User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


COVID-19 plans put to test as firefighters crowd camps for peak wildfire season
Jon Paul was leery entering his first wildfire camp of the year late last month to fight three lightning-caused fires scorching parts of a Northern California forest that hadn’t burned in 40 years.

The 54-year-old engine captain from southern Oregon knew from experience that these crowded, grimy camps can be breeding grounds for norovirus and a respiratory illness that firefighters call the “camp crud” in a normal year. He wondered what the coronavirus would do in the tent cities where hundreds of men and women eat, sleep, wash, and spend their downtime between shifts.
Mr. Paul thought about his immunocompromised wife and his 84-year-old mother back home. Then he joined the approximately 1,300 people spread across the Modoc National Forest who would provide a major test for the COVID-prevention measures that had been developed for wildland firefighters.
“We’re still first responders and we have that responsibility to go and deal with these emergencies,” he said in a recent interview. “I don’t scare easy, but I’m very wary and concerned about my surroundings. I’m still going to work and do my job.”
Mr. Paul is one of thousands of firefighters from across the United States battling dozens of wildfires burning throughout the West. It’s an inherently dangerous job that now carries the additional risk of COVID-19 transmission. Any outbreak that ripples through a camp could easily sideline crews and spread the virus across multiple fires – and back to communities across the country – as personnel transfer in and out of “hot zones” and return home.
Though most firefighters are young and fit, some will inevitably fall ill in these remote makeshift communities of shared showers and portable toilets, where medical care can be limited. The pollutants in the smoke they breathe daily also make them more susceptible to COVID-19 and can worsen the effects of the disease, according to the Centers for Disease Control and Prevention.
Also, one suspected or positive case in a camp will mean many other firefighters will need to be quarantined, unable to work. The worst-case scenario is that multiple outbreaks could hamstring the nation’s ability to respond as wildfire season peaks in August, the hottest and driest month of the year in the western United States.
The number of acres burned so far this year is below the 10-year average, but the fire outlook for August is above average in nine states, according to the National Interagency Fire Center. Twenty-two large fires were ignited on Monday alone after lightning storms passed through the Northwest.
A study published this month by researchers at Colorado State University and the U.S. Forest Service’s Rocky Mountain Research Station concluded that COVID outbreaks “could be a serious threat to the firefighting mission” and urged vigilant social distancing and screening measures in the camps.
“If simultaneous fires incurred outbreaks, the entire wildland response system could be stressed substantially, with a large portion of the workforce quarantined,” the study’s authors wrote.
This spring, the National Wildfire Coordinating Group’s Fire Management Board wrote – and has since been updating – protocols to prevent the spread of COVID-19 in fire camps, based on CDC guidelines. Though they can be adapted by managers at different fires and even by individual team, they center on some key recommendations, including the following:
- Firefighters should be screened for fever and other COVID symptoms when they arrive at camp.
- Every crew should insulate itself as a “module of one” for the fire season and limit interactions with other crews.
- Firefighters should maintain social distancing and wear face coverings when social distancing isn’t possible. Smaller satellite camps, known as spike camps, can be built to ensure enough space.
- Shared areas should be regularly cleaned and disinfected, and sharing tools and radios should be minimized.
The guidance does not include routine testing of newly arrived firefighters – a practice used for athletes at training camps and students returning to college campuses.
The Fire Management Board’s Wildland Fire Medical and Public Health Advisory Team wrote in a July 2 memo that it “does not recommend utilizing universal COVID-19 laboratory testing as a standalone risk mitigation or screening measure among wildland firefighters.” Rather, the group recommends testing an individual and directly exposed coworkers, saying that approach is in line with CDC guidance.
The lack of testing capacity and long turnaround times are factors, according to Forest Service spokesperson Dan Hottle.
The exception is Alaska, where firefighters are tested upon arrival at the airport and are quarantined in a hotel while awaiting results, which come within 24 hours, Mr. Hottle said.
Fire crews responding to early-season fires in the spring had some problems adjusting to the new protocols, according to assessments written by fire leaders and compiled by the Wildland Fire Lessons Learned Center.
Shawn Faiella, superintendent of the interagency “hotshot crew” – so named because they work the most challenging or “hottest” parts of wildfires – based at Montana’s Lolo National Forest, questioned the need to wear masks inside vehicles and the safety of bringing extra vehicles to space out firefighters traveling to a blaze. Parking extra vehicles at the scene of a fire is difficult in tight dirt roads – and would be dangerous if evacuations are necessary, he wrote.
“It’s damn tough to take these practices to the fire line,” Mr. Faiella wrote after his team responded to a 40-acre Montana fire in April.
One recommendation that fire managers say has been particularly effective is the “module of one” concept requiring crews to eat and sleep together in isolation for the entire fire season.
“Whoever came up with it, it is working,” said Mike Goicoechea, the Montana-based incident commander for the Forest Service’s Northern Region Type 1 team, which manages the nation’s largest and most complex wildfires and natural disasters. “Somebody may test positive, and you end up having to take that module out of service for 14 days. But the nice part is you’re not taking out a whole camp. ... It’s just that module.”
The total number of positive COVID cases among wildland firefighters among the various federal, state, local, and tribal agencies is not being tracked. Each fire agency has its own system for tracking and reporting COVID-19, said Jessica Gardetto, a spokesperson for the Bureau of Land Management (BLM) and the National Interagency Fire Center in Idaho.
The largest wildland firefighting agency is the Department of Agriculture’s Forest Service, with 10,000 firefighters. Another major agency is the Department of the Interior, which BLM is part of and which had more than 3,500 full-time fire employees last year. As of the first week of August, 111 Forest Service firefighters and 40 BLM firefighters (who work underneath the broader Interior Department agency) had tested positive for COVID-19, according to officials for the respective agencies.
“Considering we’ve now been experiencing fire activity for several months, this number is surprisingly low if you think about the thousands of fire personnel who’ve been suppressing wildfires this summer,” Ms. Gardetto said.
Mr. Goicoechea and his Montana team traveled north of Tucson, Arizona, on June 22 to manage a rapidly spreading fire in the Santa Catalina Mountains that required 1,200 responders at its peak. Within 2 days of the team’s arrival, his managers were overwhelmed by calls from firefighters worried or with questions about preventing the spread of COVID-19 or carrying the virus home to their families.
In an unusual move, Mr. Goicoechea called upon Montana physician – and former National Park Service ranger with wildfire experience – Harry Sibold, MD, to join the team. Physicians are rarely, if ever, part of a wildfire camp’s medical team, Mr. Goicoechea said.
Dr. Sibold gave regular coronavirus updates during morning briefings, consulted with local health officials, soothed firefighters worried about bringing the virus home to their families, and advised fire managers on how to handle scenarios that might come up.
But Dr. Sibold said he wasn’t optimistic at the beginning about keeping the coronavirus in check in a large camp in Pima County, which has the second-highest number of confirmed cases in Arizona, at the time a national COVID-19 hot spot. “I quite firmly expected that we might have two or three outbreaks,” he said.
There were no positive cases during the team’s 2-week deployment, just three or four cases in which a firefighter showed symptoms but tested negative for the virus. After the Montana team returned home, nine firefighters at the Arizona fire from other units tested positive, Mr. Goicoechea said. Contact tracers notified the Montana team, some of whom were tested. All tests returned negative.
“I can’t say enough about having that doctor to help,” Mr. Goicoechea said, suggesting other teams might consider doing the same. “We’re not the experts in a pandemic. We’re the experts with fire.”
That early success will be tested as the number of fires increases across the West, along with the number of firefighters responding to them. There were more than 15,000 firefighters and support personnel assigned to fires across the nation as of mid-August, and the success of those COVID-19 prevention protocols depend largely on them.
Mr. Paul, the Oregon firefighter, said that the guidelines were followed closely in camp, but less so out on the fire line. It also appeared to him that younger firefighters were less likely to follow the masking and social-distancing rules than the veterans like him. That worried him as he realized it wouldn’t take much to spark an outbreak that could sideline crews and cripple the ability to respond to a fire.
“We’re outside, so it definitely helps with mitigation and makes it simpler to social distance,” Mr. Paul said. “But I think if there’s a mistake made, it could happen.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Jon Paul was leery entering his first wildfire camp of the year late last month to fight three lightning-caused fires scorching parts of a Northern California forest that hadn’t burned in 40 years.

The 54-year-old engine captain from southern Oregon knew from experience that these crowded, grimy camps can be breeding grounds for norovirus and a respiratory illness that firefighters call the “camp crud” in a normal year. He wondered what the coronavirus would do in the tent cities where hundreds of men and women eat, sleep, wash, and spend their downtime between shifts.
Mr. Paul thought about his immunocompromised wife and his 84-year-old mother back home. Then he joined the approximately 1,300 people spread across the Modoc National Forest who would provide a major test for the COVID-prevention measures that had been developed for wildland firefighters.
“We’re still first responders and we have that responsibility to go and deal with these emergencies,” he said in a recent interview. “I don’t scare easy, but I’m very wary and concerned about my surroundings. I’m still going to work and do my job.”
Mr. Paul is one of thousands of firefighters from across the United States battling dozens of wildfires burning throughout the West. It’s an inherently dangerous job that now carries the additional risk of COVID-19 transmission. Any outbreak that ripples through a camp could easily sideline crews and spread the virus across multiple fires – and back to communities across the country – as personnel transfer in and out of “hot zones” and return home.
Though most firefighters are young and fit, some will inevitably fall ill in these remote makeshift communities of shared showers and portable toilets, where medical care can be limited. The pollutants in the smoke they breathe daily also make them more susceptible to COVID-19 and can worsen the effects of the disease, according to the Centers for Disease Control and Prevention.
Also, one suspected or positive case in a camp will mean many other firefighters will need to be quarantined, unable to work. The worst-case scenario is that multiple outbreaks could hamstring the nation’s ability to respond as wildfire season peaks in August, the hottest and driest month of the year in the western United States.
The number of acres burned so far this year is below the 10-year average, but the fire outlook for August is above average in nine states, according to the National Interagency Fire Center. Twenty-two large fires were ignited on Monday alone after lightning storms passed through the Northwest.
A study published this month by researchers at Colorado State University and the U.S. Forest Service’s Rocky Mountain Research Station concluded that COVID outbreaks “could be a serious threat to the firefighting mission” and urged vigilant social distancing and screening measures in the camps.
“If simultaneous fires incurred outbreaks, the entire wildland response system could be stressed substantially, with a large portion of the workforce quarantined,” the study’s authors wrote.
This spring, the National Wildfire Coordinating Group’s Fire Management Board wrote – and has since been updating – protocols to prevent the spread of COVID-19 in fire camps, based on CDC guidelines. Though they can be adapted by managers at different fires and even by individual team, they center on some key recommendations, including the following:
- Firefighters should be screened for fever and other COVID symptoms when they arrive at camp.
- Every crew should insulate itself as a “module of one” for the fire season and limit interactions with other crews.
- Firefighters should maintain social distancing and wear face coverings when social distancing isn’t possible. Smaller satellite camps, known as spike camps, can be built to ensure enough space.
- Shared areas should be regularly cleaned and disinfected, and sharing tools and radios should be minimized.
The guidance does not include routine testing of newly arrived firefighters – a practice used for athletes at training camps and students returning to college campuses.
The Fire Management Board’s Wildland Fire Medical and Public Health Advisory Team wrote in a July 2 memo that it “does not recommend utilizing universal COVID-19 laboratory testing as a standalone risk mitigation or screening measure among wildland firefighters.” Rather, the group recommends testing an individual and directly exposed coworkers, saying that approach is in line with CDC guidance.
The lack of testing capacity and long turnaround times are factors, according to Forest Service spokesperson Dan Hottle.
The exception is Alaska, where firefighters are tested upon arrival at the airport and are quarantined in a hotel while awaiting results, which come within 24 hours, Mr. Hottle said.
Fire crews responding to early-season fires in the spring had some problems adjusting to the new protocols, according to assessments written by fire leaders and compiled by the Wildland Fire Lessons Learned Center.
Shawn Faiella, superintendent of the interagency “hotshot crew” – so named because they work the most challenging or “hottest” parts of wildfires – based at Montana’s Lolo National Forest, questioned the need to wear masks inside vehicles and the safety of bringing extra vehicles to space out firefighters traveling to a blaze. Parking extra vehicles at the scene of a fire is difficult in tight dirt roads – and would be dangerous if evacuations are necessary, he wrote.
“It’s damn tough to take these practices to the fire line,” Mr. Faiella wrote after his team responded to a 40-acre Montana fire in April.
One recommendation that fire managers say has been particularly effective is the “module of one” concept requiring crews to eat and sleep together in isolation for the entire fire season.
“Whoever came up with it, it is working,” said Mike Goicoechea, the Montana-based incident commander for the Forest Service’s Northern Region Type 1 team, which manages the nation’s largest and most complex wildfires and natural disasters. “Somebody may test positive, and you end up having to take that module out of service for 14 days. But the nice part is you’re not taking out a whole camp. ... It’s just that module.”
The total number of positive COVID cases among wildland firefighters among the various federal, state, local, and tribal agencies is not being tracked. Each fire agency has its own system for tracking and reporting COVID-19, said Jessica Gardetto, a spokesperson for the Bureau of Land Management (BLM) and the National Interagency Fire Center in Idaho.
The largest wildland firefighting agency is the Department of Agriculture’s Forest Service, with 10,000 firefighters. Another major agency is the Department of the Interior, which BLM is part of and which had more than 3,500 full-time fire employees last year. As of the first week of August, 111 Forest Service firefighters and 40 BLM firefighters (who work underneath the broader Interior Department agency) had tested positive for COVID-19, according to officials for the respective agencies.
“Considering we’ve now been experiencing fire activity for several months, this number is surprisingly low if you think about the thousands of fire personnel who’ve been suppressing wildfires this summer,” Ms. Gardetto said.
Mr. Goicoechea and his Montana team traveled north of Tucson, Arizona, on June 22 to manage a rapidly spreading fire in the Santa Catalina Mountains that required 1,200 responders at its peak. Within 2 days of the team’s arrival, his managers were overwhelmed by calls from firefighters worried or with questions about preventing the spread of COVID-19 or carrying the virus home to their families.
In an unusual move, Mr. Goicoechea called upon Montana physician – and former National Park Service ranger with wildfire experience – Harry Sibold, MD, to join the team. Physicians are rarely, if ever, part of a wildfire camp’s medical team, Mr. Goicoechea said.
Dr. Sibold gave regular coronavirus updates during morning briefings, consulted with local health officials, soothed firefighters worried about bringing the virus home to their families, and advised fire managers on how to handle scenarios that might come up.
But Dr. Sibold said he wasn’t optimistic at the beginning about keeping the coronavirus in check in a large camp in Pima County, which has the second-highest number of confirmed cases in Arizona, at the time a national COVID-19 hot spot. “I quite firmly expected that we might have two or three outbreaks,” he said.
There were no positive cases during the team’s 2-week deployment, just three or four cases in which a firefighter showed symptoms but tested negative for the virus. After the Montana team returned home, nine firefighters at the Arizona fire from other units tested positive, Mr. Goicoechea said. Contact tracers notified the Montana team, some of whom were tested. All tests returned negative.
“I can’t say enough about having that doctor to help,” Mr. Goicoechea said, suggesting other teams might consider doing the same. “We’re not the experts in a pandemic. We’re the experts with fire.”
That early success will be tested as the number of fires increases across the West, along with the number of firefighters responding to them. There were more than 15,000 firefighters and support personnel assigned to fires across the nation as of mid-August, and the success of those COVID-19 prevention protocols depend largely on them.
Mr. Paul, the Oregon firefighter, said that the guidelines were followed closely in camp, but less so out on the fire line. It also appeared to him that younger firefighters were less likely to follow the masking and social-distancing rules than the veterans like him. That worried him as he realized it wouldn’t take much to spark an outbreak that could sideline crews and cripple the ability to respond to a fire.
“We’re outside, so it definitely helps with mitigation and makes it simpler to social distance,” Mr. Paul said. “But I think if there’s a mistake made, it could happen.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Jon Paul was leery entering his first wildfire camp of the year late last month to fight three lightning-caused fires scorching parts of a Northern California forest that hadn’t burned in 40 years.

The 54-year-old engine captain from southern Oregon knew from experience that these crowded, grimy camps can be breeding grounds for norovirus and a respiratory illness that firefighters call the “camp crud” in a normal year. He wondered what the coronavirus would do in the tent cities where hundreds of men and women eat, sleep, wash, and spend their downtime between shifts.
Mr. Paul thought about his immunocompromised wife and his 84-year-old mother back home. Then he joined the approximately 1,300 people spread across the Modoc National Forest who would provide a major test for the COVID-prevention measures that had been developed for wildland firefighters.
“We’re still first responders and we have that responsibility to go and deal with these emergencies,” he said in a recent interview. “I don’t scare easy, but I’m very wary and concerned about my surroundings. I’m still going to work and do my job.”
Mr. Paul is one of thousands of firefighters from across the United States battling dozens of wildfires burning throughout the West. It’s an inherently dangerous job that now carries the additional risk of COVID-19 transmission. Any outbreak that ripples through a camp could easily sideline crews and spread the virus across multiple fires – and back to communities across the country – as personnel transfer in and out of “hot zones” and return home.
Though most firefighters are young and fit, some will inevitably fall ill in these remote makeshift communities of shared showers and portable toilets, where medical care can be limited. The pollutants in the smoke they breathe daily also make them more susceptible to COVID-19 and can worsen the effects of the disease, according to the Centers for Disease Control and Prevention.
Also, one suspected or positive case in a camp will mean many other firefighters will need to be quarantined, unable to work. The worst-case scenario is that multiple outbreaks could hamstring the nation’s ability to respond as wildfire season peaks in August, the hottest and driest month of the year in the western United States.
The number of acres burned so far this year is below the 10-year average, but the fire outlook for August is above average in nine states, according to the National Interagency Fire Center. Twenty-two large fires were ignited on Monday alone after lightning storms passed through the Northwest.
A study published this month by researchers at Colorado State University and the U.S. Forest Service’s Rocky Mountain Research Station concluded that COVID outbreaks “could be a serious threat to the firefighting mission” and urged vigilant social distancing and screening measures in the camps.
“If simultaneous fires incurred outbreaks, the entire wildland response system could be stressed substantially, with a large portion of the workforce quarantined,” the study’s authors wrote.
This spring, the National Wildfire Coordinating Group’s Fire Management Board wrote – and has since been updating – protocols to prevent the spread of COVID-19 in fire camps, based on CDC guidelines. Though they can be adapted by managers at different fires and even by individual team, they center on some key recommendations, including the following:
- Firefighters should be screened for fever and other COVID symptoms when they arrive at camp.
- Every crew should insulate itself as a “module of one” for the fire season and limit interactions with other crews.
- Firefighters should maintain social distancing and wear face coverings when social distancing isn’t possible. Smaller satellite camps, known as spike camps, can be built to ensure enough space.
- Shared areas should be regularly cleaned and disinfected, and sharing tools and radios should be minimized.
The guidance does not include routine testing of newly arrived firefighters – a practice used for athletes at training camps and students returning to college campuses.
The Fire Management Board’s Wildland Fire Medical and Public Health Advisory Team wrote in a July 2 memo that it “does not recommend utilizing universal COVID-19 laboratory testing as a standalone risk mitigation or screening measure among wildland firefighters.” Rather, the group recommends testing an individual and directly exposed coworkers, saying that approach is in line with CDC guidance.
