User login
Minorities bear brunt of pediatric COVID-19 cases
Black and Hispanic children comprised significantly more cases of COVID-19, compared with White children, based on data from a large, cross-sectional study of 1,000 cases.
“Data regarding disparities in SARS-CoV-2 infection and outcomes have been, thus far, mostly limited to adults,” wrote Monika K. Goyal, MD, of Children’s National Hospital, Washington, and colleagues. “Additional data further suggest that low socioeconomic status may further exacerbate health outcomes for racial and ethnic minorities.”
In a study published in Pediatrics, the researchers conducted a cross-sectional analysis of 1,000 children from a registry of non–acutely ill pediatric patients seen at a drive-through and walk-up COVID-19 test site.
Minority, socioeconomic status affect pediatric outcomes too
The median age of the study population was 8 years, and approximately half were male.
The researchers also examined the association of median family income (MFI) using census block group estimates data from the American Community Survey (2014–2018) to represent socioeconomic status.
Infection rates were significantly higher among children in the lowest three quartiles of MFI (24%, 27%, and 38% for quartiles 3, 2, and 1, respectively), compared with the highest quartile of MFI (9%).
After adjusting for age, sex, and MFI, Hispanic children were six times more likely and non-Hispanic Black children were twice as likely to test positive for COVID-19 than non-Hispanic White children (adjusted odds ratios, 6.3 and 2.3, respectively).
The study findings were limited by several factors including the use of clinician-reported ethnicity and thus potential for misclassification, the researchers noted. In addition, the socioeconomic and racial disparities may be underestimated because these groups have less access to primary care, and the study did not allow for confounding variables including housing conditions or occupancy.
“Although it was beyond the scope of this study to understand the causes for these differential rates of infection, the causes may be multifactorial, including, but not limited to, structural factors, poorer access to health care, limited resources, and bias and discrimination,” the researchers noted. In addition, the high infection rate among minority children may be impacted by parents who are less able to telework, find child care, or avoid public transportation, Dr. Goyal and associates wrote.
Future research should address “the modifiable reasons for these observed disparities as well as their differential impact in terms of SARS-CoV-2–related morbidity and mortality outcomes to mitigate the spread of infection and its health effects,” they concluded.
How to help
“This study is important because we need to understand which groups of children are at highest risk for SARS-CoV-2 infection in order to maximize efforts for screening, allocating resources, and prioritizing vaccine administration,” Karalyn Kinsella, MD, a pediatrician in private practice in Cheshire, Conn., said in an interview.
Dr. Kinsella said she was not surprised at the higher infection rates in general in minorities and low socioeconomic groups. “We already knew that adult COVID-19 rates were higher for people in certain racial/ethnic groups and those with socioeconomic disadvantages; however, I was shocked by the percentages. That is a huge burden for a population that already has disparities in health outcomes.”
“As the authors cite, this was not a research study of why these groups were more likely to be COVID-19 positive, but they speculated that crowded living conditions, multigenerational families living together, and many minorities being essential workers unable to work from home,” said Dr. Kinsella. Additional factors contributing to higher infection rates may include limited access to care, transportation issues, insurance coverage, schedule challenges, and fear of deportation. Some of these problems might be addressed by coming into communities in mobile vans, visiting community health centers and schools with free educational materials, using masks and hand sanitizer, and offering free access to testing.
“Future studies could confirm the cause of this discrepancy, as well as study community-based interventions and their outcomes,” Dr. Kinsella said. In the meantime, a take-home message for clinicians is the need to prioritize screening, resources, and vaccines to reflect the higher rates of SARS-CoV-2 infections in children from disadvantaged racial and socioeconomic backgrounds.
The study received no outside funding. The researchers had no financial conflicts to disclose, but lead author Dr. Goyal is a member of the Pediatrics editorial board. Dr. Kinsella had no financial conflicts to disclose, but serves on the Pediatric News editorial advisory board.
SOURCE: Goyal MK et al. Pediatrics. 2020 Sep 24. doi: 10.1542/peds.2020-009951.
Black and Hispanic children comprised significantly more cases of COVID-19, compared with White children, based on data from a large, cross-sectional study of 1,000 cases.
“Data regarding disparities in SARS-CoV-2 infection and outcomes have been, thus far, mostly limited to adults,” wrote Monika K. Goyal, MD, of Children’s National Hospital, Washington, and colleagues. “Additional data further suggest that low socioeconomic status may further exacerbate health outcomes for racial and ethnic minorities.”
In a study published in Pediatrics, the researchers conducted a cross-sectional analysis of 1,000 children from a registry of non–acutely ill pediatric patients seen at a drive-through and walk-up COVID-19 test site.
Minority, socioeconomic status affect pediatric outcomes too
The median age of the study population was 8 years, and approximately half were male.
The researchers also examined the association of median family income (MFI) using census block group estimates data from the American Community Survey (2014–2018) to represent socioeconomic status.
Infection rates were significantly higher among children in the lowest three quartiles of MFI (24%, 27%, and 38% for quartiles 3, 2, and 1, respectively), compared with the highest quartile of MFI (9%).
After adjusting for age, sex, and MFI, Hispanic children were six times more likely and non-Hispanic Black children were twice as likely to test positive for COVID-19 than non-Hispanic White children (adjusted odds ratios, 6.3 and 2.3, respectively).
The study findings were limited by several factors including the use of clinician-reported ethnicity and thus potential for misclassification, the researchers noted. In addition, the socioeconomic and racial disparities may be underestimated because these groups have less access to primary care, and the study did not allow for confounding variables including housing conditions or occupancy.
“Although it was beyond the scope of this study to understand the causes for these differential rates of infection, the causes may be multifactorial, including, but not limited to, structural factors, poorer access to health care, limited resources, and bias and discrimination,” the researchers noted. In addition, the high infection rate among minority children may be impacted by parents who are less able to telework, find child care, or avoid public transportation, Dr. Goyal and associates wrote.
Future research should address “the modifiable reasons for these observed disparities as well as their differential impact in terms of SARS-CoV-2–related morbidity and mortality outcomes to mitigate the spread of infection and its health effects,” they concluded.
How to help
“This study is important because we need to understand which groups of children are at highest risk for SARS-CoV-2 infection in order to maximize efforts for screening, allocating resources, and prioritizing vaccine administration,” Karalyn Kinsella, MD, a pediatrician in private practice in Cheshire, Conn., said in an interview.
Dr. Kinsella said she was not surprised at the higher infection rates in general in minorities and low socioeconomic groups. “We already knew that adult COVID-19 rates were higher for people in certain racial/ethnic groups and those with socioeconomic disadvantages; however, I was shocked by the percentages. That is a huge burden for a population that already has disparities in health outcomes.”
“As the authors cite, this was not a research study of why these groups were more likely to be COVID-19 positive, but they speculated that crowded living conditions, multigenerational families living together, and many minorities being essential workers unable to work from home,” said Dr. Kinsella. Additional factors contributing to higher infection rates may include limited access to care, transportation issues, insurance coverage, schedule challenges, and fear of deportation. Some of these problems might be addressed by coming into communities in mobile vans, visiting community health centers and schools with free educational materials, using masks and hand sanitizer, and offering free access to testing.
“Future studies could confirm the cause of this discrepancy, as well as study community-based interventions and their outcomes,” Dr. Kinsella said. In the meantime, a take-home message for clinicians is the need to prioritize screening, resources, and vaccines to reflect the higher rates of SARS-CoV-2 infections in children from disadvantaged racial and socioeconomic backgrounds.
The study received no outside funding. The researchers had no financial conflicts to disclose, but lead author Dr. Goyal is a member of the Pediatrics editorial board. Dr. Kinsella had no financial conflicts to disclose, but serves on the Pediatric News editorial advisory board.
SOURCE: Goyal MK et al. Pediatrics. 2020 Sep 24. doi: 10.1542/peds.2020-009951.
Black and Hispanic children comprised significantly more cases of COVID-19, compared with White children, based on data from a large, cross-sectional study of 1,000 cases.
“Data regarding disparities in SARS-CoV-2 infection and outcomes have been, thus far, mostly limited to adults,” wrote Monika K. Goyal, MD, of Children’s National Hospital, Washington, and colleagues. “Additional data further suggest that low socioeconomic status may further exacerbate health outcomes for racial and ethnic minorities.”
In a study published in Pediatrics, the researchers conducted a cross-sectional analysis of 1,000 children from a registry of non–acutely ill pediatric patients seen at a drive-through and walk-up COVID-19 test site.
Minority, socioeconomic status affect pediatric outcomes too
The median age of the study population was 8 years, and approximately half were male.
The researchers also examined the association of median family income (MFI) using census block group estimates data from the American Community Survey (2014–2018) to represent socioeconomic status.
Infection rates were significantly higher among children in the lowest three quartiles of MFI (24%, 27%, and 38% for quartiles 3, 2, and 1, respectively), compared with the highest quartile of MFI (9%).
After adjusting for age, sex, and MFI, Hispanic children were six times more likely and non-Hispanic Black children were twice as likely to test positive for COVID-19 than non-Hispanic White children (adjusted odds ratios, 6.3 and 2.3, respectively).
The study findings were limited by several factors including the use of clinician-reported ethnicity and thus potential for misclassification, the researchers noted. In addition, the socioeconomic and racial disparities may be underestimated because these groups have less access to primary care, and the study did not allow for confounding variables including housing conditions or occupancy.
“Although it was beyond the scope of this study to understand the causes for these differential rates of infection, the causes may be multifactorial, including, but not limited to, structural factors, poorer access to health care, limited resources, and bias and discrimination,” the researchers noted. In addition, the high infection rate among minority children may be impacted by parents who are less able to telework, find child care, or avoid public transportation, Dr. Goyal and associates wrote.
Future research should address “the modifiable reasons for these observed disparities as well as their differential impact in terms of SARS-CoV-2–related morbidity and mortality outcomes to mitigate the spread of infection and its health effects,” they concluded.
How to help
“This study is important because we need to understand which groups of children are at highest risk for SARS-CoV-2 infection in order to maximize efforts for screening, allocating resources, and prioritizing vaccine administration,” Karalyn Kinsella, MD, a pediatrician in private practice in Cheshire, Conn., said in an interview.
Dr. Kinsella said she was not surprised at the higher infection rates in general in minorities and low socioeconomic groups. “We already knew that adult COVID-19 rates were higher for people in certain racial/ethnic groups and those with socioeconomic disadvantages; however, I was shocked by the percentages. That is a huge burden for a population that already has disparities in health outcomes.”
“As the authors cite, this was not a research study of why these groups were more likely to be COVID-19 positive, but they speculated that crowded living conditions, multigenerational families living together, and many minorities being essential workers unable to work from home,” said Dr. Kinsella. Additional factors contributing to higher infection rates may include limited access to care, transportation issues, insurance coverage, schedule challenges, and fear of deportation. Some of these problems might be addressed by coming into communities in mobile vans, visiting community health centers and schools with free educational materials, using masks and hand sanitizer, and offering free access to testing.
“Future studies could confirm the cause of this discrepancy, as well as study community-based interventions and their outcomes,” Dr. Kinsella said. In the meantime, a take-home message for clinicians is the need to prioritize screening, resources, and vaccines to reflect the higher rates of SARS-CoV-2 infections in children from disadvantaged racial and socioeconomic backgrounds.
The study received no outside funding. The researchers had no financial conflicts to disclose, but lead author Dr. Goyal is a member of the Pediatrics editorial board. Dr. Kinsella had no financial conflicts to disclose, but serves on the Pediatric News editorial advisory board.
SOURCE: Goyal MK et al. Pediatrics. 2020 Sep 24. doi: 10.1542/peds.2020-009951.
FROM PEDIATRICS
COVID-19 may discourage pediatric flu vaccination
Parents who did not vaccinate their children against influenza last year were significantly less likely to do so this year than parents whose children were vaccinated last year, based on survey data from more than 2,000 parents with babies and young children.
“Pediatric vaccination will be an important component to mitigating a dual influenza/COVID-19 epidemic,” Rebeccah L. Sokol, PhD, of Wayne State University, Detroit, and Anna H. Grummon, PhD, of Harvard School of Public Health, Boston, reported in Pediatrics.
Although the pandemic has increased acceptance of some healthy behaviors including handwashing and social distancing, the impact on influenza vaccination rates remains unknown, they said.
To assess parents’ current intentions for flu vaccination of young children this season, the researchers conducted an online survey of 2,164 parents or guardians of children aged between 6 months and 5 years in the United States. The 15-minute online survey was conducted in May 2020 and participants received gift cards. The primary outcome was the impact of the COVID-19 pandemic on parental intentions for having their child vaccinated against seasonal flu this year.
“We measured change categorically, with response options ranging from 1 (I became much less likely to get my child the flu shot next year) to 5 (I became much more likely to get my child the flu shot next year),” the researchers said.
Pandemic changes some parents’ plans
Overall, 60% of parents said that the ongoing pandemic had altered their flu vaccination intentions for their children. About 34% percent of parents whose children did not receive flu vaccine last year said they would not seek the vaccine this year because of the pandemic, compared with 25% of parents whose children received last year’s flu vaccine, a statistically significant difference (P < .001).
Approximately 21% of parents whose children received no flu vaccine last year said the pandemic made them more likely to seek vaccination for the 2020-2021 season, compared with 38% of parents whose children received last year’s flu vaccine.
“These results suggest that overall seasonal influenza vaccination rates may not increase simply because of an ongoing infectious disease pandemic. Instead, a significant predictor of future behavior remains past behavior,” Dr. Sokol and Dr. Grummon said.
The study findings were limited by several factors including the use of a convenience sample and the timing of the survey in May 2020, meaning that survey results might not be generalizable this fall as the pandemic persists, they noted. “Additionally, we assessed intentions to vaccinate; future research will clarify the COVID-19 pandemic’s influence on actual vaccination behaviors.”
The challenge of how to increase uptake of the influenza vaccine during the era of COVID-19 remains, and targeted efforts could include social norms messaging through social media, mass media, or health care providers to increase parents’ intentions to vaccinate, as well as vaccination reminders and presumptive announcements from health care providers that present vaccination as the default option, the researchers added.
Potential for ‘twindemic’ is real
The uptake of flu vaccination is especially important this year, Christopher J. Harrison, MD, director of the vaccine and treatment evaluation unit and professor of pediatrics at the University of Missouri–Kansas City, said in an interview.
“This year we are entering a flu season where the certainty of the timing as well as the potential severity of the season are not known. That said, social distancing and wearing masks – to the extent that enough people conform to COVID-19 precautions – could delay or even blunt the usual influenza season,” he noted.
Unfortunately, the Centers for Disease Control and Prevention and the Food and Drug Administration have had their credibility damaged by the challenges of creating a successful response on the fly to a uniquely multifaceted virus to which previous rules do not apply, Dr. Harrison said. In addition, public confidence was eroded when information about testing and reopening policies were released by non-CDC nonscientists and labeled “CDC recommended,” with no opportunity for the scientific community to correct inaccuracies.
“The current study reveals that public trust in influenza vaccine and indirectly in health authorities has been affected by the pandemic,” said Dr. Harrison. “Vaccine hesitancy has increased somewhat even among previous vaccine accepters. One wonders if promises of a quick COVID-19 vaccine increased mistrust of the FDA because of safety concerns, even among the most ardent provaccine population, and whether these concerns are bleeding over into influenza vaccine concerns.
“This only adds to the anxiety that families feel about visiting any medical facility for routine vaccines while the pandemic rages, and we now are in a fall SARS-CoV-2 resurgence,” he added.
Although the current study data are concerning, “there could still be a net gain of pediatric influenza vaccine uptake this season because the 34% less likely to immunize among previously nonimmunizing families would be counterbalanced by 21% of the same group being more likely to immunize their children [theoretical net loss of 13%],” Dr. Harrison explained. “But the pandemic seems to have motivated previously influenza-immunizing families, i.e. while 24% were less likely, 39% are more likely to immunize [theoretical net gain of 15%]. That said, we would still be way short of the number needed to get to herd immunity.”
Dr. Harrison said he found the findings somewhat surprising, but perhaps he should not have. “I had hoped for more acceptance rather than most people staying in their prior vaccine ‘opinion lanes,’ ending up with likely little overall net change in plans to immunize despite increased health awareness caused by a pandemic.”
However, “the U.S. population has been polarized on vaccines and particularly influenza vaccines for more than 50 years, so why would a pandemic make us less polarized, particularly when the pandemic itself has been a polarizing event?” he questioned.
The greatest barriers to flu vaccination for children this year include a lack of motivation among families to visit immunization sites, given the ongoing need for social distancing and masks, Dr. Harrison said.
“Another barrier is the waning public confidence in our medical/scientific national leaders and organizations,” he emphasized. “This makes it crucial that primary care providers step up and be extra strong vaccine advocates, despite the fact that pandemic economics and necessary safety processes have stressed providers and devastated practices. Indeed, in times of medical stress, no one gets more trust from families than their own personal provider.”
Ultimately, avenues for future research include asking diverse groups of families what they feel they need to hear to be more engaged in immunizing children against influenza. But for now, the current study findings identify that “the public is not uniformly responding to the pandemic’s influence on their likelihood of immunizing their children against influenza,” Dr. Harrison said.
“We now know the size of the problem and hopefully governments, public health organizations, pediatric advocates and clinical care givers can find ways to magnify the message that a pandemic year is not a year to avoid seasonal influenza vaccine unless one has a true contraindication,” Dr. Harrison said.
In addition, “one wonders if the poll were taken today – post the president’s COVID-19 illness – would the answers be different?” he noted.
Dr. Sokol’s work was supported in part by the Eunice Kennedy Shriver National Institute of Child Health and Human Development but otherwise had no financial conflicts to disclose. Dr. Harrison disclosed that his institution receives grant funding from Merck, Pfizer, and GlaxoSmithKline for pediatric noninfluenza vaccine studies on which he is a subinvestigator, and support from the CDC for pediatric respiratory and gastrointestinal virus surveillance studies on which he is an investigator.
SOURCE: Sokol RL, Grummon AH. Pediatrics. 2020 Sep 30. doi: 10.1542/peds.2020-022871.
Parents who did not vaccinate their children against influenza last year were significantly less likely to do so this year than parents whose children were vaccinated last year, based on survey data from more than 2,000 parents with babies and young children.
“Pediatric vaccination will be an important component to mitigating a dual influenza/COVID-19 epidemic,” Rebeccah L. Sokol, PhD, of Wayne State University, Detroit, and Anna H. Grummon, PhD, of Harvard School of Public Health, Boston, reported in Pediatrics.
Although the pandemic has increased acceptance of some healthy behaviors including handwashing and social distancing, the impact on influenza vaccination rates remains unknown, they said.
To assess parents’ current intentions for flu vaccination of young children this season, the researchers conducted an online survey of 2,164 parents or guardians of children aged between 6 months and 5 years in the United States. The 15-minute online survey was conducted in May 2020 and participants received gift cards. The primary outcome was the impact of the COVID-19 pandemic on parental intentions for having their child vaccinated against seasonal flu this year.
“We measured change categorically, with response options ranging from 1 (I became much less likely to get my child the flu shot next year) to 5 (I became much more likely to get my child the flu shot next year),” the researchers said.
Pandemic changes some parents’ plans
Overall, 60% of parents said that the ongoing pandemic had altered their flu vaccination intentions for their children. About 34% percent of parents whose children did not receive flu vaccine last year said they would not seek the vaccine this year because of the pandemic, compared with 25% of parents whose children received last year’s flu vaccine, a statistically significant difference (P < .001).
Approximately 21% of parents whose children received no flu vaccine last year said the pandemic made them more likely to seek vaccination for the 2020-2021 season, compared with 38% of parents whose children received last year’s flu vaccine.
“These results suggest that overall seasonal influenza vaccination rates may not increase simply because of an ongoing infectious disease pandemic. Instead, a significant predictor of future behavior remains past behavior,” Dr. Sokol and Dr. Grummon said.
The study findings were limited by several factors including the use of a convenience sample and the timing of the survey in May 2020, meaning that survey results might not be generalizable this fall as the pandemic persists, they noted. “Additionally, we assessed intentions to vaccinate; future research will clarify the COVID-19 pandemic’s influence on actual vaccination behaviors.”
The challenge of how to increase uptake of the influenza vaccine during the era of COVID-19 remains, and targeted efforts could include social norms messaging through social media, mass media, or health care providers to increase parents’ intentions to vaccinate, as well as vaccination reminders and presumptive announcements from health care providers that present vaccination as the default option, the researchers added.
Potential for ‘twindemic’ is real
The uptake of flu vaccination is especially important this year, Christopher J. Harrison, MD, director of the vaccine and treatment evaluation unit and professor of pediatrics at the University of Missouri–Kansas City, said in an interview.
“This year we are entering a flu season where the certainty of the timing as well as the potential severity of the season are not known. That said, social distancing and wearing masks – to the extent that enough people conform to COVID-19 precautions – could delay or even blunt the usual influenza season,” he noted.
Unfortunately, the Centers for Disease Control and Prevention and the Food and Drug Administration have had their credibility damaged by the challenges of creating a successful response on the fly to a uniquely multifaceted virus to which previous rules do not apply, Dr. Harrison said. In addition, public confidence was eroded when information about testing and reopening policies were released by non-CDC nonscientists and labeled “CDC recommended,” with no opportunity for the scientific community to correct inaccuracies.
“The current study reveals that public trust in influenza vaccine and indirectly in health authorities has been affected by the pandemic,” said Dr. Harrison. “Vaccine hesitancy has increased somewhat even among previous vaccine accepters. One wonders if promises of a quick COVID-19 vaccine increased mistrust of the FDA because of safety concerns, even among the most ardent provaccine population, and whether these concerns are bleeding over into influenza vaccine concerns.
“This only adds to the anxiety that families feel about visiting any medical facility for routine vaccines while the pandemic rages, and we now are in a fall SARS-CoV-2 resurgence,” he added.
Although the current study data are concerning, “there could still be a net gain of pediatric influenza vaccine uptake this season because the 34% less likely to immunize among previously nonimmunizing families would be counterbalanced by 21% of the same group being more likely to immunize their children [theoretical net loss of 13%],” Dr. Harrison explained. “But the pandemic seems to have motivated previously influenza-immunizing families, i.e. while 24% were less likely, 39% are more likely to immunize [theoretical net gain of 15%]. That said, we would still be way short of the number needed to get to herd immunity.”
Dr. Harrison said he found the findings somewhat surprising, but perhaps he should not have. “I had hoped for more acceptance rather than most people staying in their prior vaccine ‘opinion lanes,’ ending up with likely little overall net change in plans to immunize despite increased health awareness caused by a pandemic.”
However, “the U.S. population has been polarized on vaccines and particularly influenza vaccines for more than 50 years, so why would a pandemic make us less polarized, particularly when the pandemic itself has been a polarizing event?” he questioned.
The greatest barriers to flu vaccination for children this year include a lack of motivation among families to visit immunization sites, given the ongoing need for social distancing and masks, Dr. Harrison said.
“Another barrier is the waning public confidence in our medical/scientific national leaders and organizations,” he emphasized. “This makes it crucial that primary care providers step up and be extra strong vaccine advocates, despite the fact that pandemic economics and necessary safety processes have stressed providers and devastated practices. Indeed, in times of medical stress, no one gets more trust from families than their own personal provider.”
Ultimately, avenues for future research include asking diverse groups of families what they feel they need to hear to be more engaged in immunizing children against influenza. But for now, the current study findings identify that “the public is not uniformly responding to the pandemic’s influence on their likelihood of immunizing their children against influenza,” Dr. Harrison said.
“We now know the size of the problem and hopefully governments, public health organizations, pediatric advocates and clinical care givers can find ways to magnify the message that a pandemic year is not a year to avoid seasonal influenza vaccine unless one has a true contraindication,” Dr. Harrison said.
In addition, “one wonders if the poll were taken today – post the president’s COVID-19 illness – would the answers be different?” he noted.
Dr. Sokol’s work was supported in part by the Eunice Kennedy Shriver National Institute of Child Health and Human Development but otherwise had no financial conflicts to disclose. Dr. Harrison disclosed that his institution receives grant funding from Merck, Pfizer, and GlaxoSmithKline for pediatric noninfluenza vaccine studies on which he is a subinvestigator, and support from the CDC for pediatric respiratory and gastrointestinal virus surveillance studies on which he is an investigator.
SOURCE: Sokol RL, Grummon AH. Pediatrics. 2020 Sep 30. doi: 10.1542/peds.2020-022871.
Parents who did not vaccinate their children against influenza last year were significantly less likely to do so this year than parents whose children were vaccinated last year, based on survey data from more than 2,000 parents with babies and young children.
“Pediatric vaccination will be an important component to mitigating a dual influenza/COVID-19 epidemic,” Rebeccah L. Sokol, PhD, of Wayne State University, Detroit, and Anna H. Grummon, PhD, of Harvard School of Public Health, Boston, reported in Pediatrics.
Although the pandemic has increased acceptance of some healthy behaviors including handwashing and social distancing, the impact on influenza vaccination rates remains unknown, they said.
To assess parents’ current intentions for flu vaccination of young children this season, the researchers conducted an online survey of 2,164 parents or guardians of children aged between 6 months and 5 years in the United States. The 15-minute online survey was conducted in May 2020 and participants received gift cards. The primary outcome was the impact of the COVID-19 pandemic on parental intentions for having their child vaccinated against seasonal flu this year.
“We measured change categorically, with response options ranging from 1 (I became much less likely to get my child the flu shot next year) to 5 (I became much more likely to get my child the flu shot next year),” the researchers said.
Pandemic changes some parents’ plans
Overall, 60% of parents said that the ongoing pandemic had altered their flu vaccination intentions for their children. About 34% percent of parents whose children did not receive flu vaccine last year said they would not seek the vaccine this year because of the pandemic, compared with 25% of parents whose children received last year’s flu vaccine, a statistically significant difference (P < .001).
Approximately 21% of parents whose children received no flu vaccine last year said the pandemic made them more likely to seek vaccination for the 2020-2021 season, compared with 38% of parents whose children received last year’s flu vaccine.
“These results suggest that overall seasonal influenza vaccination rates may not increase simply because of an ongoing infectious disease pandemic. Instead, a significant predictor of future behavior remains past behavior,” Dr. Sokol and Dr. Grummon said.
The study findings were limited by several factors including the use of a convenience sample and the timing of the survey in May 2020, meaning that survey results might not be generalizable this fall as the pandemic persists, they noted. “Additionally, we assessed intentions to vaccinate; future research will clarify the COVID-19 pandemic’s influence on actual vaccination behaviors.”
The challenge of how to increase uptake of the influenza vaccine during the era of COVID-19 remains, and targeted efforts could include social norms messaging through social media, mass media, or health care providers to increase parents’ intentions to vaccinate, as well as vaccination reminders and presumptive announcements from health care providers that present vaccination as the default option, the researchers added.
Potential for ‘twindemic’ is real
The uptake of flu vaccination is especially important this year, Christopher J. Harrison, MD, director of the vaccine and treatment evaluation unit and professor of pediatrics at the University of Missouri–Kansas City, said in an interview.
“This year we are entering a flu season where the certainty of the timing as well as the potential severity of the season are not known. That said, social distancing and wearing masks – to the extent that enough people conform to COVID-19 precautions – could delay or even blunt the usual influenza season,” he noted.
Unfortunately, the Centers for Disease Control and Prevention and the Food and Drug Administration have had their credibility damaged by the challenges of creating a successful response on the fly to a uniquely multifaceted virus to which previous rules do not apply, Dr. Harrison said. In addition, public confidence was eroded when information about testing and reopening policies were released by non-CDC nonscientists and labeled “CDC recommended,” with no opportunity for the scientific community to correct inaccuracies.
“The current study reveals that public trust in influenza vaccine and indirectly in health authorities has been affected by the pandemic,” said Dr. Harrison. “Vaccine hesitancy has increased somewhat even among previous vaccine accepters. One wonders if promises of a quick COVID-19 vaccine increased mistrust of the FDA because of safety concerns, even among the most ardent provaccine population, and whether these concerns are bleeding over into influenza vaccine concerns.
“This only adds to the anxiety that families feel about visiting any medical facility for routine vaccines while the pandemic rages, and we now are in a fall SARS-CoV-2 resurgence,” he added.
Although the current study data are concerning, “there could still be a net gain of pediatric influenza vaccine uptake this season because the 34% less likely to immunize among previously nonimmunizing families would be counterbalanced by 21% of the same group being more likely to immunize their children [theoretical net loss of 13%],” Dr. Harrison explained. “But the pandemic seems to have motivated previously influenza-immunizing families, i.e. while 24% were less likely, 39% are more likely to immunize [theoretical net gain of 15%]. That said, we would still be way short of the number needed to get to herd immunity.”
