User login
Managing pain expectations is key to enhanced recovery
Planning for reduced use of opioids in pain management involves identifying appropriate patients and managing their expectations, according to according to Timothy E. Miller, MB, ChB, FRCA, of Duke University, Durham, N.C., who is president of the American Society for Enhanced Recovery.
, he said in a presentation at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education.
Dr. Miller shared a treatment algorithm for achieving optimal analgesia in patients after colorectal surgery that combines intravenous or oral analgesia with local anesthetics and additional nonopioid options. The algorithm involves choosing NSAIDs, acetaminophen, or gabapentin for IV/oral use. In addition, options for local anesthetic include with a choice of single-shot transversus abdominis plane (TAP) block.
Careful patient selection is key to an opioid-free or opioid reduced anesthetic strategy, Dr. Miller said. The appropriate patients have “no chronic opioids, no anxiety, and the desire to avoid opioid side effects,” he said.
Opioid-free or opioid-reduced strategies include realigning patient expectations to prepare for pain at a level of 2-4 on a scale of 10 as “expected and reasonable,” he said. Patients given no opioids or reduced opioids may report cramping after laparoscopic surgery, as well as shoulder pain that is referred from the CO2 bubble under the diaphragm, he said. However, opioids don’t treat the shoulder pain well, and “walking or changing position usually relieves this pain,” and it usually resolves within 24 hours, Dr. Miller noted. “Just letting the patient know what is expected in terms of pain relief in their recovery is hugely important,” he said.
The optimal analgesia after surgery is a plan that combines optimized patient comfort with the fastest functional recovery and the fewest side effects, he emphasized.
Optimized patient comfort includes optimal pain ratings at rest and with movement, a decreasing impact of pain on emotion, function, and sleep disruption, and an improvement in the patient experience, he said. The fastest functional recovery is defined as a return to drinking liquids, eating solid foods, performing activities of daily living, and maintaining normal bladder, bowel, and cognitive function. Side effects to be considered in analgesia included nausea, vomiting, sedation, ileus, itching, dizziness, and delirium, he said.
In an unpublished study, Dr. Miller and colleagues eliminated opioids intraoperatively in a series of 56 cases of laparoscopic cholecystectomy and found significantly less opioids needed in the postanesthesia care unit (PACU). In addition, opioid-free patients had significantly shorter length of stay in the PACU, he said. “We are writing this up for publication and looking into doing larger studies,” Dr. Miller said.
Questions include whether the opioid-free technique translates more broadly, he said.
In addition, it is important to continue to collect data and study methods to treat pain and reduce opioid use perioperatively, Dr. Miller said. Some ongoing concerns include data surrounding the use of gabapentin and possible association with respiratory depression, he noted. Several meta-analyses have suggested that “gabapentinoids (gabapentin, pregabalin) when given as a single dose preoperatively are associated with a decrease in postoperative pain and opioid consumption at 24 hours,” said Dr. Miller. “When gabapentinoids are included in multimodal analgesic regimens, intraoperative opioids must be reduced, and increased vigilance for respiratory depression may be warranted, especially in elderly patients,” he said.
Overall, opioid-free anesthesia is both feasible and appropriate in certain patient populations, Dr. Miller concluded. “Implement your pathway and measure your outcomes with timely feedback so you can revise your protocol based on data,” he emphasized.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Dr. Miller disclosed relationships with Edwards Lifesciences, and serving as a board member for the Perioperative Quality Initiative and as a founding member of the Morpheus Consortium.
Planning for reduced use of opioids in pain management involves identifying appropriate patients and managing their expectations, according to according to Timothy E. Miller, MB, ChB, FRCA, of Duke University, Durham, N.C., who is president of the American Society for Enhanced Recovery.
, he said in a presentation at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education.
Dr. Miller shared a treatment algorithm for achieving optimal analgesia in patients after colorectal surgery that combines intravenous or oral analgesia with local anesthetics and additional nonopioid options. The algorithm involves choosing NSAIDs, acetaminophen, or gabapentin for IV/oral use. In addition, options for local anesthetic include with a choice of single-shot transversus abdominis plane (TAP) block.
Careful patient selection is key to an opioid-free or opioid reduced anesthetic strategy, Dr. Miller said. The appropriate patients have “no chronic opioids, no anxiety, and the desire to avoid opioid side effects,” he said.
Opioid-free or opioid-reduced strategies include realigning patient expectations to prepare for pain at a level of 2-4 on a scale of 10 as “expected and reasonable,” he said. Patients given no opioids or reduced opioids may report cramping after laparoscopic surgery, as well as shoulder pain that is referred from the CO2 bubble under the diaphragm, he said. However, opioids don’t treat the shoulder pain well, and “walking or changing position usually relieves this pain,” and it usually resolves within 24 hours, Dr. Miller noted. “Just letting the patient know what is expected in terms of pain relief in their recovery is hugely important,” he said.
The optimal analgesia after surgery is a plan that combines optimized patient comfort with the fastest functional recovery and the fewest side effects, he emphasized.
Optimized patient comfort includes optimal pain ratings at rest and with movement, a decreasing impact of pain on emotion, function, and sleep disruption, and an improvement in the patient experience, he said. The fastest functional recovery is defined as a return to drinking liquids, eating solid foods, performing activities of daily living, and maintaining normal bladder, bowel, and cognitive function. Side effects to be considered in analgesia included nausea, vomiting, sedation, ileus, itching, dizziness, and delirium, he said.
In an unpublished study, Dr. Miller and colleagues eliminated opioids intraoperatively in a series of 56 cases of laparoscopic cholecystectomy and found significantly less opioids needed in the postanesthesia care unit (PACU). In addition, opioid-free patients had significantly shorter length of stay in the PACU, he said. “We are writing this up for publication and looking into doing larger studies,” Dr. Miller said.
Questions include whether the opioid-free technique translates more broadly, he said.
In addition, it is important to continue to collect data and study methods to treat pain and reduce opioid use perioperatively, Dr. Miller said. Some ongoing concerns include data surrounding the use of gabapentin and possible association with respiratory depression, he noted. Several meta-analyses have suggested that “gabapentinoids (gabapentin, pregabalin) when given as a single dose preoperatively are associated with a decrease in postoperative pain and opioid consumption at 24 hours,” said Dr. Miller. “When gabapentinoids are included in multimodal analgesic regimens, intraoperative opioids must be reduced, and increased vigilance for respiratory depression may be warranted, especially in elderly patients,” he said.
Overall, opioid-free anesthesia is both feasible and appropriate in certain patient populations, Dr. Miller concluded. “Implement your pathway and measure your outcomes with timely feedback so you can revise your protocol based on data,” he emphasized.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Dr. Miller disclosed relationships with Edwards Lifesciences, and serving as a board member for the Perioperative Quality Initiative and as a founding member of the Morpheus Consortium.
Planning for reduced use of opioids in pain management involves identifying appropriate patients and managing their expectations, according to according to Timothy E. Miller, MB, ChB, FRCA, of Duke University, Durham, N.C., who is president of the American Society for Enhanced Recovery.
, he said in a presentation at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education.
Dr. Miller shared a treatment algorithm for achieving optimal analgesia in patients after colorectal surgery that combines intravenous or oral analgesia with local anesthetics and additional nonopioid options. The algorithm involves choosing NSAIDs, acetaminophen, or gabapentin for IV/oral use. In addition, options for local anesthetic include with a choice of single-shot transversus abdominis plane (TAP) block.
Careful patient selection is key to an opioid-free or opioid reduced anesthetic strategy, Dr. Miller said. The appropriate patients have “no chronic opioids, no anxiety, and the desire to avoid opioid side effects,” he said.
Opioid-free or opioid-reduced strategies include realigning patient expectations to prepare for pain at a level of 2-4 on a scale of 10 as “expected and reasonable,” he said. Patients given no opioids or reduced opioids may report cramping after laparoscopic surgery, as well as shoulder pain that is referred from the CO2 bubble under the diaphragm, he said. However, opioids don’t treat the shoulder pain well, and “walking or changing position usually relieves this pain,” and it usually resolves within 24 hours, Dr. Miller noted. “Just letting the patient know what is expected in terms of pain relief in their recovery is hugely important,” he said.
The optimal analgesia after surgery is a plan that combines optimized patient comfort with the fastest functional recovery and the fewest side effects, he emphasized.
Optimized patient comfort includes optimal pain ratings at rest and with movement, a decreasing impact of pain on emotion, function, and sleep disruption, and an improvement in the patient experience, he said. The fastest functional recovery is defined as a return to drinking liquids, eating solid foods, performing activities of daily living, and maintaining normal bladder, bowel, and cognitive function. Side effects to be considered in analgesia included nausea, vomiting, sedation, ileus, itching, dizziness, and delirium, he said.
In an unpublished study, Dr. Miller and colleagues eliminated opioids intraoperatively in a series of 56 cases of laparoscopic cholecystectomy and found significantly less opioids needed in the postanesthesia care unit (PACU). In addition, opioid-free patients had significantly shorter length of stay in the PACU, he said. “We are writing this up for publication and looking into doing larger studies,” Dr. Miller said.
Questions include whether the opioid-free technique translates more broadly, he said.
In addition, it is important to continue to collect data and study methods to treat pain and reduce opioid use perioperatively, Dr. Miller said. Some ongoing concerns include data surrounding the use of gabapentin and possible association with respiratory depression, he noted. Several meta-analyses have suggested that “gabapentinoids (gabapentin, pregabalin) when given as a single dose preoperatively are associated with a decrease in postoperative pain and opioid consumption at 24 hours,” said Dr. Miller. “When gabapentinoids are included in multimodal analgesic regimens, intraoperative opioids must be reduced, and increased vigilance for respiratory depression may be warranted, especially in elderly patients,” he said.
Overall, opioid-free anesthesia is both feasible and appropriate in certain patient populations, Dr. Miller concluded. “Implement your pathway and measure your outcomes with timely feedback so you can revise your protocol based on data,” he emphasized.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Dr. Miller disclosed relationships with Edwards Lifesciences, and serving as a board member for the Perioperative Quality Initiative and as a founding member of the Morpheus Consortium.
FROM MISS
Pursue multimodal pain management in patients taking opioids
For surgical patients on chronic opioid therapy, , according to Stephanie B. Jones, MD, professor and chair of anesthesiology at Albany Medical College, New York.
“[With] any patient coming in for any sort of surgery, you should be considering multimodal pain management. That applies to the opioid use disorder patient as well,” Dr. Jones said in a presentation at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education.
“The challenge of opioid-tolerant patients or opioid abuse patients is twofold – tolerance and hyperalgesia,” Dr. Jones said. Patient tolerance changes how patients perceive pain and respond to medication. Clinicians need to consider the “opioid debt,” defined as the daily amount of opioid medication required by opioid-dependent patients to maintain their usual prehospitalization opioid levels, she explained. Also consider hyperalgesia, a change in pain perception “resulting in an increase in pain sensitivity to painful stimuli, thereby decreasing the analgesic effects of opioids,” Dr. Jones added.
A multimodal approach to pain management in patients on chronic opioids can include some opioids as appropriate, Dr. Jones said. Modulation of pain may draw on epidurals and nerve blocks, as well as managing CNS perception of pain through opioids or acetaminophen, and also using systemic options such as alpha-2 agonists and tramadol, she said.
Studies have shown that opioid abuse or dependence were associated with increased readmission rates, length of stay, and health care costs in surgery patients, said Dr. Jones. However, switching opioids and managing equivalents is complex, and “equianalgesic conversions serve only as a general guide to estimate opioid dose equivalents,” according to UpToDate’s, “Management of acute pain in the patient chronically using opioids,” she said.
Dr. Jones also addressed the issue of using hospitalization as an opportunity to help patients with untreated opioid use disorder. Medication-assisted options include methadone, buprenorphine, and naltrexone.
“One problem with methadone is that there are a lot of medications interactions,” she said. Buprenorphine has the advantage of being long-lasting, and is formulated with naloxone which deters injection. “Because it is a partial agonist, there is a lower risk of overdose and sedation,” and it has fewer medication interactions. However, some doctors are reluctant to prescribe it and there is some risk of medication diversion, she said.
Naltrexone is newer to the role of treating opioid use disorder, Dr. Jones said. “It can cause acute withdrawal because it is a full opioid antagonist,” she noted. However, naltrexone itself causes no withdrawal if stopped, and no respiratory depression or sedation, said Dr. Jones.
“Utilize addiction services in your hospital if you suspect a patient may be at risk for opioid use disorder,” and engage these services early, she emphasized.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Dr. Jones had no financial conflicts to disclose.
For surgical patients on chronic opioid therapy, , according to Stephanie B. Jones, MD, professor and chair of anesthesiology at Albany Medical College, New York.
“[With] any patient coming in for any sort of surgery, you should be considering multimodal pain management. That applies to the opioid use disorder patient as well,” Dr. Jones said in a presentation at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education.
“The challenge of opioid-tolerant patients or opioid abuse patients is twofold – tolerance and hyperalgesia,” Dr. Jones said. Patient tolerance changes how patients perceive pain and respond to medication. Clinicians need to consider the “opioid debt,” defined as the daily amount of opioid medication required by opioid-dependent patients to maintain their usual prehospitalization opioid levels, she explained. Also consider hyperalgesia, a change in pain perception “resulting in an increase in pain sensitivity to painful stimuli, thereby decreasing the analgesic effects of opioids,” Dr. Jones added.
A multimodal approach to pain management in patients on chronic opioids can include some opioids as appropriate, Dr. Jones said. Modulation of pain may draw on epidurals and nerve blocks, as well as managing CNS perception of pain through opioids or acetaminophen, and also using systemic options such as alpha-2 agonists and tramadol, she said.
Studies have shown that opioid abuse or dependence were associated with increased readmission rates, length of stay, and health care costs in surgery patients, said Dr. Jones. However, switching opioids and managing equivalents is complex, and “equianalgesic conversions serve only as a general guide to estimate opioid dose equivalents,” according to UpToDate’s, “Management of acute pain in the patient chronically using opioids,” she said.
Dr. Jones also addressed the issue of using hospitalization as an opportunity to help patients with untreated opioid use disorder. Medication-assisted options include methadone, buprenorphine, and naltrexone.
“One problem with methadone is that there are a lot of medications interactions,” she said. Buprenorphine has the advantage of being long-lasting, and is formulated with naloxone which deters injection. “Because it is a partial agonist, there is a lower risk of overdose and sedation,” and it has fewer medication interactions. However, some doctors are reluctant to prescribe it and there is some risk of medication diversion, she said.
Naltrexone is newer to the role of treating opioid use disorder, Dr. Jones said. “It can cause acute withdrawal because it is a full opioid antagonist,” she noted. However, naltrexone itself causes no withdrawal if stopped, and no respiratory depression or sedation, said Dr. Jones.
“Utilize addiction services in your hospital if you suspect a patient may be at risk for opioid use disorder,” and engage these services early, she emphasized.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Dr. Jones had no financial conflicts to disclose.
For surgical patients on chronic opioid therapy, , according to Stephanie B. Jones, MD, professor and chair of anesthesiology at Albany Medical College, New York.
“[With] any patient coming in for any sort of surgery, you should be considering multimodal pain management. That applies to the opioid use disorder patient as well,” Dr. Jones said in a presentation at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education.
“The challenge of opioid-tolerant patients or opioid abuse patients is twofold – tolerance and hyperalgesia,” Dr. Jones said. Patient tolerance changes how patients perceive pain and respond to medication. Clinicians need to consider the “opioid debt,” defined as the daily amount of opioid medication required by opioid-dependent patients to maintain their usual prehospitalization opioid levels, she explained. Also consider hyperalgesia, a change in pain perception “resulting in an increase in pain sensitivity to painful stimuli, thereby decreasing the analgesic effects of opioids,” Dr. Jones added.
