User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
‘Keto-like’ diet linked to doubling of heart disease risk
Consumption of a low-carbohydrate, high-fat diet, dubbed a “keto-like” diet, was associated with an increase in LDL levels and a twofold increase in the risk for future cardiovascular events, in a new observational study.
“To our knowledge this is the first study to demonstrate an association between a carbohydrate-restricted dietary platform and greater risk of atherosclerotic cardiovascular disease,” said study investigator Iulia Iatan, MD, PhD, University of British Columbia, Vancouver.
“Hypercholesterolemia occurring during a low-carb, high-fat diet should not be assumed to be benign,” she concluded.
Dr. Iatan presented the study March 5 at the joint scientific sessions of the American College of Cardiology and the World Heart Federation.
The presentation received much media attention, with headlines implying a causal relationship with cardiac events based on these observational results. But lipid expert Steven Nissen, MD, of the Cleveland Clinic, warned against paying much attention to the headlines or to the study’s conclusions.
In an interview, Dr. Nissen pointed out that the LDL increase in the “keto-like” diet group was relatively small and “certainly not enough to produce a doubling in cardiovascular risk.
“The people who were on the ‘keto-like’ diet in this study were different than those who were on the standard diet,” he said. “Those on the ‘keto-like’ diet were on it for a reason – they were more overweight, they had a higher incidence of diabetes, so their risk profile was completely different. Even though the researchers tried to adjust for other cardiovascular risk factors, there will be unmeasured confounding in a study like this.”
He said he doesn’t think this study “answers any significant questions in a way that we want to have them answered. I’m not a big fan of this type of diet, but I don’t think it doubles the risk of adverse cardiovascular events, and I don’t think this study tells us one way or another.”
For the study, Dr. Iatan and colleagues defined a low-carbohydrate, high-fat diet as consisting of no more than 25% of total daily energy from carbohydrates and more than 45% of total daily calories from fat. This is somewhat higher in carbohydrates and lower in fat than a strict ketogenic diet but could be thought of as a ‘keto-like’ diet.
They analyzed data from the UK Biobank, a large-scale prospective database with health information from over half a million people living in the United Kingdom who were followed for at least 10 years.
On enrollment in the Biobank, participants completed a one-time, self-reported 24-hour diet questionnaire and, at the same time, had blood drawn to check their levels of cholesterol. The researchers identified 305 participants whose questionnaire responses indicated that they followed a low-carbohydrate, high-fat diet. These participants were matched by age and sex with 1,220 individuals who reported being on a standard diet.
Of the study population, 73% were women and the average age was 54 years. Those on a low carbohydrate/high fat diet had a higher average body mass index (27.7 vs. 26.7) and a higher incidence of diabetes (4.9% vs. 1.7%).
Results showed that compared with participants on a standard diet, those on the “keto-like” diet had significantly higher levels of both LDL cholesterol and apolipoprotein B (ApoB).
Levels of LDL were 3.80 mmol/L (147 mg/dL) in the keto-like group vs. 3.64 mmol/L (141 mg/dL) in the standard group (P = .004). Levels of ApoB were 1.09 g/L (109 mg/dL) in the keto-like group and 1.04 g/L (104 mg/dL) in the standard group (P < .001).
After an average of 11.8 years of follow-up, 9.8% of participants on the low-carbohydrate/high-fat diet vs. 4.3% in the standard diet group experienced one of the events included in the composite event endpoint: Angina, myocardial infarction, coronary artery disease, ischemic stroke, peripheral arterial disease, or coronary/carotid revascularization.
After adjustment for other risk factors for heart disease – diabetes, hypertension, obesity, and smoking – individuals on a low-carbohydrate, high-fat diet were found to have a twofold risk of having a cardiovascular event (HR, 2.18; P < .001).
‘Closer monitoring needed’
“Our results have shown, I think for the first time, that there is an association between this increasingly popular dietary pattern and high LDL cholesterol and an increased future risk of cardiovascular events,” senior author Liam Brunham, MD, of the University of British Columbia, said in an interview. “This is concerning as there are many people out there following this type of diet, and I think it suggests there is a need for closer monitoring of these people.”
He explained that while it would be expected for cholesterol levels to rise on a high-fat diet, “there has been a perception by some that this is not worrisome as it is reflecting certain metabolic changes. What we’ve shown in this study is that if your cholesterol does increase significantly on this diet then you should not assume that this is not a problem.
“For some people with diabetes this diet can help lower blood sugar and some people can lose weight on it,” he noted, “but what our data show is that there is a subgroup of people who experience high levels of LDL and ApoB and that seems to be driving the risk.”
He pointed out that overall the mean level of LDL was only slightly increased in the individuals on the low-carb/high-fat diet but severe high cholesterol (more than 5 mmol/L or 190 mg/dL) was about doubled in that group (10% vs. 5%). And these patients had a sixfold increase in risk of cardiovascular disease (P < .001).
“This suggests that there is a subgroup of people who are susceptible to this exacerbation of hypercholesterolemia in response to a low-carb/high-fat diet.”
Dr. Brunham said his advice would be that if people choose to follow this diet, they should have their cholesterol monitored, and manage their cardiovascular risk factors.
“I wouldn’t say it is not appropriate to follow this diet based on this study,” he added. “This is just an observational study. It is not definitive. But if people do want to follow this dietary pattern because they feel there would be some benefits, then they should be aware of the potential risks and take steps to mitigate those risks.”
Jury still out
Dr. Nissen said in his view “the jury was still out” on this type of diet. “I’m open to the possibility that, particularly in the short run, a ‘keto-like’ diet may help some people lose weight and that’s a good thing. But I do not generally recommend this type of diet.”
Rather, he advises patients to follow a Mediterranean diet, which has been proven to reduce cardiovascular events in a randomized study, the PREDIMED trial.
“We can’t make decisions on what type of diet to recommend to patients based on observational studies like this where there is a lot of subtlety missing. But when studies like this are reported, the mass media seize on it. That’s not the way the public needs to be educated,” Dr. Nissen said.
“We refer to this type of study as hypothesis-generating. It raises a hypothesis. It doesn’t answer the question. It is worth looking at the question of whether a ketogenic-like diet is harmful. We don’t know at present, and I don’t think we know any more after this study,” he added.
The authors of the study reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Consumption of a low-carbohydrate, high-fat diet, dubbed a “keto-like” diet, was associated with an increase in LDL levels and a twofold increase in the risk for future cardiovascular events, in a new observational study.
“To our knowledge this is the first study to demonstrate an association between a carbohydrate-restricted dietary platform and greater risk of atherosclerotic cardiovascular disease,” said study investigator Iulia Iatan, MD, PhD, University of British Columbia, Vancouver.
“Hypercholesterolemia occurring during a low-carb, high-fat diet should not be assumed to be benign,” she concluded.
Dr. Iatan presented the study March 5 at the joint scientific sessions of the American College of Cardiology and the World Heart Federation.
The presentation received much media attention, with headlines implying a causal relationship with cardiac events based on these observational results. But lipid expert Steven Nissen, MD, of the Cleveland Clinic, warned against paying much attention to the headlines or to the study’s conclusions.
In an interview, Dr. Nissen pointed out that the LDL increase in the “keto-like” diet group was relatively small and “certainly not enough to produce a doubling in cardiovascular risk.
“The people who were on the ‘keto-like’ diet in this study were different than those who were on the standard diet,” he said. “Those on the ‘keto-like’ diet were on it for a reason – they were more overweight, they had a higher incidence of diabetes, so their risk profile was completely different. Even though the researchers tried to adjust for other cardiovascular risk factors, there will be unmeasured confounding in a study like this.”
He said he doesn’t think this study “answers any significant questions in a way that we want to have them answered. I’m not a big fan of this type of diet, but I don’t think it doubles the risk of adverse cardiovascular events, and I don’t think this study tells us one way or another.”
For the study, Dr. Iatan and colleagues defined a low-carbohydrate, high-fat diet as consisting of no more than 25% of total daily energy from carbohydrates and more than 45% of total daily calories from fat. This is somewhat higher in carbohydrates and lower in fat than a strict ketogenic diet but could be thought of as a ‘keto-like’ diet.
They analyzed data from the UK Biobank, a large-scale prospective database with health information from over half a million people living in the United Kingdom who were followed for at least 10 years.
On enrollment in the Biobank, participants completed a one-time, self-reported 24-hour diet questionnaire and, at the same time, had blood drawn to check their levels of cholesterol. The researchers identified 305 participants whose questionnaire responses indicated that they followed a low-carbohydrate, high-fat diet. These participants were matched by age and sex with 1,220 individuals who reported being on a standard diet.
Of the study population, 73% were women and the average age was 54 years. Those on a low carbohydrate/high fat diet had a higher average body mass index (27.7 vs. 26.7) and a higher incidence of diabetes (4.9% vs. 1.7%).
Results showed that compared with participants on a standard diet, those on the “keto-like” diet had significantly higher levels of both LDL cholesterol and apolipoprotein B (ApoB).
Levels of LDL were 3.80 mmol/L (147 mg/dL) in the keto-like group vs. 3.64 mmol/L (141 mg/dL) in the standard group (P = .004). Levels of ApoB were 1.09 g/L (109 mg/dL) in the keto-like group and 1.04 g/L (104 mg/dL) in the standard group (P < .001).
After an average of 11.8 years of follow-up, 9.8% of participants on the low-carbohydrate/high-fat diet vs. 4.3% in the standard diet group experienced one of the events included in the composite event endpoint: Angina, myocardial infarction, coronary artery disease, ischemic stroke, peripheral arterial disease, or coronary/carotid revascularization.
After adjustment for other risk factors for heart disease – diabetes, hypertension, obesity, and smoking – individuals on a low-carbohydrate, high-fat diet were found to have a twofold risk of having a cardiovascular event (HR, 2.18; P < .001).
‘Closer monitoring needed’
“Our results have shown, I think for the first time, that there is an association between this increasingly popular dietary pattern and high LDL cholesterol and an increased future risk of cardiovascular events,” senior author Liam Brunham, MD, of the University of British Columbia, said in an interview. “This is concerning as there are many people out there following this type of diet, and I think it suggests there is a need for closer monitoring of these people.”
He explained that while it would be expected for cholesterol levels to rise on a high-fat diet, “there has been a perception by some that this is not worrisome as it is reflecting certain metabolic changes. What we’ve shown in this study is that if your cholesterol does increase significantly on this diet then you should not assume that this is not a problem.
“For some people with diabetes this diet can help lower blood sugar and some people can lose weight on it,” he noted, “but what our data show is that there is a subgroup of people who experience high levels of LDL and ApoB and that seems to be driving the risk.”
He pointed out that overall the mean level of LDL was only slightly increased in the individuals on the low-carb/high-fat diet but severe high cholesterol (more than 5 mmol/L or 190 mg/dL) was about doubled in that group (10% vs. 5%). And these patients had a sixfold increase in risk of cardiovascular disease (P < .001).
“This suggests that there is a subgroup of people who are susceptible to this exacerbation of hypercholesterolemia in response to a low-carb/high-fat diet.”
Dr. Brunham said his advice would be that if people choose to follow this diet, they should have their cholesterol monitored, and manage their cardiovascular risk factors.
“I wouldn’t say it is not appropriate to follow this diet based on this study,” he added. “This is just an observational study. It is not definitive. But if people do want to follow this dietary pattern because they feel there would be some benefits, then they should be aware of the potential risks and take steps to mitigate those risks.”
Jury still out
Dr. Nissen said in his view “the jury was still out” on this type of diet. “I’m open to the possibility that, particularly in the short run, a ‘keto-like’ diet may help some people lose weight and that’s a good thing. But I do not generally recommend this type of diet.”
Rather, he advises patients to follow a Mediterranean diet, which has been proven to reduce cardiovascular events in a randomized study, the PREDIMED trial.
“We can’t make decisions on what type of diet to recommend to patients based on observational studies like this where there is a lot of subtlety missing. But when studies like this are reported, the mass media seize on it. That’s not the way the public needs to be educated,” Dr. Nissen said.
“We refer to this type of study as hypothesis-generating. It raises a hypothesis. It doesn’t answer the question. It is worth looking at the question of whether a ketogenic-like diet is harmful. We don’t know at present, and I don’t think we know any more after this study,” he added.
The authors of the study reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Consumption of a low-carbohydrate, high-fat diet, dubbed a “keto-like” diet, was associated with an increase in LDL levels and a twofold increase in the risk for future cardiovascular events, in a new observational study.
“To our knowledge this is the first study to demonstrate an association between a carbohydrate-restricted dietary platform and greater risk of atherosclerotic cardiovascular disease,” said study investigator Iulia Iatan, MD, PhD, University of British Columbia, Vancouver.
“Hypercholesterolemia occurring during a low-carb, high-fat diet should not be assumed to be benign,” she concluded.
Dr. Iatan presented the study March 5 at the joint scientific sessions of the American College of Cardiology and the World Heart Federation.
The presentation received much media attention, with headlines implying a causal relationship with cardiac events based on these observational results. But lipid expert Steven Nissen, MD, of the Cleveland Clinic, warned against paying much attention to the headlines or to the study’s conclusions.
In an interview, Dr. Nissen pointed out that the LDL increase in the “keto-like” diet group was relatively small and “certainly not enough to produce a doubling in cardiovascular risk.
“The people who were on the ‘keto-like’ diet in this study were different than those who were on the standard diet,” he said. “Those on the ‘keto-like’ diet were on it for a reason – they were more overweight, they had a higher incidence of diabetes, so their risk profile was completely different. Even though the researchers tried to adjust for other cardiovascular risk factors, there will be unmeasured confounding in a study like this.”
He said he doesn’t think this study “answers any significant questions in a way that we want to have them answered. I’m not a big fan of this type of diet, but I don’t think it doubles the risk of adverse cardiovascular events, and I don’t think this study tells us one way or another.”
For the study, Dr. Iatan and colleagues defined a low-carbohydrate, high-fat diet as consisting of no more than 25% of total daily energy from carbohydrates and more than 45% of total daily calories from fat. This is somewhat higher in carbohydrates and lower in fat than a strict ketogenic diet but could be thought of as a ‘keto-like’ diet.
They analyzed data from the UK Biobank, a large-scale prospective database with health information from over half a million people living in the United Kingdom who were followed for at least 10 years.
On enrollment in the Biobank, participants completed a one-time, self-reported 24-hour diet questionnaire and, at the same time, had blood drawn to check their levels of cholesterol. The researchers identified 305 participants whose questionnaire responses indicated that they followed a low-carbohydrate, high-fat diet. These participants were matched by age and sex with 1,220 individuals who reported being on a standard diet.
Of the study population, 73% were women and the average age was 54 years. Those on a low carbohydrate/high fat diet had a higher average body mass index (27.7 vs. 26.7) and a higher incidence of diabetes (4.9% vs. 1.7%).
Results showed that compared with participants on a standard diet, those on the “keto-like” diet had significantly higher levels of both LDL cholesterol and apolipoprotein B (ApoB).
Levels of LDL were 3.80 mmol/L (147 mg/dL) in the keto-like group vs. 3.64 mmol/L (141 mg/dL) in the standard group (P = .004). Levels of ApoB were 1.09 g/L (109 mg/dL) in the keto-like group and 1.04 g/L (104 mg/dL) in the standard group (P < .001).
After an average of 11.8 years of follow-up, 9.8% of participants on the low-carbohydrate/high-fat diet vs. 4.3% in the standard diet group experienced one of the events included in the composite event endpoint: Angina, myocardial infarction, coronary artery disease, ischemic stroke, peripheral arterial disease, or coronary/carotid revascularization.
After adjustment for other risk factors for heart disease – diabetes, hypertension, obesity, and smoking – individuals on a low-carbohydrate, high-fat diet were found to have a twofold risk of having a cardiovascular event (HR, 2.18; P < .001).
‘Closer monitoring needed’
“Our results have shown, I think for the first time, that there is an association between this increasingly popular dietary pattern and high LDL cholesterol and an increased future risk of cardiovascular events,” senior author Liam Brunham, MD, of the University of British Columbia, said in an interview. “This is concerning as there are many people out there following this type of diet, and I think it suggests there is a need for closer monitoring of these people.”
He explained that while it would be expected for cholesterol levels to rise on a high-fat diet, “there has been a perception by some that this is not worrisome as it is reflecting certain metabolic changes. What we’ve shown in this study is that if your cholesterol does increase significantly on this diet then you should not assume that this is not a problem.
“For some people with diabetes this diet can help lower blood sugar and some people can lose weight on it,” he noted, “but what our data show is that there is a subgroup of people who experience high levels of LDL and ApoB and that seems to be driving the risk.”
He pointed out that overall the mean level of LDL was only slightly increased in the individuals on the low-carb/high-fat diet but severe high cholesterol (more than 5 mmol/L or 190 mg/dL) was about doubled in that group (10% vs. 5%). And these patients had a sixfold increase in risk of cardiovascular disease (P < .001).
“This suggests that there is a subgroup of people who are susceptible to this exacerbation of hypercholesterolemia in response to a low-carb/high-fat diet.”
Dr. Brunham said his advice would be that if people choose to follow this diet, they should have their cholesterol monitored, and manage their cardiovascular risk factors.
“I wouldn’t say it is not appropriate to follow this diet based on this study,” he added. “This is just an observational study. It is not definitive. But if people do want to follow this dietary pattern because they feel there would be some benefits, then they should be aware of the potential risks and take steps to mitigate those risks.”
Jury still out
Dr. Nissen said in his view “the jury was still out” on this type of diet. “I’m open to the possibility that, particularly in the short run, a ‘keto-like’ diet may help some people lose weight and that’s a good thing. But I do not generally recommend this type of diet.”
Rather, he advises patients to follow a Mediterranean diet, which has been proven to reduce cardiovascular events in a randomized study, the PREDIMED trial.
