User login
Breast anatomy and augmentation in transfeminine individuals
Augmentation mammaplasty, otherwise known as a breast augmentation, is one of the most common cosmetic procedures performed in cisgender females. Gynecologists routinely perform annual breast examinations and order screening mammography in cisgender women with breast implants. Similarly, there is an increasing number of transgender women seeking breast augmentation – with approximately 60%-70% of patients having desired or undergone the procedure.1 Consequently, these patients are instructed by their surgeons to follow up with gynecologists for annual examinations and screening. While there are many similarities in technique and procedure, there are nuances in patient demographics, anatomy, and surgical technique that obstetricians/gynecologists should be aware of when examining these patients or prior to referring them to a surgeon for augmentation.2
Many patients who are dissatisfied with breast size from hormone therapy alone will seek out augmentation mammaplasty. In patients taking estrogen for hormone therapy, breast growth will commence around 2-3 months and peak over 1-2 years.3 Unlike chest surgery for transmasculine individuals, it is recommended that transfeminine patients seeking breast augmentation wait a minimum of 12 months before to surgery to allow for maximum breast enlargement. As with breast growth in cisgender females, the extent of breast development is multifactorial and varies from individual to individual. Current literature does not suggest that estrogen type or dose affects the ultimate breast size; however, younger age, tissue sensitivity, and body weight may affect breast volume.3 Referral to a genetic counselor and preoperative imaging may be necessary if a patient has a history concerning for a genetic or familial predisposition to breast cancer.
Implant selection and placement is determined by a variety of factors. While the overall principles of augmentation mammaplasty are essentially the same, there are anatomic differences in transfeminine patients that surgeons must take into consideration at the time of the consultation and during the surgery itself. For example, the pectoralis major muscle is more defined, there is a longer sternal notch-to-nipple distance, the chest wall is broader and more barrel-shaped, and there is a shorter distance between the nipple and the inframammary crease.2-4 As a result of the broader chest wall, it is extremely difficult to achieve central cleavage even with larger implant selection. The surgeon must also ensure that the nipple and areola overlie the implant centrally. Medial placement of the implant will result in lateral displacement of the nipples, which can have an unsatisfactory cosmetic appearance.
Incision location can be axillary, inframammary, or even transareolar, although the latter is less common due to the smaller areolar size and larger implant choice.3 If the inframammary incision is used, it should be placed lower than the natural inframammary fold because the distance between the inferior areolar margin and inframammary fold is shorter and will expand after the implant is placed.4 While both saline and silicone implants are available, many surgeons (myself included), favor more form-stable silicone implants. Given the association between anaplastic large-cell lymphoma and textured implants, many surgeons also use nontextured, or smooth, cohesive gel silicone implants.5
Pocket selection of the implant itself can be subglandular – directly under the breast mound – or subpectoral – behind the pectoralis muscle. For patients with a pinch test of greater than 1.5 cm (outside of the area of the breast bud), good skin softening, and marked pectoralis hypertrophy, subglandular placement is reasonable.6 In thin patients with minimal breast development, subglandular placement can result in a “double-mound” appearance and can lead to visible implant edges on the periphery.6 Use of the subpectoral plane is more common and is associated with less implant visibility due to an increased amount of soft-tissue coverage and has lower rates of capsular contracture.4 However, due to the more robust pectoralis muscle in transfeminine patients, implant displacement can occur more frequently compared to subglandular placement. The surgeon and patient must have a thorough discussion about the location of the incision, implant material, and pocket placement along with the benefits and complications of the surgical plan.
Complications of augmentation mammaplasty are rare. However, when they occur it can include capsular contracture, breast asymmetry, hematoma formation, loss of nipple sensation, implant malposition, implant displacement below the inframammary crease, implant rupture, and need for revisional surgery.7 If an obstetrician/gynecologist observes any of the aforementioned findings in a postoperative patient, consultation and referral to a plastic surgeon is imperative.
Postoperative assessment and screening are mandatory in all patients who undergo breast augmentation. It is important for the gynecologist to note the incision placement, know the type of implant used (saline or silicone), and delineate where the implant was placed. If silicone implants are used, breast MRI is more sensitive in detecting implant rupture compared to mammography alone. Given the relatively poor epidemiologic data on breast cancer in transgender women, the Endocrine Society recommends that these patients follow the same screening guidelines as cisgender women.4,6
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa.
References
1. Wierckx K et al. J Sex Med. 2014;11(5):1240-7.
2. Mehra G et al. Plast Reconstr Surg Glob Open 2021 Jan 21;9(1):e3362. doi: 10.1097/GOX.0000000000003362.
3. Schecter LS, Schechter RB. Breast and chest surgery for transgender patients. In: Ferrando CA, ed. Comprehensive Care of the Transgender Patient. Philadelphia, PA: Elsevier, 2020:73-81.
4. Colebunders B et al. Top surgery. In: Salgado CJ et al. ed. Gender Affirmation: Medical and Surgical Perspectives. New York, NY: Thieme, 2017:51-66.
5. De Boer M et al. Aesthet Surg J. 2017;37:NP83-NP87.
6. Coon D et al. Plast Reconstr Surg. 2020 Jun;145(6):1343-53.
7. Kanhai RC et al. Br J Plast Surg. 2000;53:209-11.
Augmentation mammaplasty, otherwise known as a breast augmentation, is one of the most common cosmetic procedures performed in cisgender females. Gynecologists routinely perform annual breast examinations and order screening mammography in cisgender women with breast implants. Similarly, there is an increasing number of transgender women seeking breast augmentation – with approximately 60%-70% of patients having desired or undergone the procedure.1 Consequently, these patients are instructed by their surgeons to follow up with gynecologists for annual examinations and screening. While there are many similarities in technique and procedure, there are nuances in patient demographics, anatomy, and surgical technique that obstetricians/gynecologists should be aware of when examining these patients or prior to referring them to a surgeon for augmentation.2
Many patients who are dissatisfied with breast size from hormone therapy alone will seek out augmentation mammaplasty. In patients taking estrogen for hormone therapy, breast growth will commence around 2-3 months and peak over 1-2 years.3 Unlike chest surgery for transmasculine individuals, it is recommended that transfeminine patients seeking breast augmentation wait a minimum of 12 months before to surgery to allow for maximum breast enlargement. As with breast growth in cisgender females, the extent of breast development is multifactorial and varies from individual to individual. Current literature does not suggest that estrogen type or dose affects the ultimate breast size; however, younger age, tissue sensitivity, and body weight may affect breast volume.3 Referral to a genetic counselor and preoperative imaging may be necessary if a patient has a history concerning for a genetic or familial predisposition to breast cancer.
Implant selection and placement is determined by a variety of factors. While the overall principles of augmentation mammaplasty are essentially the same, there are anatomic differences in transfeminine patients that surgeons must take into consideration at the time of the consultation and during the surgery itself. For example, the pectoralis major muscle is more defined, there is a longer sternal notch-to-nipple distance, the chest wall is broader and more barrel-shaped, and there is a shorter distance between the nipple and the inframammary crease.2-4 As a result of the broader chest wall, it is extremely difficult to achieve central cleavage even with larger implant selection. The surgeon must also ensure that the nipple and areola overlie the implant centrally. Medial placement of the implant will result in lateral displacement of the nipples, which can have an unsatisfactory cosmetic appearance.
Incision location can be axillary, inframammary, or even transareolar, although the latter is less common due to the smaller areolar size and larger implant choice.3 If the inframammary incision is used, it should be placed lower than the natural inframammary fold because the distance between the inferior areolar margin and inframammary fold is shorter and will expand after the implant is placed.4 While both saline and silicone implants are available, many surgeons (myself included), favor more form-stable silicone implants. Given the association between anaplastic large-cell lymphoma and textured implants, many surgeons also use nontextured, or smooth, cohesive gel silicone implants.5
Pocket selection of the implant itself can be subglandular – directly under the breast mound – or subpectoral – behind the pectoralis muscle. For patients with a pinch test of greater than 1.5 cm (outside of the area of the breast bud), good skin softening, and marked pectoralis hypertrophy, subglandular placement is reasonable.6 In thin patients with minimal breast development, subglandular placement can result in a “double-mound” appearance and can lead to visible implant edges on the periphery.6 Use of the subpectoral plane is more common and is associated with less implant visibility due to an increased amount of soft-tissue coverage and has lower rates of capsular contracture.4 However, due to the more robust pectoralis muscle in transfeminine patients, implant displacement can occur more frequently compared to subglandular placement. The surgeon and patient must have a thorough discussion about the location of the incision, implant material, and pocket placement along with the benefits and complications of the surgical plan.
Complications of augmentation mammaplasty are rare. However, when they occur it can include capsular contracture, breast asymmetry, hematoma formation, loss of nipple sensation, implant malposition, implant displacement below the inframammary crease, implant rupture, and need for revisional surgery.7 If an obstetrician/gynecologist observes any of the aforementioned findings in a postoperative patient, consultation and referral to a plastic surgeon is imperative.
Postoperative assessment and screening are mandatory in all patients who undergo breast augmentation. It is important for the gynecologist to note the incision placement, know the type of implant used (saline or silicone), and delineate where the implant was placed. If silicone implants are used, breast MRI is more sensitive in detecting implant rupture compared to mammography alone. Given the relatively poor epidemiologic data on breast cancer in transgender women, the Endocrine Society recommends that these patients follow the same screening guidelines as cisgender women.4,6
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa.
References
1. Wierckx K et al. J Sex Med. 2014;11(5):1240-7.
2. Mehra G et al. Plast Reconstr Surg Glob Open 2021 Jan 21;9(1):e3362. doi: 10.1097/GOX.0000000000003362.
3. Schecter LS, Schechter RB. Breast and chest surgery for transgender patients. In: Ferrando CA, ed. Comprehensive Care of the Transgender Patient. Philadelphia, PA: Elsevier, 2020:73-81.
4. Colebunders B et al. Top surgery. In: Salgado CJ et al. ed. Gender Affirmation: Medical and Surgical Perspectives. New York, NY: Thieme, 2017:51-66.
5. De Boer M et al. Aesthet Surg J. 2017;37:NP83-NP87.
6. Coon D et al. Plast Reconstr Surg. 2020 Jun;145(6):1343-53.
7. Kanhai RC et al. Br J Plast Surg. 2000;53:209-11.
Augmentation mammaplasty, otherwise known as a breast augmentation, is one of the most common cosmetic procedures performed in cisgender females. Gynecologists routinely perform annual breast examinations and order screening mammography in cisgender women with breast implants. Similarly, there is an increasing number of transgender women seeking breast augmentation – with approximately 60%-70% of patients having desired or undergone the procedure.1 Consequently, these patients are instructed by their surgeons to follow up with gynecologists for annual examinations and screening. While there are many similarities in technique and procedure, there are nuances in patient demographics, anatomy, and surgical technique that obstetricians/gynecologists should be aware of when examining these patients or prior to referring them to a surgeon for augmentation.2
Many patients who are dissatisfied with breast size from hormone therapy alone will seek out augmentation mammaplasty. In patients taking estrogen for hormone therapy, breast growth will commence around 2-3 months and peak over 1-2 years.3 Unlike chest surgery for transmasculine individuals, it is recommended that transfeminine patients seeking breast augmentation wait a minimum of 12 months before to surgery to allow for maximum breast enlargement. As with breast growth in cisgender females, the extent of breast development is multifactorial and varies from individual to individual. Current literature does not suggest that estrogen type or dose affects the ultimate breast size; however, younger age, tissue sensitivity, and body weight may affect breast volume.3 Referral to a genetic counselor and preoperative imaging may be necessary if a patient has a history concerning for a genetic or familial predisposition to breast cancer.
Implant selection and placement is determined by a variety of factors. While the overall principles of augmentation mammaplasty are essentially the same, there are anatomic differences in transfeminine patients that surgeons must take into consideration at the time of the consultation and during the surgery itself. For example, the pectoralis major muscle is more defined, there is a longer sternal notch-to-nipple distance, the chest wall is broader and more barrel-shaped, and there is a shorter distance between the nipple and the inframammary crease.2-4 As a result of the broader chest wall, it is extremely difficult to achieve central cleavage even with larger implant selection. The surgeon must also ensure that the nipple and areola overlie the implant centrally. Medial placement of the implant will result in lateral displacement of the nipples, which can have an unsatisfactory cosmetic appearance.
Incision location can be axillary, inframammary, or even transareolar, although the latter is less common due to the smaller areolar size and larger implant choice.3 If the inframammary incision is used, it should be placed lower than the natural inframammary fold because the distance between the inferior areolar margin and inframammary fold is shorter and will expand after the implant is placed.4 While both saline and silicone implants are available, many surgeons (myself included), favor more form-stable silicone implants. Given the association between anaplastic large-cell lymphoma and textured implants, many surgeons also use nontextured, or smooth, cohesive gel silicone implants.5
Pocket selection of the implant itself can be subglandular – directly under the breast mound – or subpectoral – behind the pectoralis muscle. For patients with a pinch test of greater than 1.5 cm (outside of the area of the breast bud), good skin softening, and marked pectoralis hypertrophy, subglandular placement is reasonable.6 In thin patients with minimal breast development, subglandular placement can result in a “double-mound” appearance and can lead to visible implant edges on the periphery.6 Use of the subpectoral plane is more common and is associated with less implant visibility due to an increased amount of soft-tissue coverage and has lower rates of capsular contracture.4 However, due to the more robust pectoralis muscle in transfeminine patients, implant displacement can occur more frequently compared to subglandular placement. The surgeon and patient must have a thorough discussion about the location of the incision, implant material, and pocket placement along with the benefits and complications of the surgical plan.
Complications of augmentation mammaplasty are rare. However, when they occur it can include capsular contracture, breast asymmetry, hematoma formation, loss of nipple sensation, implant malposition, implant displacement below the inframammary crease, implant rupture, and need for revisional surgery.7 If an obstetrician/gynecologist observes any of the aforementioned findings in a postoperative patient, consultation and referral to a plastic surgeon is imperative.
Postoperative assessment and screening are mandatory in all patients who undergo breast augmentation. It is important for the gynecologist to note the incision placement, know the type of implant used (saline or silicone), and delineate where the implant was placed. If silicone implants are used, breast MRI is more sensitive in detecting implant rupture compared to mammography alone. Given the relatively poor epidemiologic data on breast cancer in transgender women, the Endocrine Society recommends that these patients follow the same screening guidelines as cisgender women.4,6
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa.
References
1. Wierckx K et al. J Sex Med. 2014;11(5):1240-7.
2. Mehra G et al. Plast Reconstr Surg Glob Open 2021 Jan 21;9(1):e3362. doi: 10.1097/GOX.0000000000003362.
3. Schecter LS, Schechter RB. Breast and chest surgery for transgender patients. In: Ferrando CA, ed. Comprehensive Care of the Transgender Patient. Philadelphia, PA: Elsevier, 2020:73-81.
4. Colebunders B et al. Top surgery. In: Salgado CJ et al. ed. Gender Affirmation: Medical and Surgical Perspectives. New York, NY: Thieme, 2017:51-66.
5. De Boer M et al. Aesthet Surg J. 2017;37:NP83-NP87.
6. Coon D et al. Plast Reconstr Surg. 2020 Jun;145(6):1343-53.
7. Kanhai RC et al. Br J Plast Surg. 2000;53:209-11.
Hormones after cancer: Are they safe?
The impact of a gynecologic cancer diagnosis reaches beyond the obvious side effects of surgery, chemotherapy, and radiation. Many of our patients experience the quality-of-life–limiting side effects of abrupt hormone withdrawal as a consequence of our treatments. Assumptions are common, by both patients and providers, that hormonal therapy is unsafe after a gynecologic cancer diagnosis and that it is associated with an increased risk for recurrence. This sentiment likely originates from the fallout of the Womens’ Health Initiative (WHI) studies which showed an increased risk of breast cancer among users of combined estrogen and progesterone therapy.1 While this may be true for breast cancer risk, when initiated early, hormonal therapy is safe, even beneficial, for many patients with a history of gynecologic cancer, and can significantly improve their quality of life in addition to reducing all-cause mortality and incidence of osteoporosis, dementia, and cardiovascular disease.2
Premenopausal women undergoing surgery for endometrial cancer or preinvasive hyperplasia should be considered for ovarian preservation at the time of surgery. This strategy has been shown to be safe and not associated with an increased risk of recurrence. If oophorectomy is performed, hormonal therapy has been shown to be a safe remedy to the side effects of surgical menopause and the deleterious acceleration of bone loss and cardiovascular aging. The safety of hormone therapy for early-stage endometrial cancer has been thoroughly studied, including in a randomized controlled trial of more than 1,200 patients.3 This study showed no difference in the recurrence rate in users when compared with nonusers.
While hormone therapy is safe, from an oncologic standpoint, for women with a history of early-stage endometrial cancer other risks must also be considered. Given the association between endometrial cancer and obesity, these patients are at higher risk for venous thromboembolic (VTE) events, more so with the addition of exogenous hormone therapy. While not an overt contraindication to hormone prescription, obese patients who are prescribed these agents should be counseled regarding their risks for VTE.
The subgroup of patients with endometrial cancer in whom hormones should not be prescribed are those with advanced or recurrent disease. It is common for these tumors to express estrogen receptors, as evidenced by the responsiveness of these tumors to progesterone and antiestrogen treatments. Therefore, there is a theoretical risk for progression while using estrogen. In addition, as stated above, the risk of VTE is particularly elevated for women with metastatic malignancy receiving systemic therapies.
Cervical cancer commonly affects women of premenopausal age; therefore, early ovarian failure is particularly deleterious for this group of patients. Early-stage cervical cancer is most commonly treated with radical or extrafascial hysterectomy. Oophorectomy is not obligatory for the majority of these cases, and can be omitted in pre-, or perimenopausal patients to prevent surgical menopause. Ovarian metastases have been reported in cases of cervical adenocarcinoma, which led to the concern that ovarian preservation was not safe for this histology. However, recent data dispute this concern. A contemporary retrospective series of 105 patients with cervical adenocarcinoma identified no significant difference in overall survival when comparing those who had undergone ovarian preservation versus bilateral salpingo-oophorectomy.4
Ovarian preservation during cervical cancer surgery may not be enough to prevent early menopause. Approximately 20% of cervical cancer patients may require postoperative radiation for high- or intermediate-risk disease (such as positive lymph nodes, or adverse features in the tumor). For these women, ovarian ablation results, even if the ovaries were preserved at the time of surgery. Transposition of the ovaries to a location outside of the potential radiation fields is a strategy to mitigate this risk. To achieve this, the preserved ovaries and their vascular pedicles are skeletonized. The ovaries are then sutured to the paracolic gutter peritoneum or similar location above the pelvic brim, taking care to ensure that the vascular pedicle is not compromised or twisted. Placement of radio-opaque surgical clips on the caudad aspect of the transposed ovary aids in their identification by radiation oncologists when planning their treatment fields.
Ovarian transposition is most commonly used for women who are undergoing definitive surgery for cervical cancer. However, this strategy can also be used as a lead-in procedure for young women with advanced cervical cancer in whom definitive chemoradiation is planned. If the ovaries cannot be spared or moved out of “harm’s way” for premenopausal women undergoing treatment with definitive radiation, hormone therapy may be necessary and is safe for patients with cervical cancer, including those with adenocarcinoma. If the patient has not undergone hysterectomy, a regimen that includes a combination of estrogen and progesterone is necessary to avoid carcinogenic effects of unopposed estrogen on an intact endometrium, even after radiation has ablated those tissues.
When ovarian and fallopian cancers arise in premenopausal patients and appear confined to a single adnexa, contralateral ovarian preservation can be considered. However, for advanced disease, this is usually not possible or appropriate. Given that most ovarian cancers arise in a postmenopausal population, these patients may be preexisting users of hormone therapy. The data, including a randomized controlled trial, would suggest that it is safe to continue to use hormone therapy during or following a diagnosis of ovarian, fallopian tube, or primary peritoneal cancer and that it is not associated with worse outcomes from their cancer.5
Once again, patients should be carefully counseled about the additive risks for VTE that come from metastatic ovarian cancer, surgery via laparotomy, and exogenous hormonal therapy. However, these patients need not be subjected to an abrupt transition to menopause, because level I evidence suggests that these therapies are not associated with worse oncologic outcomes. All patients with ovarian, fallopian tube, and primary peritoneal cancer should receive genetic testing, and if deleterious mutations are found in BRCA 1 or 2 genes indicating an elevated risk for breast cancer, decision making regarding continued exogenous hormonal therapy is complicated. The most contemporary data, including long-term follow-up from the Women’s Health Initiative clinical trials, do not suggest an increased risk for breast cancer with estrogen-only preparations of hormone therapy.6 Given that most women with gynecologic cancers have undergone hysterectomy as part of their treatment, these estrogen-only preparations are appropriate for most.
For patients with rare tumors, such as endometrial stromal tumors or uterine leiomyosarcoma, the safety of exogenous hormone therapy should be dictated by the receptor profile of their particular cancer. Many of these cancers express estrogen receptors; therefore, current guidelines recommend against the use of hormones after these diagnoses when estrogen receptors are expressed.
Gynecologic cancer treatments induce many toxicities with long-term deleterious effects on quality of life. Use of hormones to mitigate the symptoms of menopause is an important tool in the toolkit for gynecologists. Assumptions should not be made that hormonal therapies are always unsafe for all of these patients. It is important to closely evaluate the patient’s tumor and other risk factors before withholding potentially valuable therapies.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Chlebowski R et al. JAMA. 2010 Oct 20;304(15):1684-92.
2. Sinno AK et al. Gynecol Oncol. 2020;157(2):303-6.
3. Barakat et al. J Clin Oncol. 2006;24(4):587-92.
4. Hu Jun et al. J Obstet Gynaecol. 2017 Nov;37(8):1065-9.
5. Eeles R et al. J Clin Oncol. 2015 Dec 10;33(35):4138-44.
6. Chlebowski R et al. JAMA Jul 28 2020;324(4):369-80.
The impact of a gynecologic cancer diagnosis reaches beyond the obvious side effects of surgery, chemotherapy, and radiation. Many of our patients experience the quality-of-life–limiting side effects of abrupt hormone withdrawal as a consequence of our treatments. Assumptions are common, by both patients and providers, that hormonal therapy is unsafe after a gynecologic cancer diagnosis and that it is associated with an increased risk for recurrence. This sentiment likely originates from the fallout of the Womens’ Health Initiative (WHI) studies which showed an increased risk of breast cancer among users of combined estrogen and progesterone therapy.1 While this may be true for breast cancer risk, when initiated early, hormonal therapy is safe, even beneficial, for many patients with a history of gynecologic cancer, and can significantly improve their quality of life in addition to reducing all-cause mortality and incidence of osteoporosis, dementia, and cardiovascular disease.2
Premenopausal women undergoing surgery for endometrial cancer or preinvasive hyperplasia should be considered for ovarian preservation at the time of surgery. This strategy has been shown to be safe and not associated with an increased risk of recurrence. If oophorectomy is performed, hormonal therapy has been shown to be a safe remedy to the side effects of surgical menopause and the deleterious acceleration of bone loss and cardiovascular aging. The safety of hormone therapy for early-stage endometrial cancer has been thoroughly studied, including in a randomized controlled trial of more than 1,200 patients.3 This study showed no difference in the recurrence rate in users when compared with nonusers.
While hormone therapy is safe, from an oncologic standpoint, for women with a history of early-stage endometrial cancer other risks must also be considered. Given the association between endometrial cancer and obesity, these patients are at higher risk for venous thromboembolic (VTE) events, more so with the addition of exogenous hormone therapy. While not an overt contraindication to hormone prescription, obese patients who are prescribed these agents should be counseled regarding their risks for VTE.
The subgroup of patients with endometrial cancer in whom hormones should not be prescribed are those with advanced or recurrent disease. It is common for these tumors to express estrogen receptors, as evidenced by the responsiveness of these tumors to progesterone and antiestrogen treatments. Therefore, there is a theoretical risk for progression while using estrogen. In addition, as stated above, the risk of VTE is particularly elevated for women with metastatic malignancy receiving systemic therapies.
Cervical cancer commonly affects women of premenopausal age; therefore, early ovarian failure is particularly deleterious for this group of patients. Early-stage cervical cancer is most commonly treated with radical or extrafascial hysterectomy. Oophorectomy is not obligatory for the majority of these cases, and can be omitted in pre-, or perimenopausal patients to prevent surgical menopause. Ovarian metastases have been reported in cases of cervical adenocarcinoma, which led to the concern that ovarian preservation was not safe for this histology. However, recent data dispute this concern. A contemporary retrospective series of 105 patients with cervical adenocarcinoma identified no significant difference in overall survival when comparing those who had undergone ovarian preservation versus bilateral salpingo-oophorectomy.4
Ovarian preservation during cervical cancer surgery may not be enough to prevent early menopause. Approximately 20% of cervical cancer patients may require postoperative radiation for high- or intermediate-risk disease (such as positive lymph nodes, or adverse features in the tumor). For these women, ovarian ablation results, even if the ovaries were preserved at the time of surgery. Transposition of the ovaries to a location outside of the potential radiation fields is a strategy to mitigate this risk. To achieve this, the preserved ovaries and their vascular pedicles are skeletonized. The ovaries are then sutured to the paracolic gutter peritoneum or similar location above the pelvic brim, taking care to ensure that the vascular pedicle is not compromised or twisted. Placement of radio-opaque surgical clips on the caudad aspect of the transposed ovary aids in their identification by radiation oncologists when planning their treatment fields.
Ovarian transposition is most commonly used for women who are undergoing definitive surgery for cervical cancer. However, this strategy can also be used as a lead-in procedure for young women with advanced cervical cancer in whom definitive chemoradiation is planned. If the ovaries cannot be spared or moved out of “harm’s way” for premenopausal women undergoing treatment with definitive radiation, hormone therapy may be necessary and is safe for patients with cervical cancer, including those with adenocarcinoma. If the patient has not undergone hysterectomy, a regimen that includes a combination of estrogen and progesterone is necessary to avoid carcinogenic effects of unopposed estrogen on an intact endometrium, even after radiation has ablated those tissues.
