User login
News and Views that Matter to Physicians
Reimbursement hurdles hinder Entresto use in HFrEF
ORLANDO – Use of sacubitril/valsartan to treat patients with heart failure with reduced ejection fraction (HFrEF) became a class I recommendation in both the U.S. and European heart failure guidelines in May 2016, but virtually all U.S. health insurers continue to regard the potent and effective sacubitril/valsartan formulation as a second-line treatment that needs special preauthorization before patients receive reimbursement for the prescription.
“What is really morally sad is that U.S. payers are requiring physicians to fill out extensive, patient-by-patient paperwork” to allow patients with HFrEF to receive health insurance coverage for sacubitril/valsartan (Entresto), Milton Packer, MD, said at the annual scientific meeting of the Heart Failure Society of America.
“It is very difficult to understand why third-party payers would intentionally try to slow adoption of this life-saving drug simply because it is considered expensive. It is much cheaper than many drugs they cover for patients with cancer that don’t work half as well,” said Dr. Packer, a cardiologist and heart failure specialist at Baylor University Medical Center in Dallas.
The “excessive paperwork” for insurers when starting patients on sacubitril/valsartan is a “new and unique phenomenon among the cardiovascular drugs I prescribe,” agreed Nancy K. Sweitzer, MD, PhD, professor and chief of cardiology at the University of Arizona in Tuscon. “This approach by insurers seems based on cost; they do not want to pay” for sacubitril/valsartan, and to successfully arrange for coverage patients need to exactly match the enrollment criteria used in the PARADIGM-HF (Prospective Comparison of ARNI [Angiotensin Receptor – Neprilysin Inhibitor] with ACEI [Angiotensin-Converting Enzyme Inhibitor] to Determine Impact on Global Mortality and Morbidity in Heart Failure Trial ), the pivotal study that supplied the evidence base for making sacubitril/valsartan a class I agent for treating HFrEF.
“I don’t put some HFrEF patients on sacubitil/valsartan just because they don’t meet the trial’s entry criteria,” Dr. Sweitzer said in an interview. “Insurers seem to scrutinize every single parameter to make sure patients match the PARADIGM-HF patients. Coverage is denied if their BNP [brain natriuretic peptide] level is too low.” Dr. Sweitzer added that in one instance she had to submit a second preauthorization to simply uptitrate the dosage of sacubitril/valsartan she wanted a patient to receive.
“Based on the data it seems like you could easily identify HFrEF patients who are good candidates for sacubitril/valsartan, but your hands are tied by payers because you can’t prescribe it until you’ve first tried something else, and even then you still need to deal with a lot of paperwork,” agreed Robert O. Bonow, MD, professor of medicine at Northwestern University in Chicago. “The paperwork burden is really cumbersome for physicians with busy practices; it impedes taking care of patients,” Dr. Bonow said in an interview.
Sales figures for sacubitril/valsartan that the drug’s manufacturer, Novartis, has reported since the agent received U.S. marketing approval a little over a year ago reflect these challenges in prescribing the compound to patients. During the first quarter of 2016, Novartis reported $17 million in worldwide sales of the agent, followed by $32 million in worldwide sales during the second quarter of 2016, through June 30. With a total of $49 million in sacubitril/valsartan sales during the first 6 months of 2016, it seems like Novartis may be challenged to meet its stated target of $200 million in total sales of the compound during 2016. In April, one commentator called the $17 million sales figure for first quarter 2016 “an astonishingly small amount for a drug that was widely expected to be a blockbuster.”
Dr. Packer has in the past been a consultant to Novartis and was one of the lead investigators for the PARADIGM-HF trial. He said that currently he has no financial relationship with Novartis but he does serve as a consultant to several other drug companies. Dr. Sweitzer has received research support from Novartis and was an investigator for PARADIGM-HF. Dr. Bonow has been a consultant to Gilead.
On Twitter @mitchelzoler
ORLANDO – Use of sacubitril/valsartan to treat patients with heart failure with reduced ejection fraction (HFrEF) became a class I recommendation in both the U.S. and European heart failure guidelines in May 2016, but virtually all U.S. health insurers continue to regard the potent and effective sacubitril/valsartan formulation as a second-line treatment that needs special preauthorization before patients receive reimbursement for the prescription.
“What is really morally sad is that U.S. payers are requiring physicians to fill out extensive, patient-by-patient paperwork” to allow patients with HFrEF to receive health insurance coverage for sacubitril/valsartan (Entresto), Milton Packer, MD, said at the annual scientific meeting of the Heart Failure Society of America.
“It is very difficult to understand why third-party payers would intentionally try to slow adoption of this life-saving drug simply because it is considered expensive. It is much cheaper than many drugs they cover for patients with cancer that don’t work half as well,” said Dr. Packer, a cardiologist and heart failure specialist at Baylor University Medical Center in Dallas.
The “excessive paperwork” for insurers when starting patients on sacubitril/valsartan is a “new and unique phenomenon among the cardiovascular drugs I prescribe,” agreed Nancy K. Sweitzer, MD, PhD, professor and chief of cardiology at the University of Arizona in Tuscon. “This approach by insurers seems based on cost; they do not want to pay” for sacubitril/valsartan, and to successfully arrange for coverage patients need to exactly match the enrollment criteria used in the PARADIGM-HF (Prospective Comparison of ARNI [Angiotensin Receptor – Neprilysin Inhibitor] with ACEI [Angiotensin-Converting Enzyme Inhibitor] to Determine Impact on Global Mortality and Morbidity in Heart Failure Trial ), the pivotal study that supplied the evidence base for making sacubitril/valsartan a class I agent for treating HFrEF.
“I don’t put some HFrEF patients on sacubitil/valsartan just because they don’t meet the trial’s entry criteria,” Dr. Sweitzer said in an interview. “Insurers seem to scrutinize every single parameter to make sure patients match the PARADIGM-HF patients. Coverage is denied if their BNP [brain natriuretic peptide] level is too low.” Dr. Sweitzer added that in one instance she had to submit a second preauthorization to simply uptitrate the dosage of sacubitril/valsartan she wanted a patient to receive.
“Based on the data it seems like you could easily identify HFrEF patients who are good candidates for sacubitril/valsartan, but your hands are tied by payers because you can’t prescribe it until you’ve first tried something else, and even then you still need to deal with a lot of paperwork,” agreed Robert O. Bonow, MD, professor of medicine at Northwestern University in Chicago. “The paperwork burden is really cumbersome for physicians with busy practices; it impedes taking care of patients,” Dr. Bonow said in an interview.
Sales figures for sacubitril/valsartan that the drug’s manufacturer, Novartis, has reported since the agent received U.S. marketing approval a little over a year ago reflect these challenges in prescribing the compound to patients. During the first quarter of 2016, Novartis reported $17 million in worldwide sales of the agent, followed by $32 million in worldwide sales during the second quarter of 2016, through June 30. With a total of $49 million in sacubitril/valsartan sales during the first 6 months of 2016, it seems like Novartis may be challenged to meet its stated target of $200 million in total sales of the compound during 2016. In April, one commentator called the $17 million sales figure for first quarter 2016 “an astonishingly small amount for a drug that was widely expected to be a blockbuster.”
Dr. Packer has in the past been a consultant to Novartis and was one of the lead investigators for the PARADIGM-HF trial. He said that currently he has no financial relationship with Novartis but he does serve as a consultant to several other drug companies. Dr. Sweitzer has received research support from Novartis and was an investigator for PARADIGM-HF. Dr. Bonow has been a consultant to Gilead.
On Twitter @mitchelzoler
ORLANDO – Use of sacubitril/valsartan to treat patients with heart failure with reduced ejection fraction (HFrEF) became a class I recommendation in both the U.S. and European heart failure guidelines in May 2016, but virtually all U.S. health insurers continue to regard the potent and effective sacubitril/valsartan formulation as a second-line treatment that needs special preauthorization before patients receive reimbursement for the prescription.
“What is really morally sad is that U.S. payers are requiring physicians to fill out extensive, patient-by-patient paperwork” to allow patients with HFrEF to receive health insurance coverage for sacubitril/valsartan (Entresto), Milton Packer, MD, said at the annual scientific meeting of the Heart Failure Society of America.
“It is very difficult to understand why third-party payers would intentionally try to slow adoption of this life-saving drug simply because it is considered expensive. It is much cheaper than many drugs they cover for patients with cancer that don’t work half as well,” said Dr. Packer, a cardiologist and heart failure specialist at Baylor University Medical Center in Dallas.
The “excessive paperwork” for insurers when starting patients on sacubitril/valsartan is a “new and unique phenomenon among the cardiovascular drugs I prescribe,” agreed Nancy K. Sweitzer, MD, PhD, professor and chief of cardiology at the University of Arizona in Tuscon. “This approach by insurers seems based on cost; they do not want to pay” for sacubitril/valsartan, and to successfully arrange for coverage patients need to exactly match the enrollment criteria used in the PARADIGM-HF (Prospective Comparison of ARNI [Angiotensin Receptor – Neprilysin Inhibitor] with ACEI [Angiotensin-Converting Enzyme Inhibitor] to Determine Impact on Global Mortality and Morbidity in Heart Failure Trial ), the pivotal study that supplied the evidence base for making sacubitril/valsartan a class I agent for treating HFrEF.
“I don’t put some HFrEF patients on sacubitil/valsartan just because they don’t meet the trial’s entry criteria,” Dr. Sweitzer said in an interview. “Insurers seem to scrutinize every single parameter to make sure patients match the PARADIGM-HF patients. Coverage is denied if their BNP [brain natriuretic peptide] level is too low.” Dr. Sweitzer added that in one instance she had to submit a second preauthorization to simply uptitrate the dosage of sacubitril/valsartan she wanted a patient to receive.
“Based on the data it seems like you could easily identify HFrEF patients who are good candidates for sacubitril/valsartan, but your hands are tied by payers because you can’t prescribe it until you’ve first tried something else, and even then you still need to deal with a lot of paperwork,” agreed Robert O. Bonow, MD, professor of medicine at Northwestern University in Chicago. “The paperwork burden is really cumbersome for physicians with busy practices; it impedes taking care of patients,” Dr. Bonow said in an interview.
Sales figures for sacubitril/valsartan that the drug’s manufacturer, Novartis, has reported since the agent received U.S. marketing approval a little over a year ago reflect these challenges in prescribing the compound to patients. During the first quarter of 2016, Novartis reported $17 million in worldwide sales of the agent, followed by $32 million in worldwide sales during the second quarter of 2016, through June 30. With a total of $49 million in sacubitril/valsartan sales during the first 6 months of 2016, it seems like Novartis may be challenged to meet its stated target of $200 million in total sales of the compound during 2016. In April, one commentator called the $17 million sales figure for first quarter 2016 “an astonishingly small amount for a drug that was widely expected to be a blockbuster.”
Dr. Packer has in the past been a consultant to Novartis and was one of the lead investigators for the PARADIGM-HF trial. He said that currently he has no financial relationship with Novartis but he does serve as a consultant to several other drug companies. Dr. Sweitzer has received research support from Novartis and was an investigator for PARADIGM-HF. Dr. Bonow has been a consultant to Gilead.
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM THE HFSA ANNUAL SCIENTIFIC MEETING
Planning, education smooth transition to longer-acting clotting factors
ORLANDO – Transitioning patients with hemophilia from standard clotting factor concentrates to newer extended half-life products takes planning, education, and a little patience, but the payoff can be better hemostasis, a hemophilia treatment specialist said.
“Real-world experience shows us that you can maintain effective protection with less infusion with these new products, but we also know that each person should be evaluated individually when determining what their specific optimal treatment is,” said Jennifer Maahs, a hemophilia nurse practitioner at the Indiana Hemophilia and Thrombosis Center in Indianapolis.
Staff and patient education about the proper use of newer extended half-life (EHL) products is the key to success, she added in an oral session at the World Federation of Hemophilia World Congress.
The new EHL products allow for longer intervals between doses, especially with EHL recombinant factor IX used to treat hemophilia B. Prophylaxis with standard factor IX concentrates requires doses of 25-40 IU/kg twice weekly; in contrasts, EHL products can be given in various doses based on patient responses of either 50 IU/kg every 7 days, 100 IU/kg every 10 days, 25-40 IU/kg every 7 days, or 50-75 IU/kg every 14 days.
In general, the longer intervals between dosing occur in adults; young children tend to require more frequent dosing and have lower levels of factor recovery, she noted.
Extended Experience
Her center currently has more than 100 patients maintained on prolonged half-life factor VIII and factor IX products.
“We have really learned a lot of lessons along the way, and we have had to modify our approach based on these lessons,” she said. “Each patient situation is unique, and everything needs to be individualized.”
Staff review the published literature to educate themselves on the EHL products and prepare answers to expected questions from patients. Ms. Maahs suggested identifying key staff who are best equipped to answer specific questions.
“From a patient standpoint, we’ve developed a patient notification letter, so for any new product that comes out – for example a new factor VIII product – the notification gets sent out factor VIII patients, and we do that for every new product that comes out,” she said.
PK OK
Pharmacokinetic (PK) analyses may also be helpful in transitioning patients to EHL products.
To test patient responses to new products, her center tests patients for recovery from 15 minutes to 1 hour post-infusion, which will provide information about how the patient may respond to the product during a bleeding episode.
If the patient is on prophylaxis they will evaluate trough effectiveness to determine that patient’s responsiveness at the lowest level prior to the next infusion. Testing at other time points may be required based on the patient’s individual clinical history.
Center staff talk with each patient to discuss his needs and capabilities. If the patient is currently being managed with on-demand therapy, the talk may center on obstacles to utilization of prophylaxis and the patient’s desired infusion interval.
