User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Developing guidance for patient movement requests
Clear guidelines in policy needed
In hospital medicine, inpatients often request more freedom to move within the hospital complex for a wide range of both benign and potentially concerning reasons, says Sara Stream, MD.
“Hospitalists are often confronted with a dilemma when considering these patient requests: how to promote patient-centered care and autonomy while balancing patient safety, concerns for hospital liability, and the delivery of timely, efficient medical care,” said Dr. Stream, a hospitalist at the VA New York Harbor Healthcare System. Guidance from medical literature and institutional policies on inpatient movement are lacking, so Dr. Stream coauthored an article seeking to develop a framework with which hospitalists can approach patient requests for liberalized movement.
The authors concluded that for a small subset of patients, liberalized movement within the hospital may be clinically feasible: those who are medically, physically, and psychiatrically stable enough to move off their assigned floors without inordinate risk. “For the rest of inpatients, movement outside their monitored inpatient settings may interfere with appropriate medical care and undermine the indications for acute hospitalization,” Dr. Stream said.
Creating institutional policy that identifies relevant clinical, legal and ethical considerations, while incorporating the varied perspectives of physicians, patients, nurses, and hospital administration/risk management will allow requests for increased movement to be evaluated systematically and transparently.
“When patients request liberalized movement, hospitalists should consider the requests systematically: first to identify the intent behind requests, and then to follow a framework to determine whether increased movement would be safe and allow appropriate medical care without creating additional risks,” Dr. Stream said.
Hospitalists should assess and compile individual patient requests for liberalized movement and work with other physicians, nurses, hospital administration, and risk management to devise pertinent policy on this issue that is specific to their institutions. “By eventually creating clear guidelines in policy, health care providers will spend less time managing each individual request to leave the floor because they have a systematic strategy for making consistent decisions about patient movement,” the authors concluded.
Reference
1. Stream S, Alfandre D. “Just Getting a Cup of Coffee” – Considering Best Practices for Patients’ Movement off the Hospital Floor. J Hosp Med. 2019 Nov. doi: 10.12788/jhm.3227.
Clear guidelines in policy needed
Clear guidelines in policy needed
In hospital medicine, inpatients often request more freedom to move within the hospital complex for a wide range of both benign and potentially concerning reasons, says Sara Stream, MD.
“Hospitalists are often confronted with a dilemma when considering these patient requests: how to promote patient-centered care and autonomy while balancing patient safety, concerns for hospital liability, and the delivery of timely, efficient medical care,” said Dr. Stream, a hospitalist at the VA New York Harbor Healthcare System. Guidance from medical literature and institutional policies on inpatient movement are lacking, so Dr. Stream coauthored an article seeking to develop a framework with which hospitalists can approach patient requests for liberalized movement.
The authors concluded that for a small subset of patients, liberalized movement within the hospital may be clinically feasible: those who are medically, physically, and psychiatrically stable enough to move off their assigned floors without inordinate risk. “For the rest of inpatients, movement outside their monitored inpatient settings may interfere with appropriate medical care and undermine the indications for acute hospitalization,” Dr. Stream said.
Creating institutional policy that identifies relevant clinical, legal and ethical considerations, while incorporating the varied perspectives of physicians, patients, nurses, and hospital administration/risk management will allow requests for increased movement to be evaluated systematically and transparently.
“When patients request liberalized movement, hospitalists should consider the requests systematically: first to identify the intent behind requests, and then to follow a framework to determine whether increased movement would be safe and allow appropriate medical care without creating additional risks,” Dr. Stream said.
Hospitalists should assess and compile individual patient requests for liberalized movement and work with other physicians, nurses, hospital administration, and risk management to devise pertinent policy on this issue that is specific to their institutions. “By eventually creating clear guidelines in policy, health care providers will spend less time managing each individual request to leave the floor because they have a systematic strategy for making consistent decisions about patient movement,” the authors concluded.
Reference
1. Stream S, Alfandre D. “Just Getting a Cup of Coffee” – Considering Best Practices for Patients’ Movement off the Hospital Floor. J Hosp Med. 2019 Nov. doi: 10.12788/jhm.3227.
In hospital medicine, inpatients often request more freedom to move within the hospital complex for a wide range of both benign and potentially concerning reasons, says Sara Stream, MD.