When ovarian and fallopian cancers arise in premenopausal patients and appear confined to a single adnexa, contralateral ovarian preservation can be considered. However, for advanced disease, this is usually not possible or appropriate. Given that most ovarian cancers arise in a postmenopausal population, these patients may be preexisting users of hormone therapy. The data, including a randomized controlled trial, would suggest that it is safe to continue to use hormone therapy during or following a diagnosis of ovarian, fallopian tube, or primary peritoneal cancer and that it is not associated with worse outcomes from their cancer.5
Once again, patients should be carefully counseled about the additive risks for VTE that come from metastatic ovarian cancer, surgery via laparotomy, and exogenous hormonal therapy. However, these patients need not be subjected to an abrupt transition to menopause, because level I evidence suggests that these therapies are not associated with worse oncologic outcomes. All patients with ovarian, fallopian tube, and primary peritoneal cancer should receive genetic testing, and if deleterious mutations are found in BRCA 1 or 2 genes indicating an elevated risk for breast cancer, decision making regarding continued exogenous hormonal therapy is complicated. The most contemporary data, including long-term follow-up from the Women’s Health Initiative clinical trials, do not suggest an increased risk for breast cancer with estrogen-only preparations of hormone therapy.6 Given that most women with gynecologic cancers have undergone hysterectomy as part of their treatment, these estrogen-only preparations are appropriate for most.
For patients with rare tumors, such as endometrial stromal tumors or uterine leiomyosarcoma, the safety of exogenous hormone therapy should be dictated by the receptor profile of their particular cancer. Many of these cancers express estrogen receptors; therefore, current guidelines recommend against the use of hormones after these diagnoses when estrogen receptors are expressed.
Gynecologic cancer treatments induce many toxicities with long-term deleterious effects on quality of life. Use of hormones to mitigate the symptoms of menopause is an important tool in the toolkit for gynecologists. Assumptions should not be made that hormonal therapies are always unsafe for all of these patients. It is important to closely evaluate the patient’s tumor and other risk factors before withholding potentially valuable therapies.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Chlebowski R et al. JAMA. 2010 Oct 20;304(15):1684-92.
2. Sinno AK et al. Gynecol Oncol. 2020;157(2):303-6.
3. Barakat et al. J Clin Oncol. 2006;24(4):587-92.
4. Hu Jun et al. J Obstet Gynaecol. 2017 Nov;37(8):1065-9.
5. Eeles R et al. J Clin Oncol. 2015 Dec 10;33(35):4138-44.
6. Chlebowski R et al. JAMA Jul 28 2020;324(4):369-80.
The impact of a gynecologic cancer diagnosis reaches beyond the obvious side effects of surgery, chemotherapy, and radiation. Many of our patients experience the quality-of-life–limiting side effects of abrupt hormone withdrawal as a consequence of our treatments. Assumptions are common, by both patients and providers, that hormonal therapy is unsafe after a gynecologic cancer diagnosis and that it is associated with an increased risk for recurrence. This sentiment likely originates from the fallout of the Womens’ Health Initiative (WHI) studies which showed an increased risk of breast cancer among users of combined estrogen and progesterone therapy.1 While this may be true for breast cancer risk, when initiated early, hormonal therapy is safe, even beneficial, for many patients with a history of gynecologic cancer, and can significantly improve their quality of life in addition to reducing all-cause mortality and incidence of osteoporosis, dementia, and cardiovascular disease.2
Premenopausal women undergoing surgery for endometrial cancer or preinvasive hyperplasia should be considered for ovarian preservation at the time of surgery. This strategy has been shown to be safe and not associated with an increased risk of recurrence. If oophorectomy is performed, hormonal therapy has been shown to be a safe remedy to the side effects of surgical menopause and the deleterious acceleration of bone loss and cardiovascular aging. The safety of hormone therapy for early-stage endometrial cancer has been thoroughly studied, including in a randomized controlled trial of more than 1,200 patients.3 This study showed no difference in the recurrence rate in users when compared with nonusers.
While hormone therapy is safe, from an oncologic standpoint, for women with a history of early-stage endometrial cancer other risks must also be considered. Given the association between endometrial cancer and obesity, these patients are at higher risk for venous thromboembolic (VTE) events, more so with the addition of exogenous hormone therapy. While not an overt contraindication to hormone prescription, obese patients who are prescribed these agents should be counseled regarding their risks for VTE.
The subgroup of patients with endometrial cancer in whom hormones should not be prescribed are those with advanced or recurrent disease. It is common for these tumors to express estrogen receptors, as evidenced by the responsiveness of these tumors to progesterone and antiestrogen treatments. Therefore, there is a theoretical risk for progression while using estrogen. In addition, as stated above, the risk of VTE is particularly elevated for women with metastatic malignancy receiving systemic therapies.
Cervical cancer commonly affects women of premenopausal age; therefore, early ovarian failure is particularly deleterious for this group of patients. Early-stage cervical cancer is most commonly treated with radical or extrafascial hysterectomy. Oophorectomy is not obligatory for the majority of these cases, and can be omitted in pre-, or perimenopausal patients to prevent surgical menopause. Ovarian metastases have been reported in cases of cervical adenocarcinoma, which led to the concern that ovarian preservation was not safe for this histology. However, recent data dispute this concern. A contemporary retrospective series of 105 patients with cervical adenocarcinoma identified no significant difference in overall survival when comparing those who had undergone ovarian preservation versus bilateral salpingo-oophorectomy.4
Ovarian preservation during cervical cancer surgery may not be enough to prevent early menopause. Approximately 20% of cervical cancer patients may require postoperative radiation for high- or intermediate-risk disease (such as positive lymph nodes, or adverse features in the tumor). For these women, ovarian ablation results, even if the ovaries were preserved at the time of surgery. Transposition of the ovaries to a location outside of the potential radiation fields is a strategy to mitigate this risk. To achieve this, the preserved ovaries and their vascular pedicles are skeletonized. The ovaries are then sutured to the paracolic gutter peritoneum or similar location above the pelvic brim, taking care to ensure that the vascular pedicle is not compromised or twisted. Placement of radio-opaque surgical clips on the caudad aspect of the transposed ovary aids in their identification by radiation oncologists when planning their treatment fields.
Ovarian transposition is most commonly used for women who are undergoing definitive surgery for cervical cancer. However, this strategy can also be used as a lead-in procedure for young women with advanced cervical cancer in whom definitive chemoradiation is planned. If the ovaries cannot be spared or moved out of “harm’s way” for premenopausal women undergoing treatment with definitive radiation, hormone therapy may be necessary and is safe for patients with cervical cancer, including those with adenocarcinoma. If the patient has not undergone hysterectomy, a regimen that includes a combination of estrogen and progesterone is necessary to avoid carcinogenic effects of unopposed estrogen on an intact endometrium, even after radiation has ablated those tissues.
When ovarian and fallopian cancers arise in premenopausal patients and appear confined to a single adnexa, contralateral ovarian preservation can be considered. However, for advanced disease, this is usually not possible or appropriate. Given that most ovarian cancers arise in a postmenopausal population, these patients may be preexisting users of hormone therapy. The data, including a randomized controlled trial, would suggest that it is safe to continue to use hormone therapy during or following a diagnosis of ovarian, fallopian tube, or primary peritoneal cancer and that it is not associated with worse outcomes from their cancer.5
Once again, patients should be carefully counseled about the additive risks for VTE that come from metastatic ovarian cancer, surgery via laparotomy, and exogenous hormonal therapy. However, these patients need not be subjected to an abrupt transition to menopause, because level I evidence suggests that these therapies are not associated with worse oncologic outcomes. All patients with ovarian, fallopian tube, and primary peritoneal cancer should receive genetic testing, and if deleterious mutations are found in BRCA 1 or 2 genes indicating an elevated risk for breast cancer, decision making regarding continued exogenous hormonal therapy is complicated. The most contemporary data, including long-term follow-up from the Women’s Health Initiative clinical trials, do not suggest an increased risk for breast cancer with estrogen-only preparations of hormone therapy.6 Given that most women with gynecologic cancers have undergone hysterectomy as part of their treatment, these estrogen-only preparations are appropriate for most.
For patients with rare tumors, such as endometrial stromal tumors or uterine leiomyosarcoma, the safety of exogenous hormone therapy should be dictated by the receptor profile of their particular cancer. Many of these cancers express estrogen receptors; therefore, current guidelines recommend against the use of hormones after these diagnoses when estrogen receptors are expressed.
Gynecologic cancer treatments induce many toxicities with long-term deleterious effects on quality of life. Use of hormones to mitigate the symptoms of menopause is an important tool in the toolkit for gynecologists. Assumptions should not be made that hormonal therapies are always unsafe for all of these patients. It is important to closely evaluate the patient’s tumor and other risk factors before withholding potentially valuable therapies.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no relevant financial disclosures. Email her at [email protected].
References
1. Chlebowski R et al. JAMA. 2010 Oct 20;304(15):1684-92.
2. Sinno AK et al. Gynecol Oncol. 2020;157(2):303-6.
3. Barakat et al. J Clin Oncol. 2006;24(4):587-92.
4. Hu Jun et al. J Obstet Gynaecol. 2017 Nov;37(8):1065-9.
5. Eeles R et al. J Clin Oncol. 2015 Dec 10;33(35):4138-44.
6. Chlebowski R et al. JAMA Jul 28 2020;324(4):369-80.
Nerve-sparing laparoscopic low anterior resection for rectal endometriosis in ten steps
Performance anxiety highly common among surgeons
a new study of surgeons in the United Kingdom shows.
“Performance anxiety or stage fright is a widely recognized problem in music and sports, and there are many similarities between these arenas and the operating theater,” first author Robert Miller, MRCS, of the Surgical Psychology and Performance Group and the department of plastic and reconstructive surgery at St. George’s Hospital NHS Trust, London, said in an interview. “We were aware of it anecdotally in a surgical context, but for one reason or another, perhaps professional pride and fear of negative perception, this is rarely openly discussed amongst surgeons.”
In the cross-sectional study, published in Annals of Surgery, Dr. Miller and colleagues surveyed surgeons in all specialties working in the United Kingdom who had at least 1 year of postgraduate surgical training.
Of a total of 631 responses received, 523 (83%) were included in the analysis. The median age of those who responded was 41.2 years, and the mean duration of surgical experience was 15.3 years (range, 1-52 years). Among them, 62% were men, and 52% were of consultant/attending grade.
All of the respondents – 100% – said they believed that performance anxiety affected surgeons, 87% reported having experienced it themselves, and 65% said they felt that performance anxiety had an effect on their surgical performance.
Both male and female surgeons who reported experiencing performance anxiety had significantly worse mental well-being, as assessed using the Short Warwick Edinburgh Mental Wellbeing Scale, compared with those who did not have performance anxiety (P < .0001 for men and P < .001 for women).
Overall, however, male surgeons had significantly better mental well-being, compared with female surgeons (P = .003), yet both genders had significantly lower mental well-being scores compared with U.K. population norms (P = .0019 for men and P = .0001 for women).
The gender differences are “clearly an important topic, which is likely multifactorial,” Dr. Miller told this news organization. “The gender well-being gap requires more in-depth research, and qualitative work involving female surgeons is critical.”
Surgical perfectionism was significantly more common among respondents who did have performance anxiety in comparison with those who did not (P < .0001).
“Although perfectionism may be a beneficial trait in surgery, our findings from hierarchical multiple regression analysis also indicate that perfectionism, [as well as] sex and experience, may drive surgical performance anxiety and help predict those experiencing [the anxiety],” the authors noted.
Performing in presence of colleagues a key trigger
By far, the leading trigger that was identified as prompting surgeon performance anxiety was the presence – and scrutiny – of colleagues within the parent specialty. This was reported by 151 respondents. Other triggers were having to perform on highly complex or high-risk cases (66 responses) and a lack of experience (30 responses).
Next to planning and preparation, opening up and talking about the anxiety and shedding light on the issue was seen as a leading strategy to help with the problem, but very few respondents reported openly sharing their struggles. Only 9% reported that they had shared it openly; 27% said they had confided in someone, and 47% did not respond to the question.
“I wish we talked about it more and shared our insecurities,” one respondent lamented. “Most of my colleagues pretend they are living gods.”
Only about 45% of respondents reported a specific technique for overcoming their anxiety. In addition to being open about the problem, other techniques included self-care, such as exercise; and distraction outside of work to get perspective; relaxation techniques such as deep or controlled breathing; music; mindfulness; and positive self-statements.
About 9% said they had received psychological counseling for performance anxiety, and only 3% reported using medication for the problem.
Anxiety a positive factor?
Surprisingly, 70% of respondents reported feeling that surgical performance anxiety could have a positive impact on surgical performance, which the authors noted is consistent with some theories.
“This may be explained by the traditional bell-curve relationship between arousal and performance, which describes a dose-dependent relationship between performance and arousal until a ‘tipping point,’ after which performance declines,” the authors explained. “A heightened awareness secondary to anxiety may be beneficial, but at high doses, anxiety can negatively affect attentional control and cause somatic symptoms.”
They noted that “the challenge would be to reap the benefits of low-level stimulation without incurring possible adverse effects.”
Dr. Miller said that, in determining whether selection bias had a role in the results, a detailed analysis showed that “our respondents were not skewed to those with only high levels of trait anxiety.
“We also had a good spread of consultants versus trainees [about half and half], and different specialties, so we feel this is likely to be a representative sample,” he told this news organization.
That being said, the results underscore the need for increased awareness – and open discussion – of the issue of surgical performance anxiety.
“Within other professions, particularly the performing arts and sports, performance psychology is becoming an integral part of training and development,” Dr. Miller said. “We feel surgeons should be supported in a similar manner.
“Surgical performance anxiety is normal for surgeons at all levels and not something to be ashamed about,” Dr. Miller added. “Talk about it, acknowledge it, and be supportive to your colleagues.”
Many keep it to themselves in ‘prevailing culture of stoicism’
Commenting on the study, Carter C. Lebares, MD, an associate professor of surgery and director of the Center for Mindfulness in Surgery, department of surgery, University of California, San Francisco, said she was not surprised to see the high rates of performance anxiety among surgeons.
“As surgeons, no matter how hard we train or how thoroughly we prepare our intellectual understanding or the patient, the disease process, and the operation, there may be surprises, unforeseen challenges, or off days,” Dr. Lebares said.
“And whatever we encounter, we are managing these things directly under the scrutiny of others – people who can affect our reputation, operating privileges, and mental health. So, I am not surprised this is a prevalent and widely recognized issue.”
Dr. Lebares noted that the reluctance to share the anxiety is part of a “challenging and recognized conundrum in both medicine and surgery and is a matter of the prevailing culture of stoicism.
“We often are called to shoulder tremendous weight intraoperatively (having perseverance, self-confidence, or sustained focus), and in owning the weight of complications (which eventually we all will have),” she said.
“So, we do need to be strong and not complain, [but] we also need to be able to set that aside [when appropriate] and ask for help or allow others to shoulder the weight for a while, and this is not [yet] a common part of surgical culture.”
Dr. Lebares added that randomized, controlled trials have shown benefits of mindfulness interventions on burnout and anxiety.
“We have observed positive effects on mental noise, self-perception, conflict resolution, and resilience in surgical residents trained in mindfulness-based cognitive skills,” she said. “[Residents] report applying these skills in the OR, in their home lives, and in how they approach their training/education.”
The authors disclosed no relevant financial relationships. Dr. Lebares has developed mindfulness-based cognitive skills training for surgeons but receives no financial compensation for the activities.
A version of this article first appeared on Medscape.com.
a new study of surgeons in the United Kingdom shows.
“Performance anxiety or stage fright is a widely recognized problem in music and sports, and there are many similarities between these arenas and the operating theater,” first author Robert Miller, MRCS, of the Surgical Psychology and Performance Group and the department of plastic and reconstructive surgery at St. George’s Hospital NHS Trust, London, said in an interview. “We were aware of it anecdotally in a surgical context, but for one reason or another, perhaps professional pride and fear of negative perception, this is rarely openly discussed amongst surgeons.”
In the cross-sectional study, published in Annals of Surgery, Dr. Miller and colleagues surveyed surgeons in all specialties working in the United Kingdom who had at least 1 year of postgraduate surgical training.
Of a total of 631 responses received, 523 (83%) were included in the analysis. The median age of those who responded was 41.2 years, and the mean duration of surgical experience was 15.3 years (range, 1-52 years). Among them, 62% were men, and 52% were of consultant/attending grade.
All of the respondents – 100% – said they believed that performance anxiety affected surgeons, 87% reported having experienced it themselves, and 65% said they felt that performance anxiety had an effect on their surgical performance.
Both male and female surgeons who reported experiencing performance anxiety had significantly worse mental well-being, as assessed using the Short Warwick Edinburgh Mental Wellbeing Scale, compared with those who did not have performance anxiety (P < .0001 for men and P < .001 for women).
Overall, however, male surgeons had significantly better mental well-being, compared with female surgeons (P = .003), yet both genders had significantly lower mental well-being scores compared with U.K. population norms (P = .0019 for men and P = .0001 for women).
The gender differences are “clearly an important topic, which is likely multifactorial,” Dr. Miller told this news organization. “The gender well-being gap requires more in-depth research, and qualitative work involving female surgeons is critical.”
Surgical perfectionism was significantly more common among respondents who did have performance anxiety in comparison with those who did not (P < .0001).
“Although perfectionism may be a beneficial trait in surgery, our findings from hierarchical multiple regression analysis also indicate that perfectionism, [as well as] sex and experience, may drive surgical performance anxiety and help predict those experiencing [the anxiety],” the authors noted.
Performing in presence of colleagues a key trigger
By far, the leading trigger that was identified as prompting surgeon performance anxiety was the presence – and scrutiny – of colleagues within the parent specialty. This was reported by 151 respondents. Other triggers were having to perform on highly complex or high-risk cases (66 responses) and a lack of experience (30 responses).
Next to planning and preparation, opening up and talking about the anxiety and shedding light on the issue was seen as a leading strategy to help with the problem, but very few respondents reported openly sharing their struggles. Only 9% reported that they had shared it openly; 27% said they had confided in someone, and 47% did not respond to the question.
“I wish we talked about it more and shared our insecurities,” one respondent lamented. “Most of my colleagues pretend they are living gods.”
Only about 45% of respondents reported a specific technique for overcoming their anxiety. In addition to being open about the problem, other techniques included self-care, such as exercise; and distraction outside of work to get perspective; relaxation techniques such as deep or controlled breathing; music; mindfulness; and positive self-statements.
About 9% said they had received psychological counseling for performance anxiety, and only 3% reported using medication for the problem.
Anxiety a positive factor?
Surprisingly, 70% of respondents reported feeling that surgical performance anxiety could have a positive impact on surgical performance, which the authors noted is consistent with some theories.
“This may be explained by the traditional bell-curve relationship between arousal and performance, which describes a dose-dependent relationship between performance and arousal until a ‘tipping point,’ after which performance declines,” the authors explained. “A heightened awareness secondary to anxiety may be beneficial, but at high doses, anxiety can negatively affect attentional control and cause somatic symptoms.”
They noted that “the challenge would be to reap the benefits of low-level stimulation without incurring possible adverse effects.”
Dr. Miller said that, in determining whether selection bias had a role in the results, a detailed analysis showed that “our respondents were not skewed to those with only high levels of trait anxiety.
“We also had a good spread of consultants versus trainees [about half and half], and different specialties, so we feel this is likely to be a representative sample,” he told this news organization.
That being said, the results underscore the need for increased awareness – and open discussion – of the issue of surgical performance anxiety.
“Within other professions, particularly the performing arts and sports, performance psychology is becoming an integral part of training and development,” Dr. Miller said. “We feel surgeons should be supported in a similar manner.
“Surgical performance anxiety is normal for surgeons at all levels and not something to be ashamed about,” Dr. Miller added. “Talk about it, acknowledge it, and be supportive to your colleagues.”
Many keep it to themselves in ‘prevailing culture of stoicism’
Commenting on the study, Carter C. Lebares, MD, an associate professor of surgery and director of the Center for Mindfulness in Surgery, department of surgery, University of California, San Francisco, said she was not surprised to see the high rates of performance anxiety among surgeons.
“As surgeons, no matter how hard we train or how thoroughly we prepare our intellectual understanding or the patient, the disease process, and the operation, there may be surprises, unforeseen challenges, or off days,” Dr. Lebares said.
“And whatever we encounter, we are managing these things directly under the scrutiny of others – people who can affect our reputation, operating privileges, and mental health. So, I am not surprised this is a prevalent and widely recognized issue.”
Dr. Lebares noted that the reluctance to share the anxiety is part of a “challenging and recognized conundrum in both medicine and surgery and is a matter of the prevailing culture of stoicism.
“We often are called to shoulder tremendous weight intraoperatively (having perseverance, self-confidence, or sustained focus), and in owning the weight of complications (which eventually we all will have),” she said.
“So, we do need to be strong and not complain, [but] we also need to be able to set that aside [when appropriate] and ask for help or allow others to shoulder the weight for a while, and this is not [yet] a common part of surgical culture.”
Dr. Lebares added that randomized, controlled trials have shown benefits of mindfulness interventions on burnout and anxiety.
“We have observed positive effects on mental noise, self-perception, conflict resolution, and resilience in surgical residents trained in mindfulness-based cognitive skills,” she said. “[Residents] report applying these skills in the OR, in their home lives, and in how they approach their training/education.”
The authors disclosed no relevant financial relationships. Dr. Lebares has developed mindfulness-based cognitive skills training for surgeons but receives no financial compensation for the activities.
A version of this article first appeared on Medscape.com.
a new study of surgeons in the United Kingdom shows.
“Performance anxiety or stage fright is a widely recognized problem in music and sports, and there are many similarities between these arenas and the operating theater,” first author Robert Miller, MRCS, of the Surgical Psychology and Performance Group and the department of plastic and reconstructive surgery at St. George’s Hospital NHS Trust, London, said in an interview. “We were aware of it anecdotally in a surgical context, but for one reason or another, perhaps professional pride and fear of negative perception, this is rarely openly discussed amongst surgeons.”
In the cross-sectional study, published in Annals of Surgery, Dr. Miller and colleagues surveyed surgeons in all specialties working in the United Kingdom who had at least 1 year of postgraduate surgical training.
Of a total of 631 responses received, 523 (83%) were included in the analysis. The median age of those who responded was 41.2 years, and the mean duration of surgical experience was 15.3 years (range, 1-52 years). Among them, 62% were men, and 52% were of consultant/attending grade.
All of the respondents – 100% – said they believed that performance anxiety affected surgeons, 87% reported having experienced it themselves, and 65% said they felt that performance anxiety had an effect on their surgical performance.
Both male and female surgeons who reported experiencing performance anxiety had significantly worse mental well-being, as assessed using the Short Warwick Edinburgh Mental Wellbeing Scale, compared with those who did not have performance anxiety (P < .0001 for men and P < .001 for women).
Overall, however, male surgeons had significantly better mental well-being, compared with female surgeons (P = .003), yet both genders had significantly lower mental well-being scores compared with U.K. population norms (P = .0019 for men and P = .0001 for women).
The gender differences are “clearly an important topic, which is likely multifactorial,” Dr. Miller told this news organization. “The gender well-being gap requires more in-depth research, and qualitative work involving female surgeons is critical.”
Surgical perfectionism was significantly more common among respondents who did have performance anxiety in comparison with those who did not (P < .0001).
“Although perfectionism may be a beneficial trait in surgery, our findings from hierarchical multiple regression analysis also indicate that perfectionism, [as well as] sex and experience, may drive surgical performance anxiety and help predict those experiencing [the anxiety],” the authors noted.
Performing in presence of colleagues a key trigger
By far, the leading trigger that was identified as prompting surgeon performance anxiety was the presence – and scrutiny – of colleagues within the parent specialty. This was reported by 151 respondents. Other triggers were having to perform on highly complex or high-risk cases (66 responses) and a lack of experience (30 responses).
Next to planning and preparation, opening up and talking about the anxiety and shedding light on the issue was seen as a leading strategy to help with the problem, but very few respondents reported openly sharing their struggles. Only 9% reported that they had shared it openly; 27% said they had confided in someone, and 47% did not respond to the question.
“I wish we talked about it more and shared our insecurities,” one respondent lamented. “Most of my colleagues pretend they are living gods.”
Only about 45% of respondents reported a specific technique for overcoming their anxiety. In addition to being open about the problem, other techniques included self-care, such as exercise; and distraction outside of work to get perspective; relaxation techniques such as deep or controlled breathing; music; mindfulness; and positive self-statements.
About 9% said they had received psychological counseling for performance anxiety, and only 3% reported using medication for the problem.
Anxiety a positive factor?
Surprisingly, 70% of respondents reported feeling that surgical performance anxiety could have a positive impact on surgical performance, which the authors noted is consistent with some theories.
“This may be explained by the traditional bell-curve relationship between arousal and performance, which describes a dose-dependent relationship between performance and arousal until a ‘tipping point,’ after which performance declines,” the authors explained. “A heightened awareness secondary to anxiety may be beneficial, but at high doses, anxiety can negatively affect attentional control and cause somatic symptoms.”
They noted that “the challenge would be to reap the benefits of low-level stimulation without incurring possible adverse effects.”
Dr. Miller said that, in determining whether selection bias had a role in the results, a detailed analysis showed that “our respondents were not skewed to those with only high levels of trait anxiety.
“We also had a good spread of consultants versus trainees [about half and half], and different specialties, so we feel this is likely to be a representative sample,” he told this news organization.
That being said, the results underscore the need for increased awareness – and open discussion – of the issue of surgical performance anxiety.
“Within other professions, particularly the performing arts and sports, performance psychology is becoming an integral part of training and development,” Dr. Miller said. “We feel surgeons should be supported in a similar manner.
“Surgical performance anxiety is normal for surgeons at all levels and not something to be ashamed about,” Dr. Miller added. “Talk about it, acknowledge it, and be supportive to your colleagues.”
Many keep it to themselves in ‘prevailing culture of stoicism’
Commenting on the study, Carter C. Lebares, MD, an associate professor of surgery and director of the Center for Mindfulness in Surgery, department of surgery, University of California, San Francisco, said she was not surprised to see the high rates of performance anxiety among surgeons.