For patients currently on prophylaxis, they discuss the current regimen frequency and dose and assess how well it’s working. Staff members also provide information about alternative approaches to therapy, and ask patients specifically about their activity levels and dates of activity, compared with currently scheduled infusion days.
Patients are also educated about the reconstitution requirements for the new product, and are told to use up any remaining concentrates before switching over to the new product.
“As we move forward, within 2 to 4 weeks of starting a new therapy, we like to obtain a trough to see how their prophylaxis is working. At that time we ask how have you been doing on the new product, are you having any breakthrough bleeding, and how are you feeling about it,” Ms. Maahs said.
Weekly phone calls to the patient during the first month are also very helpful for reinforcing information about dosing regimens for bleeding episodes, reminding patients to call in if they experience a lead, and encouraging them to keep a treatment log. The phone call can also be helpful in identifying potential product-related reactions or other issues, she said.
‘Big impact’
“What’s the impact that we’ve seen? With factor IX, it has been really big. Previous on-demand patients have agreed that, ‘gosh, I’m infusing a couple of times a month anyway,’ so starting an every 14-day prophylactic regimen seems pretty reasonable,” she said.
“We’ve had infusion schedules in children change from twice weekly to once weekly and that has really decreased the burden of disease,” she added.
A few adults, however, have gone back to standard half-life products because of concerns that they would not be able to infuse when they thought they needed treatment, she noted.
The impact of the EHL factor VIII products has been smaller, although it has allowed slight increases in the dosing intervals (from every other day to every third day in children, for example), and has overall decreased the average number of monthly infusions from about 15 to about 10.
Some adolescents and young adults, who often have been on prophylaxis for all of their lives, have experienced absent or only minimal joint disease, and some have been able to extend their dosing intervals from every 4 to every 5 to 7 days, she said.
Ms. Maahs disclosed serving on advisory committees to Baxalta, Novo Nordisk, Biogen, Genentech, and CSL, and receiving honoraria related to those activities.
ORLANDO – Transitioning patients with hemophilia from standard clotting factor concentrates to newer extended half-life products takes planning, education, and a little patience, but the payoff can be better hemostasis, a hemophilia treatment specialist said.
“Real-world experience shows us that you can maintain effective protection with less infusion with these new products, but we also know that each person should be evaluated individually when determining what their specific optimal treatment is,” said Jennifer Maahs, a hemophilia nurse practitioner at the Indiana Hemophilia and Thrombosis Center in Indianapolis.
Staff and patient education about the proper use of newer extended half-life (EHL) products is the key to success, she added in an oral session at the World Federation of Hemophilia World Congress.
The new EHL products allow for longer intervals between doses, especially with EHL recombinant factor IX used to treat hemophilia B. Prophylaxis with standard factor IX concentrates requires doses of 25-40 IU/kg twice weekly; in contrasts, EHL products can be given in various doses based on patient responses of either 50 IU/kg every 7 days, 100 IU/kg every 10 days, 25-40 IU/kg every 7 days, or 50-75 IU/kg every 14 days.
In general, the longer intervals between dosing occur in adults; young children tend to require more frequent dosing and have lower levels of factor recovery, she noted.
Extended Experience
Her center currently has more than 100 patients maintained on prolonged half-life factor VIII and factor IX products.
“We have really learned a lot of lessons along the way, and we have had to modify our approach based on these lessons,” she said. “Each patient situation is unique, and everything needs to be individualized.”
Staff review the published literature to educate themselves on the EHL products and prepare answers to expected questions from patients. Ms. Maahs suggested identifying key staff who are best equipped to answer specific questions.
“From a patient standpoint, we’ve developed a patient notification letter, so for any new product that comes out – for example a new factor VIII product – the notification gets sent out factor VIII patients, and we do that for every new product that comes out,” she said.
PK OK
Pharmacokinetic (PK) analyses may also be helpful in transitioning patients to EHL products.
To test patient responses to new products, her center tests patients for recovery from 15 minutes to 1 hour post-infusion, which will provide information about how the patient may respond to the product during a bleeding episode.
If the patient is on prophylaxis they will evaluate trough effectiveness to determine that patient’s responsiveness at the lowest level prior to the next infusion. Testing at other time points may be required based on the patient’s individual clinical history.
Center staff talk with each patient to discuss his needs and capabilities. If the patient is currently being managed with on-demand therapy, the talk may center on obstacles to utilization of prophylaxis and the patient’s desired infusion interval.
For patients currently on prophylaxis, they discuss the current regimen frequency and dose and assess how well it’s working. Staff members also provide information about alternative approaches to therapy, and ask patients specifically about their activity levels and dates of activity, compared with currently scheduled infusion days.
Patients are also educated about the reconstitution requirements for the new product, and are told to use up any remaining concentrates before switching over to the new product.
“As we move forward, within 2 to 4 weeks of starting a new therapy, we like to obtain a trough to see how their prophylaxis is working. At that time we ask how have you been doing on the new product, are you having any breakthrough bleeding, and how are you feeling about it,” Ms. Maahs said.
Weekly phone calls to the patient during the first month are also very helpful for reinforcing information about dosing regimens for bleeding episodes, reminding patients to call in if they experience a lead, and encouraging them to keep a treatment log. The phone call can also be helpful in identifying potential product-related reactions or other issues, she said.
‘Big impact’
“What’s the impact that we’ve seen? With factor IX, it has been really big. Previous on-demand patients have agreed that, ‘gosh, I’m infusing a couple of times a month anyway,’ so starting an every 14-day prophylactic regimen seems pretty reasonable,” she said.
“We’ve had infusion schedules in children change from twice weekly to once weekly and that has really decreased the burden of disease,” she added.
A few adults, however, have gone back to standard half-life products because of concerns that they would not be able to infuse when they thought they needed treatment, she noted.
The impact of the EHL factor VIII products has been smaller, although it has allowed slight increases in the dosing intervals (from every other day to every third day in children, for example), and has overall decreased the average number of monthly infusions from about 15 to about 10.
Some adolescents and young adults, who often have been on prophylaxis for all of their lives, have experienced absent or only minimal joint disease, and some have been able to extend their dosing intervals from every 4 to every 5 to 7 days, she said.
Ms. Maahs disclosed serving on advisory committees to Baxalta, Novo Nordisk, Biogen, Genentech, and CSL, and receiving honoraria related to those activities.
ORLANDO – Transitioning patients with hemophilia from standard clotting factor concentrates to newer extended half-life products takes planning, education, and a little patience, but the payoff can be better hemostasis, a hemophilia treatment specialist said.
“Real-world experience shows us that you can maintain effective protection with less infusion with these new products, but we also know that each person should be evaluated individually when determining what their specific optimal treatment is,” said Jennifer Maahs, a hemophilia nurse practitioner at the Indiana Hemophilia and Thrombosis Center in Indianapolis.
Staff and patient education about the proper use of newer extended half-life (EHL) products is the key to success, she added in an oral session at the World Federation of Hemophilia World Congress.
The new EHL products allow for longer intervals between doses, especially with EHL recombinant factor IX used to treat hemophilia B. Prophylaxis with standard factor IX concentrates requires doses of 25-40 IU/kg twice weekly; in contrasts, EHL products can be given in various doses based on patient responses of either 50 IU/kg every 7 days, 100 IU/kg every 10 days, 25-40 IU/kg every 7 days, or 50-75 IU/kg every 14 days.
In general, the longer intervals between dosing occur in adults; young children tend to require more frequent dosing and have lower levels of factor recovery, she noted.
Extended Experience
Her center currently has more than 100 patients maintained on prolonged half-life factor VIII and factor IX products.
“We have really learned a lot of lessons along the way, and we have had to modify our approach based on these lessons,” she said. “Each patient situation is unique, and everything needs to be individualized.”
Staff review the published literature to educate themselves on the EHL products and prepare answers to expected questions from patients. Ms. Maahs suggested identifying key staff who are best equipped to answer specific questions.
“From a patient standpoint, we’ve developed a patient notification letter, so for any new product that comes out – for example a new factor VIII product – the notification gets sent out factor VIII patients, and we do that for every new product that comes out,” she said.
PK OK
Pharmacokinetic (PK) analyses may also be helpful in transitioning patients to EHL products.
To test patient responses to new products, her center tests patients for recovery from 15 minutes to 1 hour post-infusion, which will provide information about how the patient may respond to the product during a bleeding episode.
If the patient is on prophylaxis they will evaluate trough effectiveness to determine that patient’s responsiveness at the lowest level prior to the next infusion. Testing at other time points may be required based on the patient’s individual clinical history.
Center staff talk with each patient to discuss his needs and capabilities. If the patient is currently being managed with on-demand therapy, the talk may center on obstacles to utilization of prophylaxis and the patient’s desired infusion interval.
For patients currently on prophylaxis, they discuss the current regimen frequency and dose and assess how well it’s working. Staff members also provide information about alternative approaches to therapy, and ask patients specifically about their activity levels and dates of activity, compared with currently scheduled infusion days.
Patients are also educated about the reconstitution requirements for the new product, and are told to use up any remaining concentrates before switching over to the new product.
“As we move forward, within 2 to 4 weeks of starting a new therapy, we like to obtain a trough to see how their prophylaxis is working. At that time we ask how have you been doing on the new product, are you having any breakthrough bleeding, and how are you feeling about it,” Ms. Maahs said.
Weekly phone calls to the patient during the first month are also very helpful for reinforcing information about dosing regimens for bleeding episodes, reminding patients to call in if they experience a lead, and encouraging them to keep a treatment log. The phone call can also be helpful in identifying potential product-related reactions or other issues, she said.
‘Big impact’
“What’s the impact that we’ve seen? With factor IX, it has been really big. Previous on-demand patients have agreed that, ‘gosh, I’m infusing a couple of times a month anyway,’ so starting an every 14-day prophylactic regimen seems pretty reasonable,” she said.
“We’ve had infusion schedules in children change from twice weekly to once weekly and that has really decreased the burden of disease,” she added.
A few adults, however, have gone back to standard half-life products because of concerns that they would not be able to infuse when they thought they needed treatment, she noted.
The impact of the EHL factor VIII products has been smaller, although it has allowed slight increases in the dosing intervals (from every other day to every third day in children, for example), and has overall decreased the average number of monthly infusions from about 15 to about 10.
Some adolescents and young adults, who often have been on prophylaxis for all of their lives, have experienced absent or only minimal joint disease, and some have been able to extend their dosing intervals from every 4 to every 5 to 7 days, she said.
Ms. Maahs disclosed serving on advisory committees to Baxalta, Novo Nordisk, Biogen, Genentech, and CSL, and receiving honoraria related to those activities.
EXPERT ANALYSIS AT WFH 2016 WORLD CONGRESS
Key clinical point: Transitioning patients to extended half-life clotting factor concentrates requires tailoring treatment to individual patients.
Major finding: Many patients can transition from on-demand dosing with factor IX to prophylaxis infusions once every 2 weeks.
Data source: Review of a hemophilia treatment center experience transitioning patients to extended half-life products.
Disclosures: Jennifer Maahs, RN-BC, disclosed serving on advisory committees to Baxalta, Novo Nordisk, Biogen, Genentech, and CSL, and receiving honoraria related to those activities.
Hospital managers identify barriers to antimicrobial stewardship
Antimicrobial stewardship programs are being introduced in hospitals internationally amidst the problem of escalating antimicrobial resistance. But sustained behavioral change in the area of antibiotic prescribing has been difficult to achieve.
While we have an understanding of doctors’ roles in antibiotic optimization within hospital contexts, the role of hospital management in successes or failures of antimicrobial stewardship programs (and optimization of antibiotics more broadly) has not been explored. Our new study published in the Journal of Hospital Infection examines this very question – the role of the manager as an enabler, or indeed a barrier, to antibiotic optimization.
Researchers in the study performed semistructured interviews with 23 hospital managers at three hospitals in two different states in Australia to specifically examine their opinions on antibiotic resistance, antibiotic governance, and their roles as senior management. The results illustrate how hospital managers prioritize financial pressures and immediate clinical demands over longer-term issues such as antibiotic prescribing and resistance. Here is an example of those pressures, described by one manager:
“I think the problem is [antimicrobial stewardship] in a competitive market. Are the waiting lists more newsworthy than antibiotic prescribing? Absolutely. You get more adverse events happening because of the waiting lists. … So, of course it’s not going to be the [antibiotic] prescribing that comes up to the top of that.” –Departmental Director
The study results also showed how managers find it challenging to comprehend, or act on the basis of, antibiotic-prescribing audits and had little faith in the value of data on antibiotic use and appropriateness. Other clinical areas with more clearly defined targets (and consequences for failing to meet targets) were prioritized over antibiotic prescribing in medical management decision making. Managers also found it difficult to influence the behavior of doctors and thought that it was a clinical responsibility to improve practice. In the words of one:
“I am a believer in delegated accountability and people on the shop floor knowing what they’re doing and being held accountable for it.” – Divisional Director
Managers perceived that there was limited accountability among doctors for antibiotic use and limited education and feedback to doctors:
“Those figures [on suboptimal prescribing] you give me, I haven’t heard them before. So, that in itself is a problem, and I would suggest you’d probably find a large number of medical staff haven’t been exposed to that.”
– Divisional Director
This study was performed in three hospitals with active antimicrobial stewardship programs. In Australia, as is becoming the pattern in countries within the Organisation for Economic Co-operation and Development (OECD), there is a legislative requirement for hospitals to have an effective antimicrobial stewardship program. And yet, meaningful sustained change in antibiotic prescribing is elusive, as evidenced by national antibiotic-prescribing data. The study results raise the important question of who is perceived as responsible for antibiotic-prescribing improvement and the actual and potential role of hospital managers in enacting change. It seems likely that both “top-down” influence (by managers and executive) and “bottom-up” influence (clinician-driven processes) will be required for effective and sustained practice change.