“Hospitalists are often confronted with a dilemma when considering these patient requests: how to promote patient-centered care and autonomy while balancing patient safety, concerns for hospital liability, and the delivery of timely, efficient medical care,” said Dr. Stream, a hospitalist at the VA New York Harbor Healthcare System. Guidance from medical literature and institutional policies on inpatient movement are lacking, so Dr. Stream coauthored an article seeking to develop a framework with which hospitalists can approach patient requests for liberalized movement.
The authors concluded that for a small subset of patients, liberalized movement within the hospital may be clinically feasible: those who are medically, physically, and psychiatrically stable enough to move off their assigned floors without inordinate risk. “For the rest of inpatients, movement outside their monitored inpatient settings may interfere with appropriate medical care and undermine the indications for acute hospitalization,” Dr. Stream said.
Creating institutional policy that identifies relevant clinical, legal and ethical considerations, while incorporating the varied perspectives of physicians, patients, nurses, and hospital administration/risk management will allow requests for increased movement to be evaluated systematically and transparently.
“When patients request liberalized movement, hospitalists should consider the requests systematically: first to identify the intent behind requests, and then to follow a framework to determine whether increased movement would be safe and allow appropriate medical care without creating additional risks,” Dr. Stream said.
Hospitalists should assess and compile individual patient requests for liberalized movement and work with other physicians, nurses, hospital administration, and risk management to devise pertinent policy on this issue that is specific to their institutions. “By eventually creating clear guidelines in policy, health care providers will spend less time managing each individual request to leave the floor because they have a systematic strategy for making consistent decisions about patient movement,” the authors concluded.
Reference
1. Stream S, Alfandre D. “Just Getting a Cup of Coffee” – Considering Best Practices for Patients’ Movement off the Hospital Floor. J Hosp Med. 2019 Nov. doi: 10.12788/jhm.3227.
CDC: Opioid prescribing and use rates down since 2010
Trends in opioid prescribing and use from 2010 to 2016 offer some encouragement, but opioid-attributable deaths continued to increase over that period, according to the Centers for Disease Control and Prevention.
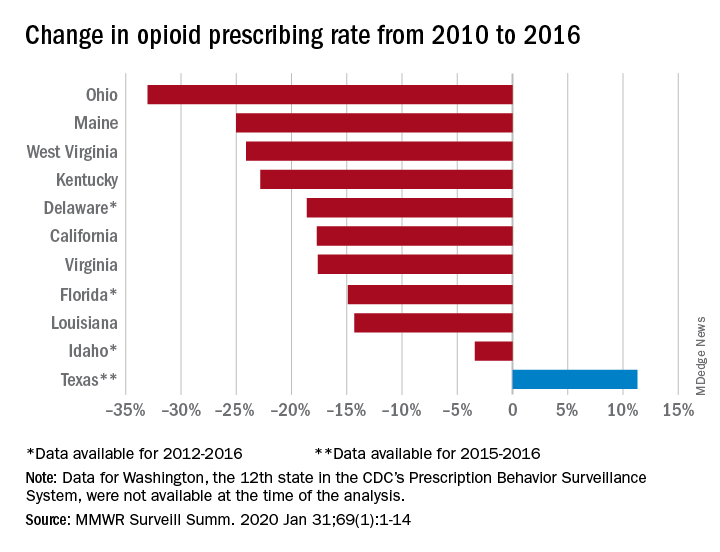
Prescribing rates dropped during that period, as did daily opioid dosage rates and the percentage of patients with high daily opioid dosages, Gail K. Strickler, PhD, of the Institute for Behavioral Health at Brandeis University in Waltham, Mass., and associates wrote in MMWR Surveillance Summaries.
Their analysis involved 11 of the 12 states (Washington was unable to provide data for the analysis) participating in the CDC’s Prescription Behavior Surveillance System, which uses data from the states’ prescription drug monitoring programs. The 11 states represented about 38% of the U.S. population in 2016.
The opioid prescribing rate fell in 10 of those 11 states, with declines varying from 3.4% in Idaho to 33.0% in Ohio. Prescribing went up in Texas by 11.3%, but the state only had data available for 2015 and 2016. Three other states – Delaware, Florida, and Idaho – were limited to data from 2012 to 2016, the investigators noted.
As for the other measures, all states showed declines for the mean daily opioid dosage. Texas had the smallest drop at 2.9% and Florida saw the largest, at 27.4%. All states also had reductions in the percentage of patients with high daily opioid dosage, with decreases varying from 5.7% in Idaho to 43.9% in Louisiana, Dr. Strickler and associates reported. A high daily dosage was defined as at least 90 morphine milligram equivalents for all class II-V opioid drugs.