“We can’t make decisions on what type of diet to recommend to patients based on observational studies like this where there is a lot of subtlety missing. But when studies like this are reported, the mass media seize on it. That’s not the way the public needs to be educated,” Dr. Nissen said.
“We refer to this type of study as hypothesis-generating. It raises a hypothesis. It doesn’t answer the question. It is worth looking at the question of whether a ketogenic-like diet is harmful. We don’t know at present, and I don’t think we know any more after this study,” he added.
The authors of the study reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM ACC 2023
Specialty and age may contribute to suicidal thoughts among physicians
A physician’s specialty can make a difference when it comes to having suicidal thoughts. Doctors who specialize in family medicine, obstetrics-gynecology, and psychiatry reported double the rates of suicidal thoughts than doctors in oncology, rheumatology, and pulmonary medicine, according to Doctors’ Burden: Medscape Physician Suicide Report 2023.
“The specialties with the highest reporting of physician suicidal thoughts are also those with the greatest physician shortages, based on the number of job openings posted by recruiting sites,” said Peter Yellowlees, MD, professor of psychiatry and chief wellness officer at UC Davis Health.
Doctors in those specialties are overworked, which can lead to burnout, he said.
There’s also a generational divide among physicians who reported suicidal thoughts. Millennials (age 27-41) and Gen-X physicians (age 42-56) were more likely to report these thoughts than were Baby Boomers (age 57-75) and the Silent Generation (age 76-95).
“Younger physicians are more burned out – they may have less control over their lives and less meaning than some older doctors who can do what they want,” said Dr. Yellowlees.
One millennial respondent commented that being on call and being required to chart detailed notes in the EHR has contributed to her burnout. “I’m more impatient and make less time and effort to see my friends and family.”
One Silent Generation respondent commented, “I am semi-retired, I take no call, I work no weekends, I provide anesthesia care in my area of special expertise, I work clinically about 46 days a year. Life is good, particularly compared to my younger colleagues who are working 60-plus hours a week with evening work, weekend work, and call. I feel really sorry for them.”
When young people enter medical school, they’re quite healthy, with low rates of depression and burnout, said Dr. Yellowlees. Yet, studies have shown that rates of burnout and suicidal thoughts increased within 2 years. “That reflects what happens when a group of idealistic young people hit a horrible system,” he said.
Who’s responsible?
Millennials were three times as likely as baby boomers to say that a medical school or health care organization should be responsible when a student or physician commits suicide.
“Young physicians may expect more of their employers than my generation did, which we see in residency programs that have unionized,” said Dr. Yellowlees, a Baby Boomer.
“As more young doctors are employed by health care organizations, they also may expect more resources to be available to them, such as wellness programs,” he added.
Younger doctors also focus more on work-life balance than older doctors, including time off and having hobbies, he said. “They are much more rational in terms of their overall beliefs and expectations than the older generation.”
Whom doctors confide in
Nearly 60% of physician-respondents with suicidal thoughts said they confided in a professional or someone they knew. Men were just as likely as women to reach out to a therapist (38%), whereas men were slightly more likely to confide in a family member and women were slightly more likely to confide in a colleague.
“It’s interesting that women are more active in seeking support at work – they often have developed a network of colleagues to support each other’s careers and whom they can confide in,” said Dr. Yellowlees.
He emphasized that 40% of physicians said they didn’t confide in anyone when they had suicidal thoughts. Of those, just over half said they could cope without professional help.
One respondent commented, “It’s just a thought; nothing I would actually do.” Another commented, “Mental health professionals can’t fix the underlying reason for the problem.”
Many doctors were concerned about risking disclosure to their medical boards (42%); that it would show up on their insurance records (33%); and that their colleagues would find out (25%), according to the report.
One respondent commented, “I don’t trust doctors to keep it to themselves.”
Another barrier doctors mentioned was a lack of time to seek help. One commented, “Time. I have none, when am I supposed to find an hour for counseling?”
A version of this article originally appeared on Medscape.com.
A physician’s specialty can make a difference when it comes to having suicidal thoughts. Doctors who specialize in family medicine, obstetrics-gynecology, and psychiatry reported double the rates of suicidal thoughts than doctors in oncology, rheumatology, and pulmonary medicine, according to Doctors’ Burden: Medscape Physician Suicide Report 2023.
“The specialties with the highest reporting of physician suicidal thoughts are also those with the greatest physician shortages, based on the number of job openings posted by recruiting sites,” said Peter Yellowlees, MD, professor of psychiatry and chief wellness officer at UC Davis Health.
Doctors in those specialties are overworked, which can lead to burnout, he said.
There’s also a generational divide among physicians who reported suicidal thoughts. Millennials (age 27-41) and Gen-X physicians (age 42-56) were more likely to report these thoughts than were Baby Boomers (age 57-75) and the Silent Generation (age 76-95).
“Younger physicians are more burned out – they may have less control over their lives and less meaning than some older doctors who can do what they want,” said Dr. Yellowlees.
One millennial respondent commented that being on call and being required to chart detailed notes in the EHR has contributed to her burnout. “I’m more impatient and make less time and effort to see my friends and family.”
One Silent Generation respondent commented, “I am semi-retired, I take no call, I work no weekends, I provide anesthesia care in my area of special expertise, I work clinically about 46 days a year. Life is good, particularly compared to my younger colleagues who are working 60-plus hours a week with evening work, weekend work, and call. I feel really sorry for them.”
When young people enter medical school, they’re quite healthy, with low rates of depression and burnout, said Dr. Yellowlees. Yet, studies have shown that rates of burnout and suicidal thoughts increased within 2 years. “That reflects what happens when a group of idealistic young people hit a horrible system,” he said.
Who’s responsible?
Millennials were three times as likely as baby boomers to say that a medical school or health care organization should be responsible when a student or physician commits suicide.
“Young physicians may expect more of their employers than my generation did, which we see in residency programs that have unionized,” said Dr. Yellowlees, a Baby Boomer.
“As more young doctors are employed by health care organizations, they also may expect more resources to be available to them, such as wellness programs,” he added.
Younger doctors also focus more on work-life balance than older doctors, including time off and having hobbies, he said. “They are much more rational in terms of their overall beliefs and expectations than the older generation.”
Whom doctors confide in
Nearly 60% of physician-respondents with suicidal thoughts said they confided in a professional or someone they knew. Men were just as likely as women to reach out to a therapist (38%), whereas men were slightly more likely to confide in a family member and women were slightly more likely to confide in a colleague.
“It’s interesting that women are more active in seeking support at work – they often have developed a network of colleagues to support each other’s careers and whom they can confide in,” said Dr. Yellowlees.
He emphasized that 40% of physicians said they didn’t confide in anyone when they had suicidal thoughts. Of those, just over half said they could cope without professional help.
One respondent commented, “It’s just a thought; nothing I would actually do.” Another commented, “Mental health professionals can’t fix the underlying reason for the problem.”
Many doctors were concerned about risking disclosure to their medical boards (42%); that it would show up on their insurance records (33%); and that their colleagues would find out (25%), according to the report.
One respondent commented, “I don’t trust doctors to keep it to themselves.”
Another barrier doctors mentioned was a lack of time to seek help. One commented, “Time. I have none, when am I supposed to find an hour for counseling?”
A version of this article originally appeared on Medscape.com.
A physician’s specialty can make a difference when it comes to having suicidal thoughts. Doctors who specialize in family medicine, obstetrics-gynecology, and psychiatry reported double the rates of suicidal thoughts than doctors in oncology, rheumatology, and pulmonary medicine, according to Doctors’ Burden: Medscape Physician Suicide Report 2023.
“The specialties with the highest reporting of physician suicidal thoughts are also those with the greatest physician shortages, based on the number of job openings posted by recruiting sites,” said Peter Yellowlees, MD, professor of psychiatry and chief wellness officer at UC Davis Health.
Doctors in those specialties are overworked, which can lead to burnout, he said.
There’s also a generational divide among physicians who reported suicidal thoughts. Millennials (age 27-41) and Gen-X physicians (age 42-56) were more likely to report these thoughts than were Baby Boomers (age 57-75) and the Silent Generation (age 76-95).
“Younger physicians are more burned out – they may have less control over their lives and less meaning than some older doctors who can do what they want,” said Dr. Yellowlees.
One millennial respondent commented that being on call and being required to chart detailed notes in the EHR has contributed to her burnout. “I’m more impatient and make less time and effort to see my friends and family.”
One Silent Generation respondent commented, “I am semi-retired, I take no call, I work no weekends, I provide anesthesia care in my area of special expertise, I work clinically about 46 days a year. Life is good, particularly compared to my younger colleagues who are working 60-plus hours a week with evening work, weekend work, and call. I feel really sorry for them.”
When young people enter medical school, they’re quite healthy, with low rates of depression and burnout, said Dr. Yellowlees. Yet, studies have shown that rates of burnout and suicidal thoughts increased within 2 years. “That reflects what happens when a group of idealistic young people hit a horrible system,” he said.
Who’s responsible?
Millennials were three times as likely as baby boomers to say that a medical school or health care organization should be responsible when a student or physician commits suicide.
“Young physicians may expect more of their employers than my generation did, which we see in residency programs that have unionized,” said Dr. Yellowlees, a Baby Boomer.
“As more young doctors are employed by health care organizations, they also may expect more resources to be available to them, such as wellness programs,” he added.
Younger doctors also focus more on work-life balance than older doctors, including time off and having hobbies, he said. “They are much more rational in terms of their overall beliefs and expectations than the older generation.”
Whom doctors confide in
Nearly 60% of physician-respondents with suicidal thoughts said they confided in a professional or someone they knew. Men were just as likely as women to reach out to a therapist (38%), whereas men were slightly more likely to confide in a family member and women were slightly more likely to confide in a colleague.
“It’s interesting that women are more active in seeking support at work – they often have developed a network of colleagues to support each other’s careers and whom they can confide in,” said Dr. Yellowlees.
He emphasized that 40% of physicians said they didn’t confide in anyone when they had suicidal thoughts. Of those, just over half said they could cope without professional help.
One respondent commented, “It’s just a thought; nothing I would actually do.” Another commented, “Mental health professionals can’t fix the underlying reason for the problem.”
Many doctors were concerned about risking disclosure to their medical boards (42%); that it would show up on their insurance records (33%); and that their colleagues would find out (25%), according to the report.
One respondent commented, “I don’t trust doctors to keep it to themselves.”
Another barrier doctors mentioned was a lack of time to seek help. One commented, “Time. I have none, when am I supposed to find an hour for counseling?”
A version of this article originally appeared on Medscape.com.
Heart-healthy actions promote longer, disease-free life
Adults who follow a heart-healthy lifestyle are more likely to live longer and to be free of chronic health conditions, based on data from a pair of related studies from the United States and United Kingdom involving nearly 200,000 individuals.
The studies, presented at the Epidemiology and Prevention/Lifestyle and Cardiometabolic Health meeting in Boston, assessed the impact of cardiovascular health on life expectancy and freedom from chronic diseases. Cardiovascular health (CVH) was based on the Life’s Essential 8 (LE8) score, a composite of health metrics released by the American Heart Association in 2022. The LE8 was developed to guide research and assessment of cardiovascular health, and includes diet, physical activity, tobacco/nicotine exposure, sleep, body mass index, non-HDL cholesterol, blood glucose, and blood pressure.
In one study, Xuan Wang, MD, a postdoctoral fellow and biostatistician in the department of epidemiology at Tulane University, New Orleans, and colleagues reviewed data from 136,599 adults in the United Kingdom Biobank who were free of cardiovascular disease, diabetes, cancer, and dementia at baseline, and for whom complete LE8 data were available.
CVH was classified as poor, intermediate, and ideal, defined as LE8 scores of less than 50, 50 to 80, and 80 or higher, respectively.
The goal of the study was to examine the role of CVH based on LE8 scores on the percentage of life expectancy free of chronic diseases.
Men and women with ideal CVH averaged 5.2 years and 6.3 years more of total life expectancy at age 50 years, compared with those with poor CVH. Out of total life expectancy, the percentage of life expectancy free of chronic diseases was 75.9% and 83.4% for men and women, respectively, compared with 64.9% and 69.4%, respectively, for men and women with poor CVH.
The researchers also found that disparities in the percentage of disease-free years for both men and women were reduced in the high CVH groups.
The findings were limited by several factors including the use of only CVD, diabetes, cancer, and dementia in the definition of “disease-free life expectancy,” the researchers noted in a press release accompanying the study. Other limitations include the lack of data on e-cigarettes, and the homogeneous White study population. More research is needed in diverse populations who experience a stronger impact from negative social determinants of health, they said.
In a second study, Hao Ma, MD, and colleagues reviewed data from 23,003 adults who participated in the National Health and Nutrition Examination Survey (NHANES) between 2005 and 2018 with mortality linked to the National Death Index through Dec. 31, 2019. The goal of the second study was to examine the association between CVH based on LE8 scores and life expectancy.
Over a median follow-up of 7.8 years, deaths occurred in 772 men and 587 women, said Dr. Ma, a postdoctoral fellow and biostatistician in epidemiology at Tulane University and coauthor on Dr. Wang’s study.
The estimated life expectancies at age 50 years for men with poor, intermediate, and ideal cardiovascular health based on the LE8 were 25.5 years, 31.2 years, and 33.1 years, respectively.
For women, the corresponding life expectancies for women at age 50 with poor, intermediate, and ideal CVH were 29.5 years, 34.2 years, and 38.4 years, respectively.
Men and women had similar gains in life expectancy from adhering to a heart-healthy lifestyle as defined by the LE8 score that reduced their risk of death from cardiovascular disease (41.8% and 44.1%, respectively).
Associations of cardiovascular health and life expectancy were similar for non-Hispanic Whites and non-Hispanic Blacks, but not among people of Mexican heritage, and more research is needed in diverse populations, the researchers wrote.
The study was limited by several factors including potential changes in cardiovascular health during the follow-up period, and by the limited analysis of racial and ethnic groups to non-Hispanic white, non-Hispanic Black, and people of Mexican heritage because of small sample sizes for other racial/ethnic groups, the researchers noted in a press release accompanying the study.
The message for clinicians and their patients is that adherence to cardiovascular health as defined by the LE8 will help not only extend life, but enhance quality of life, Dr. Xang and Dr. Ma said in an interview. “If your overall CVH score is low, we might be able to focus on one element first and improve them one by one,” they said. Sedentary lifestyle and an unhealthy diet are barriers to improving LE8 metrics that can be addressed, they added.
More research is needed to examine the effects of LE8 on high-risk patients, the researchers told this news organization. “No studies have yet focused on these patients with chronic diseases. We suspect that LE8 will play a role even in these high-risk groups,” they said. Further studies should include diverse populations and evaluations of the association between CVH change and health outcomes, they added.
“Overall, we see this 7.5-year difference [in life expectancy] going from poor to high cardiovascular health,” said Donald M. Lloyd-Jones, MD, of Northwestern University, Chicago, in a video accompanying the presentation of the study findings. The impact on life expectancy is yet another reason to motivate people to improve their cardiovascular health, said Dr. Lloyd-Jones, immediate past president of the American Heart Association and lead author on the writing group for Life’s Essential 8. “The earlier we do this, the better, and the greater the gains in life expectancy we’re likely to see in the U.S. population,” he said.
People maintaining high cardiovascular health into midlife are avoiding not only cardiovascular disease, but other chronic diseases of aging, Dr. Lloyd-Jones added. These conditions are delayed until much later in the lifespan, which allows people to enjoy better quality of life for more of their remaining years, he said.
The meeting was sponsored by the American Heart Association.
Both studies were supported by the National Heart, Lung, and Blood Institute and the National Institute of Diabetes and Digestive and Kidney Diseases, part of the National Institutes of Health; the Fogarty International Center; and the Tulane Research Centers of Excellence Awards. The researchers had no financial conflicts to disclose.
Adults who follow a heart-healthy lifestyle are more likely to live longer and to be free of chronic health conditions, based on data from a pair of related studies from the United States and United Kingdom involving nearly 200,000 individuals.
The studies, presented at the Epidemiology and Prevention/Lifestyle and Cardiometabolic Health meeting in Boston, assessed the impact of cardiovascular health on life expectancy and freedom from chronic diseases. Cardiovascular health (CVH) was based on the Life’s Essential 8 (LE8) score, a composite of health metrics released by the American Heart Association in 2022. The LE8 was developed to guide research and assessment of cardiovascular health, and includes diet, physical activity, tobacco/nicotine exposure, sleep, body mass index, non-HDL cholesterol, blood glucose, and blood pressure.
In one study, Xuan Wang, MD, a postdoctoral fellow and biostatistician in the department of epidemiology at Tulane University, New Orleans, and colleagues reviewed data from 136,599 adults in the United Kingdom Biobank who were free of cardiovascular disease, diabetes, cancer, and dementia at baseline, and for whom complete LE8 data were available.
CVH was classified as poor, intermediate, and ideal, defined as LE8 scores of less than 50, 50 to 80, and 80 or higher, respectively.
The goal of the study was to examine the role of CVH based on LE8 scores on the percentage of life expectancy free of chronic diseases.
Men and women with ideal CVH averaged 5.2 years and 6.3 years more of total life expectancy at age 50 years, compared with those with poor CVH. Out of total life expectancy, the percentage of life expectancy free of chronic diseases was 75.9% and 83.4% for men and women, respectively, compared with 64.9% and 69.4%, respectively, for men and women with poor CVH.
The researchers also found that disparities in the percentage of disease-free years for both men and women were reduced in the high CVH groups.
The findings were limited by several factors including the use of only CVD, diabetes, cancer, and dementia in the definition of “disease-free life expectancy,” the researchers noted in a press release accompanying the study. Other limitations include the lack of data on e-cigarettes, and the homogeneous White study population. More research is needed in diverse populations who experience a stronger impact from negative social determinants of health, they said.
