User login
How to choose the right vaginal moisturizer or lubricant for your patient
Vaginal dryness, encompassed in the modern term genitourinary syndrome of menopause (GSM) affects up to 40% of menopausal women and up to 60% of postmenopausal breast cancer survivors.1,2 Premenopausal women also can have vulvovaginal dryness while breastfeeding (lactational amenorrhea) and while taking low-dose contraceptives.3 Vaginal moisturizers and lubricants are the first-line treatment options for vaginal dryness, dyspareunia, and GSM.4,5 In fact, approximately two-thirds of women have reported using a vaginal lubricant in their lifetime.6 Despite such ubiquitous use, many health care providers and patients have questions about the difference between vaginal moisturizers and lubricants and how to best choose a product.
Vaginal moisturizers
Vaginal moisturizers are designed to rehydrate the vaginal epithelium. Much like facial or skin moisturizers, they are intended to be applied regularly, every 2 to 3 days, but may be applied more often depending on the severity of symptoms. Vaginal moisturizers work by increasing the fluid content of the vaginal tissue and by lowering the vaginal pH to mimic that of natural vaginal secretions. Vaginal moisturizers are typically water based and use polymers to hydrate tissues.7 They change cell morphology but do not change vaginal maturation, indicating that they bring water to the tissue but do not shift the balance between superficial and basal cells and do not increase vaginal epithelial thickness as seen with vaginal estrogen.8 Vaginal moisturizers also have been found to be a safe alternative to vaginal estrogen therapy and may improve markers of vaginal health, including vaginal moisture, vaginal fluid volume, vaginal elasticity, and premenopausal pH.9 Commercially available vaginal moisturizers have been shown to be as effective as vaginal estrogens in reducing vaginal symptoms such as itching, irritation, and dyspareunia, but some caution should be taken when interpreting these results as neither vaginal moisturizer nor vaginal estrogen tablet were more effective than placebo in a recent randomized controlled trial.10,11 Small studies on hyaluronic acid have shown efficacy for the treatment of vaginal dryness.12,13 Hyaluronic acid is commercially available as a vaginal suppository ovule and as a liquid. It may also be obtained from a reliable compounding pharmacy. Vaginal suppository ovules may be a preferable formulation for women who find the liquids messy or cumbersome to apply.
Lubricants
Lubricants differ from vaginal moisturizers because they are specifically designed to be used during intercourse to provide short-term relief from vaginal dryness. They may be water-, silicone-, mineral oil-, or plant oil-based. The use of water- and silicone-based lubricants is associated with high satisfaction for intercourse as well as masturbation.14 These products may be particularly beneficial to women whose chief complaint is dyspareunia. In fact, women with dyspareunia report more lubricant use than women without dyspareunia, and the most common reason for lubricant use among these women was to reduce or alleviate pain.15 Overall, women both with and without dyspareunia have a positive perception regarding lubricant use and prefer sexual intercourse that feels more “wet,” and women in their forties have the most positive perception about lubricant use at the time of intercourse compared with other age groups.16 Furthermore, the World Health Organization (WHO) recommends that condom-compatible lubricants be used with condoms for menopausal and postmenopausal women.17 Both water-based and silicone-based lubricants may be used with latex condoms, while oil-based lubricants should be avoided as they can degrade the latex condom. While vaginal moisturizers and lubricants technically differ based on use, patients may use one product for both purposes, and some products are marketed as both a moisturizer and lubricant.
Continue to: Providing counsel to patients...
Providing counsel to patients
Patients often seek advice on how to choose vaginal moisturizers and lubricants. Understanding the compositions of these products and their scientific evidence is useful when helping patients make informed decisions regarding their pelvic health. Most commercially available lubricants are either water- or silicone- based. In one study comparing these two types of lubricants, water-based lubricants were associated with fewer genital symptoms than silicone-based products.14 Women may want to use a natural or organic product and may prefer plant-based oils such as coconut oil or olive oil. Patients should be counseled that latex condoms are not compatible with petroleum-, mineral oil- or plant oil-based lubricants.
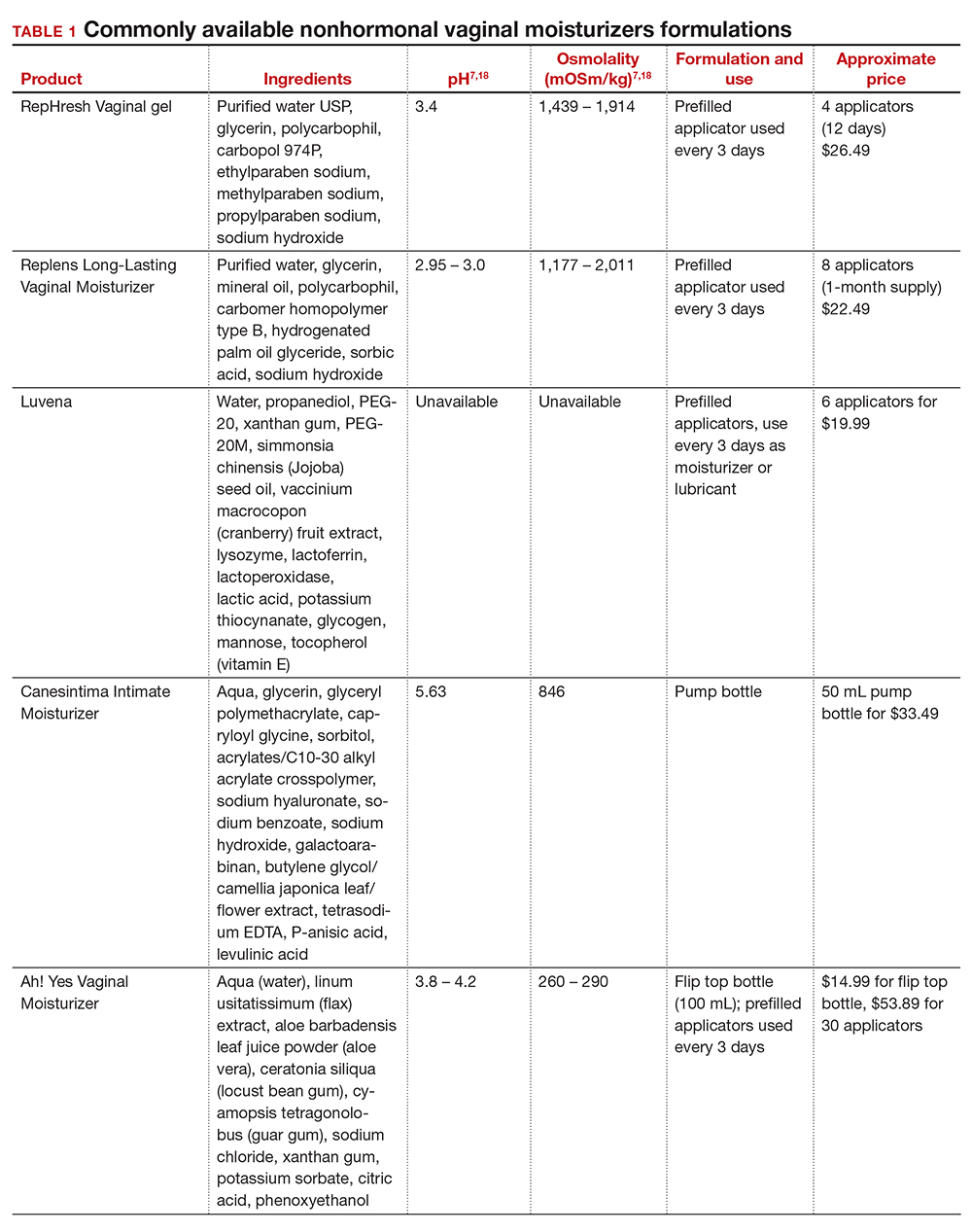
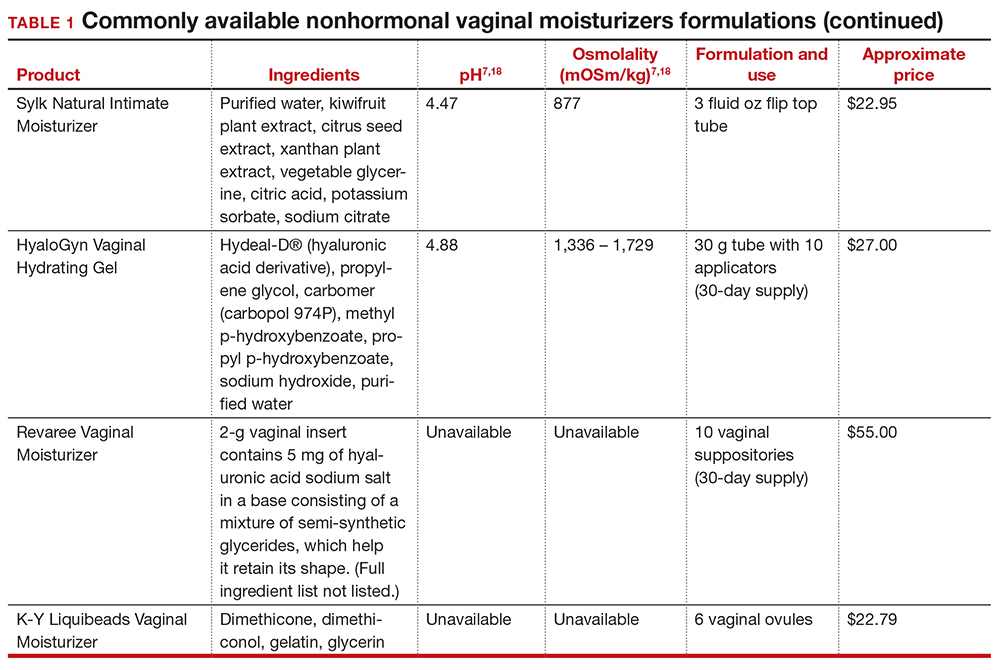
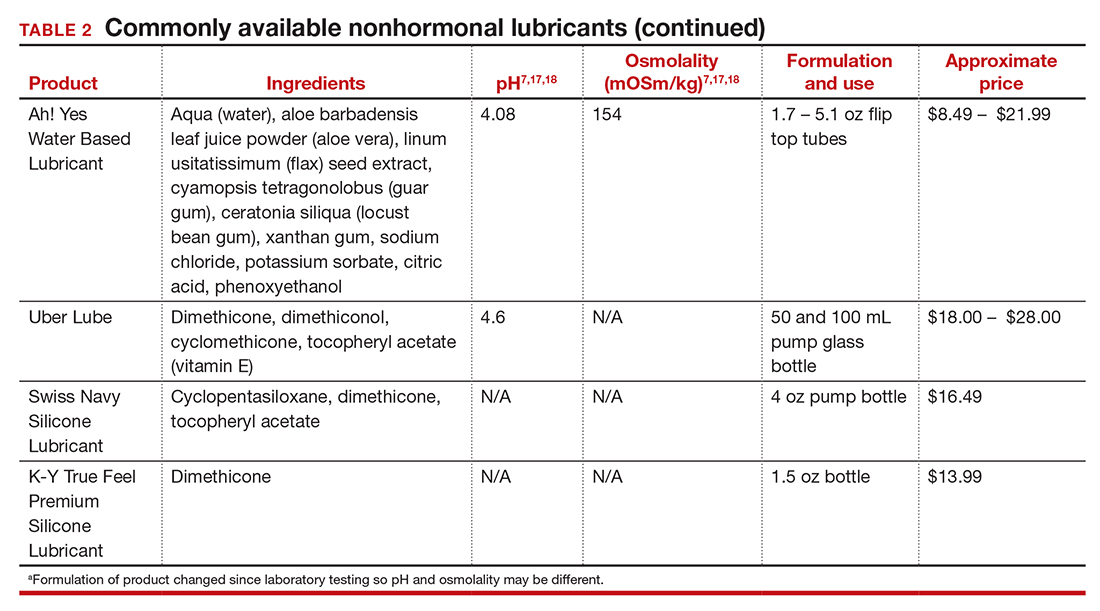
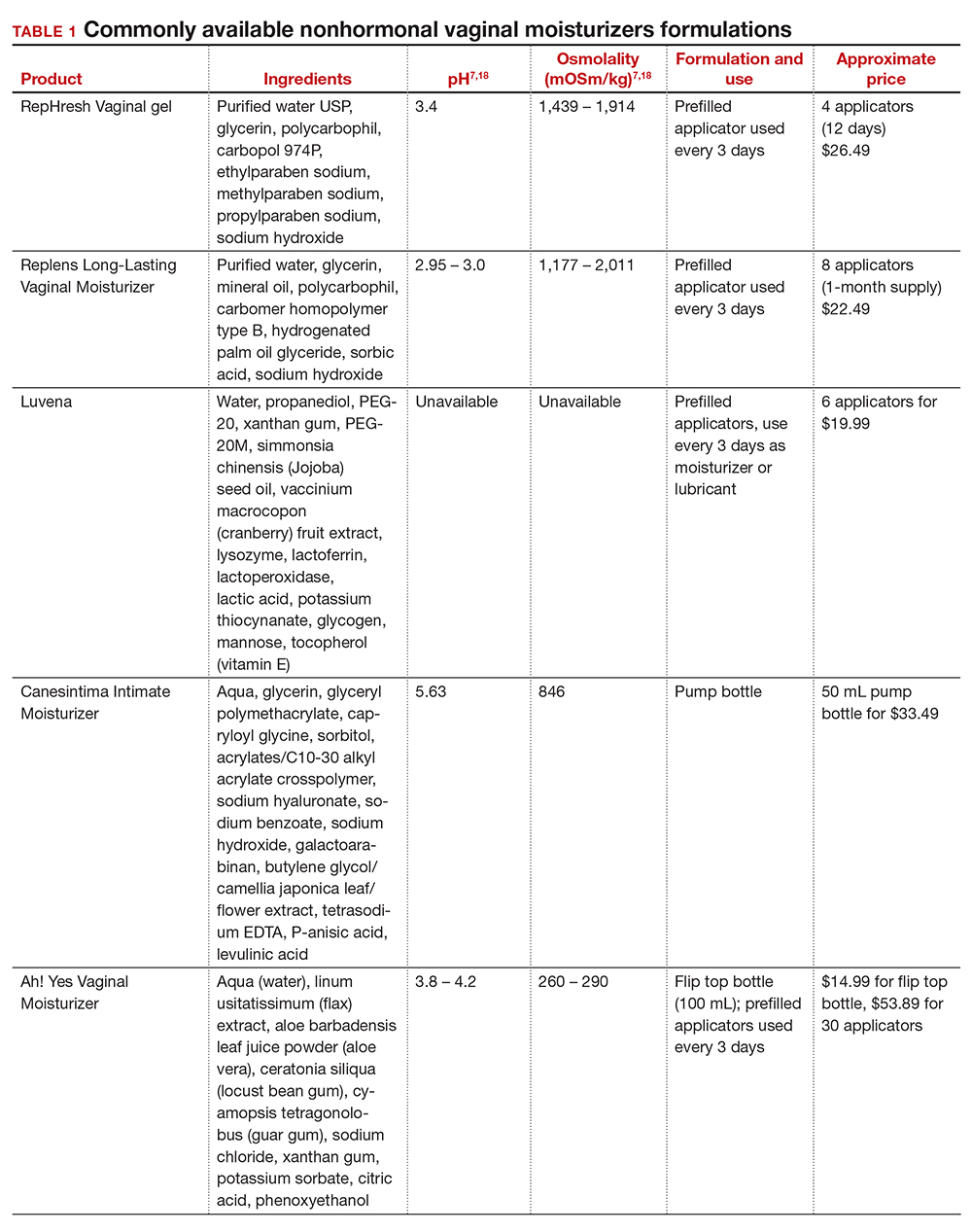
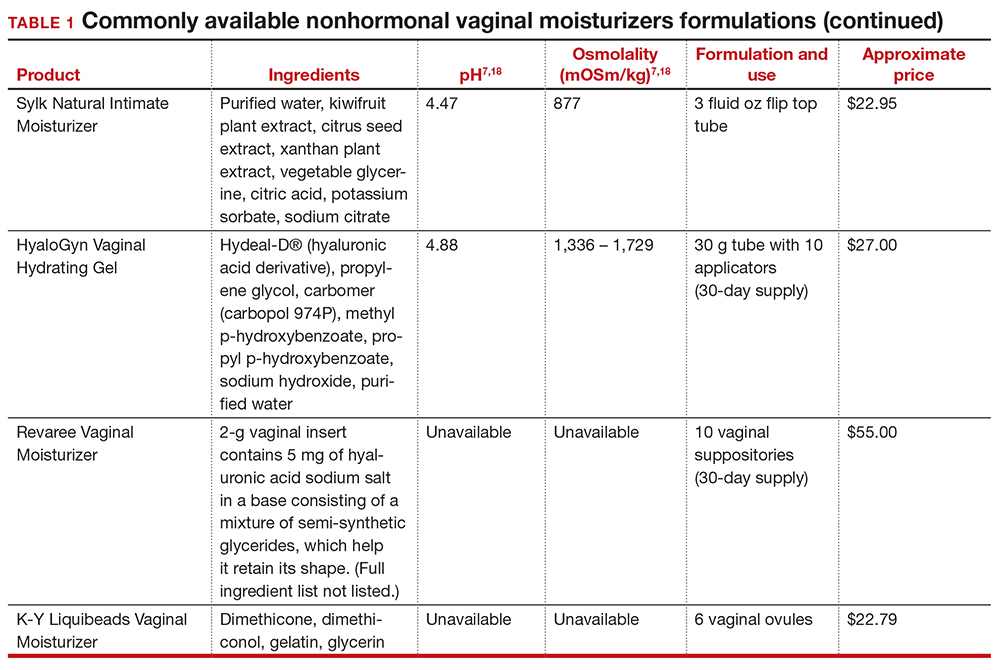
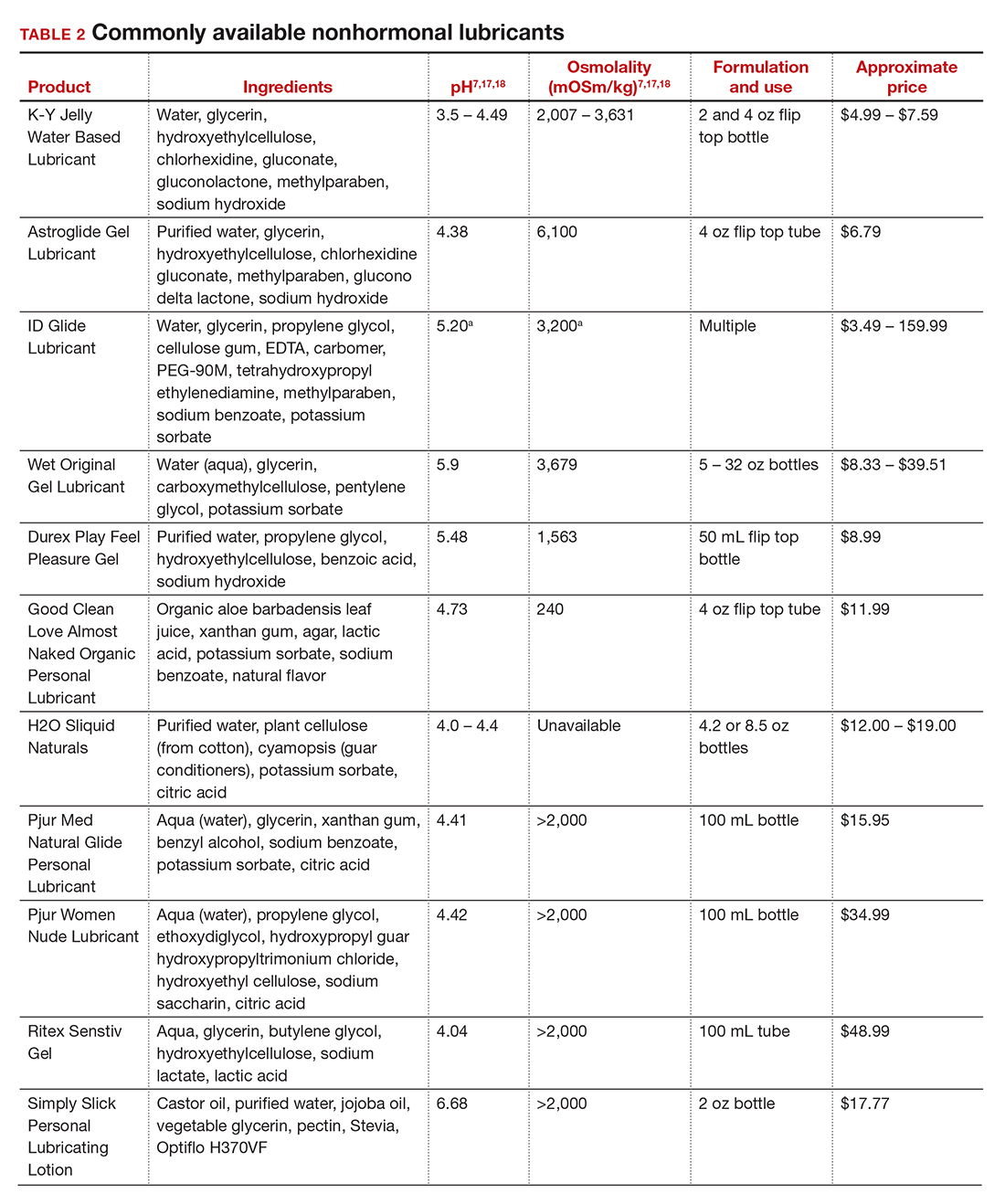
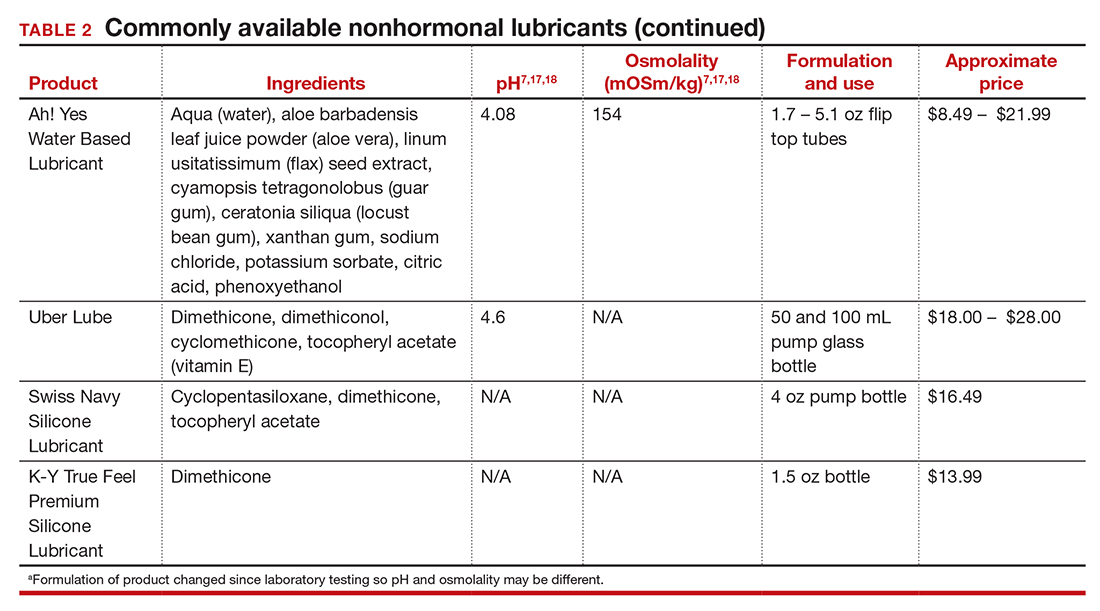
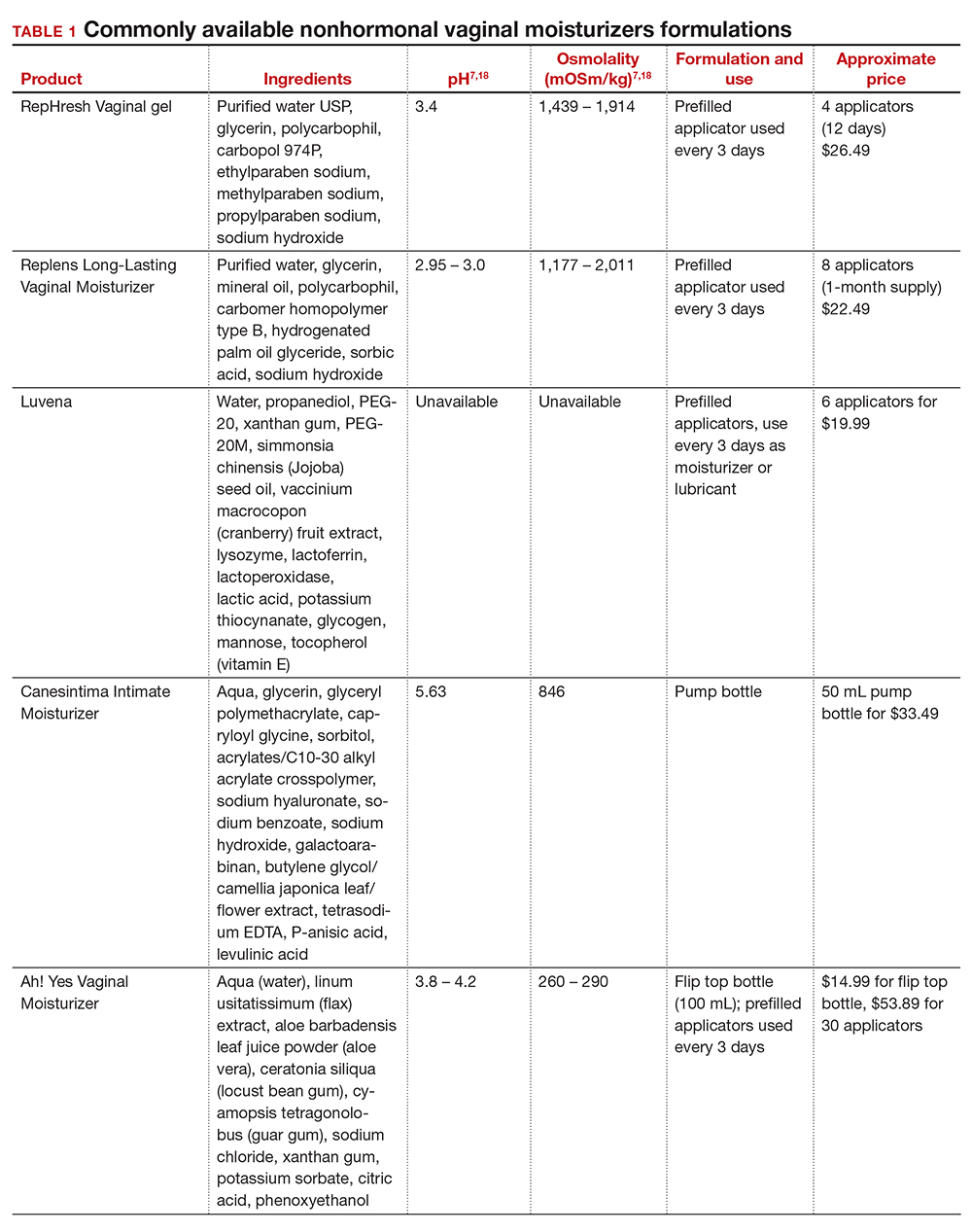
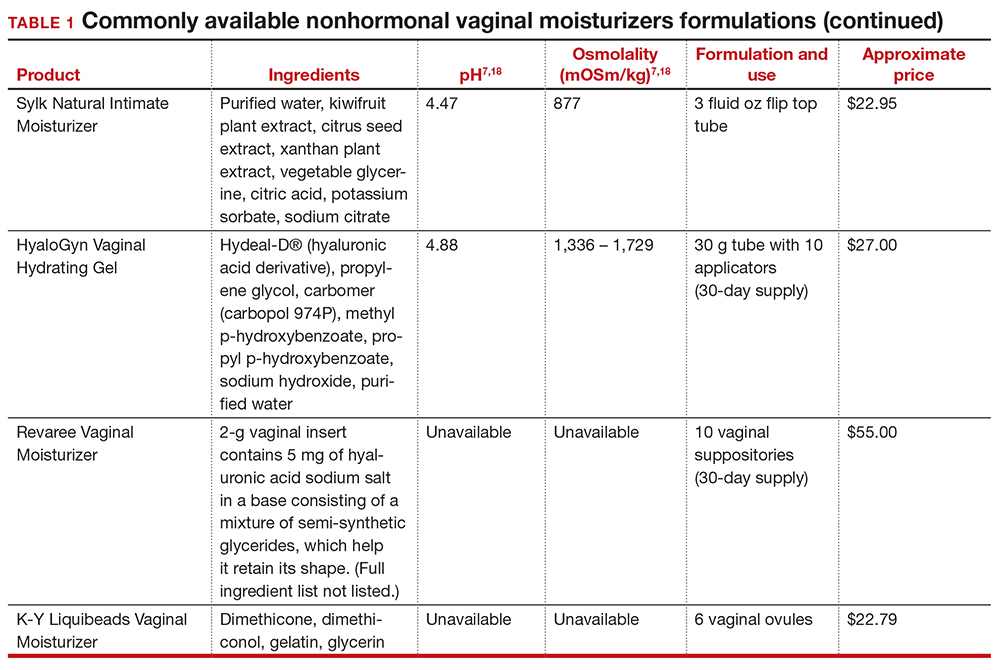
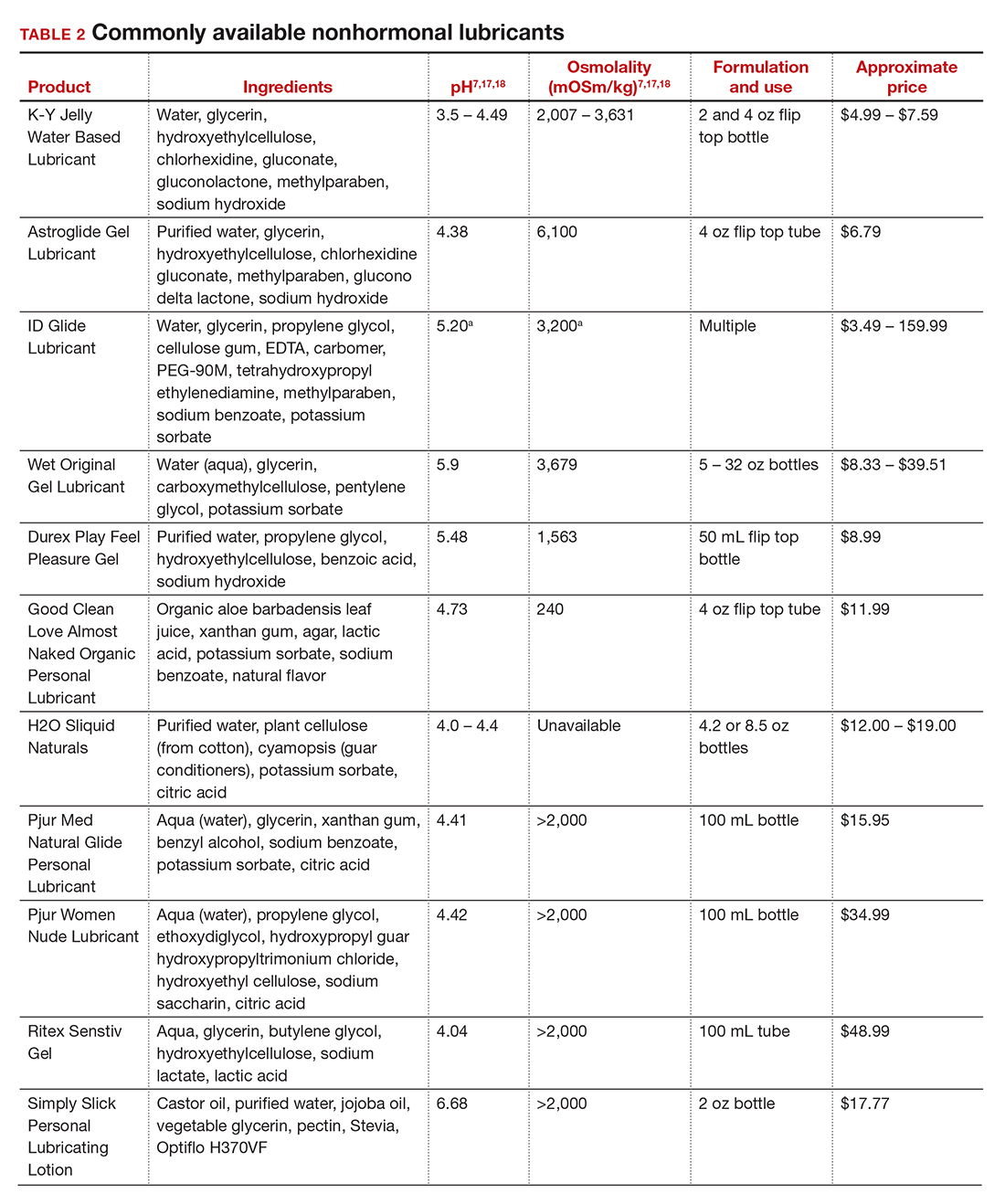
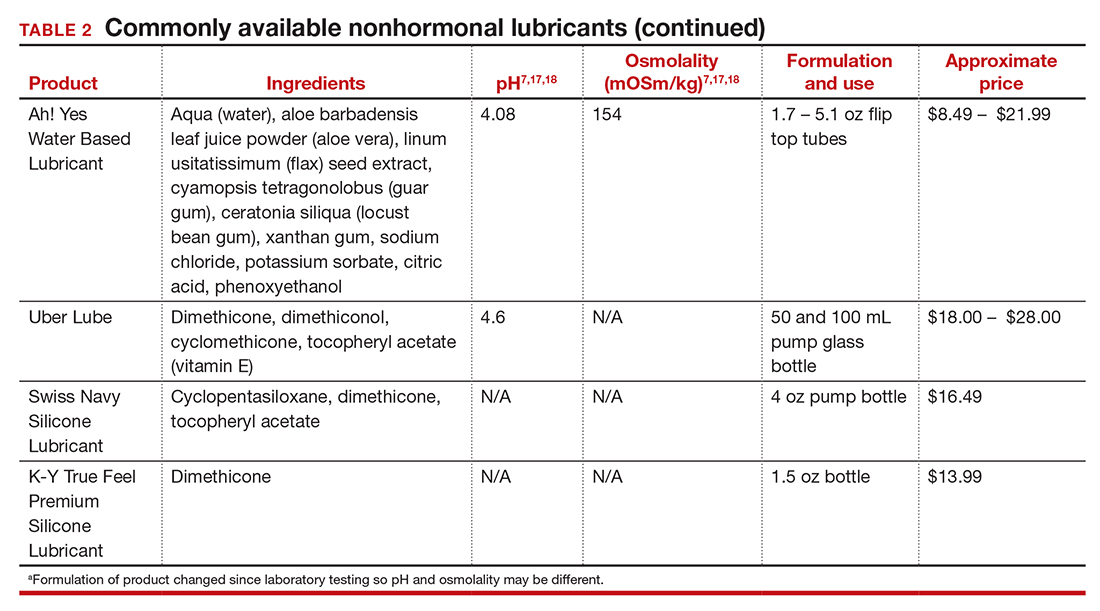
In our practice, we generally recommend silicone-based lubricants, as they are readily available and compatible with latex condoms and generally require a smaller amount than water-based lubricants. They tend to be more expensive than water-based lubricants. For vaginal moisturizers, we often recommend commercially available formulations that can be purchased at local pharmacies or drug stores. However, a patient may need to try different lubricants and moisturizers in order to find a preferred product. We have included in TABLES 1 and 27,17,18 a list of commercially available vaginal moisturizers and lubricants with ingredient list, pH, osmolality, common formulation, and cost when available, which has been compiled from WHO and published research data to help guide patient counseling.
The effects of additives
Water-based moisturizers and lubricants may contain many ingredients, such as glycerols, fragrance, flavors, sweeteners, warming or cooling agents, buffering solutions, parabens and other preservatives, and numbing agents. These substances are added to water-based products to prolong water content, alter viscosity, alter pH, achieve certain sensations, and prevent bacterial contamination.7 The addition of these substances, however, will alter osmolality and pH balance of the product, which may be of clinical consequence. Silicone- or oil-based products do not contain water and therefore do not have a pH or an osmolality value.
Hyperosmolar formulations can theoretically injure epithelial tissue. In vitro studies have shown that hyperosmotic vaginal products can induce mild to moderate irritation, while very hyperosmolar formulations can induce severe irritation and tissue damage to vaginal epithelial and cervical cells.19,20 The WHO recommends that the osmolality of a vaginal product not exceed 380 mOsm/kg, but very few commercially available products meet these criteria so, clinically, the threshold is 1,200 mOsm/kg.17 It should be noted that most commercially available products exceed the 1,200 mOsm/kg threshold. Vaginal products may be a cause for vaginal irritation and should be considered in the differential diagnosis.
The normal vaginal pH is 3.8–4.5, and vaginal products should be pH balanced to this range. The exact role of pH in these products remains poorly understood. Nonetheless, products with a pH of 3 or lower are not recommended.18 Concerns about osmolality and pH remain theoretical, as a study of 12 commercially available lubricants of varying osmolality and pH found no cytotoxic effect in vivo.18
Vaginal moisturizers and lubricants contain many inactive ingredients, the most controversial of which are parabens. These substances are used in many cosmetic products as preservatives and are weakly estrogenic. These substances have been found in breast cancer tissue, but their possible role as a carcinogen remains uncertain.21,22 Nonetheless, the use of paraben-containing products is not recommended for women who have a history of hormonally-driven cancer or who are at high risk for developing cancer.7 Many lubricants contain glycerols (glycerol, glycerine, and propylene glycol) to alter viscosity or alter the water properties. The WHO recommends limits on the content of glycerols in these products.17 Glycerols have been associated with increased risk of bacterial vaginosis (adjusted odds ratio [aOR], 11.75; 95% confidence interval [CI], 1.96–70.27), and can serve as a food source for candida species, possibly increasing risk of yeast infections.7,23 Additionally, vaginal moisturizers and lubricants may contain preservatives such as chlorhexidine, which can disrupt normal vaginal flora and may cause tissue irritation.7
Continue to: Common concerns to be aware of...
Common concerns to be aware of
Women using vaginal products may be concerned about adverse effects, such as worsening vaginal irritation or infection. Vaginal moisturizers have not been shown to have increased risk of adverse effects compared with vaginal estrogens.9,10 In vitro studies have shown that vaginal moisturizers and lubricants inhibit the growth of Escherichia coli but may also inhibit Lactobacillus crispatus.24 Clinically, vaginal moisturizers have been shown to improve signs of bacterial vaginosis and have even been used to treat bacterial vaginosis.25,26 A study of commercially available vaginal lubricants inhibited the growth of L crispatus, which may predispose to irritation and infection.27 Nonetheless, the effect of the vaginal products on the vaginal microbiome and vaginal tissue remains poorly studied. Vaginal moisturizers and lubricants, while often helpful for patients, also can potentially cause irritation or predispose to infections. Providers should consider this when evaluating patients for new onset vaginal symptoms after starting vaginal products.
Bottom line
Vaginal products such as moisturizers and lubricants are often effective treatment options for women suffering from genitourinary syndrome of menopause and may be first-line treatment options, especially for women who may wish to avoid estrogen-containing products. Vaginal moisturizers can be recommended to any women experiencing vaginal irritation due to vaginal dryness while vaginal lubricants should be recommended to sexually active women who experience dyspareunia. Clinicians need to be aware of the formulations of these products and possible side effects in order to appropriately counsel patients. ●
- Castelo-Branco C, Cancelo MJ, Villero J, et al. Management of postmenopausal vaginal atrophy and atrophic vaginitis. Maturitas. 2005;52(suppl 1):S46-S52. doi: 10.1016/j.maturitas.2005.06.014.
