User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
FDA moves to stop the spread of illicit ‘tranq’ in the U.S.
The agency issued an import alert, which gives it the power to detain raw ingredients or bulk finished product if the shipments are suspected to be in violation of the law. Xylazine was first approved by the FDA in 1972 as a sedative and analgesic for use only in animals.
It is increasingly being detected and is usually mixed with fentanyl, cocaine, methamphetamine, and other illicit drugs. A January 2023 study by Nashville-based testing company Aegis Sciences found xylazine in 413 of about 60,000 urine samples and in 25 of 39 states that submitted tests. The vast majority of xylazine-positive samples also tested positive for fentanyl.
The FDA said it would continue to ensure the availability of xylazine for veterinary use, and the American Veterinary Medicine Association said in a statement that it “supports such efforts to combat illicit drug use.”
FDA Commissioner Robert M. Califf, MD, said in a statement that the agency “remains concerned about the increasing prevalence of xylazine mixed with illicit drugs, and this action is one part of broader efforts the agency is undertaking to address this issue.”
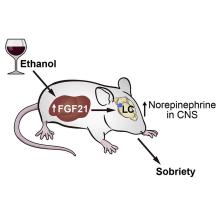
In November, the agency warned health care providers that because xylazine is not an opioid, the overdose reversal agent naloxone would not be effective. Xylazine acts as a central alpha-2-adrenergic receptor agonist in the brainstem, causing a rapid decrease in the release of norepinephrine and dopamine in the central nervous system. Its use can lead to central nervous system and respiratory depression, said the FDA.
Clinicians have scrambled to treat severe necrotic skin ulcerations that develop at injection sites.
Xylazine is relatively cheap and easy to access, said the Drug Enforcement Administration and Department of Justice in a November joint report. The drug is “readily available for purchase on other Internet sites in liquid and powder form, often with no association to the veterinary profession nor requirements to prove legitimate need,” said the Justice Department. A buyer can purchase xylazine powder online from Chinese suppliers for $6-$20 per kilogram, according to the report.
In 2021, xylazine-positive overdoses were highest in the South, which experienced a 1,127% increase from 2020, the Justice Department reported. The same year, there were 1,281 overdoses involving the substance in the Northeast and 351 in the Midwest.
There were just 34 overdoses involving xylazine in the West in 2021, but its use appears to be growing. The San Francisco Department of Public Health said it had detected low levels of xylazine in four people who died of overdoses in December and January.
“Identifying xylazine in San Francisco is concerning,” said the department in a statement, adding that it had not yet seen evidence of skin wounds in injection drug users in the city.
In late February, the Los Angeles County Department of Public Health issued a warning to first responders and health care professionals that xylazine had been detected in the area’s illicit drug supply.
The department said it will “work closely with other partners to understand the extent of the possible xylazine contamination in the illicit drug supply to increase awareness and education to the public.”
The FDA commissioner said the agency will coordinate with public health officials to more closely track xylazine.
“We will continue to use all tools at our disposal and partner with the Drug Enforcement Administration and other federal, state, local agencies, and stakeholders as appropriate to stem these illicit activities and protect public health,” said Dr. Califf.
A version of this article first appeared on Medscape.com.
The agency issued an import alert, which gives it the power to detain raw ingredients or bulk finished product if the shipments are suspected to be in violation of the law. Xylazine was first approved by the FDA in 1972 as a sedative and analgesic for use only in animals.
It is increasingly being detected and is usually mixed with fentanyl, cocaine, methamphetamine, and other illicit drugs. A January 2023 study by Nashville-based testing company Aegis Sciences found xylazine in 413 of about 60,000 urine samples and in 25 of 39 states that submitted tests. The vast majority of xylazine-positive samples also tested positive for fentanyl.
The FDA said it would continue to ensure the availability of xylazine for veterinary use, and the American Veterinary Medicine Association said in a statement that it “supports such efforts to combat illicit drug use.”
FDA Commissioner Robert M. Califf, MD, said in a statement that the agency “remains concerned about the increasing prevalence of xylazine mixed with illicit drugs, and this action is one part of broader efforts the agency is undertaking to address this issue.”
In November, the agency warned health care providers that because xylazine is not an opioid, the overdose reversal agent naloxone would not be effective. Xylazine acts as a central alpha-2-adrenergic receptor agonist in the brainstem, causing a rapid decrease in the release of norepinephrine and dopamine in the central nervous system. Its use can lead to central nervous system and respiratory depression, said the FDA.
Clinicians have scrambled to treat severe necrotic skin ulcerations that develop at injection sites.
Xylazine is relatively cheap and easy to access, said the Drug Enforcement Administration and Department of Justice in a November joint report. The drug is “readily available for purchase on other Internet sites in liquid and powder form, often with no association to the veterinary profession nor requirements to prove legitimate need,” said the Justice Department. A buyer can purchase xylazine powder online from Chinese suppliers for $6-$20 per kilogram, according to the report.
In 2021, xylazine-positive overdoses were highest in the South, which experienced a 1,127% increase from 2020, the Justice Department reported. The same year, there were 1,281 overdoses involving the substance in the Northeast and 351 in the Midwest.
There were just 34 overdoses involving xylazine in the West in 2021, but its use appears to be growing. The San Francisco Department of Public Health said it had detected low levels of xylazine in four people who died of overdoses in December and January.
“Identifying xylazine in San Francisco is concerning,” said the department in a statement, adding that it had not yet seen evidence of skin wounds in injection drug users in the city.
In late February, the Los Angeles County Department of Public Health issued a warning to first responders and health care professionals that xylazine had been detected in the area’s illicit drug supply.
The department said it will “work closely with other partners to understand the extent of the possible xylazine contamination in the illicit drug supply to increase awareness and education to the public.”
The FDA commissioner said the agency will coordinate with public health officials to more closely track xylazine.
“We will continue to use all tools at our disposal and partner with the Drug Enforcement Administration and other federal, state, local agencies, and stakeholders as appropriate to stem these illicit activities and protect public health,” said Dr. Califf.
A version of this article first appeared on Medscape.com.
The agency issued an import alert, which gives it the power to detain raw ingredients or bulk finished product if the shipments are suspected to be in violation of the law. Xylazine was first approved by the FDA in 1972 as a sedative and analgesic for use only in animals.
It is increasingly being detected and is usually mixed with fentanyl, cocaine, methamphetamine, and other illicit drugs. A January 2023 study by Nashville-based testing company Aegis Sciences found xylazine in 413 of about 60,000 urine samples and in 25 of 39 states that submitted tests. The vast majority of xylazine-positive samples also tested positive for fentanyl.
The FDA said it would continue to ensure the availability of xylazine for veterinary use, and the American Veterinary Medicine Association said in a statement that it “supports such efforts to combat illicit drug use.”
FDA Commissioner Robert M. Califf, MD, said in a statement that the agency “remains concerned about the increasing prevalence of xylazine mixed with illicit drugs, and this action is one part of broader efforts the agency is undertaking to address this issue.”
In November, the agency warned health care providers that because xylazine is not an opioid, the overdose reversal agent naloxone would not be effective. Xylazine acts as a central alpha-2-adrenergic receptor agonist in the brainstem, causing a rapid decrease in the release of norepinephrine and dopamine in the central nervous system. Its use can lead to central nervous system and respiratory depression, said the FDA.
Clinicians have scrambled to treat severe necrotic skin ulcerations that develop at injection sites.
Xylazine is relatively cheap and easy to access, said the Drug Enforcement Administration and Department of Justice in a November joint report. The drug is “readily available for purchase on other Internet sites in liquid and powder form, often with no association to the veterinary profession nor requirements to prove legitimate need,” said the Justice Department. A buyer can purchase xylazine powder online from Chinese suppliers for $6-$20 per kilogram, according to the report.
In 2021, xylazine-positive overdoses were highest in the South, which experienced a 1,127% increase from 2020, the Justice Department reported. The same year, there were 1,281 overdoses involving the substance in the Northeast and 351 in the Midwest.
There were just 34 overdoses involving xylazine in the West in 2021, but its use appears to be growing. The San Francisco Department of Public Health said it had detected low levels of xylazine in four people who died of overdoses in December and January.
“Identifying xylazine in San Francisco is concerning,” said the department in a statement, adding that it had not yet seen evidence of skin wounds in injection drug users in the city.
In late February, the Los Angeles County Department of Public Health issued a warning to first responders and health care professionals that xylazine had been detected in the area’s illicit drug supply.
The department said it will “work closely with other partners to understand the extent of the possible xylazine contamination in the illicit drug supply to increase awareness and education to the public.”
The FDA commissioner said the agency will coordinate with public health officials to more closely track xylazine.
“We will continue to use all tools at our disposal and partner with the Drug Enforcement Administration and other federal, state, local agencies, and stakeholders as appropriate to stem these illicit activities and protect public health,” said Dr. Califf.
A version of this article first appeared on Medscape.com.
Wearable fluid sensor lowers risk of HF rehospitalizations: BMAD
NEW ORLEANS – A wearable device that monitors thoracic fluid and can signal elevated levels can improve outcomes after heart failure hospitalization, according to a comparative but nonrandomized trial.
In this study, management adjustments made in response to a threshold alert from the device led to several improvements in outcome at 90 days, including a significant 38% reduction in the primary outcome of rehospitalization, relative to controls (P = .02), reported John P. Boehmer, MD, at the joint scientific sessions of the American College of Cardiology and the World Heart Federation.
The same relative risk reduction at 90 days was observed for a composite outcome of time to first hospitalization, visit to an emergency room, or death (hazard ratio, 0.62; P = .03).
Quality of life, as measured with the Kansas City Cardiomyopathy Questionnaire (KCCQ), improved steadily in both the experimental and control arm over the 90-day study, but the curves separated at about 30 days, Dr. Boehmer reported. By the end of the study, the mean KCCQ difference was 12 points favoring the experimental arm on a scale in which 5 points is considered clinically meaningful.
70% report improved quality of life
“Responder analysis revealed that nearly 70% of patients in the arm managed with the monitor reported a clinically meaningful improvement in quality of life, compared to 50% of patients in the control arm,” said Dr. Boehmer, professor of medicine and surgery at Penn State Health, Hershey.
Fluid overload is an indication of worsening disease and a frequent cause of heart failure hospitalization. The Zoll Heart Failure Monitoring System (HFMS) that was tested in this study already has regulatory approval. It is equipped to monitor several biomarkers, including heart rate and respiration rate, but its ability to measure lung fluid through low electromagnetic radiofrequency pulses was the function of interest for this study.
In this nonrandomized study, called Benefits of Microcor in Ambulatory
Decompensated Heart Failure (BMAD), a control arm was enrolled first. By monitoring the initial patients enrolled in the control arm, the investigators established a threshold of thoracic fluid that would be used to trigger an alert in the intervention arm. This ultimately was defined as 3 standard deviations from the population mean.
Patients were eligible for this study if they were discharged from a hospital with heart failure in the previous 10 days. Of exclusion criteria, a short life expectancy (< 1 year) and a wearable cardiac defibrillator were notable. Left ventricular ejection fraction (LVEF) was not considered for inclusion or exclusion.
All subjects participated in weekly phone calls and monthly office visits. However, both investigators and patients were blinded to the device data in the control arm. Conversely, subjects and investigators in the intervention arm were able to access data generated by the device through a secure website.
Of the 245 eligible patients in the control arm, 168 were available for evaluation at 90 days. Among the 249 eligible patients in the intervention arm, 176 were included in the 90-day evaluation. Of those who were not available, the most common reason was study withdrawal. About 20% died before the 90-day evaluation.
The majority of patients in both arms were in class III or IV heart failure. About half had LVEF less than 40%, and more than 40% of patients in each group had chronic kidney disease (CKD). Roughly 55% of patients were at least 65 years of age.
At 90 days, the absolute risk reduction in rehospitalization was 7%, producing a number to treat with the device of 14.3 to prevent one rehospitalization. In a subgroup stratification, the benefit was similar by age, sex, presence or absence of CKD, LVEF greater or lower than 40%, Black or non-Black race, and ischemic or nonischemic etiology.
Patient access to data considered a plus
If lack of randomization is a weakness of this study, the decision to unblind the data for both investigators and patients might not be, according to Lynne Stevenson, MD, director of the cardiomyopathy program, Vanderbilt University Medical Center, Nashville, Tenn.
“You might be criticized for this [allowing patients to monitor their data], but I actually think this is a strength of the study,” said Dr. Stevenson, who believes the growing trend to involve heart failure patients in self-management has been a positive direction in clinical care.
She indicated that, despite the potential bias derived from being aware of fluid fluctuations, this information might also be contributing to patient motivation for adherence and appropriate lifestyle modifications.
Biykem Bozkurt, MD, PhD, chair of cardiology at Baylor College of Medicine, Houston, made a similar point but for a different reason. She expressed concern about the work that monitoring the wearable device creates for clinicians. Despite the positive data generated by this study, Dr. Bozkurt said the device as used in the study demanded “a lot of clinical time and effort” when these are both in short supply.
While she called for a larger and randomized study to corroborate the results of this investigation, she also thinks that it would make sense to compare the clinical value of this device against alternative methods for monitoring heart failure, including other wearable devices. Dr. Bozkurt asserted that some of the most helpful devices from a clinical perspective might be those that patients monitor themselves.
“Hopefully in the future, we will be offering tools that provide patients information they can use without the immediate need of a clinician,” she said.
Dr. Boehmer reports financial relationships with Abbott, Boston Scientific, Medtronic, and Zoll Medical Corporation, which provided the funding for this study. Dr. Stevenson reports no potential conflicts of interest. Dr. Bozkurt reports financial relationships with Abbott, Amgen, AstraZeneca, Boehringer Ingelheim, Cardurion, LivaNova, Relypsa, Renovacor, Sanofi-Aventis, and Vifor.
NEW ORLEANS – A wearable device that monitors thoracic fluid and can signal elevated levels can improve outcomes after heart failure hospitalization, according to a comparative but nonrandomized trial.
In this study, management adjustments made in response to a threshold alert from the device led to several improvements in outcome at 90 days, including a significant 38% reduction in the primary outcome of rehospitalization, relative to controls (P = .02), reported John P. Boehmer, MD, at the joint scientific sessions of the American College of Cardiology and the World Heart Federation.
The same relative risk reduction at 90 days was observed for a composite outcome of time to first hospitalization, visit to an emergency room, or death (hazard ratio, 0.62; P = .03).
Quality of life, as measured with the Kansas City Cardiomyopathy Questionnaire (KCCQ), improved steadily in both the experimental and control arm over the 90-day study, but the curves separated at about 30 days, Dr. Boehmer reported. By the end of the study, the mean KCCQ difference was 12 points favoring the experimental arm on a scale in which 5 points is considered clinically meaningful.
70% report improved quality of life
“Responder analysis revealed that nearly 70% of patients in the arm managed with the monitor reported a clinically meaningful improvement in quality of life, compared to 50% of patients in the control arm,” said Dr. Boehmer, professor of medicine and surgery at Penn State Health, Hershey.
Fluid overload is an indication of worsening disease and a frequent cause of heart failure hospitalization. The Zoll Heart Failure Monitoring System (HFMS) that was tested in this study already has regulatory approval. It is equipped to monitor several biomarkers, including heart rate and respiration rate, but its ability to measure lung fluid through low electromagnetic radiofrequency pulses was the function of interest for this study.
In this nonrandomized study, called Benefits of Microcor in Ambulatory
Decompensated Heart Failure (BMAD), a control arm was enrolled first. By monitoring the initial patients enrolled in the control arm, the investigators established a threshold of thoracic fluid that would be used to trigger an alert in the intervention arm. This ultimately was defined as 3 standard deviations from the population mean.
Patients were eligible for this study if they were discharged from a hospital with heart failure in the previous 10 days. Of exclusion criteria, a short life expectancy (< 1 year) and a wearable cardiac defibrillator were notable. Left ventricular ejection fraction (LVEF) was not considered for inclusion or exclusion.
All subjects participated in weekly phone calls and monthly office visits. However, both investigators and patients were blinded to the device data in the control arm. Conversely, subjects and investigators in the intervention arm were able to access data generated by the device through a secure website.
Of the 245 eligible patients in the control arm, 168 were available for evaluation at 90 days. Among the 249 eligible patients in the intervention arm, 176 were included in the 90-day evaluation. Of those who were not available, the most common reason was study withdrawal. About 20% died before the 90-day evaluation.
The majority of patients in both arms were in class III or IV heart failure. About half had LVEF less than 40%, and more than 40% of patients in each group had chronic kidney disease (CKD). Roughly 55% of patients were at least 65 years of age.
At 90 days, the absolute risk reduction in rehospitalization was 7%, producing a number to treat with the device of 14.3 to prevent one rehospitalization. In a subgroup stratification, the benefit was similar by age, sex, presence or absence of CKD, LVEF greater or lower than 40%, Black or non-Black race, and ischemic or nonischemic etiology.
Patient access to data considered a plus
If lack of randomization is a weakness of this study, the decision to unblind the data for both investigators and patients might not be, according to Lynne Stevenson, MD, director of the cardiomyopathy program, Vanderbilt University Medical Center, Nashville, Tenn.
“You might be criticized for this [allowing patients to monitor their data], but I actually think this is a strength of the study,” said Dr. Stevenson, who believes the growing trend to involve heart failure patients in self-management has been a positive direction in clinical care.
She indicated that, despite the potential bias derived from being aware of fluid fluctuations, this information might also be contributing to patient motivation for adherence and appropriate lifestyle modifications.
Biykem Bozkurt, MD, PhD, chair of cardiology at Baylor College of Medicine, Houston, made a similar point but for a different reason. She expressed concern about the work that monitoring the wearable device creates for clinicians. Despite the positive data generated by this study, Dr. Bozkurt said the device as used in the study demanded “a lot of clinical time and effort” when these are both in short supply.
While she called for a larger and randomized study to corroborate the results of this investigation, she also thinks that it would make sense to compare the clinical value of this device against alternative methods for monitoring heart failure, including other wearable devices. Dr. Bozkurt asserted that some of the most helpful devices from a clinical perspective might be those that patients monitor themselves.
“Hopefully in the future, we will be offering tools that provide patients information they can use without the immediate need of a clinician,” she said.
Dr. Boehmer reports financial relationships with Abbott, Boston Scientific, Medtronic, and Zoll Medical Corporation, which provided the funding for this study. Dr. Stevenson reports no potential conflicts of interest. Dr. Bozkurt reports financial relationships with Abbott, Amgen, AstraZeneca, Boehringer Ingelheim, Cardurion, LivaNova, Relypsa, Renovacor, Sanofi-Aventis, and Vifor.
NEW ORLEANS – A wearable device that monitors thoracic fluid and can signal elevated levels can improve outcomes after heart failure hospitalization, according to a comparative but nonrandomized trial.