The lack of testing capacity and long turnaround times are factors, according to Forest Service spokesperson Dan Hottle.
The exception is Alaska, where firefighters are tested upon arrival at the airport and are quarantined in a hotel while awaiting results, which come within 24 hours, Mr. Hottle said.
Fire crews responding to early-season fires in the spring had some problems adjusting to the new protocols, according to assessments written by fire leaders and compiled by the Wildland Fire Lessons Learned Center.
Shawn Faiella, superintendent of the interagency “hotshot crew” – so named because they work the most challenging or “hottest” parts of wildfires – based at Montana’s Lolo National Forest, questioned the need to wear masks inside vehicles and the safety of bringing extra vehicles to space out firefighters traveling to a blaze. Parking extra vehicles at the scene of a fire is difficult in tight dirt roads – and would be dangerous if evacuations are necessary, he wrote.
“It’s damn tough to take these practices to the fire line,” Mr. Faiella wrote after his team responded to a 40-acre Montana fire in April.
One recommendation that fire managers say has been particularly effective is the “module of one” concept requiring crews to eat and sleep together in isolation for the entire fire season.
“Whoever came up with it, it is working,” said Mike Goicoechea, the Montana-based incident commander for the Forest Service’s Northern Region Type 1 team, which manages the nation’s largest and most complex wildfires and natural disasters. “Somebody may test positive, and you end up having to take that module out of service for 14 days. But the nice part is you’re not taking out a whole camp. ... It’s just that module.”
The total number of positive COVID cases among wildland firefighters among the various federal, state, local, and tribal agencies is not being tracked. Each fire agency has its own system for tracking and reporting COVID-19, said Jessica Gardetto, a spokesperson for the Bureau of Land Management (BLM) and the National Interagency Fire Center in Idaho.
The largest wildland firefighting agency is the Department of Agriculture’s Forest Service, with 10,000 firefighters. Another major agency is the Department of the Interior, which BLM is part of and which had more than 3,500 full-time fire employees last year. As of the first week of August, 111 Forest Service firefighters and 40 BLM firefighters (who work underneath the broader Interior Department agency) had tested positive for COVID-19, according to officials for the respective agencies.
“Considering we’ve now been experiencing fire activity for several months, this number is surprisingly low if you think about the thousands of fire personnel who’ve been suppressing wildfires this summer,” Ms. Gardetto said.
Mr. Goicoechea and his Montana team traveled north of Tucson, Arizona, on June 22 to manage a rapidly spreading fire in the Santa Catalina Mountains that required 1,200 responders at its peak. Within 2 days of the team’s arrival, his managers were overwhelmed by calls from firefighters worried or with questions about preventing the spread of COVID-19 or carrying the virus home to their families.
In an unusual move, Mr. Goicoechea called upon Montana physician – and former National Park Service ranger with wildfire experience – Harry Sibold, MD, to join the team. Physicians are rarely, if ever, part of a wildfire camp’s medical team, Mr. Goicoechea said.
Dr. Sibold gave regular coronavirus updates during morning briefings, consulted with local health officials, soothed firefighters worried about bringing the virus home to their families, and advised fire managers on how to handle scenarios that might come up.
But Dr. Sibold said he wasn’t optimistic at the beginning about keeping the coronavirus in check in a large camp in Pima County, which has the second-highest number of confirmed cases in Arizona, at the time a national COVID-19 hot spot. “I quite firmly expected that we might have two or three outbreaks,” he said.
There were no positive cases during the team’s 2-week deployment, just three or four cases in which a firefighter showed symptoms but tested negative for the virus. After the Montana team returned home, nine firefighters at the Arizona fire from other units tested positive, Mr. Goicoechea said. Contact tracers notified the Montana team, some of whom were tested. All tests returned negative.
“I can’t say enough about having that doctor to help,” Mr. Goicoechea said, suggesting other teams might consider doing the same. “We’re not the experts in a pandemic. We’re the experts with fire.”
That early success will be tested as the number of fires increases across the West, along with the number of firefighters responding to them. There were more than 15,000 firefighters and support personnel assigned to fires across the nation as of mid-August, and the success of those COVID-19 prevention protocols depend largely on them.
Mr. Paul, the Oregon firefighter, said that the guidelines were followed closely in camp, but less so out on the fire line. It also appeared to him that younger firefighters were less likely to follow the masking and social-distancing rules than the veterans like him. That worried him as he realized it wouldn’t take much to spark an outbreak that could sideline crews and cripple the ability to respond to a fire.
“We’re outside, so it definitely helps with mitigation and makes it simpler to social distance,” Mr. Paul said. “But I think if there’s a mistake made, it could happen.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
HM20 Virtual product theaters: Aug. 25-27
Aug. 25, 2020. 12:00 p.m. – 1:00 p.m. ET
Medical Product Theater: Worsening Symptoms and Hospitalization for Heart Failure: Increased Risk of Poor Outcomes and Opportunities to Enhance Care
Objectives
- Discuss hospitalization as a pivotal point in the clinical trajectory of heart failure.
- Highlight strategies for improvement and optimization of the treatment plan for patients with heart failure.
- Provide practical guidance for identifying predictors of worsening heart failure and educating on the importance of patients’ self-management.
Speaker
William T. Abraham, MD, FACP, FACC, FAHA, FESC, FRCPE
Professor of Medicine, Physiology, and Cell Biology
College of Medicine Distinguished Professor
Division of Cardiovascular Medicine
The Ohio State University,
Columbus, Ohio
Sponsored by Novartis Pharmaceuticals, and the faculty will be compensated for time.
Aug. 26, 2020. 12:00 p.m. – 1:00 p.m. ET
Commercial Product Theater: A First Choice Treatment for the Inpatient Management of Stabilized Systolic HF Patients: An Evidence-Based Approach
Description
Patients hospitalized due to heart failure with reduced ejection fraction (HFrEF) are at considerable risk of readmission and mortality. This program will review the benefits and risks of starting therapy in the hospital to help prevent rehospitalization and reduce patient mortality.
Speaker
Hameed Ali, DO, SFHM
Clinical Assistant Professor of Medicine
Baylor Scott and White Health
Dallas, Texas
Sponsored by Novartis Pharmaceuticals, and the faculty will be compensated for time.
Aug. 27, 2020. 12:00 p.m. – 1:00 p.m. ET
Commercial Product Theater: Selecting A First-Choice Therapy for Systolic HF: Meeting the Burden of Proof
Description
What is the burden of proof that needs to be met before a therapy can be selected for the treatment of systolic heart failure? Hear from Dr. Javed Butler, chairman of the Department of Medicine at the University of Mississippi Medical Center, to learn more about selecting a first-choice therapy for your patients with systolic heart failure.
In this program, Dr. Butler will discuss how aligning your therapy selection to pathophysiologic pathways for HFrEF, it is possible to reduce mortality and morbidity while providing a proven safety and tolerability profile.
Regardless of your patients’ previous heart failure treatment history, following this program, you can feel confident selecting your first-choice therapy for your patients with HFrEF.
Speaker
Javed Butler, MD, MPH, MBA
Chairman, Department of Medicine
University of Mississippi Medical Center,
Jackson, Mississippi
Sponsored by Novartis Pharmaceuticals, and the faculty will be compensated for time.
Aug. 25, 2020. 12:00 p.m. – 1:00 p.m. ET
Medical Product Theater: Worsening Symptoms and Hospitalization for Heart Failure: Increased Risk of Poor Outcomes and Opportunities to Enhance Care
Objectives
- Discuss hospitalization as a pivotal point in the clinical trajectory of heart failure.
- Highlight strategies for improvement and optimization of the treatment plan for patients with heart failure.
- Provide practical guidance for identifying predictors of worsening heart failure and educating on the importance of patients’ self-management.
Speaker
William T. Abraham, MD, FACP, FACC, FAHA, FESC, FRCPE
Professor of Medicine, Physiology, and Cell Biology
College of Medicine Distinguished Professor
Division of Cardiovascular Medicine
The Ohio State University,
Columbus, Ohio
Sponsored by Novartis Pharmaceuticals, and the faculty will be compensated for time.
Aug. 26, 2020. 12:00 p.m. – 1:00 p.m. ET
Commercial Product Theater: A First Choice Treatment for the Inpatient Management of Stabilized Systolic HF Patients: An Evidence-Based Approach
Description
Patients hospitalized due to heart failure with reduced ejection fraction (HFrEF) are at considerable risk of readmission and mortality. This program will review the benefits and risks of starting therapy in the hospital to help prevent rehospitalization and reduce patient mortality.
Speaker
Hameed Ali, DO, SFHM
Clinical Assistant Professor of Medicine
Baylor Scott and White Health
Dallas, Texas
Sponsored by Novartis Pharmaceuticals, and the faculty will be compensated for time.
Aug. 27, 2020. 12:00 p.m. – 1:00 p.m. ET
Commercial Product Theater: Selecting A First-Choice Therapy for Systolic HF: Meeting the Burden of Proof
Description
What is the burden of proof that needs to be met before a therapy can be selected for the treatment of systolic heart failure? Hear from Dr. Javed Butler, chairman of the Department of Medicine at the University of Mississippi Medical Center, to learn more about selecting a first-choice therapy for your patients with systolic heart failure.
In this program, Dr. Butler will discuss how aligning your therapy selection to pathophysiologic pathways for HFrEF, it is possible to reduce mortality and morbidity while providing a proven safety and tolerability profile.
Regardless of your patients’ previous heart failure treatment history, following this program, you can feel confident selecting your first-choice therapy for your patients with HFrEF.
Speaker
Javed Butler, MD, MPH, MBA
Chairman, Department of Medicine
University of Mississippi Medical Center,
Jackson, Mississippi
Sponsored by Novartis Pharmaceuticals, and the faculty will be compensated for time.
Aug. 25, 2020. 12:00 p.m. – 1:00 p.m. ET
Medical Product Theater: Worsening Symptoms and Hospitalization for Heart Failure: Increased Risk of Poor Outcomes and Opportunities to Enhance Care
Objectives
- Discuss hospitalization as a pivotal point in the clinical trajectory of heart failure.
- Highlight strategies for improvement and optimization of the treatment plan for patients with heart failure.
- Provide practical guidance for identifying predictors of worsening heart failure and educating on the importance of patients’ self-management.
Speaker
William T. Abraham, MD, FACP, FACC, FAHA, FESC, FRCPE
Professor of Medicine, Physiology, and Cell Biology
College of Medicine Distinguished Professor
Division of Cardiovascular Medicine
The Ohio State University,
Columbus, Ohio
Sponsored by Novartis Pharmaceuticals, and the faculty will be compensated for time.
Aug. 26, 2020. 12:00 p.m. – 1:00 p.m. ET
Commercial Product Theater: A First Choice Treatment for the Inpatient Management of Stabilized Systolic HF Patients: An Evidence-Based Approach
Description
Patients hospitalized due to heart failure with reduced ejection fraction (HFrEF) are at considerable risk of readmission and mortality. This program will review the benefits and risks of starting therapy in the hospital to help prevent rehospitalization and reduce patient mortality.
Speaker
Hameed Ali, DO, SFHM
Clinical Assistant Professor of Medicine
Baylor Scott and White Health
Dallas, Texas
Sponsored by Novartis Pharmaceuticals, and the faculty will be compensated for time.
Aug. 27, 2020. 12:00 p.m. – 1:00 p.m. ET
Commercial Product Theater: Selecting A First-Choice Therapy for Systolic HF: Meeting the Burden of Proof
Description
What is the burden of proof that needs to be met before a therapy can be selected for the treatment of systolic heart failure? Hear from Dr. Javed Butler, chairman of the Department of Medicine at the University of Mississippi Medical Center, to learn more about selecting a first-choice therapy for your patients with systolic heart failure.
In this program, Dr. Butler will discuss how aligning your therapy selection to pathophysiologic pathways for HFrEF, it is possible to reduce mortality and morbidity while providing a proven safety and tolerability profile.
Regardless of your patients’ previous heart failure treatment history, following this program, you can feel confident selecting your first-choice therapy for your patients with HFrEF.
Speaker
Javed Butler, MD, MPH, MBA
Chairman, Department of Medicine
University of Mississippi Medical Center,
Jackson, Mississippi
Sponsored by Novartis Pharmaceuticals, and the faculty will be compensated for time.
Welcome to the final week of HM20 Virtual!
Hospitalists, welcome to the final week of HM20 Virtual – the first virtual annual conference in the history of SHM. We hope you have enjoyed your experience thus far. What is most exciting about HM20 Virtual is how it exemplifies the agility and innovation that is in the hearts and minds of SHM and hospitalists all around the country and beyond. Because 2020 is shaping up to be anything but ordinary, SHM and its members have had to embrace changes on a scale that has surpassed anything we have seen in most of our careers. SHM is committed to keeping pace with the needs of hospitalists, including the use of virtual meetings to keep us all connected, informed, and engaged.
The full course of sessions for HM20 has a vast array of topics, aimed at quickly and concisely updating our members on core topics. These include clinical updates on common conditions, a half-dozen sessions dedicated to COVID-19, the ever-popular Rapid Fire sessions, an Update in Pediatric Top Articles, a High Value Care session, and special sessions on immigrant hospitalist issues and structural racism. Also included is the Best of Research and Innovations and the Annual Update in Hospital Medicine.
In addition, the “Simulive” sessions offer additional Q&A with the experts; our lineup this week includes many important clinical topics, including heart failure, glucose management, GI emergencies, drug allergies, endocrine emergencies, and balancing being a hospitalist and a parent. (Particularly challenging with COVID-19!) Of note, if you are unable to join any of these sessions live, all 3 weeks of the Simulive sessions will be available on demand after Aug. 31.
We are hopeful this new virtual format will exceed expectations for our members. Our dedicated HM20 faculty and SHM staff have worked tirelessly to make HM20 Virtual a success, and for that, we owe them our gratitude and appreciation. Since this is our “first rodeo,” we are very eager for your feedback on all aspects of this new format. The more we learn now, the better off we will all be with future offerings, so please be candid and honest. With so much change and uncertainty, we hope you continue to find SHM to be a place of consistency and stability, and the “source of truth” for all things hospital medicine.
Dr. Scheurer is chief quality officer and professor of medicine at the Medical University of South Carolina, Charleston. She is president of SHM.
Hospitalists, welcome to the final week of HM20 Virtual – the first virtual annual conference in the history of SHM. We hope you have enjoyed your experience thus far. What is most exciting about HM20 Virtual is how it exemplifies the agility and innovation that is in the hearts and minds of SHM and hospitalists all around the country and beyond. Because 2020 is shaping up to be anything but ordinary, SHM and its members have had to embrace changes on a scale that has surpassed anything we have seen in most of our careers. SHM is committed to keeping pace with the needs of hospitalists, including the use of virtual meetings to keep us all connected, informed, and engaged.
The full course of sessions for HM20 has a vast array of topics, aimed at quickly and concisely updating our members on core topics. These include clinical updates on common conditions, a half-dozen sessions dedicated to COVID-19, the ever-popular Rapid Fire sessions, an Update in Pediatric Top Articles, a High Value Care session, and special sessions on immigrant hospitalist issues and structural racism. Also included is the Best of Research and Innovations and the Annual Update in Hospital Medicine.
In addition, the “Simulive” sessions offer additional Q&A with the experts; our lineup this week includes many important clinical topics, including heart failure, glucose management, GI emergencies, drug allergies, endocrine emergencies, and balancing being a hospitalist and a parent. (Particularly challenging with COVID-19!) Of note, if you are unable to join any of these sessions live, all 3 weeks of the Simulive sessions will be available on demand after Aug. 31.
We are hopeful this new virtual format will exceed expectations for our members. Our dedicated HM20 faculty and SHM staff have worked tirelessly to make HM20 Virtual a success, and for that, we owe them our gratitude and appreciation. Since this is our “first rodeo,” we are very eager for your feedback on all aspects of this new format. The more we learn now, the better off we will all be with future offerings, so please be candid and honest. With so much change and uncertainty, we hope you continue to find SHM to be a place of consistency and stability, and the “source of truth” for all things hospital medicine.
Dr. Scheurer is chief quality officer and professor of medicine at the Medical University of South Carolina, Charleston. She is president of SHM.
Hospitalists, welcome to the final week of HM20 Virtual – the first virtual annual conference in the history of SHM. We hope you have enjoyed your experience thus far. What is most exciting about HM20 Virtual is how it exemplifies the agility and innovation that is in the hearts and minds of SHM and hospitalists all around the country and beyond. Because 2020 is shaping up to be anything but ordinary, SHM and its members have had to embrace changes on a scale that has surpassed anything we have seen in most of our careers. SHM is committed to keeping pace with the needs of hospitalists, including the use of virtual meetings to keep us all connected, informed, and engaged.
The full course of sessions for HM20 has a vast array of topics, aimed at quickly and concisely updating our members on core topics. These include clinical updates on common conditions, a half-dozen sessions dedicated to COVID-19, the ever-popular Rapid Fire sessions, an Update in Pediatric Top Articles, a High Value Care session, and special sessions on immigrant hospitalist issues and structural racism. Also included is the Best of Research and Innovations and the Annual Update in Hospital Medicine.
In addition, the “Simulive” sessions offer additional Q&A with the experts; our lineup this week includes many important clinical topics, including heart failure, glucose management, GI emergencies, drug allergies, endocrine emergencies, and balancing being a hospitalist and a parent. (Particularly challenging with COVID-19!) Of note, if you are unable to join any of these sessions live, all 3 weeks of the Simulive sessions will be available on demand after Aug. 31.
We are hopeful this new virtual format will exceed expectations for our members. Our dedicated HM20 faculty and SHM staff have worked tirelessly to make HM20 Virtual a success, and for that, we owe them our gratitude and appreciation. Since this is our “first rodeo,” we are very eager for your feedback on all aspects of this new format. The more we learn now, the better off we will all be with future offerings, so please be candid and honest. With so much change and uncertainty, we hope you continue to find SHM to be a place of consistency and stability, and the “source of truth” for all things hospital medicine.
Dr. Scheurer is chief quality officer and professor of medicine at the Medical University of South Carolina, Charleston. She is president of SHM.
Hospitalists confront administrative, financial challenges of COVID-19 crisis
Hospitalists nationwide have put in longer hours, played new clinical roles, and stretched beyond their medical specialty and comfort level to meet their hospital’s COVID-19 care demands. Can they expect some kind of financial recognition – perhaps in the form of “hazard pay” for going above and beyond – even though their institutions are experiencing negative financial fallout from the crisis?
Hospitals in regions experiencing a COVID-19 surge have limited elective procedures, discouraged non–COVID-19 admissions, and essentially entered crisis management mode. Other facilities in less hard-hit communities are also standing by, with reduced hospital census, smaller caseloads and less work to do, while trying to prepare their bottom lines for lower demand.
“This crisis has put most hospitals in financial jeopardy and that is likely to trickle down to all employees – including hospitalists,” said Ron Greeno, MD, FCCP, MHM, a past president of SHM and the society’s current senior advisor for government affairs. “But it’s not like hospitals could or would forgo an effective hospitalist program today. Hospitalists will be important players in defining the hospital’s future direction post crisis.”
That doesn’t mean tighter financials, caps on annual salary increases, or higher productivity expectations won’t be part of future conversations between hospital administrators and their hospitalists, Dr. Greeno said. Administrators are starting to look ahead to the post–COVID-19 era even as numbers of cases and rates of growth continue to rise in various regions, and Dr. Greeno sees a lot of uncertainty ahead.
