User login
‘Bane of my existence:’ The burden of Medicare Advantage denials
, a recent analysis suggests.
The report from the Office of Inspector General (OIG) of the U.S. Department of Health & Human Services found that 13% of prior authorization denials were for service requests, which included cancer care, that met Medicare coverage rules and 18% of payment denials were for claims that met Medicare coverage and MAO billing rules, delaying or halting payments for services that clinicians had provided.
MAO denials are the “bane of my existence,” said Michael Buckstein, MD, PhD, a radiation oncologist at Mount Sinai Hospital in New York.
“Working at a large hospital in a metropolitan city, we spend enormous and increasing amounts of time on prior approvals and we get denials quite frequently, which certainly can lead to delays in treatment,” said Dr. Buckstein, who reviewed the OIG report for this news organization.
According to Dr. Buckstein, once a claim is denied, staff must spend time filing and scheduling an appeal, and if the appeal is denied in a physician peer-to-peer review, staff could face secondary and tertiary appeals. “We have been living with this frustration for a long time,” Dr. Buckstein said.
Widespread and persistent problems
Medicare Advantage plans, which are approved by the Centers for Medicare & Medicaid Services but run by private companies, continue to grow in popularity.
In 2021, 26.4 million Medicare beneficiaries (42%) were enrolled in a Medicare Advantage plan, and by 2030, about 51% of all Medicare beneficiaries will be enrolled, according to estimates from the Kaiser Family Foundation.
“Although MAOs approve the vast majority of prior authorization requests and provider payment requests, MAOs also deny millions of requests each year,” the OIG wrote. “CMS’s annual audits of MAOs have highlighted widespread and persistent problems related to inappropriate denials of services and payment.”
In the current report, the OIG reviewed case files for 247 denials of prior authorization requests and 183 payment denials issued by 15 of the largest MAOs during 1 week in June of 2019.
The authors found that 13% of prior authorization denials occurred for service requests that met Medicare coverage rules, meaning these services would likely have been approved had the patient been enrolled in traditional Medicare.
The most prominent service types among these denials included imaging services, stays in postacute facilities, and injections.
In one case, for example, the MAO stated that a beneficiary would need to wait at least 1 year for a follow-up MRI because the size of the patient’s adrenal lesion (< 2 cm) was too small to warrant follow-up before 1 year. However, this restriction is not included in Medicare coverage rules. And an OIG physician panel found that the documentation in the original request demonstrated that the MRI was medically necessary to determine whether the lesion seen on an earlier CT scan was malignant.
Upon appeal, the MAO reversed its original denial.
Among the payment requests that MAOs denied, almost one in five were for claims that met Medicare coverage and billing rules, which delayed or prevented payments for services already delivered. Most payment denials were caused by human error during manual claims-processing reviews and system processing errors, the OIG report found.
In one case, for example, a MAO denied payment for radiation treatment for a patient with a tumor on the pancreas, incorrectly claiming that no prior authorization had been submitted for the service. However, the physician subsequently provided a screenshot demonstrating that the MAO had granted prior authorization for the billed claim, and the MAO reversed the denial.
Most of these prior authorization denial reversals occurred because of an appeal filed by the beneficiary or the provider, which can take weeks.
In one case, an MAO denied a request for a CT scan of the chest and pelvis for a beneficiary with endometrial cancer. It took 5 weeks for the provider to get the denial reversed. The OIG panel determined that the original request included sufficient documentation to demonstrate the CT was needed to assess the stage of the cancer and determine the appropriate course of treatment.
These denials and reversals not only waste time but may also cause harm. In a 2021 American Medical Association survey, 34% of physicians reported that prior authorization led to a serious adverse event for a patient in their care, including hospitalization, medical intervention to prevent permanent impairment, and even disability or death.
Almost 90% of the physicians surveyed described the burden associated with prior authorizations as ‘high’ or ‘extremely high.’ More specifically, physicians and their staff spend nearly 2 days a week on prior authorizations and 40% of physicians have staff who work exclusively on prior authorizations.
“It’s just not the way medicine should be practiced, especially for cancer patients who are very vulnerable and want rapid care,” Dr. Buckstein said.
Time for action
Weighing in on the OIG report, Robert E. Wailes, MD, president of the California Medical Association, noted that “it has become common practice for health insurance companies to create obstacles for patients in hopes of not having to pay for essential healthcare.”
The reason for these obstacles is simple, he said: “Fewer procedures performed translates to larger insurance company profits.”
America’s Health Insurance Plans (AHIP) defended prior authorization, saying it is “an important patient safety, cost-saving, and waste-prevention tool.”
The group also called out the OIG review for its “extraordinarily small” sample of 247 prior authorization requests over 1 week.
“Drawing far-reaching conclusions based on a very small sample of data and misleading headlines is not a productive way to improve our healthcare system for patients,” the AHIP statement reads.
But, according to Anna Schwamlein Howard, who works on policy development at the American Cancer Society Cancer Action Network, the recent OIG report is in line with previous OIG reports.
And, Ms. Howard emphasized, the current report and others like it “highlight the need for CMS to utilize its audit authority and ensure that beneficiaries have access to medically necessary treatments, particularly cancer treatments.”
Along those lines, the OIG report recommends that the CMS should issue new guidance on the appropriate use of MAO clinical criteria in medical necessity reviews, update its audit protocols to address issues identified in the report, and direct MAOs to take additional steps to identify and address vulnerabilities that can lead to manual review and system errors.
In a statement, the CMS said it is committed to oversight and enforcement of the requirements of the Medicare Advantage program and agreed with the OIG recommendations.
“Lawmakers must act now to place patient needs before corporate profits and simplify by streamlining prior authorization processes,” Dr. Wailes said.
The ACS recently released a paper on this topic entitled, “The Medicare Appeals Process: Reforms Needed to Ensure Beneficiary Access.”
A version of this article first appeared on Medscape.com.
, a recent analysis suggests.
The report from the Office of Inspector General (OIG) of the U.S. Department of Health & Human Services found that 13% of prior authorization denials were for service requests, which included cancer care, that met Medicare coverage rules and 18% of payment denials were for claims that met Medicare coverage and MAO billing rules, delaying or halting payments for services that clinicians had provided.
MAO denials are the “bane of my existence,” said Michael Buckstein, MD, PhD, a radiation oncologist at Mount Sinai Hospital in New York.
“Working at a large hospital in a metropolitan city, we spend enormous and increasing amounts of time on prior approvals and we get denials quite frequently, which certainly can lead to delays in treatment,” said Dr. Buckstein, who reviewed the OIG report for this news organization.
According to Dr. Buckstein, once a claim is denied, staff must spend time filing and scheduling an appeal, and if the appeal is denied in a physician peer-to-peer review, staff could face secondary and tertiary appeals. “We have been living with this frustration for a long time,” Dr. Buckstein said.
Widespread and persistent problems
Medicare Advantage plans, which are approved by the Centers for Medicare & Medicaid Services but run by private companies, continue to grow in popularity.
In 2021, 26.4 million Medicare beneficiaries (42%) were enrolled in a Medicare Advantage plan, and by 2030, about 51% of all Medicare beneficiaries will be enrolled, according to estimates from the Kaiser Family Foundation.
“Although MAOs approve the vast majority of prior authorization requests and provider payment requests, MAOs also deny millions of requests each year,” the OIG wrote. “CMS’s annual audits of MAOs have highlighted widespread and persistent problems related to inappropriate denials of services and payment.”
In the current report, the OIG reviewed case files for 247 denials of prior authorization requests and 183 payment denials issued by 15 of the largest MAOs during 1 week in June of 2019.
The authors found that 13% of prior authorization denials occurred for service requests that met Medicare coverage rules, meaning these services would likely have been approved had the patient been enrolled in traditional Medicare.
The most prominent service types among these denials included imaging services, stays in postacute facilities, and injections.
In one case, for example, the MAO stated that a beneficiary would need to wait at least 1 year for a follow-up MRI because the size of the patient’s adrenal lesion (< 2 cm) was too small to warrant follow-up before 1 year. However, this restriction is not included in Medicare coverage rules. And an OIG physician panel found that the documentation in the original request demonstrated that the MRI was medically necessary to determine whether the lesion seen on an earlier CT scan was malignant.
Upon appeal, the MAO reversed its original denial.
Among the payment requests that MAOs denied, almost one in five were for claims that met Medicare coverage and billing rules, which delayed or prevented payments for services already delivered. Most payment denials were caused by human error during manual claims-processing reviews and system processing errors, the OIG report found.
In one case, for example, a MAO denied payment for radiation treatment for a patient with a tumor on the pancreas, incorrectly claiming that no prior authorization had been submitted for the service. However, the physician subsequently provided a screenshot demonstrating that the MAO had granted prior authorization for the billed claim, and the MAO reversed the denial.
Most of these prior authorization denial reversals occurred because of an appeal filed by the beneficiary or the provider, which can take weeks.
In one case, an MAO denied a request for a CT scan of the chest and pelvis for a beneficiary with endometrial cancer. It took 5 weeks for the provider to get the denial reversed. The OIG panel determined that the original request included sufficient documentation to demonstrate the CT was needed to assess the stage of the cancer and determine the appropriate course of treatment.
These denials and reversals not only waste time but may also cause harm. In a 2021 American Medical Association survey, 34% of physicians reported that prior authorization led to a serious adverse event for a patient in their care, including hospitalization, medical intervention to prevent permanent impairment, and even disability or death.
Almost 90% of the physicians surveyed described the burden associated with prior authorizations as ‘high’ or ‘extremely high.’ More specifically, physicians and their staff spend nearly 2 days a week on prior authorizations and 40% of physicians have staff who work exclusively on prior authorizations.
“It’s just not the way medicine should be practiced, especially for cancer patients who are very vulnerable and want rapid care,” Dr. Buckstein said.
Time for action
Weighing in on the OIG report, Robert E. Wailes, MD, president of the California Medical Association, noted that “it has become common practice for health insurance companies to create obstacles for patients in hopes of not having to pay for essential healthcare.”
The reason for these obstacles is simple, he said: “Fewer procedures performed translates to larger insurance company profits.”
America’s Health Insurance Plans (AHIP) defended prior authorization, saying it is “an important patient safety, cost-saving, and waste-prevention tool.”
The group also called out the OIG review for its “extraordinarily small” sample of 247 prior authorization requests over 1 week.
“Drawing far-reaching conclusions based on a very small sample of data and misleading headlines is not a productive way to improve our healthcare system for patients,” the AHIP statement reads.
But, according to Anna Schwamlein Howard, who works on policy development at the American Cancer Society Cancer Action Network, the recent OIG report is in line with previous OIG reports.
And, Ms. Howard emphasized, the current report and others like it “highlight the need for CMS to utilize its audit authority and ensure that beneficiaries have access to medically necessary treatments, particularly cancer treatments.”
Along those lines, the OIG report recommends that the CMS should issue new guidance on the appropriate use of MAO clinical criteria in medical necessity reviews, update its audit protocols to address issues identified in the report, and direct MAOs to take additional steps to identify and address vulnerabilities that can lead to manual review and system errors.
In a statement, the CMS said it is committed to oversight and enforcement of the requirements of the Medicare Advantage program and agreed with the OIG recommendations.
“Lawmakers must act now to place patient needs before corporate profits and simplify by streamlining prior authorization processes,” Dr. Wailes said.
The ACS recently released a paper on this topic entitled, “The Medicare Appeals Process: Reforms Needed to Ensure Beneficiary Access.”
A version of this article first appeared on Medscape.com.
, a recent analysis suggests.
The report from the Office of Inspector General (OIG) of the U.S. Department of Health & Human Services found that 13% of prior authorization denials were for service requests, which included cancer care, that met Medicare coverage rules and 18% of payment denials were for claims that met Medicare coverage and MAO billing rules, delaying or halting payments for services that clinicians had provided.
MAO denials are the “bane of my existence,” said Michael Buckstein, MD, PhD, a radiation oncologist at Mount Sinai Hospital in New York.
“Working at a large hospital in a metropolitan city, we spend enormous and increasing amounts of time on prior approvals and we get denials quite frequently, which certainly can lead to delays in treatment,” said Dr. Buckstein, who reviewed the OIG report for this news organization.
According to Dr. Buckstein, once a claim is denied, staff must spend time filing and scheduling an appeal, and if the appeal is denied in a physician peer-to-peer review, staff could face secondary and tertiary appeals. “We have been living with this frustration for a long time,” Dr. Buckstein said.
Widespread and persistent problems
Medicare Advantage plans, which are approved by the Centers for Medicare & Medicaid Services but run by private companies, continue to grow in popularity.
In 2021, 26.4 million Medicare beneficiaries (42%) were enrolled in a Medicare Advantage plan, and by 2030, about 51% of all Medicare beneficiaries will be enrolled, according to estimates from the Kaiser Family Foundation.
“Although MAOs approve the vast majority of prior authorization requests and provider payment requests, MAOs also deny millions of requests each year,” the OIG wrote. “CMS’s annual audits of MAOs have highlighted widespread and persistent problems related to inappropriate denials of services and payment.”
In the current report, the OIG reviewed case files for 247 denials of prior authorization requests and 183 payment denials issued by 15 of the largest MAOs during 1 week in June of 2019.
The authors found that 13% of prior authorization denials occurred for service requests that met Medicare coverage rules, meaning these services would likely have been approved had the patient been enrolled in traditional Medicare.
The most prominent service types among these denials included imaging services, stays in postacute facilities, and injections.
In one case, for example, the MAO stated that a beneficiary would need to wait at least 1 year for a follow-up MRI because the size of the patient’s adrenal lesion (< 2 cm) was too small to warrant follow-up before 1 year. However, this restriction is not included in Medicare coverage rules. And an OIG physician panel found that the documentation in the original request demonstrated that the MRI was medically necessary to determine whether the lesion seen on an earlier CT scan was malignant.
Upon appeal, the MAO reversed its original denial.
Among the payment requests that MAOs denied, almost one in five were for claims that met Medicare coverage and billing rules, which delayed or prevented payments for services already delivered. Most payment denials were caused by human error during manual claims-processing reviews and system processing errors, the OIG report found.
In one case, for example, a MAO denied payment for radiation treatment for a patient with a tumor on the pancreas, incorrectly claiming that no prior authorization had been submitted for the service. However, the physician subsequently provided a screenshot demonstrating that the MAO had granted prior authorization for the billed claim, and the MAO reversed the denial.
Most of these prior authorization denial reversals occurred because of an appeal filed by the beneficiary or the provider, which can take weeks.
In one case, an MAO denied a request for a CT scan of the chest and pelvis for a beneficiary with endometrial cancer. It took 5 weeks for the provider to get the denial reversed. The OIG panel determined that the original request included sufficient documentation to demonstrate the CT was needed to assess the stage of the cancer and determine the appropriate course of treatment.
These denials and reversals not only waste time but may also cause harm. In a 2021 American Medical Association survey, 34% of physicians reported that prior authorization led to a serious adverse event for a patient in their care, including hospitalization, medical intervention to prevent permanent impairment, and even disability or death.
Almost 90% of the physicians surveyed described the burden associated with prior authorizations as ‘high’ or ‘extremely high.’ More specifically, physicians and their staff spend nearly 2 days a week on prior authorizations and 40% of physicians have staff who work exclusively on prior authorizations.
“It’s just not the way medicine should be practiced, especially for cancer patients who are very vulnerable and want rapid care,” Dr. Buckstein said.
Time for action
Weighing in on the OIG report, Robert E. Wailes, MD, president of the California Medical Association, noted that “it has become common practice for health insurance companies to create obstacles for patients in hopes of not having to pay for essential healthcare.”
The reason for these obstacles is simple, he said: “Fewer procedures performed translates to larger insurance company profits.”
America’s Health Insurance Plans (AHIP) defended prior authorization, saying it is “an important patient safety, cost-saving, and waste-prevention tool.”
The group also called out the OIG review for its “extraordinarily small” sample of 247 prior authorization requests over 1 week.
“Drawing far-reaching conclusions based on a very small sample of data and misleading headlines is not a productive way to improve our healthcare system for patients,” the AHIP statement reads.
But, according to Anna Schwamlein Howard, who works on policy development at the American Cancer Society Cancer Action Network, the recent OIG report is in line with previous OIG reports.
And, Ms. Howard emphasized, the current report and others like it “highlight the need for CMS to utilize its audit authority and ensure that beneficiaries have access to medically necessary treatments, particularly cancer treatments.”
Along those lines, the OIG report recommends that the CMS should issue new guidance on the appropriate use of MAO clinical criteria in medical necessity reviews, update its audit protocols to address issues identified in the report, and direct MAOs to take additional steps to identify and address vulnerabilities that can lead to manual review and system errors.
In a statement, the CMS said it is committed to oversight and enforcement of the requirements of the Medicare Advantage program and agreed with the OIG recommendations.
“Lawmakers must act now to place patient needs before corporate profits and simplify by streamlining prior authorization processes,” Dr. Wailes said.
The ACS recently released a paper on this topic entitled, “The Medicare Appeals Process: Reforms Needed to Ensure Beneficiary Access.”
A version of this article first appeared on Medscape.com.
Innocent doc sued after 'secret' medical expert says claim has merit
When the hospital’s trauma team could not get an IV inserted into an accident victim, they called Illinois emergency physician William Sullivan, DO, JD, for help. Dr. Sullivan, who is based in the Chicago suburb of Frankfort, inserted a central line into the patient’s leg on his first attempt – a task that took about 20 minutes.
A year later, Dr. Sullivan was shocked and angry to learn he was being sued by the trauma patient’s family. Inserting the line was his only interaction with the woman, and he had no role in her care management, he said. Yet, the suit claimed he was negligent for failing to diagnose the patient with internal bleeding and for not performing surgery.
“The lawsuit put a lot of stress on our family,” Dr. Sullivan recalled. “At the time my wife was pregnant. I was in law school, and I was also working full time in the ER to support our family. I remember my wife crying on the couch after reading the complaint and asking how the plaintiff’s attorney could get away with making the allegations he made.”
Dr. Sullivan soon learned that 15 medical providers in the patient’s medical record were named as defendants. This included the director of the radiology department, whose name was on a radiology report as “director” but who was actually out of the country when the incident occurred.
Despite some of the accusations being impossible, a medical expert had claimed there was a “meritorious claim” against every health professional named in the suit. Illinois is among the 28 states that require plaintiffs’ attorneys to file an affidavit of merit for medical malpractice claims to move forward.
Dr. Sullivan wondered who would endorse such outlandish accusations, but the expert’s identity was a mystery. According to Illinois law, About one-third of states with merit requirements permit anonymous experts, according to research and attorneys familiar with the issue.
Because the expert’s identity remains hidden, physicians have no way of knowing whether they were qualified to render an opinion, Dr. Sullivan said. The loopholes can drag out frivolous claims and waste significant time and expense, say legal experts. Frequently, it takes a year or more before innocent physicians are dismissed from unfounded lawsuits by the court or dropped when plaintiffs can’t support the claim.
“It’s hugely frustrating,” said Bruce Montoya, JD, a Colorado medical liability defense attorney. “You have an expert who is not disclosed. Further down the road, when experts are being deposed, the plaintiff does not have to reveal whether any of those testifying experts is the same one who certified the case. You never get to determine whether they, in fact, had a certificate reviewer who was legitimate.”
The laws have led to a recent outcry among physicians and fueled a revised resolution by the American College of Emergency Physicians (ACEP) denouncing anonymous affidavits of merit. (The revision has not yet been published online.)
“The minute experts are identified, they can be vetted,” said Rade B. Vukmir, MD, JD, chair of ACEP’s Medical Legal Committee. “There are reasons that you want to clarify the qualification and veracity of the witness. [Anonymous affidavits of merit] don’t allow that, and there’s something inherently wrong with that.”
Because the identities of consulting experts are unknown, it’s hard to know how many are unqualified. Expert witnesses who testify during trials, on the other hand, have long come under scrutiny for questionable qualifications. Some have come under fire for allegedly lying under oath about their experience, misrepresenting their credentials, and falsely representing their knowledge.
“Considering the known problem of potentially unethical expert witness testimony at trial, there’s is the potential likelihood that experts in anonymous affidavits of merit may sometimes lack the qualifications to give opinions,” said Dr. Vukmir, an emergency care physician in Pittsburgh.
Attorneys: Hidden experts increase costs, waste time
In Colorado, Mr. Montoya has seen firsthand how anonymous experts can prolong questionable claims and burden defendants.
Like Illinois, Colorado does not require attorneys to identify the medical experts used to fulfill its certificate of review statute. The expert consulted must have expertise in the same area of the alleged negligence, but does not have to practice in the same specialty, and the statute allows one expert to certify a lawsuit against multiple doctors.
In a recent case, Mr. Montoya represented a Denver neurosurgeon who was sued along with multiple other health care professionals. From the outset, Mr. Montoya argued the claim had no merit against the neurosurgeon, but the plaintiff’s attorney refused to dismiss the physician. Mr. Montoya asked whether the expert consulted for the certificate of merit was a neurosurgeon, but the attorney declined to disclose that information, he said.
The case progressed and Mr. Montoya eventually asked the judge to review the certificate of merit. By law, a judge can confidentially review the certificate of merit and decide whether it aligns with the state statute, but without disclosing the expert’s identity to the defense. The judge ruled the certificate appeared to conform with state law, and the case continued.
A year later, as both sides were getting ready to disclose their experts who would testify, Mr. Montoya again argued the neurosurgeon should be dropped from the suit. This time, he warned if the claim continued against the neurosurgeon, the defense would be filing a motion for summary judgment and pursuing attorney fees and costs. Colorado law allows for such fees if the filing or pursuit of an action is frivolous.
“Boom, my client was dismissed,” Mr. Montoya said. “This is a year later, after multiple conferences among the attorneys, multiple pleadings filed, expert witnesses retained to review the care, discovery exchanged, and records obtained. If we had [a stronger] certificate of review statute, it would have been a different ballgame. It’s never going to get a year down the road.”
In New York, physician defendants have experienced similar woes. The state’s law requires plaintiffs’ attorneys to certify that they consulted with a physician prior to filing the claim, and that they believe based on that discussion, there’s a reasonable basis for the claim to move forward. Attorneys are not required to disclose the expert’s identity.
The law also allows “an out,” explained Morris Auster, JD, senior vice president and chief legislative counsel for the Medical Society of the State of New York. If the attorney made three separate attempts to obtain a consultation, and all three experts would not agree to the consultation, the lawsuit can be filed anyway, he said.
“From our standpoint, it’s important to have an affidavit of merit requirement; it’s better than not having it,” Mr. Auster said. “But its effectiveness in providing control over the filing of lawsuits in New York has never been as strong as it could’ve been.”
Mr. Auster notes that New York has some of the highest liability costs in the country in addition to doctors paying some of the steepest medical liability insurance premiums.
“This really affects a lot of physicians and it’s driving physicians into employment arrangements, so they don’t have to deal with it on their own,” he said. “We support a number of measures to address these significantly high costs, and stronger certificate of merit requirements would certainly be one of those advocacy goals.”
Why are anonymous experts allowed?
Certificates of merit that shield the identity of consultants encourage a greater pool of physicians willing to review cases, said J. Matthew Dudley, JD, president of the Illinois Trial Lawyers Association. When the requirements first went into effect in Illinois, there was significant animosity among physicians toward doctors who testified in medical malpractice cases for patients, Mr. Dudley explained.
“Sometimes they would be ostracized from their professional societies, or it would hurt a referral relationship.” he said. “Over time, that animosity has lessened, but there was a concern that if the identity of physicians in certificates of merit weren’t protected, then doctors would not look at cases for patients.”
This would result in additional barriers for patients and their attorneys in pursuing their legal rights, Mr. Dudley said. He said Illinois’ certificate of merit statute is successful in fulfilling its intended purpose, and he has not seen any statistical evidence to suggest otherwise.
“It has proven effective at decreasing filings in medical malpractice and effectively screening medical malpractice cases,” he said. “Certificates of merit help to decrease filings by firms that aren’t that experienced in dealing with those kinds of cases.”
Kentucky is another state that does not require attorneys to identity the experts consulted for certificates of merit. Malpractice defense attorney Andrew DeSimone, JD, who practices in Kentucky, said this isn’t a problem since attorneys eventually must disclose the expert witnesses who will testify at trial.
“Knowing the name behind the certificate of merit is not that pertinent,” Mr. DeSimone said. “Physicians and their attorneys will ultimately have the chance to question and evaluate the expert witnesses used at trial. The certificate of merit is designed to weed out totally frivolous cases that do not have expert support. It’s not designed to be a trial on the merits.”
The belief that plaintiffs’ attorneys frequently bring weak cases and use unqualified experts to certify claims is not realistic or logical, added Sean Domnick, JD, a Florida medical malpractice attorney and vice president for the American Association for Justice. Medical malpractice cases are extremely challenging for plaintiffs – and they’re expensive, Mr. Domnick said.
“We can’t afford to take bad cases,” he said. “For me to take on a medical malpractice case, it’s not unusual for me to spend well over $100,000. Remember, if we lose, I don’t get that money back and I don’t get paid. Why in the world would a plaintiff take on that type of a burden for a case they didn’t believe in? The logic escapes me.”
In Florida, where Mr. Domnick practices, plaintiffs’ attorneys must send their certificates of merit to the defense with the expert identified. Domnick believes the requirement is a hindrance.
“It creates a delay that is unnecessary in a system that is already designed to wear our clients down,” he said. “It’s just another component that makes it harder on them.”
