User login
ERAS protocol cuts colorectal surgery morbidity, SSIs
CHICAGO – Implementing an enhanced recovery after surgery (ERAS) protocol at Canada’s second largest hospital significantly reduced morbidity and surgical site infections after elective colorectal surgery.
Rates of postoperative morbidity declined 48.7% from 27.3% before implementation to 14% after full ERAS implementation (P less than .05), while total surgical site infections fell 45% (20.2% vs. 11%; P less than .05).
Nonsignificant reductions were also seen in superficial surgical site infections (11.1% vs. 7.3%), deep SSIs (2% vs. 0.6%), and organ space SSIs (7.1% vs. 3.4%).
“Our results illustrate that using a multidisciplinary team, with attention to details and small multiple changes, aggregation of marginal gains can result in dramatic improvements in patient outcomes,” primary author Tracey Hong, R.N., said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
The ERAS protocol was implemented at Vancouver General Hospital, after ACS NSQIP risk-adjusted reports showed the 743-bed hospital had a high odds ratio of 1.50 for colorectal operative mortality.
“We had a problem,” Ms. Hong, the hospital’s quality and patient safety coordinator, said.
ERAS documents were developed, staff were educated on the protocol, intraoperative components were implemented and audited, and the full protocol was initiated in November 2013.
To explore the effects of ERAS implementation, chart reviews were conducted on 278 general surgery patients undergoing elective colorectal surgery: 99 patients before ERAS implementation (July 2011 through June 2013) and 179 patients in the first 10 months after full implementation (November 2013 through August 2014).
Laparoscopic colon resections were performed in 53% of the pre-ERAS group and 62% of the post-ERAS group, laparoscopic anterior and abdominoperineal resections in 10% and 23%, and open anterior and abdominoperineal resections in 23% and 18%, respectively. The median American Society of Anesthesiologists classification in both groups was 2.
After ERAS implementation, there was a trend for less postoperative pneumonia, unplanned intubation, ventilator use greater than 48 hours, and urinary tract infections (data not presented).
The median length of stay was reduced from 7 to 5 days, while readmissions increased from 7.1% to 11.7% (both changes were nonsignificant), according to Ms. Hong, who won the conference’s 2015 Surgical Clinical Reviewers Abstract Competition.
The reason for the increased readmissions is unclear, but opportunities to avoid preventable readmissions have been identified and are currently being worked on, she said.
Process measures showed that the goal of achieving a minimum 80% compliance from August 2014 to March 2015 was met within 4 months and sustained for the preoperative and intraoperative ERAS components, in aggregate. The aggregate postoperative components, which include early oral nutrition, early ambulation, early catheter removal, use of chewing gum, and defined discharge criteria, were the slowest to change, but are trending in the right direction, Ms. Hong said.
The key to achieving better outcomes with ERAS lies in involving a multidisciplinary team in all stages of planning and implementation, ongoing communication and sharing of results with stakeholders to foster commitment and ownership, and real-time auditing and use of plan-do-study-act cycles to enhance the rate of improvement, she said.
“It takes time to change culture; tenacity is important,” Ms. Hong added.
In a separate poster presentation, Ms. Hong and her colleagues reported compliance of ERAS components under the control of the anesthesiologist. The highest rate of compliance was seen in practices with few barriers to implementation such as active pre- and intraoperative warming (96%) and appropriate admission of antibiotics (92%) and antiemetics (86%). Conversely, rates were lower for multimodal analgesia (72%) and goal-directed fluid therapy (50%), which can be more labor intensive. Also, there is controversy around goal-directed fluid therapy’s benefit in low-risk patients, which may contribute to the lower compliance rates, the study authors noted. Overall, just under three-quarters of patients received at least four out of five components in their care.
On the basis of the success of the protocol, ERAS is now used for patients undergoing radical cystectomy, with plans to expand its use to all emergent and urgent cases within general surgery at Vancouver General as well as bariatric surgery at Richmond Hospital, also a member of Vancouver Coastal Health, Andrea Bisaillon, operations director of surgical services at Vancouver General Hospital, said in an interview.
“We’re rolling out ERAS to all the surgical patients because it’s best practice for all of surgery, not just colorectal surgery anymore,” she said.
CHICAGO – Implementing an enhanced recovery after surgery (ERAS) protocol at Canada’s second largest hospital significantly reduced morbidity and surgical site infections after elective colorectal surgery.
Rates of postoperative morbidity declined 48.7% from 27.3% before implementation to 14% after full ERAS implementation (P less than .05), while total surgical site infections fell 45% (20.2% vs. 11%; P less than .05).
Nonsignificant reductions were also seen in superficial surgical site infections (11.1% vs. 7.3%), deep SSIs (2% vs. 0.6%), and organ space SSIs (7.1% vs. 3.4%).
“Our results illustrate that using a multidisciplinary team, with attention to details and small multiple changes, aggregation of marginal gains can result in dramatic improvements in patient outcomes,” primary author Tracey Hong, R.N., said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
The ERAS protocol was implemented at Vancouver General Hospital, after ACS NSQIP risk-adjusted reports showed the 743-bed hospital had a high odds ratio of 1.50 for colorectal operative mortality.
“We had a problem,” Ms. Hong, the hospital’s quality and patient safety coordinator, said.
ERAS documents were developed, staff were educated on the protocol, intraoperative components were implemented and audited, and the full protocol was initiated in November 2013.
To explore the effects of ERAS implementation, chart reviews were conducted on 278 general surgery patients undergoing elective colorectal surgery: 99 patients before ERAS implementation (July 2011 through June 2013) and 179 patients in the first 10 months after full implementation (November 2013 through August 2014).
Laparoscopic colon resections were performed in 53% of the pre-ERAS group and 62% of the post-ERAS group, laparoscopic anterior and abdominoperineal resections in 10% and 23%, and open anterior and abdominoperineal resections in 23% and 18%, respectively. The median American Society of Anesthesiologists classification in both groups was 2.
After ERAS implementation, there was a trend for less postoperative pneumonia, unplanned intubation, ventilator use greater than 48 hours, and urinary tract infections (data not presented).
The median length of stay was reduced from 7 to 5 days, while readmissions increased from 7.1% to 11.7% (both changes were nonsignificant), according to Ms. Hong, who won the conference’s 2015 Surgical Clinical Reviewers Abstract Competition.
The reason for the increased readmissions is unclear, but opportunities to avoid preventable readmissions have been identified and are currently being worked on, she said.
Process measures showed that the goal of achieving a minimum 80% compliance from August 2014 to March 2015 was met within 4 months and sustained for the preoperative and intraoperative ERAS components, in aggregate. The aggregate postoperative components, which include early oral nutrition, early ambulation, early catheter removal, use of chewing gum, and defined discharge criteria, were the slowest to change, but are trending in the right direction, Ms. Hong said.
The key to achieving better outcomes with ERAS lies in involving a multidisciplinary team in all stages of planning and implementation, ongoing communication and sharing of results with stakeholders to foster commitment and ownership, and real-time auditing and use of plan-do-study-act cycles to enhance the rate of improvement, she said.
“It takes time to change culture; tenacity is important,” Ms. Hong added.
In a separate poster presentation, Ms. Hong and her colleagues reported compliance of ERAS components under the control of the anesthesiologist. The highest rate of compliance was seen in practices with few barriers to implementation such as active pre- and intraoperative warming (96%) and appropriate admission of antibiotics (92%) and antiemetics (86%). Conversely, rates were lower for multimodal analgesia (72%) and goal-directed fluid therapy (50%), which can be more labor intensive. Also, there is controversy around goal-directed fluid therapy’s benefit in low-risk patients, which may contribute to the lower compliance rates, the study authors noted. Overall, just under three-quarters of patients received at least four out of five components in their care.
On the basis of the success of the protocol, ERAS is now used for patients undergoing radical cystectomy, with plans to expand its use to all emergent and urgent cases within general surgery at Vancouver General as well as bariatric surgery at Richmond Hospital, also a member of Vancouver Coastal Health, Andrea Bisaillon, operations director of surgical services at Vancouver General Hospital, said in an interview.
“We’re rolling out ERAS to all the surgical patients because it’s best practice for all of surgery, not just colorectal surgery anymore,” she said.
CHICAGO – Implementing an enhanced recovery after surgery (ERAS) protocol at Canada’s second largest hospital significantly reduced morbidity and surgical site infections after elective colorectal surgery.
Rates of postoperative morbidity declined 48.7% from 27.3% before implementation to 14% after full ERAS implementation (P less than .05), while total surgical site infections fell 45% (20.2% vs. 11%; P less than .05).
Nonsignificant reductions were also seen in superficial surgical site infections (11.1% vs. 7.3%), deep SSIs (2% vs. 0.6%), and organ space SSIs (7.1% vs. 3.4%).
“Our results illustrate that using a multidisciplinary team, with attention to details and small multiple changes, aggregation of marginal gains can result in dramatic improvements in patient outcomes,” primary author Tracey Hong, R.N., said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
The ERAS protocol was implemented at Vancouver General Hospital, after ACS NSQIP risk-adjusted reports showed the 743-bed hospital had a high odds ratio of 1.50 for colorectal operative mortality.
“We had a problem,” Ms. Hong, the hospital’s quality and patient safety coordinator, said.
ERAS documents were developed, staff were educated on the protocol, intraoperative components were implemented and audited, and the full protocol was initiated in November 2013.
To explore the effects of ERAS implementation, chart reviews were conducted on 278 general surgery patients undergoing elective colorectal surgery: 99 patients before ERAS implementation (July 2011 through June 2013) and 179 patients in the first 10 months after full implementation (November 2013 through August 2014).
Laparoscopic colon resections were performed in 53% of the pre-ERAS group and 62% of the post-ERAS group, laparoscopic anterior and abdominoperineal resections in 10% and 23%, and open anterior and abdominoperineal resections in 23% and 18%, respectively. The median American Society of Anesthesiologists classification in both groups was 2.
After ERAS implementation, there was a trend for less postoperative pneumonia, unplanned intubation, ventilator use greater than 48 hours, and urinary tract infections (data not presented).
The median length of stay was reduced from 7 to 5 days, while readmissions increased from 7.1% to 11.7% (both changes were nonsignificant), according to Ms. Hong, who won the conference’s 2015 Surgical Clinical Reviewers Abstract Competition.
The reason for the increased readmissions is unclear, but opportunities to avoid preventable readmissions have been identified and are currently being worked on, she said.
Process measures showed that the goal of achieving a minimum 80% compliance from August 2014 to March 2015 was met within 4 months and sustained for the preoperative and intraoperative ERAS components, in aggregate. The aggregate postoperative components, which include early oral nutrition, early ambulation, early catheter removal, use of chewing gum, and defined discharge criteria, were the slowest to change, but are trending in the right direction, Ms. Hong said.
The key to achieving better outcomes with ERAS lies in involving a multidisciplinary team in all stages of planning and implementation, ongoing communication and sharing of results with stakeholders to foster commitment and ownership, and real-time auditing and use of plan-do-study-act cycles to enhance the rate of improvement, she said.
“It takes time to change culture; tenacity is important,” Ms. Hong added.
In a separate poster presentation, Ms. Hong and her colleagues reported compliance of ERAS components under the control of the anesthesiologist. The highest rate of compliance was seen in practices with few barriers to implementation such as active pre- and intraoperative warming (96%) and appropriate admission of antibiotics (92%) and antiemetics (86%). Conversely, rates were lower for multimodal analgesia (72%) and goal-directed fluid therapy (50%), which can be more labor intensive. Also, there is controversy around goal-directed fluid therapy’s benefit in low-risk patients, which may contribute to the lower compliance rates, the study authors noted. Overall, just under three-quarters of patients received at least four out of five components in their care.
On the basis of the success of the protocol, ERAS is now used for patients undergoing radical cystectomy, with plans to expand its use to all emergent and urgent cases within general surgery at Vancouver General as well as bariatric surgery at Richmond Hospital, also a member of Vancouver Coastal Health, Andrea Bisaillon, operations director of surgical services at Vancouver General Hospital, said in an interview.
“We’re rolling out ERAS to all the surgical patients because it’s best practice for all of surgery, not just colorectal surgery anymore,” she said.
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: Through an ERAS protocol, attention to details and small multiple changes can result in dramatic improvements in patient outcomes.
Major finding: After full ERAS implementation, rates of postoperative morbidity and total surgical site infection were reduced 48.7% and 45%, respectively.
Data source: A retrospective analysis of 278 patients undergoing elective colorectal surgery.
Disclosures: The study authors reported having no relevant financial conflicts.
VIDEO: Postoperative cognitive decline hits women hardest
WASHINGTON – Postoperative cognitive decline, which occurs in roughly 20% of elderly patients who undergo major surgery, strikes older women with greater severity than it does similarly aged men, according to a retrospective analysis of data collected from 527 older Americans.