It is also clear from the results of this study that hospital managers do not perceive clear or immediate consequences for failing to improve antibiotic prescribing, and the perceived “distant” threat of antimicrobial resistance is not prioritized among other competing pressures. In addition, the widespread nature of antibiotic use makes it difficult to audit and even more difficult to communicate the extent of the problem.
These data would suggest that to move forward we need to look at an incentive structure for antibiotic-prescribing improvements or consequences in the short term for failing to optimize antibiotic use, and clearly defined goals for antibiotic optimization in hospitals.
Jennifer Broom, MBChB, PhD, is an infectious diseases physician at the Sunshine Coast Hospital and Health Service and an associate professor of medicine at the University of Queensland, Brisbane, Australia. Alex Broom, PhD, is professor of sociology in the School of Social Sciences at the University of New South Wales, Sydney.
Antimicrobial stewardship programs are being introduced in hospitals internationally amidst the problem of escalating antimicrobial resistance. But sustained behavioral change in the area of antibiotic prescribing has been difficult to achieve.
While we have an understanding of doctors’ roles in antibiotic optimization within hospital contexts, the role of hospital management in successes or failures of antimicrobial stewardship programs (and optimization of antibiotics more broadly) has not been explored. Our new study published in the Journal of Hospital Infection examines this very question – the role of the manager as an enabler, or indeed a barrier, to antibiotic optimization.
Researchers in the study performed semistructured interviews with 23 hospital managers at three hospitals in two different states in Australia to specifically examine their opinions on antibiotic resistance, antibiotic governance, and their roles as senior management. The results illustrate how hospital managers prioritize financial pressures and immediate clinical demands over longer-term issues such as antibiotic prescribing and resistance. Here is an example of those pressures, described by one manager:
“I think the problem is [antimicrobial stewardship] in a competitive market. Are the waiting lists more newsworthy than antibiotic prescribing? Absolutely. You get more adverse events happening because of the waiting lists. … So, of course it’s not going to be the [antibiotic] prescribing that comes up to the top of that.” –Departmental Director
The study results also showed how managers find it challenging to comprehend, or act on the basis of, antibiotic-prescribing audits and had little faith in the value of data on antibiotic use and appropriateness. Other clinical areas with more clearly defined targets (and consequences for failing to meet targets) were prioritized over antibiotic prescribing in medical management decision making. Managers also found it difficult to influence the behavior of doctors and thought that it was a clinical responsibility to improve practice. In the words of one:
“I am a believer in delegated accountability and people on the shop floor knowing what they’re doing and being held accountable for it.” – Divisional Director
Managers perceived that there was limited accountability among doctors for antibiotic use and limited education and feedback to doctors:
“Those figures [on suboptimal prescribing] you give me, I haven’t heard them before. So, that in itself is a problem, and I would suggest you’d probably find a large number of medical staff haven’t been exposed to that.”
– Divisional Director
This study was performed in three hospitals with active antimicrobial stewardship programs. In Australia, as is becoming the pattern in countries within the Organisation for Economic Co-operation and Development (OECD), there is a legislative requirement for hospitals to have an effective antimicrobial stewardship program. And yet, meaningful sustained change in antibiotic prescribing is elusive, as evidenced by national antibiotic-prescribing data. The study results raise the important question of who is perceived as responsible for antibiotic-prescribing improvement and the actual and potential role of hospital managers in enacting change. It seems likely that both “top-down” influence (by managers and executive) and “bottom-up” influence (clinician-driven processes) will be required for effective and sustained practice change.
It is also clear from the results of this study that hospital managers do not perceive clear or immediate consequences for failing to improve antibiotic prescribing, and the perceived “distant” threat of antimicrobial resistance is not prioritized among other competing pressures. In addition, the widespread nature of antibiotic use makes it difficult to audit and even more difficult to communicate the extent of the problem.
These data would suggest that to move forward we need to look at an incentive structure for antibiotic-prescribing improvements or consequences in the short term for failing to optimize antibiotic use, and clearly defined goals for antibiotic optimization in hospitals.
Jennifer Broom, MBChB, PhD, is an infectious diseases physician at the Sunshine Coast Hospital and Health Service and an associate professor of medicine at the University of Queensland, Brisbane, Australia. Alex Broom, PhD, is professor of sociology in the School of Social Sciences at the University of New South Wales, Sydney.
Antimicrobial stewardship programs are being introduced in hospitals internationally amidst the problem of escalating antimicrobial resistance. But sustained behavioral change in the area of antibiotic prescribing has been difficult to achieve.
While we have an understanding of doctors’ roles in antibiotic optimization within hospital contexts, the role of hospital management in successes or failures of antimicrobial stewardship programs (and optimization of antibiotics more broadly) has not been explored. Our new study published in the Journal of Hospital Infection examines this very question – the role of the manager as an enabler, or indeed a barrier, to antibiotic optimization.
Researchers in the study performed semistructured interviews with 23 hospital managers at three hospitals in two different states in Australia to specifically examine their opinions on antibiotic resistance, antibiotic governance, and their roles as senior management. The results illustrate how hospital managers prioritize financial pressures and immediate clinical demands over longer-term issues such as antibiotic prescribing and resistance. Here is an example of those pressures, described by one manager:
“I think the problem is [antimicrobial stewardship] in a competitive market. Are the waiting lists more newsworthy than antibiotic prescribing? Absolutely. You get more adverse events happening because of the waiting lists. … So, of course it’s not going to be the [antibiotic] prescribing that comes up to the top of that.” –Departmental Director
The study results also showed how managers find it challenging to comprehend, or act on the basis of, antibiotic-prescribing audits and had little faith in the value of data on antibiotic use and appropriateness. Other clinical areas with more clearly defined targets (and consequences for failing to meet targets) were prioritized over antibiotic prescribing in medical management decision making. Managers also found it difficult to influence the behavior of doctors and thought that it was a clinical responsibility to improve practice. In the words of one:
“I am a believer in delegated accountability and people on the shop floor knowing what they’re doing and being held accountable for it.” – Divisional Director
Managers perceived that there was limited accountability among doctors for antibiotic use and limited education and feedback to doctors:
“Those figures [on suboptimal prescribing] you give me, I haven’t heard them before. So, that in itself is a problem, and I would suggest you’d probably find a large number of medical staff haven’t been exposed to that.”
– Divisional Director
This study was performed in three hospitals with active antimicrobial stewardship programs. In Australia, as is becoming the pattern in countries within the Organisation for Economic Co-operation and Development (OECD), there is a legislative requirement for hospitals to have an effective antimicrobial stewardship program. And yet, meaningful sustained change in antibiotic prescribing is elusive, as evidenced by national antibiotic-prescribing data. The study results raise the important question of who is perceived as responsible for antibiotic-prescribing improvement and the actual and potential role of hospital managers in enacting change. It seems likely that both “top-down” influence (by managers and executive) and “bottom-up” influence (clinician-driven processes) will be required for effective and sustained practice change.
It is also clear from the results of this study that hospital managers do not perceive clear or immediate consequences for failing to improve antibiotic prescribing, and the perceived “distant” threat of antimicrobial resistance is not prioritized among other competing pressures. In addition, the widespread nature of antibiotic use makes it difficult to audit and even more difficult to communicate the extent of the problem.
These data would suggest that to move forward we need to look at an incentive structure for antibiotic-prescribing improvements or consequences in the short term for failing to optimize antibiotic use, and clearly defined goals for antibiotic optimization in hospitals.
Jennifer Broom, MBChB, PhD, is an infectious diseases physician at the Sunshine Coast Hospital and Health Service and an associate professor of medicine at the University of Queensland, Brisbane, Australia. Alex Broom, PhD, is professor of sociology in the School of Social Sciences at the University of New South Wales, Sydney.
CABG best for diabetes patients with CKD – or is it?
ROME – The use of coronary artery bypass graft surgery for revascularization in patients with multivessel CAD and comorbid diabetes plus chronic kidney disease was associated with a significantly lower risk of major cardiovascular and cerebrovascular events than was PCI with first-generation drug-eluting stents in a new secondary analysis from the landmark FREEDOM trial.
“The reason for this presentation is that even though chronic kidney disease is common in patients with diabetes, until now there has not been a large study of the efficacy and safety of coronary revascularization with drug-eluting stents versus CABG in this population in a randomized trial cohort,” explained Usman Baber, MD, who reported the results at the annual congress of the European Society of Cardiology.
FREEDOM (Future Revascularization Evaluation in Patients with Diabetes Mellitus: Optimal Management of Multivessel Disease) randomized 1,900 diabetic patients with multivessel CAD to PCI or CABG. As previously reported, CABG proved superior to PCI, with a significantly lower rate of the composite primary endpoint composed of all-cause mortality, MI, or stroke (N Engl J Med. 2012 Dec 20;367[25]:2375-84).
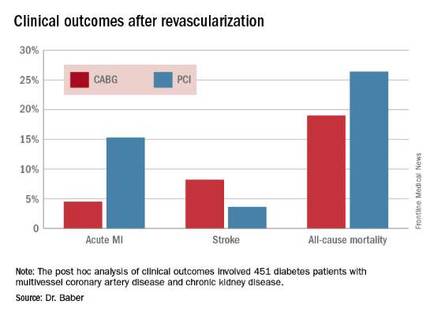
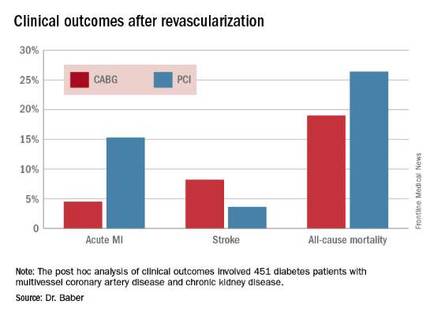
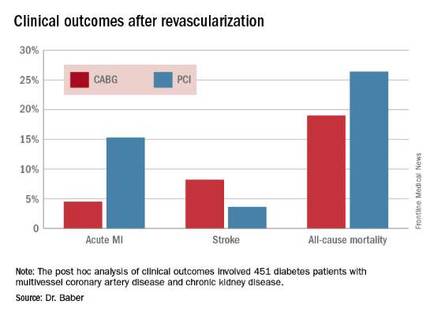
Dr. Baber presented a post hoc analysis of the 451 FREEDOM participants with baseline comorbid chronic kidney disease (CKD). Their mean SYNTAX score was 27, and their mean baseline estimated glomerular filtration rate was 44 mL/min per 1.73 m2, indicative of mild to moderate CKD.
“Only 28 patients in the FREEDOM trial had an estimated GFR below 30, therefore we can’t make any inferences about revascularization in that setting, which I think is a completely different population,” he noted.
The 5-year rate of major adverse cardiovascular and cerebrovascular events in patients with CKD was 26% in the CABG group, an absolute 9.4% less than the 35.6% rate in subjects randomized to PCI.
Roughly one-quarter of FREEDOM participants had CKD. They fared significantly worse than did those without CKD. The 5-year incidence of major adverse cardiovascular and cerebrovascular events was 30.8% in patients with CKD and 20.1% in patients without renal impairment. In a multivariate analysis adjusted for age, gender, hypertension, peripheral vascular disease, and other potential confounders, the risk of all-cause mortality was twofold higher in the CKD group. Their risk of cardiac death was increased 1.8-fold, and they were at 1.9-fold increased risk for stroke. Interestingly, however, the acute MI risk did not differ between patients with or without CKD, Dr. Baber observed.
Drilling deeper into the data, the cardiologist reported that CABG was associated with significantly lower rates of MI and a nonsignificant trend for fewer deaths, but with a significantly higher stroke rate than PCI.
One audience member rose to complain that this information won’t be helpful in counseling his diabetic patients with CKD and multivessel CAD because the choices look so grim: a higher risk of MI with percutaneous therapy, and a greater risk of stroke with surgery.
Dr. Baber replied by pointing out that the 10.8% absolute reduction in the risk of MI with CABG compared with PCI was more than twice as large as the absolute 4.6% increase in stroke risk with surgery.
“Most people would say that a heart attack is an inconvenience, and a stroke is a life-changing experience for them and their family,” said session cochair Kim A. Williams, MD, professor of medicine and chairman of cardiology at Rush University Medical Center in Chicago.
At that, Dr. Baber backtracked a bit, observing that since this was a post hoc analysis, the FREEDOM findings in patients with CKD must be viewed as hypothesis-generating rather than definitive. And, of course, contemporary second-generation drug-eluting stents have a better risk/benefit profile than do those used in FREEDOM.
“The number needed to treat/number needed to harm ratio for CABG and PCI probably ends up being roughly equal. The pertinence of an analysis like this is if you look at real-world registry-based data, you find a therapeutic nihilism that’s highly prevalent in CKD patients, where many patients who might benefit are not provided with revascularization therapy. It’s clear that we as clinicians – either because we don’t know there is a benefit or we are too concerned about potential harm – deprive patients of a treatment that might be beneficial. This analysis makes clinicians who might be concerned feel somewhat comforted that there is not unacceptable harm and that there is benefit,” Dr. Baber said.
Follow-up of FREEDOM participants continues and will be the subject of future reports, he added.
The FREEDOM trial was sponsored by the National Heart, Lung and Blood Institute. Dr. Baber reported having no financial conflicts of interest.
ROME – The use of coronary artery bypass graft surgery for revascularization in patients with multivessel CAD and comorbid diabetes plus chronic kidney disease was associated with a significantly lower risk of major cardiovascular and cerebrovascular events than was PCI with first-generation drug-eluting stents in a new secondary analysis from the landmark FREEDOM trial.