A multimodal approach to pain management in patients on chronic opioids can include some opioids as appropriate, Dr. Jones said. Modulation of pain may draw on epidurals and nerve blocks, as well as managing CNS perception of pain through opioids or acetaminophen, and also using systemic options such as alpha-2 agonists and tramadol, she said.
Studies have shown that opioid abuse or dependence were associated with increased readmission rates, length of stay, and health care costs in surgery patients, said Dr. Jones. However, switching opioids and managing equivalents is complex, and “equianalgesic conversions serve only as a general guide to estimate opioid dose equivalents,” according to UpToDate’s, “Management of acute pain in the patient chronically using opioids,” she said.
Dr. Jones also addressed the issue of using hospitalization as an opportunity to help patients with untreated opioid use disorder. Medication-assisted options include methadone, buprenorphine, and naltrexone.
“One problem with methadone is that there are a lot of medications interactions,” she said. Buprenorphine has the advantage of being long-lasting, and is formulated with naloxone which deters injection. “Because it is a partial agonist, there is a lower risk of overdose and sedation,” and it has fewer medication interactions. However, some doctors are reluctant to prescribe it and there is some risk of medication diversion, she said.
Naltrexone is newer to the role of treating opioid use disorder, Dr. Jones said. “It can cause acute withdrawal because it is a full opioid antagonist,” she noted. However, naltrexone itself causes no withdrawal if stopped, and no respiratory depression or sedation, said Dr. Jones.
“Utilize addiction services in your hospital if you suspect a patient may be at risk for opioid use disorder,” and engage these services early, she emphasized.
Global Academy for Medical Education and this news organization are owned by the same parent company.
Dr. Jones had no financial conflicts to disclose.
FROM MISS
Restriction of Foley catheters in older trauma patients improved outcomes
and led to earlier discharge, findings from a study revealed. The results of the study were reported in an abstract scheduled for release at the annual meeting of the American Academy of Orthopaedic Surgeons. The meeting was canceled because of COVID-19.
“We reduced the use of Foley catheters in our target population by more than 50%, which led to a decrease in the rate of hospital-acquired UTI and positively affected other perioperative outcomes,” reported Sanjit R. Konda, MD, an orthopedic surgeon with New York University Langone Health.
The quality initiative was introduced about 2 years ago specifically to reduce the risk of UTI in older patients admitted for femur or hip fractures. Previously at the level 1 trauma center where this quality initiative was introduced, placement of Foley catheters in these types of patients had been routine.
After the policy change, Foley catheters were only offered to these trauma patients 55 years of age or older when more than three episodes or urinary retention had been documented with a bladder scan. Urinary retention was defined as a volume of at least 600 mL.
When outcomes in 184 patients treated in the 15 months after the policy change were compared with 393 treated in the prior 38 months, Foley catheter use was substantially and significantly reduced (43.5% vs. 95.5%; P < .001), Dr. Konda said in an interview.
Although the lower rate of UTI following the policy change fell short of statistical significance (10.33% vs. 14.5%; P = .167), the policy change was associated with a decreased time to surgery (33.27 vs. 38.54 hours; P = .001), shorter length of stay (6.89 vs. 8.34 days; P < .001), and higher rate of home discharge (22.8% vs. 15.6%; P = .038).
When those who avoided a Foley catheter were compared with those who did not after the policy change, there was a significant reduction in UTI (4.81% vs. 17.4%; P = .014). In addition, patients who avoided a Foley catheter had a decreased time to surgery (P = .014), shorter length of stay (P < .001) and an almost 900% greater likelihood of home discharge (odds ratio, 9.9; P < .001).
“This quality initiative does increase the number of bladder scans required, meaning more work for nurses, but the program was developed in collaboration with our nursing staff, who were supportive of the goals,” Dr. Konda reported.
Reducing the incidence of UTI is an important initiative because the Centers for Medicare & Medicaid Services and other third-party payers employ this as a quality metric, according to Dr. Konda. This explains why hospital administrators generally embrace effective strategies to reduce UTI rates.
The improvement in outcomes, including the reduction in UTIs and length of stay, has cost implications, which will be evaluated in a future analysis, according to Dr. Konda.
Although this quality initiative was undertaken in a level 1 trauma center, Dr. Konda believes the same principles can be applied to other settings.
Jennifer A. Meddings, MD, an associate professor of medicine at the University of Michigan, Ann Arbor, agreed. Active in the evaluation of strategies to reduce hospital-acquired complications, Dr. Meddings published a study of procedural appropriateness ratings to guide strategies for improving the likelihood that catheters are employed only when needed (BMJ Qual Saf. 2019;28:56-66).
“In addition to avoiding UTI, reducing unnecessary placement of Foley catheters also eliminates the risk of trauma to the urinary tract,” Dr. Meddings said. This is a complication that is not well appreciated because the trauma is not always documented, according to Dr. Meddings, who believes increased risk of both UTI and urinary tract trauma should discourage use of Foley catheters when there is not a specific indication.
Although there are criteria other than excess bladder volume to determine when to consider a Foley catheter, Dr. Meddings encourages any systematic approach that increases the likelihood that catheters are not placed unnecessarily. She emphasized that a hip fracture by itself “is not a criterion for catheterization.”
Dr. Konda reported a financial relationship with Stryker.
and led to earlier discharge, findings from a study revealed. The results of the study were reported in an abstract scheduled for release at the annual meeting of the American Academy of Orthopaedic Surgeons. The meeting was canceled because of COVID-19.
“We reduced the use of Foley catheters in our target population by more than 50%, which led to a decrease in the rate of hospital-acquired UTI and positively affected other perioperative outcomes,” reported Sanjit R. Konda, MD, an orthopedic surgeon with New York University Langone Health.
The quality initiative was introduced about 2 years ago specifically to reduce the risk of UTI in older patients admitted for femur or hip fractures. Previously at the level 1 trauma center where this quality initiative was introduced, placement of Foley catheters in these types of patients had been routine.
After the policy change, Foley catheters were only offered to these trauma patients 55 years of age or older when more than three episodes or urinary retention had been documented with a bladder scan. Urinary retention was defined as a volume of at least 600 mL.
When outcomes in 184 patients treated in the 15 months after the policy change were compared with 393 treated in the prior 38 months, Foley catheter use was substantially and significantly reduced (43.5% vs. 95.5%; P < .001), Dr. Konda said in an interview.
Although the lower rate of UTI following the policy change fell short of statistical significance (10.33% vs. 14.5%; P = .167), the policy change was associated with a decreased time to surgery (33.27 vs. 38.54 hours; P = .001), shorter length of stay (6.89 vs. 8.34 days; P < .001), and higher rate of home discharge (22.8% vs. 15.6%; P = .038).
When those who avoided a Foley catheter were compared with those who did not after the policy change, there was a significant reduction in UTI (4.81% vs. 17.4%; P = .014). In addition, patients who avoided a Foley catheter had a decreased time to surgery (P = .014), shorter length of stay (P < .001) and an almost 900% greater likelihood of home discharge (odds ratio, 9.9; P < .001).
“This quality initiative does increase the number of bladder scans required, meaning more work for nurses, but the program was developed in collaboration with our nursing staff, who were supportive of the goals,” Dr. Konda reported.
Reducing the incidence of UTI is an important initiative because the Centers for Medicare & Medicaid Services and other third-party payers employ this as a quality metric, according to Dr. Konda. This explains why hospital administrators generally embrace effective strategies to reduce UTI rates.
The improvement in outcomes, including the reduction in UTIs and length of stay, has cost implications, which will be evaluated in a future analysis, according to Dr. Konda.
Although this quality initiative was undertaken in a level 1 trauma center, Dr. Konda believes the same principles can be applied to other settings.
Jennifer A. Meddings, MD, an associate professor of medicine at the University of Michigan, Ann Arbor, agreed. Active in the evaluation of strategies to reduce hospital-acquired complications, Dr. Meddings published a study of procedural appropriateness ratings to guide strategies for improving the likelihood that catheters are employed only when needed (BMJ Qual Saf. 2019;28:56-66).
“In addition to avoiding UTI, reducing unnecessary placement of Foley catheters also eliminates the risk of trauma to the urinary tract,” Dr. Meddings said. This is a complication that is not well appreciated because the trauma is not always documented, according to Dr. Meddings, who believes increased risk of both UTI and urinary tract trauma should discourage use of Foley catheters when there is not a specific indication.
Although there are criteria other than excess bladder volume to determine when to consider a Foley catheter, Dr. Meddings encourages any systematic approach that increases the likelihood that catheters are not placed unnecessarily. She emphasized that a hip fracture by itself “is not a criterion for catheterization.”
Dr. Konda reported a financial relationship with Stryker.
and led to earlier discharge, findings from a study revealed. The results of the study were reported in an abstract scheduled for release at the annual meeting of the American Academy of Orthopaedic Surgeons. The meeting was canceled because of COVID-19.
“We reduced the use of Foley catheters in our target population by more than 50%, which led to a decrease in the rate of hospital-acquired UTI and positively affected other perioperative outcomes,” reported Sanjit R. Konda, MD, an orthopedic surgeon with New York University Langone Health.
The quality initiative was introduced about 2 years ago specifically to reduce the risk of UTI in older patients admitted for femur or hip fractures. Previously at the level 1 trauma center where this quality initiative was introduced, placement of Foley catheters in these types of patients had been routine.
After the policy change, Foley catheters were only offered to these trauma patients 55 years of age or older when more than three episodes or urinary retention had been documented with a bladder scan. Urinary retention was defined as a volume of at least 600 mL.
When outcomes in 184 patients treated in the 15 months after the policy change were compared with 393 treated in the prior 38 months, Foley catheter use was substantially and significantly reduced (43.5% vs. 95.5%; P < .001), Dr. Konda said in an interview.
Although the lower rate of UTI following the policy change fell short of statistical significance (10.33% vs. 14.5%; P = .167), the policy change was associated with a decreased time to surgery (33.27 vs. 38.54 hours; P = .001), shorter length of stay (6.89 vs. 8.34 days; P < .001), and higher rate of home discharge (22.8% vs. 15.6%; P = .038).
When those who avoided a Foley catheter were compared with those who did not after the policy change, there was a significant reduction in UTI (4.81% vs. 17.4%; P = .014). In addition, patients who avoided a Foley catheter had a decreased time to surgery (P = .014), shorter length of stay (P < .001) and an almost 900% greater likelihood of home discharge (odds ratio, 9.9; P < .001).
“This quality initiative does increase the number of bladder scans required, meaning more work for nurses, but the program was developed in collaboration with our nursing staff, who were supportive of the goals,” Dr. Konda reported.
Reducing the incidence of UTI is an important initiative because the Centers for Medicare & Medicaid Services and other third-party payers employ this as a quality metric, according to Dr. Konda. This explains why hospital administrators generally embrace effective strategies to reduce UTI rates.
The improvement in outcomes, including the reduction in UTIs and length of stay, has cost implications, which will be evaluated in a future analysis, according to Dr. Konda.
Although this quality initiative was undertaken in a level 1 trauma center, Dr. Konda believes the same principles can be applied to other settings.
Jennifer A. Meddings, MD, an associate professor of medicine at the University of Michigan, Ann Arbor, agreed. Active in the evaluation of strategies to reduce hospital-acquired complications, Dr. Meddings published a study of procedural appropriateness ratings to guide strategies for improving the likelihood that catheters are employed only when needed (BMJ Qual Saf. 2019;28:56-66).
“In addition to avoiding UTI, reducing unnecessary placement of Foley catheters also eliminates the risk of trauma to the urinary tract,” Dr. Meddings said. This is a complication that is not well appreciated because the trauma is not always documented, according to Dr. Meddings, who believes increased risk of both UTI and urinary tract trauma should discourage use of Foley catheters when there is not a specific indication.
Although there are criteria other than excess bladder volume to determine when to consider a Foley catheter, Dr. Meddings encourages any systematic approach that increases the likelihood that catheters are not placed unnecessarily. She emphasized that a hip fracture by itself “is not a criterion for catheterization.”
Dr. Konda reported a financial relationship with Stryker.
FROM AAOS 2020
Acetaminophen plus ibuprofen cut patient-controlled morphine after total hip arthroplasty
Background: The use of multimodal non-opioid analgesics is a common practice to minimize postoperative pain and opioid analgesic use. There is limited high-quality evidence to confirm the synergistic effect and safety of acetaminophen and ibuprofen in the peripostoperative setting. The Paracetamol and NSAID in combination (PANSAID) trial investigated the analgesic efficacy and safety of four multimodal analgesic regimens after total hip arthroplasty.
Study design: Multicenter, randomized, blinded trial.
Setting: A total of six hospitals in Denmark, which represented regional and large university settings.
Synopsis: A total of 559 patients who underwent total hip arthroplasty were randomized to receive one of the following oral regimens: acetaminophen (1,000 mg) and ibuprofen (400 mg), acetaminophen (1,000 mg) and placebo, ibuprofen (400 mg) and placebo, and half-strength acetaminophen (500 mg) and ibuprofen (200 mg). One of the regimens was initiated 1 hour before surgery and continued every 6 hours for a total of 4 doses on the first postoperative day. The mean age was 67 years, and half of the patients were women.
The median morphine consumption in the 24 hours after surgery was significantly lower with full-strength acetaminophen-ibuprofen compared with acetaminophen monotherapy (20 mg vs. 36 mg, 99.6% confidence interval, 6.5-24; P < .001), which exceeded the prespecified 10-mg threshold for a minimal clinically important difference (MCID). The difference between acetaminophen-ibuprofen and ibuprofen monotherapy (20 mg vs. 26 mg) did not exceed the MCID, and was not clinically meaningful. The differences in morphine consumption with full-strength acetaminophen-ibuprofen compared to half-strength acetaminophen-ibuprofen (28 mg) and ibuprofen compared to acetaminophen monotherapy were not statistically significant.
Serious adverse events, the other primary outcome, within 90 days after surgery (15% in the ibuprofen group and 11% in the acetaminophen group, relative risk, 1.44; 97.5% CI, 0.79-2.64; P = .18) did not differ between acetaminophen monotherapy and ibuprofen monotherapy. Secondary outcomes included statistically significant analgesia (lower pain scores) at rest and with mobilization at 24 hours in the acetaminophen-ibuprofen group compared to the other groups.
An interesting observation was that acetaminophen-ibuprofen did not exceed the MCID compared to ibuprofen, which suggests that ibuprofen monotherapy may be a reasonable option for early postoperative analgesia.
Bottom line: Acetaminophen-ibuprofen reduced postoperative morphine use and had improved analgesia 24 hours after total hip arthroplasty, and was not associated with an increased 3-month risk of serious adverse events.
Citation: Thybo KH et al. Effect of combination of paracetamol (acetaminophen) and ibuprofen vs. either alone on patient-controlled morphine consumption in the first 24 hours after total hip arthroplasty. The PANSAID randomized clinical trial. JAMA. 2019;321(6):562-71.
Dr. Lambert is a hospital medicine clinician and addiction medicine specialist in the division of hospital medicine at Massachusetts General Hospital.
Background: The use of multimodal non-opioid analgesics is a common practice to minimize postoperative pain and opioid analgesic use. There is limited high-quality evidence to confirm the synergistic effect and safety of acetaminophen and ibuprofen in the peripostoperative setting. The Paracetamol and NSAID in combination (PANSAID) trial investigated the analgesic efficacy and safety of four multimodal analgesic regimens after total hip arthroplasty.
