User login
ACIP: Flu vaccines for older adults show similar safety profiles
The Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP) recommends that age-appropriate vaccines be used when possible, said Kenneth E. Schmader, MD, professor of medicine at Duke University, Durham, N.C. However, no study to date had directly compared the safety of the trivalent high dose (HD-IIV3) and adjuvanted (aIIV3) vaccines or their impact on health-related quality of life. Dr. Schmader presented findings from a randomized trial at the February ACIP meeting.
To compare the safety of the vaccines, the researchers recruited community-dwelling volunteers aged 65 years and older who were cognitively intact, not immunosuppressed, and had no contraindications for influenza vaccination. A total of 378 individuals were randomized to aIIV3 and 379 to HD-IIV3. The average age was 72 years; 80 individuals in the aIIV3 group and 83 in the HDIIV3 group were 80 years and older. The primary outcome was moderate or severe injection site pain.
Overall, the proportion of participants with moderate or severe injection site pain was not significantly different after aIIV3 vs. HD-IIV3 (3.2% vs. 5.8%).
Nine participants in the aIIV3 group and three participants in the HD-IIV3 group experienced at least one serious adverse event, but no serious adverse events were deemed vaccine related, and the occurrence of serious adverse events was not significantly different between groups.
In addition, measures of short-term, postvaccination health-related quality of life were not significantly different between the groups. Changes in scores from day 1 prevaccination to day 3 postvaccination on the EuroQOL-5 dimensions-5 levels (EQ-5D-5L) were –0.05 for both groups.
The findings were limited in part by the lack of inclusion of older adults in nursing homes or similar settings, Dr. Schmader noted. However, the results suggest that “from the standpoint of safety, either vaccine is an acceptable option for the prevention of influenza in older adults.”
Studies comparing the immunogenicity of the vaccines are ongoing, and the data should be available within the next few months, he noted.
Dr. Schmader had no financial conflicts to disclose.
The Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP) recommends that age-appropriate vaccines be used when possible, said Kenneth E. Schmader, MD, professor of medicine at Duke University, Durham, N.C. However, no study to date had directly compared the safety of the trivalent high dose (HD-IIV3) and adjuvanted (aIIV3) vaccines or their impact on health-related quality of life. Dr. Schmader presented findings from a randomized trial at the February ACIP meeting.
To compare the safety of the vaccines, the researchers recruited community-dwelling volunteers aged 65 years and older who were cognitively intact, not immunosuppressed, and had no contraindications for influenza vaccination. A total of 378 individuals were randomized to aIIV3 and 379 to HD-IIV3. The average age was 72 years; 80 individuals in the aIIV3 group and 83 in the HDIIV3 group were 80 years and older. The primary outcome was moderate or severe injection site pain.
Overall, the proportion of participants with moderate or severe injection site pain was not significantly different after aIIV3 vs. HD-IIV3 (3.2% vs. 5.8%).
Nine participants in the aIIV3 group and three participants in the HD-IIV3 group experienced at least one serious adverse event, but no serious adverse events were deemed vaccine related, and the occurrence of serious adverse events was not significantly different between groups.
In addition, measures of short-term, postvaccination health-related quality of life were not significantly different between the groups. Changes in scores from day 1 prevaccination to day 3 postvaccination on the EuroQOL-5 dimensions-5 levels (EQ-5D-5L) were –0.05 for both groups.
The findings were limited in part by the lack of inclusion of older adults in nursing homes or similar settings, Dr. Schmader noted. However, the results suggest that “from the standpoint of safety, either vaccine is an acceptable option for the prevention of influenza in older adults.”
Studies comparing the immunogenicity of the vaccines are ongoing, and the data should be available within the next few months, he noted.
Dr. Schmader had no financial conflicts to disclose.
The Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP) recommends that age-appropriate vaccines be used when possible, said Kenneth E. Schmader, MD, professor of medicine at Duke University, Durham, N.C. However, no study to date had directly compared the safety of the trivalent high dose (HD-IIV3) and adjuvanted (aIIV3) vaccines or their impact on health-related quality of life. Dr. Schmader presented findings from a randomized trial at the February ACIP meeting.
To compare the safety of the vaccines, the researchers recruited community-dwelling volunteers aged 65 years and older who were cognitively intact, not immunosuppressed, and had no contraindications for influenza vaccination. A total of 378 individuals were randomized to aIIV3 and 379 to HD-IIV3. The average age was 72 years; 80 individuals in the aIIV3 group and 83 in the HDIIV3 group were 80 years and older. The primary outcome was moderate or severe injection site pain.
Overall, the proportion of participants with moderate or severe injection site pain was not significantly different after aIIV3 vs. HD-IIV3 (3.2% vs. 5.8%).
Nine participants in the aIIV3 group and three participants in the HD-IIV3 group experienced at least one serious adverse event, but no serious adverse events were deemed vaccine related, and the occurrence of serious adverse events was not significantly different between groups.
In addition, measures of short-term, postvaccination health-related quality of life were not significantly different between the groups. Changes in scores from day 1 prevaccination to day 3 postvaccination on the EuroQOL-5 dimensions-5 levels (EQ-5D-5L) were –0.05 for both groups.
The findings were limited in part by the lack of inclusion of older adults in nursing homes or similar settings, Dr. Schmader noted. However, the results suggest that “from the standpoint of safety, either vaccine is an acceptable option for the prevention of influenza in older adults.”
Studies comparing the immunogenicity of the vaccines are ongoing, and the data should be available within the next few months, he noted.
Dr. Schmader had no financial conflicts to disclose.
FROM AN ACIP MEETING
ACIP advocates pre-exposure Ebola vaccination for high-risk groups
Vaccination against the Ebola virus is recommended for first responders, health care personnel, and laboratory workers deemed at high risk of exposure, according to the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP).
The committee voted unanimously to recommended pre-exposure vaccination with the rVSVdeltaG-ZEBOV-GP vaccine for adults aged 18 years and older who are at potential risk of exposure to the Ebola species Zaire ebolavirus because they fall into any of the following three categories:
- They are responding to an outbreak of Ebola virus disease.
- They are working as health care personnel at a federally designated Ebola Treatment Center in the United States.
- The are working in laboratories or are other staff members at biosafety-level 4 facilities in the United States.
Mary Choi, MD, of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases (NCEZID) presented data on the safety and effectiveness of the vaccine and the work group considerations in recommending vaccination in the three target populations.
In clinical trials, the most commonly reported adverse events associated with the vaccine were arthritis and arthralgia, Dr. Choi said, but the duration of those cases was limited to months and did not persist long term.
Pre-exposure vaccination for health care personnel, laboratory workers, and support staff would provide an additional layer of protection, she explained, in addition to existing safeguards such as personal protective equipment and engineering controls at the facility. The work group’s research showed that most of the target population believed that the desirable effects of that protection outweigh potentially undesirable effects, Dr. Choi noted.
Some committee members expressed concerns about vaccination of pregnant women. But the recommendations are presented as “population based, not shared decision making,” said Sharon E. Frey, MD, of Saint Louis University in St. Louis, Missouri.
Several members noted that pregnant women should not be automatically included or excluded from vaccination if they fall into a high-risk population. And the committee agreed that additional guidance in the policy note will help assess risk and that organizations will determine the risk for their employees and whether to offer the vaccine.
The FDA approved the currently available U.S. vaccine for Ebola in 2019. Merck manufactures that vaccine.
The ACIP members had no relevant financial conflicts to disclose.
Vaccination against the Ebola virus is recommended for first responders, health care personnel, and laboratory workers deemed at high risk of exposure, according to the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP).
The committee voted unanimously to recommended pre-exposure vaccination with the rVSVdeltaG-ZEBOV-GP vaccine for adults aged 18 years and older who are at potential risk of exposure to the Ebola species Zaire ebolavirus because they fall into any of the following three categories:
- They are responding to an outbreak of Ebola virus disease.
- They are working as health care personnel at a federally designated Ebola Treatment Center in the United States.
- The are working in laboratories or are other staff members at biosafety-level 4 facilities in the United States.
Mary Choi, MD, of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases (NCEZID) presented data on the safety and effectiveness of the vaccine and the work group considerations in recommending vaccination in the three target populations.
In clinical trials, the most commonly reported adverse events associated with the vaccine were arthritis and arthralgia, Dr. Choi said, but the duration of those cases was limited to months and did not persist long term.
Pre-exposure vaccination for health care personnel, laboratory workers, and support staff would provide an additional layer of protection, she explained, in addition to existing safeguards such as personal protective equipment and engineering controls at the facility. The work group’s research showed that most of the target population believed that the desirable effects of that protection outweigh potentially undesirable effects, Dr. Choi noted.
Some committee members expressed concerns about vaccination of pregnant women. But the recommendations are presented as “population based, not shared decision making,” said Sharon E. Frey, MD, of Saint Louis University in St. Louis, Missouri.
Several members noted that pregnant women should not be automatically included or excluded from vaccination if they fall into a high-risk population. And the committee agreed that additional guidance in the policy note will help assess risk and that organizations will determine the risk for their employees and whether to offer the vaccine.
The FDA approved the currently available U.S. vaccine for Ebola in 2019. Merck manufactures that vaccine.
The ACIP members had no relevant financial conflicts to disclose.
Vaccination against the Ebola virus is recommended for first responders, health care personnel, and laboratory workers deemed at high risk of exposure, according to the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices (ACIP).
The committee voted unanimously to recommended pre-exposure vaccination with the rVSVdeltaG-ZEBOV-GP vaccine for adults aged 18 years and older who are at potential risk of exposure to the Ebola species Zaire ebolavirus because they fall into any of the following three categories:
- They are responding to an outbreak of Ebola virus disease.
- They are working as health care personnel at a federally designated Ebola Treatment Center in the United States.
- The are working in laboratories or are other staff members at biosafety-level 4 facilities in the United States.
Mary Choi, MD, of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases (NCEZID) presented data on the safety and effectiveness of the vaccine and the work group considerations in recommending vaccination in the three target populations.
In clinical trials, the most commonly reported adverse events associated with the vaccine were arthritis and arthralgia, Dr. Choi said, but the duration of those cases was limited to months and did not persist long term.
Pre-exposure vaccination for health care personnel, laboratory workers, and support staff would provide an additional layer of protection, she explained, in addition to existing safeguards such as personal protective equipment and engineering controls at the facility. The work group’s research showed that most of the target population believed that the desirable effects of that protection outweigh potentially undesirable effects, Dr. Choi noted.
Some committee members expressed concerns about vaccination of pregnant women. But the recommendations are presented as “population based, not shared decision making,” said Sharon E. Frey, MD, of Saint Louis University in St. Louis, Missouri.
Several members noted that pregnant women should not be automatically included or excluded from vaccination if they fall into a high-risk population. And the committee agreed that additional guidance in the policy note will help assess risk and that organizations will determine the risk for their employees and whether to offer the vaccine.
The FDA approved the currently available U.S. vaccine for Ebola in 2019. Merck manufactures that vaccine.
The ACIP members had no relevant financial conflicts to disclose.
Shingles vaccine linked to lower stroke risk
LOS ANGELES – Prevention of shingles with the Zoster Vaccine Live may reduce the risk of subsequent stroke among older adults as well, the first study to examine this association suggests. Shingles vaccination was linked to a 20% decrease in stroke risk in people younger than 80 years of age in the large Medicare cohort study. Older participants showed a 10% reduced risk, according to data released in advance of formal presentation at this week’s International Stroke Conference, sponsored by the American Heart Association.
Reductions were seen for both ischemic and hemorrhagic events.
“Our findings might encourage people age 50 or older to get vaccinated against shingles and to prevent shingles-associated stroke risk,” Quanhe Yang, PhD, lead study author and senior scientist at the Centers for Disease Control and Prevention, said in an interview.
Dr. Yang and colleagues evaluated the only shingles vaccine available at the time of the study, Zoster Vaccine Live (Zostavax). However, the CDC now calls an adjuvanted, nonlive recombinant vaccine (Shingrix) the preferred shingles vaccine for healthy adults aged 50 years and older. Shingrix was approved in 2017. Zostavax, approved in 2006, can still be used in healthy adults aged 60 years and older, the agency states.
A reduction in inflammation from Zoster Vaccine Live may be the mechanism by which stroke risk is reduced, Dr. Yang said. The newer vaccine, which the CDC notes is more than 90% effective, might provide even greater protection against stroke, although more research is needed, he added.
Interestingly, prior research suggested that, once a person develops shingles, it may be too late. Dr. Yang and colleagues showed vaccination or antiviral treatment after a shingles episode was not effective at reducing stroke risk in research presented at the 2019 International Stroke Conference.
Shingles can present as a painful reactivation of chickenpox, also known as the varicella-zoster virus. Shingles is also common; Dr. Yang estimated one in three people who had chickenpox will develop the condition at some point in their lifetime. In addition, researchers have linked shingles to an elevated risk of stroke.
To assess the vaccine’s protective effect on stroke, Dr. Yang and colleagues reviewed health records for 1.38 million Medicare recipients. All participants were aged 66 years or older, had no history of stroke at baseline, and received the Zoster Vaccine Live during 2008-2016. The investigators compared the stroke rate in this vaccinated group with the rate in a matched control group of the same number of Medicare fee-for-service beneficiaries who did not receive the vaccination. They adjusted their analysis for age, sex, race, medications, and comorbidities.
The overall decrease of 16% in stroke risk associated with vaccination included a 12% drop in hemorrhagic stroke and 18% decrease in ischemic stroke over a median follow-up of 3.9 years follow-up (interquartile range, 2.7-5.4).
The adjusted hazard ratios comparing the vaccinated with control groups were 0.84 (95% confidence interval, 0.83-0.85) for all stroke; 0.82 (95% CI, 0.81-0.83) for acute ischemic stroke; and 0.88 (95% CI, 0.84-0.91) for hemorrhagic stroke.
The vaccinated group experienced 42,267 stroke events during that time. This rate included 33,510 acute ischemic strokes and 4,318 hemorrhagic strokes. At the same time, 48,139 strokes occurred in the control group. The breakdown included 39,334 ischemic and 4,713 hemorrhagic events.