“Despite these favorable trends ... opioid overdose deaths attributable to the most commonly prescribed opioids, the natural and semisynthetics (e.g., morphine and oxycodone), increased during 2010-2016,” they said.
It is possible that a change in mortality is lagging “behind changes in prescribing behaviors” or that “the trend in deaths related to these types of opioids has been driven by factors other than prescription opioid misuse rates, such as increasing mortality from heroin, which is frequently classified as morphine or found concomitantly with morphine postmortem, and a spike in deaths involving illicitly manufactured fentanyl combined with heroin and prescribed opioids since 2013,” the investigators suggested.
SOURCE: Strickler GK et al. MMWR Surveill Summ. 2020 Jan 31;69(1):1-14.
Trends in opioid prescribing and use from 2010 to 2016 offer some encouragement, but opioid-attributable deaths continued to increase over that period, according to the Centers for Disease Control and Prevention.
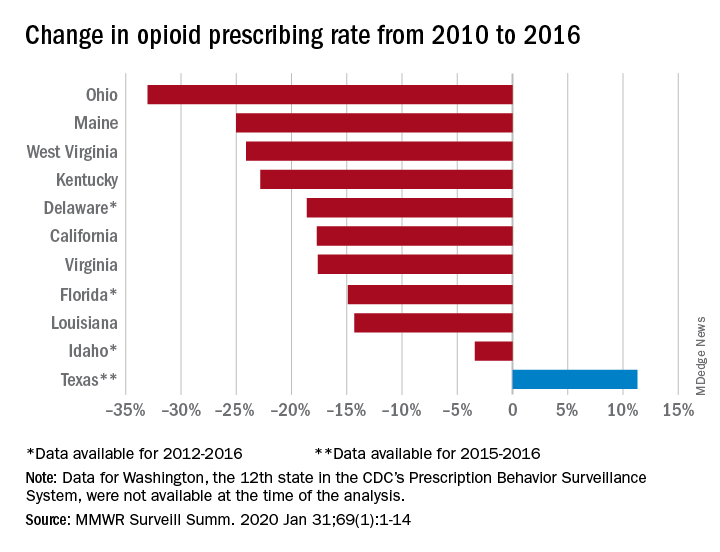
Prescribing rates dropped during that period, as did daily opioid dosage rates and the percentage of patients with high daily opioid dosages, Gail K. Strickler, PhD, of the Institute for Behavioral Health at Brandeis University in Waltham, Mass., and associates wrote in MMWR Surveillance Summaries.
Their analysis involved 11 of the 12 states (Washington was unable to provide data for the analysis) participating in the CDC’s Prescription Behavior Surveillance System, which uses data from the states’ prescription drug monitoring programs. The 11 states represented about 38% of the U.S. population in 2016.
The opioid prescribing rate fell in 10 of those 11 states, with declines varying from 3.4% in Idaho to 33.0% in Ohio. Prescribing went up in Texas by 11.3%, but the state only had data available for 2015 and 2016. Three other states – Delaware, Florida, and Idaho – were limited to data from 2012 to 2016, the investigators noted.
As for the other measures, all states showed declines for the mean daily opioid dosage. Texas had the smallest drop at 2.9% and Florida saw the largest, at 27.4%. All states also had reductions in the percentage of patients with high daily opioid dosage, with decreases varying from 5.7% in Idaho to 43.9% in Louisiana, Dr. Strickler and associates reported. A high daily dosage was defined as at least 90 morphine milligram equivalents for all class II-V opioid drugs.
“Despite these favorable trends ... opioid overdose deaths attributable to the most commonly prescribed opioids, the natural and semisynthetics (e.g., morphine and oxycodone), increased during 2010-2016,” they said.
It is possible that a change in mortality is lagging “behind changes in prescribing behaviors” or that “the trend in deaths related to these types of opioids has been driven by factors other than prescription opioid misuse rates, such as increasing mortality from heroin, which is frequently classified as morphine or found concomitantly with morphine postmortem, and a spike in deaths involving illicitly manufactured fentanyl combined with heroin and prescribed opioids since 2013,” the investigators suggested.
SOURCE: Strickler GK et al. MMWR Surveill Summ. 2020 Jan 31;69(1):1-14.
Trends in opioid prescribing and use from 2010 to 2016 offer some encouragement, but opioid-attributable deaths continued to increase over that period, according to the Centers for Disease Control and Prevention.