- Crandall C, Peterson L, Ganz PA, et al. Association of breast cancer and its therapy with menopause-related symptoms. Menopause. 2004;11:519-530. doi: 10.1097/01.gme.0000117061.40493.ab.
- Bornstein J, Goldstein AT, Stockdale CK, et al. 2015 ISSVD, ISSWSH, and IPPS Consensus Terminology and Classification of Persistant Vulvar Pain and Vulvodynia. J Sex Med. 2016;13:607-612. doi: 10.1016/j.jsxm.2016.02.167.
- American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 141: management of menopausal symptoms. Obstet Gynecol. 2014;123:202-216. doi: 10.1097/01.AOG.0000441353.20693.78.
- Faubion S, Larkin L, Stuenkel C, et al. Management of genitourinary syndrome of menopause in women with or at high risk for breast cancer: consensus recommendation from The North American Menopause Society and the International Society for the Study for Women’s Sexual Health. Menopause. 2018;25:596-608. doi: 10.1097/GME.0000000000001121.
- Herbenick D, Reece M, Schick V, et al. Women’s use and perceptions of commercial lubricants: prevalence and characteristics in a nationally representative sample of American adults. J Sex Med. 2014;11:642-652. doi: 10.1111/jsm.12427.
- Edwards D, Panay N. Treating vulvovaginal atrophy/genitourinary syndrome of menopause: how important is vaginal lubricant and moisturizer composition? Climacteric. 2016;19:151-116. doi: 10.3109/13697137.2015.1124259.
- Van der Lakk JAWN, de Bie LMT, de Leeuw H, et al. The effect of Replens on vaginal cytology in the treatment of postmenopausal atrophy: cytomorphology versus computerized cytometry. J Clin Pathol. 2002;55:446-451. doi: 10.1136/jcp.55.6.446.
- Nachtigall LE. Comparitive study: Replens versus local estrogen in menopausal women. Fertil Steril. 1994;61:178-180. doi: 10.1016/s0015-0282(16)56474-7.
- Bygdeman M, Swahn ML. Replens versus dienoestrol cream in the symptomatic treatment of vaginal atrophy in postmenopausal women. Maturitas. 1996;23:259-263. doi: 10.1016/0378-5122(95)00955-8.
- Mitchell CM, Reed SD, Diem S, et al. Efficacy of vaginal estradiol or vaginal moisturizer vs placebo for treating postmenopausal vulvovaginal symptoms. JAMA Intern Med. 2018;178:681-690. doi: 10.1001/jamainternmed.2018.0116.
- Chen J, Geng L, Song X, et al. Evaluation of the efficacy and safety of hyaluronic acid vaginal gel to ease vaginal dryness: a multicenter, randomized, controlled, open-label, parallel-group, clinical trial. J Sex Med. 2013;10:1575-1584. doi: 10.1111/jsm.12125.
- Jokar A, Davari T, Asadi N, et al. Comparison of the hyaluronic acid vaginal cream and conjugated estrogen used in treatment of vaginal atrophy of menopause women: a randomized controlled clinical trial. IJCBNM. 2016;4:69-78.
- Herbenick D, Reece M, Hensel D, et al. Association of lubricant use with women’s sexual pleasure, sexual satisfaction, and genital symptoms: a prospective daily diary study. J Sex Med. 2011;8:202-212. doi: 10.1111/j.1743-6109.2010.02067.x.
- Sutton KS, Boyer SC, Goldfinger C, et al. To lube or not to lube: experiences and perceptions of lubricant use in women with and without dyspareunia. J Sex Med. 2012;9:240-250. doi: 10.1111/j.1743-6109.2011.02543.x.
- Jozkowski KN, Herbenick D, Schick V, et al. Women’s perceptions about lubricant use and vaginal wetness during sexual activity. J Sex Med. 2013;10:484-492. doi: 10.1111/jsm.12022.
- World Health Organization. Use and procurement of additional lubricants for male and female condoms: WHO /UNFPA/FHI360 advisory note. 2012. https://www.who. int/reproductivehealth/publications/rtis/rhr12_33/en/. Accessed February 13, 2021.
- Cunha AR, Machado RM, Palmeira de Oliveira A, et al. Characterization of commercially available vaginal lubricants: a safety perspective. Pharmaceuticals. 2014;6:530-542. doi: 10.3390/pharmaceutics6030530.
- Adriaens E, Remon JP. Mucosal irritation potential of personal lubricants relates to product osmolality as detected by the slug mucosal irritation assay. Sex Transm Dis. 2008;35:512-516. doi: 10.1097/OLQ.0b013e3181644669.
- Dezzuti CS, Brown ER, Moncla B, et al. Is wetter better? An evaluation of over-the-counter personal lubricants for safety and anti-HIV activity. PLoS One. 2012;7:e48328. doi: 10.1371/journal.pone.0048328.
- Harvey PW, Everett DJ. Significance of the detection of esters of p-hydroxybenzoic acid (parabens) in human breast tumours. J Appl Toxicol. 2004:24:1-4. doi: 10.1002/jat.957.
- Darbre PD, Alijarrah A, Miller WR, et al. Concentrations of parabens in human breast tumous. J Appl Toxicol. 2004;24:5-13. doi: 10.1002/jat.958.
- Brotman RM, Ravel J, Cone RA, et al. Rapid fluctuation of the vaginal microbiota measured by Gram stain analysis. Sex Transm Infect. 2010;86:297-302. doi: 10.1136/sti.2009.040592.
- Hung KJ, Hudson P, Bergerat A, et al. Effect of commercial vaginal products on the growth of uropathogenic and commensal vaginal bacteria. Sci Rep. 2020;10:7625.
- Wu JP, Fielding SL, Fiscell K. The effect of the polycarbophil gel (Replens) on bacterial vaginosis: a pilot study. Eur J Obstet Gynecol Reprod Biol. 2007;130:132-136. doi: 10.1016/j.ejogrb.2006.01.007.
- Fiorelli A, Molteni B, Milani M. Successful treatment of bacterial vaginosis with a polycarbophil-carbopol acidic vaginal gel: results from a randomized double-bling, placebo controlled trial. Eur J Obstet Gynecol Reprod Biol. 2005;120:202-205. doi: 10.1016/j.ejogrb.2004.10.011.
- Fashemi B, Delaney ML, Onderdonk AB, et al. Effects of feminine hygiene products on the vaginal mucosal biome. Microb Ecol Health Dis. 2013;24. doi: 10.3402/mehd.v24i0.19703.
Vaginal dryness, encompassed in the modern term genitourinary syndrome of menopause (GSM) affects up to 40% of menopausal women and up to 60% of postmenopausal breast cancer survivors.1,2 Premenopausal women also can have vulvovaginal dryness while breastfeeding (lactational amenorrhea) and while taking low-dose contraceptives.3 Vaginal moisturizers and lubricants are the first-line treatment options for vaginal dryness, dyspareunia, and GSM.4,5 In fact, approximately two-thirds of women have reported using a vaginal lubricant in their lifetime.6 Despite such ubiquitous use, many health care providers and patients have questions about the difference between vaginal moisturizers and lubricants and how to best choose a product.
Vaginal moisturizers
Vaginal moisturizers are designed to rehydrate the vaginal epithelium. Much like facial or skin moisturizers, they are intended to be applied regularly, every 2 to 3 days, but may be applied more often depending on the severity of symptoms. Vaginal moisturizers work by increasing the fluid content of the vaginal tissue and by lowering the vaginal pH to mimic that of natural vaginal secretions. Vaginal moisturizers are typically water based and use polymers to hydrate tissues.7 They change cell morphology but do not change vaginal maturation, indicating that they bring water to the tissue but do not shift the balance between superficial and basal cells and do not increase vaginal epithelial thickness as seen with vaginal estrogen.8 Vaginal moisturizers also have been found to be a safe alternative to vaginal estrogen therapy and may improve markers of vaginal health, including vaginal moisture, vaginal fluid volume, vaginal elasticity, and premenopausal pH.9 Commercially available vaginal moisturizers have been shown to be as effective as vaginal estrogens in reducing vaginal symptoms such as itching, irritation, and dyspareunia, but some caution should be taken when interpreting these results as neither vaginal moisturizer nor vaginal estrogen tablet were more effective than placebo in a recent randomized controlled trial.10,11 Small studies on hyaluronic acid have shown efficacy for the treatment of vaginal dryness.12,13 Hyaluronic acid is commercially available as a vaginal suppository ovule and as a liquid. It may also be obtained from a reliable compounding pharmacy. Vaginal suppository ovules may be a preferable formulation for women who find the liquids messy or cumbersome to apply.
Lubricants
Lubricants differ from vaginal moisturizers because they are specifically designed to be used during intercourse to provide short-term relief from vaginal dryness. They may be water-, silicone-, mineral oil-, or plant oil-based. The use of water- and silicone-based lubricants is associated with high satisfaction for intercourse as well as masturbation.14 These products may be particularly beneficial to women whose chief complaint is dyspareunia. In fact, women with dyspareunia report more lubricant use than women without dyspareunia, and the most common reason for lubricant use among these women was to reduce or alleviate pain.15 Overall, women both with and without dyspareunia have a positive perception regarding lubricant use and prefer sexual intercourse that feels more “wet,” and women in their forties have the most positive perception about lubricant use at the time of intercourse compared with other age groups.16 Furthermore, the World Health Organization (WHO) recommends that condom-compatible lubricants be used with condoms for menopausal and postmenopausal women.17 Both water-based and silicone-based lubricants may be used with latex condoms, while oil-based lubricants should be avoided as they can degrade the latex condom. While vaginal moisturizers and lubricants technically differ based on use, patients may use one product for both purposes, and some products are marketed as both a moisturizer and lubricant.
Continue to: Providing counsel to patients...
Providing counsel to patients
Patients often seek advice on how to choose vaginal moisturizers and lubricants. Understanding the compositions of these products and their scientific evidence is useful when helping patients make informed decisions regarding their pelvic health. Most commercially available lubricants are either water- or silicone- based. In one study comparing these two types of lubricants, water-based lubricants were associated with fewer genital symptoms than silicone-based products.14 Women may want to use a natural or organic product and may prefer plant-based oils such as coconut oil or olive oil. Patients should be counseled that latex condoms are not compatible with petroleum-, mineral oil- or plant oil-based lubricants.
In our practice, we generally recommend silicone-based lubricants, as they are readily available and compatible with latex condoms and generally require a smaller amount than water-based lubricants. They tend to be more expensive than water-based lubricants. For vaginal moisturizers, we often recommend commercially available formulations that can be purchased at local pharmacies or drug stores. However, a patient may need to try different lubricants and moisturizers in order to find a preferred product. We have included in TABLES 1 and 27,17,18 a list of commercially available vaginal moisturizers and lubricants with ingredient list, pH, osmolality, common formulation, and cost when available, which has been compiled from WHO and published research data to help guide patient counseling.
