User login
Idarucizumab reverses dabigatran’s anticoagulant effects
TORONTO – Idarucizumab is a promising agent that quickly and safely reverses the anticoagulant effects of dabigatran whether the goal is to control serious bleeding or to permit urgent surgery, according to interim results of a multicenter trial.
Idarucizumab is a monoclonal antibody that binds to dabigatran to reverse its activity. The data, presented by Dr. V. Charles Pollack Jr. at the International Society on Thrombosis and Haemostasis congress, involved the first 90 patients of an ongoing trial with a planned enrollment of 300. The data from this trial, called REVERSE-AD, were published online simultaneously with the June 22 presentation at the congress (N. Engl. J. Med 2015 [doi:10.1056/NEJMoa1502000]).
“Non–vitamin K antagonist oral anticoagulants (NOACs) are generally safer than warfarin, and provide similar or improved efficacy in the prevention of stroke in patients with nonvalvular atrial fibrillation and in the prevention and treatment of venous thromboembolism,” Dr. Pollack said in an interview. “Nonetheless, serious bleeding events may occur with NOAC use, and patients taking one of these agents occasionally require urgent surgery or other intervention for which normal hemostasis is required,” added Dr. Pollack, chair of the department of emergency medicine at Pennsylvania Hospital in Philadelphia.
In RE-VERSE AD (a study of the reversal effects of idarucizumab on active dabigatran), the first 90 patients were divided into two distinct groups. Group A, with 51 patients, included those on dabigatran with serious bleeding. Group B, with 39 patients, required reversal of dabigatran for urgent or emergent procedures. In both, idarucizumab provided a median maximum reversal of 100% (95% confidence interval, 100-100) of the anticoagulation effect within 4 hours.
Clotting assays were normalized almost immediately in almost 90% of patients, and the effect was durable, with 80% having measured dabigatran levels reflecting no significant anticoagulation 24 hours later, Dr. Pollack said.
“Clinical outcomes were quite good in this multimorbid patient population, with restoration of hemostasis as reported by local investigators achieved in less than 12 hours when assessable, and with 92% of surgical patients being reported as having normal hemostasis at the time of the procedure,” he said.
Idarucizumab was generally well tolerated in the patient population. “There were no serious adverse events related to the reversal agent ... and only one patient experienced a thrombotic complication within 72 hours, and that patient had not been restarted on any antithrombotic medications,” Dr. Pollack said.
“The study is ongoing,” he added, “but these interim results show rather convincingly that idarucizumab completely and safely reverses the anticoagulant effects of dabigatran within minutes.”
In addition, Dr. Pollack said the availability of a specific reversal agent for dabigatran would enhance its safety margin, and thus alleviate the fears of providers who may hesitate to use a NOAC because of the lack of an “antidote.”
“In fact, most such cases can already be successfully and safely managed with general support and ‘tincture of time’ (the half-life of dabigatran is much shorter than that of warfarin), but having a specific ‘go-to’ option could streamline the care of the most significantly compromised patients,” he said.
Dr. Pollack emphasized, however, that idarucizumab is a specific reversal agent for dabigatran, not an antidote. “To me, the latter would imply that idarucizumab immediately stops bleeding associated with active use of dabigatran,” he said.
Providers should realize that while idarucizumab seems capable of removing dabigatran-induced coagulopathy from the list of concerns when managing a patient with serious bleeding or before a “sharp” procedure, bleeding is a multifaceted issue that also may be due to traumatized blood vessels, other causes of coagulopathy such as liver disease, or concurrent use of antiplatelet medications, he said.
“The patient with a serious or life-threatening bleed on dabigatran will likely need additional care to investigate and manage such concerns,” Dr. Pollack said. “But at least idarucizumab can specifically, safely, and rapidly address the primary consideration.
“The safety of anticoagulation therapy with dabigatran is further enhanced with idarucizumab, a specific reversal agent that won’t need to be used often, but the availability of which would be reassuring to prescribers,” he concluded.
Boehringer Ingelheim sponsored RE-VERSE AD. Idarucizumab was given a fast-track status by the Food and Drug Administration, and BI submitted a new drug application in March 2015, according to the company.
Dr. Pollack reported receiving personal fees from BI, Janssen, Daiichi-Sankyo, Bristol-Myers Squibb, and Pfizer. Disclosures for all the investigators are available at NEJM.org.
TORONTO – Idarucizumab is a promising agent that quickly and safely reverses the anticoagulant effects of dabigatran whether the goal is to control serious bleeding or to permit urgent surgery, according to interim results of a multicenter trial.
Idarucizumab is a monoclonal antibody that binds to dabigatran to reverse its activity. The data, presented by Dr. V. Charles Pollack Jr. at the International Society on Thrombosis and Haemostasis congress, involved the first 90 patients of an ongoing trial with a planned enrollment of 300. The data from this trial, called REVERSE-AD, were published online simultaneously with the June 22 presentation at the congress (N. Engl. J. Med 2015 [doi:10.1056/NEJMoa1502000]).
“Non–vitamin K antagonist oral anticoagulants (NOACs) are generally safer than warfarin, and provide similar or improved efficacy in the prevention of stroke in patients with nonvalvular atrial fibrillation and in the prevention and treatment of venous thromboembolism,” Dr. Pollack said in an interview. “Nonetheless, serious bleeding events may occur with NOAC use, and patients taking one of these agents occasionally require urgent surgery or other intervention for which normal hemostasis is required,” added Dr. Pollack, chair of the department of emergency medicine at Pennsylvania Hospital in Philadelphia.
In RE-VERSE AD (a study of the reversal effects of idarucizumab on active dabigatran), the first 90 patients were divided into two distinct groups. Group A, with 51 patients, included those on dabigatran with serious bleeding. Group B, with 39 patients, required reversal of dabigatran for urgent or emergent procedures. In both, idarucizumab provided a median maximum reversal of 100% (95% confidence interval, 100-100) of the anticoagulation effect within 4 hours.
Clotting assays were normalized almost immediately in almost 90% of patients, and the effect was durable, with 80% having measured dabigatran levels reflecting no significant anticoagulation 24 hours later, Dr. Pollack said.
“Clinical outcomes were quite good in this multimorbid patient population, with restoration of hemostasis as reported by local investigators achieved in less than 12 hours when assessable, and with 92% of surgical patients being reported as having normal hemostasis at the time of the procedure,” he said.
Idarucizumab was generally well tolerated in the patient population. “There were no serious adverse events related to the reversal agent ... and only one patient experienced a thrombotic complication within 72 hours, and that patient had not been restarted on any antithrombotic medications,” Dr. Pollack said.
“The study is ongoing,” he added, “but these interim results show rather convincingly that idarucizumab completely and safely reverses the anticoagulant effects of dabigatran within minutes.”
In addition, Dr. Pollack said the availability of a specific reversal agent for dabigatran would enhance its safety margin, and thus alleviate the fears of providers who may hesitate to use a NOAC because of the lack of an “antidote.”
“In fact, most such cases can already be successfully and safely managed with general support and ‘tincture of time’ (the half-life of dabigatran is much shorter than that of warfarin), but having a specific ‘go-to’ option could streamline the care of the most significantly compromised patients,” he said.
Dr. Pollack emphasized, however, that idarucizumab is a specific reversal agent for dabigatran, not an antidote. “To me, the latter would imply that idarucizumab immediately stops bleeding associated with active use of dabigatran,” he said.
Providers should realize that while idarucizumab seems capable of removing dabigatran-induced coagulopathy from the list of concerns when managing a patient with serious bleeding or before a “sharp” procedure, bleeding is a multifaceted issue that also may be due to traumatized blood vessels, other causes of coagulopathy such as liver disease, or concurrent use of antiplatelet medications, he said.
“The patient with a serious or life-threatening bleed on dabigatran will likely need additional care to investigate and manage such concerns,” Dr. Pollack said. “But at least idarucizumab can specifically, safely, and rapidly address the primary consideration.
“The safety of anticoagulation therapy with dabigatran is further enhanced with idarucizumab, a specific reversal agent that won’t need to be used often, but the availability of which would be reassuring to prescribers,” he concluded.
Boehringer Ingelheim sponsored RE-VERSE AD. Idarucizumab was given a fast-track status by the Food and Drug Administration, and BI submitted a new drug application in March 2015, according to the company.
Dr. Pollack reported receiving personal fees from BI, Janssen, Daiichi-Sankyo, Bristol-Myers Squibb, and Pfizer. Disclosures for all the investigators are available at NEJM.org.
TORONTO – Idarucizumab is a promising agent that quickly and safely reverses the anticoagulant effects of dabigatran whether the goal is to control serious bleeding or to permit urgent surgery, according to interim results of a multicenter trial.
Idarucizumab is a monoclonal antibody that binds to dabigatran to reverse its activity. The data, presented by Dr. V. Charles Pollack Jr. at the International Society on Thrombosis and Haemostasis congress, involved the first 90 patients of an ongoing trial with a planned enrollment of 300. The data from this trial, called REVERSE-AD, were published online simultaneously with the June 22 presentation at the congress (N. Engl. J. Med 2015 [doi:10.1056/NEJMoa1502000]).
“Non–vitamin K antagonist oral anticoagulants (NOACs) are generally safer than warfarin, and provide similar or improved efficacy in the prevention of stroke in patients with nonvalvular atrial fibrillation and in the prevention and treatment of venous thromboembolism,” Dr. Pollack said in an interview. “Nonetheless, serious bleeding events may occur with NOAC use, and patients taking one of these agents occasionally require urgent surgery or other intervention for which normal hemostasis is required,” added Dr. Pollack, chair of the department of emergency medicine at Pennsylvania Hospital in Philadelphia.
In RE-VERSE AD (a study of the reversal effects of idarucizumab on active dabigatran), the first 90 patients were divided into two distinct groups. Group A, with 51 patients, included those on dabigatran with serious bleeding. Group B, with 39 patients, required reversal of dabigatran for urgent or emergent procedures. In both, idarucizumab provided a median maximum reversal of 100% (95% confidence interval, 100-100) of the anticoagulation effect within 4 hours.
Clotting assays were normalized almost immediately in almost 90% of patients, and the effect was durable, with 80% having measured dabigatran levels reflecting no significant anticoagulation 24 hours later, Dr. Pollack said.
“Clinical outcomes were quite good in this multimorbid patient population, with restoration of hemostasis as reported by local investigators achieved in less than 12 hours when assessable, and with 92% of surgical patients being reported as having normal hemostasis at the time of the procedure,” he said.
Idarucizumab was generally well tolerated in the patient population. “There were no serious adverse events related to the reversal agent ... and only one patient experienced a thrombotic complication within 72 hours, and that patient had not been restarted on any antithrombotic medications,” Dr. Pollack said.
“The study is ongoing,” he added, “but these interim results show rather convincingly that idarucizumab completely and safely reverses the anticoagulant effects of dabigatran within minutes.”
In addition, Dr. Pollack said the availability of a specific reversal agent for dabigatran would enhance its safety margin, and thus alleviate the fears of providers who may hesitate to use a NOAC because of the lack of an “antidote.”
“In fact, most such cases can already be successfully and safely managed with general support and ‘tincture of time’ (the half-life of dabigatran is much shorter than that of warfarin), but having a specific ‘go-to’ option could streamline the care of the most significantly compromised patients,” he said.
Dr. Pollack emphasized, however, that idarucizumab is a specific reversal agent for dabigatran, not an antidote. “To me, the latter would imply that idarucizumab immediately stops bleeding associated with active use of dabigatran,” he said.
Providers should realize that while idarucizumab seems capable of removing dabigatran-induced coagulopathy from the list of concerns when managing a patient with serious bleeding or before a “sharp” procedure, bleeding is a multifaceted issue that also may be due to traumatized blood vessels, other causes of coagulopathy such as liver disease, or concurrent use of antiplatelet medications, he said.
“The patient with a serious or life-threatening bleed on dabigatran will likely need additional care to investigate and manage such concerns,” Dr. Pollack said. “But at least idarucizumab can specifically, safely, and rapidly address the primary consideration.
“The safety of anticoagulation therapy with dabigatran is further enhanced with idarucizumab, a specific reversal agent that won’t need to be used often, but the availability of which would be reassuring to prescribers,” he concluded.
Boehringer Ingelheim sponsored RE-VERSE AD. Idarucizumab was given a fast-track status by the Food and Drug Administration, and BI submitted a new drug application in March 2015, according to the company.
Dr. Pollack reported receiving personal fees from BI, Janssen, Daiichi-Sankyo, Bristol-Myers Squibb, and Pfizer. Disclosures for all the investigators are available at NEJM.org.
