User login
Using Telehealth Rehabilitation Therapy to Treat a Finger Flexor Tendon Repair During COVID-19
Telehealth-assisted finger rehabilitat ion therapy demonstrated good functional results following repair of a zone 2 flexor tendon laceration.
In 1948, Sterling Bunnell, MD, used the term no man’s land to describe the area between the A1 pulley at the volar aspect of the metacarpophalangeal joint and the insertion of the flexor digitorum superficialis tendons on the middle phalanx (zone 2).1 Bunnell’s description referenced the area of land in World War I between the trenches of opposing armies, and his goal was to emphasize the heightened risks of performing tendon repair in this area, as these repairs were notorious for poor outcomes. In lieu of tendon repair, Bunnell advocated treatment of tendon lacerations in this area with tendon excision and grafting.
It was not until the 1960s that researchers began to advocate for acute repair of tendons in this area.2,3 Since Verdan’s and Kleinart’s work, fastidious adherence to atraumatic technique and improvements in suture technique and rehabilitation protocols have allowed hand surgeons to repair tendons in this area with some level of success. Over the ensuing decades, acute repair of flexor tendon injuries within zone 2 has become the standard of care. The importance of meticulous technique during flexor tendon repair cannot be overemphasized; however, without appropriate hand therapy, even the most meticulous repair may fail.
COVID-19 has created significant barriers to patient care. Reducing travel and limiting face-to-face patient visits have been emphasized as methods that reduce spread of the virus, but these restrictions also prevent patients from easily accessing hand therapy. Recent adoption of telemedicine and videoconferencing technologies may help to reduce some of these barriers, but few previous studies have described the use of videoconferencing technology to supplant face-to-face hand therapy visits. This case describes the use of videoconferencing technology to provide hand therapy for a patient following repair of an acute flexor tendon laceration in zone 2.
Case Presentation
A patient aged < 50 years presented to a US Department of Veterans Affairs (VA) hand surgery clinic 2 days after sustaining a laceration to the flexor digitorum profundus (FDP) in zone 2 of the small finger while cleaning a knife. During the discussion of their treatment options and the recommended postoperative hand therapy protocol, the patient noted difficulty attending postoperative appointments due to COVID-19 as well as a lack of resources. Given these limitations and following discussion with our hand therapist, we discussed the potential for telehealth follow-up with videoconferencing. Four days following the injury, the patient underwent repair of the FDP. During surgery, the laceration was present at the level of the A3 pulley. The FDP was repaired using a 6-0 polypropylene synthetic suture for the epitendinous repair and 4-strand core suture repair using 3-0 Fiberwire suture in a modified cruciate fashion. The A2 and A4 pulleys were preserved, and venting of the pulleys was not required. At the time of surgery, the flexor digitorum superficialis and radial and ulnar digital neurovascular bundles were intact. Following surgical repair of the tendon, the patient was placed into a dorsal blocking splint with a plan for follow-up within 2 to 3 days.
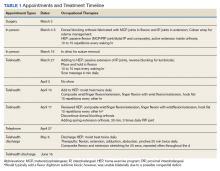
The patient attended the first postoperative visit in person on postoperative day 2. During this visit, the postoperative splint and dressings were removed, and a forearm-based dorsal blocking orthosis was fabricated using thermoplastic. At this visit, the veteran relayed concerns regarding psychosocial and resource barriers in addition to concerns surrounding COVID-19 that would prevent travel to and from hand therapy appointments. Due to these concerns, a passive-motion protocol was initiated using the Indiana manual as a guide.4 The patient returned to the hand clinic at 2 weeks after surgery for evaluation by the operating surgeon and suture removal. All visits after the suture removal were conducted via either telehealth with videoconferencing or by telephone (Table 1).
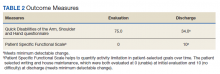
The operative team evaluated the patient 5 times following surgery. Only 2 of these visits were in-person. The patient attended 6 hand therapy sessions with 2 in-person visits to occupational therapy (Figure 1). The remaining 4 visits were conducted using videoconferencing. The patient received therapy supplies by mail as needed, and their use was reviewed in telerehabilitation sessions with videoconferencing as needed. During their postoperative course, the patient experienced little edema or scar tissue formation, and recovery was uncomplicated. The patient developed a mild extensor lag for which a proximal interphalangeal joint spring extension orthosis was provided via mail (Figure 2). The patient admitted only partial adherence with this orthosis, and at discharge, a 10-degree extensor lag remained. The patient was not concerned by this extension deficit and did not experience any associated functional deficits, demonstrated by scores on the Quick Disabilities of the Arm, Shoulder and Hand questionnaire and Patient Specific Functional Scale (Table 2).
Discussion
Few studies have been published that address the efficacy of telerehabilitation after surgical management of traumatic injuries involving the upper extremity. One Australian study performed by Worboys and colleagues concluded that utilization of telehealth services for hand therapy visits may provide accurate patient assessment with favorable patient satisfaction.5 Another study performed in the UK by Gilbert and colleagues demonstrated that videoconferencing is well received by patients, as it may offer shorter wait times, improved convenience, and reduced travel cost.
The authors noted that although videoconferencing may not completely replace in-person therapy, it could act as an adjunct.6 While these in-person visits may be necessary, particularly to establish care, at least one study has demonstrated that patients may prefer follow-up via telehealth if provided the option.7 In a randomized, controlled study performed in Norway, patients were randomized to either an in-person or video consultation with an orthopedic outpatient clinic. Of patients randomized to the in-person clinic visit, 86% preferred to have follow-up via videoconferencing.7
Previous studies have demonstrated that telehealth may produce accurate patient assessment, with relatively high patient satisfaction. Given the COVID-19 pandemic and the limitations that this crisis has placed on in-person outpatient visits, clinics that previously may have been resistant to telehealth are adapting and using the technology to meet the needs of their population.8 The present case demonstrates that videoconferencing is feasible and may lead to successful results, even for cases requiring significant hand therapy follow-up, such as flexor tendon repairs.
Conclusions
Although in-person hand therapy remains the standard of care following flexor tendon repair of the hand, situations may exist in which hand therapy conducted via telehealth is better than no hand therapy at all. The present case study highlights the use of telehealth as an acceptable supplement to in-person postoperative visits.
In our case, use of a standardized protocol with an emphasis on hand function and patient satisfaction as opposed to strict range of motion measurements produced good results. Although a specific telehealth satisfaction measure was not used in this case, commonly used questionnaires may be integrated into future visits to improve telehealth implementation and patient experience. In this specific case, the veteran felt that hand function was regained and expressed general satisfaction with the telemedicine process at the conclusion of care. While telehealth was a useful adjunct in the treatment of the present patient, further study of videoconferencing should be conducted to determine whether hand therapy conducted via telehealth could be implemented more broadly following upper extremity surgery.
1. Hege JJ. History off-hand: Bunnell’s no-man’s land. Hand (NY). 2019;14(4):570-574. doi:10.1177/1558944717744337
2. Verdan C. Primary repair of flexor tendons. J Bone Joint Surg Am. 1960;42-A:647-657.
3. Kleinert HE, Kutz JE, Ashbell TS, et al. Primary repair of lacerated flexor tendon in no man’s land (abstract). J Bone Joint Surg. 1967;49A:577.
4. Cannon NM. Diagnosis and Treatment Manual for Physicians and Therapists: Upper Extremity Rehabilitation. 4th ed. Hand Rehabilitation Center of Indiana; 2001.
5. Worboys T, Brassington M, Ward EC, Cornwell PL. Delivering occupational therapy hand assessment and treatment sessions via telehealth. J Telemed Telecare. 2018;24(3):185-192. doi:10.1177/1357633X17691861
6. Gilbert AW, Jaggi A, May CR. What is the patient acceptability of real time 1:1 videoconferencing in an orthopaedics setting? A systematic review. Physiotherapy. 2018;104(2):178-186. doi:10.1016/j.physio.2017.11.217
7. Buvik A, Bugge E, Knutsen G, Smatresk A, Wilsgaard T. Patient reported outcomes with remote orthopaedic consultations by telemedicine: A randomised controlled trial. J Telemed Telecare. 2019;25(8):451-459. doi:10.1177/1357633X18783921
8. Loeb AE, Rao SS, Ficke JR, Morris CD, Riley LH 3rd, Levin AS. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J Am Acad Orthop Surg. 2020;28(11):e469-e476. doi:10.5435/JAAOS-D-20-00380
Telehealth-assisted finger rehabilitat ion therapy demonstrated good functional results following repair of a zone 2 flexor tendon laceration.
Telehealth-assisted finger rehabilitat ion therapy demonstrated good functional results following repair of a zone 2 flexor tendon laceration.
In 1948, Sterling Bunnell, MD, used the term no man’s land to describe the area between the A1 pulley at the volar aspect of the metacarpophalangeal joint and the insertion of the flexor digitorum superficialis tendons on the middle phalanx (zone 2).1 Bunnell’s description referenced the area of land in World War I between the trenches of opposing armies, and his goal was to emphasize the heightened risks of performing tendon repair in this area, as these repairs were notorious for poor outcomes. In lieu of tendon repair, Bunnell advocated treatment of tendon lacerations in this area with tendon excision and grafting.
It was not until the 1960s that researchers began to advocate for acute repair of tendons in this area.2,3 Since Verdan’s and Kleinart’s work, fastidious adherence to atraumatic technique and improvements in suture technique and rehabilitation protocols have allowed hand surgeons to repair tendons in this area with some level of success. Over the ensuing decades, acute repair of flexor tendon injuries within zone 2 has become the standard of care. The importance of meticulous technique during flexor tendon repair cannot be overemphasized; however, without appropriate hand therapy, even the most meticulous repair may fail.
COVID-19 has created significant barriers to patient care. Reducing travel and limiting face-to-face patient visits have been emphasized as methods that reduce spread of the virus, but these restrictions also prevent patients from easily accessing hand therapy. Recent adoption of telemedicine and videoconferencing technologies may help to reduce some of these barriers, but few previous studies have described the use of videoconferencing technology to supplant face-to-face hand therapy visits. This case describes the use of videoconferencing technology to provide hand therapy for a patient following repair of an acute flexor tendon laceration in zone 2.
Case Presentation
A patient aged < 50 years presented to a US Department of Veterans Affairs (VA) hand surgery clinic 2 days after sustaining a laceration to the flexor digitorum profundus (FDP) in zone 2 of the small finger while cleaning a knife. During the discussion of their treatment options and the recommended postoperative hand therapy protocol, the patient noted difficulty attending postoperative appointments due to COVID-19 as well as a lack of resources. Given these limitations and following discussion with our hand therapist, we discussed the potential for telehealth follow-up with videoconferencing. Four days following the injury, the patient underwent repair of the FDP. During surgery, the laceration was present at the level of the A3 pulley. The FDP was repaired using a 6-0 polypropylene synthetic suture for the epitendinous repair and 4-strand core suture repair using 3-0 Fiberwire suture in a modified cruciate fashion. The A2 and A4 pulleys were preserved, and venting of the pulleys was not required. At the time of surgery, the flexor digitorum superficialis and radial and ulnar digital neurovascular bundles were intact. Following surgical repair of the tendon, the patient was placed into a dorsal blocking splint with a plan for follow-up within 2 to 3 days.
The patient attended the first postoperative visit in person on postoperative day 2. During this visit, the postoperative splint and dressings were removed, and a forearm-based dorsal blocking orthosis was fabricated using thermoplastic. At this visit, the veteran relayed concerns regarding psychosocial and resource barriers in addition to concerns surrounding COVID-19 that would prevent travel to and from hand therapy appointments. Due to these concerns, a passive-motion protocol was initiated using the Indiana manual as a guide.4 The patient returned to the hand clinic at 2 weeks after surgery for evaluation by the operating surgeon and suture removal. All visits after the suture removal were conducted via either telehealth with videoconferencing or by telephone (Table 1).
The operative team evaluated the patient 5 times following surgery. Only 2 of these visits were in-person. The patient attended 6 hand therapy sessions with 2 in-person visits to occupational therapy (Figure 1). The remaining 4 visits were conducted using videoconferencing. The patient received therapy supplies by mail as needed, and their use was reviewed in telerehabilitation sessions with videoconferencing as needed. During their postoperative course, the patient experienced little edema or scar tissue formation, and recovery was uncomplicated. The patient developed a mild extensor lag for which a proximal interphalangeal joint spring extension orthosis was provided via mail (Figure 2). The patient admitted only partial adherence with this orthosis, and at discharge, a 10-degree extensor lag remained. The patient was not concerned by this extension deficit and did not experience any associated functional deficits, demonstrated by scores on the Quick Disabilities of the Arm, Shoulder and Hand questionnaire and Patient Specific Functional Scale (Table 2).
Discussion
Few studies have been published that address the efficacy of telerehabilitation after surgical management of traumatic injuries involving the upper extremity. One Australian study performed by Worboys and colleagues concluded that utilization of telehealth services for hand therapy visits may provide accurate patient assessment with favorable patient satisfaction.5 Another study performed in the UK by Gilbert and colleagues demonstrated that videoconferencing is well received by patients, as it may offer shorter wait times, improved convenience, and reduced travel cost.
The authors noted that although videoconferencing may not completely replace in-person therapy, it could act as an adjunct.6 While these in-person visits may be necessary, particularly to establish care, at least one study has demonstrated that patients may prefer follow-up via telehealth if provided the option.7 In a randomized, controlled study performed in Norway, patients were randomized to either an in-person or video consultation with an orthopedic outpatient clinic. Of patients randomized to the in-person clinic visit, 86% preferred to have follow-up via videoconferencing.7
Previous studies have demonstrated that telehealth may produce accurate patient assessment, with relatively high patient satisfaction. Given the COVID-19 pandemic and the limitations that this crisis has placed on in-person outpatient visits, clinics that previously may have been resistant to telehealth are adapting and using the technology to meet the needs of their population.8 The present case demonstrates that videoconferencing is feasible and may lead to successful results, even for cases requiring significant hand therapy follow-up, such as flexor tendon repairs.
Conclusions
Although in-person hand therapy remains the standard of care following flexor tendon repair of the hand, situations may exist in which hand therapy conducted via telehealth is better than no hand therapy at all. The present case study highlights the use of telehealth as an acceptable supplement to in-person postoperative visits.
In our case, use of a standardized protocol with an emphasis on hand function and patient satisfaction as opposed to strict range of motion measurements produced good results. Although a specific telehealth satisfaction measure was not used in this case, commonly used questionnaires may be integrated into future visits to improve telehealth implementation and patient experience. In this specific case, the veteran felt that hand function was regained and expressed general satisfaction with the telemedicine process at the conclusion of care. While telehealth was a useful adjunct in the treatment of the present patient, further study of videoconferencing should be conducted to determine whether hand therapy conducted via telehealth could be implemented more broadly following upper extremity surgery.
In 1948, Sterling Bunnell, MD, used the term no man’s land to describe the area between the A1 pulley at the volar aspect of the metacarpophalangeal joint and the insertion of the flexor digitorum superficialis tendons on the middle phalanx (zone 2).1 Bunnell’s description referenced the area of land in World War I between the trenches of opposing armies, and his goal was to emphasize the heightened risks of performing tendon repair in this area, as these repairs were notorious for poor outcomes. In lieu of tendon repair, Bunnell advocated treatment of tendon lacerations in this area with tendon excision and grafting.
It was not until the 1960s that researchers began to advocate for acute repair of tendons in this area.2,3 Since Verdan’s and Kleinart’s work, fastidious adherence to atraumatic technique and improvements in suture technique and rehabilitation protocols have allowed hand surgeons to repair tendons in this area with some level of success. Over the ensuing decades, acute repair of flexor tendon injuries within zone 2 has become the standard of care. The importance of meticulous technique during flexor tendon repair cannot be overemphasized; however, without appropriate hand therapy, even the most meticulous repair may fail.
COVID-19 has created significant barriers to patient care. Reducing travel and limiting face-to-face patient visits have been emphasized as methods that reduce spread of the virus, but these restrictions also prevent patients from easily accessing hand therapy. Recent adoption of telemedicine and videoconferencing technologies may help to reduce some of these barriers, but few previous studies have described the use of videoconferencing technology to supplant face-to-face hand therapy visits. This case describes the use of videoconferencing technology to provide hand therapy for a patient following repair of an acute flexor tendon laceration in zone 2.
Case Presentation
A patient aged < 50 years presented to a US Department of Veterans Affairs (VA) hand surgery clinic 2 days after sustaining a laceration to the flexor digitorum profundus (FDP) in zone 2 of the small finger while cleaning a knife. During the discussion of their treatment options and the recommended postoperative hand therapy protocol, the patient noted difficulty attending postoperative appointments due to COVID-19 as well as a lack of resources. Given these limitations and following discussion with our hand therapist, we discussed the potential for telehealth follow-up with videoconferencing. Four days following the injury, the patient underwent repair of the FDP. During surgery, the laceration was present at the level of the A3 pulley. The FDP was repaired using a 6-0 polypropylene synthetic suture for the epitendinous repair and 4-strand core suture repair using 3-0 Fiberwire suture in a modified cruciate fashion. The A2 and A4 pulleys were preserved, and venting of the pulleys was not required. At the time of surgery, the flexor digitorum superficialis and radial and ulnar digital neurovascular bundles were intact. Following surgical repair of the tendon, the patient was placed into a dorsal blocking splint with a plan for follow-up within 2 to 3 days.
The patient attended the first postoperative visit in person on postoperative day 2. During this visit, the postoperative splint and dressings were removed, and a forearm-based dorsal blocking orthosis was fabricated using thermoplastic. At this visit, the veteran relayed concerns regarding psychosocial and resource barriers in addition to concerns surrounding COVID-19 that would prevent travel to and from hand therapy appointments. Due to these concerns, a passive-motion protocol was initiated using the Indiana manual as a guide.4 The patient returned to the hand clinic at 2 weeks after surgery for evaluation by the operating surgeon and suture removal. All visits after the suture removal were conducted via either telehealth with videoconferencing or by telephone (Table 1).
The operative team evaluated the patient 5 times following surgery. Only 2 of these visits were in-person. The patient attended 6 hand therapy sessions with 2 in-person visits to occupational therapy (Figure 1). The remaining 4 visits were conducted using videoconferencing. The patient received therapy supplies by mail as needed, and their use was reviewed in telerehabilitation sessions with videoconferencing as needed. During their postoperative course, the patient experienced little edema or scar tissue formation, and recovery was uncomplicated. The patient developed a mild extensor lag for which a proximal interphalangeal joint spring extension orthosis was provided via mail (Figure 2). The patient admitted only partial adherence with this orthosis, and at discharge, a 10-degree extensor lag remained. The patient was not concerned by this extension deficit and did not experience any associated functional deficits, demonstrated by scores on the Quick Disabilities of the Arm, Shoulder and Hand questionnaire and Patient Specific Functional Scale (Table 2).
Discussion
Few studies have been published that address the efficacy of telerehabilitation after surgical management of traumatic injuries involving the upper extremity. One Australian study performed by Worboys and colleagues concluded that utilization of telehealth services for hand therapy visits may provide accurate patient assessment with favorable patient satisfaction.5 Another study performed in the UK by Gilbert and colleagues demonstrated that videoconferencing is well received by patients, as it may offer shorter wait times, improved convenience, and reduced travel cost.
The authors noted that although videoconferencing may not completely replace in-person therapy, it could act as an adjunct.6 While these in-person visits may be necessary, particularly to establish care, at least one study has demonstrated that patients may prefer follow-up via telehealth if provided the option.7 In a randomized, controlled study performed in Norway, patients were randomized to either an in-person or video consultation with an orthopedic outpatient clinic. Of patients randomized to the in-person clinic visit, 86% preferred to have follow-up via videoconferencing.7
Previous studies have demonstrated that telehealth may produce accurate patient assessment, with relatively high patient satisfaction. Given the COVID-19 pandemic and the limitations that this crisis has placed on in-person outpatient visits, clinics that previously may have been resistant to telehealth are adapting and using the technology to meet the needs of their population.8 The present case demonstrates that videoconferencing is feasible and may lead to successful results, even for cases requiring significant hand therapy follow-up, such as flexor tendon repairs.
Conclusions
Although in-person hand therapy remains the standard of care following flexor tendon repair of the hand, situations may exist in which hand therapy conducted via telehealth is better than no hand therapy at all. The present case study highlights the use of telehealth as an acceptable supplement to in-person postoperative visits.
In our case, use of a standardized protocol with an emphasis on hand function and patient satisfaction as opposed to strict range of motion measurements produced good results. Although a specific telehealth satisfaction measure was not used in this case, commonly used questionnaires may be integrated into future visits to improve telehealth implementation and patient experience. In this specific case, the veteran felt that hand function was regained and expressed general satisfaction with the telemedicine process at the conclusion of care. While telehealth was a useful adjunct in the treatment of the present patient, further study of videoconferencing should be conducted to determine whether hand therapy conducted via telehealth could be implemented more broadly following upper extremity surgery.
1. Hege JJ. History off-hand: Bunnell’s no-man’s land. Hand (NY). 2019;14(4):570-574. doi:10.1177/1558944717744337
2. Verdan C. Primary repair of flexor tendons. J Bone Joint Surg Am. 1960;42-A:647-657.
3. Kleinert HE, Kutz JE, Ashbell TS, et al. Primary repair of lacerated flexor tendon in no man’s land (abstract). J Bone Joint Surg. 1967;49A:577.
4. Cannon NM. Diagnosis and Treatment Manual for Physicians and Therapists: Upper Extremity Rehabilitation. 4th ed. Hand Rehabilitation Center of Indiana; 2001.
5. Worboys T, Brassington M, Ward EC, Cornwell PL. Delivering occupational therapy hand assessment and treatment sessions via telehealth. J Telemed Telecare. 2018;24(3):185-192. doi:10.1177/1357633X17691861
6. Gilbert AW, Jaggi A, May CR. What is the patient acceptability of real time 1:1 videoconferencing in an orthopaedics setting? A systematic review. Physiotherapy. 2018;104(2):178-186. doi:10.1016/j.physio.2017.11.217
7. Buvik A, Bugge E, Knutsen G, Smatresk A, Wilsgaard T. Patient reported outcomes with remote orthopaedic consultations by telemedicine: A randomised controlled trial. J Telemed Telecare. 2019;25(8):451-459. doi:10.1177/1357633X18783921
8. Loeb AE, Rao SS, Ficke JR, Morris CD, Riley LH 3rd, Levin AS. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J Am Acad Orthop Surg. 2020;28(11):e469-e476. doi:10.5435/JAAOS-D-20-00380
1. Hege JJ. History off-hand: Bunnell’s no-man’s land. Hand (NY). 2019;14(4):570-574. doi:10.1177/1558944717744337
2. Verdan C. Primary repair of flexor tendons. J Bone Joint Surg Am. 1960;42-A:647-657.
3. Kleinert HE, Kutz JE, Ashbell TS, et al. Primary repair of lacerated flexor tendon in no man’s land (abstract). J Bone Joint Surg. 1967;49A:577.
4. Cannon NM. Diagnosis and Treatment Manual for Physicians and Therapists: Upper Extremity Rehabilitation. 4th ed. Hand Rehabilitation Center of Indiana; 2001.
5. Worboys T, Brassington M, Ward EC, Cornwell PL. Delivering occupational therapy hand assessment and treatment sessions via telehealth. J Telemed Telecare. 2018;24(3):185-192. doi:10.1177/1357633X17691861
6. Gilbert AW, Jaggi A, May CR. What is the patient acceptability of real time 1:1 videoconferencing in an orthopaedics setting? A systematic review. Physiotherapy. 2018;104(2):178-186. doi:10.1016/j.physio.2017.11.217
7. Buvik A, Bugge E, Knutsen G, Smatresk A, Wilsgaard T. Patient reported outcomes with remote orthopaedic consultations by telemedicine: A randomised controlled trial. J Telemed Telecare. 2019;25(8):451-459. doi:10.1177/1357633X18783921
8. Loeb AE, Rao SS, Ficke JR, Morris CD, Riley LH 3rd, Levin AS. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J Am Acad Orthop Surg. 2020;28(11):e469-e476. doi:10.5435/JAAOS-D-20-00380
Review of Efficacy and Safety of Spinal Cord Stimulation in Veterans
Lower back pain (LBP) affects an estimated 9.4% of the global population and has resulted in more years lived with disability than any other health condition.1 LBP affects a wide range of populations, but US veterans have been shown to have significantly higher rates of back pain than nonveterans. The National Institutes of Health reports that 65.6% of veterans experience chronic pain; 9.1% of veterans experience severe, chronic pain.2 Chronic back pain is treated by a range of methods, including medications, surgery, physical therapy (PT), patient education, and behavioral therapy.3 However, chronic neuropathic back pain has been shown to have limited responsiveness to medication.4
Neuropathic pain is caused by lesions in the somatosensory nervous system, resulting in spontaneous pain and amplified pain responses to both painful and nonpainful stimuli.5 The most common location for neuropathic pain is the back and legs. Between 10% and 40% of people who undergo lumbosacral spine surgery to treat neuropathic radicular pain will experience further neuropathic pain.6 This condition is referred to as failed back surgery syndrome or postlaminectomy syndrome (PLS). While neuropathic back pain has had limited responsiveness to medication and repeated lumbosacral spine surgery, spinal cord stimulation (SCS) has shown promise as an effective form of pain treatment for those experiencing PLS and other spine disorders.7-10 In addition, SCS therapy has had a very low incidence of complications, which may be on the decline with recent technological advancements.11 Patients with a diagnosis of PLS, LBP, or complex regional pain syndrome (CRPS) who have not responded to medications, therapy, and/or injections for ≥ 6 months were eligible for a trial of SCS therapy. Trial leads were placed via the percutaneous route with the battery strapped to the waistline for 3 to 5 days and were removed in clinic. Patients who experienced > 60% pain relief and functional improvement received a SCS implant.
