User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Children and COVID: New cases up by 50%
The latest increase in new child COVID-19 cases seems to be picking up steam, rising by 50% in the last week, according to the American Academy of Pediatrics and the Children’s Hospital Association.
That 50% week-to-week change follows increases of 17%, 44%, 12%, and 28% since the nationwide weekly total fell to its low point for the year (25,915) in the beginning of April, the AAP and CHA said in their weekly COVID report.
Regionally, the distribution of those 93,000 COVID cases was fairly even. The Northeast, which saw the biggest jump for the week, and the Midwest were both around 25,000 new cases, while the South had about 20,000 and the West was lowest with 18,000 or so. At the state/territory level, the largest percent increases over the last 2 weeks were found in Maine and Puerto Rico, with Massachusetts and Vermont just a step behind, the AAP/CHA data show.
In cumulative terms, there have been over 13.1 million cases of COVID-19 among children in the United States, with pediatric cases representing 19.0% of all cases since the pandemic began, the two organizations reported. They also noted a number of important limitations: New York state has never reported cases by age, several states have stopped updating their online dashboards, and states apply a variety of age ranges to define children (Alabama has the smallest range, 0-14 years; South Carolina, Tennessee, and West Virginia the largest, 0-20).
By comparison, the Centers for Disease Control and Prevention put the total number of cases in children aged 0-17 at 12.7 million, although that figure is based on a cumulative number of 73.4 million cases among all ages, which is well short of the reported total of almost 82.4 million as of May 16. COVID cases in children have led to 1,536 deaths so far, the CDC said.
The recent upward trend in new cases also can be seen in the CDC’s data, which show the weekly rate rising from 35 per 100,000 population on March 26 to 102 per 100,000 on May 7 in children aged 0-14 years, with commensurate increases seen among older children over the same period. In turn, the rate of new admissions for children aged 0-17 has gone from a low of 0.13 per 100,000 as late as April 10 up to 0.23 on May 13, the CDC said on its COVID Data Tracker.
One thing not going up these days is vaccinations among the youngest eligible children. The number of 5- to 11-year-olds receiving their initial dose was down to 40,000 for the week of May 5-11, the fewest since the vaccine was approved for that age group. For a change of pace, the number increased among children aged 12-17, as 37,000 got initial vaccinations that week, compared with 29,000 a week earlier, the AAP said in its weekly vaccination report.
The latest increase in new child COVID-19 cases seems to be picking up steam, rising by 50% in the last week, according to the American Academy of Pediatrics and the Children’s Hospital Association.
That 50% week-to-week change follows increases of 17%, 44%, 12%, and 28% since the nationwide weekly total fell to its low point for the year (25,915) in the beginning of April, the AAP and CHA said in their weekly COVID report.
Regionally, the distribution of those 93,000 COVID cases was fairly even. The Northeast, which saw the biggest jump for the week, and the Midwest were both around 25,000 new cases, while the South had about 20,000 and the West was lowest with 18,000 or so. At the state/territory level, the largest percent increases over the last 2 weeks were found in Maine and Puerto Rico, with Massachusetts and Vermont just a step behind, the AAP/CHA data show.
In cumulative terms, there have been over 13.1 million cases of COVID-19 among children in the United States, with pediatric cases representing 19.0% of all cases since the pandemic began, the two organizations reported. They also noted a number of important limitations: New York state has never reported cases by age, several states have stopped updating their online dashboards, and states apply a variety of age ranges to define children (Alabama has the smallest range, 0-14 years; South Carolina, Tennessee, and West Virginia the largest, 0-20).
By comparison, the Centers for Disease Control and Prevention put the total number of cases in children aged 0-17 at 12.7 million, although that figure is based on a cumulative number of 73.4 million cases among all ages, which is well short of the reported total of almost 82.4 million as of May 16. COVID cases in children have led to 1,536 deaths so far, the CDC said.
The recent upward trend in new cases also can be seen in the CDC’s data, which show the weekly rate rising from 35 per 100,000 population on March 26 to 102 per 100,000 on May 7 in children aged 0-14 years, with commensurate increases seen among older children over the same period. In turn, the rate of new admissions for children aged 0-17 has gone from a low of 0.13 per 100,000 as late as April 10 up to 0.23 on May 13, the CDC said on its COVID Data Tracker.
One thing not going up these days is vaccinations among the youngest eligible children. The number of 5- to 11-year-olds receiving their initial dose was down to 40,000 for the week of May 5-11, the fewest since the vaccine was approved for that age group. For a change of pace, the number increased among children aged 12-17, as 37,000 got initial vaccinations that week, compared with 29,000 a week earlier, the AAP said in its weekly vaccination report.
The latest increase in new child COVID-19 cases seems to be picking up steam, rising by 50% in the last week, according to the American Academy of Pediatrics and the Children’s Hospital Association.
That 50% week-to-week change follows increases of 17%, 44%, 12%, and 28% since the nationwide weekly total fell to its low point for the year (25,915) in the beginning of April, the AAP and CHA said in their weekly COVID report.
Regionally, the distribution of those 93,000 COVID cases was fairly even. The Northeast, which saw the biggest jump for the week, and the Midwest were both around 25,000 new cases, while the South had about 20,000 and the West was lowest with 18,000 or so. At the state/territory level, the largest percent increases over the last 2 weeks were found in Maine and Puerto Rico, with Massachusetts and Vermont just a step behind, the AAP/CHA data show.
In cumulative terms, there have been over 13.1 million cases of COVID-19 among children in the United States, with pediatric cases representing 19.0% of all cases since the pandemic began, the two organizations reported. They also noted a number of important limitations: New York state has never reported cases by age, several states have stopped updating their online dashboards, and states apply a variety of age ranges to define children (Alabama has the smallest range, 0-14 years; South Carolina, Tennessee, and West Virginia the largest, 0-20).
By comparison, the Centers for Disease Control and Prevention put the total number of cases in children aged 0-17 at 12.7 million, although that figure is based on a cumulative number of 73.4 million cases among all ages, which is well short of the reported total of almost 82.4 million as of May 16. COVID cases in children have led to 1,536 deaths so far, the CDC said.
The recent upward trend in new cases also can be seen in the CDC’s data, which show the weekly rate rising from 35 per 100,000 population on March 26 to 102 per 100,000 on May 7 in children aged 0-14 years, with commensurate increases seen among older children over the same period. In turn, the rate of new admissions for children aged 0-17 has gone from a low of 0.13 per 100,000 as late as April 10 up to 0.23 on May 13, the CDC said on its COVID Data Tracker.
One thing not going up these days is vaccinations among the youngest eligible children. The number of 5- to 11-year-olds receiving their initial dose was down to 40,000 for the week of May 5-11, the fewest since the vaccine was approved for that age group. For a change of pace, the number increased among children aged 12-17, as 37,000 got initial vaccinations that week, compared with 29,000 a week earlier, the AAP said in its weekly vaccination report.
HPV strains covered by the vaccine have declined greatly in the U.S.
Twelve years after the human papillomavirus (HPV) vaccination program was introduced in the United States, the overall prevalence of cancer-causing HPV strains covered by the vaccine dropped by 85% among females – 90% among vaccinated females and 74% among unvaccinated females – a strong sign of herd immunity, a new analysis of a nationally representative database is showing.
“HPV vaccination is working well,” Hannah Rosenblum, MD, Centers for Disease Control and Prevention, Atlanta, told this news organization in an email.
“Twelve years after introduction of HPV vaccination in the United States, national data demonstrate increasing impact among females and strong herd effects among unvaccinated females,” she added. “[Although] vaccination coverage and completion of the recommended dose in the United States is lower than coverage with other adolescent vaccinations, HPV vaccination is the best way to prevent HPV infections that can lead to several cancers in both females and males.”
The study was published online in Annals of Internal Medicine.
NHANES survey
The authors used data from the National Health and Nutrition Examination Survey (NHANES) to examine the four HPV types in the quadrivalent vaccine before 2003 and 2006 (the pre-vaccine era) and then again between 2007-2010, 2011-2014, and 2015-2018 (the vaccine era). For females, they analyzed demographic and HPV prevalence data across each 4-year era.
“Analyses were limited to sexually experienced participants, to ensure that all those included had an opportunity for HPV exposure, and to participants aged 14-24 years with adequate self-collected cervicovaginal specimens,” the authors explain.
This resulted in a sample size of 3,197 females. Demographic and HPV prevalence data were also collected from males but only during the 2013-2016 era, because those are the only years for which male HPV typing data are available in NHANES. Again, analyses were limited to sexually experienced males aged 14-24 years with adequate self-collected penile specimens, which resulted in a sample size of 661 males.
Over the 12 years of follow-up for females, there was a steady increase in females reporting having received at least one dose of the HPV vaccine – from slightly over 25% during 2007-12 to 59% during 2015-2018. The percentage of males who reported having at least one HPV dose also increased, from 29.5% in 2016 to 34.5% in 2018.
During the earliest vaccine era (2007-2010), the prevalence of the four HPV strains covered by the vaccine was 7.3% among vaccinated females, compared with 20.4% among unvaccinated females. “By 2015 to 2018, the prevalence was 2.8% (prevalence ratio, 0.16; 95% confidence interval, 0.07-0.39). The prevalence of the four vaccine-covered types was only 1.9% in vaccinated females, compared with 4.8% in unvaccinated females (PR, 0.40; 95% CI, 0.11-1.41).
In contrast, the prevalence of HPV types that were not covered by the vaccine showed little change – from 51.1% in the pre-vaccine era to 47.6% during 2015-2018 (PR, 0.93; 95% CI, 0.80-1.08). The authors considered this a good sign because it indicates that vaccine-type HPV infections are not being replaced with other oncogenic HPV infections. Between 2013 and 2016, the difference in the prevalence of the four HPV vaccine types was smaller at 1.8% among vaccinated males and 3.5% among unvaccinated males (PR, 0.49; 95% CI, 0.11-2.20).
Again, the prevalence of non-HPV vaccine types was not significantly different between vaccinated and unvaccinated males: 30.7% versus 34.3%.
During the vaccine era, effectiveness for females ranged from 60% to 84%. For males, vaccine effectiveness could only be evaluated for the single 4-year period from 2013 to 2016, and it was estimated at 51%. Dr. Rosenblum noted that vaccine efficacy estimates were lower on this national survey than the almost 100% efficacy rates observed in clinical trials in both males and females.
“This might be due in part to many participants receiving the vaccine at an older age than is recommended when they could have been infected [with HPV] at the time of vaccination,” Dr. Rosenblum said. She also noted that because males were incorporated into the HPV vaccination program years after females, they likely also experienced strong herd effects from the vaccine, making it challenging to estimate vaccine effectiveness.
Dr. Rosenblum also noted that there have already been documented declines in cervical precancers and high-grade vulvar and vaginal precancers, as well as genital warts and juvenile-onset recurrent respiratory papillomatosis. At the same time, the incidence of cervical precancers has recently declined among U.S. females in their late teens and early 20s – “likely reflecting the impact of vaccination,” she said.
“This study is good news for the United States HPV vaccination program, and all efforts are needed to ensure that children and adolescents receive routinely recommended vaccinations [including vaccination against HPV],” Dr. Rosenblum added.
Editorial comment
Commenting on the findings, Rebecca Perkins, MD, Boston University School of Medicine, and colleagues point out that the COVID-19 pandemic has led to disruptions in HPV vaccination programs and has reversed much of the progress made in recent years. “During the pandemic, providers and health systems have deprioritized adolescent vaccination and particularly HPV vaccination, which in turn has led to more severe drops for HPV vaccination than for other adolescent vaccinations, and for adolescent vaccination, compared with early childhood and adult vaccinations,” Dr. Perkins and colleagues write in an accompanying editorial.
Thus, the need to compensate for the cumulative deficit of missed vaccinations over the past 2 years has created a “serious and urgent threat” to cancer prevention efforts – “a shortfall from which it may take a decade to recover,” the editorialists predict. To try and reverse this trend, several practices have been shown to improve HPV vaccination rates.
The first is a strong provider recommendation such as, “Your child is due for an HPV vaccine today.” The second is to give standing orders to allow nurses and medical assistants to administer vaccinations without requiring intervention by a physician. Lastly, programs to remind patients when vaccines are due and to recall them for appointments also work well.
“Using evidence-based methods and redoubling our efforts to prioritize HPV vaccination will be crucial to ensuring that we do not lose a generation to preventable HPV-associated cancer,” write Dr. Perkins and colleagues.
The study authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Twelve years after the human papillomavirus (HPV) vaccination program was introduced in the United States, the overall prevalence of cancer-causing HPV strains covered by the vaccine dropped by 85% among females – 90% among vaccinated females and 74% among unvaccinated females – a strong sign of herd immunity, a new analysis of a nationally representative database is showing.
“HPV vaccination is working well,” Hannah Rosenblum, MD, Centers for Disease Control and Prevention, Atlanta, told this news organization in an email.
“Twelve years after introduction of HPV vaccination in the United States, national data demonstrate increasing impact among females and strong herd effects among unvaccinated females,” she added. “[Although] vaccination coverage and completion of the recommended dose in the United States is lower than coverage with other adolescent vaccinations, HPV vaccination is the best way to prevent HPV infections that can lead to several cancers in both females and males.”
The study was published online in Annals of Internal Medicine.
NHANES survey
The authors used data from the National Health and Nutrition Examination Survey (NHANES) to examine the four HPV types in the quadrivalent vaccine before 2003 and 2006 (the pre-vaccine era) and then again between 2007-2010, 2011-2014, and 2015-2018 (the vaccine era). For females, they analyzed demographic and HPV prevalence data across each 4-year era.
“Analyses were limited to sexually experienced participants, to ensure that all those included had an opportunity for HPV exposure, and to participants aged 14-24 years with adequate self-collected cervicovaginal specimens,” the authors explain.
This resulted in a sample size of 3,197 females. Demographic and HPV prevalence data were also collected from males but only during the 2013-2016 era, because those are the only years for which male HPV typing data are available in NHANES. Again, analyses were limited to sexually experienced males aged 14-24 years with adequate self-collected penile specimens, which resulted in a sample size of 661 males.
Over the 12 years of follow-up for females, there was a steady increase in females reporting having received at least one dose of the HPV vaccine – from slightly over 25% during 2007-12 to 59% during 2015-2018. The percentage of males who reported having at least one HPV dose also increased, from 29.5% in 2016 to 34.5% in 2018.
During the earliest vaccine era (2007-2010), the prevalence of the four HPV strains covered by the vaccine was 7.3% among vaccinated females, compared with 20.4% among unvaccinated females. “By 2015 to 2018, the prevalence was 2.8% (prevalence ratio, 0.16; 95% confidence interval, 0.07-0.39). The prevalence of the four vaccine-covered types was only 1.9% in vaccinated females, compared with 4.8% in unvaccinated females (PR, 0.40; 95% CI, 0.11-1.41).
In contrast, the prevalence of HPV types that were not covered by the vaccine showed little change – from 51.1% in the pre-vaccine era to 47.6% during 2015-2018 (PR, 0.93; 95% CI, 0.80-1.08). The authors considered this a good sign because it indicates that vaccine-type HPV infections are not being replaced with other oncogenic HPV infections. Between 2013 and 2016, the difference in the prevalence of the four HPV vaccine types was smaller at 1.8% among vaccinated males and 3.5% among unvaccinated males (PR, 0.49; 95% CI, 0.11-2.20).
Again, the prevalence of non-HPV vaccine types was not significantly different between vaccinated and unvaccinated males: 30.7% versus 34.3%.
During the vaccine era, effectiveness for females ranged from 60% to 84%. For males, vaccine effectiveness could only be evaluated for the single 4-year period from 2013 to 2016, and it was estimated at 51%. Dr. Rosenblum noted that vaccine efficacy estimates were lower on this national survey than the almost 100% efficacy rates observed in clinical trials in both males and females.
“This might be due in part to many participants receiving the vaccine at an older age than is recommended when they could have been infected [with HPV] at the time of vaccination,” Dr. Rosenblum said. She also noted that because males were incorporated into the HPV vaccination program years after females, they likely also experienced strong herd effects from the vaccine, making it challenging to estimate vaccine effectiveness.
Dr. Rosenblum also noted that there have already been documented declines in cervical precancers and high-grade vulvar and vaginal precancers, as well as genital warts and juvenile-onset recurrent respiratory papillomatosis. At the same time, the incidence of cervical precancers has recently declined among U.S. females in their late teens and early 20s – “likely reflecting the impact of vaccination,” she said.
“This study is good news for the United States HPV vaccination program, and all efforts are needed to ensure that children and adolescents receive routinely recommended vaccinations [including vaccination against HPV],” Dr. Rosenblum added.
