User login
Official Newspaper of the American College of Surgeons
Opioids still overprescribed for postop pain management
Most patients use far less opioids than they are prescribed after hernia and other abdominal surgery, resulting in substantial waste and potential diversion, a prospective cohort study has found.
In an evaluation of 176 narcotic-naive patients who underwent surgery in a over the 14-day postdischarge study period was 30 morphine milligram equivalents (MME) but the median prescription was 150 MME, reported Wen Hui Tan, MD, and her research team at Washington University, St. Louis. The report was published in the Journal of the American College of Surgeons.
Overall, 76.7% of patients reported being satisfied or very satisfied with their postoperative pain management. Some patients (n = 31, 17.6%) reported not filling their prescription or not taking any of their prescribed opioid pain medications at all.
Sixty-nine percent of the surgeries were laparoscopic. A variety of abdominal procedures were represented, including hiatal hernia repair, inguinal hernia repair, and cholecystectomy. The median age was 60 years. Of postoperative pain prescriptions, 67% were for hydrocodone-acetaminophen and most of the remainder were for oxycodone-acetaminophen or oxycodone alone. The median prescription was for the equivalent of 20 5-mg oxycodone pills, while the median consumption in the first 7 postoperative days was 3.7 pills. Only 4.5% of patients received a refill.
The findings are consistent with numerous studies of different types of operations showing that patients often don’t use all of the opioid medications they are prescribed for pain control after surgery.
“Now that opioid pain medications can no longer be refilled with a pharmacy via telephone, overprescription may also be partially driven by a desire to prevent future inconvenience and workload of office staff from patients requesting refills. However, the rising numbers of opioid-related unintentional deaths over the last decade point to the fact that overprescription has serious potential consequences,” the researchers wrote.
They reported having no potential conflicts of interest.
SOURCE: Tan et al. J Am Coll Surg 2018 May 7. doi: 10.1016/j.jamcollsurg.2018.04.032.
Most patients use far less opioids than they are prescribed after hernia and other abdominal surgery, resulting in substantial waste and potential diversion, a prospective cohort study has found.
In an evaluation of 176 narcotic-naive patients who underwent surgery in a over the 14-day postdischarge study period was 30 morphine milligram equivalents (MME) but the median prescription was 150 MME, reported Wen Hui Tan, MD, and her research team at Washington University, St. Louis. The report was published in the Journal of the American College of Surgeons.
Overall, 76.7% of patients reported being satisfied or very satisfied with their postoperative pain management. Some patients (n = 31, 17.6%) reported not filling their prescription or not taking any of their prescribed opioid pain medications at all.
Sixty-nine percent of the surgeries were laparoscopic. A variety of abdominal procedures were represented, including hiatal hernia repair, inguinal hernia repair, and cholecystectomy. The median age was 60 years. Of postoperative pain prescriptions, 67% were for hydrocodone-acetaminophen and most of the remainder were for oxycodone-acetaminophen or oxycodone alone. The median prescription was for the equivalent of 20 5-mg oxycodone pills, while the median consumption in the first 7 postoperative days was 3.7 pills. Only 4.5% of patients received a refill.
The findings are consistent with numerous studies of different types of operations showing that patients often don’t use all of the opioid medications they are prescribed for pain control after surgery.
“Now that opioid pain medications can no longer be refilled with a pharmacy via telephone, overprescription may also be partially driven by a desire to prevent future inconvenience and workload of office staff from patients requesting refills. However, the rising numbers of opioid-related unintentional deaths over the last decade point to the fact that overprescription has serious potential consequences,” the researchers wrote.
They reported having no potential conflicts of interest.
SOURCE: Tan et al. J Am Coll Surg 2018 May 7. doi: 10.1016/j.jamcollsurg.2018.04.032.
Most patients use far less opioids than they are prescribed after hernia and other abdominal surgery, resulting in substantial waste and potential diversion, a prospective cohort study has found.
In an evaluation of 176 narcotic-naive patients who underwent surgery in a over the 14-day postdischarge study period was 30 morphine milligram equivalents (MME) but the median prescription was 150 MME, reported Wen Hui Tan, MD, and her research team at Washington University, St. Louis. The report was published in the Journal of the American College of Surgeons.
Overall, 76.7% of patients reported being satisfied or very satisfied with their postoperative pain management. Some patients (n = 31, 17.6%) reported not filling their prescription or not taking any of their prescribed opioid pain medications at all.
Sixty-nine percent of the surgeries were laparoscopic. A variety of abdominal procedures were represented, including hiatal hernia repair, inguinal hernia repair, and cholecystectomy. The median age was 60 years. Of postoperative pain prescriptions, 67% were for hydrocodone-acetaminophen and most of the remainder were for oxycodone-acetaminophen or oxycodone alone. The median prescription was for the equivalent of 20 5-mg oxycodone pills, while the median consumption in the first 7 postoperative days was 3.7 pills. Only 4.5% of patients received a refill.
The findings are consistent with numerous studies of different types of operations showing that patients often don’t use all of the opioid medications they are prescribed for pain control after surgery.
“Now that opioid pain medications can no longer be refilled with a pharmacy via telephone, overprescription may also be partially driven by a desire to prevent future inconvenience and workload of office staff from patients requesting refills. However, the rising numbers of opioid-related unintentional deaths over the last decade point to the fact that overprescription has serious potential consequences,” the researchers wrote.
They reported having no potential conflicts of interest.
SOURCE: Tan et al. J Am Coll Surg 2018 May 7. doi: 10.1016/j.jamcollsurg.2018.04.032.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: For postoperative recovery, a survey showed that far more opioids are prescribed than are consumed.
Major finding: On average, surgical patients went home with opioid prescriptions of 150 MME but took a median of 30 MME.
Study details: Prospective cohort study.
Disclosures: The authors report no potential conflicts of interest.
Source: Tan et al. J Am Coll Surg 2018 May 7. doi: 10.1016/j.jamcollsurg.2018.04.032.
Eleven on a scale of 1 to 10
I literally rode into the sunset recently as I finished my tour of duty as one of the Director examiners for the American Board of Surgery. I was heading out of St. Louis westward toward my home in Kansas. It was a 9-hour drive, which gave me plenty of time to reflect on the 6 years I shared the responsibility of administering the certifying exam known by most surgeons as “the oral exam.”
Over the last dozen years, Directors V. Suzanne Klimberg and Karen J. Brasel, along with former Executive Director Frank Lewis, a team of psychometricians at the Board, and members of the certification committee of the Board, worked tirelessly to create a testing instrument as fair and statistically sound as possible given the inherently qualitative exam. I believe they did a magnificent job. Gone are the legends of yesteryear where candidates were subjected to the whims of whatever crossed the mind of the examiners, including their prejudices about the “right” answer. The oral exam now represents a well-constructed survey of surgical judgment issues that have been thoroughly vetted.
Being an examiner for the orals means you arrive Sunday afternoon before the exams that are given over the next two and a half days. Each examiner undergoes an overview briefing on Sunday afternoon and then studies “the book” for that test’s content usually until late into the night. This book is an impressive document.
We arise around 0530 to attend a breakfast meeting, which includes breaking into our six-person teams and going over each question that will be given that day. At 0800, the first candidates for the first session walk into a room and meet the two surgeons who will make some of the most important decisions affecting that candidate’s career. If you rate the intensity of this moment on a scale of 1 to 10, this is an 11 for both candidates and examiners. No one in the room knows how it will turn out because every session has its own twists and turns. Everyone there wants to see a passing score, but the two examiners know that they must make a decision that is safe for the public and fair for the candidate.
Twelve exams are given per team per day except for the final day which has only six. So, each team examines 30 candidates over 3 days. I’ve opened a door and shaken the moist hand of 438 candidates. I’ve seen every sort of emotion during those sessions. I’ve had moments of great joy and times of profound sadness as candidates respond to the questions. I’ve always tried to be friendly, but just like surgery, it is a serious business and decisions have to be made. That means ignoring one’s hopes and acting on the best facts available at the moment. Most surgeons remember their oral examiners and what they were asked for a lifetime. I know I do.
I could write a book on this experience (I won’t, though). But as I reflect on my time as a Director, what stands out in my mind are the associate examiners with whom I’ve worked. These surgeons are invited to participate and receive no compensation. It’s 3 days out of their lives, and because they don’t give the exam as frequently as the Directors do, the amount of study and effort is greater for them. Each is selected because he or she is considered to be a thoughtful surgeon with high standards. These surgeons do this job because they care about quality in our profession.
Most of the associates I have worked with are far more accomplished than I. I was once paired with a renowned breast surgeon (okay, it was Kelly K. Hunt). My ego was at great risk because I knew how accomplished she was. But like all the other associates, she was gracious and hard working. We rarely work with another Director, but Anne G. Rizzo, who later became a Director, and I did an exam together. She was a dazzling questioner with very high standards. In other words, she was typical of the people I met. My first associate (also later a Director) was Reid Adams. He was great; I was nervous. My last associate was Marc L. Melcher, a transplant surgeon who asked penetrating questions in a calm manner. I wish I could name each of my associates and thank them for making my work so much better, for teaching me things I didn’t know, for deepening my own knowledge, and serving in a hard job with grace. This column can’t be that long, but you all know who you are. Thank you.
At the end of the day, I believe the oral exam to be a great thing for our profession. When you think about the number of patients potentially affected throughout a surgeon’s career, the impact of decisions made on the day of the exam can be enormous. Given that, over a 20-year career, a surgeon may operate on 25,000 patients, a summative check on a surgeon’s judgment and knowledge is important. Each year, the ABS adjudicates on some 1,100 surgeons. A single year’s set of surgeons over the following 20-year period translates into 27.5 million patients. I hope we never stop doing the orals because of cost, time, or convenience. The exam is just too important to our profession to risk forgoing this last, big step before a surgeon is presented to the world as “certified.”
I literally rode into the sunset recently as I finished my tour of duty as one of the Director examiners for the American Board of Surgery. I was heading out of St. Louis westward toward my home in Kansas. It was a 9-hour drive, which gave me plenty of time to reflect on the 6 years I shared the responsibility of administering the certifying exam known by most surgeons as “the oral exam.”
Over the last dozen years, Directors V. Suzanne Klimberg and Karen J. Brasel, along with former Executive Director Frank Lewis, a team of psychometricians at the Board, and members of the certification committee of the Board, worked tirelessly to create a testing instrument as fair and statistically sound as possible given the inherently qualitative exam. I believe they did a magnificent job. Gone are the legends of yesteryear where candidates were subjected to the whims of whatever crossed the mind of the examiners, including their prejudices about the “right” answer. The oral exam now represents a well-constructed survey of surgical judgment issues that have been thoroughly vetted.
Being an examiner for the orals means you arrive Sunday afternoon before the exams that are given over the next two and a half days. Each examiner undergoes an overview briefing on Sunday afternoon and then studies “the book” for that test’s content usually until late into the night. This book is an impressive document.
We arise around 0530 to attend a breakfast meeting, which includes breaking into our six-person teams and going over each question that will be given that day. At 0800, the first candidates for the first session walk into a room and meet the two surgeons who will make some of the most important decisions affecting that candidate’s career. If you rate the intensity of this moment on a scale of 1 to 10, this is an 11 for both candidates and examiners. No one in the room knows how it will turn out because every session has its own twists and turns. Everyone there wants to see a passing score, but the two examiners know that they must make a decision that is safe for the public and fair for the candidate.
Twelve exams are given per team per day except for the final day which has only six. So, each team examines 30 candidates over 3 days. I’ve opened a door and shaken the moist hand of 438 candidates. I’ve seen every sort of emotion during those sessions. I’ve had moments of great joy and times of profound sadness as candidates respond to the questions. I’ve always tried to be friendly, but just like surgery, it is a serious business and decisions have to be made. That means ignoring one’s hopes and acting on the best facts available at the moment. Most surgeons remember their oral examiners and what they were asked for a lifetime. I know I do.
I could write a book on this experience (I won’t, though). But as I reflect on my time as a Director, what stands out in my mind are the associate examiners with whom I’ve worked. These surgeons are invited to participate and receive no compensation. It’s 3 days out of their lives, and because they don’t give the exam as frequently as the Directors do, the amount of study and effort is greater for them. Each is selected because he or she is considered to be a thoughtful surgeon with high standards. These surgeons do this job because they care about quality in our profession.
Most of the associates I have worked with are far more accomplished than I. I was once paired with a renowned breast surgeon (okay, it was Kelly K. Hunt). My ego was at great risk because I knew how accomplished she was. But like all the other associates, she was gracious and hard working. We rarely work with another Director, but Anne G. Rizzo, who later became a Director, and I did an exam together. She was a dazzling questioner with very high standards. In other words, she was typical of the people I met. My first associate (also later a Director) was Reid Adams. He was great; I was nervous. My last associate was Marc L. Melcher, a transplant surgeon who asked penetrating questions in a calm manner. I wish I could name each of my associates and thank them for making my work so much better, for teaching me things I didn’t know, for deepening my own knowledge, and serving in a hard job with grace. This column can’t be that long, but you all know who you are. Thank you.
At the end of the day, I believe the oral exam to be a great thing for our profession. When you think about the number of patients potentially affected throughout a surgeon’s career, the impact of decisions made on the day of the exam can be enormous. Given that, over a 20-year career, a surgeon may operate on 25,000 patients, a summative check on a surgeon’s judgment and knowledge is important. Each year, the ABS adjudicates on some 1,100 surgeons. A single year’s set of surgeons over the following 20-year period translates into 27.5 million patients. I hope we never stop doing the orals because of cost, time, or convenience. The exam is just too important to our profession to risk forgoing this last, big step before a surgeon is presented to the world as “certified.”
I literally rode into the sunset recently as I finished my tour of duty as one of the Director examiners for the American Board of Surgery. I was heading out of St. Louis westward toward my home in Kansas. It was a 9-hour drive, which gave me plenty of time to reflect on the 6 years I shared the responsibility of administering the certifying exam known by most surgeons as “the oral exam.”
Over the last dozen years, Directors V. Suzanne Klimberg and Karen J. Brasel, along with former Executive Director Frank Lewis, a team of psychometricians at the Board, and members of the certification committee of the Board, worked tirelessly to create a testing instrument as fair and statistically sound as possible given the inherently qualitative exam. I believe they did a magnificent job. Gone are the legends of yesteryear where candidates were subjected to the whims of whatever crossed the mind of the examiners, including their prejudices about the “right” answer. The oral exam now represents a well-constructed survey of surgical judgment issues that have been thoroughly vetted.
Being an examiner for the orals means you arrive Sunday afternoon before the exams that are given over the next two and a half days. Each examiner undergoes an overview briefing on Sunday afternoon and then studies “the book” for that test’s content usually until late into the night. This book is an impressive document.