“The reason for this presentation is that even though chronic kidney disease is common in patients with diabetes, until now there has not been a large study of the efficacy and safety of coronary revascularization with drug-eluting stents versus CABG in this population in a randomized trial cohort,” explained Usman Baber, MD, who reported the results at the annual congress of the European Society of Cardiology.
FREEDOM (Future Revascularization Evaluation in Patients with Diabetes Mellitus: Optimal Management of Multivessel Disease) randomized 1,900 diabetic patients with multivessel CAD to PCI or CABG. As previously reported, CABG proved superior to PCI, with a significantly lower rate of the composite primary endpoint composed of all-cause mortality, MI, or stroke (N Engl J Med. 2012 Dec 20;367[25]:2375-84).
Dr. Baber presented a post hoc analysis of the 451 FREEDOM participants with baseline comorbid chronic kidney disease (CKD). Their mean SYNTAX score was 27, and their mean baseline estimated glomerular filtration rate was 44 mL/min per 1.73 m2, indicative of mild to moderate CKD.
“Only 28 patients in the FREEDOM trial had an estimated GFR below 30, therefore we can’t make any inferences about revascularization in that setting, which I think is a completely different population,” he noted.
The 5-year rate of major adverse cardiovascular and cerebrovascular events in patients with CKD was 26% in the CABG group, an absolute 9.4% less than the 35.6% rate in subjects randomized to PCI.
Roughly one-quarter of FREEDOM participants had CKD. They fared significantly worse than did those without CKD. The 5-year incidence of major adverse cardiovascular and cerebrovascular events was 30.8% in patients with CKD and 20.1% in patients without renal impairment. In a multivariate analysis adjusted for age, gender, hypertension, peripheral vascular disease, and other potential confounders, the risk of all-cause mortality was twofold higher in the CKD group. Their risk of cardiac death was increased 1.8-fold, and they were at 1.9-fold increased risk for stroke. Interestingly, however, the acute MI risk did not differ between patients with or without CKD, Dr. Baber observed.
Drilling deeper into the data, the cardiologist reported that CABG was associated with significantly lower rates of MI and a nonsignificant trend for fewer deaths, but with a significantly higher stroke rate than PCI.
One audience member rose to complain that this information won’t be helpful in counseling his diabetic patients with CKD and multivessel CAD because the choices look so grim: a higher risk of MI with percutaneous therapy, and a greater risk of stroke with surgery.
Dr. Baber replied by pointing out that the 10.8% absolute reduction in the risk of MI with CABG compared with PCI was more than twice as large as the absolute 4.6% increase in stroke risk with surgery.
“Most people would say that a heart attack is an inconvenience, and a stroke is a life-changing experience for them and their family,” said session cochair Kim A. Williams, MD, professor of medicine and chairman of cardiology at Rush University Medical Center in Chicago.
At that, Dr. Baber backtracked a bit, observing that since this was a post hoc analysis, the FREEDOM findings in patients with CKD must be viewed as hypothesis-generating rather than definitive. And, of course, contemporary second-generation drug-eluting stents have a better risk/benefit profile than do those used in FREEDOM.
“The number needed to treat/number needed to harm ratio for CABG and PCI probably ends up being roughly equal. The pertinence of an analysis like this is if you look at real-world registry-based data, you find a therapeutic nihilism that’s highly prevalent in CKD patients, where many patients who might benefit are not provided with revascularization therapy. It’s clear that we as clinicians – either because we don’t know there is a benefit or we are too concerned about potential harm – deprive patients of a treatment that might be beneficial. This analysis makes clinicians who might be concerned feel somewhat comforted that there is not unacceptable harm and that there is benefit,” Dr. Baber said.
Follow-up of FREEDOM participants continues and will be the subject of future reports, he added.
The FREEDOM trial was sponsored by the National Heart, Lung and Blood Institute. Dr. Baber reported having no financial conflicts of interest.
ROME – The use of coronary artery bypass graft surgery for revascularization in patients with multivessel CAD and comorbid diabetes plus chronic kidney disease was associated with a significantly lower risk of major cardiovascular and cerebrovascular events than was PCI with first-generation drug-eluting stents in a new secondary analysis from the landmark FREEDOM trial.
“The reason for this presentation is that even though chronic kidney disease is common in patients with diabetes, until now there has not been a large study of the efficacy and safety of coronary revascularization with drug-eluting stents versus CABG in this population in a randomized trial cohort,” explained Usman Baber, MD, who reported the results at the annual congress of the European Society of Cardiology.
FREEDOM (Future Revascularization Evaluation in Patients with Diabetes Mellitus: Optimal Management of Multivessel Disease) randomized 1,900 diabetic patients with multivessel CAD to PCI or CABG. As previously reported, CABG proved superior to PCI, with a significantly lower rate of the composite primary endpoint composed of all-cause mortality, MI, or stroke (N Engl J Med. 2012 Dec 20;367[25]:2375-84).
Dr. Baber presented a post hoc analysis of the 451 FREEDOM participants with baseline comorbid chronic kidney disease (CKD). Their mean SYNTAX score was 27, and their mean baseline estimated glomerular filtration rate was 44 mL/min per 1.73 m2, indicative of mild to moderate CKD.
“Only 28 patients in the FREEDOM trial had an estimated GFR below 30, therefore we can’t make any inferences about revascularization in that setting, which I think is a completely different population,” he noted.
The 5-year rate of major adverse cardiovascular and cerebrovascular events in patients with CKD was 26% in the CABG group, an absolute 9.4% less than the 35.6% rate in subjects randomized to PCI.
Roughly one-quarter of FREEDOM participants had CKD. They fared significantly worse than did those without CKD. The 5-year incidence of major adverse cardiovascular and cerebrovascular events was 30.8% in patients with CKD and 20.1% in patients without renal impairment. In a multivariate analysis adjusted for age, gender, hypertension, peripheral vascular disease, and other potential confounders, the risk of all-cause mortality was twofold higher in the CKD group. Their risk of cardiac death was increased 1.8-fold, and they were at 1.9-fold increased risk for stroke. Interestingly, however, the acute MI risk did not differ between patients with or without CKD, Dr. Baber observed.
Drilling deeper into the data, the cardiologist reported that CABG was associated with significantly lower rates of MI and a nonsignificant trend for fewer deaths, but with a significantly higher stroke rate than PCI.
One audience member rose to complain that this information won’t be helpful in counseling his diabetic patients with CKD and multivessel CAD because the choices look so grim: a higher risk of MI with percutaneous therapy, and a greater risk of stroke with surgery.
Dr. Baber replied by pointing out that the 10.8% absolute reduction in the risk of MI with CABG compared with PCI was more than twice as large as the absolute 4.6% increase in stroke risk with surgery.
“Most people would say that a heart attack is an inconvenience, and a stroke is a life-changing experience for them and their family,” said session cochair Kim A. Williams, MD, professor of medicine and chairman of cardiology at Rush University Medical Center in Chicago.
At that, Dr. Baber backtracked a bit, observing that since this was a post hoc analysis, the FREEDOM findings in patients with CKD must be viewed as hypothesis-generating rather than definitive. And, of course, contemporary second-generation drug-eluting stents have a better risk/benefit profile than do those used in FREEDOM.
“The number needed to treat/number needed to harm ratio for CABG and PCI probably ends up being roughly equal. The pertinence of an analysis like this is if you look at real-world registry-based data, you find a therapeutic nihilism that’s highly prevalent in CKD patients, where many patients who might benefit are not provided with revascularization therapy. It’s clear that we as clinicians – either because we don’t know there is a benefit or we are too concerned about potential harm – deprive patients of a treatment that might be beneficial. This analysis makes clinicians who might be concerned feel somewhat comforted that there is not unacceptable harm and that there is benefit,” Dr. Baber said.
Follow-up of FREEDOM participants continues and will be the subject of future reports, he added.
The FREEDOM trial was sponsored by the National Heart, Lung and Blood Institute. Dr. Baber reported having no financial conflicts of interest.
AT THE ESC CONGRESS 2016
Key clinical point: Coronary artery bypass graft surgery resulted in fewer myocardial infarctions but more strokes than did percutaneous coronary intervention at 5 years of follow-up in diabetic patients with multivessel coronary artery disease and chronic kidney disease.
Major finding: The cumulative MI rates in patients randomized to CABG versus PCI were 4.5% and 15.3%, respectively, while the stroke rates were 8.2% versus 3.6%.
Data source: A post hoc analysis of clinical outcomes in 451 diabetic patients with multivessel CAD and chronic kidney disease who were randomized to CABG or PCI in the prospective multicenter FREEDOM trial.
Disclosures: The FREEDOM trial was sponsored by the National Heart, Lung, and Blood Institute. The presenter reported having no financial conflicts of interest.
Aspirin not prescribed appropriately to cut cardiovascular risk in diabetes
MUNICH – Many patients with diabetes who could benefit from low-dose aspirin therapy may not be getting it – and many who are getting aspirin should not be, according to data presented at the annual meeting of the European Association for the Study of Diabetes.
A large, randomized trial concluded that 21% of diabetes patients who qualified for aspirin therapy for cardiovascular risk reduction were not getting it, and that it was contraindicated in almost 60% of those who were taking it, Lauren Crain, PhD, reported at the meeting.
Balancing the risks and benefits of aspirin therapy is not an easy challenge, said Dr. Crain, a health behavior researcher at HealthPartners Institute, Minneapolis. The clinical information necessary for the assessment is “rather lengthy, and not always readily available in primary care settings,” she said, and it’s clear from this study that clinicians could use some help in this area. Unfortunately, the electronic algorithm tested, which was meant to improve appropriate aspirin prescribing, didn’t improve the situation very much.
“At the final visit in the diabetes group [after the algorithm was employed], the total proportion of patients using aspirin was higher than at the first visit,” Dr. Crain noted. “However, that was the case regardless of whether patients were over- or underusing aspirin at the first visit.”
The aspirin findings were part of a large, randomized trial testing the algorithm as a way to reduce cardiovascular risk factors. The study was conducted in 19 primary care practices.
The decision-making algorithm, Cardiovascular Wizard, uses electronic health records to identify and advise patients with uncontrolled cardiovascular risk factors. Priorities and clinical recommendations are displayed for the provider and patient in the hope of facilitating shared decision making, Dr. Crain said.
One of the Wizard’s algorithms concerns aspirin prescribing. It is programmed with data from the United States Preventive Services Task Force, and recommends aspirin if cardiovascular risk scores are high and if consistent with providing a benefit greater than the risk of gastrointestinal bleeding. Aspirin is not recommended if the benefit is determined to be low or if major contraindications are present, including anticoagulant use or history of intracerebral hemorrhage.
The tool also alerts providers to the presence of other potential risks including aspirin allergy or intolerance, history of GI bleeds or risk conditions, and the concomitant use of nonsteroidal anti-inflammatory drugs.
The study comprised 11,000 adults, 4,000 of whom had diabetes. The remainder had high-risk, reversible cardiovascular risk factors (hypertension, dyslipidemia, or tobacco use). Each group was randomized to either cardiovascular risk assessment by usual care or with the Cardiovascular Wizard program.
The aspirin substudy looked at aspirin use at the baseline visit and the patient’s final, 1-year follow-up visit. At both visits, aspirin use was documented, and the clinician used the Wizard to assess whether or not it was indicated.
At the baseline visit, 71% of the diabetes group was using aspirin. However, according to the Wizard tool, more than one-third of them should not have been taking it – and among these, 57% were doing so. Among the remaining two-thirds of patients, all of whom should have been using aspirin, 21% were not taking it, Dr. Crain said.
Among the patients with reversible high-risk factors, 27% were using aspirin. However, according to the Wizard tool, the drug was contraindicated in 34% of those patients. “Most importantly, however, among those for whom aspirin was indicated, only 25% were using it – so, we’re talking about a 75% underusage,” Dr. Crain said.
By the 1-year follow-up visit, the situation was not much changed, despite the tool’s recommendations. Among those with diabetes, 56% in the usual care group and 60% in Wizard group were still overusing aspirin. Underuse was occurring in 21% of the usual care group and 17% of the Wizard group.
Patients with reversible high-risk factors fared a little better at 1 year, especially those who, at baseline, should have been taking aspirin but were not. Among these, 10% in the usual care group and 13% in the Wizard group had started taking aspirin.
The results were a bit of a disappointment, Dr. Crain said, but they don’t invalidate the investigators’ faith in an algorithmic advising system.
“We do think that electronic health record tools like this can help providers follow guidelines and improve the quality of their aspirin recommendations and prescribing, and hopefully reduce cardiovascular events and aspirin-related hazards,” she said. “Unfortunately, that didn’t happen here in the diabetes patients,” and the results in the second group were not stellar.
She added that the Wizard development team will be tweaking the tool to clarify some of the choices available as it guides patients and providers through the algorithm, in hopes of improving its efficacy.
Dr. Crain made no financial disclosures.
On Twitter @alz_gal
MUNICH – Many patients with diabetes who could benefit from low-dose aspirin therapy may not be getting it – and many who are getting aspirin should not be, according to data presented at the annual meeting of the European Association for the Study of Diabetes.
A large, randomized trial concluded that 21% of diabetes patients who qualified for aspirin therapy for cardiovascular risk reduction were not getting it, and that it was contraindicated in almost 60% of those who were taking it, Lauren Crain, PhD, reported at the meeting.