Editorial comment
Commenting on the findings, Rebecca Perkins, MD, Boston University School of Medicine, and colleagues point out that the COVID-19 pandemic has led to disruptions in HPV vaccination programs and has reversed much of the progress made in recent years. “During the pandemic, providers and health systems have deprioritized adolescent vaccination and particularly HPV vaccination, which in turn has led to more severe drops for HPV vaccination than for other adolescent vaccinations, and for adolescent vaccination, compared with early childhood and adult vaccinations,” Dr. Perkins and colleagues write in an accompanying editorial.
Thus, the need to compensate for the cumulative deficit of missed vaccinations over the past 2 years has created a “serious and urgent threat” to cancer prevention efforts – “a shortfall from which it may take a decade to recover,” the editorialists predict. To try and reverse this trend, several practices have been shown to improve HPV vaccination rates.
The first is a strong provider recommendation such as, “Your child is due for an HPV vaccine today.” The second is to give standing orders to allow nurses and medical assistants to administer vaccinations without requiring intervention by a physician. Lastly, programs to remind patients when vaccines are due and to recall them for appointments also work well.
“Using evidence-based methods and redoubling our efforts to prioritize HPV vaccination will be crucial to ensuring that we do not lose a generation to preventable HPV-associated cancer,” write Dr. Perkins and colleagues.
The study authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Twelve years after the human papillomavirus (HPV) vaccination program was introduced in the United States, the overall prevalence of cancer-causing HPV strains covered by the vaccine dropped by 85% among females – 90% among vaccinated females and 74% among unvaccinated females – a strong sign of herd immunity, a new analysis of a nationally representative database is showing.
“HPV vaccination is working well,” Hannah Rosenblum, MD, Centers for Disease Control and Prevention, Atlanta, told this news organization in an email.
“Twelve years after introduction of HPV vaccination in the United States, national data demonstrate increasing impact among females and strong herd effects among unvaccinated females,” she added. “[Although] vaccination coverage and completion of the recommended dose in the United States is lower than coverage with other adolescent vaccinations, HPV vaccination is the best way to prevent HPV infections that can lead to several cancers in both females and males.”
The study was published online in Annals of Internal Medicine.
NHANES survey
The authors used data from the National Health and Nutrition Examination Survey (NHANES) to examine the four HPV types in the quadrivalent vaccine before 2003 and 2006 (the pre-vaccine era) and then again between 2007-2010, 2011-2014, and 2015-2018 (the vaccine era). For females, they analyzed demographic and HPV prevalence data across each 4-year era.
“Analyses were limited to sexually experienced participants, to ensure that all those included had an opportunity for HPV exposure, and to participants aged 14-24 years with adequate self-collected cervicovaginal specimens,” the authors explain.
This resulted in a sample size of 3,197 females. Demographic and HPV prevalence data were also collected from males but only during the 2013-2016 era, because those are the only years for which male HPV typing data are available in NHANES. Again, analyses were limited to sexually experienced males aged 14-24 years with adequate self-collected penile specimens, which resulted in a sample size of 661 males.
Over the 12 years of follow-up for females, there was a steady increase in females reporting having received at least one dose of the HPV vaccine – from slightly over 25% during 2007-12 to 59% during 2015-2018. The percentage of males who reported having at least one HPV dose also increased, from 29.5% in 2016 to 34.5% in 2018.
During the earliest vaccine era (2007-2010), the prevalence of the four HPV strains covered by the vaccine was 7.3% among vaccinated females, compared with 20.4% among unvaccinated females. “By 2015 to 2018, the prevalence was 2.8% (prevalence ratio, 0.16; 95% confidence interval, 0.07-0.39). The prevalence of the four vaccine-covered types was only 1.9% in vaccinated females, compared with 4.8% in unvaccinated females (PR, 0.40; 95% CI, 0.11-1.41).
In contrast, the prevalence of HPV types that were not covered by the vaccine showed little change – from 51.1% in the pre-vaccine era to 47.6% during 2015-2018 (PR, 0.93; 95% CI, 0.80-1.08). The authors considered this a good sign because it indicates that vaccine-type HPV infections are not being replaced with other oncogenic HPV infections. Between 2013 and 2016, the difference in the prevalence of the four HPV vaccine types was smaller at 1.8% among vaccinated males and 3.5% among unvaccinated males (PR, 0.49; 95% CI, 0.11-2.20).
Again, the prevalence of non-HPV vaccine types was not significantly different between vaccinated and unvaccinated males: 30.7% versus 34.3%.
During the vaccine era, effectiveness for females ranged from 60% to 84%. For males, vaccine effectiveness could only be evaluated for the single 4-year period from 2013 to 2016, and it was estimated at 51%. Dr. Rosenblum noted that vaccine efficacy estimates were lower on this national survey than the almost 100% efficacy rates observed in clinical trials in both males and females.
“This might be due in part to many participants receiving the vaccine at an older age than is recommended when they could have been infected [with HPV] at the time of vaccination,” Dr. Rosenblum said. She also noted that because males were incorporated into the HPV vaccination program years after females, they likely also experienced strong herd effects from the vaccine, making it challenging to estimate vaccine effectiveness.
Dr. Rosenblum also noted that there have already been documented declines in cervical precancers and high-grade vulvar and vaginal precancers, as well as genital warts and juvenile-onset recurrent respiratory papillomatosis. At the same time, the incidence of cervical precancers has recently declined among U.S. females in their late teens and early 20s – “likely reflecting the impact of vaccination,” she said.
“This study is good news for the United States HPV vaccination program, and all efforts are needed to ensure that children and adolescents receive routinely recommended vaccinations [including vaccination against HPV],” Dr. Rosenblum added.
Editorial comment
Commenting on the findings, Rebecca Perkins, MD, Boston University School of Medicine, and colleagues point out that the COVID-19 pandemic has led to disruptions in HPV vaccination programs and has reversed much of the progress made in recent years. “During the pandemic, providers and health systems have deprioritized adolescent vaccination and particularly HPV vaccination, which in turn has led to more severe drops for HPV vaccination than for other adolescent vaccinations, and for adolescent vaccination, compared with early childhood and adult vaccinations,” Dr. Perkins and colleagues write in an accompanying editorial.
Thus, the need to compensate for the cumulative deficit of missed vaccinations over the past 2 years has created a “serious and urgent threat” to cancer prevention efforts – “a shortfall from which it may take a decade to recover,” the editorialists predict. To try and reverse this trend, several practices have been shown to improve HPV vaccination rates.
The first is a strong provider recommendation such as, “Your child is due for an HPV vaccine today.” The second is to give standing orders to allow nurses and medical assistants to administer vaccinations without requiring intervention by a physician. Lastly, programs to remind patients when vaccines are due and to recall them for appointments also work well.
“Using evidence-based methods and redoubling our efforts to prioritize HPV vaccination will be crucial to ensuring that we do not lose a generation to preventable HPV-associated cancer,” write Dr. Perkins and colleagues.
The study authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE
Pfizer COVID vaccine performs well in youth with rheumatic diseases
The Pfizer-BioNTech mRNA vaccine (Comirnaty) showed a good safety profile with minimal short-term side effects and no negative impact on disease activity in a cohort of adolescents and young adults with rheumatic diseases, according to research presented at the annual scientific meeting of the Childhood Arthritis and Rheumatology Research Alliance, held virtually this year.
Only 3% of patients experience a severe transient adverse event, according to Merav Heshin-Bekenstein, MD, of Dana-Dwek Children’s Hospital at the Tel Aviv Sourasky Medical Center in Israel. The findings were published in Rheumatology.
“We found that the mRNA Pfizer vaccine was immunogenic and induced an adequate humoral immune response in adolescent patients,” Dr. Heshin-Bekenstein told CARRA attendees. “It was definitely comparable to healthy controls and practically all patients were seropositive following the second vaccine, except for one patient with long-standing systemic sclerosis.”
The findings were not necessarily surprising but were encouraging to Melissa S. Oliver, MD, assistant professor of clinical pediatrics in the division of pediatric rheumatology at Indiana University, Indianapolis. Dr. Oliver wasn’t part of the study team.
“We know that the COVID vaccines in healthy adolescents have shown good efficacy with minimal side effects, and it’s good to see that this study showed that in those with rheumatic diseases on immunosuppressive therapy,” Dr. Oliver told this news organization.
Until now, the data on COVID-19 vaccines in teens with rheumatic illnesses has been limited, she said, so “many pediatric rheumatologists only have the data from adult studies to go on or personal experience with their own cohort of patients.”
But the high immunogenicity seen in the study was a pleasant surprise to Beth H. Rutstein, MD, assistant professor of clinical pediatrics in the division of rheumatology at Children’s Hospital of Philadelphia and the Perelman School of Medicine at the University of Pennsylvania.
“I was both surprised and thrilled with Dr. Heshin-Bekenstein’s findings suggesting near-universal seroconversion for patients with rheumatic disease regardless of underlying diagnosis or immunomodulatory therapy regimen, as much of the adult data has suggested a poorer seroconversion rate” and lower antibody titers in adults with similar illnesses, Dr. Rutstein said in an interview.
The study “provides essential reassurance that vaccination against COVID-19 does not increase the risk of disease flare or worsen disease severity scores,” said Dr. Rutstein, who was not associated with the research. “Rather than speaking purely anecdotally with our patients and their families, we can refer to the science – which is always more reassuring for both our patients and ourselves.”
Study included diverse conditions and therapies
Risk factors for poor outcomes with COVID-19 in children include obesity, cardiovascular disease, chronic lung disease, diabetes, and asthma, Dr. Heshin-Bekenstein told CARRA attendees. Multisystem inflammatory syndrome in children (MIS-C) and long COVID are also potential complications of COVID-19 with less understood risk factors.
Although COVID-19 is most often mild in children, certain severe, systemic rheumatic diseases increase hospitalization risk, including systemic lupus erythematosus (SLE) and vasculitis. Evidence has also shown that COVID-19 infection increases the risk of disease flare in teens with juvenile-onset rheumatic diseases, so it’s “crucial to prevent COVID-19 disease in this population,” Dr. Heshin-Bekenstein said.
Her study therefore aimed to assess the safety and immunogenicity of the Pfizer mRNA vaccine for teens with juvenile-onset rheumatic diseases and those taking immunomodulatory medications. The international prospective multicenter study ran from April to November 2021 at three pediatric rheumatology clinics in Israel and one in Slovenia. Endpoints included short-term side effects, vaccination impact on clinical disease activity, immunogenicity at 2-9 weeks after the second dose, and, secondarily, efficacy against COVID-19 infection.
The 91 participants included adolescents aged 12-18 and young adults aged 18-21. Nearly half of the participants (46%) had juvenile idiopathic arthritis (JIA), and 14% had SLE. Other participants’ conditions included systemic vasculitis, idiopathic uveitis, inflammatory bowel disease–related arthritis, systemic or localized scleroderma, juvenile dermatomyositis, or an autoinflammatory disease. Participants’ mean disease duration was 4.8 years.
The researchers compared the patients with a control group of 40 individuals with similar demographics but without rheumatic disease. The researchers used the LIAISON quantitative assay to assess serum IgG antibody levels against the SARS-CoV-2 spike protein in both groups.
Eight in 10 participants with rheumatic disease were taking an immunomodulatory medication, including a conventional synthetic disease-modifying antirheumatic drug (csDMARD) in 40%, a biologic DMARD in 37%, tumor necrosis factor (TNF) inhibitors in 32%, hydroxychloroquine (HCQ) in 19%, glucocorticoids in 14%, and mycophenolate in 11%. A smaller proportion were on other biologics: JAK inhibitors in 6.6%, anti-CD20 drugs in 4.4%, and an IL-6 inhibitor in 1%.
Side effects similar in both groups
None of the side effects reported by participants were statistically different between those with rheumatic disease and the control group. Localized pain was the most common side effect, reported by 73%-79% of participants after each dose. About twice as many participants with rheumatic disease experienced muscle aches and joint pains, compared with the control group, but the differences were not significant. Fever occurred more often in those with rheumatic disease (6%, five cases) than without (3%, one case). One-third of those with rheumatic disease felt tiredness, compared with 20% of the control group.
None of the healthy controls were hospitalized after vaccination, but three rheumatic patients were, including two after the first dose. Both were 17 years old, had systemic vasculitis with granulomatosis with polyangiitis (GPA), and were taking rituximab (Rituxan). One patient experienced acute onset of chronic renal failure, fever, dehydration, and high C-reactive protein within hours of vaccination. The other experienced new onset of pulmonary hemorrhage a week after vaccination.
In addition, a 14-year-old female with lupus, taking only HCQ, went to the emergency department with fever, headache, vomiting, and joint pain 1 day after the second vaccine dose. She had normal inflammatory markers and no change in disease activity score, and she was discharged with low-dose steroids tapered after 2 weeks.
Immune response high in patients with rheumatic disease
Immunogenicity was similar in both groups, with 97% seropositivity in the rheumatic disease group and 100% in the control group. Average IgG titers were 242 in the rheumatic group and 388 in the control group (P < .0001). Seropositivity was 88% in those taking mycophenolate with another drug (100% with mycophenolate monotherapy), 90% with HCQ, 94% with any csDMARDs and another drug (100% with csDMARD monotherapy), and 100% for all other drugs. During 3 months’ follow-up after vaccination, there were no COVID-19 cases among the participants.
Dr. Heshin-Bekenstein noted that their results showed better immunogenicity in teens, compared with adults, for two specific drugs. Seropositivity in teens taking methotrexate (Rheumatrex, Trexall) or rituximab was 100% in this study, compared with 84% in adults taking methotrexate and 39% in adults taking rituximab in a previous study. However, only three patients in this study were taking rituximab, and only seven were taking methotrexate.
The study’s heterogenous population was both a strength and a weakness of the study. “Due to the diversity of rheumatic diseases and medications included in this cohort, it was not possible to draw significant conclusions regarding the impact of the immunomodulatory medications and type of disease” on titers, Dr. Heshin-Bekenstein told attendees.
Still, “I think as pediatric rheumatologists, we can feel reassured in recommending the COVID-19 vaccine to our patients,” Dr. Oliver said. “I will add that every patient is different, and everyone should have a conversation with their physician about receiving the COVID-19 vaccine.” Dr. Oliver said she discusses vaccination, including COVID vaccination, with every patient, and it’s been challenging to address concerns in the midst of so much misinformation circulating about the vaccine.
These findings do raise questions about whether it’s still necessary to hold immunomodulatory medications to get the vaccine,” Dr. Rutstein said.
“Many families are nervous to pause their medications before and after the vaccine as is currently recommended for many therapies by the American College of Rheumatology, and I do share that concern for some of my patients with more clinically unstable disease, so I try to work with each family to decide on best timing and have delayed or deferred the series until some patients are on a steady dose of a new immunomodulatory medication if it has been recently started,” Dr. Rutstein said. “This is one of the reasons why Dr. Heshin-Bekenstein’s study is so important – we may be holding medications that can be safely continued and even further decrease the risk of disease flare.”
None of the physicians have disclosed any relevant financial relationships.
A version of this article first appeared on Medscape.com.
The Pfizer-BioNTech mRNA vaccine (Comirnaty) showed a good safety profile with minimal short-term side effects and no negative impact on disease activity in a cohort of adolescents and young adults with rheumatic diseases, according to research presented at the annual scientific meeting of the Childhood Arthritis and Rheumatology Research Alliance, held virtually this year.
Only 3% of patients experience a severe transient adverse event, according to Merav Heshin-Bekenstein, MD, of Dana-Dwek Children’s Hospital at the Tel Aviv Sourasky Medical Center in Israel. The findings were published in Rheumatology.
“We found that the mRNA Pfizer vaccine was immunogenic and induced an adequate humoral immune response in adolescent patients,” Dr. Heshin-Bekenstein told CARRA attendees. “It was definitely comparable to healthy controls and practically all patients were seropositive following the second vaccine, except for one patient with long-standing systemic sclerosis.”
The findings were not necessarily surprising but were encouraging to Melissa S. Oliver, MD, assistant professor of clinical pediatrics in the division of pediatric rheumatology at Indiana University, Indianapolis. Dr. Oliver wasn’t part of the study team.
“We know that the COVID vaccines in healthy adolescents have shown good efficacy with minimal side effects, and it’s good to see that this study showed that in those with rheumatic diseases on immunosuppressive therapy,” Dr. Oliver told this news organization.
Until now, the data on COVID-19 vaccines in teens with rheumatic illnesses has been limited, she said, so “many pediatric rheumatologists only have the data from adult studies to go on or personal experience with their own cohort of patients.”
But the high immunogenicity seen in the study was a pleasant surprise to Beth H. Rutstein, MD, assistant professor of clinical pediatrics in the division of rheumatology at Children’s Hospital of Philadelphia and the Perelman School of Medicine at the University of Pennsylvania.
“I was both surprised and thrilled with Dr. Heshin-Bekenstein’s findings suggesting near-universal seroconversion for patients with rheumatic disease regardless of underlying diagnosis or immunomodulatory therapy regimen, as much of the adult data has suggested a poorer seroconversion rate” and lower antibody titers in adults with similar illnesses, Dr. Rutstein said in an interview.