“As surgeons, no matter how hard we train or how thoroughly we prepare our intellectual understanding or the patient, the disease process, and the operation, there may be surprises, unforeseen challenges, or off days,” Dr. Lebares said.
“And whatever we encounter, we are managing these things directly under the scrutiny of others – people who can affect our reputation, operating privileges, and mental health. So, I am not surprised this is a prevalent and widely recognized issue.”
Dr. Lebares noted that the reluctance to share the anxiety is part of a “challenging and recognized conundrum in both medicine and surgery and is a matter of the prevailing culture of stoicism.
“We often are called to shoulder tremendous weight intraoperatively (having perseverance, self-confidence, or sustained focus), and in owning the weight of complications (which eventually we all will have),” she said.
“So, we do need to be strong and not complain, [but] we also need to be able to set that aside [when appropriate] and ask for help or allow others to shoulder the weight for a while, and this is not [yet] a common part of surgical culture.”
Dr. Lebares added that randomized, controlled trials have shown benefits of mindfulness interventions on burnout and anxiety.
“We have observed positive effects on mental noise, self-perception, conflict resolution, and resilience in surgical residents trained in mindfulness-based cognitive skills,” she said. “[Residents] report applying these skills in the OR, in their home lives, and in how they approach their training/education.”
The authors disclosed no relevant financial relationships. Dr. Lebares has developed mindfulness-based cognitive skills training for surgeons but receives no financial compensation for the activities.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF SURGERY
POISE-3 backs wider use of tranexamic acid in noncardiac surgery
The antifibrinolytic tranexamic acid (TXA) reduced serious bleeding without a significant effect on major vascular outcomes in patients undergoing noncardiac surgery at risk for these complications in the POISE-3 trial.
TXA cut the primary efficacy outcome of life-threatening, major, and critical organ bleeding at 30 days by 24% compared with placebo (9.1% vs. 11.7%; hazard ratio [HR], 0.76; P < .0001).
The primary safety outcome of myocardial injury after noncardiac surgery (MINS), nonhemorrhagic stroke, peripheral arterial thrombosis, and symptomatic proximal venous thromboembolism (VTE) at 30 days occurred in 14.2% vs.. 13.9% of patients, respectively (HR, 1.023). This failed, however, to meet the study›s threshold to prove TXA noninferior to placebo (one-sided P = .044).
There was no increased risk for death or stroke with TXA, according to results published April 2 in the New England Journal of Medicine.
Principal investigator P.J. Devereaux, MD, PhD, Population Health Research Institute and McMaster University, Hamilton, Ontario, Canada, pointed out that there is only a 4.4% probability that the composite vascular outcome hazard ratio was above the noninferiority margin and that just 10 events separated the two groups (649 vs.. 639).
“Healthcare providers and patients will have to weigh a clear beneficial reduction in the composite bleeding outcome, which is an absolute difference of 2.7%, a result that was highly statistically significant, versus a low probability of a small increase in risk of the composite vascular endpoint, with an absolute difference of 0.3%,” a nonsignificant result, Dr. Devereaux said during the formal presentation of the results at the hybrid annual scientific sessions of the American College of Cardiology.
The findings, he said, should also be put in the context that 300 million adults have a major surgery each year worldwide and most don’t receive TXA. At the same time, there’s an annual global shortage of 30 million blood product units, and surgical bleeding accounts for up to 40% of all transfusions.
“POISE-3 identifies that use of TXA could avoid upwards of 8 million bleeding events resulting in transfusion on an annual basis, indicating potential for large public health and clinical benefit if TXA become standard practice in noncardiac surgery,” Dr. Devereaux said during the late-breaking trial session.
TXA is indicated for heavy menstrual bleeding and hemophilia and has been used in cardiac surgery, but it is increasingly being used in noncardiac surgeries. As previously reported, POISE showed that the beta-blocker metoprolol lowered the risk for myocardial infarction (MI) but increased the risk for severe stroke and overall death, whereas in POISE-2, perioperative low-dose aspirin lowered the risk for MI but was linked to more major bleeding.
The cumulative data have not shown an increased risk for thrombotic events in other settings, Dr. Devereaux told this news organization.
“I’m a cardiologist, and I think that we’ve been guilty at times of always only focusing on the thrombotic side of the equation and ignoring that bleeding is a very important aspect of the circulatory system,” he said. “And I think this shows for the first time clear unequivocal evidence that there’s a cheap, very encouraging, safe way to prevent this.”
“An important point is that if you can give tranexamic acid and prevent bleeding in your cardiac patients having noncardiac surgery, then you can prevent the delay of reinitiating their anticoagulants and their antiplatelets after surgery and getting them back on the medications that are important for them to prevent their cardiovascular event,” Dr. Devereaux added.
Discussant Michael J. Mack, MD, commented that TXA, widely used in cardiac surgery, is an old, inexpensive drug that “should be more widely used in noncardiac surgery.” Dr. Mack, from Baylor Scott & White Health, Dallas, added that he would limit it to major noncardiac surgery.
International trial
PeriOperative ISchemic Evaluation-3 (POISE-3) investigators at 114 hospitals in 22 countries (including countries in North and South America, Europe, and Africa; Russia; India; and Australia) randomly assigned 9,535 patients, aged 45 years or older, with or at risk for cardiovascular and bleeding complications to receive a TXA 1-g intravenous bolus or placebo at the start and end of inpatient noncardiac surgery.
Patients taking at least one long-term antihypertensive medication were also randomly assigned to a perioperative hypotension- or hypertension-avoidance strategy, which differ in the use of antihypertensives on the morning of surgery and the first 2 days after surgery, and in the target mean arterial pressure during surgery. Results from these cohorts will be presented in a separate session on April 4.
The study had planned to enroll 10,000 patients but was stopped early by the steering committee because of financial constraints resulting from slow enrollment during the pandemic. The decision was made without knowledge of the trial results but with knowledge that aggregate composite bleeding and vascular outcomes were higher than originally estimated, Dr. Devereaux noted.
Among all participants, the mean age was 70 years, 56% were male, almost a third had coronary artery disease, 15% had peripheral artery disease, and 8% had a prior stroke. About 80% were undergoing major surgery. Adherence to the study medications was 96.3% in both groups.
Secondary bleeding outcomes were lower in the TXA and placebo groups, including bleeding independently associated with mortality after surgery (8.7% vs. 11.3%), life-threatening bleeding (1.6% vs. 1.7%), major bleeding (7.6% vs. 10.4%), and critical organ bleeding (0.3% vs. 0.4%).
Importantly, the TXA group had significantly lower rates of International Society on Thrombosis and Haemostasis major bleeding (6.6% vs. 8.7%; P = .0001) and the need for transfusion of 1 or more units of packed red blood cells (9.4% vs. 12.0%; P <.0001), Dr. Devereaux noted.
In terms of secondary vascular outcomes, there were no significant differences between the TXA and placebo groups in rates of MINS (12.8% vs. 12.6%), MINS not fulfilling definition of MI (both 11.5%), MI (1.4% vs. 1.1%), and the net risk-benefit outcome (a composite of vascular death and nonfatal life-threatening, major, or critical organ bleeding, MINS, stroke, peripheral arterial thrombosis, and symptomatic proximal VTE; 20.7% vs. 21.9%).
The two groups had similar rates of all-cause (1.1% vs. 1.2%) and vascular (0.5% vs. 0.6%) mortality.
There also were no significant differences in other tertiary outcomes, such as acute kidney injury (14.1% vs. 13.7%), rehospitalization for vascular reasons (1.8% vs. 1.6%), or seizures (0.2% vs. <0.1%). The latter has been a concern, with the risk reported to increase with higher doses.
Subgroup analyses
Preplanned subgroup analyses showed a benefit for TXA over placebo for the primary efficacy outcome in orthopedic and nonorthopedic surgery and in patients with hemoglobin level below 120 g/L or 120 g/L or higher, with an estimated glomerular filtration rate less than 45 mL/min/1.73 m 2 or 45 mL/min/1.73 m 2 or higher, or with an N-terminal pro– B-type natriuretic peptide level below 200 ng/L or 200 ng/L or higher.
For the primary safety outcome, the benefit favored placebo but the interaction was not statistically significant for any of the four subgroups.
A post hoc subgroup analysis also showed similar results across the major categories of surgery, including general, vascular, urologic, and gynecologic, Dr. Devereaux told this news organization.
Although TXA is commonly used in orthopedic procedures, Dr. Devereaux noted, in other types of surgeries, “it’s not used at all.” But because TXA “is so cheap, and we can apply it to a broad population, even at an economic level it looks like it’s a winner to give to almost all patients having noncardiac surgery.”
The team also recently published a risk prediction tool that can help estimate a patient’s baseline risk for bleeding.
“So just using a model, which will bring together the patient’s type of surgery and their risk factors, you can look to see, okay, this is enough risk of bleeding, I’m just going to give tranexamic acid,” he said. “We will also be doing economic analyses because blood is also not cheap.”
The study was funded by the Canadian Institutes of Health Research, National Health and Medical Research Council (Australia), and the Research Grant Council (Hong Kong). Dr. Devereaux reports research/research grants from Abbott Diagnostics, Philips Healthcare, Roche Diagnostics, and Siemens. Dr. Mack reports receiving research grants from Abbott Vascular, Edwards Lifesciences, and Medtronic.
A version of this article first appeared on Medscape.com.
The antifibrinolytic tranexamic acid (TXA) reduced serious bleeding without a significant effect on major vascular outcomes in patients undergoing noncardiac surgery at risk for these complications in the POISE-3 trial.
TXA cut the primary efficacy outcome of life-threatening, major, and critical organ bleeding at 30 days by 24% compared with placebo (9.1% vs. 11.7%; hazard ratio [HR], 0.76; P < .0001).
The primary safety outcome of myocardial injury after noncardiac surgery (MINS), nonhemorrhagic stroke, peripheral arterial thrombosis, and symptomatic proximal venous thromboembolism (VTE) at 30 days occurred in 14.2% vs.. 13.9% of patients, respectively (HR, 1.023). This failed, however, to meet the study›s threshold to prove TXA noninferior to placebo (one-sided P = .044).
There was no increased risk for death or stroke with TXA, according to results published April 2 in the New England Journal of Medicine.
Principal investigator P.J. Devereaux, MD, PhD, Population Health Research Institute and McMaster University, Hamilton, Ontario, Canada, pointed out that there is only a 4.4% probability that the composite vascular outcome hazard ratio was above the noninferiority margin and that just 10 events separated the two groups (649 vs.. 639).
“Healthcare providers and patients will have to weigh a clear beneficial reduction in the composite bleeding outcome, which is an absolute difference of 2.7%, a result that was highly statistically significant, versus a low probability of a small increase in risk of the composite vascular endpoint, with an absolute difference of 0.3%,” a nonsignificant result, Dr. Devereaux said during the formal presentation of the results at the hybrid annual scientific sessions of the American College of Cardiology.
The findings, he said, should also be put in the context that 300 million adults have a major surgery each year worldwide and most don’t receive TXA. At the same time, there’s an annual global shortage of 30 million blood product units, and surgical bleeding accounts for up to 40% of all transfusions.
“POISE-3 identifies that use of TXA could avoid upwards of 8 million bleeding events resulting in transfusion on an annual basis, indicating potential for large public health and clinical benefit if TXA become standard practice in noncardiac surgery,” Dr. Devereaux said during the late-breaking trial session.
TXA is indicated for heavy menstrual bleeding and hemophilia and has been used in cardiac surgery, but it is increasingly being used in noncardiac surgeries. As previously reported, POISE showed that the beta-blocker metoprolol lowered the risk for myocardial infarction (MI) but increased the risk for severe stroke and overall death, whereas in POISE-2, perioperative low-dose aspirin lowered the risk for MI but was linked to more major bleeding.
The cumulative data have not shown an increased risk for thrombotic events in other settings, Dr. Devereaux told this news organization.
“I’m a cardiologist, and I think that we’ve been guilty at times of always only focusing on the thrombotic side of the equation and ignoring that bleeding is a very important aspect of the circulatory system,” he said. “And I think this shows for the first time clear unequivocal evidence that there’s a cheap, very encouraging, safe way to prevent this.”
“An important point is that if you can give tranexamic acid and prevent bleeding in your cardiac patients having noncardiac surgery, then you can prevent the delay of reinitiating their anticoagulants and their antiplatelets after surgery and getting them back on the medications that are important for them to prevent their cardiovascular event,” Dr. Devereaux added.
Discussant Michael J. Mack, MD, commented that TXA, widely used in cardiac surgery, is an old, inexpensive drug that “should be more widely used in noncardiac surgery.” Dr. Mack, from Baylor Scott & White Health, Dallas, added that he would limit it to major noncardiac surgery.
International trial
PeriOperative ISchemic Evaluation-3 (POISE-3) investigators at 114 hospitals in 22 countries (including countries in North and South America, Europe, and Africa; Russia; India; and Australia) randomly assigned 9,535 patients, aged 45 years or older, with or at risk for cardiovascular and bleeding complications to receive a TXA 1-g intravenous bolus or placebo at the start and end of inpatient noncardiac surgery.
Patients taking at least one long-term antihypertensive medication were also randomly assigned to a perioperative hypotension- or hypertension-avoidance strategy, which differ in the use of antihypertensives on the morning of surgery and the first 2 days after surgery, and in the target mean arterial pressure during surgery. Results from these cohorts will be presented in a separate session on April 4.
The study had planned to enroll 10,000 patients but was stopped early by the steering committee because of financial constraints resulting from slow enrollment during the pandemic. The decision was made without knowledge of the trial results but with knowledge that aggregate composite bleeding and vascular outcomes were higher than originally estimated, Dr. Devereaux noted.
Among all participants, the mean age was 70 years, 56% were male, almost a third had coronary artery disease, 15% had peripheral artery disease, and 8% had a prior stroke. About 80% were undergoing major surgery. Adherence to the study medications was 96.3% in both groups.
Secondary bleeding outcomes were lower in the TXA and placebo groups, including bleeding independently associated with mortality after surgery (8.7% vs. 11.3%), life-threatening bleeding (1.6% vs. 1.7%), major bleeding (7.6% vs. 10.4%), and critical organ bleeding (0.3% vs. 0.4%).
Importantly, the TXA group had significantly lower rates of International Society on Thrombosis and Haemostasis major bleeding (6.6% vs. 8.7%; P = .0001) and the need for transfusion of 1 or more units of packed red blood cells (9.4% vs. 12.0%; P <.0001), Dr. Devereaux noted.
In terms of secondary vascular outcomes, there were no significant differences between the TXA and placebo groups in rates of MINS (12.8% vs. 12.6%), MINS not fulfilling definition of MI (both 11.5%), MI (1.4% vs. 1.1%), and the net risk-benefit outcome (a composite of vascular death and nonfatal life-threatening, major, or critical organ bleeding, MINS, stroke, peripheral arterial thrombosis, and symptomatic proximal VTE; 20.7% vs. 21.9%).
The two groups had similar rates of all-cause (1.1% vs. 1.2%) and vascular (0.5% vs. 0.6%) mortality.
There also were no significant differences in other tertiary outcomes, such as acute kidney injury (14.1% vs. 13.7%), rehospitalization for vascular reasons (1.8% vs. 1.6%), or seizures (0.2% vs. <0.1%). The latter has been a concern, with the risk reported to increase with higher doses.
Subgroup analyses
Preplanned subgroup analyses showed a benefit for TXA over placebo for the primary efficacy outcome in orthopedic and nonorthopedic surgery and in patients with hemoglobin level below 120 g/L or 120 g/L or higher, with an estimated glomerular filtration rate less than 45 mL/min/1.73 m 2 or 45 mL/min/1.73 m 2 or higher, or with an N-terminal pro– B-type natriuretic peptide level below 200 ng/L or 200 ng/L or higher.
For the primary safety outcome, the benefit favored placebo but the interaction was not statistically significant for any of the four subgroups.
A post hoc subgroup analysis also showed similar results across the major categories of surgery, including general, vascular, urologic, and gynecologic, Dr. Devereaux told this news organization.
Although TXA is commonly used in orthopedic procedures, Dr. Devereaux noted, in other types of surgeries, “it’s not used at all.” But because TXA “is so cheap, and we can apply it to a broad population, even at an economic level it looks like it’s a winner to give to almost all patients having noncardiac surgery.”
The team also recently published a risk prediction tool that can help estimate a patient’s baseline risk for bleeding.
“So just using a model, which will bring together the patient’s type of surgery and their risk factors, you can look to see, okay, this is enough risk of bleeding, I’m just going to give tranexamic acid,” he said. “We will also be doing economic analyses because blood is also not cheap.”
The study was funded by the Canadian Institutes of Health Research, National Health and Medical Research Council (Australia), and the Research Grant Council (Hong Kong). Dr. Devereaux reports research/research grants from Abbott Diagnostics, Philips Healthcare, Roche Diagnostics, and Siemens. Dr. Mack reports receiving research grants from Abbott Vascular, Edwards Lifesciences, and Medtronic.
A version of this article first appeared on Medscape.com.
The antifibrinolytic tranexamic acid (TXA) reduced serious bleeding without a significant effect on major vascular outcomes in patients undergoing noncardiac surgery at risk for these complications in the POISE-3 trial.
TXA cut the primary efficacy outcome of life-threatening, major, and critical organ bleeding at 30 days by 24% compared with placebo (9.1% vs. 11.7%; hazard ratio [HR], 0.76; P < .0001).
The primary safety outcome of myocardial injury after noncardiac surgery (MINS), nonhemorrhagic stroke, peripheral arterial thrombosis, and symptomatic proximal venous thromboembolism (VTE) at 30 days occurred in 14.2% vs.. 13.9% of patients, respectively (HR, 1.023). This failed, however, to meet the study›s threshold to prove TXA noninferior to placebo (one-sided P = .044).
There was no increased risk for death or stroke with TXA, according to results published April 2 in the New England Journal of Medicine.
Principal investigator P.J. Devereaux, MD, PhD, Population Health Research Institute and McMaster University, Hamilton, Ontario, Canada, pointed out that there is only a 4.4% probability that the composite vascular outcome hazard ratio was above the noninferiority margin and that just 10 events separated the two groups (649 vs.. 639).
“Healthcare providers and patients will have to weigh a clear beneficial reduction in the composite bleeding outcome, which is an absolute difference of 2.7%, a result that was highly statistically significant, versus a low probability of a small increase in risk of the composite vascular endpoint, with an absolute difference of 0.3%,” a nonsignificant result, Dr. Devereaux said during the formal presentation of the results at the hybrid annual scientific sessions of the American College of Cardiology.
The findings, he said, should also be put in the context that 300 million adults have a major surgery each year worldwide and most don’t receive TXA. At the same time, there’s an annual global shortage of 30 million blood product units, and surgical bleeding accounts for up to 40% of all transfusions.
“POISE-3 identifies that use of TXA could avoid upwards of 8 million bleeding events resulting in transfusion on an annual basis, indicating potential for large public health and clinical benefit if TXA become standard practice in noncardiac surgery,” Dr. Devereaux said during the late-breaking trial session.
TXA is indicated for heavy menstrual bleeding and hemophilia and has been used in cardiac surgery, but it is increasingly being used in noncardiac surgeries. As previously reported, POISE showed that the beta-blocker metoprolol lowered the risk for myocardial infarction (MI) but increased the risk for severe stroke and overall death, whereas in POISE-2, perioperative low-dose aspirin lowered the risk for MI but was linked to more major bleeding.
The cumulative data have not shown an increased risk for thrombotic events in other settings, Dr. Devereaux told this news organization.
“I’m a cardiologist, and I think that we’ve been guilty at times of always only focusing on the thrombotic side of the equation and ignoring that bleeding is a very important aspect of the circulatory system,” he said. “And I think this shows for the first time clear unequivocal evidence that there’s a cheap, very encouraging, safe way to prevent this.”
“An important point is that if you can give tranexamic acid and prevent bleeding in your cardiac patients having noncardiac surgery, then you can prevent the delay of reinitiating their anticoagulants and their antiplatelets after surgery and getting them back on the medications that are important for them to prevent their cardiovascular event,” Dr. Devereaux added.
Discussant Michael J. Mack, MD, commented that TXA, widely used in cardiac surgery, is an old, inexpensive drug that “should be more widely used in noncardiac surgery.” Dr. Mack, from Baylor Scott & White Health, Dallas, added that he would limit it to major noncardiac surgery.
International trial
PeriOperative ISchemic Evaluation-3 (POISE-3) investigators at 114 hospitals in 22 countries (including countries in North and South America, Europe, and Africa; Russia; India; and Australia) randomly assigned 9,535 patients, aged 45 years or older, with or at risk for cardiovascular and bleeding complications to receive a TXA 1-g intravenous bolus or placebo at the start and end of inpatient noncardiac surgery.
Patients taking at least one long-term antihypertensive medication were also randomly assigned to a perioperative hypotension- or hypertension-avoidance strategy, which differ in the use of antihypertensives on the morning of surgery and the first 2 days after surgery, and in the target mean arterial pressure during surgery. Results from these cohorts will be presented in a separate session on April 4.
The study had planned to enroll 10,000 patients but was stopped early by the steering committee because of financial constraints resulting from slow enrollment during the pandemic. The decision was made without knowledge of the trial results but with knowledge that aggregate composite bleeding and vascular outcomes were higher than originally estimated, Dr. Devereaux noted.
Among all participants, the mean age was 70 years, 56% were male, almost a third had coronary artery disease, 15% had peripheral artery disease, and 8% had a prior stroke. About 80% were undergoing major surgery. Adherence to the study medications was 96.3% in both groups.
Secondary bleeding outcomes were lower in the TXA and placebo groups, including bleeding independently associated with mortality after surgery (8.7% vs. 11.3%), life-threatening bleeding (1.6% vs. 1.7%), major bleeding (7.6% vs. 10.4%), and critical organ bleeding (0.3% vs. 0.4%).
Importantly, the TXA group had significantly lower rates of International Society on Thrombosis and Haemostasis major bleeding (6.6% vs. 8.7%; P = .0001) and the need for transfusion of 1 or more units of packed red blood cells (9.4% vs. 12.0%; P <.0001), Dr. Devereaux noted.
In terms of secondary vascular outcomes, there were no significant differences between the TXA and placebo groups in rates of MINS (12.8% vs. 12.6%), MINS not fulfilling definition of MI (both 11.5%), MI (1.4% vs. 1.1%), and the net risk-benefit outcome (a composite of vascular death and nonfatal life-threatening, major, or critical organ bleeding, MINS, stroke, peripheral arterial thrombosis, and symptomatic proximal VTE; 20.7% vs. 21.9%).
The two groups had similar rates of all-cause (1.1% vs. 1.2%) and vascular (0.5% vs. 0.6%) mortality.
There also were no significant differences in other tertiary outcomes, such as acute kidney injury (14.1% vs. 13.7%), rehospitalization for vascular reasons (1.8% vs. 1.6%), or seizures (0.2% vs. <0.1%). The latter has been a concern, with the risk reported to increase with higher doses.
Subgroup analyses
Preplanned subgroup analyses showed a benefit for TXA over placebo for the primary efficacy outcome in orthopedic and nonorthopedic surgery and in patients with hemoglobin level below 120 g/L or 120 g/L or higher, with an estimated glomerular filtration rate less than 45 mL/min/1.73 m 2 or 45 mL/min/1.73 m 2 or higher, or with an N-terminal pro– B-type natriuretic peptide level below 200 ng/L or 200 ng/L or higher.
For the primary safety outcome, the benefit favored placebo but the interaction was not statistically significant for any of the four subgroups.
A post hoc subgroup analysis also showed similar results across the major categories of surgery, including general, vascular, urologic, and gynecologic, Dr. Devereaux told this news organization.
Although TXA is commonly used in orthopedic procedures, Dr. Devereaux noted, in other types of surgeries, “it’s not used at all.” But because TXA “is so cheap, and we can apply it to a broad population, even at an economic level it looks like it’s a winner to give to almost all patients having noncardiac surgery.”
The team also recently published a risk prediction tool that can help estimate a patient’s baseline risk for bleeding.
“So just using a model, which will bring together the patient’s type of surgery and their risk factors, you can look to see, okay, this is enough risk of bleeding, I’m just going to give tranexamic acid,” he said. “We will also be doing economic analyses because blood is also not cheap.”
The study was funded by the Canadian Institutes of Health Research, National Health and Medical Research Council (Australia), and the Research Grant Council (Hong Kong). Dr. Devereaux reports research/research grants from Abbott Diagnostics, Philips Healthcare, Roche Diagnostics, and Siemens. Dr. Mack reports receiving research grants from Abbott Vascular, Edwards Lifesciences, and Medtronic.
A version of this article first appeared on Medscape.com.
FROM ACC 2022
Reporting from: 48th annual scientific meeting of the Society of Gynecologic Surgeons
Wednesday, March 30. Day 3 of SGS.
The final day of #SGS2022 began with the last round of oral and video presentations on topics including: the efficacy and safety of restrictive blood transfusion protocols in gynecologic surgical patients, restricted opioid use following midurethral sling procedures, and the efficacy of trigger point injections for myofascial pelvic pain. Next, the prestigious Distinguished Surgeon Award was presented to Dr. Jeffrey Cornella, professor of Obstetrics and Gynecology at Mayo Clinic College of Medicine, for his contributions to the field of gynecologic surgery.
This was followed by the passing of the presidential gavel from current SGS president Dr. Carl Zimmerman to incoming president Dr. Cheryl Iglesia, Director of Female Pelvic Medicine and Reconstructive Surgery at MedStar Washington Hospital Center, Washington DC, and Director of the National Center for Advanced Pelvic Surgery (NCAPS) at Medstar Health. Dr. Iglesia has been internationally and nationally recognized for her work in advancing the field of pelvic surgery and urogynecology through extensive research, clinical excellence, and support of medical education.
Needless to say, #SGS2022 was a huge success! While many of us are sad to leave San Antonio today, we are returning to our respective programs feeling motivated and rejuvenated. There is nothing more inspiring than spending time with such a highly committed group of physicians who strive to improve patient care through their excellent contributions to research and medical education. I am grateful for the new mentors, colleagues, and friends I have met at this meeting.