Study design: Multicenter, randomized, blinded trial.
Setting: A total of six hospitals in Denmark, which represented regional and large university settings.
Synopsis: A total of 559 patients who underwent total hip arthroplasty were randomized to receive one of the following oral regimens: acetaminophen (1,000 mg) and ibuprofen (400 mg), acetaminophen (1,000 mg) and placebo, ibuprofen (400 mg) and placebo, and half-strength acetaminophen (500 mg) and ibuprofen (200 mg). One of the regimens was initiated 1 hour before surgery and continued every 6 hours for a total of 4 doses on the first postoperative day. The mean age was 67 years, and half of the patients were women.
The median morphine consumption in the 24 hours after surgery was significantly lower with full-strength acetaminophen-ibuprofen compared with acetaminophen monotherapy (20 mg vs. 36 mg, 99.6% confidence interval, 6.5-24; P < .001), which exceeded the prespecified 10-mg threshold for a minimal clinically important difference (MCID). The difference between acetaminophen-ibuprofen and ibuprofen monotherapy (20 mg vs. 26 mg) did not exceed the MCID, and was not clinically meaningful. The differences in morphine consumption with full-strength acetaminophen-ibuprofen compared to half-strength acetaminophen-ibuprofen (28 mg) and ibuprofen compared to acetaminophen monotherapy were not statistically significant.
Serious adverse events, the other primary outcome, within 90 days after surgery (15% in the ibuprofen group and 11% in the acetaminophen group, relative risk, 1.44; 97.5% CI, 0.79-2.64; P = .18) did not differ between acetaminophen monotherapy and ibuprofen monotherapy. Secondary outcomes included statistically significant analgesia (lower pain scores) at rest and with mobilization at 24 hours in the acetaminophen-ibuprofen group compared to the other groups.
An interesting observation was that acetaminophen-ibuprofen did not exceed the MCID compared to ibuprofen, which suggests that ibuprofen monotherapy may be a reasonable option for early postoperative analgesia.
Bottom line: Acetaminophen-ibuprofen reduced postoperative morphine use and had improved analgesia 24 hours after total hip arthroplasty, and was not associated with an increased 3-month risk of serious adverse events.
Citation: Thybo KH et al. Effect of combination of paracetamol (acetaminophen) and ibuprofen vs. either alone on patient-controlled morphine consumption in the first 24 hours after total hip arthroplasty. The PANSAID randomized clinical trial. JAMA. 2019;321(6):562-71.
Dr. Lambert is a hospital medicine clinician and addiction medicine specialist in the division of hospital medicine at Massachusetts General Hospital.
Background: The use of multimodal non-opioid analgesics is a common practice to minimize postoperative pain and opioid analgesic use. There is limited high-quality evidence to confirm the synergistic effect and safety of acetaminophen and ibuprofen in the peripostoperative setting. The Paracetamol and NSAID in combination (PANSAID) trial investigated the analgesic efficacy and safety of four multimodal analgesic regimens after total hip arthroplasty.
Study design: Multicenter, randomized, blinded trial.
Setting: A total of six hospitals in Denmark, which represented regional and large university settings.
Synopsis: A total of 559 patients who underwent total hip arthroplasty were randomized to receive one of the following oral regimens: acetaminophen (1,000 mg) and ibuprofen (400 mg), acetaminophen (1,000 mg) and placebo, ibuprofen (400 mg) and placebo, and half-strength acetaminophen (500 mg) and ibuprofen (200 mg). One of the regimens was initiated 1 hour before surgery and continued every 6 hours for a total of 4 doses on the first postoperative day. The mean age was 67 years, and half of the patients were women.
The median morphine consumption in the 24 hours after surgery was significantly lower with full-strength acetaminophen-ibuprofen compared with acetaminophen monotherapy (20 mg vs. 36 mg, 99.6% confidence interval, 6.5-24; P < .001), which exceeded the prespecified 10-mg threshold for a minimal clinically important difference (MCID). The difference between acetaminophen-ibuprofen and ibuprofen monotherapy (20 mg vs. 26 mg) did not exceed the MCID, and was not clinically meaningful. The differences in morphine consumption with full-strength acetaminophen-ibuprofen compared to half-strength acetaminophen-ibuprofen (28 mg) and ibuprofen compared to acetaminophen monotherapy were not statistically significant.
Serious adverse events, the other primary outcome, within 90 days after surgery (15% in the ibuprofen group and 11% in the acetaminophen group, relative risk, 1.44; 97.5% CI, 0.79-2.64; P = .18) did not differ between acetaminophen monotherapy and ibuprofen monotherapy. Secondary outcomes included statistically significant analgesia (lower pain scores) at rest and with mobilization at 24 hours in the acetaminophen-ibuprofen group compared to the other groups.
An interesting observation was that acetaminophen-ibuprofen did not exceed the MCID compared to ibuprofen, which suggests that ibuprofen monotherapy may be a reasonable option for early postoperative analgesia.
Bottom line: Acetaminophen-ibuprofen reduced postoperative morphine use and had improved analgesia 24 hours after total hip arthroplasty, and was not associated with an increased 3-month risk of serious adverse events.
Citation: Thybo KH et al. Effect of combination of paracetamol (acetaminophen) and ibuprofen vs. either alone on patient-controlled morphine consumption in the first 24 hours after total hip arthroplasty. The PANSAID randomized clinical trial. JAMA. 2019;321(6):562-71.
Dr. Lambert is a hospital medicine clinician and addiction medicine specialist in the division of hospital medicine at Massachusetts General Hospital.
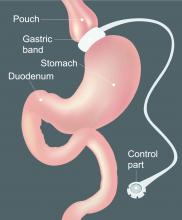
The hospitalized postbariatric surgery patient
What every hospitalist should know
With the prevalence of obesity worldwide topping 650 million people1 and nearly 40% of U.S. adults having obesity,2 bariatric surgery is increasingly used to treat this disease and its associated comorbidities.
The American Society for Metabolic & Bariatric Surgery estimates that 228,000 bariatric procedures were performed on Americans in 2017, up from 158,000 in 2011.3 Despite lowering the risks of diabetes, stroke, myocardial infarction, cancer, and all-cause mortality,4 bariatric surgery is associated with increased health care use. Neovius et al. found that people who underwent bariatric surgery used 54 mean cumulative hospital days in the 20 years following their procedures, compared with just 40 inpatient days used by controls.5
Although hospitalists are caring for increasing numbers of patients who have undergone bariatric surgery, many of us may not be aware of some of the things that can lead to hospitalization or otherwise affect inpatient medical care. Here are a few points to keep in mind the next time you care for an inpatient with prior bariatric surgery.
Pharmacokinetics change after surgery
Gastrointestinal anatomy necessarily changes after bariatric surgery and can affect the oral absorption of drugs. Because gastric motility may be impaired and the pH in the stomach is increased after bariatric surgery, the disintegration and dissolution of immediate-release solid pills or caps may be compromised.
It is therefore prudent to crush solid forms or switch to liquid or chewable formulations of immediate-release drugs for the first few weeks to months after surgery. Enteric-coated or long-acting drug formulations should not be crushed and should generally be avoided in patients who have undergone bypass procedures such as Roux-en-Y gastric bypass (RYGB) or biliopancreatic diversion with duodenal switch (BPD/DS), as they can demonstrate either enhanced or diminished absorption (depending on the drug).
Reduced intestinal transit times and changes in intestinal pH can alter the absorption of certain drugs as well, and the expression of some drug transporter proteins and enzymes such as the CYP3A4 variant of cytochrome P450 – which is estimated to metabolize up to half of currently available drugs – varies between the upper and the lower small intestine, potentially leading to increased bioavailability of medications metabolized by this enzyme in patients who have undergone bypass surgeries.
Interestingly, longer-term studies have reexamined drug absorption in patients 2-4 years after RYGB and found that initially-increased drug plasma levels often return to preoperative levels or even lower over time,6 likely because of adaptive changes in the GI tract. Because research on the pharmacokinetics of individual drugs after bariatric surgery is lacking, the hospitalist should be aware that the bioavailability of oral drugs is often altered and should monitor patients for the desired therapeutic effect as well as potential toxicities for any drug administered to postbariatric surgery patients.
Finally, note that nonsteroidal anti-inflammatory drugs (NSAIDs), aspirin, and corticosteroids should be avoided after bariatric surgery unless the benefit clearly outweighs the risk, as they increase the risk of ulcers even in patients without underlying surgical disruptions to the gastric mucosa.
Micronutrient deficiencies are common and can occur at any time
While many clinicians recognize that vitamin deficiencies can occur after weight loss surgeries which bypass the duodenum, such as the RYGB or the BPD/DS, it is important to note that vitamin and mineral deficiencies occur commonly even in patients with intact intestinal absorption such as those who underwent sleeve gastrectomy (SG) and even despite regained weight due to greater volumes of food (and micronutrient) intake over time.
The most common vitamin deficiencies include iron, vitamin B12, thiamine (vitamin B1), and vitamin D, but deficiencies in other vitamins and minerals may found as well. Anemia, bone fractures, heart failure, and encephalopathy can all be related to postoperative vitamin deficiencies. Most bariatric surgery patients should have micronutrient levels monitored on a yearly basis and should be taking at least a multivitamin with minerals (including zinc, copper, selenium and iron), a form of vitamin B12, and vitamin D with calcium supplementation. Additional supplements may be appropriate depending on the type of surgery the patient had or whether a deficiency is found.
The differential diagnosis for abdominal pain after bariatric surgery is unique
While the usual suspects such as diverticulitis or gastritis should be considered in postbariatric surgery patients just as in others, a few specific complications can arise after weight loss surgery.
Marginal ulcerations (ulcers at the surgical anastomotic sites) have been reported in up to a third of patients complaining of abdominal pain or dysphagia after RYGB, with tobacco, alcohol, or NSAID use conferring even greater risk.7 Early upper endoscopy may be warranted in symptomatic patients.
Small bowel obstruction (SBO) may occur due to surgical adhesions as in other patients, but catastrophic internal hernias with associated volvulus can occur due to specific anatomical defects that are created by the RYGB and BPD/DS procedures. CT imaging is insensitive and can miss up to 30% of these cases,8 and nasogastric tubes placed blindly for decompression of an SBO can lead to perforation of the end of the alimentary limb at the gastric pouch outlet, so post-RYGB or BPD/DS patients presenting with signs of small bowel obstruction should have an early surgical consult for expeditious surgical management rather than a trial of conservative medical management.9
Cholelithiasis is a very common postoperative complication, occurring in about 25% of SG patients and 32% of RYGB patients in the first year following surgery. The risk of gallstone formation can be significantly reduced with the postoperative use of ursodeoxycholic acid.10
Onset of abdominal cramping, nausea and diarrhea (sometimes accompanied by vasomotor symptoms) within 15-60 minutes of eating may be due to early dumping syndrome. Rapid delivery of food from the gastric pouch into the small intestine causes the release of gut peptides and an osmotic fluid shift into the intestinal lumen that can trigger these symptoms even in patients with a preserved pyloric sphincter, such as those who underwent SG. Simply eliminating sugars and simple carbohydrates from the diet usually resolves the problem, and eliminating lactose can often be helpful as well.
Postprandial hyperinsulinemic hypoglycemia (“late dumping syndrome”) can develop years after surgery
Vasomotor symptoms such as flushing/sweating, shaking, tachycardia/palpitations, lightheadedness, or difficulty concentrating occurring 1-3 hours after a meal should prompt blood glucose testing, as delayed hypoglycemia can occur after a large insulin surge.
Most commonly seen after RYGB, late dumping syndrome, like early dumping syndrome, can often be managed by eliminating sugars and simple carbohydrates from the diet. The onset of late dumping syndrome has been reported as late as 8 years after surgery,11 so the etiology of symptoms can be elusive. If the diagnosis is unclear, an oral glucose tolerance test may be helpful.
Alcohol use disorder is more prevalent after weight loss surgery
Changes to the gastrointestinal anatomy allow for more rapid absorption of ethanol into the bloodstream, making the drug more potent in postop patients. Simultaneously, many patients who undergo bariatric surgery have a history of using food to buffer negative emotions. Abruptly depriving them of that comfort in the context of the increased potency of alcohol could potentially leave bariatric surgery patients vulnerable to the development of alcohol use disorder, even when they did not misuse alcohol preoperatively.
Of note, alcohol misuse becomes more prevalent after the first postoperative year.12 Screening for alcohol misuse on admission to the hospital is wise in all cases, but perhaps even more so in the postbariatric surgery patient. If a patient does report excessive alcohol use, keep possible thiamine deficiency in mind.
The risk of suicide and self-harm increases after bariatric surgery
While all-cause mortality rates decrease after bariatric surgery compared with matched controls, the risk of suicide and nonfatal self-harm increases.
About half of bariatric surgery patients with nonfatal events have substance misuse.13 Notably, several studies have found reduced plasma levels of SSRIs in patients after RYGB,6 so pharmacotherapy for mood disorders could be less effective after bariatric surgery as well. The hospitalist could positively impact patients by screening for both substance misuse and depression and by having a low threshold for referral to a mental health professional.
As we see ever-increasing numbers of inpatients who have a history of bariatric surgery, being aware of these common and important complications can help today’s hospitalist provide the best care possible.
Dr. Kerns is a hospitalist and codirector of bariatric surgery at the Washington DC VA Medical Center.
References
1. Obesity and overweight. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Published Feb 16, 2018.
2. Hales CM et al. Prevalence of obesity among adults and youth: United States, 2015-2016. NCHS data brief, no 288. Hyattsville, MD: National Center for Health Statistics. 2017.
3. Estimate of Bariatric Surgery Numbers, 2011-2018. ASMBS.org. Published June 2018.
4. Sjöström L. Review of the key results from the Swedish Obese Subjects (SOS) trial – a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013 Mar;273(3):219-34. doi: 10.1111/joim.12012.
5. Neovius M et al. Health care use during 20 years following bariatric surgery. JAMA. 2012 Sep 19; 308(11):1132-41. doi: 10.1001/2012.jama.11792.
6. Azran C. et al. Oral drug therapy following bariatric surgery: An overview of fundamentals, literature and clinical recommendations. Obes Rev. 2016 Nov;17(11):1050-66. doi: 10.1111/obr.12434.
7. El-hayek KM et al. Marginal ulcer after Roux-en-Y gastric bypass: What have we really learned? Surg Endosc. 2012 Oct;26(10):2789-96. Epub 2012 Apr 28. (Abstract presented at Society of American Gastrointestinal and Endoscopic Surgeons 2012 annual meeting, San Diego.) 8. Iannelli A et al. Internal hernia after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Obes Surg. 2006;16:1265-71. doi: 10.1381/096089206778663689.
9. Lim R et al. Early and late complications of bariatric operation. Trauma Surg Acute Care Open. 2018 Oct 9;3(1): e000219. doi: 10.1136/tsaco-2018-000219.
10. Coupaye M et al. Evaluation of incidence of cholelithiasis after bariatric surgery in subjects treated or not treated with ursodeoxycholic acid. Surg Obes Relat Dis. 2017;13(4):681-5. doi: 10.1016/j.soard.2016.11.022.
11. Eisenberg D et al. ASMBS position statement on postprandial hyperinsulinemic hypoglycemia after bariatric surgery. Surg Obes Relat Dis. 2017 Mar;13(3):371-8. doi: 10.1016/j.soard.2016.12.005.
12. King WC et al. Prevalence of alcohol use disorders before and after bariatric surgery. JAMA. 2012 Jun 20;307(23):2516-25. doi: 10.1001/jama.2012.6147.
