User login
Formerly Skin & Allergy News
ass lick
assault rifle
balls
ballsac
black jack
bleach
Boko Haram
bondage
causas
cheap
child abuse
cocaine
compulsive behaviors
cost of miracles
cunt
Daech
display network stats
drug paraphernalia
explosion
fart
fda and death
fda AND warn
fda AND warning
fda AND warns
feom
fuck
gambling
gfc
gun
human trafficking
humira AND expensive
illegal
ISIL
ISIS
Islamic caliphate
Islamic state
madvocate
masturbation
mixed martial arts
MMA
molestation
national rifle association
NRA
nsfw
nuccitelli
pedophile
pedophilia
poker
porn
porn
pornography
psychedelic drug
recreational drug
sex slave rings
shit
slot machine
snort
substance abuse
terrorism
terrorist
texarkana
Texas hold 'em
UFC
section[contains(@class, 'nav-hidden')]
section[contains(@class, 'nav-hidden active')]
The leading independent newspaper covering dermatology news and commentary.
FDA okays Palforzia, first drug for peanut allergy in children
The Food and Drug Administration has approved the first drug to combat peanut allergy in children, (Palforzia, Aimmune Therapeutics), although those who take it must continue to avoid peanuts in their diets.
The peanut (Arachis hypogaea) allergen powder is also the first drug ever approved to treat a food allergy. It is not a cure, but it mitigates allergic reactions, including anaphylaxis, that may occur with accidental exposure to peanuts, the FDA said in a news release.
Treatment with the oral powder, which is mixed into semisolid food – such as applesauce or yogurt – can be started in children aged 4 through 17 years who have a confirmed peanut allergy and then continued as a maintenance medication. Some 1 million American children have peanut allergy, and only a fifth will outgrow the allergy, the agency said.
“Because there is no cure, allergic individuals must strictly avoid exposure to prevent severe and potentially life-threatening reactions,” said Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, in the statement.
An FDA advisory panel backed the medication in September 2019, but some committee members expressed concern about the large number of children in clinical trials who required epinephrine after receiving a dose of Palforzia.
The initial dose phase is given on a single day, while updosing consists of 11 increasing doses over several months. If the patient tolerates the first administration of an increased dose level, they may continue that dose daily at home. Daily maintenance begins after the completion of all updosing levels.
Palforzia will be available only through specially certified health care providers, health care settings, and pharmacies to patients enrolled in the REMS program, the agency said. Also, the initial dose escalation and first dose of each updosing level can be given only in a certified setting.
The agency said that patients or parents or caregivers must be counseled on the need for constant availability of injectable epinephrine, the need for continued dietary peanut avoidance, and on how to recognize the signs and symptoms of anaphylaxis.
‘Eagerly’ awaited
Palforzia’s effectiveness was based on a randomized, double-blind, placebo-controlled study involving about 500 peanut-allergic individuals that found that 67.2% of allergic patients tolerated an oral challenge with a single 600-mg dose of peanut protein with no more than mild allergic symptoms after 6 months of maintenance treatment, compared with 4% of placebo recipients, the FDA said.
In two double-blind, placebo-controlled studies looking at safety, the most commonly reported side effects among about 700 individuals involved in the research were abdominal pain, vomiting, nausea, tingling in the mouth, itching (including in the mouth and ears), cough, runny nose, throat irritation and tightness, hives, wheezing and shortness of breath, and anaphylaxis.
Palforzia should not be given to those with uncontrolled asthma and can’t be used for emergency treatment of allergic reactions, including anaphylaxis.
“The food allergy community has been eagerly awaiting an FDA-approved treatment that can help mitigate allergic reactions to peanut and, as allergists, we want nothing more than to have a treatment option to offer our patients that has demonstrated both the safety and efficacy to truly impact the lives of patients who live with peanut allergy,” said Christina Ciaccio, MD, chief of Allergy/Immunology and Pediatric Pulmonary Medicine at the University of Chicago Medical Center and Biological Sciences, in a company statement from Aimmune. “With today’s approval of Palforzia, we can – for the first time – offer children and teens with peanut allergy a proven medicine that employs an established therapeutic approach.”
This article first appeared on Medscape.com.
The Food and Drug Administration has approved the first drug to combat peanut allergy in children, (Palforzia, Aimmune Therapeutics), although those who take it must continue to avoid peanuts in their diets.
The peanut (Arachis hypogaea) allergen powder is also the first drug ever approved to treat a food allergy. It is not a cure, but it mitigates allergic reactions, including anaphylaxis, that may occur with accidental exposure to peanuts, the FDA said in a news release.
Treatment with the oral powder, which is mixed into semisolid food – such as applesauce or yogurt – can be started in children aged 4 through 17 years who have a confirmed peanut allergy and then continued as a maintenance medication. Some 1 million American children have peanut allergy, and only a fifth will outgrow the allergy, the agency said.
“Because there is no cure, allergic individuals must strictly avoid exposure to prevent severe and potentially life-threatening reactions,” said Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, in the statement.
An FDA advisory panel backed the medication in September 2019, but some committee members expressed concern about the large number of children in clinical trials who required epinephrine after receiving a dose of Palforzia.
The initial dose phase is given on a single day, while updosing consists of 11 increasing doses over several months. If the patient tolerates the first administration of an increased dose level, they may continue that dose daily at home. Daily maintenance begins after the completion of all updosing levels.
Palforzia will be available only through specially certified health care providers, health care settings, and pharmacies to patients enrolled in the REMS program, the agency said. Also, the initial dose escalation and first dose of each updosing level can be given only in a certified setting.
The agency said that patients or parents or caregivers must be counseled on the need for constant availability of injectable epinephrine, the need for continued dietary peanut avoidance, and on how to recognize the signs and symptoms of anaphylaxis.
‘Eagerly’ awaited
Palforzia’s effectiveness was based on a randomized, double-blind, placebo-controlled study involving about 500 peanut-allergic individuals that found that 67.2% of allergic patients tolerated an oral challenge with a single 600-mg dose of peanut protein with no more than mild allergic symptoms after 6 months of maintenance treatment, compared with 4% of placebo recipients, the FDA said.
In two double-blind, placebo-controlled studies looking at safety, the most commonly reported side effects among about 700 individuals involved in the research were abdominal pain, vomiting, nausea, tingling in the mouth, itching (including in the mouth and ears), cough, runny nose, throat irritation and tightness, hives, wheezing and shortness of breath, and anaphylaxis.
Palforzia should not be given to those with uncontrolled asthma and can’t be used for emergency treatment of allergic reactions, including anaphylaxis.
“The food allergy community has been eagerly awaiting an FDA-approved treatment that can help mitigate allergic reactions to peanut and, as allergists, we want nothing more than to have a treatment option to offer our patients that has demonstrated both the safety and efficacy to truly impact the lives of patients who live with peanut allergy,” said Christina Ciaccio, MD, chief of Allergy/Immunology and Pediatric Pulmonary Medicine at the University of Chicago Medical Center and Biological Sciences, in a company statement from Aimmune. “With today’s approval of Palforzia, we can – for the first time – offer children and teens with peanut allergy a proven medicine that employs an established therapeutic approach.”
This article first appeared on Medscape.com.
The Food and Drug Administration has approved the first drug to combat peanut allergy in children, (Palforzia, Aimmune Therapeutics), although those who take it must continue to avoid peanuts in their diets.
The peanut (Arachis hypogaea) allergen powder is also the first drug ever approved to treat a food allergy. It is not a cure, but it mitigates allergic reactions, including anaphylaxis, that may occur with accidental exposure to peanuts, the FDA said in a news release.
Treatment with the oral powder, which is mixed into semisolid food – such as applesauce or yogurt – can be started in children aged 4 through 17 years who have a confirmed peanut allergy and then continued as a maintenance medication. Some 1 million American children have peanut allergy, and only a fifth will outgrow the allergy, the agency said.
“Because there is no cure, allergic individuals must strictly avoid exposure to prevent severe and potentially life-threatening reactions,” said Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, in the statement.
An FDA advisory panel backed the medication in September 2019, but some committee members expressed concern about the large number of children in clinical trials who required epinephrine after receiving a dose of Palforzia.
The initial dose phase is given on a single day, while updosing consists of 11 increasing doses over several months. If the patient tolerates the first administration of an increased dose level, they may continue that dose daily at home. Daily maintenance begins after the completion of all updosing levels.
Palforzia will be available only through specially certified health care providers, health care settings, and pharmacies to patients enrolled in the REMS program, the agency said. Also, the initial dose escalation and first dose of each updosing level can be given only in a certified setting.
The agency said that patients or parents or caregivers must be counseled on the need for constant availability of injectable epinephrine, the need for continued dietary peanut avoidance, and on how to recognize the signs and symptoms of anaphylaxis.
‘Eagerly’ awaited
Palforzia’s effectiveness was based on a randomized, double-blind, placebo-controlled study involving about 500 peanut-allergic individuals that found that 67.2% of allergic patients tolerated an oral challenge with a single 600-mg dose of peanut protein with no more than mild allergic symptoms after 6 months of maintenance treatment, compared with 4% of placebo recipients, the FDA said.
In two double-blind, placebo-controlled studies looking at safety, the most commonly reported side effects among about 700 individuals involved in the research were abdominal pain, vomiting, nausea, tingling in the mouth, itching (including in the mouth and ears), cough, runny nose, throat irritation and tightness, hives, wheezing and shortness of breath, and anaphylaxis.
Palforzia should not be given to those with uncontrolled asthma and can’t be used for emergency treatment of allergic reactions, including anaphylaxis.
“The food allergy community has been eagerly awaiting an FDA-approved treatment that can help mitigate allergic reactions to peanut and, as allergists, we want nothing more than to have a treatment option to offer our patients that has demonstrated both the safety and efficacy to truly impact the lives of patients who live with peanut allergy,” said Christina Ciaccio, MD, chief of Allergy/Immunology and Pediatric Pulmonary Medicine at the University of Chicago Medical Center and Biological Sciences, in a company statement from Aimmune. “With today’s approval of Palforzia, we can – for the first time – offer children and teens with peanut allergy a proven medicine that employs an established therapeutic approach.”
This article first appeared on Medscape.com.
HHS declares coronavirus emergency, orders quarantine
The federal government declared a formal public health emergency on Jan. 31 to aid in the response to the 2019 Novel Coronavirus (2019-nCoV). The declaration, issued by Health and Human Services Secretary Alex. M. Azar II gives state, tribal, and local health departments additional flexibility to request assistance from the federal government in responding to the coronavirus.
"While this virus poses a serious public health threat, the risk to the American public remains low at this time, and we are working to keep this risk low."*
2019-nCoV—the first such action taken by the Centers for Disease Control and Prevention in more than 50 years.
“This decision is based on the current scientific facts,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during a press briefing Jan. 31. “While we understand the action seems drastic, our goal today, tomorrow, and always continues to be the safety of the American public. We would rather be remembered for over-reacting than under-reacting.”
These actions come on the heels of the World Health Organization’s Jan. 30 declaration of 2019-nCoV as a public health emergency of international concern, and from a recent spike in cases reported by Chinese health officials. “Every day this week China has reported additional cases,” Dr. Messonnier said. “Today’s numbers are a 26% increase since yesterday. Over the course of the last week, there have been nearly 7,000 new cases reported. This tells us the virus is continuing to spread rapidly in China. The reported deaths have continued to rise as well. In addition, locations outside China have continued to report cases. There have been an increasing number of reports of person-to-person spread, and now, most recently, a report in the New England Journal of Medicine of asymptomatic spread.”
The quarantine of passengers will last 14 days from when the plane left Wuhan, China. Martin Cetron, MD, who directs the CDC’s Division of Global Migration and Quarantine, said that the quarantine order “offers the greatest level of protection for the American public in preventing introduction and spread. That is our primary concern. Prior epidemics suggest that when people are properly informed, they’re usually very compliant with this request to restrict their movement. This allows someone who would become symptomatic to be rapidly identified. Offering early, rapid diagnosis of their illness could alleviate a lot of anxiety and uncertainty. In addition, this is a protective effect on family members. No individual wants to be the source of introducing or exposing a family member or a loved one to their virus. Additionally, this is part of their civic responsibility to protect their communities.”
* This story was updated on 01/31/2020.
The federal government declared a formal public health emergency on Jan. 31 to aid in the response to the 2019 Novel Coronavirus (2019-nCoV). The declaration, issued by Health and Human Services Secretary Alex. M. Azar II gives state, tribal, and local health departments additional flexibility to request assistance from the federal government in responding to the coronavirus.
"While this virus poses a serious public health threat, the risk to the American public remains low at this time, and we are working to keep this risk low."*
2019-nCoV—the first such action taken by the Centers for Disease Control and Prevention in more than 50 years.
“This decision is based on the current scientific facts,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during a press briefing Jan. 31. “While we understand the action seems drastic, our goal today, tomorrow, and always continues to be the safety of the American public. We would rather be remembered for over-reacting than under-reacting.”
These actions come on the heels of the World Health Organization’s Jan. 30 declaration of 2019-nCoV as a public health emergency of international concern, and from a recent spike in cases reported by Chinese health officials. “Every day this week China has reported additional cases,” Dr. Messonnier said. “Today’s numbers are a 26% increase since yesterday. Over the course of the last week, there have been nearly 7,000 new cases reported. This tells us the virus is continuing to spread rapidly in China. The reported deaths have continued to rise as well. In addition, locations outside China have continued to report cases. There have been an increasing number of reports of person-to-person spread, and now, most recently, a report in the New England Journal of Medicine of asymptomatic spread.”
The quarantine of passengers will last 14 days from when the plane left Wuhan, China. Martin Cetron, MD, who directs the CDC’s Division of Global Migration and Quarantine, said that the quarantine order “offers the greatest level of protection for the American public in preventing introduction and spread. That is our primary concern. Prior epidemics suggest that when people are properly informed, they’re usually very compliant with this request to restrict their movement. This allows someone who would become symptomatic to be rapidly identified. Offering early, rapid diagnosis of their illness could alleviate a lot of anxiety and uncertainty. In addition, this is a protective effect on family members. No individual wants to be the source of introducing or exposing a family member or a loved one to their virus. Additionally, this is part of their civic responsibility to protect their communities.”
* This story was updated on 01/31/2020.
The federal government declared a formal public health emergency on Jan. 31 to aid in the response to the 2019 Novel Coronavirus (2019-nCoV). The declaration, issued by Health and Human Services Secretary Alex. M. Azar II gives state, tribal, and local health departments additional flexibility to request assistance from the federal government in responding to the coronavirus.
"While this virus poses a serious public health threat, the risk to the American public remains low at this time, and we are working to keep this risk low."*
2019-nCoV—the first such action taken by the Centers for Disease Control and Prevention in more than 50 years.
“This decision is based on the current scientific facts,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during a press briefing Jan. 31. “While we understand the action seems drastic, our goal today, tomorrow, and always continues to be the safety of the American public. We would rather be remembered for over-reacting than under-reacting.”
These actions come on the heels of the World Health Organization’s Jan. 30 declaration of 2019-nCoV as a public health emergency of international concern, and from a recent spike in cases reported by Chinese health officials. “Every day this week China has reported additional cases,” Dr. Messonnier said. “Today’s numbers are a 26% increase since yesterday. Over the course of the last week, there have been nearly 7,000 new cases reported. This tells us the virus is continuing to spread rapidly in China. The reported deaths have continued to rise as well. In addition, locations outside China have continued to report cases. There have been an increasing number of reports of person-to-person spread, and now, most recently, a report in the New England Journal of Medicine of asymptomatic spread.”