The effectiveness of SCS has been demonstrated in a nonveteran population, but it has not been studied in a veteran population.12 US Department of Veterans Affairs (VA) health care coverage is different from Medicare and private insurance in that it is classified as a benefit and not insurance. The goals of treatment at the VA may include considerations in addition to feeling better, and patient presentations may not align with those in the private sector.
We hypothesize that SCS is both a safe and beneficial treatment option for veterans with chronic intractable spine and/or extremity pain. The purpose of this study was to determine the efficacy and safety of SCS in a veteran population.
Methods
The efficacy and safety of SCS was determined via a retrospective study. Inclusion criteria for the study consisted of any Southeastern Louisiana Veterans Health Care System (SLVHCS) patient who had an SCS trial and/or implant from 2008 to 2020. Eligible veterans must have had chronic pain for at least 6 months and had previously tried multiple medications, PT, transcutaneous nerve stimulation, facet injections, epidural steroid injections, or surgery without success. For medication therapy to be considered unsuccessful, it must have included acetaminophen, nonsteroidal anti-inflammatory drugs, and ≥ 1 adjuvant medication (gabapentin, duloxetine, amitriptyline, lidocaine, and menthol). A diagnosis of chronic LBP, PLS, cervical or lumbar spondylosis with radiculopathy, complex regional pain syndrome, or chronic pain syndrome was required for eligibility. Patients whose pain decreased by > 60% and had functional improvement in a 3- to 5-day trial received SCS implantation with percutaneous leads by a pain physician or paddle lead by a neurosurgeon.
The SLVHCS Institutional Review Board approved this study. Electronic health records were reviewed to determine patient age, anthropometric data, and date of SCS implantation. Patients were then called and interviewed to complete a survey. After obtaining verbal consent to the study, subjects were surveyed regarding whether the patient would recommend the procedure to peers, adverse effects (AEs) or complications, and the ability to decrease opiates if applicable. A verbal Pain Outcome Questionnaire (POQ) assessment of activities of daily living also was given during the phone interview regarding pain levels before SCS and at the time of the phone interview.13 (eAppendix available at doi:10.12788/fp.0204) Following the survey, a chart review was performed to corroborate the given AEs or complications and opiate use information. Before and after results of the POQ were compared via a paired sample t test, and P values < .05 were considered significant. Analyses were performed by IBM SPSS, version 26.
The primary outcome measure for this study was whether veterans would recommend SCS to their peers; in our view, this categorical outcome measure seemed to be more valuable to share with future patients who might be candidates for SCS. Since VA health care coverage and goals of treatment may be different from a nonveteran population, we opted to use this primary measure to decrease the possibility of confounding variables.
Secondary outcome measures included changes in POC scores, improvements in activities of daily living, and decreases in use of opioid pain medications.
POQ responses were recorded during the telephone interviews (0 to 10 scale). A paired sample t test was conducted to compare pain levels before and after SCS implant. Pain levels were gathered in the single phone call. Patient opioid usage, if applicable, was assessed by converting medications to morphine milligram equivalent dosing (MMED). Since patients who were on chronic opioids took multiple formulations, we changed the total daily dose to all morphine; for this study, morphine was considered equivalent to hydrocodone, and oxycodone was 1.5x morphine.
Results
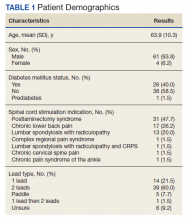
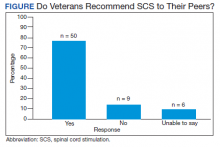
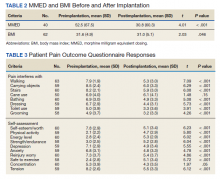
Of the 90 SLVHCS patients who received an SCS implant between 2008 and 2020, 76 were reached by telephone and 65 had their responses recorded in the study. Of the 11 patients who were not included, 5 had the SCS removed; it is unclear whether these veterans would have recommended the treatment. Four were unable to quantify pain and/or SCS effects, and 2 were excluded due to a dementia diagnosis years after the implant. The mean (SD) age of participants was 63.9 (10.3) years. Forty percent of patients had a diabetes mellitus diagnosis and 1 had prediabetes. Patients’ most common qualifying diagnosis for SCS was PLS (47.7%) followed by chronic LBP (26.2%). A percutaneous 2-lead technique was the most common type of SCS type used (60.0%) followed by 1-lead (21.5%). The most common SCS manufacturer was Boston Scientific (87.7%)(Table 1). Most veterans (76.9%) recommended SCS to their peers; 13.8% did not recommend SCS; 9.2% were undecided and stated that they were unable to recommend because they did not want to persuade a peer to get SCS (Figure).
There was a statistically significant decrease in opioid use for the 40 veterans for whom pain medication was converted (P < .001)(Table 2). Six patients reported using opioids at some point but could not remember their dose, and no records were found in their chart review, so they were not included in the MMED analysis. In that group, 4 patients reported using opioids before SCS but discontinued the opioid use after SCS implantation, and 2 patients noted using opioids before SCS and concomitantly. Eighteen subjects reported no opioid use at any point before or after SCS (Table 3).
There were few life-threatening complications of SCS. Three veterans developed skin dehiscence; 2 had dehiscence at the battery/generator site, and 1 had dehiscence at the lead anchor site. Two patients with dehiscence also had morbid obesity, and the third had postoperative malnourishment. The dehiscence occurred 3 and 8 months postoperation. All 3 patients with dehiscence had the SCS explanted, though they were eager to get a new SCS implanted as soon as possible because SCS was their most successful treatment to date.
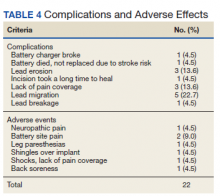
Twenty of the 64 veterans surveyed reported other complications of SCS, including lead migration, lack of pain coverage, paresthesia and numbness, soreness around generator site, SCS shocking patient when performing full thoracic spine flexion, and shingles at the battery site (Table 4). There were 11 explants among the 76 veterans contacted. The primary reason for explant was lack of pain coverage.
Patient concerns included pain with sitting in chairs due to tenderness around the implant, SCS helping with physical pain but not mental pain, SCS only working during the day and not helping with sleep, and patients lacking education regarding possible complications of SCS.
Discussion
In this nonrandomized retrospective review, SCS was shown to be an effective treatment for intractable spine and/or extremity pain. Veterans’ pain levels were significantly reduced following SCS implantation, and more than three-fourths of veterans recommended SCS to their peers. We used the recommendation of SCS to peers as the most important metric regarding the effectiveness of SCS, as this measure was felt to be more valuable to share with future patients; furthermore, categorical analysis has been shown to be more valuable than ordinal pain scales to measure pain.14 In addition to wanting to expand the available research to the general public, we wanted a measure that we could easily relay to our patient population regarding SCS.
The explant rate of 14.5% among surveyed veterans falls at the higher end of the normal ranges found in previous studies of long-term SCS outcomes.15-17 One possible reason for the higher rate is that we did not differentiate based on the reason for the explant (ie, no benefit, further surgery needed for underlying medical condition, or SCS-specific complications). Another possible contributing factor to the higher than expected explant rate is the geographic location in the New Orleans metro area; New Orleans is considered to have one of the highest rates of obesity in the United States and obesity typically has other diseases associated with it such as hypertension and diabetes mellitus.
Limitations
Limitations of the study include the relatively low number of subjects, subjective nature of the interview questions, and the patients’ answers. Typically the POQ has been used as a prospective assessment of pain; whether it is valid in a retrospective analysis is not clear. While there was a statistically significant decrease of opioid use after getting SCS, this study can only show correlation, not causation. During the study period, there has been a drastic change in opioid prescribing patterns and efforts to decrease the amount of opioids prescribed.
Subjects also were asked to rate their pain and quality of life before SCS. Some subjects had SCS implantation up to 10 years prior to the phone interview. The variable amount of time between SCS implantation and interview likely affected subjects’ responses. Chronic pain is a moving target. Patients have good days and bad days that would likely change opinions on SCS benefits on a single phone interview. Some patients needed battery replacements at the time of the interview (battery life averaged about 3 to 5 years in our study population) and were asked to report current levels of pain from the perspective of when their batteries were still functional, further affecting results.
Conclusions
SCS was shown to improve the quality of life of US veterans at SLVHCS across a wide variety of metrics, including activities of daily living, as well as mental and physical health. For veterans with chronic intractable pain who have tried and failed more conservative treatments, SCS is a great treatment.
1. Hoy DG, Smith E, Cross M, et al. The global burden of musculoskeletal conditions for 2010: an overview of methods. Ann Rheum Dis. 2014;73(6):982-989 doi:10.1136/annrheumdis-2013-204344
2. Nahin RL. Severe pain in veterans: the effect of age and sex, and comparisons with the general population. J Pain. 2017;18(3):247-254. doi:10.1016/j.jpain.2016.10.021
3. Institute of Medicine (US) Committee on Advancing Pain Research, Care, and Education. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: National Academies Press; 2011.
4. Finnerup NB, Attal N, Haroutounian S, et al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. 2015;14(2):162-173. doi:10.1016/S1474-4422(14)70251-0
5. Costigan M, Scholz J, Woolf CJ. Neuropathic pain: a maladaptive response of the nervous system to damage. Annu Rev Neurosci. 2009;32:1-32. doi:10.1146/annurev.neuro.051508.135531
6. Wilkinson HA. The Failed Back Syndrome: Etiology and Therapy. 2nd ed. Harper & Row; 1991.
7. Kumar K, Taylor RS, Jacques L, et al. Spinal cord stimulation versus conventional medical management for neuropathic pain: a multicentre randomised controlled trial in patients with failed back surgery syndrome. Pain. 2007;132(1-2):179-188. doi:10.1016/j.pain.2007.07.028
8. North RB, Kidd DH, Farrokhi F, Piantadosi SA. Spinal cord stimulation versus repeated lumbosacral spine surgery for chronic pain: a randomized, controlled trial. Neurosurgery. 2005;56(1):98-107. doi:10.1227/01.neu.0000144839.65524.e0
9. Geurts JW, Smits H, Kemler MA, Brunner F, Kessels AG, van Kleef M. Spinal cord stimulation for complex regional pain syndrome type I: a prospective cohort study with long-term follow-up. Neuromodulation. 2013;16(6):523-529. doi:10.1111/ner.12024
10. Kumar K, Rizvi S, Bnurs SB. Spinal cord stimulation is effective in management of complex regional pain syndrome I: fact or fiction. Neurosurgery. 2011;69(3):566-5580. doi:10.1227/NEU.0b013e3182181e60
11. Mekhail NA, Mathews M, Nageeb F, Guirguis M, Mekhail MN, Cheng J. Retrospective review of 707 cases of spinal cord stimulation: indications and complications. Pain Pract. 2011;11(2):148-153. doi:10.1111/j.1533-2500.2010.00407.x
12. Veizi E, Hayek SM, North J, et al. Spinal cord stimulation (SCS) with anatomically guided (3D) neural targeting shows superior chronic axial low back pain relief compared to traditional SCS-LUMINA Study. Pain Med. 2017;18(8):1534-1548. doi:10.1093/pm/pnw286
13. Gordon DB, Polomano RC, Pellino TA, et al. Revised American Pain Society Patient Outcome Questionnaire (APS-POQ-R) for quality improvement of pain management in hospitalized adults: preliminary psychometric evaluation. J Pain. 2010;11(11):1172-1186. doi:10.1016/j.jpain.2010.02.012
14. Kennedy DJ, Schneider B. Lies, damn lies, and statistic: a commentary. Pain Med. 2020;21(10):2052-2054. doi:10.1093/pm/pnaa287
15. Van Buyten JP, Wille F, Smet I, et al. Therapy-related explants after spinal cord stimulation: results of an international retrospective chart review study. Neuromodulation. 2017;20(7):642-649. doi:10.1111/ner.12642
16. Hayek SM, Veizi E, Hanes M. Treatment-limiting complications of percutaneous spinal cord stimulator implants: a review of eight years of experience from an academic center database. Neuromodulation. 2015;18(7):603-609. doi:10.1111/ner.12312
17. Pope JE, Deer TR, Falowski S, et al. Multicenter retrospective study of neurostimulation with exit of therapy by explant. Neuromodulation. 2017;20(6):543-552. doi:10.1111/ner.12634
Lower back pain (LBP) affects an estimated 9.4% of the global population and has resulted in more years lived with disability than any other health condition.1 LBP affects a wide range of populations, but US veterans have been shown to have significantly higher rates of back pain than nonveterans. The National Institutes of Health reports that 65.6% of veterans experience chronic pain; 9.1% of veterans experience severe, chronic pain.2 Chronic back pain is treated by a range of methods, including medications, surgery, physical therapy (PT), patient education, and behavioral therapy.3 However, chronic neuropathic back pain has been shown to have limited responsiveness to medication.4
Neuropathic pain is caused by lesions in the somatosensory nervous system, resulting in spontaneous pain and amplified pain responses to both painful and nonpainful stimuli.5 The most common location for neuropathic pain is the back and legs. Between 10% and 40% of people who undergo lumbosacral spine surgery to treat neuropathic radicular pain will experience further neuropathic pain.6 This condition is referred to as failed back surgery syndrome or postlaminectomy syndrome (PLS). While neuropathic back pain has had limited responsiveness to medication and repeated lumbosacral spine surgery, spinal cord stimulation (SCS) has shown promise as an effective form of pain treatment for those experiencing PLS and other spine disorders.7-10 In addition, SCS therapy has had a very low incidence of complications, which may be on the decline with recent technological advancements.11 Patients with a diagnosis of PLS, LBP, or complex regional pain syndrome (CRPS) who have not responded to medications, therapy, and/or injections for ≥ 6 months were eligible for a trial of SCS therapy. Trial leads were placed via the percutaneous route with the battery strapped to the waistline for 3 to 5 days and were removed in clinic. Patients who experienced > 60% pain relief and functional improvement received a SCS implant.
The effectiveness of SCS has been demonstrated in a nonveteran population, but it has not been studied in a veteran population.12 US Department of Veterans Affairs (VA) health care coverage is different from Medicare and private insurance in that it is classified as a benefit and not insurance. The goals of treatment at the VA may include considerations in addition to feeling better, and patient presentations may not align with those in the private sector.
We hypothesize that SCS is both a safe and beneficial treatment option for veterans with chronic intractable spine and/or extremity pain. The purpose of this study was to determine the efficacy and safety of SCS in a veteran population.
Methods
The efficacy and safety of SCS was determined via a retrospective study. Inclusion criteria for the study consisted of any Southeastern Louisiana Veterans Health Care System (SLVHCS) patient who had an SCS trial and/or implant from 2008 to 2020. Eligible veterans must have had chronic pain for at least 6 months and had previously tried multiple medications, PT, transcutaneous nerve stimulation, facet injections, epidural steroid injections, or surgery without success. For medication therapy to be considered unsuccessful, it must have included acetaminophen, nonsteroidal anti-inflammatory drugs, and ≥ 1 adjuvant medication (gabapentin, duloxetine, amitriptyline, lidocaine, and menthol). A diagnosis of chronic LBP, PLS, cervical or lumbar spondylosis with radiculopathy, complex regional pain syndrome, or chronic pain syndrome was required for eligibility. Patients whose pain decreased by > 60% and had functional improvement in a 3- to 5-day trial received SCS implantation with percutaneous leads by a pain physician or paddle lead by a neurosurgeon.
The SLVHCS Institutional Review Board approved this study. Electronic health records were reviewed to determine patient age, anthropometric data, and date of SCS implantation. Patients were then called and interviewed to complete a survey. After obtaining verbal consent to the study, subjects were surveyed regarding whether the patient would recommend the procedure to peers, adverse effects (AEs) or complications, and the ability to decrease opiates if applicable. A verbal Pain Outcome Questionnaire (POQ) assessment of activities of daily living also was given during the phone interview regarding pain levels before SCS and at the time of the phone interview.13 (eAppendix available at doi:10.12788/fp.0204) Following the survey, a chart review was performed to corroborate the given AEs or complications and opiate use information. Before and after results of the POQ were compared via a paired sample t test, and P values < .05 were considered significant. Analyses were performed by IBM SPSS, version 26.
The primary outcome measure for this study was whether veterans would recommend SCS to their peers; in our view, this categorical outcome measure seemed to be more valuable to share with future patients who might be candidates for SCS. Since VA health care coverage and goals of treatment may be different from a nonveteran population, we opted to use this primary measure to decrease the possibility of confounding variables.
Secondary outcome measures included changes in POC scores, improvements in activities of daily living, and decreases in use of opioid pain medications.
POQ responses were recorded during the telephone interviews (0 to 10 scale). A paired sample t test was conducted to compare pain levels before and after SCS implant. Pain levels were gathered in the single phone call. Patient opioid usage, if applicable, was assessed by converting medications to morphine milligram equivalent dosing (MMED). Since patients who were on chronic opioids took multiple formulations, we changed the total daily dose to all morphine; for this study, morphine was considered equivalent to hydrocodone, and oxycodone was 1.5x morphine.
Results
Of the 90 SLVHCS patients who received an SCS implant between 2008 and 2020, 76 were reached by telephone and 65 had their responses recorded in the study. Of the 11 patients who were not included, 5 had the SCS removed; it is unclear whether these veterans would have recommended the treatment. Four were unable to quantify pain and/or SCS effects, and 2 were excluded due to a dementia diagnosis years after the implant. The mean (SD) age of participants was 63.9 (10.3) years. Forty percent of patients had a diabetes mellitus diagnosis and 1 had prediabetes. Patients’ most common qualifying diagnosis for SCS was PLS (47.7%) followed by chronic LBP (26.2%). A percutaneous 2-lead technique was the most common type of SCS type used (60.0%) followed by 1-lead (21.5%). The most common SCS manufacturer was Boston Scientific (87.7%)(Table 1). Most veterans (76.9%) recommended SCS to their peers; 13.8% did not recommend SCS; 9.2% were undecided and stated that they were unable to recommend because they did not want to persuade a peer to get SCS (Figure).
There was a statistically significant decrease in opioid use for the 40 veterans for whom pain medication was converted (P < .001)(Table 2). Six patients reported using opioids at some point but could not remember their dose, and no records were found in their chart review, so they were not included in the MMED analysis. In that group, 4 patients reported using opioids before SCS but discontinued the opioid use after SCS implantation, and 2 patients noted using opioids before SCS and concomitantly. Eighteen subjects reported no opioid use at any point before or after SCS (Table 3).
There were few life-threatening complications of SCS. Three veterans developed skin dehiscence; 2 had dehiscence at the battery/generator site, and 1 had dehiscence at the lead anchor site. Two patients with dehiscence also had morbid obesity, and the third had postoperative malnourishment. The dehiscence occurred 3 and 8 months postoperation. All 3 patients with dehiscence had the SCS explanted, though they were eager to get a new SCS implanted as soon as possible because SCS was their most successful treatment to date.
Twenty of the 64 veterans surveyed reported other complications of SCS, including lead migration, lack of pain coverage, paresthesia and numbness, soreness around generator site, SCS shocking patient when performing full thoracic spine flexion, and shingles at the battery site (Table 4). There were 11 explants among the 76 veterans contacted. The primary reason for explant was lack of pain coverage.
Patient concerns included pain with sitting in chairs due to tenderness around the implant, SCS helping with physical pain but not mental pain, SCS only working during the day and not helping with sleep, and patients lacking education regarding possible complications of SCS.
Discussion
In this nonrandomized retrospective review, SCS was shown to be an effective treatment for intractable spine and/or extremity pain. Veterans’ pain levels were significantly reduced following SCS implantation, and more than three-fourths of veterans recommended SCS to their peers. We used the recommendation of SCS to peers as the most important metric regarding the effectiveness of SCS, as this measure was felt to be more valuable to share with future patients; furthermore, categorical analysis has been shown to be more valuable than ordinal pain scales to measure pain.14 In addition to wanting to expand the available research to the general public, we wanted a measure that we could easily relay to our patient population regarding SCS.
The explant rate of 14.5% among surveyed veterans falls at the higher end of the normal ranges found in previous studies of long-term SCS outcomes.15-17 One possible reason for the higher rate is that we did not differentiate based on the reason for the explant (ie, no benefit, further surgery needed for underlying medical condition, or SCS-specific complications). Another possible contributing factor to the higher than expected explant rate is the geographic location in the New Orleans metro area; New Orleans is considered to have one of the highest rates of obesity in the United States and obesity typically has other diseases associated with it such as hypertension and diabetes mellitus.
Limitations
Limitations of the study include the relatively low number of subjects, subjective nature of the interview questions, and the patients’ answers. Typically the POQ has been used as a prospective assessment of pain; whether it is valid in a retrospective analysis is not clear. While there was a statistically significant decrease of opioid use after getting SCS, this study can only show correlation, not causation. During the study period, there has been a drastic change in opioid prescribing patterns and efforts to decrease the amount of opioids prescribed.
Subjects also were asked to rate their pain and quality of life before SCS. Some subjects had SCS implantation up to 10 years prior to the phone interview. The variable amount of time between SCS implantation and interview likely affected subjects’ responses. Chronic pain is a moving target. Patients have good days and bad days that would likely change opinions on SCS benefits on a single phone interview. Some patients needed battery replacements at the time of the interview (battery life averaged about 3 to 5 years in our study population) and were asked to report current levels of pain from the perspective of when their batteries were still functional, further affecting results.
Conclusions
SCS was shown to improve the quality of life of US veterans at SLVHCS across a wide variety of metrics, including activities of daily living, as well as mental and physical health. For veterans with chronic intractable pain who have tried and failed more conservative treatments, SCS is a great treatment.
Lower back pain (LBP) affects an estimated 9.4% of the global population and has resulted in more years lived with disability than any other health condition.1 LBP affects a wide range of populations, but US veterans have been shown to have significantly higher rates of back pain than nonveterans. The National Institutes of Health reports that 65.6% of veterans experience chronic pain; 9.1% of veterans experience severe, chronic pain.2 Chronic back pain is treated by a range of methods, including medications, surgery, physical therapy (PT), patient education, and behavioral therapy.3 However, chronic neuropathic back pain has been shown to have limited responsiveness to medication.4
Neuropathic pain is caused by lesions in the somatosensory nervous system, resulting in spontaneous pain and amplified pain responses to both painful and nonpainful stimuli.5 The most common location for neuropathic pain is the back and legs. Between 10% and 40% of people who undergo lumbosacral spine surgery to treat neuropathic radicular pain will experience further neuropathic pain.6 This condition is referred to as failed back surgery syndrome or postlaminectomy syndrome (PLS). While neuropathic back pain has had limited responsiveness to medication and repeated lumbosacral spine surgery, spinal cord stimulation (SCS) has shown promise as an effective form of pain treatment for those experiencing PLS and other spine disorders.7-10 In addition, SCS therapy has had a very low incidence of complications, which may be on the decline with recent technological advancements.11 Patients with a diagnosis of PLS, LBP, or complex regional pain syndrome (CRPS) who have not responded to medications, therapy, and/or injections for ≥ 6 months were eligible for a trial of SCS therapy. Trial leads were placed via the percutaneous route with the battery strapped to the waistline for 3 to 5 days and were removed in clinic. Patients who experienced > 60% pain relief and functional improvement received a SCS implant.
The effectiveness of SCS has been demonstrated in a nonveteran population, but it has not been studied in a veteran population.12 US Department of Veterans Affairs (VA) health care coverage is different from Medicare and private insurance in that it is classified as a benefit and not insurance. The goals of treatment at the VA may include considerations in addition to feeling better, and patient presentations may not align with those in the private sector.
We hypothesize that SCS is both a safe and beneficial treatment option for veterans with chronic intractable spine and/or extremity pain. The purpose of this study was to determine the efficacy and safety of SCS in a veteran population.
Methods
The efficacy and safety of SCS was determined via a retrospective study. Inclusion criteria for the study consisted of any Southeastern Louisiana Veterans Health Care System (SLVHCS) patient who had an SCS trial and/or implant from 2008 to 2020. Eligible veterans must have had chronic pain for at least 6 months and had previously tried multiple medications, PT, transcutaneous nerve stimulation, facet injections, epidural steroid injections, or surgery without success. For medication therapy to be considered unsuccessful, it must have included acetaminophen, nonsteroidal anti-inflammatory drugs, and ≥ 1 adjuvant medication (gabapentin, duloxetine, amitriptyline, lidocaine, and menthol). A diagnosis of chronic LBP, PLS, cervical or lumbar spondylosis with radiculopathy, complex regional pain syndrome, or chronic pain syndrome was required for eligibility. Patients whose pain decreased by > 60% and had functional improvement in a 3- to 5-day trial received SCS implantation with percutaneous leads by a pain physician or paddle lead by a neurosurgeon.