“We looked at the sex difference in postoperative cognitive decline and Alzheimer’s disease because of the sex difference in Alzheimer’s disease, where about two-thirds of patients are women,” Dr. Katie J. Schenning said in an interview during the Alzheimer’s Association International Conference 2015. “We know that a lot of the pathologic changes that happen to the brain after anesthesia and surgery are similar to the changes that happen in Alzheimer’s disease patients. But at this point that is all we can say about a link between the two. It is currently unknown whether there is a clear relationship between postoperative cognitive decline and Alzheimer’s disease,” said Dr. Schenning, an anesthesiologist at Oregon Health & Science University in Portland.
She and her associates studied data collected longitudinally from two cohorts, the Oregon Brain Aging Study and the Intelligent Systems for Assessment of Aging Changes. At baseline, the average age of the enrollees in the combined group was 83 years, and just under two-thirds were women. During follow-up, 182 of the participants underwent a total of 331 major surgeries, with some undergoing more than one surgery. The most common form of surgery was orthopedic, done in one-third of the patients, followed by general surgery, in a quarter.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The researchers running both studies collected data annually from participants using a battery of neuropsychological evaluations, brain MRIs, and information on their general health. Retrospective analysis of the data showed that following surgery, people showed evidence of statistically significant and clinically meaningful declines in several measures, compared with those who did not undergo surgery, including deficits measured by the Mini-Mental State Examination, instrumental activities of daily living, and logical memory delayed recall. The trajectory of these declines was significantly steeper in women following surgery, compared with men following surgery, Dr. Schenning reported in a poster at the meeting. In addition, the MRI scans showed ventricular enlargement in the postsurgical women but not in men, a change that is characteristic of neuropathology.
“Women who underwent surgery had a more rapid rate of decline in measures of cognition and function than women who did not have surgery, and it affected women in more categories than in men,” Dr. Schenning said.
The risk for postoperative cognitive decline “is one of the things that patients should take into consideration before undergoing elective surgery, especially if they are older or have pre-existing cognitive impairment,” Dr. Schenning suggested. The enhanced risk for postsurgical cognitive decline faced by older women and even the somewhat lesser risk that exists for older men “is certainly something that patients should discuss with their surgeon, anesthesiologist, and family members,” she said.
Dr. Schenning had no disclosures.
On Twitter @mitchelzoler
WASHINGTON – Postoperative cognitive decline, which occurs in roughly 20% of elderly patients who undergo major surgery, strikes older women with greater severity than it does similarly aged men, according to a retrospective analysis of data collected from 527 older Americans.
“We looked at the sex difference in postoperative cognitive decline and Alzheimer’s disease because of the sex difference in Alzheimer’s disease, where about two-thirds of patients are women,” Dr. Katie J. Schenning said in an interview during the Alzheimer’s Association International Conference 2015. “We know that a lot of the pathologic changes that happen to the brain after anesthesia and surgery are similar to the changes that happen in Alzheimer’s disease patients. But at this point that is all we can say about a link between the two. It is currently unknown whether there is a clear relationship between postoperative cognitive decline and Alzheimer’s disease,” said Dr. Schenning, an anesthesiologist at Oregon Health & Science University in Portland.
She and her associates studied data collected longitudinally from two cohorts, the Oregon Brain Aging Study and the Intelligent Systems for Assessment of Aging Changes. At baseline, the average age of the enrollees in the combined group was 83 years, and just under two-thirds were women. During follow-up, 182 of the participants underwent a total of 331 major surgeries, with some undergoing more than one surgery. The most common form of surgery was orthopedic, done in one-third of the patients, followed by general surgery, in a quarter.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The researchers running both studies collected data annually from participants using a battery of neuropsychological evaluations, brain MRIs, and information on their general health. Retrospective analysis of the data showed that following surgery, people showed evidence of statistically significant and clinically meaningful declines in several measures, compared with those who did not undergo surgery, including deficits measured by the Mini-Mental State Examination, instrumental activities of daily living, and logical memory delayed recall. The trajectory of these declines was significantly steeper in women following surgery, compared with men following surgery, Dr. Schenning reported in a poster at the meeting. In addition, the MRI scans showed ventricular enlargement in the postsurgical women but not in men, a change that is characteristic of neuropathology.
“Women who underwent surgery had a more rapid rate of decline in measures of cognition and function than women who did not have surgery, and it affected women in more categories than in men,” Dr. Schenning said.
The risk for postoperative cognitive decline “is one of the things that patients should take into consideration before undergoing elective surgery, especially if they are older or have pre-existing cognitive impairment,” Dr. Schenning suggested. The enhanced risk for postsurgical cognitive decline faced by older women and even the somewhat lesser risk that exists for older men “is certainly something that patients should discuss with their surgeon, anesthesiologist, and family members,” she said.
Dr. Schenning had no disclosures.
On Twitter @mitchelzoler
WASHINGTON – Postoperative cognitive decline, which occurs in roughly 20% of elderly patients who undergo major surgery, strikes older women with greater severity than it does similarly aged men, according to a retrospective analysis of data collected from 527 older Americans.
“We looked at the sex difference in postoperative cognitive decline and Alzheimer’s disease because of the sex difference in Alzheimer’s disease, where about two-thirds of patients are women,” Dr. Katie J. Schenning said in an interview during the Alzheimer’s Association International Conference 2015. “We know that a lot of the pathologic changes that happen to the brain after anesthesia and surgery are similar to the changes that happen in Alzheimer’s disease patients. But at this point that is all we can say about a link between the two. It is currently unknown whether there is a clear relationship between postoperative cognitive decline and Alzheimer’s disease,” said Dr. Schenning, an anesthesiologist at Oregon Health & Science University in Portland.
She and her associates studied data collected longitudinally from two cohorts, the Oregon Brain Aging Study and the Intelligent Systems for Assessment of Aging Changes. At baseline, the average age of the enrollees in the combined group was 83 years, and just under two-thirds were women. During follow-up, 182 of the participants underwent a total of 331 major surgeries, with some undergoing more than one surgery. The most common form of surgery was orthopedic, done in one-third of the patients, followed by general surgery, in a quarter.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The researchers running both studies collected data annually from participants using a battery of neuropsychological evaluations, brain MRIs, and information on their general health. Retrospective analysis of the data showed that following surgery, people showed evidence of statistically significant and clinically meaningful declines in several measures, compared with those who did not undergo surgery, including deficits measured by the Mini-Mental State Examination, instrumental activities of daily living, and logical memory delayed recall. The trajectory of these declines was significantly steeper in women following surgery, compared with men following surgery, Dr. Schenning reported in a poster at the meeting. In addition, the MRI scans showed ventricular enlargement in the postsurgical women but not in men, a change that is characteristic of neuropathology.
“Women who underwent surgery had a more rapid rate of decline in measures of cognition and function than women who did not have surgery, and it affected women in more categories than in men,” Dr. Schenning said.
The risk for postoperative cognitive decline “is one of the things that patients should take into consideration before undergoing elective surgery, especially if they are older or have pre-existing cognitive impairment,” Dr. Schenning suggested. The enhanced risk for postsurgical cognitive decline faced by older women and even the somewhat lesser risk that exists for older men “is certainly something that patients should discuss with their surgeon, anesthesiologist, and family members,” she said.
Dr. Schenning had no disclosures.
On Twitter @mitchelzoler
AT AAIC 2015
CABG costs more in patients with diabetes
The rate of diabetic coronary artery bypass graft patients has increased more than fivefold in recent decades, and these patients are more likely to have worse outcomes and higher treatment costs, a study showed.
The percentage of patients who had diabetes among all those undergoing coronary artery bypass grafting (CABG) increased from 7% in the 1970s to 37% in the 2000s, according to a database study of 55,501 patients operated on at the Cleveland Clinic.
Patients were identified and preoperative, operative, and postoperative variables were identified, resulting in 45,139 nondiabetic patients assessed and 10,362 diabetic patients (defined as those diabetic patients pharmacologically treated with either insulin or an oral agent) evaluated. The endpoints assessed were in-hospital adverse outcomes as determined by the Society of Thoracic Surgeons National Database, in-hospital direct technical costs, and time-related mortality, according to Dr. Sajjad Raza and his colleagues at the Cleveland Clinic in the August issue of the Journal of Thoracic and Cardiovascular Surgery (150:294-301).
Compared with nondiabetics, diabetic patients undergoing CABG were older and were more likely to be overweight, to be women, and to have a history of heart failure, peripheral arterial disease, carotid disease, hypertension, renal failure, stroke, and advanced coronary artery disease. Over time, the cardiovascular risk profile of the entire population changed, becoming even more pronounced for all patients, but more so for diabetics.
Overall long-term survival at 6 months and at 1, 5 10, 15, and 20 years for diabetic patients was 95%, 94%, 80%, 54%, 31%, and 18%, respectively, compared with 97%, 97%, 90%, 76%, 59%, and 42% for nondiabetic patients, a significant difference at P <.0001.
Propensity matching of similar diabetic and nondiabetic patients showed that deep sternal wound infection and stroke occurred significantly more often in diabetics, although there were no significant differences in cost remaining after matching, even though the length of stay greater than 14 days remained higher for diabetic patients.
Among diabetics, overall survival at 6 months and at 1, 5, 10, 15, and 20 years after CABG was 95%, 94%, 80%, 54%, 31%, and 18%, respectively, compared with overall survival in nondiabetics at 97%, 97%, 90%, 76%, 59%, and 42%, respectively, a significant difference (P <.0001).
“Although long-term survival after CABG is worse in diabetics and high-risk nondiabetics, it is important to note that, in general, high-risk patients reap the greatest survival benefit from CABG. Moreover, using surgical techniques that are associated with better long-term survival after CABG in diabetics could further enhance this survival benefit,” Dr. Raza and his colleagues wrote.
“Diabetes is both a marker for high-risk, resource-intensive, and expensive care after CABG and an independent risk factor for reduced long-term survival,” they added. “Diabetic patients and those with a similar high-risk profile set to undergo CABG should be made aware that their risks of postoperative complications are higher than average, and measures should be taken to reduce their postoperative complications,” Dr. Raza and his colleagues concluded.
The authors reported that they had no relevant conflicts of interest.
Patients with diabetes, with or without metabolic syndrome, represent an increasing challenge for cardiac surgery. CABG has been shown to convey a mortality benefit in such patients who also have multivessel disease. This study confirms what most clinicians already know – that the outcomes of patients with diabetes are worse than those in nondiabetic patients, according to Dr. Mani Arsalan and Dr. Michael Mack. “What is particularly important about this study, however, is that it is a single institutional experience with known surgical excellence and a very meticulous and complete outcomes database,” they wrote (J. Thorac. Cardiovasc. Surg. 2015;150:284-5).
Given their findings and the fact that CABG can be expected to remain the mainstay of treatment of multivessel disease in diabetics because of the results of the FREEDOM (Future Revascularization Evaluation in Patients With Diabetes Mellitus: Optimal Management of Multivessel Disease) trial, surgeons should pay increased attention to the details of the procedure for these patients. There should be an increased use of bilateral internal mammary arteries, which has been distressingly low, and yet can provide a 23% mortality benefit. “Two arteries are better than one.” Despite the increased risk of deep sternal infection, “the use of skeletonized bilateral internal mammary arteries in young, nonobese diabetic patients with a greater than 10-year life expectancy seems a reasonable risk to take,” Dr. Arsalan and Dr. Mack wrote. In addition, where possible, reaching satisfactory glycemic control before surgery can help decrease early complications. “The weight may be increasingly on our patients, but the real weight is on us as surgeons to help improve their early and long-term survival,” they concluded.
Dr. Arsalan and Dr. Mack are cardiovascular surgeons at Baylor Scott & White Health, Dallas. Their remarks were part of an invited commentary published with the paper.
Patients with diabetes, with or without metabolic syndrome, represent an increasing challenge for cardiac surgery. CABG has been shown to convey a mortality benefit in such patients who also have multivessel disease. This study confirms what most clinicians already know – that the outcomes of patients with diabetes are worse than those in nondiabetic patients, according to Dr. Mani Arsalan and Dr. Michael Mack. “What is particularly important about this study, however, is that it is a single institutional experience with known surgical excellence and a very meticulous and complete outcomes database,” they wrote (J. Thorac. Cardiovasc. Surg. 2015;150:284-5).
Given their findings and the fact that CABG can be expected to remain the mainstay of treatment of multivessel disease in diabetics because of the results of the FREEDOM (Future Revascularization Evaluation in Patients With Diabetes Mellitus: Optimal Management of Multivessel Disease) trial, surgeons should pay increased attention to the details of the procedure for these patients. There should be an increased use of bilateral internal mammary arteries, which has been distressingly low, and yet can provide a 23% mortality benefit. “Two arteries are better than one.” Despite the increased risk of deep sternal infection, “the use of skeletonized bilateral internal mammary arteries in young, nonobese diabetic patients with a greater than 10-year life expectancy seems a reasonable risk to take,” Dr. Arsalan and Dr. Mack wrote. In addition, where possible, reaching satisfactory glycemic control before surgery can help decrease early complications. “The weight may be increasingly on our patients, but the real weight is on us as surgeons to help improve their early and long-term survival,” they concluded.