The quarantine of passengers will last 14 days from when the plane left Wuhan, China. Martin Cetron, MD, who directs the CDC’s Division of Global Migration and Quarantine, said that the quarantine order “offers the greatest level of protection for the American public in preventing introduction and spread. That is our primary concern. Prior epidemics suggest that when people are properly informed, they’re usually very compliant with this request to restrict their movement. This allows someone who would become symptomatic to be rapidly identified. Offering early, rapid diagnosis of their illness could alleviate a lot of anxiety and uncertainty. In addition, this is a protective effect on family members. No individual wants to be the source of introducing or exposing a family member or a loved one to their virus. Additionally, this is part of their civic responsibility to protect their communities.”
* This story was updated on 01/31/2020.
Is anxiety about the coronavirus out of proportion?
A number of years ago, a patient I was treating mentioned that she was not eating tomatoes. There had been stories in the news about people contracting bacterial infections from tomatoes, but I paused for a moment, then asked her: “Have there been any contaminated tomatoes here in Maryland?” There had not been and I was still happily eating salsa, but my patient thought about this differently: If disease-causing tomatoes were to come to our state, someone would be the first person to become ill. She did not want to take any risks. My patient, however, was a heavy smoker and already grappling with health issues that were caused by smoking, so I found her choice of what she should worry about and how it influenced her behavior to be perplexing. I realize it’s not the same; nicotine is an addiction, while tomatoes remain a choice for most of us, and it’s common for people to worry about very unlikely events even when we are surrounded by very real and statistically more probable threats to our well-being.
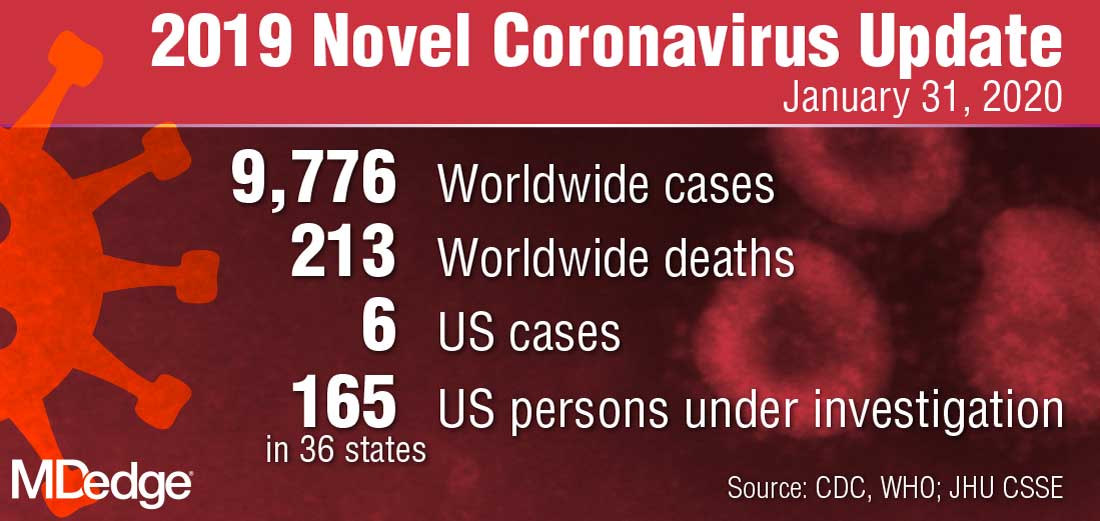
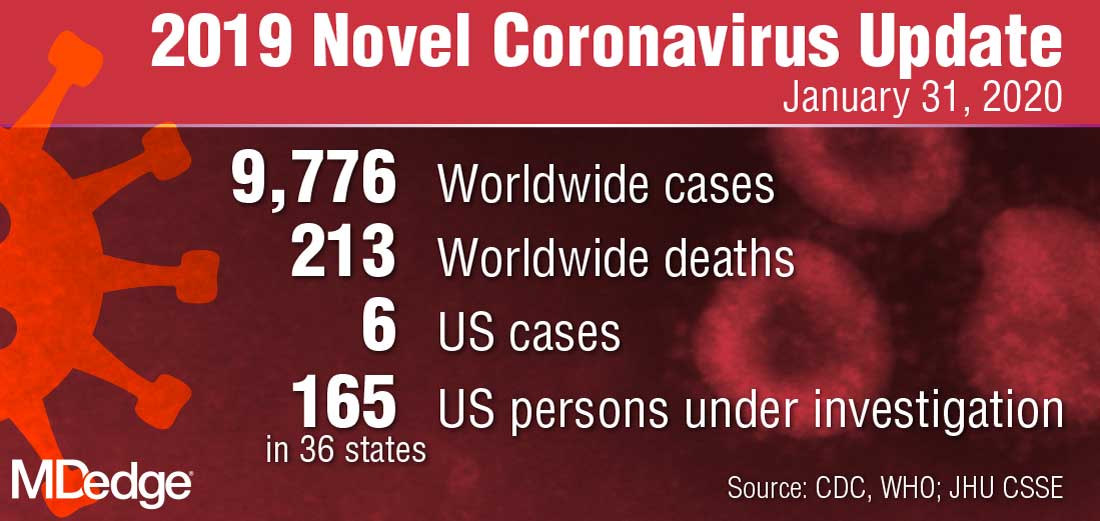
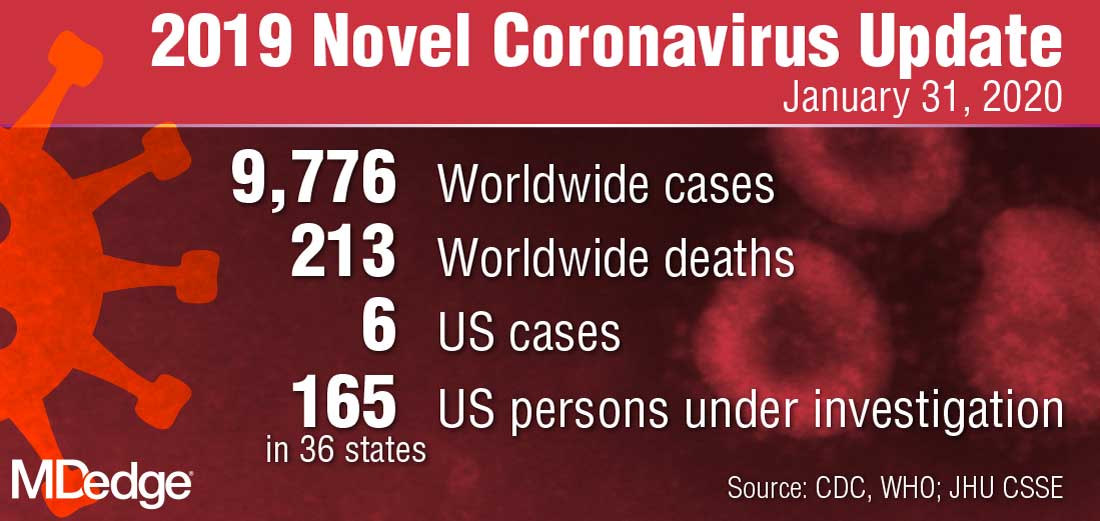
Today’s news reports are filled with stories about 2019 Novel Coronavirus (2019-nCoV), an illness that started in Wuhan, China; as of Jan. 31, 2020, there were 9,776 confirmed cases and 213 deaths. There have been an additional 118 cases reported outside of mainland China, including 6 in the United States, and no one outside of China has died.
The response to the virus has been remarkable: Wuhan, a city of more than 11 million inhabitants, is on lockdown, as are 15 other cities in China; 46 million people have been affected, the largest quarantine in human history. Travel is restricted in parts of China, airports all over the world are screening those who fly in from Wuhan, foreign governments are bringing their citizens home from Wuhan, and even Starbucks has temporarily closed half its stores in China. The economics of containing this virus are astounding.
In the meantime, the Centers for Disease Control and Prevention reports that, as of the week of Jan. 25, there have been 19 million cases of the flu in the United States. Of those stricken, 180,000 people have been hospitalized and 10,000 have died, including 68 pediatric patients. No cities are on lockdown, public transportation runs as usual, airports don’t screen passengers for flu symptoms, and Starbucks continues to serve vanilla lattes to any willing customer. Anxiety about illness is not new; we’ve seen it with SARS, Ebola, measles, and even around Chipotle’s food poisoning cases – to name just a few recent scares. We have also seen a lot of media on vaping-related deaths, and as of early January 2020, vaping-related illnesses affected 2,602 people with 59 deaths. It has been a topic of discussion among legislators, with an emphasis on either outlawing the flavoring that might appeal to younger people or simply outlawing e-cigarettes. No one, however, is talking about outlawing regular cigarettes, despite the fact that many people have switched from cigarettes to vaping products as a way to quit smoking. So, while vaping has caused 59 deaths since 2018, cigarettes are responsible for 480,000 fatalities a year in the United States and smokers live, on average, 10 years less than nonsmokers.
So what fuels anxiety about the latest health scare, and why aren’t we more anxious about the more common causes of premature mortality? Certainly, the newness and the unknown are factors in the coronavirus scare. It’s not certain how this illness was introduced into the human population, although one theory is that it started with the consumption of bats who carry the virus. It’s spreading fast, and in some people, it has been lethal. The incubation period is not known, or whether it is contagious before symptoms appear. Coronavirus is getting a lot of public health attention and the World Health Organization just announced that the virus is a public health emergency of international concern. On the televised news on Jan. 29, 2020, coronavirus was the top story in the United States, even though an impeachment trial is in progress for our country’s president.
The public health response of locking down cities may help contain the outbreak and prevent a global epidemic, although millions of people had already left Wuhan, so the heavy-handed attempt to prevent spread of the virus may well be too late. In the case of the Ebola virus – a much more lethal disease that was also thought to be introduced by bats – public health measures certainly curtailed global spread, and the epidemic of 2014-2016 was limited to 28,600 cases and 11,325 deaths, nearly all of them in West Africa.
Most of the things that cause people to die are not new and are not topics the media chooses to sensationalize. Dissemination of news has changed over the decades, with so much more of it, instant reports on social media, and competition for viewers that leads journalists to pull at our emotions. And while we may, or may not, get flu shots and avoid those who have the flu, how and where we position both our anxiety and our resources does not always make sense. Certainly some people are predisposed to worry about both common and uncommon dangers, while others seem never to worry and engage in acts that many of us would consider dangerous. If we are looking for logic, it may be hard to find – there are those who would happily go bungee jumping but wouldn’t dream of leaving the house out without hand sanitizer.
The repercussions from this massive response to the Wuhan coronavirus are significant. For the millions of people on lockdown in China, each day gets emotionally harder; some may begin to have issues procuring food, and the financial losses for the economy will be significant. It’s not really possible to know yet if this response is warranted; we do know that infectious diseases can kill millions. The AIDS pandemic has taken the lives of 36 million people since 1981, and the influenza pandemic of 1918 resulted in an estimated 20 million to 50 million deaths after infecting 500 million people. Still, one might wonder if other, more mundane causes of morbidity and mortality – the ones that no longer garner our dread or make it to the front pages – might also be worthy of more hype and resources.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
A number of years ago, a patient I was treating mentioned that she was not eating tomatoes. There had been stories in the news about people contracting bacterial infections from tomatoes, but I paused for a moment, then asked her: “Have there been any contaminated tomatoes here in Maryland?” There had not been and I was still happily eating salsa, but my patient thought about this differently: If disease-causing tomatoes were to come to our state, someone would be the first person to become ill. She did not want to take any risks. My patient, however, was a heavy smoker and already grappling with health issues that were caused by smoking, so I found her choice of what she should worry about and how it influenced her behavior to be perplexing. I realize it’s not the same; nicotine is an addiction, while tomatoes remain a choice for most of us, and it’s common for people to worry about very unlikely events even when we are surrounded by very real and statistically more probable threats to our well-being.
Today’s news reports are filled with stories about 2019 Novel Coronavirus (2019-nCoV), an illness that started in Wuhan, China; as of Jan. 31, 2020, there were 9,776 confirmed cases and 213 deaths. There have been an additional 118 cases reported outside of mainland China, including 6 in the United States, and no one outside of China has died.
The response to the virus has been remarkable: Wuhan, a city of more than 11 million inhabitants, is on lockdown, as are 15 other cities in China; 46 million people have been affected, the largest quarantine in human history. Travel is restricted in parts of China, airports all over the world are screening those who fly in from Wuhan, foreign governments are bringing their citizens home from Wuhan, and even Starbucks has temporarily closed half its stores in China. The economics of containing this virus are astounding.
In the meantime, the Centers for Disease Control and Prevention reports that, as of the week of Jan. 25, there have been 19 million cases of the flu in the United States. Of those stricken, 180,000 people have been hospitalized and 10,000 have died, including 68 pediatric patients. No cities are on lockdown, public transportation runs as usual, airports don’t screen passengers for flu symptoms, and Starbucks continues to serve vanilla lattes to any willing customer. Anxiety about illness is not new; we’ve seen it with SARS, Ebola, measles, and even around Chipotle’s food poisoning cases – to name just a few recent scares. We have also seen a lot of media on vaping-related deaths, and as of early January 2020, vaping-related illnesses affected 2,602 people with 59 deaths. It has been a topic of discussion among legislators, with an emphasis on either outlawing the flavoring that might appeal to younger people or simply outlawing e-cigarettes. No one, however, is talking about outlawing regular cigarettes, despite the fact that many people have switched from cigarettes to vaping products as a way to quit smoking. So, while vaping has caused 59 deaths since 2018, cigarettes are responsible for 480,000 fatalities a year in the United States and smokers live, on average, 10 years less than nonsmokers.
So what fuels anxiety about the latest health scare, and why aren’t we more anxious about the more common causes of premature mortality? Certainly, the newness and the unknown are factors in the coronavirus scare. It’s not certain how this illness was introduced into the human population, although one theory is that it started with the consumption of bats who carry the virus. It’s spreading fast, and in some people, it has been lethal. The incubation period is not known, or whether it is contagious before symptoms appear. Coronavirus is getting a lot of public health attention and the World Health Organization just announced that the virus is a public health emergency of international concern. On the televised news on Jan. 29, 2020, coronavirus was the top story in the United States, even though an impeachment trial is in progress for our country’s president.
The public health response of locking down cities may help contain the outbreak and prevent a global epidemic, although millions of people had already left Wuhan, so the heavy-handed attempt to prevent spread of the virus may well be too late. In the case of the Ebola virus – a much more lethal disease that was also thought to be introduced by bats – public health measures certainly curtailed global spread, and the epidemic of 2014-2016 was limited to 28,600 cases and 11,325 deaths, nearly all of them in West Africa.
Most of the things that cause people to die are not new and are not topics the media chooses to sensationalize. Dissemination of news has changed over the decades, with so much more of it, instant reports on social media, and competition for viewers that leads journalists to pull at our emotions. And while we may, or may not, get flu shots and avoid those who have the flu, how and where we position both our anxiety and our resources does not always make sense. Certainly some people are predisposed to worry about both common and uncommon dangers, while others seem never to worry and engage in acts that many of us would consider dangerous. If we are looking for logic, it may be hard to find – there are those who would happily go bungee jumping but wouldn’t dream of leaving the house out without hand sanitizer.
