User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Psychological difficulties persist among patients with IBD
Psychological issues in patients with inflammatory bowel disease should be addressed at both personal and systemic levels, according to a review of current literature.
In a review published in the Journal of Clinical Gastroenterology, researchers highlighted data on the burden of mental disorders in inflammatory bowel disease (IBD) patients and presented several strategies for addressing them.
“From a systems perspective, underrecognized and/or suboptimally treated mental health problems in patients with IBD are associated with increased disability, poorer adherence, and more admissions and surgeries, driving increased health care utilization and costs,” Maia S. Kredentser, PhD, of the University of Manitoba, Winnipeg, and colleagues wrote, citing a 2018 study’s findings.
“There is ample evidence for a higher prevalence of mental disorders in IBD, in particular depression and anxiety, compared with the general population,” the authors wrote.
They cited a recent population-based study in which the incident rate ratios were significantly higher for IBD patients, compared with matched controls for depression (IRR, 1.58), anxiety disorder (IRR, 1.39), bipolar disorder (IRR, 1.82), and schizophrenia (IRR, 1.64).
Mental disorders associated with IBD also include issues of body image and sexuality. Although research on the impact of disease activity on sexual function is inconsistent, one study suggested that body image “may be an important target of treatment in women reporting poor quality of life and psychological distress,” the researchers noted. A French study from 2017 published in the Journal of Crohn’s and Colitis showed that approximately half of men and women reported problems with erectile or sexual dysfunction.
Issues related to environmental stressors may contribute to IBD by promoting chronic inflammation, the researchers wrote. For example, data from longitudinal, population-based research suggest that adverse childhood experiences can promote proinflammatory states across inflammatory illnesses. Research has also suggested that people with IBD have higher rates of these adverse childhood experiences than the general population. However, data also show that many are able to cope and adapt: “Many patients with IBD are resilient, experience growth, and in fact, thrive,” the researchers added. One longitudinal study suggested that patients with IBD who identified with “thriving” had “stronger coping efficacy (the perceived ability to meet illness demands), illness acceptance, and social support and lower depression” and that this was associated with life satisfaction 6 months later.
Fatigue also has been shown to be a factor for patients with IBD. The researchers cited one population-based study showing fatigue in 57%-72% of IBD patients with active disease. IBD patients with quiescent disease also report fatigue. The psychological and behavioral factors driving fatigue could be related to mental disorders or other factors such as suboptimal sleep, stress, and use of caffeine and alcohol, they noted. Management strategies include improving sleep hygiene and evaluation of mental health concerns.
Seek complete picture before treatment
“Addressing psychological comorbidity in IBD requires individual and systemic approaches focused on both the prevention and treatment of mental health concerns,” the researchers wrote. “Because of the pervasiveness of psychological comorbidities in IBD, and recent evidence that they may be part of the disease process itself, assessment of psychological functioning in IBD is considered an essential aspect of disease management.”
Evidence-based psychological interventions include cognitive-behavioral therapy, which includes training in relaxation; treatment with clinical hypnosis; and encouraging mindfulness through acceptance and commitment therapy, which focuses on developing psychological flexibility to cope with suffering. In addition, a small but evolving body of research shows some benefit to motivational interviewing (a strategy focused on behavior change) for IBD patients. Notably, one review of four studies showed benefits of motivational interviewing for improving medication adherence and advice seeking, the researchers reported.
Although several psychological treatment options exist for addressing mental health issues in IBD, randomized trials are needed. “To facilitate this important research and optimize patient care, the integration of psychologists and other mental health providers into IBD care is considered best practice and provides exciting opportunities for improving patient care and outcomes,” the researchers concluded.
Address mental health to ease disease burden
“There is a large burden of mental health issues in patients with inflammatory bowel disease, with depression and anxiety leading the way,” Kim L. Isaacs, MD, of the University of North Carolina at Chapel Hill, said in an interview.
“There are multiple reasons for this, including dealing with chronic pain, social concerns around using the bathroom, body-image issues due to surgery, and drug side effects. There is increasing evidence that the inflammatory process in IBD may be driving some of the changes in the brain which lead to further mental health dysfunction,” she noted.
“Addressing depression, anxiety, [and] sleep disturbance in patients will not only improve quality of life from a mental health perspective but has been shown to improve control of disease,” Dr. Isaacs emphasized.
“Small things like increased medication compliance have a large impact on disease management and decreased need for hospitalization and hospitalization,” said Dr. Isaacs. “As gastroenterologists we need to expand our focus beyond the gut and address the emotional needs of our patients – identifying those patients who need increased mental health support.”
Barriers to better care
The greatest barriers to treating mental health issues in IBD patients are time and knowledge, said Dr. Isaacs. “Many gastroenterologists have limited time in the office to do more than address the acute issues of the patients such as rectal bleeding and worsening diarrhea. It takes time and trust to explore what is going on in a patient’s life. Is the patient anxious and depressed? How are they coping with their current disease manifestations? Simple screening tools may help with this, but then there need to be resources to support interventions.”
Some IBD practices, especially academic ones, have a psychologist in the IBD center or one that’s readily available for consultation. “This is an investment for the practice that may reduce significantly disease burden. The IBD specialty home model includes resources for management of psychiatric issues and nutritional concerns as well as disease management,” she added.
More research in several areas can help reduce the mental health burden of IBD. “On the immunology/biology side, understanding how the microbiome affects the brain/gut may allow for more directed mental health treatment. On the disease management side, larger trials directed at psychiatric interventions may help to determine which therapy is best for each patient,” Dr. Isaacs said. “Further work developing health care systems, such as the medical home, that allow for maximum disease management and decreased system costs will go far in implementation of models of care that address the needs of the entire patient with inflammatory bowel disease.”
The review received no outside funding. The researchers had no financial conflicts to disclose. Dr. Isaacs disclosed consulting on the data safety monitoring board for Janssen.
Psychological issues in patients with inflammatory bowel disease should be addressed at both personal and systemic levels, according to a review of current literature.
In a review published in the Journal of Clinical Gastroenterology, researchers highlighted data on the burden of mental disorders in inflammatory bowel disease (IBD) patients and presented several strategies for addressing them.
“From a systems perspective, underrecognized and/or suboptimally treated mental health problems in patients with IBD are associated with increased disability, poorer adherence, and more admissions and surgeries, driving increased health care utilization and costs,” Maia S. Kredentser, PhD, of the University of Manitoba, Winnipeg, and colleagues wrote, citing a 2018 study’s findings.
“There is ample evidence for a higher prevalence of mental disorders in IBD, in particular depression and anxiety, compared with the general population,” the authors wrote.
They cited a recent population-based study in which the incident rate ratios were significantly higher for IBD patients, compared with matched controls for depression (IRR, 1.58), anxiety disorder (IRR, 1.39), bipolar disorder (IRR, 1.82), and schizophrenia (IRR, 1.64).
Mental disorders associated with IBD also include issues of body image and sexuality. Although research on the impact of disease activity on sexual function is inconsistent, one study suggested that body image “may be an important target of treatment in women reporting poor quality of life and psychological distress,” the researchers noted. A French study from 2017 published in the Journal of Crohn’s and Colitis showed that approximately half of men and women reported problems with erectile or sexual dysfunction.
Issues related to environmental stressors may contribute to IBD by promoting chronic inflammation, the researchers wrote. For example, data from longitudinal, population-based research suggest that adverse childhood experiences can promote proinflammatory states across inflammatory illnesses. Research has also suggested that people with IBD have higher rates of these adverse childhood experiences than the general population. However, data also show that many are able to cope and adapt: “Many patients with IBD are resilient, experience growth, and in fact, thrive,” the researchers added. One longitudinal study suggested that patients with IBD who identified with “thriving” had “stronger coping efficacy (the perceived ability to meet illness demands), illness acceptance, and social support and lower depression” and that this was associated with life satisfaction 6 months later.
Fatigue also has been shown to be a factor for patients with IBD. The researchers cited one population-based study showing fatigue in 57%-72% of IBD patients with active disease. IBD patients with quiescent disease also report fatigue. The psychological and behavioral factors driving fatigue could be related to mental disorders or other factors such as suboptimal sleep, stress, and use of caffeine and alcohol, they noted. Management strategies include improving sleep hygiene and evaluation of mental health concerns.
Seek complete picture before treatment
“Addressing psychological comorbidity in IBD requires individual and systemic approaches focused on both the prevention and treatment of mental health concerns,” the researchers wrote. “Because of the pervasiveness of psychological comorbidities in IBD, and recent evidence that they may be part of the disease process itself, assessment of psychological functioning in IBD is considered an essential aspect of disease management.”
Evidence-based psychological interventions include cognitive-behavioral therapy, which includes training in relaxation; treatment with clinical hypnosis; and encouraging mindfulness through acceptance and commitment therapy, which focuses on developing psychological flexibility to cope with suffering. In addition, a small but evolving body of research shows some benefit to motivational interviewing (a strategy focused on behavior change) for IBD patients. Notably, one review of four studies showed benefits of motivational interviewing for improving medication adherence and advice seeking, the researchers reported.
Although several psychological treatment options exist for addressing mental health issues in IBD, randomized trials are needed. “To facilitate this important research and optimize patient care, the integration of psychologists and other mental health providers into IBD care is considered best practice and provides exciting opportunities for improving patient care and outcomes,” the researchers concluded.
Address mental health to ease disease burden
“There is a large burden of mental health issues in patients with inflammatory bowel disease, with depression and anxiety leading the way,” Kim L. Isaacs, MD, of the University of North Carolina at Chapel Hill, said in an interview.
“There are multiple reasons for this, including dealing with chronic pain, social concerns around using the bathroom, body-image issues due to surgery, and drug side effects. There is increasing evidence that the inflammatory process in IBD may be driving some of the changes in the brain which lead to further mental health dysfunction,” she noted.
“Addressing depression, anxiety, [and] sleep disturbance in patients will not only improve quality of life from a mental health perspective but has been shown to improve control of disease,” Dr. Isaacs emphasized.
“Small things like increased medication compliance have a large impact on disease management and decreased need for hospitalization and hospitalization,” said Dr. Isaacs. “As gastroenterologists we need to expand our focus beyond the gut and address the emotional needs of our patients – identifying those patients who need increased mental health support.”
Barriers to better care
The greatest barriers to treating mental health issues in IBD patients are time and knowledge, said Dr. Isaacs. “Many gastroenterologists have limited time in the office to do more than address the acute issues of the patients such as rectal bleeding and worsening diarrhea. It takes time and trust to explore what is going on in a patient’s life. Is the patient anxious and depressed? How are they coping with their current disease manifestations? Simple screening tools may help with this, but then there need to be resources to support interventions.”
Some IBD practices, especially academic ones, have a psychologist in the IBD center or one that’s readily available for consultation. “This is an investment for the practice that may reduce significantly disease burden. The IBD specialty home model includes resources for management of psychiatric issues and nutritional concerns as well as disease management,” she added.
More research in several areas can help reduce the mental health burden of IBD. “On the immunology/biology side, understanding how the microbiome affects the brain/gut may allow for more directed mental health treatment. On the disease management side, larger trials directed at psychiatric interventions may help to determine which therapy is best for each patient,” Dr. Isaacs said. “Further work developing health care systems, such as the medical home, that allow for maximum disease management and decreased system costs will go far in implementation of models of care that address the needs of the entire patient with inflammatory bowel disease.”
The review received no outside funding. The researchers had no financial conflicts to disclose. Dr. Isaacs disclosed consulting on the data safety monitoring board for Janssen.
Psychological issues in patients with inflammatory bowel disease should be addressed at both personal and systemic levels, according to a review of current literature.
In a review published in the Journal of Clinical Gastroenterology, researchers highlighted data on the burden of mental disorders in inflammatory bowel disease (IBD) patients and presented several strategies for addressing them.
“From a systems perspective, underrecognized and/or suboptimally treated mental health problems in patients with IBD are associated with increased disability, poorer adherence, and more admissions and surgeries, driving increased health care utilization and costs,” Maia S. Kredentser, PhD, of the University of Manitoba, Winnipeg, and colleagues wrote, citing a 2018 study’s findings.
“There is ample evidence for a higher prevalence of mental disorders in IBD, in particular depression and anxiety, compared with the general population,” the authors wrote.
They cited a recent population-based study in which the incident rate ratios were significantly higher for IBD patients, compared with matched controls for depression (IRR, 1.58), anxiety disorder (IRR, 1.39), bipolar disorder (IRR, 1.82), and schizophrenia (IRR, 1.64).
Mental disorders associated with IBD also include issues of body image and sexuality. Although research on the impact of disease activity on sexual function is inconsistent, one study suggested that body image “may be an important target of treatment in women reporting poor quality of life and psychological distress,” the researchers noted. A French study from 2017 published in the Journal of Crohn’s and Colitis showed that approximately half of men and women reported problems with erectile or sexual dysfunction.
Issues related to environmental stressors may contribute to IBD by promoting chronic inflammation, the researchers wrote. For example, data from longitudinal, population-based research suggest that adverse childhood experiences can promote proinflammatory states across inflammatory illnesses. Research has also suggested that people with IBD have higher rates of these adverse childhood experiences than the general population. However, data also show that many are able to cope and adapt: “Many patients with IBD are resilient, experience growth, and in fact, thrive,” the researchers added. One longitudinal study suggested that patients with IBD who identified with “thriving” had “stronger coping efficacy (the perceived ability to meet illness demands), illness acceptance, and social support and lower depression” and that this was associated with life satisfaction 6 months later.
Fatigue also has been shown to be a factor for patients with IBD. The researchers cited one population-based study showing fatigue in 57%-72% of IBD patients with active disease. IBD patients with quiescent disease also report fatigue. The psychological and behavioral factors driving fatigue could be related to mental disorders or other factors such as suboptimal sleep, stress, and use of caffeine and alcohol, they noted. Management strategies include improving sleep hygiene and evaluation of mental health concerns.
Seek complete picture before treatment
“Addressing psychological comorbidity in IBD requires individual and systemic approaches focused on both the prevention and treatment of mental health concerns,” the researchers wrote. “Because of the pervasiveness of psychological comorbidities in IBD, and recent evidence that they may be part of the disease process itself, assessment of psychological functioning in IBD is considered an essential aspect of disease management.”
Evidence-based psychological interventions include cognitive-behavioral therapy, which includes training in relaxation; treatment with clinical hypnosis; and encouraging mindfulness through acceptance and commitment therapy, which focuses on developing psychological flexibility to cope with suffering. In addition, a small but evolving body of research shows some benefit to motivational interviewing (a strategy focused on behavior change) for IBD patients. Notably, one review of four studies showed benefits of motivational interviewing for improving medication adherence and advice seeking, the researchers reported.
Although several psychological treatment options exist for addressing mental health issues in IBD, randomized trials are needed. “To facilitate this important research and optimize patient care, the integration of psychologists and other mental health providers into IBD care is considered best practice and provides exciting opportunities for improving patient care and outcomes,” the researchers concluded.
Address mental health to ease disease burden
“There is a large burden of mental health issues in patients with inflammatory bowel disease, with depression and anxiety leading the way,” Kim L. Isaacs, MD, of the University of North Carolina at Chapel Hill, said in an interview.
“There are multiple reasons for this, including dealing with chronic pain, social concerns around using the bathroom, body-image issues due to surgery, and drug side effects. There is increasing evidence that the inflammatory process in IBD may be driving some of the changes in the brain which lead to further mental health dysfunction,” she noted.
“Addressing depression, anxiety, [and] sleep disturbance in patients will not only improve quality of life from a mental health perspective but has been shown to improve control of disease,” Dr. Isaacs emphasized.
“Small things like increased medication compliance have a large impact on disease management and decreased need for hospitalization and hospitalization,” said Dr. Isaacs. “As gastroenterologists we need to expand our focus beyond the gut and address the emotional needs of our patients – identifying those patients who need increased mental health support.”
Barriers to better care
The greatest barriers to treating mental health issues in IBD patients are time and knowledge, said Dr. Isaacs. “Many gastroenterologists have limited time in the office to do more than address the acute issues of the patients such as rectal bleeding and worsening diarrhea. It takes time and trust to explore what is going on in a patient’s life. Is the patient anxious and depressed? How are they coping with their current disease manifestations? Simple screening tools may help with this, but then there need to be resources to support interventions.”
Some IBD practices, especially academic ones, have a psychologist in the IBD center or one that’s readily available for consultation. “This is an investment for the practice that may reduce significantly disease burden. The IBD specialty home model includes resources for management of psychiatric issues and nutritional concerns as well as disease management,” she added.
More research in several areas can help reduce the mental health burden of IBD. “On the immunology/biology side, understanding how the microbiome affects the brain/gut may allow for more directed mental health treatment. On the disease management side, larger trials directed at psychiatric interventions may help to determine which therapy is best for each patient,” Dr. Isaacs said. “Further work developing health care systems, such as the medical home, that allow for maximum disease management and decreased system costs will go far in implementation of models of care that address the needs of the entire patient with inflammatory bowel disease.”
The review received no outside funding. The researchers had no financial conflicts to disclose. Dr. Isaacs disclosed consulting on the data safety monitoring board for Janssen.
FROM THE JOURNAL OF CLINICAL GASTROENTEROLOGY
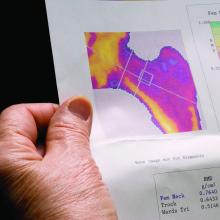
Bone loss common in kidney stone patients, yet rarely detected
Almost one in four men and women diagnosed with kidney stones have osteoporosis or a history of fracture at the time of their diagnosis, yet fewer than 10% undergo bone mineral density (BMD) screening, a retrospective analysis of a Veterans Health Administration database shows.
Because the majority of those analyzed in the VA dataset were men, this means that middle-aged and older men with kidney stones have about the same risk for osteoporosis as postmenopausal women do, but BMD screening for such men is not currently recommended, the study notes.
“These findings suggest that the risk of osteoporosis or fractures in patients with kidney stone disease is not restricted to postmenopausal women but is also observed in men, a group that is less well recognized to be at risk,” Calyani Ganesan, MD, of Stanford (Calif.) University and colleagues say in their article, published online March 3 in the Journal of Bone and Mineral Research.
“We hope this work raises awareness regarding the possibility of reduced bone strength in patients with kidney stones, [and] in our future work, we hope to identify which patients with kidney stones are at higher risk for osteoporosis or fracture to help guide bone density screening efforts by clinicians in this population,” Dr. Ganesan added in a statement.
VA dataset: Just 9.1% had DXA after kidney stone diagnosed
A total of 531,431 patients with a history of kidney stone disease were identified in the VA dataset. Of these, 23.6% either had been diagnosed with osteoporosis or had a history of fracture around the time of their kidney stone diagnosis. The most common diagnosis was a non-hip fracture, seen in 19% of patients, Dr. Ganesan and colleagues note, followed by osteoporosis in 6.1%, and hip fracture in 2.1%.
The mean age of the patients who concurrently had received a diagnosis of kidney stone disease and osteoporosis or had a fracture history was 64.2 years. In this cohort, more than 91% were men. The majority of the patients were White.
Among some 462,681 patients who had no prior history of either osteoporosis or fracture before their diagnosis of kidney stones, only 9.1% had undergone dual-energy x-ray absorptiometry (DXA) screening for BMD in the 5 years after their kidney stone diagnosis.
“Of those who completed DXA ... 20% were subsequently diagnosed with osteoporosis,” the authors note – 19% with non-hip fracture, and 2.4% with hip fracture.
Importantly, 85% of patients with kidney stone disease who were screened with DXA and were later diagnosed with osteoporosis were men.
“Given that almost 20% of patients in our cohort had a non-hip fracture, we contend that osteoporosis is underdiagnosed and undertreated in older men with kidney stone disease,” the authors stress.
Perform DXA screen in older men, even in absence of hypercalciuria
The authors also explain that the most common metabolic abnormality associated with kidney stones is high urine calcium excretion, or hypercalciuria.
“In a subset of patients with kidney stones, dysregulated calcium homeostasis may be present in which calcium is resorbed from bone and excreted into the urine, which can lead to osteoporosis and the formation of calcium stones,” they explain.
However, when they carried out a 24-hour assessment of urine calcium excretion on a small subset of patients with kidney stones, “we found no correlation between osteoporosis and the level of 24-hour urine calcium excretion,” they point out.
Even when the authors excluded patients who were taking a thiazide diuretic – a class of drugs that decreases urine calcium excretion – there was no correlation between osteoporosis and the level of 24-hour urine calcium excretion.
The investigators suggest it is possible that, in the majority of patients with kidney stones, the cause of hypercalciuria is more closely related to overabsorption of calcium from the gut, not to overresorption of calcium from the bone.
“Nonetheless, our findings indicate that patients with kidney stone disease could benefit from DXA screening even in the absence of hypercalciuria,” they state.
“And our findings provide support for wider use of bone mineral density screening in patients with kidney stone disease, including middle-aged and older men, for whom efforts to mitigate risks of osteoporosis and fractures are not commonly emphasized,” they reaffirm.
The study was funded by the VA Merit Review and the National Institute of Diabetes and Digestive and Kidney Diseases. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Almost one in four men and women diagnosed with kidney stones have osteoporosis or a history of fracture at the time of their diagnosis, yet fewer than 10% undergo bone mineral density (BMD) screening, a retrospective analysis of a Veterans Health Administration database shows.
Because the majority of those analyzed in the VA dataset were men, this means that middle-aged and older men with kidney stones have about the same risk for osteoporosis as postmenopausal women do, but BMD screening for such men is not currently recommended, the study notes.
“These findings suggest that the risk of osteoporosis or fractures in patients with kidney stone disease is not restricted to postmenopausal women but is also observed in men, a group that is less well recognized to be at risk,” Calyani Ganesan, MD, of Stanford (Calif.) University and colleagues say in their article, published online March 3 in the Journal of Bone and Mineral Research.
“We hope this work raises awareness regarding the possibility of reduced bone strength in patients with kidney stones, [and] in our future work, we hope to identify which patients with kidney stones are at higher risk for osteoporosis or fracture to help guide bone density screening efforts by clinicians in this population,” Dr. Ganesan added in a statement.
VA dataset: Just 9.1% had DXA after kidney stone diagnosed
A total of 531,431 patients with a history of kidney stone disease were identified in the VA dataset. Of these, 23.6% either had been diagnosed with osteoporosis or had a history of fracture around the time of their kidney stone diagnosis. The most common diagnosis was a non-hip fracture, seen in 19% of patients, Dr. Ganesan and colleagues note, followed by osteoporosis in 6.1%, and hip fracture in 2.1%.
The mean age of the patients who concurrently had received a diagnosis of kidney stone disease and osteoporosis or had a fracture history was 64.2 years. In this cohort, more than 91% were men. The majority of the patients were White.
Among some 462,681 patients who had no prior history of either osteoporosis or fracture before their diagnosis of kidney stones, only 9.1% had undergone dual-energy x-ray absorptiometry (DXA) screening for BMD in the 5 years after their kidney stone diagnosis.
“Of those who completed DXA ... 20% were subsequently diagnosed with osteoporosis,” the authors note – 19% with non-hip fracture, and 2.4% with hip fracture.
Importantly, 85% of patients with kidney stone disease who were screened with DXA and were later diagnosed with osteoporosis were men.
“Given that almost 20% of patients in our cohort had a non-hip fracture, we contend that osteoporosis is underdiagnosed and undertreated in older men with kidney stone disease,” the authors stress.
Perform DXA screen in older men, even in absence of hypercalciuria
The authors also explain that the most common metabolic abnormality associated with kidney stones is high urine calcium excretion, or hypercalciuria.
“In a subset of patients with kidney stones, dysregulated calcium homeostasis may be present in which calcium is resorbed from bone and excreted into the urine, which can lead to osteoporosis and the formation of calcium stones,” they explain.
However, when they carried out a 24-hour assessment of urine calcium excretion on a small subset of patients with kidney stones, “we found no correlation between osteoporosis and the level of 24-hour urine calcium excretion,” they point out.
Even when the authors excluded patients who were taking a thiazide diuretic – a class of drugs that decreases urine calcium excretion – there was no correlation between osteoporosis and the level of 24-hour urine calcium excretion.
The investigators suggest it is possible that, in the majority of patients with kidney stones, the cause of hypercalciuria is more closely related to overabsorption of calcium from the gut, not to overresorption of calcium from the bone.
“Nonetheless, our findings indicate that patients with kidney stone disease could benefit from DXA screening even in the absence of hypercalciuria,” they state.
“And our findings provide support for wider use of bone mineral density screening in patients with kidney stone disease, including middle-aged and older men, for whom efforts to mitigate risks of osteoporosis and fractures are not commonly emphasized,” they reaffirm.
