User login
Diabetes Hub contains news and clinical review articles for physicians seeking the most up-to-date information on the rapidly evolving options for treating and preventing Type 2 Diabetes in at-risk patients. The Diabetes Hub is powered by Frontline Medical Communications.
Nomogram may direct diabetes patients to best operation
PHILADELPHIA – A nomogram that assigns a disease severity score to individuals with type 2 diabetes may provide a tool that helps surgeons, endocrinologists, and primary care physicians determine which weight-loss surgical procedure would be most effective, according to an analysis of 900 patients from Cleveland Clinic and University Hospital Clinic, Barcelona, reported at the annual meeting of the American Surgical Association.
“This is the largest reported cohort with long-term glycemic follow-up data that categorizes diabetes into three validated stages of severity to guide procedure selection,” said Ali Aminian, MD, of Cleveland Clinic. The study also highlighted the importance of surgery in early diabetes. The study involved a modeling cohort of 659 patients who had bariatric procedures at Cleveland Clinic from 2005 to 2011 and a separate data set of 241 patients from Barcelona to validate the findings. Roux-en-Y gastric bypass (RYGB) was performed in 78% of the Cleveland Clinic group and 49% of the Barcelona group, with the remainder having sleeve gastrectomy (SG).
RYGB and SG account for more than 95% of all bariatric procedures in people with type 2 diabetes, Dr. Aminian said, but outcomes of clinical trials have been variable, some reporting up to half of patients having long-term relapses. The Cleveland Clinic study involved all patients with type 2 diabetes who had RYGB or SG from 2005 to 2011 with 5 years or more of glycemic data, with a median follow-up of 7 years. The study used American Diabetes Association targets to define remission and glycemic control.
“Long-term response after bariatric surgery in patients with diabetes significantly differs according to diabetes severity,” Dr. Aminian said. “For example, the outcome of surgery in a patient who has diabetes for 2 years is significantly different than a patient who has diabetes for 15 years taking three medications, including insulin.”
The researchers generated the nomogram based on these four independent preoperative factors:
- Number of preoperative diabetes medications (P less than .0001).
- Insulin use (P = .002).
- Duration of diabetes (P less than .0001).
- Glycemic control (P = .002).
“These factors are readily available in clinical practice and are considered a proxy of functional pancreatic beta-cell reserve,” Dr. Aminian said. The nomogram scores the severity of each factor on a scale of 0 to 100. For example, one preoperative medication scores 12, but five scores 63; duration of diabetes of 1 year scores five points, but 16 years scores 60. The patient’s total points represent the Individualized Metabolic Surgery score.
The researchers assigned three categories: A score of 25 or less represents mild disease, a score of 25-95 represents moderate, and 95 to the maximum 180 is severe disease.
Based on the Cleveland Clinic and Barcelona cohorts, the researchers next developed recommendations for average risk patients in each category.
RYGB is “suggested” in mild disease based on remission rates of 92% in the Cleveland subgroup and 91% in the Barcelona subgroup vs. SG remission rates of 74% and 91%, respectively. On the other end of the spectrum, in patients with severe diabetes, both procedures were less effective in achieving long-term diabetes remission. The disparities were more pronounced for the moderate group: 60% and 70% for RYGB and 25% and 56% for SG in the Cleveland Clinic and Barcelona subgroups, respectively. Hence the nomogram highly “recommends” RYGB. An online calculator to determine Individualized Metabolic Surgery score is available at http://riskcalc.org/Metabolic_Surgery_Score/.
“Obviously, this is the first attempt toward individualized procedure selection and more work needs to be done,” Dr. Aminian said. “Our findings also highlight the importance of surgical intervention in early stages of diabetes in order to achieve sustainable remission.”
In his discussion, Matthew M. Hutter, MD, FACS, of Harvard Medical School, Boston, offered to “quibble” with Dr. Aminian’s conclusions. “I challenge you on your conclusion for the mild and severe categories,” Dr. Hutter said. “My rate-of-cure data makes me want to recommend bypass for any patient with diabetes – mild, moderate or severe.”
Dr. Aminian acknowledged that the number of SG cases in the severe subgroup – 51 – was not great, and long-term diabetes remission was comparable between the two procedures. The key distinguishing measure in the severe category was a net 8% difference between two procedures in glycemic control at last follow-up. “This is the difference that we must decide whether it’s clinically important or not – whether we’re willing to recommend a riskier procedure for an extra 8% achieving glycemic control,” Dr. Aminian said. “If someone thinks it’s worth the risk, then they may suggest gastric bypass. If someone thinks it’s not worth the risk, then they may suggest a sleeve gastrectomy. But, we should remember that patients in the severe group are very high-risk patients.”
Dr. Aminian reported no financial disclosures. Dr. Hutter disclosed receiving conference reimbursement from Olympus.
The complete manuscript of this study and its presentation at the American Surgical Association’s 137th Annual Meeting, April 2017, in Philadelphia, Pennsylvania, is to be published in Annals of Surgery pending editorial review.
PHILADELPHIA – A nomogram that assigns a disease severity score to individuals with type 2 diabetes may provide a tool that helps surgeons, endocrinologists, and primary care physicians determine which weight-loss surgical procedure would be most effective, according to an analysis of 900 patients from Cleveland Clinic and University Hospital Clinic, Barcelona, reported at the annual meeting of the American Surgical Association.
“This is the largest reported cohort with long-term glycemic follow-up data that categorizes diabetes into three validated stages of severity to guide procedure selection,” said Ali Aminian, MD, of Cleveland Clinic. The study also highlighted the importance of surgery in early diabetes. The study involved a modeling cohort of 659 patients who had bariatric procedures at Cleveland Clinic from 2005 to 2011 and a separate data set of 241 patients from Barcelona to validate the findings. Roux-en-Y gastric bypass (RYGB) was performed in 78% of the Cleveland Clinic group and 49% of the Barcelona group, with the remainder having sleeve gastrectomy (SG).
RYGB and SG account for more than 95% of all bariatric procedures in people with type 2 diabetes, Dr. Aminian said, but outcomes of clinical trials have been variable, some reporting up to half of patients having long-term relapses. The Cleveland Clinic study involved all patients with type 2 diabetes who had RYGB or SG from 2005 to 2011 with 5 years or more of glycemic data, with a median follow-up of 7 years. The study used American Diabetes Association targets to define remission and glycemic control.
“Long-term response after bariatric surgery in patients with diabetes significantly differs according to diabetes severity,” Dr. Aminian said. “For example, the outcome of surgery in a patient who has diabetes for 2 years is significantly different than a patient who has diabetes for 15 years taking three medications, including insulin.”
The researchers generated the nomogram based on these four independent preoperative factors:
- Number of preoperative diabetes medications (P less than .0001).
- Insulin use (P = .002).
- Duration of diabetes (P less than .0001).
- Glycemic control (P = .002).
“These factors are readily available in clinical practice and are considered a proxy of functional pancreatic beta-cell reserve,” Dr. Aminian said. The nomogram scores the severity of each factor on a scale of 0 to 100. For example, one preoperative medication scores 12, but five scores 63; duration of diabetes of 1 year scores five points, but 16 years scores 60. The patient’s total points represent the Individualized Metabolic Surgery score.
The researchers assigned three categories: A score of 25 or less represents mild disease, a score of 25-95 represents moderate, and 95 to the maximum 180 is severe disease.
Based on the Cleveland Clinic and Barcelona cohorts, the researchers next developed recommendations for average risk patients in each category.
RYGB is “suggested” in mild disease based on remission rates of 92% in the Cleveland subgroup and 91% in the Barcelona subgroup vs. SG remission rates of 74% and 91%, respectively. On the other end of the spectrum, in patients with severe diabetes, both procedures were less effective in achieving long-term diabetes remission. The disparities were more pronounced for the moderate group: 60% and 70% for RYGB and 25% and 56% for SG in the Cleveland Clinic and Barcelona subgroups, respectively. Hence the nomogram highly “recommends” RYGB. An online calculator to determine Individualized Metabolic Surgery score is available at http://riskcalc.org/Metabolic_Surgery_Score/.
“Obviously, this is the first attempt toward individualized procedure selection and more work needs to be done,” Dr. Aminian said. “Our findings also highlight the importance of surgical intervention in early stages of diabetes in order to achieve sustainable remission.”
In his discussion, Matthew M. Hutter, MD, FACS, of Harvard Medical School, Boston, offered to “quibble” with Dr. Aminian’s conclusions. “I challenge you on your conclusion for the mild and severe categories,” Dr. Hutter said. “My rate-of-cure data makes me want to recommend bypass for any patient with diabetes – mild, moderate or severe.”
Dr. Aminian acknowledged that the number of SG cases in the severe subgroup – 51 – was not great, and long-term diabetes remission was comparable between the two procedures. The key distinguishing measure in the severe category was a net 8% difference between two procedures in glycemic control at last follow-up. “This is the difference that we must decide whether it’s clinically important or not – whether we’re willing to recommend a riskier procedure for an extra 8% achieving glycemic control,” Dr. Aminian said. “If someone thinks it’s worth the risk, then they may suggest gastric bypass. If someone thinks it’s not worth the risk, then they may suggest a sleeve gastrectomy. But, we should remember that patients in the severe group are very high-risk patients.”
Dr. Aminian reported no financial disclosures. Dr. Hutter disclosed receiving conference reimbursement from Olympus.
The complete manuscript of this study and its presentation at the American Surgical Association’s 137th Annual Meeting, April 2017, in Philadelphia, Pennsylvania, is to be published in Annals of Surgery pending editorial review.
PHILADELPHIA – A nomogram that assigns a disease severity score to individuals with type 2 diabetes may provide a tool that helps surgeons, endocrinologists, and primary care physicians determine which weight-loss surgical procedure would be most effective, according to an analysis of 900 patients from Cleveland Clinic and University Hospital Clinic, Barcelona, reported at the annual meeting of the American Surgical Association.
“This is the largest reported cohort with long-term glycemic follow-up data that categorizes diabetes into three validated stages of severity to guide procedure selection,” said Ali Aminian, MD, of Cleveland Clinic. The study also highlighted the importance of surgery in early diabetes. The study involved a modeling cohort of 659 patients who had bariatric procedures at Cleveland Clinic from 2005 to 2011 and a separate data set of 241 patients from Barcelona to validate the findings. Roux-en-Y gastric bypass (RYGB) was performed in 78% of the Cleveland Clinic group and 49% of the Barcelona group, with the remainder having sleeve gastrectomy (SG).
RYGB and SG account for more than 95% of all bariatric procedures in people with type 2 diabetes, Dr. Aminian said, but outcomes of clinical trials have been variable, some reporting up to half of patients having long-term relapses. The Cleveland Clinic study involved all patients with type 2 diabetes who had RYGB or SG from 2005 to 2011 with 5 years or more of glycemic data, with a median follow-up of 7 years. The study used American Diabetes Association targets to define remission and glycemic control.
“Long-term response after bariatric surgery in patients with diabetes significantly differs according to diabetes severity,” Dr. Aminian said. “For example, the outcome of surgery in a patient who has diabetes for 2 years is significantly different than a patient who has diabetes for 15 years taking three medications, including insulin.”
The researchers generated the nomogram based on these four independent preoperative factors:
- Number of preoperative diabetes medications (P less than .0001).
- Insulin use (P = .002).
- Duration of diabetes (P less than .0001).
- Glycemic control (P = .002).
“These factors are readily available in clinical practice and are considered a proxy of functional pancreatic beta-cell reserve,” Dr. Aminian said. The nomogram scores the severity of each factor on a scale of 0 to 100. For example, one preoperative medication scores 12, but five scores 63; duration of diabetes of 1 year scores five points, but 16 years scores 60. The patient’s total points represent the Individualized Metabolic Surgery score.
The researchers assigned three categories: A score of 25 or less represents mild disease, a score of 25-95 represents moderate, and 95 to the maximum 180 is severe disease.
Based on the Cleveland Clinic and Barcelona cohorts, the researchers next developed recommendations for average risk patients in each category.
RYGB is “suggested” in mild disease based on remission rates of 92% in the Cleveland subgroup and 91% in the Barcelona subgroup vs. SG remission rates of 74% and 91%, respectively. On the other end of the spectrum, in patients with severe diabetes, both procedures were less effective in achieving long-term diabetes remission. The disparities were more pronounced for the moderate group: 60% and 70% for RYGB and 25% and 56% for SG in the Cleveland Clinic and Barcelona subgroups, respectively. Hence the nomogram highly “recommends” RYGB. An online calculator to determine Individualized Metabolic Surgery score is available at http://riskcalc.org/Metabolic_Surgery_Score/.
“Obviously, this is the first attempt toward individualized procedure selection and more work needs to be done,” Dr. Aminian said. “Our findings also highlight the importance of surgical intervention in early stages of diabetes in order to achieve sustainable remission.”
In his discussion, Matthew M. Hutter, MD, FACS, of Harvard Medical School, Boston, offered to “quibble” with Dr. Aminian’s conclusions. “I challenge you on your conclusion for the mild and severe categories,” Dr. Hutter said. “My rate-of-cure data makes me want to recommend bypass for any patient with diabetes – mild, moderate or severe.”