Balancing the risks and benefits of aspirin therapy is not an easy challenge, said Dr. Crain, a health behavior researcher at HealthPartners Institute, Minneapolis. The clinical information necessary for the assessment is “rather lengthy, and not always readily available in primary care settings,” she said, and it’s clear from this study that clinicians could use some help in this area. Unfortunately, the electronic algorithm tested, which was meant to improve appropriate aspirin prescribing, didn’t improve the situation very much.
“At the final visit in the diabetes group [after the algorithm was employed], the total proportion of patients using aspirin was higher than at the first visit,” Dr. Crain noted. “However, that was the case regardless of whether patients were over- or underusing aspirin at the first visit.”
The aspirin findings were part of a large, randomized trial testing the algorithm as a way to reduce cardiovascular risk factors. The study was conducted in 19 primary care practices.
The decision-making algorithm, Cardiovascular Wizard, uses electronic health records to identify and advise patients with uncontrolled cardiovascular risk factors. Priorities and clinical recommendations are displayed for the provider and patient in the hope of facilitating shared decision making, Dr. Crain said.
One of the Wizard’s algorithms concerns aspirin prescribing. It is programmed with data from the United States Preventive Services Task Force, and recommends aspirin if cardiovascular risk scores are high and if consistent with providing a benefit greater than the risk of gastrointestinal bleeding. Aspirin is not recommended if the benefit is determined to be low or if major contraindications are present, including anticoagulant use or history of intracerebral hemorrhage.
The tool also alerts providers to the presence of other potential risks including aspirin allergy or intolerance, history of GI bleeds or risk conditions, and the concomitant use of nonsteroidal anti-inflammatory drugs.
The study comprised 11,000 adults, 4,000 of whom had diabetes. The remainder had high-risk, reversible cardiovascular risk factors (hypertension, dyslipidemia, or tobacco use). Each group was randomized to either cardiovascular risk assessment by usual care or with the Cardiovascular Wizard program.
The aspirin substudy looked at aspirin use at the baseline visit and the patient’s final, 1-year follow-up visit. At both visits, aspirin use was documented, and the clinician used the Wizard to assess whether or not it was indicated.
At the baseline visit, 71% of the diabetes group was using aspirin. However, according to the Wizard tool, more than one-third of them should not have been taking it – and among these, 57% were doing so. Among the remaining two-thirds of patients, all of whom should have been using aspirin, 21% were not taking it, Dr. Crain said.
Among the patients with reversible high-risk factors, 27% were using aspirin. However, according to the Wizard tool, the drug was contraindicated in 34% of those patients. “Most importantly, however, among those for whom aspirin was indicated, only 25% were using it – so, we’re talking about a 75% underusage,” Dr. Crain said.
By the 1-year follow-up visit, the situation was not much changed, despite the tool’s recommendations. Among those with diabetes, 56% in the usual care group and 60% in Wizard group were still overusing aspirin. Underuse was occurring in 21% of the usual care group and 17% of the Wizard group.
Patients with reversible high-risk factors fared a little better at 1 year, especially those who, at baseline, should have been taking aspirin but were not. Among these, 10% in the usual care group and 13% in the Wizard group had started taking aspirin.
The results were a bit of a disappointment, Dr. Crain said, but they don’t invalidate the investigators’ faith in an algorithmic advising system.
“We do think that electronic health record tools like this can help providers follow guidelines and improve the quality of their aspirin recommendations and prescribing, and hopefully reduce cardiovascular events and aspirin-related hazards,” she said. “Unfortunately, that didn’t happen here in the diabetes patients,” and the results in the second group were not stellar.
She added that the Wizard development team will be tweaking the tool to clarify some of the choices available as it guides patients and providers through the algorithm, in hopes of improving its efficacy.
Dr. Crain made no financial disclosures.
On Twitter @alz_gal
MUNICH – Many patients with diabetes who could benefit from low-dose aspirin therapy may not be getting it – and many who are getting aspirin should not be, according to data presented at the annual meeting of the European Association for the Study of Diabetes.
A large, randomized trial concluded that 21% of diabetes patients who qualified for aspirin therapy for cardiovascular risk reduction were not getting it, and that it was contraindicated in almost 60% of those who were taking it, Lauren Crain, PhD, reported at the meeting.
Balancing the risks and benefits of aspirin therapy is not an easy challenge, said Dr. Crain, a health behavior researcher at HealthPartners Institute, Minneapolis. The clinical information necessary for the assessment is “rather lengthy, and not always readily available in primary care settings,” she said, and it’s clear from this study that clinicians could use some help in this area. Unfortunately, the electronic algorithm tested, which was meant to improve appropriate aspirin prescribing, didn’t improve the situation very much.
“At the final visit in the diabetes group [after the algorithm was employed], the total proportion of patients using aspirin was higher than at the first visit,” Dr. Crain noted. “However, that was the case regardless of whether patients were over- or underusing aspirin at the first visit.”
The aspirin findings were part of a large, randomized trial testing the algorithm as a way to reduce cardiovascular risk factors. The study was conducted in 19 primary care practices.
The decision-making algorithm, Cardiovascular Wizard, uses electronic health records to identify and advise patients with uncontrolled cardiovascular risk factors. Priorities and clinical recommendations are displayed for the provider and patient in the hope of facilitating shared decision making, Dr. Crain said.
One of the Wizard’s algorithms concerns aspirin prescribing. It is programmed with data from the United States Preventive Services Task Force, and recommends aspirin if cardiovascular risk scores are high and if consistent with providing a benefit greater than the risk of gastrointestinal bleeding. Aspirin is not recommended if the benefit is determined to be low or if major contraindications are present, including anticoagulant use or history of intracerebral hemorrhage.
The tool also alerts providers to the presence of other potential risks including aspirin allergy or intolerance, history of GI bleeds or risk conditions, and the concomitant use of nonsteroidal anti-inflammatory drugs.
The study comprised 11,000 adults, 4,000 of whom had diabetes. The remainder had high-risk, reversible cardiovascular risk factors (hypertension, dyslipidemia, or tobacco use). Each group was randomized to either cardiovascular risk assessment by usual care or with the Cardiovascular Wizard program.
The aspirin substudy looked at aspirin use at the baseline visit and the patient’s final, 1-year follow-up visit. At both visits, aspirin use was documented, and the clinician used the Wizard to assess whether or not it was indicated.
At the baseline visit, 71% of the diabetes group was using aspirin. However, according to the Wizard tool, more than one-third of them should not have been taking it – and among these, 57% were doing so. Among the remaining two-thirds of patients, all of whom should have been using aspirin, 21% were not taking it, Dr. Crain said.
Among the patients with reversible high-risk factors, 27% were using aspirin. However, according to the Wizard tool, the drug was contraindicated in 34% of those patients. “Most importantly, however, among those for whom aspirin was indicated, only 25% were using it – so, we’re talking about a 75% underusage,” Dr. Crain said.
By the 1-year follow-up visit, the situation was not much changed, despite the tool’s recommendations. Among those with diabetes, 56% in the usual care group and 60% in Wizard group were still overusing aspirin. Underuse was occurring in 21% of the usual care group and 17% of the Wizard group.
Patients with reversible high-risk factors fared a little better at 1 year, especially those who, at baseline, should have been taking aspirin but were not. Among these, 10% in the usual care group and 13% in the Wizard group had started taking aspirin.
The results were a bit of a disappointment, Dr. Crain said, but they don’t invalidate the investigators’ faith in an algorithmic advising system.
“We do think that electronic health record tools like this can help providers follow guidelines and improve the quality of their aspirin recommendations and prescribing, and hopefully reduce cardiovascular events and aspirin-related hazards,” she said. “Unfortunately, that didn’t happen here in the diabetes patients,” and the results in the second group were not stellar.
She added that the Wizard development team will be tweaking the tool to clarify some of the choices available as it guides patients and providers through the algorithm, in hopes of improving its efficacy.
Dr. Crain made no financial disclosures.
On Twitter @alz_gal
AT EASD 2016
Key clinical point: Many diabetes patients who should be taking aspirin for cardiovascular risk reduction are not doing so, and many who should not be taking it are.
Major finding: Aspirin was underused in 21% of diabetes patients and overused in 57% of patients.
Data source: A randomized study of 11,000 patients.
Disclosures: Dr. Lauren Crain had no financial disclosures.
Nearly half of patients readmitted after liver transplant
Nearly half of patients were readmitted to the hospital within 90 days of liver transplantation, according to a single-center retrospective study.
“As readmission portends decreased survival, an emphasis should be placed on identifying and optimizing those at increased risk. If readmission does occur, however, it presents an opportunity to intervene, as virtually no patients died during initial readmission,” Madhukar S. Patel, MD, and his associates at Massachusetts General Hospital, Boston, wrote online in HPB.
Long wait times for liver transplantation in this part of the country lead to “high patient acuity,” the researchers noted. To better understand the correlates and consequences of posttransplant readmissions, they reviewed the records for 325 adults who underwent liver transplantation at their hospital between 2005 and 2015. Patients averaged 56 years old and had awaited transplant for a mean of 1 year (standard deviation, 506 days). Their average MELD (Model for End-Stage Liver Disease) scores were 30.3 at transplant (SD, 5.8), and 16.9 (SD, 9.4) on postoperative day 5. Their average hospital length of stay was 12 days, the investigators reported (HPB. 2016 Sep 15. doi: 10.1016/j.hpb.2016.08.003). A total of 149 patients (46%) were readmitted within 90 days of discharge, most often for infections (28% of readmissions), followed by medication issues (19%) and biliary complications (11%). The strongest predictor of posttransplant readmission was hepatitis C virus (HCV) infection, which more than doubled the odds of readmission, compared with alcoholic liver disease (odds ratio, 2.37; 95% confidence interval, 1.44-3.91; P = .001). Transplantees with HCV might benefit from closer outpatient follow-up to detect worsening liver function, diagnostic algorithms to help prevent unnecessary readmissions, and associated nosocomial infections, and pre- and posttransplant direct-acting antiviral therapy, “although the impact [of direct-acting antiviral] therapy on readmissions] is unknown at this time,” the investigators said.
The multivariable analysis also linked readmissions to longer hospital stays (OR, 1.03; P = .04), while age and male sex were protective factors, the investigators said. “Although speculative, it is possible that these factors may be protective due to differences in social support structures upon discharge,” they wrote, noting that women are more likely than men to outlive their partners and thus to live alone in later life.
Readmission within 90 days was associated with a significantly lower rate of survival at 5 years (75% vs. 88% for patients who were not readmitted; P = .008). But only one patient died during the initial readmission, “suggesting that when readmission does occur, it may be an opportunity to intervene,” the researchers said. Strategies include earlier extubation and removal of indwelling catheters, decreasing levels of immunosuppression, lowering treatment thresholds, and shifting patients with laboratory abnormalities to the outpatient setting, they noted. “At our center a process has been initiated in which the inpatient transplant attending surgeon directly passes off discharged patients to the outpatient team,” the investigators wrote. “Additionally, for patients discharged to an acute rehabilitation facility, a specific transplant physician point of contact is provided to the team at the rehab center in case any questions or issues arise [after] discharge. Although these strategies are a reasonable starting point, follow-up studies remain necessary in order to evaluate the impact of these interventions in this patient cohort.”
The researchers reported no funding sources and had no relevant financial disclosures.
Nearly half of patients were readmitted to the hospital within 90 days of liver transplantation, according to a single-center retrospective study.
“As readmission portends decreased survival, an emphasis should be placed on identifying and optimizing those at increased risk. If readmission does occur, however, it presents an opportunity to intervene, as virtually no patients died during initial readmission,” Madhukar S. Patel, MD, and his associates at Massachusetts General Hospital, Boston, wrote online in HPB.
Long wait times for liver transplantation in this part of the country lead to “high patient acuity,” the researchers noted. To better understand the correlates and consequences of posttransplant readmissions, they reviewed the records for 325 adults who underwent liver transplantation at their hospital between 2005 and 2015. Patients averaged 56 years old and had awaited transplant for a mean of 1 year (standard deviation, 506 days). Their average MELD (Model for End-Stage Liver Disease) scores were 30.3 at transplant (SD, 5.8), and 16.9 (SD, 9.4) on postoperative day 5. Their average hospital length of stay was 12 days, the investigators reported (HPB. 2016 Sep 15. doi: 10.1016/j.hpb.2016.08.003). A total of 149 patients (46%) were readmitted within 90 days of discharge, most often for infections (28% of readmissions), followed by medication issues (19%) and biliary complications (11%). The strongest predictor of posttransplant readmission was hepatitis C virus (HCV) infection, which more than doubled the odds of readmission, compared with alcoholic liver disease (odds ratio, 2.37; 95% confidence interval, 1.44-3.91; P = .001). Transplantees with HCV might benefit from closer outpatient follow-up to detect worsening liver function, diagnostic algorithms to help prevent unnecessary readmissions, and associated nosocomial infections, and pre- and posttransplant direct-acting antiviral therapy, “although the impact [of direct-acting antiviral] therapy on readmissions] is unknown at this time,” the investigators said.
The multivariable analysis also linked readmissions to longer hospital stays (OR, 1.03; P = .04), while age and male sex were protective factors, the investigators said. “Although speculative, it is possible that these factors may be protective due to differences in social support structures upon discharge,” they wrote, noting that women are more likely than men to outlive their partners and thus to live alone in later life.
Readmission within 90 days was associated with a significantly lower rate of survival at 5 years (75% vs. 88% for patients who were not readmitted; P = .008). But only one patient died during the initial readmission, “suggesting that when readmission does occur, it may be an opportunity to intervene,” the researchers said. Strategies include earlier extubation and removal of indwelling catheters, decreasing levels of immunosuppression, lowering treatment thresholds, and shifting patients with laboratory abnormalities to the outpatient setting, they noted. “At our center a process has been initiated in which the inpatient transplant attending surgeon directly passes off discharged patients to the outpatient team,” the investigators wrote. “Additionally, for patients discharged to an acute rehabilitation facility, a specific transplant physician point of contact is provided to the team at the rehab center in case any questions or issues arise [after] discharge. Although these strategies are a reasonable starting point, follow-up studies remain necessary in order to evaluate the impact of these interventions in this patient cohort.”