“Approximately 1 million people in the United States get shingles each year, yet there is a vaccine to help prevent it,” Dr. Yang stated in a news release. “Our study results may encourage people ages 50 and older to follow the recommendation and get vaccinated against shingles. You are reducing the risk of shingles, and at the same time, you may be reducing your risk of stroke.”
“Further studies are needed to confirm our findings of association between Zostavax vaccine and risk of stroke,” Dr. Yang said.
Because the CDC Advisory Committee on Immunization Practices recommended Shingrix vaccine only for healthy adults 50 years and older in 2017, there were insufficient data in Medicare to study the association between that vaccine and risk of stroke at the time of the current study.
“However, two doses of Shingrix are more than 90% effective at preventing shingles and postherpetic neuralgia, and higher than that of Zostavax,” Dr. Yang said.
‘Very intriguing’ research
“This is a very interesting study,” Ralph L. Sacco, MD, past president of the American Heart Association, said in a video commentary released in advance of the conference. It was a very large sample, he noted, and those older than age 60 years who had the vaccine were protected with a lower risk for both ischemic and hemorrhagic stroke.
“So it is very intriguing,” added Dr. Sacco, chairman of the department of neurology at the University of Miami. “We know things like shingles can increase inflammation and increase the risk of stroke,” Dr. Sacco said, “but this is the first time in a very large Medicare database that it was shown that those who had the vaccine had a lower risk of stroke.”
The CDC funded this study. Dr. Yang and Dr. Sacco have disclosed no relevant financial relationships.
SOURCE: Yang Q et al. ISC 2020, Abstract TP493.
This article first appeared on Medscape.com.
LOS ANGELES – Prevention of shingles with the Zoster Vaccine Live may reduce the risk of subsequent stroke among older adults as well, the first study to examine this association suggests. Shingles vaccination was linked to a 20% decrease in stroke risk in people younger than 80 years of age in the large Medicare cohort study. Older participants showed a 10% reduced risk, according to data released in advance of formal presentation at this week’s International Stroke Conference, sponsored by the American Heart Association.
Reductions were seen for both ischemic and hemorrhagic events.
“Our findings might encourage people age 50 or older to get vaccinated against shingles and to prevent shingles-associated stroke risk,” Quanhe Yang, PhD, lead study author and senior scientist at the Centers for Disease Control and Prevention, said in an interview.
Dr. Yang and colleagues evaluated the only shingles vaccine available at the time of the study, Zoster Vaccine Live (Zostavax). However, the CDC now calls an adjuvanted, nonlive recombinant vaccine (Shingrix) the preferred shingles vaccine for healthy adults aged 50 years and older. Shingrix was approved in 2017. Zostavax, approved in 2006, can still be used in healthy adults aged 60 years and older, the agency states.
A reduction in inflammation from Zoster Vaccine Live may be the mechanism by which stroke risk is reduced, Dr. Yang said. The newer vaccine, which the CDC notes is more than 90% effective, might provide even greater protection against stroke, although more research is needed, he added.
Interestingly, prior research suggested that, once a person develops shingles, it may be too late. Dr. Yang and colleagues showed vaccination or antiviral treatment after a shingles episode was not effective at reducing stroke risk in research presented at the 2019 International Stroke Conference.
Shingles can present as a painful reactivation of chickenpox, also known as the varicella-zoster virus. Shingles is also common; Dr. Yang estimated one in three people who had chickenpox will develop the condition at some point in their lifetime. In addition, researchers have linked shingles to an elevated risk of stroke.
To assess the vaccine’s protective effect on stroke, Dr. Yang and colleagues reviewed health records for 1.38 million Medicare recipients. All participants were aged 66 years or older, had no history of stroke at baseline, and received the Zoster Vaccine Live during 2008-2016. The investigators compared the stroke rate in this vaccinated group with the rate in a matched control group of the same number of Medicare fee-for-service beneficiaries who did not receive the vaccination. They adjusted their analysis for age, sex, race, medications, and comorbidities.
The overall decrease of 16% in stroke risk associated with vaccination included a 12% drop in hemorrhagic stroke and 18% decrease in ischemic stroke over a median follow-up of 3.9 years follow-up (interquartile range, 2.7-5.4).
The adjusted hazard ratios comparing the vaccinated with control groups were 0.84 (95% confidence interval, 0.83-0.85) for all stroke; 0.82 (95% CI, 0.81-0.83) for acute ischemic stroke; and 0.88 (95% CI, 0.84-0.91) for hemorrhagic stroke.
The vaccinated group experienced 42,267 stroke events during that time. This rate included 33,510 acute ischemic strokes and 4,318 hemorrhagic strokes. At the same time, 48,139 strokes occurred in the control group. The breakdown included 39,334 ischemic and 4,713 hemorrhagic events.
“Approximately 1 million people in the United States get shingles each year, yet there is a vaccine to help prevent it,” Dr. Yang stated in a news release. “Our study results may encourage people ages 50 and older to follow the recommendation and get vaccinated against shingles. You are reducing the risk of shingles, and at the same time, you may be reducing your risk of stroke.”
“Further studies are needed to confirm our findings of association between Zostavax vaccine and risk of stroke,” Dr. Yang said.
Because the CDC Advisory Committee on Immunization Practices recommended Shingrix vaccine only for healthy adults 50 years and older in 2017, there were insufficient data in Medicare to study the association between that vaccine and risk of stroke at the time of the current study.
“However, two doses of Shingrix are more than 90% effective at preventing shingles and postherpetic neuralgia, and higher than that of Zostavax,” Dr. Yang said.
‘Very intriguing’ research
“This is a very interesting study,” Ralph L. Sacco, MD, past president of the American Heart Association, said in a video commentary released in advance of the conference. It was a very large sample, he noted, and those older than age 60 years who had the vaccine were protected with a lower risk for both ischemic and hemorrhagic stroke.
“So it is very intriguing,” added Dr. Sacco, chairman of the department of neurology at the University of Miami. “We know things like shingles can increase inflammation and increase the risk of stroke,” Dr. Sacco said, “but this is the first time in a very large Medicare database that it was shown that those who had the vaccine had a lower risk of stroke.”
The CDC funded this study. Dr. Yang and Dr. Sacco have disclosed no relevant financial relationships.
SOURCE: Yang Q et al. ISC 2020, Abstract TP493.
This article first appeared on Medscape.com.
LOS ANGELES – Prevention of shingles with the Zoster Vaccine Live may reduce the risk of subsequent stroke among older adults as well, the first study to examine this association suggests. Shingles vaccination was linked to a 20% decrease in stroke risk in people younger than 80 years of age in the large Medicare cohort study. Older participants showed a 10% reduced risk, according to data released in advance of formal presentation at this week’s International Stroke Conference, sponsored by the American Heart Association.
Reductions were seen for both ischemic and hemorrhagic events.
“Our findings might encourage people age 50 or older to get vaccinated against shingles and to prevent shingles-associated stroke risk,” Quanhe Yang, PhD, lead study author and senior scientist at the Centers for Disease Control and Prevention, said in an interview.
Dr. Yang and colleagues evaluated the only shingles vaccine available at the time of the study, Zoster Vaccine Live (Zostavax). However, the CDC now calls an adjuvanted, nonlive recombinant vaccine (Shingrix) the preferred shingles vaccine for healthy adults aged 50 years and older. Shingrix was approved in 2017. Zostavax, approved in 2006, can still be used in healthy adults aged 60 years and older, the agency states.
A reduction in inflammation from Zoster Vaccine Live may be the mechanism by which stroke risk is reduced, Dr. Yang said. The newer vaccine, which the CDC notes is more than 90% effective, might provide even greater protection against stroke, although more research is needed, he added.
Interestingly, prior research suggested that, once a person develops shingles, it may be too late. Dr. Yang and colleagues showed vaccination or antiviral treatment after a shingles episode was not effective at reducing stroke risk in research presented at the 2019 International Stroke Conference.
Shingles can present as a painful reactivation of chickenpox, also known as the varicella-zoster virus. Shingles is also common; Dr. Yang estimated one in three people who had chickenpox will develop the condition at some point in their lifetime. In addition, researchers have linked shingles to an elevated risk of stroke.
To assess the vaccine’s protective effect on stroke, Dr. Yang and colleagues reviewed health records for 1.38 million Medicare recipients. All participants were aged 66 years or older, had no history of stroke at baseline, and received the Zoster Vaccine Live during 2008-2016. The investigators compared the stroke rate in this vaccinated group with the rate in a matched control group of the same number of Medicare fee-for-service beneficiaries who did not receive the vaccination. They adjusted their analysis for age, sex, race, medications, and comorbidities.
The overall decrease of 16% in stroke risk associated with vaccination included a 12% drop in hemorrhagic stroke and 18% decrease in ischemic stroke over a median follow-up of 3.9 years follow-up (interquartile range, 2.7-5.4).
The adjusted hazard ratios comparing the vaccinated with control groups were 0.84 (95% confidence interval, 0.83-0.85) for all stroke; 0.82 (95% CI, 0.81-0.83) for acute ischemic stroke; and 0.88 (95% CI, 0.84-0.91) for hemorrhagic stroke.
The vaccinated group experienced 42,267 stroke events during that time. This rate included 33,510 acute ischemic strokes and 4,318 hemorrhagic strokes. At the same time, 48,139 strokes occurred in the control group. The breakdown included 39,334 ischemic and 4,713 hemorrhagic events.
“Approximately 1 million people in the United States get shingles each year, yet there is a vaccine to help prevent it,” Dr. Yang stated in a news release. “Our study results may encourage people ages 50 and older to follow the recommendation and get vaccinated against shingles. You are reducing the risk of shingles, and at the same time, you may be reducing your risk of stroke.”
“Further studies are needed to confirm our findings of association between Zostavax vaccine and risk of stroke,” Dr. Yang said.
Because the CDC Advisory Committee on Immunization Practices recommended Shingrix vaccine only for healthy adults 50 years and older in 2017, there were insufficient data in Medicare to study the association between that vaccine and risk of stroke at the time of the current study.
“However, two doses of Shingrix are more than 90% effective at preventing shingles and postherpetic neuralgia, and higher than that of Zostavax,” Dr. Yang said.
‘Very intriguing’ research
“This is a very interesting study,” Ralph L. Sacco, MD, past president of the American Heart Association, said in a video commentary released in advance of the conference. It was a very large sample, he noted, and those older than age 60 years who had the vaccine were protected with a lower risk for both ischemic and hemorrhagic stroke.
“So it is very intriguing,” added Dr. Sacco, chairman of the department of neurology at the University of Miami. “We know things like shingles can increase inflammation and increase the risk of stroke,” Dr. Sacco said, “but this is the first time in a very large Medicare database that it was shown that those who had the vaccine had a lower risk of stroke.”
The CDC funded this study. Dr. Yang and Dr. Sacco have disclosed no relevant financial relationships.
SOURCE: Yang Q et al. ISC 2020, Abstract TP493.
This article first appeared on Medscape.com.
REPORTING FROM ISC 2020
To Improve TB Vaccination, Change The Way It’s Given?
The standard intradermal route of delivery for Bacille Calmette–Guérin (BCG) does not necessarily generate a strong enough response from lung T-cells, the researchers say. They hypothesized that administering BCG by IV or aerosol might be more effective.
They gave a group of rhesus macaques the BGC vaccine by intradermal, aerosol, or IV routes, then assessed immune responses in blood and fluid drawn from the lungs over a 24-week follow-up. Six months after vaccination, the researchers injected the vaccinated animals with a virulent strain of Mycobacterium tuberculosis (M tuberculosis) and tracked infection and disease development over 3 months.
The IV vaccination resulted in the highest durable levels of T-cells in blood and lungs. Nine of 10 animals vaccinated via IV were highly protected; 6 showed no detectable infection in any tissue tested and 3 had only very low counts of M tuberculosis in lung tissue. All unvaccinated animals and those immunized via intradermal or aerosol routes showed signs of significantly greater infection.
Upping the dose did not improve protection. The IV BCG group showed 90% protection at a threshold as low as 50 colony-forming units (the standard human ID dose is 5 x 105 CFUs).
The researchers say several unique quantitative and qualitative differences in the immune responses may underlie protection. Perhaps most noteworthy, they say, was the large population of T- cells in the tissue across all lung parenchyma lobes.
The study provides a “paradigm shift,” the researchers conclude, adding that the IV route may also improve the protective capacity of other vaccines.
The standard intradermal route of delivery for Bacille Calmette–Guérin (BCG) does not necessarily generate a strong enough response from lung T-cells, the researchers say. They hypothesized that administering BCG by IV or aerosol might be more effective.
They gave a group of rhesus macaques the BGC vaccine by intradermal, aerosol, or IV routes, then assessed immune responses in blood and fluid drawn from the lungs over a 24-week follow-up. Six months after vaccination, the researchers injected the vaccinated animals with a virulent strain of Mycobacterium tuberculosis (M tuberculosis) and tracked infection and disease development over 3 months.
The IV vaccination resulted in the highest durable levels of T-cells in blood and lungs. Nine of 10 animals vaccinated via IV were highly protected; 6 showed no detectable infection in any tissue tested and 3 had only very low counts of M tuberculosis in lung tissue. All unvaccinated animals and those immunized via intradermal or aerosol routes showed signs of significantly greater infection.
Upping the dose did not improve protection. The IV BCG group showed 90% protection at a threshold as low as 50 colony-forming units (the standard human ID dose is 5 x 105 CFUs).
The researchers say several unique quantitative and qualitative differences in the immune responses may underlie protection. Perhaps most noteworthy, they say, was the large population of T- cells in the tissue across all lung parenchyma lobes.
The study provides a “paradigm shift,” the researchers conclude, adding that the IV route may also improve the protective capacity of other vaccines.
The standard intradermal route of delivery for Bacille Calmette–Guérin (BCG) does not necessarily generate a strong enough response from lung T-cells, the researchers say. They hypothesized that administering BCG by IV or aerosol might be more effective.
They gave a group of rhesus macaques the BGC vaccine by intradermal, aerosol, or IV routes, then assessed immune responses in blood and fluid drawn from the lungs over a 24-week follow-up. Six months after vaccination, the researchers injected the vaccinated animals with a virulent strain of Mycobacterium tuberculosis (M tuberculosis) and tracked infection and disease development over 3 months.