In a second study, Hao Ma, MD, and colleagues reviewed data from 23,003 adults who participated in the National Health and Nutrition Examination Survey (NHANES) between 2005 and 2018 with mortality linked to the National Death Index through Dec. 31, 2019. The goal of the second study was to examine the association between CVH based on LE8 scores and life expectancy.
Over a median follow-up of 7.8 years, deaths occurred in 772 men and 587 women, said Dr. Ma, a postdoctoral fellow and biostatistician in epidemiology at Tulane University and coauthor on Dr. Wang’s study.
The estimated life expectancies at age 50 years for men with poor, intermediate, and ideal cardiovascular health based on the LE8 were 25.5 years, 31.2 years, and 33.1 years, respectively.
For women, the corresponding life expectancies for women at age 50 with poor, intermediate, and ideal CVH were 29.5 years, 34.2 years, and 38.4 years, respectively.
Men and women had similar gains in life expectancy from adhering to a heart-healthy lifestyle as defined by the LE8 score that reduced their risk of death from cardiovascular disease (41.8% and 44.1%, respectively).
Associations of cardiovascular health and life expectancy were similar for non-Hispanic Whites and non-Hispanic Blacks, but not among people of Mexican heritage, and more research is needed in diverse populations, the researchers wrote.
The study was limited by several factors including potential changes in cardiovascular health during the follow-up period, and by the limited analysis of racial and ethnic groups to non-Hispanic white, non-Hispanic Black, and people of Mexican heritage because of small sample sizes for other racial/ethnic groups, the researchers noted in a press release accompanying the study.
The message for clinicians and their patients is that adherence to cardiovascular health as defined by the LE8 will help not only extend life, but enhance quality of life, Dr. Xang and Dr. Ma said in an interview. “If your overall CVH score is low, we might be able to focus on one element first and improve them one by one,” they said. Sedentary lifestyle and an unhealthy diet are barriers to improving LE8 metrics that can be addressed, they added.
More research is needed to examine the effects of LE8 on high-risk patients, the researchers told this news organization. “No studies have yet focused on these patients with chronic diseases. We suspect that LE8 will play a role even in these high-risk groups,” they said. Further studies should include diverse populations and evaluations of the association between CVH change and health outcomes, they added.
“Overall, we see this 7.5-year difference [in life expectancy] going from poor to high cardiovascular health,” said Donald M. Lloyd-Jones, MD, of Northwestern University, Chicago, in a video accompanying the presentation of the study findings. The impact on life expectancy is yet another reason to motivate people to improve their cardiovascular health, said Dr. Lloyd-Jones, immediate past president of the American Heart Association and lead author on the writing group for Life’s Essential 8. “The earlier we do this, the better, and the greater the gains in life expectancy we’re likely to see in the U.S. population,” he said.
People maintaining high cardiovascular health into midlife are avoiding not only cardiovascular disease, but other chronic diseases of aging, Dr. Lloyd-Jones added. These conditions are delayed until much later in the lifespan, which allows people to enjoy better quality of life for more of their remaining years, he said.
The meeting was sponsored by the American Heart Association.
Both studies were supported by the National Heart, Lung, and Blood Institute and the National Institute of Diabetes and Digestive and Kidney Diseases, part of the National Institutes of Health; the Fogarty International Center; and the Tulane Research Centers of Excellence Awards. The researchers had no financial conflicts to disclose.
Adults who follow a heart-healthy lifestyle are more likely to live longer and to be free of chronic health conditions, based on data from a pair of related studies from the United States and United Kingdom involving nearly 200,000 individuals.
The studies, presented at the Epidemiology and Prevention/Lifestyle and Cardiometabolic Health meeting in Boston, assessed the impact of cardiovascular health on life expectancy and freedom from chronic diseases. Cardiovascular health (CVH) was based on the Life’s Essential 8 (LE8) score, a composite of health metrics released by the American Heart Association in 2022. The LE8 was developed to guide research and assessment of cardiovascular health, and includes diet, physical activity, tobacco/nicotine exposure, sleep, body mass index, non-HDL cholesterol, blood glucose, and blood pressure.
In one study, Xuan Wang, MD, a postdoctoral fellow and biostatistician in the department of epidemiology at Tulane University, New Orleans, and colleagues reviewed data from 136,599 adults in the United Kingdom Biobank who were free of cardiovascular disease, diabetes, cancer, and dementia at baseline, and for whom complete LE8 data were available.
CVH was classified as poor, intermediate, and ideal, defined as LE8 scores of less than 50, 50 to 80, and 80 or higher, respectively.
The goal of the study was to examine the role of CVH based on LE8 scores on the percentage of life expectancy free of chronic diseases.
Men and women with ideal CVH averaged 5.2 years and 6.3 years more of total life expectancy at age 50 years, compared with those with poor CVH. Out of total life expectancy, the percentage of life expectancy free of chronic diseases was 75.9% and 83.4% for men and women, respectively, compared with 64.9% and 69.4%, respectively, for men and women with poor CVH.
The researchers also found that disparities in the percentage of disease-free years for both men and women were reduced in the high CVH groups.
The findings were limited by several factors including the use of only CVD, diabetes, cancer, and dementia in the definition of “disease-free life expectancy,” the researchers noted in a press release accompanying the study. Other limitations include the lack of data on e-cigarettes, and the homogeneous White study population. More research is needed in diverse populations who experience a stronger impact from negative social determinants of health, they said.
In a second study, Hao Ma, MD, and colleagues reviewed data from 23,003 adults who participated in the National Health and Nutrition Examination Survey (NHANES) between 2005 and 2018 with mortality linked to the National Death Index through Dec. 31, 2019. The goal of the second study was to examine the association between CVH based on LE8 scores and life expectancy.
Over a median follow-up of 7.8 years, deaths occurred in 772 men and 587 women, said Dr. Ma, a postdoctoral fellow and biostatistician in epidemiology at Tulane University and coauthor on Dr. Wang’s study.
The estimated life expectancies at age 50 years for men with poor, intermediate, and ideal cardiovascular health based on the LE8 were 25.5 years, 31.2 years, and 33.1 years, respectively.
For women, the corresponding life expectancies for women at age 50 with poor, intermediate, and ideal CVH were 29.5 years, 34.2 years, and 38.4 years, respectively.
Men and women had similar gains in life expectancy from adhering to a heart-healthy lifestyle as defined by the LE8 score that reduced their risk of death from cardiovascular disease (41.8% and 44.1%, respectively).
Associations of cardiovascular health and life expectancy were similar for non-Hispanic Whites and non-Hispanic Blacks, but not among people of Mexican heritage, and more research is needed in diverse populations, the researchers wrote.
The study was limited by several factors including potential changes in cardiovascular health during the follow-up period, and by the limited analysis of racial and ethnic groups to non-Hispanic white, non-Hispanic Black, and people of Mexican heritage because of small sample sizes for other racial/ethnic groups, the researchers noted in a press release accompanying the study.
The message for clinicians and their patients is that adherence to cardiovascular health as defined by the LE8 will help not only extend life, but enhance quality of life, Dr. Xang and Dr. Ma said in an interview. “If your overall CVH score is low, we might be able to focus on one element first and improve them one by one,” they said. Sedentary lifestyle and an unhealthy diet are barriers to improving LE8 metrics that can be addressed, they added.
More research is needed to examine the effects of LE8 on high-risk patients, the researchers told this news organization. “No studies have yet focused on these patients with chronic diseases. We suspect that LE8 will play a role even in these high-risk groups,” they said. Further studies should include diverse populations and evaluations of the association between CVH change and health outcomes, they added.
“Overall, we see this 7.5-year difference [in life expectancy] going from poor to high cardiovascular health,” said Donald M. Lloyd-Jones, MD, of Northwestern University, Chicago, in a video accompanying the presentation of the study findings. The impact on life expectancy is yet another reason to motivate people to improve their cardiovascular health, said Dr. Lloyd-Jones, immediate past president of the American Heart Association and lead author on the writing group for Life’s Essential 8. “The earlier we do this, the better, and the greater the gains in life expectancy we’re likely to see in the U.S. population,” he said.
People maintaining high cardiovascular health into midlife are avoiding not only cardiovascular disease, but other chronic diseases of aging, Dr. Lloyd-Jones added. These conditions are delayed until much later in the lifespan, which allows people to enjoy better quality of life for more of their remaining years, he said.
The meeting was sponsored by the American Heart Association.
Both studies were supported by the National Heart, Lung, and Blood Institute and the National Institute of Diabetes and Digestive and Kidney Diseases, part of the National Institutes of Health; the Fogarty International Center; and the Tulane Research Centers of Excellence Awards. The researchers had no financial conflicts to disclose.
FROM EPI/LIFESTYLE 2023
Keto/paleo diets ‘lower quality than others,’ and bad for planet
suggests a new analysis that reveals meat-based, as well as keto and paleo diets, to be the worst on both measures.
The research was published online in The American Journal of Clinical Nutrition.
To obtain a real-world view on the environmental and health impact of diets as consumed by U.S. adults, the team examined a nationally representative survey of the 1-day eating habits of more than 16,000 individuals.
This revealed that the best quality diet was pescatarian, followed by vegetarian and vegan diets. Omnivore diets, although less healthy, tended to score better than keto and paleo diets, which were the lowest ranked.
Both keto and paleo diets tend to be higher in animal foods and lower in plant foods than other popular diets, the researchers explain in their study, and they both have been associated with negative effects on blood lipids, specifically increased LDL cholesterol, raising concern about the long-term health outcomes associated with these diets.”
Analysis of the environmental impact of the different eating patterns showed that the vegan diet had the lowest carbon footprint, followed by the vegetarian and pescatarian diets. The omnivore, paleo, and keto diets had a far higher carbon footprint, with that of the keto diet more than four times greater than that for a vegan diet.
“Climate change is arguably one of the most pressing problems of our time, and a lot of people are interested in moving to a plant-based diet,” said senior author Diego Rose, PhD, MPH, RD, in a press release.
“Based on our results, that would reduce your footprint and be generally healthy,” noted Dr. Rose, nutrition program director, Tulane University, New Orleans.
To determine the carbon footprint and quality of popular diets as they are consumed by U.S. adults, Keelia O’Malley, PhD, MPH, Amelia Willits-Smith, PhD, MSc, and Dr. Rose, all with Tulane University, studied 24-hour recall data from the ongoing, nationally representative National Health and Nutrition Examination Survey (NHANES) for the years 2005-2010.
The data, which was captured by trained interviewers using a validated tool, was matched with the U.S. Department of Agriculture Food Patterns Equivalents Database to categorize the participants into one of six mutually exclusive categories: vegan, vegetarian, pescatarian, keto, paleo, or omnivore.
The omnivore category included anyone who did not fit into any of the preceding categories.
The environmental impact of the diets was then calculated by matching the established greenhouse gas emissions (GHGE) of over 300 commodities to foods listed on the NHANES, which was then summarized for each individual to give a carbon footprint for their 1-day diet.
Finally, the quality of their diet was estimated using the 2010 versions of the Healthy Eating Index and the Alternate Healthy Eating Index, both of which award a score to food components based on their impact on health.
Overall, 16,412 individuals were included in the analysis, of whom 52.1% were female.
The most common diet was omnivore, which was followed by 83.6% of respondents, followed by vegetarian (7.5%), pescatarian (4.7%), vegan (0.7%), keto (0.4%), and paleo diets (0.3%).
The lowest carbon footprint was seen with a vegan diet, at an average of 0.69 kg of carbon dioxide equivalents per 1,000 kcal consumed, followed by a vegetarian diet (1.16 kg of carbon dioxide equivalents per 1,000 kcal) and pescatarian diet (1.66 kg of carbon dioxide equivalents per 1,000 kcal).
The highest carbon footprints were observed with the omnivore (2.23 kg of carbon dioxide equivalents per 1,000 kcal), paleo (2.62 kg of carbon dioxide equivalents per 1,000 kcal), and keto diets (2.91 kg of carbon dioxide equivalents per 1,000 kcal).
In terms of diet quality, the pescatarian diet was ranked the highest on both eating index scores, followed by the vegetarian, then vegan, diets. The order of the three lowest scores depended on the index used, with either the keto or paleo diet deemed to be the worst quality.
Analysis of individuals following an omnivore diet suggested that those who ate in line with the DASH or Mediterranean diets had higher diet quality, as well as a lower environmental impact, than other people within the group.
Hence, Dr. Rose observed, “Our research ... shows there is a way to improve your health and footprint without giving up meat entirely.”
The researchers acknowledge that the use of 1-day diets has limitations, including that whatever individuals may have eaten during those 24 hours may not correspond to their overall day-in, day-out diet.
The study was supported by the Wellcome Trust. Dr. Rose declares relationships with the Center for Biological Diversity, the NCI, and the Health Resources and Services Administration. Dr. Willits-Smith has received funding from CBD and NCI. Dr. O’Malley has received funding from HRSA.
A version of this article first appeared on Medscape.com.
suggests a new analysis that reveals meat-based, as well as keto and paleo diets, to be the worst on both measures.
The research was published online in The American Journal of Clinical Nutrition.
To obtain a real-world view on the environmental and health impact of diets as consumed by U.S. adults, the team examined a nationally representative survey of the 1-day eating habits of more than 16,000 individuals.
This revealed that the best quality diet was pescatarian, followed by vegetarian and vegan diets. Omnivore diets, although less healthy, tended to score better than keto and paleo diets, which were the lowest ranked.
Both keto and paleo diets tend to be higher in animal foods and lower in plant foods than other popular diets, the researchers explain in their study, and they both have been associated with negative effects on blood lipids, specifically increased LDL cholesterol, raising concern about the long-term health outcomes associated with these diets.”
Analysis of the environmental impact of the different eating patterns showed that the vegan diet had the lowest carbon footprint, followed by the vegetarian and pescatarian diets. The omnivore, paleo, and keto diets had a far higher carbon footprint, with that of the keto diet more than four times greater than that for a vegan diet.
“Climate change is arguably one of the most pressing problems of our time, and a lot of people are interested in moving to a plant-based diet,” said senior author Diego Rose, PhD, MPH, RD, in a press release.
“Based on our results, that would reduce your footprint and be generally healthy,” noted Dr. Rose, nutrition program director, Tulane University, New Orleans.
To determine the carbon footprint and quality of popular diets as they are consumed by U.S. adults, Keelia O’Malley, PhD, MPH, Amelia Willits-Smith, PhD, MSc, and Dr. Rose, all with Tulane University, studied 24-hour recall data from the ongoing, nationally representative National Health and Nutrition Examination Survey (NHANES) for the years 2005-2010.
The data, which was captured by trained interviewers using a validated tool, was matched with the U.S. Department of Agriculture Food Patterns Equivalents Database to categorize the participants into one of six mutually exclusive categories: vegan, vegetarian, pescatarian, keto, paleo, or omnivore.
The omnivore category included anyone who did not fit into any of the preceding categories.
The environmental impact of the diets was then calculated by matching the established greenhouse gas emissions (GHGE) of over 300 commodities to foods listed on the NHANES, which was then summarized for each individual to give a carbon footprint for their 1-day diet.
Finally, the quality of their diet was estimated using the 2010 versions of the Healthy Eating Index and the Alternate Healthy Eating Index, both of which award a score to food components based on their impact on health.
Overall, 16,412 individuals were included in the analysis, of whom 52.1% were female.
The most common diet was omnivore, which was followed by 83.6% of respondents, followed by vegetarian (7.5%), pescatarian (4.7%), vegan (0.7%), keto (0.4%), and paleo diets (0.3%).
The lowest carbon footprint was seen with a vegan diet, at an average of 0.69 kg of carbon dioxide equivalents per 1,000 kcal consumed, followed by a vegetarian diet (1.16 kg of carbon dioxide equivalents per 1,000 kcal) and pescatarian diet (1.66 kg of carbon dioxide equivalents per 1,000 kcal).
The highest carbon footprints were observed with the omnivore (2.23 kg of carbon dioxide equivalents per 1,000 kcal), paleo (2.62 kg of carbon dioxide equivalents per 1,000 kcal), and keto diets (2.91 kg of carbon dioxide equivalents per 1,000 kcal).
In terms of diet quality, the pescatarian diet was ranked the highest on both eating index scores, followed by the vegetarian, then vegan, diets. The order of the three lowest scores depended on the index used, with either the keto or paleo diet deemed to be the worst quality.
Analysis of individuals following an omnivore diet suggested that those who ate in line with the DASH or Mediterranean diets had higher diet quality, as well as a lower environmental impact, than other people within the group.
Hence, Dr. Rose observed, “Our research ... shows there is a way to improve your health and footprint without giving up meat entirely.”
The researchers acknowledge that the use of 1-day diets has limitations, including that whatever individuals may have eaten during those 24 hours may not correspond to their overall day-in, day-out diet.
The study was supported by the Wellcome Trust. Dr. Rose declares relationships with the Center for Biological Diversity, the NCI, and the Health Resources and Services Administration. Dr. Willits-Smith has received funding from CBD and NCI. Dr. O’Malley has received funding from HRSA.
A version of this article first appeared on Medscape.com.
suggests a new analysis that reveals meat-based, as well as keto and paleo diets, to be the worst on both measures.
The research was published online in The American Journal of Clinical Nutrition.
To obtain a real-world view on the environmental and health impact of diets as consumed by U.S. adults, the team examined a nationally representative survey of the 1-day eating habits of more than 16,000 individuals.
This revealed that the best quality diet was pescatarian, followed by vegetarian and vegan diets. Omnivore diets, although less healthy, tended to score better than keto and paleo diets, which were the lowest ranked.
Both keto and paleo diets tend to be higher in animal foods and lower in plant foods than other popular diets, the researchers explain in their study, and they both have been associated with negative effects on blood lipids, specifically increased LDL cholesterol, raising concern about the long-term health outcomes associated with these diets.”