AT 2015 ISTH CONGRESS
Key clinical point: The investigational monoclonal antibody idarucizumab reversed the anticoagulant effects of dabigatran.
Major finding: Idarucizumab provided a median maximum dabigatran reversal of 100% (95% CI, 100-100) of the anticoagulation effect within 4 hours in an interim analysis.
Data source: RE-VERSE AD, a prospective cohort study in which 90 patients treated with dabigatran who had uncontrolled bleeding or required emergency surgery or procedures were given 5.0 g idarucizumab.
Disclosures: Boehringer Ingelheim sponsored RE-VERSE AD. Dr. Pollack reported receiving personal fees from Boehringer Ingelheim, Janssen, Daiichi-Sankyo, Bristol-Myers Squibb, and Pfizer. Disclosures for all the investigators are available at NEJM.org.
Decompressive brain surgery carries high complication risk
VIENNA – Decompressive hemicraniectomy for malignant middle cerebral artery infarction was associated with high rates of in-hospital and late complications in a clinical practice setting, according to research reported at the annual European Stroke Conference.
The retrospective findings showed that 88.1% of the 48 patients who underwent the surgery experienced complications such as intracranial hemorrhage (ICH) or symptomatic epilepsy while hospitalized, and 89.5% experienced complications in the later months of their recovery.
While these complication rates are higher than those seen in the randomized controlled clinical studies, the operation still proved life saving for many, with in-hospital and overall mortality rates of 12.5% and 14.6%, respectively, which is similar to the mortality rate seen in the DESTINY trial (Stroke 2007;38:2518-25) after 6 months.
“Patients who underwent [decompressive hemicraniectomy] are a complication-prone collective”, said Dr. Hans-Werner Pledl, resident physician at the department of neurology, UniversitätsMedizin Mannheim, University of Heidelberg (Germany). “Especially in the elderly, recovery stays limited in relevant factors such as ambulation and conversation for self-sufficiency,” he added.
To date, four clinical trials – DECIMAL (Stroke 2007;38:2506-17), HAMLET (Lancet Neurol 2009;8:326-33) and DESTINY and DESTINY II (Int J Stroke 2011;6:79-86) – have looked at the efficacy and safety of DHC in small numbers of patients with life-threatening middle cerebral artery (MCA) infarction. Of these, only DESTINY II included patients over 60 years of age so while there was evidence that the pressure-relieving surgery reduced mortality if performed early, albeit with an increase in functional disability, experience in older patients was less clear. To look at the complication rates in a real-world practice setting, Dr. Pledl of University Hospital Mannheim’s stroke unit, examined the medical records of 48 patients with MCA infarction who underwent DHC between 2008 and 2014. At the time of admission, the 21 male and 27 female patients were aged 28 to 70 years, with the mean age being 57 years. Dr. Pledl noted that two out of every five (41.7%) patients was over the age of 60 years.
On average, patients were referred to the stroke unit within 3 hours and 44 minutes of the incident event, but some were seen within 30 minutes and others within 5 days. A total of 43.8% of patients had an MCA infarction involving the dominant hemisphere and just under 60% received thrombolytic therapy with rtPA. The median time to surgery was 1.3 days, with just over one-fifth (21.7%) of patients undergoing DHC more than 48 hours after their stroke.
The median National Institutes of Health Stroke Scale scores at admission and discharge were 19 and 18, respectively, while the modified Rankin Scale (mRS) score was 5 at both time points. The Barthel Index was 0 at admission, signifying that the patient was heavily dependent on a carer to perform basic living activities, and 7.5 at discharge, indicating some only marginal improvement in patients’ independence.
The majority (75%) of patients achieved reasonable recovery with early (phase B) rehabilitation, 44% with continued poststroke (phase C) rehabilitation, and 6% were able to become self-sufficient and some even returning to work (phase D). “Remarkably, nearly half (48.9%) of patients return home after rehabilitation and do not stay in a clinical or institutional care facility,” Dr. Pledl said.
In-hospital neurological or psychiatric complications included ICH (seven patients), symptomatic epilepsy (six patients), and delirium (five patients). Perioperative complications included meningitis (three patients), wound healing disorders (three patients), and two patients had epidural hemorrhage (EDH). Common infections included pneumonia (13 patients) and urinary tract infections (UTI, eight patients), and other complications included anemia (14 patients) and cardiac complications (nine patients).
During the recovery phase, the most common neurological or psychiatric complications were central pain syndrome and symptomatic epilepsy, affecting nine patients each. Patients again experienced EDH (five patients), with some cases of hydrocephalus (four patients) and wound-healing problems (three patients). UTIs were the most common type of infection, seen in 14 patients. Other late complications included dysphagia (41.7%) and tracheostomy (35.4%), and post-rehab depression (54.2%).
Dr. Pledl suggested that the findings could be used to help better inform patients and their carers so they can have “realistic expectations” of the procedure’s likely outcomes and decide whether or not to have the surgery performed. These “real world” data could also help physicians to be more aware of the likely complications and perhaps address them in some way so that they have minimal impact on patients’ quality of life.
Although patients who experienced complications in this study were not asked if they regretted the decision to undergo the surgery, there is evidence to show that patients and carers can accept a significant level of disability without having significantly impaired quality of life. Nevertheless, the decision on whether DHC should be performed should be made on an individual case basis, especially in older patients, Dr. Pledl concluded.
The next step is to see if there are any subgroups of patients who might fare better or worse after DHC and hopefully identify some predictive imaging markers that could help the decision-making process.
Dr. Pledl reported no conflicts.
VIENNA – Decompressive hemicraniectomy for malignant middle cerebral artery infarction was associated with high rates of in-hospital and late complications in a clinical practice setting, according to research reported at the annual European Stroke Conference.
The retrospective findings showed that 88.1% of the 48 patients who underwent the surgery experienced complications such as intracranial hemorrhage (ICH) or symptomatic epilepsy while hospitalized, and 89.5% experienced complications in the later months of their recovery.
While these complication rates are higher than those seen in the randomized controlled clinical studies, the operation still proved life saving for many, with in-hospital and overall mortality rates of 12.5% and 14.6%, respectively, which is similar to the mortality rate seen in the DESTINY trial (Stroke 2007;38:2518-25) after 6 months.
“Patients who underwent [decompressive hemicraniectomy] are a complication-prone collective”, said Dr. Hans-Werner Pledl, resident physician at the department of neurology, UniversitätsMedizin Mannheim, University of Heidelberg (Germany). “Especially in the elderly, recovery stays limited in relevant factors such as ambulation and conversation for self-sufficiency,” he added.
To date, four clinical trials – DECIMAL (Stroke 2007;38:2506-17), HAMLET (Lancet Neurol 2009;8:326-33) and DESTINY and DESTINY II (Int J Stroke 2011;6:79-86) – have looked at the efficacy and safety of DHC in small numbers of patients with life-threatening middle cerebral artery (MCA) infarction. Of these, only DESTINY II included patients over 60 years of age so while there was evidence that the pressure-relieving surgery reduced mortality if performed early, albeit with an increase in functional disability, experience in older patients was less clear. To look at the complication rates in a real-world practice setting, Dr. Pledl of University Hospital Mannheim’s stroke unit, examined the medical records of 48 patients with MCA infarction who underwent DHC between 2008 and 2014. At the time of admission, the 21 male and 27 female patients were aged 28 to 70 years, with the mean age being 57 years. Dr. Pledl noted that two out of every five (41.7%) patients was over the age of 60 years.
On average, patients were referred to the stroke unit within 3 hours and 44 minutes of the incident event, but some were seen within 30 minutes and others within 5 days. A total of 43.8% of patients had an MCA infarction involving the dominant hemisphere and just under 60% received thrombolytic therapy with rtPA. The median time to surgery was 1.3 days, with just over one-fifth (21.7%) of patients undergoing DHC more than 48 hours after their stroke.
The median National Institutes of Health Stroke Scale scores at admission and discharge were 19 and 18, respectively, while the modified Rankin Scale (mRS) score was 5 at both time points. The Barthel Index was 0 at admission, signifying that the patient was heavily dependent on a carer to perform basic living activities, and 7.5 at discharge, indicating some only marginal improvement in patients’ independence.
The majority (75%) of patients achieved reasonable recovery with early (phase B) rehabilitation, 44% with continued poststroke (phase C) rehabilitation, and 6% were able to become self-sufficient and some even returning to work (phase D). “Remarkably, nearly half (48.9%) of patients return home after rehabilitation and do not stay in a clinical or institutional care facility,” Dr. Pledl said.
In-hospital neurological or psychiatric complications included ICH (seven patients), symptomatic epilepsy (six patients), and delirium (five patients). Perioperative complications included meningitis (three patients), wound healing disorders (three patients), and two patients had epidural hemorrhage (EDH). Common infections included pneumonia (13 patients) and urinary tract infections (UTI, eight patients), and other complications included anemia (14 patients) and cardiac complications (nine patients).
During the recovery phase, the most common neurological or psychiatric complications were central pain syndrome and symptomatic epilepsy, affecting nine patients each. Patients again experienced EDH (five patients), with some cases of hydrocephalus (four patients) and wound-healing problems (three patients). UTIs were the most common type of infection, seen in 14 patients. Other late complications included dysphagia (41.7%) and tracheostomy (35.4%), and post-rehab depression (54.2%).
Dr. Pledl suggested that the findings could be used to help better inform patients and their carers so they can have “realistic expectations” of the procedure’s likely outcomes and decide whether or not to have the surgery performed. These “real world” data could also help physicians to be more aware of the likely complications and perhaps address them in some way so that they have minimal impact on patients’ quality of life.
Although patients who experienced complications in this study were not asked if they regretted the decision to undergo the surgery, there is evidence to show that patients and carers can accept a significant level of disability without having significantly impaired quality of life. Nevertheless, the decision on whether DHC should be performed should be made on an individual case basis, especially in older patients, Dr. Pledl concluded.
The next step is to see if there are any subgroups of patients who might fare better or worse after DHC and hopefully identify some predictive imaging markers that could help the decision-making process.
Dr. Pledl reported no conflicts.
VIENNA – Decompressive hemicraniectomy for malignant middle cerebral artery infarction was associated with high rates of in-hospital and late complications in a clinical practice setting, according to research reported at the annual European Stroke Conference.
The retrospective findings showed that 88.1% of the 48 patients who underwent the surgery experienced complications such as intracranial hemorrhage (ICH) or symptomatic epilepsy while hospitalized, and 89.5% experienced complications in the later months of their recovery.
While these complication rates are higher than those seen in the randomized controlled clinical studies, the operation still proved life saving for many, with in-hospital and overall mortality rates of 12.5% and 14.6%, respectively, which is similar to the mortality rate seen in the DESTINY trial (Stroke 2007;38:2518-25) after 6 months.
“Patients who underwent [decompressive hemicraniectomy] are a complication-prone collective”, said Dr. Hans-Werner Pledl, resident physician at the department of neurology, UniversitätsMedizin Mannheim, University of Heidelberg (Germany). “Especially in the elderly, recovery stays limited in relevant factors such as ambulation and conversation for self-sufficiency,” he added.
To date, four clinical trials – DECIMAL (Stroke 2007;38:2506-17), HAMLET (Lancet Neurol 2009;8:326-33) and DESTINY and DESTINY II (Int J Stroke 2011;6:79-86) – have looked at the efficacy and safety of DHC in small numbers of patients with life-threatening middle cerebral artery (MCA) infarction. Of these, only DESTINY II included patients over 60 years of age so while there was evidence that the pressure-relieving surgery reduced mortality if performed early, albeit with an increase in functional disability, experience in older patients was less clear. To look at the complication rates in a real-world practice setting, Dr. Pledl of University Hospital Mannheim’s stroke unit, examined the medical records of 48 patients with MCA infarction who underwent DHC between 2008 and 2014. At the time of admission, the 21 male and 27 female patients were aged 28 to 70 years, with the mean age being 57 years. Dr. Pledl noted that two out of every five (41.7%) patients was over the age of 60 years.
On average, patients were referred to the stroke unit within 3 hours and 44 minutes of the incident event, but some were seen within 30 minutes and others within 5 days. A total of 43.8% of patients had an MCA infarction involving the dominant hemisphere and just under 60% received thrombolytic therapy with rtPA. The median time to surgery was 1.3 days, with just over one-fifth (21.7%) of patients undergoing DHC more than 48 hours after their stroke.