The researchers reported no funding sources and had no relevant financial disclosures.
Nearly half of patients were readmitted to the hospital within 90 days of liver transplantation, according to a single-center retrospective study.
“As readmission portends decreased survival, an emphasis should be placed on identifying and optimizing those at increased risk. If readmission does occur, however, it presents an opportunity to intervene, as virtually no patients died during initial readmission,” Madhukar S. Patel, MD, and his associates at Massachusetts General Hospital, Boston, wrote online in HPB.
Long wait times for liver transplantation in this part of the country lead to “high patient acuity,” the researchers noted. To better understand the correlates and consequences of posttransplant readmissions, they reviewed the records for 325 adults who underwent liver transplantation at their hospital between 2005 and 2015. Patients averaged 56 years old and had awaited transplant for a mean of 1 year (standard deviation, 506 days). Their average MELD (Model for End-Stage Liver Disease) scores were 30.3 at transplant (SD, 5.8), and 16.9 (SD, 9.4) on postoperative day 5. Their average hospital length of stay was 12 days, the investigators reported (HPB. 2016 Sep 15. doi: 10.1016/j.hpb.2016.08.003). A total of 149 patients (46%) were readmitted within 90 days of discharge, most often for infections (28% of readmissions), followed by medication issues (19%) and biliary complications (11%). The strongest predictor of posttransplant readmission was hepatitis C virus (HCV) infection, which more than doubled the odds of readmission, compared with alcoholic liver disease (odds ratio, 2.37; 95% confidence interval, 1.44-3.91; P = .001). Transplantees with HCV might benefit from closer outpatient follow-up to detect worsening liver function, diagnostic algorithms to help prevent unnecessary readmissions, and associated nosocomial infections, and pre- and posttransplant direct-acting antiviral therapy, “although the impact [of direct-acting antiviral] therapy on readmissions] is unknown at this time,” the investigators said.
The multivariable analysis also linked readmissions to longer hospital stays (OR, 1.03; P = .04), while age and male sex were protective factors, the investigators said. “Although speculative, it is possible that these factors may be protective due to differences in social support structures upon discharge,” they wrote, noting that women are more likely than men to outlive their partners and thus to live alone in later life.
Readmission within 90 days was associated with a significantly lower rate of survival at 5 years (75% vs. 88% for patients who were not readmitted; P = .008). But only one patient died during the initial readmission, “suggesting that when readmission does occur, it may be an opportunity to intervene,” the researchers said. Strategies include earlier extubation and removal of indwelling catheters, decreasing levels of immunosuppression, lowering treatment thresholds, and shifting patients with laboratory abnormalities to the outpatient setting, they noted. “At our center a process has been initiated in which the inpatient transplant attending surgeon directly passes off discharged patients to the outpatient team,” the investigators wrote. “Additionally, for patients discharged to an acute rehabilitation facility, a specific transplant physician point of contact is provided to the team at the rehab center in case any questions or issues arise [after] discharge. Although these strategies are a reasonable starting point, follow-up studies remain necessary in order to evaluate the impact of these interventions in this patient cohort.”
The researchers reported no funding sources and had no relevant financial disclosures.
FROM HPB
Key clinical point: Nearly half of liver recipients at Massachusetts General Hospital were readmitted within 90 days.
Major finding: A total of 46% of patients were readmitted, with hepatitis C virus infection being the strongest predictor of readmission (odds ratio, 2.37, compared with alcoholic liver disease).
Data source: A single-center retrospective study of 325 liver transplant patients between 2005 and 2015.
Disclosures: The researchers reported no funding sources and had no relevant financial disclosures.
Benefits of early endovascular thrombectomy outlined in five trials
For patients with large-vessel ischemic stroke, endovascular thrombectomy produces better functional outcomes at 90 days than does optimal medical therapy, as long as the procedure is started within 7.3 hours of symptom onset, according to a report published online Sept. 27 in JAMA.
The benefit of thrombectomy was greatest when the procedure was begun under 2 hours from symptom onset, and it became nonsignificant after 7 hours and 18 minutes elapsed. This emphasizes “the importance of programs to enhance patient awareness, out-of-hospital care, and in-hospital management to shorten symptom onset-to-treatment times,” wrote Jeffrey L. Saver, MD, of the University of California, Los Angeles, and his associates.
Five major randomized trials have demonstrated the benefit of second-generation endovascular recanalization therapies over medical therapy in this patient population, but uncertainties persist regarding the timing of the intervention. For example, practice guidelines in the United States recommend thrombectomy until 6 hours after symptom onset, but the Food and Drug Administration allows thrombectomy devices to be used up to 8 hours after symptom onset and Canadian guidelines recommend the procedure for selected patients up to 12 hours after symptom onset.
The investigators for the five trials formed the Highly Effective Reperfusion Evaluated in Multiple Endovascular Stroke Trials (HERMES) collaboration to pool their individual patient data and perform a meta-analysis to clarify the issue of timing. They assessed patients’ functional independence at 90 days using the modified Rankin Score (mRS). The study participants included 634 patients who had been randomly assigned to endovascular thrombectomy and 653 randomly assigned to medical therapy.
The intervention correlated with a substantially lower degree of patient disability at 90 days than did medical therapy: the mean mRS was 2.9 in the thrombectomy group and 3.6 in the medical therapy group. In addition, increasing delays in treatment were associated with higher levels of residual disability in the thrombectomy group but not in the medical therapy group, the investigators reported.
“Based on the current study, and assuming the findings are generalizable to the population of patients with acute ischemic stroke due to large-vessel occlusion, among every 1,000 patients achieving substantial endovascular reperfusion, for every 15-minute faster ED door-to-reperfusion time, an estimated 39 patients would have a less-disabled outcome at 3 months, including 25 more who would achieve functional independence (mRS 0-2),” Dr. Saver and his associates wrote (JAMA. 2016;316[12]:1279-88).
These findings reinforce current recommendations to attempt endovascular thrombectomy when the procedure can be initiated within 6 hours of symptom onset, and they also “provide evidence that potentially supports strengthening of the recommendation for treatment from 6 through 7.3 hours after symptom onset,” they added.
No specific sponsor of this study was cited. Dr. Saver reported ties to Medtronic, Stryker, Cognition Medical, Covidien, Neuravi, BrainsGate, Pfizer, Bristol-Myers Squibb, Boehringer Ingelheim, ZZ Biotech, St. Jude Medical, and Genentech. His associates reported ties to numerous industry sources.
Earlier thrombectomy has such a profound effect on stroke patients’ outcomes that substantial changes in the current medical system are warranted to shorten these times even further. In this study, median time from symptom onset to randomization was approximately 3 hours, median time to arterial puncture was approximately 4 hours, and median time to reperfusion was nearly 5 hours.
Reducing the number of patients who are transferred from community hospitals to facilities with stroke centers would shorten door-to-reperfusion time a great deal. It is estimated that direct transport to stroke centers would allow endovascular thrombectomy for an additional 13% of stroke patients. Telemedicine, mobile stroke units, and out-of-hospital administration of tissue plasminogen activator are other possibilities that should be investigated.
Steven Warach, MD, PhD, and S. Claiborne Johnston, MD, PhD, are with the University of Texas at Austin. They reported having no relevant financial disclosures. Dr. Warach and Dr. Johnston made these remarks in an editorial (JAMA. 2016;316[12]:1265-6) accompanying Dr. Saver’s report.
Earlier thrombectomy has such a profound effect on stroke patients’ outcomes that substantial changes in the current medical system are warranted to shorten these times even further. In this study, median time from symptom onset to randomization was approximately 3 hours, median time to arterial puncture was approximately 4 hours, and median time to reperfusion was nearly 5 hours.
Reducing the number of patients who are transferred from community hospitals to facilities with stroke centers would shorten door-to-reperfusion time a great deal. It is estimated that direct transport to stroke centers would allow endovascular thrombectomy for an additional 13% of stroke patients. Telemedicine, mobile stroke units, and out-of-hospital administration of tissue plasminogen activator are other possibilities that should be investigated.
Steven Warach, MD, PhD, and S. Claiborne Johnston, MD, PhD, are with the University of Texas at Austin. They reported having no relevant financial disclosures. Dr. Warach and Dr. Johnston made these remarks in an editorial (JAMA. 2016;316[12]:1265-6) accompanying Dr. Saver’s report.
Earlier thrombectomy has such a profound effect on stroke patients’ outcomes that substantial changes in the current medical system are warranted to shorten these times even further. In this study, median time from symptom onset to randomization was approximately 3 hours, median time to arterial puncture was approximately 4 hours, and median time to reperfusion was nearly 5 hours.
Reducing the number of patients who are transferred from community hospitals to facilities with stroke centers would shorten door-to-reperfusion time a great deal. It is estimated that direct transport to stroke centers would allow endovascular thrombectomy for an additional 13% of stroke patients. Telemedicine, mobile stroke units, and out-of-hospital administration of tissue plasminogen activator are other possibilities that should be investigated.
Steven Warach, MD, PhD, and S. Claiborne Johnston, MD, PhD, are with the University of Texas at Austin. They reported having no relevant financial disclosures. Dr. Warach and Dr. Johnston made these remarks in an editorial (JAMA. 2016;316[12]:1265-6) accompanying Dr. Saver’s report.
For patients with large-vessel ischemic stroke, endovascular thrombectomy produces better functional outcomes at 90 days than does optimal medical therapy, as long as the procedure is started within 7.3 hours of symptom onset, according to a report published online Sept. 27 in JAMA.
The benefit of thrombectomy was greatest when the procedure was begun under 2 hours from symptom onset, and it became nonsignificant after 7 hours and 18 minutes elapsed. This emphasizes “the importance of programs to enhance patient awareness, out-of-hospital care, and in-hospital management to shorten symptom onset-to-treatment times,” wrote Jeffrey L. Saver, MD, of the University of California, Los Angeles, and his associates.
Five major randomized trials have demonstrated the benefit of second-generation endovascular recanalization therapies over medical therapy in this patient population, but uncertainties persist regarding the timing of the intervention. For example, practice guidelines in the United States recommend thrombectomy until 6 hours after symptom onset, but the Food and Drug Administration allows thrombectomy devices to be used up to 8 hours after symptom onset and Canadian guidelines recommend the procedure for selected patients up to 12 hours after symptom onset.
The investigators for the five trials formed the Highly Effective Reperfusion Evaluated in Multiple Endovascular Stroke Trials (HERMES) collaboration to pool their individual patient data and perform a meta-analysis to clarify the issue of timing. They assessed patients’ functional independence at 90 days using the modified Rankin Score (mRS). The study participants included 634 patients who had been randomly assigned to endovascular thrombectomy and 653 randomly assigned to medical therapy.
The intervention correlated with a substantially lower degree of patient disability at 90 days than did medical therapy: the mean mRS was 2.9 in the thrombectomy group and 3.6 in the medical therapy group. In addition, increasing delays in treatment were associated with higher levels of residual disability in the thrombectomy group but not in the medical therapy group, the investigators reported.
“Based on the current study, and assuming the findings are generalizable to the population of patients with acute ischemic stroke due to large-vessel occlusion, among every 1,000 patients achieving substantial endovascular reperfusion, for every 15-minute faster ED door-to-reperfusion time, an estimated 39 patients would have a less-disabled outcome at 3 months, including 25 more who would achieve functional independence (mRS 0-2),” Dr. Saver and his associates wrote (JAMA. 2016;316[12]:1279-88).
These findings reinforce current recommendations to attempt endovascular thrombectomy when the procedure can be initiated within 6 hours of symptom onset, and they also “provide evidence that potentially supports strengthening of the recommendation for treatment from 6 through 7.3 hours after symptom onset,” they added.
No specific sponsor of this study was cited. Dr. Saver reported ties to Medtronic, Stryker, Cognition Medical, Covidien, Neuravi, BrainsGate, Pfizer, Bristol-Myers Squibb, Boehringer Ingelheim, ZZ Biotech, St. Jude Medical, and Genentech. His associates reported ties to numerous industry sources.
For patients with large-vessel ischemic stroke, endovascular thrombectomy produces better functional outcomes at 90 days than does optimal medical therapy, as long as the procedure is started within 7.3 hours of symptom onset, according to a report published online Sept. 27 in JAMA.
The benefit of thrombectomy was greatest when the procedure was begun under 2 hours from symptom onset, and it became nonsignificant after 7 hours and 18 minutes elapsed. This emphasizes “the importance of programs to enhance patient awareness, out-of-hospital care, and in-hospital management to shorten symptom onset-to-treatment times,” wrote Jeffrey L. Saver, MD, of the University of California, Los Angeles, and his associates.
Five major randomized trials have demonstrated the benefit of second-generation endovascular recanalization therapies over medical therapy in this patient population, but uncertainties persist regarding the timing of the intervention. For example, practice guidelines in the United States recommend thrombectomy until 6 hours after symptom onset, but the Food and Drug Administration allows thrombectomy devices to be used up to 8 hours after symptom onset and Canadian guidelines recommend the procedure for selected patients up to 12 hours after symptom onset.
The investigators for the five trials formed the Highly Effective Reperfusion Evaluated in Multiple Endovascular Stroke Trials (HERMES) collaboration to pool their individual patient data and perform a meta-analysis to clarify the issue of timing. They assessed patients’ functional independence at 90 days using the modified Rankin Score (mRS). The study participants included 634 patients who had been randomly assigned to endovascular thrombectomy and 653 randomly assigned to medical therapy.