Analysis of the environmental impact of the different eating patterns showed that the vegan diet had the lowest carbon footprint, followed by the vegetarian and pescatarian diets. The omnivore, paleo, and keto diets had a far higher carbon footprint, with that of the keto diet more than four times greater than that for a vegan diet.
“Climate change is arguably one of the most pressing problems of our time, and a lot of people are interested in moving to a plant-based diet,” said senior author Diego Rose, PhD, MPH, RD, in a press release.
“Based on our results, that would reduce your footprint and be generally healthy,” noted Dr. Rose, nutrition program director, Tulane University, New Orleans.
To determine the carbon footprint and quality of popular diets as they are consumed by U.S. adults, Keelia O’Malley, PhD, MPH, Amelia Willits-Smith, PhD, MSc, and Dr. Rose, all with Tulane University, studied 24-hour recall data from the ongoing, nationally representative National Health and Nutrition Examination Survey (NHANES) for the years 2005-2010.
The data, which was captured by trained interviewers using a validated tool, was matched with the U.S. Department of Agriculture Food Patterns Equivalents Database to categorize the participants into one of six mutually exclusive categories: vegan, vegetarian, pescatarian, keto, paleo, or omnivore.
The omnivore category included anyone who did not fit into any of the preceding categories.
The environmental impact of the diets was then calculated by matching the established greenhouse gas emissions (GHGE) of over 300 commodities to foods listed on the NHANES, which was then summarized for each individual to give a carbon footprint for their 1-day diet.
Finally, the quality of their diet was estimated using the 2010 versions of the Healthy Eating Index and the Alternate Healthy Eating Index, both of which award a score to food components based on their impact on health.
Overall, 16,412 individuals were included in the analysis, of whom 52.1% were female.
The most common diet was omnivore, which was followed by 83.6% of respondents, followed by vegetarian (7.5%), pescatarian (4.7%), vegan (0.7%), keto (0.4%), and paleo diets (0.3%).
The lowest carbon footprint was seen with a vegan diet, at an average of 0.69 kg of carbon dioxide equivalents per 1,000 kcal consumed, followed by a vegetarian diet (1.16 kg of carbon dioxide equivalents per 1,000 kcal) and pescatarian diet (1.66 kg of carbon dioxide equivalents per 1,000 kcal).
The highest carbon footprints were observed with the omnivore (2.23 kg of carbon dioxide equivalents per 1,000 kcal), paleo (2.62 kg of carbon dioxide equivalents per 1,000 kcal), and keto diets (2.91 kg of carbon dioxide equivalents per 1,000 kcal).
In terms of diet quality, the pescatarian diet was ranked the highest on both eating index scores, followed by the vegetarian, then vegan, diets. The order of the three lowest scores depended on the index used, with either the keto or paleo diet deemed to be the worst quality.
Analysis of individuals following an omnivore diet suggested that those who ate in line with the DASH or Mediterranean diets had higher diet quality, as well as a lower environmental impact, than other people within the group.
Hence, Dr. Rose observed, “Our research ... shows there is a way to improve your health and footprint without giving up meat entirely.”
The researchers acknowledge that the use of 1-day diets has limitations, including that whatever individuals may have eaten during those 24 hours may not correspond to their overall day-in, day-out diet.
The study was supported by the Wellcome Trust. Dr. Rose declares relationships with the Center for Biological Diversity, the NCI, and the Health Resources and Services Administration. Dr. Willits-Smith has received funding from CBD and NCI. Dr. O’Malley has received funding from HRSA.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF CLINICAL NUTRITION
Even mild COVID is hard on the brain
early research suggests.
“Our results suggest a severe pattern of changes in how the brain communicates as well as its structure, mainly in people with anxiety and depression with long-COVID syndrome, which affects so many people,” study investigator Clarissa Yasuda, MD, PhD, from University of Campinas, São Paulo, said in a news release.
“The magnitude of these changes suggests that they could lead to problems with memory and thinking skills, so we need to be exploring holistic treatments even for people mildly affected by COVID-19,” Dr. Yasuda added.
The findings were released March 6 ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology.
Brain shrinkage
Some studies have shown a high prevalence of symptoms of anxiety and depression in COVID-19 survivors, but few have investigated the associated cerebral changes, Dr. Yasuda told this news organization.
The study included 254 adults (177 women, 77 men, median age 41 years) who had mild COVID-19 a median of 82 days earlier. A total of 102 had symptoms of both anxiety and depression, and 152 had no such symptoms.
On brain imaging, those with COVID-19 and anxiety and depression had atrophy in the limbic area of the brain, which plays a role in memory and emotional processing.
No shrinkage in this area was evident in people who had COVID-19 without anxiety and depression or in a healthy control group of individuals without COVID-19.
The researchers also observed a “severe” pattern of abnormal cerebral functional connectivity in those with COVID-19 and anxiety and depression.
In this functional connectivity analysis, individuals with COVID-19 and anxiety and depression had widespread functional changes in each of the 12 networks assessed, while those with COVID-19 but without symptoms of anxiety and depression showed changes in only 5 networks.
Mechanisms unclear
“Unfortunately, the underpinning mechanisms associated with brain changes and neuropsychiatric dysfunction after COVID-19 infection are unclear,” Dr. Yasuda told this news organization.
“Some studies have demonstrated an association between symptoms of anxiety and depression with inflammation. However, we hypothesize that these cerebral alterations may result from a more complex interaction of social, psychological, and systemic stressors, including inflammation. It is indeed intriguing that such alterations are present in individuals who presented mild acute infection,” Dr. Yasuda added.
“Symptoms of anxiety and depression are frequently observed after COVID-19 and are part of long-COVID syndrome for some individuals. These symptoms require adequate treatment to improve the quality of life, cognition, and work capacity,” she said.
Treating these symptoms may induce “brain plasticity, which may result in some degree of gray matter increase and eventually prevent further structural and functional damage,” Dr. Yasuda said.
A limitation of the study was that symptoms of anxiety and depression were self-reported, meaning people may have misjudged or misreported symptoms.
Commenting on the findings for this news organization, Cyrus Raji, MD, PhD, with the Mallinckrodt Institute of Radiology, Washington University, St. Louis, said the idea that COVID-19 is bad for the brain isn’t new. Dr. Raji was not involved with the study.
Early in the pandemic, Dr. Raji and colleagues published a paper detailing COVID-19’s effects on the brain, and Dr. Raji followed it up with a TED talk on the subject.
“Within the growing framework of what we already know about COVID-19 infection and its adverse effects on the brain, this work incrementally adds to this knowledge by identifying functional and structural neuroimaging abnormalities related to anxiety and depression in persons suffering from COVID-19 infection,” Dr. Raji said.
The study was supported by the São Paulo Research Foundation. The authors have no relevant disclosures. Raji is a consultant for Brainreader, Apollo Health, Pacific Neuroscience Foundation, and Neurevolution LLC.
early research suggests.
“Our results suggest a severe pattern of changes in how the brain communicates as well as its structure, mainly in people with anxiety and depression with long-COVID syndrome, which affects so many people,” study investigator Clarissa Yasuda, MD, PhD, from University of Campinas, São Paulo, said in a news release.
“The magnitude of these changes suggests that they could lead to problems with memory and thinking skills, so we need to be exploring holistic treatments even for people mildly affected by COVID-19,” Dr. Yasuda added.
The findings were released March 6 ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology.
Brain shrinkage
Some studies have shown a high prevalence of symptoms of anxiety and depression in COVID-19 survivors, but few have investigated the associated cerebral changes, Dr. Yasuda told this news organization.
The study included 254 adults (177 women, 77 men, median age 41 years) who had mild COVID-19 a median of 82 days earlier. A total of 102 had symptoms of both anxiety and depression, and 152 had no such symptoms.
On brain imaging, those with COVID-19 and anxiety and depression had atrophy in the limbic area of the brain, which plays a role in memory and emotional processing.
No shrinkage in this area was evident in people who had COVID-19 without anxiety and depression or in a healthy control group of individuals without COVID-19.
The researchers also observed a “severe” pattern of abnormal cerebral functional connectivity in those with COVID-19 and anxiety and depression.
In this functional connectivity analysis, individuals with COVID-19 and anxiety and depression had widespread functional changes in each of the 12 networks assessed, while those with COVID-19 but without symptoms of anxiety and depression showed changes in only 5 networks.
Mechanisms unclear
“Unfortunately, the underpinning mechanisms associated with brain changes and neuropsychiatric dysfunction after COVID-19 infection are unclear,” Dr. Yasuda told this news organization.
“Some studies have demonstrated an association between symptoms of anxiety and depression with inflammation. However, we hypothesize that these cerebral alterations may result from a more complex interaction of social, psychological, and systemic stressors, including inflammation. It is indeed intriguing that such alterations are present in individuals who presented mild acute infection,” Dr. Yasuda added.
“Symptoms of anxiety and depression are frequently observed after COVID-19 and are part of long-COVID syndrome for some individuals. These symptoms require adequate treatment to improve the quality of life, cognition, and work capacity,” she said.
Treating these symptoms may induce “brain plasticity, which may result in some degree of gray matter increase and eventually prevent further structural and functional damage,” Dr. Yasuda said.
A limitation of the study was that symptoms of anxiety and depression were self-reported, meaning people may have misjudged or misreported symptoms.
Commenting on the findings for this news organization, Cyrus Raji, MD, PhD, with the Mallinckrodt Institute of Radiology, Washington University, St. Louis, said the idea that COVID-19 is bad for the brain isn’t new. Dr. Raji was not involved with the study.
Early in the pandemic, Dr. Raji and colleagues published a paper detailing COVID-19’s effects on the brain, and Dr. Raji followed it up with a TED talk on the subject.
“Within the growing framework of what we already know about COVID-19 infection and its adverse effects on the brain, this work incrementally adds to this knowledge by identifying functional and structural neuroimaging abnormalities related to anxiety and depression in persons suffering from COVID-19 infection,” Dr. Raji said.
The study was supported by the São Paulo Research Foundation. The authors have no relevant disclosures. Raji is a consultant for Brainreader, Apollo Health, Pacific Neuroscience Foundation, and Neurevolution LLC.
early research suggests.
“Our results suggest a severe pattern of changes in how the brain communicates as well as its structure, mainly in people with anxiety and depression with long-COVID syndrome, which affects so many people,” study investigator Clarissa Yasuda, MD, PhD, from University of Campinas, São Paulo, said in a news release.
“The magnitude of these changes suggests that they could lead to problems with memory and thinking skills, so we need to be exploring holistic treatments even for people mildly affected by COVID-19,” Dr. Yasuda added.
The findings were released March 6 ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology.
Brain shrinkage
Some studies have shown a high prevalence of symptoms of anxiety and depression in COVID-19 survivors, but few have investigated the associated cerebral changes, Dr. Yasuda told this news organization.
The study included 254 adults (177 women, 77 men, median age 41 years) who had mild COVID-19 a median of 82 days earlier. A total of 102 had symptoms of both anxiety and depression, and 152 had no such symptoms.
On brain imaging, those with COVID-19 and anxiety and depression had atrophy in the limbic area of the brain, which plays a role in memory and emotional processing.
No shrinkage in this area was evident in people who had COVID-19 without anxiety and depression or in a healthy control group of individuals without COVID-19.
The researchers also observed a “severe” pattern of abnormal cerebral functional connectivity in those with COVID-19 and anxiety and depression.
In this functional connectivity analysis, individuals with COVID-19 and anxiety and depression had widespread functional changes in each of the 12 networks assessed, while those with COVID-19 but without symptoms of anxiety and depression showed changes in only 5 networks.
Mechanisms unclear
“Unfortunately, the underpinning mechanisms associated with brain changes and neuropsychiatric dysfunction after COVID-19 infection are unclear,” Dr. Yasuda told this news organization.
“Some studies have demonstrated an association between symptoms of anxiety and depression with inflammation. However, we hypothesize that these cerebral alterations may result from a more complex interaction of social, psychological, and systemic stressors, including inflammation. It is indeed intriguing that such alterations are present in individuals who presented mild acute infection,” Dr. Yasuda added.
“Symptoms of anxiety and depression are frequently observed after COVID-19 and are part of long-COVID syndrome for some individuals. These symptoms require adequate treatment to improve the quality of life, cognition, and work capacity,” she said.
Treating these symptoms may induce “brain plasticity, which may result in some degree of gray matter increase and eventually prevent further structural and functional damage,” Dr. Yasuda said.
A limitation of the study was that symptoms of anxiety and depression were self-reported, meaning people may have misjudged or misreported symptoms.
Commenting on the findings for this news organization, Cyrus Raji, MD, PhD, with the Mallinckrodt Institute of Radiology, Washington University, St. Louis, said the idea that COVID-19 is bad for the brain isn’t new. Dr. Raji was not involved with the study.
Early in the pandemic, Dr. Raji and colleagues published a paper detailing COVID-19’s effects on the brain, and Dr. Raji followed it up with a TED talk on the subject.
“Within the growing framework of what we already know about COVID-19 infection and its adverse effects on the brain, this work incrementally adds to this knowledge by identifying functional and structural neuroimaging abnormalities related to anxiety and depression in persons suffering from COVID-19 infection,” Dr. Raji said.
The study was supported by the São Paulo Research Foundation. The authors have no relevant disclosures. Raji is a consultant for Brainreader, Apollo Health, Pacific Neuroscience Foundation, and Neurevolution LLC.
High CV risk factor burden in young adults a ‘smoldering’ crisis
New data show a high and rising burden of most cardiovascular (CV) risk factors among young adults aged 20-44 years in the United States.
In this age group, over the past 10 years, there has been an increase in the prevalence of diabetes and obesity, no improvement in the prevalence of hypertension, and a decrease in the prevalence of hyperlipidemia.
Yet medical treatment rates for CV risk factors are “surprisingly” low among young adults, study investigator Rishi Wadhera, MD, with Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, told this news organization.
The findings are “extremely concerning. We’re witnessing a smoldering public health crisis. The onset of these risk factors earlier in life is associated with a higher lifetime risk of heart disease and potentially life-threatening,” Dr. Wadhera added.
The study was presented March 5 at the joint scientific sessions of the American College of Cardiology and the World Heart Federation and was simultaneously published in JAMA.
The burden of CV risk factors among young adults is “unacceptably high and increasing,” write the co-authors of a JAMA editorial.
“The time is now for aggressive preventive measures in young adults. Without immediate action there will continue to be a rise in heart disease and the burden it places on patients, families, and communities,” say Norrina Allen, PhD, and John Wilkins, MD, with Northwestern University, Chicago.
Preventing a tsunami of heart disease
The findings stem from a cross-sectional study of 12,294 U.S. adults aged 20-44 years (mean age, 32; 51% women) who participated in National Health and Nutrition Examination Survey (NHANES) cycles for 2009-2010 to 2017-2020.
Overall, the prevalence of hypertension was 9.3% in 2009-2010 and increased to 11.5% in 2017-2020. The prevalence of diabetes rose from 3.0% to 4.1%, and the prevalence of obesity rose from 32.7% to 40.9%. The prevalence of hyperlipidemia decreased from 40.5% to 36.1%.
Black adults consistently had high rates of hypertension during the study period – 16.2% in 2009-2010 and 20.1% in 2017-2020 – and significant increases in hypertension occurred among Mexican American adults (from 6.5% to 9.5%) and other Hispanic adults (from 4.4% to 10.5%), while Mexican American adults had a significant uptick in diabetes (from 4.3% to 7.5%).
Equally concerning, said Dr. Wadhera, is the fact that only about 55% of young adults with hypertension were receiving antihypertensive medication, and just 1 in 2 young adults with diabetes were receiving treatment. “These low rates were driven, in part, by many young adults not being aware of their diagnosis,” he noted.
The NHANES data also show that the percentage of young adults who were treated for hypertension and who achieved blood pressure control did not change significantly over the study period (65.0% in 2009-2010 and 74.8% in 2017-2020). Blood sugar control among young adults being treated for diabetes remained suboptimal throughout the study period (45.5% in 2009-2010 and 56.6% in 2017-2020).
“The fact that blood pressure control and glycemic control are so poor is really worrisome,” Jeffrey Berger, MD, director of the Center for the Prevention of Cardiovascular Disease at NYU Langone Heart, who wasn’t involved in the study, told this news organization.
“Even in the lipid control, while it did get a little bit better, it’s still only around 30%-40%. So, I think we have ways to go as a society,” Dr. Berger noted.
Double down on screening
Dr. Wadhera said “we need to double down on efforts to screen for and treat cardiovascular risk factors like high blood pressure and diabetes in young adults. We need to intensify clinical and public health interventions focused on primordial and primary prevention in young adults now so that we can avoid a tsunami of cardiovascular disease in the long term.”
“It’s critically important that young adults speak with their health care provider about whether – and when – they should undergo screening for high blood pressure, diabetes, and high cholesterol,” Dr. Wadhera added.
Dr. Berger said one problem is that younger people often have a “superman or superwoman” view and don’t comprehend that they are at risk for some of these conditions. Studies such as this “reinforce the idea that it’s never too young to be checked out.”
As a cardiologist who specializes in cardiovascular prevention, Dr. Berger said he sometimes hears patients say things like, “I don’t ever want to need a cardiologist,” or “I hope I never need a cardiologist.”
“My response is, ‘There are many different types of cardiologists,’ and I think it would really be helpful for many people to see a prevention-focused cardiologist way before they have problems,” he said in an interview.
“As a system, medicine has become very good at treating patients with different diseases. I think we need to get better in terms of preventing some of these problems,” Dr. Berger added.
In their editorial, Dr. Allen and Dr. Wilkins say the “foundation of cardiovascular health begins early in life. These worsening trends in risk factors highlight the importance of focusing on prevention in adolescence and young adulthood in order to promote cardiovascular health across the lifetime.”
