine is the most important element in drug addiction. What this study showed is that in the pediatric population, about 60% of what is prescribed is left over.”
As part of a larger ongoing project, Dr. Yaster, professor of pediatric anesthesiology, critical care medicine, and pain management at Johns Hopkins University Hospital, Baltimore, Md., and his associates recruited 433 English-speaking inpatients who were given opioids on discharge from the university’s pediatric hospital. All prescriptions were analyzed by the investigators following discharge for drug, formulation, and amount dispensed. Parents of the patients were interviewed within 2 days of discharge and again up to 2 weeks after discharge to determine if the prescription was filled, to determine pain control on a 4-point Likert scale, how long opioids were used, the amount of medication left at completion of therapy, if patients were given instructions about how to dispose of leftover drug, and if the remaining medications were discarded.
Of the 433 parents, 292 (67%) completed both sets of interviews. The average age of patients was 11 years and their average weight was 44 kg. The majority of patients (89%) were prescribed oxycodone, a liquid formulation 44% of the time. A minority (5%) did not fill their prescriptions, 25% misidentified or did not know the name of their prescription opioid, and patients took opioids for an average of 5 days. “We need to know more about what the prescribers are thinking when they prescribe,” Dr. Yaster said. “Do they actually believe that [patients are] going to take the medicine for 10 days?”
Nearly half of the time (47%), parents rated pain control as “excellent,” followed by “good” (34%), “fair” (10%), or poor (0%). The remaining 9% gave no response. At 2 weeks, an average of 36 opioid tablets and an average of 67 mL of opioid liquid medication remained unused. Overall, patients used only 42% of their prescribed amount.
The researchers also found that 82% of parents were not provided instructions as to what to do with leftover medicine, and only 6% actually did dispose of it. “That means that all that leftover medicine is in people’s medicine cabinets,” Dr. Yaster said. “The study also found that almost half of patients had a teenage sibling. That’s the target population of drug abuse.”
Dr. Yaster reported having no financial disclosures. One of the study authors was Aaron Hsu, a medical student at Johns Hopkins.
SAN DIEGO – Pediatric clinicians are dispensing more medicine than needed to treat pain and may be contributing to the epidemic of nonmedical use of prescription opioids, results from a prospective cohort study suggest.
“On the one hand, we have an ethical and more responsibility to treat pain,” Dr. Myron Yaster said in an interview at the annual meeting of the American Society of Anesthesiologists. “I think we’re doing a pretty good job of that. But there’s also a societal issue in what happens to medicines that are left over. That leftover medicine is the most important element in drug addiction. What this study showed is that in the pediatric population, about 60% of what is prescribed is left over.”
As part of a larger ongoing project, Dr. Yaster, professor of pediatric anesthesiology, critical care medicine, and pain management at Johns Hopkins University Hospital, Baltimore, Md., and his associates recruited 433 English-speaking inpatients who were given opioids on discharge from the university’s pediatric hospital. All prescriptions were analyzed by the investigators following discharge for drug, formulation, and amount dispensed. Parents of the patients were interviewed within 2 days of discharge and again up to 2 weeks after discharge to determine if the prescription was filled, to determine pain control on a 4-point Likert scale, how long opioids were used, the amount of medication left at completion of therapy, if patients were given instructions about how to dispose of leftover drug, and if the remaining medications were discarded.
Of the 433 parents, 292 (67%) completed both sets of interviews. The average age of patients was 11 years and their average weight was 44 kg. The majority of patients (89%) were prescribed oxycodone, a liquid formulation 44% of the time. A minority (5%) did not fill their prescriptions, 25% misidentified or did not know the name of their prescription opioid, and patients took opioids for an average of 5 days. “We need to know more about what the prescribers are thinking when they prescribe,” Dr. Yaster said. “Do they actually believe that [patients are] going to take the medicine for 10 days?”
Nearly half of the time (47%), parents rated pain control as “excellent,” followed by “good” (34%), “fair” (10%), or poor (0%). The remaining 9% gave no response. At 2 weeks, an average of 36 opioid tablets and an average of 67 mL of opioid liquid medication remained unused. Overall, patients used only 42% of their prescribed amount.