We arise around 0530 to attend a breakfast meeting, which includes breaking into our six-person teams and going over each question that will be given that day. At 0800, the first candidates for the first session walk into a room and meet the two surgeons who will make some of the most important decisions affecting that candidate’s career. If you rate the intensity of this moment on a scale of 1 to 10, this is an 11 for both candidates and examiners. No one in the room knows how it will turn out because every session has its own twists and turns. Everyone there wants to see a passing score, but the two examiners know that they must make a decision that is safe for the public and fair for the candidate.
Twelve exams are given per team per day except for the final day which has only six. So, each team examines 30 candidates over 3 days. I’ve opened a door and shaken the moist hand of 438 candidates. I’ve seen every sort of emotion during those sessions. I’ve had moments of great joy and times of profound sadness as candidates respond to the questions. I’ve always tried to be friendly, but just like surgery, it is a serious business and decisions have to be made. That means ignoring one’s hopes and acting on the best facts available at the moment. Most surgeons remember their oral examiners and what they were asked for a lifetime. I know I do.
I could write a book on this experience (I won’t, though). But as I reflect on my time as a Director, what stands out in my mind are the associate examiners with whom I’ve worked. These surgeons are invited to participate and receive no compensation. It’s 3 days out of their lives, and because they don’t give the exam as frequently as the Directors do, the amount of study and effort is greater for them. Each is selected because he or she is considered to be a thoughtful surgeon with high standards. These surgeons do this job because they care about quality in our profession.
Most of the associates I have worked with are far more accomplished than I. I was once paired with a renowned breast surgeon (okay, it was Kelly K. Hunt). My ego was at great risk because I knew how accomplished she was. But like all the other associates, she was gracious and hard working. We rarely work with another Director, but Anne G. Rizzo, who later became a Director, and I did an exam together. She was a dazzling questioner with very high standards. In other words, she was typical of the people I met. My first associate (also later a Director) was Reid Adams. He was great; I was nervous. My last associate was Marc L. Melcher, a transplant surgeon who asked penetrating questions in a calm manner. I wish I could name each of my associates and thank them for making my work so much better, for teaching me things I didn’t know, for deepening my own knowledge, and serving in a hard job with grace. This column can’t be that long, but you all know who you are. Thank you.
At the end of the day, I believe the oral exam to be a great thing for our profession. When you think about the number of patients potentially affected throughout a surgeon’s career, the impact of decisions made on the day of the exam can be enormous. Given that, over a 20-year career, a surgeon may operate on 25,000 patients, a summative check on a surgeon’s judgment and knowledge is important. Each year, the ABS adjudicates on some 1,100 surgeons. A single year’s set of surgeons over the following 20-year period translates into 27.5 million patients. I hope we never stop doing the orals because of cost, time, or convenience. The exam is just too important to our profession to risk forgoing this last, big step before a surgeon is presented to the world as “certified.”
Sarcopenia had minor impact on hernia repair SSIs
according to findings from a prospective, single-institution study.
Steve R. Siegal, MD, and his colleagues at the Oregon Health & Science University, Portland, wrote in Hernia that risk factors for postoperative complications after hernia repair established in the literature include uncontrolled diabetes, active tobacco use, prior hernia repair, active infection, and obesity. Sarcopenia occurs in many physiological or pathological states, not only in the elderly but also in cases of immunosuppression, cirrhosis, trauma, prolonged immobility, and malignancy. Many opportunities exist for sarcopenia and hernia surgery to coincide but the role of sarcopenia in hernia repair outcomes has not been much studied.
The investigators began with the hypothesis that sarcopenia in hernia patients would lead to worse postoperative outcomes given the large metabolic requirement for postoperative healing of hernia defects and abdominal wall reconstruction.
The study involved 135 patients who underwent ventral hernia repair, 27% of whom had sarcopenia. The literature-based definition of sarcopenia was a muscle index cutoff of less than 52.4 cm2/m2 for men and less than 38.5 cm2/m2 for women. The investigators noted that the index cutoff was validated in oncology patients. Patients underwent a preoperative CT scan to assess muscle mass. The study group included patients with ventral hernia repair with or without mesh, component separation/abdominal wall reconstruction, and a hernia defect of 2 cm or larger.
With data on variables including gender, diabetes status, body mass index (BMI), chronic obstructive pulmonary disease (COPD), wound class, alcohol abuse status, and prior wound infections, the investigators created a multivariate model to look at primary outcomes of surgical site infection (SSI), surgical site occurrences (wound complications, other infections) and hernia recurrence. Secondary outcomes included length of hospital stay, morbidities, and other postoperative complications.
Patients with sarcopenia were more likely to have lower BMI (median 29.6 kg/m2 vs. 36.6 kg/m2), to be slightly older (median 63.1 vs. 59.2 years), and to have a history of immunosuppression (29.7% vs. 11.2%). The differences for the other variables (diabetes, tobacco use, COPD) were not significant.
The surprising finding was that sarcopenia was not significantly correlated with SSIs (P = 0.140), other complications (P = 0.113), or recurrence (P = 0.895) after ventral hernia repair. In-hospital morbidities and length of hospital stay did not differ significantly between the sarcopenic and nonsarcopenic patients. But sarcopenia combined with other factors did have an impact on outcomes. After adjustment for BMI and diabetes and critical care status, muscle mass as a continuous variable “was notable for a 1.44 increased odds [95% confidence interval, 1.00-2.07; P = 0.049] of inpatient morbidity with every decrease of 10 cm2/m2 of muscle index,” Dr. Siegal and his associates wrote.
The nonsignificant results of this study may be explained by the markedly lower BMI in the sarcopenic group, which could have been protective against worse outcomes, the investigators noted. However, they concluded, “Sarcopenia may still be a factor in adverse perioperative outcomes, but the established muscle index cutoff value may be inappropriately applied to benign patients, such as our ventral hernia cohort results in this study.”
The investigators declared no conflicts of interest and received no outside funding for this study.
SOURCE: Siegal SR et al. Hernia. 2018 May 11. doi: 10.1007/s10029-018-1770-8.
according to findings from a prospective, single-institution study.
Steve R. Siegal, MD, and his colleagues at the Oregon Health & Science University, Portland, wrote in Hernia that risk factors for postoperative complications after hernia repair established in the literature include uncontrolled diabetes, active tobacco use, prior hernia repair, active infection, and obesity. Sarcopenia occurs in many physiological or pathological states, not only in the elderly but also in cases of immunosuppression, cirrhosis, trauma, prolonged immobility, and malignancy. Many opportunities exist for sarcopenia and hernia surgery to coincide but the role of sarcopenia in hernia repair outcomes has not been much studied.
The investigators began with the hypothesis that sarcopenia in hernia patients would lead to worse postoperative outcomes given the large metabolic requirement for postoperative healing of hernia defects and abdominal wall reconstruction.
The study involved 135 patients who underwent ventral hernia repair, 27% of whom had sarcopenia. The literature-based definition of sarcopenia was a muscle index cutoff of less than 52.4 cm2/m2 for men and less than 38.5 cm2/m2 for women. The investigators noted that the index cutoff was validated in oncology patients. Patients underwent a preoperative CT scan to assess muscle mass. The study group included patients with ventral hernia repair with or without mesh, component separation/abdominal wall reconstruction, and a hernia defect of 2 cm or larger.
With data on variables including gender, diabetes status, body mass index (BMI), chronic obstructive pulmonary disease (COPD), wound class, alcohol abuse status, and prior wound infections, the investigators created a multivariate model to look at primary outcomes of surgical site infection (SSI), surgical site occurrences (wound complications, other infections) and hernia recurrence. Secondary outcomes included length of hospital stay, morbidities, and other postoperative complications.
Patients with sarcopenia were more likely to have lower BMI (median 29.6 kg/m2 vs. 36.6 kg/m2), to be slightly older (median 63.1 vs. 59.2 years), and to have a history of immunosuppression (29.7% vs. 11.2%). The differences for the other variables (diabetes, tobacco use, COPD) were not significant.
The surprising finding was that sarcopenia was not significantly correlated with SSIs (P = 0.140), other complications (P = 0.113), or recurrence (P = 0.895) after ventral hernia repair. In-hospital morbidities and length of hospital stay did not differ significantly between the sarcopenic and nonsarcopenic patients. But sarcopenia combined with other factors did have an impact on outcomes. After adjustment for BMI and diabetes and critical care status, muscle mass as a continuous variable “was notable for a 1.44 increased odds [95% confidence interval, 1.00-2.07; P = 0.049] of inpatient morbidity with every decrease of 10 cm2/m2 of muscle index,” Dr. Siegal and his associates wrote.
The nonsignificant results of this study may be explained by the markedly lower BMI in the sarcopenic group, which could have been protective against worse outcomes, the investigators noted. However, they concluded, “Sarcopenia may still be a factor in adverse perioperative outcomes, but the established muscle index cutoff value may be inappropriately applied to benign patients, such as our ventral hernia cohort results in this study.”
The investigators declared no conflicts of interest and received no outside funding for this study.
SOURCE: Siegal SR et al. Hernia. 2018 May 11. doi: 10.1007/s10029-018-1770-8.
according to findings from a prospective, single-institution study.
Steve R. Siegal, MD, and his colleagues at the Oregon Health & Science University, Portland, wrote in Hernia that risk factors for postoperative complications after hernia repair established in the literature include uncontrolled diabetes, active tobacco use, prior hernia repair, active infection, and obesity. Sarcopenia occurs in many physiological or pathological states, not only in the elderly but also in cases of immunosuppression, cirrhosis, trauma, prolonged immobility, and malignancy. Many opportunities exist for sarcopenia and hernia surgery to coincide but the role of sarcopenia in hernia repair outcomes has not been much studied.
The investigators began with the hypothesis that sarcopenia in hernia patients would lead to worse postoperative outcomes given the large metabolic requirement for postoperative healing of hernia defects and abdominal wall reconstruction.
The study involved 135 patients who underwent ventral hernia repair, 27% of whom had sarcopenia. The literature-based definition of sarcopenia was a muscle index cutoff of less than 52.4 cm2/m2 for men and less than 38.5 cm2/m2 for women. The investigators noted that the index cutoff was validated in oncology patients. Patients underwent a preoperative CT scan to assess muscle mass. The study group included patients with ventral hernia repair with or without mesh, component separation/abdominal wall reconstruction, and a hernia defect of 2 cm or larger.
With data on variables including gender, diabetes status, body mass index (BMI), chronic obstructive pulmonary disease (COPD), wound class, alcohol abuse status, and prior wound infections, the investigators created a multivariate model to look at primary outcomes of surgical site infection (SSI), surgical site occurrences (wound complications, other infections) and hernia recurrence. Secondary outcomes included length of hospital stay, morbidities, and other postoperative complications.
Patients with sarcopenia were more likely to have lower BMI (median 29.6 kg/m2 vs. 36.6 kg/m2), to be slightly older (median 63.1 vs. 59.2 years), and to have a history of immunosuppression (29.7% vs. 11.2%). The differences for the other variables (diabetes, tobacco use, COPD) were not significant.
The surprising finding was that sarcopenia was not significantly correlated with SSIs (P = 0.140), other complications (P = 0.113), or recurrence (P = 0.895) after ventral hernia repair. In-hospital morbidities and length of hospital stay did not differ significantly between the sarcopenic and nonsarcopenic patients. But sarcopenia combined with other factors did have an impact on outcomes. After adjustment for BMI and diabetes and critical care status, muscle mass as a continuous variable “was notable for a 1.44 increased odds [95% confidence interval, 1.00-2.07; P = 0.049] of inpatient morbidity with every decrease of 10 cm2/m2 of muscle index,” Dr. Siegal and his associates wrote.
The nonsignificant results of this study may be explained by the markedly lower BMI in the sarcopenic group, which could have been protective against worse outcomes, the investigators noted. However, they concluded, “Sarcopenia may still be a factor in adverse perioperative outcomes, but the established muscle index cutoff value may be inappropriately applied to benign patients, such as our ventral hernia cohort results in this study.”
The investigators declared no conflicts of interest and received no outside funding for this study.
SOURCE: Siegal SR et al. Hernia. 2018 May 11. doi: 10.1007/s10029-018-1770-8.
FROM HERNIA
Key clinical point: Sarcopenia was not correlated with surgical site infections, other complications, or recurrence after ventral hernia repair.
Major finding: After adjustment for body mass index and diabetes and critical care status, muscle mass as a continuous variable was notable for a 1.44 increased odds of inpatient morbidity.
Study details: A prospective, single-institution study of 135 patients who had ventral hernia repair, 27% of whom were sarcopenic.
Disclosures: The investigators declared no conflicts of interest and received no outside funding for this study.
Source: Siegal SR et al. Hernia. 2018 May 11. doi: 10.1007/s10029-018-1770-8.
Teaching opportunities of live surgery broadcasts debated
SAN DIEGO – Two thoracic societies are being challenged to review their rejection of at medical meetings.
The American Association for Thoracic Surgery and Society of Thoracic Surgeons “should modify their stance on live surgery as an educational tool like almost all of their sister organizations,” said Joseph E. Bavaria, MD, FACS, of the University of Pennsylvania, Philadelphia. “Presently, it is effectively a ban on the practice. But there are no data to suggest that it does harm to patients if done with proper constraints.”
Live broadcasts of surgeries at medical meetings are both common and controversial. Dr. Bavaria listed numerous recent thoracic meetings in Europe and Canada that featured live broadcasts. But, he noted, the AATS and STS are not supportive of the trend.
In a policy amended in 2017, the AATS states, among other things, that “national and international cardiothoracic societies should consider prohibiting live surgery broadcasts to large audiences at their annual meetings.” The STS policy, amended in 2016, is nearly identical. However, it adds language specifying that “violation of these guidelines may lead to disciplinary action by the Society.”
Both the AATS and STS policies state that surgeons should not take part in live broadcasts of operations that are intended for the public. And both policies say “generally, recorded broadcasts, either edited or unedited, are preferable to live surgery broadcasts because recordings intended for later broadcast pose fewer risks of harm to patients.”
The policies don’t elaborate on how a live broadcast of an operation might be more harmful than one aired at a later time. “Where are the data to support this statement?” Dr. Bavaria asked. “Is this what we call the expert opinion of a few people with gray hair? Our European and Canadian colleagues certainly don’t agree with [the policies] and might take issue with our sanctimonious lecturing that’s not supported by any data whatsoever.”
He pointed to a 2011 study that examined 250 cardiac procedures that were broadcast live to 32 scientific meetings. Researchers found that “there is no evidence for an excess perioperative risk for patients operated under the conditions of live broadcasting” (Eur J Cardiothorac Surg. 2011;40[2]:367-71).
A member of the audience at the AATS session pointed out that the study may be misleading because only top surgeons may be willing to perform procedures live on television. Dr. Bavaria responded by noting that the outcomes of surgeries performed on live video were not worse.