The IV vaccination resulted in the highest durable levels of T-cells in blood and lungs. Nine of 10 animals vaccinated via IV were highly protected; 6 showed no detectable infection in any tissue tested and 3 had only very low counts of M tuberculosis in lung tissue. All unvaccinated animals and those immunized via intradermal or aerosol routes showed signs of significantly greater infection.
Upping the dose did not improve protection. The IV BCG group showed 90% protection at a threshold as low as 50 colony-forming units (the standard human ID dose is 5 x 105 CFUs).
The researchers say several unique quantitative and qualitative differences in the immune responses may underlie protection. Perhaps most noteworthy, they say, was the large population of T- cells in the tissue across all lung parenchyma lobes.
The study provides a “paradigm shift,” the researchers conclude, adding that the IV route may also improve the protective capacity of other vaccines.
Vaccinating most girls could eliminate cervical cancer within a century
Cervical cancer is the second most common cancer among women in lower- and middle-income countries, but universal human papillomavirus vaccination for girls would reduce new cervical cancer cases by about 90% over the next century, according to researchers.
Adding twice-lifetime cervical screening with human papillomavirus (HPV) testing would further reduce the incidence of cervical cancer, including in countries with the highest burden, the researchers reported in The Lancet.
Marc Brisson, PhD, of Laval University, Quebec City, and colleagues conducted this study using three models identified by the World Health Organization. The models were used to project reductions in cervical cancer incidence for women in 78 low- and middle-income countries based on the following HPV vaccination and screening scenarios:
- Universal girls-only vaccination at age 9 years, assuming 90% of girls vaccinated and a vaccine that is perfectly effective
- Girls-only vaccination plus cervical screening with HPV testing at age 35 years
- Girls-only vaccination plus screening at ages 35 and 45.
All three scenarios modeled would result in the elimination of cervical cancer, Dr. Brisson and colleagues found. Elimination was defined as four or fewer new cases per 100,000 women-years.
The simplest scenario, universal girls-only vaccination, was predicted to reduce age-standardized cervical cancer incidence from 19.8 cases per 100,000 women-years to 2.1 cases per 100,000 women-years (89.4% reduction) by 2120. That amounts to about 61 million potential cases avoided, with elimination targets reached in 60% of the countries studied.
HPV vaccination plus one-time screening was predicted to reduce the incidence of cervical cancer to 1.0 case per 100,000 women-years (95.0% reduction), and HPV vaccination plus twice-lifetime screening was predicted to reduce the incidence to 0.7 cases per 100,000 women-years (96.7% reduction).
Dr. Brisson and colleagues reported that, for the countries with the highest burden of cervical cancer (more than 25 cases per 100,000 women-years), adding screening would be necessary to achieve elimination.
To meet the same targets across all 78 countries, “our models predict that scale-up of both girls-only HPV vaccination and twice-lifetime screening is necessary, with 90% HPV vaccination coverage, 90% screening uptake, and long-term protection against HPV types 16, 18, 31, 33, 45, 52, and 58,” the researchers wrote.
Dr. Brisson and colleagues claimed that a strength of this study is the modeling approach, which compared three models “that have been extensively peer reviewed and validated with postvaccination surveillance data.”
The researchers acknowledged, however, that their modeling could not account for variations in sexual behavior from country to country, and the study was not designed to anticipate behavioral or technological changes that could affect cervical cancer incidence in the decades to come.
The study was funded by the WHO, the United Nations, and the Canadian and Australian governments. The WHO contributed to the study design, data analysis and interpretation, and writing of the manuscript. Two study authors reported receiving indirect industry funding for a cervical screening trial in Australia.
SOURCE: Brisson M et al. Lancet. 2020 Jan 30. doi: 10.1016/S0140-6736(20)30068-4.
Cervical cancer is the second most common cancer among women in lower- and middle-income countries, but universal human papillomavirus vaccination for girls would reduce new cervical cancer cases by about 90% over the next century, according to researchers.
Adding twice-lifetime cervical screening with human papillomavirus (HPV) testing would further reduce the incidence of cervical cancer, including in countries with the highest burden, the researchers reported in The Lancet.
Marc Brisson, PhD, of Laval University, Quebec City, and colleagues conducted this study using three models identified by the World Health Organization. The models were used to project reductions in cervical cancer incidence for women in 78 low- and middle-income countries based on the following HPV vaccination and screening scenarios:
- Universal girls-only vaccination at age 9 years, assuming 90% of girls vaccinated and a vaccine that is perfectly effective
- Girls-only vaccination plus cervical screening with HPV testing at age 35 years
- Girls-only vaccination plus screening at ages 35 and 45.
All three scenarios modeled would result in the elimination of cervical cancer, Dr. Brisson and colleagues found. Elimination was defined as four or fewer new cases per 100,000 women-years.
The simplest scenario, universal girls-only vaccination, was predicted to reduce age-standardized cervical cancer incidence from 19.8 cases per 100,000 women-years to 2.1 cases per 100,000 women-years (89.4% reduction) by 2120. That amounts to about 61 million potential cases avoided, with elimination targets reached in 60% of the countries studied.
HPV vaccination plus one-time screening was predicted to reduce the incidence of cervical cancer to 1.0 case per 100,000 women-years (95.0% reduction), and HPV vaccination plus twice-lifetime screening was predicted to reduce the incidence to 0.7 cases per 100,000 women-years (96.7% reduction).
Dr. Brisson and colleagues reported that, for the countries with the highest burden of cervical cancer (more than 25 cases per 100,000 women-years), adding screening would be necessary to achieve elimination.
To meet the same targets across all 78 countries, “our models predict that scale-up of both girls-only HPV vaccination and twice-lifetime screening is necessary, with 90% HPV vaccination coverage, 90% screening uptake, and long-term protection against HPV types 16, 18, 31, 33, 45, 52, and 58,” the researchers wrote.
Dr. Brisson and colleagues claimed that a strength of this study is the modeling approach, which compared three models “that have been extensively peer reviewed and validated with postvaccination surveillance data.”
The researchers acknowledged, however, that their modeling could not account for variations in sexual behavior from country to country, and the study was not designed to anticipate behavioral or technological changes that could affect cervical cancer incidence in the decades to come.
The study was funded by the WHO, the United Nations, and the Canadian and Australian governments. The WHO contributed to the study design, data analysis and interpretation, and writing of the manuscript. Two study authors reported receiving indirect industry funding for a cervical screening trial in Australia.
SOURCE: Brisson M et al. Lancet. 2020 Jan 30. doi: 10.1016/S0140-6736(20)30068-4.
Cervical cancer is the second most common cancer among women in lower- and middle-income countries, but universal human papillomavirus vaccination for girls would reduce new cervical cancer cases by about 90% over the next century, according to researchers.
Adding twice-lifetime cervical screening with human papillomavirus (HPV) testing would further reduce the incidence of cervical cancer, including in countries with the highest burden, the researchers reported in The Lancet.
Marc Brisson, PhD, of Laval University, Quebec City, and colleagues conducted this study using three models identified by the World Health Organization. The models were used to project reductions in cervical cancer incidence for women in 78 low- and middle-income countries based on the following HPV vaccination and screening scenarios:
- Universal girls-only vaccination at age 9 years, assuming 90% of girls vaccinated and a vaccine that is perfectly effective
- Girls-only vaccination plus cervical screening with HPV testing at age 35 years
- Girls-only vaccination plus screening at ages 35 and 45.
All three scenarios modeled would result in the elimination of cervical cancer, Dr. Brisson and colleagues found. Elimination was defined as four or fewer new cases per 100,000 women-years.
The simplest scenario, universal girls-only vaccination, was predicted to reduce age-standardized cervical cancer incidence from 19.8 cases per 100,000 women-years to 2.1 cases per 100,000 women-years (89.4% reduction) by 2120. That amounts to about 61 million potential cases avoided, with elimination targets reached in 60% of the countries studied.
HPV vaccination plus one-time screening was predicted to reduce the incidence of cervical cancer to 1.0 case per 100,000 women-years (95.0% reduction), and HPV vaccination plus twice-lifetime screening was predicted to reduce the incidence to 0.7 cases per 100,000 women-years (96.7% reduction).
Dr. Brisson and colleagues reported that, for the countries with the highest burden of cervical cancer (more than 25 cases per 100,000 women-years), adding screening would be necessary to achieve elimination.
To meet the same targets across all 78 countries, “our models predict that scale-up of both girls-only HPV vaccination and twice-lifetime screening is necessary, with 90% HPV vaccination coverage, 90% screening uptake, and long-term protection against HPV types 16, 18, 31, 33, 45, 52, and 58,” the researchers wrote.
Dr. Brisson and colleagues claimed that a strength of this study is the modeling approach, which compared three models “that have been extensively peer reviewed and validated with postvaccination surveillance data.”
The researchers acknowledged, however, that their modeling could not account for variations in sexual behavior from country to country, and the study was not designed to anticipate behavioral or technological changes that could affect cervical cancer incidence in the decades to come.
The study was funded by the WHO, the United Nations, and the Canadian and Australian governments. The WHO contributed to the study design, data analysis and interpretation, and writing of the manuscript. Two study authors reported receiving indirect industry funding for a cervical screening trial in Australia.
SOURCE: Brisson M et al. Lancet. 2020 Jan 30. doi: 10.1016/S0140-6736(20)30068-4.
FROM THE LANCET
Delaying flu vaccine didn’t drop fever rate for childhood immunizations
according to a randomized trial.
An increased risk for febrile seizures had been seen when the three vaccines were administered together, wrote Emmanuel B. Walter, MD, MPH, and coauthors, so they constructed a trial that compared a simultaneous administration strategy that delayed inactivated influenza vaccine (IIV) administration by about 2 weeks.
In all, 221 children aged 12-16 months were enrolled in the randomized study. A total of 110 children received quadrivalent IIV (IIV4), DTaP, and 13-valent pneumococcal conjugate vaccine (PCV13) simultaneously and returned for a dental health education visit 2 weeks later. For 111 children, DTaP and PCV13 were administered at study visit 1, and IIV4 was given along with dental health education 2 weeks later. Most children in both groups also received at least one nonstudy vaccine at the first study visit. Eleven children in the simultaneous group and four in the sequential group didn’t complete the study.
There was no difference between study groups in the combined rates of fever on the first 2 days after study visits 1 and 2 taken together: 8% of children in the simultaneous group and 9% of those in the sequential group had fever of 38° C or higher (adjusted relative risk, 0.87; 95% confidence interval, 0.36-2.10).
However, children in the simultaneous group were more likely to receive antipyretic medication in the first 2 days after visit 1 (37% versus 22%; P = .020), reported Dr. Walter, professor of pediatrics at Duke University, Durham, N.C., and coauthors. Because it’s rare for febrile seizures to occur after immunization, the authors didn’t make the occurrence of febrile seizure a primary or secondary endpoint of the study; no seizures occurred in study participants. They did hypothesize that the total proportion of children having fever would be higher in the simultaneous than in the sequential group – a hypothesis not supported by the study findings.
Children were excluded, or their study vaccinations were delayed, if they had received antipyretic medication within the 72 hours preceding the visit or at the study visit, or if they had a temperature of 38° C or more.
Parents monitored participants’ temperatures for 8 days after visits by using a study-provided temporal thermometer once daily at about the same time, and also by checking the temperature if their child felt feverish. Parents also recorded any antipyretic use, medical care, other symptoms, and febrile seizures.
The study was stopped earlier than anticipated because unexpectedly high levels of influenza activity made it unethical to delay influenza immunization, explained Dr. Walter and coauthors.
Participants were a median 15 months old; most were non-Hispanic white and had private insurance. Most participants didn’t attend day care.
“Nearly all fever episodes and days of fever on days 1-2 after the study visits occurred after visit 1,” reported Dr. Walter and coinvestigators. They saw no difference between groups in the proportion of children who had a fever of 38.6° C on days 1-2 after either study visit.
The mean peak temperature – about 38.5° C – on combined study visits 1 and 2 didn’t differ between groups. Similarly, for those participants who had a fever, the mean postvisit fever duration of 1.3 days was identical between groups.
Parents also were asked about their perceptions of the vaccination schedule their children received. Over half of parents overall (56%) reported that they disliked having to bring their child in for two separate clinic visits, with more parents in the sequential group than the simultaneous group reporting this (65% versus 48%).
Generalizability of the findings and comparison with previous studies are limited, noted Dr. Walter and coinvestigators, because the composition of influenza vaccine varies from year to year. No signal for seizures was seen in the Vaccine Safety Datalink after IIV during the 2017-2018 influenza season, wrote the investigators. The 2010-2011 influenza season’s IIV formulation was associated with increased febrile seizure risk, indicating that the IIV formulation for that year may have been more pyrogenic than the 2017-2018 formulation.
Also, children deemed at higher risk of febrile seizure were excluded from the study, so findings may have limited applicability to these children. The lack of parental blinding also may have influenced antipyretic administration or other symptom reporting, although objective temperature measurement should not have been affected by the lack of blinding, wrote Dr. Walker and collaborators.
The study was funded by the Centers for Disease Control and Prevention. One coauthor reported potential conflicts of interest from financial support received from GlaxoSmithKline, Sanofi Pasteur, Pfizer, Merck, Protein Science, Dynavax, and Medimmune. The remaining authors have no relevant financial disclosures.
SOURCE: Walter EB et al. Pediatrics. 2020;145(3):e20191909.
according to a randomized trial.
An increased risk for febrile seizures had been seen when the three vaccines were administered together, wrote Emmanuel B. Walter, MD, MPH, and coauthors, so they constructed a trial that compared a simultaneous administration strategy that delayed inactivated influenza vaccine (IIV) administration by about 2 weeks.
In all, 221 children aged 12-16 months were enrolled in the randomized study. A total of 110 children received quadrivalent IIV (IIV4), DTaP, and 13-valent pneumococcal conjugate vaccine (PCV13) simultaneously and returned for a dental health education visit 2 weeks later. For 111 children, DTaP and PCV13 were administered at study visit 1, and IIV4 was given along with dental health education 2 weeks later. Most children in both groups also received at least one nonstudy vaccine at the first study visit. Eleven children in the simultaneous group and four in the sequential group didn’t complete the study.