Dr. Harrison said he found the findings somewhat surprising, but perhaps he should not have. “I had hoped for more acceptance rather than most people staying in their prior vaccine ‘opinion lanes,’ ending up with likely little overall net change in plans to immunize despite increased health awareness caused by a pandemic.”
However, “the U.S. population has been polarized on vaccines and particularly influenza vaccines for more than 50 years, so why would a pandemic make us less polarized, particularly when the pandemic itself has been a polarizing event?” he questioned.
The greatest barriers to flu vaccination for children this year include a lack of motivation among families to visit immunization sites, given the ongoing need for social distancing and masks, Dr. Harrison said.
“Another barrier is the waning public confidence in our medical/scientific national leaders and organizations,” he emphasized. “This makes it crucial that primary care providers step up and be extra strong vaccine advocates, despite the fact that pandemic economics and necessary safety processes have stressed providers and devastated practices. Indeed, in times of medical stress, no one gets more trust from families than their own personal provider.”
Ultimately, avenues for future research include asking diverse groups of families what they feel they need to hear to be more engaged in immunizing children against influenza. But for now, the current study findings identify that “the public is not uniformly responding to the pandemic’s influence on their likelihood of immunizing their children against influenza,” Dr. Harrison said.
“We now know the size of the problem and hopefully governments, public health organizations, pediatric advocates and clinical care givers can find ways to magnify the message that a pandemic year is not a year to avoid seasonal influenza vaccine unless one has a true contraindication,” Dr. Harrison said.
In addition, “one wonders if the poll were taken today – post the president’s COVID-19 illness – would the answers be different?” he noted.
Dr. Sokol’s work was supported in part by the Eunice Kennedy Shriver National Institute of Child Health and Human Development but otherwise had no financial conflicts to disclose. Dr. Harrison disclosed that his institution receives grant funding from Merck, Pfizer, and GlaxoSmithKline for pediatric noninfluenza vaccine studies on which he is a subinvestigator, and support from the CDC for pediatric respiratory and gastrointestinal virus surveillance studies on which he is an investigator.
SOURCE: Sokol RL, Grummon AH. Pediatrics. 2020 Sep 30. doi: 10.1542/peds.2020-022871.
FROM PEDIATRICS
FDA updates info on postmarketing surveillance study of Essure
The Food and Drug Administration has updated its page on Essure information for patients and health care providers to add additional information on adverse events reported by its manufacturer.
Essure was a permanent implantable birth control device approved by the FDA in 2002. FDA ordered Bayer in 2016 to conduct a postmarket surveillance study of Essure following reports of safety concerns, and expanded the study from 3 years to 5 years in 2018. Bayer voluntarily removed Essure from the market at the end of 2018, citing low sales after a “black box” warning was placed on the device. All devices were returned to the company by the end of 2019.
Bayer is required to report variances in Medical Device Reporting (MDR) requirements of Essure related to litigation to the FDA, which includes adverse events such death, serious injury, and “malfunction that would be likely to cause or contribute to a death or serious injury if the malfunction were to recur.” The reports are limited to events Bayer becomes aware of between November 2016 and November 2020. Bayer will continue to provide these reports until April 2021.
The FDA emphasized that the collected data are based on social media reports and already may be reported to the FDA, rather than being a collection of new events. “The limited information provided in the reports prevents the ability to draw any conclusions as to whether the device, or its removal, caused or contributed to any of the events in the reports,” Benjamin Fisher, PhD, director of the Reproductive, Gastro-Renal, Urological, General Hospital Device and Human Factors Office in the Center for Devices and Radiological Health, said in an FDA In Brief statement on Aug. 11.
The FDA first uploaded an Essure MDR variance spreadsheet in August 2020, listing 1,453 events, consisting of 53 reports of deaths, 1,376 reports of serious injury, and 24 reports of device malfunction that occurred as of June 2020. In September 2020, FDA uploaded a second variance spreadsheet, which added another 1,934 events that occurred as of July.
Interim analysis of postmarketing surveillance study
An interim analysis of 1,128 patients from 67 centers in the Essure postmarket surveillance study, which compared women who received Essure with those who received laparoscopic tubal sterilization, revealed that 94.6% (265 of 280 patients) in the Essure group had a successful implantation of the device, compared with 99.6% of women who achieved bilateral tubal occlusion from laparoscopic tubal sterilization.
Regarding safety, 9.1% of women in the Essure group and 4.5% in the laparoscopic tubal sterilization group reported chronic lower abdominal and/or pelvic pain, and 16.3% in the Essure group and 10.2% in the laparoscopic tubal sterilization group reported new or worsening abnormal uterine bleeding. In the Essure group, 22.3% of women said they experienced hypersensitivity, an allergic reaction, and new “autoimmune-like reactions” compared with 12.5% of women in the laparoscopic tubal sterilization group.
The interim analysis also showed 19.7% of women in the Essure group and 3.0% in the laparoscopic tubal sterilization group underwent gynecologic surgical procedures, which were “driven primarily by Essure removal and endometrial ablation procedures in Essure patients.” Device removal occurred in 6.8% of women with the Essure device.
Consistent data on Essure
An FDA search of the Manufacturer and User Facility Device Experience (MAUDE) database in January of 2020 revealed 47,856 medical device reports of Essure between November 2002 and December 2019. The most common adverse events observed during this period were:
- Pain or abdominal pain (32,901 cases).
- Heavy or irregular menses (14,573 cases). Headache (8,570 cases).
- Device fragment or foreign body in a patient (8,501 cases).
- Perforation (7,825 cases).
- Fatigue (7,083 cases).
- Gain or loss in weight (5,980 cases).
- Anxiety and/or depression (5,366 cases).
- Rash and/or hypersensitivity (5,077 cases)
- Hair loss (4,999 cases).
Problems with the device itself included reports of:
- Device incompatibility such as an allergy (7,515 cases).
- The device migrating (4,535 cases).
- The device breaking or fracturing (2,297 cases).
- The device dislodging or dislocating (1,797 cases).
- Improper operation including implant failure and pregnancy (1,058 cases).
In 2019, Essure received 15,083 medical device reports, an increase from 6,000 reports in 2018 and 11,854 reports in 2017.
To date, nearly 39,000 women in the United States have made claims to injuries related to the Essure device. In August, Bayer announced it would pay approximately $1.6 billion U.S. dollars to settle 90% of these cases in exchange for claimants to “dismiss their cases or not file.” Bayer also said in a press release that the settlement is not an admission of wrongdoing or liability on the part of the company.
In an interview, Catherine Cansino, MD, MPH, of the department of obstetrics and gynecology at the University of California, Davis, said the latest adverse event reports show “consistent info from [the] MAUDE database when comparing 2019 to previous years, highlighting most common problems related to pain and heavy or irregular bleeding.”
She emphasized ob.gyns with patients who have an Essure device should “consider Essure-related etiology that may necessitate device removal when evaluating patients with gynecological problems, especially with regard to abdominal/pelvic pain and heavy/irregular bleeding.”
Dr. Cansino reported no relevant financial disclosures. She is a member of the Ob.Gyn. News Editorial Advisory Board.
The Food and Drug Administration has updated its page on Essure information for patients and health care providers to add additional information on adverse events reported by its manufacturer.
Essure was a permanent implantable birth control device approved by the FDA in 2002. FDA ordered Bayer in 2016 to conduct a postmarket surveillance study of Essure following reports of safety concerns, and expanded the study from 3 years to 5 years in 2018. Bayer voluntarily removed Essure from the market at the end of 2018, citing low sales after a “black box” warning was placed on the device. All devices were returned to the company by the end of 2019.
Bayer is required to report variances in Medical Device Reporting (MDR) requirements of Essure related to litigation to the FDA, which includes adverse events such death, serious injury, and “malfunction that would be likely to cause or contribute to a death or serious injury if the malfunction were to recur.” The reports are limited to events Bayer becomes aware of between November 2016 and November 2020. Bayer will continue to provide these reports until April 2021.
The FDA emphasized that the collected data are based on social media reports and already may be reported to the FDA, rather than being a collection of new events. “The limited information provided in the reports prevents the ability to draw any conclusions as to whether the device, or its removal, caused or contributed to any of the events in the reports,” Benjamin Fisher, PhD, director of the Reproductive, Gastro-Renal, Urological, General Hospital Device and Human Factors Office in the Center for Devices and Radiological Health, said in an FDA In Brief statement on Aug. 11.
The FDA first uploaded an Essure MDR variance spreadsheet in August 2020, listing 1,453 events, consisting of 53 reports of deaths, 1,376 reports of serious injury, and 24 reports of device malfunction that occurred as of June 2020. In September 2020, FDA uploaded a second variance spreadsheet, which added another 1,934 events that occurred as of July.
Interim analysis of postmarketing surveillance study
An interim analysis of 1,128 patients from 67 centers in the Essure postmarket surveillance study, which compared women who received Essure with those who received laparoscopic tubal sterilization, revealed that 94.6% (265 of 280 patients) in the Essure group had a successful implantation of the device, compared with 99.6% of women who achieved bilateral tubal occlusion from laparoscopic tubal sterilization.
Regarding safety, 9.1% of women in the Essure group and 4.5% in the laparoscopic tubal sterilization group reported chronic lower abdominal and/or pelvic pain, and 16.3% in the Essure group and 10.2% in the laparoscopic tubal sterilization group reported new or worsening abnormal uterine bleeding. In the Essure group, 22.3% of women said they experienced hypersensitivity, an allergic reaction, and new “autoimmune-like reactions” compared with 12.5% of women in the laparoscopic tubal sterilization group.
The interim analysis also showed 19.7% of women in the Essure group and 3.0% in the laparoscopic tubal sterilization group underwent gynecologic surgical procedures, which were “driven primarily by Essure removal and endometrial ablation procedures in Essure patients.” Device removal occurred in 6.8% of women with the Essure device.
Consistent data on Essure
An FDA search of the Manufacturer and User Facility Device Experience (MAUDE) database in January of 2020 revealed 47,856 medical device reports of Essure between November 2002 and December 2019. The most common adverse events observed during this period were:
- Pain or abdominal pain (32,901 cases).
- Heavy or irregular menses (14,573 cases). Headache (8,570 cases).
- Device fragment or foreign body in a patient (8,501 cases).
- Perforation (7,825 cases).
- Fatigue (7,083 cases).
- Gain or loss in weight (5,980 cases).
- Anxiety and/or depression (5,366 cases).
- Rash and/or hypersensitivity (5,077 cases)
- Hair loss (4,999 cases).
Problems with the device itself included reports of:
- Device incompatibility such as an allergy (7,515 cases).
- The device migrating (4,535 cases).
- The device breaking or fracturing (2,297 cases).
- The device dislodging or dislocating (1,797 cases).
- Improper operation including implant failure and pregnancy (1,058 cases).
In 2019, Essure received 15,083 medical device reports, an increase from 6,000 reports in 2018 and 11,854 reports in 2017.
To date, nearly 39,000 women in the United States have made claims to injuries related to the Essure device. In August, Bayer announced it would pay approximately $1.6 billion U.S. dollars to settle 90% of these cases in exchange for claimants to “dismiss their cases or not file.” Bayer also said in a press release that the settlement is not an admission of wrongdoing or liability on the part of the company.
In an interview, Catherine Cansino, MD, MPH, of the department of obstetrics and gynecology at the University of California, Davis, said the latest adverse event reports show “consistent info from [the] MAUDE database when comparing 2019 to previous years, highlighting most common problems related to pain and heavy or irregular bleeding.”
She emphasized ob.gyns with patients who have an Essure device should “consider Essure-related etiology that may necessitate device removal when evaluating patients with gynecological problems, especially with regard to abdominal/pelvic pain and heavy/irregular bleeding.”
Dr. Cansino reported no relevant financial disclosures. She is a member of the Ob.Gyn. News Editorial Advisory Board.
The Food and Drug Administration has updated its page on Essure information for patients and health care providers to add additional information on adverse events reported by its manufacturer.
Essure was a permanent implantable birth control device approved by the FDA in 2002. FDA ordered Bayer in 2016 to conduct a postmarket surveillance study of Essure following reports of safety concerns, and expanded the study from 3 years to 5 years in 2018. Bayer voluntarily removed Essure from the market at the end of 2018, citing low sales after a “black box” warning was placed on the device. All devices were returned to the company by the end of 2019.
Bayer is required to report variances in Medical Device Reporting (MDR) requirements of Essure related to litigation to the FDA, which includes adverse events such death, serious injury, and “malfunction that would be likely to cause or contribute to a death or serious injury if the malfunction were to recur.” The reports are limited to events Bayer becomes aware of between November 2016 and November 2020. Bayer will continue to provide these reports until April 2021.
The FDA emphasized that the collected data are based on social media reports and already may be reported to the FDA, rather than being a collection of new events. “The limited information provided in the reports prevents the ability to draw any conclusions as to whether the device, or its removal, caused or contributed to any of the events in the reports,” Benjamin Fisher, PhD, director of the Reproductive, Gastro-Renal, Urological, General Hospital Device and Human Factors Office in the Center for Devices and Radiological Health, said in an FDA In Brief statement on Aug. 11.
The FDA first uploaded an Essure MDR variance spreadsheet in August 2020, listing 1,453 events, consisting of 53 reports of deaths, 1,376 reports of serious injury, and 24 reports of device malfunction that occurred as of June 2020. In September 2020, FDA uploaded a second variance spreadsheet, which added another 1,934 events that occurred as of July.
Interim analysis of postmarketing surveillance study
An interim analysis of 1,128 patients from 67 centers in the Essure postmarket surveillance study, which compared women who received Essure with those who received laparoscopic tubal sterilization, revealed that 94.6% (265 of 280 patients) in the Essure group had a successful implantation of the device, compared with 99.6% of women who achieved bilateral tubal occlusion from laparoscopic tubal sterilization.
Regarding safety, 9.1% of women in the Essure group and 4.5% in the laparoscopic tubal sterilization group reported chronic lower abdominal and/or pelvic pain, and 16.3% in the Essure group and 10.2% in the laparoscopic tubal sterilization group reported new or worsening abnormal uterine bleeding. In the Essure group, 22.3% of women said they experienced hypersensitivity, an allergic reaction, and new “autoimmune-like reactions” compared with 12.5% of women in the laparoscopic tubal sterilization group.
The interim analysis also showed 19.7% of women in the Essure group and 3.0% in the laparoscopic tubal sterilization group underwent gynecologic surgical procedures, which were “driven primarily by Essure removal and endometrial ablation procedures in Essure patients.” Device removal occurred in 6.8% of women with the Essure device.
Consistent data on Essure
An FDA search of the Manufacturer and User Facility Device Experience (MAUDE) database in January of 2020 revealed 47,856 medical device reports of Essure between November 2002 and December 2019. The most common adverse events observed during this period were:
- Pain or abdominal pain (32,901 cases).
- Heavy or irregular menses (14,573 cases). Headache (8,570 cases).
- Device fragment or foreign body in a patient (8,501 cases).
- Perforation (7,825 cases).
- Fatigue (7,083 cases).
- Gain or loss in weight (5,980 cases).
- Anxiety and/or depression (5,366 cases).
- Rash and/or hypersensitivity (5,077 cases)
- Hair loss (4,999 cases).
Problems with the device itself included reports of:
- Device incompatibility such as an allergy (7,515 cases).
- The device migrating (4,535 cases).
- The device breaking or fracturing (2,297 cases).
- The device dislodging or dislocating (1,797 cases).
- Improper operation including implant failure and pregnancy (1,058 cases).
In 2019, Essure received 15,083 medical device reports, an increase from 6,000 reports in 2018 and 11,854 reports in 2017.
To date, nearly 39,000 women in the United States have made claims to injuries related to the Essure device. In August, Bayer announced it would pay approximately $1.6 billion U.S. dollars to settle 90% of these cases in exchange for claimants to “dismiss their cases or not file.” Bayer also said in a press release that the settlement is not an admission of wrongdoing or liability on the part of the company.
In an interview, Catherine Cansino, MD, MPH, of the department of obstetrics and gynecology at the University of California, Davis, said the latest adverse event reports show “consistent info from [the] MAUDE database when comparing 2019 to previous years, highlighting most common problems related to pain and heavy or irregular bleeding.”
She emphasized ob.gyns with patients who have an Essure device should “consider Essure-related etiology that may necessitate device removal when evaluating patients with gynecological problems, especially with regard to abdominal/pelvic pain and heavy/irregular bleeding.”
Dr. Cansino reported no relevant financial disclosures. She is a member of the Ob.Gyn. News Editorial Advisory Board.
More female specialists, but gender gap persists in pay, survey finds
More female physicians are becoming specialists, a Medscape survey finds, and five specialties have seen particularly large increases during the last 5 years.
Obstetrician/gynecologists and pediatricians had the largest female representation at 58% and those percentages were both up from 50% in 2015, according to the Medscape Female Physician Compensation Report 2020.
Rheumatology saw a dramatic jump in numbers of women from 29% in 2015 to 54% now. Dermatology increased from 32% to 49%, and family medicine rose from 35% to 43% during that time.
Specialist pay gap narrows slightly
The gender gap was the same this year in primary care — women made 25% less ($212,000 vs. $264,000).
The gap in specialists narrowed slightly. Women made 31% less this year ($286,000 vs $375,000) instead of the 33% less reported in last year’s survey, a difference of $89,000 this year.
The gender pay gap was consistent across all race and age groups and was consistent in responses about net worth. Whereas 57% of male physicians had a net worth of $1 million or more, only 40% of female physicians did. Twice as many male physicians as female physicians had a net worth of more than $5 million (10% vs. 5%).
“Many physicians expect the gender pay gap to narrow in the coming years,” John Prescott, MD, chief academic officer of the Association of American Medical Colleges, said in an interview.
“Yet, it is a challenging task, requiring an institutional commitment to transparency, cross-campus collaboration, ongoing communication, dedicated resources, and enlightened leadership,” he said.
Female physicians working in office-based, solo practices made the most overall at $290,000; women in outpatient settings made the least at $223,000.
The survey included more than 4,500 responses. The responses were collected during the early part of the year and do not reflect changes in income expected from the COVID-19 pandemic.
An analysis in Health Affairs, for instance, predicted that primary care practices would lose $67,774 in gross revenue per full-time-equivalent physician in calendar year 2020 because of the pandemic.
Most physicians did not experience a significant financial loss in 2019, but COVID-19 may, at least temporarily, change those answers in next year’s report, physicians predicted.
Women more likely than men to live above their means
More women this year (39%) said they live below their means than answered that way last year (31%). Female physicians were more likely to say they lived above their means than were their male counterparts (8% vs. 6%).
Greenwald Wealth Management in St. Louis Park, Minn., says aiming for putting away 20% of total gross salary is a good financial goal.
Women in this year’s survey spent about 7% less time seeing patients than did their male counterparts (35.9 hours a week vs. 38.8). The average for all physicians was 37.8 hours a week. Add the 15.6 average hours per week physicians spend on paperwork, and they are putting in 53-hour workweeks on average overall.
Asked what parts of their job they found most rewarding, women were more likely than were men to say “gratitude/relationships with patients” (31% vs. 25%). They were less likely than were men to answer that the most rewarding part was “being very good at what I do/finding answers/diagnoses” (22% vs. 25%) or “making good money at a job I like” (9% vs. 13%).
Most female physicians — and physicians overall — said they would choose medicine again. But two specialties saw a substantial increase in that answer.
This year, 79% of those in physical medicine and rehabilitation said they would choose medicine again (compared with 66% last year) and 84% of gastroenterologists answered that way (compared with 76% in 2019).
Psychiatrists, however, were in the group least likely to say they would choose their specialty again along with those in internal medicine, family medicine, and diabetes and endocrinology.
Female physicians in orthopedics, radiology, and dermatology were most likely to choose their specialties again (91% - 92%).
Female physicians were less likely to use physician assistants in their practices than were their male colleagues (31% vs. 38%) but more likely to use NPs (52% vs. 50%). More than a third (38%) of male and female physicians reported they use neither.
A version of this article originally appeared on Medscape.com.
More female physicians are becoming specialists, a Medscape survey finds, and five specialties have seen particularly large increases during the last 5 years.
Obstetrician/gynecologists and pediatricians had the largest female representation at 58% and those percentages were both up from 50% in 2015, according to the Medscape Female Physician Compensation Report 2020.
Rheumatology saw a dramatic jump in numbers of women from 29% in 2015 to 54% now. Dermatology increased from 32% to 49%, and family medicine rose from 35% to 43% during that time.
Specialist pay gap narrows slightly
The gender gap was the same this year in primary care — women made 25% less ($212,000 vs. $264,000).
The gap in specialists narrowed slightly. Women made 31% less this year ($286,000 vs $375,000) instead of the 33% less reported in last year’s survey, a difference of $89,000 this year.
The gender pay gap was consistent across all race and age groups and was consistent in responses about net worth. Whereas 57% of male physicians had a net worth of $1 million or more, only 40% of female physicians did. Twice as many male physicians as female physicians had a net worth of more than $5 million (10% vs. 5%).
“Many physicians expect the gender pay gap to narrow in the coming years,” John Prescott, MD, chief academic officer of the Association of American Medical Colleges, said in an interview.
“Yet, it is a challenging task, requiring an institutional commitment to transparency, cross-campus collaboration, ongoing communication, dedicated resources, and enlightened leadership,” he said.
Female physicians working in office-based, solo practices made the most overall at $290,000; women in outpatient settings made the least at $223,000.
The survey included more than 4,500 responses. The responses were collected during the early part of the year and do not reflect changes in income expected from the COVID-19 pandemic.
An analysis in Health Affairs, for instance, predicted that primary care practices would lose $67,774 in gross revenue per full-time-equivalent physician in calendar year 2020 because of the pandemic.
Most physicians did not experience a significant financial loss in 2019, but COVID-19 may, at least temporarily, change those answers in next year’s report, physicians predicted.
Women more likely than men to live above their means
More women this year (39%) said they live below their means than answered that way last year (31%). Female physicians were more likely to say they lived above their means than were their male counterparts (8% vs. 6%).
Greenwald Wealth Management in St. Louis Park, Minn., says aiming for putting away 20% of total gross salary is a good financial goal.
Women in this year’s survey spent about 7% less time seeing patients than did their male counterparts (35.9 hours a week vs. 38.8). The average for all physicians was 37.8 hours a week. Add the 15.6 average hours per week physicians spend on paperwork, and they are putting in 53-hour workweeks on average overall.
Asked what parts of their job they found most rewarding, women were more likely than were men to say “gratitude/relationships with patients” (31% vs. 25%). They were less likely than were men to answer that the most rewarding part was “being very good at what I do/finding answers/diagnoses” (22% vs. 25%) or “making good money at a job I like” (9% vs. 13%).
Most female physicians — and physicians overall — said they would choose medicine again. But two specialties saw a substantial increase in that answer.
This year, 79% of those in physical medicine and rehabilitation said they would choose medicine again (compared with 66% last year) and 84% of gastroenterologists answered that way (compared with 76% in 2019).
Psychiatrists, however, were in the group least likely to say they would choose their specialty again along with those in internal medicine, family medicine, and diabetes and endocrinology.
Female physicians in orthopedics, radiology, and dermatology were most likely to choose their specialties again (91% - 92%).
Female physicians were less likely to use physician assistants in their practices than were their male colleagues (31% vs. 38%) but more likely to use NPs (52% vs. 50%). More than a third (38%) of male and female physicians reported they use neither.
A version of this article originally appeared on Medscape.com.
More female physicians are becoming specialists, a Medscape survey finds, and five specialties have seen particularly large increases during the last 5 years.
Obstetrician/gynecologists and pediatricians had the largest female representation at 58% and those percentages were both up from 50% in 2015, according to the Medscape Female Physician Compensation Report 2020.
Rheumatology saw a dramatic jump in numbers of women from 29% in 2015 to 54% now. Dermatology increased from 32% to 49%, and family medicine rose from 35% to 43% during that time.
Specialist pay gap narrows slightly
The gender gap was the same this year in primary care — women made 25% less ($212,000 vs. $264,000).
The gap in specialists narrowed slightly. Women made 31% less this year ($286,000 vs $375,000) instead of the 33% less reported in last year’s survey, a difference of $89,000 this year.
The gender pay gap was consistent across all race and age groups and was consistent in responses about net worth. Whereas 57% of male physicians had a net worth of $1 million or more, only 40% of female physicians did. Twice as many male physicians as female physicians had a net worth of more than $5 million (10% vs. 5%).
“Many physicians expect the gender pay gap to narrow in the coming years,” John Prescott, MD, chief academic officer of the Association of American Medical Colleges, said in an interview.
“Yet, it is a challenging task, requiring an institutional commitment to transparency, cross-campus collaboration, ongoing communication, dedicated resources, and enlightened leadership,” he said.
Female physicians working in office-based, solo practices made the most overall at $290,000; women in outpatient settings made the least at $223,000.
The survey included more than 4,500 responses. The responses were collected during the early part of the year and do not reflect changes in income expected from the COVID-19 pandemic.
An analysis in Health Affairs, for instance, predicted that primary care practices would lose $67,774 in gross revenue per full-time-equivalent physician in calendar year 2020 because of the pandemic.
Most physicians did not experience a significant financial loss in 2019, but COVID-19 may, at least temporarily, change those answers in next year’s report, physicians predicted.
Women more likely than men to live above their means
More women this year (39%) said they live below their means than answered that way last year (31%). Female physicians were more likely to say they lived above their means than were their male counterparts (8% vs. 6%).
Greenwald Wealth Management in St. Louis Park, Minn., says aiming for putting away 20% of total gross salary is a good financial goal.
Women in this year’s survey spent about 7% less time seeing patients than did their male counterparts (35.9 hours a week vs. 38.8). The average for all physicians was 37.8 hours a week. Add the 15.6 average hours per week physicians spend on paperwork, and they are putting in 53-hour workweeks on average overall.
Asked what parts of their job they found most rewarding, women were more likely than were men to say “gratitude/relationships with patients” (31% vs. 25%). They were less likely than were men to answer that the most rewarding part was “being very good at what I do/finding answers/diagnoses” (22% vs. 25%) or “making good money at a job I like” (9% vs. 13%).
Most female physicians — and physicians overall — said they would choose medicine again. But two specialties saw a substantial increase in that answer.
This year, 79% of those in physical medicine and rehabilitation said they would choose medicine again (compared with 66% last year) and 84% of gastroenterologists answered that way (compared with 76% in 2019).
Psychiatrists, however, were in the group least likely to say they would choose their specialty again along with those in internal medicine, family medicine, and diabetes and endocrinology.
Female physicians in orthopedics, radiology, and dermatology were most likely to choose their specialties again (91% - 92%).
Female physicians were less likely to use physician assistants in their practices than were their male colleagues (31% vs. 38%) but more likely to use NPs (52% vs. 50%). More than a third (38%) of male and female physicians reported they use neither.
A version of this article originally appeared on Medscape.com.
Effect of a Smartphone App Plus an Accelerometer on Physical Activity and Functional Recovery During Hospitalization After Orthopedic Surgery
Study Overview
Objective. To investigate the potential of Hospital Fit (a smartphone application with an accelerometer) to enhance physical activity levels and functional recovery following orthopedic surgery.
Design. Nonrandomized, quasi-experimental pilot study.
Settings and participants. Patients scheduled for an elective total knee arthroplasty (TKA) or total hip arthroplasty (THA) at the orthopedic ward of Maastricht University Medical Center in Maastricht, the Netherlands, were invited to participate. Patients scheduled for surgery between January 2017 and December 2018 were recruited for the control group at a rate of 1 patient per week (due to a limited number of accelerometers available). After development of Hospital Fit was completed in December 2018 (and sufficient accelerators had become available), patients scheduled for surgery between February 2019 and May 2019 were recruited for the intervention group. The ratio of patients included in the control and intervention group was set at 2:1, respectively.
At preoperative physiotherapy screenings (scheduled 6 weeks before surgery), patients received verbal and written information about the study. Patients were eligible if they met the following inclusion criteria: receiving physiotherapy after elective TKA or THA; able to walk independently 2 weeks prior to surgery, as scored on the Functional Ambulation Categories (FAC > 3); were expected to be discharged to their own home; were aged 18 years and older; and had a sufficient understanding of the Dutch language. Exclusion criteria were: the presence of contraindications to walking or wearing an accelerometer on the upper leg; admission to the intensive care unit; impaired cognition (delirium/dementia), as reported by the attending doctor; a life expectancy of less than 3 months; and previous participation in this study. Patients were contacted on the day of their surgery, and written informed consent was obtained prior to the initiation of any study activities.