Skeptics have also expressed concern about the potential for sensationalism in live broadcasts and the drive for participants to make a splash: “the demands of ‘the performance,’ including questions and discussion with the audience, may divert the surgeon’s attention and produce an inferior outcome,” wrote three physicians in 2011 (J Surg Educ. 2011 Jan-Feb; 68[1]:58-61).
The trio also expressed worry about safety risks posed by extra equipment and extra people in the operating room during a live broadcast. However, Dr. Bavaria said the crowded conditions of an operation observed in person – instead of via video – could be worse: “You don’t have a sterile environment, you have people hanging around all over. A moderated live session could be better for the surgeon and the patient, rather than having a bunch of people in the room.”
Dr. Bavaria was also asked why surgeries couldn’t be recorded for airing later instead of being broadcast live, as this approach “takes you out of the nexus of having two masters, the patient and the audience.” In response, Dr. Bavaria said editing takes extra time in order to capture the nuances of the live procedure.
Dr. Bavaria reports no relevant disclosures.
Peter Angelos, MD, FACS, is the Linda Kohler Anderson Professor of Surgery and Surgical Ethics, chief of endocrine surgery, and associate director of the MacLean Center for Clinical Medical Ethics at the University of Chicago. Dr. Angelos has no disclosures.
Peter Angelos, MD, FACS, is the Linda Kohler Anderson Professor of Surgery and Surgical Ethics, chief of endocrine surgery, and associate director of the MacLean Center for Clinical Medical Ethics at the University of Chicago. Dr. Angelos has no disclosures.
Peter Angelos, MD, FACS, is the Linda Kohler Anderson Professor of Surgery and Surgical Ethics, chief of endocrine surgery, and associate director of the MacLean Center for Clinical Medical Ethics at the University of Chicago. Dr. Angelos has no disclosures.
SAN DIEGO – Two thoracic societies are being challenged to review their rejection of at medical meetings.
The American Association for Thoracic Surgery and Society of Thoracic Surgeons “should modify their stance on live surgery as an educational tool like almost all of their sister organizations,” said Joseph E. Bavaria, MD, FACS, of the University of Pennsylvania, Philadelphia. “Presently, it is effectively a ban on the practice. But there are no data to suggest that it does harm to patients if done with proper constraints.”
Live broadcasts of surgeries at medical meetings are both common and controversial. Dr. Bavaria listed numerous recent thoracic meetings in Europe and Canada that featured live broadcasts. But, he noted, the AATS and STS are not supportive of the trend.
In a policy amended in 2017, the AATS states, among other things, that “national and international cardiothoracic societies should consider prohibiting live surgery broadcasts to large audiences at their annual meetings.” The STS policy, amended in 2016, is nearly identical. However, it adds language specifying that “violation of these guidelines may lead to disciplinary action by the Society.”
Both the AATS and STS policies state that surgeons should not take part in live broadcasts of operations that are intended for the public. And both policies say “generally, recorded broadcasts, either edited or unedited, are preferable to live surgery broadcasts because recordings intended for later broadcast pose fewer risks of harm to patients.”
The policies don’t elaborate on how a live broadcast of an operation might be more harmful than one aired at a later time. “Where are the data to support this statement?” Dr. Bavaria asked. “Is this what we call the expert opinion of a few people with gray hair? Our European and Canadian colleagues certainly don’t agree with [the policies] and might take issue with our sanctimonious lecturing that’s not supported by any data whatsoever.”
He pointed to a 2011 study that examined 250 cardiac procedures that were broadcast live to 32 scientific meetings. Researchers found that “there is no evidence for an excess perioperative risk for patients operated under the conditions of live broadcasting” (Eur J Cardiothorac Surg. 2011;40[2]:367-71).
A member of the audience at the AATS session pointed out that the study may be misleading because only top surgeons may be willing to perform procedures live on television. Dr. Bavaria responded by noting that the outcomes of surgeries performed on live video were not worse.
Skeptics have also expressed concern about the potential for sensationalism in live broadcasts and the drive for participants to make a splash: “the demands of ‘the performance,’ including questions and discussion with the audience, may divert the surgeon’s attention and produce an inferior outcome,” wrote three physicians in 2011 (J Surg Educ. 2011 Jan-Feb; 68[1]:58-61).
The trio also expressed worry about safety risks posed by extra equipment and extra people in the operating room during a live broadcast. However, Dr. Bavaria said the crowded conditions of an operation observed in person – instead of via video – could be worse: “You don’t have a sterile environment, you have people hanging around all over. A moderated live session could be better for the surgeon and the patient, rather than having a bunch of people in the room.”
Dr. Bavaria was also asked why surgeries couldn’t be recorded for airing later instead of being broadcast live, as this approach “takes you out of the nexus of having two masters, the patient and the audience.” In response, Dr. Bavaria said editing takes extra time in order to capture the nuances of the live procedure.
Dr. Bavaria reports no relevant disclosures.
SAN DIEGO – Two thoracic societies are being challenged to review their rejection of at medical meetings.
The American Association for Thoracic Surgery and Society of Thoracic Surgeons “should modify their stance on live surgery as an educational tool like almost all of their sister organizations,” said Joseph E. Bavaria, MD, FACS, of the University of Pennsylvania, Philadelphia. “Presently, it is effectively a ban on the practice. But there are no data to suggest that it does harm to patients if done with proper constraints.”
Live broadcasts of surgeries at medical meetings are both common and controversial. Dr. Bavaria listed numerous recent thoracic meetings in Europe and Canada that featured live broadcasts. But, he noted, the AATS and STS are not supportive of the trend.
In a policy amended in 2017, the AATS states, among other things, that “national and international cardiothoracic societies should consider prohibiting live surgery broadcasts to large audiences at their annual meetings.” The STS policy, amended in 2016, is nearly identical. However, it adds language specifying that “violation of these guidelines may lead to disciplinary action by the Society.”
Both the AATS and STS policies state that surgeons should not take part in live broadcasts of operations that are intended for the public. And both policies say “generally, recorded broadcasts, either edited or unedited, are preferable to live surgery broadcasts because recordings intended for later broadcast pose fewer risks of harm to patients.”
The policies don’t elaborate on how a live broadcast of an operation might be more harmful than one aired at a later time. “Where are the data to support this statement?” Dr. Bavaria asked. “Is this what we call the expert opinion of a few people with gray hair? Our European and Canadian colleagues certainly don’t agree with [the policies] and might take issue with our sanctimonious lecturing that’s not supported by any data whatsoever.”
He pointed to a 2011 study that examined 250 cardiac procedures that were broadcast live to 32 scientific meetings. Researchers found that “there is no evidence for an excess perioperative risk for patients operated under the conditions of live broadcasting” (Eur J Cardiothorac Surg. 2011;40[2]:367-71).
A member of the audience at the AATS session pointed out that the study may be misleading because only top surgeons may be willing to perform procedures live on television. Dr. Bavaria responded by noting that the outcomes of surgeries performed on live video were not worse.
Skeptics have also expressed concern about the potential for sensationalism in live broadcasts and the drive for participants to make a splash: “the demands of ‘the performance,’ including questions and discussion with the audience, may divert the surgeon’s attention and produce an inferior outcome,” wrote three physicians in 2011 (J Surg Educ. 2011 Jan-Feb; 68[1]:58-61).
The trio also expressed worry about safety risks posed by extra equipment and extra people in the operating room during a live broadcast. However, Dr. Bavaria said the crowded conditions of an operation observed in person – instead of via video – could be worse: “You don’t have a sterile environment, you have people hanging around all over. A moderated live session could be better for the surgeon and the patient, rather than having a bunch of people in the room.”
Dr. Bavaria was also asked why surgeries couldn’t be recorded for airing later instead of being broadcast live, as this approach “takes you out of the nexus of having two masters, the patient and the audience.” In response, Dr. Bavaria said editing takes extra time in order to capture the nuances of the live procedure.
Dr. Bavaria reports no relevant disclosures.
REPORTING FROM AATS
Peer mentorship, groups help combat burnout in female physicians
NEW YORK – Female physicians are at higher risk for burnout compared with their male counterparts, and the reasons and potential solutions for the problem were addressed at a symposium during the annual meeting of the American Psychiatric Association.
The work environment for women has improved over time, but lingering implicit and unconscious biases are part of the reason for the high burnout rate among women who are physicians, as are some inherent biological differences, according to Cynthia M. Stonnington, MD, of the Mayo Clinic, Phoenix.
In this video interview, Dr. Stonnington, symposium chair, discussed potential solutions, including facilitated peer mentorship and group support. She also reviewed recent data on how group support can be of benefit, and noted that “there is power in numbers.
“,” she said.
Dr. Stonnington reported having no disclosures.
NEW YORK – Female physicians are at higher risk for burnout compared with their male counterparts, and the reasons and potential solutions for the problem were addressed at a symposium during the annual meeting of the American Psychiatric Association.
The work environment for women has improved over time, but lingering implicit and unconscious biases are part of the reason for the high burnout rate among women who are physicians, as are some inherent biological differences, according to Cynthia M. Stonnington, MD, of the Mayo Clinic, Phoenix.
In this video interview, Dr. Stonnington, symposium chair, discussed potential solutions, including facilitated peer mentorship and group support. She also reviewed recent data on how group support can be of benefit, and noted that “there is power in numbers.
“,” she said.
Dr. Stonnington reported having no disclosures.
NEW YORK – Female physicians are at higher risk for burnout compared with their male counterparts, and the reasons and potential solutions for the problem were addressed at a symposium during the annual meeting of the American Psychiatric Association.
The work environment for women has improved over time, but lingering implicit and unconscious biases are part of the reason for the high burnout rate among women who are physicians, as are some inherent biological differences, according to Cynthia M. Stonnington, MD, of the Mayo Clinic, Phoenix.
In this video interview, Dr. Stonnington, symposium chair, discussed potential solutions, including facilitated peer mentorship and group support. She also reviewed recent data on how group support can be of benefit, and noted that “there is power in numbers.
“,” she said.
Dr. Stonnington reported having no disclosures.
REPORTING FROM APA
Hospital safety program curbs surgical site infections
The Agency for Healthcare Research and Quality (AHRQ) designed the program to reduce surgical site infections (SSIs), which are harmful to patients and expensive for the health care system, wrote Della M. Lin, MD, of Johns Hopkins University, Baltimore, and the department of surgery at the University of Hawaii, Honolulu, and her colleagues.
In a study published in the Journal of the American College of Surgeons, the researchers reviewed data from a statewide intervention conducted at 15 hospitals in Hawaii from January 2013 to June 2015. The intervention included the Comprehensive Unit-based Safety Program and individualized interventions for each hospital to help reduce SSIs. The primary outcome was the number of colorectal SSIs. A secondary outcome of hospital safety culture was assessed using the AHRQ Hospital Survey on Patient Safety Culture. The participating hospitals ranged from a 25-bed critical-access hospital to a 533-bed academic medical center.
Overall, the colorectal SSI rate decreased significantly (from 12% to 5%) from the first quarter of 2013 to the second quarter of 2015, with a significant linear decrease over the study period. The rate of superficial SSIs decreased significantly, falling from 8% to 3%. However, the rate of deep SSIs was not significantly different before and after the intervention program (2% vs. 0%), nor was the organ space SSI rate (3% vs. 2%). The standardized infection ratio decreased from 1.83 to 0.92.
The culture of safety in the hospitals improved, but more modestly, in 10 of 12 areas that were measured over the study period.
The overall perception of patient safety improved from 49% to 53%, teamwork across different units improved from 49% to 54%, management and support for patient safety improved from 53% to 60%, and nonpunitive response to errors improved from 36% to 40%.
In addition, communication and openness improved from 50% to 53%, frequency of reported events improved from 51% to 60%, feedback and communication about errors improved from 52% to 59%, organizational learning and continuous improvement increased from 59% to 70%, teamwork within units improved from 68% to 75%, and expectations and actions by supervisors and managers to promote safety improved from 58% to 64%. Staff responses reflect agreement on improvement in the areas of issues of communication, feedback mechanisms, and teamwork, but the change in culture was not on the order of the SSI change.
The most common interventions to reduce SSIs were the use of reliable chlorhexidine wash or wipe before surgery/surgical prep; appropriate use of antibiotics with respect to selection, dosage, and timing; standardized postsurgical debriefing; and differentiating clean/dirty/clean in the use of anastomosis trays and closing trays.
One bundle component, the implementation of the standard operating room debrief, was found to be of particular value to participants. The investigators noted that debrief questions such as “What went well?” and “What needs to be improved?” had “encouraged new processes of thinking beyond first-order problem solving. The debrief challenge embraced by the teams emphasized that ‘bundles’ did not consist of only technical interventions [e.g. clean/dirty trays, chlorhexidine gluconate wipes in preop], but embedded culture interventions—new processes for problem solving.”
The study findings were limited by several factors, such as the use of public SSI data that were not audited for accuracy and the inability to monitor the reliability of the implementation of the various interventions, the researchers said. In addition, “In this current study, there was a change in SSI rates and a change in safety culture, but correlations between the two were negligible or weak for most domains of safety culture,” they noted. The question of sustainability of the SSI improvement without the concomitant staff support of culture change was not addressed by the investigators.
However, the results suggest that a 62% decrease is robust, and that for some hospitals with a low volume of colorectal cases, “teams could attend to iteratively reduce surgical harm beyond SSI,” the researchers wrote.
The study was supported in part by the AHRQ. Dr. Lin disclosed serving as a board member and as a paid independent contractor to the Hawaii Medical Service Association. Her coauthors had no financial conflicts to disclose.
SOURCE: Lin DM et al. J Am Coll Surg. 2018 May 18. doi: 10.1016/j.jamcollsurg.2018.04.031.
The Agency for Healthcare Research and Quality (AHRQ) designed the program to reduce surgical site infections (SSIs), which are harmful to patients and expensive for the health care system, wrote Della M. Lin, MD, of Johns Hopkins University, Baltimore, and the department of surgery at the University of Hawaii, Honolulu, and her colleagues.
In a study published in the Journal of the American College of Surgeons, the researchers reviewed data from a statewide intervention conducted at 15 hospitals in Hawaii from January 2013 to June 2015. The intervention included the Comprehensive Unit-based Safety Program and individualized interventions for each hospital to help reduce SSIs. The primary outcome was the number of colorectal SSIs. A secondary outcome of hospital safety culture was assessed using the AHRQ Hospital Survey on Patient Safety Culture. The participating hospitals ranged from a 25-bed critical-access hospital to a 533-bed academic medical center.
Overall, the colorectal SSI rate decreased significantly (from 12% to 5%) from the first quarter of 2013 to the second quarter of 2015, with a significant linear decrease over the study period. The rate of superficial SSIs decreased significantly, falling from 8% to 3%. However, the rate of deep SSIs was not significantly different before and after the intervention program (2% vs. 0%), nor was the organ space SSI rate (3% vs. 2%). The standardized infection ratio decreased from 1.83 to 0.92.
The culture of safety in the hospitals improved, but more modestly, in 10 of 12 areas that were measured over the study period.