In this study, management adjustments made in response to a threshold alert from the device led to several improvements in outcome at 90 days, including a significant 38% reduction in the primary outcome of rehospitalization, relative to controls (P = .02), reported John P. Boehmer, MD, at the joint scientific sessions of the American College of Cardiology and the World Heart Federation.
The same relative risk reduction at 90 days was observed for a composite outcome of time to first hospitalization, visit to an emergency room, or death (hazard ratio, 0.62; P = .03).
Quality of life, as measured with the Kansas City Cardiomyopathy Questionnaire (KCCQ), improved steadily in both the experimental and control arm over the 90-day study, but the curves separated at about 30 days, Dr. Boehmer reported. By the end of the study, the mean KCCQ difference was 12 points favoring the experimental arm on a scale in which 5 points is considered clinically meaningful.
70% report improved quality of life
“Responder analysis revealed that nearly 70% of patients in the arm managed with the monitor reported a clinically meaningful improvement in quality of life, compared to 50% of patients in the control arm,” said Dr. Boehmer, professor of medicine and surgery at Penn State Health, Hershey.
Fluid overload is an indication of worsening disease and a frequent cause of heart failure hospitalization. The Zoll Heart Failure Monitoring System (HFMS) that was tested in this study already has regulatory approval. It is equipped to monitor several biomarkers, including heart rate and respiration rate, but its ability to measure lung fluid through low electromagnetic radiofrequency pulses was the function of interest for this study.
In this nonrandomized study, called Benefits of Microcor in Ambulatory
Decompensated Heart Failure (BMAD), a control arm was enrolled first. By monitoring the initial patients enrolled in the control arm, the investigators established a threshold of thoracic fluid that would be used to trigger an alert in the intervention arm. This ultimately was defined as 3 standard deviations from the population mean.
Patients were eligible for this study if they were discharged from a hospital with heart failure in the previous 10 days. Of exclusion criteria, a short life expectancy (< 1 year) and a wearable cardiac defibrillator were notable. Left ventricular ejection fraction (LVEF) was not considered for inclusion or exclusion.
All subjects participated in weekly phone calls and monthly office visits. However, both investigators and patients were blinded to the device data in the control arm. Conversely, subjects and investigators in the intervention arm were able to access data generated by the device through a secure website.
Of the 245 eligible patients in the control arm, 168 were available for evaluation at 90 days. Among the 249 eligible patients in the intervention arm, 176 were included in the 90-day evaluation. Of those who were not available, the most common reason was study withdrawal. About 20% died before the 90-day evaluation.
The majority of patients in both arms were in class III or IV heart failure. About half had LVEF less than 40%, and more than 40% of patients in each group had chronic kidney disease (CKD). Roughly 55% of patients were at least 65 years of age.
At 90 days, the absolute risk reduction in rehospitalization was 7%, producing a number to treat with the device of 14.3 to prevent one rehospitalization. In a subgroup stratification, the benefit was similar by age, sex, presence or absence of CKD, LVEF greater or lower than 40%, Black or non-Black race, and ischemic or nonischemic etiology.
Patient access to data considered a plus
If lack of randomization is a weakness of this study, the decision to unblind the data for both investigators and patients might not be, according to Lynne Stevenson, MD, director of the cardiomyopathy program, Vanderbilt University Medical Center, Nashville, Tenn.
“You might be criticized for this [allowing patients to monitor their data], but I actually think this is a strength of the study,” said Dr. Stevenson, who believes the growing trend to involve heart failure patients in self-management has been a positive direction in clinical care.
She indicated that, despite the potential bias derived from being aware of fluid fluctuations, this information might also be contributing to patient motivation for adherence and appropriate lifestyle modifications.
Biykem Bozkurt, MD, PhD, chair of cardiology at Baylor College of Medicine, Houston, made a similar point but for a different reason. She expressed concern about the work that monitoring the wearable device creates for clinicians. Despite the positive data generated by this study, Dr. Bozkurt said the device as used in the study demanded “a lot of clinical time and effort” when these are both in short supply.
While she called for a larger and randomized study to corroborate the results of this investigation, she also thinks that it would make sense to compare the clinical value of this device against alternative methods for monitoring heart failure, including other wearable devices. Dr. Bozkurt asserted that some of the most helpful devices from a clinical perspective might be those that patients monitor themselves.
“Hopefully in the future, we will be offering tools that provide patients information they can use without the immediate need of a clinician,” she said.
Dr. Boehmer reports financial relationships with Abbott, Boston Scientific, Medtronic, and Zoll Medical Corporation, which provided the funding for this study. Dr. Stevenson reports no potential conflicts of interest. Dr. Bozkurt reports financial relationships with Abbott, Amgen, AstraZeneca, Boehringer Ingelheim, Cardurion, LivaNova, Relypsa, Renovacor, Sanofi-Aventis, and Vifor.
AT ACC 2023
FREEDOM COVID: Full-dose anticoagulation cut mortality but missed primary endpoint
Study conducted in noncritically ill
NEW ORLEANS – In the international FREEDOM COVID trial that randomized non–critically ill hospitalized patients, a therapeutic dose of anticoagulation relative to a prophylactic dose significantly reduced death from COVID-19 at 30 days, even as a larger composite primary endpoint was missed.
The mortality reduction suggests therapeutic-dose anticoagulation “may improve outcomes in non–critically ill patients hospitalized with COVID-19 who are at increased risk for adverse events but do not yet require ICU-level of care,” reported Valentin Fuster, MD, PhD, at the joint scientific sessions of the American College of Cardiology and the World Heart Federation.
These data provide a suggestion rather than a demonstration of benefit because the primary composite endpoint of all-cause mortality, intubation requiring mechanical ventilation, systemic thromboembolism or ischemic stroke at 30 days was not met. Although this 30-day outcome was lower on the therapeutic dose (11.3% vs. 13.2%), the difference was only a trend (hazard ratio, 0.85; P = .11), said Dr. Fuster, physician-in-chief, Mount Sinai Hospital, New York.
Missed primary endpoint blamed on low events
The declining severity of more recent COVID-19 variants (the trial was conducted from August 2022 to September 2022) might be one explanation that the primary endpoint was not met, but the more likely explanation is the relatively good health status – and therefore a low risk of events – among patients randomized in India, 1 of 10 participating countries.
India accounted for roughly 40% of the total number of 3,398 patients in the intention-to-treat population. In India, the rates of events were 0.7 and 1.3 in the prophylactic and therapeutic anticoagulation arms, respectively. In contrast, they were 17.5 and 9.5, respectively in the United States. In combined data from the other eight countries, the rates were 22.78 and 20.4, respectively.
“These results emphasize that varying country-specific thresholds for hospitalization may affect patient prognosis and the potential utility of advanced therapies” Dr. Fuster said.
In fact, the therapeutic anticoagulation was linked to a nonsignificant twofold increase in the risk of the primary outcome in India (HR, 2.01; 95% confidence interval, 0.57-7.13) when outcomes were stratified by country. In the United States, where there was a much higher incidence of events, therapeutic anticoagulation was associated with a nearly 50% reduction (HR, 0.53; 95% CI, 0.31-0.91).
In the remaining countries, which included those in Latin America and Europe as well as the city of Hong Kong, the primary outcome was reduced numerically but not statistically by therapeutic relative to prophylactic anticoagulation (HR, 0.89; 95% CI, 0.71-1.11).
Enoxaparin and apixaban are studied
In FREEDOM COVID, patients were randomized to a therapeutic dose of the low-molecular-weight heparin (LMWH) enoxaparin (1 mg/kg every 12 hours), a prophylactic dose of enoxaparin (40 mg once daily), or a therapeutic dose of the direct factor Xa inhibitor apixaban (5 mg every 12 hours). Lower doses of enoxaparin and apixaban were used for those with renal impairment, and lower doses of apixaban were employed for elderly patients (≥ 80 years) and those with low body weight (≤ 60 kg).
The major inclusion criteria were confirmed COVID-19 infection with symptomatic systemic involvement. The major exclusion criteria were need for ICU level of care or active bleeding.
The therapeutic anticoagulation arms performed similarly and were combined for comparison to the prophylactic arm. Despite the failure to show a difference in the primary outcome, the rate of 30-day mortality was substantially lower in the therapeutic arm (4.9% vs. 7.0%), translating into a 30% risk reduction (HR, 0.70; P = .01).
Therapeutic anticoagulation was also associated with a lower rate of intubation/mechanical ventilation (6.4% vs. 8.4%) that reached statistical significance (HR, 0.75; P = .03). The risk reduction was also significant for a combination of these endpoints (HR, 0.77; P = .03).
The lower proportion of patients who eventually required ICU-level of care (9.9% vs. 11.7%) showed a trend in favor of therapeutic anticoagulation (HR, 0.84; P = .11).
Bleeding rates did not differ between arms
Bleeding Academic Research Consortium major bleeding types 3 and 5 were slightly numerically higher in the group randomized to therapeutic enoxaparin (0.5%) than prophylactic enoxaparin (0.1%) and therapeutic apixaban (0.3%), but the differences between any groups were not significant.
Numerous anticoagulation trials in patients with COVID-19 have been published previously. One 2021 trial published in the New England Journal of Medicine also suggested benefit from a therapeutic relative to prophylactic anticoagulation. In that trial, which compared heparin to usual-care thromboprophylaxis, benefits were derived from a Bayesian analysis. Significant differences were not shown for death or other major outcome assessed individually.
Even though this more recent trial missed its primary endpoint, Gregg Stone, MD, a coauthor of this study and a colleague of Dr. Fuster at the Mount Sinai School of Medicine, New York, reiterated that these results support routine anticoagulation in hospitalized COVID-19 patients.
“These are robust reductions in mortality and intubation rates, which are the most serious outcomes,” said Dr. Stone, who is first author of the paper, which was published in the Journal of the American College of Cardiology immediately after Dr. Fuster’s presentation.
COVID-19 has proven to be a very thrombogenic virus, but the literature has not been wholly consistent on which anticoagulation treatment provides the best balance of benefits and risks, according to Julia Grapsa, MD, PhD, attending cardiologist, Guys and St. Thomas Hospital, London. She said that this randomized trial, despite its failure to meet the primary endpoint, is useful.
“This demonstrates that a therapeutic dose of enoxaparin is likely to improve outcomes over a prophylactic dose with a low risk of bleeding,” Dr. Grapsa said. On the basis of the randomized study, “I feel more confident with this approach.”
Dr. Fuster reported no potential conflicts of interest. Dr. Stone has financial relationships with more than 30 companies that make pharmaceuticals and medical devices. Dr. Grapsa reported no potential conflicts of interest.
Study conducted in noncritically ill
Study conducted in noncritically ill
NEW ORLEANS – In the international FREEDOM COVID trial that randomized non–critically ill hospitalized patients, a therapeutic dose of anticoagulation relative to a prophylactic dose significantly reduced death from COVID-19 at 30 days, even as a larger composite primary endpoint was missed.
The mortality reduction suggests therapeutic-dose anticoagulation “may improve outcomes in non–critically ill patients hospitalized with COVID-19 who are at increased risk for adverse events but do not yet require ICU-level of care,” reported Valentin Fuster, MD, PhD, at the joint scientific sessions of the American College of Cardiology and the World Heart Federation.
These data provide a suggestion rather than a demonstration of benefit because the primary composite endpoint of all-cause mortality, intubation requiring mechanical ventilation, systemic thromboembolism or ischemic stroke at 30 days was not met. Although this 30-day outcome was lower on the therapeutic dose (11.3% vs. 13.2%), the difference was only a trend (hazard ratio, 0.85; P = .11), said Dr. Fuster, physician-in-chief, Mount Sinai Hospital, New York.
Missed primary endpoint blamed on low events
The declining severity of more recent COVID-19 variants (the trial was conducted from August 2022 to September 2022) might be one explanation that the primary endpoint was not met, but the more likely explanation is the relatively good health status – and therefore a low risk of events – among patients randomized in India, 1 of 10 participating countries.
India accounted for roughly 40% of the total number of 3,398 patients in the intention-to-treat population. In India, the rates of events were 0.7 and 1.3 in the prophylactic and therapeutic anticoagulation arms, respectively. In contrast, they were 17.5 and 9.5, respectively in the United States. In combined data from the other eight countries, the rates were 22.78 and 20.4, respectively.
“These results emphasize that varying country-specific thresholds for hospitalization may affect patient prognosis and the potential utility of advanced therapies” Dr. Fuster said.
In fact, the therapeutic anticoagulation was linked to a nonsignificant twofold increase in the risk of the primary outcome in India (HR, 2.01; 95% confidence interval, 0.57-7.13) when outcomes were stratified by country. In the United States, where there was a much higher incidence of events, therapeutic anticoagulation was associated with a nearly 50% reduction (HR, 0.53; 95% CI, 0.31-0.91).
In the remaining countries, which included those in Latin America and Europe as well as the city of Hong Kong, the primary outcome was reduced numerically but not statistically by therapeutic relative to prophylactic anticoagulation (HR, 0.89; 95% CI, 0.71-1.11).
Enoxaparin and apixaban are studied
In FREEDOM COVID, patients were randomized to a therapeutic dose of the low-molecular-weight heparin (LMWH) enoxaparin (1 mg/kg every 12 hours), a prophylactic dose of enoxaparin (40 mg once daily), or a therapeutic dose of the direct factor Xa inhibitor apixaban (5 mg every 12 hours). Lower doses of enoxaparin and apixaban were used for those with renal impairment, and lower doses of apixaban were employed for elderly patients (≥ 80 years) and those with low body weight (≤ 60 kg).
The major inclusion criteria were confirmed COVID-19 infection with symptomatic systemic involvement. The major exclusion criteria were need for ICU level of care or active bleeding.
The therapeutic anticoagulation arms performed similarly and were combined for comparison to the prophylactic arm. Despite the failure to show a difference in the primary outcome, the rate of 30-day mortality was substantially lower in the therapeutic arm (4.9% vs. 7.0%), translating into a 30% risk reduction (HR, 0.70; P = .01).
Therapeutic anticoagulation was also associated with a lower rate of intubation/mechanical ventilation (6.4% vs. 8.4%) that reached statistical significance (HR, 0.75; P = .03). The risk reduction was also significant for a combination of these endpoints (HR, 0.77; P = .03).
The lower proportion of patients who eventually required ICU-level of care (9.9% vs. 11.7%) showed a trend in favor of therapeutic anticoagulation (HR, 0.84; P = .11).
Bleeding rates did not differ between arms
Bleeding Academic Research Consortium major bleeding types 3 and 5 were slightly numerically higher in the group randomized to therapeutic enoxaparin (0.5%) than prophylactic enoxaparin (0.1%) and therapeutic apixaban (0.3%), but the differences between any groups were not significant.
Numerous anticoagulation trials in patients with COVID-19 have been published previously. One 2021 trial published in the New England Journal of Medicine also suggested benefit from a therapeutic relative to prophylactic anticoagulation. In that trial, which compared heparin to usual-care thromboprophylaxis, benefits were derived from a Bayesian analysis. Significant differences were not shown for death or other major outcome assessed individually.
Even though this more recent trial missed its primary endpoint, Gregg Stone, MD, a coauthor of this study and a colleague of Dr. Fuster at the Mount Sinai School of Medicine, New York, reiterated that these results support routine anticoagulation in hospitalized COVID-19 patients.
“These are robust reductions in mortality and intubation rates, which are the most serious outcomes,” said Dr. Stone, who is first author of the paper, which was published in the Journal of the American College of Cardiology immediately after Dr. Fuster’s presentation.
COVID-19 has proven to be a very thrombogenic virus, but the literature has not been wholly consistent on which anticoagulation treatment provides the best balance of benefits and risks, according to Julia Grapsa, MD, PhD, attending cardiologist, Guys and St. Thomas Hospital, London. She said that this randomized trial, despite its failure to meet the primary endpoint, is useful.
“This demonstrates that a therapeutic dose of enoxaparin is likely to improve outcomes over a prophylactic dose with a low risk of bleeding,” Dr. Grapsa said. On the basis of the randomized study, “I feel more confident with this approach.”
Dr. Fuster reported no potential conflicts of interest. Dr. Stone has financial relationships with more than 30 companies that make pharmaceuticals and medical devices. Dr. Grapsa reported no potential conflicts of interest.
NEW ORLEANS – In the international FREEDOM COVID trial that randomized non–critically ill hospitalized patients, a therapeutic dose of anticoagulation relative to a prophylactic dose significantly reduced death from COVID-19 at 30 days, even as a larger composite primary endpoint was missed.
The mortality reduction suggests therapeutic-dose anticoagulation “may improve outcomes in non–critically ill patients hospitalized with COVID-19 who are at increased risk for adverse events but do not yet require ICU-level of care,” reported Valentin Fuster, MD, PhD, at the joint scientific sessions of the American College of Cardiology and the World Heart Federation.
These data provide a suggestion rather than a demonstration of benefit because the primary composite endpoint of all-cause mortality, intubation requiring mechanical ventilation, systemic thromboembolism or ischemic stroke at 30 days was not met. Although this 30-day outcome was lower on the therapeutic dose (11.3% vs. 13.2%), the difference was only a trend (hazard ratio, 0.85; P = .11), said Dr. Fuster, physician-in-chief, Mount Sinai Hospital, New York.
Missed primary endpoint blamed on low events
The declining severity of more recent COVID-19 variants (the trial was conducted from August 2022 to September 2022) might be one explanation that the primary endpoint was not met, but the more likely explanation is the relatively good health status – and therefore a low risk of events – among patients randomized in India, 1 of 10 participating countries.
India accounted for roughly 40% of the total number of 3,398 patients in the intention-to-treat population. In India, the rates of events were 0.7 and 1.3 in the prophylactic and therapeutic anticoagulation arms, respectively. In contrast, they were 17.5 and 9.5, respectively in the United States. In combined data from the other eight countries, the rates were 22.78 and 20.4, respectively.
“These results emphasize that varying country-specific thresholds for hospitalization may affect patient prognosis and the potential utility of advanced therapies” Dr. Fuster said.
In fact, the therapeutic anticoagulation was linked to a nonsignificant twofold increase in the risk of the primary outcome in India (HR, 2.01; 95% confidence interval, 0.57-7.13) when outcomes were stratified by country. In the United States, where there was a much higher incidence of events, therapeutic anticoagulation was associated with a nearly 50% reduction (HR, 0.53; 95% CI, 0.31-0.91).
In the remaining countries, which included those in Latin America and Europe as well as the city of Hong Kong, the primary outcome was reduced numerically but not statistically by therapeutic relative to prophylactic anticoagulation (HR, 0.89; 95% CI, 0.71-1.11).