Dr. Aminian acknowledged that the number of SG cases in the severe subgroup – 51 – was not great, and long-term diabetes remission was comparable between the two procedures. The key distinguishing measure in the severe category was a net 8% difference between two procedures in glycemic control at last follow-up. “This is the difference that we must decide whether it’s clinically important or not – whether we’re willing to recommend a riskier procedure for an extra 8% achieving glycemic control,” Dr. Aminian said. “If someone thinks it’s worth the risk, then they may suggest gastric bypass. If someone thinks it’s not worth the risk, then they may suggest a sleeve gastrectomy. But, we should remember that patients in the severe group are very high-risk patients.”
Dr. Aminian reported no financial disclosures. Dr. Hutter disclosed receiving conference reimbursement from Olympus.
The complete manuscript of this study and its presentation at the American Surgical Association’s 137th Annual Meeting, April 2017, in Philadelphia, Pennsylvania, is to be published in Annals of Surgery pending editorial review.
AT THE ASA ANNUAL MEETING
Key clinical point: A nomogram has been developed that assigns an Individualized Metabolic Surgery score to individuals with type 2 diabetes to help determine which type of bariatric procedure would provide best outcomes.
Major finding: In mild diabetes (Individualized Metabolic Surgery score less than or equal to 25), Roux-en-Y gastric bypass and sleeve gastrectomy significantly improve diabetes. For patients with severe diabetes (IMS Score greater than 95), both procedures have similarly low efficacy for diabetes remission.
Data source: Analysis of 900 patients with type 2 diabetes who had either Roux-en-Y gastric bypass or sleeve gastrectomy with a minimum 5-year follow-up.
Disclosure: Dr. Aminian reported no financial disclosures. Dr. Hutter disclosed receiving conference reimbursement from Olympus.
Small study: Vitamin D repletion may decrease insulin resistance
WASHINGTON – Normalizing vitamin D levels correlated with lower insulin resistance and decreased adipose fibrosis in obese patients, according to a study presented at the Eastern regional meeting of the American Federation for Medical Research.
Approximately 86 million U.S. patients have prediabetes, according to Diabetes Report Card 2014, the most recent estimates from the Centers for Disease Control and Prevention. Vitamin D therapy may be able to help lower that number and prevent diabetes in some patients, Jee Young You, MD, a research fellow at Albert Einstein College of Medicine, New York, said at the meeting.
“When there’s increased adiposity, there is reduction of the blood flow which will further lead to inflammation, macrophage infiltration, and fibrosis, which all together leads to insulin resistance,” Dr. You said. “It is shown that there are vitamin D receptors present on adipocytes, so we hypothesize repleting vitamin D will help in reducing this inflammation.”
In a double blind study, Dr. You and her colleagues randomized 11 obese patients, with an average body mass index of 34 kg/m2, insulin resistance, and vitamin D deficiency to vitamin D repletion therapy. Eight similar patients served as controls. The average age was 43 years.
Patients in the test group were placed on a step schedule for vitamin D supplementation. For 3 months, they received 40,000 IU of vitamin D3 weekly in an effort to reach a target 25-hydroxyvitamin D level of greater than 30 ng/ml. Patients then received another 3 months of the same supplementation with an aim to reach a target level of greater than 50 ng/ml.
“We wanted to see if there was a dose dependent effect for vitamin D in patients,” Dr. You said.
Endogenous glucose production decreased by 24% (P = .04) after normalization of vitamin D levels. Patients who received placebo saw an increase in endogenous glucose, pointing to lower hepatic insulin sensitivity, Dr. You said.
When the vitamin D receptors are activated, they inhibit the profibrotic pathways like TGFb-1, Dr. You explained, decreasing fibrosis.
The researchers also found a decrease in profibrotic gene expression in TGFb-1, HiF-1, MMP7, and Collagen I, V, and VI.
However, while testing for reduction in profibrotic gene expression in whole fat, the investigators found that there was no additional improvement after the first round of vitamin D therapy, leading them to assert that raising vitamin D levels above the normal range does not give any additional benefit.
[email protected]
On Twitter @eaztweets
WASHINGTON – Normalizing vitamin D levels correlated with lower insulin resistance and decreased adipose fibrosis in obese patients, according to a study presented at the Eastern regional meeting of the American Federation for Medical Research.
Approximately 86 million U.S. patients have prediabetes, according to Diabetes Report Card 2014, the most recent estimates from the Centers for Disease Control and Prevention. Vitamin D therapy may be able to help lower that number and prevent diabetes in some patients, Jee Young You, MD, a research fellow at Albert Einstein College of Medicine, New York, said at the meeting.
“When there’s increased adiposity, there is reduction of the blood flow which will further lead to inflammation, macrophage infiltration, and fibrosis, which all together leads to insulin resistance,” Dr. You said. “It is shown that there are vitamin D receptors present on adipocytes, so we hypothesize repleting vitamin D will help in reducing this inflammation.”
In a double blind study, Dr. You and her colleagues randomized 11 obese patients, with an average body mass index of 34 kg/m2, insulin resistance, and vitamin D deficiency to vitamin D repletion therapy. Eight similar patients served as controls. The average age was 43 years.
Patients in the test group were placed on a step schedule for vitamin D supplementation. For 3 months, they received 40,000 IU of vitamin D3 weekly in an effort to reach a target 25-hydroxyvitamin D level of greater than 30 ng/ml. Patients then received another 3 months of the same supplementation with an aim to reach a target level of greater than 50 ng/ml.
“We wanted to see if there was a dose dependent effect for vitamin D in patients,” Dr. You said.
Endogenous glucose production decreased by 24% (P = .04) after normalization of vitamin D levels. Patients who received placebo saw an increase in endogenous glucose, pointing to lower hepatic insulin sensitivity, Dr. You said.
When the vitamin D receptors are activated, they inhibit the profibrotic pathways like TGFb-1, Dr. You explained, decreasing fibrosis.
The researchers also found a decrease in profibrotic gene expression in TGFb-1, HiF-1, MMP7, and Collagen I, V, and VI.
However, while testing for reduction in profibrotic gene expression in whole fat, the investigators found that there was no additional improvement after the first round of vitamin D therapy, leading them to assert that raising vitamin D levels above the normal range does not give any additional benefit.
[email protected]
On Twitter @eaztweets
WASHINGTON – Normalizing vitamin D levels correlated with lower insulin resistance and decreased adipose fibrosis in obese patients, according to a study presented at the Eastern regional meeting of the American Federation for Medical Research.
Approximately 86 million U.S. patients have prediabetes, according to Diabetes Report Card 2014, the most recent estimates from the Centers for Disease Control and Prevention. Vitamin D therapy may be able to help lower that number and prevent diabetes in some patients, Jee Young You, MD, a research fellow at Albert Einstein College of Medicine, New York, said at the meeting.
“When there’s increased adiposity, there is reduction of the blood flow which will further lead to inflammation, macrophage infiltration, and fibrosis, which all together leads to insulin resistance,” Dr. You said. “It is shown that there are vitamin D receptors present on adipocytes, so we hypothesize repleting vitamin D will help in reducing this inflammation.”
In a double blind study, Dr. You and her colleagues randomized 11 obese patients, with an average body mass index of 34 kg/m2, insulin resistance, and vitamin D deficiency to vitamin D repletion therapy. Eight similar patients served as controls. The average age was 43 years.
Patients in the test group were placed on a step schedule for vitamin D supplementation. For 3 months, they received 40,000 IU of vitamin D3 weekly in an effort to reach a target 25-hydroxyvitamin D level of greater than 30 ng/ml. Patients then received another 3 months of the same supplementation with an aim to reach a target level of greater than 50 ng/ml.
“We wanted to see if there was a dose dependent effect for vitamin D in patients,” Dr. You said.
Endogenous glucose production decreased by 24% (P = .04) after normalization of vitamin D levels. Patients who received placebo saw an increase in endogenous glucose, pointing to lower hepatic insulin sensitivity, Dr. You said.
When the vitamin D receptors are activated, they inhibit the profibrotic pathways like TGFb-1, Dr. You explained, decreasing fibrosis.
The researchers also found a decrease in profibrotic gene expression in TGFb-1, HiF-1, MMP7, and Collagen I, V, and VI.
However, while testing for reduction in profibrotic gene expression in whole fat, the investigators found that there was no additional improvement after the first round of vitamin D therapy, leading them to assert that raising vitamin D levels above the normal range does not give any additional benefit.
[email protected]
On Twitter @eaztweets
AT THE AFMR EASTERN REGIONAL MEETING
Key clinical point:
Major finding: Of the 19 patients studied, expression of profibrotic genes TGFb-1, HiF-1, MMP7, and Collagen I, V, and VI in those given vitamin D therapy decreased 0.81, 0.72, 0.62,. 0.56, 0.56, and 0.43 times, respectively (P less than .05).
Data source: Randomized, double blind, placebo-controlled study of 19 obese, insulin resistant, vitamin D deficient patients.
Disclosures: The investigators reported no relevant conflicts of interest.
Shared-savings ESRD organization reduced missed treatments, hospitalizations
SAN DIEGO – In the first year since Delaware Valley Nephrology joined an end–stage renal disease seamless care organization, patient hospitalizations have declined by 40% and rehospitalizations by 20%, according to Edward R. Jones, MD.
At the annual meeting of the American College of Physicians, Dr. Jones, a nephrologist at a Philadelphia-based practice, described his experience with the alternative payment model, which focuses on managing costs while providing better health outcomes.
More than 15 months ago, Dr. Jones and seven other nephrologists in his practice partnered with Fresenius Medical Care to form an ESCO with two other nephrology groups, amounting to 45 physicians who work out of 30 dialysis units in 14 hospitals and care for 1,000 patients.
It became one of 13 ESCOs that have been operating nationwide since October 2015. The ESCOs share savings with the Centers for Medicare & Medicaid Services if matched beneficiaries’ expenditures decrease and quality is maintained or improved, and it shares losses if beneficiaries’ expenditures increase.
To be eligible for participation in the ESCO, patients must be enrolled in Medicare Parts A and B and have Medicare as their primary payer. They are ineligible if they are enrolled in a Medicare Advantage plan. Patients must not have received a kidney transplant in the last 12 months and must receive at least 51% of annual dialysis services in the ESCO’s market area.
“The governing structure of the ESCO was critical as we put it together,” Dr. Jones said. “We insisted that a nephrologist be at the table of the governing body, as well as a consumer advocate, and no one controls more than 50% of the vote.
“The concept here is that a benchmark for spending is set,” he explained. “If your spending is less than the benchmark expenditure, there are shared savings. The opposite occurs if there are losses, so it’s a fairly straightforward program.”
To illustrate how the ESCO works, he discussed a hypothetical model in which the ESCO used $50 million of expenditures from 2012 to 2015.
“If the actual ESCO expenditures are $47 million, there are $3 million in potential shared savings,” Dr. Jones explained. “It’s potential because two things are necessary. First, you have to have hit at least 1% savings or 1% loss. This allows for any random outcomes. Of $3 million of potential shared savings, CMS keeps 25%.
“The remaining shared savings depends on where you hit on the metric performance,” he continued. “In the first year, it’s a pay for reporting [system], so all we had to do is hit three measures. So, the first year was great.”
In the second year of ESCO participation, centers have to perform in the 90th percentile on 16 metrics to get full shared savings. Drawn from Medicare claims and medical records, the list of metrics includes diabetic foot exam, medication reconciliation, and advanced care planning, and it accounts for 50% of the score. Surveys of person- and caregiver-centered experience outcomes compose 33% of the score.
“These metrics are compared to all other metrics throughout the country,” Dr. Jones said. “Wherever you fall, you generate a certain number of points, between 0 and 2. It’s tied to quality and outcomes. If you’re in the 90th percentile you get all 2 points. If you’re below the 50th percentile, you get no points.”
The goal of the ESCO is to achieve the minimal savings rate, to maximize achievement of quality metrics, and to reduce expenses below the set benchmark. In Dr. Jones’ practice area, ESRD care costs about $87,000 per patient per year – 34% are related to inpatient costs, and 30% are related to dialysis costs.
Keys to a successful ESCO include “a cooperative and engaged nephrologist” and the ability to gather analytics.
“There is no way that a practice of my size has the capability of generating the analytics to be able to risk-stratify patients,” he said. “Who is likely to be readmitted? We put all of our effort into those folks. Medication reconciliation accounts for a lot of rehospitalization. We spend a lot of time on that.”
There is also increased use of care navigators. “Our goal is for patients to call the care navigators before they call the nephrologist,” Dr. Jones said. “We have safety net clinics that are open 24/7. So, if a patient comes in on a Saturday or Sunday, we can divert the patient to those areas.”
In the first year since joining the ESCO, patient hospitalizations at Dr. Jones’ practice have declined by 40%, and rehospitalizations have dropped by 20%.
“Importantly, we know that when a patient is not in his dialysis chair within 15 minutes, the care navigator calls him,” he said. “The number of missed treatments is down dramatically.”