Intervention. Once enrolled, all patients followed a standardized clinical care pathway for TKA or THA (see original article for additional details). Postoperative physiotherapy was administered to all participating patients, starting within 4 hours after surgery. The physiotherapy treatment was aimed at increasing physical activity levels and enhancing functional recovery. Control group patients only received physiotherapy (twice daily, 30 minutes per session) and had their physical activity levels monitored with an accelerometer, without receiving feedback, until functional recovery was achieved, as measured with the modified Iowa Level of Assistance Scale (mILAS). Intervention group patients used Hospital Fit in addition to physiotherapy. Hospital Fit consists of a smartphone-based app, connected to a MOX activity monitor via Bluetooth (device contains a tri-axial accelerometer sensor in a small waterproof housing attached to the upper leg). Hospital Fit enables objective activity monitoring, provides patients and their physiotherapists insights and real-time feedback on the number of minutes spent standing and walking per day, and offers a tailored exercise program supported by videos aimed at stimulating self-management.
Measures. The primary outcome measure was the time spent physically active (total number of minutes standing and walking) per day until discharge. Physical activity was monitored 24 hours a day; days with ≥ 20 hours of wear time were considered valid measurement days and were included in the analysis. After the last treatment session, the accelerometer was removed, and the raw tri-axial accelerometer data were uploaded and processed to classify minutes as “active” (standing and walking) or “sedentary” (lying and sitting). The secondary outcome measures were the achievement of functional recovery on postoperative day 1 (POD1). Functional recovery was assessed by the physiotherapist during each treatment session using the mILAS and was reported in the electronic health record. In the intervention group, it was also reported in the app. The achievement of functional recovery on POD1 was defined as having reached a total mILAS-score of 0 on or before POD1, using a dichotomized outcome (0 = mILAS = 0 > POD1; 1 = mILAS = 0 ≤ POD1).
The independent variables measured were: Hospital Fit use (control versus the intervention group), age, sex, body mass index (BMI), type of surgery (TKA or THA), and comorbidities assessed by the American Society of Anesthesiologists (ASA) classification (ASA class ≤ 2 versus ASA class = 3; a higher score indicates being less fit for surgery). The medical and demographic data measured were the type of walking aid used and length of stay, with the day of surgery being defined as day 1.
Analysis. Data analysis was performed according to the intention-to-treat principle. Missing values were not substituted; drop-outs were not replaced. Descriptive statistics were presented as means (SD) or as 95% confidence intervals (CI) for continuous variables. The median and interquartile ranges (IQR) were used to present non-normally distributed data. The frequencies and percentages were used to present categorical variables. A multiple linear regression analysis was performed to determine the association between the time spent physically active per day and Hospital Fit use, corrected for potential confounding factors (age, sex, BMI, ASA class, and type of surgery). A multiple logistic regression analysis was performed additionally to determine the association between the achievement of functional recovery on POD1 and Hospital Fit use, corrected for potential confounding factors. For all statistical analyses, the level of significance was set at P < 0.05. All statistical analyses were performed using SPSS (version 23.0.0.2; IBM Corporation, Armonk, NY).
Main results. Ninety-seven patients were recruited; after excluding 9 patients because of missing data, 88 were included for analysis, with 61 (69%) in the control group and 27 (31%) in the intervention group. A median (IQR) number of 1.00 (0) valid measurement days (≥ 20 hr wear time) was collected. Physical activity data for 84 patients (95%) was available on POD1 (n = 61 control group, n = 23 intervention group). On postoperative day 2 (POD2), the majority of patients were discharged (n = 61, 69%), and data for only 23 patients (26%) were available (n = 17 control, n = 6 intervention). From postoperative day 3 to day 7, data of valid measurement days were available for just 1 patient (intervention group). Due to the large reduction in valid measurement days from POD2 onward, data from these days were not included in the analysis.
Results of the multiple linear regression analysis showed that, corrected for age, patients who used Hospital Fit stood and walked an average of 28.43 minutes (95% CI, 5.55-51.32) more on POD1 than patients who did not use Hospital Fit. Also, the model showed that an increase in age led to a decrease in the number of minutes standing and walking on POD1. The results of the multiple logistic regression analysis also showed that, corrected for ASA class, the odds of achieving functional recovery on POD1 were 3.08 times higher (95% CI, 1.14-8.31) for patients who used Hospital Fit compared to patients who did not use Hospital Fit. Including ASA class in the model shows that a lower ASA class increased the odds ratio for a functional recovery on POD1.
Conclusion. A smartphone app combined with an accelerometer demonstrates the potential to enhance patients’ physical activity levels and functional recovery during hospitalization following joint replacement surgery.
Commentary
Although the beneficial effects of physical activity during hospitalization after surgery are well documented, patients continue to spend between 92% and 96% of their time lying or sitting.1-3 Therefore, strategies aimed at increasing the amount of time spent standing and walking are needed. Postoperative physiotherapy aims to enhance physical activity levels and functional recovery of activities of daily living, which are essential to function independently at home.4-7 Physiotherapists may be able to advise patients more effectively on their physical activity behavior if continuous physical activity monitoring with real-time feedback is implemented in standard care. Although mobile health (mHealth) tools are being used to monitor physical activity in support of outpatient physiotherapy within the orthopedic rehabilitation pathway,8-10 there is currently no mHealth tool available that offers hospitalized patients and their physiotherapists essential strategies to enhance their physical activity levels and support their recovery process. In addition, because hospitalized patients frequently use walking aids and often have impaired gait, the algorithm of most available activity monitors is not validated for use in this population.
This study, therefore, is an important contribution to the literature, as it describes a preliminary evaluation of a novel mHealth tool—Hospital Fit—consisting of a smartphone application connected to an accelerometer whose algorithm has been validated to differentiate between lying/sitting and standing/walking among hospitalized patients. Briefly, results from this study showed an increase in the time spent standing and walking, as well as higher odds of functional recovery on POD1 from the introduction of Hospital Fit. While guidelines on the recommended amount of physical activity during hospitalization do not yet exist, an average improvement of 28 minutes (39%) standing and walking on POD1 can be considered a clinically relevant contribution to prevent the negative effects of inactivity.
This study has limitations, particularly related to the study design, which is acknowledged by the authors. The current study was a nonrandomized, quasi-experimental pilot study implemented at a single medical center, and therefore, the results have limited generalizability and more importantly, may not only be attributable to the introduction of Hospital Fit. In addition, as there was lag in patient recruitment where patients were initially selected for the control group over the course of 1 year, followed by selection of patients for the intervention group over 4 months (once Hospital Fit was developed), it is possible that awareness on the importance of physical activity during hospitalization increased among patients and health care professionals, which may have resulted in a bias in favor of the intervention group (and thus a potentially slight overestimation of results). Also, as individual functionalities of Hospital Fit were not investigated, relationships between each functionality and physical activity could not be established. As the authors indicated, future research is needed to determine the effectiveness of Hospital Fit (ie, a larger, cluster randomized controlled trial in a population of hospitalized patients with a longer length of stay). This study design would also enable investigation of the effect of individual functionalities of Hospital Fit on physical activity.
Applications for Clinical Practice
mHealth tools have the potential to increase patient awareness, support personalized care, and stimulate self-management. This study highlights the potential for a novel mHealth tool—Hospital Fit—to improve the amount of physical activity and shorten the time to functional recovery in hospitalized patients following orthopedic surgery. Further, mHealth tools like Hospital Fit may have a greater impact when the hospital stay of a patient permits the use of the tool for a longer period of time. More broadly, continuous objective monitoring through mHealth tools may provide patients and their physiotherapists enhanced and more detailed data to support and create more personalized recovery goals and related strategies.
Katrina F. Mateo, PhD, MPH
1. Brown CJ, Roth DL, Allman RM. Validation of use of wireless monitors to measure levels of mobility during hospitalization. J Rehabil Res Dev. 2008;45:551-558.
2. Pedersen MM, Bodilsen AC, Petersen J, et al. Twenty-four-hour mobility during acute hospitalization in older medical patients. J Gerontol Ser A Biol Sci Med Sci. 2013;68:331–337.
3. Evensen S, Sletvold O, Lydersen S, Taraldsen K. Physical activity among hospitalized older adults – an observational study. BMC Geriatr. 2017;17:110.
4. Engdal M, Foss OA, Taraldsen K, et al. Daily physical activity in total hip arthroplasty patients undergoing different surgical approaches: a cohort study. Am J Phys Med Rehabil. 2017;96:473-478.
5. Hoogeboom TJ, Dronkers JJ, Hulzebos EH, van Meeteren NL. Merits of exercise therapy before and after major surgery. Curr Opin Anaesthesiol. 2014;27:161-166.
6. Hoogeboom TJ, van Meeteren NL, Schank K, et al. Risk factors for delayed inpatient functional recovery after total knee arthroplasty. Biomed Res Int. 2015:2015:167643.
7. Lenssen AF, Crijns YH, Waltje EM, et al. Efficiency of immediate postoperative inpatient physical therapy following total knee arthroplasty: an RCT. BMC Musculoskelet Disord. 2006;7:71.
8. Ramkumar PN, Haeberle HS, Ramanathan D, et al. Remote patient monitoring using mobile health for total knee arthroplasty: validation of a wearable and machine learning-based surveillance platform. J Arthroplast. 2019;34:2253-2259.
9. Ramkumar PN, Haeberle HS, Bloomfield MR, et al. Artificial Intelligence and arthroplasty at a single institution: Real-world applications of machine learning to big data, value-based care, mobile health, and remote patient monitoring. J Arthroplast. 2019;34:2204-2209.
10. Correia FD, Nogueira A, Magalhães I, et al, et al. Medium-term outcomes of digital versus conventional home-based rehabilitation after total knee arthroplasty: prospective, parallel-group feasibility study. JMIR Rehabil Assist Technol. 2019;6:e13111.
Study Overview
Objective. To investigate the potential of Hospital Fit (a smartphone application with an accelerometer) to enhance physical activity levels and functional recovery following orthopedic surgery.
Design. Nonrandomized, quasi-experimental pilot study.
Settings and participants. Patients scheduled for an elective total knee arthroplasty (TKA) or total hip arthroplasty (THA) at the orthopedic ward of Maastricht University Medical Center in Maastricht, the Netherlands, were invited to participate. Patients scheduled for surgery between January 2017 and December 2018 were recruited for the control group at a rate of 1 patient per week (due to a limited number of accelerometers available). After development of Hospital Fit was completed in December 2018 (and sufficient accelerators had become available), patients scheduled for surgery between February 2019 and May 2019 were recruited for the intervention group. The ratio of patients included in the control and intervention group was set at 2:1, respectively.
At preoperative physiotherapy screenings (scheduled 6 weeks before surgery), patients received verbal and written information about the study. Patients were eligible if they met the following inclusion criteria: receiving physiotherapy after elective TKA or THA; able to walk independently 2 weeks prior to surgery, as scored on the Functional Ambulation Categories (FAC > 3); were expected to be discharged to their own home; were aged 18 years and older; and had a sufficient understanding of the Dutch language. Exclusion criteria were: the presence of contraindications to walking or wearing an accelerometer on the upper leg; admission to the intensive care unit; impaired cognition (delirium/dementia), as reported by the attending doctor; a life expectancy of less than 3 months; and previous participation in this study. Patients were contacted on the day of their surgery, and written informed consent was obtained prior to the initiation of any study activities.
Intervention. Once enrolled, all patients followed a standardized clinical care pathway for TKA or THA (see original article for additional details). Postoperative physiotherapy was administered to all participating patients, starting within 4 hours after surgery. The physiotherapy treatment was aimed at increasing physical activity levels and enhancing functional recovery. Control group patients only received physiotherapy (twice daily, 30 minutes per session) and had their physical activity levels monitored with an accelerometer, without receiving feedback, until functional recovery was achieved, as measured with the modified Iowa Level of Assistance Scale (mILAS). Intervention group patients used Hospital Fit in addition to physiotherapy. Hospital Fit consists of a smartphone-based app, connected to a MOX activity monitor via Bluetooth (device contains a tri-axial accelerometer sensor in a small waterproof housing attached to the upper leg). Hospital Fit enables objective activity monitoring, provides patients and their physiotherapists insights and real-time feedback on the number of minutes spent standing and walking per day, and offers a tailored exercise program supported by videos aimed at stimulating self-management.
Measures. The primary outcome measure was the time spent physically active (total number of minutes standing and walking) per day until discharge. Physical activity was monitored 24 hours a day; days with ≥ 20 hours of wear time were considered valid measurement days and were included in the analysis. After the last treatment session, the accelerometer was removed, and the raw tri-axial accelerometer data were uploaded and processed to classify minutes as “active” (standing and walking) or “sedentary” (lying and sitting). The secondary outcome measures were the achievement of functional recovery on postoperative day 1 (POD1). Functional recovery was assessed by the physiotherapist during each treatment session using the mILAS and was reported in the electronic health record. In the intervention group, it was also reported in the app. The achievement of functional recovery on POD1 was defined as having reached a total mILAS-score of 0 on or before POD1, using a dichotomized outcome (0 = mILAS = 0 > POD1; 1 = mILAS = 0 ≤ POD1).
The independent variables measured were: Hospital Fit use (control versus the intervention group), age, sex, body mass index (BMI), type of surgery (TKA or THA), and comorbidities assessed by the American Society of Anesthesiologists (ASA) classification (ASA class ≤ 2 versus ASA class = 3; a higher score indicates being less fit for surgery). The medical and demographic data measured were the type of walking aid used and length of stay, with the day of surgery being defined as day 1.
Analysis. Data analysis was performed according to the intention-to-treat principle. Missing values were not substituted; drop-outs were not replaced. Descriptive statistics were presented as means (SD) or as 95% confidence intervals (CI) for continuous variables. The median and interquartile ranges (IQR) were used to present non-normally distributed data. The frequencies and percentages were used to present categorical variables. A multiple linear regression analysis was performed to determine the association between the time spent physically active per day and Hospital Fit use, corrected for potential confounding factors (age, sex, BMI, ASA class, and type of surgery). A multiple logistic regression analysis was performed additionally to determine the association between the achievement of functional recovery on POD1 and Hospital Fit use, corrected for potential confounding factors. For all statistical analyses, the level of significance was set at P < 0.05. All statistical analyses were performed using SPSS (version 23.0.0.2; IBM Corporation, Armonk, NY).
Main results. Ninety-seven patients were recruited; after excluding 9 patients because of missing data, 88 were included for analysis, with 61 (69%) in the control group and 27 (31%) in the intervention group. A median (IQR) number of 1.00 (0) valid measurement days (≥ 20 hr wear time) was collected. Physical activity data for 84 patients (95%) was available on POD1 (n = 61 control group, n = 23 intervention group). On postoperative day 2 (POD2), the majority of patients were discharged (n = 61, 69%), and data for only 23 patients (26%) were available (n = 17 control, n = 6 intervention). From postoperative day 3 to day 7, data of valid measurement days were available for just 1 patient (intervention group). Due to the large reduction in valid measurement days from POD2 onward, data from these days were not included in the analysis.
Results of the multiple linear regression analysis showed that, corrected for age, patients who used Hospital Fit stood and walked an average of 28.43 minutes (95% CI, 5.55-51.32) more on POD1 than patients who did not use Hospital Fit. Also, the model showed that an increase in age led to a decrease in the number of minutes standing and walking on POD1. The results of the multiple logistic regression analysis also showed that, corrected for ASA class, the odds of achieving functional recovery on POD1 were 3.08 times higher (95% CI, 1.14-8.31) for patients who used Hospital Fit compared to patients who did not use Hospital Fit. Including ASA class in the model shows that a lower ASA class increased the odds ratio for a functional recovery on POD1.
Conclusion. A smartphone app combined with an accelerometer demonstrates the potential to enhance patients’ physical activity levels and functional recovery during hospitalization following joint replacement surgery.
Commentary
Although the beneficial effects of physical activity during hospitalization after surgery are well documented, patients continue to spend between 92% and 96% of their time lying or sitting.1-3 Therefore, strategies aimed at increasing the amount of time spent standing and walking are needed. Postoperative physiotherapy aims to enhance physical activity levels and functional recovery of activities of daily living, which are essential to function independently at home.4-7 Physiotherapists may be able to advise patients more effectively on their physical activity behavior if continuous physical activity monitoring with real-time feedback is implemented in standard care. Although mobile health (mHealth) tools are being used to monitor physical activity in support of outpatient physiotherapy within the orthopedic rehabilitation pathway,8-10 there is currently no mHealth tool available that offers hospitalized patients and their physiotherapists essential strategies to enhance their physical activity levels and support their recovery process. In addition, because hospitalized patients frequently use walking aids and often have impaired gait, the algorithm of most available activity monitors is not validated for use in this population.
This study, therefore, is an important contribution to the literature, as it describes a preliminary evaluation of a novel mHealth tool—Hospital Fit—consisting of a smartphone application connected to an accelerometer whose algorithm has been validated to differentiate between lying/sitting and standing/walking among hospitalized patients. Briefly, results from this study showed an increase in the time spent standing and walking, as well as higher odds of functional recovery on POD1 from the introduction of Hospital Fit. While guidelines on the recommended amount of physical activity during hospitalization do not yet exist, an average improvement of 28 minutes (39%) standing and walking on POD1 can be considered a clinically relevant contribution to prevent the negative effects of inactivity.
This study has limitations, particularly related to the study design, which is acknowledged by the authors. The current study was a nonrandomized, quasi-experimental pilot study implemented at a single medical center, and therefore, the results have limited generalizability and more importantly, may not only be attributable to the introduction of Hospital Fit. In addition, as there was lag in patient recruitment where patients were initially selected for the control group over the course of 1 year, followed by selection of patients for the intervention group over 4 months (once Hospital Fit was developed), it is possible that awareness on the importance of physical activity during hospitalization increased among patients and health care professionals, which may have resulted in a bias in favor of the intervention group (and thus a potentially slight overestimation of results). Also, as individual functionalities of Hospital Fit were not investigated, relationships between each functionality and physical activity could not be established. As the authors indicated, future research is needed to determine the effectiveness of Hospital Fit (ie, a larger, cluster randomized controlled trial in a population of hospitalized patients with a longer length of stay). This study design would also enable investigation of the effect of individual functionalities of Hospital Fit on physical activity.
Applications for Clinical Practice
mHealth tools have the potential to increase patient awareness, support personalized care, and stimulate self-management. This study highlights the potential for a novel mHealth tool—Hospital Fit—to improve the amount of physical activity and shorten the time to functional recovery in hospitalized patients following orthopedic surgery. Further, mHealth tools like Hospital Fit may have a greater impact when the hospital stay of a patient permits the use of the tool for a longer period of time. More broadly, continuous objective monitoring through mHealth tools may provide patients and their physiotherapists enhanced and more detailed data to support and create more personalized recovery goals and related strategies.
Katrina F. Mateo, PhD, MPH
Study Overview
Objective. To investigate the potential of Hospital Fit (a smartphone application with an accelerometer) to enhance physical activity levels and functional recovery following orthopedic surgery.
Design. Nonrandomized, quasi-experimental pilot study.
Settings and participants. Patients scheduled for an elective total knee arthroplasty (TKA) or total hip arthroplasty (THA) at the orthopedic ward of Maastricht University Medical Center in Maastricht, the Netherlands, were invited to participate. Patients scheduled for surgery between January 2017 and December 2018 were recruited for the control group at a rate of 1 patient per week (due to a limited number of accelerometers available). After development of Hospital Fit was completed in December 2018 (and sufficient accelerators had become available), patients scheduled for surgery between February 2019 and May 2019 were recruited for the intervention group. The ratio of patients included in the control and intervention group was set at 2:1, respectively.
At preoperative physiotherapy screenings (scheduled 6 weeks before surgery), patients received verbal and written information about the study. Patients were eligible if they met the following inclusion criteria: receiving physiotherapy after elective TKA or THA; able to walk independently 2 weeks prior to surgery, as scored on the Functional Ambulation Categories (FAC > 3); were expected to be discharged to their own home; were aged 18 years and older; and had a sufficient understanding of the Dutch language. Exclusion criteria were: the presence of contraindications to walking or wearing an accelerometer on the upper leg; admission to the intensive care unit; impaired cognition (delirium/dementia), as reported by the attending doctor; a life expectancy of less than 3 months; and previous participation in this study. Patients were contacted on the day of their surgery, and written informed consent was obtained prior to the initiation of any study activities.
Intervention. Once enrolled, all patients followed a standardized clinical care pathway for TKA or THA (see original article for additional details). Postoperative physiotherapy was administered to all participating patients, starting within 4 hours after surgery. The physiotherapy treatment was aimed at increasing physical activity levels and enhancing functional recovery. Control group patients only received physiotherapy (twice daily, 30 minutes per session) and had their physical activity levels monitored with an accelerometer, without receiving feedback, until functional recovery was achieved, as measured with the modified Iowa Level of Assistance Scale (mILAS). Intervention group patients used Hospital Fit in addition to physiotherapy. Hospital Fit consists of a smartphone-based app, connected to a MOX activity monitor via Bluetooth (device contains a tri-axial accelerometer sensor in a small waterproof housing attached to the upper leg). Hospital Fit enables objective activity monitoring, provides patients and their physiotherapists insights and real-time feedback on the number of minutes spent standing and walking per day, and offers a tailored exercise program supported by videos aimed at stimulating self-management.
Measures. The primary outcome measure was the time spent physically active (total number of minutes standing and walking) per day until discharge. Physical activity was monitored 24 hours a day; days with ≥ 20 hours of wear time were considered valid measurement days and were included in the analysis. After the last treatment session, the accelerometer was removed, and the raw tri-axial accelerometer data were uploaded and processed to classify minutes as “active” (standing and walking) or “sedentary” (lying and sitting). The secondary outcome measures were the achievement of functional recovery on postoperative day 1 (POD1). Functional recovery was assessed by the physiotherapist during each treatment session using the mILAS and was reported in the electronic health record. In the intervention group, it was also reported in the app. The achievement of functional recovery on POD1 was defined as having reached a total mILAS-score of 0 on or before POD1, using a dichotomized outcome (0 = mILAS = 0 > POD1; 1 = mILAS = 0 ≤ POD1).
The independent variables measured were: Hospital Fit use (control versus the intervention group), age, sex, body mass index (BMI), type of surgery (TKA or THA), and comorbidities assessed by the American Society of Anesthesiologists (ASA) classification (ASA class ≤ 2 versus ASA class = 3; a higher score indicates being less fit for surgery). The medical and demographic data measured were the type of walking aid used and length of stay, with the day of surgery being defined as day 1.
Analysis. Data analysis was performed according to the intention-to-treat principle. Missing values were not substituted; drop-outs were not replaced. Descriptive statistics were presented as means (SD) or as 95% confidence intervals (CI) for continuous variables. The median and interquartile ranges (IQR) were used to present non-normally distributed data. The frequencies and percentages were used to present categorical variables. A multiple linear regression analysis was performed to determine the association between the time spent physically active per day and Hospital Fit use, corrected for potential confounding factors (age, sex, BMI, ASA class, and type of surgery). A multiple logistic regression analysis was performed additionally to determine the association between the achievement of functional recovery on POD1 and Hospital Fit use, corrected for potential confounding factors. For all statistical analyses, the level of significance was set at P < 0.05. All statistical analyses were performed using SPSS (version 23.0.0.2; IBM Corporation, Armonk, NY).
Main results. Ninety-seven patients were recruited; after excluding 9 patients because of missing data, 88 were included for analysis, with 61 (69%) in the control group and 27 (31%) in the intervention group. A median (IQR) number of 1.00 (0) valid measurement days (≥ 20 hr wear time) was collected. Physical activity data for 84 patients (95%) was available on POD1 (n = 61 control group, n = 23 intervention group). On postoperative day 2 (POD2), the majority of patients were discharged (n = 61, 69%), and data for only 23 patients (26%) were available (n = 17 control, n = 6 intervention). From postoperative day 3 to day 7, data of valid measurement days were available for just 1 patient (intervention group). Due to the large reduction in valid measurement days from POD2 onward, data from these days were not included in the analysis.
Results of the multiple linear regression analysis showed that, corrected for age, patients who used Hospital Fit stood and walked an average of 28.43 minutes (95% CI, 5.55-51.32) more on POD1 than patients who did not use Hospital Fit. Also, the model showed that an increase in age led to a decrease in the number of minutes standing and walking on POD1. The results of the multiple logistic regression analysis also showed that, corrected for ASA class, the odds of achieving functional recovery on POD1 were 3.08 times higher (95% CI, 1.14-8.31) for patients who used Hospital Fit compared to patients who did not use Hospital Fit. Including ASA class in the model shows that a lower ASA class increased the odds ratio for a functional recovery on POD1.
Conclusion. A smartphone app combined with an accelerometer demonstrates the potential to enhance patients’ physical activity levels and functional recovery during hospitalization following joint replacement surgery.
Commentary
Although the beneficial effects of physical activity during hospitalization after surgery are well documented, patients continue to spend between 92% and 96% of their time lying or sitting.1-3 Therefore, strategies aimed at increasing the amount of time spent standing and walking are needed. Postoperative physiotherapy aims to enhance physical activity levels and functional recovery of activities of daily living, which are essential to function independently at home.4-7 Physiotherapists may be able to advise patients more effectively on their physical activity behavior if continuous physical activity monitoring with real-time feedback is implemented in standard care. Although mobile health (mHealth) tools are being used to monitor physical activity in support of outpatient physiotherapy within the orthopedic rehabilitation pathway,8-10 there is currently no mHealth tool available that offers hospitalized patients and their physiotherapists essential strategies to enhance their physical activity levels and support their recovery process. In addition, because hospitalized patients frequently use walking aids and often have impaired gait, the algorithm of most available activity monitors is not validated for use in this population.
This study, therefore, is an important contribution to the literature, as it describes a preliminary evaluation of a novel mHealth tool—Hospital Fit—consisting of a smartphone application connected to an accelerometer whose algorithm has been validated to differentiate between lying/sitting and standing/walking among hospitalized patients. Briefly, results from this study showed an increase in the time spent standing and walking, as well as higher odds of functional recovery on POD1 from the introduction of Hospital Fit. While guidelines on the recommended amount of physical activity during hospitalization do not yet exist, an average improvement of 28 minutes (39%) standing and walking on POD1 can be considered a clinically relevant contribution to prevent the negative effects of inactivity.
This study has limitations, particularly related to the study design, which is acknowledged by the authors. The current study was a nonrandomized, quasi-experimental pilot study implemented at a single medical center, and therefore, the results have limited generalizability and more importantly, may not only be attributable to the introduction of Hospital Fit. In addition, as there was lag in patient recruitment where patients were initially selected for the control group over the course of 1 year, followed by selection of patients for the intervention group over 4 months (once Hospital Fit was developed), it is possible that awareness on the importance of physical activity during hospitalization increased among patients and health care professionals, which may have resulted in a bias in favor of the intervention group (and thus a potentially slight overestimation of results). Also, as individual functionalities of Hospital Fit were not investigated, relationships between each functionality and physical activity could not be established. As the authors indicated, future research is needed to determine the effectiveness of Hospital Fit (ie, a larger, cluster randomized controlled trial in a population of hospitalized patients with a longer length of stay). This study design would also enable investigation of the effect of individual functionalities of Hospital Fit on physical activity.
Applications for Clinical Practice
mHealth tools have the potential to increase patient awareness, support personalized care, and stimulate self-management. This study highlights the potential for a novel mHealth tool—Hospital Fit—to improve the amount of physical activity and shorten the time to functional recovery in hospitalized patients following orthopedic surgery. Further, mHealth tools like Hospital Fit may have a greater impact when the hospital stay of a patient permits the use of the tool for a longer period of time. More broadly, continuous objective monitoring through mHealth tools may provide patients and their physiotherapists enhanced and more detailed data to support and create more personalized recovery goals and related strategies.
Katrina F. Mateo, PhD, MPH
1. Brown CJ, Roth DL, Allman RM. Validation of use of wireless monitors to measure levels of mobility during hospitalization. J Rehabil Res Dev. 2008;45:551-558.
2. Pedersen MM, Bodilsen AC, Petersen J, et al. Twenty-four-hour mobility during acute hospitalization in older medical patients. J Gerontol Ser A Biol Sci Med Sci. 2013;68:331–337.