Dr. Arsalan and Dr. Mack are cardiovascular surgeons at Baylor Scott & White Health, Dallas. Their remarks were part of an invited commentary published with the paper.
Patients with diabetes, with or without metabolic syndrome, represent an increasing challenge for cardiac surgery. CABG has been shown to convey a mortality benefit in such patients who also have multivessel disease. This study confirms what most clinicians already know – that the outcomes of patients with diabetes are worse than those in nondiabetic patients, according to Dr. Mani Arsalan and Dr. Michael Mack. “What is particularly important about this study, however, is that it is a single institutional experience with known surgical excellence and a very meticulous and complete outcomes database,” they wrote (J. Thorac. Cardiovasc. Surg. 2015;150:284-5).
Given their findings and the fact that CABG can be expected to remain the mainstay of treatment of multivessel disease in diabetics because of the results of the FREEDOM (Future Revascularization Evaluation in Patients With Diabetes Mellitus: Optimal Management of Multivessel Disease) trial, surgeons should pay increased attention to the details of the procedure for these patients. There should be an increased use of bilateral internal mammary arteries, which has been distressingly low, and yet can provide a 23% mortality benefit. “Two arteries are better than one.” Despite the increased risk of deep sternal infection, “the use of skeletonized bilateral internal mammary arteries in young, nonobese diabetic patients with a greater than 10-year life expectancy seems a reasonable risk to take,” Dr. Arsalan and Dr. Mack wrote. In addition, where possible, reaching satisfactory glycemic control before surgery can help decrease early complications. “The weight may be increasingly on our patients, but the real weight is on us as surgeons to help improve their early and long-term survival,” they concluded.
Dr. Arsalan and Dr. Mack are cardiovascular surgeons at Baylor Scott & White Health, Dallas. Their remarks were part of an invited commentary published with the paper.
The rate of diabetic coronary artery bypass graft patients has increased more than fivefold in recent decades, and these patients are more likely to have worse outcomes and higher treatment costs, a study showed.
The percentage of patients who had diabetes among all those undergoing coronary artery bypass grafting (CABG) increased from 7% in the 1970s to 37% in the 2000s, according to a database study of 55,501 patients operated on at the Cleveland Clinic.
Patients were identified and preoperative, operative, and postoperative variables were identified, resulting in 45,139 nondiabetic patients assessed and 10,362 diabetic patients (defined as those diabetic patients pharmacologically treated with either insulin or an oral agent) evaluated. The endpoints assessed were in-hospital adverse outcomes as determined by the Society of Thoracic Surgeons National Database, in-hospital direct technical costs, and time-related mortality, according to Dr. Sajjad Raza and his colleagues at the Cleveland Clinic in the August issue of the Journal of Thoracic and Cardiovascular Surgery (150:294-301).
Compared with nondiabetics, diabetic patients undergoing CABG were older and were more likely to be overweight, to be women, and to have a history of heart failure, peripheral arterial disease, carotid disease, hypertension, renal failure, stroke, and advanced coronary artery disease. Over time, the cardiovascular risk profile of the entire population changed, becoming even more pronounced for all patients, but more so for diabetics.
Overall long-term survival at 6 months and at 1, 5 10, 15, and 20 years for diabetic patients was 95%, 94%, 80%, 54%, 31%, and 18%, respectively, compared with 97%, 97%, 90%, 76%, 59%, and 42% for nondiabetic patients, a significant difference at P <.0001.
Propensity matching of similar diabetic and nondiabetic patients showed that deep sternal wound infection and stroke occurred significantly more often in diabetics, although there were no significant differences in cost remaining after matching, even though the length of stay greater than 14 days remained higher for diabetic patients.
Among diabetics, overall survival at 6 months and at 1, 5, 10, 15, and 20 years after CABG was 95%, 94%, 80%, 54%, 31%, and 18%, respectively, compared with overall survival in nondiabetics at 97%, 97%, 90%, 76%, 59%, and 42%, respectively, a significant difference (P <.0001).
“Although long-term survival after CABG is worse in diabetics and high-risk nondiabetics, it is important to note that, in general, high-risk patients reap the greatest survival benefit from CABG. Moreover, using surgical techniques that are associated with better long-term survival after CABG in diabetics could further enhance this survival benefit,” Dr. Raza and his colleagues wrote.
“Diabetes is both a marker for high-risk, resource-intensive, and expensive care after CABG and an independent risk factor for reduced long-term survival,” they added. “Diabetic patients and those with a similar high-risk profile set to undergo CABG should be made aware that their risks of postoperative complications are higher than average, and measures should be taken to reduce their postoperative complications,” Dr. Raza and his colleagues concluded.
The authors reported that they had no relevant conflicts of interest.
The rate of diabetic coronary artery bypass graft patients has increased more than fivefold in recent decades, and these patients are more likely to have worse outcomes and higher treatment costs, a study showed.
The percentage of patients who had diabetes among all those undergoing coronary artery bypass grafting (CABG) increased from 7% in the 1970s to 37% in the 2000s, according to a database study of 55,501 patients operated on at the Cleveland Clinic.
Patients were identified and preoperative, operative, and postoperative variables were identified, resulting in 45,139 nondiabetic patients assessed and 10,362 diabetic patients (defined as those diabetic patients pharmacologically treated with either insulin or an oral agent) evaluated. The endpoints assessed were in-hospital adverse outcomes as determined by the Society of Thoracic Surgeons National Database, in-hospital direct technical costs, and time-related mortality, according to Dr. Sajjad Raza and his colleagues at the Cleveland Clinic in the August issue of the Journal of Thoracic and Cardiovascular Surgery (150:294-301).
Compared with nondiabetics, diabetic patients undergoing CABG were older and were more likely to be overweight, to be women, and to have a history of heart failure, peripheral arterial disease, carotid disease, hypertension, renal failure, stroke, and advanced coronary artery disease. Over time, the cardiovascular risk profile of the entire population changed, becoming even more pronounced for all patients, but more so for diabetics.
Overall long-term survival at 6 months and at 1, 5 10, 15, and 20 years for diabetic patients was 95%, 94%, 80%, 54%, 31%, and 18%, respectively, compared with 97%, 97%, 90%, 76%, 59%, and 42% for nondiabetic patients, a significant difference at P <.0001.
Propensity matching of similar diabetic and nondiabetic patients showed that deep sternal wound infection and stroke occurred significantly more often in diabetics, although there were no significant differences in cost remaining after matching, even though the length of stay greater than 14 days remained higher for diabetic patients.
Among diabetics, overall survival at 6 months and at 1, 5, 10, 15, and 20 years after CABG was 95%, 94%, 80%, 54%, 31%, and 18%, respectively, compared with overall survival in nondiabetics at 97%, 97%, 90%, 76%, 59%, and 42%, respectively, a significant difference (P <.0001).
“Although long-term survival after CABG is worse in diabetics and high-risk nondiabetics, it is important to note that, in general, high-risk patients reap the greatest survival benefit from CABG. Moreover, using surgical techniques that are associated with better long-term survival after CABG in diabetics could further enhance this survival benefit,” Dr. Raza and his colleagues wrote.
“Diabetes is both a marker for high-risk, resource-intensive, and expensive care after CABG and an independent risk factor for reduced long-term survival,” they added. “Diabetic patients and those with a similar high-risk profile set to undergo CABG should be made aware that their risks of postoperative complications are higher than average, and measures should be taken to reduce their postoperative complications,” Dr. Raza and his colleagues concluded.
The authors reported that they had no relevant conflicts of interest.
FROM JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: The percentage of CABG patients with diabetes increased from 7% in the 1970s to 37% in the 2000s. The risk/benefit ratio warrants greater use of bilateral mammary arteries except in obese women with diabetes.
Major finding: Diabetic patients had significantly worse outcomes than nondiabetics with regard to hospital death, deep sternal wound infections, strokes, and renal failure as well as hospital stay and costs.
Data source: A retrospective analysis of a prospective database of patients undergoing first-time CABG at the Cleveland Clinic from 1972 to 2011.
Disclosures: The authors reported that they had no relevant conflicts of interest.
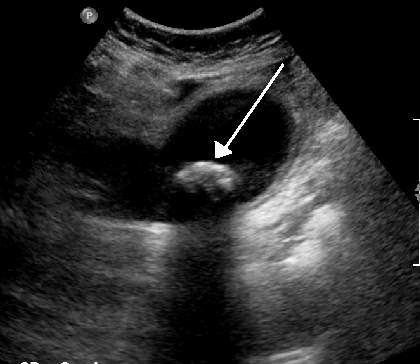
Surgical follow-up after ED cholelithiasis episode cuts long-term costs, complications
Patients who don’t receive surgical follow-up after an emergency department visit for cholelithiasis are at increased risk for further ED visits, extraneous imaging, and complications from the disease and from emergent cholecystectomy, according to the findings of a retrospective study.
“Our study identifies lack of surgical follow-up [as] a major contributor to the failure to perform cholecystecomy and highlights the importance of prompt surgical evaluation,” stated Taylor P. Williams of the University of Texas Medical Branch (UTMB), Galveston, and co-investigators.
Between August 2009 and May 2014, 71 patients were discharged from the ED at UTMB with a diagnosis of symptomatic gallstones. The study charted the care of these patients for a follow-up period of 2 years, and the findings were published the August issue of the Journal of Surgical Research (2015;197:318-23).
The mean age of patients was 41 years; 86% were women, and 49% were white. A majority of the patients (56.3%) had no health insurance, while 11.3% had Medicare, 11.3% were on Medicaid, and 21.1% had private insurance.
Of the 71 patients, 18 (25.4%) had outpatient surgical follow-up after an ED visit for a cholelithiasis episode, and they saw the surgeon an average of 7.7 days after the initial ED visit. In the 9 patients who then had an elective cholecystectomy, 8 of these operations occurred within a month of the initital ED visit.
A total of 53 (74.6%) had no immediate surgical follow-up after their ED visit.
The 62 patients who did not have a cholecystectomy had a different trajectory of care than did those who had surgery soon after their ED visit. Of the non-cholecystectomy group, 14.5% of this group eventually had outpatient surgical follow-up within a mean time of 137 days and 37.1% had repeat visits to the ED for gallstone symptoms (17.7% had two or more additional ED visits). Over half of those visits resulted in additional CT or ultrasound imaging. A total of 8 (12.9%) of the total group ended up with an emergent cholecystectomy.
The investigators looked at factors associated with surgical follow-up and eventual or emergent cholecystectomy. Laboratory values, demographics, and radiographic findings were similar between those who underwent cholecystectomy and those who did not. Patients with insurance were more likely to achieve surgical follow-up and more likely to have an elective cholecystectomy. Nausea and vomiting on presentation at the initial ED visit were associated with a greater likelihood of having a cholecystectomy.
The study showed that the 71 patients who presented at the ED with symptoms of cholelithiasis had a similar number of elective and emergent cholecystectomies. But those who did not pursue follow-up and delayed in having surgery incurred additional risks and costs.
A limitation of the study, according to the investigators, is that it involves a small sample from a single center in a community with a high proportion of patients who lack health insurance. In addition, UTMB protocol for acute gallbladder disease leads to a higher rate of admissions than is typical in the United States.
The investigators concluded that “lack of appropriate follow-up leads to multiple ED visits, high rates of emergent cholecystectomy, and redundant radiographic studies, increasing the cost of care and quality of life of those patients. Our data contribute to the literature supporting early surgical follow-up and elective cholecystectomy in preventing repeat ED visits and development of gallstone-related complications in patients presenting to the ED with symptomatic gallstones not severe enough to require emergency admission.”
The investigators had no relevant disclosures.
Patients who don’t receive surgical follow-up after an emergency department visit for cholelithiasis are at increased risk for further ED visits, extraneous imaging, and complications from the disease and from emergent cholecystectomy, according to the findings of a retrospective study.
“Our study identifies lack of surgical follow-up [as] a major contributor to the failure to perform cholecystecomy and highlights the importance of prompt surgical evaluation,” stated Taylor P. Williams of the University of Texas Medical Branch (UTMB), Galveston, and co-investigators.
Between August 2009 and May 2014, 71 patients were discharged from the ED at UTMB with a diagnosis of symptomatic gallstones. The study charted the care of these patients for a follow-up period of 2 years, and the findings were published the August issue of the Journal of Surgical Research (2015;197:318-23).
The mean age of patients was 41 years; 86% were women, and 49% were white. A majority of the patients (56.3%) had no health insurance, while 11.3% had Medicare, 11.3% were on Medicaid, and 21.1% had private insurance.
Of the 71 patients, 18 (25.4%) had outpatient surgical follow-up after an ED visit for a cholelithiasis episode, and they saw the surgeon an average of 7.7 days after the initial ED visit. In the 9 patients who then had an elective cholecystectomy, 8 of these operations occurred within a month of the initital ED visit.
A total of 53 (74.6%) had no immediate surgical follow-up after their ED visit.