Dr. Jones reported owning stock in Cytosorbents. He also serves as a consultant for Fresenius Medical Care, Fresenius Medical Services, Physicians Choice Dialysis, and Reliant Renal Care. He is also an advisory board member for Cytosorbents and Fresenius.
SAN DIEGO – In the first year since Delaware Valley Nephrology joined an end–stage renal disease seamless care organization, patient hospitalizations have declined by 40% and rehospitalizations by 20%, according to Edward R. Jones, MD.
At the annual meeting of the American College of Physicians, Dr. Jones, a nephrologist at a Philadelphia-based practice, described his experience with the alternative payment model, which focuses on managing costs while providing better health outcomes.
More than 15 months ago, Dr. Jones and seven other nephrologists in his practice partnered with Fresenius Medical Care to form an ESCO with two other nephrology groups, amounting to 45 physicians who work out of 30 dialysis units in 14 hospitals and care for 1,000 patients.
It became one of 13 ESCOs that have been operating nationwide since October 2015. The ESCOs share savings with the Centers for Medicare & Medicaid Services if matched beneficiaries’ expenditures decrease and quality is maintained or improved, and it shares losses if beneficiaries’ expenditures increase.
To be eligible for participation in the ESCO, patients must be enrolled in Medicare Parts A and B and have Medicare as their primary payer. They are ineligible if they are enrolled in a Medicare Advantage plan. Patients must not have received a kidney transplant in the last 12 months and must receive at least 51% of annual dialysis services in the ESCO’s market area.
“The governing structure of the ESCO was critical as we put it together,” Dr. Jones said. “We insisted that a nephrologist be at the table of the governing body, as well as a consumer advocate, and no one controls more than 50% of the vote.
“The concept here is that a benchmark for spending is set,” he explained. “If your spending is less than the benchmark expenditure, there are shared savings. The opposite occurs if there are losses, so it’s a fairly straightforward program.”
To illustrate how the ESCO works, he discussed a hypothetical model in which the ESCO used $50 million of expenditures from 2012 to 2015.
“If the actual ESCO expenditures are $47 million, there are $3 million in potential shared savings,” Dr. Jones explained. “It’s potential because two things are necessary. First, you have to have hit at least 1% savings or 1% loss. This allows for any random outcomes. Of $3 million of potential shared savings, CMS keeps 25%.
“The remaining shared savings depends on where you hit on the metric performance,” he continued. “In the first year, it’s a pay for reporting [system], so all we had to do is hit three measures. So, the first year was great.”
In the second year of ESCO participation, centers have to perform in the 90th percentile on 16 metrics to get full shared savings. Drawn from Medicare claims and medical records, the list of metrics includes diabetic foot exam, medication reconciliation, and advanced care planning, and it accounts for 50% of the score. Surveys of person- and caregiver-centered experience outcomes compose 33% of the score.
“These metrics are compared to all other metrics throughout the country,” Dr. Jones said. “Wherever you fall, you generate a certain number of points, between 0 and 2. It’s tied to quality and outcomes. If you’re in the 90th percentile you get all 2 points. If you’re below the 50th percentile, you get no points.”
The goal of the ESCO is to achieve the minimal savings rate, to maximize achievement of quality metrics, and to reduce expenses below the set benchmark. In Dr. Jones’ practice area, ESRD care costs about $87,000 per patient per year – 34% are related to inpatient costs, and 30% are related to dialysis costs.
Keys to a successful ESCO include “a cooperative and engaged nephrologist” and the ability to gather analytics.
“There is no way that a practice of my size has the capability of generating the analytics to be able to risk-stratify patients,” he said. “Who is likely to be readmitted? We put all of our effort into those folks. Medication reconciliation accounts for a lot of rehospitalization. We spend a lot of time on that.”
There is also increased use of care navigators. “Our goal is for patients to call the care navigators before they call the nephrologist,” Dr. Jones said. “We have safety net clinics that are open 24/7. So, if a patient comes in on a Saturday or Sunday, we can divert the patient to those areas.”
In the first year since joining the ESCO, patient hospitalizations at Dr. Jones’ practice have declined by 40%, and rehospitalizations have dropped by 20%.
“Importantly, we know that when a patient is not in his dialysis chair within 15 minutes, the care navigator calls him,” he said. “The number of missed treatments is down dramatically.”
Dr. Jones reported owning stock in Cytosorbents. He also serves as a consultant for Fresenius Medical Care, Fresenius Medical Services, Physicians Choice Dialysis, and Reliant Renal Care. He is also an advisory board member for Cytosorbents and Fresenius.
SAN DIEGO – In the first year since Delaware Valley Nephrology joined an end–stage renal disease seamless care organization, patient hospitalizations have declined by 40% and rehospitalizations by 20%, according to Edward R. Jones, MD.
At the annual meeting of the American College of Physicians, Dr. Jones, a nephrologist at a Philadelphia-based practice, described his experience with the alternative payment model, which focuses on managing costs while providing better health outcomes.
More than 15 months ago, Dr. Jones and seven other nephrologists in his practice partnered with Fresenius Medical Care to form an ESCO with two other nephrology groups, amounting to 45 physicians who work out of 30 dialysis units in 14 hospitals and care for 1,000 patients.
It became one of 13 ESCOs that have been operating nationwide since October 2015. The ESCOs share savings with the Centers for Medicare & Medicaid Services if matched beneficiaries’ expenditures decrease and quality is maintained or improved, and it shares losses if beneficiaries’ expenditures increase.
To be eligible for participation in the ESCO, patients must be enrolled in Medicare Parts A and B and have Medicare as their primary payer. They are ineligible if they are enrolled in a Medicare Advantage plan. Patients must not have received a kidney transplant in the last 12 months and must receive at least 51% of annual dialysis services in the ESCO’s market area.
“The governing structure of the ESCO was critical as we put it together,” Dr. Jones said. “We insisted that a nephrologist be at the table of the governing body, as well as a consumer advocate, and no one controls more than 50% of the vote.
“The concept here is that a benchmark for spending is set,” he explained. “If your spending is less than the benchmark expenditure, there are shared savings. The opposite occurs if there are losses, so it’s a fairly straightforward program.”
To illustrate how the ESCO works, he discussed a hypothetical model in which the ESCO used $50 million of expenditures from 2012 to 2015.
“If the actual ESCO expenditures are $47 million, there are $3 million in potential shared savings,” Dr. Jones explained. “It’s potential because two things are necessary. First, you have to have hit at least 1% savings or 1% loss. This allows for any random outcomes. Of $3 million of potential shared savings, CMS keeps 25%.
“The remaining shared savings depends on where you hit on the metric performance,” he continued. “In the first year, it’s a pay for reporting [system], so all we had to do is hit three measures. So, the first year was great.”
In the second year of ESCO participation, centers have to perform in the 90th percentile on 16 metrics to get full shared savings. Drawn from Medicare claims and medical records, the list of metrics includes diabetic foot exam, medication reconciliation, and advanced care planning, and it accounts for 50% of the score. Surveys of person- and caregiver-centered experience outcomes compose 33% of the score.
“These metrics are compared to all other metrics throughout the country,” Dr. Jones said. “Wherever you fall, you generate a certain number of points, between 0 and 2. It’s tied to quality and outcomes. If you’re in the 90th percentile you get all 2 points. If you’re below the 50th percentile, you get no points.”
The goal of the ESCO is to achieve the minimal savings rate, to maximize achievement of quality metrics, and to reduce expenses below the set benchmark. In Dr. Jones’ practice area, ESRD care costs about $87,000 per patient per year – 34% are related to inpatient costs, and 30% are related to dialysis costs.
Keys to a successful ESCO include “a cooperative and engaged nephrologist” and the ability to gather analytics.
“There is no way that a practice of my size has the capability of generating the analytics to be able to risk-stratify patients,” he said. “Who is likely to be readmitted? We put all of our effort into those folks. Medication reconciliation accounts for a lot of rehospitalization. We spend a lot of time on that.”
There is also increased use of care navigators. “Our goal is for patients to call the care navigators before they call the nephrologist,” Dr. Jones said. “We have safety net clinics that are open 24/7. So, if a patient comes in on a Saturday or Sunday, we can divert the patient to those areas.”
In the first year since joining the ESCO, patient hospitalizations at Dr. Jones’ practice have declined by 40%, and rehospitalizations have dropped by 20%.
“Importantly, we know that when a patient is not in his dialysis chair within 15 minutes, the care navigator calls him,” he said. “The number of missed treatments is down dramatically.”
Dr. Jones reported owning stock in Cytosorbents. He also serves as a consultant for Fresenius Medical Care, Fresenius Medical Services, Physicians Choice Dialysis, and Reliant Renal Care. He is also an advisory board member for Cytosorbents and Fresenius.
EXPERT ANALYSIS AT ACP INTERNAL MEDICINE
Both diabetes types increase markedly among youths
The annual incidence of both types 1 and 2 diabetes markedly increased among youths between 2002 and 2012, especially among those in minority racial and ethnic groups, according to a report published online April 13 in the New England Journal of Medicine.
Researchers analyzed trends in diabetes incidence in the observational Search for Diabetes in Youth study, which conducts annual population-based case ascertainment of the disease in people aged 0-20 years. SEARCH is funded by the Centers for Disease Control and Prevention and the National Institute of Diabetes and Digestive and Kidney Diseases.
In this analysis of SEARCH data, there were 11,245 youths with type 1 diabetes in 54,239,600 person-years of surveillance and 2,846 with type 2 diabetes in 28,029,000 person-years of surveillance.
“We estimated that approximately 15,900 cases of type 1 diabetes were diagnosed annually in the U.S. in the 2002-2003 period, and this number increased to 17,900 annually in the 2011-2012 period. Overall, the adjusted annual relative increase in the incidence of type 1 diabetes was 1.8%,” noted Elizabeth J. Mayer-Davis, PhD, of the departments of nutrition and medicine, University of North Carolina, Chapel Hill, and her associates (N Engl J Med. 2017 April 13. doi: 101056/NEJMoa1610187).
Similarly, they estimated that approximately 3,800 cases of type 2 diabetes were diagnosed in the first year of the study, increasing to 5,300 in the final year. The annual relative increase in type 2 diabetes was 4.8%.
The rate of increase varied across the five major ethnic groups studied: non-Hispanic whites, non-Hispanic blacks, Hispanics, Asians or Pacific Islanders, and Native Americans. Type 1 diabetes incidence rose rapidly among Hispanic youths, and type 2 diabetes rose rapidly in all racial and ethnic groups other than whites, with the greatest rate of increase among Native Americans.
These increases suggest “a growing disease burden that will not be shared equally” because of differences among ethnic groups in barriers to care, methods of treatment, and clinical outcomes. “These findings highlight the critical need to identify approaches to reduce disparities among racial and ethnic groups,” Dr. Mayer-Davis and her associates noted.
The National Institute of Diabetes and Digestive and Kidney Diseases and the Centers for Disease Control and Prevention funded the study. Dr. Mayer-Davis reported having no relevant disclosures. One of her associates reported serving as a consultant to Denka-Seiken and MedTest DX.
This study by Mayer-Davis et al. provides the most current data available on the incidence of diabetes in this age group.
The consequence of this increase in diabetes among youths is that the overall disease burden on public health is actually increasing, despite improvements in mortality and CVD rates among older diabetes patients.
According to the 2015 Global Burden of Disease report, the number of years lived with disability has increased by 32.5% and the number of years of life lost has increased by 25.4%.
What do the marked increase in the incidence of diabetes and more people at risk imply about therapy? Data from two large studies over the past several decades support that intensive glycemic control improved outcomes in persons with type 1 or type 2 diabetes mellitus. But what is missing, despite a growing understanding about the pathogenesis of each condition, is knowledge about how best to lower the number of new cases and how best to treat problems once they arise in persons with diabetes.
It is clear that we are far from controlling the negative effects of diabetes on health worldwide. As the prevalence increases, we clearly need new approaches to reduce the burden of this disease on public health.
Julie R. Ingelfinger, M.D., and John A. Jarcho, M.D., are deputy editors of The New England Journal of Medicine. They reported having no relevant disclosures. Dr. Ingelfinger and Dr. Jarcho made these remarks in an editorial accompanying Dr. Mayer-Davis’s report (N Engl J Med. 2017 April 13. doi: 10.1056/NEJMe1616575).
This study by Mayer-Davis et al. provides the most current data available on the incidence of diabetes in this age group.
The consequence of this increase in diabetes among youths is that the overall disease burden on public health is actually increasing, despite improvements in mortality and CVD rates among older diabetes patients.
According to the 2015 Global Burden of Disease report, the number of years lived with disability has increased by 32.5% and the number of years of life lost has increased by 25.4%.
What do the marked increase in the incidence of diabetes and more people at risk imply about therapy? Data from two large studies over the past several decades support that intensive glycemic control improved outcomes in persons with type 1 or type 2 diabetes mellitus. But what is missing, despite a growing understanding about the pathogenesis of each condition, is knowledge about how best to lower the number of new cases and how best to treat problems once they arise in persons with diabetes.