3. Evensen S, Sletvold O, Lydersen S, Taraldsen K. Physical activity among hospitalized older adults – an observational study. BMC Geriatr. 2017;17:110.
4. Engdal M, Foss OA, Taraldsen K, et al. Daily physical activity in total hip arthroplasty patients undergoing different surgical approaches: a cohort study. Am J Phys Med Rehabil. 2017;96:473-478.
5. Hoogeboom TJ, Dronkers JJ, Hulzebos EH, van Meeteren NL. Merits of exercise therapy before and after major surgery. Curr Opin Anaesthesiol. 2014;27:161-166.
6. Hoogeboom TJ, van Meeteren NL, Schank K, et al. Risk factors for delayed inpatient functional recovery after total knee arthroplasty. Biomed Res Int. 2015:2015:167643.
7. Lenssen AF, Crijns YH, Waltje EM, et al. Efficiency of immediate postoperative inpatient physical therapy following total knee arthroplasty: an RCT. BMC Musculoskelet Disord. 2006;7:71.
8. Ramkumar PN, Haeberle HS, Ramanathan D, et al. Remote patient monitoring using mobile health for total knee arthroplasty: validation of a wearable and machine learning-based surveillance platform. J Arthroplast. 2019;34:2253-2259.
9. Ramkumar PN, Haeberle HS, Bloomfield MR, et al. Artificial Intelligence and arthroplasty at a single institution: Real-world applications of machine learning to big data, value-based care, mobile health, and remote patient monitoring. J Arthroplast. 2019;34:2204-2209.
10. Correia FD, Nogueira A, Magalhães I, et al, et al. Medium-term outcomes of digital versus conventional home-based rehabilitation after total knee arthroplasty: prospective, parallel-group feasibility study. JMIR Rehabil Assist Technol. 2019;6:e13111.
1. Brown CJ, Roth DL, Allman RM. Validation of use of wireless monitors to measure levels of mobility during hospitalization. J Rehabil Res Dev. 2008;45:551-558.
2. Pedersen MM, Bodilsen AC, Petersen J, et al. Twenty-four-hour mobility during acute hospitalization in older medical patients. J Gerontol Ser A Biol Sci Med Sci. 2013;68:331–337.
3. Evensen S, Sletvold O, Lydersen S, Taraldsen K. Physical activity among hospitalized older adults – an observational study. BMC Geriatr. 2017;17:110.
4. Engdal M, Foss OA, Taraldsen K, et al. Daily physical activity in total hip arthroplasty patients undergoing different surgical approaches: a cohort study. Am J Phys Med Rehabil. 2017;96:473-478.
5. Hoogeboom TJ, Dronkers JJ, Hulzebos EH, van Meeteren NL. Merits of exercise therapy before and after major surgery. Curr Opin Anaesthesiol. 2014;27:161-166.
6. Hoogeboom TJ, van Meeteren NL, Schank K, et al. Risk factors for delayed inpatient functional recovery after total knee arthroplasty. Biomed Res Int. 2015:2015:167643.
7. Lenssen AF, Crijns YH, Waltje EM, et al. Efficiency of immediate postoperative inpatient physical therapy following total knee arthroplasty: an RCT. BMC Musculoskelet Disord. 2006;7:71.
8. Ramkumar PN, Haeberle HS, Ramanathan D, et al. Remote patient monitoring using mobile health for total knee arthroplasty: validation of a wearable and machine learning-based surveillance platform. J Arthroplast. 2019;34:2253-2259.
9. Ramkumar PN, Haeberle HS, Bloomfield MR, et al. Artificial Intelligence and arthroplasty at a single institution: Real-world applications of machine learning to big data, value-based care, mobile health, and remote patient monitoring. J Arthroplast. 2019;34:2204-2209.
10. Correia FD, Nogueira A, Magalhães I, et al, et al. Medium-term outcomes of digital versus conventional home-based rehabilitation after total knee arthroplasty: prospective, parallel-group feasibility study. JMIR Rehabil Assist Technol. 2019;6:e13111.
2020-2021 respiratory viral season: Onset, presentations, and testing likely to differ in pandemic
Respiratory virus seasons usually follow a fairly well-known pattern. Enterovirus 68 (EV-D68) is a summer-to-early fall virus with biennial peak years. Rhinovirus (HRv) and adenovirus (Adv) occur nearly year-round but may have small upticks in the first month or so that children return to school. Early in the school year, upper respiratory infections from both HRv and Adv and viral sore throats from Adv are common, with conjunctivitis from Adv outbreaks in some years. October to November is human parainfluenza (HPiV) 1 and 2 season, often presenting as croup. Human metapneumovirus infections span October through April. In late November to December, influenza begins, usually with an A type, later transitioning to a B type in February through April. Also in December, respiratory syncytial virus (RSV) starts, characteristically with bronchiolitis presentations, peaking in February to March and tapering off in May. In late March to April, HPiV 3 also appears for 4-6 weeks.

Will 2020-2021 be different?
Summer was remarkably free of expected enterovirus activity, suggesting that the seasonal parade may differ this year. Remember that the 2019-2020 respiratory season suddenly and nearly completely stopped in March because of social distancing and lockdowns needed to address the SARS-CoV-2 pandemic.
The mild influenza season in the southern hemisphere suggests that our influenza season also could be mild. But perhaps not – most southern hemisphere countries that are surveyed for influenza activities had the most intense SARS-CoV-2 mitigations, making the observed mildness potentially related more to social mitigation than less virulent influenza strains. If so, southern hemisphere influenza data may not apply to the United States, where social distancing and masks are ignored or used inconsistently by almost half the population.
Further, the stop-and-go pattern of in-person school/college attendance adds to uncertainties for the usual orderly virus-specific seasonality. The result may be multiple stop-and-go “pop-up” or “mini” outbreaks for any given virus potentially reflected as exaggerated local or regional differences in circulation of various viruses. The erratic seasonality also would increase coinfections, which could present with more severe or different symptoms.
SARS-CoV-2’s potential interaction
Will the relatively mild presentations for most children with SARS-CoV-2 hold up in the setting of coinfections or sequential respiratory viral infections? Could SARS-CoV-2 cause worse/more prolonged symptoms or more sequelae if paired simultaneously or in tandem with a traditional respiratory virus? To date, data on the frequency and severity of SARS-CoV-2 coinfections are conflicting and sparse, but it appears that non-SARS-CoV-2 viruses can be involved in 15%-50% pediatric acute respiratory infections.1,2
However, it may not be important to know about coinfecting viruses other than influenza (can be treated) or SARS-CoV-2 (needs quarantine and contact tracing), unless symptoms are atypical or more severe than usual. For example, a young child with bronchiolitis is most likely infected with RSV, but HPiV, influenza, metapneumovirus, HRv, and even SARS-CoV-2 can cause bronchiolitis. Even so, testing outpatients for RSV or non-influenza is not routine or even clinically helpful. Supportive treatment and restriction from daycare attendance are sufficient management for outpatient ARIs whether presenting as bronchiolitis or not.
Considerations for SARS-CoV-2 testing: Outpatient bronchiolitis
If a child presents with classic bronchiolitis but has above moderate to severe symptoms, is SARS-CoV-2 a consideration? Perhaps, if SARS-CoV-2 acts similarly to non-SARS-CoV-2s.
A recent report from the 30th Multicenter Airway Research Collaboration (MARC-30) surveillance study (2007-2014) of children hospitalized with clinical bronchiolitis evaluated respiratory viruses, including RSV and the four common non-SARS coronaviruses using molecular testing.3 Among 1,880 subjects, a CoV (alpha CoV: NL63 or 229E, or beta CoV: KKU1 or OC43) was detected in 12%. Yet most had only RSV (n = 1,661); 32 had only CoV (n = 32). But note that 219 had both.
Bronchiolitis subjects with CoV were older – median 3.7 (1.4-5.8) vs. 2.8 (1.9-7.2) years – and more likely male than were RSV subjects (68% vs. 58%). OC43 was most frequent followed by equal numbers of HKU1 and NL63, while 229E was the least frequent. Medical utilization and severity did not differ among the CoVs, or between RSV+CoV vs. RSV alone, unless one considered CoV viral load as a variable. ICU use increased when the polymerase chain reaction cycle threshold result indicated a high CoV viral load.
These data suggest CoVs are not infrequent coinfectors with RSV in bronchiolitis – and that SARS-CoV-2 is the same. Therefore, a bronchiolitis presentation doesn’t necessarily take us off the hook for the need to consider SARS-CoV-2 testing, particularly in the somewhat older bronchiolitis patient with more than mild symptoms.
Considerations for SARS-CoV-2 testing: Outpatient influenza-like illness
In 2020-2021, the Centers for Disease Control and Prevention recommends considering empiric antiviral treatment for ILIs (fever plus either cough or sore throat) based upon our clinical judgement, even in non-high-risk children.4
While pediatric COVID-19 illnesses are predominantly asymptomatic or mild, a febrile ARI is also a SARS-CoV-2 compatible presentation. So, if all we use is our clinical judgment, how do we know if the febrile ARI is due to influenza or SARS-CoV-2 or both? At least one study used a highly sensitive and specific molecular influenza test to show that the accuracy of clinically diagnosing influenza in children is not much better than flipping a coin and would lead to potential antiviral overuse.5
So, it seems ideal to test for influenza when possible. Point-of-care (POC) tests are frequently used for outpatients. Eight POC Clinical Laboratory Improvement Amendments (CLIA)–waived kits, some also detecting RSV, are available but most have modest sensitivity (60%-80%) compared with lab-based molecular tests.6 That said, if supplies and kits for one of the POC tests are available to us during these SARS-CoV-2 stressed times (back orders seem more common this year), a positive influenza test in the first 48 hours of symptoms confirms the option to prescribe an antiviral. Yet how will we have confidence that the febrile ARI is not also partly due to SARS-CoV-2? Currently febrile ARIs usually are considered SARS-CoV-2 and the children are sent for SARS-CoV-2 testing. During influenza season, it seems we will need to continue to send febrile outpatients for SARS-CoV-2 testing, even if POC influenza positive, via whatever mechanisms are available as time goes on.
We expect more rapid pediatric testing modalities for SARS-CoV-2 (maybe even saliva tests) to become available over the next months. Indeed, rapid antigen tests and rapid molecular tests are being evaluated in adults and seem destined for CLIA waivers as POC tests, and even home testing kits. Pediatric approvals hopefully also will occur. So, the pathways for SARS-CoV-2 testing available now will likely change over this winter. But be aware that supplies/kits will be prioritized to locations within high need areas and bulk purchase contracts. So POC kits may remain scarce for practices, meaning a reference laboratory still could be the way to go for SARS-CoV-2 for at least the rest of 2020. Reference labs are becoming creative as well; one combined detection of influenza A, influenza B, RSV, and SARS-CoV-2 into one test, and hopes to get approval for swab collection that can be done by families at home and mailed in.
Summary
Expect variations on the traditional parade of seasonal respiratory viruses, with increased numbers of coinfections. Choosing the outpatient who needs influenza testing is the same as in past years, although we have CDC permissive recommendations to prescribe antivirals for any outpatient ILI within the first 48 hours of symptoms. Still, POC testing for influenza remains potentially valuable in the ILI patient. The choice of whether and how to test for SARS-CoV-2 given its potential to be a primary or coinfecting agent in presentations linked more closely to a traditional virus (e.g. RSV bronchiolitis) will be a test of our clinical judgement until more data and easier testing are available. Further complicating coinfection recognition is the fact that many sick visits occur by telehealth and much testing is done at drive-through SARS-CoV-2 testing facilities with no clinician exam. Unless we are liberal in SARS-CoV-2 testing, detecting SARS-CoV-2 coinfections is easier said than done given its usually mild presentation being overshadowed by any coinfecting virus.
But understanding who has SARS-CoV-2, even as a coinfection, still is essential in controlling the pandemic. We will need to be vigilant for evolving approaches to SARS-CoV-2 testing in the context of symptomatic ARI presentations, knowing this will likely remain a moving target for the foreseeable future.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospital-Kansas City, Mo. Children’s Mercy Hospital receives grant funding to study two candidate RSV vaccines. The hospital also receives CDC funding under the New Vaccine Surveillance Network for multicenter surveillance of acute respiratory infections, including influenza, RSV, and parainfluenza virus. Email Dr. Harrison at [email protected].
References
1. Pediatrics. 2020;146(1):e20200961.
2. JAMA. 2020 May 26;323(20):2085-6.
3. Pediatrics. 2020. doi: 10.1542/peds.2020-1267.
4. www.cdc.gov/flu/professionals/antivirals/summary-clinicians.htm.
5. J. Pediatr. 2020. doi: 10.1016/j.jpeds.2020.08.007.
6. www.cdc.gov/flu/professionals/diagnosis/table-nucleic-acid-detection.html.
Respiratory virus seasons usually follow a fairly well-known pattern. Enterovirus 68 (EV-D68) is a summer-to-early fall virus with biennial peak years. Rhinovirus (HRv) and adenovirus (Adv) occur nearly year-round but may have small upticks in the first month or so that children return to school. Early in the school year, upper respiratory infections from both HRv and Adv and viral sore throats from Adv are common, with conjunctivitis from Adv outbreaks in some years. October to November is human parainfluenza (HPiV) 1 and 2 season, often presenting as croup. Human metapneumovirus infections span October through April. In late November to December, influenza begins, usually with an A type, later transitioning to a B type in February through April. Also in December, respiratory syncytial virus (RSV) starts, characteristically with bronchiolitis presentations, peaking in February to March and tapering off in May. In late March to April, HPiV 3 also appears for 4-6 weeks.

Will 2020-2021 be different?
Summer was remarkably free of expected enterovirus activity, suggesting that the seasonal parade may differ this year. Remember that the 2019-2020 respiratory season suddenly and nearly completely stopped in March because of social distancing and lockdowns needed to address the SARS-CoV-2 pandemic.
The mild influenza season in the southern hemisphere suggests that our influenza season also could be mild. But perhaps not – most southern hemisphere countries that are surveyed for influenza activities had the most intense SARS-CoV-2 mitigations, making the observed mildness potentially related more to social mitigation than less virulent influenza strains. If so, southern hemisphere influenza data may not apply to the United States, where social distancing and masks are ignored or used inconsistently by almost half the population.
Further, the stop-and-go pattern of in-person school/college attendance adds to uncertainties for the usual orderly virus-specific seasonality. The result may be multiple stop-and-go “pop-up” or “mini” outbreaks for any given virus potentially reflected as exaggerated local or regional differences in circulation of various viruses. The erratic seasonality also would increase coinfections, which could present with more severe or different symptoms.
SARS-CoV-2’s potential interaction
Will the relatively mild presentations for most children with SARS-CoV-2 hold up in the setting of coinfections or sequential respiratory viral infections? Could SARS-CoV-2 cause worse/more prolonged symptoms or more sequelae if paired simultaneously or in tandem with a traditional respiratory virus? To date, data on the frequency and severity of SARS-CoV-2 coinfections are conflicting and sparse, but it appears that non-SARS-CoV-2 viruses can be involved in 15%-50% pediatric acute respiratory infections.1,2
However, it may not be important to know about coinfecting viruses other than influenza (can be treated) or SARS-CoV-2 (needs quarantine and contact tracing), unless symptoms are atypical or more severe than usual. For example, a young child with bronchiolitis is most likely infected with RSV, but HPiV, influenza, metapneumovirus, HRv, and even SARS-CoV-2 can cause bronchiolitis. Even so, testing outpatients for RSV or non-influenza is not routine or even clinically helpful. Supportive treatment and restriction from daycare attendance are sufficient management for outpatient ARIs whether presenting as bronchiolitis or not.
Considerations for SARS-CoV-2 testing: Outpatient bronchiolitis
If a child presents with classic bronchiolitis but has above moderate to severe symptoms, is SARS-CoV-2 a consideration? Perhaps, if SARS-CoV-2 acts similarly to non-SARS-CoV-2s.
A recent report from the 30th Multicenter Airway Research Collaboration (MARC-30) surveillance study (2007-2014) of children hospitalized with clinical bronchiolitis evaluated respiratory viruses, including RSV and the four common non-SARS coronaviruses using molecular testing.3 Among 1,880 subjects, a CoV (alpha CoV: NL63 or 229E, or beta CoV: KKU1 or OC43) was detected in 12%. Yet most had only RSV (n = 1,661); 32 had only CoV (n = 32). But note that 219 had both.
Bronchiolitis subjects with CoV were older – median 3.7 (1.4-5.8) vs. 2.8 (1.9-7.2) years – and more likely male than were RSV subjects (68% vs. 58%). OC43 was most frequent followed by equal numbers of HKU1 and NL63, while 229E was the least frequent. Medical utilization and severity did not differ among the CoVs, or between RSV+CoV vs. RSV alone, unless one considered CoV viral load as a variable. ICU use increased when the polymerase chain reaction cycle threshold result indicated a high CoV viral load.
These data suggest CoVs are not infrequent coinfectors with RSV in bronchiolitis – and that SARS-CoV-2 is the same. Therefore, a bronchiolitis presentation doesn’t necessarily take us off the hook for the need to consider SARS-CoV-2 testing, particularly in the somewhat older bronchiolitis patient with more than mild symptoms.
Considerations for SARS-CoV-2 testing: Outpatient influenza-like illness
In 2020-2021, the Centers for Disease Control and Prevention recommends considering empiric antiviral treatment for ILIs (fever plus either cough or sore throat) based upon our clinical judgement, even in non-high-risk children.4
While pediatric COVID-19 illnesses are predominantly asymptomatic or mild, a febrile ARI is also a SARS-CoV-2 compatible presentation. So, if all we use is our clinical judgment, how do we know if the febrile ARI is due to influenza or SARS-CoV-2 or both? At least one study used a highly sensitive and specific molecular influenza test to show that the accuracy of clinically diagnosing influenza in children is not much better than flipping a coin and would lead to potential antiviral overuse.5
So, it seems ideal to test for influenza when possible. Point-of-care (POC) tests are frequently used for outpatients. Eight POC Clinical Laboratory Improvement Amendments (CLIA)–waived kits, some also detecting RSV, are available but most have modest sensitivity (60%-80%) compared with lab-based molecular tests.6 That said, if supplies and kits for one of the POC tests are available to us during these SARS-CoV-2 stressed times (back orders seem more common this year), a positive influenza test in the first 48 hours of symptoms confirms the option to prescribe an antiviral. Yet how will we have confidence that the febrile ARI is not also partly due to SARS-CoV-2? Currently febrile ARIs usually are considered SARS-CoV-2 and the children are sent for SARS-CoV-2 testing. During influenza season, it seems we will need to continue to send febrile outpatients for SARS-CoV-2 testing, even if POC influenza positive, via whatever mechanisms are available as time goes on.
We expect more rapid pediatric testing modalities for SARS-CoV-2 (maybe even saliva tests) to become available over the next months. Indeed, rapid antigen tests and rapid molecular tests are being evaluated in adults and seem destined for CLIA waivers as POC tests, and even home testing kits. Pediatric approvals hopefully also will occur. So, the pathways for SARS-CoV-2 testing available now will likely change over this winter. But be aware that supplies/kits will be prioritized to locations within high need areas and bulk purchase contracts. So POC kits may remain scarce for practices, meaning a reference laboratory still could be the way to go for SARS-CoV-2 for at least the rest of 2020. Reference labs are becoming creative as well; one combined detection of influenza A, influenza B, RSV, and SARS-CoV-2 into one test, and hopes to get approval for swab collection that can be done by families at home and mailed in.
Summary
Expect variations on the traditional parade of seasonal respiratory viruses, with increased numbers of coinfections. Choosing the outpatient who needs influenza testing is the same as in past years, although we have CDC permissive recommendations to prescribe antivirals for any outpatient ILI within the first 48 hours of symptoms. Still, POC testing for influenza remains potentially valuable in the ILI patient. The choice of whether and how to test for SARS-CoV-2 given its potential to be a primary or coinfecting agent in presentations linked more closely to a traditional virus (e.g. RSV bronchiolitis) will be a test of our clinical judgement until more data and easier testing are available. Further complicating coinfection recognition is the fact that many sick visits occur by telehealth and much testing is done at drive-through SARS-CoV-2 testing facilities with no clinician exam. Unless we are liberal in SARS-CoV-2 testing, detecting SARS-CoV-2 coinfections is easier said than done given its usually mild presentation being overshadowed by any coinfecting virus.
But understanding who has SARS-CoV-2, even as a coinfection, still is essential in controlling the pandemic. We will need to be vigilant for evolving approaches to SARS-CoV-2 testing in the context of symptomatic ARI presentations, knowing this will likely remain a moving target for the foreseeable future.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospital-Kansas City, Mo. Children’s Mercy Hospital receives grant funding to study two candidate RSV vaccines. The hospital also receives CDC funding under the New Vaccine Surveillance Network for multicenter surveillance of acute respiratory infections, including influenza, RSV, and parainfluenza virus. Email Dr. Harrison at [email protected].
References
1. Pediatrics. 2020;146(1):e20200961.
2. JAMA. 2020 May 26;323(20):2085-6.
3. Pediatrics. 2020. doi: 10.1542/peds.2020-1267.
4. www.cdc.gov/flu/professionals/antivirals/summary-clinicians.htm.
5. J. Pediatr. 2020. doi: 10.1016/j.jpeds.2020.08.007.
6. www.cdc.gov/flu/professionals/diagnosis/table-nucleic-acid-detection.html.
Respiratory virus seasons usually follow a fairly well-known pattern. Enterovirus 68 (EV-D68) is a summer-to-early fall virus with biennial peak years. Rhinovirus (HRv) and adenovirus (Adv) occur nearly year-round but may have small upticks in the first month or so that children return to school. Early in the school year, upper respiratory infections from both HRv and Adv and viral sore throats from Adv are common, with conjunctivitis from Adv outbreaks in some years. October to November is human parainfluenza (HPiV) 1 and 2 season, often presenting as croup. Human metapneumovirus infections span October through April. In late November to December, influenza begins, usually with an A type, later transitioning to a B type in February through April. Also in December, respiratory syncytial virus (RSV) starts, characteristically with bronchiolitis presentations, peaking in February to March and tapering off in May. In late March to April, HPiV 3 also appears for 4-6 weeks.

Will 2020-2021 be different?
Summer was remarkably free of expected enterovirus activity, suggesting that the seasonal parade may differ this year. Remember that the 2019-2020 respiratory season suddenly and nearly completely stopped in March because of social distancing and lockdowns needed to address the SARS-CoV-2 pandemic.
The mild influenza season in the southern hemisphere suggests that our influenza season also could be mild. But perhaps not – most southern hemisphere countries that are surveyed for influenza activities had the most intense SARS-CoV-2 mitigations, making the observed mildness potentially related more to social mitigation than less virulent influenza strains. If so, southern hemisphere influenza data may not apply to the United States, where social distancing and masks are ignored or used inconsistently by almost half the population.
Further, the stop-and-go pattern of in-person school/college attendance adds to uncertainties for the usual orderly virus-specific seasonality. The result may be multiple stop-and-go “pop-up” or “mini” outbreaks for any given virus potentially reflected as exaggerated local or regional differences in circulation of various viruses. The erratic seasonality also would increase coinfections, which could present with more severe or different symptoms.
SARS-CoV-2’s potential interaction
Will the relatively mild presentations for most children with SARS-CoV-2 hold up in the setting of coinfections or sequential respiratory viral infections? Could SARS-CoV-2 cause worse/more prolonged symptoms or more sequelae if paired simultaneously or in tandem with a traditional respiratory virus? To date, data on the frequency and severity of SARS-CoV-2 coinfections are conflicting and sparse, but it appears that non-SARS-CoV-2 viruses can be involved in 15%-50% pediatric acute respiratory infections.1,2
However, it may not be important to know about coinfecting viruses other than influenza (can be treated) or SARS-CoV-2 (needs quarantine and contact tracing), unless symptoms are atypical or more severe than usual. For example, a young child with bronchiolitis is most likely infected with RSV, but HPiV, influenza, metapneumovirus, HRv, and even SARS-CoV-2 can cause bronchiolitis. Even so, testing outpatients for RSV or non-influenza is not routine or even clinically helpful. Supportive treatment and restriction from daycare attendance are sufficient management for outpatient ARIs whether presenting as bronchiolitis or not.
Considerations for SARS-CoV-2 testing: Outpatient bronchiolitis
If a child presents with classic bronchiolitis but has above moderate to severe symptoms, is SARS-CoV-2 a consideration? Perhaps, if SARS-CoV-2 acts similarly to non-SARS-CoV-2s.
A recent report from the 30th Multicenter Airway Research Collaboration (MARC-30) surveillance study (2007-2014) of children hospitalized with clinical bronchiolitis evaluated respiratory viruses, including RSV and the four common non-SARS coronaviruses using molecular testing.3 Among 1,880 subjects, a CoV (alpha CoV: NL63 or 229E, or beta CoV: KKU1 or OC43) was detected in 12%. Yet most had only RSV (n = 1,661); 32 had only CoV (n = 32). But note that 219 had both.
Bronchiolitis subjects with CoV were older – median 3.7 (1.4-5.8) vs. 2.8 (1.9-7.2) years – and more likely male than were RSV subjects (68% vs. 58%). OC43 was most frequent followed by equal numbers of HKU1 and NL63, while 229E was the least frequent. Medical utilization and severity did not differ among the CoVs, or between RSV+CoV vs. RSV alone, unless one considered CoV viral load as a variable. ICU use increased when the polymerase chain reaction cycle threshold result indicated a high CoV viral load.
These data suggest CoVs are not infrequent coinfectors with RSV in bronchiolitis – and that SARS-CoV-2 is the same. Therefore, a bronchiolitis presentation doesn’t necessarily take us off the hook for the need to consider SARS-CoV-2 testing, particularly in the somewhat older bronchiolitis patient with more than mild symptoms.
Considerations for SARS-CoV-2 testing: Outpatient influenza-like illness
In 2020-2021, the Centers for Disease Control and Prevention recommends considering empiric antiviral treatment for ILIs (fever plus either cough or sore throat) based upon our clinical judgement, even in non-high-risk children.4
While pediatric COVID-19 illnesses are predominantly asymptomatic or mild, a febrile ARI is also a SARS-CoV-2 compatible presentation. So, if all we use is our clinical judgment, how do we know if the febrile ARI is due to influenza or SARS-CoV-2 or both? At least one study used a highly sensitive and specific molecular influenza test to show that the accuracy of clinically diagnosing influenza in children is not much better than flipping a coin and would lead to potential antiviral overuse.5
So, it seems ideal to test for influenza when possible. Point-of-care (POC) tests are frequently used for outpatients. Eight POC Clinical Laboratory Improvement Amendments (CLIA)–waived kits, some also detecting RSV, are available but most have modest sensitivity (60%-80%) compared with lab-based molecular tests.6 That said, if supplies and kits for one of the POC tests are available to us during these SARS-CoV-2 stressed times (back orders seem more common this year), a positive influenza test in the first 48 hours of symptoms confirms the option to prescribe an antiviral. Yet how will we have confidence that the febrile ARI is not also partly due to SARS-CoV-2? Currently febrile ARIs usually are considered SARS-CoV-2 and the children are sent for SARS-CoV-2 testing. During influenza season, it seems we will need to continue to send febrile outpatients for SARS-CoV-2 testing, even if POC influenza positive, via whatever mechanisms are available as time goes on.
We expect more rapid pediatric testing modalities for SARS-CoV-2 (maybe even saliva tests) to become available over the next months. Indeed, rapid antigen tests and rapid molecular tests are being evaluated in adults and seem destined for CLIA waivers as POC tests, and even home testing kits. Pediatric approvals hopefully also will occur. So, the pathways for SARS-CoV-2 testing available now will likely change over this winter. But be aware that supplies/kits will be prioritized to locations within high need areas and bulk purchase contracts. So POC kits may remain scarce for practices, meaning a reference laboratory still could be the way to go for SARS-CoV-2 for at least the rest of 2020. Reference labs are becoming creative as well; one combined detection of influenza A, influenza B, RSV, and SARS-CoV-2 into one test, and hopes to get approval for swab collection that can be done by families at home and mailed in.
