User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
CDC signs off on COVID boosters in children ages 5-11
Centers for Disease Control and Prevention Director Rochelle Walensky, MD, signed off May 19 on an advisory panel’s recommendation that children ages 5 to 11 years should receive a Pfizer-BioNTech COVID-19 vaccine booster dose at least 5 months after completion of the primary series.
The CDC’s Advisory Committee on Immunization Practices (ACIP) voted 11:1, with one abstention, on a question about whether it recommended these additional shots in this age group.
The U.S. Food and Drug Administration on May 17 amended the emergency use authorization (EUA) for the Pfizer-BioNTech COVID-19 vaccine to cover a single booster dose for administration to individuals 5 through 11 years of age.
At the request of CDC staff, ACIP members considered whether there should be softer wording for this recommendation, stating that children in this age group “may” receive a booster. This kind of phrasing would better reflect uncertainty about the course of COVID in the months ahead and allow flexibility for a stronger recommendation in the fall.
ACIP panelists and members of key groups argued strongly for a “should” recommendation, despite the uncertainties.
They also called for stronger efforts to make sure eligible children received their initial COVID-19 shots. Data gathered between November and April show only 14.4% of children ages 5 to 11 in rural areas have received at least one dose of COVID-19 vaccination, with top rates of 39.8% in large urban communities and 36% in larger suburban regions, CDC staff said.
CDC staff also said nearly 40% of parents in rural areas reported that their children’s pediatricians did not recommend COVID-19 vaccinations, compared with only 8% of parents in urban communities. These figures concerned ACIP members and liaisons from medical associations who take part in the panel’s deliberations but not in its votes.
“People will hear the word ‘m-a-y’ as ‘m-e-h’,” said Patricia Stinchfield, RN, MS, who served as the liaison for National Association of Pediatric Nurse Practitioners to ACIP. “I think we need to add urgency” to efforts to increase use of COVID vaccinations, she said.
Voting no on Thursday was Helen Keipp Talbot, MD, of Vanderbilt University. She explained after the vote that she is in favor of having young children vaccinated, but she’s concerned about the low rates of initial uptake of the COVID-19 shots.
“Boosters are great once we’ve gotten everyone their first round,” she said. “That needs to be our priority in this.”
Sandra Fryhofer, MD, the American Medical Association’s liaison to ACIP, stressed the add-on benefits from more widespread vaccination of children against COVID. Dr. Fryhofer said she serves adults in her practice as an internal medicine physician, with many of her patients being at high risk for complications from COVID.
Too many people are assuming the spread of infections in the community has lessened the risk of the virus, Dr. Fryhofer said.
“Not everyone’s had COVID yet, and my patients will be likely to get COVID if their grandchildren get it. We’re going through pandemic fatigue in this country,” she said. “Unfortunately, masks are now more off than on. Winter’s coming. They’re more variants” of the virus likely to emerge.
The data emerging so far suggests COVID vaccines will become a three-dose medicine, as is already accepted for other shots like hepatitis B vaccine, Dr. Fryhofer said.
Data gathered to date show the vaccine decreases risk of hospitalization for COVID and for complications such as multisystem inflammatory syndrome in children (MIS-C), she said.
“The bottom line is children in this age group are getting COVID,” Dr. Fryhofer said of the 5- to 11-year-olds. “Some do fine. Some are getting real sick. Some are hospitalized, some have died.”
At the meeting, CDC staff cited data from a paper published in the New England Journal of Medicine in March showing that vaccination had reduced the risk of hospitalization for COVID-19 among children 5 to 11 years of age by two-thirds during the Omicron period; most children with critical COVID-19 were unvaccinated.
COVID-19 led to 66 deaths among children ages 5 to 11 in the October 2020 to October 2021 timeframe, said ACIP member Matthew F. Daley, MD, of Kaiser Permanente Colorado during a presentation to his fellow panel members.
Parents may underestimate children’s risk from COVID and thus hold off on vaccinations, stressed AMA President Gerald E. Harmon, MD, in a statement issued after the meeting.
“It is concerning that only 1 in 3 children between the ages of 5 and 11 in the United States have received two doses of the vaccine, in part because parents believe them to be at lower risk for severe disease than adults,” Dr. Harmon said. “But the Omicron variant brought about change that should alter that calculus.”
Responding to early data
As Dr. Fryhofer put it, the medical community has been learning in “real time” about how COVID vaccines work and how to use them.
The EUA granted on May 17 for booster shots for children ages 5 to 11 was based on an analysis of immune response data in a subset of children from an ongoing randomized placebo-controlled trial, the FDA said.
Antibody responses were evaluated in 67 study participants who received a booster dose 7 to 9 months after completing a two-dose primary series of the Pfizer-BioNTech COVID-19 Vaccine. The EUA for the booster shot was intended to respond to emerging data that suggest that vaccine effectiveness against COVID-19 wanes after the second dose of the vaccine, the FDA said.
CDC seeks help tracking vaccine complications
At the ACIP meeting, a top CDC vaccine-safety official, Tom Shimabukuro, MD, MPH, MBA, asked physicians to make sure their patients know about the agency’s V-Safe program for gathering reports from the public about their experiences with COVID vaccines. This is intended to help the CDC monitor for side effects of these medications.
“We need your help,” he said during a presentation about adverse events reported to date in children ages 5 to 11 who took the Pfizer vaccine.
About 18.1 million doses of Pfizer-BioNTech vaccine have been administered to children ages 5 to 11 years in the United States so far. Most of the reports of adverse events following vaccination were not serious, he said. But there were 20 reports of myocarditis verified to meet CDC case definition among children ages 5 to 11 years.
One case involved a death with histopathologic evidence of myocarditis on autopsy. The CDC continues to assist with case review, he said.
A version of this article first appeared on Medscape.com.
Centers for Disease Control and Prevention Director Rochelle Walensky, MD, signed off May 19 on an advisory panel’s recommendation that children ages 5 to 11 years should receive a Pfizer-BioNTech COVID-19 vaccine booster dose at least 5 months after completion of the primary series.
The CDC’s Advisory Committee on Immunization Practices (ACIP) voted 11:1, with one abstention, on a question about whether it recommended these additional shots in this age group.
The U.S. Food and Drug Administration on May 17 amended the emergency use authorization (EUA) for the Pfizer-BioNTech COVID-19 vaccine to cover a single booster dose for administration to individuals 5 through 11 years of age.
At the request of CDC staff, ACIP members considered whether there should be softer wording for this recommendation, stating that children in this age group “may” receive a booster. This kind of phrasing would better reflect uncertainty about the course of COVID in the months ahead and allow flexibility for a stronger recommendation in the fall.
ACIP panelists and members of key groups argued strongly for a “should” recommendation, despite the uncertainties.
They also called for stronger efforts to make sure eligible children received their initial COVID-19 shots. Data gathered between November and April show only 14.4% of children ages 5 to 11 in rural areas have received at least one dose of COVID-19 vaccination, with top rates of 39.8% in large urban communities and 36% in larger suburban regions, CDC staff said.
CDC staff also said nearly 40% of parents in rural areas reported that their children’s pediatricians did not recommend COVID-19 vaccinations, compared with only 8% of parents in urban communities. These figures concerned ACIP members and liaisons from medical associations who take part in the panel’s deliberations but not in its votes.
“People will hear the word ‘m-a-y’ as ‘m-e-h’,” said Patricia Stinchfield, RN, MS, who served as the liaison for National Association of Pediatric Nurse Practitioners to ACIP. “I think we need to add urgency” to efforts to increase use of COVID vaccinations, she said.
Voting no on Thursday was Helen Keipp Talbot, MD, of Vanderbilt University. She explained after the vote that she is in favor of having young children vaccinated, but she’s concerned about the low rates of initial uptake of the COVID-19 shots.
“Boosters are great once we’ve gotten everyone their first round,” she said. “That needs to be our priority in this.”
Sandra Fryhofer, MD, the American Medical Association’s liaison to ACIP, stressed the add-on benefits from more widespread vaccination of children against COVID. Dr. Fryhofer said she serves adults in her practice as an internal medicine physician, with many of her patients being at high risk for complications from COVID.
Too many people are assuming the spread of infections in the community has lessened the risk of the virus, Dr. Fryhofer said.
“Not everyone’s had COVID yet, and my patients will be likely to get COVID if their grandchildren get it. We’re going through pandemic fatigue in this country,” she said. “Unfortunately, masks are now more off than on. Winter’s coming. They’re more variants” of the virus likely to emerge.
The data emerging so far suggests COVID vaccines will become a three-dose medicine, as is already accepted for other shots like hepatitis B vaccine, Dr. Fryhofer said.
Data gathered to date show the vaccine decreases risk of hospitalization for COVID and for complications such as multisystem inflammatory syndrome in children (MIS-C), she said.
“The bottom line is children in this age group are getting COVID,” Dr. Fryhofer said of the 5- to 11-year-olds. “Some do fine. Some are getting real sick. Some are hospitalized, some have died.”
At the meeting, CDC staff cited data from a paper published in the New England Journal of Medicine in March showing that vaccination had reduced the risk of hospitalization for COVID-19 among children 5 to 11 years of age by two-thirds during the Omicron period; most children with critical COVID-19 were unvaccinated.
COVID-19 led to 66 deaths among children ages 5 to 11 in the October 2020 to October 2021 timeframe, said ACIP member Matthew F. Daley, MD, of Kaiser Permanente Colorado during a presentation to his fellow panel members.
Parents may underestimate children’s risk from COVID and thus hold off on vaccinations, stressed AMA President Gerald E. Harmon, MD, in a statement issued after the meeting.
“It is concerning that only 1 in 3 children between the ages of 5 and 11 in the United States have received two doses of the vaccine, in part because parents believe them to be at lower risk for severe disease than adults,” Dr. Harmon said. “But the Omicron variant brought about change that should alter that calculus.”
Responding to early data
As Dr. Fryhofer put it, the medical community has been learning in “real time” about how COVID vaccines work and how to use them.
The EUA granted on May 17 for booster shots for children ages 5 to 11 was based on an analysis of immune response data in a subset of children from an ongoing randomized placebo-controlled trial, the FDA said.
Antibody responses were evaluated in 67 study participants who received a booster dose 7 to 9 months after completing a two-dose primary series of the Pfizer-BioNTech COVID-19 Vaccine. The EUA for the booster shot was intended to respond to emerging data that suggest that vaccine effectiveness against COVID-19 wanes after the second dose of the vaccine, the FDA said.
CDC seeks help tracking vaccine complications
At the ACIP meeting, a top CDC vaccine-safety official, Tom Shimabukuro, MD, MPH, MBA, asked physicians to make sure their patients know about the agency’s V-Safe program for gathering reports from the public about their experiences with COVID vaccines. This is intended to help the CDC monitor for side effects of these medications.
“We need your help,” he said during a presentation about adverse events reported to date in children ages 5 to 11 who took the Pfizer vaccine.
About 18.1 million doses of Pfizer-BioNTech vaccine have been administered to children ages 5 to 11 years in the United States so far. Most of the reports of adverse events following vaccination were not serious, he said. But there were 20 reports of myocarditis verified to meet CDC case definition among children ages 5 to 11 years.
One case involved a death with histopathologic evidence of myocarditis on autopsy. The CDC continues to assist with case review, he said.
A version of this article first appeared on Medscape.com.
Centers for Disease Control and Prevention Director Rochelle Walensky, MD, signed off May 19 on an advisory panel’s recommendation that children ages 5 to 11 years should receive a Pfizer-BioNTech COVID-19 vaccine booster dose at least 5 months after completion of the primary series.
The CDC’s Advisory Committee on Immunization Practices (ACIP) voted 11:1, with one abstention, on a question about whether it recommended these additional shots in this age group.
The U.S. Food and Drug Administration on May 17 amended the emergency use authorization (EUA) for the Pfizer-BioNTech COVID-19 vaccine to cover a single booster dose for administration to individuals 5 through 11 years of age.
At the request of CDC staff, ACIP members considered whether there should be softer wording for this recommendation, stating that children in this age group “may” receive a booster. This kind of phrasing would better reflect uncertainty about the course of COVID in the months ahead and allow flexibility for a stronger recommendation in the fall.
ACIP panelists and members of key groups argued strongly for a “should” recommendation, despite the uncertainties.
They also called for stronger efforts to make sure eligible children received their initial COVID-19 shots. Data gathered between November and April show only 14.4% of children ages 5 to 11 in rural areas have received at least one dose of COVID-19 vaccination, with top rates of 39.8% in large urban communities and 36% in larger suburban regions, CDC staff said.
CDC staff also said nearly 40% of parents in rural areas reported that their children’s pediatricians did not recommend COVID-19 vaccinations, compared with only 8% of parents in urban communities. These figures concerned ACIP members and liaisons from medical associations who take part in the panel’s deliberations but not in its votes.
“People will hear the word ‘m-a-y’ as ‘m-e-h’,” said Patricia Stinchfield, RN, MS, who served as the liaison for National Association of Pediatric Nurse Practitioners to ACIP. “I think we need to add urgency” to efforts to increase use of COVID vaccinations, she said.
Voting no on Thursday was Helen Keipp Talbot, MD, of Vanderbilt University. She explained after the vote that she is in favor of having young children vaccinated, but she’s concerned about the low rates of initial uptake of the COVID-19 shots.
“Boosters are great once we’ve gotten everyone their first round,” she said. “That needs to be our priority in this.”
Sandra Fryhofer, MD, the American Medical Association’s liaison to ACIP, stressed the add-on benefits from more widespread vaccination of children against COVID. Dr. Fryhofer said she serves adults in her practice as an internal medicine physician, with many of her patients being at high risk for complications from COVID.
Too many people are assuming the spread of infections in the community has lessened the risk of the virus, Dr. Fryhofer said.
“Not everyone’s had COVID yet, and my patients will be likely to get COVID if their grandchildren get it. We’re going through pandemic fatigue in this country,” she said. “Unfortunately, masks are now more off than on. Winter’s coming. They’re more variants” of the virus likely to emerge.
The data emerging so far suggests COVID vaccines will become a three-dose medicine, as is already accepted for other shots like hepatitis B vaccine, Dr. Fryhofer said.
Data gathered to date show the vaccine decreases risk of hospitalization for COVID and for complications such as multisystem inflammatory syndrome in children (MIS-C), she said.
“The bottom line is children in this age group are getting COVID,” Dr. Fryhofer said of the 5- to 11-year-olds. “Some do fine. Some are getting real sick. Some are hospitalized, some have died.”
At the meeting, CDC staff cited data from a paper published in the New England Journal of Medicine in March showing that vaccination had reduced the risk of hospitalization for COVID-19 among children 5 to 11 years of age by two-thirds during the Omicron period; most children with critical COVID-19 were unvaccinated.
COVID-19 led to 66 deaths among children ages 5 to 11 in the October 2020 to October 2021 timeframe, said ACIP member Matthew F. Daley, MD, of Kaiser Permanente Colorado during a presentation to his fellow panel members.
Parents may underestimate children’s risk from COVID and thus hold off on vaccinations, stressed AMA President Gerald E. Harmon, MD, in a statement issued after the meeting.
“It is concerning that only 1 in 3 children between the ages of 5 and 11 in the United States have received two doses of the vaccine, in part because parents believe them to be at lower risk for severe disease than adults,” Dr. Harmon said. “But the Omicron variant brought about change that should alter that calculus.”
Responding to early data
As Dr. Fryhofer put it, the medical community has been learning in “real time” about how COVID vaccines work and how to use them.
The EUA granted on May 17 for booster shots for children ages 5 to 11 was based on an analysis of immune response data in a subset of children from an ongoing randomized placebo-controlled trial, the FDA said.
Antibody responses were evaluated in 67 study participants who received a booster dose 7 to 9 months after completing a two-dose primary series of the Pfizer-BioNTech COVID-19 Vaccine. The EUA for the booster shot was intended to respond to emerging data that suggest that vaccine effectiveness against COVID-19 wanes after the second dose of the vaccine, the FDA said.