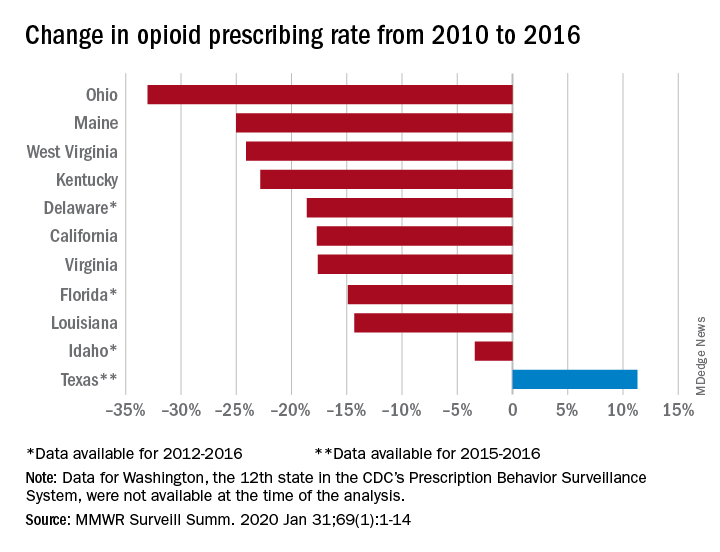
Prescribing rates dropped during that period, as did daily opioid dosage rates and the percentage of patients with high daily opioid dosages, Gail K. Strickler, PhD, of the Institute for Behavioral Health at Brandeis University in Waltham, Mass., and associates wrote in MMWR Surveillance Summaries.
Their analysis involved 11 of the 12 states (Washington was unable to provide data for the analysis) participating in the CDC’s Prescription Behavior Surveillance System, which uses data from the states’ prescription drug monitoring programs. The 11 states represented about 38% of the U.S. population in 2016.
The opioid prescribing rate fell in 10 of those 11 states, with declines varying from 3.4% in Idaho to 33.0% in Ohio. Prescribing went up in Texas by 11.3%, but the state only had data available for 2015 and 2016. Three other states – Delaware, Florida, and Idaho – were limited to data from 2012 to 2016, the investigators noted.
As for the other measures, all states showed declines for the mean daily opioid dosage. Texas had the smallest drop at 2.9% and Florida saw the largest, at 27.4%. All states also had reductions in the percentage of patients with high daily opioid dosage, with decreases varying from 5.7% in Idaho to 43.9% in Louisiana, Dr. Strickler and associates reported. A high daily dosage was defined as at least 90 morphine milligram equivalents for all class II-V opioid drugs.
“Despite these favorable trends ... opioid overdose deaths attributable to the most commonly prescribed opioids, the natural and semisynthetics (e.g., morphine and oxycodone), increased during 2010-2016,” they said.
It is possible that a change in mortality is lagging “behind changes in prescribing behaviors” or that “the trend in deaths related to these types of opioids has been driven by factors other than prescription opioid misuse rates, such as increasing mortality from heroin, which is frequently classified as morphine or found concomitantly with morphine postmortem, and a spike in deaths involving illicitly manufactured fentanyl combined with heroin and prescribed opioids since 2013,” the investigators suggested.
SOURCE: Strickler GK et al. MMWR Surveill Summ. 2020 Jan 31;69(1):1-14.
FROM MMWR SURVEILLANCE SUMMARIES
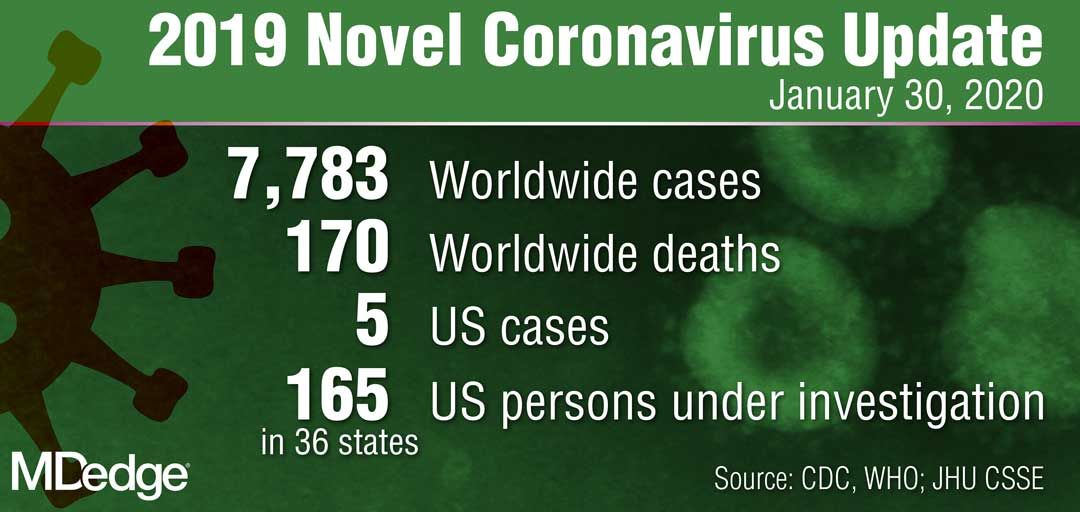
WHO declares public health emergency for novel coronavirus
Amid the rising spread of the 2019 Novel Coronavirus (2019-nCoV),
The declaration was made during a press briefing on Jan. 30 after a week of growing concern and pressure on WHO to designate the virus at a higher emergency level. WHO’s Emergency Committee made the nearly unanimous decision after considering the increasing number of coronavirus cases in China, the rising infections outside of China, and the questionable measures some countries are taking regarding travel, said committee chair Didier Houssin, MD, said during the press conference.