The researchers also found that 82% of parents were not provided instructions as to what to do with leftover medicine, and only 6% actually did dispose of it. “That means that all that leftover medicine is in people’s medicine cabinets,” Dr. Yaster said. “The study also found that almost half of patients had a teenage sibling. That’s the target population of drug abuse.”
Dr. Yaster reported having no financial disclosures. One of the study authors was Aaron Hsu, a medical student at Johns Hopkins.
AT THE ASA ANNUAL MEETING
Key clinical point: Clinicians dispense more opioids than needed to treat pediatric pain.
Major finding: The majority of patients (89%) were prescribed oxycodone, and overall they used only 42% of the opioids they were prescribed.
Data source: A prospective study based on responses from 292 parents of children who were discharged from a university pediatric hospital with an opioid prescription.
Disclosures: Dr. Yaster reported having no financial disclosures.
Readmission after esophagectomy raises mortality
About one in five patients who have surgery to remove part or all of the esophagus return to the hospital for complications within 30 days, and when they do their chance of death increases fivefold, compared with those who don’t return to the hospital, investigators at the University of Virginia Health System reported in the Journal of Thoracic and Cardiovascular Surgery (2015;150:1254-60).
“Early recognition of life-threatening readmission diagnoses is essential in order to provide optimal care,” said lead author Dr. Yinin Hu and colleagues. Esophageal cancer is the fastest-growing cancer in the United States, so the study investigators set out to closely examine the reasons for readmissions and death after surgery.
The study identified 1,688 patients in the Surveillance, Epidemiology, and End Results (SEER)-Medicare database aged 66 or older who had surgery for esophageal cancer from 2000 to 2009. The overall 30-day mortality was 6.9%, and the 90-day mortality was 13.9%.
After excluding in-hospital deaths, the investigators’ readmission analysis included 1,543 patients. In this group, overall 90-day mortality following discharge was 6.4%, and the readmission rate within 30 days of discharge was 20.7%
The 90-day mortality for patients who were readmitted was more than four times that for those who were not readmitted, 16.3% vs. 3.8%; their in-hospital mortality was 8.8%. About one-third of readmissions were to facilities different from where patients had the index esophagectomy, and those patients were about seven times more likely to be transferred after readmission than patients admitted to the same facility, 15% vs. 1.9%. Risk-adjusted mortality did not vary significantly across providers.
The most frequent reasons for readmission were pneumonia (11.8%), malnutrition/dehydration (8.1%), pleural effusion (97.5%), and aspiration pneumonitis (6.8%). “Notably, more than one in five patients readmitted with a pulmonary diagnosis subsequently died within 90 days of the operation,” Dr. Hu and coauthors said, indicating that readmissions for pulmonary complications carried the worst prognosis.
This is the first study to demonstrate the gravity of pulmonary readmissions within 30 days of discharge, Dr. Hu and coauthors said. “Patients with nonspecific dyspneic symptoms or small pleural effusions should receive aggressive care upon readmission, as more than 20% will not survive the next few months,” Dr. Hu and coauthors said. “These results reinforce the notion that a fairly benign readmitting diagnosis is often an indicator of a much more severe root process.”
Among nonpulmonary reasons for readmission, dehydration and malnutrition carried the highest risk for death. “While there are many interventions that can promote postoperative nutrition, a readmission due to poor dietary tolerance often indicates other complications such as infection, stenosis, or anastomotic leak,” Dr. Hu and coauthors said. They suggested a thorough root-cause analysis should be part of every readmission.
The study also analyzed the hospital length of stay (LOS) as a predictor for readmission. The median LOS was 13 days, but the most common LOS was 9 days. “In general, the probability of readmission increases with increasing postoperative LOS,” Dr. Hu and colleagues said.
The authors reported no disclosures. Dr. Yinin Hu received funding from the National Institutes of Health and coauthor Dr. Benjamin Kozower received funding from the Agency for Healthcare Research and Quality.