Summary
Expect variations on the traditional parade of seasonal respiratory viruses, with increased numbers of coinfections. Choosing the outpatient who needs influenza testing is the same as in past years, although we have CDC permissive recommendations to prescribe antivirals for any outpatient ILI within the first 48 hours of symptoms. Still, POC testing for influenza remains potentially valuable in the ILI patient. The choice of whether and how to test for SARS-CoV-2 given its potential to be a primary or coinfecting agent in presentations linked more closely to a traditional virus (e.g. RSV bronchiolitis) will be a test of our clinical judgement until more data and easier testing are available. Further complicating coinfection recognition is the fact that many sick visits occur by telehealth and much testing is done at drive-through SARS-CoV-2 testing facilities with no clinician exam. Unless we are liberal in SARS-CoV-2 testing, detecting SARS-CoV-2 coinfections is easier said than done given its usually mild presentation being overshadowed by any coinfecting virus.
But understanding who has SARS-CoV-2, even as a coinfection, still is essential in controlling the pandemic. We will need to be vigilant for evolving approaches to SARS-CoV-2 testing in the context of symptomatic ARI presentations, knowing this will likely remain a moving target for the foreseeable future.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospital-Kansas City, Mo. Children’s Mercy Hospital receives grant funding to study two candidate RSV vaccines. The hospital also receives CDC funding under the New Vaccine Surveillance Network for multicenter surveillance of acute respiratory infections, including influenza, RSV, and parainfluenza virus. Email Dr. Harrison at [email protected].
References
1. Pediatrics. 2020;146(1):e20200961.
2. JAMA. 2020 May 26;323(20):2085-6.
3. Pediatrics. 2020. doi: 10.1542/peds.2020-1267.
4. www.cdc.gov/flu/professionals/antivirals/summary-clinicians.htm.
5. J. Pediatr. 2020. doi: 10.1016/j.jpeds.2020.08.007.
6. www.cdc.gov/flu/professionals/diagnosis/table-nucleic-acid-detection.html.
Even in a virtual environment, the Society of Gynecologic Surgeons delivers without a “glitch”
Earlier this year, I was honored to serve as the Scientific Program Chair for the 46th Annual Scientific Meeting of the Society of Gynecologic Surgeons (SGS). This year’s meeting was the first ever (and hopefully last) “virtual” scientific meeting, which consisted of a hybrid of prerecorded and live presentations. Although faculty and attendees were not able to be together physically, the essence of the lively SGS meetings came through loud and clear. We still had “discussants” comment on the oral presentations and ask questions of the presenters. These questions and answers were all done live—without a glitch! Many thanks to all who made this meeting possible.
In addition to the outstanding abstract and video presentations, there were 4 superb postgraduate courses:
- Mikio Nihira, MD, chaired “Enhanced recovery after surgery: Overcoming barriers to implementation.”
- Charles Hanes, MD, headed up “It’s all about the apex: The key to successful POP surgery.”
- Cara King, DO, MS, led “Total laparoscopic hysterectomy: Pushing the envelope.”
- Vincent Lucente, MD, chaired “Transvaginal reconstructive pelvic surgery using graft augmentation post-FDA.”
Many special thanks to Dr. Lucente who transformed his course into a wonderful article for this special section of
One of our exceptional keynote speakers was Marc Beer (a serial entrepreneur and cofounder, chairman, and CEO of Renovia, Inc.), whose talk was entitled “A primer on medical device innovation—How to avoid common pitfalls while realizing your vision.” Mr. Beer has turned this topic into a unique article for this special section (see next month’s issue for Part 2).
Our TeLinde Lecture, entitled “Artificial intelligence in surgery,” was delivered by the dynamic Vicente Gracias, MD, professor of surgery at Robert Wood Johnson University Hospital, New Brunswick, New Jersey. We also held 2 live panel discussions that were very popular. The first, “Work-life balance and gynecologic surgery,” featured various perspectives from Drs. Kristie Green, Sally Huber, Catherine Matthews, and Charles Rardin. The second panel discussion, entitled “Understanding, managing, and benefiting from your e-presence,” by experts Heather Schueppert; Chief Marketing Officer at Unified Physician Management, Brad Bowman, MD; and Peter Lotze, MD. Both of these panel discussions are included in this special section as well.
I hope you enjoy the content of this special section of
Earlier this year, I was honored to serve as the Scientific Program Chair for the 46th Annual Scientific Meeting of the Society of Gynecologic Surgeons (SGS). This year’s meeting was the first ever (and hopefully last) “virtual” scientific meeting, which consisted of a hybrid of prerecorded and live presentations. Although faculty and attendees were not able to be together physically, the essence of the lively SGS meetings came through loud and clear. We still had “discussants” comment on the oral presentations and ask questions of the presenters. These questions and answers were all done live—without a glitch! Many thanks to all who made this meeting possible.
In addition to the outstanding abstract and video presentations, there were 4 superb postgraduate courses:
- Mikio Nihira, MD, chaired “Enhanced recovery after surgery: Overcoming barriers to implementation.”
- Charles Hanes, MD, headed up “It’s all about the apex: The key to successful POP surgery.”
- Cara King, DO, MS, led “Total laparoscopic hysterectomy: Pushing the envelope.”
- Vincent Lucente, MD, chaired “Transvaginal reconstructive pelvic surgery using graft augmentation post-FDA.”
Many special thanks to Dr. Lucente who transformed his course into a wonderful article for this special section of
One of our exceptional keynote speakers was Marc Beer (a serial entrepreneur and cofounder, chairman, and CEO of Renovia, Inc.), whose talk was entitled “A primer on medical device innovation—How to avoid common pitfalls while realizing your vision.” Mr. Beer has turned this topic into a unique article for this special section (see next month’s issue for Part 2).
Our TeLinde Lecture, entitled “Artificial intelligence in surgery,” was delivered by the dynamic Vicente Gracias, MD, professor of surgery at Robert Wood Johnson University Hospital, New Brunswick, New Jersey. We also held 2 live panel discussions that were very popular. The first, “Work-life balance and gynecologic surgery,” featured various perspectives from Drs. Kristie Green, Sally Huber, Catherine Matthews, and Charles Rardin. The second panel discussion, entitled “Understanding, managing, and benefiting from your e-presence,” by experts Heather Schueppert; Chief Marketing Officer at Unified Physician Management, Brad Bowman, MD; and Peter Lotze, MD. Both of these panel discussions are included in this special section as well.
I hope you enjoy the content of this special section of
Earlier this year, I was honored to serve as the Scientific Program Chair for the 46th Annual Scientific Meeting of the Society of Gynecologic Surgeons (SGS). This year’s meeting was the first ever (and hopefully last) “virtual” scientific meeting, which consisted of a hybrid of prerecorded and live presentations. Although faculty and attendees were not able to be together physically, the essence of the lively SGS meetings came through loud and clear. We still had “discussants” comment on the oral presentations and ask questions of the presenters. These questions and answers were all done live—without a glitch! Many thanks to all who made this meeting possible.
In addition to the outstanding abstract and video presentations, there were 4 superb postgraduate courses:
- Mikio Nihira, MD, chaired “Enhanced recovery after surgery: Overcoming barriers to implementation.”
- Charles Hanes, MD, headed up “It’s all about the apex: The key to successful POP surgery.”
- Cara King, DO, MS, led “Total laparoscopic hysterectomy: Pushing the envelope.”
- Vincent Lucente, MD, chaired “Transvaginal reconstructive pelvic surgery using graft augmentation post-FDA.”
Many special thanks to Dr. Lucente who transformed his course into a wonderful article for this special section of
One of our exceptional keynote speakers was Marc Beer (a serial entrepreneur and cofounder, chairman, and CEO of Renovia, Inc.), whose talk was entitled “A primer on medical device innovation—How to avoid common pitfalls while realizing your vision.” Mr. Beer has turned this topic into a unique article for this special section (see next month’s issue for Part 2).
Our TeLinde Lecture, entitled “Artificial intelligence in surgery,” was delivered by the dynamic Vicente Gracias, MD, professor of surgery at Robert Wood Johnson University Hospital, New Brunswick, New Jersey. We also held 2 live panel discussions that were very popular. The first, “Work-life balance and gynecologic surgery,” featured various perspectives from Drs. Kristie Green, Sally Huber, Catherine Matthews, and Charles Rardin. The second panel discussion, entitled “Understanding, managing, and benefiting from your e-presence,” by experts Heather Schueppert; Chief Marketing Officer at Unified Physician Management, Brad Bowman, MD; and Peter Lotze, MD. Both of these panel discussions are included in this special section as well.
I hope you enjoy the content of this special section of
Researchers examine learning curve for gender-affirming vaginoplasty
research suggests. For one surgeon, certain adverse events, including the need for revision surgery, were less likely after 50 cases.
“As surgical programs evolve, the important question becomes: At what case threshold are cases performed safely, efficiently, and with favorable outcomes?” said Cecile A. Ferrando, MD, MPH, program director of the female pelvic medicine and reconstructive surgery fellowship at Cleveland Clinic and director of the transgender surgery and medicine program in the Cleveland Clinic’s Center for LGBT Care.
The answer could guide training for future surgeons, Dr. Ferrando said at the virtual annual scientific meeting of the Society of Gynecologic Surgeons. Future studies should include patient-centered outcomes and data from multiple centers, other doctors said.
Transgender women who opt to surgically transition may undergo vaginoplasty. Although many reports describe surgical techniques, “there is a paucity of evidence-based data as well as few reports on outcomes,” Dr. Ferrando noted.
To describe perioperative adverse events related to vaginoplasty performed for gender affirmation and determine a minimum number of cases needed to reduce their likelihood, Dr. Ferrando performed a retrospective study of 76 patients. The patients underwent surgery between December 2015 and March 2019 and had 6-month postoperative outcomes available. Dr. Ferrando performed the procedures.
Dr. Ferrando evaluated outcomes after increments of 10 cases. After 50 cases, the median surgical time decreased to approximately 180 minutes, which an informal survey of surgeons suggested was efficient, and the rates of adverse events were similar to those in other studies. Dr. Ferrando compared outcomes from the first 50 cases with outcomes from the 26 cases that followed.
Overall, the patients had a mean age of 41 years. The first 50 patients were older on average (44 years vs. 35 years). About 83% underwent full-depth vaginoplasty. The incidence of intraoperative and immediate postoperative events was low and did not differ between the two groups. Rates of delayed postoperative events – those occurring 30 or more days after surgery – did significantly differ between the two groups, however.
After 50 cases, there was a lower incidence of urinary stream abnormalities (7.7% vs. 16.3%), introital stenosis (3.9% vs. 12%), and revision surgery (that is, elective, cosmetic, or functional revision within 6 months; 19.2% vs. 44%), compared with the first 50 cases.
The study did not include patient-centered outcomes and the results may have limited generalizability, Dr. Ferrando noted. “The incidence of serious adverse events related to vaginoplasty is low while minor events are common,” she said. “A 50-case minimum may be an adequate case number target for postgraduate trainees learning how to do this surgery.”
“I learned that the incidence of serious complications, like injuries during the surgery, or serious events immediately after surgery was quite low, which was reassuring,” Dr. Ferrando said in a later interview. “The cosmetic result and detail that is involved with the surgery – something that is very important to patients – that skill set takes time and experience to refine.”
Subsequent studies should include patient-centered outcomes, which may help surgeons understand potential “sources of consternation for patients,” such as persistent corporal tissue, poor aesthetics, vaginal stenosis, urinary meatus location, and clitoral hooding, Joseph J. Pariser, MD, commented in an interview. Dr. Pariser, a urologist who specializes in gender care at the University of Minnesota in Minneapolis, in 2019 reviewed safety outcomes from published case series.
“In my own practice, precise placement of the urethra, familiarity with landmarks during canal dissection, and rapidity of working through steps of the surgery have all dramatically improved as our experience at University of Minnesota performing primary vaginoplasty has grown,” Dr. Pariser said.
Optimal case thresholds may vary depending on a surgeon’s background, Rachel M. Whynott, MD, a reproductive endocrinology and infertility fellow at the University of Iowa in Iowa City, said in an interview. At the University of Kansas in Kansas City, a multidisciplinary team that includes a gynecologist, a reconstructive urologist, and a plastic surgeon performs the procedure.
Dr. Whynott and colleagues recently published a retrospective study that evaluated surgical aptitude over time in a male-to-female penoscrotal vaginoplasty program . Their analysis of 43 cases identified a learning curve that was reflected in overall time in the operating room and time to neoclitoral sensation.
Investigators are “trying to add to the growing body of literature about this procedure and how we can best go about improving outcomes for our patients and improving this surgery,” Dr. Whynott said. A study that includes data from multiple centers would be useful, she added.
Dr. Ferrando disclosed authorship royalties from UpToDate. Dr. Pariser and Dr. Whynott had no relevant financial disclosures.
SOURCE: Ferrando C. SGS 2020, Abstract 09.
research suggests. For one surgeon, certain adverse events, including the need for revision surgery, were less likely after 50 cases.
“As surgical programs evolve, the important question becomes: At what case threshold are cases performed safely, efficiently, and with favorable outcomes?” said Cecile A. Ferrando, MD, MPH, program director of the female pelvic medicine and reconstructive surgery fellowship at Cleveland Clinic and director of the transgender surgery and medicine program in the Cleveland Clinic’s Center for LGBT Care.
The answer could guide training for future surgeons, Dr. Ferrando said at the virtual annual scientific meeting of the Society of Gynecologic Surgeons. Future studies should include patient-centered outcomes and data from multiple centers, other doctors said.
Transgender women who opt to surgically transition may undergo vaginoplasty. Although many reports describe surgical techniques, “there is a paucity of evidence-based data as well as few reports on outcomes,” Dr. Ferrando noted.
To describe perioperative adverse events related to vaginoplasty performed for gender affirmation and determine a minimum number of cases needed to reduce their likelihood, Dr. Ferrando performed a retrospective study of 76 patients. The patients underwent surgery between December 2015 and March 2019 and had 6-month postoperative outcomes available. Dr. Ferrando performed the procedures.
Dr. Ferrando evaluated outcomes after increments of 10 cases. After 50 cases, the median surgical time decreased to approximately 180 minutes, which an informal survey of surgeons suggested was efficient, and the rates of adverse events were similar to those in other studies. Dr. Ferrando compared outcomes from the first 50 cases with outcomes from the 26 cases that followed.
Overall, the patients had a mean age of 41 years. The first 50 patients were older on average (44 years vs. 35 years). About 83% underwent full-depth vaginoplasty. The incidence of intraoperative and immediate postoperative events was low and did not differ between the two groups. Rates of delayed postoperative events – those occurring 30 or more days after surgery – did significantly differ between the two groups, however.
After 50 cases, there was a lower incidence of urinary stream abnormalities (7.7% vs. 16.3%), introital stenosis (3.9% vs. 12%), and revision surgery (that is, elective, cosmetic, or functional revision within 6 months; 19.2% vs. 44%), compared with the first 50 cases.
The study did not include patient-centered outcomes and the results may have limited generalizability, Dr. Ferrando noted. “The incidence of serious adverse events related to vaginoplasty is low while minor events are common,” she said. “A 50-case minimum may be an adequate case number target for postgraduate trainees learning how to do this surgery.”
“I learned that the incidence of serious complications, like injuries during the surgery, or serious events immediately after surgery was quite low, which was reassuring,” Dr. Ferrando said in a later interview. “The cosmetic result and detail that is involved with the surgery – something that is very important to patients – that skill set takes time and experience to refine.”
Subsequent studies should include patient-centered outcomes, which may help surgeons understand potential “sources of consternation for patients,” such as persistent corporal tissue, poor aesthetics, vaginal stenosis, urinary meatus location, and clitoral hooding, Joseph J. Pariser, MD, commented in an interview. Dr. Pariser, a urologist who specializes in gender care at the University of Minnesota in Minneapolis, in 2019 reviewed safety outcomes from published case series.
“In my own practice, precise placement of the urethra, familiarity with landmarks during canal dissection, and rapidity of working through steps of the surgery have all dramatically improved as our experience at University of Minnesota performing primary vaginoplasty has grown,” Dr. Pariser said.
Optimal case thresholds may vary depending on a surgeon’s background, Rachel M. Whynott, MD, a reproductive endocrinology and infertility fellow at the University of Iowa in Iowa City, said in an interview. At the University of Kansas in Kansas City, a multidisciplinary team that includes a gynecologist, a reconstructive urologist, and a plastic surgeon performs the procedure.
Dr. Whynott and colleagues recently published a retrospective study that evaluated surgical aptitude over time in a male-to-female penoscrotal vaginoplasty program . Their analysis of 43 cases identified a learning curve that was reflected in overall time in the operating room and time to neoclitoral sensation.
Investigators are “trying to add to the growing body of literature about this procedure and how we can best go about improving outcomes for our patients and improving this surgery,” Dr. Whynott said. A study that includes data from multiple centers would be useful, she added.
Dr. Ferrando disclosed authorship royalties from UpToDate. Dr. Pariser and Dr. Whynott had no relevant financial disclosures.
SOURCE: Ferrando C. SGS 2020, Abstract 09.
research suggests. For one surgeon, certain adverse events, including the need for revision surgery, were less likely after 50 cases.
“As surgical programs evolve, the important question becomes: At what case threshold are cases performed safely, efficiently, and with favorable outcomes?” said Cecile A. Ferrando, MD, MPH, program director of the female pelvic medicine and reconstructive surgery fellowship at Cleveland Clinic and director of the transgender surgery and medicine program in the Cleveland Clinic’s Center for LGBT Care.
The answer could guide training for future surgeons, Dr. Ferrando said at the virtual annual scientific meeting of the Society of Gynecologic Surgeons. Future studies should include patient-centered outcomes and data from multiple centers, other doctors said.
Transgender women who opt to surgically transition may undergo vaginoplasty. Although many reports describe surgical techniques, “there is a paucity of evidence-based data as well as few reports on outcomes,” Dr. Ferrando noted.
To describe perioperative adverse events related to vaginoplasty performed for gender affirmation and determine a minimum number of cases needed to reduce their likelihood, Dr. Ferrando performed a retrospective study of 76 patients. The patients underwent surgery between December 2015 and March 2019 and had 6-month postoperative outcomes available. Dr. Ferrando performed the procedures.
Dr. Ferrando evaluated outcomes after increments of 10 cases. After 50 cases, the median surgical time decreased to approximately 180 minutes, which an informal survey of surgeons suggested was efficient, and the rates of adverse events were similar to those in other studies. Dr. Ferrando compared outcomes from the first 50 cases with outcomes from the 26 cases that followed.
Overall, the patients had a mean age of 41 years. The first 50 patients were older on average (44 years vs. 35 years). About 83% underwent full-depth vaginoplasty. The incidence of intraoperative and immediate postoperative events was low and did not differ between the two groups. Rates of delayed postoperative events – those occurring 30 or more days after surgery – did significantly differ between the two groups, however.
After 50 cases, there was a lower incidence of urinary stream abnormalities (7.7% vs. 16.3%), introital stenosis (3.9% vs. 12%), and revision surgery (that is, elective, cosmetic, or functional revision within 6 months; 19.2% vs. 44%), compared with the first 50 cases.
The study did not include patient-centered outcomes and the results may have limited generalizability, Dr. Ferrando noted. “The incidence of serious adverse events related to vaginoplasty is low while minor events are common,” she said. “A 50-case minimum may be an adequate case number target for postgraduate trainees learning how to do this surgery.”
“I learned that the incidence of serious complications, like injuries during the surgery, or serious events immediately after surgery was quite low, which was reassuring,” Dr. Ferrando said in a later interview. “The cosmetic result and detail that is involved with the surgery – something that is very important to patients – that skill set takes time and experience to refine.”
Subsequent studies should include patient-centered outcomes, which may help surgeons understand potential “sources of consternation for patients,” such as persistent corporal tissue, poor aesthetics, vaginal stenosis, urinary meatus location, and clitoral hooding, Joseph J. Pariser, MD, commented in an interview. Dr. Pariser, a urologist who specializes in gender care at the University of Minnesota in Minneapolis, in 2019 reviewed safety outcomes from published case series.
“In my own practice, precise placement of the urethra, familiarity with landmarks during canal dissection, and rapidity of working through steps of the surgery have all dramatically improved as our experience at University of Minnesota performing primary vaginoplasty has grown,” Dr. Pariser said.
Optimal case thresholds may vary depending on a surgeon’s background, Rachel M. Whynott, MD, a reproductive endocrinology and infertility fellow at the University of Iowa in Iowa City, said in an interview. At the University of Kansas in Kansas City, a multidisciplinary team that includes a gynecologist, a reconstructive urologist, and a plastic surgeon performs the procedure.
Dr. Whynott and colleagues recently published a retrospective study that evaluated surgical aptitude over time in a male-to-female penoscrotal vaginoplasty program . Their analysis of 43 cases identified a learning curve that was reflected in overall time in the operating room and time to neoclitoral sensation.
Investigators are “trying to add to the growing body of literature about this procedure and how we can best go about improving outcomes for our patients and improving this surgery,” Dr. Whynott said. A study that includes data from multiple centers would be useful, she added.
Dr. Ferrando disclosed authorship royalties from UpToDate. Dr. Pariser and Dr. Whynott had no relevant financial disclosures.
SOURCE: Ferrando C. SGS 2020, Abstract 09.
FROM SGS 2020
Transvaginal reconstructive surgery for POP: Innovative approach to graft augmentation in the post-mesh era
Pelvic organ prolapse (POP) is a common occurrence over the course of a woman’s lifetime, especially in parous women (up to 50% of women who have given birth).1 The anterior vaginal wall is the most common site of POP and has the highest recurrence rate of up to 70%.2 The risk of developing POP increases with age, obesity, White race, family history, and prior pelvic surgery, such as hysterectomy. It affects more than 3 million women in the United States alone, often negatively impacting sexual function and overall quality of life.3,4
Because women are living longer than ever before and are more active in their senior years, a long-lasting, durable surgical repair is desirable, if not necessary. To be cost-effective and to avoid general anesthesia, the surgical approach ideally should be vaginal.
Biologic and synthetic grafts to augment transvaginal repair traditionally are used to improve on the well-recognized high failure rate of native-tissue repair that is often seen at both short-term and medium-term follow-up.5 The failure rate is commonly referenced as 30% to 40% at 2-year follow-up and 61% to 70% at 5-year follow-up, well-established by the results of the OPTIMAL randomized clinical trial.6 The more recent Descent trial likewise demonstrates a higher failure rate of native-tissue repair versus transvaginal mesh repair at a shorter term of 30 to 42 months.7 Furthermore, the use of permanent versus absorbable suture in suspension of the vaginal apex is associated with lower short-term failure rates.8
Despite this Level I evidence that demonstrates a clear advantage for obtaining a longer or more durable repair with permanent materials, native-tissue repairs with absorbable suture are still performed routinely. Since the US Food and Drug Administration (FDA) ordered that the use of transvaginal surgical mesh augmentation for pelvic reconstructive surgery be discontinued, it is more important than ever to explore evolving alternative native-tissue augmentation repair techniques that hopefully can preserve the advantages and merits of vaginal surgery and achieve longer durability.9
Biologic graft augmentation use in transvaginal reconstruction
All biologic grafts, including allografts derived from human tissue and xenografts derived from animal tissue, are acellular constructs composed of extracellular matrix (ECM) that acts as scaffolding for the host tissue. The ECM is predominantly composed of collagen (types I and III) and noncollagenous fibronectin, laminin, and glycosaminoglycans in various amounts depending on the source tissue. The 3D presentation of ECM’s complex molecules allows for rapid repopulation of host cells and revascularization with eventual regeneration.
Once a biologic graft is placed surgically, the body’s response to the scaffold ECM mimics the normal wound-healing process, beginning with fibrin-rich matrix hemostasis and the subsequent innate immune response of neutrophil and M1 macrophage infiltration. M1 macrophages are proinflammatory and clear cellular debris and begin the process of graft scaffold degradation. The host tissue then begins the process of remodeling through pro-remodeling M2 macrophages and stem cell recruitment, proliferation, and differentiation.10 As the biologic graft provides initial structure and strength for pelvic repairs, the ideal ECM scaffold would not degrade before the host is able to fully undergo regeneration and maintain its structure and strength.
Biologic grafts differ in source (allograft or xenograft), type (pericardium, dermis, or bladder), developmental stage (fetal or adult), decellularization processing, and sterilization techniques. These 5 aspects determine the distinct 3D ECM scaffold structure, strength, and longevity. If the ECM scaffold is damaged or retains noncollagenous proteins during the preparation process, an inflammatory response is triggered in which the graft is degraded, resorbed, and replaced with scar tissue. Furthermore, certain processing techniques aimed at extending the ECM’s durability—that is, cross-linking collagen—results in the foreign body response in which there is no vascular infiltration or cellular penetration of the graft and a collagen capsule is created around the empty matrix.11 To avoid resorption or encapsulation of the graft, the ECM scaffolds of biologic grafts must be optimized to induce regeneration.
Continue to: Choosing surgical POP repair...
Choosing surgical POP repair
The decision to undergo surgical treatment for prolapse is a shared decision-making process between the patient and surgeon and always should be individualized. The type of procedure and the surgical approach will depend on the patient’s goals, the degree of prolapse, clinical history, risk tolerance, the surgeon’s skill set, and whether or not there is an indication or relative contraindication for uterine removal at the time of prolapse repair.
While the FDA’s order does not apply to transabdominally placed surgical mesh, such as sacrocolpopexy, not all patients are ideal candidates for an abdominal sacrocolpopexy. Most notable are women with a history of multiple prior abdominal surgeries with higher rates of intraperitoneal adhesions. Ideally, to be cost-effective and to avoid general anesthesia, the surgical approach should be vaginal whenever possible.
Biologic versus native-tissue grafts
Currently, only low-quality evidence exists that compares the outcomes of biologic grafts with traditional native-tissue repairs in POP. Studies have been limited by poor reporting of methods, inconsistency in technique and materials used, and imprecise definitions. One Cochrane Review on the surgical management of POP concluded that biologic graft augmentation was associated with a lower failure rate (18%) within 1 to 2 years when compared with a traditional anterior colporrhaphy (28%).12
Based on consideration of all Cochrane Database Reviews and recent large systematic reviews, there clearly is a paucity of information on which to draw well-defined conclusions regarding the advantage of biomaterials in prolapse surgery.12-14 This is due in part to the variation in graft material used and the surgical technique employed.
Similarly, evidence is lacking regarding the superiority of one type of biologic graft over another. Furthermore, some of the grafts previously studied are no longer on the market.15 With the FDA’s removal of all transvaginal mesh, including xenografts, only allografts are available for pelvic floor reconstruction. Currently, only 3 commercial manufacturers market allografts for pelvic floor reconstruction. Each allograft is available in various sizes and all can be trimmed at the time of the surgical procedure to customize both the size and shape to fit the individual patient.
A novel technique using Axis Dermis and polypropylene suture
One of the commercially available allografts, Axis Dermis (Coloplast), is non–cross-linked and is derived from human cadaveric dermal tissue from the back and dorsum of the upper leg. It is sterilized by a proprietary Tutoplast️ sterilization process that uses gamma irradiation to inactivate and prevent the transmission of pathogens. This unique technique involving solvent dehydration means the graft is never freeze dried; thus, the natural tissue matrix is preserved.
Additionally, the allograft is antigen-free, which decreases the risk of tissue reaction (scarring/fibrosis) and aids in the process of host tissue remodeling; invasion by growth factors, blood cells, collagen, elastin, and neovascularization. This natural tissue remodeling facilitates the anticipated “reabsorption” of the graft by the host tissue, leaving the patient with a tissue scaffold, that is, a stronger layer of “fascia” beneath the muscularis.16 As a result of this “biocompatible” graft, the host tissue remodeling has been shown in the rat model to involve early cellular infiltration and angiogenesis (in the first week after implantation), that leads to an organized cellular architecture with greater tensile strength by week 4, and ultimately inability to distinguish host collagen from the implant by 8 to 12 weeks.17,18
Continue to: Steps in performing the technique...
Steps in performing the technique
To ensure that the graft is placed adjacent to the vaginal serosa, a full-thickness dissection is carried out to enter the true vesicovaginal space, which lies below all 4 histologic layers of the vagina (nonkeratinized stratified squamous epithelium, lamina propria, muscularis, and serosa). For the anterior dissection, a Tuohy epidural needle is used to achieve an accurate and consistent depth when injecting fluid (hydrodissection) to enter this true pelvic space (FIGURE 1). Correct entry into the vesicovaginal space can be confirmed visually by the presence of adipose tissue.