The repercussions from this massive response to the Wuhan coronavirus are significant. For the millions of people on lockdown in China, each day gets emotionally harder; some may begin to have issues procuring food, and the financial losses for the economy will be significant. It’s not really possible to know yet if this response is warranted; we do know that infectious diseases can kill millions. The AIDS pandemic has taken the lives of 36 million people since 1981, and the influenza pandemic of 1918 resulted in an estimated 20 million to 50 million deaths after infecting 500 million people. Still, one might wonder if other, more mundane causes of morbidity and mortality – the ones that no longer garner our dread or make it to the front pages – might also be worthy of more hype and resources.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
A number of years ago, a patient I was treating mentioned that she was not eating tomatoes. There had been stories in the news about people contracting bacterial infections from tomatoes, but I paused for a moment, then asked her: “Have there been any contaminated tomatoes here in Maryland?” There had not been and I was still happily eating salsa, but my patient thought about this differently: If disease-causing tomatoes were to come to our state, someone would be the first person to become ill. She did not want to take any risks. My patient, however, was a heavy smoker and already grappling with health issues that were caused by smoking, so I found her choice of what she should worry about and how it influenced her behavior to be perplexing. I realize it’s not the same; nicotine is an addiction, while tomatoes remain a choice for most of us, and it’s common for people to worry about very unlikely events even when we are surrounded by very real and statistically more probable threats to our well-being.
Today’s news reports are filled with stories about 2019 Novel Coronavirus (2019-nCoV), an illness that started in Wuhan, China; as of Jan. 31, 2020, there were 9,776 confirmed cases and 213 deaths. There have been an additional 118 cases reported outside of mainland China, including 6 in the United States, and no one outside of China has died.
The response to the virus has been remarkable: Wuhan, a city of more than 11 million inhabitants, is on lockdown, as are 15 other cities in China; 46 million people have been affected, the largest quarantine in human history. Travel is restricted in parts of China, airports all over the world are screening those who fly in from Wuhan, foreign governments are bringing their citizens home from Wuhan, and even Starbucks has temporarily closed half its stores in China. The economics of containing this virus are astounding.
In the meantime, the Centers for Disease Control and Prevention reports that, as of the week of Jan. 25, there have been 19 million cases of the flu in the United States. Of those stricken, 180,000 people have been hospitalized and 10,000 have died, including 68 pediatric patients. No cities are on lockdown, public transportation runs as usual, airports don’t screen passengers for flu symptoms, and Starbucks continues to serve vanilla lattes to any willing customer. Anxiety about illness is not new; we’ve seen it with SARS, Ebola, measles, and even around Chipotle’s food poisoning cases – to name just a few recent scares. We have also seen a lot of media on vaping-related deaths, and as of early January 2020, vaping-related illnesses affected 2,602 people with 59 deaths. It has been a topic of discussion among legislators, with an emphasis on either outlawing the flavoring that might appeal to younger people or simply outlawing e-cigarettes. No one, however, is talking about outlawing regular cigarettes, despite the fact that many people have switched from cigarettes to vaping products as a way to quit smoking. So, while vaping has caused 59 deaths since 2018, cigarettes are responsible for 480,000 fatalities a year in the United States and smokers live, on average, 10 years less than nonsmokers.
So what fuels anxiety about the latest health scare, and why aren’t we more anxious about the more common causes of premature mortality? Certainly, the newness and the unknown are factors in the coronavirus scare. It’s not certain how this illness was introduced into the human population, although one theory is that it started with the consumption of bats who carry the virus. It’s spreading fast, and in some people, it has been lethal. The incubation period is not known, or whether it is contagious before symptoms appear. Coronavirus is getting a lot of public health attention and the World Health Organization just announced that the virus is a public health emergency of international concern. On the televised news on Jan. 29, 2020, coronavirus was the top story in the United States, even though an impeachment trial is in progress for our country’s president.
The public health response of locking down cities may help contain the outbreak and prevent a global epidemic, although millions of people had already left Wuhan, so the heavy-handed attempt to prevent spread of the virus may well be too late. In the case of the Ebola virus – a much more lethal disease that was also thought to be introduced by bats – public health measures certainly curtailed global spread, and the epidemic of 2014-2016 was limited to 28,600 cases and 11,325 deaths, nearly all of them in West Africa.
Most of the things that cause people to die are not new and are not topics the media chooses to sensationalize. Dissemination of news has changed over the decades, with so much more of it, instant reports on social media, and competition for viewers that leads journalists to pull at our emotions. And while we may, or may not, get flu shots and avoid those who have the flu, how and where we position both our anxiety and our resources does not always make sense. Certainly some people are predisposed to worry about both common and uncommon dangers, while others seem never to worry and engage in acts that many of us would consider dangerous. If we are looking for logic, it may be hard to find – there are those who would happily go bungee jumping but wouldn’t dream of leaving the house out without hand sanitizer.
The repercussions from this massive response to the Wuhan coronavirus are significant. For the millions of people on lockdown in China, each day gets emotionally harder; some may begin to have issues procuring food, and the financial losses for the economy will be significant. It’s not really possible to know yet if this response is warranted; we do know that infectious diseases can kill millions. The AIDS pandemic has taken the lives of 36 million people since 1981, and the influenza pandemic of 1918 resulted in an estimated 20 million to 50 million deaths after infecting 500 million people. Still, one might wonder if other, more mundane causes of morbidity and mortality – the ones that no longer garner our dread or make it to the front pages – might also be worthy of more hype and resources.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
Systemic therapy options for pediatric skin diseases are improving
ORLANDO – Because Food and Drug Administration–approved treatment options for medications. However, this scenario is changing, A. Yasmine Kirkorian, MD, said at the ODAC Dermatology, Aesthetic & Surgical Conference.
“I really would like to emphasize that children with severe disease need to be treated,” added Dr. Kirkorian, a pediatric dermatologist at George Washington University, Washington, and Children’s National Health System, where she is interim chief of the division of dermatology.
Current on-label systemic therapies for pediatric skin disease include etanercept for psoriasis (4 years and older), ustekinumab for psoriasis (12 years and older), adalimumab for hidradenitis suppurativa (12 years and older), and omalizumab for chronic idiopathic urticaria (12 years and older). A new addition to the list is dupilumab, which was approved for children and adolescents with atopic dermatitis (AD) aged 12 years and older in 2019, she noted.
Dupilumab is currently being studied in children aged 6 months to 12 years, and other clinical trials are evaluating more options for pediatric patients with AD, alopecia areata, and psoriasis. They include a clinical trial of the oral Janus kinase 3 (JAK3) inhibitor PF-06651600 in patients aged 12 years and older with alopecia areata. Six biologic therapies are being evaluated for psoriasis in patients beginning at 6 years: ixekizumab, secukinumab, ustekinumab, guselkumab, brodalumab, and apremilast.
Some systemic therapies are off-label “but used all the time” for dermatologic diseases in pediatrics, Dr. Kirkorian noted. One example is methotrexate, which is approved by the FDA for acute lymphoblastic leukemia, meningeal leukemia, and juvenile idiopathic arthritis down to infancy. Having existing efficacy and safety data for a medication in a pediatric population, even for a different disease, can be helpful when counseling parents of children with severe dermatologic disease. “If you have something, even in an older population of children, it can be reassuring, or you can use evidence from other diseases,” she said.
While methotrexate is a cheap option and approved by the FDA for other pediatric indications down to infancy, the cons of using it to treat AD in pediatric patients are numerous. Treatment requires a number of blood draws for lab testing, which can be discouraging for younger patients, and the reported adverse effect profile may be concerning to some parents, while “in practice doesn’t really occur,” she said. Methotrexate is a teratogen so is not appropriate for teenagers who are sexually active and not using contraception.
The “biggest problem,” though, is the issue of whether methotrexate is effective, since it doesn’t always work for AD, Dr. Kirkorian said. “Even at the highest doses, I often feel that we fail the atopic children,” as opposed to using it to treat psoriasis, “where you know I’m going to get you on something that works.”
In contrast, cyclosporine is FDA approved down to infancy, and works quickly as a bridge to other therapy, and is not expensive, Dr. Kirkorian said. Cons include the need for blood draws, blood pressure checks, drug interactions, and adverse effects, she noted, adding that she tries to use cyclosporine as a bridge to on-label and off-label dupilumab.
Even with FDA approval for dupilumab down to age 12 years, she said it can be difficult to get insurance approval for the on-label treatment for patients in this age group with AD, before they first fail other therapies (even with off-label systemic drugs). For patients under age 12 years, getting approval is even more challenging and requires rigorous documentation of what therapies the child has failed, and how it has affected their quality of life, she said.
“If you send in a letter to the insurance company without an IGA [Investigator Global Assessment] or SCORAD, you’re going to get rejected,” Dr. Kirkorian said. In addition to those two measures, she provides “everything else,” including the impact of the disease on quality of life of patients, and school, she said, adding, “Did they miss school, did they get hospitalized for infections? And do they have comorbid diseases that might help you get approval?”
In pediatric patients with psoriasis, common issues are more likely to be about how insurance dictates step therapy. She has often found that young children may stop responding to etanercept after a few years, which can justify a switch to ustekinumab or a new treatment in a clinical trial, she said. Adolescents with psoriasis can receive ustekinumab, which is approved for psoriasis in patients aged 12-17 years, she said, noting that the infrequent ustekinumab dosing schedule is often beneficial in this population.
When all other approved options fail for young patients with psoriasis, justifying off-label use isn’t always easy. “You just have to make a justification based on the literature, even though it’s off label,” citing available safety information for other diseases, and “demonstrate over and over the impact on quality of life,” which works “most of the time,” Dr. Kirkorian said.
She reported having no conflicts of interest.
ORLANDO – Because Food and Drug Administration–approved treatment options for medications. However, this scenario is changing, A. Yasmine Kirkorian, MD, said at the ODAC Dermatology, Aesthetic & Surgical Conference.
“I really would like to emphasize that children with severe disease need to be treated,” added Dr. Kirkorian, a pediatric dermatologist at George Washington University, Washington, and Children’s National Health System, where she is interim chief of the division of dermatology.
Current on-label systemic therapies for pediatric skin disease include etanercept for psoriasis (4 years and older), ustekinumab for psoriasis (12 years and older), adalimumab for hidradenitis suppurativa (12 years and older), and omalizumab for chronic idiopathic urticaria (12 years and older). A new addition to the list is dupilumab, which was approved for children and adolescents with atopic dermatitis (AD) aged 12 years and older in 2019, she noted.
Dupilumab is currently being studied in children aged 6 months to 12 years, and other clinical trials are evaluating more options for pediatric patients with AD, alopecia areata, and psoriasis. They include a clinical trial of the oral Janus kinase 3 (JAK3) inhibitor PF-06651600 in patients aged 12 years and older with alopecia areata. Six biologic therapies are being evaluated for psoriasis in patients beginning at 6 years: ixekizumab, secukinumab, ustekinumab, guselkumab, brodalumab, and apremilast.
Some systemic therapies are off-label “but used all the time” for dermatologic diseases in pediatrics, Dr. Kirkorian noted. One example is methotrexate, which is approved by the FDA for acute lymphoblastic leukemia, meningeal leukemia, and juvenile idiopathic arthritis down to infancy. Having existing efficacy and safety data for a medication in a pediatric population, even for a different disease, can be helpful when counseling parents of children with severe dermatologic disease. “If you have something, even in an older population of children, it can be reassuring, or you can use evidence from other diseases,” she said.
While methotrexate is a cheap option and approved by the FDA for other pediatric indications down to infancy, the cons of using it to treat AD in pediatric patients are numerous. Treatment requires a number of blood draws for lab testing, which can be discouraging for younger patients, and the reported adverse effect profile may be concerning to some parents, while “in practice doesn’t really occur,” she said. Methotrexate is a teratogen so is not appropriate for teenagers who are sexually active and not using contraception.
The “biggest problem,” though, is the issue of whether methotrexate is effective, since it doesn’t always work for AD, Dr. Kirkorian said. “Even at the highest doses, I often feel that we fail the atopic children,” as opposed to using it to treat psoriasis, “where you know I’m going to get you on something that works.”
In contrast, cyclosporine is FDA approved down to infancy, and works quickly as a bridge to other therapy, and is not expensive, Dr. Kirkorian said. Cons include the need for blood draws, blood pressure checks, drug interactions, and adverse effects, she noted, adding that she tries to use cyclosporine as a bridge to on-label and off-label dupilumab.
Even with FDA approval for dupilumab down to age 12 years, she said it can be difficult to get insurance approval for the on-label treatment for patients in this age group with AD, before they first fail other therapies (even with off-label systemic drugs). For patients under age 12 years, getting approval is even more challenging and requires rigorous documentation of what therapies the child has failed, and how it has affected their quality of life, she said.
“If you send in a letter to the insurance company without an IGA [Investigator Global Assessment] or SCORAD, you’re going to get rejected,” Dr. Kirkorian said. In addition to those two measures, she provides “everything else,” including the impact of the disease on quality of life of patients, and school, she said, adding, “Did they miss school, did they get hospitalized for infections? And do they have comorbid diseases that might help you get approval?”
In pediatric patients with psoriasis, common issues are more likely to be about how insurance dictates step therapy. She has often found that young children may stop responding to etanercept after a few years, which can justify a switch to ustekinumab or a new treatment in a clinical trial, she said. Adolescents with psoriasis can receive ustekinumab, which is approved for psoriasis in patients aged 12-17 years, she said, noting that the infrequent ustekinumab dosing schedule is often beneficial in this population.
When all other approved options fail for young patients with psoriasis, justifying off-label use isn’t always easy. “You just have to make a justification based on the literature, even though it’s off label,” citing available safety information for other diseases, and “demonstrate over and over the impact on quality of life,” which works “most of the time,” Dr. Kirkorian said.
She reported having no conflicts of interest.
ORLANDO – Because Food and Drug Administration–approved treatment options for medications. However, this scenario is changing, A. Yasmine Kirkorian, MD, said at the ODAC Dermatology, Aesthetic & Surgical Conference.
“I really would like to emphasize that children with severe disease need to be treated,” added Dr. Kirkorian, a pediatric dermatologist at George Washington University, Washington, and Children’s National Health System, where she is interim chief of the division of dermatology.
Current on-label systemic therapies for pediatric skin disease include etanercept for psoriasis (4 years and older), ustekinumab for psoriasis (12 years and older), adalimumab for hidradenitis suppurativa (12 years and older), and omalizumab for chronic idiopathic urticaria (12 years and older). A new addition to the list is dupilumab, which was approved for children and adolescents with atopic dermatitis (AD) aged 12 years and older in 2019, she noted.
Dupilumab is currently being studied in children aged 6 months to 12 years, and other clinical trials are evaluating more options for pediatric patients with AD, alopecia areata, and psoriasis. They include a clinical trial of the oral Janus kinase 3 (JAK3) inhibitor PF-06651600 in patients aged 12 years and older with alopecia areata. Six biologic therapies are being evaluated for psoriasis in patients beginning at 6 years: ixekizumab, secukinumab, ustekinumab, guselkumab, brodalumab, and apremilast.
Some systemic therapies are off-label “but used all the time” for dermatologic diseases in pediatrics, Dr. Kirkorian noted. One example is methotrexate, which is approved by the FDA for acute lymphoblastic leukemia, meningeal leukemia, and juvenile idiopathic arthritis down to infancy. Having existing efficacy and safety data for a medication in a pediatric population, even for a different disease, can be helpful when counseling parents of children with severe dermatologic disease. “If you have something, even in an older population of children, it can be reassuring, or you can use evidence from other diseases,” she said.
While methotrexate is a cheap option and approved by the FDA for other pediatric indications down to infancy, the cons of using it to treat AD in pediatric patients are numerous. Treatment requires a number of blood draws for lab testing, which can be discouraging for younger patients, and the reported adverse effect profile may be concerning to some parents, while “in practice doesn’t really occur,” she said. Methotrexate is a teratogen so is not appropriate for teenagers who are sexually active and not using contraception.
The “biggest problem,” though, is the issue of whether methotrexate is effective, since it doesn’t always work for AD, Dr. Kirkorian said. “Even at the highest doses, I often feel that we fail the atopic children,” as opposed to using it to treat psoriasis, “where you know I’m going to get you on something that works.”