The findings of this study may indicate that patients who stay in the hospital longer have underlying issues that did not surface during their admission for the operation, Dr. Anthony W. Kim of Yale University, New Haven, Conn., said in his invited commentary (J Thorac Cardiovasc Surg. 2015;150:1030-1). “Therefore, rather than employing a prevention of a failure-to-rescue strategy during a readmission, it may be worthwhile to enact a prevention-of-readmission strategy triggered by a longer than typical [length of stay],” Dr. Kim said. He suggested the root-cause analysis should begin in the hospital on the day after the patient exceeds the median length of stay.

|
Dr. Anthony W. Kim |
But citing the law of unintended consequences, Dr. Kim warns against using readmission as a quality metric as well a instrument to dictate reimbursement. “The law of unintended consequences dictates that when a readmission is taken out of context, using this measure raises the potential conflict of interest between doing what is right for the patient and achieving a specific milestone that may not be in the best interest of an individual patient,” he said. “Discharging a patient early perhaps to the exclusion of adequately addressing inpatient issues for the purposes of achieving a target [length of stay] is perhaps the prime example of these conflicting interests.”
Because of the difficult recovery course after esophagectomy, some readmissions are “necessary, beneficial and, unequivocally, the right decision,” Dr. Kim said. “Ironically, one of the unintended consequences of this article may be that it exposes the fact that until a better system of recording and scrutinizing readmissions exists, governing organizations should exercise considerable caution when assessing a surgeon, hospital, or system and their readmissions,” he said.
To paraphrase the sociologist Robert K. Merton, who devised the law of unintended consequences, the existing state of knowledge limits one’s ability to anticipate the consequences of action. The authors of this study “have added immensely to a body of knowledge that is still growing and deserves ongoing study if policy is to be based upon it,” Dr. Kim said.
Dr. Kim had no disclosures.
The findings of this study may indicate that patients who stay in the hospital longer have underlying issues that did not surface during their admission for the operation, Dr. Anthony W. Kim of Yale University, New Haven, Conn., said in his invited commentary (J Thorac Cardiovasc Surg. 2015;150:1030-1). “Therefore, rather than employing a prevention of a failure-to-rescue strategy during a readmission, it may be worthwhile to enact a prevention-of-readmission strategy triggered by a longer than typical [length of stay],” Dr. Kim said. He suggested the root-cause analysis should begin in the hospital on the day after the patient exceeds the median length of stay.

|
Dr. Anthony W. Kim |
But citing the law of unintended consequences, Dr. Kim warns against using readmission as a quality metric as well a instrument to dictate reimbursement. “The law of unintended consequences dictates that when a readmission is taken out of context, using this measure raises the potential conflict of interest between doing what is right for the patient and achieving a specific milestone that may not be in the best interest of an individual patient,” he said. “Discharging a patient early perhaps to the exclusion of adequately addressing inpatient issues for the purposes of achieving a target [length of stay] is perhaps the prime example of these conflicting interests.”
Because of the difficult recovery course after esophagectomy, some readmissions are “necessary, beneficial and, unequivocally, the right decision,” Dr. Kim said. “Ironically, one of the unintended consequences of this article may be that it exposes the fact that until a better system of recording and scrutinizing readmissions exists, governing organizations should exercise considerable caution when assessing a surgeon, hospital, or system and their readmissions,” he said.
To paraphrase the sociologist Robert K. Merton, who devised the law of unintended consequences, the existing state of knowledge limits one’s ability to anticipate the consequences of action. The authors of this study “have added immensely to a body of knowledge that is still growing and deserves ongoing study if policy is to be based upon it,” Dr. Kim said.
Dr. Kim had no disclosures.
The findings of this study may indicate that patients who stay in the hospital longer have underlying issues that did not surface during their admission for the operation, Dr. Anthony W. Kim of Yale University, New Haven, Conn., said in his invited commentary (J Thorac Cardiovasc Surg. 2015;150:1030-1). “Therefore, rather than employing a prevention of a failure-to-rescue strategy during a readmission, it may be worthwhile to enact a prevention-of-readmission strategy triggered by a longer than typical [length of stay],” Dr. Kim said. He suggested the root-cause analysis should begin in the hospital on the day after the patient exceeds the median length of stay.