CDC seeks help tracking vaccine complications
At the ACIP meeting, a top CDC vaccine-safety official, Tom Shimabukuro, MD, MPH, MBA, asked physicians to make sure their patients know about the agency’s V-Safe program for gathering reports from the public about their experiences with COVID vaccines. This is intended to help the CDC monitor for side effects of these medications.
“We need your help,” he said during a presentation about adverse events reported to date in children ages 5 to 11 who took the Pfizer vaccine.
About 18.1 million doses of Pfizer-BioNTech vaccine have been administered to children ages 5 to 11 years in the United States so far. Most of the reports of adverse events following vaccination were not serious, he said. But there were 20 reports of myocarditis verified to meet CDC case definition among children ages 5 to 11 years.
One case involved a death with histopathologic evidence of myocarditis on autopsy. The CDC continues to assist with case review, he said.
A version of this article first appeared on Medscape.com.
Pancreatic involvement in COVID-19: What do we know?
MADRID – It involves the relationship between COVID-19 and new diagnoses of diabetes and blood glucose disorders, among others, in the post–COVID-19 period. These topics were addressed at the XXXIII National Congress of the Spanish Diabetes Society. They were also the central theme of the inaugural conference, Pancreatic Involvement During COVID-19: From Preclinical Studies to Clinical Relevance, which was led by Alexander Kleger, MD, PhD, head of the department of pancreatology at the Ulm (Germany) University Clinic for Internal Medicine.
The chair of the scientific committee of the congress, Franz Martín, MD, launched the conference by noting that the work of Dr. Kleger and his team has made it possible to ascertain that SARS-CoV-2 can infect pancreatic beta cells that produce insulin. This observation may help in understanding why patients with COVID-19 sometimes experience symptoms related to greater difficulty regulating blood glucose.
“In addition, the German expert and his group have described the abnormalities that occur in beta cells when they are infected by SARS-CoV-2, something especially important, given that knowledge of these abnormalities may be of great importance to understanding the possible appearance of more cases of diabetes in the future,” Dr. Martín added.
“Our data identify the human pancreas as a target of SARS-CoV-2 infection and suggest that pancreatic beta cell involvement could contribute to the metabolic dysregulation seen in COVID-19 patients,” Dr. Kleger pointed out.
In his speech, Dr. Kleger reviewed the evidence on the effects of SARS-CoV-2 that has been garnered since the start of the pandemic, and he presented his research group’s findings on the impact at the pancreatic level.
“Since March 2020, it has been seen that COVID-19 affected the pancreas, and studies published in August of that same year clearly spoke of both a worsening of diabetes and an increase in new cases of this disease diagnosed after SARS-CoV-2 infection. Also, the data showed how hospitalized patients with no previous history of diabetes experienced rapid increases in glucose levels 5 days after admission,” Dr. Kleger said.
Angiotensin-converting enzyme 2
As an example of the pace at which evidence on the pancreatic impact of this virus has been evolving, Dr. Kleger referred to early studies that found no angiotensin-converting enzyme 2 receptor on cells of the endocrine and exocrine pancreas. “To our surprise, in our work, we did observe the obvious presence of angiotensin-converting enzyme 2 specifically expressed in human pancreatic beta cells, something confirmed by other investigations. Another surprising aspect was verifying that the viral infection lasts longer in the pancreas than in the lungs,” said the expert.
These findings caused the researchers to realize that SARS-CoV-2 may be directly or indirectly associated with diabetes. “It is currently the subject of debate whether it may be a direct effect, infecting or directly reaching the pancreatic beta cells, or whether this involvement is a result of the effect of the infection at systemic level, in the context of the cytokine storm and the proinflammatory environment derived from it. Our current challenge is to confirm whether this virus can really replicate in pancreatic beta cells and to assess the possible existence of reinfections, among other aspects,” said Dr. Kleger.
Along with these “developing areas of knowledge,” there are several certainties regarding the link between diabetes and COVID-19. Dr. Kleger summarized the most relevant one. “Preexisting diabetes is known to be a highly prevalent comorbidity seen in 11%-22% of patients and increases the risk of severe disease and mortality.
“SARS-CoV-2 infection has also been shown to affect the exocrine pancreas, manifesting as pancreatitis in 5% of critically ill patients with COVID-19, as well as enlargement of the pancreas and abnormal levels of amylase or lipase in 7.5%-17% of patients.
“Furthermore, it is obvious that SARS-CoV-2 infection produces glycometabolic dysfunction in these patients, with increased hyperglycemia in people with type 2 diabetes and ketoacidosis in 2%-6.4% of patients with and without diabetes.”
After recovery
The most recent research reveals the persistence of this dysregulation long after recovery from COVID-19. “We’ve seen that in a significant proportion of patients, hyperglycemia is maintained for some time; in the specific case of hospitalized patients [without the need for assisted ventilation or other intensive care requirements], for up to more than 2 months after overcoming the illness.
“In the same way, there are studies that have shown that insulin resistance and hyperstimulation of pancreatic beta cells remain at pathological levels in the post–COVID-19 phase. And in line with increased insulin resistance, signs of hyperinflammation have also been detected in these patients.”
Dr. Kleger noted that another research area is the increased incidence of newly diagnosed diabetes after recovery from SARS-CoV-2 infection, “something that seems to be correlated with how severely the disease has been experienced and also depending on whether hospitalization or intensive care was needed. Likewise, retrospective studies have shown that the risk of developing type 2 diabetes is higher in COVID-19 patients, compared with those with other respiratory infections. Regarding the incidence of type 1 diabetes, there is evidence, particularly in the case of children, of a clear correlation between the pandemic waves and the increase in cases.
“Therefore, and in view of this data, we could say that, with regard to the involvement of SARS-CoV-2 in pancreatic beta cells, something is up, but we are not yet able to fully understand what it is. What can be confirmed based on the numerous studies carried out in this regard is that COVID-19 produces a metabolic dysregulation [hyperglycemia, insulin resistance, diabetic ketoacidosis] which in turn favors the development of diabetes in patients with no history of this disease,” said Dr. Kleger.
“Likewise, everything points to the existence of a definitively feasible infection in pancreatic beta cells associated with SARS-CoV-2, but there are still unknown aspects of the physiology that explain this effect that remain the subject of debate and deserve future studies,” he concluded.
Consequences of the pandemic
The experts agreed that, although COVID-19 is no longer at the center of specialist care, it is still a subject of investigation. On the conference’s opening day, an update was made on the approach to diabetes.
Care activity is gradually recovering as the time that professionals devote to COVID-19 care is reduced, “but it will take time to catch up with the care activities not carried out during the pandemic, and, unfortunately, in the coming years, we will see the repercussion of the lack or reduction of care during these years,” stressed the SED chair, Antonio Pérez Pérez, MD, director of endocrinology and nutrition of Hospital de la Santa Creu i Sant Pau, Barcelona.
Dr. Pérez stressed that the pandemic has revealed health system deficiencies in diabetes care. He added that the impact of COVID-19 on diabetes (resulting from the effects of the infection itself or from the inadequacy of prevention, diagnosis, and treatment measures) fostered a deterioration of metabolic control and a delay in the diagnosis of the disease and its complications.
“All this contributes to the fact that we currently continue to see patients with complications, especially in the case of type 2 diabetes, with more serious decompensations and diagnoses in more advanced stages of the disease. This impact has been more significant in older people from disadvantaged areas and with less capacity for self-monitoring and self-adjustment of treatment,” he added.
Describing lessons learned through the experiences accumulated in diabetes care during the pandemic, Dr. Pérez highlighted the push for virtual consultations, accessibility to drugs prescribed in electronic prescriptions, and the use of educational resources online and of telemedicine tools. “The need to invest in the health sector has also been assumed, endowing it with robustness in well-trained health personnel, to promote health education, boost efficient health organization, and invest in innovation aimed at facilitating care.”
Dr. Kleger and Dr. Pérez disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com. This article was translated from the Medscape Spanish edition.
MADRID – It involves the relationship between COVID-19 and new diagnoses of diabetes and blood glucose disorders, among others, in the post–COVID-19 period. These topics were addressed at the XXXIII National Congress of the Spanish Diabetes Society. They were also the central theme of the inaugural conference, Pancreatic Involvement During COVID-19: From Preclinical Studies to Clinical Relevance, which was led by Alexander Kleger, MD, PhD, head of the department of pancreatology at the Ulm (Germany) University Clinic for Internal Medicine.
The chair of the scientific committee of the congress, Franz Martín, MD, launched the conference by noting that the work of Dr. Kleger and his team has made it possible to ascertain that SARS-CoV-2 can infect pancreatic beta cells that produce insulin. This observation may help in understanding why patients with COVID-19 sometimes experience symptoms related to greater difficulty regulating blood glucose.
“In addition, the German expert and his group have described the abnormalities that occur in beta cells when they are infected by SARS-CoV-2, something especially important, given that knowledge of these abnormalities may be of great importance to understanding the possible appearance of more cases of diabetes in the future,” Dr. Martín added.
“Our data identify the human pancreas as a target of SARS-CoV-2 infection and suggest that pancreatic beta cell involvement could contribute to the metabolic dysregulation seen in COVID-19 patients,” Dr. Kleger pointed out.
In his speech, Dr. Kleger reviewed the evidence on the effects of SARS-CoV-2 that has been garnered since the start of the pandemic, and he presented his research group’s findings on the impact at the pancreatic level.
“Since March 2020, it has been seen that COVID-19 affected the pancreas, and studies published in August of that same year clearly spoke of both a worsening of diabetes and an increase in new cases of this disease diagnosed after SARS-CoV-2 infection. Also, the data showed how hospitalized patients with no previous history of diabetes experienced rapid increases in glucose levels 5 days after admission,” Dr. Kleger said.
Angiotensin-converting enzyme 2
As an example of the pace at which evidence on the pancreatic impact of this virus has been evolving, Dr. Kleger referred to early studies that found no angiotensin-converting enzyme 2 receptor on cells of the endocrine and exocrine pancreas. “To our surprise, in our work, we did observe the obvious presence of angiotensin-converting enzyme 2 specifically expressed in human pancreatic beta cells, something confirmed by other investigations. Another surprising aspect was verifying that the viral infection lasts longer in the pancreas than in the lungs,” said the expert.
These findings caused the researchers to realize that SARS-CoV-2 may be directly or indirectly associated with diabetes. “It is currently the subject of debate whether it may be a direct effect, infecting or directly reaching the pancreatic beta cells, or whether this involvement is a result of the effect of the infection at systemic level, in the context of the cytokine storm and the proinflammatory environment derived from it. Our current challenge is to confirm whether this virus can really replicate in pancreatic beta cells and to assess the possible existence of reinfections, among other aspects,” said Dr. Kleger.
Along with these “developing areas of knowledge,” there are several certainties regarding the link between diabetes and COVID-19. Dr. Kleger summarized the most relevant one. “Preexisting diabetes is known to be a highly prevalent comorbidity seen in 11%-22% of patients and increases the risk of severe disease and mortality.
“SARS-CoV-2 infection has also been shown to affect the exocrine pancreas, manifesting as pancreatitis in 5% of critically ill patients with COVID-19, as well as enlargement of the pancreas and abnormal levels of amylase or lipase in 7.5%-17% of patients.
“Furthermore, it is obvious that SARS-CoV-2 infection produces glycometabolic dysfunction in these patients, with increased hyperglycemia in people with type 2 diabetes and ketoacidosis in 2%-6.4% of patients with and without diabetes.”
After recovery
The most recent research reveals the persistence of this dysregulation long after recovery from COVID-19. “We’ve seen that in a significant proportion of patients, hyperglycemia is maintained for some time; in the specific case of hospitalized patients [without the need for assisted ventilation or other intensive care requirements], for up to more than 2 months after overcoming the illness.
“In the same way, there are studies that have shown that insulin resistance and hyperstimulation of pancreatic beta cells remain at pathological levels in the post–COVID-19 phase. And in line with increased insulin resistance, signs of hyperinflammation have also been detected in these patients.”
Dr. Kleger noted that another research area is the increased incidence of newly diagnosed diabetes after recovery from SARS-CoV-2 infection, “something that seems to be correlated with how severely the disease has been experienced and also depending on whether hospitalization or intensive care was needed. Likewise, retrospective studies have shown that the risk of developing type 2 diabetes is higher in COVID-19 patients, compared with those with other respiratory infections. Regarding the incidence of type 1 diabetes, there is evidence, particularly in the case of children, of a clear correlation between the pandemic waves and the increase in cases.
“Therefore, and in view of this data, we could say that, with regard to the involvement of SARS-CoV-2 in pancreatic beta cells, something is up, but we are not yet able to fully understand what it is. What can be confirmed based on the numerous studies carried out in this regard is that COVID-19 produces a metabolic dysregulation [hyperglycemia, insulin resistance, diabetic ketoacidosis] which in turn favors the development of diabetes in patients with no history of this disease,” said Dr. Kleger.
“Likewise, everything points to the existence of a definitively feasible infection in pancreatic beta cells associated with SARS-CoV-2, but there are still unknown aspects of the physiology that explain this effect that remain the subject of debate and deserve future studies,” he concluded.
Consequences of the pandemic
The experts agreed that, although COVID-19 is no longer at the center of specialist care, it is still a subject of investigation. On the conference’s opening day, an update was made on the approach to diabetes.
Care activity is gradually recovering as the time that professionals devote to COVID-19 care is reduced, “but it will take time to catch up with the care activities not carried out during the pandemic, and, unfortunately, in the coming years, we will see the repercussion of the lack or reduction of care during these years,” stressed the SED chair, Antonio Pérez Pérez, MD, director of endocrinology and nutrition of Hospital de la Santa Creu i Sant Pau, Barcelona.
Dr. Pérez stressed that the pandemic has revealed health system deficiencies in diabetes care. He added that the impact of COVID-19 on diabetes (resulting from the effects of the infection itself or from the inadequacy of prevention, diagnosis, and treatment measures) fostered a deterioration of metabolic control and a delay in the diagnosis of the disease and its complications.
“All this contributes to the fact that we currently continue to see patients with complications, especially in the case of type 2 diabetes, with more serious decompensations and diagnoses in more advanced stages of the disease. This impact has been more significant in older people from disadvantaged areas and with less capacity for self-monitoring and self-adjustment of treatment,” he added.
Describing lessons learned through the experiences accumulated in diabetes care during the pandemic, Dr. Pérez highlighted the push for virtual consultations, accessibility to drugs prescribed in electronic prescriptions, and the use of educational resources online and of telemedicine tools. “The need to invest in the health sector has also been assumed, endowing it with robustness in well-trained health personnel, to promote health education, boost efficient health organization, and invest in innovation aimed at facilitating care.”
Dr. Kleger and Dr. Pérez disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com. This article was translated from the Medscape Spanish edition.
MADRID – It involves the relationship between COVID-19 and new diagnoses of diabetes and blood glucose disorders, among others, in the post–COVID-19 period. These topics were addressed at the XXXIII National Congress of the Spanish Diabetes Society. They were also the central theme of the inaugural conference, Pancreatic Involvement During COVID-19: From Preclinical Studies to Clinical Relevance, which was led by Alexander Kleger, MD, PhD, head of the department of pancreatology at the Ulm (Germany) University Clinic for Internal Medicine.
The chair of the scientific committee of the congress, Franz Martín, MD, launched the conference by noting that the work of Dr. Kleger and his team has made it possible to ascertain that SARS-CoV-2 can infect pancreatic beta cells that produce insulin. This observation may help in understanding why patients with COVID-19 sometimes experience symptoms related to greater difficulty regulating blood glucose.
“In addition, the German expert and his group have described the abnormalities that occur in beta cells when they are infected by SARS-CoV-2, something especially important, given that knowledge of these abnormalities may be of great importance to understanding the possible appearance of more cases of diabetes in the future,” Dr. Martín added.