In contrast, cyclosporine is FDA approved down to infancy, and works quickly as a bridge to other therapy, and is not expensive, Dr. Kirkorian said. Cons include the need for blood draws, blood pressure checks, drug interactions, and adverse effects, she noted, adding that she tries to use cyclosporine as a bridge to on-label and off-label dupilumab.
Even with FDA approval for dupilumab down to age 12 years, she said it can be difficult to get insurance approval for the on-label treatment for patients in this age group with AD, before they first fail other therapies (even with off-label systemic drugs). For patients under age 12 years, getting approval is even more challenging and requires rigorous documentation of what therapies the child has failed, and how it has affected their quality of life, she said.
“If you send in a letter to the insurance company without an IGA [Investigator Global Assessment] or SCORAD, you’re going to get rejected,” Dr. Kirkorian said. In addition to those two measures, she provides “everything else,” including the impact of the disease on quality of life of patients, and school, she said, adding, “Did they miss school, did they get hospitalized for infections? And do they have comorbid diseases that might help you get approval?”
In pediatric patients with psoriasis, common issues are more likely to be about how insurance dictates step therapy. She has often found that young children may stop responding to etanercept after a few years, which can justify a switch to ustekinumab or a new treatment in a clinical trial, she said. Adolescents with psoriasis can receive ustekinumab, which is approved for psoriasis in patients aged 12-17 years, she said, noting that the infrequent ustekinumab dosing schedule is often beneficial in this population.
When all other approved options fail for young patients with psoriasis, justifying off-label use isn’t always easy. “You just have to make a justification based on the literature, even though it’s off label,” citing available safety information for other diseases, and “demonstrate over and over the impact on quality of life,” which works “most of the time,” Dr. Kirkorian said.
She reported having no conflicts of interest.
EXPERT ANALYSIS FROM ODAC 2020
WHO declares public health emergency for novel coronavirus
Amid the rising spread of the 2019 Novel Coronavirus (2019-nCoV),
The declaration was made during a press briefing on Jan. 30 after a week of growing concern and pressure on WHO to designate the virus at a higher emergency level. WHO’s Emergency Committee made the nearly unanimous decision after considering the increasing number of coronavirus cases in China, the rising infections outside of China, and the questionable measures some countries are taking regarding travel, said committee chair Didier Houssin, MD, said during the press conference.
As of Jan. 30, there were 8,236 confirmed cases of the coronavirus in China and 171 deaths, with another 112 cases identified outside of China in 21 other countries.
“Declaring a Public Health Emergency of International Concern is likely to facilitate [WHO’s] leadership role for public health measures, holding countries to account concerning additional measures they may take regarding travel, trade, quarantine or screening, research efforts, global coordination and anticipation of economic impact [and] support to vulnerable states,” Dr. Houssin said during the press conference. “Declaring a PHEIC should certainly not be seen as manifestation of distrust in the Chinese authorities and people which are doing tremendous efforts on the frontlines of this outbreak, with transparency, and let us hope, with success.”
What happens next?
Once a PHEIC is declared, WHO launches a series of steps, including the release of temporary recommendations for the affected country on health measures to implement and guidance for other countries on preventing and reducing the international spread of the disease, WHO spokesman Tarik Jasarevic said in an interview.
“The purpose of declaring a PHEIC is to advise the world on what measures need to be taken to enhance global health security by preventing international transmission of an infectious hazard,” he said.
Following the Jan. 30 press conference, WHO released temporary guidance for China and for other countries regarding identifying, managing, containing, and preventing the virus. China is advised to continue updating the population about the outbreak, continue enhancing its public health measures for containment and surveillance of cases, and to continue collaboration with WHO and other partners to investigate the epidemiology and evolution of the outbreak and share data on all human cases.
Other countries should be prepared for containment, including the active surveillance, early detection, isolation, case management, and prevention of virus transmission and to share full data with WHO, according to the recommendations.
Under the International Health Regulations (IHR), countries are required to share information and data with WHO. Additionally, WHO leaders advised the global community to support low- and middle-income countries with their response to the coronavirus and to facilitate diagnostics, potential vaccines, and therapeutics in these areas.
The IHR requires that countries implementing health measures that go beyond what WHO recommends must send to WHO the public health rationale and justification within 48 hours of their implementation for WHO review, Mr. Jasarevic noted.
“WHO is obliged to share the information about measures and the justification received with other countries involved,” he said.
PHEIC travel and resource impact
Declaration of a PHEIC means WHO will now oversee any travel restrictions made by other countries in response to 2019-nCoV. The agency recommends that countries conduct a risk and cost-benefit analysis before enacting travel restrictions and other countries are required to inform WHO about any travel measures taken.
“Countries will be asked to provide public health justification for any travel or trade measures that are not scientifically based, such as refusal of entry of suspect cases or unaffected persons to affected areas,” Mr. Jasarevic said in an interview.
As far as resources, the PHEIC mechanism is not a fundraising mechanism, but some donors might consider a PHEIC declaration as a trigger for releasing additional funding to respond to the health threat, he said.
Allison T. Chamberlain, PhD, acting director for the Emory Center for Public Health Preparedness and Research at the Emory Rollins School of Public Health in Atlanta, said national governments and nongovernmental aid organizations are among the most affected by a PHEIC because they are looked at to provide assistance to the most heavily affected areas and to bolster public health preparedness within their own borders.
“In terms of resources that are deployed, a Public Health Emergency of International Concern raises levels of international support and commitment to stopping the emergency,” Dr. Chamberlain said in an interview. “By doing so, it gives countries the needed flexibility to release financial resources of their own accord to support things like response teams that might go into heavily affected areas to assist, for instance.”
WHO Director-General Dr. Tedros Adhanom Ghebreyesus stressed that cooperation among countries is key during the PHEIC.
“We can only stop it together,” he said during the press conference. “This is the time for facts, not fear. This is the time for science, not rumors. This is the time for solidarity, not stigma.”
This is the sixth PHEIC declared by WHO in the last 10 years. Such declarations were made for the 2009 H1NI influenza pandemic, the 2014 polio resurgence, the 2014 Ebola outbreak in West Africa, the 2016 Zika virus, and the 2019 Kivu Ebola outbreak in the Democratic Republic of Congo.
Amid the rising spread of the 2019 Novel Coronavirus (2019-nCoV),
The declaration was made during a press briefing on Jan. 30 after a week of growing concern and pressure on WHO to designate the virus at a higher emergency level. WHO’s Emergency Committee made the nearly unanimous decision after considering the increasing number of coronavirus cases in China, the rising infections outside of China, and the questionable measures some countries are taking regarding travel, said committee chair Didier Houssin, MD, said during the press conference.
As of Jan. 30, there were 8,236 confirmed cases of the coronavirus in China and 171 deaths, with another 112 cases identified outside of China in 21 other countries.
“Declaring a Public Health Emergency of International Concern is likely to facilitate [WHO’s] leadership role for public health measures, holding countries to account concerning additional measures they may take regarding travel, trade, quarantine or screening, research efforts, global coordination and anticipation of economic impact [and] support to vulnerable states,” Dr. Houssin said during the press conference. “Declaring a PHEIC should certainly not be seen as manifestation of distrust in the Chinese authorities and people which are doing tremendous efforts on the frontlines of this outbreak, with transparency, and let us hope, with success.”
What happens next?
Once a PHEIC is declared, WHO launches a series of steps, including the release of temporary recommendations for the affected country on health measures to implement and guidance for other countries on preventing and reducing the international spread of the disease, WHO spokesman Tarik Jasarevic said in an interview.
“The purpose of declaring a PHEIC is to advise the world on what measures need to be taken to enhance global health security by preventing international transmission of an infectious hazard,” he said.
Following the Jan. 30 press conference, WHO released temporary guidance for China and for other countries regarding identifying, managing, containing, and preventing the virus. China is advised to continue updating the population about the outbreak, continue enhancing its public health measures for containment and surveillance of cases, and to continue collaboration with WHO and other partners to investigate the epidemiology and evolution of the outbreak and share data on all human cases.
Other countries should be prepared for containment, including the active surveillance, early detection, isolation, case management, and prevention of virus transmission and to share full data with WHO, according to the recommendations.
Under the International Health Regulations (IHR), countries are required to share information and data with WHO. Additionally, WHO leaders advised the global community to support low- and middle-income countries with their response to the coronavirus and to facilitate diagnostics, potential vaccines, and therapeutics in these areas.
The IHR requires that countries implementing health measures that go beyond what WHO recommends must send to WHO the public health rationale and justification within 48 hours of their implementation for WHO review, Mr. Jasarevic noted.
“WHO is obliged to share the information about measures and the justification received with other countries involved,” he said.
PHEIC travel and resource impact
Declaration of a PHEIC means WHO will now oversee any travel restrictions made by other countries in response to 2019-nCoV. The agency recommends that countries conduct a risk and cost-benefit analysis before enacting travel restrictions and other countries are required to inform WHO about any travel measures taken.
“Countries will be asked to provide public health justification for any travel or trade measures that are not scientifically based, such as refusal of entry of suspect cases or unaffected persons to affected areas,” Mr. Jasarevic said in an interview.
As far as resources, the PHEIC mechanism is not a fundraising mechanism, but some donors might consider a PHEIC declaration as a trigger for releasing additional funding to respond to the health threat, he said.
Allison T. Chamberlain, PhD, acting director for the Emory Center for Public Health Preparedness and Research at the Emory Rollins School of Public Health in Atlanta, said national governments and nongovernmental aid organizations are among the most affected by a PHEIC because they are looked at to provide assistance to the most heavily affected areas and to bolster public health preparedness within their own borders.
“In terms of resources that are deployed, a Public Health Emergency of International Concern raises levels of international support and commitment to stopping the emergency,” Dr. Chamberlain said in an interview. “By doing so, it gives countries the needed flexibility to release financial resources of their own accord to support things like response teams that might go into heavily affected areas to assist, for instance.”
WHO Director-General Dr. Tedros Adhanom Ghebreyesus stressed that cooperation among countries is key during the PHEIC.
“We can only stop it together,” he said during the press conference. “This is the time for facts, not fear. This is the time for science, not rumors. This is the time for solidarity, not stigma.”
This is the sixth PHEIC declared by WHO in the last 10 years. Such declarations were made for the 2009 H1NI influenza pandemic, the 2014 polio resurgence, the 2014 Ebola outbreak in West Africa, the 2016 Zika virus, and the 2019 Kivu Ebola outbreak in the Democratic Republic of Congo.
Amid the rising spread of the 2019 Novel Coronavirus (2019-nCoV),
The declaration was made during a press briefing on Jan. 30 after a week of growing concern and pressure on WHO to designate the virus at a higher emergency level. WHO’s Emergency Committee made the nearly unanimous decision after considering the increasing number of coronavirus cases in China, the rising infections outside of China, and the questionable measures some countries are taking regarding travel, said committee chair Didier Houssin, MD, said during the press conference.
As of Jan. 30, there were 8,236 confirmed cases of the coronavirus in China and 171 deaths, with another 112 cases identified outside of China in 21 other countries.
“Declaring a Public Health Emergency of International Concern is likely to facilitate [WHO’s] leadership role for public health measures, holding countries to account concerning additional measures they may take regarding travel, trade, quarantine or screening, research efforts, global coordination and anticipation of economic impact [and] support to vulnerable states,” Dr. Houssin said during the press conference. “Declaring a PHEIC should certainly not be seen as manifestation of distrust in the Chinese authorities and people which are doing tremendous efforts on the frontlines of this outbreak, with transparency, and let us hope, with success.”
What happens next?
Once a PHEIC is declared, WHO launches a series of steps, including the release of temporary recommendations for the affected country on health measures to implement and guidance for other countries on preventing and reducing the international spread of the disease, WHO spokesman Tarik Jasarevic said in an interview.
“The purpose of declaring a PHEIC is to advise the world on what measures need to be taken to enhance global health security by preventing international transmission of an infectious hazard,” he said.
Following the Jan. 30 press conference, WHO released temporary guidance for China and for other countries regarding identifying, managing, containing, and preventing the virus. China is advised to continue updating the population about the outbreak, continue enhancing its public health measures for containment and surveillance of cases, and to continue collaboration with WHO and other partners to investigate the epidemiology and evolution of the outbreak and share data on all human cases.
Other countries should be prepared for containment, including the active surveillance, early detection, isolation, case management, and prevention of virus transmission and to share full data with WHO, according to the recommendations.
Under the International Health Regulations (IHR), countries are required to share information and data with WHO. Additionally, WHO leaders advised the global community to support low- and middle-income countries with their response to the coronavirus and to facilitate diagnostics, potential vaccines, and therapeutics in these areas.
The IHR requires that countries implementing health measures that go beyond what WHO recommends must send to WHO the public health rationale and justification within 48 hours of their implementation for WHO review, Mr. Jasarevic noted.
“WHO is obliged to share the information about measures and the justification received with other countries involved,” he said.
PHEIC travel and resource impact
Declaration of a PHEIC means WHO will now oversee any travel restrictions made by other countries in response to 2019-nCoV. The agency recommends that countries conduct a risk and cost-benefit analysis before enacting travel restrictions and other countries are required to inform WHO about any travel measures taken.
“Countries will be asked to provide public health justification for any travel or trade measures that are not scientifically based, such as refusal of entry of suspect cases or unaffected persons to affected areas,” Mr. Jasarevic said in an interview.
As far as resources, the PHEIC mechanism is not a fundraising mechanism, but some donors might consider a PHEIC declaration as a trigger for releasing additional funding to respond to the health threat, he said.
Allison T. Chamberlain, PhD, acting director for the Emory Center for Public Health Preparedness and Research at the Emory Rollins School of Public Health in Atlanta, said national governments and nongovernmental aid organizations are among the most affected by a PHEIC because they are looked at to provide assistance to the most heavily affected areas and to bolster public health preparedness within their own borders.
“In terms of resources that are deployed, a Public Health Emergency of International Concern raises levels of international support and commitment to stopping the emergency,” Dr. Chamberlain said in an interview. “By doing so, it gives countries the needed flexibility to release financial resources of their own accord to support things like response teams that might go into heavily affected areas to assist, for instance.”
WHO Director-General Dr. Tedros Adhanom Ghebreyesus stressed that cooperation among countries is key during the PHEIC.
“We can only stop it together,” he said during the press conference. “This is the time for facts, not fear. This is the time for science, not rumors. This is the time for solidarity, not stigma.”
This is the sixth PHEIC declared by WHO in the last 10 years. Such declarations were made for the 2009 H1NI influenza pandemic, the 2014 polio resurgence, the 2014 Ebola outbreak in West Africa, the 2016 Zika virus, and the 2019 Kivu Ebola outbreak in the Democratic Republic of Congo.
2019 Novel Coronavirus: Frequently asked questions for clinicians
The 2019 Novel Coronavirus (2019-nCoV) outbreak has unfolded so rapidly that many clinicians are scrambling to stay on top of it. Here are the answers to some frequently asked questions about how to prepare your clinic to respond to this outbreak.
Keep in mind that the outbreak is moving rapidly. Though scientific and epidemiologic knowledge has increased at unprecedented speed, there is much we don’t know, and some of what we think we know will change. Follow the links for the most up-to-date information.
What should our clinic do first?
Plan ahead with the following:
- Develop a plan for office staff to take travel histories from anyone with a respiratory illness and provide training for those who need it. Travel history at present should include asking about travel to China in the past 14 days, specifically Wuhan city or Hubei province.
- Review up-to-date infection control practices with all office staff and provide training for those who need it.
- Take an inventory of supplies of personal protective equipment (PPE), such as gowns, gloves, masks, eye protection, and N95 respirators or powered air-purifying respirators (PAPRs), and order items that are missing or low in stock.
- Fit-test users of N95 masks for maximal effectiveness.