|
Dr. Anthony W. Kim |
But citing the law of unintended consequences, Dr. Kim warns against using readmission as a quality metric as well a instrument to dictate reimbursement. “The law of unintended consequences dictates that when a readmission is taken out of context, using this measure raises the potential conflict of interest between doing what is right for the patient and achieving a specific milestone that may not be in the best interest of an individual patient,” he said. “Discharging a patient early perhaps to the exclusion of adequately addressing inpatient issues for the purposes of achieving a target [length of stay] is perhaps the prime example of these conflicting interests.”
Because of the difficult recovery course after esophagectomy, some readmissions are “necessary, beneficial and, unequivocally, the right decision,” Dr. Kim said. “Ironically, one of the unintended consequences of this article may be that it exposes the fact that until a better system of recording and scrutinizing readmissions exists, governing organizations should exercise considerable caution when assessing a surgeon, hospital, or system and their readmissions,” he said.
To paraphrase the sociologist Robert K. Merton, who devised the law of unintended consequences, the existing state of knowledge limits one’s ability to anticipate the consequences of action. The authors of this study “have added immensely to a body of knowledge that is still growing and deserves ongoing study if policy is to be based upon it,” Dr. Kim said.
Dr. Kim had no disclosures.
About one in five patients who have surgery to remove part or all of the esophagus return to the hospital for complications within 30 days, and when they do their chance of death increases fivefold, compared with those who don’t return to the hospital, investigators at the University of Virginia Health System reported in the Journal of Thoracic and Cardiovascular Surgery (2015;150:1254-60).
“Early recognition of life-threatening readmission diagnoses is essential in order to provide optimal care,” said lead author Dr. Yinin Hu and colleagues. Esophageal cancer is the fastest-growing cancer in the United States, so the study investigators set out to closely examine the reasons for readmissions and death after surgery.
The study identified 1,688 patients in the Surveillance, Epidemiology, and End Results (SEER)-Medicare database aged 66 or older who had surgery for esophageal cancer from 2000 to 2009. The overall 30-day mortality was 6.9%, and the 90-day mortality was 13.9%.
After excluding in-hospital deaths, the investigators’ readmission analysis included 1,543 patients. In this group, overall 90-day mortality following discharge was 6.4%, and the readmission rate within 30 days of discharge was 20.7%
The 90-day mortality for patients who were readmitted was more than four times that for those who were not readmitted, 16.3% vs. 3.8%; their in-hospital mortality was 8.8%. About one-third of readmissions were to facilities different from where patients had the index esophagectomy, and those patients were about seven times more likely to be transferred after readmission than patients admitted to the same facility, 15% vs. 1.9%. Risk-adjusted mortality did not vary significantly across providers.
The most frequent reasons for readmission were pneumonia (11.8%), malnutrition/dehydration (8.1%), pleural effusion (97.5%), and aspiration pneumonitis (6.8%). “Notably, more than one in five patients readmitted with a pulmonary diagnosis subsequently died within 90 days of the operation,” Dr. Hu and coauthors said, indicating that readmissions for pulmonary complications carried the worst prognosis.
This is the first study to demonstrate the gravity of pulmonary readmissions within 30 days of discharge, Dr. Hu and coauthors said. “Patients with nonspecific dyspneic symptoms or small pleural effusions should receive aggressive care upon readmission, as more than 20% will not survive the next few months,” Dr. Hu and coauthors said. “These results reinforce the notion that a fairly benign readmitting diagnosis is often an indicator of a much more severe root process.”
Among nonpulmonary reasons for readmission, dehydration and malnutrition carried the highest risk for death. “While there are many interventions that can promote postoperative nutrition, a readmission due to poor dietary tolerance often indicates other complications such as infection, stenosis, or anastomotic leak,” Dr. Hu and coauthors said. They suggested a thorough root-cause analysis should be part of every readmission.
The study also analyzed the hospital length of stay (LOS) as a predictor for readmission. The median LOS was 13 days, but the most common LOS was 9 days. “In general, the probability of readmission increases with increasing postoperative LOS,” Dr. Hu and colleagues said.