“Our data identify the human pancreas as a target of SARS-CoV-2 infection and suggest that pancreatic beta cell involvement could contribute to the metabolic dysregulation seen in COVID-19 patients,” Dr. Kleger pointed out.
In his speech, Dr. Kleger reviewed the evidence on the effects of SARS-CoV-2 that has been garnered since the start of the pandemic, and he presented his research group’s findings on the impact at the pancreatic level.
“Since March 2020, it has been seen that COVID-19 affected the pancreas, and studies published in August of that same year clearly spoke of both a worsening of diabetes and an increase in new cases of this disease diagnosed after SARS-CoV-2 infection. Also, the data showed how hospitalized patients with no previous history of diabetes experienced rapid increases in glucose levels 5 days after admission,” Dr. Kleger said.
Angiotensin-converting enzyme 2
As an example of the pace at which evidence on the pancreatic impact of this virus has been evolving, Dr. Kleger referred to early studies that found no angiotensin-converting enzyme 2 receptor on cells of the endocrine and exocrine pancreas. “To our surprise, in our work, we did observe the obvious presence of angiotensin-converting enzyme 2 specifically expressed in human pancreatic beta cells, something confirmed by other investigations. Another surprising aspect was verifying that the viral infection lasts longer in the pancreas than in the lungs,” said the expert.
These findings caused the researchers to realize that SARS-CoV-2 may be directly or indirectly associated with diabetes. “It is currently the subject of debate whether it may be a direct effect, infecting or directly reaching the pancreatic beta cells, or whether this involvement is a result of the effect of the infection at systemic level, in the context of the cytokine storm and the proinflammatory environment derived from it. Our current challenge is to confirm whether this virus can really replicate in pancreatic beta cells and to assess the possible existence of reinfections, among other aspects,” said Dr. Kleger.
Along with these “developing areas of knowledge,” there are several certainties regarding the link between diabetes and COVID-19. Dr. Kleger summarized the most relevant one. “Preexisting diabetes is known to be a highly prevalent comorbidity seen in 11%-22% of patients and increases the risk of severe disease and mortality.
“SARS-CoV-2 infection has also been shown to affect the exocrine pancreas, manifesting as pancreatitis in 5% of critically ill patients with COVID-19, as well as enlargement of the pancreas and abnormal levels of amylase or lipase in 7.5%-17% of patients.
“Furthermore, it is obvious that SARS-CoV-2 infection produces glycometabolic dysfunction in these patients, with increased hyperglycemia in people with type 2 diabetes and ketoacidosis in 2%-6.4% of patients with and without diabetes.”
After recovery
The most recent research reveals the persistence of this dysregulation long after recovery from COVID-19. “We’ve seen that in a significant proportion of patients, hyperglycemia is maintained for some time; in the specific case of hospitalized patients [without the need for assisted ventilation or other intensive care requirements], for up to more than 2 months after overcoming the illness.
“In the same way, there are studies that have shown that insulin resistance and hyperstimulation of pancreatic beta cells remain at pathological levels in the post–COVID-19 phase. And in line with increased insulin resistance, signs of hyperinflammation have also been detected in these patients.”
Dr. Kleger noted that another research area is the increased incidence of newly diagnosed diabetes after recovery from SARS-CoV-2 infection, “something that seems to be correlated with how severely the disease has been experienced and also depending on whether hospitalization or intensive care was needed. Likewise, retrospective studies have shown that the risk of developing type 2 diabetes is higher in COVID-19 patients, compared with those with other respiratory infections. Regarding the incidence of type 1 diabetes, there is evidence, particularly in the case of children, of a clear correlation between the pandemic waves and the increase in cases.
“Therefore, and in view of this data, we could say that, with regard to the involvement of SARS-CoV-2 in pancreatic beta cells, something is up, but we are not yet able to fully understand what it is. What can be confirmed based on the numerous studies carried out in this regard is that COVID-19 produces a metabolic dysregulation [hyperglycemia, insulin resistance, diabetic ketoacidosis] which in turn favors the development of diabetes in patients with no history of this disease,” said Dr. Kleger.
“Likewise, everything points to the existence of a definitively feasible infection in pancreatic beta cells associated with SARS-CoV-2, but there are still unknown aspects of the physiology that explain this effect that remain the subject of debate and deserve future studies,” he concluded.
Consequences of the pandemic
The experts agreed that, although COVID-19 is no longer at the center of specialist care, it is still a subject of investigation. On the conference’s opening day, an update was made on the approach to diabetes.
Care activity is gradually recovering as the time that professionals devote to COVID-19 care is reduced, “but it will take time to catch up with the care activities not carried out during the pandemic, and, unfortunately, in the coming years, we will see the repercussion of the lack or reduction of care during these years,” stressed the SED chair, Antonio Pérez Pérez, MD, director of endocrinology and nutrition of Hospital de la Santa Creu i Sant Pau, Barcelona.
Dr. Pérez stressed that the pandemic has revealed health system deficiencies in diabetes care. He added that the impact of COVID-19 on diabetes (resulting from the effects of the infection itself or from the inadequacy of prevention, diagnosis, and treatment measures) fostered a deterioration of metabolic control and a delay in the diagnosis of the disease and its complications.
“All this contributes to the fact that we currently continue to see patients with complications, especially in the case of type 2 diabetes, with more serious decompensations and diagnoses in more advanced stages of the disease. This impact has been more significant in older people from disadvantaged areas and with less capacity for self-monitoring and self-adjustment of treatment,” he added.
Describing lessons learned through the experiences accumulated in diabetes care during the pandemic, Dr. Pérez highlighted the push for virtual consultations, accessibility to drugs prescribed in electronic prescriptions, and the use of educational resources online and of telemedicine tools. “The need to invest in the health sector has also been assumed, endowing it with robustness in well-trained health personnel, to promote health education, boost efficient health organization, and invest in innovation aimed at facilitating care.”
Dr. Kleger and Dr. Pérez disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com. This article was translated from the Medscape Spanish edition.
Some smokers don’t get lung cancer; genetics might explain it
These people have genes that help limit mutations to DNA that would turn cells malignant and make them grow into tumors, the researchers say.
Scientists have long suspected that smoking leads to lung cancer by triggering DNA mutations in healthy cells. But it was hard for them to identify the mutations in healthy cells that might help predict future cancer risk, Jan Vijg, PhD, a senior author of the study and researcher at the University School of Medicine, Shanghai, China, said in a statement.
His team used a process called single-cell whole genome sequencing to examine cells lining the lungs of 19 smokers and 14 nonsmokers ranging in age from their pre-teens to their mid-80s. The cells came from patients who had tissue samples collected from their lungs during diagnostic testing unrelated to cancer. The scientists reported their findings in Nature Genetics.
The researchers specifically looked at cells lining the lungs because these cells can survive for years and build up mutations over time that are linked to aging and smoking.
“Of all the lung’s cell types, these are among the most likely to become cancerous,” says Simon Spivack, MD, a senior author of the study and professor at the Albert Einstein College of Medicine, New York.
Smokers had far more gene mutations that can cause lung cancer than nonsmokers, the analysis found.
“This experimentally confirms that smoking increases lung cancer risk by increasing the frequency of mutations, as previously hypothesized,” says Dr. Spivack. “This is likely one reason why so few nonsmokers get lung cancer, while 10 to 20 percent of lifelong smokers do.”
Among the smokers, people had smoked a maximum of 116 pack-years. A pack-year is the equivalent of smoking one pack a day for a year. The number of mutations detected in smokers’ lung cells increased in direct proportion to the number of pack-years they smoked.
But after 23 pack-years, the lung cells in smokers didn’t appear to add more mutations, the researchers report, suggesting that some people’s genes might make them more likely to fight mutations.
“The heaviest smokers did not have the highest mutation burden,” says Dr. Spivack. “Our data suggest that these individuals may have survived for so long in spite of their heavy smoking because they managed to suppress further mutation accumulation.”
While it’s possible these findings could one day help doctors come up with better ways to screen for lung cancer and treat the disease, that’s still a long way off. Many more lab tests and larger studies will be needed to better pinpoint which smokers might be more prone to lung cancer and why.
A version of this article first appeared on WebMD.com.
These people have genes that help limit mutations to DNA that would turn cells malignant and make them grow into tumors, the researchers say.
Scientists have long suspected that smoking leads to lung cancer by triggering DNA mutations in healthy cells. But it was hard for them to identify the mutations in healthy cells that might help predict future cancer risk, Jan Vijg, PhD, a senior author of the study and researcher at the University School of Medicine, Shanghai, China, said in a statement.
His team used a process called single-cell whole genome sequencing to examine cells lining the lungs of 19 smokers and 14 nonsmokers ranging in age from their pre-teens to their mid-80s. The cells came from patients who had tissue samples collected from their lungs during diagnostic testing unrelated to cancer. The scientists reported their findings in Nature Genetics.
The researchers specifically looked at cells lining the lungs because these cells can survive for years and build up mutations over time that are linked to aging and smoking.
“Of all the lung’s cell types, these are among the most likely to become cancerous,” says Simon Spivack, MD, a senior author of the study and professor at the Albert Einstein College of Medicine, New York.
Smokers had far more gene mutations that can cause lung cancer than nonsmokers, the analysis found.
“This experimentally confirms that smoking increases lung cancer risk by increasing the frequency of mutations, as previously hypothesized,” says Dr. Spivack. “This is likely one reason why so few nonsmokers get lung cancer, while 10 to 20 percent of lifelong smokers do.”
Among the smokers, people had smoked a maximum of 116 pack-years. A pack-year is the equivalent of smoking one pack a day for a year. The number of mutations detected in smokers’ lung cells increased in direct proportion to the number of pack-years they smoked.
But after 23 pack-years, the lung cells in smokers didn’t appear to add more mutations, the researchers report, suggesting that some people’s genes might make them more likely to fight mutations.
“The heaviest smokers did not have the highest mutation burden,” says Dr. Spivack. “Our data suggest that these individuals may have survived for so long in spite of their heavy smoking because they managed to suppress further mutation accumulation.”
While it’s possible these findings could one day help doctors come up with better ways to screen for lung cancer and treat the disease, that’s still a long way off. Many more lab tests and larger studies will be needed to better pinpoint which smokers might be more prone to lung cancer and why.
A version of this article first appeared on WebMD.com.
These people have genes that help limit mutations to DNA that would turn cells malignant and make them grow into tumors, the researchers say.
Scientists have long suspected that smoking leads to lung cancer by triggering DNA mutations in healthy cells. But it was hard for them to identify the mutations in healthy cells that might help predict future cancer risk, Jan Vijg, PhD, a senior author of the study and researcher at the University School of Medicine, Shanghai, China, said in a statement.
His team used a process called single-cell whole genome sequencing to examine cells lining the lungs of 19 smokers and 14 nonsmokers ranging in age from their pre-teens to their mid-80s. The cells came from patients who had tissue samples collected from their lungs during diagnostic testing unrelated to cancer. The scientists reported their findings in Nature Genetics.
The researchers specifically looked at cells lining the lungs because these cells can survive for years and build up mutations over time that are linked to aging and smoking.
“Of all the lung’s cell types, these are among the most likely to become cancerous,” says Simon Spivack, MD, a senior author of the study and professor at the Albert Einstein College of Medicine, New York.
Smokers had far more gene mutations that can cause lung cancer than nonsmokers, the analysis found.
“This experimentally confirms that smoking increases lung cancer risk by increasing the frequency of mutations, as previously hypothesized,” says Dr. Spivack. “This is likely one reason why so few nonsmokers get lung cancer, while 10 to 20 percent of lifelong smokers do.”
Among the smokers, people had smoked a maximum of 116 pack-years. A pack-year is the equivalent of smoking one pack a day for a year. The number of mutations detected in smokers’ lung cells increased in direct proportion to the number of pack-years they smoked.
But after 23 pack-years, the lung cells in smokers didn’t appear to add more mutations, the researchers report, suggesting that some people’s genes might make them more likely to fight mutations.
“The heaviest smokers did not have the highest mutation burden,” says Dr. Spivack. “Our data suggest that these individuals may have survived for so long in spite of their heavy smoking because they managed to suppress further mutation accumulation.”
While it’s possible these findings could one day help doctors come up with better ways to screen for lung cancer and treat the disease, that’s still a long way off. Many more lab tests and larger studies will be needed to better pinpoint which smokers might be more prone to lung cancer and why.
A version of this article first appeared on WebMD.com.
FROM NATURE GENETICS
Could new therapy for food ‘cues’ improve weight loss?
An intensive 1-year behavior therapy program aimed at changing a person’s response to food “cues” might help people with obesity lose a modest amount of weight, a randomized clinical trial suggests.
“Patients who are food-cue sensitive often feel out of control with their eating; they cannot resist food and/or cannot stop thinking about food,” said lead author Kerri N. Boutelle, PhD.
“Behavioral weight loss skills are not sufficient for these individuals,” so they designed this new approach, Dr. Boutelle, of the University of California, San Diego, explained in a press release.
The regulation of cues (ROC) intervention trains individuals to respond to their hunger and to resist eating highly craved foods (internal management), in contrast to behavioral weight loss programs that focus on counting calories (external management), Dr. Boutelle explained in an email.
The results of the Providing Adult Collaborative Interventions for Ideal Changes (PACIFIC) clinical trial, including follow-up out to 2 years, were published in JAMA Network Open.
Patients in the behavioral weight loss therapy group or the combined ROC and behavioral weight loss therapy group lost more weight at 6 months than patients in the ROC group – but then they slowly regained weight (whereas patients in the ROC group did not).
At 24 months, the three groups had a similar modest weight loss, compared with a control group that did not lose weight.
“We believe these internal management strategies are more durable over time,” said Dr. Boutelle.
However, two obesity experts, who helped develop the Canadian Adult Obesity Clinical Practice Guidelines, cautioned in emails that the intervention is very labor-intensive with less than 5% weight loss.
Four interventions
The trial was conducted at the Center for Healthy Eating and Activity Research at the University of California, San Diego, from December 2015 to December 2019.
Researchers randomized 271 adults with a mean BMI of 35 kg/m2 to one of four interventions:
- Regulation of cues: Patients were not given a prescribed diet but instead were given skills to tolerate cravings and respond better to hunger or satiety cues.
- Behavioral weight loss therapy: Patients were advised to follow a balanced, calorie-deficit diet based on their weight and given related skills.
- Combined regulation of cues plus behavioral weight loss therapy.
- Control: Patients received information about nutrition and stress management plus mindfulness training and were encouraged to find social support.
Therapy was given as 26 group sessions, 90 minutes each, over 12 months, with 16 weekly sessions, four biweekly sessions, and six monthly booster sessions.
Participants were asked to take part in 150 minutes of moderate to high intensity exercise each week and aim for 10,000 steps per day. All patients except those in the control group received a pedometer.
The patients were a mean age of 46 years, 82% were women and 62% were White.
At the end of the 12-month intervention, mean BMI had dropped by –1.18 kg/m2 in the ROC group and by –1.58 kg/m2 and –1.56 kg/m2 in the other two groups, compared with the control group, where BMI was virtually unchanged.
At 24 months follow-up, mean BMI was similar (roughly 33.5 kg/m2) in the ROC, the behavioral weight loss therapy, and the ROC plus behavioral weight loss therapy groups.
There was weight regain from 12 months in the latter two groups but not in the ROC group.
‘Nice study, but not practical’
“This is a nice study, but in no way is it practical,” Sean Wharton, MD, summarized.
“I think it may have difficulty finding its way into everyday practice,” said Dr. Wharton, adjunct professor at McMaster University, Hamilton, Ontario.
Also, “it does not compare ROC to pharmacotherapy,” he added, which is “quickly becoming the gold standard for obesity management. We have learned that adding intensive behavioral therapy – more visits and possibly a liquid diet as part of the weight management and some light group counseling – to pharmacotherapy does not add much.”