The effects of additives
Water-based moisturizers and lubricants may contain many ingredients, such as glycerols, fragrance, flavors, sweeteners, warming or cooling agents, buffering solutions, parabens and other preservatives, and numbing agents. These substances are added to water-based products to prolong water content, alter viscosity, alter pH, achieve certain sensations, and prevent bacterial contamination.7 The addition of these substances, however, will alter osmolality and pH balance of the product, which may be of clinical consequence. Silicone- or oil-based products do not contain water and therefore do not have a pH or an osmolality value.
Hyperosmolar formulations can theoretically injure epithelial tissue. In vitro studies have shown that hyperosmotic vaginal products can induce mild to moderate irritation, while very hyperosmolar formulations can induce severe irritation and tissue damage to vaginal epithelial and cervical cells.19,20 The WHO recommends that the osmolality of a vaginal product not exceed 380 mOsm/kg, but very few commercially available products meet these criteria so, clinically, the threshold is 1,200 mOsm/kg.17 It should be noted that most commercially available products exceed the 1,200 mOsm/kg threshold. Vaginal products may be a cause for vaginal irritation and should be considered in the differential diagnosis.
The normal vaginal pH is 3.8–4.5, and vaginal products should be pH balanced to this range. The exact role of pH in these products remains poorly understood. Nonetheless, products with a pH of 3 or lower are not recommended.18 Concerns about osmolality and pH remain theoretical, as a study of 12 commercially available lubricants of varying osmolality and pH found no cytotoxic effect in vivo.18
Vaginal moisturizers and lubricants contain many inactive ingredients, the most controversial of which are parabens. These substances are used in many cosmetic products as preservatives and are weakly estrogenic. These substances have been found in breast cancer tissue, but their possible role as a carcinogen remains uncertain.21,22 Nonetheless, the use of paraben-containing products is not recommended for women who have a history of hormonally-driven cancer or who are at high risk for developing cancer.7 Many lubricants contain glycerols (glycerol, glycerine, and propylene glycol) to alter viscosity or alter the water properties. The WHO recommends limits on the content of glycerols in these products.17 Glycerols have been associated with increased risk of bacterial vaginosis (adjusted odds ratio [aOR], 11.75; 95% confidence interval [CI], 1.96–70.27), and can serve as a food source for candida species, possibly increasing risk of yeast infections.7,23 Additionally, vaginal moisturizers and lubricants may contain preservatives such as chlorhexidine, which can disrupt normal vaginal flora and may cause tissue irritation.7
Continue to: Common concerns to be aware of...
Common concerns to be aware of
Women using vaginal products may be concerned about adverse effects, such as worsening vaginal irritation or infection. Vaginal moisturizers have not been shown to have increased risk of adverse effects compared with vaginal estrogens.9,10 In vitro studies have shown that vaginal moisturizers and lubricants inhibit the growth of Escherichia coli but may also inhibit Lactobacillus crispatus.24 Clinically, vaginal moisturizers have been shown to improve signs of bacterial vaginosis and have even been used to treat bacterial vaginosis.25,26 A study of commercially available vaginal lubricants inhibited the growth of L crispatus, which may predispose to irritation and infection.27 Nonetheless, the effect of the vaginal products on the vaginal microbiome and vaginal tissue remains poorly studied. Vaginal moisturizers and lubricants, while often helpful for patients, also can potentially cause irritation or predispose to infections. Providers should consider this when evaluating patients for new onset vaginal symptoms after starting vaginal products.
Bottom line
Vaginal products such as moisturizers and lubricants are often effective treatment options for women suffering from genitourinary syndrome of menopause and may be first-line treatment options, especially for women who may wish to avoid estrogen-containing products. Vaginal moisturizers can be recommended to any women experiencing vaginal irritation due to vaginal dryness while vaginal lubricants should be recommended to sexually active women who experience dyspareunia. Clinicians need to be aware of the formulations of these products and possible side effects in order to appropriately counsel patients. ●
Vaginal dryness, encompassed in the modern term genitourinary syndrome of menopause (GSM) affects up to 40% of menopausal women and up to 60% of postmenopausal breast cancer survivors.1,2 Premenopausal women also can have vulvovaginal dryness while breastfeeding (lactational amenorrhea) and while taking low-dose contraceptives.3 Vaginal moisturizers and lubricants are the first-line treatment options for vaginal dryness, dyspareunia, and GSM.4,5 In fact, approximately two-thirds of women have reported using a vaginal lubricant in their lifetime.6 Despite such ubiquitous use, many health care providers and patients have questions about the difference between vaginal moisturizers and lubricants and how to best choose a product.
Vaginal moisturizers
Vaginal moisturizers are designed to rehydrate the vaginal epithelium. Much like facial or skin moisturizers, they are intended to be applied regularly, every 2 to 3 days, but may be applied more often depending on the severity of symptoms. Vaginal moisturizers work by increasing the fluid content of the vaginal tissue and by lowering the vaginal pH to mimic that of natural vaginal secretions. Vaginal moisturizers are typically water based and use polymers to hydrate tissues.7 They change cell morphology but do not change vaginal maturation, indicating that they bring water to the tissue but do not shift the balance between superficial and basal cells and do not increase vaginal epithelial thickness as seen with vaginal estrogen.8 Vaginal moisturizers also have been found to be a safe alternative to vaginal estrogen therapy and may improve markers of vaginal health, including vaginal moisture, vaginal fluid volume, vaginal elasticity, and premenopausal pH.9 Commercially available vaginal moisturizers have been shown to be as effective as vaginal estrogens in reducing vaginal symptoms such as itching, irritation, and dyspareunia, but some caution should be taken when interpreting these results as neither vaginal moisturizer nor vaginal estrogen tablet were more effective than placebo in a recent randomized controlled trial.10,11 Small studies on hyaluronic acid have shown efficacy for the treatment of vaginal dryness.12,13 Hyaluronic acid is commercially available as a vaginal suppository ovule and as a liquid. It may also be obtained from a reliable compounding pharmacy. Vaginal suppository ovules may be a preferable formulation for women who find the liquids messy or cumbersome to apply.
Lubricants
Lubricants differ from vaginal moisturizers because they are specifically designed to be used during intercourse to provide short-term relief from vaginal dryness. They may be water-, silicone-, mineral oil-, or plant oil-based. The use of water- and silicone-based lubricants is associated with high satisfaction for intercourse as well as masturbation.14 These products may be particularly beneficial to women whose chief complaint is dyspareunia. In fact, women with dyspareunia report more lubricant use than women without dyspareunia, and the most common reason for lubricant use among these women was to reduce or alleviate pain.15 Overall, women both with and without dyspareunia have a positive perception regarding lubricant use and prefer sexual intercourse that feels more “wet,” and women in their forties have the most positive perception about lubricant use at the time of intercourse compared with other age groups.16 Furthermore, the World Health Organization (WHO) recommends that condom-compatible lubricants be used with condoms for menopausal and postmenopausal women.17 Both water-based and silicone-based lubricants may be used with latex condoms, while oil-based lubricants should be avoided as they can degrade the latex condom. While vaginal moisturizers and lubricants technically differ based on use, patients may use one product for both purposes, and some products are marketed as both a moisturizer and lubricant.
Continue to: Providing counsel to patients...
Providing counsel to patients
Patients often seek advice on how to choose vaginal moisturizers and lubricants. Understanding the compositions of these products and their scientific evidence is useful when helping patients make informed decisions regarding their pelvic health. Most commercially available lubricants are either water- or silicone- based. In one study comparing these two types of lubricants, water-based lubricants were associated with fewer genital symptoms than silicone-based products.14 Women may want to use a natural or organic product and may prefer plant-based oils such as coconut oil or olive oil. Patients should be counseled that latex condoms are not compatible with petroleum-, mineral oil- or plant oil-based lubricants.
In our practice, we generally recommend silicone-based lubricants, as they are readily available and compatible with latex condoms and generally require a smaller amount than water-based lubricants. They tend to be more expensive than water-based lubricants. For vaginal moisturizers, we often recommend commercially available formulations that can be purchased at local pharmacies or drug stores. However, a patient may need to try different lubricants and moisturizers in order to find a preferred product. We have included in TABLES 1 and 27,17,18 a list of commercially available vaginal moisturizers and lubricants with ingredient list, pH, osmolality, common formulation, and cost when available, which has been compiled from WHO and published research data to help guide patient counseling.
The effects of additives
Water-based moisturizers and lubricants may contain many ingredients, such as glycerols, fragrance, flavors, sweeteners, warming or cooling agents, buffering solutions, parabens and other preservatives, and numbing agents. These substances are added to water-based products to prolong water content, alter viscosity, alter pH, achieve certain sensations, and prevent bacterial contamination.7 The addition of these substances, however, will alter osmolality and pH balance of the product, which may be of clinical consequence. Silicone- or oil-based products do not contain water and therefore do not have a pH or an osmolality value.
Hyperosmolar formulations can theoretically injure epithelial tissue. In vitro studies have shown that hyperosmotic vaginal products can induce mild to moderate irritation, while very hyperosmolar formulations can induce severe irritation and tissue damage to vaginal epithelial and cervical cells.19,20 The WHO recommends that the osmolality of a vaginal product not exceed 380 mOsm/kg, but very few commercially available products meet these criteria so, clinically, the threshold is 1,200 mOsm/kg.17 It should be noted that most commercially available products exceed the 1,200 mOsm/kg threshold. Vaginal products may be a cause for vaginal irritation and should be considered in the differential diagnosis.
The normal vaginal pH is 3.8–4.5, and vaginal products should be pH balanced to this range. The exact role of pH in these products remains poorly understood. Nonetheless, products with a pH of 3 or lower are not recommended.18 Concerns about osmolality and pH remain theoretical, as a study of 12 commercially available lubricants of varying osmolality and pH found no cytotoxic effect in vivo.18
Vaginal moisturizers and lubricants contain many inactive ingredients, the most controversial of which are parabens. These substances are used in many cosmetic products as preservatives and are weakly estrogenic. These substances have been found in breast cancer tissue, but their possible role as a carcinogen remains uncertain.21,22 Nonetheless, the use of paraben-containing products is not recommended for women who have a history of hormonally-driven cancer or who are at high risk for developing cancer.7 Many lubricants contain glycerols (glycerol, glycerine, and propylene glycol) to alter viscosity or alter the water properties. The WHO recommends limits on the content of glycerols in these products.17 Glycerols have been associated with increased risk of bacterial vaginosis (adjusted odds ratio [aOR], 11.75; 95% confidence interval [CI], 1.96–70.27), and can serve as a food source for candida species, possibly increasing risk of yeast infections.7,23 Additionally, vaginal moisturizers and lubricants may contain preservatives such as chlorhexidine, which can disrupt normal vaginal flora and may cause tissue irritation.7
Continue to: Common concerns to be aware of...
Common concerns to be aware of
Women using vaginal products may be concerned about adverse effects, such as worsening vaginal irritation or infection. Vaginal moisturizers have not been shown to have increased risk of adverse effects compared with vaginal estrogens.9,10 In vitro studies have shown that vaginal moisturizers and lubricants inhibit the growth of Escherichia coli but may also inhibit Lactobacillus crispatus.24 Clinically, vaginal moisturizers have been shown to improve signs of bacterial vaginosis and have even been used to treat bacterial vaginosis.25,26 A study of commercially available vaginal lubricants inhibited the growth of L crispatus, which may predispose to irritation and infection.27 Nonetheless, the effect of the vaginal products on the vaginal microbiome and vaginal tissue remains poorly studied. Vaginal moisturizers and lubricants, while often helpful for patients, also can potentially cause irritation or predispose to infections. Providers should consider this when evaluating patients for new onset vaginal symptoms after starting vaginal products.
Bottom line
Vaginal products such as moisturizers and lubricants are often effective treatment options for women suffering from genitourinary syndrome of menopause and may be first-line treatment options, especially for women who may wish to avoid estrogen-containing products. Vaginal moisturizers can be recommended to any women experiencing vaginal irritation due to vaginal dryness while vaginal lubricants should be recommended to sexually active women who experience dyspareunia. Clinicians need to be aware of the formulations of these products and possible side effects in order to appropriately counsel patients. ●
- Castelo-Branco C, Cancelo MJ, Villero J, et al. Management of postmenopausal vaginal atrophy and atrophic vaginitis. Maturitas. 2005;52(suppl 1):S46-S52. doi: 10.1016/j.maturitas.2005.06.014.
- Crandall C, Peterson L, Ganz PA, et al. Association of breast cancer and its therapy with menopause-related symptoms. Menopause. 2004;11:519-530. doi: 10.1097/01.gme.0000117061.40493.ab.
- Bornstein J, Goldstein AT, Stockdale CK, et al. 2015 ISSVD, ISSWSH, and IPPS Consensus Terminology and Classification of Persistant Vulvar Pain and Vulvodynia. J Sex Med. 2016;13:607-612. doi: 10.1016/j.jsxm.2016.02.167.
- American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 141: management of menopausal symptoms. Obstet Gynecol. 2014;123:202-216. doi: 10.1097/01.AOG.0000441353.20693.78.
- Faubion S, Larkin L, Stuenkel C, et al. Management of genitourinary syndrome of menopause in women with or at high risk for breast cancer: consensus recommendation from The North American Menopause Society and the International Society for the Study for Women’s Sexual Health. Menopause. 2018;25:596-608. doi: 10.1097/GME.0000000000001121.
- Herbenick D, Reece M, Schick V, et al. Women’s use and perceptions of commercial lubricants: prevalence and characteristics in a nationally representative sample of American adults. J Sex Med. 2014;11:642-652. doi: 10.1111/jsm.12427.
- Edwards D, Panay N. Treating vulvovaginal atrophy/genitourinary syndrome of menopause: how important is vaginal lubricant and moisturizer composition? Climacteric. 2016;19:151-116. doi: 10.3109/13697137.2015.1124259.
- Van der Lakk JAWN, de Bie LMT, de Leeuw H, et al. The effect of Replens on vaginal cytology in the treatment of postmenopausal atrophy: cytomorphology versus computerized cytometry. J Clin Pathol. 2002;55:446-451. doi: 10.1136/jcp.55.6.446.
- Nachtigall LE. Comparitive study: Replens versus local estrogen in menopausal women. Fertil Steril. 1994;61:178-180. doi: 10.1016/s0015-0282(16)56474-7.
- Bygdeman M, Swahn ML. Replens versus dienoestrol cream in the symptomatic treatment of vaginal atrophy in postmenopausal women. Maturitas. 1996;23:259-263. doi: 10.1016/0378-5122(95)00955-8.
- Mitchell CM, Reed SD, Diem S, et al. Efficacy of vaginal estradiol or vaginal moisturizer vs placebo for treating postmenopausal vulvovaginal symptoms. JAMA Intern Med. 2018;178:681-690. doi: 10.1001/jamainternmed.2018.0116.
- Chen J, Geng L, Song X, et al. Evaluation of the efficacy and safety of hyaluronic acid vaginal gel to ease vaginal dryness: a multicenter, randomized, controlled, open-label, parallel-group, clinical trial. J Sex Med. 2013;10:1575-1584. doi: 10.1111/jsm.12125.
- Jokar A, Davari T, Asadi N, et al. Comparison of the hyaluronic acid vaginal cream and conjugated estrogen used in treatment of vaginal atrophy of menopause women: a randomized controlled clinical trial. IJCBNM. 2016;4:69-78.
- Herbenick D, Reece M, Hensel D, et al. Association of lubricant use with women’s sexual pleasure, sexual satisfaction, and genital symptoms: a prospective daily diary study. J Sex Med. 2011;8:202-212. doi: 10.1111/j.1743-6109.2010.02067.x.
- Sutton KS, Boyer SC, Goldfinger C, et al. To lube or not to lube: experiences and perceptions of lubricant use in women with and without dyspareunia. J Sex Med. 2012;9:240-250. doi: 10.1111/j.1743-6109.2011.02543.x.
- Jozkowski KN, Herbenick D, Schick V, et al. Women’s perceptions about lubricant use and vaginal wetness during sexual activity. J Sex Med. 2013;10:484-492. doi: 10.1111/jsm.12022.
- World Health Organization. Use and procurement of additional lubricants for male and female condoms: WHO /UNFPA/FHI360 advisory note. 2012. https://www.who. int/reproductivehealth/publications/rtis/rhr12_33/en/. Accessed February 13, 2021.
- Cunha AR, Machado RM, Palmeira de Oliveira A, et al. Characterization of commercially available vaginal lubricants: a safety perspective. Pharmaceuticals. 2014;6:530-542. doi: 10.3390/pharmaceutics6030530.
- Adriaens E, Remon JP. Mucosal irritation potential of personal lubricants relates to product osmolality as detected by the slug mucosal irritation assay. Sex Transm Dis. 2008;35:512-516. doi: 10.1097/OLQ.0b013e3181644669.
- Dezzuti CS, Brown ER, Moncla B, et al. Is wetter better? An evaluation of over-the-counter personal lubricants for safety and anti-HIV activity. PLoS One. 2012;7:e48328. doi: 10.1371/journal.pone.0048328.
- Harvey PW, Everett DJ. Significance of the detection of esters of p-hydroxybenzoic acid (parabens) in human breast tumours. J Appl Toxicol. 2004:24:1-4. doi: 10.1002/jat.957.
- Darbre PD, Alijarrah A, Miller WR, et al. Concentrations of parabens in human breast tumous. J Appl Toxicol. 2004;24:5-13. doi: 10.1002/jat.958.
- Brotman RM, Ravel J, Cone RA, et al. Rapid fluctuation of the vaginal microbiota measured by Gram stain analysis. Sex Transm Infect. 2010;86:297-302. doi: 10.1136/sti.2009.040592.
- Hung KJ, Hudson P, Bergerat A, et al. Effect of commercial vaginal products on the growth of uropathogenic and commensal vaginal bacteria. Sci Rep. 2020;10:7625.
- Wu JP, Fielding SL, Fiscell K. The effect of the polycarbophil gel (Replens) on bacterial vaginosis: a pilot study. Eur J Obstet Gynecol Reprod Biol. 2007;130:132-136. doi: 10.1016/j.ejogrb.2006.01.007.
- Fiorelli A, Molteni B, Milani M. Successful treatment of bacterial vaginosis with a polycarbophil-carbopol acidic vaginal gel: results from a randomized double-bling, placebo controlled trial. Eur J Obstet Gynecol Reprod Biol. 2005;120:202-205. doi: 10.1016/j.ejogrb.2004.10.011.
- Fashemi B, Delaney ML, Onderdonk AB, et al. Effects of feminine hygiene products on the vaginal mucosal biome. Microb Ecol Health Dis. 2013;24. doi: 10.3402/mehd.v24i0.19703.
- Castelo-Branco C, Cancelo MJ, Villero J, et al. Management of postmenopausal vaginal atrophy and atrophic vaginitis. Maturitas. 2005;52(suppl 1):S46-S52. doi: 10.1016/j.maturitas.2005.06.014.
- Crandall C, Peterson L, Ganz PA, et al. Association of breast cancer and its therapy with menopause-related symptoms. Menopause. 2004;11:519-530. doi: 10.1097/01.gme.0000117061.40493.ab.
- Bornstein J, Goldstein AT, Stockdale CK, et al. 2015 ISSVD, ISSWSH, and IPPS Consensus Terminology and Classification of Persistant Vulvar Pain and Vulvodynia. J Sex Med. 2016;13:607-612. doi: 10.1016/j.jsxm.2016.02.167.
- American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 141: management of menopausal symptoms. Obstet Gynecol. 2014;123:202-216. doi: 10.1097/01.AOG.0000441353.20693.78.
- Faubion S, Larkin L, Stuenkel C, et al. Management of genitourinary syndrome of menopause in women with or at high risk for breast cancer: consensus recommendation from The North American Menopause Society and the International Society for the Study for Women’s Sexual Health. Menopause. 2018;25:596-608. doi: 10.1097/GME.0000000000001121.
- Herbenick D, Reece M, Schick V, et al. Women’s use and perceptions of commercial lubricants: prevalence and characteristics in a nationally representative sample of American adults. J Sex Med. 2014;11:642-652. doi: 10.1111/jsm.12427.
- Edwards D, Panay N. Treating vulvovaginal atrophy/genitourinary syndrome of menopause: how important is vaginal lubricant and moisturizer composition? Climacteric. 2016;19:151-116. doi: 10.3109/13697137.2015.1124259.
- Van der Lakk JAWN, de Bie LMT, de Leeuw H, et al. The effect of Replens on vaginal cytology in the treatment of postmenopausal atrophy: cytomorphology versus computerized cytometry. J Clin Pathol. 2002;55:446-451. doi: 10.1136/jcp.55.6.446.
- Nachtigall LE. Comparitive study: Replens versus local estrogen in menopausal women. Fertil Steril. 1994;61:178-180. doi: 10.1016/s0015-0282(16)56474-7.
- Bygdeman M, Swahn ML. Replens versus dienoestrol cream in the symptomatic treatment of vaginal atrophy in postmenopausal women. Maturitas. 1996;23:259-263. doi: 10.1016/0378-5122(95)00955-8.
- Mitchell CM, Reed SD, Diem S, et al. Efficacy of vaginal estradiol or vaginal moisturizer vs placebo for treating postmenopausal vulvovaginal symptoms. JAMA Intern Med. 2018;178:681-690. doi: 10.1001/jamainternmed.2018.0116.
- Chen J, Geng L, Song X, et al. Evaluation of the efficacy and safety of hyaluronic acid vaginal gel to ease vaginal dryness: a multicenter, randomized, controlled, open-label, parallel-group, clinical trial. J Sex Med. 2013;10:1575-1584. doi: 10.1111/jsm.12125.
- Jokar A, Davari T, Asadi N, et al. Comparison of the hyaluronic acid vaginal cream and conjugated estrogen used in treatment of vaginal atrophy of menopause women: a randomized controlled clinical trial. IJCBNM. 2016;4:69-78.
- Herbenick D, Reece M, Hensel D, et al. Association of lubricant use with women’s sexual pleasure, sexual satisfaction, and genital symptoms: a prospective daily diary study. J Sex Med. 2011;8:202-212. doi: 10.1111/j.1743-6109.2010.02067.x.
- Sutton KS, Boyer SC, Goldfinger C, et al. To lube or not to lube: experiences and perceptions of lubricant use in women with and without dyspareunia. J Sex Med. 2012;9:240-250. doi: 10.1111/j.1743-6109.2011.02543.x.
- Jozkowski KN, Herbenick D, Schick V, et al. Women’s perceptions about lubricant use and vaginal wetness during sexual activity. J Sex Med. 2013;10:484-492. doi: 10.1111/jsm.12022.
- World Health Organization. Use and procurement of additional lubricants for male and female condoms: WHO /UNFPA/FHI360 advisory note. 2012. https://www.who. int/reproductivehealth/publications/rtis/rhr12_33/en/. Accessed February 13, 2021.
- Cunha AR, Machado RM, Palmeira de Oliveira A, et al. Characterization of commercially available vaginal lubricants: a safety perspective. Pharmaceuticals. 2014;6:530-542. doi: 10.3390/pharmaceutics6030530.
- Adriaens E, Remon JP. Mucosal irritation potential of personal lubricants relates to product osmolality as detected by the slug mucosal irritation assay. Sex Transm Dis. 2008;35:512-516. doi: 10.1097/OLQ.0b013e3181644669.
- Dezzuti CS, Brown ER, Moncla B, et al. Is wetter better? An evaluation of over-the-counter personal lubricants for safety and anti-HIV activity. PLoS One. 2012;7:e48328. doi: 10.1371/journal.pone.0048328.
- Harvey PW, Everett DJ. Significance of the detection of esters of p-hydroxybenzoic acid (parabens) in human breast tumours. J Appl Toxicol. 2004:24:1-4. doi: 10.1002/jat.957.
- Darbre PD, Alijarrah A, Miller WR, et al. Concentrations of parabens in human breast tumous. J Appl Toxicol. 2004;24:5-13. doi: 10.1002/jat.958.
- Brotman RM, Ravel J, Cone RA, et al. Rapid fluctuation of the vaginal microbiota measured by Gram stain analysis. Sex Transm Infect. 2010;86:297-302. doi: 10.1136/sti.2009.040592.
- Hung KJ, Hudson P, Bergerat A, et al. Effect of commercial vaginal products on the growth of uropathogenic and commensal vaginal bacteria. Sci Rep. 2020;10:7625.
- Wu JP, Fielding SL, Fiscell K. The effect of the polycarbophil gel (Replens) on bacterial vaginosis: a pilot study. Eur J Obstet Gynecol Reprod Biol. 2007;130:132-136. doi: 10.1016/j.ejogrb.2006.01.007.
- Fiorelli A, Molteni B, Milani M. Successful treatment of bacterial vaginosis with a polycarbophil-carbopol acidic vaginal gel: results from a randomized double-bling, placebo controlled trial. Eur J Obstet Gynecol Reprod Biol. 2005;120:202-205. doi: 10.1016/j.ejogrb.2004.10.011.
- Fashemi B, Delaney ML, Onderdonk AB, et al. Effects of feminine hygiene products on the vaginal mucosal biome. Microb Ecol Health Dis. 2013;24. doi: 10.3402/mehd.v24i0.19703.
The Cures Act: Is the “cure” worse than the disease?
There is a sudden spill of icy anxiety down your spine as you pick up your phone in your shaking hands. It’s 6 p.m.; your doctor’s office is closed. You open the message, and your worst fears are confirmed ... the cancer is back.