The study was funded by the VA Merit Review and the National Institute of Diabetes and Digestive and Kidney Diseases. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Almost one in four men and women diagnosed with kidney stones have osteoporosis or a history of fracture at the time of their diagnosis, yet fewer than 10% undergo bone mineral density (BMD) screening, a retrospective analysis of a Veterans Health Administration database shows.
Because the majority of those analyzed in the VA dataset were men, this means that middle-aged and older men with kidney stones have about the same risk for osteoporosis as postmenopausal women do, but BMD screening for such men is not currently recommended, the study notes.
“These findings suggest that the risk of osteoporosis or fractures in patients with kidney stone disease is not restricted to postmenopausal women but is also observed in men, a group that is less well recognized to be at risk,” Calyani Ganesan, MD, of Stanford (Calif.) University and colleagues say in their article, published online March 3 in the Journal of Bone and Mineral Research.
“We hope this work raises awareness regarding the possibility of reduced bone strength in patients with kidney stones, [and] in our future work, we hope to identify which patients with kidney stones are at higher risk for osteoporosis or fracture to help guide bone density screening efforts by clinicians in this population,” Dr. Ganesan added in a statement.
VA dataset: Just 9.1% had DXA after kidney stone diagnosed
A total of 531,431 patients with a history of kidney stone disease were identified in the VA dataset. Of these, 23.6% either had been diagnosed with osteoporosis or had a history of fracture around the time of their kidney stone diagnosis. The most common diagnosis was a non-hip fracture, seen in 19% of patients, Dr. Ganesan and colleagues note, followed by osteoporosis in 6.1%, and hip fracture in 2.1%.
The mean age of the patients who concurrently had received a diagnosis of kidney stone disease and osteoporosis or had a fracture history was 64.2 years. In this cohort, more than 91% were men. The majority of the patients were White.
Among some 462,681 patients who had no prior history of either osteoporosis or fracture before their diagnosis of kidney stones, only 9.1% had undergone dual-energy x-ray absorptiometry (DXA) screening for BMD in the 5 years after their kidney stone diagnosis.
“Of those who completed DXA ... 20% were subsequently diagnosed with osteoporosis,” the authors note – 19% with non-hip fracture, and 2.4% with hip fracture.
Importantly, 85% of patients with kidney stone disease who were screened with DXA and were later diagnosed with osteoporosis were men.
“Given that almost 20% of patients in our cohort had a non-hip fracture, we contend that osteoporosis is underdiagnosed and undertreated in older men with kidney stone disease,” the authors stress.
Perform DXA screen in older men, even in absence of hypercalciuria
The authors also explain that the most common metabolic abnormality associated with kidney stones is high urine calcium excretion, or hypercalciuria.
“In a subset of patients with kidney stones, dysregulated calcium homeostasis may be present in which calcium is resorbed from bone and excreted into the urine, which can lead to osteoporosis and the formation of calcium stones,” they explain.
However, when they carried out a 24-hour assessment of urine calcium excretion on a small subset of patients with kidney stones, “we found no correlation between osteoporosis and the level of 24-hour urine calcium excretion,” they point out.
Even when the authors excluded patients who were taking a thiazide diuretic – a class of drugs that decreases urine calcium excretion – there was no correlation between osteoporosis and the level of 24-hour urine calcium excretion.
The investigators suggest it is possible that, in the majority of patients with kidney stones, the cause of hypercalciuria is more closely related to overabsorption of calcium from the gut, not to overresorption of calcium from the bone.
“Nonetheless, our findings indicate that patients with kidney stone disease could benefit from DXA screening even in the absence of hypercalciuria,” they state.
“And our findings provide support for wider use of bone mineral density screening in patients with kidney stone disease, including middle-aged and older men, for whom efforts to mitigate risks of osteoporosis and fractures are not commonly emphasized,” they reaffirm.
The study was funded by the VA Merit Review and the National Institute of Diabetes and Digestive and Kidney Diseases. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pediatric TB – more work needed, especially with HIV-coinfection
Despite recent advances in the diagnosis, treatment, and prevention of pediatric tuberculosis in children living with HIV (CLHIV) and HIV-exposed uninfected children (HEU), several unmet needs remain, including studies evaluating the feasibility of shortened TB treatment regimens.
“Children living with HIV contribute disproportionately to pediatric TB mortality rates, accounting for 16% of child TB deaths, and many cases are underdiagnosed and underreported,” said Nicole Salazar-Austin, MD, of Johns Hopkins University in Baltimore. She provided an update on pediatric TB prevention and treatment during an educational symposium at this year’s virtual Conference on Retroviruses & Opportunistic Infections.
Dr. Salazar-Austin summarized current diagnostics for pediatric TB and reviewed options for the prevention and treatment of TB in CLHIV and HEU.
TB and CLHIV
Presently, TB is the most common opportunistic infection among CLHIV, and those with severe immune suppression have a fivefold greater risk of TB disease. While antiretroviral therapy (ART) is highly protective against TB disease in CLHIV, only about 50% of eligible children receive ART.
Dr. Salazar-Austin explained that many individuals with TB/HIV coinfection are unaware of their coinfection and not receiving treatment. Despite recommendations, TB preventive therapy is poorly implemented in CLHIV, especially in high-burden settings.
Pediatric TB diagnosis
Smear microscopy, culture, and Xpert MTB/RIF Ultra are the main diagnostic modalities for pediatric TB. The Xpert MTB/RIF test is an automated PCR-based assay that simultaneously and rapidly detects Mycobacterium tuberculosis complex and resistance to rifampin. The test is currently recommended by the World Health Organization as the initial diagnostic method for presumptive TB cases in both adults and children.
However, under optimal conditions, only 40% of TB cases will be detected. This is in part due to limited implementation of sputum collection procedures, but recent evidence has shown that collection of multiple specimens improves sensitivity for both culture and Xpert MTB/RIF Ultra across all specimen types, Dr. Salazar-Austin explained.
In 2020, the WHO endorsed the use of stool samples for the diagnosis of pediatric pulmonary TB. Stool Xpert is an emerging alternative, noninvasive method for ruling in pediatric TB disease, and has shown sensitivity and specificity similar to that of Xpert MTB/RIF Ultra.
“TB diagnostics have limited sensitivity in children, and efforts are ongoing to maximize current diagnostics, but new diagnostics are needed,” said Dr. Salazar-Austin.
Pediatric TB treatment
Despite the high frequency of TB as an opportunistic infection in CLHIV, current data on co-treatment strategies are limited.
Dolutegravir-based regimens are the preferred first-line regimen for CLHIV. In June 2020, the Food and Drug Administration approved the dispersible dolutegravir tablet, and it is expected to become widely available in 2021.
In children with TB/HIV coinfection who receive dolutegravir and rifampicin, dolutegravir is typically dosed twice daily because of a known drug interaction, based on data from the ODYSSEY study. The WHO recommendations for treatment of pediatric TB/HIV coinfection were recently updated to reflect twice-daily dosing of dolutegravir.
Despite these new recommendations, data are currently limited, and observational pharmacokinetic studies evaluating twice daily dolutegravir with TB treatment in young children are needed.
“More work is needed to evaluate the drug-drug interactions and proper dosing of rifamycins with dolutegravir for the treatment and prevention of TB in CLHIV,” Dr. Salazar-Austin said.
Based on data from TBTC Study 31/ACTG A5349, high-dose rifapentine (a rifamycin) with moxifloxacin (a fluoroquinolone) was noninferior to rifapentine alone in newly diagnosed, culture positive, drug-susceptible TB in children 12 years and older.
Whether rifapentine and moxifloxacin (RPT-Mox) can be used in children under 12 years remains unknown, but future studies may help answer this question, Dr. Salazar-Austin noted. The FDA has restricted the use of fluoroquinolones in children because of a possible effect on cartilage development, she explained.
Furthermore, recent data from the SHINE trial suggested that shortened treatment regimens may hold promise for children with TB.
“While shortened TB treatment regimens hold promise, much work needs to be done in children to implement RPT-Mox, but the results from SHINE can be implemented rapidly,” Dr. Salazar-Austin said.
Dr. Salazar-Austin disclosed no conflicts of interest. The presentation was funded by NICHD, UNITAID, Fogarty Institute, and the IMPAACT network.
Despite recent advances in the diagnosis, treatment, and prevention of pediatric tuberculosis in children living with HIV (CLHIV) and HIV-exposed uninfected children (HEU), several unmet needs remain, including studies evaluating the feasibility of shortened TB treatment regimens.
“Children living with HIV contribute disproportionately to pediatric TB mortality rates, accounting for 16% of child TB deaths, and many cases are underdiagnosed and underreported,” said Nicole Salazar-Austin, MD, of Johns Hopkins University in Baltimore. She provided an update on pediatric TB prevention and treatment during an educational symposium at this year’s virtual Conference on Retroviruses & Opportunistic Infections.
Dr. Salazar-Austin summarized current diagnostics for pediatric TB and reviewed options for the prevention and treatment of TB in CLHIV and HEU.
TB and CLHIV
Presently, TB is the most common opportunistic infection among CLHIV, and those with severe immune suppression have a fivefold greater risk of TB disease. While antiretroviral therapy (ART) is highly protective against TB disease in CLHIV, only about 50% of eligible children receive ART.
Dr. Salazar-Austin explained that many individuals with TB/HIV coinfection are unaware of their coinfection and not receiving treatment. Despite recommendations, TB preventive therapy is poorly implemented in CLHIV, especially in high-burden settings.
Pediatric TB diagnosis
Smear microscopy, culture, and Xpert MTB/RIF Ultra are the main diagnostic modalities for pediatric TB. The Xpert MTB/RIF test is an automated PCR-based assay that simultaneously and rapidly detects Mycobacterium tuberculosis complex and resistance to rifampin. The test is currently recommended by the World Health Organization as the initial diagnostic method for presumptive TB cases in both adults and children.
However, under optimal conditions, only 40% of TB cases will be detected. This is in part due to limited implementation of sputum collection procedures, but recent evidence has shown that collection of multiple specimens improves sensitivity for both culture and Xpert MTB/RIF Ultra across all specimen types, Dr. Salazar-Austin explained.
In 2020, the WHO endorsed the use of stool samples for the diagnosis of pediatric pulmonary TB. Stool Xpert is an emerging alternative, noninvasive method for ruling in pediatric TB disease, and has shown sensitivity and specificity similar to that of Xpert MTB/RIF Ultra.
“TB diagnostics have limited sensitivity in children, and efforts are ongoing to maximize current diagnostics, but new diagnostics are needed,” said Dr. Salazar-Austin.
Pediatric TB treatment
Despite the high frequency of TB as an opportunistic infection in CLHIV, current data on co-treatment strategies are limited.
Dolutegravir-based regimens are the preferred first-line regimen for CLHIV. In June 2020, the Food and Drug Administration approved the dispersible dolutegravir tablet, and it is expected to become widely available in 2021.
In children with TB/HIV coinfection who receive dolutegravir and rifampicin, dolutegravir is typically dosed twice daily because of a known drug interaction, based on data from the ODYSSEY study. The WHO recommendations for treatment of pediatric TB/HIV coinfection were recently updated to reflect twice-daily dosing of dolutegravir.
Despite these new recommendations, data are currently limited, and observational pharmacokinetic studies evaluating twice daily dolutegravir with TB treatment in young children are needed.
“More work is needed to evaluate the drug-drug interactions and proper dosing of rifamycins with dolutegravir for the treatment and prevention of TB in CLHIV,” Dr. Salazar-Austin said.
Based on data from TBTC Study 31/ACTG A5349, high-dose rifapentine (a rifamycin) with moxifloxacin (a fluoroquinolone) was noninferior to rifapentine alone in newly diagnosed, culture positive, drug-susceptible TB in children 12 years and older.
Whether rifapentine and moxifloxacin (RPT-Mox) can be used in children under 12 years remains unknown, but future studies may help answer this question, Dr. Salazar-Austin noted. The FDA has restricted the use of fluoroquinolones in children because of a possible effect on cartilage development, she explained.
Furthermore, recent data from the SHINE trial suggested that shortened treatment regimens may hold promise for children with TB.
“While shortened TB treatment regimens hold promise, much work needs to be done in children to implement RPT-Mox, but the results from SHINE can be implemented rapidly,” Dr. Salazar-Austin said.
Dr. Salazar-Austin disclosed no conflicts of interest. The presentation was funded by NICHD, UNITAID, Fogarty Institute, and the IMPAACT network.
Despite recent advances in the diagnosis, treatment, and prevention of pediatric tuberculosis in children living with HIV (CLHIV) and HIV-exposed uninfected children (HEU), several unmet needs remain, including studies evaluating the feasibility of shortened TB treatment regimens.
“Children living with HIV contribute disproportionately to pediatric TB mortality rates, accounting for 16% of child TB deaths, and many cases are underdiagnosed and underreported,” said Nicole Salazar-Austin, MD, of Johns Hopkins University in Baltimore. She provided an update on pediatric TB prevention and treatment during an educational symposium at this year’s virtual Conference on Retroviruses & Opportunistic Infections.
Dr. Salazar-Austin summarized current diagnostics for pediatric TB and reviewed options for the prevention and treatment of TB in CLHIV and HEU.
TB and CLHIV
Presently, TB is the most common opportunistic infection among CLHIV, and those with severe immune suppression have a fivefold greater risk of TB disease. While antiretroviral therapy (ART) is highly protective against TB disease in CLHIV, only about 50% of eligible children receive ART.
Dr. Salazar-Austin explained that many individuals with TB/HIV coinfection are unaware of their coinfection and not receiving treatment. Despite recommendations, TB preventive therapy is poorly implemented in CLHIV, especially in high-burden settings.
Pediatric TB diagnosis
Smear microscopy, culture, and Xpert MTB/RIF Ultra are the main diagnostic modalities for pediatric TB. The Xpert MTB/RIF test is an automated PCR-based assay that simultaneously and rapidly detects Mycobacterium tuberculosis complex and resistance to rifampin. The test is currently recommended by the World Health Organization as the initial diagnostic method for presumptive TB cases in both adults and children.
However, under optimal conditions, only 40% of TB cases will be detected. This is in part due to limited implementation of sputum collection procedures, but recent evidence has shown that collection of multiple specimens improves sensitivity for both culture and Xpert MTB/RIF Ultra across all specimen types, Dr. Salazar-Austin explained.
In 2020, the WHO endorsed the use of stool samples for the diagnosis of pediatric pulmonary TB. Stool Xpert is an emerging alternative, noninvasive method for ruling in pediatric TB disease, and has shown sensitivity and specificity similar to that of Xpert MTB/RIF Ultra.
“TB diagnostics have limited sensitivity in children, and efforts are ongoing to maximize current diagnostics, but new diagnostics are needed,” said Dr. Salazar-Austin.
Pediatric TB treatment
Despite the high frequency of TB as an opportunistic infection in CLHIV, current data on co-treatment strategies are limited.
Dolutegravir-based regimens are the preferred first-line regimen for CLHIV. In June 2020, the Food and Drug Administration approved the dispersible dolutegravir tablet, and it is expected to become widely available in 2021.
In children with TB/HIV coinfection who receive dolutegravir and rifampicin, dolutegravir is typically dosed twice daily because of a known drug interaction, based on data from the ODYSSEY study. The WHO recommendations for treatment of pediatric TB/HIV coinfection were recently updated to reflect twice-daily dosing of dolutegravir.
Despite these new recommendations, data are currently limited, and observational pharmacokinetic studies evaluating twice daily dolutegravir with TB treatment in young children are needed.
“More work is needed to evaluate the drug-drug interactions and proper dosing of rifamycins with dolutegravir for the treatment and prevention of TB in CLHIV,” Dr. Salazar-Austin said.
Based on data from TBTC Study 31/ACTG A5349, high-dose rifapentine (a rifamycin) with moxifloxacin (a fluoroquinolone) was noninferior to rifapentine alone in newly diagnosed, culture positive, drug-susceptible TB in children 12 years and older.
Whether rifapentine and moxifloxacin (RPT-Mox) can be used in children under 12 years remains unknown, but future studies may help answer this question, Dr. Salazar-Austin noted. The FDA has restricted the use of fluoroquinolones in children because of a possible effect on cartilage development, she explained.
Furthermore, recent data from the SHINE trial suggested that shortened treatment regimens may hold promise for children with TB.
“While shortened TB treatment regimens hold promise, much work needs to be done in children to implement RPT-Mox, but the results from SHINE can be implemented rapidly,” Dr. Salazar-Austin said.
Dr. Salazar-Austin disclosed no conflicts of interest. The presentation was funded by NICHD, UNITAID, Fogarty Institute, and the IMPAACT network.
FROM CROI 2021
Are long-acting injectables the future of TB treatment?
Long-acting injectable (LAI) drug formulations represent a promising new strategy for the prevention and treatment of tuberculosis in women and children, according to an online presentation at the Conference on Retroviruses & Opportunistic Infections, held virtually.
“As a delivery strategy, LAIs hold the potential to unlock a vast chemical space of lipophilic compounds with very potent anti-TB activity that would otherwise not be developed due to poor predicted oral bioavailability,” explained presenter Eric Nuermberger, MD.
He summarized current preventive treatment options for TB and reviewed the potential impact of LAI formulations on TB therapy. In addition, he identified key challenges for future LAI development and proposed a new development path for clinical implementation.
Current TB preventive therapies
Despite widespread availability, the uptake of TB preventive therapy is poor and currently lags behind global targets. One key barrier to widespread uptake is the long duration of treatment, which may hinder patient adherence to therapy.
While shorter preventive regimens, such as 1 month of daily isoniazid plus rifapentine, show similar efficacy and higher completion rates, further shortening of therapy and reducing clinic visits are the most direct methods to increase adherence and treatment completion rates, Dr. Nuermberger said.
LAI drugs
LAI drug formulations allow for slow release of suitable drugs from a depot injected subcutaneously or intramuscularly.
The goal of LAI formulations is to free patients from the daily burden of oral administration. Other potential benefits include better adherence and efficacy, drug exposure, and the potential to overcome intrinsic poor oral bioavailability by bypassing the GI tract entirely.
Potential indications for LAIs include treatment of latent tuberculosis infection (LTBI), and as continuous therapy in people living with HIV in high-burden settings. There is also potential for treating younger children, such as household contacts, who have difficulty taking oral medications.
“We’ve already seen LAIs revolutionize other areas, such as psychiatry and contraception, and we appear to have another revolution in HIV prevention and treatment,” Dr. Nuermberger explained.
Not all existing TB drugs are suitable for LAI formulations, but drugs such as rifapentine, rifabutin, delamanid, and bedaquiline, show more promise than isoniazid or rifampin because of their physiochemical composition. Of all, bedaquiline may offer the best profile for LAI formulation, Dr. Nuermberger said.
Early proof-of-concept in vivo studies have shown potential use of LAI bedaquiline for TB prevention in both drug-sensitive and drug-resistant TB contacts. Translational PK modeling and simulation predicted that a 1-g intramuscular injection of LAI bedaquiline could maintain therapeutic plasma concentrations in humans for greater than 1 month.
Dr. Nuermberger noted that novel diarylquinoline-based therapies, currently in phase 1 studies, may be even better candidates for LAI-based TB preventive therapy. Early data suggests these compounds may be 10-20 times more potent and have a lower CV risk profile than that of bedaquiline.
Considerations for development and implementation
“Despite the promising potential of long-acting injectables for TB, we are still in the very early stages,” said Dr. Nuermberger.
Ensuring and optimizing acceptance of LAI formulations, especially in at-risk populations, will be very important, he explained. Early involvement of children and pregnant women in studies of who may benefit most from LAI drugs will also be essential.
Other important considerations include cost-effectiveness, particularly in at-risk and vulnerable populations. Furthermore, new dedicated research and development programs are needed to continue to develop more drug candidates suitable for LAI.
“Long-acting formulations hold enormous promise to be transformative for combating TB, through simplification of delivery and overcoming issues of adherence that can compromise success of current interventions,” said Andrew Owen, PhD, of the University of Liverpool (England).
“The ability to deliver an entire course of drug in a single visit promises to ensure missed doses don’t compromise outcomes or place unnecessary selective pressure in favor of drug resistance,” Dr. Owen said.
“Recent studies showing the value of one-month oral treatment regimens for LTBI make long-acting formulations seem more realistic and drugs such as long-acting bedaquiline put a one-shot regimen within reach,” Charles W. Flexner, MD, of Johns Hopkins University, Baltimore, said in an interview.
While no LAIs have been approved for TB, Dr. Nuermberger was optimistic that the recent success of LAI formulations for HIV treatment and prevention will catalyze further efforts in the TB landscape.
Dr. Nuermberger disclosed research support from Janssen Pharmaceuticals, TB Alliance, and the Gates Medical Research Institute. The presentation was sponsored by Janssen Pharmaceuticals, Johns Hopkins CFAR, NIH, Unitaid, and the TB Alliance.
Long-acting injectable (LAI) drug formulations represent a promising new strategy for the prevention and treatment of tuberculosis in women and children, according to an online presentation at the Conference on Retroviruses & Opportunistic Infections, held virtually.
“As a delivery strategy, LAIs hold the potential to unlock a vast chemical space of lipophilic compounds with very potent anti-TB activity that would otherwise not be developed due to poor predicted oral bioavailability,” explained presenter Eric Nuermberger, MD.
He summarized current preventive treatment options for TB and reviewed the potential impact of LAI formulations on TB therapy. In addition, he identified key challenges for future LAI development and proposed a new development path for clinical implementation.
Current TB preventive therapies
Despite widespread availability, the uptake of TB preventive therapy is poor and currently lags behind global targets. One key barrier to widespread uptake is the long duration of treatment, which may hinder patient adherence to therapy.
While shorter preventive regimens, such as 1 month of daily isoniazid plus rifapentine, show similar efficacy and higher completion rates, further shortening of therapy and reducing clinic visits are the most direct methods to increase adherence and treatment completion rates, Dr. Nuermberger said.
LAI drugs
LAI drug formulations allow for slow release of suitable drugs from a depot injected subcutaneously or intramuscularly.
The goal of LAI formulations is to free patients from the daily burden of oral administration. Other potential benefits include better adherence and efficacy, drug exposure, and the potential to overcome intrinsic poor oral bioavailability by bypassing the GI tract entirely.
Potential indications for LAIs include treatment of latent tuberculosis infection (LTBI), and as continuous therapy in people living with HIV in high-burden settings. There is also potential for treating younger children, such as household contacts, who have difficulty taking oral medications.
“We’ve already seen LAIs revolutionize other areas, such as psychiatry and contraception, and we appear to have another revolution in HIV prevention and treatment,” Dr. Nuermberger explained.
Not all existing TB drugs are suitable for LAI formulations, but drugs such as rifapentine, rifabutin, delamanid, and bedaquiline, show more promise than isoniazid or rifampin because of their physiochemical composition. Of all, bedaquiline may offer the best profile for LAI formulation, Dr. Nuermberger said.
Early proof-of-concept in vivo studies have shown potential use of LAI bedaquiline for TB prevention in both drug-sensitive and drug-resistant TB contacts. Translational PK modeling and simulation predicted that a 1-g intramuscular injection of LAI bedaquiline could maintain therapeutic plasma concentrations in humans for greater than 1 month.
Dr. Nuermberger noted that novel diarylquinoline-based therapies, currently in phase 1 studies, may be even better candidates for LAI-based TB preventive therapy. Early data suggests these compounds may be 10-20 times more potent and have a lower CV risk profile than that of bedaquiline.
Considerations for development and implementation
“Despite the promising potential of long-acting injectables for TB, we are still in the very early stages,” said Dr. Nuermberger.
Ensuring and optimizing acceptance of LAI formulations, especially in at-risk populations, will be very important, he explained. Early involvement of children and pregnant women in studies of who may benefit most from LAI drugs will also be essential.
Other important considerations include cost-effectiveness, particularly in at-risk and vulnerable populations. Furthermore, new dedicated research and development programs are needed to continue to develop more drug candidates suitable for LAI.
“Long-acting formulations hold enormous promise to be transformative for combating TB, through simplification of delivery and overcoming issues of adherence that can compromise success of current interventions,” said Andrew Owen, PhD, of the University of Liverpool (England).
“The ability to deliver an entire course of drug in a single visit promises to ensure missed doses don’t compromise outcomes or place unnecessary selective pressure in favor of drug resistance,” Dr. Owen said.
“Recent studies showing the value of one-month oral treatment regimens for LTBI make long-acting formulations seem more realistic and drugs such as long-acting bedaquiline put a one-shot regimen within reach,” Charles W. Flexner, MD, of Johns Hopkins University, Baltimore, said in an interview.
While no LAIs have been approved for TB, Dr. Nuermberger was optimistic that the recent success of LAI formulations for HIV treatment and prevention will catalyze further efforts in the TB landscape.
Dr. Nuermberger disclosed research support from Janssen Pharmaceuticals, TB Alliance, and the Gates Medical Research Institute. The presentation was sponsored by Janssen Pharmaceuticals, Johns Hopkins CFAR, NIH, Unitaid, and the TB Alliance.
Long-acting injectable (LAI) drug formulations represent a promising new strategy for the prevention and treatment of tuberculosis in women and children, according to an online presentation at the Conference on Retroviruses & Opportunistic Infections, held virtually.
“As a delivery strategy, LAIs hold the potential to unlock a vast chemical space of lipophilic compounds with very potent anti-TB activity that would otherwise not be developed due to poor predicted oral bioavailability,” explained presenter Eric Nuermberger, MD.
He summarized current preventive treatment options for TB and reviewed the potential impact of LAI formulations on TB therapy. In addition, he identified key challenges for future LAI development and proposed a new development path for clinical implementation.
Current TB preventive therapies
Despite widespread availability, the uptake of TB preventive therapy is poor and currently lags behind global targets. One key barrier to widespread uptake is the long duration of treatment, which may hinder patient adherence to therapy.
While shorter preventive regimens, such as 1 month of daily isoniazid plus rifapentine, show similar efficacy and higher completion rates, further shortening of therapy and reducing clinic visits are the most direct methods to increase adherence and treatment completion rates, Dr. Nuermberger said.
LAI drugs
LAI drug formulations allow for slow release of suitable drugs from a depot injected subcutaneously or intramuscularly.
The goal of LAI formulations is to free patients from the daily burden of oral administration. Other potential benefits include better adherence and efficacy, drug exposure, and the potential to overcome intrinsic poor oral bioavailability by bypassing the GI tract entirely.
Potential indications for LAIs include treatment of latent tuberculosis infection (LTBI), and as continuous therapy in people living with HIV in high-burden settings. There is also potential for treating younger children, such as household contacts, who have difficulty taking oral medications.
“We’ve already seen LAIs revolutionize other areas, such as psychiatry and contraception, and we appear to have another revolution in HIV prevention and treatment,” Dr. Nuermberger explained.
Not all existing TB drugs are suitable for LAI formulations, but drugs such as rifapentine, rifabutin, delamanid, and bedaquiline, show more promise than isoniazid or rifampin because of their physiochemical composition. Of all, bedaquiline may offer the best profile for LAI formulation, Dr. Nuermberger said.
Early proof-of-concept in vivo studies have shown potential use of LAI bedaquiline for TB prevention in both drug-sensitive and drug-resistant TB contacts. Translational PK modeling and simulation predicted that a 1-g intramuscular injection of LAI bedaquiline could maintain therapeutic plasma concentrations in humans for greater than 1 month.