However, Dr. Wharton conceded that if an individual did not want, or could not take, pharmacotherapy and had access to ROC sessions, this might be a good option.
“The challenge will be offering this labor-intensive tool to 40% of Americans living with obesity,” he said.
The ROC intervention “is very different than a GP’s office that may see a patient two to three times/year max, with limited supports,” Dr. Wharton pointed out.
“It is labor-intensive, not reproducible in most places, and cannot be sustained forever. There is no evidence that the learning remains past the treatment interval. For example, 2 to 3 years later, are patients still adhering to ROC? Is weight still decreased or do they need to come to classes every month forever?”
‘Modest weight loss, doubtful long-term benefits’
Similarly, Arya M. Sharma, MD, said: “While this [ROC] approach may be helpful for some individuals, given the rather modest weight loss achieved (despite considerable efforts and a cash incentive), the long-term clinical benefits remain doubtful.”
The weight loss of less than 5% over 24 months is “in the ballpark of other behavioral weight-loss interventions,” said Dr. Sharma, of the University of Edmonton, Alberta, and past scientific director of Obesity Canada.
“I’m not convinced” about less weight regain, he added. “The difference between the groups is minimal. While this approach may well help individuals better deal with food cues, it does not change the underlying biology of weight regain.”
“This approach at best may help prevent future weight gain in susceptible individuals,” he speculated. “I would consider this more as a weight-stabilization than a weight-loss strategy.”
Next steps
Insurance doesn’t always cover weight loss with a mental health professional, Dr. Boutelle agreed. “However, there are eating disorder categories that also apply to many of our food-cue-sensitive patients, including binge eating,” she noted.
“We believe that ROC is an alternative model for weight loss that could be offered to patients who are interested or for whom behavioral weight loss has not been successful ... who are highly food-cue-responsive.”
The group is writing a manual about the ROC program to disseminate to other behavior therapists. They are also studying ROC in another clinical trial, Solutions for Hunger and Regulating Eating (SHARE). The ROC program is being offered at the UC San Diego Center for Healthy Eating and Activity Research, of which Dr. Boutelle is director.
The study was supported by grants from the National Institutes of Health. The researchers have reported no relevant financial relationships. Dr. Wharton has reported receiving honoraria and travel expenses and has participated in academic advisory boards for Novo Nordisk, Bausch Health, Eli Lilly, and Janssen. He is the medical director of a medical clinic specializing in weight management and diabetes. Dr. Sharma has reported receiving speakers bureau and consulting fees from Novo Nordisk, Bausch Pharmaceuticals, and AstraZeneca.
A version of this article first appeared on Medscape.com.
An intensive 1-year behavior therapy program aimed at changing a person’s response to food “cues” might help people with obesity lose a modest amount of weight, a randomized clinical trial suggests.
“Patients who are food-cue sensitive often feel out of control with their eating; they cannot resist food and/or cannot stop thinking about food,” said lead author Kerri N. Boutelle, PhD.
“Behavioral weight loss skills are not sufficient for these individuals,” so they designed this new approach, Dr. Boutelle, of the University of California, San Diego, explained in a press release.
The regulation of cues (ROC) intervention trains individuals to respond to their hunger and to resist eating highly craved foods (internal management), in contrast to behavioral weight loss programs that focus on counting calories (external management), Dr. Boutelle explained in an email.
The results of the Providing Adult Collaborative Interventions for Ideal Changes (PACIFIC) clinical trial, including follow-up out to 2 years, were published in JAMA Network Open.
Patients in the behavioral weight loss therapy group or the combined ROC and behavioral weight loss therapy group lost more weight at 6 months than patients in the ROC group – but then they slowly regained weight (whereas patients in the ROC group did not).
At 24 months, the three groups had a similar modest weight loss, compared with a control group that did not lose weight.
“We believe these internal management strategies are more durable over time,” said Dr. Boutelle.
However, two obesity experts, who helped develop the Canadian Adult Obesity Clinical Practice Guidelines, cautioned in emails that the intervention is very labor-intensive with less than 5% weight loss.
Four interventions
The trial was conducted at the Center for Healthy Eating and Activity Research at the University of California, San Diego, from December 2015 to December 2019.
Researchers randomized 271 adults with a mean BMI of 35 kg/m2 to one of four interventions:
- Regulation of cues: Patients were not given a prescribed diet but instead were given skills to tolerate cravings and respond better to hunger or satiety cues.
- Behavioral weight loss therapy: Patients were advised to follow a balanced, calorie-deficit diet based on their weight and given related skills.
- Combined regulation of cues plus behavioral weight loss therapy.
- Control: Patients received information about nutrition and stress management plus mindfulness training and were encouraged to find social support.
Therapy was given as 26 group sessions, 90 minutes each, over 12 months, with 16 weekly sessions, four biweekly sessions, and six monthly booster sessions.
Participants were asked to take part in 150 minutes of moderate to high intensity exercise each week and aim for 10,000 steps per day. All patients except those in the control group received a pedometer.
The patients were a mean age of 46 years, 82% were women and 62% were White.
At the end of the 12-month intervention, mean BMI had dropped by –1.18 kg/m2 in the ROC group and by –1.58 kg/m2 and –1.56 kg/m2 in the other two groups, compared with the control group, where BMI was virtually unchanged.
At 24 months follow-up, mean BMI was similar (roughly 33.5 kg/m2) in the ROC, the behavioral weight loss therapy, and the ROC plus behavioral weight loss therapy groups.
There was weight regain from 12 months in the latter two groups but not in the ROC group.
‘Nice study, but not practical’
“This is a nice study, but in no way is it practical,” Sean Wharton, MD, summarized.
“I think it may have difficulty finding its way into everyday practice,” said Dr. Wharton, adjunct professor at McMaster University, Hamilton, Ontario.
Also, “it does not compare ROC to pharmacotherapy,” he added, which is “quickly becoming the gold standard for obesity management. We have learned that adding intensive behavioral therapy – more visits and possibly a liquid diet as part of the weight management and some light group counseling – to pharmacotherapy does not add much.”
However, Dr. Wharton conceded that if an individual did not want, or could not take, pharmacotherapy and had access to ROC sessions, this might be a good option.
“The challenge will be offering this labor-intensive tool to 40% of Americans living with obesity,” he said.
The ROC intervention “is very different than a GP’s office that may see a patient two to three times/year max, with limited supports,” Dr. Wharton pointed out.
“It is labor-intensive, not reproducible in most places, and cannot be sustained forever. There is no evidence that the learning remains past the treatment interval. For example, 2 to 3 years later, are patients still adhering to ROC? Is weight still decreased or do they need to come to classes every month forever?”
‘Modest weight loss, doubtful long-term benefits’
Similarly, Arya M. Sharma, MD, said: “While this [ROC] approach may be helpful for some individuals, given the rather modest weight loss achieved (despite considerable efforts and a cash incentive), the long-term clinical benefits remain doubtful.”
The weight loss of less than 5% over 24 months is “in the ballpark of other behavioral weight-loss interventions,” said Dr. Sharma, of the University of Edmonton, Alberta, and past scientific director of Obesity Canada.
“I’m not convinced” about less weight regain, he added. “The difference between the groups is minimal. While this approach may well help individuals better deal with food cues, it does not change the underlying biology of weight regain.”
“This approach at best may help prevent future weight gain in susceptible individuals,” he speculated. “I would consider this more as a weight-stabilization than a weight-loss strategy.”
Next steps
Insurance doesn’t always cover weight loss with a mental health professional, Dr. Boutelle agreed. “However, there are eating disorder categories that also apply to many of our food-cue-sensitive patients, including binge eating,” she noted.
“We believe that ROC is an alternative model for weight loss that could be offered to patients who are interested or for whom behavioral weight loss has not been successful ... who are highly food-cue-responsive.”
The group is writing a manual about the ROC program to disseminate to other behavior therapists. They are also studying ROC in another clinical trial, Solutions for Hunger and Regulating Eating (SHARE). The ROC program is being offered at the UC San Diego Center for Healthy Eating and Activity Research, of which Dr. Boutelle is director.
The study was supported by grants from the National Institutes of Health. The researchers have reported no relevant financial relationships. Dr. Wharton has reported receiving honoraria and travel expenses and has participated in academic advisory boards for Novo Nordisk, Bausch Health, Eli Lilly, and Janssen. He is the medical director of a medical clinic specializing in weight management and diabetes. Dr. Sharma has reported receiving speakers bureau and consulting fees from Novo Nordisk, Bausch Pharmaceuticals, and AstraZeneca.
A version of this article first appeared on Medscape.com.
An intensive 1-year behavior therapy program aimed at changing a person’s response to food “cues” might help people with obesity lose a modest amount of weight, a randomized clinical trial suggests.
“Patients who are food-cue sensitive often feel out of control with their eating; they cannot resist food and/or cannot stop thinking about food,” said lead author Kerri N. Boutelle, PhD.
“Behavioral weight loss skills are not sufficient for these individuals,” so they designed this new approach, Dr. Boutelle, of the University of California, San Diego, explained in a press release.
The regulation of cues (ROC) intervention trains individuals to respond to their hunger and to resist eating highly craved foods (internal management), in contrast to behavioral weight loss programs that focus on counting calories (external management), Dr. Boutelle explained in an email.
The results of the Providing Adult Collaborative Interventions for Ideal Changes (PACIFIC) clinical trial, including follow-up out to 2 years, were published in JAMA Network Open.
Patients in the behavioral weight loss therapy group or the combined ROC and behavioral weight loss therapy group lost more weight at 6 months than patients in the ROC group – but then they slowly regained weight (whereas patients in the ROC group did not).
At 24 months, the three groups had a similar modest weight loss, compared with a control group that did not lose weight.
“We believe these internal management strategies are more durable over time,” said Dr. Boutelle.
However, two obesity experts, who helped develop the Canadian Adult Obesity Clinical Practice Guidelines, cautioned in emails that the intervention is very labor-intensive with less than 5% weight loss.
Four interventions
The trial was conducted at the Center for Healthy Eating and Activity Research at the University of California, San Diego, from December 2015 to December 2019.
Researchers randomized 271 adults with a mean BMI of 35 kg/m2 to one of four interventions:
- Regulation of cues: Patients were not given a prescribed diet but instead were given skills to tolerate cravings and respond better to hunger or satiety cues.
- Behavioral weight loss therapy: Patients were advised to follow a balanced, calorie-deficit diet based on their weight and given related skills.
- Combined regulation of cues plus behavioral weight loss therapy.
- Control: Patients received information about nutrition and stress management plus mindfulness training and were encouraged to find social support.
Therapy was given as 26 group sessions, 90 minutes each, over 12 months, with 16 weekly sessions, four biweekly sessions, and six monthly booster sessions.
Participants were asked to take part in 150 minutes of moderate to high intensity exercise each week and aim for 10,000 steps per day. All patients except those in the control group received a pedometer.
The patients were a mean age of 46 years, 82% were women and 62% were White.
At the end of the 12-month intervention, mean BMI had dropped by –1.18 kg/m2 in the ROC group and by –1.58 kg/m2 and –1.56 kg/m2 in the other two groups, compared with the control group, where BMI was virtually unchanged.
At 24 months follow-up, mean BMI was similar (roughly 33.5 kg/m2) in the ROC, the behavioral weight loss therapy, and the ROC plus behavioral weight loss therapy groups.
There was weight regain from 12 months in the latter two groups but not in the ROC group.
‘Nice study, but not practical’
“This is a nice study, but in no way is it practical,” Sean Wharton, MD, summarized.
“I think it may have difficulty finding its way into everyday practice,” said Dr. Wharton, adjunct professor at McMaster University, Hamilton, Ontario.
Also, “it does not compare ROC to pharmacotherapy,” he added, which is “quickly becoming the gold standard for obesity management. We have learned that adding intensive behavioral therapy – more visits and possibly a liquid diet as part of the weight management and some light group counseling – to pharmacotherapy does not add much.”
However, Dr. Wharton conceded that if an individual did not want, or could not take, pharmacotherapy and had access to ROC sessions, this might be a good option.
“The challenge will be offering this labor-intensive tool to 40% of Americans living with obesity,” he said.
The ROC intervention “is very different than a GP’s office that may see a patient two to three times/year max, with limited supports,” Dr. Wharton pointed out.
“It is labor-intensive, not reproducible in most places, and cannot be sustained forever. There is no evidence that the learning remains past the treatment interval. For example, 2 to 3 years later, are patients still adhering to ROC? Is weight still decreased or do they need to come to classes every month forever?”
‘Modest weight loss, doubtful long-term benefits’
Similarly, Arya M. Sharma, MD, said: “While this [ROC] approach may be helpful for some individuals, given the rather modest weight loss achieved (despite considerable efforts and a cash incentive), the long-term clinical benefits remain doubtful.”
The weight loss of less than 5% over 24 months is “in the ballpark of other behavioral weight-loss interventions,” said Dr. Sharma, of the University of Edmonton, Alberta, and past scientific director of Obesity Canada.
“I’m not convinced” about less weight regain, he added. “The difference between the groups is minimal. While this approach may well help individuals better deal with food cues, it does not change the underlying biology of weight regain.”
“This approach at best may help prevent future weight gain in susceptible individuals,” he speculated. “I would consider this more as a weight-stabilization than a weight-loss strategy.”
Next steps
Insurance doesn’t always cover weight loss with a mental health professional, Dr. Boutelle agreed. “However, there are eating disorder categories that also apply to many of our food-cue-sensitive patients, including binge eating,” she noted.
“We believe that ROC is an alternative model for weight loss that could be offered to patients who are interested or for whom behavioral weight loss has not been successful ... who are highly food-cue-responsive.”
The group is writing a manual about the ROC program to disseminate to other behavior therapists. They are also studying ROC in another clinical trial, Solutions for Hunger and Regulating Eating (SHARE). The ROC program is being offered at the UC San Diego Center for Healthy Eating and Activity Research, of which Dr. Boutelle is director.
The study was supported by grants from the National Institutes of Health. The researchers have reported no relevant financial relationships. Dr. Wharton has reported receiving honoraria and travel expenses and has participated in academic advisory boards for Novo Nordisk, Bausch Health, Eli Lilly, and Janssen. He is the medical director of a medical clinic specializing in weight management and diabetes. Dr. Sharma has reported receiving speakers bureau and consulting fees from Novo Nordisk, Bausch Pharmaceuticals, and AstraZeneca.
A version of this article first appeared on Medscape.com.
Updated AHA/ASA guideline changes care for spontaneous intracerebral hemorrhage
Many strategies widely considered “standard care” for managing spontaneous intracerebral hemorrhage (ICH) are not as effective as previously thought and are no longer recommended in updated guidelines from the American Heart Association/American Stroke Association (ASA).
Compression stockings, antiseizure medication, and steroid treatment are among the treatments with uncertain effectiveness, the writing group says.
The 2022 Guideline for the Management of Patients With Spontaneous ICH was published online in Stroke. The 80-page document contains major changes and refinements to the 2015 guideline on ICH management.
“Advances have been made in an array of fields related to ICH, including the organization of regional health care systems, reversal of the negative effects of blood thinners, minimally invasive surgical procedures, and the underlying disease in small blood vessels,” Steven M. Greenberg, MD, PhD, chair of the guideline writing group with Harvard Medical School and Massachusetts General Hospital, both in Boston, said in a news release.
“We’ve updated sections across the board. There’s probably no area that went untouched with some tweaking and new evidence added that led to some changes in level of evidence or strength of a recommendation,” Dr. Greenberg added in an interview with this news organization.
“Each section comes with knowledge gaps, and it wasn’t hard to come up with knowledge gaps in every section,” Dr. Greenberg acknowledged.
Time-honored treatments no more?
Among the key updates are changes to some “time-honored” treatments that continue to be used with some “regularity” for patients with ICH, yet appear to confer either no benefit or harm, Dr. Greenberg said.