There was no difference between study groups in the combined rates of fever on the first 2 days after study visits 1 and 2 taken together: 8% of children in the simultaneous group and 9% of those in the sequential group had fever of 38° C or higher (adjusted relative risk, 0.87; 95% confidence interval, 0.36-2.10).
However, children in the simultaneous group were more likely to receive antipyretic medication in the first 2 days after visit 1 (37% versus 22%; P = .020), reported Dr. Walter, professor of pediatrics at Duke University, Durham, N.C., and coauthors. Because it’s rare for febrile seizures to occur after immunization, the authors didn’t make the occurrence of febrile seizure a primary or secondary endpoint of the study; no seizures occurred in study participants. They did hypothesize that the total proportion of children having fever would be higher in the simultaneous than in the sequential group – a hypothesis not supported by the study findings.
Children were excluded, or their study vaccinations were delayed, if they had received antipyretic medication within the 72 hours preceding the visit or at the study visit, or if they had a temperature of 38° C or more.
Parents monitored participants’ temperatures for 8 days after visits by using a study-provided temporal thermometer once daily at about the same time, and also by checking the temperature if their child felt feverish. Parents also recorded any antipyretic use, medical care, other symptoms, and febrile seizures.
The study was stopped earlier than anticipated because unexpectedly high levels of influenza activity made it unethical to delay influenza immunization, explained Dr. Walter and coauthors.
Participants were a median 15 months old; most were non-Hispanic white and had private insurance. Most participants didn’t attend day care.
“Nearly all fever episodes and days of fever on days 1-2 after the study visits occurred after visit 1,” reported Dr. Walter and coinvestigators. They saw no difference between groups in the proportion of children who had a fever of 38.6° C on days 1-2 after either study visit.
The mean peak temperature – about 38.5° C – on combined study visits 1 and 2 didn’t differ between groups. Similarly, for those participants who had a fever, the mean postvisit fever duration of 1.3 days was identical between groups.
Parents also were asked about their perceptions of the vaccination schedule their children received. Over half of parents overall (56%) reported that they disliked having to bring their child in for two separate clinic visits, with more parents in the sequential group than the simultaneous group reporting this (65% versus 48%).
Generalizability of the findings and comparison with previous studies are limited, noted Dr. Walter and coinvestigators, because the composition of influenza vaccine varies from year to year. No signal for seizures was seen in the Vaccine Safety Datalink after IIV during the 2017-2018 influenza season, wrote the investigators. The 2010-2011 influenza season’s IIV formulation was associated with increased febrile seizure risk, indicating that the IIV formulation for that year may have been more pyrogenic than the 2017-2018 formulation.
Also, children deemed at higher risk of febrile seizure were excluded from the study, so findings may have limited applicability to these children. The lack of parental blinding also may have influenced antipyretic administration or other symptom reporting, although objective temperature measurement should not have been affected by the lack of blinding, wrote Dr. Walker and collaborators.
The study was funded by the Centers for Disease Control and Prevention. One coauthor reported potential conflicts of interest from financial support received from GlaxoSmithKline, Sanofi Pasteur, Pfizer, Merck, Protein Science, Dynavax, and Medimmune. The remaining authors have no relevant financial disclosures.
SOURCE: Walter EB et al. Pediatrics. 2020;145(3):e20191909.
according to a randomized trial.
An increased risk for febrile seizures had been seen when the three vaccines were administered together, wrote Emmanuel B. Walter, MD, MPH, and coauthors, so they constructed a trial that compared a simultaneous administration strategy that delayed inactivated influenza vaccine (IIV) administration by about 2 weeks.
In all, 221 children aged 12-16 months were enrolled in the randomized study. A total of 110 children received quadrivalent IIV (IIV4), DTaP, and 13-valent pneumococcal conjugate vaccine (PCV13) simultaneously and returned for a dental health education visit 2 weeks later. For 111 children, DTaP and PCV13 were administered at study visit 1, and IIV4 was given along with dental health education 2 weeks later. Most children in both groups also received at least one nonstudy vaccine at the first study visit. Eleven children in the simultaneous group and four in the sequential group didn’t complete the study.
There was no difference between study groups in the combined rates of fever on the first 2 days after study visits 1 and 2 taken together: 8% of children in the simultaneous group and 9% of those in the sequential group had fever of 38° C or higher (adjusted relative risk, 0.87; 95% confidence interval, 0.36-2.10).
However, children in the simultaneous group were more likely to receive antipyretic medication in the first 2 days after visit 1 (37% versus 22%; P = .020), reported Dr. Walter, professor of pediatrics at Duke University, Durham, N.C., and coauthors. Because it’s rare for febrile seizures to occur after immunization, the authors didn’t make the occurrence of febrile seizure a primary or secondary endpoint of the study; no seizures occurred in study participants. They did hypothesize that the total proportion of children having fever would be higher in the simultaneous than in the sequential group – a hypothesis not supported by the study findings.
Children were excluded, or their study vaccinations were delayed, if they had received antipyretic medication within the 72 hours preceding the visit or at the study visit, or if they had a temperature of 38° C or more.
Parents monitored participants’ temperatures for 8 days after visits by using a study-provided temporal thermometer once daily at about the same time, and also by checking the temperature if their child felt feverish. Parents also recorded any antipyretic use, medical care, other symptoms, and febrile seizures.
The study was stopped earlier than anticipated because unexpectedly high levels of influenza activity made it unethical to delay influenza immunization, explained Dr. Walter and coauthors.
Participants were a median 15 months old; most were non-Hispanic white and had private insurance. Most participants didn’t attend day care.
“Nearly all fever episodes and days of fever on days 1-2 after the study visits occurred after visit 1,” reported Dr. Walter and coinvestigators. They saw no difference between groups in the proportion of children who had a fever of 38.6° C on days 1-2 after either study visit.
The mean peak temperature – about 38.5° C – on combined study visits 1 and 2 didn’t differ between groups. Similarly, for those participants who had a fever, the mean postvisit fever duration of 1.3 days was identical between groups.
Parents also were asked about their perceptions of the vaccination schedule their children received. Over half of parents overall (56%) reported that they disliked having to bring their child in for two separate clinic visits, with more parents in the sequential group than the simultaneous group reporting this (65% versus 48%).
Generalizability of the findings and comparison with previous studies are limited, noted Dr. Walter and coinvestigators, because the composition of influenza vaccine varies from year to year. No signal for seizures was seen in the Vaccine Safety Datalink after IIV during the 2017-2018 influenza season, wrote the investigators. The 2010-2011 influenza season’s IIV formulation was associated with increased febrile seizure risk, indicating that the IIV formulation for that year may have been more pyrogenic than the 2017-2018 formulation.
Also, children deemed at higher risk of febrile seizure were excluded from the study, so findings may have limited applicability to these children. The lack of parental blinding also may have influenced antipyretic administration or other symptom reporting, although objective temperature measurement should not have been affected by the lack of blinding, wrote Dr. Walker and collaborators.
The study was funded by the Centers for Disease Control and Prevention. One coauthor reported potential conflicts of interest from financial support received from GlaxoSmithKline, Sanofi Pasteur, Pfizer, Merck, Protein Science, Dynavax, and Medimmune. The remaining authors have no relevant financial disclosures.
SOURCE: Walter EB et al. Pediatrics. 2020;145(3):e20191909.
FROM PEDIATRICS
Key clinical point: Fevers were no less common when influenza vaccine was delayed for children receiving DTaP and pneumococcal vaccinations.
Major finding: There was no difference between study groups in the combined rates of fever on the first 2 days after study visits 1 and 2 taken together: 8% of children in the simultaneous group and 9% of those in the sequential group had fever of 38° C or higher (adjusted relative risk, 0.87).
Study details: Randomized, nonblinded trial of 221 children aged 12-16 months receiving scheduled vaccinations.
Disclosures: The study was funded by the Centers for Disease Control and Prevention. One coauthor reported financial support received from GlaxoSmithKline, Sanofi Pasteur, Pfizer, Merck, Protein Science, Dynavax, and Medimmune.
Source: Walter EB et al. Pediatrics. 2020;145(3):e20191909.
Measles, scarlet fever among infectious diseases to watch for in 2020
ORLANDO – – leading into 2020, Justin Finch, MD, said at the ODAC Dermatology, Aesthetic, & Surgical Conference.
While group A streptococcus has declined over the past century, there has been “an unprecedented” resurgence in severe, invasive group A streptococcal infections and severe epidemics of scarlet fever worldwide, including in industrialized regions like the United Kingdom. Shedding some light on why this may be occurring, Dr. Finch referred to a recently published population-based molecular epidemiologic study identified a new dominant emm1UK lineage of Streptococcus pyogenes associated with such cases in England (Lancet Infect Dis. 2019 Nov;19(11):1209-18). This new lineage of S. pyogenes was genotypically distinct from other emm1 isolates and had greatly increased expression of the streptococcal pyrogenic exotoxin A, one of the exotoxins responsible for the clinical features of scarlet fever.
“We have not, to my knowledge, seen the strain yet in the United States,” said Dr. Finch, of Central Connecticut Dermatology in Cromwell. “Have it on your radar. With all of the worldwide travel patterns, I expect that you will see this in the United States at some point in the not-too-distant future.”
Also in 2019, promising data on the safety and effectiveness of the recombinant herpes zoster vaccine in immunocompromised patients became available for the first time. A randomized clinical trial published in JAMA of 1,846 patients who were immunosuppressed after autologous hematopoietic stem cell transplantation and received two doses of a recombinant zoster vaccine found that the patients had a reduced incidence of herpes zoster after a median follow-up of 21 months (JAMA. 2019 Jul 9;322[2]:123-33). The study found that the recombinant vaccine was both safe and effective in these immunocompromised patients, “so we can easily generalize this to our dermatology population as well,” Dr. Finch said. In comparing the live attenuated and recombinant vaccines, he noted the recombinant vaccine requires two doses but appears to be slightly more effective. “The number needed to treat to prevent [one case] of zoster is about half as high as that for the live vaccine, and most importantly for us is, it’s safe in immunocompromised patients.”
2019 also saw a record high in the number of measles cases in the United States, the highest since 1993, Dr. Finch pointed out. Most cases were seen in the area in and around New York City, but the percentage of people across the United States who are vaccinated against measles is below the threshold for herd immunity to protect immunocompromised patients. Measles requires a population vaccination rate of 94%, and less than half of U.S. counties in 2014 and 2015 reached that vaccination rate.
“Furthermore, if we look at that over the last 20 years, comparing the domestic measles cases to imported measles cases, we are increasingly breeding these measles epidemics right here at home, whereas they used to be imported from throughout the world,” said Dr. Finch. Patients with measles can be treated with vitamin A, he added, referring to a Cochrane review showing that 200,000 units of vitamin A given daily for 2 days decreased the mortality rate of measles by about 80%. Measles is on the Centers for Disease Control and Prevention’s list of reportable diseases, so should be reported to local health authorities, and will be followed up with confirmatory testing.
In 2019, a study examining herd protection of oral human papillomavirus infection in men and women compared the prevalence of oral HPV infection based on the 4 HPV types present in the quadrivalent HPV vaccine with 33 nonvaccine types from 2009 to 2016. There was no change in the prevalence of nonvaccine type oral HPV infections among men who were unvaccinated, but the prevalence of oral HPV infections because of the four strains in the quadrivalent HPV vaccine declined from 2.7% in 2009-2010 to 1.6% in 2015-2016 (JAMA. 2019 Sep 10;322[10]:977-9). Among unvaccinated women, the prevalence of nonvaccine- and vaccine-type oral HPV infections did not change between the two time periods.
“Notably, this only occurred in men,” Dr. Finch said. Herd immunity is being achieved in men “because we’re vaccinating all women, [but] we’re not seeing that herd immunity in women. Which begs the question: Why are we still vaccinating only half of our population?”
One study published in 2019 (Br J Dermatol. 2019 Nov;181[5]:1093-5) described a patient with CARD9 mutations, which predispose individuals to deep invasive infections – a disseminated Microsporum infection in this case, Dr. Finch said. “You shouldn’t see that,” he added, noting that these mutations are known to predispose individuals to severe Trichophyton infections and familial candidiasis.
“What I think is interesting about this is that, as we look forward to 2020, we’re going to increasingly see studies like this that are identifying specific mutations in our community that underlie a lot of these weird infections,” he added. “I wouldn’t be surprised if within the span of our careers, we find that a lot of those severe treatment-refractory reports that so commonly plague your everyday clinic have some underlying, specific immunity.”
Dr. Finch reported no relevant conflicts of interest.
ORLANDO – – leading into 2020, Justin Finch, MD, said at the ODAC Dermatology, Aesthetic, & Surgical Conference.
While group A streptococcus has declined over the past century, there has been “an unprecedented” resurgence in severe, invasive group A streptococcal infections and severe epidemics of scarlet fever worldwide, including in industrialized regions like the United Kingdom. Shedding some light on why this may be occurring, Dr. Finch referred to a recently published population-based molecular epidemiologic study identified a new dominant emm1UK lineage of Streptococcus pyogenes associated with such cases in England (Lancet Infect Dis. 2019 Nov;19(11):1209-18). This new lineage of S. pyogenes was genotypically distinct from other emm1 isolates and had greatly increased expression of the streptococcal pyrogenic exotoxin A, one of the exotoxins responsible for the clinical features of scarlet fever.
“We have not, to my knowledge, seen the strain yet in the United States,” said Dr. Finch, of Central Connecticut Dermatology in Cromwell. “Have it on your radar. With all of the worldwide travel patterns, I expect that you will see this in the United States at some point in the not-too-distant future.”