Thank you to the Society of Gynecologic Surgeons and OBG Management for giving me the opportunity to reflect on my experience at #SGS2022, as well as the companies that support the Fellows Scholar program.
I can’t wait to attend the 49th Annual Scientific Meeting in Tuscon, Arizona, in 2023!
Tuesday, March 29, 2022. Day 2 of SGS.
The second day of #SGS2022 began with several academic roundtables on a variety of topics including hysteroscopy, uterine-preserving prolapse surgeries, how to select patients for vaginal hysterectomy, and the role of minimally invasive surgery in transabdominal cerclage. The general session continued with more outstanding poster and video presentations that were followed by the annual presidential address. SGS president Dr. Carl Zimmerman spoke about the changing surgical landscape and SGS’s commitment to improving surgical education: “The women of America and the world deserve better.” He went on to announce the creation of a presidential task force on surgical training, whose members will include: Dr. Ted Anderson, Dr. Emily Weber LeBrun, and Dr. Mike Moen.
This year’s TeLinde Lecture was given by the executive director of the American College of Surgeons, Dr. Dr. Patricia Turner. Her talk was entitled, “Surgeons: More to Unite Us Than Divide Us.” Dr. Turner began by reminding us of the shared history between general surgery and gynecologic surgery. In fact, the American College of Surgeons was founded by gynecologist Dr. Franklin H. Martin. She went on to thoughtfully discuss the need to rethink surgical training and the way we assess surgical trainees. She highlighted the importance of collaboration between all surgical specialties to improve surgical education, improve outcomes, and advocate for patients. “In order to heal all, we have to have ALL surgeons at the table.”
Today’s general session was concluded with a panel discussion on “Operating Room Safety and Efficiency” in which Dr. Kenneth Catchpole, Dr. Teodor Grantcharov, and Dr. Jason Wright shared some interesting ideas on how we can improve patient care in the operating room. The afternoon continued with a number of social activities, providing an opportunity to enjoy the beautiful landscape of San Antonio, Texas, including: a tour of Eisenhower park, kayaking on the Guadelupe River, and the SGS golf tournament.
The fun continued into the evening at the annual “SGS’ Got Talent” in which participants could be spotted in cowboy hats, bandanas, and boots. The night was filled with food, drinks, laughter, and line dancing! #SGS2022
Monday, March 28, 2022. Day 1 of SGS.
“How do you become brave? How do you become an advocate? How do you make a change?” These are just some of the questions asked during our thought-provoking early morning session entitled, “Healthcare Inequity Awareness—A Conversation to Empower Providers and Enhance the Patient Experience” at this year’s annual scientific meeting of the Society of Gynecologic Surgeons #SGS2022. The panelists, which included Dr. Olivia Cardenas-Trowers, Dr. Maria Florian-Rodriguez, and Dr. Tristi Muir, emphasized the importance of acknowledging our own bias as physicians, as well as the role structural racism plays in the health care access and outcomes of our patients. We were reminded that “Diversity, Equity, Inclusion (aka DEI) is a journey. It is progress over time, not over night.”
Following the early morning panel, the 48th annual scientific meeting officially began with a brief welcome and recognition of new SGS members by current president Dr. Carl Zimmerman and scientific program committee chair Dr. Oz Harmanli. The rest of the morning session was filled with outstanding oral and video presentations on topics ranging from the role of oophorectomy in patients with breast cancer, creating simulation models to enhance medical education, and tips for navigating the altered retroperitoneum.
Next, the Mark D. Walters endowed lecture was given by Dr. Marta A. Crispens, entitled “Restructuring Gynecologic Surgical Education: It’s a Matter of Equity.” In her exceptionally powerful address, Dr. Crispens began by discussing the historical context in which the fields of obstetrics and gynecology were combined and comparing it to a shift in current practice toward a national decrease in number of hysterectomies and an increase in the complexity of surgical cases. She highlighted the well-studied fact that low-volume surgeons have higher complication rates and that many new ObGyn residency graduates perform only 3 to 4 hysterectomies annually during the first few years of practice. Finally, she asserted that, by separating the practices of obstetrics and gynecology, we can improve surgical education and the quality of surgical care for our patients. The audience’s enthusiasm was undeniable, resulting in resounding applause and a standing ovation.
The afternoon was filled with unique opportunities for fellows, including: the Fellow’s Pelvic Research Network (FPRN) meeting, an incredibly informative panel on how to navigate the first year out of fellowship with Dr. Mireille Truong, Dr. Christine Foley, and Dr. Jon Pennycuff, and finally, the Mentorship Mingle.
The first day was concluded with the President’s Award Ceremony in which Dr. John DeLancey was presented with the illustrious President’s Award, followed by the President’s Reception with food, drinks, and lively conversation. Looking forward to day 2 of #SGS2022. @gynsurgery
Wednesday, March 30. Day 3 of SGS.
The final day of #SGS2022 began with the last round of oral and video presentations on topics including: the efficacy and safety of restrictive blood transfusion protocols in gynecologic surgical patients, restricted opioid use following midurethral sling procedures, and the efficacy of trigger point injections for myofascial pelvic pain. Next, the prestigious Distinguished Surgeon Award was presented to Dr. Jeffrey Cornella, professor of Obstetrics and Gynecology at Mayo Clinic College of Medicine, for his contributions to the field of gynecologic surgery.
This was followed by the passing of the presidential gavel from current SGS president Dr. Carl Zimmerman to incoming president Dr. Cheryl Iglesia, Director of Female Pelvic Medicine and Reconstructive Surgery at MedStar Washington Hospital Center, Washington DC, and Director of the National Center for Advanced Pelvic Surgery (NCAPS) at Medstar Health. Dr. Iglesia has been internationally and nationally recognized for her work in advancing the field of pelvic surgery and urogynecology through extensive research, clinical excellence, and support of medical education.
Needless to say, #SGS2022 was a huge success! While many of us are sad to leave San Antonio today, we are returning to our respective programs feeling motivated and rejuvenated. There is nothing more inspiring than spending time with such a highly committed group of physicians who strive to improve patient care through their excellent contributions to research and medical education. I am grateful for the new mentors, colleagues, and friends I have met at this meeting.
Thank you to the Society of Gynecologic Surgeons and OBG Management for giving me the opportunity to reflect on my experience at #SGS2022, as well as the companies that support the Fellows Scholar program.
I can’t wait to attend the 49th Annual Scientific Meeting in Tuscon, Arizona, in 2023!
Tuesday, March 29, 2022. Day 2 of SGS.
The second day of #SGS2022 began with several academic roundtables on a variety of topics including hysteroscopy, uterine-preserving prolapse surgeries, how to select patients for vaginal hysterectomy, and the role of minimally invasive surgery in transabdominal cerclage. The general session continued with more outstanding poster and video presentations that were followed by the annual presidential address. SGS president Dr. Carl Zimmerman spoke about the changing surgical landscape and SGS’s commitment to improving surgical education: “The women of America and the world deserve better.” He went on to announce the creation of a presidential task force on surgical training, whose members will include: Dr. Ted Anderson, Dr. Emily Weber LeBrun, and Dr. Mike Moen.
This year’s TeLinde Lecture was given by the executive director of the American College of Surgeons, Dr. Dr. Patricia Turner. Her talk was entitled, “Surgeons: More to Unite Us Than Divide Us.” Dr. Turner began by reminding us of the shared history between general surgery and gynecologic surgery. In fact, the American College of Surgeons was founded by gynecologist Dr. Franklin H. Martin. She went on to thoughtfully discuss the need to rethink surgical training and the way we assess surgical trainees. She highlighted the importance of collaboration between all surgical specialties to improve surgical education, improve outcomes, and advocate for patients. “In order to heal all, we have to have ALL surgeons at the table.”
Today’s general session was concluded with a panel discussion on “Operating Room Safety and Efficiency” in which Dr. Kenneth Catchpole, Dr. Teodor Grantcharov, and Dr. Jason Wright shared some interesting ideas on how we can improve patient care in the operating room. The afternoon continued with a number of social activities, providing an opportunity to enjoy the beautiful landscape of San Antonio, Texas, including: a tour of Eisenhower park, kayaking on the Guadelupe River, and the SGS golf tournament.
The fun continued into the evening at the annual “SGS’ Got Talent” in which participants could be spotted in cowboy hats, bandanas, and boots. The night was filled with food, drinks, laughter, and line dancing! #SGS2022
Monday, March 28, 2022. Day 1 of SGS.
“How do you become brave? How do you become an advocate? How do you make a change?” These are just some of the questions asked during our thought-provoking early morning session entitled, “Healthcare Inequity Awareness—A Conversation to Empower Providers and Enhance the Patient Experience” at this year’s annual scientific meeting of the Society of Gynecologic Surgeons #SGS2022. The panelists, which included Dr. Olivia Cardenas-Trowers, Dr. Maria Florian-Rodriguez, and Dr. Tristi Muir, emphasized the importance of acknowledging our own bias as physicians, as well as the role structural racism plays in the health care access and outcomes of our patients. We were reminded that “Diversity, Equity, Inclusion (aka DEI) is a journey. It is progress over time, not over night.”
Following the early morning panel, the 48th annual scientific meeting officially began with a brief welcome and recognition of new SGS members by current president Dr. Carl Zimmerman and scientific program committee chair Dr. Oz Harmanli. The rest of the morning session was filled with outstanding oral and video presentations on topics ranging from the role of oophorectomy in patients with breast cancer, creating simulation models to enhance medical education, and tips for navigating the altered retroperitoneum.
Next, the Mark D. Walters endowed lecture was given by Dr. Marta A. Crispens, entitled “Restructuring Gynecologic Surgical Education: It’s a Matter of Equity.” In her exceptionally powerful address, Dr. Crispens began by discussing the historical context in which the fields of obstetrics and gynecology were combined and comparing it to a shift in current practice toward a national decrease in number of hysterectomies and an increase in the complexity of surgical cases. She highlighted the well-studied fact that low-volume surgeons have higher complication rates and that many new ObGyn residency graduates perform only 3 to 4 hysterectomies annually during the first few years of practice. Finally, she asserted that, by separating the practices of obstetrics and gynecology, we can improve surgical education and the quality of surgical care for our patients. The audience’s enthusiasm was undeniable, resulting in resounding applause and a standing ovation.
The afternoon was filled with unique opportunities for fellows, including: the Fellow’s Pelvic Research Network (FPRN) meeting, an incredibly informative panel on how to navigate the first year out of fellowship with Dr. Mireille Truong, Dr. Christine Foley, and Dr. Jon Pennycuff, and finally, the Mentorship Mingle.
The first day was concluded with the President’s Award Ceremony in which Dr. John DeLancey was presented with the illustrious President’s Award, followed by the President’s Reception with food, drinks, and lively conversation. Looking forward to day 2 of #SGS2022. @gynsurgery
Wednesday, March 30. Day 3 of SGS.
The final day of #SGS2022 began with the last round of oral and video presentations on topics including: the efficacy and safety of restrictive blood transfusion protocols in gynecologic surgical patients, restricted opioid use following midurethral sling procedures, and the efficacy of trigger point injections for myofascial pelvic pain. Next, the prestigious Distinguished Surgeon Award was presented to Dr. Jeffrey Cornella, professor of Obstetrics and Gynecology at Mayo Clinic College of Medicine, for his contributions to the field of gynecologic surgery.
This was followed by the passing of the presidential gavel from current SGS president Dr. Carl Zimmerman to incoming president Dr. Cheryl Iglesia, Director of Female Pelvic Medicine and Reconstructive Surgery at MedStar Washington Hospital Center, Washington DC, and Director of the National Center for Advanced Pelvic Surgery (NCAPS) at Medstar Health. Dr. Iglesia has been internationally and nationally recognized for her work in advancing the field of pelvic surgery and urogynecology through extensive research, clinical excellence, and support of medical education.
Needless to say, #SGS2022 was a huge success! While many of us are sad to leave San Antonio today, we are returning to our respective programs feeling motivated and rejuvenated. There is nothing more inspiring than spending time with such a highly committed group of physicians who strive to improve patient care through their excellent contributions to research and medical education. I am grateful for the new mentors, colleagues, and friends I have met at this meeting.
Thank you to the Society of Gynecologic Surgeons and OBG Management for giving me the opportunity to reflect on my experience at #SGS2022, as well as the companies that support the Fellows Scholar program.
I can’t wait to attend the 49th Annual Scientific Meeting in Tuscon, Arizona, in 2023!
Tuesday, March 29, 2022. Day 2 of SGS.
The second day of #SGS2022 began with several academic roundtables on a variety of topics including hysteroscopy, uterine-preserving prolapse surgeries, how to select patients for vaginal hysterectomy, and the role of minimally invasive surgery in transabdominal cerclage. The general session continued with more outstanding poster and video presentations that were followed by the annual presidential address. SGS president Dr. Carl Zimmerman spoke about the changing surgical landscape and SGS’s commitment to improving surgical education: “The women of America and the world deserve better.” He went on to announce the creation of a presidential task force on surgical training, whose members will include: Dr. Ted Anderson, Dr. Emily Weber LeBrun, and Dr. Mike Moen.
This year’s TeLinde Lecture was given by the executive director of the American College of Surgeons, Dr. Dr. Patricia Turner. Her talk was entitled, “Surgeons: More to Unite Us Than Divide Us.” Dr. Turner began by reminding us of the shared history between general surgery and gynecologic surgery. In fact, the American College of Surgeons was founded by gynecologist Dr. Franklin H. Martin. She went on to thoughtfully discuss the need to rethink surgical training and the way we assess surgical trainees. She highlighted the importance of collaboration between all surgical specialties to improve surgical education, improve outcomes, and advocate for patients. “In order to heal all, we have to have ALL surgeons at the table.”
Today’s general session was concluded with a panel discussion on “Operating Room Safety and Efficiency” in which Dr. Kenneth Catchpole, Dr. Teodor Grantcharov, and Dr. Jason Wright shared some interesting ideas on how we can improve patient care in the operating room. The afternoon continued with a number of social activities, providing an opportunity to enjoy the beautiful landscape of San Antonio, Texas, including: a tour of Eisenhower park, kayaking on the Guadelupe River, and the SGS golf tournament.
The fun continued into the evening at the annual “SGS’ Got Talent” in which participants could be spotted in cowboy hats, bandanas, and boots. The night was filled with food, drinks, laughter, and line dancing! #SGS2022
Monday, March 28, 2022. Day 1 of SGS.
“How do you become brave? How do you become an advocate? How do you make a change?” These are just some of the questions asked during our thought-provoking early morning session entitled, “Healthcare Inequity Awareness—A Conversation to Empower Providers and Enhance the Patient Experience” at this year’s annual scientific meeting of the Society of Gynecologic Surgeons #SGS2022. The panelists, which included Dr. Olivia Cardenas-Trowers, Dr. Maria Florian-Rodriguez, and Dr. Tristi Muir, emphasized the importance of acknowledging our own bias as physicians, as well as the role structural racism plays in the health care access and outcomes of our patients. We were reminded that “Diversity, Equity, Inclusion (aka DEI) is a journey. It is progress over time, not over night.”
Following the early morning panel, the 48th annual scientific meeting officially began with a brief welcome and recognition of new SGS members by current president Dr. Carl Zimmerman and scientific program committee chair Dr. Oz Harmanli. The rest of the morning session was filled with outstanding oral and video presentations on topics ranging from the role of oophorectomy in patients with breast cancer, creating simulation models to enhance medical education, and tips for navigating the altered retroperitoneum.
Next, the Mark D. Walters endowed lecture was given by Dr. Marta A. Crispens, entitled “Restructuring Gynecologic Surgical Education: It’s a Matter of Equity.” In her exceptionally powerful address, Dr. Crispens began by discussing the historical context in which the fields of obstetrics and gynecology were combined and comparing it to a shift in current practice toward a national decrease in number of hysterectomies and an increase in the complexity of surgical cases. She highlighted the well-studied fact that low-volume surgeons have higher complication rates and that many new ObGyn residency graduates perform only 3 to 4 hysterectomies annually during the first few years of practice. Finally, she asserted that, by separating the practices of obstetrics and gynecology, we can improve surgical education and the quality of surgical care for our patients. The audience’s enthusiasm was undeniable, resulting in resounding applause and a standing ovation.
The afternoon was filled with unique opportunities for fellows, including: the Fellow’s Pelvic Research Network (FPRN) meeting, an incredibly informative panel on how to navigate the first year out of fellowship with Dr. Mireille Truong, Dr. Christine Foley, and Dr. Jon Pennycuff, and finally, the Mentorship Mingle.
The first day was concluded with the President’s Award Ceremony in which Dr. John DeLancey was presented with the illustrious President’s Award, followed by the President’s Reception with food, drinks, and lively conversation. Looking forward to day 2 of #SGS2022. @gynsurgery
Fertility after tubal ligation – It’s a matter of ‘AGE’
Despite the original intent of permanent contraception, tubal sterilization regret is experienced by 2%-26% of women as demonstrated by the United States Collaborative Review of Sterilization “CREST” 14-year study (Obstet Gynecol. 1999 Jun;93[6]:889-95). Regret appears to be higher in the United States than Europe and in resource-limited countries and is more common in women who are less than age 30, African-American, and unmarried. Nevertheless, requests for tubal reversal are estimated to be between 1% and 4% (Contraception. 1981 Jun;23[6]:579-89). The alternative option for fertility is in vitro fertilization (IVF) and this month’s column considers the pros and cons of both methods.
The procedure of tubal reanastomosis involves removing abnormal tissue and reapproximating the healthy tubal segments with attention to minimize adhesion formation through continued gentle irrigation. The surgery involves microsuturing using 6-0 to 10-0 sutures. Tubal patency can be confirmed during the procedure and with a subsequent hysterosalpingogram. While time from sterilization and the type of sterilization technique are factors that may influence the success rate of tubal reanastomosis, the age of the woman is the most predictive for pregnancy outcome.
In the original CREST study, the risk of ectopic pregnancy following tubal reanastomosis was contingent on the method of sterilization: Bipolar electrosurgery resulted in the highest probability of ectopic pregnancy (17.1 per 1,000 procedures at 10 years after permanent contraception), while postpartum partial salpingectomy resulted in the lowest (1.5 per 1,000 procedures at 10 years after permanent contraception) (N Engl J Med. 1997;336[11]:762). Comparatively, the ectopic pregnancy rate during an IVF cycle was 1.9% for pregnancies from transfers of fresh cleavage embryo, followed by transfers of frozen cleavage embryo (1.7%), transfers of fresh blastocyst (1.3%), and transfers of frozen blastocyst (0.8%) (Hum Reprod. 2015;30[9]:2048-54).
Reports vary regarding pregnancy rates from tubal reanastomosis. Prior use of rings and clips for sterilization appear to yield the highest outcomes as opposed to the use of electrocautery. In one large Canadian cohort study of over 300,000 women, those aged 15-30 years, 30-33 years, and 34-49 years had a conception rate of 73%, 64%, and 46%, respectively (Obstet Gynecol. 2003;101[4]:677-84). Most pregnancies were within 2 years after reversal and 48% of women achieved a delivery. Of interest, 23% of patients subsequently underwent another sterilization.
An Australian study of nearly 2,000 women found an overall cumulative live-delivery rate of 20% within the first year after reversal, 40% at 2 years, 51% at 5 years, and 52% at 10 years. As expected, the 5-year cumulative live-delivery rate was significantly lower in women who were aged 40-44 years (26%), compared with younger women. For all women below age 40 years, the live-delivery rate was approximately 50% within 5 years after tubal reanastomosis, while the rate halves after the age of 40 (Fertil Steril. 2015 Oct;104[4]:921-6).
To compare tubal reanastomosis with IVF, a retrospective cohort study of 163 patients demonstrated the cumulative delivery rate over 72 months was comparable for IVF vs. sterilization reversal (52% vs. 60%). The only significant difference was in a subset of patients aged <37 years (52% after IVF and 72% after reversal) and the lower cost of surgery. The authors advocated laparoscopic sterilization reversal in women younger than 37 years who have ≥4 cm of residual tube with IVF as the better alternative for all other women (Hum Reprod. 2007;22[10]:2660).
Indeed, tubal length is another important factor in successful reversal. The pregnancy rate after tubal anastomosis is 75% in women with tubal length of 4 cm or more, but only 19% in those with shorter tubes (Fertil Steril. 1987;48[1]:13-7). The literature does suggest equivalent pregnancy rates after laparoscopic tubal anastomosis and conventional microsurgical anastomosis. Although the laparoscopic approach may be more economical, it is more demanding technically than an open microsurgical procedure.
Tubal reanastomosis can also be performed using robot-assisted laparoscopy. In preliminary studies, robotic surgery appears to have a similar success rate and a shorter recovery time, but longer operative times and higher costs (Obstet Gynecol. 2007;109[6]:1375; Fertil Steril. 2008;90[4]:1175).
To educate women on the success of IVF based on individual characteristics, a valuable tool to approximate the cumulative outcome for a live birth following one cycle of IVF is offered by the Society for Assisted Reproductive Technology. To clarify, a cycle of IVF consists of one egg retrieval and the ultimate transfer of all embryos produced, i.e., fresh and frozen. The website also includes estimations of success following a second and third IVF cycle.
The woman’s age is a significant predictor of IVF success. Ovarian aging is currently best measured by combining chronologic age, antral follicle count (AFC) by transvaginal pelvic ultrasound, and serum anti-Müllerian hormone (AMH). Natural fecundity begins to decline, on average, above age 32-33 years. An AFC less than 11 reflects diminished ovarian reserve (DOR) and less than 6 is severe. AMH levels below 1.6 ng/mL have been shown to reduce the number of eggs retrieved with IVF, while levels below 0.4 ng/mL are very low. Very low AMH levels negatively affect the outcome of IVF cycles as demonstrated in the SART data study from a population of women with a mean age of 39.4 years: Cycle cancellation was 54%; of all retrieval attempts, no oocytes were obtained in 5.4%, and no embryo transfer occurred in 25.1% of cycles; the live birth rate per embryo transfer was 20.5% (9.5% per cycle start and 16.3% per retrieval) from a mean age of 36.8 years (Fertil Steril. 2016 Feb;105[2]:385-93.e3). The predictive ability of AMH on the live birth rate from IVF cycles was also shown in a study of over 85,000 women (Fertil Steril. 2018;109:258-65).
While low AMH has been shown to lessen a successful outcome from IVF, there appears to be no difference in natural pregnancy rates in women aged 30-44 years irrespective of AMH levels (JAMA. 2017;318[14]:1367-76). Of importance, the use of AMH in a population at low risk for DOR will yield a larger number of false-positive results (i.e., characterizing a woman as DOR when in fact she has normal ovarian reserve). Further, users of hormonal contraceptives have a 25.2% lower mean AMH level than nonusers.
When a patient is considering tubal reanastomosis vs. IVF, a useful acronym to remember is to check “AGE” – the A is for AMH because severely diminished ovarian reserve will reduce success with IVF as shown by the SART calculator; the G represents guy, i.e., ensuring a reasonably normal sperm analysis; and E stands for eggs representing ovulation function. In a woman who is anovulatory and who will require fertility medication, it would be reasonable to consider IVF given the need for ovarian stimulation. As in females, advanced paternal age has demonstrated a decline in fertility and sperm analysis parameters. Men above age 45 take approximately five times as long to achieve a pregnancy, compared with men less than 25 years of age. Further, there is evidence for advanced paternal age increasing risk of miscarriage, preterm birth, and birth defects. Men older than 40-45 years have twice the risk of an autistic child and five times the risk of having a child with schizophrenia (Transl Psychiatry 2017;7: e1019; Am J Psychiatry. 2002;159:1528-33).
To conclude, the data support consideration for sterilization reversal in women less than age 37 years with more than 4 cm of residual functional fallopian tube and the prior use of rings or clip sterilization. In other women, IVF may be the better option, particularly when ovulation dysfunction and/or male factor is present. IVF also offers the advantage of maintaining contraception and gender determination. However, given that AMH does not appear to reduce natural fertility, unlike during its effect during an IVF cycle, the option of tubal reversal may be more favorable in women with severe DOR.
Dr. Trolice is director of the IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
Despite the original intent of permanent contraception, tubal sterilization regret is experienced by 2%-26% of women as demonstrated by the United States Collaborative Review of Sterilization “CREST” 14-year study (Obstet Gynecol. 1999 Jun;93[6]:889-95). Regret appears to be higher in the United States than Europe and in resource-limited countries and is more common in women who are less than age 30, African-American, and unmarried. Nevertheless, requests for tubal reversal are estimated to be between 1% and 4% (Contraception. 1981 Jun;23[6]:579-89). The alternative option for fertility is in vitro fertilization (IVF) and this month’s column considers the pros and cons of both methods.
The procedure of tubal reanastomosis involves removing abnormal tissue and reapproximating the healthy tubal segments with attention to minimize adhesion formation through continued gentle irrigation. The surgery involves microsuturing using 6-0 to 10-0 sutures. Tubal patency can be confirmed during the procedure and with a subsequent hysterosalpingogram. While time from sterilization and the type of sterilization technique are factors that may influence the success rate of tubal reanastomosis, the age of the woman is the most predictive for pregnancy outcome.
In the original CREST study, the risk of ectopic pregnancy following tubal reanastomosis was contingent on the method of sterilization: Bipolar electrosurgery resulted in the highest probability of ectopic pregnancy (17.1 per 1,000 procedures at 10 years after permanent contraception), while postpartum partial salpingectomy resulted in the lowest (1.5 per 1,000 procedures at 10 years after permanent contraception) (N Engl J Med. 1997;336[11]:762). Comparatively, the ectopic pregnancy rate during an IVF cycle was 1.9% for pregnancies from transfers of fresh cleavage embryo, followed by transfers of frozen cleavage embryo (1.7%), transfers of fresh blastocyst (1.3%), and transfers of frozen blastocyst (0.8%) (Hum Reprod. 2015;30[9]:2048-54).
Reports vary regarding pregnancy rates from tubal reanastomosis. Prior use of rings and clips for sterilization appear to yield the highest outcomes as opposed to the use of electrocautery. In one large Canadian cohort study of over 300,000 women, those aged 15-30 years, 30-33 years, and 34-49 years had a conception rate of 73%, 64%, and 46%, respectively (Obstet Gynecol. 2003;101[4]:677-84). Most pregnancies were within 2 years after reversal and 48% of women achieved a delivery. Of interest, 23% of patients subsequently underwent another sterilization.