The SLVHCS Institutional Review Board approved this study. Electronic health records were reviewed to determine patient age, anthropometric data, and date of SCS implantation. Patients were then called and interviewed to complete a survey. After obtaining verbal consent to the study, subjects were surveyed regarding whether the patient would recommend the procedure to peers, adverse effects (AEs) or complications, and the ability to decrease opiates if applicable. A verbal Pain Outcome Questionnaire (POQ) assessment of activities of daily living also was given during the phone interview regarding pain levels before SCS and at the time of the phone interview.13 (eAppendix available at doi:10.12788/fp.0204) Following the survey, a chart review was performed to corroborate the given AEs or complications and opiate use information. Before and after results of the POQ were compared via a paired sample t test, and P values < .05 were considered significant. Analyses were performed by IBM SPSS, version 26.
The primary outcome measure for this study was whether veterans would recommend SCS to their peers; in our view, this categorical outcome measure seemed to be more valuable to share with future patients who might be candidates for SCS. Since VA health care coverage and goals of treatment may be different from a nonveteran population, we opted to use this primary measure to decrease the possibility of confounding variables.
Secondary outcome measures included changes in POC scores, improvements in activities of daily living, and decreases in use of opioid pain medications.
POQ responses were recorded during the telephone interviews (0 to 10 scale). A paired sample t test was conducted to compare pain levels before and after SCS implant. Pain levels were gathered in the single phone call. Patient opioid usage, if applicable, was assessed by converting medications to morphine milligram equivalent dosing (MMED). Since patients who were on chronic opioids took multiple formulations, we changed the total daily dose to all morphine; for this study, morphine was considered equivalent to hydrocodone, and oxycodone was 1.5x morphine.
Results
Of the 90 SLVHCS patients who received an SCS implant between 2008 and 2020, 76 were reached by telephone and 65 had their responses recorded in the study. Of the 11 patients who were not included, 5 had the SCS removed; it is unclear whether these veterans would have recommended the treatment. Four were unable to quantify pain and/or SCS effects, and 2 were excluded due to a dementia diagnosis years after the implant. The mean (SD) age of participants was 63.9 (10.3) years. Forty percent of patients had a diabetes mellitus diagnosis and 1 had prediabetes. Patients’ most common qualifying diagnosis for SCS was PLS (47.7%) followed by chronic LBP (26.2%). A percutaneous 2-lead technique was the most common type of SCS type used (60.0%) followed by 1-lead (21.5%). The most common SCS manufacturer was Boston Scientific (87.7%)(Table 1). Most veterans (76.9%) recommended SCS to their peers; 13.8% did not recommend SCS; 9.2% were undecided and stated that they were unable to recommend because they did not want to persuade a peer to get SCS (Figure).
There was a statistically significant decrease in opioid use for the 40 veterans for whom pain medication was converted (P < .001)(Table 2). Six patients reported using opioids at some point but could not remember their dose, and no records were found in their chart review, so they were not included in the MMED analysis. In that group, 4 patients reported using opioids before SCS but discontinued the opioid use after SCS implantation, and 2 patients noted using opioids before SCS and concomitantly. Eighteen subjects reported no opioid use at any point before or after SCS (Table 3).
There were few life-threatening complications of SCS. Three veterans developed skin dehiscence; 2 had dehiscence at the battery/generator site, and 1 had dehiscence at the lead anchor site. Two patients with dehiscence also had morbid obesity, and the third had postoperative malnourishment. The dehiscence occurred 3 and 8 months postoperation. All 3 patients with dehiscence had the SCS explanted, though they were eager to get a new SCS implanted as soon as possible because SCS was their most successful treatment to date.
Twenty of the 64 veterans surveyed reported other complications of SCS, including lead migration, lack of pain coverage, paresthesia and numbness, soreness around generator site, SCS shocking patient when performing full thoracic spine flexion, and shingles at the battery site (Table 4). There were 11 explants among the 76 veterans contacted. The primary reason for explant was lack of pain coverage.
Patient concerns included pain with sitting in chairs due to tenderness around the implant, SCS helping with physical pain but not mental pain, SCS only working during the day and not helping with sleep, and patients lacking education regarding possible complications of SCS.
Discussion
In this nonrandomized retrospective review, SCS was shown to be an effective treatment for intractable spine and/or extremity pain. Veterans’ pain levels were significantly reduced following SCS implantation, and more than three-fourths of veterans recommended SCS to their peers. We used the recommendation of SCS to peers as the most important metric regarding the effectiveness of SCS, as this measure was felt to be more valuable to share with future patients; furthermore, categorical analysis has been shown to be more valuable than ordinal pain scales to measure pain.14 In addition to wanting to expand the available research to the general public, we wanted a measure that we could easily relay to our patient population regarding SCS.
The explant rate of 14.5% among surveyed veterans falls at the higher end of the normal ranges found in previous studies of long-term SCS outcomes.15-17 One possible reason for the higher rate is that we did not differentiate based on the reason for the explant (ie, no benefit, further surgery needed for underlying medical condition, or SCS-specific complications). Another possible contributing factor to the higher than expected explant rate is the geographic location in the New Orleans metro area; New Orleans is considered to have one of the highest rates of obesity in the United States and obesity typically has other diseases associated with it such as hypertension and diabetes mellitus.
Limitations
Limitations of the study include the relatively low number of subjects, subjective nature of the interview questions, and the patients’ answers. Typically the POQ has been used as a prospective assessment of pain; whether it is valid in a retrospective analysis is not clear. While there was a statistically significant decrease of opioid use after getting SCS, this study can only show correlation, not causation. During the study period, there has been a drastic change in opioid prescribing patterns and efforts to decrease the amount of opioids prescribed.
Subjects also were asked to rate their pain and quality of life before SCS. Some subjects had SCS implantation up to 10 years prior to the phone interview. The variable amount of time between SCS implantation and interview likely affected subjects’ responses. Chronic pain is a moving target. Patients have good days and bad days that would likely change opinions on SCS benefits on a single phone interview. Some patients needed battery replacements at the time of the interview (battery life averaged about 3 to 5 years in our study population) and were asked to report current levels of pain from the perspective of when their batteries were still functional, further affecting results.
Conclusions
SCS was shown to improve the quality of life of US veterans at SLVHCS across a wide variety of metrics, including activities of daily living, as well as mental and physical health. For veterans with chronic intractable pain who have tried and failed more conservative treatments, SCS is a great treatment.
1. Hoy DG, Smith E, Cross M, et al. The global burden of musculoskeletal conditions for 2010: an overview of methods. Ann Rheum Dis. 2014;73(6):982-989 doi:10.1136/annrheumdis-2013-204344
2. Nahin RL. Severe pain in veterans: the effect of age and sex, and comparisons with the general population. J Pain. 2017;18(3):247-254. doi:10.1016/j.jpain.2016.10.021
3. Institute of Medicine (US) Committee on Advancing Pain Research, Care, and Education. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: National Academies Press; 2011.
4. Finnerup NB, Attal N, Haroutounian S, et al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. 2015;14(2):162-173. doi:10.1016/S1474-4422(14)70251-0
5. Costigan M, Scholz J, Woolf CJ. Neuropathic pain: a maladaptive response of the nervous system to damage. Annu Rev Neurosci. 2009;32:1-32. doi:10.1146/annurev.neuro.051508.135531
6. Wilkinson HA. The Failed Back Syndrome: Etiology and Therapy. 2nd ed. Harper & Row; 1991.
7. Kumar K, Taylor RS, Jacques L, et al. Spinal cord stimulation versus conventional medical management for neuropathic pain: a multicentre randomised controlled trial in patients with failed back surgery syndrome. Pain. 2007;132(1-2):179-188. doi:10.1016/j.pain.2007.07.028
8. North RB, Kidd DH, Farrokhi F, Piantadosi SA. Spinal cord stimulation versus repeated lumbosacral spine surgery for chronic pain: a randomized, controlled trial. Neurosurgery. 2005;56(1):98-107. doi:10.1227/01.neu.0000144839.65524.e0
9. Geurts JW, Smits H, Kemler MA, Brunner F, Kessels AG, van Kleef M. Spinal cord stimulation for complex regional pain syndrome type I: a prospective cohort study with long-term follow-up. Neuromodulation. 2013;16(6):523-529. doi:10.1111/ner.12024
10. Kumar K, Rizvi S, Bnurs SB. Spinal cord stimulation is effective in management of complex regional pain syndrome I: fact or fiction. Neurosurgery. 2011;69(3):566-5580. doi:10.1227/NEU.0b013e3182181e60
11. Mekhail NA, Mathews M, Nageeb F, Guirguis M, Mekhail MN, Cheng J. Retrospective review of 707 cases of spinal cord stimulation: indications and complications. Pain Pract. 2011;11(2):148-153. doi:10.1111/j.1533-2500.2010.00407.x
12. Veizi E, Hayek SM, North J, et al. Spinal cord stimulation (SCS) with anatomically guided (3D) neural targeting shows superior chronic axial low back pain relief compared to traditional SCS-LUMINA Study. Pain Med. 2017;18(8):1534-1548. doi:10.1093/pm/pnw286
13. Gordon DB, Polomano RC, Pellino TA, et al. Revised American Pain Society Patient Outcome Questionnaire (APS-POQ-R) for quality improvement of pain management in hospitalized adults: preliminary psychometric evaluation. J Pain. 2010;11(11):1172-1186. doi:10.1016/j.jpain.2010.02.012
14. Kennedy DJ, Schneider B. Lies, damn lies, and statistic: a commentary. Pain Med. 2020;21(10):2052-2054. doi:10.1093/pm/pnaa287
15. Van Buyten JP, Wille F, Smet I, et al. Therapy-related explants after spinal cord stimulation: results of an international retrospective chart review study. Neuromodulation. 2017;20(7):642-649. doi:10.1111/ner.12642
16. Hayek SM, Veizi E, Hanes M. Treatment-limiting complications of percutaneous spinal cord stimulator implants: a review of eight years of experience from an academic center database. Neuromodulation. 2015;18(7):603-609. doi:10.1111/ner.12312
17. Pope JE, Deer TR, Falowski S, et al. Multicenter retrospective study of neurostimulation with exit of therapy by explant. Neuromodulation. 2017;20(6):543-552. doi:10.1111/ner.12634
1. Hoy DG, Smith E, Cross M, et al. The global burden of musculoskeletal conditions for 2010: an overview of methods. Ann Rheum Dis. 2014;73(6):982-989 doi:10.1136/annrheumdis-2013-204344
2. Nahin RL. Severe pain in veterans: the effect of age and sex, and comparisons with the general population. J Pain. 2017;18(3):247-254. doi:10.1016/j.jpain.2016.10.021
3. Institute of Medicine (US) Committee on Advancing Pain Research, Care, and Education. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: National Academies Press; 2011.
4. Finnerup NB, Attal N, Haroutounian S, et al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. 2015;14(2):162-173. doi:10.1016/S1474-4422(14)70251-0
5. Costigan M, Scholz J, Woolf CJ. Neuropathic pain: a maladaptive response of the nervous system to damage. Annu Rev Neurosci. 2009;32:1-32. doi:10.1146/annurev.neuro.051508.135531
6. Wilkinson HA. The Failed Back Syndrome: Etiology and Therapy. 2nd ed. Harper & Row; 1991.
7. Kumar K, Taylor RS, Jacques L, et al. Spinal cord stimulation versus conventional medical management for neuropathic pain: a multicentre randomised controlled trial in patients with failed back surgery syndrome. Pain. 2007;132(1-2):179-188. doi:10.1016/j.pain.2007.07.028
8. North RB, Kidd DH, Farrokhi F, Piantadosi SA. Spinal cord stimulation versus repeated lumbosacral spine surgery for chronic pain: a randomized, controlled trial. Neurosurgery. 2005;56(1):98-107. doi:10.1227/01.neu.0000144839.65524.e0
9. Geurts JW, Smits H, Kemler MA, Brunner F, Kessels AG, van Kleef M. Spinal cord stimulation for complex regional pain syndrome type I: a prospective cohort study with long-term follow-up. Neuromodulation. 2013;16(6):523-529. doi:10.1111/ner.12024
10. Kumar K, Rizvi S, Bnurs SB. Spinal cord stimulation is effective in management of complex regional pain syndrome I: fact or fiction. Neurosurgery. 2011;69(3):566-5580. doi:10.1227/NEU.0b013e3182181e60
11. Mekhail NA, Mathews M, Nageeb F, Guirguis M, Mekhail MN, Cheng J. Retrospective review of 707 cases of spinal cord stimulation: indications and complications. Pain Pract. 2011;11(2):148-153. doi:10.1111/j.1533-2500.2010.00407.x
12. Veizi E, Hayek SM, North J, et al. Spinal cord stimulation (SCS) with anatomically guided (3D) neural targeting shows superior chronic axial low back pain relief compared to traditional SCS-LUMINA Study. Pain Med. 2017;18(8):1534-1548. doi:10.1093/pm/pnw286
13. Gordon DB, Polomano RC, Pellino TA, et al. Revised American Pain Society Patient Outcome Questionnaire (APS-POQ-R) for quality improvement of pain management in hospitalized adults: preliminary psychometric evaluation. J Pain. 2010;11(11):1172-1186. doi:10.1016/j.jpain.2010.02.012
14. Kennedy DJ, Schneider B. Lies, damn lies, and statistic: a commentary. Pain Med. 2020;21(10):2052-2054. doi:10.1093/pm/pnaa287
15. Van Buyten JP, Wille F, Smet I, et al. Therapy-related explants after spinal cord stimulation: results of an international retrospective chart review study. Neuromodulation. 2017;20(7):642-649. doi:10.1111/ner.12642
16. Hayek SM, Veizi E, Hanes M. Treatment-limiting complications of percutaneous spinal cord stimulator implants: a review of eight years of experience from an academic center database. Neuromodulation. 2015;18(7):603-609. doi:10.1111/ner.12312
17. Pope JE, Deer TR, Falowski S, et al. Multicenter retrospective study of neurostimulation with exit of therapy by explant. Neuromodulation. 2017;20(6):543-552. doi:10.1111/ner.12634
‘Baby-wearing’ poses serious injury risks for infants, ED data show
Baby-wearing – carrying a child against your body in a sling, soft carrier, or other device – is associated with benefits like reduced crying and increased breastfeeding, studies have shown.
But this practice also entails risks. Babies can fall out of carriers, or be injured when an adult carrying them falls, for example.
researchers estimated in a study presented at the annual meeting of the American Academy of Pediatrics.
To characterize the epidemiology of these injuries, Samantha J. Rowe, MD, chief resident physician at Walter Reed National Military Medical Center in Bethesda, Md., and colleagues analyzed data from the National Electronic Injury Surveillance System between 2011 and 2020.
They included in their analysis data from patients aged 5 years and younger who sustained an injury associated with a baby-wearing product. Baby harnesses, carriers, slings, framed baby carriers, and soft baby carriers were among the devices included in the study. The researchers used 601 cases to generate national estimates.
An estimated 14,024 patients presented to EDs because of baby-wearing injuries, and 52% of the injuries occurred when a patient fell from the product.
Most injuries (61%) occurred in children aged 5 months and younger; 19.3% of these infants required hospitalization, most often for head injuries.
The investigators found that about 22% of the injuries were associated with a caregiver falling, noted Rachel Y. Moon, MD, who was not involved in the study.
“Carrying a baby changes your center of gravity – and can also obscure your vision of where you’re walking, so adults who use these devices should be cognizant of this,” said Dr. Moon, with the University of Virginia, Charlottesville.
Dr. Rowe often practiced baby-wearing with her daughter, and found that it was beneficial. And studies have demonstrated various benefits of baby-wearing, including improved thermoregulation and glycemic control.
Still, the new analysis illustrates the potential for baby-wearing products “to cause serious injury, especially in infants 5 months and younger,” Dr. Rowe said. “We need to provide more education to caregivers on safe baby-wearing and continue to improve our safety standards for baby-wearing products.”
Study coauthor Patrick T. Reeves, MD, with the Naval Medical Center at San Diego, offered additional guidance in a news release: “Like when buying a new pair of shoes, parents must be educated on the proper sizing, selection, and wear of baby carriers to prevent injury to themselves and their child.”
Parents also need to ensure that the child’s nose and mouth are not obstructed, Dr. Moon
In a recent article discussing the possible benefits of baby-wearing in terms of helping with breastfeeding, Dr. Moon also pointed out further safety considerations: “No matter which carrier is used, for safety reasons, we need to remind parents that the baby should be positioned so that the head is upright and the nose and mouth are not obstructed.”
The researchers and Dr. Moon had no relevant financial disclosures.
Baby-wearing – carrying a child against your body in a sling, soft carrier, or other device – is associated with benefits like reduced crying and increased breastfeeding, studies have shown.
But this practice also entails risks. Babies can fall out of carriers, or be injured when an adult carrying them falls, for example.
researchers estimated in a study presented at the annual meeting of the American Academy of Pediatrics.
To characterize the epidemiology of these injuries, Samantha J. Rowe, MD, chief resident physician at Walter Reed National Military Medical Center in Bethesda, Md., and colleagues analyzed data from the National Electronic Injury Surveillance System between 2011 and 2020.
They included in their analysis data from patients aged 5 years and younger who sustained an injury associated with a baby-wearing product. Baby harnesses, carriers, slings, framed baby carriers, and soft baby carriers were among the devices included in the study. The researchers used 601 cases to generate national estimates.
An estimated 14,024 patients presented to EDs because of baby-wearing injuries, and 52% of the injuries occurred when a patient fell from the product.
Most injuries (61%) occurred in children aged 5 months and younger; 19.3% of these infants required hospitalization, most often for head injuries.
The investigators found that about 22% of the injuries were associated with a caregiver falling, noted Rachel Y. Moon, MD, who was not involved in the study.
“Carrying a baby changes your center of gravity – and can also obscure your vision of where you’re walking, so adults who use these devices should be cognizant of this,” said Dr. Moon, with the University of Virginia, Charlottesville.
Dr. Rowe often practiced baby-wearing with her daughter, and found that it was beneficial. And studies have demonstrated various benefits of baby-wearing, including improved thermoregulation and glycemic control.
Still, the new analysis illustrates the potential for baby-wearing products “to cause serious injury, especially in infants 5 months and younger,” Dr. Rowe said. “We need to provide more education to caregivers on safe baby-wearing and continue to improve our safety standards for baby-wearing products.”
Study coauthor Patrick T. Reeves, MD, with the Naval Medical Center at San Diego, offered additional guidance in a news release: “Like when buying a new pair of shoes, parents must be educated on the proper sizing, selection, and wear of baby carriers to prevent injury to themselves and their child.”
Parents also need to ensure that the child’s nose and mouth are not obstructed, Dr. Moon
In a recent article discussing the possible benefits of baby-wearing in terms of helping with breastfeeding, Dr. Moon also pointed out further safety considerations: “No matter which carrier is used, for safety reasons, we need to remind parents that the baby should be positioned so that the head is upright and the nose and mouth are not obstructed.”
The researchers and Dr. Moon had no relevant financial disclosures.
Baby-wearing – carrying a child against your body in a sling, soft carrier, or other device – is associated with benefits like reduced crying and increased breastfeeding, studies have shown.
But this practice also entails risks. Babies can fall out of carriers, or be injured when an adult carrying them falls, for example.
researchers estimated in a study presented at the annual meeting of the American Academy of Pediatrics.
To characterize the epidemiology of these injuries, Samantha J. Rowe, MD, chief resident physician at Walter Reed National Military Medical Center in Bethesda, Md., and colleagues analyzed data from the National Electronic Injury Surveillance System between 2011 and 2020.
They included in their analysis data from patients aged 5 years and younger who sustained an injury associated with a baby-wearing product. Baby harnesses, carriers, slings, framed baby carriers, and soft baby carriers were among the devices included in the study. The researchers used 601 cases to generate national estimates.
An estimated 14,024 patients presented to EDs because of baby-wearing injuries, and 52% of the injuries occurred when a patient fell from the product.
Most injuries (61%) occurred in children aged 5 months and younger; 19.3% of these infants required hospitalization, most often for head injuries.
The investigators found that about 22% of the injuries were associated with a caregiver falling, noted Rachel Y. Moon, MD, who was not involved in the study.
“Carrying a baby changes your center of gravity – and can also obscure your vision of where you’re walking, so adults who use these devices should be cognizant of this,” said Dr. Moon, with the University of Virginia, Charlottesville.
Dr. Rowe often practiced baby-wearing with her daughter, and found that it was beneficial. And studies have demonstrated various benefits of baby-wearing, including improved thermoregulation and glycemic control.
Still, the new analysis illustrates the potential for baby-wearing products “to cause serious injury, especially in infants 5 months and younger,” Dr. Rowe said. “We need to provide more education to caregivers on safe baby-wearing and continue to improve our safety standards for baby-wearing products.”
Study coauthor Patrick T. Reeves, MD, with the Naval Medical Center at San Diego, offered additional guidance in a news release: “Like when buying a new pair of shoes, parents must be educated on the proper sizing, selection, and wear of baby carriers to prevent injury to themselves and their child.”
Parents also need to ensure that the child’s nose and mouth are not obstructed, Dr. Moon
In a recent article discussing the possible benefits of baby-wearing in terms of helping with breastfeeding, Dr. Moon also pointed out further safety considerations: “No matter which carrier is used, for safety reasons, we need to remind parents that the baby should be positioned so that the head is upright and the nose and mouth are not obstructed.”
The researchers and Dr. Moon had no relevant financial disclosures.
FROM AAP 2021
Pediatricians can effectively promote gun safety
When pediatricians and other pediatric providers are given training and resource materials, levels of firearm screenings and anticipatory guidance about firearm safety increase significantly, according to two new studies presented at the annual meeting of the American Academy of Pediatrics.
“With the rise in firearm sales and injuries during the COVID-19 pandemic, it is more important than ever that pediatricians address the firearm epidemic,” said Alexandra Byrne, MD, a pediatric resident at the University of Florida in Gainesville, who presented one of the studies.
There were 4.3 million more firearms purchased from March through July 2020 than expected, a recent study estimates, and 4,075 more firearm injuries than expected from April through July 2020.
In states with more excess purchases, firearm injuries related to domestic violence increased in April (rate ratio, 2.60; 95% CI, 1.32-5.93) and May (RR, 1.79; 95% CI, 1.19-2.91) 2020. However, excess gun purchases had no effect on rates of firearm violence outside the home.
In addition to the link between firearms in the home and domestic violence, they are also linked to a three- to fourfold greater risk for teen suicide, and both depression and suicidal thoughts have risen in teens during the pandemic.
“The data are pretty clear that if you have an unlocked, loaded weapon in your home, and you have a kid who’s depressed or anxious or dysregulated or doing maladaptive things for the pandemic, they’re much more likely to inadvertently take their own or someone else’s life by grabbing [a gun],” said Cora Breuner, MD, MPH, professor of pediatrics at Seattle Children’s Hospital.
However, there is no difference in gun ownership or gun-safety measures between homes with and without at-risk children, previous research shows.
Training, guidance, and locks
Previous research has also shown that there has been a reluctance by pediatricians to conduct firearm screenings and counsel parents about gun safety in the home.
For their two-step program, Dr. Byrne’s team used a plan-do-study-act approach. They started by providing training on firearm safety, evidence-based recommendations for firearm screening, and anticipatory guidance regarding safe firearm storage to members of the general pediatrics division at the University of Florida. And they supplied clinics with free firearm locks.
Next they supplied clinics with posters and educational cards from the Be SMART campaign, an initiative of the Everytown for Gun Safety Support Fund, which provides materials for anyone, including physicians, to use.
During their study, the researchers sent three anonymous six-question online surveys – at baseline and 3 to 4 months after each of the two steps – to pediatric residents, physician assistants, advanced practice registered nurses, and attendings to assess the project. There were 52 responses to the first survey, for a response rate of 58.4%, 42 responses to the second survey, for a response rate of 47.2%, and 23 responses to the third survey, for a rate of response 25.8%.