Dr. Nuermberger noted that novel diarylquinoline-based therapies, currently in phase 1 studies, may be even better candidates for LAI-based TB preventive therapy. Early data suggests these compounds may be 10-20 times more potent and have a lower CV risk profile than that of bedaquiline.
Considerations for development and implementation
“Despite the promising potential of long-acting injectables for TB, we are still in the very early stages,” said Dr. Nuermberger.
Ensuring and optimizing acceptance of LAI formulations, especially in at-risk populations, will be very important, he explained. Early involvement of children and pregnant women in studies of who may benefit most from LAI drugs will also be essential.
Other important considerations include cost-effectiveness, particularly in at-risk and vulnerable populations. Furthermore, new dedicated research and development programs are needed to continue to develop more drug candidates suitable for LAI.
“Long-acting formulations hold enormous promise to be transformative for combating TB, through simplification of delivery and overcoming issues of adherence that can compromise success of current interventions,” said Andrew Owen, PhD, of the University of Liverpool (England).
“The ability to deliver an entire course of drug in a single visit promises to ensure missed doses don’t compromise outcomes or place unnecessary selective pressure in favor of drug resistance,” Dr. Owen said.
“Recent studies showing the value of one-month oral treatment regimens for LTBI make long-acting formulations seem more realistic and drugs such as long-acting bedaquiline put a one-shot regimen within reach,” Charles W. Flexner, MD, of Johns Hopkins University, Baltimore, said in an interview.
While no LAIs have been approved for TB, Dr. Nuermberger was optimistic that the recent success of LAI formulations for HIV treatment and prevention will catalyze further efforts in the TB landscape.
Dr. Nuermberger disclosed research support from Janssen Pharmaceuticals, TB Alliance, and the Gates Medical Research Institute. The presentation was sponsored by Janssen Pharmaceuticals, Johns Hopkins CFAR, NIH, Unitaid, and the TB Alliance.
FROM CROI 2021
Five-day course of oral antiviral appears to stop SARS-CoV-2 in its tracks
A single pill of the investigational drug molnupiravir taken twice a day for 5 days eliminated SARS-CoV-2 from the nasopharynx of 49 participants.
That led Carlos del Rio, MD, distinguished professor of medicine at Emory University, Atlanta, to suggest a future in which a drug like molnupiravir could be taken in the first few days of symptoms to prevent severe disease, similar to Tamiflu for influenza.
“I think it’s critically important,” he said of the data. Emory University was involved in the trial of molnupiravir but Dr. del Rio was not part of that team. “This drug offers the first antiviral oral drug that then could be used in an outpatient setting.”
Still, Dr. del Rio said it’s too soon to call this particular drug the breakthrough clinicians need to keep people out of the ICU. “It has the potential to be practice changing; it’s not practice changing at the moment.”
Wendy Painter, MD, of Ridgeback Biotherapeutics, who presented the data at the Conference on Retroviruses and Opportunistic Infections, agreed. While the data are promising, “We will need to see if people get better from actual illness” to assess the real value of the drug in clinical care.
“That’s a phase 3 objective we’ll need to prove,” she said in an interview.
Phase 2/3 efficacy and safety studies of the drug are now underway in hospitalized and nonhospitalized patients.
In a brief prerecorded presentation of the data, Dr. Painter laid out what researchers know so far: Preclinical studies suggest that molnupiravir is effective against a number of viruses, including coronaviruses and specifically SARS-CoV-2. It prevents a virus from replicating by inducing viral error catastrophe (Proc Natl Acad Sci U S A. 2002 Oct 15;99[21]:13374-6) – essentially overloading the virus with replication and mutation until the virus burns itself out and can’t produce replicable copies.
In this phase 2a, randomized, double-blind, controlled trial, researchers recruited 202 adults who were treated at an outpatient clinic with fever or other symptoms of a respiratory virus and confirmed SARS-CoV-2 infection by day 4. Participants were randomly assigned to three different groups: 200 mg of molnupiravir, 400 mg, or 800 mg. The 200-mg arm was matched 1:1 with a placebo-controlled group, and the other two groups had three participants in the active group for every one control.
Participants took the pills twice daily for 5 days, and then were followed for a total of 28 days to monitor for complications or adverse events. At days 3, 5, 7, 14, and 28, researchers also took nasopharyngeal swabs for polymerase chain reaction tests, to sequence the virus, and to grow cultures of SARS-CoV-2 to see if the virus that’s present is actually capable of infecting others.
Notably, the pills do not have to be refrigerated at any point in the process, alleviating the cold-chain challenges that have plagued vaccines.
“There’s an urgent need for an easily produced, transported, stored, and administered antiviral drug against SARS-CoV-2,” Dr. Painter said.
Of the 202 people recruited, 182 had swabs that could be evaluated, of which 78 showed infection at baseline. The results are based on labs of those 78 participants.
By day 3, 28% of patients in the placebo arm had SARS-CoV-2 in their nasopharynx, compared with 20.4% of patients receiving any dose of molnupiravir. But by day 5, none of the participants receiving the active drug had evidence of SARS-CoV-2 in their nasopharynx. In comparison, 24% of people in the placebo arm still had detectable virus.
Halfway through the treatment course, differences in the presence of infectious virus were already evident. By day 3 of the 5-day course, 36.4% of participants in the 200-mg group had detectable virus in the nasopharynx, compared with 21% in the 400-mg group and just 12.5% in the 800-mg group. And although the reduction in SARS-CoV-2 was noticeable in the 200-mg and the 400-mg arms, it was only statistically significant in the 800-mg arm.
In contrast, by the end of the 5 days in the placebo groups, infectious virus varied from 18.2% in the 200-mg placebo group to 30% in the 800-mg group. This points out the variability of the disease course of SARS-CoV-2.
“You just don’t know” which infections will lead to serious disease, Dr. Painter said in an interview. “And don’t you wish we did?”
Seven participants discontinued treatment, though only four experienced adverse events. Three of those discontinued the trial because of adverse events. The study is still blinded, so it’s unclear what those events were, but Dr. Painter said that they were not thought to be related to the study drug.
The bottom line, said Dr. Painter, was that people treated with molnupiravir had starkly different outcomes in lab measures during the study.
“An average of 10 days after symptom onset, 24% of placebo patients remained culture positive” for SARS-CoV-2 – meaning there wasn’t just virus in the nasopharynx, but it was capable of replicating, Dr. Painter said. “In contrast, no infectious virus could be recovered at study day 5 in any molnupiravir-treated patients.”
A version of this article first appeared on Medscape.com.
A single pill of the investigational drug molnupiravir taken twice a day for 5 days eliminated SARS-CoV-2 from the nasopharynx of 49 participants.
That led Carlos del Rio, MD, distinguished professor of medicine at Emory University, Atlanta, to suggest a future in which a drug like molnupiravir could be taken in the first few days of symptoms to prevent severe disease, similar to Tamiflu for influenza.
“I think it’s critically important,” he said of the data. Emory University was involved in the trial of molnupiravir but Dr. del Rio was not part of that team. “This drug offers the first antiviral oral drug that then could be used in an outpatient setting.”
Still, Dr. del Rio said it’s too soon to call this particular drug the breakthrough clinicians need to keep people out of the ICU. “It has the potential to be practice changing; it’s not practice changing at the moment.”
Wendy Painter, MD, of Ridgeback Biotherapeutics, who presented the data at the Conference on Retroviruses and Opportunistic Infections, agreed. While the data are promising, “We will need to see if people get better from actual illness” to assess the real value of the drug in clinical care.
“That’s a phase 3 objective we’ll need to prove,” she said in an interview.
Phase 2/3 efficacy and safety studies of the drug are now underway in hospitalized and nonhospitalized patients.
In a brief prerecorded presentation of the data, Dr. Painter laid out what researchers know so far: Preclinical studies suggest that molnupiravir is effective against a number of viruses, including coronaviruses and specifically SARS-CoV-2. It prevents a virus from replicating by inducing viral error catastrophe (Proc Natl Acad Sci U S A. 2002 Oct 15;99[21]:13374-6) – essentially overloading the virus with replication and mutation until the virus burns itself out and can’t produce replicable copies.
In this phase 2a, randomized, double-blind, controlled trial, researchers recruited 202 adults who were treated at an outpatient clinic with fever or other symptoms of a respiratory virus and confirmed SARS-CoV-2 infection by day 4. Participants were randomly assigned to three different groups: 200 mg of molnupiravir, 400 mg, or 800 mg. The 200-mg arm was matched 1:1 with a placebo-controlled group, and the other two groups had three participants in the active group for every one control.
Participants took the pills twice daily for 5 days, and then were followed for a total of 28 days to monitor for complications or adverse events. At days 3, 5, 7, 14, and 28, researchers also took nasopharyngeal swabs for polymerase chain reaction tests, to sequence the virus, and to grow cultures of SARS-CoV-2 to see if the virus that’s present is actually capable of infecting others.
Notably, the pills do not have to be refrigerated at any point in the process, alleviating the cold-chain challenges that have plagued vaccines.
“There’s an urgent need for an easily produced, transported, stored, and administered antiviral drug against SARS-CoV-2,” Dr. Painter said.
Of the 202 people recruited, 182 had swabs that could be evaluated, of which 78 showed infection at baseline. The results are based on labs of those 78 participants.
By day 3, 28% of patients in the placebo arm had SARS-CoV-2 in their nasopharynx, compared with 20.4% of patients receiving any dose of molnupiravir. But by day 5, none of the participants receiving the active drug had evidence of SARS-CoV-2 in their nasopharynx. In comparison, 24% of people in the placebo arm still had detectable virus.
Halfway through the treatment course, differences in the presence of infectious virus were already evident. By day 3 of the 5-day course, 36.4% of participants in the 200-mg group had detectable virus in the nasopharynx, compared with 21% in the 400-mg group and just 12.5% in the 800-mg group. And although the reduction in SARS-CoV-2 was noticeable in the 200-mg and the 400-mg arms, it was only statistically significant in the 800-mg arm.
In contrast, by the end of the 5 days in the placebo groups, infectious virus varied from 18.2% in the 200-mg placebo group to 30% in the 800-mg group. This points out the variability of the disease course of SARS-CoV-2.
“You just don’t know” which infections will lead to serious disease, Dr. Painter said in an interview. “And don’t you wish we did?”
Seven participants discontinued treatment, though only four experienced adverse events. Three of those discontinued the trial because of adverse events. The study is still blinded, so it’s unclear what those events were, but Dr. Painter said that they were not thought to be related to the study drug.
The bottom line, said Dr. Painter, was that people treated with molnupiravir had starkly different outcomes in lab measures during the study.
“An average of 10 days after symptom onset, 24% of placebo patients remained culture positive” for SARS-CoV-2 – meaning there wasn’t just virus in the nasopharynx, but it was capable of replicating, Dr. Painter said. “In contrast, no infectious virus could be recovered at study day 5 in any molnupiravir-treated patients.”
A version of this article first appeared on Medscape.com.
A single pill of the investigational drug molnupiravir taken twice a day for 5 days eliminated SARS-CoV-2 from the nasopharynx of 49 participants.
That led Carlos del Rio, MD, distinguished professor of medicine at Emory University, Atlanta, to suggest a future in which a drug like molnupiravir could be taken in the first few days of symptoms to prevent severe disease, similar to Tamiflu for influenza.
“I think it’s critically important,” he said of the data. Emory University was involved in the trial of molnupiravir but Dr. del Rio was not part of that team. “This drug offers the first antiviral oral drug that then could be used in an outpatient setting.”
Still, Dr. del Rio said it’s too soon to call this particular drug the breakthrough clinicians need to keep people out of the ICU. “It has the potential to be practice changing; it’s not practice changing at the moment.”
Wendy Painter, MD, of Ridgeback Biotherapeutics, who presented the data at the Conference on Retroviruses and Opportunistic Infections, agreed. While the data are promising, “We will need to see if people get better from actual illness” to assess the real value of the drug in clinical care.
“That’s a phase 3 objective we’ll need to prove,” she said in an interview.
Phase 2/3 efficacy and safety studies of the drug are now underway in hospitalized and nonhospitalized patients.
In a brief prerecorded presentation of the data, Dr. Painter laid out what researchers know so far: Preclinical studies suggest that molnupiravir is effective against a number of viruses, including coronaviruses and specifically SARS-CoV-2. It prevents a virus from replicating by inducing viral error catastrophe (Proc Natl Acad Sci U S A. 2002 Oct 15;99[21]:13374-6) – essentially overloading the virus with replication and mutation until the virus burns itself out and can’t produce replicable copies.
In this phase 2a, randomized, double-blind, controlled trial, researchers recruited 202 adults who were treated at an outpatient clinic with fever or other symptoms of a respiratory virus and confirmed SARS-CoV-2 infection by day 4. Participants were randomly assigned to three different groups: 200 mg of molnupiravir, 400 mg, or 800 mg. The 200-mg arm was matched 1:1 with a placebo-controlled group, and the other two groups had three participants in the active group for every one control.
Participants took the pills twice daily for 5 days, and then were followed for a total of 28 days to monitor for complications or adverse events. At days 3, 5, 7, 14, and 28, researchers also took nasopharyngeal swabs for polymerase chain reaction tests, to sequence the virus, and to grow cultures of SARS-CoV-2 to see if the virus that’s present is actually capable of infecting others.
Notably, the pills do not have to be refrigerated at any point in the process, alleviating the cold-chain challenges that have plagued vaccines.
“There’s an urgent need for an easily produced, transported, stored, and administered antiviral drug against SARS-CoV-2,” Dr. Painter said.
Of the 202 people recruited, 182 had swabs that could be evaluated, of which 78 showed infection at baseline. The results are based on labs of those 78 participants.
By day 3, 28% of patients in the placebo arm had SARS-CoV-2 in their nasopharynx, compared with 20.4% of patients receiving any dose of molnupiravir. But by day 5, none of the participants receiving the active drug had evidence of SARS-CoV-2 in their nasopharynx. In comparison, 24% of people in the placebo arm still had detectable virus.
Halfway through the treatment course, differences in the presence of infectious virus were already evident. By day 3 of the 5-day course, 36.4% of participants in the 200-mg group had detectable virus in the nasopharynx, compared with 21% in the 400-mg group and just 12.5% in the 800-mg group. And although the reduction in SARS-CoV-2 was noticeable in the 200-mg and the 400-mg arms, it was only statistically significant in the 800-mg arm.
In contrast, by the end of the 5 days in the placebo groups, infectious virus varied from 18.2% in the 200-mg placebo group to 30% in the 800-mg group. This points out the variability of the disease course of SARS-CoV-2.
“You just don’t know” which infections will lead to serious disease, Dr. Painter said in an interview. “And don’t you wish we did?”
Seven participants discontinued treatment, though only four experienced adverse events. Three of those discontinued the trial because of adverse events. The study is still blinded, so it’s unclear what those events were, but Dr. Painter said that they were not thought to be related to the study drug.
The bottom line, said Dr. Painter, was that people treated with molnupiravir had starkly different outcomes in lab measures during the study.
“An average of 10 days after symptom onset, 24% of placebo patients remained culture positive” for SARS-CoV-2 – meaning there wasn’t just virus in the nasopharynx, but it was capable of replicating, Dr. Painter said. “In contrast, no infectious virus could be recovered at study day 5 in any molnupiravir-treated patients.”
A version of this article first appeared on Medscape.com.
Novel oral agent effective in teens with atopic dermatitis
Abrocitinib, an investigational drug proven to be a safe and effective treatment for moderate to severe atopic dermatitis (AD) in adults 18 years and older, is also safe and effective in patients aged 12-17 years, according to a randomized trial of the oral, once-daily Janus kinase (JAK) 1 selective inhibitor, used in combination with medicated topical therapy.
The results, from the phase 3 JADE TEEN study, were presented during an oral abstract session at the annual meeting of the American Academy of Allergy, Asthma, and Immunology, held virtually this year.
“We’re very excited about the introduction of oral JAKs into our armamentarium for atopic dermatitis,” lead author Lawrence Eichenfield, MD, professor of dermatology and pediatrics, University of California, San Diego, and chief of pediatric and adolescent dermatology, Rady Children’s Hospital, also in San Diego, said in an interview.
AD ranges in severity, and there is a great deal of moderate to severe AD that has a tremendous negative impact on the individual, Dr. Eichenfield said. “Traditionally we have treated it with intermittent topical corticosteroids, but this has left a significant percentage of patients without long-term disease control.”
JAK inhibitors are effective mediators of the inflammation response that occurs in moderate to severe AD. They inhibit the stimulation of the JAK pathway and allow anti-inflammatory effects and therefore have potential, especially in more severe disease, Dr. Eichenfield said.
In the current study, which is a spin-off of the original study that looked at abrocitinib in adults, he and his team randomly assigned 285 teens (mean age, 14.9 years; 50.9% male; 56.1% White) with moderate to severe AD to receive one of the following treatments for 12 weeks: abrocitinib 200 mg plus topical therapy (95); abrocitinib 100 mg plus topical therapy (95); or placebo, which consisted of topical therapy alone (95).
The primary endpoints were an Investigator’s Global Assessment response of clear or almost clear (scores of 0 and 1, respectively), with an improvement of at least 2 points, and an improvement in Eczema Area and Severity Index score of at least 75% at week 12.
Secondary endpoints included an improvement in Peak Pruritus Numerical Rating Scale (PP-NRS) response of at least 4 points at week 12.
The teens who received abrocitinib along with medicated topical therapy showed significant improvement in the severity of their AD at the end of the 12-week period, compared with those in the placebo group.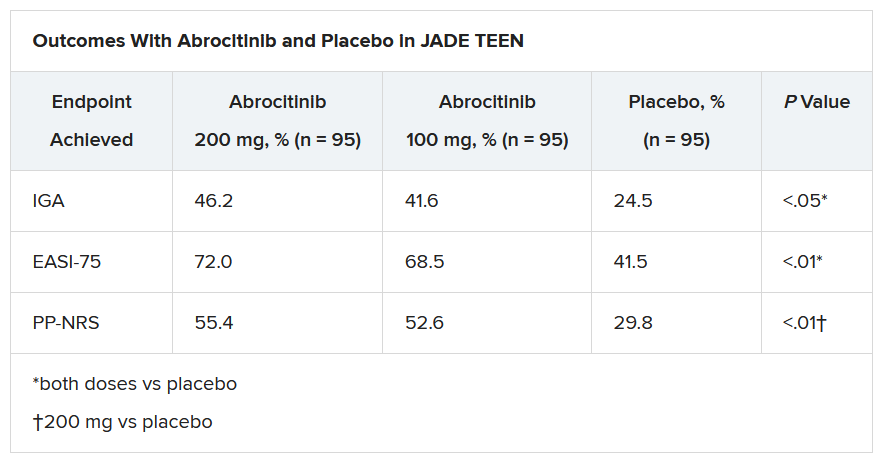
“The percentage of patients achieving essentially no itch, as captured in the fact that more than half of those on the higher dose of abrocitinib made it to no itch, is a new data point and is important to note,” Dr. Eichenfield said. “A lot of the other medicines don’t really get a significant percentage of the population to an itch score of 0 to 1. This drug brought about a rapid and profound itch relief.”
He added: “The results from JADE TEEN extend the drug’s utility in this younger population and show that abrocitinib performs the same with regard to efficacy and safety in the teenagers. Having atopic dermatitis that does not respond to treatment is especially hard for adolescents, but now we know that abrocitinib will be safe and effective and so we now have something to offer these kids.”
“Abrocitinib achieved a good response in this study that was statistically significant, compared to standard treatment,” Jonathan A. Bernstein, MD, professor of medicine at the University of Cincinnati, commented in an interview.
“JAK inhibitors are very promising, and this study adds to that promise. They play an important role in atopic dermatitis, so obviously, teenagers with AD represent an important population,” said Dr. Bernstein, who was not part of the study. “These results are very encouraging, and I think that we will probably see some of these JAK inhibitors approved by the FDA, if not this year, probably next.”
The study was sponsored by Pfizer. Dr. Eichenfield serves as an investigator, speaker, and consultant for Pfizer; and as an investigator, speaker, consultant, and/or is on a data safety monitoring board for AbbVie, Almirall, Amgen, Arcutis, Asana, Dermavant, Dermira, Forte, Galderma, Ichnos/Glenmark, Incyte, LEO, Lilly, L’Oreal, Novartis, Regeneron, Sanofi-Genzyme, and Verrica. Dr. Bernstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Abrocitinib, an investigational drug proven to be a safe and effective treatment for moderate to severe atopic dermatitis (AD) in adults 18 years and older, is also safe and effective in patients aged 12-17 years, according to a randomized trial of the oral, once-daily Janus kinase (JAK) 1 selective inhibitor, used in combination with medicated topical therapy.
The results, from the phase 3 JADE TEEN study, were presented during an oral abstract session at the annual meeting of the American Academy of Allergy, Asthma, and Immunology, held virtually this year.
“We’re very excited about the introduction of oral JAKs into our armamentarium for atopic dermatitis,” lead author Lawrence Eichenfield, MD, professor of dermatology and pediatrics, University of California, San Diego, and chief of pediatric and adolescent dermatology, Rady Children’s Hospital, also in San Diego, said in an interview.
AD ranges in severity, and there is a great deal of moderate to severe AD that has a tremendous negative impact on the individual, Dr. Eichenfield said. “Traditionally we have treated it with intermittent topical corticosteroids, but this has left a significant percentage of patients without long-term disease control.”
JAK inhibitors are effective mediators of the inflammation response that occurs in moderate to severe AD. They inhibit the stimulation of the JAK pathway and allow anti-inflammatory effects and therefore have potential, especially in more severe disease, Dr. Eichenfield said.
In the current study, which is a spin-off of the original study that looked at abrocitinib in adults, he and his team randomly assigned 285 teens (mean age, 14.9 years; 50.9% male; 56.1% White) with moderate to severe AD to receive one of the following treatments for 12 weeks: abrocitinib 200 mg plus topical therapy (95); abrocitinib 100 mg plus topical therapy (95); or placebo, which consisted of topical therapy alone (95).
The primary endpoints were an Investigator’s Global Assessment response of clear or almost clear (scores of 0 and 1, respectively), with an improvement of at least 2 points, and an improvement in Eczema Area and Severity Index score of at least 75% at week 12.
Secondary endpoints included an improvement in Peak Pruritus Numerical Rating Scale (PP-NRS) response of at least 4 points at week 12.
The teens who received abrocitinib along with medicated topical therapy showed significant improvement in the severity of their AD at the end of the 12-week period, compared with those in the placebo group.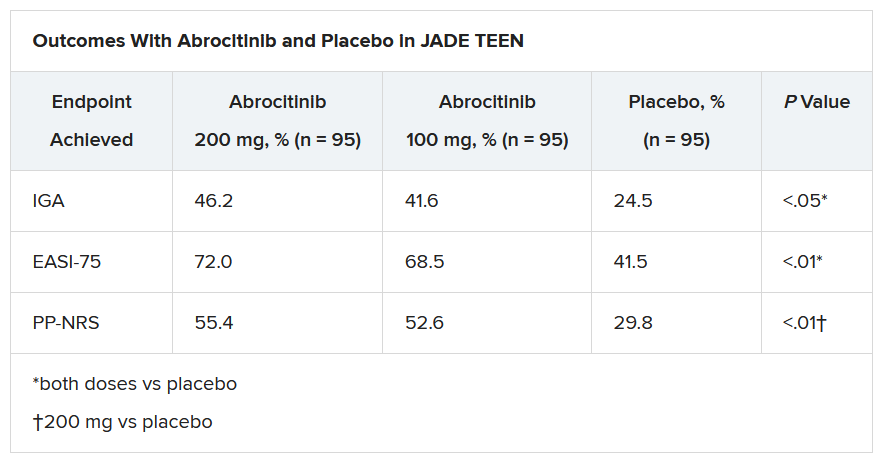
“The percentage of patients achieving essentially no itch, as captured in the fact that more than half of those on the higher dose of abrocitinib made it to no itch, is a new data point and is important to note,” Dr. Eichenfield said. “A lot of the other medicines don’t really get a significant percentage of the population to an itch score of 0 to 1. This drug brought about a rapid and profound itch relief.”
He added: “The results from JADE TEEN extend the drug’s utility in this younger population and show that abrocitinib performs the same with regard to efficacy and safety in the teenagers. Having atopic dermatitis that does not respond to treatment is especially hard for adolescents, but now we know that abrocitinib will be safe and effective and so we now have something to offer these kids.”
“Abrocitinib achieved a good response in this study that was statistically significant, compared to standard treatment,” Jonathan A. Bernstein, MD, professor of medicine at the University of Cincinnati, commented in an interview.
“JAK inhibitors are very promising, and this study adds to that promise. They play an important role in atopic dermatitis, so obviously, teenagers with AD represent an important population,” said Dr. Bernstein, who was not part of the study. “These results are very encouraging, and I think that we will probably see some of these JAK inhibitors approved by the FDA, if not this year, probably next.”
The study was sponsored by Pfizer. Dr. Eichenfield serves as an investigator, speaker, and consultant for Pfizer; and as an investigator, speaker, consultant, and/or is on a data safety monitoring board for AbbVie, Almirall, Amgen, Arcutis, Asana, Dermavant, Dermira, Forte, Galderma, Ichnos/Glenmark, Incyte, LEO, Lilly, L’Oreal, Novartis, Regeneron, Sanofi-Genzyme, and Verrica. Dr. Bernstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Abrocitinib, an investigational drug proven to be a safe and effective treatment for moderate to severe atopic dermatitis (AD) in adults 18 years and older, is also safe and effective in patients aged 12-17 years, according to a randomized trial of the oral, once-daily Janus kinase (JAK) 1 selective inhibitor, used in combination with medicated topical therapy.
The results, from the phase 3 JADE TEEN study, were presented during an oral abstract session at the annual meeting of the American Academy of Allergy, Asthma, and Immunology, held virtually this year.
“We’re very excited about the introduction of oral JAKs into our armamentarium for atopic dermatitis,” lead author Lawrence Eichenfield, MD, professor of dermatology and pediatrics, University of California, San Diego, and chief of pediatric and adolescent dermatology, Rady Children’s Hospital, also in San Diego, said in an interview.
AD ranges in severity, and there is a great deal of moderate to severe AD that has a tremendous negative impact on the individual, Dr. Eichenfield said. “Traditionally we have treated it with intermittent topical corticosteroids, but this has left a significant percentage of patients without long-term disease control.”
JAK inhibitors are effective mediators of the inflammation response that occurs in moderate to severe AD. They inhibit the stimulation of the JAK pathway and allow anti-inflammatory effects and therefore have potential, especially in more severe disease, Dr. Eichenfield said.
In the current study, which is a spin-off of the original study that looked at abrocitinib in adults, he and his team randomly assigned 285 teens (mean age, 14.9 years; 50.9% male; 56.1% White) with moderate to severe AD to receive one of the following treatments for 12 weeks: abrocitinib 200 mg plus topical therapy (95); abrocitinib 100 mg plus topical therapy (95); or placebo, which consisted of topical therapy alone (95).
The primary endpoints were an Investigator’s Global Assessment response of clear or almost clear (scores of 0 and 1, respectively), with an improvement of at least 2 points, and an improvement in Eczema Area and Severity Index score of at least 75% at week 12.
Secondary endpoints included an improvement in Peak Pruritus Numerical Rating Scale (PP-NRS) response of at least 4 points at week 12.
The teens who received abrocitinib along with medicated topical therapy showed significant improvement in the severity of their AD at the end of the 12-week period, compared with those in the placebo group.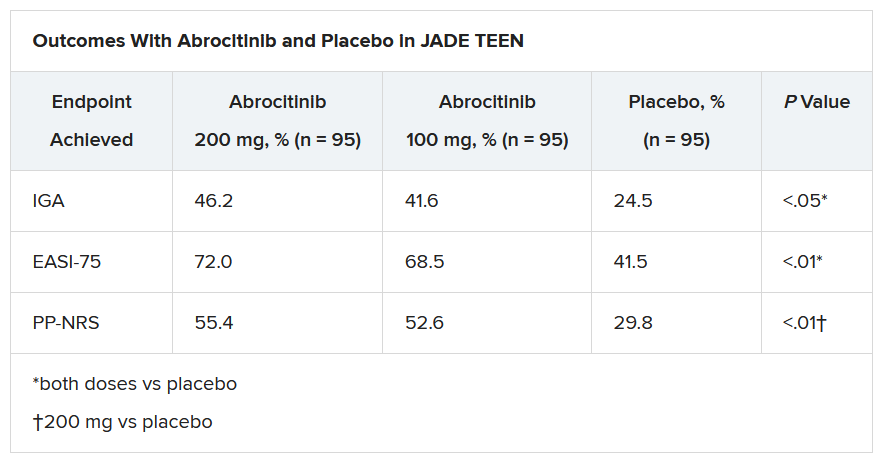
“The percentage of patients achieving essentially no itch, as captured in the fact that more than half of those on the higher dose of abrocitinib made it to no itch, is a new data point and is important to note,” Dr. Eichenfield said. “A lot of the other medicines don’t really get a significant percentage of the population to an itch score of 0 to 1. This drug brought about a rapid and profound itch relief.”
He added: “The results from JADE TEEN extend the drug’s utility in this younger population and show that abrocitinib performs the same with regard to efficacy and safety in the teenagers. Having atopic dermatitis that does not respond to treatment is especially hard for adolescents, but now we know that abrocitinib will be safe and effective and so we now have something to offer these kids.”
“Abrocitinib achieved a good response in this study that was statistically significant, compared to standard treatment,” Jonathan A. Bernstein, MD, professor of medicine at the University of Cincinnati, commented in an interview.
“JAK inhibitors are very promising, and this study adds to that promise. They play an important role in atopic dermatitis, so obviously, teenagers with AD represent an important population,” said Dr. Bernstein, who was not part of the study. “These results are very encouraging, and I think that we will probably see some of these JAK inhibitors approved by the FDA, if not this year, probably next.”
The study was sponsored by Pfizer. Dr. Eichenfield serves as an investigator, speaker, and consultant for Pfizer; and as an investigator, speaker, consultant, and/or is on a data safety monitoring board for AbbVie, Almirall, Amgen, Arcutis, Asana, Dermavant, Dermira, Forte, Galderma, Ichnos/Glenmark, Incyte, LEO, Lilly, L’Oreal, Novartis, Regeneron, Sanofi-Genzyme, and Verrica. Dr. Bernstein disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Slow-growing lesion on eyebrow
A 51-year-old woman presented to the family medicine clinic for evaluation of a slightly tender skin lesion on her left eyebrow. The lesion had been slowly growing for a year.
The patient’s family history included multiple family members with colon or breast cancer and other relatives with pancreatic and prostate cancer. A colonoscopy performed a year earlier on the patient was negative. The patient’s past medical history included hypertension, major depressive disorder, hyperlipidemia, and venous insufficiency. She also had a colon polyp history.
Physical examination of the eyebrow showed a 3-mm papule that was firm on palpation. Dermoscopy of the lesion revealed a yellow papule with