The overall perception of patient safety improved from 49% to 53%, teamwork across different units improved from 49% to 54%, management and support for patient safety improved from 53% to 60%, and nonpunitive response to errors improved from 36% to 40%.
In addition, communication and openness improved from 50% to 53%, frequency of reported events improved from 51% to 60%, feedback and communication about errors improved from 52% to 59%, organizational learning and continuous improvement increased from 59% to 70%, teamwork within units improved from 68% to 75%, and expectations and actions by supervisors and managers to promote safety improved from 58% to 64%. Staff responses reflect agreement on improvement in the areas of issues of communication, feedback mechanisms, and teamwork, but the change in culture was not on the order of the SSI change.
The most common interventions to reduce SSIs were the use of reliable chlorhexidine wash or wipe before surgery/surgical prep; appropriate use of antibiotics with respect to selection, dosage, and timing; standardized postsurgical debriefing; and differentiating clean/dirty/clean in the use of anastomosis trays and closing trays.
One bundle component, the implementation of the standard operating room debrief, was found to be of particular value to participants. The investigators noted that debrief questions such as “What went well?” and “What needs to be improved?” had “encouraged new processes of thinking beyond first-order problem solving. The debrief challenge embraced by the teams emphasized that ‘bundles’ did not consist of only technical interventions [e.g. clean/dirty trays, chlorhexidine gluconate wipes in preop], but embedded culture interventions—new processes for problem solving.”
The study findings were limited by several factors, such as the use of public SSI data that were not audited for accuracy and the inability to monitor the reliability of the implementation of the various interventions, the researchers said. In addition, “In this current study, there was a change in SSI rates and a change in safety culture, but correlations between the two were negligible or weak for most domains of safety culture,” they noted. The question of sustainability of the SSI improvement without the concomitant staff support of culture change was not addressed by the investigators.
However, the results suggest that a 62% decrease is robust, and that for some hospitals with a low volume of colorectal cases, “teams could attend to iteratively reduce surgical harm beyond SSI,” the researchers wrote.
The study was supported in part by the AHRQ. Dr. Lin disclosed serving as a board member and as a paid independent contractor to the Hawaii Medical Service Association. Her coauthors had no financial conflicts to disclose.
SOURCE: Lin DM et al. J Am Coll Surg. 2018 May 18. doi: 10.1016/j.jamcollsurg.2018.04.031.
The Agency for Healthcare Research and Quality (AHRQ) designed the program to reduce surgical site infections (SSIs), which are harmful to patients and expensive for the health care system, wrote Della M. Lin, MD, of Johns Hopkins University, Baltimore, and the department of surgery at the University of Hawaii, Honolulu, and her colleagues.
In a study published in the Journal of the American College of Surgeons, the researchers reviewed data from a statewide intervention conducted at 15 hospitals in Hawaii from January 2013 to June 2015. The intervention included the Comprehensive Unit-based Safety Program and individualized interventions for each hospital to help reduce SSIs. The primary outcome was the number of colorectal SSIs. A secondary outcome of hospital safety culture was assessed using the AHRQ Hospital Survey on Patient Safety Culture. The participating hospitals ranged from a 25-bed critical-access hospital to a 533-bed academic medical center.
Overall, the colorectal SSI rate decreased significantly (from 12% to 5%) from the first quarter of 2013 to the second quarter of 2015, with a significant linear decrease over the study period. The rate of superficial SSIs decreased significantly, falling from 8% to 3%. However, the rate of deep SSIs was not significantly different before and after the intervention program (2% vs. 0%), nor was the organ space SSI rate (3% vs. 2%). The standardized infection ratio decreased from 1.83 to 0.92.
The culture of safety in the hospitals improved, but more modestly, in 10 of 12 areas that were measured over the study period.
The overall perception of patient safety improved from 49% to 53%, teamwork across different units improved from 49% to 54%, management and support for patient safety improved from 53% to 60%, and nonpunitive response to errors improved from 36% to 40%.
In addition, communication and openness improved from 50% to 53%, frequency of reported events improved from 51% to 60%, feedback and communication about errors improved from 52% to 59%, organizational learning and continuous improvement increased from 59% to 70%, teamwork within units improved from 68% to 75%, and expectations and actions by supervisors and managers to promote safety improved from 58% to 64%. Staff responses reflect agreement on improvement in the areas of issues of communication, feedback mechanisms, and teamwork, but the change in culture was not on the order of the SSI change.
The most common interventions to reduce SSIs were the use of reliable chlorhexidine wash or wipe before surgery/surgical prep; appropriate use of antibiotics with respect to selection, dosage, and timing; standardized postsurgical debriefing; and differentiating clean/dirty/clean in the use of anastomosis trays and closing trays.
One bundle component, the implementation of the standard operating room debrief, was found to be of particular value to participants. The investigators noted that debrief questions such as “What went well?” and “What needs to be improved?” had “encouraged new processes of thinking beyond first-order problem solving. The debrief challenge embraced by the teams emphasized that ‘bundles’ did not consist of only technical interventions [e.g. clean/dirty trays, chlorhexidine gluconate wipes in preop], but embedded culture interventions—new processes for problem solving.”
The study findings were limited by several factors, such as the use of public SSI data that were not audited for accuracy and the inability to monitor the reliability of the implementation of the various interventions, the researchers said. In addition, “In this current study, there was a change in SSI rates and a change in safety culture, but correlations between the two were negligible or weak for most domains of safety culture,” they noted. The question of sustainability of the SSI improvement without the concomitant staff support of culture change was not addressed by the investigators.
However, the results suggest that a 62% decrease is robust, and that for some hospitals with a low volume of colorectal cases, “teams could attend to iteratively reduce surgical harm beyond SSI,” the researchers wrote.
The study was supported in part by the AHRQ. Dr. Lin disclosed serving as a board member and as a paid independent contractor to the Hawaii Medical Service Association. Her coauthors had no financial conflicts to disclose.
SOURCE: Lin DM et al. J Am Coll Surg. 2018 May 18. doi: 10.1016/j.jamcollsurg.2018.04.031.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: Hospital participation in an Agency for Healthcare Research and Quality safety program improved safety culture and reduced surgical site infections.
Major finding: Surgical site infections among colorectal surgery patients decreased by 61.7% after the intervention.
Study details: The data come from a cohort study of 15 hospitals in Hawaii from January 2013 to June 2015.
Disclosures: The study was supported in part by the AHRQ. Dr. Lin disclosed serving as a board member and as a paid independent contractor to the Hawaii Medical Service Association. Her coauthors had no financial conflicts to disclose.
Source: Lin DM et al. J Am Coll Surg. 2018 May 18. doi: 10.1016/j.jamcollsurg.2018.04.031.
Postop delirium management proposed as hospital performance measure
A study suggests that outcome measures, and assessment of hospital performance.
Lead author Julia R. Berian, MD, of the University of Chicago Medical Center and her colleagues wrote, “Postoperative delirium has been associated with mortality, morbidity, prolonged length of stay, and increased costs of care. Furthermore, postoperative delirium may be associated with long-term cognitive and functional decline. However, postoperative delirium has not been incorporated as an outcome measure into major surgical quality registries. Approximately one-third of hospitalized delirium is believed to be preventable, making postoperative delirium an ideal target for surgical quality improvement efforts,” Dr. Berian and her colleagues reported in the Annals of Surgery.
The Geriatric Surgery Pilot data abstractors were instructed to assign postoperative delirium if the medical record words indicating an acute confusional stat such a mental status change, confusion, disorientation, agitation, delirium, and inappropriate behavior. Data were collected from the period 2 hours after surgery to exclude effects of the pharmacologic agents of anesthesia. Delirium status was ascertained as a binary outcome (Yes/No).
Postoperative delirium was observed in 2,427 patients for an average, unadjusted rate of 12.0%. Investigators identified 20 risk factors markedly associated with delirium. The strongest predictors included preoperative cognitive impairment, preoperative use of mobility aid, surrogate consent form, ASA class 4 or greater, age 80 years and older, preoperative sepsis, and fall history within 1 year. Patients with delirium generally were older than patients without delirium were and accounted for a greater proportion of emergency cases. Postoperative hospital length of stay was about 4 days longer on average for patients with delirium, compared with those without delirium.
By specialty, the highest rates of postoperative delirium occurred following cardiothoracic (13.7%), orthopedic (13.0%), and general surgeries (13.0%). Study authors found varied associated risk for postoperative delirium within each surgical specialty. For example, in general surgery, the risk for postoperative delirium with partial mastectomy was low, compared with a mid-level risk in the repair of a recurrent, incarcerated, or strangulated inguinal hernia and a high-level risk in Whipple operations.
The model developed to measure delirium management success in 30 hospitals found that adjusted delirium rates ranged from 3.2% to 27.5%, with eight poor- and five excellent-performing outliers. Authors noted that their model demonstrated good calibration and discrimination. Examination of changes in the Bayesian Information Criteria indicates that as few as 10-12 variables may suffice in building a parsimonious model with “an excellent fit.”
Study authors noted that screening for postoperative delirium in older adults is likely in the best interests of patients. However, they also mentioned that such screening may identify cases of postoperative delirium that were previously unrecognized, resulting in higher rates. In addition, the inclusion of only ACS NSQIP hospitals and the voluntary participation may mean a biased dataset. No one delirium prevention intervention was implemented across the hospitals and so the study doesn’t indicate why some hospitals are more successful than are others. Chart-based identification of patients who have delirium needs further study to assess validity.
Authors concluded that one solution may be to “standardize and consistently employ delirium screening in high-risk patients across hospitals, as has been advocated by a coalition of interdisciplinary experts in geriatric care.”
This project is funded in part by a grant from the John A. Hartford Foundation. The authors declare no conflict of interests.
SOURCE: Berlan JR et al. Ann Surg. 2017 July 24. doi: 10.1097/SLA.0000000000002436
A study suggests that outcome measures, and assessment of hospital performance.
Lead author Julia R. Berian, MD, of the University of Chicago Medical Center and her colleagues wrote, “Postoperative delirium has been associated with mortality, morbidity, prolonged length of stay, and increased costs of care. Furthermore, postoperative delirium may be associated with long-term cognitive and functional decline. However, postoperative delirium has not been incorporated as an outcome measure into major surgical quality registries. Approximately one-third of hospitalized delirium is believed to be preventable, making postoperative delirium an ideal target for surgical quality improvement efforts,” Dr. Berian and her colleagues reported in the Annals of Surgery.
The Geriatric Surgery Pilot data abstractors were instructed to assign postoperative delirium if the medical record words indicating an acute confusional stat such a mental status change, confusion, disorientation, agitation, delirium, and inappropriate behavior. Data were collected from the period 2 hours after surgery to exclude effects of the pharmacologic agents of anesthesia. Delirium status was ascertained as a binary outcome (Yes/No).
Postoperative delirium was observed in 2,427 patients for an average, unadjusted rate of 12.0%. Investigators identified 20 risk factors markedly associated with delirium. The strongest predictors included preoperative cognitive impairment, preoperative use of mobility aid, surrogate consent form, ASA class 4 or greater, age 80 years and older, preoperative sepsis, and fall history within 1 year. Patients with delirium generally were older than patients without delirium were and accounted for a greater proportion of emergency cases. Postoperative hospital length of stay was about 4 days longer on average for patients with delirium, compared with those without delirium.
By specialty, the highest rates of postoperative delirium occurred following cardiothoracic (13.7%), orthopedic (13.0%), and general surgeries (13.0%). Study authors found varied associated risk for postoperative delirium within each surgical specialty. For example, in general surgery, the risk for postoperative delirium with partial mastectomy was low, compared with a mid-level risk in the repair of a recurrent, incarcerated, or strangulated inguinal hernia and a high-level risk in Whipple operations.
The model developed to measure delirium management success in 30 hospitals found that adjusted delirium rates ranged from 3.2% to 27.5%, with eight poor- and five excellent-performing outliers. Authors noted that their model demonstrated good calibration and discrimination. Examination of changes in the Bayesian Information Criteria indicates that as few as 10-12 variables may suffice in building a parsimonious model with “an excellent fit.”
Study authors noted that screening for postoperative delirium in older adults is likely in the best interests of patients. However, they also mentioned that such screening may identify cases of postoperative delirium that were previously unrecognized, resulting in higher rates. In addition, the inclusion of only ACS NSQIP hospitals and the voluntary participation may mean a biased dataset. No one delirium prevention intervention was implemented across the hospitals and so the study doesn’t indicate why some hospitals are more successful than are others. Chart-based identification of patients who have delirium needs further study to assess validity.
Authors concluded that one solution may be to “standardize and consistently employ delirium screening in high-risk patients across hospitals, as has been advocated by a coalition of interdisciplinary experts in geriatric care.”
This project is funded in part by a grant from the John A. Hartford Foundation. The authors declare no conflict of interests.
SOURCE: Berlan JR et al. Ann Surg. 2017 July 24. doi: 10.1097/SLA.0000000000002436
A study suggests that outcome measures, and assessment of hospital performance.
Lead author Julia R. Berian, MD, of the University of Chicago Medical Center and her colleagues wrote, “Postoperative delirium has been associated with mortality, morbidity, prolonged length of stay, and increased costs of care. Furthermore, postoperative delirium may be associated with long-term cognitive and functional decline. However, postoperative delirium has not been incorporated as an outcome measure into major surgical quality registries. Approximately one-third of hospitalized delirium is believed to be preventable, making postoperative delirium an ideal target for surgical quality improvement efforts,” Dr. Berian and her colleagues reported in the Annals of Surgery.
The Geriatric Surgery Pilot data abstractors were instructed to assign postoperative delirium if the medical record words indicating an acute confusional stat such a mental status change, confusion, disorientation, agitation, delirium, and inappropriate behavior. Data were collected from the period 2 hours after surgery to exclude effects of the pharmacologic agents of anesthesia. Delirium status was ascertained as a binary outcome (Yes/No).
Postoperative delirium was observed in 2,427 patients for an average, unadjusted rate of 12.0%. Investigators identified 20 risk factors markedly associated with delirium. The strongest predictors included preoperative cognitive impairment, preoperative use of mobility aid, surrogate consent form, ASA class 4 or greater, age 80 years and older, preoperative sepsis, and fall history within 1 year. Patients with delirium generally were older than patients without delirium were and accounted for a greater proportion of emergency cases. Postoperative hospital length of stay was about 4 days longer on average for patients with delirium, compared with those without delirium.
By specialty, the highest rates of postoperative delirium occurred following cardiothoracic (13.7%), orthopedic (13.0%), and general surgeries (13.0%). Study authors found varied associated risk for postoperative delirium within each surgical specialty. For example, in general surgery, the risk for postoperative delirium with partial mastectomy was low, compared with a mid-level risk in the repair of a recurrent, incarcerated, or strangulated inguinal hernia and a high-level risk in Whipple operations.