An Australian study of nearly 2,000 women found an overall cumulative live-delivery rate of 20% within the first year after reversal, 40% at 2 years, 51% at 5 years, and 52% at 10 years. As expected, the 5-year cumulative live-delivery rate was significantly lower in women who were aged 40-44 years (26%), compared with younger women. For all women below age 40 years, the live-delivery rate was approximately 50% within 5 years after tubal reanastomosis, while the rate halves after the age of 40 (Fertil Steril. 2015 Oct;104[4]:921-6).
To compare tubal reanastomosis with IVF, a retrospective cohort study of 163 patients demonstrated the cumulative delivery rate over 72 months was comparable for IVF vs. sterilization reversal (52% vs. 60%). The only significant difference was in a subset of patients aged <37 years (52% after IVF and 72% after reversal) and the lower cost of surgery. The authors advocated laparoscopic sterilization reversal in women younger than 37 years who have ≥4 cm of residual tube with IVF as the better alternative for all other women (Hum Reprod. 2007;22[10]:2660).
Indeed, tubal length is another important factor in successful reversal. The pregnancy rate after tubal anastomosis is 75% in women with tubal length of 4 cm or more, but only 19% in those with shorter tubes (Fertil Steril. 1987;48[1]:13-7). The literature does suggest equivalent pregnancy rates after laparoscopic tubal anastomosis and conventional microsurgical anastomosis. Although the laparoscopic approach may be more economical, it is more demanding technically than an open microsurgical procedure.
Tubal reanastomosis can also be performed using robot-assisted laparoscopy. In preliminary studies, robotic surgery appears to have a similar success rate and a shorter recovery time, but longer operative times and higher costs (Obstet Gynecol. 2007;109[6]:1375; Fertil Steril. 2008;90[4]:1175).
To educate women on the success of IVF based on individual characteristics, a valuable tool to approximate the cumulative outcome for a live birth following one cycle of IVF is offered by the Society for Assisted Reproductive Technology. To clarify, a cycle of IVF consists of one egg retrieval and the ultimate transfer of all embryos produced, i.e., fresh and frozen. The website also includes estimations of success following a second and third IVF cycle.
The woman’s age is a significant predictor of IVF success. Ovarian aging is currently best measured by combining chronologic age, antral follicle count (AFC) by transvaginal pelvic ultrasound, and serum anti-Müllerian hormone (AMH). Natural fecundity begins to decline, on average, above age 32-33 years. An AFC less than 11 reflects diminished ovarian reserve (DOR) and less than 6 is severe. AMH levels below 1.6 ng/mL have been shown to reduce the number of eggs retrieved with IVF, while levels below 0.4 ng/mL are very low. Very low AMH levels negatively affect the outcome of IVF cycles as demonstrated in the SART data study from a population of women with a mean age of 39.4 years: Cycle cancellation was 54%; of all retrieval attempts, no oocytes were obtained in 5.4%, and no embryo transfer occurred in 25.1% of cycles; the live birth rate per embryo transfer was 20.5% (9.5% per cycle start and 16.3% per retrieval) from a mean age of 36.8 years (Fertil Steril. 2016 Feb;105[2]:385-93.e3). The predictive ability of AMH on the live birth rate from IVF cycles was also shown in a study of over 85,000 women (Fertil Steril. 2018;109:258-65).
While low AMH has been shown to lessen a successful outcome from IVF, there appears to be no difference in natural pregnancy rates in women aged 30-44 years irrespective of AMH levels (JAMA. 2017;318[14]:1367-76). Of importance, the use of AMH in a population at low risk for DOR will yield a larger number of false-positive results (i.e., characterizing a woman as DOR when in fact she has normal ovarian reserve). Further, users of hormonal contraceptives have a 25.2% lower mean AMH level than nonusers.
When a patient is considering tubal reanastomosis vs. IVF, a useful acronym to remember is to check “AGE” – the A is for AMH because severely diminished ovarian reserve will reduce success with IVF as shown by the SART calculator; the G represents guy, i.e., ensuring a reasonably normal sperm analysis; and E stands for eggs representing ovulation function. In a woman who is anovulatory and who will require fertility medication, it would be reasonable to consider IVF given the need for ovarian stimulation. As in females, advanced paternal age has demonstrated a decline in fertility and sperm analysis parameters. Men above age 45 take approximately five times as long to achieve a pregnancy, compared with men less than 25 years of age. Further, there is evidence for advanced paternal age increasing risk of miscarriage, preterm birth, and birth defects. Men older than 40-45 years have twice the risk of an autistic child and five times the risk of having a child with schizophrenia (Transl Psychiatry 2017;7: e1019; Am J Psychiatry. 2002;159:1528-33).
To conclude, the data support consideration for sterilization reversal in women less than age 37 years with more than 4 cm of residual functional fallopian tube and the prior use of rings or clip sterilization. In other women, IVF may be the better option, particularly when ovulation dysfunction and/or male factor is present. IVF also offers the advantage of maintaining contraception and gender determination. However, given that AMH does not appear to reduce natural fertility, unlike during its effect during an IVF cycle, the option of tubal reversal may be more favorable in women with severe DOR.
Dr. Trolice is director of the IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
Despite the original intent of permanent contraception, tubal sterilization regret is experienced by 2%-26% of women as demonstrated by the United States Collaborative Review of Sterilization “CREST” 14-year study (Obstet Gynecol. 1999 Jun;93[6]:889-95). Regret appears to be higher in the United States than Europe and in resource-limited countries and is more common in women who are less than age 30, African-American, and unmarried. Nevertheless, requests for tubal reversal are estimated to be between 1% and 4% (Contraception. 1981 Jun;23[6]:579-89). The alternative option for fertility is in vitro fertilization (IVF) and this month’s column considers the pros and cons of both methods.
The procedure of tubal reanastomosis involves removing abnormal tissue and reapproximating the healthy tubal segments with attention to minimize adhesion formation through continued gentle irrigation. The surgery involves microsuturing using 6-0 to 10-0 sutures. Tubal patency can be confirmed during the procedure and with a subsequent hysterosalpingogram. While time from sterilization and the type of sterilization technique are factors that may influence the success rate of tubal reanastomosis, the age of the woman is the most predictive for pregnancy outcome.
In the original CREST study, the risk of ectopic pregnancy following tubal reanastomosis was contingent on the method of sterilization: Bipolar electrosurgery resulted in the highest probability of ectopic pregnancy (17.1 per 1,000 procedures at 10 years after permanent contraception), while postpartum partial salpingectomy resulted in the lowest (1.5 per 1,000 procedures at 10 years after permanent contraception) (N Engl J Med. 1997;336[11]:762). Comparatively, the ectopic pregnancy rate during an IVF cycle was 1.9% for pregnancies from transfers of fresh cleavage embryo, followed by transfers of frozen cleavage embryo (1.7%), transfers of fresh blastocyst (1.3%), and transfers of frozen blastocyst (0.8%) (Hum Reprod. 2015;30[9]:2048-54).
Reports vary regarding pregnancy rates from tubal reanastomosis. Prior use of rings and clips for sterilization appear to yield the highest outcomes as opposed to the use of electrocautery. In one large Canadian cohort study of over 300,000 women, those aged 15-30 years, 30-33 years, and 34-49 years had a conception rate of 73%, 64%, and 46%, respectively (Obstet Gynecol. 2003;101[4]:677-84). Most pregnancies were within 2 years after reversal and 48% of women achieved a delivery. Of interest, 23% of patients subsequently underwent another sterilization.
An Australian study of nearly 2,000 women found an overall cumulative live-delivery rate of 20% within the first year after reversal, 40% at 2 years, 51% at 5 years, and 52% at 10 years. As expected, the 5-year cumulative live-delivery rate was significantly lower in women who were aged 40-44 years (26%), compared with younger women. For all women below age 40 years, the live-delivery rate was approximately 50% within 5 years after tubal reanastomosis, while the rate halves after the age of 40 (Fertil Steril. 2015 Oct;104[4]:921-6).
To compare tubal reanastomosis with IVF, a retrospective cohort study of 163 patients demonstrated the cumulative delivery rate over 72 months was comparable for IVF vs. sterilization reversal (52% vs. 60%). The only significant difference was in a subset of patients aged <37 years (52% after IVF and 72% after reversal) and the lower cost of surgery. The authors advocated laparoscopic sterilization reversal in women younger than 37 years who have ≥4 cm of residual tube with IVF as the better alternative for all other women (Hum Reprod. 2007;22[10]:2660).
Indeed, tubal length is another important factor in successful reversal. The pregnancy rate after tubal anastomosis is 75% in women with tubal length of 4 cm or more, but only 19% in those with shorter tubes (Fertil Steril. 1987;48[1]:13-7). The literature does suggest equivalent pregnancy rates after laparoscopic tubal anastomosis and conventional microsurgical anastomosis. Although the laparoscopic approach may be more economical, it is more demanding technically than an open microsurgical procedure.
Tubal reanastomosis can also be performed using robot-assisted laparoscopy. In preliminary studies, robotic surgery appears to have a similar success rate and a shorter recovery time, but longer operative times and higher costs (Obstet Gynecol. 2007;109[6]:1375; Fertil Steril. 2008;90[4]:1175).
To educate women on the success of IVF based on individual characteristics, a valuable tool to approximate the cumulative outcome for a live birth following one cycle of IVF is offered by the Society for Assisted Reproductive Technology. To clarify, a cycle of IVF consists of one egg retrieval and the ultimate transfer of all embryos produced, i.e., fresh and frozen. The website also includes estimations of success following a second and third IVF cycle.
The woman’s age is a significant predictor of IVF success. Ovarian aging is currently best measured by combining chronologic age, antral follicle count (AFC) by transvaginal pelvic ultrasound, and serum anti-Müllerian hormone (AMH). Natural fecundity begins to decline, on average, above age 32-33 years. An AFC less than 11 reflects diminished ovarian reserve (DOR) and less than 6 is severe. AMH levels below 1.6 ng/mL have been shown to reduce the number of eggs retrieved with IVF, while levels below 0.4 ng/mL are very low. Very low AMH levels negatively affect the outcome of IVF cycles as demonstrated in the SART data study from a population of women with a mean age of 39.4 years: Cycle cancellation was 54%; of all retrieval attempts, no oocytes were obtained in 5.4%, and no embryo transfer occurred in 25.1% of cycles; the live birth rate per embryo transfer was 20.5% (9.5% per cycle start and 16.3% per retrieval) from a mean age of 36.8 years (Fertil Steril. 2016 Feb;105[2]:385-93.e3). The predictive ability of AMH on the live birth rate from IVF cycles was also shown in a study of over 85,000 women (Fertil Steril. 2018;109:258-65).
While low AMH has been shown to lessen a successful outcome from IVF, there appears to be no difference in natural pregnancy rates in women aged 30-44 years irrespective of AMH levels (JAMA. 2017;318[14]:1367-76). Of importance, the use of AMH in a population at low risk for DOR will yield a larger number of false-positive results (i.e., characterizing a woman as DOR when in fact she has normal ovarian reserve). Further, users of hormonal contraceptives have a 25.2% lower mean AMH level than nonusers.
When a patient is considering tubal reanastomosis vs. IVF, a useful acronym to remember is to check “AGE” – the A is for AMH because severely diminished ovarian reserve will reduce success with IVF as shown by the SART calculator; the G represents guy, i.e., ensuring a reasonably normal sperm analysis; and E stands for eggs representing ovulation function. In a woman who is anovulatory and who will require fertility medication, it would be reasonable to consider IVF given the need for ovarian stimulation. As in females, advanced paternal age has demonstrated a decline in fertility and sperm analysis parameters. Men above age 45 take approximately five times as long to achieve a pregnancy, compared with men less than 25 years of age. Further, there is evidence for advanced paternal age increasing risk of miscarriage, preterm birth, and birth defects. Men older than 40-45 years have twice the risk of an autistic child and five times the risk of having a child with schizophrenia (Transl Psychiatry 2017;7: e1019; Am J Psychiatry. 2002;159:1528-33).
To conclude, the data support consideration for sterilization reversal in women less than age 37 years with more than 4 cm of residual functional fallopian tube and the prior use of rings or clip sterilization. In other women, IVF may be the better option, particularly when ovulation dysfunction and/or male factor is present. IVF also offers the advantage of maintaining contraception and gender determination. However, given that AMH does not appear to reduce natural fertility, unlike during its effect during an IVF cycle, the option of tubal reversal may be more favorable in women with severe DOR.
Dr. Trolice is director of the IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
Complex surgery 10 times more likely with some ovarian tumors
according to a report at the Society of Gynecologic Oncology annual meeting.
Investigators found that women with those features, compared with those without them, are 10 times more likely to have a high-complexity surgery and almost 27 times more likely to have something other than a complete (RD0) resection.
The findings speak to a common dilemma in advanced ovarian cancer, whether women should have surgery or chemotherapy first. Part of the decision hinges on the likelihood of surgical success, explained lead investigator Diogo Torres, MD, a gynecologic oncologist at Ochsner Health in New Orleans.
He and his team concluded that “preoperative CT imaging combined with tumor molecular subtyping can identify a subset of women for whom successful primary surgery is unlikely. Preoperative tumor sampling may be useful in advanced [ovarian cancer] to better triage these cases to alternative approaches.”
For years “we’ve been trying to figure out” how best to make the call between primary debulking and neoadjuvant chemotherapy, said Pamela T. Soliman, MD, MPH,a gynecologic oncologist at the University of Texas MD Anderson Cancer Center, Houston, who discussed the abstract at the meeting.
Imaging alone or CA-125 are often used to make the decision, but they’re unreliable. Diagnostic laparoscopy is accurate, but it isn’t used much, she said.
What’s unique about Dr. Torres’s approach is that, by including tumor subtype, it incorporates tumor biology. It makes sense because his team previously found that women with mesenchymal (MES) tumors are more likely than those with other subtypes to have upper abdominal and miliary disease.
The approach needs validation in a larger study, but “I really commend” the team “for incorporating biology into the decision-making because it is clearly a step in the right direction,” Dr. Soliman said.
The study included 129 women who underwent primary debulking surgery for stage 3c or 4 high-grade serous ovarian cancer; 46x women (36%) had MES tumors according to RNA profiling of surgical specimens.
Preoperative CTs were reviewed to assess diaphragmatic disease; gastrohepatic/portahepatis lesions; root of superior mesenteric artery involvement; presence of moderate to severe ascites; intrahepatic lesions, and diffuse peritoneal thickening greater than 4 mm.
Fifty-nine women (46%) were classified as “CT high,” meaning that they had two or more of those findings. Women with no more than one were categorized as “CT low.”
Patients with MES tumors and CT-high disease had the lowest rates of complete resections, 8% versus 46% for the entire cohort and 72% for non-MES, CT-low women. MES, CT-high women were also the most likely to have high-complexity surgery (81% versus 35% in the non-MES, CT-low group).
Adjusting for age, stage, and American Society of Anesthesiologists score, the odds of high-complexity surgery were 9.53 times higher and the odds of something less than a complete resection were 26.73 times greater in MES, CT-high patients, compared with non-MES, CT-low women.
“Further studies are needed to evaluate and validate this model using preoperative biopsy specimens” instead of surgical specimens, the investigators said.
No funding was reported for the work. Dr. Torres didn’t have any disclosures. Dr. Soliman is an adviser for Eisai and Amgen, a consultant for Medscape, and receives research funding from Novartis and Incyte.
according to a report at the Society of Gynecologic Oncology annual meeting.
Investigators found that women with those features, compared with those without them, are 10 times more likely to have a high-complexity surgery and almost 27 times more likely to have something other than a complete (RD0) resection.
The findings speak to a common dilemma in advanced ovarian cancer, whether women should have surgery or chemotherapy first. Part of the decision hinges on the likelihood of surgical success, explained lead investigator Diogo Torres, MD, a gynecologic oncologist at Ochsner Health in New Orleans.
He and his team concluded that “preoperative CT imaging combined with tumor molecular subtyping can identify a subset of women for whom successful primary surgery is unlikely. Preoperative tumor sampling may be useful in advanced [ovarian cancer] to better triage these cases to alternative approaches.”
For years “we’ve been trying to figure out” how best to make the call between primary debulking and neoadjuvant chemotherapy, said Pamela T. Soliman, MD, MPH,a gynecologic oncologist at the University of Texas MD Anderson Cancer Center, Houston, who discussed the abstract at the meeting.
Imaging alone or CA-125 are often used to make the decision, but they’re unreliable. Diagnostic laparoscopy is accurate, but it isn’t used much, she said.
What’s unique about Dr. Torres’s approach is that, by including tumor subtype, it incorporates tumor biology. It makes sense because his team previously found that women with mesenchymal (MES) tumors are more likely than those with other subtypes to have upper abdominal and miliary disease.
The approach needs validation in a larger study, but “I really commend” the team “for incorporating biology into the decision-making because it is clearly a step in the right direction,” Dr. Soliman said.
The study included 129 women who underwent primary debulking surgery for stage 3c or 4 high-grade serous ovarian cancer; 46x women (36%) had MES tumors according to RNA profiling of surgical specimens.
Preoperative CTs were reviewed to assess diaphragmatic disease; gastrohepatic/portahepatis lesions; root of superior mesenteric artery involvement; presence of moderate to severe ascites; intrahepatic lesions, and diffuse peritoneal thickening greater than 4 mm.
Fifty-nine women (46%) were classified as “CT high,” meaning that they had two or more of those findings. Women with no more than one were categorized as “CT low.”
Patients with MES tumors and CT-high disease had the lowest rates of complete resections, 8% versus 46% for the entire cohort and 72% for non-MES, CT-low women. MES, CT-high women were also the most likely to have high-complexity surgery (81% versus 35% in the non-MES, CT-low group).
Adjusting for age, stage, and American Society of Anesthesiologists score, the odds of high-complexity surgery were 9.53 times higher and the odds of something less than a complete resection were 26.73 times greater in MES, CT-high patients, compared with non-MES, CT-low women.
“Further studies are needed to evaluate and validate this model using preoperative biopsy specimens” instead of surgical specimens, the investigators said.
No funding was reported for the work. Dr. Torres didn’t have any disclosures. Dr. Soliman is an adviser for Eisai and Amgen, a consultant for Medscape, and receives research funding from Novartis and Incyte.
according to a report at the Society of Gynecologic Oncology annual meeting.
Investigators found that women with those features, compared with those without them, are 10 times more likely to have a high-complexity surgery and almost 27 times more likely to have something other than a complete (RD0) resection.
The findings speak to a common dilemma in advanced ovarian cancer, whether women should have surgery or chemotherapy first. Part of the decision hinges on the likelihood of surgical success, explained lead investigator Diogo Torres, MD, a gynecologic oncologist at Ochsner Health in New Orleans.
He and his team concluded that “preoperative CT imaging combined with tumor molecular subtyping can identify a subset of women for whom successful primary surgery is unlikely. Preoperative tumor sampling may be useful in advanced [ovarian cancer] to better triage these cases to alternative approaches.”
For years “we’ve been trying to figure out” how best to make the call between primary debulking and neoadjuvant chemotherapy, said Pamela T. Soliman, MD, MPH,a gynecologic oncologist at the University of Texas MD Anderson Cancer Center, Houston, who discussed the abstract at the meeting.
Imaging alone or CA-125 are often used to make the decision, but they’re unreliable. Diagnostic laparoscopy is accurate, but it isn’t used much, she said.
What’s unique about Dr. Torres’s approach is that, by including tumor subtype, it incorporates tumor biology. It makes sense because his team previously found that women with mesenchymal (MES) tumors are more likely than those with other subtypes to have upper abdominal and miliary disease.
The approach needs validation in a larger study, but “I really commend” the team “for incorporating biology into the decision-making because it is clearly a step in the right direction,” Dr. Soliman said.
The study included 129 women who underwent primary debulking surgery for stage 3c or 4 high-grade serous ovarian cancer; 46x women (36%) had MES tumors according to RNA profiling of surgical specimens.
Preoperative CTs were reviewed to assess diaphragmatic disease; gastrohepatic/portahepatis lesions; root of superior mesenteric artery involvement; presence of moderate to severe ascites; intrahepatic lesions, and diffuse peritoneal thickening greater than 4 mm.
Fifty-nine women (46%) were classified as “CT high,” meaning that they had two or more of those findings. Women with no more than one were categorized as “CT low.”
Patients with MES tumors and CT-high disease had the lowest rates of complete resections, 8% versus 46% for the entire cohort and 72% for non-MES, CT-low women. MES, CT-high women were also the most likely to have high-complexity surgery (81% versus 35% in the non-MES, CT-low group).
Adjusting for age, stage, and American Society of Anesthesiologists score, the odds of high-complexity surgery were 9.53 times higher and the odds of something less than a complete resection were 26.73 times greater in MES, CT-high patients, compared with non-MES, CT-low women.
“Further studies are needed to evaluate and validate this model using preoperative biopsy specimens” instead of surgical specimens, the investigators said.
No funding was reported for the work. Dr. Torres didn’t have any disclosures. Dr. Soliman is an adviser for Eisai and Amgen, a consultant for Medscape, and receives research funding from Novartis and Incyte.
FROM SGO 2022
Racial disparities seen in pediatric postoperative mortality rates
Among Black and White children, higher socioeconomic status (SES) was associated with lower pediatric postoperative mortality, according to a cohort study published in JAMA Network Open. However, this association was not equitable when comparing Black and White children.
The results showed that postoperative mortality rates were significantly higher in Black children in the highest income category, compared with White children in the same category.
“[We] assessed whether increasing family SES is associated with lower pediatric postoperative mortality and, if so, whether this association is equitable among Black and White children,” Brittany L. Willer, MD, of Nationwide Children’s Hospital in Columbus, Ohio, and colleagues wrote.
The researchers retrospectively analyzed data from 51 pediatric tertiary care hospitals apart of the Children’s Hospital Association Pediatric Health Information System. The cohort included children younger than 18 years who underwent inpatient surgical procedures between January 2004 and December 2020.
The exposures of interest were race and parental income quartile; the primary endpoint was risk-adjusted in-hospital mortality rates by race and parental income quartile.
Results
The study cohort included 1,378,111 participants, including 248,464 (18.0%) Black and 1,129,647 (82.0%) White children, respectively.
The overall mortality rate was 1.2%, and rates decreased as income quartile increased (1.4% in quartile 1 [lowest income]; 1.3% in quartile 2; 1.0% in quartile 3; and 0.9% in quartile 4 [highest income]; P < .001).
Among participants in the three lowest income quartiles, Black children had 33% greater odds of postoperative death versus White children (adjusted odds ratio, 1.33; 95% confidence interval, 1.27-1.39; P < .001). This difference persisted in children in the highest income quartile (aOR, 1.39; 95% CI, 1.25-1.54; P < .001).
In addition, postoperative mortality rates in Black children in the highest income quartile (1.30%; 95% CI, 1.19%-1.42%) were similar to those of White children in the lowest income quartile (1.20%; 95% CI, 1.16%-1.25%).
“These findings suggest that increasing family SES did not provide equitable advantage to Black, compared with White children, and interventions that target socioeconomic inequities alone may not fully address persistent racial disparities in pediatric postoperative mortality,” wrote Dr. Willer and colleagues. “A multifaceted approach that includes dismantling of socioeconomic barriers, equitable availability of comprehensive pediatric surgical care, and personalized care for children of all races is needed.”
The researchers acknowledged that a potential limitation of the study was the use of zip code–level median household income as a proxy for family SES.
A perspective
In an interview, Timothy Joos, MD, a Seattle internist and pediatrician in private practice, said “there is a fair dose of racism and classism inside all of us – recognizing and coming to terms with it are steps toward improving equity issues.
“As providers, we have to remind ourselves to give our most prompt and thorough care to the patients with the most acute and severe illnesses,” Dr. Joos said. “As organizations, we have to pursue feedback from all our clients, but with special outreach to those that are used to not having their voices heard.”
No funding sources were reported. The authors reported no relevant disclosures. Dr. Joos is a member of the Pediatric News editorial advisory board but had no other disclosures.
Among Black and White children, higher socioeconomic status (SES) was associated with lower pediatric postoperative mortality, according to a cohort study published in JAMA Network Open. However, this association was not equitable when comparing Black and White children.
The results showed that postoperative mortality rates were significantly higher in Black children in the highest income category, compared with White children in the same category.
“[We] assessed whether increasing family SES is associated with lower pediatric postoperative mortality and, if so, whether this association is equitable among Black and White children,” Brittany L. Willer, MD, of Nationwide Children’s Hospital in Columbus, Ohio, and colleagues wrote.
The researchers retrospectively analyzed data from 51 pediatric tertiary care hospitals apart of the Children’s Hospital Association Pediatric Health Information System. The cohort included children younger than 18 years who underwent inpatient surgical procedures between January 2004 and December 2020.
The exposures of interest were race and parental income quartile; the primary endpoint was risk-adjusted in-hospital mortality rates by race and parental income quartile.
Results
The study cohort included 1,378,111 participants, including 248,464 (18.0%) Black and 1,129,647 (82.0%) White children, respectively.
The overall mortality rate was 1.2%, and rates decreased as income quartile increased (1.4% in quartile 1 [lowest income]; 1.3% in quartile 2; 1.0% in quartile 3; and 0.9% in quartile 4 [highest income]; P < .001).
Among participants in the three lowest income quartiles, Black children had 33% greater odds of postoperative death versus White children (adjusted odds ratio, 1.33; 95% confidence interval, 1.27-1.39; P < .001). This difference persisted in children in the highest income quartile (aOR, 1.39; 95% CI, 1.25-1.54; P < .001).
In addition, postoperative mortality rates in Black children in the highest income quartile (1.30%; 95% CI, 1.19%-1.42%) were similar to those of White children in the lowest income quartile (1.20%; 95% CI, 1.16%-1.25%).