Even prior to the crisis, he noted, hospital margins had been falling, while the cost of labor, including hospitalist labor, was going up. That was pointing toward an inevitable collision, which has only intensified with the new financial crisis facing hospitals – created by SARS-CoV-2 and by policies such as shutting down elective surgeries in anticipation of a COVID-19 patient surge that, for some institutions, may never come.
Brian Harte, MD, MHM, president of Cleveland Clinic Akron General and a past president of SHM, said that the Cleveland Clinic system has been planning since January its response to the coming crisis. “Governor Mike DeWine and the state Department of Health led the way in flattening the curve in Ohio. We engaged our hospitalists in brainstorming solutions. They have been excellent partners,” he said.
Approaching the crisis with a sense of urgency from the outset, the Cleveland Clinic built a COVID-19 surge team and incident command structure, with nursing, infectious diseases, critical care and hospital medicine represented. “We used that time to get ready for what was coming. We worked on streamlining consultant work flows.”
But utilization numbers are off in almost every service line, Dr. Harte said. “It has forced us to look at things we’ve always talked about, including greater use of telemedicine and exploring other ways of caring for patients, such as increased use of evening hours.”
Cleveland Clinic contracts with Sound Physicians of Tacoma, Wash., for its hospitalist coverage. “We have an excellent working relationship with Sound at the local, regional, and national levels, with common goals for quality and utilization. We tried to involve our hospitalists as early as possible in planning. We needed them to step in and role model and lead the way,” Dr. Harte said, for everybody’s anxiety levels.
“We’re still in the process of understanding the long-term financial impact of the epidemic,” Dr. Harte added. “But at this point I see no reason to think our relationship with our hospitalists needs to change. We’re the stewards of long-term finances. We’ll need to keep a close eye on this. But we’re committed to working through this together.”
Hazard pay for frontline health care workers was included in the COVID-19 relief package assembled in mid-May by Democrats in the House of Representatives. The $3 trillion HEROES Act includes $200 billion to award hazard pay to essential workers, including those in the health field, but Senate Majority Leader Mitch McConnell (R-Ky.) declared the legislation “dead on arrival” in the Senate.
Supplementary hazard payments made by hospitals to their hospitalists as a reward for sacrifices they made in the crisis is an interesting question, Dr. Greeno noted, and it’s definitely on the table at some hospitals. “But I think it is going to be a tough ask in these times.”
Dr. Harte said he has not offered nor been asked about hazard pay for hospitalists. Cleveland Clinic Akron General made a strategic decision that hazard pay was not going to be part of its response to the pandemic. Other hospital administrators interviewed for this article concur.
Hospitals respond to the fiscal crisis
Hospitals in other parts of the country also report significant fiscal fallout from the COVID-19 crisis, with predictions that 100 or more hospitals may be forced to close. Jeff Dye, president of the New Mexico Hospital Association, told the Albuquerque Journal on May 1 that hospitals in his state have been squeezed on all sides by increased costs, patients delaying routine care, and public health orders restricting elective surgeries. New Mexico hospitals, especially in rural areas, face incredible financial strain.
The University of Virginia Medical Center, Charlottesville, recently announced 20% reductions in total compensation for its providers through July 31, along with suspension of retirement contributions. Those changes won’t affect team members caring for COVID-19 patients. And the Spectrum Health Medical Group of 15 hospitals in western Michigan, according to Michigan Public Radio, told its doctors they either needed to sign “contract addendums” giving the system more control over their hours – or face a 25% pay cut, or worse.
Cheyenne (Wyo.) Regional Medical Center issued a statement April 24 that it expected losses of $10 million for the month of April. “CRMC, like every other hospital in Wyoming, is certainly feeling the financial impact that COVID-19 is having,” CEO Tim Thornell told the Cowboy State Daily on April 24. That includes a 30% reduction in inpatient care and 50% reduction in outpatient care, while the hospital has only had a handful of COVID-19 patients at any time. Capital projects are now on hold, overtime is limited, and a hiring freeze is in effect.
“We’re certainly prepared for a larger surge, which hasn’t come yet,” Mr. Thornell said in an interview. CRMC’s ICU was split to create a nine-bed dedicated COVID-19 unit. Intensivists see most of the critical care patients, while the hospital’s 15 directly-employed hospitalists are treating all of the non-ICU COVID-19 patients. “Among themselves, the hospitalists volunteered who would work on the unit. We’ve been fortunate enough to have enough volunteers and enough PPE [personal protective equipment],” he said.
Preparing for the COVID-19 pandemic has strengthened the medical center’s relationship with its hospitalists, Mr. Thornell explained. “Hospitalists are key to our operations, involved in so much that happens here. We’re trying to staff to volume with decreased utilization. We’ve scaled back, which only makes fiscal sense. Now, how do we reinfuse patients back into the mix? Our hospitalists are paid by the number of shifts, and as you distribute shift reductions over 15 providers, it shouldn’t be an intolerable burden.” But two open hospitalist positions have not been filled, he noted.
CRMC is trying to approach these changes with a Lean perspective, Mr. Thornell said. “We had already adopted a Lean program, but this has been a chance to go through a life-altering circumstance using the tools of Lean planning and applying them instantaneously.”
Providers step up
At Emory Healthcare in Atlanta, a major center for COVID-19 cases, communication has been essential in the crisis, said Bryce Gartland, MD, SFHM, Emory’s hospital group president and cochief of clinical operations. “Our group was prepared for a significant influx of patients. Like every other institution, we made the decision to postpone elective care, with a resulting plummet in volume,” he said.
As COVID-19 patients entered the Emory system, frontline hospitalists stepped up to care for those patients. “We’ve had ample providers in terms of clinical care. We guaranteed our physicians’ base compensation. They have flexed teams up and down as needed.” Advanced practice professionals also stepped up to bridge gaps.
With regard to the return of volumes of non–COVID-19 patients, the jury’s still out, Dr. Gartland said. “None of us has a crystal ball, and there are tremendous variables and decision points that will have significant impact. We have started to see numbers of time-sensitive and essential cases increase as of the first week of May.”
What lies ahead will likely include some rightsizing to future volumes. On top of that, the broader economic pressures on hospitals from high rates of unemployment, uninsured patients, bad debt, and charity care will push health care systems to significantly address costs and infrastructure, he said. “We’re still early in planning, and striving to maintain flexibility and nimbleness, given the uncertainties to this early understanding of our new normal. No hospital is immune from the financial impact. We’ll see and hear about more of these conversations in the months ahead.”
But the experience has also generated some positives, Dr. Gartland noted. “Things like telehealth, which we’ve been talking about for years but previously faced barriers to widespread adoption.” Now with COVID-19, the federal government issued waivers, and barriers – both internal and external – came down. “With telehealth, what will the role and deployment of hospitalists look like in this new model? How will traditional productivity expectations change, or the numbers and types of providers? This will make the relationship and partnership between hospitalist groups and hospital administrators ever more important as we consider the evolution toward new care models.”
Dr. Gartland said that “one of the great things about hospital medicine as a field is its flexibility and adaptability. Where there have been gaps, hospitalists were quick to step in. As long as hospital medicine continues to embrace those kinds of behaviors, it will be successful.” But if the conversation with hospitals is just about money, it will be harder, he acknowledged. “Where there is this kind of disruption in our usual way of doing things, there are also tremendous opportunities for care model innovation. I would encourage hospitalist groups to try to be true value partners.”
Command center mode
Like other physicians in hospital C-suites, Chad Whelan MD, FACP, SFHM, chief executive officer of Banner–University Medicine in Tucson, Ariz., led his two hospitals into command center mode when the crisis hit, planning for a surge of COVID-19 cases that could overwhelm hospital capacity.
“In terms of our hospitalists, we leaned in to them hard in the beginning, preparing them to supervise other physicians who came in to help if needed,” he said. “Our [non–COVID-19] census is down, revenues are down, and the implications are enormous – like nothing we’ve ever seen before.”
“We’re fortunate that we’re part of the Banner health system. We made a decision that we would essentially keep our physicians financially protected through this crisis,” Dr. Whelan said. “In return, we called on them to step up and be on the front lines and to put in enormous hours for planning. We asked them to consider: How could you contribute if the surge comes?”
He affirmed that hospital medicine has been a major part of his medical center’s planning and implementation. “I’ve been overwhelmed by the degree to which the entire delivery team has rallied around the pandemic, with everybody saying they want to keep people safe and be part of the solution. We have always had hospitalist leaders at the table as we’ve planned our response and as decisions were made,” said Dr. Whelan, a practicing hospitalist and teaching service attending since 2000 until he assumed his current executive position in Arizona 18 months ago.
“While we have kept people whole during the immediate crisis, we have acknowledged that we don’t know what our recovery will look like. What if [non–COVID-19] volume doesn’t return? That keeps me awake at night,” he said. “I have talked to our physician leadership in hospital medicine and more broadly. We need to ask ourselves many questions, including: do we have the right levels of staffing? Is this the time to consider alternate models of staffing, for example, advanced practice providers? And does the compensation plan need adjustments?”
Dr. Whelan thinks that the COVID-19 crisis is an opportunity for hospital medicine to more rapidly explore different models and to ask what additional value hospitalists can bring to the care model. “For example, what would it mean to redefine the hospitalist’s scope of practice as an acute medicine specialist, not defined by the hospital’s four walls?” he noted.
“One of the reasons our smaller hospital reached capacity with COVID-19 patients was the skilled nursing facility located a few hundred feet away that turned into a hot spot. If we had imported the hospital medicine model virtually into that SNF early on, could there have been a different scenario? Have we thought through what that would have even looked like?” Dr. Whelan asked.
He challenges the hospital medicine field, once it gets to the other side of this crisis, to not fall back on old way of doing things. “Instead, let’s use this time to create a better model today,” he said. “That’s what we’re trying to do at a system level at Banner, with our hospital medicine groups partnering with the hospital. I want to see our hospitalists create and thrive in that new model.”
Hospitalists nationwide have put in longer hours, played new clinical roles, and stretched beyond their medical specialty and comfort level to meet their hospital’s COVID-19 care demands. Can they expect some kind of financial recognition – perhaps in the form of “hazard pay” for going above and beyond – even though their institutions are experiencing negative financial fallout from the crisis?
Hospitals in regions experiencing a COVID-19 surge have limited elective procedures, discouraged non–COVID-19 admissions, and essentially entered crisis management mode. Other facilities in less hard-hit communities are also standing by, with reduced hospital census, smaller caseloads and less work to do, while trying to prepare their bottom lines for lower demand.
“This crisis has put most hospitals in financial jeopardy and that is likely to trickle down to all employees – including hospitalists,” said Ron Greeno, MD, FCCP, MHM, a past president of SHM and the society’s current senior advisor for government affairs. “But it’s not like hospitals could or would forgo an effective hospitalist program today. Hospitalists will be important players in defining the hospital’s future direction post crisis.”
That doesn’t mean tighter financials, caps on annual salary increases, or higher productivity expectations won’t be part of future conversations between hospital administrators and their hospitalists, Dr. Greeno said. Administrators are starting to look ahead to the post–COVID-19 era even as numbers of cases and rates of growth continue to rise in various regions, and Dr. Greeno sees a lot of uncertainty ahead.
Even prior to the crisis, he noted, hospital margins had been falling, while the cost of labor, including hospitalist labor, was going up. That was pointing toward an inevitable collision, which has only intensified with the new financial crisis facing hospitals – created by SARS-CoV-2 and by policies such as shutting down elective surgeries in anticipation of a COVID-19 patient surge that, for some institutions, may never come.
Brian Harte, MD, MHM, president of Cleveland Clinic Akron General and a past president of SHM, said that the Cleveland Clinic system has been planning since January its response to the coming crisis. “Governor Mike DeWine and the state Department of Health led the way in flattening the curve in Ohio. We engaged our hospitalists in brainstorming solutions. They have been excellent partners,” he said.
Approaching the crisis with a sense of urgency from the outset, the Cleveland Clinic built a COVID-19 surge team and incident command structure, with nursing, infectious diseases, critical care and hospital medicine represented. “We used that time to get ready for what was coming. We worked on streamlining consultant work flows.”
But utilization numbers are off in almost every service line, Dr. Harte said. “It has forced us to look at things we’ve always talked about, including greater use of telemedicine and exploring other ways of caring for patients, such as increased use of evening hours.”
Cleveland Clinic contracts with Sound Physicians of Tacoma, Wash., for its hospitalist coverage. “We have an excellent working relationship with Sound at the local, regional, and national levels, with common goals for quality and utilization. We tried to involve our hospitalists as early as possible in planning. We needed them to step in and role model and lead the way,” Dr. Harte said, for everybody’s anxiety levels.
“We’re still in the process of understanding the long-term financial impact of the epidemic,” Dr. Harte added. “But at this point I see no reason to think our relationship with our hospitalists needs to change. We’re the stewards of long-term finances. We’ll need to keep a close eye on this. But we’re committed to working through this together.”
Hazard pay for frontline health care workers was included in the COVID-19 relief package assembled in mid-May by Democrats in the House of Representatives. The $3 trillion HEROES Act includes $200 billion to award hazard pay to essential workers, including those in the health field, but Senate Majority Leader Mitch McConnell (R-Ky.) declared the legislation “dead on arrival” in the Senate.
Supplementary hazard payments made by hospitals to their hospitalists as a reward for sacrifices they made in the crisis is an interesting question, Dr. Greeno noted, and it’s definitely on the table at some hospitals. “But I think it is going to be a tough ask in these times.”
Dr. Harte said he has not offered nor been asked about hazard pay for hospitalists. Cleveland Clinic Akron General made a strategic decision that hazard pay was not going to be part of its response to the pandemic. Other hospital administrators interviewed for this article concur.
Hospitals respond to the fiscal crisis
Hospitals in other parts of the country also report significant fiscal fallout from the COVID-19 crisis, with predictions that 100 or more hospitals may be forced to close. Jeff Dye, president of the New Mexico Hospital Association, told the Albuquerque Journal on May 1 that hospitals in his state have been squeezed on all sides by increased costs, patients delaying routine care, and public health orders restricting elective surgeries. New Mexico hospitals, especially in rural areas, face incredible financial strain.
The University of Virginia Medical Center, Charlottesville, recently announced 20% reductions in total compensation for its providers through July 31, along with suspension of retirement contributions. Those changes won’t affect team members caring for COVID-19 patients. And the Spectrum Health Medical Group of 15 hospitals in western Michigan, according to Michigan Public Radio, told its doctors they either needed to sign “contract addendums” giving the system more control over their hours – or face a 25% pay cut, or worse.
Cheyenne (Wyo.) Regional Medical Center issued a statement April 24 that it expected losses of $10 million for the month of April. “CRMC, like every other hospital in Wyoming, is certainly feeling the financial impact that COVID-19 is having,” CEO Tim Thornell told the Cowboy State Daily on April 24. That includes a 30% reduction in inpatient care and 50% reduction in outpatient care, while the hospital has only had a handful of COVID-19 patients at any time. Capital projects are now on hold, overtime is limited, and a hiring freeze is in effect.
“We’re certainly prepared for a larger surge, which hasn’t come yet,” Mr. Thornell said in an interview. CRMC’s ICU was split to create a nine-bed dedicated COVID-19 unit. Intensivists see most of the critical care patients, while the hospital’s 15 directly-employed hospitalists are treating all of the non-ICU COVID-19 patients. “Among themselves, the hospitalists volunteered who would work on the unit. We’ve been fortunate enough to have enough volunteers and enough PPE [personal protective equipment],” he said.
Preparing for the COVID-19 pandemic has strengthened the medical center’s relationship with its hospitalists, Mr. Thornell explained. “Hospitalists are key to our operations, involved in so much that happens here. We’re trying to staff to volume with decreased utilization. We’ve scaled back, which only makes fiscal sense. Now, how do we reinfuse patients back into the mix? Our hospitalists are paid by the number of shifts, and as you distribute shift reductions over 15 providers, it shouldn’t be an intolerable burden.” But two open hospitalist positions have not been filled, he noted.
CRMC is trying to approach these changes with a Lean perspective, Mr. Thornell said. “We had already adopted a Lean program, but this has been a chance to go through a life-altering circumstance using the tools of Lean planning and applying them instantaneously.”
Providers step up
At Emory Healthcare in Atlanta, a major center for COVID-19 cases, communication has been essential in the crisis, said Bryce Gartland, MD, SFHM, Emory’s hospital group president and cochief of clinical operations. “Our group was prepared for a significant influx of patients. Like every other institution, we made the decision to postpone elective care, with a resulting plummet in volume,” he said.
As COVID-19 patients entered the Emory system, frontline hospitalists stepped up to care for those patients. “We’ve had ample providers in terms of clinical care. We guaranteed our physicians’ base compensation. They have flexed teams up and down as needed.” Advanced practice professionals also stepped up to bridge gaps.
With regard to the return of volumes of non–COVID-19 patients, the jury’s still out, Dr. Gartland said. “None of us has a crystal ball, and there are tremendous variables and decision points that will have significant impact. We have started to see numbers of time-sensitive and essential cases increase as of the first week of May.”
What lies ahead will likely include some rightsizing to future volumes. On top of that, the broader economic pressures on hospitals from high rates of unemployment, uninsured patients, bad debt, and charity care will push health care systems to significantly address costs and infrastructure, he said. “We’re still early in planning, and striving to maintain flexibility and nimbleness, given the uncertainties to this early understanding of our new normal. No hospital is immune from the financial impact. We’ll see and hear about more of these conversations in the months ahead.”
But the experience has also generated some positives, Dr. Gartland noted. “Things like telehealth, which we’ve been talking about for years but previously faced barriers to widespread adoption.” Now with COVID-19, the federal government issued waivers, and barriers – both internal and external – came down. “With telehealth, what will the role and deployment of hospitalists look like in this new model? How will traditional productivity expectations change, or the numbers and types of providers? This will make the relationship and partnership between hospitalist groups and hospital administrators ever more important as we consider the evolution toward new care models.”
Dr. Gartland said that “one of the great things about hospital medicine as a field is its flexibility and adaptability. Where there have been gaps, hospitalists were quick to step in. As long as hospital medicine continues to embrace those kinds of behaviors, it will be successful.” But if the conversation with hospitals is just about money, it will be harder, he acknowledged. “Where there is this kind of disruption in our usual way of doing things, there are also tremendous opportunities for care model innovation. I would encourage hospitalist groups to try to be true value partners.”
Command center mode
Like other physicians in hospital C-suites, Chad Whelan MD, FACP, SFHM, chief executive officer of Banner–University Medicine in Tucson, Ariz., led his two hospitals into command center mode when the crisis hit, planning for a surge of COVID-19 cases that could overwhelm hospital capacity.
“In terms of our hospitalists, we leaned in to them hard in the beginning, preparing them to supervise other physicians who came in to help if needed,” he said. “Our [non–COVID-19] census is down, revenues are down, and the implications are enormous – like nothing we’ve ever seen before.”
“We’re fortunate that we’re part of the Banner health system. We made a decision that we would essentially keep our physicians financially protected through this crisis,” Dr. Whelan said. “In return, we called on them to step up and be on the front lines and to put in enormous hours for planning. We asked them to consider: How could you contribute if the surge comes?”
He affirmed that hospital medicine has been a major part of his medical center’s planning and implementation. “I’ve been overwhelmed by the degree to which the entire delivery team has rallied around the pandemic, with everybody saying they want to keep people safe and be part of the solution. We have always had hospitalist leaders at the table as we’ve planned our response and as decisions were made,” said Dr. Whelan, a practicing hospitalist and teaching service attending since 2000 until he assumed his current executive position in Arizona 18 months ago.