The model developed to measure delirium management success in 30 hospitals found that adjusted delirium rates ranged from 3.2% to 27.5%, with eight poor- and five excellent-performing outliers. Authors noted that their model demonstrated good calibration and discrimination. Examination of changes in the Bayesian Information Criteria indicates that as few as 10-12 variables may suffice in building a parsimonious model with “an excellent fit.”
Study authors noted that screening for postoperative delirium in older adults is likely in the best interests of patients. However, they also mentioned that such screening may identify cases of postoperative delirium that were previously unrecognized, resulting in higher rates. In addition, the inclusion of only ACS NSQIP hospitals and the voluntary participation may mean a biased dataset. No one delirium prevention intervention was implemented across the hospitals and so the study doesn’t indicate why some hospitals are more successful than are others. Chart-based identification of patients who have delirium needs further study to assess validity.
Authors concluded that one solution may be to “standardize and consistently employ delirium screening in high-risk patients across hospitals, as has been advocated by a coalition of interdisciplinary experts in geriatric care.”
This project is funded in part by a grant from the John A. Hartford Foundation. The authors declare no conflict of interests.
SOURCE: Berlan JR et al. Ann Surg. 2017 July 24. doi: 10.1097/SLA.0000000000002436
FROM ANNALS OF SURGERY
Key clinical point: Through predictive modeling, the study identified 20 risk factors markedly associated with delirium that can be used to identify high-risk patients.
Major finding: Among the 2,427 patients who experienced delirium, 35% had preoperative cognitive impairment, 30 % had a surrogate sign the consent form, and 32% experienced serious postoperative complications or death.
Study details: An analysis of 2,427 elderly patients at 30 hospitals through data from the ACS NSQIP Geriatric Surgery Pilot Project.
Disclosures: This project is funded in part by a grant from the John A. Hartford Foundation. The authors declare no conflict of interests.
Source: Berian JR et al. Ann Surg. 2017Jul 24. doi: 10.1097/SLA.0000000000002436
The diagnosis and treatment of ureteral injury
A gynecologic surgeon learns very early in his/her career to respect the ureter. Whether from the procedure being performed (endometriosis surgery, hysterectomy, myomectomy for ligamentous fibroids, salpingo-oophorectomy, excision of ovarian remnants, adhesiolysis), blood loss that obscures visualization and must be controlled, or use of energy for cutting, desiccation, and coagulation leading to potential lateral tissue damage, ureteral injury is a well-known complication. Even normal anatomic variations may put some women at greater risk; according to Hurd et al. (Am J Obstet Gynecol. 2001;184:336-9). In a small subset of women, the distance between the cervix and the ureter may be less than 0.5 cm.
As a practicing minimally invasive gynecologic surgeon for the past 30 years, and an early adapter to laparoscopic hysterectomy, I remember quite well the recommendation to always dissect out ureters at time of the procedure. At present, most will agree that selective dissection is safe and thus, more desirable, as bleeding, damage secondary to desiccation, and ureter devascularization with subsequent necrosis are all increased with ureterolysis.
I agree with Dr. Kenton and Dr. Mueller that ureteral stenting has not been shown to significantly decrease ureteral injury rates. Often times, with loss of peristalsis secondary to stent placement, locating the ureter may be even more difficult. Recent advances using lighted stents or indocyanine green, which fluoresces in response to near-infrared laser and can be injected into the ureter via the ureteral catheter tip, are still in the feasibility phase of evaluation and can be costly.
As most urogenital fistulae are secondary to unrecognized injuries at time of surgery, and due to the fact that intraoperative recognition of the injury allows for primary repair, thus, decreasing the rate of secondary surgery and the associated increased morbidity, I recommend cystoscopy to check for ureteral jets (ureteral efflux) be performed when there is concern regarding ureter compromise.
Currently, I utilize a 70° cystoscope to visualize the ureters. While in the past, I have used intravenous indigo carmine, methylene blue, or fluorescein sodium, I currently use Pyridium (phenazopyridine) 200 mg taken by mouth 1 hour prior to the procedure.
Unfortunately, ureteral jetting still may be noted despite partial ligation, laceration, or desiccation of the ureter.
If ureteral injury is not recognized at time of surgery, it can lead to various postoperative symptoms. If there is a ureteral defect, the patient may note profuse wound leakage, increased abdominal fluid, or a urinoma, ileus, fever, peritonitis, or hematuria. With ureteral obstruction, flank or abdominal pain or anuria can be noted; while, with fistula formation, the patient will likely present with urinary incontinence or watery vaginal discharge.
Dr. Miller is a minimally invasive gynecologic surgeon in Naperville, Ill., and a past president of the AAGL.
A gynecologic surgeon learns very early in his/her career to respect the ureter. Whether from the procedure being performed (endometriosis surgery, hysterectomy, myomectomy for ligamentous fibroids, salpingo-oophorectomy, excision of ovarian remnants, adhesiolysis), blood loss that obscures visualization and must be controlled, or use of energy for cutting, desiccation, and coagulation leading to potential lateral tissue damage, ureteral injury is a well-known complication. Even normal anatomic variations may put some women at greater risk; according to Hurd et al. (Am J Obstet Gynecol. 2001;184:336-9). In a small subset of women, the distance between the cervix and the ureter may be less than 0.5 cm.
As a practicing minimally invasive gynecologic surgeon for the past 30 years, and an early adapter to laparoscopic hysterectomy, I remember quite well the recommendation to always dissect out ureters at time of the procedure. At present, most will agree that selective dissection is safe and thus, more desirable, as bleeding, damage secondary to desiccation, and ureter devascularization with subsequent necrosis are all increased with ureterolysis.
I agree with Dr. Kenton and Dr. Mueller that ureteral stenting has not been shown to significantly decrease ureteral injury rates. Often times, with loss of peristalsis secondary to stent placement, locating the ureter may be even more difficult. Recent advances using lighted stents or indocyanine green, which fluoresces in response to near-infrared laser and can be injected into the ureter via the ureteral catheter tip, are still in the feasibility phase of evaluation and can be costly.
As most urogenital fistulae are secondary to unrecognized injuries at time of surgery, and due to the fact that intraoperative recognition of the injury allows for primary repair, thus, decreasing the rate of secondary surgery and the associated increased morbidity, I recommend cystoscopy to check for ureteral jets (ureteral efflux) be performed when there is concern regarding ureter compromise.
Currently, I utilize a 70° cystoscope to visualize the ureters. While in the past, I have used intravenous indigo carmine, methylene blue, or fluorescein sodium, I currently use Pyridium (phenazopyridine) 200 mg taken by mouth 1 hour prior to the procedure.
Unfortunately, ureteral jetting still may be noted despite partial ligation, laceration, or desiccation of the ureter.
If ureteral injury is not recognized at time of surgery, it can lead to various postoperative symptoms. If there is a ureteral defect, the patient may note profuse wound leakage, increased abdominal fluid, or a urinoma, ileus, fever, peritonitis, or hematuria. With ureteral obstruction, flank or abdominal pain or anuria can be noted; while, with fistula formation, the patient will likely present with urinary incontinence or watery vaginal discharge.
Dr. Miller is a minimally invasive gynecologic surgeon in Naperville, Ill., and a past president of the AAGL.
A gynecologic surgeon learns very early in his/her career to respect the ureter. Whether from the procedure being performed (endometriosis surgery, hysterectomy, myomectomy for ligamentous fibroids, salpingo-oophorectomy, excision of ovarian remnants, adhesiolysis), blood loss that obscures visualization and must be controlled, or use of energy for cutting, desiccation, and coagulation leading to potential lateral tissue damage, ureteral injury is a well-known complication. Even normal anatomic variations may put some women at greater risk; according to Hurd et al. (Am J Obstet Gynecol. 2001;184:336-9). In a small subset of women, the distance between the cervix and the ureter may be less than 0.5 cm.
As a practicing minimally invasive gynecologic surgeon for the past 30 years, and an early adapter to laparoscopic hysterectomy, I remember quite well the recommendation to always dissect out ureters at time of the procedure. At present, most will agree that selective dissection is safe and thus, more desirable, as bleeding, damage secondary to desiccation, and ureter devascularization with subsequent necrosis are all increased with ureterolysis.
I agree with Dr. Kenton and Dr. Mueller that ureteral stenting has not been shown to significantly decrease ureteral injury rates. Often times, with loss of peristalsis secondary to stent placement, locating the ureter may be even more difficult. Recent advances using lighted stents or indocyanine green, which fluoresces in response to near-infrared laser and can be injected into the ureter via the ureteral catheter tip, are still in the feasibility phase of evaluation and can be costly.
As most urogenital fistulae are secondary to unrecognized injuries at time of surgery, and due to the fact that intraoperative recognition of the injury allows for primary repair, thus, decreasing the rate of secondary surgery and the associated increased morbidity, I recommend cystoscopy to check for ureteral jets (ureteral efflux) be performed when there is concern regarding ureter compromise.
Currently, I utilize a 70° cystoscope to visualize the ureters. While in the past, I have used intravenous indigo carmine, methylene blue, or fluorescein sodium, I currently use Pyridium (phenazopyridine) 200 mg taken by mouth 1 hour prior to the procedure.
Unfortunately, ureteral jetting still may be noted despite partial ligation, laceration, or desiccation of the ureter.
If ureteral injury is not recognized at time of surgery, it can lead to various postoperative symptoms. If there is a ureteral defect, the patient may note profuse wound leakage, increased abdominal fluid, or a urinoma, ileus, fever, peritonitis, or hematuria. With ureteral obstruction, flank or abdominal pain or anuria can be noted; while, with fistula formation, the patient will likely present with urinary incontinence or watery vaginal discharge.
Dr. Miller is a minimally invasive gynecologic surgeon in Naperville, Ill., and a past president of the AAGL.
MDR Candida auris is on the move
MADRID – The anticipated global emergence of multidrug resistant Candida auris is now an established fact, but a case study presented at the European Society of Clinical Microbiology and Infectious Diseases annual congress demonstrates just how devastating an outbreak can be to a medical facility and its surgical ICU patients.
The dangerous invasive infection is spreading through Asia, Europe, and the Americas, causing potentially fatal candidemias and proving devilishly difficult to eradicate in health care facilities once it becomes established.
Several multidrug resistant (MDR) C. auris outbreaks were reported at the ECCMID meeting. Most troubling: a continuing outbreak in a hospital in Valencia, Spain, in which 17 patients have died – a 41% fatality rate among those who developed a fulminant C. auris candidemia, Javier Pemán, MD, said at the meeting. The strain appeared to be a clonal population not previously identified in published reports.
“C. auris is hard to remove from the hospital environment,” once it becomes established, said Dr. Pemán of La Fe University and Polytechnic Hospital, Valencia. “When an outbreak lasts for months, as ours has, it is difficult, but necessary, to maintain control measures, identify it early in the lab, and isolate and treat patients early with combination therapy.”
He and his team have relied primarily on a combination of amphotericin B and echinocandin (AMB+ECN), although, he added, the optimal dosing and treatment time aren’t known, and many C. auris isolates are echinocandin resistant.
MDR C. auris first appearedin Tokyo in 2009. It then spread to South Korea around 2011, and then appeared across Asia and Western Europe. Its first appearance in Spain was the 2016 Le Fe outbreak.
According to the Centers for Disease Control and Prevention, single cases have appeared in Austria, Belgium, Malaysia, Norway, and the United Arab Emirates. Canada, Colombia, France, Germany, India, Israel, Japan, Kenya, Kuwait, Oman, Pakistan, Panama, South Korea, South Africa, Spain, the United Arab Emirates, the United Kingdom, and Venezuela have experienced multiple outbreaks.
The CDC has recorded 257 confirmed and 30 probable cases of MDR C. auris in the United States as of March 31, 2018. Most of these occurred in New York City and New Jersey; a number of patients had recent stays in hospitals in India, Pakistan, South Africa, the UAE, and Venezuela.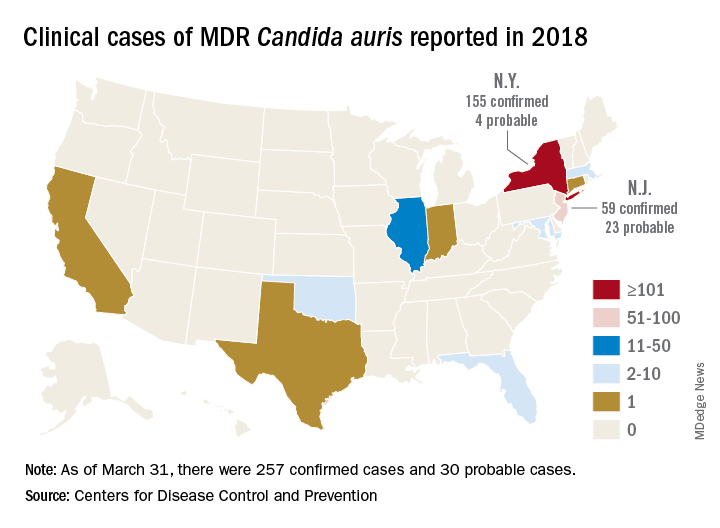
Jacques Meis, MD, of the department of medical microbiology and infectious diseases at Canisius Wilhelmina Hospital, Nijmegen, the Netherlands, set the stage for an extended discussion of C. auris at the meeting.
“This is a multidrug resistant yeast that has emerged in the last decade. Some rare isolates are resistant to all three major antifungal classes. Unlike other Candida species, it seems to persist for prolonged periods in health care environments and to colonize patients’ skin. It behaves rather like resistant bacteria.”
Once established in a health care setting – often an intensive care ward – C. auris poses major infection controls challenges and can be very hard to identify and eradicate, said Dr. Meis.
The identification problem is well known. The 2016 CDC alert noted that “commercially available biochemical-based tests, including API strips and VITEK-2, used in many U.S. laboratories to identify fungi, cannot differentiate C. auris from related species. Because of these challenges, clinical laboratories have misidentified the organism as C. haemulonii and Saccharomyces cerevisiae.”
“It’s often misidentified as other Candida species or as Saccharomyces when we investigate with biochemical methods. C. auris is best identified using Matrix Assisted Laser Desorption/Ionization time of flight mass spectrometry (MALDI-TOF),” said Dr. Meis.
Among the presentations at ECCMID were a report of a U.K. outbreak that affected 70 patients in a neuroscience ICU. It was traced to axillary skin-surface temperature probes, and eradicated only after those probes were removed. More than 90% of the isolates were resistant to fluconazole, voriconazole, and posaconazole; 18% were amphotericin resistant.
A poster described the microbiological characteristics of 50 C. auris isolates taken from 11 hospitals in Korea.
Dr. Pemán described the outbreak in Valencia, which began in April 2016; the report was simultaneously published in the online journal Mycoses (2018 Apr 14. doi: 10.1111/myc.12781).