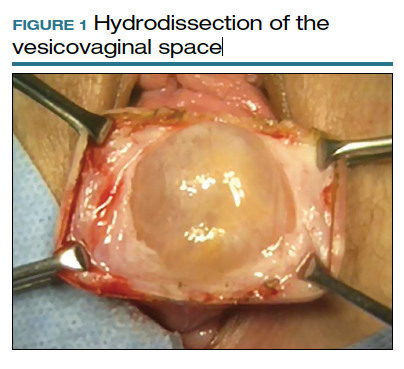
Many pelvic surgeons use the sacrospinous ligament (SSL) as a strong and reliable point of attachment for vaginal prolapse repair. It can be approached either anteriorly or posteriorly with careful dissection. Permanent suture (0-Prolene) is used to “bridge” the attachment between the SSL, the Axis Dermis graft, and the cervix (or vaginal apex). The suture is placed in the middle third and lower half of the ligament to avoid injury to nearby neurovascular structures.
While the surgeon may use any suture-capturing device, we prefer the Anchosure System (Neomedic). This device delivers a small anchor securely into the ligament through a single point of entry, minimizing the risk of postoperative pain for the patient. A 6 cm x 8 cm size Axis Dermis graft is then trimmed to meet the specifications of the patient’s anatomy.
Most commonly, we measure, mark, and trim the body of the graft to 5.5 cm in length with a width of 3 cm. The bilateral arms are approximately 1 cm in width and comprise the remaining length of the 8 cm graft (FIGURE 2). As shown in Figure 2, pre-made holes are marked and punched out using a large hollow needle. These serve as the points of attachment for the permanent suture to be “weaved” into the graft arms and delayed absorbable “tacking suture” to be attached from the pubocervical fascia at the bladder neck to the distal end of the graft. This facilitates fixation of the graft in the midline of the anterior vaginal wall, overlying any central distention-type defect.
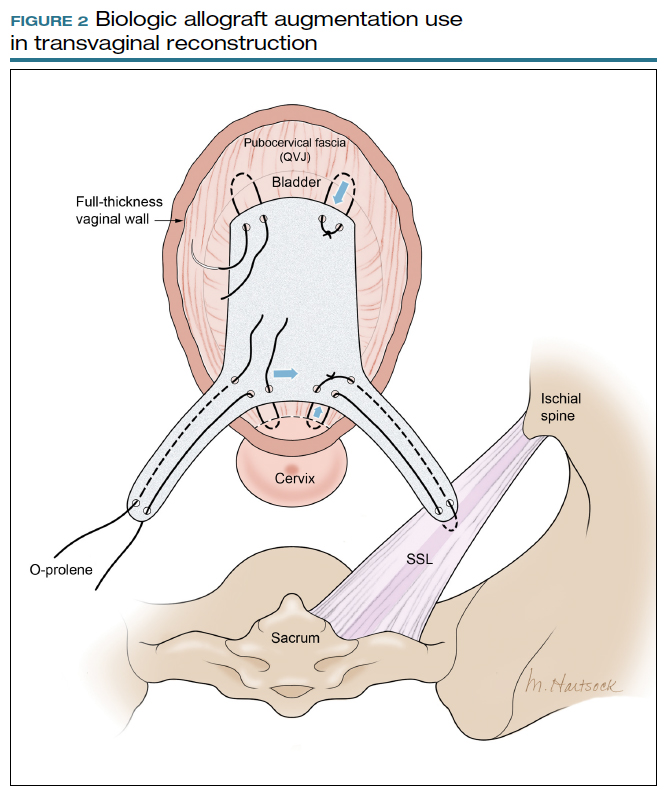
Finally, following attachment of the SSL permanent suture to the distal graft arm, this suture is then attached to the proximal U-shaped end of the graft body (in the midline), followed by a deep and secure bite through the cervix (or vaginal vault apex) and back through the proximal graft. These SSL suspension sutures are then tied such that the distal arms of the graft advance down to the ligament. Care is taken not to tie down to the SSL itself, rather until the cervix (or apex) is reduced to its normal anatomical location.
After the graft is secured in place, the full-thickness vaginal wall is closed with delayed absorbable suture. Sterile 1-inch ribbon packing is placed in the vagina immediately to close any dead space between the vagina and the graft to decrease the risk of seroma or hematoma formation.
This newly developed technique, like many surgeries for POP, requires extensive knowledge of pelvic anatomy and skill in vaginal surgery, and we recommend referral to a subspecialist in Female Pelvic Medicine and Reconstructive Surgery.

Continue to: Upcoming plans to share outcomes data...
Upcoming plans to share outcomes data
We are in the process of performing a retrospective review of all of the cases we have performed at our institution using this technique of permanent suture bridging to the SSL within the arm of the biograft. Given the relatively recent FDA announcement, we have yet to establish any long-term outcomes data. However, the preliminary results at 6-month follow-up are promising and demonstrate a low (2.6%) failure rate, without significant safety concerns. We hope to publish these data as well as more data on longitudinal outcomes in the future.
In summary
Many women are at risk for native-tissue repair failure or are not well suited for an abdominal procedure to correct their pelvic support defect and restore their quality of life. As expert pelvic surgeons, we play an important role in the search for innovative solutions for these women. There is ample opportunity for future research and clinical trials to determine the best biologic materials and their optimal use in pelvic reconstructive surgery.
Originally, polypropylene mesh was designed for use in augmenting abdominal hernia repairs and later was adapted by manufacturers for use in POP repair. The FDA removal from the market of existing transvaginal synthetic mesh kits was a unique catalyst that challenged our community to develop transvaginal repairs using biologic grafts that are genuinely tailored to the unique needs of the female pelvic anatomy. ●
- Maher C, Feiner B, Baessler K. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013:CD004014.
- Weber AM, Walters MD, Piedmonte MR, et al. Anterior colporrhaphy: a randomized trial of three surgical techniques. Am J Obstet Gynecol. 2001;185:1299-1304.
- Walters MD, Ridgeway BM. Surgical treatment of vaginal apex prolapse. Obstet Gynecol. 2013;121(2 pt 1):354-374.
- Meister MRL, Sutcliffe S, Lowder JL. Definitions of apical vaginal support loss: a systematic review. Am J Obstet Gynecol. 2017;216:232. e1-232.e14.
- Cox A, Herschorn S. Evaluation of current biologic meshes in pelvic organ prolapse repair. Curr Urol Rep. 2012;13:247-255.
- Jelovsek JE, Barber M, Brubaker K, et al. Effect of uterosacral ligament suspension vs sacrospinous ligament fixation with or without perioperative behavioral therapy for pelvic organ vaginal prolapse on surgical outcomes and prolapse symptoms at 5 years in the OPTIMAL randomized clinical trial. JAMA. 2018:319:1554-1565.
- Bowen ST, Moalli P, Abramowitch S, et al. Outcomes of the defining mechanisms of anterior vaginal wall descent trial [abstract 15]. Am J Obstet Gynecol. 2020;222:S770-S771.
- Chung CP, Miskimins R, Kuehl TJ, et al. Permanent suture used in uterosacral ligament suspension offers better anatomical support than delayed absorbable suture. Int Urogynecol J. 2012;23:223-227.
- US Food and Drug Administration. FDA takes action to protect women’s health, orders manufacturers of surgical mesh intended for transvaginal repair of pelvic organ prolapse to stop selling all devices. https://www.fda.gov/news-events/press-announcements/fda-takes-action-protect-womens-health-orders-manufacturers-surgical -mesh-intended-transvaginal. April 16, 2019. Accessed September 1, 2020.
- Londono R, Badylak SF. Biologic scaffolds for regenerative medicine: mechanisms of in vivo remodeling. Ann Biomed Eng. 2015;43:577-592.
- Cornwell KG, Landsman A, James KS. Extracellular matrix biomaterials for soft tissue repair. Clin Podiatr Med Surg. 2009;26: 507-523.
- Maher CM, Feiner B, Baessler K, et al. Surgical management of pelvic organ prolapse in women: the updated summary version Cochrane review. Int Urogynecol J. 2011;22:1445-1447.
- Maher C, Feiner B, Baessler K, et al. Surgery for women with anterior compartment prolapse. Cochrane Database Syst Rev. 2016;11:CD004014.
- Maher C, Feiner B, Baessler K, et al. Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. Cochrane Database Syst Rev. 2016;2:CD012179.
- Rosenblatt P, Von Bargen E. Use of biologic grafts in pelvic organ prolapse surgery. Contemporary OB/GYN. 2017;62:14-19.
- Greenspan DC, Hernandez R, Faleris J. Histology of surgically implanted Tutoplast processed dermis. http://www.zimmerbiomet .co.il/images/lib_artHistologyDermis%2010.pdf. Accessed September 2, 2020.
- Williams D. Revisiting the definition of biocompatibility. Med Device Technol. 2003;14:10-13.
- Nosti PA, Carter CM, Sokol AI, et al. Transvaginal versus transabdominal placement of synthetic mesh at time of sacrocolpopexy. Female Pelvic Med Reconstr Surg. 2016;22:151-155.
Pelvic organ prolapse (POP) is a common occurrence over the course of a woman’s lifetime, especially in parous women (up to 50% of women who have given birth).1 The anterior vaginal wall is the most common site of POP and has the highest recurrence rate of up to 70%.2 The risk of developing POP increases with age, obesity, White race, family history, and prior pelvic surgery, such as hysterectomy. It affects more than 3 million women in the United States alone, often negatively impacting sexual function and overall quality of life.3,4
Because women are living longer than ever before and are more active in their senior years, a long-lasting, durable surgical repair is desirable, if not necessary. To be cost-effective and to avoid general anesthesia, the surgical approach ideally should be vaginal.
Biologic and synthetic grafts to augment transvaginal repair traditionally are used to improve on the well-recognized high failure rate of native-tissue repair that is often seen at both short-term and medium-term follow-up.5 The failure rate is commonly referenced as 30% to 40% at 2-year follow-up and 61% to 70% at 5-year follow-up, well-established by the results of the OPTIMAL randomized clinical trial.6 The more recent Descent trial likewise demonstrates a higher failure rate of native-tissue repair versus transvaginal mesh repair at a shorter term of 30 to 42 months.7 Furthermore, the use of permanent versus absorbable suture in suspension of the vaginal apex is associated with lower short-term failure rates.8
Despite this Level I evidence that demonstrates a clear advantage for obtaining a longer or more durable repair with permanent materials, native-tissue repairs with absorbable suture are still performed routinely. Since the US Food and Drug Administration (FDA) ordered that the use of transvaginal surgical mesh augmentation for pelvic reconstructive surgery be discontinued, it is more important than ever to explore evolving alternative native-tissue augmentation repair techniques that hopefully can preserve the advantages and merits of vaginal surgery and achieve longer durability.9
Biologic graft augmentation use in transvaginal reconstruction
All biologic grafts, including allografts derived from human tissue and xenografts derived from animal tissue, are acellular constructs composed of extracellular matrix (ECM) that acts as scaffolding for the host tissue. The ECM is predominantly composed of collagen (types I and III) and noncollagenous fibronectin, laminin, and glycosaminoglycans in various amounts depending on the source tissue. The 3D presentation of ECM’s complex molecules allows for rapid repopulation of host cells and revascularization with eventual regeneration.
Once a biologic graft is placed surgically, the body’s response to the scaffold ECM mimics the normal wound-healing process, beginning with fibrin-rich matrix hemostasis and the subsequent innate immune response of neutrophil and M1 macrophage infiltration. M1 macrophages are proinflammatory and clear cellular debris and begin the process of graft scaffold degradation. The host tissue then begins the process of remodeling through pro-remodeling M2 macrophages and stem cell recruitment, proliferation, and differentiation.10 As the biologic graft provides initial structure and strength for pelvic repairs, the ideal ECM scaffold would not degrade before the host is able to fully undergo regeneration and maintain its structure and strength.
Biologic grafts differ in source (allograft or xenograft), type (pericardium, dermis, or bladder), developmental stage (fetal or adult), decellularization processing, and sterilization techniques. These 5 aspects determine the distinct 3D ECM scaffold structure, strength, and longevity. If the ECM scaffold is damaged or retains noncollagenous proteins during the preparation process, an inflammatory response is triggered in which the graft is degraded, resorbed, and replaced with scar tissue. Furthermore, certain processing techniques aimed at extending the ECM’s durability—that is, cross-linking collagen—results in the foreign body response in which there is no vascular infiltration or cellular penetration of the graft and a collagen capsule is created around the empty matrix.11 To avoid resorption or encapsulation of the graft, the ECM scaffolds of biologic grafts must be optimized to induce regeneration.
Continue to: Choosing surgical POP repair...
Choosing surgical POP repair
The decision to undergo surgical treatment for prolapse is a shared decision-making process between the patient and surgeon and always should be individualized. The type of procedure and the surgical approach will depend on the patient’s goals, the degree of prolapse, clinical history, risk tolerance, the surgeon’s skill set, and whether or not there is an indication or relative contraindication for uterine removal at the time of prolapse repair.
While the FDA’s order does not apply to transabdominally placed surgical mesh, such as sacrocolpopexy, not all patients are ideal candidates for an abdominal sacrocolpopexy. Most notable are women with a history of multiple prior abdominal surgeries with higher rates of intraperitoneal adhesions. Ideally, to be cost-effective and to avoid general anesthesia, the surgical approach should be vaginal whenever possible.
Biologic versus native-tissue grafts
Currently, only low-quality evidence exists that compares the outcomes of biologic grafts with traditional native-tissue repairs in POP. Studies have been limited by poor reporting of methods, inconsistency in technique and materials used, and imprecise definitions. One Cochrane Review on the surgical management of POP concluded that biologic graft augmentation was associated with a lower failure rate (18%) within 1 to 2 years when compared with a traditional anterior colporrhaphy (28%).12
Based on consideration of all Cochrane Database Reviews and recent large systematic reviews, there clearly is a paucity of information on which to draw well-defined conclusions regarding the advantage of biomaterials in prolapse surgery.12-14 This is due in part to the variation in graft material used and the surgical technique employed.
Similarly, evidence is lacking regarding the superiority of one type of biologic graft over another. Furthermore, some of the grafts previously studied are no longer on the market.15 With the FDA’s removal of all transvaginal mesh, including xenografts, only allografts are available for pelvic floor reconstruction. Currently, only 3 commercial manufacturers market allografts for pelvic floor reconstruction. Each allograft is available in various sizes and all can be trimmed at the time of the surgical procedure to customize both the size and shape to fit the individual patient.
A novel technique using Axis Dermis and polypropylene suture
One of the commercially available allografts, Axis Dermis (Coloplast), is non–cross-linked and is derived from human cadaveric dermal tissue from the back and dorsum of the upper leg. It is sterilized by a proprietary Tutoplast️ sterilization process that uses gamma irradiation to inactivate and prevent the transmission of pathogens. This unique technique involving solvent dehydration means the graft is never freeze dried; thus, the natural tissue matrix is preserved.
Additionally, the allograft is antigen-free, which decreases the risk of tissue reaction (scarring/fibrosis) and aids in the process of host tissue remodeling; invasion by growth factors, blood cells, collagen, elastin, and neovascularization. This natural tissue remodeling facilitates the anticipated “reabsorption” of the graft by the host tissue, leaving the patient with a tissue scaffold, that is, a stronger layer of “fascia” beneath the muscularis.16 As a result of this “biocompatible” graft, the host tissue remodeling has been shown in the rat model to involve early cellular infiltration and angiogenesis (in the first week after implantation), that leads to an organized cellular architecture with greater tensile strength by week 4, and ultimately inability to distinguish host collagen from the implant by 8 to 12 weeks.17,18
Continue to: Steps in performing the technique...
Steps in performing the technique
To ensure that the graft is placed adjacent to the vaginal serosa, a full-thickness dissection is carried out to enter the true vesicovaginal space, which lies below all 4 histologic layers of the vagina (nonkeratinized stratified squamous epithelium, lamina propria, muscularis, and serosa). For the anterior dissection, a Tuohy epidural needle is used to achieve an accurate and consistent depth when injecting fluid (hydrodissection) to enter this true pelvic space (FIGURE 1). Correct entry into the vesicovaginal space can be confirmed visually by the presence of adipose tissue.
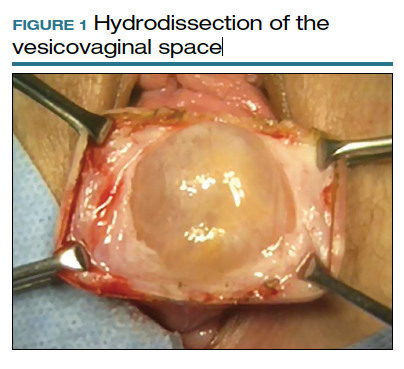
Many pelvic surgeons use the sacrospinous ligament (SSL) as a strong and reliable point of attachment for vaginal prolapse repair. It can be approached either anteriorly or posteriorly with careful dissection. Permanent suture (0-Prolene) is used to “bridge” the attachment between the SSL, the Axis Dermis graft, and the cervix (or vaginal apex). The suture is placed in the middle third and lower half of the ligament to avoid injury to nearby neurovascular structures.
While the surgeon may use any suture-capturing device, we prefer the Anchosure System (Neomedic). This device delivers a small anchor securely into the ligament through a single point of entry, minimizing the risk of postoperative pain for the patient. A 6 cm x 8 cm size Axis Dermis graft is then trimmed to meet the specifications of the patient’s anatomy.
Most commonly, we measure, mark, and trim the body of the graft to 5.5 cm in length with a width of 3 cm. The bilateral arms are approximately 1 cm in width and comprise the remaining length of the 8 cm graft (FIGURE 2). As shown in Figure 2, pre-made holes are marked and punched out using a large hollow needle. These serve as the points of attachment for the permanent suture to be “weaved” into the graft arms and delayed absorbable “tacking suture” to be attached from the pubocervical fascia at the bladder neck to the distal end of the graft. This facilitates fixation of the graft in the midline of the anterior vaginal wall, overlying any central distention-type defect.
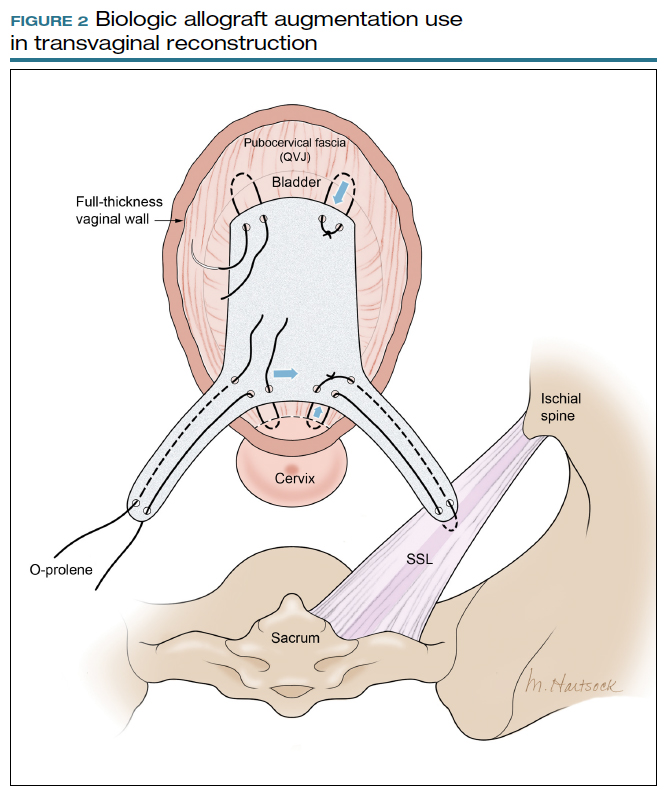
Finally, following attachment of the SSL permanent suture to the distal graft arm, this suture is then attached to the proximal U-shaped end of the graft body (in the midline), followed by a deep and secure bite through the cervix (or vaginal vault apex) and back through the proximal graft. These SSL suspension sutures are then tied such that the distal arms of the graft advance down to the ligament. Care is taken not to tie down to the SSL itself, rather until the cervix (or apex) is reduced to its normal anatomical location.
After the graft is secured in place, the full-thickness vaginal wall is closed with delayed absorbable suture. Sterile 1-inch ribbon packing is placed in the vagina immediately to close any dead space between the vagina and the graft to decrease the risk of seroma or hematoma formation.
This newly developed technique, like many surgeries for POP, requires extensive knowledge of pelvic anatomy and skill in vaginal surgery, and we recommend referral to a subspecialist in Female Pelvic Medicine and Reconstructive Surgery.

Continue to: Upcoming plans to share outcomes data...
Upcoming plans to share outcomes data
We are in the process of performing a retrospective review of all of the cases we have performed at our institution using this technique of permanent suture bridging to the SSL within the arm of the biograft. Given the relatively recent FDA announcement, we have yet to establish any long-term outcomes data. However, the preliminary results at 6-month follow-up are promising and demonstrate a low (2.6%) failure rate, without significant safety concerns. We hope to publish these data as well as more data on longitudinal outcomes in the future.
In summary
Many women are at risk for native-tissue repair failure or are not well suited for an abdominal procedure to correct their pelvic support defect and restore their quality of life. As expert pelvic surgeons, we play an important role in the search for innovative solutions for these women. There is ample opportunity for future research and clinical trials to determine the best biologic materials and their optimal use in pelvic reconstructive surgery.
Originally, polypropylene mesh was designed for use in augmenting abdominal hernia repairs and later was adapted by manufacturers for use in POP repair. The FDA removal from the market of existing transvaginal synthetic mesh kits was a unique catalyst that challenged our community to develop transvaginal repairs using biologic grafts that are genuinely tailored to the unique needs of the female pelvic anatomy. ●
Pelvic organ prolapse (POP) is a common occurrence over the course of a woman’s lifetime, especially in parous women (up to 50% of women who have given birth).1 The anterior vaginal wall is the most common site of POP and has the highest recurrence rate of up to 70%.2 The risk of developing POP increases with age, obesity, White race, family history, and prior pelvic surgery, such as hysterectomy. It affects more than 3 million women in the United States alone, often negatively impacting sexual function and overall quality of life.3,4
Because women are living longer than ever before and are more active in their senior years, a long-lasting, durable surgical repair is desirable, if not necessary. To be cost-effective and to avoid general anesthesia, the surgical approach ideally should be vaginal.
Biologic and synthetic grafts to augment transvaginal repair traditionally are used to improve on the well-recognized high failure rate of native-tissue repair that is often seen at both short-term and medium-term follow-up.5 The failure rate is commonly referenced as 30% to 40% at 2-year follow-up and 61% to 70% at 5-year follow-up, well-established by the results of the OPTIMAL randomized clinical trial.6 The more recent Descent trial likewise demonstrates a higher failure rate of native-tissue repair versus transvaginal mesh repair at a shorter term of 30 to 42 months.7 Furthermore, the use of permanent versus absorbable suture in suspension of the vaginal apex is associated with lower short-term failure rates.8
Despite this Level I evidence that demonstrates a clear advantage for obtaining a longer or more durable repair with permanent materials, native-tissue repairs with absorbable suture are still performed routinely. Since the US Food and Drug Administration (FDA) ordered that the use of transvaginal surgical mesh augmentation for pelvic reconstructive surgery be discontinued, it is more important than ever to explore evolving alternative native-tissue augmentation repair techniques that hopefully can preserve the advantages and merits of vaginal surgery and achieve longer durability.9
Biologic graft augmentation use in transvaginal reconstruction
All biologic grafts, including allografts derived from human tissue and xenografts derived from animal tissue, are acellular constructs composed of extracellular matrix (ECM) that acts as scaffolding for the host tissue. The ECM is predominantly composed of collagen (types I and III) and noncollagenous fibronectin, laminin, and glycosaminoglycans in various amounts depending on the source tissue. The 3D presentation of ECM’s complex molecules allows for rapid repopulation of host cells and revascularization with eventual regeneration.
Once a biologic graft is placed surgically, the body’s response to the scaffold ECM mimics the normal wound-healing process, beginning with fibrin-rich matrix hemostasis and the subsequent innate immune response of neutrophil and M1 macrophage infiltration. M1 macrophages are proinflammatory and clear cellular debris and begin the process of graft scaffold degradation. The host tissue then begins the process of remodeling through pro-remodeling M2 macrophages and stem cell recruitment, proliferation, and differentiation.10 As the biologic graft provides initial structure and strength for pelvic repairs, the ideal ECM scaffold would not degrade before the host is able to fully undergo regeneration and maintain its structure and strength.
Biologic grafts differ in source (allograft or xenograft), type (pericardium, dermis, or bladder), developmental stage (fetal or adult), decellularization processing, and sterilization techniques. These 5 aspects determine the distinct 3D ECM scaffold structure, strength, and longevity. If the ECM scaffold is damaged or retains noncollagenous proteins during the preparation process, an inflammatory response is triggered in which the graft is degraded, resorbed, and replaced with scar tissue. Furthermore, certain processing techniques aimed at extending the ECM’s durability—that is, cross-linking collagen—results in the foreign body response in which there is no vascular infiltration or cellular penetration of the graft and a collagen capsule is created around the empty matrix.11 To avoid resorption or encapsulation of the graft, the ECM scaffolds of biologic grafts must be optimized to induce regeneration.
Continue to: Choosing surgical POP repair...
Choosing surgical POP repair
The decision to undergo surgical treatment for prolapse is a shared decision-making process between the patient and surgeon and always should be individualized. The type of procedure and the surgical approach will depend on the patient’s goals, the degree of prolapse, clinical history, risk tolerance, the surgeon’s skill set, and whether or not there is an indication or relative contraindication for uterine removal at the time of prolapse repair.
While the FDA’s order does not apply to transabdominally placed surgical mesh, such as sacrocolpopexy, not all patients are ideal candidates for an abdominal sacrocolpopexy. Most notable are women with a history of multiple prior abdominal surgeries with higher rates of intraperitoneal adhesions. Ideally, to be cost-effective and to avoid general anesthesia, the surgical approach should be vaginal whenever possible.
Biologic versus native-tissue grafts
Currently, only low-quality evidence exists that compares the outcomes of biologic grafts with traditional native-tissue repairs in POP. Studies have been limited by poor reporting of methods, inconsistency in technique and materials used, and imprecise definitions. One Cochrane Review on the surgical management of POP concluded that biologic graft augmentation was associated with a lower failure rate (18%) within 1 to 2 years when compared with a traditional anterior colporrhaphy (28%).12
Based on consideration of all Cochrane Database Reviews and recent large systematic reviews, there clearly is a paucity of information on which to draw well-defined conclusions regarding the advantage of biomaterials in prolapse surgery.12-14 This is due in part to the variation in graft material used and the surgical technique employed.
Similarly, evidence is lacking regarding the superiority of one type of biologic graft over another. Furthermore, some of the grafts previously studied are no longer on the market.15 With the FDA’s removal of all transvaginal mesh, including xenografts, only allografts are available for pelvic floor reconstruction. Currently, only 3 commercial manufacturers market allografts for pelvic floor reconstruction. Each allograft is available in various sizes and all can be trimmed at the time of the surgical procedure to customize both the size and shape to fit the individual patient.
A novel technique using Axis Dermis and polypropylene suture
One of the commercially available allografts, Axis Dermis (Coloplast), is non–cross-linked and is derived from human cadaveric dermal tissue from the back and dorsum of the upper leg. It is sterilized by a proprietary Tutoplast️ sterilization process that uses gamma irradiation to inactivate and prevent the transmission of pathogens. This unique technique involving solvent dehydration means the graft is never freeze dried; thus, the natural tissue matrix is preserved.
Additionally, the allograft is antigen-free, which decreases the risk of tissue reaction (scarring/fibrosis) and aids in the process of host tissue remodeling; invasion by growth factors, blood cells, collagen, elastin, and neovascularization. This natural tissue remodeling facilitates the anticipated “reabsorption” of the graft by the host tissue, leaving the patient with a tissue scaffold, that is, a stronger layer of “fascia” beneath the muscularis.16 As a result of this “biocompatible” graft, the host tissue remodeling has been shown in the rat model to involve early cellular infiltration and angiogenesis (in the first week after implantation), that leads to an organized cellular architecture with greater tensile strength by week 4, and ultimately inability to distinguish host collagen from the implant by 8 to 12 weeks.17,18
Continue to: Steps in performing the technique...
Steps in performing the technique
To ensure that the graft is placed adjacent to the vaginal serosa, a full-thickness dissection is carried out to enter the true vesicovaginal space, which lies below all 4 histologic layers of the vagina (nonkeratinized stratified squamous epithelium, lamina propria, muscularis, and serosa). For the anterior dissection, a Tuohy epidural needle is used to achieve an accurate and consistent depth when injecting fluid (hydrodissection) to enter this true pelvic space (FIGURE 1). Correct entry into the vesicovaginal space can be confirmed visually by the presence of adipose tissue.