For example, for emergency or critical care treatment of ICH, prophylactic corticosteroids or continuous hyperosmolar therapy is not recommended, because it appears to have no benefit for outcome, while use of platelet transfusions outside the setting of emergency surgery or severe thrombocytopenia appears to worsen outcome, the authors say.
Use of graduated knee- or thigh-high compression stockings alone is not an effective prophylactic therapy for prevention of deep vein thrombosis (DVT). Instead, intermittent pneumatic compression (IPC) starting on the day of diagnosis is now recommended for DVT prophylaxis.
“This is an area where we still have a lot of exploration to do. It is unclear whether even specialized compression devices reduce the risks of deep vein thrombosis or improve the overall health of people with a brain bleed,” Dr. Greenberg said in the release.
The new guidance advises against use of antiseizure or antidepressant medications for ICH patients in whom there is no evidence of seizures or depression.
In clinical trials, antiseizure medication did not contribute to improvements in functionality or long-term seizure control, and the use of antidepressants increased the chance of bone fractures, the authors say.
The guideline also provides updated recommendations for acute reversal of anticoagulation after ICH. It highlights the use of protein complex concentrate for reversal of vitamin K antagonists, such as warfarin; idarucizumab for reversal of the thrombin inhibitor dabigatran; and andexanet alfa for reversal of factor Xa inhibitors, such as rivaroxaban, apixaban, and edoxaban.
For acute blood pressure lowering after mild to moderate ICH, treatment regimens that limit blood pressure variability and achieve smooth, sustained blood pressure control appear to reduce hematoma expansion and yield better functional outcome, the guideline says.
It also notes that minimally invasive approaches for hematoma evacuation, compared with medical management alone‚ have been shown to reduce mortality.
For patients with cerebellar hemorrhage, indications for immediate surgical evacuation with or without an external ventricular drain to reduce mortality now include larger volume (> 15 mL) in addition to previously recommended indications of neurologic deterioration, brainstem compression, and hydrocephalus, the authors note.
However, a “major knowledge gap is whether we can improve functional outcome with hematoma evacuation,” Dr. Greenberg said.
Multidisciplinary care
For rehabilitation after ICH, the guideline reinforces the importance of having a multidisciplinary team to develop a comprehensive plan for recovery.
Starting rehabilitation activities such as stretching and functional task training may be considered 24 to 48 hours following mild or moderate ICH. However, early aggressive mobilization within the first 24 hours has been linked to an increased risk of death within 14 days after an ICH, the guideline says.
Knowledge gaps include how soon it’s safe to return to work, drive, and participate in other social engagements. Recommendations on sexual activity and exercise levels that are safe after a stroke are also needed.
“People need additional help with these lifestyle changes, whether it’s moving around more, curbing their alcohol use, or eating healthier foods. This all happens after they leave the hospital, and we need to be sure we are empowering families with the information they may need to be properly supportive,” Dr. Greenberg says in the release.
The guideline points to the patient’s home caregiver as a “key and sometimes overlooked” member of the care team. It recommends psychosocial education, practical support, and training for the caregiver to improve the patient’s balance, activity level, and overall quality of life.
Opportunity for prevention?
The guideline also suggests there may be an opportunity to prevent ICH in some people through neuroimaging markers.
While neuroimaging is not routinely performed as a part of risk stratification for primary ICH risk, damage to small blood vessels that is associated with ICH may be evident on MRI that could signal future ICH risk, the guideline says.
“We added to the guidelines for the first time a section on mostly imaging markers of risk for having a first-ever hemorrhage,” Dr. Greenberg said in an interview.
“We don’t make any recommendations as to how to act on these markers because there is a knowledge gap. The hope is that we’ll see growth in our ability to predict first-ever hemorrhage and be able to do things to prevent first-ever hemorrhage,” he said.
“We believe the wide range of knowledge set forth in the new guideline will translate into meaningful improvements in ICH care,” Dr. Greenberg adds in the release.
The updated guideline has been endorsed by the American Association of Neurological Surgeons and Congress of Neurological Surgeons, the Society of Vascular and Interventional Neurology, and the Neurocritical Care Society. The American Academy of Neurology has affirmed the value of this statement as an educational tool for neurologists.
This research had no commercial funding. Dr. Greenberg has disclosed no relevant financial relationships. A complete list of disclosures for the guideline group is available with the original article.
A version of this article first appeared on Medscape.com.
Many strategies widely considered “standard care” for managing spontaneous intracerebral hemorrhage (ICH) are not as effective as previously thought and are no longer recommended in updated guidelines from the American Heart Association/American Stroke Association (ASA).
Compression stockings, antiseizure medication, and steroid treatment are among the treatments with uncertain effectiveness, the writing group says.
The 2022 Guideline for the Management of Patients With Spontaneous ICH was published online in Stroke. The 80-page document contains major changes and refinements to the 2015 guideline on ICH management.
“Advances have been made in an array of fields related to ICH, including the organization of regional health care systems, reversal of the negative effects of blood thinners, minimally invasive surgical procedures, and the underlying disease in small blood vessels,” Steven M. Greenberg, MD, PhD, chair of the guideline writing group with Harvard Medical School and Massachusetts General Hospital, both in Boston, said in a news release.
“We’ve updated sections across the board. There’s probably no area that went untouched with some tweaking and new evidence added that led to some changes in level of evidence or strength of a recommendation,” Dr. Greenberg added in an interview with this news organization.
“Each section comes with knowledge gaps, and it wasn’t hard to come up with knowledge gaps in every section,” Dr. Greenberg acknowledged.
Time-honored treatments no more?
Among the key updates are changes to some “time-honored” treatments that continue to be used with some “regularity” for patients with ICH, yet appear to confer either no benefit or harm, Dr. Greenberg said.
For example, for emergency or critical care treatment of ICH, prophylactic corticosteroids or continuous hyperosmolar therapy is not recommended, because it appears to have no benefit for outcome, while use of platelet transfusions outside the setting of emergency surgery or severe thrombocytopenia appears to worsen outcome, the authors say.
Use of graduated knee- or thigh-high compression stockings alone is not an effective prophylactic therapy for prevention of deep vein thrombosis (DVT). Instead, intermittent pneumatic compression (IPC) starting on the day of diagnosis is now recommended for DVT prophylaxis.
“This is an area where we still have a lot of exploration to do. It is unclear whether even specialized compression devices reduce the risks of deep vein thrombosis or improve the overall health of people with a brain bleed,” Dr. Greenberg said in the release.
The new guidance advises against use of antiseizure or antidepressant medications for ICH patients in whom there is no evidence of seizures or depression.
In clinical trials, antiseizure medication did not contribute to improvements in functionality or long-term seizure control, and the use of antidepressants increased the chance of bone fractures, the authors say.
The guideline also provides updated recommendations for acute reversal of anticoagulation after ICH. It highlights the use of protein complex concentrate for reversal of vitamin K antagonists, such as warfarin; idarucizumab for reversal of the thrombin inhibitor dabigatran; and andexanet alfa for reversal of factor Xa inhibitors, such as rivaroxaban, apixaban, and edoxaban.
For acute blood pressure lowering after mild to moderate ICH, treatment regimens that limit blood pressure variability and achieve smooth, sustained blood pressure control appear to reduce hematoma expansion and yield better functional outcome, the guideline says.
It also notes that minimally invasive approaches for hematoma evacuation, compared with medical management alone‚ have been shown to reduce mortality.
For patients with cerebellar hemorrhage, indications for immediate surgical evacuation with or without an external ventricular drain to reduce mortality now include larger volume (> 15 mL) in addition to previously recommended indications of neurologic deterioration, brainstem compression, and hydrocephalus, the authors note.
However, a “major knowledge gap is whether we can improve functional outcome with hematoma evacuation,” Dr. Greenberg said.
Multidisciplinary care
For rehabilitation after ICH, the guideline reinforces the importance of having a multidisciplinary team to develop a comprehensive plan for recovery.
Starting rehabilitation activities such as stretching and functional task training may be considered 24 to 48 hours following mild or moderate ICH. However, early aggressive mobilization within the first 24 hours has been linked to an increased risk of death within 14 days after an ICH, the guideline says.
Knowledge gaps include how soon it’s safe to return to work, drive, and participate in other social engagements. Recommendations on sexual activity and exercise levels that are safe after a stroke are also needed.
“People need additional help with these lifestyle changes, whether it’s moving around more, curbing their alcohol use, or eating healthier foods. This all happens after they leave the hospital, and we need to be sure we are empowering families with the information they may need to be properly supportive,” Dr. Greenberg says in the release.
The guideline points to the patient’s home caregiver as a “key and sometimes overlooked” member of the care team. It recommends psychosocial education, practical support, and training for the caregiver to improve the patient’s balance, activity level, and overall quality of life.
Opportunity for prevention?
The guideline also suggests there may be an opportunity to prevent ICH in some people through neuroimaging markers.
While neuroimaging is not routinely performed as a part of risk stratification for primary ICH risk, damage to small blood vessels that is associated with ICH may be evident on MRI that could signal future ICH risk, the guideline says.
“We added to the guidelines for the first time a section on mostly imaging markers of risk for having a first-ever hemorrhage,” Dr. Greenberg said in an interview.
“We don’t make any recommendations as to how to act on these markers because there is a knowledge gap. The hope is that we’ll see growth in our ability to predict first-ever hemorrhage and be able to do things to prevent first-ever hemorrhage,” he said.
“We believe the wide range of knowledge set forth in the new guideline will translate into meaningful improvements in ICH care,” Dr. Greenberg adds in the release.
The updated guideline has been endorsed by the American Association of Neurological Surgeons and Congress of Neurological Surgeons, the Society of Vascular and Interventional Neurology, and the Neurocritical Care Society. The American Academy of Neurology has affirmed the value of this statement as an educational tool for neurologists.
This research had no commercial funding. Dr. Greenberg has disclosed no relevant financial relationships. A complete list of disclosures for the guideline group is available with the original article.
A version of this article first appeared on Medscape.com.
Many strategies widely considered “standard care” for managing spontaneous intracerebral hemorrhage (ICH) are not as effective as previously thought and are no longer recommended in updated guidelines from the American Heart Association/American Stroke Association (ASA).
Compression stockings, antiseizure medication, and steroid treatment are among the treatments with uncertain effectiveness, the writing group says.
The 2022 Guideline for the Management of Patients With Spontaneous ICH was published online in Stroke. The 80-page document contains major changes and refinements to the 2015 guideline on ICH management.
“Advances have been made in an array of fields related to ICH, including the organization of regional health care systems, reversal of the negative effects of blood thinners, minimally invasive surgical procedures, and the underlying disease in small blood vessels,” Steven M. Greenberg, MD, PhD, chair of the guideline writing group with Harvard Medical School and Massachusetts General Hospital, both in Boston, said in a news release.
“We’ve updated sections across the board. There’s probably no area that went untouched with some tweaking and new evidence added that led to some changes in level of evidence or strength of a recommendation,” Dr. Greenberg added in an interview with this news organization.
“Each section comes with knowledge gaps, and it wasn’t hard to come up with knowledge gaps in every section,” Dr. Greenberg acknowledged.
Time-honored treatments no more?
Among the key updates are changes to some “time-honored” treatments that continue to be used with some “regularity” for patients with ICH, yet appear to confer either no benefit or harm, Dr. Greenberg said.
For example, for emergency or critical care treatment of ICH, prophylactic corticosteroids or continuous hyperosmolar therapy is not recommended, because it appears to have no benefit for outcome, while use of platelet transfusions outside the setting of emergency surgery or severe thrombocytopenia appears to worsen outcome, the authors say.
Use of graduated knee- or thigh-high compression stockings alone is not an effective prophylactic therapy for prevention of deep vein thrombosis (DVT). Instead, intermittent pneumatic compression (IPC) starting on the day of diagnosis is now recommended for DVT prophylaxis.
“This is an area where we still have a lot of exploration to do. It is unclear whether even specialized compression devices reduce the risks of deep vein thrombosis or improve the overall health of people with a brain bleed,” Dr. Greenberg said in the release.
The new guidance advises against use of antiseizure or antidepressant medications for ICH patients in whom there is no evidence of seizures or depression.
In clinical trials, antiseizure medication did not contribute to improvements in functionality or long-term seizure control, and the use of antidepressants increased the chance of bone fractures, the authors say.
The guideline also provides updated recommendations for acute reversal of anticoagulation after ICH. It highlights the use of protein complex concentrate for reversal of vitamin K antagonists, such as warfarin; idarucizumab for reversal of the thrombin inhibitor dabigatran; and andexanet alfa for reversal of factor Xa inhibitors, such as rivaroxaban, apixaban, and edoxaban.
For acute blood pressure lowering after mild to moderate ICH, treatment regimens that limit blood pressure variability and achieve smooth, sustained blood pressure control appear to reduce hematoma expansion and yield better functional outcome, the guideline says.
It also notes that minimally invasive approaches for hematoma evacuation, compared with medical management alone‚ have been shown to reduce mortality.
For patients with cerebellar hemorrhage, indications for immediate surgical evacuation with or without an external ventricular drain to reduce mortality now include larger volume (> 15 mL) in addition to previously recommended indications of neurologic deterioration, brainstem compression, and hydrocephalus, the authors note.
However, a “major knowledge gap is whether we can improve functional outcome with hematoma evacuation,” Dr. Greenberg said.
Multidisciplinary care
For rehabilitation after ICH, the guideline reinforces the importance of having a multidisciplinary team to develop a comprehensive plan for recovery.
Starting rehabilitation activities such as stretching and functional task training may be considered 24 to 48 hours following mild or moderate ICH. However, early aggressive mobilization within the first 24 hours has been linked to an increased risk of death within 14 days after an ICH, the guideline says.
Knowledge gaps include how soon it’s safe to return to work, drive, and participate in other social engagements. Recommendations on sexual activity and exercise levels that are safe after a stroke are also needed.
“People need additional help with these lifestyle changes, whether it’s moving around more, curbing their alcohol use, or eating healthier foods. This all happens after they leave the hospital, and we need to be sure we are empowering families with the information they may need to be properly supportive,” Dr. Greenberg says in the release.
The guideline points to the patient’s home caregiver as a “key and sometimes overlooked” member of the care team. It recommends psychosocial education, practical support, and training for the caregiver to improve the patient’s balance, activity level, and overall quality of life.
Opportunity for prevention?
The guideline also suggests there may be an opportunity to prevent ICH in some people through neuroimaging markers.
While neuroimaging is not routinely performed as a part of risk stratification for primary ICH risk, damage to small blood vessels that is associated with ICH may be evident on MRI that could signal future ICH risk, the guideline says.
“We added to the guidelines for the first time a section on mostly imaging markers of risk for having a first-ever hemorrhage,” Dr. Greenberg said in an interview.
“We don’t make any recommendations as to how to act on these markers because there is a knowledge gap. The hope is that we’ll see growth in our ability to predict first-ever hemorrhage and be able to do things to prevent first-ever hemorrhage,” he said.
“We believe the wide range of knowledge set forth in the new guideline will translate into meaningful improvements in ICH care,” Dr. Greenberg adds in the release.
The updated guideline has been endorsed by the American Association of Neurological Surgeons and Congress of Neurological Surgeons, the Society of Vascular and Interventional Neurology, and the Neurocritical Care Society. The American Academy of Neurology has affirmed the value of this statement as an educational tool for neurologists.
This research had no commercial funding. Dr. Greenberg has disclosed no relevant financial relationships. A complete list of disclosures for the guideline group is available with the original article.
A version of this article first appeared on Medscape.com.
Finding ‘bright lights’: Why family physician continues to love practicing mid-career
A few years ago I tracked down my medical school interviewer to thank him for giving me the opportunity to do what I felt I was called to do. I was surprised that, after 15 years, he actually remembered me and remembered details like walking to the courtyard to meet my father who’d driven me to the interview.
Sharing my gratitude and letting him know I was happy felt important to me.