It is clear that we are far from controlling the negative effects of diabetes on health worldwide. As the prevalence increases, we clearly need new approaches to reduce the burden of this disease on public health.
Julie R. Ingelfinger, M.D., and John A. Jarcho, M.D., are deputy editors of The New England Journal of Medicine. They reported having no relevant disclosures. Dr. Ingelfinger and Dr. Jarcho made these remarks in an editorial accompanying Dr. Mayer-Davis’s report (N Engl J Med. 2017 April 13. doi: 10.1056/NEJMe1616575).
This study by Mayer-Davis et al. provides the most current data available on the incidence of diabetes in this age group.
The consequence of this increase in diabetes among youths is that the overall disease burden on public health is actually increasing, despite improvements in mortality and CVD rates among older diabetes patients.
According to the 2015 Global Burden of Disease report, the number of years lived with disability has increased by 32.5% and the number of years of life lost has increased by 25.4%.
What do the marked increase in the incidence of diabetes and more people at risk imply about therapy? Data from two large studies over the past several decades support that intensive glycemic control improved outcomes in persons with type 1 or type 2 diabetes mellitus. But what is missing, despite a growing understanding about the pathogenesis of each condition, is knowledge about how best to lower the number of new cases and how best to treat problems once they arise in persons with diabetes.
It is clear that we are far from controlling the negative effects of diabetes on health worldwide. As the prevalence increases, we clearly need new approaches to reduce the burden of this disease on public health.
Julie R. Ingelfinger, M.D., and John A. Jarcho, M.D., are deputy editors of The New England Journal of Medicine. They reported having no relevant disclosures. Dr. Ingelfinger and Dr. Jarcho made these remarks in an editorial accompanying Dr. Mayer-Davis’s report (N Engl J Med. 2017 April 13. doi: 10.1056/NEJMe1616575).
The annual incidence of both types 1 and 2 diabetes markedly increased among youths between 2002 and 2012, especially among those in minority racial and ethnic groups, according to a report published online April 13 in the New England Journal of Medicine.
Researchers analyzed trends in diabetes incidence in the observational Search for Diabetes in Youth study, which conducts annual population-based case ascertainment of the disease in people aged 0-20 years. SEARCH is funded by the Centers for Disease Control and Prevention and the National Institute of Diabetes and Digestive and Kidney Diseases.
In this analysis of SEARCH data, there were 11,245 youths with type 1 diabetes in 54,239,600 person-years of surveillance and 2,846 with type 2 diabetes in 28,029,000 person-years of surveillance.
“We estimated that approximately 15,900 cases of type 1 diabetes were diagnosed annually in the U.S. in the 2002-2003 period, and this number increased to 17,900 annually in the 2011-2012 period. Overall, the adjusted annual relative increase in the incidence of type 1 diabetes was 1.8%,” noted Elizabeth J. Mayer-Davis, PhD, of the departments of nutrition and medicine, University of North Carolina, Chapel Hill, and her associates (N Engl J Med. 2017 April 13. doi: 101056/NEJMoa1610187).
Similarly, they estimated that approximately 3,800 cases of type 2 diabetes were diagnosed in the first year of the study, increasing to 5,300 in the final year. The annual relative increase in type 2 diabetes was 4.8%.
The rate of increase varied across the five major ethnic groups studied: non-Hispanic whites, non-Hispanic blacks, Hispanics, Asians or Pacific Islanders, and Native Americans. Type 1 diabetes incidence rose rapidly among Hispanic youths, and type 2 diabetes rose rapidly in all racial and ethnic groups other than whites, with the greatest rate of increase among Native Americans.
These increases suggest “a growing disease burden that will not be shared equally” because of differences among ethnic groups in barriers to care, methods of treatment, and clinical outcomes. “These findings highlight the critical need to identify approaches to reduce disparities among racial and ethnic groups,” Dr. Mayer-Davis and her associates noted.
The National Institute of Diabetes and Digestive and Kidney Diseases and the Centers for Disease Control and Prevention funded the study. Dr. Mayer-Davis reported having no relevant disclosures. One of her associates reported serving as a consultant to Denka-Seiken and MedTest DX.
The annual incidence of both types 1 and 2 diabetes markedly increased among youths between 2002 and 2012, especially among those in minority racial and ethnic groups, according to a report published online April 13 in the New England Journal of Medicine.
Researchers analyzed trends in diabetes incidence in the observational Search for Diabetes in Youth study, which conducts annual population-based case ascertainment of the disease in people aged 0-20 years. SEARCH is funded by the Centers for Disease Control and Prevention and the National Institute of Diabetes and Digestive and Kidney Diseases.
In this analysis of SEARCH data, there were 11,245 youths with type 1 diabetes in 54,239,600 person-years of surveillance and 2,846 with type 2 diabetes in 28,029,000 person-years of surveillance.
“We estimated that approximately 15,900 cases of type 1 diabetes were diagnosed annually in the U.S. in the 2002-2003 period, and this number increased to 17,900 annually in the 2011-2012 period. Overall, the adjusted annual relative increase in the incidence of type 1 diabetes was 1.8%,” noted Elizabeth J. Mayer-Davis, PhD, of the departments of nutrition and medicine, University of North Carolina, Chapel Hill, and her associates (N Engl J Med. 2017 April 13. doi: 101056/NEJMoa1610187).
Similarly, they estimated that approximately 3,800 cases of type 2 diabetes were diagnosed in the first year of the study, increasing to 5,300 in the final year. The annual relative increase in type 2 diabetes was 4.8%.
The rate of increase varied across the five major ethnic groups studied: non-Hispanic whites, non-Hispanic blacks, Hispanics, Asians or Pacific Islanders, and Native Americans. Type 1 diabetes incidence rose rapidly among Hispanic youths, and type 2 diabetes rose rapidly in all racial and ethnic groups other than whites, with the greatest rate of increase among Native Americans.
These increases suggest “a growing disease burden that will not be shared equally” because of differences among ethnic groups in barriers to care, methods of treatment, and clinical outcomes. “These findings highlight the critical need to identify approaches to reduce disparities among racial and ethnic groups,” Dr. Mayer-Davis and her associates noted.
The National Institute of Diabetes and Digestive and Kidney Diseases and the Centers for Disease Control and Prevention funded the study. Dr. Mayer-Davis reported having no relevant disclosures. One of her associates reported serving as a consultant to Denka-Seiken and MedTest DX.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Both types 1 and 2 diabetes increased markedly among youths between 2002 and 2012, especially among those in minority racial and ethnic groups.
Major finding: The incidence of type 1 diabetes increased an estimated 1.8% per year and that of type 2 diabetes increased 4.8% per year between 2002 and 2012.
Data source: An observational study assessing a nationally representative sample of youths aged 0-20 years in five states, including 11,245 with type 1 and 2,846 with type 2 diabetes.
Disclosures: The National Institute of Diabetes and Digestive and Kidney Diseases and the Centers for Disease Control and Prevention funded the study. Dr. Mayer-Davis reported having no relevant disclosures. One of her associates reported serving as a consultant to Denka-Seiken and MedTest DX.
Metformin linked with better survival in RCC patients with diabetes
Metformin use was associated with better survival for patients with renal cell carcinoma and diabetes in a meta-analysis, investigators report.
Yang Li, MD, and associates at Chongqing (China) Medical University, performed a pooled analysis of data from 254,329 patients with both localized and metastatic renal cell carcinoma, and found the risk of mortality was reduced in patients exposed to metformin (hazard ratio, 0.41; P less than .001).
However, there was significant heterogeneity among the eight eligible studies included in the meta-analysis, Dr. Li and associates reported (Int Urol Nephrol. 2017 Mar 7. doi: 10.1007/s11255-017-1548-4).
In a subgroup analysis, the association held in patients with localized disease, but was not significant in those with metastatic disease.
The current meta-analysis suggests that the use of metformin could improve the survival of kidney cancer patients, particularly those with localized disease; however, further studies are needed, the investigators conclude.
The authors declared that they had no conflicts of interest.
Metformin use was associated with better survival for patients with renal cell carcinoma and diabetes in a meta-analysis, investigators report.
Yang Li, MD, and associates at Chongqing (China) Medical University, performed a pooled analysis of data from 254,329 patients with both localized and metastatic renal cell carcinoma, and found the risk of mortality was reduced in patients exposed to metformin (hazard ratio, 0.41; P less than .001).
However, there was significant heterogeneity among the eight eligible studies included in the meta-analysis, Dr. Li and associates reported (Int Urol Nephrol. 2017 Mar 7. doi: 10.1007/s11255-017-1548-4).
In a subgroup analysis, the association held in patients with localized disease, but was not significant in those with metastatic disease.
The current meta-analysis suggests that the use of metformin could improve the survival of kidney cancer patients, particularly those with localized disease; however, further studies are needed, the investigators conclude.
The authors declared that they had no conflicts of interest.
Metformin use was associated with better survival for patients with renal cell carcinoma and diabetes in a meta-analysis, investigators report.
Yang Li, MD, and associates at Chongqing (China) Medical University, performed a pooled analysis of data from 254,329 patients with both localized and metastatic renal cell carcinoma, and found the risk of mortality was reduced in patients exposed to metformin (hazard ratio, 0.41; P less than .001).
However, there was significant heterogeneity among the eight eligible studies included in the meta-analysis, Dr. Li and associates reported (Int Urol Nephrol. 2017 Mar 7. doi: 10.1007/s11255-017-1548-4).
In a subgroup analysis, the association held in patients with localized disease, but was not significant in those with metastatic disease.
The current meta-analysis suggests that the use of metformin could improve the survival of kidney cancer patients, particularly those with localized disease; however, further studies are needed, the investigators conclude.
The authors declared that they had no conflicts of interest.
Key clinical point:
Major finding: In a pooled analysis of data from eight studies, the risk of mortality was reduced in patients exposed to metformin (hazard ratio, 0.41; P less than .001).
Data source: A meta-analysis of eight studies including 254,329 patients with renal cell carcinoma.
Disclosures: The authors declared that they had no conflicts of interest.
Weight fluctuations linked to higher mortality, CV events
Weight fluctuations – like the typical pattern of weight loss followed by partial or total regain that affects most people attempting to lose weight – are strongly associated with higher mortality, more cardiovascular events, and new-onset diabetes, according to an analysis of the Treating to New Targets trial published online April 6 in the New England Journal of Medicine.
Weight loss is commonly prescribed as a lifestyle intervention to improve health, especially cardiovascular health. However, “the usual pattern for most patients ... is weight loss followed by weight gain” (also termed weight cycling), which has been linked to poor cardiovascular outcomes, especially when the pattern is repeated over time, said Sripal Bangalore, MD, of New York University, and his coinvestigators.
The primary outcome measure – the composite rate of death from coronary heart disease, nonfatal MI, resuscitated cardiac arrest, revascularization, or angina – was significantly associated with weight fluctuations in a dose-dependent fashion so that greater degrees of variability in body weight were linked to higher event rates (N Engl J Med. 2017 April 6. doi: 10.1056/NEJMoa1606148).
“When compared with the lowest quintile, patients with the highest quintile of variability had an increase in the risk of any coronary event of 64%, an increase in the risk of any cardiovascular event of 85%, an increase in the risk of death of 124%, an increase in the risk of MI of 117%, an increase in the risk of stroke of 136%, and an increase in the risk of new-onset diabetes of 78%, independent of traditional risk factors,” Dr. Bangalore and his associates reported.
This association remained strong regardless of the patients’ weight at baseline, consistent among those of normal body weight and those who were overweight or obese. And the association also persisted across multiple sensitivity analyses.
This study was supported by Pfizer. Dr. Bangalore reported serving as a consultant to Pfizer, Daiichi-Sankyo, Boehringer Ingelheim, Merck, Menarini, Gilead, and Abbott Vascular; his associates reported ties to numerous industry sources.
Weight fluctuations – like the typical pattern of weight loss followed by partial or total regain that affects most people attempting to lose weight – are strongly associated with higher mortality, more cardiovascular events, and new-onset diabetes, according to an analysis of the Treating to New Targets trial published online April 6 in the New England Journal of Medicine.
Weight loss is commonly prescribed as a lifestyle intervention to improve health, especially cardiovascular health. However, “the usual pattern for most patients ... is weight loss followed by weight gain” (also termed weight cycling), which has been linked to poor cardiovascular outcomes, especially when the pattern is repeated over time, said Sripal Bangalore, MD, of New York University, and his coinvestigators.
The primary outcome measure – the composite rate of death from coronary heart disease, nonfatal MI, resuscitated cardiac arrest, revascularization, or angina – was significantly associated with weight fluctuations in a dose-dependent fashion so that greater degrees of variability in body weight were linked to higher event rates (N Engl J Med. 2017 April 6. doi: 10.1056/NEJMoa1606148).
“When compared with the lowest quintile, patients with the highest quintile of variability had an increase in the risk of any coronary event of 64%, an increase in the risk of any cardiovascular event of 85%, an increase in the risk of death of 124%, an increase in the risk of MI of 117%, an increase in the risk of stroke of 136%, and an increase in the risk of new-onset diabetes of 78%, independent of traditional risk factors,” Dr. Bangalore and his associates reported.