Hidden experts may insulate plaintiffs’ attorneys from liability
Dr. Sullivan, the Illinois emergency physician, was ultimately dismissed from the multiparty lawsuit, but not for roughly 18 months. After the dismissal, he fought back. He sued the plaintiff’s law firm for malicious prosecution, negligence in hiring, and relying on the opinion of an expert who was unqualified to render an opinion against an emergency physician.
The law firm, however, argued that it was immune from liability because it reasonably relied on the expert’s opinion as required by Illinois law. A trial court agreed with the plaintiffs’ firm. The judge denied Dr. Sullivan’s request to identify the expert, ruling there was no finding that the affidavit was untrue or made without reasonable cause. Dr. Sullivan appealed, and the appellate court upheld the trial’s court decision.
“As happened with my case, law firms can use the affidavit as a defense against countersuits or motions for sanctions,” Dr. Sullivan said. “Although the certificate of merit is intended to prevent attorneys from filing frivolous cases, it can also have the opposite effect of helping to insulate plaintiff attorneys from liability for filing a frivolous lawsuit.”
In Colorado, complaints about the state’s certificate of merit statute have gone before the Colorado Supreme Court. In one case, a lower court ruled that a certificate of merit was deficient because the consultants were not chiropractors. In another case, a nurse defendant argued the claim’s certificate of review was insufficient because the consulting expert was a physician.
In both instances, Colorado judges held the state’s statute does not require consultants to be in the same profession or the same specialty as the health professional defendant.
In New York, meanwhile, Mr. Auster said several bills to strengthen the state’s certificate of merit requirements have failed in recent years.
“It’s hard to say whether it will improve anytime soon,” he said. “The trial lawyers are a very powerful advocacy force in the state, and they tend to oppose even the slightest of changes in civil liability. [In addition], some of these issues have been put on a lower tier because of trying to manage the pandemic.”
Ultimately, Dr. Sullivan said that courts and legislatures need to strongly consider the ethics of allowing anonymous experts to provide testimony against defendant physicians.
“I also think we need to consider how the notion of a secret expert comports with a defendant physician’s due process,” he said. “If an expert’s opinion is appropriate, why would there be a need to shroud one’s identity in a veil of secrecy?”
A version of this article first appeared on Medscape.com.
When the hospital’s trauma team could not get an IV inserted into an accident victim, they called Illinois emergency physician William Sullivan, DO, JD, for help. Dr. Sullivan, who is based in the Chicago suburb of Frankfort, inserted a central line into the patient’s leg on his first attempt – a task that took about 20 minutes.
A year later, Dr. Sullivan was shocked and angry to learn he was being sued by the trauma patient’s family. Inserting the line was his only interaction with the woman, and he had no role in her care management, he said. Yet, the suit claimed he was negligent for failing to diagnose the patient with internal bleeding and for not performing surgery.
“The lawsuit put a lot of stress on our family,” Dr. Sullivan recalled. “At the time my wife was pregnant. I was in law school, and I was also working full time in the ER to support our family. I remember my wife crying on the couch after reading the complaint and asking how the plaintiff’s attorney could get away with making the allegations he made.”
Dr. Sullivan soon learned that 15 medical providers in the patient’s medical record were named as defendants. This included the director of the radiology department, whose name was on a radiology report as “director” but who was actually out of the country when the incident occurred.
Despite some of the accusations being impossible, a medical expert had claimed there was a “meritorious claim” against every health professional named in the suit. Illinois is among the 28 states that require plaintiffs’ attorneys to file an affidavit of merit for medical malpractice claims to move forward.
Dr. Sullivan wondered who would endorse such outlandish accusations, but the expert’s identity was a mystery. According to Illinois law, About one-third of states with merit requirements permit anonymous experts, according to research and attorneys familiar with the issue.
Because the expert’s identity remains hidden, physicians have no way of knowing whether they were qualified to render an opinion, Dr. Sullivan said. The loopholes can drag out frivolous claims and waste significant time and expense, say legal experts. Frequently, it takes a year or more before innocent physicians are dismissed from unfounded lawsuits by the court or dropped when plaintiffs can’t support the claim.
“It’s hugely frustrating,” said Bruce Montoya, JD, a Colorado medical liability defense attorney. “You have an expert who is not disclosed. Further down the road, when experts are being deposed, the plaintiff does not have to reveal whether any of those testifying experts is the same one who certified the case. You never get to determine whether they, in fact, had a certificate reviewer who was legitimate.”
The laws have led to a recent outcry among physicians and fueled a revised resolution by the American College of Emergency Physicians (ACEP) denouncing anonymous affidavits of merit. (The revision has not yet been published online.)
“The minute experts are identified, they can be vetted,” said Rade B. Vukmir, MD, JD, chair of ACEP’s Medical Legal Committee. “There are reasons that you want to clarify the qualification and veracity of the witness. [Anonymous affidavits of merit] don’t allow that, and there’s something inherently wrong with that.”
Because the identities of consulting experts are unknown, it’s hard to know how many are unqualified. Expert witnesses who testify during trials, on the other hand, have long come under scrutiny for questionable qualifications. Some have come under fire for allegedly lying under oath about their experience, misrepresenting their credentials, and falsely representing their knowledge.
“Considering the known problem of potentially unethical expert witness testimony at trial, there’s is the potential likelihood that experts in anonymous affidavits of merit may sometimes lack the qualifications to give opinions,” said Dr. Vukmir, an emergency care physician in Pittsburgh.
Attorneys: Hidden experts increase costs, waste time
In Colorado, Mr. Montoya has seen firsthand how anonymous experts can prolong questionable claims and burden defendants.
Like Illinois, Colorado does not require attorneys to identify the medical experts used to fulfill its certificate of review statute. The expert consulted must have expertise in the same area of the alleged negligence, but does not have to practice in the same specialty, and the statute allows one expert to certify a lawsuit against multiple doctors.
In a recent case, Mr. Montoya represented a Denver neurosurgeon who was sued along with multiple other health care professionals. From the outset, Mr. Montoya argued the claim had no merit against the neurosurgeon, but the plaintiff’s attorney refused to dismiss the physician. Mr. Montoya asked whether the expert consulted for the certificate of merit was a neurosurgeon, but the attorney declined to disclose that information, he said.
The case progressed and Mr. Montoya eventually asked the judge to review the certificate of merit. By law, a judge can confidentially review the certificate of merit and decide whether it aligns with the state statute, but without disclosing the expert’s identity to the defense. The judge ruled the certificate appeared to conform with state law, and the case continued.
A year later, as both sides were getting ready to disclose their experts who would testify, Mr. Montoya again argued the neurosurgeon should be dropped from the suit. This time, he warned if the claim continued against the neurosurgeon, the defense would be filing a motion for summary judgment and pursuing attorney fees and costs. Colorado law allows for such fees if the filing or pursuit of an action is frivolous.
“Boom, my client was dismissed,” Mr. Montoya said. “This is a year later, after multiple conferences among the attorneys, multiple pleadings filed, expert witnesses retained to review the care, discovery exchanged, and records obtained. If we had [a stronger] certificate of review statute, it would have been a different ballgame. It’s never going to get a year down the road.”
In New York, physician defendants have experienced similar woes. The state’s law requires plaintiffs’ attorneys to certify that they consulted with a physician prior to filing the claim, and that they believe based on that discussion, there’s a reasonable basis for the claim to move forward. Attorneys are not required to disclose the expert’s identity.
The law also allows “an out,” explained Morris Auster, JD, senior vice president and chief legislative counsel for the Medical Society of the State of New York. If the attorney made three separate attempts to obtain a consultation, and all three experts would not agree to the consultation, the lawsuit can be filed anyway, he said.
“From our standpoint, it’s important to have an affidavit of merit requirement; it’s better than not having it,” Mr. Auster said. “But its effectiveness in providing control over the filing of lawsuits in New York has never been as strong as it could’ve been.”
Mr. Auster notes that New York has some of the highest liability costs in the country in addition to doctors paying some of the steepest medical liability insurance premiums.
“This really affects a lot of physicians and it’s driving physicians into employment arrangements, so they don’t have to deal with it on their own,” he said. “We support a number of measures to address these significantly high costs, and stronger certificate of merit requirements would certainly be one of those advocacy goals.”
Why are anonymous experts allowed?
Certificates of merit that shield the identity of consultants encourage a greater pool of physicians willing to review cases, said J. Matthew Dudley, JD, president of the Illinois Trial Lawyers Association. When the requirements first went into effect in Illinois, there was significant animosity among physicians toward doctors who testified in medical malpractice cases for patients, Mr. Dudley explained.
“Sometimes they would be ostracized from their professional societies, or it would hurt a referral relationship.” he said. “Over time, that animosity has lessened, but there was a concern that if the identity of physicians in certificates of merit weren’t protected, then doctors would not look at cases for patients.”
This would result in additional barriers for patients and their attorneys in pursuing their legal rights, Mr. Dudley said. He said Illinois’ certificate of merit statute is successful in fulfilling its intended purpose, and he has not seen any statistical evidence to suggest otherwise.
“It has proven effective at decreasing filings in medical malpractice and effectively screening medical malpractice cases,” he said. “Certificates of merit help to decrease filings by firms that aren’t that experienced in dealing with those kinds of cases.”
Kentucky is another state that does not require attorneys to identity the experts consulted for certificates of merit. Malpractice defense attorney Andrew DeSimone, JD, who practices in Kentucky, said this isn’t a problem since attorneys eventually must disclose the expert witnesses who will testify at trial.
“Knowing the name behind the certificate of merit is not that pertinent,” Mr. DeSimone said. “Physicians and their attorneys will ultimately have the chance to question and evaluate the expert witnesses used at trial. The certificate of merit is designed to weed out totally frivolous cases that do not have expert support. It’s not designed to be a trial on the merits.”
The belief that plaintiffs’ attorneys frequently bring weak cases and use unqualified experts to certify claims is not realistic or logical, added Sean Domnick, JD, a Florida medical malpractice attorney and vice president for the American Association for Justice. Medical malpractice cases are extremely challenging for plaintiffs – and they’re expensive, Mr. Domnick said.
“We can’t afford to take bad cases,” he said. “For me to take on a medical malpractice case, it’s not unusual for me to spend well over $100,000. Remember, if we lose, I don’t get that money back and I don’t get paid. Why in the world would a plaintiff take on that type of a burden for a case they didn’t believe in? The logic escapes me.”
In Florida, where Mr. Domnick practices, plaintiffs’ attorneys must send their certificates of merit to the defense with the expert identified. Domnick believes the requirement is a hindrance.
“It creates a delay that is unnecessary in a system that is already designed to wear our clients down,” he said. “It’s just another component that makes it harder on them.”
Hidden experts may insulate plaintiffs’ attorneys from liability
Dr. Sullivan, the Illinois emergency physician, was ultimately dismissed from the multiparty lawsuit, but not for roughly 18 months. After the dismissal, he fought back. He sued the plaintiff’s law firm for malicious prosecution, negligence in hiring, and relying on the opinion of an expert who was unqualified to render an opinion against an emergency physician.
The law firm, however, argued that it was immune from liability because it reasonably relied on the expert’s opinion as required by Illinois law. A trial court agreed with the plaintiffs’ firm. The judge denied Dr. Sullivan’s request to identify the expert, ruling there was no finding that the affidavit was untrue or made without reasonable cause. Dr. Sullivan appealed, and the appellate court upheld the trial’s court decision.
“As happened with my case, law firms can use the affidavit as a defense against countersuits or motions for sanctions,” Dr. Sullivan said. “Although the certificate of merit is intended to prevent attorneys from filing frivolous cases, it can also have the opposite effect of helping to insulate plaintiff attorneys from liability for filing a frivolous lawsuit.”
In Colorado, complaints about the state’s certificate of merit statute have gone before the Colorado Supreme Court. In one case, a lower court ruled that a certificate of merit was deficient because the consultants were not chiropractors. In another case, a nurse defendant argued the claim’s certificate of review was insufficient because the consulting expert was a physician.
In both instances, Colorado judges held the state’s statute does not require consultants to be in the same profession or the same specialty as the health professional defendant.
In New York, meanwhile, Mr. Auster said several bills to strengthen the state’s certificate of merit requirements have failed in recent years.
“It’s hard to say whether it will improve anytime soon,” he said. “The trial lawyers are a very powerful advocacy force in the state, and they tend to oppose even the slightest of changes in civil liability. [In addition], some of these issues have been put on a lower tier because of trying to manage the pandemic.”
Ultimately, Dr. Sullivan said that courts and legislatures need to strongly consider the ethics of allowing anonymous experts to provide testimony against defendant physicians.
“I also think we need to consider how the notion of a secret expert comports with a defendant physician’s due process,” he said. “If an expert’s opinion is appropriate, why would there be a need to shroud one’s identity in a veil of secrecy?”
A version of this article first appeared on Medscape.com.
When the hospital’s trauma team could not get an IV inserted into an accident victim, they called Illinois emergency physician William Sullivan, DO, JD, for help. Dr. Sullivan, who is based in the Chicago suburb of Frankfort, inserted a central line into the patient’s leg on his first attempt – a task that took about 20 minutes.
A year later, Dr. Sullivan was shocked and angry to learn he was being sued by the trauma patient’s family. Inserting the line was his only interaction with the woman, and he had no role in her care management, he said. Yet, the suit claimed he was negligent for failing to diagnose the patient with internal bleeding and for not performing surgery.
“The lawsuit put a lot of stress on our family,” Dr. Sullivan recalled. “At the time my wife was pregnant. I was in law school, and I was also working full time in the ER to support our family. I remember my wife crying on the couch after reading the complaint and asking how the plaintiff’s attorney could get away with making the allegations he made.”
Dr. Sullivan soon learned that 15 medical providers in the patient’s medical record were named as defendants. This included the director of the radiology department, whose name was on a radiology report as “director” but who was actually out of the country when the incident occurred.
Despite some of the accusations being impossible, a medical expert had claimed there was a “meritorious claim” against every health professional named in the suit. Illinois is among the 28 states that require plaintiffs’ attorneys to file an affidavit of merit for medical malpractice claims to move forward.
Dr. Sullivan wondered who would endorse such outlandish accusations, but the expert’s identity was a mystery. According to Illinois law, About one-third of states with merit requirements permit anonymous experts, according to research and attorneys familiar with the issue.
Because the expert’s identity remains hidden, physicians have no way of knowing whether they were qualified to render an opinion, Dr. Sullivan said. The loopholes can drag out frivolous claims and waste significant time and expense, say legal experts. Frequently, it takes a year or more before innocent physicians are dismissed from unfounded lawsuits by the court or dropped when plaintiffs can’t support the claim.
“It’s hugely frustrating,” said Bruce Montoya, JD, a Colorado medical liability defense attorney. “You have an expert who is not disclosed. Further down the road, when experts are being deposed, the plaintiff does not have to reveal whether any of those testifying experts is the same one who certified the case. You never get to determine whether they, in fact, had a certificate reviewer who was legitimate.”
The laws have led to a recent outcry among physicians and fueled a revised resolution by the American College of Emergency Physicians (ACEP) denouncing anonymous affidavits of merit. (The revision has not yet been published online.)
“The minute experts are identified, they can be vetted,” said Rade B. Vukmir, MD, JD, chair of ACEP’s Medical Legal Committee. “There are reasons that you want to clarify the qualification and veracity of the witness. [Anonymous affidavits of merit] don’t allow that, and there’s something inherently wrong with that.”
Because the identities of consulting experts are unknown, it’s hard to know how many are unqualified. Expert witnesses who testify during trials, on the other hand, have long come under scrutiny for questionable qualifications. Some have come under fire for allegedly lying under oath about their experience, misrepresenting their credentials, and falsely representing their knowledge.
“Considering the known problem of potentially unethical expert witness testimony at trial, there’s is the potential likelihood that experts in anonymous affidavits of merit may sometimes lack the qualifications to give opinions,” said Dr. Vukmir, an emergency care physician in Pittsburgh.
Attorneys: Hidden experts increase costs, waste time
In Colorado, Mr. Montoya has seen firsthand how anonymous experts can prolong questionable claims and burden defendants.
Like Illinois, Colorado does not require attorneys to identify the medical experts used to fulfill its certificate of review statute. The expert consulted must have expertise in the same area of the alleged negligence, but does not have to practice in the same specialty, and the statute allows one expert to certify a lawsuit against multiple doctors.
In a recent case, Mr. Montoya represented a Denver neurosurgeon who was sued along with multiple other health care professionals. From the outset, Mr. Montoya argued the claim had no merit against the neurosurgeon, but the plaintiff’s attorney refused to dismiss the physician. Mr. Montoya asked whether the expert consulted for the certificate of merit was a neurosurgeon, but the attorney declined to disclose that information, he said.
The case progressed and Mr. Montoya eventually asked the judge to review the certificate of merit. By law, a judge can confidentially review the certificate of merit and decide whether it aligns with the state statute, but without disclosing the expert’s identity to the defense. The judge ruled the certificate appeared to conform with state law, and the case continued.
A year later, as both sides were getting ready to disclose their experts who would testify, Mr. Montoya again argued the neurosurgeon should be dropped from the suit. This time, he warned if the claim continued against the neurosurgeon, the defense would be filing a motion for summary judgment and pursuing attorney fees and costs. Colorado law allows for such fees if the filing or pursuit of an action is frivolous.
“Boom, my client was dismissed,” Mr. Montoya said. “This is a year later, after multiple conferences among the attorneys, multiple pleadings filed, expert witnesses retained to review the care, discovery exchanged, and records obtained. If we had [a stronger] certificate of review statute, it would have been a different ballgame. It’s never going to get a year down the road.”
In New York, physician defendants have experienced similar woes. The state’s law requires plaintiffs’ attorneys to certify that they consulted with a physician prior to filing the claim, and that they believe based on that discussion, there’s a reasonable basis for the claim to move forward. Attorneys are not required to disclose the expert’s identity.
The law also allows “an out,” explained Morris Auster, JD, senior vice president and chief legislative counsel for the Medical Society of the State of New York. If the attorney made three separate attempts to obtain a consultation, and all three experts would not agree to the consultation, the lawsuit can be filed anyway, he said.
“From our standpoint, it’s important to have an affidavit of merit requirement; it’s better than not having it,” Mr. Auster said. “But its effectiveness in providing control over the filing of lawsuits in New York has never been as strong as it could’ve been.”
Mr. Auster notes that New York has some of the highest liability costs in the country in addition to doctors paying some of the steepest medical liability insurance premiums.
“This really affects a lot of physicians and it’s driving physicians into employment arrangements, so they don’t have to deal with it on their own,” he said. “We support a number of measures to address these significantly high costs, and stronger certificate of merit requirements would certainly be one of those advocacy goals.”
Why are anonymous experts allowed?
Certificates of merit that shield the identity of consultants encourage a greater pool of physicians willing to review cases, said J. Matthew Dudley, JD, president of the Illinois Trial Lawyers Association. When the requirements first went into effect in Illinois, there was significant animosity among physicians toward doctors who testified in medical malpractice cases for patients, Mr. Dudley explained.
“Sometimes they would be ostracized from their professional societies, or it would hurt a referral relationship.” he said. “Over time, that animosity has lessened, but there was a concern that if the identity of physicians in certificates of merit weren’t protected, then doctors would not look at cases for patients.”
This would result in additional barriers for patients and their attorneys in pursuing their legal rights, Mr. Dudley said. He said Illinois’ certificate of merit statute is successful in fulfilling its intended purpose, and he has not seen any statistical evidence to suggest otherwise.
“It has proven effective at decreasing filings in medical malpractice and effectively screening medical malpractice cases,” he said. “Certificates of merit help to decrease filings by firms that aren’t that experienced in dealing with those kinds of cases.”
Kentucky is another state that does not require attorneys to identity the experts consulted for certificates of merit. Malpractice defense attorney Andrew DeSimone, JD, who practices in Kentucky, said this isn’t a problem since attorneys eventually must disclose the expert witnesses who will testify at trial.
“Knowing the name behind the certificate of merit is not that pertinent,” Mr. DeSimone said. “Physicians and their attorneys will ultimately have the chance to question and evaluate the expert witnesses used at trial. The certificate of merit is designed to weed out totally frivolous cases that do not have expert support. It’s not designed to be a trial on the merits.”
The belief that plaintiffs’ attorneys frequently bring weak cases and use unqualified experts to certify claims is not realistic or logical, added Sean Domnick, JD, a Florida medical malpractice attorney and vice president for the American Association for Justice. Medical malpractice cases are extremely challenging for plaintiffs – and they’re expensive, Mr. Domnick said.
“We can’t afford to take bad cases,” he said. “For me to take on a medical malpractice case, it’s not unusual for me to spend well over $100,000. Remember, if we lose, I don’t get that money back and I don’t get paid. Why in the world would a plaintiff take on that type of a burden for a case they didn’t believe in? The logic escapes me.”
In Florida, where Mr. Domnick practices, plaintiffs’ attorneys must send their certificates of merit to the defense with the expert identified. Domnick believes the requirement is a hindrance.
“It creates a delay that is unnecessary in a system that is already designed to wear our clients down,” he said. “It’s just another component that makes it harder on them.”
Hidden experts may insulate plaintiffs’ attorneys from liability
Dr. Sullivan, the Illinois emergency physician, was ultimately dismissed from the multiparty lawsuit, but not for roughly 18 months. After the dismissal, he fought back. He sued the plaintiff’s law firm for malicious prosecution, negligence in hiring, and relying on the opinion of an expert who was unqualified to render an opinion against an emergency physician.
The law firm, however, argued that it was immune from liability because it reasonably relied on the expert’s opinion as required by Illinois law. A trial court agreed with the plaintiffs’ firm. The judge denied Dr. Sullivan’s request to identify the expert, ruling there was no finding that the affidavit was untrue or made without reasonable cause. Dr. Sullivan appealed, and the appellate court upheld the trial’s court decision.
“As happened with my case, law firms can use the affidavit as a defense against countersuits or motions for sanctions,” Dr. Sullivan said. “Although the certificate of merit is intended to prevent attorneys from filing frivolous cases, it can also have the opposite effect of helping to insulate plaintiff attorneys from liability for filing a frivolous lawsuit.”
In Colorado, complaints about the state’s certificate of merit statute have gone before the Colorado Supreme Court. In one case, a lower court ruled that a certificate of merit was deficient because the consultants were not chiropractors. In another case, a nurse defendant argued the claim’s certificate of review was insufficient because the consulting expert was a physician.
In both instances, Colorado judges held the state’s statute does not require consultants to be in the same profession or the same specialty as the health professional defendant.
In New York, meanwhile, Mr. Auster said several bills to strengthen the state’s certificate of merit requirements have failed in recent years.
“It’s hard to say whether it will improve anytime soon,” he said. “The trial lawyers are a very powerful advocacy force in the state, and they tend to oppose even the slightest of changes in civil liability. [In addition], some of these issues have been put on a lower tier because of trying to manage the pandemic.”
Ultimately, Dr. Sullivan said that courts and legislatures need to strongly consider the ethics of allowing anonymous experts to provide testimony against defendant physicians.
“I also think we need to consider how the notion of a secret expert comports with a defendant physician’s due process,” he said. “If an expert’s opinion is appropriate, why would there be a need to shroud one’s identity in a veil of secrecy?”
A version of this article first appeared on Medscape.com.
‘Together, we can demand improvements’: Stanford Health Care’s residents vote to join union
More than 81% of the health system’s resident physicians voted to join the union; the decision garnered 835 yes votes and 214 no votes, according to a CIR-SEIU announcement. The largest housestaff union in the United States and a local of the Service Employees International Union (SEIU), CIR-SEIU represents more than 20,000 resident physicians and fellows.
“With its successful representation with the Committee of Interns and Residents, Stanford housestaff now join the strong community of allied unions and fellow health care workers such as the Committee for Recognition of Nursing Achievement (CRONA), an independent union of Stanford nurses,” according to CIR-SEIU.
“We are organizing not only for a new economic contract that enables all potential housestaff and their families to afford living in the Bay Area but also for a new social contract that redefines how we are valued by the hospital system,” Ben Solomon, MD, PhD, a third-year resident physician in pediatrics at Stanford Medicine and a member of CIR-SEIU, said in an interview.
“This includes advocating for more humane working hours, reasonable parental leave, and childcare support, as well as resources to combat burnout in young physicians,” he added.
Lisa Kim, a spokesperson for Stanford Health Care, told this news organization that “a majority of residents and fellows at Stanford Health Care voted in favor of unionization. Of 1,478 total residents and fellows, 835 voted in favor. CIR/SEIU will be certified as the exclusive bargaining representative for all residents and fellows. Stanford Health Care does not plan to contest the election results.”
“As we begin the collective bargaining process, our goal remains unchanged: providing our residents and fellows with a world-class training experience. We will bring this same focus to negotiations as we strive to support their development as physician leaders,” she added.
The National Labor Relations Board (NLRB) must certify the election results before they are considered final, per CIR-SEIU. An independent federal agency, the NLRB safeguards employees’ rights to organize and determines whether union participation is appropriate while also preventing and remedying unfair labor practices committed by private sector employers and unions.
Concerns date back to initial COVID-19 vaccine rollout
The residents delivered a formal demand to Stanford Health Care to recognize the union in February; their request was not accepted by the health system. The residents’ concerns date as far back as the availability of the COVID-19 vaccines at the end of 2020.
Of the health system’s 5,000 doses, only seven residents and fellows were included in the initial round.
Niraj Sehgal, MD, chief medical officer for Stanford Health Care, apologized in a letter to the graduate medical education community, posted by Palo Alto Weekly, which revealed the root causes to be an algorithm used by the hospital and the age of the residents.