- Plan where a potential patient would be isolated while obtaining expert advice.
- Know whom to contact at the state or local health department if you have a patient with the appropriate travel history.
The Centers for Disease Control and Prevention has prepared a toolkit to help frontline health care professionals prepare for this virus. Providers need to stay up to date on the latest recommendations, as the situation is changing rapidly.
When should I suspect 2019-nCoV illness, and what should I do?
Take the following steps to assess the concern and respond:
- If a patient with respiratory illness has traveled to China in the past 14 days, immediately put a mask on the patient and move the individual to a private room. Use a negative-pressure room if available.
- Put on appropriate PPE (including gloves, gown, eye protection, and mask) for contact, droplet, and airborne precautions. CDC recommends an N95 respirator mask if available, although we don’t know yet if there is true airborne spread.
- Obtain an accurate travel history, including dates and cities. (Tip: Get the correct spelling, as the English spelling of cities in China can cause confusion.)
- If the patient meets the current CDC definition of “person under investigation” or PUI, or if you need guidance on how to proceed, notify infection control (if you are in a facility that has it) and call your state or local health department immediately.
- Contact public health authorities who can help decide whether the patient should be admitted to airborne isolation or monitored at home with appropriate precautions.
What is the definition of a PUI?
The current definition of a PUI is a person who has fever and symptoms of a respiratory infection (cough, shortness of breath) AND who has EITHER been in Wuhan city or Hubei province in the past 14 days OR had close contact with a person either under investigation for 2019-nCoV infection or with confirmed infection. The definition of a PUI will change over time, so check this link.
How can I test for 2019-nCoV?
As of Jan. 30, 2020, testing is by polymerase chain reaction (PCR) and is available in the United States only through the CDC in Atlanta. Testing should soon be available in state health department laboratories. If public health authorities decide that your patient should be tested, they will instruct you on which samples to obtain.
The full sequence of 2019-nCoV has been shared, so some reference laboratories may develop and validate tests, ideally with assistance from CDC. If testing becomes available, make certain that it is a reputable lab that has carefully validated the test.
Should I test for other viruses?
Because the symptoms of 2019-nCoV infection overlap with those of influenza and other respiratory viruses, PCR testing for other viruses should be considered if it will change management (i.e., change the decision to provide influenza antivirals). Use appropriate PPE while collecting specimens, including eye protection. If 2019-nCoV is a consideration, you may want to send the specimen to a hospital lab for testing, where the sample will be processed under a biosafety hood, rather than doing point-of-care testing in the office.
How dangerous is 2019-nCoV?
The current estimated mortality rate is 2%-3%. That is probably an overestimate, as those with severe disease and those who die are more likely to be tested and reported early in an epidemic.
Our current knowledge is based on preliminary reports from hospitalized patients and will probably change. From the speed of spread and a single family cluster, it seems likely that there are milder cases and perhaps asymptomatic infection.
What else do I need to know about coronaviruses?
Coronaviruses are a large and diverse group of viruses, many of which are animal viruses. Before the discovery of the 2019-nCoV, six coronaviruses were known to infect humans. Four of these (HKU1, NL63, OC43, and 229E) predominantly caused mild to moderate upper respiratory illness, and they are thought to be responsible for 10%-30% of colds. They occasionally cause viral pneumonia and can be detected by some commercial multiplex panels.
Two other coronaviruses have caused outbreaks of severe respiratory illness in people: SARS, which emerged in Southern China in 2002, and MERS in the Middle East, in 2012. Unlike SARS, sporadic cases of MERS continue to occur.
The current outbreak is caused by 2019-nCoV, a previously unknown beta coronavirus. It is most closely related (~96%) to a bat virus and shares about 80% sequence homology with SARS CoV.
Andrew T. Pavia, MD, is the George and Esther Gross Presidential Professor and chief of the division of pediatric infectious disease in the department of pediatrics at the University of Utah, Salt Lake City. He is also director of hospital epidemiology and associate director of antimicrobial stewardship at Primary Children’s Hospital, Salt Lake City. Dr. Pavia has disclosed that he has served as a consultant for Genentech, Merck, and Seqirus and that he has served as associate editor for The Sanford Guide.
This article first appeared on Medscape.com.
The 2019 Novel Coronavirus (2019-nCoV) outbreak has unfolded so rapidly that many clinicians are scrambling to stay on top of it. Here are the answers to some frequently asked questions about how to prepare your clinic to respond to this outbreak.
Keep in mind that the outbreak is moving rapidly. Though scientific and epidemiologic knowledge has increased at unprecedented speed, there is much we don’t know, and some of what we think we know will change. Follow the links for the most up-to-date information.
What should our clinic do first?
Plan ahead with the following:
- Develop a plan for office staff to take travel histories from anyone with a respiratory illness and provide training for those who need it. Travel history at present should include asking about travel to China in the past 14 days, specifically Wuhan city or Hubei province.
- Review up-to-date infection control practices with all office staff and provide training for those who need it.
- Take an inventory of supplies of personal protective equipment (PPE), such as gowns, gloves, masks, eye protection, and N95 respirators or powered air-purifying respirators (PAPRs), and order items that are missing or low in stock.
- Fit-test users of N95 masks for maximal effectiveness.
- Plan where a potential patient would be isolated while obtaining expert advice.
- Know whom to contact at the state or local health department if you have a patient with the appropriate travel history.
The Centers for Disease Control and Prevention has prepared a toolkit to help frontline health care professionals prepare for this virus. Providers need to stay up to date on the latest recommendations, as the situation is changing rapidly.
When should I suspect 2019-nCoV illness, and what should I do?
Take the following steps to assess the concern and respond:
- If a patient with respiratory illness has traveled to China in the past 14 days, immediately put a mask on the patient and move the individual to a private room. Use a negative-pressure room if available.
- Put on appropriate PPE (including gloves, gown, eye protection, and mask) for contact, droplet, and airborne precautions. CDC recommends an N95 respirator mask if available, although we don’t know yet if there is true airborne spread.
- Obtain an accurate travel history, including dates and cities. (Tip: Get the correct spelling, as the English spelling of cities in China can cause confusion.)
- If the patient meets the current CDC definition of “person under investigation” or PUI, or if you need guidance on how to proceed, notify infection control (if you are in a facility that has it) and call your state or local health department immediately.
- Contact public health authorities who can help decide whether the patient should be admitted to airborne isolation or monitored at home with appropriate precautions.
What is the definition of a PUI?
The current definition of a PUI is a person who has fever and symptoms of a respiratory infection (cough, shortness of breath) AND who has EITHER been in Wuhan city or Hubei province in the past 14 days OR had close contact with a person either under investigation for 2019-nCoV infection or with confirmed infection. The definition of a PUI will change over time, so check this link.
How can I test for 2019-nCoV?
As of Jan. 30, 2020, testing is by polymerase chain reaction (PCR) and is available in the United States only through the CDC in Atlanta. Testing should soon be available in state health department laboratories. If public health authorities decide that your patient should be tested, they will instruct you on which samples to obtain.
The full sequence of 2019-nCoV has been shared, so some reference laboratories may develop and validate tests, ideally with assistance from CDC. If testing becomes available, make certain that it is a reputable lab that has carefully validated the test.
Should I test for other viruses?
Because the symptoms of 2019-nCoV infection overlap with those of influenza and other respiratory viruses, PCR testing for other viruses should be considered if it will change management (i.e., change the decision to provide influenza antivirals). Use appropriate PPE while collecting specimens, including eye protection. If 2019-nCoV is a consideration, you may want to send the specimen to a hospital lab for testing, where the sample will be processed under a biosafety hood, rather than doing point-of-care testing in the office.
How dangerous is 2019-nCoV?
The current estimated mortality rate is 2%-3%. That is probably an overestimate, as those with severe disease and those who die are more likely to be tested and reported early in an epidemic.
Our current knowledge is based on preliminary reports from hospitalized patients and will probably change. From the speed of spread and a single family cluster, it seems likely that there are milder cases and perhaps asymptomatic infection.
What else do I need to know about coronaviruses?
Coronaviruses are a large and diverse group of viruses, many of which are animal viruses. Before the discovery of the 2019-nCoV, six coronaviruses were known to infect humans. Four of these (HKU1, NL63, OC43, and 229E) predominantly caused mild to moderate upper respiratory illness, and they are thought to be responsible for 10%-30% of colds. They occasionally cause viral pneumonia and can be detected by some commercial multiplex panels.
Two other coronaviruses have caused outbreaks of severe respiratory illness in people: SARS, which emerged in Southern China in 2002, and MERS in the Middle East, in 2012. Unlike SARS, sporadic cases of MERS continue to occur.
The current outbreak is caused by 2019-nCoV, a previously unknown beta coronavirus. It is most closely related (~96%) to a bat virus and shares about 80% sequence homology with SARS CoV.
Andrew T. Pavia, MD, is the George and Esther Gross Presidential Professor and chief of the division of pediatric infectious disease in the department of pediatrics at the University of Utah, Salt Lake City. He is also director of hospital epidemiology and associate director of antimicrobial stewardship at Primary Children’s Hospital, Salt Lake City. Dr. Pavia has disclosed that he has served as a consultant for Genentech, Merck, and Seqirus and that he has served as associate editor for The Sanford Guide.
This article first appeared on Medscape.com.
The 2019 Novel Coronavirus (2019-nCoV) outbreak has unfolded so rapidly that many clinicians are scrambling to stay on top of it. Here are the answers to some frequently asked questions about how to prepare your clinic to respond to this outbreak.
Keep in mind that the outbreak is moving rapidly. Though scientific and epidemiologic knowledge has increased at unprecedented speed, there is much we don’t know, and some of what we think we know will change. Follow the links for the most up-to-date information.
What should our clinic do first?
Plan ahead with the following:
- Develop a plan for office staff to take travel histories from anyone with a respiratory illness and provide training for those who need it. Travel history at present should include asking about travel to China in the past 14 days, specifically Wuhan city or Hubei province.
- Review up-to-date infection control practices with all office staff and provide training for those who need it.
- Take an inventory of supplies of personal protective equipment (PPE), such as gowns, gloves, masks, eye protection, and N95 respirators or powered air-purifying respirators (PAPRs), and order items that are missing or low in stock.
- Fit-test users of N95 masks for maximal effectiveness.
- Plan where a potential patient would be isolated while obtaining expert advice.
- Know whom to contact at the state or local health department if you have a patient with the appropriate travel history.
The Centers for Disease Control and Prevention has prepared a toolkit to help frontline health care professionals prepare for this virus. Providers need to stay up to date on the latest recommendations, as the situation is changing rapidly.
When should I suspect 2019-nCoV illness, and what should I do?
Take the following steps to assess the concern and respond:
- If a patient with respiratory illness has traveled to China in the past 14 days, immediately put a mask on the patient and move the individual to a private room. Use a negative-pressure room if available.
- Put on appropriate PPE (including gloves, gown, eye protection, and mask) for contact, droplet, and airborne precautions. CDC recommends an N95 respirator mask if available, although we don’t know yet if there is true airborne spread.
- Obtain an accurate travel history, including dates and cities. (Tip: Get the correct spelling, as the English spelling of cities in China can cause confusion.)
- If the patient meets the current CDC definition of “person under investigation” or PUI, or if you need guidance on how to proceed, notify infection control (if you are in a facility that has it) and call your state or local health department immediately.
- Contact public health authorities who can help decide whether the patient should be admitted to airborne isolation or monitored at home with appropriate precautions.
What is the definition of a PUI?
The current definition of a PUI is a person who has fever and symptoms of a respiratory infection (cough, shortness of breath) AND who has EITHER been in Wuhan city or Hubei province in the past 14 days OR had close contact with a person either under investigation for 2019-nCoV infection or with confirmed infection. The definition of a PUI will change over time, so check this link.
How can I test for 2019-nCoV?
As of Jan. 30, 2020, testing is by polymerase chain reaction (PCR) and is available in the United States only through the CDC in Atlanta. Testing should soon be available in state health department laboratories. If public health authorities decide that your patient should be tested, they will instruct you on which samples to obtain.
The full sequence of 2019-nCoV has been shared, so some reference laboratories may develop and validate tests, ideally with assistance from CDC. If testing becomes available, make certain that it is a reputable lab that has carefully validated the test.
Should I test for other viruses?
Because the symptoms of 2019-nCoV infection overlap with those of influenza and other respiratory viruses, PCR testing for other viruses should be considered if it will change management (i.e., change the decision to provide influenza antivirals). Use appropriate PPE while collecting specimens, including eye protection. If 2019-nCoV is a consideration, you may want to send the specimen to a hospital lab for testing, where the sample will be processed under a biosafety hood, rather than doing point-of-care testing in the office.
How dangerous is 2019-nCoV?
The current estimated mortality rate is 2%-3%. That is probably an overestimate, as those with severe disease and those who die are more likely to be tested and reported early in an epidemic.
Our current knowledge is based on preliminary reports from hospitalized patients and will probably change. From the speed of spread and a single family cluster, it seems likely that there are milder cases and perhaps asymptomatic infection.
What else do I need to know about coronaviruses?
Coronaviruses are a large and diverse group of viruses, many of which are animal viruses. Before the discovery of the 2019-nCoV, six coronaviruses were known to infect humans. Four of these (HKU1, NL63, OC43, and 229E) predominantly caused mild to moderate upper respiratory illness, and they are thought to be responsible for 10%-30% of colds. They occasionally cause viral pneumonia and can be detected by some commercial multiplex panels.
Two other coronaviruses have caused outbreaks of severe respiratory illness in people: SARS, which emerged in Southern China in 2002, and MERS in the Middle East, in 2012. Unlike SARS, sporadic cases of MERS continue to occur.
The current outbreak is caused by 2019-nCoV, a previously unknown beta coronavirus. It is most closely related (~96%) to a bat virus and shares about 80% sequence homology with SARS CoV.
Andrew T. Pavia, MD, is the George and Esther Gross Presidential Professor and chief of the division of pediatric infectious disease in the department of pediatrics at the University of Utah, Salt Lake City. He is also director of hospital epidemiology and associate director of antimicrobial stewardship at Primary Children’s Hospital, Salt Lake City. Dr. Pavia has disclosed that he has served as a consultant for Genentech, Merck, and Seqirus and that he has served as associate editor for The Sanford Guide.
This article first appeared on Medscape.com.
CDC: First person-to-person spread of novel coronavirus in U.S.
A Chicago woman in her 60s who tested positive for the 2019 Novel Coronavirus (2019-nCoV) after returning from Wuhan, China, earlier this month has infected her husband, becoming the first known instance of person-to-person transmission of the 2019-nCoV in the United States.
“Limited person-to-person spread of this new virus outside of China has already been seen in nine close contacts, where travelers were infected and transmitted the virus to someone else,” Robert R. Redfield, MD, director of the Centers for Disease Control and Prevention, said during a press briefing on Jan. 30, 2020. “However, the full picture of how easy and how sustainable this virus can spread is unclear. Today’s news underscores the important risk-dependent exposure. The vast majority of Americans have not had recent travel to China, where sustained human-to-human transmission is occurring. Individuals who are close personal contacts of cases, though, could have a risk.”
The affected man, also in his 60s, is the spouse of the first confirmed travel-associated case of 2019-nCoV to be reported in the state of Illinois, according to Ngozi O. Ezike, MD, director of the Illinois Department of Public Health. The man had no history of recent travel to China. “This person-to-person spread was between two very close contacts: a wife and husband,” said Dr. Ezike, who added that 21 individuals in the state are under investigation for 2019-nCoV. “The virus is not spreading widely across the community. At this time, we are not recommending that people in the general public take additional precautions such as canceling activities or avoiding going out. While there is concern with this second case, public health officials are actively monitoring close contacts, including health care workers, and we believe that people in Illinois are at low risk.”