The index case was a 66-year-old man with hepatocellular carcinoma who underwent a liver resection at Hospital Le Fe in April 2016. During his stay in the surgical ICU (SICU), he developed a fungal infection from an unknown, highly fluconazole-resistant yeast. The pathogen was twice misidentified, first as C. haemulonii and then as S. cerevisiae.
Three weeks later, the patient in the adjacent bed developed a similar infection. Sequencing of the internal transcribed spacer confirmed both as a Candida isolate – an organism previously unknown in Spain.
The SICU setup was apparently very conducive to the C. auris life cycle, Dr. Pemán said. It’s a relatively open ward divided into three rooms with 12 beds in each. There are no isolation beds, and dozens of workers have access to the ward every day, including clinical and cleaning staff.
After identifying the second isolate, Dr. Pemán said, infection control staff went into action. They instituted contact precautions in the SICU, and took regular cultures from newly admitted patients and cultures of every SICU patient every 7 days.
“We also started an intense search for more cases throughout the hospital and in 101 SICU workers. Of 305 samples from hands and ears, we found nothing.” They reviewed all the prior fluconazole-resistant Candida isolates; C. auris was not present in the hospital before the index case.
Three weeks after case 2, six new SICU patients tested positive for C. auris (two blood cultures, one vascular line, one respiratory specimen, two rectal swabs, and one urinary tract sample).
“We reinforced contact precautions in colonized and infected patients and started a twice-daily environmental cleaning practice with quaternary ammonium around them,” said Dr. Pemán. They instituted a proactive hospital-wide hand hygiene campaign and spread the word about the outbreak.
By July, there were 11 new colonized patients, 3 of whom developed candidemia. These patients were grouped in the same SICU ward and underwent daily skin treatments with 4% aqueous chlorhexidine wipes.
The environmental inspection found C. auris on beds, tables, walls, and the floor all around infected patients. The pathogen also was living on IV pumps, computer keyboards, and bedside tables. Blood pressure cuffs were a favorite haunt: 19 of 36 samples in the adjacent ICU were positive. These data were separately reported at ECCMID.
Despite all of these efforts at eradication, infections continued to rise. By November, there were 24 newly colonized patients and nine new candidemia episodes in SICU and regular ICU patients. In December, a new infection control bundle began: A surveillance nurse in the C. auris SICU ward was in charge of compliance; any patient with any yeast growth in culture was isolated, and staff used 2% alcohol chlorhexidine wipes before and after IV catheter handling. Staff also washed down all surfaces three times daily with a disinfectant.
Patients could leave isolation after three consecutive C. auris–negative cultures. After discharge, an ultraviolet light decontamination procedure disinfected each patient room.
The pathogen was almost unbelievably resilient, Dr. Pemán noted in the Mycoses article. “In some cases, C. auris was recovered from walls after cleaning with cationic surface–active products ... it was not known until very recently that these products, as well as quaternary ammonium disinfectants, cannot effectively remove C. auris from surfaces.”
As a result of the previous measures, the outbreak slowed down during December 2016, with two new candidemia cases, but by February, the outbreak resumed with 50 new cases and 18 candidemias detected. Cases continued to emerge throughout 2017.
By September 2017, 250 patients had been colonized; 116 of these were included in the Mycoses report. There were 30 episodes of candidemia (26%); of these, 17 died by 30 days (41.4%). Spondylodiscitis and endocarditis each developed in two patients and one developed ventriculitis.
A separate poster by Dr. Pemán and his colleagues gave more details:
• A 52-year-old woman with C. auris–induced endocarditis died after 4 weeks of treatment with AMB+ECN and flucytosine. She had undergone a prosthetic heart valve placement for Ebstein’s anomaly.
• A 71-year-old man with hydrocephalus developed a C. auris–induced infection of his ventriculoperitoneal shunt; he also had undergone cardiovascular surgery and had an ischemic cardiomyopathy. He died despite shunt removal and 8 weeks of AMB+ECN.
• A 71-year-old man who underwent cardiovascular surgery and received a prosthetic heart valve developed endocarditis. He is alive and at last report, on week 26 of AMB+ECN, flucytosine, and isavuconazole.
• A 68-year-old man who underwent abdominal surgery for hepatocellular carcinoma developed spondylodiscitis and is alive after 24 weeks of AMB+ECN.
• A 48-year old female multiple trauma patient developed spondylodiscitis and is alive after 48 weeks of treatment with AMB+ECN.
A multivariate analysis determined that antibacterial treatment increased the risk of candidemia by almost 30 times (odds ratio, 29.59). The next highest risk was neutropenia (OR, 20.7) and then simply being a hospital and SICU patient. Dr. Pemán’s poster said, “In the 16 months before the index case, La Fe recorded 89 candidemias, none caused by C. auris. In the 16 months afterward, there were 154 candidemias, largely C. auris. Before April 2016, C. parapsilosis accounted for the largest portion of candidemias (46%) followed by C. albicans. After the index case, C. auris accounted for 42%, followed by C. parapsilosis (21%) and C. albicans (18%).”
Because of its fluconazole resistance, patients with C. auris received a combined antifungal treatment of liposomal amphotericin B 3 mg/kg per day for 5 days, and a standard dose of echinocandin for 3 weeks. Many C. auris strains are echinocandin resistant, Dr. Pemán noted. This particular strain was clonal, different from any other previously reported, he said.
“Our results confirm those previously reported by other authors, that C. auris is grouped in different independent clusters according to its geographical origin. Although all Spanish isolates were genotypically distinct from Indian, Omani, U.K., and Venezuelan isolates, there seems to be some connection with South African isolates.”
Hospital Le Fe continues to struggle with C. auris. As of March, 335 patients have tested positive for the pathogen, and 80 have developed candidemias.
“We feel we may be approaching the end of this episode, but it’s really not possible to be sure,” he said.
Dr. Pemán had no relevant financial disclosures.
SOURCE: ECCMID 2018 Peman et al. S0067.
MADRID – The anticipated global emergence of multidrug resistant Candida auris is now an established fact, but a case study presented at the European Society of Clinical Microbiology and Infectious Diseases annual congress demonstrates just how devastating an outbreak can be to a medical facility and its surgical ICU patients.
The dangerous invasive infection is spreading through Asia, Europe, and the Americas, causing potentially fatal candidemias and proving devilishly difficult to eradicate in health care facilities once it becomes established.
Several multidrug resistant (MDR) C. auris outbreaks were reported at the ECCMID meeting. Most troubling: a continuing outbreak in a hospital in Valencia, Spain, in which 17 patients have died – a 41% fatality rate among those who developed a fulminant C. auris candidemia, Javier Pemán, MD, said at the meeting. The strain appeared to be a clonal population not previously identified in published reports.
“C. auris is hard to remove from the hospital environment,” once it becomes established, said Dr. Pemán of La Fe University and Polytechnic Hospital, Valencia. “When an outbreak lasts for months, as ours has, it is difficult, but necessary, to maintain control measures, identify it early in the lab, and isolate and treat patients early with combination therapy.”
He and his team have relied primarily on a combination of amphotericin B and echinocandin (AMB+ECN), although, he added, the optimal dosing and treatment time aren’t known, and many C. auris isolates are echinocandin resistant.
MDR C. auris first appearedin Tokyo in 2009. It then spread to South Korea around 2011, and then appeared across Asia and Western Europe. Its first appearance in Spain was the 2016 Le Fe outbreak.
According to the Centers for Disease Control and Prevention, single cases have appeared in Austria, Belgium, Malaysia, Norway, and the United Arab Emirates. Canada, Colombia, France, Germany, India, Israel, Japan, Kenya, Kuwait, Oman, Pakistan, Panama, South Korea, South Africa, Spain, the United Arab Emirates, the United Kingdom, and Venezuela have experienced multiple outbreaks.
The CDC has recorded 257 confirmed and 30 probable cases of MDR C. auris in the United States as of March 31, 2018. Most of these occurred in New York City and New Jersey; a number of patients had recent stays in hospitals in India, Pakistan, South Africa, the UAE, and Venezuela.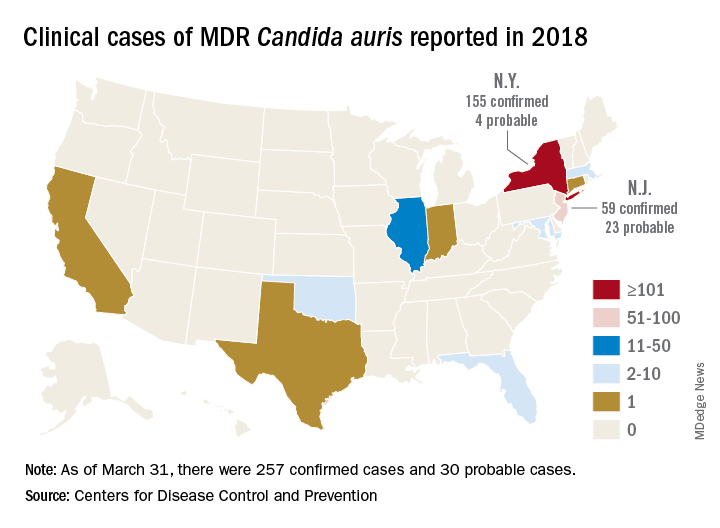
Jacques Meis, MD, of the department of medical microbiology and infectious diseases at Canisius Wilhelmina Hospital, Nijmegen, the Netherlands, set the stage for an extended discussion of C. auris at the meeting.
“This is a multidrug resistant yeast that has emerged in the last decade. Some rare isolates are resistant to all three major antifungal classes. Unlike other Candida species, it seems to persist for prolonged periods in health care environments and to colonize patients’ skin. It behaves rather like resistant bacteria.”
Once established in a health care setting – often an intensive care ward – C. auris poses major infection controls challenges and can be very hard to identify and eradicate, said Dr. Meis.
The identification problem is well known. The 2016 CDC alert noted that “commercially available biochemical-based tests, including API strips and VITEK-2, used in many U.S. laboratories to identify fungi, cannot differentiate C. auris from related species. Because of these challenges, clinical laboratories have misidentified the organism as C. haemulonii and Saccharomyces cerevisiae.”
“It’s often misidentified as other Candida species or as Saccharomyces when we investigate with biochemical methods. C. auris is best identified using Matrix Assisted Laser Desorption/Ionization time of flight mass spectrometry (MALDI-TOF),” said Dr. Meis.
Among the presentations at ECCMID were a report of a U.K. outbreak that affected 70 patients in a neuroscience ICU. It was traced to axillary skin-surface temperature probes, and eradicated only after those probes were removed. More than 90% of the isolates were resistant to fluconazole, voriconazole, and posaconazole; 18% were amphotericin resistant.
A poster described the microbiological characteristics of 50 C. auris isolates taken from 11 hospitals in Korea.
Dr. Pemán described the outbreak in Valencia, which began in April 2016; the report was simultaneously published in the online journal Mycoses (2018 Apr 14. doi: 10.1111/myc.12781).
The index case was a 66-year-old man with hepatocellular carcinoma who underwent a liver resection at Hospital Le Fe in April 2016. During his stay in the surgical ICU (SICU), he developed a fungal infection from an unknown, highly fluconazole-resistant yeast. The pathogen was twice misidentified, first as C. haemulonii and then as S. cerevisiae.
Three weeks later, the patient in the adjacent bed developed a similar infection. Sequencing of the internal transcribed spacer confirmed both as a Candida isolate – an organism previously unknown in Spain.
The SICU setup was apparently very conducive to the C. auris life cycle, Dr. Pemán said. It’s a relatively open ward divided into three rooms with 12 beds in each. There are no isolation beds, and dozens of workers have access to the ward every day, including clinical and cleaning staff.
After identifying the second isolate, Dr. Pemán said, infection control staff went into action. They instituted contact precautions in the SICU, and took regular cultures from newly admitted patients and cultures of every SICU patient every 7 days.
“We also started an intense search for more cases throughout the hospital and in 101 SICU workers. Of 305 samples from hands and ears, we found nothing.” They reviewed all the prior fluconazole-resistant Candida isolates; C. auris was not present in the hospital before the index case.
Three weeks after case 2, six new SICU patients tested positive for C. auris (two blood cultures, one vascular line, one respiratory specimen, two rectal swabs, and one urinary tract sample).
“We reinforced contact precautions in colonized and infected patients and started a twice-daily environmental cleaning practice with quaternary ammonium around them,” said Dr. Pemán. They instituted a proactive hospital-wide hand hygiene campaign and spread the word about the outbreak.
By July, there were 11 new colonized patients, 3 of whom developed candidemia. These patients were grouped in the same SICU ward and underwent daily skin treatments with 4% aqueous chlorhexidine wipes.
The environmental inspection found C. auris on beds, tables, walls, and the floor all around infected patients. The pathogen also was living on IV pumps, computer keyboards, and bedside tables. Blood pressure cuffs were a favorite haunt: 19 of 36 samples in the adjacent ICU were positive. These data were separately reported at ECCMID.
Despite all of these efforts at eradication, infections continued to rise. By November, there were 24 newly colonized patients and nine new candidemia episodes in SICU and regular ICU patients. In December, a new infection control bundle began: A surveillance nurse in the C. auris SICU ward was in charge of compliance; any patient with any yeast growth in culture was isolated, and staff used 2% alcohol chlorhexidine wipes before and after IV catheter handling. Staff also washed down all surfaces three times daily with a disinfectant.
Patients could leave isolation after three consecutive C. auris–negative cultures. After discharge, an ultraviolet light decontamination procedure disinfected each patient room.
The pathogen was almost unbelievably resilient, Dr. Pemán noted in the Mycoses article. “In some cases, C. auris was recovered from walls after cleaning with cationic surface–active products ... it was not known until very recently that these products, as well as quaternary ammonium disinfectants, cannot effectively remove C. auris from surfaces.”
As a result of the previous measures, the outbreak slowed down during December 2016, with two new candidemia cases, but by February, the outbreak resumed with 50 new cases and 18 candidemias detected. Cases continued to emerge throughout 2017.
By September 2017, 250 patients had been colonized; 116 of these were included in the Mycoses report. There were 30 episodes of candidemia (26%); of these, 17 died by 30 days (41.4%). Spondylodiscitis and endocarditis each developed in two patients and one developed ventriculitis.
A separate poster by Dr. Pemán and his colleagues gave more details:
• A 52-year-old woman with C. auris–induced endocarditis died after 4 weeks of treatment with AMB+ECN and flucytosine. She had undergone a prosthetic heart valve placement for Ebstein’s anomaly.
• A 71-year-old man with hydrocephalus developed a C. auris–induced infection of his ventriculoperitoneal shunt; he also had undergone cardiovascular surgery and had an ischemic cardiomyopathy. He died despite shunt removal and 8 weeks of AMB+ECN.
• A 71-year-old man who underwent cardiovascular surgery and received a prosthetic heart valve developed endocarditis. He is alive and at last report, on week 26 of AMB+ECN, flucytosine, and isavuconazole.