Or is it? You’re not sure. The biopsy sure sounds bad. But you’re an English teacher, not a doctor, and you spend the rest of the night Googling words like “tubulovillous” and “high-grade dysplasia.” You sit awake, terrified in front of the computer screen desperately trying to make sense of the possibly life-changing results. You wish you knew someone who could help you understand; you consider calling your doctor’s emergency line, or your cousin who is an ophthalmologist – anybody who can help you make sense of the results.
Or imagine another scenario: you’re a trans teen who has asked your doctor to refer to you by your preferred pronouns. You’re still presenting as your birth sex, in part because your family would disown you if they knew, and you’re not financially or emotionally ready for that step. You feel proud of yourself for advocating for your needs to your long-time physician, and excited about the resources they’ve included in your after visit summary and the referrals they’d made to gender-confirming specialists.
When you get home, you are confronted with a terrible reality that your doctor’s notes, orders, and recommendations are immediately viewable to anybody with your MyChart login – your parents knew the second your doctor signed the note. They received the notification, logged on as your guardians, and you have effectively been “outed” by the physician who took and oath to care for you and who you trusted implicitly.
How the Cures Act is affecting patients
While these examples may sound extreme, they are becoming more and more commonplace thanks to a recently enacted 21st Century Cures Act. The act was originally written to improve communication between physicians and patients. Part of the act stipulates that nearly all medical information – from notes to biopsies to lab results – must be available within 24 hours, published to a patient portal and a notification be sent to the patient by phone.
Oftentimes, this occurs before the ordering physician has even seen the results, much less interpreted them and made a plan for the patient. What happens now, not long after its enactment date, when it has become clear that the Cures Act is causing extreme harm to our patients?
Take, for example, the real example of a physician whose patient found out about her own intrauterine fetal demise by way of an EMR text message alert of “new imaging results!” sent directly to her phone. Or a physician colleague who witnessed firsthand the intrusive unhelpfulness of the Cures Act when she was informed via patient portal releasing her imaging information that she had a large, possibly malignant breast mass. “No phone call,” she said. “No human being for questions or comfort. Just a notification on my phone.”
The stories about the impact of the Cures Act across the medical community are an endless stream of anxiety, hurt, and broken trust. The relationship between a physician and a patient should be sacred, bolstered by communication and mutual respect.
In many ways, the new act feels like a third party to the patient-physician relationship – a digital imposter, oftentimes blurting out personal and life-altering medical information without any of the finesse, context, and perspective of an experienced physician.
Breaking ‘bad news’ to a patient
In training, some residents are taught how to “break bad news” to a patient. Some good practices for doing this are to have information available for the patient, provide emotional support, have a plan for their next steps already formulated, and call the appropriate specialist ahead of time if you can.
Above all, it’s most important to let the patient be the one to direct their own care. Give them time to ask questions and answer them honestly and clearly. Ask them how much they want to know and help them to understand the complex change in their usual state of health.
Now, unless physicians are keeping a very close eye on their inbox, results are slipping out to patients in a void. The bad news conversations aren’t happening at all, or if they are, they’re happening at 8 p.m. on a phone call after an exhausted physician ends their shift but has to slog through their results bin, calling all the patients who shouldn’t have to find out their results in solitude.
Reaching out to these patients immediately is an honorable, kind thing to, but for a physician, knowing they need to beat the patient to opening an email creates anxiety. Plus, making these calls at whatever hour the results are released to a patient is another burden added to doctors’ already-full plates.
Interpreting results
None of us want to harm our patients. All of us want to be there for them. But this act stands in the way of delivering quality, humanizing medical care.
It is true that patients have a right to access their own medical information. It is also true that waiting anxiously on results can cause undue harm to a patient. But the across-the-board, breakneck speed of information release mandated in this act causes irreparable harm not only to patients, but to the patient-physician relationship.
No patient should find out their cancer recurred while checking their emails at their desk. No patient should first learn of a life-altering diagnosis by way of scrolling through their smartphone in bed. The role of a physician is more than just a healer – we should also be educators, interpreters, partners and, first and foremost, advocates for our patients’ needs.
Our patients are depending on us to stand up and speak out about necessary changes to this act. Result releases should be delayed until they are viewed by a physician. Our patients deserve the dignity and opportunity of a conversation with their medical provider about their test results, and physicians deserve the chance to interpret results and frame the conversation in a way which is conducive to patient understanding and healing.
Dr. Persampiere is a first-year resident in the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece. You can contact them at [email protected].
There is a sudden spill of icy anxiety down your spine as you pick up your phone in your shaking hands. It’s 6 p.m.; your doctor’s office is closed. You open the message, and your worst fears are confirmed ... the cancer is back.
Or is it? You’re not sure. The biopsy sure sounds bad. But you’re an English teacher, not a doctor, and you spend the rest of the night Googling words like “tubulovillous” and “high-grade dysplasia.” You sit awake, terrified in front of the computer screen desperately trying to make sense of the possibly life-changing results. You wish you knew someone who could help you understand; you consider calling your doctor’s emergency line, or your cousin who is an ophthalmologist – anybody who can help you make sense of the results.
Or imagine another scenario: you’re a trans teen who has asked your doctor to refer to you by your preferred pronouns. You’re still presenting as your birth sex, in part because your family would disown you if they knew, and you’re not financially or emotionally ready for that step. You feel proud of yourself for advocating for your needs to your long-time physician, and excited about the resources they’ve included in your after visit summary and the referrals they’d made to gender-confirming specialists.
When you get home, you are confronted with a terrible reality that your doctor’s notes, orders, and recommendations are immediately viewable to anybody with your MyChart login – your parents knew the second your doctor signed the note. They received the notification, logged on as your guardians, and you have effectively been “outed” by the physician who took and oath to care for you and who you trusted implicitly.
How the Cures Act is affecting patients
While these examples may sound extreme, they are becoming more and more commonplace thanks to a recently enacted 21st Century Cures Act. The act was originally written to improve communication between physicians and patients. Part of the act stipulates that nearly all medical information – from notes to biopsies to lab results – must be available within 24 hours, published to a patient portal and a notification be sent to the patient by phone.
Oftentimes, this occurs before the ordering physician has even seen the results, much less interpreted them and made a plan for the patient. What happens now, not long after its enactment date, when it has become clear that the Cures Act is causing extreme harm to our patients?
Take, for example, the real example of a physician whose patient found out about her own intrauterine fetal demise by way of an EMR text message alert of “new imaging results!” sent directly to her phone. Or a physician colleague who witnessed firsthand the intrusive unhelpfulness of the Cures Act when she was informed via patient portal releasing her imaging information that she had a large, possibly malignant breast mass. “No phone call,” she said. “No human being for questions or comfort. Just a notification on my phone.”
The stories about the impact of the Cures Act across the medical community are an endless stream of anxiety, hurt, and broken trust. The relationship between a physician and a patient should be sacred, bolstered by communication and mutual respect.
In many ways, the new act feels like a third party to the patient-physician relationship – a digital imposter, oftentimes blurting out personal and life-altering medical information without any of the finesse, context, and perspective of an experienced physician.
Breaking ‘bad news’ to a patient
In training, some residents are taught how to “break bad news” to a patient. Some good practices for doing this are to have information available for the patient, provide emotional support, have a plan for their next steps already formulated, and call the appropriate specialist ahead of time if you can.
Above all, it’s most important to let the patient be the one to direct their own care. Give them time to ask questions and answer them honestly and clearly. Ask them how much they want to know and help them to understand the complex change in their usual state of health.
Now, unless physicians are keeping a very close eye on their inbox, results are slipping out to patients in a void. The bad news conversations aren’t happening at all, or if they are, they’re happening at 8 p.m. on a phone call after an exhausted physician ends their shift but has to slog through their results bin, calling all the patients who shouldn’t have to find out their results in solitude.
Reaching out to these patients immediately is an honorable, kind thing to, but for a physician, knowing they need to beat the patient to opening an email creates anxiety. Plus, making these calls at whatever hour the results are released to a patient is another burden added to doctors’ already-full plates.
Interpreting results
None of us want to harm our patients. All of us want to be there for them. But this act stands in the way of delivering quality, humanizing medical care.
It is true that patients have a right to access their own medical information. It is also true that waiting anxiously on results can cause undue harm to a patient. But the across-the-board, breakneck speed of information release mandated in this act causes irreparable harm not only to patients, but to the patient-physician relationship.
No patient should find out their cancer recurred while checking their emails at their desk. No patient should first learn of a life-altering diagnosis by way of scrolling through their smartphone in bed. The role of a physician is more than just a healer – we should also be educators, interpreters, partners and, first and foremost, advocates for our patients’ needs.
Our patients are depending on us to stand up and speak out about necessary changes to this act. Result releases should be delayed until they are viewed by a physician. Our patients deserve the dignity and opportunity of a conversation with their medical provider about their test results, and physicians deserve the chance to interpret results and frame the conversation in a way which is conducive to patient understanding and healing.
Dr. Persampiere is a first-year resident in the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece. You can contact them at [email protected].
There is a sudden spill of icy anxiety down your spine as you pick up your phone in your shaking hands. It’s 6 p.m.; your doctor’s office is closed. You open the message, and your worst fears are confirmed ... the cancer is back.
Or is it? You’re not sure. The biopsy sure sounds bad. But you’re an English teacher, not a doctor, and you spend the rest of the night Googling words like “tubulovillous” and “high-grade dysplasia.” You sit awake, terrified in front of the computer screen desperately trying to make sense of the possibly life-changing results. You wish you knew someone who could help you understand; you consider calling your doctor’s emergency line, or your cousin who is an ophthalmologist – anybody who can help you make sense of the results.
Or imagine another scenario: you’re a trans teen who has asked your doctor to refer to you by your preferred pronouns. You’re still presenting as your birth sex, in part because your family would disown you if they knew, and you’re not financially or emotionally ready for that step. You feel proud of yourself for advocating for your needs to your long-time physician, and excited about the resources they’ve included in your after visit summary and the referrals they’d made to gender-confirming specialists.
When you get home, you are confronted with a terrible reality that your doctor’s notes, orders, and recommendations are immediately viewable to anybody with your MyChart login – your parents knew the second your doctor signed the note. They received the notification, logged on as your guardians, and you have effectively been “outed” by the physician who took and oath to care for you and who you trusted implicitly.
How the Cures Act is affecting patients
While these examples may sound extreme, they are becoming more and more commonplace thanks to a recently enacted 21st Century Cures Act. The act was originally written to improve communication between physicians and patients. Part of the act stipulates that nearly all medical information – from notes to biopsies to lab results – must be available within 24 hours, published to a patient portal and a notification be sent to the patient by phone.
Oftentimes, this occurs before the ordering physician has even seen the results, much less interpreted them and made a plan for the patient. What happens now, not long after its enactment date, when it has become clear that the Cures Act is causing extreme harm to our patients?
Take, for example, the real example of a physician whose patient found out about her own intrauterine fetal demise by way of an EMR text message alert of “new imaging results!” sent directly to her phone. Or a physician colleague who witnessed firsthand the intrusive unhelpfulness of the Cures Act when she was informed via patient portal releasing her imaging information that she had a large, possibly malignant breast mass. “No phone call,” she said. “No human being for questions or comfort. Just a notification on my phone.”
The stories about the impact of the Cures Act across the medical community are an endless stream of anxiety, hurt, and broken trust. The relationship between a physician and a patient should be sacred, bolstered by communication and mutual respect.
In many ways, the new act feels like a third party to the patient-physician relationship – a digital imposter, oftentimes blurting out personal and life-altering medical information without any of the finesse, context, and perspective of an experienced physician.
Breaking ‘bad news’ to a patient
In training, some residents are taught how to “break bad news” to a patient. Some good practices for doing this are to have information available for the patient, provide emotional support, have a plan for their next steps already formulated, and call the appropriate specialist ahead of time if you can.
Above all, it’s most important to let the patient be the one to direct their own care. Give them time to ask questions and answer them honestly and clearly. Ask them how much they want to know and help them to understand the complex change in their usual state of health.
Now, unless physicians are keeping a very close eye on their inbox, results are slipping out to patients in a void. The bad news conversations aren’t happening at all, or if they are, they’re happening at 8 p.m. on a phone call after an exhausted physician ends their shift but has to slog through their results bin, calling all the patients who shouldn’t have to find out their results in solitude.
Reaching out to these patients immediately is an honorable, kind thing to, but for a physician, knowing they need to beat the patient to opening an email creates anxiety. Plus, making these calls at whatever hour the results are released to a patient is another burden added to doctors’ already-full plates.
Interpreting results
None of us want to harm our patients. All of us want to be there for them. But this act stands in the way of delivering quality, humanizing medical care.
It is true that patients have a right to access their own medical information. It is also true that waiting anxiously on results can cause undue harm to a patient. But the across-the-board, breakneck speed of information release mandated in this act causes irreparable harm not only to patients, but to the patient-physician relationship.
No patient should find out their cancer recurred while checking their emails at their desk. No patient should first learn of a life-altering diagnosis by way of scrolling through their smartphone in bed. The role of a physician is more than just a healer – we should also be educators, interpreters, partners and, first and foremost, advocates for our patients’ needs.
Our patients are depending on us to stand up and speak out about necessary changes to this act. Result releases should be delayed until they are viewed by a physician. Our patients deserve the dignity and opportunity of a conversation with their medical provider about their test results, and physicians deserve the chance to interpret results and frame the conversation in a way which is conducive to patient understanding and healing.
Dr. Persampiere is a first-year resident in the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece. You can contact them at [email protected].
Vaginoplasty basics – what every gynecologist needs to know
Feminizing gender affirmation surgery is a complex genital surgery that most commonly involves removal of natal male genitalia (testes, penile urethra, a majority of the glans penis, penile shaft) and construction of the vulva and/or neovagina utilizing scrotal and penile shaft tissue. Other surgical procedures can also involve using a peritoneal flap or a portion of the small bowel or sigmoid colon to create the neovaginal canal. As with any major surgical procedure, complications do occur, and these can range from minor to major; intraoperative to postoperative. For the purposes of this article, the focus shall be on postoperative complications. Most postoperative complications occur within the first 4 months of the surgery and include vaginal stenosis, genitourinary fistula formation, urinary stream abnormalities, and sexual dysfunction.1 Minor complications that can be managed in the office include granulation tissue treatment, vaginitis, and hair growth in the neovagina. It is important to note that, if any complication occurs, it is essential to refer to the patient’s original surgeon or to a surgeon with expertise in vaginoplasty techniques and postoperative management.2
For patients who undergo vaginoplasty, or a creation of a neovaginal canal, postoperative dilation is necessary to maintain patency. The frequency and duration of dilation are often determined by each individual surgeon or surgical practice as there is no universal, evidence-based standard to guide recommendations on dilation. Failure to maintain a dilation schedule can result in neovaginal stenosis and inability to engage in penetrative vaginal intercourse (if patients desire). Dilation can be difficult.
Challenges with dilation can occur for a variety of reasons: pain, history of trauma, pelvic floor dysfunction, lack of privacy or a supportive environment, or change in personal goals.3 If the underlying cause is related to pelvic floor dysfunction, postoperative pelvic floor therapy has demonstrated improvement in dilation.4 Additionally, routine douching is required for vaginal hygiene. Unlike natal vaginas, neovaginas do not usually contain mucosa, with the exception of a colonic interposition vaginoplasty, and routine douching with soapy water can help prevent a buildup of lubricant and debris.
If a patient reports abnormal discharge, an exam of the vulva and neovagina is warranted. Many patients are able to tolerate a speculum examination. If a patient has undergone a penile inversion vaginoplasty, the microbiome of the neovagina is quite different than that of a natal vagina and most common causes of abnormal discharge often include retained lubricant, keratin debris, sebum, or semen.5 During a speculum exam, the provider may notice granulation tissue, which is often another cause of persistent vaginal discharge, vaginal bleeding, or pain during dilation. Depending on the patient’s symptoms and quantity of granulation tissue present, it can often resolve spontaneously. Persistent granulation tissue can be treated with silver nitrate. An alternative to silver nitrate is using medical grade honey or a course of a mild-strength topical steroid cream or ointment.5 In some cases, abnormal discharge may be the result of a fistula. If a fistula is noted the patient should be immediately referred back to the original surgeon or to a urogynecologist and/or colorectal surgeon for evaluation and management.
While this surgery often falls outside of the scope of practice of the general obstetrician-gynecologist, most patients will seek the care of a general obstetrician-gynecologist in the postoperative period. It is therefore imperative that obstetrician-gynecologists have a basic understanding of the surgical procedure and the aftercare involved.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa. Email her at [email protected].
References
1. Gaither TW et al. J Urol. 2018;199(3):760-5.
2. Ferrando CA and Bowers ML. In: Ferrando CA, ed. “Comprehensive care of the transgender patient” Philadelphia: Elsevier, 2020, p. 82-92.
3. Chi AC et al. Complications of vaginoplasty. In: Niklavsky D and Blakely SA, eds. “Urological care for the transgender patient: A comprehensive guide” Switzerland: Springer Nature, 2021 p. 83-97.
4. Jiang D et al. Obstet Gynecol. 2019;133(5):1003-11.
5. Obedin-Maliver J and Haan GD. Gynecologic care for transgender patients. In: Ferrando CA, ed. “Comprehensive care of the transgender patient” Philadelphia: Elsevier, 2020, p. 131-51.
Feminizing gender affirmation surgery is a complex genital surgery that most commonly involves removal of natal male genitalia (testes, penile urethra, a majority of the glans penis, penile shaft) and construction of the vulva and/or neovagina utilizing scrotal and penile shaft tissue. Other surgical procedures can also involve using a peritoneal flap or a portion of the small bowel or sigmoid colon to create the neovaginal canal. As with any major surgical procedure, complications do occur, and these can range from minor to major; intraoperative to postoperative. For the purposes of this article, the focus shall be on postoperative complications. Most postoperative complications occur within the first 4 months of the surgery and include vaginal stenosis, genitourinary fistula formation, urinary stream abnormalities, and sexual dysfunction.1 Minor complications that can be managed in the office include granulation tissue treatment, vaginitis, and hair growth in the neovagina. It is important to note that, if any complication occurs, it is essential to refer to the patient’s original surgeon or to a surgeon with expertise in vaginoplasty techniques and postoperative management.2
For patients who undergo vaginoplasty, or a creation of a neovaginal canal, postoperative dilation is necessary to maintain patency. The frequency and duration of dilation are often determined by each individual surgeon or surgical practice as there is no universal, evidence-based standard to guide recommendations on dilation. Failure to maintain a dilation schedule can result in neovaginal stenosis and inability to engage in penetrative vaginal intercourse (if patients desire). Dilation can be difficult.
Challenges with dilation can occur for a variety of reasons: pain, history of trauma, pelvic floor dysfunction, lack of privacy or a supportive environment, or change in personal goals.3 If the underlying cause is related to pelvic floor dysfunction, postoperative pelvic floor therapy has demonstrated improvement in dilation.4 Additionally, routine douching is required for vaginal hygiene. Unlike natal vaginas, neovaginas do not usually contain mucosa, with the exception of a colonic interposition vaginoplasty, and routine douching with soapy water can help prevent a buildup of lubricant and debris.
If a patient reports abnormal discharge, an exam of the vulva and neovagina is warranted. Many patients are able to tolerate a speculum examination. If a patient has undergone a penile inversion vaginoplasty, the microbiome of the neovagina is quite different than that of a natal vagina and most common causes of abnormal discharge often include retained lubricant, keratin debris, sebum, or semen.5 During a speculum exam, the provider may notice granulation tissue, which is often another cause of persistent vaginal discharge, vaginal bleeding, or pain during dilation. Depending on the patient’s symptoms and quantity of granulation tissue present, it can often resolve spontaneously. Persistent granulation tissue can be treated with silver nitrate. An alternative to silver nitrate is using medical grade honey or a course of a mild-strength topical steroid cream or ointment.5 In some cases, abnormal discharge may be the result of a fistula. If a fistula is noted the patient should be immediately referred back to the original surgeon or to a urogynecologist and/or colorectal surgeon for evaluation and management.
While this surgery often falls outside of the scope of practice of the general obstetrician-gynecologist, most patients will seek the care of a general obstetrician-gynecologist in the postoperative period. It is therefore imperative that obstetrician-gynecologists have a basic understanding of the surgical procedure and the aftercare involved.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa. Email her at [email protected].
References
1. Gaither TW et al. J Urol. 2018;199(3):760-5.
2. Ferrando CA and Bowers ML. In: Ferrando CA, ed. “Comprehensive care of the transgender patient” Philadelphia: Elsevier, 2020, p. 82-92.
3. Chi AC et al. Complications of vaginoplasty. In: Niklavsky D and Blakely SA, eds. “Urological care for the transgender patient: A comprehensive guide” Switzerland: Springer Nature, 2021 p. 83-97.
4. Jiang D et al. Obstet Gynecol. 2019;133(5):1003-11.
5. Obedin-Maliver J and Haan GD. Gynecologic care for transgender patients. In: Ferrando CA, ed. “Comprehensive care of the transgender patient” Philadelphia: Elsevier, 2020, p. 131-51.
Feminizing gender affirmation surgery is a complex genital surgery that most commonly involves removal of natal male genitalia (testes, penile urethra, a majority of the glans penis, penile shaft) and construction of the vulva and/or neovagina utilizing scrotal and penile shaft tissue. Other surgical procedures can also involve using a peritoneal flap or a portion of the small bowel or sigmoid colon to create the neovaginal canal. As with any major surgical procedure, complications do occur, and these can range from minor to major; intraoperative to postoperative. For the purposes of this article, the focus shall be on postoperative complications. Most postoperative complications occur within the first 4 months of the surgery and include vaginal stenosis, genitourinary fistula formation, urinary stream abnormalities, and sexual dysfunction.1 Minor complications that can be managed in the office include granulation tissue treatment, vaginitis, and hair growth in the neovagina. It is important to note that, if any complication occurs, it is essential to refer to the patient’s original surgeon or to a surgeon with expertise in vaginoplasty techniques and postoperative management.2
For patients who undergo vaginoplasty, or a creation of a neovaginal canal, postoperative dilation is necessary to maintain patency. The frequency and duration of dilation are often determined by each individual surgeon or surgical practice as there is no universal, evidence-based standard to guide recommendations on dilation. Failure to maintain a dilation schedule can result in neovaginal stenosis and inability to engage in penetrative vaginal intercourse (if patients desire). Dilation can be difficult.
Challenges with dilation can occur for a variety of reasons: pain, history of trauma, pelvic floor dysfunction, lack of privacy or a supportive environment, or change in personal goals.3 If the underlying cause is related to pelvic floor dysfunction, postoperative pelvic floor therapy has demonstrated improvement in dilation.4 Additionally, routine douching is required for vaginal hygiene. Unlike natal vaginas, neovaginas do not usually contain mucosa, with the exception of a colonic interposition vaginoplasty, and routine douching with soapy water can help prevent a buildup of lubricant and debris.
If a patient reports abnormal discharge, an exam of the vulva and neovagina is warranted. Many patients are able to tolerate a speculum examination. If a patient has undergone a penile inversion vaginoplasty, the microbiome of the neovagina is quite different than that of a natal vagina and most common causes of abnormal discharge often include retained lubricant, keratin debris, sebum, or semen.5 During a speculum exam, the provider may notice granulation tissue, which is often another cause of persistent vaginal discharge, vaginal bleeding, or pain during dilation. Depending on the patient’s symptoms and quantity of granulation tissue present, it can often resolve spontaneously. Persistent granulation tissue can be treated with silver nitrate. An alternative to silver nitrate is using medical grade honey or a course of a mild-strength topical steroid cream or ointment.5 In some cases, abnormal discharge may be the result of a fistula. If a fistula is noted the patient should be immediately referred back to the original surgeon or to a urogynecologist and/or colorectal surgeon for evaluation and management.
While this surgery often falls outside of the scope of practice of the general obstetrician-gynecologist, most patients will seek the care of a general obstetrician-gynecologist in the postoperative period. It is therefore imperative that obstetrician-gynecologists have a basic understanding of the surgical procedure and the aftercare involved.
Dr. Brandt is an ob.gyn. and fellowship-trained gender-affirming surgeon in West Reading, Pa. Email her at [email protected].
References
1. Gaither TW et al. J Urol. 2018;199(3):760-5.
2. Ferrando CA and Bowers ML. In: Ferrando CA, ed. “Comprehensive care of the transgender patient” Philadelphia: Elsevier, 2020, p. 82-92.
3. Chi AC et al. Complications of vaginoplasty. In: Niklavsky D and Blakely SA, eds. “Urological care for the transgender patient: A comprehensive guide” Switzerland: Springer Nature, 2021 p. 83-97.
4. Jiang D et al. Obstet Gynecol. 2019;133(5):1003-11.
5. Obedin-Maliver J and Haan GD. Gynecologic care for transgender patients. In: Ferrando CA, ed. “Comprehensive care of the transgender patient” Philadelphia: Elsevier, 2020, p. 131-51.
HHS prohibits discrimination against LGBTQ patients: Action reverses Trump-era policy
The Biden administration is reversing a Trump-era policy that allowed health care providers to bar services to lesbian, gay, bisexual, transgender, or queer (LGBTQ) patients.
The U.S. Department of Health and Human Services gave notice on Monday that it would interpret the Affordable Care Act’s Section 1557 – which bars discrimination on the basis of sex – to include discrimination on the basis of sexual orientation or gender identity. The department said its position is consistent with a June 2020 U.S. Supreme Court ruling in Bostock v. Clayton County, GA. The ruling determined that the Civil Rights Act’s prohibition of employment discrimination on the basis of sex includes sexual orientation and gender identity.