The 62 patients who did not have a cholecystectomy had a different trajectory of care than did those who had surgery soon after their ED visit. Of the non-cholecystectomy group, 14.5% of this group eventually had outpatient surgical follow-up within a mean time of 137 days and 37.1% had repeat visits to the ED for gallstone symptoms (17.7% had two or more additional ED visits). Over half of those visits resulted in additional CT or ultrasound imaging. A total of 8 (12.9%) of the total group ended up with an emergent cholecystectomy.
The investigators looked at factors associated with surgical follow-up and eventual or emergent cholecystectomy. Laboratory values, demographics, and radiographic findings were similar between those who underwent cholecystectomy and those who did not. Patients with insurance were more likely to achieve surgical follow-up and more likely to have an elective cholecystectomy. Nausea and vomiting on presentation at the initial ED visit were associated with a greater likelihood of having a cholecystectomy.
The study showed that the 71 patients who presented at the ED with symptoms of cholelithiasis had a similar number of elective and emergent cholecystectomies. But those who did not pursue follow-up and delayed in having surgery incurred additional risks and costs.
A limitation of the study, according to the investigators, is that it involves a small sample from a single center in a community with a high proportion of patients who lack health insurance. In addition, UTMB protocol for acute gallbladder disease leads to a higher rate of admissions than is typical in the United States.
The investigators concluded that “lack of appropriate follow-up leads to multiple ED visits, high rates of emergent cholecystectomy, and redundant radiographic studies, increasing the cost of care and quality of life of those patients. Our data contribute to the literature supporting early surgical follow-up and elective cholecystectomy in preventing repeat ED visits and development of gallstone-related complications in patients presenting to the ED with symptomatic gallstones not severe enough to require emergency admission.”
The investigators had no relevant disclosures.
Patients who don’t receive surgical follow-up after an emergency department visit for cholelithiasis are at increased risk for further ED visits, extraneous imaging, and complications from the disease and from emergent cholecystectomy, according to the findings of a retrospective study.
“Our study identifies lack of surgical follow-up [as] a major contributor to the failure to perform cholecystecomy and highlights the importance of prompt surgical evaluation,” stated Taylor P. Williams of the University of Texas Medical Branch (UTMB), Galveston, and co-investigators.
Between August 2009 and May 2014, 71 patients were discharged from the ED at UTMB with a diagnosis of symptomatic gallstones. The study charted the care of these patients for a follow-up period of 2 years, and the findings were published the August issue of the Journal of Surgical Research (2015;197:318-23).
The mean age of patients was 41 years; 86% were women, and 49% were white. A majority of the patients (56.3%) had no health insurance, while 11.3% had Medicare, 11.3% were on Medicaid, and 21.1% had private insurance.
Of the 71 patients, 18 (25.4%) had outpatient surgical follow-up after an ED visit for a cholelithiasis episode, and they saw the surgeon an average of 7.7 days after the initial ED visit. In the 9 patients who then had an elective cholecystectomy, 8 of these operations occurred within a month of the initital ED visit.
A total of 53 (74.6%) had no immediate surgical follow-up after their ED visit.
The 62 patients who did not have a cholecystectomy had a different trajectory of care than did those who had surgery soon after their ED visit. Of the non-cholecystectomy group, 14.5% of this group eventually had outpatient surgical follow-up within a mean time of 137 days and 37.1% had repeat visits to the ED for gallstone symptoms (17.7% had two or more additional ED visits). Over half of those visits resulted in additional CT or ultrasound imaging. A total of 8 (12.9%) of the total group ended up with an emergent cholecystectomy.
The investigators looked at factors associated with surgical follow-up and eventual or emergent cholecystectomy. Laboratory values, demographics, and radiographic findings were similar between those who underwent cholecystectomy and those who did not. Patients with insurance were more likely to achieve surgical follow-up and more likely to have an elective cholecystectomy. Nausea and vomiting on presentation at the initial ED visit were associated with a greater likelihood of having a cholecystectomy.
The study showed that the 71 patients who presented at the ED with symptoms of cholelithiasis had a similar number of elective and emergent cholecystectomies. But those who did not pursue follow-up and delayed in having surgery incurred additional risks and costs.
A limitation of the study, according to the investigators, is that it involves a small sample from a single center in a community with a high proportion of patients who lack health insurance. In addition, UTMB protocol for acute gallbladder disease leads to a higher rate of admissions than is typical in the United States.
The investigators concluded that “lack of appropriate follow-up leads to multiple ED visits, high rates of emergent cholecystectomy, and redundant radiographic studies, increasing the cost of care and quality of life of those patients. Our data contribute to the literature supporting early surgical follow-up and elective cholecystectomy in preventing repeat ED visits and development of gallstone-related complications in patients presenting to the ED with symptomatic gallstones not severe enough to require emergency admission.”
The investigators had no relevant disclosures.
FROM JOURNAL OF SURGICAL RESEARCH
Key clinical point: Surgical follow-up after a patient presents at the ED with symptomatic cholelithiasis is critical in reducing ED visits, complications, and costs for gallbladder disease.
Major finding: Of those patients who did not have elective surgery, 37.1% had repeat visits to the ED for gallstone symptoms, 17.7% of which had two or more additional ED visits, and over half of those additional visits resulted in CT or ultrasound imaging.
Data source: A single-center study of 71 patients presenting to the emergency department with symptomatic cholelithiasis and followed for up to 2 years.
Disclosures: The investigators had no relevant disclosures.
SVS: Beta-blockers cut stroke, death risk in carotid stenting
CHICAGO – Carotid artery stenting is safer if patients have been on beta-blockers for at least a month beforehand, according to a review of 5,248 stent cases during 2005-2014.
“Compared to non-users, patients on long-term beta-blockers are at 34% less risk of stroke and death after carotid artery stenting [odds ratio, 0.66; 95% confidence interval, 0.46-0.95; P = .025], and this risk reduction is amplified to 65% in patients with postop hypertension [OR, 0.35; 95% CI, 0.17-0.73; P = .005]. Beta-blockers significantly reduce the stroke and death risk ... and should be investigated prospectively for potential use during” carotid artery stenting (CAS), said senior investigator Dr. Mahmoud Malas, director of endovascular surgery and associate professor of surgery at Johns Hopkins Bayview Medical Center in Baltimore.
In the study, long-term beta-blocker use was not associated with post-procedure hypotension in the study. Among patients who developed it, however, beta-blockers were associated with a 48% reduction in the risk of stroke or death at 30 days (OR, 0.52; 95% CI, 0.28-0.98; P = .43).
“We think” the benefits are due to “up-regulation of adrenergic receptors. We think also there is better baroreceptor reflex sensitivity.” Long-term use of beta-blockers reduces heart rate variability, as well, and decreases the risk of hyperperfusion fourfold, Dr. Malas said at the meeting hosted by the Society for Vascular Surgery.
The researchers looked into the issue because they are trying to find a way to make CAS safer in the wake of the Carotid Revascularization Endarterectomy versus Stent Trial (CREST) and others that have shown increased risk compared with carotid endarterectomy.
The subjects were all captured in SVS’s Vascular Quality Initiative database; 2,152 were not on beta-blockers before CAS, 259 were on them for less than 30 days, and 2,837 were on them for more than 30 days. There were no statistical between-group differences in lesion sites, approach (femoral in almost all the cases), or contrast volume used in surgery, a marker of case complexity.
Long-term users had more diabetes, hypertension, coronary artery disease, and congestive heart failure, whereas short term users were more symptomatic; those and other differences were controlled for on multivariate analysis. Aspirin, clopidogrel, and statin use were similar between the groups. About two-thirds of the subjects were men, and the average age in the study was about 70 years old.
Overall, the 30-day stroke and death rate was 3.4% (minor stroke 1.5%, major 0.9%, and death 1.2%).
Predictors of postoperative stroke or death at 30 days included symptomatic status, age, diabetes, and perioperative hypotension and hypertension. Prior carotid endarterectomy and distal embolic protection were both protective.
The investigators have no disclosures.
CHICAGO – Carotid artery stenting is safer if patients have been on beta-blockers for at least a month beforehand, according to a review of 5,248 stent cases during 2005-2014.
“Compared to non-users, patients on long-term beta-blockers are at 34% less risk of stroke and death after carotid artery stenting [odds ratio, 0.66; 95% confidence interval, 0.46-0.95; P = .025], and this risk reduction is amplified to 65% in patients with postop hypertension [OR, 0.35; 95% CI, 0.17-0.73; P = .005]. Beta-blockers significantly reduce the stroke and death risk ... and should be investigated prospectively for potential use during” carotid artery stenting (CAS), said senior investigator Dr. Mahmoud Malas, director of endovascular surgery and associate professor of surgery at Johns Hopkins Bayview Medical Center in Baltimore.
In the study, long-term beta-blocker use was not associated with post-procedure hypotension in the study. Among patients who developed it, however, beta-blockers were associated with a 48% reduction in the risk of stroke or death at 30 days (OR, 0.52; 95% CI, 0.28-0.98; P = .43).
“We think” the benefits are due to “up-regulation of adrenergic receptors. We think also there is better baroreceptor reflex sensitivity.” Long-term use of beta-blockers reduces heart rate variability, as well, and decreases the risk of hyperperfusion fourfold, Dr. Malas said at the meeting hosted by the Society for Vascular Surgery.
The researchers looked into the issue because they are trying to find a way to make CAS safer in the wake of the Carotid Revascularization Endarterectomy versus Stent Trial (CREST) and others that have shown increased risk compared with carotid endarterectomy.
The subjects were all captured in SVS’s Vascular Quality Initiative database; 2,152 were not on beta-blockers before CAS, 259 were on them for less than 30 days, and 2,837 were on them for more than 30 days. There were no statistical between-group differences in lesion sites, approach (femoral in almost all the cases), or contrast volume used in surgery, a marker of case complexity.
Long-term users had more diabetes, hypertension, coronary artery disease, and congestive heart failure, whereas short term users were more symptomatic; those and other differences were controlled for on multivariate analysis. Aspirin, clopidogrel, and statin use were similar between the groups. About two-thirds of the subjects were men, and the average age in the study was about 70 years old.
Overall, the 30-day stroke and death rate was 3.4% (minor stroke 1.5%, major 0.9%, and death 1.2%).
Predictors of postoperative stroke or death at 30 days included symptomatic status, age, diabetes, and perioperative hypotension and hypertension. Prior carotid endarterectomy and distal embolic protection were both protective.
The investigators have no disclosures.
CHICAGO – Carotid artery stenting is safer if patients have been on beta-blockers for at least a month beforehand, according to a review of 5,248 stent cases during 2005-2014.
“Compared to non-users, patients on long-term beta-blockers are at 34% less risk of stroke and death after carotid artery stenting [odds ratio, 0.66; 95% confidence interval, 0.46-0.95; P = .025], and this risk reduction is amplified to 65% in patients with postop hypertension [OR, 0.35; 95% CI, 0.17-0.73; P = .005]. Beta-blockers significantly reduce the stroke and death risk ... and should be investigated prospectively for potential use during” carotid artery stenting (CAS), said senior investigator Dr. Mahmoud Malas, director of endovascular surgery and associate professor of surgery at Johns Hopkins Bayview Medical Center in Baltimore.
In the study, long-term beta-blocker use was not associated with post-procedure hypotension in the study. Among patients who developed it, however, beta-blockers were associated with a 48% reduction in the risk of stroke or death at 30 days (OR, 0.52; 95% CI, 0.28-0.98; P = .43).
“We think” the benefits are due to “up-regulation of adrenergic receptors. We think also there is better baroreceptor reflex sensitivity.” Long-term use of beta-blockers reduces heart rate variability, as well, and decreases the risk of hyperperfusion fourfold, Dr. Malas said at the meeting hosted by the Society for Vascular Surgery.
The researchers looked into the issue because they are trying to find a way to make CAS safer in the wake of the Carotid Revascularization Endarterectomy versus Stent Trial (CREST) and others that have shown increased risk compared with carotid endarterectomy.
The subjects were all captured in SVS’s Vascular Quality Initiative database; 2,152 were not on beta-blockers before CAS, 259 were on them for less than 30 days, and 2,837 were on them for more than 30 days. There were no statistical between-group differences in lesion sites, approach (femoral in almost all the cases), or contrast volume used in surgery, a marker of case complexity.
Long-term users had more diabetes, hypertension, coronary artery disease, and congestive heart failure, whereas short term users were more symptomatic; those and other differences were controlled for on multivariate analysis. Aspirin, clopidogrel, and statin use were similar between the groups. About two-thirds of the subjects were men, and the average age in the study was about 70 years old.
Overall, the 30-day stroke and death rate was 3.4% (minor stroke 1.5%, major 0.9%, and death 1.2%).
Predictors of postoperative stroke or death at 30 days included symptomatic status, age, diabetes, and perioperative hypotension and hypertension. Prior carotid endarterectomy and distal embolic protection were both protective.
The investigators have no disclosures.
AT THE 2015 VASCULAR ANNUAL MEETING
Key clinical point: Carotid artery stenting is safer if patients have been on beta-blockers for at least a month beforehand.
Major finding: The risk of stroke or death after carotid artery stenting is reduced by 34% when patients are on long-term beta-blockers preoperatively.