This association remained strong regardless of the patients’ weight at baseline, consistent among those of normal body weight and those who were overweight or obese. And the association also persisted across multiple sensitivity analyses.
This study was supported by Pfizer. Dr. Bangalore reported serving as a consultant to Pfizer, Daiichi-Sankyo, Boehringer Ingelheim, Merck, Menarini, Gilead, and Abbott Vascular; his associates reported ties to numerous industry sources.
Weight fluctuations – like the typical pattern of weight loss followed by partial or total regain that affects most people attempting to lose weight – are strongly associated with higher mortality, more cardiovascular events, and new-onset diabetes, according to an analysis of the Treating to New Targets trial published online April 6 in the New England Journal of Medicine.
Weight loss is commonly prescribed as a lifestyle intervention to improve health, especially cardiovascular health. However, “the usual pattern for most patients ... is weight loss followed by weight gain” (also termed weight cycling), which has been linked to poor cardiovascular outcomes, especially when the pattern is repeated over time, said Sripal Bangalore, MD, of New York University, and his coinvestigators.
The primary outcome measure – the composite rate of death from coronary heart disease, nonfatal MI, resuscitated cardiac arrest, revascularization, or angina – was significantly associated with weight fluctuations in a dose-dependent fashion so that greater degrees of variability in body weight were linked to higher event rates (N Engl J Med. 2017 April 6. doi: 10.1056/NEJMoa1606148).
“When compared with the lowest quintile, patients with the highest quintile of variability had an increase in the risk of any coronary event of 64%, an increase in the risk of any cardiovascular event of 85%, an increase in the risk of death of 124%, an increase in the risk of MI of 117%, an increase in the risk of stroke of 136%, and an increase in the risk of new-onset diabetes of 78%, independent of traditional risk factors,” Dr. Bangalore and his associates reported.
This association remained strong regardless of the patients’ weight at baseline, consistent among those of normal body weight and those who were overweight or obese. And the association also persisted across multiple sensitivity analyses.
This study was supported by Pfizer. Dr. Bangalore reported serving as a consultant to Pfizer, Daiichi-Sankyo, Boehringer Ingelheim, Merck, Menarini, Gilead, and Abbott Vascular; his associates reported ties to numerous industry sources.
Key clinical point: Weight fluctuations are strongly associated with higher mortality, more cardiovascular events, and new-onset diabetes.
Major finding: Patients with the highest quintile of weight variability had increased risks of coronary events (64%), cardiovascular events (85%), death (124%), MI (117%), stroke (136%), and new-onset diabetes (78%).
Data source: A secondary analysis of data for 9,509 adults with coronary artery disease participating in the Treating to New Targets trial of cholesterol therapy.
Disclosures: This study was supported by Pfizer. Dr. Bangalore reported serving as a consultant to Pfizer, Daiichi-Sankyo, Boehringer Ingelheim, Merck, Menarini, Gilead, and Abbott Vascular; his associates reported ties to numerous industry sources.
Gliflozins’ heart failure protection in type 2 diabetes confirmed
WASHINGTON – The remarkable and unexpected findings first reported from the EMPA-REG OUTCOME trial in late 2015 – that treatment of type 2 diabetes patients with the SGLT-2 inhibitor empagliflozin led to significantly reduced rates of heart failure hospitalization and all-cause death – received its first major confirmation in an analysis of observational data collected from more than 300,000 patients with type 2 diabetes treated in six countries including the United States.
The new findings also, for the first time, extended the EMPA-REG OUTCOME results (N Engl J Med. 2015 Nov 26;373[22]:2117-28) beyond empagliflozin with evidence that the heart failure and mortality benefit also occurred with other drugs from the sodium glucose cotransporter–2 (SGLT-2) inhibitor class, specifically canagliflozin and dapagliflozin, Mikhail Kosiborod, MD, said at the annual meeting of the American College of Cardiology.
The analysis showed that type 2 diabetes patients who were newly started on treatment with one of these SGLT-2 inhibitors had during follow-up a 39% reduced rate of heart failure hospitalizations, a 51% reduced mortality rate, and a 46% reduced rate of the combined endpoint of heart failure hospitalization or death, compared with patients treated with any other type of oral glucose-lowering drug, reported Dr. Kosiborod. The risk reductions were “remarkably similar to those seen in EMPA-REG OUTCOME,” he noted.
The findings address three “key questions” raised by the EMPA-REG OUTCOME results, Dr. Kosiborod, a cardiologist and professor of medicine at Saint Luke’s Mid America Heart Institute in Kansas City, Mo., said in an interview:
• Is this a class effect? The data “seem to suggest that the benefits seen in the EMPA-REG OUTCOME study are likely a class effect.” The study population of 154,523 patients in the heart failure hospitalization analysis who began treatment with an SGLT-2 inhibitor included 53% who received canagliflozin (Invokana), 42% who received dapagliflozin (Farxiga), and 6% who received empagliflozin (Jardiance) (percentages total 101% because of rounding). Dr. Kosiborod also highlighted that within several of the six countries that contributed data to this analysis – the United States, Denmark, Germany, Norway, Sweden, and the United Kingdom – the percentages of patients on each of these three drugs varied substantially, but despite that the relative reduced risks for heart failure hospitalization and mortality were roughly the same within each country, giving further credence to the notion that a class effect exists.
• Do lower-risk patients benefit? “The benefits of SGLT-2 inhibitor treatment appeared to extend to lower risk patients” than those enrolled in EMPA-REG OUTCOME. In the randomized trial, which enrolled 7,028 patients, more than 99% had established cardiovascular disease. In the new analysis patients had a 13% prevalence of any cardiovascular disease at baseline, and the prevalence of heart failure was 3%.
• Is this relevant to clinical practice? Unlike the highly selected patients entered in the EMPA-REG OUTCOME trial, the patients started on an SGLT-2 inhibitor in the observational study were unselected and came from routine practice situations, “suggesting that the benefits seen in EMPA-REG OUTCOME translate into real-world clinical practice,” Dr. Kosiborod said. “With these data we see for the first time in a large number of patients from multiple countries important evidence suggesting that the SGLT-2 inhibitors may provide in the real world a similar benefit to what was observed in EMPA-REG OUTCOME.”
“The lesson from Dr. Kosiborod’s study is that among patients with type 2 diabetes, treatment with an SGLT-2 inhibitor seems to result in lowered rates of heart failure hospitalizations and mortality, and it’s a safe class of drugs. In the past, we worried about worsening heart failure in patients at risk for developing heart failure” such as patients with type 2 diabetes, said Adrian F. Hernandez, MD, professor of medicine and a cardiologist at Duke University in Durham, N.C. The new data make it seem like using an SGLT-2 inhibitor to treat patients with type 2 diabetes “is an appropriate strategy.” But Dr. Hernandez added that in his opinion metformin remains the top drug for type 2 diabetes, while SGLT-2 inhibitors are now “the next drug class to add,” he said in an interview.
Dr. Kosiborod had a somewhat different take. “If a patient with type 2 diabetes did not want to enter a trial or couldn’t get into a trial and fit the profile of a patient who could benefit, I would absolutely treat that patient with an SGLT-2 inhibitor. I’m using these medications clinically as a cardiologist,” he said. “Treatments that have significant benefits for important outcomes should be prioritized over treatments that may reduce hemoglobin A1c but do not have similar benefits.”
The CVD-REAL (Comparative Effectiveness of Cardiovascular Outcomes in New Users of SGLT-2 Inhibitors) study used data from adult, previously untreated patients with type 2 diabetes in national registries from the five included European countries. U.S. data were from the Truven Health MarketScan database and from Medicare. This produced a total pool of 160,010 patients who began treatment on an SGLT-2 inhibitor and 1,139,905 patients who began treatment with another oral antidiabetes drug.
Dr. Kosiborod and his associates then performed propensity-score matching to identify 154,523 patients started on an SGLT-2 inhibitor who each closely matched a patient from the other subgroup for baseline demographic and clinical features, producing an analysis dataset of just over 309,000 matched patients. The average age of the included patients was 57 years; 45% were women. During follow-up, 961 patients had a heart failure hospitalization and 1,334 patients died.
Dr. Kosiborod noted that while a potential limitation to his findings is residual confounding not eliminated by the propensity score matching, he was confident about the results because the incidence of other outcomes not expected to be influenced by treatment with SGLT-2 inhibitors were similar in the two study subgroups, suggesting that the linkages between the kind of drug used and differences in heart failure hospitalization rates and in mortality weren’t spurious.
“If there was residual confounding, you’d expect to see similar associations for other endpoints, which we didn’t see,” he said. In addition, the heart failure hospitalization rate differences seen between the SGLT-2 inhibitor recipients and the other patients were consistent in a trio of sensitivity analyses, further buttressing the findings’ plausibility.
CVD-REAL was sponsored by AstraZeneca, the company that markets dapagliflozin (Farxiga). Dr. Kosiborod has been a consultant to and/or received research funding from AstraZeneca, Boehringer Ingelheim, Sanofi-Aventis and Gilead. Dr. Hernandez has received honoraria and/or research support from AstraZeneca, Amgen, Janssen, Merck, Novartis, and Portola. Several of the coauthors on the CVD-REAL study were AstraZeneca employees.
[email protected]
On Twitter @mitchelzoler
WASHINGTON – The remarkable and unexpected findings first reported from the EMPA-REG OUTCOME trial in late 2015 – that treatment of type 2 diabetes patients with the SGLT-2 inhibitor empagliflozin led to significantly reduced rates of heart failure hospitalization and all-cause death – received its first major confirmation in an analysis of observational data collected from more than 300,000 patients with type 2 diabetes treated in six countries including the United States.
The new findings also, for the first time, extended the EMPA-REG OUTCOME results (N Engl J Med. 2015 Nov 26;373[22]:2117-28) beyond empagliflozin with evidence that the heart failure and mortality benefit also occurred with other drugs from the sodium glucose cotransporter–2 (SGLT-2) inhibitor class, specifically canagliflozin and dapagliflozin, Mikhail Kosiborod, MD, said at the annual meeting of the American College of Cardiology.
The analysis showed that type 2 diabetes patients who were newly started on treatment with one of these SGLT-2 inhibitors had during follow-up a 39% reduced rate of heart failure hospitalizations, a 51% reduced mortality rate, and a 46% reduced rate of the combined endpoint of heart failure hospitalization or death, compared with patients treated with any other type of oral glucose-lowering drug, reported Dr. Kosiborod. The risk reductions were “remarkably similar to those seen in EMPA-REG OUTCOME,” he noted.
The findings address three “key questions” raised by the EMPA-REG OUTCOME results, Dr. Kosiborod, a cardiologist and professor of medicine at Saint Luke’s Mid America Heart Institute in Kansas City, Mo., said in an interview:
• Is this a class effect? The data “seem to suggest that the benefits seen in the EMPA-REG OUTCOME study are likely a class effect.” The study population of 154,523 patients in the heart failure hospitalization analysis who began treatment with an SGLT-2 inhibitor included 53% who received canagliflozin (Invokana), 42% who received dapagliflozin (Farxiga), and 6% who received empagliflozin (Jardiance) (percentages total 101% because of rounding). Dr. Kosiborod also highlighted that within several of the six countries that contributed data to this analysis – the United States, Denmark, Germany, Norway, Sweden, and the United Kingdom – the percentages of patients on each of these three drugs varied substantially, but despite that the relative reduced risks for heart failure hospitalization and mortality were roughly the same within each country, giving further credence to the notion that a class effect exists.
• Do lower-risk patients benefit? “The benefits of SGLT-2 inhibitor treatment appeared to extend to lower risk patients” than those enrolled in EMPA-REG OUTCOME. In the randomized trial, which enrolled 7,028 patients, more than 99% had established cardiovascular disease. In the new analysis patients had a 13% prevalence of any cardiovascular disease at baseline, and the prevalence of heart failure was 3%.
• Is this relevant to clinical practice? Unlike the highly selected patients entered in the EMPA-REG OUTCOME trial, the patients started on an SGLT-2 inhibitor in the observational study were unselected and came from routine practice situations, “suggesting that the benefits seen in EMPA-REG OUTCOME translate into real-world clinical practice,” Dr. Kosiborod said. “With these data we see for the first time in a large number of patients from multiple countries important evidence suggesting that the SGLT-2 inhibitors may provide in the real world a similar benefit to what was observed in EMPA-REG OUTCOME.”
“The lesson from Dr. Kosiborod’s study is that among patients with type 2 diabetes, treatment with an SGLT-2 inhibitor seems to result in lowered rates of heart failure hospitalizations and mortality, and it’s a safe class of drugs. In the past, we worried about worsening heart failure in patients at risk for developing heart failure” such as patients with type 2 diabetes, said Adrian F. Hernandez, MD, professor of medicine and a cardiologist at Duke University in Durham, N.C. The new data make it seem like using an SGLT-2 inhibitor to treat patients with type 2 diabetes “is an appropriate strategy.” But Dr. Hernandez added that in his opinion metformin remains the top drug for type 2 diabetes, while SGLT-2 inhibitors are now “the next drug class to add,” he said in an interview.