“These findings suggest that increasing family SES did not provide equitable advantage to Black, compared with White children, and interventions that target socioeconomic inequities alone may not fully address persistent racial disparities in pediatric postoperative mortality,” wrote Dr. Willer and colleagues. “A multifaceted approach that includes dismantling of socioeconomic barriers, equitable availability of comprehensive pediatric surgical care, and personalized care for children of all races is needed.”
The researchers acknowledged that a potential limitation of the study was the use of zip code–level median household income as a proxy for family SES.
A perspective
In an interview, Timothy Joos, MD, a Seattle internist and pediatrician in private practice, said “there is a fair dose of racism and classism inside all of us – recognizing and coming to terms with it are steps toward improving equity issues.
“As providers, we have to remind ourselves to give our most prompt and thorough care to the patients with the most acute and severe illnesses,” Dr. Joos said. “As organizations, we have to pursue feedback from all our clients, but with special outreach to those that are used to not having their voices heard.”
No funding sources were reported. The authors reported no relevant disclosures. Dr. Joos is a member of the Pediatric News editorial advisory board but had no other disclosures.
Among Black and White children, higher socioeconomic status (SES) was associated with lower pediatric postoperative mortality, according to a cohort study published in JAMA Network Open. However, this association was not equitable when comparing Black and White children.
The results showed that postoperative mortality rates were significantly higher in Black children in the highest income category, compared with White children in the same category.
“[We] assessed whether increasing family SES is associated with lower pediatric postoperative mortality and, if so, whether this association is equitable among Black and White children,” Brittany L. Willer, MD, of Nationwide Children’s Hospital in Columbus, Ohio, and colleagues wrote.
The researchers retrospectively analyzed data from 51 pediatric tertiary care hospitals apart of the Children’s Hospital Association Pediatric Health Information System. The cohort included children younger than 18 years who underwent inpatient surgical procedures between January 2004 and December 2020.
The exposures of interest were race and parental income quartile; the primary endpoint was risk-adjusted in-hospital mortality rates by race and parental income quartile.
Results
The study cohort included 1,378,111 participants, including 248,464 (18.0%) Black and 1,129,647 (82.0%) White children, respectively.
The overall mortality rate was 1.2%, and rates decreased as income quartile increased (1.4% in quartile 1 [lowest income]; 1.3% in quartile 2; 1.0% in quartile 3; and 0.9% in quartile 4 [highest income]; P < .001).
Among participants in the three lowest income quartiles, Black children had 33% greater odds of postoperative death versus White children (adjusted odds ratio, 1.33; 95% confidence interval, 1.27-1.39; P < .001). This difference persisted in children in the highest income quartile (aOR, 1.39; 95% CI, 1.25-1.54; P < .001).
In addition, postoperative mortality rates in Black children in the highest income quartile (1.30%; 95% CI, 1.19%-1.42%) were similar to those of White children in the lowest income quartile (1.20%; 95% CI, 1.16%-1.25%).
“These findings suggest that increasing family SES did not provide equitable advantage to Black, compared with White children, and interventions that target socioeconomic inequities alone may not fully address persistent racial disparities in pediatric postoperative mortality,” wrote Dr. Willer and colleagues. “A multifaceted approach that includes dismantling of socioeconomic barriers, equitable availability of comprehensive pediatric surgical care, and personalized care for children of all races is needed.”
The researchers acknowledged that a potential limitation of the study was the use of zip code–level median household income as a proxy for family SES.
A perspective
In an interview, Timothy Joos, MD, a Seattle internist and pediatrician in private practice, said “there is a fair dose of racism and classism inside all of us – recognizing and coming to terms with it are steps toward improving equity issues.
“As providers, we have to remind ourselves to give our most prompt and thorough care to the patients with the most acute and severe illnesses,” Dr. Joos said. “As organizations, we have to pursue feedback from all our clients, but with special outreach to those that are used to not having their voices heard.”
No funding sources were reported. The authors reported no relevant disclosures. Dr. Joos is a member of the Pediatric News editorial advisory board but had no other disclosures.
FROM JAMA NETWORK OPEN
Acute STEMI During the COVID-19 Pandemic at a Regional Hospital: Incidence, Clinical Characteristics, and Outcomes
From the Department of Medicine, Medical College of Georgia at the Augusta University-University of Georgia Medical Partnership, Athens, GA (Syed H. Ali, Syed Hyder, and Dr. Murrow), and the Department of Cardiology, Piedmont Heart Institute, Piedmont Athens Regional, Athens, GA (Dr. Murrow and Mrs. Davis).
Abstract
Objectives: The aim of this study was to describe the characteristics and in-hospital outcomes of patients with acute ST-segment elevation myocardial infarction (STEMI) during the early COVID-19 pandemic at Piedmont Athens Regional (PAR), a 330-bed tertiary referral center in Northeast Georgia.
Methods: A retrospective study was conducted at PAR to evaluate patients with acute STEMI admitted over an 8-week period during the initial COVID-19 outbreak. This study group was compared to patients admitted during the corresponding period in 2019. The primary endpoint of this study was defined as a composite of sustained ventricular arrhythmia, congestive heart failure (CHF) with pulmonary congestion, and/or in-hospital mortality.
Results: This study cohort was composed of 64 patients with acute STEMI; 30 patients (46.9%) were hospitalized during the COVID-19 pandemic. Patients with STEMI in both the COVID-19 and control groups had similar comorbidities, Killip classification score, and clinical presentations. The median (interquartile range) time from symptom onset to reperfusion (total ischemic time) increased from 99.5 minutes (84.8-132) in 2019 to 149 minutes (96.3-231.8; P = .032) in 2020. Hospitalization during the COVID-19 period was associated with an increased risk for combined in-hospital outcome (odds ratio, 3.96; P = .046).
Conclusion: Patients with STEMI admitted during the first wave of the COVID-19 outbreak experienced longer total ischemic time and increased risk for combined in-hospital outcomes compared to patients admitted during the corresponding period in 2019.
Keywords: myocardial infarction, acute coronary syndrome, hospitalization, outcomes.
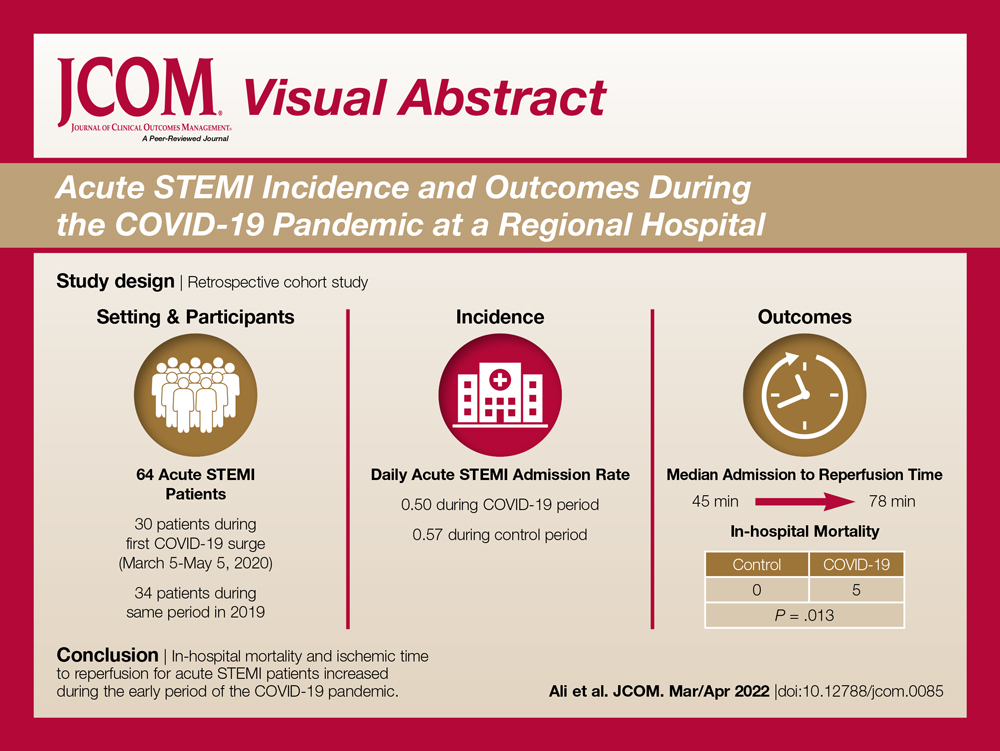
The emergence of the SARS-Cov-2 virus in December 2019 caused a worldwide shift in resource allocation and the restructuring of health care systems within the span of a few months. With the rapid spread of infection, the World Health Organization officially declared a pandemic in March 2020. The pandemic led to the deferral and cancellation of in-person patient visits, routine diagnostic studies, and nonessential surgeries and procedures. This response occurred secondary to a joint effort to reduce transmission via stay-at-home mandates and appropriate social distancing.1
Alongside the reduction in elective procedures and health care visits, significant reductions in hospitalization rates due to decreases in acute ST-segment elevation myocardial infarction (STEMI) and catheterization laboratory utilization have been reported in many studies from around the world.2-7 Comprehensive data demonstrating the impact of the COVID-19 pandemic on acute STEMI patient characteristics, clinical presentation, and in-hospital outcomes are lacking. Although patients with previously diagnosed cardiovascular disease are more likely to encounter worse outcomes in the setting of COVID-19, there may also be an indirect impact of the pandemic on high-risk patients, including those without the infection.8 Several theories have been hypothesized to explain this phenomenon. One theory postulates that the fear of contracting the virus during hospitalization is great enough to prevent patients from seeking care.2 Another theory suggests that the increased utilization of telemedicine prevents exacerbation of chronic conditions and the need for hospitalization.9 Contrary to this trend, previous studies have shown an increased incidence of acute STEMI following stressful events such as natural disasters.10
The aim of this study was to describe trends pertaining to clinical characteristics and in-hospital outcomes of patients with acute STEMI during the early COVID-19 pandemic at Piedmont Athens Regional (PAR), a 330-bed tertiary referral center in Northeast Georgia.
Methods
A retrospective cohort study was conducted at PAR to evaluate patients with STEMI admitted to the cardiovascular intensive care unit over an 8-week period (March 5 to May 5, 2020) during the COVID-19 outbreak. COVID-19 was declared a national emergency on March 13, 2020, in the United States. The institutional review board at PAR approved the study; the need for individual consent was waived under the condition that participant data would undergo de-identification and be strictly safeguarded.
Data Collection
Because there are seasonal variations in cardiovascular admissions, patient data from a control period (March 9 to May 9, 2019) were obtained to compare with data from the 2020 period. The number of patients with the diagnosis of acute STEMI during the COVID-19 period was recorded. Demographic data, clinical characteristics, and primary angiographic findings were gathered for all patients. Time from symptom onset to hospital admission and time from hospital admission to reperfusion (defined as door-to-balloon time) were documented for each patient. Killip classification was used to assess patients’ clinical status on admission. Length of stay was determined as days from hospital admission to discharge or death (if occurring during the same hospitalization).
Adverse in-hospital complications were also recorded. These were selected based on inclusion of the following categories of acute STEMI complications: ischemic, mechanical, arrhythmic, embolic, and inflammatory. The following complications occurred in our patient cohort: sustained ventricular arrhythmia, congestive heart failure (CHF) defined as congestion requiring intravenous diuretics, re-infarction, mechanical complications (free-wall rupture, ventricular septal defect, or mitral regurgitation), second- or third-degree atrioventricular block, atrial fibrillation, stroke, mechanical ventilation, major bleeding, pericarditis, cardiogenic shock, cardiac arrest, and in-hospital mortality. The primary outcome of this study was defined as a composite of sustained ventricular arrhythmia, CHF with congestion requiring intravenous diuretics, and/or in-hospital mortality. Ventricular arrythmia and CHF were included in the composite outcome because they are defined as the 2 most common causes of sudden cardiac death following acute STEMI.11,12
Statistical Analysis
Normally distributed continuous variables and categorical variables were compared using the paired t-test. A 2-sided P value <.05 was considered to be statistically significant. Mean admission rates for acute STEMI hospitalizations were determined by dividing the number of admissions by the number of days in each time period. The daily rate of COVID-19 cases per 100,000 individuals was obtained from the Centers for Disease Control and Prevention COVID-19 database. All data analyses were performed using Microsoft Excel.
Results
The study cohort consisted of 64 patients, of whom 30 (46.9%) were hospitalized between March 5 and May 5, 2020, and 34 (53.1%) who were admitted during the analogous time period in 2019. This reflected a 6% decrease in STEMI admissions at PAR in the COVID-19 cohort.
Acute STEMI Hospitalization Rates and COVID-19 Incidence
The mean daily acute STEMI admission rate was 0.50 during the study period compared to 0.57 during the control period. During the study period in 2020 in the state of Georgia, the daily rate of newly confirmed COVID-19 cases ranged from 0.194 per 100,000 on March 5 to 8.778 per 100,000 on May 5. Results of COVID-19 testing were available for 9 STEMI patients, and of these 0 tests were positive.
Baseline Characteristics
Baseline characteristics of the acute STEMI cohorts are presented in Table 1. Approximately 75% were male; median (interquartile range [IQR]) age was 60 (51-72) years. There were no significant differences in age and gender between the study periods. Three-quarters of patients had a history of hypertension, and 87.5% had a history of dyslipidemia. There was no significant difference in baseline comorbidity profiles between the 2 study periods; therefore, our sample populations shared similar characteristics.
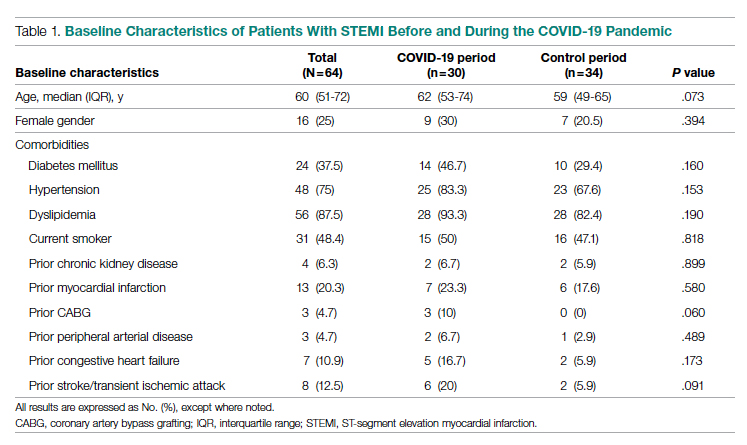
Clinical Presentation
Significant differences were observed regarding the time intervals of STEMI patients in the COVID-19 period and the control period (Table 2). Median time from symptom onset to hospital admission (patient delay) was extended from 57.5 minutes (IQR, 40.3-106) in 2019 to 93 minutes (IQR, 48.8-132) in 2020; however, this difference was not statistically significant (P = .697). Median time from hospital admission to reperfusion (system delay) was prolonged from 45 minutes (IQR, 28-61) in 2019 to 78 minutes (IQR, 50-110) in 2020 (P < .001). Overall time from symptom onset to reperfusion (total ischemic time) increased from 99.5 minutes (IQR, 84.8-132) in 2019 to 149 minutes (IQR, 96.3-231.8) in 2020 (P = .032).
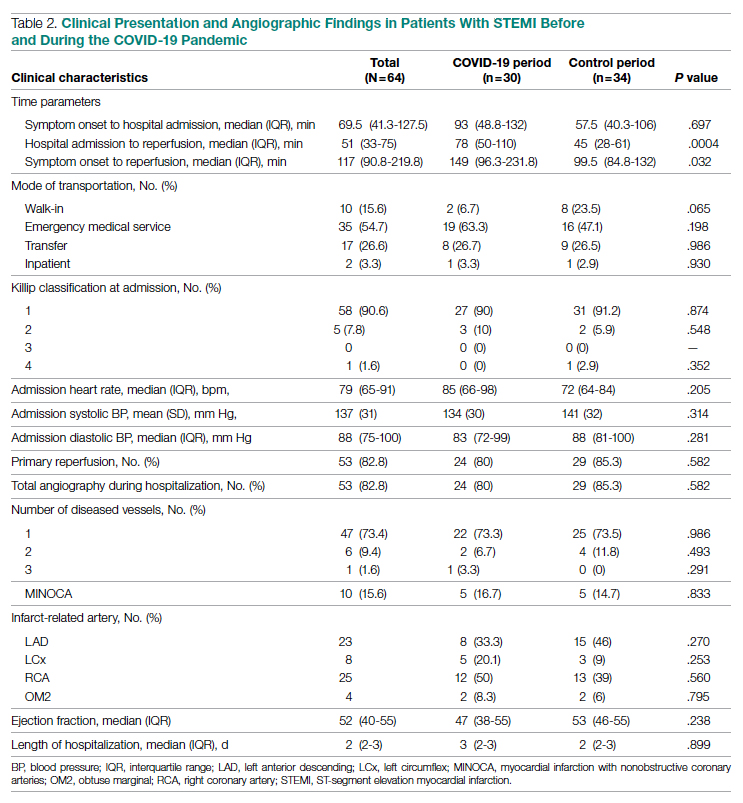
Regarding mode of transportation, 23.5% of patients in 2019 were walk-in admissions to the emergency department. During the COVID-19 period, walk-in admissions decreased to 6.7% (P = .065). There were no significant differences between emergency medical service, transfer, or in-patient admissions for STEMI cases between the 2 study periods.
Killip classification scores were calculated for all patients on admission; 90.6% of patients were classified as Killip Class 1. There was no significant difference between hemodynamic presentations during the COVID-19 period compared to the control period.
Angiographic Data
Overall, 53 (82.8%) patients admitted with acute STEMI underwent coronary angiography during their hospital stay. The proportion of patients who underwent primary reperfusion was greater in the control period than in the COVID-19 period (85.3% vs 80%; P = .582). Angiographic characteristics and findings were similar between the 2 study groups (Table 2).
In-Hospital Outcomes
In-hospital outcome data were available for all patients. As shown in Table 3, hospitalization during the COVID-19 period was independently associated with an increased risk for combined in-hospital outcome (odds ratio, 3.96; P = .046). The rate of in-hospital mortality was greater in the COVID-19 period (P = .013). We found no significant difference when comparing secondary outcomes from admissions during the COVID-19 period and the control period in 2019. For the 5 patients who died during the study period, the primary diagnosis at death was acute STEMI complicated by CHF (3 patients) or cardiogenic shock (2 patients).
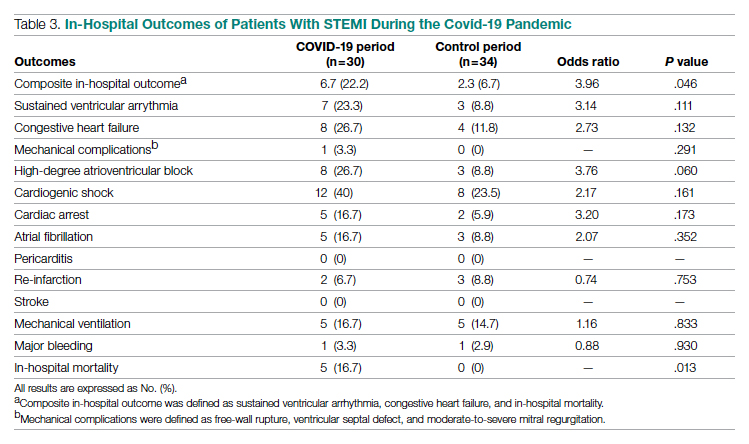
Discussion
This single-center retrospective study at PAR looks at the impact of COVID-19 on hospitalizations for acute STEMI during the initial peak of the pandemic. The key findings of this study show a significant increase in ischemic time parameters (symptom onset to reperfusion, hospital admission to reperfusion), in-hospital mortality, and combined in-hospital outcomes.
There was a 49.5-minute increase in total ischemic time noted in this study (P = .032). Though there was a numerical increase in time of symptom onset to hospital admission by 23.5 minutes, this difference was not statistically significant (P = .697). However, this study observed a statistically significant 33-minute increase in ischemic time from hospital admission to reperfusion (P < .001). Multiple studies globally have found a similar increase in total ischemic times, including those conducted in China and Europe.13-15 Every level of potential delay must be considered, including pre-hospital, triage and emergency department, and/or reperfusion team. Pre-hospital sources of delays that have been suggested include “stay-at-home” orders and apprehension to seek medical care due to concern about contracting the virus or overwhelming the health care facilities. There was a clinically significant 4-fold decrease in the number of walk-in acute STEMI cases in the study period. In 2019, there were 8 walk-in cases compared to 2 cases in 2020 (P = .065). However, this change was not statistically significant. In-hospital/systemic sources of delays have been mentioned in other studies; they include increased time taken to rule out COVID-19 (nasopharyngeal swab/chest x-ray) and increased time due to the need for intensive gowning and gloving procedures by staff. It was difficult to objectively determine the sources of system delay by the reperfusion team due to a lack of quantitative data.
In the current study, we found a significant increase in in-hospital mortality during the COVID-19 period compared to a parallel time frame in 2019. This finding is contrary to a multicenter study from Spain that reported no difference in in-hospital outcomes or mortality rates among all acute coronary syndrome cases.16 The worsening outcomes and prognosis may simply be a result of increased ischemic time; however, the virus that causes COVID-19 itself may play a role as well. Studies have found that SARS-Cov-2 infection places patients at greater risk for cardiovascular conditions such as hypercoagulability, myocarditis, and arrhythmias.17 In our study, however, there were no acute STEMI patients who tested positive for COVID-19. Therefore, we cannot discuss the impact of increased thrombus burden in patients with COVID-19. Piedmont Healthcare published a STEMI treatment protocol in May 2020 that advised increased use of tissue plasminogen activator (tPA) in COVID-19-positive cases; during the study period, however, there were no occasions when tPA use was deemed appropriate based on clinical judgment.
Our findings align with previous studies that describe an increase in combined in-hospital adverse outcomes during the COVID-19 era. Previous studies detected a higher rate of complications in the COVID-19 cohort, but in the current study, the adverse in-hospital course is unrelated to underlying infection.18,19 This study reports a higher incidence of major in-hospital outcomes, including a 65% increase in the rate of combined in-hospital outcomes, which is similar to a multicenter study conducted in Israel.19 There was a 2.3-fold numerical increase in sustained ventricular arrhythmias and a 2.5-fold numerical increase in the incidence of cardiac arrest in the study period. This phenomenon was observed despite a similar rate of reperfusion procedures in both groups.
Acute STEMI is a highly fatal condition with an incidence of 8.5 in 10,000 annually in the United States. While studies across the world have shown a 25% to 40% reduction in the rate of hospitalized acute coronary syndrome cases during the COVID-19 pandemic, the decrease from 34 to 30 STEMI admissions at PAR is not statistically significant.20 Possible reasons for the reduction globally include increased out-of-hospital mortality and decreased incidence of acute STEMI across the general population as a result of improved access to telemedicine or decreased levels of life stressors.20
In summary, there was an increase in ischemic time to reperfusion, in-hospital mortality, and combined in-hospital outcomes for acute STEMI patients at PAR during the COVID period.
Limitations
This study has several limitations. This is a single-center study, so the sample size is small and may not be generalizable to a larger population. This is a retrospective observational study, so causation cannot be inferred. This study analyzed ischemic time parameters as average rates over time rather than in an interrupted time series. Post-reperfusion outcomes were limited to hospital stay. Post-hospital follow-up would provide a better picture of the effects of STEMI intervention. There is no account of patients who died out-of-hospital secondary to acute STEMI. COVID-19 testing was not introduced until midway in our study period. Therefore, we cannot rule out the possibility of the SARS-Cov-2 virus inciting acute STEMI and subsequently leading to worse outcomes and poor prognosis.
Conclusions
This study provides an analysis of the incidence, characteristics, and clinical outcomes of patients presenting with acute STEMI during the early period of the COVID-19 pandemic. In-hospital mortality and ischemic time to reperfusion increased while combined in-hospital outcomes worsened.
Acknowledgment: The authors thank Piedmont Athens Regional IRB for approving this project and allowing access to patient data.
Corresponding author: Syed H. Ali; Department of Medicine, Medical College of Georgia at the Augusta University-University of Georgia Medical Partnership, 30606, Athens, GA; [email protected]
Disclosures: None reported.
doi:10.12788/jcom.0085
1. Bhatt AS, Moscone A, McElrath EE, et al. Fewer hospitalizations for acute cardiovascular conditions during the COVID-19 pandemic. J Am Coll Cardiol. 2020;76(3):280-288. doi:10.1016/j.jacc.2020.05.038
2. Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJR. Decline of acute coronary syndrome admissions in Austria since the outbreak of Covid-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41:1852-1853. doi:10.1093/eurheartj/ehaa314
3. De Rosa S, Spaccarotella C, Basso C, et al. Reduction of hospitalizations for myocardial infarction in Italy in the Covid-19 era. Eur Heart J. 2020;41(22):2083-2088.