The study “provides essential reassurance that vaccination against COVID-19 does not increase the risk of disease flare or worsen disease severity scores,” said Dr. Rutstein, who was not associated with the research. “Rather than speaking purely anecdotally with our patients and their families, we can refer to the science – which is always more reassuring for both our patients and ourselves.”
Study included diverse conditions and therapies
Risk factors for poor outcomes with COVID-19 in children include obesity, cardiovascular disease, chronic lung disease, diabetes, and asthma, Dr. Heshin-Bekenstein told CARRA attendees. Multisystem inflammatory syndrome in children (MIS-C) and long COVID are also potential complications of COVID-19 with less understood risk factors.
Although COVID-19 is most often mild in children, certain severe, systemic rheumatic diseases increase hospitalization risk, including systemic lupus erythematosus (SLE) and vasculitis. Evidence has also shown that COVID-19 infection increases the risk of disease flare in teens with juvenile-onset rheumatic diseases, so it’s “crucial to prevent COVID-19 disease in this population,” Dr. Heshin-Bekenstein said.
Her study therefore aimed to assess the safety and immunogenicity of the Pfizer mRNA vaccine for teens with juvenile-onset rheumatic diseases and those taking immunomodulatory medications. The international prospective multicenter study ran from April to November 2021 at three pediatric rheumatology clinics in Israel and one in Slovenia. Endpoints included short-term side effects, vaccination impact on clinical disease activity, immunogenicity at 2-9 weeks after the second dose, and, secondarily, efficacy against COVID-19 infection.
The 91 participants included adolescents aged 12-18 and young adults aged 18-21. Nearly half of the participants (46%) had juvenile idiopathic arthritis (JIA), and 14% had SLE. Other participants’ conditions included systemic vasculitis, idiopathic uveitis, inflammatory bowel disease–related arthritis, systemic or localized scleroderma, juvenile dermatomyositis, or an autoinflammatory disease. Participants’ mean disease duration was 4.8 years.
The researchers compared the patients with a control group of 40 individuals with similar demographics but without rheumatic disease. The researchers used the LIAISON quantitative assay to assess serum IgG antibody levels against the SARS-CoV-2 spike protein in both groups.
Eight in 10 participants with rheumatic disease were taking an immunomodulatory medication, including a conventional synthetic disease-modifying antirheumatic drug (csDMARD) in 40%, a biologic DMARD in 37%, tumor necrosis factor (TNF) inhibitors in 32%, hydroxychloroquine (HCQ) in 19%, glucocorticoids in 14%, and mycophenolate in 11%. A smaller proportion were on other biologics: JAK inhibitors in 6.6%, anti-CD20 drugs in 4.4%, and an IL-6 inhibitor in 1%.
Side effects similar in both groups
None of the side effects reported by participants were statistically different between those with rheumatic disease and the control group. Localized pain was the most common side effect, reported by 73%-79% of participants after each dose. About twice as many participants with rheumatic disease experienced muscle aches and joint pains, compared with the control group, but the differences were not significant. Fever occurred more often in those with rheumatic disease (6%, five cases) than without (3%, one case). One-third of those with rheumatic disease felt tiredness, compared with 20% of the control group.
None of the healthy controls were hospitalized after vaccination, but three rheumatic patients were, including two after the first dose. Both were 17 years old, had systemic vasculitis with granulomatosis with polyangiitis (GPA), and were taking rituximab (Rituxan). One patient experienced acute onset of chronic renal failure, fever, dehydration, and high C-reactive protein within hours of vaccination. The other experienced new onset of pulmonary hemorrhage a week after vaccination.
In addition, a 14-year-old female with lupus, taking only HCQ, went to the emergency department with fever, headache, vomiting, and joint pain 1 day after the second vaccine dose. She had normal inflammatory markers and no change in disease activity score, and she was discharged with low-dose steroids tapered after 2 weeks.
Immune response high in patients with rheumatic disease
Immunogenicity was similar in both groups, with 97% seropositivity in the rheumatic disease group and 100% in the control group. Average IgG titers were 242 in the rheumatic group and 388 in the control group (P < .0001). Seropositivity was 88% in those taking mycophenolate with another drug (100% with mycophenolate monotherapy), 90% with HCQ, 94% with any csDMARDs and another drug (100% with csDMARD monotherapy), and 100% for all other drugs. During 3 months’ follow-up after vaccination, there were no COVID-19 cases among the participants.
Dr. Heshin-Bekenstein noted that their results showed better immunogenicity in teens, compared with adults, for two specific drugs. Seropositivity in teens taking methotrexate (Rheumatrex, Trexall) or rituximab was 100% in this study, compared with 84% in adults taking methotrexate and 39% in adults taking rituximab in a previous study. However, only three patients in this study were taking rituximab, and only seven were taking methotrexate.
The study’s heterogenous population was both a strength and a weakness of the study. “Due to the diversity of rheumatic diseases and medications included in this cohort, it was not possible to draw significant conclusions regarding the impact of the immunomodulatory medications and type of disease” on titers, Dr. Heshin-Bekenstein told attendees.
Still, “I think as pediatric rheumatologists, we can feel reassured in recommending the COVID-19 vaccine to our patients,” Dr. Oliver said. “I will add that every patient is different, and everyone should have a conversation with their physician about receiving the COVID-19 vaccine.” Dr. Oliver said she discusses vaccination, including COVID vaccination, with every patient, and it’s been challenging to address concerns in the midst of so much misinformation circulating about the vaccine.
These findings do raise questions about whether it’s still necessary to hold immunomodulatory medications to get the vaccine,” Dr. Rutstein said.
“Many families are nervous to pause their medications before and after the vaccine as is currently recommended for many therapies by the American College of Rheumatology, and I do share that concern for some of my patients with more clinically unstable disease, so I try to work with each family to decide on best timing and have delayed or deferred the series until some patients are on a steady dose of a new immunomodulatory medication if it has been recently started,” Dr. Rutstein said. “This is one of the reasons why Dr. Heshin-Bekenstein’s study is so important – we may be holding medications that can be safely continued and even further decrease the risk of disease flare.”
None of the physicians have disclosed any relevant financial relationships.
A version of this article first appeared on Medscape.com.
The Pfizer-BioNTech mRNA vaccine (Comirnaty) showed a good safety profile with minimal short-term side effects and no negative impact on disease activity in a cohort of adolescents and young adults with rheumatic diseases, according to research presented at the annual scientific meeting of the Childhood Arthritis and Rheumatology Research Alliance, held virtually this year.
Only 3% of patients experience a severe transient adverse event, according to Merav Heshin-Bekenstein, MD, of Dana-Dwek Children’s Hospital at the Tel Aviv Sourasky Medical Center in Israel. The findings were published in Rheumatology.
“We found that the mRNA Pfizer vaccine was immunogenic and induced an adequate humoral immune response in adolescent patients,” Dr. Heshin-Bekenstein told CARRA attendees. “It was definitely comparable to healthy controls and practically all patients were seropositive following the second vaccine, except for one patient with long-standing systemic sclerosis.”
The findings were not necessarily surprising but were encouraging to Melissa S. Oliver, MD, assistant professor of clinical pediatrics in the division of pediatric rheumatology at Indiana University, Indianapolis. Dr. Oliver wasn’t part of the study team.
“We know that the COVID vaccines in healthy adolescents have shown good efficacy with minimal side effects, and it’s good to see that this study showed that in those with rheumatic diseases on immunosuppressive therapy,” Dr. Oliver told this news organization.
Until now, the data on COVID-19 vaccines in teens with rheumatic illnesses has been limited, she said, so “many pediatric rheumatologists only have the data from adult studies to go on or personal experience with their own cohort of patients.”
But the high immunogenicity seen in the study was a pleasant surprise to Beth H. Rutstein, MD, assistant professor of clinical pediatrics in the division of rheumatology at Children’s Hospital of Philadelphia and the Perelman School of Medicine at the University of Pennsylvania.
“I was both surprised and thrilled with Dr. Heshin-Bekenstein’s findings suggesting near-universal seroconversion for patients with rheumatic disease regardless of underlying diagnosis or immunomodulatory therapy regimen, as much of the adult data has suggested a poorer seroconversion rate” and lower antibody titers in adults with similar illnesses, Dr. Rutstein said in an interview.
The study “provides essential reassurance that vaccination against COVID-19 does not increase the risk of disease flare or worsen disease severity scores,” said Dr. Rutstein, who was not associated with the research. “Rather than speaking purely anecdotally with our patients and their families, we can refer to the science – which is always more reassuring for both our patients and ourselves.”
Study included diverse conditions and therapies
Risk factors for poor outcomes with COVID-19 in children include obesity, cardiovascular disease, chronic lung disease, diabetes, and asthma, Dr. Heshin-Bekenstein told CARRA attendees. Multisystem inflammatory syndrome in children (MIS-C) and long COVID are also potential complications of COVID-19 with less understood risk factors.
Although COVID-19 is most often mild in children, certain severe, systemic rheumatic diseases increase hospitalization risk, including systemic lupus erythematosus (SLE) and vasculitis. Evidence has also shown that COVID-19 infection increases the risk of disease flare in teens with juvenile-onset rheumatic diseases, so it’s “crucial to prevent COVID-19 disease in this population,” Dr. Heshin-Bekenstein said.
Her study therefore aimed to assess the safety and immunogenicity of the Pfizer mRNA vaccine for teens with juvenile-onset rheumatic diseases and those taking immunomodulatory medications. The international prospective multicenter study ran from April to November 2021 at three pediatric rheumatology clinics in Israel and one in Slovenia. Endpoints included short-term side effects, vaccination impact on clinical disease activity, immunogenicity at 2-9 weeks after the second dose, and, secondarily, efficacy against COVID-19 infection.
The 91 participants included adolescents aged 12-18 and young adults aged 18-21. Nearly half of the participants (46%) had juvenile idiopathic arthritis (JIA), and 14% had SLE. Other participants’ conditions included systemic vasculitis, idiopathic uveitis, inflammatory bowel disease–related arthritis, systemic or localized scleroderma, juvenile dermatomyositis, or an autoinflammatory disease. Participants’ mean disease duration was 4.8 years.
The researchers compared the patients with a control group of 40 individuals with similar demographics but without rheumatic disease. The researchers used the LIAISON quantitative assay to assess serum IgG antibody levels against the SARS-CoV-2 spike protein in both groups.
Eight in 10 participants with rheumatic disease were taking an immunomodulatory medication, including a conventional synthetic disease-modifying antirheumatic drug (csDMARD) in 40%, a biologic DMARD in 37%, tumor necrosis factor (TNF) inhibitors in 32%, hydroxychloroquine (HCQ) in 19%, glucocorticoids in 14%, and mycophenolate in 11%. A smaller proportion were on other biologics: JAK inhibitors in 6.6%, anti-CD20 drugs in 4.4%, and an IL-6 inhibitor in 1%.
Side effects similar in both groups
None of the side effects reported by participants were statistically different between those with rheumatic disease and the control group. Localized pain was the most common side effect, reported by 73%-79% of participants after each dose. About twice as many participants with rheumatic disease experienced muscle aches and joint pains, compared with the control group, but the differences were not significant. Fever occurred more often in those with rheumatic disease (6%, five cases) than without (3%, one case). One-third of those with rheumatic disease felt tiredness, compared with 20% of the control group.
None of the healthy controls were hospitalized after vaccination, but three rheumatic patients were, including two after the first dose. Both were 17 years old, had systemic vasculitis with granulomatosis with polyangiitis (GPA), and were taking rituximab (Rituxan). One patient experienced acute onset of chronic renal failure, fever, dehydration, and high C-reactive protein within hours of vaccination. The other experienced new onset of pulmonary hemorrhage a week after vaccination.
In addition, a 14-year-old female with lupus, taking only HCQ, went to the emergency department with fever, headache, vomiting, and joint pain 1 day after the second vaccine dose. She had normal inflammatory markers and no change in disease activity score, and she was discharged with low-dose steroids tapered after 2 weeks.
Immune response high in patients with rheumatic disease
Immunogenicity was similar in both groups, with 97% seropositivity in the rheumatic disease group and 100% in the control group. Average IgG titers were 242 in the rheumatic group and 388 in the control group (P < .0001). Seropositivity was 88% in those taking mycophenolate with another drug (100% with mycophenolate monotherapy), 90% with HCQ, 94% with any csDMARDs and another drug (100% with csDMARD monotherapy), and 100% for all other drugs. During 3 months’ follow-up after vaccination, there were no COVID-19 cases among the participants.
Dr. Heshin-Bekenstein noted that their results showed better immunogenicity in teens, compared with adults, for two specific drugs. Seropositivity in teens taking methotrexate (Rheumatrex, Trexall) or rituximab was 100% in this study, compared with 84% in adults taking methotrexate and 39% in adults taking rituximab in a previous study. However, only three patients in this study were taking rituximab, and only seven were taking methotrexate.
The study’s heterogenous population was both a strength and a weakness of the study. “Due to the diversity of rheumatic diseases and medications included in this cohort, it was not possible to draw significant conclusions regarding the impact of the immunomodulatory medications and type of disease” on titers, Dr. Heshin-Bekenstein told attendees.
Still, “I think as pediatric rheumatologists, we can feel reassured in recommending the COVID-19 vaccine to our patients,” Dr. Oliver said. “I will add that every patient is different, and everyone should have a conversation with their physician about receiving the COVID-19 vaccine.” Dr. Oliver said she discusses vaccination, including COVID vaccination, with every patient, and it’s been challenging to address concerns in the midst of so much misinformation circulating about the vaccine.
These findings do raise questions about whether it’s still necessary to hold immunomodulatory medications to get the vaccine,” Dr. Rutstein said.
“Many families are nervous to pause their medications before and after the vaccine as is currently recommended for many therapies by the American College of Rheumatology, and I do share that concern for some of my patients with more clinically unstable disease, so I try to work with each family to decide on best timing and have delayed or deferred the series until some patients are on a steady dose of a new immunomodulatory medication if it has been recently started,” Dr. Rutstein said. “This is one of the reasons why Dr. Heshin-Bekenstein’s study is so important – we may be holding medications that can be safely continued and even further decrease the risk of disease flare.”
None of the physicians have disclosed any relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CARRA 2022
Ondansetron use for acute gastroenteritis in children accelerates
Use of oral ondansetron for acute gastroenteritis in children in an emergency setting increased significantly between 2006 and 2018, but use of intravenous fluids remained consistent, based on data from a cross-sectional analysis.
Recommendations for managing acute gastroenteritis in children include oral rehydration therapy for mild to moderate cases and intravenous rehydration for severe cases, Brett Burstein, MDCM, of McGill University, Montreal, and colleagues wrote.
Oral ondansetron has been shown to reduce vomiting and the need for intravenous rehydration, as well as reduce the need for hospitalization in children with evidence of dehydration, but has no significant benefits for children who are not dehydrated, the researchers noted.
“Given the high prevalence and costs associated with acute gastroenteritis treatment for children, understanding national trends in management in a broad, generalizable sample is important,” they wrote.
In a study published in JAMA Network Open, the researchers identified data from the National Hospital Ambulatory Medical Care Survey from Jan. 1, 2006, to Dec. 31, 2018. They analyzed ED visits by individuals younger than 18 years with either a primary discharge diagnosis of acute gastroenteritis or a primary diagnosis of nausea, vomiting, diarrhea, or dehydration with a secondary diagnosis of acute gastroenteritis. The study population included 4,122 patients with a mean age of 4.8 years. Approximately 85% of the visits were to nonacademic EDs, and 80% were to nonpediatric EDs.
Overall, ED visits for acute gastroenteritis increased over time, from 1.23 million in 2006 to 1.87 million in 2018 (P = .03 for trend). ED visits for acute gastroenteritis also increased significantly as a proportion of all ED pediatric visits, from 4.7% in 2006 to 5.6% in 2018 (P = .02 for trend).
Notably, the use of ondansetron increased from 10.6% in 2006 to 59.2% in 2018; however, intravenous rehydration and hospitalizations remained consistent over the study period, the researchers wrote. Approximately half of children who received intravenous fluids (53.9%) and those hospitalized (49.1%) also received ondansetron.
“Approximately half of children administered intravenous fluids or hospitalized did not receive ondansetron, suggesting that many children without dehydration receive ondansetron with limited benefit, whereas those most likely to benefit receive intravenous fluids without an adequate trial of ondansetron and oral rehydration therapy,” the researchers wrote in their discussion of the findings.
The study findings were limited by several factors including the lack of data on detailed patient-level information such as severity of dehydration, the researchers noted. Other limitations include lack of data on return visits and lack of data on the route of medication administration, which means that the perceived lack of benefit from ondansetron may be the result of children treated with both intravenous ondansetron and fluids, they said.