Enoxaparin and apixaban are studied
In FREEDOM COVID, patients were randomized to a therapeutic dose of the low-molecular-weight heparin (LMWH) enoxaparin (1 mg/kg every 12 hours), a prophylactic dose of enoxaparin (40 mg once daily), or a therapeutic dose of the direct factor Xa inhibitor apixaban (5 mg every 12 hours). Lower doses of enoxaparin and apixaban were used for those with renal impairment, and lower doses of apixaban were employed for elderly patients (≥ 80 years) and those with low body weight (≤ 60 kg).
The major inclusion criteria were confirmed COVID-19 infection with symptomatic systemic involvement. The major exclusion criteria were need for ICU level of care or active bleeding.
The therapeutic anticoagulation arms performed similarly and were combined for comparison to the prophylactic arm. Despite the failure to show a difference in the primary outcome, the rate of 30-day mortality was substantially lower in the therapeutic arm (4.9% vs. 7.0%), translating into a 30% risk reduction (HR, 0.70; P = .01).
Therapeutic anticoagulation was also associated with a lower rate of intubation/mechanical ventilation (6.4% vs. 8.4%) that reached statistical significance (HR, 0.75; P = .03). The risk reduction was also significant for a combination of these endpoints (HR, 0.77; P = .03).
The lower proportion of patients who eventually required ICU-level of care (9.9% vs. 11.7%) showed a trend in favor of therapeutic anticoagulation (HR, 0.84; P = .11).
Bleeding rates did not differ between arms
Bleeding Academic Research Consortium major bleeding types 3 and 5 were slightly numerically higher in the group randomized to therapeutic enoxaparin (0.5%) than prophylactic enoxaparin (0.1%) and therapeutic apixaban (0.3%), but the differences between any groups were not significant.
Numerous anticoagulation trials in patients with COVID-19 have been published previously. One 2021 trial published in the New England Journal of Medicine also suggested benefit from a therapeutic relative to prophylactic anticoagulation. In that trial, which compared heparin to usual-care thromboprophylaxis, benefits were derived from a Bayesian analysis. Significant differences were not shown for death or other major outcome assessed individually.
Even though this more recent trial missed its primary endpoint, Gregg Stone, MD, a coauthor of this study and a colleague of Dr. Fuster at the Mount Sinai School of Medicine, New York, reiterated that these results support routine anticoagulation in hospitalized COVID-19 patients.
“These are robust reductions in mortality and intubation rates, which are the most serious outcomes,” said Dr. Stone, who is first author of the paper, which was published in the Journal of the American College of Cardiology immediately after Dr. Fuster’s presentation.
COVID-19 has proven to be a very thrombogenic virus, but the literature has not been wholly consistent on which anticoagulation treatment provides the best balance of benefits and risks, according to Julia Grapsa, MD, PhD, attending cardiologist, Guys and St. Thomas Hospital, London. She said that this randomized trial, despite its failure to meet the primary endpoint, is useful.
“This demonstrates that a therapeutic dose of enoxaparin is likely to improve outcomes over a prophylactic dose with a low risk of bleeding,” Dr. Grapsa said. On the basis of the randomized study, “I feel more confident with this approach.”
Dr. Fuster reported no potential conflicts of interest. Dr. Stone has financial relationships with more than 30 companies that make pharmaceuticals and medical devices. Dr. Grapsa reported no potential conflicts of interest.
AT ACC 2023
Clinician violence: Virtual reality to the rescue?
This discussion was recorded on Feb. 21, 2023. This transcript has been edited for clarity.
Robert D. Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical adviser for Medscape Emergency Medicine. Welcome, Dr. Salazar. It’s a pleasure to have you join us today.
Gilberto A. Salazar, MD: The pleasure is all mine, Dr. Glatter. Thank you so much for having me.
Dr. Glatter: This is such an important topic, as you can imagine. Workplace violence is affecting so many providers in hospital emergency departments but also throughout other parts of the hospital.
First, can you describe how the virtual reality (VR) program was designed that you developed and what type of situations it simulates?
Dr. Salazar: We worked in conjunction with the University of Texas at Dallas. They help people like me, subject matter experts in health care, to bring ideas to reality. I worked very closely with a group of engineers from their department in designing a module specifically designed to tackle, as you mentioned, one of our biggest threats in workplace violence.
We decided to bring in a series of competencies and proficiencies that we wanted to bring into the virtual reality space. In leveraging the technology and the expertise from UT Dallas, we were able to make that happen.
Dr. Glatter: I think it’s important to understand, in terms of virtual reality, what type of environment the program creates. Can you describe what a provider who puts the goggles on is experiencing? Do they feel anything? Is there technology that enables this?
Dr. Salazar: Yes, absolutely. We were able to bring to reality a series of scenarios very common from what you and I see in the emergency department on a daily basis. We wanted to immerse a learner into that specific environment. We didn’t feel that a module or something on a computer or a slide set could really bring the reality of what it’s like to interact with a patient who may be escalating or may be aggressive.
We are immersing learners into an actual hospital room to our specifications, very similar to exactly where we practice each and every day, and taking the learners through different situations that we designed with various levels of escalation and aggression, and asking the learner to manage that situation as best as they possibly can using the competencies and proficiencies that we taught them.
Dr. Glatter: Haptic feedback is an important part of the program and also the approach and technique that you’re using. Can you describe what haptic feedback means and what people actually feel?
Dr. Salazar: Absolutely. One of the most unfortunate things in my professional career is physical abuse suffered by people like me and you and our colleagues, nursing personnel, technicians, and others, resulting in injury.
We wanted to provide the most realistic experience that we could design. Haptics engage digital senses other than your auditory and your visuals. They really engage your tactile senses. These haptic vests and gloves and technology allow us to provide a third set of sensory stimuli for the learner.
At one of the modules, we have an actual physical assault that takes place, and the learner is actually able to feel in their body the strikes – of course, not painful – but just bringing in those senses and that stimulus, really leaving the learner with an experience that’s going to be long-lasting.
Dr. Glatter: Feeling that stimulus certainly affects your vital signs. Do you monitor a provider’s vital signs, such as their blood pressure and heart rate, as the situation and the threat escalate? That could potentially trigger some issues in people with prior PTSD or people with other mental health issues. Has that ever been considered in the design of your program?
Dr. Salazar: Yes, 100%. The beautiful thing about haptics is that they can be tailored to our specific parameters. The sensory stimulus that’s provided is actually very mild. It feels more like a tap than an actual strike. It just reminds us that when we’re having or experiencing an actual physical attack, we’re really engaging the senses.
We have an emergency physician or an EMT-paramedic on site at all times during the training so that we can monitor our subjects and make sure that they’re comfortable and healthy.
Dr. Glatter: Do they have actual sensors attached to their bodies that are part of your program or distinct in terms of monitoring their vital signs?
Dr. Salazar: It’s completely different. We have two different systems that we are planning on utilizing. Frankly, in the final version of this virtual reality module, we may not even involve the haptics. We’re going to study it and see how our learners behave and how much information they’re able to acquire and retain.
It may be very possible that just the visuals – the auditory and the immersion taking place within the hospital room – may be enough. It’s very possible that, in the next final version of this, we may find that haptics bring in quite a bit of value, and we may incorporate that. If that is the case, then we will, of course, acquire different technology to monitor the patient’s vital signs.
Dr. Glatter: Clearly, when situations escalate in the department, everyone gets more concerned about the patient, but providers are part of this equation, as you allude to.
In 2022, there was a poll by the American College of Emergency Physicians that stated that 85% of emergency physicians reported an increase in violent activity in their ERs in the past 5 years. Nearly two-thirds of nearly 3,000 emergency physicians surveyed reported being assaulted in the past year. This is an important module that we integrate into training providers in terms of these types of tense situations that can result not only in mental anguish but also in physical injury.
Dr. Salazar: One hundred percent. I frankly got tired of seeing my friends and my colleagues suffer both the physical and mental effects of verbal and physical abuse, and I wanted to design a project that was very patient centric while allowing our personnel to really manage these situations a little bit better.
Frankly, we don’t receive great training in this space, and I wanted to rewrite that narrative and make things better for our clinicians out there while remaining patient centric. I wanted to do something about it, and hopefully this dream will become a reality.
Dr. Glatter: Absolutely. There are other data from the Bureau of Labor Statistics stating that health care workers are five times more likely than employees in any other area of work to experience workplace violence. This could, again, range from verbal to physical violence. This is a very important module that you’re developing.
Are there any thoughts to extend this to active-shooter scenarios or any other high-stakes scenarios that you can imagine in the department?
Dr. Salazar: We’re actually working with the same developer that’s helping us with this VR module in developing a mass-casualty incident module so that we can get better training in responding to these very unfortunate high-stakes situations.
Dr. Glatter: In terms of using the module remotely, certainly not requiring resources or having to be in a physical place, can providers in your plan be able to take such a headset home and practice on their own in the sense of being able to deal with a situation? Would this be more reserved for in-department use?
Dr. Salazar: That’s a phenomenal question. I wanted to create the most flexible module that I possibly could. Ideally, a dream scenario is leveraging a simulation center at an academic center and not just do the VR module but also have a brief didactics incorporating a small slide set, some feedback, and some standardized patients. I wanted it to be flexible enough so that folks here in my state, a different state, or even internationally could take advantage of this technology and do it from the comfort of their home.
As you mentioned, this is going to strike some people. It’s going to hit them heavier than others in terms of prior experience as PTSD. For some people, it may be more comfortable to do it in the comfort of their homes. I wanted to create something very flexible and dynamic.
Dr. Glatter: I think that’s ideal. Just one other point. Can you discuss the different levels of competencies involved in this module and how that would be attained?
Dr. Salazar: It’s all evidence based, so we borrowed from literature and the specialties of emergency medicine. We collaborated with psychiatrists within our medical center. We looked at all available literature and methods, proficiencies, competencies, and best practices, and we took all of them together to form something that we think is organized and concise.
We were able to create our own algorithm, but it’s not brand new. We’re just borrowing what we think is the best to create something that the majority of health care personnel are going to be able to relate to and be able to really be proficient at.
This includes things like active listening, bargaining, how to respond, where to put yourself in a situation, and the best possible situation to respond to a scenario, how to prevent things – how to get out of a chokehold, for example. We’re borrowing from several different disciplines and creating something that can be very concise and organized.
Dr. Glatter: Does this program that you’ve developed allow the provider to get feedback in the sense that when they’re in such a danger, their life could be at risk? For example, if they don’t remove themselves in a certain amount of time, this could be lethal.
Dr. Salazar: Yes, 100%. Probably the one thing that differentiates our project from any others is the ability to customize the experience so that a learner who is doing the things that we ask them to do in terms of safety and response is able to get out of a situation successfully within the environment. If they don’t, they get some kind of feedback.
Not to spoil the surprise here, but we’re going to be doing things like looking at decibel meters to see what the volume in the room is doing and how you’re managing the volume and the stimulation within the room. If you are able to maintain the decibel readings at a specific level, you’re going to succeed through the module. If you don’t, we keep the patient escalation going.
Dr. Glatter: There is a debrief built into this type of approach where, in other words, learning points are emphasized – where you could have done better and such.
Dr. Salazar: Yes, absolutely. We are going to be able to get individualized data for each learner so that we can tailor the debrief to their own performance and be able to give them actionable items to work on. It’s a debrief that’s productive and individualized, and folks can walk away with something useful in the end.
Dr. Glatter: Are the data shared or confidential at present?
Dr. Salazar: At this very moment, the data are confidential. We are going to look at how to best use this. We’re hoping to eventually write this up and see how this information can be best used to train personnel.
Eventually, we may see that some of the advice that we’re giving is very common to most folks. Others may require some individualized type of feedback. That said, it remains to be seen, but right now, it’s confidential.
Dr. Glatter: Is this currently being implemented as part of your curriculum for emergency medicine residents?
Dr. Salazar: We’re going to study it first. We’re very excited to include our emergency medicine residents as one of our cohorts that’s going to be undergoing the module, and we’re going to be studying other forms of workplace violence mitigation strategies. We’re really excited about the possibility of this eventually becoming the standard of education for not only our emergency medicine residents, but also health care personnel all over the world.
Dr. Glatter: I’m glad you mentioned that, because obviously nurses, clerks in the department, and anyone who’s working in the department, for that matter, and who interfaces with patients really should undergo such training.
Dr. Salazar: Absolutely. The folks at intake, at check-in, and at kiosks. Do they go through a separate area for screening? You’re absolutely right. There are many folks who interface with patients and all of us are potential victims of workplace violence. We want to give our health care family the best opportunity to succeed in these situations.
Dr. Glatter:: Absolutely. Even EMS providers, being on the front lines and encountering patients in such situations, would benefit, in my opinion.
Dr. Salazar: Yes, absolutely. Behavioral health emergencies and organically induced altered mental status results in injury, both physical and mental, to EMS professionals as well, and there’s good evidence of that. I’ll be very glad to see this type of education make it out to our initial and continuing education efforts for EMS as well.
Dr. Glatter: I want to thank you. This has been very helpful. It’s such an important task that you’ve started to explore, and I look forward to follow-up on this. Again, thank you for your time.
Dr. Salazar: It was my pleasure. Thank you so much for having me.
Dr. Glatter is an attending physician at Lenox Hill Hospital in New York City and assistant professor of emergency medicine at Zucker School of Medicine at Hofstra/Northwell in Hempstead, N.Y. He is an editorial adviser and hosts the Hot Topics in EM series on Medscape. He is also a medical contributor for Forbes. Dr. Salazar is a board-certified emergency physician and associate professor at UT Southwestern Medicine Center in Dallas. He is involved with the UTSW Emergency Medicine Education Program and serves as the medical director to teach both initial and continuing the emergency medicine education for emergency medical technicians and paramedics, which trains most of the Dallas Fire Rescue personnel and the vast majority for EMS providers in the Dallas County. In addition, he serves as an associate chief of service at Parkland’s emergency department, and liaison to surgical services. A version of this article originally appeared on Medscape.com.
This discussion was recorded on Feb. 21, 2023. This transcript has been edited for clarity.
Robert D. Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical adviser for Medscape Emergency Medicine. Welcome, Dr. Salazar. It’s a pleasure to have you join us today.
Gilberto A. Salazar, MD: The pleasure is all mine, Dr. Glatter. Thank you so much for having me.
Dr. Glatter: This is such an important topic, as you can imagine. Workplace violence is affecting so many providers in hospital emergency departments but also throughout other parts of the hospital.
First, can you describe how the virtual reality (VR) program was designed that you developed and what type of situations it simulates?
Dr. Salazar: We worked in conjunction with the University of Texas at Dallas. They help people like me, subject matter experts in health care, to bring ideas to reality. I worked very closely with a group of engineers from their department in designing a module specifically designed to tackle, as you mentioned, one of our biggest threats in workplace violence.
We decided to bring in a series of competencies and proficiencies that we wanted to bring into the virtual reality space. In leveraging the technology and the expertise from UT Dallas, we were able to make that happen.
Dr. Glatter: I think it’s important to understand, in terms of virtual reality, what type of environment the program creates. Can you describe what a provider who puts the goggles on is experiencing? Do they feel anything? Is there technology that enables this?
Dr. Salazar: Yes, absolutely. We were able to bring to reality a series of scenarios very common from what you and I see in the emergency department on a daily basis. We wanted to immerse a learner into that specific environment. We didn’t feel that a module or something on a computer or a slide set could really bring the reality of what it’s like to interact with a patient who may be escalating or may be aggressive.
We are immersing learners into an actual hospital room to our specifications, very similar to exactly where we practice each and every day, and taking the learners through different situations that we designed with various levels of escalation and aggression, and asking the learner to manage that situation as best as they possibly can using the competencies and proficiencies that we taught them.
Dr. Glatter: Haptic feedback is an important part of the program and also the approach and technique that you’re using. Can you describe what haptic feedback means and what people actually feel?
Dr. Salazar: Absolutely. One of the most unfortunate things in my professional career is physical abuse suffered by people like me and you and our colleagues, nursing personnel, technicians, and others, resulting in injury.
We wanted to provide the most realistic experience that we could design. Haptics engage digital senses other than your auditory and your visuals. They really engage your tactile senses. These haptic vests and gloves and technology allow us to provide a third set of sensory stimuli for the learner.
At one of the modules, we have an actual physical assault that takes place, and the learner is actually able to feel in their body the strikes – of course, not painful – but just bringing in those senses and that stimulus, really leaving the learner with an experience that’s going to be long-lasting.
Dr. Glatter: Feeling that stimulus certainly affects your vital signs. Do you monitor a provider’s vital signs, such as their blood pressure and heart rate, as the situation and the threat escalate? That could potentially trigger some issues in people with prior PTSD or people with other mental health issues. Has that ever been considered in the design of your program?
Dr. Salazar: Yes, 100%. The beautiful thing about haptics is that they can be tailored to our specific parameters. The sensory stimulus that’s provided is actually very mild. It feels more like a tap than an actual strike. It just reminds us that when we’re having or experiencing an actual physical attack, we’re really engaging the senses.
We have an emergency physician or an EMT-paramedic on site at all times during the training so that we can monitor our subjects and make sure that they’re comfortable and healthy.
Dr. Glatter: Do they have actual sensors attached to their bodies that are part of your program or distinct in terms of monitoring their vital signs?
Dr. Salazar: It’s completely different. We have two different systems that we are planning on utilizing. Frankly, in the final version of this virtual reality module, we may not even involve the haptics. We’re going to study it and see how our learners behave and how much information they’re able to acquire and retain.
It may be very possible that just the visuals – the auditory and the immersion taking place within the hospital room – may be enough. It’s very possible that, in the next final version of this, we may find that haptics bring in quite a bit of value, and we may incorporate that. If that is the case, then we will, of course, acquire different technology to monitor the patient’s vital signs.
Dr. Glatter: Clearly, when situations escalate in the department, everyone gets more concerned about the patient, but providers are part of this equation, as you allude to.
In 2022, there was a poll by the American College of Emergency Physicians that stated that 85% of emergency physicians reported an increase in violent activity in their ERs in the past 5 years. Nearly two-thirds of nearly 3,000 emergency physicians surveyed reported being assaulted in the past year. This is an important module that we integrate into training providers in terms of these types of tense situations that can result not only in mental anguish but also in physical injury.
Dr. Salazar: One hundred percent. I frankly got tired of seeing my friends and my colleagues suffer both the physical and mental effects of verbal and physical abuse, and I wanted to design a project that was very patient centric while allowing our personnel to really manage these situations a little bit better.
Frankly, we don’t receive great training in this space, and I wanted to rewrite that narrative and make things better for our clinicians out there while remaining patient centric. I wanted to do something about it, and hopefully this dream will become a reality.
Dr. Glatter: Absolutely. There are other data from the Bureau of Labor Statistics stating that health care workers are five times more likely than employees in any other area of work to experience workplace violence. This could, again, range from verbal to physical violence. This is a very important module that you’re developing.