13. Neovius M et al. Risk of suicide and non-fatal self-harm after bariatric surgery: Results from two matched cohort studies. Lancet Diabetes Endocrinol. 2018 Mar;6(3):197-207. doi: 10.1016/S2213-8587(17)30437-0.
What every hospitalist should know
What every hospitalist should know
With the prevalence of obesity worldwide topping 650 million people1 and nearly 40% of U.S. adults having obesity,2 bariatric surgery is increasingly used to treat this disease and its associated comorbidities.
The American Society for Metabolic & Bariatric Surgery estimates that 228,000 bariatric procedures were performed on Americans in 2017, up from 158,000 in 2011.3 Despite lowering the risks of diabetes, stroke, myocardial infarction, cancer, and all-cause mortality,4 bariatric surgery is associated with increased health care use. Neovius et al. found that people who underwent bariatric surgery used 54 mean cumulative hospital days in the 20 years following their procedures, compared with just 40 inpatient days used by controls.5
Although hospitalists are caring for increasing numbers of patients who have undergone bariatric surgery, many of us may not be aware of some of the things that can lead to hospitalization or otherwise affect inpatient medical care. Here are a few points to keep in mind the next time you care for an inpatient with prior bariatric surgery.
Pharmacokinetics change after surgery
Gastrointestinal anatomy necessarily changes after bariatric surgery and can affect the oral absorption of drugs. Because gastric motility may be impaired and the pH in the stomach is increased after bariatric surgery, the disintegration and dissolution of immediate-release solid pills or caps may be compromised.
It is therefore prudent to crush solid forms or switch to liquid or chewable formulations of immediate-release drugs for the first few weeks to months after surgery. Enteric-coated or long-acting drug formulations should not be crushed and should generally be avoided in patients who have undergone bypass procedures such as Roux-en-Y gastric bypass (RYGB) or biliopancreatic diversion with duodenal switch (BPD/DS), as they can demonstrate either enhanced or diminished absorption (depending on the drug).
Reduced intestinal transit times and changes in intestinal pH can alter the absorption of certain drugs as well, and the expression of some drug transporter proteins and enzymes such as the CYP3A4 variant of cytochrome P450 – which is estimated to metabolize up to half of currently available drugs – varies between the upper and the lower small intestine, potentially leading to increased bioavailability of medications metabolized by this enzyme in patients who have undergone bypass surgeries.
Interestingly, longer-term studies have reexamined drug absorption in patients 2-4 years after RYGB and found that initially-increased drug plasma levels often return to preoperative levels or even lower over time,6 likely because of adaptive changes in the GI tract. Because research on the pharmacokinetics of individual drugs after bariatric surgery is lacking, the hospitalist should be aware that the bioavailability of oral drugs is often altered and should monitor patients for the desired therapeutic effect as well as potential toxicities for any drug administered to postbariatric surgery patients.
Finally, note that nonsteroidal anti-inflammatory drugs (NSAIDs), aspirin, and corticosteroids should be avoided after bariatric surgery unless the benefit clearly outweighs the risk, as they increase the risk of ulcers even in patients without underlying surgical disruptions to the gastric mucosa.
Micronutrient deficiencies are common and can occur at any time
While many clinicians recognize that vitamin deficiencies can occur after weight loss surgeries which bypass the duodenum, such as the RYGB or the BPD/DS, it is important to note that vitamin and mineral deficiencies occur commonly even in patients with intact intestinal absorption such as those who underwent sleeve gastrectomy (SG) and even despite regained weight due to greater volumes of food (and micronutrient) intake over time.
The most common vitamin deficiencies include iron, vitamin B12, thiamine (vitamin B1), and vitamin D, but deficiencies in other vitamins and minerals may found as well. Anemia, bone fractures, heart failure, and encephalopathy can all be related to postoperative vitamin deficiencies. Most bariatric surgery patients should have micronutrient levels monitored on a yearly basis and should be taking at least a multivitamin with minerals (including zinc, copper, selenium and iron), a form of vitamin B12, and vitamin D with calcium supplementation. Additional supplements may be appropriate depending on the type of surgery the patient had or whether a deficiency is found.
The differential diagnosis for abdominal pain after bariatric surgery is unique
While the usual suspects such as diverticulitis or gastritis should be considered in postbariatric surgery patients just as in others, a few specific complications can arise after weight loss surgery.
Marginal ulcerations (ulcers at the surgical anastomotic sites) have been reported in up to a third of patients complaining of abdominal pain or dysphagia after RYGB, with tobacco, alcohol, or NSAID use conferring even greater risk.7 Early upper endoscopy may be warranted in symptomatic patients.
Small bowel obstruction (SBO) may occur due to surgical adhesions as in other patients, but catastrophic internal hernias with associated volvulus can occur due to specific anatomical defects that are created by the RYGB and BPD/DS procedures. CT imaging is insensitive and can miss up to 30% of these cases,8 and nasogastric tubes placed blindly for decompression of an SBO can lead to perforation of the end of the alimentary limb at the gastric pouch outlet, so post-RYGB or BPD/DS patients presenting with signs of small bowel obstruction should have an early surgical consult for expeditious surgical management rather than a trial of conservative medical management.9
Cholelithiasis is a very common postoperative complication, occurring in about 25% of SG patients and 32% of RYGB patients in the first year following surgery. The risk of gallstone formation can be significantly reduced with the postoperative use of ursodeoxycholic acid.10
Onset of abdominal cramping, nausea and diarrhea (sometimes accompanied by vasomotor symptoms) within 15-60 minutes of eating may be due to early dumping syndrome. Rapid delivery of food from the gastric pouch into the small intestine causes the release of gut peptides and an osmotic fluid shift into the intestinal lumen that can trigger these symptoms even in patients with a preserved pyloric sphincter, such as those who underwent SG. Simply eliminating sugars and simple carbohydrates from the diet usually resolves the problem, and eliminating lactose can often be helpful as well.
Postprandial hyperinsulinemic hypoglycemia (“late dumping syndrome”) can develop years after surgery
Vasomotor symptoms such as flushing/sweating, shaking, tachycardia/palpitations, lightheadedness, or difficulty concentrating occurring 1-3 hours after a meal should prompt blood glucose testing, as delayed hypoglycemia can occur after a large insulin surge.
Most commonly seen after RYGB, late dumping syndrome, like early dumping syndrome, can often be managed by eliminating sugars and simple carbohydrates from the diet. The onset of late dumping syndrome has been reported as late as 8 years after surgery,11 so the etiology of symptoms can be elusive. If the diagnosis is unclear, an oral glucose tolerance test may be helpful.
Alcohol use disorder is more prevalent after weight loss surgery
Changes to the gastrointestinal anatomy allow for more rapid absorption of ethanol into the bloodstream, making the drug more potent in postop patients. Simultaneously, many patients who undergo bariatric surgery have a history of using food to buffer negative emotions. Abruptly depriving them of that comfort in the context of the increased potency of alcohol could potentially leave bariatric surgery patients vulnerable to the development of alcohol use disorder, even when they did not misuse alcohol preoperatively.
Of note, alcohol misuse becomes more prevalent after the first postoperative year.12 Screening for alcohol misuse on admission to the hospital is wise in all cases, but perhaps even more so in the postbariatric surgery patient. If a patient does report excessive alcohol use, keep possible thiamine deficiency in mind.
The risk of suicide and self-harm increases after bariatric surgery
While all-cause mortality rates decrease after bariatric surgery compared with matched controls, the risk of suicide and nonfatal self-harm increases.
About half of bariatric surgery patients with nonfatal events have substance misuse.13 Notably, several studies have found reduced plasma levels of SSRIs in patients after RYGB,6 so pharmacotherapy for mood disorders could be less effective after bariatric surgery as well. The hospitalist could positively impact patients by screening for both substance misuse and depression and by having a low threshold for referral to a mental health professional.
As we see ever-increasing numbers of inpatients who have a history of bariatric surgery, being aware of these common and important complications can help today’s hospitalist provide the best care possible.
Dr. Kerns is a hospitalist and codirector of bariatric surgery at the Washington DC VA Medical Center.
References
1. Obesity and overweight. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Published Feb 16, 2018.
2. Hales CM et al. Prevalence of obesity among adults and youth: United States, 2015-2016. NCHS data brief, no 288. Hyattsville, MD: National Center for Health Statistics. 2017.
3. Estimate of Bariatric Surgery Numbers, 2011-2018. ASMBS.org. Published June 2018.
4. Sjöström L. Review of the key results from the Swedish Obese Subjects (SOS) trial – a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013 Mar;273(3):219-34. doi: 10.1111/joim.12012.
5. Neovius M et al. Health care use during 20 years following bariatric surgery. JAMA. 2012 Sep 19; 308(11):1132-41. doi: 10.1001/2012.jama.11792.
6. Azran C. et al. Oral drug therapy following bariatric surgery: An overview of fundamentals, literature and clinical recommendations. Obes Rev. 2016 Nov;17(11):1050-66. doi: 10.1111/obr.12434.
7. El-hayek KM et al. Marginal ulcer after Roux-en-Y gastric bypass: What have we really learned? Surg Endosc. 2012 Oct;26(10):2789-96. Epub 2012 Apr 28. (Abstract presented at Society of American Gastrointestinal and Endoscopic Surgeons 2012 annual meeting, San Diego.) 8. Iannelli A et al. Internal hernia after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Obes Surg. 2006;16:1265-71. doi: 10.1381/096089206778663689.
9. Lim R et al. Early and late complications of bariatric operation. Trauma Surg Acute Care Open. 2018 Oct 9;3(1): e000219. doi: 10.1136/tsaco-2018-000219.
10. Coupaye M et al. Evaluation of incidence of cholelithiasis after bariatric surgery in subjects treated or not treated with ursodeoxycholic acid. Surg Obes Relat Dis. 2017;13(4):681-5. doi: 10.1016/j.soard.2016.11.022.
11. Eisenberg D et al. ASMBS position statement on postprandial hyperinsulinemic hypoglycemia after bariatric surgery. Surg Obes Relat Dis. 2017 Mar;13(3):371-8. doi: 10.1016/j.soard.2016.12.005.
12. King WC et al. Prevalence of alcohol use disorders before and after bariatric surgery. JAMA. 2012 Jun 20;307(23):2516-25. doi: 10.1001/jama.2012.6147.
13. Neovius M et al. Risk of suicide and non-fatal self-harm after bariatric surgery: Results from two matched cohort studies. Lancet Diabetes Endocrinol. 2018 Mar;6(3):197-207. doi: 10.1016/S2213-8587(17)30437-0.
With the prevalence of obesity worldwide topping 650 million people1 and nearly 40% of U.S. adults having obesity,2 bariatric surgery is increasingly used to treat this disease and its associated comorbidities.
The American Society for Metabolic & Bariatric Surgery estimates that 228,000 bariatric procedures were performed on Americans in 2017, up from 158,000 in 2011.3 Despite lowering the risks of diabetes, stroke, myocardial infarction, cancer, and all-cause mortality,4 bariatric surgery is associated with increased health care use. Neovius et al. found that people who underwent bariatric surgery used 54 mean cumulative hospital days in the 20 years following their procedures, compared with just 40 inpatient days used by controls.5
Although hospitalists are caring for increasing numbers of patients who have undergone bariatric surgery, many of us may not be aware of some of the things that can lead to hospitalization or otherwise affect inpatient medical care. Here are a few points to keep in mind the next time you care for an inpatient with prior bariatric surgery.
Pharmacokinetics change after surgery
Gastrointestinal anatomy necessarily changes after bariatric surgery and can affect the oral absorption of drugs. Because gastric motility may be impaired and the pH in the stomach is increased after bariatric surgery, the disintegration and dissolution of immediate-release solid pills or caps may be compromised.
It is therefore prudent to crush solid forms or switch to liquid or chewable formulations of immediate-release drugs for the first few weeks to months after surgery. Enteric-coated or long-acting drug formulations should not be crushed and should generally be avoided in patients who have undergone bypass procedures such as Roux-en-Y gastric bypass (RYGB) or biliopancreatic diversion with duodenal switch (BPD/DS), as they can demonstrate either enhanced or diminished absorption (depending on the drug).
Reduced intestinal transit times and changes in intestinal pH can alter the absorption of certain drugs as well, and the expression of some drug transporter proteins and enzymes such as the CYP3A4 variant of cytochrome P450 – which is estimated to metabolize up to half of currently available drugs – varies between the upper and the lower small intestine, potentially leading to increased bioavailability of medications metabolized by this enzyme in patients who have undergone bypass surgeries.
Interestingly, longer-term studies have reexamined drug absorption in patients 2-4 years after RYGB and found that initially-increased drug plasma levels often return to preoperative levels or even lower over time,6 likely because of adaptive changes in the GI tract. Because research on the pharmacokinetics of individual drugs after bariatric surgery is lacking, the hospitalist should be aware that the bioavailability of oral drugs is often altered and should monitor patients for the desired therapeutic effect as well as potential toxicities for any drug administered to postbariatric surgery patients.
Finally, note that nonsteroidal anti-inflammatory drugs (NSAIDs), aspirin, and corticosteroids should be avoided after bariatric surgery unless the benefit clearly outweighs the risk, as they increase the risk of ulcers even in patients without underlying surgical disruptions to the gastric mucosa.
Micronutrient deficiencies are common and can occur at any time
While many clinicians recognize that vitamin deficiencies can occur after weight loss surgeries which bypass the duodenum, such as the RYGB or the BPD/DS, it is important to note that vitamin and mineral deficiencies occur commonly even in patients with intact intestinal absorption such as those who underwent sleeve gastrectomy (SG) and even despite regained weight due to greater volumes of food (and micronutrient) intake over time.
The most common vitamin deficiencies include iron, vitamin B12, thiamine (vitamin B1), and vitamin D, but deficiencies in other vitamins and minerals may found as well. Anemia, bone fractures, heart failure, and encephalopathy can all be related to postoperative vitamin deficiencies. Most bariatric surgery patients should have micronutrient levels monitored on a yearly basis and should be taking at least a multivitamin with minerals (including zinc, copper, selenium and iron), a form of vitamin B12, and vitamin D with calcium supplementation. Additional supplements may be appropriate depending on the type of surgery the patient had or whether a deficiency is found.
The differential diagnosis for abdominal pain after bariatric surgery is unique
While the usual suspects such as diverticulitis or gastritis should be considered in postbariatric surgery patients just as in others, a few specific complications can arise after weight loss surgery.
Marginal ulcerations (ulcers at the surgical anastomotic sites) have been reported in up to a third of patients complaining of abdominal pain or dysphagia after RYGB, with tobacco, alcohol, or NSAID use conferring even greater risk.7 Early upper endoscopy may be warranted in symptomatic patients.
Small bowel obstruction (SBO) may occur due to surgical adhesions as in other patients, but catastrophic internal hernias with associated volvulus can occur due to specific anatomical defects that are created by the RYGB and BPD/DS procedures. CT imaging is insensitive and can miss up to 30% of these cases,8 and nasogastric tubes placed blindly for decompression of an SBO can lead to perforation of the end of the alimentary limb at the gastric pouch outlet, so post-RYGB or BPD/DS patients presenting with signs of small bowel obstruction should have an early surgical consult for expeditious surgical management rather than a trial of conservative medical management.9
Cholelithiasis is a very common postoperative complication, occurring in about 25% of SG patients and 32% of RYGB patients in the first year following surgery. The risk of gallstone formation can be significantly reduced with the postoperative use of ursodeoxycholic acid.10
Onset of abdominal cramping, nausea and diarrhea (sometimes accompanied by vasomotor symptoms) within 15-60 minutes of eating may be due to early dumping syndrome. Rapid delivery of food from the gastric pouch into the small intestine causes the release of gut peptides and an osmotic fluid shift into the intestinal lumen that can trigger these symptoms even in patients with a preserved pyloric sphincter, such as those who underwent SG. Simply eliminating sugars and simple carbohydrates from the diet usually resolves the problem, and eliminating lactose can often be helpful as well.