“While we have kept people whole during the immediate crisis, we have acknowledged that we don’t know what our recovery will look like. What if [non–COVID-19] volume doesn’t return? That keeps me awake at night,” he said. “I have talked to our physician leadership in hospital medicine and more broadly. We need to ask ourselves many questions, including: do we have the right levels of staffing? Is this the time to consider alternate models of staffing, for example, advanced practice providers? And does the compensation plan need adjustments?”
Dr. Whelan thinks that the COVID-19 crisis is an opportunity for hospital medicine to more rapidly explore different models and to ask what additional value hospitalists can bring to the care model. “For example, what would it mean to redefine the hospitalist’s scope of practice as an acute medicine specialist, not defined by the hospital’s four walls?” he noted.
“One of the reasons our smaller hospital reached capacity with COVID-19 patients was the skilled nursing facility located a few hundred feet away that turned into a hot spot. If we had imported the hospital medicine model virtually into that SNF early on, could there have been a different scenario? Have we thought through what that would have even looked like?” Dr. Whelan asked.
He challenges the hospital medicine field, once it gets to the other side of this crisis, to not fall back on old way of doing things. “Instead, let’s use this time to create a better model today,” he said. “That’s what we’re trying to do at a system level at Banner, with our hospital medicine groups partnering with the hospital. I want to see our hospitalists create and thrive in that new model.”
Hospitalists nationwide have put in longer hours, played new clinical roles, and stretched beyond their medical specialty and comfort level to meet their hospital’s COVID-19 care demands. Can they expect some kind of financial recognition – perhaps in the form of “hazard pay” for going above and beyond – even though their institutions are experiencing negative financial fallout from the crisis?
Hospitals in regions experiencing a COVID-19 surge have limited elective procedures, discouraged non–COVID-19 admissions, and essentially entered crisis management mode. Other facilities in less hard-hit communities are also standing by, with reduced hospital census, smaller caseloads and less work to do, while trying to prepare their bottom lines for lower demand.
“This crisis has put most hospitals in financial jeopardy and that is likely to trickle down to all employees – including hospitalists,” said Ron Greeno, MD, FCCP, MHM, a past president of SHM and the society’s current senior advisor for government affairs. “But it’s not like hospitals could or would forgo an effective hospitalist program today. Hospitalists will be important players in defining the hospital’s future direction post crisis.”
That doesn’t mean tighter financials, caps on annual salary increases, or higher productivity expectations won’t be part of future conversations between hospital administrators and their hospitalists, Dr. Greeno said. Administrators are starting to look ahead to the post–COVID-19 era even as numbers of cases and rates of growth continue to rise in various regions, and Dr. Greeno sees a lot of uncertainty ahead.
Even prior to the crisis, he noted, hospital margins had been falling, while the cost of labor, including hospitalist labor, was going up. That was pointing toward an inevitable collision, which has only intensified with the new financial crisis facing hospitals – created by SARS-CoV-2 and by policies such as shutting down elective surgeries in anticipation of a COVID-19 patient surge that, for some institutions, may never come.
Brian Harte, MD, MHM, president of Cleveland Clinic Akron General and a past president of SHM, said that the Cleveland Clinic system has been planning since January its response to the coming crisis. “Governor Mike DeWine and the state Department of Health led the way in flattening the curve in Ohio. We engaged our hospitalists in brainstorming solutions. They have been excellent partners,” he said.
Approaching the crisis with a sense of urgency from the outset, the Cleveland Clinic built a COVID-19 surge team and incident command structure, with nursing, infectious diseases, critical care and hospital medicine represented. “We used that time to get ready for what was coming. We worked on streamlining consultant work flows.”
But utilization numbers are off in almost every service line, Dr. Harte said. “It has forced us to look at things we’ve always talked about, including greater use of telemedicine and exploring other ways of caring for patients, such as increased use of evening hours.”
Cleveland Clinic contracts with Sound Physicians of Tacoma, Wash., for its hospitalist coverage. “We have an excellent working relationship with Sound at the local, regional, and national levels, with common goals for quality and utilization. We tried to involve our hospitalists as early as possible in planning. We needed them to step in and role model and lead the way,” Dr. Harte said, for everybody’s anxiety levels.
“We’re still in the process of understanding the long-term financial impact of the epidemic,” Dr. Harte added. “But at this point I see no reason to think our relationship with our hospitalists needs to change. We’re the stewards of long-term finances. We’ll need to keep a close eye on this. But we’re committed to working through this together.”
Hazard pay for frontline health care workers was included in the COVID-19 relief package assembled in mid-May by Democrats in the House of Representatives. The $3 trillion HEROES Act includes $200 billion to award hazard pay to essential workers, including those in the health field, but Senate Majority Leader Mitch McConnell (R-Ky.) declared the legislation “dead on arrival” in the Senate.
Supplementary hazard payments made by hospitals to their hospitalists as a reward for sacrifices they made in the crisis is an interesting question, Dr. Greeno noted, and it’s definitely on the table at some hospitals. “But I think it is going to be a tough ask in these times.”
Dr. Harte said he has not offered nor been asked about hazard pay for hospitalists. Cleveland Clinic Akron General made a strategic decision that hazard pay was not going to be part of its response to the pandemic. Other hospital administrators interviewed for this article concur.
Hospitals respond to the fiscal crisis
Hospitals in other parts of the country also report significant fiscal fallout from the COVID-19 crisis, with predictions that 100 or more hospitals may be forced to close. Jeff Dye, president of the New Mexico Hospital Association, told the Albuquerque Journal on May 1 that hospitals in his state have been squeezed on all sides by increased costs, patients delaying routine care, and public health orders restricting elective surgeries. New Mexico hospitals, especially in rural areas, face incredible financial strain.
The University of Virginia Medical Center, Charlottesville, recently announced 20% reductions in total compensation for its providers through July 31, along with suspension of retirement contributions. Those changes won’t affect team members caring for COVID-19 patients. And the Spectrum Health Medical Group of 15 hospitals in western Michigan, according to Michigan Public Radio, told its doctors they either needed to sign “contract addendums” giving the system more control over their hours – or face a 25% pay cut, or worse.
Cheyenne (Wyo.) Regional Medical Center issued a statement April 24 that it expected losses of $10 million for the month of April. “CRMC, like every other hospital in Wyoming, is certainly feeling the financial impact that COVID-19 is having,” CEO Tim Thornell told the Cowboy State Daily on April 24. That includes a 30% reduction in inpatient care and 50% reduction in outpatient care, while the hospital has only had a handful of COVID-19 patients at any time. Capital projects are now on hold, overtime is limited, and a hiring freeze is in effect.
“We’re certainly prepared for a larger surge, which hasn’t come yet,” Mr. Thornell said in an interview. CRMC’s ICU was split to create a nine-bed dedicated COVID-19 unit. Intensivists see most of the critical care patients, while the hospital’s 15 directly-employed hospitalists are treating all of the non-ICU COVID-19 patients. “Among themselves, the hospitalists volunteered who would work on the unit. We’ve been fortunate enough to have enough volunteers and enough PPE [personal protective equipment],” he said.
Preparing for the COVID-19 pandemic has strengthened the medical center’s relationship with its hospitalists, Mr. Thornell explained. “Hospitalists are key to our operations, involved in so much that happens here. We’re trying to staff to volume with decreased utilization. We’ve scaled back, which only makes fiscal sense. Now, how do we reinfuse patients back into the mix? Our hospitalists are paid by the number of shifts, and as you distribute shift reductions over 15 providers, it shouldn’t be an intolerable burden.” But two open hospitalist positions have not been filled, he noted.
CRMC is trying to approach these changes with a Lean perspective, Mr. Thornell said. “We had already adopted a Lean program, but this has been a chance to go through a life-altering circumstance using the tools of Lean planning and applying them instantaneously.”
Providers step up
At Emory Healthcare in Atlanta, a major center for COVID-19 cases, communication has been essential in the crisis, said Bryce Gartland, MD, SFHM, Emory’s hospital group president and cochief of clinical operations. “Our group was prepared for a significant influx of patients. Like every other institution, we made the decision to postpone elective care, with a resulting plummet in volume,” he said.
As COVID-19 patients entered the Emory system, frontline hospitalists stepped up to care for those patients. “We’ve had ample providers in terms of clinical care. We guaranteed our physicians’ base compensation. They have flexed teams up and down as needed.” Advanced practice professionals also stepped up to bridge gaps.
With regard to the return of volumes of non–COVID-19 patients, the jury’s still out, Dr. Gartland said. “None of us has a crystal ball, and there are tremendous variables and decision points that will have significant impact. We have started to see numbers of time-sensitive and essential cases increase as of the first week of May.”
What lies ahead will likely include some rightsizing to future volumes. On top of that, the broader economic pressures on hospitals from high rates of unemployment, uninsured patients, bad debt, and charity care will push health care systems to significantly address costs and infrastructure, he said. “We’re still early in planning, and striving to maintain flexibility and nimbleness, given the uncertainties to this early understanding of our new normal. No hospital is immune from the financial impact. We’ll see and hear about more of these conversations in the months ahead.”
But the experience has also generated some positives, Dr. Gartland noted. “Things like telehealth, which we’ve been talking about for years but previously faced barriers to widespread adoption.” Now with COVID-19, the federal government issued waivers, and barriers – both internal and external – came down. “With telehealth, what will the role and deployment of hospitalists look like in this new model? How will traditional productivity expectations change, or the numbers and types of providers? This will make the relationship and partnership between hospitalist groups and hospital administrators ever more important as we consider the evolution toward new care models.”
Dr. Gartland said that “one of the great things about hospital medicine as a field is its flexibility and adaptability. Where there have been gaps, hospitalists were quick to step in. As long as hospital medicine continues to embrace those kinds of behaviors, it will be successful.” But if the conversation with hospitals is just about money, it will be harder, he acknowledged. “Where there is this kind of disruption in our usual way of doing things, there are also tremendous opportunities for care model innovation. I would encourage hospitalist groups to try to be true value partners.”
Command center mode
Like other physicians in hospital C-suites, Chad Whelan MD, FACP, SFHM, chief executive officer of Banner–University Medicine in Tucson, Ariz., led his two hospitals into command center mode when the crisis hit, planning for a surge of COVID-19 cases that could overwhelm hospital capacity.
“In terms of our hospitalists, we leaned in to them hard in the beginning, preparing them to supervise other physicians who came in to help if needed,” he said. “Our [non–COVID-19] census is down, revenues are down, and the implications are enormous – like nothing we’ve ever seen before.”
“We’re fortunate that we’re part of the Banner health system. We made a decision that we would essentially keep our physicians financially protected through this crisis,” Dr. Whelan said. “In return, we called on them to step up and be on the front lines and to put in enormous hours for planning. We asked them to consider: How could you contribute if the surge comes?”
He affirmed that hospital medicine has been a major part of his medical center’s planning and implementation. “I’ve been overwhelmed by the degree to which the entire delivery team has rallied around the pandemic, with everybody saying they want to keep people safe and be part of the solution. We have always had hospitalist leaders at the table as we’ve planned our response and as decisions were made,” said Dr. Whelan, a practicing hospitalist and teaching service attending since 2000 until he assumed his current executive position in Arizona 18 months ago.
“While we have kept people whole during the immediate crisis, we have acknowledged that we don’t know what our recovery will look like. What if [non–COVID-19] volume doesn’t return? That keeps me awake at night,” he said. “I have talked to our physician leadership in hospital medicine and more broadly. We need to ask ourselves many questions, including: do we have the right levels of staffing? Is this the time to consider alternate models of staffing, for example, advanced practice providers? And does the compensation plan need adjustments?”
Dr. Whelan thinks that the COVID-19 crisis is an opportunity for hospital medicine to more rapidly explore different models and to ask what additional value hospitalists can bring to the care model. “For example, what would it mean to redefine the hospitalist’s scope of practice as an acute medicine specialist, not defined by the hospital’s four walls?” he noted.
“One of the reasons our smaller hospital reached capacity with COVID-19 patients was the skilled nursing facility located a few hundred feet away that turned into a hot spot. If we had imported the hospital medicine model virtually into that SNF early on, could there have been a different scenario? Have we thought through what that would have even looked like?” Dr. Whelan asked.
He challenges the hospital medicine field, once it gets to the other side of this crisis, to not fall back on old way of doing things. “Instead, let’s use this time to create a better model today,” he said. “That’s what we’re trying to do at a system level at Banner, with our hospital medicine groups partnering with the hospital. I want to see our hospitalists create and thrive in that new model.”
Performance status, molecular testing key to metastatic cancer prognosis
according to Sam Brondfield, MD, MA, an inpatient medical oncologist at the University of California, San Francisco.
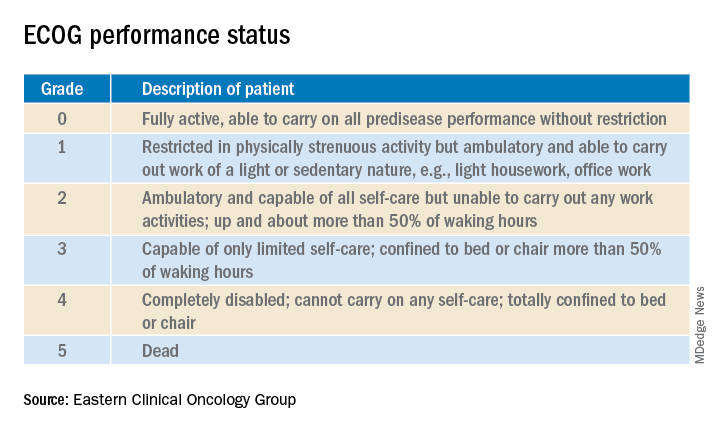
Oncologists have at their fingertips a voluminous and ever-growing body of clinical trials data to draw on for prognostication. Yet many hospitalists will be surprised to learn that this wealth of information is of little value in the inpatient settings where they work, he said at HM20 Virtual, hosted by the Society of Hospital Medicine.
“The applicability of clinical trials data to hospitalized patients is generally poor. That’s an important caveat to keep in mind,” Dr. Brondfield said.
Enrollment in clinical trials is usually restricted to patients with a score of 0 or 1 on the Eastern Clinical Oncology Group Performance Status, meaning their cancer is causing minimal or no disruption to their life (see graphic). Sometimes trials will include patients with a performance status of 2 on the ECOG scale, a tool developed nearly 40 years ago, but clinical trials virtually never enroll those with an ECOG status of 3 or 4. Yet most hospitalized patients with metastatic cancer have an ECOG performance status of 3 or worse. Thus, the clinical trials outcome data are of little relevance.
“In oncology the distinction between ECOG 2 and 3 is very important,” Dr. Brondfield emphasized.
When he talks about treatment options with hospitalized patients who have metastatic cancer and poor performance status – that is, ECOG 3 or 4 – he’ll often say: “Assuming you feel better and can go home, that’s when these clinical trial data may apply better to you.”
Dr. Brondfield cautioned against quoting the National Cancer Institute’s Surveillance, Epidemiology and End Results (SEER) 5-year overall survival data when hospitalized patients with advanced cancer ask how long they have to live. For one thing, the national average 5-year overall survival figure is hardly an individualized assessment. Plus, oncology is a fast-moving field in which important treatment advances occur all the time, and the SEER data lag far behind. For example, when Dr. Brondfield recently looked up the current SEER 5-year survival for patients diagnosed with metastatic non–small cell lung cancer (NSCLC), the figure quoted was less than 6%, and it was drawn from data accrued in 2009-2015. That simply doesn’t reflect contemporary practice.
Indeed, it’s no longer true that the average survival of patients with metastatic NSCLC is less than a year. In the practice-changing KEYNOTE-189 randomized trial, which accrued participants in 2016-2017, the median overall survival of patients randomized to pembrolizumab (Keytruda) plus standard cytotoxic chemotherapy was 22 months, compared with 11 months with chemotherapy plus placebo (J Clin Oncol. 2020 May 10. doi: 10.1200/JCO.19.03136). As a result, immunotherapy with a programmed death–1 inhibitor such as pembrolizumab in combination with chemotherapy is now standard practice in patients with metastatic NSCLC without targetable mutations.
Performance status guides treatment decision-making
Hospitalists can help oncologists in decision-making regarding whether to offer palliative systemic therapy to patients with advanced metastatic cancer and poor performance status by determining whether that status is caused by the cancer itself or some other cause that’s not easily reversible, such as liver failure.
Take, for example, the inpatient with advanced SCLC. This is an aggressive and chemosensitive cancer. Dr. Brondfield said he is among many medical oncologists who are convinced that, if poor performance status in a patient with advanced SCLC is caused by the cancer itself, prompt initiation of inpatient chemotherapy should be recommended to elicit a response that improves quality of life and performance status in the short term. If, on the other hand, the poor performance status is caused by organ failure or some other issue that can’t easily be improved, hospice may be more appropriate.
“The contour of SCLC over time is that despite its treatment responsiveness it inevitably recurs. But with chemotherapy you can give people in this situation months of quality time, so we generally try to treat these sorts of patients,” Dr. Brondfield explained.
The National Comprehensive Cancer Network guidelines upon which oncologists rely leave lots of room for interpretation regarding the appropriateness of inpatient chemotherapy in patients with advanced cancer and poor patient performance status. Citing “knowledge that’s been passed down across oncology generations,” Dr. Brondfield said he and many of his colleagues believe early palliative supportive care rather than systemic cytotoxic cancer-directed therapy is appropriate for patients with poor performance status who have one of several specific relatively nonchemoresponsive types of metastatic cancer. These include esophageal, gastric, and head and neck cancers.
On the other hand, advanced SCLC isn’t the only type of metastatic cancer that’s so chemosensitive that he and many other oncologists believe aggressive chemotherapy should be offered even in the face of poor patient performance status attributable to the cancer itself.
Take, for example, colorectal cancer with no more than five metastases to the lung or liver, provided those metastases are treatable with resection or radiation. “Those patients are actually curable at a high rate. They have about a 30%-40% cure rate. So those patients, even if they have poor performance status, if we can get them up for surgery or radiation, we usually do try to treat them aggressively,” Dr. Brondfield said.
There are other often chemoresponsive metastatic cancers for which oncologists frequently recommend aggressive treatment to improve quality of life in patients with poor performance status. These cancers include aggressive lymphomas, which are actually often curable; multiple myeloma; testicular and germ cell cancers; NSCLC with a targetable mutation, which is often responsive to oral medications; and prostate and well-differentiated thyroid cancers, which can usually be treated with hormone- or iodine-based therapies rather than more toxic intravenous cytotoxic chemotherapy.
The impact of inpatient palliative chemotherapy in patients with poor performance status and advanced solid cancers not on the short list of highly chemosensitive cancers has not been well studied. A recent retrospective study of 228 such patients who received inpatient palliative chemotherapy at a large Brazilian academic medical center provided little reason for enthusiasm regarding the practice. Survival was short, with 30- and 60-day survival rates of 56% and 39%, respectively. Plus, 30% of patients were admitted to the ICU, where they received aggressive and costly end-of-life care. The investigators found these results suggestive of overprescribing of inpatient palliative chemotherapy (BMC Palliat Care. 2019 May 20;18[1]:42. doi: 10.1186/s12904-019-0427-4).
Of note, the investigators found in a multivariate analysis that an elevated bilirubin was associated with a 217% increased risk of 30-day mortality, and hypercalcemia was associated with a 119% increased risk.
“That’s something to take into account when these decisions are being made,” Dr. Brondfield advised.