4. Wilson SJ, Connolly MJ, Elghamry Z, et al. Effect of the COVID-19 pandemic on ST-segment-elevation myocardial infarction presentations and in-hospital outcomes. Circ Cardiovasc Interv. 2020; 13(7):e009438. doi:10.1161/CIRCINTERVENTIONS.120.009438
5. Mafham MM, Spata E, Goldacre R, et al. Covid-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396 (10248):381-389. doi:10.1016/S0140-6736(20)31356-8
6. Bhatt AS, Moscone A, McElrath EE, et al. Fewer Hospitalizations for acute cardiovascular conditions during the COVID-19 pandemic. J Am Coll Cardiol. 2020;76(3):280-288. doi:10.1016/j.jacc.2020.05.038
7. Tam CF, Cheung KS, Lam S, et al. Impact of Coronavirus disease 2019 (Covid-19) outbreak on ST-segment elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13(4):e006631. doi:10.1161/CIRCOUTCOMES.120.006631
8. Clerkin KJ, Fried JA, Raikhelkar J, et al. Coronavirus disease 2019 (COVID-19) and cardiovascular disease. Circulation. 2020;141:1648-1655. doi:10.1161/CIRCULATIONAHA.120.046941
9. Ebinger JE, Shah PK. Declining admissions for acute cardiovascular illness: The Covid-19 paradox. J Am Coll Cardiol. 2020;76(3):289-291. doi:10.1016/j.jacc.2020.05.039
10 Leor J, Poole WK, Kloner RA. Sudden cardiac death triggered by an earthquake. N Engl J Med. 1996;334(7):413-419. doi:10.1056/NEJM199602153340701
11. Hiramori K. Major causes of death from acute myocardial infarction in a coronary care unit. Jpn Circ J. 1987;51(9):1041-1047. doi:10.1253/jcj.51.1041
12. Bui AH, Waks JW. Risk stratification of sudden cardiac death after acute myocardial infarction. J Innov Card Rhythm Manag. 2018;9(2):3035-3049. doi:10.19102/icrm.2018.090201
13. Xiang D, Xiang X, Zhang W, et al. Management and outcomes of patients with STEMI during the COVID-19 pandemic in China. J Am Coll Cardiol. 2020;76(11):1318-1324. doi:10.1016/j.jacc.2020.06.039
14. Hakim R, Motreff P, Rangé G. COVID-19 and STEMI. [Article in French]. Ann Cardiol Angeiol (Paris). 2020;69(6):355-359. doi:10.1016/j.ancard.2020.09.034
15. Soylu K, Coksevim M, Yanık A, Bugra Cerik I, Aksan G. Effect of Covid-19 pandemic process on STEMI patients timeline. Int J Clin Pract. 2021;75(5):e14005. doi:10.1111/ijcp.14005
16. Salinas P, Travieso A, Vergara-Uzcategui C, et al. Clinical profile and 30-day mortality of invasively managed patients with suspected acute coronary syndrome during the COVID-19 outbreak. Int Heart J. 2021;62(2):274-281. doi:10.1536/ihj.20-574
17. Hu Y, Sun J, Dai Z, et al. Prevalence and severity of corona virus disease 2019 (Covid-19): a systematic review and meta-analysis. J Clin Virol. 2020;127:104371. doi:10.1016/j.jcv.2020.104371
18. Rodriguez-Leor O, Cid Alvarez AB, Perez de Prado A, et al. In-hospital outcomes of COVID-19 ST-elevation myocardial infarction patients. EuroIntervention. 2021;16(17):1426-1433. doi:10.4244/EIJ-D-20-00935
19. Fardman A, Zahger D, Orvin K, et al. Acute myocardial infarction in the Covid-19 era: incidence, clinical characteristics and in-hospital outcomes—A multicenter registry. PLoS ONE. 2021;16(6): e0253524. doi:10.1371/journal.pone.0253524
20. Pessoa-Amorim G, Camm CF, Gajendragadkar P, et al. Admission of patients with STEMI since the outbreak of the COVID-19 pandemic: a survey by the European Society of Cardiology. Eur Heart J Qual Care Clin Outcomes. 2020;6(3):210-216. doi:10.1093/ehjqcco/qcaa046
From the Department of Medicine, Medical College of Georgia at the Augusta University-University of Georgia Medical Partnership, Athens, GA (Syed H. Ali, Syed Hyder, and Dr. Murrow), and the Department of Cardiology, Piedmont Heart Institute, Piedmont Athens Regional, Athens, GA (Dr. Murrow and Mrs. Davis).
Abstract
Objectives: The aim of this study was to describe the characteristics and in-hospital outcomes of patients with acute ST-segment elevation myocardial infarction (STEMI) during the early COVID-19 pandemic at Piedmont Athens Regional (PAR), a 330-bed tertiary referral center in Northeast Georgia.
Methods: A retrospective study was conducted at PAR to evaluate patients with acute STEMI admitted over an 8-week period during the initial COVID-19 outbreak. This study group was compared to patients admitted during the corresponding period in 2019. The primary endpoint of this study was defined as a composite of sustained ventricular arrhythmia, congestive heart failure (CHF) with pulmonary congestion, and/or in-hospital mortality.
Results: This study cohort was composed of 64 patients with acute STEMI; 30 patients (46.9%) were hospitalized during the COVID-19 pandemic. Patients with STEMI in both the COVID-19 and control groups had similar comorbidities, Killip classification score, and clinical presentations. The median (interquartile range) time from symptom onset to reperfusion (total ischemic time) increased from 99.5 minutes (84.8-132) in 2019 to 149 minutes (96.3-231.8; P = .032) in 2020. Hospitalization during the COVID-19 period was associated with an increased risk for combined in-hospital outcome (odds ratio, 3.96; P = .046).
Conclusion: Patients with STEMI admitted during the first wave of the COVID-19 outbreak experienced longer total ischemic time and increased risk for combined in-hospital outcomes compared to patients admitted during the corresponding period in 2019.
Keywords: myocardial infarction, acute coronary syndrome, hospitalization, outcomes.
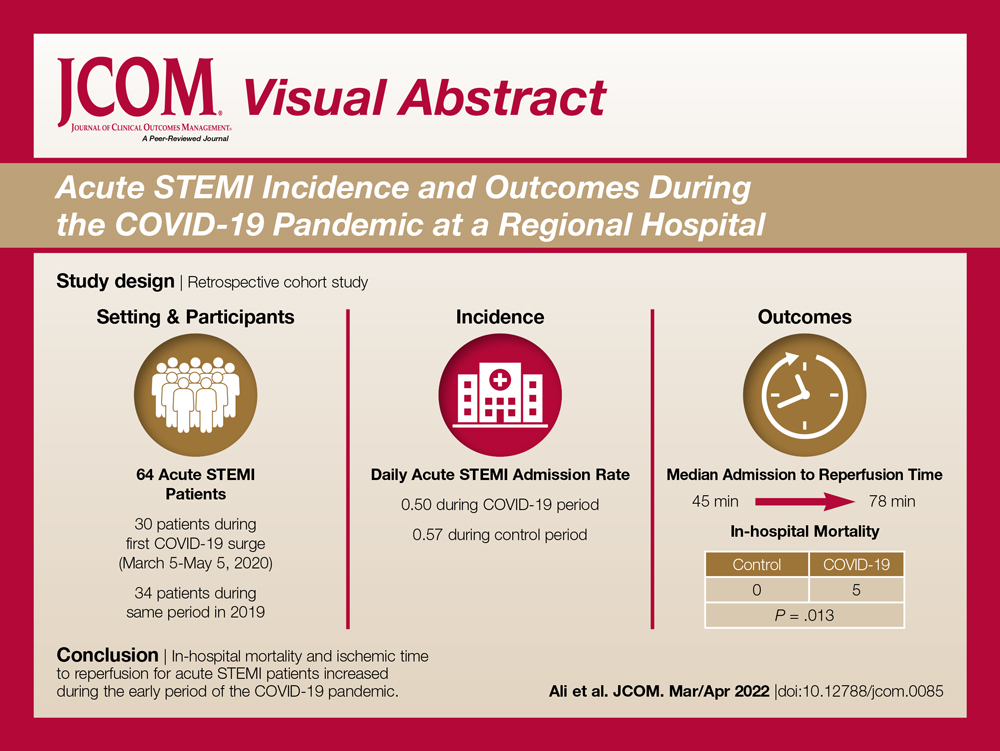
The emergence of the SARS-Cov-2 virus in December 2019 caused a worldwide shift in resource allocation and the restructuring of health care systems within the span of a few months. With the rapid spread of infection, the World Health Organization officially declared a pandemic in March 2020. The pandemic led to the deferral and cancellation of in-person patient visits, routine diagnostic studies, and nonessential surgeries and procedures. This response occurred secondary to a joint effort to reduce transmission via stay-at-home mandates and appropriate social distancing.1
Alongside the reduction in elective procedures and health care visits, significant reductions in hospitalization rates due to decreases in acute ST-segment elevation myocardial infarction (STEMI) and catheterization laboratory utilization have been reported in many studies from around the world.2-7 Comprehensive data demonstrating the impact of the COVID-19 pandemic on acute STEMI patient characteristics, clinical presentation, and in-hospital outcomes are lacking. Although patients with previously diagnosed cardiovascular disease are more likely to encounter worse outcomes in the setting of COVID-19, there may also be an indirect impact of the pandemic on high-risk patients, including those without the infection.8 Several theories have been hypothesized to explain this phenomenon. One theory postulates that the fear of contracting the virus during hospitalization is great enough to prevent patients from seeking care.2 Another theory suggests that the increased utilization of telemedicine prevents exacerbation of chronic conditions and the need for hospitalization.9 Contrary to this trend, previous studies have shown an increased incidence of acute STEMI following stressful events such as natural disasters.10
The aim of this study was to describe trends pertaining to clinical characteristics and in-hospital outcomes of patients with acute STEMI during the early COVID-19 pandemic at Piedmont Athens Regional (PAR), a 330-bed tertiary referral center in Northeast Georgia.
Methods
A retrospective cohort study was conducted at PAR to evaluate patients with STEMI admitted to the cardiovascular intensive care unit over an 8-week period (March 5 to May 5, 2020) during the COVID-19 outbreak. COVID-19 was declared a national emergency on March 13, 2020, in the United States. The institutional review board at PAR approved the study; the need for individual consent was waived under the condition that participant data would undergo de-identification and be strictly safeguarded.
Data Collection
Because there are seasonal variations in cardiovascular admissions, patient data from a control period (March 9 to May 9, 2019) were obtained to compare with data from the 2020 period. The number of patients with the diagnosis of acute STEMI during the COVID-19 period was recorded. Demographic data, clinical characteristics, and primary angiographic findings were gathered for all patients. Time from symptom onset to hospital admission and time from hospital admission to reperfusion (defined as door-to-balloon time) were documented for each patient. Killip classification was used to assess patients’ clinical status on admission. Length of stay was determined as days from hospital admission to discharge or death (if occurring during the same hospitalization).
Adverse in-hospital complications were also recorded. These were selected based on inclusion of the following categories of acute STEMI complications: ischemic, mechanical, arrhythmic, embolic, and inflammatory. The following complications occurred in our patient cohort: sustained ventricular arrhythmia, congestive heart failure (CHF) defined as congestion requiring intravenous diuretics, re-infarction, mechanical complications (free-wall rupture, ventricular septal defect, or mitral regurgitation), second- or third-degree atrioventricular block, atrial fibrillation, stroke, mechanical ventilation, major bleeding, pericarditis, cardiogenic shock, cardiac arrest, and in-hospital mortality. The primary outcome of this study was defined as a composite of sustained ventricular arrhythmia, CHF with congestion requiring intravenous diuretics, and/or in-hospital mortality. Ventricular arrythmia and CHF were included in the composite outcome because they are defined as the 2 most common causes of sudden cardiac death following acute STEMI.11,12
Statistical Analysis
Normally distributed continuous variables and categorical variables were compared using the paired t-test. A 2-sided P value <.05 was considered to be statistically significant. Mean admission rates for acute STEMI hospitalizations were determined by dividing the number of admissions by the number of days in each time period. The daily rate of COVID-19 cases per 100,000 individuals was obtained from the Centers for Disease Control and Prevention COVID-19 database. All data analyses were performed using Microsoft Excel.
Results
The study cohort consisted of 64 patients, of whom 30 (46.9%) were hospitalized between March 5 and May 5, 2020, and 34 (53.1%) who were admitted during the analogous time period in 2019. This reflected a 6% decrease in STEMI admissions at PAR in the COVID-19 cohort.
Acute STEMI Hospitalization Rates and COVID-19 Incidence
The mean daily acute STEMI admission rate was 0.50 during the study period compared to 0.57 during the control period. During the study period in 2020 in the state of Georgia, the daily rate of newly confirmed COVID-19 cases ranged from 0.194 per 100,000 on March 5 to 8.778 per 100,000 on May 5. Results of COVID-19 testing were available for 9 STEMI patients, and of these 0 tests were positive.
Baseline Characteristics
Baseline characteristics of the acute STEMI cohorts are presented in Table 1. Approximately 75% were male; median (interquartile range [IQR]) age was 60 (51-72) years. There were no significant differences in age and gender between the study periods. Three-quarters of patients had a history of hypertension, and 87.5% had a history of dyslipidemia. There was no significant difference in baseline comorbidity profiles between the 2 study periods; therefore, our sample populations shared similar characteristics.
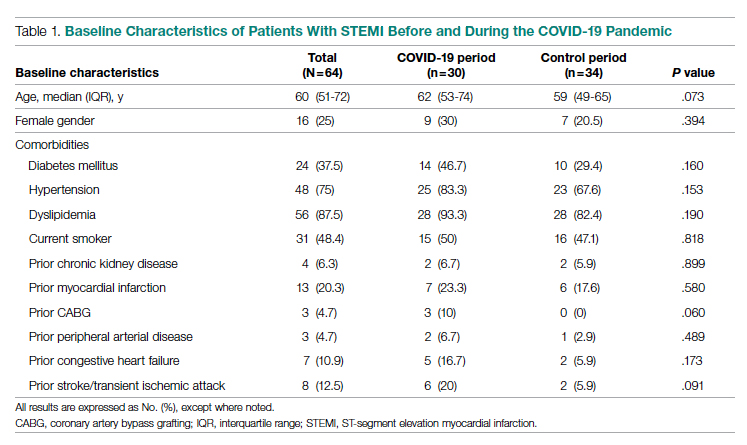
Clinical Presentation
Significant differences were observed regarding the time intervals of STEMI patients in the COVID-19 period and the control period (Table 2). Median time from symptom onset to hospital admission (patient delay) was extended from 57.5 minutes (IQR, 40.3-106) in 2019 to 93 minutes (IQR, 48.8-132) in 2020; however, this difference was not statistically significant (P = .697). Median time from hospital admission to reperfusion (system delay) was prolonged from 45 minutes (IQR, 28-61) in 2019 to 78 minutes (IQR, 50-110) in 2020 (P < .001). Overall time from symptom onset to reperfusion (total ischemic time) increased from 99.5 minutes (IQR, 84.8-132) in 2019 to 149 minutes (IQR, 96.3-231.8) in 2020 (P = .032).
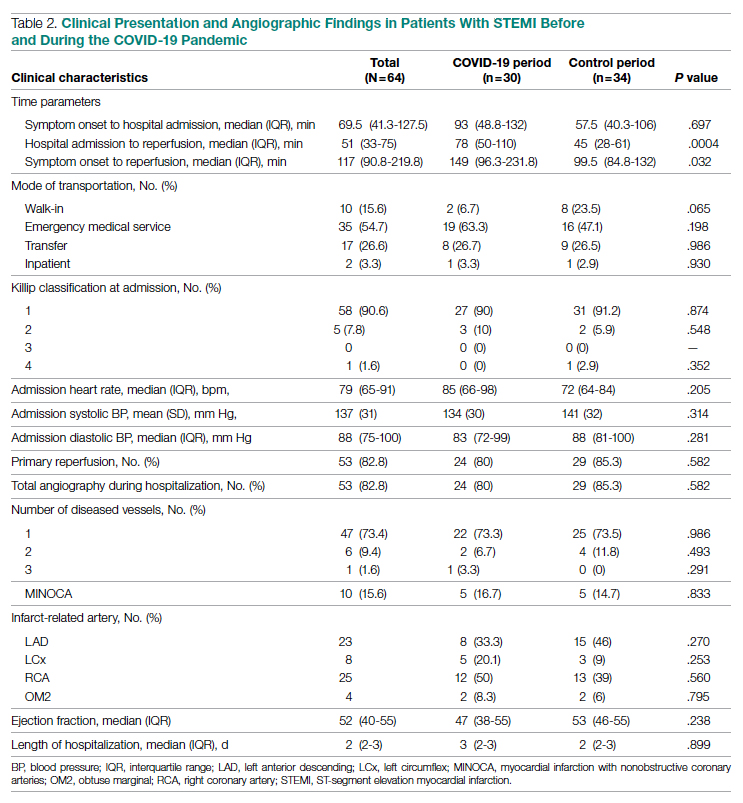
Regarding mode of transportation, 23.5% of patients in 2019 were walk-in admissions to the emergency department. During the COVID-19 period, walk-in admissions decreased to 6.7% (P = .065). There were no significant differences between emergency medical service, transfer, or in-patient admissions for STEMI cases between the 2 study periods.
Killip classification scores were calculated for all patients on admission; 90.6% of patients were classified as Killip Class 1. There was no significant difference between hemodynamic presentations during the COVID-19 period compared to the control period.
Angiographic Data
Overall, 53 (82.8%) patients admitted with acute STEMI underwent coronary angiography during their hospital stay. The proportion of patients who underwent primary reperfusion was greater in the control period than in the COVID-19 period (85.3% vs 80%; P = .582). Angiographic characteristics and findings were similar between the 2 study groups (Table 2).
In-Hospital Outcomes
In-hospital outcome data were available for all patients. As shown in Table 3, hospitalization during the COVID-19 period was independently associated with an increased risk for combined in-hospital outcome (odds ratio, 3.96; P = .046). The rate of in-hospital mortality was greater in the COVID-19 period (P = .013). We found no significant difference when comparing secondary outcomes from admissions during the COVID-19 period and the control period in 2019. For the 5 patients who died during the study period, the primary diagnosis at death was acute STEMI complicated by CHF (3 patients) or cardiogenic shock (2 patients).
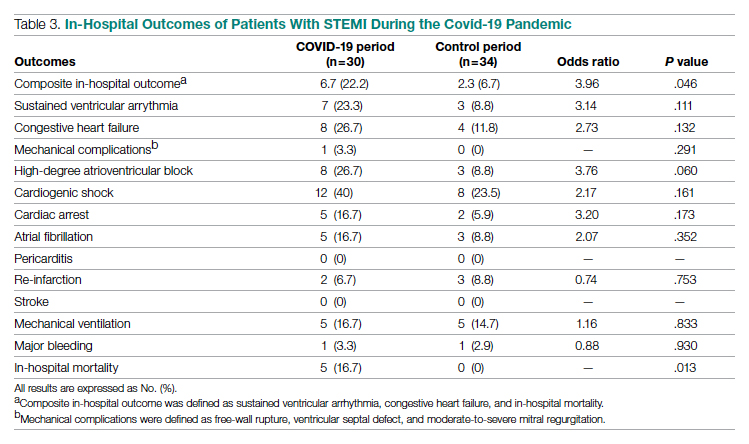
Discussion
This single-center retrospective study at PAR looks at the impact of COVID-19 on hospitalizations for acute STEMI during the initial peak of the pandemic. The key findings of this study show a significant increase in ischemic time parameters (symptom onset to reperfusion, hospital admission to reperfusion), in-hospital mortality, and combined in-hospital outcomes.
There was a 49.5-minute increase in total ischemic time noted in this study (P = .032). Though there was a numerical increase in time of symptom onset to hospital admission by 23.5 minutes, this difference was not statistically significant (P = .697). However, this study observed a statistically significant 33-minute increase in ischemic time from hospital admission to reperfusion (P < .001). Multiple studies globally have found a similar increase in total ischemic times, including those conducted in China and Europe.13-15 Every level of potential delay must be considered, including pre-hospital, triage and emergency department, and/or reperfusion team. Pre-hospital sources of delays that have been suggested include “stay-at-home” orders and apprehension to seek medical care due to concern about contracting the virus or overwhelming the health care facilities. There was a clinically significant 4-fold decrease in the number of walk-in acute STEMI cases in the study period. In 2019, there were 8 walk-in cases compared to 2 cases in 2020 (P = .065). However, this change was not statistically significant. In-hospital/systemic sources of delays have been mentioned in other studies; they include increased time taken to rule out COVID-19 (nasopharyngeal swab/chest x-ray) and increased time due to the need for intensive gowning and gloving procedures by staff. It was difficult to objectively determine the sources of system delay by the reperfusion team due to a lack of quantitative data.
In the current study, we found a significant increase in in-hospital mortality during the COVID-19 period compared to a parallel time frame in 2019. This finding is contrary to a multicenter study from Spain that reported no difference in in-hospital outcomes or mortality rates among all acute coronary syndrome cases.16 The worsening outcomes and prognosis may simply be a result of increased ischemic time; however, the virus that causes COVID-19 itself may play a role as well. Studies have found that SARS-Cov-2 infection places patients at greater risk for cardiovascular conditions such as hypercoagulability, myocarditis, and arrhythmias.17 In our study, however, there were no acute STEMI patients who tested positive for COVID-19. Therefore, we cannot discuss the impact of increased thrombus burden in patients with COVID-19. Piedmont Healthcare published a STEMI treatment protocol in May 2020 that advised increased use of tissue plasminogen activator (tPA) in COVID-19-positive cases; during the study period, however, there were no occasions when tPA use was deemed appropriate based on clinical judgment.
Our findings align with previous studies that describe an increase in combined in-hospital adverse outcomes during the COVID-19 era. Previous studies detected a higher rate of complications in the COVID-19 cohort, but in the current study, the adverse in-hospital course is unrelated to underlying infection.18,19 This study reports a higher incidence of major in-hospital outcomes, including a 65% increase in the rate of combined in-hospital outcomes, which is similar to a multicenter study conducted in Israel.19 There was a 2.3-fold numerical increase in sustained ventricular arrhythmias and a 2.5-fold numerical increase in the incidence of cardiac arrest in the study period. This phenomenon was observed despite a similar rate of reperfusion procedures in both groups.
Acute STEMI is a highly fatal condition with an incidence of 8.5 in 10,000 annually in the United States. While studies across the world have shown a 25% to 40% reduction in the rate of hospitalized acute coronary syndrome cases during the COVID-19 pandemic, the decrease from 34 to 30 STEMI admissions at PAR is not statistically significant.20 Possible reasons for the reduction globally include increased out-of-hospital mortality and decreased incidence of acute STEMI across the general population as a result of improved access to telemedicine or decreased levels of life stressors.20
In summary, there was an increase in ischemic time to reperfusion, in-hospital mortality, and combined in-hospital outcomes for acute STEMI patients at PAR during the COVID period.
Limitations
This study has several limitations. This is a single-center study, so the sample size is small and may not be generalizable to a larger population. This is a retrospective observational study, so causation cannot be inferred. This study analyzed ischemic time parameters as average rates over time rather than in an interrupted time series. Post-reperfusion outcomes were limited to hospital stay. Post-hospital follow-up would provide a better picture of the effects of STEMI intervention. There is no account of patients who died out-of-hospital secondary to acute STEMI. COVID-19 testing was not introduced until midway in our study period. Therefore, we cannot rule out the possibility of the SARS-Cov-2 virus inciting acute STEMI and subsequently leading to worse outcomes and poor prognosis.
Conclusions
This study provides an analysis of the incidence, characteristics, and clinical outcomes of patients presenting with acute STEMI during the early period of the COVID-19 pandemic. In-hospital mortality and ischemic time to reperfusion increased while combined in-hospital outcomes worsened.
Acknowledgment: The authors thank Piedmont Athens Regional IRB for approving this project and allowing access to patient data.
Corresponding author: Syed H. Ali; Department of Medicine, Medical College of Georgia at the Augusta University-University of Georgia Medical Partnership, 30606, Athens, GA; [email protected]
Disclosures: None reported.
doi:10.12788/jcom.0085
From the Department of Medicine, Medical College of Georgia at the Augusta University-University of Georgia Medical Partnership, Athens, GA (Syed H. Ali, Syed Hyder, and Dr. Murrow), and the Department of Cardiology, Piedmont Heart Institute, Piedmont Athens Regional, Athens, GA (Dr. Murrow and Mrs. Davis).
Abstract
Objectives: The aim of this study was to describe the characteristics and in-hospital outcomes of patients with acute ST-segment elevation myocardial infarction (STEMI) during the early COVID-19 pandemic at Piedmont Athens Regional (PAR), a 330-bed tertiary referral center in Northeast Georgia.
Methods: A retrospective study was conducted at PAR to evaluate patients with acute STEMI admitted over an 8-week period during the initial COVID-19 outbreak. This study group was compared to patients admitted during the corresponding period in 2019. The primary endpoint of this study was defined as a composite of sustained ventricular arrhythmia, congestive heart failure (CHF) with pulmonary congestion, and/or in-hospital mortality.
Results: This study cohort was composed of 64 patients with acute STEMI; 30 patients (46.9%) were hospitalized during the COVID-19 pandemic. Patients with STEMI in both the COVID-19 and control groups had similar comorbidities, Killip classification score, and clinical presentations. The median (interquartile range) time from symptom onset to reperfusion (total ischemic time) increased from 99.5 minutes (84.8-132) in 2019 to 149 minutes (96.3-231.8; P = .032) in 2020. Hospitalization during the COVID-19 period was associated with an increased risk for combined in-hospital outcome (odds ratio, 3.96; P = .046).
Conclusion: Patients with STEMI admitted during the first wave of the COVID-19 outbreak experienced longer total ischemic time and increased risk for combined in-hospital outcomes compared to patients admitted during the corresponding period in 2019.
Keywords: myocardial infarction, acute coronary syndrome, hospitalization, outcomes.