Choosing to practice family medicine has a lot to do with why I am happy in my career today.
One of my frustrations with health care had been its emphasis on treatment of sickness, rather than a broader one that incorporated prevention of sickness. During my third year of medical school, I was following a family and sports medicine faculty member who was focusing on aspects of lifestyle medicine to help a patient remain active and age gracefully. Seeing opportunities to practice preventative medicine in family medicine made me realize the specialty was the perfect fit for me.
Food as medicine
While participating in rotations I also realized you can find a subspecialty within family medicine.
During my fourth year of medical school, I followed an attending who was seeing a patient for hypertension, prediabetes and hypercholesterolemia. The attending told the patient to eat “healthier,” gave her a handout, and scheduled a follow up appointment for 6 months later.
My thoughts were: “That’s it? That’s how we counsel patients to improve their dietary habits?”
As the patient was leaving the exam room, I asked her what type of oil she cooked with, and I proceeded to share culinary tips from my mother – who was a self-taught and early adopter of the food-as-medicine movement.
Once I started my residency, I knew I’d want to incorporate lifestyle and dietary approaches at many of my patient visits.
I scheduled patients every month to monitor their weight, follow up on chronic conditions, but more importantly, to engage them in their health and empower them to make small lifestyle changes each month and report their efforts. I felt like I was their health coach and cheerleader.
My career in family medicine
Entering the job market allowed me to form my philosophy of treating patients with a mind, body, and spirit approach. I chose to practice value-based care, which aligns with my lifestyle and preventative medicine approach .
I currently practice in a small family medicine–only clinic that is part of a larger multispecialty system. Primary care specialties in my organization are valued, respected and central to a patient’s well being and care. We are encouraged to spend time with patients, assess barriers to care and work collaboratively with our healthcare team, so that preventative medicine approaches take the lead in a patient’s health. This supportive culture and environment is one where my passion for food as medicine has thrived.
One day I forgot to pack a lunch and instead brought a grocery bag of items to make a salad. When I realized I made too much, I sent an email to my staff to get some “free salad in my office.” This serendipitous moment started an informal office “salad club” each week. Continued support from my staff and leadership, allowed me to consider further extending this teaching to my patients and my colleagues.
Three years ago, I helped adopt a sustainable plant-forward menu for our physician meetings, complete with a recipe from the menu for physicians to replicate at home or give to their patients.
I also pursued adoption of shared medical appointments for our medical group. These appointments apply the “see one, do one, teach one” model in medicine, but with culinary medicine as the focus.
Knowing that my patients are all connected to their families through food, I sought this as an opportunity to dive in further with wellness opportunities at their next meal. After almost 2 years of working on this project, I was able to host my first shared medical appointment with a group of patients on March 12, 2020. The next day schools closed, lockdowns occurred, and the world changed.
Opportunities highlighted by the pandemic
We always knew health care was broken but adding the increasingly longer hours and COVID vaccine–hesitant patients that the pandemic brought made everything look dark at times. What has helped me stay hopeful and energetic for system changes is feeling gratitude and seeking bright lights.
My experiences seeing patients in telehealth visits are examples of some of the bright lights I found in the pandemic. During these visits, patients showed me something from their pantry, and we’d go over nutritional labels together.
Additionally, my patients became engaged with their own conditions and wanted to improve them because of news articles highlighting risk factors for COVID-19, such as obesity. I had an active audience when it came to talking about food-as-medicine approaches to improving risk factors and immunity. And since everyone was listening, I didn’t stop at food. I also talked about physical health, stress resiliency, planetary diets, sleep, connections, and lastly vaccines!
Once the vaccines were distributed, I naturally gravitated to having those conversations with patients and colleagues and on social media. Plus, the pandemic gave us moments of simple times to slow down, take more rests, be less overscheduled, consider work-life priorities, and, lastly, to be okay with not being totally okay.
In practicing primary care, we have a unique role in seeing medicine from a whole body, whole person, whole family perspective. There is an opportunity to highlight what is broken in medicine and aim to make it whole.
I’m currently looking at shared medical appointments as a new standard way to provide care to all patients, because it improves access, provides better quality visits and aligns my values, mission, and purpose.
In the midst of the pandemic, I helped advocate for a sustainable plant-forward menu that was launched throughout four different hospitals in the Sharp HealthCare system, in California, in 2020. Knowing that patients were served a menu I played a role in, gave me solace.
As part of the hospital food and nutrition team, I am grateful for the opportunity I have to work on a broader mission to address social determinants of health and seek opportunities to help the system work for our patients.
Public health communication has been lacking in the pandemic, but another bright light is that we were still the trusted messengers to our patients and our communities. I’m continually honored and humbled to be trusted with a whole family’s health.
Dr. Neison practices family medicine and culinary medicine at Sharp Rees-Stealy Medical Group in San Diego, and is cochair of climate and planetary health for SRS Medical Group. You can follow her on Instagram, LinkedIn, and Facebook @Flavors4WellnessMD.
A few years ago I tracked down my medical school interviewer to thank him for giving me the opportunity to do what I felt I was called to do. I was surprised that, after 15 years, he actually remembered me and remembered details like walking to the courtyard to meet my father who’d driven me to the interview.
Sharing my gratitude and letting him know I was happy felt important to me.
Choosing to practice family medicine has a lot to do with why I am happy in my career today.
One of my frustrations with health care had been its emphasis on treatment of sickness, rather than a broader one that incorporated prevention of sickness. During my third year of medical school, I was following a family and sports medicine faculty member who was focusing on aspects of lifestyle medicine to help a patient remain active and age gracefully. Seeing opportunities to practice preventative medicine in family medicine made me realize the specialty was the perfect fit for me.
Food as medicine
While participating in rotations I also realized you can find a subspecialty within family medicine.
During my fourth year of medical school, I followed an attending who was seeing a patient for hypertension, prediabetes and hypercholesterolemia. The attending told the patient to eat “healthier,” gave her a handout, and scheduled a follow up appointment for 6 months later.
My thoughts were: “That’s it? That’s how we counsel patients to improve their dietary habits?”
As the patient was leaving the exam room, I asked her what type of oil she cooked with, and I proceeded to share culinary tips from my mother – who was a self-taught and early adopter of the food-as-medicine movement.
Once I started my residency, I knew I’d want to incorporate lifestyle and dietary approaches at many of my patient visits.
I scheduled patients every month to monitor their weight, follow up on chronic conditions, but more importantly, to engage them in their health and empower them to make small lifestyle changes each month and report their efforts. I felt like I was their health coach and cheerleader.
My career in family medicine
Entering the job market allowed me to form my philosophy of treating patients with a mind, body, and spirit approach. I chose to practice value-based care, which aligns with my lifestyle and preventative medicine approach .
I currently practice in a small family medicine–only clinic that is part of a larger multispecialty system. Primary care specialties in my organization are valued, respected and central to a patient’s well being and care. We are encouraged to spend time with patients, assess barriers to care and work collaboratively with our healthcare team, so that preventative medicine approaches take the lead in a patient’s health. This supportive culture and environment is one where my passion for food as medicine has thrived.
One day I forgot to pack a lunch and instead brought a grocery bag of items to make a salad. When I realized I made too much, I sent an email to my staff to get some “free salad in my office.” This serendipitous moment started an informal office “salad club” each week. Continued support from my staff and leadership, allowed me to consider further extending this teaching to my patients and my colleagues.
Three years ago, I helped adopt a sustainable plant-forward menu for our physician meetings, complete with a recipe from the menu for physicians to replicate at home or give to their patients.
I also pursued adoption of shared medical appointments for our medical group. These appointments apply the “see one, do one, teach one” model in medicine, but with culinary medicine as the focus.
Knowing that my patients are all connected to their families through food, I sought this as an opportunity to dive in further with wellness opportunities at their next meal. After almost 2 years of working on this project, I was able to host my first shared medical appointment with a group of patients on March 12, 2020. The next day schools closed, lockdowns occurred, and the world changed.
Opportunities highlighted by the pandemic
We always knew health care was broken but adding the increasingly longer hours and COVID vaccine–hesitant patients that the pandemic brought made everything look dark at times. What has helped me stay hopeful and energetic for system changes is feeling gratitude and seeking bright lights.
My experiences seeing patients in telehealth visits are examples of some of the bright lights I found in the pandemic. During these visits, patients showed me something from their pantry, and we’d go over nutritional labels together.
Additionally, my patients became engaged with their own conditions and wanted to improve them because of news articles highlighting risk factors for COVID-19, such as obesity. I had an active audience when it came to talking about food-as-medicine approaches to improving risk factors and immunity. And since everyone was listening, I didn’t stop at food. I also talked about physical health, stress resiliency, planetary diets, sleep, connections, and lastly vaccines!
Once the vaccines were distributed, I naturally gravitated to having those conversations with patients and colleagues and on social media. Plus, the pandemic gave us moments of simple times to slow down, take more rests, be less overscheduled, consider work-life priorities, and, lastly, to be okay with not being totally okay.
In practicing primary care, we have a unique role in seeing medicine from a whole body, whole person, whole family perspective. There is an opportunity to highlight what is broken in medicine and aim to make it whole.
I’m currently looking at shared medical appointments as a new standard way to provide care to all patients, because it improves access, provides better quality visits and aligns my values, mission, and purpose.
In the midst of the pandemic, I helped advocate for a sustainable plant-forward menu that was launched throughout four different hospitals in the Sharp HealthCare system, in California, in 2020. Knowing that patients were served a menu I played a role in, gave me solace.
As part of the hospital food and nutrition team, I am grateful for the opportunity I have to work on a broader mission to address social determinants of health and seek opportunities to help the system work for our patients.
Public health communication has been lacking in the pandemic, but another bright light is that we were still the trusted messengers to our patients and our communities. I’m continually honored and humbled to be trusted with a whole family’s health.
Dr. Neison practices family medicine and culinary medicine at Sharp Rees-Stealy Medical Group in San Diego, and is cochair of climate and planetary health for SRS Medical Group. You can follow her on Instagram, LinkedIn, and Facebook @Flavors4WellnessMD.
A few years ago I tracked down my medical school interviewer to thank him for giving me the opportunity to do what I felt I was called to do. I was surprised that, after 15 years, he actually remembered me and remembered details like walking to the courtyard to meet my father who’d driven me to the interview.
Sharing my gratitude and letting him know I was happy felt important to me.
Choosing to practice family medicine has a lot to do with why I am happy in my career today.
One of my frustrations with health care had been its emphasis on treatment of sickness, rather than a broader one that incorporated prevention of sickness. During my third year of medical school, I was following a family and sports medicine faculty member who was focusing on aspects of lifestyle medicine to help a patient remain active and age gracefully. Seeing opportunities to practice preventative medicine in family medicine made me realize the specialty was the perfect fit for me.
Food as medicine
While participating in rotations I also realized you can find a subspecialty within family medicine.
During my fourth year of medical school, I followed an attending who was seeing a patient for hypertension, prediabetes and hypercholesterolemia. The attending told the patient to eat “healthier,” gave her a handout, and scheduled a follow up appointment for 6 months later.
My thoughts were: “That’s it? That’s how we counsel patients to improve their dietary habits?”
As the patient was leaving the exam room, I asked her what type of oil she cooked with, and I proceeded to share culinary tips from my mother – who was a self-taught and early adopter of the food-as-medicine movement.
Once I started my residency, I knew I’d want to incorporate lifestyle and dietary approaches at many of my patient visits.
I scheduled patients every month to monitor their weight, follow up on chronic conditions, but more importantly, to engage them in their health and empower them to make small lifestyle changes each month and report their efforts. I felt like I was their health coach and cheerleader.
My career in family medicine
Entering the job market allowed me to form my philosophy of treating patients with a mind, body, and spirit approach. I chose to practice value-based care, which aligns with my lifestyle and preventative medicine approach .
I currently practice in a small family medicine–only clinic that is part of a larger multispecialty system. Primary care specialties in my organization are valued, respected and central to a patient’s well being and care. We are encouraged to spend time with patients, assess barriers to care and work collaboratively with our healthcare team, so that preventative medicine approaches take the lead in a patient’s health. This supportive culture and environment is one where my passion for food as medicine has thrived.
One day I forgot to pack a lunch and instead brought a grocery bag of items to make a salad. When I realized I made too much, I sent an email to my staff to get some “free salad in my office.” This serendipitous moment started an informal office “salad club” each week. Continued support from my staff and leadership, allowed me to consider further extending this teaching to my patients and my colleagues.
Three years ago, I helped adopt a sustainable plant-forward menu for our physician meetings, complete with a recipe from the menu for physicians to replicate at home or give to their patients.
I also pursued adoption of shared medical appointments for our medical group. These appointments apply the “see one, do one, teach one” model in medicine, but with culinary medicine as the focus.
Knowing that my patients are all connected to their families through food, I sought this as an opportunity to dive in further with wellness opportunities at their next meal. After almost 2 years of working on this project, I was able to host my first shared medical appointment with a group of patients on March 12, 2020. The next day schools closed, lockdowns occurred, and the world changed.
Opportunities highlighted by the pandemic
We always knew health care was broken but adding the increasingly longer hours and COVID vaccine–hesitant patients that the pandemic brought made everything look dark at times. What has helped me stay hopeful and energetic for system changes is feeling gratitude and seeking bright lights.
My experiences seeing patients in telehealth visits are examples of some of the bright lights I found in the pandemic. During these visits, patients showed me something from their pantry, and we’d go over nutritional labels together.
Additionally, my patients became engaged with their own conditions and wanted to improve them because of news articles highlighting risk factors for COVID-19, such as obesity. I had an active audience when it came to talking about food-as-medicine approaches to improving risk factors and immunity. And since everyone was listening, I didn’t stop at food. I also talked about physical health, stress resiliency, planetary diets, sleep, connections, and lastly vaccines!
Once the vaccines were distributed, I naturally gravitated to having those conversations with patients and colleagues and on social media. Plus, the pandemic gave us moments of simple times to slow down, take more rests, be less overscheduled, consider work-life priorities, and, lastly, to be okay with not being totally okay.
In practicing primary care, we have a unique role in seeing medicine from a whole body, whole person, whole family perspective. There is an opportunity to highlight what is broken in medicine and aim to make it whole.
I’m currently looking at shared medical appointments as a new standard way to provide care to all patients, because it improves access, provides better quality visits and aligns my values, mission, and purpose.
In the midst of the pandemic, I helped advocate for a sustainable plant-forward menu that was launched throughout four different hospitals in the Sharp HealthCare system, in California, in 2020. Knowing that patients were served a menu I played a role in, gave me solace.
As part of the hospital food and nutrition team, I am grateful for the opportunity I have to work on a broader mission to address social determinants of health and seek opportunities to help the system work for our patients.
Public health communication has been lacking in the pandemic, but another bright light is that we were still the trusted messengers to our patients and our communities. I’m continually honored and humbled to be trusted with a whole family’s health.
Dr. Neison practices family medicine and culinary medicine at Sharp Rees-Stealy Medical Group in San Diego, and is cochair of climate and planetary health for SRS Medical Group. You can follow her on Instagram, LinkedIn, and Facebook @Flavors4WellnessMD.