In response to an audience comment that oncologists often seem overly optimistic about prognosis, Dr. Brondfield observed, “I think it’s very common for there to be a disagreement between the oncologist wanting to be aggressive for a sick inpatient and the hospitalist or generalist provider thinking: ‘This person looks way too sick for chemotherapy.’ ”
For this reason he is a firm believer in having multidisciplinary conversations regarding prognosis in challenging situations involving hospitalized patients with advanced cancer. An oncologist can bring to such discussions a detailed understanding of clinical trial and molecular data as well as information about the patient’s response to the first round of therapy. But lots of other factors are relevant to prognosis, including nutritional status, comorbidities, and the intuitive eyeball test of how a patient might do. The patient’s family, primary care provider, oncologist, the hospitalist, and the palliative care team will have perspectives of their own.
Molecular testing is now the norm in metastatic cancers
These days oncologists order molecular testing for most patients with metastatic carcinomas to determine eligibility for targeted therapy, suitability for participation in clinical trials, prognostication, and/or assistance in determining the site of origin if that’s unclear.
A single-pass fine needle aspiration biopsy doesn’t provide enough tissue for molecular testing. It’s therefore important to order initially a multipass fine needle aspiration to avoid the need for a repeat biopsy, which is uncomfortable for the patient and can delay diagnosis and treatment.
Dr. Brondfield advised waiting for molecular testing results to come in before trying to prognosticate in patients with a metastatic cancer for which targetable mutations might be present. Survival rates can vary substantially depending upon those test results. Take, for example, metastatic NSCLC: Just within the past year, clinical trials have been published reporting overall survival rates of 39 months in patients with treatable mutations in epidermal growth factor receptor, 42 months with anaplastic lymphoma kinase mutations, and 51 months in patients whose tumor signature features mutations in c-ros oncogene 1, as compared with 22 months with no targetable mutations in the KEYNOTE-189 trial.
“There’s a lot of heterogeneity around how metastatic tumors behave and respond to therapy. Not all metastatic cancers are the same,” the oncologist emphasized.
according to Sam Brondfield, MD, MA, an inpatient medical oncologist at the University of California, San Francisco.
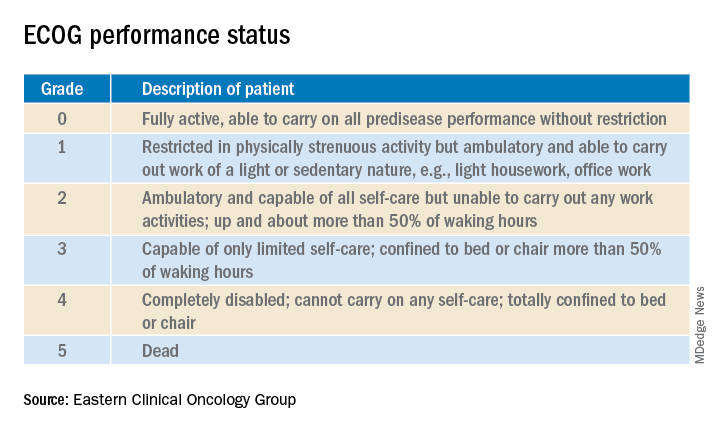
Oncologists have at their fingertips a voluminous and ever-growing body of clinical trials data to draw on for prognostication. Yet many hospitalists will be surprised to learn that this wealth of information is of little value in the inpatient settings where they work, he said at HM20 Virtual, hosted by the Society of Hospital Medicine.
“The applicability of clinical trials data to hospitalized patients is generally poor. That’s an important caveat to keep in mind,” Dr. Brondfield said.
Enrollment in clinical trials is usually restricted to patients with a score of 0 or 1 on the Eastern Clinical Oncology Group Performance Status, meaning their cancer is causing minimal or no disruption to their life (see graphic). Sometimes trials will include patients with a performance status of 2 on the ECOG scale, a tool developed nearly 40 years ago, but clinical trials virtually never enroll those with an ECOG status of 3 or 4. Yet most hospitalized patients with metastatic cancer have an ECOG performance status of 3 or worse. Thus, the clinical trials outcome data are of little relevance.
“In oncology the distinction between ECOG 2 and 3 is very important,” Dr. Brondfield emphasized.
When he talks about treatment options with hospitalized patients who have metastatic cancer and poor performance status – that is, ECOG 3 or 4 – he’ll often say: “Assuming you feel better and can go home, that’s when these clinical trial data may apply better to you.”
Dr. Brondfield cautioned against quoting the National Cancer Institute’s Surveillance, Epidemiology and End Results (SEER) 5-year overall survival data when hospitalized patients with advanced cancer ask how long they have to live. For one thing, the national average 5-year overall survival figure is hardly an individualized assessment. Plus, oncology is a fast-moving field in which important treatment advances occur all the time, and the SEER data lag far behind. For example, when Dr. Brondfield recently looked up the current SEER 5-year survival for patients diagnosed with metastatic non–small cell lung cancer (NSCLC), the figure quoted was less than 6%, and it was drawn from data accrued in 2009-2015. That simply doesn’t reflect contemporary practice.
Indeed, it’s no longer true that the average survival of patients with metastatic NSCLC is less than a year. In the practice-changing KEYNOTE-189 randomized trial, which accrued participants in 2016-2017, the median overall survival of patients randomized to pembrolizumab (Keytruda) plus standard cytotoxic chemotherapy was 22 months, compared with 11 months with chemotherapy plus placebo (J Clin Oncol. 2020 May 10. doi: 10.1200/JCO.19.03136). As a result, immunotherapy with a programmed death–1 inhibitor such as pembrolizumab in combination with chemotherapy is now standard practice in patients with metastatic NSCLC without targetable mutations.
Performance status guides treatment decision-making
Hospitalists can help oncologists in decision-making regarding whether to offer palliative systemic therapy to patients with advanced metastatic cancer and poor performance status by determining whether that status is caused by the cancer itself or some other cause that’s not easily reversible, such as liver failure.
Take, for example, the inpatient with advanced SCLC. This is an aggressive and chemosensitive cancer. Dr. Brondfield said he is among many medical oncologists who are convinced that, if poor performance status in a patient with advanced SCLC is caused by the cancer itself, prompt initiation of inpatient chemotherapy should be recommended to elicit a response that improves quality of life and performance status in the short term. If, on the other hand, the poor performance status is caused by organ failure or some other issue that can’t easily be improved, hospice may be more appropriate.
“The contour of SCLC over time is that despite its treatment responsiveness it inevitably recurs. But with chemotherapy you can give people in this situation months of quality time, so we generally try to treat these sorts of patients,” Dr. Brondfield explained.
The National Comprehensive Cancer Network guidelines upon which oncologists rely leave lots of room for interpretation regarding the appropriateness of inpatient chemotherapy in patients with advanced cancer and poor patient performance status. Citing “knowledge that’s been passed down across oncology generations,” Dr. Brondfield said he and many of his colleagues believe early palliative supportive care rather than systemic cytotoxic cancer-directed therapy is appropriate for patients with poor performance status who have one of several specific relatively nonchemoresponsive types of metastatic cancer. These include esophageal, gastric, and head and neck cancers.
On the other hand, advanced SCLC isn’t the only type of metastatic cancer that’s so chemosensitive that he and many other oncologists believe aggressive chemotherapy should be offered even in the face of poor patient performance status attributable to the cancer itself.
Take, for example, colorectal cancer with no more than five metastases to the lung or liver, provided those metastases are treatable with resection or radiation. “Those patients are actually curable at a high rate. They have about a 30%-40% cure rate. So those patients, even if they have poor performance status, if we can get them up for surgery or radiation, we usually do try to treat them aggressively,” Dr. Brondfield said.
There are other often chemoresponsive metastatic cancers for which oncologists frequently recommend aggressive treatment to improve quality of life in patients with poor performance status. These cancers include aggressive lymphomas, which are actually often curable; multiple myeloma; testicular and germ cell cancers; NSCLC with a targetable mutation, which is often responsive to oral medications; and prostate and well-differentiated thyroid cancers, which can usually be treated with hormone- or iodine-based therapies rather than more toxic intravenous cytotoxic chemotherapy.
The impact of inpatient palliative chemotherapy in patients with poor performance status and advanced solid cancers not on the short list of highly chemosensitive cancers has not been well studied. A recent retrospective study of 228 such patients who received inpatient palliative chemotherapy at a large Brazilian academic medical center provided little reason for enthusiasm regarding the practice. Survival was short, with 30- and 60-day survival rates of 56% and 39%, respectively. Plus, 30% of patients were admitted to the ICU, where they received aggressive and costly end-of-life care. The investigators found these results suggestive of overprescribing of inpatient palliative chemotherapy (BMC Palliat Care. 2019 May 20;18[1]:42. doi: 10.1186/s12904-019-0427-4).
Of note, the investigators found in a multivariate analysis that an elevated bilirubin was associated with a 217% increased risk of 30-day mortality, and hypercalcemia was associated with a 119% increased risk.
“That’s something to take into account when these decisions are being made,” Dr. Brondfield advised.
In response to an audience comment that oncologists often seem overly optimistic about prognosis, Dr. Brondfield observed, “I think it’s very common for there to be a disagreement between the oncologist wanting to be aggressive for a sick inpatient and the hospitalist or generalist provider thinking: ‘This person looks way too sick for chemotherapy.’ ”
For this reason he is a firm believer in having multidisciplinary conversations regarding prognosis in challenging situations involving hospitalized patients with advanced cancer. An oncologist can bring to such discussions a detailed understanding of clinical trial and molecular data as well as information about the patient’s response to the first round of therapy. But lots of other factors are relevant to prognosis, including nutritional status, comorbidities, and the intuitive eyeball test of how a patient might do. The patient’s family, primary care provider, oncologist, the hospitalist, and the palliative care team will have perspectives of their own.
Molecular testing is now the norm in metastatic cancers
These days oncologists order molecular testing for most patients with metastatic carcinomas to determine eligibility for targeted therapy, suitability for participation in clinical trials, prognostication, and/or assistance in determining the site of origin if that’s unclear.
A single-pass fine needle aspiration biopsy doesn’t provide enough tissue for molecular testing. It’s therefore important to order initially a multipass fine needle aspiration to avoid the need for a repeat biopsy, which is uncomfortable for the patient and can delay diagnosis and treatment.
Dr. Brondfield advised waiting for molecular testing results to come in before trying to prognosticate in patients with a metastatic cancer for which targetable mutations might be present. Survival rates can vary substantially depending upon those test results. Take, for example, metastatic NSCLC: Just within the past year, clinical trials have been published reporting overall survival rates of 39 months in patients with treatable mutations in epidermal growth factor receptor, 42 months with anaplastic lymphoma kinase mutations, and 51 months in patients whose tumor signature features mutations in c-ros oncogene 1, as compared with 22 months with no targetable mutations in the KEYNOTE-189 trial.
“There’s a lot of heterogeneity around how metastatic tumors behave and respond to therapy. Not all metastatic cancers are the same,” the oncologist emphasized.
according to Sam Brondfield, MD, MA, an inpatient medical oncologist at the University of California, San Francisco.
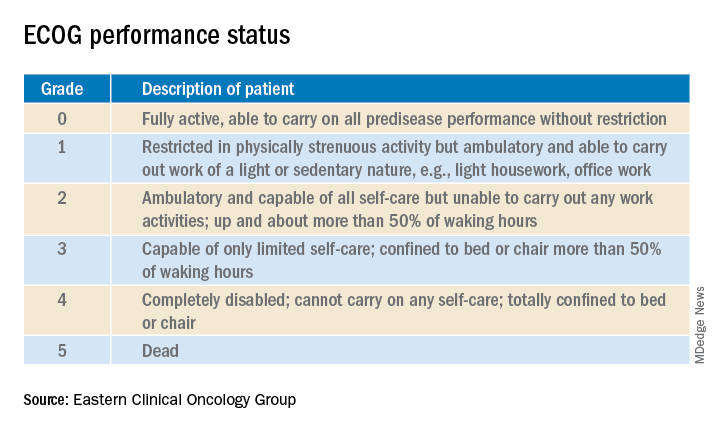
Oncologists have at their fingertips a voluminous and ever-growing body of clinical trials data to draw on for prognostication. Yet many hospitalists will be surprised to learn that this wealth of information is of little value in the inpatient settings where they work, he said at HM20 Virtual, hosted by the Society of Hospital Medicine.
“The applicability of clinical trials data to hospitalized patients is generally poor. That’s an important caveat to keep in mind,” Dr. Brondfield said.
Enrollment in clinical trials is usually restricted to patients with a score of 0 or 1 on the Eastern Clinical Oncology Group Performance Status, meaning their cancer is causing minimal or no disruption to their life (see graphic). Sometimes trials will include patients with a performance status of 2 on the ECOG scale, a tool developed nearly 40 years ago, but clinical trials virtually never enroll those with an ECOG status of 3 or 4. Yet most hospitalized patients with metastatic cancer have an ECOG performance status of 3 or worse. Thus, the clinical trials outcome data are of little relevance.
“In oncology the distinction between ECOG 2 and 3 is very important,” Dr. Brondfield emphasized.
When he talks about treatment options with hospitalized patients who have metastatic cancer and poor performance status – that is, ECOG 3 or 4 – he’ll often say: “Assuming you feel better and can go home, that’s when these clinical trial data may apply better to you.”
Dr. Brondfield cautioned against quoting the National Cancer Institute’s Surveillance, Epidemiology and End Results (SEER) 5-year overall survival data when hospitalized patients with advanced cancer ask how long they have to live. For one thing, the national average 5-year overall survival figure is hardly an individualized assessment. Plus, oncology is a fast-moving field in which important treatment advances occur all the time, and the SEER data lag far behind. For example, when Dr. Brondfield recently looked up the current SEER 5-year survival for patients diagnosed with metastatic non–small cell lung cancer (NSCLC), the figure quoted was less than 6%, and it was drawn from data accrued in 2009-2015. That simply doesn’t reflect contemporary practice.
Indeed, it’s no longer true that the average survival of patients with metastatic NSCLC is less than a year. In the practice-changing KEYNOTE-189 randomized trial, which accrued participants in 2016-2017, the median overall survival of patients randomized to pembrolizumab (Keytruda) plus standard cytotoxic chemotherapy was 22 months, compared with 11 months with chemotherapy plus placebo (J Clin Oncol. 2020 May 10. doi: 10.1200/JCO.19.03136). As a result, immunotherapy with a programmed death–1 inhibitor such as pembrolizumab in combination with chemotherapy is now standard practice in patients with metastatic NSCLC without targetable mutations.
Performance status guides treatment decision-making
Hospitalists can help oncologists in decision-making regarding whether to offer palliative systemic therapy to patients with advanced metastatic cancer and poor performance status by determining whether that status is caused by the cancer itself or some other cause that’s not easily reversible, such as liver failure.
Take, for example, the inpatient with advanced SCLC. This is an aggressive and chemosensitive cancer. Dr. Brondfield said he is among many medical oncologists who are convinced that, if poor performance status in a patient with advanced SCLC is caused by the cancer itself, prompt initiation of inpatient chemotherapy should be recommended to elicit a response that improves quality of life and performance status in the short term. If, on the other hand, the poor performance status is caused by organ failure or some other issue that can’t easily be improved, hospice may be more appropriate.
“The contour of SCLC over time is that despite its treatment responsiveness it inevitably recurs. But with chemotherapy you can give people in this situation months of quality time, so we generally try to treat these sorts of patients,” Dr. Brondfield explained.
The National Comprehensive Cancer Network guidelines upon which oncologists rely leave lots of room for interpretation regarding the appropriateness of inpatient chemotherapy in patients with advanced cancer and poor patient performance status. Citing “knowledge that’s been passed down across oncology generations,” Dr. Brondfield said he and many of his colleagues believe early palliative supportive care rather than systemic cytotoxic cancer-directed therapy is appropriate for patients with poor performance status who have one of several specific relatively nonchemoresponsive types of metastatic cancer. These include esophageal, gastric, and head and neck cancers.
On the other hand, advanced SCLC isn’t the only type of metastatic cancer that’s so chemosensitive that he and many other oncologists believe aggressive chemotherapy should be offered even in the face of poor patient performance status attributable to the cancer itself.
Take, for example, colorectal cancer with no more than five metastases to the lung or liver, provided those metastases are treatable with resection or radiation. “Those patients are actually curable at a high rate. They have about a 30%-40% cure rate. So those patients, even if they have poor performance status, if we can get them up for surgery or radiation, we usually do try to treat them aggressively,” Dr. Brondfield said.
There are other often chemoresponsive metastatic cancers for which oncologists frequently recommend aggressive treatment to improve quality of life in patients with poor performance status. These cancers include aggressive lymphomas, which are actually often curable; multiple myeloma; testicular and germ cell cancers; NSCLC with a targetable mutation, which is often responsive to oral medications; and prostate and well-differentiated thyroid cancers, which can usually be treated with hormone- or iodine-based therapies rather than more toxic intravenous cytotoxic chemotherapy.
The impact of inpatient palliative chemotherapy in patients with poor performance status and advanced solid cancers not on the short list of highly chemosensitive cancers has not been well studied. A recent retrospective study of 228 such patients who received inpatient palliative chemotherapy at a large Brazilian academic medical center provided little reason for enthusiasm regarding the practice. Survival was short, with 30- and 60-day survival rates of 56% and 39%, respectively. Plus, 30% of patients were admitted to the ICU, where they received aggressive and costly end-of-life care. The investigators found these results suggestive of overprescribing of inpatient palliative chemotherapy (BMC Palliat Care. 2019 May 20;18[1]:42. doi: 10.1186/s12904-019-0427-4).
Of note, the investigators found in a multivariate analysis that an elevated bilirubin was associated with a 217% increased risk of 30-day mortality, and hypercalcemia was associated with a 119% increased risk.
“That’s something to take into account when these decisions are being made,” Dr. Brondfield advised.
In response to an audience comment that oncologists often seem overly optimistic about prognosis, Dr. Brondfield observed, “I think it’s very common for there to be a disagreement between the oncologist wanting to be aggressive for a sick inpatient and the hospitalist or generalist provider thinking: ‘This person looks way too sick for chemotherapy.’ ”
For this reason he is a firm believer in having multidisciplinary conversations regarding prognosis in challenging situations involving hospitalized patients with advanced cancer. An oncologist can bring to such discussions a detailed understanding of clinical trial and molecular data as well as information about the patient’s response to the first round of therapy. But lots of other factors are relevant to prognosis, including nutritional status, comorbidities, and the intuitive eyeball test of how a patient might do. The patient’s family, primary care provider, oncologist, the hospitalist, and the palliative care team will have perspectives of their own.
Molecular testing is now the norm in metastatic cancers
These days oncologists order molecular testing for most patients with metastatic carcinomas to determine eligibility for targeted therapy, suitability for participation in clinical trials, prognostication, and/or assistance in determining the site of origin if that’s unclear.
A single-pass fine needle aspiration biopsy doesn’t provide enough tissue for molecular testing. It’s therefore important to order initially a multipass fine needle aspiration to avoid the need for a repeat biopsy, which is uncomfortable for the patient and can delay diagnosis and treatment.
Dr. Brondfield advised waiting for molecular testing results to come in before trying to prognosticate in patients with a metastatic cancer for which targetable mutations might be present. Survival rates can vary substantially depending upon those test results. Take, for example, metastatic NSCLC: Just within the past year, clinical trials have been published reporting overall survival rates of 39 months in patients with treatable mutations in epidermal growth factor receptor, 42 months with anaplastic lymphoma kinase mutations, and 51 months in patients whose tumor signature features mutations in c-ros oncogene 1, as compared with 22 months with no targetable mutations in the KEYNOTE-189 trial.