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Sebaceous carcinoma
A rapid teledermatology consultation helped us to determine that this was a sebaceous lesion, but its location and the overlying telangiectasia raised concerns for malignancy. After shared decision-making with the patient, she agreed to proceed with a biopsy. We first made an incision into the lesion, which was hard, demonstrating that it was not cystic. A shave biopsy was then completed. The dermatopathology findings showed clear-cell change consisting of bubbly or foamy cytoplasm, with scalloping of the nuclei, which is characteristic of a sebaceous origin. There were tumor cells that were enlarged with pleomorphism, multiple nucleoli, and scattered mitotic figures. These findings pointed to a diagnosis of sebaceous carcinoma.
Sebaceous carcinomas most commonly manifest on the eyelids. They can originate from the Meibomian glands as well as from pilosebaceous glands at other sites on the body.1 They are rare, accounting for only 1% to 5% of eyelid malignancies, and occur in approximately 2 per 1 million people.1 Tumors can invade locally and metastasize, particularly to surrounding lymph nodes. Periocular pathology may sometimes lead to misdiagnosis, which contributes to a mortality rate that has been reported as high as 20%.1 Suspicion for malignancy may arise due to ulceration, bleeding, pain, or rapid growth.
A lesson in considering the full differential
While sebaceous lesions on the eyelid and eyebrow are often benign, this case underscored the importance of considering the more worrisome elements in the differential. The differential diagnosis for lesions in the area of the eye include the following:
Sebaceous hyperplasia is a common condition (typically among older patients) in which sebaceous glands increase in size and number.2 The classic clinical feature is yellow or skin-colored papules. The lesions typically manifest on the face—particularly on the forehead. They are benign and often have a central umbilication.2
Sebaceous adenomas are benign tumors that may manifest as tan, skin-colored, pink, or yellow papules or nodules.2 The lesions are usually asymptomatic, small, and slow growing.2
Continue to: Basal and squamous cell carcinomas
Basal and squamous cell carcinomas. Basal cell carcinomas often feature translucent lesions on areas of the skin that are exposed to sunlight. These lesions often have slightly rolled border edges or overlying branching telangiectasia and may be nodular.3 Squamous cell carcinomas often feature scaled, reddened patches that may become tender and ulcerate.4
Hordeolums and chalazions. A hordeolum (or stye) is a painful, acute, localized swelling of the eyelid.5 These often develop externally at the lid margin from infection of the follicle. A chalazion is characterized by a persistent, nontender mass that results from small, noninfectious obstruction of the Meibomian glands with secondary granulomatous inflammation.5
Dermoscopy can (and did) help with the Dx
Dermoscopy can help confirm whether a lesion has a sebaceous origin because it would show yellow globules with “crown vessel” telangiectasias that classically do not cross midline.6 Unfortunately, the findings of yellow globules and dermal vessels do not adequately differentiate benign from malignant lesions.6 Carcinomas can manifest in an undifferentiated way early in their course.
Sebaceous carcinomas can be associated with the autosomal dominant Muir-Torre syndrome, a subset of the Lynch syndrome.7,8 Colorectal and genitourinary carcinomas are the most common internal malignancies seen in patients with Muir-Torre syndrome.9
Patients benefit from Mohs surgery
Treatment outcomes for sebaceous carcinoma appear to be improved by Mohs surgery. In a recent review of 1265 patients with early-stage sebaceous carcinomas, Su et al found that 234 patients who were treated with Mohs surgery had improved overall survival, compared with 1031 who were treated with surgical excision.10
Continue to: Our patient
Our patient was referred to a Mohs surgeon who removed the lesion (FIGURES 2 and 3). Given the overall small tumor size, a sentinel lymph node biopsy was not necessary. Because of the patient’s family history, which was suggestive of a genetic predisposition to cancer, she requested a clinical genetics consultation for definitive testing. She went on to pursue genetic testing, which came back negative for Lynch syndrome genes.