“Ondansetron-supported oral rehydration therapy for appropriately selected children can achieve intravenous rehydration rates of 9%, more than threefold lower than 2018 national estimates,” and more initiatives are needed to optimize ondansetron and reduce the excessive use of intravenous fluids, the researchers concluded.
Emergency care setting may promote IV fluid use
“Acute gastroenteritis has remained a major cause of pediatric morbidity and mortality worldwide with significant costs for the health care system,” Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice who was not involved in the current study, said in an interview. “The authors highlight that although ondansetron use for acute gastroenteritis in the ED has increased substantially, there are still a number of children who receive intravenous fluids in the ED without a trial of ondansetron and [oral rehydration therapy] first. For the individual patient, it is not surprising that the fast-paced culture of the ED doesn’t cater to a watchful waiting approach. This highlights the need for a more protocol-based algorithm for care of these patients upon check-in.
“Often the practice in the ED is a single dose of ondansetron, followed by attempts at oral rehydration 30 minutes later,” said Dr. Joos. “It would be interesting to know the extent that outpatient clinics are practicing this model prior to sending the patient on to the ED. Despite it becoming a common practice, there is still ongoing research into the efficacy and safety of multidose oral ondansetron at home in reducing ED visits/hospitalizations.”
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose. Lead author Dr. Burstein received a career award from the Quebec Health Research Fund.
Use of oral ondansetron for acute gastroenteritis in children in an emergency setting increased significantly between 2006 and 2018, but use of intravenous fluids remained consistent, based on data from a cross-sectional analysis.
Recommendations for managing acute gastroenteritis in children include oral rehydration therapy for mild to moderate cases and intravenous rehydration for severe cases, Brett Burstein, MDCM, of McGill University, Montreal, and colleagues wrote.
Oral ondansetron has been shown to reduce vomiting and the need for intravenous rehydration, as well as reduce the need for hospitalization in children with evidence of dehydration, but has no significant benefits for children who are not dehydrated, the researchers noted.
“Given the high prevalence and costs associated with acute gastroenteritis treatment for children, understanding national trends in management in a broad, generalizable sample is important,” they wrote.
In a study published in JAMA Network Open, the researchers identified data from the National Hospital Ambulatory Medical Care Survey from Jan. 1, 2006, to Dec. 31, 2018. They analyzed ED visits by individuals younger than 18 years with either a primary discharge diagnosis of acute gastroenteritis or a primary diagnosis of nausea, vomiting, diarrhea, or dehydration with a secondary diagnosis of acute gastroenteritis. The study population included 4,122 patients with a mean age of 4.8 years. Approximately 85% of the visits were to nonacademic EDs, and 80% were to nonpediatric EDs.
Overall, ED visits for acute gastroenteritis increased over time, from 1.23 million in 2006 to 1.87 million in 2018 (P = .03 for trend). ED visits for acute gastroenteritis also increased significantly as a proportion of all ED pediatric visits, from 4.7% in 2006 to 5.6% in 2018 (P = .02 for trend).
Notably, the use of ondansetron increased from 10.6% in 2006 to 59.2% in 2018; however, intravenous rehydration and hospitalizations remained consistent over the study period, the researchers wrote. Approximately half of children who received intravenous fluids (53.9%) and those hospitalized (49.1%) also received ondansetron.
“Approximately half of children administered intravenous fluids or hospitalized did not receive ondansetron, suggesting that many children without dehydration receive ondansetron with limited benefit, whereas those most likely to benefit receive intravenous fluids without an adequate trial of ondansetron and oral rehydration therapy,” the researchers wrote in their discussion of the findings.
The study findings were limited by several factors including the lack of data on detailed patient-level information such as severity of dehydration, the researchers noted. Other limitations include lack of data on return visits and lack of data on the route of medication administration, which means that the perceived lack of benefit from ondansetron may be the result of children treated with both intravenous ondansetron and fluids, they said.
“Ondansetron-supported oral rehydration therapy for appropriately selected children can achieve intravenous rehydration rates of 9%, more than threefold lower than 2018 national estimates,” and more initiatives are needed to optimize ondansetron and reduce the excessive use of intravenous fluids, the researchers concluded.
Emergency care setting may promote IV fluid use
“Acute gastroenteritis has remained a major cause of pediatric morbidity and mortality worldwide with significant costs for the health care system,” Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice who was not involved in the current study, said in an interview. “The authors highlight that although ondansetron use for acute gastroenteritis in the ED has increased substantially, there are still a number of children who receive intravenous fluids in the ED without a trial of ondansetron and [oral rehydration therapy] first. For the individual patient, it is not surprising that the fast-paced culture of the ED doesn’t cater to a watchful waiting approach. This highlights the need for a more protocol-based algorithm for care of these patients upon check-in.
“Often the practice in the ED is a single dose of ondansetron, followed by attempts at oral rehydration 30 minutes later,” said Dr. Joos. “It would be interesting to know the extent that outpatient clinics are practicing this model prior to sending the patient on to the ED. Despite it becoming a common practice, there is still ongoing research into the efficacy and safety of multidose oral ondansetron at home in reducing ED visits/hospitalizations.”
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose. Lead author Dr. Burstein received a career award from the Quebec Health Research Fund.
Use of oral ondansetron for acute gastroenteritis in children in an emergency setting increased significantly between 2006 and 2018, but use of intravenous fluids remained consistent, based on data from a cross-sectional analysis.
Recommendations for managing acute gastroenteritis in children include oral rehydration therapy for mild to moderate cases and intravenous rehydration for severe cases, Brett Burstein, MDCM, of McGill University, Montreal, and colleagues wrote.
Oral ondansetron has been shown to reduce vomiting and the need for intravenous rehydration, as well as reduce the need for hospitalization in children with evidence of dehydration, but has no significant benefits for children who are not dehydrated, the researchers noted.
“Given the high prevalence and costs associated with acute gastroenteritis treatment for children, understanding national trends in management in a broad, generalizable sample is important,” they wrote.
In a study published in JAMA Network Open, the researchers identified data from the National Hospital Ambulatory Medical Care Survey from Jan. 1, 2006, to Dec. 31, 2018. They analyzed ED visits by individuals younger than 18 years with either a primary discharge diagnosis of acute gastroenteritis or a primary diagnosis of nausea, vomiting, diarrhea, or dehydration with a secondary diagnosis of acute gastroenteritis. The study population included 4,122 patients with a mean age of 4.8 years. Approximately 85% of the visits were to nonacademic EDs, and 80% were to nonpediatric EDs.
Overall, ED visits for acute gastroenteritis increased over time, from 1.23 million in 2006 to 1.87 million in 2018 (P = .03 for trend). ED visits for acute gastroenteritis also increased significantly as a proportion of all ED pediatric visits, from 4.7% in 2006 to 5.6% in 2018 (P = .02 for trend).
Notably, the use of ondansetron increased from 10.6% in 2006 to 59.2% in 2018; however, intravenous rehydration and hospitalizations remained consistent over the study period, the researchers wrote. Approximately half of children who received intravenous fluids (53.9%) and those hospitalized (49.1%) also received ondansetron.
“Approximately half of children administered intravenous fluids or hospitalized did not receive ondansetron, suggesting that many children without dehydration receive ondansetron with limited benefit, whereas those most likely to benefit receive intravenous fluids without an adequate trial of ondansetron and oral rehydration therapy,” the researchers wrote in their discussion of the findings.
The study findings were limited by several factors including the lack of data on detailed patient-level information such as severity of dehydration, the researchers noted. Other limitations include lack of data on return visits and lack of data on the route of medication administration, which means that the perceived lack of benefit from ondansetron may be the result of children treated with both intravenous ondansetron and fluids, they said.
“Ondansetron-supported oral rehydration therapy for appropriately selected children can achieve intravenous rehydration rates of 9%, more than threefold lower than 2018 national estimates,” and more initiatives are needed to optimize ondansetron and reduce the excessive use of intravenous fluids, the researchers concluded.
Emergency care setting may promote IV fluid use
“Acute gastroenteritis has remained a major cause of pediatric morbidity and mortality worldwide with significant costs for the health care system,” Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice who was not involved in the current study, said in an interview. “The authors highlight that although ondansetron use for acute gastroenteritis in the ED has increased substantially, there are still a number of children who receive intravenous fluids in the ED without a trial of ondansetron and [oral rehydration therapy] first. For the individual patient, it is not surprising that the fast-paced culture of the ED doesn’t cater to a watchful waiting approach. This highlights the need for a more protocol-based algorithm for care of these patients upon check-in.
“Often the practice in the ED is a single dose of ondansetron, followed by attempts at oral rehydration 30 minutes later,” said Dr. Joos. “It would be interesting to know the extent that outpatient clinics are practicing this model prior to sending the patient on to the ED. Despite it becoming a common practice, there is still ongoing research into the efficacy and safety of multidose oral ondansetron at home in reducing ED visits/hospitalizations.”
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose. Lead author Dr. Burstein received a career award from the Quebec Health Research Fund.
FROM JAMA NETWORK OPEN
Race-based spirometry may lead to missed diagnoses
SAN FRANCISCO – It may be time to move beyond relying largely on spirometry to distinguish between healthy and abnormal lung function in diverse populations.
That conclusion comes from investigators who looked at patients with ostensibly normal spirometry values in a large population-based study and found that using standard equations to adjust for racial differences in lung-function measures appeared to miss emphysema in a significant proportion of Black patients.
“Our traditional measures of lung health based on spirometry may be under-recognizing impaired respiratory health in Black adults and particularly Black men,” said lead author Gabrielle Liu, MD, a fellow in the division of pulmonary and critical care medicine at the Northwestern University Feinberg School of Medicine, Chicago.
“CT imaging may be useful in the evaluation of those with suspected impaired respiratory health and normal spirometry,” she said in an oral abstract session at the American Thoracic Society International Conference 2022.
Dr. Liu and colleagues studied the association between self-identified race and visually identified emphysema among 2,674 participants in the Coronary Artery Risk Development in Young Adults (CARDIA) study. The patients had CT scans at a mean age of 50 and spirometry at a mean age of 55.
Racial differences
The investigators found that among men with forced expiratory volume in 1 second (FEV1) ranging from 100% to 120% of predicted according to race-adjusted formulas, 14.6% of Black men had emphysema, compared with only 1.7% of White men (P < .001). Respective emphysema rates in Black women and White women were 3.8% and 1.9%; this difference was not statistically significant.
Among patients with FEV1 80% to 99% of predicted according to race-specific measures, 15.5% of Black men had emphysema, compared with 4% of White men (P < .001). Respective rates of emphysema were 6.9% for Black women versus 3.2% for White women (P = .025).
When the investigators applied race-neutral spirometry reference equations to the same population, they found that it attenuated but did not completely eliminate the racial disparity in emphysema prevalence among patients with FEV1, ranging from 80% to 120% of predicted.
Relic of the past
The results suggest that race-based adjustments of spirometry measures are a relic of less enlightened times, said Adam Gaffney, MD, MPH, assistant professor of medicine at Harvard Medical School, Boston, and a pulmonologist and critical care physician at Cambridge Health Alliance, Massachusetts.
“If the average lower lung function of Black people is being driven by adversity, structural racism, and deprivation, that means that race-specific equations are normalizing that adversity,” he said in an interview.
“In my opinion, it is time to move beyond race-based equations in clinical pulmonary medicine, particularly in the context of patients with established lung disease in whom use of race-based equations might actually lead to undertreatment,” said Dr. Gaffney, who was not involved in the study.
Dr. Liu agreed that it’s time to move to race-neutral measures and that the whole concept of race-based differences is flawed.
“The long-standing structural inequities in health likely made the reference populations have lower lung function than among Whites,” she told this news organization.
Dr. Liu said that evaluation of lung function should not rely on spirometry alone, but should also include – when appropriate – CT scans, as well as improved understanding of how symptoms may be predictive for poor outcomes.
The study was supported by grants from the National Institutes of Health. Dr. Liu and Dr. Gaffney have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – It may be time to move beyond relying largely on spirometry to distinguish between healthy and abnormal lung function in diverse populations.
That conclusion comes from investigators who looked at patients with ostensibly normal spirometry values in a large population-based study and found that using standard equations to adjust for racial differences in lung-function measures appeared to miss emphysema in a significant proportion of Black patients.
“Our traditional measures of lung health based on spirometry may be under-recognizing impaired respiratory health in Black adults and particularly Black men,” said lead author Gabrielle Liu, MD, a fellow in the division of pulmonary and critical care medicine at the Northwestern University Feinberg School of Medicine, Chicago.
“CT imaging may be useful in the evaluation of those with suspected impaired respiratory health and normal spirometry,” she said in an oral abstract session at the American Thoracic Society International Conference 2022.
Dr. Liu and colleagues studied the association between self-identified race and visually identified emphysema among 2,674 participants in the Coronary Artery Risk Development in Young Adults (CARDIA) study. The patients had CT scans at a mean age of 50 and spirometry at a mean age of 55.
Racial differences
The investigators found that among men with forced expiratory volume in 1 second (FEV1) ranging from 100% to 120% of predicted according to race-adjusted formulas, 14.6% of Black men had emphysema, compared with only 1.7% of White men (P < .001). Respective emphysema rates in Black women and White women were 3.8% and 1.9%; this difference was not statistically significant.
Among patients with FEV1 80% to 99% of predicted according to race-specific measures, 15.5% of Black men had emphysema, compared with 4% of White men (P < .001). Respective rates of emphysema were 6.9% for Black women versus 3.2% for White women (P = .025).
When the investigators applied race-neutral spirometry reference equations to the same population, they found that it attenuated but did not completely eliminate the racial disparity in emphysema prevalence among patients with FEV1, ranging from 80% to 120% of predicted.
Relic of the past
The results suggest that race-based adjustments of spirometry measures are a relic of less enlightened times, said Adam Gaffney, MD, MPH, assistant professor of medicine at Harvard Medical School, Boston, and a pulmonologist and critical care physician at Cambridge Health Alliance, Massachusetts.
“If the average lower lung function of Black people is being driven by adversity, structural racism, and deprivation, that means that race-specific equations are normalizing that adversity,” he said in an interview.
“In my opinion, it is time to move beyond race-based equations in clinical pulmonary medicine, particularly in the context of patients with established lung disease in whom use of race-based equations might actually lead to undertreatment,” said Dr. Gaffney, who was not involved in the study.
Dr. Liu agreed that it’s time to move to race-neutral measures and that the whole concept of race-based differences is flawed.
“The long-standing structural inequities in health likely made the reference populations have lower lung function than among Whites,” she told this news organization.
Dr. Liu said that evaluation of lung function should not rely on spirometry alone, but should also include – when appropriate – CT scans, as well as improved understanding of how symptoms may be predictive for poor outcomes.
The study was supported by grants from the National Institutes of Health. Dr. Liu and Dr. Gaffney have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – It may be time to move beyond relying largely on spirometry to distinguish between healthy and abnormal lung function in diverse populations.
That conclusion comes from investigators who looked at patients with ostensibly normal spirometry values in a large population-based study and found that using standard equations to adjust for racial differences in lung-function measures appeared to miss emphysema in a significant proportion of Black patients.
“Our traditional measures of lung health based on spirometry may be under-recognizing impaired respiratory health in Black adults and particularly Black men,” said lead author Gabrielle Liu, MD, a fellow in the division of pulmonary and critical care medicine at the Northwestern University Feinberg School of Medicine, Chicago.
“CT imaging may be useful in the evaluation of those with suspected impaired respiratory health and normal spirometry,” she said in an oral abstract session at the American Thoracic Society International Conference 2022.
Dr. Liu and colleagues studied the association between self-identified race and visually identified emphysema among 2,674 participants in the Coronary Artery Risk Development in Young Adults (CARDIA) study. The patients had CT scans at a mean age of 50 and spirometry at a mean age of 55.
Racial differences
The investigators found that among men with forced expiratory volume in 1 second (FEV1) ranging from 100% to 120% of predicted according to race-adjusted formulas, 14.6% of Black men had emphysema, compared with only 1.7% of White men (P < .001). Respective emphysema rates in Black women and White women were 3.8% and 1.9%; this difference was not statistically significant.
Among patients with FEV1 80% to 99% of predicted according to race-specific measures, 15.5% of Black men had emphysema, compared with 4% of White men (P < .001). Respective rates of emphysema were 6.9% for Black women versus 3.2% for White women (P = .025).
When the investigators applied race-neutral spirometry reference equations to the same population, they found that it attenuated but did not completely eliminate the racial disparity in emphysema prevalence among patients with FEV1, ranging from 80% to 120% of predicted.
Relic of the past
The results suggest that race-based adjustments of spirometry measures are a relic of less enlightened times, said Adam Gaffney, MD, MPH, assistant professor of medicine at Harvard Medical School, Boston, and a pulmonologist and critical care physician at Cambridge Health Alliance, Massachusetts.