Data source: Review of 5,248 stent cases during 2005-2014
Disclosures: The investigators have no disclosures.
SVS: Stroke reduction outweighs bleeding risk of dual antiplatelet therapy in CEA
CHICAGO – Don’t automatically discontinue dual antiplatelet therapy for carotid endarterectomy because the neuroprotective effects may outweigh the bleeding risks, researchers concluded after a review of more than 28,000 patients who underwent the procedure during 2003-2014.
They found in the study that the 7,059 patients on perioperative dual antiplatelet therapy with clopidogrel (Plavix) and aspirin had about a 40% reduction in transient ischemic attacks (TIAs), strokes, and stroke-related deaths when compared with the 21,624 patients on aspirin alone.
The investigators found on multivariate analysis that bleeding bad enough for a return trip to the operating room was more common in their dual antiplatelet group (odds ratio, 1.73; P < .01), but they felt the neuroprotective effect was probably worth the “slightly increased bleeding risk.” Earlier research suggests that about half of vascular surgeons will discontinue clopidogrel a week or so before carotid endarterectomy (CEA) because of bleeding risks (Eur. J. Vasc. Endovasc. Surg. 2009;38:402-7).
“Although dual therapy increases perioperative bleeding, it confers an overall benefit by reducing stroke and death. Patients taking dual therapy at the time of CEA should continue treatment preoperatively. This study also suggests that initiating dual therapy is beneficial for asymptomatic patients,” lead investigator Dr. Douglas Jones of the New York Presbyterian Hospital in New York said at the meeting hosted by the Society for Vascular Surgery.
The team used the Society for Vascular Surgery’s (SVS) Vascular Quality Initiative database. Patients were about 70 years old on average and about 60% were men. Dual-therapy patients had more coronary artery disease, congestive heart failure, chronic obstructive pulmonary disease, and diabetes.
On multivariate analysis to control for those differences, dual therapy was protective against TIA or stroke (OR, 0.60; P < .01); ipsilateral TIA or stroke (OR, 0.68; P = .05); stroke (OR, 0.62; P = .04); and stroke death (OR, 0.65; P = .03). It did not protect against myocardial infarction.
“More than 95% of patients received heparin for these cases,” said Dr. Jones, noting that protamine-reversal after the case “had the greatest protective effect” against major bleeding, which is consistent with previous reports. Protamine reversal reduced it by more than 50% (OR, 0.44; P < .01).
The results, for the most part, were similar on propensity matching of 4,548 patients on dual therapy to 4,548 on aspirin alone, all of whom had CEA after 2010. Dual-therapy patients were about twice as likely to return to the operating room for bleeding (1.3% vs. 0.7%), but also had fewer thrombotic complications (for instance, stroke 0.6% vs. 1.0% in the aspirin cohort).
Asymptomatic patients on dual therapy were again about twice as likely to return to surgery for major bleeding, but half as likely to have a stroke. Bleeding was more common in symptomatic dual therapy patients, as well, but for reasons that aren’t clear, a trend toward fewer thrombotic events in symptomatic patients on propensity matching did not reach statistical significance. “The protective effect was greatest among asymptomatic patients,” Dr. Jones said.
Patients on dual therapy were also more likely to have a drain placed, but drain placement did not protect against reoperation for bleeding (OR, 1.06; P = .75).
Dr. Jones has no disclosures. Other investigators disclosed consulting fees from Medtronic, Volcano, Bard, and AnGes.
CHICAGO – Don’t automatically discontinue dual antiplatelet therapy for carotid endarterectomy because the neuroprotective effects may outweigh the bleeding risks, researchers concluded after a review of more than 28,000 patients who underwent the procedure during 2003-2014.
They found in the study that the 7,059 patients on perioperative dual antiplatelet therapy with clopidogrel (Plavix) and aspirin had about a 40% reduction in transient ischemic attacks (TIAs), strokes, and stroke-related deaths when compared with the 21,624 patients on aspirin alone.
The investigators found on multivariate analysis that bleeding bad enough for a return trip to the operating room was more common in their dual antiplatelet group (odds ratio, 1.73; P < .01), but they felt the neuroprotective effect was probably worth the “slightly increased bleeding risk.” Earlier research suggests that about half of vascular surgeons will discontinue clopidogrel a week or so before carotid endarterectomy (CEA) because of bleeding risks (Eur. J. Vasc. Endovasc. Surg. 2009;38:402-7).
“Although dual therapy increases perioperative bleeding, it confers an overall benefit by reducing stroke and death. Patients taking dual therapy at the time of CEA should continue treatment preoperatively. This study also suggests that initiating dual therapy is beneficial for asymptomatic patients,” lead investigator Dr. Douglas Jones of the New York Presbyterian Hospital in New York said at the meeting hosted by the Society for Vascular Surgery.
The team used the Society for Vascular Surgery’s (SVS) Vascular Quality Initiative database. Patients were about 70 years old on average and about 60% were men. Dual-therapy patients had more coronary artery disease, congestive heart failure, chronic obstructive pulmonary disease, and diabetes.
On multivariate analysis to control for those differences, dual therapy was protective against TIA or stroke (OR, 0.60; P < .01); ipsilateral TIA or stroke (OR, 0.68; P = .05); stroke (OR, 0.62; P = .04); and stroke death (OR, 0.65; P = .03). It did not protect against myocardial infarction.
“More than 95% of patients received heparin for these cases,” said Dr. Jones, noting that protamine-reversal after the case “had the greatest protective effect” against major bleeding, which is consistent with previous reports. Protamine reversal reduced it by more than 50% (OR, 0.44; P < .01).
The results, for the most part, were similar on propensity matching of 4,548 patients on dual therapy to 4,548 on aspirin alone, all of whom had CEA after 2010. Dual-therapy patients were about twice as likely to return to the operating room for bleeding (1.3% vs. 0.7%), but also had fewer thrombotic complications (for instance, stroke 0.6% vs. 1.0% in the aspirin cohort).
Asymptomatic patients on dual therapy were again about twice as likely to return to surgery for major bleeding, but half as likely to have a stroke. Bleeding was more common in symptomatic dual therapy patients, as well, but for reasons that aren’t clear, a trend toward fewer thrombotic events in symptomatic patients on propensity matching did not reach statistical significance. “The protective effect was greatest among asymptomatic patients,” Dr. Jones said.
Patients on dual therapy were also more likely to have a drain placed, but drain placement did not protect against reoperation for bleeding (OR, 1.06; P = .75).
Dr. Jones has no disclosures. Other investigators disclosed consulting fees from Medtronic, Volcano, Bard, and AnGes.
CHICAGO – Don’t automatically discontinue dual antiplatelet therapy for carotid endarterectomy because the neuroprotective effects may outweigh the bleeding risks, researchers concluded after a review of more than 28,000 patients who underwent the procedure during 2003-2014.
They found in the study that the 7,059 patients on perioperative dual antiplatelet therapy with clopidogrel (Plavix) and aspirin had about a 40% reduction in transient ischemic attacks (TIAs), strokes, and stroke-related deaths when compared with the 21,624 patients on aspirin alone.
The investigators found on multivariate analysis that bleeding bad enough for a return trip to the operating room was more common in their dual antiplatelet group (odds ratio, 1.73; P < .01), but they felt the neuroprotective effect was probably worth the “slightly increased bleeding risk.” Earlier research suggests that about half of vascular surgeons will discontinue clopidogrel a week or so before carotid endarterectomy (CEA) because of bleeding risks (Eur. J. Vasc. Endovasc. Surg. 2009;38:402-7).
“Although dual therapy increases perioperative bleeding, it confers an overall benefit by reducing stroke and death. Patients taking dual therapy at the time of CEA should continue treatment preoperatively. This study also suggests that initiating dual therapy is beneficial for asymptomatic patients,” lead investigator Dr. Douglas Jones of the New York Presbyterian Hospital in New York said at the meeting hosted by the Society for Vascular Surgery.
The team used the Society for Vascular Surgery’s (SVS) Vascular Quality Initiative database. Patients were about 70 years old on average and about 60% were men. Dual-therapy patients had more coronary artery disease, congestive heart failure, chronic obstructive pulmonary disease, and diabetes.
On multivariate analysis to control for those differences, dual therapy was protective against TIA or stroke (OR, 0.60; P < .01); ipsilateral TIA or stroke (OR, 0.68; P = .05); stroke (OR, 0.62; P = .04); and stroke death (OR, 0.65; P = .03). It did not protect against myocardial infarction.
“More than 95% of patients received heparin for these cases,” said Dr. Jones, noting that protamine-reversal after the case “had the greatest protective effect” against major bleeding, which is consistent with previous reports. Protamine reversal reduced it by more than 50% (OR, 0.44; P < .01).
The results, for the most part, were similar on propensity matching of 4,548 patients on dual therapy to 4,548 on aspirin alone, all of whom had CEA after 2010. Dual-therapy patients were about twice as likely to return to the operating room for bleeding (1.3% vs. 0.7%), but also had fewer thrombotic complications (for instance, stroke 0.6% vs. 1.0% in the aspirin cohort).
Asymptomatic patients on dual therapy were again about twice as likely to return to surgery for major bleeding, but half as likely to have a stroke. Bleeding was more common in symptomatic dual therapy patients, as well, but for reasons that aren’t clear, a trend toward fewer thrombotic events in symptomatic patients on propensity matching did not reach statistical significance. “The protective effect was greatest among asymptomatic patients,” Dr. Jones said.
Patients on dual therapy were also more likely to have a drain placed, but drain placement did not protect against reoperation for bleeding (OR, 1.06; P = .75).
Dr. Jones has no disclosures. Other investigators disclosed consulting fees from Medtronic, Volcano, Bard, and AnGes.
AT THE 2015 VASCULAR ANNUAL MEETING
Key clinical point: Strokes are less likely after CEA if patients are on perioperative clopidogrel and aspirin.
Major finding: On multivariate analysis, dual therapy was protective against TIA or stroke (OR, 0.60; P < .01); ipsilateral TIA or stroke (OR, 0.68; P = .05); stroke (OR, 0.62, P = .04); and stroke death (OR, 0.65; P = .03).
Data source: Review of more than 28,000 carotid endarterectomy patients
Disclosures: The presenter has no disclosures. Other investigators disclosed consulting fees from Medtronic, Volcano, Bard, and AnGes.
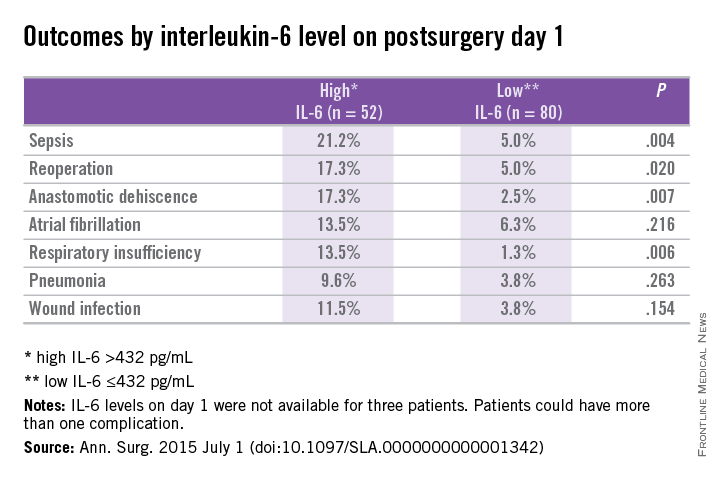
Elevated IL-6 linked to complications after major abdominal surgery
On postoperative day 1, elevated interleukin-6 level was associated with postoperative complications, according to a single-center cohort study of patients who had major abdominal surgery.
“Up to 28% of patients undergoing major abdominal surgery experience postoperative complications, including wound infection, sepsis, anastomotic dehiscence, pneumonia,cardiovascular or respiratory events, and mortality” but an accurate means of identifying those in the risk category would contribute the development of prevention stratetgies, the investigators wrote.
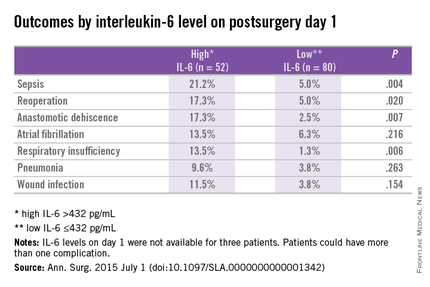
Previous studies of cardiothoracic surgery have supported an association of systemic inflammation to poor outcomes. Dr. Thijs Rettig and colleagues at St. Antonius Hospital, Nieuwegein, the Netherlands, sought to clarify if markers of inflammation and major abdominal surgery correlate with outcomes. Their results were published in the July issue of Annals of Surgery.
Researchers conducted a prospective cohort study at a single center using data obtained from the Myocardial Injury and Complications after major abdominal surgery (MICOLON) study. Participants in the MICOLON study were individuals aged 45 years or older who underwent elective major abdominal surgery. Other inclusion criteria included major cardiovascular (CV) risk factors, coronary artery disease, cerebrovascular accident, diabetes, renal insufficiency, atrial fibrillation, left ventricular dysfunction, aortic valve stenosis, or two minor CV risk factors.