Are there any thoughts to extend this to active-shooter scenarios or any other high-stakes scenarios that you can imagine in the department?
Dr. Salazar: We’re actually working with the same developer that’s helping us with this VR module in developing a mass-casualty incident module so that we can get better training in responding to these very unfortunate high-stakes situations.
Dr. Glatter: In terms of using the module remotely, certainly not requiring resources or having to be in a physical place, can providers in your plan be able to take such a headset home and practice on their own in the sense of being able to deal with a situation? Would this be more reserved for in-department use?
Dr. Salazar: That’s a phenomenal question. I wanted to create the most flexible module that I possibly could. Ideally, a dream scenario is leveraging a simulation center at an academic center and not just do the VR module but also have a brief didactics incorporating a small slide set, some feedback, and some standardized patients. I wanted it to be flexible enough so that folks here in my state, a different state, or even internationally could take advantage of this technology and do it from the comfort of their home.
As you mentioned, this is going to strike some people. It’s going to hit them heavier than others in terms of prior experience as PTSD. For some people, it may be more comfortable to do it in the comfort of their homes. I wanted to create something very flexible and dynamic.
Dr. Glatter: I think that’s ideal. Just one other point. Can you discuss the different levels of competencies involved in this module and how that would be attained?
Dr. Salazar: It’s all evidence based, so we borrowed from literature and the specialties of emergency medicine. We collaborated with psychiatrists within our medical center. We looked at all available literature and methods, proficiencies, competencies, and best practices, and we took all of them together to form something that we think is organized and concise.
We were able to create our own algorithm, but it’s not brand new. We’re just borrowing what we think is the best to create something that the majority of health care personnel are going to be able to relate to and be able to really be proficient at.
This includes things like active listening, bargaining, how to respond, where to put yourself in a situation, and the best possible situation to respond to a scenario, how to prevent things – how to get out of a chokehold, for example. We’re borrowing from several different disciplines and creating something that can be very concise and organized.
Dr. Glatter: Does this program that you’ve developed allow the provider to get feedback in the sense that when they’re in such a danger, their life could be at risk? For example, if they don’t remove themselves in a certain amount of time, this could be lethal.
Dr. Salazar: Yes, 100%. Probably the one thing that differentiates our project from any others is the ability to customize the experience so that a learner who is doing the things that we ask them to do in terms of safety and response is able to get out of a situation successfully within the environment. If they don’t, they get some kind of feedback.
Not to spoil the surprise here, but we’re going to be doing things like looking at decibel meters to see what the volume in the room is doing and how you’re managing the volume and the stimulation within the room. If you are able to maintain the decibel readings at a specific level, you’re going to succeed through the module. If you don’t, we keep the patient escalation going.
Dr. Glatter: There is a debrief built into this type of approach where, in other words, learning points are emphasized – where you could have done better and such.
Dr. Salazar: Yes, absolutely. We are going to be able to get individualized data for each learner so that we can tailor the debrief to their own performance and be able to give them actionable items to work on. It’s a debrief that’s productive and individualized, and folks can walk away with something useful in the end.
Dr. Glatter: Are the data shared or confidential at present?
Dr. Salazar: At this very moment, the data are confidential. We are going to look at how to best use this. We’re hoping to eventually write this up and see how this information can be best used to train personnel.
Eventually, we may see that some of the advice that we’re giving is very common to most folks. Others may require some individualized type of feedback. That said, it remains to be seen, but right now, it’s confidential.
Dr. Glatter: Is this currently being implemented as part of your curriculum for emergency medicine residents?
Dr. Salazar: We’re going to study it first. We’re very excited to include our emergency medicine residents as one of our cohorts that’s going to be undergoing the module, and we’re going to be studying other forms of workplace violence mitigation strategies. We’re really excited about the possibility of this eventually becoming the standard of education for not only our emergency medicine residents, but also health care personnel all over the world.
Dr. Glatter: I’m glad you mentioned that, because obviously nurses, clerks in the department, and anyone who’s working in the department, for that matter, and who interfaces with patients really should undergo such training.
Dr. Salazar: Absolutely. The folks at intake, at check-in, and at kiosks. Do they go through a separate area for screening? You’re absolutely right. There are many folks who interface with patients and all of us are potential victims of workplace violence. We want to give our health care family the best opportunity to succeed in these situations.
Dr. Glatter:: Absolutely. Even EMS providers, being on the front lines and encountering patients in such situations, would benefit, in my opinion.
Dr. Salazar: Yes, absolutely. Behavioral health emergencies and organically induced altered mental status results in injury, both physical and mental, to EMS professionals as well, and there’s good evidence of that. I’ll be very glad to see this type of education make it out to our initial and continuing education efforts for EMS as well.
Dr. Glatter: I want to thank you. This has been very helpful. It’s such an important task that you’ve started to explore, and I look forward to follow-up on this. Again, thank you for your time.
Dr. Salazar: It was my pleasure. Thank you so much for having me.
Dr. Glatter is an attending physician at Lenox Hill Hospital in New York City and assistant professor of emergency medicine at Zucker School of Medicine at Hofstra/Northwell in Hempstead, N.Y. He is an editorial adviser and hosts the Hot Topics in EM series on Medscape. He is also a medical contributor for Forbes. Dr. Salazar is a board-certified emergency physician and associate professor at UT Southwestern Medicine Center in Dallas. He is involved with the UTSW Emergency Medicine Education Program and serves as the medical director to teach both initial and continuing the emergency medicine education for emergency medical technicians and paramedics, which trains most of the Dallas Fire Rescue personnel and the vast majority for EMS providers in the Dallas County. In addition, he serves as an associate chief of service at Parkland’s emergency department, and liaison to surgical services. A version of this article originally appeared on Medscape.com.
This discussion was recorded on Feb. 21, 2023. This transcript has been edited for clarity.
Robert D. Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical adviser for Medscape Emergency Medicine. Welcome, Dr. Salazar. It’s a pleasure to have you join us today.
Gilberto A. Salazar, MD: The pleasure is all mine, Dr. Glatter. Thank you so much for having me.
Dr. Glatter: This is such an important topic, as you can imagine. Workplace violence is affecting so many providers in hospital emergency departments but also throughout other parts of the hospital.
First, can you describe how the virtual reality (VR) program was designed that you developed and what type of situations it simulates?
Dr. Salazar: We worked in conjunction with the University of Texas at Dallas. They help people like me, subject matter experts in health care, to bring ideas to reality. I worked very closely with a group of engineers from their department in designing a module specifically designed to tackle, as you mentioned, one of our biggest threats in workplace violence.
We decided to bring in a series of competencies and proficiencies that we wanted to bring into the virtual reality space. In leveraging the technology and the expertise from UT Dallas, we were able to make that happen.
Dr. Glatter: I think it’s important to understand, in terms of virtual reality, what type of environment the program creates. Can you describe what a provider who puts the goggles on is experiencing? Do they feel anything? Is there technology that enables this?
Dr. Salazar: Yes, absolutely. We were able to bring to reality a series of scenarios very common from what you and I see in the emergency department on a daily basis. We wanted to immerse a learner into that specific environment. We didn’t feel that a module or something on a computer or a slide set could really bring the reality of what it’s like to interact with a patient who may be escalating or may be aggressive.
We are immersing learners into an actual hospital room to our specifications, very similar to exactly where we practice each and every day, and taking the learners through different situations that we designed with various levels of escalation and aggression, and asking the learner to manage that situation as best as they possibly can using the competencies and proficiencies that we taught them.
Dr. Glatter: Haptic feedback is an important part of the program and also the approach and technique that you’re using. Can you describe what haptic feedback means and what people actually feel?
Dr. Salazar: Absolutely. One of the most unfortunate things in my professional career is physical abuse suffered by people like me and you and our colleagues, nursing personnel, technicians, and others, resulting in injury.
We wanted to provide the most realistic experience that we could design. Haptics engage digital senses other than your auditory and your visuals. They really engage your tactile senses. These haptic vests and gloves and technology allow us to provide a third set of sensory stimuli for the learner.
At one of the modules, we have an actual physical assault that takes place, and the learner is actually able to feel in their body the strikes – of course, not painful – but just bringing in those senses and that stimulus, really leaving the learner with an experience that’s going to be long-lasting.
Dr. Glatter: Feeling that stimulus certainly affects your vital signs. Do you monitor a provider’s vital signs, such as their blood pressure and heart rate, as the situation and the threat escalate? That could potentially trigger some issues in people with prior PTSD or people with other mental health issues. Has that ever been considered in the design of your program?
Dr. Salazar: Yes, 100%. The beautiful thing about haptics is that they can be tailored to our specific parameters. The sensory stimulus that’s provided is actually very mild. It feels more like a tap than an actual strike. It just reminds us that when we’re having or experiencing an actual physical attack, we’re really engaging the senses.
We have an emergency physician or an EMT-paramedic on site at all times during the training so that we can monitor our subjects and make sure that they’re comfortable and healthy.
Dr. Glatter: Do they have actual sensors attached to their bodies that are part of your program or distinct in terms of monitoring their vital signs?
Dr. Salazar: It’s completely different. We have two different systems that we are planning on utilizing. Frankly, in the final version of this virtual reality module, we may not even involve the haptics. We’re going to study it and see how our learners behave and how much information they’re able to acquire and retain.
It may be very possible that just the visuals – the auditory and the immersion taking place within the hospital room – may be enough. It’s very possible that, in the next final version of this, we may find that haptics bring in quite a bit of value, and we may incorporate that. If that is the case, then we will, of course, acquire different technology to monitor the patient’s vital signs.
Dr. Glatter: Clearly, when situations escalate in the department, everyone gets more concerned about the patient, but providers are part of this equation, as you allude to.
In 2022, there was a poll by the American College of Emergency Physicians that stated that 85% of emergency physicians reported an increase in violent activity in their ERs in the past 5 years. Nearly two-thirds of nearly 3,000 emergency physicians surveyed reported being assaulted in the past year. This is an important module that we integrate into training providers in terms of these types of tense situations that can result not only in mental anguish but also in physical injury.
Dr. Salazar: One hundred percent. I frankly got tired of seeing my friends and my colleagues suffer both the physical and mental effects of verbal and physical abuse, and I wanted to design a project that was very patient centric while allowing our personnel to really manage these situations a little bit better.
Frankly, we don’t receive great training in this space, and I wanted to rewrite that narrative and make things better for our clinicians out there while remaining patient centric. I wanted to do something about it, and hopefully this dream will become a reality.
Dr. Glatter: Absolutely. There are other data from the Bureau of Labor Statistics stating that health care workers are five times more likely than employees in any other area of work to experience workplace violence. This could, again, range from verbal to physical violence. This is a very important module that you’re developing.
Are there any thoughts to extend this to active-shooter scenarios or any other high-stakes scenarios that you can imagine in the department?
Dr. Salazar: We’re actually working with the same developer that’s helping us with this VR module in developing a mass-casualty incident module so that we can get better training in responding to these very unfortunate high-stakes situations.
Dr. Glatter: In terms of using the module remotely, certainly not requiring resources or having to be in a physical place, can providers in your plan be able to take such a headset home and practice on their own in the sense of being able to deal with a situation? Would this be more reserved for in-department use?
Dr. Salazar: That’s a phenomenal question. I wanted to create the most flexible module that I possibly could. Ideally, a dream scenario is leveraging a simulation center at an academic center and not just do the VR module but also have a brief didactics incorporating a small slide set, some feedback, and some standardized patients. I wanted it to be flexible enough so that folks here in my state, a different state, or even internationally could take advantage of this technology and do it from the comfort of their home.
As you mentioned, this is going to strike some people. It’s going to hit them heavier than others in terms of prior experience as PTSD. For some people, it may be more comfortable to do it in the comfort of their homes. I wanted to create something very flexible and dynamic.
Dr. Glatter: I think that’s ideal. Just one other point. Can you discuss the different levels of competencies involved in this module and how that would be attained?
Dr. Salazar: It’s all evidence based, so we borrowed from literature and the specialties of emergency medicine. We collaborated with psychiatrists within our medical center. We looked at all available literature and methods, proficiencies, competencies, and best practices, and we took all of them together to form something that we think is organized and concise.
We were able to create our own algorithm, but it’s not brand new. We’re just borrowing what we think is the best to create something that the majority of health care personnel are going to be able to relate to and be able to really be proficient at.
This includes things like active listening, bargaining, how to respond, where to put yourself in a situation, and the best possible situation to respond to a scenario, how to prevent things – how to get out of a chokehold, for example. We’re borrowing from several different disciplines and creating something that can be very concise and organized.
Dr. Glatter: Does this program that you’ve developed allow the provider to get feedback in the sense that when they’re in such a danger, their life could be at risk? For example, if they don’t remove themselves in a certain amount of time, this could be lethal.
Dr. Salazar: Yes, 100%. Probably the one thing that differentiates our project from any others is the ability to customize the experience so that a learner who is doing the things that we ask them to do in terms of safety and response is able to get out of a situation successfully within the environment. If they don’t, they get some kind of feedback.
Not to spoil the surprise here, but we’re going to be doing things like looking at decibel meters to see what the volume in the room is doing and how you’re managing the volume and the stimulation within the room. If you are able to maintain the decibel readings at a specific level, you’re going to succeed through the module. If you don’t, we keep the patient escalation going.
Dr. Glatter: There is a debrief built into this type of approach where, in other words, learning points are emphasized – where you could have done better and such.
Dr. Salazar: Yes, absolutely. We are going to be able to get individualized data for each learner so that we can tailor the debrief to their own performance and be able to give them actionable items to work on. It’s a debrief that’s productive and individualized, and folks can walk away with something useful in the end.
Dr. Glatter: Are the data shared or confidential at present?
Dr. Salazar: At this very moment, the data are confidential. We are going to look at how to best use this. We’re hoping to eventually write this up and see how this information can be best used to train personnel.
Eventually, we may see that some of the advice that we’re giving is very common to most folks. Others may require some individualized type of feedback. That said, it remains to be seen, but right now, it’s confidential.
Dr. Glatter: Is this currently being implemented as part of your curriculum for emergency medicine residents?
Dr. Salazar: We’re going to study it first. We’re very excited to include our emergency medicine residents as one of our cohorts that’s going to be undergoing the module, and we’re going to be studying other forms of workplace violence mitigation strategies. We’re really excited about the possibility of this eventually becoming the standard of education for not only our emergency medicine residents, but also health care personnel all over the world.
Dr. Glatter: I’m glad you mentioned that, because obviously nurses, clerks in the department, and anyone who’s working in the department, for that matter, and who interfaces with patients really should undergo such training.
Dr. Salazar: Absolutely. The folks at intake, at check-in, and at kiosks. Do they go through a separate area for screening? You’re absolutely right. There are many folks who interface with patients and all of us are potential victims of workplace violence. We want to give our health care family the best opportunity to succeed in these situations.
Dr. Glatter:: Absolutely. Even EMS providers, being on the front lines and encountering patients in such situations, would benefit, in my opinion.
Dr. Salazar: Yes, absolutely. Behavioral health emergencies and organically induced altered mental status results in injury, both physical and mental, to EMS professionals as well, and there’s good evidence of that. I’ll be very glad to see this type of education make it out to our initial and continuing education efforts for EMS as well.
Dr. Glatter: I want to thank you. This has been very helpful. It’s such an important task that you’ve started to explore, and I look forward to follow-up on this. Again, thank you for your time.
Dr. Salazar: It was my pleasure. Thank you so much for having me.
Dr. Glatter is an attending physician at Lenox Hill Hospital in New York City and assistant professor of emergency medicine at Zucker School of Medicine at Hofstra/Northwell in Hempstead, N.Y. He is an editorial adviser and hosts the Hot Topics in EM series on Medscape. He is also a medical contributor for Forbes. Dr. Salazar is a board-certified emergency physician and associate professor at UT Southwestern Medicine Center in Dallas. He is involved with the UTSW Emergency Medicine Education Program and serves as the medical director to teach both initial and continuing the emergency medicine education for emergency medical technicians and paramedics, which trains most of the Dallas Fire Rescue personnel and the vast majority for EMS providers in the Dallas County. In addition, he serves as an associate chief of service at Parkland’s emergency department, and liaison to surgical services. A version of this article originally appeared on Medscape.com.
Buprenorphine proves effective for fentanyl users in the ED
based on data from nearly 900 individuals.
California EDs include a facilitation program known as CA Bridge for the treatment of opioid use disorder. Guidelines for CA Bridge call for high-dose buprenorphine to treat patients in drug withdrawal, with doses starting at 8-16 mg, Hannah Snyder, MD, of the University of California, San Francisco, and colleagues wrote.
“Buprenorphine has been repeatedly shown to save lives and prevent overdoses,” Dr. Snyder said in an interview. “We know that emergency department–initiated buprenorphine is an essential tool for increasing access. In the era of fentanyl, both patients and providers have expressed concerns that buprenorphine may not work as well as it did when patients were more likely to be using heroin or opioid pills.
“This retrospective cohort study provides additional information about emergency department buprenorphine as fentanyl becomes increasingly prevalent.”
In a research letter published in JAMA Network Open, the investigators reviewed data from the electronic health records of 896 patients who presented with opioid use disorder (OUD) at 16 CA Bridge EDs between Jan. 1, 2020, and April 30, 2020. All patients with OUD were included regardless of chief concern, current treatment, treatment desires, or withdrawal. A total of 87 individuals reported fentanyl use; if no fentanyl use was reported, the patient was classified as not using fentanyl. The median age of the patients was 35 years, two thirds were male, approximately 46% were White and non-Hispanic, and 30% had unstable housing.
The primary outcome was follow-up engagement at 7-14 days and 25-37 days.
A total of 492 patients received buprenorphine, including 44 fentanyl users, and 439 initiated high doses of 8-32 mg. At a 30-day follow-up, eight patients had precipitated withdrawal, including two cases in fentanyl users; none of these cases required hospital admission.
The follow-up engagement was similar for both groups, with adjusted odds ratios of 0.60 for administered buprenorphine at the initial ED encounter, 1.09 for 7-day follow-up, and 1.33 for 30-day follow-up.
The findings were limited by the retrospective design and use of clinical documentation, which likely resulted in underreporting of fentanyl use and follow-up, the researchers noted. However, the results supported the effectiveness of buprenorphine for ED patients in withdrawal with a history of fentanyl exposure.
“We were pleased to see that precipitated withdrawal was relatively uncommon in this study, and that patients who did and did not use fentanyl followed up at similar rates,” said Dr. Snyder. “This aligns with our clinical experience and prior research showing that emergency department buprenorphine starts continue to be an essential tool.”