The vote by Stanford Health Care’s residents comes a day after nurses at Stanford and Lucile Packard Children’s hospitals ratified a new contract with their union after a strike for better working conditions and higher pay stretched on for a week, reported Palo Alto Online.
Part of a growing trend
Dr. Solomon got involved in the unionization effort at Stanford Health Care “to have a say in working conditions for residents and fellows,” he said. “As individuals, it’s virtually impossible to make demands to our hospital without risking our careers, but together we can demand improvements on the job and in patient care.”
The health system’s inability to extend COVID-19 vaccines during the initial rollout, “despite our role working with COVID patients on the frontlines,” spurred his involvement in the union effort, said Dr. Solomon.
In the short term, the union will be involved in negotiating its first contract, he said. “However, in the long term, we are committed to supporting the unionization efforts of residents and fellows across the country, including partnering with many housestaff unions here in California.”
Stanford Health Care’s residents are participating in a growing trend. In Worcester, Mass., UMass Medical School’s 613 residents and fellow physicians, who are also represented by CIR-SEIU, had their union certified by the Massachusetts Department of Labor Relations in March 2021, reported the (Worcester) Telegram & Gazette.
Other unionization efforts across the country include a supermajority of 85 interns, residents, and fellows employed by Keck School of Medicine of University of Southern California , who requested that Los Angeles County+USC Medical Center recognize their union, per an announcement. That’s in addition to residents at University of Vermont Medical Center, who announced their intention to unionize in March, reported VTDigger.org.
A version of this article first appeared on Medscape.com.
More than 81% of the health system’s resident physicians voted to join the union; the decision garnered 835 yes votes and 214 no votes, according to a CIR-SEIU announcement. The largest housestaff union in the United States and a local of the Service Employees International Union (SEIU), CIR-SEIU represents more than 20,000 resident physicians and fellows.
“With its successful representation with the Committee of Interns and Residents, Stanford housestaff now join the strong community of allied unions and fellow health care workers such as the Committee for Recognition of Nursing Achievement (CRONA), an independent union of Stanford nurses,” according to CIR-SEIU.
“We are organizing not only for a new economic contract that enables all potential housestaff and their families to afford living in the Bay Area but also for a new social contract that redefines how we are valued by the hospital system,” Ben Solomon, MD, PhD, a third-year resident physician in pediatrics at Stanford Medicine and a member of CIR-SEIU, said in an interview.
“This includes advocating for more humane working hours, reasonable parental leave, and childcare support, as well as resources to combat burnout in young physicians,” he added.
Lisa Kim, a spokesperson for Stanford Health Care, told this news organization that “a majority of residents and fellows at Stanford Health Care voted in favor of unionization. Of 1,478 total residents and fellows, 835 voted in favor. CIR/SEIU will be certified as the exclusive bargaining representative for all residents and fellows. Stanford Health Care does not plan to contest the election results.”
“As we begin the collective bargaining process, our goal remains unchanged: providing our residents and fellows with a world-class training experience. We will bring this same focus to negotiations as we strive to support their development as physician leaders,” she added.
The National Labor Relations Board (NLRB) must certify the election results before they are considered final, per CIR-SEIU. An independent federal agency, the NLRB safeguards employees’ rights to organize and determines whether union participation is appropriate while also preventing and remedying unfair labor practices committed by private sector employers and unions.
Concerns date back to initial COVID-19 vaccine rollout
The residents delivered a formal demand to Stanford Health Care to recognize the union in February; their request was not accepted by the health system. The residents’ concerns date as far back as the availability of the COVID-19 vaccines at the end of 2020.
Of the health system’s 5,000 doses, only seven residents and fellows were included in the initial round.
Niraj Sehgal, MD, chief medical officer for Stanford Health Care, apologized in a letter to the graduate medical education community, posted by Palo Alto Weekly, which revealed the root causes to be an algorithm used by the hospital and the age of the residents.
The vote by Stanford Health Care’s residents comes a day after nurses at Stanford and Lucile Packard Children’s hospitals ratified a new contract with their union after a strike for better working conditions and higher pay stretched on for a week, reported Palo Alto Online.
Part of a growing trend
Dr. Solomon got involved in the unionization effort at Stanford Health Care “to have a say in working conditions for residents and fellows,” he said. “As individuals, it’s virtually impossible to make demands to our hospital without risking our careers, but together we can demand improvements on the job and in patient care.”
The health system’s inability to extend COVID-19 vaccines during the initial rollout, “despite our role working with COVID patients on the frontlines,” spurred his involvement in the union effort, said Dr. Solomon.
In the short term, the union will be involved in negotiating its first contract, he said. “However, in the long term, we are committed to supporting the unionization efforts of residents and fellows across the country, including partnering with many housestaff unions here in California.”
Stanford Health Care’s residents are participating in a growing trend. In Worcester, Mass., UMass Medical School’s 613 residents and fellow physicians, who are also represented by CIR-SEIU, had their union certified by the Massachusetts Department of Labor Relations in March 2021, reported the (Worcester) Telegram & Gazette.
Other unionization efforts across the country include a supermajority of 85 interns, residents, and fellows employed by Keck School of Medicine of University of Southern California , who requested that Los Angeles County+USC Medical Center recognize their union, per an announcement. That’s in addition to residents at University of Vermont Medical Center, who announced their intention to unionize in March, reported VTDigger.org.
A version of this article first appeared on Medscape.com.
More than 81% of the health system’s resident physicians voted to join the union; the decision garnered 835 yes votes and 214 no votes, according to a CIR-SEIU announcement. The largest housestaff union in the United States and a local of the Service Employees International Union (SEIU), CIR-SEIU represents more than 20,000 resident physicians and fellows.
“With its successful representation with the Committee of Interns and Residents, Stanford housestaff now join the strong community of allied unions and fellow health care workers such as the Committee for Recognition of Nursing Achievement (CRONA), an independent union of Stanford nurses,” according to CIR-SEIU.
“We are organizing not only for a new economic contract that enables all potential housestaff and their families to afford living in the Bay Area but also for a new social contract that redefines how we are valued by the hospital system,” Ben Solomon, MD, PhD, a third-year resident physician in pediatrics at Stanford Medicine and a member of CIR-SEIU, said in an interview.
“This includes advocating for more humane working hours, reasonable parental leave, and childcare support, as well as resources to combat burnout in young physicians,” he added.
Lisa Kim, a spokesperson for Stanford Health Care, told this news organization that “a majority of residents and fellows at Stanford Health Care voted in favor of unionization. Of 1,478 total residents and fellows, 835 voted in favor. CIR/SEIU will be certified as the exclusive bargaining representative for all residents and fellows. Stanford Health Care does not plan to contest the election results.”
“As we begin the collective bargaining process, our goal remains unchanged: providing our residents and fellows with a world-class training experience. We will bring this same focus to negotiations as we strive to support their development as physician leaders,” she added.
The National Labor Relations Board (NLRB) must certify the election results before they are considered final, per CIR-SEIU. An independent federal agency, the NLRB safeguards employees’ rights to organize and determines whether union participation is appropriate while also preventing and remedying unfair labor practices committed by private sector employers and unions.
Concerns date back to initial COVID-19 vaccine rollout
The residents delivered a formal demand to Stanford Health Care to recognize the union in February; their request was not accepted by the health system. The residents’ concerns date as far back as the availability of the COVID-19 vaccines at the end of 2020.
Of the health system’s 5,000 doses, only seven residents and fellows were included in the initial round.
Niraj Sehgal, MD, chief medical officer for Stanford Health Care, apologized in a letter to the graduate medical education community, posted by Palo Alto Weekly, which revealed the root causes to be an algorithm used by the hospital and the age of the residents.
The vote by Stanford Health Care’s residents comes a day after nurses at Stanford and Lucile Packard Children’s hospitals ratified a new contract with their union after a strike for better working conditions and higher pay stretched on for a week, reported Palo Alto Online.
Part of a growing trend
Dr. Solomon got involved in the unionization effort at Stanford Health Care “to have a say in working conditions for residents and fellows,” he said. “As individuals, it’s virtually impossible to make demands to our hospital without risking our careers, but together we can demand improvements on the job and in patient care.”
The health system’s inability to extend COVID-19 vaccines during the initial rollout, “despite our role working with COVID patients on the frontlines,” spurred his involvement in the union effort, said Dr. Solomon.
In the short term, the union will be involved in negotiating its first contract, he said. “However, in the long term, we are committed to supporting the unionization efforts of residents and fellows across the country, including partnering with many housestaff unions here in California.”
Stanford Health Care’s residents are participating in a growing trend. In Worcester, Mass., UMass Medical School’s 613 residents and fellow physicians, who are also represented by CIR-SEIU, had their union certified by the Massachusetts Department of Labor Relations in March 2021, reported the (Worcester) Telegram & Gazette.
Other unionization efforts across the country include a supermajority of 85 interns, residents, and fellows employed by Keck School of Medicine of University of Southern California , who requested that Los Angeles County+USC Medical Center recognize their union, per an announcement. That’s in addition to residents at University of Vermont Medical Center, who announced their intention to unionize in March, reported VTDigger.org.
A version of this article first appeared on Medscape.com.
Docs find new and better ways to cut EHR documentation time
About 60% of physicians cite documenting information in the electronic health record and other paperwork as major contributors to burnout. Physicians have been working with a variety of ways to reduce their documentation burdens; could one of them be right for you?
The first is widely used speech-to-text software, which requires the doctors to manually enter the text into the EHR; the second uses artificial intelligence (AI) to not only turn speech into text but to also automatically organize it and enter it into the EHR.
These AI solutions, which are only a few years old, are widely considered to be a work in progress – but many doctors who have used these products are impressed.
Other people do the documenting: On-site scribes
“It’s estimated that now one in five to one in eight doctors use scribes,” said Jeffrey A. Gold, MD, an internist who has studied the phenomenon. Utilization is already very high in emergency medicine and has been surging in specialties such as orthopedic surgery; it is also growing in primary care.
Scribes work with the doctor and enter information into the EHR. Their numbers have reportedly been rising in recent years, as more doctors look for ways to cut back on their documentation, according to Dr. Gold, vice chair for quality and safety at the department of medicine at Oregon Health and Science University, Portland.
The price tag of $33,000 a year or more for an on-site scribe is a major barrier. And because the typical scribe only works for 1-1.5 years, they must be constantly hired and trained, which is done by scribing services such as Scrivas in Miami.
However, Scrivas CEO Fernando G. Mendoza, MD, said scribes typically pay for themselves because they allow physicians to see more patients. Scribes can save doctors 2-3 hours of work per day, increase reimbursement by around 20% by producing more detailed notes, and improve satisfaction for both patients and doctors, according to several studies. In one study, physician documentation time significantly decreased, averaging 3 minutes per patient and 36 minutes per session.
Despite these possible savings, many health systems resisted hiring scribes for their employed physicians until the past few years, according to Kevin Brady, president of Physicians Angels, a scribing service based in Toledo, Ohio. “They figured they’d just spent millions on EHRs and didn’t want to spend any more,” he said. “They were also waiting for the EHR vendors to simplify documentation, but that never happened.”
Mr. Brady said what finally convinced many systems to invest in scribes was the need to reduce physician turnover and improve recruitment. Newly minted physicians often look for jobs that don’t interfere with their leisure time.
On-site scribes
On-site scribes accompany the doctor into the exam room and type the note during the encounter. Typically, the note is completed when the encounter is over, allowing for orders to be carried out immediately.
The traditional scribe is a premed student who wants to get acquainted with medicine and is thus willing to make a fairly low income. This career trajectory is the reason scribes have a high turnover. As demand surged, the scribe pool was supplemented with students aspiring to other health care professions like nursing, and even with people who want to make a career of scribing.
Since scribes have to set aside time for studying, scribe companies provide each physician-customer with one or two backup scribes. Dr. Mendoza bills his scribes as “personal assistants” who can do some nonclinical tasks beyond filling in the EHR, such as reminding doctors about the need to order a test or check in on another patient briefly before moving on to the next exam room.
Dr. Gold, however, warned against allowing “functional creep,” where scribes are asked to carry out tasks beyond their abilities, such as interpreting medical data. He added that doctors are expected to read through and sign all scribe-generated orders.
Some practices grow their own scribes, cross-training their medical assistants (MAs) to do the work. This addresses the turnover problem and could reduce costs. MAs already know clinical terms and how the doctor works, and they may be able to get special training at a local community college. However, some MAs do not want this extra work, and in any case, the work would take them away from other duties.
How often do physicians use their scribes? “Our doctors generally use them for all of their visits, but surgeons tend to limit use to their clinic days when they’re not in surgery,” said Tony Andrulonis, MD, president of ScribeAmerica in Fort Lauderdale, Fla.
Virtual scribes work off-site
Virtual scribes, who operate remotely from the doctor and can cost up to $10 less per hour than on-site scribes, got a boost during the COVID-19 pandemic because they fit well with telemedicine visits. Furthermore, the growing availability of virtual scribes from abroad has made scribes even more affordable.
“When doctors could no longer work on-site due to the pandemic, they replaced their on-site scribes with virtual scribes, and to some extent this trend is still going on,” Dr. Gold said.
One downside with virtual scribes is that they cannot do many of the extra tasks that on-site scribes can do. However, they are often a necessity in rural areas where on-site scribes are not available. In addition to having an audio-video connection, they may also just be on audio in areas where internet reception is poor or the patient wants privacy, Dr. Andrulonis said.
Mr. Brady said Physicians Angels uses offshore scribes from India. The company charges $16-$18 per hour, compared with $26-$28 per hour for U.S.-based virtual scribes. He said well over half of his clients are family physicians, who appreciate the lower cost.
Another advantage of offshore scribes is slower turnover and full-time availability. Mr. Brady said his scribes usually stay with the company for 5-6 years and are always available. “This is their full-time job,” Brady said.
Mr. Brady said when large organizations arrange with his company for scribes, often the goal is that the scribes pay for themselves. “They’ll tell their doctors: ‘We’ll let you have scribes as long as you see one or two more patients a day,’ ” he said. Mr. Brady then helps the organization reach that goal, which he said is easily achievable, except when doctors have no clear incentive to see more patients. He also works with clients on other goals, such as higher quality of life or time saved.
Speech-to-text software
For years, doctors have been using speech-to-text software to transform their speech into notes. They speak into the microphone, calling out punctuation and referring to prep-made templates for routine tasks. As they speak, the text appears on a screen. They can correct the text if necessary, and then they must put that information into the EHR.
Speech-to-text systems are used by more physicians than those using human scribes. Nuance’s Dragon Medical One system is the most popular, with more than 1000 large healthcare organizations signed up. Competitors include Dolbey, Entrada, and nVoq.
Prices are just a fraction of the cost of a human scribe. Dolbey’s Fusion Narrate system, for example, costs about $800-$850 a year per user. Doctors should shop around for these systems, because prices can vary by 30%-50%, said Wayne Kaniewski, MD, a retired family and urgent care physician and now owner and CEO of Twin Cities EMR Consulting in Minneapolis.
As a contracted reseller of the nVoq and Dolbey systems, Dr. Kaniewski provides training and support. During 13 years in business, he said machine dictation systems have become faster, more accurate, and, thanks to cloud-based technology, easier to set up.
Digital assistants
AI software, also known as digital assistants, takes speech-to-text software to the next logical step – organizing and automatically entering the information into the EHR. Using ambient technology, a smartphone captures the physician-patient conversation in the exam room, extracts the needed information, and distributes it in the EHR.
The cost is about one-sixth that of a human scribe, but higher than the cost for speech-to-text software because the technology still makes errors and requires a human at the software company to guide the process.
Currently about 10 companies sell digital scribes, including Nuance’s Dragon Medical One, NoteSwift, DeepScribe, and ScribeAmerica. These systems can be connected to the major EHR systems, and in some cases EHR systems have agreements with digital scribe vendors so that their systems can be seamlessly connected.
“DAX software can understand nonlinear conversations – the way normal conversations bounce from topic to topic,” said Kenneth Harper, general manager of Nuance’s Ambient Clinical Intelligence Division. “This level of technology was not possible 5 years ago.”
Mr. Harper said DAX saves doctors 6 minutes per patient on average, and 70% of doctors using it reported less burnout and fatigue. Kansas University Medical Center has been testing DAX with physicians there. Many of them no longer need to write up their notes after hours, said Denton Shanks, DO, the medical center’s digital health medical director.
One of the things Dr. Shanks likes about DAX is that it remembers all the details of a visit. As a family physician, “there are something like 15 different problems that come up in one typical visit. Before, I had to carry those problems in my head, and when I wrote up my notes at the end of the day, I might have forgotten a few of them. Not so with DAX.”
Dr. Shanks knows he has to speak clearly and unambiguously when using DAX. “DAX can only document what it hears, so I describe what I am looking at in a physical exam or I might further explain the patient’s account so DAX can pick up on it.”
Are digital assistants ready for doctors?
Since a human at the software company is needed to guide the system, it takes a few hours for the digital assistant to complete entries into the EHR, but vendors are looking for ways to eliminate human guidance.
“We’re definitely moving toward digital scribes, but we’re not there yet,” Dr. Gold said, pointing to a 2018 study that found a significantly higher error rate for speech recognition software than for human scribes.
Dr. Kaniewski added that digital scribes pick up a great deal of irrelevant information, making for a bloated note. “Clinicians must then edit the note down, which is more work than just dictating a concise note,” he said.
Many doctors, however, are happy with these new systems. Steven Y. Lin, MD, a family physician who has been testing a digital scribe system with 40 fellow clinicians at Stanford (Calif.) Health Care, said 95% of clinicians who stayed with the trial are continuing to use the system, but he concedes that there was a relatively high dropout rate. “These people felt that they had lost control of the process when using the software.”
Furthermore, Dr. Lin is concerned that using a digital scribe may eliminate doctors’ crucial step of sitting down and writing the clinical note. Here “doctors bring together everything they have heard and then come up with the diagnosis and treatment.” He recognized that doctors could still take this step when reviewing the digital note, but it would be easy to skip.
What is the future for documentation aids?
Increasingly more doctors are finding ways to expedite documentation tasks. Speech-to-text software is still the most popular solution, but more physicians are now using human scribes, driven by the decisions of some large organizations to start paying for them.
However, these physicians are often expected to work harder in order for the scribes to pay for themselves, which is a solution that could, ironically, add to burnout rather than alleviate it.
Digital assistants answer these concerns because they are more affordable and are supposed to do all the work of human scribes. This software parses the physician-patient conversation into a clinical note and other data and deposits them directly into the EHR.
Most experts think digital assistants will eventually meet their promise, but it is widely thought that they’re not ready yet. It will be up to vendors like Nuance to convince skeptics that their products are ready for doctors.
A version of this article first appeared on Medscape.com.
About 60% of physicians cite documenting information in the electronic health record and other paperwork as major contributors to burnout. Physicians have been working with a variety of ways to reduce their documentation burdens; could one of them be right for you?
The first is widely used speech-to-text software, which requires the doctors to manually enter the text into the EHR; the second uses artificial intelligence (AI) to not only turn speech into text but to also automatically organize it and enter it into the EHR.
These AI solutions, which are only a few years old, are widely considered to be a work in progress – but many doctors who have used these products are impressed.
Other people do the documenting: On-site scribes
“It’s estimated that now one in five to one in eight doctors use scribes,” said Jeffrey A. Gold, MD, an internist who has studied the phenomenon. Utilization is already very high in emergency medicine and has been surging in specialties such as orthopedic surgery; it is also growing in primary care.
Scribes work with the doctor and enter information into the EHR. Their numbers have reportedly been rising in recent years, as more doctors look for ways to cut back on their documentation, according to Dr. Gold, vice chair for quality and safety at the department of medicine at Oregon Health and Science University, Portland.
The price tag of $33,000 a year or more for an on-site scribe is a major barrier. And because the typical scribe only works for 1-1.5 years, they must be constantly hired and trained, which is done by scribing services such as Scrivas in Miami.
However, Scrivas CEO Fernando G. Mendoza, MD, said scribes typically pay for themselves because they allow physicians to see more patients. Scribes can save doctors 2-3 hours of work per day, increase reimbursement by around 20% by producing more detailed notes, and improve satisfaction for both patients and doctors, according to several studies. In one study, physician documentation time significantly decreased, averaging 3 minutes per patient and 36 minutes per session.
Despite these possible savings, many health systems resisted hiring scribes for their employed physicians until the past few years, according to Kevin Brady, president of Physicians Angels, a scribing service based in Toledo, Ohio. “They figured they’d just spent millions on EHRs and didn’t want to spend any more,” he said. “They were also waiting for the EHR vendors to simplify documentation, but that never happened.”
Mr. Brady said what finally convinced many systems to invest in scribes was the need to reduce physician turnover and improve recruitment. Newly minted physicians often look for jobs that don’t interfere with their leisure time.
On-site scribes
On-site scribes accompany the doctor into the exam room and type the note during the encounter. Typically, the note is completed when the encounter is over, allowing for orders to be carried out immediately.
The traditional scribe is a premed student who wants to get acquainted with medicine and is thus willing to make a fairly low income. This career trajectory is the reason scribes have a high turnover. As demand surged, the scribe pool was supplemented with students aspiring to other health care professions like nursing, and even with people who want to make a career of scribing.
Since scribes have to set aside time for studying, scribe companies provide each physician-customer with one or two backup scribes. Dr. Mendoza bills his scribes as “personal assistants” who can do some nonclinical tasks beyond filling in the EHR, such as reminding doctors about the need to order a test or check in on another patient briefly before moving on to the next exam room.
Dr. Gold, however, warned against allowing “functional creep,” where scribes are asked to carry out tasks beyond their abilities, such as interpreting medical data. He added that doctors are expected to read through and sign all scribe-generated orders.
Some practices grow their own scribes, cross-training their medical assistants (MAs) to do the work. This addresses the turnover problem and could reduce costs. MAs already know clinical terms and how the doctor works, and they may be able to get special training at a local community college. However, some MAs do not want this extra work, and in any case, the work would take them away from other duties.
How often do physicians use their scribes? “Our doctors generally use them for all of their visits, but surgeons tend to limit use to their clinic days when they’re not in surgery,” said Tony Andrulonis, MD, president of ScribeAmerica in Fort Lauderdale, Fla.
Virtual scribes work off-site
Virtual scribes, who operate remotely from the doctor and can cost up to $10 less per hour than on-site scribes, got a boost during the COVID-19 pandemic because they fit well with telemedicine visits. Furthermore, the growing availability of virtual scribes from abroad has made scribes even more affordable.
“When doctors could no longer work on-site due to the pandemic, they replaced their on-site scribes with virtual scribes, and to some extent this trend is still going on,” Dr. Gold said.
One downside with virtual scribes is that they cannot do many of the extra tasks that on-site scribes can do. However, they are often a necessity in rural areas where on-site scribes are not available. In addition to having an audio-video connection, they may also just be on audio in areas where internet reception is poor or the patient wants privacy, Dr. Andrulonis said.
Mr. Brady said Physicians Angels uses offshore scribes from India. The company charges $16-$18 per hour, compared with $26-$28 per hour for U.S.-based virtual scribes. He said well over half of his clients are family physicians, who appreciate the lower cost.
Another advantage of offshore scribes is slower turnover and full-time availability. Mr. Brady said his scribes usually stay with the company for 5-6 years and are always available. “This is their full-time job,” Brady said.
Mr. Brady said when large organizations arrange with his company for scribes, often the goal is that the scribes pay for themselves. “They’ll tell their doctors: ‘We’ll let you have scribes as long as you see one or two more patients a day,’ ” he said. Mr. Brady then helps the organization reach that goal, which he said is easily achievable, except when doctors have no clear incentive to see more patients. He also works with clients on other goals, such as higher quality of life or time saved.
Speech-to-text software
For years, doctors have been using speech-to-text software to transform their speech into notes. They speak into the microphone, calling out punctuation and referring to prep-made templates for routine tasks. As they speak, the text appears on a screen. They can correct the text if necessary, and then they must put that information into the EHR.
Speech-to-text systems are used by more physicians than those using human scribes. Nuance’s Dragon Medical One system is the most popular, with more than 1000 large healthcare organizations signed up. Competitors include Dolbey, Entrada, and nVoq.
Prices are just a fraction of the cost of a human scribe. Dolbey’s Fusion Narrate system, for example, costs about $800-$850 a year per user. Doctors should shop around for these systems, because prices can vary by 30%-50%, said Wayne Kaniewski, MD, a retired family and urgent care physician and now owner and CEO of Twin Cities EMR Consulting in Minneapolis.
As a contracted reseller of the nVoq and Dolbey systems, Dr. Kaniewski provides training and support. During 13 years in business, he said machine dictation systems have become faster, more accurate, and, thanks to cloud-based technology, easier to set up.
Digital assistants
AI software, also known as digital assistants, takes speech-to-text software to the next logical step – organizing and automatically entering the information into the EHR. Using ambient technology, a smartphone captures the physician-patient conversation in the exam room, extracts the needed information, and distributes it in the EHR.
The cost is about one-sixth that of a human scribe, but higher than the cost for speech-to-text software because the technology still makes errors and requires a human at the software company to guide the process.
Currently about 10 companies sell digital scribes, including Nuance’s Dragon Medical One, NoteSwift, DeepScribe, and ScribeAmerica. These systems can be connected to the major EHR systems, and in some cases EHR systems have agreements with digital scribe vendors so that their systems can be seamlessly connected.