The dermatologist recommended yearly skin examination for 5 years for the patient.

1. Kahana A, Pribila HT, Nelson CC, et al. Sebaceous cell carcinoma. In: Levin LA, Albert DM, eds. Ocular Disease: Mechanisms and Management. Saunders/Elsevier; 2010:396-407.
2. Iacobelli J, Harvey NT, Wood BA. Sebaceous lesions of the skin. Pathology. 2017;49:688-697.
3. Marzuka AG, Book SE. Basal cell carcinoma: pathogenesis, epidemiology, clinical features, diagnosis, histopathology, and management. Yale J Biol Med. 2015;88:167-179.
4. Smith H, Patel A. When to suspect a non-melanoma skin cancer. BMJ. 2020;368:m692.
5. Sun MT, Huang S, Huilgol SC, et al. Eyelid lesions in general practice. Aust J Gen Pract. 2019;48:509-514.
6. Kim NH, Zell DS, Kolm I, et al. The dermoscopic differential diagnosis of yellow lobularlike structures. Arch Dermatol. 2008;144:962.
7. EG, Bell AJY, Barlow KA. Multiple primary carcinomata of the colon, duodenum, and larynx associated with kerato-acanthomata of the face. Br J Surg. 1967;54:191-195.
8. Torre D. Multiple sebaceous tumors. Arch Dermatol. 1968;98:549-55.
9. Cohen PR, Kohn SR, Kurzrock R. Association of sebaceous gland tumors and internal malignancy: the Muir-Torre syndrome. Am J Med. 1991;90:606-613.
10. Su C, Nguyen KA, Bai HX, et al. Comparison of Mohs surgery and surgical excision in the treatment of localized sebaceous carcinoma. Dermatol Surg. 2019;45:1125-1135.
A 51-year-old woman presented to the family medicine clinic for evaluation of a slightly tender skin lesion on her left eyebrow. The lesion had been slowly growing for a year.
The patient’s family history included multiple family members with colon or breast cancer and other relatives with pancreatic and prostate cancer. A colonoscopy performed a year earlier on the patient was negative. The patient’s past medical history included hypertension, major depressive disorder, hyperlipidemia, and venous insufficiency. She also had a colon polyp history.
Physical examination of the eyebrow showed a 3-mm papule that was firm on palpation. Dermoscopy of the lesion revealed a yellow papule with