Dr. Kosiborod had a somewhat different take. “If a patient with type 2 diabetes did not want to enter a trial or couldn’t get into a trial and fit the profile of a patient who could benefit, I would absolutely treat that patient with an SGLT-2 inhibitor. I’m using these medications clinically as a cardiologist,” he said. “Treatments that have significant benefits for important outcomes should be prioritized over treatments that may reduce hemoglobin A1c but do not have similar benefits.”
The CVD-REAL (Comparative Effectiveness of Cardiovascular Outcomes in New Users of SGLT-2 Inhibitors) study used data from adult, previously untreated patients with type 2 diabetes in national registries from the five included European countries. U.S. data were from the Truven Health MarketScan database and from Medicare. This produced a total pool of 160,010 patients who began treatment on an SGLT-2 inhibitor and 1,139,905 patients who began treatment with another oral antidiabetes drug.
Dr. Kosiborod and his associates then performed propensity-score matching to identify 154,523 patients started on an SGLT-2 inhibitor who each closely matched a patient from the other subgroup for baseline demographic and clinical features, producing an analysis dataset of just over 309,000 matched patients. The average age of the included patients was 57 years; 45% were women. During follow-up, 961 patients had a heart failure hospitalization and 1,334 patients died.
Dr. Kosiborod noted that while a potential limitation to his findings is residual confounding not eliminated by the propensity score matching, he was confident about the results because the incidence of other outcomes not expected to be influenced by treatment with SGLT-2 inhibitors were similar in the two study subgroups, suggesting that the linkages between the kind of drug used and differences in heart failure hospitalization rates and in mortality weren’t spurious.
“If there was residual confounding, you’d expect to see similar associations for other endpoints, which we didn’t see,” he said. In addition, the heart failure hospitalization rate differences seen between the SGLT-2 inhibitor recipients and the other patients were consistent in a trio of sensitivity analyses, further buttressing the findings’ plausibility.
CVD-REAL was sponsored by AstraZeneca, the company that markets dapagliflozin (Farxiga). Dr. Kosiborod has been a consultant to and/or received research funding from AstraZeneca, Boehringer Ingelheim, Sanofi-Aventis and Gilead. Dr. Hernandez has received honoraria and/or research support from AstraZeneca, Amgen, Janssen, Merck, Novartis, and Portola. Several of the coauthors on the CVD-REAL study were AstraZeneca employees.
[email protected]
On Twitter @mitchelzoler
WASHINGTON – The remarkable and unexpected findings first reported from the EMPA-REG OUTCOME trial in late 2015 – that treatment of type 2 diabetes patients with the SGLT-2 inhibitor empagliflozin led to significantly reduced rates of heart failure hospitalization and all-cause death – received its first major confirmation in an analysis of observational data collected from more than 300,000 patients with type 2 diabetes treated in six countries including the United States.
The new findings also, for the first time, extended the EMPA-REG OUTCOME results (N Engl J Med. 2015 Nov 26;373[22]:2117-28) beyond empagliflozin with evidence that the heart failure and mortality benefit also occurred with other drugs from the sodium glucose cotransporter–2 (SGLT-2) inhibitor class, specifically canagliflozin and dapagliflozin, Mikhail Kosiborod, MD, said at the annual meeting of the American College of Cardiology.
The analysis showed that type 2 diabetes patients who were newly started on treatment with one of these SGLT-2 inhibitors had during follow-up a 39% reduced rate of heart failure hospitalizations, a 51% reduced mortality rate, and a 46% reduced rate of the combined endpoint of heart failure hospitalization or death, compared with patients treated with any other type of oral glucose-lowering drug, reported Dr. Kosiborod. The risk reductions were “remarkably similar to those seen in EMPA-REG OUTCOME,” he noted.
The findings address three “key questions” raised by the EMPA-REG OUTCOME results, Dr. Kosiborod, a cardiologist and professor of medicine at Saint Luke’s Mid America Heart Institute in Kansas City, Mo., said in an interview:
• Is this a class effect? The data “seem to suggest that the benefits seen in the EMPA-REG OUTCOME study are likely a class effect.” The study population of 154,523 patients in the heart failure hospitalization analysis who began treatment with an SGLT-2 inhibitor included 53% who received canagliflozin (Invokana), 42% who received dapagliflozin (Farxiga), and 6% who received empagliflozin (Jardiance) (percentages total 101% because of rounding). Dr. Kosiborod also highlighted that within several of the six countries that contributed data to this analysis – the United States, Denmark, Germany, Norway, Sweden, and the United Kingdom – the percentages of patients on each of these three drugs varied substantially, but despite that the relative reduced risks for heart failure hospitalization and mortality were roughly the same within each country, giving further credence to the notion that a class effect exists.
• Do lower-risk patients benefit? “The benefits of SGLT-2 inhibitor treatment appeared to extend to lower risk patients” than those enrolled in EMPA-REG OUTCOME. In the randomized trial, which enrolled 7,028 patients, more than 99% had established cardiovascular disease. In the new analysis patients had a 13% prevalence of any cardiovascular disease at baseline, and the prevalence of heart failure was 3%.
• Is this relevant to clinical practice? Unlike the highly selected patients entered in the EMPA-REG OUTCOME trial, the patients started on an SGLT-2 inhibitor in the observational study were unselected and came from routine practice situations, “suggesting that the benefits seen in EMPA-REG OUTCOME translate into real-world clinical practice,” Dr. Kosiborod said. “With these data we see for the first time in a large number of patients from multiple countries important evidence suggesting that the SGLT-2 inhibitors may provide in the real world a similar benefit to what was observed in EMPA-REG OUTCOME.”
“The lesson from Dr. Kosiborod’s study is that among patients with type 2 diabetes, treatment with an SGLT-2 inhibitor seems to result in lowered rates of heart failure hospitalizations and mortality, and it’s a safe class of drugs. In the past, we worried about worsening heart failure in patients at risk for developing heart failure” such as patients with type 2 diabetes, said Adrian F. Hernandez, MD, professor of medicine and a cardiologist at Duke University in Durham, N.C. The new data make it seem like using an SGLT-2 inhibitor to treat patients with type 2 diabetes “is an appropriate strategy.” But Dr. Hernandez added that in his opinion metformin remains the top drug for type 2 diabetes, while SGLT-2 inhibitors are now “the next drug class to add,” he said in an interview.
Dr. Kosiborod had a somewhat different take. “If a patient with type 2 diabetes did not want to enter a trial or couldn’t get into a trial and fit the profile of a patient who could benefit, I would absolutely treat that patient with an SGLT-2 inhibitor. I’m using these medications clinically as a cardiologist,” he said. “Treatments that have significant benefits for important outcomes should be prioritized over treatments that may reduce hemoglobin A1c but do not have similar benefits.”
The CVD-REAL (Comparative Effectiveness of Cardiovascular Outcomes in New Users of SGLT-2 Inhibitors) study used data from adult, previously untreated patients with type 2 diabetes in national registries from the five included European countries. U.S. data were from the Truven Health MarketScan database and from Medicare. This produced a total pool of 160,010 patients who began treatment on an SGLT-2 inhibitor and 1,139,905 patients who began treatment with another oral antidiabetes drug.
Dr. Kosiborod and his associates then performed propensity-score matching to identify 154,523 patients started on an SGLT-2 inhibitor who each closely matched a patient from the other subgroup for baseline demographic and clinical features, producing an analysis dataset of just over 309,000 matched patients. The average age of the included patients was 57 years; 45% were women. During follow-up, 961 patients had a heart failure hospitalization and 1,334 patients died.
Dr. Kosiborod noted that while a potential limitation to his findings is residual confounding not eliminated by the propensity score matching, he was confident about the results because the incidence of other outcomes not expected to be influenced by treatment with SGLT-2 inhibitors were similar in the two study subgroups, suggesting that the linkages between the kind of drug used and differences in heart failure hospitalization rates and in mortality weren’t spurious.
“If there was residual confounding, you’d expect to see similar associations for other endpoints, which we didn’t see,” he said. In addition, the heart failure hospitalization rate differences seen between the SGLT-2 inhibitor recipients and the other patients were consistent in a trio of sensitivity analyses, further buttressing the findings’ plausibility.
CVD-REAL was sponsored by AstraZeneca, the company that markets dapagliflozin (Farxiga). Dr. Kosiborod has been a consultant to and/or received research funding from AstraZeneca, Boehringer Ingelheim, Sanofi-Aventis and Gilead. Dr. Hernandez has received honoraria and/or research support from AstraZeneca, Amgen, Janssen, Merck, Novartis, and Portola. Several of the coauthors on the CVD-REAL study were AstraZeneca employees.
[email protected]
On Twitter @mitchelzoler
AT ACC 17
Key clinical point:
Major finding: Treatment with an SGLT-2 inhibitor was associated with a significant 39% reduction in heart failure hospitalizations compared with other antidiabetes drugs.
Data source: CVD-REAL, which used observational data collected from 309,046 patients with type 2 diabetes in six countries.
Disclosures: CVD-REAL was sponsored by AstraZeneca, the company that markets dapagliflozin (Farxiga). Dr. Kosiborod has been a consultant to AstraZeneca and to several other drug companies, and he has received research funding from AstraZeneca, Boehringer Ingelheim, Sanofi-Aventis and Gilead. Dr. Hernandez has received honoraria and research support from AstraZeneca and has also received honoraria from Amgen, Janssen, Merck, and Novartis, and has also received research support from Amgen, Bayer, Merck, and Portola. Several of the coauthors on the CVD-REAL study were AstraZeneca employees.
In type 2 diabetes, chronotype may affect depressive symptoms
ORLANDO – For patients with type 2 diabetes, larks may have an edge on owls when it comes to mood, according to a new study. Significantly more depressive symptoms were seen in owls – individuals whose sleep time preference, or chronotype, was later-to-bed and later-to-rise – in a cohort of 476 patients with type 2 diabetes.
In work that accounted for regional differences in chronotype by drawing from two different geographic regions, a later chronotype was associated with a higher score on the Center for Epidemiologic Studies Depression scale (CES-D), after controlling for potentially confounding factors (P = .045 for each cohort).
The study’s senior author, Sirimon Reutrakul, MD, of the faculty of medicine at Mahidol University, Bangkok, Thailand, said that previous work had also shown that when depression in patients with diabetes is untreated, self-care and blood glucose control can suffer, and more complications of diabetes are seen.
Dr. Reutrakul’s facility teamed with Rush University School of Medicine in Chicago, administering questionnaires designed to assess where patients fell along the morningness-eveningness scale. For the Chicago cohort (n = 194, 70% female), the Morningness-Eveningness Questionnaire (MEQ) was administered, while the Thailand cohort (n = 282, 57% female) completed the Composite Score of Morningness (CSM). Both groups completed the CES-D to assess depressive symptoms and the Pittsburgh Sleep Quality Index (PSQI); hemoglobin A1c values for both groups were ascertained by medical record review.
The mean age for the two cohorts was similar (Chicago, 58.3 plus or minus 13.0 years; Thailand, 55.7 plus or minus 11.6 years). The Chicago patients who scored higher on the CES-D, indicating that they had more depressive symptoms, were more likely to have a later chronotype on unadjusted analysis (P = .001). They were also likely to be younger (P = .005) and to have poorer sleep quality (P less than .001). Patients with more depressive symptoms were significantly more likely to be female, non-white, to use insulin, and to have poor glycemic control.
For the patients in Thailand, more depressive symptoms were also associated with a later chronotype on unadjusted analysis (P less than .001); younger age (P = .019), and poor sleep quality (P less than .001) were also associated with more depressive symptoms. Correction for a number of potentially confounding variables yielded modest statistical significance (P = .045) of the depressive symptoms-later chronotype relationship in both cohorts.
The Chicago patients were at approximately latitude 42N, while the patients in Thailand were at about latitude 13N, much closer to the equator. Populations that live closer to the equator, where days and nights are of approximately equal length year-round, tend to have more larks than owls, wrote Dr. Reutrakul and her colleagues.
In these two cohorts, which differed both by ethnic composition and geographic distance from the equator, “later chronotype was found to be independently associated with depressive symptoms” for patients with type 2 diabetes, wrote Dr. Reutrakul and her coauthors in the abstract accompanying the presentation. “In addition, sleep disturbances, more prevalent in evening types, have been associated with depression,” which is common in type 2 diabetes, the investigators wrote.
Dr. Reutrakul acknowledged that the work found an “only modest,” though consistent, association between eveningness and depressive symptoms. “We need further research to explore a combination of interventions that help with circadian timing, such as light therapy and melatonin,” she said in a press statement preceding her presentation. “Learning more about the relationship between depression and circadian functioning might help us figure out strategies to improve physical and mental health for patients with diabetes…We need further research to explore a combination of interventions that help with circadian timing, such as light therapy and melatonin,” Dr. Reutrakul said.
Dr. Reutrakul reported financial relationships with Medtronic Minimed, Novo Nordisk, Merck, and Sanofi.