The message for clinicians: “If a patient presents to the emergency department in objective opioid withdrawal and desires buprenorphine, they should be offered treatment in that moment,” Dr. Snyder said. “Treatment protocols used by hospitals in this study are available online. Emergency departments can offer compassionate and evidence-based treatment initiation 24 hours a day, 7 days a week, 365 days a year.”
More data needed on dosing strategies
“We need additional research to determine best practices for patients who use fentanyl and want to start buprenorphine, but are not yet in withdrawal,” Dr. Snyder said. “Doses of buprenorphine like those in this study are only appropriate for patients who are in withdrawal with objective signs, so some patients may struggle to wait long enough after their last use to go into sufficient withdrawal.”
Precipitated withdrawal does occur in some cases, said Dr. Snyder. “If it does, the emergency department is a very good place to manage it. We need additional research to determine best practices in management to make patients as comfortable as possible, including additional high-dose buprenorphine as well as additional adjunctive agents.”
Findings support buprenorphine
“The classic approach to buprenorphine initiation, which emerged from psychiatry outpatient office visits, is to start with very small doses of buprenorphine [2-4 mg] and titrate up slowly,” Reuben J. Strayer, MD, said in an interview.
“This dose range turns out to be the ‘sour spot’ most likely to cause the most important complication around buprenorphine initiation–precipitated withdrawal,” said Dr. Strayer, the director of addiction medicine in the emergency medicine department at Maimonides Medical Center, New York.
“One of the current focus areas of OUD treatment research is determining how to initiate buprenorphine without entailing a period of spontaneous withdrawal and without causing precipitated withdrawal,” Strayer explained. “The two primary strategies are low-dose buprenorphine initiation [LDBI, less than 2 mg, sometimes called microdosing] and high-dose [HDBI, ≥ 16 mg] buprenorphine initiation. HDBI is attractive because the primary treatment of buprenorphine-precipitated withdrawal is more buprenorphine.
“Additionally, using a high dose up front immediately transitions the patient to therapeutic blood levels, which protects the patient from withdrawal, cravings, and overdose from dangerous opioids (heroin, fentanyl, oxycodone).”
However, “the contamination and now replacement of heroin with fentanyl in the street drug supply has challenged buprenorphine initiation, because fentanyl, when used chronically, accumulates in the body and leaks into the bloodstream slowly over time, preventing the opioid washout that is required to eliminate the risk of precipitated withdrawal when buprenorphine is administered,” said Dr. Strayer.
The current study demonstrates that patients who are initiated with a first dose of 8-16 mg buprenorphine are unlikely to experience precipitated withdrawal and are successfully transitioned to buprenorphine maintenance and clinic follow-up, Dr. Snyder said, but he was surprised by the low rate of precipitated withdrawal in the current study, “which is discordant with what is being anecdotally reported across the country.”
However, the take-home message for clinicians is the support for the initiation of buprenorphine in emergency department settings at a starting dose of 8-16 mg, regardless of reported fentanyl use, he said. “Given the huge impact buprenorphine therapy has on OUD-related mortality, clinicians should make every effort to initiate buprenorphine for OUD patients at every opportunity, and precipitated withdrawal is very unlikely in appropriately selected patients.
“Many clinicians remain reluctant to initiate buprenorphine in ED settings for unfamiliarity with the drug, fear of precipitated withdrawal, or concerns around the certainty of outpatient follow-up,” Dr. Snyder said. “Education, encouragement, systems programming, such as including decision support within the electronic health record, and role-modeling from local champions will promote wider adoption of this lifesaving practice.”
Looking ahead, “more research, including prospective research, is needed to refine best practices around buprenorphine administration,” said Dr. Snyder. Questions to address include which patients are most at risk for precipitated withdrawal and whether there are alternatives to standard initiation dosing that are sufficiently unlikely to cause precipitated withdrawal. “Possibly effective alternatives include buprenorphine initiation by administration of long-acting injectable depot buprenorphine, which accumulates slowly, potentially avoiding precipitated withdrawal, as well as a slow intravenous buprenorphine infusion such as 9 mg given over 12 hours.”
The study received no outside funding. Dr. Snyder disclosed grants from the Substance Abuse and Mental Health Services Administration and the California Department of Health Care Services during the study. Dr. Strayer reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
based on data from nearly 900 individuals.
California EDs include a facilitation program known as CA Bridge for the treatment of opioid use disorder. Guidelines for CA Bridge call for high-dose buprenorphine to treat patients in drug withdrawal, with doses starting at 8-16 mg, Hannah Snyder, MD, of the University of California, San Francisco, and colleagues wrote.
“Buprenorphine has been repeatedly shown to save lives and prevent overdoses,” Dr. Snyder said in an interview. “We know that emergency department–initiated buprenorphine is an essential tool for increasing access. In the era of fentanyl, both patients and providers have expressed concerns that buprenorphine may not work as well as it did when patients were more likely to be using heroin or opioid pills.
“This retrospective cohort study provides additional information about emergency department buprenorphine as fentanyl becomes increasingly prevalent.”
In a research letter published in JAMA Network Open, the investigators reviewed data from the electronic health records of 896 patients who presented with opioid use disorder (OUD) at 16 CA Bridge EDs between Jan. 1, 2020, and April 30, 2020. All patients with OUD were included regardless of chief concern, current treatment, treatment desires, or withdrawal. A total of 87 individuals reported fentanyl use; if no fentanyl use was reported, the patient was classified as not using fentanyl. The median age of the patients was 35 years, two thirds were male, approximately 46% were White and non-Hispanic, and 30% had unstable housing.
The primary outcome was follow-up engagement at 7-14 days and 25-37 days.
A total of 492 patients received buprenorphine, including 44 fentanyl users, and 439 initiated high doses of 8-32 mg. At a 30-day follow-up, eight patients had precipitated withdrawal, including two cases in fentanyl users; none of these cases required hospital admission.
The follow-up engagement was similar for both groups, with adjusted odds ratios of 0.60 for administered buprenorphine at the initial ED encounter, 1.09 for 7-day follow-up, and 1.33 for 30-day follow-up.
The findings were limited by the retrospective design and use of clinical documentation, which likely resulted in underreporting of fentanyl use and follow-up, the researchers noted. However, the results supported the effectiveness of buprenorphine for ED patients in withdrawal with a history of fentanyl exposure.
“We were pleased to see that precipitated withdrawal was relatively uncommon in this study, and that patients who did and did not use fentanyl followed up at similar rates,” said Dr. Snyder. “This aligns with our clinical experience and prior research showing that emergency department buprenorphine starts continue to be an essential tool.”
The message for clinicians: “If a patient presents to the emergency department in objective opioid withdrawal and desires buprenorphine, they should be offered treatment in that moment,” Dr. Snyder said. “Treatment protocols used by hospitals in this study are available online. Emergency departments can offer compassionate and evidence-based treatment initiation 24 hours a day, 7 days a week, 365 days a year.”
More data needed on dosing strategies
“We need additional research to determine best practices for patients who use fentanyl and want to start buprenorphine, but are not yet in withdrawal,” Dr. Snyder said. “Doses of buprenorphine like those in this study are only appropriate for patients who are in withdrawal with objective signs, so some patients may struggle to wait long enough after their last use to go into sufficient withdrawal.”
Precipitated withdrawal does occur in some cases, said Dr. Snyder. “If it does, the emergency department is a very good place to manage it. We need additional research to determine best practices in management to make patients as comfortable as possible, including additional high-dose buprenorphine as well as additional adjunctive agents.”
Findings support buprenorphine
“The classic approach to buprenorphine initiation, which emerged from psychiatry outpatient office visits, is to start with very small doses of buprenorphine [2-4 mg] and titrate up slowly,” Reuben J. Strayer, MD, said in an interview.
“This dose range turns out to be the ‘sour spot’ most likely to cause the most important complication around buprenorphine initiation–precipitated withdrawal,” said Dr. Strayer, the director of addiction medicine in the emergency medicine department at Maimonides Medical Center, New York.
“One of the current focus areas of OUD treatment research is determining how to initiate buprenorphine without entailing a period of spontaneous withdrawal and without causing precipitated withdrawal,” Strayer explained. “The two primary strategies are low-dose buprenorphine initiation [LDBI, less than 2 mg, sometimes called microdosing] and high-dose [HDBI, ≥ 16 mg] buprenorphine initiation. HDBI is attractive because the primary treatment of buprenorphine-precipitated withdrawal is more buprenorphine.
“Additionally, using a high dose up front immediately transitions the patient to therapeutic blood levels, which protects the patient from withdrawal, cravings, and overdose from dangerous opioids (heroin, fentanyl, oxycodone).”
However, “the contamination and now replacement of heroin with fentanyl in the street drug supply has challenged buprenorphine initiation, because fentanyl, when used chronically, accumulates in the body and leaks into the bloodstream slowly over time, preventing the opioid washout that is required to eliminate the risk of precipitated withdrawal when buprenorphine is administered,” said Dr. Strayer.
The current study demonstrates that patients who are initiated with a first dose of 8-16 mg buprenorphine are unlikely to experience precipitated withdrawal and are successfully transitioned to buprenorphine maintenance and clinic follow-up, Dr. Snyder said, but he was surprised by the low rate of precipitated withdrawal in the current study, “which is discordant with what is being anecdotally reported across the country.”
However, the take-home message for clinicians is the support for the initiation of buprenorphine in emergency department settings at a starting dose of 8-16 mg, regardless of reported fentanyl use, he said. “Given the huge impact buprenorphine therapy has on OUD-related mortality, clinicians should make every effort to initiate buprenorphine for OUD patients at every opportunity, and precipitated withdrawal is very unlikely in appropriately selected patients.
“Many clinicians remain reluctant to initiate buprenorphine in ED settings for unfamiliarity with the drug, fear of precipitated withdrawal, or concerns around the certainty of outpatient follow-up,” Dr. Snyder said. “Education, encouragement, systems programming, such as including decision support within the electronic health record, and role-modeling from local champions will promote wider adoption of this lifesaving practice.”
Looking ahead, “more research, including prospective research, is needed to refine best practices around buprenorphine administration,” said Dr. Snyder. Questions to address include which patients are most at risk for precipitated withdrawal and whether there are alternatives to standard initiation dosing that are sufficiently unlikely to cause precipitated withdrawal. “Possibly effective alternatives include buprenorphine initiation by administration of long-acting injectable depot buprenorphine, which accumulates slowly, potentially avoiding precipitated withdrawal, as well as a slow intravenous buprenorphine infusion such as 9 mg given over 12 hours.”
The study received no outside funding. Dr. Snyder disclosed grants from the Substance Abuse and Mental Health Services Administration and the California Department of Health Care Services during the study. Dr. Strayer reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
based on data from nearly 900 individuals.
California EDs include a facilitation program known as CA Bridge for the treatment of opioid use disorder. Guidelines for CA Bridge call for high-dose buprenorphine to treat patients in drug withdrawal, with doses starting at 8-16 mg, Hannah Snyder, MD, of the University of California, San Francisco, and colleagues wrote.
“Buprenorphine has been repeatedly shown to save lives and prevent overdoses,” Dr. Snyder said in an interview. “We know that emergency department–initiated buprenorphine is an essential tool for increasing access. In the era of fentanyl, both patients and providers have expressed concerns that buprenorphine may not work as well as it did when patients were more likely to be using heroin or opioid pills.
“This retrospective cohort study provides additional information about emergency department buprenorphine as fentanyl becomes increasingly prevalent.”
In a research letter published in JAMA Network Open, the investigators reviewed data from the electronic health records of 896 patients who presented with opioid use disorder (OUD) at 16 CA Bridge EDs between Jan. 1, 2020, and April 30, 2020. All patients with OUD were included regardless of chief concern, current treatment, treatment desires, or withdrawal. A total of 87 individuals reported fentanyl use; if no fentanyl use was reported, the patient was classified as not using fentanyl. The median age of the patients was 35 years, two thirds were male, approximately 46% were White and non-Hispanic, and 30% had unstable housing.
The primary outcome was follow-up engagement at 7-14 days and 25-37 days.
A total of 492 patients received buprenorphine, including 44 fentanyl users, and 439 initiated high doses of 8-32 mg. At a 30-day follow-up, eight patients had precipitated withdrawal, including two cases in fentanyl users; none of these cases required hospital admission.
The follow-up engagement was similar for both groups, with adjusted odds ratios of 0.60 for administered buprenorphine at the initial ED encounter, 1.09 for 7-day follow-up, and 1.33 for 30-day follow-up.
The findings were limited by the retrospective design and use of clinical documentation, which likely resulted in underreporting of fentanyl use and follow-up, the researchers noted. However, the results supported the effectiveness of buprenorphine for ED patients in withdrawal with a history of fentanyl exposure.
“We were pleased to see that precipitated withdrawal was relatively uncommon in this study, and that patients who did and did not use fentanyl followed up at similar rates,” said Dr. Snyder. “This aligns with our clinical experience and prior research showing that emergency department buprenorphine starts continue to be an essential tool.”
The message for clinicians: “If a patient presents to the emergency department in objective opioid withdrawal and desires buprenorphine, they should be offered treatment in that moment,” Dr. Snyder said. “Treatment protocols used by hospitals in this study are available online. Emergency departments can offer compassionate and evidence-based treatment initiation 24 hours a day, 7 days a week, 365 days a year.”
More data needed on dosing strategies
“We need additional research to determine best practices for patients who use fentanyl and want to start buprenorphine, but are not yet in withdrawal,” Dr. Snyder said. “Doses of buprenorphine like those in this study are only appropriate for patients who are in withdrawal with objective signs, so some patients may struggle to wait long enough after their last use to go into sufficient withdrawal.”
Precipitated withdrawal does occur in some cases, said Dr. Snyder. “If it does, the emergency department is a very good place to manage it. We need additional research to determine best practices in management to make patients as comfortable as possible, including additional high-dose buprenorphine as well as additional adjunctive agents.”
Findings support buprenorphine
“The classic approach to buprenorphine initiation, which emerged from psychiatry outpatient office visits, is to start with very small doses of buprenorphine [2-4 mg] and titrate up slowly,” Reuben J. Strayer, MD, said in an interview.
“This dose range turns out to be the ‘sour spot’ most likely to cause the most important complication around buprenorphine initiation–precipitated withdrawal,” said Dr. Strayer, the director of addiction medicine in the emergency medicine department at Maimonides Medical Center, New York.
“One of the current focus areas of OUD treatment research is determining how to initiate buprenorphine without entailing a period of spontaneous withdrawal and without causing precipitated withdrawal,” Strayer explained. “The two primary strategies are low-dose buprenorphine initiation [LDBI, less than 2 mg, sometimes called microdosing] and high-dose [HDBI, ≥ 16 mg] buprenorphine initiation. HDBI is attractive because the primary treatment of buprenorphine-precipitated withdrawal is more buprenorphine.
“Additionally, using a high dose up front immediately transitions the patient to therapeutic blood levels, which protects the patient from withdrawal, cravings, and overdose from dangerous opioids (heroin, fentanyl, oxycodone).”
However, “the contamination and now replacement of heroin with fentanyl in the street drug supply has challenged buprenorphine initiation, because fentanyl, when used chronically, accumulates in the body and leaks into the bloodstream slowly over time, preventing the opioid washout that is required to eliminate the risk of precipitated withdrawal when buprenorphine is administered,” said Dr. Strayer.
The current study demonstrates that patients who are initiated with a first dose of 8-16 mg buprenorphine are unlikely to experience precipitated withdrawal and are successfully transitioned to buprenorphine maintenance and clinic follow-up, Dr. Snyder said, but he was surprised by the low rate of precipitated withdrawal in the current study, “which is discordant with what is being anecdotally reported across the country.”
However, the take-home message for clinicians is the support for the initiation of buprenorphine in emergency department settings at a starting dose of 8-16 mg, regardless of reported fentanyl use, he said. “Given the huge impact buprenorphine therapy has on OUD-related mortality, clinicians should make every effort to initiate buprenorphine for OUD patients at every opportunity, and precipitated withdrawal is very unlikely in appropriately selected patients.
“Many clinicians remain reluctant to initiate buprenorphine in ED settings for unfamiliarity with the drug, fear of precipitated withdrawal, or concerns around the certainty of outpatient follow-up,” Dr. Snyder said. “Education, encouragement, systems programming, such as including decision support within the electronic health record, and role-modeling from local champions will promote wider adoption of this lifesaving practice.”
Looking ahead, “more research, including prospective research, is needed to refine best practices around buprenorphine administration,” said Dr. Snyder. Questions to address include which patients are most at risk for precipitated withdrawal and whether there are alternatives to standard initiation dosing that are sufficiently unlikely to cause precipitated withdrawal. “Possibly effective alternatives include buprenorphine initiation by administration of long-acting injectable depot buprenorphine, which accumulates slowly, potentially avoiding precipitated withdrawal, as well as a slow intravenous buprenorphine infusion such as 9 mg given over 12 hours.”
The study received no outside funding. Dr. Snyder disclosed grants from the Substance Abuse and Mental Health Services Administration and the California Department of Health Care Services during the study. Dr. Strayer reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Who can sue docs for wrongful death? Some states are trying to expand that group
In addition, the types of emotional damage that physicians can be sued for is expanding in pockets across the nation. The latest effort to expand the capacity to sue, a bill in New York state, failed when it was not signed by the governor – but a toned-down bill is in the works.
The impact of New York’s proposed expansion of wrongful death lawsuits would have been widespread. The New York legislation would have expanded the definition of “close family members” to include spouses, domestic partners, children, parents, stepparents, siblings, grandparents, and perhaps more. Additionally, lawsuits could have allowed juries to determine “close family members” of the deceased patient on the basis of specific circumstances of the person’s relationship with the decedent.
Currently, every state allows a wrongful death claim to be filed by immediate family members. If the patient who died was married, a surviving spouse could bring the lawsuit. If the patient had been unmarried, an adult child could bring the lawsuit in some states. A parent typically brings a lawsuit if their minor child has died from alleged wrongful death. In some states, one member of a civil union or domestic partnership may bring a wrongful death lawsuit. And if a single adult has no children or spouse/partner, more distant family members, including aunts, uncles, siblings, or grandparents, may file the suit.
The New York bill would also have expanded compensable damages to include loss of affection and companionship, and it would have expanded emotional damages, which are not currently included in New York. It would also have extended the statute of limitations of a wrongful death claim from 2 years to 3.5 years.
In general, in states that allow emotional distress to be included in wrongful death lawsuits, attorneys must demonstrate that survivors have suffered mental harm, such as depression, loss of sleep, fear, and anger, says Russ Haven, JD, general counsel for the New York Public Interest Research Group. While mental harm is not particularly easy to prove, attorneys must show that survivors have ongoing distress that is the direct result of the loss of the loved one and that the distress is significant enough to severely affect their quality of life.