The median National Institutes of Health Stroke Scale scores at admission and discharge were 19 and 18, respectively, while the modified Rankin Scale (mRS) score was 5 at both time points. The Barthel Index was 0 at admission, signifying that the patient was heavily dependent on a carer to perform basic living activities, and 7.5 at discharge, indicating some only marginal improvement in patients’ independence.
The majority (75%) of patients achieved reasonable recovery with early (phase B) rehabilitation, 44% with continued poststroke (phase C) rehabilitation, and 6% were able to become self-sufficient and some even returning to work (phase D). “Remarkably, nearly half (48.9%) of patients return home after rehabilitation and do not stay in a clinical or institutional care facility,” Dr. Pledl said.
In-hospital neurological or psychiatric complications included ICH (seven patients), symptomatic epilepsy (six patients), and delirium (five patients). Perioperative complications included meningitis (three patients), wound healing disorders (three patients), and two patients had epidural hemorrhage (EDH). Common infections included pneumonia (13 patients) and urinary tract infections (UTI, eight patients), and other complications included anemia (14 patients) and cardiac complications (nine patients).
During the recovery phase, the most common neurological or psychiatric complications were central pain syndrome and symptomatic epilepsy, affecting nine patients each. Patients again experienced EDH (five patients), with some cases of hydrocephalus (four patients) and wound-healing problems (three patients). UTIs were the most common type of infection, seen in 14 patients. Other late complications included dysphagia (41.7%) and tracheostomy (35.4%), and post-rehab depression (54.2%).
Dr. Pledl suggested that the findings could be used to help better inform patients and their carers so they can have “realistic expectations” of the procedure’s likely outcomes and decide whether or not to have the surgery performed. These “real world” data could also help physicians to be more aware of the likely complications and perhaps address them in some way so that they have minimal impact on patients’ quality of life.
Although patients who experienced complications in this study were not asked if they regretted the decision to undergo the surgery, there is evidence to show that patients and carers can accept a significant level of disability without having significantly impaired quality of life. Nevertheless, the decision on whether DHC should be performed should be made on an individual case basis, especially in older patients, Dr. Pledl concluded.
The next step is to see if there are any subgroups of patients who might fare better or worse after DHC and hopefully identify some predictive imaging markers that could help the decision-making process.
Dr. Pledl reported no conflicts.
AT THE EUROPEAN STROKE CONFERENCE
Key clinical point: The high risk of complications associated with decompressive hemicraniectomy for malignant middle cerebral artery infarction warrants appropriate counseling and individualized therapeutic decision-making.
Major finding: The in-hospital and late complication rates associated with decompressive hemicraniectomy for malignant middle cerebral artery infarction were 88.1% and 89.5%, respectively.
Data source: Retrospective, observational, single-center study of 48 patients who underwent decompressive hemicrainiectomy between 2008 and 2014.
Disclosures: Dr. Pledl reported no conflicts.
Communication failures behind many surgical ‘never events’
Poor communication remains at the heart of most surgical “never events” (i.e., preventable events), say the authors of a systematic review that estimates around 500 wrong-site surgeries and 5,000 retained surgical items incidents still happen each year in the United States.
The review of 138 empirical studies of wrong-site surgery, retained surgical items, and surgical fires, published between 2004 and 2014, found wrong-site surgery occurred roughly once per 100,000 surgical procedures, and retained surgical items incidents at a rate of 1.32 events per 10,000 procedures, with unknown data on the per-procedure incidence of surgical fire, according to data published online June 10 in JAMA Surgery.
“A frequently reported cause of wrong-site surgery across 28 identified analyses was communication problems, including miscommunications among staff, missing information that should have been available to the operating room staff, surgical team members not speaking up when they noticed that a procedure targeted the wrong side, and a surgeon ignoring surgical team members who questioned laterality,” wrote Susanne Hempel, PhD, of the Southern California Evidence-Based Practice Center, Santa Monica, and her coauthors.
They found that very few evaluations of interventions designed specifically to reduce the incidence of never events were conclusive, although they pointed out that given the rarity of these events, it was methodologically challenging to assess the effectiveness of these interventions (JAMA Surg. 2015 June 10 [doi:10.1001/jamasurg.2015.0301]).
The Department of Veterans Affairs supported the study. There were no conflicts of interest declared.
Poor communication remains at the heart of most surgical “never events” (i.e., preventable events), say the authors of a systematic review that estimates around 500 wrong-site surgeries and 5,000 retained surgical items incidents still happen each year in the United States.
The review of 138 empirical studies of wrong-site surgery, retained surgical items, and surgical fires, published between 2004 and 2014, found wrong-site surgery occurred roughly once per 100,000 surgical procedures, and retained surgical items incidents at a rate of 1.32 events per 10,000 procedures, with unknown data on the per-procedure incidence of surgical fire, according to data published online June 10 in JAMA Surgery.
“A frequently reported cause of wrong-site surgery across 28 identified analyses was communication problems, including miscommunications among staff, missing information that should have been available to the operating room staff, surgical team members not speaking up when they noticed that a procedure targeted the wrong side, and a surgeon ignoring surgical team members who questioned laterality,” wrote Susanne Hempel, PhD, of the Southern California Evidence-Based Practice Center, Santa Monica, and her coauthors.
They found that very few evaluations of interventions designed specifically to reduce the incidence of never events were conclusive, although they pointed out that given the rarity of these events, it was methodologically challenging to assess the effectiveness of these interventions (JAMA Surg. 2015 June 10 [doi:10.1001/jamasurg.2015.0301]).
The Department of Veterans Affairs supported the study. There were no conflicts of interest declared.
Poor communication remains at the heart of most surgical “never events” (i.e., preventable events), say the authors of a systematic review that estimates around 500 wrong-site surgeries and 5,000 retained surgical items incidents still happen each year in the United States.
The review of 138 empirical studies of wrong-site surgery, retained surgical items, and surgical fires, published between 2004 and 2014, found wrong-site surgery occurred roughly once per 100,000 surgical procedures, and retained surgical items incidents at a rate of 1.32 events per 10,000 procedures, with unknown data on the per-procedure incidence of surgical fire, according to data published online June 10 in JAMA Surgery.
“A frequently reported cause of wrong-site surgery across 28 identified analyses was communication problems, including miscommunications among staff, missing information that should have been available to the operating room staff, surgical team members not speaking up when they noticed that a procedure targeted the wrong side, and a surgeon ignoring surgical team members who questioned laterality,” wrote Susanne Hempel, PhD, of the Southern California Evidence-Based Practice Center, Santa Monica, and her coauthors.
They found that very few evaluations of interventions designed specifically to reduce the incidence of never events were conclusive, although they pointed out that given the rarity of these events, it was methodologically challenging to assess the effectiveness of these interventions (JAMA Surg. 2015 June 10 [doi:10.1001/jamasurg.2015.0301]).
The Department of Veterans Affairs supported the study. There were no conflicts of interest declared.
FROM JAMA SURGERY
Key clinical point: Around 500 wrong-site surgeries and 5,000 retained surgical items incidents still happen each year, many caused by inadequate communication.
Major finding: Wrong-site surgery occurs roughly once per 100,000 surgical procedures, and retained surgical items incidents occur at a rate of 1.32 events per 10,000 procedures.
Data source: Systematic review of 138 empirical studies.
Disclosures: The Department of Veterans Affairs supported the study. There were no conflicts of interest declared.
ERAS protocol superior for postop cystectomy pain management
NEW ORLEANS – The enhanced recovery after surgery (ERAS) protocol resulted in significantly less opioid use for pain management for radical cystectomy patients, compared with traditional postop approaches, according to Dr. Hooman Djaladat.
“The whole idea behind the ERAS protocol was to diminish hospital stay and send the patients home sooner, with no increase in complications or readmission rates,” said Dr. Djaladat, associate professor of clinical urology at the University of Southern California, Los Angeles.
ERAS protocols are multimodal perioperative care pathways, the aim of which is early recovery after surgery by maintaining preoperative organ function and reducing the profound stress response following surgery. The key elements of ERAS protocols include preoperative counseling, optimization of nutrition, standardized analgesic and anesthetic regimens, and early mobilization.
Opioids have traditionally been the standard for pain management after radical cystectomy (RC) for bladder cancer, but opioid use is often accompanied by side effects such as respiratory depression, nausea, vomiting, confusion, and ileus – the leading cause of prolonged hospital stay.
Dr. Djaladat and his colleagues at USC compared the amount of opioid use, pain score, and postoperative ileus in consecutive ERAS and traditional postop RC patients at USC, and presented their findings in a poster at the annual meeting of the American Urological Association.
Study Methods
Dr. Djaladat and his colleagues retrospectively evaluated 205 open-RC patients, 124 of whom underwent pain management as outlined by ERAS protocol (May 2012 to December 2013) and 81 who underwent traditional pain management with opioids (February 2010 to September 2013); the two groups were matched according to patient demographics, and those with a history of opioid use prior to surgery were not included in the study.
Traditional pain management protocol relied primarily on intravenous and epidural opioids, with acetaminophen and ketorolac as supplements as needed. Patient-controlled analgesia also was used if necessary.
The ERAS protocol utilized predominantly acetaminophen and ketorolac started intraoperatively, supplemented by consistent use of local anesthetic through subfascial catheters. Opioids were used only for breakthrough pain.
All opioids used (oxycodone, hydromorphone, tramadol, hydrocodone, morphine, and fentanyl) were converted to intravenous morphine equivalents. Opioid use and pain scores were examined and compared up to postoperative day 4.
“Bottom line, a traditional pathway has been mostly opioid controlled, but ERAS protocol is mostly focused on nonopioid control,” said Dr. Djaladat. “We believe that opioids cause a lot of problems.”
Results
Length of hospital stay in the ERAS cohort was half that in the traditional cohort (4 days vs. 8 days, P < .0001). Additionally, mean morphine equivalent use in the ERAS group was about one-quarter of that observed in the traditional patients (4.9 mg/day vs. 20.87 mg/day, P < .0001).
Postoperative ileus was higher in the traditional group, compared with the ERAS group (22.2% vs. 7.3%, P < .0028). “One of the most important contributing factors to decreased ileus is less narcotic,” he said.
ERAS patients reported higher mean visual analogous (VAS) pain scores per day than traditional patients (3.1 vs. 1.14 on a 4-point scale, P < .0001). VAS scores are the modality by which patients’ pain is measured subjectively. However, Dr. Djaladat suggested in an interview that the statistically significant difference in VAS scores did not necessarily reflect a substantial difference in pain from a clinical perspective.
Dr. Djaladat and his colleagues observed that patients on ERAS protocol used significantly fewer opioid analgesics, which may have potentially contributed to decreased postoperative ileus and shorter lengths of hospital stay, he suggested. They affirm, however, that multi-institutional studies would aid in externally validating these results.
“We find that ERAS is sufficient to manage pain immediately and at the time of discharge, with less narcotic use, in patients who have just undergone radical cystectomy,” Dr. Djaladat reported.
Dr. Djaladat disclosed no relevant financial relationships.
NEW ORLEANS – The enhanced recovery after surgery (ERAS) protocol resulted in significantly less opioid use for pain management for radical cystectomy patients, compared with traditional postop approaches, according to Dr. Hooman Djaladat.
“The whole idea behind the ERAS protocol was to diminish hospital stay and send the patients home sooner, with no increase in complications or readmission rates,” said Dr. Djaladat, associate professor of clinical urology at the University of Southern California, Los Angeles.
ERAS protocols are multimodal perioperative care pathways, the aim of which is early recovery after surgery by maintaining preoperative organ function and reducing the profound stress response following surgery. The key elements of ERAS protocols include preoperative counseling, optimization of nutrition, standardized analgesic and anesthetic regimens, and early mobilization.
Opioids have traditionally been the standard for pain management after radical cystectomy (RC) for bladder cancer, but opioid use is often accompanied by side effects such as respiratory depression, nausea, vomiting, confusion, and ileus – the leading cause of prolonged hospital stay.
Dr. Djaladat and his colleagues at USC compared the amount of opioid use, pain score, and postoperative ileus in consecutive ERAS and traditional postop RC patients at USC, and presented their findings in a poster at the annual meeting of the American Urological Association.
Study Methods
Dr. Djaladat and his colleagues retrospectively evaluated 205 open-RC patients, 124 of whom underwent pain management as outlined by ERAS protocol (May 2012 to December 2013) and 81 who underwent traditional pain management with opioids (February 2010 to September 2013); the two groups were matched according to patient demographics, and those with a history of opioid use prior to surgery were not included in the study.