The intervention correlated with a substantially lower degree of patient disability at 90 days than did medical therapy: the mean mRS was 2.9 in the thrombectomy group and 3.6 in the medical therapy group. In addition, increasing delays in treatment were associated with higher levels of residual disability in the thrombectomy group but not in the medical therapy group, the investigators reported.
“Based on the current study, and assuming the findings are generalizable to the population of patients with acute ischemic stroke due to large-vessel occlusion, among every 1,000 patients achieving substantial endovascular reperfusion, for every 15-minute faster ED door-to-reperfusion time, an estimated 39 patients would have a less-disabled outcome at 3 months, including 25 more who would achieve functional independence (mRS 0-2),” Dr. Saver and his associates wrote (JAMA. 2016;316[12]:1279-88).
These findings reinforce current recommendations to attempt endovascular thrombectomy when the procedure can be initiated within 6 hours of symptom onset, and they also “provide evidence that potentially supports strengthening of the recommendation for treatment from 6 through 7.3 hours after symptom onset,” they added.
No specific sponsor of this study was cited. Dr. Saver reported ties to Medtronic, Stryker, Cognition Medical, Covidien, Neuravi, BrainsGate, Pfizer, Bristol-Myers Squibb, Boehringer Ingelheim, ZZ Biotech, St. Jude Medical, and Genentech. His associates reported ties to numerous industry sources.
FROM JAMA
Key clinical point: Endovascular thrombectomy started within 7.3 hours of symptom onset for large-vessel ischemic stroke produces better outcomes than does optimal medical therapy.
Major finding: For every 15-minute shorter door-to-reperfusion time, an estimated 39 patients would have a less-disabled outcome at 3 months, including 25 more who would achieve functional independence.
Data source: A meta-analysis of pooled data from five randomized clinical trials involving 1,287 patients.
Disclosures: No specific sponsor of this study was cited. Dr. Saver reported ties to Medtronic, Stryker, Cognition Medical, Covidien, Neuravi, BrainsGate, Pfizer, Bristol Myers Squibb, Boehringer Ingelheim, ZZ Biotech, St. Jude Medical, and Genentech. His associates reported ties to numerous industry sources.
Early intensive prophylaxis provides better QoL in hemophilia
ORLANDO – Boys with hemophilia have a better quality of life when they are managed with intensive bleeding prophylaxis with clotting factor concentrates rather than on-demand therapy, results of an international study suggest.
An analysis of pooled data from six studies conducted in eight countries showed that boys with severe hemophilia who received limited on-demand factor replacement had significantly lower health-related quality of life (HRQoL) scores than did boys treated prophylactically, reported Victoria Price, MB, of Dalhousie University, Halifax, N.S., and colleagues.
“Early initiation of intensive prophylaxis has the greatest impact on HRQoL in boys with severe hemophilia. HRQoL in boys with severe hemophilia exposed to early initiation of intensive prophylaxis is comparable to boys with mild hemophilia receiving on-demand therapy,” they wrote in a scientific poster presented at the World Federation of Hemophilia World Congress.
In countries where patients have access to safe clotting factor concentrates, prophylaxis has become the standard of care for management of hemophilia A and B, because it has been shown to reduce the frequency of bleeds. But because of the small sample sizes in most studies of hemophilia, it has been difficult to determine whether prophylaxis actually has a significant effect on HRQoL, the investigators noted.
To get an answer to that question, they looked at data from six studies in boys younger than 18 that measured HRQoL using the same standard instrument, the Canadian Haemophilia Outcomes–Kids’ Life Assessment Tool (CHO-KLAT). The studies were conducted in Brazil, Canada, China, France, Germany, the Netherlands, Spain, and the United Kingdom.
Patients in the studies were grouped into one of five categories:
• Early initiation with intensive prophylaxis (Germany, the Netherlands, Spain, UK)
• Gradual initiation with intensive prophylaxis (Canada, France)
• Late initiation with limited prophylaxis (Brazil, China)
• On-demand with good access to factor (Canada and European nations)
• On-demand with variable or limited access to factor (Brazil and China).
Data on a total of 254 boys with severe hemophilia were analyzed and compared with estimated scores from boys with mild hemophilia in the pooled dataset.
Of the boys with severe hemophilia, 220 (86.6% had hemophilia A, and 34 (13.4%) had hemophilia B. They ranged in age from 4.4 to 17.9 years; 21 of the boys were younger than 7 years.
The investigators found that in a linear regression model, patients with early initiation and intensive prophylaxis had the highest CHO-KLAT scores, followed by those who had gradual initiation with intensive prophylaxis (P = .003), late initiation/limited prophylaxis (P = .005), on-demand with good access (P = .008) and, lastly, on-demand with limited access to factor (P less than .001)
The authors noted that the differences by treatment group in the analysis were defined by expert consensus, and may not reflect changes in treatment protocols over the last 10 years. The studies were published between 2006 and 2016.
“Despite this limitation, important differences were observed between groups,” they wrote.
The studies were supported by grants from the Canadian Haemophilia Society and the Society of Haemophilia Clinic Directors of Canada, Bayer, Baxalta, and CSL Behring. The authors did not report conflict of interest disclosures.
ORLANDO – Boys with hemophilia have a better quality of life when they are managed with intensive bleeding prophylaxis with clotting factor concentrates rather than on-demand therapy, results of an international study suggest.
An analysis of pooled data from six studies conducted in eight countries showed that boys with severe hemophilia who received limited on-demand factor replacement had significantly lower health-related quality of life (HRQoL) scores than did boys treated prophylactically, reported Victoria Price, MB, of Dalhousie University, Halifax, N.S., and colleagues.
“Early initiation of intensive prophylaxis has the greatest impact on HRQoL in boys with severe hemophilia. HRQoL in boys with severe hemophilia exposed to early initiation of intensive prophylaxis is comparable to boys with mild hemophilia receiving on-demand therapy,” they wrote in a scientific poster presented at the World Federation of Hemophilia World Congress.
In countries where patients have access to safe clotting factor concentrates, prophylaxis has become the standard of care for management of hemophilia A and B, because it has been shown to reduce the frequency of bleeds. But because of the small sample sizes in most studies of hemophilia, it has been difficult to determine whether prophylaxis actually has a significant effect on HRQoL, the investigators noted.
To get an answer to that question, they looked at data from six studies in boys younger than 18 that measured HRQoL using the same standard instrument, the Canadian Haemophilia Outcomes–Kids’ Life Assessment Tool (CHO-KLAT). The studies were conducted in Brazil, Canada, China, France, Germany, the Netherlands, Spain, and the United Kingdom.
Patients in the studies were grouped into one of five categories:
• Early initiation with intensive prophylaxis (Germany, the Netherlands, Spain, UK)
• Gradual initiation with intensive prophylaxis (Canada, France)
• Late initiation with limited prophylaxis (Brazil, China)
• On-demand with good access to factor (Canada and European nations)
• On-demand with variable or limited access to factor (Brazil and China).
Data on a total of 254 boys with severe hemophilia were analyzed and compared with estimated scores from boys with mild hemophilia in the pooled dataset.
Of the boys with severe hemophilia, 220 (86.6% had hemophilia A, and 34 (13.4%) had hemophilia B. They ranged in age from 4.4 to 17.9 years; 21 of the boys were younger than 7 years.
The investigators found that in a linear regression model, patients with early initiation and intensive prophylaxis had the highest CHO-KLAT scores, followed by those who had gradual initiation with intensive prophylaxis (P = .003), late initiation/limited prophylaxis (P = .005), on-demand with good access (P = .008) and, lastly, on-demand with limited access to factor (P less than .001)
The authors noted that the differences by treatment group in the analysis were defined by expert consensus, and may not reflect changes in treatment protocols over the last 10 years. The studies were published between 2006 and 2016.
“Despite this limitation, important differences were observed between groups,” they wrote.
The studies were supported by grants from the Canadian Haemophilia Society and the Society of Haemophilia Clinic Directors of Canada, Bayer, Baxalta, and CSL Behring. The authors did not report conflict of interest disclosures.
ORLANDO – Boys with hemophilia have a better quality of life when they are managed with intensive bleeding prophylaxis with clotting factor concentrates rather than on-demand therapy, results of an international study suggest.
An analysis of pooled data from six studies conducted in eight countries showed that boys with severe hemophilia who received limited on-demand factor replacement had significantly lower health-related quality of life (HRQoL) scores than did boys treated prophylactically, reported Victoria Price, MB, of Dalhousie University, Halifax, N.S., and colleagues.
“Early initiation of intensive prophylaxis has the greatest impact on HRQoL in boys with severe hemophilia. HRQoL in boys with severe hemophilia exposed to early initiation of intensive prophylaxis is comparable to boys with mild hemophilia receiving on-demand therapy,” they wrote in a scientific poster presented at the World Federation of Hemophilia World Congress.
In countries where patients have access to safe clotting factor concentrates, prophylaxis has become the standard of care for management of hemophilia A and B, because it has been shown to reduce the frequency of bleeds. But because of the small sample sizes in most studies of hemophilia, it has been difficult to determine whether prophylaxis actually has a significant effect on HRQoL, the investigators noted.
To get an answer to that question, they looked at data from six studies in boys younger than 18 that measured HRQoL using the same standard instrument, the Canadian Haemophilia Outcomes–Kids’ Life Assessment Tool (CHO-KLAT). The studies were conducted in Brazil, Canada, China, France, Germany, the Netherlands, Spain, and the United Kingdom.
Patients in the studies were grouped into one of five categories:
• Early initiation with intensive prophylaxis (Germany, the Netherlands, Spain, UK)
• Gradual initiation with intensive prophylaxis (Canada, France)
• Late initiation with limited prophylaxis (Brazil, China)
• On-demand with good access to factor (Canada and European nations)
• On-demand with variable or limited access to factor (Brazil and China).
Data on a total of 254 boys with severe hemophilia were analyzed and compared with estimated scores from boys with mild hemophilia in the pooled dataset.
Of the boys with severe hemophilia, 220 (86.6% had hemophilia A, and 34 (13.4%) had hemophilia B. They ranged in age from 4.4 to 17.9 years; 21 of the boys were younger than 7 years.
The investigators found that in a linear regression model, patients with early initiation and intensive prophylaxis had the highest CHO-KLAT scores, followed by those who had gradual initiation with intensive prophylaxis (P = .003), late initiation/limited prophylaxis (P = .005), on-demand with good access (P = .008) and, lastly, on-demand with limited access to factor (P less than .001)
The authors noted that the differences by treatment group in the analysis were defined by expert consensus, and may not reflect changes in treatment protocols over the last 10 years. The studies were published between 2006 and 2016.
“Despite this limitation, important differences were observed between groups,” they wrote.
The studies were supported by grants from the Canadian Haemophilia Society and the Society of Haemophilia Clinic Directors of Canada, Bayer, Baxalta, and CSL Behring. The authors did not report conflict of interest disclosures.
AT WFH 2016 WORLD CONGRESS
Key clinical point: Early initiation of intensive bleeding prophylaxis was associated with significantly better health-related quality of life (HRQoL).
Major finding: Boys with severe hemophilia started early on intensive prophylaxis had HRQoL comparable to that of boys with mild hemophilia with good access to factor.
Data source: Pooled analysis of six studies comprising 254 boys with severe hemophilia.
Disclosures: The studies were supported by grants from the Canadian Haemophilia Society and the Society of Haemophilia Clinic Directors of Canada, Bayer, Baxalta, and CSL Behring. The authors did not report conflict of interest disclosures.
Feds require more transparent reporting of clinical trial results
New federal regulations aim to strengthen the current requirements on reporting of clinical trial information.
The new rule offers a checklist to help determine which clinical trials are subject to regulations and who is responsible for information that appears on ClinicalTrials.gov. In addition, the rule does the following:
• Expands the scope of trials for which results must be submitted to include Food and Drug Administration–regulated products that have not yet been approved, licensed, or cleared.
• Requires additional information be submitted to ClinicalTrials.gov, including demographic information about trial participants.
• Expands adverse-event reporting.
• Adds potential penalties for noncompliance.
Simultaneously, the National Institutes of Health issued a complimentary policy for all trials it funds, regardless of whether the trials would be subject to the final rule.
Current federal requirements for reporting of clinical trial information were originally enacted as part of the FDA Amendments Act of 2007. However, a 2015 analysis of trials listed on ClinicalTrials.gov from 2007 to 2012 found a woeful lack of compliance: Study results were posted for 13% of trials covered by reporting requirements (N Engl J Med. 2015;372:1031-9).
“Organizations will need to ensure that their systems, procedures, and organizational values all promote complete and timely clinical trial reporting,” wrote Deborah Zarin, MD, of the National Library of Medicine, Bethesda, Md., and her colleagues in a special report on the final rule (N Engl J Med. 2016 Sep 16. doi: 10.1056/NEJMsr1611785). “In the end, the parties responsible for clinical trials will be held accountable by the public.”
The final rule applies to most interventional studies of drugs, biologics, and devices regulated by FDA, but it will not apply to phase I trials of pharmaceuticals or small feasibility studies of devices. It specifies how and when information collected in a clinical trial should be collected and submitted to ClinicalTrials.gov but does not dictate how clinical trials should be designed or conducted.
“Expanding the registration information in ClinicalTrials.gov improves people’s ability to find clinical trials in which they may be able to participate and access investigational therapies,” NIH officials said in a statement. “More information about the scientific results of trials, whether positive or negative, may help inform healthcare providers and patients regarding medical decisions. Additional information will help researchers avoid unnecessary duplication of studies, focus on areas in need of study and improve study design, ultimately advancing the development of clinical interventions.”