Jennifer Layden, MD, state epidemiologist at the Illinois Department of Public Health, said that the infected Chicago woman returned from Wuhan, China on Jan. 13, 2020. She is hospitalized in stable condition “and continues to do well,” Dr. Layden said. “Public health officials have been actively and closely monitoring individuals who had contacts with her, including her husband, who had close contact for symptoms. He recently began reporting symptoms and was immediately admitted to the hospital and placed in an isolation room, where he is in stable condition. We are actively monitoring individuals such as health care workers, household contacts, and others who were in contact with either of the confirmed cases in the goal to contain and reduce the risk of additional transmission.”
Nancy Messonnier, MD, director, National Center for Immunization and Respiratory Diseases, expects that more cases of 2019-nCoV will transpire in the United States.
“More cases means the potential for more person-to-person spread,” Dr. Messonnier said. “We’re trying to strike a balance in our response right now. We want to be aggressive, but we want our actions to be evidence-based and appropriate for the current circumstance. For example, CDC does not currently recommend use of face masks for the general public. The virus is not spreading in the general community.”
A Chicago woman in her 60s who tested positive for the 2019 Novel Coronavirus (2019-nCoV) after returning from Wuhan, China, earlier this month has infected her husband, becoming the first known instance of person-to-person transmission of the 2019-nCoV in the United States.
“Limited person-to-person spread of this new virus outside of China has already been seen in nine close contacts, where travelers were infected and transmitted the virus to someone else,” Robert R. Redfield, MD, director of the Centers for Disease Control and Prevention, said during a press briefing on Jan. 30, 2020. “However, the full picture of how easy and how sustainable this virus can spread is unclear. Today’s news underscores the important risk-dependent exposure. The vast majority of Americans have not had recent travel to China, where sustained human-to-human transmission is occurring. Individuals who are close personal contacts of cases, though, could have a risk.”
The affected man, also in his 60s, is the spouse of the first confirmed travel-associated case of 2019-nCoV to be reported in the state of Illinois, according to Ngozi O. Ezike, MD, director of the Illinois Department of Public Health. The man had no history of recent travel to China. “This person-to-person spread was between two very close contacts: a wife and husband,” said Dr. Ezike, who added that 21 individuals in the state are under investigation for 2019-nCoV. “The virus is not spreading widely across the community. At this time, we are not recommending that people in the general public take additional precautions such as canceling activities or avoiding going out. While there is concern with this second case, public health officials are actively monitoring close contacts, including health care workers, and we believe that people in Illinois are at low risk.”
Jennifer Layden, MD, state epidemiologist at the Illinois Department of Public Health, said that the infected Chicago woman returned from Wuhan, China on Jan. 13, 2020. She is hospitalized in stable condition “and continues to do well,” Dr. Layden said. “Public health officials have been actively and closely monitoring individuals who had contacts with her, including her husband, who had close contact for symptoms. He recently began reporting symptoms and was immediately admitted to the hospital and placed in an isolation room, where he is in stable condition. We are actively monitoring individuals such as health care workers, household contacts, and others who were in contact with either of the confirmed cases in the goal to contain and reduce the risk of additional transmission.”
Nancy Messonnier, MD, director, National Center for Immunization and Respiratory Diseases, expects that more cases of 2019-nCoV will transpire in the United States.
“More cases means the potential for more person-to-person spread,” Dr. Messonnier said. “We’re trying to strike a balance in our response right now. We want to be aggressive, but we want our actions to be evidence-based and appropriate for the current circumstance. For example, CDC does not currently recommend use of face masks for the general public. The virus is not spreading in the general community.”
A Chicago woman in her 60s who tested positive for the 2019 Novel Coronavirus (2019-nCoV) after returning from Wuhan, China, earlier this month has infected her husband, becoming the first known instance of person-to-person transmission of the 2019-nCoV in the United States.
“Limited person-to-person spread of this new virus outside of China has already been seen in nine close contacts, where travelers were infected and transmitted the virus to someone else,” Robert R. Redfield, MD, director of the Centers for Disease Control and Prevention, said during a press briefing on Jan. 30, 2020. “However, the full picture of how easy and how sustainable this virus can spread is unclear. Today’s news underscores the important risk-dependent exposure. The vast majority of Americans have not had recent travel to China, where sustained human-to-human transmission is occurring. Individuals who are close personal contacts of cases, though, could have a risk.”
The affected man, also in his 60s, is the spouse of the first confirmed travel-associated case of 2019-nCoV to be reported in the state of Illinois, according to Ngozi O. Ezike, MD, director of the Illinois Department of Public Health. The man had no history of recent travel to China. “This person-to-person spread was between two very close contacts: a wife and husband,” said Dr. Ezike, who added that 21 individuals in the state are under investigation for 2019-nCoV. “The virus is not spreading widely across the community. At this time, we are not recommending that people in the general public take additional precautions such as canceling activities or avoiding going out. While there is concern with this second case, public health officials are actively monitoring close contacts, including health care workers, and we believe that people in Illinois are at low risk.”
Jennifer Layden, MD, state epidemiologist at the Illinois Department of Public Health, said that the infected Chicago woman returned from Wuhan, China on Jan. 13, 2020. She is hospitalized in stable condition “and continues to do well,” Dr. Layden said. “Public health officials have been actively and closely monitoring individuals who had contacts with her, including her husband, who had close contact for symptoms. He recently began reporting symptoms and was immediately admitted to the hospital and placed in an isolation room, where he is in stable condition. We are actively monitoring individuals such as health care workers, household contacts, and others who were in contact with either of the confirmed cases in the goal to contain and reduce the risk of additional transmission.”
Nancy Messonnier, MD, director, National Center for Immunization and Respiratory Diseases, expects that more cases of 2019-nCoV will transpire in the United States.
“More cases means the potential for more person-to-person spread,” Dr. Messonnier said. “We’re trying to strike a balance in our response right now. We want to be aggressive, but we want our actions to be evidence-based and appropriate for the current circumstance. For example, CDC does not currently recommend use of face masks for the general public. The virus is not spreading in the general community.”
Lasers expunge mucosal tattoos
, researchers reported.
Mucocutaneous tattoos are relatively rare, and lasers have been used for their removal, but cases and results have not been well documented, wrote Hao Feng, MD, then of the Laser & Skin Surgery Center of New York, and the department of dermatology, New York University, and coauthors.
In a report published in Lasers in Surgery and Medicine, the clinicians noted significant improvement with no scarring or dyspigmentation at 1 month after the last treatment session in two patients, with mucosal tattoos that had not been previously treated.
In one case, a healthy 19-year-old woman with Fitzpatrick skin type II presented for removal of a 6‐month‐old, black tattoo on the mucosal surface of her lower lip. She received six treatment sessions at months 0, 1, 3, 5, 7, and 12 with a QS 694‐nm ruby laser at settings of 6-mm spot size, 20-nanosecond pulse duration, and 3.0-3.5 J/cm2.
In a second case, a 30‐year‐old man with Fitzpatrick skin type IV presented for removal of a 10‐year‐old black tattoo on his left buccal mucosa. He received one treatment with 755-nm alexandrite picosecond lasers at settings of 2.5-mm spot size, 500-picosecond pulse duration, and 3.36 J/cm2.
Both patients experienced local mild discomfort, erythema, and edema after treatment.
“Older tattoos respond better and quicker on the skin to laser treatments, and it is likely the reason why the buccal mucosa tattoo (10 years) resolved with a single treatment whereas the lower lip tattoo (6 months) required six treatments,” the authors noted.
Mucosal tattoos, they added, “tend to respond better, faster, and with less unwanted side effects than tattoos on the skin. This may relate to the fact that mucosal skin is thinner, non-keratinized, well‐vascularized, and contains less melanin content.”
As to which laser is the best choice for removing mucosal tattoos, the authors noted that it is unclear, but while they said they have been using picosecond lasers for tattoo removals, QS lasers “remain excellent treatment modalities,” they wrote.
“Given the excellent clinical response combined with lack of scarring and dyspigmentation in our highly satisfied patients, it is the authors’ opinion that laser treatment should be considered as the first‐line treatment in removing unwanted cosmetic mucosal tattoos. This can be accomplished with various wavelengths in the picosecond and nanosecond domains,” they concluded.
Dr. Feng, who is now director of laser surgery and cosmetic dermatology at the University of Connecticut Health Center, Farmington, disclosed serving as a consultant and medical monitor for Cytrellis Biosystems. Another author disclosed serving on the advisory boards for Cytrellis, Syneron Candela, and Cynosure; owning stocks or having stock options with Cytrellis; and investing in Syneron Candela, Cynosure, and Cytrellis. The remaining two authors had no disclosures.
SOURCE: Feng H et al. Lasers Surg Med. 2019 Dec 30. doi: 10.1002/lsm.23207.
, researchers reported.
Mucocutaneous tattoos are relatively rare, and lasers have been used for their removal, but cases and results have not been well documented, wrote Hao Feng, MD, then of the Laser & Skin Surgery Center of New York, and the department of dermatology, New York University, and coauthors.
In a report published in Lasers in Surgery and Medicine, the clinicians noted significant improvement with no scarring or dyspigmentation at 1 month after the last treatment session in two patients, with mucosal tattoos that had not been previously treated.
In one case, a healthy 19-year-old woman with Fitzpatrick skin type II presented for removal of a 6‐month‐old, black tattoo on the mucosal surface of her lower lip. She received six treatment sessions at months 0, 1, 3, 5, 7, and 12 with a QS 694‐nm ruby laser at settings of 6-mm spot size, 20-nanosecond pulse duration, and 3.0-3.5 J/cm2.
In a second case, a 30‐year‐old man with Fitzpatrick skin type IV presented for removal of a 10‐year‐old black tattoo on his left buccal mucosa. He received one treatment with 755-nm alexandrite picosecond lasers at settings of 2.5-mm spot size, 500-picosecond pulse duration, and 3.36 J/cm2.
Both patients experienced local mild discomfort, erythema, and edema after treatment.
“Older tattoos respond better and quicker on the skin to laser treatments, and it is likely the reason why the buccal mucosa tattoo (10 years) resolved with a single treatment whereas the lower lip tattoo (6 months) required six treatments,” the authors noted.
Mucosal tattoos, they added, “tend to respond better, faster, and with less unwanted side effects than tattoos on the skin. This may relate to the fact that mucosal skin is thinner, non-keratinized, well‐vascularized, and contains less melanin content.”
As to which laser is the best choice for removing mucosal tattoos, the authors noted that it is unclear, but while they said they have been using picosecond lasers for tattoo removals, QS lasers “remain excellent treatment modalities,” they wrote.
“Given the excellent clinical response combined with lack of scarring and dyspigmentation in our highly satisfied patients, it is the authors’ opinion that laser treatment should be considered as the first‐line treatment in removing unwanted cosmetic mucosal tattoos. This can be accomplished with various wavelengths in the picosecond and nanosecond domains,” they concluded.
Dr. Feng, who is now director of laser surgery and cosmetic dermatology at the University of Connecticut Health Center, Farmington, disclosed serving as a consultant and medical monitor for Cytrellis Biosystems. Another author disclosed serving on the advisory boards for Cytrellis, Syneron Candela, and Cynosure; owning stocks or having stock options with Cytrellis; and investing in Syneron Candela, Cynosure, and Cytrellis. The remaining two authors had no disclosures.
SOURCE: Feng H et al. Lasers Surg Med. 2019 Dec 30. doi: 10.1002/lsm.23207.
, researchers reported.
Mucocutaneous tattoos are relatively rare, and lasers have been used for their removal, but cases and results have not been well documented, wrote Hao Feng, MD, then of the Laser & Skin Surgery Center of New York, and the department of dermatology, New York University, and coauthors.
In a report published in Lasers in Surgery and Medicine, the clinicians noted significant improvement with no scarring or dyspigmentation at 1 month after the last treatment session in two patients, with mucosal tattoos that had not been previously treated.
In one case, a healthy 19-year-old woman with Fitzpatrick skin type II presented for removal of a 6‐month‐old, black tattoo on the mucosal surface of her lower lip. She received six treatment sessions at months 0, 1, 3, 5, 7, and 12 with a QS 694‐nm ruby laser at settings of 6-mm spot size, 20-nanosecond pulse duration, and 3.0-3.5 J/cm2.
In a second case, a 30‐year‐old man with Fitzpatrick skin type IV presented for removal of a 10‐year‐old black tattoo on his left buccal mucosa. He received one treatment with 755-nm alexandrite picosecond lasers at settings of 2.5-mm spot size, 500-picosecond pulse duration, and 3.36 J/cm2.
Both patients experienced local mild discomfort, erythema, and edema after treatment.
“Older tattoos respond better and quicker on the skin to laser treatments, and it is likely the reason why the buccal mucosa tattoo (10 years) resolved with a single treatment whereas the lower lip tattoo (6 months) required six treatments,” the authors noted.
Mucosal tattoos, they added, “tend to respond better, faster, and with less unwanted side effects than tattoos on the skin. This may relate to the fact that mucosal skin is thinner, non-keratinized, well‐vascularized, and contains less melanin content.”
As to which laser is the best choice for removing mucosal tattoos, the authors noted that it is unclear, but while they said they have been using picosecond lasers for tattoo removals, QS lasers “remain excellent treatment modalities,” they wrote.
“Given the excellent clinical response combined with lack of scarring and dyspigmentation in our highly satisfied patients, it is the authors’ opinion that laser treatment should be considered as the first‐line treatment in removing unwanted cosmetic mucosal tattoos. This can be accomplished with various wavelengths in the picosecond and nanosecond domains,” they concluded.
Dr. Feng, who is now director of laser surgery and cosmetic dermatology at the University of Connecticut Health Center, Farmington, disclosed serving as a consultant and medical monitor for Cytrellis Biosystems. Another author disclosed serving on the advisory boards for Cytrellis, Syneron Candela, and Cynosure; owning stocks or having stock options with Cytrellis; and investing in Syneron Candela, Cynosure, and Cytrellis. The remaining two authors had no disclosures.
SOURCE: Feng H et al. Lasers Surg Med. 2019 Dec 30. doi: 10.1002/lsm.23207.
FROM LASERS IN SURGERY AND MEDICINE
Be ready for patient questions on sunscreen safety, SPF choice
ORLANDO – Dermatologists should be well versed in addressing common concerns that patients, family members, and the media have about photoprotection, Adam Friedman, MD, advised at the ODAC Dermatology, Aesthetic, & Surgical Conference.
“Know the controversies. Be armed and ready when these patients come to your office with questions,” Dr. Friedman, professor and interim chair of dermatology at George Washington University, Washington, said in an interview at the meeting, where he presented on issues related to photoprotection.
Sunscreen SPFs above 50 don’t technically provide a “meaningful” increase in ultraviolet protection, given that this value relates to filtering about 98% of UVB, but they still can provide some benefit, which has to do with real-world human error, Dr. Friedman said.
“Most people don’t use sunscreens the right way,” meaning they don’t apply enough to achieve the SPF listed, he added in the interview. “A higher SPF is meaningful, because if they apply less [sunscreen], they actually still are in that safety window,” with the higher SPF sunscreen. (The American Academy of Dermatology recommends an SPF of 30 or higher.) Several studies have shown that a SPF of 70 or 100 is superior to 50, likely because of this “dilutional” effect.
Patients may have concerns about the effects of sunscreen on vitamin D production, the environment, and hair loss, and whether they have endocrine disrupting effects, added Dr. Friedman, who is also the medical director of the meeting.