The authors reported no disclosures. Dr. Yinin Hu received funding from the National Institutes of Health and coauthor Dr. Benjamin Kozower received funding from the Agency for Healthcare Research and Quality.
About one in five patients who have surgery to remove part or all of the esophagus return to the hospital for complications within 30 days, and when they do their chance of death increases fivefold, compared with those who don’t return to the hospital, investigators at the University of Virginia Health System reported in the Journal of Thoracic and Cardiovascular Surgery (2015;150:1254-60).
“Early recognition of life-threatening readmission diagnoses is essential in order to provide optimal care,” said lead author Dr. Yinin Hu and colleagues. Esophageal cancer is the fastest-growing cancer in the United States, so the study investigators set out to closely examine the reasons for readmissions and death after surgery.
The study identified 1,688 patients in the Surveillance, Epidemiology, and End Results (SEER)-Medicare database aged 66 or older who had surgery for esophageal cancer from 2000 to 2009. The overall 30-day mortality was 6.9%, and the 90-day mortality was 13.9%.
After excluding in-hospital deaths, the investigators’ readmission analysis included 1,543 patients. In this group, overall 90-day mortality following discharge was 6.4%, and the readmission rate within 30 days of discharge was 20.7%
The 90-day mortality for patients who were readmitted was more than four times that for those who were not readmitted, 16.3% vs. 3.8%; their in-hospital mortality was 8.8%. About one-third of readmissions were to facilities different from where patients had the index esophagectomy, and those patients were about seven times more likely to be transferred after readmission than patients admitted to the same facility, 15% vs. 1.9%. Risk-adjusted mortality did not vary significantly across providers.
The most frequent reasons for readmission were pneumonia (11.8%), malnutrition/dehydration (8.1%), pleural effusion (97.5%), and aspiration pneumonitis (6.8%). “Notably, more than one in five patients readmitted with a pulmonary diagnosis subsequently died within 90 days of the operation,” Dr. Hu and coauthors said, indicating that readmissions for pulmonary complications carried the worst prognosis.
This is the first study to demonstrate the gravity of pulmonary readmissions within 30 days of discharge, Dr. Hu and coauthors said. “Patients with nonspecific dyspneic symptoms or small pleural effusions should receive aggressive care upon readmission, as more than 20% will not survive the next few months,” Dr. Hu and coauthors said. “These results reinforce the notion that a fairly benign readmitting diagnosis is often an indicator of a much more severe root process.”
Among nonpulmonary reasons for readmission, dehydration and malnutrition carried the highest risk for death. “While there are many interventions that can promote postoperative nutrition, a readmission due to poor dietary tolerance often indicates other complications such as infection, stenosis, or anastomotic leak,” Dr. Hu and coauthors said. They suggested a thorough root-cause analysis should be part of every readmission.
The study also analyzed the hospital length of stay (LOS) as a predictor for readmission. The median LOS was 13 days, but the most common LOS was 9 days. “In general, the probability of readmission increases with increasing postoperative LOS,” Dr. Hu and colleagues said.
The authors reported no disclosures. Dr. Yinin Hu received funding from the National Institutes of Health and coauthor Dr. Benjamin Kozower received funding from the Agency for Healthcare Research and Quality.
Key clinical point: Patients readmitted after esophagectomy are at a greater than fourfold higher risk of death than patients who do not need readmission.
Major finding: The 90-day mortality for patients who were readmitted was greater than four times that for those who were not readmitted, 16.3% vs. 3.8%.
Data source: Analysis of 1,688 patients in the SEER-Medicare database aged 66 or older who had surgery for esophageal cancer from 2000 to 2009.
Disclosures: The authors had no disclosures. Lead author Dr. Yinin Hu received funding from the National Institutes of Health and coauthor Dr. Benjamin Kozower received funding from the Agency for Healthcare Research and Quality.
FDA okays prophylactic Pradaxa for VTE in hip replacement
The Food and Drug Administration has approved dabigatran for the prevention of deep venous thrombosis and pulmonary embolism for patients after hip replacement surgery.