“If the average lower lung function of Black people is being driven by adversity, structural racism, and deprivation, that means that race-specific equations are normalizing that adversity,” he said in an interview.
“In my opinion, it is time to move beyond race-based equations in clinical pulmonary medicine, particularly in the context of patients with established lung disease in whom use of race-based equations might actually lead to undertreatment,” said Dr. Gaffney, who was not involved in the study.
Dr. Liu agreed that it’s time to move to race-neutral measures and that the whole concept of race-based differences is flawed.
“The long-standing structural inequities in health likely made the reference populations have lower lung function than among Whites,” she told this news organization.
Dr. Liu said that evaluation of lung function should not rely on spirometry alone, but should also include – when appropriate – CT scans, as well as improved understanding of how symptoms may be predictive for poor outcomes.
The study was supported by grants from the National Institutes of Health. Dr. Liu and Dr. Gaffney have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ATS 2022
Recurrent Arciform Plaque on the Face
The Diagnosis: Lupus Erythematosus Tumidus
Histopathologic evaluation of a punch biopsy revealed focal dermal mucin deposition and CD123+ discrete clusters of plasmacytoid dendritic cells without interface changes (Figure 1), favoring a diagnosis of lupus erythematosus tumidus (LET) in our patient. There was no clinical improvement in symptoms when she previously was treated with topical antifungals or class III corticosteroid creams. Tacrolimus ointment 0.1% twice daily for 1 month did not result in substantial improvement in the appearance of the plaque, and it spontaneously resolved after 2 to 3 months. She declined treatment with hydroxychloroquine.
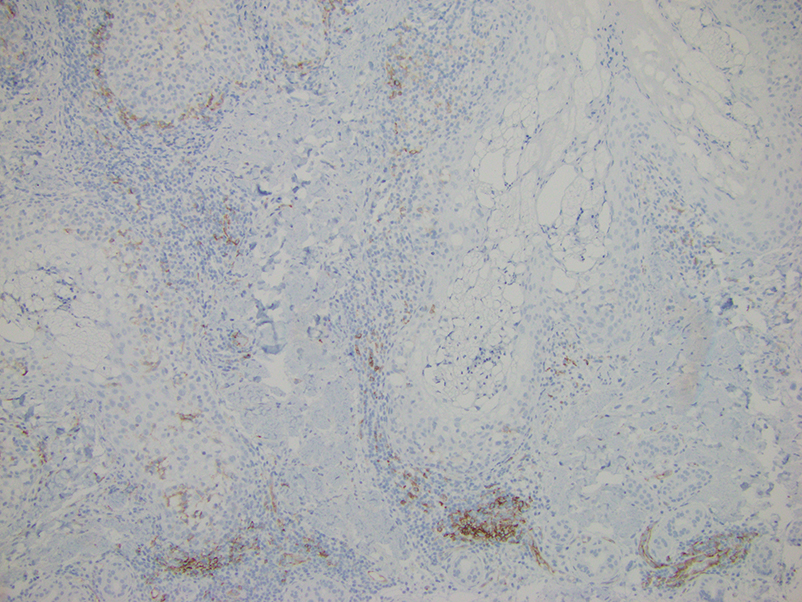
Lupus erythematosus tumidus is an uncommon subtype of chronic cutaneous lupus erythematosus with no distinct etiology. It is clinically characterized by edematous, urticarial, single or multiple plaques with a smooth surface affecting sun-exposed areas that can last for months to years.1 In contrast to other variations of chronic cutaneous lupus such as discoid lupus erythematosus, LET lesions lack surface papulosquamous features such as scaling, atrophy, and follicular plugging.1-4 Based solely on histologic findings, LET may be indistinguishable from reticular erythematous mucinosis and Jessner lymphocytic infiltration of the skin (JLIS) due to a similar lack of epidermal involvement and presence of a perivascular lymphocytic infiltrate (Figure 2).
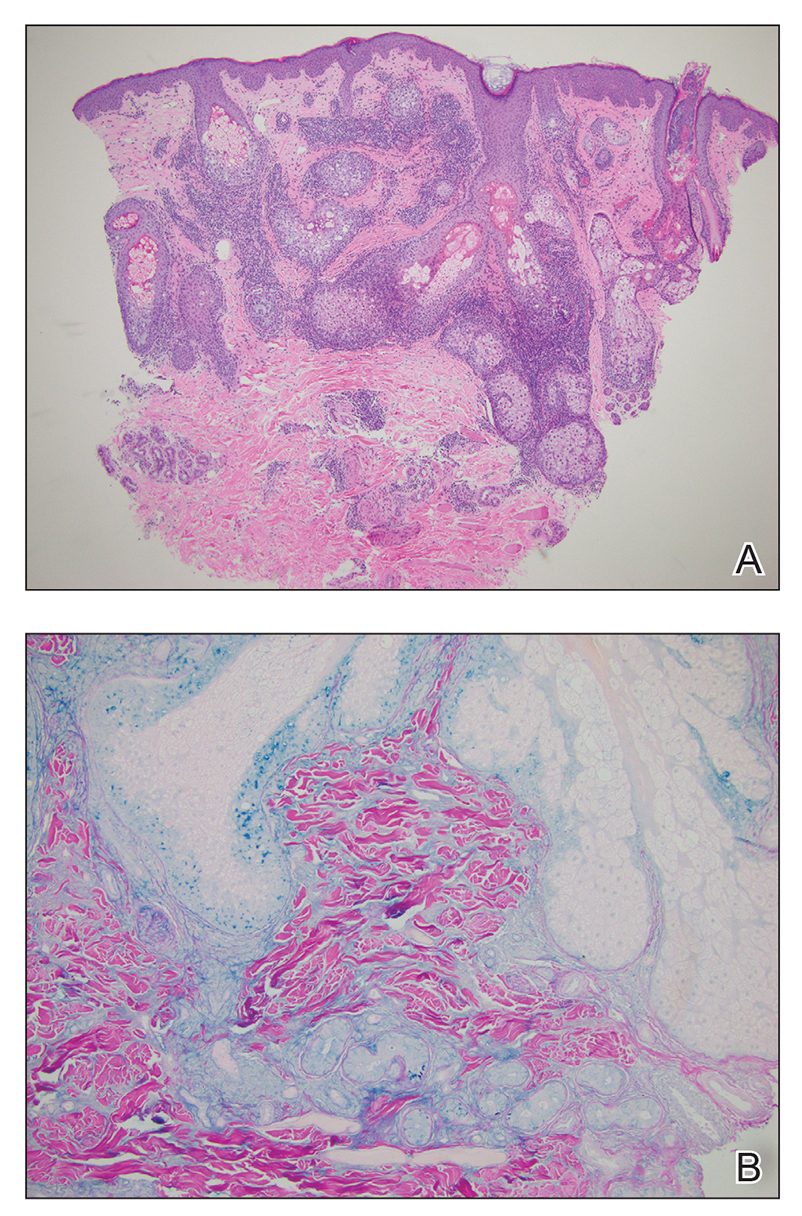
The average age at disease onset is 36 years, nearly the same as that described in discoid lupus erythematosus.4 Lupus erythematosus tumidus has a favorable prognosis and commonly presents without other autoimmune signs, serologic abnormalities, or gender preference, with concomitant systemic lupus erythematosus sometimes reported.5
The absence of clinical and histological epidermal involvement are the most important clues to aid in the diagnosis. It has been postulated that JLIS could be an early cutaneous manifestation of LET.6 The differential diagnosis also may include erythema annulare centrifugum, granuloma annulare, and urticarial vasculitis. Lesions typically respond well to photoprotection, topical corticosteroids, and/or antimalarials. The addition of tacrolimus ointment 0.1% may result in complete regression without recurrence.7
Erythema annulare centrifugum is a reactive erythema that classically begins as a pink papule that gradually enlarges to form an annular erythematous plaque with a fine trailing scale that may recur.8 The histopathology of erythema annulare centrifugum shares features seen in LET, making the diagnosis difficult; however, secondary changes to the epidermis (eg, spongiosis, hyperkeratosis) may be seen. This condition has been associated with lymphoproliferative malignancies.8
Reticular erythematous mucinosis is clinically distinguished from LET, as it presents as reticular, rather than arciform, erythematous macules, papules, or plaques that may be asymptomatic or pruritic.9 Histopathology typically shows more superficial mucin deposition than in LET as well as superficial to mid-dermal perivascular and periadnexal lymphocytic infiltrates. Reticular erythematous mucinosis more frequently is reported in women in their 30s and 40s and has been associated with UV exposure and hormonal triggers, such as oral contraceptive medications and pregnancy.9
Granuloma annulare typically presents as asymptomatic, erythematous, annular plaques or papules in young women.10 There are several histologic subtypes that show focal collagen degeneration, inflammation with palisaded or interstitial histiocytes, and mucin deposition, regardless of clinical presentation. Granuloma annulare has been associated with systemic diseases including type 2 diabetes mellitus and thyroid disease. Localized granuloma annulare most commonly presents on the dorsal aspects of the hands or feet.10
We present a case of LET on the face. Although histologically similar to other dermatoses, LET often lacks epidermal involvement and presents on sun-exposed areas of the body. Jessner lymphocytic infiltration of the skin also should be considered in the differential, as there is an overlap of clinical and histopathological features; JLIS lacks mucin deposits.6 This case reinforces the importance of correlating clinical with histopathologic findings. Our patient was treated with tacrolimus ointment 0.1%, and the plaque eventually resolved in 2 to 3 months without recurrence. This condition should be included in the differential diagnosis of recurring annular plaques on sunexposed areas, particularly in middle-aged adults, even in the absence of systemic involvement.
- Liu E, Daze RP, Moon S. Tumid lupus erythematosus: a rare and distinctive variant of cutaneous lupus erythematosus masquerading as urticarial vasculitis. Cureus. 2020;12:E8305. doi:10.7759/cureus.8305
- Saleh D, Crane JS. Tumid lupus erythematosus. In: StatPearls. StatPearls Publishing; 2020.
- Verma P, Sharma S, Yadav P, et al. Tumid lupus erythematosus: an intriguing dermatopathological connotation treated successfully with topical tacrolimus and hydroxychloroquine combination. Indian J Dermatol. 2014;59:210. doi:10.4103/0019-5154.127716
- Kuhn A, Bein D, Bonsmann G. The 100th anniversary of lupus erythematosus tumidus. Autoimmun Rev. 2009;8:441-448. doi:10.1016/j. autrev.2008.12.010
- Jatwani K, Chugh K, Osholowu OS, et al. Tumid lupus erythematosus and systemic lupus erythematosus: a report on their rare coexistence. Cureus. 2020;12:E7545. doi:10.7759/cureus.7545
- Tomasini D, Mentzel T, Hantschke M, et al. Plasmacytoid dendritic cells: an overview of their presence and distribution in different inflammatory skin diseases, with special emphasis on Jessner’s lymphocytic infiltrate of the skin and cutaneous lupus erythematosus. J Cutan Pathol. 2010;37:1132-1139. doi:10.1111/j.1600-0560.2010.01587.x
- Patsinakidis N, Kautz O, Gibbs BF, et al. Lupus erythematosus tumidus: clinical perspectives. Clin Cosmet Investig Dermatol. 2019;12:707-719. doi:10.2147/CCID.S166723
- Mu EW, Sanchez M, Mir A, et al. Paraneoplastic erythema annulare centrifugum eruption (PEACE). Dermatol Online J. 2015;21:13030/ qt6053h29n.
- Ocanha-Xavier JP, Cola-Senra CO, Xavier-Junior JCC. Reticular erythematous mucinosis: literature review and case report of a 24-year-old patient with systemic erythematosus lupus. Lupus. 2021;30:325-335. doi:10.1177/0961203320965702 10. Keimig EL. Granuloma annulare. Dermatol Clin. 2015;33:315-329. doi:10.1016/j.det.2015.03.001
The Diagnosis: Lupus Erythematosus Tumidus
Histopathologic evaluation of a punch biopsy revealed focal dermal mucin deposition and CD123+ discrete clusters of plasmacytoid dendritic cells without interface changes (Figure 1), favoring a diagnosis of lupus erythematosus tumidus (LET) in our patient. There was no clinical improvement in symptoms when she previously was treated with topical antifungals or class III corticosteroid creams. Tacrolimus ointment 0.1% twice daily for 1 month did not result in substantial improvement in the appearance of the plaque, and it spontaneously resolved after 2 to 3 months. She declined treatment with hydroxychloroquine.
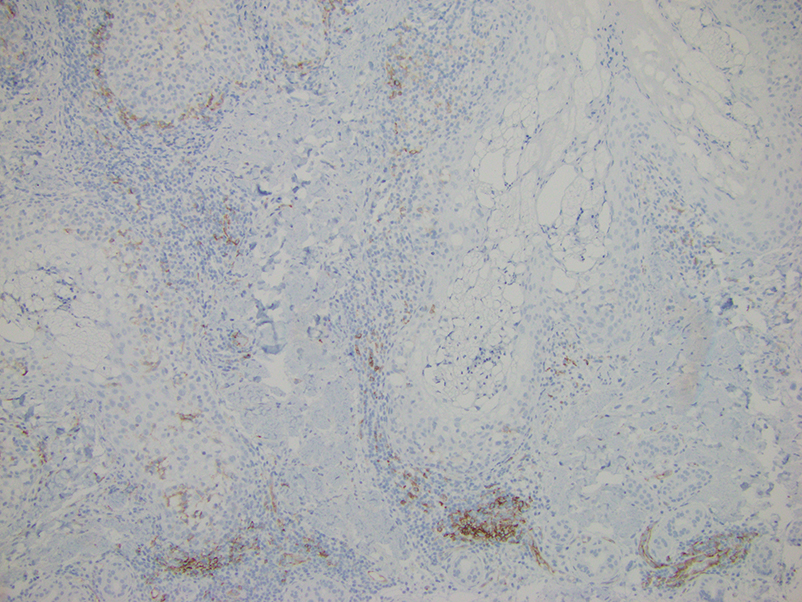
Lupus erythematosus tumidus is an uncommon subtype of chronic cutaneous lupus erythematosus with no distinct etiology. It is clinically characterized by edematous, urticarial, single or multiple plaques with a smooth surface affecting sun-exposed areas that can last for months to years.1 In contrast to other variations of chronic cutaneous lupus such as discoid lupus erythematosus, LET lesions lack surface papulosquamous features such as scaling, atrophy, and follicular plugging.1-4 Based solely on histologic findings, LET may be indistinguishable from reticular erythematous mucinosis and Jessner lymphocytic infiltration of the skin (JLIS) due to a similar lack of epidermal involvement and presence of a perivascular lymphocytic infiltrate (Figure 2).