Postprandial hyperinsulinemic hypoglycemia (“late dumping syndrome”) can develop years after surgery
Vasomotor symptoms such as flushing/sweating, shaking, tachycardia/palpitations, lightheadedness, or difficulty concentrating occurring 1-3 hours after a meal should prompt blood glucose testing, as delayed hypoglycemia can occur after a large insulin surge.
Most commonly seen after RYGB, late dumping syndrome, like early dumping syndrome, can often be managed by eliminating sugars and simple carbohydrates from the diet. The onset of late dumping syndrome has been reported as late as 8 years after surgery,11 so the etiology of symptoms can be elusive. If the diagnosis is unclear, an oral glucose tolerance test may be helpful.
Alcohol use disorder is more prevalent after weight loss surgery
Changes to the gastrointestinal anatomy allow for more rapid absorption of ethanol into the bloodstream, making the drug more potent in postop patients. Simultaneously, many patients who undergo bariatric surgery have a history of using food to buffer negative emotions. Abruptly depriving them of that comfort in the context of the increased potency of alcohol could potentially leave bariatric surgery patients vulnerable to the development of alcohol use disorder, even when they did not misuse alcohol preoperatively.
Of note, alcohol misuse becomes more prevalent after the first postoperative year.12 Screening for alcohol misuse on admission to the hospital is wise in all cases, but perhaps even more so in the postbariatric surgery patient. If a patient does report excessive alcohol use, keep possible thiamine deficiency in mind.
The risk of suicide and self-harm increases after bariatric surgery
While all-cause mortality rates decrease after bariatric surgery compared with matched controls, the risk of suicide and nonfatal self-harm increases.
About half of bariatric surgery patients with nonfatal events have substance misuse.13 Notably, several studies have found reduced plasma levels of SSRIs in patients after RYGB,6 so pharmacotherapy for mood disorders could be less effective after bariatric surgery as well. The hospitalist could positively impact patients by screening for both substance misuse and depression and by having a low threshold for referral to a mental health professional.
As we see ever-increasing numbers of inpatients who have a history of bariatric surgery, being aware of these common and important complications can help today’s hospitalist provide the best care possible.
Dr. Kerns is a hospitalist and codirector of bariatric surgery at the Washington DC VA Medical Center.
References
1. Obesity and overweight. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Published Feb 16, 2018.
2. Hales CM et al. Prevalence of obesity among adults and youth: United States, 2015-2016. NCHS data brief, no 288. Hyattsville, MD: National Center for Health Statistics. 2017.
3. Estimate of Bariatric Surgery Numbers, 2011-2018. ASMBS.org. Published June 2018.
4. Sjöström L. Review of the key results from the Swedish Obese Subjects (SOS) trial – a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013 Mar;273(3):219-34. doi: 10.1111/joim.12012.
5. Neovius M et al. Health care use during 20 years following bariatric surgery. JAMA. 2012 Sep 19; 308(11):1132-41. doi: 10.1001/2012.jama.11792.
6. Azran C. et al. Oral drug therapy following bariatric surgery: An overview of fundamentals, literature and clinical recommendations. Obes Rev. 2016 Nov;17(11):1050-66. doi: 10.1111/obr.12434.
7. El-hayek KM et al. Marginal ulcer after Roux-en-Y gastric bypass: What have we really learned? Surg Endosc. 2012 Oct;26(10):2789-96. Epub 2012 Apr 28. (Abstract presented at Society of American Gastrointestinal and Endoscopic Surgeons 2012 annual meeting, San Diego.) 8. Iannelli A et al. Internal hernia after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Obes Surg. 2006;16:1265-71. doi: 10.1381/096089206778663689.
9. Lim R et al. Early and late complications of bariatric operation. Trauma Surg Acute Care Open. 2018 Oct 9;3(1): e000219. doi: 10.1136/tsaco-2018-000219.
10. Coupaye M et al. Evaluation of incidence of cholelithiasis after bariatric surgery in subjects treated or not treated with ursodeoxycholic acid. Surg Obes Relat Dis. 2017;13(4):681-5. doi: 10.1016/j.soard.2016.11.022.
11. Eisenberg D et al. ASMBS position statement on postprandial hyperinsulinemic hypoglycemia after bariatric surgery. Surg Obes Relat Dis. 2017 Mar;13(3):371-8. doi: 10.1016/j.soard.2016.12.005.
12. King WC et al. Prevalence of alcohol use disorders before and after bariatric surgery. JAMA. 2012 Jun 20;307(23):2516-25. doi: 10.1001/jama.2012.6147.
13. Neovius M et al. Risk of suicide and non-fatal self-harm after bariatric surgery: Results from two matched cohort studies. Lancet Diabetes Endocrinol. 2018 Mar;6(3):197-207. doi: 10.1016/S2213-8587(17)30437-0.
Cultivating patient activation through technology
Tech alone is not enough
Patient activation refers to an individual’s knowledge, skill, and confidence in managing their health and health care, according to a recent BMJ editorial. It’s recognized as a critical aspect of high-quality, patient-centered health care – patient activation has the potential to improve patient outcomes while reducing costs.
Total knee replacement offers a great opportunity to study patient activation, said editorial lead author Jesse I. Wolfstadt, MD, MS, FRCSC, of the University of Toronto. “It may help address the one in five patients who are unsatisfied with their knee replacement despite an otherwise technically sound procedure.”
The authors considered some patient activation studies that have shown positive results for cultivating activation through technology. In one, patients engaging with a bedside multimedia intervention on a tablet after undergoing knee replacement reported better pain scores, length of stay, knee function, and satisfaction with care. Another study showed patients who received automated text messages after joint replacement improved time spent on home exercises, decreased their use of narcotics, and had fewer calls to the surgeon’s office.
But “negative mobile app studies seem to suggest that when technologies are used as a passive educational intervention, patient activation may suffer,” according to the editorial. “One possible key ingredient to successful patient activation is the engagement of the health care team that is facilitated through mobile technology. ... Mobile apps and other technological interventions also must have clear goals if they are to be used successfully; and these goals are likely to differ for different patient populations and disease processes.”
Technology alone is not enough to affect patient activation, Dr. Wolfstadt said. “The key to success will likely involve tailoring interventions to individual patients and facilitating increased engagement with the health care team. You can’t just give a patient an app or other form of technology and expect it to replace the function of patient-clinician communication/interaction.”
Reference
1. Wolfstadt JI et ak. Improving patient outcomes following total joint arthroplasty: Is there an app for that? BMJ Qual Saf. 2019 May 2019. doi: 10.1136/bmjqs-2019-009571.
Tech alone is not enough
Tech alone is not enough
Patient activation refers to an individual’s knowledge, skill, and confidence in managing their health and health care, according to a recent BMJ editorial. It’s recognized as a critical aspect of high-quality, patient-centered health care – patient activation has the potential to improve patient outcomes while reducing costs.
Total knee replacement offers a great opportunity to study patient activation, said editorial lead author Jesse I. Wolfstadt, MD, MS, FRCSC, of the University of Toronto. “It may help address the one in five patients who are unsatisfied with their knee replacement despite an otherwise technically sound procedure.”
The authors considered some patient activation studies that have shown positive results for cultivating activation through technology. In one, patients engaging with a bedside multimedia intervention on a tablet after undergoing knee replacement reported better pain scores, length of stay, knee function, and satisfaction with care. Another study showed patients who received automated text messages after joint replacement improved time spent on home exercises, decreased their use of narcotics, and had fewer calls to the surgeon’s office.
But “negative mobile app studies seem to suggest that when technologies are used as a passive educational intervention, patient activation may suffer,” according to the editorial. “One possible key ingredient to successful patient activation is the engagement of the health care team that is facilitated through mobile technology. ... Mobile apps and other technological interventions also must have clear goals if they are to be used successfully; and these goals are likely to differ for different patient populations and disease processes.”
Technology alone is not enough to affect patient activation, Dr. Wolfstadt said. “The key to success will likely involve tailoring interventions to individual patients and facilitating increased engagement with the health care team. You can’t just give a patient an app or other form of technology and expect it to replace the function of patient-clinician communication/interaction.”
Reference
1. Wolfstadt JI et ak. Improving patient outcomes following total joint arthroplasty: Is there an app for that? BMJ Qual Saf. 2019 May 2019. doi: 10.1136/bmjqs-2019-009571.
Patient activation refers to an individual’s knowledge, skill, and confidence in managing their health and health care, according to a recent BMJ editorial. It’s recognized as a critical aspect of high-quality, patient-centered health care – patient activation has the potential to improve patient outcomes while reducing costs.
Total knee replacement offers a great opportunity to study patient activation, said editorial lead author Jesse I. Wolfstadt, MD, MS, FRCSC, of the University of Toronto. “It may help address the one in five patients who are unsatisfied with their knee replacement despite an otherwise technically sound procedure.”
The authors considered some patient activation studies that have shown positive results for cultivating activation through technology. In one, patients engaging with a bedside multimedia intervention on a tablet after undergoing knee replacement reported better pain scores, length of stay, knee function, and satisfaction with care. Another study showed patients who received automated text messages after joint replacement improved time spent on home exercises, decreased their use of narcotics, and had fewer calls to the surgeon’s office.
But “negative mobile app studies seem to suggest that when technologies are used as a passive educational intervention, patient activation may suffer,” according to the editorial. “One possible key ingredient to successful patient activation is the engagement of the health care team that is facilitated through mobile technology. ... Mobile apps and other technological interventions also must have clear goals if they are to be used successfully; and these goals are likely to differ for different patient populations and disease processes.”
Technology alone is not enough to affect patient activation, Dr. Wolfstadt said. “The key to success will likely involve tailoring interventions to individual patients and facilitating increased engagement with the health care team. You can’t just give a patient an app or other form of technology and expect it to replace the function of patient-clinician communication/interaction.”
Reference
1. Wolfstadt JI et ak. Improving patient outcomes following total joint arthroplasty: Is there an app for that? BMJ Qual Saf. 2019 May 2019. doi: 10.1136/bmjqs-2019-009571.
New ASH guideline: VTE prophylaxis after major surgery
ORLANDO – The latest American Society of Hematology guideline on venous thromboembolism (VTE) tackles 30 key questions regarding prophylaxis in hospitalized patients undergoing surgery, according to the chair of the guideline panel, who highlighted 9 of those questions during a special session at the society’s annual meeting.
The clinical practice guideline, published just about a week before the annual meeting of the American Society of Hematology, focuses mainly on pharmacologic prophylaxis in specific surgical settings, said David R. Anderson, MD, dean of the faculty of medicine of Dalhousie University, Halifax, N.S.
“Our guidelines focused upon clinically important symptomatic outcomes, with less emphasis being placed on asymptomatic deep vein thrombosis detected by screening tests,” Dr. Anderson said.
At the special education session, Dr. Anderson highlighted several specific recommendations on prophylaxis in surgical patients.
Pharmacologic prophylaxis is not recommended for patients experiencing major trauma deemed to be at high risk of bleeding. Its use does reduce risk of symptomatic pulmonary embolism (PE) and deep vein thrombosis (DVT) by about 10 events per 1,000 patients treated; however, Dr. Anderson said, the panel’s opinion was that this benefit was outweighed by increased risk of major bleeding, at 24 events per 1,000 patients treated.
“We do recommend, however that this risk of bleeding must be reevaluated over the course of recovery of patients, and this may change the decision around this intervention over time,” Dr. Anderson told attendees at the special session.
That’s because pharmacologic prophylaxis is recommended in surgical patients at low to moderate risk of bleeding. In this scenario, the incremental risk of major bleeding (14 events per 1,000 patients treated) is outweighed by the benefit of the reduction of symptomatic VTE events, according to Dr. Anderson.
When pharmacologic prophylaxis is used, the panel recommends combined prophylaxis – mechanical prophylaxis in addition to pharmacologic prophylaxis – especially in those patients at high or very high risk of VTE. Evidence shows that the combination approach significantly reduces risk of PE, and strongly suggests it may also reduce risk of symptomatic proximal DVT, Dr. Anderson said.
In surgical patients not receiving pharmacologic prophylaxis, mechanical prophylaxis is recommended over no mechanical prophylaxis, he added. Moreover, in those patients receiving mechanical prophylaxis, the ASH panel recommends use of intermittent compression devices over graduated compression stockings.
The panel comes out against prophylactic inferior vena cava (IVC) filter insertion in the guidelines. Dr. Anderson said that the “small reduction” in PE risk seen in observational studies is outweighed by increased risk of DVT, and a resulting trend for increased mortality, associated with insertion of the devices.
“We did not consider other risks of IVC filters such as filter embolization or perforation, which again would be complications that would support our recommendation against routine use of these devices in patients undergoing major surgery,” he said.
In terms of the type of pharmacologic prophylaxis to use, the panel said low-molecular-weight heparin or unfractionated heparin would be reasonable choices in this setting. Available data do not demonstrate any significant differences between these choices for major clinical outcomes, Dr. Anderson added.
The guideline also addresses duration of pharmacologic prophylaxis, stating that extended prophylaxis – of at least 3 weeks – is favored over short-term prophylaxis, or up to 2 weeks of treatment. The extended approach significantly reduces risk of symptomatic PE and proximal DVT, though most of the supporting data come from studies of major joint arthroplasty and major general surgical procedures for patients with cancer. “We need more studies in other clinical areas to examine this particular question,” Dr. Anderson said.
The guideline on prophylaxis in surgical patients was published in Blood Advances (2019 Dec 3;3[23]:3898-944). Six other ASH VTE guidelines, all published in 2018, covered prophylaxis in medical patients, diagnosis, VTE in pregnancy, optimal anticoagulation, heparin-induced thrombocytopenia, and pediatric considerations. The guidelines are available on the ASH website.
Dr. Anderson reported having no relevant conflicts of interest.
ORLANDO – The latest American Society of Hematology guideline on venous thromboembolism (VTE) tackles 30 key questions regarding prophylaxis in hospitalized patients undergoing surgery, according to the chair of the guideline panel, who highlighted 9 of those questions during a special session at the society’s annual meeting.
The clinical practice guideline, published just about a week before the annual meeting of the American Society of Hematology, focuses mainly on pharmacologic prophylaxis in specific surgical settings, said David R. Anderson, MD, dean of the faculty of medicine of Dalhousie University, Halifax, N.S.
“Our guidelines focused upon clinically important symptomatic outcomes, with less emphasis being placed on asymptomatic deep vein thrombosis detected by screening tests,” Dr. Anderson said.
At the special education session, Dr. Anderson highlighted several specific recommendations on prophylaxis in surgical patients.
Pharmacologic prophylaxis is not recommended for patients experiencing major trauma deemed to be at high risk of bleeding. Its use does reduce risk of symptomatic pulmonary embolism (PE) and deep vein thrombosis (DVT) by about 10 events per 1,000 patients treated; however, Dr. Anderson said, the panel’s opinion was that this benefit was outweighed by increased risk of major bleeding, at 24 events per 1,000 patients treated.
“We do recommend, however that this risk of bleeding must be reevaluated over the course of recovery of patients, and this may change the decision around this intervention over time,” Dr. Anderson told attendees at the special session.
That’s because pharmacologic prophylaxis is recommended in surgical patients at low to moderate risk of bleeding. In this scenario, the incremental risk of major bleeding (14 events per 1,000 patients treated) is outweighed by the benefit of the reduction of symptomatic VTE events, according to Dr. Anderson.