The study was funded by a grant from the National Heart, Lung, and Blood Institute. Dr. Wadhera has served as a consultant for Abbott and CVS Health. Dr. Wilkins has received personal fees from 3M. Dr. Berger has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New data show a high and rising burden of most cardiovascular (CV) risk factors among young adults aged 20-44 years in the United States.
In this age group, over the past 10 years, there has been an increase in the prevalence of diabetes and obesity, no improvement in the prevalence of hypertension, and a decrease in the prevalence of hyperlipidemia.
Yet medical treatment rates for CV risk factors are “surprisingly” low among young adults, study investigator Rishi Wadhera, MD, with Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, told this news organization.
The findings are “extremely concerning. We’re witnessing a smoldering public health crisis. The onset of these risk factors earlier in life is associated with a higher lifetime risk of heart disease and potentially life-threatening,” Dr. Wadhera added.
The study was presented March 5 at the joint scientific sessions of the American College of Cardiology and the World Heart Federation and was simultaneously published in JAMA.
The burden of CV risk factors among young adults is “unacceptably high and increasing,” write the co-authors of a JAMA editorial.
“The time is now for aggressive preventive measures in young adults. Without immediate action there will continue to be a rise in heart disease and the burden it places on patients, families, and communities,” say Norrina Allen, PhD, and John Wilkins, MD, with Northwestern University, Chicago.
Preventing a tsunami of heart disease
The findings stem from a cross-sectional study of 12,294 U.S. adults aged 20-44 years (mean age, 32; 51% women) who participated in National Health and Nutrition Examination Survey (NHANES) cycles for 2009-2010 to 2017-2020.
Overall, the prevalence of hypertension was 9.3% in 2009-2010 and increased to 11.5% in 2017-2020. The prevalence of diabetes rose from 3.0% to 4.1%, and the prevalence of obesity rose from 32.7% to 40.9%. The prevalence of hyperlipidemia decreased from 40.5% to 36.1%.
Black adults consistently had high rates of hypertension during the study period – 16.2% in 2009-2010 and 20.1% in 2017-2020 – and significant increases in hypertension occurred among Mexican American adults (from 6.5% to 9.5%) and other Hispanic adults (from 4.4% to 10.5%), while Mexican American adults had a significant uptick in diabetes (from 4.3% to 7.5%).
Equally concerning, said Dr. Wadhera, is the fact that only about 55% of young adults with hypertension were receiving antihypertensive medication, and just 1 in 2 young adults with diabetes were receiving treatment. “These low rates were driven, in part, by many young adults not being aware of their diagnosis,” he noted.
The NHANES data also show that the percentage of young adults who were treated for hypertension and who achieved blood pressure control did not change significantly over the study period (65.0% in 2009-2010 and 74.8% in 2017-2020). Blood sugar control among young adults being treated for diabetes remained suboptimal throughout the study period (45.5% in 2009-2010 and 56.6% in 2017-2020).
“The fact that blood pressure control and glycemic control are so poor is really worrisome,” Jeffrey Berger, MD, director of the Center for the Prevention of Cardiovascular Disease at NYU Langone Heart, who wasn’t involved in the study, told this news organization.
“Even in the lipid control, while it did get a little bit better, it’s still only around 30%-40%. So, I think we have ways to go as a society,” Dr. Berger noted.
Double down on screening
Dr. Wadhera said “we need to double down on efforts to screen for and treat cardiovascular risk factors like high blood pressure and diabetes in young adults. We need to intensify clinical and public health interventions focused on primordial and primary prevention in young adults now so that we can avoid a tsunami of cardiovascular disease in the long term.”
“It’s critically important that young adults speak with their health care provider about whether – and when – they should undergo screening for high blood pressure, diabetes, and high cholesterol,” Dr. Wadhera added.
Dr. Berger said one problem is that younger people often have a “superman or superwoman” view and don’t comprehend that they are at risk for some of these conditions. Studies such as this “reinforce the idea that it’s never too young to be checked out.”
As a cardiologist who specializes in cardiovascular prevention, Dr. Berger said he sometimes hears patients say things like, “I don’t ever want to need a cardiologist,” or “I hope I never need a cardiologist.”
“My response is, ‘There are many different types of cardiologists,’ and I think it would really be helpful for many people to see a prevention-focused cardiologist way before they have problems,” he said in an interview.
“As a system, medicine has become very good at treating patients with different diseases. I think we need to get better in terms of preventing some of these problems,” Dr. Berger added.
In their editorial, Dr. Allen and Dr. Wilkins say the “foundation of cardiovascular health begins early in life. These worsening trends in risk factors highlight the importance of focusing on prevention in adolescence and young adulthood in order to promote cardiovascular health across the lifetime.”
The study was funded by a grant from the National Heart, Lung, and Blood Institute. Dr. Wadhera has served as a consultant for Abbott and CVS Health. Dr. Wilkins has received personal fees from 3M. Dr. Berger has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New data show a high and rising burden of most cardiovascular (CV) risk factors among young adults aged 20-44 years in the United States.
In this age group, over the past 10 years, there has been an increase in the prevalence of diabetes and obesity, no improvement in the prevalence of hypertension, and a decrease in the prevalence of hyperlipidemia.
Yet medical treatment rates for CV risk factors are “surprisingly” low among young adults, study investigator Rishi Wadhera, MD, with Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, told this news organization.
The findings are “extremely concerning. We’re witnessing a smoldering public health crisis. The onset of these risk factors earlier in life is associated with a higher lifetime risk of heart disease and potentially life-threatening,” Dr. Wadhera added.
The study was presented March 5 at the joint scientific sessions of the American College of Cardiology and the World Heart Federation and was simultaneously published in JAMA.
The burden of CV risk factors among young adults is “unacceptably high and increasing,” write the co-authors of a JAMA editorial.
“The time is now for aggressive preventive measures in young adults. Without immediate action there will continue to be a rise in heart disease and the burden it places on patients, families, and communities,” say Norrina Allen, PhD, and John Wilkins, MD, with Northwestern University, Chicago.
Preventing a tsunami of heart disease
The findings stem from a cross-sectional study of 12,294 U.S. adults aged 20-44 years (mean age, 32; 51% women) who participated in National Health and Nutrition Examination Survey (NHANES) cycles for 2009-2010 to 2017-2020.
Overall, the prevalence of hypertension was 9.3% in 2009-2010 and increased to 11.5% in 2017-2020. The prevalence of diabetes rose from 3.0% to 4.1%, and the prevalence of obesity rose from 32.7% to 40.9%. The prevalence of hyperlipidemia decreased from 40.5% to 36.1%.
Black adults consistently had high rates of hypertension during the study period – 16.2% in 2009-2010 and 20.1% in 2017-2020 – and significant increases in hypertension occurred among Mexican American adults (from 6.5% to 9.5%) and other Hispanic adults (from 4.4% to 10.5%), while Mexican American adults had a significant uptick in diabetes (from 4.3% to 7.5%).
Equally concerning, said Dr. Wadhera, is the fact that only about 55% of young adults with hypertension were receiving antihypertensive medication, and just 1 in 2 young adults with diabetes were receiving treatment. “These low rates were driven, in part, by many young adults not being aware of their diagnosis,” he noted.
The NHANES data also show that the percentage of young adults who were treated for hypertension and who achieved blood pressure control did not change significantly over the study period (65.0% in 2009-2010 and 74.8% in 2017-2020). Blood sugar control among young adults being treated for diabetes remained suboptimal throughout the study period (45.5% in 2009-2010 and 56.6% in 2017-2020).
“The fact that blood pressure control and glycemic control are so poor is really worrisome,” Jeffrey Berger, MD, director of the Center for the Prevention of Cardiovascular Disease at NYU Langone Heart, who wasn’t involved in the study, told this news organization.
“Even in the lipid control, while it did get a little bit better, it’s still only around 30%-40%. So, I think we have ways to go as a society,” Dr. Berger noted.
Double down on screening
Dr. Wadhera said “we need to double down on efforts to screen for and treat cardiovascular risk factors like high blood pressure and diabetes in young adults. We need to intensify clinical and public health interventions focused on primordial and primary prevention in young adults now so that we can avoid a tsunami of cardiovascular disease in the long term.”
“It’s critically important that young adults speak with their health care provider about whether – and when – they should undergo screening for high blood pressure, diabetes, and high cholesterol,” Dr. Wadhera added.
Dr. Berger said one problem is that younger people often have a “superman or superwoman” view and don’t comprehend that they are at risk for some of these conditions. Studies such as this “reinforce the idea that it’s never too young to be checked out.”
As a cardiologist who specializes in cardiovascular prevention, Dr. Berger said he sometimes hears patients say things like, “I don’t ever want to need a cardiologist,” or “I hope I never need a cardiologist.”
“My response is, ‘There are many different types of cardiologists,’ and I think it would really be helpful for many people to see a prevention-focused cardiologist way before they have problems,” he said in an interview.
“As a system, medicine has become very good at treating patients with different diseases. I think we need to get better in terms of preventing some of these problems,” Dr. Berger added.
In their editorial, Dr. Allen and Dr. Wilkins say the “foundation of cardiovascular health begins early in life. These worsening trends in risk factors highlight the importance of focusing on prevention in adolescence and young adulthood in order to promote cardiovascular health across the lifetime.”
The study was funded by a grant from the National Heart, Lung, and Blood Institute. Dr. Wadhera has served as a consultant for Abbott and CVS Health. Dr. Wilkins has received personal fees from 3M. Dr. Berger has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ACC 2023
OTC budesonide-formoterol for asthma could save lives, money
, according to a computer modeling study presented at the American Academy of Allergy, Asthma, and Immunology 2023 annual meeting in San Antonio.
Asthma affects 25 million people, about 1 in 13, in the United States. About 28% are uninsured or underinsured, and 70% have mild asthma. Many are using a $30 inhaled epinephrine product (Primatene Mist) – the only FDA-approved asthma inhaler available without a prescription, said Marcus Shaker, MD, MS, professor of pediatrics and medicine at Geisel School of Medicine at Dartmouth, and clinician at Dartmouth Health Children’s, N.H.
A new version of Primatene Mist was reintroduced on the market in 2018 after the product was pulled for containing chlorofluorocarbons in 2011, but it is not recommended by professional medical societies because of safety concerns over epinephrine’s adverse effects, such as increased heart rate and blood pressure.
Drugs in its class (bronchodilators) have long been associated with a higher risk for death or near-death.
Meanwhile, research more than 2 decades ago linked regular use of low-dose inhaled corticosteroids with reduced risk for asthma death.
More recently, two large studies (SYGMA 1 and SYGMA 2) compared maintenance therapy with a low-dose inhaled corticosteroid (budesonide) vs. on-demand treatment with an inhaler containing both a corticosteroid (budesonide) and a long-acting bronchodilator (formoterol).
“Using as-needed budesonide-formoterol led to outcomes that are almost as good as taking a maintenance budesonide dose every day,” said Dr. Shaker.
The Global Initiative for Asthma guidelines now recommend this approach – as-needed inhaled corticosteroids (ICS) plus long-acting bronchodilators – for adults with mild asthma. In the United States, however, the National Heart, Lung, and Blood Institute still suggests daily ICS plus quick-relief therapy as needed.
Dr. Shaker and colleagues used computer modeling to compare the cost-effectiveness of as-needed budesonide-formoterol vs. over-the-counter inhaled epinephrine in underinsured U.S. adults who were self-managing their mild asthma. The study randomly assigned these individuals into three groups: OTC inhaled epinephrine (current reality), OTC budesonide-formoterol (not yet available), or no OTC option. The model assumed that patients treated for an exacerbation were referred to a health care provider and started a regimen of ICS plus as-needed rescue therapy.
In this analysis, which has been submitted for publication, the OTC budesonide-formoterol strategy was associated with 12,495 fewer deaths, prevented nearly 14 million severe asthma exacerbations, and saved more than $68 billion. And “when we looked at OTC budesonide-formoterol vs. having no OTC option at all, budesonide-formoterol was similarly cost-effective,” said Dr. Shaker, who presented the results at an AAAAI oral abstract session.
The cost savings emerged even though in the United States asthma controller therapies (for example, fluticasone) cost about 10 times more than rescue therapies (for instance, salbutamol, OTC epinephrine).
Nevertheless, the results make sense. “If you’re using Primatene Mist, your health costs are predicted to be much greater because you’re going to be in the hospital more. Your asthma is not going to be well-controlled,” Thanai Pongdee, MD, an allergist-immunologist with the Mayo Clinic in Rochester, Minn., told this news organization. “It’s not only the cost of your ER visit but also the cost of loss of work or school, and loss of daily productivity. There are all these associated costs.”
The analysis “is certainly something policy makers could take a look at,” he said.
He noted that current use of budesonide-formoterol is stymied by difficulties with insurance coverage. The difficulties stem from a mismatch between the updated recommendation for as-needed use and the description printed on the brand-name product (Symbicort).
“On the product label, it says Symbicort should be used on a daily basis,” Dr. Pongdee said. “But if a prescription comes through and says you’re going to use this ‘as needed,’ the health plan may say that’s not appropriate because that’s not on the product label.”
Given these access challenges with the all-in-one inhaler, other researchers have developed a workaround – asking patients to continue their usual care (that is, using a rescue inhaler as needed) but to also administer a controller medication after each rescue. When tested in Black and Latino patients with moderate to severe asthma, this easy strategy (patient activated reliever-triggered inhaled corticosteroid, or PARTICS) reduced severe asthma exacerbations about as well as the all-in-one inhaler.
If the all-in-one budesonide-formoterol does become available OTC, Dr. Shaker stressed that it “would not be a substitute for seeing an allergist and getting appropriate medical care and an evaluation and all the rest. But it’s better than the status quo. It’s the sort of thing where the perfect is not the enemy of the good,” he said.
Dr. Shaker is the AAAAI cochair of the Joint Task Force on Practice Parameters and serves as an editorial board member of the Journal of Allergy and Clinical Immunology in Practice. He is also an associate editor of the Annals of Allergy, Asthma, and Immunology. Dr. Pongdee serves as an at-large director on the AAAAI board of directors. He receives grant funding from GlaxoSmithKline, and Mayo Clinic is a trial site for GlaxoSmithKline and AstraZeneca.
A version of this article first appeared on Medscape.com.
, according to a computer modeling study presented at the American Academy of Allergy, Asthma, and Immunology 2023 annual meeting in San Antonio.
Asthma affects 25 million people, about 1 in 13, in the United States. About 28% are uninsured or underinsured, and 70% have mild asthma. Many are using a $30 inhaled epinephrine product (Primatene Mist) – the only FDA-approved asthma inhaler available without a prescription, said Marcus Shaker, MD, MS, professor of pediatrics and medicine at Geisel School of Medicine at Dartmouth, and clinician at Dartmouth Health Children’s, N.H.
A new version of Primatene Mist was reintroduced on the market in 2018 after the product was pulled for containing chlorofluorocarbons in 2011, but it is not recommended by professional medical societies because of safety concerns over epinephrine’s adverse effects, such as increased heart rate and blood pressure.
Drugs in its class (bronchodilators) have long been associated with a higher risk for death or near-death.
Meanwhile, research more than 2 decades ago linked regular use of low-dose inhaled corticosteroids with reduced risk for asthma death.
More recently, two large studies (SYGMA 1 and SYGMA 2) compared maintenance therapy with a low-dose inhaled corticosteroid (budesonide) vs. on-demand treatment with an inhaler containing both a corticosteroid (budesonide) and a long-acting bronchodilator (formoterol).
“Using as-needed budesonide-formoterol led to outcomes that are almost as good as taking a maintenance budesonide dose every day,” said Dr. Shaker.
The Global Initiative for Asthma guidelines now recommend this approach – as-needed inhaled corticosteroids (ICS) plus long-acting bronchodilators – for adults with mild asthma. In the United States, however, the National Heart, Lung, and Blood Institute still suggests daily ICS plus quick-relief therapy as needed.
Dr. Shaker and colleagues used computer modeling to compare the cost-effectiveness of as-needed budesonide-formoterol vs. over-the-counter inhaled epinephrine in underinsured U.S. adults who were self-managing their mild asthma. The study randomly assigned these individuals into three groups: OTC inhaled epinephrine (current reality), OTC budesonide-formoterol (not yet available), or no OTC option. The model assumed that patients treated for an exacerbation were referred to a health care provider and started a regimen of ICS plus as-needed rescue therapy.
In this analysis, which has been submitted for publication, the OTC budesonide-formoterol strategy was associated with 12,495 fewer deaths, prevented nearly 14 million severe asthma exacerbations, and saved more than $68 billion. And “when we looked at OTC budesonide-formoterol vs. having no OTC option at all, budesonide-formoterol was similarly cost-effective,” said Dr. Shaker, who presented the results at an AAAAI oral abstract session.
The cost savings emerged even though in the United States asthma controller therapies (for example, fluticasone) cost about 10 times more than rescue therapies (for instance, salbutamol, OTC epinephrine).
Nevertheless, the results make sense. “If you’re using Primatene Mist, your health costs are predicted to be much greater because you’re going to be in the hospital more. Your asthma is not going to be well-controlled,” Thanai Pongdee, MD, an allergist-immunologist with the Mayo Clinic in Rochester, Minn., told this news organization. “It’s not only the cost of your ER visit but also the cost of loss of work or school, and loss of daily productivity. There are all these associated costs.”
The analysis “is certainly something policy makers could take a look at,” he said.
He noted that current use of budesonide-formoterol is stymied by difficulties with insurance coverage. The difficulties stem from a mismatch between the updated recommendation for as-needed use and the description printed on the brand-name product (Symbicort).
“On the product label, it says Symbicort should be used on a daily basis,” Dr. Pongdee said. “But if a prescription comes through and says you’re going to use this ‘as needed,’ the health plan may say that’s not appropriate because that’s not on the product label.”