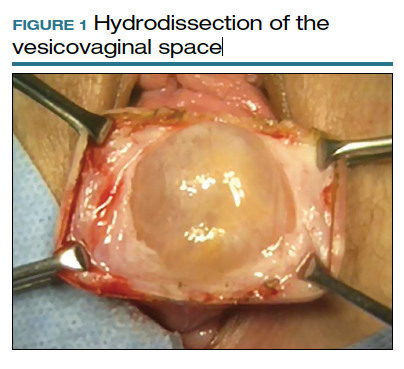
Many pelvic surgeons use the sacrospinous ligament (SSL) as a strong and reliable point of attachment for vaginal prolapse repair. It can be approached either anteriorly or posteriorly with careful dissection. Permanent suture (0-Prolene) is used to “bridge” the attachment between the SSL, the Axis Dermis graft, and the cervix (or vaginal apex). The suture is placed in the middle third and lower half of the ligament to avoid injury to nearby neurovascular structures.
While the surgeon may use any suture-capturing device, we prefer the Anchosure System (Neomedic). This device delivers a small anchor securely into the ligament through a single point of entry, minimizing the risk of postoperative pain for the patient. A 6 cm x 8 cm size Axis Dermis graft is then trimmed to meet the specifications of the patient’s anatomy.
Most commonly, we measure, mark, and trim the body of the graft to 5.5 cm in length with a width of 3 cm. The bilateral arms are approximately 1 cm in width and comprise the remaining length of the 8 cm graft (FIGURE 2). As shown in Figure 2, pre-made holes are marked and punched out using a large hollow needle. These serve as the points of attachment for the permanent suture to be “weaved” into the graft arms and delayed absorbable “tacking suture” to be attached from the pubocervical fascia at the bladder neck to the distal end of the graft. This facilitates fixation of the graft in the midline of the anterior vaginal wall, overlying any central distention-type defect.
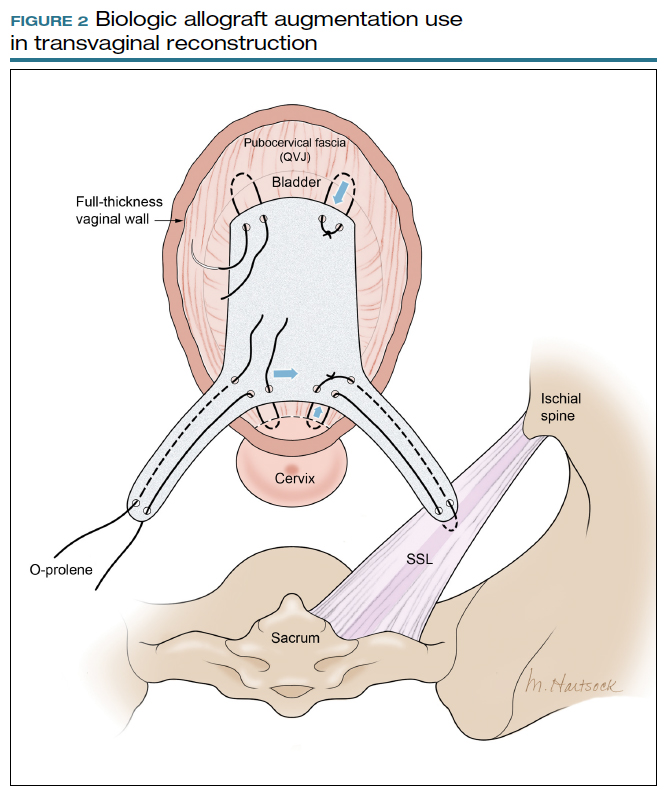
Finally, following attachment of the SSL permanent suture to the distal graft arm, this suture is then attached to the proximal U-shaped end of the graft body (in the midline), followed by a deep and secure bite through the cervix (or vaginal vault apex) and back through the proximal graft. These SSL suspension sutures are then tied such that the distal arms of the graft advance down to the ligament. Care is taken not to tie down to the SSL itself, rather until the cervix (or apex) is reduced to its normal anatomical location.
After the graft is secured in place, the full-thickness vaginal wall is closed with delayed absorbable suture. Sterile 1-inch ribbon packing is placed in the vagina immediately to close any dead space between the vagina and the graft to decrease the risk of seroma or hematoma formation.
This newly developed technique, like many surgeries for POP, requires extensive knowledge of pelvic anatomy and skill in vaginal surgery, and we recommend referral to a subspecialist in Female Pelvic Medicine and Reconstructive Surgery.

Continue to: Upcoming plans to share outcomes data...
Upcoming plans to share outcomes data
We are in the process of performing a retrospective review of all of the cases we have performed at our institution using this technique of permanent suture bridging to the SSL within the arm of the biograft. Given the relatively recent FDA announcement, we have yet to establish any long-term outcomes data. However, the preliminary results at 6-month follow-up are promising and demonstrate a low (2.6%) failure rate, without significant safety concerns. We hope to publish these data as well as more data on longitudinal outcomes in the future.
In summary
Many women are at risk for native-tissue repair failure or are not well suited for an abdominal procedure to correct their pelvic support defect and restore their quality of life. As expert pelvic surgeons, we play an important role in the search for innovative solutions for these women. There is ample opportunity for future research and clinical trials to determine the best biologic materials and their optimal use in pelvic reconstructive surgery.
Originally, polypropylene mesh was designed for use in augmenting abdominal hernia repairs and later was adapted by manufacturers for use in POP repair. The FDA removal from the market of existing transvaginal synthetic mesh kits was a unique catalyst that challenged our community to develop transvaginal repairs using biologic grafts that are genuinely tailored to the unique needs of the female pelvic anatomy. ●
- Maher C, Feiner B, Baessler K. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013:CD004014.
- Weber AM, Walters MD, Piedmonte MR, et al. Anterior colporrhaphy: a randomized trial of three surgical techniques. Am J Obstet Gynecol. 2001;185:1299-1304.
- Walters MD, Ridgeway BM. Surgical treatment of vaginal apex prolapse. Obstet Gynecol. 2013;121(2 pt 1):354-374.
- Meister MRL, Sutcliffe S, Lowder JL. Definitions of apical vaginal support loss: a systematic review. Am J Obstet Gynecol. 2017;216:232. e1-232.e14.
- Cox A, Herschorn S. Evaluation of current biologic meshes in pelvic organ prolapse repair. Curr Urol Rep. 2012;13:247-255.
- Jelovsek JE, Barber M, Brubaker K, et al. Effect of uterosacral ligament suspension vs sacrospinous ligament fixation with or without perioperative behavioral therapy for pelvic organ vaginal prolapse on surgical outcomes and prolapse symptoms at 5 years in the OPTIMAL randomized clinical trial. JAMA. 2018:319:1554-1565.
- Bowen ST, Moalli P, Abramowitch S, et al. Outcomes of the defining mechanisms of anterior vaginal wall descent trial [abstract 15]. Am J Obstet Gynecol. 2020;222:S770-S771.
- Chung CP, Miskimins R, Kuehl TJ, et al. Permanent suture used in uterosacral ligament suspension offers better anatomical support than delayed absorbable suture. Int Urogynecol J. 2012;23:223-227.
- US Food and Drug Administration. FDA takes action to protect women’s health, orders manufacturers of surgical mesh intended for transvaginal repair of pelvic organ prolapse to stop selling all devices. https://www.fda.gov/news-events/press-announcements/fda-takes-action-protect-womens-health-orders-manufacturers-surgical -mesh-intended-transvaginal. April 16, 2019. Accessed September 1, 2020.
- Londono R, Badylak SF. Biologic scaffolds for regenerative medicine: mechanisms of in vivo remodeling. Ann Biomed Eng. 2015;43:577-592.
- Cornwell KG, Landsman A, James KS. Extracellular matrix biomaterials for soft tissue repair. Clin Podiatr Med Surg. 2009;26: 507-523.
- Maher CM, Feiner B, Baessler K, et al. Surgical management of pelvic organ prolapse in women: the updated summary version Cochrane review. Int Urogynecol J. 2011;22:1445-1447.
- Maher C, Feiner B, Baessler K, et al. Surgery for women with anterior compartment prolapse. Cochrane Database Syst Rev. 2016;11:CD004014.
- Maher C, Feiner B, Baessler K, et al. Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. Cochrane Database Syst Rev. 2016;2:CD012179.
- Rosenblatt P, Von Bargen E. Use of biologic grafts in pelvic organ prolapse surgery. Contemporary OB/GYN. 2017;62:14-19.
- Greenspan DC, Hernandez R, Faleris J. Histology of surgically implanted Tutoplast processed dermis. http://www.zimmerbiomet .co.il/images/lib_artHistologyDermis%2010.pdf. Accessed September 2, 2020.
- Williams D. Revisiting the definition of biocompatibility. Med Device Technol. 2003;14:10-13.
- Nosti PA, Carter CM, Sokol AI, et al. Transvaginal versus transabdominal placement of synthetic mesh at time of sacrocolpopexy. Female Pelvic Med Reconstr Surg. 2016;22:151-155.
- Maher C, Feiner B, Baessler K. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013:CD004014.
- Weber AM, Walters MD, Piedmonte MR, et al. Anterior colporrhaphy: a randomized trial of three surgical techniques. Am J Obstet Gynecol. 2001;185:1299-1304.
- Walters MD, Ridgeway BM. Surgical treatment of vaginal apex prolapse. Obstet Gynecol. 2013;121(2 pt 1):354-374.
- Meister MRL, Sutcliffe S, Lowder JL. Definitions of apical vaginal support loss: a systematic review. Am J Obstet Gynecol. 2017;216:232. e1-232.e14.
- Cox A, Herschorn S. Evaluation of current biologic meshes in pelvic organ prolapse repair. Curr Urol Rep. 2012;13:247-255.
- Jelovsek JE, Barber M, Brubaker K, et al. Effect of uterosacral ligament suspension vs sacrospinous ligament fixation with or without perioperative behavioral therapy for pelvic organ vaginal prolapse on surgical outcomes and prolapse symptoms at 5 years in the OPTIMAL randomized clinical trial. JAMA. 2018:319:1554-1565.
- Bowen ST, Moalli P, Abramowitch S, et al. Outcomes of the defining mechanisms of anterior vaginal wall descent trial [abstract 15]. Am J Obstet Gynecol. 2020;222:S770-S771.
- Chung CP, Miskimins R, Kuehl TJ, et al. Permanent suture used in uterosacral ligament suspension offers better anatomical support than delayed absorbable suture. Int Urogynecol J. 2012;23:223-227.
- US Food and Drug Administration. FDA takes action to protect women’s health, orders manufacturers of surgical mesh intended for transvaginal repair of pelvic organ prolapse to stop selling all devices. https://www.fda.gov/news-events/press-announcements/fda-takes-action-protect-womens-health-orders-manufacturers-surgical -mesh-intended-transvaginal. April 16, 2019. Accessed September 1, 2020.
- Londono R, Badylak SF. Biologic scaffolds for regenerative medicine: mechanisms of in vivo remodeling. Ann Biomed Eng. 2015;43:577-592.
- Cornwell KG, Landsman A, James KS. Extracellular matrix biomaterials for soft tissue repair. Clin Podiatr Med Surg. 2009;26: 507-523.
- Maher CM, Feiner B, Baessler K, et al. Surgical management of pelvic organ prolapse in women: the updated summary version Cochrane review. Int Urogynecol J. 2011;22:1445-1447.
- Maher C, Feiner B, Baessler K, et al. Surgery for women with anterior compartment prolapse. Cochrane Database Syst Rev. 2016;11:CD004014.
- Maher C, Feiner B, Baessler K, et al. Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. Cochrane Database Syst Rev. 2016;2:CD012179.
- Rosenblatt P, Von Bargen E. Use of biologic grafts in pelvic organ prolapse surgery. Contemporary OB/GYN. 2017;62:14-19.
- Greenspan DC, Hernandez R, Faleris J. Histology of surgically implanted Tutoplast processed dermis. http://www.zimmerbiomet .co.il/images/lib_artHistologyDermis%2010.pdf. Accessed September 2, 2020.
- Williams D. Revisiting the definition of biocompatibility. Med Device Technol. 2003;14:10-13.
- Nosti PA, Carter CM, Sokol AI, et al. Transvaginal versus transabdominal placement of synthetic mesh at time of sacrocolpopexy. Female Pelvic Med Reconstr Surg. 2016;22:151-155.
How to build your identity as a physician online
To have a thriving business in today’s world, a functioning website is crucial to the overall business health. For a medical practice in general, and for its physicians specifically, it is one of the first steps for maintaining a practice. But to grow that practice, it is crucial to take the steps beyond just having a website. Growth requires website optimization for search engines, an expanding referral base, and the knowledge to use web tools and social media at your disposal to promote the practice and its physicians. In this roundtable, several marketing experts and web-savvy physicians discuss using available tools to best position and grow a practice.
Choosing a web upgrade
Patrick J. Culligan, MD: Peter, can you start us off by describing your relationship with Heather, and how your practice benefitted from her expertise?
Peter M. Lotze, MD: Sure. I am a urogynecologist in the competitive market of pelvic reconstructive surgery in Houston, Texas. Within that market, my main approach was to reach out to other physicians to refer patients to my practice. It generally would work, but took increasingly greater amounts of time to call these physicians up, write them letters, and maintain relationships. I felt that the large, national practice group that I am in did not have a significant web presence optimized to promote my practice, which makes it difficult for patients seeking your services to find you in their search for a doctor. It is helpful for patients to be able to understand from your website who you are, what you do, and what their experience may be like.
Glaring to me was that a web search specific for me or things that I do, would not produce our company’s results until page 2 or more on Google. This can be devastating for a practice because most people don’t go past the first page, and you can end up with fewer self-referrals, which should be a significant portion of new patients to your practice. I knew I needed guidance; I knew of Heather’s expertise given her exceptional past work building marketing strategies.
Digital go-tos for marketing
Heather Schueppert: Yes, I was pleased to work with Dr. Lotze, and at the time was a marketing consultant for practices such as his. But gone are the days of printed material—brochures, pamphlets, or even billboards—to effectively promote a business, or in this case, a practice. What still withstands the test of time, however, as the number 1 marketing referral source is word of mouth—from your trusted friend, family member, or coworker.
It is now proven that the number 2 most trusted form of advertising, the most persuasive and the most motivating, is online marketing.1 It is the “digital word of mouth”—the review. Patients are actively online, and a strong digital presence is critical to provide that direct value to retain and grow your patient base.
Continue to: Foundations of private practice reach out...
Foundations of private practice reach out
There are 3 important areas that I consider the foundation of any private practice marketing strategy (TABLE). First is an updated website that is search engine optimized (SEO). You can’t just set it and forget it, it needs to be an updated website. The algorithms for search engines are changing constantly to try to make it as fair and relevant as possible for patients or consumers to find the businesses they are searching for online.
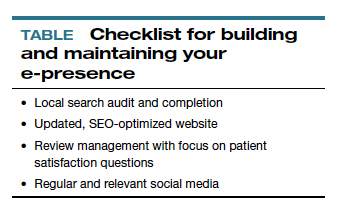
The second area is review management, and for a physician, or even a care center, to do this on your own is a daunting task. It is a critical component, however, to making sure that your reputation out there, that online word of mouth, is as high a star rating as possible.
The third component is local search, which is basically a form of SEO that helps businesses show up in relevant local searches. We are all familiar with the search, “find a restaurant near me,” anything that pushes those search engines to find something local.
Those are what I call the effective triad: that updated website, the review management, and the local search, and all of these are tied together. I think Dr. Lotze and his practice did these effectively well, and I believe that he achieved his goals for the longer term.
Review/reputation management
Dr. Culligan: Brad, is there something that doctors may not know about Healthgrades, and are there opportunities to take full advantage of this physician-rating site?
Brad Bowman, MD: I agree with everything that Dr. Lotze and Heather have said. Start with yourself—what is it that you want to be, the one thing you want to stand for? Get your own marketing, your website right, then, the point is, once you do all that and you are number 1 in SEO, you are still only going to get about 25% of the people looking for you by name to come to your website. The other 75% are going to look at all the other different sites that are out there to provide information to consumers. So the question becomes what do you do with all these other third-party sites? Healthgrades is the most comprehensive and has the highest traffic of the third-party “find a doctor” sites. In 2020, half of all Americans who go to a doctor will use Healthgrades at some point to help select and connect with that doctor.
Physicians have their focus on the quality of the care they provide. Patients, however, focus on the quality of the entire health care experience. Did I get better? How long did I have to wait? Was the office staff helpful? Scarily enough, we still spend more time shopping for a refrigerator or mattress than we do shopping for a doctor. We still tend to think that all doctors are the same. It is the reality of how we have been trained by our insurance companies and by the health care system. That is why getting your marketing right and getting what is it that you want to be known for out there is important, so that you can get the types of patients you want.
Listings management is very important. Make sure that you are findable everywhere. There are services that will do this: Doctor.com, Reputation.com, and many others. They can help you make sure you get all your basic materials right: addresses, phone numbers, your picture. Because 75% of people are going to end up on third-party websites, if your phone number is wrong there, you could lose that patient.
Then the second piece of working with third-party sites is reputation management. Physician reviews are not a bad thing, they are the new word of mouth, as Heather pointed out. Most (80%) of the reviews are going to be positive. The others will be negative, and that is okay. It is important that you get at least 1 or 2 reviews on all the different sites. We know from Healthgrades.com that going from zero reviews to 1 review will increase your call volume by 60%. If you have the choice between 2 physicians and one practice looks like people have been there before, you will go to that one.
You can learn from reviews as well, consumers provide valid feedback. Best practice is to respond to every positive and negative review. Thank them, indicate that you have listened to them, and address any concerns as necessary.
Continue to: Dr. Lotze...
Dr. Lotze: As an example, one of the paramount things that Heather introduced me to was the third party I use to run my website. That company sends a HIPAA-compliant review out to each patient we have seen that day and gives them the opportunity to rate our services and leave comments. If a patient brings up a concern, we can respond immediately, which is important. Patients appreciate feeling that they have been heard. Typically, communicating with a patient will turn the 3-star review into a 5-star as she follows up with the practice.
Ms. Schueppert: Timeliness is important. And just to mention, there certainly is a time commitment to this (and it is a marathon versus a sprint) and there is some financial investment to get it going, but it could truly be detrimental to a practice if you decide not to do anything at all.
Dr. Bowman: Agencies can really help with the time commitment.
Handling bad reviews
Dr. Culligan: What about that person who seems to have it out for you, perhaps giving you multiple bad reviews?
Dr. Bowman: I have seen this before. At Healthgrades, we recently analyzed 8.4 million patient reviews to see what people wrote about.2 The first thing they will talk about is quality of care as they see it. Did I get better or not? You can’t “fix” every patient; there will be some that you cannot help. The next thing patients comment on is bedside manner. With negative reviews, you will see more comments about the office staff.2
A single negative review actually helps make the positive ones look more credible. But if you do believe someone is trolling you, we can flag it and will investigate to the best of our ability. (Different sites likely have different editorial policies.) For example, we look at the IP addresses of all reviews, and if multiple reviews are coming from the same location, we would only let one through, overwriting the previous review from that address.
Patients just want to be heard. We have seen people change their views, based on how their review is handled and responded to.
Dr. Lotze: Is there a response by the physician that you think tends to work better in terms of resolving the issue that can minimize a perceived caustic reaction to a patient’s criticism?
Dr. Bowman: First, just like with any stressful situation, take a deep breath and respond when you feel like you can be constructive. When you do respond, be gracious. Thank them for their feedback. Make sure you reference something about their concern: “I understand that you had to wait longer than you would have liked.” Acknowledge the problem they reference, and then just apologize: “I’m sorry we didn’t meet your expectations.” Then, if they waited too long for example, “We have a new system where no one should have to wait more than 30 minutes….” You can respond privately or publically. Generally, public responses are better as it shows other consumers that you are willing to listen and consider their point of view.
Continue to: The next phase at Healthgrades...
The next phase at Healthgrades
Dr. Culligan: Do you see changes to the way physician-rating sites are working now? Are we going to stay status quo over the next 10 years, or do you see frontiers in how your site is going to develop?
Dr. Bowman: For Healthgrades, we rely on quantitative and objective measures, not just the qualitative. We are investing heavily right now in trying to help consumers understand what are the relative volumes of different procedures or different patient types that each individual doctor sees. Orthopedics is an easy example—if you have a knee problem, you want to go to someone who specializes in knees. Our job is to help consumers easily identify, “This is a shoulder doctor, this is a knee doctor, and this is why that matters.”
In the meantime, as a physician, you can always go into our site and state your care philosophy, identifying what is the sort of patient that you like to treat. Transparency is good for everyone, and especially physicians. It helps the right patient show up for you, and it helps you do a better job providing referrals.
Social media: Avoid pitfalls, and use it to your benefit
Dr. Lotze: Branding was one of the things that I was confused about, and Heather really helped me out. As physicians, we put ourselves out there on our websites, which we try to make professional sources of information for patients. But patients often want to see what else they can find out about us, including Healthgrades and social media. I think the thing that is important to know with social media is that it is a place where people learn about you as a person. Your social media should be another avenue of promotion. Whether it is your personal or professional Facebook page, people are going to see those sites. You have an opportunity to promote yourself as a good physician and a good person with a wholesome practice that you want people to come to. If a physician is posting questionable things about themselves on any kind of social media, it could be perceived as inappropriate by the patient. That can impact how patients think of you as a person, and how they are going to grade you. If people lose sight of who you are due to a questionable social media posting, everything else (SEO, the website) can be for naught.
Dr. Culligan: What are the most important social media tools to invest your time in?
Ms. Schueppert: Before anybody jumps into social media, I firmly recommend that you make sure your local search and your Google 3-pack is set up—which is basically a method Google uses to display the top 3 results on its listings page. Then make sure you have a review management system in place. Make sure you have that updated website. Those are the foundational elements. Once you have that going, social media is the next added layer to that digital presence.
I usually recommend LinkedIn. It is huge because you are staying in contact with your colleagues, that business-to-business type of connection. It remains a way for physicians to set themselves up as experts in their level of specialty.
From there, it’s either Instagram or Facebook. If you are serving more of the younger generations, the millennials and younger, then Instagram is the way to go. If you are focusing on your 40+, 50+, they are going to be far more on Facebook.
Continue to: Dr. Lotze...
Dr. Lotze: For me, a Facebook page was a great place to start. The cost of those Google ads—the first things we see at the top of a Google search in their own separate box—is significant. If a practice has that kind of money to invest, great; it is an instant way to be first on the page during a search. But there are more cost-effective ways of doing that, especially as you are getting your name out. Facebook provides, at a smaller cost, promotion of whatever it is that you are seeking to promote. You can find people within a certain zip code, for instance, and use a Facebook ad campaign that can drive people to your Facebook page—which should have both routinely updated new posts and a link to your website. The posts should be interesting topics relevant to the patients you wish to treat (avoiding personal stories or controversial discussions). You can put a post together, or you can have a third-party service do this. People who follow your page will get reminders of you and your practice with each new post. As your page followers increase, your Facebook rank will improve, and your page will more likely be discovered by Facebook searches for your services. With an added link to your office practice website, those patients go straight to your site without getting lost in the noise of Google search results.
For Instagram, a short video or an interesting picture, along with a brief statement, are the essentials. You can add a single link. Marketing here is by direct messaging or having patients going to your website through a link. Instagram, like Facebook, offers analytics to help show you what your audience likes to read about, improving the quality of your posts and increasing number of followers.
YouTube is the number 2 search engine behind Google. A Google search for your field of medicine may be filled with pages of competitors. However, YouTube has a much lower volume of competing practices, making it easier for patients to find you. The only downside to YouTube is that it will list your video along with other competing videos, which can draw attention away from your practice.
If you want to promote your website or practice with video, using a company such as Vimeo is a better choice compared with YouTube, as YouTube gets credit for video views—which improves YouTube’s SEO and not your own website. Vimeo allows for your website to get credit each time the video is watched. Regardless of where you place your videos, make them short and to the point, with links to your website. Videos only need to be long enough to get your message across and stimulate interest in your practice.
If you can have a blog on your website, it also will help with SEO. What a search engine like Google wants to see is that a patient is on your web page and looking at something for at least 60 seconds. If so, the website is deemed to have information that is relevant, improving your SEO ranking.
Finally, Twitter also can be used for getting messaging out and for branding. The problem with it is that many people go to Twitter to follow a Hollywood celebrity, a sports star, or are looking for mass communication. There is less interest on Twitter for physician outreach.
Continue to: Measuring ROI...
Measuring ROI
Dr. Culligan: What’s the best way to track your return on investment?
Dr. Lotze: First for me was to find out what didn’t work in the office and fix that before really promoting my practice. It’s about the global experience for a patient, as Brad mentioned. As a marketing expert, Heather met with me to understand my goals. She then called my office as a patient to set up an appointment and went through that entire office experience. We identified issues needing improvement.
The next step was to develop a working relationship with my webmaster—someone who can help manage Internet image and SEO. Together, you will develop goals for what the SEO should promote specific to your practice. Once a good SEO program is in place, your website’s ranking will go up—although it can take a minimum of 6 months to see a significant increase. To help understand your website’s performance, your webmaster should provide you with reports on your site’s analytics.
As you go through this process, it is great to have a marketing expert to be the point person. You will work closely together for a while, but eventually you can back off over time. The time and expense you invest on the front end have huge rewards on the back end. Currently, I still spend a reasonable amount of money every month. I have a high self-referral base because of these efforts, however, which results in more patient surgeries and easily covers my expenses. It is money well invested. My website traffic increased by 268% over 2 years (FIGURE). I’ll propose that currently more than half of my patients are self-referrals due to online marketing.
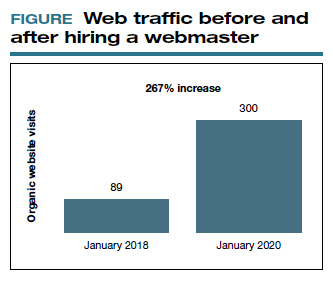
Ms. Schueppert: The only thing I would add is training your front staff. They are checking people in, taking appointments, checking your patients out. Have them be mindful that there are campaigns going on, whether it is a social media push, or a new video that went on the website. They can ask, “How did you hear about us?” when a new patient calls.
Dr. Bowman: Unless you are a large university hospital, where the analytics get significantly more advanced in terms of measuring return on investment (ROI), I think you should just be looking at your schedule and looking at your monthly billings and seeing how they change over time. You can calculate how much a new patient is worth because you can figure out how many patients you have and how much you bill and what your profits are.
Dr. Culligan: For those of us who are hospital employees, you can try to convince the hospital that you can do a detailed ROI analysis, or you can just look at it like (say it’s $3,000 per month), how many surgeries does this project have to generate before the hospital makes that back? The answer is a fraction of 1 case.
Thank you to all of you for your expertise on this roundtable.
- Anderson A. Online reviews vs. word of mouth: Which one is more important. https://www.revlocal.com/blog/reviewandreputationmanagement/onlinereviewsvswordofmouthwhichoneismoreimportant. Accessed July 17, 2020.
- 2020 Patient sentiment report. Healthgrades; Medical Group Management Association. https://www.healthgrades.com/content /patientsentimentreport. Accessed July 17, 2020
To have a thriving business in today’s world, a functioning website is crucial to the overall business health. For a medical practice in general, and for its physicians specifically, it is one of the first steps for maintaining a practice. But to grow that practice, it is crucial to take the steps beyond just having a website. Growth requires website optimization for search engines, an expanding referral base, and the knowledge to use web tools and social media at your disposal to promote the practice and its physicians. In this roundtable, several marketing experts and web-savvy physicians discuss using available tools to best position and grow a practice.
Choosing a web upgrade
Patrick J. Culligan, MD: Peter, can you start us off by describing your relationship with Heather, and how your practice benefitted from her expertise?
Peter M. Lotze, MD: Sure. I am a urogynecologist in the competitive market of pelvic reconstructive surgery in Houston, Texas. Within that market, my main approach was to reach out to other physicians to refer patients to my practice. It generally would work, but took increasingly greater amounts of time to call these physicians up, write them letters, and maintain relationships. I felt that the large, national practice group that I am in did not have a significant web presence optimized to promote my practice, which makes it difficult for patients seeking your services to find you in their search for a doctor. It is helpful for patients to be able to understand from your website who you are, what you do, and what their experience may be like.
Glaring to me was that a web search specific for me or things that I do, would not produce our company’s results until page 2 or more on Google. This can be devastating for a practice because most people don’t go past the first page, and you can end up with fewer self-referrals, which should be a significant portion of new patients to your practice. I knew I needed guidance; I knew of Heather’s expertise given her exceptional past work building marketing strategies.