When pharmacologic prophylaxis is used, the panel recommends combined prophylaxis – mechanical prophylaxis in addition to pharmacologic prophylaxis – especially in those patients at high or very high risk of VTE. Evidence shows that the combination approach significantly reduces risk of PE, and strongly suggests it may also reduce risk of symptomatic proximal DVT, Dr. Anderson said.
In surgical patients not receiving pharmacologic prophylaxis, mechanical prophylaxis is recommended over no mechanical prophylaxis, he added. Moreover, in those patients receiving mechanical prophylaxis, the ASH panel recommends use of intermittent compression devices over graduated compression stockings.
The panel comes out against prophylactic inferior vena cava (IVC) filter insertion in the guidelines. Dr. Anderson said that the “small reduction” in PE risk seen in observational studies is outweighed by increased risk of DVT, and a resulting trend for increased mortality, associated with insertion of the devices.
“We did not consider other risks of IVC filters such as filter embolization or perforation, which again would be complications that would support our recommendation against routine use of these devices in patients undergoing major surgery,” he said.
In terms of the type of pharmacologic prophylaxis to use, the panel said low-molecular-weight heparin or unfractionated heparin would be reasonable choices in this setting. Available data do not demonstrate any significant differences between these choices for major clinical outcomes, Dr. Anderson added.
The guideline also addresses duration of pharmacologic prophylaxis, stating that extended prophylaxis – of at least 3 weeks – is favored over short-term prophylaxis, or up to 2 weeks of treatment. The extended approach significantly reduces risk of symptomatic PE and proximal DVT, though most of the supporting data come from studies of major joint arthroplasty and major general surgical procedures for patients with cancer. “We need more studies in other clinical areas to examine this particular question,” Dr. Anderson said.
The guideline on prophylaxis in surgical patients was published in Blood Advances (2019 Dec 3;3[23]:3898-944). Six other ASH VTE guidelines, all published in 2018, covered prophylaxis in medical patients, diagnosis, VTE in pregnancy, optimal anticoagulation, heparin-induced thrombocytopenia, and pediatric considerations. The guidelines are available on the ASH website.
Dr. Anderson reported having no relevant conflicts of interest.
ORLANDO – The latest American Society of Hematology guideline on venous thromboembolism (VTE) tackles 30 key questions regarding prophylaxis in hospitalized patients undergoing surgery, according to the chair of the guideline panel, who highlighted 9 of those questions during a special session at the society’s annual meeting.
The clinical practice guideline, published just about a week before the annual meeting of the American Society of Hematology, focuses mainly on pharmacologic prophylaxis in specific surgical settings, said David R. Anderson, MD, dean of the faculty of medicine of Dalhousie University, Halifax, N.S.
“Our guidelines focused upon clinically important symptomatic outcomes, with less emphasis being placed on asymptomatic deep vein thrombosis detected by screening tests,” Dr. Anderson said.
At the special education session, Dr. Anderson highlighted several specific recommendations on prophylaxis in surgical patients.
Pharmacologic prophylaxis is not recommended for patients experiencing major trauma deemed to be at high risk of bleeding. Its use does reduce risk of symptomatic pulmonary embolism (PE) and deep vein thrombosis (DVT) by about 10 events per 1,000 patients treated; however, Dr. Anderson said, the panel’s opinion was that this benefit was outweighed by increased risk of major bleeding, at 24 events per 1,000 patients treated.
“We do recommend, however that this risk of bleeding must be reevaluated over the course of recovery of patients, and this may change the decision around this intervention over time,” Dr. Anderson told attendees at the special session.
That’s because pharmacologic prophylaxis is recommended in surgical patients at low to moderate risk of bleeding. In this scenario, the incremental risk of major bleeding (14 events per 1,000 patients treated) is outweighed by the benefit of the reduction of symptomatic VTE events, according to Dr. Anderson.
When pharmacologic prophylaxis is used, the panel recommends combined prophylaxis – mechanical prophylaxis in addition to pharmacologic prophylaxis – especially in those patients at high or very high risk of VTE. Evidence shows that the combination approach significantly reduces risk of PE, and strongly suggests it may also reduce risk of symptomatic proximal DVT, Dr. Anderson said.
In surgical patients not receiving pharmacologic prophylaxis, mechanical prophylaxis is recommended over no mechanical prophylaxis, he added. Moreover, in those patients receiving mechanical prophylaxis, the ASH panel recommends use of intermittent compression devices over graduated compression stockings.
The panel comes out against prophylactic inferior vena cava (IVC) filter insertion in the guidelines. Dr. Anderson said that the “small reduction” in PE risk seen in observational studies is outweighed by increased risk of DVT, and a resulting trend for increased mortality, associated with insertion of the devices.
“We did not consider other risks of IVC filters such as filter embolization or perforation, which again would be complications that would support our recommendation against routine use of these devices in patients undergoing major surgery,” he said.
In terms of the type of pharmacologic prophylaxis to use, the panel said low-molecular-weight heparin or unfractionated heparin would be reasonable choices in this setting. Available data do not demonstrate any significant differences between these choices for major clinical outcomes, Dr. Anderson added.
The guideline also addresses duration of pharmacologic prophylaxis, stating that extended prophylaxis – of at least 3 weeks – is favored over short-term prophylaxis, or up to 2 weeks of treatment. The extended approach significantly reduces risk of symptomatic PE and proximal DVT, though most of the supporting data come from studies of major joint arthroplasty and major general surgical procedures for patients with cancer. “We need more studies in other clinical areas to examine this particular question,” Dr. Anderson said.
The guideline on prophylaxis in surgical patients was published in Blood Advances (2019 Dec 3;3[23]:3898-944). Six other ASH VTE guidelines, all published in 2018, covered prophylaxis in medical patients, diagnosis, VTE in pregnancy, optimal anticoagulation, heparin-induced thrombocytopenia, and pediatric considerations. The guidelines are available on the ASH website.
Dr. Anderson reported having no relevant conflicts of interest.
EXPERT ANALYSIS FROM ASH 2019
Transfusion-related lung injury is on the rise in elderly patients
SAN ANTONIO – Although there has been a general decline in transfusion-related anaphylaxis and acute infections over time among hospitalized older adults in the United States, incidence rates for both transfusion-related acute lung injury and transfusion-associated circulatory overload have risen over the last decade, according to researchers from the Food and Drug Administration.
Mikhail Menis, PharmD, an epidemiologist at the FDA Center for Biologics Evaluation and Research (CBER) and colleagues queried large Medicare databases to assess trends in transfusion-related adverse events among adults aged 65 years and older.
The investigators saw “substantially higher risk of all outcomes among immunocompromised beneficiaries, which could be related to higher blood use of all blood components, especially platelets, underlying conditions such as malignancies, and treatments such as chemotherapy or radiation, which need further investigation,” Dr. Menis said at the annual meeting of AABB, the group formerly known as the American Association of Blood Banks.
He reported data from a series of studies on four categories of transfusion-related events that may be life-threatening or fatal: transfusion-related anaphylaxis (TRA), transfusion-related acute lung injury (TRALI), transfusion-associated circulatory overload (TACO), and acute infection following transfusion (AIFT).
For each type of event, the researchers looked at overall incidence and the incidence by immune status, calendar year, blood components transfused, number of units transfused, age, sex, and race.
Anaphylaxis (TRA)
TRA may be caused by preformed immunoglobin E (IgE) antibodies to proteins in the plasma in transfused blood products or by preformed IgA antibodies in patients who are likely IgA deficient, Dr. Menis said.
The overall incidence of TRA among 8,833,817 inpatient transfusions stays for elderly beneficiaries from 2012 through 2018 was 7.1 per 100,000 stays. The rate was higher for immunocompromised patients, at 9.6, than it was among nonimmunocompromised patients, at 6.5.
The rates varied by every subgroup measured except immune status. Annual rates showed a downward trend, from 8.7 per 100,000 in 2012, to 5.1 in 2017 and 6.4 in 2018. The decline in occurrence may be caused by a decline in inpatient blood utilization during the study period, particularly among immunocompromised patients.
TRA rates increased with five or more units transfused. The risk was significantly reduced in the oldest group of patients versus the youngest (P less than .001), which supports the immune-based mechanism of action of anaphylaxis, Dr. Menis said.
They also found that TRA rates were substantially higher among patients who had received platelet and/or plasma transfusions, compared with patients who received only red blood cells (RBCs).
Additionally, risk for TRA was significantly higher among men than it was among women (9.3 vs. 5.4) and among white versus nonwhite patients (7.8 vs. 3.8).
The evidence suggested TRA cases are likely to be severe in this population, with inpatient mortality of 7.1%, and hospital stays of 7 days or longer in about 58% of cases, indicating the importance of TRA prevention, Dr. Menis said.
The investigators plan to perform multivariate regression analyses to assess potential risk factors, including underlying comorbidities and health histories for TRA occurrence for both the overall population and by immune status.
Acute lung injury (TRALI)
TRALI is a rare but serious adverse event, a clinical syndrome with onset within 6 hours of transfusion that presents as acute hypoxemia, respiratory distress, and noncardiogenic pulmonary edema.
Among 17,771,193 total inpatient transfusion stays, the overall incidence of TRALI was 33.2 per 100,000. The rate was 55.9 for immunocompromised patients versus 28.4 for nonimmunocompromised patients. The rate ratio was 2.0 (P less than .001).
The difference by immune status may be caused by higher blood utilizations with more units transfused per stay among immunocompromised patients, a higher incidence of prior transfusions among these patients, higher use of irradiated blood components that may lead to accumulation of proinflammatory mediators in blood products during storage, or underlying comorbidities.
The overall rate increased from 14.3 in 2007 to 56.4 in 2018. The rates increased proportionally among both immunocompromised and nonimmunocompromised patients.
As with TRA, the incidence of TRALI was higher in patients with five or more units transfused, while the incidence declined with age, likely caused by declining blood use and age-related changes in neutrophil function, Dr. Menis said.
TRALI rates were slightly higher among men than among women, as well as higher among white patients than among nonwhite patients.
Overall, TRALI rates were higher for patients who received platelets either alone or in combination with RBCs and/or plasma. The highest rates were among patients who received RBCs, plasma and platelets.
Dr. Menis called for studies to determine what effects the processing and storage of blood components may have on TRALI occurrence; he and his colleagues also are planning regression analyses to assess potential risk factors for this complication.
Circulatory overload (TACO)
TACO is one of the leading reported causes of transfusion-related fatalities in the U.S., with onset usually occurring within 6 hours of transfusion, presenting as acute respiratory distress with dyspnea, orthopnea, increased blood pressure, and cardiogenic pulmonary edema.
The overall incidence of TACO among hospitalized patients aged 65 years and older from 2011 through 2018 was 86.3 per 100,000 stays. The incidences were 128.3 in immunocompromised and 76.0 in nonimmunocompromised patients. The rate ratio for TACO in immunocompromised versus nonimmunocompromised patients was 1.70 (P less than .001).
Overall incidence rates of TACO rose from 62 per 100,000 stays in 2011 to 119.8 in 2018. As with other adverse events, incident rates rose with the number of units transfused.
Rates of TACO were significantly higher among women than they were among men (94.6 vs. 75.9 per 100,000; P less than .001), which could be caused by the higher mean age of women and/or a lower tolerance for increased blood volume from transfusion.
The study results also suggested that TACO and TRALI may coexist, based on evidence that 3.5% of all TACO stays also had diagnostic codes for TRALI. The frequency of co-occurrence of these two adverse events also increased over time, which may be caused by improved awareness, Dr. Menis said.
Infections (AIFT)
Acute infections following transfusion can lead to prolonged hospitalizations, sepsis, septic shock, and death. Those most at risk include elderly and immunocompromised patients because of high utilization of blood products, comorbidities, and decreased immune function.
Among 8,833,817 stays, the overall rate per 100,000 stays was 2.1. The rate for immunocompromised patients was 5.4, compared with 1.2 for nonimmunocompromised patients, for a rate ratio of 4.4 (P less than .001).
The incidence rate declined significantly (P = .03) over the study period, with the 3 latest years having the lowest rates.
Rates increased substantially among immunocompromised patients by the number of units transfused, but remained relatively stable among nonimmunocompromised patients.
Infection rates declined with age, from 2.7 per 100,000 stays for patients aged 65-68 years to 1.2 per 100,000 for those aged 85 years and older.
As with other adverse events, AIFT rates were likely related to the blood components transfused, with substantially higher rates for stays during which platelets were transfused either alone or with RBCs, compared with RBCs alone. This could be caused by the room-temperature storage of platelets and higher number of platelets units transfused, compared with RBCs alone, especially among immunocompromised patients.
In all, 51.9% of AIFT cases also had sepsis noted in the medical record, indicating high severity and emphasizing the importance of AIFT prevention, Dr. Menis said.
The studies were funded by the FDA, and Dr. Menis is an FDA employee. He reported having no conflicts of interest.
SAN ANTONIO – Although there has been a general decline in transfusion-related anaphylaxis and acute infections over time among hospitalized older adults in the United States, incidence rates for both transfusion-related acute lung injury and transfusion-associated circulatory overload have risen over the last decade, according to researchers from the Food and Drug Administration.
Mikhail Menis, PharmD, an epidemiologist at the FDA Center for Biologics Evaluation and Research (CBER) and colleagues queried large Medicare databases to assess trends in transfusion-related adverse events among adults aged 65 years and older.
The investigators saw “substantially higher risk of all outcomes among immunocompromised beneficiaries, which could be related to higher blood use of all blood components, especially platelets, underlying conditions such as malignancies, and treatments such as chemotherapy or radiation, which need further investigation,” Dr. Menis said at the annual meeting of AABB, the group formerly known as the American Association of Blood Banks.
He reported data from a series of studies on four categories of transfusion-related events that may be life-threatening or fatal: transfusion-related anaphylaxis (TRA), transfusion-related acute lung injury (TRALI), transfusion-associated circulatory overload (TACO), and acute infection following transfusion (AIFT).
For each type of event, the researchers looked at overall incidence and the incidence by immune status, calendar year, blood components transfused, number of units transfused, age, sex, and race.
Anaphylaxis (TRA)
TRA may be caused by preformed immunoglobin E (IgE) antibodies to proteins in the plasma in transfused blood products or by preformed IgA antibodies in patients who are likely IgA deficient, Dr. Menis said.
The overall incidence of TRA among 8,833,817 inpatient transfusions stays for elderly beneficiaries from 2012 through 2018 was 7.1 per 100,000 stays. The rate was higher for immunocompromised patients, at 9.6, than it was among nonimmunocompromised patients, at 6.5.
The rates varied by every subgroup measured except immune status. Annual rates showed a downward trend, from 8.7 per 100,000 in 2012, to 5.1 in 2017 and 6.4 in 2018. The decline in occurrence may be caused by a decline in inpatient blood utilization during the study period, particularly among immunocompromised patients.
TRA rates increased with five or more units transfused. The risk was significantly reduced in the oldest group of patients versus the youngest (P less than .001), which supports the immune-based mechanism of action of anaphylaxis, Dr. Menis said.
They also found that TRA rates were substantially higher among patients who had received platelet and/or plasma transfusions, compared with patients who received only red blood cells (RBCs).
Additionally, risk for TRA was significantly higher among men than it was among women (9.3 vs. 5.4) and among white versus nonwhite patients (7.8 vs. 3.8).
The evidence suggested TRA cases are likely to be severe in this population, with inpatient mortality of 7.1%, and hospital stays of 7 days or longer in about 58% of cases, indicating the importance of TRA prevention, Dr. Menis said.