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Sebaceous carcinoma
A rapid teledermatology consultation helped us to determine that this was a sebaceous lesion, but its location and the overlying telangiectasia raised concerns for malignancy. After shared decision-making with the patient, she agreed to proceed with a biopsy. We first made an incision into the lesion, which was hard, demonstrating that it was not cystic. A shave biopsy was then completed. The dermatopathology findings showed clear-cell change consisting of bubbly or foamy cytoplasm, with scalloping of the nuclei, which is characteristic of a sebaceous origin. There were tumor cells that were enlarged with pleomorphism, multiple nucleoli, and scattered mitotic figures. These findings pointed to a diagnosis of sebaceous carcinoma.
Sebaceous carcinomas most commonly manifest on the eyelids. They can originate from the Meibomian glands as well as from pilosebaceous glands at other sites on the body.1 They are rare, accounting for only 1% to 5% of eyelid malignancies, and occur in approximately 2 per 1 million people.1 Tumors can invade locally and metastasize, particularly to surrounding lymph nodes. Periocular pathology may sometimes lead to misdiagnosis, which contributes to a mortality rate that has been reported as high as 20%.1 Suspicion for malignancy may arise due to ulceration, bleeding, pain, or rapid growth.
A lesson in considering the full differential
While sebaceous lesions on the eyelid and eyebrow are often benign, this case underscored the importance of considering the more worrisome elements in the differential. The differential diagnosis for lesions in the area of the eye include the following:
Sebaceous hyperplasia is a common condition (typically among older patients) in which sebaceous glands increase in size and number.2 The classic clinical feature is yellow or skin-colored papules. The lesions typically manifest on the face—particularly on the forehead. They are benign and often have a central umbilication.2
Sebaceous adenomas are benign tumors that may manifest as tan, skin-colored, pink, or yellow papules or nodules.2 The lesions are usually asymptomatic, small, and slow growing.2
Continue to: Basal and squamous cell carcinomas
Basal and squamous cell carcinomas. Basal cell carcinomas often feature translucent lesions on areas of the skin that are exposed to sunlight. These lesions often have slightly rolled border edges or overlying branching telangiectasia and may be nodular.3 Squamous cell carcinomas often feature scaled, reddened patches that may become tender and ulcerate.4
Hordeolums and chalazions. A hordeolum (or stye) is a painful, acute, localized swelling of the eyelid.5 These often develop externally at the lid margin from infection of the follicle. A chalazion is characterized by a persistent, nontender mass that results from small, noninfectious obstruction of the Meibomian glands with secondary granulomatous inflammation.5
Dermoscopy can (and did) help with the Dx
Dermoscopy can help confirm whether a lesion has a sebaceous origin because it would show yellow globules with “crown vessel” telangiectasias that classically do not cross midline.6 Unfortunately, the findings of yellow globules and dermal vessels do not adequately differentiate benign from malignant lesions.6 Carcinomas can manifest in an undifferentiated way early in their course.
Sebaceous carcinomas can be associated with the autosomal dominant Muir-Torre syndrome, a subset of the Lynch syndrome.7,8 Colorectal and genitourinary carcinomas are the most common internal malignancies seen in patients with Muir-Torre syndrome.9
Patients benefit from Mohs surgery
Treatment outcomes for sebaceous carcinoma appear to be improved by Mohs surgery. In a recent review of 1265 patients with early-stage sebaceous carcinomas, Su et al found that 234 patients who were treated with Mohs surgery had improved overall survival, compared with 1031 who were treated with surgical excision.10
Continue to: Our patient
Our patient was referred to a Mohs surgeon who removed the lesion (FIGURES 2 and 3). Given the overall small tumor size, a sentinel lymph node biopsy was not necessary. Because of the patient’s family history, which was suggestive of a genetic predisposition to cancer, she requested a clinical genetics consultation for definitive testing. She went on to pursue genetic testing, which came back negative for Lynch syndrome genes.

The dermatologist recommended yearly skin examination for 5 years for the patient.

A 51-year-old woman presented to the family medicine clinic for evaluation of a slightly tender skin lesion on her left eyebrow. The lesion had been slowly growing for a year.
The patient’s family history included multiple family members with colon or breast cancer and other relatives with pancreatic and prostate cancer. A colonoscopy performed a year earlier on the patient was negative. The patient’s past medical history included hypertension, major depressive disorder, hyperlipidemia, and venous insufficiency. She also had a colon polyp history.
Physical examination of the eyebrow showed a 3-mm papule that was firm on palpation. Dermoscopy of the lesion revealed a yellow papule with

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Sebaceous carcinoma
A rapid teledermatology consultation helped us to determine that this was a sebaceous lesion, but its location and the overlying telangiectasia raised concerns for malignancy. After shared decision-making with the patient, she agreed to proceed with a biopsy. We first made an incision into the lesion, which was hard, demonstrating that it was not cystic. A shave biopsy was then completed. The dermatopathology findings showed clear-cell change consisting of bubbly or foamy cytoplasm, with scalloping of the nuclei, which is characteristic of a sebaceous origin. There were tumor cells that were enlarged with pleomorphism, multiple nucleoli, and scattered mitotic figures. These findings pointed to a diagnosis of sebaceous carcinoma.
Sebaceous carcinomas most commonly manifest on the eyelids. They can originate from the Meibomian glands as well as from pilosebaceous glands at other sites on the body.1 They are rare, accounting for only 1% to 5% of eyelid malignancies, and occur in approximately 2 per 1 million people.1 Tumors can invade locally and metastasize, particularly to surrounding lymph nodes. Periocular pathology may sometimes lead to misdiagnosis, which contributes to a mortality rate that has been reported as high as 20%.1 Suspicion for malignancy may arise due to ulceration, bleeding, pain, or rapid growth.
A lesson in considering the full differential
While sebaceous lesions on the eyelid and eyebrow are often benign, this case underscored the importance of considering the more worrisome elements in the differential. The differential diagnosis for lesions in the area of the eye include the following:
Sebaceous hyperplasia is a common condition (typically among older patients) in which sebaceous glands increase in size and number.2 The classic clinical feature is yellow or skin-colored papules. The lesions typically manifest on the face—particularly on the forehead. They are benign and often have a central umbilication.2
Sebaceous adenomas are benign tumors that may manifest as tan, skin-colored, pink, or yellow papules or nodules.2 The lesions are usually asymptomatic, small, and slow growing.2
Continue to: Basal and squamous cell carcinomas
Basal and squamous cell carcinomas. Basal cell carcinomas often feature translucent lesions on areas of the skin that are exposed to sunlight. These lesions often have slightly rolled border edges or overlying branching telangiectasia and may be nodular.3 Squamous cell carcinomas often feature scaled, reddened patches that may become tender and ulcerate.4
Hordeolums and chalazions. A hordeolum (or stye) is a painful, acute, localized swelling of the eyelid.5 These often develop externally at the lid margin from infection of the follicle. A chalazion is characterized by a persistent, nontender mass that results from small, noninfectious obstruction of the Meibomian glands with secondary granulomatous inflammation.5
Dermoscopy can (and did) help with the Dx
Dermoscopy can help confirm whether a lesion has a sebaceous origin because it would show yellow globules with “crown vessel” telangiectasias that classically do not cross midline.6 Unfortunately, the findings of yellow globules and dermal vessels do not adequately differentiate benign from malignant lesions.6 Carcinomas can manifest in an undifferentiated way early in their course.
Sebaceous carcinomas can be associated with the autosomal dominant Muir-Torre syndrome, a subset of the Lynch syndrome.7,8 Colorectal and genitourinary carcinomas are the most common internal malignancies seen in patients with Muir-Torre syndrome.9
Patients benefit from Mohs surgery
Treatment outcomes for sebaceous carcinoma appear to be improved by Mohs surgery. In a recent review of 1265 patients with early-stage sebaceous carcinomas, Su et al found that 234 patients who were treated with Mohs surgery had improved overall survival, compared with 1031 who were treated with surgical excision.10
Continue to: Our patient
Our patient was referred to a Mohs surgeon who removed the lesion (FIGURES 2 and 3). Given the overall small tumor size, a sentinel lymph node biopsy was not necessary. Because of the patient’s family history, which was suggestive of a genetic predisposition to cancer, she requested a clinical genetics consultation for definitive testing. She went on to pursue genetic testing, which came back negative for Lynch syndrome genes.

The dermatologist recommended yearly skin examination for 5 years for the patient.

1. Kahana A, Pribila HT, Nelson CC, et al. Sebaceous cell carcinoma. In: Levin LA, Albert DM, eds. Ocular Disease: Mechanisms and Management. Saunders/Elsevier; 2010:396-407.
2. Iacobelli J, Harvey NT, Wood BA. Sebaceous lesions of the skin. Pathology. 2017;49:688-697.
3. Marzuka AG, Book SE. Basal cell carcinoma: pathogenesis, epidemiology, clinical features, diagnosis, histopathology, and management. Yale J Biol Med. 2015;88:167-179.
4. Smith H, Patel A. When to suspect a non-melanoma skin cancer. BMJ. 2020;368:m692.
5. Sun MT, Huang S, Huilgol SC, et al. Eyelid lesions in general practice. Aust J Gen Pract. 2019;48:509-514.
6. Kim NH, Zell DS, Kolm I, et al. The dermoscopic differential diagnosis of yellow lobularlike structures. Arch Dermatol. 2008;144:962.
7. EG, Bell AJY, Barlow KA. Multiple primary carcinomata of the colon, duodenum, and larynx associated with kerato-acanthomata of the face. Br J Surg. 1967;54:191-195.
8. Torre D. Multiple sebaceous tumors. Arch Dermatol. 1968;98:549-55.
9. Cohen PR, Kohn SR, Kurzrock R. Association of sebaceous gland tumors and internal malignancy: the Muir-Torre syndrome. Am J Med. 1991;90:606-613.
10. Su C, Nguyen KA, Bai HX, et al. Comparison of Mohs surgery and surgical excision in the treatment of localized sebaceous carcinoma. Dermatol Surg. 2019;45:1125-1135.
1. Kahana A, Pribila HT, Nelson CC, et al. Sebaceous cell carcinoma. In: Levin LA, Albert DM, eds. Ocular Disease: Mechanisms and Management. Saunders/Elsevier; 2010:396-407.
2. Iacobelli J, Harvey NT, Wood BA. Sebaceous lesions of the skin. Pathology. 2017;49:688-697.
3. Marzuka AG, Book SE. Basal cell carcinoma: pathogenesis, epidemiology, clinical features, diagnosis, histopathology, and management. Yale J Biol Med. 2015;88:167-179.
4. Smith H, Patel A. When to suspect a non-melanoma skin cancer. BMJ. 2020;368:m692.
5. Sun MT, Huang S, Huilgol SC, et al. Eyelid lesions in general practice. Aust J Gen Pract. 2019;48:509-514.
6. Kim NH, Zell DS, Kolm I, et al. The dermoscopic differential diagnosis of yellow lobularlike structures. Arch Dermatol. 2008;144:962.
7. EG, Bell AJY, Barlow KA. Multiple primary carcinomata of the colon, duodenum, and larynx associated with kerato-acanthomata of the face. Br J Surg. 1967;54:191-195.
8. Torre D. Multiple sebaceous tumors. Arch Dermatol. 1968;98:549-55.
9. Cohen PR, Kohn SR, Kurzrock R. Association of sebaceous gland tumors and internal malignancy: the Muir-Torre syndrome. Am J Med. 1991;90:606-613.
10. Su C, Nguyen KA, Bai HX, et al. Comparison of Mohs surgery and surgical excision in the treatment of localized sebaceous carcinoma. Dermatol Surg. 2019;45:1125-1135.
New skin papules
A 49-year-old woman with a history of end-stage renal disease, uncontrolled type 2 diabetes, and congestive heart failure visited the hospital for an acute heart failure exacerbation secondary to missed dialysis appointments. On admission, her provider noted that she had tender, pruritic lesions on the extensor surface of her arms. She said they had appeared 2 to 3 months after she started dialysis. She had attempted to control the pain and pruritus with over-the-counter topical hydrocortisone and oral diphenhydramine but nothing provided relief. She was recommended for follow-up at the hospital for further examination and biopsy of one of her lesions.
At this follow-up visit, the patient noted that the lesions had spread to her left knee. Multiple firm discrete papules and nodules, with central hyperkeratotic plugs, were noted along the extensor surfaces of her forearms, left extensor knee, and around her ankles (FIGURES 1A and 1B). Some of the lesions were tender. Examination of the rest of her skin was normal. A punch biopsy was obtained.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Kyrle disease
The patient’s end-stage renal disease and type 2 diabetes—along with findings from the physical examination—led us to suspect Kyrle disease. The punch biopsy, as well as the characteristic keratotic plugs (FIGURE 2) within epidermal invagination that was bordered by hyperkeratotic epidermis, confirmed the diagnosis.