Inhibition of cutaneous vitamin D synthesis after using sunscreen can vary, based on whether a person has properly applied sunscreen, the season, latitude, and an individual’s age and obesity level. Patients with low vitamin D levels can use a vitamin D supplement to achieve sufficient levels, and patients concerned about the impact of sunscreen and vitamin D can be advised to take 600 IU of vitamin D3 a day, according to Dr. Friedman. Some studies have suggested that UVB exposure and risk of certain cancers are inversely correlated, implicating cutaneous vitamin D synthesis (J Clin Transl Endocrinol. 2014 Oct 5;1[4]:179-86). But correlation does not equal causation, he pointed out.
Other concerns stem from the potential for oxybenzone, a UVA/UVB filter in more than 70% of sunscreens, to act as an endocrine disruptor in people and whether it is potentially damaging the environment. The data driving these concerns “stem from the bench, not the real world,” Dr. Friedman said. While topical application of oxybenzone can result in systemic absorption, and even though it’s been detected in waters that are heavily populated or where people go on vacation, there is no evidence demonstrating toxicity to humans or the coral reefs. “At least the information we have to date says they don’t,” he added.
In a randomized clinical trial recently published in JAMA, Food and Drug Administration investigators found that systemic skin absorption with geometric mean plasma concentrations greater than 0.5 ng/mL with six active ingredients in sunscreen that were tested, including oxybenzone (JAMA. 2020;323[3]:256-7). The study was part of an FDA proposed rule requesting additional information on sunscreen ingredients; the plasma concentrations exceeded the level at which further safety studies could potentially be waived.
The study, Dr. Friedman said, “only demonstrated the ability to detect these UV filters at very small concentrations in the blood. They have yet to show any meaningful biologic correlation to these findings.”
For those patients who prefer not to use chemical filters, Dr. Friedman suggests recommending mineral-based sunscreens, of which he said micro- and nanoparticulate formulations offer the best cosmesis by sitting more evenly on the skin, being more amenable to thinner and less-lipophilic vehicles, and limiting visible light scattering (thereby limiting the unsightly white appearance) – while maintaining UV scattering efficacy. However, controversy has emerged as there are past studies that posit the theoretical danger of nanoparticles in sunscreens, given their potential to penetrate the skin and enter cells.
But continually emerging evidence has shown that commercially available nanosunscreens are safe, with no toxicity even at the cellular level when applied to the skin in sunscreen or in cosmetics. “All evidence to date suggests they do not do this,” Dr. Friedman said, noting that, in Europe, the European Commission’s Scientific Committee on Consumer Safety has stated that nanoparticles below a concentration of 25% in sunscreens is safe, “just don’t put them in aerosolized forms.”
Lastly, while some recent studies have detected titanium dioxide on the hair shafts of patients with and without frontal fibrosing alopecia, Dr. Friedman noted more evidence is needed before recommending that these patients avoid using sunscreen (Br J Dermatol. 2019 Jul;181[1]:216-7). “Correlation does not mean causation, and the current dogma is that there’s no connection between these two,” he commented.
Dr. Friedman reported consulting and advisory board relationships with numerous companies; he also reported speaking for Regeneron, Abbvie, and Dermira, and receiving grants with Pfizer and DF Pharma.
ORLANDO – Dermatologists should be well versed in addressing common concerns that patients, family members, and the media have about photoprotection, Adam Friedman, MD, advised at the ODAC Dermatology, Aesthetic, & Surgical Conference.
“Know the controversies. Be armed and ready when these patients come to your office with questions,” Dr. Friedman, professor and interim chair of dermatology at George Washington University, Washington, said in an interview at the meeting, where he presented on issues related to photoprotection.
Sunscreen SPFs above 50 don’t technically provide a “meaningful” increase in ultraviolet protection, given that this value relates to filtering about 98% of UVB, but they still can provide some benefit, which has to do with real-world human error, Dr. Friedman said.
“Most people don’t use sunscreens the right way,” meaning they don’t apply enough to achieve the SPF listed, he added in the interview. “A higher SPF is meaningful, because if they apply less [sunscreen], they actually still are in that safety window,” with the higher SPF sunscreen. (The American Academy of Dermatology recommends an SPF of 30 or higher.) Several studies have shown that a SPF of 70 or 100 is superior to 50, likely because of this “dilutional” effect.
Patients may have concerns about the effects of sunscreen on vitamin D production, the environment, and hair loss, and whether they have endocrine disrupting effects, added Dr. Friedman, who is also the medical director of the meeting.
Inhibition of cutaneous vitamin D synthesis after using sunscreen can vary, based on whether a person has properly applied sunscreen, the season, latitude, and an individual’s age and obesity level. Patients with low vitamin D levels can use a vitamin D supplement to achieve sufficient levels, and patients concerned about the impact of sunscreen and vitamin D can be advised to take 600 IU of vitamin D3 a day, according to Dr. Friedman. Some studies have suggested that UVB exposure and risk of certain cancers are inversely correlated, implicating cutaneous vitamin D synthesis (J Clin Transl Endocrinol. 2014 Oct 5;1[4]:179-86). But correlation does not equal causation, he pointed out.
Other concerns stem from the potential for oxybenzone, a UVA/UVB filter in more than 70% of sunscreens, to act as an endocrine disruptor in people and whether it is potentially damaging the environment. The data driving these concerns “stem from the bench, not the real world,” Dr. Friedman said. While topical application of oxybenzone can result in systemic absorption, and even though it’s been detected in waters that are heavily populated or where people go on vacation, there is no evidence demonstrating toxicity to humans or the coral reefs. “At least the information we have to date says they don’t,” he added.
In a randomized clinical trial recently published in JAMA, Food and Drug Administration investigators found that systemic skin absorption with geometric mean plasma concentrations greater than 0.5 ng/mL with six active ingredients in sunscreen that were tested, including oxybenzone (JAMA. 2020;323[3]:256-7). The study was part of an FDA proposed rule requesting additional information on sunscreen ingredients; the plasma concentrations exceeded the level at which further safety studies could potentially be waived.
The study, Dr. Friedman said, “only demonstrated the ability to detect these UV filters at very small concentrations in the blood. They have yet to show any meaningful biologic correlation to these findings.”
For those patients who prefer not to use chemical filters, Dr. Friedman suggests recommending mineral-based sunscreens, of which he said micro- and nanoparticulate formulations offer the best cosmesis by sitting more evenly on the skin, being more amenable to thinner and less-lipophilic vehicles, and limiting visible light scattering (thereby limiting the unsightly white appearance) – while maintaining UV scattering efficacy. However, controversy has emerged as there are past studies that posit the theoretical danger of nanoparticles in sunscreens, given their potential to penetrate the skin and enter cells.
But continually emerging evidence has shown that commercially available nanosunscreens are safe, with no toxicity even at the cellular level when applied to the skin in sunscreen or in cosmetics. “All evidence to date suggests they do not do this,” Dr. Friedman said, noting that, in Europe, the European Commission’s Scientific Committee on Consumer Safety has stated that nanoparticles below a concentration of 25% in sunscreens is safe, “just don’t put them in aerosolized forms.”
Lastly, while some recent studies have detected titanium dioxide on the hair shafts of patients with and without frontal fibrosing alopecia, Dr. Friedman noted more evidence is needed before recommending that these patients avoid using sunscreen (Br J Dermatol. 2019 Jul;181[1]:216-7). “Correlation does not mean causation, and the current dogma is that there’s no connection between these two,” he commented.
Dr. Friedman reported consulting and advisory board relationships with numerous companies; he also reported speaking for Regeneron, Abbvie, and Dermira, and receiving grants with Pfizer and DF Pharma.
ORLANDO – Dermatologists should be well versed in addressing common concerns that patients, family members, and the media have about photoprotection, Adam Friedman, MD, advised at the ODAC Dermatology, Aesthetic, & Surgical Conference.
“Know the controversies. Be armed and ready when these patients come to your office with questions,” Dr. Friedman, professor and interim chair of dermatology at George Washington University, Washington, said in an interview at the meeting, where he presented on issues related to photoprotection.
Sunscreen SPFs above 50 don’t technically provide a “meaningful” increase in ultraviolet protection, given that this value relates to filtering about 98% of UVB, but they still can provide some benefit, which has to do with real-world human error, Dr. Friedman said.
“Most people don’t use sunscreens the right way,” meaning they don’t apply enough to achieve the SPF listed, he added in the interview. “A higher SPF is meaningful, because if they apply less [sunscreen], they actually still are in that safety window,” with the higher SPF sunscreen. (The American Academy of Dermatology recommends an SPF of 30 or higher.) Several studies have shown that a SPF of 70 or 100 is superior to 50, likely because of this “dilutional” effect.
Patients may have concerns about the effects of sunscreen on vitamin D production, the environment, and hair loss, and whether they have endocrine disrupting effects, added Dr. Friedman, who is also the medical director of the meeting.
Inhibition of cutaneous vitamin D synthesis after using sunscreen can vary, based on whether a person has properly applied sunscreen, the season, latitude, and an individual’s age and obesity level. Patients with low vitamin D levels can use a vitamin D supplement to achieve sufficient levels, and patients concerned about the impact of sunscreen and vitamin D can be advised to take 600 IU of vitamin D3 a day, according to Dr. Friedman. Some studies have suggested that UVB exposure and risk of certain cancers are inversely correlated, implicating cutaneous vitamin D synthesis (J Clin Transl Endocrinol. 2014 Oct 5;1[4]:179-86). But correlation does not equal causation, he pointed out.
Other concerns stem from the potential for oxybenzone, a UVA/UVB filter in more than 70% of sunscreens, to act as an endocrine disruptor in people and whether it is potentially damaging the environment. The data driving these concerns “stem from the bench, not the real world,” Dr. Friedman said. While topical application of oxybenzone can result in systemic absorption, and even though it’s been detected in waters that are heavily populated or where people go on vacation, there is no evidence demonstrating toxicity to humans or the coral reefs. “At least the information we have to date says they don’t,” he added.
In a randomized clinical trial recently published in JAMA, Food and Drug Administration investigators found that systemic skin absorption with geometric mean plasma concentrations greater than 0.5 ng/mL with six active ingredients in sunscreen that were tested, including oxybenzone (JAMA. 2020;323[3]:256-7). The study was part of an FDA proposed rule requesting additional information on sunscreen ingredients; the plasma concentrations exceeded the level at which further safety studies could potentially be waived.
The study, Dr. Friedman said, “only demonstrated the ability to detect these UV filters at very small concentrations in the blood. They have yet to show any meaningful biologic correlation to these findings.”
For those patients who prefer not to use chemical filters, Dr. Friedman suggests recommending mineral-based sunscreens, of which he said micro- and nanoparticulate formulations offer the best cosmesis by sitting more evenly on the skin, being more amenable to thinner and less-lipophilic vehicles, and limiting visible light scattering (thereby limiting the unsightly white appearance) – while maintaining UV scattering efficacy. However, controversy has emerged as there are past studies that posit the theoretical danger of nanoparticles in sunscreens, given their potential to penetrate the skin and enter cells.
But continually emerging evidence has shown that commercially available nanosunscreens are safe, with no toxicity even at the cellular level when applied to the skin in sunscreen or in cosmetics. “All evidence to date suggests they do not do this,” Dr. Friedman said, noting that, in Europe, the European Commission’s Scientific Committee on Consumer Safety has stated that nanoparticles below a concentration of 25% in sunscreens is safe, “just don’t put them in aerosolized forms.”
Lastly, while some recent studies have detected titanium dioxide on the hair shafts of patients with and without frontal fibrosing alopecia, Dr. Friedman noted more evidence is needed before recommending that these patients avoid using sunscreen (Br J Dermatol. 2019 Jul;181[1]:216-7). “Correlation does not mean causation, and the current dogma is that there’s no connection between these two,” he commented.
Dr. Friedman reported consulting and advisory board relationships with numerous companies; he also reported speaking for Regeneron, Abbvie, and Dermira, and receiving grants with Pfizer and DF Pharma.
EXPERT ANALYSIS FROM ODAC 2020
Docs weigh pulling out of MIPS over paltry payments
If you’ve knocked yourself out to earn a Merit-Based Incentive Payment System (MIPS) bonus payment, it’s pretty safe to say that getting a 1.68% payment boost probably didn’t feel like a “win” that was worth the effort.
And although it saved you from having a negative 5% payment adjustment, many physicians don’t feel that it was worth the effort.
On Jan. 6, the Centers for Medicare & Medicaid Services announced the 2020 payouts for MIPS.
Based on 2018 participation, the bonus for those who scored a perfect 100 is only a 1.68% boost in Medicare reimbursement, slightly lower than last year’s 1.88%. This decline comes as no surprise as the agency leader admits: “As the program matures, we expect that the increases in the performance thresholds in future program years will create a smaller distribution of positive payment adjustments.” Overall, more than 97% of participants avoided having a negative 5% payment adjustment.
Indeed, these bonus monies are based on a short-term appropriation of extra funds from Congress. After these temporary funds are no longer available, there will be little, if any, monies to distribute as the program is based on a “losers-feed-the-winners” construct.
It may be very tempting for many physicians to decide to ignore MIPS, with the rationale that 1.68% is not worth the effort. But don’t let your foot off the gas pedal yet, since the penalty for not participating in 2020 is a substantial 9%.
However, it is certainly time to reconsider efforts to participate at the highest level.
Should you or shouldn’t you bother with MIPS?
Let’s say you have $75,000 in revenue from Medicare Part B per year. Depending on the services you offer in your practice, that equates to 500-750 encounters with Medicare beneficiaries per year. (A reminder that MIPS affects only Part B; Medicare Advantage plans do not partake in the program.)
The recent announcement reveals that perfection would equate to an additional $1,260 per year. That’s only if you received the full 100 points; if you were simply an “exceptional performer,” the government will allot an additional $157. That’s less than you get paid for a single office visit.
The difference between perfection and compliance is approximately $1,000. Failure to participate, however, knocks $6,750 off your bottom line. Clearly, that’s a substantial financial loss that would affect most practices. Obviously, the numbers change if you have higher – or lower – Medicare revenue, but it’s important to do the math.
Why? Physicians are spending a significant amount of money to comply with the program requirements. This includes substantial payments to registries – typically $200 to >$1,000 per year – to report the quality measures for the program; electronic health record (EHR) systems, many of which require additional funding for the “upgrade” to a MIPS-compatible system, are also a sizable investment.
These hard costs pale in comparison with the time spent on understanding the ever-changing requirements of the program and the process by which your practice will implement them. Take, for example, something as innocuous as the required “Support Electronic Referral Loops by Receiving and Incorporating Health Information.”
You first must understand the elements of the measure: What is a “referral loop?” When do we need to generate one? To whom shall it be sent? What needs to be included in “health information?” What is the electronic address to which we should route the information? How do we obtain that address? Then you must determine how your EHR system captures and reports it.
Only then comes the hard part: How are we going to implement this? That’s only one of more than a dozen required elements: six quality measures, two (to four) improvement activities, and four promoting interoperability requirements. Each one of these elements has a host of requirements, all listed on multipage specification sheets.
The government does not seem to be listening. John Cullen, MD, president of the American Academy of Family Physicians, testified at the Senate Finance Committee in May 2019 that MIPS “has created a burdensome and extremely complex program that has increased practice costs ... ” Yet, later that year, CMS issued another hefty ruling that outlines significant changes to the program, despite the fact that it’s in its fourth performance year.
Turning frustration into action
Frustration or even anger may be one reaction, but now is an opportune time to determine your investment in the program. At a minimum, it’s vital to understand and meet the threshold to avoid the penalty. It’s been shifting to date, but it’s now set at 9% for perpetuity.
First, it’s crucial to check on your participation status. CMS revealed that the participation database was recently corrected for so-called inconsistencies, so it pays to double-check. It only takes seconds: Insert your NPI in the QPP Participation Status Tool to determine your eligibility for 2020.