“DAX software can understand nonlinear conversations – the way normal conversations bounce from topic to topic,” said Kenneth Harper, general manager of Nuance’s Ambient Clinical Intelligence Division. “This level of technology was not possible 5 years ago.”
Mr. Harper said DAX saves doctors 6 minutes per patient on average, and 70% of doctors using it reported less burnout and fatigue. Kansas University Medical Center has been testing DAX with physicians there. Many of them no longer need to write up their notes after hours, said Denton Shanks, DO, the medical center’s digital health medical director.
One of the things Dr. Shanks likes about DAX is that it remembers all the details of a visit. As a family physician, “there are something like 15 different problems that come up in one typical visit. Before, I had to carry those problems in my head, and when I wrote up my notes at the end of the day, I might have forgotten a few of them. Not so with DAX.”
Dr. Shanks knows he has to speak clearly and unambiguously when using DAX. “DAX can only document what it hears, so I describe what I am looking at in a physical exam or I might further explain the patient’s account so DAX can pick up on it.”
Are digital assistants ready for doctors?
Since a human at the software company is needed to guide the system, it takes a few hours for the digital assistant to complete entries into the EHR, but vendors are looking for ways to eliminate human guidance.
“We’re definitely moving toward digital scribes, but we’re not there yet,” Dr. Gold said, pointing to a 2018 study that found a significantly higher error rate for speech recognition software than for human scribes.
Dr. Kaniewski added that digital scribes pick up a great deal of irrelevant information, making for a bloated note. “Clinicians must then edit the note down, which is more work than just dictating a concise note,” he said.
Many doctors, however, are happy with these new systems. Steven Y. Lin, MD, a family physician who has been testing a digital scribe system with 40 fellow clinicians at Stanford (Calif.) Health Care, said 95% of clinicians who stayed with the trial are continuing to use the system, but he concedes that there was a relatively high dropout rate. “These people felt that they had lost control of the process when using the software.”
Furthermore, Dr. Lin is concerned that using a digital scribe may eliminate doctors’ crucial step of sitting down and writing the clinical note. Here “doctors bring together everything they have heard and then come up with the diagnosis and treatment.” He recognized that doctors could still take this step when reviewing the digital note, but it would be easy to skip.
What is the future for documentation aids?
Increasingly more doctors are finding ways to expedite documentation tasks. Speech-to-text software is still the most popular solution, but more physicians are now using human scribes, driven by the decisions of some large organizations to start paying for them.
However, these physicians are often expected to work harder in order for the scribes to pay for themselves, which is a solution that could, ironically, add to burnout rather than alleviate it.
Digital assistants answer these concerns because they are more affordable and are supposed to do all the work of human scribes. This software parses the physician-patient conversation into a clinical note and other data and deposits them directly into the EHR.
Most experts think digital assistants will eventually meet their promise, but it is widely thought that they’re not ready yet. It will be up to vendors like Nuance to convince skeptics that their products are ready for doctors.
A version of this article first appeared on Medscape.com.
About 60% of physicians cite documenting information in the electronic health record and other paperwork as major contributors to burnout. Physicians have been working with a variety of ways to reduce their documentation burdens; could one of them be right for you?
The first is widely used speech-to-text software, which requires the doctors to manually enter the text into the EHR; the second uses artificial intelligence (AI) to not only turn speech into text but to also automatically organize it and enter it into the EHR.
These AI solutions, which are only a few years old, are widely considered to be a work in progress – but many doctors who have used these products are impressed.
Other people do the documenting: On-site scribes
“It’s estimated that now one in five to one in eight doctors use scribes,” said Jeffrey A. Gold, MD, an internist who has studied the phenomenon. Utilization is already very high in emergency medicine and has been surging in specialties such as orthopedic surgery; it is also growing in primary care.
Scribes work with the doctor and enter information into the EHR. Their numbers have reportedly been rising in recent years, as more doctors look for ways to cut back on their documentation, according to Dr. Gold, vice chair for quality and safety at the department of medicine at Oregon Health and Science University, Portland.
The price tag of $33,000 a year or more for an on-site scribe is a major barrier. And because the typical scribe only works for 1-1.5 years, they must be constantly hired and trained, which is done by scribing services such as Scrivas in Miami.
However, Scrivas CEO Fernando G. Mendoza, MD, said scribes typically pay for themselves because they allow physicians to see more patients. Scribes can save doctors 2-3 hours of work per day, increase reimbursement by around 20% by producing more detailed notes, and improve satisfaction for both patients and doctors, according to several studies. In one study, physician documentation time significantly decreased, averaging 3 minutes per patient and 36 minutes per session.
Despite these possible savings, many health systems resisted hiring scribes for their employed physicians until the past few years, according to Kevin Brady, president of Physicians Angels, a scribing service based in Toledo, Ohio. “They figured they’d just spent millions on EHRs and didn’t want to spend any more,” he said. “They were also waiting for the EHR vendors to simplify documentation, but that never happened.”
Mr. Brady said what finally convinced many systems to invest in scribes was the need to reduce physician turnover and improve recruitment. Newly minted physicians often look for jobs that don’t interfere with their leisure time.
On-site scribes
On-site scribes accompany the doctor into the exam room and type the note during the encounter. Typically, the note is completed when the encounter is over, allowing for orders to be carried out immediately.
The traditional scribe is a premed student who wants to get acquainted with medicine and is thus willing to make a fairly low income. This career trajectory is the reason scribes have a high turnover. As demand surged, the scribe pool was supplemented with students aspiring to other health care professions like nursing, and even with people who want to make a career of scribing.
Since scribes have to set aside time for studying, scribe companies provide each physician-customer with one or two backup scribes. Dr. Mendoza bills his scribes as “personal assistants” who can do some nonclinical tasks beyond filling in the EHR, such as reminding doctors about the need to order a test or check in on another patient briefly before moving on to the next exam room.
Dr. Gold, however, warned against allowing “functional creep,” where scribes are asked to carry out tasks beyond their abilities, such as interpreting medical data. He added that doctors are expected to read through and sign all scribe-generated orders.
Some practices grow their own scribes, cross-training their medical assistants (MAs) to do the work. This addresses the turnover problem and could reduce costs. MAs already know clinical terms and how the doctor works, and they may be able to get special training at a local community college. However, some MAs do not want this extra work, and in any case, the work would take them away from other duties.
How often do physicians use their scribes? “Our doctors generally use them for all of their visits, but surgeons tend to limit use to their clinic days when they’re not in surgery,” said Tony Andrulonis, MD, president of ScribeAmerica in Fort Lauderdale, Fla.
Virtual scribes work off-site
Virtual scribes, who operate remotely from the doctor and can cost up to $10 less per hour than on-site scribes, got a boost during the COVID-19 pandemic because they fit well with telemedicine visits. Furthermore, the growing availability of virtual scribes from abroad has made scribes even more affordable.
“When doctors could no longer work on-site due to the pandemic, they replaced their on-site scribes with virtual scribes, and to some extent this trend is still going on,” Dr. Gold said.
One downside with virtual scribes is that they cannot do many of the extra tasks that on-site scribes can do. However, they are often a necessity in rural areas where on-site scribes are not available. In addition to having an audio-video connection, they may also just be on audio in areas where internet reception is poor or the patient wants privacy, Dr. Andrulonis said.
Mr. Brady said Physicians Angels uses offshore scribes from India. The company charges $16-$18 per hour, compared with $26-$28 per hour for U.S.-based virtual scribes. He said well over half of his clients are family physicians, who appreciate the lower cost.
Another advantage of offshore scribes is slower turnover and full-time availability. Mr. Brady said his scribes usually stay with the company for 5-6 years and are always available. “This is their full-time job,” Brady said.
Mr. Brady said when large organizations arrange with his company for scribes, often the goal is that the scribes pay for themselves. “They’ll tell their doctors: ‘We’ll let you have scribes as long as you see one or two more patients a day,’ ” he said. Mr. Brady then helps the organization reach that goal, which he said is easily achievable, except when doctors have no clear incentive to see more patients. He also works with clients on other goals, such as higher quality of life or time saved.
Speech-to-text software
For years, doctors have been using speech-to-text software to transform their speech into notes. They speak into the microphone, calling out punctuation and referring to prep-made templates for routine tasks. As they speak, the text appears on a screen. They can correct the text if necessary, and then they must put that information into the EHR.
Speech-to-text systems are used by more physicians than those using human scribes. Nuance’s Dragon Medical One system is the most popular, with more than 1000 large healthcare organizations signed up. Competitors include Dolbey, Entrada, and nVoq.
Prices are just a fraction of the cost of a human scribe. Dolbey’s Fusion Narrate system, for example, costs about $800-$850 a year per user. Doctors should shop around for these systems, because prices can vary by 30%-50%, said Wayne Kaniewski, MD, a retired family and urgent care physician and now owner and CEO of Twin Cities EMR Consulting in Minneapolis.
As a contracted reseller of the nVoq and Dolbey systems, Dr. Kaniewski provides training and support. During 13 years in business, he said machine dictation systems have become faster, more accurate, and, thanks to cloud-based technology, easier to set up.
Digital assistants
AI software, also known as digital assistants, takes speech-to-text software to the next logical step – organizing and automatically entering the information into the EHR. Using ambient technology, a smartphone captures the physician-patient conversation in the exam room, extracts the needed information, and distributes it in the EHR.
The cost is about one-sixth that of a human scribe, but higher than the cost for speech-to-text software because the technology still makes errors and requires a human at the software company to guide the process.
Currently about 10 companies sell digital scribes, including Nuance’s Dragon Medical One, NoteSwift, DeepScribe, and ScribeAmerica. These systems can be connected to the major EHR systems, and in some cases EHR systems have agreements with digital scribe vendors so that their systems can be seamlessly connected.
“DAX software can understand nonlinear conversations – the way normal conversations bounce from topic to topic,” said Kenneth Harper, general manager of Nuance’s Ambient Clinical Intelligence Division. “This level of technology was not possible 5 years ago.”
Mr. Harper said DAX saves doctors 6 minutes per patient on average, and 70% of doctors using it reported less burnout and fatigue. Kansas University Medical Center has been testing DAX with physicians there. Many of them no longer need to write up their notes after hours, said Denton Shanks, DO, the medical center’s digital health medical director.
One of the things Dr. Shanks likes about DAX is that it remembers all the details of a visit. As a family physician, “there are something like 15 different problems that come up in one typical visit. Before, I had to carry those problems in my head, and when I wrote up my notes at the end of the day, I might have forgotten a few of them. Not so with DAX.”
Dr. Shanks knows he has to speak clearly and unambiguously when using DAX. “DAX can only document what it hears, so I describe what I am looking at in a physical exam or I might further explain the patient’s account so DAX can pick up on it.”
Are digital assistants ready for doctors?
Since a human at the software company is needed to guide the system, it takes a few hours for the digital assistant to complete entries into the EHR, but vendors are looking for ways to eliminate human guidance.
“We’re definitely moving toward digital scribes, but we’re not there yet,” Dr. Gold said, pointing to a 2018 study that found a significantly higher error rate for speech recognition software than for human scribes.
Dr. Kaniewski added that digital scribes pick up a great deal of irrelevant information, making for a bloated note. “Clinicians must then edit the note down, which is more work than just dictating a concise note,” he said.
Many doctors, however, are happy with these new systems. Steven Y. Lin, MD, a family physician who has been testing a digital scribe system with 40 fellow clinicians at Stanford (Calif.) Health Care, said 95% of clinicians who stayed with the trial are continuing to use the system, but he concedes that there was a relatively high dropout rate. “These people felt that they had lost control of the process when using the software.”
Furthermore, Dr. Lin is concerned that using a digital scribe may eliminate doctors’ crucial step of sitting down and writing the clinical note. Here “doctors bring together everything they have heard and then come up with the diagnosis and treatment.” He recognized that doctors could still take this step when reviewing the digital note, but it would be easy to skip.
What is the future for documentation aids?
Increasingly more doctors are finding ways to expedite documentation tasks. Speech-to-text software is still the most popular solution, but more physicians are now using human scribes, driven by the decisions of some large organizations to start paying for them.
However, these physicians are often expected to work harder in order for the scribes to pay for themselves, which is a solution that could, ironically, add to burnout rather than alleviate it.
Digital assistants answer these concerns because they are more affordable and are supposed to do all the work of human scribes. This software parses the physician-patient conversation into a clinical note and other data and deposits them directly into the EHR.
Most experts think digital assistants will eventually meet their promise, but it is widely thought that they’re not ready yet. It will be up to vendors like Nuance to convince skeptics that their products are ready for doctors.
A version of this article first appeared on Medscape.com.
How Dermatology Residents Can Best Serve the Needs of the LGBT Community
The chances are good that at least one patient you saw today could have been provided a better environment to foster your patient-physician relationship. A 2020 Gallup poll revealed that an estimated 5.6% of US adults identified as lesbian, gay, bisexual, and transgender (LGBT).1 Based on the estimated US population of 331.7 million individuals on December 3, 2020, this means that approximately 18.6 million identified as LGBT and could potentially require health care services.2 These numbers highlight the increasing need within the medical community to provide quality and accessible care to the LGBT community, and dermatologists have a role to play. They treat conditions that are apparent to the patient and others around them, attracting those that may not be motivated to see different physicians. They can not only help with skin diseases that affect all patients but also can train other physicians to screen for some dermatologic diseases that may have a higher prevalence within the LGBT community. Dermatologists have a unique opportunity to help patients better reflect themselves through both surgical and nonsurgical modalities.
Demographics and Definitions
To discuss this topic effectively, it is important to define LGBT terms (Table).3 As a disclaimer, language is fluid. Despite a word or term currently being used and accepted, it quickly can become obsolete. A clinician can always do research, follow the lead of the patient, and respectfully ask questions if there is ever confusion surrounding terminology. Patients do not expect every physician they encounter to be an expert in this subject. What is most important is that patients are approached with an open mind and humility with the goal of providing optimal care.
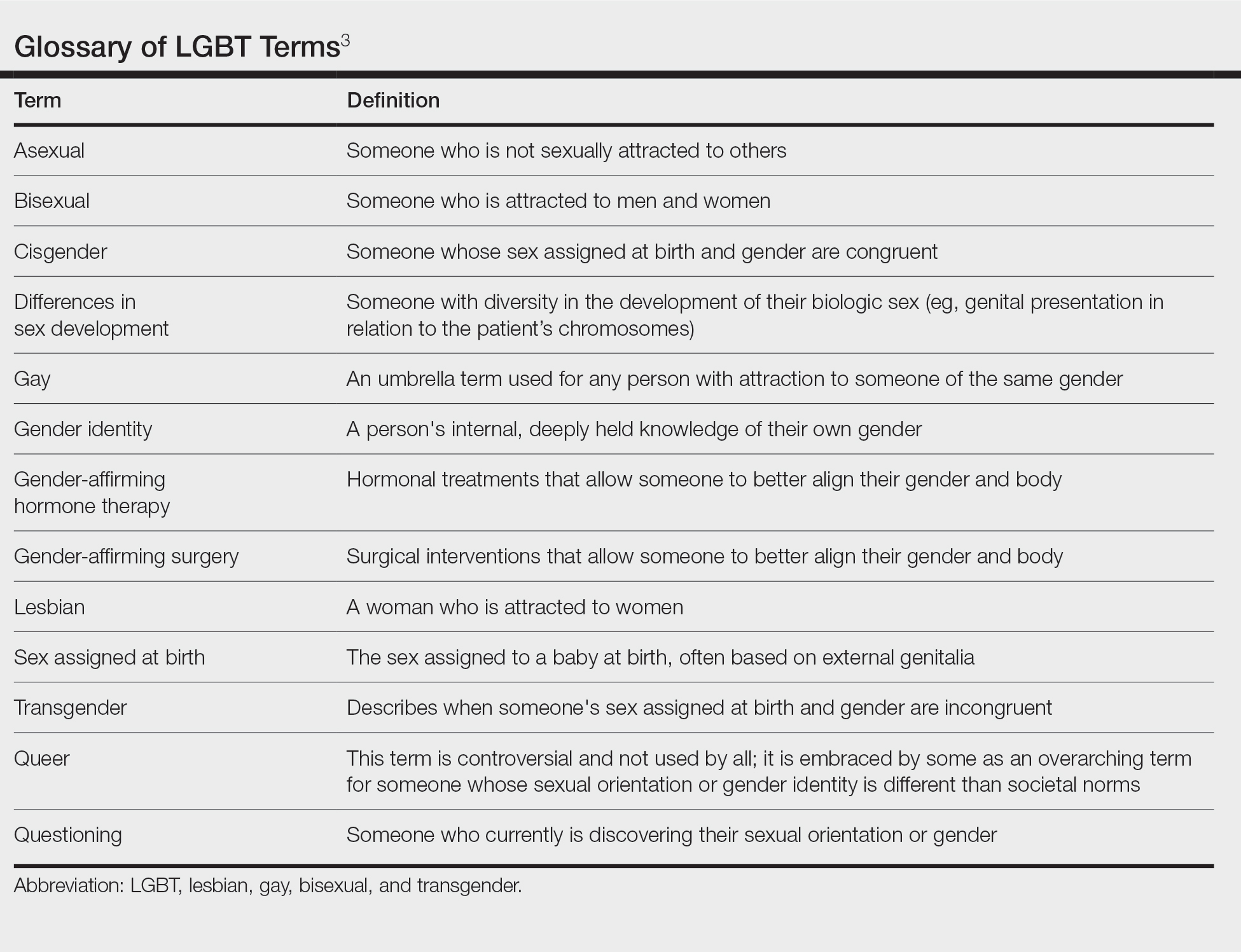
Although the federal government now uses the term sexual and gender minorities (SGM), the more specific terms lesbian, gay, bisexual, and transgender usually are preferred.3,4 Other letters are at times added to the acronym LGBT, including Q for questioning or queer, I for intersex, and A for asexual; all of these letters are under the larger SGM umbrella. Because LGBT is the most commonly used acronym in the daily vernacular, it will be the default for this article.
A term describing sexual orientation does not necessarily describe sexual practices. A woman who identifies as straight may have sex with both men and women, and a gay man may not have sex at all. To be more descriptive regarding sexual practices, one may use the terms men who have sex with men or women who have sex with women.3 Because of this nuance, it is important to elicit a sexual history when speaking to all patients in a forward nonjudgmental manner.
The term transgender is used to describe people whose gender identity differs from the sex they were assigned at birth. Two examples of transgender individuals would be transgender women who were assigned male at birth and transgender men who were assigned female at birth. The term transgender is used in opposition to the term cisgender, which is applied to a person whose gender and sex assigned at birth align.3 When a transgender patient presents to a physician, they may want to discuss methods of gender affirmation or transitioning. These terms encompass any action a person may take to align their body or gender expression with that of the gender they identify with. This could be in the form of gender-affirming hormone therapy (ie, estrogen or testosterone treatment) or gender-affirming surgery (ie, “top” and “bottom” surgeries, in which someone surgically treats their chest or genitals, respectively).3
Creating a Safe Space
The physician is responsible for providing a safe space for patients to disclose medically pertinent information. It is then the job of the dermatologist to be cognizant of health concerns that directly affect the LGBT population and to be prepared if one of these concerns should arise. A safe space consists of both the physical location in which the patient encounter will occur and the people that will be conducting and assisting in the patient encounter. Safe spaces provide a patient with reassurance that they will receive care in a judgement-free location. To create a safe space, both the physical and interpersonal aspects must be addressed to provide an environment that strengthens the patient-physician alliance.
Dermatology residents often spend more time with patients than their attending physicians, providing them the opportunity to foster robust relationships with those served. Although they may not be able to change the physical environment, residents can advocate for patients in their departments and show solidarity in subtle ways. One way to show support for the LGBT community is to publicly display a symbol of solidarity, which could be done by wearing a symbol of support on a white coat lapel. Although there are many designs and styles to choose from, one example is the American Medical Student Association pins that combine the caduceus (a common symbol for medicine) with a rainbow design.5 Whichever symbol is chosen, this small gesture allows patients to immediately know that their physician is an ally. Residents also can encourage their department to add a rainbow flag, a pink triangle, or another symbol somewhere prominent in the check-in area that conveys a message of support.6 Many institutions require residents to perform quality improvement projects. The resident can make a substantial difference in their patients’ experiences by revising their office’s intake forms as a quality improvement project, which can be done by including a section on assigned sex at birth separate from gender.7 When inquiring about gender, in addition to “male” and “female,” a space can be left for people that do not identify with the traditional binary. When asking about sexual orientation, inclusive language options can be provided with additional space for self-identification. Finally, residents can incorporate pronouns below their name in their email signature to normalize this disclosure of information.8 These small changes can have a substantial impact on the health care experience of SGM patients.
Medical Problems Encountered
The previously described changes can be implemented by residents to provide better care to SGM patients, a group usually considered to be more burdened by physical and psychological diseases.9 Furthermore, dermatologists can provide care for these patients in ways that other physicians cannot. There are special considerations for LGBT patients, as some dermatologic conditions may be more common in this patient population.
Prior studies have shown that men who have sex with men have a higher rate of HIV and other sexually transmitted infections, methicillin-resistant Staphylococcus aureus skin infections, and potentially nonmelanoma skin cancer.10-14 Transgender women also have been found to have higher rates of HIV, in addition to a higher incidence of anal human papillomavirus.15,16 Women who have sex with women have been shown to see physicians less frequently and to be less up to date on their pertinent cancer-related screenings.10,17 Although these associations should not dictate the patient encounter, awareness of them will lead to better patient care. Such awareness also can provide further motivation for dermatologists to discuss safe sexual practices, potential initiation of pre-exposure prophylactic antiretroviral therapy, sun-protective practices, and the importance of following up with a primary physician for examinations and age-specific cancer screening.
Transgender patients may present with unique dermatologic concerns. For transgender male patients, testosterone therapy can cause acne breakouts and androgenetic alopecia. Usually considered worse during the start of treatment, hormone-related acne can be managed with topical retinoids, topical and oral antibiotics, and isotretinoin (if severe).18,19 The iPLEDGE system necessary for prescribing isotretinoin to patients in the United States recently has changed its language to “patients who can get pregnant” and “patients who cannot get pregnant,” following urging by the medical community for inclusivity and progress.20,21 This change creates an inclusive space where registration is no longer centered around gender and instead focuses on the presence of anatomy. Although androgenetic alopecia is a side effect of hormone therapy, it may not be unwanted.18 Discussion about patient desires is important. If the alopecia is unwanted, the Endocrine Society recommends treating cisgender and transgender patients the same in terms of treatment modalities.22
Transgender female patients also can experience dermatologic manifestations of gender-affirming hormone therapy. Melasma may develop secondary to estrogen replacement and can be treated with topical bleaching creams, lasers, and phototherapy.23 Hair removal may be pursued for patients with refractory unwanted body hair, with laser hair removal being the most commonly pursued treatment. Patients also may desire cosmetic procedures, such as botulinum toxin or fillers, to augment their physical appearance.24 Providing these services to patients may allow them to better express themselves and live authentically.
Final Thoughts
There is no way to summarize the experience of everyone within a community. Each person has different thoughts, values, and goals. It also is impossible to encompass every topic that is important for SGM patients. The goal of this article is to empower clinicians to be comfortable discussing issues related to sexuality and gender while also offering resources to learn more, allowing optimal care to be provided to this population. Thus, this article is not comprehensive. There are articles to provide further resources and education, such as the continuing medical education series by Yeung et al10,25 in the Journal of the American Academy of Dermatology, as well as organizations within medicine, such as the GLMA: Health Professionals Advancing LGBTQ Equality (https://www.glma.org/), and in dermatology, such as GALDA, the Gay and Lesbian Dermatology Association (https://www.glderm.org/). By providing a safe space for our patients and learning about specific health-related risk factors, dermatologists can provide the best possible care to the LGBT community.
Acknowledgments—I thank Warren R. Heymann, MD (Camden, New Jersey), and Howa Yeung, MD, MSc (Atlanta, Georgia), for their guidance and mentorship in the creation of this article.
- Jones JM. LGBT identification rises to 5.6% in latest U.S. estimate. Gallup website. Published February 24, 2021. Accessed March 22, 2022. https://news.gallup.com/poll/329708/lgbt-identification-rises-latest-estimate.aspx
- U.S. and world population clock. US Census Bureau website. Accessed March 22, 2022. https://www.census.gov/popclock/
- National LGBTQIA+ Health Education Center. LGBTQIA+ glossary of terms for health care teams. Published February 2, 2022. Accessed April 11, 2022. https://www.lgbtqiahealtheducation.org/wp-content/uploads/2020/02/Glossary-2022.02.22-1.pdf
- National Institutes of Health Sexual and Gender Minority Research Coordinating Committee. NIH FY 2016-2020 strategic plan to advance research on the health and well-being of sexual and gender minorities. NIH website. Accessed March 23, 2022. https://www.edi.nih.gov/sites/default/files/EDI_Public_files/sgm-strategic-plan.pdf
- Caduceus pin—rainbow. American Medical Student Association website. Accessed March 23, 2022. https://www.amsa.org/member-center/store/Caduceus-Pin-Rainbow-p67375123
- 10 tips for caring for LGBTQIA+ patients. Nurse.org website. Accessed March 23, 2022. https://nurse.org/articles/culturally-competent-healthcare-for-LGBTQ-patients/
- Cartron AM, Raiciulescu S, Trinidad JC. Culturally competent care for LGBT patients in dermatology clinics. J Drugs Dermatol. 2020;19:786-787.