Traditional pain management protocol relied primarily on intravenous and epidural opioids, with acetaminophen and ketorolac as supplements as needed. Patient-controlled analgesia also was used if necessary.
The ERAS protocol utilized predominantly acetaminophen and ketorolac started intraoperatively, supplemented by consistent use of local anesthetic through subfascial catheters. Opioids were used only for breakthrough pain.
All opioids used (oxycodone, hydromorphone, tramadol, hydrocodone, morphine, and fentanyl) were converted to intravenous morphine equivalents. Opioid use and pain scores were examined and compared up to postoperative day 4.
“Bottom line, a traditional pathway has been mostly opioid controlled, but ERAS protocol is mostly focused on nonopioid control,” said Dr. Djaladat. “We believe that opioids cause a lot of problems.”
Results
Length of hospital stay in the ERAS cohort was half that in the traditional cohort (4 days vs. 8 days, P < .0001). Additionally, mean morphine equivalent use in the ERAS group was about one-quarter of that observed in the traditional patients (4.9 mg/day vs. 20.87 mg/day, P < .0001).
Postoperative ileus was higher in the traditional group, compared with the ERAS group (22.2% vs. 7.3%, P < .0028). “One of the most important contributing factors to decreased ileus is less narcotic,” he said.
ERAS patients reported higher mean visual analogous (VAS) pain scores per day than traditional patients (3.1 vs. 1.14 on a 4-point scale, P < .0001). VAS scores are the modality by which patients’ pain is measured subjectively. However, Dr. Djaladat suggested in an interview that the statistically significant difference in VAS scores did not necessarily reflect a substantial difference in pain from a clinical perspective.
Dr. Djaladat and his colleagues observed that patients on ERAS protocol used significantly fewer opioid analgesics, which may have potentially contributed to decreased postoperative ileus and shorter lengths of hospital stay, he suggested. They affirm, however, that multi-institutional studies would aid in externally validating these results.
“We find that ERAS is sufficient to manage pain immediately and at the time of discharge, with less narcotic use, in patients who have just undergone radical cystectomy,” Dr. Djaladat reported.
Dr. Djaladat disclosed no relevant financial relationships.
NEW ORLEANS – The enhanced recovery after surgery (ERAS) protocol resulted in significantly less opioid use for pain management for radical cystectomy patients, compared with traditional postop approaches, according to Dr. Hooman Djaladat.
“The whole idea behind the ERAS protocol was to diminish hospital stay and send the patients home sooner, with no increase in complications or readmission rates,” said Dr. Djaladat, associate professor of clinical urology at the University of Southern California, Los Angeles.
ERAS protocols are multimodal perioperative care pathways, the aim of which is early recovery after surgery by maintaining preoperative organ function and reducing the profound stress response following surgery. The key elements of ERAS protocols include preoperative counseling, optimization of nutrition, standardized analgesic and anesthetic regimens, and early mobilization.
Opioids have traditionally been the standard for pain management after radical cystectomy (RC) for bladder cancer, but opioid use is often accompanied by side effects such as respiratory depression, nausea, vomiting, confusion, and ileus – the leading cause of prolonged hospital stay.
Dr. Djaladat and his colleagues at USC compared the amount of opioid use, pain score, and postoperative ileus in consecutive ERAS and traditional postop RC patients at USC, and presented their findings in a poster at the annual meeting of the American Urological Association.
Study Methods
Dr. Djaladat and his colleagues retrospectively evaluated 205 open-RC patients, 124 of whom underwent pain management as outlined by ERAS protocol (May 2012 to December 2013) and 81 who underwent traditional pain management with opioids (February 2010 to September 2013); the two groups were matched according to patient demographics, and those with a history of opioid use prior to surgery were not included in the study.
Traditional pain management protocol relied primarily on intravenous and epidural opioids, with acetaminophen and ketorolac as supplements as needed. Patient-controlled analgesia also was used if necessary.
The ERAS protocol utilized predominantly acetaminophen and ketorolac started intraoperatively, supplemented by consistent use of local anesthetic through subfascial catheters. Opioids were used only for breakthrough pain.
All opioids used (oxycodone, hydromorphone, tramadol, hydrocodone, morphine, and fentanyl) were converted to intravenous morphine equivalents. Opioid use and pain scores were examined and compared up to postoperative day 4.
“Bottom line, a traditional pathway has been mostly opioid controlled, but ERAS protocol is mostly focused on nonopioid control,” said Dr. Djaladat. “We believe that opioids cause a lot of problems.”
Results
Length of hospital stay in the ERAS cohort was half that in the traditional cohort (4 days vs. 8 days, P < .0001). Additionally, mean morphine equivalent use in the ERAS group was about one-quarter of that observed in the traditional patients (4.9 mg/day vs. 20.87 mg/day, P < .0001).
Postoperative ileus was higher in the traditional group, compared with the ERAS group (22.2% vs. 7.3%, P < .0028). “One of the most important contributing factors to decreased ileus is less narcotic,” he said.
ERAS patients reported higher mean visual analogous (VAS) pain scores per day than traditional patients (3.1 vs. 1.14 on a 4-point scale, P < .0001). VAS scores are the modality by which patients’ pain is measured subjectively. However, Dr. Djaladat suggested in an interview that the statistically significant difference in VAS scores did not necessarily reflect a substantial difference in pain from a clinical perspective.
Dr. Djaladat and his colleagues observed that patients on ERAS protocol used significantly fewer opioid analgesics, which may have potentially contributed to decreased postoperative ileus and shorter lengths of hospital stay, he suggested. They affirm, however, that multi-institutional studies would aid in externally validating these results.
“We find that ERAS is sufficient to manage pain immediately and at the time of discharge, with less narcotic use, in patients who have just undergone radical cystectomy,” Dr. Djaladat reported.
Dr. Djaladat disclosed no relevant financial relationships.
AT THE AUA ANNUAL MEETING
Key clinical point: Consider ERAS protocol for patients after radical cystectomy to reduce hospital stays and complications.
Major finding: Length of hospital stay in the ERAS cohort was half that in the traditional cohort (4 vs. 8 days). Mean morphine equivalent use in the ERAS group was about one-quarter of that observed in the traditional patients (4.9 vs. 20.87 mg/day).
Data source: Comparative study of 205 well matched, open radical cystectomy patients, 124 of whom underwent pain management as outlined by ERAS protocol and 81 who underwent traditional pain management with opioids.
Disclosures: Dr. Djaladat disclosed no relevant financial relationships.
AACE: How to safely skip radioactive iodine for low-grade thyroid cancer
NASHVILLE, TENN. – Patients with stage I or II differentiated thyroid cancers do not need radioactive iodine treatment if their nonsuppressed thyroglobulin level is less than 2 ng/mL 2 weeks after surgery, according to Dr. Kathleen Hands.
When that’s the case, “I know the patient had an excellent surgery and will have an excellent prognosis with an extremely low likelihood of recurrence over the next 10 years without radioactive iodine. These patients can be managed safely and effectively without radioactive iodine in a community setting,” said Dr. Hands, a thyroidologist who practices in San Antonio.
It’s common for patients in the United States to receive iodine-131 (I-131) after surgery for low-risk thyroid cancers “despite the abundance of evidence” showing that it does them no good and may cause harm and despite guidelines calling for conservative use of I-131, she said (World. J. Surg. 2002;26:879-85).
“It’s a habit,” a holdover from decades ago “when we didn’t actually have good surgical technique. We need to [heed recent data] and step away from what we did in the 60s, 70s, and 80s and get into the 21st century. We should stop using radioactive iodine in these low-risk patients,” Dr. Hands said at the American Association of Clinical Endocrinologists annual meeting.
Among radioactive iodine’s drawbacks are its expense and sometimes salivary and lacrimal problems associated with its use. Earlier in her career, “I personally had two of my cases” – 19 and 22 years old – “develop acute myelogenous leukemia [shortly] after I-131, one of whom succumbed. I took that very seriously. I’ve become very conservative in the use of this drug. Ablation should be restricted to patients with incomplete surgical excision or poor prognostic factors for recurrence or death,” she said.
This advice is backed up by findings from her review of 378 patients who underwent surgery for differentiated thyroid cancer, with MACIS (metastasis, age, completeness of resection, invasion, and size) scores below 7, meaning low-intermediate-risk disease. Patients ranged from 18 to 79 years old. The majority were women, and about a third had multifocal disease. Tumor sizes ranged from 0.8 mm to 4.0 cm. Twenty-one patients under 45 years old had lymph node metastases of less than 5 mm.
The patients had nonsuppressed thyroglobulin levels below 2 ng/mL 2 weeks after surgery. They opted against I-131, and were started on levothyroxine. There’s been no recurrence of disease in the group after 8 years’ follow-up; thyroglobulin was undetectable in 72% by 2 years. Those in whom thyroglobulin remained detectable had thyroglobulin velocities below 10% over a period of 5 years.
“Nonsuppressed thyroglobulin” means that the patients were not put on thyroxine right after surgery, so that Dr. Hands could get an idea if any tumor was left 2 weeks later. They also weren’t put on low-iodine diets in the interim, she said, because she had no intention of giving them I-131.
To get the most out of the approach, patients need excellent and complete surgeries. That means that endocrinologists should learn to perform preoperative neck ultrasounds – or refer to someone who can – to give surgeons a heads-up about tumor location, size, shape, and invasiveness, as well as lymph node involvement, calcifications, and other issues. “This is the kind of information your surgeon needs” to do a good job, Dr. Hands said.
She said she doesn’t worry about hypothyroidism when patients don’t get thyroxine right after surgery. Manipulation of the thyroid during surgery releases hormone into the system, and “I think that tides them over; It’s a long-acting hormone. Patients tolerate not having replacement immediately [after surgery],” Dr. Hands said.
There was no funding for the project, and Dr. Hands said she had no relevant financial disclosures.
NASHVILLE, TENN. – Patients with stage I or II differentiated thyroid cancers do not need radioactive iodine treatment if their nonsuppressed thyroglobulin level is less than 2 ng/mL 2 weeks after surgery, according to Dr. Kathleen Hands.
When that’s the case, “I know the patient had an excellent surgery and will have an excellent prognosis with an extremely low likelihood of recurrence over the next 10 years without radioactive iodine. These patients can be managed safely and effectively without radioactive iodine in a community setting,” said Dr. Hands, a thyroidologist who practices in San Antonio.
It’s common for patients in the United States to receive iodine-131 (I-131) after surgery for low-risk thyroid cancers “despite the abundance of evidence” showing that it does them no good and may cause harm and despite guidelines calling for conservative use of I-131, she said (World. J. Surg. 2002;26:879-85).
“It’s a habit,” a holdover from decades ago “when we didn’t actually have good surgical technique. We need to [heed recent data] and step away from what we did in the 60s, 70s, and 80s and get into the 21st century. We should stop using radioactive iodine in these low-risk patients,” Dr. Hands said at the American Association of Clinical Endocrinologists annual meeting.
Among radioactive iodine’s drawbacks are its expense and sometimes salivary and lacrimal problems associated with its use. Earlier in her career, “I personally had two of my cases” – 19 and 22 years old – “develop acute myelogenous leukemia [shortly] after I-131, one of whom succumbed. I took that very seriously. I’ve become very conservative in the use of this drug. Ablation should be restricted to patients with incomplete surgical excision or poor prognostic factors for recurrence or death,” she said.
This advice is backed up by findings from her review of 378 patients who underwent surgery for differentiated thyroid cancer, with MACIS (metastasis, age, completeness of resection, invasion, and size) scores below 7, meaning low-intermediate-risk disease. Patients ranged from 18 to 79 years old. The majority were women, and about a third had multifocal disease. Tumor sizes ranged from 0.8 mm to 4.0 cm. Twenty-one patients under 45 years old had lymph node metastases of less than 5 mm.
The patients had nonsuppressed thyroglobulin levels below 2 ng/mL 2 weeks after surgery. They opted against I-131, and were started on levothyroxine. There’s been no recurrence of disease in the group after 8 years’ follow-up; thyroglobulin was undetectable in 72% by 2 years. Those in whom thyroglobulin remained detectable had thyroglobulin velocities below 10% over a period of 5 years.
“Nonsuppressed thyroglobulin” means that the patients were not put on thyroxine right after surgery, so that Dr. Hands could get an idea if any tumor was left 2 weeks later. They also weren’t put on low-iodine diets in the interim, she said, because she had no intention of giving them I-131.