“The mission of our Department is to enhance the health and well-being of all Americans, no matter their gender identity or sexual orientation,” said HHS Assistant Secretary for Health Rachel Levine, MD, in a statement released Monday.
“All people need access to health care services to fix a broken bone, protect their heart health, and screen for cancer risk,” she said. “No one should be discriminated against when seeking medical services because of who they are.”
Many physician organizations applauded the decision.
“The Biden administration did the right thing by terminating a short-lived effort to allow discrimination based on gender or sexual orientation when seeking health care,” said Susan R. Bailey, MD, president of the American Medical Association, in a statement.
When, in 2019, the Trump administration proposed to allow providers to deny care to LGBTQ people, the AMA said in a letter to the HHS that its interpretation “was contrary to the intent and the plain language of the law.”
Now, said Bailey, the AMA welcomes the Biden administration’s interpretation. It “is a victory for health equity and ends a dismal chapter in which a federal agency sought to remove civil rights protections,” she said.
An alliance of patient groups – including the American Cancer Society, the American Cancer Society Cancer Action Network, the American Heart Association, the American Lung Association, the Epilepsy Foundation, the National Multiple Sclerosis Society, and the National Organization for Rare Disorders – also applauded the new policy. “This community already faces significant health disparities,” the groups noted in a statement. People with chronic illness such as HIV and cancer “need to be able to access care quickly and without fear of discrimination,” they said.
The groups had filed a friend of the court brief in a case against the Trump administration rule.
“We welcome this positive step to ensure access is preserved without hindrance, as intended by the health care law,” they said.
Twenty-two states and Washington, D.C. – led by former California Attorney General Xavier Becerra, who is now HHS secretary – sued the Trump administration in July 2020, aiming to overturn the rule.
Chase Strangio, deputy director for Trans Justice with the American Civil Liberties Union LGBTQ & HIV Project, noted that the HHS announcement was crucial in the face of efforts in multiple states to bar health care for transgender youth. “The Biden administration has affirmed what courts have said for decades: Discrimination against LGBTQ people is against the law. It also affirms what transgender people have long said: Gender-affirming care is life-saving care,” he said in a statement.
Lambda Legal, which led another lawsuit against the Trump administration rule, said it welcomed the HHS action but noted in a statement by the organization’s senior attorney, Omar Gonzalez-Pagan, that it “does not address significant aspects of the Trump-era rule that we and others have challenged in court.”
The Trump rule also “limited the remedies available to people who face health disparities, limited access to health care for people with Limited English Proficiency, unlawfully incorporated religious exemptions, and dramatically reduced the number of health care entities and insurance subject to the rule, all of which today’s action does not address,” said Gonzalez-Pagan.
“We encourage Secretary Xavier Becerra and the Biden administration to take additional steps to ensure that all LGBTQ people are completely covered wherever and whenever they may encounter discrimination during some of the most delicate and precarious moments of their lives: When seeking health care,” he said.
A version of this article first appeared on Medscape.com.
The Biden administration is reversing a Trump-era policy that allowed health care providers to bar services to lesbian, gay, bisexual, transgender, or queer (LGBTQ) patients.
The U.S. Department of Health and Human Services gave notice on Monday that it would interpret the Affordable Care Act’s Section 1557 – which bars discrimination on the basis of sex – to include discrimination on the basis of sexual orientation or gender identity. The department said its position is consistent with a June 2020 U.S. Supreme Court ruling in Bostock v. Clayton County, GA. The ruling determined that the Civil Rights Act’s prohibition of employment discrimination on the basis of sex includes sexual orientation and gender identity.
“The mission of our Department is to enhance the health and well-being of all Americans, no matter their gender identity or sexual orientation,” said HHS Assistant Secretary for Health Rachel Levine, MD, in a statement released Monday.
“All people need access to health care services to fix a broken bone, protect their heart health, and screen for cancer risk,” she said. “No one should be discriminated against when seeking medical services because of who they are.”
Many physician organizations applauded the decision.
“The Biden administration did the right thing by terminating a short-lived effort to allow discrimination based on gender or sexual orientation when seeking health care,” said Susan R. Bailey, MD, president of the American Medical Association, in a statement.
When, in 2019, the Trump administration proposed to allow providers to deny care to LGBTQ people, the AMA said in a letter to the HHS that its interpretation “was contrary to the intent and the plain language of the law.”
Now, said Bailey, the AMA welcomes the Biden administration’s interpretation. It “is a victory for health equity and ends a dismal chapter in which a federal agency sought to remove civil rights protections,” she said.
An alliance of patient groups – including the American Cancer Society, the American Cancer Society Cancer Action Network, the American Heart Association, the American Lung Association, the Epilepsy Foundation, the National Multiple Sclerosis Society, and the National Organization for Rare Disorders – also applauded the new policy. “This community already faces significant health disparities,” the groups noted in a statement. People with chronic illness such as HIV and cancer “need to be able to access care quickly and without fear of discrimination,” they said.
The groups had filed a friend of the court brief in a case against the Trump administration rule.
“We welcome this positive step to ensure access is preserved without hindrance, as intended by the health care law,” they said.
Twenty-two states and Washington, D.C. – led by former California Attorney General Xavier Becerra, who is now HHS secretary – sued the Trump administration in July 2020, aiming to overturn the rule.
Chase Strangio, deputy director for Trans Justice with the American Civil Liberties Union LGBTQ & HIV Project, noted that the HHS announcement was crucial in the face of efforts in multiple states to bar health care for transgender youth. “The Biden administration has affirmed what courts have said for decades: Discrimination against LGBTQ people is against the law. It also affirms what transgender people have long said: Gender-affirming care is life-saving care,” he said in a statement.
Lambda Legal, which led another lawsuit against the Trump administration rule, said it welcomed the HHS action but noted in a statement by the organization’s senior attorney, Omar Gonzalez-Pagan, that it “does not address significant aspects of the Trump-era rule that we and others have challenged in court.”
The Trump rule also “limited the remedies available to people who face health disparities, limited access to health care for people with Limited English Proficiency, unlawfully incorporated religious exemptions, and dramatically reduced the number of health care entities and insurance subject to the rule, all of which today’s action does not address,” said Gonzalez-Pagan.
“We encourage Secretary Xavier Becerra and the Biden administration to take additional steps to ensure that all LGBTQ people are completely covered wherever and whenever they may encounter discrimination during some of the most delicate and precarious moments of their lives: When seeking health care,” he said.
A version of this article first appeared on Medscape.com.
The Biden administration is reversing a Trump-era policy that allowed health care providers to bar services to lesbian, gay, bisexual, transgender, or queer (LGBTQ) patients.
The U.S. Department of Health and Human Services gave notice on Monday that it would interpret the Affordable Care Act’s Section 1557 – which bars discrimination on the basis of sex – to include discrimination on the basis of sexual orientation or gender identity. The department said its position is consistent with a June 2020 U.S. Supreme Court ruling in Bostock v. Clayton County, GA. The ruling determined that the Civil Rights Act’s prohibition of employment discrimination on the basis of sex includes sexual orientation and gender identity.
“The mission of our Department is to enhance the health and well-being of all Americans, no matter their gender identity or sexual orientation,” said HHS Assistant Secretary for Health Rachel Levine, MD, in a statement released Monday.
“All people need access to health care services to fix a broken bone, protect their heart health, and screen for cancer risk,” she said. “No one should be discriminated against when seeking medical services because of who they are.”
Many physician organizations applauded the decision.
“The Biden administration did the right thing by terminating a short-lived effort to allow discrimination based on gender or sexual orientation when seeking health care,” said Susan R. Bailey, MD, president of the American Medical Association, in a statement.
When, in 2019, the Trump administration proposed to allow providers to deny care to LGBTQ people, the AMA said in a letter to the HHS that its interpretation “was contrary to the intent and the plain language of the law.”
Now, said Bailey, the AMA welcomes the Biden administration’s interpretation. It “is a victory for health equity and ends a dismal chapter in which a federal agency sought to remove civil rights protections,” she said.
An alliance of patient groups – including the American Cancer Society, the American Cancer Society Cancer Action Network, the American Heart Association, the American Lung Association, the Epilepsy Foundation, the National Multiple Sclerosis Society, and the National Organization for Rare Disorders – also applauded the new policy. “This community already faces significant health disparities,” the groups noted in a statement. People with chronic illness such as HIV and cancer “need to be able to access care quickly and without fear of discrimination,” they said.
The groups had filed a friend of the court brief in a case against the Trump administration rule.
“We welcome this positive step to ensure access is preserved without hindrance, as intended by the health care law,” they said.
Twenty-two states and Washington, D.C. – led by former California Attorney General Xavier Becerra, who is now HHS secretary – sued the Trump administration in July 2020, aiming to overturn the rule.
Chase Strangio, deputy director for Trans Justice with the American Civil Liberties Union LGBTQ & HIV Project, noted that the HHS announcement was crucial in the face of efforts in multiple states to bar health care for transgender youth. “The Biden administration has affirmed what courts have said for decades: Discrimination against LGBTQ people is against the law. It also affirms what transgender people have long said: Gender-affirming care is life-saving care,” he said in a statement.
Lambda Legal, which led another lawsuit against the Trump administration rule, said it welcomed the HHS action but noted in a statement by the organization’s senior attorney, Omar Gonzalez-Pagan, that it “does not address significant aspects of the Trump-era rule that we and others have challenged in court.”
The Trump rule also “limited the remedies available to people who face health disparities, limited access to health care for people with Limited English Proficiency, unlawfully incorporated religious exemptions, and dramatically reduced the number of health care entities and insurance subject to the rule, all of which today’s action does not address,” said Gonzalez-Pagan.
“We encourage Secretary Xavier Becerra and the Biden administration to take additional steps to ensure that all LGBTQ people are completely covered wherever and whenever they may encounter discrimination during some of the most delicate and precarious moments of their lives: When seeking health care,” he said.
A version of this article first appeared on Medscape.com.
Parental attitudes to kids’ sexual orientation: Unexpected findings
For gay and lesbian individuals, consistency in parents’ attitudes toward their child’s sexual orientation, even when they are negative, is an important factor in positive mental health outcomes, new research shows.
Study investigator Matthew Verdun, MS, a licensed marriage and family therapist and doctoral student at the Chicago School of Professional Psychology at Los Angeles, California, found that gays and lesbians whose parents were not supportive of their sexual orientation could still have good outcomes.
The findings were presented at the annual meeting of the American Psychiatric Association, which was held as a virtual live event.
High rates of mental illness
Research shows that members of the gay and lesbian community experience higher rates of mental illness and substance use disorders and that psychological well-being declines during periods close to when sexual orientation is disclosed.
Mr. Verdun referred to a theory in the literature of homosexual identity formation that describes how individuals go through six stages: confusion, comparison, tolerance, acceptance, pride, and synthesis.
Research shows a U-shaped relationship between subjective reports of well-being at these six stages. The lowest rates occur during the identity comparison and identity tolerance stages.
“Those stages roughly correspond with the time when people would disclose their sexual orientation to parents and family members. The time when a person discloses is probably one of the most anxious times in their life; it’s also where their rate of well-being is the lowest,” said Mr. Verdun.
Mr. Verdun said he “wanted to know what happens when a parent is supportive or rejecting at that moment, but also what happens over time.”
To determine whether parental support affects depression, anxiety, or substance abuse in members of the gay and lesbian community, Mr. Verdun studied 175 individuals who self-identified as gay or lesbian (77 males and 98 females) and were recruited via social media. Most (70.3%) were of White race or ethnicity.
Participants completed surveys asking about their parents’ initial and current level of support regarding their sexual orientation. They also completed the nine-item Patient Health Questionnaire (PHQ-9), the seven-item General Anxiety Disorder (GAD-7), and the 20-item Drug Abuse Screening Tool (DAST-20).
The investigators categorized participants into one of three groups on the basis of parental support:
- Consistently positive.
- Negative to positive.
- Consistently negative.
A fourth group, positive to negative, was excluded from the analysis because it was too small.
Mr. Verdun was unable analyze results for substance abuse. “The DAST-20 results violated the assumption of homogeneity of variances, which meant the analysis could result in error,” he explained.
Analyses for the PHQ-9 and GAD-7 showed that the consistently positive group had the lowest symptom scores.
“People whose parents were accepting had the lowest scores for anxiety and depression,” said Mr. Verdun.
For both the PHQ and GAD, the findings were significant (P < .05) for the consistently positive and the consistently negative groups in comparison with the negative to positive group.
The difference between the consistently positive and the consistently negative groups was not statistically significant.
Surprise finding
Previous research has shown that current levels of parental support relate to better mental health, so Mr. Verdun initially thought children whose parents were consistently supportive or those whose parents became supportive over time would have the best mental health outcomes.
“But, interestingly, what I found was that people whose parents vacillated between being accepting and rejecting over time actually had significantly more mental health symptoms at the time of the assessment than people whose parents were consistently accepting or consistently rejecting,” he said.
Although the study provided evidence of better outcomes for those with consistently unsupportive parents, Mr. Verdun believes some hypotheses are worthy of further research.
One is that people with unsupportive parents receive support elsewhere and could, for example, turn to peers, teachers, or other community members, including faith leaders, and that symptoms of mental illness may improve with such support, said Mr. Verdun.
These individuals may also develop ways to “buffer their mental health symptoms,” possibly by cultivating meaningful relationships “where they’re seen as a complete and total person, not just in terms of their sexual orientation,” he said.
Gay and lesbian individuals may also benefit from “healing activities,” which might include engagement and involvement in their community, such as performing volunteer work and learning about the history of their community, said Mr. Verdun.
Mental health providers can play a role in creating a positive environment by referring patients to support groups, to centers that cater to gays and lesbians, to faith communities, or by encouraging recreational activities, said Mr. Verdun.
Clinicians can also help gay and lesbian patients determine how and when to safely disclose their sexual orientation, he said.
The study did not include bisexual or transsexual individuals because processes of identifying sexual orientation differ for those persons, said Mr. Verdun.
“I would like to conduct future research that includes bisexual, trans people, and intersectional groups within the LGBTQIA [lesbian, gay, bisexual, transgender, queer, intersex, asexual] community,” he said.
Important research
Commenting on the study, Jeffrey Borenstein, MD, president and CEO of the Brain and Behavior Research Foundation and editor-in-chief of Psychiatric News, said the work is “extremely important and that it has the potential to lead to clinical guidance.”
The finding that levels of depression and anxiety were lower in children whose parents were accepting of their sexual orientation is not surprising, said Dr. Borenstein. “It’s common sense, but it’s always good to have such a finding demonstrate it,” he said.
Parents who understand this relationship may be better able to help their child who is depressed or anxious, he added.
Dr. Borenstein agreed that further research is needed regarding the finding of benefits from consistent parenting, even when that parenting involves rejection.
Such research might uncover “what types of other supports these individuals have that allow for lower levels of depression and anxiety,” he said.
“For this population, the risk of mental health issues is higher, and the risk of suicide is higher, so anything we can do to provide support and improved treatment is extremely important,” he said.
A version of this article first appeared on Medscape.com.
For gay and lesbian individuals, consistency in parents’ attitudes toward their child’s sexual orientation, even when they are negative, is an important factor in positive mental health outcomes, new research shows.
Study investigator Matthew Verdun, MS, a licensed marriage and family therapist and doctoral student at the Chicago School of Professional Psychology at Los Angeles, California, found that gays and lesbians whose parents were not supportive of their sexual orientation could still have good outcomes.
The findings were presented at the annual meeting of the American Psychiatric Association, which was held as a virtual live event.
High rates of mental illness
Research shows that members of the gay and lesbian community experience higher rates of mental illness and substance use disorders and that psychological well-being declines during periods close to when sexual orientation is disclosed.
Mr. Verdun referred to a theory in the literature of homosexual identity formation that describes how individuals go through six stages: confusion, comparison, tolerance, acceptance, pride, and synthesis.
Research shows a U-shaped relationship between subjective reports of well-being at these six stages. The lowest rates occur during the identity comparison and identity tolerance stages.
“Those stages roughly correspond with the time when people would disclose their sexual orientation to parents and family members. The time when a person discloses is probably one of the most anxious times in their life; it’s also where their rate of well-being is the lowest,” said Mr. Verdun.
Mr. Verdun said he “wanted to know what happens when a parent is supportive or rejecting at that moment, but also what happens over time.”
To determine whether parental support affects depression, anxiety, or substance abuse in members of the gay and lesbian community, Mr. Verdun studied 175 individuals who self-identified as gay or lesbian (77 males and 98 females) and were recruited via social media. Most (70.3%) were of White race or ethnicity.
Participants completed surveys asking about their parents’ initial and current level of support regarding their sexual orientation. They also completed the nine-item Patient Health Questionnaire (PHQ-9), the seven-item General Anxiety Disorder (GAD-7), and the 20-item Drug Abuse Screening Tool (DAST-20).
The investigators categorized participants into one of three groups on the basis of parental support:
- Consistently positive.
- Negative to positive.
- Consistently negative.
A fourth group, positive to negative, was excluded from the analysis because it was too small.
Mr. Verdun was unable analyze results for substance abuse. “The DAST-20 results violated the assumption of homogeneity of variances, which meant the analysis could result in error,” he explained.
Analyses for the PHQ-9 and GAD-7 showed that the consistently positive group had the lowest symptom scores.
“People whose parents were accepting had the lowest scores for anxiety and depression,” said Mr. Verdun.
For both the PHQ and GAD, the findings were significant (P < .05) for the consistently positive and the consistently negative groups in comparison with the negative to positive group.
The difference between the consistently positive and the consistently negative groups was not statistically significant.
Surprise finding
Previous research has shown that current levels of parental support relate to better mental health, so Mr. Verdun initially thought children whose parents were consistently supportive or those whose parents became supportive over time would have the best mental health outcomes.
“But, interestingly, what I found was that people whose parents vacillated between being accepting and rejecting over time actually had significantly more mental health symptoms at the time of the assessment than people whose parents were consistently accepting or consistently rejecting,” he said.
Although the study provided evidence of better outcomes for those with consistently unsupportive parents, Mr. Verdun believes some hypotheses are worthy of further research.
One is that people with unsupportive parents receive support elsewhere and could, for example, turn to peers, teachers, or other community members, including faith leaders, and that symptoms of mental illness may improve with such support, said Mr. Verdun.
These individuals may also develop ways to “buffer their mental health symptoms,” possibly by cultivating meaningful relationships “where they’re seen as a complete and total person, not just in terms of their sexual orientation,” he said.
Gay and lesbian individuals may also benefit from “healing activities,” which might include engagement and involvement in their community, such as performing volunteer work and learning about the history of their community, said Mr. Verdun.
Mental health providers can play a role in creating a positive environment by referring patients to support groups, to centers that cater to gays and lesbians, to faith communities, or by encouraging recreational activities, said Mr. Verdun.
Clinicians can also help gay and lesbian patients determine how and when to safely disclose their sexual orientation, he said.
The study did not include bisexual or transsexual individuals because processes of identifying sexual orientation differ for those persons, said Mr. Verdun.
“I would like to conduct future research that includes bisexual, trans people, and intersectional groups within the LGBTQIA [lesbian, gay, bisexual, transgender, queer, intersex, asexual] community,” he said.
Important research
Commenting on the study, Jeffrey Borenstein, MD, president and CEO of the Brain and Behavior Research Foundation and editor-in-chief of Psychiatric News, said the work is “extremely important and that it has the potential to lead to clinical guidance.”
The finding that levels of depression and anxiety were lower in children whose parents were accepting of their sexual orientation is not surprising, said Dr. Borenstein. “It’s common sense, but it’s always good to have such a finding demonstrate it,” he said.
Parents who understand this relationship may be better able to help their child who is depressed or anxious, he added.
Dr. Borenstein agreed that further research is needed regarding the finding of benefits from consistent parenting, even when that parenting involves rejection.
Such research might uncover “what types of other supports these individuals have that allow for lower levels of depression and anxiety,” he said.
“For this population, the risk of mental health issues is higher, and the risk of suicide is higher, so anything we can do to provide support and improved treatment is extremely important,” he said.
A version of this article first appeared on Medscape.com.
For gay and lesbian individuals, consistency in parents’ attitudes toward their child’s sexual orientation, even when they are negative, is an important factor in positive mental health outcomes, new research shows.
Study investigator Matthew Verdun, MS, a licensed marriage and family therapist and doctoral student at the Chicago School of Professional Psychology at Los Angeles, California, found that gays and lesbians whose parents were not supportive of their sexual orientation could still have good outcomes.
The findings were presented at the annual meeting of the American Psychiatric Association, which was held as a virtual live event.
High rates of mental illness
Research shows that members of the gay and lesbian community experience higher rates of mental illness and substance use disorders and that psychological well-being declines during periods close to when sexual orientation is disclosed.
Mr. Verdun referred to a theory in the literature of homosexual identity formation that describes how individuals go through six stages: confusion, comparison, tolerance, acceptance, pride, and synthesis.
Research shows a U-shaped relationship between subjective reports of well-being at these six stages. The lowest rates occur during the identity comparison and identity tolerance stages.
“Those stages roughly correspond with the time when people would disclose their sexual orientation to parents and family members. The time when a person discloses is probably one of the most anxious times in their life; it’s also where their rate of well-being is the lowest,” said Mr. Verdun.
Mr. Verdun said he “wanted to know what happens when a parent is supportive or rejecting at that moment, but also what happens over time.”
To determine whether parental support affects depression, anxiety, or substance abuse in members of the gay and lesbian community, Mr. Verdun studied 175 individuals who self-identified as gay or lesbian (77 males and 98 females) and were recruited via social media. Most (70.3%) were of White race or ethnicity.
Participants completed surveys asking about their parents’ initial and current level of support regarding their sexual orientation. They also completed the nine-item Patient Health Questionnaire (PHQ-9), the seven-item General Anxiety Disorder (GAD-7), and the 20-item Drug Abuse Screening Tool (DAST-20).
The investigators categorized participants into one of three groups on the basis of parental support:
- Consistently positive.
- Negative to positive.
- Consistently negative.
A fourth group, positive to negative, was excluded from the analysis because it was too small.
Mr. Verdun was unable analyze results for substance abuse. “The DAST-20 results violated the assumption of homogeneity of variances, which meant the analysis could result in error,” he explained.
Analyses for the PHQ-9 and GAD-7 showed that the consistently positive group had the lowest symptom scores.
“People whose parents were accepting had the lowest scores for anxiety and depression,” said Mr. Verdun.
For both the PHQ and GAD, the findings were significant (P < .05) for the consistently positive and the consistently negative groups in comparison with the negative to positive group.
The difference between the consistently positive and the consistently negative groups was not statistically significant.
Surprise finding
Previous research has shown that current levels of parental support relate to better mental health, so Mr. Verdun initially thought children whose parents were consistently supportive or those whose parents became supportive over time would have the best mental health outcomes.
“But, interestingly, what I found was that people whose parents vacillated between being accepting and rejecting over time actually had significantly more mental health symptoms at the time of the assessment than people whose parents were consistently accepting or consistently rejecting,” he said.
Although the study provided evidence of better outcomes for those with consistently unsupportive parents, Mr. Verdun believes some hypotheses are worthy of further research.
One is that people with unsupportive parents receive support elsewhere and could, for example, turn to peers, teachers, or other community members, including faith leaders, and that symptoms of mental illness may improve with such support, said Mr. Verdun.
These individuals may also develop ways to “buffer their mental health symptoms,” possibly by cultivating meaningful relationships “where they’re seen as a complete and total person, not just in terms of their sexual orientation,” he said.
Gay and lesbian individuals may also benefit from “healing activities,” which might include engagement and involvement in their community, such as performing volunteer work and learning about the history of their community, said Mr. Verdun.
Mental health providers can play a role in creating a positive environment by referring patients to support groups, to centers that cater to gays and lesbians, to faith communities, or by encouraging recreational activities, said Mr. Verdun.
Clinicians can also help gay and lesbian patients determine how and when to safely disclose their sexual orientation, he said.
The study did not include bisexual or transsexual individuals because processes of identifying sexual orientation differ for those persons, said Mr. Verdun.
“I would like to conduct future research that includes bisexual, trans people, and intersectional groups within the LGBTQIA [lesbian, gay, bisexual, transgender, queer, intersex, asexual] community,” he said.
Important research
Commenting on the study, Jeffrey Borenstein, MD, president and CEO of the Brain and Behavior Research Foundation and editor-in-chief of Psychiatric News, said the work is “extremely important and that it has the potential to lead to clinical guidance.”
The finding that levels of depression and anxiety were lower in children whose parents were accepting of their sexual orientation is not surprising, said Dr. Borenstein. “It’s common sense, but it’s always good to have such a finding demonstrate it,” he said.
Parents who understand this relationship may be better able to help their child who is depressed or anxious, he added.
Dr. Borenstein agreed that further research is needed regarding the finding of benefits from consistent parenting, even when that parenting involves rejection.
Such research might uncover “what types of other supports these individuals have that allow for lower levels of depression and anxiety,” he said.
“For this population, the risk of mental health issues is higher, and the risk of suicide is higher, so anything we can do to provide support and improved treatment is extremely important,” he said.
A version of this article first appeared on Medscape.com.