The program nearly doubled screenings during well-child visits and dramatically increased the proportion of families who received a firearm lock when they told providers they had a firearm at home.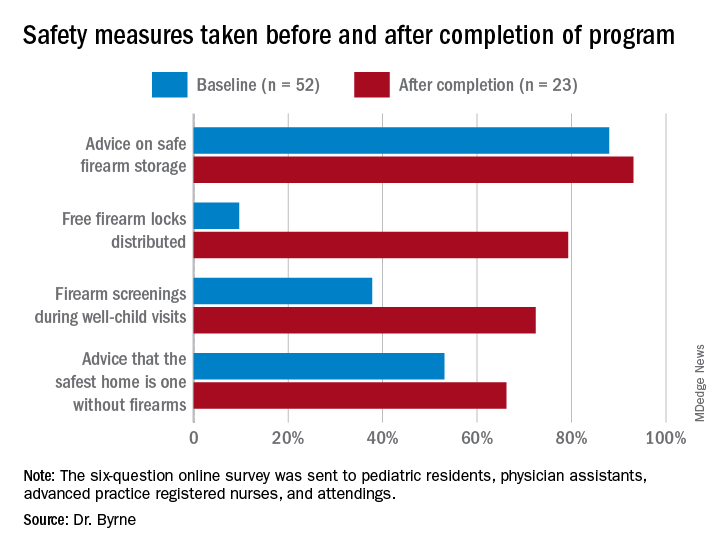
Previous research has shown “a significant increase in safe firearm storage when firearm locks were provided to families in clinic compared to verbal counseling alone,” Dr. Byrne said. “We know that safe firearm storage reduces injuries. Roughly one in three children in the United States lives in a home with a firearm. Individuals with a firearm are at two times the risk of homicide and three to four times the risk of suicide, so it is essential we further study how pediatricians can be most effective when it comes to firearm counseling.”
The difference in lock distribution as a result of the program is a “tremendous increase,” said Christopher S. Greeley, MD, MS, chief of the division of public health pediatrics at Texas Children’s Hospital and professor of pediatrics at Baylor College of Medicine in Houston, who was not involved in the research.
“Locks could go a long way to minimizing the risk,” he said in an interview, adding that nearly half of all teen suicide deaths that occurred over a decade in Houston involved a firearm.
Adding a social-history component
A program to increase firearm screening was also presented at the AAP conference.
After random review of medical records from 30 patients admitted to the hospital documented zero firearm screenings, Marjorie Farrington, MD, and Samantha Gunkelman, MD, from Akron Children’s Hospital in Ohio, implemented a program that they hope will increase firearm screenings during inpatient admissions to at least 50%.
They started their ongoing program in April 2020 by adding a social-history component to the history and physical (H&P) exam template and educating residents on how to screen and included guidance on safe firearm storage.
They also had physicians with firearm expertise give gun-safety lectures, and they plan to involve the Family Resource Center at their hospital in the creation of resources that can be incorporated into discharge instructions.
From April 2020 to June 2021, after the addition to the H&P template, 63% of the 5196 patients admitted to the hospital underwent a firearm screening. Of the 25% of patients who reported guns at home, 3% were not storing their firearms safely.
The pair used the “Store It Safe” Physician Handout provided by the Ohio chapter of the AAP.
Many pediatricians and pediatric trainees are not comfortable counseling on firearm safety, often a result of inadequate training on the topic.
The BulletPoints Project — developed by the Violence Prevention Research Program at the University of California, Davis — can also help physicians talk to patients about guns.
“Many pediatricians and pediatric trainees are not comfortable counseling on firearm safety, often a result of inadequate training on the topic,” Dr. Byrne said in an interview. “Additionally, it is a challenging topic that can often be met with resistance from patients and families. Lack of time during visits is also a huge barrier.”
Lack of training is an obstacle to greater firearm screenings, Dr. Greeley agreed, as are the feeling that guidance simply won’t make a difference and concerns about political pressure and divineness. The lack of research on firearm injuries and the impact of firearm screenings and anticipatory guidance is a challenge, he added, although that is starting to change.
Pediatricians need education on how to make a difference when it comes to firearm safety, and should follow AAP guidelines, Dr. Greeley said.
Counseling on firearm safety is in the same category as immunizations, seatbelts, substance use, helmets, and other public-health issues that are important to address at visits, regardless of how difficult it might be, Dr. Breuner told this news organization.
“It is our mission, as pediatricians, to provide every ounce of prevention in our well-child and anticipatory guidance visits,” she said. “It’s our job, so we shouldn’t shy away from it even though it’s hard.”
Doctors are more comfortable discussing firearm safety if they are firearm owners, previous research has shown, so she advises pediatricians who feel unqualified to discuss firearms to seek guidance from their peers on how to approach screenings and anticipatory guidance, she noted.
The firearm study being done in an academic center gives me great pause. The populations are often very different than private practice.
Both of these studies were conducted at single institutions and might not reflect what would work in private clinics.
“The firearm study being done in an academic center gives me great pause,” Dr. Greeley said. “The populations are often very different than private practice. I think that there is still a lot that remains unknown about decreasing household firearm injury and death.”
And the degree to which findings from these two gun-safety programs can be generalized to other academic centers or children’s hospitals is unclear.
“There are states where, I suspect, firearm screening is much more common. Some states have very pro-firearm cultures and others are anti-firearm,” Dr. Greeley said. “There are also likely differences within states,” particularly between urban and rural regions.
“Firearms are often a very personal issue for families, and pediatricians in ‘pro-firearm’ communities may have greater resistance to working on this,” he pointed out.
Nevertheless, Dr. Greeley said, “this is a promising strategy that could be part of a broad injury prevention initiative.”
Neither study noted any external funding. Dr. Byrne is a member of the Moms Demand Action Gainesville Chapter, which donated the firearm locks for the project. Dr. Breuner, Dr. Greeley, and Dr. Farrington have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
When pediatricians and other pediatric providers are given training and resource materials, levels of firearm screenings and anticipatory guidance about firearm safety increase significantly, according to two new studies presented at the annual meeting of the American Academy of Pediatrics.
“With the rise in firearm sales and injuries during the COVID-19 pandemic, it is more important than ever that pediatricians address the firearm epidemic,” said Alexandra Byrne, MD, a pediatric resident at the University of Florida in Gainesville, who presented one of the studies.
There were 4.3 million more firearms purchased from March through July 2020 than expected, a recent study estimates, and 4,075 more firearm injuries than expected from April through July 2020.
In states with more excess purchases, firearm injuries related to domestic violence increased in April (rate ratio, 2.60; 95% CI, 1.32-5.93) and May (RR, 1.79; 95% CI, 1.19-2.91) 2020. However, excess gun purchases had no effect on rates of firearm violence outside the home.
In addition to the link between firearms in the home and domestic violence, they are also linked to a three- to fourfold greater risk for teen suicide, and both depression and suicidal thoughts have risen in teens during the pandemic.
“The data are pretty clear that if you have an unlocked, loaded weapon in your home, and you have a kid who’s depressed or anxious or dysregulated or doing maladaptive things for the pandemic, they’re much more likely to inadvertently take their own or someone else’s life by grabbing [a gun],” said Cora Breuner, MD, MPH, professor of pediatrics at Seattle Children’s Hospital.
However, there is no difference in gun ownership or gun-safety measures between homes with and without at-risk children, previous research shows.
Training, guidance, and locks
Previous research has also shown that there has been a reluctance by pediatricians to conduct firearm screenings and counsel parents about gun safety in the home.
For their two-step program, Dr. Byrne’s team used a plan-do-study-act approach. They started by providing training on firearm safety, evidence-based recommendations for firearm screening, and anticipatory guidance regarding safe firearm storage to members of the general pediatrics division at the University of Florida. And they supplied clinics with free firearm locks.
Next they supplied clinics with posters and educational cards from the Be SMART campaign, an initiative of the Everytown for Gun Safety Support Fund, which provides materials for anyone, including physicians, to use.
During their study, the researchers sent three anonymous six-question online surveys – at baseline and 3 to 4 months after each of the two steps – to pediatric residents, physician assistants, advanced practice registered nurses, and attendings to assess the project. There were 52 responses to the first survey, for a response rate of 58.4%, 42 responses to the second survey, for a response rate of 47.2%, and 23 responses to the third survey, for a rate of response 25.8%.
The program nearly doubled screenings during well-child visits and dramatically increased the proportion of families who received a firearm lock when they told providers they had a firearm at home.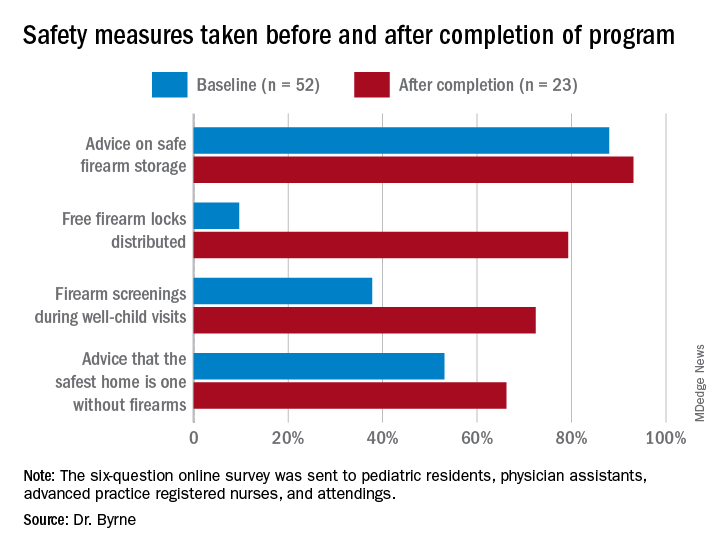
Previous research has shown “a significant increase in safe firearm storage when firearm locks were provided to families in clinic compared to verbal counseling alone,” Dr. Byrne said. “We know that safe firearm storage reduces injuries. Roughly one in three children in the United States lives in a home with a firearm. Individuals with a firearm are at two times the risk of homicide and three to four times the risk of suicide, so it is essential we further study how pediatricians can be most effective when it comes to firearm counseling.”
The difference in lock distribution as a result of the program is a “tremendous increase,” said Christopher S. Greeley, MD, MS, chief of the division of public health pediatrics at Texas Children’s Hospital and professor of pediatrics at Baylor College of Medicine in Houston, who was not involved in the research.
“Locks could go a long way to minimizing the risk,” he said in an interview, adding that nearly half of all teen suicide deaths that occurred over a decade in Houston involved a firearm.
Adding a social-history component
A program to increase firearm screening was also presented at the AAP conference.
After random review of medical records from 30 patients admitted to the hospital documented zero firearm screenings, Marjorie Farrington, MD, and Samantha Gunkelman, MD, from Akron Children’s Hospital in Ohio, implemented a program that they hope will increase firearm screenings during inpatient admissions to at least 50%.
They started their ongoing program in April 2020 by adding a social-history component to the history and physical (H&P) exam template and educating residents on how to screen and included guidance on safe firearm storage.
They also had physicians with firearm expertise give gun-safety lectures, and they plan to involve the Family Resource Center at their hospital in the creation of resources that can be incorporated into discharge instructions.
From April 2020 to June 2021, after the addition to the H&P template, 63% of the 5196 patients admitted to the hospital underwent a firearm screening. Of the 25% of patients who reported guns at home, 3% were not storing their firearms safely.
The pair used the “Store It Safe” Physician Handout provided by the Ohio chapter of the AAP.
Many pediatricians and pediatric trainees are not comfortable counseling on firearm safety, often a result of inadequate training on the topic.
The BulletPoints Project — developed by the Violence Prevention Research Program at the University of California, Davis — can also help physicians talk to patients about guns.
“Many pediatricians and pediatric trainees are not comfortable counseling on firearm safety, often a result of inadequate training on the topic,” Dr. Byrne said in an interview. “Additionally, it is a challenging topic that can often be met with resistance from patients and families. Lack of time during visits is also a huge barrier.”
Lack of training is an obstacle to greater firearm screenings, Dr. Greeley agreed, as are the feeling that guidance simply won’t make a difference and concerns about political pressure and divineness. The lack of research on firearm injuries and the impact of firearm screenings and anticipatory guidance is a challenge, he added, although that is starting to change.
Pediatricians need education on how to make a difference when it comes to firearm safety, and should follow AAP guidelines, Dr. Greeley said.
Counseling on firearm safety is in the same category as immunizations, seatbelts, substance use, helmets, and other public-health issues that are important to address at visits, regardless of how difficult it might be, Dr. Breuner told this news organization.
“It is our mission, as pediatricians, to provide every ounce of prevention in our well-child and anticipatory guidance visits,” she said. “It’s our job, so we shouldn’t shy away from it even though it’s hard.”
Doctors are more comfortable discussing firearm safety if they are firearm owners, previous research has shown, so she advises pediatricians who feel unqualified to discuss firearms to seek guidance from their peers on how to approach screenings and anticipatory guidance, she noted.
The firearm study being done in an academic center gives me great pause. The populations are often very different than private practice.
Both of these studies were conducted at single institutions and might not reflect what would work in private clinics.
“The firearm study being done in an academic center gives me great pause,” Dr. Greeley said. “The populations are often very different than private practice. I think that there is still a lot that remains unknown about decreasing household firearm injury and death.”
And the degree to which findings from these two gun-safety programs can be generalized to other academic centers or children’s hospitals is unclear.
“There are states where, I suspect, firearm screening is much more common. Some states have very pro-firearm cultures and others are anti-firearm,” Dr. Greeley said. “There are also likely differences within states,” particularly between urban and rural regions.
“Firearms are often a very personal issue for families, and pediatricians in ‘pro-firearm’ communities may have greater resistance to working on this,” he pointed out.
Nevertheless, Dr. Greeley said, “this is a promising strategy that could be part of a broad injury prevention initiative.”
Neither study noted any external funding. Dr. Byrne is a member of the Moms Demand Action Gainesville Chapter, which donated the firearm locks for the project. Dr. Breuner, Dr. Greeley, and Dr. Farrington have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
When pediatricians and other pediatric providers are given training and resource materials, levels of firearm screenings and anticipatory guidance about firearm safety increase significantly, according to two new studies presented at the annual meeting of the American Academy of Pediatrics.
“With the rise in firearm sales and injuries during the COVID-19 pandemic, it is more important than ever that pediatricians address the firearm epidemic,” said Alexandra Byrne, MD, a pediatric resident at the University of Florida in Gainesville, who presented one of the studies.
There were 4.3 million more firearms purchased from March through July 2020 than expected, a recent study estimates, and 4,075 more firearm injuries than expected from April through July 2020.
In states with more excess purchases, firearm injuries related to domestic violence increased in April (rate ratio, 2.60; 95% CI, 1.32-5.93) and May (RR, 1.79; 95% CI, 1.19-2.91) 2020. However, excess gun purchases had no effect on rates of firearm violence outside the home.
In addition to the link between firearms in the home and domestic violence, they are also linked to a three- to fourfold greater risk for teen suicide, and both depression and suicidal thoughts have risen in teens during the pandemic.
“The data are pretty clear that if you have an unlocked, loaded weapon in your home, and you have a kid who’s depressed or anxious or dysregulated or doing maladaptive things for the pandemic, they’re much more likely to inadvertently take their own or someone else’s life by grabbing [a gun],” said Cora Breuner, MD, MPH, professor of pediatrics at Seattle Children’s Hospital.
However, there is no difference in gun ownership or gun-safety measures between homes with and without at-risk children, previous research shows.
Training, guidance, and locks
Previous research has also shown that there has been a reluctance by pediatricians to conduct firearm screenings and counsel parents about gun safety in the home.
For their two-step program, Dr. Byrne’s team used a plan-do-study-act approach. They started by providing training on firearm safety, evidence-based recommendations for firearm screening, and anticipatory guidance regarding safe firearm storage to members of the general pediatrics division at the University of Florida. And they supplied clinics with free firearm locks.
Next they supplied clinics with posters and educational cards from the Be SMART campaign, an initiative of the Everytown for Gun Safety Support Fund, which provides materials for anyone, including physicians, to use.
During their study, the researchers sent three anonymous six-question online surveys – at baseline and 3 to 4 months after each of the two steps – to pediatric residents, physician assistants, advanced practice registered nurses, and attendings to assess the project. There were 52 responses to the first survey, for a response rate of 58.4%, 42 responses to the second survey, for a response rate of 47.2%, and 23 responses to the third survey, for a rate of response 25.8%.
The program nearly doubled screenings during well-child visits and dramatically increased the proportion of families who received a firearm lock when they told providers they had a firearm at home.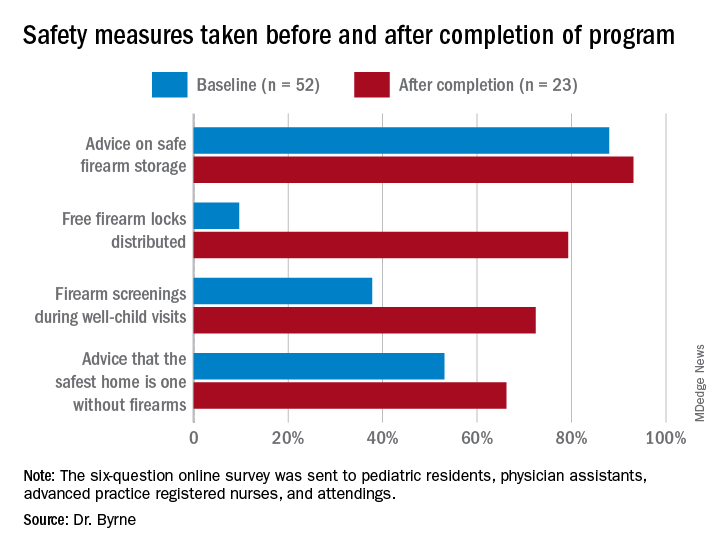
Previous research has shown “a significant increase in safe firearm storage when firearm locks were provided to families in clinic compared to verbal counseling alone,” Dr. Byrne said. “We know that safe firearm storage reduces injuries. Roughly one in three children in the United States lives in a home with a firearm. Individuals with a firearm are at two times the risk of homicide and three to four times the risk of suicide, so it is essential we further study how pediatricians can be most effective when it comes to firearm counseling.”
The difference in lock distribution as a result of the program is a “tremendous increase,” said Christopher S. Greeley, MD, MS, chief of the division of public health pediatrics at Texas Children’s Hospital and professor of pediatrics at Baylor College of Medicine in Houston, who was not involved in the research.
“Locks could go a long way to minimizing the risk,” he said in an interview, adding that nearly half of all teen suicide deaths that occurred over a decade in Houston involved a firearm.
Adding a social-history component
A program to increase firearm screening was also presented at the AAP conference.
After random review of medical records from 30 patients admitted to the hospital documented zero firearm screenings, Marjorie Farrington, MD, and Samantha Gunkelman, MD, from Akron Children’s Hospital in Ohio, implemented a program that they hope will increase firearm screenings during inpatient admissions to at least 50%.
They started their ongoing program in April 2020 by adding a social-history component to the history and physical (H&P) exam template and educating residents on how to screen and included guidance on safe firearm storage.
They also had physicians with firearm expertise give gun-safety lectures, and they plan to involve the Family Resource Center at their hospital in the creation of resources that can be incorporated into discharge instructions.
From April 2020 to June 2021, after the addition to the H&P template, 63% of the 5196 patients admitted to the hospital underwent a firearm screening. Of the 25% of patients who reported guns at home, 3% were not storing their firearms safely.
The pair used the “Store It Safe” Physician Handout provided by the Ohio chapter of the AAP.
Many pediatricians and pediatric trainees are not comfortable counseling on firearm safety, often a result of inadequate training on the topic.
The BulletPoints Project — developed by the Violence Prevention Research Program at the University of California, Davis — can also help physicians talk to patients about guns.
“Many pediatricians and pediatric trainees are not comfortable counseling on firearm safety, often a result of inadequate training on the topic,” Dr. Byrne said in an interview. “Additionally, it is a challenging topic that can often be met with resistance from patients and families. Lack of time during visits is also a huge barrier.”
Lack of training is an obstacle to greater firearm screenings, Dr. Greeley agreed, as are the feeling that guidance simply won’t make a difference and concerns about political pressure and divineness. The lack of research on firearm injuries and the impact of firearm screenings and anticipatory guidance is a challenge, he added, although that is starting to change.
Pediatricians need education on how to make a difference when it comes to firearm safety, and should follow AAP guidelines, Dr. Greeley said.
Counseling on firearm safety is in the same category as immunizations, seatbelts, substance use, helmets, and other public-health issues that are important to address at visits, regardless of how difficult it might be, Dr. Breuner told this news organization.
“It is our mission, as pediatricians, to provide every ounce of prevention in our well-child and anticipatory guidance visits,” she said. “It’s our job, so we shouldn’t shy away from it even though it’s hard.”
Doctors are more comfortable discussing firearm safety if they are firearm owners, previous research has shown, so she advises pediatricians who feel unqualified to discuss firearms to seek guidance from their peers on how to approach screenings and anticipatory guidance, she noted.
The firearm study being done in an academic center gives me great pause. The populations are often very different than private practice.
Both of these studies were conducted at single institutions and might not reflect what would work in private clinics.
“The firearm study being done in an academic center gives me great pause,” Dr. Greeley said. “The populations are often very different than private practice. I think that there is still a lot that remains unknown about decreasing household firearm injury and death.”
And the degree to which findings from these two gun-safety programs can be generalized to other academic centers or children’s hospitals is unclear.
“There are states where, I suspect, firearm screening is much more common. Some states have very pro-firearm cultures and others are anti-firearm,” Dr. Greeley said. “There are also likely differences within states,” particularly between urban and rural regions.
“Firearms are often a very personal issue for families, and pediatricians in ‘pro-firearm’ communities may have greater resistance to working on this,” he pointed out.
Nevertheless, Dr. Greeley said, “this is a promising strategy that could be part of a broad injury prevention initiative.”
Neither study noted any external funding. Dr. Byrne is a member of the Moms Demand Action Gainesville Chapter, which donated the firearm locks for the project. Dr. Breuner, Dr. Greeley, and Dr. Farrington have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AAP 2021
Med student’s skills put to the test saving life of accident victim
Third-year medical student Liz Groesbeck was like other excited Las Vegas Raiders fans recently headed to the first full-capacity game in the new Allegiant Stadium since the team moved to “Sin City.” She was in an Uber on a first date just blocks from the game that would pit her Raiders against the Seattle Seahawks when she saw a man on the ground and people gathered around him.
Abandoning her keys, cellphone, and date in the Uber, Ms. Groesbeck popped out to see if she could help. The Uber had been stuck in traffic, so Ms. Groesbeck thought she’d still be able to jump back in the car if she wasn’t needed.
Then she heard screams. “That didn’t concern me. People scream whenever anything unexpected happens,” said the 28-year-old student from the Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas (UNLV). But the screams were only a small indication of what she would discover on closer inspection. The arm of the middle-aged man lying on the ground was detached. An abandoned gold SUV remained on the curb nearby. It would turn out to be a hit-and-run of pedestrians by a driver later charged by police with DUI.
“I was one of the first people there,” Ms. Groesbeck recounted for this news organization. “I knew this guy did not just fall. I told someone to call EMS and I got someone to take his wife somewhere else [away from the bloody scene]. She was obviously very distraught. …At a couple of points she was hysterical.”
Next, Ms. Groesbeck, who, ironically, had finished her emergency general surgery rotation the day before, focused on the patient. Kneeling beside him, she determined that the immediate priorities were to stop the bleeding and clear his airway. “He was barely breathing,” she recounted. Another student who Ms. Groesbeck believes was pursuing a medical degree — there wasn’t time for formal introductions — offered to help, along with bystanders headed to the game.
“The crowd was very energetic. It was a beautiful thing.” Ms. Groesbeck cited the spirit of saving lives that developed from the October 1, 2017, Las Vegas country music festival shooting. “People are very willing to try to help others in any way they can.”
MS. Groesbeck, leading the effort, asked for belts, “and bystanders immediately provided that,” and the other student followed Ms. Groesbeck’s directions to apply tourniquets with the help of those around her. With the blood loss being stemmed, Ms. Groesbeck’s next priority was making sure the patient could breathe.
Appealing for clothing to clear the man’s airway, “five shirts were handed in a circle to me.” She only needed one jersey to scoop the blood out of his mouth manually to free his airway.
She overruled well-meaning suggestions to lay the man on his side — which she was concerned could paralyze him — or use a straw to help him breathe. “I did not want to stick anything down his throat.” Meanwhile, there was so much traffic that night around Allegiant Stadium that when the ambulance couldn’t get any closer the firefighters and paramedics exited the vehicle and ran to the scene.
From training to practice
The decisions Ms. Groesbeck made until they could arrive called upon her years of training to be a doctor, and specifically an EMT certification course she had to pass before beginning medical school, she said.
She credits the life-saving methods she learned in that course to Douglas Fraser, MD, FACS, associate professor of surgery at UNLV and University Medical Center (UMC) trauma medical director. He happened to be the attending physician when the accident victim was admitted to the hospital that night in critical condition. The man’s wife also was injured, but not to the extent of her husband.
Dr. Fraser said he didn’t know at the time that his student had been involved in saving the man’s life until Ms. Groesbeck reached out to say thanks for teaching her what to do in an emergency. “I [first] was overly impressed that she did that. Students are so busy; they move after they graduate or finish their rotations. You don’t get to see them time and time again; your short time with them could have a lasting impact and that is my goal,” Dr. Fraser told this news organization.
“They rarely thank you or reflect back. It renewed my sense that I want to teach more, to see the positive impact it had on Elizabeth” and other students, he said.