To get the most out of the approach, patients need excellent and complete surgeries. That means that endocrinologists should learn to perform preoperative neck ultrasounds – or refer to someone who can – to give surgeons a heads-up about tumor location, size, shape, and invasiveness, as well as lymph node involvement, calcifications, and other issues. “This is the kind of information your surgeon needs” to do a good job, Dr. Hands said.
She said she doesn’t worry about hypothyroidism when patients don’t get thyroxine right after surgery. Manipulation of the thyroid during surgery releases hormone into the system, and “I think that tides them over; It’s a long-acting hormone. Patients tolerate not having replacement immediately [after surgery],” Dr. Hands said.
There was no funding for the project, and Dr. Hands said she had no relevant financial disclosures.
NASHVILLE, TENN. – Patients with stage I or II differentiated thyroid cancers do not need radioactive iodine treatment if their nonsuppressed thyroglobulin level is less than 2 ng/mL 2 weeks after surgery, according to Dr. Kathleen Hands.
When that’s the case, “I know the patient had an excellent surgery and will have an excellent prognosis with an extremely low likelihood of recurrence over the next 10 years without radioactive iodine. These patients can be managed safely and effectively without radioactive iodine in a community setting,” said Dr. Hands, a thyroidologist who practices in San Antonio.
It’s common for patients in the United States to receive iodine-131 (I-131) after surgery for low-risk thyroid cancers “despite the abundance of evidence” showing that it does them no good and may cause harm and despite guidelines calling for conservative use of I-131, she said (World. J. Surg. 2002;26:879-85).
“It’s a habit,” a holdover from decades ago “when we didn’t actually have good surgical technique. We need to [heed recent data] and step away from what we did in the 60s, 70s, and 80s and get into the 21st century. We should stop using radioactive iodine in these low-risk patients,” Dr. Hands said at the American Association of Clinical Endocrinologists annual meeting.
Among radioactive iodine’s drawbacks are its expense and sometimes salivary and lacrimal problems associated with its use. Earlier in her career, “I personally had two of my cases” – 19 and 22 years old – “develop acute myelogenous leukemia [shortly] after I-131, one of whom succumbed. I took that very seriously. I’ve become very conservative in the use of this drug. Ablation should be restricted to patients with incomplete surgical excision or poor prognostic factors for recurrence or death,” she said.
This advice is backed up by findings from her review of 378 patients who underwent surgery for differentiated thyroid cancer, with MACIS (metastasis, age, completeness of resection, invasion, and size) scores below 7, meaning low-intermediate-risk disease. Patients ranged from 18 to 79 years old. The majority were women, and about a third had multifocal disease. Tumor sizes ranged from 0.8 mm to 4.0 cm. Twenty-one patients under 45 years old had lymph node metastases of less than 5 mm.
The patients had nonsuppressed thyroglobulin levels below 2 ng/mL 2 weeks after surgery. They opted against I-131, and were started on levothyroxine. There’s been no recurrence of disease in the group after 8 years’ follow-up; thyroglobulin was undetectable in 72% by 2 years. Those in whom thyroglobulin remained detectable had thyroglobulin velocities below 10% over a period of 5 years.
“Nonsuppressed thyroglobulin” means that the patients were not put on thyroxine right after surgery, so that Dr. Hands could get an idea if any tumor was left 2 weeks later. They also weren’t put on low-iodine diets in the interim, she said, because she had no intention of giving them I-131.
To get the most out of the approach, patients need excellent and complete surgeries. That means that endocrinologists should learn to perform preoperative neck ultrasounds – or refer to someone who can – to give surgeons a heads-up about tumor location, size, shape, and invasiveness, as well as lymph node involvement, calcifications, and other issues. “This is the kind of information your surgeon needs” to do a good job, Dr. Hands said.
She said she doesn’t worry about hypothyroidism when patients don’t get thyroxine right after surgery. Manipulation of the thyroid during surgery releases hormone into the system, and “I think that tides them over; It’s a long-acting hormone. Patients tolerate not having replacement immediately [after surgery],” Dr. Hands said.
There was no funding for the project, and Dr. Hands said she had no relevant financial disclosures.
AT AACE 2015
Key clinical point: Thyroid cancer patients do not need radioactive iodine treatment if their nonsuppressed thyroglobulin is less than 2 ng/mL 2 weeks after surgery.
Major finding: Among 378 patients whose nonsuppressed thyroglobulin levels were below 2 ng/mL 2 weeks after removal of low-risk differentiated thyroid cancers, there were zero recurrences over 8 years of follow-up.
Data source: A single-center, retrospective study.
Disclosures: The investigator said she had no relevant financial disclosures and no outside funding.
Warfarin bridge therapy ups bleeding risk, with no reduction in VTE
Bridge therapy for warfarin patients undergoing invasive therapy is unnecessary for most, said investigators who found an increased risk of bleeding associated with the use of short-acting anticoagulant at the time of the procedure.
A retrospective cohort study of 1,812 procedures in 1,178 patients – most of whom were considered to be at low risk of venous thromboembolism recurrence – showed a 17-fold increase in the risk of clinically relevant bleeding in the group that received bridge anticoagulant therapy, compared with the group that didn’t (2.7% vs. 0.2%).
There was, however, no significant difference in the rate of recurrent venous thromboembolism between the bridge-therapy and non–bridge-therapy groups (0 vs. 3), and no deaths were observed in either group, according to an article published online May 26 (JAMA Intern. Med. [doi:10.1001/jamainternmed.2015.1843].
“Our results confirm and strengthen the findings of those previous studies and highlight the need for a risk categorization scheme that identifies patients at highest risk for recurrent VTE who may benefit from bridge therapy,” wrote Thomas Delate, Ph.D., from Kaiser Permanente Colorado, and coauthors.
The study was conducted and supported by Kaiser Permanente Colorado. One author reported consultancies with Astra-Zeneca, Boehringer-Ingelheim, Pfizer, and Sanofi.
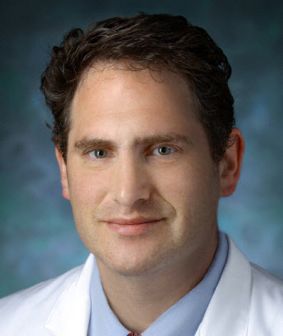
|
| Dr. Daniel J. Brotman |
There are undoubtedly some patients at such high risk for recurrent venous thromboembolism that bridge therapy is a necessary evil, such as those with acute VTE in the preceding month and those with a prior pattern of brisk VTE recurrence during short-term interruption of anticoagulation therapy.
However, for the vast majority of patients receiving oral anticoagulants for VTE, it is probably safer to simply allow the oral anticoagulant to wash out before the procedure and, if indicated based on the type of surgery, to use routine prophylactic-dose anticoagulation therapy afterward.
Dr. Daniel J. Brotman and Dr. Michael B. Streiff are from Johns Hopkins University, Baltimore. These comments are taken from an accompanying editorial (JAMA Intern. Med. 2015 May 26 [doi:10.1001/jamainternmed.2015.1858]). Dr Streiff declared research funding from Bristol-Myers Squibb and Portola and consultancies for Boehringer-Ingelheim, Daiichi-Sankyo, Eisai, Janssen HealthCare, Pfizer, and Sanofi.
|
| Dr. Daniel J. Brotman |
There are undoubtedly some patients at such high risk for recurrent venous thromboembolism that bridge therapy is a necessary evil, such as those with acute VTE in the preceding month and those with a prior pattern of brisk VTE recurrence during short-term interruption of anticoagulation therapy.
However, for the vast majority of patients receiving oral anticoagulants for VTE, it is probably safer to simply allow the oral anticoagulant to wash out before the procedure and, if indicated based on the type of surgery, to use routine prophylactic-dose anticoagulation therapy afterward.
Dr. Daniel J. Brotman and Dr. Michael B. Streiff are from Johns Hopkins University, Baltimore. These comments are taken from an accompanying editorial (JAMA Intern. Med. 2015 May 26 [doi:10.1001/jamainternmed.2015.1858]). Dr Streiff declared research funding from Bristol-Myers Squibb and Portola and consultancies for Boehringer-Ingelheim, Daiichi-Sankyo, Eisai, Janssen HealthCare, Pfizer, and Sanofi.
|
| Dr. Daniel J. Brotman |
There are undoubtedly some patients at such high risk for recurrent venous thromboembolism that bridge therapy is a necessary evil, such as those with acute VTE in the preceding month and those with a prior pattern of brisk VTE recurrence during short-term interruption of anticoagulation therapy.
However, for the vast majority of patients receiving oral anticoagulants for VTE, it is probably safer to simply allow the oral anticoagulant to wash out before the procedure and, if indicated based on the type of surgery, to use routine prophylactic-dose anticoagulation therapy afterward.
Dr. Daniel J. Brotman and Dr. Michael B. Streiff are from Johns Hopkins University, Baltimore. These comments are taken from an accompanying editorial (JAMA Intern. Med. 2015 May 26 [doi:10.1001/jamainternmed.2015.1858]). Dr Streiff declared research funding from Bristol-Myers Squibb and Portola and consultancies for Boehringer-Ingelheim, Daiichi-Sankyo, Eisai, Janssen HealthCare, Pfizer, and Sanofi.
Bridge therapy for warfarin patients undergoing invasive therapy is unnecessary for most, said investigators who found an increased risk of bleeding associated with the use of short-acting anticoagulant at the time of the procedure.
A retrospective cohort study of 1,812 procedures in 1,178 patients – most of whom were considered to be at low risk of venous thromboembolism recurrence – showed a 17-fold increase in the risk of clinically relevant bleeding in the group that received bridge anticoagulant therapy, compared with the group that didn’t (2.7% vs. 0.2%).
There was, however, no significant difference in the rate of recurrent venous thromboembolism between the bridge-therapy and non–bridge-therapy groups (0 vs. 3), and no deaths were observed in either group, according to an article published online May 26 (JAMA Intern. Med. [doi:10.1001/jamainternmed.2015.1843].
“Our results confirm and strengthen the findings of those previous studies and highlight the need for a risk categorization scheme that identifies patients at highest risk for recurrent VTE who may benefit from bridge therapy,” wrote Thomas Delate, Ph.D., from Kaiser Permanente Colorado, and coauthors.
The study was conducted and supported by Kaiser Permanente Colorado. One author reported consultancies with Astra-Zeneca, Boehringer-Ingelheim, Pfizer, and Sanofi.
Bridge therapy for warfarin patients undergoing invasive therapy is unnecessary for most, said investigators who found an increased risk of bleeding associated with the use of short-acting anticoagulant at the time of the procedure.
A retrospective cohort study of 1,812 procedures in 1,178 patients – most of whom were considered to be at low risk of venous thromboembolism recurrence – showed a 17-fold increase in the risk of clinically relevant bleeding in the group that received bridge anticoagulant therapy, compared with the group that didn’t (2.7% vs. 0.2%).
There was, however, no significant difference in the rate of recurrent venous thromboembolism between the bridge-therapy and non–bridge-therapy groups (0 vs. 3), and no deaths were observed in either group, according to an article published online May 26 (JAMA Intern. Med. [doi:10.1001/jamainternmed.2015.1843].
“Our results confirm and strengthen the findings of those previous studies and highlight the need for a risk categorization scheme that identifies patients at highest risk for recurrent VTE who may benefit from bridge therapy,” wrote Thomas Delate, Ph.D., from Kaiser Permanente Colorado, and coauthors.
The study was conducted and supported by Kaiser Permanente Colorado. One author reported consultancies with Astra-Zeneca, Boehringer-Ingelheim, Pfizer, and Sanofi.
Key clinical point: Bridge therapy for warfarin patients undergoing invasive therapy is associated with an increased risk of bleeding without a reduction in thromboembolism risk.
Major finding: Patients given bridge therapy during invasive therapy had a 17-fold increase in the risk of clinically significant bleeding.
Data source: A retrospective cohort study of 1,812 procedures in 1,178 patients.
Disclosures: The study was conducted and supported by Kaiser Permanente Colorado. One author reported consultancies with AstraZeneca, Boehringer-Ingelheim, Pfizer, and Sanofi.
APA: Honest talk about opioid dependence encouraged
TORONTO – More than half of patients in a random sample of individuals seeking treatment for opioid dependence started their journey to addiction with a legitimate medical need for painkillers, according to Dr. Christopher Chiodo.
With the rising morbidity, mortality, and costs associated with opioid dependence, it’s time for physicians to take a closer look at their prescribing habits, said Dr. Chiodo, an orthopedic surgeon at the Brigham and Women’s Faulkner Hospital, Boston.