Mr. Haven gives an example of emotional distress: “We worked with a woman who lost her fiancé in a motor vehicle accident,” he says. “The funeral ended up on the day she had scheduled her wedding dress fitting. A situation like that causes a good deal of lasting emotional distress.”
Expanding family members who can bring the lawsuit
The fact that a fiancé could be included in a wrongful death settlement is another aspect of the New York bill that was central to arguments both for and against the expansion of family members who can make claims. “We think a modern society includes unmarried partners, grandparents, siblings, and others,” says Mr. Haven.
“The language of who is a close family member might seem clear, but to a defense attorney, it isn’t,” says Tom Stebbins, executive director of the Lawsuit Reform Alliance of New York. “This could end up being a situation where someone has 40 grandchildren, and all could be considered close family members.”
Many states currently allow damages for claims of grief and mental anguish resulting from a wrongful death.
In her recent veto of the Grieving Families Act, New York Gov. Kathy Hochul took fire for her choices. The bill represented years of effort by the state legislature to expand the qualifiers for wrongful death lawsuits. Those supporting what ultimately became Senate Bill S74A believed they finally had the law over the finish line. Those opposed breathed a sigh of relief when the bill was vetoed.
Had Gov. Hochul signed Bill 274A, the effect on costs would have been enormous for physicians. New York already has the highest cumulative medical liability payouts in the nation, according to the Medical Society of the State of New York.
The MSSNY was among many parties that fought against the law. The Greater New York Hospital Association, insurance companies, the Defense Association of New York, and the New York Conference of Mayors all joined in lobbying against the bill.
“Gov. Hochul, in her veto message, correctly noted that the proposed New York legislation represented an extraordinary departure from New York’s wrongful death jurisprudence,” says Remi Stone, director of government relations at The Doctors Company, part of the TDC Group. “I would add that while there are some other states that allow grief damages, none are as wide-ranging as the proposed legislation.”
The NYPIRG, the AARP, and the New York Immigration Coalition supported the bill. In a statement following the veto, the New York State Trial Lawyers Association said: “By vetoing the Grieving Families Act, Gov. Hochul has sided with insurance companies, the health care industry, big corporations, and anyone else who doesn’t want to be held accountable for the negligent killing of a person. This bill passed with overwhelming bipartisan support and would rectify over a century of injustice.”
Following Gov. Hochul’s veto, the bill’s proponents and the state legislature vowed to return to the drawing board and construct a bill that the governor would eventually approve. For now, however, the controversial legislation has been put to rest.
Mr. Haven and the NYPIRG argue that New York lags behind many other states in allowing survivors to claim loss for their emotional distress. “When there is relationship loss, it has a great impact on your life,” Mr. Haven says, “and this goes beyond simply the financial impact.”
“The bill was well intended but completely vague on who could bring lawsuits and would have increased medical malpractice insurance by far too much,” says MSSNY President Parag Mehta, MD. “For safety net hospitals, one lawsuit would halt their ability to provide many programs aimed at underserved populations.”
Peter Kolbert, JD, senior vice president of claim and litigation services at Healthcare Risk Advisors (part of the TDC Group), had this to say: “The current ‘recoverable’ damages in New York in a wrongful death case include loss of guidance and support for minor children of a decedent. Those damages have been sustained at $2 million per child. It is rationally very challenging, if not impossible, to distinguish between those damages and the proposed damages that the very same people would have been entitled to under the proposed statute.”
What will happen in the future?
While the veto has stalled New York’s wrongful death expansion for now, supporters in and out of the legislature remain determined to continue their fight. “Advocates argue that the bill would have brought the state in line with wrongful death law in others,” says Brian Whitelaw, JD, a partner at Michigan’s Foley, Baron, Metzger & Juip. “But if the bill had become law as written, the economic impact would have been substantial.”
Mr. Whitelaw says that such wide-ranging lawsuits can have consequences that extend far beyond physicians’ insurance premiums. “This could impact the average person on the street’s ability to obtain the medical care they need, because doctors will go elsewhere to practice,” he says. “Beyond impacting the health care system, it can hurt small businesses as well.”
Mr. Haven says supporters of the expansion are far from finished with their efforts. “New York’s current law dates back to 1847, and it was cutting edge then,” he says. “It was designed for an agrarian society where if the husband died, his widow and children wouldn’t become destitute. Now, 175 years later, we realize that the law has biases, and tort law has evolved. The state needs to evolve as well.”
For his part, Dr. Mehta is open to a dialogue with lawmakers to revise the law in a manner agreeable to all parties. “We want to work together to make the system right,” he says. “The liability system in New York needs an overall holistic change, and we are available at any time to have discussions. The vetoed bill was a Band-Aid and didn’t address the main, underlying issues in the state.”
Mr. Stebbins, too, says he would like to continue the debate over how an expansion should look. “We hope to go through a discussion on caps to these suits,” he explains. “We have already seen the cap of $10 million broken four times in the past few years through nuclear verdicts. That’s something we need to address.”
Given the legislature’s overwhelming support for the bill, some version of it will likely make another appearance in the coming session. Whether or not it can strike the middle ground that will make all parties happy – including the governor – is yet to be seen. “Is it wrong to seek compensation for pain and suffering from a wrongful death?” asks Mr. Whitelaw. “No. But there must be limits to such laws, or where does it end?”
A version of this article first appeared on Medscape.com.
In addition, the types of emotional damage that physicians can be sued for is expanding in pockets across the nation. The latest effort to expand the capacity to sue, a bill in New York state, failed when it was not signed by the governor – but a toned-down bill is in the works.
The impact of New York’s proposed expansion of wrongful death lawsuits would have been widespread. The New York legislation would have expanded the definition of “close family members” to include spouses, domestic partners, children, parents, stepparents, siblings, grandparents, and perhaps more. Additionally, lawsuits could have allowed juries to determine “close family members” of the deceased patient on the basis of specific circumstances of the person’s relationship with the decedent.
Currently, every state allows a wrongful death claim to be filed by immediate family members. If the patient who died was married, a surviving spouse could bring the lawsuit. If the patient had been unmarried, an adult child could bring the lawsuit in some states. A parent typically brings a lawsuit if their minor child has died from alleged wrongful death. In some states, one member of a civil union or domestic partnership may bring a wrongful death lawsuit. And if a single adult has no children or spouse/partner, more distant family members, including aunts, uncles, siblings, or grandparents, may file the suit.
The New York bill would also have expanded compensable damages to include loss of affection and companionship, and it would have expanded emotional damages, which are not currently included in New York. It would also have extended the statute of limitations of a wrongful death claim from 2 years to 3.5 years.
In general, in states that allow emotional distress to be included in wrongful death lawsuits, attorneys must demonstrate that survivors have suffered mental harm, such as depression, loss of sleep, fear, and anger, says Russ Haven, JD, general counsel for the New York Public Interest Research Group. While mental harm is not particularly easy to prove, attorneys must show that survivors have ongoing distress that is the direct result of the loss of the loved one and that the distress is significant enough to severely affect their quality of life.
Mr. Haven gives an example of emotional distress: “We worked with a woman who lost her fiancé in a motor vehicle accident,” he says. “The funeral ended up on the day she had scheduled her wedding dress fitting. A situation like that causes a good deal of lasting emotional distress.”
Expanding family members who can bring the lawsuit
The fact that a fiancé could be included in a wrongful death settlement is another aspect of the New York bill that was central to arguments both for and against the expansion of family members who can make claims. “We think a modern society includes unmarried partners, grandparents, siblings, and others,” says Mr. Haven.
“The language of who is a close family member might seem clear, but to a defense attorney, it isn’t,” says Tom Stebbins, executive director of the Lawsuit Reform Alliance of New York. “This could end up being a situation where someone has 40 grandchildren, and all could be considered close family members.”
Many states currently allow damages for claims of grief and mental anguish resulting from a wrongful death.
In her recent veto of the Grieving Families Act, New York Gov. Kathy Hochul took fire for her choices. The bill represented years of effort by the state legislature to expand the qualifiers for wrongful death lawsuits. Those supporting what ultimately became Senate Bill S74A believed they finally had the law over the finish line. Those opposed breathed a sigh of relief when the bill was vetoed.
Had Gov. Hochul signed Bill 274A, the effect on costs would have been enormous for physicians. New York already has the highest cumulative medical liability payouts in the nation, according to the Medical Society of the State of New York.
The MSSNY was among many parties that fought against the law. The Greater New York Hospital Association, insurance companies, the Defense Association of New York, and the New York Conference of Mayors all joined in lobbying against the bill.
“Gov. Hochul, in her veto message, correctly noted that the proposed New York legislation represented an extraordinary departure from New York’s wrongful death jurisprudence,” says Remi Stone, director of government relations at The Doctors Company, part of the TDC Group. “I would add that while there are some other states that allow grief damages, none are as wide-ranging as the proposed legislation.”
The NYPIRG, the AARP, and the New York Immigration Coalition supported the bill. In a statement following the veto, the New York State Trial Lawyers Association said: “By vetoing the Grieving Families Act, Gov. Hochul has sided with insurance companies, the health care industry, big corporations, and anyone else who doesn’t want to be held accountable for the negligent killing of a person. This bill passed with overwhelming bipartisan support and would rectify over a century of injustice.”
Following Gov. Hochul’s veto, the bill’s proponents and the state legislature vowed to return to the drawing board and construct a bill that the governor would eventually approve. For now, however, the controversial legislation has been put to rest.
Mr. Haven and the NYPIRG argue that New York lags behind many other states in allowing survivors to claim loss for their emotional distress. “When there is relationship loss, it has a great impact on your life,” Mr. Haven says, “and this goes beyond simply the financial impact.”
“The bill was well intended but completely vague on who could bring lawsuits and would have increased medical malpractice insurance by far too much,” says MSSNY President Parag Mehta, MD. “For safety net hospitals, one lawsuit would halt their ability to provide many programs aimed at underserved populations.”
Peter Kolbert, JD, senior vice president of claim and litigation services at Healthcare Risk Advisors (part of the TDC Group), had this to say: “The current ‘recoverable’ damages in New York in a wrongful death case include loss of guidance and support for minor children of a decedent. Those damages have been sustained at $2 million per child. It is rationally very challenging, if not impossible, to distinguish between those damages and the proposed damages that the very same people would have been entitled to under the proposed statute.”
What will happen in the future?
While the veto has stalled New York’s wrongful death expansion for now, supporters in and out of the legislature remain determined to continue their fight. “Advocates argue that the bill would have brought the state in line with wrongful death law in others,” says Brian Whitelaw, JD, a partner at Michigan’s Foley, Baron, Metzger & Juip. “But if the bill had become law as written, the economic impact would have been substantial.”
Mr. Whitelaw says that such wide-ranging lawsuits can have consequences that extend far beyond physicians’ insurance premiums. “This could impact the average person on the street’s ability to obtain the medical care they need, because doctors will go elsewhere to practice,” he says. “Beyond impacting the health care system, it can hurt small businesses as well.”
Mr. Haven says supporters of the expansion are far from finished with their efforts. “New York’s current law dates back to 1847, and it was cutting edge then,” he says. “It was designed for an agrarian society where if the husband died, his widow and children wouldn’t become destitute. Now, 175 years later, we realize that the law has biases, and tort law has evolved. The state needs to evolve as well.”
For his part, Dr. Mehta is open to a dialogue with lawmakers to revise the law in a manner agreeable to all parties. “We want to work together to make the system right,” he says. “The liability system in New York needs an overall holistic change, and we are available at any time to have discussions. The vetoed bill was a Band-Aid and didn’t address the main, underlying issues in the state.”
Mr. Stebbins, too, says he would like to continue the debate over how an expansion should look. “We hope to go through a discussion on caps to these suits,” he explains. “We have already seen the cap of $10 million broken four times in the past few years through nuclear verdicts. That’s something we need to address.”
Given the legislature’s overwhelming support for the bill, some version of it will likely make another appearance in the coming session. Whether or not it can strike the middle ground that will make all parties happy – including the governor – is yet to be seen. “Is it wrong to seek compensation for pain and suffering from a wrongful death?” asks Mr. Whitelaw. “No. But there must be limits to such laws, or where does it end?”
A version of this article first appeared on Medscape.com.
In addition, the types of emotional damage that physicians can be sued for is expanding in pockets across the nation. The latest effort to expand the capacity to sue, a bill in New York state, failed when it was not signed by the governor – but a toned-down bill is in the works.
The impact of New York’s proposed expansion of wrongful death lawsuits would have been widespread. The New York legislation would have expanded the definition of “close family members” to include spouses, domestic partners, children, parents, stepparents, siblings, grandparents, and perhaps more. Additionally, lawsuits could have allowed juries to determine “close family members” of the deceased patient on the basis of specific circumstances of the person’s relationship with the decedent.
Currently, every state allows a wrongful death claim to be filed by immediate family members. If the patient who died was married, a surviving spouse could bring the lawsuit. If the patient had been unmarried, an adult child could bring the lawsuit in some states. A parent typically brings a lawsuit if their minor child has died from alleged wrongful death. In some states, one member of a civil union or domestic partnership may bring a wrongful death lawsuit. And if a single adult has no children or spouse/partner, more distant family members, including aunts, uncles, siblings, or grandparents, may file the suit.
The New York bill would also have expanded compensable damages to include loss of affection and companionship, and it would have expanded emotional damages, which are not currently included in New York. It would also have extended the statute of limitations of a wrongful death claim from 2 years to 3.5 years.
In general, in states that allow emotional distress to be included in wrongful death lawsuits, attorneys must demonstrate that survivors have suffered mental harm, such as depression, loss of sleep, fear, and anger, says Russ Haven, JD, general counsel for the New York Public Interest Research Group. While mental harm is not particularly easy to prove, attorneys must show that survivors have ongoing distress that is the direct result of the loss of the loved one and that the distress is significant enough to severely affect their quality of life.
Mr. Haven gives an example of emotional distress: “We worked with a woman who lost her fiancé in a motor vehicle accident,” he says. “The funeral ended up on the day she had scheduled her wedding dress fitting. A situation like that causes a good deal of lasting emotional distress.”
Expanding family members who can bring the lawsuit
The fact that a fiancé could be included in a wrongful death settlement is another aspect of the New York bill that was central to arguments both for and against the expansion of family members who can make claims. “We think a modern society includes unmarried partners, grandparents, siblings, and others,” says Mr. Haven.
“The language of who is a close family member might seem clear, but to a defense attorney, it isn’t,” says Tom Stebbins, executive director of the Lawsuit Reform Alliance of New York. “This could end up being a situation where someone has 40 grandchildren, and all could be considered close family members.”
Many states currently allow damages for claims of grief and mental anguish resulting from a wrongful death.
In her recent veto of the Grieving Families Act, New York Gov. Kathy Hochul took fire for her choices. The bill represented years of effort by the state legislature to expand the qualifiers for wrongful death lawsuits. Those supporting what ultimately became Senate Bill S74A believed they finally had the law over the finish line. Those opposed breathed a sigh of relief when the bill was vetoed.
Had Gov. Hochul signed Bill 274A, the effect on costs would have been enormous for physicians. New York already has the highest cumulative medical liability payouts in the nation, according to the Medical Society of the State of New York.
The MSSNY was among many parties that fought against the law. The Greater New York Hospital Association, insurance companies, the Defense Association of New York, and the New York Conference of Mayors all joined in lobbying against the bill.
“Gov. Hochul, in her veto message, correctly noted that the proposed New York legislation represented an extraordinary departure from New York’s wrongful death jurisprudence,” says Remi Stone, director of government relations at The Doctors Company, part of the TDC Group. “I would add that while there are some other states that allow grief damages, none are as wide-ranging as the proposed legislation.”
The NYPIRG, the AARP, and the New York Immigration Coalition supported the bill. In a statement following the veto, the New York State Trial Lawyers Association said: “By vetoing the Grieving Families Act, Gov. Hochul has sided with insurance companies, the health care industry, big corporations, and anyone else who doesn’t want to be held accountable for the negligent killing of a person. This bill passed with overwhelming bipartisan support and would rectify over a century of injustice.”
Following Gov. Hochul’s veto, the bill’s proponents and the state legislature vowed to return to the drawing board and construct a bill that the governor would eventually approve. For now, however, the controversial legislation has been put to rest.
Mr. Haven and the NYPIRG argue that New York lags behind many other states in allowing survivors to claim loss for their emotional distress. “When there is relationship loss, it has a great impact on your life,” Mr. Haven says, “and this goes beyond simply the financial impact.”
“The bill was well intended but completely vague on who could bring lawsuits and would have increased medical malpractice insurance by far too much,” says MSSNY President Parag Mehta, MD. “For safety net hospitals, one lawsuit would halt their ability to provide many programs aimed at underserved populations.”
Peter Kolbert, JD, senior vice president of claim and litigation services at Healthcare Risk Advisors (part of the TDC Group), had this to say: “The current ‘recoverable’ damages in New York in a wrongful death case include loss of guidance and support for minor children of a decedent. Those damages have been sustained at $2 million per child. It is rationally very challenging, if not impossible, to distinguish between those damages and the proposed damages that the very same people would have been entitled to under the proposed statute.”
What will happen in the future?
While the veto has stalled New York’s wrongful death expansion for now, supporters in and out of the legislature remain determined to continue their fight. “Advocates argue that the bill would have brought the state in line with wrongful death law in others,” says Brian Whitelaw, JD, a partner at Michigan’s Foley, Baron, Metzger & Juip. “But if the bill had become law as written, the economic impact would have been substantial.”
Mr. Whitelaw says that such wide-ranging lawsuits can have consequences that extend far beyond physicians’ insurance premiums. “This could impact the average person on the street’s ability to obtain the medical care they need, because doctors will go elsewhere to practice,” he says. “Beyond impacting the health care system, it can hurt small businesses as well.”
Mr. Haven says supporters of the expansion are far from finished with their efforts. “New York’s current law dates back to 1847, and it was cutting edge then,” he says. “It was designed for an agrarian society where if the husband died, his widow and children wouldn’t become destitute. Now, 175 years later, we realize that the law has biases, and tort law has evolved. The state needs to evolve as well.”
For his part, Dr. Mehta is open to a dialogue with lawmakers to revise the law in a manner agreeable to all parties. “We want to work together to make the system right,” he says. “The liability system in New York needs an overall holistic change, and we are available at any time to have discussions. The vetoed bill was a Band-Aid and didn’t address the main, underlying issues in the state.”
Mr. Stebbins, too, says he would like to continue the debate over how an expansion should look. “We hope to go through a discussion on caps to these suits,” he explains. “We have already seen the cap of $10 million broken four times in the past few years through nuclear verdicts. That’s something we need to address.”
Given the legislature’s overwhelming support for the bill, some version of it will likely make another appearance in the coming session. Whether or not it can strike the middle ground that will make all parties happy – including the governor – is yet to be seen. “Is it wrong to seek compensation for pain and suffering from a wrongful death?” asks Mr. Whitelaw. “No. But there must be limits to such laws, or where does it end?”