Itching at night
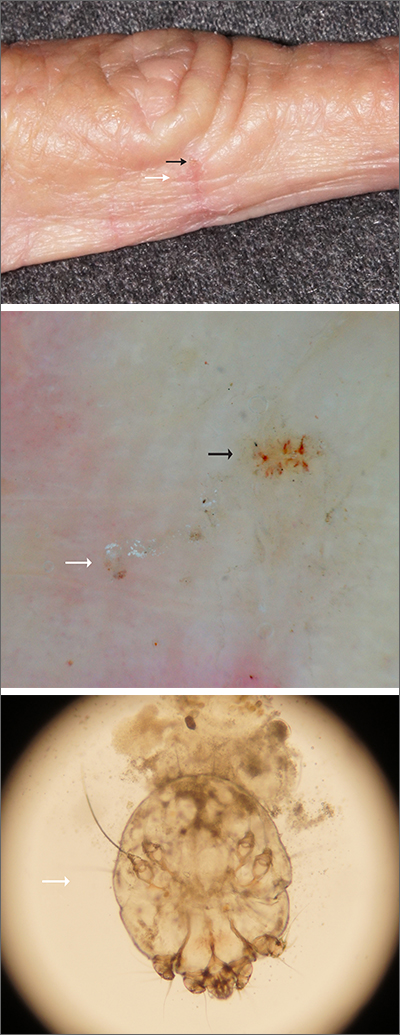
Microscopic evaluation of a dermoscopy-guided skin scraping revealed that this was a case of scabies.
Classically, patients with scabies have many excoriated papules or plaques on their hands, genitals, and trunk with itching so intense that their sleep is interrupted. However, scabies can also be diagnosed in patients who complain of itching but also have very subtle skin findings, such as a small dry patch or fissure (as in this case). Such subtle findings can be easily mistaken for mild hand dermatitis.
In the elderly, itching without a significant rash can arise from many causes. A short list includes dry skin, medications, kidney disease, liver disease, and of course, various dermatologic conditions. Dermoscopy is a sensitive and specific tool for investigating itching and areas of suspected infestation with mites.1 A mite appears as an oval on dermoscopy, but the most recognizable part is the head and front legs, which appear as a single gray triangle. The photo shows that the most erythematous area around a burrow (black arrows) is an excellent place to start when looking through the dermatoscope. In this case, an area of broken skin was connected to a haphazard tunnel that ultimately led to the mite (white arrows).
Scabies may be effectively treated with topical permethrin 5% applied over every inch of the body from the top of the neck to the tips of the toes.
This topical treatment is left on for at least 8 hours and reapplied a week later. Also, remember to take a careful history of close contacts so that others who are affected may receive treatment.
This patient was treated with permethrin, as was her adult son who lived at home with her and had similar itching. Permethrin comes in 60 g tubes, which is enough to treat 1 adult twice. After 6 weeks, all itching symptoms in the patient had cleared.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
1. Dupuy A, Dehen L, Bourrat E, et al. Accuracy of standard dermoscopy for diagnosing scabies. J Am Acad Dermatol. 2007;56:53-62. doi: 10.1016/j.jaad.2006.07.025
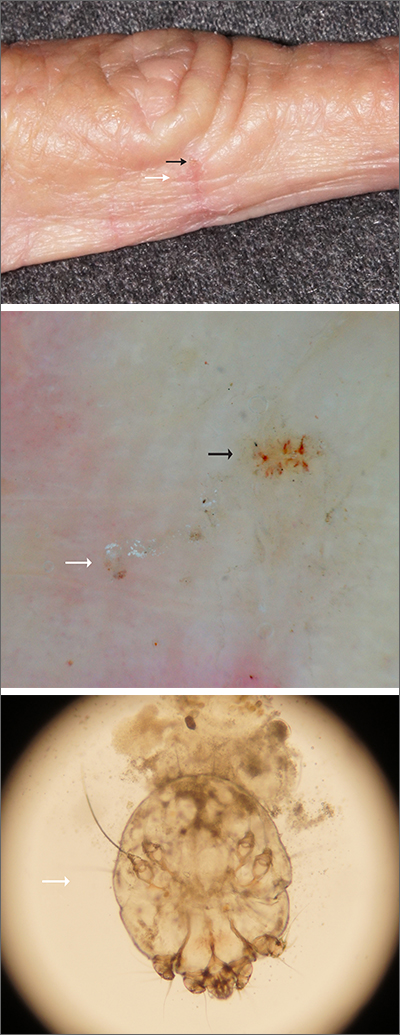
Microscopic evaluation of a dermoscopy-guided skin scraping revealed that this was a case of scabies.
Classically, patients with scabies have many excoriated papules or plaques on their hands, genitals, and trunk with itching so intense that their sleep is interrupted. However, scabies can also be diagnosed in patients who complain of itching but also have very subtle skin findings, such as a small dry patch or fissure (as in this case). Such subtle findings can be easily mistaken for mild hand dermatitis.
In the elderly, itching without a significant rash can arise from many causes. A short list includes dry skin, medications, kidney disease, liver disease, and of course, various dermatologic conditions. Dermoscopy is a sensitive and specific tool for investigating itching and areas of suspected infestation with mites.1 A mite appears as an oval on dermoscopy, but the most recognizable part is the head and front legs, which appear as a single gray triangle. The photo shows that the most erythematous area around a burrow (black arrows) is an excellent place to start when looking through the dermatoscope. In this case, an area of broken skin was connected to a haphazard tunnel that ultimately led to the mite (white arrows).
Scabies may be effectively treated with topical permethrin 5% applied over every inch of the body from the top of the neck to the tips of the toes.
This topical treatment is left on for at least 8 hours and reapplied a week later. Also, remember to take a careful history of close contacts so that others who are affected may receive treatment.
This patient was treated with permethrin, as was her adult son who lived at home with her and had similar itching. Permethrin comes in 60 g tubes, which is enough to treat 1 adult twice. After 6 weeks, all itching symptoms in the patient had cleared.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
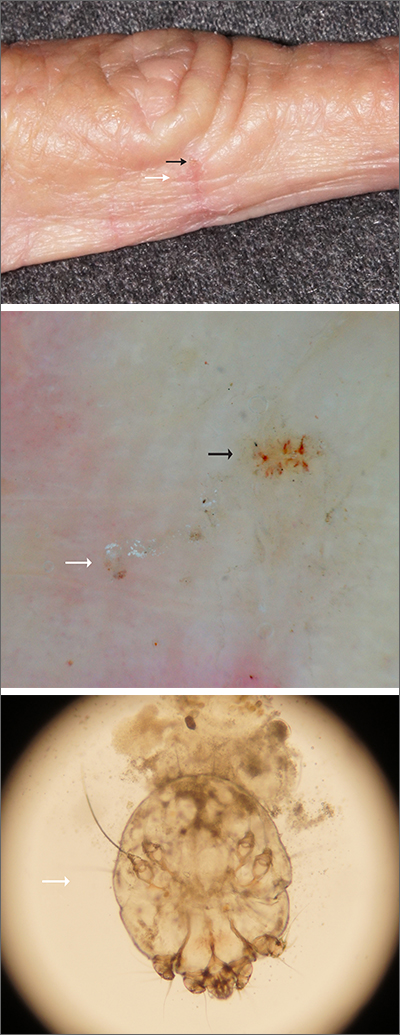
Microscopic evaluation of a dermoscopy-guided skin scraping revealed that this was a case of scabies.
Classically, patients with scabies have many excoriated papules or plaques on their hands, genitals, and trunk with itching so intense that their sleep is interrupted. However, scabies can also be diagnosed in patients who complain of itching but also have very subtle skin findings, such as a small dry patch or fissure (as in this case). Such subtle findings can be easily mistaken for mild hand dermatitis.
In the elderly, itching without a significant rash can arise from many causes. A short list includes dry skin, medications, kidney disease, liver disease, and of course, various dermatologic conditions. Dermoscopy is a sensitive and specific tool for investigating itching and areas of suspected infestation with mites.1 A mite appears as an oval on dermoscopy, but the most recognizable part is the head and front legs, which appear as a single gray triangle. The photo shows that the most erythematous area around a burrow (black arrows) is an excellent place to start when looking through the dermatoscope. In this case, an area of broken skin was connected to a haphazard tunnel that ultimately led to the mite (white arrows).
Scabies may be effectively treated with topical permethrin 5% applied over every inch of the body from the top of the neck to the tips of the toes.
This topical treatment is left on for at least 8 hours and reapplied a week later. Also, remember to take a careful history of close contacts so that others who are affected may receive treatment.
This patient was treated with permethrin, as was her adult son who lived at home with her and had similar itching. Permethrin comes in 60 g tubes, which is enough to treat 1 adult twice. After 6 weeks, all itching symptoms in the patient had cleared.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
1. Dupuy A, Dehen L, Bourrat E, et al. Accuracy of standard dermoscopy for diagnosing scabies. J Am Acad Dermatol. 2007;56:53-62. doi: 10.1016/j.jaad.2006.07.025
1. Dupuy A, Dehen L, Bourrat E, et al. Accuracy of standard dermoscopy for diagnosing scabies. J Am Acad Dermatol. 2007;56:53-62. doi: 10.1016/j.jaad.2006.07.025
Omicron breakthrough cases boost protection, studies say
two preprint studies show.
The University of Washington, Seattle, working with Vir Biotechnology of San Francisco, looked at blood samples of vaccinated people who had breakthrough cases of Delta or Omicron and compared the samples with three other groups: people who caught COVID and were later vaccinated, vaccinated people who were never infected, and people who were infected and never vaccinated.
The vaccinated people who had a breakthrough case of Omicron produced antibodies that helped protect against coronavirus variants, whereas unvaccinated people who caught Omicron didn’t produce as many antibodies, the study showed.
BioNTech, the German biotechnology company, found that people who’d been double and triple vaccinated and then became infected with Omicron had a better B-cell response than people who’d gotten a booster shot but had not been infected.
The University of Washington research team also came up with similar findings about B cells.
The findings don’t mean people should deliberately try to become infected with COVID, said Alexandra Walls, PhD, one of the University of Washington scientists, according to Business Standard.
But the study does indicate “that we are at the point where we may want to consider having a different vaccine to boost people,” said David Veesler, PhD, of the University of Washington team.
“We should think about breakthrough infections as essentially equivalent to another dose of vaccine,” John Wherry, PhD, a professor and director of the Institute for Immunology at the University of Pennsylvania, Philadelphia, told Business Standard. Dr. Wherry was not involved in the studies but reviewed the BioNTech study.
A version of this article first appeared on WebMD.com.
two preprint studies show.
The University of Washington, Seattle, working with Vir Biotechnology of San Francisco, looked at blood samples of vaccinated people who had breakthrough cases of Delta or Omicron and compared the samples with three other groups: people who caught COVID and were later vaccinated, vaccinated people who were never infected, and people who were infected and never vaccinated.
The vaccinated people who had a breakthrough case of Omicron produced antibodies that helped protect against coronavirus variants, whereas unvaccinated people who caught Omicron didn’t produce as many antibodies, the study showed.
BioNTech, the German biotechnology company, found that people who’d been double and triple vaccinated and then became infected with Omicron had a better B-cell response than people who’d gotten a booster shot but had not been infected.
The University of Washington research team also came up with similar findings about B cells.
The findings don’t mean people should deliberately try to become infected with COVID, said Alexandra Walls, PhD, one of the University of Washington scientists, according to Business Standard.
But the study does indicate “that we are at the point where we may want to consider having a different vaccine to boost people,” said David Veesler, PhD, of the University of Washington team.
“We should think about breakthrough infections as essentially equivalent to another dose of vaccine,” John Wherry, PhD, a professor and director of the Institute for Immunology at the University of Pennsylvania, Philadelphia, told Business Standard. Dr. Wherry was not involved in the studies but reviewed the BioNTech study.
A version of this article first appeared on WebMD.com.
two preprint studies show.
The University of Washington, Seattle, working with Vir Biotechnology of San Francisco, looked at blood samples of vaccinated people who had breakthrough cases of Delta or Omicron and compared the samples with three other groups: people who caught COVID and were later vaccinated, vaccinated people who were never infected, and people who were infected and never vaccinated.
The vaccinated people who had a breakthrough case of Omicron produced antibodies that helped protect against coronavirus variants, whereas unvaccinated people who caught Omicron didn’t produce as many antibodies, the study showed.
BioNTech, the German biotechnology company, found that people who’d been double and triple vaccinated and then became infected with Omicron had a better B-cell response than people who’d gotten a booster shot but had not been infected.
The University of Washington research team also came up with similar findings about B cells.
The findings don’t mean people should deliberately try to become infected with COVID, said Alexandra Walls, PhD, one of the University of Washington scientists, according to Business Standard.
But the study does indicate “that we are at the point where we may want to consider having a different vaccine to boost people,” said David Veesler, PhD, of the University of Washington team.
“We should think about breakthrough infections as essentially equivalent to another dose of vaccine,” John Wherry, PhD, a professor and director of the Institute for Immunology at the University of Pennsylvania, Philadelphia, told Business Standard. Dr. Wherry was not involved in the studies but reviewed the BioNTech study.
A version of this article first appeared on WebMD.com.
Spell it out: Writing out common medical terms boosts patient understanding, says study
MI. HTN. hx. Although these abbreviations might make it easier for physicians and other health care professionals to create and consume clinical documentation, the shorthand confuses patients, according to a study published in JAMA Network Open.
Researchers, who conducted clinical trials at three hospitals, found that expansion of 10 common medical abbreviations and acronyms in patient health records significantly increased overall comprehension.
Corresponding author Lisa Grossman Liu, PhD, MD, of Columbia University, New York, told this news organization that “comprehension of abbreviations was much lower than we expected and much lower than the clinicians who participated in this study expected.”
This discovery is particularly relevant in this era of digital care, where providers are now communicating with patients electronically more than ever before – and are required by rules emanating from the 21st Century Cures Act to provide online access to electronic health records.
Using elongated terms
Although the study found that expansion of medical abbreviations and acronyms can improve patient understanding, identifying all of the medical abbreviations that exist is difficult because the terms vary by specialty and geography. The fact that many abbreviations and acronyms have multiple meanings complicates matters even more. For example, the abbreviation PA has 128 possible meanings, Dr. Grossman Liu pointed out.
Technology, fortunately, has advanced in the last few years and is on the cusp of providing a solution. Artificial intelligence systems could help to develop large compendiums of abbreviations and acronyms and then machine learning could elongate the words.
“We’re almost to the point where we have these automated systems that can actually expand abbreviations pretty well and with a great degree of accuracy and ... where those can actually be used in medicine to help with patient communication,” Dr. Grossman Liu said.
Such intervention, however, is not a cure-all.
“There are abbreviations that are really hard to understand even after you expand them, such as MI for myocardial infarction, which is really a tough term all around. It means heart attack. So even if you tell patients, MI means myocardial infarction, they’re still not going to understand it,” Dr. Grossman Liu said.
On the flip side, patients are likely to understand some abbreviations such as hrs, which stands for hours, without elongating the words.
Moving from in-person to online communication
A look at the evolution of clinical documentation explains how this abbreviation problem came to fruition. Prior to this digital age where providers communicate with patients through portals, secure messaging, and other electronic methods, patients and providers would talk face to face. Now, however, electronic written communication is becoming the norm.
“We are not only seeing direct written communication through things like messaging systems or email, but also patients are now reading their medical records online and you can consider that as a form of communication,” Dr. Grossman Liu said. “It’s really interesting that the electronic health record itself has essentially become a medium for communication between patients and providers when previously it was only a way for providers to communicate with themselves and document patient care. So, clinicians use abbreviations because they aren’t intending for patients to see the records.”
Requiring physicians to use complete words in clinical documentation now that electronic records are relied on for patient communication, however, is not a practical solution.
“Abbreviations are so commonly used because they are more efficient to read and more efficient to write. We really shouldn’t be putting the onus on providers to spell out all the abbreviations in their notes. That’s realistically not going to work, because it compromises clinical efficiency,” Dr. Grossman Liu said.
While physicians should not be forced to use complete words in documentation, they should be wary of patients’ unfamiliarity with abbreviations as they communicate in person.
“I use terms like ED constantly when I talk to patients, and it turns out that only 67% of patients understand what you’re talking about when you say ED in reference to the emergency department. So it’s important to be mindful of that,” Dr. Grossman Liu concluded.
A version of this article first appeared on Medscape.com.
MI. HTN. hx. Although these abbreviations might make it easier for physicians and other health care professionals to create and consume clinical documentation, the shorthand confuses patients, according to a study published in JAMA Network Open.