“You guys are on the back end, taking care of these poor individuals,” Dr. Chiodo told a room full of addiction specialists. “I’m on the front end. I’m the one giving out the prescriptions to patients who are becoming addicted.”
The journey to dependence
In an effort to better understand the role physicians play in the origins of patients’ addiction, Dr. Chiodo and his colleagues at the Brigham and Women’s hospital studied 50 consecutive patients (64% male; mean age, 40 years) being treated for opioid addiction at the hospital’s outpatient center.
Based on an anonymous written survey, the investigators found that 58% of patients received their first opioids from a doctor’s prescription, an additional 28% got the drugs from family and friends, and 14% got them from dealers or other sources.
“There are a lot of patients, for whom we are starting this process. … I’m certainly not going to use the word ‘responsible’ for it, but we’re starting the process,” Dr. Chiodo said at the annual meeting of the American Psychiatric Association.
Orthopedic surgeons weren’t actually the biggest prescribers: 36% of patients reported getting the prescription from a primary care doctor, 7% from a dentist, 7% from an orthopedic surgeon, 14% from general surgeons, and the remaining 36% from other clinicians or from multiple physicians (for example, through doctor shopping).
Perhaps of most concern, at the time the patients reported first considering themselves addicted to opioids, 45% were still getting their drugs from doctors.
The pressures to overprescribe
Many doctors overprescribe just to avoid being called in the middle of the night by a patient in pain. “It’s the low road,” he said.
Other pressures that increase prescribing include patient expectations, increasing surgical volume, and the lack of a longitudinal relationship with patients who are often being treated for acute problems.
“Typical orthopedic office encounters involve patients in pain, quick visits, and we don’t have a longitudinal relationship with these patients – we don’t know who they are, what their personal values are, or their coping or anxiety scores,” Dr. Chiodo said.
Perhaps one of the strongest issues in overprescribing is the desire to avoid complaints, he said.
“You’re doing everything you can to avoid having to confront the patients, so you take the easier road and give them a prescription, and hope they give you a better review in the hospital and on the Internet,” said Dr. Chiodo.
Recent studies have estimated the total annual cost in the United States of opioid abuse to be between $18 billion and $72 billion per year. As well, the United States consumes 80% of the global opioid supply and 99% of global hydrocodone. Studies have shown that patients are more likely to complain about doctors who don’t give them pain medications.
Have the talk
Just prescribing fewer opioids isn’t the only answer, said Dr. Chiodo. What is needed is more dialogue with patients about their pain expectations and their need for opioids.
“I give them 2 weeks [after surgery], and maybe one more prescription to carry them through the third week, but when you get that call, you need to tell your patient that it’s OK to be having some pain,” Dr. Chiodo said. “Half of the time, that’s enough for them; they sigh and say they don’t want the prescription for another week.”
Sometime what is needed – and this is a harder talk to have, said Dr. Chiodo – is an honest suggestion to patients that they are at risk for addiction. “You’re prescribing something very powerful for pain that is affecting their life, and I think we need to talk to our patients more.”
During the Q&A period, Dr. Stephen Frye, a psychiatrist from Las Vegas, suggested that much of this musculoskeletal pain can be better managed with medicinal marijuana.
“Let me assure you that marijuana, which is medically now allowed in 24 states, is really valuable medicine, remarkably safe, you cannot die from it, you cannot OD from it. … This is excellent medication for these problems,” Dr. Frye said.
Dr. Chiodo reported no relevant financial disclosures.
TORONTO – More than half of patients in a random sample of individuals seeking treatment for opioid dependence started their journey to addiction with a legitimate medical need for painkillers, according to Dr. Christopher Chiodo.
With the rising morbidity, mortality, and costs associated with opioid dependence, it’s time for physicians to take a closer look at their prescribing habits, said Dr. Chiodo, an orthopedic surgeon at the Brigham and Women’s Faulkner Hospital, Boston.
“You guys are on the back end, taking care of these poor individuals,” Dr. Chiodo told a room full of addiction specialists. “I’m on the front end. I’m the one giving out the prescriptions to patients who are becoming addicted.”
The journey to dependence
In an effort to better understand the role physicians play in the origins of patients’ addiction, Dr. Chiodo and his colleagues at the Brigham and Women’s hospital studied 50 consecutive patients (64% male; mean age, 40 years) being treated for opioid addiction at the hospital’s outpatient center.
Based on an anonymous written survey, the investigators found that 58% of patients received their first opioids from a doctor’s prescription, an additional 28% got the drugs from family and friends, and 14% got them from dealers or other sources.
“There are a lot of patients, for whom we are starting this process. … I’m certainly not going to use the word ‘responsible’ for it, but we’re starting the process,” Dr. Chiodo said at the annual meeting of the American Psychiatric Association.
Orthopedic surgeons weren’t actually the biggest prescribers: 36% of patients reported getting the prescription from a primary care doctor, 7% from a dentist, 7% from an orthopedic surgeon, 14% from general surgeons, and the remaining 36% from other clinicians or from multiple physicians (for example, through doctor shopping).
Perhaps of most concern, at the time the patients reported first considering themselves addicted to opioids, 45% were still getting their drugs from doctors.
The pressures to overprescribe
Many doctors overprescribe just to avoid being called in the middle of the night by a patient in pain. “It’s the low road,” he said.
Other pressures that increase prescribing include patient expectations, increasing surgical volume, and the lack of a longitudinal relationship with patients who are often being treated for acute problems.
“Typical orthopedic office encounters involve patients in pain, quick visits, and we don’t have a longitudinal relationship with these patients – we don’t know who they are, what their personal values are, or their coping or anxiety scores,” Dr. Chiodo said.
Perhaps one of the strongest issues in overprescribing is the desire to avoid complaints, he said.
“You’re doing everything you can to avoid having to confront the patients, so you take the easier road and give them a prescription, and hope they give you a better review in the hospital and on the Internet,” said Dr. Chiodo.
Recent studies have estimated the total annual cost in the United States of opioid abuse to be between $18 billion and $72 billion per year. As well, the United States consumes 80% of the global opioid supply and 99% of global hydrocodone. Studies have shown that patients are more likely to complain about doctors who don’t give them pain medications.
Have the talk
Just prescribing fewer opioids isn’t the only answer, said Dr. Chiodo. What is needed is more dialogue with patients about their pain expectations and their need for opioids.
“I give them 2 weeks [after surgery], and maybe one more prescription to carry them through the third week, but when you get that call, you need to tell your patient that it’s OK to be having some pain,” Dr. Chiodo said. “Half of the time, that’s enough for them; they sigh and say they don’t want the prescription for another week.”
Sometime what is needed – and this is a harder talk to have, said Dr. Chiodo – is an honest suggestion to patients that they are at risk for addiction. “You’re prescribing something very powerful for pain that is affecting their life, and I think we need to talk to our patients more.”
During the Q&A period, Dr. Stephen Frye, a psychiatrist from Las Vegas, suggested that much of this musculoskeletal pain can be better managed with medicinal marijuana.
“Let me assure you that marijuana, which is medically now allowed in 24 states, is really valuable medicine, remarkably safe, you cannot die from it, you cannot OD from it. … This is excellent medication for these problems,” Dr. Frye said.
Dr. Chiodo reported no relevant financial disclosures.
TORONTO – More than half of patients in a random sample of individuals seeking treatment for opioid dependence started their journey to addiction with a legitimate medical need for painkillers, according to Dr. Christopher Chiodo.
With the rising morbidity, mortality, and costs associated with opioid dependence, it’s time for physicians to take a closer look at their prescribing habits, said Dr. Chiodo, an orthopedic surgeon at the Brigham and Women’s Faulkner Hospital, Boston.
“You guys are on the back end, taking care of these poor individuals,” Dr. Chiodo told a room full of addiction specialists. “I’m on the front end. I’m the one giving out the prescriptions to patients who are becoming addicted.”
The journey to dependence
In an effort to better understand the role physicians play in the origins of patients’ addiction, Dr. Chiodo and his colleagues at the Brigham and Women’s hospital studied 50 consecutive patients (64% male; mean age, 40 years) being treated for opioid addiction at the hospital’s outpatient center.
Based on an anonymous written survey, the investigators found that 58% of patients received their first opioids from a doctor’s prescription, an additional 28% got the drugs from family and friends, and 14% got them from dealers or other sources.
“There are a lot of patients, for whom we are starting this process. … I’m certainly not going to use the word ‘responsible’ for it, but we’re starting the process,” Dr. Chiodo said at the annual meeting of the American Psychiatric Association.
Orthopedic surgeons weren’t actually the biggest prescribers: 36% of patients reported getting the prescription from a primary care doctor, 7% from a dentist, 7% from an orthopedic surgeon, 14% from general surgeons, and the remaining 36% from other clinicians or from multiple physicians (for example, through doctor shopping).
Perhaps of most concern, at the time the patients reported first considering themselves addicted to opioids, 45% were still getting their drugs from doctors.
The pressures to overprescribe
Many doctors overprescribe just to avoid being called in the middle of the night by a patient in pain. “It’s the low road,” he said.
Other pressures that increase prescribing include patient expectations, increasing surgical volume, and the lack of a longitudinal relationship with patients who are often being treated for acute problems.
“Typical orthopedic office encounters involve patients in pain, quick visits, and we don’t have a longitudinal relationship with these patients – we don’t know who they are, what their personal values are, or their coping or anxiety scores,” Dr. Chiodo said.
Perhaps one of the strongest issues in overprescribing is the desire to avoid complaints, he said.
“You’re doing everything you can to avoid having to confront the patients, so you take the easier road and give them a prescription, and hope they give you a better review in the hospital and on the Internet,” said Dr. Chiodo.
Recent studies have estimated the total annual cost in the United States of opioid abuse to be between $18 billion and $72 billion per year. As well, the United States consumes 80% of the global opioid supply and 99% of global hydrocodone. Studies have shown that patients are more likely to complain about doctors who don’t give them pain medications.
Have the talk
Just prescribing fewer opioids isn’t the only answer, said Dr. Chiodo. What is needed is more dialogue with patients about their pain expectations and their need for opioids.
“I give them 2 weeks [after surgery], and maybe one more prescription to carry them through the third week, but when you get that call, you need to tell your patient that it’s OK to be having some pain,” Dr. Chiodo said. “Half of the time, that’s enough for them; they sigh and say they don’t want the prescription for another week.”
Sometime what is needed – and this is a harder talk to have, said Dr. Chiodo – is an honest suggestion to patients that they are at risk for addiction. “You’re prescribing something very powerful for pain that is affecting their life, and I think we need to talk to our patients more.”
During the Q&A period, Dr. Stephen Frye, a psychiatrist from Las Vegas, suggested that much of this musculoskeletal pain can be better managed with medicinal marijuana.
“Let me assure you that marijuana, which is medically now allowed in 24 states, is really valuable medicine, remarkably safe, you cannot die from it, you cannot OD from it. … This is excellent medication for these problems,” Dr. Frye said.
Dr. Chiodo reported no relevant financial disclosures.
AT THE APA ANNUAL MEETING
Key clinical point: Physicians are overprescribing opioids, starting many patients on the road to opioid dependence.
Major finding: In a random sample of patients receiving treatment for opioid dependence, 58% received their first opioids from a doctor’s prescription. At the time they considered themselves addicted, 45% were still being prescribed opioids.
Data source: An observational study of 50 people.
Disclosures: Dr. Chiodo reported no relevant financial disclosures.
Autar scale helps identify DVT risk, prevent DVT
The Autar scale is a successful tool for identifying orthopedic surgery patients at risk for deep vein thrombosis (DVT) – and can prevent DVT when patients follow prophylactic measures corresponding with their DVT risk level, according to researchers.
The study comprised 216 patients who were undergoing orthopedic surgery to the lower extremities in Henan, China. They were divided into a control group and an intervention group, consisting of 106 and 110 patients, respectively. Researchers used the Autar scale to assess the risk of a DVT occurring in all of the patients.
The scale is used mainly for evaluating the probability of DVT in a hospitalized patient undergoing surgery. It includes seven risk categories and 41 items, and is used to assign scores to patients indicating whether they are at no, low, moderate, or high risk of DVT.
Specific preventive measures were implemented among the intervention group’s members based on the Autar scale scores of each of these patients. The scores of patients in the control group were not used to implement DVT prophylaxis. Such patients, however, did receive routine nursing and mechanical and pharmacological prophylactic measures, if clinical experience and basic information caused their health care providers to identify them as being at high risk for DVT.