• A 68-year-old man who underwent abdominal surgery for hepatocellular carcinoma developed spondylodiscitis and is alive after 24 weeks of AMB+ECN.
• A 48-year old female multiple trauma patient developed spondylodiscitis and is alive after 48 weeks of treatment with AMB+ECN.
A multivariate analysis determined that antibacterial treatment increased the risk of candidemia by almost 30 times (odds ratio, 29.59). The next highest risk was neutropenia (OR, 20.7) and then simply being a hospital and SICU patient. Dr. Pemán’s poster said, “In the 16 months before the index case, La Fe recorded 89 candidemias, none caused by C. auris. In the 16 months afterward, there were 154 candidemias, largely C. auris. Before April 2016, C. parapsilosis accounted for the largest portion of candidemias (46%) followed by C. albicans. After the index case, C. auris accounted for 42%, followed by C. parapsilosis (21%) and C. albicans (18%).”
Because of its fluconazole resistance, patients with C. auris received a combined antifungal treatment of liposomal amphotericin B 3 mg/kg per day for 5 days, and a standard dose of echinocandin for 3 weeks. Many C. auris strains are echinocandin resistant, Dr. Pemán noted. This particular strain was clonal, different from any other previously reported, he said.
“Our results confirm those previously reported by other authors, that C. auris is grouped in different independent clusters according to its geographical origin. Although all Spanish isolates were genotypically distinct from Indian, Omani, U.K., and Venezuelan isolates, there seems to be some connection with South African isolates.”
Hospital Le Fe continues to struggle with C. auris. As of March, 335 patients have tested positive for the pathogen, and 80 have developed candidemias.
“We feel we may be approaching the end of this episode, but it’s really not possible to be sure,” he said.
Dr. Pemán had no relevant financial disclosures.
SOURCE: ECCMID 2018 Peman et al. S0067.
MADRID – The anticipated global emergence of multidrug resistant Candida auris is now an established fact, but a case study presented at the European Society of Clinical Microbiology and Infectious Diseases annual congress demonstrates just how devastating an outbreak can be to a medical facility and its surgical ICU patients.
The dangerous invasive infection is spreading through Asia, Europe, and the Americas, causing potentially fatal candidemias and proving devilishly difficult to eradicate in health care facilities once it becomes established.
Several multidrug resistant (MDR) C. auris outbreaks were reported at the ECCMID meeting. Most troubling: a continuing outbreak in a hospital in Valencia, Spain, in which 17 patients have died – a 41% fatality rate among those who developed a fulminant C. auris candidemia, Javier Pemán, MD, said at the meeting. The strain appeared to be a clonal population not previously identified in published reports.
“C. auris is hard to remove from the hospital environment,” once it becomes established, said Dr. Pemán of La Fe University and Polytechnic Hospital, Valencia. “When an outbreak lasts for months, as ours has, it is difficult, but necessary, to maintain control measures, identify it early in the lab, and isolate and treat patients early with combination therapy.”
He and his team have relied primarily on a combination of amphotericin B and echinocandin (AMB+ECN), although, he added, the optimal dosing and treatment time aren’t known, and many C. auris isolates are echinocandin resistant.
MDR C. auris first appearedin Tokyo in 2009. It then spread to South Korea around 2011, and then appeared across Asia and Western Europe. Its first appearance in Spain was the 2016 Le Fe outbreak.
According to the Centers for Disease Control and Prevention, single cases have appeared in Austria, Belgium, Malaysia, Norway, and the United Arab Emirates. Canada, Colombia, France, Germany, India, Israel, Japan, Kenya, Kuwait, Oman, Pakistan, Panama, South Korea, South Africa, Spain, the United Arab Emirates, the United Kingdom, and Venezuela have experienced multiple outbreaks.
The CDC has recorded 257 confirmed and 30 probable cases of MDR C. auris in the United States as of March 31, 2018. Most of these occurred in New York City and New Jersey; a number of patients had recent stays in hospitals in India, Pakistan, South Africa, the UAE, and Venezuela.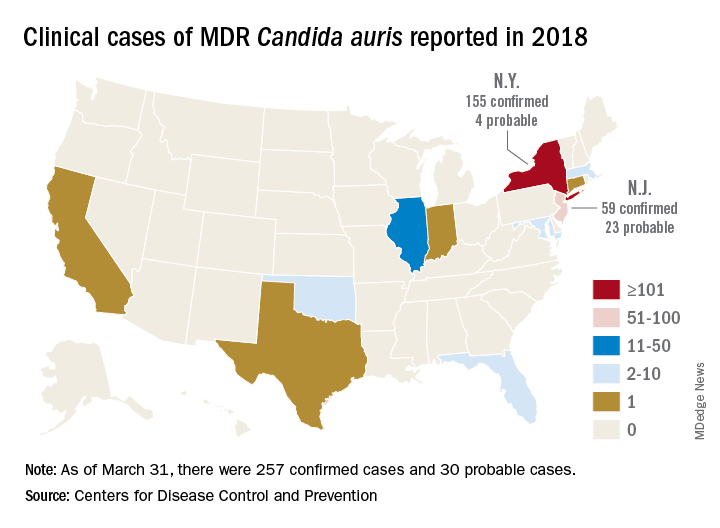
Jacques Meis, MD, of the department of medical microbiology and infectious diseases at Canisius Wilhelmina Hospital, Nijmegen, the Netherlands, set the stage for an extended discussion of C. auris at the meeting.
“This is a multidrug resistant yeast that has emerged in the last decade. Some rare isolates are resistant to all three major antifungal classes. Unlike other Candida species, it seems to persist for prolonged periods in health care environments and to colonize patients’ skin. It behaves rather like resistant bacteria.”
Once established in a health care setting – often an intensive care ward – C. auris poses major infection controls challenges and can be very hard to identify and eradicate, said Dr. Meis.
The identification problem is well known. The 2016 CDC alert noted that “commercially available biochemical-based tests, including API strips and VITEK-2, used in many U.S. laboratories to identify fungi, cannot differentiate C. auris from related species. Because of these challenges, clinical laboratories have misidentified the organism as C. haemulonii and Saccharomyces cerevisiae.”
“It’s often misidentified as other Candida species or as Saccharomyces when we investigate with biochemical methods. C. auris is best identified using Matrix Assisted Laser Desorption/Ionization time of flight mass spectrometry (MALDI-TOF),” said Dr. Meis.
Among the presentations at ECCMID were a report of a U.K. outbreak that affected 70 patients in a neuroscience ICU. It was traced to axillary skin-surface temperature probes, and eradicated only after those probes were removed. More than 90% of the isolates were resistant to fluconazole, voriconazole, and posaconazole; 18% were amphotericin resistant.
A poster described the microbiological characteristics of 50 C. auris isolates taken from 11 hospitals in Korea.
Dr. Pemán described the outbreak in Valencia, which began in April 2016; the report was simultaneously published in the online journal Mycoses (2018 Apr 14. doi: 10.1111/myc.12781).
The index case was a 66-year-old man with hepatocellular carcinoma who underwent a liver resection at Hospital Le Fe in April 2016. During his stay in the surgical ICU (SICU), he developed a fungal infection from an unknown, highly fluconazole-resistant yeast. The pathogen was twice misidentified, first as C. haemulonii and then as S. cerevisiae.
Three weeks later, the patient in the adjacent bed developed a similar infection. Sequencing of the internal transcribed spacer confirmed both as a Candida isolate – an organism previously unknown in Spain.
The SICU setup was apparently very conducive to the C. auris life cycle, Dr. Pemán said. It’s a relatively open ward divided into three rooms with 12 beds in each. There are no isolation beds, and dozens of workers have access to the ward every day, including clinical and cleaning staff.
After identifying the second isolate, Dr. Pemán said, infection control staff went into action. They instituted contact precautions in the SICU, and took regular cultures from newly admitted patients and cultures of every SICU patient every 7 days.
“We also started an intense search for more cases throughout the hospital and in 101 SICU workers. Of 305 samples from hands and ears, we found nothing.” They reviewed all the prior fluconazole-resistant Candida isolates; C. auris was not present in the hospital before the index case.
Three weeks after case 2, six new SICU patients tested positive for C. auris (two blood cultures, one vascular line, one respiratory specimen, two rectal swabs, and one urinary tract sample).
“We reinforced contact precautions in colonized and infected patients and started a twice-daily environmental cleaning practice with quaternary ammonium around them,” said Dr. Pemán. They instituted a proactive hospital-wide hand hygiene campaign and spread the word about the outbreak.
By July, there were 11 new colonized patients, 3 of whom developed candidemia. These patients were grouped in the same SICU ward and underwent daily skin treatments with 4% aqueous chlorhexidine wipes.
The environmental inspection found C. auris on beds, tables, walls, and the floor all around infected patients. The pathogen also was living on IV pumps, computer keyboards, and bedside tables. Blood pressure cuffs were a favorite haunt: 19 of 36 samples in the adjacent ICU were positive. These data were separately reported at ECCMID.
Despite all of these efforts at eradication, infections continued to rise. By November, there were 24 newly colonized patients and nine new candidemia episodes in SICU and regular ICU patients. In December, a new infection control bundle began: A surveillance nurse in the C. auris SICU ward was in charge of compliance; any patient with any yeast growth in culture was isolated, and staff used 2% alcohol chlorhexidine wipes before and after IV catheter handling. Staff also washed down all surfaces three times daily with a disinfectant.
Patients could leave isolation after three consecutive C. auris–negative cultures. After discharge, an ultraviolet light decontamination procedure disinfected each patient room.
The pathogen was almost unbelievably resilient, Dr. Pemán noted in the Mycoses article. “In some cases, C. auris was recovered from walls after cleaning with cationic surface–active products ... it was not known until very recently that these products, as well as quaternary ammonium disinfectants, cannot effectively remove C. auris from surfaces.”
As a result of the previous measures, the outbreak slowed down during December 2016, with two new candidemia cases, but by February, the outbreak resumed with 50 new cases and 18 candidemias detected. Cases continued to emerge throughout 2017.
By September 2017, 250 patients had been colonized; 116 of these were included in the Mycoses report. There were 30 episodes of candidemia (26%); of these, 17 died by 30 days (41.4%). Spondylodiscitis and endocarditis each developed in two patients and one developed ventriculitis.
A separate poster by Dr. Pemán and his colleagues gave more details:
• A 52-year-old woman with C. auris–induced endocarditis died after 4 weeks of treatment with AMB+ECN and flucytosine. She had undergone a prosthetic heart valve placement for Ebstein’s anomaly.
• A 71-year-old man with hydrocephalus developed a C. auris–induced infection of his ventriculoperitoneal shunt; he also had undergone cardiovascular surgery and had an ischemic cardiomyopathy. He died despite shunt removal and 8 weeks of AMB+ECN.
• A 71-year-old man who underwent cardiovascular surgery and received a prosthetic heart valve developed endocarditis. He is alive and at last report, on week 26 of AMB+ECN, flucytosine, and isavuconazole.
• A 68-year-old man who underwent abdominal surgery for hepatocellular carcinoma developed spondylodiscitis and is alive after 24 weeks of AMB+ECN.
• A 48-year old female multiple trauma patient developed spondylodiscitis and is alive after 48 weeks of treatment with AMB+ECN.
A multivariate analysis determined that antibacterial treatment increased the risk of candidemia by almost 30 times (odds ratio, 29.59). The next highest risk was neutropenia (OR, 20.7) and then simply being a hospital and SICU patient. Dr. Pemán’s poster said, “In the 16 months before the index case, La Fe recorded 89 candidemias, none caused by C. auris. In the 16 months afterward, there were 154 candidemias, largely C. auris. Before April 2016, C. parapsilosis accounted for the largest portion of candidemias (46%) followed by C. albicans. After the index case, C. auris accounted for 42%, followed by C. parapsilosis (21%) and C. albicans (18%).”
Because of its fluconazole resistance, patients with C. auris received a combined antifungal treatment of liposomal amphotericin B 3 mg/kg per day for 5 days, and a standard dose of echinocandin for 3 weeks. Many C. auris strains are echinocandin resistant, Dr. Pemán noted. This particular strain was clonal, different from any other previously reported, he said.
“Our results confirm those previously reported by other authors, that C. auris is grouped in different independent clusters according to its geographical origin. Although all Spanish isolates were genotypically distinct from Indian, Omani, U.K., and Venezuelan isolates, there seems to be some connection with South African isolates.”
Hospital Le Fe continues to struggle with C. auris. As of March, 335 patients have tested positive for the pathogen, and 80 have developed candidemias.
“We feel we may be approaching the end of this episode, but it’s really not possible to be sure,” he said.
Dr. Pemán had no relevant financial disclosures.
SOURCE: ECCMID 2018 Peman et al. S0067.
REPORTING FROM ECCMID 2018
Drugmakers blamed for blocking generics have cost U.S. billions
Makers of brand-name drugs called out by the Trump administration for potentially stalling generic competition have hiked their prices by double-digit percentages since 2012 and cost Medicare and Medicaid nearly $12 billion in 2016, a Kaiser Health News analysis has found.
As part of President Donald Trump’s promise to curb high drug prices, the Food and Drug Administration posted a list of pharmaceutical companies that makers of generics allege refused to let them buy the drug samples needed to develop their products. For approval, the FDA requires so-called bioequivalence testing using samples to demonstrate that generics are the same as their branded counterparts.
The analysis shows that drug companies that may have engaged in what FDA Commissioner Scott Gottlieb, MD, called “shenanigans” to delay the entrance of cheaper competitors onto the market have indeed raised prices and cost taxpayers more money over time.
The FDA listed more than 50 drugs whose manufacturers have withheld or refused to sell samples and cited 164 inquiries for help obtaining them. Thirteen of these pleas from makers of generics pertained to Celgene’s blockbuster cancer drug Revlimid (lenalidomide), which accounted for 63% of Celgene’s revenue in the first quarter of 2018, according to a company press release.
The brand-name drug companies “wouldn’t put so much effort into fighting off competition if these weren’t [such] lucrative sources of revenue,” said Ameet Sarpatwari, JD, PhD, of Harvard Medical School in Boston. “In the case of a blockbuster drug, that can be hundreds of millions of dollars of revenue for the brand-name drugs and almost the same cost to the health care system.”
Indeed, a KHN analysis found that 47 of the drugs cost Medicare and Medicaid almost $12 billion in 2016. The spending totals don’t include rebates, which drugmakers return to the government after paying for the drugs upfront but are not public. The rebates ranged from 9.5% to 26.3% for Medicare Part D in 2014, the most recent year that data are available.
The remaining drugs do not appear in the Medicare and Medicaid data.
By delaying development of generics, drugmakers can maintain their monopolies and keep prices high. Most of the drugs cost Medicare Part D more in 2016 than they did in 2012, for an average spending increase of about 60% more per unit. This excludes drugs that don’t appear in the 2012 Medicare Part D data.