In terms of the emergency situation she navigated, Dr. Fraser said he was very proud of his student, but was also concerned she could have gotten hurt herself in the middle of a busy intersection. “She was selfless and put herself in harm’s way to help someone.” He also noted it was the first time he knew of a student putting her skills to the test so soon after learning them. “It was a good outcome and she truly provided lifesaving care to this victim.”
He attributed her training to the Stop the Bleed program, which began after the Sandy Hook tragedy in 2012. UNLV requires new med students to complete the American College of Surgeons’ first aid program to learn how to stop the bleeding of a severely injured person by applying tourniquets and pressure. “You have to stop the bleeding right away…and look to see whether their airway is open and if it’s not, open their airway or you won’t have a patient very long. I know she did that. These are the two most important lifesaving skills that she did.”
Medical students are often called upon as doctors by their family and friends, Dr. Fraser continued. “Everyone looks to you. It can happen on an airplane; you can be anywhere. She heard a person was in need and jumped to action and was able to use the training her school provided and was able to put it to good use.”
Not her first call to action
Just the week before the incident, Ms. Groesbeck was on clinical rotations at UMC helping in the emergency and operating rooms. “She was always very engaged and mature beyond her years,” Dr. Fraser said. “She definitely had that ‘it’ factor. She was sincere with patients and their families and performed well in the operating room. …She was very comfortable around the patients; very comfortable in stressful situations.”
He added, “I look forward to her participating in trauma surgery rotations in the near future.”
In the meantime, Ms. Groesbeck was pleased to learn that the man she saved survived and thrilled to be part of that effort. As of press time, he had not contacted her. Nor has the other student who helped save his life.
“A lot of people stepped up and donated their time to help. He got lucky on a very unlucky day,” Ms. Groesbeck said.
She recalled a previous accident victim years ago who wasn’t as lucky. On the way to pick up her white coat for the ceremony before her first year of medical school, she came upon a car that had flipped upside down. “It sheared the roof away. I checked on the restrained passenger. He was partially scalped. The windows were broken and I climbed in next to him.” This time, she used her own shirt to hold pressure on the wound. “He, unfortunately did not make it.” There was nothing she could have done, she was told.
“That one got me mentally. Very graphic imaging was stuck in my head,” Ms. Groesbeck said. With a masters in neuroscience, she was accustomed to seeing the brain, “but not like this. I felt sad he passed in such a violent way.” So the more recent life-saving experience was redemptive, she said. “I’ve been through hell and back.”
And she’s still on track to become the doctor she envisioned as a child, mummifying her cats with gauze wraps and covering her little sister with adhesive bandages. “It felt good knowing what I could do,” Ms. Groesbeck said. “I’m glad this [man] made it. He got lucky and he could go home to his family. I was not positive when he left in the ambulance. It was a huge relief.”
Of her role in the episode and her future career ambitions, Ms. Groesbeck noted: “We are studying all the time. It’s not very rewarding. But this, not thinking but having sprung into action, doing the right thing and he could go home to his family a week later. It’s things like this that make the endless hours of studying worth it. I feel like I accomplished something.”
A version of this article first appeared on Medscape.com.
Third-year medical student Liz Groesbeck was like other excited Las Vegas Raiders fans recently headed to the first full-capacity game in the new Allegiant Stadium since the team moved to “Sin City.” She was in an Uber on a first date just blocks from the game that would pit her Raiders against the Seattle Seahawks when she saw a man on the ground and people gathered around him.
Abandoning her keys, cellphone, and date in the Uber, Ms. Groesbeck popped out to see if she could help. The Uber had been stuck in traffic, so Ms. Groesbeck thought she’d still be able to jump back in the car if she wasn’t needed.
Then she heard screams. “That didn’t concern me. People scream whenever anything unexpected happens,” said the 28-year-old student from the Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas (UNLV). But the screams were only a small indication of what she would discover on closer inspection. The arm of the middle-aged man lying on the ground was detached. An abandoned gold SUV remained on the curb nearby. It would turn out to be a hit-and-run of pedestrians by a driver later charged by police with DUI.
“I was one of the first people there,” Ms. Groesbeck recounted for this news organization. “I knew this guy did not just fall. I told someone to call EMS and I got someone to take his wife somewhere else [away from the bloody scene]. She was obviously very distraught. …At a couple of points she was hysterical.”
Next, Ms. Groesbeck, who, ironically, had finished her emergency general surgery rotation the day before, focused on the patient. Kneeling beside him, she determined that the immediate priorities were to stop the bleeding and clear his airway. “He was barely breathing,” she recounted. Another student who Ms. Groesbeck believes was pursuing a medical degree — there wasn’t time for formal introductions — offered to help, along with bystanders headed to the game.
“The crowd was very energetic. It was a beautiful thing.” Ms. Groesbeck cited the spirit of saving lives that developed from the October 1, 2017, Las Vegas country music festival shooting. “People are very willing to try to help others in any way they can.”
MS. Groesbeck, leading the effort, asked for belts, “and bystanders immediately provided that,” and the other student followed Ms. Groesbeck’s directions to apply tourniquets with the help of those around her. With the blood loss being stemmed, Ms. Groesbeck’s next priority was making sure the patient could breathe.
Appealing for clothing to clear the man’s airway, “five shirts were handed in a circle to me.” She only needed one jersey to scoop the blood out of his mouth manually to free his airway.
She overruled well-meaning suggestions to lay the man on his side — which she was concerned could paralyze him — or use a straw to help him breathe. “I did not want to stick anything down his throat.” Meanwhile, there was so much traffic that night around Allegiant Stadium that when the ambulance couldn’t get any closer the firefighters and paramedics exited the vehicle and ran to the scene.
From training to practice
The decisions Ms. Groesbeck made until they could arrive called upon her years of training to be a doctor, and specifically an EMT certification course she had to pass before beginning medical school, she said.
She credits the life-saving methods she learned in that course to Douglas Fraser, MD, FACS, associate professor of surgery at UNLV and University Medical Center (UMC) trauma medical director. He happened to be the attending physician when the accident victim was admitted to the hospital that night in critical condition. The man’s wife also was injured, but not to the extent of her husband.
Dr. Fraser said he didn’t know at the time that his student had been involved in saving the man’s life until Ms. Groesbeck reached out to say thanks for teaching her what to do in an emergency. “I [first] was overly impressed that she did that. Students are so busy; they move after they graduate or finish their rotations. You don’t get to see them time and time again; your short time with them could have a lasting impact and that is my goal,” Dr. Fraser told this news organization.
“They rarely thank you or reflect back. It renewed my sense that I want to teach more, to see the positive impact it had on Elizabeth” and other students, he said.
In terms of the emergency situation she navigated, Dr. Fraser said he was very proud of his student, but was also concerned she could have gotten hurt herself in the middle of a busy intersection. “She was selfless and put herself in harm’s way to help someone.” He also noted it was the first time he knew of a student putting her skills to the test so soon after learning them. “It was a good outcome and she truly provided lifesaving care to this victim.”
He attributed her training to the Stop the Bleed program, which began after the Sandy Hook tragedy in 2012. UNLV requires new med students to complete the American College of Surgeons’ first aid program to learn how to stop the bleeding of a severely injured person by applying tourniquets and pressure. “You have to stop the bleeding right away…and look to see whether their airway is open and if it’s not, open their airway or you won’t have a patient very long. I know she did that. These are the two most important lifesaving skills that she did.”
Medical students are often called upon as doctors by their family and friends, Dr. Fraser continued. “Everyone looks to you. It can happen on an airplane; you can be anywhere. She heard a person was in need and jumped to action and was able to use the training her school provided and was able to put it to good use.”
Not her first call to action
Just the week before the incident, Ms. Groesbeck was on clinical rotations at UMC helping in the emergency and operating rooms. “She was always very engaged and mature beyond her years,” Dr. Fraser said. “She definitely had that ‘it’ factor. She was sincere with patients and their families and performed well in the operating room. …She was very comfortable around the patients; very comfortable in stressful situations.”
He added, “I look forward to her participating in trauma surgery rotations in the near future.”
In the meantime, Ms. Groesbeck was pleased to learn that the man she saved survived and thrilled to be part of that effort. As of press time, he had not contacted her. Nor has the other student who helped save his life.
“A lot of people stepped up and donated their time to help. He got lucky on a very unlucky day,” Ms. Groesbeck said.
She recalled a previous accident victim years ago who wasn’t as lucky. On the way to pick up her white coat for the ceremony before her first year of medical school, she came upon a car that had flipped upside down. “It sheared the roof away. I checked on the restrained passenger. He was partially scalped. The windows were broken and I climbed in next to him.” This time, she used her own shirt to hold pressure on the wound. “He, unfortunately did not make it.” There was nothing she could have done, she was told.
“That one got me mentally. Very graphic imaging was stuck in my head,” Ms. Groesbeck said. With a masters in neuroscience, she was accustomed to seeing the brain, “but not like this. I felt sad he passed in such a violent way.” So the more recent life-saving experience was redemptive, she said. “I’ve been through hell and back.”
And she’s still on track to become the doctor she envisioned as a child, mummifying her cats with gauze wraps and covering her little sister with adhesive bandages. “It felt good knowing what I could do,” Ms. Groesbeck said. “I’m glad this [man] made it. He got lucky and he could go home to his family. I was not positive when he left in the ambulance. It was a huge relief.”
Of her role in the episode and her future career ambitions, Ms. Groesbeck noted: “We are studying all the time. It’s not very rewarding. But this, not thinking but having sprung into action, doing the right thing and he could go home to his family a week later. It’s things like this that make the endless hours of studying worth it. I feel like I accomplished something.”
A version of this article first appeared on Medscape.com.
Third-year medical student Liz Groesbeck was like other excited Las Vegas Raiders fans recently headed to the first full-capacity game in the new Allegiant Stadium since the team moved to “Sin City.” She was in an Uber on a first date just blocks from the game that would pit her Raiders against the Seattle Seahawks when she saw a man on the ground and people gathered around him.
Abandoning her keys, cellphone, and date in the Uber, Ms. Groesbeck popped out to see if she could help. The Uber had been stuck in traffic, so Ms. Groesbeck thought she’d still be able to jump back in the car if she wasn’t needed.
Then she heard screams. “That didn’t concern me. People scream whenever anything unexpected happens,” said the 28-year-old student from the Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas (UNLV). But the screams were only a small indication of what she would discover on closer inspection. The arm of the middle-aged man lying on the ground was detached. An abandoned gold SUV remained on the curb nearby. It would turn out to be a hit-and-run of pedestrians by a driver later charged by police with DUI.
“I was one of the first people there,” Ms. Groesbeck recounted for this news organization. “I knew this guy did not just fall. I told someone to call EMS and I got someone to take his wife somewhere else [away from the bloody scene]. She was obviously very distraught. …At a couple of points she was hysterical.”
Next, Ms. Groesbeck, who, ironically, had finished her emergency general surgery rotation the day before, focused on the patient. Kneeling beside him, she determined that the immediate priorities were to stop the bleeding and clear his airway. “He was barely breathing,” she recounted. Another student who Ms. Groesbeck believes was pursuing a medical degree — there wasn’t time for formal introductions — offered to help, along with bystanders headed to the game.
“The crowd was very energetic. It was a beautiful thing.” Ms. Groesbeck cited the spirit of saving lives that developed from the October 1, 2017, Las Vegas country music festival shooting. “People are very willing to try to help others in any way they can.”
MS. Groesbeck, leading the effort, asked for belts, “and bystanders immediately provided that,” and the other student followed Ms. Groesbeck’s directions to apply tourniquets with the help of those around her. With the blood loss being stemmed, Ms. Groesbeck’s next priority was making sure the patient could breathe.
Appealing for clothing to clear the man’s airway, “five shirts were handed in a circle to me.” She only needed one jersey to scoop the blood out of his mouth manually to free his airway.
She overruled well-meaning suggestions to lay the man on his side — which she was concerned could paralyze him — or use a straw to help him breathe. “I did not want to stick anything down his throat.” Meanwhile, there was so much traffic that night around Allegiant Stadium that when the ambulance couldn’t get any closer the firefighters and paramedics exited the vehicle and ran to the scene.
From training to practice
The decisions Ms. Groesbeck made until they could arrive called upon her years of training to be a doctor, and specifically an EMT certification course she had to pass before beginning medical school, she said.
She credits the life-saving methods she learned in that course to Douglas Fraser, MD, FACS, associate professor of surgery at UNLV and University Medical Center (UMC) trauma medical director. He happened to be the attending physician when the accident victim was admitted to the hospital that night in critical condition. The man’s wife also was injured, but not to the extent of her husband.
Dr. Fraser said he didn’t know at the time that his student had been involved in saving the man’s life until Ms. Groesbeck reached out to say thanks for teaching her what to do in an emergency. “I [first] was overly impressed that she did that. Students are so busy; they move after they graduate or finish their rotations. You don’t get to see them time and time again; your short time with them could have a lasting impact and that is my goal,” Dr. Fraser told this news organization.
“They rarely thank you or reflect back. It renewed my sense that I want to teach more, to see the positive impact it had on Elizabeth” and other students, he said.
In terms of the emergency situation she navigated, Dr. Fraser said he was very proud of his student, but was also concerned she could have gotten hurt herself in the middle of a busy intersection. “She was selfless and put herself in harm’s way to help someone.” He also noted it was the first time he knew of a student putting her skills to the test so soon after learning them. “It was a good outcome and she truly provided lifesaving care to this victim.”
He attributed her training to the Stop the Bleed program, which began after the Sandy Hook tragedy in 2012. UNLV requires new med students to complete the American College of Surgeons’ first aid program to learn how to stop the bleeding of a severely injured person by applying tourniquets and pressure. “You have to stop the bleeding right away…and look to see whether their airway is open and if it’s not, open their airway or you won’t have a patient very long. I know she did that. These are the two most important lifesaving skills that she did.”
Medical students are often called upon as doctors by their family and friends, Dr. Fraser continued. “Everyone looks to you. It can happen on an airplane; you can be anywhere. She heard a person was in need and jumped to action and was able to use the training her school provided and was able to put it to good use.”
Not her first call to action
Just the week before the incident, Ms. Groesbeck was on clinical rotations at UMC helping in the emergency and operating rooms. “She was always very engaged and mature beyond her years,” Dr. Fraser said. “She definitely had that ‘it’ factor. She was sincere with patients and their families and performed well in the operating room. …She was very comfortable around the patients; very comfortable in stressful situations.”
He added, “I look forward to her participating in trauma surgery rotations in the near future.”
In the meantime, Ms. Groesbeck was pleased to learn that the man she saved survived and thrilled to be part of that effort. As of press time, he had not contacted her. Nor has the other student who helped save his life.
“A lot of people stepped up and donated their time to help. He got lucky on a very unlucky day,” Ms. Groesbeck said.
She recalled a previous accident victim years ago who wasn’t as lucky. On the way to pick up her white coat for the ceremony before her first year of medical school, she came upon a car that had flipped upside down. “It sheared the roof away. I checked on the restrained passenger. He was partially scalped. The windows were broken and I climbed in next to him.” This time, she used her own shirt to hold pressure on the wound. “He, unfortunately did not make it.” There was nothing she could have done, she was told.
“That one got me mentally. Very graphic imaging was stuck in my head,” Ms. Groesbeck said. With a masters in neuroscience, she was accustomed to seeing the brain, “but not like this. I felt sad he passed in such a violent way.” So the more recent life-saving experience was redemptive, she said. “I’ve been through hell and back.”
And she’s still on track to become the doctor she envisioned as a child, mummifying her cats with gauze wraps and covering her little sister with adhesive bandages. “It felt good knowing what I could do,” Ms. Groesbeck said. “I’m glad this [man] made it. He got lucky and he could go home to his family. I was not positive when he left in the ambulance. It was a huge relief.”
Of her role in the episode and her future career ambitions, Ms. Groesbeck noted: “We are studying all the time. It’s not very rewarding. But this, not thinking but having sprung into action, doing the right thing and he could go home to his family a week later. It’s things like this that make the endless hours of studying worth it. I feel like I accomplished something.”
A version of this article first appeared on Medscape.com.
Trauma, psychiatric comorbidities tied to functional motor disorders
Most adults with functional motor disorders (FMDs) report a history of psychological or physical trauma 6 months before the onset of symptoms, a retrospective study of 482 individuals suggests. Those challenges prevent more than half of those patients – most of whom are women – from working, the researchers found.
“This finding points to the huge socioeconomical burden of FMD and emphasizes the need for better diagnostic procedure and active management,” wrote Béatrice Garcin, MD, of Sorbonne Université, Paris, and associates.
FMDs are a common presentation of functional neurologic disorders, but clinical characteristics of FMDs are not well understood because large series of consecutive patients are limited, Dr. Garcin and associates said.
In the study, published in the Journal of Psychosomatic Research, the investigators reviewed data from consecutive patients with FMD who were seen at a single hospital in France between 2008 and 2016. Half of the patients had functional motor weakness (241) and half had functional movement disorders (241). All of the patients had been referred for transcranial magnetic stimulation (TMS) as treatment for FMD.
The median age of the patients was 40 years, the median age at the onset of symptoms was 35.5 years, and 74% were women. The most common clinical presentations were tremor and dystonia (83.4%), and no demographic differences were observed between patients with functional motor weakness and functional movement disorders. Symptoms were bilateral in about half of the patients (51.7%), with left- and right-sided symptoms in 28.2% and 20.1%, respectively.
More than 80% of the patients reported a history of trauma within 6 months of the onset of their symptoms, mainly psychological trauma (50.6%). Another 20.1% reported a physical trauma, and 8.7% reported trauma from surgical procedures.
In addition, about two-thirds (66.4%) had psychiatric comorbidities; 52.7% of these were mood disorders: 49.3% depression and 3.3% bipolar disorder. “However, these results about psychiatric comorbidities should be taken with caution,” the researchers emphasized. “ and psychiatric diagnosis may lack precision because of the absence of systematic psychiatric interviews and psychiatric questionnaires in the present study.”
No significant differences appeared between the motor weakness and movement disorders groups in terms of occupation, level of education, medical somatic history, symptom onset, psychiatric comorbidities, or self-reported history of trauma. Patients in the motor weakness group were significantly younger at the time of TMS treatment and had a shorter disease duration prior to that treatment. No differences were noted between the groups with regard to clinical FMD phenotypes.
The study findings were limited by several factors, including the potential selection bias because of enrollment at a neurology referral center, lack of a control group, and underrepresentation of children and older adults, the researchers noted. Also, symptom severity was not assessed and could not be compared among phenotypes or demographic groups.
However, the results contribute to the characterization of FMD patients. “Future studies are needed to clarify the characteristics of FMD patients and the consequences of their symptoms on disability and work status,” they said.
The study received no outside funding. Lead author Dr. Garcin had no disclosures.
Most adults with functional motor disorders (FMDs) report a history of psychological or physical trauma 6 months before the onset of symptoms, a retrospective study of 482 individuals suggests. Those challenges prevent more than half of those patients – most of whom are women – from working, the researchers found.
“This finding points to the huge socioeconomical burden of FMD and emphasizes the need for better diagnostic procedure and active management,” wrote Béatrice Garcin, MD, of Sorbonne Université, Paris, and associates.
FMDs are a common presentation of functional neurologic disorders, but clinical characteristics of FMDs are not well understood because large series of consecutive patients are limited, Dr. Garcin and associates said.
In the study, published in the Journal of Psychosomatic Research, the investigators reviewed data from consecutive patients with FMD who were seen at a single hospital in France between 2008 and 2016. Half of the patients had functional motor weakness (241) and half had functional movement disorders (241). All of the patients had been referred for transcranial magnetic stimulation (TMS) as treatment for FMD.
The median age of the patients was 40 years, the median age at the onset of symptoms was 35.5 years, and 74% were women. The most common clinical presentations were tremor and dystonia (83.4%), and no demographic differences were observed between patients with functional motor weakness and functional movement disorders. Symptoms were bilateral in about half of the patients (51.7%), with left- and right-sided symptoms in 28.2% and 20.1%, respectively.
More than 80% of the patients reported a history of trauma within 6 months of the onset of their symptoms, mainly psychological trauma (50.6%). Another 20.1% reported a physical trauma, and 8.7% reported trauma from surgical procedures.
In addition, about two-thirds (66.4%) had psychiatric comorbidities; 52.7% of these were mood disorders: 49.3% depression and 3.3% bipolar disorder. “However, these results about psychiatric comorbidities should be taken with caution,” the researchers emphasized. “ and psychiatric diagnosis may lack precision because of the absence of systematic psychiatric interviews and psychiatric questionnaires in the present study.”
No significant differences appeared between the motor weakness and movement disorders groups in terms of occupation, level of education, medical somatic history, symptom onset, psychiatric comorbidities, or self-reported history of trauma. Patients in the motor weakness group were significantly younger at the time of TMS treatment and had a shorter disease duration prior to that treatment. No differences were noted between the groups with regard to clinical FMD phenotypes.
The study findings were limited by several factors, including the potential selection bias because of enrollment at a neurology referral center, lack of a control group, and underrepresentation of children and older adults, the researchers noted. Also, symptom severity was not assessed and could not be compared among phenotypes or demographic groups.
However, the results contribute to the characterization of FMD patients. “Future studies are needed to clarify the characteristics of FMD patients and the consequences of their symptoms on disability and work status,” they said.
The study received no outside funding. Lead author Dr. Garcin had no disclosures.
Most adults with functional motor disorders (FMDs) report a history of psychological or physical trauma 6 months before the onset of symptoms, a retrospective study of 482 individuals suggests. Those challenges prevent more than half of those patients – most of whom are women – from working, the researchers found.
“This finding points to the huge socioeconomical burden of FMD and emphasizes the need for better diagnostic procedure and active management,” wrote Béatrice Garcin, MD, of Sorbonne Université, Paris, and associates.
FMDs are a common presentation of functional neurologic disorders, but clinical characteristics of FMDs are not well understood because large series of consecutive patients are limited, Dr. Garcin and associates said.
In the study, published in the Journal of Psychosomatic Research, the investigators reviewed data from consecutive patients with FMD who were seen at a single hospital in France between 2008 and 2016. Half of the patients had functional motor weakness (241) and half had functional movement disorders (241). All of the patients had been referred for transcranial magnetic stimulation (TMS) as treatment for FMD.
The median age of the patients was 40 years, the median age at the onset of symptoms was 35.5 years, and 74% were women. The most common clinical presentations were tremor and dystonia (83.4%), and no demographic differences were observed between patients with functional motor weakness and functional movement disorders. Symptoms were bilateral in about half of the patients (51.7%), with left- and right-sided symptoms in 28.2% and 20.1%, respectively.
More than 80% of the patients reported a history of trauma within 6 months of the onset of their symptoms, mainly psychological trauma (50.6%). Another 20.1% reported a physical trauma, and 8.7% reported trauma from surgical procedures.
In addition, about two-thirds (66.4%) had psychiatric comorbidities; 52.7% of these were mood disorders: 49.3% depression and 3.3% bipolar disorder. “However, these results about psychiatric comorbidities should be taken with caution,” the researchers emphasized. “ and psychiatric diagnosis may lack precision because of the absence of systematic psychiatric interviews and psychiatric questionnaires in the present study.”
No significant differences appeared between the motor weakness and movement disorders groups in terms of occupation, level of education, medical somatic history, symptom onset, psychiatric comorbidities, or self-reported history of trauma. Patients in the motor weakness group were significantly younger at the time of TMS treatment and had a shorter disease duration prior to that treatment. No differences were noted between the groups with regard to clinical FMD phenotypes.
The study findings were limited by several factors, including the potential selection bias because of enrollment at a neurology referral center, lack of a control group, and underrepresentation of children and older adults, the researchers noted. Also, symptom severity was not assessed and could not be compared among phenotypes or demographic groups.
However, the results contribute to the characterization of FMD patients. “Future studies are needed to clarify the characteristics of FMD patients and the consequences of their symptoms on disability and work status,” they said.
The study received no outside funding. Lead author Dr. Garcin had no disclosures.
FROM THE JOURNAL OF PSYCHOSOMATIC RESEARCH
Veteran and Provider Perspectives on Telehealth for Vocational Rehabilitation Services
Vocational rehabilitation (VR) interventions are offered through Compensated Work Therapy (CWT) as part of clinical care in the Veterans Health Administration (VHA) to improve employment and quality of life outcomes for veterans with life-altering disabilities.1–5 CWT vocational services range from assessment, vocational counseling, and treatment plan development to job placement, coaching, and follow-along support.1 However, many veterans receive care in community-based clinics that are not staffed with a VR specialist (VRS) to provide these services.6–8 Telehealth may increase patient access to VR, especially for rural veterans and those with travel barriers, but it is not known whether veterans and VRS would find this to be a satisfactory service delivery method.8,9 This paper examines veteran and VRS provider perspectives on VR provided by telehealth (VRtele) as part of a VHA clinical demonstration project. To our knowledge, this is the first report of using real-time, clinic-based VRtele.