The Autar scale’s efficacy was confirmed by the fact that “the number of patients with DVT was in line with the number of high-risk patients in both groups,” according to Hui-Zhen Yin and Professor Ci-Ming Shan of Zhengzhou (China) University.
The numbers of DVTs that occurred in each group were significantly different from each other; 1.82% of patients in the intervention group got DVTs, compared to 9.43% of patients in the control group. Therefore, the study showed that the Autar scale is useful not only for predicting DVT, but also for preventing its incidence when patients receive the appropriate prophylactic and nursing interventions, the researchers noted.
They recommend wide use of the scale, because they believe it is “a comprehensive and valid instrument that improves the consistency of nursing assessment and creates a reference for preventing DVT in nursing practice.”
Read the full study in International Journal of Nursing Sciences (doi:10.1016/j.ijnss.2015.04.003).
The Autar scale is a successful tool for identifying orthopedic surgery patients at risk for deep vein thrombosis (DVT) – and can prevent DVT when patients follow prophylactic measures corresponding with their DVT risk level, according to researchers.
The study comprised 216 patients who were undergoing orthopedic surgery to the lower extremities in Henan, China. They were divided into a control group and an intervention group, consisting of 106 and 110 patients, respectively. Researchers used the Autar scale to assess the risk of a DVT occurring in all of the patients.
The scale is used mainly for evaluating the probability of DVT in a hospitalized patient undergoing surgery. It includes seven risk categories and 41 items, and is used to assign scores to patients indicating whether they are at no, low, moderate, or high risk of DVT.
Specific preventive measures were implemented among the intervention group’s members based on the Autar scale scores of each of these patients. The scores of patients in the control group were not used to implement DVT prophylaxis. Such patients, however, did receive routine nursing and mechanical and pharmacological prophylactic measures, if clinical experience and basic information caused their health care providers to identify them as being at high risk for DVT.
The Autar scale’s efficacy was confirmed by the fact that “the number of patients with DVT was in line with the number of high-risk patients in both groups,” according to Hui-Zhen Yin and Professor Ci-Ming Shan of Zhengzhou (China) University.
The numbers of DVTs that occurred in each group were significantly different from each other; 1.82% of patients in the intervention group got DVTs, compared to 9.43% of patients in the control group. Therefore, the study showed that the Autar scale is useful not only for predicting DVT, but also for preventing its incidence when patients receive the appropriate prophylactic and nursing interventions, the researchers noted.
They recommend wide use of the scale, because they believe it is “a comprehensive and valid instrument that improves the consistency of nursing assessment and creates a reference for preventing DVT in nursing practice.”
Read the full study in International Journal of Nursing Sciences (doi:10.1016/j.ijnss.2015.04.003).
The Autar scale is a successful tool for identifying orthopedic surgery patients at risk for deep vein thrombosis (DVT) – and can prevent DVT when patients follow prophylactic measures corresponding with their DVT risk level, according to researchers.
The study comprised 216 patients who were undergoing orthopedic surgery to the lower extremities in Henan, China. They were divided into a control group and an intervention group, consisting of 106 and 110 patients, respectively. Researchers used the Autar scale to assess the risk of a DVT occurring in all of the patients.
The scale is used mainly for evaluating the probability of DVT in a hospitalized patient undergoing surgery. It includes seven risk categories and 41 items, and is used to assign scores to patients indicating whether they are at no, low, moderate, or high risk of DVT.
Specific preventive measures were implemented among the intervention group’s members based on the Autar scale scores of each of these patients. The scores of patients in the control group were not used to implement DVT prophylaxis. Such patients, however, did receive routine nursing and mechanical and pharmacological prophylactic measures, if clinical experience and basic information caused their health care providers to identify them as being at high risk for DVT.
The Autar scale’s efficacy was confirmed by the fact that “the number of patients with DVT was in line with the number of high-risk patients in both groups,” according to Hui-Zhen Yin and Professor Ci-Ming Shan of Zhengzhou (China) University.
The numbers of DVTs that occurred in each group were significantly different from each other; 1.82% of patients in the intervention group got DVTs, compared to 9.43% of patients in the control group. Therefore, the study showed that the Autar scale is useful not only for predicting DVT, but also for preventing its incidence when patients receive the appropriate prophylactic and nursing interventions, the researchers noted.
They recommend wide use of the scale, because they believe it is “a comprehensive and valid instrument that improves the consistency of nursing assessment and creates a reference for preventing DVT in nursing practice.”
Read the full study in International Journal of Nursing Sciences (doi:10.1016/j.ijnss.2015.04.003).
Oral cancer survival lower with positive margins, public insurance
In patients who underwent surgical treatment for stage I or II oral cavity squamous cell cancer, positive tumor margin, the use of radiation or chemotherapy, treatment in a nonacademic facility, and having public health insurance were significantly associated with lower 5-year survival rates, according to a retrospective analysis published online in the JAMA Otolaryngology–Head & Neck Surgery.
The findings suggest that some factors associated with lower 5-year survival rates “may be targets for quality improvement efforts,” wrote Alexander L. Luryi of Yale University, New Haven, Conn., and colleagues.
Seventy percent of 6,830 patients who underwent surgery for stage I or II oral cavity squamous cell cancer (OCSCC) from 2003 to 2006 survived 5 years, according to information from the National Cancer Data Base.
Multivariate analysis showed higher survival rates were significantly associated with neck dissection (hazard ratio, 0.85; P = .003). Lower survival rates were significantly associated with radiation therapy (HR, 1.31; P < .001), chemotherapy (HR, 1.34; P = .03), nonprivate insurance (HR Medicaid, 1.96; HR Medicare, 1.45; P < .001), and nonacademic treatment facility (HR, 1.13; P = .03).
Care at academic centers compared with nonacademic centers was associated with improved survival, possibly due to health care provider expertise, the study authors noted (JAMA Otolaryngol. Head Neck Surg. 2015 May 14 [doi:10.1001/jamaoto.2015.0719]).
Survival rates were lower in patients treated at nonacademic cancer centers, but multivariate analysis showed no association between facility-based case volume and survival. Patients insured through Medicaid and Medicare had significantly lower 5-year survival rates (P < .001 for both). That finding may be the result of inconsistent treatment and follow-up, the investigators said, or worse baseline health among that patient population.
Controversy exists over the relationship between positive margins and outcomes, and the implications for aggressiveness of surgery. The study found positive margins were significantly associated with poorer outcomes, the researchers noted, which supports the use of aggressive surgery in early OCSCC to achieve negative margins.
Radiation and chemotherapy were linked to worse outcomes, and those therapies were possibly indicators of less aggressive resection in localized disease. The analysis could not adjust for potential confounding effects of perineural and lymphovascular invasion, because the information was not recorded in the National Cancer Data Base.
The study indicated a positive impact by neck dissection on survival. Patients with occult neck disease who underwent neck dissection likely would have been restaged to stage III or higher and removed from the early stage sample, the authors explained, which would account for higher survival rates for those remaining. Prospective trials are needed to determine the role of elective neck dissection in early OCSCC, the researchers added.
The William U. Gardner Memorial Research Fund at Yale University supported the study. Dr. Luryi and coauthors reported having no disclosures.
In patients who underwent surgical treatment for stage I or II oral cavity squamous cell cancer, positive tumor margin, the use of radiation or chemotherapy, treatment in a nonacademic facility, and having public health insurance were significantly associated with lower 5-year survival rates, according to a retrospective analysis published online in the JAMA Otolaryngology–Head & Neck Surgery.
The findings suggest that some factors associated with lower 5-year survival rates “may be targets for quality improvement efforts,” wrote Alexander L. Luryi of Yale University, New Haven, Conn., and colleagues.
Seventy percent of 6,830 patients who underwent surgery for stage I or II oral cavity squamous cell cancer (OCSCC) from 2003 to 2006 survived 5 years, according to information from the National Cancer Data Base.
Multivariate analysis showed higher survival rates were significantly associated with neck dissection (hazard ratio, 0.85; P = .003). Lower survival rates were significantly associated with radiation therapy (HR, 1.31; P < .001), chemotherapy (HR, 1.34; P = .03), nonprivate insurance (HR Medicaid, 1.96; HR Medicare, 1.45; P < .001), and nonacademic treatment facility (HR, 1.13; P = .03).
Care at academic centers compared with nonacademic centers was associated with improved survival, possibly due to health care provider expertise, the study authors noted (JAMA Otolaryngol. Head Neck Surg. 2015 May 14 [doi:10.1001/jamaoto.2015.0719]).
Survival rates were lower in patients treated at nonacademic cancer centers, but multivariate analysis showed no association between facility-based case volume and survival. Patients insured through Medicaid and Medicare had significantly lower 5-year survival rates (P < .001 for both). That finding may be the result of inconsistent treatment and follow-up, the investigators said, or worse baseline health among that patient population.
Controversy exists over the relationship between positive margins and outcomes, and the implications for aggressiveness of surgery. The study found positive margins were significantly associated with poorer outcomes, the researchers noted, which supports the use of aggressive surgery in early OCSCC to achieve negative margins.
Radiation and chemotherapy were linked to worse outcomes, and those therapies were possibly indicators of less aggressive resection in localized disease. The analysis could not adjust for potential confounding effects of perineural and lymphovascular invasion, because the information was not recorded in the National Cancer Data Base.
The study indicated a positive impact by neck dissection on survival. Patients with occult neck disease who underwent neck dissection likely would have been restaged to stage III or higher and removed from the early stage sample, the authors explained, which would account for higher survival rates for those remaining. Prospective trials are needed to determine the role of elective neck dissection in early OCSCC, the researchers added.
The William U. Gardner Memorial Research Fund at Yale University supported the study. Dr. Luryi and coauthors reported having no disclosures.
In patients who underwent surgical treatment for stage I or II oral cavity squamous cell cancer, positive tumor margin, the use of radiation or chemotherapy, treatment in a nonacademic facility, and having public health insurance were significantly associated with lower 5-year survival rates, according to a retrospective analysis published online in the JAMA Otolaryngology–Head & Neck Surgery.
The findings suggest that some factors associated with lower 5-year survival rates “may be targets for quality improvement efforts,” wrote Alexander L. Luryi of Yale University, New Haven, Conn., and colleagues.
Seventy percent of 6,830 patients who underwent surgery for stage I or II oral cavity squamous cell cancer (OCSCC) from 2003 to 2006 survived 5 years, according to information from the National Cancer Data Base.
Multivariate analysis showed higher survival rates were significantly associated with neck dissection (hazard ratio, 0.85; P = .003). Lower survival rates were significantly associated with radiation therapy (HR, 1.31; P < .001), chemotherapy (HR, 1.34; P = .03), nonprivate insurance (HR Medicaid, 1.96; HR Medicare, 1.45; P < .001), and nonacademic treatment facility (HR, 1.13; P = .03).
Care at academic centers compared with nonacademic centers was associated with improved survival, possibly due to health care provider expertise, the study authors noted (JAMA Otolaryngol. Head Neck Surg. 2015 May 14 [doi:10.1001/jamaoto.2015.0719]).
Survival rates were lower in patients treated at nonacademic cancer centers, but multivariate analysis showed no association between facility-based case volume and survival. Patients insured through Medicaid and Medicare had significantly lower 5-year survival rates (P < .001 for both). That finding may be the result of inconsistent treatment and follow-up, the investigators said, or worse baseline health among that patient population.
Controversy exists over the relationship between positive margins and outcomes, and the implications for aggressiveness of surgery. The study found positive margins were significantly associated with poorer outcomes, the researchers noted, which supports the use of aggressive surgery in early OCSCC to achieve negative margins.
Radiation and chemotherapy were linked to worse outcomes, and those therapies were possibly indicators of less aggressive resection in localized disease. The analysis could not adjust for potential confounding effects of perineural and lymphovascular invasion, because the information was not recorded in the National Cancer Data Base.
The study indicated a positive impact by neck dissection on survival. Patients with occult neck disease who underwent neck dissection likely would have been restaged to stage III or higher and removed from the early stage sample, the authors explained, which would account for higher survival rates for those remaining. Prospective trials are needed to determine the role of elective neck dissection in early OCSCC, the researchers added.
The William U. Gardner Memorial Research Fund at Yale University supported the study. Dr. Luryi and coauthors reported having no disclosures.
FROM JAMA OTOLARYNGOLOGY–HEAD & NECK SURGERY
Key clinical point: Treatment factors such as neck dissection, tumor margins, type of insurance, and health care facility impact 5-year survival after surgery for early stage oral cavity cancer.
Major finding: Radiation, chemotherapy, positive tumor margin, nonacademic facility, and nonprivate insurance were significantly associated with lower 5-year survival.