“There’s a lot of heterogeneity around how metastatic tumors behave and respond to therapy. Not all metastatic cancers are the same,” the oncologist emphasized.
FROM HM20 VIRTUAL
Oleander extract for COVID-19? That’s a hard ‘no’ experts say
“Though renowned for its beauty and use in landscaping, this Mediterranean shrub is responsible for cases of accidental poisoning across the globe. All parts of the plant are poisonous,” Cassandra Quave, PhD, ethnobotanist and herbarium curator at Emory University, Atlanta, cautioned in an article in The Conversation, an independent, not-for-profit publication.
Oleandrin has properties similar to digoxin; the onset of toxicity occurs several hours after consumption.
The first symptoms of oleandrin poisoning may be gastrointestinal, such as nausea, vomiting, abdominal pain, diarrhea (which may contain blood), and loss of appetite.
After these first symptoms, the heart may be affected by tachyarrhythmia, bradyarrhythmia, premature ventricular contractions, or atrioventricular blockage. Xanthopsia (yellow vision), a burning sensation in the eyes, paralysis of the gastrointestinal tract, and respiratory symptoms may also occur.
Oleandrin poisoning may affect the central nervous system, as evidenced by drowsiness, tremors, seizures, collapse, and coma leading to death. When applied to the skin, oleander sap can cause skin irritations and allergic reactions characterized by dermatitis.
Diagnosis of oleandrin poisoning is mainly made on the basis of a description of the plant, how much of it was ingested, how much time has elapsed since ingestion, and symptoms. Confirmation of oleandrin in blood involves fluorescence polarization immunoassay, digoxin immunoassay, or liquid chromatography-electrospray tandem mass spectrometry.
Neither oleander nor oleandrin is approved by regulatory agencies as a prescription drug or dietary supplement.
In vitro study
Oleandrin for COVID-19 made headlines after President Trump met in the Oval Office with Andrew Whitney, vice chairman and director of Phoenix Biotechnology, along with Housing and Urban Development Secretary Ben Carson, MD, and MyPillow founder/CEO Mike Lindell, a strong supporter of Trump and an investor in the biotech company, to learn about oleandrin, which Whitney called a “cure” for COVID-19, Axios reported.
In an in vitro study, researchers from Phoenix Biotechnology and the University of Texas Medical Branch, Galveston, tested oleandrin against SARS-CoV-2 in cultured Vero cells.
“When administered both before and after virus infection, nanogram doses of oleandrin significantly inhibited replication by 45 to 3000-fold,” the researchers said in an article posted on bioRxiv, a free online archive and distribution service for unpublished preprints in the life sciences. The study has not been peer reviewed.
On the basis of these in vitro findings, the researchers said the plant extract has “potential to prevent disease and virus spread in persons recently exposed to SARS-CoV-2, as well as to prevent severe disease in persons at high risk.”
But it’s a far cry from test tube to human, one expert cautioned.
“This is an understatement: Care must be taken when inferring potential therapeutic benefits from in vitro antiviral effects,” Harlan Krumholz, MD, cardiologist and director, Yale New Haven Hospital Center for Outcomes Research and Evaluation, New Haven, Connecticut, told Medscape Medical News.
“There is a chasm between a single in vitro study and any use in humans outside of a protocol. People should be cautioned about that distance and the need [to] avoid such remedies unless part of a credible research project,” said Krumholz.
Yet Lindell told Axios that, in the Oval Office meeting, Trump expressed enthusiasm for the Food and Drug Administration to allow oleandrin to be marketed as a dietary supplement or approved for COVID-19.
“This is really just nonsense and a distraction,” Jonathan Reiner, MD, of George Washington University Medical Center, Washington, DC, said on CNN.
This article first appeared on Medscape.com.
“Though renowned for its beauty and use in landscaping, this Mediterranean shrub is responsible for cases of accidental poisoning across the globe. All parts of the plant are poisonous,” Cassandra Quave, PhD, ethnobotanist and herbarium curator at Emory University, Atlanta, cautioned in an article in The Conversation, an independent, not-for-profit publication.
Oleandrin has properties similar to digoxin; the onset of toxicity occurs several hours after consumption.
The first symptoms of oleandrin poisoning may be gastrointestinal, such as nausea, vomiting, abdominal pain, diarrhea (which may contain blood), and loss of appetite.
After these first symptoms, the heart may be affected by tachyarrhythmia, bradyarrhythmia, premature ventricular contractions, or atrioventricular blockage. Xanthopsia (yellow vision), a burning sensation in the eyes, paralysis of the gastrointestinal tract, and respiratory symptoms may also occur.
Oleandrin poisoning may affect the central nervous system, as evidenced by drowsiness, tremors, seizures, collapse, and coma leading to death. When applied to the skin, oleander sap can cause skin irritations and allergic reactions characterized by dermatitis.
Diagnosis of oleandrin poisoning is mainly made on the basis of a description of the plant, how much of it was ingested, how much time has elapsed since ingestion, and symptoms. Confirmation of oleandrin in blood involves fluorescence polarization immunoassay, digoxin immunoassay, or liquid chromatography-electrospray tandem mass spectrometry.
Neither oleander nor oleandrin is approved by regulatory agencies as a prescription drug or dietary supplement.
In vitro study
Oleandrin for COVID-19 made headlines after President Trump met in the Oval Office with Andrew Whitney, vice chairman and director of Phoenix Biotechnology, along with Housing and Urban Development Secretary Ben Carson, MD, and MyPillow founder/CEO Mike Lindell, a strong supporter of Trump and an investor in the biotech company, to learn about oleandrin, which Whitney called a “cure” for COVID-19, Axios reported.
In an in vitro study, researchers from Phoenix Biotechnology and the University of Texas Medical Branch, Galveston, tested oleandrin against SARS-CoV-2 in cultured Vero cells.
“When administered both before and after virus infection, nanogram doses of oleandrin significantly inhibited replication by 45 to 3000-fold,” the researchers said in an article posted on bioRxiv, a free online archive and distribution service for unpublished preprints in the life sciences. The study has not been peer reviewed.
On the basis of these in vitro findings, the researchers said the plant extract has “potential to prevent disease and virus spread in persons recently exposed to SARS-CoV-2, as well as to prevent severe disease in persons at high risk.”
But it’s a far cry from test tube to human, one expert cautioned.
“This is an understatement: Care must be taken when inferring potential therapeutic benefits from in vitro antiviral effects,” Harlan Krumholz, MD, cardiologist and director, Yale New Haven Hospital Center for Outcomes Research and Evaluation, New Haven, Connecticut, told Medscape Medical News.
“There is a chasm between a single in vitro study and any use in humans outside of a protocol. People should be cautioned about that distance and the need [to] avoid such remedies unless part of a credible research project,” said Krumholz.
Yet Lindell told Axios that, in the Oval Office meeting, Trump expressed enthusiasm for the Food and Drug Administration to allow oleandrin to be marketed as a dietary supplement or approved for COVID-19.
“This is really just nonsense and a distraction,” Jonathan Reiner, MD, of George Washington University Medical Center, Washington, DC, said on CNN.
This article first appeared on Medscape.com.
“Though renowned for its beauty and use in landscaping, this Mediterranean shrub is responsible for cases of accidental poisoning across the globe. All parts of the plant are poisonous,” Cassandra Quave, PhD, ethnobotanist and herbarium curator at Emory University, Atlanta, cautioned in an article in The Conversation, an independent, not-for-profit publication.
Oleandrin has properties similar to digoxin; the onset of toxicity occurs several hours after consumption.
The first symptoms of oleandrin poisoning may be gastrointestinal, such as nausea, vomiting, abdominal pain, diarrhea (which may contain blood), and loss of appetite.
After these first symptoms, the heart may be affected by tachyarrhythmia, bradyarrhythmia, premature ventricular contractions, or atrioventricular blockage. Xanthopsia (yellow vision), a burning sensation in the eyes, paralysis of the gastrointestinal tract, and respiratory symptoms may also occur.
Oleandrin poisoning may affect the central nervous system, as evidenced by drowsiness, tremors, seizures, collapse, and coma leading to death. When applied to the skin, oleander sap can cause skin irritations and allergic reactions characterized by dermatitis.
Diagnosis of oleandrin poisoning is mainly made on the basis of a description of the plant, how much of it was ingested, how much time has elapsed since ingestion, and symptoms. Confirmation of oleandrin in blood involves fluorescence polarization immunoassay, digoxin immunoassay, or liquid chromatography-electrospray tandem mass spectrometry.
Neither oleander nor oleandrin is approved by regulatory agencies as a prescription drug or dietary supplement.
In vitro study
Oleandrin for COVID-19 made headlines after President Trump met in the Oval Office with Andrew Whitney, vice chairman and director of Phoenix Biotechnology, along with Housing and Urban Development Secretary Ben Carson, MD, and MyPillow founder/CEO Mike Lindell, a strong supporter of Trump and an investor in the biotech company, to learn about oleandrin, which Whitney called a “cure” for COVID-19, Axios reported.
In an in vitro study, researchers from Phoenix Biotechnology and the University of Texas Medical Branch, Galveston, tested oleandrin against SARS-CoV-2 in cultured Vero cells.
“When administered both before and after virus infection, nanogram doses of oleandrin significantly inhibited replication by 45 to 3000-fold,” the researchers said in an article posted on bioRxiv, a free online archive and distribution service for unpublished preprints in the life sciences. The study has not been peer reviewed.
On the basis of these in vitro findings, the researchers said the plant extract has “potential to prevent disease and virus spread in persons recently exposed to SARS-CoV-2, as well as to prevent severe disease in persons at high risk.”
But it’s a far cry from test tube to human, one expert cautioned.
“This is an understatement: Care must be taken when inferring potential therapeutic benefits from in vitro antiviral effects,” Harlan Krumholz, MD, cardiologist and director, Yale New Haven Hospital Center for Outcomes Research and Evaluation, New Haven, Connecticut, told Medscape Medical News.
“There is a chasm between a single in vitro study and any use in humans outside of a protocol. People should be cautioned about that distance and the need [to] avoid such remedies unless part of a credible research project,” said Krumholz.
Yet Lindell told Axios that, in the Oval Office meeting, Trump expressed enthusiasm for the Food and Drug Administration to allow oleandrin to be marketed as a dietary supplement or approved for COVID-19.
“This is really just nonsense and a distraction,” Jonathan Reiner, MD, of George Washington University Medical Center, Washington, DC, said on CNN.
This article first appeared on Medscape.com.
Pulmonary rehab reduces COPD readmissions
Pulmonary rehabilitation reduces the likelihood that patients with chronic obstructive pulmonary disease (COPD) will be readmitted to the hospital in the year after discharge by 33%, new research shows, but few patients participate in those programs.
In fact, in a retrospective cohort of 197,376 patients from 4446 hospitals, only 1.5% of patients initiated pulmonary rehabilitation in the 90 days after hospital discharge.
“This is a striking finding,” said Mihaela Stefan, PhD, from the University of Massachusetts Medical School–Baystate in Springfield. “Our study demonstrates that we need to increase access to rehabilitation to reduce the risk of readmissions.”
Not enough patients are initiating rehabilitation, but the onus is not only on them; the system is failing them. “We wanted to understand how much pulmonary rehabilitation lowers the readmission rate,” Stefan told Medscape Medical News.
So she and her colleagues examined the records of patients who were hospitalized for COPD in 2014 to see whether they had begun rehabilitation in the 90 days after discharge and whether they were readmitted to the hospital in the subsequent 12 months.
Patients who were unlikely to initiate pulmonary rehabilitation — such as those with dementia or metastatic cancer and those discharged to hospice care or a nursing home — were excluded from the analysis, Stefan said during her presentation at the study results at the virtual American Thoracic Society (ATS) 2020 International Conference.
The risk analysis was complex because many patients died before the year was out, and “a patient who dies has no risk of being readmitted,” she explained. Selection bias was also a factor because patients who do pulmonary rehab tend to be in better shape.
The researchers used propensity score matching and Anderson–Gill models of cumulative rehospitalizations or death at 1 year with time-varying exposure to pulmonary rehabilitation to account for clustering of individual events and adjust for covariates. “It was a complicated risk analysis,” she said.
In the year after discharge, 130,660 patients (66%) were readmitted to the hospital. The rate of rehospitalization was lower for those who initiated rehabilitation than for those who did not (59% vs 66%), as was the mean number of readmissions per patient (1.4 vs 1.8).
Rehabilitation was associated with a lower risk for readmission or death (hazard ratio, 0.67; 95% CI, 0.66 - 0.69).
“We know the referral rates are low and that pulmonary rehabilitation is effective in clinical trials,” said Stefan, and now “we see that pulmonary rehabilitation is effective when you look at patients in real life.”
From a provider perspective, “we need to make sure that hospitals get more money for pulmonary rehabilitation. Cardiac rehabilitation is paid for,” she explained. "But pulmonary rehab is not a lucrative business. I don›t know why the CMS pays more for cardiac."
A rehabilitation program generally consists of 36 sessions, held two or three times a week, and many patients can’t afford that on their own, she noted. Transportation is another huge issue.
A recent study in which semi-structured interviews were conducted with 15 COPD patients showed that the main barriers to enrollment in a pulmonary rehabilitation program are lack of awareness, family obligations, transportation, and lack of motivation, said Stefan, who was involved in that research.
Telehealth rehabilitation programs might become more available in the near future, given the COVID pandemic. But “currently, Medicare doesn’t pay for telerehab,” she said. Virtual sessions might attract more patients, but lack of computer access and training could present another barrier for some.
PAH rehab
Uptake for pulmonary rehabilitation is as low for patients with pulmonary arterial hypertension (PAH) as it is for those with COPD, according to another study presented at the virtual ATS meeting.
An examination of the electronic health records of 111,356 veterans who experienced incident PAH from 2010 to 2016 showed that only 1,737 (1.6%) followed through on pulmonary rehabilitation.
“Exercise therapy is safe and effective at improving outcomes,” lead author Thomas Cascino, MD, from the University of Michigan in Ann Arbor, said in an ATS press release. “Recognizing that it is being underutilized is a necessary first step in working toward increasing patient access to rehab.
His group is currently working on a trial for home-based rehabilitation “using wearable technology as a means to expand access for people unable to come to center-based rehab for a variety of reasons,” he explained.
“The goal of all our treatments is to help people feel better and live longer,” Cascino added.
Stefan and Cascino have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Pulmonary rehabilitation reduces the likelihood that patients with chronic obstructive pulmonary disease (COPD) will be readmitted to the hospital in the year after discharge by 33%, new research shows, but few patients participate in those programs.
In fact, in a retrospective cohort of 197,376 patients from 4446 hospitals, only 1.5% of patients initiated pulmonary rehabilitation in the 90 days after hospital discharge.
“This is a striking finding,” said Mihaela Stefan, PhD, from the University of Massachusetts Medical School–Baystate in Springfield. “Our study demonstrates that we need to increase access to rehabilitation to reduce the risk of readmissions.”
Not enough patients are initiating rehabilitation, but the onus is not only on them; the system is failing them. “We wanted to understand how much pulmonary rehabilitation lowers the readmission rate,” Stefan told Medscape Medical News.
So she and her colleagues examined the records of patients who were hospitalized for COPD in 2014 to see whether they had begun rehabilitation in the 90 days after discharge and whether they were readmitted to the hospital in the subsequent 12 months.
Patients who were unlikely to initiate pulmonary rehabilitation — such as those with dementia or metastatic cancer and those discharged to hospice care or a nursing home — were excluded from the analysis, Stefan said during her presentation at the study results at the virtual American Thoracic Society (ATS) 2020 International Conference.
The risk analysis was complex because many patients died before the year was out, and “a patient who dies has no risk of being readmitted,” she explained. Selection bias was also a factor because patients who do pulmonary rehab tend to be in better shape.
The researchers used propensity score matching and Anderson–Gill models of cumulative rehospitalizations or death at 1 year with time-varying exposure to pulmonary rehabilitation to account for clustering of individual events and adjust for covariates. “It was a complicated risk analysis,” she said.
In the year after discharge, 130,660 patients (66%) were readmitted to the hospital. The rate of rehospitalization was lower for those who initiated rehabilitation than for those who did not (59% vs 66%), as was the mean number of readmissions per patient (1.4 vs 1.8).
Rehabilitation was associated with a lower risk for readmission or death (hazard ratio, 0.67; 95% CI, 0.66 - 0.69).
“We know the referral rates are low and that pulmonary rehabilitation is effective in clinical trials,” said Stefan, and now “we see that pulmonary rehabilitation is effective when you look at patients in real life.”
From a provider perspective, “we need to make sure that hospitals get more money for pulmonary rehabilitation. Cardiac rehabilitation is paid for,” she explained. "But pulmonary rehab is not a lucrative business. I don›t know why the CMS pays more for cardiac."
A rehabilitation program generally consists of 36 sessions, held two or three times a week, and many patients can’t afford that on their own, she noted. Transportation is another huge issue.
A recent study in which semi-structured interviews were conducted with 15 COPD patients showed that the main barriers to enrollment in a pulmonary rehabilitation program are lack of awareness, family obligations, transportation, and lack of motivation, said Stefan, who was involved in that research.
Telehealth rehabilitation programs might become more available in the near future, given the COVID pandemic. But “currently, Medicare doesn’t pay for telerehab,” she said. Virtual sessions might attract more patients, but lack of computer access and training could present another barrier for some.
PAH rehab
Uptake for pulmonary rehabilitation is as low for patients with pulmonary arterial hypertension (PAH) as it is for those with COPD, according to another study presented at the virtual ATS meeting.
An examination of the electronic health records of 111,356 veterans who experienced incident PAH from 2010 to 2016 showed that only 1,737 (1.6%) followed through on pulmonary rehabilitation.
“Exercise therapy is safe and effective at improving outcomes,” lead author Thomas Cascino, MD, from the University of Michigan in Ann Arbor, said in an ATS press release. “Recognizing that it is being underutilized is a necessary first step in working toward increasing patient access to rehab.
His group is currently working on a trial for home-based rehabilitation “using wearable technology as a means to expand access for people unable to come to center-based rehab for a variety of reasons,” he explained.
“The goal of all our treatments is to help people feel better and live longer,” Cascino added.
Stefan and Cascino have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Pulmonary rehabilitation reduces the likelihood that patients with chronic obstructive pulmonary disease (COPD) will be readmitted to the hospital in the year after discharge by 33%, new research shows, but few patients participate in those programs.
In fact, in a retrospective cohort of 197,376 patients from 4446 hospitals, only 1.5% of patients initiated pulmonary rehabilitation in the 90 days after hospital discharge.
“This is a striking finding,” said Mihaela Stefan, PhD, from the University of Massachusetts Medical School–Baystate in Springfield. “Our study demonstrates that we need to increase access to rehabilitation to reduce the risk of readmissions.”
Not enough patients are initiating rehabilitation, but the onus is not only on them; the system is failing them. “We wanted to understand how much pulmonary rehabilitation lowers the readmission rate,” Stefan told Medscape Medical News.
So she and her colleagues examined the records of patients who were hospitalized for COPD in 2014 to see whether they had begun rehabilitation in the 90 days after discharge and whether they were readmitted to the hospital in the subsequent 12 months.