- Wareham J. Should you put pronouns in email signatures and social media bios? Forbes website. Published Dec 30, 2019. Accessed March 23, 2022. https://www.forbes.com/sites/jamiewareham/2020/12/30/should-you-put-pronouns-in-email-signatures-and-social-media-bios/?sh=5b74f1246320
- Hafeez H, Zeshan M, Tahir MA, et al. Healthcare disparities among lesbian, gay, bisexual, and transgender youth: a literature review. Cureus. 2017;9:E1184.
- Yeung H, Luk KM, Chen SC, et al. Dermatologic care for lesbian, gay, bisexual, and transgender persons. part II. epidemiology, screening, and disease prevention. J Am Acad Dermatol. 2019;80:591-602.
- Centers for Disease Control and Prevention. CDC fact sheet: HIV among gay and bisexual men. CDC website. Accessed April 14, 2022. https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/cdc-msm-508.pdf
- Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2016. CDC website. Accessed April 14, 2022. https://www.cdc.gov/std/stats16/CDC_2016_STDS_Report-for508WebSep21_2017_1644.pdf
- Galindo GR, Casey AJ, Yeung A, et al. Community associated methicillin resistant Staphylococcus aureus among New York City men who have sex with men: qualitative research findings and implications for public health practice. J Community Health. 2012;37:458-467.
- Blashill AJ. Indoor tanning and skin cancer risk among diverse US youth: results from a national sample. JAMA Dermatol. 2017;153:344-345.
- Herbst JH, Jacobs ED, Finlayson TJ, et al. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 2008;12:1-17.
- Uaamnuichai S, Panyakhamlerd K, Suwan A, et al. Neovaginal and anal high-risk human papillomavirus DNA among Thai transgender women in gender health clinics. Sex Transm Dis. 2021;48:547-549.
- Valanis BG, Bowen DJ, Bassford T, et al. Sexual orientation and health: comparisons in the women’s health initiative sample. Arch Fam Med. 2000;9:843-853.
- Wierckx K, Van de Peer F, Verhaeghe E, et al. Short- and long-term clinical skin effects of testosterone treatment in trans men. J Sex Med. 2014;11:222-229.
- Turrion-Merino L, Urech-Garcia-de-la-Vega M, Miguel-Gomez L, et al. Severe acne in female-to-male transgender patients. JAMA Dermatol. 2015;151:1260-1261.
- Questions and answers on the iPLEDGE REMS. US Food and Drug Administration website. Published October 12, 2021. Accessed March 23, 2022. https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/questions-and-answers-ipledge-rems#:~:text=The%20modification%20will%20become%20effective,verify%20authorization%20to%20dispense%20isotretinoin
- Gao JL, Thoreson N, Dommasch ED. Navigating iPLEDGE enrollment for transgender and gender diverse patients: a guide for providing culturally competent care. J Am Acad Dermatol. 2021;85:790-791.
- Hembree WC, Cohen-Kettenis PT, Gooren L, et al. Endocrine treatment of gender-dysphoric/gender-incongruent persons: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2017;102:3869-3903.
- Garcia-Rodriguez L, Spiegel JH. Melasma in a transgender woman. Am J Otolaryngol. 2018;39:788-790.
- Ginsberg BA, Calderon M, Seminara NM, et al. A potential role for the dermatologist in the physical transformation of transgender people: a survey of attitudes and practices within the transgender community.J Am Acad Dermatol. 2016;74:303-308.
- Yeung H, Luk KM, Chen SC, et al. Dermatologic care for lesbian,gay, bisexual, and transgender persons. part I. terminology, demographics, health disparities, and approaches to care. J Am Acad Dermatol. 2019;80:581-589.
The chances are good that at least one patient you saw today could have been provided a better environment to foster your patient-physician relationship. A 2020 Gallup poll revealed that an estimated 5.6% of US adults identified as lesbian, gay, bisexual, and transgender (LGBT).1 Based on the estimated US population of 331.7 million individuals on December 3, 2020, this means that approximately 18.6 million identified as LGBT and could potentially require health care services.2 These numbers highlight the increasing need within the medical community to provide quality and accessible care to the LGBT community, and dermatologists have a role to play. They treat conditions that are apparent to the patient and others around them, attracting those that may not be motivated to see different physicians. They can not only help with skin diseases that affect all patients but also can train other physicians to screen for some dermatologic diseases that may have a higher prevalence within the LGBT community. Dermatologists have a unique opportunity to help patients better reflect themselves through both surgical and nonsurgical modalities.
Demographics and Definitions
To discuss this topic effectively, it is important to define LGBT terms (Table).3 As a disclaimer, language is fluid. Despite a word or term currently being used and accepted, it quickly can become obsolete. A clinician can always do research, follow the lead of the patient, and respectfully ask questions if there is ever confusion surrounding terminology. Patients do not expect every physician they encounter to be an expert in this subject. What is most important is that patients are approached with an open mind and humility with the goal of providing optimal care.
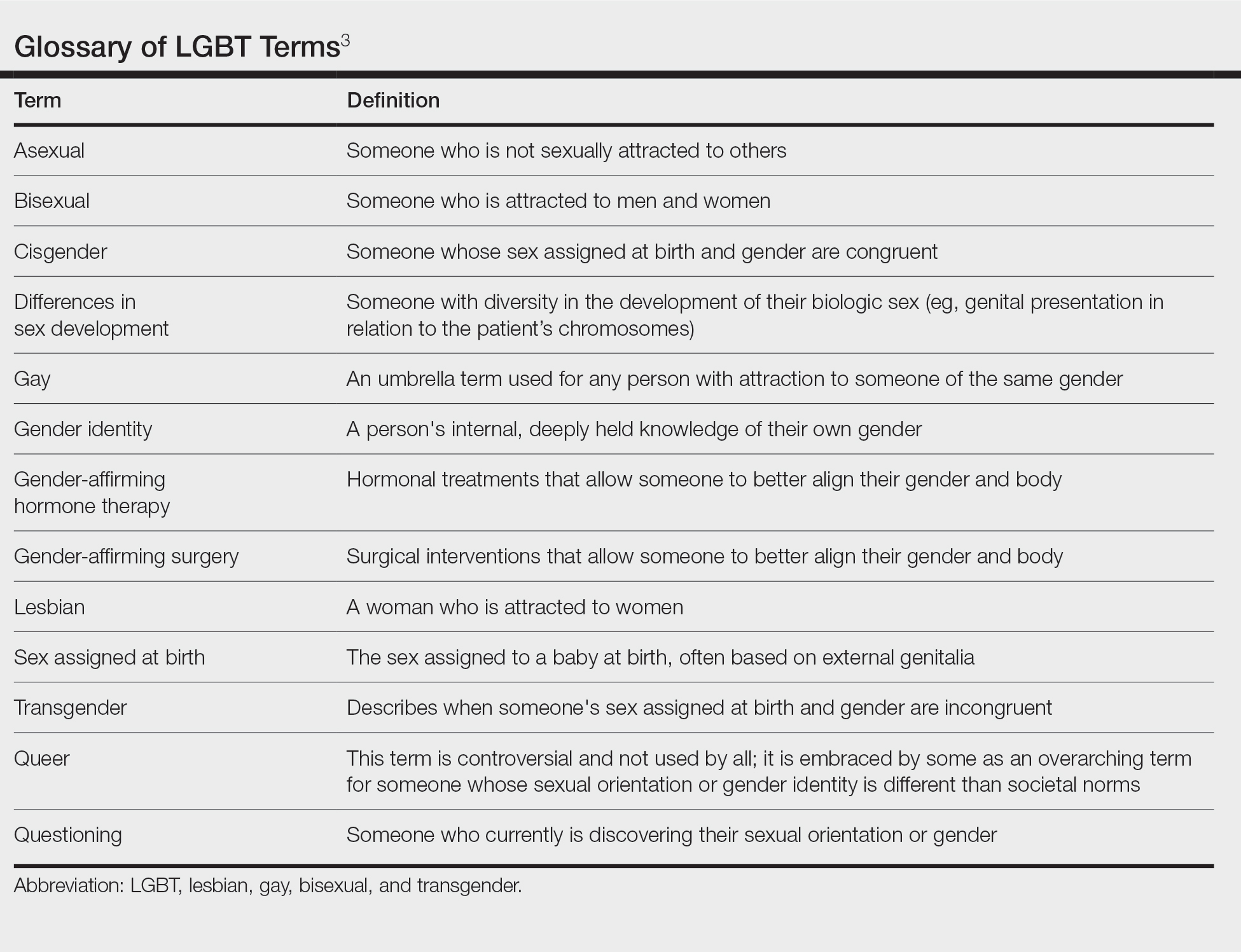
Although the federal government now uses the term sexual and gender minorities (SGM), the more specific terms lesbian, gay, bisexual, and transgender usually are preferred.3,4 Other letters are at times added to the acronym LGBT, including Q for questioning or queer, I for intersex, and A for asexual; all of these letters are under the larger SGM umbrella. Because LGBT is the most commonly used acronym in the daily vernacular, it will be the default for this article.
A term describing sexual orientation does not necessarily describe sexual practices. A woman who identifies as straight may have sex with both men and women, and a gay man may not have sex at all. To be more descriptive regarding sexual practices, one may use the terms men who have sex with men or women who have sex with women.3 Because of this nuance, it is important to elicit a sexual history when speaking to all patients in a forward nonjudgmental manner.
The term transgender is used to describe people whose gender identity differs from the sex they were assigned at birth. Two examples of transgender individuals would be transgender women who were assigned male at birth and transgender men who were assigned female at birth. The term transgender is used in opposition to the term cisgender, which is applied to a person whose gender and sex assigned at birth align.3 When a transgender patient presents to a physician, they may want to discuss methods of gender affirmation or transitioning. These terms encompass any action a person may take to align their body or gender expression with that of the gender they identify with. This could be in the form of gender-affirming hormone therapy (ie, estrogen or testosterone treatment) or gender-affirming surgery (ie, “top” and “bottom” surgeries, in which someone surgically treats their chest or genitals, respectively).3
Creating a Safe Space
The physician is responsible for providing a safe space for patients to disclose medically pertinent information. It is then the job of the dermatologist to be cognizant of health concerns that directly affect the LGBT population and to be prepared if one of these concerns should arise. A safe space consists of both the physical location in which the patient encounter will occur and the people that will be conducting and assisting in the patient encounter. Safe spaces provide a patient with reassurance that they will receive care in a judgement-free location. To create a safe space, both the physical and interpersonal aspects must be addressed to provide an environment that strengthens the patient-physician alliance.
Dermatology residents often spend more time with patients than their attending physicians, providing them the opportunity to foster robust relationships with those served. Although they may not be able to change the physical environment, residents can advocate for patients in their departments and show solidarity in subtle ways. One way to show support for the LGBT community is to publicly display a symbol of solidarity, which could be done by wearing a symbol of support on a white coat lapel. Although there are many designs and styles to choose from, one example is the American Medical Student Association pins that combine the caduceus (a common symbol for medicine) with a rainbow design.5 Whichever symbol is chosen, this small gesture allows patients to immediately know that their physician is an ally. Residents also can encourage their department to add a rainbow flag, a pink triangle, or another symbol somewhere prominent in the check-in area that conveys a message of support.6 Many institutions require residents to perform quality improvement projects. The resident can make a substantial difference in their patients’ experiences by revising their office’s intake forms as a quality improvement project, which can be done by including a section on assigned sex at birth separate from gender.7 When inquiring about gender, in addition to “male” and “female,” a space can be left for people that do not identify with the traditional binary. When asking about sexual orientation, inclusive language options can be provided with additional space for self-identification. Finally, residents can incorporate pronouns below their name in their email signature to normalize this disclosure of information.8 These small changes can have a substantial impact on the health care experience of SGM patients.
Medical Problems Encountered
The previously described changes can be implemented by residents to provide better care to SGM patients, a group usually considered to be more burdened by physical and psychological diseases.9 Furthermore, dermatologists can provide care for these patients in ways that other physicians cannot. There are special considerations for LGBT patients, as some dermatologic conditions may be more common in this patient population.
Prior studies have shown that men who have sex with men have a higher rate of HIV and other sexually transmitted infections, methicillin-resistant Staphylococcus aureus skin infections, and potentially nonmelanoma skin cancer.10-14 Transgender women also have been found to have higher rates of HIV, in addition to a higher incidence of anal human papillomavirus.15,16 Women who have sex with women have been shown to see physicians less frequently and to be less up to date on their pertinent cancer-related screenings.10,17 Although these associations should not dictate the patient encounter, awareness of them will lead to better patient care. Such awareness also can provide further motivation for dermatologists to discuss safe sexual practices, potential initiation of pre-exposure prophylactic antiretroviral therapy, sun-protective practices, and the importance of following up with a primary physician for examinations and age-specific cancer screening.
Transgender patients may present with unique dermatologic concerns. For transgender male patients, testosterone therapy can cause acne breakouts and androgenetic alopecia. Usually considered worse during the start of treatment, hormone-related acne can be managed with topical retinoids, topical and oral antibiotics, and isotretinoin (if severe).18,19 The iPLEDGE system necessary for prescribing isotretinoin to patients in the United States recently has changed its language to “patients who can get pregnant” and “patients who cannot get pregnant,” following urging by the medical community for inclusivity and progress.20,21 This change creates an inclusive space where registration is no longer centered around gender and instead focuses on the presence of anatomy. Although androgenetic alopecia is a side effect of hormone therapy, it may not be unwanted.18 Discussion about patient desires is important. If the alopecia is unwanted, the Endocrine Society recommends treating cisgender and transgender patients the same in terms of treatment modalities.22
Transgender female patients also can experience dermatologic manifestations of gender-affirming hormone therapy. Melasma may develop secondary to estrogen replacement and can be treated with topical bleaching creams, lasers, and phototherapy.23 Hair removal may be pursued for patients with refractory unwanted body hair, with laser hair removal being the most commonly pursued treatment. Patients also may desire cosmetic procedures, such as botulinum toxin or fillers, to augment their physical appearance.24 Providing these services to patients may allow them to better express themselves and live authentically.
Final Thoughts
There is no way to summarize the experience of everyone within a community. Each person has different thoughts, values, and goals. It also is impossible to encompass every topic that is important for SGM patients. The goal of this article is to empower clinicians to be comfortable discussing issues related to sexuality and gender while also offering resources to learn more, allowing optimal care to be provided to this population. Thus, this article is not comprehensive. There are articles to provide further resources and education, such as the continuing medical education series by Yeung et al10,25 in the Journal of the American Academy of Dermatology, as well as organizations within medicine, such as the GLMA: Health Professionals Advancing LGBTQ Equality (https://www.glma.org/), and in dermatology, such as GALDA, the Gay and Lesbian Dermatology Association (https://www.glderm.org/). By providing a safe space for our patients and learning about specific health-related risk factors, dermatologists can provide the best possible care to the LGBT community.
Acknowledgments—I thank Warren R. Heymann, MD (Camden, New Jersey), and Howa Yeung, MD, MSc (Atlanta, Georgia), for their guidance and mentorship in the creation of this article.
The chances are good that at least one patient you saw today could have been provided a better environment to foster your patient-physician relationship. A 2020 Gallup poll revealed that an estimated 5.6% of US adults identified as lesbian, gay, bisexual, and transgender (LGBT).1 Based on the estimated US population of 331.7 million individuals on December 3, 2020, this means that approximately 18.6 million identified as LGBT and could potentially require health care services.2 These numbers highlight the increasing need within the medical community to provide quality and accessible care to the LGBT community, and dermatologists have a role to play. They treat conditions that are apparent to the patient and others around them, attracting those that may not be motivated to see different physicians. They can not only help with skin diseases that affect all patients but also can train other physicians to screen for some dermatologic diseases that may have a higher prevalence within the LGBT community. Dermatologists have a unique opportunity to help patients better reflect themselves through both surgical and nonsurgical modalities.
Demographics and Definitions
To discuss this topic effectively, it is important to define LGBT terms (Table).3 As a disclaimer, language is fluid. Despite a word or term currently being used and accepted, it quickly can become obsolete. A clinician can always do research, follow the lead of the patient, and respectfully ask questions if there is ever confusion surrounding terminology. Patients do not expect every physician they encounter to be an expert in this subject. What is most important is that patients are approached with an open mind and humility with the goal of providing optimal care.
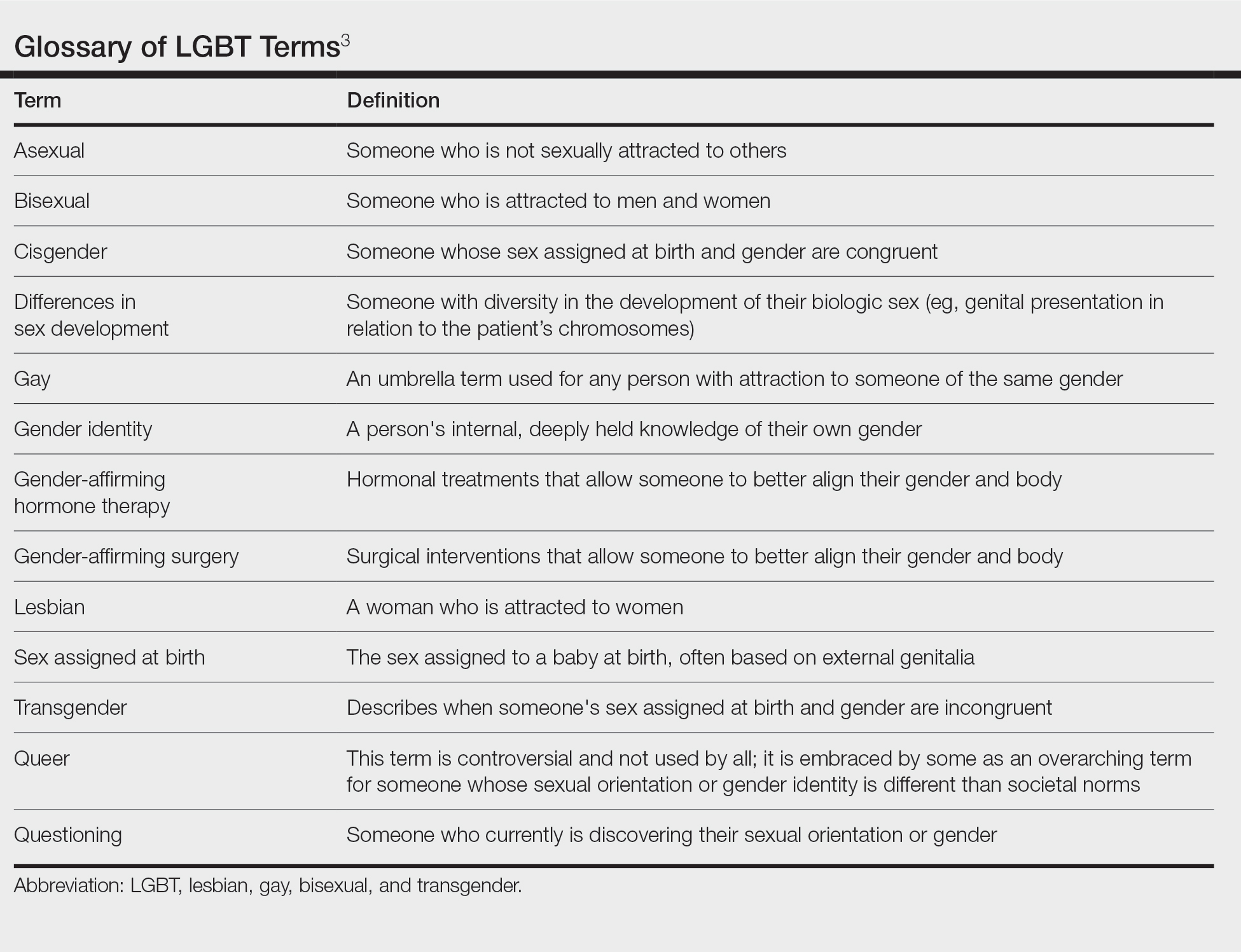
Although the federal government now uses the term sexual and gender minorities (SGM), the more specific terms lesbian, gay, bisexual, and transgender usually are preferred.3,4 Other letters are at times added to the acronym LGBT, including Q for questioning or queer, I for intersex, and A for asexual; all of these letters are under the larger SGM umbrella. Because LGBT is the most commonly used acronym in the daily vernacular, it will be the default for this article.
A term describing sexual orientation does not necessarily describe sexual practices. A woman who identifies as straight may have sex with both men and women, and a gay man may not have sex at all. To be more descriptive regarding sexual practices, one may use the terms men who have sex with men or women who have sex with women.3 Because of this nuance, it is important to elicit a sexual history when speaking to all patients in a forward nonjudgmental manner.
The term transgender is used to describe people whose gender identity differs from the sex they were assigned at birth. Two examples of transgender individuals would be transgender women who were assigned male at birth and transgender men who were assigned female at birth. The term transgender is used in opposition to the term cisgender, which is applied to a person whose gender and sex assigned at birth align.3 When a transgender patient presents to a physician, they may want to discuss methods of gender affirmation or transitioning. These terms encompass any action a person may take to align their body or gender expression with that of the gender they identify with. This could be in the form of gender-affirming hormone therapy (ie, estrogen or testosterone treatment) or gender-affirming surgery (ie, “top” and “bottom” surgeries, in which someone surgically treats their chest or genitals, respectively).3
Creating a Safe Space
The physician is responsible for providing a safe space for patients to disclose medically pertinent information. It is then the job of the dermatologist to be cognizant of health concerns that directly affect the LGBT population and to be prepared if one of these concerns should arise. A safe space consists of both the physical location in which the patient encounter will occur and the people that will be conducting and assisting in the patient encounter. Safe spaces provide a patient with reassurance that they will receive care in a judgement-free location. To create a safe space, both the physical and interpersonal aspects must be addressed to provide an environment that strengthens the patient-physician alliance.
Dermatology residents often spend more time with patients than their attending physicians, providing them the opportunity to foster robust relationships with those served. Although they may not be able to change the physical environment, residents can advocate for patients in their departments and show solidarity in subtle ways. One way to show support for the LGBT community is to publicly display a symbol of solidarity, which could be done by wearing a symbol of support on a white coat lapel. Although there are many designs and styles to choose from, one example is the American Medical Student Association pins that combine the caduceus (a common symbol for medicine) with a rainbow design.5 Whichever symbol is chosen, this small gesture allows patients to immediately know that their physician is an ally. Residents also can encourage their department to add a rainbow flag, a pink triangle, or another symbol somewhere prominent in the check-in area that conveys a message of support.6 Many institutions require residents to perform quality improvement projects. The resident can make a substantial difference in their patients’ experiences by revising their office’s intake forms as a quality improvement project, which can be done by including a section on assigned sex at birth separate from gender.7 When inquiring about gender, in addition to “male” and “female,” a space can be left for people that do not identify with the traditional binary. When asking about sexual orientation, inclusive language options can be provided with additional space for self-identification. Finally, residents can incorporate pronouns below their name in their email signature to normalize this disclosure of information.8 These small changes can have a substantial impact on the health care experience of SGM patients.
Medical Problems Encountered
The previously described changes can be implemented by residents to provide better care to SGM patients, a group usually considered to be more burdened by physical and psychological diseases.9 Furthermore, dermatologists can provide care for these patients in ways that other physicians cannot. There are special considerations for LGBT patients, as some dermatologic conditions may be more common in this patient population.
Prior studies have shown that men who have sex with men have a higher rate of HIV and other sexually transmitted infections, methicillin-resistant Staphylococcus aureus skin infections, and potentially nonmelanoma skin cancer.10-14 Transgender women also have been found to have higher rates of HIV, in addition to a higher incidence of anal human papillomavirus.15,16 Women who have sex with women have been shown to see physicians less frequently and to be less up to date on their pertinent cancer-related screenings.10,17 Although these associations should not dictate the patient encounter, awareness of them will lead to better patient care. Such awareness also can provide further motivation for dermatologists to discuss safe sexual practices, potential initiation of pre-exposure prophylactic antiretroviral therapy, sun-protective practices, and the importance of following up with a primary physician for examinations and age-specific cancer screening.
Transgender patients may present with unique dermatologic concerns. For transgender male patients, testosterone therapy can cause acne breakouts and androgenetic alopecia. Usually considered worse during the start of treatment, hormone-related acne can be managed with topical retinoids, topical and oral antibiotics, and isotretinoin (if severe).18,19 The iPLEDGE system necessary for prescribing isotretinoin to patients in the United States recently has changed its language to “patients who can get pregnant” and “patients who cannot get pregnant,” following urging by the medical community for inclusivity and progress.20,21 This change creates an inclusive space where registration is no longer centered around gender and instead focuses on the presence of anatomy. Although androgenetic alopecia is a side effect of hormone therapy, it may not be unwanted.18 Discussion about patient desires is important. If the alopecia is unwanted, the Endocrine Society recommends treating cisgender and transgender patients the same in terms of treatment modalities.22
Transgender female patients also can experience dermatologic manifestations of gender-affirming hormone therapy. Melasma may develop secondary to estrogen replacement and can be treated with topical bleaching creams, lasers, and phototherapy.23 Hair removal may be pursued for patients with refractory unwanted body hair, with laser hair removal being the most commonly pursued treatment. Patients also may desire cosmetic procedures, such as botulinum toxin or fillers, to augment their physical appearance.24 Providing these services to patients may allow them to better express themselves and live authentically.