Methods
The Rural Veterans Supported Employment Telerehabilitation Initiative (RVSETI) was conducted as a field-initiated demonstration project at 2 US Department of Veterans Affairs (VA) medical centers (VAMCs) in Florida between 2014 and 2016: James A. Haley Veterans’ Hospital & Clinics (Tampa) and Malcom Randall VAMC (Gainesville). This retrospective evaluation of its first year did not require institutional review board approval as it was determined to be a quality improvement project by the local research service.
The patient population for the project was veterans with disabilities who were referred by clinical consults to the CWT service, a recovery-oriented vocational program. During the project years, veterans were offered the option of receiving VR services, such as supported employment, community-based employment services, or vocational assistance, through VRtele rather than traditional face-to-face meetings. The specific interventions delivered included patient orientation, interview assessment, treatment plan development, referral activities, vocational counseling, assessment of workplace for accommodation needs, vocational case management, and other employment supports. VR staff participating in the project included 2 VR supervisors, 1 supported employment mentor trainer, and 5 VRSs.
Each clinic was set up for VRtele, and codes were added to the electronic health record (EHR) to ensure proper documentation. Participating VRSs completed teleconferencing training, including a skills assessment using the equipment for real-time, high-quality video streaming over an encrypted network to provide services in a patient’s home or other remote locations. VRS staff provided veterans with instructions on using a VA-provided tablet or their own device and assisted them with establishing connectivity with the network. Video equipment included speakers, camera, and headphones connected to the desktop computer or laptop of the VRS. A patient’s first VRtele
Demographic data, primary diagnosis, VR usage data, and zip codes of participating veterans were extracted from the EHR. Veterans completed a 2-part satisfaction survey administered 90 days after enrollment and at discharge. Part 1 was composed of 15 items, most with a 5-point Likert scale (higher ratings indicated greater satisfaction), on various aspects of the VRtele experience, such as audio and video quality and wait times.10 Part 2 addressed VR services and the VRS and consisted of 8 Likert scale items with the option to add a comment for each and 2 open-ended items that asked the participant to list what they liked best and least about VRtele.
Semistructured, in-person 30- to 60-minute interviews were conducted with VRSs at the initiation of VRtele
After ≥ 2 months of VRtele use
Analyses
Descriptive statistics were used for EHR data and satisfaction surveys. For qualitative analysis, each transcript was read in full by 2 researchers to get an overview of the data, and a rapid analysis approach was used to identify central themes focused on how technology was used and the experiences of the participants.11,12 Relevant text for each topic was tabulated, and a summary table was created that highlighted overlapping ideas discussed by the interviewees as well as differences.
Results
Of the 22 veterans who participated in the project, 11 completed satisfaction surveys and 4 participated in qualitative interviews. The rural and nonrural groups did not differ demographically or by diagnosis, which was predominantly mental health related. Only 1 veteran in each group owned a tablet; the majority of both groups required VA-issued devices: 80% (n = 8) rural and 91.7% (n = 11) nonrural. The number of VRtele sessions for the groups also was similar, 53 for rural and 60 for nonrural, as was the mean (SD) number of sessions per veteran: 5.3 (SD, 3.2) rural and 5.0 (SD, 2.5) urban. Overall, 63 miles per session were saved, mostly for rural veterans, and the number of mean (SD) miles saved per veteran was greater for rural than nonrural veterans: 379.2 (243.0) and 256.1 (275.9), respectively. One veteran who moved to a different state during the program continued VRtele at the new location. In a qualitative sampling of 5 VRtele sessions, all the VRSs used office desktop computers.
Level of satisfaction with aspects of VRtele related to the technology rated was consistently > 4 on the Likert scale. The lowest mean (SD) ratings were 4.2 (1.0) for audio quality and 4.4 (0.5) for video quality, and the highest rating was given for equipment operation explanation and privacy was respected, 4.9 (0.3) for both. All questions related to satisfaction with services were also rated high: The mean (SD) lowest ratings were 4.3 (1.0) given to both vocational needs 4.3 (1.0) and tasks effectively helped achieve goals 4.3 (0.7). The highest mean (SD) ratings were 4.6 (0.5) given to VR program service explained and 4.7 (0.5) for appointment timeliness.
Qualitative Results
At first, some VRSs thought the teleconferencing system might be difficult or awkward to use, but they found it easier to set up than expected and seamless to use. VRS staff reported being surprised at how well it worked despite some issues that occurred with loading the software. Once loaded, however, the connection worked well, one VRS noting that following step-by-step instructions solved the problem. Some VRSs indicated they did not invite all the veterans on their caseload to participate in VRtele due to concerns with the patient’s familiarity with technology, but one VRS stated, “I haven’t had anybody that failed to do a [session] that I couldn’t get them up and running within a few minutes.”
When working in the community, VRSs reported using laptops for VRtele but found that these devices were unreliable due to lack of internet access and were slow to start; several VRSs thought tablets would have been more helpful. Some veterans reported technical glitches, lack of comfort with technology, or a problem with sound due to a tablet’s protective case blocking the speakers. To solve the sound issue, a veteran used headphones. This veteran also explained that the log-on process required a new password every time, so he would keep a pen and paper ready to write it down. Because signing in and setting up takes a little time, this veteran and his VRS agreed to start connecting 5 minutes before their meeting time to allow for that set- up time.
Initially, some VRSs expressed concern that transitioning to VRtele would affect the quality of interactions with the veterans. However, VRSs also identified strengths of VRtele, including flexibility, saved time, and increased interaction. One VRS discussed a veteran’s adaptation by saying, “I think he feels even more involved in his plan [and] enjoys the increased interaction.” Veterans reported enjoying using tablets and identified the main strength of VRtele as being able to talk face-to-face with the VRS. Echoing the VRSs, veterans reported teleconferencing saved time by avoiding travel and enabled spontaneous meetings. One of the veterans summed up the benefits of using VRtele: “I’d rather just connect. It’s going to take us 40 to 50 minutes [to meet in person] when we can just connect right here and it takes 15 to 20. We don’t have to go through the driving.… So this right here, doing it ahead of time and having the appointment, it’s a lot easier.”
In their interviews, VRSs talked about enjoying VRtele. A VRS explained: “It makes it a lot easier. It makes me feel less guilty. This way [veterans] don’t have to use their gas money, use their time. I know [the veteran] had something else he needed to do today.” Thus, both veterans and VRSs were satisfied with their VRtele experiences.
Discussion
This first report on the perspective of providers and veterans using VRtele suggests that it is a viable option for service delivery and that is highly satisfactory for serving veterans with disabilities, many of whom live in rural areas or have travel barriers. These findings are consistent with data on telerehabilitation for veterans with cognitive, physical, and mental disabilities.13-22 Further, the data support the notion of using VRtele to facilitate long-term VR follow-up for persons with disabilities, as illustrated by successful continuation of vocational services after a veteran moved out of state.23
Similar to other reports, our experience highlighted 2 factors that affect successful VRtele: (1) Troubleshooting technology barriers for both VR providers and clients; and (2) supportive leadership to facilitate implementation
Changes to technology and increased usage of VA Video Connect may indicate that the barriers identified from the earlier process described here have been diminished or eliminated. More evaluation is needed to assess whether system upgrades have increased ease of use and access for veterans with disabilities.
Conclusions
Encouragingly, this clinical demonstration project showed that both providers and clients recognize the benefits of VRtele. Patient satisfaction and decreased travel costs were clear advantages to using VRtele for this small group of veterans who had barriers to care due to travel or disability barriers. As this program evaluation was limited by a small sample, absence of a comparison group, and lack of outcome data (eg, employment rates, hours, wages, retention), future research is needed on implementation and outcomes of VRtele
Acknowledgments
The authors thank Lynn Dirk, MAMC, for substantial editorial assistance. This material was based on work supported by Rural Veterans Supported Employment TeleRehabilitation Initiative (RVSETI), funded by the VA Office of Rural Health (Project # N08-FY14Q3-S2-P01222) and by support of the VA Health Services Research and Development Service. This work was presented in part at the 114th Annual Meeting of the American Anthropological Association at Denver, Colorado, November 21, 2015; a field-based Health Services Research and Development Service meeting, US Department of Veterans Affairs at Washington, DC, September 12, 2016; and the 2016 Annual Conference of the American Congress for Rehabilitation Medicine at Chicago, Illinois, October-November 2016.
1. Abraham KM, Yosef M, Resnick SG, Zivin K. Competitive employment outcomes among veterans in VHA therapeutic and supported employment services programs. Psychiatr Serv. 2017;68(9):938-946. doi:10.1176/appi.ps.201600412
2. Davis LL, Kyriakides TC, Suris AM, et al. Effect of evidence-based supported employment vs transitional work on achieving steady work among veterans with posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatry. 2018;75(4):316. doi:10.1001/jamapsychiatry.2017.4472
3. Ottomanelli L, Goetz LL, Suris A, et al. Effectiveness of supported employment for veterans with spinal cord injuries: results from a randomized multisite study. Arch Phys Med Rehabil. 2012;93(5):740-747. doi:10.1016/j.apmr.2012.01.002
4. Ottomanelli L, Goetz LL, Barnett SD, et al. Individual placement and support in spinal cord injury: a longitudinal observational study of employment outcomes. Arch Phys Med Rehabil. 2017;98(8):1567-1575. doi:10.1016/j.apmr.2016.12.010
5. Cotner BA, Ottomanelli L, O’Connor DR, Njoh EN, Barnett SD, Miech EJ. Quality of life outcomes for veterans with spinal cord injury receiving individual placement and support (IPS). Top Spinal Cord Inj Rehabil. 2018;24(4):325-335. doi:10.1310/sci17-00046
6. Metzel DS, Giordano A. Locations of employment services and people with disabilities: a geographical analysis of accessibility. J Disabil Policy Stud. 2007;18(2):88-97. doi:10.1177/10442073070180020501
7. Landon T, Connor A, McKnight-Lizotte M, Peña J. Rehabilitation counseling in rural settings: a phenomenological study on barriers and supports. J Rehabil. 2019;85(2):47-57.
8. Riemer-Reiss M. Vocational rehabilitation counseling at a distance: Challenges, strategies and ethics to consider. J Rehabil. 2000;66(1):11-17.
9. Schmeler MR, Schein RM, McCue M, Betz K. Telerehabilitation clinical and vocational applications for assistive technology: research, opportunities, and challenges. Int J Telerehabilitation. 2009;1(1):59-72.
10. Levy CE, Silverman E, Jia H, Geiss M, Omura D. Effects of physical therapy delivery via home video telerehabilitation on functional and health-related quality of life outcomes. J Rehabil Res Dev. 2015;52(3):361-370. doi:10.1682/JRRD.2014.10.0239
11. McMullen CK, Ash JS, Sittig DF, et al. Rapid assessment of clinical information systems in the healthcare setting: an efficient method for time-pressed evaluation. Methods Inf Med. 2011;50(4):299-307. doi:10.3414/ME10-01-0042
12. Averill JB. Matrix analysis as a complementary analytic strategy in qualitative inquiry. Qual Health Res. 2002;12(6):855-866.
13. Egede LE, Acierno R, Knapp RG, et al. Psychotherapy for depression in older veterans via telemedicine: a randomised, open-label, non-inferiority trial. Lancet Psychiatry. 2015;2(8):693-701. doi:10.1016/S2215-0366(15)00122-4
14. Fortney JC, Pyne JM, Edlund MJ, et al. A randomized trial of telemedicine-based collaborative care for depression. J Gen Intern Med. 2007;22(8):1086-1093. doi:10.1007/s11606-007-0201-9
15. Fortney JC, Pyne JM, Kimbrell TA, et al. Telemedicine-based collaborative care for posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatry. 2015;72(1):58. doi:10.1001/jamapsychiatry.2014.1575
16. Grubbs KM, Fortney JC, Dean T, Williams JS, Godleski L. A comparison of mental health diagnoses treated via interactive video and face to face in the Veterans Healthcare Administration. Telemed E-Health. 2015;21(7):564-566. doi:10.1089/tmj.2014.0152
17. Agostini M, Moja L, Banzi R, et al. Telerehabilitation and recovery of motor function: a systematic review and meta-analysis. J Telemed Telecare. 2015;21(4):202-213. doi:10.1177/1357633X15572201
18. Bergquist TF, Thompson K, Gehl C, Munoz Pineda J. Satisfaction ratings after receiving internet-based cognitive rehabilitation in persons with memory impairments after severe acquired brain injury. Telemed E-Health. 2010;16(4):417-423. doi:10.1089/tmj.2009.0118
19. Brennan DM, Georgeadis AC, Baron CR, Barker LM. The effect of videoconference-based telerehabilitation on story retelling performance by brain-injured subjects and its implications for remote speech-language therapy. Telemed J E Health. 2004;10(2):147-154. doi:10.1089/tmj.2004.10.147
20. Dallolio L, Menarini M, China S, et al. Functional and clinical outcomes of telemedicine in patients with spinal cord injury. Arch Phys Med Rehabil. 2008;89(12):2332-2341. doi:10.1016/j.apmr.2008.06.012
21. Houlihan BV, Jette A, Friedman RH, et al. A pilot study of a telehealth intervention for persons with spinal cord dysfunction. Spinal Cord. 2013;51(9):715-720.doi:10.1038/sc.2013.45
22. Smith MW, Hill ML, Hopkins KL, Kiratli BJ, Cronkite RC. A modeled analysis of telehealth methods for treating pressure ulcers after spinal cord injury. Int J Telemed Appl. 2012;2012:1-10. doi:10.1155/2012/729492
23. Balcazar FE, Keys CB, Davis M, Lardon C, Jones C. Strengths and challenges of intervention research in vocational rehabilitation: an illustration of agency-university collaboration. J Rehabil. 2005;71(2):40-48.
24. Martinez RN, Hogan TP, Balbale S, et al. Sociotechnical perspective on implementing clinical video telehealth for veterans with spinal cord injuries and disorders. Telemed J E Health. 2017;23(7):567-576. doi:10.1089/tmj.2016.0200
25. Martinez RN, Hogan TP, Lones K, et al. Evaluation and treatment of mild traumatic brain injury through the implementation of clinical video telehealth: provider perspectives from the Veterans Health Administration. PM R. 2017;9(3):231-240. doi:10.1016/j.pmrj.2016.07.002
26. Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020;26(5):309-313. doi:10.1177/1357633X20916567
27. Cowper-Ripley DC, Jia H, Wang X, et al. Trends in VA telerehabilitation patients and encounters over time and by rurality. Fed Pract. 2019; 36(3):122-128.
28. US Department of Veterans Affairs. Veterans VA Video Connect. Published May 22, 2020. Accessed May 29, 2020. https://mobile.va.gov/app/va-video-connect#AppDescription.
29. US Department of Veterans Affairs. VA telehealth at home. Accessed May 29, 2020. https://telehealth.va.gov/type/home
Vocational rehabilitation (VR) interventions are offered through Compensated Work Therapy (CWT) as part of clinical care in the Veterans Health Administration (VHA) to improve employment and quality of life outcomes for veterans with life-altering disabilities.1–5 CWT vocational services range from assessment, vocational counseling, and treatment plan development to job placement, coaching, and follow-along support.1 However, many veterans receive care in community-based clinics that are not staffed with a VR specialist (VRS) to provide these services.6–8 Telehealth may increase patient access to VR, especially for rural veterans and those with travel barriers, but it is not known whether veterans and VRS would find this to be a satisfactory service delivery method.8,9 This paper examines veteran and VRS provider perspectives on VR provided by telehealth (VRtele) as part of a VHA clinical demonstration project. To our knowledge, this is the first report of using real-time, clinic-based VRtele.
Methods
The Rural Veterans Supported Employment Telerehabilitation Initiative (RVSETI) was conducted as a field-initiated demonstration project at 2 US Department of Veterans Affairs (VA) medical centers (VAMCs) in Florida between 2014 and 2016: James A. Haley Veterans’ Hospital & Clinics (Tampa) and Malcom Randall VAMC (Gainesville). This retrospective evaluation of its first year did not require institutional review board approval as it was determined to be a quality improvement project by the local research service.
The patient population for the project was veterans with disabilities who were referred by clinical consults to the CWT service, a recovery-oriented vocational program. During the project years, veterans were offered the option of receiving VR services, such as supported employment, community-based employment services, or vocational assistance, through VRtele rather than traditional face-to-face meetings. The specific interventions delivered included patient orientation, interview assessment, treatment plan development, referral activities, vocational counseling, assessment of workplace for accommodation needs, vocational case management, and other employment supports. VR staff participating in the project included 2 VR supervisors, 1 supported employment mentor trainer, and 5 VRSs.
Each clinic was set up for VRtele, and codes were added to the electronic health record (EHR) to ensure proper documentation. Participating VRSs completed teleconferencing training, including a skills assessment using the equipment for real-time, high-quality video streaming over an encrypted network to provide services in a patient’s home or other remote locations. VRS staff provided veterans with instructions on using a VA-provided tablet or their own device and assisted them with establishing connectivity with the network. Video equipment included speakers, camera, and headphones connected to the desktop computer or laptop of the VRS. A patient’s first VRtele
Demographic data, primary diagnosis, VR usage data, and zip codes of participating veterans were extracted from the EHR. Veterans completed a 2-part satisfaction survey administered 90 days after enrollment and at discharge. Part 1 was composed of 15 items, most with a 5-point Likert scale (higher ratings indicated greater satisfaction), on various aspects of the VRtele experience, such as audio and video quality and wait times.10 Part 2 addressed VR services and the VRS and consisted of 8 Likert scale items with the option to add a comment for each and 2 open-ended items that asked the participant to list what they liked best and least about VRtele.
Semistructured, in-person 30- to 60-minute interviews were conducted with VRSs at the initiation of VRtele
After ≥ 2 months of VRtele use
Analyses
Descriptive statistics were used for EHR data and satisfaction surveys. For qualitative analysis, each transcript was read in full by 2 researchers to get an overview of the data, and a rapid analysis approach was used to identify central themes focused on how technology was used and the experiences of the participants.11,12 Relevant text for each topic was tabulated, and a summary table was created that highlighted overlapping ideas discussed by the interviewees as well as differences.
Results
Of the 22 veterans who participated in the project, 11 completed satisfaction surveys and 4 participated in qualitative interviews. The rural and nonrural groups did not differ demographically or by diagnosis, which was predominantly mental health related. Only 1 veteran in each group owned a tablet; the majority of both groups required VA-issued devices: 80% (n = 8) rural and 91.7% (n = 11) nonrural. The number of VRtele sessions for the groups also was similar, 53 for rural and 60 for nonrural, as was the mean (SD) number of sessions per veteran: 5.3 (SD, 3.2) rural and 5.0 (SD, 2.5) urban. Overall, 63 miles per session were saved, mostly for rural veterans, and the number of mean (SD) miles saved per veteran was greater for rural than nonrural veterans: 379.2 (243.0) and 256.1 (275.9), respectively. One veteran who moved to a different state during the program continued VRtele at the new location. In a qualitative sampling of 5 VRtele sessions, all the VRSs used office desktop computers.
Level of satisfaction with aspects of VRtele related to the technology rated was consistently > 4 on the Likert scale. The lowest mean (SD) ratings were 4.2 (1.0) for audio quality and 4.4 (0.5) for video quality, and the highest rating was given for equipment operation explanation and privacy was respected, 4.9 (0.3) for both. All questions related to satisfaction with services were also rated high: The mean (SD) lowest ratings were 4.3 (1.0) given to both vocational needs 4.3 (1.0) and tasks effectively helped achieve goals 4.3 (0.7). The highest mean (SD) ratings were 4.6 (0.5) given to VR program service explained and 4.7 (0.5) for appointment timeliness.
Qualitative Results
At first, some VRSs thought the teleconferencing system might be difficult or awkward to use, but they found it easier to set up than expected and seamless to use. VRS staff reported being surprised at how well it worked despite some issues that occurred with loading the software. Once loaded, however, the connection worked well, one VRS noting that following step-by-step instructions solved the problem. Some VRSs indicated they did not invite all the veterans on their caseload to participate in VRtele due to concerns with the patient’s familiarity with technology, but one VRS stated, “I haven’t had anybody that failed to do a [session] that I couldn’t get them up and running within a few minutes.”
When working in the community, VRSs reported using laptops for VRtele but found that these devices were unreliable due to lack of internet access and were slow to start; several VRSs thought tablets would have been more helpful. Some veterans reported technical glitches, lack of comfort with technology, or a problem with sound due to a tablet’s protective case blocking the speakers. To solve the sound issue, a veteran used headphones. This veteran also explained that the log-on process required a new password every time, so he would keep a pen and paper ready to write it down. Because signing in and setting up takes a little time, this veteran and his VRS agreed to start connecting 5 minutes before their meeting time to allow for that set- up time.
Initially, some VRSs expressed concern that transitioning to VRtele would affect the quality of interactions with the veterans. However, VRSs also identified strengths of VRtele, including flexibility, saved time, and increased interaction. One VRS discussed a veteran’s adaptation by saying, “I think he feels even more involved in his plan [and] enjoys the increased interaction.” Veterans reported enjoying using tablets and identified the main strength of VRtele as being able to talk face-to-face with the VRS. Echoing the VRSs, veterans reported teleconferencing saved time by avoiding travel and enabled spontaneous meetings. One of the veterans summed up the benefits of using VRtele: “I’d rather just connect. It’s going to take us 40 to 50 minutes [to meet in person] when we can just connect right here and it takes 15 to 20. We don’t have to go through the driving.… So this right here, doing it ahead of time and having the appointment, it’s a lot easier.”
In their interviews, VRSs talked about enjoying VRtele. A VRS explained: “It makes it a lot easier. It makes me feel less guilty. This way [veterans] don’t have to use their gas money, use their time. I know [the veteran] had something else he needed to do today.” Thus, both veterans and VRSs were satisfied with their VRtele experiences.
Discussion
This first report on the perspective of providers and veterans using VRtele suggests that it is a viable option for service delivery and that is highly satisfactory for serving veterans with disabilities, many of whom live in rural areas or have travel barriers. These findings are consistent with data on telerehabilitation for veterans with cognitive, physical, and mental disabilities.13-22 Further, the data support the notion of using VRtele to facilitate long-term VR follow-up for persons with disabilities, as illustrated by successful continuation of vocational services after a veteran moved out of state.23
Similar to other reports, our experience highlighted 2 factors that affect successful VRtele: (1) Troubleshooting technology barriers for both VR providers and clients; and (2) supportive leadership to facilitate implementation
Changes to technology and increased usage of VA Video Connect may indicate that the barriers identified from the earlier process described here have been diminished or eliminated. More evaluation is needed to assess whether system upgrades have increased ease of use and access for veterans with disabilities.
Conclusions
Encouragingly, this clinical demonstration project showed that both providers and clients recognize the benefits of VRtele. Patient satisfaction and decreased travel costs were clear advantages to using VRtele for this small group of veterans who had barriers to care due to travel or disability barriers. As this program evaluation was limited by a small sample, absence of a comparison group, and lack of outcome data (eg, employment rates, hours, wages, retention), future research is needed on implementation and outcomes of VRtele
Acknowledgments
The authors thank Lynn Dirk, MAMC, for substantial editorial assistance. This material was based on work supported by Rural Veterans Supported Employment TeleRehabilitation Initiative (RVSETI), funded by the VA Office of Rural Health (Project # N08-FY14Q3-S2-P01222) and by support of the VA Health Services Research and Development Service. This work was presented in part at the 114th Annual Meeting of the American Anthropological Association at Denver, Colorado, November 21, 2015; a field-based Health Services Research and Development Service meeting, US Department of Veterans Affairs at Washington, DC, September 12, 2016; and the 2016 Annual Conference of the American Congress for Rehabilitation Medicine at Chicago, Illinois, October-November 2016.
Vocational rehabilitation (VR) interventions are offered through Compensated Work Therapy (CWT) as part of clinical care in the Veterans Health Administration (VHA) to improve employment and quality of life outcomes for veterans with life-altering disabilities.1–5 CWT vocational services range from assessment, vocational counseling, and treatment plan development to job placement, coaching, and follow-along support.1 However, many veterans receive care in community-based clinics that are not staffed with a VR specialist (VRS) to provide these services.6–8 Telehealth may increase patient access to VR, especially for rural veterans and those with travel barriers, but it is not known whether veterans and VRS would find this to be a satisfactory service delivery method.8,9 This paper examines veteran and VRS provider perspectives on VR provided by telehealth (VRtele) as part of a VHA clinical demonstration project. To our knowledge, this is the first report of using real-time, clinic-based VRtele.
Methods
The Rural Veterans Supported Employment Telerehabilitation Initiative (RVSETI) was conducted as a field-initiated demonstration project at 2 US Department of Veterans Affairs (VA) medical centers (VAMCs) in Florida between 2014 and 2016: James A. Haley Veterans’ Hospital & Clinics (Tampa) and Malcom Randall VAMC (Gainesville). This retrospective evaluation of its first year did not require institutional review board approval as it was determined to be a quality improvement project by the local research service.