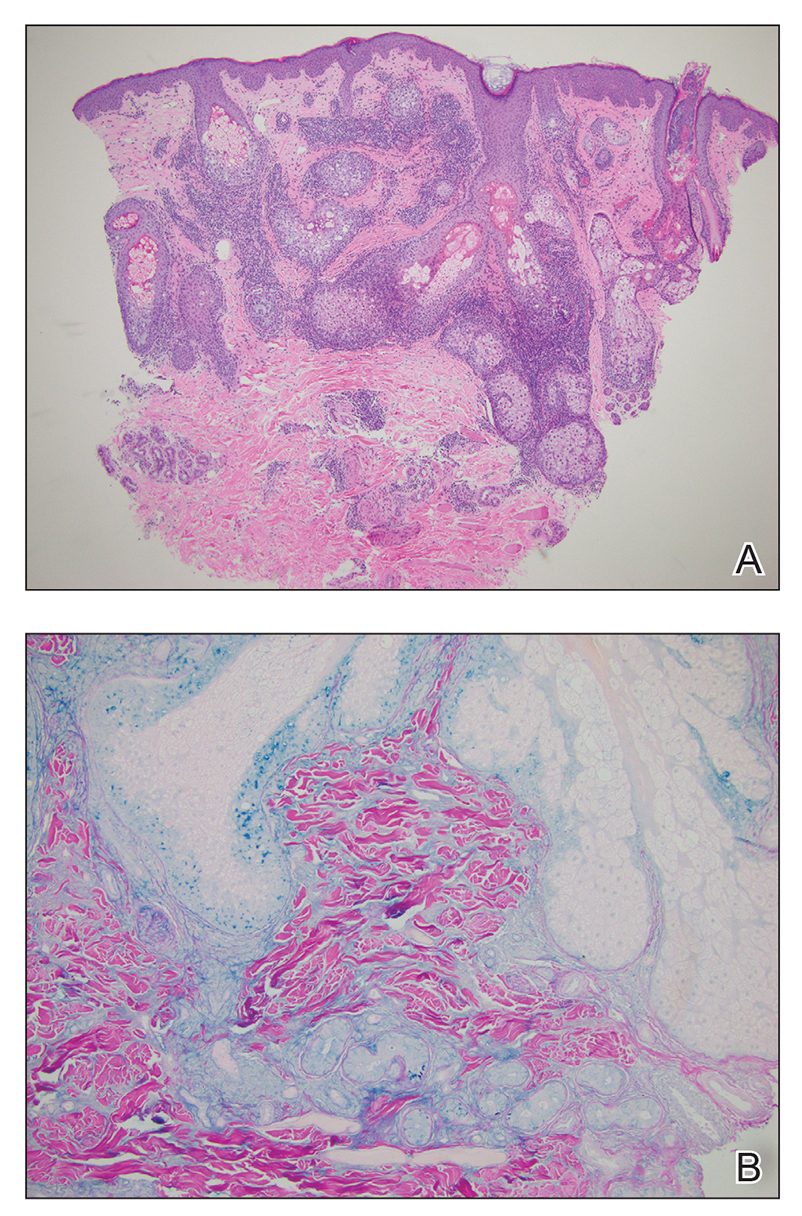
The average age at disease onset is 36 years, nearly the same as that described in discoid lupus erythematosus.4 Lupus erythematosus tumidus has a favorable prognosis and commonly presents without other autoimmune signs, serologic abnormalities, or gender preference, with concomitant systemic lupus erythematosus sometimes reported.5
The absence of clinical and histological epidermal involvement are the most important clues to aid in the diagnosis. It has been postulated that JLIS could be an early cutaneous manifestation of LET.6 The differential diagnosis also may include erythema annulare centrifugum, granuloma annulare, and urticarial vasculitis. Lesions typically respond well to photoprotection, topical corticosteroids, and/or antimalarials. The addition of tacrolimus ointment 0.1% may result in complete regression without recurrence.7
Erythema annulare centrifugum is a reactive erythema that classically begins as a pink papule that gradually enlarges to form an annular erythematous plaque with a fine trailing scale that may recur.8 The histopathology of erythema annulare centrifugum shares features seen in LET, making the diagnosis difficult; however, secondary changes to the epidermis (eg, spongiosis, hyperkeratosis) may be seen. This condition has been associated with lymphoproliferative malignancies.8
Reticular erythematous mucinosis is clinically distinguished from LET, as it presents as reticular, rather than arciform, erythematous macules, papules, or plaques that may be asymptomatic or pruritic.9 Histopathology typically shows more superficial mucin deposition than in LET as well as superficial to mid-dermal perivascular and periadnexal lymphocytic infiltrates. Reticular erythematous mucinosis more frequently is reported in women in their 30s and 40s and has been associated with UV exposure and hormonal triggers, such as oral contraceptive medications and pregnancy.9
Granuloma annulare typically presents as asymptomatic, erythematous, annular plaques or papules in young women.10 There are several histologic subtypes that show focal collagen degeneration, inflammation with palisaded or interstitial histiocytes, and mucin deposition, regardless of clinical presentation. Granuloma annulare has been associated with systemic diseases including type 2 diabetes mellitus and thyroid disease. Localized granuloma annulare most commonly presents on the dorsal aspects of the hands or feet.10
We present a case of LET on the face. Although histologically similar to other dermatoses, LET often lacks epidermal involvement and presents on sun-exposed areas of the body. Jessner lymphocytic infiltration of the skin also should be considered in the differential, as there is an overlap of clinical and histopathological features; JLIS lacks mucin deposits.6 This case reinforces the importance of correlating clinical with histopathologic findings. Our patient was treated with tacrolimus ointment 0.1%, and the plaque eventually resolved in 2 to 3 months without recurrence. This condition should be included in the differential diagnosis of recurring annular plaques on sunexposed areas, particularly in middle-aged adults, even in the absence of systemic involvement.
The Diagnosis: Lupus Erythematosus Tumidus
Histopathologic evaluation of a punch biopsy revealed focal dermal mucin deposition and CD123+ discrete clusters of plasmacytoid dendritic cells without interface changes (Figure 1), favoring a diagnosis of lupus erythematosus tumidus (LET) in our patient. There was no clinical improvement in symptoms when she previously was treated with topical antifungals or class III corticosteroid creams. Tacrolimus ointment 0.1% twice daily for 1 month did not result in substantial improvement in the appearance of the plaque, and it spontaneously resolved after 2 to 3 months. She declined treatment with hydroxychloroquine.
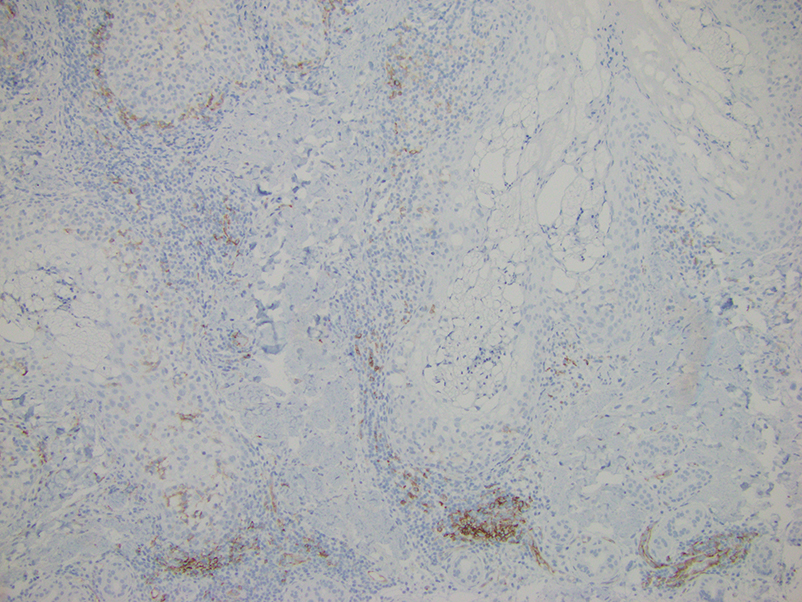
Lupus erythematosus tumidus is an uncommon subtype of chronic cutaneous lupus erythematosus with no distinct etiology. It is clinically characterized by edematous, urticarial, single or multiple plaques with a smooth surface affecting sun-exposed areas that can last for months to years.1 In contrast to other variations of chronic cutaneous lupus such as discoid lupus erythematosus, LET lesions lack surface papulosquamous features such as scaling, atrophy, and follicular plugging.1-4 Based solely on histologic findings, LET may be indistinguishable from reticular erythematous mucinosis and Jessner lymphocytic infiltration of the skin (JLIS) due to a similar lack of epidermal involvement and presence of a perivascular lymphocytic infiltrate (Figure 2).
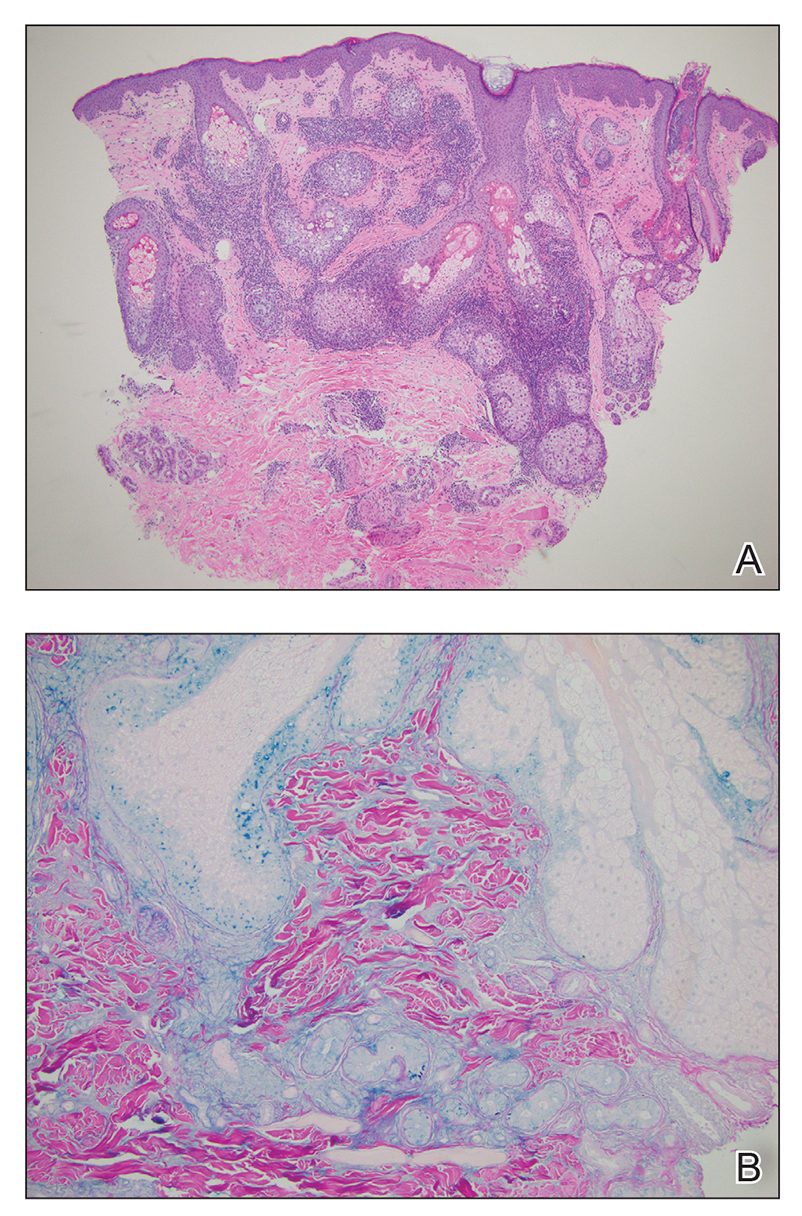
The average age at disease onset is 36 years, nearly the same as that described in discoid lupus erythematosus.4 Lupus erythematosus tumidus has a favorable prognosis and commonly presents without other autoimmune signs, serologic abnormalities, or gender preference, with concomitant systemic lupus erythematosus sometimes reported.5
The absence of clinical and histological epidermal involvement are the most important clues to aid in the diagnosis. It has been postulated that JLIS could be an early cutaneous manifestation of LET.6 The differential diagnosis also may include erythema annulare centrifugum, granuloma annulare, and urticarial vasculitis. Lesions typically respond well to photoprotection, topical corticosteroids, and/or antimalarials. The addition of tacrolimus ointment 0.1% may result in complete regression without recurrence.7
Erythema annulare centrifugum is a reactive erythema that classically begins as a pink papule that gradually enlarges to form an annular erythematous plaque with a fine trailing scale that may recur.8 The histopathology of erythema annulare centrifugum shares features seen in LET, making the diagnosis difficult; however, secondary changes to the epidermis (eg, spongiosis, hyperkeratosis) may be seen. This condition has been associated with lymphoproliferative malignancies.8
Reticular erythematous mucinosis is clinically distinguished from LET, as it presents as reticular, rather than arciform, erythematous macules, papules, or plaques that may be asymptomatic or pruritic.9 Histopathology typically shows more superficial mucin deposition than in LET as well as superficial to mid-dermal perivascular and periadnexal lymphocytic infiltrates. Reticular erythematous mucinosis more frequently is reported in women in their 30s and 40s and has been associated with UV exposure and hormonal triggers, such as oral contraceptive medications and pregnancy.9
Granuloma annulare typically presents as asymptomatic, erythematous, annular plaques or papules in young women.10 There are several histologic subtypes that show focal collagen degeneration, inflammation with palisaded or interstitial histiocytes, and mucin deposition, regardless of clinical presentation. Granuloma annulare has been associated with systemic diseases including type 2 diabetes mellitus and thyroid disease. Localized granuloma annulare most commonly presents on the dorsal aspects of the hands or feet.10
We present a case of LET on the face. Although histologically similar to other dermatoses, LET often lacks epidermal involvement and presents on sun-exposed areas of the body. Jessner lymphocytic infiltration of the skin also should be considered in the differential, as there is an overlap of clinical and histopathological features; JLIS lacks mucin deposits.6 This case reinforces the importance of correlating clinical with histopathologic findings. Our patient was treated with tacrolimus ointment 0.1%, and the plaque eventually resolved in 2 to 3 months without recurrence. This condition should be included in the differential diagnosis of recurring annular plaques on sunexposed areas, particularly in middle-aged adults, even in the absence of systemic involvement.
- Liu E, Daze RP, Moon S. Tumid lupus erythematosus: a rare and distinctive variant of cutaneous lupus erythematosus masquerading as urticarial vasculitis. Cureus. 2020;12:E8305. doi:10.7759/cureus.8305
- Saleh D, Crane JS. Tumid lupus erythematosus. In: StatPearls. StatPearls Publishing; 2020.
- Verma P, Sharma S, Yadav P, et al. Tumid lupus erythematosus: an intriguing dermatopathological connotation treated successfully with topical tacrolimus and hydroxychloroquine combination. Indian J Dermatol. 2014;59:210. doi:10.4103/0019-5154.127716
- Kuhn A, Bein D, Bonsmann G. The 100th anniversary of lupus erythematosus tumidus. Autoimmun Rev. 2009;8:441-448. doi:10.1016/j. autrev.2008.12.010
- Jatwani K, Chugh K, Osholowu OS, et al. Tumid lupus erythematosus and systemic lupus erythematosus: a report on their rare coexistence. Cureus. 2020;12:E7545. doi:10.7759/cureus.7545
- Tomasini D, Mentzel T, Hantschke M, et al. Plasmacytoid dendritic cells: an overview of their presence and distribution in different inflammatory skin diseases, with special emphasis on Jessner’s lymphocytic infiltrate of the skin and cutaneous lupus erythematosus. J Cutan Pathol. 2010;37:1132-1139. doi:10.1111/j.1600-0560.2010.01587.x
- Patsinakidis N, Kautz O, Gibbs BF, et al. Lupus erythematosus tumidus: clinical perspectives. Clin Cosmet Investig Dermatol. 2019;12:707-719. doi:10.2147/CCID.S166723
- Mu EW, Sanchez M, Mir A, et al. Paraneoplastic erythema annulare centrifugum eruption (PEACE). Dermatol Online J. 2015;21:13030/ qt6053h29n.
- Ocanha-Xavier JP, Cola-Senra CO, Xavier-Junior JCC. Reticular erythematous mucinosis: literature review and case report of a 24-year-old patient with systemic erythematosus lupus. Lupus. 2021;30:325-335. doi:10.1177/0961203320965702 10. Keimig EL. Granuloma annulare. Dermatol Clin. 2015;33:315-329. doi:10.1016/j.det.2015.03.001
- Liu E, Daze RP, Moon S. Tumid lupus erythematosus: a rare and distinctive variant of cutaneous lupus erythematosus masquerading as urticarial vasculitis. Cureus. 2020;12:E8305. doi:10.7759/cureus.8305
- Saleh D, Crane JS. Tumid lupus erythematosus. In: StatPearls. StatPearls Publishing; 2020.
- Verma P, Sharma S, Yadav P, et al. Tumid lupus erythematosus: an intriguing dermatopathological connotation treated successfully with topical tacrolimus and hydroxychloroquine combination. Indian J Dermatol. 2014;59:210. doi:10.4103/0019-5154.127716
- Kuhn A, Bein D, Bonsmann G. The 100th anniversary of lupus erythematosus tumidus. Autoimmun Rev. 2009;8:441-448. doi:10.1016/j. autrev.2008.12.010
- Jatwani K, Chugh K, Osholowu OS, et al. Tumid lupus erythematosus and systemic lupus erythematosus: a report on their rare coexistence. Cureus. 2020;12:E7545. doi:10.7759/cureus.7545
- Tomasini D, Mentzel T, Hantschke M, et al. Plasmacytoid dendritic cells: an overview of their presence and distribution in different inflammatory skin diseases, with special emphasis on Jessner’s lymphocytic infiltrate of the skin and cutaneous lupus erythematosus. J Cutan Pathol. 2010;37:1132-1139. doi:10.1111/j.1600-0560.2010.01587.x
- Patsinakidis N, Kautz O, Gibbs BF, et al. Lupus erythematosus tumidus: clinical perspectives. Clin Cosmet Investig Dermatol. 2019;12:707-719. doi:10.2147/CCID.S166723
- Mu EW, Sanchez M, Mir A, et al. Paraneoplastic erythema annulare centrifugum eruption (PEACE). Dermatol Online J. 2015;21:13030/ qt6053h29n.
- Ocanha-Xavier JP, Cola-Senra CO, Xavier-Junior JCC. Reticular erythematous mucinosis: literature review and case report of a 24-year-old patient with systemic erythematosus lupus. Lupus. 2021;30:325-335. doi:10.1177/0961203320965702 10. Keimig EL. Granuloma annulare. Dermatol Clin. 2015;33:315-329. doi:10.1016/j.det.2015.03.001
An otherwise healthy 31-year-old woman presented with a gradual growth of a semiannular, arciform, mildly pruritic plaque around the mouth of 10 years’ duration that recurred biannually, persisted for a few months, and spontaneously remitted without residual scarring. She denied joint pain, muscle aches, sores in the mouth, personal or family history of autoimmune diseases, or other remarkable review of systems. Physical examination revealed a welldefined, edematous, smooth, arciform plaque on the face with no mucous membrane involvement. Laboratory evaluation, including complete blood cell count, comprehensive metabolic panel, and antinuclear antibody titer, was unremarkable. A punch biopsy was obtained.