Final Thoughts
There is no way to summarize the experience of everyone within a community. Each person has different thoughts, values, and goals. It also is impossible to encompass every topic that is important for SGM patients. The goal of this article is to empower clinicians to be comfortable discussing issues related to sexuality and gender while also offering resources to learn more, allowing optimal care to be provided to this population. Thus, this article is not comprehensive. There are articles to provide further resources and education, such as the continuing medical education series by Yeung et al10,25 in the Journal of the American Academy of Dermatology, as well as organizations within medicine, such as the GLMA: Health Professionals Advancing LGBTQ Equality (https://www.glma.org/), and in dermatology, such as GALDA, the Gay and Lesbian Dermatology Association (https://www.glderm.org/). By providing a safe space for our patients and learning about specific health-related risk factors, dermatologists can provide the best possible care to the LGBT community.
Acknowledgments—I thank Warren R. Heymann, MD (Camden, New Jersey), and Howa Yeung, MD, MSc (Atlanta, Georgia), for their guidance and mentorship in the creation of this article.
- Jones JM. LGBT identification rises to 5.6% in latest U.S. estimate. Gallup website. Published February 24, 2021. Accessed March 22, 2022. https://news.gallup.com/poll/329708/lgbt-identification-rises-latest-estimate.aspx
- U.S. and world population clock. US Census Bureau website. Accessed March 22, 2022. https://www.census.gov/popclock/
- National LGBTQIA+ Health Education Center. LGBTQIA+ glossary of terms for health care teams. Published February 2, 2022. Accessed April 11, 2022. https://www.lgbtqiahealtheducation.org/wp-content/uploads/2020/02/Glossary-2022.02.22-1.pdf
- National Institutes of Health Sexual and Gender Minority Research Coordinating Committee. NIH FY 2016-2020 strategic plan to advance research on the health and well-being of sexual and gender minorities. NIH website. Accessed March 23, 2022. https://www.edi.nih.gov/sites/default/files/EDI_Public_files/sgm-strategic-plan.pdf
- Caduceus pin—rainbow. American Medical Student Association website. Accessed March 23, 2022. https://www.amsa.org/member-center/store/Caduceus-Pin-Rainbow-p67375123
- 10 tips for caring for LGBTQIA+ patients. Nurse.org website. Accessed March 23, 2022. https://nurse.org/articles/culturally-competent-healthcare-for-LGBTQ-patients/
- Cartron AM, Raiciulescu S, Trinidad JC. Culturally competent care for LGBT patients in dermatology clinics. J Drugs Dermatol. 2020;19:786-787.
- Wareham J. Should you put pronouns in email signatures and social media bios? Forbes website. Published Dec 30, 2019. Accessed March 23, 2022. https://www.forbes.com/sites/jamiewareham/2020/12/30/should-you-put-pronouns-in-email-signatures-and-social-media-bios/?sh=5b74f1246320
- Hafeez H, Zeshan M, Tahir MA, et al. Healthcare disparities among lesbian, gay, bisexual, and transgender youth: a literature review. Cureus. 2017;9:E1184.
- Yeung H, Luk KM, Chen SC, et al. Dermatologic care for lesbian, gay, bisexual, and transgender persons. part II. epidemiology, screening, and disease prevention. J Am Acad Dermatol. 2019;80:591-602.
- Centers for Disease Control and Prevention. CDC fact sheet: HIV among gay and bisexual men. CDC website. Accessed April 14, 2022. https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/cdc-msm-508.pdf
- Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2016. CDC website. Accessed April 14, 2022. https://www.cdc.gov/std/stats16/CDC_2016_STDS_Report-for508WebSep21_2017_1644.pdf
- Galindo GR, Casey AJ, Yeung A, et al. Community associated methicillin resistant Staphylococcus aureus among New York City men who have sex with men: qualitative research findings and implications for public health practice. J Community Health. 2012;37:458-467.
- Blashill AJ. Indoor tanning and skin cancer risk among diverse US youth: results from a national sample. JAMA Dermatol. 2017;153:344-345.
- Herbst JH, Jacobs ED, Finlayson TJ, et al. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 2008;12:1-17.
- Uaamnuichai S, Panyakhamlerd K, Suwan A, et al. Neovaginal and anal high-risk human papillomavirus DNA among Thai transgender women in gender health clinics. Sex Transm Dis. 2021;48:547-549.
- Valanis BG, Bowen DJ, Bassford T, et al. Sexual orientation and health: comparisons in the women’s health initiative sample. Arch Fam Med. 2000;9:843-853.
- Wierckx K, Van de Peer F, Verhaeghe E, et al. Short- and long-term clinical skin effects of testosterone treatment in trans men. J Sex Med. 2014;11:222-229.
- Turrion-Merino L, Urech-Garcia-de-la-Vega M, Miguel-Gomez L, et al. Severe acne in female-to-male transgender patients. JAMA Dermatol. 2015;151:1260-1261.
- Questions and answers on the iPLEDGE REMS. US Food and Drug Administration website. Published October 12, 2021. Accessed March 23, 2022. https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/questions-and-answers-ipledge-rems#:~:text=The%20modification%20will%20become%20effective,verify%20authorization%20to%20dispense%20isotretinoin
- Gao JL, Thoreson N, Dommasch ED. Navigating iPLEDGE enrollment for transgender and gender diverse patients: a guide for providing culturally competent care. J Am Acad Dermatol. 2021;85:790-791.
- Hembree WC, Cohen-Kettenis PT, Gooren L, et al. Endocrine treatment of gender-dysphoric/gender-incongruent persons: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2017;102:3869-3903.
- Garcia-Rodriguez L, Spiegel JH. Melasma in a transgender woman. Am J Otolaryngol. 2018;39:788-790.
- Ginsberg BA, Calderon M, Seminara NM, et al. A potential role for the dermatologist in the physical transformation of transgender people: a survey of attitudes and practices within the transgender community.J Am Acad Dermatol. 2016;74:303-308.
- Yeung H, Luk KM, Chen SC, et al. Dermatologic care for lesbian,gay, bisexual, and transgender persons. part I. terminology, demographics, health disparities, and approaches to care. J Am Acad Dermatol. 2019;80:581-589.
- Jones JM. LGBT identification rises to 5.6% in latest U.S. estimate. Gallup website. Published February 24, 2021. Accessed March 22, 2022. https://news.gallup.com/poll/329708/lgbt-identification-rises-latest-estimate.aspx
- U.S. and world population clock. US Census Bureau website. Accessed March 22, 2022. https://www.census.gov/popclock/
- National LGBTQIA+ Health Education Center. LGBTQIA+ glossary of terms for health care teams. Published February 2, 2022. Accessed April 11, 2022. https://www.lgbtqiahealtheducation.org/wp-content/uploads/2020/02/Glossary-2022.02.22-1.pdf
- National Institutes of Health Sexual and Gender Minority Research Coordinating Committee. NIH FY 2016-2020 strategic plan to advance research on the health and well-being of sexual and gender minorities. NIH website. Accessed March 23, 2022. https://www.edi.nih.gov/sites/default/files/EDI_Public_files/sgm-strategic-plan.pdf
- Caduceus pin—rainbow. American Medical Student Association website. Accessed March 23, 2022. https://www.amsa.org/member-center/store/Caduceus-Pin-Rainbow-p67375123
- 10 tips for caring for LGBTQIA+ patients. Nurse.org website. Accessed March 23, 2022. https://nurse.org/articles/culturally-competent-healthcare-for-LGBTQ-patients/
- Cartron AM, Raiciulescu S, Trinidad JC. Culturally competent care for LGBT patients in dermatology clinics. J Drugs Dermatol. 2020;19:786-787.
- Wareham J. Should you put pronouns in email signatures and social media bios? Forbes website. Published Dec 30, 2019. Accessed March 23, 2022. https://www.forbes.com/sites/jamiewareham/2020/12/30/should-you-put-pronouns-in-email-signatures-and-social-media-bios/?sh=5b74f1246320
- Hafeez H, Zeshan M, Tahir MA, et al. Healthcare disparities among lesbian, gay, bisexual, and transgender youth: a literature review. Cureus. 2017;9:E1184.
- Yeung H, Luk KM, Chen SC, et al. Dermatologic care for lesbian, gay, bisexual, and transgender persons. part II. epidemiology, screening, and disease prevention. J Am Acad Dermatol. 2019;80:591-602.
- Centers for Disease Control and Prevention. CDC fact sheet: HIV among gay and bisexual men. CDC website. Accessed April 14, 2022. https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/cdc-msm-508.pdf
- Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2016. CDC website. Accessed April 14, 2022. https://www.cdc.gov/std/stats16/CDC_2016_STDS_Report-for508WebSep21_2017_1644.pdf
- Galindo GR, Casey AJ, Yeung A, et al. Community associated methicillin resistant Staphylococcus aureus among New York City men who have sex with men: qualitative research findings and implications for public health practice. J Community Health. 2012;37:458-467.
- Blashill AJ. Indoor tanning and skin cancer risk among diverse US youth: results from a national sample. JAMA Dermatol. 2017;153:344-345.
- Herbst JH, Jacobs ED, Finlayson TJ, et al. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 2008;12:1-17.
- Uaamnuichai S, Panyakhamlerd K, Suwan A, et al. Neovaginal and anal high-risk human papillomavirus DNA among Thai transgender women in gender health clinics. Sex Transm Dis. 2021;48:547-549.
- Valanis BG, Bowen DJ, Bassford T, et al. Sexual orientation and health: comparisons in the women’s health initiative sample. Arch Fam Med. 2000;9:843-853.
- Wierckx K, Van de Peer F, Verhaeghe E, et al. Short- and long-term clinical skin effects of testosterone treatment in trans men. J Sex Med. 2014;11:222-229.
- Turrion-Merino L, Urech-Garcia-de-la-Vega M, Miguel-Gomez L, et al. Severe acne in female-to-male transgender patients. JAMA Dermatol. 2015;151:1260-1261.
- Questions and answers on the iPLEDGE REMS. US Food and Drug Administration website. Published October 12, 2021. Accessed March 23, 2022. https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/questions-and-answers-ipledge-rems#:~:text=The%20modification%20will%20become%20effective,verify%20authorization%20to%20dispense%20isotretinoin
- Gao JL, Thoreson N, Dommasch ED. Navigating iPLEDGE enrollment for transgender and gender diverse patients: a guide for providing culturally competent care. J Am Acad Dermatol. 2021;85:790-791.
- Hembree WC, Cohen-Kettenis PT, Gooren L, et al. Endocrine treatment of gender-dysphoric/gender-incongruent persons: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2017;102:3869-3903.
- Garcia-Rodriguez L, Spiegel JH. Melasma in a transgender woman. Am J Otolaryngol. 2018;39:788-790.
- Ginsberg BA, Calderon M, Seminara NM, et al. A potential role for the dermatologist in the physical transformation of transgender people: a survey of attitudes and practices within the transgender community.J Am Acad Dermatol. 2016;74:303-308.
- Yeung H, Luk KM, Chen SC, et al. Dermatologic care for lesbian,gay, bisexual, and transgender persons. part I. terminology, demographics, health disparities, and approaches to care. J Am Acad Dermatol. 2019;80:581-589.
Resident Pearl
- Because of the longitudinal relationships dermatology residents make with their patients, they have a unique opportunity to provide a safe space and life-changing care to patients within the lesbian, gay, bisexual, and transgender community.
How old is too old to work as a doctor?
Air traffic controllers face mandatory retirement at age 56, with exceptions up to 61. Commercial airline pilots must bow out at 65; same for foreign service employees. Physicians, however, have no age limit, regardless of specialty.
As the profession rapidly ages – some 30% of the physician workforce is currently a senior, according to the American Medical Association – the topic of whether or not there should be a standard measure or age for retirement is front and center. The AMA’s Council on Medical Education formed a workgroup to look into the issue in 2015 and 2018, and in 2021, delegates adopted a set of guidelines for screening and assessing physicians, but stopped short of a mandate.
Mark Katlic, MD, chair of surgery at Lifebridge Health System, Baltimore, has devoted a decade to studying this topic. “I’m a bit of an outlier looking into this,” he says. “The public is unaware and seemingly unconcerned about the issue. Even among the medical profession, there’s been a series of fits and starts to develop a cohesive approach.”
One of the reasons guidelines – mandatory or otherwise – have been tough to come by is that aging brings with it a huge degree of variability. “If you look at a group of 80-year-olds, there will be much more variability than within a group of 40-year-olds,” Dr. Katlic pointed out.
Indeed, some 80-year-olds can easily continue to teach college courses, keep up in 10K running races, or perform delicate surgeries. Yet others in their peer group might struggle to properly button a shirt, walk a flight of stairs, or remember yesterday’s meals. Functional age is not the same as chronological age.
Frank Stockdale, MD, PhD, an 86-year-old practicing oncologist at Stanford (Calif.) University Health, counts himself in the camp opposed to age-based assessments. “It’s age discrimination,” he says. “Physicians receive assessments throughout their careers as part of the accreditation process – there’s no need to change that as doctors reach a certain age.”
Dr. Stockdale suggests that in many cases, malpractice suits are filed against mid-career doctors, not those of advanced age. “If you’re using the argument that there is an accumulation of deficits with age, the fact is that those deficits begin well before your 70s,” he said. “It’s better to have a uniform screening policy and begin at a much younger age.”
At Stanford, in fact, there was a former assessment policy that included cognitive testing, but physicians were successful in seeing that portion of testing eliminated. “It is a physical examination, by a physician of choice, certifying that for the privileges requested there is no physical or mental reason the candidate cannot safely perform them,” Dr. Stockdale explained.
In some cases, medical staffs have filed lawsuits to fight age-related testing. In New Haven, Conn., for instance, the U.S. Equal Employment Opportunity Commission (EEOC) filed a suit in 2020 on behalf of the Yale New Haven Hospital staff, alleging a discriminatory “late career practitioner policy.”
A similar case in Minnesota reached a settlement in 2021, providing monetary relief to staff impacted by out-of-pocket costs for the assessment, in addition to requiring that the hospital in question report to the EEOC any complaints related to age discrimination.
James Ellison, MD, MPH, chair in Memory Care and Geriatrics with ChristianaCare in Wilmington, Del., points out that aging can bring benefits for practicing physicians. “Age is very individualized and there are good and bad consequences,” he said. “Experience can build knowledge and confidence and expertise, and it does improve diagnostic accuracy.”
On the flip side, however, age-related brain changes include loss of volume and lower levels of some neurotransmitters, resulting in cognitive changes. “Functional changes occur too,” Dr. Ellison said.
“Just as some aging athletes may lose a degree of speed, strength, and flexibility, and some aging scientists may lose a part of their former cognitive speed, flexibility, and mental strength, aging health care providers can lose some of the physical coordination, strength, and visual acuity necessary to perform demanding surgical operations. They can also lose some of the processing speed, working memory, and executive function that allows them to excel in cognitive professional tasks.”
An estimated 5.8 million Americans age 65 and older have Alzheimer’s dementia, according to the Alzheimer’s Association.
Picking an arbitrary age for mandatory retirement isn’t the right approach for physicians, said Dr. Katlic. Rather, he said, the answer is to establish late-practitioner screening programs. “Very few hospitals have them, however,” he pointed out. “We do [at Lifebridge Health], and so do a few dozen others, but that’s out of hundreds.”
Instead, what typically plays out is that hospital staff might begin to notice a decline in a colleague. Things like a disheveled appearance or lack of hygiene, or trouble with memory, such as getting lost en route back to his or her office. Even dangerous behaviors such as nodding off during a procedure are not unheard of.
There are many examples of physician decline that fly under the radar. “Unfortunately, it’s unusual for cognitively impaired health care providers to recognize and report their own difficulties,” said Dr. Ellison. “Although peers are expected to report cognitively impaired colleagues, they often fail to do so. In some other countries, age-based assessment is an accepted policy. In the U.S., this is not a uniform policy.”
Sometimes physicians can remain on the job in spite of decline thanks to certain “props,” according to Dr. Ellison. “Good procedures, efficient supports, and various workarounds compensate,” he said, “but often are not sufficient to maintain high-quality practice.”
Most often, these situations play out slowly, until the problem becomes glaringly obvious and potentially dangerous, and someone in a position of power must step in.
“Often, it’s hearsay from a nurse or another staff member, and then a hospital president or chief of staff must make a career-affecting decision for the doctor in question,” said Dr. Katlic.
Because there is little self- or colleague policing – and barring official or binding guidelines on the aging physician issue – both Dr. Katlic and Dr. Ellison are proponents of late-career screening.
How screening can help
As it stands, Dr. Katlic maintains that the profession isn’t doing enough to ensure public safety. “We have peer review and recertification processes, but when you get down to it, we don’t police ourselves well,” he said. “All physicians are assessed throughout their careers as part of the hospital accreditation process, which is fair and adequate.”
Dr. Katlic said that there are three main benchmarks that physicians should be able to meet at an agreed upon age: a physical exam, a neurocognitive screening, and an eye exam. “At some reasonable age, I personally believe these exams should take place,” he said. “We can allow doctors to pick their own practitioners for the eye and physical exams, but the neurocognitive exam should be completed by a PhD neuropsychologist.”
At Lifebridge, for instance, these screenings begin at age 75 and take place every 2 years, during the recredentialing process. It applies to all specialties, not just surgeons. “Surgery is a little different in that it requires fine motor skills in addition to the others we test, but you want any physician to be cognitively intact,” Dr. Katlic pointed out. “All doctors need the ability to make decisions quickly, often under noisy, distracting conditions.”
Dr. Ellison supports applying the screenings to all specialties. “Let’s not forget that all physicians must be alert to the many ways in which their patients reveal what needs attention, evaluation, and treatment,” he said. “Some health care tasks could be performed without visual input; for example, perhaps psychotherapy could be provided competently by a clinician who lacks visual acuity. Auditory input might not be necessary for reading x-rays – but the information a health care provider gets from their eyes and ears is important, not just for surgeons.”
University of California San Diego has established what it calls its Physician Assessment and Clinical Education (PACE) program. One of the nation’s oldest and largest such programs, the hospital founded PACE in 1996. Most physicians taking part arrive as a requirement of disciplinary action from the state medical board, but a small percentage self-refers.
PACE involves two phases. The first is a 2-day set of tests and measures core competency knowledge. Phase 2 is more comprehensive and lasts 5 days. Here, within their specialty, physicians participate in the activities of the corresponding residency program. Faculty evaluates the physician, and a multidisciplinary team meets to review all the findings of the combined phases.
Depending on the results, doctors may face remediation steps that range from programs to address performance deficiencies to residency-level clinical experiences. According to a paper on the program published by the institution, “most physicians referred to the PACE program are found to have mild to moderate performance dyscompetence.”
In the case of the 2021 guidelines adopted by AMA delegates, there are nine principles for assessment. They should be evidence-based, ethical, relevant, accountable, fair and equitable, transparent, supportive, and nonburdensome, and should afford physicians due process protections.
Looking ahead
Even Dr. Katlic worries about the possibility of Congress intervening to establish federal-level, mandatory retirement age. “This just doesn’t make sense for our profession given the great variability we see,” he said. “My biggest hope is that more individual hospitals will institute these screenings.”
As the physician population ages – and the influx of new doctors shrinks – the slope becomes even more slippery. The AMA is predicting a physician shortage of nearly 40,000 by the year 2034. This strengthens arguments to keep existing physicians practicing for as long as possible and might make institutions less likely to screen.
It’s all a delicate balancing act and a continuing work in progress, said Dr. Ellison. “Ultimately, I believe we need to find a way to understand and address the possible implications for public safety, while at the same time protecting the privacy and dignity of our valued older physicians and other health care providers.”
A version of this article first appeared on Medscape.com.
Air traffic controllers face mandatory retirement at age 56, with exceptions up to 61. Commercial airline pilots must bow out at 65; same for foreign service employees. Physicians, however, have no age limit, regardless of specialty.
As the profession rapidly ages – some 30% of the physician workforce is currently a senior, according to the American Medical Association – the topic of whether or not there should be a standard measure or age for retirement is front and center. The AMA’s Council on Medical Education formed a workgroup to look into the issue in 2015 and 2018, and in 2021, delegates adopted a set of guidelines for screening and assessing physicians, but stopped short of a mandate.
Mark Katlic, MD, chair of surgery at Lifebridge Health System, Baltimore, has devoted a decade to studying this topic. “I’m a bit of an outlier looking into this,” he says. “The public is unaware and seemingly unconcerned about the issue. Even among the medical profession, there’s been a series of fits and starts to develop a cohesive approach.”
One of the reasons guidelines – mandatory or otherwise – have been tough to come by is that aging brings with it a huge degree of variability. “If you look at a group of 80-year-olds, there will be much more variability than within a group of 40-year-olds,” Dr. Katlic pointed out.
Indeed, some 80-year-olds can easily continue to teach college courses, keep up in 10K running races, or perform delicate surgeries. Yet others in their peer group might struggle to properly button a shirt, walk a flight of stairs, or remember yesterday’s meals. Functional age is not the same as chronological age.
Frank Stockdale, MD, PhD, an 86-year-old practicing oncologist at Stanford (Calif.) University Health, counts himself in the camp opposed to age-based assessments. “It’s age discrimination,” he says. “Physicians receive assessments throughout their careers as part of the accreditation process – there’s no need to change that as doctors reach a certain age.”
Dr. Stockdale suggests that in many cases, malpractice suits are filed against mid-career doctors, not those of advanced age. “If you’re using the argument that there is an accumulation of deficits with age, the fact is that those deficits begin well before your 70s,” he said. “It’s better to have a uniform screening policy and begin at a much younger age.”
At Stanford, in fact, there was a former assessment policy that included cognitive testing, but physicians were successful in seeing that portion of testing eliminated. “It is a physical examination, by a physician of choice, certifying that for the privileges requested there is no physical or mental reason the candidate cannot safely perform them,” Dr. Stockdale explained.
In some cases, medical staffs have filed lawsuits to fight age-related testing. In New Haven, Conn., for instance, the U.S. Equal Employment Opportunity Commission (EEOC) filed a suit in 2020 on behalf of the Yale New Haven Hospital staff, alleging a discriminatory “late career practitioner policy.”
A similar case in Minnesota reached a settlement in 2021, providing monetary relief to staff impacted by out-of-pocket costs for the assessment, in addition to requiring that the hospital in question report to the EEOC any complaints related to age discrimination.
James Ellison, MD, MPH, chair in Memory Care and Geriatrics with ChristianaCare in Wilmington, Del., points out that aging can bring benefits for practicing physicians. “Age is very individualized and there are good and bad consequences,” he said. “Experience can build knowledge and confidence and expertise, and it does improve diagnostic accuracy.”
On the flip side, however, age-related brain changes include loss of volume and lower levels of some neurotransmitters, resulting in cognitive changes. “Functional changes occur too,” Dr. Ellison said.
“Just as some aging athletes may lose a degree of speed, strength, and flexibility, and some aging scientists may lose a part of their former cognitive speed, flexibility, and mental strength, aging health care providers can lose some of the physical coordination, strength, and visual acuity necessary to perform demanding surgical operations. They can also lose some of the processing speed, working memory, and executive function that allows them to excel in cognitive professional tasks.”
An estimated 5.8 million Americans age 65 and older have Alzheimer’s dementia, according to the Alzheimer’s Association.
Picking an arbitrary age for mandatory retirement isn’t the right approach for physicians, said Dr. Katlic. Rather, he said, the answer is to establish late-practitioner screening programs. “Very few hospitals have them, however,” he pointed out. “We do [at Lifebridge Health], and so do a few dozen others, but that’s out of hundreds.”
Instead, what typically plays out is that hospital staff might begin to notice a decline in a colleague. Things like a disheveled appearance or lack of hygiene, or trouble with memory, such as getting lost en route back to his or her office. Even dangerous behaviors such as nodding off during a procedure are not unheard of.
There are many examples of physician decline that fly under the radar. “Unfortunately, it’s unusual for cognitively impaired health care providers to recognize and report their own difficulties,” said Dr. Ellison. “Although peers are expected to report cognitively impaired colleagues, they often fail to do so. In some other countries, age-based assessment is an accepted policy. In the U.S., this is not a uniform policy.”
Sometimes physicians can remain on the job in spite of decline thanks to certain “props,” according to Dr. Ellison. “Good procedures, efficient supports, and various workarounds compensate,” he said, “but often are not sufficient to maintain high-quality practice.”
Most often, these situations play out slowly, until the problem becomes glaringly obvious and potentially dangerous, and someone in a position of power must step in.
“Often, it’s hearsay from a nurse or another staff member, and then a hospital president or chief of staff must make a career-affecting decision for the doctor in question,” said Dr. Katlic.
Because there is little self- or colleague policing – and barring official or binding guidelines on the aging physician issue – both Dr. Katlic and Dr. Ellison are proponents of late-career screening.
How screening can help
As it stands, Dr. Katlic maintains that the profession isn’t doing enough to ensure public safety. “We have peer review and recertification processes, but when you get down to it, we don’t police ourselves well,” he said. “All physicians are assessed throughout their careers as part of the hospital accreditation process, which is fair and adequate.”
Dr. Katlic said that there are three main benchmarks that physicians should be able to meet at an agreed upon age: a physical exam, a neurocognitive screening, and an eye exam. “At some reasonable age, I personally believe these exams should take place,” he said. “We can allow doctors to pick their own practitioners for the eye and physical exams, but the neurocognitive exam should be completed by a PhD neuropsychologist.”
At Lifebridge, for instance, these screenings begin at age 75 and take place every 2 years, during the recredentialing process. It applies to all specialties, not just surgeons. “Surgery is a little different in that it requires fine motor skills in addition to the others we test, but you want any physician to be cognitively intact,” Dr. Katlic pointed out. “All doctors need the ability to make decisions quickly, often under noisy, distracting conditions.”