The investigators plan to perform multivariate regression analyses to assess potential risk factors, including underlying comorbidities and health histories for TRA occurrence for both the overall population and by immune status.
Acute lung injury (TRALI)
TRALI is a rare but serious adverse event, a clinical syndrome with onset within 6 hours of transfusion that presents as acute hypoxemia, respiratory distress, and noncardiogenic pulmonary edema.
Among 17,771,193 total inpatient transfusion stays, the overall incidence of TRALI was 33.2 per 100,000. The rate was 55.9 for immunocompromised patients versus 28.4 for nonimmunocompromised patients. The rate ratio was 2.0 (P less than .001).
The difference by immune status may be caused by higher blood utilizations with more units transfused per stay among immunocompromised patients, a higher incidence of prior transfusions among these patients, higher use of irradiated blood components that may lead to accumulation of proinflammatory mediators in blood products during storage, or underlying comorbidities.
The overall rate increased from 14.3 in 2007 to 56.4 in 2018. The rates increased proportionally among both immunocompromised and nonimmunocompromised patients.
As with TRA, the incidence of TRALI was higher in patients with five or more units transfused, while the incidence declined with age, likely caused by declining blood use and age-related changes in neutrophil function, Dr. Menis said.
TRALI rates were slightly higher among men than among women, as well as higher among white patients than among nonwhite patients.
Overall, TRALI rates were higher for patients who received platelets either alone or in combination with RBCs and/or plasma. The highest rates were among patients who received RBCs, plasma and platelets.
Dr. Menis called for studies to determine what effects the processing and storage of blood components may have on TRALI occurrence; he and his colleagues also are planning regression analyses to assess potential risk factors for this complication.
Circulatory overload (TACO)
TACO is one of the leading reported causes of transfusion-related fatalities in the U.S., with onset usually occurring within 6 hours of transfusion, presenting as acute respiratory distress with dyspnea, orthopnea, increased blood pressure, and cardiogenic pulmonary edema.
The overall incidence of TACO among hospitalized patients aged 65 years and older from 2011 through 2018 was 86.3 per 100,000 stays. The incidences were 128.3 in immunocompromised and 76.0 in nonimmunocompromised patients. The rate ratio for TACO in immunocompromised versus nonimmunocompromised patients was 1.70 (P less than .001).
Overall incidence rates of TACO rose from 62 per 100,000 stays in 2011 to 119.8 in 2018. As with other adverse events, incident rates rose with the number of units transfused.
Rates of TACO were significantly higher among women than they were among men (94.6 vs. 75.9 per 100,000; P less than .001), which could be caused by the higher mean age of women and/or a lower tolerance for increased blood volume from transfusion.
The study results also suggested that TACO and TRALI may coexist, based on evidence that 3.5% of all TACO stays also had diagnostic codes for TRALI. The frequency of co-occurrence of these two adverse events also increased over time, which may be caused by improved awareness, Dr. Menis said.
Infections (AIFT)
Acute infections following transfusion can lead to prolonged hospitalizations, sepsis, septic shock, and death. Those most at risk include elderly and immunocompromised patients because of high utilization of blood products, comorbidities, and decreased immune function.
Among 8,833,817 stays, the overall rate per 100,000 stays was 2.1. The rate for immunocompromised patients was 5.4, compared with 1.2 for nonimmunocompromised patients, for a rate ratio of 4.4 (P less than .001).
The incidence rate declined significantly (P = .03) over the study period, with the 3 latest years having the lowest rates.
Rates increased substantially among immunocompromised patients by the number of units transfused, but remained relatively stable among nonimmunocompromised patients.
Infection rates declined with age, from 2.7 per 100,000 stays for patients aged 65-68 years to 1.2 per 100,000 for those aged 85 years and older.
As with other adverse events, AIFT rates were likely related to the blood components transfused, with substantially higher rates for stays during which platelets were transfused either alone or with RBCs, compared with RBCs alone. This could be caused by the room-temperature storage of platelets and higher number of platelets units transfused, compared with RBCs alone, especially among immunocompromised patients.
In all, 51.9% of AIFT cases also had sepsis noted in the medical record, indicating high severity and emphasizing the importance of AIFT prevention, Dr. Menis said.
The studies were funded by the FDA, and Dr. Menis is an FDA employee. He reported having no conflicts of interest.
SAN ANTONIO – Although there has been a general decline in transfusion-related anaphylaxis and acute infections over time among hospitalized older adults in the United States, incidence rates for both transfusion-related acute lung injury and transfusion-associated circulatory overload have risen over the last decade, according to researchers from the Food and Drug Administration.
Mikhail Menis, PharmD, an epidemiologist at the FDA Center for Biologics Evaluation and Research (CBER) and colleagues queried large Medicare databases to assess trends in transfusion-related adverse events among adults aged 65 years and older.
The investigators saw “substantially higher risk of all outcomes among immunocompromised beneficiaries, which could be related to higher blood use of all blood components, especially platelets, underlying conditions such as malignancies, and treatments such as chemotherapy or radiation, which need further investigation,” Dr. Menis said at the annual meeting of AABB, the group formerly known as the American Association of Blood Banks.
He reported data from a series of studies on four categories of transfusion-related events that may be life-threatening or fatal: transfusion-related anaphylaxis (TRA), transfusion-related acute lung injury (TRALI), transfusion-associated circulatory overload (TACO), and acute infection following transfusion (AIFT).
For each type of event, the researchers looked at overall incidence and the incidence by immune status, calendar year, blood components transfused, number of units transfused, age, sex, and race.
Anaphylaxis (TRA)
TRA may be caused by preformed immunoglobin E (IgE) antibodies to proteins in the plasma in transfused blood products or by preformed IgA antibodies in patients who are likely IgA deficient, Dr. Menis said.
The overall incidence of TRA among 8,833,817 inpatient transfusions stays for elderly beneficiaries from 2012 through 2018 was 7.1 per 100,000 stays. The rate was higher for immunocompromised patients, at 9.6, than it was among nonimmunocompromised patients, at 6.5.
The rates varied by every subgroup measured except immune status. Annual rates showed a downward trend, from 8.7 per 100,000 in 2012, to 5.1 in 2017 and 6.4 in 2018. The decline in occurrence may be caused by a decline in inpatient blood utilization during the study period, particularly among immunocompromised patients.
TRA rates increased with five or more units transfused. The risk was significantly reduced in the oldest group of patients versus the youngest (P less than .001), which supports the immune-based mechanism of action of anaphylaxis, Dr. Menis said.
They also found that TRA rates were substantially higher among patients who had received platelet and/or plasma transfusions, compared with patients who received only red blood cells (RBCs).
Additionally, risk for TRA was significantly higher among men than it was among women (9.3 vs. 5.4) and among white versus nonwhite patients (7.8 vs. 3.8).
The evidence suggested TRA cases are likely to be severe in this population, with inpatient mortality of 7.1%, and hospital stays of 7 days or longer in about 58% of cases, indicating the importance of TRA prevention, Dr. Menis said.
The investigators plan to perform multivariate regression analyses to assess potential risk factors, including underlying comorbidities and health histories for TRA occurrence for both the overall population and by immune status.
Acute lung injury (TRALI)
TRALI is a rare but serious adverse event, a clinical syndrome with onset within 6 hours of transfusion that presents as acute hypoxemia, respiratory distress, and noncardiogenic pulmonary edema.
Among 17,771,193 total inpatient transfusion stays, the overall incidence of TRALI was 33.2 per 100,000. The rate was 55.9 for immunocompromised patients versus 28.4 for nonimmunocompromised patients. The rate ratio was 2.0 (P less than .001).
The difference by immune status may be caused by higher blood utilizations with more units transfused per stay among immunocompromised patients, a higher incidence of prior transfusions among these patients, higher use of irradiated blood components that may lead to accumulation of proinflammatory mediators in blood products during storage, or underlying comorbidities.
The overall rate increased from 14.3 in 2007 to 56.4 in 2018. The rates increased proportionally among both immunocompromised and nonimmunocompromised patients.
As with TRA, the incidence of TRALI was higher in patients with five or more units transfused, while the incidence declined with age, likely caused by declining blood use and age-related changes in neutrophil function, Dr. Menis said.
TRALI rates were slightly higher among men than among women, as well as higher among white patients than among nonwhite patients.
Overall, TRALI rates were higher for patients who received platelets either alone or in combination with RBCs and/or plasma. The highest rates were among patients who received RBCs, plasma and platelets.
Dr. Menis called for studies to determine what effects the processing and storage of blood components may have on TRALI occurrence; he and his colleagues also are planning regression analyses to assess potential risk factors for this complication.
Circulatory overload (TACO)
TACO is one of the leading reported causes of transfusion-related fatalities in the U.S., with onset usually occurring within 6 hours of transfusion, presenting as acute respiratory distress with dyspnea, orthopnea, increased blood pressure, and cardiogenic pulmonary edema.
The overall incidence of TACO among hospitalized patients aged 65 years and older from 2011 through 2018 was 86.3 per 100,000 stays. The incidences were 128.3 in immunocompromised and 76.0 in nonimmunocompromised patients. The rate ratio for TACO in immunocompromised versus nonimmunocompromised patients was 1.70 (P less than .001).
Overall incidence rates of TACO rose from 62 per 100,000 stays in 2011 to 119.8 in 2018. As with other adverse events, incident rates rose with the number of units transfused.
Rates of TACO were significantly higher among women than they were among men (94.6 vs. 75.9 per 100,000; P less than .001), which could be caused by the higher mean age of women and/or a lower tolerance for increased blood volume from transfusion.
The study results also suggested that TACO and TRALI may coexist, based on evidence that 3.5% of all TACO stays also had diagnostic codes for TRALI. The frequency of co-occurrence of these two adverse events also increased over time, which may be caused by improved awareness, Dr. Menis said.
Infections (AIFT)
Acute infections following transfusion can lead to prolonged hospitalizations, sepsis, septic shock, and death. Those most at risk include elderly and immunocompromised patients because of high utilization of blood products, comorbidities, and decreased immune function.
Among 8,833,817 stays, the overall rate per 100,000 stays was 2.1. The rate for immunocompromised patients was 5.4, compared with 1.2 for nonimmunocompromised patients, for a rate ratio of 4.4 (P less than .001).
The incidence rate declined significantly (P = .03) over the study period, with the 3 latest years having the lowest rates.
Rates increased substantially among immunocompromised patients by the number of units transfused, but remained relatively stable among nonimmunocompromised patients.
Infection rates declined with age, from 2.7 per 100,000 stays for patients aged 65-68 years to 1.2 per 100,000 for those aged 85 years and older.
As with other adverse events, AIFT rates were likely related to the blood components transfused, with substantially higher rates for stays during which platelets were transfused either alone or with RBCs, compared with RBCs alone. This could be caused by the room-temperature storage of platelets and higher number of platelets units transfused, compared with RBCs alone, especially among immunocompromised patients.
In all, 51.9% of AIFT cases also had sepsis noted in the medical record, indicating high severity and emphasizing the importance of AIFT prevention, Dr. Menis said.
The studies were funded by the FDA, and Dr. Menis is an FDA employee. He reported having no conflicts of interest.
REPORTING FROM AABB 2019
Storytelling tool can assist elderly in the ICU
SAN FRANCISCO – A “Best Case/Worst Case” (BCWC) framework tool has been adapted for use with geriatric trauma patients in the ICU, where it can help track a patient’s progress and enable better communication with patients and loved ones. The tool relies on a combination of graphics and text that surgeons update daily during rounds, and creates a longitudinal view of a patient’s trajectory during their stay in the ICU.
– for example, after a complication has arisen.
“Each day during rounds, the ICU team records important events on the graphic aid that change the patient’s course. The team draws a star to represent the best case, and a line to represent prognostic uncertainty. The attending trauma surgeon then uses the geriatric trauma outcome score, their knowledge of the health state of the patient, and their own clinical experience to tell a story about treatments, recovery, and outcomes if everything goes as well as we might hope. This story is written down in the best-case scenario box,” Christopher Zimmerman, MD, a general surgery resident at the University of Wisconsin–Madison, said during a presentation about the BCWC tool at the annual clinical congress of the American College of Surgeons
“We often like to talk to patients and their families [about best- and worst-case scenarios] anyway, but [the research team] have tried to formalize it,” said Tam Pham, MD, professor of surgery at the University of Washington, in an interview. Dr. Pham comoderated the session where the research was presented.
“When we’re able to communicate where the uncertainty is and where the boundaries are around the course of care and possible outcomes, we can build an alliance with patients and families that will be helpful when there is a big decision to make, say about a laparotomy for a perforated viscus,” said Dr. Zimmerman.
Dr. Zimmerman gave an example of a patient who came into the ICU after suffering multiple fractures from falling down a set of stairs. The team created an initial BCWC with a hoped-for best-case scenario. Later, the patient developed hypoxemic respiratory failure and had to be intubated overnight. “This event is recorded on the graphic, and her star representing the best case has changed position, the line representing uncertainty has shortened, and the contents of her best-case scenario has changed. Each day in rounds, this process is repeated,” said Dr. Zimmerman.
Palliative care physicians, education experts, and surgeons at the University of Wisconsin–Madison developed the tool in an effort to reduce unwanted care at the end of life, in the context of high-risk surgeries. The researchers adapted the tool to the trauma setting by gathering six focus groups of trauma practitioners at the University of Wisconsin; University of Texas, Dallas; and Oregon Health & Science University, Portland. They modified the tool after incorporating comments, and then iteratively modified it through tasks carried out in the ICU as part of a qualitative improvement initiative at the University of Wisconsin–Madison. They generated a change to the tool, implemented it in the ICU during subsequent rounds, then collected observations and field notes, then revised and repeated the process, streamlining it to fit into the ICU environment, according to Dr. Zimmerman.
The back side of the tool is available for family members to write important details about their loved ones, leading insight into the patient’s personality and desires, such as favorite music or affection for a family pet.
The work was supported by the National Institutes of Health. Dr. Zimmerman and Dr. Pham have no relevant financial disclosures.
SOURCE: Zimmerman C et al. Clinical Congress 2019, Abstract.
SAN FRANCISCO – A “Best Case/Worst Case” (BCWC) framework tool has been adapted for use with geriatric trauma patients in the ICU, where it can help track a patient’s progress and enable better communication with patients and loved ones. The tool relies on a combination of graphics and text that surgeons update daily during rounds, and creates a longitudinal view of a patient’s trajectory during their stay in the ICU.
– for example, after a complication has arisen.
“Each day during rounds, the ICU team records important events on the graphic aid that change the patient’s course. The team draws a star to represent the best case, and a line to represent prognostic uncertainty. The attending trauma surgeon then uses the geriatric trauma outcome score, their knowledge of the health state of the patient, and their own clinical experience to tell a story about treatments, recovery, and outcomes if everything goes as well as we might hope. This story is written down in the best-case scenario box,” Christopher Zimmerman, MD, a general surgery resident at the University of Wisconsin–Madison, said during a presentation about the BCWC tool at the annual clinical congress of the American College of Surgeons
“We often like to talk to patients and their families [about best- and worst-case scenarios] anyway, but [the research team] have tried to formalize it,” said Tam Pham, MD, professor of surgery at the University of Washington, in an interview. Dr. Pham comoderated the session where the research was presented.
“When we’re able to communicate where the uncertainty is and where the boundaries are around the course of care and possible outcomes, we can build an alliance with patients and families that will be helpful when there is a big decision to make, say about a laparotomy for a perforated viscus,” said Dr. Zimmerman.