Success in LGBTQ+ medicine requires awareness of risk
Patients who are transgender, for instance, are nine times more likely to commit suicide than the general population (2015 U.S. Transgender Survey (USTS). Inter-university Consortium for Political and Social Research. 2019 May 22. doi: 10.3886/ICPSR37229.v1), and those who are also Black have an estimated HIV prevalence of 62%, demonstrating the cumulative, negative health effects of intersectionality (www.cdc.gov/hiv/group/gender/transgender/hiv-prevalence.html).
“Experiences with marginalization and stigma directly relate to some of the poor physical and mental health outcomes that these patients experience,” Megan McNamara, MD, said during a presentation at the American College of Physicians annual Internal Medicine meeting.
Dr. McNamara, who is director of the Gender Identity Veteran’s Experience (GIVE) Clinic, Veterans Affairs Northeast Ohio Healthcare System, Cleveland, offered a brief guide to managing LGBTQ+ patients. She emphasized increased rates of psychological distress and substance abuse, and encouraged familiarity with specific risks associated with three subgroups: men who have sex with men (MSM), women who have sex with women (WSW), and those who are transgender.
Men who have sex with men
According to Dr. McNamara, preexposure prophylaxis (PrEP) should be offered based on Centers for Disease Control and Prevention eligibility criteria, which require that the patient is HIV negative, has had a male sex partner in the past 6 months, is not in a monogamous relationship, and has had anal sex or a bacterial sexually transmitted infection in the past 6 months. The two PrEP options, emtricitabine/tenofovir disoproxil fumarate and emtricitabine/tenofovir alafenamide, are equally effective and have similar safety profiles, Dr. McNamara said, but patients with impaired renal function should receive the alafenamide formulation.
Dr. McNamara also advised screening gay men for extragenital STIs, noting a 13.3% increased risk. When asked about anal Pap testing for HPV, Dr. McNamara called the subject “very controversial,” and ultimately recommended against it, citing a lack of data linking anal HPV infection and dysplasia with later development of rectal carcinoma, as well as the nonactionable impact of a positive result.
“For me, the issue is ... if [a positive anal Pap test] is not going to change my management, if I don’t know that the anal HPV that I diagnose will result in cancer, should I continue to monitor it?” Dr. McNamara said.
Women who have sex with women
Beyond higher rates of psychological distress and substance abuse among lesbian and bisexual women, Dr. McNamara described increased risks of overweight and obesity, higher rates of smoking, and lower rates of Pap testing, all of which should prompt clinicians to advise accordingly, with cervical cancer screening in alignment with guidelines. Clinicians should also discuss HPV vaccination with patients, taking care to weigh benefits and risks, as “catch-up” HPV vaccination is not unilaterally recommended for adults older than 26 years.
Transgender patients
Discussing transgender patients, Dr. McNamara focused on cross-sex hormone therapy (CSHT), first noting the significant psychological benefits, including improvements in depression, somatization, interpersonal sensitivity, hostility, anxiety, phobic anxiety/agoraphobia, and quality of life.
According to Dr. McNamara, CSHT is relatively simple and may be safely administered by primary care providers. For transmasculine patients, testosterone supplementation is all that is needed, whereas transfeminine patients will require spironolactone or GnRH agonists to reduce testosterone and estradiol to increase feminizing hormones to pubertal levels.
CSHT is not without risks, Dr. McNamara said, including “very high” risks of erythrocytosis among transmasculine patients and venous thromboembolic disease among transfeminine patients; but these risks need to be considered in the context of an approximate 40% suicide rate among transgender individuals.
“I can tell you in my own practice that these [suicide] data ring true,” Dr. McNamara said. “Many, many of my patients have attempted suicide, so [CSHT] is something that you really want to think about right away.”
Even when additional risk factors are present, such as preexisting cardiovascular disease, Dr. McNamara suggested that “there are very few absolute contraindications to CSHT,” and described it as a “life-sustaining treatment” that should be viewed analogously with any other long-term management strategy, such as therapy for diabetes or hypertension.
Fostering a transgender-friendly practice
In an interview, Nicole Nisly, MD, codirector of the LGBTQ+ Clinic at the University of Iowa Hospitals and Clinics, Iowa City, reflected upon Dr. McNamara’s presentation, noting that primary care providers – with a little education – are the best candidates to care for transgender patients.
“I think [primary care providers] do a better job [caring for transgender patients] than endocrinologists, honestly, because they can provide care for the whole person,” Dr. Nisly said. “They can do a Pap, they can do STI screening, they can assess mood, they can [evaluate] safety, and the whole person, as opposed to endocrinologists, who do hormone therapy, but somebody else does everything else.”
Dr. Nisly emphasized the importance of personalizing care for transgender individuals, which depends upon a welcoming practice environment, with careful attention to language.
Foremost, Dr. Nisly recommended asking patients for their preferred name, sexual orientation, and gender identity.
“One of the most difficult things [for transgender patients] is to see notes with the wrong name – the name that makes them feel uncomfortable – or the wrong pronoun,” Dr. Nisly said. “That’s very important to the community.”
Dr. Nisly also recommended an alternative term for cross-sex hormone therapy.
“I hate cross-sex hormone therapy terminology, honestly,” Dr. Nisly said. “I just think it’s so unwelcoming, and I think most of our patients don’t like the terminology, so we use ‘gender-affirming hormone therapy.’”
Dr. Nisly explained that the term “cross-sex” assumes a conventional definition of sex, which is inherently flawed.
When discussing certain medical risk factors, such as pregnancy or HIV, it is helpful to know “sex assigned at birth” for both patients and their sexual partners, Dr. Nisly said. It’s best to ask in this way, instead of using terms like “boyfriend” or “girlfriend,” as “sex assigned at birth” is “terminology the community recognizes, affirms, and feels comfortable with.”
Concerning management of medical risk factors, Dr. Nisly offered some additional perspectives.
For one, she recommended giving PrEP to any patient who has a desire to be on PrEP, noting that this desire can indicate a change in future sexual practices, which the CDC criteria do not anticipate. She also advised in-hospital self-swabbing for extragenital STIs, as this can increase patient comfort and adherence. And, in contrast with Dr. McNamara, Dr. Nisly recommended anal Pap screening for any man that has sex with men and anyone with HIV of any gender. She noted that rates of anal dysplasia are “pretty high” among men who have sex with men, and that detection may reduce cancer risk.
For clinicians who would like to learn more about caring for transgender patients, Dr. Nisly recommended that they start by reading the World Professional Association for Transgender Health guidelines.
“It’s about 300 pages,” Dr. Nisly said, “but it is great.”
Dr. McNamara and Dr. Nisly reported no conflicts of interest.
Patients who are transgender, for instance, are nine times more likely to commit suicide than the general population (2015 U.S. Transgender Survey (USTS). Inter-university Consortium for Political and Social Research. 2019 May 22. doi: 10.3886/ICPSR37229.v1), and those who are also Black have an estimated HIV prevalence of 62%, demonstrating the cumulative, negative health effects of intersectionality (www.cdc.gov/hiv/group/gender/transgender/hiv-prevalence.html).
“Experiences with marginalization and stigma directly relate to some of the poor physical and mental health outcomes that these patients experience,” Megan McNamara, MD, said during a presentation at the American College of Physicians annual Internal Medicine meeting.
Dr. McNamara, who is director of the Gender Identity Veteran’s Experience (GIVE) Clinic, Veterans Affairs Northeast Ohio Healthcare System, Cleveland, offered a brief guide to managing LGBTQ+ patients. She emphasized increased rates of psychological distress and substance abuse, and encouraged familiarity with specific risks associated with three subgroups: men who have sex with men (MSM), women who have sex with women (WSW), and those who are transgender.
Men who have sex with men
According to Dr. McNamara, preexposure prophylaxis (PrEP) should be offered based on Centers for Disease Control and Prevention eligibility criteria, which require that the patient is HIV negative, has had a male sex partner in the past 6 months, is not in a monogamous relationship, and has had anal sex or a bacterial sexually transmitted infection in the past 6 months. The two PrEP options, emtricitabine/tenofovir disoproxil fumarate and emtricitabine/tenofovir alafenamide, are equally effective and have similar safety profiles, Dr. McNamara said, but patients with impaired renal function should receive the alafenamide formulation.
Dr. McNamara also advised screening gay men for extragenital STIs, noting a 13.3% increased risk. When asked about anal Pap testing for HPV, Dr. McNamara called the subject “very controversial,” and ultimately recommended against it, citing a lack of data linking anal HPV infection and dysplasia with later development of rectal carcinoma, as well as the nonactionable impact of a positive result.
“For me, the issue is ... if [a positive anal Pap test] is not going to change my management, if I don’t know that the anal HPV that I diagnose will result in cancer, should I continue to monitor it?” Dr. McNamara said.
Women who have sex with women
Beyond higher rates of psychological distress and substance abuse among lesbian and bisexual women, Dr. McNamara described increased risks of overweight and obesity, higher rates of smoking, and lower rates of Pap testing, all of which should prompt clinicians to advise accordingly, with cervical cancer screening in alignment with guidelines. Clinicians should also discuss HPV vaccination with patients, taking care to weigh benefits and risks, as “catch-up” HPV vaccination is not unilaterally recommended for adults older than 26 years.
Transgender patients
Discussing transgender patients, Dr. McNamara focused on cross-sex hormone therapy (CSHT), first noting the significant psychological benefits, including improvements in depression, somatization, interpersonal sensitivity, hostility, anxiety, phobic anxiety/agoraphobia, and quality of life.
According to Dr. McNamara, CSHT is relatively simple and may be safely administered by primary care providers. For transmasculine patients, testosterone supplementation is all that is needed, whereas transfeminine patients will require spironolactone or GnRH agonists to reduce testosterone and estradiol to increase feminizing hormones to pubertal levels.
CSHT is not without risks, Dr. McNamara said, including “very high” risks of erythrocytosis among transmasculine patients and venous thromboembolic disease among transfeminine patients; but these risks need to be considered in the context of an approximate 40% suicide rate among transgender individuals.
“I can tell you in my own practice that these [suicide] data ring true,” Dr. McNamara said. “Many, many of my patients have attempted suicide, so [CSHT] is something that you really want to think about right away.”
Even when additional risk factors are present, such as preexisting cardiovascular disease, Dr. McNamara suggested that “there are very few absolute contraindications to CSHT,” and described it as a “life-sustaining treatment” that should be viewed analogously with any other long-term management strategy, such as therapy for diabetes or hypertension.
Fostering a transgender-friendly practice
In an interview, Nicole Nisly, MD, codirector of the LGBTQ+ Clinic at the University of Iowa Hospitals and Clinics, Iowa City, reflected upon Dr. McNamara’s presentation, noting that primary care providers – with a little education – are the best candidates to care for transgender patients.
“I think [primary care providers] do a better job [caring for transgender patients] than endocrinologists, honestly, because they can provide care for the whole person,” Dr. Nisly said. “They can do a Pap, they can do STI screening, they can assess mood, they can [evaluate] safety, and the whole person, as opposed to endocrinologists, who do hormone therapy, but somebody else does everything else.”
Dr. Nisly emphasized the importance of personalizing care for transgender individuals, which depends upon a welcoming practice environment, with careful attention to language.
Foremost, Dr. Nisly recommended asking patients for their preferred name, sexual orientation, and gender identity.
“One of the most difficult things [for transgender patients] is to see notes with the wrong name – the name that makes them feel uncomfortable – or the wrong pronoun,” Dr. Nisly said. “That’s very important to the community.”
Dr. Nisly also recommended an alternative term for cross-sex hormone therapy.
“I hate cross-sex hormone therapy terminology, honestly,” Dr. Nisly said. “I just think it’s so unwelcoming, and I think most of our patients don’t like the terminology, so we use ‘gender-affirming hormone therapy.’”
Dr. Nisly explained that the term “cross-sex” assumes a conventional definition of sex, which is inherently flawed.
When discussing certain medical risk factors, such as pregnancy or HIV, it is helpful to know “sex assigned at birth” for both patients and their sexual partners, Dr. Nisly said. It’s best to ask in this way, instead of using terms like “boyfriend” or “girlfriend,” as “sex assigned at birth” is “terminology the community recognizes, affirms, and feels comfortable with.”
Concerning management of medical risk factors, Dr. Nisly offered some additional perspectives.
For one, she recommended giving PrEP to any patient who has a desire to be on PrEP, noting that this desire can indicate a change in future sexual practices, which the CDC criteria do not anticipate. She also advised in-hospital self-swabbing for extragenital STIs, as this can increase patient comfort and adherence. And, in contrast with Dr. McNamara, Dr. Nisly recommended anal Pap screening for any man that has sex with men and anyone with HIV of any gender. She noted that rates of anal dysplasia are “pretty high” among men who have sex with men, and that detection may reduce cancer risk.
For clinicians who would like to learn more about caring for transgender patients, Dr. Nisly recommended that they start by reading the World Professional Association for Transgender Health guidelines.
“It’s about 300 pages,” Dr. Nisly said, “but it is great.”
Dr. McNamara and Dr. Nisly reported no conflicts of interest.
Patients who are transgender, for instance, are nine times more likely to commit suicide than the general population (2015 U.S. Transgender Survey (USTS). Inter-university Consortium for Political and Social Research. 2019 May 22. doi: 10.3886/ICPSR37229.v1), and those who are also Black have an estimated HIV prevalence of 62%, demonstrating the cumulative, negative health effects of intersectionality (www.cdc.gov/hiv/group/gender/transgender/hiv-prevalence.html).
“Experiences with marginalization and stigma directly relate to some of the poor physical and mental health outcomes that these patients experience,” Megan McNamara, MD, said during a presentation at the American College of Physicians annual Internal Medicine meeting.
Dr. McNamara, who is director of the Gender Identity Veteran’s Experience (GIVE) Clinic, Veterans Affairs Northeast Ohio Healthcare System, Cleveland, offered a brief guide to managing LGBTQ+ patients. She emphasized increased rates of psychological distress and substance abuse, and encouraged familiarity with specific risks associated with three subgroups: men who have sex with men (MSM), women who have sex with women (WSW), and those who are transgender.
Men who have sex with men
According to Dr. McNamara, preexposure prophylaxis (PrEP) should be offered based on Centers for Disease Control and Prevention eligibility criteria, which require that the patient is HIV negative, has had a male sex partner in the past 6 months, is not in a monogamous relationship, and has had anal sex or a bacterial sexually transmitted infection in the past 6 months. The two PrEP options, emtricitabine/tenofovir disoproxil fumarate and emtricitabine/tenofovir alafenamide, are equally effective and have similar safety profiles, Dr. McNamara said, but patients with impaired renal function should receive the alafenamide formulation.
Dr. McNamara also advised screening gay men for extragenital STIs, noting a 13.3% increased risk. When asked about anal Pap testing for HPV, Dr. McNamara called the subject “very controversial,” and ultimately recommended against it, citing a lack of data linking anal HPV infection and dysplasia with later development of rectal carcinoma, as well as the nonactionable impact of a positive result.
“For me, the issue is ... if [a positive anal Pap test] is not going to change my management, if I don’t know that the anal HPV that I diagnose will result in cancer, should I continue to monitor it?” Dr. McNamara said.
Women who have sex with women
Beyond higher rates of psychological distress and substance abuse among lesbian and bisexual women, Dr. McNamara described increased risks of overweight and obesity, higher rates of smoking, and lower rates of Pap testing, all of which should prompt clinicians to advise accordingly, with cervical cancer screening in alignment with guidelines. Clinicians should also discuss HPV vaccination with patients, taking care to weigh benefits and risks, as “catch-up” HPV vaccination is not unilaterally recommended for adults older than 26 years.
Transgender patients
Discussing transgender patients, Dr. McNamara focused on cross-sex hormone therapy (CSHT), first noting the significant psychological benefits, including improvements in depression, somatization, interpersonal sensitivity, hostility, anxiety, phobic anxiety/agoraphobia, and quality of life.
According to Dr. McNamara, CSHT is relatively simple and may be safely administered by primary care providers. For transmasculine patients, testosterone supplementation is all that is needed, whereas transfeminine patients will require spironolactone or GnRH agonists to reduce testosterone and estradiol to increase feminizing hormones to pubertal levels.
CSHT is not without risks, Dr. McNamara said, including “very high” risks of erythrocytosis among transmasculine patients and venous thromboembolic disease among transfeminine patients; but these risks need to be considered in the context of an approximate 40% suicide rate among transgender individuals.
“I can tell you in my own practice that these [suicide] data ring true,” Dr. McNamara said. “Many, many of my patients have attempted suicide, so [CSHT] is something that you really want to think about right away.”
Even when additional risk factors are present, such as preexisting cardiovascular disease, Dr. McNamara suggested that “there are very few absolute contraindications to CSHT,” and described it as a “life-sustaining treatment” that should be viewed analogously with any other long-term management strategy, such as therapy for diabetes or hypertension.
Fostering a transgender-friendly practice
In an interview, Nicole Nisly, MD, codirector of the LGBTQ+ Clinic at the University of Iowa Hospitals and Clinics, Iowa City, reflected upon Dr. McNamara’s presentation, noting that primary care providers – with a little education – are the best candidates to care for transgender patients.
“I think [primary care providers] do a better job [caring for transgender patients] than endocrinologists, honestly, because they can provide care for the whole person,” Dr. Nisly said. “They can do a Pap, they can do STI screening, they can assess mood, they can [evaluate] safety, and the whole person, as opposed to endocrinologists, who do hormone therapy, but somebody else does everything else.”
Dr. Nisly emphasized the importance of personalizing care for transgender individuals, which depends upon a welcoming practice environment, with careful attention to language.
Foremost, Dr. Nisly recommended asking patients for their preferred name, sexual orientation, and gender identity.
“One of the most difficult things [for transgender patients] is to see notes with the wrong name – the name that makes them feel uncomfortable – or the wrong pronoun,” Dr. Nisly said. “That’s very important to the community.”
Dr. Nisly also recommended an alternative term for cross-sex hormone therapy.
“I hate cross-sex hormone therapy terminology, honestly,” Dr. Nisly said. “I just think it’s so unwelcoming, and I think most of our patients don’t like the terminology, so we use ‘gender-affirming hormone therapy.’”
Dr. Nisly explained that the term “cross-sex” assumes a conventional definition of sex, which is inherently flawed.
When discussing certain medical risk factors, such as pregnancy or HIV, it is helpful to know “sex assigned at birth” for both patients and their sexual partners, Dr. Nisly said. It’s best to ask in this way, instead of using terms like “boyfriend” or “girlfriend,” as “sex assigned at birth” is “terminology the community recognizes, affirms, and feels comfortable with.”
Concerning management of medical risk factors, Dr. Nisly offered some additional perspectives.
For one, she recommended giving PrEP to any patient who has a desire to be on PrEP, noting that this desire can indicate a change in future sexual practices, which the CDC criteria do not anticipate. She also advised in-hospital self-swabbing for extragenital STIs, as this can increase patient comfort and adherence. And, in contrast with Dr. McNamara, Dr. Nisly recommended anal Pap screening for any man that has sex with men and anyone with HIV of any gender. She noted that rates of anal dysplasia are “pretty high” among men who have sex with men, and that detection may reduce cancer risk.
For clinicians who would like to learn more about caring for transgender patients, Dr. Nisly recommended that they start by reading the World Professional Association for Transgender Health guidelines.
“It’s about 300 pages,” Dr. Nisly said, “but it is great.”
Dr. McNamara and Dr. Nisly reported no conflicts of interest.
FROM INTERNAL MEDICINE 2021
Transgender hormone therapy linked to blood pressure changes
Transgender people treated with gender-affirming hormone therapy show distinctive changes in blood pressure that begin soon after treatment initiation and do not subside over years of treatment, according to the largest and longest observational study to date to look at the issue.
“Many physicians may not be aware of the changes to blood pressure in trans patients who start hormone therapy,” senior author Michael S. Irwig, MD, director of transgender medicine at Beth Israel Deaconess Medical Center in Boston, told this news organization.
“The take-away message for physicians is to monitor blood pressure both before and after starting hormone therapy in transgender patients, as over a third of transgender individuals had stage 1 hypertension before starting hormone therapy, and many had their blood pressure increase after starting hormone therapy.”
Mean blood pressure increases in transgender males, decreases in females
In the study, published in Hypertension, Katherine Banks, MD, George Washington University, Washington, and colleagues, followed 470 transgender adult patients for up to 5 years.
The mean systolic blood pressure levels in transgender female patients (male at birth) significantly decreased compared with baseline within a few months of them starting gender-affirming hormone treatment.
Conversely, the systolic blood pressure levels in transgender males (females at birth) who were treated with testosterone increased over the same period.
There were no significant changes in the groups in terms of diastolic blood pressure, consistent with other studies.
“Our study is the first to describe the time course of the blood pressure effects of gender-affirming hormone therapy and to compare the rates of elevated blood pressure and stage 1 and stage 2 hypertension using blood pressure readings from gender-diverse individuals pre- and post–gender-affirming hormone therapy,” the authors note.
Gender-affirming hormone therapy – which has been prescribed to transgender patients for more than 25 years – typically involves a combination of estrogen and an anti-androgen for males transitioning to female, while the therapy for those transitioning to male generally only involves testosterone.
The therapy has previously been linked to various cardiac effects, with evidence showing transgender men have as much as a 5-times greater risk of heart attack versus cisgender women, the authors note.
Although the American Heart Association issued a 2020 Scientific Statement addressing the cardiovascular disease risk, evidence on the effects specifically on blood pressure in transgender patients has been inconsistent.
For the new study, Dr. Banks and colleagues enrolled 247 transgender females and 223 transgender males who were treated between 2007 and 2015 at two medical centers in Washington, D.C. Of the individuals, who had a mean age of 27.8, about 27% were non-White and 16% were Latinx.
They had blood pressure measurements taken at baseline and at follow-up clinical visits for up to 57 months following the initiation of gender-affirming hormone therapy.
Over the follow-up period, the transgender females had decreases in mean systolic blood pressure of 4.0 mm Hg within 2 to 4 months of starting hormone therapy (P < .0001) and mean declines of 6.0 mm Hg were further observed at 11 to 21 months compared with baseline.
In transgender males, the mean systolic blood pressure increased by 2.6 mm Hg at 2 to 4 months (P = .02), and by 2.9 mm Hg at 11 to 21 months after starting therapy.
Furthermore, “although the average increase in systolic blood pressure was 2.6 mm Hg in transgender men within 2 to 4 months, some patients had much higher increases,” Dr. Irwig noted.
As many as 40% of transgender men had stage 1 hypertension after 11 to 21 months of hormone therapy.
The blood pressure changes in transgender males and females were observed across all three racial ethnic groups of Whites, Blacks, and Latinx, and the changes remained consistent throughout the entire follow-up period of approximately 5 years while hormone therapy was continued.
In addition to the changes after therapy initiation, the researchers note that more than one-third of individuals in both groups had stage 1 hypertension even before starting hormone therapy.
The findings are a concern in light of “clear evidence linking hypertension and higher blood pressure with cardiovascular events such as stroke and heart attacks,” Dr. Irwig said.
Protective effects for transgender females?
Transgender females showed as much as a 47% decrease in the prevalence of stage 2 hypertension, from 19% to 10%, within 2 to 4 months of treatment with gender-affirming hormone therapy (P = .001), and the rate declined further to 8% at 11 to 21 months, suggesting a protective effect of the treatment.
“The rate of stage 2 hypertension did drop in transgender feminine individuals, which could be protective and lower their risk for cardiovascular events,” Dr. Irwig said.
“This was not a surprise, as lowering testosterone and the use of spironolactone can lower blood pressure,” he noted.
Exceptions in both groups
Of note, a sizable proportion of patients had blood pressure changes that were in fact the opposite of the patterns seen in the majority of their gender group.
Specifically, while 42% to 53% of the transgender females had systolic blood pressure readings of at least 5 mm Hg lower than their baseline readings, up to 32% had increases of at least 5 mm Hg compared to baseline readings.
Likewise, whereas 41% to 59% of transgender males had increases of at least 5 mm Hg compared with baseline, up to 35% had levels that were at least 5 mm Hg lower than baseline.
“It was a surprise that over a quarter of individuals had changes opposite to the mean changes,” Dr. Irwig said.
The differing blood pressure changes underscore that “more research is needed to determine which formulations of estrogen, testosterone, and antiandrogens are optimal regarding blood pressure and cardiovascular health, especially in older individuals,” the authors note.
Gender-affirming hormone therapy formulations differ
Various formulations for gender-affirming hormone regimens are available, including oral, transdermal, sublingual, and intramuscular preparations.
In the study, 77% to 91% of transgender males were on intramuscular testosterone injections, with the rest on transdermal formulations, and 92% of transgender female patients were started on oral estradiol, with mean doses generally increasing over time.
The study’s results are consistent with evidence from other studies, with 7 of 8 involving transgender males showing mean increases in systolic blood pressure ranging from 1 to 14 mm Hg.
Previous research supports cardiovascular risk
As reported by this news organization, other emerging research on cardiovascular risks to transgender people include a recent study showing more than 10% of transgender males were found to have hematocrit levels that could put them at risk for blood clots.
And further research on transgender youth also shows concerning elevations in lipids and other cardiovascular risks.
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Transgender people treated with gender-affirming hormone therapy show distinctive changes in blood pressure that begin soon after treatment initiation and do not subside over years of treatment, according to the largest and longest observational study to date to look at the issue.
“Many physicians may not be aware of the changes to blood pressure in trans patients who start hormone therapy,” senior author Michael S. Irwig, MD, director of transgender medicine at Beth Israel Deaconess Medical Center in Boston, told this news organization.