[email protected]
On Twitter @karioakes
ORLANDO – For patients with type 2 diabetes, larks may have an edge on owls when it comes to mood, according to a new study. Significantly more depressive symptoms were seen in owls – individuals whose sleep time preference, or chronotype, was later-to-bed and later-to-rise – in a cohort of 476 patients with type 2 diabetes.
In work that accounted for regional differences in chronotype by drawing from two different geographic regions, a later chronotype was associated with a higher score on the Center for Epidemiologic Studies Depression scale (CES-D), after controlling for potentially confounding factors (P = .045 for each cohort).
The study’s senior author, Sirimon Reutrakul, MD, of the faculty of medicine at Mahidol University, Bangkok, Thailand, said that previous work had also shown that when depression in patients with diabetes is untreated, self-care and blood glucose control can suffer, and more complications of diabetes are seen.
Dr. Reutrakul’s facility teamed with Rush University School of Medicine in Chicago, administering questionnaires designed to assess where patients fell along the morningness-eveningness scale. For the Chicago cohort (n = 194, 70% female), the Morningness-Eveningness Questionnaire (MEQ) was administered, while the Thailand cohort (n = 282, 57% female) completed the Composite Score of Morningness (CSM). Both groups completed the CES-D to assess depressive symptoms and the Pittsburgh Sleep Quality Index (PSQI); hemoglobin A1c values for both groups were ascertained by medical record review.
The mean age for the two cohorts was similar (Chicago, 58.3 plus or minus 13.0 years; Thailand, 55.7 plus or minus 11.6 years). The Chicago patients who scored higher on the CES-D, indicating that they had more depressive symptoms, were more likely to have a later chronotype on unadjusted analysis (P = .001). They were also likely to be younger (P = .005) and to have poorer sleep quality (P less than .001). Patients with more depressive symptoms were significantly more likely to be female, non-white, to use insulin, and to have poor glycemic control.
For the patients in Thailand, more depressive symptoms were also associated with a later chronotype on unadjusted analysis (P less than .001); younger age (P = .019), and poor sleep quality (P less than .001) were also associated with more depressive symptoms. Correction for a number of potentially confounding variables yielded modest statistical significance (P = .045) of the depressive symptoms-later chronotype relationship in both cohorts.
The Chicago patients were at approximately latitude 42N, while the patients in Thailand were at about latitude 13N, much closer to the equator. Populations that live closer to the equator, where days and nights are of approximately equal length year-round, tend to have more larks than owls, wrote Dr. Reutrakul and her colleagues.
In these two cohorts, which differed both by ethnic composition and geographic distance from the equator, “later chronotype was found to be independently associated with depressive symptoms” for patients with type 2 diabetes, wrote Dr. Reutrakul and her coauthors in the abstract accompanying the presentation. “In addition, sleep disturbances, more prevalent in evening types, have been associated with depression,” which is common in type 2 diabetes, the investigators wrote.
Dr. Reutrakul acknowledged that the work found an “only modest,” though consistent, association between eveningness and depressive symptoms. “We need further research to explore a combination of interventions that help with circadian timing, such as light therapy and melatonin,” she said in a press statement preceding her presentation. “Learning more about the relationship between depression and circadian functioning might help us figure out strategies to improve physical and mental health for patients with diabetes…We need further research to explore a combination of interventions that help with circadian timing, such as light therapy and melatonin,” Dr. Reutrakul said.
Dr. Reutrakul reported financial relationships with Medtronic Minimed, Novo Nordisk, Merck, and Sanofi.
[email protected]
On Twitter @karioakes
ORLANDO – For patients with type 2 diabetes, larks may have an edge on owls when it comes to mood, according to a new study. Significantly more depressive symptoms were seen in owls – individuals whose sleep time preference, or chronotype, was later-to-bed and later-to-rise – in a cohort of 476 patients with type 2 diabetes.
In work that accounted for regional differences in chronotype by drawing from two different geographic regions, a later chronotype was associated with a higher score on the Center for Epidemiologic Studies Depression scale (CES-D), after controlling for potentially confounding factors (P = .045 for each cohort).
The study’s senior author, Sirimon Reutrakul, MD, of the faculty of medicine at Mahidol University, Bangkok, Thailand, said that previous work had also shown that when depression in patients with diabetes is untreated, self-care and blood glucose control can suffer, and more complications of diabetes are seen.
Dr. Reutrakul’s facility teamed with Rush University School of Medicine in Chicago, administering questionnaires designed to assess where patients fell along the morningness-eveningness scale. For the Chicago cohort (n = 194, 70% female), the Morningness-Eveningness Questionnaire (MEQ) was administered, while the Thailand cohort (n = 282, 57% female) completed the Composite Score of Morningness (CSM). Both groups completed the CES-D to assess depressive symptoms and the Pittsburgh Sleep Quality Index (PSQI); hemoglobin A1c values for both groups were ascertained by medical record review.
The mean age for the two cohorts was similar (Chicago, 58.3 plus or minus 13.0 years; Thailand, 55.7 plus or minus 11.6 years). The Chicago patients who scored higher on the CES-D, indicating that they had more depressive symptoms, were more likely to have a later chronotype on unadjusted analysis (P = .001). They were also likely to be younger (P = .005) and to have poorer sleep quality (P less than .001). Patients with more depressive symptoms were significantly more likely to be female, non-white, to use insulin, and to have poor glycemic control.
For the patients in Thailand, more depressive symptoms were also associated with a later chronotype on unadjusted analysis (P less than .001); younger age (P = .019), and poor sleep quality (P less than .001) were also associated with more depressive symptoms. Correction for a number of potentially confounding variables yielded modest statistical significance (P = .045) of the depressive symptoms-later chronotype relationship in both cohorts.
The Chicago patients were at approximately latitude 42N, while the patients in Thailand were at about latitude 13N, much closer to the equator. Populations that live closer to the equator, where days and nights are of approximately equal length year-round, tend to have more larks than owls, wrote Dr. Reutrakul and her colleagues.
In these two cohorts, which differed both by ethnic composition and geographic distance from the equator, “later chronotype was found to be independently associated with depressive symptoms” for patients with type 2 diabetes, wrote Dr. Reutrakul and her coauthors in the abstract accompanying the presentation. “In addition, sleep disturbances, more prevalent in evening types, have been associated with depression,” which is common in type 2 diabetes, the investigators wrote.
Dr. Reutrakul acknowledged that the work found an “only modest,” though consistent, association between eveningness and depressive symptoms. “We need further research to explore a combination of interventions that help with circadian timing, such as light therapy and melatonin,” she said in a press statement preceding her presentation. “Learning more about the relationship between depression and circadian functioning might help us figure out strategies to improve physical and mental health for patients with diabetes…We need further research to explore a combination of interventions that help with circadian timing, such as light therapy and melatonin,” Dr. Reutrakul said.
Dr. Reutrakul reported financial relationships with Medtronic Minimed, Novo Nordisk, Merck, and Sanofi.
[email protected]
On Twitter @karioakes
AT ENDO 2017
Key clinical point:
Major finding: Later chronotype was associated with more depressive symptoms in 2 cohorts with type 2 diabetes (P = .045)
Data source: Cross-sectional study of 476 patients with type 2 diabetes in Chicago and Thailand..
Disclosures: Dr. Reutrakul reported financial relationships with Medtronic Minimed, Merck, Novo Nordisk, and Sanofi.
Osteoarthritis’ link to metabolic syndrome tied to body weight, BMI
The metabolic syndrome’s association with the development of osteoarthritis appears to occur primarily through the influence of factors related to body weight or body mass index, according to an analysis of data from the longitudinal Framingham osteoarthritis study.
Jingbo Niu, DSc, of the Clinical Epidemiology Research and Training Unit at Boston University, and her colleagues found that while the presence of the metabolic syndrome (MetS) and its individual components – central obesity, dyslipidemia, impaired fasting glucose, and hypertension – were associated with a risk of both radiographic osteoarthritis (ROA) and symptomatic OA (SxOA), all associations besides high blood pressure (particularly diastolic blood pressure) disappeared after they adjusted for body mass index (BMI) or body weight (Arthritis Rheumatol. 2017 Mar 3. doi: 10.1002/art.40087).
The research team analyzed 991 participants of the 1992-1995 Framingham Offspring Cohort who did not have existing OA at baseline. Average age was 54.2 years; 55.1% were women. According to Adult Treatment Panel III criteria, 27% of the men and 23% of the women had MetS. Those who had MetS were older, had a higher BMI, and were less likely to drink alcohol or have a college education.
In 2002-2005, the cohort underwent follow-up for the presence of OA. The incidence of ROA in the cohort was 9.8% (78 of 800 knees) in men and 10.5% (105 of 1,003 knees) in women. ROA occurred when a knee without previous radiographic evidence of OA developed a Kellgren and Lawrence score of 2 or higher, and SxOA occurred when a knee developed ROA together with knee pain.
After adjusting for age, education, smoking status, alcohol consumption, and physical activity, the researchers found that MetS, abdominal obesity, and low high-density lipoprotein cholesterol were significantly associated with incident ROA among men. Among women, abdominal obesity and high blood pressure were associated with incident ROA, while MetS was not. However, after adjustment for body weight or BMI, none of the associations remained significant.
The incidence of SxOA was 6.3% (53 of 837 knees) in men and 7.2% (75 of 1,037 knees) in women. Incident SxOA was significantly associated with MetS in women and with the MetS components of abdominal obesity and high blood pressure in both men and women before adjustment for BMI or body weight. However, only an association between diastolic blood pressure and incident SxOA persisted in both sexes after adjustment for body weight, the study authors noted.
“High blood pressure is another MetS component associated with OA in previous studies before adjusting for BMI ... While we found [diastolic blood pressure] was related to incident SxOA even after adjustment for BMI, the relation of [systolic blood pressure] and incident SxOA was nearly significant also, suggesting that both might be related to SxOA,” the study authors wrote.
But a cross-sectional analysis of the relationship would be challenging to interpret, they said, since treatment for SxOA included NSAIDs, which are known to raise blood pressure.
The National Institutes of Health supported the study. The authors declared having no conflicts of interest.
The OA incidence reported in the Framingham study is particularly noteworthy because it shows that preexisting MetS and its components are risk factors for subsequent symptomatic OA and not just radiographic OA, which seems to indicate the existence of common risk factors for both MetS and OA in a manner such that OA could be just a late-occurring component of MetS.
But it may be most appropriate to consider metabolic OA as a complication of MetS, similar to cardiovascular disease.
The fact that any component of MetS remained significantly associated with symptomatic OA after adjustment for BMI and body weight argued strongly for a metabolic driver of OA pathophysiology when considering the likely confounding of body weight between mechanical and metabolic processes.
Nevertheless, carefully designed studies are needed to determine the relative impact of increased body mass in MetS on joint loading versus metabolic derangements, including systemic inflammation, to rule in or out the effects of altered metabolism on incident OA risk independent of biomechanics.
This knowledge would help a great deal toward understanding metabolic OA and other phenotypes as well as for the development of rational treatment approaches.
Thomas Appleton, MD, PhD, of Western University in London, Ont., and his colleagues made these comments in an editorial (Arthritis Rheumatol. 2017 Mar 7. doi: 10.1002/art.40089). They declared having no conflicts of interest to relevant to their editorial.
The OA incidence reported in the Framingham study is particularly noteworthy because it shows that preexisting MetS and its components are risk factors for subsequent symptomatic OA and not just radiographic OA, which seems to indicate the existence of common risk factors for both MetS and OA in a manner such that OA could be just a late-occurring component of MetS.
But it may be most appropriate to consider metabolic OA as a complication of MetS, similar to cardiovascular disease.
The fact that any component of MetS remained significantly associated with symptomatic OA after adjustment for BMI and body weight argued strongly for a metabolic driver of OA pathophysiology when considering the likely confounding of body weight between mechanical and metabolic processes.
Nevertheless, carefully designed studies are needed to determine the relative impact of increased body mass in MetS on joint loading versus metabolic derangements, including systemic inflammation, to rule in or out the effects of altered metabolism on incident OA risk independent of biomechanics.
This knowledge would help a great deal toward understanding metabolic OA and other phenotypes as well as for the development of rational treatment approaches.
Thomas Appleton, MD, PhD, of Western University in London, Ont., and his colleagues made these comments in an editorial (Arthritis Rheumatol. 2017 Mar 7. doi: 10.1002/art.40089). They declared having no conflicts of interest to relevant to their editorial.
The OA incidence reported in the Framingham study is particularly noteworthy because it shows that preexisting MetS and its components are risk factors for subsequent symptomatic OA and not just radiographic OA, which seems to indicate the existence of common risk factors for both MetS and OA in a manner such that OA could be just a late-occurring component of MetS.
But it may be most appropriate to consider metabolic OA as a complication of MetS, similar to cardiovascular disease.
The fact that any component of MetS remained significantly associated with symptomatic OA after adjustment for BMI and body weight argued strongly for a metabolic driver of OA pathophysiology when considering the likely confounding of body weight between mechanical and metabolic processes.
Nevertheless, carefully designed studies are needed to determine the relative impact of increased body mass in MetS on joint loading versus metabolic derangements, including systemic inflammation, to rule in or out the effects of altered metabolism on incident OA risk independent of biomechanics.