Also in 2019, promising data on the safety and effectiveness of the recombinant herpes zoster vaccine in immunocompromised patients became available for the first time. A randomized clinical trial published in JAMA of 1,846 patients who were immunosuppressed after autologous hematopoietic stem cell transplantation and received two doses of a recombinant zoster vaccine found that the patients had a reduced incidence of herpes zoster after a median follow-up of 21 months (JAMA. 2019 Jul 9;322[2]:123-33). The study found that the recombinant vaccine was both safe and effective in these immunocompromised patients, “so we can easily generalize this to our dermatology population as well,” Dr. Finch said. In comparing the live attenuated and recombinant vaccines, he noted the recombinant vaccine requires two doses but appears to be slightly more effective. “The number needed to treat to prevent [one case] of zoster is about half as high as that for the live vaccine, and most importantly for us is, it’s safe in immunocompromised patients.”
2019 also saw a record high in the number of measles cases in the United States, the highest since 1993, Dr. Finch pointed out. Most cases were seen in the area in and around New York City, but the percentage of people across the United States who are vaccinated against measles is below the threshold for herd immunity to protect immunocompromised patients. Measles requires a population vaccination rate of 94%, and less than half of U.S. counties in 2014 and 2015 reached that vaccination rate.
“Furthermore, if we look at that over the last 20 years, comparing the domestic measles cases to imported measles cases, we are increasingly breeding these measles epidemics right here at home, whereas they used to be imported from throughout the world,” said Dr. Finch. Patients with measles can be treated with vitamin A, he added, referring to a Cochrane review showing that 200,000 units of vitamin A given daily for 2 days decreased the mortality rate of measles by about 80%. Measles is on the Centers for Disease Control and Prevention’s list of reportable diseases, so should be reported to local health authorities, and will be followed up with confirmatory testing.
In 2019, a study examining herd protection of oral human papillomavirus infection in men and women compared the prevalence of oral HPV infection based on the 4 HPV types present in the quadrivalent HPV vaccine with 33 nonvaccine types from 2009 to 2016. There was no change in the prevalence of nonvaccine type oral HPV infections among men who were unvaccinated, but the prevalence of oral HPV infections because of the four strains in the quadrivalent HPV vaccine declined from 2.7% in 2009-2010 to 1.6% in 2015-2016 (JAMA. 2019 Sep 10;322[10]:977-9). Among unvaccinated women, the prevalence of nonvaccine- and vaccine-type oral HPV infections did not change between the two time periods.
“Notably, this only occurred in men,” Dr. Finch said. Herd immunity is being achieved in men “because we’re vaccinating all women, [but] we’re not seeing that herd immunity in women. Which begs the question: Why are we still vaccinating only half of our population?”
One study published in 2019 (Br J Dermatol. 2019 Nov;181[5]:1093-5) described a patient with CARD9 mutations, which predispose individuals to deep invasive infections – a disseminated Microsporum infection in this case, Dr. Finch said. “You shouldn’t see that,” he added, noting that these mutations are known to predispose individuals to severe Trichophyton infections and familial candidiasis.
“What I think is interesting about this is that, as we look forward to 2020, we’re going to increasingly see studies like this that are identifying specific mutations in our community that underlie a lot of these weird infections,” he added. “I wouldn’t be surprised if within the span of our careers, we find that a lot of those severe treatment-refractory reports that so commonly plague your everyday clinic have some underlying, specific immunity.”
Dr. Finch reported no relevant conflicts of interest.
ORLANDO – – leading into 2020, Justin Finch, MD, said at the ODAC Dermatology, Aesthetic, & Surgical Conference.
While group A streptococcus has declined over the past century, there has been “an unprecedented” resurgence in severe, invasive group A streptococcal infections and severe epidemics of scarlet fever worldwide, including in industrialized regions like the United Kingdom. Shedding some light on why this may be occurring, Dr. Finch referred to a recently published population-based molecular epidemiologic study identified a new dominant emm1UK lineage of Streptococcus pyogenes associated with such cases in England (Lancet Infect Dis. 2019 Nov;19(11):1209-18). This new lineage of S. pyogenes was genotypically distinct from other emm1 isolates and had greatly increased expression of the streptococcal pyrogenic exotoxin A, one of the exotoxins responsible for the clinical features of scarlet fever.
“We have not, to my knowledge, seen the strain yet in the United States,” said Dr. Finch, of Central Connecticut Dermatology in Cromwell. “Have it on your radar. With all of the worldwide travel patterns, I expect that you will see this in the United States at some point in the not-too-distant future.”
Also in 2019, promising data on the safety and effectiveness of the recombinant herpes zoster vaccine in immunocompromised patients became available for the first time. A randomized clinical trial published in JAMA of 1,846 patients who were immunosuppressed after autologous hematopoietic stem cell transplantation and received two doses of a recombinant zoster vaccine found that the patients had a reduced incidence of herpes zoster after a median follow-up of 21 months (JAMA. 2019 Jul 9;322[2]:123-33). The study found that the recombinant vaccine was both safe and effective in these immunocompromised patients, “so we can easily generalize this to our dermatology population as well,” Dr. Finch said. In comparing the live attenuated and recombinant vaccines, he noted the recombinant vaccine requires two doses but appears to be slightly more effective. “The number needed to treat to prevent [one case] of zoster is about half as high as that for the live vaccine, and most importantly for us is, it’s safe in immunocompromised patients.”
2019 also saw a record high in the number of measles cases in the United States, the highest since 1993, Dr. Finch pointed out. Most cases were seen in the area in and around New York City, but the percentage of people across the United States who are vaccinated against measles is below the threshold for herd immunity to protect immunocompromised patients. Measles requires a population vaccination rate of 94%, and less than half of U.S. counties in 2014 and 2015 reached that vaccination rate.
“Furthermore, if we look at that over the last 20 years, comparing the domestic measles cases to imported measles cases, we are increasingly breeding these measles epidemics right here at home, whereas they used to be imported from throughout the world,” said Dr. Finch. Patients with measles can be treated with vitamin A, he added, referring to a Cochrane review showing that 200,000 units of vitamin A given daily for 2 days decreased the mortality rate of measles by about 80%. Measles is on the Centers for Disease Control and Prevention’s list of reportable diseases, so should be reported to local health authorities, and will be followed up with confirmatory testing.
In 2019, a study examining herd protection of oral human papillomavirus infection in men and women compared the prevalence of oral HPV infection based on the 4 HPV types present in the quadrivalent HPV vaccine with 33 nonvaccine types from 2009 to 2016. There was no change in the prevalence of nonvaccine type oral HPV infections among men who were unvaccinated, but the prevalence of oral HPV infections because of the four strains in the quadrivalent HPV vaccine declined from 2.7% in 2009-2010 to 1.6% in 2015-2016 (JAMA. 2019 Sep 10;322[10]:977-9). Among unvaccinated women, the prevalence of nonvaccine- and vaccine-type oral HPV infections did not change between the two time periods.
“Notably, this only occurred in men,” Dr. Finch said. Herd immunity is being achieved in men “because we’re vaccinating all women, [but] we’re not seeing that herd immunity in women. Which begs the question: Why are we still vaccinating only half of our population?”
One study published in 2019 (Br J Dermatol. 2019 Nov;181[5]:1093-5) described a patient with CARD9 mutations, which predispose individuals to deep invasive infections – a disseminated Microsporum infection in this case, Dr. Finch said. “You shouldn’t see that,” he added, noting that these mutations are known to predispose individuals to severe Trichophyton infections and familial candidiasis.
“What I think is interesting about this is that, as we look forward to 2020, we’re going to increasingly see studies like this that are identifying specific mutations in our community that underlie a lot of these weird infections,” he added. “I wouldn’t be surprised if within the span of our careers, we find that a lot of those severe treatment-refractory reports that so commonly plague your everyday clinic have some underlying, specific immunity.”
Dr. Finch reported no relevant conflicts of interest.
REPORTING FROM ODAC 2020
FDA approves novel pandemic influenza vaccine
The Food and Drug Administration has approved the first and only adjuvanted, cell-based pandemic vaccine to provide active immunization against the influenza A virus H5N1 strain.
Influenza A (H5N1) monovalent vaccine, adjuvanted (Audenz, Seqirus) is for use in individuals aged 6 months and older. It’s designed to be rapidly deployed to help protect the U.S. population and can be stockpiled for first responders in the event of a pandemic.
The vaccine and formulated prefilled syringes used in the vaccine are produced in a state-of-the-art production facility built and supported through a multiyear public-private partnership between Seqirus and the Biomedical Advanced Research and Development Authority (BARDA), part of the Office of the Assistant Secretary for Preparedness and Response at the U.S. Department of Health & Human Services.
“Pandemic influenza viruses can be deadly and spread rapidly, making production of safe, effective vaccines essential in saving lives,” BARDA Director Rick Bright, PhD, said in a company news release.
“With this licensure – the latest FDA-approved vaccine to prevent H5N1 influenza — we celebrate a decade-long partnership to achieve health security goals set by the National Strategy for Pandemic Influenza and the 2019 Executive Order to speed the availability of influenza vaccine. Ultimately, this latest licensure means we can protect more people in an influenza pandemic,” said Bright.
“The approval of Audenz represents a key advance in influenza prevention and pandemic preparedness, combining leading-edge, cell-based manufacturing and adjuvant technologies,” Russell Basser, MD, chief scientist and senior vice president of research and development at Seqirus, said in the news release. “This pandemic influenza vaccine exemplifies our commitment to developing innovative technologies that can help provide rapid response during a pandemic emergency.”
Audenz had FDA fast track designation, a process designed to facilitate the development and expedite the review of drugs to treat serious conditions and fill an unmet medical need.
This article first appeared on Medscape.com.
The Food and Drug Administration has approved the first and only adjuvanted, cell-based pandemic vaccine to provide active immunization against the influenza A virus H5N1 strain.
Influenza A (H5N1) monovalent vaccine, adjuvanted (Audenz, Seqirus) is for use in individuals aged 6 months and older. It’s designed to be rapidly deployed to help protect the U.S. population and can be stockpiled for first responders in the event of a pandemic.
The vaccine and formulated prefilled syringes used in the vaccine are produced in a state-of-the-art production facility built and supported through a multiyear public-private partnership between Seqirus and the Biomedical Advanced Research and Development Authority (BARDA), part of the Office of the Assistant Secretary for Preparedness and Response at the U.S. Department of Health & Human Services.
“Pandemic influenza viruses can be deadly and spread rapidly, making production of safe, effective vaccines essential in saving lives,” BARDA Director Rick Bright, PhD, said in a company news release.
“With this licensure – the latest FDA-approved vaccine to prevent H5N1 influenza — we celebrate a decade-long partnership to achieve health security goals set by the National Strategy for Pandemic Influenza and the 2019 Executive Order to speed the availability of influenza vaccine. Ultimately, this latest licensure means we can protect more people in an influenza pandemic,” said Bright.
“The approval of Audenz represents a key advance in influenza prevention and pandemic preparedness, combining leading-edge, cell-based manufacturing and adjuvant technologies,” Russell Basser, MD, chief scientist and senior vice president of research and development at Seqirus, said in the news release. “This pandemic influenza vaccine exemplifies our commitment to developing innovative technologies that can help provide rapid response during a pandemic emergency.”
Audenz had FDA fast track designation, a process designed to facilitate the development and expedite the review of drugs to treat serious conditions and fill an unmet medical need.
This article first appeared on Medscape.com.
The Food and Drug Administration has approved the first and only adjuvanted, cell-based pandemic vaccine to provide active immunization against the influenza A virus H5N1 strain.
Influenza A (H5N1) monovalent vaccine, adjuvanted (Audenz, Seqirus) is for use in individuals aged 6 months and older. It’s designed to be rapidly deployed to help protect the U.S. population and can be stockpiled for first responders in the event of a pandemic.
The vaccine and formulated prefilled syringes used in the vaccine are produced in a state-of-the-art production facility built and supported through a multiyear public-private partnership between Seqirus and the Biomedical Advanced Research and Development Authority (BARDA), part of the Office of the Assistant Secretary for Preparedness and Response at the U.S. Department of Health & Human Services.
“Pandemic influenza viruses can be deadly and spread rapidly, making production of safe, effective vaccines essential in saving lives,” BARDA Director Rick Bright, PhD, said in a company news release.
“With this licensure – the latest FDA-approved vaccine to prevent H5N1 influenza — we celebrate a decade-long partnership to achieve health security goals set by the National Strategy for Pandemic Influenza and the 2019 Executive Order to speed the availability of influenza vaccine. Ultimately, this latest licensure means we can protect more people in an influenza pandemic,” said Bright.
“The approval of Audenz represents a key advance in influenza prevention and pandemic preparedness, combining leading-edge, cell-based manufacturing and adjuvant technologies,” Russell Basser, MD, chief scientist and senior vice president of research and development at Seqirus, said in the news release. “This pandemic influenza vaccine exemplifies our commitment to developing innovative technologies that can help provide rapid response during a pandemic emergency.”
Audenz had FDA fast track designation, a process designed to facilitate the development and expedite the review of drugs to treat serious conditions and fill an unmet medical need.
This article first appeared on Medscape.com.
ACIP updates recommendations for adult vaccines
The Centers for Disease Control and Prevention has released an updated schedule for adult vaccines. The update includes changes regarding the administration of several vaccines, including those for influenza, human papillomavirus (HPV), hepatitis A and B, and meningitis B, as well as the pneumococcal 13-valent conjugate (PCV13) vaccine.
The schedule, revised annually by the Advisory Committee on Immunization Practices (ACIP) of the CDC, was simultaneously published online February 3, 2020, in the Annals of Internal Medicine and on the CDC website.
Perhaps the change most likely to raise questions is that concerning the PCV13 vaccine. “Owing to a decline in prevalence of the types covered by the PCV13 vaccine, this is no longer routinely recommended for all persons age 65 and older,” senior author Mark Freedman, DVM, MPH, of the immunization services division at the National Center for Immunization and Respiratory Disease, said in an interview.
For purposes of shared clinical decision, however, it should be discussed with previously unvaccinated seniors who do not have risk factors, such as an immunocompromising condition, a cerebrospinal fluid leak, or a cochlear implant.
“But the circumstances for use of the vaccine are not always clear even based on the detailed list of considerations provided, because it’s impossible to think of every conceivable combination of risk factors,” Mr. Freedman added.
Possible beneficiaries of this vaccine are vulnerable elderly people living in nursing homes and long-term care facilities and those living in or traveling to settings in which the rate of pediatric PCV13 uptake is low or zero.