Dr. Zimmerman gave an example of a patient who came into the ICU after suffering multiple fractures from falling down a set of stairs. The team created an initial BCWC with a hoped-for best-case scenario. Later, the patient developed hypoxemic respiratory failure and had to be intubated overnight. “This event is recorded on the graphic, and her star representing the best case has changed position, the line representing uncertainty has shortened, and the contents of her best-case scenario has changed. Each day in rounds, this process is repeated,” said Dr. Zimmerman.
Palliative care physicians, education experts, and surgeons at the University of Wisconsin–Madison developed the tool in an effort to reduce unwanted care at the end of life, in the context of high-risk surgeries. The researchers adapted the tool to the trauma setting by gathering six focus groups of trauma practitioners at the University of Wisconsin; University of Texas, Dallas; and Oregon Health & Science University, Portland. They modified the tool after incorporating comments, and then iteratively modified it through tasks carried out in the ICU as part of a qualitative improvement initiative at the University of Wisconsin–Madison. They generated a change to the tool, implemented it in the ICU during subsequent rounds, then collected observations and field notes, then revised and repeated the process, streamlining it to fit into the ICU environment, according to Dr. Zimmerman.
The back side of the tool is available for family members to write important details about their loved ones, leading insight into the patient’s personality and desires, such as favorite music or affection for a family pet.
The work was supported by the National Institutes of Health. Dr. Zimmerman and Dr. Pham have no relevant financial disclosures.
SOURCE: Zimmerman C et al. Clinical Congress 2019, Abstract.
SAN FRANCISCO – A “Best Case/Worst Case” (BCWC) framework tool has been adapted for use with geriatric trauma patients in the ICU, where it can help track a patient’s progress and enable better communication with patients and loved ones. The tool relies on a combination of graphics and text that surgeons update daily during rounds, and creates a longitudinal view of a patient’s trajectory during their stay in the ICU.
– for example, after a complication has arisen.
“Each day during rounds, the ICU team records important events on the graphic aid that change the patient’s course. The team draws a star to represent the best case, and a line to represent prognostic uncertainty. The attending trauma surgeon then uses the geriatric trauma outcome score, their knowledge of the health state of the patient, and their own clinical experience to tell a story about treatments, recovery, and outcomes if everything goes as well as we might hope. This story is written down in the best-case scenario box,” Christopher Zimmerman, MD, a general surgery resident at the University of Wisconsin–Madison, said during a presentation about the BCWC tool at the annual clinical congress of the American College of Surgeons
“We often like to talk to patients and their families [about best- and worst-case scenarios] anyway, but [the research team] have tried to formalize it,” said Tam Pham, MD, professor of surgery at the University of Washington, in an interview. Dr. Pham comoderated the session where the research was presented.
“When we’re able to communicate where the uncertainty is and where the boundaries are around the course of care and possible outcomes, we can build an alliance with patients and families that will be helpful when there is a big decision to make, say about a laparotomy for a perforated viscus,” said Dr. Zimmerman.
Dr. Zimmerman gave an example of a patient who came into the ICU after suffering multiple fractures from falling down a set of stairs. The team created an initial BCWC with a hoped-for best-case scenario. Later, the patient developed hypoxemic respiratory failure and had to be intubated overnight. “This event is recorded on the graphic, and her star representing the best case has changed position, the line representing uncertainty has shortened, and the contents of her best-case scenario has changed. Each day in rounds, this process is repeated,” said Dr. Zimmerman.
Palliative care physicians, education experts, and surgeons at the University of Wisconsin–Madison developed the tool in an effort to reduce unwanted care at the end of life, in the context of high-risk surgeries. The researchers adapted the tool to the trauma setting by gathering six focus groups of trauma practitioners at the University of Wisconsin; University of Texas, Dallas; and Oregon Health & Science University, Portland. They modified the tool after incorporating comments, and then iteratively modified it through tasks carried out in the ICU as part of a qualitative improvement initiative at the University of Wisconsin–Madison. They generated a change to the tool, implemented it in the ICU during subsequent rounds, then collected observations and field notes, then revised and repeated the process, streamlining it to fit into the ICU environment, according to Dr. Zimmerman.
The back side of the tool is available for family members to write important details about their loved ones, leading insight into the patient’s personality and desires, such as favorite music or affection for a family pet.
The work was supported by the National Institutes of Health. Dr. Zimmerman and Dr. Pham have no relevant financial disclosures.
SOURCE: Zimmerman C et al. Clinical Congress 2019, Abstract.
REPORTING FROM CLINICAL CONGRESS 2019
Automated ventilation outperformed nurses in post-op cardiac care
MADRID – In patients managed on mechanical ventilation in an intensive care unit following cardiac surgery, a fully automated system provides more reliable ventilatory support than highly experienced ICU nurses, suggest results of a randomized trial.
The study’s control group received usual care, which means that nurses adjusted mechanical ventilation manually in response to respiratory rate, tidal volume, positive end-respiratory pressure (PEEP), and other factors to maintain ventilation within parameters associated with safe respiration. The experimental group was managed with a fully automated closed-loop system to make these adjustments without any nurse intervention.
For those in the experimental group “the proportion of time in the optimal zone was increased and the proportion of time in the unsafe zone was decreased” relative to those randomized to conventional nursing care, Marcus J. Schultz, MD, reported at the annual congress of the European Respiratory Society.
Conducted at a hospital with an experienced ICU staff, the study had a control arm that was managed by “dedicated nurses who, I can tell you, are very eager to provide the best level of care possible,” said Dr. Schultz, professor of experimental intensive care, University of Amsterdam, the Netherlands..
The investigator-initiated POSITiVE trial randomized 220 cardiac surgery patients scheduled to receive postoperative mechanical ventilation in the ICU. Exclusions included those with class III or higher chronic obstructive pulmonary disease (COPD), a requirement for extracorporeal membrane oxygenation (ECMO), or a history of lung surgery.
The primary endpoint was the proportion of time spent in an optimal zone, an acceptable zone, or a dangerous zone of ventilation based on predefined values for tidal volume, maximum airway pressure, end-tidal CO2, and oxygen saturation (SpO2).
The greatest between-group difference was seen in the proportion of time spent in the optimal zone. This climbed from approximately 35% in the control arm to slightly more than 70% in the experimental arm, a significant difference. The proportion of time in the dangerous zone was reduced from approximately 6% in the control arm to 3% in the automated arm. On average nurse-managed patients spent nearly 60% of the time in the acceptable zone versus less than 30% of those in the automated experimental arm.
A heat map using green, yellow, and red to represent optimal, acceptable, and dangerous zones, respectively, for individual participants in the trial provided a more stark global impression. For the control group, the heat map was primarily yellow with scattered dashes of green and red. For the experimental group, the map was primarily green with dashes of yellow and a much smaller number of red dashes relative to the control group.
In addition, the time to spontaneous breathing was 38% shorter for those randomized to automated ventilation than to conventional care, a significant difference.
There are now many devices marketed for automated ventilation, according to Dr. Schultz. The device used in this study was the proprietary INTELLiVENT-ASV system, marketed by Hamilton Medical, which was selected based on prior satisfactory experience. Although not unique, this system has sophisticated software to adjust ventilation to reach targets set by the clinician on the basis of information it is receiving from physiologic sensors for such variables as respiratory rate, tidal volume, and inspiratory pressure.
“It is frequently adjusting the PEEP levels to reach the lowest driving pressure,” said Dr. Schultz. Among its many other features, it also “gives spontaneous breathing trials automatically.”
Uncomplicated patients were selected purposefully to test this system, but Dr. Schultz said that a second trial, called POSITiVE 2, is now being planned that will enroll more complex patients. Keeping complex patients within the optimal zone as defined by tidal volume and other critical variables has the potential to reduce the lung damage that is known to occur when these are not optimized.
“Applying safe ventilatory support in clinical practice remains a serious challenge and is extremely time consuming,” Dr. Schultz said. He reported that fully automated ventilation appears to be reliable, and “it takes out the human factor” in regard to diligence in monitoring and potential for error.
Overall, these results support the potential for a fully automated system to improve optimal ventilatory support, reduce risk of lung injury, and reduce staffing required for monitoring of mechanical ventilation, according to Dr. Schultz.
Relative costs were not evaluated in this analysis, but might be another factor relevant to the value of fully automated ventilation in ICU patients.
MADRID – In patients managed on mechanical ventilation in an intensive care unit following cardiac surgery, a fully automated system provides more reliable ventilatory support than highly experienced ICU nurses, suggest results of a randomized trial.
The study’s control group received usual care, which means that nurses adjusted mechanical ventilation manually in response to respiratory rate, tidal volume, positive end-respiratory pressure (PEEP), and other factors to maintain ventilation within parameters associated with safe respiration. The experimental group was managed with a fully automated closed-loop system to make these adjustments without any nurse intervention.
For those in the experimental group “the proportion of time in the optimal zone was increased and the proportion of time in the unsafe zone was decreased” relative to those randomized to conventional nursing care, Marcus J. Schultz, MD, reported at the annual congress of the European Respiratory Society.
Conducted at a hospital with an experienced ICU staff, the study had a control arm that was managed by “dedicated nurses who, I can tell you, are very eager to provide the best level of care possible,” said Dr. Schultz, professor of experimental intensive care, University of Amsterdam, the Netherlands..
The investigator-initiated POSITiVE trial randomized 220 cardiac surgery patients scheduled to receive postoperative mechanical ventilation in the ICU. Exclusions included those with class III or higher chronic obstructive pulmonary disease (COPD), a requirement for extracorporeal membrane oxygenation (ECMO), or a history of lung surgery.
The primary endpoint was the proportion of time spent in an optimal zone, an acceptable zone, or a dangerous zone of ventilation based on predefined values for tidal volume, maximum airway pressure, end-tidal CO2, and oxygen saturation (SpO2).
The greatest between-group difference was seen in the proportion of time spent in the optimal zone. This climbed from approximately 35% in the control arm to slightly more than 70% in the experimental arm, a significant difference. The proportion of time in the dangerous zone was reduced from approximately 6% in the control arm to 3% in the automated arm. On average nurse-managed patients spent nearly 60% of the time in the acceptable zone versus less than 30% of those in the automated experimental arm.
A heat map using green, yellow, and red to represent optimal, acceptable, and dangerous zones, respectively, for individual participants in the trial provided a more stark global impression. For the control group, the heat map was primarily yellow with scattered dashes of green and red. For the experimental group, the map was primarily green with dashes of yellow and a much smaller number of red dashes relative to the control group.
In addition, the time to spontaneous breathing was 38% shorter for those randomized to automated ventilation than to conventional care, a significant difference.
There are now many devices marketed for automated ventilation, according to Dr. Schultz. The device used in this study was the proprietary INTELLiVENT-ASV system, marketed by Hamilton Medical, which was selected based on prior satisfactory experience. Although not unique, this system has sophisticated software to adjust ventilation to reach targets set by the clinician on the basis of information it is receiving from physiologic sensors for such variables as respiratory rate, tidal volume, and inspiratory pressure.
“It is frequently adjusting the PEEP levels to reach the lowest driving pressure,” said Dr. Schultz. Among its many other features, it also “gives spontaneous breathing trials automatically.”
Uncomplicated patients were selected purposefully to test this system, but Dr. Schultz said that a second trial, called POSITiVE 2, is now being planned that will enroll more complex patients. Keeping complex patients within the optimal zone as defined by tidal volume and other critical variables has the potential to reduce the lung damage that is known to occur when these are not optimized.
“Applying safe ventilatory support in clinical practice remains a serious challenge and is extremely time consuming,” Dr. Schultz said. He reported that fully automated ventilation appears to be reliable, and “it takes out the human factor” in regard to diligence in monitoring and potential for error.
Overall, these results support the potential for a fully automated system to improve optimal ventilatory support, reduce risk of lung injury, and reduce staffing required for monitoring of mechanical ventilation, according to Dr. Schultz.
Relative costs were not evaluated in this analysis, but might be another factor relevant to the value of fully automated ventilation in ICU patients.
MADRID – In patients managed on mechanical ventilation in an intensive care unit following cardiac surgery, a fully automated system provides more reliable ventilatory support than highly experienced ICU nurses, suggest results of a randomized trial.
The study’s control group received usual care, which means that nurses adjusted mechanical ventilation manually in response to respiratory rate, tidal volume, positive end-respiratory pressure (PEEP), and other factors to maintain ventilation within parameters associated with safe respiration. The experimental group was managed with a fully automated closed-loop system to make these adjustments without any nurse intervention.
For those in the experimental group “the proportion of time in the optimal zone was increased and the proportion of time in the unsafe zone was decreased” relative to those randomized to conventional nursing care, Marcus J. Schultz, MD, reported at the annual congress of the European Respiratory Society.
Conducted at a hospital with an experienced ICU staff, the study had a control arm that was managed by “dedicated nurses who, I can tell you, are very eager to provide the best level of care possible,” said Dr. Schultz, professor of experimental intensive care, University of Amsterdam, the Netherlands..
The investigator-initiated POSITiVE trial randomized 220 cardiac surgery patients scheduled to receive postoperative mechanical ventilation in the ICU. Exclusions included those with class III or higher chronic obstructive pulmonary disease (COPD), a requirement for extracorporeal membrane oxygenation (ECMO), or a history of lung surgery.
The primary endpoint was the proportion of time spent in an optimal zone, an acceptable zone, or a dangerous zone of ventilation based on predefined values for tidal volume, maximum airway pressure, end-tidal CO2, and oxygen saturation (SpO2).
The greatest between-group difference was seen in the proportion of time spent in the optimal zone. This climbed from approximately 35% in the control arm to slightly more than 70% in the experimental arm, a significant difference. The proportion of time in the dangerous zone was reduced from approximately 6% in the control arm to 3% in the automated arm. On average nurse-managed patients spent nearly 60% of the time in the acceptable zone versus less than 30% of those in the automated experimental arm.
A heat map using green, yellow, and red to represent optimal, acceptable, and dangerous zones, respectively, for individual participants in the trial provided a more stark global impression. For the control group, the heat map was primarily yellow with scattered dashes of green and red. For the experimental group, the map was primarily green with dashes of yellow and a much smaller number of red dashes relative to the control group.
In addition, the time to spontaneous breathing was 38% shorter for those randomized to automated ventilation than to conventional care, a significant difference.
There are now many devices marketed for automated ventilation, according to Dr. Schultz. The device used in this study was the proprietary INTELLiVENT-ASV system, marketed by Hamilton Medical, which was selected based on prior satisfactory experience. Although not unique, this system has sophisticated software to adjust ventilation to reach targets set by the clinician on the basis of information it is receiving from physiologic sensors for such variables as respiratory rate, tidal volume, and inspiratory pressure.
“It is frequently adjusting the PEEP levels to reach the lowest driving pressure,” said Dr. Schultz. Among its many other features, it also “gives spontaneous breathing trials automatically.”
Uncomplicated patients were selected purposefully to test this system, but Dr. Schultz said that a second trial, called POSITiVE 2, is now being planned that will enroll more complex patients. Keeping complex patients within the optimal zone as defined by tidal volume and other critical variables has the potential to reduce the lung damage that is known to occur when these are not optimized.
“Applying safe ventilatory support in clinical practice remains a serious challenge and is extremely time consuming,” Dr. Schultz said. He reported that fully automated ventilation appears to be reliable, and “it takes out the human factor” in regard to diligence in monitoring and potential for error.
Overall, these results support the potential for a fully automated system to improve optimal ventilatory support, reduce risk of lung injury, and reduce staffing required for monitoring of mechanical ventilation, according to Dr. Schultz.
Relative costs were not evaluated in this analysis, but might be another factor relevant to the value of fully automated ventilation in ICU patients.
REPORTING FROM ERS 2019