Dr. Ellison supports applying the screenings to all specialties. “Let’s not forget that all physicians must be alert to the many ways in which their patients reveal what needs attention, evaluation, and treatment,” he said. “Some health care tasks could be performed without visual input; for example, perhaps psychotherapy could be provided competently by a clinician who lacks visual acuity. Auditory input might not be necessary for reading x-rays – but the information a health care provider gets from their eyes and ears is important, not just for surgeons.”
University of California San Diego has established what it calls its Physician Assessment and Clinical Education (PACE) program. One of the nation’s oldest and largest such programs, the hospital founded PACE in 1996. Most physicians taking part arrive as a requirement of disciplinary action from the state medical board, but a small percentage self-refers.
PACE involves two phases. The first is a 2-day set of tests and measures core competency knowledge. Phase 2 is more comprehensive and lasts 5 days. Here, within their specialty, physicians participate in the activities of the corresponding residency program. Faculty evaluates the physician, and a multidisciplinary team meets to review all the findings of the combined phases.
Depending on the results, doctors may face remediation steps that range from programs to address performance deficiencies to residency-level clinical experiences. According to a paper on the program published by the institution, “most physicians referred to the PACE program are found to have mild to moderate performance dyscompetence.”
In the case of the 2021 guidelines adopted by AMA delegates, there are nine principles for assessment. They should be evidence-based, ethical, relevant, accountable, fair and equitable, transparent, supportive, and nonburdensome, and should afford physicians due process protections.
Looking ahead
Even Dr. Katlic worries about the possibility of Congress intervening to establish federal-level, mandatory retirement age. “This just doesn’t make sense for our profession given the great variability we see,” he said. “My biggest hope is that more individual hospitals will institute these screenings.”
As the physician population ages – and the influx of new doctors shrinks – the slope becomes even more slippery. The AMA is predicting a physician shortage of nearly 40,000 by the year 2034. This strengthens arguments to keep existing physicians practicing for as long as possible and might make institutions less likely to screen.
It’s all a delicate balancing act and a continuing work in progress, said Dr. Ellison. “Ultimately, I believe we need to find a way to understand and address the possible implications for public safety, while at the same time protecting the privacy and dignity of our valued older physicians and other health care providers.”
A version of this article first appeared on Medscape.com.
Air traffic controllers face mandatory retirement at age 56, with exceptions up to 61. Commercial airline pilots must bow out at 65; same for foreign service employees. Physicians, however, have no age limit, regardless of specialty.
As the profession rapidly ages – some 30% of the physician workforce is currently a senior, according to the American Medical Association – the topic of whether or not there should be a standard measure or age for retirement is front and center. The AMA’s Council on Medical Education formed a workgroup to look into the issue in 2015 and 2018, and in 2021, delegates adopted a set of guidelines for screening and assessing physicians, but stopped short of a mandate.
Mark Katlic, MD, chair of surgery at Lifebridge Health System, Baltimore, has devoted a decade to studying this topic. “I’m a bit of an outlier looking into this,” he says. “The public is unaware and seemingly unconcerned about the issue. Even among the medical profession, there’s been a series of fits and starts to develop a cohesive approach.”
One of the reasons guidelines – mandatory or otherwise – have been tough to come by is that aging brings with it a huge degree of variability. “If you look at a group of 80-year-olds, there will be much more variability than within a group of 40-year-olds,” Dr. Katlic pointed out.
Indeed, some 80-year-olds can easily continue to teach college courses, keep up in 10K running races, or perform delicate surgeries. Yet others in their peer group might struggle to properly button a shirt, walk a flight of stairs, or remember yesterday’s meals. Functional age is not the same as chronological age.
Frank Stockdale, MD, PhD, an 86-year-old practicing oncologist at Stanford (Calif.) University Health, counts himself in the camp opposed to age-based assessments. “It’s age discrimination,” he says. “Physicians receive assessments throughout their careers as part of the accreditation process – there’s no need to change that as doctors reach a certain age.”
Dr. Stockdale suggests that in many cases, malpractice suits are filed against mid-career doctors, not those of advanced age. “If you’re using the argument that there is an accumulation of deficits with age, the fact is that those deficits begin well before your 70s,” he said. “It’s better to have a uniform screening policy and begin at a much younger age.”
At Stanford, in fact, there was a former assessment policy that included cognitive testing, but physicians were successful in seeing that portion of testing eliminated. “It is a physical examination, by a physician of choice, certifying that for the privileges requested there is no physical or mental reason the candidate cannot safely perform them,” Dr. Stockdale explained.
In some cases, medical staffs have filed lawsuits to fight age-related testing. In New Haven, Conn., for instance, the U.S. Equal Employment Opportunity Commission (EEOC) filed a suit in 2020 on behalf of the Yale New Haven Hospital staff, alleging a discriminatory “late career practitioner policy.”
A similar case in Minnesota reached a settlement in 2021, providing monetary relief to staff impacted by out-of-pocket costs for the assessment, in addition to requiring that the hospital in question report to the EEOC any complaints related to age discrimination.
James Ellison, MD, MPH, chair in Memory Care and Geriatrics with ChristianaCare in Wilmington, Del., points out that aging can bring benefits for practicing physicians. “Age is very individualized and there are good and bad consequences,” he said. “Experience can build knowledge and confidence and expertise, and it does improve diagnostic accuracy.”
On the flip side, however, age-related brain changes include loss of volume and lower levels of some neurotransmitters, resulting in cognitive changes. “Functional changes occur too,” Dr. Ellison said.
“Just as some aging athletes may lose a degree of speed, strength, and flexibility, and some aging scientists may lose a part of their former cognitive speed, flexibility, and mental strength, aging health care providers can lose some of the physical coordination, strength, and visual acuity necessary to perform demanding surgical operations. They can also lose some of the processing speed, working memory, and executive function that allows them to excel in cognitive professional tasks.”
An estimated 5.8 million Americans age 65 and older have Alzheimer’s dementia, according to the Alzheimer’s Association.
Picking an arbitrary age for mandatory retirement isn’t the right approach for physicians, said Dr. Katlic. Rather, he said, the answer is to establish late-practitioner screening programs. “Very few hospitals have them, however,” he pointed out. “We do [at Lifebridge Health], and so do a few dozen others, but that’s out of hundreds.”
Instead, what typically plays out is that hospital staff might begin to notice a decline in a colleague. Things like a disheveled appearance or lack of hygiene, or trouble with memory, such as getting lost en route back to his or her office. Even dangerous behaviors such as nodding off during a procedure are not unheard of.
There are many examples of physician decline that fly under the radar. “Unfortunately, it’s unusual for cognitively impaired health care providers to recognize and report their own difficulties,” said Dr. Ellison. “Although peers are expected to report cognitively impaired colleagues, they often fail to do so. In some other countries, age-based assessment is an accepted policy. In the U.S., this is not a uniform policy.”
Sometimes physicians can remain on the job in spite of decline thanks to certain “props,” according to Dr. Ellison. “Good procedures, efficient supports, and various workarounds compensate,” he said, “but often are not sufficient to maintain high-quality practice.”
Most often, these situations play out slowly, until the problem becomes glaringly obvious and potentially dangerous, and someone in a position of power must step in.
“Often, it’s hearsay from a nurse or another staff member, and then a hospital president or chief of staff must make a career-affecting decision for the doctor in question,” said Dr. Katlic.
Because there is little self- or colleague policing – and barring official or binding guidelines on the aging physician issue – both Dr. Katlic and Dr. Ellison are proponents of late-career screening.
How screening can help
As it stands, Dr. Katlic maintains that the profession isn’t doing enough to ensure public safety. “We have peer review and recertification processes, but when you get down to it, we don’t police ourselves well,” he said. “All physicians are assessed throughout their careers as part of the hospital accreditation process, which is fair and adequate.”
Dr. Katlic said that there are three main benchmarks that physicians should be able to meet at an agreed upon age: a physical exam, a neurocognitive screening, and an eye exam. “At some reasonable age, I personally believe these exams should take place,” he said. “We can allow doctors to pick their own practitioners for the eye and physical exams, but the neurocognitive exam should be completed by a PhD neuropsychologist.”
At Lifebridge, for instance, these screenings begin at age 75 and take place every 2 years, during the recredentialing process. It applies to all specialties, not just surgeons. “Surgery is a little different in that it requires fine motor skills in addition to the others we test, but you want any physician to be cognitively intact,” Dr. Katlic pointed out. “All doctors need the ability to make decisions quickly, often under noisy, distracting conditions.”
Dr. Ellison supports applying the screenings to all specialties. “Let’s not forget that all physicians must be alert to the many ways in which their patients reveal what needs attention, evaluation, and treatment,” he said. “Some health care tasks could be performed without visual input; for example, perhaps psychotherapy could be provided competently by a clinician who lacks visual acuity. Auditory input might not be necessary for reading x-rays – but the information a health care provider gets from their eyes and ears is important, not just for surgeons.”
University of California San Diego has established what it calls its Physician Assessment and Clinical Education (PACE) program. One of the nation’s oldest and largest such programs, the hospital founded PACE in 1996. Most physicians taking part arrive as a requirement of disciplinary action from the state medical board, but a small percentage self-refers.
PACE involves two phases. The first is a 2-day set of tests and measures core competency knowledge. Phase 2 is more comprehensive and lasts 5 days. Here, within their specialty, physicians participate in the activities of the corresponding residency program. Faculty evaluates the physician, and a multidisciplinary team meets to review all the findings of the combined phases.
Depending on the results, doctors may face remediation steps that range from programs to address performance deficiencies to residency-level clinical experiences. According to a paper on the program published by the institution, “most physicians referred to the PACE program are found to have mild to moderate performance dyscompetence.”
In the case of the 2021 guidelines adopted by AMA delegates, there are nine principles for assessment. They should be evidence-based, ethical, relevant, accountable, fair and equitable, transparent, supportive, and nonburdensome, and should afford physicians due process protections.
Looking ahead
Even Dr. Katlic worries about the possibility of Congress intervening to establish federal-level, mandatory retirement age. “This just doesn’t make sense for our profession given the great variability we see,” he said. “My biggest hope is that more individual hospitals will institute these screenings.”
As the physician population ages – and the influx of new doctors shrinks – the slope becomes even more slippery. The AMA is predicting a physician shortage of nearly 40,000 by the year 2034. This strengthens arguments to keep existing physicians practicing for as long as possible and might make institutions less likely to screen.
It’s all a delicate balancing act and a continuing work in progress, said Dr. Ellison. “Ultimately, I believe we need to find a way to understand and address the possible implications for public safety, while at the same time protecting the privacy and dignity of our valued older physicians and other health care providers.”
A version of this article first appeared on Medscape.com.
30 years of fake nursing ends with 7-year prison sentence
A Canadian woman who officials allege faked being a registered nurse for some 30 years in Canada and the United States is scheduled to appear in court next month after being sentenced to 7 years in prison.
She was previously sentenced April 22 in an Ontario court after she pled guilty in January to seven offenses, including impersonation, assault with a weapon, and assault, according to CBC Radio-Canada.
Ms. Cleroux, who uses several aliases, had a long history of deception in three provinces in Canada, as well as in Colorado and Florida. The sentencing in Ontario stemmed from incidents at a medical and dental clinic in Ottawa last year, which included administration of medications to patients through needle injections, Ottawa Police reported in a press statement obtained by this news organization.
Authorities charged Ms. Cleroux in September with assault with a weapon and criminal negligence causing bodily harm, along with “personation to gain advantage,” obtaining by false pretense, and using a forged document, this news organization reported.
Ms. Cleroux has been in custody since her arrest by Ottawa Police in August.
The Vancouver Police Department (VPD) charged Ms. Cleroux last year with fraud of over $5,000 and personation with intent. VPD investigated claims that an employee at BC Women’s Hospital fraudulently identified herself as a nurse while working there between June 2020 and June 2021, according to a VPD press release.
Nursing colleges in British Columbia and Ontario issued warnings that she had used aliases and purported to be a registered nurse to gain employment. The aliases included Melanie Thompson, Melanie Smith, and Melanie Cleroux.
Ms. Cleroux was believed to be a student in a nursing school in Colorado, but she only completed 2 years of a 4-year nursing course and was never certified as a nurse, according to CBC. Her criminal record dates back 30 years and includes 67 adult convictions and other convictions in her youth, CBC reported.
A version of this article first appeared on Medscape.com.
A Canadian woman who officials allege faked being a registered nurse for some 30 years in Canada and the United States is scheduled to appear in court next month after being sentenced to 7 years in prison.
She was previously sentenced April 22 in an Ontario court after she pled guilty in January to seven offenses, including impersonation, assault with a weapon, and assault, according to CBC Radio-Canada.
Ms. Cleroux, who uses several aliases, had a long history of deception in three provinces in Canada, as well as in Colorado and Florida. The sentencing in Ontario stemmed from incidents at a medical and dental clinic in Ottawa last year, which included administration of medications to patients through needle injections, Ottawa Police reported in a press statement obtained by this news organization.
Authorities charged Ms. Cleroux in September with assault with a weapon and criminal negligence causing bodily harm, along with “personation to gain advantage,” obtaining by false pretense, and using a forged document, this news organization reported.
Ms. Cleroux has been in custody since her arrest by Ottawa Police in August.
The Vancouver Police Department (VPD) charged Ms. Cleroux last year with fraud of over $5,000 and personation with intent. VPD investigated claims that an employee at BC Women’s Hospital fraudulently identified herself as a nurse while working there between June 2020 and June 2021, according to a VPD press release.
Nursing colleges in British Columbia and Ontario issued warnings that she had used aliases and purported to be a registered nurse to gain employment. The aliases included Melanie Thompson, Melanie Smith, and Melanie Cleroux.
Ms. Cleroux was believed to be a student in a nursing school in Colorado, but she only completed 2 years of a 4-year nursing course and was never certified as a nurse, according to CBC. Her criminal record dates back 30 years and includes 67 adult convictions and other convictions in her youth, CBC reported.
A version of this article first appeared on Medscape.com.
A Canadian woman who officials allege faked being a registered nurse for some 30 years in Canada and the United States is scheduled to appear in court next month after being sentenced to 7 years in prison.
She was previously sentenced April 22 in an Ontario court after she pled guilty in January to seven offenses, including impersonation, assault with a weapon, and assault, according to CBC Radio-Canada.
Ms. Cleroux, who uses several aliases, had a long history of deception in three provinces in Canada, as well as in Colorado and Florida. The sentencing in Ontario stemmed from incidents at a medical and dental clinic in Ottawa last year, which included administration of medications to patients through needle injections, Ottawa Police reported in a press statement obtained by this news organization.
Authorities charged Ms. Cleroux in September with assault with a weapon and criminal negligence causing bodily harm, along with “personation to gain advantage,” obtaining by false pretense, and using a forged document, this news organization reported.
Ms. Cleroux has been in custody since her arrest by Ottawa Police in August.
The Vancouver Police Department (VPD) charged Ms. Cleroux last year with fraud of over $5,000 and personation with intent. VPD investigated claims that an employee at BC Women’s Hospital fraudulently identified herself as a nurse while working there between June 2020 and June 2021, according to a VPD press release.
Nursing colleges in British Columbia and Ontario issued warnings that she had used aliases and purported to be a registered nurse to gain employment. The aliases included Melanie Thompson, Melanie Smith, and Melanie Cleroux.
Ms. Cleroux was believed to be a student in a nursing school in Colorado, but she only completed 2 years of a 4-year nursing course and was never certified as a nurse, according to CBC. Her criminal record dates back 30 years and includes 67 adult convictions and other convictions in her youth, CBC reported.
A version of this article first appeared on Medscape.com.
Three in four U.S. doctors are employed by hospitals, corporate entities: Report
Marcus Welby, MD, was a fictitious hometown doctor featured in a TV drama with the same name that was shown on ABC from 1969 to 1976. Played by actor Robert Young, Dr. Welby treated his patients through their bouts with breast cancer, impotence, and Alzheimer’s disease.
, according to a recent report sponsored by the Physicians Advocacy Institute and prepared by consulting firm Avalere Health.
“COVID-19 drove physicians to leave private practice for employment at an even more rapid pace than we’ve seen in recent years, and these trends continued to accelerate in 2021,” Kelly Kenney, chief executive officer of Physicians Advocacy Institute, said in an announcement. “This study underscores the fact that physicians across the nation are facing severe burnout and strain. The pressures of the pandemic forced many independent physicians to make difficult decisions to sell their practices, health insurers, or other corporate entities.”
Corporate entities are defined in the report as health insurers, private equity firms, and umbrella corporate entities that own multiple physician practices.
“The pandemic has been just brutal ... for nurses and physicians who are caring for patients,” Ms. Kenney told this news organization. “Between the financial stress that the pandemic certainly had on practices, because they certainly had little revenue for a while, and then also we know that the stress that physicians have felt mentally, you can’t overstate that.”
More than half of physician practices owned by hospitals, corporate entities
The Physicians Advocacy Institute has tracked changes in physician employment consistently since 2012, said Ms. Kenney. In 2012, 25% of physicians were employed; that has jumped to nearly 74%, which means the past decade has brought a world of change to the nation’s physicians.
“These are essentially small-business people ... and they were primarily trained to care for patients,” said Ms. Kenney, referring to physicians in independent practice. Still, she understands why physicians would seek employment in the face of “the crushing kind of pressure of having to deal with 20 different payers, pay overhead, and keep the lights on [at the practice].”
According to the report, 108,700 physicians left independent practice to enter employment with hospitals or other corporate entities in the 3-year period that ended in 2021. Seventy-six percent of that shift to employed status among physicians has occurred since the start of the COVID-19 pandemic in March 2020.
From a regional perspective, the report found continued growth among employed physicians across all U.S. regions in the last half of 2020. Hospital- or corporate-owned physician practices increased between 28% and 44%, while the percentage of hospital- or corporate-employed physicians increased between 13% and 24%.
Eighty percent of physicians in the Midwest are employed by hospitals or corporations, which leads the rest of the country, per the report. That’s followed by the Northeast, the West, and the South. Overall, the number of physicians working for such entities increased in all regions.
The report revealed that physician employment by corporations such as health insurers and venture capital firms grew from 92,400 in January 2019 to 142,900 in January 2022.
Hospitals and corporate entities acquired 36,200 physician practices (representing 38% growth) between 2019 and 2021, and the majority of these moves occurred since the pandemic’s start, according to the report.
Value-based care, venture capital firms driving change
Ms. Kenney pointed to value-based care as driving much of this activity by hospitals. “We all embrace [value-based payment], because we need to get a handle on cost, and we want better quality [but] those trends tend to favor integrated systems and systems that can handle a lot of risk and populations of patients.”
Still, the moves by private equity firms and health insurers in this space is relatively new, said Ms. Kenney, who added that her organization started tracking this trend 3 years ago. She pointed to a “marked acceleration” in the trend toward employing physicians and the sale of practices in the 18 months following the pandemic’s start; nonhospital corporate entities drove that steep increase, she said.
Ms. Kenney calls for further study and “guardrails” to respond to “that force in the health care system,” referring to the acquisition of practices by entities such as private equity firms. “Are these big [health care] systems going to continue to see patients in underserved areas, rural areas, and Medicaid patients if it doesn’t make sense financially to do so?
“That’s what we’re teeing up with this research,” added Ms. Kenney. “We are providing information that starts some conversations around what we might want to think about in terms of policies to ensure that we don’t impact patients’ access to care.”
The Physicians Advocacy Institute represents more than 170,000 physicians and medical students. Avalere Health used the IQVIA OneKey database for the report. The researchers studied the 3-year period from Jan. 1, 2019, to Jan. 1, 2022.
A version of this article first appeared on Medscape.com.
Marcus Welby, MD, was a fictitious hometown doctor featured in a TV drama with the same name that was shown on ABC from 1969 to 1976. Played by actor Robert Young, Dr. Welby treated his patients through their bouts with breast cancer, impotence, and Alzheimer’s disease.
, according to a recent report sponsored by the Physicians Advocacy Institute and prepared by consulting firm Avalere Health.
“COVID-19 drove physicians to leave private practice for employment at an even more rapid pace than we’ve seen in recent years, and these trends continued to accelerate in 2021,” Kelly Kenney, chief executive officer of Physicians Advocacy Institute, said in an announcement. “This study underscores the fact that physicians across the nation are facing severe burnout and strain. The pressures of the pandemic forced many independent physicians to make difficult decisions to sell their practices, health insurers, or other corporate entities.”
Corporate entities are defined in the report as health insurers, private equity firms, and umbrella corporate entities that own multiple physician practices.
“The pandemic has been just brutal ... for nurses and physicians who are caring for patients,” Ms. Kenney told this news organization. “Between the financial stress that the pandemic certainly had on practices, because they certainly had little revenue for a while, and then also we know that the stress that physicians have felt mentally, you can’t overstate that.”
More than half of physician practices owned by hospitals, corporate entities
The Physicians Advocacy Institute has tracked changes in physician employment consistently since 2012, said Ms. Kenney. In 2012, 25% of physicians were employed; that has jumped to nearly 74%, which means the past decade has brought a world of change to the nation’s physicians.
“These are essentially small-business people ... and they were primarily trained to care for patients,” said Ms. Kenney, referring to physicians in independent practice. Still, she understands why physicians would seek employment in the face of “the crushing kind of pressure of having to deal with 20 different payers, pay overhead, and keep the lights on [at the practice].”
According to the report, 108,700 physicians left independent practice to enter employment with hospitals or other corporate entities in the 3-year period that ended in 2021. Seventy-six percent of that shift to employed status among physicians has occurred since the start of the COVID-19 pandemic in March 2020.
From a regional perspective, the report found continued growth among employed physicians across all U.S. regions in the last half of 2020. Hospital- or corporate-owned physician practices increased between 28% and 44%, while the percentage of hospital- or corporate-employed physicians increased between 13% and 24%.
Eighty percent of physicians in the Midwest are employed by hospitals or corporations, which leads the rest of the country, per the report. That’s followed by the Northeast, the West, and the South. Overall, the number of physicians working for such entities increased in all regions.
The report revealed that physician employment by corporations such as health insurers and venture capital firms grew from 92,400 in January 2019 to 142,900 in January 2022.
Hospitals and corporate entities acquired 36,200 physician practices (representing 38% growth) between 2019 and 2021, and the majority of these moves occurred since the pandemic’s start, according to the report.
Value-based care, venture capital firms driving change
Ms. Kenney pointed to value-based care as driving much of this activity by hospitals. “We all embrace [value-based payment], because we need to get a handle on cost, and we want better quality [but] those trends tend to favor integrated systems and systems that can handle a lot of risk and populations of patients.”
Still, the moves by private equity firms and health insurers in this space is relatively new, said Ms. Kenney, who added that her organization started tracking this trend 3 years ago. She pointed to a “marked acceleration” in the trend toward employing physicians and the sale of practices in the 18 months following the pandemic’s start; nonhospital corporate entities drove that steep increase, she said.
Ms. Kenney calls for further study and “guardrails” to respond to “that force in the health care system,” referring to the acquisition of practices by entities such as private equity firms. “Are these big [health care] systems going to continue to see patients in underserved areas, rural areas, and Medicaid patients if it doesn’t make sense financially to do so?
“That’s what we’re teeing up with this research,” added Ms. Kenney. “We are providing information that starts some conversations around what we might want to think about in terms of policies to ensure that we don’t impact patients’ access to care.”
The Physicians Advocacy Institute represents more than 170,000 physicians and medical students. Avalere Health used the IQVIA OneKey database for the report. The researchers studied the 3-year period from Jan. 1, 2019, to Jan. 1, 2022.
A version of this article first appeared on Medscape.com.
Marcus Welby, MD, was a fictitious hometown doctor featured in a TV drama with the same name that was shown on ABC from 1969 to 1976. Played by actor Robert Young, Dr. Welby treated his patients through their bouts with breast cancer, impotence, and Alzheimer’s disease.
, according to a recent report sponsored by the Physicians Advocacy Institute and prepared by consulting firm Avalere Health.
“COVID-19 drove physicians to leave private practice for employment at an even more rapid pace than we’ve seen in recent years, and these trends continued to accelerate in 2021,” Kelly Kenney, chief executive officer of Physicians Advocacy Institute, said in an announcement. “This study underscores the fact that physicians across the nation are facing severe burnout and strain. The pressures of the pandemic forced many independent physicians to make difficult decisions to sell their practices, health insurers, or other corporate entities.”
Corporate entities are defined in the report as health insurers, private equity firms, and umbrella corporate entities that own multiple physician practices.
“The pandemic has been just brutal ... for nurses and physicians who are caring for patients,” Ms. Kenney told this news organization. “Between the financial stress that the pandemic certainly had on practices, because they certainly had little revenue for a while, and then also we know that the stress that physicians have felt mentally, you can’t overstate that.”
More than half of physician practices owned by hospitals, corporate entities
The Physicians Advocacy Institute has tracked changes in physician employment consistently since 2012, said Ms. Kenney. In 2012, 25% of physicians were employed; that has jumped to nearly 74%, which means the past decade has brought a world of change to the nation’s physicians.
“These are essentially small-business people ... and they were primarily trained to care for patients,” said Ms. Kenney, referring to physicians in independent practice. Still, she understands why physicians would seek employment in the face of “the crushing kind of pressure of having to deal with 20 different payers, pay overhead, and keep the lights on [at the practice].”