Kyrle disease (also known as hyperkeratosis follicularis et follicularis in cutem penetrans) is a rare skin condition. It is 1 of 4 skin conditions that are classified as perforating skin disorders; the other 3 are elastosis perforans serpiginosa, reactive perforating collagenosis, and perforating folliculitis (TABLE1,2).3 Perforating skin disorders share the common characteristic of transepidermal elimination of material from the upper dermis.4 These disorders are typically classified based on the nature of the eliminated material and the type of epidermal disruption.5

There are 2 forms of Kyrle disease: an inherited form often seen in childhood that is not associated with systemic disease and an acquired form that occurs in adulthood, most commonly among women ages 35 to 70 years who have systemic disease.3,4,6 The acquired form of Kyrle disease is associated with diabetes and renal failure, but there is a lack of data on its pathogenesis.7,8
Characteristic findings include discrete pruritic, dry papules and nodules with central keratotic plugs that are occasionally tender. These can manifest over the extensor surface of the extremities, trunk, face, and scalp.4,7,9 Lesions most commonly manifest on the extensor surfaces of the lower extremities.
Other conditions that feature pruritic lesions
In addition to the other perforating skin disorders described in the TABLE,1,2 the differential for Kyrle disease includes the following:
Prurigo nodularis (PN) is a skin disorder in which the manifestation of extremely pruritic nodules leads to vigorous scratching and secondary infections. These lesions typically have a grouped and symmetrically distributed appearance. They often appear on extensor surfaces of upper and lower extremities.10 PN has no known etiology, but like Kyrle disease, is associated with renal failure. Biopsy can help to distinguish PN from Kyrle disease.
Continue to: Hypertrophic lichen planus
Hypertrophic lichen planus is a pruritic skin disorder characterized by the “6 Ps”: planar, purple, polygonal, pruritic, papules, and plaques. These lesions can mimic the early stages of Kyrle disease.11 However, in the later stages of Kyrle disease, discrete papules with hyperkeratotic plugs develop, whereas large plaques will be seen with lichen planus.
Keratosis pilaris (KP) is an extremely common, yet benign, disorder in which hair follicles become keratinized.12 KP can feature rough papules that are often described as “goosebumps” or having a sandpaper–like appearance. These papules often affect the upper arms. KP usually manifests in adolescents or young adults and tends to improve with age.12 The lesions are typically smaller than those seen in Kyrle disease and are asymptomatic. In addition, KP is not associated with systemic disease.
Target symptoms and any underlying conditions
In patients who have an acquired form of the disease, symptoms may improve by
For patients whose Kyrle disease is inherited or whose underlying condition is not easily treated, there are a number of treatment options to consider. First-line treatment includes topical keratolytics (salicylic acid and urea), topical retinoids, and ultraviolet light therapy.5,7 Systemic retinoids, topical steroids, cryotherapy, electrosurgery, CO2 laser surgery, and surgical excision have also been used with some success.7,14 Oral histamines and emollients also may help to relieve the pruritus. Lesions often recur upon discontinuation of therapy.
Our patient was referred to Dermatology for ultraviolet light therapy. She was also treated with topical 12% ammonium lactate twice daily. Within a few months, she reported improvement of her symptoms.
1. Rapini R. Perforating disorders. Plastic Surgery Key. Published April 22, 2017. Accessed February 18, 2021. https://plasticsurgerykey.com/perforating-disorders/
2. Patterson JW. The perforating disorders. J Am Acad Dermatol. 1984;10:561-581
3. Azad K, Hajirnis K, Sawant S, et al. Kyrle’s disease. Indian Dermatol Online J. 2013;4:378-379.
4. Arora K, Hajirnis KA, Sawant S, et al. Perforating disorders of the skin. Indian J Pathol Microbiol. 2013;56:355-358.
5. Ataseven A, Ozturk P, Kucukosmanoglu I, et al. Kyrle’s disease. BMJ Case Rep. 2014;2014: bcr2013009905.
6. Cunningham SR, Walsh M, Matthews R. Kyrle’s disease. J Am Acad Dermatol. 1987;16(pt 1):117-123.
7. Nair PA, Jivani NB, Diwan NG. Kyrle’s disease in a patient of diabetes mellitus and chronic renal failure on dialysis. J Family Med Prim Care. 2015;4:284-286.
8. Hurwitz RM, Melton ME, Creech FT 3rd, et al. Perforating folliculitis in association with hemodialysis. Am J Dermatopathol. 1982;4:101-108.
9. Kolla PK, Desai M, Pathapati RM, et al. Cutaneous manifestations in patients with chronic kidney disease on maintenance hemodialysis. ISRN Dermatol. 2012;2012:679619.
10. Lee MR, Shumack S. Prurigo nodularis: a review. Australas J Dermatol. 2005;46:211-220.
11. Usatine RP, Tinitigan M. Diagnosis and treatment of lichen planus. Am Fam Physician. 2011;84:53-60.
12. Thomas M, Khopkar US. Keratosis pilaris revisited: is it more than just a follicular keratosis? Int J Trichology. 2012;4:255-258.
13. Chang P, Fernández V. Acquired perforating disease: report of nine cases. Int J Dermatol. 1993;32:874-876.
14. Wagner G, Sachse MM. Acquired reactive perforating dermatosis. J Dtsch Dermatol Ges. 2013;11:723-729.
A 49-year-old woman with a history of end-stage renal disease, uncontrolled type 2 diabetes, and congestive heart failure visited the hospital for an acute heart failure exacerbation secondary to missed dialysis appointments. On admission, her provider noted that she had tender, pruritic lesions on the extensor surface of her arms. She said they had appeared 2 to 3 months after she started dialysis. She had attempted to control the pain and pruritus with over-the-counter topical hydrocortisone and oral diphenhydramine but nothing provided relief. She was recommended for follow-up at the hospital for further examination and biopsy of one of her lesions.
At this follow-up visit, the patient noted that the lesions had spread to her left knee. Multiple firm discrete papules and nodules, with central hyperkeratotic plugs, were noted along the extensor surfaces of her forearms, left extensor knee, and around her ankles (FIGURES 1A and 1B). Some of the lesions were tender. Examination of the rest of her skin was normal. A punch biopsy was obtained.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Kyrle disease
The patient’s end-stage renal disease and type 2 diabetes—along with findings from the physical examination—led us to suspect Kyrle disease. The punch biopsy, as well as the characteristic keratotic plugs (FIGURE 2) within epidermal invagination that was bordered by hyperkeratotic epidermis, confirmed the diagnosis.

Kyrle disease (also known as hyperkeratosis follicularis et follicularis in cutem penetrans) is a rare skin condition. It is 1 of 4 skin conditions that are classified as perforating skin disorders; the other 3 are elastosis perforans serpiginosa, reactive perforating collagenosis, and perforating folliculitis (TABLE1,2).3 Perforating skin disorders share the common characteristic of transepidermal elimination of material from the upper dermis.4 These disorders are typically classified based on the nature of the eliminated material and the type of epidermal disruption.5

There are 2 forms of Kyrle disease: an inherited form often seen in childhood that is not associated with systemic disease and an acquired form that occurs in adulthood, most commonly among women ages 35 to 70 years who have systemic disease.3,4,6 The acquired form of Kyrle disease is associated with diabetes and renal failure, but there is a lack of data on its pathogenesis.7,8
Characteristic findings include discrete pruritic, dry papules and nodules with central keratotic plugs that are occasionally tender. These can manifest over the extensor surface of the extremities, trunk, face, and scalp.4,7,9 Lesions most commonly manifest on the extensor surfaces of the lower extremities.
Other conditions that feature pruritic lesions
In addition to the other perforating skin disorders described in the TABLE,1,2 the differential for Kyrle disease includes the following:
Prurigo nodularis (PN) is a skin disorder in which the manifestation of extremely pruritic nodules leads to vigorous scratching and secondary infections. These lesions typically have a grouped and symmetrically distributed appearance. They often appear on extensor surfaces of upper and lower extremities.10 PN has no known etiology, but like Kyrle disease, is associated with renal failure. Biopsy can help to distinguish PN from Kyrle disease.
Continue to: Hypertrophic lichen planus
Hypertrophic lichen planus is a pruritic skin disorder characterized by the “6 Ps”: planar, purple, polygonal, pruritic, papules, and plaques. These lesions can mimic the early stages of Kyrle disease.11 However, in the later stages of Kyrle disease, discrete papules with hyperkeratotic plugs develop, whereas large plaques will be seen with lichen planus.
Keratosis pilaris (KP) is an extremely common, yet benign, disorder in which hair follicles become keratinized.12 KP can feature rough papules that are often described as “goosebumps” or having a sandpaper–like appearance. These papules often affect the upper arms. KP usually manifests in adolescents or young adults and tends to improve with age.12 The lesions are typically smaller than those seen in Kyrle disease and are asymptomatic. In addition, KP is not associated with systemic disease.
Target symptoms and any underlying conditions
In patients who have an acquired form of the disease, symptoms may improve by
For patients whose Kyrle disease is inherited or whose underlying condition is not easily treated, there are a number of treatment options to consider. First-line treatment includes topical keratolytics (salicylic acid and urea), topical retinoids, and ultraviolet light therapy.5,7 Systemic retinoids, topical steroids, cryotherapy, electrosurgery, CO2 laser surgery, and surgical excision have also been used with some success.7,14 Oral histamines and emollients also may help to relieve the pruritus. Lesions often recur upon discontinuation of therapy.
Our patient was referred to Dermatology for ultraviolet light therapy. She was also treated with topical 12% ammonium lactate twice daily. Within a few months, she reported improvement of her symptoms.
A 49-year-old woman with a history of end-stage renal disease, uncontrolled type 2 diabetes, and congestive heart failure visited the hospital for an acute heart failure exacerbation secondary to missed dialysis appointments. On admission, her provider noted that she had tender, pruritic lesions on the extensor surface of her arms. She said they had appeared 2 to 3 months after she started dialysis. She had attempted to control the pain and pruritus with over-the-counter topical hydrocortisone and oral diphenhydramine but nothing provided relief. She was recommended for follow-up at the hospital for further examination and biopsy of one of her lesions.
At this follow-up visit, the patient noted that the lesions had spread to her left knee. Multiple firm discrete papules and nodules, with central hyperkeratotic plugs, were noted along the extensor surfaces of her forearms, left extensor knee, and around her ankles (FIGURES 1A and 1B). Some of the lesions were tender. Examination of the rest of her skin was normal. A punch biopsy was obtained.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Kyrle disease
The patient’s end-stage renal disease and type 2 diabetes—along with findings from the physical examination—led us to suspect Kyrle disease. The punch biopsy, as well as the characteristic keratotic plugs (FIGURE 2) within epidermal invagination that was bordered by hyperkeratotic epidermis, confirmed the diagnosis.

Kyrle disease (also known as hyperkeratosis follicularis et follicularis in cutem penetrans) is a rare skin condition. It is 1 of 4 skin conditions that are classified as perforating skin disorders; the other 3 are elastosis perforans serpiginosa, reactive perforating collagenosis, and perforating folliculitis (TABLE1,2).3 Perforating skin disorders share the common characteristic of transepidermal elimination of material from the upper dermis.4 These disorders are typically classified based on the nature of the eliminated material and the type of epidermal disruption.5