Given these access challenges with the all-in-one inhaler, other researchers have developed a workaround – asking patients to continue their usual care (that is, using a rescue inhaler as needed) but to also administer a controller medication after each rescue. When tested in Black and Latino patients with moderate to severe asthma, this easy strategy (patient activated reliever-triggered inhaled corticosteroid, or PARTICS) reduced severe asthma exacerbations about as well as the all-in-one inhaler.
If the all-in-one budesonide-formoterol does become available OTC, Dr. Shaker stressed that it “would not be a substitute for seeing an allergist and getting appropriate medical care and an evaluation and all the rest. But it’s better than the status quo. It’s the sort of thing where the perfect is not the enemy of the good,” he said.
Dr. Shaker is the AAAAI cochair of the Joint Task Force on Practice Parameters and serves as an editorial board member of the Journal of Allergy and Clinical Immunology in Practice. He is also an associate editor of the Annals of Allergy, Asthma, and Immunology. Dr. Pongdee serves as an at-large director on the AAAAI board of directors. He receives grant funding from GlaxoSmithKline, and Mayo Clinic is a trial site for GlaxoSmithKline and AstraZeneca.
A version of this article first appeared on Medscape.com.
, according to a computer modeling study presented at the American Academy of Allergy, Asthma, and Immunology 2023 annual meeting in San Antonio.
Asthma affects 25 million people, about 1 in 13, in the United States. About 28% are uninsured or underinsured, and 70% have mild asthma. Many are using a $30 inhaled epinephrine product (Primatene Mist) – the only FDA-approved asthma inhaler available without a prescription, said Marcus Shaker, MD, MS, professor of pediatrics and medicine at Geisel School of Medicine at Dartmouth, and clinician at Dartmouth Health Children’s, N.H.
A new version of Primatene Mist was reintroduced on the market in 2018 after the product was pulled for containing chlorofluorocarbons in 2011, but it is not recommended by professional medical societies because of safety concerns over epinephrine’s adverse effects, such as increased heart rate and blood pressure.
Drugs in its class (bronchodilators) have long been associated with a higher risk for death or near-death.
Meanwhile, research more than 2 decades ago linked regular use of low-dose inhaled corticosteroids with reduced risk for asthma death.
More recently, two large studies (SYGMA 1 and SYGMA 2) compared maintenance therapy with a low-dose inhaled corticosteroid (budesonide) vs. on-demand treatment with an inhaler containing both a corticosteroid (budesonide) and a long-acting bronchodilator (formoterol).
“Using as-needed budesonide-formoterol led to outcomes that are almost as good as taking a maintenance budesonide dose every day,” said Dr. Shaker.
The Global Initiative for Asthma guidelines now recommend this approach – as-needed inhaled corticosteroids (ICS) plus long-acting bronchodilators – for adults with mild asthma. In the United States, however, the National Heart, Lung, and Blood Institute still suggests daily ICS plus quick-relief therapy as needed.
Dr. Shaker and colleagues used computer modeling to compare the cost-effectiveness of as-needed budesonide-formoterol vs. over-the-counter inhaled epinephrine in underinsured U.S. adults who were self-managing their mild asthma. The study randomly assigned these individuals into three groups: OTC inhaled epinephrine (current reality), OTC budesonide-formoterol (not yet available), or no OTC option. The model assumed that patients treated for an exacerbation were referred to a health care provider and started a regimen of ICS plus as-needed rescue therapy.
In this analysis, which has been submitted for publication, the OTC budesonide-formoterol strategy was associated with 12,495 fewer deaths, prevented nearly 14 million severe asthma exacerbations, and saved more than $68 billion. And “when we looked at OTC budesonide-formoterol vs. having no OTC option at all, budesonide-formoterol was similarly cost-effective,” said Dr. Shaker, who presented the results at an AAAAI oral abstract session.
The cost savings emerged even though in the United States asthma controller therapies (for example, fluticasone) cost about 10 times more than rescue therapies (for instance, salbutamol, OTC epinephrine).
Nevertheless, the results make sense. “If you’re using Primatene Mist, your health costs are predicted to be much greater because you’re going to be in the hospital more. Your asthma is not going to be well-controlled,” Thanai Pongdee, MD, an allergist-immunologist with the Mayo Clinic in Rochester, Minn., told this news organization. “It’s not only the cost of your ER visit but also the cost of loss of work or school, and loss of daily productivity. There are all these associated costs.”
The analysis “is certainly something policy makers could take a look at,” he said.
He noted that current use of budesonide-formoterol is stymied by difficulties with insurance coverage. The difficulties stem from a mismatch between the updated recommendation for as-needed use and the description printed on the brand-name product (Symbicort).
“On the product label, it says Symbicort should be used on a daily basis,” Dr. Pongdee said. “But if a prescription comes through and says you’re going to use this ‘as needed,’ the health plan may say that’s not appropriate because that’s not on the product label.”
Given these access challenges with the all-in-one inhaler, other researchers have developed a workaround – asking patients to continue their usual care (that is, using a rescue inhaler as needed) but to also administer a controller medication after each rescue. When tested in Black and Latino patients with moderate to severe asthma, this easy strategy (patient activated reliever-triggered inhaled corticosteroid, or PARTICS) reduced severe asthma exacerbations about as well as the all-in-one inhaler.
If the all-in-one budesonide-formoterol does become available OTC, Dr. Shaker stressed that it “would not be a substitute for seeing an allergist and getting appropriate medical care and an evaluation and all the rest. But it’s better than the status quo. It’s the sort of thing where the perfect is not the enemy of the good,” he said.
Dr. Shaker is the AAAAI cochair of the Joint Task Force on Practice Parameters and serves as an editorial board member of the Journal of Allergy and Clinical Immunology in Practice. He is also an associate editor of the Annals of Allergy, Asthma, and Immunology. Dr. Pongdee serves as an at-large director on the AAAAI board of directors. He receives grant funding from GlaxoSmithKline, and Mayo Clinic is a trial site for GlaxoSmithKline and AstraZeneca.
A version of this article first appeared on Medscape.com.
FROM AAAAI 2023
EoE: One-food elimination works as well as six-food elimination
according to a new report.
A one-food elimination diet (1FED) led to histologic remission in 34% of patients, as determined on the basis of eosinophil count at 6 weeks, and in 40% of patients who followed a six-food elimination diet (6FED) – a nonstatistical difference, the research team wrote.
“The takeaway message is that one-food (milk) elimination is an effective treatment and a reasonable first-line treatment for EoE,” senior study author Marc Rothenberg, MD, PhD, a professor of pediatrics and director of the allergy and immunology division at the Cincinnati Center for Eosinophilic Disorders at Cincinnati Children’s Hospital Medical Center, said in an interview.
“The study was designed by the Consortium of Eosinophilic Disease Researchers (CEGIR), which includes the nation’s top institutions working with patient advocacy groups, together with the National Institutes of Health,” he said. “The group, under advice from patients, determined that it was an important question to research if one-food elimination would be effective – and how effective – compared with six-food elimination.”
The study was published in The Lancet Gastroenterology and Hepatology.
Studying EOE and food elimination
Previous studies have found that eliminating six common foods that trigger esophageal injury – milk, eggs, wheat, soy, fish, and nuts – can substantially reduce EoE symptoms. The 6FED has become a common approach to managing the disease.
In recent years, however, researchers have conducted small, nonrandomized studies of the less restrictive 1FED and have found some success.
In a multisite, randomized trial, Dr. Rothenberg and colleagues compared the 6FED with the 1FED among 129 adults aged 18-60 years with a confirmed EoE diagnosis, active EoE symptoms, and a high number of eosinophils in esophageal tissue. The participants enrolled at 1 of 10 U.S. medical centers that participate in CEGIR, which is part of the NIH-funded Rare Diseases Clinical Research Network.
Between 2016 and 2019, 67 participants were assigned to the 1FED group, which eliminated only animal milk from the diet, and 62 participants were assigned to the 6FED group, which eliminated milk, eggs, wheat, soy, fish/shellfish, and peanuts/tree nuts. After following the diet for 6 weeks, participants underwent an upper endoscopy exam and esophageal tissue biopsy. The primary endpoint was the proportion of patients with histologic remission, or a peak count of less than 15 eosinophils per high-power field (eos/hpf).
If the number of eosinophils indicated that EoE was in remission, the participant exited the study. If EoE wasn’t in remission, those who were on 1FED could proceed to 6FED, and those who were on 6FED could take fluticasone propionate 880 mcg two times per day with an unrestricted diet. Both groups followed the protocols for 6 weeks and underwent another exam with tissue biopsy.
At 6 weeks, 25 patients (40%) on 6FED and 23 patients (34%) on 1FED achieved histologic remission. The difference was not statistically significant.
There were also no significant differences between the groups at stricter thresholds for partial remission, defined as peak counts of 10 eos/hpf or less and 6 eos/hpf or less. The rate of complete remission (at a peak count of ≤ 1 eos/hpf) favored 6FED, at 19% versus 6% among 1FED.
The two diets had a similar impact across several other measures, including reduction in peak eosinophil counts, reduction in EoE symptoms, and improvement in quality of life. For 6FED versus 1FED, the mean changes from baseline in the Eosinophilic Esophagitis Histology Scoring System were –0.23 versus –0.15. In addition, the mean changes in the Eosinophilic Esophagitis Endoscopic Reference Score were 1 versus –0.6, and in the Eosinophilic Esophagitis Activity Index, they were –8.2 versus –3. None of the differences were significant.
Among the patients who didn’t respond to 1FED, 21 opted to follow 6FED in the study’s second phase. Of those patients, nine (43%) attained remission after following the more restrictive diet. Among the 11 patients who didn’t initially respond to 6FED and who opted to receive fluticasone propionate, nine patients (82%) achieved remission.
“We examined a series of validated endpoints that have not previously been examined in diet trials,” Dr. Rothenberg said. “We are surprised to see that one food was equally effective as six foods.”
Incorporating food elimination therapy
Dr. Rothenberg and colleagues are continuing their research into EoE and food-elimination diets, with a strong focus on furthering diet therapy. In particular, the research team wants to understand how to potentially add milk – and other foods – back to the diet.
Wael Sayej, MD, associate professor of pediatrics at the University of Massachusetts Baystate Regional Campus, Springfield, has found success with the one-food elimination diet among children with EoE, he said in an interview.
In a retrospective study, Dr. Sayej and colleagues found that a one-food elimination diet was an effective first-line treatment option for pediatric patients.
“Once we get past the one-food or two-food elimination, it becomes much more difficult and cumbersome for patients to follow,” said Dr. Sayej, who is also a pediatric gastroenterologist with Baystate Health in Springfield and who wasn’t involved with the CEGIR study. “Obviously, I prefer my patients to follow a strict dairy-free diet as long-term therapy, rather than have them on a medication for the rest of their life.”
Dr. Sayej advises patients to follow the one-food elimination diet in his practice. If patients aren’t responsive, he offers options for additional dietary elimination or initiation of steroid therapy.
“The most important thing about initiating dietary elimination therapy is to take the time to educate the patient and family about the disease, the risks or complications associated with untreated disease, and the pros and cons of the treatment options,” he said.
The study was cofunded by the National Institute of Allergy and Infectious Diseases, the National Center for Advancing Translational Sciences, and the National Institute of Diabetes and Digestive and Kidney Diseases. The authors have research, consultant, and leadership relationships with several pharmaceutical companies and organizations not related to this study. Dr. Sayej disclosed no relevant financial relationships.
according to a new report.
A one-food elimination diet (1FED) led to histologic remission in 34% of patients, as determined on the basis of eosinophil count at 6 weeks, and in 40% of patients who followed a six-food elimination diet (6FED) – a nonstatistical difference, the research team wrote.
“The takeaway message is that one-food (milk) elimination is an effective treatment and a reasonable first-line treatment for EoE,” senior study author Marc Rothenberg, MD, PhD, a professor of pediatrics and director of the allergy and immunology division at the Cincinnati Center for Eosinophilic Disorders at Cincinnati Children’s Hospital Medical Center, said in an interview.
“The study was designed by the Consortium of Eosinophilic Disease Researchers (CEGIR), which includes the nation’s top institutions working with patient advocacy groups, together with the National Institutes of Health,” he said. “The group, under advice from patients, determined that it was an important question to research if one-food elimination would be effective – and how effective – compared with six-food elimination.”
The study was published in The Lancet Gastroenterology and Hepatology.
Studying EOE and food elimination
Previous studies have found that eliminating six common foods that trigger esophageal injury – milk, eggs, wheat, soy, fish, and nuts – can substantially reduce EoE symptoms. The 6FED has become a common approach to managing the disease.
In recent years, however, researchers have conducted small, nonrandomized studies of the less restrictive 1FED and have found some success.
In a multisite, randomized trial, Dr. Rothenberg and colleagues compared the 6FED with the 1FED among 129 adults aged 18-60 years with a confirmed EoE diagnosis, active EoE symptoms, and a high number of eosinophils in esophageal tissue. The participants enrolled at 1 of 10 U.S. medical centers that participate in CEGIR, which is part of the NIH-funded Rare Diseases Clinical Research Network.
Between 2016 and 2019, 67 participants were assigned to the 1FED group, which eliminated only animal milk from the diet, and 62 participants were assigned to the 6FED group, which eliminated milk, eggs, wheat, soy, fish/shellfish, and peanuts/tree nuts. After following the diet for 6 weeks, participants underwent an upper endoscopy exam and esophageal tissue biopsy. The primary endpoint was the proportion of patients with histologic remission, or a peak count of less than 15 eosinophils per high-power field (eos/hpf).
If the number of eosinophils indicated that EoE was in remission, the participant exited the study. If EoE wasn’t in remission, those who were on 1FED could proceed to 6FED, and those who were on 6FED could take fluticasone propionate 880 mcg two times per day with an unrestricted diet. Both groups followed the protocols for 6 weeks and underwent another exam with tissue biopsy.
At 6 weeks, 25 patients (40%) on 6FED and 23 patients (34%) on 1FED achieved histologic remission. The difference was not statistically significant.
There were also no significant differences between the groups at stricter thresholds for partial remission, defined as peak counts of 10 eos/hpf or less and 6 eos/hpf or less. The rate of complete remission (at a peak count of ≤ 1 eos/hpf) favored 6FED, at 19% versus 6% among 1FED.
The two diets had a similar impact across several other measures, including reduction in peak eosinophil counts, reduction in EoE symptoms, and improvement in quality of life. For 6FED versus 1FED, the mean changes from baseline in the Eosinophilic Esophagitis Histology Scoring System were –0.23 versus –0.15. In addition, the mean changes in the Eosinophilic Esophagitis Endoscopic Reference Score were 1 versus –0.6, and in the Eosinophilic Esophagitis Activity Index, they were –8.2 versus –3. None of the differences were significant.
Among the patients who didn’t respond to 1FED, 21 opted to follow 6FED in the study’s second phase. Of those patients, nine (43%) attained remission after following the more restrictive diet. Among the 11 patients who didn’t initially respond to 6FED and who opted to receive fluticasone propionate, nine patients (82%) achieved remission.
“We examined a series of validated endpoints that have not previously been examined in diet trials,” Dr. Rothenberg said. “We are surprised to see that one food was equally effective as six foods.”
Incorporating food elimination therapy
Dr. Rothenberg and colleagues are continuing their research into EoE and food-elimination diets, with a strong focus on furthering diet therapy. In particular, the research team wants to understand how to potentially add milk – and other foods – back to the diet.
Wael Sayej, MD, associate professor of pediatrics at the University of Massachusetts Baystate Regional Campus, Springfield, has found success with the one-food elimination diet among children with EoE, he said in an interview.
In a retrospective study, Dr. Sayej and colleagues found that a one-food elimination diet was an effective first-line treatment option for pediatric patients.
“Once we get past the one-food or two-food elimination, it becomes much more difficult and cumbersome for patients to follow,” said Dr. Sayej, who is also a pediatric gastroenterologist with Baystate Health in Springfield and who wasn’t involved with the CEGIR study. “Obviously, I prefer my patients to follow a strict dairy-free diet as long-term therapy, rather than have them on a medication for the rest of their life.”
Dr. Sayej advises patients to follow the one-food elimination diet in his practice. If patients aren’t responsive, he offers options for additional dietary elimination or initiation of steroid therapy.
“The most important thing about initiating dietary elimination therapy is to take the time to educate the patient and family about the disease, the risks or complications associated with untreated disease, and the pros and cons of the treatment options,” he said.
The study was cofunded by the National Institute of Allergy and Infectious Diseases, the National Center for Advancing Translational Sciences, and the National Institute of Diabetes and Digestive and Kidney Diseases. The authors have research, consultant, and leadership relationships with several pharmaceutical companies and organizations not related to this study. Dr. Sayej disclosed no relevant financial relationships.
according to a new report.
A one-food elimination diet (1FED) led to histologic remission in 34% of patients, as determined on the basis of eosinophil count at 6 weeks, and in 40% of patients who followed a six-food elimination diet (6FED) – a nonstatistical difference, the research team wrote.
“The takeaway message is that one-food (milk) elimination is an effective treatment and a reasonable first-line treatment for EoE,” senior study author Marc Rothenberg, MD, PhD, a professor of pediatrics and director of the allergy and immunology division at the Cincinnati Center for Eosinophilic Disorders at Cincinnati Children’s Hospital Medical Center, said in an interview.
“The study was designed by the Consortium of Eosinophilic Disease Researchers (CEGIR), which includes the nation’s top institutions working with patient advocacy groups, together with the National Institutes of Health,” he said. “The group, under advice from patients, determined that it was an important question to research if one-food elimination would be effective – and how effective – compared with six-food elimination.”
The study was published in The Lancet Gastroenterology and Hepatology.
Studying EOE and food elimination
Previous studies have found that eliminating six common foods that trigger esophageal injury – milk, eggs, wheat, soy, fish, and nuts – can substantially reduce EoE symptoms. The 6FED has become a common approach to managing the disease.