The patient population for the project was veterans with disabilities who were referred by clinical consults to the CWT service, a recovery-oriented vocational program. During the project years, veterans were offered the option of receiving VR services, such as supported employment, community-based employment services, or vocational assistance, through VRtele rather than traditional face-to-face meetings. The specific interventions delivered included patient orientation, interview assessment, treatment plan development, referral activities, vocational counseling, assessment of workplace for accommodation needs, vocational case management, and other employment supports. VR staff participating in the project included 2 VR supervisors, 1 supported employment mentor trainer, and 5 VRSs.
Each clinic was set up for VRtele, and codes were added to the electronic health record (EHR) to ensure proper documentation. Participating VRSs completed teleconferencing training, including a skills assessment using the equipment for real-time, high-quality video streaming over an encrypted network to provide services in a patient’s home or other remote locations. VRS staff provided veterans with instructions on using a VA-provided tablet or their own device and assisted them with establishing connectivity with the network. Video equipment included speakers, camera, and headphones connected to the desktop computer or laptop of the VRS. A patient’s first VRtele
Demographic data, primary diagnosis, VR usage data, and zip codes of participating veterans were extracted from the EHR. Veterans completed a 2-part satisfaction survey administered 90 days after enrollment and at discharge. Part 1 was composed of 15 items, most with a 5-point Likert scale (higher ratings indicated greater satisfaction), on various aspects of the VRtele experience, such as audio and video quality and wait times.10 Part 2 addressed VR services and the VRS and consisted of 8 Likert scale items with the option to add a comment for each and 2 open-ended items that asked the participant to list what they liked best and least about VRtele.
Semistructured, in-person 30- to 60-minute interviews were conducted with VRSs at the initiation of VRtele
After ≥ 2 months of VRtele use
Analyses
Descriptive statistics were used for EHR data and satisfaction surveys. For qualitative analysis, each transcript was read in full by 2 researchers to get an overview of the data, and a rapid analysis approach was used to identify central themes focused on how technology was used and the experiences of the participants.11,12 Relevant text for each topic was tabulated, and a summary table was created that highlighted overlapping ideas discussed by the interviewees as well as differences.
Results
Of the 22 veterans who participated in the project, 11 completed satisfaction surveys and 4 participated in qualitative interviews. The rural and nonrural groups did not differ demographically or by diagnosis, which was predominantly mental health related. Only 1 veteran in each group owned a tablet; the majority of both groups required VA-issued devices: 80% (n = 8) rural and 91.7% (n = 11) nonrural. The number of VRtele sessions for the groups also was similar, 53 for rural and 60 for nonrural, as was the mean (SD) number of sessions per veteran: 5.3 (SD, 3.2) rural and 5.0 (SD, 2.5) urban. Overall, 63 miles per session were saved, mostly for rural veterans, and the number of mean (SD) miles saved per veteran was greater for rural than nonrural veterans: 379.2 (243.0) and 256.1 (275.9), respectively. One veteran who moved to a different state during the program continued VRtele at the new location. In a qualitative sampling of 5 VRtele sessions, all the VRSs used office desktop computers.
Level of satisfaction with aspects of VRtele related to the technology rated was consistently > 4 on the Likert scale. The lowest mean (SD) ratings were 4.2 (1.0) for audio quality and 4.4 (0.5) for video quality, and the highest rating was given for equipment operation explanation and privacy was respected, 4.9 (0.3) for both. All questions related to satisfaction with services were also rated high: The mean (SD) lowest ratings were 4.3 (1.0) given to both vocational needs 4.3 (1.0) and tasks effectively helped achieve goals 4.3 (0.7). The highest mean (SD) ratings were 4.6 (0.5) given to VR program service explained and 4.7 (0.5) for appointment timeliness.
Qualitative Results
At first, some VRSs thought the teleconferencing system might be difficult or awkward to use, but they found it easier to set up than expected and seamless to use. VRS staff reported being surprised at how well it worked despite some issues that occurred with loading the software. Once loaded, however, the connection worked well, one VRS noting that following step-by-step instructions solved the problem. Some VRSs indicated they did not invite all the veterans on their caseload to participate in VRtele due to concerns with the patient’s familiarity with technology, but one VRS stated, “I haven’t had anybody that failed to do a [session] that I couldn’t get them up and running within a few minutes.”
When working in the community, VRSs reported using laptops for VRtele but found that these devices were unreliable due to lack of internet access and were slow to start; several VRSs thought tablets would have been more helpful. Some veterans reported technical glitches, lack of comfort with technology, or a problem with sound due to a tablet’s protective case blocking the speakers. To solve the sound issue, a veteran used headphones. This veteran also explained that the log-on process required a new password every time, so he would keep a pen and paper ready to write it down. Because signing in and setting up takes a little time, this veteran and his VRS agreed to start connecting 5 minutes before their meeting time to allow for that set- up time.
Initially, some VRSs expressed concern that transitioning to VRtele would affect the quality of interactions with the veterans. However, VRSs also identified strengths of VRtele, including flexibility, saved time, and increased interaction. One VRS discussed a veteran’s adaptation by saying, “I think he feels even more involved in his plan [and] enjoys the increased interaction.” Veterans reported enjoying using tablets and identified the main strength of VRtele as being able to talk face-to-face with the VRS. Echoing the VRSs, veterans reported teleconferencing saved time by avoiding travel and enabled spontaneous meetings. One of the veterans summed up the benefits of using VRtele: “I’d rather just connect. It’s going to take us 40 to 50 minutes [to meet in person] when we can just connect right here and it takes 15 to 20. We don’t have to go through the driving.… So this right here, doing it ahead of time and having the appointment, it’s a lot easier.”
In their interviews, VRSs talked about enjoying VRtele. A VRS explained: “It makes it a lot easier. It makes me feel less guilty. This way [veterans] don’t have to use their gas money, use their time. I know [the veteran] had something else he needed to do today.” Thus, both veterans and VRSs were satisfied with their VRtele experiences.
Discussion
This first report on the perspective of providers and veterans using VRtele suggests that it is a viable option for service delivery and that is highly satisfactory for serving veterans with disabilities, many of whom live in rural areas or have travel barriers. These findings are consistent with data on telerehabilitation for veterans with cognitive, physical, and mental disabilities.13-22 Further, the data support the notion of using VRtele to facilitate long-term VR follow-up for persons with disabilities, as illustrated by successful continuation of vocational services after a veteran moved out of state.23
Similar to other reports, our experience highlighted 2 factors that affect successful VRtele: (1) Troubleshooting technology barriers for both VR providers and clients; and (2) supportive leadership to facilitate implementation
Changes to technology and increased usage of VA Video Connect may indicate that the barriers identified from the earlier process described here have been diminished or eliminated. More evaluation is needed to assess whether system upgrades have increased ease of use and access for veterans with disabilities.
Conclusions
Encouragingly, this clinical demonstration project showed that both providers and clients recognize the benefits of VRtele. Patient satisfaction and decreased travel costs were clear advantages to using VRtele for this small group of veterans who had barriers to care due to travel or disability barriers. As this program evaluation was limited by a small sample, absence of a comparison group, and lack of outcome data (eg, employment rates, hours, wages, retention), future research is needed on implementation and outcomes of VRtele
Acknowledgments
The authors thank Lynn Dirk, MAMC, for substantial editorial assistance. This material was based on work supported by Rural Veterans Supported Employment TeleRehabilitation Initiative (RVSETI), funded by the VA Office of Rural Health (Project # N08-FY14Q3-S2-P01222) and by support of the VA Health Services Research and Development Service. This work was presented in part at the 114th Annual Meeting of the American Anthropological Association at Denver, Colorado, November 21, 2015; a field-based Health Services Research and Development Service meeting, US Department of Veterans Affairs at Washington, DC, September 12, 2016; and the 2016 Annual Conference of the American Congress for Rehabilitation Medicine at Chicago, Illinois, October-November 2016.
1. Abraham KM, Yosef M, Resnick SG, Zivin K. Competitive employment outcomes among veterans in VHA therapeutic and supported employment services programs. Psychiatr Serv. 2017;68(9):938-946. doi:10.1176/appi.ps.201600412
2. Davis LL, Kyriakides TC, Suris AM, et al. Effect of evidence-based supported employment vs transitional work on achieving steady work among veterans with posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatry. 2018;75(4):316. doi:10.1001/jamapsychiatry.2017.4472
3. Ottomanelli L, Goetz LL, Suris A, et al. Effectiveness of supported employment for veterans with spinal cord injuries: results from a randomized multisite study. Arch Phys Med Rehabil. 2012;93(5):740-747. doi:10.1016/j.apmr.2012.01.002
4. Ottomanelli L, Goetz LL, Barnett SD, et al. Individual placement and support in spinal cord injury: a longitudinal observational study of employment outcomes. Arch Phys Med Rehabil. 2017;98(8):1567-1575. doi:10.1016/j.apmr.2016.12.010
5. Cotner BA, Ottomanelli L, O’Connor DR, Njoh EN, Barnett SD, Miech EJ. Quality of life outcomes for veterans with spinal cord injury receiving individual placement and support (IPS). Top Spinal Cord Inj Rehabil. 2018;24(4):325-335. doi:10.1310/sci17-00046
6. Metzel DS, Giordano A. Locations of employment services and people with disabilities: a geographical analysis of accessibility. J Disabil Policy Stud. 2007;18(2):88-97. doi:10.1177/10442073070180020501
7. Landon T, Connor A, McKnight-Lizotte M, Peña J. Rehabilitation counseling in rural settings: a phenomenological study on barriers and supports. J Rehabil. 2019;85(2):47-57.
8. Riemer-Reiss M. Vocational rehabilitation counseling at a distance: Challenges, strategies and ethics to consider. J Rehabil. 2000;66(1):11-17.
9. Schmeler MR, Schein RM, McCue M, Betz K. Telerehabilitation clinical and vocational applications for assistive technology: research, opportunities, and challenges. Int J Telerehabilitation. 2009;1(1):59-72.
10. Levy CE, Silverman E, Jia H, Geiss M, Omura D. Effects of physical therapy delivery via home video telerehabilitation on functional and health-related quality of life outcomes. J Rehabil Res Dev. 2015;52(3):361-370. doi:10.1682/JRRD.2014.10.0239
11. McMullen CK, Ash JS, Sittig DF, et al. Rapid assessment of clinical information systems in the healthcare setting: an efficient method for time-pressed evaluation. Methods Inf Med. 2011;50(4):299-307. doi:10.3414/ME10-01-0042
12. Averill JB. Matrix analysis as a complementary analytic strategy in qualitative inquiry. Qual Health Res. 2002;12(6):855-866.
13. Egede LE, Acierno R, Knapp RG, et al. Psychotherapy for depression in older veterans via telemedicine: a randomised, open-label, non-inferiority trial. Lancet Psychiatry. 2015;2(8):693-701. doi:10.1016/S2215-0366(15)00122-4
14. Fortney JC, Pyne JM, Edlund MJ, et al. A randomized trial of telemedicine-based collaborative care for depression. J Gen Intern Med. 2007;22(8):1086-1093. doi:10.1007/s11606-007-0201-9
15. Fortney JC, Pyne JM, Kimbrell TA, et al. Telemedicine-based collaborative care for posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatry. 2015;72(1):58. doi:10.1001/jamapsychiatry.2014.1575
16. Grubbs KM, Fortney JC, Dean T, Williams JS, Godleski L. A comparison of mental health diagnoses treated via interactive video and face to face in the Veterans Healthcare Administration. Telemed E-Health. 2015;21(7):564-566. doi:10.1089/tmj.2014.0152
17. Agostini M, Moja L, Banzi R, et al. Telerehabilitation and recovery of motor function: a systematic review and meta-analysis. J Telemed Telecare. 2015;21(4):202-213. doi:10.1177/1357633X15572201
18. Bergquist TF, Thompson K, Gehl C, Munoz Pineda J. Satisfaction ratings after receiving internet-based cognitive rehabilitation in persons with memory impairments after severe acquired brain injury. Telemed E-Health. 2010;16(4):417-423. doi:10.1089/tmj.2009.0118
19. Brennan DM, Georgeadis AC, Baron CR, Barker LM. The effect of videoconference-based telerehabilitation on story retelling performance by brain-injured subjects and its implications for remote speech-language therapy. Telemed J E Health. 2004;10(2):147-154. doi:10.1089/tmj.2004.10.147
20. Dallolio L, Menarini M, China S, et al. Functional and clinical outcomes of telemedicine in patients with spinal cord injury. Arch Phys Med Rehabil. 2008;89(12):2332-2341. doi:10.1016/j.apmr.2008.06.012
21. Houlihan BV, Jette A, Friedman RH, et al. A pilot study of a telehealth intervention for persons with spinal cord dysfunction. Spinal Cord. 2013;51(9):715-720.doi:10.1038/sc.2013.45
22. Smith MW, Hill ML, Hopkins KL, Kiratli BJ, Cronkite RC. A modeled analysis of telehealth methods for treating pressure ulcers after spinal cord injury. Int J Telemed Appl. 2012;2012:1-10. doi:10.1155/2012/729492
23. Balcazar FE, Keys CB, Davis M, Lardon C, Jones C. Strengths and challenges of intervention research in vocational rehabilitation: an illustration of agency-university collaboration. J Rehabil. 2005;71(2):40-48.
24. Martinez RN, Hogan TP, Balbale S, et al. Sociotechnical perspective on implementing clinical video telehealth for veterans with spinal cord injuries and disorders. Telemed J E Health. 2017;23(7):567-576. doi:10.1089/tmj.2016.0200
25. Martinez RN, Hogan TP, Lones K, et al. Evaluation and treatment of mild traumatic brain injury through the implementation of clinical video telehealth: provider perspectives from the Veterans Health Administration. PM R. 2017;9(3):231-240. doi:10.1016/j.pmrj.2016.07.002
26. Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020;26(5):309-313. doi:10.1177/1357633X20916567
27. Cowper-Ripley DC, Jia H, Wang X, et al. Trends in VA telerehabilitation patients and encounters over time and by rurality. Fed Pract. 2019; 36(3):122-128.
28. US Department of Veterans Affairs. Veterans VA Video Connect. Published May 22, 2020. Accessed May 29, 2020. https://mobile.va.gov/app/va-video-connect#AppDescription.
29. US Department of Veterans Affairs. VA telehealth at home. Accessed May 29, 2020. https://telehealth.va.gov/type/home
1. Abraham KM, Yosef M, Resnick SG, Zivin K. Competitive employment outcomes among veterans in VHA therapeutic and supported employment services programs. Psychiatr Serv. 2017;68(9):938-946. doi:10.1176/appi.ps.201600412
2. Davis LL, Kyriakides TC, Suris AM, et al. Effect of evidence-based supported employment vs transitional work on achieving steady work among veterans with posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatry. 2018;75(4):316. doi:10.1001/jamapsychiatry.2017.4472
3. Ottomanelli L, Goetz LL, Suris A, et al. Effectiveness of supported employment for veterans with spinal cord injuries: results from a randomized multisite study. Arch Phys Med Rehabil. 2012;93(5):740-747. doi:10.1016/j.apmr.2012.01.002
4. Ottomanelli L, Goetz LL, Barnett SD, et al. Individual placement and support in spinal cord injury: a longitudinal observational study of employment outcomes. Arch Phys Med Rehabil. 2017;98(8):1567-1575. doi:10.1016/j.apmr.2016.12.010
5. Cotner BA, Ottomanelli L, O’Connor DR, Njoh EN, Barnett SD, Miech EJ. Quality of life outcomes for veterans with spinal cord injury receiving individual placement and support (IPS). Top Spinal Cord Inj Rehabil. 2018;24(4):325-335. doi:10.1310/sci17-00046
6. Metzel DS, Giordano A. Locations of employment services and people with disabilities: a geographical analysis of accessibility. J Disabil Policy Stud. 2007;18(2):88-97. doi:10.1177/10442073070180020501
7. Landon T, Connor A, McKnight-Lizotte M, Peña J. Rehabilitation counseling in rural settings: a phenomenological study on barriers and supports. J Rehabil. 2019;85(2):47-57.
8. Riemer-Reiss M. Vocational rehabilitation counseling at a distance: Challenges, strategies and ethics to consider. J Rehabil. 2000;66(1):11-17.
9. Schmeler MR, Schein RM, McCue M, Betz K. Telerehabilitation clinical and vocational applications for assistive technology: research, opportunities, and challenges. Int J Telerehabilitation. 2009;1(1):59-72.
10. Levy CE, Silverman E, Jia H, Geiss M, Omura D. Effects of physical therapy delivery via home video telerehabilitation on functional and health-related quality of life outcomes. J Rehabil Res Dev. 2015;52(3):361-370. doi:10.1682/JRRD.2014.10.0239
11. McMullen CK, Ash JS, Sittig DF, et al. Rapid assessment of clinical information systems in the healthcare setting: an efficient method for time-pressed evaluation. Methods Inf Med. 2011;50(4):299-307. doi:10.3414/ME10-01-0042
12. Averill JB. Matrix analysis as a complementary analytic strategy in qualitative inquiry. Qual Health Res. 2002;12(6):855-866.
13. Egede LE, Acierno R, Knapp RG, et al. Psychotherapy for depression in older veterans via telemedicine: a randomised, open-label, non-inferiority trial. Lancet Psychiatry. 2015;2(8):693-701. doi:10.1016/S2215-0366(15)00122-4
14. Fortney JC, Pyne JM, Edlund MJ, et al. A randomized trial of telemedicine-based collaborative care for depression. J Gen Intern Med. 2007;22(8):1086-1093. doi:10.1007/s11606-007-0201-9
15. Fortney JC, Pyne JM, Kimbrell TA, et al. Telemedicine-based collaborative care for posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatry. 2015;72(1):58. doi:10.1001/jamapsychiatry.2014.1575
16. Grubbs KM, Fortney JC, Dean T, Williams JS, Godleski L. A comparison of mental health diagnoses treated via interactive video and face to face in the Veterans Healthcare Administration. Telemed E-Health. 2015;21(7):564-566. doi:10.1089/tmj.2014.0152
17. Agostini M, Moja L, Banzi R, et al. Telerehabilitation and recovery of motor function: a systematic review and meta-analysis. J Telemed Telecare. 2015;21(4):202-213. doi:10.1177/1357633X15572201
18. Bergquist TF, Thompson K, Gehl C, Munoz Pineda J. Satisfaction ratings after receiving internet-based cognitive rehabilitation in persons with memory impairments after severe acquired brain injury. Telemed E-Health. 2010;16(4):417-423. doi:10.1089/tmj.2009.0118
19. Brennan DM, Georgeadis AC, Baron CR, Barker LM. The effect of videoconference-based telerehabilitation on story retelling performance by brain-injured subjects and its implications for remote speech-language therapy. Telemed J E Health. 2004;10(2):147-154. doi:10.1089/tmj.2004.10.147
20. Dallolio L, Menarini M, China S, et al. Functional and clinical outcomes of telemedicine in patients with spinal cord injury. Arch Phys Med Rehabil. 2008;89(12):2332-2341. doi:10.1016/j.apmr.2008.06.012
21. Houlihan BV, Jette A, Friedman RH, et al. A pilot study of a telehealth intervention for persons with spinal cord dysfunction. Spinal Cord. 2013;51(9):715-720.doi:10.1038/sc.2013.45
22. Smith MW, Hill ML, Hopkins KL, Kiratli BJ, Cronkite RC. A modeled analysis of telehealth methods for treating pressure ulcers after spinal cord injury. Int J Telemed Appl. 2012;2012:1-10. doi:10.1155/2012/729492
23. Balcazar FE, Keys CB, Davis M, Lardon C, Jones C. Strengths and challenges of intervention research in vocational rehabilitation: an illustration of agency-university collaboration. J Rehabil. 2005;71(2):40-48.
24. Martinez RN, Hogan TP, Balbale S, et al. Sociotechnical perspective on implementing clinical video telehealth for veterans with spinal cord injuries and disorders. Telemed J E Health. 2017;23(7):567-576. doi:10.1089/tmj.2016.0200
25. Martinez RN, Hogan TP, Lones K, et al. Evaluation and treatment of mild traumatic brain injury through the implementation of clinical video telehealth: provider perspectives from the Veterans Health Administration. PM R. 2017;9(3):231-240. doi:10.1016/j.pmrj.2016.07.002
26. Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020;26(5):309-313. doi:10.1177/1357633X20916567
27. Cowper-Ripley DC, Jia H, Wang X, et al. Trends in VA telerehabilitation patients and encounters over time and by rurality. Fed Pract. 2019; 36(3):122-128.
28. US Department of Veterans Affairs. Veterans VA Video Connect. Published May 22, 2020. Accessed May 29, 2020. https://mobile.va.gov/app/va-video-connect#AppDescription.
29. US Department of Veterans Affairs. VA telehealth at home. Accessed May 29, 2020. https://telehealth.va.gov/type/home
Study calls for sex-specific concussion management in adolescent soccer players
A large study of adolescent soccer players in Michigan revealed key differences in concussion injury metrics among males and females, underscoring a need to develop sex-specific approaches to managing injury in the sport.
Sport-related concussion (SRC) is a specific concern in young female athletes, study authors Abigail C. Bretzin, PhD, and colleagues noted in their paper, which appears in JAMA Network Open. Previous surveillance studies on SRC at the high school and college level have reported higher rates of injury risk and longer recovery outcomes in female soccer athletes. Taking a deeper dive into these trends, the investigators explored whether sex-associated differences existed in SRC, addressing the mechanics, management, and recovery from SRC.
“This is an area that is remarkably underresearched,” William Stewart, MBChB, PhD, the study’s corresponding author, said in an interview. Prior studies of males and females have shown that female axons are thinner, with fewer microtubules or internal scaffolding than male axons. This potentially increases risk of shear injury in females. Limited research has also cited differences in concussion risk across the menstrual cycle in female athletes.
Reporting system targets four injury areas
The investigators conducted a high school injury surveillance project in 43,741 male and 39,637 female soccer athletes participating in the Michigan High School Athletic Association (MHSAA) Head Injury Reporting System. The study included students from 9th to 12th grade, spanning from the beginning of academic year 2016-2017 to the end of academic year 2018-2019. Since 2015, the state has mandated high schools to submit data to MHSAA.
MHSAA captures data on four categories: person-to-person contact, person-to-object contact, person-to-playing surface contact, or uncertain about cause of the event. Study outcomes included details regarding injury mechanism, immediate management, and return-to-play time for each documented SRC.
Investigators reported notable differences among male and female players. Documented SRC risk was 1.88 times higher among adolescent girls than boys across all academic years (RR, 1.88; 95% CI, 1.69-2.09; P < .001). They also cited inconsistencies in distribution of injury mechanisms among the sexes. Females were most likely to suffer injury from equipment contact such as heading a ball (41.9%), whereas male players commonly sustained SRC from contact with another player (48.4%). The authors suggested that “female soccer athletes have lower neck strength and girth, compared with male athletes, with these variables inversely associated with linear and rotational head acceleration after soccer ball heading.”
Boys had greater odds of immediate removal from play and but also returned to the sport 2 days sooner than girls. “The possibility exists, therefore, that this longer recovery time might, in part, be reflective of our observed differences in immediate care, in particular removal from play,” the authors wrote. Immediate removal from play was also more common in cases where an athletic trainer played a part in evaluating players for SRC.
Eliminating the one-size-fits-all approach
Current concussion management is based on a “one-size-fits-all” model, said Dr. Stewart. Male and female athletes are treated following a common concussion management protocol, covering concussion detection through to rehabilitation. “This model of management is based on research that is almost exclusively in male athletes.”
What the study showed is this one-size-fits-all approach may be flawed, letting down female athletes. “We should be pursuing more research in sex differences in concussion and, importantly, putting these into practice in sex-specific concussion management protocols,” he suggested.
Future studies should also look at the effects of athletic trainer employment on SRC metrics. “Although this was a large, statewide epidemiological study of reported SRC in adolescent soccer athletes, inclusive of high schools with and without access to athletic trainers, the Head Injury Reporting System did not include information on the whether there were athletic trainer services available at each school, including specific athletic training services for soccer,” wrote the investigators, in citing the study’s limitations.
Girls report symptoms more often
“The researchers are to be commended for taking a prospective approach to address this common observation in high school sports,” said Keith J. Loud, MD, MSc, FAAP, a sports pediatrician at Children’s Hospital at Dartmouth-Hitchcock in Manchester, N.H. The results are “entirely believable,” said Dr. Loud, who was not affiliated with the study. “We have long postulated differences in neurophysiology, neck strength, style of play, and tendency to report as explanations for the observation that girls in high school soccer are diagnosed with more concussions than boys.”
The findings suggest that boys play more aggressively, but sustain fewer concussions, he added. Girls in the meantime, are more likely to speak up about their injury.
“Concussion diagnosis still relies to a large degree on the athlete to report symptoms, which is one of our hypotheses as to why girls seem to sustain more concussions – they report symptoms more often. That could also be why they have a prolonged recovery,” offered Dr. Loud. A main limitation of this study is it can’t overcome this reporting bias.
Dr. Loud was also concerned that girls were less likely to be removed from game play, even though they apparently sustained more concussions. “Perhaps that is because their injuries are less obvious on the field, and they are diagnosed when reported after the games.”