Data source: Retrospective study of 6,830 patients in National Cancer Data Base who underwent surgery to treat stage I or II oral cavity squamous cell cancer.
Disclosures: The William U. Gardner Memorial Research Fund at Yale University supported the study. Dr. Luryi and coauthors reported having no disclosures.
Weekend surgery safer with more nurses, EMR use
SAN DIEGO – More nurses, robust ancillary services, and an electronic medical record (EMR) helped reduce hospital length of stay when an urgent general surgery procedure was performed on the weekend. When these surgeon-independent resources were present, hospitals were able to overcome the weekend effect.
When a patient needs urgent surgery over the weekend, the result can be increased length of stay, higher charges, increased major and minor complications, and even increased mortality. Overall, patients admitted on the weekend have worse outcomes than do those admitted on a weekday. Factors contributing to the weekend effect for hospitals in one state were explored in a presentation at the American Surgical Association annual meeting.
“Not all hospitals are created equal in their ability to avoid the weekend effect,” noted presenter Matthew Zapf, a second-year medical student at Stritch School of Medicine, Loyola University Chicago. The work of Mr. Zapf and his colleagues at the university showed that hospitals with full electronic medical records, increased nurse-to-bed ratios, pain and wound management services, and home health programs were more likely to overcome the weekend effect, as defined by length of stay for specific urgent and emergent surgical procedures.
The study used Florida’s Healthcare Cost and Utilization Project State Inpatient Dataset (HCUP-SID), an all-payer dataset, and linked that information to Florida’s American Hospital Association annual survey database, which assesses hospital characteristics. Outcomes were assessed for cholecystectomy, hernia repair for obstructed or gangrenous hernias, and appendectomy for 126,666 people aged 18-90 years. To ensure that the study captured just urgent or emergency procedures, only procedures performed within 2 days of hospital admission were included.
By assessing whether length of stay was longer for weekend vs. weekday admissions for these procedures, the researchers identified which hospitals demonstrated the weekend effect. Of the 197 acute care hospitals identified, 117 performed more than 10 emergent cases per year and were included in the analysis. The presence or absence of a weekend effect was recorded for each hospital for each year of the study. Hospital characteristics were assessed for association with the weekend effect for a given facility in a given year.
None of the 117 hospitals were free of the weekend effect – an outcome that had not been anticipated by the study authors. “I was shocked by the fact that nobody was immune to the weekend effect,” Dr. Anai Kothari said in an interview. Dr. Kothari, also of Loyola University Chicago and first author of the study, said that 41 of the hospitals had a persistent weekend effect through all years of the study. Seventeen hospitals overcame the weekend effect during the time period studied, while 21 others developed the weekend effect during this time. Most hospitals (n = 87) oscillated between states, exhibiting a weekend effect only in some years.
Institutions with an EMR in place during the study period had an odds ratio (OR) of nearly 5 of being able to overcome the weekend effect (P = .010). The EMR, said Dr. Kothari, is especially helpful in effecting safe care transitions. “We are going to see a strong effect, especially in situations where there’s a care transition” as institutions learn how to make full use of the EMR, he said.
Inpatient resources linked with overcoming the weekend effect included a higher ratio of registered nurses to beds (P = .0036), a physical rehabilitation program (P = .017), and a pain management program (P = .001). After-care resources in the form of home health (P = .001) and wound management (P = .043) also contributed significantly to being able to overcome the weekend effect.
Discussant Dr. Lena Napolitano of the University of Michigan commented on the “incredibly robust statistical analysis” performed by the study investigators.
How, she asked, did investigators select median length of stay as the marker for outcomes, when an extended stay over the weekend may just represent poor discharge planning, and not really represent increased adverse outcomes? Senior author Dr. Paul Kuo of Loyola University Chicago replied: “We put a lot of thought into this. We found that length of stay was predictive of each outcome during modeling.”
Study limitations included the fact that data were administrative and were drawn from a single state. It was not possible, for example, to differentiate weekend vs. weekday distribution of resources at a given institution. The next steps will include searching for richer data sources to explore the full set of hospital resources that contribute to patient outcomes for urgent surgeries, said Dr. Kothari.
The authors reported no disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 135th Annual Meeting, April 2015, in San Diego, California, are anticipated to be published in the Annals of Surgery pending editorial review.
SAN DIEGO – More nurses, robust ancillary services, and an electronic medical record (EMR) helped reduce hospital length of stay when an urgent general surgery procedure was performed on the weekend. When these surgeon-independent resources were present, hospitals were able to overcome the weekend effect.
When a patient needs urgent surgery over the weekend, the result can be increased length of stay, higher charges, increased major and minor complications, and even increased mortality. Overall, patients admitted on the weekend have worse outcomes than do those admitted on a weekday. Factors contributing to the weekend effect for hospitals in one state were explored in a presentation at the American Surgical Association annual meeting.
“Not all hospitals are created equal in their ability to avoid the weekend effect,” noted presenter Matthew Zapf, a second-year medical student at Stritch School of Medicine, Loyola University Chicago. The work of Mr. Zapf and his colleagues at the university showed that hospitals with full electronic medical records, increased nurse-to-bed ratios, pain and wound management services, and home health programs were more likely to overcome the weekend effect, as defined by length of stay for specific urgent and emergent surgical procedures.
The study used Florida’s Healthcare Cost and Utilization Project State Inpatient Dataset (HCUP-SID), an all-payer dataset, and linked that information to Florida’s American Hospital Association annual survey database, which assesses hospital characteristics. Outcomes were assessed for cholecystectomy, hernia repair for obstructed or gangrenous hernias, and appendectomy for 126,666 people aged 18-90 years. To ensure that the study captured just urgent or emergency procedures, only procedures performed within 2 days of hospital admission were included.
By assessing whether length of stay was longer for weekend vs. weekday admissions for these procedures, the researchers identified which hospitals demonstrated the weekend effect. Of the 197 acute care hospitals identified, 117 performed more than 10 emergent cases per year and were included in the analysis. The presence or absence of a weekend effect was recorded for each hospital for each year of the study. Hospital characteristics were assessed for association with the weekend effect for a given facility in a given year.
None of the 117 hospitals were free of the weekend effect – an outcome that had not been anticipated by the study authors. “I was shocked by the fact that nobody was immune to the weekend effect,” Dr. Anai Kothari said in an interview. Dr. Kothari, also of Loyola University Chicago and first author of the study, said that 41 of the hospitals had a persistent weekend effect through all years of the study. Seventeen hospitals overcame the weekend effect during the time period studied, while 21 others developed the weekend effect during this time. Most hospitals (n = 87) oscillated between states, exhibiting a weekend effect only in some years.
Institutions with an EMR in place during the study period had an odds ratio (OR) of nearly 5 of being able to overcome the weekend effect (P = .010). The EMR, said Dr. Kothari, is especially helpful in effecting safe care transitions. “We are going to see a strong effect, especially in situations where there’s a care transition” as institutions learn how to make full use of the EMR, he said.
Inpatient resources linked with overcoming the weekend effect included a higher ratio of registered nurses to beds (P = .0036), a physical rehabilitation program (P = .017), and a pain management program (P = .001). After-care resources in the form of home health (P = .001) and wound management (P = .043) also contributed significantly to being able to overcome the weekend effect.
Discussant Dr. Lena Napolitano of the University of Michigan commented on the “incredibly robust statistical analysis” performed by the study investigators.
How, she asked, did investigators select median length of stay as the marker for outcomes, when an extended stay over the weekend may just represent poor discharge planning, and not really represent increased adverse outcomes? Senior author Dr. Paul Kuo of Loyola University Chicago replied: “We put a lot of thought into this. We found that length of stay was predictive of each outcome during modeling.”
Study limitations included the fact that data were administrative and were drawn from a single state. It was not possible, for example, to differentiate weekend vs. weekday distribution of resources at a given institution. The next steps will include searching for richer data sources to explore the full set of hospital resources that contribute to patient outcomes for urgent surgeries, said Dr. Kothari.
The authors reported no disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 135th Annual Meeting, April 2015, in San Diego, California, are anticipated to be published in the Annals of Surgery pending editorial review.
SAN DIEGO – More nurses, robust ancillary services, and an electronic medical record (EMR) helped reduce hospital length of stay when an urgent general surgery procedure was performed on the weekend. When these surgeon-independent resources were present, hospitals were able to overcome the weekend effect.
When a patient needs urgent surgery over the weekend, the result can be increased length of stay, higher charges, increased major and minor complications, and even increased mortality. Overall, patients admitted on the weekend have worse outcomes than do those admitted on a weekday. Factors contributing to the weekend effect for hospitals in one state were explored in a presentation at the American Surgical Association annual meeting.
“Not all hospitals are created equal in their ability to avoid the weekend effect,” noted presenter Matthew Zapf, a second-year medical student at Stritch School of Medicine, Loyola University Chicago. The work of Mr. Zapf and his colleagues at the university showed that hospitals with full electronic medical records, increased nurse-to-bed ratios, pain and wound management services, and home health programs were more likely to overcome the weekend effect, as defined by length of stay for specific urgent and emergent surgical procedures.
The study used Florida’s Healthcare Cost and Utilization Project State Inpatient Dataset (HCUP-SID), an all-payer dataset, and linked that information to Florida’s American Hospital Association annual survey database, which assesses hospital characteristics. Outcomes were assessed for cholecystectomy, hernia repair for obstructed or gangrenous hernias, and appendectomy for 126,666 people aged 18-90 years. To ensure that the study captured just urgent or emergency procedures, only procedures performed within 2 days of hospital admission were included.
By assessing whether length of stay was longer for weekend vs. weekday admissions for these procedures, the researchers identified which hospitals demonstrated the weekend effect. Of the 197 acute care hospitals identified, 117 performed more than 10 emergent cases per year and were included in the analysis. The presence or absence of a weekend effect was recorded for each hospital for each year of the study. Hospital characteristics were assessed for association with the weekend effect for a given facility in a given year.
None of the 117 hospitals were free of the weekend effect – an outcome that had not been anticipated by the study authors. “I was shocked by the fact that nobody was immune to the weekend effect,” Dr. Anai Kothari said in an interview. Dr. Kothari, also of Loyola University Chicago and first author of the study, said that 41 of the hospitals had a persistent weekend effect through all years of the study. Seventeen hospitals overcame the weekend effect during the time period studied, while 21 others developed the weekend effect during this time. Most hospitals (n = 87) oscillated between states, exhibiting a weekend effect only in some years.
Institutions with an EMR in place during the study period had an odds ratio (OR) of nearly 5 of being able to overcome the weekend effect (P = .010). The EMR, said Dr. Kothari, is especially helpful in effecting safe care transitions. “We are going to see a strong effect, especially in situations where there’s a care transition” as institutions learn how to make full use of the EMR, he said.
Inpatient resources linked with overcoming the weekend effect included a higher ratio of registered nurses to beds (P = .0036), a physical rehabilitation program (P = .017), and a pain management program (P = .001). After-care resources in the form of home health (P = .001) and wound management (P = .043) also contributed significantly to being able to overcome the weekend effect.
Discussant Dr. Lena Napolitano of the University of Michigan commented on the “incredibly robust statistical analysis” performed by the study investigators.
How, she asked, did investigators select median length of stay as the marker for outcomes, when an extended stay over the weekend may just represent poor discharge planning, and not really represent increased adverse outcomes? Senior author Dr. Paul Kuo of Loyola University Chicago replied: “We put a lot of thought into this. We found that length of stay was predictive of each outcome during modeling.”
Study limitations included the fact that data were administrative and were drawn from a single state. It was not possible, for example, to differentiate weekend vs. weekday distribution of resources at a given institution. The next steps will include searching for richer data sources to explore the full set of hospital resources that contribute to patient outcomes for urgent surgeries, said Dr. Kothari.
The authors reported no disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 135th Annual Meeting, April 2015, in San Diego, California, are anticipated to be published in the Annals of Surgery pending editorial review.
AT THE ASA ANNUAL MEETING
Key clinical point: Surgeon-independent factors impacted patient outcomes for urgent surgical procedures.
Major finding: Facilities with an electronic medical record, higher nurse-to-bed ratios, and strong ancillary services were significantly less likely to exhibit the weekend effect for urgent surgical procedures, as measured by patient length of stay.
Data source: Healthcare Cost and Utilization Project State Inpatient Dataset and American Hospital Association Annual Survey database for the state of Florida for 2007-2011.
Disclosures: The authors reported no disclosures.