Patients who were unlikely to initiate pulmonary rehabilitation — such as those with dementia or metastatic cancer and those discharged to hospice care or a nursing home — were excluded from the analysis, Stefan said during her presentation at the study results at the virtual American Thoracic Society (ATS) 2020 International Conference.
The risk analysis was complex because many patients died before the year was out, and “a patient who dies has no risk of being readmitted,” she explained. Selection bias was also a factor because patients who do pulmonary rehab tend to be in better shape.
The researchers used propensity score matching and Anderson–Gill models of cumulative rehospitalizations or death at 1 year with time-varying exposure to pulmonary rehabilitation to account for clustering of individual events and adjust for covariates. “It was a complicated risk analysis,” she said.
In the year after discharge, 130,660 patients (66%) were readmitted to the hospital. The rate of rehospitalization was lower for those who initiated rehabilitation than for those who did not (59% vs 66%), as was the mean number of readmissions per patient (1.4 vs 1.8).
Rehabilitation was associated with a lower risk for readmission or death (hazard ratio, 0.67; 95% CI, 0.66 - 0.69).
“We know the referral rates are low and that pulmonary rehabilitation is effective in clinical trials,” said Stefan, and now “we see that pulmonary rehabilitation is effective when you look at patients in real life.”
From a provider perspective, “we need to make sure that hospitals get more money for pulmonary rehabilitation. Cardiac rehabilitation is paid for,” she explained. "But pulmonary rehab is not a lucrative business. I don›t know why the CMS pays more for cardiac."
A rehabilitation program generally consists of 36 sessions, held two or three times a week, and many patients can’t afford that on their own, she noted. Transportation is another huge issue.
A recent study in which semi-structured interviews were conducted with 15 COPD patients showed that the main barriers to enrollment in a pulmonary rehabilitation program are lack of awareness, family obligations, transportation, and lack of motivation, said Stefan, who was involved in that research.
Telehealth rehabilitation programs might become more available in the near future, given the COVID pandemic. But “currently, Medicare doesn’t pay for telerehab,” she said. Virtual sessions might attract more patients, but lack of computer access and training could present another barrier for some.
PAH rehab
Uptake for pulmonary rehabilitation is as low for patients with pulmonary arterial hypertension (PAH) as it is for those with COPD, according to another study presented at the virtual ATS meeting.
An examination of the electronic health records of 111,356 veterans who experienced incident PAH from 2010 to 2016 showed that only 1,737 (1.6%) followed through on pulmonary rehabilitation.
“Exercise therapy is safe and effective at improving outcomes,” lead author Thomas Cascino, MD, from the University of Michigan in Ann Arbor, said in an ATS press release. “Recognizing that it is being underutilized is a necessary first step in working toward increasing patient access to rehab.
His group is currently working on a trial for home-based rehabilitation “using wearable technology as a means to expand access for people unable to come to center-based rehab for a variety of reasons,” he explained.
“The goal of all our treatments is to help people feel better and live longer,” Cascino added.
Stefan and Cascino have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
PHM20 Virtual: Can’t miss heart disease for hospitalists
PHM20 Virtual session title
Can’t Miss Heart Disease for Hospitalists
Presenter
Erich Maul, DO, MPH, FAAP, SFHM
Session summary
Dr. Erich Maul, professor of pediatrics, medical director for progressive care and acute care, and chief of hospital pediatrics at Kentucky Children’s Hospital, Lexington, presented an engaging, case-based approach to evaluate heart disease when “on call.” He iterated the importance of recognizing congenital heart disease, especially since 25% of these patients usually need surgical intervention within the first month of diagnosis and about 50% of congenital heart disease patients do not have a murmur.
Presenting cases seen during a busy hospitalist call night, Dr. Maul highlighted that patients can present with signs of heart failure, cyanosis, sepsis or hypoperfusion, failure to thrive, and respiratory distress or failure. He discussed the presentation, epidemiology, diagnosis, treatment, and prognosis. He also provided examples of common arrhythmias and provided refreshers on management using basic life support (BLS) and pediatric advanced life support.
Key takeaways
- Always start with the nine steps to resuscitation: ABC (airway, breathing, circulation), ABC, oxygen, access, monitoring.
- Early BLS is important.
- Congenital heart disease often presents with either cyanosis, hypoperfusion, failure to thrive, or respiratory distress.
Dr. Tantoco is an academic med-peds hospitalist practicing at Northwestern Memorial Hospital and Ann & Robert H. Lurie Children’s Hospital of Chicago. She is an instructor of medicine (hospital medicine) and pediatrics at Northwestern University, Chicago.
PHM20 Virtual session title
Can’t Miss Heart Disease for Hospitalists
Presenter
Erich Maul, DO, MPH, FAAP, SFHM
Session summary
Dr. Erich Maul, professor of pediatrics, medical director for progressive care and acute care, and chief of hospital pediatrics at Kentucky Children’s Hospital, Lexington, presented an engaging, case-based approach to evaluate heart disease when “on call.” He iterated the importance of recognizing congenital heart disease, especially since 25% of these patients usually need surgical intervention within the first month of diagnosis and about 50% of congenital heart disease patients do not have a murmur.
Presenting cases seen during a busy hospitalist call night, Dr. Maul highlighted that patients can present with signs of heart failure, cyanosis, sepsis or hypoperfusion, failure to thrive, and respiratory distress or failure. He discussed the presentation, epidemiology, diagnosis, treatment, and prognosis. He also provided examples of common arrhythmias and provided refreshers on management using basic life support (BLS) and pediatric advanced life support.
Key takeaways
- Always start with the nine steps to resuscitation: ABC (airway, breathing, circulation), ABC, oxygen, access, monitoring.
- Early BLS is important.
- Congenital heart disease often presents with either cyanosis, hypoperfusion, failure to thrive, or respiratory distress.
Dr. Tantoco is an academic med-peds hospitalist practicing at Northwestern Memorial Hospital and Ann & Robert H. Lurie Children’s Hospital of Chicago. She is an instructor of medicine (hospital medicine) and pediatrics at Northwestern University, Chicago.
PHM20 Virtual session title
Can’t Miss Heart Disease for Hospitalists
Presenter
Erich Maul, DO, MPH, FAAP, SFHM
Session summary
Dr. Erich Maul, professor of pediatrics, medical director for progressive care and acute care, and chief of hospital pediatrics at Kentucky Children’s Hospital, Lexington, presented an engaging, case-based approach to evaluate heart disease when “on call.” He iterated the importance of recognizing congenital heart disease, especially since 25% of these patients usually need surgical intervention within the first month of diagnosis and about 50% of congenital heart disease patients do not have a murmur.
Presenting cases seen during a busy hospitalist call night, Dr. Maul highlighted that patients can present with signs of heart failure, cyanosis, sepsis or hypoperfusion, failure to thrive, and respiratory distress or failure. He discussed the presentation, epidemiology, diagnosis, treatment, and prognosis. He also provided examples of common arrhythmias and provided refreshers on management using basic life support (BLS) and pediatric advanced life support.
Key takeaways
- Always start with the nine steps to resuscitation: ABC (airway, breathing, circulation), ABC, oxygen, access, monitoring.
- Early BLS is important.
- Congenital heart disease often presents with either cyanosis, hypoperfusion, failure to thrive, or respiratory distress.
Dr. Tantoco is an academic med-peds hospitalist practicing at Northwestern Memorial Hospital and Ann & Robert H. Lurie Children’s Hospital of Chicago. She is an instructor of medicine (hospital medicine) and pediatrics at Northwestern University, Chicago.
COVID-19 child case count now over 400,000
according to a new report from the American Academy of Pediatrics and the Children’s Hospital Association.
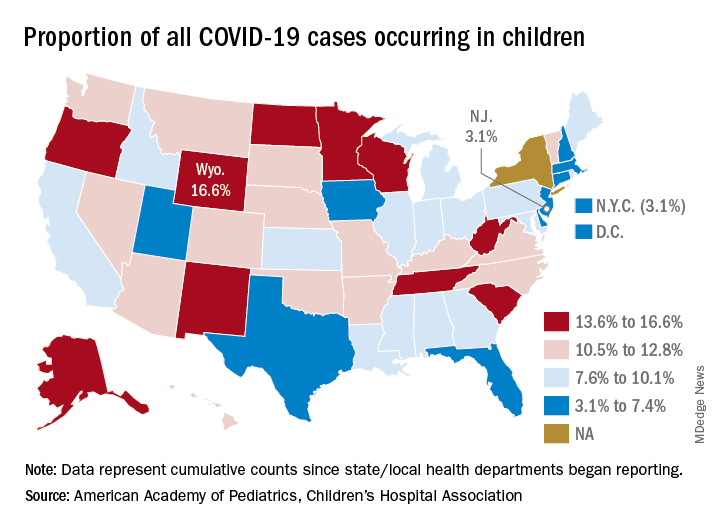
The 406,000 children who have tested positive for COVID-19 represent 9.1% of all cases reported so far by 49 states (New York does not provide age distribution), New York City, the District of Columbia, Puerto Rico, and Guam. Since the proportion of child cases also was 9.1% on Aug. 6, the most recent week is the first without an increase since tracking began in mid-April, the report shows.
State-level data show that Wyoming has the highest percentage of child cases (16.6%) after Alabama changed its “definition of child case from 0-24 to 0-17 years, resulting in a downward revision of cumulative child cases,” the AAP and the CHA said. Alabama’s proportion of such cases dropped from 22.5% to 9.0%.
New Jersey had the lowest rate (3.1%) again this week, along with New York City, but both were up slightly from the week before, when New Jersey was at 2.9% and N.Y.C. was 3.0%. The only states, other than Alabama, that saw declines over the last week were Arkansas, Massachusetts, Mississippi, South Dakota, Texas, and West Virginia. Texas, however, has reported age for only 8% of its confirmed cases, the report noted.
The overall rate of child COVID-19 cases as of Aug. 13 was 538 per 100,000 children, up from 500.7 per 100,000 a week earlier. Arizona was again highest among the states with a rate of 1,254 per 100,000 (up from 1,206) and Vermont was lowest at 121, although Puerto Rico (114) and Guam (88) were lower still, the AAP/CHA data indicate.
For the nine states that report testing information for children, Arizona has the highest positivity rate at 18.3% and West Virginia has the lowest at 3.6%. Data on hospitalizations – available from 21 states and N.Y.C. – show that 3,849 children have been admitted, with rates varying from 0.2% of children in Hawaii to 8.8% in the Big Apple, according to the report.
More specific information on child cases, such as symptoms or underlying conditions, is not being provided by states at this time, the AAP and CHA pointed out.
according to a new report from the American Academy of Pediatrics and the Children’s Hospital Association.
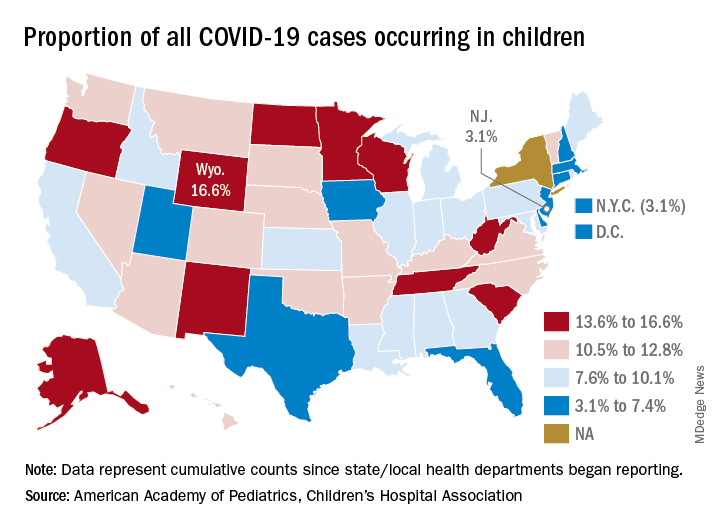
The 406,000 children who have tested positive for COVID-19 represent 9.1% of all cases reported so far by 49 states (New York does not provide age distribution), New York City, the District of Columbia, Puerto Rico, and Guam. Since the proportion of child cases also was 9.1% on Aug. 6, the most recent week is the first without an increase since tracking began in mid-April, the report shows.
State-level data show that Wyoming has the highest percentage of child cases (16.6%) after Alabama changed its “definition of child case from 0-24 to 0-17 years, resulting in a downward revision of cumulative child cases,” the AAP and the CHA said. Alabama’s proportion of such cases dropped from 22.5% to 9.0%.
New Jersey had the lowest rate (3.1%) again this week, along with New York City, but both were up slightly from the week before, when New Jersey was at 2.9% and N.Y.C. was 3.0%. The only states, other than Alabama, that saw declines over the last week were Arkansas, Massachusetts, Mississippi, South Dakota, Texas, and West Virginia. Texas, however, has reported age for only 8% of its confirmed cases, the report noted.
The overall rate of child COVID-19 cases as of Aug. 13 was 538 per 100,000 children, up from 500.7 per 100,000 a week earlier. Arizona was again highest among the states with a rate of 1,254 per 100,000 (up from 1,206) and Vermont was lowest at 121, although Puerto Rico (114) and Guam (88) were lower still, the AAP/CHA data indicate.
For the nine states that report testing information for children, Arizona has the highest positivity rate at 18.3% and West Virginia has the lowest at 3.6%. Data on hospitalizations – available from 21 states and N.Y.C. – show that 3,849 children have been admitted, with rates varying from 0.2% of children in Hawaii to 8.8% in the Big Apple, according to the report.
More specific information on child cases, such as symptoms or underlying conditions, is not being provided by states at this time, the AAP and CHA pointed out.
according to a new report from the American Academy of Pediatrics and the Children’s Hospital Association.
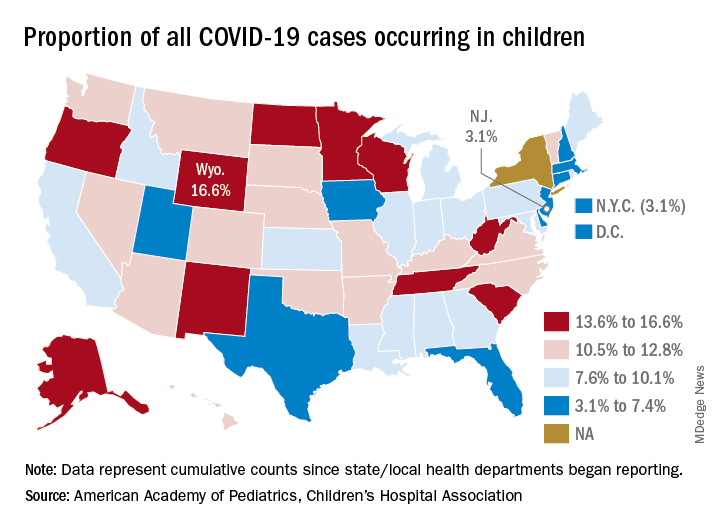
The 406,000 children who have tested positive for COVID-19 represent 9.1% of all cases reported so far by 49 states (New York does not provide age distribution), New York City, the District of Columbia, Puerto Rico, and Guam. Since the proportion of child cases also was 9.1% on Aug. 6, the most recent week is the first without an increase since tracking began in mid-April, the report shows.
State-level data show that Wyoming has the highest percentage of child cases (16.6%) after Alabama changed its “definition of child case from 0-24 to 0-17 years, resulting in a downward revision of cumulative child cases,” the AAP and the CHA said. Alabama’s proportion of such cases dropped from 22.5% to 9.0%.
New Jersey had the lowest rate (3.1%) again this week, along with New York City, but both were up slightly from the week before, when New Jersey was at 2.9% and N.Y.C. was 3.0%. The only states, other than Alabama, that saw declines over the last week were Arkansas, Massachusetts, Mississippi, South Dakota, Texas, and West Virginia. Texas, however, has reported age for only 8% of its confirmed cases, the report noted.
The overall rate of child COVID-19 cases as of Aug. 13 was 538 per 100,000 children, up from 500.7 per 100,000 a week earlier. Arizona was again highest among the states with a rate of 1,254 per 100,000 (up from 1,206) and Vermont was lowest at 121, although Puerto Rico (114) and Guam (88) were lower still, the AAP/CHA data indicate.
For the nine states that report testing information for children, Arizona has the highest positivity rate at 18.3% and West Virginia has the lowest at 3.6%. Data on hospitalizations – available from 21 states and N.Y.C. – show that 3,849 children have been admitted, with rates varying from 0.2% of children in Hawaii to 8.8% in the Big Apple, according to the report.
More specific information on child cases, such as symptoms or underlying conditions, is not being provided by states at this time, the AAP and CHA pointed out.
Are aging physicians a burden?
The evaluation of physicians with alleged cognitive decline
As forensic evaluators, we are often asked to review and assess the cognition of aging colleagues. The premise often involves a minor mistake, a poor choice of words, or a lapse in judgment. A physician gets reported for having difficulty using a new electronic form, forgetting the dose of a brand new medication, or getting upset in a public setting. Those behaviors often lead to mandatory psychiatric evaluations. Those requirements are often perceived by the provider as an insult, and betrayal by peers despite many years of dedicated work.
Interestingly, we have noticed many independent evaluators and hospital administrators using this opportunity to send many of our colleagues to pasture. There seems to be an unspoken rule among some forensic evaluators that physicians should represent some form of apex of humanity, beyond reproach, and beyond any fault. Those evaluators will point to any mistake on cognitive scales as proof that the aging physician is no longer safe to practice.1 Forgetting that Jill is from Illinois in the Saint Louis University Mental Status Examination test or how to copy a three-dimensional cube on the Montreal Cognitive Assessment can cost someone their license.2 We are also aware of some evaluators even taking the step further and opining that physicians not only need to score adequately but also demonstrate cognition significantly above average to maintain their privileges.
There is certainly significant appeal in setting a high bar for physicians. In many ways, physicians are characterized in society by their astuteness, intelligence, and high ethical standards. Patients place their lives in the hands of physicians and should trust that those physicians have the cognitive tools to heal them. It could almost seem evident that physicians should have high IQs, score perfectly on screening tools for dementia, and complete a mandatory psychiatric evaluation without any reproach. Yet the reality is often more complex.
We have two main concerns about the idea that we should be intransigent with aging physicians. The first one is the vast differential diagnosis for minor mistakes. An aging physician refusing to comply with a new form or yelling at a clerk once when asked to learn a new electronic medical record are inappropriate though not specific assessments for dementia. Similarly, having significant difficulty learning a new electronic medical record system more often is a sign of ageism rather than cognitive impairment. Subsequently, when arriving for their evaluation, forgetting the date is a common sign of anxiety. A relatable analogy would be to compare the mistake with a medical student forgetting part of the anatomy while questioning by an attending during surgery. Imagine such medical students being referred to mandatory psychiatric evaluation when failing to answer a question during rounds.
In our practice, the most common reason for those minor mistakes during our clinical evaluation is anxiety. After all, patients who present for problems completely unrelated to cognitive decline make similar mistakes. Psychological stressors in physicians require no introduction. The concept is so prevalent and pervasive that it has its own name, “burnout.” Imagine having dedicated most of one’s life to a profession then being enumerated a list of complaints, having one’s privileges put on hold, then being told to complete an independent psychiatric evaluation. If burnout is in part caused by a lack of control, unclear job expectations, rapidly changing models of health care, and dysfunctional workplace dynamics, imagine the consequence of such a referral.