“The take-away message for physicians is to monitor blood pressure both before and after starting hormone therapy in transgender patients, as over a third of transgender individuals had stage 1 hypertension before starting hormone therapy, and many had their blood pressure increase after starting hormone therapy.”
Mean blood pressure increases in transgender males, decreases in females
In the study, published in Hypertension, Katherine Banks, MD, George Washington University, Washington, and colleagues, followed 470 transgender adult patients for up to 5 years.
The mean systolic blood pressure levels in transgender female patients (male at birth) significantly decreased compared with baseline within a few months of them starting gender-affirming hormone treatment.
Conversely, the systolic blood pressure levels in transgender males (females at birth) who were treated with testosterone increased over the same period.
There were no significant changes in the groups in terms of diastolic blood pressure, consistent with other studies.
“Our study is the first to describe the time course of the blood pressure effects of gender-affirming hormone therapy and to compare the rates of elevated blood pressure and stage 1 and stage 2 hypertension using blood pressure readings from gender-diverse individuals pre- and post–gender-affirming hormone therapy,” the authors note.
Gender-affirming hormone therapy – which has been prescribed to transgender patients for more than 25 years – typically involves a combination of estrogen and an anti-androgen for males transitioning to female, while the therapy for those transitioning to male generally only involves testosterone.
The therapy has previously been linked to various cardiac effects, with evidence showing transgender men have as much as a 5-times greater risk of heart attack versus cisgender women, the authors note.
Although the American Heart Association issued a 2020 Scientific Statement addressing the cardiovascular disease risk, evidence on the effects specifically on blood pressure in transgender patients has been inconsistent.
For the new study, Dr. Banks and colleagues enrolled 247 transgender females and 223 transgender males who were treated between 2007 and 2015 at two medical centers in Washington, D.C. Of the individuals, who had a mean age of 27.8, about 27% were non-White and 16% were Latinx.
They had blood pressure measurements taken at baseline and at follow-up clinical visits for up to 57 months following the initiation of gender-affirming hormone therapy.
Over the follow-up period, the transgender females had decreases in mean systolic blood pressure of 4.0 mm Hg within 2 to 4 months of starting hormone therapy (P < .0001) and mean declines of 6.0 mm Hg were further observed at 11 to 21 months compared with baseline.
In transgender males, the mean systolic blood pressure increased by 2.6 mm Hg at 2 to 4 months (P = .02), and by 2.9 mm Hg at 11 to 21 months after starting therapy.
Furthermore, “although the average increase in systolic blood pressure was 2.6 mm Hg in transgender men within 2 to 4 months, some patients had much higher increases,” Dr. Irwig noted.
As many as 40% of transgender men had stage 1 hypertension after 11 to 21 months of hormone therapy.
The blood pressure changes in transgender males and females were observed across all three racial ethnic groups of Whites, Blacks, and Latinx, and the changes remained consistent throughout the entire follow-up period of approximately 5 years while hormone therapy was continued.
In addition to the changes after therapy initiation, the researchers note that more than one-third of individuals in both groups had stage 1 hypertension even before starting hormone therapy.
The findings are a concern in light of “clear evidence linking hypertension and higher blood pressure with cardiovascular events such as stroke and heart attacks,” Dr. Irwig said.
Protective effects for transgender females?
Transgender females showed as much as a 47% decrease in the prevalence of stage 2 hypertension, from 19% to 10%, within 2 to 4 months of treatment with gender-affirming hormone therapy (P = .001), and the rate declined further to 8% at 11 to 21 months, suggesting a protective effect of the treatment.
“The rate of stage 2 hypertension did drop in transgender feminine individuals, which could be protective and lower their risk for cardiovascular events,” Dr. Irwig said.
“This was not a surprise, as lowering testosterone and the use of spironolactone can lower blood pressure,” he noted.
Exceptions in both groups
Of note, a sizable proportion of patients had blood pressure changes that were in fact the opposite of the patterns seen in the majority of their gender group.
Specifically, while 42% to 53% of the transgender females had systolic blood pressure readings of at least 5 mm Hg lower than their baseline readings, up to 32% had increases of at least 5 mm Hg compared to baseline readings.
Likewise, whereas 41% to 59% of transgender males had increases of at least 5 mm Hg compared with baseline, up to 35% had levels that were at least 5 mm Hg lower than baseline.
“It was a surprise that over a quarter of individuals had changes opposite to the mean changes,” Dr. Irwig said.
The differing blood pressure changes underscore that “more research is needed to determine which formulations of estrogen, testosterone, and antiandrogens are optimal regarding blood pressure and cardiovascular health, especially in older individuals,” the authors note.
Gender-affirming hormone therapy formulations differ
Various formulations for gender-affirming hormone regimens are available, including oral, transdermal, sublingual, and intramuscular preparations.
In the study, 77% to 91% of transgender males were on intramuscular testosterone injections, with the rest on transdermal formulations, and 92% of transgender female patients were started on oral estradiol, with mean doses generally increasing over time.
The study’s results are consistent with evidence from other studies, with 7 of 8 involving transgender males showing mean increases in systolic blood pressure ranging from 1 to 14 mm Hg.
Previous research supports cardiovascular risk
As reported by this news organization, other emerging research on cardiovascular risks to transgender people include a recent study showing more than 10% of transgender males were found to have hematocrit levels that could put them at risk for blood clots.
And further research on transgender youth also shows concerning elevations in lipids and other cardiovascular risks.
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Transgender people treated with gender-affirming hormone therapy show distinctive changes in blood pressure that begin soon after treatment initiation and do not subside over years of treatment, according to the largest and longest observational study to date to look at the issue.
“Many physicians may not be aware of the changes to blood pressure in trans patients who start hormone therapy,” senior author Michael S. Irwig, MD, director of transgender medicine at Beth Israel Deaconess Medical Center in Boston, told this news organization.
“The take-away message for physicians is to monitor blood pressure both before and after starting hormone therapy in transgender patients, as over a third of transgender individuals had stage 1 hypertension before starting hormone therapy, and many had their blood pressure increase after starting hormone therapy.”
Mean blood pressure increases in transgender males, decreases in females
In the study, published in Hypertension, Katherine Banks, MD, George Washington University, Washington, and colleagues, followed 470 transgender adult patients for up to 5 years.
The mean systolic blood pressure levels in transgender female patients (male at birth) significantly decreased compared with baseline within a few months of them starting gender-affirming hormone treatment.
Conversely, the systolic blood pressure levels in transgender males (females at birth) who were treated with testosterone increased over the same period.
There were no significant changes in the groups in terms of diastolic blood pressure, consistent with other studies.
“Our study is the first to describe the time course of the blood pressure effects of gender-affirming hormone therapy and to compare the rates of elevated blood pressure and stage 1 and stage 2 hypertension using blood pressure readings from gender-diverse individuals pre- and post–gender-affirming hormone therapy,” the authors note.
Gender-affirming hormone therapy – which has been prescribed to transgender patients for more than 25 years – typically involves a combination of estrogen and an anti-androgen for males transitioning to female, while the therapy for those transitioning to male generally only involves testosterone.
The therapy has previously been linked to various cardiac effects, with evidence showing transgender men have as much as a 5-times greater risk of heart attack versus cisgender women, the authors note.
Although the American Heart Association issued a 2020 Scientific Statement addressing the cardiovascular disease risk, evidence on the effects specifically on blood pressure in transgender patients has been inconsistent.
For the new study, Dr. Banks and colleagues enrolled 247 transgender females and 223 transgender males who were treated between 2007 and 2015 at two medical centers in Washington, D.C. Of the individuals, who had a mean age of 27.8, about 27% were non-White and 16% were Latinx.
They had blood pressure measurements taken at baseline and at follow-up clinical visits for up to 57 months following the initiation of gender-affirming hormone therapy.
Over the follow-up period, the transgender females had decreases in mean systolic blood pressure of 4.0 mm Hg within 2 to 4 months of starting hormone therapy (P < .0001) and mean declines of 6.0 mm Hg were further observed at 11 to 21 months compared with baseline.
In transgender males, the mean systolic blood pressure increased by 2.6 mm Hg at 2 to 4 months (P = .02), and by 2.9 mm Hg at 11 to 21 months after starting therapy.
Furthermore, “although the average increase in systolic blood pressure was 2.6 mm Hg in transgender men within 2 to 4 months, some patients had much higher increases,” Dr. Irwig noted.
As many as 40% of transgender men had stage 1 hypertension after 11 to 21 months of hormone therapy.
The blood pressure changes in transgender males and females were observed across all three racial ethnic groups of Whites, Blacks, and Latinx, and the changes remained consistent throughout the entire follow-up period of approximately 5 years while hormone therapy was continued.
In addition to the changes after therapy initiation, the researchers note that more than one-third of individuals in both groups had stage 1 hypertension even before starting hormone therapy.
The findings are a concern in light of “clear evidence linking hypertension and higher blood pressure with cardiovascular events such as stroke and heart attacks,” Dr. Irwig said.
Protective effects for transgender females?
Transgender females showed as much as a 47% decrease in the prevalence of stage 2 hypertension, from 19% to 10%, within 2 to 4 months of treatment with gender-affirming hormone therapy (P = .001), and the rate declined further to 8% at 11 to 21 months, suggesting a protective effect of the treatment.
“The rate of stage 2 hypertension did drop in transgender feminine individuals, which could be protective and lower their risk for cardiovascular events,” Dr. Irwig said.
“This was not a surprise, as lowering testosterone and the use of spironolactone can lower blood pressure,” he noted.
Exceptions in both groups
Of note, a sizable proportion of patients had blood pressure changes that were in fact the opposite of the patterns seen in the majority of their gender group.
Specifically, while 42% to 53% of the transgender females had systolic blood pressure readings of at least 5 mm Hg lower than their baseline readings, up to 32% had increases of at least 5 mm Hg compared to baseline readings.
Likewise, whereas 41% to 59% of transgender males had increases of at least 5 mm Hg compared with baseline, up to 35% had levels that were at least 5 mm Hg lower than baseline.
“It was a surprise that over a quarter of individuals had changes opposite to the mean changes,” Dr. Irwig said.
The differing blood pressure changes underscore that “more research is needed to determine which formulations of estrogen, testosterone, and antiandrogens are optimal regarding blood pressure and cardiovascular health, especially in older individuals,” the authors note.
Gender-affirming hormone therapy formulations differ
Various formulations for gender-affirming hormone regimens are available, including oral, transdermal, sublingual, and intramuscular preparations.
In the study, 77% to 91% of transgender males were on intramuscular testosterone injections, with the rest on transdermal formulations, and 92% of transgender female patients were started on oral estradiol, with mean doses generally increasing over time.
The study’s results are consistent with evidence from other studies, with 7 of 8 involving transgender males showing mean increases in systolic blood pressure ranging from 1 to 14 mm Hg.
Previous research supports cardiovascular risk
As reported by this news organization, other emerging research on cardiovascular risks to transgender people include a recent study showing more than 10% of transgender males were found to have hematocrit levels that could put them at risk for blood clots.
And further research on transgender youth also shows concerning elevations in lipids and other cardiovascular risks.
The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Helping your patients navigate the coming out process
“Mom, Dad: I’m gay.” Saying these words can be difficult for anyone but especially for adolescents and young adults. The process of coming out is one filled with anticipation, angst, and hopefully relief. However, this process is not a one-time event but rather something that LGBTQ adolescents and young adults have to face every time they meet someone new or are placed in a new situation. They have to decide if that new person can be trusted with their very personal information.
Coming out is a process that begins months to years before the adolescent or young adult utters the words above. The first step in the coming out process is accepting one’s sexual orientation and/or gender identity. This period of time can be somewhat tumultuous, filled with a mix of emotions ranging from fear to excitement. The adolescent or young adult may need support in coming to terms with who they are as their authentic self. This can take the role of a therapist, a trusted friend, or a trusted family member. There may even be times that the adolescent or young adult’s physician is the only person that they are out to besides their friends. Therefore, you can play a very important role in helping your adolescent and young adult patients as they navigate the journey of coming out.
One of the most important ways that physicians can help adolescents and young adults is to spend time alone with them at as many visits as you can. This gives the patient the time to discuss confidential matters with you, including their sexual orientation and/or gender identity. It is possible that the chronic abdominal pain that your adolescent patient is experiencing may not represent an organic abdominal problem but could represent a manifestation of anxiety because that patient is afraid of his/her parent(s) finding out that he/she identifies as LGBTQ. If one of your patients comes out to you, it is important that you validate for your patient that they are normal as who they are. In addition, you can thank your patient for trusting you with that information and let them know that you are there to support them in whatever way they feel appropriate. Just as important is that you work with the adolescent on a plan for their other concerns that respects their right to privacy in regard to their gender identity and/or sexual orientation.
The adolescent or young adult should always be in control of who knows about their gender identity and/or sexual orientation. Ideally, they should also always be the one who shares that information with others. Many times, parents may react positively to finding out that their child identifies as LGBTQ and want to share that information with their friends or family members. Alternatively, the parent could use the patient’s sexual orientation or gender identity negatively against them to their family and/or friends. As the physician, you can help counsel the family that it should always be their child who gets to share that information and when it is shared.
So how can you support your LGBTQ patients as they navigate the coming out process? First, when you find out from your patient that they identify as LGBTQ, ensure that you ask them who knows about their identity. This prevents inadvertent disclosures to the parent/guardian when the patient is not ready for them to know. Second, discuss with the patient if he/she needs any resources related to their sexual orientation and/or gender identity. This includes things such as the names of local LGBTQ youth organizations or the phone number for the Trevor Project suicide hotline, for example. Third, ensure that your office and staff are a welcoming and affirmative environment for your patients. A 2017 survey by the Human Rights Campaign found that only 8% of transgender or gender-diverse adolescents and young adults were out to all of their physicians and only 5% of LGB adolescents and young adults were out to all of their physicians.1 This is likely because of past negative experiences these patients have had with previous physicians. A 2017 study from the Center for American Progress found that 8% of LGB patients and 29% of transgender or gender-diverse patients said that a doctor or health care provider had refused to see them because of their actual or perceived identity.2 Lastly, you could offer to help facilitate a discussion between the patient and his/her parents in relation to his/her sexual orientation and/or gender identity.
In summary, pediatricians can play an important role in the coming out process of their LGBTQ patients. Your office is an important source of support for the physical and mental health of these patients as they navigate this journey. You can also be a strong advocate for these patients to their parents and families. I think that we all can agree that our patients deserve better than only feeling comfortable to be out to 5%-8% of their physicians.
Dr. Cooper is assistant professor of pediatrics at the University of Texas, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas. Contact him at [email protected].
References
1. Human Rights Campaign 2018 LGBTQ Youth Report.
2. Mirza SA and Rooney C. “Discrimination prevents LGBTQ people from accessing health care.” Center for American Progress. 2018 Jan 18.
“Mom, Dad: I’m gay.” Saying these words can be difficult for anyone but especially for adolescents and young adults. The process of coming out is one filled with anticipation, angst, and hopefully relief. However, this process is not a one-time event but rather something that LGBTQ adolescents and young adults have to face every time they meet someone new or are placed in a new situation. They have to decide if that new person can be trusted with their very personal information.
Coming out is a process that begins months to years before the adolescent or young adult utters the words above. The first step in the coming out process is accepting one’s sexual orientation and/or gender identity. This period of time can be somewhat tumultuous, filled with a mix of emotions ranging from fear to excitement. The adolescent or young adult may need support in coming to terms with who they are as their authentic self. This can take the role of a therapist, a trusted friend, or a trusted family member. There may even be times that the adolescent or young adult’s physician is the only person that they are out to besides their friends. Therefore, you can play a very important role in helping your adolescent and young adult patients as they navigate the journey of coming out.
One of the most important ways that physicians can help adolescents and young adults is to spend time alone with them at as many visits as you can. This gives the patient the time to discuss confidential matters with you, including their sexual orientation and/or gender identity. It is possible that the chronic abdominal pain that your adolescent patient is experiencing may not represent an organic abdominal problem but could represent a manifestation of anxiety because that patient is afraid of his/her parent(s) finding out that he/she identifies as LGBTQ. If one of your patients comes out to you, it is important that you validate for your patient that they are normal as who they are. In addition, you can thank your patient for trusting you with that information and let them know that you are there to support them in whatever way they feel appropriate. Just as important is that you work with the adolescent on a plan for their other concerns that respects their right to privacy in regard to their gender identity and/or sexual orientation.
The adolescent or young adult should always be in control of who knows about their gender identity and/or sexual orientation. Ideally, they should also always be the one who shares that information with others. Many times, parents may react positively to finding out that their child identifies as LGBTQ and want to share that information with their friends or family members. Alternatively, the parent could use the patient’s sexual orientation or gender identity negatively against them to their family and/or friends. As the physician, you can help counsel the family that it should always be their child who gets to share that information and when it is shared.
So how can you support your LGBTQ patients as they navigate the coming out process? First, when you find out from your patient that they identify as LGBTQ, ensure that you ask them who knows about their identity. This prevents inadvertent disclosures to the parent/guardian when the patient is not ready for them to know. Second, discuss with the patient if he/she needs any resources related to their sexual orientation and/or gender identity. This includes things such as the names of local LGBTQ youth organizations or the phone number for the Trevor Project suicide hotline, for example. Third, ensure that your office and staff are a welcoming and affirmative environment for your patients. A 2017 survey by the Human Rights Campaign found that only 8% of transgender or gender-diverse adolescents and young adults were out to all of their physicians and only 5% of LGB adolescents and young adults were out to all of their physicians.1 This is likely because of past negative experiences these patients have had with previous physicians. A 2017 study from the Center for American Progress found that 8% of LGB patients and 29% of transgender or gender-diverse patients said that a doctor or health care provider had refused to see them because of their actual or perceived identity.2 Lastly, you could offer to help facilitate a discussion between the patient and his/her parents in relation to his/her sexual orientation and/or gender identity.
In summary, pediatricians can play an important role in the coming out process of their LGBTQ patients. Your office is an important source of support for the physical and mental health of these patients as they navigate this journey. You can also be a strong advocate for these patients to their parents and families. I think that we all can agree that our patients deserve better than only feeling comfortable to be out to 5%-8% of their physicians.
Dr. Cooper is assistant professor of pediatrics at the University of Texas, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas. Contact him at [email protected].
References
1. Human Rights Campaign 2018 LGBTQ Youth Report.
2. Mirza SA and Rooney C. “Discrimination prevents LGBTQ people from accessing health care.” Center for American Progress. 2018 Jan 18.
“Mom, Dad: I’m gay.” Saying these words can be difficult for anyone but especially for adolescents and young adults. The process of coming out is one filled with anticipation, angst, and hopefully relief. However, this process is not a one-time event but rather something that LGBTQ adolescents and young adults have to face every time they meet someone new or are placed in a new situation. They have to decide if that new person can be trusted with their very personal information.
Coming out is a process that begins months to years before the adolescent or young adult utters the words above. The first step in the coming out process is accepting one’s sexual orientation and/or gender identity. This period of time can be somewhat tumultuous, filled with a mix of emotions ranging from fear to excitement. The adolescent or young adult may need support in coming to terms with who they are as their authentic self. This can take the role of a therapist, a trusted friend, or a trusted family member. There may even be times that the adolescent or young adult’s physician is the only person that they are out to besides their friends. Therefore, you can play a very important role in helping your adolescent and young adult patients as they navigate the journey of coming out.
One of the most important ways that physicians can help adolescents and young adults is to spend time alone with them at as many visits as you can. This gives the patient the time to discuss confidential matters with you, including their sexual orientation and/or gender identity. It is possible that the chronic abdominal pain that your adolescent patient is experiencing may not represent an organic abdominal problem but could represent a manifestation of anxiety because that patient is afraid of his/her parent(s) finding out that he/she identifies as LGBTQ. If one of your patients comes out to you, it is important that you validate for your patient that they are normal as who they are. In addition, you can thank your patient for trusting you with that information and let them know that you are there to support them in whatever way they feel appropriate. Just as important is that you work with the adolescent on a plan for their other concerns that respects their right to privacy in regard to their gender identity and/or sexual orientation.
The adolescent or young adult should always be in control of who knows about their gender identity and/or sexual orientation. Ideally, they should also always be the one who shares that information with others. Many times, parents may react positively to finding out that their child identifies as LGBTQ and want to share that information with their friends or family members. Alternatively, the parent could use the patient’s sexual orientation or gender identity negatively against them to their family and/or friends. As the physician, you can help counsel the family that it should always be their child who gets to share that information and when it is shared.
So how can you support your LGBTQ patients as they navigate the coming out process? First, when you find out from your patient that they identify as LGBTQ, ensure that you ask them who knows about their identity. This prevents inadvertent disclosures to the parent/guardian when the patient is not ready for them to know. Second, discuss with the patient if he/she needs any resources related to their sexual orientation and/or gender identity. This includes things such as the names of local LGBTQ youth organizations or the phone number for the Trevor Project suicide hotline, for example. Third, ensure that your office and staff are a welcoming and affirmative environment for your patients. A 2017 survey by the Human Rights Campaign found that only 8% of transgender or gender-diverse adolescents and young adults were out to all of their physicians and only 5% of LGB adolescents and young adults were out to all of their physicians.1 This is likely because of past negative experiences these patients have had with previous physicians. A 2017 study from the Center for American Progress found that 8% of LGB patients and 29% of transgender or gender-diverse patients said that a doctor or health care provider had refused to see them because of their actual or perceived identity.2 Lastly, you could offer to help facilitate a discussion between the patient and his/her parents in relation to his/her sexual orientation and/or gender identity.
In summary, pediatricians can play an important role in the coming out process of their LGBTQ patients. Your office is an important source of support for the physical and mental health of these patients as they navigate this journey. You can also be a strong advocate for these patients to their parents and families. I think that we all can agree that our patients deserve better than only feeling comfortable to be out to 5%-8% of their physicians.
Dr. Cooper is assistant professor of pediatrics at the University of Texas, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas. Contact him at [email protected].
References
1. Human Rights Campaign 2018 LGBTQ Youth Report.
2. Mirza SA and Rooney C. “Discrimination prevents LGBTQ people from accessing health care.” Center for American Progress. 2018 Jan 18.
How physicians can provide better care to transgender patients
People who identify as transgender experience many health disparities, in addition to lack of access to quality care. The most commonly cited barrier is the lack of providers who are knowledgeable about transgender health care, according to past surveys.
Even those who do seek care often have unpleasant experiences. A 2015 survey conducted by the National Center for Transgender Equality found that 33% of those who saw a health care provider reported at least one unfavorable experience related to being transgender, such as being verbally harassed or refused treatment because of their gender identity. In fact, 23% of those surveyed say they did not seek health care they needed in the past year because of fear of being mistreated as a transgender person.
This interview has been edited for length and clarity.
Question: Surveys have shown that many people who identify as transgender will seek only transition care, not primary or preventive care. Why is that?
Dr. Brandt: My answer is multifactorial. Transgender patients do seek primary care – just not as readily. There’s a lot of misconceptions about health care needs for the LGBT community in general. For example, lesbian or bisexual women may be not as well informed about the need for Pap smears compared with their heterosexual counterparts. These misconceptions are further exacerbated in the transgender community.
The fact that a lot of patients seek only transition-related care, but not preventive services, such as primary care and gynecologic care, is also related to fears of discrimination and lack of education of providers. These patients are afraid when they walk into an office that they will be misgendered or their physician won’t be familiar with their health care needs.
What can clinics and clinicians do to create a safe and welcoming environment?
Dr. Brandt: It starts with educating office staff about terminology and gender identities.
A key feature of our EHR is the sexual orientation and gender identity platform, which asks questions about a patient’s gender identity, sexual orientation, sex assigned at birth, and organ inventory. These data are then found in the patient information tab and are just as relevant as their insurance status, age, and date of birth.
There are many ways a doctor’s office can signal to patients that they are inclusive. They can hang LGBTQ-friendly flags or symbols or a sign saying, “We have an anti-discrimination policy” in the waiting room. A welcoming environment can also be achieved by revising patient questionnaires or forms so that they aren’t gender-specific or binary.
Given that the patient may have limited contact with a primary care clinician, how do you prioritize what you address during the visit?
Dr. Brandt: Similar to cisgender patients, it depends initially on the age of the patient and the reason for the visit. The priorities of an otherwise healthy transgender patient in their 20s are going to be largely the same as for a cisgender patient of the same age. As patients age in the primary care world, you’re addressing more issues, such as colorectal screening, lipid disorders, and mammograms, and that doesn’t change. For the most part, the problems that you address should be specific for that age group.
It becomes more complicated when you add in factors such as hormone therapy and whether patients have had any type of gender-affirming surgery. Those things can change the usual recommendations for screening or risk assessment. We try to figure out what routine health maintenance and cancer screening a patient needs based on age and risk factors, in addition to hormone status and surgical state.
Do you think that many physicians are educated about the care of underserved populations such as transgender patients?
Dr. Brandt: Yes and no. We are definitely getting better at it. For example, the American College of Obstetricians and Gynecologists published a committee opinion highlighting transgender care. So organizations are starting to prioritize these populations and recognize that they are, in fact, underserved and they have special health care needs.
However, the knowledge gaps are still pretty big. I get calls daily from providers asking questions about how to manage patients on hormones, or how to examine a patient who has undergone a vaginoplasty. I hear a lot of horror stories from transgender patients who had their hormones stopped for absurd and medically misinformed reasons.
But I definitely think it’s getting better and it’s being addressed at all levels – the medical school level, the residency level, and the attending level. It just takes time to inform people and for people to get used to the health care needs of these patients.