Digital go-tos for marketing
Heather Schueppert: Yes, I was pleased to work with Dr. Lotze, and at the time was a marketing consultant for practices such as his. But gone are the days of printed material—brochures, pamphlets, or even billboards—to effectively promote a business, or in this case, a practice. What still withstands the test of time, however, as the number 1 marketing referral source is word of mouth—from your trusted friend, family member, or coworker.
It is now proven that the number 2 most trusted form of advertising, the most persuasive and the most motivating, is online marketing.1 It is the “digital word of mouth”—the review. Patients are actively online, and a strong digital presence is critical to provide that direct value to retain and grow your patient base.
Continue to: Foundations of private practice reach out...
Foundations of private practice reach out
There are 3 important areas that I consider the foundation of any private practice marketing strategy (TABLE). First is an updated website that is search engine optimized (SEO). You can’t just set it and forget it, it needs to be an updated website. The algorithms for search engines are changing constantly to try to make it as fair and relevant as possible for patients or consumers to find the businesses they are searching for online.
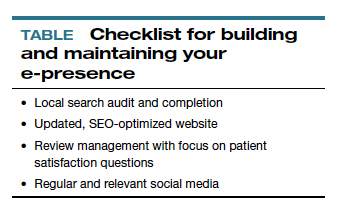
The second area is review management, and for a physician, or even a care center, to do this on your own is a daunting task. It is a critical component, however, to making sure that your reputation out there, that online word of mouth, is as high a star rating as possible.
The third component is local search, which is basically a form of SEO that helps businesses show up in relevant local searches. We are all familiar with the search, “find a restaurant near me,” anything that pushes those search engines to find something local.
Those are what I call the effective triad: that updated website, the review management, and the local search, and all of these are tied together. I think Dr. Lotze and his practice did these effectively well, and I believe that he achieved his goals for the longer term.
Review/reputation management
Dr. Culligan: Brad, is there something that doctors may not know about Healthgrades, and are there opportunities to take full advantage of this physician-rating site?
Brad Bowman, MD: I agree with everything that Dr. Lotze and Heather have said. Start with yourself—what is it that you want to be, the one thing you want to stand for? Get your own marketing, your website right, then, the point is, once you do all that and you are number 1 in SEO, you are still only going to get about 25% of the people looking for you by name to come to your website. The other 75% are going to look at all the other different sites that are out there to provide information to consumers. So the question becomes what do you do with all these other third-party sites? Healthgrades is the most comprehensive and has the highest traffic of the third-party “find a doctor” sites. In 2020, half of all Americans who go to a doctor will use Healthgrades at some point to help select and connect with that doctor.
Physicians have their focus on the quality of the care they provide. Patients, however, focus on the quality of the entire health care experience. Did I get better? How long did I have to wait? Was the office staff helpful? Scarily enough, we still spend more time shopping for a refrigerator or mattress than we do shopping for a doctor. We still tend to think that all doctors are the same. It is the reality of how we have been trained by our insurance companies and by the health care system. That is why getting your marketing right and getting what is it that you want to be known for out there is important, so that you can get the types of patients you want.
Listings management is very important. Make sure that you are findable everywhere. There are services that will do this: Doctor.com, Reputation.com, and many others. They can help you make sure you get all your basic materials right: addresses, phone numbers, your picture. Because 75% of people are going to end up on third-party websites, if your phone number is wrong there, you could lose that patient.
Then the second piece of working with third-party sites is reputation management. Physician reviews are not a bad thing, they are the new word of mouth, as Heather pointed out. Most (80%) of the reviews are going to be positive. The others will be negative, and that is okay. It is important that you get at least 1 or 2 reviews on all the different sites. We know from Healthgrades.com that going from zero reviews to 1 review will increase your call volume by 60%. If you have the choice between 2 physicians and one practice looks like people have been there before, you will go to that one.
You can learn from reviews as well, consumers provide valid feedback. Best practice is to respond to every positive and negative review. Thank them, indicate that you have listened to them, and address any concerns as necessary.
Continue to: Dr. Lotze...
Dr. Lotze: As an example, one of the paramount things that Heather introduced me to was the third party I use to run my website. That company sends a HIPAA-compliant review out to each patient we have seen that day and gives them the opportunity to rate our services and leave comments. If a patient brings up a concern, we can respond immediately, which is important. Patients appreciate feeling that they have been heard. Typically, communicating with a patient will turn the 3-star review into a 5-star as she follows up with the practice.
Ms. Schueppert: Timeliness is important. And just to mention, there certainly is a time commitment to this (and it is a marathon versus a sprint) and there is some financial investment to get it going, but it could truly be detrimental to a practice if you decide not to do anything at all.
Dr. Bowman: Agencies can really help with the time commitment.
Handling bad reviews
Dr. Culligan: What about that person who seems to have it out for you, perhaps giving you multiple bad reviews?
Dr. Bowman: I have seen this before. At Healthgrades, we recently analyzed 8.4 million patient reviews to see what people wrote about.2 The first thing they will talk about is quality of care as they see it. Did I get better or not? You can’t “fix” every patient; there will be some that you cannot help. The next thing patients comment on is bedside manner. With negative reviews, you will see more comments about the office staff.2
A single negative review actually helps make the positive ones look more credible. But if you do believe someone is trolling you, we can flag it and will investigate to the best of our ability. (Different sites likely have different editorial policies.) For example, we look at the IP addresses of all reviews, and if multiple reviews are coming from the same location, we would only let one through, overwriting the previous review from that address.
Patients just want to be heard. We have seen people change their views, based on how their review is handled and responded to.
Dr. Lotze: Is there a response by the physician that you think tends to work better in terms of resolving the issue that can minimize a perceived caustic reaction to a patient’s criticism?
Dr. Bowman: First, just like with any stressful situation, take a deep breath and respond when you feel like you can be constructive. When you do respond, be gracious. Thank them for their feedback. Make sure you reference something about their concern: “I understand that you had to wait longer than you would have liked.” Acknowledge the problem they reference, and then just apologize: “I’m sorry we didn’t meet your expectations.” Then, if they waited too long for example, “We have a new system where no one should have to wait more than 30 minutes….” You can respond privately or publically. Generally, public responses are better as it shows other consumers that you are willing to listen and consider their point of view.
Continue to: The next phase at Healthgrades...
The next phase at Healthgrades
Dr. Culligan: Do you see changes to the way physician-rating sites are working now? Are we going to stay status quo over the next 10 years, or do you see frontiers in how your site is going to develop?
Dr. Bowman: For Healthgrades, we rely on quantitative and objective measures, not just the qualitative. We are investing heavily right now in trying to help consumers understand what are the relative volumes of different procedures or different patient types that each individual doctor sees. Orthopedics is an easy example—if you have a knee problem, you want to go to someone who specializes in knees. Our job is to help consumers easily identify, “This is a shoulder doctor, this is a knee doctor, and this is why that matters.”
In the meantime, as a physician, you can always go into our site and state your care philosophy, identifying what is the sort of patient that you like to treat. Transparency is good for everyone, and especially physicians. It helps the right patient show up for you, and it helps you do a better job providing referrals.
Social media: Avoid pitfalls, and use it to your benefit
Dr. Lotze: Branding was one of the things that I was confused about, and Heather really helped me out. As physicians, we put ourselves out there on our websites, which we try to make professional sources of information for patients. But patients often want to see what else they can find out about us, including Healthgrades and social media. I think the thing that is important to know with social media is that it is a place where people learn about you as a person. Your social media should be another avenue of promotion. Whether it is your personal or professional Facebook page, people are going to see those sites. You have an opportunity to promote yourself as a good physician and a good person with a wholesome practice that you want people to come to. If a physician is posting questionable things about themselves on any kind of social media, it could be perceived as inappropriate by the patient. That can impact how patients think of you as a person, and how they are going to grade you. If people lose sight of who you are due to a questionable social media posting, everything else (SEO, the website) can be for naught.
Dr. Culligan: What are the most important social media tools to invest your time in?
Ms. Schueppert: Before anybody jumps into social media, I firmly recommend that you make sure your local search and your Google 3-pack is set up—which is basically a method Google uses to display the top 3 results on its listings page. Then make sure you have a review management system in place. Make sure you have that updated website. Those are the foundational elements. Once you have that going, social media is the next added layer to that digital presence.
I usually recommend LinkedIn. It is huge because you are staying in contact with your colleagues, that business-to-business type of connection. It remains a way for physicians to set themselves up as experts in their level of specialty.
From there, it’s either Instagram or Facebook. If you are serving more of the younger generations, the millennials and younger, then Instagram is the way to go. If you are focusing on your 40+, 50+, they are going to be far more on Facebook.
Continue to: Dr. Lotze...
Dr. Lotze: For me, a Facebook page was a great place to start. The cost of those Google ads—the first things we see at the top of a Google search in their own separate box—is significant. If a practice has that kind of money to invest, great; it is an instant way to be first on the page during a search. But there are more cost-effective ways of doing that, especially as you are getting your name out. Facebook provides, at a smaller cost, promotion of whatever it is that you are seeking to promote. You can find people within a certain zip code, for instance, and use a Facebook ad campaign that can drive people to your Facebook page—which should have both routinely updated new posts and a link to your website. The posts should be interesting topics relevant to the patients you wish to treat (avoiding personal stories or controversial discussions). You can put a post together, or you can have a third-party service do this. People who follow your page will get reminders of you and your practice with each new post. As your page followers increase, your Facebook rank will improve, and your page will more likely be discovered by Facebook searches for your services. With an added link to your office practice website, those patients go straight to your site without getting lost in the noise of Google search results.
For Instagram, a short video or an interesting picture, along with a brief statement, are the essentials. You can add a single link. Marketing here is by direct messaging or having patients going to your website through a link. Instagram, like Facebook, offers analytics to help show you what your audience likes to read about, improving the quality of your posts and increasing number of followers.
YouTube is the number 2 search engine behind Google. A Google search for your field of medicine may be filled with pages of competitors. However, YouTube has a much lower volume of competing practices, making it easier for patients to find you. The only downside to YouTube is that it will list your video along with other competing videos, which can draw attention away from your practice.
If you want to promote your website or practice with video, using a company such as Vimeo is a better choice compared with YouTube, as YouTube gets credit for video views—which improves YouTube’s SEO and not your own website. Vimeo allows for your website to get credit each time the video is watched. Regardless of where you place your videos, make them short and to the point, with links to your website. Videos only need to be long enough to get your message across and stimulate interest in your practice.
If you can have a blog on your website, it also will help with SEO. What a search engine like Google wants to see is that a patient is on your web page and looking at something for at least 60 seconds. If so, the website is deemed to have information that is relevant, improving your SEO ranking.
Finally, Twitter also can be used for getting messaging out and for branding. The problem with it is that many people go to Twitter to follow a Hollywood celebrity, a sports star, or are looking for mass communication. There is less interest on Twitter for physician outreach.
Continue to: Measuring ROI...
Measuring ROI
Dr. Culligan: What’s the best way to track your return on investment?
Dr. Lotze: First for me was to find out what didn’t work in the office and fix that before really promoting my practice. It’s about the global experience for a patient, as Brad mentioned. As a marketing expert, Heather met with me to understand my goals. She then called my office as a patient to set up an appointment and went through that entire office experience. We identified issues needing improvement.
The next step was to develop a working relationship with my webmaster—someone who can help manage Internet image and SEO. Together, you will develop goals for what the SEO should promote specific to your practice. Once a good SEO program is in place, your website’s ranking will go up—although it can take a minimum of 6 months to see a significant increase. To help understand your website’s performance, your webmaster should provide you with reports on your site’s analytics.
As you go through this process, it is great to have a marketing expert to be the point person. You will work closely together for a while, but eventually you can back off over time. The time and expense you invest on the front end have huge rewards on the back end. Currently, I still spend a reasonable amount of money every month. I have a high self-referral base because of these efforts, however, which results in more patient surgeries and easily covers my expenses. It is money well invested. My website traffic increased by 268% over 2 years (FIGURE). I’ll propose that currently more than half of my patients are self-referrals due to online marketing.
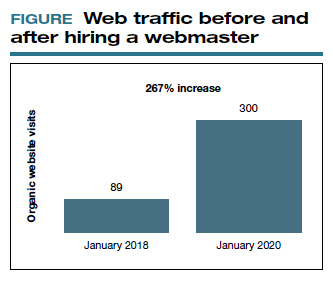
Ms. Schueppert: The only thing I would add is training your front staff. They are checking people in, taking appointments, checking your patients out. Have them be mindful that there are campaigns going on, whether it is a social media push, or a new video that went on the website. They can ask, “How did you hear about us?” when a new patient calls.
Dr. Bowman: Unless you are a large university hospital, where the analytics get significantly more advanced in terms of measuring return on investment (ROI), I think you should just be looking at your schedule and looking at your monthly billings and seeing how they change over time. You can calculate how much a new patient is worth because you can figure out how many patients you have and how much you bill and what your profits are.
Dr. Culligan: For those of us who are hospital employees, you can try to convince the hospital that you can do a detailed ROI analysis, or you can just look at it like (say it’s $3,000 per month), how many surgeries does this project have to generate before the hospital makes that back? The answer is a fraction of 1 case.
Thank you to all of you for your expertise on this roundtable.
To have a thriving business in today’s world, a functioning website is crucial to the overall business health. For a medical practice in general, and for its physicians specifically, it is one of the first steps for maintaining a practice. But to grow that practice, it is crucial to take the steps beyond just having a website. Growth requires website optimization for search engines, an expanding referral base, and the knowledge to use web tools and social media at your disposal to promote the practice and its physicians. In this roundtable, several marketing experts and web-savvy physicians discuss using available tools to best position and grow a practice.
Choosing a web upgrade
Patrick J. Culligan, MD: Peter, can you start us off by describing your relationship with Heather, and how your practice benefitted from her expertise?
Peter M. Lotze, MD: Sure. I am a urogynecologist in the competitive market of pelvic reconstructive surgery in Houston, Texas. Within that market, my main approach was to reach out to other physicians to refer patients to my practice. It generally would work, but took increasingly greater amounts of time to call these physicians up, write them letters, and maintain relationships. I felt that the large, national practice group that I am in did not have a significant web presence optimized to promote my practice, which makes it difficult for patients seeking your services to find you in their search for a doctor. It is helpful for patients to be able to understand from your website who you are, what you do, and what their experience may be like.
Glaring to me was that a web search specific for me or things that I do, would not produce our company’s results until page 2 or more on Google. This can be devastating for a practice because most people don’t go past the first page, and you can end up with fewer self-referrals, which should be a significant portion of new patients to your practice. I knew I needed guidance; I knew of Heather’s expertise given her exceptional past work building marketing strategies.
Digital go-tos for marketing
Heather Schueppert: Yes, I was pleased to work with Dr. Lotze, and at the time was a marketing consultant for practices such as his. But gone are the days of printed material—brochures, pamphlets, or even billboards—to effectively promote a business, or in this case, a practice. What still withstands the test of time, however, as the number 1 marketing referral source is word of mouth—from your trusted friend, family member, or coworker.
It is now proven that the number 2 most trusted form of advertising, the most persuasive and the most motivating, is online marketing.1 It is the “digital word of mouth”—the review. Patients are actively online, and a strong digital presence is critical to provide that direct value to retain and grow your patient base.
Continue to: Foundations of private practice reach out...
Foundations of private practice reach out
There are 3 important areas that I consider the foundation of any private practice marketing strategy (TABLE). First is an updated website that is search engine optimized (SEO). You can’t just set it and forget it, it needs to be an updated website. The algorithms for search engines are changing constantly to try to make it as fair and relevant as possible for patients or consumers to find the businesses they are searching for online.
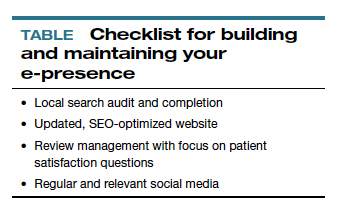
The second area is review management, and for a physician, or even a care center, to do this on your own is a daunting task. It is a critical component, however, to making sure that your reputation out there, that online word of mouth, is as high a star rating as possible.
The third component is local search, which is basically a form of SEO that helps businesses show up in relevant local searches. We are all familiar with the search, “find a restaurant near me,” anything that pushes those search engines to find something local.
Those are what I call the effective triad: that updated website, the review management, and the local search, and all of these are tied together. I think Dr. Lotze and his practice did these effectively well, and I believe that he achieved his goals for the longer term.
Review/reputation management
Dr. Culligan: Brad, is there something that doctors may not know about Healthgrades, and are there opportunities to take full advantage of this physician-rating site?
Brad Bowman, MD: I agree with everything that Dr. Lotze and Heather have said. Start with yourself—what is it that you want to be, the one thing you want to stand for? Get your own marketing, your website right, then, the point is, once you do all that and you are number 1 in SEO, you are still only going to get about 25% of the people looking for you by name to come to your website. The other 75% are going to look at all the other different sites that are out there to provide information to consumers. So the question becomes what do you do with all these other third-party sites? Healthgrades is the most comprehensive and has the highest traffic of the third-party “find a doctor” sites. In 2020, half of all Americans who go to a doctor will use Healthgrades at some point to help select and connect with that doctor.
Physicians have their focus on the quality of the care they provide. Patients, however, focus on the quality of the entire health care experience. Did I get better? How long did I have to wait? Was the office staff helpful? Scarily enough, we still spend more time shopping for a refrigerator or mattress than we do shopping for a doctor. We still tend to think that all doctors are the same. It is the reality of how we have been trained by our insurance companies and by the health care system. That is why getting your marketing right and getting what is it that you want to be known for out there is important, so that you can get the types of patients you want.
Listings management is very important. Make sure that you are findable everywhere. There are services that will do this: Doctor.com, Reputation.com, and many others. They can help you make sure you get all your basic materials right: addresses, phone numbers, your picture. Because 75% of people are going to end up on third-party websites, if your phone number is wrong there, you could lose that patient.
Then the second piece of working with third-party sites is reputation management. Physician reviews are not a bad thing, they are the new word of mouth, as Heather pointed out. Most (80%) of the reviews are going to be positive. The others will be negative, and that is okay. It is important that you get at least 1 or 2 reviews on all the different sites. We know from Healthgrades.com that going from zero reviews to 1 review will increase your call volume by 60%. If you have the choice between 2 physicians and one practice looks like people have been there before, you will go to that one.
You can learn from reviews as well, consumers provide valid feedback. Best practice is to respond to every positive and negative review. Thank them, indicate that you have listened to them, and address any concerns as necessary.
Continue to: Dr. Lotze...
Dr. Lotze: As an example, one of the paramount things that Heather introduced me to was the third party I use to run my website. That company sends a HIPAA-compliant review out to each patient we have seen that day and gives them the opportunity to rate our services and leave comments. If a patient brings up a concern, we can respond immediately, which is important. Patients appreciate feeling that they have been heard. Typically, communicating with a patient will turn the 3-star review into a 5-star as she follows up with the practice.
Ms. Schueppert: Timeliness is important. And just to mention, there certainly is a time commitment to this (and it is a marathon versus a sprint) and there is some financial investment to get it going, but it could truly be detrimental to a practice if you decide not to do anything at all.
Dr. Bowman: Agencies can really help with the time commitment.
Handling bad reviews
Dr. Culligan: What about that person who seems to have it out for you, perhaps giving you multiple bad reviews?
Dr. Bowman: I have seen this before. At Healthgrades, we recently analyzed 8.4 million patient reviews to see what people wrote about.2 The first thing they will talk about is quality of care as they see it. Did I get better or not? You can’t “fix” every patient; there will be some that you cannot help. The next thing patients comment on is bedside manner. With negative reviews, you will see more comments about the office staff.2
A single negative review actually helps make the positive ones look more credible. But if you do believe someone is trolling you, we can flag it and will investigate to the best of our ability. (Different sites likely have different editorial policies.) For example, we look at the IP addresses of all reviews, and if multiple reviews are coming from the same location, we would only let one through, overwriting the previous review from that address.
Patients just want to be heard. We have seen people change their views, based on how their review is handled and responded to.
Dr. Lotze: Is there a response by the physician that you think tends to work better in terms of resolving the issue that can minimize a perceived caustic reaction to a patient’s criticism?
Dr. Bowman: First, just like with any stressful situation, take a deep breath and respond when you feel like you can be constructive. When you do respond, be gracious. Thank them for their feedback. Make sure you reference something about their concern: “I understand that you had to wait longer than you would have liked.” Acknowledge the problem they reference, and then just apologize: “I’m sorry we didn’t meet your expectations.” Then, if they waited too long for example, “We have a new system where no one should have to wait more than 30 minutes….” You can respond privately or publically. Generally, public responses are better as it shows other consumers that you are willing to listen and consider their point of view.
Continue to: The next phase at Healthgrades...
The next phase at Healthgrades
Dr. Culligan: Do you see changes to the way physician-rating sites are working now? Are we going to stay status quo over the next 10 years, or do you see frontiers in how your site is going to develop?
Dr. Bowman: For Healthgrades, we rely on quantitative and objective measures, not just the qualitative. We are investing heavily right now in trying to help consumers understand what are the relative volumes of different procedures or different patient types that each individual doctor sees. Orthopedics is an easy example—if you have a knee problem, you want to go to someone who specializes in knees. Our job is to help consumers easily identify, “This is a shoulder doctor, this is a knee doctor, and this is why that matters.”
In the meantime, as a physician, you can always go into our site and state your care philosophy, identifying what is the sort of patient that you like to treat. Transparency is good for everyone, and especially physicians. It helps the right patient show up for you, and it helps you do a better job providing referrals.
Social media: Avoid pitfalls, and use it to your benefit
Dr. Lotze: Branding was one of the things that I was confused about, and Heather really helped me out. As physicians, we put ourselves out there on our websites, which we try to make professional sources of information for patients. But patients often want to see what else they can find out about us, including Healthgrades and social media. I think the thing that is important to know with social media is that it is a place where people learn about you as a person. Your social media should be another avenue of promotion. Whether it is your personal or professional Facebook page, people are going to see those sites. You have an opportunity to promote yourself as a good physician and a good person with a wholesome practice that you want people to come to. If a physician is posting questionable things about themselves on any kind of social media, it could be perceived as inappropriate by the patient. That can impact how patients think of you as a person, and how they are going to grade you. If people lose sight of who you are due to a questionable social media posting, everything else (SEO, the website) can be for naught.
Dr. Culligan: What are the most important social media tools to invest your time in?
Ms. Schueppert: Before anybody jumps into social media, I firmly recommend that you make sure your local search and your Google 3-pack is set up—which is basically a method Google uses to display the top 3 results on its listings page. Then make sure you have a review management system in place. Make sure you have that updated website. Those are the foundational elements. Once you have that going, social media is the next added layer to that digital presence.
I usually recommend LinkedIn. It is huge because you are staying in contact with your colleagues, that business-to-business type of connection. It remains a way for physicians to set themselves up as experts in their level of specialty.
From there, it’s either Instagram or Facebook. If you are serving more of the younger generations, the millennials and younger, then Instagram is the way to go. If you are focusing on your 40+, 50+, they are going to be far more on Facebook.
Continue to: Dr. Lotze...
Dr. Lotze: For me, a Facebook page was a great place to start. The cost of those Google ads—the first things we see at the top of a Google search in their own separate box—is significant. If a practice has that kind of money to invest, great; it is an instant way to be first on the page during a search. But there are more cost-effective ways of doing that, especially as you are getting your name out. Facebook provides, at a smaller cost, promotion of whatever it is that you are seeking to promote. You can find people within a certain zip code, for instance, and use a Facebook ad campaign that can drive people to your Facebook page—which should have both routinely updated new posts and a link to your website. The posts should be interesting topics relevant to the patients you wish to treat (avoiding personal stories or controversial discussions). You can put a post together, or you can have a third-party service do this. People who follow your page will get reminders of you and your practice with each new post. As your page followers increase, your Facebook rank will improve, and your page will more likely be discovered by Facebook searches for your services. With an added link to your office practice website, those patients go straight to your site without getting lost in the noise of Google search results.
For Instagram, a short video or an interesting picture, along with a brief statement, are the essentials. You can add a single link. Marketing here is by direct messaging or having patients going to your website through a link. Instagram, like Facebook, offers analytics to help show you what your audience likes to read about, improving the quality of your posts and increasing number of followers.
YouTube is the number 2 search engine behind Google. A Google search for your field of medicine may be filled with pages of competitors. However, YouTube has a much lower volume of competing practices, making it easier for patients to find you. The only downside to YouTube is that it will list your video along with other competing videos, which can draw attention away from your practice.
If you want to promote your website or practice with video, using a company such as Vimeo is a better choice compared with YouTube, as YouTube gets credit for video views—which improves YouTube’s SEO and not your own website. Vimeo allows for your website to get credit each time the video is watched. Regardless of where you place your videos, make them short and to the point, with links to your website. Videos only need to be long enough to get your message across and stimulate interest in your practice.
If you can have a blog on your website, it also will help with SEO. What a search engine like Google wants to see is that a patient is on your web page and looking at something for at least 60 seconds. If so, the website is deemed to have information that is relevant, improving your SEO ranking.
Finally, Twitter also can be used for getting messaging out and for branding. The problem with it is that many people go to Twitter to follow a Hollywood celebrity, a sports star, or are looking for mass communication. There is less interest on Twitter for physician outreach.
Continue to: Measuring ROI...
Measuring ROI
Dr. Culligan: What’s the best way to track your return on investment?
Dr. Lotze: First for me was to find out what didn’t work in the office and fix that before really promoting my practice. It’s about the global experience for a patient, as Brad mentioned. As a marketing expert, Heather met with me to understand my goals. She then called my office as a patient to set up an appointment and went through that entire office experience. We identified issues needing improvement.
The next step was to develop a working relationship with my webmaster—someone who can help manage Internet image and SEO. Together, you will develop goals for what the SEO should promote specific to your practice. Once a good SEO program is in place, your website’s ranking will go up—although it can take a minimum of 6 months to see a significant increase. To help understand your website’s performance, your webmaster should provide you with reports on your site’s analytics.
As you go through this process, it is great to have a marketing expert to be the point person. You will work closely together for a while, but eventually you can back off over time. The time and expense you invest on the front end have huge rewards on the back end. Currently, I still spend a reasonable amount of money every month. I have a high self-referral base because of these efforts, however, which results in more patient surgeries and easily covers my expenses. It is money well invested. My website traffic increased by 268% over 2 years (FIGURE). I’ll propose that currently more than half of my patients are self-referrals due to online marketing.
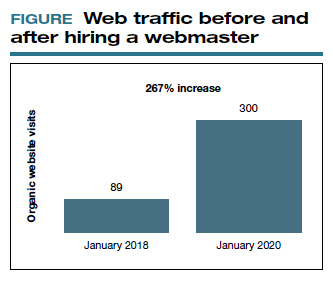
Ms. Schueppert: The only thing I would add is training your front staff. They are checking people in, taking appointments, checking your patients out. Have them be mindful that there are campaigns going on, whether it is a social media push, or a new video that went on the website. They can ask, “How did you hear about us?” when a new patient calls.
Dr. Bowman: Unless you are a large university hospital, where the analytics get significantly more advanced in terms of measuring return on investment (ROI), I think you should just be looking at your schedule and looking at your monthly billings and seeing how they change over time. You can calculate how much a new patient is worth because you can figure out how many patients you have and how much you bill and what your profits are.
Dr. Culligan: For those of us who are hospital employees, you can try to convince the hospital that you can do a detailed ROI analysis, or you can just look at it like (say it’s $3,000 per month), how many surgeries does this project have to generate before the hospital makes that back? The answer is a fraction of 1 case.
Thank you to all of you for your expertise on this roundtable.
- Anderson A. Online reviews vs. word of mouth: Which one is more important. https://www.revlocal.com/blog/reviewandreputationmanagement/onlinereviewsvswordofmouthwhichoneismoreimportant. Accessed July 17, 2020.
- 2020 Patient sentiment report. Healthgrades; Medical Group Management Association. https://www.healthgrades.com/content /patientsentimentreport. Accessed July 17, 2020
- Anderson A. Online reviews vs. word of mouth: Which one is more important. https://www.revlocal.com/blog/reviewandreputationmanagement/onlinereviewsvswordofmouthwhichoneismoreimportant. Accessed July 17, 2020.
- 2020 Patient sentiment report. Healthgrades; Medical Group Management Association. https://www.healthgrades.com/content /patientsentimentreport. Accessed July 17, 2020