A version of this article first appeared on Medscape.com.
Telehealth doctor indicted on health care fraud, opioid distribution charges
Sangita Patel, MD, 50, practiced at Advance Medical Home Physicians in Troy.
According to court documents, between July 2020 and June 2022 Patel was responsible for submitting Medicare claims for improper telehealth visits she didn’t conduct herself.
Dr. Patel, who accepted patients who paid in cash as well as those with Medicare and Medicaid coverage, billed approximately $3.4 million to Medicare between 2018 and 2022, according to court documents. An unusual number of these visits were billed using complex codes, an indication of health care fraud. The investigation also found that on many days, Dr. Patel billed for more than 24 hours of services. During this period, according to the document, 76% of Dr. Patel’s Medicare reimbursements were for telehealth.
Prosecutors say that Dr. Patel prescribed Schedule II controlled substances to more than 90% of the patients in these telehealth visits. She delegated her prescription authority to an unlicensed medical assistant. Through undercover visits and cell site search warrant data, the investigation found that Dr. Patel directed patients to contact, via cell phone, this assistant, who then entered electronic prescriptions into the electronic medical records system. Dr. Patel then signed the prescriptions and sent them to the pharmacies without ever interacting with the patients. Prosecutors also used text messages, obtained by search warrant, between Dr. Patel and her assistant and between the assistant and undercover informers to build their case.
Dr. Patel is also accused of referring patients to other providers, who in turn billed Medicare for claims associated with those patients. Advance Medical received $143,000 from these providers, potentially in violation of anti-kickback laws, according to bank records obtained by subpoena.
If convicted, Dr. Patel could be sentenced to up to 10 years in federal prison.
A version of this article first appeared on Medscape.com.
Sangita Patel, MD, 50, practiced at Advance Medical Home Physicians in Troy.
According to court documents, between July 2020 and June 2022 Patel was responsible for submitting Medicare claims for improper telehealth visits she didn’t conduct herself.
Dr. Patel, who accepted patients who paid in cash as well as those with Medicare and Medicaid coverage, billed approximately $3.4 million to Medicare between 2018 and 2022, according to court documents. An unusual number of these visits were billed using complex codes, an indication of health care fraud. The investigation also found that on many days, Dr. Patel billed for more than 24 hours of services. During this period, according to the document, 76% of Dr. Patel’s Medicare reimbursements were for telehealth.
Prosecutors say that Dr. Patel prescribed Schedule II controlled substances to more than 90% of the patients in these telehealth visits. She delegated her prescription authority to an unlicensed medical assistant. Through undercover visits and cell site search warrant data, the investigation found that Dr. Patel directed patients to contact, via cell phone, this assistant, who then entered electronic prescriptions into the electronic medical records system. Dr. Patel then signed the prescriptions and sent them to the pharmacies without ever interacting with the patients. Prosecutors also used text messages, obtained by search warrant, between Dr. Patel and her assistant and between the assistant and undercover informers to build their case.
Dr. Patel is also accused of referring patients to other providers, who in turn billed Medicare for claims associated with those patients. Advance Medical received $143,000 from these providers, potentially in violation of anti-kickback laws, according to bank records obtained by subpoena.
If convicted, Dr. Patel could be sentenced to up to 10 years in federal prison.
A version of this article first appeared on Medscape.com.
Sangita Patel, MD, 50, practiced at Advance Medical Home Physicians in Troy.
According to court documents, between July 2020 and June 2022 Patel was responsible for submitting Medicare claims for improper telehealth visits she didn’t conduct herself.
Dr. Patel, who accepted patients who paid in cash as well as those with Medicare and Medicaid coverage, billed approximately $3.4 million to Medicare between 2018 and 2022, according to court documents. An unusual number of these visits were billed using complex codes, an indication of health care fraud. The investigation also found that on many days, Dr. Patel billed for more than 24 hours of services. During this period, according to the document, 76% of Dr. Patel’s Medicare reimbursements were for telehealth.
Prosecutors say that Dr. Patel prescribed Schedule II controlled substances to more than 90% of the patients in these telehealth visits. She delegated her prescription authority to an unlicensed medical assistant. Through undercover visits and cell site search warrant data, the investigation found that Dr. Patel directed patients to contact, via cell phone, this assistant, who then entered electronic prescriptions into the electronic medical records system. Dr. Patel then signed the prescriptions and sent them to the pharmacies without ever interacting with the patients. Prosecutors also used text messages, obtained by search warrant, between Dr. Patel and her assistant and between the assistant and undercover informers to build their case.
Dr. Patel is also accused of referring patients to other providers, who in turn billed Medicare for claims associated with those patients. Advance Medical received $143,000 from these providers, potentially in violation of anti-kickback laws, according to bank records obtained by subpoena.
If convicted, Dr. Patel could be sentenced to up to 10 years in federal prison.
A version of this article first appeared on Medscape.com.
Migraine after concussion linked to worse outcomes
researchers have found.
“Early assessment of headache – and whether it has migraine features – after concussion can be helpful in predicting which children are at risk for poor outcomes and identifying children who require targeted intervention,” said senior author Keith Owen Yeates, PhD, the Ronald and Irene Ward Chair in Pediatric Brain Injury Professor and head of the department of psychology at the University of Calgary (Alta.). “Posttraumatic headache, especially when it involves migraine features, is a strong predictor of persisting symptoms and poorer quality of life after childhood concussion.”
Approximately 840,000 children per year visit an emergency department in the United States after having a traumatic brain injury. As many as 90% of those visits are considered to involve a concussion, according to the investigators. Although most children recover quickly, approximately one-third continue to report symptoms a month after the event.
Posttraumatic headache occurs in up to 90% of children, most commonly with features of migraine.
The new study, published in JAMA Network Open, was a secondary analysis of the Advancing Concussion Assessment in Pediatrics (A-CAP) prospective cohort study. The study was conducted at five emergency departments in Canada from September 2016 to July 2019 and included children and adolescents aged 8-17 years who presented with acute concussion or an orthopedic injury.
Children were included in the concussion group if they had a history of blunt head trauma resulting in at least one of three criteria consistent with the World Health Organization definition of mild traumatic brain injury. The criteria include loss of consciousness for less than 30 minutes, a Glasgow Coma Scale score of 13 or 14, or at least one acute sign or symptom of concussion, as noted by emergency clinicians.
Patients were excluded from the concussion group if they had deteriorating neurologic status, underwent neurosurgical intervention, had posttraumatic amnesia that lasted more than 24 hours, or had a score higher than 4 on the Abbreviated Injury Scale (AIS). The orthopedic injury group included patients without symptoms of concussion and with blunt trauma associated with an AIS 13 score of 4 or less. Patients were excluded from both groups if they had an overnight hospitalization for traumatic brain injury, a concussion within the past 3 months, or a neurodevelopmental disorder.
The researchers analyzed data from 928 children of 967 enrolled in the study. The median age was 12.2 years, and 41.3% were female. The final study cohort included 239 children with orthopedic injuries but no headache, 160 with a concussion and no headache, 134 with a concussion and nonmigraine headaches, and 254 with a concussion and migraine headaches.
Children with posttraumatic migraines 10 days after a concussion had the most severe symptoms and worst quality of life 3 months following their head trauma, the researchers found. Children without headaches within 10 days after concussion had the best 3-month outcomes, comparable to those with orthopedic injuries alone.
The researchers said the strengths of their study included its large population and its inclusion of various causes of head trauma, not just sports-related concussions. Limitations included self-reports of headaches instead of a physician diagnosis and lack of control for clinical interventions that might have affected the outcomes.
Charles Tator, MD, PhD, director of the Canadian Concussion Centre at Toronto Western Hospital, said the findings were unsurprising.
“Headaches are the most common symptom after concussion,” Dr. Tator, who was not involved in the latest research, told this news organization. “In my practice and research with concussed kids 11 and up and with adults, those with preconcussion history of migraine are the most difficult to treat because their headaches don’t improve unless specific measures are taken.”
Dr. Tator, who also is a professor of neurosurgery at the University of Toronto, said clinicians who treat concussions must determine which type of headaches children are experiencing – and refer as early as possible for migraine prevention or treatment and medication, as warranted.
“Early recognition after concussion that migraine headaches are occurring will save kids a lot of suffering,” he said.
The study was supported by a Canadian Institute of Health Research Foundation Grant and by funds from the Alberta Children’s Hospital Foundation and the Alberta Children’s Hospital Research Institute. Dr. Tator has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
researchers have found.
“Early assessment of headache – and whether it has migraine features – after concussion can be helpful in predicting which children are at risk for poor outcomes and identifying children who require targeted intervention,” said senior author Keith Owen Yeates, PhD, the Ronald and Irene Ward Chair in Pediatric Brain Injury Professor and head of the department of psychology at the University of Calgary (Alta.). “Posttraumatic headache, especially when it involves migraine features, is a strong predictor of persisting symptoms and poorer quality of life after childhood concussion.”
Approximately 840,000 children per year visit an emergency department in the United States after having a traumatic brain injury. As many as 90% of those visits are considered to involve a concussion, according to the investigators. Although most children recover quickly, approximately one-third continue to report symptoms a month after the event.
Posttraumatic headache occurs in up to 90% of children, most commonly with features of migraine.
The new study, published in JAMA Network Open, was a secondary analysis of the Advancing Concussion Assessment in Pediatrics (A-CAP) prospective cohort study. The study was conducted at five emergency departments in Canada from September 2016 to July 2019 and included children and adolescents aged 8-17 years who presented with acute concussion or an orthopedic injury.
Children were included in the concussion group if they had a history of blunt head trauma resulting in at least one of three criteria consistent with the World Health Organization definition of mild traumatic brain injury. The criteria include loss of consciousness for less than 30 minutes, a Glasgow Coma Scale score of 13 or 14, or at least one acute sign or symptom of concussion, as noted by emergency clinicians.
Patients were excluded from the concussion group if they had deteriorating neurologic status, underwent neurosurgical intervention, had posttraumatic amnesia that lasted more than 24 hours, or had a score higher than 4 on the Abbreviated Injury Scale (AIS). The orthopedic injury group included patients without symptoms of concussion and with blunt trauma associated with an AIS 13 score of 4 or less. Patients were excluded from both groups if they had an overnight hospitalization for traumatic brain injury, a concussion within the past 3 months, or a neurodevelopmental disorder.
The researchers analyzed data from 928 children of 967 enrolled in the study. The median age was 12.2 years, and 41.3% were female. The final study cohort included 239 children with orthopedic injuries but no headache, 160 with a concussion and no headache, 134 with a concussion and nonmigraine headaches, and 254 with a concussion and migraine headaches.
Children with posttraumatic migraines 10 days after a concussion had the most severe symptoms and worst quality of life 3 months following their head trauma, the researchers found. Children without headaches within 10 days after concussion had the best 3-month outcomes, comparable to those with orthopedic injuries alone.
The researchers said the strengths of their study included its large population and its inclusion of various causes of head trauma, not just sports-related concussions. Limitations included self-reports of headaches instead of a physician diagnosis and lack of control for clinical interventions that might have affected the outcomes.
Charles Tator, MD, PhD, director of the Canadian Concussion Centre at Toronto Western Hospital, said the findings were unsurprising.
“Headaches are the most common symptom after concussion,” Dr. Tator, who was not involved in the latest research, told this news organization. “In my practice and research with concussed kids 11 and up and with adults, those with preconcussion history of migraine are the most difficult to treat because their headaches don’t improve unless specific measures are taken.”
Dr. Tator, who also is a professor of neurosurgery at the University of Toronto, said clinicians who treat concussions must determine which type of headaches children are experiencing – and refer as early as possible for migraine prevention or treatment and medication, as warranted.
“Early recognition after concussion that migraine headaches are occurring will save kids a lot of suffering,” he said.
The study was supported by a Canadian Institute of Health Research Foundation Grant and by funds from the Alberta Children’s Hospital Foundation and the Alberta Children’s Hospital Research Institute. Dr. Tator has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
researchers have found.
“Early assessment of headache – and whether it has migraine features – after concussion can be helpful in predicting which children are at risk for poor outcomes and identifying children who require targeted intervention,” said senior author Keith Owen Yeates, PhD, the Ronald and Irene Ward Chair in Pediatric Brain Injury Professor and head of the department of psychology at the University of Calgary (Alta.). “Posttraumatic headache, especially when it involves migraine features, is a strong predictor of persisting symptoms and poorer quality of life after childhood concussion.”
Approximately 840,000 children per year visit an emergency department in the United States after having a traumatic brain injury. As many as 90% of those visits are considered to involve a concussion, according to the investigators. Although most children recover quickly, approximately one-third continue to report symptoms a month after the event.
Posttraumatic headache occurs in up to 90% of children, most commonly with features of migraine.
The new study, published in JAMA Network Open, was a secondary analysis of the Advancing Concussion Assessment in Pediatrics (A-CAP) prospective cohort study. The study was conducted at five emergency departments in Canada from September 2016 to July 2019 and included children and adolescents aged 8-17 years who presented with acute concussion or an orthopedic injury.
Children were included in the concussion group if they had a history of blunt head trauma resulting in at least one of three criteria consistent with the World Health Organization definition of mild traumatic brain injury. The criteria include loss of consciousness for less than 30 minutes, a Glasgow Coma Scale score of 13 or 14, or at least one acute sign or symptom of concussion, as noted by emergency clinicians.
Patients were excluded from the concussion group if they had deteriorating neurologic status, underwent neurosurgical intervention, had posttraumatic amnesia that lasted more than 24 hours, or had a score higher than 4 on the Abbreviated Injury Scale (AIS). The orthopedic injury group included patients without symptoms of concussion and with blunt trauma associated with an AIS 13 score of 4 or less. Patients were excluded from both groups if they had an overnight hospitalization for traumatic brain injury, a concussion within the past 3 months, or a neurodevelopmental disorder.
The researchers analyzed data from 928 children of 967 enrolled in the study. The median age was 12.2 years, and 41.3% were female. The final study cohort included 239 children with orthopedic injuries but no headache, 160 with a concussion and no headache, 134 with a concussion and nonmigraine headaches, and 254 with a concussion and migraine headaches.
Children with posttraumatic migraines 10 days after a concussion had the most severe symptoms and worst quality of life 3 months following their head trauma, the researchers found. Children without headaches within 10 days after concussion had the best 3-month outcomes, comparable to those with orthopedic injuries alone.
The researchers said the strengths of their study included its large population and its inclusion of various causes of head trauma, not just sports-related concussions. Limitations included self-reports of headaches instead of a physician diagnosis and lack of control for clinical interventions that might have affected the outcomes.
Charles Tator, MD, PhD, director of the Canadian Concussion Centre at Toronto Western Hospital, said the findings were unsurprising.
“Headaches are the most common symptom after concussion,” Dr. Tator, who was not involved in the latest research, told this news organization. “In my practice and research with concussed kids 11 and up and with adults, those with preconcussion history of migraine are the most difficult to treat because their headaches don’t improve unless specific measures are taken.”
Dr. Tator, who also is a professor of neurosurgery at the University of Toronto, said clinicians who treat concussions must determine which type of headaches children are experiencing – and refer as early as possible for migraine prevention or treatment and medication, as warranted.
“Early recognition after concussion that migraine headaches are occurring will save kids a lot of suffering,” he said.
The study was supported by a Canadian Institute of Health Research Foundation Grant and by funds from the Alberta Children’s Hospital Foundation and the Alberta Children’s Hospital Research Institute. Dr. Tator has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
We have seen the future of healthy muffins, and its name is Roselle
Get ‘em while they’re hot … for your health
Today on the Eating Channel, it’s a very special episode of “Much Ado About Muffin.”
The muffin. For some of us, it’s a good way to pretend we’re not having dessert for breakfast. A bran muffin can be loaded with calcium and fiber, and our beloved blueberry is full of yummy antioxidants and vitamins. Definitely not dessert.
Well, the muffin denial can stop there because there’s a new flavor on the scene, and research suggests it may actually be healthy. (Disclaimer: Muffin may not be considered healthy in Norway.) This new muffin has a name, Roselle, that comes from the calyx extract used in it, which is found in the Hibiscus sabdariffa plant of the same name.
Now, when it comes to new foods, especially ones that are supposed to be healthy, the No. 1 criteria is the same: It has to taste good. Researchers at the Norwegian University of Science and Technology and Amity University in India agreed, but they also set out to make it nutritionally valuable and give it a long shelf life without the addition of preservatives.
Sounds like a tall order, but they figured it out.
Not only is it tasty, but the properties of it could rival your morning multivitamin. Hibiscus extract has huge amounts of antioxidants, like phenolics, which are believed to help prevent cell membrane damage. Foods like vegetables, flax seed, and whole grains also have these antioxidants, but why not just have a Roselle muffin instead? You also get a dose of ascorbic acid without the glass of OJ in the morning.
The ascorbic acid, however, is not there just to help you. It also helps to check the researcher’s third box, shelf life. These naturally rosy-colored pastries will stay mold-free for 6 days without refrigeration at room temperature and without added preservatives.
Our guess, though, is they won’t be on the kitchen counter long enough to find out.
A sobering proposition
If Hollywood is to be believed, there’s no amount of drunkenness that can’t be cured with a cup of coffee or a stern slap in the face. Unfortunately, here in the real world the only thing that can make you less drunk is time. Maybe next time you’ll stop after that seventh Manhattan.
But what if we could beat time? What if there’s an actual sobriety drug out there?
Say hello to fibroblast growth factor 21. Although the liver already does good work filtering out what is essentially poison, it then goes the extra mile and produces fibroblast growth factor 21 (or, as her friends call her, FGF21), a hormone that suppresses the desire to drink, makes you desire water, and protects the liver all at the same time.
Now, FGF21 in its current role is great, but if you’ve ever seen or been a drunk person before, you’ve experienced the lack of interest in listening to reason, especially when it comes from within our own bodies. Who are you to tell us what to do, body? You’re not the boss of us! So a group of scientists decided to push the limits of FGF21. Could it do more than it already does?
First off, they genetically altered a group of mice so that they didn’t produce FGF21 on their own. Then they got them drunk. We’re going to assume they built a scale model of the bar from Cheers and had the mice filter in through the front door as they served their subjects beer out of tiny little glasses.
Once the mice were nice and liquored up, some were given a treatment of FGF21 while others were given a placebo. Lo and behold, the mice given FGF21 recovered about 50% faster than those that received the control treatment. Not exactly instant, but 50% is nothing to sniff at.
Before you bring your FGF21 supplement to the bar, though, this research only applies to mice. We don’t know if it works in people. And make sure you stick to booze. If your choice of intoxication is a bit more exotic, FGF21 isn’t going to do anything for you. Yes, the scientists tried. Yes, those mice are living a very interesting life. And yes, we are jealous of drugged-up lab mice.