Interleukin-6 (IL-6), tumor necrosis factor (TNF)-alpha, and C-reactive protein (CRP) levels were obtained at baseline and postoperative days 1, 3, and 7 in 137 patients. Systemic inflammatory response syndrome (SIRS) scores were calculated within 48 hours of surgery.
Primary endpoints were 30-day mortality, sepsis, pneumonia, wound infection, anastomotic dehiscence, reoperation, new-onset atrial fibrillation, respiratory insufficiency, congestive heart failure, and myocardial infarction. Data were also collected on length of stay and patients were followed up at 30 days postoperatively for further complications.
With a mean age of 68 years, 59% of patients were male and 30% (n = 40) had an ASA score of 3 or higher. Colorectal (50%), gastroesophageal (22%), and pancreatic (10%) surgery were the most common procedures performed. After excluding 2 patients from analysis for elevated baseline IL-6, 135 patients were analyzed.
At least one postoperative complication was observed in 29% (n = 39) of study subjects with a mean onset of 5 days after surgery. Use of preoperative steroids, aspirin, and statins were not associated with complications; however, blood loss and longer surgery duration where associated with worse outcomes.
In patients with and without complications, differences in IL-6 levels were observed at day 1 at 596 pg/mL vs. 303 pg/mL (P < .01), day 3 at 128 pg/mL vs. 69 pg/mL (P < .01), and day 7 at 76 pg/mL vs. 27 pg/mL (P = .02).
On day 1, CRP was similar in both groups (90 mg/L vs. 78 mg/L; P = .131), but on days 3 (223 mg/L vs. 131 mg/L; P < .001) and 7 (131 mg/L vs. 63 mg/L; P < .001) differences were observed.
Differences in TNF-alpha were observed between groups on day 7 (0.5 pg/mL vs. 0, P < .01). The two groups demonstrated similar leukocyte counts postoperatively.
Prediction for postoperative complications was associated with an IL-6 of 432 pg/mL at day 1, which was 70% specific and 64% sensitive, and had a positive predictive value (PPV) of 44% and negative predictive value (NPV) of 84%. A longer hospital stay of 12 days vs. 7 days (P < .001) was associated with high IL-6 (> 432 pg/mL) vs. a low IL-6 (< 432 pg/mL) at day 1.
Elevated IL-6 level on postoperative day 1 was independently associated with postoperative complications by multivariant regression analysis (AOR: 3.3; 95% confidence interval, 1.3-8.5; P < .02).
The researchers concluded that an increased IL-6 level on postoperative day 1 was associated with increased length of stay and threefold increased risk of complications after major abdominal surgery. They further continued, “It is plausible that early recognition of postoperative complications optimizes the chance of better outcome. One way to enhance early detection of complications is using inflammatory markers as predictors of outcome.”
The authors reported no conflicts of interest.
On postoperative day 1, elevated interleukin-6 level was associated with postoperative complications, according to a single-center cohort study of patients who had major abdominal surgery.
“Up to 28% of patients undergoing major abdominal surgery experience postoperative complications, including wound infection, sepsis, anastomotic dehiscence, pneumonia,cardiovascular or respiratory events, and mortality” but an accurate means of identifying those in the risk category would contribute the development of prevention stratetgies, the investigators wrote.
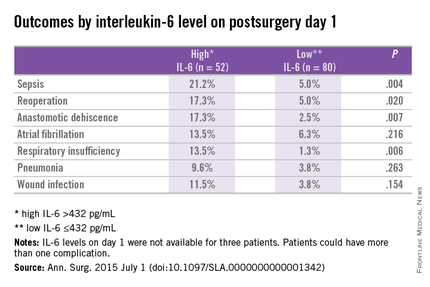
Previous studies of cardiothoracic surgery have supported an association of systemic inflammation to poor outcomes. Dr. Thijs Rettig and colleagues at St. Antonius Hospital, Nieuwegein, the Netherlands, sought to clarify if markers of inflammation and major abdominal surgery correlate with outcomes. Their results were published in the July issue of Annals of Surgery.
Researchers conducted a prospective cohort study at a single center using data obtained from the Myocardial Injury and Complications after major abdominal surgery (MICOLON) study. Participants in the MICOLON study were individuals aged 45 years or older who underwent elective major abdominal surgery. Other inclusion criteria included major cardiovascular (CV) risk factors, coronary artery disease, cerebrovascular accident, diabetes, renal insufficiency, atrial fibrillation, left ventricular dysfunction, aortic valve stenosis, or two minor CV risk factors.
Interleukin-6 (IL-6), tumor necrosis factor (TNF)-alpha, and C-reactive protein (CRP) levels were obtained at baseline and postoperative days 1, 3, and 7 in 137 patients. Systemic inflammatory response syndrome (SIRS) scores were calculated within 48 hours of surgery.
Primary endpoints were 30-day mortality, sepsis, pneumonia, wound infection, anastomotic dehiscence, reoperation, new-onset atrial fibrillation, respiratory insufficiency, congestive heart failure, and myocardial infarction. Data were also collected on length of stay and patients were followed up at 30 days postoperatively for further complications.
With a mean age of 68 years, 59% of patients were male and 30% (n = 40) had an ASA score of 3 or higher. Colorectal (50%), gastroesophageal (22%), and pancreatic (10%) surgery were the most common procedures performed. After excluding 2 patients from analysis for elevated baseline IL-6, 135 patients were analyzed.
At least one postoperative complication was observed in 29% (n = 39) of study subjects with a mean onset of 5 days after surgery. Use of preoperative steroids, aspirin, and statins were not associated with complications; however, blood loss and longer surgery duration where associated with worse outcomes.
In patients with and without complications, differences in IL-6 levels were observed at day 1 at 596 pg/mL vs. 303 pg/mL (P < .01), day 3 at 128 pg/mL vs. 69 pg/mL (P < .01), and day 7 at 76 pg/mL vs. 27 pg/mL (P = .02).
On day 1, CRP was similar in both groups (90 mg/L vs. 78 mg/L; P = .131), but on days 3 (223 mg/L vs. 131 mg/L; P < .001) and 7 (131 mg/L vs. 63 mg/L; P < .001) differences were observed.
Differences in TNF-alpha were observed between groups on day 7 (0.5 pg/mL vs. 0, P < .01). The two groups demonstrated similar leukocyte counts postoperatively.
Prediction for postoperative complications was associated with an IL-6 of 432 pg/mL at day 1, which was 70% specific and 64% sensitive, and had a positive predictive value (PPV) of 44% and negative predictive value (NPV) of 84%. A longer hospital stay of 12 days vs. 7 days (P < .001) was associated with high IL-6 (> 432 pg/mL) vs. a low IL-6 (< 432 pg/mL) at day 1.
Elevated IL-6 level on postoperative day 1 was independently associated with postoperative complications by multivariant regression analysis (AOR: 3.3; 95% confidence interval, 1.3-8.5; P < .02).
The researchers concluded that an increased IL-6 level on postoperative day 1 was associated with increased length of stay and threefold increased risk of complications after major abdominal surgery. They further continued, “It is plausible that early recognition of postoperative complications optimizes the chance of better outcome. One way to enhance early detection of complications is using inflammatory markers as predictors of outcome.”
The authors reported no conflicts of interest.
On postoperative day 1, elevated interleukin-6 level was associated with postoperative complications, according to a single-center cohort study of patients who had major abdominal surgery.
“Up to 28% of patients undergoing major abdominal surgery experience postoperative complications, including wound infection, sepsis, anastomotic dehiscence, pneumonia,cardiovascular or respiratory events, and mortality” but an accurate means of identifying those in the risk category would contribute the development of prevention stratetgies, the investigators wrote.
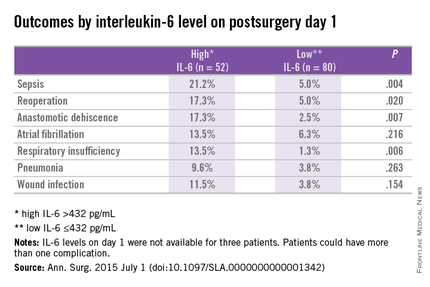
Previous studies of cardiothoracic surgery have supported an association of systemic inflammation to poor outcomes. Dr. Thijs Rettig and colleagues at St. Antonius Hospital, Nieuwegein, the Netherlands, sought to clarify if markers of inflammation and major abdominal surgery correlate with outcomes. Their results were published in the July issue of Annals of Surgery.
Researchers conducted a prospective cohort study at a single center using data obtained from the Myocardial Injury and Complications after major abdominal surgery (MICOLON) study. Participants in the MICOLON study were individuals aged 45 years or older who underwent elective major abdominal surgery. Other inclusion criteria included major cardiovascular (CV) risk factors, coronary artery disease, cerebrovascular accident, diabetes, renal insufficiency, atrial fibrillation, left ventricular dysfunction, aortic valve stenosis, or two minor CV risk factors.
Interleukin-6 (IL-6), tumor necrosis factor (TNF)-alpha, and C-reactive protein (CRP) levels were obtained at baseline and postoperative days 1, 3, and 7 in 137 patients. Systemic inflammatory response syndrome (SIRS) scores were calculated within 48 hours of surgery.
Primary endpoints were 30-day mortality, sepsis, pneumonia, wound infection, anastomotic dehiscence, reoperation, new-onset atrial fibrillation, respiratory insufficiency, congestive heart failure, and myocardial infarction. Data were also collected on length of stay and patients were followed up at 30 days postoperatively for further complications.
With a mean age of 68 years, 59% of patients were male and 30% (n = 40) had an ASA score of 3 or higher. Colorectal (50%), gastroesophageal (22%), and pancreatic (10%) surgery were the most common procedures performed. After excluding 2 patients from analysis for elevated baseline IL-6, 135 patients were analyzed.
At least one postoperative complication was observed in 29% (n = 39) of study subjects with a mean onset of 5 days after surgery. Use of preoperative steroids, aspirin, and statins were not associated with complications; however, blood loss and longer surgery duration where associated with worse outcomes.
In patients with and without complications, differences in IL-6 levels were observed at day 1 at 596 pg/mL vs. 303 pg/mL (P < .01), day 3 at 128 pg/mL vs. 69 pg/mL (P < .01), and day 7 at 76 pg/mL vs. 27 pg/mL (P = .02).
On day 1, CRP was similar in both groups (90 mg/L vs. 78 mg/L; P = .131), but on days 3 (223 mg/L vs. 131 mg/L; P < .001) and 7 (131 mg/L vs. 63 mg/L; P < .001) differences were observed.
Differences in TNF-alpha were observed between groups on day 7 (0.5 pg/mL vs. 0, P < .01). The two groups demonstrated similar leukocyte counts postoperatively.
Prediction for postoperative complications was associated with an IL-6 of 432 pg/mL at day 1, which was 70% specific and 64% sensitive, and had a positive predictive value (PPV) of 44% and negative predictive value (NPV) of 84%. A longer hospital stay of 12 days vs. 7 days (P < .001) was associated with high IL-6 (> 432 pg/mL) vs. a low IL-6 (< 432 pg/mL) at day 1.
Elevated IL-6 level on postoperative day 1 was independently associated with postoperative complications by multivariant regression analysis (AOR: 3.3; 95% confidence interval, 1.3-8.5; P < .02).
The researchers concluded that an increased IL-6 level on postoperative day 1 was associated with increased length of stay and threefold increased risk of complications after major abdominal surgery. They further continued, “It is plausible that early recognition of postoperative complications optimizes the chance of better outcome. One way to enhance early detection of complications is using inflammatory markers as predictors of outcome.”
The authors reported no conflicts of interest.
FROM ANNALS OF SURGERY
Key clinical point: Postoperative complications after major abdominal surgery are associated with elevated IL-6.
Major finding: Elevated IL-6 level on postoperative day 1 was independently associated with postoperative complications by multivariant regression analysis (P < .02).
Data source: Prospective cohort study at a single center using data from the Myocardial Injury and Postoperative Complications after major abdominal surgery (MICOLON) study.
Disclosures: The authors reported no conflicts of interest.
Risk of major bleeding is decreased when AF patients do not receive bridging anticoagulation
TORONTO – Forgoing bridging anticoagulation in patients with atrial fibrillation (AF) is noninferior to perioperative bridging with low-molecular-weight heparin for the prevention of arterial thromboembolism and decreases the risk of major bleeding.
Those results emerged from trial data presented at the International Society on Thrombosis and Haemostasis congress and published simultaneously in the New England Journal of Medicine. Study investigator Dr. Thomas Ortel, chief of the division of hematology at Duke University Medical Center, Durham, N.C., discussed results of the BRIDGE (Effectiveness of Bridging Anticoagulation for Surgery) trial, which evaluated the safety and efficacy of bridging anticoagulant therapy.
Bridging anticoagulation is frequently used in patients taking chronic oral anticoagulant therapy who need their anticoagulation transiently held for an operation or invasive procedure. The need for bridging anticoagulation never has been shown definitively, however, Dr. Ortel said in an interview.