In 2020, the threshold to avoid the penalty is 45 points. To get the 45 points, practices must participate in two improvement activities, which is not difficult as there are 118 options. That will garner 15 points. Then there are 45 points available from the quality category; you need at least 30 to reach the 45-point threshold for penalty avoidance.
Smart MIPS hacks that can help you
To obtain the additional 30 points, turn your attention to the quality category. There are 268 quality measures; choose at least six to measure. If you report directly from your EHR system, you’ll get a bonus point for each reported measure, plus one just for trying. (There are a few other opportunities for bonus points, such as improving your scores over last year.) Those bonus points give you a base with which to work, but getting to 45 will require effort to report successfully on at least a couple of the measures.
The quality category has a total of 100 points available, which are converted to 45 toward your composite score. Since you need 30 to reach that magical 45 (if 15 were attained from improvement activities), that means you must come up with 75 points in the quality category. Between the bonus points and measuring a handful of measures successfully through the year, you’ll achieve this threshold.
There are two other categories in the program: promoting interoperability (PI) and cost. The PI category mirrors the old “meaningful use” program; however, it has become increasingly difficult over the years. If you think that you can meet the required elements, you can pick up 25 more points toward your composite score.
Cost is a bit of an unknown, as the scoring is based on a retrospective review of your claims. You’ll likely pick up a few more points on this 15-point category, but there’s no method to determine performance until after the reporting period. Therefore, be cautious about relying on this category.
The best MIPS hack, however, is if you are a small practice. CMS – remarkably – defines a “small practice” as 15 or fewer eligible professionals. If you qualify under this paradigm, you have multiple options to ease compliance:
Apply for a “hardship exemption” simply on the basis of being small; the exemption relates to the promoting operability category, shifting those points to the quality category.
Gain three points per quality measure, regardless of data completeness; this compares to just one point for other physicians.
Capture all of the points available from the Improvement Activities category by confirming participation with just a single activity. (This also applies to all physicians in rural or Health Professional Shortage Areas.)
In the event that you don’t qualify as a “small practice” or you’re still falling short of the requirements, CMS allows for the ultimate “out”: You can apply for exemption on the basis of an “extreme and uncontrollable circumstance.” The applications for these exceptions open this summer.
Unless you qualify for the program exemption, it’s important to keep pace with the program to ensure that you reach the 45-point threshold. It may not, however, be worthwhile to gear up for all 100 points unless your estimate of the potential return – and what it costs you to get there – reveals otherwise. MIPS is not going anywhere; the program is written into the law.
But that doesn’t mean that CMS can’t make tweaks and updates. Hopefully, the revisions won’t create even more administrative burden as the program is quickly turning into a big stick with only a small carrot at the end.
Elizabeth Woodcock is president of Woodcock & Associates in Atlanta. She has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
If you’ve knocked yourself out to earn a Merit-Based Incentive Payment System (MIPS) bonus payment, it’s pretty safe to say that getting a 1.68% payment boost probably didn’t feel like a “win” that was worth the effort.
And although it saved you from having a negative 5% payment adjustment, many physicians don’t feel that it was worth the effort.
On Jan. 6, the Centers for Medicare & Medicaid Services announced the 2020 payouts for MIPS.
Based on 2018 participation, the bonus for those who scored a perfect 100 is only a 1.68% boost in Medicare reimbursement, slightly lower than last year’s 1.88%. This decline comes as no surprise as the agency leader admits: “As the program matures, we expect that the increases in the performance thresholds in future program years will create a smaller distribution of positive payment adjustments.” Overall, more than 97% of participants avoided having a negative 5% payment adjustment.
Indeed, these bonus monies are based on a short-term appropriation of extra funds from Congress. After these temporary funds are no longer available, there will be little, if any, monies to distribute as the program is based on a “losers-feed-the-winners” construct.
It may be very tempting for many physicians to decide to ignore MIPS, with the rationale that 1.68% is not worth the effort. But don’t let your foot off the gas pedal yet, since the penalty for not participating in 2020 is a substantial 9%.
However, it is certainly time to reconsider efforts to participate at the highest level.
Should you or shouldn’t you bother with MIPS?
Let’s say you have $75,000 in revenue from Medicare Part B per year. Depending on the services you offer in your practice, that equates to 500-750 encounters with Medicare beneficiaries per year. (A reminder that MIPS affects only Part B; Medicare Advantage plans do not partake in the program.)
The recent announcement reveals that perfection would equate to an additional $1,260 per year. That’s only if you received the full 100 points; if you were simply an “exceptional performer,” the government will allot an additional $157. That’s less than you get paid for a single office visit.
The difference between perfection and compliance is approximately $1,000. Failure to participate, however, knocks $6,750 off your bottom line. Clearly, that’s a substantial financial loss that would affect most practices. Obviously, the numbers change if you have higher – or lower – Medicare revenue, but it’s important to do the math.
Why? Physicians are spending a significant amount of money to comply with the program requirements. This includes substantial payments to registries – typically $200 to >$1,000 per year – to report the quality measures for the program; electronic health record (EHR) systems, many of which require additional funding for the “upgrade” to a MIPS-compatible system, are also a sizable investment.
These hard costs pale in comparison with the time spent on understanding the ever-changing requirements of the program and the process by which your practice will implement them. Take, for example, something as innocuous as the required “Support Electronic Referral Loops by Receiving and Incorporating Health Information.”
You first must understand the elements of the measure: What is a “referral loop?” When do we need to generate one? To whom shall it be sent? What needs to be included in “health information?” What is the electronic address to which we should route the information? How do we obtain that address? Then you must determine how your EHR system captures and reports it.
Only then comes the hard part: How are we going to implement this? That’s only one of more than a dozen required elements: six quality measures, two (to four) improvement activities, and four promoting interoperability requirements. Each one of these elements has a host of requirements, all listed on multipage specification sheets.
The government does not seem to be listening. John Cullen, MD, president of the American Academy of Family Physicians, testified at the Senate Finance Committee in May 2019 that MIPS “has created a burdensome and extremely complex program that has increased practice costs ... ” Yet, later that year, CMS issued another hefty ruling that outlines significant changes to the program, despite the fact that it’s in its fourth performance year.
Turning frustration into action
Frustration or even anger may be one reaction, but now is an opportune time to determine your investment in the program. At a minimum, it’s vital to understand and meet the threshold to avoid the penalty. It’s been shifting to date, but it’s now set at 9% for perpetuity.
First, it’s crucial to check on your participation status. CMS revealed that the participation database was recently corrected for so-called inconsistencies, so it pays to double-check. It only takes seconds: Insert your NPI in the QPP Participation Status Tool to determine your eligibility for 2020.
In 2020, the threshold to avoid the penalty is 45 points. To get the 45 points, practices must participate in two improvement activities, which is not difficult as there are 118 options. That will garner 15 points. Then there are 45 points available from the quality category; you need at least 30 to reach the 45-point threshold for penalty avoidance.
Smart MIPS hacks that can help you
To obtain the additional 30 points, turn your attention to the quality category. There are 268 quality measures; choose at least six to measure. If you report directly from your EHR system, you’ll get a bonus point for each reported measure, plus one just for trying. (There are a few other opportunities for bonus points, such as improving your scores over last year.) Those bonus points give you a base with which to work, but getting to 45 will require effort to report successfully on at least a couple of the measures.
The quality category has a total of 100 points available, which are converted to 45 toward your composite score. Since you need 30 to reach that magical 45 (if 15 were attained from improvement activities), that means you must come up with 75 points in the quality category. Between the bonus points and measuring a handful of measures successfully through the year, you’ll achieve this threshold.
There are two other categories in the program: promoting interoperability (PI) and cost. The PI category mirrors the old “meaningful use” program; however, it has become increasingly difficult over the years. If you think that you can meet the required elements, you can pick up 25 more points toward your composite score.
Cost is a bit of an unknown, as the scoring is based on a retrospective review of your claims. You’ll likely pick up a few more points on this 15-point category, but there’s no method to determine performance until after the reporting period. Therefore, be cautious about relying on this category.
The best MIPS hack, however, is if you are a small practice. CMS – remarkably – defines a “small practice” as 15 or fewer eligible professionals. If you qualify under this paradigm, you have multiple options to ease compliance:
Apply for a “hardship exemption” simply on the basis of being small; the exemption relates to the promoting operability category, shifting those points to the quality category.
Gain three points per quality measure, regardless of data completeness; this compares to just one point for other physicians.
Capture all of the points available from the Improvement Activities category by confirming participation with just a single activity. (This also applies to all physicians in rural or Health Professional Shortage Areas.)
In the event that you don’t qualify as a “small practice” or you’re still falling short of the requirements, CMS allows for the ultimate “out”: You can apply for exemption on the basis of an “extreme and uncontrollable circumstance.” The applications for these exceptions open this summer.
Unless you qualify for the program exemption, it’s important to keep pace with the program to ensure that you reach the 45-point threshold. It may not, however, be worthwhile to gear up for all 100 points unless your estimate of the potential return – and what it costs you to get there – reveals otherwise. MIPS is not going anywhere; the program is written into the law.
But that doesn’t mean that CMS can’t make tweaks and updates. Hopefully, the revisions won’t create even more administrative burden as the program is quickly turning into a big stick with only a small carrot at the end.
Elizabeth Woodcock is president of Woodcock & Associates in Atlanta. She has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
If you’ve knocked yourself out to earn a Merit-Based Incentive Payment System (MIPS) bonus payment, it’s pretty safe to say that getting a 1.68% payment boost probably didn’t feel like a “win” that was worth the effort.
And although it saved you from having a negative 5% payment adjustment, many physicians don’t feel that it was worth the effort.
On Jan. 6, the Centers for Medicare & Medicaid Services announced the 2020 payouts for MIPS.
Based on 2018 participation, the bonus for those who scored a perfect 100 is only a 1.68% boost in Medicare reimbursement, slightly lower than last year’s 1.88%. This decline comes as no surprise as the agency leader admits: “As the program matures, we expect that the increases in the performance thresholds in future program years will create a smaller distribution of positive payment adjustments.” Overall, more than 97% of participants avoided having a negative 5% payment adjustment.
Indeed, these bonus monies are based on a short-term appropriation of extra funds from Congress. After these temporary funds are no longer available, there will be little, if any, monies to distribute as the program is based on a “losers-feed-the-winners” construct.
It may be very tempting for many physicians to decide to ignore MIPS, with the rationale that 1.68% is not worth the effort. But don’t let your foot off the gas pedal yet, since the penalty for not participating in 2020 is a substantial 9%.
However, it is certainly time to reconsider efforts to participate at the highest level.
Should you or shouldn’t you bother with MIPS?
Let’s say you have $75,000 in revenue from Medicare Part B per year. Depending on the services you offer in your practice, that equates to 500-750 encounters with Medicare beneficiaries per year. (A reminder that MIPS affects only Part B; Medicare Advantage plans do not partake in the program.)
The recent announcement reveals that perfection would equate to an additional $1,260 per year. That’s only if you received the full 100 points; if you were simply an “exceptional performer,” the government will allot an additional $157. That’s less than you get paid for a single office visit.
The difference between perfection and compliance is approximately $1,000. Failure to participate, however, knocks $6,750 off your bottom line. Clearly, that’s a substantial financial loss that would affect most practices. Obviously, the numbers change if you have higher – or lower – Medicare revenue, but it’s important to do the math.
Why? Physicians are spending a significant amount of money to comply with the program requirements. This includes substantial payments to registries – typically $200 to >$1,000 per year – to report the quality measures for the program; electronic health record (EHR) systems, many of which require additional funding for the “upgrade” to a MIPS-compatible system, are also a sizable investment.
These hard costs pale in comparison with the time spent on understanding the ever-changing requirements of the program and the process by which your practice will implement them. Take, for example, something as innocuous as the required “Support Electronic Referral Loops by Receiving and Incorporating Health Information.”
You first must understand the elements of the measure: What is a “referral loop?” When do we need to generate one? To whom shall it be sent? What needs to be included in “health information?” What is the electronic address to which we should route the information? How do we obtain that address? Then you must determine how your EHR system captures and reports it.
Only then comes the hard part: How are we going to implement this? That’s only one of more than a dozen required elements: six quality measures, two (to four) improvement activities, and four promoting interoperability requirements. Each one of these elements has a host of requirements, all listed on multipage specification sheets.
The government does not seem to be listening. John Cullen, MD, president of the American Academy of Family Physicians, testified at the Senate Finance Committee in May 2019 that MIPS “has created a burdensome and extremely complex program that has increased practice costs ... ” Yet, later that year, CMS issued another hefty ruling that outlines significant changes to the program, despite the fact that it’s in its fourth performance year.
Turning frustration into action
Frustration or even anger may be one reaction, but now is an opportune time to determine your investment in the program. At a minimum, it’s vital to understand and meet the threshold to avoid the penalty. It’s been shifting to date, but it’s now set at 9% for perpetuity.
First, it’s crucial to check on your participation status. CMS revealed that the participation database was recently corrected for so-called inconsistencies, so it pays to double-check. It only takes seconds: Insert your NPI in the QPP Participation Status Tool to determine your eligibility for 2020.
In 2020, the threshold to avoid the penalty is 45 points. To get the 45 points, practices must participate in two improvement activities, which is not difficult as there are 118 options. That will garner 15 points. Then there are 45 points available from the quality category; you need at least 30 to reach the 45-point threshold for penalty avoidance.
Smart MIPS hacks that can help you
To obtain the additional 30 points, turn your attention to the quality category. There are 268 quality measures; choose at least six to measure. If you report directly from your EHR system, you’ll get a bonus point for each reported measure, plus one just for trying. (There are a few other opportunities for bonus points, such as improving your scores over last year.) Those bonus points give you a base with which to work, but getting to 45 will require effort to report successfully on at least a couple of the measures.
The quality category has a total of 100 points available, which are converted to 45 toward your composite score. Since you need 30 to reach that magical 45 (if 15 were attained from improvement activities), that means you must come up with 75 points in the quality category. Between the bonus points and measuring a handful of measures successfully through the year, you’ll achieve this threshold.
There are two other categories in the program: promoting interoperability (PI) and cost. The PI category mirrors the old “meaningful use” program; however, it has become increasingly difficult over the years. If you think that you can meet the required elements, you can pick up 25 more points toward your composite score.
Cost is a bit of an unknown, as the scoring is based on a retrospective review of your claims. You’ll likely pick up a few more points on this 15-point category, but there’s no method to determine performance until after the reporting period. Therefore, be cautious about relying on this category.
The best MIPS hack, however, is if you are a small practice. CMS – remarkably – defines a “small practice” as 15 or fewer eligible professionals. If you qualify under this paradigm, you have multiple options to ease compliance:
Apply for a “hardship exemption” simply on the basis of being small; the exemption relates to the promoting operability category, shifting those points to the quality category.
Gain three points per quality measure, regardless of data completeness; this compares to just one point for other physicians.
Capture all of the points available from the Improvement Activities category by confirming participation with just a single activity. (This also applies to all physicians in rural or Health Professional Shortage Areas.)
In the event that you don’t qualify as a “small practice” or you’re still falling short of the requirements, CMS allows for the ultimate “out”: You can apply for exemption on the basis of an “extreme and uncontrollable circumstance.” The applications for these exceptions open this summer.
Unless you qualify for the program exemption, it’s important to keep pace with the program to ensure that you reach the 45-point threshold. It may not, however, be worthwhile to gear up for all 100 points unless your estimate of the potential return – and what it costs you to get there – reveals otherwise. MIPS is not going anywhere; the program is written into the law.
But that doesn’t mean that CMS can’t make tweaks and updates. Hopefully, the revisions won’t create even more administrative burden as the program is quickly turning into a big stick with only a small carrot at the end.
Elizabeth Woodcock is president of Woodcock & Associates in Atlanta. She has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.