All adults in this age group should continue to receive a single dose of the pneumococcal 23-valent polysaccharide vaccine.*
HPV
The advisory committee now recommends catch-up immunization for women and men through age 26 years (the previous cutoff for men was 21). And in another new recommendation, the ACIP advises considering vaccination for some patients aged 27-45 years who have not been adequately vaccinated.
“Most people ages 27-45 do not need vaccination, but some may benefit,” Mr. Freedman said. “For example, somebody who’s been in a prior long-term monogamous relationship and suddenly finds himself with a new sexual partner.”
“That makes very good sense for older people who haven’t been vaccinated and might continue to be exposed to HPV,” Daniel M. Musher, MD, a professor of medicine at Baylor College of Medicine and an infectious diseases physician at the Michael E. DeBakey Veterans Affairs Medical Center, both in Houston, said in an interview.
Here again, the ACIP advises taking a shared decision-making approach, with clinicians discussing the merits of vaccination in this and other scenarios with patients according to the talking points outlined in the HPV section.
Influenza, hepatitis A and B
For the 2019-2020 influenza season, routine influenza vaccination is recommended for all persons aged 6 months or older who have no contraindications. Where more than one appropriate option is available, the ACIP does not recommend any product over another.
Routine hepatitis A vaccination is recommended for all persons aged 1 year or older who have HIV infection regardless of their level of immune suppression.
For hepatitis B, a new addition to the list of vulnerable patients who may possibly benefit from vaccination is pregnant women at risk for infection or an adverse infection-related pregnancy outcome. Whereas older formulations are safe, the ACIP does not recommend the HepB-CpG (Heplisav-B) vaccine during pregnancy, owing to the fact that safety data are lacking.
Meningitis B
Individuals aged 10 years or older who have complement deficiency, who use a complement inhibitor, who have asplenia, or who are microbiologists should receive a meningitis B booster dose 1 year following completion of a primary series. After that, they should receive booster doses every 2-3 years for as long they are at elevated risk.
Vaccination should be discussed with individuals aged 16-23 years even if they are not at increased risk for meningococcal disease. Persons aged 10 years or older whom public health authorities deem to be at increased risk during an outbreak should have a one-time booster dose if at least 1 year has elapsed since completion of a meningitis B primary series.
Td/Tdap, varicella
The ACIP now recommends that either the Td or Tdap vaccine be given in cases in which currently just the Td vaccine is recommended; that is, for the 10-year booster shot as well as for tetanus prophylaxis in wound management and the catch-up immunization schedule, including that for pregnant women.
Vaccination against varicella should be considered for HIV-infected individuals who are without evidence of varicella immunity and whose CD4 counts are at least 200 cells/mL.
Dr. Musher, who was not involved in drafting the recommendations, takes issue generally with the addition of shared clinical decision making on vaccination. “Shared decision making is a problem for anyone practicing medicine. It places a terrible burden [on] the doctors to discuss these options with patients at great length. Most patients want the doctor to make the decision.”
In his view, this approach makes little sense in the case of the PCV13 vaccine because the strains it covers have disappeared from the population through the widespread vaccination of children. “But discussions are important for some vaccines, such as the herpes zoster vaccine, since patients can have a terrible reaction to the first dose and refuse to have the second,” he said.
Some of these new recommendations were released in 2019 after ACIP members met to vote on them in February, June, and October.
As in previous years, the schedule has been streamlined for easier reference. Physicians are reminded to closely read the details in the vaccine notes, as these specify who needs what vaccine, when, and at what dose.
The ACIP develops its recommendations after reviewing vaccine-related data, including the data regarding the epidemiology and burden of the vaccine-preventable disease, vaccine effectiveness and safety, the quality of evidence, implementability, and the economics of immunization policy.
The authors have received grants and expense payments from public and not-for-profit institutions. One coauthor has received fees from ACI Clinical for data and safety monitoring in an immunization trial. Dr. Musher has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Correction, 3/31/20: An earlier version of this article misstated the recommendation for administration of the pneumococcal 23-valent polysaccharide vaccine. All adults in this age group should continue to receive a single dose of this vaccine.
The Centers for Disease Control and Prevention has released an updated schedule for adult vaccines. The update includes changes regarding the administration of several vaccines, including those for influenza, human papillomavirus (HPV), hepatitis A and B, and meningitis B, as well as the pneumococcal 13-valent conjugate (PCV13) vaccine.
The schedule, revised annually by the Advisory Committee on Immunization Practices (ACIP) of the CDC, was simultaneously published online February 3, 2020, in the Annals of Internal Medicine and on the CDC website.
Perhaps the change most likely to raise questions is that concerning the PCV13 vaccine. “Owing to a decline in prevalence of the types covered by the PCV13 vaccine, this is no longer routinely recommended for all persons age 65 and older,” senior author Mark Freedman, DVM, MPH, of the immunization services division at the National Center for Immunization and Respiratory Disease, said in an interview.
For purposes of shared clinical decision, however, it should be discussed with previously unvaccinated seniors who do not have risk factors, such as an immunocompromising condition, a cerebrospinal fluid leak, or a cochlear implant.
“But the circumstances for use of the vaccine are not always clear even based on the detailed list of considerations provided, because it’s impossible to think of every conceivable combination of risk factors,” Mr. Freedman added.
Possible beneficiaries of this vaccine are vulnerable elderly people living in nursing homes and long-term care facilities and those living in or traveling to settings in which the rate of pediatric PCV13 uptake is low or zero.
All adults in this age group should continue to receive a single dose of the pneumococcal 23-valent polysaccharide vaccine.*
HPV
The advisory committee now recommends catch-up immunization for women and men through age 26 years (the previous cutoff for men was 21). And in another new recommendation, the ACIP advises considering vaccination for some patients aged 27-45 years who have not been adequately vaccinated.
“Most people ages 27-45 do not need vaccination, but some may benefit,” Mr. Freedman said. “For example, somebody who’s been in a prior long-term monogamous relationship and suddenly finds himself with a new sexual partner.”
“That makes very good sense for older people who haven’t been vaccinated and might continue to be exposed to HPV,” Daniel M. Musher, MD, a professor of medicine at Baylor College of Medicine and an infectious diseases physician at the Michael E. DeBakey Veterans Affairs Medical Center, both in Houston, said in an interview.
Here again, the ACIP advises taking a shared decision-making approach, with clinicians discussing the merits of vaccination in this and other scenarios with patients according to the talking points outlined in the HPV section.
Influenza, hepatitis A and B
For the 2019-2020 influenza season, routine influenza vaccination is recommended for all persons aged 6 months or older who have no contraindications. Where more than one appropriate option is available, the ACIP does not recommend any product over another.
Routine hepatitis A vaccination is recommended for all persons aged 1 year or older who have HIV infection regardless of their level of immune suppression.
For hepatitis B, a new addition to the list of vulnerable patients who may possibly benefit from vaccination is pregnant women at risk for infection or an adverse infection-related pregnancy outcome. Whereas older formulations are safe, the ACIP does not recommend the HepB-CpG (Heplisav-B) vaccine during pregnancy, owing to the fact that safety data are lacking.
Meningitis B
Individuals aged 10 years or older who have complement deficiency, who use a complement inhibitor, who have asplenia, or who are microbiologists should receive a meningitis B booster dose 1 year following completion of a primary series. After that, they should receive booster doses every 2-3 years for as long they are at elevated risk.
Vaccination should be discussed with individuals aged 16-23 years even if they are not at increased risk for meningococcal disease. Persons aged 10 years or older whom public health authorities deem to be at increased risk during an outbreak should have a one-time booster dose if at least 1 year has elapsed since completion of a meningitis B primary series.
Td/Tdap, varicella
The ACIP now recommends that either the Td or Tdap vaccine be given in cases in which currently just the Td vaccine is recommended; that is, for the 10-year booster shot as well as for tetanus prophylaxis in wound management and the catch-up immunization schedule, including that for pregnant women.
Vaccination against varicella should be considered for HIV-infected individuals who are without evidence of varicella immunity and whose CD4 counts are at least 200 cells/mL.
Dr. Musher, who was not involved in drafting the recommendations, takes issue generally with the addition of shared clinical decision making on vaccination. “Shared decision making is a problem for anyone practicing medicine. It places a terrible burden [on] the doctors to discuss these options with patients at great length. Most patients want the doctor to make the decision.”
In his view, this approach makes little sense in the case of the PCV13 vaccine because the strains it covers have disappeared from the population through the widespread vaccination of children. “But discussions are important for some vaccines, such as the herpes zoster vaccine, since patients can have a terrible reaction to the first dose and refuse to have the second,” he said.
Some of these new recommendations were released in 2019 after ACIP members met to vote on them in February, June, and October.
As in previous years, the schedule has been streamlined for easier reference. Physicians are reminded to closely read the details in the vaccine notes, as these specify who needs what vaccine, when, and at what dose.
The ACIP develops its recommendations after reviewing vaccine-related data, including the data regarding the epidemiology and burden of the vaccine-preventable disease, vaccine effectiveness and safety, the quality of evidence, implementability, and the economics of immunization policy.
The authors have received grants and expense payments from public and not-for-profit institutions. One coauthor has received fees from ACI Clinical for data and safety monitoring in an immunization trial. Dr. Musher has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Correction, 3/31/20: An earlier version of this article misstated the recommendation for administration of the pneumococcal 23-valent polysaccharide vaccine. All adults in this age group should continue to receive a single dose of this vaccine.
The Centers for Disease Control and Prevention has released an updated schedule for adult vaccines. The update includes changes regarding the administration of several vaccines, including those for influenza, human papillomavirus (HPV), hepatitis A and B, and meningitis B, as well as the pneumococcal 13-valent conjugate (PCV13) vaccine.
The schedule, revised annually by the Advisory Committee on Immunization Practices (ACIP) of the CDC, was simultaneously published online February 3, 2020, in the Annals of Internal Medicine and on the CDC website.
Perhaps the change most likely to raise questions is that concerning the PCV13 vaccine. “Owing to a decline in prevalence of the types covered by the PCV13 vaccine, this is no longer routinely recommended for all persons age 65 and older,” senior author Mark Freedman, DVM, MPH, of the immunization services division at the National Center for Immunization and Respiratory Disease, said in an interview.
For purposes of shared clinical decision, however, it should be discussed with previously unvaccinated seniors who do not have risk factors, such as an immunocompromising condition, a cerebrospinal fluid leak, or a cochlear implant.
“But the circumstances for use of the vaccine are not always clear even based on the detailed list of considerations provided, because it’s impossible to think of every conceivable combination of risk factors,” Mr. Freedman added.
Possible beneficiaries of this vaccine are vulnerable elderly people living in nursing homes and long-term care facilities and those living in or traveling to settings in which the rate of pediatric PCV13 uptake is low or zero.
All adults in this age group should continue to receive a single dose of the pneumococcal 23-valent polysaccharide vaccine.*
HPV
The advisory committee now recommends catch-up immunization for women and men through age 26 years (the previous cutoff for men was 21). And in another new recommendation, the ACIP advises considering vaccination for some patients aged 27-45 years who have not been adequately vaccinated.
“Most people ages 27-45 do not need vaccination, but some may benefit,” Mr. Freedman said. “For example, somebody who’s been in a prior long-term monogamous relationship and suddenly finds himself with a new sexual partner.”
“That makes very good sense for older people who haven’t been vaccinated and might continue to be exposed to HPV,” Daniel M. Musher, MD, a professor of medicine at Baylor College of Medicine and an infectious diseases physician at the Michael E. DeBakey Veterans Affairs Medical Center, both in Houston, said in an interview.
Here again, the ACIP advises taking a shared decision-making approach, with clinicians discussing the merits of vaccination in this and other scenarios with patients according to the talking points outlined in the HPV section.
Influenza, hepatitis A and B
For the 2019-2020 influenza season, routine influenza vaccination is recommended for all persons aged 6 months or older who have no contraindications. Where more than one appropriate option is available, the ACIP does not recommend any product over another.
Routine hepatitis A vaccination is recommended for all persons aged 1 year or older who have HIV infection regardless of their level of immune suppression.
For hepatitis B, a new addition to the list of vulnerable patients who may possibly benefit from vaccination is pregnant women at risk for infection or an adverse infection-related pregnancy outcome. Whereas older formulations are safe, the ACIP does not recommend the HepB-CpG (Heplisav-B) vaccine during pregnancy, owing to the fact that safety data are lacking.
Meningitis B
Individuals aged 10 years or older who have complement deficiency, who use a complement inhibitor, who have asplenia, or who are microbiologists should receive a meningitis B booster dose 1 year following completion of a primary series. After that, they should receive booster doses every 2-3 years for as long they are at elevated risk.
Vaccination should be discussed with individuals aged 16-23 years even if they are not at increased risk for meningococcal disease. Persons aged 10 years or older whom public health authorities deem to be at increased risk during an outbreak should have a one-time booster dose if at least 1 year has elapsed since completion of a meningitis B primary series.
Td/Tdap, varicella
The ACIP now recommends that either the Td or Tdap vaccine be given in cases in which currently just the Td vaccine is recommended; that is, for the 10-year booster shot as well as for tetanus prophylaxis in wound management and the catch-up immunization schedule, including that for pregnant women.
Vaccination against varicella should be considered for HIV-infected individuals who are without evidence of varicella immunity and whose CD4 counts are at least 200 cells/mL.
Dr. Musher, who was not involved in drafting the recommendations, takes issue generally with the addition of shared clinical decision making on vaccination. “Shared decision making is a problem for anyone practicing medicine. It places a terrible burden [on] the doctors to discuss these options with patients at great length. Most patients want the doctor to make the decision.”
In his view, this approach makes little sense in the case of the PCV13 vaccine because the strains it covers have disappeared from the population through the widespread vaccination of children. “But discussions are important for some vaccines, such as the herpes zoster vaccine, since patients can have a terrible reaction to the first dose and refuse to have the second,” he said.
Some of these new recommendations were released in 2019 after ACIP members met to vote on them in February, June, and October.
As in previous years, the schedule has been streamlined for easier reference. Physicians are reminded to closely read the details in the vaccine notes, as these specify who needs what vaccine, when, and at what dose.