Researchers, who conducted clinical trials at three hospitals, found that expansion of 10 common medical abbreviations and acronyms in patient health records significantly increased overall comprehension.
Corresponding author Lisa Grossman Liu, PhD, MD, of Columbia University, New York, told this news organization that “comprehension of abbreviations was much lower than we expected and much lower than the clinicians who participated in this study expected.”
This discovery is particularly relevant in this era of digital care, where providers are now communicating with patients electronically more than ever before – and are required by rules emanating from the 21st Century Cures Act to provide online access to electronic health records.
Using elongated terms
Although the study found that expansion of medical abbreviations and acronyms can improve patient understanding, identifying all of the medical abbreviations that exist is difficult because the terms vary by specialty and geography. The fact that many abbreviations and acronyms have multiple meanings complicates matters even more. For example, the abbreviation PA has 128 possible meanings, Dr. Grossman Liu pointed out.
Technology, fortunately, has advanced in the last few years and is on the cusp of providing a solution. Artificial intelligence systems could help to develop large compendiums of abbreviations and acronyms and then machine learning could elongate the words.
“We’re almost to the point where we have these automated systems that can actually expand abbreviations pretty well and with a great degree of accuracy and ... where those can actually be used in medicine to help with patient communication,” Dr. Grossman Liu said.
Such intervention, however, is not a cure-all.
“There are abbreviations that are really hard to understand even after you expand them, such as MI for myocardial infarction, which is really a tough term all around. It means heart attack. So even if you tell patients, MI means myocardial infarction, they’re still not going to understand it,” Dr. Grossman Liu said.
On the flip side, patients are likely to understand some abbreviations such as hrs, which stands for hours, without elongating the words.
Moving from in-person to online communication
A look at the evolution of clinical documentation explains how this abbreviation problem came to fruition. Prior to this digital age where providers communicate with patients through portals, secure messaging, and other electronic methods, patients and providers would talk face to face. Now, however, electronic written communication is becoming the norm.
“We are not only seeing direct written communication through things like messaging systems or email, but also patients are now reading their medical records online and you can consider that as a form of communication,” Dr. Grossman Liu said. “It’s really interesting that the electronic health record itself has essentially become a medium for communication between patients and providers when previously it was only a way for providers to communicate with themselves and document patient care. So, clinicians use abbreviations because they aren’t intending for patients to see the records.”
Requiring physicians to use complete words in clinical documentation now that electronic records are relied on for patient communication, however, is not a practical solution.
“Abbreviations are so commonly used because they are more efficient to read and more efficient to write. We really shouldn’t be putting the onus on providers to spell out all the abbreviations in their notes. That’s realistically not going to work, because it compromises clinical efficiency,” Dr. Grossman Liu said.
While physicians should not be forced to use complete words in documentation, they should be wary of patients’ unfamiliarity with abbreviations as they communicate in person.
“I use terms like ED constantly when I talk to patients, and it turns out that only 67% of patients understand what you’re talking about when you say ED in reference to the emergency department. So it’s important to be mindful of that,” Dr. Grossman Liu concluded.
A version of this article first appeared on Medscape.com.
MI. HTN. hx. Although these abbreviations might make it easier for physicians and other health care professionals to create and consume clinical documentation, the shorthand confuses patients, according to a study published in JAMA Network Open.
Researchers, who conducted clinical trials at three hospitals, found that expansion of 10 common medical abbreviations and acronyms in patient health records significantly increased overall comprehension.
Corresponding author Lisa Grossman Liu, PhD, MD, of Columbia University, New York, told this news organization that “comprehension of abbreviations was much lower than we expected and much lower than the clinicians who participated in this study expected.”
This discovery is particularly relevant in this era of digital care, where providers are now communicating with patients electronically more than ever before – and are required by rules emanating from the 21st Century Cures Act to provide online access to electronic health records.
Using elongated terms
Although the study found that expansion of medical abbreviations and acronyms can improve patient understanding, identifying all of the medical abbreviations that exist is difficult because the terms vary by specialty and geography. The fact that many abbreviations and acronyms have multiple meanings complicates matters even more. For example, the abbreviation PA has 128 possible meanings, Dr. Grossman Liu pointed out.
Technology, fortunately, has advanced in the last few years and is on the cusp of providing a solution. Artificial intelligence systems could help to develop large compendiums of abbreviations and acronyms and then machine learning could elongate the words.
“We’re almost to the point where we have these automated systems that can actually expand abbreviations pretty well and with a great degree of accuracy and ... where those can actually be used in medicine to help with patient communication,” Dr. Grossman Liu said.
Such intervention, however, is not a cure-all.
“There are abbreviations that are really hard to understand even after you expand them, such as MI for myocardial infarction, which is really a tough term all around. It means heart attack. So even if you tell patients, MI means myocardial infarction, they’re still not going to understand it,” Dr. Grossman Liu said.
On the flip side, patients are likely to understand some abbreviations such as hrs, which stands for hours, without elongating the words.
Moving from in-person to online communication
A look at the evolution of clinical documentation explains how this abbreviation problem came to fruition. Prior to this digital age where providers communicate with patients through portals, secure messaging, and other electronic methods, patients and providers would talk face to face. Now, however, electronic written communication is becoming the norm.
“We are not only seeing direct written communication through things like messaging systems or email, but also patients are now reading their medical records online and you can consider that as a form of communication,” Dr. Grossman Liu said. “It’s really interesting that the electronic health record itself has essentially become a medium for communication between patients and providers when previously it was only a way for providers to communicate with themselves and document patient care. So, clinicians use abbreviations because they aren’t intending for patients to see the records.”
Requiring physicians to use complete words in clinical documentation now that electronic records are relied on for patient communication, however, is not a practical solution.
“Abbreviations are so commonly used because they are more efficient to read and more efficient to write. We really shouldn’t be putting the onus on providers to spell out all the abbreviations in their notes. That’s realistically not going to work, because it compromises clinical efficiency,” Dr. Grossman Liu said.
While physicians should not be forced to use complete words in documentation, they should be wary of patients’ unfamiliarity with abbreviations as they communicate in person.
“I use terms like ED constantly when I talk to patients, and it turns out that only 67% of patients understand what you’re talking about when you say ED in reference to the emergency department. So it’s important to be mindful of that,” Dr. Grossman Liu concluded.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Fewer than half of preschool care programs meet activity guidelines
Only 43% of early child care programs in the United States met guidelines for both sufficient opportunities outdoors and 60-90 minutes of physical activity daily, according to researchers.
To date, no national study has examined these factors, according to Maria H. Boyle, MS, RD, with Abt Associates in Cambridge, Mass., and colleagues. They conducted the study published online in Pediatrics.
The results came “even employing a relatively lenient interpretation of the guidance,” the authors noted, and have particular significance because about 60% of preschool children in the United States are enrolled in center-based care.
Nearly three-fourths of the programs (74%) met the outdoor-opportunities guideline, but only 50% met the physical activity guideline.
Caring for Our Children (CFOC) guidance from the American Academy of Pediatrics recommends at least two outdoor physical activity opportunities (weather permitting) and at least 60-90 minutes allotted for moderate and vigorous physical activities each day during care for children aged 1-6 years.
Still, “children are frequently observed to be sedentary or inactive when in child care settings,” the authors wrote.
They found that some of the main barriers included weather and staff not joining outdoor play.
The researchers used the Study of Nutrition and Activity in Child Care Settings (SNACS), which assesses opportunities for physical activity opportunities and sedentary occasions for children aged 1-5 years at programs participating in the U.S. Department of Agriculture Child and Adult Care Food Program.
Their sample included 227 classrooms: 96 in child care centers and 131 in Head Start programs.
On 1 day (from February to July 2017) an observer in each sampled classroom recorded whether there were designated outdoor and indoor spaces for physical activity, whether that was a playground or other outdoor play space, such as a field, grassy area, or other open area, or parking lot used for play.
They looked for a separate indoor room or gym for active play and how many minutes the class spent in these spaces, and whether there were physical activity facilitators. They made note of barriers, including weather that was too hot or too cold or involved precipitation.
The data show that while almost all programs observed (97%) had dedicated outdoor play space, only 34% had a separate dedicated indoor play space – a gym, for example, or another room separate from main classrooms.
“Of those without a separate indoor play space, virtually all (99.8%) indicated a classroom was available for indoor play.”
Weather and staff not participating in play are barriers
After adjustment for program characteristics, weather barriers resulted in an average 74 fewer minutes daily allotted to physical activity (P < .001).
Another large barrier was staff not participating in play. That was associated with 31 fewer minutes per day allotted for physical activity (P < .001).
“Given the critical role of child care staff as gatekeepers in allowing and encouraging physical activity, it is as important to measure sedentary time when children are not permitted to be active as to measure time when they have opportunity to be active,” the authors wrote. “Best practice guidelines emphasize limiting time children are expected to stay seated during care.”
William Roberts, MD, professor in the department of family medicine and community health at the University of Minnesota in Minneapolis, said in an interview that the findings in this paper help quantify a public health concern as inactivity early sets a harmful precedent.
“Inactive kids too often become inactive adults subject to the long list of noncommunicable chronic diseases associated with lack of regular exercise,” he said.
Lack of movement in childhood, in a program setting or at home, contributes to the obesity epidemic, he pointed out.
“They also do not develop the motor and social skills associated with free play and physical activity,” he said.
He said the findings in this study can guide questions when choosing a child care program. He noted that parents should ask: “What are the opportunities for free play and physical activity?”
The authors and Dr. Roberts declared no relevant financial relationships.
Only 43% of early child care programs in the United States met guidelines for both sufficient opportunities outdoors and 60-90 minutes of physical activity daily, according to researchers.
To date, no national study has examined these factors, according to Maria H. Boyle, MS, RD, with Abt Associates in Cambridge, Mass., and colleagues. They conducted the study published online in Pediatrics.
The results came “even employing a relatively lenient interpretation of the guidance,” the authors noted, and have particular significance because about 60% of preschool children in the United States are enrolled in center-based care.
Nearly three-fourths of the programs (74%) met the outdoor-opportunities guideline, but only 50% met the physical activity guideline.
Caring for Our Children (CFOC) guidance from the American Academy of Pediatrics recommends at least two outdoor physical activity opportunities (weather permitting) and at least 60-90 minutes allotted for moderate and vigorous physical activities each day during care for children aged 1-6 years.
Still, “children are frequently observed to be sedentary or inactive when in child care settings,” the authors wrote.
They found that some of the main barriers included weather and staff not joining outdoor play.
The researchers used the Study of Nutrition and Activity in Child Care Settings (SNACS), which assesses opportunities for physical activity opportunities and sedentary occasions for children aged 1-5 years at programs participating in the U.S. Department of Agriculture Child and Adult Care Food Program.
Their sample included 227 classrooms: 96 in child care centers and 131 in Head Start programs.
On 1 day (from February to July 2017) an observer in each sampled classroom recorded whether there were designated outdoor and indoor spaces for physical activity, whether that was a playground or other outdoor play space, such as a field, grassy area, or other open area, or parking lot used for play.
They looked for a separate indoor room or gym for active play and how many minutes the class spent in these spaces, and whether there were physical activity facilitators. They made note of barriers, including weather that was too hot or too cold or involved precipitation.
The data show that while almost all programs observed (97%) had dedicated outdoor play space, only 34% had a separate dedicated indoor play space – a gym, for example, or another room separate from main classrooms.
“Of those without a separate indoor play space, virtually all (99.8%) indicated a classroom was available for indoor play.”
Weather and staff not participating in play are barriers
After adjustment for program characteristics, weather barriers resulted in an average 74 fewer minutes daily allotted to physical activity (P < .001).
Another large barrier was staff not participating in play. That was associated with 31 fewer minutes per day allotted for physical activity (P < .001).
“Given the critical role of child care staff as gatekeepers in allowing and encouraging physical activity, it is as important to measure sedentary time when children are not permitted to be active as to measure time when they have opportunity to be active,” the authors wrote. “Best practice guidelines emphasize limiting time children are expected to stay seated during care.”
William Roberts, MD, professor in the department of family medicine and community health at the University of Minnesota in Minneapolis, said in an interview that the findings in this paper help quantify a public health concern as inactivity early sets a harmful precedent.
“Inactive kids too often become inactive adults subject to the long list of noncommunicable chronic diseases associated with lack of regular exercise,” he said.
Lack of movement in childhood, in a program setting or at home, contributes to the obesity epidemic, he pointed out.
“They also do not develop the motor and social skills associated with free play and physical activity,” he said.
He said the findings in this study can guide questions when choosing a child care program. He noted that parents should ask: “What are the opportunities for free play and physical activity?”
The authors and Dr. Roberts declared no relevant financial relationships.
Only 43% of early child care programs in the United States met guidelines for both sufficient opportunities outdoors and 60-90 minutes of physical activity daily, according to researchers.
To date, no national study has examined these factors, according to Maria H. Boyle, MS, RD, with Abt Associates in Cambridge, Mass., and colleagues. They conducted the study published online in Pediatrics.
The results came “even employing a relatively lenient interpretation of the guidance,” the authors noted, and have particular significance because about 60% of preschool children in the United States are enrolled in center-based care.
Nearly three-fourths of the programs (74%) met the outdoor-opportunities guideline, but only 50% met the physical activity guideline.
Caring for Our Children (CFOC) guidance from the American Academy of Pediatrics recommends at least two outdoor physical activity opportunities (weather permitting) and at least 60-90 minutes allotted for moderate and vigorous physical activities each day during care for children aged 1-6 years.
Still, “children are frequently observed to be sedentary or inactive when in child care settings,” the authors wrote.
They found that some of the main barriers included weather and staff not joining outdoor play.
The researchers used the Study of Nutrition and Activity in Child Care Settings (SNACS), which assesses opportunities for physical activity opportunities and sedentary occasions for children aged 1-5 years at programs participating in the U.S. Department of Agriculture Child and Adult Care Food Program.
Their sample included 227 classrooms: 96 in child care centers and 131 in Head Start programs.
On 1 day (from February to July 2017) an observer in each sampled classroom recorded whether there were designated outdoor and indoor spaces for physical activity, whether that was a playground or other outdoor play space, such as a field, grassy area, or other open area, or parking lot used for play.
They looked for a separate indoor room or gym for active play and how many minutes the class spent in these spaces, and whether there were physical activity facilitators. They made note of barriers, including weather that was too hot or too cold or involved precipitation.
The data show that while almost all programs observed (97%) had dedicated outdoor play space, only 34% had a separate dedicated indoor play space – a gym, for example, or another room separate from main classrooms.
“Of those without a separate indoor play space, virtually all (99.8%) indicated a classroom was available for indoor play.”
Weather and staff not participating in play are barriers
After adjustment for program characteristics, weather barriers resulted in an average 74 fewer minutes daily allotted to physical activity (P < .001).
Another large barrier was staff not participating in play. That was associated with 31 fewer minutes per day allotted for physical activity (P < .001).
“Given the critical role of child care staff as gatekeepers in allowing and encouraging physical activity, it is as important to measure sedentary time when children are not permitted to be active as to measure time when they have opportunity to be active,” the authors wrote. “Best practice guidelines emphasize limiting time children are expected to stay seated during care.”
William Roberts, MD, professor in the department of family medicine and community health at the University of Minnesota in Minneapolis, said in an interview that the findings in this paper help quantify a public health concern as inactivity early sets a harmful precedent.
“Inactive kids too often become inactive adults subject to the long list of noncommunicable chronic diseases associated with lack of regular exercise,” he said.
Lack of movement in childhood, in a program setting or at home, contributes to the obesity epidemic, he pointed out.
“They also do not develop the motor and social skills associated with free play and physical activity,” he said.
He said the findings in this study can guide questions when choosing a child care program. He noted that parents should ask: “What are the opportunities for free play and physical activity?”
The authors and Dr. Roberts declared no relevant financial relationships.
FROM PEDIATRICS