This knowledge would help a great deal toward understanding metabolic OA and other phenotypes as well as for the development of rational treatment approaches.
Thomas Appleton, MD, PhD, of Western University in London, Ont., and his colleagues made these comments in an editorial (Arthritis Rheumatol. 2017 Mar 7. doi: 10.1002/art.40089). They declared having no conflicts of interest to relevant to their editorial.
The metabolic syndrome’s association with the development of osteoarthritis appears to occur primarily through the influence of factors related to body weight or body mass index, according to an analysis of data from the longitudinal Framingham osteoarthritis study.
Jingbo Niu, DSc, of the Clinical Epidemiology Research and Training Unit at Boston University, and her colleagues found that while the presence of the metabolic syndrome (MetS) and its individual components – central obesity, dyslipidemia, impaired fasting glucose, and hypertension – were associated with a risk of both radiographic osteoarthritis (ROA) and symptomatic OA (SxOA), all associations besides high blood pressure (particularly diastolic blood pressure) disappeared after they adjusted for body mass index (BMI) or body weight (Arthritis Rheumatol. 2017 Mar 3. doi: 10.1002/art.40087).
The research team analyzed 991 participants of the 1992-1995 Framingham Offspring Cohort who did not have existing OA at baseline. Average age was 54.2 years; 55.1% were women. According to Adult Treatment Panel III criteria, 27% of the men and 23% of the women had MetS. Those who had MetS were older, had a higher BMI, and were less likely to drink alcohol or have a college education.
In 2002-2005, the cohort underwent follow-up for the presence of OA. The incidence of ROA in the cohort was 9.8% (78 of 800 knees) in men and 10.5% (105 of 1,003 knees) in women. ROA occurred when a knee without previous radiographic evidence of OA developed a Kellgren and Lawrence score of 2 or higher, and SxOA occurred when a knee developed ROA together with knee pain.
After adjusting for age, education, smoking status, alcohol consumption, and physical activity, the researchers found that MetS, abdominal obesity, and low high-density lipoprotein cholesterol were significantly associated with incident ROA among men. Among women, abdominal obesity and high blood pressure were associated with incident ROA, while MetS was not. However, after adjustment for body weight or BMI, none of the associations remained significant.
The incidence of SxOA was 6.3% (53 of 837 knees) in men and 7.2% (75 of 1,037 knees) in women. Incident SxOA was significantly associated with MetS in women and with the MetS components of abdominal obesity and high blood pressure in both men and women before adjustment for BMI or body weight. However, only an association between diastolic blood pressure and incident SxOA persisted in both sexes after adjustment for body weight, the study authors noted.
“High blood pressure is another MetS component associated with OA in previous studies before adjusting for BMI ... While we found [diastolic blood pressure] was related to incident SxOA even after adjustment for BMI, the relation of [systolic blood pressure] and incident SxOA was nearly significant also, suggesting that both might be related to SxOA,” the study authors wrote.
But a cross-sectional analysis of the relationship would be challenging to interpret, they said, since treatment for SxOA included NSAIDs, which are known to raise blood pressure.
The National Institutes of Health supported the study. The authors declared having no conflicts of interest.
The metabolic syndrome’s association with the development of osteoarthritis appears to occur primarily through the influence of factors related to body weight or body mass index, according to an analysis of data from the longitudinal Framingham osteoarthritis study.
Jingbo Niu, DSc, of the Clinical Epidemiology Research and Training Unit at Boston University, and her colleagues found that while the presence of the metabolic syndrome (MetS) and its individual components – central obesity, dyslipidemia, impaired fasting glucose, and hypertension – were associated with a risk of both radiographic osteoarthritis (ROA) and symptomatic OA (SxOA), all associations besides high blood pressure (particularly diastolic blood pressure) disappeared after they adjusted for body mass index (BMI) or body weight (Arthritis Rheumatol. 2017 Mar 3. doi: 10.1002/art.40087).
The research team analyzed 991 participants of the 1992-1995 Framingham Offspring Cohort who did not have existing OA at baseline. Average age was 54.2 years; 55.1% were women. According to Adult Treatment Panel III criteria, 27% of the men and 23% of the women had MetS. Those who had MetS were older, had a higher BMI, and were less likely to drink alcohol or have a college education.
In 2002-2005, the cohort underwent follow-up for the presence of OA. The incidence of ROA in the cohort was 9.8% (78 of 800 knees) in men and 10.5% (105 of 1,003 knees) in women. ROA occurred when a knee without previous radiographic evidence of OA developed a Kellgren and Lawrence score of 2 or higher, and SxOA occurred when a knee developed ROA together with knee pain.
After adjusting for age, education, smoking status, alcohol consumption, and physical activity, the researchers found that MetS, abdominal obesity, and low high-density lipoprotein cholesterol were significantly associated with incident ROA among men. Among women, abdominal obesity and high blood pressure were associated with incident ROA, while MetS was not. However, after adjustment for body weight or BMI, none of the associations remained significant.
The incidence of SxOA was 6.3% (53 of 837 knees) in men and 7.2% (75 of 1,037 knees) in women. Incident SxOA was significantly associated with MetS in women and with the MetS components of abdominal obesity and high blood pressure in both men and women before adjustment for BMI or body weight. However, only an association between diastolic blood pressure and incident SxOA persisted in both sexes after adjustment for body weight, the study authors noted.
“High blood pressure is another MetS component associated with OA in previous studies before adjusting for BMI ... While we found [diastolic blood pressure] was related to incident SxOA even after adjustment for BMI, the relation of [systolic blood pressure] and incident SxOA was nearly significant also, suggesting that both might be related to SxOA,” the study authors wrote.
But a cross-sectional analysis of the relationship would be challenging to interpret, they said, since treatment for SxOA included NSAIDs, which are known to raise blood pressure.
The National Institutes of Health supported the study. The authors declared having no conflicts of interest.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point: There is no strong association between the metabolic syndrome (MetS) and OA after adjustment for BMI or body weight.
Major finding: Components of MetS were initially associated with incident radiographic and symptomatic OA, but after adjustment for BMI or body weight, most of the associations were weak and insignificant. However, an association between the MetS and high blood pressure persisted in both sexes.
Data source: An analysis of 991 participants of the 1992-1995 Framingham Offspring Cohort who did not have existing OA at baseline and were followed for 10 years.
Disclosures: The National Institutes of Health supported the study. The authors declared having no conflicts of interest.
Humira Pen topped per-person drug spending in 2016
Humira Pen (adalimumab) was the most expensive drug in 2016 when ranked by spending per person, according to pharmacy benefits manager Express Scripts.
Total spending per person with employer-sponsored insurance was $45.11 last year for Humira Pen, which is indicated for rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, Crohn’s disease, ulcerative colitis, and plaque psoriasis. Next in spending per person was Enbrel (etanercept) – another drug for arthritis, psoriatic arthritis, ankylosing spondylitis, and psoriasis – at $26.82, followed by the diabetes drug Lantus (insulin glargine) and two multiple sclerosis drugs: Tecfidera (dimethyl fumarate) and Copaxone (glatiramer), Express Scripts said in its “2016 Drug Trend Report.”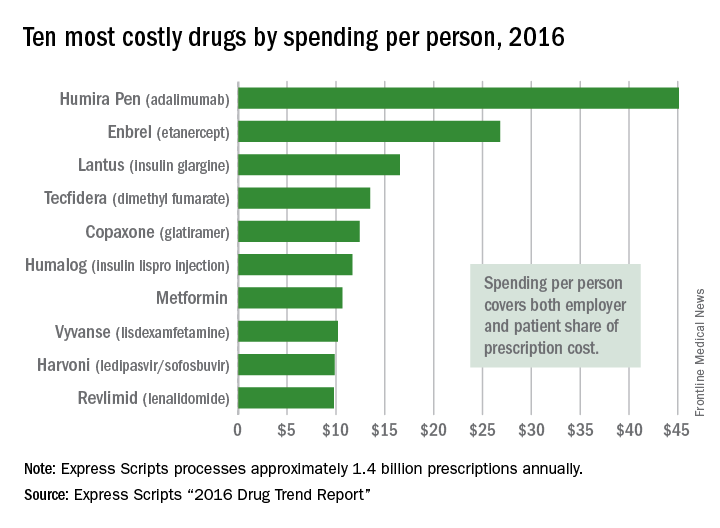
Humira Pen had the next-largest increase from 2015 – a mere 28% – while the hepatitis C drug Harvoni (ledipasvir/sofisbuvir) had the largest decrease in per-person spending among the top 10, dropping 54%, the report noted.
Express Scripts processes approximately 1.4 billion prescriptions annually for 85 million insured members from 3,000 client companies.
Humira Pen (adalimumab) was the most expensive drug in 2016 when ranked by spending per person, according to pharmacy benefits manager Express Scripts.
Total spending per person with employer-sponsored insurance was $45.11 last year for Humira Pen, which is indicated for rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, Crohn’s disease, ulcerative colitis, and plaque psoriasis. Next in spending per person was Enbrel (etanercept) – another drug for arthritis, psoriatic arthritis, ankylosing spondylitis, and psoriasis – at $26.82, followed by the diabetes drug Lantus (insulin glargine) and two multiple sclerosis drugs: Tecfidera (dimethyl fumarate) and Copaxone (glatiramer), Express Scripts said in its “2016 Drug Trend Report.”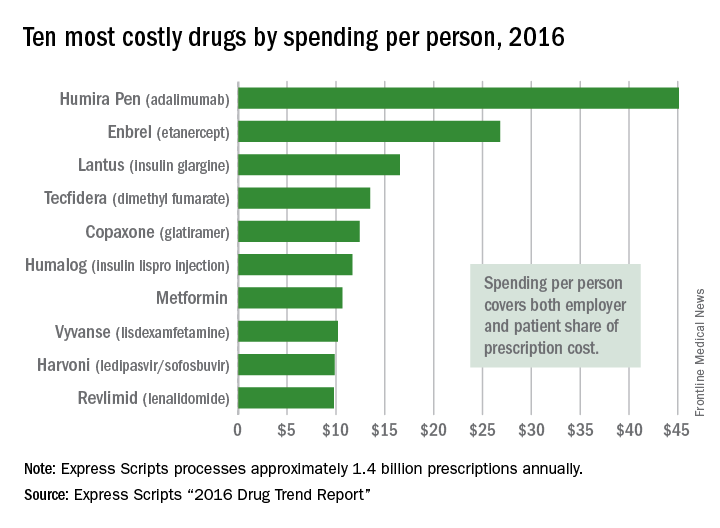
Humira Pen had the next-largest increase from 2015 – a mere 28% – while the hepatitis C drug Harvoni (ledipasvir/sofisbuvir) had the largest decrease in per-person spending among the top 10, dropping 54%, the report noted.
Express Scripts processes approximately 1.4 billion prescriptions annually for 85 million insured members from 3,000 client companies.
Humira Pen (adalimumab) was the most expensive drug in 2016 when ranked by spending per person, according to pharmacy benefits manager Express Scripts.
Total spending per person with employer-sponsored insurance was $45.11 last year for Humira Pen, which is indicated for rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, Crohn’s disease, ulcerative colitis, and plaque psoriasis. Next in spending per person was Enbrel (etanercept) – another drug for arthritis, psoriatic arthritis, ankylosing spondylitis, and psoriasis – at $26.82, followed by the diabetes drug Lantus (insulin glargine) and two multiple sclerosis drugs: Tecfidera (dimethyl fumarate) and Copaxone (glatiramer), Express Scripts said in its “2016 Drug Trend Report.”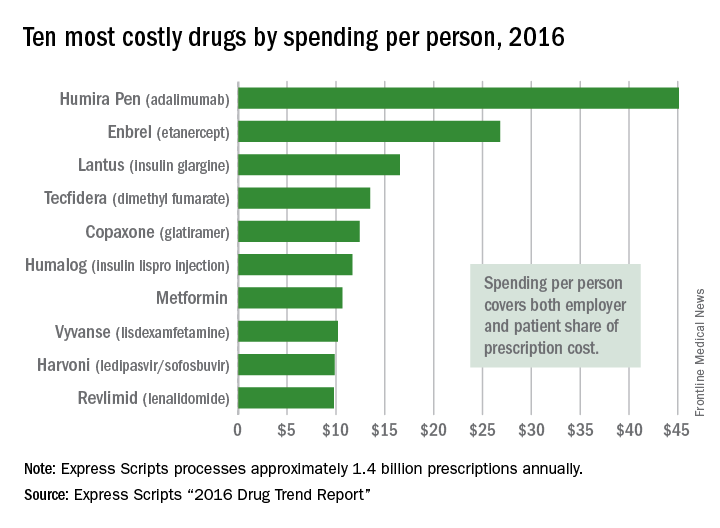
Humira Pen had the next-largest increase from 2015 – a mere 28% – while the hepatitis C drug Harvoni (ledipasvir/sofisbuvir) had the largest decrease in per-person spending among the top 10, dropping 54%, the report noted.
Express Scripts processes approximately 1.4 billion prescriptions annually for 85 million insured members from 3,000 client companies.