What should physicians keep in mind when treating patients who identify as transgender?
Dr. Brandt: First and foremost, understanding the terminology and the difference between gender identity, sex, and sexual orientation. Being familiar with that language and being able to speak that language very comfortably and not being awkward about it is a really important thing for primary care physicians and indeed any physician who treats transgender patients.
Physicians should also be aware that any underserved population has higher rates of mental health issues, such as depression and anxiety. Obviously, that goes along with being underserved and the stigma and the disparities that exist for these patients. Having providers educate themselves about what those disparities are and how they impact a patient’s daily life and health is paramount to knowing how to treat patients.
What are your top health concerns for these patients and how do you address them?
Dr. Brandt: I think mental health and safety is probably the number one for me. About 41% of transgender adults have attempted suicide. That number is roughly 51% in transgender youth. That is an astonishing number. These patients have much higher rates of domestic violence, intimate partner violence, and sexual assault, especially trans women and trans women of color. So understanding those statistics is huge.
Obesity, smoking, and substance abuse are my next three. Again, those are things that should be addressed at any visit, regardless of the gender identity or sexual orientation of the patient, but those rates are particularly high in this population.
Fertility and long-term care for patients should be addressed. Many patients who identify as transgender are told they can’t have a family. As a primary care physician, you may see a patient before they are seen by an ob.gyn. or surgeon. Talking about what a patient’s long-term life goals are with fertility and family planning, and what that looks like for them, is a big thing for me. Other providers may not feel that’s a concern, but I believe it should be discussed before initiation of hormone therapy, which can significantly impact fertility in some patients.
Are there nuances to the physical examination that primary care physicians should be aware of when dealing with transmasculine patients vs. transfeminine patients?
Dr. Brandt: Absolutely. And this interview can’t cover the scope of those nuances. An example that comes to mind is the genital exam. For transgender women who have undergone a vaginoplasty, the pelvic exam can be very affirming. Whereas for transgender men, a gynecologic exam can significantly exacerbate dysphoria and there are ways to conduct the exam to limit this discomfort and avoid creating a traumatic experience for the patient. It’s important to be aware that the genital exam, or any type of genitourinary exam, can be either affirming or not affirming.
Sexually transmitted infections are up in the general population, and the trans population is at even higher risk. What should physicians think about when they assess this risk?
Dr. Brandt: It’s really important for primary care clinicians and for gynecologists to learn to be comfortable talking about sexual practices, because what people do behind closed doors is really a key to how to counsel patients about safe sex.
People are well aware of the need to have safe sex. However, depending on the type of sex that you’re having, what body parts go where, what is truly safe can vary and people may not know, for example, to wear a condom when sex toys are involved or that a transgender male on testosterone can become pregnant during penile-vaginal intercourse. Providers really should be very educated on the array of sexual practices that people have and how to counsel them about those. They should know how to ask patients the gender identity of their sexual partners, the sexual orientation of their partners, and what parts go where during sex.
Providers should also talk to patients about PrEP [pre-exposure prophylaxis], whether they identify as cisgender or transgender. My trans patients tend to be a lot more educated about PrEP than other patients. It’s something that many of the residents, even in a standard gynecologic clinic, for example, don’t talk to cisgender patients about because of the stigma surrounding HIV. Many providers still think that the only people who are at risk for HIV are men who have sex with men. And while those rates are higher in some populations, depending on sexual practices, those aren’t the only patients who qualify for PrEP.
Overall, in order to counsel patients about STIs and safe sexual practices, providers should learn to be comfortable talking about sex.
Do you have any strategies on how to make the appointment more successful in addressing those issues?
Dr. Brandt: Bedside manner is a hard thing to teach, and comfort in talking about sex, gender identity, and sexual orientation can vary – but there are a lot of continuing medical education courses that physicians can utilize through the World Professional Association for Transgender Health.
If providers start to notice an influx of patients who identify as transgender or if they want to start seeing transgender patients, it’s really important for them to have that training before they start interacting with patients. In all of medicine, we sort of learn as we go, but this patient population has been subjected to discrimination, violence, error, and misgendering. They have dealt with providers who didn’t understand their health care needs. While this field is evolving, knowing how to appropriately address a patient (using their correct name, pronouns, etc.) is an absolute must.
That needs to be part of a provider’s routine vernacular and not something that they sort of stumble through. You can scare a patient away as soon as they walk into the office with an uneducated front desk staff and things that are seen in the office. Seeking out those educational tools, being aware of your own deficits as a provider and the educational needs of your office, and addressing those needs is really key.
A version of this article first appeared on Medscape.com.
People who identify as transgender experience many health disparities, in addition to lack of access to quality care. The most commonly cited barrier is the lack of providers who are knowledgeable about transgender health care, according to past surveys.
Even those who do seek care often have unpleasant experiences. A 2015 survey conducted by the National Center for Transgender Equality found that 33% of those who saw a health care provider reported at least one unfavorable experience related to being transgender, such as being verbally harassed or refused treatment because of their gender identity. In fact, 23% of those surveyed say they did not seek health care they needed in the past year because of fear of being mistreated as a transgender person.
This interview has been edited for length and clarity.
Question: Surveys have shown that many people who identify as transgender will seek only transition care, not primary or preventive care. Why is that?
Dr. Brandt: My answer is multifactorial. Transgender patients do seek primary care – just not as readily. There’s a lot of misconceptions about health care needs for the LGBT community in general. For example, lesbian or bisexual women may be not as well informed about the need for Pap smears compared with their heterosexual counterparts. These misconceptions are further exacerbated in the transgender community.
The fact that a lot of patients seek only transition-related care, but not preventive services, such as primary care and gynecologic care, is also related to fears of discrimination and lack of education of providers. These patients are afraid when they walk into an office that they will be misgendered or their physician won’t be familiar with their health care needs.
What can clinics and clinicians do to create a safe and welcoming environment?
Dr. Brandt: It starts with educating office staff about terminology and gender identities.
A key feature of our EHR is the sexual orientation and gender identity platform, which asks questions about a patient’s gender identity, sexual orientation, sex assigned at birth, and organ inventory. These data are then found in the patient information tab and are just as relevant as their insurance status, age, and date of birth.
There are many ways a doctor’s office can signal to patients that they are inclusive. They can hang LGBTQ-friendly flags or symbols or a sign saying, “We have an anti-discrimination policy” in the waiting room. A welcoming environment can also be achieved by revising patient questionnaires or forms so that they aren’t gender-specific or binary.
Given that the patient may have limited contact with a primary care clinician, how do you prioritize what you address during the visit?
Dr. Brandt: Similar to cisgender patients, it depends initially on the age of the patient and the reason for the visit. The priorities of an otherwise healthy transgender patient in their 20s are going to be largely the same as for a cisgender patient of the same age. As patients age in the primary care world, you’re addressing more issues, such as colorectal screening, lipid disorders, and mammograms, and that doesn’t change. For the most part, the problems that you address should be specific for that age group.
It becomes more complicated when you add in factors such as hormone therapy and whether patients have had any type of gender-affirming surgery. Those things can change the usual recommendations for screening or risk assessment. We try to figure out what routine health maintenance and cancer screening a patient needs based on age and risk factors, in addition to hormone status and surgical state.
Do you think that many physicians are educated about the care of underserved populations such as transgender patients?
Dr. Brandt: Yes and no. We are definitely getting better at it. For example, the American College of Obstetricians and Gynecologists published a committee opinion highlighting transgender care. So organizations are starting to prioritize these populations and recognize that they are, in fact, underserved and they have special health care needs.
However, the knowledge gaps are still pretty big. I get calls daily from providers asking questions about how to manage patients on hormones, or how to examine a patient who has undergone a vaginoplasty. I hear a lot of horror stories from transgender patients who had their hormones stopped for absurd and medically misinformed reasons.
But I definitely think it’s getting better and it’s being addressed at all levels – the medical school level, the residency level, and the attending level. It just takes time to inform people and for people to get used to the health care needs of these patients.
What should physicians keep in mind when treating patients who identify as transgender?
Dr. Brandt: First and foremost, understanding the terminology and the difference between gender identity, sex, and sexual orientation. Being familiar with that language and being able to speak that language very comfortably and not being awkward about it is a really important thing for primary care physicians and indeed any physician who treats transgender patients.
Physicians should also be aware that any underserved population has higher rates of mental health issues, such as depression and anxiety. Obviously, that goes along with being underserved and the stigma and the disparities that exist for these patients. Having providers educate themselves about what those disparities are and how they impact a patient’s daily life and health is paramount to knowing how to treat patients.
What are your top health concerns for these patients and how do you address them?
Dr. Brandt: I think mental health and safety is probably the number one for me. About 41% of transgender adults have attempted suicide. That number is roughly 51% in transgender youth. That is an astonishing number. These patients have much higher rates of domestic violence, intimate partner violence, and sexual assault, especially trans women and trans women of color. So understanding those statistics is huge.
Obesity, smoking, and substance abuse are my next three. Again, those are things that should be addressed at any visit, regardless of the gender identity or sexual orientation of the patient, but those rates are particularly high in this population.
Fertility and long-term care for patients should be addressed. Many patients who identify as transgender are told they can’t have a family. As a primary care physician, you may see a patient before they are seen by an ob.gyn. or surgeon. Talking about what a patient’s long-term life goals are with fertility and family planning, and what that looks like for them, is a big thing for me. Other providers may not feel that’s a concern, but I believe it should be discussed before initiation of hormone therapy, which can significantly impact fertility in some patients.
Are there nuances to the physical examination that primary care physicians should be aware of when dealing with transmasculine patients vs. transfeminine patients?
Dr. Brandt: Absolutely. And this interview can’t cover the scope of those nuances. An example that comes to mind is the genital exam. For transgender women who have undergone a vaginoplasty, the pelvic exam can be very affirming. Whereas for transgender men, a gynecologic exam can significantly exacerbate dysphoria and there are ways to conduct the exam to limit this discomfort and avoid creating a traumatic experience for the patient. It’s important to be aware that the genital exam, or any type of genitourinary exam, can be either affirming or not affirming.
Sexually transmitted infections are up in the general population, and the trans population is at even higher risk. What should physicians think about when they assess this risk?
Dr. Brandt: It’s really important for primary care clinicians and for gynecologists to learn to be comfortable talking about sexual practices, because what people do behind closed doors is really a key to how to counsel patients about safe sex.
People are well aware of the need to have safe sex. However, depending on the type of sex that you’re having, what body parts go where, what is truly safe can vary and people may not know, for example, to wear a condom when sex toys are involved or that a transgender male on testosterone can become pregnant during penile-vaginal intercourse. Providers really should be very educated on the array of sexual practices that people have and how to counsel them about those. They should know how to ask patients the gender identity of their sexual partners, the sexual orientation of their partners, and what parts go where during sex.
Providers should also talk to patients about PrEP [pre-exposure prophylaxis], whether they identify as cisgender or transgender. My trans patients tend to be a lot more educated about PrEP than other patients. It’s something that many of the residents, even in a standard gynecologic clinic, for example, don’t talk to cisgender patients about because of the stigma surrounding HIV. Many providers still think that the only people who are at risk for HIV are men who have sex with men. And while those rates are higher in some populations, depending on sexual practices, those aren’t the only patients who qualify for PrEP.
Overall, in order to counsel patients about STIs and safe sexual practices, providers should learn to be comfortable talking about sex.
Do you have any strategies on how to make the appointment more successful in addressing those issues?
Dr. Brandt: Bedside manner is a hard thing to teach, and comfort in talking about sex, gender identity, and sexual orientation can vary – but there are a lot of continuing medical education courses that physicians can utilize through the World Professional Association for Transgender Health.
If providers start to notice an influx of patients who identify as transgender or if they want to start seeing transgender patients, it’s really important for them to have that training before they start interacting with patients. In all of medicine, we sort of learn as we go, but this patient population has been subjected to discrimination, violence, error, and misgendering. They have dealt with providers who didn’t understand their health care needs. While this field is evolving, knowing how to appropriately address a patient (using their correct name, pronouns, etc.) is an absolute must.
That needs to be part of a provider’s routine vernacular and not something that they sort of stumble through. You can scare a patient away as soon as they walk into the office with an uneducated front desk staff and things that are seen in the office. Seeking out those educational tools, being aware of your own deficits as a provider and the educational needs of your office, and addressing those needs is really key.
A version of this article first appeared on Medscape.com.
People who identify as transgender experience many health disparities, in addition to lack of access to quality care. The most commonly cited barrier is the lack of providers who are knowledgeable about transgender health care, according to past surveys.
Even those who do seek care often have unpleasant experiences. A 2015 survey conducted by the National Center for Transgender Equality found that 33% of those who saw a health care provider reported at least one unfavorable experience related to being transgender, such as being verbally harassed or refused treatment because of their gender identity. In fact, 23% of those surveyed say they did not seek health care they needed in the past year because of fear of being mistreated as a transgender person.
This interview has been edited for length and clarity.
Question: Surveys have shown that many people who identify as transgender will seek only transition care, not primary or preventive care. Why is that?
Dr. Brandt: My answer is multifactorial. Transgender patients do seek primary care – just not as readily. There’s a lot of misconceptions about health care needs for the LGBT community in general. For example, lesbian or bisexual women may be not as well informed about the need for Pap smears compared with their heterosexual counterparts. These misconceptions are further exacerbated in the transgender community.
The fact that a lot of patients seek only transition-related care, but not preventive services, such as primary care and gynecologic care, is also related to fears of discrimination and lack of education of providers. These patients are afraid when they walk into an office that they will be misgendered or their physician won’t be familiar with their health care needs.
What can clinics and clinicians do to create a safe and welcoming environment?
Dr. Brandt: It starts with educating office staff about terminology and gender identities.
A key feature of our EHR is the sexual orientation and gender identity platform, which asks questions about a patient’s gender identity, sexual orientation, sex assigned at birth, and organ inventory. These data are then found in the patient information tab and are just as relevant as their insurance status, age, and date of birth.
There are many ways a doctor’s office can signal to patients that they are inclusive. They can hang LGBTQ-friendly flags or symbols or a sign saying, “We have an anti-discrimination policy” in the waiting room. A welcoming environment can also be achieved by revising patient questionnaires or forms so that they aren’t gender-specific or binary.
Given that the patient may have limited contact with a primary care clinician, how do you prioritize what you address during the visit?
Dr. Brandt: Similar to cisgender patients, it depends initially on the age of the patient and the reason for the visit. The priorities of an otherwise healthy transgender patient in their 20s are going to be largely the same as for a cisgender patient of the same age. As patients age in the primary care world, you’re addressing more issues, such as colorectal screening, lipid disorders, and mammograms, and that doesn’t change. For the most part, the problems that you address should be specific for that age group.
It becomes more complicated when you add in factors such as hormone therapy and whether patients have had any type of gender-affirming surgery. Those things can change the usual recommendations for screening or risk assessment. We try to figure out what routine health maintenance and cancer screening a patient needs based on age and risk factors, in addition to hormone status and surgical state.
Do you think that many physicians are educated about the care of underserved populations such as transgender patients?
Dr. Brandt: Yes and no. We are definitely getting better at it. For example, the American College of Obstetricians and Gynecologists published a committee opinion highlighting transgender care. So organizations are starting to prioritize these populations and recognize that they are, in fact, underserved and they have special health care needs.
However, the knowledge gaps are still pretty big. I get calls daily from providers asking questions about how to manage patients on hormones, or how to examine a patient who has undergone a vaginoplasty. I hear a lot of horror stories from transgender patients who had their hormones stopped for absurd and medically misinformed reasons.
But I definitely think it’s getting better and it’s being addressed at all levels – the medical school level, the residency level, and the attending level. It just takes time to inform people and for people to get used to the health care needs of these patients.
What should physicians keep in mind when treating patients who identify as transgender?
Dr. Brandt: First and foremost, understanding the terminology and the difference between gender identity, sex, and sexual orientation. Being familiar with that language and being able to speak that language very comfortably and not being awkward about it is a really important thing for primary care physicians and indeed any physician who treats transgender patients.
Physicians should also be aware that any underserved population has higher rates of mental health issues, such as depression and anxiety. Obviously, that goes along with being underserved and the stigma and the disparities that exist for these patients. Having providers educate themselves about what those disparities are and how they impact a patient’s daily life and health is paramount to knowing how to treat patients.
What are your top health concerns for these patients and how do you address them?
Dr. Brandt: I think mental health and safety is probably the number one for me. About 41% of transgender adults have attempted suicide. That number is roughly 51% in transgender youth. That is an astonishing number. These patients have much higher rates of domestic violence, intimate partner violence, and sexual assault, especially trans women and trans women of color. So understanding those statistics is huge.
Obesity, smoking, and substance abuse are my next three. Again, those are things that should be addressed at any visit, regardless of the gender identity or sexual orientation of the patient, but those rates are particularly high in this population.
Fertility and long-term care for patients should be addressed. Many patients who identify as transgender are told they can’t have a family. As a primary care physician, you may see a patient before they are seen by an ob.gyn. or surgeon. Talking about what a patient’s long-term life goals are with fertility and family planning, and what that looks like for them, is a big thing for me. Other providers may not feel that’s a concern, but I believe it should be discussed before initiation of hormone therapy, which can significantly impact fertility in some patients.
Are there nuances to the physical examination that primary care physicians should be aware of when dealing with transmasculine patients vs. transfeminine patients?
Dr. Brandt: Absolutely. And this interview can’t cover the scope of those nuances. An example that comes to mind is the genital exam. For transgender women who have undergone a vaginoplasty, the pelvic exam can be very affirming. Whereas for transgender men, a gynecologic exam can significantly exacerbate dysphoria and there are ways to conduct the exam to limit this discomfort and avoid creating a traumatic experience for the patient. It’s important to be aware that the genital exam, or any type of genitourinary exam, can be either affirming or not affirming.
Sexually transmitted infections are up in the general population, and the trans population is at even higher risk. What should physicians think about when they assess this risk?
Dr. Brandt: It’s really important for primary care clinicians and for gynecologists to learn to be comfortable talking about sexual practices, because what people do behind closed doors is really a key to how to counsel patients about safe sex.
People are well aware of the need to have safe sex. However, depending on the type of sex that you’re having, what body parts go where, what is truly safe can vary and people may not know, for example, to wear a condom when sex toys are involved or that a transgender male on testosterone can become pregnant during penile-vaginal intercourse. Providers really should be very educated on the array of sexual practices that people have and how to counsel them about those. They should know how to ask patients the gender identity of their sexual partners, the sexual orientation of their partners, and what parts go where during sex.
Providers should also talk to patients about PrEP [pre-exposure prophylaxis], whether they identify as cisgender or transgender. My trans patients tend to be a lot more educated about PrEP than other patients. It’s something that many of the residents, even in a standard gynecologic clinic, for example, don’t talk to cisgender patients about because of the stigma surrounding HIV. Many providers still think that the only people who are at risk for HIV are men who have sex with men. And while those rates are higher in some populations, depending on sexual practices, those aren’t the only patients who qualify for PrEP.
Overall, in order to counsel patients about STIs and safe sexual practices, providers should learn to be comfortable talking about sex.
Do you have any strategies on how to make the appointment more successful in addressing those issues?
Dr. Brandt: Bedside manner is a hard thing to teach, and comfort in talking about sex, gender identity, and sexual orientation can vary – but there are a lot of continuing medical education courses that physicians can utilize through the World Professional Association for Transgender Health.
If providers start to notice an influx of patients who identify as transgender or if they want to start seeing transgender patients, it’s really important for them to have that training before they start interacting with patients. In all of medicine, we sort of learn as we go, but this patient population has been subjected to discrimination, violence, error, and misgendering. They have dealt with providers who didn’t understand their health care needs. While this field is evolving, knowing how to appropriately address a patient (using their correct name, pronouns, etc.) is an absolute must.
That needs to be part of a provider’s routine vernacular and not something that they sort of stumble through. You can scare a patient away as soon as they walk into the office with an uneducated front desk staff and things that are seen in the office. Seeking out those educational tools, being aware of your own deficits as a provider and the educational needs of your office, and addressing those needs is really key.
A version of this article first appeared on Medscape.com.
Arkansas first state to ban transgender medical treatments for youths
Arkansas has become the first state to pass a law prohibiting doctors from giving gender-affirming medical treatments to transgender youths, CNN reported.
Gov. Asa Hutchinson had vetoed the bill on April 5, calling it a “product of the cultural war in America.” But on April 6, the state House and Senate voted to override the veto, making it state law, CNN reported.
At least 17 other states are considering similar legislation, but the Arkansas bill was the first to reach the governor’s desk, the Washington Post reported.
The bill bans doctors from prescribing puberty blockers, hormone therapies, or genital-altering surgeries for anybody under 18. Ever referring a youth for such treatment from another doctor is prohibited.
“It is of grave concern to the General Assembly that the medical community is allowing individuals who experience distress at identifying with their biological sex to be subjects of irreversible and drastic nongenital gender reassignment surgery and irreversible, permanently sterilizing genital gender reassignment surgery, despite the lack of studies showing that the benefits of such extreme interventions outweigh the risks,” the text of the bill said.
Gov. Hutchinson, a Republican, had called the measure a “vast government overreach” in announcing his veto.
“The bill is overbroad, extreme, and does not grandfather those young people who are currently under hormone treatment,” Gov. Hutchinson said. “The young people who are currently under a doctor’s care will be without treatment when this law goes into effect. That means they will be looking to the black market or go out of state ... to find the treatment that they want and need. This is not the right path to put them on.”
Many medical groups have come out against this kind of legislation. The American Academy of Child and Adolescent Psychiatry says it “strongly opposes any efforts – legal, legislative, and otherwise – to block access to these recognized interventions.”
Chase Strangio, the deputy director for transgender justice with the American Civil Liberty Union’s LGBTQ & HIV Project, complimented Gov. Hutchinson for his veto. On April 6, he said the ACLU is preparing to challenge the bill in court, CNN said.
A version of this article first appeared on Medscape.com.
Arkansas has become the first state to pass a law prohibiting doctors from giving gender-affirming medical treatments to transgender youths, CNN reported.
Gov. Asa Hutchinson had vetoed the bill on April 5, calling it a “product of the cultural war in America.” But on April 6, the state House and Senate voted to override the veto, making it state law, CNN reported.
At least 17 other states are considering similar legislation, but the Arkansas bill was the first to reach the governor’s desk, the Washington Post reported.
The bill bans doctors from prescribing puberty blockers, hormone therapies, or genital-altering surgeries for anybody under 18. Ever referring a youth for such treatment from another doctor is prohibited.
“It is of grave concern to the General Assembly that the medical community is allowing individuals who experience distress at identifying with their biological sex to be subjects of irreversible and drastic nongenital gender reassignment surgery and irreversible, permanently sterilizing genital gender reassignment surgery, despite the lack of studies showing that the benefits of such extreme interventions outweigh the risks,” the text of the bill said.
Gov. Hutchinson, a Republican, had called the measure a “vast government overreach” in announcing his veto.
“The bill is overbroad, extreme, and does not grandfather those young people who are currently under hormone treatment,” Gov. Hutchinson said. “The young people who are currently under a doctor’s care will be without treatment when this law goes into effect. That means they will be looking to the black market or go out of state ... to find the treatment that they want and need. This is not the right path to put them on.”
Many medical groups have come out against this kind of legislation. The American Academy of Child and Adolescent Psychiatry says it “strongly opposes any efforts – legal, legislative, and otherwise – to block access to these recognized interventions.”
Chase Strangio, the deputy director for transgender justice with the American Civil Liberty Union’s LGBTQ & HIV Project, complimented Gov. Hutchinson for his veto. On April 6, he said the ACLU is preparing to challenge the bill in court, CNN said.
A version of this article first appeared on Medscape.com.
Arkansas has become the first state to pass a law prohibiting doctors from giving gender-affirming medical treatments to transgender youths, CNN reported.
Gov. Asa Hutchinson had vetoed the bill on April 5, calling it a “product of the cultural war in America.” But on April 6, the state House and Senate voted to override the veto, making it state law, CNN reported.
At least 17 other states are considering similar legislation, but the Arkansas bill was the first to reach the governor’s desk, the Washington Post reported.
The bill bans doctors from prescribing puberty blockers, hormone therapies, or genital-altering surgeries for anybody under 18. Ever referring a youth for such treatment from another doctor is prohibited.
“It is of grave concern to the General Assembly that the medical community is allowing individuals who experience distress at identifying with their biological sex to be subjects of irreversible and drastic nongenital gender reassignment surgery and irreversible, permanently sterilizing genital gender reassignment surgery, despite the lack of studies showing that the benefits of such extreme interventions outweigh the risks,” the text of the bill said.
Gov. Hutchinson, a Republican, had called the measure a “vast government overreach” in announcing his veto.
“The bill is overbroad, extreme, and does not grandfather those young people who are currently under hormone treatment,” Gov. Hutchinson said. “The young people who are currently under a doctor’s care will be without treatment when this law goes into effect. That means they will be looking to the black market or go out of state ... to find the treatment that they want and need. This is not the right path to put them on.”
Many medical groups have come out against this kind of legislation. The American Academy of Child and Adolescent Psychiatry says it “strongly opposes any efforts – legal, legislative, and otherwise – to block access to these recognized interventions.”
Chase Strangio, the deputy director for transgender justice with the American Civil Liberty Union’s LGBTQ & HIV Project, complimented Gov. Hutchinson for his veto. On April 6, he said the ACLU is preparing to challenge the bill in court, CNN said.
A version of this article first appeared on Medscape.com.