Revlimid cost Medicare Part D $2.7 billion in 2016, trailing only Harvoni (ledipasvir and sofosbuvir), which treats hepatitis C and is not on the FDA’s new list. The cost of Revlimid, which faces no competition from generics, has jumped 40% per unit in just 4 years, the Medicare data show, and cost $75,200/beneficiary in 2016.
Some drugs on the FDA’s list, including Celgene’s, are part of a safety program that can require restricted distribution of brand-name drugs that have serious risks or addictive qualities. Drugmakers with products in the safety program sometimes say they can’t provide samples unless the generics manufacturer jumps through a series of hoops “that generic companies find hard or impossible to comply with,” Dr. Gottlieb said in a statement.
The Department of Health & Human Services Office of Inspector General issued a report in 2013 that said the FDA couldn’t prove that the program actually improved safety, and Dr. Sarpatwari said there’s evidence drugmakers are abusing it to stave off competition from generics.
Dr. Gottlieb said the FDA will be notifying the Federal Trade Commission about pleas for help from would-be generics manufacturers about obtaining samples, and he encouraged the manufacturers to do the same if they suspect they’re being thwarted by anticompetitive practices.
Celgene spokesman Greg Geissman said the company has sold samples to generics manufacturers and will continue to do so. He stressed maintaining a balance of innovation, generic competition, and safety.
“Even a single dose of thalidomide, the active ingredient in Thalomid, can cause irreversible, debilitating birth defects if not properly handled and dispensed. Revlimid and Pomalyst (pomalidomide) are believed to have similar risks,” Mr. Geissman said.
The highest number of pleas for help related to Actelion Pharmaceuticals’ pulmonary hypertension drug Tracleer (bosentan). In 2016, that drug cost Medicare $90,700/patient and more than $304 million overall. Meanwhile, spending per unit jumped 52% from 2012 through 2016.
Actelion was acquired by Johnson & Johnson’s pharmaceutical arm, Janssen, in 2017.
Actelion spokeswoman Colleen Wilson said that the company “cooperate[s]” with makers of generic drugs and “has responded to all requests it has received directly from generic manufacturers seeking access to its medications for bioequivalence testing.”
PhRMA, the trade group for makers of brand-name pharmaceuticals, said the FDA’s list was somewhat unfair because it lacked context and responses from those it represents.
“While we must continue to foster a competitive marketplace, PhRMA is concerned that FDA’s release of the ‘inquiries’ it has received lacks proper context and conflates a number of divergent scenarios,” said PhRMA spokesman Andrew Powaleny.
Congress is considering the CREATES Act, which stands for “Creating and Restoring Equal Access to Equivalent Samples” and would foster competition in part by allowing generics manufacturers to sue brand-name drug manufacturers to compel them to provide samples.
The bill’s sponsor, Sen. Patrick Leahy (D-Vt.), said more transparency from the FDA is helpful, but more work from the agency is needed to end the anticompetitive tactics. “With billions of dollars at stake, a database alone will not stop this behavior,” Sen. Leahy said.
Cosponsor Sen. Chuck Grassley (R-Iowa), chairman of the Judiciary Committee, expressed similar sentiments, telling KHN: “The CREATES Act is necessary because it would serve as a strong deterrent to pharmaceutical companies that engage in anticompetitive practices to keep low-cost generic drugs off the market.”
The FDA hasn’t come out in support of CREATES. “They should know that this is going to require a legislative solution,” Dr. Sarpatwari said. “Why are they not stepping into this arena and saying that?”
KHN’s coverage of prescription drug development, costs and pricing is supported by the Laura and John Arnold Foundation. Kaiser Health News (hyperlink to khn.org) is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Makers of brand-name drugs called out by the Trump administration for potentially stalling generic competition have hiked their prices by double-digit percentages since 2012 and cost Medicare and Medicaid nearly $12 billion in 2016, a Kaiser Health News analysis has found.
As part of President Donald Trump’s promise to curb high drug prices, the Food and Drug Administration posted a list of pharmaceutical companies that makers of generics allege refused to let them buy the drug samples needed to develop their products. For approval, the FDA requires so-called bioequivalence testing using samples to demonstrate that generics are the same as their branded counterparts.
The analysis shows that drug companies that may have engaged in what FDA Commissioner Scott Gottlieb, MD, called “shenanigans” to delay the entrance of cheaper competitors onto the market have indeed raised prices and cost taxpayers more money over time.
The FDA listed more than 50 drugs whose manufacturers have withheld or refused to sell samples and cited 164 inquiries for help obtaining them. Thirteen of these pleas from makers of generics pertained to Celgene’s blockbuster cancer drug Revlimid (lenalidomide), which accounted for 63% of Celgene’s revenue in the first quarter of 2018, according to a company press release.
The brand-name drug companies “wouldn’t put so much effort into fighting off competition if these weren’t [such] lucrative sources of revenue,” said Ameet Sarpatwari, JD, PhD, of Harvard Medical School in Boston. “In the case of a blockbuster drug, that can be hundreds of millions of dollars of revenue for the brand-name drugs and almost the same cost to the health care system.”
Indeed, a KHN analysis found that 47 of the drugs cost Medicare and Medicaid almost $12 billion in 2016. The spending totals don’t include rebates, which drugmakers return to the government after paying for the drugs upfront but are not public. The rebates ranged from 9.5% to 26.3% for Medicare Part D in 2014, the most recent year that data are available.
The remaining drugs do not appear in the Medicare and Medicaid data.
By delaying development of generics, drugmakers can maintain their monopolies and keep prices high. Most of the drugs cost Medicare Part D more in 2016 than they did in 2012, for an average spending increase of about 60% more per unit. This excludes drugs that don’t appear in the 2012 Medicare Part D data.
Revlimid cost Medicare Part D $2.7 billion in 2016, trailing only Harvoni (ledipasvir and sofosbuvir), which treats hepatitis C and is not on the FDA’s new list. The cost of Revlimid, which faces no competition from generics, has jumped 40% per unit in just 4 years, the Medicare data show, and cost $75,200/beneficiary in 2016.
Some drugs on the FDA’s list, including Celgene’s, are part of a safety program that can require restricted distribution of brand-name drugs that have serious risks or addictive qualities. Drugmakers with products in the safety program sometimes say they can’t provide samples unless the generics manufacturer jumps through a series of hoops “that generic companies find hard or impossible to comply with,” Dr. Gottlieb said in a statement.
The Department of Health & Human Services Office of Inspector General issued a report in 2013 that said the FDA couldn’t prove that the program actually improved safety, and Dr. Sarpatwari said there’s evidence drugmakers are abusing it to stave off competition from generics.
Dr. Gottlieb said the FDA will be notifying the Federal Trade Commission about pleas for help from would-be generics manufacturers about obtaining samples, and he encouraged the manufacturers to do the same if they suspect they’re being thwarted by anticompetitive practices.
Celgene spokesman Greg Geissman said the company has sold samples to generics manufacturers and will continue to do so. He stressed maintaining a balance of innovation, generic competition, and safety.
“Even a single dose of thalidomide, the active ingredient in Thalomid, can cause irreversible, debilitating birth defects if not properly handled and dispensed. Revlimid and Pomalyst (pomalidomide) are believed to have similar risks,” Mr. Geissman said.
The highest number of pleas for help related to Actelion Pharmaceuticals’ pulmonary hypertension drug Tracleer (bosentan). In 2016, that drug cost Medicare $90,700/patient and more than $304 million overall. Meanwhile, spending per unit jumped 52% from 2012 through 2016.
Actelion was acquired by Johnson & Johnson’s pharmaceutical arm, Janssen, in 2017.
Actelion spokeswoman Colleen Wilson said that the company “cooperate[s]” with makers of generic drugs and “has responded to all requests it has received directly from generic manufacturers seeking access to its medications for bioequivalence testing.”
PhRMA, the trade group for makers of brand-name pharmaceuticals, said the FDA’s list was somewhat unfair because it lacked context and responses from those it represents.
“While we must continue to foster a competitive marketplace, PhRMA is concerned that FDA’s release of the ‘inquiries’ it has received lacks proper context and conflates a number of divergent scenarios,” said PhRMA spokesman Andrew Powaleny.
Congress is considering the CREATES Act, which stands for “Creating and Restoring Equal Access to Equivalent Samples” and would foster competition in part by allowing generics manufacturers to sue brand-name drug manufacturers to compel them to provide samples.
The bill’s sponsor, Sen. Patrick Leahy (D-Vt.), said more transparency from the FDA is helpful, but more work from the agency is needed to end the anticompetitive tactics. “With billions of dollars at stake, a database alone will not stop this behavior,” Sen. Leahy said.
Cosponsor Sen. Chuck Grassley (R-Iowa), chairman of the Judiciary Committee, expressed similar sentiments, telling KHN: “The CREATES Act is necessary because it would serve as a strong deterrent to pharmaceutical companies that engage in anticompetitive practices to keep low-cost generic drugs off the market.”
The FDA hasn’t come out in support of CREATES. “They should know that this is going to require a legislative solution,” Dr. Sarpatwari said. “Why are they not stepping into this arena and saying that?”
KHN’s coverage of prescription drug development, costs and pricing is supported by the Laura and John Arnold Foundation. Kaiser Health News (hyperlink to khn.org) is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Makers of brand-name drugs called out by the Trump administration for potentially stalling generic competition have hiked their prices by double-digit percentages since 2012 and cost Medicare and Medicaid nearly $12 billion in 2016, a Kaiser Health News analysis has found.
As part of President Donald Trump’s promise to curb high drug prices, the Food and Drug Administration posted a list of pharmaceutical companies that makers of generics allege refused to let them buy the drug samples needed to develop their products. For approval, the FDA requires so-called bioequivalence testing using samples to demonstrate that generics are the same as their branded counterparts.
The analysis shows that drug companies that may have engaged in what FDA Commissioner Scott Gottlieb, MD, called “shenanigans” to delay the entrance of cheaper competitors onto the market have indeed raised prices and cost taxpayers more money over time.
The FDA listed more than 50 drugs whose manufacturers have withheld or refused to sell samples and cited 164 inquiries for help obtaining them. Thirteen of these pleas from makers of generics pertained to Celgene’s blockbuster cancer drug Revlimid (lenalidomide), which accounted for 63% of Celgene’s revenue in the first quarter of 2018, according to a company press release.
The brand-name drug companies “wouldn’t put so much effort into fighting off competition if these weren’t [such] lucrative sources of revenue,” said Ameet Sarpatwari, JD, PhD, of Harvard Medical School in Boston. “In the case of a blockbuster drug, that can be hundreds of millions of dollars of revenue for the brand-name drugs and almost the same cost to the health care system.”
Indeed, a KHN analysis found that 47 of the drugs cost Medicare and Medicaid almost $12 billion in 2016. The spending totals don’t include rebates, which drugmakers return to the government after paying for the drugs upfront but are not public. The rebates ranged from 9.5% to 26.3% for Medicare Part D in 2014, the most recent year that data are available.
The remaining drugs do not appear in the Medicare and Medicaid data.
By delaying development of generics, drugmakers can maintain their monopolies and keep prices high. Most of the drugs cost Medicare Part D more in 2016 than they did in 2012, for an average spending increase of about 60% more per unit. This excludes drugs that don’t appear in the 2012 Medicare Part D data.
Revlimid cost Medicare Part D $2.7 billion in 2016, trailing only Harvoni (ledipasvir and sofosbuvir), which treats hepatitis C and is not on the FDA’s new list. The cost of Revlimid, which faces no competition from generics, has jumped 40% per unit in just 4 years, the Medicare data show, and cost $75,200/beneficiary in 2016.
Some drugs on the FDA’s list, including Celgene’s, are part of a safety program that can require restricted distribution of brand-name drugs that have serious risks or addictive qualities. Drugmakers with products in the safety program sometimes say they can’t provide samples unless the generics manufacturer jumps through a series of hoops “that generic companies find hard or impossible to comply with,” Dr. Gottlieb said in a statement.
The Department of Health & Human Services Office of Inspector General issued a report in 2013 that said the FDA couldn’t prove that the program actually improved safety, and Dr. Sarpatwari said there’s evidence drugmakers are abusing it to stave off competition from generics.
Dr. Gottlieb said the FDA will be notifying the Federal Trade Commission about pleas for help from would-be generics manufacturers about obtaining samples, and he encouraged the manufacturers to do the same if they suspect they’re being thwarted by anticompetitive practices.
Celgene spokesman Greg Geissman said the company has sold samples to generics manufacturers and will continue to do so. He stressed maintaining a balance of innovation, generic competition, and safety.
“Even a single dose of thalidomide, the active ingredient in Thalomid, can cause irreversible, debilitating birth defects if not properly handled and dispensed. Revlimid and Pomalyst (pomalidomide) are believed to have similar risks,” Mr. Geissman said.
The highest number of pleas for help related to Actelion Pharmaceuticals’ pulmonary hypertension drug Tracleer (bosentan). In 2016, that drug cost Medicare $90,700/patient and more than $304 million overall. Meanwhile, spending per unit jumped 52% from 2012 through 2016.
Actelion was acquired by Johnson & Johnson’s pharmaceutical arm, Janssen, in 2017.
Actelion spokeswoman Colleen Wilson said that the company “cooperate[s]” with makers of generic drugs and “has responded to all requests it has received directly from generic manufacturers seeking access to its medications for bioequivalence testing.”
PhRMA, the trade group for makers of brand-name pharmaceuticals, said the FDA’s list was somewhat unfair because it lacked context and responses from those it represents.
“While we must continue to foster a competitive marketplace, PhRMA is concerned that FDA’s release of the ‘inquiries’ it has received lacks proper context and conflates a number of divergent scenarios,” said PhRMA spokesman Andrew Powaleny.
Congress is considering the CREATES Act, which stands for “Creating and Restoring Equal Access to Equivalent Samples” and would foster competition in part by allowing generics manufacturers to sue brand-name drug manufacturers to compel them to provide samples.
The bill’s sponsor, Sen. Patrick Leahy (D-Vt.), said more transparency from the FDA is helpful, but more work from the agency is needed to end the anticompetitive tactics. “With billions of dollars at stake, a database alone will not stop this behavior,” Sen. Leahy said.
Cosponsor Sen. Chuck Grassley (R-Iowa), chairman of the Judiciary Committee, expressed similar sentiments, telling KHN: “The CREATES Act is necessary because it would serve as a strong deterrent to pharmaceutical companies that engage in anticompetitive practices to keep low-cost generic drugs off the market.”
The FDA hasn’t come out in support of CREATES. “They should know that this is going to require a legislative solution,” Dr. Sarpatwari said. “Why are they not stepping into this arena and saying that?”
KHN’s coverage of prescription drug development, costs and pricing is supported by the Laura and John Arnold Foundation. Kaiser Health News (hyperlink to khn.org) is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.