Dr. Stewart reported receiving grants from The Football Association and National Health Service Research Scotland during the study. He also served as a nonremunerated member of the Fédération Internationale de Football Association Independent Football Concussion Advisory Group and the Football Association Expert Panel on Concussion and Head Injury in Football. None of the other authors had disclosures.
A large study of adolescent soccer players in Michigan revealed key differences in concussion injury metrics among males and females, underscoring a need to develop sex-specific approaches to managing injury in the sport.
Sport-related concussion (SRC) is a specific concern in young female athletes, study authors Abigail C. Bretzin, PhD, and colleagues noted in their paper, which appears in JAMA Network Open. Previous surveillance studies on SRC at the high school and college level have reported higher rates of injury risk and longer recovery outcomes in female soccer athletes. Taking a deeper dive into these trends, the investigators explored whether sex-associated differences existed in SRC, addressing the mechanics, management, and recovery from SRC.
“This is an area that is remarkably underresearched,” William Stewart, MBChB, PhD, the study’s corresponding author, said in an interview. Prior studies of males and females have shown that female axons are thinner, with fewer microtubules or internal scaffolding than male axons. This potentially increases risk of shear injury in females. Limited research has also cited differences in concussion risk across the menstrual cycle in female athletes.
Reporting system targets four injury areas
The investigators conducted a high school injury surveillance project in 43,741 male and 39,637 female soccer athletes participating in the Michigan High School Athletic Association (MHSAA) Head Injury Reporting System. The study included students from 9th to 12th grade, spanning from the beginning of academic year 2016-2017 to the end of academic year 2018-2019. Since 2015, the state has mandated high schools to submit data to MHSAA.
MHSAA captures data on four categories: person-to-person contact, person-to-object contact, person-to-playing surface contact, or uncertain about cause of the event. Study outcomes included details regarding injury mechanism, immediate management, and return-to-play time for each documented SRC.
Investigators reported notable differences among male and female players. Documented SRC risk was 1.88 times higher among adolescent girls than boys across all academic years (RR, 1.88; 95% CI, 1.69-2.09; P < .001). They also cited inconsistencies in distribution of injury mechanisms among the sexes. Females were most likely to suffer injury from equipment contact such as heading a ball (41.9%), whereas male players commonly sustained SRC from contact with another player (48.4%). The authors suggested that “female soccer athletes have lower neck strength and girth, compared with male athletes, with these variables inversely associated with linear and rotational head acceleration after soccer ball heading.”
Boys had greater odds of immediate removal from play and but also returned to the sport 2 days sooner than girls. “The possibility exists, therefore, that this longer recovery time might, in part, be reflective of our observed differences in immediate care, in particular removal from play,” the authors wrote. Immediate removal from play was also more common in cases where an athletic trainer played a part in evaluating players for SRC.
Eliminating the one-size-fits-all approach
Current concussion management is based on a “one-size-fits-all” model, said Dr. Stewart. Male and female athletes are treated following a common concussion management protocol, covering concussion detection through to rehabilitation. “This model of management is based on research that is almost exclusively in male athletes.”
What the study showed is this one-size-fits-all approach may be flawed, letting down female athletes. “We should be pursuing more research in sex differences in concussion and, importantly, putting these into practice in sex-specific concussion management protocols,” he suggested.
Future studies should also look at the effects of athletic trainer employment on SRC metrics. “Although this was a large, statewide epidemiological study of reported SRC in adolescent soccer athletes, inclusive of high schools with and without access to athletic trainers, the Head Injury Reporting System did not include information on the whether there were athletic trainer services available at each school, including specific athletic training services for soccer,” wrote the investigators, in citing the study’s limitations.
Girls report symptoms more often
“The researchers are to be commended for taking a prospective approach to address this common observation in high school sports,” said Keith J. Loud, MD, MSc, FAAP, a sports pediatrician at Children’s Hospital at Dartmouth-Hitchcock in Manchester, N.H. The results are “entirely believable,” said Dr. Loud, who was not affiliated with the study. “We have long postulated differences in neurophysiology, neck strength, style of play, and tendency to report as explanations for the observation that girls in high school soccer are diagnosed with more concussions than boys.”
The findings suggest that boys play more aggressively, but sustain fewer concussions, he added. Girls in the meantime, are more likely to speak up about their injury.
“Concussion diagnosis still relies to a large degree on the athlete to report symptoms, which is one of our hypotheses as to why girls seem to sustain more concussions – they report symptoms more often. That could also be why they have a prolonged recovery,” offered Dr. Loud. A main limitation of this study is it can’t overcome this reporting bias.
Dr. Loud was also concerned that girls were less likely to be removed from game play, even though they apparently sustained more concussions. “Perhaps that is because their injuries are less obvious on the field, and they are diagnosed when reported after the games.”
Dr. Stewart reported receiving grants from The Football Association and National Health Service Research Scotland during the study. He also served as a nonremunerated member of the Fédération Internationale de Football Association Independent Football Concussion Advisory Group and the Football Association Expert Panel on Concussion and Head Injury in Football. None of the other authors had disclosures.
A large study of adolescent soccer players in Michigan revealed key differences in concussion injury metrics among males and females, underscoring a need to develop sex-specific approaches to managing injury in the sport.
Sport-related concussion (SRC) is a specific concern in young female athletes, study authors Abigail C. Bretzin, PhD, and colleagues noted in their paper, which appears in JAMA Network Open. Previous surveillance studies on SRC at the high school and college level have reported higher rates of injury risk and longer recovery outcomes in female soccer athletes. Taking a deeper dive into these trends, the investigators explored whether sex-associated differences existed in SRC, addressing the mechanics, management, and recovery from SRC.
“This is an area that is remarkably underresearched,” William Stewart, MBChB, PhD, the study’s corresponding author, said in an interview. Prior studies of males and females have shown that female axons are thinner, with fewer microtubules or internal scaffolding than male axons. This potentially increases risk of shear injury in females. Limited research has also cited differences in concussion risk across the menstrual cycle in female athletes.
Reporting system targets four injury areas
The investigators conducted a high school injury surveillance project in 43,741 male and 39,637 female soccer athletes participating in the Michigan High School Athletic Association (MHSAA) Head Injury Reporting System. The study included students from 9th to 12th grade, spanning from the beginning of academic year 2016-2017 to the end of academic year 2018-2019. Since 2015, the state has mandated high schools to submit data to MHSAA.
MHSAA captures data on four categories: person-to-person contact, person-to-object contact, person-to-playing surface contact, or uncertain about cause of the event. Study outcomes included details regarding injury mechanism, immediate management, and return-to-play time for each documented SRC.
Investigators reported notable differences among male and female players. Documented SRC risk was 1.88 times higher among adolescent girls than boys across all academic years (RR, 1.88; 95% CI, 1.69-2.09; P < .001). They also cited inconsistencies in distribution of injury mechanisms among the sexes. Females were most likely to suffer injury from equipment contact such as heading a ball (41.9%), whereas male players commonly sustained SRC from contact with another player (48.4%). The authors suggested that “female soccer athletes have lower neck strength and girth, compared with male athletes, with these variables inversely associated with linear and rotational head acceleration after soccer ball heading.”
Boys had greater odds of immediate removal from play and but also returned to the sport 2 days sooner than girls. “The possibility exists, therefore, that this longer recovery time might, in part, be reflective of our observed differences in immediate care, in particular removal from play,” the authors wrote. Immediate removal from play was also more common in cases where an athletic trainer played a part in evaluating players for SRC.
Eliminating the one-size-fits-all approach
Current concussion management is based on a “one-size-fits-all” model, said Dr. Stewart. Male and female athletes are treated following a common concussion management protocol, covering concussion detection through to rehabilitation. “This model of management is based on research that is almost exclusively in male athletes.”
What the study showed is this one-size-fits-all approach may be flawed, letting down female athletes. “We should be pursuing more research in sex differences in concussion and, importantly, putting these into practice in sex-specific concussion management protocols,” he suggested.
Future studies should also look at the effects of athletic trainer employment on SRC metrics. “Although this was a large, statewide epidemiological study of reported SRC in adolescent soccer athletes, inclusive of high schools with and without access to athletic trainers, the Head Injury Reporting System did not include information on the whether there were athletic trainer services available at each school, including specific athletic training services for soccer,” wrote the investigators, in citing the study’s limitations.
Girls report symptoms more often
“The researchers are to be commended for taking a prospective approach to address this common observation in high school sports,” said Keith J. Loud, MD, MSc, FAAP, a sports pediatrician at Children’s Hospital at Dartmouth-Hitchcock in Manchester, N.H. The results are “entirely believable,” said Dr. Loud, who was not affiliated with the study. “We have long postulated differences in neurophysiology, neck strength, style of play, and tendency to report as explanations for the observation that girls in high school soccer are diagnosed with more concussions than boys.”
The findings suggest that boys play more aggressively, but sustain fewer concussions, he added. Girls in the meantime, are more likely to speak up about their injury.
“Concussion diagnosis still relies to a large degree on the athlete to report symptoms, which is one of our hypotheses as to why girls seem to sustain more concussions – they report symptoms more often. That could also be why they have a prolonged recovery,” offered Dr. Loud. A main limitation of this study is it can’t overcome this reporting bias.
Dr. Loud was also concerned that girls were less likely to be removed from game play, even though they apparently sustained more concussions. “Perhaps that is because their injuries are less obvious on the field, and they are diagnosed when reported after the games.”
Dr. Stewart reported receiving grants from The Football Association and National Health Service Research Scotland during the study. He also served as a nonremunerated member of the Fédération Internationale de Football Association Independent Football Concussion Advisory Group and the Football Association Expert Panel on Concussion and Head Injury in Football. None of the other authors had disclosures.
FROM JAMA NETWORK OPEN
U.S. suicide rate in 2019 took first downturn in 14 years
In 2019, the U.S. suicide rate dropped for the first time in 14 years, driven largely by a significant decline in firearm-related deaths, according to a new analysis of National Vital Statistics System data.
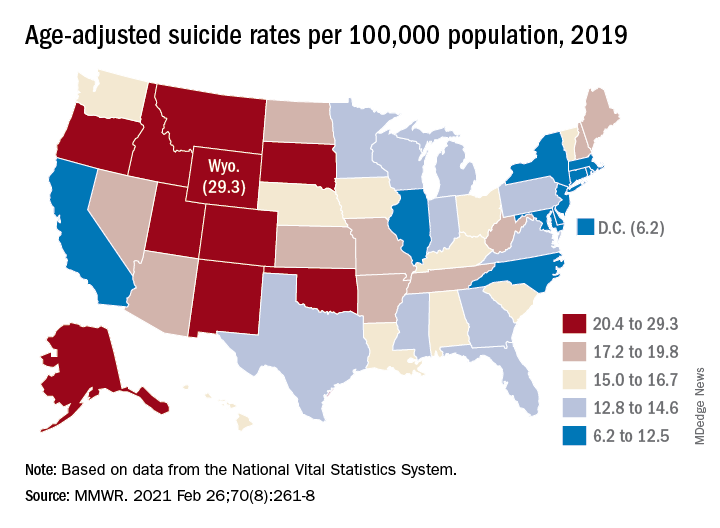
Since firearms are the “most common and most lethal” mechanism of suicide, the drop in deaths is “particularly encouraging,” Deborah M. Stone, ScD, MSW, MPH, and associates wrote in the Morbidity and Mortality Weekly Report.
The national suicide rate decreased from 14.2 per 100,000 population in 2018 to 13.9 per 100,000 in 2019, a statistically significant drop of 2.1% that reversed a 20-year trend that saw the rate increase by 33% since 1999, they said.
The rate for firearm use, which is involved in half of all suicides, declined from 7.0 per 100,000 to 6.8, for a significant change of 2.9%, said Dr. Stone and associates at the Centers for Disease Control and Prevention’s National Center for Injury Prevention and Control.
The only other method with a drop in suicide rate from 2018 to 2019 was suffocation – the second most common mechanism of injury – but the relative change of 2.3% was not significant, they noted.
Significant declines also occurred in several subgroups: Whites; those aged 15-24, 55-64, and 65-74 years; and those living in counties classified as large fringe metropolitan or micropolitan (urban cluster of ≥ 10,000 but less than 50,000 population), they said, based on data from the National Vital Statistics System.
the investigators wrote.
The states with significant increases were Hawaii (30.3%) and Nebraska (20.1%), while declines in the suicide rate were significant in five states – Idaho, Indiana, Massachusetts, North Carolina, and Virginia, Dr. Stone and associates reported. Altogether, the rate fell in 31 states, increased in 18, and did not change in 2.
The significance of those changes varied between males and females. Declines were significant for females in Indiana, Massachusetts, and Washington, and for males in Florida, Kentucky, Massachusetts, North Carolina, and West Virginia. Minnesota was the only state with a significant increase among females, with Hawaii and Wyoming posting increases for males, they said.
As the response to the COVID-19 pandemic continues, the investigators pointed out, “prevention is more important than ever. Past research indicates that suicide rates remain stable or decline during infrastructure disruption (e.g., natural disasters), only to rise afterwards as the longer-term sequelae unfold in persons, families, and communities.”
In 2019, the U.S. suicide rate dropped for the first time in 14 years, driven largely by a significant decline in firearm-related deaths, according to a new analysis of National Vital Statistics System data.
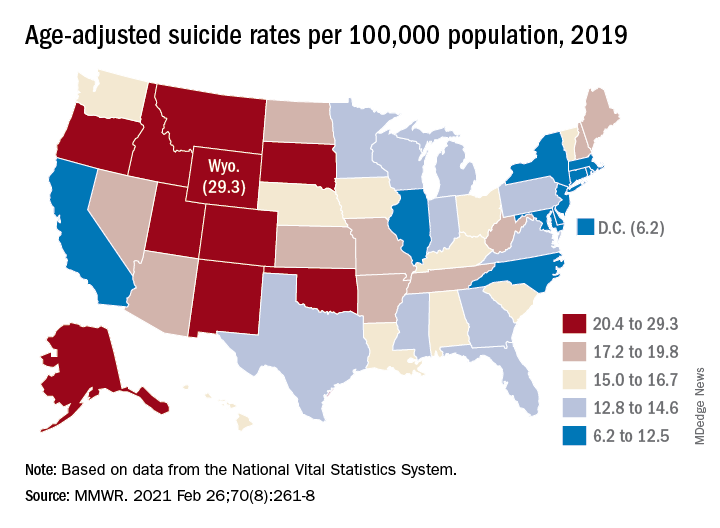
Since firearms are the “most common and most lethal” mechanism of suicide, the drop in deaths is “particularly encouraging,” Deborah M. Stone, ScD, MSW, MPH, and associates wrote in the Morbidity and Mortality Weekly Report.
The national suicide rate decreased from 14.2 per 100,000 population in 2018 to 13.9 per 100,000 in 2019, a statistically significant drop of 2.1% that reversed a 20-year trend that saw the rate increase by 33% since 1999, they said.
The rate for firearm use, which is involved in half of all suicides, declined from 7.0 per 100,000 to 6.8, for a significant change of 2.9%, said Dr. Stone and associates at the Centers for Disease Control and Prevention’s National Center for Injury Prevention and Control.
The only other method with a drop in suicide rate from 2018 to 2019 was suffocation – the second most common mechanism of injury – but the relative change of 2.3% was not significant, they noted.
Significant declines also occurred in several subgroups: Whites; those aged 15-24, 55-64, and 65-74 years; and those living in counties classified as large fringe metropolitan or micropolitan (urban cluster of ≥ 10,000 but less than 50,000 population), they said, based on data from the National Vital Statistics System.
the investigators wrote.
The states with significant increases were Hawaii (30.3%) and Nebraska (20.1%), while declines in the suicide rate were significant in five states – Idaho, Indiana, Massachusetts, North Carolina, and Virginia, Dr. Stone and associates reported. Altogether, the rate fell in 31 states, increased in 18, and did not change in 2.
The significance of those changes varied between males and females. Declines were significant for females in Indiana, Massachusetts, and Washington, and for males in Florida, Kentucky, Massachusetts, North Carolina, and West Virginia. Minnesota was the only state with a significant increase among females, with Hawaii and Wyoming posting increases for males, they said.
As the response to the COVID-19 pandemic continues, the investigators pointed out, “prevention is more important than ever. Past research indicates that suicide rates remain stable or decline during infrastructure disruption (e.g., natural disasters), only to rise afterwards as the longer-term sequelae unfold in persons, families, and communities.”
In 2019, the U.S. suicide rate dropped for the first time in 14 years, driven largely by a significant decline in firearm-related deaths, according to a new analysis of National Vital Statistics System data.
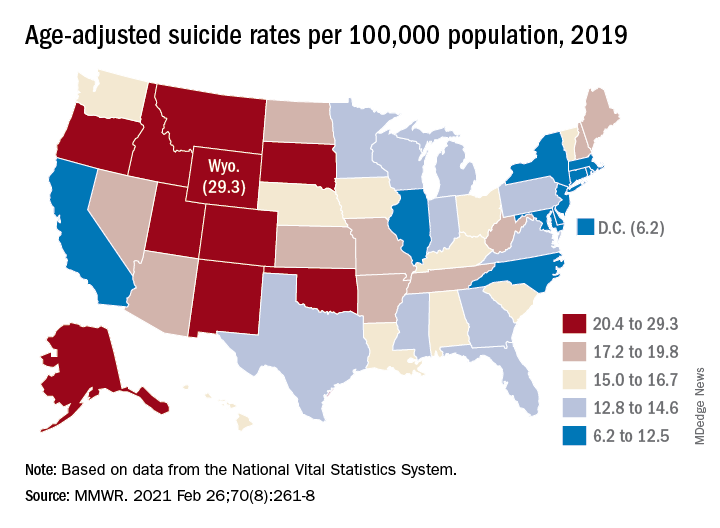
Since firearms are the “most common and most lethal” mechanism of suicide, the drop in deaths is “particularly encouraging,” Deborah M. Stone, ScD, MSW, MPH, and associates wrote in the Morbidity and Mortality Weekly Report.
The national suicide rate decreased from 14.2 per 100,000 population in 2018 to 13.9 per 100,000 in 2019, a statistically significant drop of 2.1% that reversed a 20-year trend that saw the rate increase by 33% since 1999, they said.
The rate for firearm use, which is involved in half of all suicides, declined from 7.0 per 100,000 to 6.8, for a significant change of 2.9%, said Dr. Stone and associates at the Centers for Disease Control and Prevention’s National Center for Injury Prevention and Control.
The only other method with a drop in suicide rate from 2018 to 2019 was suffocation – the second most common mechanism of injury – but the relative change of 2.3% was not significant, they noted.
Significant declines also occurred in several subgroups: Whites; those aged 15-24, 55-64, and 65-74 years; and those living in counties classified as large fringe metropolitan or micropolitan (urban cluster of ≥ 10,000 but less than 50,000 population), they said, based on data from the National Vital Statistics System.
the investigators wrote.
The states with significant increases were Hawaii (30.3%) and Nebraska (20.1%), while declines in the suicide rate were significant in five states – Idaho, Indiana, Massachusetts, North Carolina, and Virginia, Dr. Stone and associates reported. Altogether, the rate fell in 31 states, increased in 18, and did not change in 2.
The significance of those changes varied between males and females. Declines were significant for females in Indiana, Massachusetts, and Washington, and for males in Florida, Kentucky, Massachusetts, North Carolina, and West Virginia. Minnesota was the only state with a significant increase among females, with Hawaii and Wyoming posting increases for males, they said.
As the response to the COVID-19 pandemic continues, the investigators pointed out, “prevention is more important than ever. Past research indicates that suicide rates remain stable or decline during infrastructure disruption (e.g., natural disasters), only to rise afterwards as the longer-term sequelae unfold in persons, families, and communities.”
FROM MMWR
Child abuse visits to EDs declined in 2020, but not admissions
but the visits in 2020 were significantly more likely to result in hospitalization, based on analysis of a national ED database.

The number of ED visits involving child abuse and neglect was down by 53% during the 4-week period from March 29 to April 25, 2020, compared with the 4 weeks from March 31 to April 27, 2019. The proportion of those ED visits that ended in hospitalizations, however, increased from 2.1% in 2019 to 3.2% in 2020, Elizabeth Swedo, MD, and associates at the Centers for Disease Control and Prevention said in the Morbidity and Mortality Weekly Report.
“ED visits related to suspected or confirmed child abuse and neglect decreased beginning the week of March 15, 2020, coinciding with the declaration of a national emergency related to COVID-19 and implementation of community mitigation measures,” they wrote.
An earlier study involving the same database (the National Syndromic Surveillance Program) showed that, over the two same 4-week periods, the volume of all ED visits in 2020 was down 72% for children aged 10 years and younger and 71% for those aged 11-14 years.
In the current study, however, all age subgroups had significant increases in hospital admissions. The proportion of ED visits related to child abuse and neglect that resulted in hospitalization rose from 3.5% in 2019 to 5.3% in 2020 among ages 0-4 years, 0.7% to 1.3% for ages 5-11 years, and 1.6% to 2.2% for adolescents aged 12-17, Dr. Swedo and associates reported.
The absence of a corresponding drop in hospitalizations may be tied to risk factors related to the pandemic, “such as loss of income, increased stress related to parental child care and schooling responsibilities, and increased substance use and mental health conditions among adults,” the investigators added.
The National Syndromic Surveillance Program receives daily data from 3,310 EDs in 47 states, but the number of facilities meeting the investigators’ criteria averaged 2,970 a week for the 8 weeks of the study period.
SOURCE: Swedo E et al. MMWR. 2020 Dec. 11;69(49):1841-7.
but the visits in 2020 were significantly more likely to result in hospitalization, based on analysis of a national ED database.

The number of ED visits involving child abuse and neglect was down by 53% during the 4-week period from March 29 to April 25, 2020, compared with the 4 weeks from March 31 to April 27, 2019. The proportion of those ED visits that ended in hospitalizations, however, increased from 2.1% in 2019 to 3.2% in 2020, Elizabeth Swedo, MD, and associates at the Centers for Disease Control and Prevention said in the Morbidity and Mortality Weekly Report.
“ED visits related to suspected or confirmed child abuse and neglect decreased beginning the week of March 15, 2020, coinciding with the declaration of a national emergency related to COVID-19 and implementation of community mitigation measures,” they wrote.
An earlier study involving the same database (the National Syndromic Surveillance Program) showed that, over the two same 4-week periods, the volume of all ED visits in 2020 was down 72% for children aged 10 years and younger and 71% for those aged 11-14 years.
In the current study, however, all age subgroups had significant increases in hospital admissions. The proportion of ED visits related to child abuse and neglect that resulted in hospitalization rose from 3.5% in 2019 to 5.3% in 2020 among ages 0-4 years, 0.7% to 1.3% for ages 5-11 years, and 1.6% to 2.2% for adolescents aged 12-17, Dr. Swedo and associates reported.
The absence of a corresponding drop in hospitalizations may be tied to risk factors related to the pandemic, “such as loss of income, increased stress related to parental child care and schooling responsibilities, and increased substance use and mental health conditions among adults,” the investigators added.
The National Syndromic Surveillance Program receives daily data from 3,310 EDs in 47 states, but the number of facilities meeting the investigators’ criteria averaged 2,970 a week for the 8 weeks of the study period.
SOURCE: Swedo E et al. MMWR. 2020 Dec. 11;69(49):1841-7.
but the visits in 2020 were significantly more likely to result in hospitalization, based on analysis of a national ED database.

The number of ED visits involving child abuse and neglect was down by 53% during the 4-week period from March 29 to April 25, 2020, compared with the 4 weeks from March 31 to April 27, 2019. The proportion of those ED visits that ended in hospitalizations, however, increased from 2.1% in 2019 to 3.2% in 2020, Elizabeth Swedo, MD, and associates at the Centers for Disease Control and Prevention said in the Morbidity and Mortality Weekly Report.
“ED visits related to suspected or confirmed child abuse and neglect decreased beginning the week of March 15, 2020, coinciding with the declaration of a national emergency related to COVID-19 and implementation of community mitigation measures,” they wrote.
An earlier study involving the same database (the National Syndromic Surveillance Program) showed that, over the two same 4-week periods, the volume of all ED visits in 2020 was down 72% for children aged 10 years and younger and 71% for those aged 11-14 years.
In the current study, however, all age subgroups had significant increases in hospital admissions. The proportion of ED visits related to child abuse and neglect that resulted in hospitalization rose from 3.5% in 2019 to 5.3% in 2020 among ages 0-4 years, 0.7% to 1.3% for ages 5-11 years, and 1.6% to 2.2% for adolescents aged 12-17, Dr. Swedo and associates reported.
The absence of a corresponding drop in hospitalizations may be tied to risk factors related to the pandemic, “such as loss of income, increased stress related to parental child care and schooling responsibilities, and increased substance use and mental health conditions among adults,” the investigators added.
The National Syndromic Surveillance Program receives daily data from 3,310 EDs in 47 states, but the number of facilities meeting the investigators’ criteria averaged 2,970 a week for the 8 weeks of the study period.
SOURCE: Swedo E et al. MMWR. 2020 Dec. 11;69(49):1841-7.
FROM MMWR