The militant evaluator will use jargon to vilify the reviewed physician. If the physician complains too voraciously, he will be described as having signs of frontotemporal dementia. If the physician comes with a written list of rebuttals, he will be described as having memory problems requiring aids. If the physician is demoralized and quiet, he will be described as being withdrawn and apathetic. If the physician refuses to use or has difficulty with new forms or electronic systems, he will be described as having “impaired executive function,” an ominous term that surely should not be associated with a practicing physician.
The second concern arises from problems with the validity and use of diagnoses like mild cognitive impairment (MCI). MCI is considered to be a transition stage when one maintains “normal activities of daily living, and normal general cognitive function.”3 The American Psychiatric Association Textbook of Psychiatry mentions that there are “however, many cases of nonprogressive MCI.” Should a disorder with generally normal cognition and unclear progression to a more severe disorder require one to be dispensed of their privileges? Should any disorder trump an assessment of functioning?
It is our experience that many if not most physicians’ practice of medicine is not a job but a profession that defines who they are. As such, their occupational habits are an overly repeated and ingrained series of maneuvers analogous to so-called muscle memory. This kind of ritualistic pattern is precisely the kind of cognition that may persist as one starts to have some deficits. This requires the evaluator to be particularly sensitive and cognizant that one may still be able to perform professionally despite some mild but notable deficits. While it is facile to diagnose someone with MCI and justify removing their license, a review of their actual clinical skills is, despite being more time consuming, more pertinent to the evaluation.
In practice, we find that many cases lie in a gray area, which is hard to define. Physicians may come to our office for an evaluation after having said something odd at work. Maybe they misdosed a medication on one occasion. Maybe they wrote the wrong year on a chart. However, if the physician was 30 years old, would we consider any one of those incidents significant? As a psychiatrist rather than a physician practicing the specialty in review, it is particularly hard and sometimes unwise to condone or sanction individual incidents.
Evaluators find solace in neuropsychological testing. However the relevance to the safety of patients is unclear. Many of those tests end up being a simple proxy for age. A physicians’ ability to sort words or cards at a certain speed might correlate to cognitive performance but has unclear significance to the ability to care for patients. Using such tests becomes a de facto age limit on the practice of medicine. It seems essential to expand and refine our repertoire of evaluation tools for the assessment of physicians. As when we perform capacity evaluation in the hospital, we enlist the assistance of the treating team in understanding the questions being asked for a patient, medical boards could consider creating independent multidisciplinary teams where psychiatry has a seat along with the relevant specialties of the evaluee. Likewise, the assessment would benefit from a broad review of the physicians’ general practice rather than the more typical review of one or two incidents.
We are promoting a more individualized approach by medical boards to the many issues of the aging physician. Retiring is no longer the dream of older physicians, but rather working in the suitable position where their contributions, clinical experience, and wisdom are positive contributions to patient care. Furthermore, we encourage medical boards to consider more nuanced decisions. A binary approach fits few cases that we see. Surgeons are a prime example of this. A surgeon in the early stages of Parkinsonism may be unfit to perform surgery but very capable of continuing to contribute to the well-being of patients in other forms of clinical work, including postsurgical care that doesn’t involve physical dexterity. Similarly, medical boards could consider other forms of partial restrictions, including a ban on procedures, a ban on hospital privileges, as well as required supervision or working in teams. Accumulated clinical wisdom allows older physicians to be excellent mentors and educators for younger doctors. There is no simple method to predict which physicians may have the early stages of a progressive dementia, and which may have a stable MCI. A yearly reevaluation if there are no further complaints, is the best approach to determine progression of cognitive problems.
Few crises like the current COVID-19 pandemic can better remind us of the importance of the place of medicine in society. Many states have encouraged retired physicians to contribute their knowledge and expertise, putting themselves in particular risk because of their age. It is a good time to be reminded that we owe them significant respect and care when deciding to remove their license. We are encouraged by the diligent efforts of medical boards in supervising our colleagues but warn against zealot evaluators who use this opportunity to force physicians into retirement. We also encourage medical boards to expand their tools and approaches when facing such cases, as mislabeled cognitive diagnoses can be an easy scapegoat of a poor understanding of the more important psychological and biological factors in the evaluation.
References
1. Tariq SH et al. Am J Geriatr Psychiatry. 2006;14:900-10.
2. Nasreddine Z. mocatest.org. Version 2004 Nov 7.
3. Hales RE et al. The American Psychiatric Publishing Textbook of Psychiatry. Washington: American Psychiatric Association Publishing, 2014.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings in chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer, 2019). He has no disclosures.
Dr. Abrams is a forensic psychiatrist and attorney in San Diego. He is an expert in addictionology, behavioral toxicology, psychopharmacology and correctional mental health. He holds a teaching positions at the University of California, San Diego. Among his writings are chapters about competency in national textbooks. Dr. Abrams has no disclosures.
The evaluation of physicians with alleged cognitive decline
The evaluation of physicians with alleged cognitive decline
As forensic evaluators, we are often asked to review and assess the cognition of aging colleagues. The premise often involves a minor mistake, a poor choice of words, or a lapse in judgment. A physician gets reported for having difficulty using a new electronic form, forgetting the dose of a brand new medication, or getting upset in a public setting. Those behaviors often lead to mandatory psychiatric evaluations. Those requirements are often perceived by the provider as an insult, and betrayal by peers despite many years of dedicated work.
Interestingly, we have noticed many independent evaluators and hospital administrators using this opportunity to send many of our colleagues to pasture. There seems to be an unspoken rule among some forensic evaluators that physicians should represent some form of apex of humanity, beyond reproach, and beyond any fault. Those evaluators will point to any mistake on cognitive scales as proof that the aging physician is no longer safe to practice.1 Forgetting that Jill is from Illinois in the Saint Louis University Mental Status Examination test or how to copy a three-dimensional cube on the Montreal Cognitive Assessment can cost someone their license.2 We are also aware of some evaluators even taking the step further and opining that physicians not only need to score adequately but also demonstrate cognition significantly above average to maintain their privileges.
There is certainly significant appeal in setting a high bar for physicians. In many ways, physicians are characterized in society by their astuteness, intelligence, and high ethical standards. Patients place their lives in the hands of physicians and should trust that those physicians have the cognitive tools to heal them. It could almost seem evident that physicians should have high IQs, score perfectly on screening tools for dementia, and complete a mandatory psychiatric evaluation without any reproach. Yet the reality is often more complex.
We have two main concerns about the idea that we should be intransigent with aging physicians. The first one is the vast differential diagnosis for minor mistakes. An aging physician refusing to comply with a new form or yelling at a clerk once when asked to learn a new electronic medical record are inappropriate though not specific assessments for dementia. Similarly, having significant difficulty learning a new electronic medical record system more often is a sign of ageism rather than cognitive impairment. Subsequently, when arriving for their evaluation, forgetting the date is a common sign of anxiety. A relatable analogy would be to compare the mistake with a medical student forgetting part of the anatomy while questioning by an attending during surgery. Imagine such medical students being referred to mandatory psychiatric evaluation when failing to answer a question during rounds.
In our practice, the most common reason for those minor mistakes during our clinical evaluation is anxiety. After all, patients who present for problems completely unrelated to cognitive decline make similar mistakes. Psychological stressors in physicians require no introduction. The concept is so prevalent and pervasive that it has its own name, “burnout.” Imagine having dedicated most of one’s life to a profession then being enumerated a list of complaints, having one’s privileges put on hold, then being told to complete an independent psychiatric evaluation. If burnout is in part caused by a lack of control, unclear job expectations, rapidly changing models of health care, and dysfunctional workplace dynamics, imagine the consequence of such a referral.
The militant evaluator will use jargon to vilify the reviewed physician. If the physician complains too voraciously, he will be described as having signs of frontotemporal dementia. If the physician comes with a written list of rebuttals, he will be described as having memory problems requiring aids. If the physician is demoralized and quiet, he will be described as being withdrawn and apathetic. If the physician refuses to use or has difficulty with new forms or electronic systems, he will be described as having “impaired executive function,” an ominous term that surely should not be associated with a practicing physician.
The second concern arises from problems with the validity and use of diagnoses like mild cognitive impairment (MCI). MCI is considered to be a transition stage when one maintains “normal activities of daily living, and normal general cognitive function.”3 The American Psychiatric Association Textbook of Psychiatry mentions that there are “however, many cases of nonprogressive MCI.” Should a disorder with generally normal cognition and unclear progression to a more severe disorder require one to be dispensed of their privileges? Should any disorder trump an assessment of functioning?
It is our experience that many if not most physicians’ practice of medicine is not a job but a profession that defines who they are. As such, their occupational habits are an overly repeated and ingrained series of maneuvers analogous to so-called muscle memory. This kind of ritualistic pattern is precisely the kind of cognition that may persist as one starts to have some deficits. This requires the evaluator to be particularly sensitive and cognizant that one may still be able to perform professionally despite some mild but notable deficits. While it is facile to diagnose someone with MCI and justify removing their license, a review of their actual clinical skills is, despite being more time consuming, more pertinent to the evaluation.
In practice, we find that many cases lie in a gray area, which is hard to define. Physicians may come to our office for an evaluation after having said something odd at work. Maybe they misdosed a medication on one occasion. Maybe they wrote the wrong year on a chart. However, if the physician was 30 years old, would we consider any one of those incidents significant? As a psychiatrist rather than a physician practicing the specialty in review, it is particularly hard and sometimes unwise to condone or sanction individual incidents.
Evaluators find solace in neuropsychological testing. However the relevance to the safety of patients is unclear. Many of those tests end up being a simple proxy for age. A physicians’ ability to sort words or cards at a certain speed might correlate to cognitive performance but has unclear significance to the ability to care for patients. Using such tests becomes a de facto age limit on the practice of medicine. It seems essential to expand and refine our repertoire of evaluation tools for the assessment of physicians. As when we perform capacity evaluation in the hospital, we enlist the assistance of the treating team in understanding the questions being asked for a patient, medical boards could consider creating independent multidisciplinary teams where psychiatry has a seat along with the relevant specialties of the evaluee. Likewise, the assessment would benefit from a broad review of the physicians’ general practice rather than the more typical review of one or two incidents.
We are promoting a more individualized approach by medical boards to the many issues of the aging physician. Retiring is no longer the dream of older physicians, but rather working in the suitable position where their contributions, clinical experience, and wisdom are positive contributions to patient care. Furthermore, we encourage medical boards to consider more nuanced decisions. A binary approach fits few cases that we see. Surgeons are a prime example of this. A surgeon in the early stages of Parkinsonism may be unfit to perform surgery but very capable of continuing to contribute to the well-being of patients in other forms of clinical work, including postsurgical care that doesn’t involve physical dexterity. Similarly, medical boards could consider other forms of partial restrictions, including a ban on procedures, a ban on hospital privileges, as well as required supervision or working in teams. Accumulated clinical wisdom allows older physicians to be excellent mentors and educators for younger doctors. There is no simple method to predict which physicians may have the early stages of a progressive dementia, and which may have a stable MCI. A yearly reevaluation if there are no further complaints, is the best approach to determine progression of cognitive problems.
Few crises like the current COVID-19 pandemic can better remind us of the importance of the place of medicine in society. Many states have encouraged retired physicians to contribute their knowledge and expertise, putting themselves in particular risk because of their age. It is a good time to be reminded that we owe them significant respect and care when deciding to remove their license. We are encouraged by the diligent efforts of medical boards in supervising our colleagues but warn against zealot evaluators who use this opportunity to force physicians into retirement. We also encourage medical boards to expand their tools and approaches when facing such cases, as mislabeled cognitive diagnoses can be an easy scapegoat of a poor understanding of the more important psychological and biological factors in the evaluation.
References
1. Tariq SH et al. Am J Geriatr Psychiatry. 2006;14:900-10.
2. Nasreddine Z. mocatest.org. Version 2004 Nov 7.
3. Hales RE et al. The American Psychiatric Publishing Textbook of Psychiatry. Washington: American Psychiatric Association Publishing, 2014.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings in chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer, 2019). He has no disclosures.
Dr. Abrams is a forensic psychiatrist and attorney in San Diego. He is an expert in addictionology, behavioral toxicology, psychopharmacology and correctional mental health. He holds a teaching positions at the University of California, San Diego. Among his writings are chapters about competency in national textbooks. Dr. Abrams has no disclosures.
As forensic evaluators, we are often asked to review and assess the cognition of aging colleagues. The premise often involves a minor mistake, a poor choice of words, or a lapse in judgment. A physician gets reported for having difficulty using a new electronic form, forgetting the dose of a brand new medication, or getting upset in a public setting. Those behaviors often lead to mandatory psychiatric evaluations. Those requirements are often perceived by the provider as an insult, and betrayal by peers despite many years of dedicated work.
Interestingly, we have noticed many independent evaluators and hospital administrators using this opportunity to send many of our colleagues to pasture. There seems to be an unspoken rule among some forensic evaluators that physicians should represent some form of apex of humanity, beyond reproach, and beyond any fault. Those evaluators will point to any mistake on cognitive scales as proof that the aging physician is no longer safe to practice.1 Forgetting that Jill is from Illinois in the Saint Louis University Mental Status Examination test or how to copy a three-dimensional cube on the Montreal Cognitive Assessment can cost someone their license.2 We are also aware of some evaluators even taking the step further and opining that physicians not only need to score adequately but also demonstrate cognition significantly above average to maintain their privileges.
There is certainly significant appeal in setting a high bar for physicians. In many ways, physicians are characterized in society by their astuteness, intelligence, and high ethical standards. Patients place their lives in the hands of physicians and should trust that those physicians have the cognitive tools to heal them. It could almost seem evident that physicians should have high IQs, score perfectly on screening tools for dementia, and complete a mandatory psychiatric evaluation without any reproach. Yet the reality is often more complex.
We have two main concerns about the idea that we should be intransigent with aging physicians. The first one is the vast differential diagnosis for minor mistakes. An aging physician refusing to comply with a new form or yelling at a clerk once when asked to learn a new electronic medical record are inappropriate though not specific assessments for dementia. Similarly, having significant difficulty learning a new electronic medical record system more often is a sign of ageism rather than cognitive impairment. Subsequently, when arriving for their evaluation, forgetting the date is a common sign of anxiety. A relatable analogy would be to compare the mistake with a medical student forgetting part of the anatomy while questioning by an attending during surgery. Imagine such medical students being referred to mandatory psychiatric evaluation when failing to answer a question during rounds.
In our practice, the most common reason for those minor mistakes during our clinical evaluation is anxiety. After all, patients who present for problems completely unrelated to cognitive decline make similar mistakes. Psychological stressors in physicians require no introduction. The concept is so prevalent and pervasive that it has its own name, “burnout.” Imagine having dedicated most of one’s life to a profession then being enumerated a list of complaints, having one’s privileges put on hold, then being told to complete an independent psychiatric evaluation. If burnout is in part caused by a lack of control, unclear job expectations, rapidly changing models of health care, and dysfunctional workplace dynamics, imagine the consequence of such a referral.
The militant evaluator will use jargon to vilify the reviewed physician. If the physician complains too voraciously, he will be described as having signs of frontotemporal dementia. If the physician comes with a written list of rebuttals, he will be described as having memory problems requiring aids. If the physician is demoralized and quiet, he will be described as being withdrawn and apathetic. If the physician refuses to use or has difficulty with new forms or electronic systems, he will be described as having “impaired executive function,” an ominous term that surely should not be associated with a practicing physician.
The second concern arises from problems with the validity and use of diagnoses like mild cognitive impairment (MCI). MCI is considered to be a transition stage when one maintains “normal activities of daily living, and normal general cognitive function.”3 The American Psychiatric Association Textbook of Psychiatry mentions that there are “however, many cases of nonprogressive MCI.” Should a disorder with generally normal cognition and unclear progression to a more severe disorder require one to be dispensed of their privileges? Should any disorder trump an assessment of functioning?
It is our experience that many if not most physicians’ practice of medicine is not a job but a profession that defines who they are. As such, their occupational habits are an overly repeated and ingrained series of maneuvers analogous to so-called muscle memory. This kind of ritualistic pattern is precisely the kind of cognition that may persist as one starts to have some deficits. This requires the evaluator to be particularly sensitive and cognizant that one may still be able to perform professionally despite some mild but notable deficits. While it is facile to diagnose someone with MCI and justify removing their license, a review of their actual clinical skills is, despite being more time consuming, more pertinent to the evaluation.
In practice, we find that many cases lie in a gray area, which is hard to define. Physicians may come to our office for an evaluation after having said something odd at work. Maybe they misdosed a medication on one occasion. Maybe they wrote the wrong year on a chart. However, if the physician was 30 years old, would we consider any one of those incidents significant? As a psychiatrist rather than a physician practicing the specialty in review, it is particularly hard and sometimes unwise to condone or sanction individual incidents.
Evaluators find solace in neuropsychological testing. However the relevance to the safety of patients is unclear. Many of those tests end up being a simple proxy for age. A physicians’ ability to sort words or cards at a certain speed might correlate to cognitive performance but has unclear significance to the ability to care for patients. Using such tests becomes a de facto age limit on the practice of medicine. It seems essential to expand and refine our repertoire of evaluation tools for the assessment of physicians. As when we perform capacity evaluation in the hospital, we enlist the assistance of the treating team in understanding the questions being asked for a patient, medical boards could consider creating independent multidisciplinary teams where psychiatry has a seat along with the relevant specialties of the evaluee. Likewise, the assessment would benefit from a broad review of the physicians’ general practice rather than the more typical review of one or two incidents.
We are promoting a more individualized approach by medical boards to the many issues of the aging physician. Retiring is no longer the dream of older physicians, but rather working in the suitable position where their contributions, clinical experience, and wisdom are positive contributions to patient care. Furthermore, we encourage medical boards to consider more nuanced decisions. A binary approach fits few cases that we see. Surgeons are a prime example of this. A surgeon in the early stages of Parkinsonism may be unfit to perform surgery but very capable of continuing to contribute to the well-being of patients in other forms of clinical work, including postsurgical care that doesn’t involve physical dexterity. Similarly, medical boards could consider other forms of partial restrictions, including a ban on procedures, a ban on hospital privileges, as well as required supervision or working in teams. Accumulated clinical wisdom allows older physicians to be excellent mentors and educators for younger doctors. There is no simple method to predict which physicians may have the early stages of a progressive dementia, and which may have a stable MCI. A yearly reevaluation if there are no further complaints, is the best approach to determine progression of cognitive problems.
Few crises like the current COVID-19 pandemic can better remind us of the importance of the place of medicine in society. Many states have encouraged retired physicians to contribute their knowledge and expertise, putting themselves in particular risk because of their age. It is a good time to be reminded that we owe them significant respect and care when deciding to remove their license. We are encouraged by the diligent efforts of medical boards in supervising our colleagues but warn against zealot evaluators who use this opportunity to force physicians into retirement. We also encourage medical boards to expand their tools and approaches when facing such cases, as mislabeled cognitive diagnoses can be an easy scapegoat of a poor understanding of the more important psychological and biological factors in the evaluation.
References
1. Tariq SH et al. Am J Geriatr Psychiatry. 2006;14:900-10.
2. Nasreddine Z. mocatest.org. Version 2004 Nov 7.
3. Hales RE et al. The American Psychiatric Publishing Textbook of Psychiatry. Washington: American Psychiatric Association Publishing, 2014.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings in chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer, 2019). He has no disclosures.
Dr. Abrams is a forensic psychiatrist and attorney in San Diego. He is an expert in addictionology, behavioral toxicology, psychopharmacology and correctional mental health. He holds a teaching positions at the University of California, San Diego. Among his writings are chapters about competency in national textbooks. Dr. Abrams has no disclosures.