“This is the first prospective, randomized, placebo-controlled, double-blind clinical trial to investigate the role of bridging anticoagulant therapy in patients with AF on chronic anticoagulation with warfarin who need the anticoagulant therapy held for an elective operation or invasive procedure,” he said.
Dr. Ortel and his coauthors evaluated 1,884 patients in the trial, which compared bridging and no bridging in patients with nonvalvular/valvular AF or atrial flutter who required warfarin interruption for elective surgery. The median age was 72.7 years, and 73% of patients were male. A total of 336 patients had a history of stroke or transient ischemic attack.
After stopping warfarin 5 days before the procedure, study participants received dalteparin 100 IU/kg (934 patients) or matching placebo (950 patients) for 3 days before and 5-9 days after the procedure. Dalteparin/placebo was resumed 12-24 hours after minor surgery and 48-72 hours after major surgery.
Warfarin was resumed 24 hours or less after the procedure. Follow-up lasted 30 ± 7 days after the procedure. Primary outcomes were arterial thromboembolism and major bleeding. Secondary outcomes were minor bleeding, death, myocardial infarction, and venous thromboembolism.
Protocol adherence occurred in 81% of patients before the procedure, and in 94.5% of patients post procedure.
The incidence of arterial thromboembolism was 0.4% in the no-bridging group, compared with 0.3% in the bridging group (95% confidence interval, –0.6 to 0.8; P = .01 for noninferiority). The incidence of major bleeding was 1.3% in the no-bridging group and 3.2% in the bridging group (relative risk, 0.41; 95% CI, 0.20-0.78; P = .005 for superiority).
“Current practice guidelines provide weak and inconsistent recommendations concerning the need for bridging anticoagulation,” Dr. Ortel said. “This study provides the highest level of evidence to support a strong recommendation concerning the role of bridging in this patient population.”
It is estimated that approximately one in six warfarin-treated patients with AF will need anticoagulation transiently held for an elective operation or invasive procedure each year, making this a common clinical scenario for providers, Dr. Ortel said. Knowing the findings from the BRIDGE trial will help guide clinicians in making decisions when this situation arises in their patients, he concluded.
“With the introduction of the direct oral anticoagulants, we will now need to develop periprocedural approaches to manage patients on a variety of different agents,” he said. “Warfarin continues to be extensively used in many of these patients, however, and the BRIDGE trial will contribute to improved management for these individuals.”
In response to an audience member’s question about which patients should receive bridging anticoagulation, Dr. Ortel said that “right now, our data would suggest that for AF patients, we don’t need to bridge.”
“I can’t say that, necessarily, for prosthetic heart valves or for venous thromboembolism. I think some of the recommendations that you’ve seen in the guidelines where people try to stratify this by how recently they had thromboembolism or by what type of heart valve they have – those might be the higher-risk patients to consider. But that’s all based on existing guidelines and no prospective data, so I feel comfortable telling you who you don’t need to bridge in, but I’m not going to tell you who you should,” he added.
The BRIDGE Trial was sponsored by the National Heart, Lung, and Blood Institute. Dr. Ortel disclosed grant/research support from Eisai Co. Ltd and Pfizer Inc.
TORONTO – Forgoing bridging anticoagulation in patients with atrial fibrillation (AF) is noninferior to perioperative bridging with low-molecular-weight heparin for the prevention of arterial thromboembolism and decreases the risk of major bleeding.
Those results emerged from trial data presented at the International Society on Thrombosis and Haemostasis congress and published simultaneously in the New England Journal of Medicine. Study investigator Dr. Thomas Ortel, chief of the division of hematology at Duke University Medical Center, Durham, N.C., discussed results of the BRIDGE (Effectiveness of Bridging Anticoagulation for Surgery) trial, which evaluated the safety and efficacy of bridging anticoagulant therapy.
Bridging anticoagulation is frequently used in patients taking chronic oral anticoagulant therapy who need their anticoagulation transiently held for an operation or invasive procedure. The need for bridging anticoagulation never has been shown definitively, however, Dr. Ortel said in an interview.
“This is the first prospective, randomized, placebo-controlled, double-blind clinical trial to investigate the role of bridging anticoagulant therapy in patients with AF on chronic anticoagulation with warfarin who need the anticoagulant therapy held for an elective operation or invasive procedure,” he said.
Dr. Ortel and his coauthors evaluated 1,884 patients in the trial, which compared bridging and no bridging in patients with nonvalvular/valvular AF or atrial flutter who required warfarin interruption for elective surgery. The median age was 72.7 years, and 73% of patients were male. A total of 336 patients had a history of stroke or transient ischemic attack.
After stopping warfarin 5 days before the procedure, study participants received dalteparin 100 IU/kg (934 patients) or matching placebo (950 patients) for 3 days before and 5-9 days after the procedure. Dalteparin/placebo was resumed 12-24 hours after minor surgery and 48-72 hours after major surgery.
Warfarin was resumed 24 hours or less after the procedure. Follow-up lasted 30 ± 7 days after the procedure. Primary outcomes were arterial thromboembolism and major bleeding. Secondary outcomes were minor bleeding, death, myocardial infarction, and venous thromboembolism.
Protocol adherence occurred in 81% of patients before the procedure, and in 94.5% of patients post procedure.
The incidence of arterial thromboembolism was 0.4% in the no-bridging group, compared with 0.3% in the bridging group (95% confidence interval, –0.6 to 0.8; P = .01 for noninferiority). The incidence of major bleeding was 1.3% in the no-bridging group and 3.2% in the bridging group (relative risk, 0.41; 95% CI, 0.20-0.78; P = .005 for superiority).
“Current practice guidelines provide weak and inconsistent recommendations concerning the need for bridging anticoagulation,” Dr. Ortel said. “This study provides the highest level of evidence to support a strong recommendation concerning the role of bridging in this patient population.”
It is estimated that approximately one in six warfarin-treated patients with AF will need anticoagulation transiently held for an elective operation or invasive procedure each year, making this a common clinical scenario for providers, Dr. Ortel said. Knowing the findings from the BRIDGE trial will help guide clinicians in making decisions when this situation arises in their patients, he concluded.
“With the introduction of the direct oral anticoagulants, we will now need to develop periprocedural approaches to manage patients on a variety of different agents,” he said. “Warfarin continues to be extensively used in many of these patients, however, and the BRIDGE trial will contribute to improved management for these individuals.”
In response to an audience member’s question about which patients should receive bridging anticoagulation, Dr. Ortel said that “right now, our data would suggest that for AF patients, we don’t need to bridge.”
“I can’t say that, necessarily, for prosthetic heart valves or for venous thromboembolism. I think some of the recommendations that you’ve seen in the guidelines where people try to stratify this by how recently they had thromboembolism or by what type of heart valve they have – those might be the higher-risk patients to consider. But that’s all based on existing guidelines and no prospective data, so I feel comfortable telling you who you don’t need to bridge in, but I’m not going to tell you who you should,” he added.
The BRIDGE Trial was sponsored by the National Heart, Lung, and Blood Institute. Dr. Ortel disclosed grant/research support from Eisai Co. Ltd and Pfizer Inc.
TORONTO – Forgoing bridging anticoagulation in patients with atrial fibrillation (AF) is noninferior to perioperative bridging with low-molecular-weight heparin for the prevention of arterial thromboembolism and decreases the risk of major bleeding.
Those results emerged from trial data presented at the International Society on Thrombosis and Haemostasis congress and published simultaneously in the New England Journal of Medicine. Study investigator Dr. Thomas Ortel, chief of the division of hematology at Duke University Medical Center, Durham, N.C., discussed results of the BRIDGE (Effectiveness of Bridging Anticoagulation for Surgery) trial, which evaluated the safety and efficacy of bridging anticoagulant therapy.
Bridging anticoagulation is frequently used in patients taking chronic oral anticoagulant therapy who need their anticoagulation transiently held for an operation or invasive procedure. The need for bridging anticoagulation never has been shown definitively, however, Dr. Ortel said in an interview.
“This is the first prospective, randomized, placebo-controlled, double-blind clinical trial to investigate the role of bridging anticoagulant therapy in patients with AF on chronic anticoagulation with warfarin who need the anticoagulant therapy held for an elective operation or invasive procedure,” he said.
Dr. Ortel and his coauthors evaluated 1,884 patients in the trial, which compared bridging and no bridging in patients with nonvalvular/valvular AF or atrial flutter who required warfarin interruption for elective surgery. The median age was 72.7 years, and 73% of patients were male. A total of 336 patients had a history of stroke or transient ischemic attack.
After stopping warfarin 5 days before the procedure, study participants received dalteparin 100 IU/kg (934 patients) or matching placebo (950 patients) for 3 days before and 5-9 days after the procedure. Dalteparin/placebo was resumed 12-24 hours after minor surgery and 48-72 hours after major surgery.
Warfarin was resumed 24 hours or less after the procedure. Follow-up lasted 30 ± 7 days after the procedure. Primary outcomes were arterial thromboembolism and major bleeding. Secondary outcomes were minor bleeding, death, myocardial infarction, and venous thromboembolism.
Protocol adherence occurred in 81% of patients before the procedure, and in 94.5% of patients post procedure.
The incidence of arterial thromboembolism was 0.4% in the no-bridging group, compared with 0.3% in the bridging group (95% confidence interval, –0.6 to 0.8; P = .01 for noninferiority). The incidence of major bleeding was 1.3% in the no-bridging group and 3.2% in the bridging group (relative risk, 0.41; 95% CI, 0.20-0.78; P = .005 for superiority).
“Current practice guidelines provide weak and inconsistent recommendations concerning the need for bridging anticoagulation,” Dr. Ortel said. “This study provides the highest level of evidence to support a strong recommendation concerning the role of bridging in this patient population.”
It is estimated that approximately one in six warfarin-treated patients with AF will need anticoagulation transiently held for an elective operation or invasive procedure each year, making this a common clinical scenario for providers, Dr. Ortel said. Knowing the findings from the BRIDGE trial will help guide clinicians in making decisions when this situation arises in their patients, he concluded.
“With the introduction of the direct oral anticoagulants, we will now need to develop periprocedural approaches to manage patients on a variety of different agents,” he said. “Warfarin continues to be extensively used in many of these patients, however, and the BRIDGE trial will contribute to improved management for these individuals.”
In response to an audience member’s question about which patients should receive bridging anticoagulation, Dr. Ortel said that “right now, our data would suggest that for AF patients, we don’t need to bridge.”
“I can’t say that, necessarily, for prosthetic heart valves or for venous thromboembolism. I think some of the recommendations that you’ve seen in the guidelines where people try to stratify this by how recently they had thromboembolism or by what type of heart valve they have – those might be the higher-risk patients to consider. But that’s all based on existing guidelines and no prospective data, so I feel comfortable telling you who you don’t need to bridge in, but I’m not going to tell you who you should,” he added.
The BRIDGE Trial was sponsored by the National Heart, Lung, and Blood Institute. Dr. Ortel disclosed grant/research support from Eisai Co. Ltd and Pfizer Inc.
FROM 2015 ISTH CONGRESS
Key clinical point: Forgoing bridging anticoagulation in patients with atrial fibrillation is noninferior to perioperative bridging for preventing arterial thromboembolism and decreasing the risk of major bleeding.
Major finding: The incidence of arterial thromboembolism was 0.4% vs. 0.3% in the no-bridging and bridging groups, respectively. The incidence of major bleeding was 1.3% in the no-bridging group and 3.2% in the bridging group.
Data source: A prospective, randomized, placebo-controlled, double-blind trial of 1,884 patients with nonvalvular/valvular AF or atrial flutter who required warfarin interruption for elective surgery.
Disclosures: The BRIDGE Trial was sponsored by the National Heart, Lung, and Blood Institute. Dr. Ortel disclosed grant/research support from Eisai Co. Ltd and Pfizer Inc.
CMS proposes comprehensive care initiative for hip and knee replacements
The Centers for Medicare & Medicaid Services has proposed a Comprehensive Care for Joint Replacement payment model to improve patient outcomes from hip and knee replacement surgery, the agency announced July 9.
Under the proposed rule, the hospital in which the surgery takes place would be responsible for cost and quality of care from the time of surgery through 90 days after the procedure, or an “episode” of care. Then, based on cost performance and the quality of care delivered, the facility would either receive a financial reward or be required to repay Medicare for a portion of the costs, CMS said in a statement.
“This payment would give hospitals an incentive to work with physicians, home health agencies, and nursing facilities to make sure beneficiaries receive the coordinated care they need with the goal of reducing avoidable hospitalizations and complications,” the agency said.
The new model is an effort to improve the lack of coordinated care that may lead to postsurgery complications and high readmission rates in Medicare beneficiaries who receive these procedures.
“Joint replacements are the most commonly performed Medicare inpatient surgery and their utilization is predicted to continue to grow,” CMS said. “They can require long recoveries that may include extensive rehabilitation or other post-acute care, which provides many opportunities to reward providers that improve patient outcomes.”