The FDA’s approval was based on the results of two randomized, double-blind, phase III trials in patients undergoing total hip replacement, Boehringer Ingelheim, the manufacturer of the direct thrombin inhibitor, announced.
In RE-NOVATE I, the first trial, 3,494 patients were randomly assigned to three groups receiving prophylactic treatment with one of two doses of dabigatran (220 mg or 150 mg) once daily, or to the low-molecular-weight heparin enoxaparin at 40 mg once daily for 28-35 days. The first study drug arm was given 110 mg on the day of surgery and 220 mg daily thereafter; the second study drug arm received a dose of 75 mg on the day of surgery and 150 mg daily thereafter. Patients taking the dabigatran (Pradaxa) at 220 mg had a lower composite total of venous thromboembolism (VTE) and all-cause mortality (6.0%) than did those on enoxaparin 40 mg (6.7%), meeting the noninferiority mark (Lancet. 2007 Sep 15;370[9591]:949-56).
In RE-NOVATE II, 2,055 patients were randomly assigned prophylactic treatment for 28-35 days with the study drug dosed at 220 mg once daily, or enoxaparin 40 mg once daily. Patients receiving the study drug were treated with a dose of 110 mg on the day of surgery and 220 mg daily thereafter. The composite total of VTE and all-cause death occurred in 7.7% of patients in the study group vs. 8.8% of patients in the enoxaparin group, which was within the margin for noninferiority (Thromb Haemost. 2011 Apr;105[4]:721-9).
However, there were higher rates of major bleeding in RE-NOVATE I (2.0%, 1.6%) and II (1.4%, 0.9%) with 220 mg vs. enoxaparin. In both studies, the rate of major gastrointestinal bleeds in patients was the same (0.1%) for both the study and control drugs. The rate of any GI bleeds was 1.4% for the study drug and 0.9% for enoxaparin. The most common adverse events in both studies were GI disorders. The incidence rate was the same across all treatment groups (39.5%). Dyspepsia occurred more frequently in patients receiving the study drug (4.1%), compared with those taking enoxaparin (3.8%). Gastritislike symptoms were less common in patients receiving the study drug (0.6%), compared with enoxaparin (1.0%). Clinical myocardial infarction was reported in two (0.1%) study patients and six (0.3%) enoxaparin patients.
Pradaxa was initially indicated by the FDA in 2010 to reduce stroke and systemic embolism risk in patients with nonvalvular atrial fibrillation. In 2014, the FDA approved two additional indications for the drug for the treatment of VTE in patients treated with a parenteral anticoagulant for 5-10 day and to reduce the risk of recurrent VTE in patients who have been previously treated.
On Twitter @whitneymcknight
The Food and Drug Administration has approved dabigatran for the prevention of deep venous thrombosis and pulmonary embolism for patients after hip replacement surgery.
The FDA’s approval was based on the results of two randomized, double-blind, phase III trials in patients undergoing total hip replacement, Boehringer Ingelheim, the manufacturer of the direct thrombin inhibitor, announced.
In RE-NOVATE I, the first trial, 3,494 patients were randomly assigned to three groups receiving prophylactic treatment with one of two doses of dabigatran (220 mg or 150 mg) once daily, or to the low-molecular-weight heparin enoxaparin at 40 mg once daily for 28-35 days. The first study drug arm was given 110 mg on the day of surgery and 220 mg daily thereafter; the second study drug arm received a dose of 75 mg on the day of surgery and 150 mg daily thereafter. Patients taking the dabigatran (Pradaxa) at 220 mg had a lower composite total of venous thromboembolism (VTE) and all-cause mortality (6.0%) than did those on enoxaparin 40 mg (6.7%), meeting the noninferiority mark (Lancet. 2007 Sep 15;370[9591]:949-56).
In RE-NOVATE II, 2,055 patients were randomly assigned prophylactic treatment for 28-35 days with the study drug dosed at 220 mg once daily, or enoxaparin 40 mg once daily. Patients receiving the study drug were treated with a dose of 110 mg on the day of surgery and 220 mg daily thereafter. The composite total of VTE and all-cause death occurred in 7.7% of patients in the study group vs. 8.8% of patients in the enoxaparin group, which was within the margin for noninferiority (Thromb Haemost. 2011 Apr;105[4]:721-9).