RaDonda Vaught sentenced to probation for patient death
Before sentencing, a tearful Ms. Vaught, 38, asked for leniency and apologized for the first time to the Murphey family. “I’m sorry I haven’t said this sooner. I’m sorry for what you lost. Your mother, wife, grandmother did not deserve that…I’m sorry you have not heard from me before. I am never, ever forgetting my role in this.”
The sentencing also included statements from family members about the impact on them and Ms. Murphey’s husband. They said Ms. Murphey wouldn’t have wanted Ms. Vaught to serve prison time but her husband wanted the maximum sentence.
The testimony also centered on a perjury charge against Ms. Vaught in 2020 that stemmed from a gun permit she was denied because she failed to report she was under indictment for a felony or any crime that could result in prison time.
In reading her sentencing decision, Judge Jennifer Smith noted that Ms. Vaught, a former ICU nurse at Vanderbilt University Medical Center, “will never again be in the position to do this fatal error,” as she was stripped of her nursing license.
“[Ms. Vaught had] no sustained intent to violate the law, is highly amenable to correction, has no criminal record, is removed from the healthcare setting, and she will never practice nursing again,” said Judge Smith. “This situation will never be repeated by Ms. Vaught.”
The judge also hoped that her decision would have wider implications. Ms. Smith said going forward, she hoped changes in medical policies, including how medications are stored, “will mitigate this from ever happening again.”
After issuing the sentence of 3 years supervised probation with diversion — meaning the conviction can be dismissed at a later date — Ms. Vaught openly wept in court.
Outside of the courtroom, nurses from around the country who gathered for the verdict cheered loudly.
Ms. Vaught was found guilty March 25 of two felonies, criminally negligent homicide, and gross neglect for making a fatal medication mistake that cost Murphey her life. Ms. Murphey was supposed to receive Versed (midazolam) to ease her anxiety, but was given the paralytic drug vecuronium, which prevented her from breathing. She had entered the hospital with a brain injury, according to news reports.
Ms. Vaught was fired from the hospital and last summer, the Tennessee Board of Nursing unanimously voted to revoke her license.
After several hours of testimony from witnesses and Vaught, summation by the attorneys, and a period of personal deliberation, Judge Smith pronounced the sentence. The defense had argued for probation and the prosecution suggested 3 to 6 years, but left the time in custody up to the judge.
Previous reports indicated that Ms. Vaught might face up to 8 years in prison for the error.
The trial included testimony from a few nurse witnesses who painted Ms. Vaughn as a caring, compassionate nurse who went above and beyond for her patients — and quickly admitted her responsibility in the medical error that led to Ms. Murphey’s death.
Ms. Vaught told the court that “caring for the patient and the family is an integral part of my daily life. I care for people as if I was one [of them]. That day I let Charlene Murphey down. I let her family down. I let myself down.”
She said she lost more than her license and her career after the incident. “I will never be the same. When Ms. Murphey died a part of me died with her,” she said, sniffling and having to stop several times during her testimony to compose herself.
“I have replayed my mistakes over and over again…This has been the most horrifying experience of my life and at the same time the most humbling experience of my life.”
But Ms. Vaught also argued for leniency, “I will never be able to practice nursing again. I am not a threat to public safety.” She also expressed her concern about the effect of her case on healthcare workers and patients.
Outside the courthouse, supporters of Ms. Vaught wearing purple “Nurse Strong” T-shirts, among others, sat on the lawn while others advocated in favor of the RN and waited for the verdict to be announced.
A version of this article first appeared on Medscape.com.
Before sentencing, a tearful Ms. Vaught, 38, asked for leniency and apologized for the first time to the Murphey family. “I’m sorry I haven’t said this sooner. I’m sorry for what you lost. Your mother, wife, grandmother did not deserve that…I’m sorry you have not heard from me before. I am never, ever forgetting my role in this.”
The sentencing also included statements from family members about the impact on them and Ms. Murphey’s husband. They said Ms. Murphey wouldn’t have wanted Ms. Vaught to serve prison time but her husband wanted the maximum sentence.
The testimony also centered on a perjury charge against Ms. Vaught in 2020 that stemmed from a gun permit she was denied because she failed to report she was under indictment for a felony or any crime that could result in prison time.
In reading her sentencing decision, Judge Jennifer Smith noted that Ms. Vaught, a former ICU nurse at Vanderbilt University Medical Center, “will never again be in the position to do this fatal error,” as she was stripped of her nursing license.
“[Ms. Vaught had] no sustained intent to violate the law, is highly amenable to correction, has no criminal record, is removed from the healthcare setting, and she will never practice nursing again,” said Judge Smith. “This situation will never be repeated by Ms. Vaught.”
The judge also hoped that her decision would have wider implications. Ms. Smith said going forward, she hoped changes in medical policies, including how medications are stored, “will mitigate this from ever happening again.”
After issuing the sentence of 3 years supervised probation with diversion — meaning the conviction can be dismissed at a later date — Ms. Vaught openly wept in court.
Outside of the courtroom, nurses from around the country who gathered for the verdict cheered loudly.
Ms. Vaught was found guilty March 25 of two felonies, criminally negligent homicide, and gross neglect for making a fatal medication mistake that cost Murphey her life. Ms. Murphey was supposed to receive Versed (midazolam) to ease her anxiety, but was given the paralytic drug vecuronium, which prevented her from breathing. She had entered the hospital with a brain injury, according to news reports.
Ms. Vaught was fired from the hospital and last summer, the Tennessee Board of Nursing unanimously voted to revoke her license.
After several hours of testimony from witnesses and Vaught, summation by the attorneys, and a period of personal deliberation, Judge Smith pronounced the sentence. The defense had argued for probation and the prosecution suggested 3 to 6 years, but left the time in custody up to the judge.
Previous reports indicated that Ms. Vaught might face up to 8 years in prison for the error.
The trial included testimony from a few nurse witnesses who painted Ms. Vaughn as a caring, compassionate nurse who went above and beyond for her patients — and quickly admitted her responsibility in the medical error that led to Ms. Murphey’s death.
Ms. Vaught told the court that “caring for the patient and the family is an integral part of my daily life. I care for people as if I was one [of them]. That day I let Charlene Murphey down. I let her family down. I let myself down.”
She said she lost more than her license and her career after the incident. “I will never be the same. When Ms. Murphey died a part of me died with her,” she said, sniffling and having to stop several times during her testimony to compose herself.
“I have replayed my mistakes over and over again…This has been the most horrifying experience of my life and at the same time the most humbling experience of my life.”
But Ms. Vaught also argued for leniency, “I will never be able to practice nursing again. I am not a threat to public safety.” She also expressed her concern about the effect of her case on healthcare workers and patients.
Outside the courthouse, supporters of Ms. Vaught wearing purple “Nurse Strong” T-shirts, among others, sat on the lawn while others advocated in favor of the RN and waited for the verdict to be announced.
A version of this article first appeared on Medscape.com.
Before sentencing, a tearful Ms. Vaught, 38, asked for leniency and apologized for the first time to the Murphey family. “I’m sorry I haven’t said this sooner. I’m sorry for what you lost. Your mother, wife, grandmother did not deserve that…I’m sorry you have not heard from me before. I am never, ever forgetting my role in this.”
The sentencing also included statements from family members about the impact on them and Ms. Murphey’s husband. They said Ms. Murphey wouldn’t have wanted Ms. Vaught to serve prison time but her husband wanted the maximum sentence.
The testimony also centered on a perjury charge against Ms. Vaught in 2020 that stemmed from a gun permit she was denied because she failed to report she was under indictment for a felony or any crime that could result in prison time.
In reading her sentencing decision, Judge Jennifer Smith noted that Ms. Vaught, a former ICU nurse at Vanderbilt University Medical Center, “will never again be in the position to do this fatal error,” as she was stripped of her nursing license.
“[Ms. Vaught had] no sustained intent to violate the law, is highly amenable to correction, has no criminal record, is removed from the healthcare setting, and she will never practice nursing again,” said Judge Smith. “This situation will never be repeated by Ms. Vaught.”
The judge also hoped that her decision would have wider implications. Ms. Smith said going forward, she hoped changes in medical policies, including how medications are stored, “will mitigate this from ever happening again.”
After issuing the sentence of 3 years supervised probation with diversion — meaning the conviction can be dismissed at a later date — Ms. Vaught openly wept in court.
Outside of the courtroom, nurses from around the country who gathered for the verdict cheered loudly.
Ms. Vaught was found guilty March 25 of two felonies, criminally negligent homicide, and gross neglect for making a fatal medication mistake that cost Murphey her life. Ms. Murphey was supposed to receive Versed (midazolam) to ease her anxiety, but was given the paralytic drug vecuronium, which prevented her from breathing. She had entered the hospital with a brain injury, according to news reports.
Ms. Vaught was fired from the hospital and last summer, the Tennessee Board of Nursing unanimously voted to revoke her license.
After several hours of testimony from witnesses and Vaught, summation by the attorneys, and a period of personal deliberation, Judge Smith pronounced the sentence. The defense had argued for probation and the prosecution suggested 3 to 6 years, but left the time in custody up to the judge.
Previous reports indicated that Ms. Vaught might face up to 8 years in prison for the error.
The trial included testimony from a few nurse witnesses who painted Ms. Vaughn as a caring, compassionate nurse who went above and beyond for her patients — and quickly admitted her responsibility in the medical error that led to Ms. Murphey’s death.
Ms. Vaught told the court that “caring for the patient and the family is an integral part of my daily life. I care for people as if I was one [of them]. That day I let Charlene Murphey down. I let her family down. I let myself down.”
She said she lost more than her license and her career after the incident. “I will never be the same. When Ms. Murphey died a part of me died with her,” she said, sniffling and having to stop several times during her testimony to compose herself.
“I have replayed my mistakes over and over again…This has been the most horrifying experience of my life and at the same time the most humbling experience of my life.”
But Ms. Vaught also argued for leniency, “I will never be able to practice nursing again. I am not a threat to public safety.” She also expressed her concern about the effect of her case on healthcare workers and patients.
Outside the courthouse, supporters of Ms. Vaught wearing purple “Nurse Strong” T-shirts, among others, sat on the lawn while others advocated in favor of the RN and waited for the verdict to be announced.
A version of this article first appeared on Medscape.com.
Nurses under fire: The stress of medical malpractice
Just because nurses are sued less often than doctors doesn’t mean that their actions aren’t a focus of a large number of medical malpractice lawsuits. A condition known as medical malpractice stress syndrome (MMSS) is increasingly being recognized as affecting medical professionals who are subjected to litigation.
According to a 2019 report by CRICO, the risk management arm of Harvard’s medical facilities, nursing was a “primary service” in 34% of cases with a high-severity injury and in 44% of cases that were closed with a payment. And even though nurses were named as defendants only 14% of the time, likely because many nurses don’t have their own personal malpractice coverage, their hospitals or facilities were sued in most of these cases – making the nurses important witnesses for the defense.
We have every reason to believe that things have gotten worse since the CRICO study was published. Chronic nursing shortages were exacerbated during the COVID pandemic, and we have seen a large number of nurses leave the workforce altogether. In a recent survey of nurses by Hospital IQ, 90% of respondents said they were considering leaving the nursing profession in the next year, with 71% of nurses who have more than 15 years of nursing experience thinking about leaving within the next few months.
Those remaining are faced with increased workloads and extra shifts – often mandated – and working with too little sleep. Their commitment to their mission is heroic, but they are only human; it’s hard to imagine the number of errors, the number of bad outcomes, and the number of lawsuits going anywhere but up.
And of course, the entire profession has been fixated on the recent case of the Tennessee nurse who was prosecuted criminally and convicted in connection with a fatal medication error.
These are all reasons to expect that an increasing number of nurses are going to be trying to cope with symptoms of MMSS. Too many of them will initially be viewed by lawyers or claims professionals as simply defensive, arrogant, or difficult to work with. In fact, it’s impossible to know how many cases are settled just to avoid the risk of such a “difficult client” being deposed.
These caring, hard-working, and committed individuals have had their lives shaken in ways that they never expected. Nurses with MMSS need support, but traditional psychotherapy, with a diffuse focus and long-time horizon, is not the most effective option. What’s necessary is practical support that is short term, goal oriented, and tailored to the specifics of the pending litigation process.
Most important, they need to know that they are not experiencing this alone, that MMSS is a common phenomenon, and that a productive coaching relationship can be highly effective.
When approached and supported effectively, nurses – and indeed all medical professionals – can regain their confidence and focus, continue having productive professional and personal lives, and reduce the likelihood of a downhill spiral. And it makes it more likely that they’ll remain in the profession rather than becoming just another statistic in the ever-worsening shortage of nurses in the United States.
Signs of MMSS in nurses
Mixed with their feelings of anxiety and depression, nurses with MMSS often have thoughts such as:
- Am I going to lose my license?
- Am I going to lose my job?
- Will my reputation be destroyed? Will I ever be able to work as a nurse again?
- What am I going to do for a living?
- If I lose everything, will my spouse divorce me? Will I lose my kids?
- I don’t think I did anything wrong, but what if I’m still found to be at fault?
- Did I miss something? Did I make a mistake? Was there something more that I should have done?
- What’s going to happen next? What else could go wrong?
- Are there more people out there who are going to sue me?
- Everything feels overwhelming and out of control.
- My entire identity is now in question.
- How do I get this case out of my head? I can’t focus on anything else.
- I’m developing medical problems of my own.
- I’m having difficulty focusing at work and relating to patients; how do I know who’s going to sue me next?
- I wish that I could escape it all; I feel like killing myself.
Gail Fiore is president of The Winning Focus, which works with physicians and other professionals involved in litigation who are having difficulty coping with stress, anxiety, and other emotional issues. A version of this article first appeared on Medscape.com.
Just because nurses are sued less often than doctors doesn’t mean that their actions aren’t a focus of a large number of medical malpractice lawsuits. A condition known as medical malpractice stress syndrome (MMSS) is increasingly being recognized as affecting medical professionals who are subjected to litigation.
According to a 2019 report by CRICO, the risk management arm of Harvard’s medical facilities, nursing was a “primary service” in 34% of cases with a high-severity injury and in 44% of cases that were closed with a payment. And even though nurses were named as defendants only 14% of the time, likely because many nurses don’t have their own personal malpractice coverage, their hospitals or facilities were sued in most of these cases – making the nurses important witnesses for the defense.
We have every reason to believe that things have gotten worse since the CRICO study was published. Chronic nursing shortages were exacerbated during the COVID pandemic, and we have seen a large number of nurses leave the workforce altogether. In a recent survey of nurses by Hospital IQ, 90% of respondents said they were considering leaving the nursing profession in the next year, with 71% of nurses who have more than 15 years of nursing experience thinking about leaving within the next few months.
Those remaining are faced with increased workloads and extra shifts – often mandated – and working with too little sleep. Their commitment to their mission is heroic, but they are only human; it’s hard to imagine the number of errors, the number of bad outcomes, and the number of lawsuits going anywhere but up.
And of course, the entire profession has been fixated on the recent case of the Tennessee nurse who was prosecuted criminally and convicted in connection with a fatal medication error.
These are all reasons to expect that an increasing number of nurses are going to be trying to cope with symptoms of MMSS. Too many of them will initially be viewed by lawyers or claims professionals as simply defensive, arrogant, or difficult to work with. In fact, it’s impossible to know how many cases are settled just to avoid the risk of such a “difficult client” being deposed.
These caring, hard-working, and committed individuals have had their lives shaken in ways that they never expected. Nurses with MMSS need support, but traditional psychotherapy, with a diffuse focus and long-time horizon, is not the most effective option. What’s necessary is practical support that is short term, goal oriented, and tailored to the specifics of the pending litigation process.
Most important, they need to know that they are not experiencing this alone, that MMSS is a common phenomenon, and that a productive coaching relationship can be highly effective.
When approached and supported effectively, nurses – and indeed all medical professionals – can regain their confidence and focus, continue having productive professional and personal lives, and reduce the likelihood of a downhill spiral. And it makes it more likely that they’ll remain in the profession rather than becoming just another statistic in the ever-worsening shortage of nurses in the United States.
Signs of MMSS in nurses
Mixed with their feelings of anxiety and depression, nurses with MMSS often have thoughts such as:
- Am I going to lose my license?
- Am I going to lose my job?
- Will my reputation be destroyed? Will I ever be able to work as a nurse again?
- What am I going to do for a living?