Read the proposed rule here: https://s3.amazonaws.com/public-inspection.federalregister.gov/2015-17190.pdf
The Centers for Medicare & Medicaid Services has proposed a Comprehensive Care for Joint Replacement payment model to improve patient outcomes from hip and knee replacement surgery, the agency announced July 9.
Under the proposed rule, the hospital in which the surgery takes place would be responsible for cost and quality of care from the time of surgery through 90 days after the procedure, or an “episode” of care. Then, based on cost performance and the quality of care delivered, the facility would either receive a financial reward or be required to repay Medicare for a portion of the costs, CMS said in a statement.
“This payment would give hospitals an incentive to work with physicians, home health agencies, and nursing facilities to make sure beneficiaries receive the coordinated care they need with the goal of reducing avoidable hospitalizations and complications,” the agency said.
The new model is an effort to improve the lack of coordinated care that may lead to postsurgery complications and high readmission rates in Medicare beneficiaries who receive these procedures.
“Joint replacements are the most commonly performed Medicare inpatient surgery and their utilization is predicted to continue to grow,” CMS said. “They can require long recoveries that may include extensive rehabilitation or other post-acute care, which provides many opportunities to reward providers that improve patient outcomes.”
Read the proposed rule here: https://s3.amazonaws.com/public-inspection.federalregister.gov/2015-17190.pdf
The Centers for Medicare & Medicaid Services has proposed a Comprehensive Care for Joint Replacement payment model to improve patient outcomes from hip and knee replacement surgery, the agency announced July 9.
Under the proposed rule, the hospital in which the surgery takes place would be responsible for cost and quality of care from the time of surgery through 90 days after the procedure, or an “episode” of care. Then, based on cost performance and the quality of care delivered, the facility would either receive a financial reward or be required to repay Medicare for a portion of the costs, CMS said in a statement.
“This payment would give hospitals an incentive to work with physicians, home health agencies, and nursing facilities to make sure beneficiaries receive the coordinated care they need with the goal of reducing avoidable hospitalizations and complications,” the agency said.
The new model is an effort to improve the lack of coordinated care that may lead to postsurgery complications and high readmission rates in Medicare beneficiaries who receive these procedures.
“Joint replacements are the most commonly performed Medicare inpatient surgery and their utilization is predicted to continue to grow,” CMS said. “They can require long recoveries that may include extensive rehabilitation or other post-acute care, which provides many opportunities to reward providers that improve patient outcomes.”
Read the proposed rule here: https://s3.amazonaws.com/public-inspection.federalregister.gov/2015-17190.pdf
Cefazolin ranks sixth as cause of drug-induced liver injury
A single intravenous infusion of cefazolin can cause drug-induced liver injury, and the antibiotic ranked sixth among pharmacologic causes of hepatic injury in an analysis of 1,212 patients.
“Cephalosporins appear to be a relatively common cause of antibiotic-associated liver injury,” said Dr. Saleh Alqahtani at the University of Texas Southwestern in Dallas and his associates. “The latency period is typically 1-3 weeks after exposure, and patients may not become symptomatic until after the antibiotic is stopped – this is particularly true in the unique clinical syndrome in which a single infusion of cefazolin leads to drug-induced liver injury.”
Cephalosporins have been reported as rare causes of drug-induced liver injury (DILI), but most data come from single case reports, the researchers said. To study causes of DILI, they analyzed cases from the Drug-Induced Livery Injury Network, an ongoing prospective study at eight U.S. medical centers. Enrolled patients had strong clinical suspicion for liver injury caused by a drug or an herbal agent. Liver injury was defined based on specific criteria for liver enzymes, alkaline phosphatase, or total bilirubin levels, or as an international normalized ratio greater than 1.5 that was accompanied by elevated liver enzymes or ALP. Patients were followed for at least 6 months after their baseline visit (Clin. Gastroenterol. Hepatol. 2014 Dec. 17 [doi: 10.1016/j.cgh.2015.01.010]).
Among the 1,212 cases of DILI in the analysis, one-third were linked to antimicrobial therapies, including 41 (3.3%) in which cephalosporins were implicated, the investigators reported. Nineteen of the cases were tied to a single dose of intravenous cefazolin given before surgery. These patients developed cholestatic or mixed hepatocellular-cholestatic injury 1-3 weeks after the cefazolin infusion. They almost always had jaundice and pruritus, and usually also had fever and nausea. Signs and symptoms were self-limiting, resolving within a few days to a few weeks.
“Because of confusion about the specific diagnosis, patients underwent substantial diagnostic testing (including multiple computed tomography scans, magnetic resonance imaging scans, endoscopic retrograde cholangiopancreatography exams, liver biopsies, and others), which often were unnecessary,” and in some cases led to severe complications, the investigators said.
The study also identified barriers to identifying cefazolin as a cause of DILI, they said. Patients often did not know they had received the antibiotic, and clinicians, including study investigators, often did not know that cefazolin could cause DILI. In more than half of cases, DILI was linked to cefazolin only after careful medical record reviews. “For these reasons, we speculate that cefazolin is and has been underappreciated as a cause of DILI,” the researchers noted. “The appearance of jaundice and pruritus 1-3 weeks after minor surgery should lead to a search of surgical records and medications that might have been given during surgery. These results also imply that the merits of routine use of cefazolin at the time of uncomplicated surgery should be reconsidered carefully.”
Two patients died after receiving cephalosporins other than cefazolin, and another patient developed severe liver injury, the researchers said. “However, in each of the fatal cases, patients had a complicated clinical course, with a severe hypersensitivity reaction on top of an underlying liver disease. Therefore, we urge caution in concluding that non-cefazolin cephalosporin-induced DILI may be severe or fatal,” they said. “Because cephalosporins are used commonly in clinical practice, it is likely that the overall mortality rate associated with cephalosporin use is low, but not nil, and it may be more likely in patients with underlying disorders.”
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institutes of Health, the National Cancer Institute, and by six Clinical and Translational Science Award grants. The investigators reported having no conflicts of interest.
A single intravenous infusion of cefazolin can cause drug-induced liver injury, and the antibiotic ranked sixth among pharmacologic causes of hepatic injury in an analysis of 1,212 patients.
“Cephalosporins appear to be a relatively common cause of antibiotic-associated liver injury,” said Dr. Saleh Alqahtani at the University of Texas Southwestern in Dallas and his associates. “The latency period is typically 1-3 weeks after exposure, and patients may not become symptomatic until after the antibiotic is stopped – this is particularly true in the unique clinical syndrome in which a single infusion of cefazolin leads to drug-induced liver injury.”
Cephalosporins have been reported as rare causes of drug-induced liver injury (DILI), but most data come from single case reports, the researchers said. To study causes of DILI, they analyzed cases from the Drug-Induced Livery Injury Network, an ongoing prospective study at eight U.S. medical centers. Enrolled patients had strong clinical suspicion for liver injury caused by a drug or an herbal agent. Liver injury was defined based on specific criteria for liver enzymes, alkaline phosphatase, or total bilirubin levels, or as an international normalized ratio greater than 1.5 that was accompanied by elevated liver enzymes or ALP. Patients were followed for at least 6 months after their baseline visit (Clin. Gastroenterol. Hepatol. 2014 Dec. 17 [doi: 10.1016/j.cgh.2015.01.010]).
Among the 1,212 cases of DILI in the analysis, one-third were linked to antimicrobial therapies, including 41 (3.3%) in which cephalosporins were implicated, the investigators reported. Nineteen of the cases were tied to a single dose of intravenous cefazolin given before surgery. These patients developed cholestatic or mixed hepatocellular-cholestatic injury 1-3 weeks after the cefazolin infusion. They almost always had jaundice and pruritus, and usually also had fever and nausea. Signs and symptoms were self-limiting, resolving within a few days to a few weeks.
“Because of confusion about the specific diagnosis, patients underwent substantial diagnostic testing (including multiple computed tomography scans, magnetic resonance imaging scans, endoscopic retrograde cholangiopancreatography exams, liver biopsies, and others), which often were unnecessary,” and in some cases led to severe complications, the investigators said.
The study also identified barriers to identifying cefazolin as a cause of DILI, they said. Patients often did not know they had received the antibiotic, and clinicians, including study investigators, often did not know that cefazolin could cause DILI. In more than half of cases, DILI was linked to cefazolin only after careful medical record reviews. “For these reasons, we speculate that cefazolin is and has been underappreciated as a cause of DILI,” the researchers noted. “The appearance of jaundice and pruritus 1-3 weeks after minor surgery should lead to a search of surgical records and medications that might have been given during surgery. These results also imply that the merits of routine use of cefazolin at the time of uncomplicated surgery should be reconsidered carefully.”
Two patients died after receiving cephalosporins other than cefazolin, and another patient developed severe liver injury, the researchers said. “However, in each of the fatal cases, patients had a complicated clinical course, with a severe hypersensitivity reaction on top of an underlying liver disease. Therefore, we urge caution in concluding that non-cefazolin cephalosporin-induced DILI may be severe or fatal,” they said. “Because cephalosporins are used commonly in clinical practice, it is likely that the overall mortality rate associated with cephalosporin use is low, but not nil, and it may be more likely in patients with underlying disorders.”
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institutes of Health, the National Cancer Institute, and by six Clinical and Translational Science Award grants. The investigators reported having no conflicts of interest.
A single intravenous infusion of cefazolin can cause drug-induced liver injury, and the antibiotic ranked sixth among pharmacologic causes of hepatic injury in an analysis of 1,212 patients.
“Cephalosporins appear to be a relatively common cause of antibiotic-associated liver injury,” said Dr. Saleh Alqahtani at the University of Texas Southwestern in Dallas and his associates. “The latency period is typically 1-3 weeks after exposure, and patients may not become symptomatic until after the antibiotic is stopped – this is particularly true in the unique clinical syndrome in which a single infusion of cefazolin leads to drug-induced liver injury.”
Cephalosporins have been reported as rare causes of drug-induced liver injury (DILI), but most data come from single case reports, the researchers said. To study causes of DILI, they analyzed cases from the Drug-Induced Livery Injury Network, an ongoing prospective study at eight U.S. medical centers. Enrolled patients had strong clinical suspicion for liver injury caused by a drug or an herbal agent. Liver injury was defined based on specific criteria for liver enzymes, alkaline phosphatase, or total bilirubin levels, or as an international normalized ratio greater than 1.5 that was accompanied by elevated liver enzymes or ALP. Patients were followed for at least 6 months after their baseline visit (Clin. Gastroenterol. Hepatol. 2014 Dec. 17 [doi: 10.1016/j.cgh.2015.01.010]).
Among the 1,212 cases of DILI in the analysis, one-third were linked to antimicrobial therapies, including 41 (3.3%) in which cephalosporins were implicated, the investigators reported. Nineteen of the cases were tied to a single dose of intravenous cefazolin given before surgery. These patients developed cholestatic or mixed hepatocellular-cholestatic injury 1-3 weeks after the cefazolin infusion. They almost always had jaundice and pruritus, and usually also had fever and nausea. Signs and symptoms were self-limiting, resolving within a few days to a few weeks.
“Because of confusion about the specific diagnosis, patients underwent substantial diagnostic testing (including multiple computed tomography scans, magnetic resonance imaging scans, endoscopic retrograde cholangiopancreatography exams, liver biopsies, and others), which often were unnecessary,” and in some cases led to severe complications, the investigators said.
The study also identified barriers to identifying cefazolin as a cause of DILI, they said. Patients often did not know they had received the antibiotic, and clinicians, including study investigators, often did not know that cefazolin could cause DILI. In more than half of cases, DILI was linked to cefazolin only after careful medical record reviews. “For these reasons, we speculate that cefazolin is and has been underappreciated as a cause of DILI,” the researchers noted. “The appearance of jaundice and pruritus 1-3 weeks after minor surgery should lead to a search of surgical records and medications that might have been given during surgery. These results also imply that the merits of routine use of cefazolin at the time of uncomplicated surgery should be reconsidered carefully.”
Two patients died after receiving cephalosporins other than cefazolin, and another patient developed severe liver injury, the researchers said. “However, in each of the fatal cases, patients had a complicated clinical course, with a severe hypersensitivity reaction on top of an underlying liver disease. Therefore, we urge caution in concluding that non-cefazolin cephalosporin-induced DILI may be severe or fatal,” they said. “Because cephalosporins are used commonly in clinical practice, it is likely that the overall mortality rate associated with cephalosporin use is low, but not nil, and it may be more likely in patients with underlying disorders.”
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institutes of Health, the National Cancer Institute, and by six Clinical and Translational Science Award grants. The investigators reported having no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: A single dose of cefazolin can cause drug-induced liver injury (DILI), and the agent is implicated more often than previously thought.
Major finding: Cefazolin ranked sixth among causes of DILI, and signs and symptoms began 1-3 weeks after initial exposure.
Data source: Registry-based study of 1,212 cases of DILI.
Disclosures: The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institutes of Health, the National Cancer Institute, and by Clinical and Translational Science Award grants. The investigators reported having no conflicts of interest.