The ACIP develops its recommendations after reviewing vaccine-related data, including the data regarding the epidemiology and burden of the vaccine-preventable disease, vaccine effectiveness and safety, the quality of evidence, implementability, and the economics of immunization policy.
The authors have received grants and expense payments from public and not-for-profit institutions. One coauthor has received fees from ACI Clinical for data and safety monitoring in an immunization trial. Dr. Musher has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Correction, 3/31/20: An earlier version of this article misstated the recommendation for administration of the pneumococcal 23-valent polysaccharide vaccine. All adults in this age group should continue to receive a single dose of this vaccine.
56-year-old woman • worsening pain in left upper arm • influenza vaccination in the arm a few days prior to pain onset • Dx?
THE CASE
A 56-year-old woman presented with a 3-day complaint of worsening left upper arm pain. She denied having any specific initiating factors but reported receiving an influenza vaccination in the arm a few days prior to the onset of pain. The patient did not have any associated numbness or tingling in the arm. She reported that the pain was worse with movement—especially abduction. The patient reported taking an over-the-counter nonsteroidal anti-inflammatory drug (NSAID) without much relief.
On physical examination, the patient had difficulty with active range of motion and had erythema, swelling, and tenderness to palpation along the subacromial space and the proximal deltoid. Further examination of the shoulder revealed a positive Neer Impingement Test and a positive Hawkins–Kennedy Test. (For more on these tests, visit “MSK Clinic: Evaluating shoulder pain using IPASS.”). The patient demonstrated full passive range of motion, but her pain was exacerbated with abduction.
THE DIAGNOSIS
In light of the soft-tissue findings and the absence of trauma, magnetic resonance imaging (MRI), rather than an x-ray, of the upper extremity was ordered. Imaging revealed subacromial subdeltoid bursal inflammation (FIGURE).
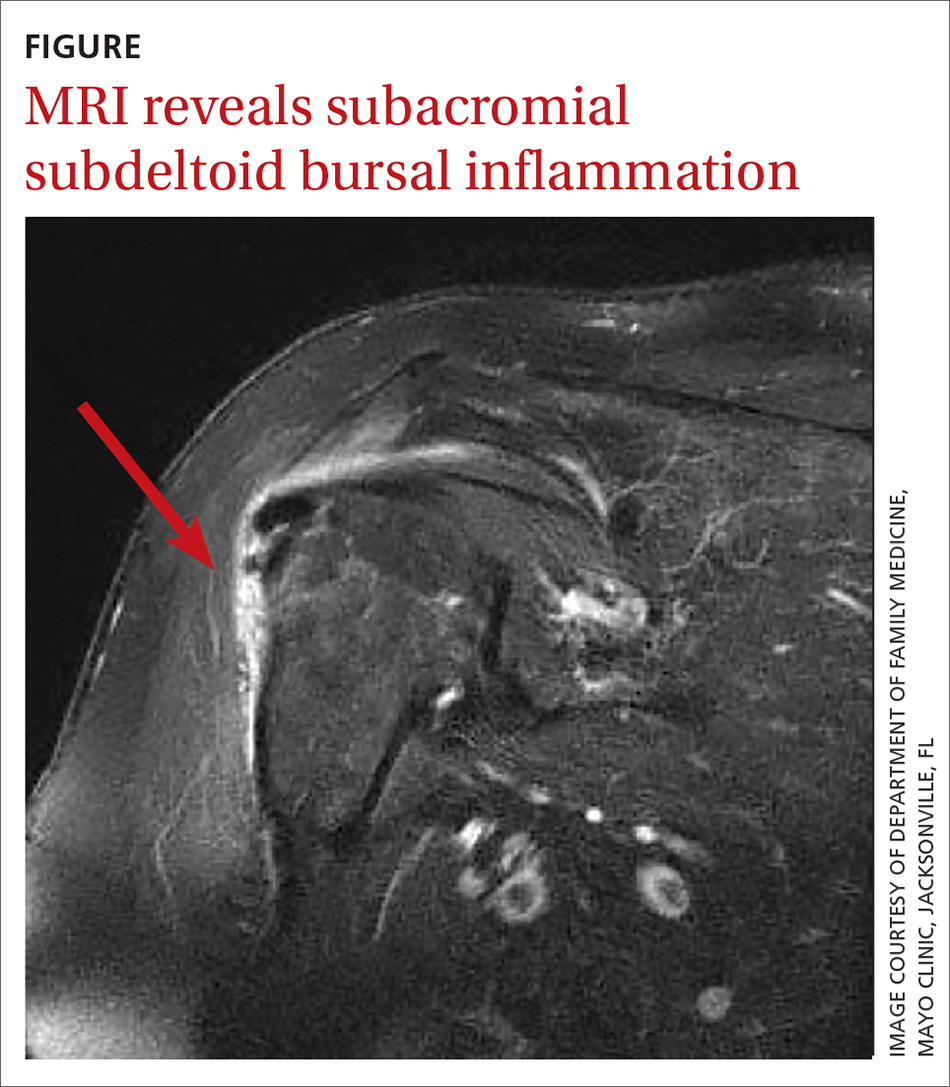
DISCUSSION
Shoulder injury related to vaccine administration (SIRVA) is the result of accidental injection of a vaccine into the tissue lying underneath the deltoid muscle or joint space, leading to a suspected immune-mediated inflammatory reaction.
A report from the National Vaccine Advisory Committee of the US Department of Health & Human Services showed an increase in the number of reported cases of SIRVA (59 reported cases in 2011-2014 and 202 cases reported in 2016).1 Additionally, in 2016 more than $29 million was awarded in compensation to patients with SIRVA.1,2 In a 2011 report, an Institute of Medicine committee found convincing evidence of a causal relationship between injection of vaccine, independent of the antigen involved, and deltoid bursitis, or frozen shoulder, characterized by shoulder pain and loss of motion.3
A review of 13 cases revealed that 50% of the patients reported pain immediately after the injection and 90% had developed pain within 24 hours.2 On physical exam, a limited range of motion and pain were the most common findings, while weakness and sensory changes were uncommon. In some cases, the pain lasted several years and 30% of the patients required surgery. Forty-six percent of the patients reported apprehension concerning the administration of the vaccine, specifically that the injection was administered “too high” into the deltoid.2
In the review of cases, routine x-rays of the shoulder did not provide beneficial diagnostic information; however, when an MRI was performed, it revealed fluid collections in the deep deltoid or overlying the rotator cuff tendons; bursitis; tendonitis; and rotator cuff tears.2
Continue to: Management of SIRVA
Management of SIRVA
Management of SIRVA is similar to that of other shoulder injuries. Treatment may include icing the shoulder, NSAIDs, intra-articular steroid injections, and physical therapy. If conservative management does not resolve the patient’s pain and improve function, then a consult with an orthopedic surgeon is recommended to determine if surgical intervention is required.
Another case report from Japan reported that a 45-year-old woman developed acute pain following a third injection of Cervarix, the prophylactic human papillomavirus-16/18 vaccine. An x-ray was ordered and was normal, but an MRI revealed acute subacromial bursitis. In an attempt to relieve the pain and improve her mobility, multiple cortisone injections were administered and physical therapy was performed. Despite the conservative treatment efforts, she continued to have pain and limited mobility in the shoulder 6 months following the onset of symptoms. As a result, the patient underwent arthroscopic synovectomy and subacromial decompression. One week following the surgery, the patient’s pain improved and at 1 year she had no pain and full range of motion.4
Prevention of SIRVA
By using appropriate techniques when administering intramuscular vaccinations, SIRVA can be prevented. The manufacturer recommended route of administration is based on studies showing maximum safety and immunogenicity, and should therefore be followed by the individual administering the vaccine.5 The Centers for Disease Control and Prevention recommends using a 22- to 25-gauge needle that is long enough to reach into the muscle and may range from ⅝" to 1½" depending on the patient’s weight.6 The vaccine should be injected at a 90° angle into the central and thickest portion of the deltoid muscle, about 2" below the acromion process and above the level of the axilla.5
Our patient’s outcome. The patient’s symptoms resolved within 10 days of receiving a steroid injection into the subacromial space. Although this case was the result of the influenza vaccine, any intramuscularly injected vaccine could lead to SIRVA.
THE TAKEAWAY
Inappropriate administration of routine intramuscularly injected vaccinations can lead to significant patient harm, including pain and disability. It is important for physicians to be aware of SIRVA and to be able to identify the signs and symptoms. Although an MRI of the shoulder is helpful in confirming the diagnosis, it is not necessary if the physician takes a thorough history and performs a comprehensive shoulder exam. Routine x-rays do not provide any beneficial clinical information.
CORRESPONDENCE
Bryan Farford, DO, Department of Family Medicine, Mayo Clinic, Davis Building, 4500 San Pablo Road South #358, Jacksonville, FL 32224; [email protected]
1. Nair N. Update on SIRVA National Vaccine Advisory Committee. U.S. Department of Health & Human Services. Health Resources and Services Administration (HRSA). www.hhs.gov/sites/default/files/Nair_Special%20Highlight_SIRVA%20remediated.pdf. Accessed January 14, 2020.
2. Atanasoff S, Ryan T, Lightfoot R, et al. Shoulder injury related to vaccine administration (SIRVA). Vaccine. 2010;28:8049-8052.
3. Institute of Medicine of the National Academies. Adverse Effects of Vaccines: Evidence and Causality. Washington DC: The National Academies Press; 2011.
4. Uchida S, Sakai A, Nakamura T. Subacromial bursitis following human papilloma virus vaccine misinjection. Vaccine. 2012;31:27-30.
5. Meissner HC. Shoulder injury related to vaccine administration reported more frequently. AAP News. September 1, 2017. www.aappublications.org/news/2017/09/01/IDSnapshot082917. Accessed January 14, 2020.
6. Immunization Action Coalition. How to administer intramuscular and subcutaneous vaccine injections to adults. https://www.immunize.org/catg.d/p2020a.pdf. Accessed January 14, 2020.
THE CASE
A 56-year-old woman presented with a 3-day complaint of worsening left upper arm pain. She denied having any specific initiating factors but reported receiving an influenza vaccination in the arm a few days prior to the onset of pain. The patient did not have any associated numbness or tingling in the arm. She reported that the pain was worse with movement—especially abduction. The patient reported taking an over-the-counter nonsteroidal anti-inflammatory drug (NSAID) without much relief.
On physical examination, the patient had difficulty with active range of motion and had erythema, swelling, and tenderness to palpation along the subacromial space and the proximal deltoid. Further examination of the shoulder revealed a positive Neer Impingement Test and a positive Hawkins–Kennedy Test. (For more on these tests, visit “MSK Clinic: Evaluating shoulder pain using IPASS.”). The patient demonstrated full passive range of motion, but her pain was exacerbated with abduction.
THE DIAGNOSIS
In light of the soft-tissue findings and the absence of trauma, magnetic resonance imaging (MRI), rather than an x-ray, of the upper extremity was ordered. Imaging revealed subacromial subdeltoid bursal inflammation (FIGURE).
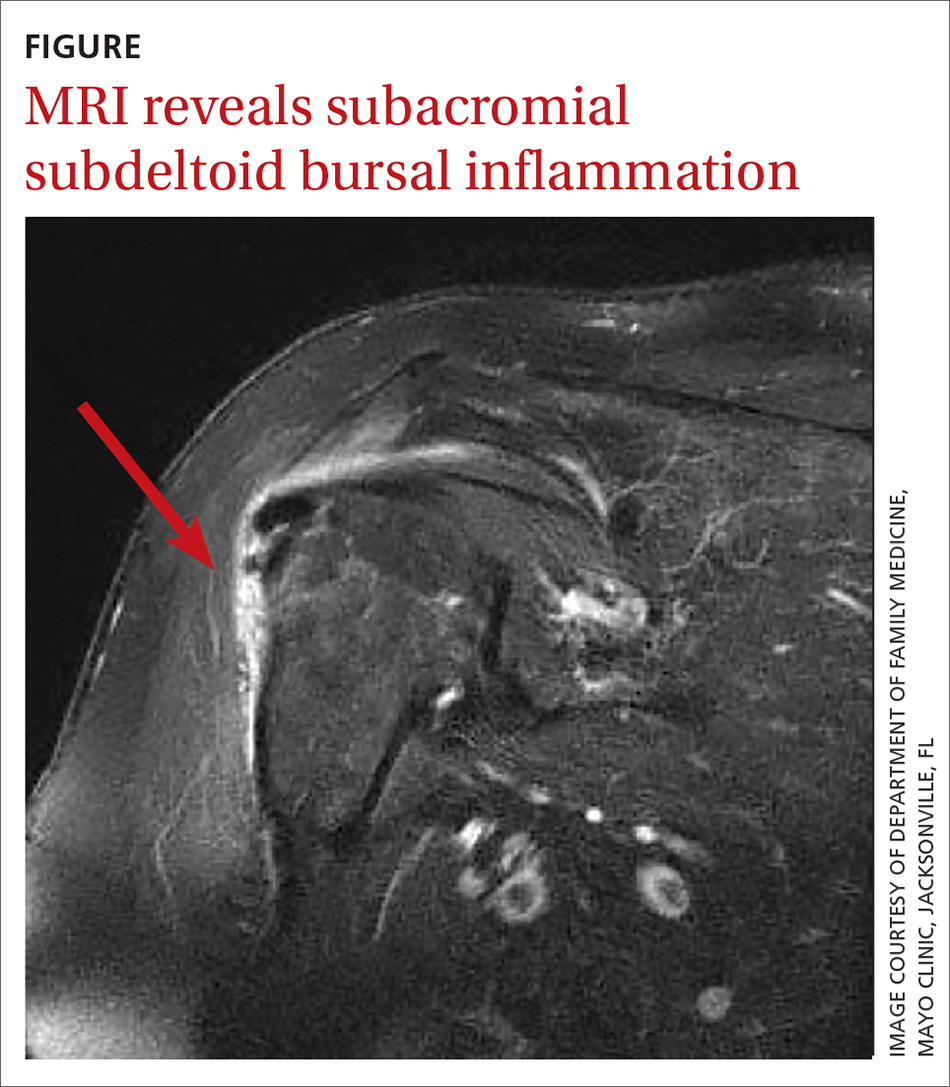
DISCUSSION
Shoulder injury related to vaccine administration (SIRVA) is the result of accidental injection of a vaccine into the tissue lying underneath the deltoid muscle or joint space, leading to a suspected immune-mediated inflammatory reaction.