In recent years, however, researchers have conducted small, nonrandomized studies of the less restrictive 1FED and have found some success.
In a multisite, randomized trial, Dr. Rothenberg and colleagues compared the 6FED with the 1FED among 129 adults aged 18-60 years with a confirmed EoE diagnosis, active EoE symptoms, and a high number of eosinophils in esophageal tissue. The participants enrolled at 1 of 10 U.S. medical centers that participate in CEGIR, which is part of the NIH-funded Rare Diseases Clinical Research Network.
Between 2016 and 2019, 67 participants were assigned to the 1FED group, which eliminated only animal milk from the diet, and 62 participants were assigned to the 6FED group, which eliminated milk, eggs, wheat, soy, fish/shellfish, and peanuts/tree nuts. After following the diet for 6 weeks, participants underwent an upper endoscopy exam and esophageal tissue biopsy. The primary endpoint was the proportion of patients with histologic remission, or a peak count of less than 15 eosinophils per high-power field (eos/hpf).
If the number of eosinophils indicated that EoE was in remission, the participant exited the study. If EoE wasn’t in remission, those who were on 1FED could proceed to 6FED, and those who were on 6FED could take fluticasone propionate 880 mcg two times per day with an unrestricted diet. Both groups followed the protocols for 6 weeks and underwent another exam with tissue biopsy.
At 6 weeks, 25 patients (40%) on 6FED and 23 patients (34%) on 1FED achieved histologic remission. The difference was not statistically significant.
There were also no significant differences between the groups at stricter thresholds for partial remission, defined as peak counts of 10 eos/hpf or less and 6 eos/hpf or less. The rate of complete remission (at a peak count of ≤ 1 eos/hpf) favored 6FED, at 19% versus 6% among 1FED.
The two diets had a similar impact across several other measures, including reduction in peak eosinophil counts, reduction in EoE symptoms, and improvement in quality of life. For 6FED versus 1FED, the mean changes from baseline in the Eosinophilic Esophagitis Histology Scoring System were –0.23 versus –0.15. In addition, the mean changes in the Eosinophilic Esophagitis Endoscopic Reference Score were 1 versus –0.6, and in the Eosinophilic Esophagitis Activity Index, they were –8.2 versus –3. None of the differences were significant.
Among the patients who didn’t respond to 1FED, 21 opted to follow 6FED in the study’s second phase. Of those patients, nine (43%) attained remission after following the more restrictive diet. Among the 11 patients who didn’t initially respond to 6FED and who opted to receive fluticasone propionate, nine patients (82%) achieved remission.
“We examined a series of validated endpoints that have not previously been examined in diet trials,” Dr. Rothenberg said. “We are surprised to see that one food was equally effective as six foods.”
Incorporating food elimination therapy
Dr. Rothenberg and colleagues are continuing their research into EoE and food-elimination diets, with a strong focus on furthering diet therapy. In particular, the research team wants to understand how to potentially add milk – and other foods – back to the diet.
Wael Sayej, MD, associate professor of pediatrics at the University of Massachusetts Baystate Regional Campus, Springfield, has found success with the one-food elimination diet among children with EoE, he said in an interview.
In a retrospective study, Dr. Sayej and colleagues found that a one-food elimination diet was an effective first-line treatment option for pediatric patients.
“Once we get past the one-food or two-food elimination, it becomes much more difficult and cumbersome for patients to follow,” said Dr. Sayej, who is also a pediatric gastroenterologist with Baystate Health in Springfield and who wasn’t involved with the CEGIR study. “Obviously, I prefer my patients to follow a strict dairy-free diet as long-term therapy, rather than have them on a medication for the rest of their life.”
Dr. Sayej advises patients to follow the one-food elimination diet in his practice. If patients aren’t responsive, he offers options for additional dietary elimination or initiation of steroid therapy.
“The most important thing about initiating dietary elimination therapy is to take the time to educate the patient and family about the disease, the risks or complications associated with untreated disease, and the pros and cons of the treatment options,” he said.
The study was cofunded by the National Institute of Allergy and Infectious Diseases, the National Center for Advancing Translational Sciences, and the National Institute of Diabetes and Digestive and Kidney Diseases. The authors have research, consultant, and leadership relationships with several pharmaceutical companies and organizations not related to this study. Dr. Sayej disclosed no relevant financial relationships.
FROM THE LANCET GASTROENTEROLOGY AND HEPATOLOGY
Med center and top cardio surgeon must pay $8.5 million for fraud, concurrent surgeries
the Department of Justice (DOJ) announced.
The lawsuit alleges that James L. Luketich, MD, the longtime chair of the school’s cardiothoracic surgery department, regularly performed up to three complex surgical procedures simultaneously, moving among multiple operating rooms and attending to matters other than patient care. The investigation began after Jonathan D’Cunha, MD, a former UPMC surgeon, raised concerns about his colleague’s surgical scheduling and billing practices.
Dr. Luketich’s overbooking of procedures led to patients enduring hours of medically unnecessary anesthesia time and risking surgical complications, according to court documents.
In addition, the complaint states that these practices violated the False Claims Act, which prohibits “teaching physicians” like Dr. Luketich from billing Medicare and other government health plans for “concurrent surgeries” – regulations federal authorities say UPMC leadership were aware of and the University of Pittsburgh Physicians (UPP), also named in the suit, permitted Dr. Luketich to skirt.
The whistleblower provision of the False Claims Act allows private parties to file an action on behalf of the United States and receive a portion of the recovery to help deter health care fraud, says the DOJ.
The defendants previously asked the court to dismiss the case, but a judge denied the request in June 2022.
Paul Wood, vice president and chief communications officer for UPMC, told this news organization that the lawsuit pertained to Dr. Luketich’s “most complicated, team-based surgical procedures.”
“At issue was compliance with the Centers for Medicare & Medicaid Services’ (CMS’s) Teaching Physician Regulation and related billing guidance as well as with UPMC’s internal surgical policies,” he said.
“While UPMC continues to believe Dr. Luketich’s surgical practice complies with CMS requirements, it has agreed to [the settlement] to avoid the distraction and expense of further litigation,” said Mr. Wood, adding that all parties agree that UPMC can seek clarity from CMS regarding future billing of these surgeries.
Efrem Grail, JD, Dr. Luketich’s attorney, said in an interview that he and Dr. Luketich are pleased that the settlement puts an end to the case and that he hopes the United States will issue “authoritative guidance” on billing regulations for teaching physicians, something medical schools and hospitals have sought for years.
Dr. Luketich, UPMC, and UPP face more legal challenges from a separate medical malpractice lawsuit. In March 2018, Bernadette Fedorka underwent a lung transplant at UPMC. Although Dr. Luketich did not perform the surgery, Ms. Fedorka alleges that his poor leadership caused understaffing of the lung transplant program and contributed to surgical complications, including a 4-inch piece of wire left in her neck.
Ms. Fedorka claims that suboxone impaired Dr. Luketich’s decision-making. He began taking the drug in 2008 to manage the pain from a slipped disc injury after a history of prescription drug abuse. Both UPMC and Dr. Luketich have denied the validity of Ms. Fedorka’s claims.
The malpractice suit centers on a recording of a conversation between Dr. Luketich and David Wilson, MD, who prescribed the suboxone and treated the surgeon’s opioid use disorder for several years. Dr. Luketich has accused former colleagues, Dr. D’Cunha and Lara Schaheen, MD, of illegally recording the private conversation that discussed Dr. Luketich’s suboxone prescription – something both physicians deny.
For the billing fraud case, Dr. Luketich has agreed to complete a corrective action plan and submit to a third-party audit of his Medicare billings for 1 year.
“This is an important settlement and a just conclusion to the United States’ investigation into Dr. Luketich’s surgical and billing practices and UPMC and UPP’s acceptance of those practices,” Acting U.S. Attorney Troy Rivetti said in a statement that, “no medical provider – however renowned – is excepted from scrutiny or above the law.”
A version of this article first appeared on Medscape.com.
the Department of Justice (DOJ) announced.
The lawsuit alleges that James L. Luketich, MD, the longtime chair of the school’s cardiothoracic surgery department, regularly performed up to three complex surgical procedures simultaneously, moving among multiple operating rooms and attending to matters other than patient care. The investigation began after Jonathan D’Cunha, MD, a former UPMC surgeon, raised concerns about his colleague’s surgical scheduling and billing practices.
Dr. Luketich’s overbooking of procedures led to patients enduring hours of medically unnecessary anesthesia time and risking surgical complications, according to court documents.
In addition, the complaint states that these practices violated the False Claims Act, which prohibits “teaching physicians” like Dr. Luketich from billing Medicare and other government health plans for “concurrent surgeries” – regulations federal authorities say UPMC leadership were aware of and the University of Pittsburgh Physicians (UPP), also named in the suit, permitted Dr. Luketich to skirt.
The whistleblower provision of the False Claims Act allows private parties to file an action on behalf of the United States and receive a portion of the recovery to help deter health care fraud, says the DOJ.
The defendants previously asked the court to dismiss the case, but a judge denied the request in June 2022.
Paul Wood, vice president and chief communications officer for UPMC, told this news organization that the lawsuit pertained to Dr. Luketich’s “most complicated, team-based surgical procedures.”
“At issue was compliance with the Centers for Medicare & Medicaid Services’ (CMS’s) Teaching Physician Regulation and related billing guidance as well as with UPMC’s internal surgical policies,” he said.
“While UPMC continues to believe Dr. Luketich’s surgical practice complies with CMS requirements, it has agreed to [the settlement] to avoid the distraction and expense of further litigation,” said Mr. Wood, adding that all parties agree that UPMC can seek clarity from CMS regarding future billing of these surgeries.
Efrem Grail, JD, Dr. Luketich’s attorney, said in an interview that he and Dr. Luketich are pleased that the settlement puts an end to the case and that he hopes the United States will issue “authoritative guidance” on billing regulations for teaching physicians, something medical schools and hospitals have sought for years.
Dr. Luketich, UPMC, and UPP face more legal challenges from a separate medical malpractice lawsuit. In March 2018, Bernadette Fedorka underwent a lung transplant at UPMC. Although Dr. Luketich did not perform the surgery, Ms. Fedorka alleges that his poor leadership caused understaffing of the lung transplant program and contributed to surgical complications, including a 4-inch piece of wire left in her neck.
Ms. Fedorka claims that suboxone impaired Dr. Luketich’s decision-making. He began taking the drug in 2008 to manage the pain from a slipped disc injury after a history of prescription drug abuse. Both UPMC and Dr. Luketich have denied the validity of Ms. Fedorka’s claims.
The malpractice suit centers on a recording of a conversation between Dr. Luketich and David Wilson, MD, who prescribed the suboxone and treated the surgeon’s opioid use disorder for several years. Dr. Luketich has accused former colleagues, Dr. D’Cunha and Lara Schaheen, MD, of illegally recording the private conversation that discussed Dr. Luketich’s suboxone prescription – something both physicians deny.
For the billing fraud case, Dr. Luketich has agreed to complete a corrective action plan and submit to a third-party audit of his Medicare billings for 1 year.
“This is an important settlement and a just conclusion to the United States’ investigation into Dr. Luketich’s surgical and billing practices and UPMC and UPP’s acceptance of those practices,” Acting U.S. Attorney Troy Rivetti said in a statement that, “no medical provider – however renowned – is excepted from scrutiny or above the law.”
A version of this article first appeared on Medscape.com.
the Department of Justice (DOJ) announced.
The lawsuit alleges that James L. Luketich, MD, the longtime chair of the school’s cardiothoracic surgery department, regularly performed up to three complex surgical procedures simultaneously, moving among multiple operating rooms and attending to matters other than patient care. The investigation began after Jonathan D’Cunha, MD, a former UPMC surgeon, raised concerns about his colleague’s surgical scheduling and billing practices.
Dr. Luketich’s overbooking of procedures led to patients enduring hours of medically unnecessary anesthesia time and risking surgical complications, according to court documents.
In addition, the complaint states that these practices violated the False Claims Act, which prohibits “teaching physicians” like Dr. Luketich from billing Medicare and other government health plans for “concurrent surgeries” – regulations federal authorities say UPMC leadership were aware of and the University of Pittsburgh Physicians (UPP), also named in the suit, permitted Dr. Luketich to skirt.
The whistleblower provision of the False Claims Act allows private parties to file an action on behalf of the United States and receive a portion of the recovery to help deter health care fraud, says the DOJ.
The defendants previously asked the court to dismiss the case, but a judge denied the request in June 2022.
Paul Wood, vice president and chief communications officer for UPMC, told this news organization that the lawsuit pertained to Dr. Luketich’s “most complicated, team-based surgical procedures.”
“At issue was compliance with the Centers for Medicare & Medicaid Services’ (CMS’s) Teaching Physician Regulation and related billing guidance as well as with UPMC’s internal surgical policies,” he said.
“While UPMC continues to believe Dr. Luketich’s surgical practice complies with CMS requirements, it has agreed to [the settlement] to avoid the distraction and expense of further litigation,” said Mr. Wood, adding that all parties agree that UPMC can seek clarity from CMS regarding future billing of these surgeries.
Efrem Grail, JD, Dr. Luketich’s attorney, said in an interview that he and Dr. Luketich are pleased that the settlement puts an end to the case and that he hopes the United States will issue “authoritative guidance” on billing regulations for teaching physicians, something medical schools and hospitals have sought for years.
Dr. Luketich, UPMC, and UPP face more legal challenges from a separate medical malpractice lawsuit. In March 2018, Bernadette Fedorka underwent a lung transplant at UPMC. Although Dr. Luketich did not perform the surgery, Ms. Fedorka alleges that his poor leadership caused understaffing of the lung transplant program and contributed to surgical complications, including a 4-inch piece of wire left in her neck.
Ms. Fedorka claims that suboxone impaired Dr. Luketich’s decision-making. He began taking the drug in 2008 to manage the pain from a slipped disc injury after a history of prescription drug abuse. Both UPMC and Dr. Luketich have denied the validity of Ms. Fedorka’s claims.
The malpractice suit centers on a recording of a conversation between Dr. Luketich and David Wilson, MD, who prescribed the suboxone and treated the surgeon’s opioid use disorder for several years. Dr. Luketich has accused former colleagues, Dr. D’Cunha and Lara Schaheen, MD, of illegally recording the private conversation that discussed Dr. Luketich’s suboxone prescription – something both physicians deny.
For the billing fraud case, Dr. Luketich has agreed to complete a corrective action plan and submit to a third-party audit of his Medicare billings for 1 year.
“This is an important settlement and a just conclusion to the United States’ investigation into Dr. Luketich’s surgical and billing practices and UPMC and UPP’s acceptance of those practices,” Acting U.S. Attorney Troy Rivetti said in a statement that, “no medical provider – however renowned – is excepted from scrutiny or above the law.”
A version of this article first appeared on Medscape.com.
Distinct suicidal thought patterns flag those at highest risk
Long-term assessment of suicide risk and ideation in older adults may help identify distinct ideation patterns and predict potential future suicidal behavior, new research suggests.
Investigators studied over 300 older adults, assessing suicidal ideation and behavior for up to 14 years at least once annually. They then identified four suicidal ideation profiles.
They found that In turn, fast-remitting ideators were at higher risk in comparison to low/nonideators with no attempts or suicide.
Chronic severe ideators also showed the most severe levels of dysfunction across personality, social characteristics, and impulsivity measures, while highly variable and fast-remitting ideators displayed more specific deficits.
“We identified longitudinal ideation profiles that convey differential risk of future suicidal behavior to help clinicians recognize high suicide risk patients for preventing suicide,” said lead author Hanga Galfalvy, PhD, associate professor, department of psychiatry, Columbia University Irving Medical Center, New York.
“Clinicians should repeatedly assess suicidal ideation and ask not only about current ideation but also about the worst ideation since the last visit [because] similar levels of ideation during a single assessment can belong to very different risk profiles,” said Dr. Galfalvy, also a professor of biostatistics and a coinvestigator in the Conte Center for Suicide Prevention at Columbia University.
The study was published online in the Journal of Clinical Psychiatry.
Vulnerable population
“Older adults in most countries, including the U.S., are at the highest risk of dying of suicide out of all age groups,” said Dr. Galfalvy. “A significant number of depressed older adults experience thoughts of killing themselves, but fortunately, only a few transition from suicidal thoughts to behavior.”
Senior author Katalin Szanto, MD, professor of psychiatry, University of Pittsburgh, said in an interview that currently established clinical and psychosocial suicide risk factors have “low predictive value and provide little insight into the high suicide rate in the elderly.”
These traditional risk factors “poorly distinguish between suicide ideators and suicide attempters and do not take into consideration the heterogeneity of suicidal behavior,” said Dr. Szanto, principal investigator at the University of Pittsburgh’s Longitudinal research Program in Late-Life Suicide, where the study was conducted.
“Suicidal ideation measured at one time point – current or lifetime – may not be enough to accurately predict suicide risk,” the investigators wrote.
The current study, a collaboration between investigators from the Longitudinal Research Program in Late-Life Suicide and the Conte Center for Suicide Prevention, investigates “profiles of suicidal thoughts and behavior in patients with late-life depression over a longer period of time,” Dr. Galfalvy said.
The researchers used latent profile analysis (LPA) in a cohort of adults with nonpsychotic unipolar depression (aged 50-93 years; n = 337; mean age, 65.12 years) to “identify distinct ideation profiles and their clinical correlates” and to “test the profiles’ association with the risk of suicidal behavior before and during follow-up.”
LPA is “a data-driven method of grouping individuals into subgroups, based on quantitative characteristics,” Dr. Galfalvy explained.