“Many U.S. academic medical centers, including those that conduct the most clinical trials, will find that the majority of their clinical trials fall under the [FDA Amendments Act], the NIH policy, or both,” Dr. Zarin and her colleagues wrote. “We hope that sponsors and other relevant entities will go considerably above and beyond the minimum requirements and expectations, making an effort to honor the contributions of all study participants and ensure that others in the scientific community have access to complete and high-quality information about every clinical trial under their stewardship.”
The final rule was published in the Federal Register on Sept. 21 and becomes effective on Jan. 18, 2017.
New federal regulations aim to strengthen the current requirements on reporting of clinical trial information.
The new rule offers a checklist to help determine which clinical trials are subject to regulations and who is responsible for information that appears on ClinicalTrials.gov. In addition, the rule does the following:
• Expands the scope of trials for which results must be submitted to include Food and Drug Administration–regulated products that have not yet been approved, licensed, or cleared.
• Requires additional information be submitted to ClinicalTrials.gov, including demographic information about trial participants.
• Expands adverse-event reporting.
• Adds potential penalties for noncompliance.
Simultaneously, the National Institutes of Health issued a complimentary policy for all trials it funds, regardless of whether the trials would be subject to the final rule.
Current federal requirements for reporting of clinical trial information were originally enacted as part of the FDA Amendments Act of 2007. However, a 2015 analysis of trials listed on ClinicalTrials.gov from 2007 to 2012 found a woeful lack of compliance: Study results were posted for 13% of trials covered by reporting requirements (N Engl J Med. 2015;372:1031-9).
“Organizations will need to ensure that their systems, procedures, and organizational values all promote complete and timely clinical trial reporting,” wrote Deborah Zarin, MD, of the National Library of Medicine, Bethesda, Md., and her colleagues in a special report on the final rule (N Engl J Med. 2016 Sep 16. doi: 10.1056/NEJMsr1611785). “In the end, the parties responsible for clinical trials will be held accountable by the public.”
The final rule applies to most interventional studies of drugs, biologics, and devices regulated by FDA, but it will not apply to phase I trials of pharmaceuticals or small feasibility studies of devices. It specifies how and when information collected in a clinical trial should be collected and submitted to ClinicalTrials.gov but does not dictate how clinical trials should be designed or conducted.
“Expanding the registration information in ClinicalTrials.gov improves people’s ability to find clinical trials in which they may be able to participate and access investigational therapies,” NIH officials said in a statement. “More information about the scientific results of trials, whether positive or negative, may help inform healthcare providers and patients regarding medical decisions. Additional information will help researchers avoid unnecessary duplication of studies, focus on areas in need of study and improve study design, ultimately advancing the development of clinical interventions.”
“Many U.S. academic medical centers, including those that conduct the most clinical trials, will find that the majority of their clinical trials fall under the [FDA Amendments Act], the NIH policy, or both,” Dr. Zarin and her colleagues wrote. “We hope that sponsors and other relevant entities will go considerably above and beyond the minimum requirements and expectations, making an effort to honor the contributions of all study participants and ensure that others in the scientific community have access to complete and high-quality information about every clinical trial under their stewardship.”
The final rule was published in the Federal Register on Sept. 21 and becomes effective on Jan. 18, 2017.
New federal regulations aim to strengthen the current requirements on reporting of clinical trial information.
The new rule offers a checklist to help determine which clinical trials are subject to regulations and who is responsible for information that appears on ClinicalTrials.gov. In addition, the rule does the following:
• Expands the scope of trials for which results must be submitted to include Food and Drug Administration–regulated products that have not yet been approved, licensed, or cleared.
• Requires additional information be submitted to ClinicalTrials.gov, including demographic information about trial participants.
• Expands adverse-event reporting.
• Adds potential penalties for noncompliance.
Simultaneously, the National Institutes of Health issued a complimentary policy for all trials it funds, regardless of whether the trials would be subject to the final rule.
Current federal requirements for reporting of clinical trial information were originally enacted as part of the FDA Amendments Act of 2007. However, a 2015 analysis of trials listed on ClinicalTrials.gov from 2007 to 2012 found a woeful lack of compliance: Study results were posted for 13% of trials covered by reporting requirements (N Engl J Med. 2015;372:1031-9).
“Organizations will need to ensure that their systems, procedures, and organizational values all promote complete and timely clinical trial reporting,” wrote Deborah Zarin, MD, of the National Library of Medicine, Bethesda, Md., and her colleagues in a special report on the final rule (N Engl J Med. 2016 Sep 16. doi: 10.1056/NEJMsr1611785). “In the end, the parties responsible for clinical trials will be held accountable by the public.”
The final rule applies to most interventional studies of drugs, biologics, and devices regulated by FDA, but it will not apply to phase I trials of pharmaceuticals or small feasibility studies of devices. It specifies how and when information collected in a clinical trial should be collected and submitted to ClinicalTrials.gov but does not dictate how clinical trials should be designed or conducted.
“Expanding the registration information in ClinicalTrials.gov improves people’s ability to find clinical trials in which they may be able to participate and access investigational therapies,” NIH officials said in a statement. “More information about the scientific results of trials, whether positive or negative, may help inform healthcare providers and patients regarding medical decisions. Additional information will help researchers avoid unnecessary duplication of studies, focus on areas in need of study and improve study design, ultimately advancing the development of clinical interventions.”
“Many U.S. academic medical centers, including those that conduct the most clinical trials, will find that the majority of their clinical trials fall under the [FDA Amendments Act], the NIH policy, or both,” Dr. Zarin and her colleagues wrote. “We hope that sponsors and other relevant entities will go considerably above and beyond the minimum requirements and expectations, making an effort to honor the contributions of all study participants and ensure that others in the scientific community have access to complete and high-quality information about every clinical trial under their stewardship.”
The final rule was published in the Federal Register on Sept. 21 and becomes effective on Jan. 18, 2017.
MRSA patients report signs of stigma tied to illness
About half of individuals infected with methicillin-resistant Staphylococcus aureus report feeling stigmatized in interactions with hospital staff, data from a survey of 61 adult patients show.
“Hospital care for people who carry MRSA calls for a dedicated and patient-centered approach in both the way the care is delivered ... as well as the way the care is organized at the institutional level,” wrote Babette Rump, MD, of the Regional Health Service Utrecht region, Zeist, the Netherlands, and her coauthors (J Hosp Infect. 2016. doi: 10.1016/j.jhin.2016.09.010). “Prevention of unnecessary intrusive measures, while as the same time applying appropriate precautionary measures, is key to successful and respectful MRSA management.”
Dr. Rump and her associates set out to identify and quantify stigma tied to MRSA and “explore its association with mental health within a country with a MRSA ‘search and destroy’ policy.” In the Netherlands and Scandinavian countries, this policy includes isolating MRSA carriers, wearing personal protective equipment, and disinfecting the room after patients are discharged (Antimicrob Resist Infect Control. 2014 Jan 15;3[1]3). The U.S. Centers for Disease Control and Prevention, in its 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings, recommends similar methods, including application of infection control precautions during patient care and environmental measures, such as cleaning and disinfection of the patient care environment and dedicated single-patient use of noncritical equipment.
In the current study, 60-item questionnaires were provided to all adult patients at two hospitals and two regional health services who had acquired MRSA between Oct. 1, 2013, and April 1, 2014. Stigma was assessed using the 40-item Berger HIV Stigma Scale, reported Dr. Rump.
Overall, 56% of survey respondents reported stigma, including 14% who reported clear stigma and 42% who reported suggestive stigma. The remaining 44% reported no stigma. A total of 80% of the patients received MRSA eradication treatment, which was strongly associated with higher stigma, the researchers noted.
Written comments provided by 40 patients (68%) along with the questionnaires “offer valuable insights to set the focus for improvement,” the researchers said.
The most frequent comments involved patients’ perceived organizational problems with the hospital (8 patients), lack of staff knowledge (4 patients), as well as little attention paid to patient perspectives (4 patients) and unnecessarily intrusive treatments (3 patients). Also of note, 5 patients blamed and 2 “shamed” the hospital as their source of MRSA.
The results were limited by several factors, including the small study size, the researchers wrote. However, the findings suggest that “a substantial proportion of people that carry MRSA experience signs of stigma and that anticipation on MRSA-associated stigma is warranted,” they said.
The researchers had no financial conflicts to disclose.
About half of individuals infected with methicillin-resistant Staphylococcus aureus report feeling stigmatized in interactions with hospital staff, data from a survey of 61 adult patients show.
“Hospital care for people who carry MRSA calls for a dedicated and patient-centered approach in both the way the care is delivered ... as well as the way the care is organized at the institutional level,” wrote Babette Rump, MD, of the Regional Health Service Utrecht region, Zeist, the Netherlands, and her coauthors (J Hosp Infect. 2016. doi: 10.1016/j.jhin.2016.09.010). “Prevention of unnecessary intrusive measures, while as the same time applying appropriate precautionary measures, is key to successful and respectful MRSA management.”
Dr. Rump and her associates set out to identify and quantify stigma tied to MRSA and “explore its association with mental health within a country with a MRSA ‘search and destroy’ policy.” In the Netherlands and Scandinavian countries, this policy includes isolating MRSA carriers, wearing personal protective equipment, and disinfecting the room after patients are discharged (Antimicrob Resist Infect Control. 2014 Jan 15;3[1]3). The U.S. Centers for Disease Control and Prevention, in its 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings, recommends similar methods, including application of infection control precautions during patient care and environmental measures, such as cleaning and disinfection of the patient care environment and dedicated single-patient use of noncritical equipment.
In the current study, 60-item questionnaires were provided to all adult patients at two hospitals and two regional health services who had acquired MRSA between Oct. 1, 2013, and April 1, 2014. Stigma was assessed using the 40-item Berger HIV Stigma Scale, reported Dr. Rump.
Overall, 56% of survey respondents reported stigma, including 14% who reported clear stigma and 42% who reported suggestive stigma. The remaining 44% reported no stigma. A total of 80% of the patients received MRSA eradication treatment, which was strongly associated with higher stigma, the researchers noted.
Written comments provided by 40 patients (68%) along with the questionnaires “offer valuable insights to set the focus for improvement,” the researchers said.
The most frequent comments involved patients’ perceived organizational problems with the hospital (8 patients), lack of staff knowledge (4 patients), as well as little attention paid to patient perspectives (4 patients) and unnecessarily intrusive treatments (3 patients). Also of note, 5 patients blamed and 2 “shamed” the hospital as their source of MRSA.
The results were limited by several factors, including the small study size, the researchers wrote. However, the findings suggest that “a substantial proportion of people that carry MRSA experience signs of stigma and that anticipation on MRSA-associated stigma is warranted,” they said.
The researchers had no financial conflicts to disclose.
About half of individuals infected with methicillin-resistant Staphylococcus aureus report feeling stigmatized in interactions with hospital staff, data from a survey of 61 adult patients show.
“Hospital care for people who carry MRSA calls for a dedicated and patient-centered approach in both the way the care is delivered ... as well as the way the care is organized at the institutional level,” wrote Babette Rump, MD, of the Regional Health Service Utrecht region, Zeist, the Netherlands, and her coauthors (J Hosp Infect. 2016. doi: 10.1016/j.jhin.2016.09.010). “Prevention of unnecessary intrusive measures, while as the same time applying appropriate precautionary measures, is key to successful and respectful MRSA management.”
Dr. Rump and her associates set out to identify and quantify stigma tied to MRSA and “explore its association with mental health within a country with a MRSA ‘search and destroy’ policy.” In the Netherlands and Scandinavian countries, this policy includes isolating MRSA carriers, wearing personal protective equipment, and disinfecting the room after patients are discharged (Antimicrob Resist Infect Control. 2014 Jan 15;3[1]3). The U.S. Centers for Disease Control and Prevention, in its 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings, recommends similar methods, including application of infection control precautions during patient care and environmental measures, such as cleaning and disinfection of the patient care environment and dedicated single-patient use of noncritical equipment.
In the current study, 60-item questionnaires were provided to all adult patients at two hospitals and two regional health services who had acquired MRSA between Oct. 1, 2013, and April 1, 2014. Stigma was assessed using the 40-item Berger HIV Stigma Scale, reported Dr. Rump.
Overall, 56% of survey respondents reported stigma, including 14% who reported clear stigma and 42% who reported suggestive stigma. The remaining 44% reported no stigma. A total of 80% of the patients received MRSA eradication treatment, which was strongly associated with higher stigma, the researchers noted.
Written comments provided by 40 patients (68%) along with the questionnaires “offer valuable insights to set the focus for improvement,” the researchers said.
The most frequent comments involved patients’ perceived organizational problems with the hospital (8 patients), lack of staff knowledge (4 patients), as well as little attention paid to patient perspectives (4 patients) and unnecessarily intrusive treatments (3 patients). Also of note, 5 patients blamed and 2 “shamed” the hospital as their source of MRSA.
The results were limited by several factors, including the small study size, the researchers wrote. However, the findings suggest that “a substantial proportion of people that carry MRSA experience signs of stigma and that anticipation on MRSA-associated stigma is warranted,” they said.
The researchers had no financial conflicts to disclose.
FROM THE JOURNAL OF HOSPITAL INFECTION
Key clinical point: Adults with methicillin-resistant Staphylococcus aureus (MRSA) are susceptible to stigma.
Major finding: Approximately half (56%) of adults being treated for MRSA reported stigma associated with their illness.
Data source: A cross-sectional study including 61 adults with MRSA.
Disclosures: The researchers had no financial conflicts to disclose.