- If I lose everything, will my spouse divorce me? Will I lose my kids?
- I don’t think I did anything wrong, but what if I’m still found to be at fault?
- Did I miss something? Did I make a mistake? Was there something more that I should have done?
- What’s going to happen next? What else could go wrong?
- Are there more people out there who are going to sue me?
- Everything feels overwhelming and out of control.
- My entire identity is now in question.
- How do I get this case out of my head? I can’t focus on anything else.
- I’m developing medical problems of my own.
- I’m having difficulty focusing at work and relating to patients; how do I know who’s going to sue me next?
- I wish that I could escape it all; I feel like killing myself.
Gail Fiore is president of The Winning Focus, which works with physicians and other professionals involved in litigation who are having difficulty coping with stress, anxiety, and other emotional issues. A version of this article first appeared on Medscape.com.
Just because nurses are sued less often than doctors doesn’t mean that their actions aren’t a focus of a large number of medical malpractice lawsuits. A condition known as medical malpractice stress syndrome (MMSS) is increasingly being recognized as affecting medical professionals who are subjected to litigation.
According to a 2019 report by CRICO, the risk management arm of Harvard’s medical facilities, nursing was a “primary service” in 34% of cases with a high-severity injury and in 44% of cases that were closed with a payment. And even though nurses were named as defendants only 14% of the time, likely because many nurses don’t have their own personal malpractice coverage, their hospitals or facilities were sued in most of these cases – making the nurses important witnesses for the defense.
We have every reason to believe that things have gotten worse since the CRICO study was published. Chronic nursing shortages were exacerbated during the COVID pandemic, and we have seen a large number of nurses leave the workforce altogether. In a recent survey of nurses by Hospital IQ, 90% of respondents said they were considering leaving the nursing profession in the next year, with 71% of nurses who have more than 15 years of nursing experience thinking about leaving within the next few months.
Those remaining are faced with increased workloads and extra shifts – often mandated – and working with too little sleep. Their commitment to their mission is heroic, but they are only human; it’s hard to imagine the number of errors, the number of bad outcomes, and the number of lawsuits going anywhere but up.
And of course, the entire profession has been fixated on the recent case of the Tennessee nurse who was prosecuted criminally and convicted in connection with a fatal medication error.
These are all reasons to expect that an increasing number of nurses are going to be trying to cope with symptoms of MMSS. Too many of them will initially be viewed by lawyers or claims professionals as simply defensive, arrogant, or difficult to work with. In fact, it’s impossible to know how many cases are settled just to avoid the risk of such a “difficult client” being deposed.
These caring, hard-working, and committed individuals have had their lives shaken in ways that they never expected. Nurses with MMSS need support, but traditional psychotherapy, with a diffuse focus and long-time horizon, is not the most effective option. What’s necessary is practical support that is short term, goal oriented, and tailored to the specifics of the pending litigation process.
Most important, they need to know that they are not experiencing this alone, that MMSS is a common phenomenon, and that a productive coaching relationship can be highly effective.
When approached and supported effectively, nurses – and indeed all medical professionals – can regain their confidence and focus, continue having productive professional and personal lives, and reduce the likelihood of a downhill spiral. And it makes it more likely that they’ll remain in the profession rather than becoming just another statistic in the ever-worsening shortage of nurses in the United States.
Signs of MMSS in nurses
Mixed with their feelings of anxiety and depression, nurses with MMSS often have thoughts such as:
- Am I going to lose my license?
- Am I going to lose my job?
- Will my reputation be destroyed? Will I ever be able to work as a nurse again?
- What am I going to do for a living?
- If I lose everything, will my spouse divorce me? Will I lose my kids?
- I don’t think I did anything wrong, but what if I’m still found to be at fault?
- Did I miss something? Did I make a mistake? Was there something more that I should have done?
- What’s going to happen next? What else could go wrong?
- Are there more people out there who are going to sue me?
- Everything feels overwhelming and out of control.
- My entire identity is now in question.
- How do I get this case out of my head? I can’t focus on anything else.
- I’m developing medical problems of my own.
- I’m having difficulty focusing at work and relating to patients; how do I know who’s going to sue me next?
- I wish that I could escape it all; I feel like killing myself.
Gail Fiore is president of The Winning Focus, which works with physicians and other professionals involved in litigation who are having difficulty coping with stress, anxiety, and other emotional issues. A version of this article first appeared on Medscape.com.
Using anti-inflammatory drugs may prolong back pain
A new study questions the conventional wisdom of using steroids and anti-inflammatory drugs like ibuprofen to treat low back pain if exercise and other nondrug therapies don’t work right away.
Those medications offer relief from acute pain but may actually increase a person’s chances of developing chronic pain, said the investigators for a study published in Science Translational Medicine. The study results indicate that
“For many decades it’s been standard medical practice to treat pain with anti-inflammatory drugs,” Jeffrey Mogil, PhD, a psychology professor at McGill University, Montreal, said in a school news release. “But we found that this short-term fix could lead to longer-term problems.”
Researchers looked at low back pain because it’s so common, with 25% of U.S. adults saying they had low back pain in the previous 3 months, according to the Centers for Disease Control and Prevention. Acute back pain is defined as lasting less than 4 weeks while chronic back pain lasts more than 12 weeks.
By examining blood samples, researchers discovered that people whose low back pain was resolved had high inflammation driven by neutrophils, a type of white blood cell that helps the body fight infection, the study said.
“Neutrophils dominate the early stages of inflammation and set the stage for repair of tissue damage. Inflammation occurs for a reason, and it looks like it’s dangerous to interfere with it,” Dr. Mogil said in the news release.
The research team found that blocking neutrophils in mice prolonged pain in the animals up to 10-fold. Pain also was prolonged when the mice were given anti-inflammatory drugs and steroids, the news release says.
McGill University said other studies support the findings. The school cited an analysis of 500,000 people in the United Kingdom. The analysis found that those taking anti-inflammatory drugs for pain were more likely to have pain 2 to 10 years later.
While saying the study suggests it’s time to reconsider how pain is treated, the researchers called for clinical trials on humans, not just observations of people with low back pain.
Experts warned about accepting the results without further investigation.
“It’s intriguing but requires further study,” Steven J. Atlas, MD, director of the Primary Care Research & Quality Improvement Network at Massachusetts General Hospital, Boston, told The New York Times.
A version of this article first appeared on WebMD.com.
A new study questions the conventional wisdom of using steroids and anti-inflammatory drugs like ibuprofen to treat low back pain if exercise and other nondrug therapies don’t work right away.
Those medications offer relief from acute pain but may actually increase a person’s chances of developing chronic pain, said the investigators for a study published in Science Translational Medicine. The study results indicate that
“For many decades it’s been standard medical practice to treat pain with anti-inflammatory drugs,” Jeffrey Mogil, PhD, a psychology professor at McGill University, Montreal, said in a school news release. “But we found that this short-term fix could lead to longer-term problems.”
Researchers looked at low back pain because it’s so common, with 25% of U.S. adults saying they had low back pain in the previous 3 months, according to the Centers for Disease Control and Prevention. Acute back pain is defined as lasting less than 4 weeks while chronic back pain lasts more than 12 weeks.
By examining blood samples, researchers discovered that people whose low back pain was resolved had high inflammation driven by neutrophils, a type of white blood cell that helps the body fight infection, the study said.
“Neutrophils dominate the early stages of inflammation and set the stage for repair of tissue damage. Inflammation occurs for a reason, and it looks like it’s dangerous to interfere with it,” Dr. Mogil said in the news release.
The research team found that blocking neutrophils in mice prolonged pain in the animals up to 10-fold. Pain also was prolonged when the mice were given anti-inflammatory drugs and steroids, the news release says.
McGill University said other studies support the findings. The school cited an analysis of 500,000 people in the United Kingdom. The analysis found that those taking anti-inflammatory drugs for pain were more likely to have pain 2 to 10 years later.
While saying the study suggests it’s time to reconsider how pain is treated, the researchers called for clinical trials on humans, not just observations of people with low back pain.
Experts warned about accepting the results without further investigation.
“It’s intriguing but requires further study,” Steven J. Atlas, MD, director of the Primary Care Research & Quality Improvement Network at Massachusetts General Hospital, Boston, told The New York Times.
A version of this article first appeared on WebMD.com.
A new study questions the conventional wisdom of using steroids and anti-inflammatory drugs like ibuprofen to treat low back pain if exercise and other nondrug therapies don’t work right away.
Those medications offer relief from acute pain but may actually increase a person’s chances of developing chronic pain, said the investigators for a study published in Science Translational Medicine. The study results indicate that
“For many decades it’s been standard medical practice to treat pain with anti-inflammatory drugs,” Jeffrey Mogil, PhD, a psychology professor at McGill University, Montreal, said in a school news release. “But we found that this short-term fix could lead to longer-term problems.”
Researchers looked at low back pain because it’s so common, with 25% of U.S. adults saying they had low back pain in the previous 3 months, according to the Centers for Disease Control and Prevention. Acute back pain is defined as lasting less than 4 weeks while chronic back pain lasts more than 12 weeks.
By examining blood samples, researchers discovered that people whose low back pain was resolved had high inflammation driven by neutrophils, a type of white blood cell that helps the body fight infection, the study said.
“Neutrophils dominate the early stages of inflammation and set the stage for repair of tissue damage. Inflammation occurs for a reason, and it looks like it’s dangerous to interfere with it,” Dr. Mogil said in the news release.
The research team found that blocking neutrophils in mice prolonged pain in the animals up to 10-fold. Pain also was prolonged when the mice were given anti-inflammatory drugs and steroids, the news release says.
McGill University said other studies support the findings. The school cited an analysis of 500,000 people in the United Kingdom. The analysis found that those taking anti-inflammatory drugs for pain were more likely to have pain 2 to 10 years later.
While saying the study suggests it’s time to reconsider how pain is treated, the researchers called for clinical trials on humans, not just observations of people with low back pain.
Experts warned about accepting the results without further investigation.
“It’s intriguing but requires further study,” Steven J. Atlas, MD, director of the Primary Care Research & Quality Improvement Network at Massachusetts General Hospital, Boston, told The New York Times.
A version of this article first appeared on WebMD.com.
FROM SCIENCE TRANSLATIONAL MEDICINE
Sex toys for science
California researchers are seeking women willing to use sex toys for science.
“We have not had good-quality studies with the use of modern vibrators,” Alexandra Dubinskaya, MD, an obstetrician who is leading the study, said in an interview.
Vibrators of various kinds have been used by women for centuries if not millennia. More than half of women in the United States have at least some experience with the devices.
Victorian-era physicians are said to have routinely prescribed multiple types of vibrators to treat “female hysteria,” although the frequency with which vibrators were recommended for therapeutic purposes has been questioned.
Still, Dr. Dubinskaya said vibrators have a long history of use as therapy – with some evidence of success.
She and her colleagues reviewed the medical literature and found that studies generally supported the use of vibrators for increased blood flow in pelvic tissues, improved sexual function, including orgasms, and possibly urinary incontinence by helping to strengthen the pelvic floor. They also appear to boost desire, arousal, and genital sensation.
For the new study, Dr. Dubinskaya and her colleagues hope to eventually include 100 women between the ages of 18 and 99 years. Each will receive a commercially available genital vibrator and instructions to use the device to reach orgasm three times per week for 3 to 4 months. The researchers will track any changes in sexual function, pelvic prolapse, urinary continence, and other measures of pelvic and sexual health.
The goal of the study, Dr. Dubinskaya said, is to provide prospective data for clinicians who might consider recommending vibrators to their patients – a list that includes urologists, gynecologists, and experts in sexual medicine.
These clinicians “are frequently the first to encounter questions on women’s sexual function, pelvic floor problems, and vulvar health,” Dr. Dubinskaya said. She noted that such questions are common.
Asking women to consider using vibrators might seem too sensitive a subject in a clinical setting, but Dr. Dubinskaya said data indicate that women are receptive to the suggestion.
Debra Lynne Herbenick, PhD, director of the Center for Sexual Health Promotion and a professor of public health at Indiana University, Indianapolis, who has studied vibrator use in the United States, said the research could make a valuable contribution to sexual health.
“This study is an important next step because it is a prospective study and will be able to assess changes in sexual and pelvic floor function over time in relation to vibrator use,” Dr. Herbenick said. Owing to the limited quality of the currently available evidence, these data have the potential “to support clinicians’ recommendations and also their communication with patients.”
Dr. Dubinskaya and Dr. Herbenick reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
California researchers are seeking women willing to use sex toys for science.
“We have not had good-quality studies with the use of modern vibrators,” Alexandra Dubinskaya, MD, an obstetrician who is leading the study, said in an interview.
Vibrators of various kinds have been used by women for centuries if not millennia. More than half of women in the United States have at least some experience with the devices.
Victorian-era physicians are said to have routinely prescribed multiple types of vibrators to treat “female hysteria,” although the frequency with which vibrators were recommended for therapeutic purposes has been questioned.
Still, Dr. Dubinskaya said vibrators have a long history of use as therapy – with some evidence of success.
She and her colleagues reviewed the medical literature and found that studies generally supported the use of vibrators for increased blood flow in pelvic tissues, improved sexual function, including orgasms, and possibly urinary incontinence by helping to strengthen the pelvic floor. They also appear to boost desire, arousal, and genital sensation.
For the new study, Dr. Dubinskaya and her colleagues hope to eventually include 100 women between the ages of 18 and 99 years. Each will receive a commercially available genital vibrator and instructions to use the device to reach orgasm three times per week for 3 to 4 months. The researchers will track any changes in sexual function, pelvic prolapse, urinary continence, and other measures of pelvic and sexual health.
The goal of the study, Dr. Dubinskaya said, is to provide prospective data for clinicians who might consider recommending vibrators to their patients – a list that includes urologists, gynecologists, and experts in sexual medicine.
These clinicians “are frequently the first to encounter questions on women’s sexual function, pelvic floor problems, and vulvar health,” Dr. Dubinskaya said. She noted that such questions are common.
Asking women to consider using vibrators might seem too sensitive a subject in a clinical setting, but Dr. Dubinskaya said data indicate that women are receptive to the suggestion.
Debra Lynne Herbenick, PhD, director of the Center for Sexual Health Promotion and a professor of public health at Indiana University, Indianapolis, who has studied vibrator use in the United States, said the research could make a valuable contribution to sexual health.
“This study is an important next step because it is a prospective study and will be able to assess changes in sexual and pelvic floor function over time in relation to vibrator use,” Dr. Herbenick said. Owing to the limited quality of the currently available evidence, these data have the potential “to support clinicians’ recommendations and also their communication with patients.”
Dr. Dubinskaya and Dr. Herbenick reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
California researchers are seeking women willing to use sex toys for science.
“We have not had good-quality studies with the use of modern vibrators,” Alexandra Dubinskaya, MD, an obstetrician who is leading the study, said in an interview.
Vibrators of various kinds have been used by women for centuries if not millennia. More than half of women in the United States have at least some experience with the devices.
Victorian-era physicians are said to have routinely prescribed multiple types of vibrators to treat “female hysteria,” although the frequency with which vibrators were recommended for therapeutic purposes has been questioned.
Still, Dr. Dubinskaya said vibrators have a long history of use as therapy – with some evidence of success.
She and her colleagues reviewed the medical literature and found that studies generally supported the use of vibrators for increased blood flow in pelvic tissues, improved sexual function, including orgasms, and possibly urinary incontinence by helping to strengthen the pelvic floor. They also appear to boost desire, arousal, and genital sensation.
For the new study, Dr. Dubinskaya and her colleagues hope to eventually include 100 women between the ages of 18 and 99 years. Each will receive a commercially available genital vibrator and instructions to use the device to reach orgasm three times per week for 3 to 4 months. The researchers will track any changes in sexual function, pelvic prolapse, urinary continence, and other measures of pelvic and sexual health.
The goal of the study, Dr. Dubinskaya said, is to provide prospective data for clinicians who might consider recommending vibrators to their patients – a list that includes urologists, gynecologists, and experts in sexual medicine.
These clinicians “are frequently the first to encounter questions on women’s sexual function, pelvic floor problems, and vulvar health,” Dr. Dubinskaya said. She noted that such questions are common.
Asking women to consider using vibrators might seem too sensitive a subject in a clinical setting, but Dr. Dubinskaya said data indicate that women are receptive to the suggestion.
Debra Lynne Herbenick, PhD, director of the Center for Sexual Health Promotion and a professor of public health at Indiana University, Indianapolis, who has studied vibrator use in the United States, said the research could make a valuable contribution to sexual health.
“This study is an important next step because it is a prospective study and will be able to assess changes in sexual and pelvic floor function over time in relation to vibrator use,” Dr. Herbenick said. Owing to the limited quality of the currently available evidence, these data have the potential “to support clinicians’ recommendations and also their communication with patients.”
Dr. Dubinskaya and Dr. Herbenick reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.