The LPA yielded four profiles of ideation.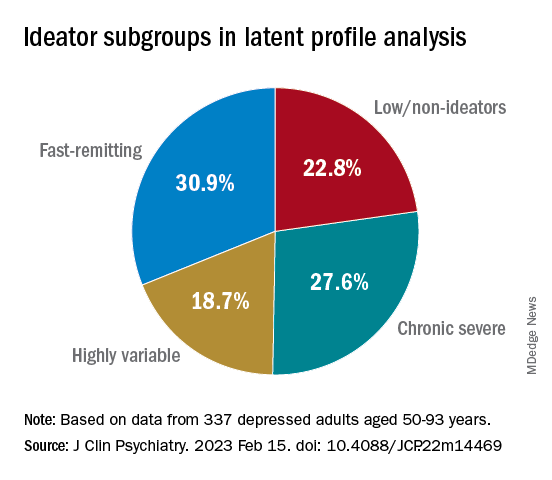
At baseline, the researchers assessed the presence or absence of suicidal behavior history and the number and lethality of attempts. They prospectively assessed suicidal ideation and attempts at least once annually thereafter over a period ranging from 3 months to 14 years (median, 3 years; IQR, 1.6-4 years).
At baseline and at follow-ups, they assessed ideation severity.
They also assessed depression severity, impulsivity, and personality measures, as well as perception of social support, social problem solving, cognitive performance, and physical comorbidities.
Personalized prevention
Of the original cohort, 92 patients died during the follow-up period, with 13 dying of suicide (or suspected suicide).
Over half (60%) of the chronic severe as well as the highly variable groups and almost half (48%) of the fast-remitting group had a history of past suicide attempt – all significantly higher than the low-nonideators (0%).
Despite comparable current ideation severity at baseline, the risk of suicide attempt/death was greater for chronic severe ideators versus fast-remitting ideators, but not greater than for highly variable ideators. On the other hand, highly variable ideators were at greater risk, compared with fast-remitting ideators.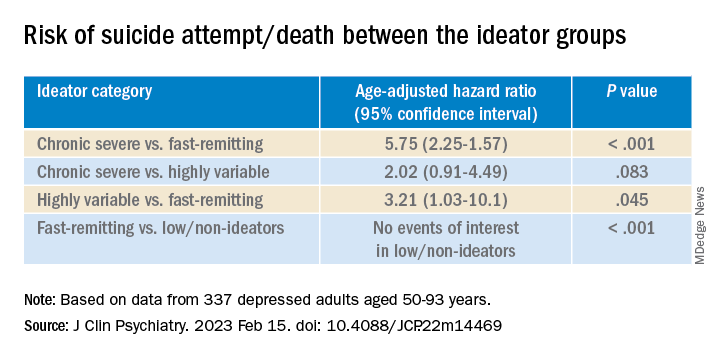
Cognitive factors “did not significantly discriminate between the ideation profiles, although ... lower global cognitive performance predicted suicidal behavior during follow-up,” the authors wrote.
This finding “aligns with prior studies indicating that late-life suicidal behavior but not ideation may be related to cognition ... and instead, ideation and cognition may act as independent risk factors for suicidal behavior,” they added.
“Patients in the fluctuating ideator group generally had moderate or high levels of worst suicidal ideation between visits, but not when asked about current ideation levels at the time of the follow-up assessment,” Dr. Galfalvy noted. “For them, the time frame of the question made a difference as to the level of ideation reported.”
The study “identified several clinical differences among these subgroups which could lead to more personalized suicide prevention efforts and further research into the heterogeneity of suicidal behavior,” she suggested.
New insight
Commenting on the study, Ari Cuperfain, MD, of the University of Toronto said the study “adds to the nuanced understanding of how changes in suicidal ideation over time can lead to suicidal actions and behavior.”
The study “sheds light on the notion of how older adults who die by suicide can demonstrate a greater degree of premeditated intent relative to younger cohorts, with chronic severe ideators portending the highest risk for suicide in this sample,” added Dr. Cuperfain, who was not involved with the current research.
“Overall, the paper highlights the importance of both screening for current levels of suicidal ideation in addition to the evolution of suicidal ideation in developing a risk assessment and in finding interventions to reduce this risk when it is most prominent,” he stated.
The research was supported by the National Institutes of Health. The authors and Dr. Cuperfain disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Long-term assessment of suicide risk and ideation in older adults may help identify distinct ideation patterns and predict potential future suicidal behavior, new research suggests.
Investigators studied over 300 older adults, assessing suicidal ideation and behavior for up to 14 years at least once annually. They then identified four suicidal ideation profiles.
They found that In turn, fast-remitting ideators were at higher risk in comparison to low/nonideators with no attempts or suicide.
Chronic severe ideators also showed the most severe levels of dysfunction across personality, social characteristics, and impulsivity measures, while highly variable and fast-remitting ideators displayed more specific deficits.
“We identified longitudinal ideation profiles that convey differential risk of future suicidal behavior to help clinicians recognize high suicide risk patients for preventing suicide,” said lead author Hanga Galfalvy, PhD, associate professor, department of psychiatry, Columbia University Irving Medical Center, New York.
“Clinicians should repeatedly assess suicidal ideation and ask not only about current ideation but also about the worst ideation since the last visit [because] similar levels of ideation during a single assessment can belong to very different risk profiles,” said Dr. Galfalvy, also a professor of biostatistics and a coinvestigator in the Conte Center for Suicide Prevention at Columbia University.
The study was published online in the Journal of Clinical Psychiatry.
Vulnerable population
“Older adults in most countries, including the U.S., are at the highest risk of dying of suicide out of all age groups,” said Dr. Galfalvy. “A significant number of depressed older adults experience thoughts of killing themselves, but fortunately, only a few transition from suicidal thoughts to behavior.”
Senior author Katalin Szanto, MD, professor of psychiatry, University of Pittsburgh, said in an interview that currently established clinical and psychosocial suicide risk factors have “low predictive value and provide little insight into the high suicide rate in the elderly.”
These traditional risk factors “poorly distinguish between suicide ideators and suicide attempters and do not take into consideration the heterogeneity of suicidal behavior,” said Dr. Szanto, principal investigator at the University of Pittsburgh’s Longitudinal research Program in Late-Life Suicide, where the study was conducted.
“Suicidal ideation measured at one time point – current or lifetime – may not be enough to accurately predict suicide risk,” the investigators wrote.
The current study, a collaboration between investigators from the Longitudinal Research Program in Late-Life Suicide and the Conte Center for Suicide Prevention, investigates “profiles of suicidal thoughts and behavior in patients with late-life depression over a longer period of time,” Dr. Galfalvy said.
The researchers used latent profile analysis (LPA) in a cohort of adults with nonpsychotic unipolar depression (aged 50-93 years; n = 337; mean age, 65.12 years) to “identify distinct ideation profiles and their clinical correlates” and to “test the profiles’ association with the risk of suicidal behavior before and during follow-up.”
LPA is “a data-driven method of grouping individuals into subgroups, based on quantitative characteristics,” Dr. Galfalvy explained.
The LPA yielded four profiles of ideation.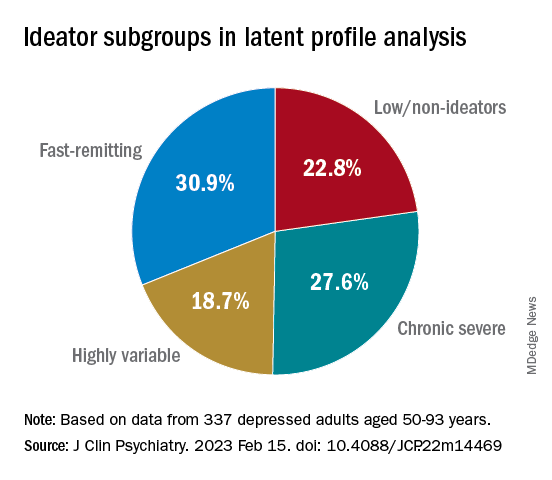
At baseline, the researchers assessed the presence or absence of suicidal behavior history and the number and lethality of attempts. They prospectively assessed suicidal ideation and attempts at least once annually thereafter over a period ranging from 3 months to 14 years (median, 3 years; IQR, 1.6-4 years).
At baseline and at follow-ups, they assessed ideation severity.
They also assessed depression severity, impulsivity, and personality measures, as well as perception of social support, social problem solving, cognitive performance, and physical comorbidities.
Personalized prevention
Of the original cohort, 92 patients died during the follow-up period, with 13 dying of suicide (or suspected suicide).
Over half (60%) of the chronic severe as well as the highly variable groups and almost half (48%) of the fast-remitting group had a history of past suicide attempt – all significantly higher than the low-nonideators (0%).
Despite comparable current ideation severity at baseline, the risk of suicide attempt/death was greater for chronic severe ideators versus fast-remitting ideators, but not greater than for highly variable ideators. On the other hand, highly variable ideators were at greater risk, compared with fast-remitting ideators.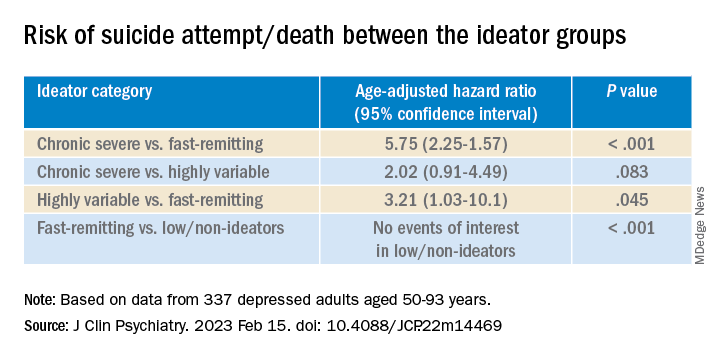
Cognitive factors “did not significantly discriminate between the ideation profiles, although ... lower global cognitive performance predicted suicidal behavior during follow-up,” the authors wrote.
This finding “aligns with prior studies indicating that late-life suicidal behavior but not ideation may be related to cognition ... and instead, ideation and cognition may act as independent risk factors for suicidal behavior,” they added.
“Patients in the fluctuating ideator group generally had moderate or high levels of worst suicidal ideation between visits, but not when asked about current ideation levels at the time of the follow-up assessment,” Dr. Galfalvy noted. “For them, the time frame of the question made a difference as to the level of ideation reported.”
The study “identified several clinical differences among these subgroups which could lead to more personalized suicide prevention efforts and further research into the heterogeneity of suicidal behavior,” she suggested.
New insight
Commenting on the study, Ari Cuperfain, MD, of the University of Toronto said the study “adds to the nuanced understanding of how changes in suicidal ideation over time can lead to suicidal actions and behavior.”
The study “sheds light on the notion of how older adults who die by suicide can demonstrate a greater degree of premeditated intent relative to younger cohorts, with chronic severe ideators portending the highest risk for suicide in this sample,” added Dr. Cuperfain, who was not involved with the current research.
“Overall, the paper highlights the importance of both screening for current levels of suicidal ideation in addition to the evolution of suicidal ideation in developing a risk assessment and in finding interventions to reduce this risk when it is most prominent,” he stated.
The research was supported by the National Institutes of Health. The authors and Dr. Cuperfain disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Long-term assessment of suicide risk and ideation in older adults may help identify distinct ideation patterns and predict potential future suicidal behavior, new research suggests.
Investigators studied over 300 older adults, assessing suicidal ideation and behavior for up to 14 years at least once annually. They then identified four suicidal ideation profiles.
They found that In turn, fast-remitting ideators were at higher risk in comparison to low/nonideators with no attempts or suicide.
Chronic severe ideators also showed the most severe levels of dysfunction across personality, social characteristics, and impulsivity measures, while highly variable and fast-remitting ideators displayed more specific deficits.
“We identified longitudinal ideation profiles that convey differential risk of future suicidal behavior to help clinicians recognize high suicide risk patients for preventing suicide,” said lead author Hanga Galfalvy, PhD, associate professor, department of psychiatry, Columbia University Irving Medical Center, New York.
“Clinicians should repeatedly assess suicidal ideation and ask not only about current ideation but also about the worst ideation since the last visit [because] similar levels of ideation during a single assessment can belong to very different risk profiles,” said Dr. Galfalvy, also a professor of biostatistics and a coinvestigator in the Conte Center for Suicide Prevention at Columbia University.
The study was published online in the Journal of Clinical Psychiatry.
Vulnerable population
“Older adults in most countries, including the U.S., are at the highest risk of dying of suicide out of all age groups,” said Dr. Galfalvy. “A significant number of depressed older adults experience thoughts of killing themselves, but fortunately, only a few transition from suicidal thoughts to behavior.”
Senior author Katalin Szanto, MD, professor of psychiatry, University of Pittsburgh, said in an interview that currently established clinical and psychosocial suicide risk factors have “low predictive value and provide little insight into the high suicide rate in the elderly.”
These traditional risk factors “poorly distinguish between suicide ideators and suicide attempters and do not take into consideration the heterogeneity of suicidal behavior,” said Dr. Szanto, principal investigator at the University of Pittsburgh’s Longitudinal research Program in Late-Life Suicide, where the study was conducted.
“Suicidal ideation measured at one time point – current or lifetime – may not be enough to accurately predict suicide risk,” the investigators wrote.
The current study, a collaboration between investigators from the Longitudinal Research Program in Late-Life Suicide and the Conte Center for Suicide Prevention, investigates “profiles of suicidal thoughts and behavior in patients with late-life depression over a longer period of time,” Dr. Galfalvy said.
The researchers used latent profile analysis (LPA) in a cohort of adults with nonpsychotic unipolar depression (aged 50-93 years; n = 337; mean age, 65.12 years) to “identify distinct ideation profiles and their clinical correlates” and to “test the profiles’ association with the risk of suicidal behavior before and during follow-up.”
LPA is “a data-driven method of grouping individuals into subgroups, based on quantitative characteristics,” Dr. Galfalvy explained.
The LPA yielded four profiles of ideation.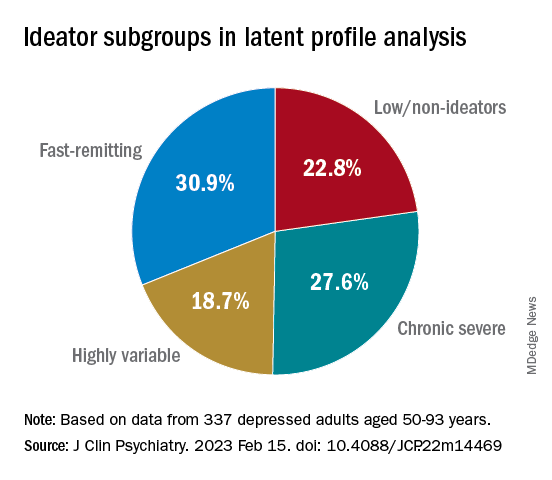
At baseline, the researchers assessed the presence or absence of suicidal behavior history and the number and lethality of attempts. They prospectively assessed suicidal ideation and attempts at least once annually thereafter over a period ranging from 3 months to 14 years (median, 3 years; IQR, 1.6-4 years).
At baseline and at follow-ups, they assessed ideation severity.
They also assessed depression severity, impulsivity, and personality measures, as well as perception of social support, social problem solving, cognitive performance, and physical comorbidities.
Personalized prevention
Of the original cohort, 92 patients died during the follow-up period, with 13 dying of suicide (or suspected suicide).
Over half (60%) of the chronic severe as well as the highly variable groups and almost half (48%) of the fast-remitting group had a history of past suicide attempt – all significantly higher than the low-nonideators (0%).
Despite comparable current ideation severity at baseline, the risk of suicide attempt/death was greater for chronic severe ideators versus fast-remitting ideators, but not greater than for highly variable ideators. On the other hand, highly variable ideators were at greater risk, compared with fast-remitting ideators.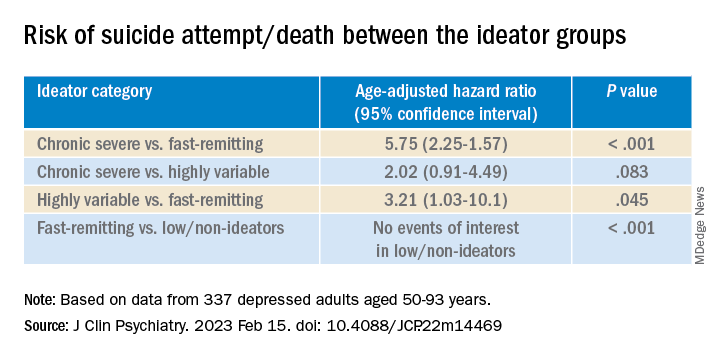
Cognitive factors “did not significantly discriminate between the ideation profiles, although ... lower global cognitive performance predicted suicidal behavior during follow-up,” the authors wrote.
This finding “aligns with prior studies indicating that late-life suicidal behavior but not ideation may be related to cognition ... and instead, ideation and cognition may act as independent risk factors for suicidal behavior,” they added.
“Patients in the fluctuating ideator group generally had moderate or high levels of worst suicidal ideation between visits, but not when asked about current ideation levels at the time of the follow-up assessment,” Dr. Galfalvy noted. “For them, the time frame of the question made a difference as to the level of ideation reported.”
The study “identified several clinical differences among these subgroups which could lead to more personalized suicide prevention efforts and further research into the heterogeneity of suicidal behavior,” she suggested.
New insight
Commenting on the study, Ari Cuperfain, MD, of the University of Toronto said the study “adds to the nuanced understanding of how changes in suicidal ideation over time can lead to suicidal actions and behavior.”
The study “sheds light on the notion of how older adults who die by suicide can demonstrate a greater degree of premeditated intent relative to younger cohorts, with chronic severe ideators portending the highest risk for suicide in this sample,” added Dr. Cuperfain, who was not involved with the current research.
“Overall, the paper highlights the importance of both screening for current levels of suicidal ideation in addition to the evolution of suicidal ideation in developing a risk assessment and in finding interventions to reduce this risk when it is most prominent,” he stated.
The research was supported by the National Institutes of Health. The authors and Dr. Cuperfain disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL PSYCHIATRY