A report from the National Vaccine Advisory Committee of the US Department of Health & Human Services showed an increase in the number of reported cases of SIRVA (59 reported cases in 2011-2014 and 202 cases reported in 2016).1 Additionally, in 2016 more than $29 million was awarded in compensation to patients with SIRVA.1,2 In a 2011 report, an Institute of Medicine committee found convincing evidence of a causal relationship between injection of vaccine, independent of the antigen involved, and deltoid bursitis, or frozen shoulder, characterized by shoulder pain and loss of motion.3
A review of 13 cases revealed that 50% of the patients reported pain immediately after the injection and 90% had developed pain within 24 hours.2 On physical exam, a limited range of motion and pain were the most common findings, while weakness and sensory changes were uncommon. In some cases, the pain lasted several years and 30% of the patients required surgery. Forty-six percent of the patients reported apprehension concerning the administration of the vaccine, specifically that the injection was administered “too high” into the deltoid.2
In the review of cases, routine x-rays of the shoulder did not provide beneficial diagnostic information; however, when an MRI was performed, it revealed fluid collections in the deep deltoid or overlying the rotator cuff tendons; bursitis; tendonitis; and rotator cuff tears.2
Continue to: Management of SIRVA
Management of SIRVA
Management of SIRVA is similar to that of other shoulder injuries. Treatment may include icing the shoulder, NSAIDs, intra-articular steroid injections, and physical therapy. If conservative management does not resolve the patient’s pain and improve function, then a consult with an orthopedic surgeon is recommended to determine if surgical intervention is required.
Another case report from Japan reported that a 45-year-old woman developed acute pain following a third injection of Cervarix, the prophylactic human papillomavirus-16/18 vaccine. An x-ray was ordered and was normal, but an MRI revealed acute subacromial bursitis. In an attempt to relieve the pain and improve her mobility, multiple cortisone injections were administered and physical therapy was performed. Despite the conservative treatment efforts, she continued to have pain and limited mobility in the shoulder 6 months following the onset of symptoms. As a result, the patient underwent arthroscopic synovectomy and subacromial decompression. One week following the surgery, the patient’s pain improved and at 1 year she had no pain and full range of motion.4
Prevention of SIRVA
By using appropriate techniques when administering intramuscular vaccinations, SIRVA can be prevented. The manufacturer recommended route of administration is based on studies showing maximum safety and immunogenicity, and should therefore be followed by the individual administering the vaccine.5 The Centers for Disease Control and Prevention recommends using a 22- to 25-gauge needle that is long enough to reach into the muscle and may range from ⅝" to 1½" depending on the patient’s weight.6 The vaccine should be injected at a 90° angle into the central and thickest portion of the deltoid muscle, about 2" below the acromion process and above the level of the axilla.5
Our patient’s outcome. The patient’s symptoms resolved within 10 days of receiving a steroid injection into the subacromial space. Although this case was the result of the influenza vaccine, any intramuscularly injected vaccine could lead to SIRVA.
THE TAKEAWAY
Inappropriate administration of routine intramuscularly injected vaccinations can lead to significant patient harm, including pain and disability. It is important for physicians to be aware of SIRVA and to be able to identify the signs and symptoms. Although an MRI of the shoulder is helpful in confirming the diagnosis, it is not necessary if the physician takes a thorough history and performs a comprehensive shoulder exam. Routine x-rays do not provide any beneficial clinical information.
CORRESPONDENCE
Bryan Farford, DO, Department of Family Medicine, Mayo Clinic, Davis Building, 4500 San Pablo Road South #358, Jacksonville, FL 32224; [email protected]
THE CASE
A 56-year-old woman presented with a 3-day complaint of worsening left upper arm pain. She denied having any specific initiating factors but reported receiving an influenza vaccination in the arm a few days prior to the onset of pain. The patient did not have any associated numbness or tingling in the arm. She reported that the pain was worse with movement—especially abduction. The patient reported taking an over-the-counter nonsteroidal anti-inflammatory drug (NSAID) without much relief.
On physical examination, the patient had difficulty with active range of motion and had erythema, swelling, and tenderness to palpation along the subacromial space and the proximal deltoid. Further examination of the shoulder revealed a positive Neer Impingement Test and a positive Hawkins–Kennedy Test. (For more on these tests, visit “MSK Clinic: Evaluating shoulder pain using IPASS.”). The patient demonstrated full passive range of motion, but her pain was exacerbated with abduction.
THE DIAGNOSIS
In light of the soft-tissue findings and the absence of trauma, magnetic resonance imaging (MRI), rather than an x-ray, of the upper extremity was ordered. Imaging revealed subacromial subdeltoid bursal inflammation (FIGURE).
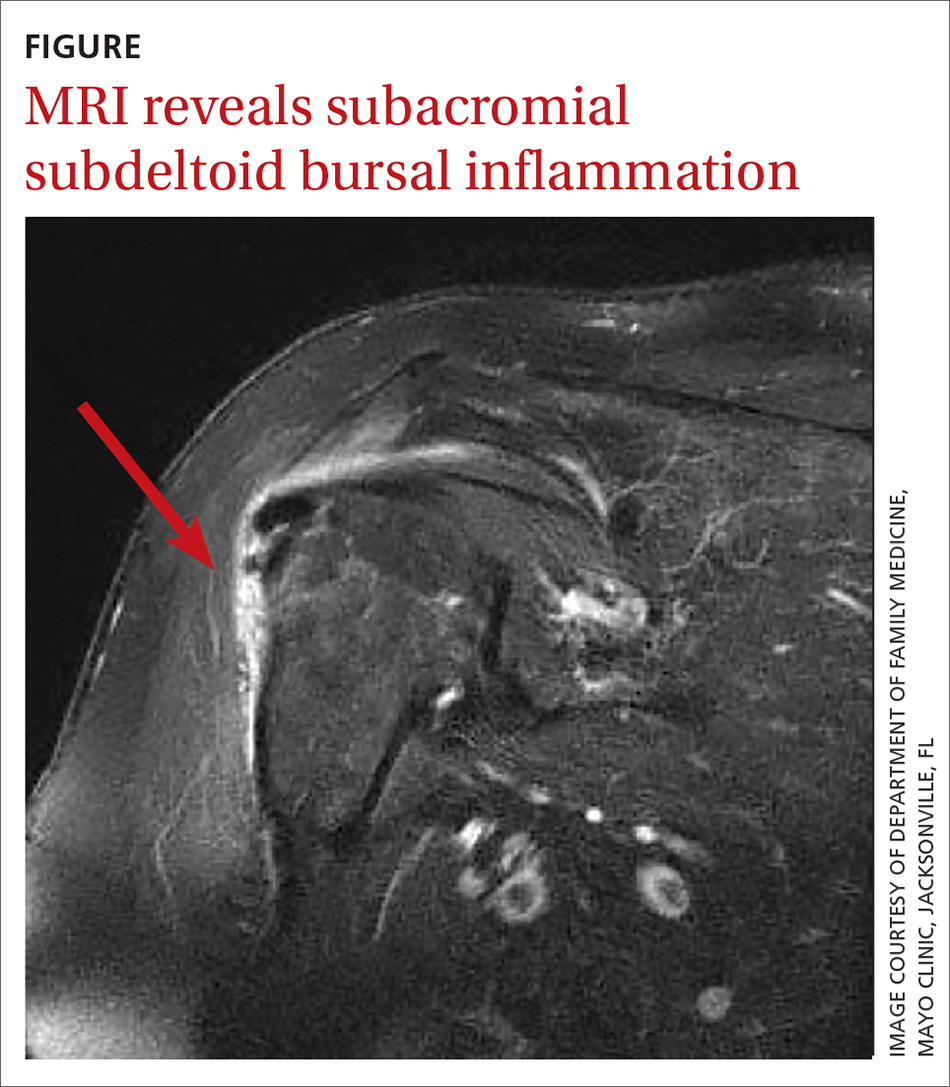
DISCUSSION
Shoulder injury related to vaccine administration (SIRVA) is the result of accidental injection of a vaccine into the tissue lying underneath the deltoid muscle or joint space, leading to a suspected immune-mediated inflammatory reaction.
A report from the National Vaccine Advisory Committee of the US Department of Health & Human Services showed an increase in the number of reported cases of SIRVA (59 reported cases in 2011-2014 and 202 cases reported in 2016).1 Additionally, in 2016 more than $29 million was awarded in compensation to patients with SIRVA.1,2 In a 2011 report, an Institute of Medicine committee found convincing evidence of a causal relationship between injection of vaccine, independent of the antigen involved, and deltoid bursitis, or frozen shoulder, characterized by shoulder pain and loss of motion.3
A review of 13 cases revealed that 50% of the patients reported pain immediately after the injection and 90% had developed pain within 24 hours.2 On physical exam, a limited range of motion and pain were the most common findings, while weakness and sensory changes were uncommon. In some cases, the pain lasted several years and 30% of the patients required surgery. Forty-six percent of the patients reported apprehension concerning the administration of the vaccine, specifically that the injection was administered “too high” into the deltoid.2
In the review of cases, routine x-rays of the shoulder did not provide beneficial diagnostic information; however, when an MRI was performed, it revealed fluid collections in the deep deltoid or overlying the rotator cuff tendons; bursitis; tendonitis; and rotator cuff tears.2
Continue to: Management of SIRVA
Management of SIRVA
Management of SIRVA is similar to that of other shoulder injuries. Treatment may include icing the shoulder, NSAIDs, intra-articular steroid injections, and physical therapy. If conservative management does not resolve the patient’s pain and improve function, then a consult with an orthopedic surgeon is recommended to determine if surgical intervention is required.
Another case report from Japan reported that a 45-year-old woman developed acute pain following a third injection of Cervarix, the prophylactic human papillomavirus-16/18 vaccine. An x-ray was ordered and was normal, but an MRI revealed acute subacromial bursitis. In an attempt to relieve the pain and improve her mobility, multiple cortisone injections were administered and physical therapy was performed. Despite the conservative treatment efforts, she continued to have pain and limited mobility in the shoulder 6 months following the onset of symptoms. As a result, the patient underwent arthroscopic synovectomy and subacromial decompression. One week following the surgery, the patient’s pain improved and at 1 year she had no pain and full range of motion.4
Prevention of SIRVA
By using appropriate techniques when administering intramuscular vaccinations, SIRVA can be prevented. The manufacturer recommended route of administration is based on studies showing maximum safety and immunogenicity, and should therefore be followed by the individual administering the vaccine.5 The Centers for Disease Control and Prevention recommends using a 22- to 25-gauge needle that is long enough to reach into the muscle and may range from ⅝" to 1½" depending on the patient’s weight.6 The vaccine should be injected at a 90° angle into the central and thickest portion of the deltoid muscle, about 2" below the acromion process and above the level of the axilla.5
Our patient’s outcome. The patient’s symptoms resolved within 10 days of receiving a steroid injection into the subacromial space. Although this case was the result of the influenza vaccine, any intramuscularly injected vaccine could lead to SIRVA.
THE TAKEAWAY
Inappropriate administration of routine intramuscularly injected vaccinations can lead to significant patient harm, including pain and disability. It is important for physicians to be aware of SIRVA and to be able to identify the signs and symptoms. Although an MRI of the shoulder is helpful in confirming the diagnosis, it is not necessary if the physician takes a thorough history and performs a comprehensive shoulder exam. Routine x-rays do not provide any beneficial clinical information.
CORRESPONDENCE
Bryan Farford, DO, Department of Family Medicine, Mayo Clinic, Davis Building, 4500 San Pablo Road South #358, Jacksonville, FL 32224; [email protected]
1. Nair N. Update on SIRVA National Vaccine Advisory Committee. U.S. Department of Health & Human Services. Health Resources and Services Administration (HRSA). www.hhs.gov/sites/default/files/Nair_Special%20Highlight_SIRVA%20remediated.pdf. Accessed January 14, 2020.
2. Atanasoff S, Ryan T, Lightfoot R, et al. Shoulder injury related to vaccine administration (SIRVA). Vaccine. 2010;28:8049-8052.
3. Institute of Medicine of the National Academies. Adverse Effects of Vaccines: Evidence and Causality. Washington DC: The National Academies Press; 2011.
4. Uchida S, Sakai A, Nakamura T. Subacromial bursitis following human papilloma virus vaccine misinjection. Vaccine. 2012;31:27-30.
5. Meissner HC. Shoulder injury related to vaccine administration reported more frequently. AAP News. September 1, 2017. www.aappublications.org/news/2017/09/01/IDSnapshot082917. Accessed January 14, 2020.
6. Immunization Action Coalition. How to administer intramuscular and subcutaneous vaccine injections to adults. https://www.immunize.org/catg.d/p2020a.pdf. Accessed January 14, 2020.
1. Nair N. Update on SIRVA National Vaccine Advisory Committee. U.S. Department of Health & Human Services. Health Resources and Services Administration (HRSA). www.hhs.gov/sites/default/files/Nair_Special%20Highlight_SIRVA%20remediated.pdf. Accessed January 14, 2020.
2. Atanasoff S, Ryan T, Lightfoot R, et al. Shoulder injury related to vaccine administration (SIRVA). Vaccine. 2010;28:8049-8052.
3. Institute of Medicine of the National Academies. Adverse Effects of Vaccines: Evidence and Causality. Washington DC: The National Academies Press; 2011.
4. Uchida S, Sakai A, Nakamura T. Subacromial bursitis following human papilloma virus vaccine misinjection. Vaccine. 2012;31:27-30.
5. Meissner HC. Shoulder injury related to vaccine administration reported more frequently. AAP News. September 1, 2017. www.aappublications.org/news/2017/09/01/IDSnapshot082917. Accessed January 14, 2020.
6. Immunization Action Coalition. How to administer intramuscular and subcutaneous vaccine injections to adults. https://www.immunize.org/catg.d/p2020a.pdf. Accessed January 14, 2020.