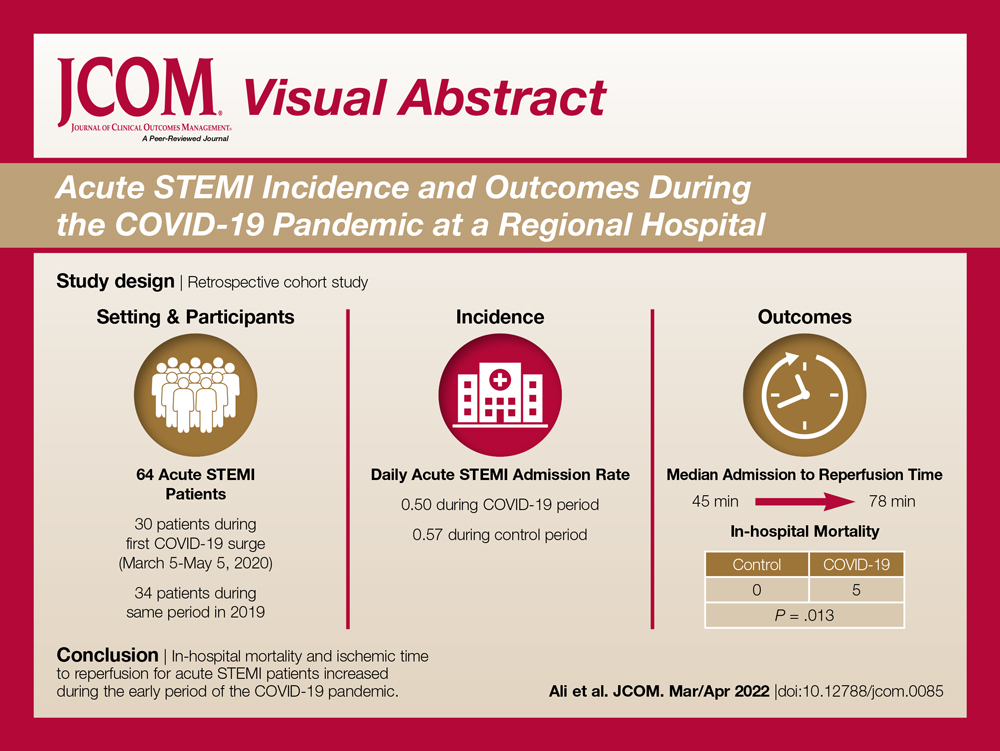
The emergence of the SARS-Cov-2 virus in December 2019 caused a worldwide shift in resource allocation and the restructuring of health care systems within the span of a few months. With the rapid spread of infection, the World Health Organization officially declared a pandemic in March 2020. The pandemic led to the deferral and cancellation of in-person patient visits, routine diagnostic studies, and nonessential surgeries and procedures. This response occurred secondary to a joint effort to reduce transmission via stay-at-home mandates and appropriate social distancing.1
Alongside the reduction in elective procedures and health care visits, significant reductions in hospitalization rates due to decreases in acute ST-segment elevation myocardial infarction (STEMI) and catheterization laboratory utilization have been reported in many studies from around the world.2-7 Comprehensive data demonstrating the impact of the COVID-19 pandemic on acute STEMI patient characteristics, clinical presentation, and in-hospital outcomes are lacking. Although patients with previously diagnosed cardiovascular disease are more likely to encounter worse outcomes in the setting of COVID-19, there may also be an indirect impact of the pandemic on high-risk patients, including those without the infection.8 Several theories have been hypothesized to explain this phenomenon. One theory postulates that the fear of contracting the virus during hospitalization is great enough to prevent patients from seeking care.2 Another theory suggests that the increased utilization of telemedicine prevents exacerbation of chronic conditions and the need for hospitalization.9 Contrary to this trend, previous studies have shown an increased incidence of acute STEMI following stressful events such as natural disasters.10
The aim of this study was to describe trends pertaining to clinical characteristics and in-hospital outcomes of patients with acute STEMI during the early COVID-19 pandemic at Piedmont Athens Regional (PAR), a 330-bed tertiary referral center in Northeast Georgia.
Methods
A retrospective cohort study was conducted at PAR to evaluate patients with STEMI admitted to the cardiovascular intensive care unit over an 8-week period (March 5 to May 5, 2020) during the COVID-19 outbreak. COVID-19 was declared a national emergency on March 13, 2020, in the United States. The institutional review board at PAR approved the study; the need for individual consent was waived under the condition that participant data would undergo de-identification and be strictly safeguarded.
Data Collection
Because there are seasonal variations in cardiovascular admissions, patient data from a control period (March 9 to May 9, 2019) were obtained to compare with data from the 2020 period. The number of patients with the diagnosis of acute STEMI during the COVID-19 period was recorded. Demographic data, clinical characteristics, and primary angiographic findings were gathered for all patients. Time from symptom onset to hospital admission and time from hospital admission to reperfusion (defined as door-to-balloon time) were documented for each patient. Killip classification was used to assess patients’ clinical status on admission. Length of stay was determined as days from hospital admission to discharge or death (if occurring during the same hospitalization).
Adverse in-hospital complications were also recorded. These were selected based on inclusion of the following categories of acute STEMI complications: ischemic, mechanical, arrhythmic, embolic, and inflammatory. The following complications occurred in our patient cohort: sustained ventricular arrhythmia, congestive heart failure (CHF) defined as congestion requiring intravenous diuretics, re-infarction, mechanical complications (free-wall rupture, ventricular septal defect, or mitral regurgitation), second- or third-degree atrioventricular block, atrial fibrillation, stroke, mechanical ventilation, major bleeding, pericarditis, cardiogenic shock, cardiac arrest, and in-hospital mortality. The primary outcome of this study was defined as a composite of sustained ventricular arrhythmia, CHF with congestion requiring intravenous diuretics, and/or in-hospital mortality. Ventricular arrythmia and CHF were included in the composite outcome because they are defined as the 2 most common causes of sudden cardiac death following acute STEMI.11,12
Statistical Analysis
Normally distributed continuous variables and categorical variables were compared using the paired t-test. A 2-sided P value <.05 was considered to be statistically significant. Mean admission rates for acute STEMI hospitalizations were determined by dividing the number of admissions by the number of days in each time period. The daily rate of COVID-19 cases per 100,000 individuals was obtained from the Centers for Disease Control and Prevention COVID-19 database. All data analyses were performed using Microsoft Excel.
Results
The study cohort consisted of 64 patients, of whom 30 (46.9%) were hospitalized between March 5 and May 5, 2020, and 34 (53.1%) who were admitted during the analogous time period in 2019. This reflected a 6% decrease in STEMI admissions at PAR in the COVID-19 cohort.
Acute STEMI Hospitalization Rates and COVID-19 Incidence
The mean daily acute STEMI admission rate was 0.50 during the study period compared to 0.57 during the control period. During the study period in 2020 in the state of Georgia, the daily rate of newly confirmed COVID-19 cases ranged from 0.194 per 100,000 on March 5 to 8.778 per 100,000 on May 5. Results of COVID-19 testing were available for 9 STEMI patients, and of these 0 tests were positive.
Baseline Characteristics
Baseline characteristics of the acute STEMI cohorts are presented in Table 1. Approximately 75% were male; median (interquartile range [IQR]) age was 60 (51-72) years. There were no significant differences in age and gender between the study periods. Three-quarters of patients had a history of hypertension, and 87.5% had a history of dyslipidemia. There was no significant difference in baseline comorbidity profiles between the 2 study periods; therefore, our sample populations shared similar characteristics.
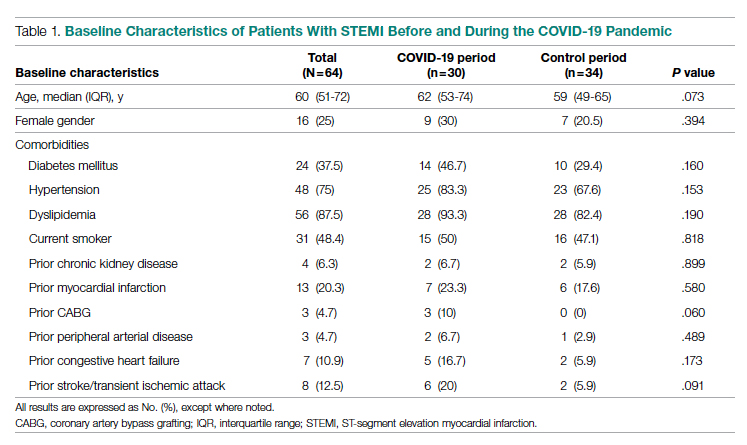
Clinical Presentation
Significant differences were observed regarding the time intervals of STEMI patients in the COVID-19 period and the control period (Table 2). Median time from symptom onset to hospital admission (patient delay) was extended from 57.5 minutes (IQR, 40.3-106) in 2019 to 93 minutes (IQR, 48.8-132) in 2020; however, this difference was not statistically significant (P = .697). Median time from hospital admission to reperfusion (system delay) was prolonged from 45 minutes (IQR, 28-61) in 2019 to 78 minutes (IQR, 50-110) in 2020 (P < .001). Overall time from symptom onset to reperfusion (total ischemic time) increased from 99.5 minutes (IQR, 84.8-132) in 2019 to 149 minutes (IQR, 96.3-231.8) in 2020 (P = .032).
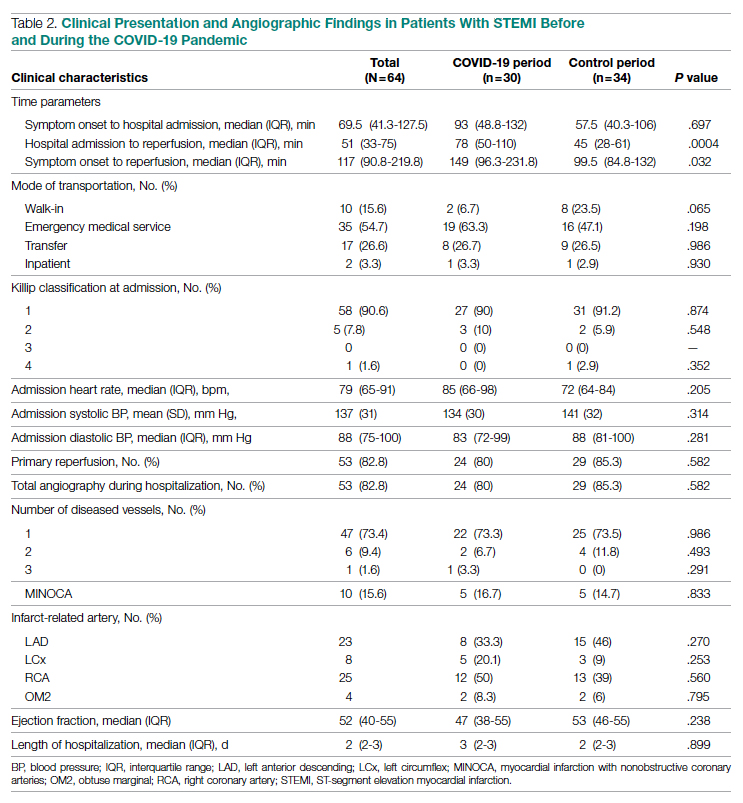
Regarding mode of transportation, 23.5% of patients in 2019 were walk-in admissions to the emergency department. During the COVID-19 period, walk-in admissions decreased to 6.7% (P = .065). There were no significant differences between emergency medical service, transfer, or in-patient admissions for STEMI cases between the 2 study periods.
Killip classification scores were calculated for all patients on admission; 90.6% of patients were classified as Killip Class 1. There was no significant difference between hemodynamic presentations during the COVID-19 period compared to the control period.
Angiographic Data
Overall, 53 (82.8%) patients admitted with acute STEMI underwent coronary angiography during their hospital stay. The proportion of patients who underwent primary reperfusion was greater in the control period than in the COVID-19 period (85.3% vs 80%; P = .582). Angiographic characteristics and findings were similar between the 2 study groups (Table 2).
In-Hospital Outcomes
In-hospital outcome data were available for all patients. As shown in Table 3, hospitalization during the COVID-19 period was independently associated with an increased risk for combined in-hospital outcome (odds ratio, 3.96; P = .046). The rate of in-hospital mortality was greater in the COVID-19 period (P = .013). We found no significant difference when comparing secondary outcomes from admissions during the COVID-19 period and the control period in 2019. For the 5 patients who died during the study period, the primary diagnosis at death was acute STEMI complicated by CHF (3 patients) or cardiogenic shock (2 patients).
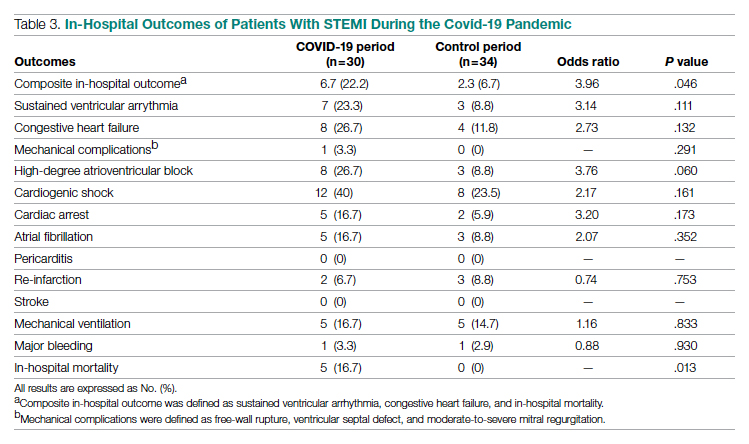
Discussion
This single-center retrospective study at PAR looks at the impact of COVID-19 on hospitalizations for acute STEMI during the initial peak of the pandemic. The key findings of this study show a significant increase in ischemic time parameters (symptom onset to reperfusion, hospital admission to reperfusion), in-hospital mortality, and combined in-hospital outcomes.
There was a 49.5-minute increase in total ischemic time noted in this study (P = .032). Though there was a numerical increase in time of symptom onset to hospital admission by 23.5 minutes, this difference was not statistically significant (P = .697). However, this study observed a statistically significant 33-minute increase in ischemic time from hospital admission to reperfusion (P < .001). Multiple studies globally have found a similar increase in total ischemic times, including those conducted in China and Europe.13-15 Every level of potential delay must be considered, including pre-hospital, triage and emergency department, and/or reperfusion team. Pre-hospital sources of delays that have been suggested include “stay-at-home” orders and apprehension to seek medical care due to concern about contracting the virus or overwhelming the health care facilities. There was a clinically significant 4-fold decrease in the number of walk-in acute STEMI cases in the study period. In 2019, there were 8 walk-in cases compared to 2 cases in 2020 (P = .065). However, this change was not statistically significant. In-hospital/systemic sources of delays have been mentioned in other studies; they include increased time taken to rule out COVID-19 (nasopharyngeal swab/chest x-ray) and increased time due to the need for intensive gowning and gloving procedures by staff. It was difficult to objectively determine the sources of system delay by the reperfusion team due to a lack of quantitative data.
In the current study, we found a significant increase in in-hospital mortality during the COVID-19 period compared to a parallel time frame in 2019. This finding is contrary to a multicenter study from Spain that reported no difference in in-hospital outcomes or mortality rates among all acute coronary syndrome cases.16 The worsening outcomes and prognosis may simply be a result of increased ischemic time; however, the virus that causes COVID-19 itself may play a role as well. Studies have found that SARS-Cov-2 infection places patients at greater risk for cardiovascular conditions such as hypercoagulability, myocarditis, and arrhythmias.17 In our study, however, there were no acute STEMI patients who tested positive for COVID-19. Therefore, we cannot discuss the impact of increased thrombus burden in patients with COVID-19. Piedmont Healthcare published a STEMI treatment protocol in May 2020 that advised increased use of tissue plasminogen activator (tPA) in COVID-19-positive cases; during the study period, however, there were no occasions when tPA use was deemed appropriate based on clinical judgment.
Our findings align with previous studies that describe an increase in combined in-hospital adverse outcomes during the COVID-19 era. Previous studies detected a higher rate of complications in the COVID-19 cohort, but in the current study, the adverse in-hospital course is unrelated to underlying infection.18,19 This study reports a higher incidence of major in-hospital outcomes, including a 65% increase in the rate of combined in-hospital outcomes, which is similar to a multicenter study conducted in Israel.19 There was a 2.3-fold numerical increase in sustained ventricular arrhythmias and a 2.5-fold numerical increase in the incidence of cardiac arrest in the study period. This phenomenon was observed despite a similar rate of reperfusion procedures in both groups.
Acute STEMI is a highly fatal condition with an incidence of 8.5 in 10,000 annually in the United States. While studies across the world have shown a 25% to 40% reduction in the rate of hospitalized acute coronary syndrome cases during the COVID-19 pandemic, the decrease from 34 to 30 STEMI admissions at PAR is not statistically significant.20 Possible reasons for the reduction globally include increased out-of-hospital mortality and decreased incidence of acute STEMI across the general population as a result of improved access to telemedicine or decreased levels of life stressors.20
In summary, there was an increase in ischemic time to reperfusion, in-hospital mortality, and combined in-hospital outcomes for acute STEMI patients at PAR during the COVID period.
Limitations
This study has several limitations. This is a single-center study, so the sample size is small and may not be generalizable to a larger population. This is a retrospective observational study, so causation cannot be inferred. This study analyzed ischemic time parameters as average rates over time rather than in an interrupted time series. Post-reperfusion outcomes were limited to hospital stay. Post-hospital follow-up would provide a better picture of the effects of STEMI intervention. There is no account of patients who died out-of-hospital secondary to acute STEMI. COVID-19 testing was not introduced until midway in our study period. Therefore, we cannot rule out the possibility of the SARS-Cov-2 virus inciting acute STEMI and subsequently leading to worse outcomes and poor prognosis.
Conclusions
This study provides an analysis of the incidence, characteristics, and clinical outcomes of patients presenting with acute STEMI during the early period of the COVID-19 pandemic. In-hospital mortality and ischemic time to reperfusion increased while combined in-hospital outcomes worsened.
Acknowledgment: The authors thank Piedmont Athens Regional IRB for approving this project and allowing access to patient data.
Corresponding author: Syed H. Ali; Department of Medicine, Medical College of Georgia at the Augusta University-University of Georgia Medical Partnership, 30606, Athens, GA; [email protected]
Disclosures: None reported.
doi:10.12788/jcom.0085
1. Bhatt AS, Moscone A, McElrath EE, et al. Fewer hospitalizations for acute cardiovascular conditions during the COVID-19 pandemic. J Am Coll Cardiol. 2020;76(3):280-288. doi:10.1016/j.jacc.2020.05.038
2. Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJR. Decline of acute coronary syndrome admissions in Austria since the outbreak of Covid-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41:1852-1853. doi:10.1093/eurheartj/ehaa314
3. De Rosa S, Spaccarotella C, Basso C, et al. Reduction of hospitalizations for myocardial infarction in Italy in the Covid-19 era. Eur Heart J. 2020;41(22):2083-2088.
4. Wilson SJ, Connolly MJ, Elghamry Z, et al. Effect of the COVID-19 pandemic on ST-segment-elevation myocardial infarction presentations and in-hospital outcomes. Circ Cardiovasc Interv. 2020; 13(7):e009438. doi:10.1161/CIRCINTERVENTIONS.120.009438
5. Mafham MM, Spata E, Goldacre R, et al. Covid-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396 (10248):381-389. doi:10.1016/S0140-6736(20)31356-8
6. Bhatt AS, Moscone A, McElrath EE, et al. Fewer Hospitalizations for acute cardiovascular conditions during the COVID-19 pandemic. J Am Coll Cardiol. 2020;76(3):280-288. doi:10.1016/j.jacc.2020.05.038
7. Tam CF, Cheung KS, Lam S, et al. Impact of Coronavirus disease 2019 (Covid-19) outbreak on ST-segment elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13(4):e006631. doi:10.1161/CIRCOUTCOMES.120.006631
8. Clerkin KJ, Fried JA, Raikhelkar J, et al. Coronavirus disease 2019 (COVID-19) and cardiovascular disease. Circulation. 2020;141:1648-1655. doi:10.1161/CIRCULATIONAHA.120.046941
9. Ebinger JE, Shah PK. Declining admissions for acute cardiovascular illness: The Covid-19 paradox. J Am Coll Cardiol. 2020;76(3):289-291. doi:10.1016/j.jacc.2020.05.039
10 Leor J, Poole WK, Kloner RA. Sudden cardiac death triggered by an earthquake. N Engl J Med. 1996;334(7):413-419. doi:10.1056/NEJM199602153340701
11. Hiramori K. Major causes of death from acute myocardial infarction in a coronary care unit. Jpn Circ J. 1987;51(9):1041-1047. doi:10.1253/jcj.51.1041
12. Bui AH, Waks JW. Risk stratification of sudden cardiac death after acute myocardial infarction. J Innov Card Rhythm Manag. 2018;9(2):3035-3049. doi:10.19102/icrm.2018.090201
13. Xiang D, Xiang X, Zhang W, et al. Management and outcomes of patients with STEMI during the COVID-19 pandemic in China. J Am Coll Cardiol. 2020;76(11):1318-1324. doi:10.1016/j.jacc.2020.06.039
14. Hakim R, Motreff P, Rangé G. COVID-19 and STEMI. [Article in French]. Ann Cardiol Angeiol (Paris). 2020;69(6):355-359. doi:10.1016/j.ancard.2020.09.034
15. Soylu K, Coksevim M, Yanık A, Bugra Cerik I, Aksan G. Effect of Covid-19 pandemic process on STEMI patients timeline. Int J Clin Pract. 2021;75(5):e14005. doi:10.1111/ijcp.14005
16. Salinas P, Travieso A, Vergara-Uzcategui C, et al. Clinical profile and 30-day mortality of invasively managed patients with suspected acute coronary syndrome during the COVID-19 outbreak. Int Heart J. 2021;62(2):274-281. doi:10.1536/ihj.20-574
17. Hu Y, Sun J, Dai Z, et al. Prevalence and severity of corona virus disease 2019 (Covid-19): a systematic review and meta-analysis. J Clin Virol. 2020;127:104371. doi:10.1016/j.jcv.2020.104371
18. Rodriguez-Leor O, Cid Alvarez AB, Perez de Prado A, et al. In-hospital outcomes of COVID-19 ST-elevation myocardial infarction patients. EuroIntervention. 2021;16(17):1426-1433. doi:10.4244/EIJ-D-20-00935
19. Fardman A, Zahger D, Orvin K, et al. Acute myocardial infarction in the Covid-19 era: incidence, clinical characteristics and in-hospital outcomes—A multicenter registry. PLoS ONE. 2021;16(6): e0253524. doi:10.1371/journal.pone.0253524
20. Pessoa-Amorim G, Camm CF, Gajendragadkar P, et al. Admission of patients with STEMI since the outbreak of the COVID-19 pandemic: a survey by the European Society of Cardiology. Eur Heart J Qual Care Clin Outcomes. 2020;6(3):210-216. doi:10.1093/ehjqcco/qcaa046
1. Bhatt AS, Moscone A, McElrath EE, et al. Fewer hospitalizations for acute cardiovascular conditions during the COVID-19 pandemic. J Am Coll Cardiol. 2020;76(3):280-288. doi:10.1016/j.jacc.2020.05.038
2. Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJR. Decline of acute coronary syndrome admissions in Austria since the outbreak of Covid-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41:1852-1853. doi:10.1093/eurheartj/ehaa314
3. De Rosa S, Spaccarotella C, Basso C, et al. Reduction of hospitalizations for myocardial infarction in Italy in the Covid-19 era. Eur Heart J. 2020;41(22):2083-2088.
4. Wilson SJ, Connolly MJ, Elghamry Z, et al. Effect of the COVID-19 pandemic on ST-segment-elevation myocardial infarction presentations and in-hospital outcomes. Circ Cardiovasc Interv. 2020; 13(7):e009438. doi:10.1161/CIRCINTERVENTIONS.120.009438
5. Mafham MM, Spata E, Goldacre R, et al. Covid-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396 (10248):381-389. doi:10.1016/S0140-6736(20)31356-8
6. Bhatt AS, Moscone A, McElrath EE, et al. Fewer Hospitalizations for acute cardiovascular conditions during the COVID-19 pandemic. J Am Coll Cardiol. 2020;76(3):280-288. doi:10.1016/j.jacc.2020.05.038
7. Tam CF, Cheung KS, Lam S, et al. Impact of Coronavirus disease 2019 (Covid-19) outbreak on ST-segment elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13(4):e006631. doi:10.1161/CIRCOUTCOMES.120.006631
8. Clerkin KJ, Fried JA, Raikhelkar J, et al. Coronavirus disease 2019 (COVID-19) and cardiovascular disease. Circulation. 2020;141:1648-1655. doi:10.1161/CIRCULATIONAHA.120.046941
9. Ebinger JE, Shah PK. Declining admissions for acute cardiovascular illness: The Covid-19 paradox. J Am Coll Cardiol. 2020;76(3):289-291. doi:10.1016/j.jacc.2020.05.039
10 Leor J, Poole WK, Kloner RA. Sudden cardiac death triggered by an earthquake. N Engl J Med. 1996;334(7):413-419. doi:10.1056/NEJM199602153340701
11. Hiramori K. Major causes of death from acute myocardial infarction in a coronary care unit. Jpn Circ J. 1987;51(9):1041-1047. doi:10.1253/jcj.51.1041
12. Bui AH, Waks JW. Risk stratification of sudden cardiac death after acute myocardial infarction. J Innov Card Rhythm Manag. 2018;9(2):3035-3049. doi:10.19102/icrm.2018.090201
13. Xiang D, Xiang X, Zhang W, et al. Management and outcomes of patients with STEMI during the COVID-19 pandemic in China. J Am Coll Cardiol. 2020;76(11):1318-1324. doi:10.1016/j.jacc.2020.06.039
14. Hakim R, Motreff P, Rangé G. COVID-19 and STEMI. [Article in French]. Ann Cardiol Angeiol (Paris). 2020;69(6):355-359. doi:10.1016/j.ancard.2020.09.034
15. Soylu K, Coksevim M, Yanık A, Bugra Cerik I, Aksan G. Effect of Covid-19 pandemic process on STEMI patients timeline. Int J Clin Pract. 2021;75(5):e14005. doi:10.1111/ijcp.14005
16. Salinas P, Travieso A, Vergara-Uzcategui C, et al. Clinical profile and 30-day mortality of invasively managed patients with suspected acute coronary syndrome during the COVID-19 outbreak. Int Heart J. 2021;62(2):274-281. doi:10.1536/ihj.20-574
17. Hu Y, Sun J, Dai Z, et al. Prevalence and severity of corona virus disease 2019 (Covid-19): a systematic review and meta-analysis. J Clin Virol. 2020;127:104371. doi:10.1016/j.jcv.2020.104371
18. Rodriguez-Leor O, Cid Alvarez AB, Perez de Prado A, et al. In-hospital outcomes of COVID-19 ST-elevation myocardial infarction patients. EuroIntervention. 2021;16(17):1426-1433. doi:10.4244/EIJ-D-20-00935
19. Fardman A, Zahger D, Orvin K, et al. Acute myocardial infarction in the Covid-19 era: incidence, clinical characteristics and in-hospital outcomes—A multicenter registry. PLoS ONE. 2021;16(6): e0253524. doi:10.1371/journal.pone.0253524
20. Pessoa-Amorim G, Camm CF, Gajendragadkar P, et al. Admission of patients with STEMI since the outbreak of the COVID-19 pandemic: a survey by the European Society of Cardiology. Eur Heart J Qual Care Clin Outcomes. 2020;6(3):210-216. doi:10.1093/ehjqcco/qcaa046