There are 2 forms of Kyrle disease: an inherited form often seen in childhood that is not associated with systemic disease and an acquired form that occurs in adulthood, most commonly among women ages 35 to 70 years who have systemic disease.3,4,6 The acquired form of Kyrle disease is associated with diabetes and renal failure, but there is a lack of data on its pathogenesis.7,8
Characteristic findings include discrete pruritic, dry papules and nodules with central keratotic plugs that are occasionally tender. These can manifest over the extensor surface of the extremities, trunk, face, and scalp.4,7,9 Lesions most commonly manifest on the extensor surfaces of the lower extremities.
Other conditions that feature pruritic lesions
In addition to the other perforating skin disorders described in the TABLE,1,2 the differential for Kyrle disease includes the following:
Prurigo nodularis (PN) is a skin disorder in which the manifestation of extremely pruritic nodules leads to vigorous scratching and secondary infections. These lesions typically have a grouped and symmetrically distributed appearance. They often appear on extensor surfaces of upper and lower extremities.10 PN has no known etiology, but like Kyrle disease, is associated with renal failure. Biopsy can help to distinguish PN from Kyrle disease.
Continue to: Hypertrophic lichen planus
Hypertrophic lichen planus is a pruritic skin disorder characterized by the “6 Ps”: planar, purple, polygonal, pruritic, papules, and plaques. These lesions can mimic the early stages of Kyrle disease.11 However, in the later stages of Kyrle disease, discrete papules with hyperkeratotic plugs develop, whereas large plaques will be seen with lichen planus.
Keratosis pilaris (KP) is an extremely common, yet benign, disorder in which hair follicles become keratinized.12 KP can feature rough papules that are often described as “goosebumps” or having a sandpaper–like appearance. These papules often affect the upper arms. KP usually manifests in adolescents or young adults and tends to improve with age.12 The lesions are typically smaller than those seen in Kyrle disease and are asymptomatic. In addition, KP is not associated with systemic disease.
Target symptoms and any underlying conditions
In patients who have an acquired form of the disease, symptoms may improve by
For patients whose Kyrle disease is inherited or whose underlying condition is not easily treated, there are a number of treatment options to consider. First-line treatment includes topical keratolytics (salicylic acid and urea), topical retinoids, and ultraviolet light therapy.5,7 Systemic retinoids, topical steroids, cryotherapy, electrosurgery, CO2 laser surgery, and surgical excision have also been used with some success.7,14 Oral histamines and emollients also may help to relieve the pruritus. Lesions often recur upon discontinuation of therapy.
Our patient was referred to Dermatology for ultraviolet light therapy. She was also treated with topical 12% ammonium lactate twice daily. Within a few months, she reported improvement of her symptoms.
1. Rapini R. Perforating disorders. Plastic Surgery Key. Published April 22, 2017. Accessed February 18, 2021. https://plasticsurgerykey.com/perforating-disorders/
2. Patterson JW. The perforating disorders. J Am Acad Dermatol. 1984;10:561-581
3. Azad K, Hajirnis K, Sawant S, et al. Kyrle’s disease. Indian Dermatol Online J. 2013;4:378-379.
4. Arora K, Hajirnis KA, Sawant S, et al. Perforating disorders of the skin. Indian J Pathol Microbiol. 2013;56:355-358.
5. Ataseven A, Ozturk P, Kucukosmanoglu I, et al. Kyrle’s disease. BMJ Case Rep. 2014;2014: bcr2013009905.
6. Cunningham SR, Walsh M, Matthews R. Kyrle’s disease. J Am Acad Dermatol. 1987;16(pt 1):117-123.
7. Nair PA, Jivani NB, Diwan NG. Kyrle’s disease in a patient of diabetes mellitus and chronic renal failure on dialysis. J Family Med Prim Care. 2015;4:284-286.
8. Hurwitz RM, Melton ME, Creech FT 3rd, et al. Perforating folliculitis in association with hemodialysis. Am J Dermatopathol. 1982;4:101-108.
9. Kolla PK, Desai M, Pathapati RM, et al. Cutaneous manifestations in patients with chronic kidney disease on maintenance hemodialysis. ISRN Dermatol. 2012;2012:679619.
10. Lee MR, Shumack S. Prurigo nodularis: a review. Australas J Dermatol. 2005;46:211-220.
11. Usatine RP, Tinitigan M. Diagnosis and treatment of lichen planus. Am Fam Physician. 2011;84:53-60.
12. Thomas M, Khopkar US. Keratosis pilaris revisited: is it more than just a follicular keratosis? Int J Trichology. 2012;4:255-258.
13. Chang P, Fernández V. Acquired perforating disease: report of nine cases. Int J Dermatol. 1993;32:874-876.
14. Wagner G, Sachse MM. Acquired reactive perforating dermatosis. J Dtsch Dermatol Ges. 2013;11:723-729.
1. Rapini R. Perforating disorders. Plastic Surgery Key. Published April 22, 2017. Accessed February 18, 2021. https://plasticsurgerykey.com/perforating-disorders/
2. Patterson JW. The perforating disorders. J Am Acad Dermatol. 1984;10:561-581
3. Azad K, Hajirnis K, Sawant S, et al. Kyrle’s disease. Indian Dermatol Online J. 2013;4:378-379.
4. Arora K, Hajirnis KA, Sawant S, et al. Perforating disorders of the skin. Indian J Pathol Microbiol. 2013;56:355-358.
5. Ataseven A, Ozturk P, Kucukosmanoglu I, et al. Kyrle’s disease. BMJ Case Rep. 2014;2014: bcr2013009905.
6. Cunningham SR, Walsh M, Matthews R. Kyrle’s disease. J Am Acad Dermatol. 1987;16(pt 1):117-123.
7. Nair PA, Jivani NB, Diwan NG. Kyrle’s disease in a patient of diabetes mellitus and chronic renal failure on dialysis. J Family Med Prim Care. 2015;4:284-286.
8. Hurwitz RM, Melton ME, Creech FT 3rd, et al. Perforating folliculitis in association with hemodialysis. Am J Dermatopathol. 1982;4:101-108.
9. Kolla PK, Desai M, Pathapati RM, et al. Cutaneous manifestations in patients with chronic kidney disease on maintenance hemodialysis. ISRN Dermatol. 2012;2012:679619.
10. Lee MR, Shumack S. Prurigo nodularis: a review. Australas J Dermatol. 2005;46:211-220.
11. Usatine RP, Tinitigan M. Diagnosis and treatment of lichen planus. Am Fam Physician. 2011;84:53-60.
12. Thomas M, Khopkar US. Keratosis pilaris revisited: is it more than just a follicular keratosis? Int J Trichology. 2012;4:255-258.
13. Chang P, Fernández V. Acquired perforating disease: report of nine cases. Int J Dermatol. 1993;32:874-876.
14. Wagner G, Sachse MM. Acquired reactive perforating dermatosis. J Dtsch Dermatol Ges. 2013;11:723-729.
Big data ‘clinch’ link between high glycemic index diets and CVD
People who mostly ate foods with a low glycemic index had a lower likelihood of premature death and major cardiovascular disease (CVD) events, compared with those whose diet included more “poor-quality” food with a high glycemic index.
The results from the global PURE study of nearly 120,000 people provide evidence that helps cement glycemic index as a key measure of dietary health.
This new analysis from PURE (Prospective Urban and Rural Epidemiological Study) – a massive prospective epidemiologic study – shows people with a diet in the highest quintile of glycemic index had a significant 25% higher rate of combined total deaths and major CVD events during a median follow-up of nearly 10 years, compared with those with a diet in the lowest glycemic index quintile, in the report published online on Feb. 24, 2021, in the New England Journal of Medicine.
David J.A. Jenkins, MD, PhD, DSc, lead author, said people do not necessarily need to closely track the glycemic index of what they eat to follow the guidance that lower is better.
The link between lower glycemic load and fewer CVD events was even stronger among people with an established history of CVD at study entry. In this subset, which included 9% of the total cohort, people in the highest quintile for glycemic index consumption had a 51% higher rate of the composite primary endpoint, compared with those in the lowest quintile, in an analysis that adjusted for several potential confounders.
A simple but accurate and effective public health message is to follow existing dietary recommendations to eat better-quality food – more unprocessed fruits, vegetables, legumes, and whole grains – Dr. Jenkins advised. Those who prefer a more detailed approach could use the comprehensive glycemic index tables compiled by researchers at the University of Sydney.
‘All carbohydrates are not the same’
“What we’re saying is that all carbohydrates are not the same. Some seem to increase the risk for CVD, and others seem protective. This is not new, but worth restating in an era of low-carb and no-carb diets,” said Dr. Jenkins.
Low-glycemic-index foods are generally unprocessed foods in their native state, including fruits, vegetables, legumes, and unrefined whole grains. High-glycemic-index foods contain processed and refined carbohydrates that deliver jolts of glucose soon after eating, as the sugar in these carbohydrates quickly moves from the gut to the bloodstream.
An association between a diet with a lower glycemic index and better outcomes had appeared in prior reports from other studies, but not as unambiguously as in the new data from PURE, likely because of fewer study participants in previous studies.
Another feature of PURE that adds to the generalizability of the findings is the diversity of adults included in the study, from 20 countries on five continents.
“This clinches it,” Dr. Jenkins declared in an interview.
New PURE data tip the evidence balance
The NEJM article includes a new meta-analysis that adds the PURE findings to data from two large prior reports that were each less conclusive. The new calculation with the PURE numbers helps establish a clearer association between a diet with a higher glycemic index and the endpoint of CVD death, showing an overall 26% increase in the outcome.
The PURE data are especially informative because the investigators collected additional information on a range of potential confounders they incorporated into their analyses.
“We were able to include a lot of documentation on many potential confounders. That’s a strength of our data,” noted Dr. Jenkins, a professor of nutritional science and medicine at the University of Toronto.
“The present data, along with prior publications from PURE and several other studies, emphasize that consumption of poor quality carbohydrates is likely to be more adverse than the consumption of most fats in the diet,” said senior author Salim Yusuf, MD, DPhil, professor of medicine and executive director of the Population Health Research Institute at McMaster University, Hamilton, Ont.
“This calls for a fundamental shift in our thinking of what types of diet are likely to be harmful and what types neutral or beneficial,” Dr. Yusuf said in a statement from his institution.
Higher BMI associated with greater glycemic index effect
Another important analysis in the new report calculated the impact of a higher glycemic index diet among people with a body mass index (BMI) of less than 25 kg/m2 as well as higher BMIs.
Among people in the lower BMI subgroup, greater intake of high-glycemic-index foods showed slightly more incident primary outcome events. In contrast, people with a BMI of 25 or greater showed a steady increment in primary outcome events as the glycemic index of their diet increased.
People with higher BMIs in the quartile that ate the greatest amount of high-glycemic =-index foods had a significant 38% higher rate of primary outcome events, compared with people with similar BMIs in the lowest quartile for high-glycemic-index intake.
However, the study showed no impact on the primary association of high glycemic index and increased adverse outcomes by exercise habits, smoking, use of blood pressure medications, or use of statins.
The new report complements a separate analysis from PURE published just a few weeks earlier in the BMJ that established a significant association between increased consumption of whole grains and fewer CVD events, compared with people who had more refined grains in their diet, as reported by this news organization.
This prior report on whole versus refined grains, which Dr. Jenkins coauthored, looked at carbohydrate quality using a two-pronged approach, while glycemic index is a continuous variable that provides more nuance and takes into account carbohydrates from sources other than grains, Dr. Jenkins said.
PURE enrolled roughly 225,000 people aged 35-70 years at entry. The glycemic index analysis focused on 119,575 people who had data available for the primary outcome. During a median follow-up of 9.5 years, these people had 14,075 primary outcome events, including 8,780 deaths.
Analyses that looked at the individual outcomes that comprised the composite endpoint showed significant associations between a high-glycemic-index diet and total mortality, CVD death, non-CVD death, and stroke, but showed no significant link with myocardial infarction or heart failure. These findings are consistent with prior results of other studies that showed a stronger link between stroke and a high glycemic index diet, compared with other nonfatal CVD events.
Dr. Jenkins suggested that the significant excess of non-CVD deaths linked with a high-glycemic-index diet may stem from the impact of this type of diet on cancer-associated mortality.
PURE received partial funding through unrestricted grants from several drug companies. Dr. Jenkins has reported receiving gifts from several food-related trade associations and food companies, as well as research grants from two legume-oriented trade associations.
A version of this article first appeared on Medscape.com.
People who mostly ate foods with a low glycemic index had a lower likelihood of premature death and major cardiovascular disease (CVD) events, compared with those whose diet included more “poor-quality” food with a high glycemic index.
The results from the global PURE study of nearly 120,000 people provide evidence that helps cement glycemic index as a key measure of dietary health.
This new analysis from PURE (Prospective Urban and Rural Epidemiological Study) – a massive prospective epidemiologic study – shows people with a diet in the highest quintile of glycemic index had a significant 25% higher rate of combined total deaths and major CVD events during a median follow-up of nearly 10 years, compared with those with a diet in the lowest glycemic index quintile, in the report published online on Feb. 24, 2021, in the New England Journal of Medicine.
David J.A. Jenkins, MD, PhD, DSc, lead author, said people do not necessarily need to closely track the glycemic index of what they eat to follow the guidance that lower is better.
The link between lower glycemic load and fewer CVD events was even stronger among people with an established history of CVD at study entry. In this subset, which included 9% of the total cohort, people in the highest quintile for glycemic index consumption had a 51% higher rate of the composite primary endpoint, compared with those in the lowest quintile, in an analysis that adjusted for several potential confounders.
A simple but accurate and effective public health message is to follow existing dietary recommendations to eat better-quality food – more unprocessed fruits, vegetables, legumes, and whole grains – Dr. Jenkins advised. Those who prefer a more detailed approach could use the comprehensive glycemic index tables compiled by researchers at the University of Sydney.
‘All carbohydrates are not the same’
“What we’re saying is that all carbohydrates are not the same. Some seem to increase the risk for CVD, and others seem protective. This is not new, but worth restating in an era of low-carb and no-carb diets,” said Dr. Jenkins.
Low-glycemic-index foods are generally unprocessed foods in their native state, including fruits, vegetables, legumes, and unrefined whole grains. High-glycemic-index foods contain processed and refined carbohydrates that deliver jolts of glucose soon after eating, as the sugar in these carbohydrates quickly moves from the gut to the bloodstream.
An association between a diet with a lower glycemic index and better outcomes had appeared in prior reports from other studies, but not as unambiguously as in the new data from PURE, likely because of fewer study participants in previous studies.
Another feature of PURE that adds to the generalizability of the findings is the diversity of adults included in the study, from 20 countries on five continents.
“This clinches it,” Dr. Jenkins declared in an interview.
New PURE data tip the evidence balance
The NEJM article includes a new meta-analysis that adds the PURE findings to data from two large prior reports that were each less conclusive. The new calculation with the PURE numbers helps establish a clearer association between a diet with a higher glycemic index and the endpoint of CVD death, showing an overall 26% increase in the outcome.
The PURE data are especially informative because the investigators collected additional information on a range of potential confounders they incorporated into their analyses.
“We were able to include a lot of documentation on many potential confounders. That’s a strength of our data,” noted Dr. Jenkins, a professor of nutritional science and medicine at the University of Toronto.
“The present data, along with prior publications from PURE and several other studies, emphasize that consumption of poor quality carbohydrates is likely to be more adverse than the consumption of most fats in the diet,” said senior author Salim Yusuf, MD, DPhil, professor of medicine and executive director of the Population Health Research Institute at McMaster University, Hamilton, Ont.
“This calls for a fundamental shift in our thinking of what types of diet are likely to be harmful and what types neutral or beneficial,” Dr. Yusuf said in a statement from his institution.
Higher BMI associated with greater glycemic index effect
Another important analysis in the new report calculated the impact of a higher glycemic index diet among people with a body mass index (BMI) of less than 25 kg/m2 as well as higher BMIs.
Among people in the lower BMI subgroup, greater intake of high-glycemic-index foods showed slightly more incident primary outcome events. In contrast, people with a BMI of 25 or greater showed a steady increment in primary outcome events as the glycemic index of their diet increased.
People with higher BMIs in the quartile that ate the greatest amount of high-glycemic =-index foods had a significant 38% higher rate of primary outcome events, compared with people with similar BMIs in the lowest quartile for high-glycemic-index intake.
However, the study showed no impact on the primary association of high glycemic index and increased adverse outcomes by exercise habits, smoking, use of blood pressure medications, or use of statins.
The new report complements a separate analysis from PURE published just a few weeks earlier in the BMJ that established a significant association between increased consumption of whole grains and fewer CVD events, compared with people who had more refined grains in their diet, as reported by this news organization.
This prior report on whole versus refined grains, which Dr. Jenkins coauthored, looked at carbohydrate quality using a two-pronged approach, while glycemic index is a continuous variable that provides more nuance and takes into account carbohydrates from sources other than grains, Dr. Jenkins said.
PURE enrolled roughly 225,000 people aged 35-70 years at entry. The glycemic index analysis focused on 119,575 people who had data available for the primary outcome. During a median follow-up of 9.5 years, these people had 14,075 primary outcome events, including 8,780 deaths.
Analyses that looked at the individual outcomes that comprised the composite endpoint showed significant associations between a high-glycemic-index diet and total mortality, CVD death, non-CVD death, and stroke, but showed no significant link with myocardial infarction or heart failure. These findings are consistent with prior results of other studies that showed a stronger link between stroke and a high glycemic index diet, compared with other nonfatal CVD events.
Dr. Jenkins suggested that the significant excess of non-CVD deaths linked with a high-glycemic-index diet may stem from the impact of this type of diet on cancer-associated mortality.
PURE received partial funding through unrestricted grants from several drug companies. Dr. Jenkins has reported receiving gifts from several food-related trade associations and food companies, as well as research grants from two legume-oriented trade associations.
A version of this article first appeared on Medscape.com.
People who mostly ate foods with a low glycemic index had a lower likelihood of premature death and major cardiovascular disease (CVD) events, compared with those whose diet included more “poor-quality” food with a high glycemic index.
The results from the global PURE study of nearly 120,000 people provide evidence that helps cement glycemic index as a key measure of dietary health.
This new analysis from PURE (Prospective Urban and Rural Epidemiological Study) – a massive prospective epidemiologic study – shows people with a diet in the highest quintile of glycemic index had a significant 25% higher rate of combined total deaths and major CVD events during a median follow-up of nearly 10 years, compared with those with a diet in the lowest glycemic index quintile, in the report published online on Feb. 24, 2021, in the New England Journal of Medicine.
David J.A. Jenkins, MD, PhD, DSc, lead author, said people do not necessarily need to closely track the glycemic index of what they eat to follow the guidance that lower is better.
The link between lower glycemic load and fewer CVD events was even stronger among people with an established history of CVD at study entry. In this subset, which included 9% of the total cohort, people in the highest quintile for glycemic index consumption had a 51% higher rate of the composite primary endpoint, compared with those in the lowest quintile, in an analysis that adjusted for several potential confounders.
A simple but accurate and effective public health message is to follow existing dietary recommendations to eat better-quality food – more unprocessed fruits, vegetables, legumes, and whole grains – Dr. Jenkins advised. Those who prefer a more detailed approach could use the comprehensive glycemic index tables compiled by researchers at the University of Sydney.
‘All carbohydrates are not the same’
“What we’re saying is that all carbohydrates are not the same. Some seem to increase the risk for CVD, and others seem protective. This is not new, but worth restating in an era of low-carb and no-carb diets,” said Dr. Jenkins.
Low-glycemic-index foods are generally unprocessed foods in their native state, including fruits, vegetables, legumes, and unrefined whole grains. High-glycemic-index foods contain processed and refined carbohydrates that deliver jolts of glucose soon after eating, as the sugar in these carbohydrates quickly moves from the gut to the bloodstream.
An association between a diet with a lower glycemic index and better outcomes had appeared in prior reports from other studies, but not as unambiguously as in the new data from PURE, likely because of fewer study participants in previous studies.
Another feature of PURE that adds to the generalizability of the findings is the diversity of adults included in the study, from 20 countries on five continents.
“This clinches it,” Dr. Jenkins declared in an interview.
New PURE data tip the evidence balance
The NEJM article includes a new meta-analysis that adds the PURE findings to data from two large prior reports that were each less conclusive. The new calculation with the PURE numbers helps establish a clearer association between a diet with a higher glycemic index and the endpoint of CVD death, showing an overall 26% increase in the outcome.
The PURE data are especially informative because the investigators collected additional information on a range of potential confounders they incorporated into their analyses.
“We were able to include a lot of documentation on many potential confounders. That’s a strength of our data,” noted Dr. Jenkins, a professor of nutritional science and medicine at the University of Toronto.
“The present data, along with prior publications from PURE and several other studies, emphasize that consumption of poor quality carbohydrates is likely to be more adverse than the consumption of most fats in the diet,” said senior author Salim Yusuf, MD, DPhil, professor of medicine and executive director of the Population Health Research Institute at McMaster University, Hamilton, Ont.
“This calls for a fundamental shift in our thinking of what types of diet are likely to be harmful and what types neutral or beneficial,” Dr. Yusuf said in a statement from his institution.
Higher BMI associated with greater glycemic index effect
Another important analysis in the new report calculated the impact of a higher glycemic index diet among people with a body mass index (BMI) of less than 25 kg/m2 as well as higher BMIs.
Among people in the lower BMI subgroup, greater intake of high-glycemic-index foods showed slightly more incident primary outcome events. In contrast, people with a BMI of 25 or greater showed a steady increment in primary outcome events as the glycemic index of their diet increased.
People with higher BMIs in the quartile that ate the greatest amount of high-glycemic =-index foods had a significant 38% higher rate of primary outcome events, compared with people with similar BMIs in the lowest quartile for high-glycemic-index intake.
However, the study showed no impact on the primary association of high glycemic index and increased adverse outcomes by exercise habits, smoking, use of blood pressure medications, or use of statins.
The new report complements a separate analysis from PURE published just a few weeks earlier in the BMJ that established a significant association between increased consumption of whole grains and fewer CVD events, compared with people who had more refined grains in their diet, as reported by this news organization.
This prior report on whole versus refined grains, which Dr. Jenkins coauthored, looked at carbohydrate quality using a two-pronged approach, while glycemic index is a continuous variable that provides more nuance and takes into account carbohydrates from sources other than grains, Dr. Jenkins said.
PURE enrolled roughly 225,000 people aged 35-70 years at entry. The glycemic index analysis focused on 119,575 people who had data available for the primary outcome. During a median follow-up of 9.5 years, these people had 14,075 primary outcome events, including 8,780 deaths.
Analyses that looked at the individual outcomes that comprised the composite endpoint showed significant associations between a high-glycemic-index diet and total mortality, CVD death, non-CVD death, and stroke, but showed no significant link with myocardial infarction or heart failure. These findings are consistent with prior results of other studies that showed a stronger link between stroke and a high glycemic index diet, compared with other nonfatal CVD events.
Dr. Jenkins suggested that the significant excess of non-CVD deaths linked with a high-glycemic-index diet may stem from the impact of this type of diet on cancer-associated mortality.
PURE received partial funding through unrestricted grants from several drug companies. Dr. Jenkins has reported receiving gifts from several food-related trade associations and food companies, as well as research grants from two legume-oriented trade associations.
A version of this article first appeared on Medscape.com.
Painless Mobile Nodule on the Shoulder
The Diagnosis: Cutaneous Metaplastic Synovial Cyst
Gross examination of the excised nodule revealed a 2.5×1.2×1.0-cm, intact, gray-white, thin-walled, smooth-lined nodule filled with clear mucinouslike material. Hematoxylin and eosin-stained sections demonstrated a dermal-based cystlike structure composed of a lining of connective tissue with hyalinized material and fibrin as well as spindle and epithelioid cells with a mild mixed inflammatory infiltrate (Figure). These histopathologic findings led to the diagnosis of cutaneous metaplastic synovial cyst (CMSC).
Cutaneous metaplastic synovial cyst, also known as synovial metaplasia of the skin, is an uncommon benign cystic lesion that was first reported by Gonzalez et al1 in 1987. Histologically, CMSC lacks an epithelial lining and therefore is not a true cyst but rather a pseudocyst.2 Clinically, the lesion typically presents as a solitary subcutaneous nodule that may be tender or painless. In a literature review of CMSC cases performed by Fukuyama et al,3 distribution of reported cases according to body site varied; however, limbs were found to be the most commonly involved area. A PubMed search of articles indexed for MEDLINE as well as a Google Scholar search using the term cutaneous metaplastic synovial cyst revealed at least 37 cases reported in the English-language literature,3-9 including our present case. The pathogenesis remains uncertain; however, a majority of previously reported cases of CMSC characteristically have been associated with a pre-existing lesion, with most presentations developing at surgical scar sites secondary to operation or trauma.5 Relative tissue fragility secondary to rheumatoid arthritis10 and Ehlers-Danlos syndrome9,11,12 has been linked to CMSC in some documented reports, while a minority of cases report no antecedent events triggering formation of the lesion.13-15
As evidenced by our patient, CMSC clinically mimics several other benign entities; histopathologic examination is necessary to confirm the diagnosis. Although nodular hidradenoma also may clinically present as a solitary firm intradermal nodule, microscopy reveals a dermal-based lobulated tumor containing cystic spaces and solid areas composed of basophilic polyhedral cells and round glycogen-filled clear cells.16 Epidermoid cysts are differentiated from CMSC by the presence of a cyst wall lining composed of stratified squamous epithelium and associated laminated keratin within the lumen,17 which corresponds to its pearly white appearance on gross examination. Cutaneous ciliated cysts predominantly occur on the lower extremities of young women and are lined by simple cuboidal or columnar ciliated cells that resemble müllerian epithelium.18 Similar to CMSC, ganglion cysts are pseudocysts that lack a true epithelial lining but differ in appearance due to their mucin-filled synovial-lined sac.19 Additionally, ganglion cysts most often occur on the dorsal and volar aspects of the wrist.
Excisional biopsy is indicated as the preferred treatment of CMSC, given the lesion's benign behavior and low recurrence rate.6 Our case highlights this rare entity and reinforces its inclusion in the differential diagnosis of subcutaneous mobile nodules, especially in the setting of prior tissue injury secondary to trauma, surgical procedures, or conditions such as rheumatoid arthritis or Ehlers-Danlos syndrome. Unlike most previously reported cases, our patient reported no preceding tissue injury associated with formation of the lesion, and she was largely asymptomatic on presentation. Considering the limited number of CMSC cases demonstrated in the literature, it is important to continue reporting new cases to better understand characteristics and presentations of this uncommon lesion.
- Gonzalez JG, Ghiselli RW, Santa Cruz DJ. Synovial metaplasia of the skin. Am J Surg Pathol. 1987;11:343-350.
- Calonje E, Brenn T, Lazar A, et al. Cutaneous cysts. In: Calonje E, Brenn T, Lazar A, et al. McKee's Pathology of the Skin. 5th ed. Elsevier Limited; 2020:1680-1697.
- Fukuyama M, Sato Y, Hayakawa J, et al. Cutaneous metaplastic synovial cyst: case report and literature review from the dermatological point of view. Keio J Med. 2016;66:9-13.
- Karaytug K, Kapicioglu M, Can N, et al. Unprecedented recurrence of carpal tunnel syndrome by metaplastic synovial cyst in the carpal tunnel. Acta Orthop Traumatol Turc. 2019;53:230-232.
- Martelli SJ, Silveira FM, Carvalho PH, et al. Asymptomatic subcutaneous swelling of lower face. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019;128:101-105.
- Majdi M, Saffar H, Ghanadan A. Cutaneous metaplastic synovial cyst: a case report. Iran J Pathol. 2016;11:423-426.
- Ramachandra S, Rao L, Al-Kindi M. Cutaneous metaplastic synovial cyst. Sultan Qaboos Univ Med J. 2016;16:E117-E118.
- Heidarian A, Xie Q, Banihashemi A. Cutaneous metaplastic synovial cyst presenting as an axillary mass after modified mastectomy and adjuvant radiotherapy. Am J Clin Pathol. 2016;146:S2.
- Fernandez-Flores A, Barja-Lopez JM. Cutaneous metaplastic synovial cyst in Ehlers-Danlos syndrome. J Cutan Pathol. 2020;47:729-733.
- Choonhakarn C, Tang S. Cutaneous metaplastic synovial cyst. J Dermatol. 2003;30:480-484.
- Guala A, Viglio S, Ottinetti A, et al. Cutaneous metaplastic synovial cyst in Ehlers-Danlos syndrome: report of a second case. Am J Dermatopathol. 2008;30:59-61.
- Nieto S, Buezo GF, Jones-Caballero M, et al. Cutaneous metaplastic synovial cyst in an Ehlers-Danlos patient. Am J Dermatopathol. 1997;19:407-410.
- Goiriz R, Rios-Buceta L, Alonso-Perez A, et al. Cutaneous metaplastic synovial cyst. J Am Acad Dermatol. 2005;53:180-181.
- Kim BC, Choi WJ, Park EJ, et al. Cutaneous metaplastic synovial cyst of the first metatarsal head area. Ann Dermatol. 2011;23(suppl 2):S165-S168.
- Yang HC, Tsai YJ, Hu SL, et al. Cutaneous metaplastic synovial cyst--a case report and review of literature. Dermatol Sinica. 2003;21:275-279.
- Kataria SP, Singh G, Batra A, et al. Nodular hidradenoma: a series of five cases in male subjects and review of literature. Adv Cytol Pathol. 2018;3:46-47.
- Mohamed Haflah N, Mohd Kassim A, Hassan Shukur M. Giant epidermoid cyst of the thigh. Malays Orthop J. 2011;5:17-19.
- Torisu-Itakura H, Itakura E, Horiuchi R, et al. Cutaneous ciliated cyst on the leg of a woman of menopausal age. Acta Derm Venereol. 2009;89:323-324.
- Fullen DR. Cysts and sinuses. In: Busam K, ed. Dermatopathology. Saunders; 2010:300-330.
The Diagnosis: Cutaneous Metaplastic Synovial Cyst
Gross examination of the excised nodule revealed a 2.5×1.2×1.0-cm, intact, gray-white, thin-walled, smooth-lined nodule filled with clear mucinouslike material. Hematoxylin and eosin-stained sections demonstrated a dermal-based cystlike structure composed of a lining of connective tissue with hyalinized material and fibrin as well as spindle and epithelioid cells with a mild mixed inflammatory infiltrate (Figure). These histopathologic findings led to the diagnosis of cutaneous metaplastic synovial cyst (CMSC).
Cutaneous metaplastic synovial cyst, also known as synovial metaplasia of the skin, is an uncommon benign cystic lesion that was first reported by Gonzalez et al1 in 1987. Histologically, CMSC lacks an epithelial lining and therefore is not a true cyst but rather a pseudocyst.2 Clinically, the lesion typically presents as a solitary subcutaneous nodule that may be tender or painless. In a literature review of CMSC cases performed by Fukuyama et al,3 distribution of reported cases according to body site varied; however, limbs were found to be the most commonly involved area. A PubMed search of articles indexed for MEDLINE as well as a Google Scholar search using the term cutaneous metaplastic synovial cyst revealed at least 37 cases reported in the English-language literature,3-9 including our present case. The pathogenesis remains uncertain; however, a majority of previously reported cases of CMSC characteristically have been associated with a pre-existing lesion, with most presentations developing at surgical scar sites secondary to operation or trauma.5 Relative tissue fragility secondary to rheumatoid arthritis10 and Ehlers-Danlos syndrome9,11,12 has been linked to CMSC in some documented reports, while a minority of cases report no antecedent events triggering formation of the lesion.13-15
As evidenced by our patient, CMSC clinically mimics several other benign entities; histopathologic examination is necessary to confirm the diagnosis. Although nodular hidradenoma also may clinically present as a solitary firm intradermal nodule, microscopy reveals a dermal-based lobulated tumor containing cystic spaces and solid areas composed of basophilic polyhedral cells and round glycogen-filled clear cells.16 Epidermoid cysts are differentiated from CMSC by the presence of a cyst wall lining composed of stratified squamous epithelium and associated laminated keratin within the lumen,17 which corresponds to its pearly white appearance on gross examination. Cutaneous ciliated cysts predominantly occur on the lower extremities of young women and are lined by simple cuboidal or columnar ciliated cells that resemble müllerian epithelium.18 Similar to CMSC, ganglion cysts are pseudocysts that lack a true epithelial lining but differ in appearance due to their mucin-filled synovial-lined sac.19 Additionally, ganglion cysts most often occur on the dorsal and volar aspects of the wrist.
Excisional biopsy is indicated as the preferred treatment of CMSC, given the lesion's benign behavior and low recurrence rate.6 Our case highlights this rare entity and reinforces its inclusion in the differential diagnosis of subcutaneous mobile nodules, especially in the setting of prior tissue injury secondary to trauma, surgical procedures, or conditions such as rheumatoid arthritis or Ehlers-Danlos syndrome. Unlike most previously reported cases, our patient reported no preceding tissue injury associated with formation of the lesion, and she was largely asymptomatic on presentation. Considering the limited number of CMSC cases demonstrated in the literature, it is important to continue reporting new cases to better understand characteristics and presentations of this uncommon lesion.
The Diagnosis: Cutaneous Metaplastic Synovial Cyst
Gross examination of the excised nodule revealed a 2.5×1.2×1.0-cm, intact, gray-white, thin-walled, smooth-lined nodule filled with clear mucinouslike material. Hematoxylin and eosin-stained sections demonstrated a dermal-based cystlike structure composed of a lining of connective tissue with hyalinized material and fibrin as well as spindle and epithelioid cells with a mild mixed inflammatory infiltrate (Figure). These histopathologic findings led to the diagnosis of cutaneous metaplastic synovial cyst (CMSC).
Cutaneous metaplastic synovial cyst, also known as synovial metaplasia of the skin, is an uncommon benign cystic lesion that was first reported by Gonzalez et al1 in 1987. Histologically, CMSC lacks an epithelial lining and therefore is not a true cyst but rather a pseudocyst.2 Clinically, the lesion typically presents as a solitary subcutaneous nodule that may be tender or painless. In a literature review of CMSC cases performed by Fukuyama et al,3 distribution of reported cases according to body site varied; however, limbs were found to be the most commonly involved area. A PubMed search of articles indexed for MEDLINE as well as a Google Scholar search using the term cutaneous metaplastic synovial cyst revealed at least 37 cases reported in the English-language literature,3-9 including our present case. The pathogenesis remains uncertain; however, a majority of previously reported cases of CMSC characteristically have been associated with a pre-existing lesion, with most presentations developing at surgical scar sites secondary to operation or trauma.5 Relative tissue fragility secondary to rheumatoid arthritis10 and Ehlers-Danlos syndrome9,11,12 has been linked to CMSC in some documented reports, while a minority of cases report no antecedent events triggering formation of the lesion.13-15
As evidenced by our patient, CMSC clinically mimics several other benign entities; histopathologic examination is necessary to confirm the diagnosis. Although nodular hidradenoma also may clinically present as a solitary firm intradermal nodule, microscopy reveals a dermal-based lobulated tumor containing cystic spaces and solid areas composed of basophilic polyhedral cells and round glycogen-filled clear cells.16 Epidermoid cysts are differentiated from CMSC by the presence of a cyst wall lining composed of stratified squamous epithelium and associated laminated keratin within the lumen,17 which corresponds to its pearly white appearance on gross examination. Cutaneous ciliated cysts predominantly occur on the lower extremities of young women and are lined by simple cuboidal or columnar ciliated cells that resemble müllerian epithelium.18 Similar to CMSC, ganglion cysts are pseudocysts that lack a true epithelial lining but differ in appearance due to their mucin-filled synovial-lined sac.19 Additionally, ganglion cysts most often occur on the dorsal and volar aspects of the wrist.
Excisional biopsy is indicated as the preferred treatment of CMSC, given the lesion's benign behavior and low recurrence rate.6 Our case highlights this rare entity and reinforces its inclusion in the differential diagnosis of subcutaneous mobile nodules, especially in the setting of prior tissue injury secondary to trauma, surgical procedures, or conditions such as rheumatoid arthritis or Ehlers-Danlos syndrome. Unlike most previously reported cases, our patient reported no preceding tissue injury associated with formation of the lesion, and she was largely asymptomatic on presentation. Considering the limited number of CMSC cases demonstrated in the literature, it is important to continue reporting new cases to better understand characteristics and presentations of this uncommon lesion.
- Gonzalez JG, Ghiselli RW, Santa Cruz DJ. Synovial metaplasia of the skin. Am J Surg Pathol. 1987;11:343-350.
- Calonje E, Brenn T, Lazar A, et al. Cutaneous cysts. In: Calonje E, Brenn T, Lazar A, et al. McKee's Pathology of the Skin. 5th ed. Elsevier Limited; 2020:1680-1697.
- Fukuyama M, Sato Y, Hayakawa J, et al. Cutaneous metaplastic synovial cyst: case report and literature review from the dermatological point of view. Keio J Med. 2016;66:9-13.
- Karaytug K, Kapicioglu M, Can N, et al. Unprecedented recurrence of carpal tunnel syndrome by metaplastic synovial cyst in the carpal tunnel. Acta Orthop Traumatol Turc. 2019;53:230-232.
- Martelli SJ, Silveira FM, Carvalho PH, et al. Asymptomatic subcutaneous swelling of lower face. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019;128:101-105.
- Majdi M, Saffar H, Ghanadan A. Cutaneous metaplastic synovial cyst: a case report. Iran J Pathol. 2016;11:423-426.
- Ramachandra S, Rao L, Al-Kindi M. Cutaneous metaplastic synovial cyst. Sultan Qaboos Univ Med J. 2016;16:E117-E118.
- Heidarian A, Xie Q, Banihashemi A. Cutaneous metaplastic synovial cyst presenting as an axillary mass after modified mastectomy and adjuvant radiotherapy. Am J Clin Pathol. 2016;146:S2.
- Fernandez-Flores A, Barja-Lopez JM. Cutaneous metaplastic synovial cyst in Ehlers-Danlos syndrome. J Cutan Pathol. 2020;47:729-733.
- Choonhakarn C, Tang S. Cutaneous metaplastic synovial cyst. J Dermatol. 2003;30:480-484.
- Guala A, Viglio S, Ottinetti A, et al. Cutaneous metaplastic synovial cyst in Ehlers-Danlos syndrome: report of a second case. Am J Dermatopathol. 2008;30:59-61.
- Nieto S, Buezo GF, Jones-Caballero M, et al. Cutaneous metaplastic synovial cyst in an Ehlers-Danlos patient. Am J Dermatopathol. 1997;19:407-410.
- Goiriz R, Rios-Buceta L, Alonso-Perez A, et al. Cutaneous metaplastic synovial cyst. J Am Acad Dermatol. 2005;53:180-181.
- Kim BC, Choi WJ, Park EJ, et al. Cutaneous metaplastic synovial cyst of the first metatarsal head area. Ann Dermatol. 2011;23(suppl 2):S165-S168.
- Yang HC, Tsai YJ, Hu SL, et al. Cutaneous metaplastic synovial cyst--a case report and review of literature. Dermatol Sinica. 2003;21:275-279.
- Kataria SP, Singh G, Batra A, et al. Nodular hidradenoma: a series of five cases in male subjects and review of literature. Adv Cytol Pathol. 2018;3:46-47.
- Mohamed Haflah N, Mohd Kassim A, Hassan Shukur M. Giant epidermoid cyst of the thigh. Malays Orthop J. 2011;5:17-19.
- Torisu-Itakura H, Itakura E, Horiuchi R, et al. Cutaneous ciliated cyst on the leg of a woman of menopausal age. Acta Derm Venereol. 2009;89:323-324.
- Fullen DR. Cysts and sinuses. In: Busam K, ed. Dermatopathology. Saunders; 2010:300-330.
- Gonzalez JG, Ghiselli RW, Santa Cruz DJ. Synovial metaplasia of the skin. Am J Surg Pathol. 1987;11:343-350.
- Calonje E, Brenn T, Lazar A, et al. Cutaneous cysts. In: Calonje E, Brenn T, Lazar A, et al. McKee's Pathology of the Skin. 5th ed. Elsevier Limited; 2020:1680-1697.
- Fukuyama M, Sato Y, Hayakawa J, et al. Cutaneous metaplastic synovial cyst: case report and literature review from the dermatological point of view. Keio J Med. 2016;66:9-13.
- Karaytug K, Kapicioglu M, Can N, et al. Unprecedented recurrence of carpal tunnel syndrome by metaplastic synovial cyst in the carpal tunnel. Acta Orthop Traumatol Turc. 2019;53:230-232.
- Martelli SJ, Silveira FM, Carvalho PH, et al. Asymptomatic subcutaneous swelling of lower face. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019;128:101-105.
- Majdi M, Saffar H, Ghanadan A. Cutaneous metaplastic synovial cyst: a case report. Iran J Pathol. 2016;11:423-426.
- Ramachandra S, Rao L, Al-Kindi M. Cutaneous metaplastic synovial cyst. Sultan Qaboos Univ Med J. 2016;16:E117-E118.
- Heidarian A, Xie Q, Banihashemi A. Cutaneous metaplastic synovial cyst presenting as an axillary mass after modified mastectomy and adjuvant radiotherapy. Am J Clin Pathol. 2016;146:S2.
- Fernandez-Flores A, Barja-Lopez JM. Cutaneous metaplastic synovial cyst in Ehlers-Danlos syndrome. J Cutan Pathol. 2020;47:729-733.
- Choonhakarn C, Tang S. Cutaneous metaplastic synovial cyst. J Dermatol. 2003;30:480-484.
- Guala A, Viglio S, Ottinetti A, et al. Cutaneous metaplastic synovial cyst in Ehlers-Danlos syndrome: report of a second case. Am J Dermatopathol. 2008;30:59-61.
- Nieto S, Buezo GF, Jones-Caballero M, et al. Cutaneous metaplastic synovial cyst in an Ehlers-Danlos patient. Am J Dermatopathol. 1997;19:407-410.
- Goiriz R, Rios-Buceta L, Alonso-Perez A, et al. Cutaneous metaplastic synovial cyst. J Am Acad Dermatol. 2005;53:180-181.
- Kim BC, Choi WJ, Park EJ, et al. Cutaneous metaplastic synovial cyst of the first metatarsal head area. Ann Dermatol. 2011;23(suppl 2):S165-S168.
- Yang HC, Tsai YJ, Hu SL, et al. Cutaneous metaplastic synovial cyst--a case report and review of literature. Dermatol Sinica. 2003;21:275-279.
- Kataria SP, Singh G, Batra A, et al. Nodular hidradenoma: a series of five cases in male subjects and review of literature. Adv Cytol Pathol. 2018;3:46-47.
- Mohamed Haflah N, Mohd Kassim A, Hassan Shukur M. Giant epidermoid cyst of the thigh. Malays Orthop J. 2011;5:17-19.
- Torisu-Itakura H, Itakura E, Horiuchi R, et al. Cutaneous ciliated cyst on the leg of a woman of menopausal age. Acta Derm Venereol. 2009;89:323-324.
- Fullen DR. Cysts and sinuses. In: Busam K, ed. Dermatopathology. Saunders; 2010:300-330.
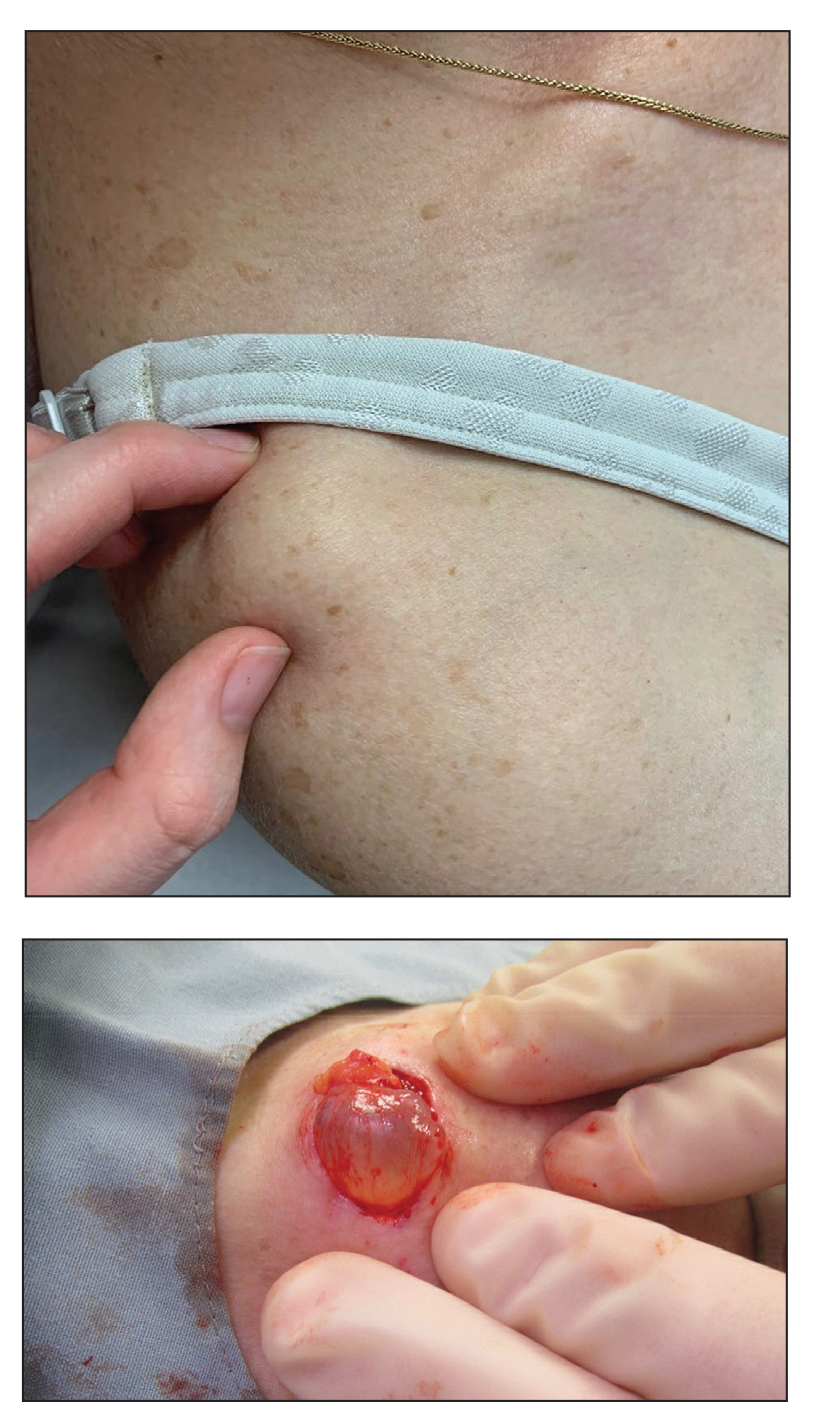
A 70-year-old woman presented to the outpatient dermatology clinic with an acute-onset lesion on the right shoulder. She first noticed a “cyst” developing in the area approximately 3 weeks prior but noted that it may have been present longer. The lesion was bothersome when her undergarments rubbed against it, but she otherwise denied pain, increase in size, or drainage from the site. Her medical history was remarkable for a proliferating trichilemmal tumor on the right parietal scalp treated with Mohs surgery approximately 13 years prior to presentation. She had no personal or family history of skin cancer. Physical examination revealed a 2.5-cm, mobile, nontender, flesh-colored subcutaneous nodule on the right shoulder (top); no ulceration, bleeding, or drainage was present. The surrounding skin demonstrated no clinical changes. The patient was scheduled for outpatient surgical excision of the nodule, which initially was suspected to be a lipoma. During the excision, a translucent cystlike nodule (bottom) was gently dissected and sent for histopathologic examination.