According to the report, 108,700 physicians left independent practice to enter employment with hospitals or other corporate entities in the 3-year period that ended in 2021. Seventy-six percent of that shift to employed status among physicians has occurred since the start of the COVID-19 pandemic in March 2020.
From a regional perspective, the report found continued growth among employed physicians across all U.S. regions in the last half of 2020. Hospital- or corporate-owned physician practices increased between 28% and 44%, while the percentage of hospital- or corporate-employed physicians increased between 13% and 24%.
Eighty percent of physicians in the Midwest are employed by hospitals or corporations, which leads the rest of the country, per the report. That’s followed by the Northeast, the West, and the South. Overall, the number of physicians working for such entities increased in all regions.
The report revealed that physician employment by corporations such as health insurers and venture capital firms grew from 92,400 in January 2019 to 142,900 in January 2022.
Hospitals and corporate entities acquired 36,200 physician practices (representing 38% growth) between 2019 and 2021, and the majority of these moves occurred since the pandemic’s start, according to the report.
Value-based care, venture capital firms driving change
Ms. Kenney pointed to value-based care as driving much of this activity by hospitals. “We all embrace [value-based payment], because we need to get a handle on cost, and we want better quality [but] those trends tend to favor integrated systems and systems that can handle a lot of risk and populations of patients.”
Still, the moves by private equity firms and health insurers in this space is relatively new, said Ms. Kenney, who added that her organization started tracking this trend 3 years ago. She pointed to a “marked acceleration” in the trend toward employing physicians and the sale of practices in the 18 months following the pandemic’s start; nonhospital corporate entities drove that steep increase, she said.
Ms. Kenney calls for further study and “guardrails” to respond to “that force in the health care system,” referring to the acquisition of practices by entities such as private equity firms. “Are these big [health care] systems going to continue to see patients in underserved areas, rural areas, and Medicaid patients if it doesn’t make sense financially to do so?
“That’s what we’re teeing up with this research,” added Ms. Kenney. “We are providing information that starts some conversations around what we might want to think about in terms of policies to ensure that we don’t impact patients’ access to care.”
The Physicians Advocacy Institute represents more than 170,000 physicians and medical students. Avalere Health used the IQVIA OneKey database for the report. The researchers studied the 3-year period from Jan. 1, 2019, to Jan. 1, 2022.
A version of this article first appeared on Medscape.com.
Cancer hospitals often mark up drug prices, ignore price transparency rules
Among those that do provide this information, new research shows that hospitals substantially mark up prices for top-selling cancer therapies relative to acquisition costs. Median drug price markups across NCI centers and payers ranged from nearly 120% to more than 600%.
As a result, “the total price for an entire treatment course could vary on the order of hundreds of thousands of dollars,” Roy Xiao, MD, department of otolaryngology–head and neck surgery, Massachusetts Eye and Ear Infirmary, Boston, said in an interview.
The study was published online in JAMA Internal Medicine.
Manufacturers often price novel anticancer therapies at more than $100,000 per year, but less is known about how much hospitals mark up these prices for patients with private health insurance and how much negotiated prices vary across centers and payers.
Dr. Xiao and colleagues analyzed private payer-specific negotiated prices for the top 25 parenteral cancer therapies by Medicare Part B spending in 2019 using publicly available hospital price transparency files for 61 NCI-designated cancer centers.
Fewer than half of the centers (44.3%) disclosed payer-specific negotiated prices for at least one top-selling cancer drug. Disclosure rates for different drugs ranged from 21.3% (13 centers) for rituximab with hyaluronidase to 42.6% (26 centers) for rituximab, bevacizumab, or leuprolide.
The researchers also found a wide variation in negotiated prices for cancer therapies across hospitals. Across-center price ratios – defined as the ratio between the 90th and 10th percentile median price per unit – ranged from 2.2 ($16 vs. $36 for pembrolizumab 1 mg) and 15.8 ($247 vs. $3,914 for leuprolide 7.5 mg).
Payer-specific prices also varied considerably between payers at the same center. Among all centers, the median within-center price ratios for cancer therapies ranged from 1.8 (brentuximab) to 2.5 (bevacizumab).
As for the extent of cancer therapy markups, median price markups across centers and payers ranged from 118% (sipuleucel-T) to 634% (leuprolide) more than the estimated cost paid by hospitals.
Conservative estimates of acquisition costs and payer-specific prices yielded markups ranging from 42.1% (sipuleucel-T) to 234.1% (leuprolide).
The authors also provided examples of how these variations might affect the total cost of treatment. For instance, the median total price variation across centers to treat metastatic non–small cell lung cancer with pembrolizumab was $168,405. At one institution, the within-center median price variation for daratumumab as third-line therapy for multiple myeloma was $174,225.
To reduce the financial burden of cancer treatment for patients, the authors suggested implementing public policies “to discourage or prevent excessive hospital price markups on parenteral chemotherapeutics.”
To promote hospital compliance with transparency regulations, in January 2022, the Centers for Medicare & Medicare Services increased penalties for nondisclosure from a fixed maximum of $300 per day to up to $5,500 per day, based on hospital bed size, which would total over $2 million per year, Dr. Xiao said in an interview.
“We would expect that this significant financial penalty would encourage more consistent reporting,” he said.
The study had no specific funding. Dr. Xiao has disclosed no relevant disclosures.
A version of this article first appeared on Medscape.com.
Among those that do provide this information, new research shows that hospitals substantially mark up prices for top-selling cancer therapies relative to acquisition costs. Median drug price markups across NCI centers and payers ranged from nearly 120% to more than 600%.
As a result, “the total price for an entire treatment course could vary on the order of hundreds of thousands of dollars,” Roy Xiao, MD, department of otolaryngology–head and neck surgery, Massachusetts Eye and Ear Infirmary, Boston, said in an interview.
The study was published online in JAMA Internal Medicine.
Manufacturers often price novel anticancer therapies at more than $100,000 per year, but less is known about how much hospitals mark up these prices for patients with private health insurance and how much negotiated prices vary across centers and payers.
Dr. Xiao and colleagues analyzed private payer-specific negotiated prices for the top 25 parenteral cancer therapies by Medicare Part B spending in 2019 using publicly available hospital price transparency files for 61 NCI-designated cancer centers.
Fewer than half of the centers (44.3%) disclosed payer-specific negotiated prices for at least one top-selling cancer drug. Disclosure rates for different drugs ranged from 21.3% (13 centers) for rituximab with hyaluronidase to 42.6% (26 centers) for rituximab, bevacizumab, or leuprolide.
The researchers also found a wide variation in negotiated prices for cancer therapies across hospitals. Across-center price ratios – defined as the ratio between the 90th and 10th percentile median price per unit – ranged from 2.2 ($16 vs. $36 for pembrolizumab 1 mg) and 15.8 ($247 vs. $3,914 for leuprolide 7.5 mg).
Payer-specific prices also varied considerably between payers at the same center. Among all centers, the median within-center price ratios for cancer therapies ranged from 1.8 (brentuximab) to 2.5 (bevacizumab).
As for the extent of cancer therapy markups, median price markups across centers and payers ranged from 118% (sipuleucel-T) to 634% (leuprolide) more than the estimated cost paid by hospitals.
Conservative estimates of acquisition costs and payer-specific prices yielded markups ranging from 42.1% (sipuleucel-T) to 234.1% (leuprolide).
The authors also provided examples of how these variations might affect the total cost of treatment. For instance, the median total price variation across centers to treat metastatic non–small cell lung cancer with pembrolizumab was $168,405. At one institution, the within-center median price variation for daratumumab as third-line therapy for multiple myeloma was $174,225.
To reduce the financial burden of cancer treatment for patients, the authors suggested implementing public policies “to discourage or prevent excessive hospital price markups on parenteral chemotherapeutics.”
To promote hospital compliance with transparency regulations, in January 2022, the Centers for Medicare & Medicare Services increased penalties for nondisclosure from a fixed maximum of $300 per day to up to $5,500 per day, based on hospital bed size, which would total over $2 million per year, Dr. Xiao said in an interview.
“We would expect that this significant financial penalty would encourage more consistent reporting,” he said.
The study had no specific funding. Dr. Xiao has disclosed no relevant disclosures.
A version of this article first appeared on Medscape.com.
Among those that do provide this information, new research shows that hospitals substantially mark up prices for top-selling cancer therapies relative to acquisition costs. Median drug price markups across NCI centers and payers ranged from nearly 120% to more than 600%.
As a result, “the total price for an entire treatment course could vary on the order of hundreds of thousands of dollars,” Roy Xiao, MD, department of otolaryngology–head and neck surgery, Massachusetts Eye and Ear Infirmary, Boston, said in an interview.
The study was published online in JAMA Internal Medicine.
Manufacturers often price novel anticancer therapies at more than $100,000 per year, but less is known about how much hospitals mark up these prices for patients with private health insurance and how much negotiated prices vary across centers and payers.
Dr. Xiao and colleagues analyzed private payer-specific negotiated prices for the top 25 parenteral cancer therapies by Medicare Part B spending in 2019 using publicly available hospital price transparency files for 61 NCI-designated cancer centers.
Fewer than half of the centers (44.3%) disclosed payer-specific negotiated prices for at least one top-selling cancer drug. Disclosure rates for different drugs ranged from 21.3% (13 centers) for rituximab with hyaluronidase to 42.6% (26 centers) for rituximab, bevacizumab, or leuprolide.
The researchers also found a wide variation in negotiated prices for cancer therapies across hospitals. Across-center price ratios – defined as the ratio between the 90th and 10th percentile median price per unit – ranged from 2.2 ($16 vs. $36 for pembrolizumab 1 mg) and 15.8 ($247 vs. $3,914 for leuprolide 7.5 mg).
Payer-specific prices also varied considerably between payers at the same center. Among all centers, the median within-center price ratios for cancer therapies ranged from 1.8 (brentuximab) to 2.5 (bevacizumab).
As for the extent of cancer therapy markups, median price markups across centers and payers ranged from 118% (sipuleucel-T) to 634% (leuprolide) more than the estimated cost paid by hospitals.
Conservative estimates of acquisition costs and payer-specific prices yielded markups ranging from 42.1% (sipuleucel-T) to 234.1% (leuprolide).
The authors also provided examples of how these variations might affect the total cost of treatment. For instance, the median total price variation across centers to treat metastatic non–small cell lung cancer with pembrolizumab was $168,405. At one institution, the within-center median price variation for daratumumab as third-line therapy for multiple myeloma was $174,225.
To reduce the financial burden of cancer treatment for patients, the authors suggested implementing public policies “to discourage or prevent excessive hospital price markups on parenteral chemotherapeutics.”
To promote hospital compliance with transparency regulations, in January 2022, the Centers for Medicare & Medicare Services increased penalties for nondisclosure from a fixed maximum of $300 per day to up to $5,500 per day, based on hospital bed size, which would total over $2 million per year, Dr. Xiao said in an interview.
“We would expect that this significant financial penalty would encourage more consistent reporting,” he said.
The study had no specific funding. Dr. Xiao has disclosed no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM JAMA INTERNAL MEDICINE
Are free lunches back? Docs start seeing drug reps again
In their heyday, drug reps had big expense budgets and would wine and dine physicians, golf with them, and give gifts to their potential physician clients.
But in 2002, pressure from Congress and increased scrutiny from the American Medical Association prompted the Pharmaceutical Research and Manufacturers of America to adopt a set of voluntary ethical codes to regulate the gifts given to physicians. Now, physicians must report even small gifts or meals to the National Practitioner Data Bank.
Before the restrictions, physician/pharmaceutical rep relationships relied on face-to-face meetings. These included lunches with a limited budget or sharing a cup of coffee during a morning visit to a practice. The parties got to know each other, which led to trust and long-term relationships.
During the COVID-19 pandemic, everything changed. “It was culture shock for us,” admitted Craig F, a career pharmaceutical rep. “We didn’t know what we were going to do.”
The pharmaceutical industry pivoted and quickly got up to speed with Zoom, Microsoft Teams, and the like. “We began by reaching out to doctors via email and cell phones to set up virtual meetings,” Craig said. “Most of the doctors were working from home, doing telehealth whenever possible. For new sales reps, this was particularly difficult, because they couldn’t visit offices and get to know doctors.”
Many physicians didn’t want to devote time to Zoom meetings with pharma reps. “We worked around their schedules, and sometimes this even looked like Sunday calls,” he said.
As vaccination levels increased and medical offices began to reopen, so too did some of the old-school, face-to-face pharma rep/doctor meetings. But most proceeded with caution. “Some pharmaceutical companies didn’t put reps back into the field until the fall of 2020,” said Craig. “If we weren’t welcome in an office, we didn’t push it.”
Once much of the population was vaccinated, the thaw began in earnest, although the drug reps continued to tread cautiously, mask up, and respect the wishes of physicians. Today, Craig estimated that about two-thirds of his appointments are in person.
Still, it’s unlikely that the drug rep–supplied “free staff lunch” will ever regain its former popularity. Medical office staff are still keeping distance, owing to COVID; office schedules may be more crowded and may not allow the time; and many physicians are still nervous about having to report “gifts” or “paid lunches” from pharma.
The post-COVID paradigm shift
The pandemic put a dent in the pharma rep/doctor relationship, said Suzy Jackson, managing director of life sciences at Accenture and an author of The “New” Rules of Healthcare Provider Engagement . “COVID started moving power away from reps because they lost the ability to simply wander into a building and have a conversation with a health care provider. We’re seeing the pandemic evolve the meeting model into a hybrid in-person and virtual.”
“Many doctors are operating in a slower fashion because they’re balancing a hybrid model with patients, as well,” said Craig. “Some of my visits now involve talking to nurses or front-office staff, not getting in to see the doctors.”
The push from some doctors to see reps virtually as opposed to in person is a challenge for the pharma companies. “We get more done in person, so virtual is not our favorite way to do business,” said Craig. “But we’re thankful for any time we can get with doctors, so when they ask to do virtual, we agree.”
Still, the Accenture survey offered good news for pharma reps: Only 4% of respondents didn’t want to continue with in-person meetings at all. “I think of this as a positive,” Ms. Jackson said. “It shows that physicians value these relationships, if they’re done in the right way.”
But a survey by Boston Consulting Group confirms that virtual visits are likely to continue. BCG’s Doctors’ Changing Expectations of Pharma Are Here to Stay revealed that three-quarters of respondent physicians prefer to maintain or increase the amount of virtual engagements with pharma reps after becoming accustomed to the practice during the pandemic.
Under these changing scenarios, said Ms. Jackson, pharma reps have to think about more meaningful ways to engage with doctors.
“I feel that doctors are more crunched for time now, managing hybrid environments,” Craig said. “They have less time and want more patient-specific information that leads to fewer calls back to their offices.”
More physicians now value webinars, virtual training, and speaker programs. Virtual channels, the survey found, “give physicians access to the information they need in an easy and convenient manner.”
Still, physicians have noted that the survey indicated that email communications from pharma reps had increased. Often, physicians found the useful information buried in irrelevant “clutter.”
Restrictions on drug reps became tighter
In the 20 years since the guidelines came into existence, PhRMA has continued to strengthen the codes. In 2009, PhRMA issued new recommendations surrounding noneducational gifts and placed a cap of $100 for meals, drug samples, and other items. In 2022, they added layers to the code that focus on speaker programs. For instance, while companies can provide “modest” meals to attendees as an incidental courtesy, pharma reps can no longer pay for or provide alcohol in conjunction with these programs.
The rules vary from state to state. In Minnesota, for instance, gifts from pharma companies cannot exceed $50 per year. Some institutions – such as the Cleveland Clinic – have even stricter rules. “When we have conventions, we put up signage reminding doctors from the strictest states that they can’t even accept a cup of coffee from a rep,” said Craig.
However, COVID hasn’t completely changed doctor/pharma relationships. In Ms. Jackson’s words, “In spite of the shift to a more hybrid model, this is a very human relationship yielding real human results.”
A version of this article first appeared on Medscape.com.
In their heyday, drug reps had big expense budgets and would wine and dine physicians, golf with them, and give gifts to their potential physician clients.
But in 2002, pressure from Congress and increased scrutiny from the American Medical Association prompted the Pharmaceutical Research and Manufacturers of America to adopt a set of voluntary ethical codes to regulate the gifts given to physicians. Now, physicians must report even small gifts or meals to the National Practitioner Data Bank.
Before the restrictions, physician/pharmaceutical rep relationships relied on face-to-face meetings. These included lunches with a limited budget or sharing a cup of coffee during a morning visit to a practice. The parties got to know each other, which led to trust and long-term relationships.
During the COVID-19 pandemic, everything changed. “It was culture shock for us,” admitted Craig F, a career pharmaceutical rep. “We didn’t know what we were going to do.”
The pharmaceutical industry pivoted and quickly got up to speed with Zoom, Microsoft Teams, and the like. “We began by reaching out to doctors via email and cell phones to set up virtual meetings,” Craig said. “Most of the doctors were working from home, doing telehealth whenever possible. For new sales reps, this was particularly difficult, because they couldn’t visit offices and get to know doctors.”
Many physicians didn’t want to devote time to Zoom meetings with pharma reps. “We worked around their schedules, and sometimes this even looked like Sunday calls,” he said.
As vaccination levels increased and medical offices began to reopen, so too did some of the old-school, face-to-face pharma rep/doctor meetings. But most proceeded with caution. “Some pharmaceutical companies didn’t put reps back into the field until the fall of 2020,” said Craig. “If we weren’t welcome in an office, we didn’t push it.”
Once much of the population was vaccinated, the thaw began in earnest, although the drug reps continued to tread cautiously, mask up, and respect the wishes of physicians. Today, Craig estimated that about two-thirds of his appointments are in person.
Still, it’s unlikely that the drug rep–supplied “free staff lunch” will ever regain its former popularity. Medical office staff are still keeping distance, owing to COVID; office schedules may be more crowded and may not allow the time; and many physicians are still nervous about having to report “gifts” or “paid lunches” from pharma.
The post-COVID paradigm shift
The pandemic put a dent in the pharma rep/doctor relationship, said Suzy Jackson, managing director of life sciences at Accenture and an author of The “New” Rules of Healthcare Provider Engagement . “COVID started moving power away from reps because they lost the ability to simply wander into a building and have a conversation with a health care provider. We’re seeing the pandemic evolve the meeting model into a hybrid in-person and virtual.”
“Many doctors are operating in a slower fashion because they’re balancing a hybrid model with patients, as well,” said Craig. “Some of my visits now involve talking to nurses or front-office staff, not getting in to see the doctors.”
The push from some doctors to see reps virtually as opposed to in person is a challenge for the pharma companies. “We get more done in person, so virtual is not our favorite way to do business,” said Craig. “But we’re thankful for any time we can get with doctors, so when they ask to do virtual, we agree.”
Still, the Accenture survey offered good news for pharma reps: Only 4% of respondents didn’t want to continue with in-person meetings at all. “I think of this as a positive,” Ms. Jackson said. “It shows that physicians value these relationships, if they’re done in the right way.”
But a survey by Boston Consulting Group confirms that virtual visits are likely to continue. BCG’s Doctors’ Changing Expectations of Pharma Are Here to Stay revealed that three-quarters of respondent physicians prefer to maintain or increase the amount of virtual engagements with pharma reps after becoming accustomed to the practice during the pandemic.
Under these changing scenarios, said Ms. Jackson, pharma reps have to think about more meaningful ways to engage with doctors.
“I feel that doctors are more crunched for time now, managing hybrid environments,” Craig said. “They have less time and want more patient-specific information that leads to fewer calls back to their offices.”
More physicians now value webinars, virtual training, and speaker programs. Virtual channels, the survey found, “give physicians access to the information they need in an easy and convenient manner.”
Still, physicians have noted that the survey indicated that email communications from pharma reps had increased. Often, physicians found the useful information buried in irrelevant “clutter.”
Restrictions on drug reps became tighter
In the 20 years since the guidelines came into existence, PhRMA has continued to strengthen the codes. In 2009, PhRMA issued new recommendations surrounding noneducational gifts and placed a cap of $100 for meals, drug samples, and other items. In 2022, they added layers to the code that focus on speaker programs. For instance, while companies can provide “modest” meals to attendees as an incidental courtesy, pharma reps can no longer pay for or provide alcohol in conjunction with these programs.
The rules vary from state to state. In Minnesota, for instance, gifts from pharma companies cannot exceed $50 per year. Some institutions – such as the Cleveland Clinic – have even stricter rules. “When we have conventions, we put up signage reminding doctors from the strictest states that they can’t even accept a cup of coffee from a rep,” said Craig.
However, COVID hasn’t completely changed doctor/pharma relationships. In Ms. Jackson’s words, “In spite of the shift to a more hybrid model, this is a very human relationship yielding real human results.”
A version of this article first appeared on Medscape.com.
In their heyday, drug reps had big expense budgets and would wine and dine physicians, golf with them, and give gifts to their potential physician clients.
But in 2002, pressure from Congress and increased scrutiny from the American Medical Association prompted the Pharmaceutical Research and Manufacturers of America to adopt a set of voluntary ethical codes to regulate the gifts given to physicians. Now, physicians must report even small gifts or meals to the National Practitioner Data Bank.
Before the restrictions, physician/pharmaceutical rep relationships relied on face-to-face meetings. These included lunches with a limited budget or sharing a cup of coffee during a morning visit to a practice. The parties got to know each other, which led to trust and long-term relationships.
During the COVID-19 pandemic, everything changed. “It was culture shock for us,” admitted Craig F, a career pharmaceutical rep. “We didn’t know what we were going to do.”
The pharmaceutical industry pivoted and quickly got up to speed with Zoom, Microsoft Teams, and the like. “We began by reaching out to doctors via email and cell phones to set up virtual meetings,” Craig said. “Most of the doctors were working from home, doing telehealth whenever possible. For new sales reps, this was particularly difficult, because they couldn’t visit offices and get to know doctors.”
Many physicians didn’t want to devote time to Zoom meetings with pharma reps. “We worked around their schedules, and sometimes this even looked like Sunday calls,” he said.
As vaccination levels increased and medical offices began to reopen, so too did some of the old-school, face-to-face pharma rep/doctor meetings. But most proceeded with caution. “Some pharmaceutical companies didn’t put reps back into the field until the fall of 2020,” said Craig. “If we weren’t welcome in an office, we didn’t push it.”
Once much of the population was vaccinated, the thaw began in earnest, although the drug reps continued to tread cautiously, mask up, and respect the wishes of physicians. Today, Craig estimated that about two-thirds of his appointments are in person.
Still, it’s unlikely that the drug rep–supplied “free staff lunch” will ever regain its former popularity. Medical office staff are still keeping distance, owing to COVID; office schedules may be more crowded and may not allow the time; and many physicians are still nervous about having to report “gifts” or “paid lunches” from pharma.
The post-COVID paradigm shift
The pandemic put a dent in the pharma rep/doctor relationship, said Suzy Jackson, managing director of life sciences at Accenture and an author of The “New” Rules of Healthcare Provider Engagement . “COVID started moving power away from reps because they lost the ability to simply wander into a building and have a conversation with a health care provider. We’re seeing the pandemic evolve the meeting model into a hybrid in-person and virtual.”
“Many doctors are operating in a slower fashion because they’re balancing a hybrid model with patients, as well,” said Craig. “Some of my visits now involve talking to nurses or front-office staff, not getting in to see the doctors.”
The push from some doctors to see reps virtually as opposed to in person is a challenge for the pharma companies. “We get more done in person, so virtual is not our favorite way to do business,” said Craig. “But we’re thankful for any time we can get with doctors, so when they ask to do virtual, we agree.”
Still, the Accenture survey offered good news for pharma reps: Only 4% of respondents didn’t want to continue with in-person meetings at all. “I think of this as a positive,” Ms. Jackson said. “It shows that physicians value these relationships, if they’re done in the right way.”
But a survey by Boston Consulting Group confirms that virtual visits are likely to continue. BCG’s Doctors’ Changing Expectations of Pharma Are Here to Stay revealed that three-quarters of respondent physicians prefer to maintain or increase the amount of virtual engagements with pharma reps after becoming accustomed to the practice during the pandemic.
Under these changing scenarios, said Ms. Jackson, pharma reps have to think about more meaningful ways to engage with doctors.
“I feel that doctors are more crunched for time now, managing hybrid environments,” Craig said. “They have less time and want more patient-specific information that leads to fewer calls back to their offices.”
More physicians now value webinars, virtual training, and speaker programs. Virtual channels, the survey found, “give physicians access to the information they need in an easy and convenient manner.”
Still, physicians have noted that the survey indicated that email communications from pharma reps had increased. Often, physicians found the useful information buried in irrelevant “clutter.”
Restrictions on drug reps became tighter
In the 20 years since the guidelines came into existence, PhRMA has continued to strengthen the codes. In 2009, PhRMA issued new recommendations surrounding noneducational gifts and placed a cap of $100 for meals, drug samples, and other items. In 2022, they added layers to the code that focus on speaker programs. For instance, while companies can provide “modest” meals to attendees as an incidental courtesy, pharma reps can no longer pay for or provide alcohol in conjunction with these programs.
The rules vary from state to state. In Minnesota, for instance, gifts from pharma companies cannot exceed $50 per year. Some institutions – such as the Cleveland Clinic – have even stricter rules. “When we have conventions, we put up signage reminding doctors from the strictest states that they can’t even accept a cup of coffee from a rep,” said Craig.
However, COVID hasn’t completely changed doctor/pharma relationships. In Ms. Jackson’s words, “In spite of the shift to a more hybrid model, this is a very human relationship yielding real human results.”
A version of this article first appeared on Medscape.com.