However, there were higher rates of major bleeding in RE-NOVATE I (2.0%, 1.6%) and II (1.4%, 0.9%) with 220 mg vs. enoxaparin. In both studies, the rate of major gastrointestinal bleeds in patients was the same (0.1%) for both the study and control drugs. The rate of any GI bleeds was 1.4% for the study drug and 0.9% for enoxaparin. The most common adverse events in both studies were GI disorders. The incidence rate was the same across all treatment groups (39.5%). Dyspepsia occurred more frequently in patients receiving the study drug (4.1%), compared with those taking enoxaparin (3.8%). Gastritislike symptoms were less common in patients receiving the study drug (0.6%), compared with enoxaparin (1.0%). Clinical myocardial infarction was reported in two (0.1%) study patients and six (0.3%) enoxaparin patients.
Pradaxa was initially indicated by the FDA in 2010 to reduce stroke and systemic embolism risk in patients with nonvalvular atrial fibrillation. In 2014, the FDA approved two additional indications for the drug for the treatment of VTE in patients treated with a parenteral anticoagulant for 5-10 day and to reduce the risk of recurrent VTE in patients who have been previously treated.
On Twitter @whitneymcknight
The Food and Drug Administration has approved dabigatran for the prevention of deep venous thrombosis and pulmonary embolism for patients after hip replacement surgery.
The FDA’s approval was based on the results of two randomized, double-blind, phase III trials in patients undergoing total hip replacement, Boehringer Ingelheim, the manufacturer of the direct thrombin inhibitor, announced.
In RE-NOVATE I, the first trial, 3,494 patients were randomly assigned to three groups receiving prophylactic treatment with one of two doses of dabigatran (220 mg or 150 mg) once daily, or to the low-molecular-weight heparin enoxaparin at 40 mg once daily for 28-35 days. The first study drug arm was given 110 mg on the day of surgery and 220 mg daily thereafter; the second study drug arm received a dose of 75 mg on the day of surgery and 150 mg daily thereafter. Patients taking the dabigatran (Pradaxa) at 220 mg had a lower composite total of venous thromboembolism (VTE) and all-cause mortality (6.0%) than did those on enoxaparin 40 mg (6.7%), meeting the noninferiority mark (Lancet. 2007 Sep 15;370[9591]:949-56).
In RE-NOVATE II, 2,055 patients were randomly assigned prophylactic treatment for 28-35 days with the study drug dosed at 220 mg once daily, or enoxaparin 40 mg once daily. Patients receiving the study drug were treated with a dose of 110 mg on the day of surgery and 220 mg daily thereafter. The composite total of VTE and all-cause death occurred in 7.7% of patients in the study group vs. 8.8% of patients in the enoxaparin group, which was within the margin for noninferiority (Thromb Haemost. 2011 Apr;105[4]:721-9).
However, there were higher rates of major bleeding in RE-NOVATE I (2.0%, 1.6%) and II (1.4%, 0.9%) with 220 mg vs. enoxaparin. In both studies, the rate of major gastrointestinal bleeds in patients was the same (0.1%) for both the study and control drugs. The rate of any GI bleeds was 1.4% for the study drug and 0.9% for enoxaparin. The most common adverse events in both studies were GI disorders. The incidence rate was the same across all treatment groups (39.5%). Dyspepsia occurred more frequently in patients receiving the study drug (4.1%), compared with those taking enoxaparin (3.8%). Gastritislike symptoms were less common in patients receiving the study drug (0.6%), compared with enoxaparin (1.0%). Clinical myocardial infarction was reported in two (0.1%) study patients and six (0.3%) enoxaparin patients.
Pradaxa was initially indicated by the FDA in 2010 to reduce stroke and systemic embolism risk in patients with nonvalvular atrial fibrillation. In 2014, the FDA approved two additional indications for the drug for the treatment of VTE in patients treated with a parenteral anticoagulant for 5-10 day and to reduce the risk of recurrent VTE in patients who have been previously treated.
On Twitter @whitneymcknight