Supersize your imagination, shrink your snacks
Have you ever heard of the meal-recall effect? Did you know that, in England, a biscuit is really a cookie? Did you also know that the magazine Bon Appétit is not the same as the peer-reviewed journal Appetite? We do … now.
The meal-recall effect is the subsequent reduction in snacking that comes from remembering a recent meal. It was used to great effect in a recent study conducted at the University of Cambridge, which is in England, where they feed their experimental humans cookies but, for some reason, call them biscuits.
For the first part of the study, the participants were invited to dine at Che Laboratory, where they “were given a microwave ready meal of rice and sauce and a cup of water,” according to a statement from the university. As our Uncle Ernie would say, “Gourmet all the way.”
The test subjects were instructed not to eat anything for 3 hours and “then invited back to the lab to perform imagination tasks.” Those who did come back were randomly divided into five different groups, each with a different task:
- Imagine moving their recent lunch at the lab around a plate.
- Recall eating their recent lunch in detail.
- Imagine that the lunch was twice as big and filling as it really was.
- Look at a photograph of spaghetti hoops in tomato sauce and write a description of it before imagining moving the food around a plate.
- Look at a photo of paper clips and rubber bands and imagine moving them around.
Now, at last, we get to the biscuits/cookies, which were the subject of a taste test that “was simply a rouse for covertly assessing snacking,” the investigators explained. As part of that test, participants were told they could eat as many biscuits as they wanted.
When the tables were cleared and the leftovers examined, the group that imagined spaghetti hoops had eaten the most biscuits (75.9 g), followed by the group that imagined paper clips (75.5 g), the moving-their-lunch-around-the-plate group (72.0 g), and the group that relived eating their lunch (70.0 g).
In a victory for the meal-recall effect, the people who imagined their meal being twice as big ate the fewest biscuits (51.1 g). “Your mind can be more powerful than your stomach in dictating how much you eat,” lead author Joanna Szypula, PhD, said in the university statement.
Oh! One more thing. The study appeared in Appetite, which is a peer-reviewed journal, not in Bon Appétit, which is not a peer-reviewed journal. Thanks to the fine folks at both publications for pointing that out to us.
Get ‘em while they’re hot … for your health
Today on the Eating Channel, it’s a very special episode of “Much Ado About Muffin.”
The muffin. For some of us, it’s a good way to pretend we’re not having dessert for breakfast. A bran muffin can be loaded with calcium and fiber, and our beloved blueberry is full of yummy antioxidants and vitamins. Definitely not dessert.
Well, the muffin denial can stop there because there’s a new flavor on the scene, and research suggests it may actually be healthy. (Disclaimer: Muffin may not be considered healthy in Norway.) This new muffin has a name, Roselle, that comes from the calyx extract used in it, which is found in the Hibiscus sabdariffa plant of the same name.
Now, when it comes to new foods, especially ones that are supposed to be healthy, the No. 1 criteria is the same: It has to taste good. Researchers at the Norwegian University of Science and Technology and Amity University in India agreed, but they also set out to make it nutritionally valuable and give it a long shelf life without the addition of preservatives.
Sounds like a tall order, but they figured it out.
Not only is it tasty, but the properties of it could rival your morning multivitamin. Hibiscus extract has huge amounts of antioxidants, like phenolics, which are believed to help prevent cell membrane damage. Foods like vegetables, flax seed, and whole grains also have these antioxidants, but why not just have a Roselle muffin instead? You also get a dose of ascorbic acid without the glass of OJ in the morning.
The ascorbic acid, however, is not there just to help you. It also helps to check the researcher’s third box, shelf life. These naturally rosy-colored pastries will stay mold-free for 6 days without refrigeration at room temperature and without added preservatives.
Our guess, though, is they won’t be on the kitchen counter long enough to find out.
A sobering proposition
If Hollywood is to be believed, there’s no amount of drunkenness that can’t be cured with a cup of coffee or a stern slap in the face. Unfortunately, here in the real world the only thing that can make you less drunk is time. Maybe next time you’ll stop after that seventh Manhattan.
But what if we could beat time? What if there’s an actual sobriety drug out there?
Say hello to fibroblast growth factor 21. Although the liver already does good work filtering out what is essentially poison, it then goes the extra mile and produces fibroblast growth factor 21 (or, as her friends call her, FGF21), a hormone that suppresses the desire to drink, makes you desire water, and protects the liver all at the same time.
Now, FGF21 in its current role is great, but if you’ve ever seen or been a drunk person before, you’ve experienced the lack of interest in listening to reason, especially when it comes from within our own bodies. Who are you to tell us what to do, body? You’re not the boss of us! So a group of scientists decided to push the limits of FGF21. Could it do more than it already does?
First off, they genetically altered a group of mice so that they didn’t produce FGF21 on their own. Then they got them drunk. We’re going to assume they built a scale model of the bar from Cheers and had the mice filter in through the front door as they served their subjects beer out of tiny little glasses.
Once the mice were nice and liquored up, some were given a treatment of FGF21 while others were given a placebo. Lo and behold, the mice given FGF21 recovered about 50% faster than those that received the control treatment. Not exactly instant, but 50% is nothing to sniff at.
Before you bring your FGF21 supplement to the bar, though, this research only applies to mice. We don’t know if it works in people. And make sure you stick to booze. If your choice of intoxication is a bit more exotic, FGF21 isn’t going to do anything for you. Yes, the scientists tried. Yes, those mice are living a very interesting life. And yes, we are jealous of drugged-up lab mice.
Supersize your imagination, shrink your snacks
Have you ever heard of the meal-recall effect? Did you know that, in England, a biscuit is really a cookie? Did you also know that the magazine Bon Appétit is not the same as the peer-reviewed journal Appetite? We do … now.
The meal-recall effect is the subsequent reduction in snacking that comes from remembering a recent meal. It was used to great effect in a recent study conducted at the University of Cambridge, which is in England, where they feed their experimental humans cookies but, for some reason, call them biscuits.
For the first part of the study, the participants were invited to dine at Che Laboratory, where they “were given a microwave ready meal of rice and sauce and a cup of water,” according to a statement from the university. As our Uncle Ernie would say, “Gourmet all the way.”
The test subjects were instructed not to eat anything for 3 hours and “then invited back to the lab to perform imagination tasks.” Those who did come back were randomly divided into five different groups, each with a different task:
- Imagine moving their recent lunch at the lab around a plate.
- Recall eating their recent lunch in detail.
- Imagine that the lunch was twice as big and filling as it really was.
- Look at a photograph of spaghetti hoops in tomato sauce and write a description of it before imagining moving the food around a plate.
- Look at a photo of paper clips and rubber bands and imagine moving them around.
Now, at last, we get to the biscuits/cookies, which were the subject of a taste test that “was simply a rouse for covertly assessing snacking,” the investigators explained. As part of that test, participants were told they could eat as many biscuits as they wanted.
When the tables were cleared and the leftovers examined, the group that imagined spaghetti hoops had eaten the most biscuits (75.9 g), followed by the group that imagined paper clips (75.5 g), the moving-their-lunch-around-the-plate group (72.0 g), and the group that relived eating their lunch (70.0 g).
In a victory for the meal-recall effect, the people who imagined their meal being twice as big ate the fewest biscuits (51.1 g). “Your mind can be more powerful than your stomach in dictating how much you eat,” lead author Joanna Szypula, PhD, said in the university statement.
Oh! One more thing. The study appeared in Appetite, which is a peer-reviewed journal, not in Bon Appétit, which is not a peer-reviewed journal. Thanks to the fine folks at both publications for pointing that out to us.
Get ‘em while they’re hot … for your health
Today on the Eating Channel, it’s a very special episode of “Much Ado About Muffin.”
The muffin. For some of us, it’s a good way to pretend we’re not having dessert for breakfast. A bran muffin can be loaded with calcium and fiber, and our beloved blueberry is full of yummy antioxidants and vitamins. Definitely not dessert.
Well, the muffin denial can stop there because there’s a new flavor on the scene, and research suggests it may actually be healthy. (Disclaimer: Muffin may not be considered healthy in Norway.) This new muffin has a name, Roselle, that comes from the calyx extract used in it, which is found in the Hibiscus sabdariffa plant of the same name.
Now, when it comes to new foods, especially ones that are supposed to be healthy, the No. 1 criteria is the same: It has to taste good. Researchers at the Norwegian University of Science and Technology and Amity University in India agreed, but they also set out to make it nutritionally valuable and give it a long shelf life without the addition of preservatives.
Sounds like a tall order, but they figured it out.
Not only is it tasty, but the properties of it could rival your morning multivitamin. Hibiscus extract has huge amounts of antioxidants, like phenolics, which are believed to help prevent cell membrane damage. Foods like vegetables, flax seed, and whole grains also have these antioxidants, but why not just have a Roselle muffin instead? You also get a dose of ascorbic acid without the glass of OJ in the morning.
The ascorbic acid, however, is not there just to help you. It also helps to check the researcher’s third box, shelf life. These naturally rosy-colored pastries will stay mold-free for 6 days without refrigeration at room temperature and without added preservatives.
Our guess, though, is they won’t be on the kitchen counter long enough to find out.
A sobering proposition
If Hollywood is to be believed, there’s no amount of drunkenness that can’t be cured with a cup of coffee or a stern slap in the face. Unfortunately, here in the real world the only thing that can make you less drunk is time. Maybe next time you’ll stop after that seventh Manhattan.
But what if we could beat time? What if there’s an actual sobriety drug out there?
Say hello to fibroblast growth factor 21. Although the liver already does good work filtering out what is essentially poison, it then goes the extra mile and produces fibroblast growth factor 21 (or, as her friends call her, FGF21), a hormone that suppresses the desire to drink, makes you desire water, and protects the liver all at the same time.
Now, FGF21 in its current role is great, but if you’ve ever seen or been a drunk person before, you’ve experienced the lack of interest in listening to reason, especially when it comes from within our own bodies. Who are you to tell us what to do, body? You’re not the boss of us! So a group of scientists decided to push the limits of FGF21. Could it do more than it already does?
First off, they genetically altered a group of mice so that they didn’t produce FGF21 on their own. Then they got them drunk. We’re going to assume they built a scale model of the bar from Cheers and had the mice filter in through the front door as they served their subjects beer out of tiny little glasses.
Once the mice were nice and liquored up, some were given a treatment of FGF21 while others were given a placebo. Lo and behold, the mice given FGF21 recovered about 50% faster than those that received the control treatment. Not exactly instant, but 50% is nothing to sniff at.
Before you bring your FGF21 supplement to the bar, though, this research only applies to mice. We don’t know if it works in people. And make sure you stick to booze. If your choice of intoxication is a bit more exotic, FGF21 isn’t going to do anything for you. Yes, the scientists tried. Yes, those mice are living a very interesting life. And yes, we are jealous of drugged-up lab mice.
Supersize your imagination, shrink your snacks
Have you ever heard of the meal-recall effect? Did you know that, in England, a biscuit is really a cookie? Did you also know that the magazine Bon Appétit is not the same as the peer-reviewed journal Appetite? We do … now.
The meal-recall effect is the subsequent reduction in snacking that comes from remembering a recent meal. It was used to great effect in a recent study conducted at the University of Cambridge, which is in England, where they feed their experimental humans cookies but, for some reason, call them biscuits.
For the first part of the study, the participants were invited to dine at Che Laboratory, where they “were given a microwave ready meal of rice and sauce and a cup of water,” according to a statement from the university. As our Uncle Ernie would say, “Gourmet all the way.”
The test subjects were instructed not to eat anything for 3 hours and “then invited back to the lab to perform imagination tasks.” Those who did come back were randomly divided into five different groups, each with a different task:
- Imagine moving their recent lunch at the lab around a plate.
- Recall eating their recent lunch in detail.
- Imagine that the lunch was twice as big and filling as it really was.
- Look at a photograph of spaghetti hoops in tomato sauce and write a description of it before imagining moving the food around a plate.
- Look at a photo of paper clips and rubber bands and imagine moving them around.
Now, at last, we get to the biscuits/cookies, which were the subject of a taste test that “was simply a rouse for covertly assessing snacking,” the investigators explained. As part of that test, participants were told they could eat as many biscuits as they wanted.
When the tables were cleared and the leftovers examined, the group that imagined spaghetti hoops had eaten the most biscuits (75.9 g), followed by the group that imagined paper clips (75.5 g), the moving-their-lunch-around-the-plate group (72.0 g), and the group that relived eating their lunch (70.0 g).
In a victory for the meal-recall effect, the people who imagined their meal being twice as big ate the fewest biscuits (51.1 g). “Your mind can be more powerful than your stomach in dictating how much you eat,” lead author Joanna Szypula, PhD, said in the university statement.
Oh! One more thing. The study appeared in Appetite, which is a peer-reviewed journal, not in Bon Appétit, which is not a peer-reviewed journal. Thanks to the fine folks at both publications for pointing that out to us.
APA releases updated eating disorder guidelines
The updated guidelines focus primarily on anorexia nervosa (AN), bulimia nervosa (BN), and binge-eating disorder (BED) and include recommendations for screening and treatment.
“Eating disorders often are unrecognized and untreated,” Catherine Crone, MD, chair of the guideline writing group, said in a statement from APA. “This guideline and supplementary resources are intended to serve as a practical tool for clinicians, to help with screening, diagnosis, and providing evidence-based treatment for eating disorders.”
Approximately one in five children worldwide are at risk for developing an eating disorder and U.S. medical admissions for adolescents with restrictive eating disorders more than doubled during the pandemic.
The economic cost of eating disorders in the United States from 2018 to 2019 was an estimated $64.7 billion, the report notes, with an additional $326.5 billion attributable to reductions in well-being associated with eating disorders.
The executive summary of the updated guidelines was published online in The American Journal of Psychiatry.
The practice guideline, which was approved at the 2021 APA annual meeting, features 16 recommendations for clinicians, including screening patients for eating disorders as part of an initial psychiatric evaluation and conducting comprehensive patient evaluations that incorporate laboratory tests and electrocardiograms.
Recommendations also include setting individualized weight goals for patients with anorexia and incorporating family-based therapy as part of a treatment plan for adolescents with anorexia or bulimia.
“This practice guideline aims to help clinicians improve care for their patients by reviewing current evidence and providing evidence-based statements that are intended to enhance knowledge, increase assessment, and optimize treatment of eating disorders,” the authors wrote.
A range of other resources were released with the new guidelines to provide clinicians with support to implement the recommendations, including a pocket guide for clinicians, continuing medical education activities, and slides. The association is also launching a pocket guide for patients and families and an interactive tool kit with a screening assessment calculator.
The APA guidelines follow the 2021 release by the American Academy of Pediatrics on diagnosing and managing eating disorders in children and adolescents.
The development of the guidelines was supported by a grant from the Council of Medical Specialty Societies.
A version of this article first appeared on Medscape.com.
The updated guidelines focus primarily on anorexia nervosa (AN), bulimia nervosa (BN), and binge-eating disorder (BED) and include recommendations for screening and treatment.
“Eating disorders often are unrecognized and untreated,” Catherine Crone, MD, chair of the guideline writing group, said in a statement from APA. “This guideline and supplementary resources are intended to serve as a practical tool for clinicians, to help with screening, diagnosis, and providing evidence-based treatment for eating disorders.”
Approximately one in five children worldwide are at risk for developing an eating disorder and U.S. medical admissions for adolescents with restrictive eating disorders more than doubled during the pandemic.
The economic cost of eating disorders in the United States from 2018 to 2019 was an estimated $64.7 billion, the report notes, with an additional $326.5 billion attributable to reductions in well-being associated with eating disorders.
The executive summary of the updated guidelines was published online in The American Journal of Psychiatry.
The practice guideline, which was approved at the 2021 APA annual meeting, features 16 recommendations for clinicians, including screening patients for eating disorders as part of an initial psychiatric evaluation and conducting comprehensive patient evaluations that incorporate laboratory tests and electrocardiograms.
Recommendations also include setting individualized weight goals for patients with anorexia and incorporating family-based therapy as part of a treatment plan for adolescents with anorexia or bulimia.
“This practice guideline aims to help clinicians improve care for their patients by reviewing current evidence and providing evidence-based statements that are intended to enhance knowledge, increase assessment, and optimize treatment of eating disorders,” the authors wrote.
A range of other resources were released with the new guidelines to provide clinicians with support to implement the recommendations, including a pocket guide for clinicians, continuing medical education activities, and slides. The association is also launching a pocket guide for patients and families and an interactive tool kit with a screening assessment calculator.
The APA guidelines follow the 2021 release by the American Academy of Pediatrics on diagnosing and managing eating disorders in children and adolescents.
The development of the guidelines was supported by a grant from the Council of Medical Specialty Societies.
A version of this article first appeared on Medscape.com.
The updated guidelines focus primarily on anorexia nervosa (AN), bulimia nervosa (BN), and binge-eating disorder (BED) and include recommendations for screening and treatment.
“Eating disorders often are unrecognized and untreated,” Catherine Crone, MD, chair of the guideline writing group, said in a statement from APA. “This guideline and supplementary resources are intended to serve as a practical tool for clinicians, to help with screening, diagnosis, and providing evidence-based treatment for eating disorders.”
Approximately one in five children worldwide are at risk for developing an eating disorder and U.S. medical admissions for adolescents with restrictive eating disorders more than doubled during the pandemic.
The economic cost of eating disorders in the United States from 2018 to 2019 was an estimated $64.7 billion, the report notes, with an additional $326.5 billion attributable to reductions in well-being associated with eating disorders.
The executive summary of the updated guidelines was published online in The American Journal of Psychiatry.
The practice guideline, which was approved at the 2021 APA annual meeting, features 16 recommendations for clinicians, including screening patients for eating disorders as part of an initial psychiatric evaluation and conducting comprehensive patient evaluations that incorporate laboratory tests and electrocardiograms.
Recommendations also include setting individualized weight goals for patients with anorexia and incorporating family-based therapy as part of a treatment plan for adolescents with anorexia or bulimia.
“This practice guideline aims to help clinicians improve care for their patients by reviewing current evidence and providing evidence-based statements that are intended to enhance knowledge, increase assessment, and optimize treatment of eating disorders,” the authors wrote.
A range of other resources were released with the new guidelines to provide clinicians with support to implement the recommendations, including a pocket guide for clinicians, continuing medical education activities, and slides. The association is also launching a pocket guide for patients and families and an interactive tool kit with a screening assessment calculator.
The APA guidelines follow the 2021 release by the American Academy of Pediatrics on diagnosing and managing eating disorders in children and adolescents.
The development of the guidelines was supported by a grant from the Council of Medical Specialty Societies.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF PSYCHIATRY