As of Jan. 30, there were 8,236 confirmed cases of the coronavirus in China and 171 deaths, with another 112 cases identified outside of China in 21 other countries.
“Declaring a Public Health Emergency of International Concern is likely to facilitate [WHO’s] leadership role for public health measures, holding countries to account concerning additional measures they may take regarding travel, trade, quarantine or screening, research efforts, global coordination and anticipation of economic impact [and] support to vulnerable states,” Dr. Houssin said during the press conference. “Declaring a PHEIC should certainly not be seen as manifestation of distrust in the Chinese authorities and people which are doing tremendous efforts on the frontlines of this outbreak, with transparency, and let us hope, with success.”
What happens next?
Once a PHEIC is declared, WHO launches a series of steps, including the release of temporary recommendations for the affected country on health measures to implement and guidance for other countries on preventing and reducing the international spread of the disease, WHO spokesman Tarik Jasarevic said in an interview.
“The purpose of declaring a PHEIC is to advise the world on what measures need to be taken to enhance global health security by preventing international transmission of an infectious hazard,” he said.
Following the Jan. 30 press conference, WHO released temporary guidance for China and for other countries regarding identifying, managing, containing, and preventing the virus. China is advised to continue updating the population about the outbreak, continue enhancing its public health measures for containment and surveillance of cases, and to continue collaboration with WHO and other partners to investigate the epidemiology and evolution of the outbreak and share data on all human cases.
Other countries should be prepared for containment, including the active surveillance, early detection, isolation, case management, and prevention of virus transmission and to share full data with WHO, according to the recommendations.
Under the International Health Regulations (IHR), countries are required to share information and data with WHO. Additionally, WHO leaders advised the global community to support low- and middle-income countries with their response to the coronavirus and to facilitate diagnostics, potential vaccines, and therapeutics in these areas.
The IHR requires that countries implementing health measures that go beyond what WHO recommends must send to WHO the public health rationale and justification within 48 hours of their implementation for WHO review, Mr. Jasarevic noted.
“WHO is obliged to share the information about measures and the justification received with other countries involved,” he said.
PHEIC travel and resource impact
Declaration of a PHEIC means WHO will now oversee any travel restrictions made by other countries in response to 2019-nCoV. The agency recommends that countries conduct a risk and cost-benefit analysis before enacting travel restrictions and other countries are required to inform WHO about any travel measures taken.
“Countries will be asked to provide public health justification for any travel or trade measures that are not scientifically based, such as refusal of entry of suspect cases or unaffected persons to affected areas,” Mr. Jasarevic said in an interview.
As far as resources, the PHEIC mechanism is not a fundraising mechanism, but some donors might consider a PHEIC declaration as a trigger for releasing additional funding to respond to the health threat, he said.
Allison T. Chamberlain, PhD, acting director for the Emory Center for Public Health Preparedness and Research at the Emory Rollins School of Public Health in Atlanta, said national governments and nongovernmental aid organizations are among the most affected by a PHEIC because they are looked at to provide assistance to the most heavily affected areas and to bolster public health preparedness within their own borders.
“In terms of resources that are deployed, a Public Health Emergency of International Concern raises levels of international support and commitment to stopping the emergency,” Dr. Chamberlain said in an interview. “By doing so, it gives countries the needed flexibility to release financial resources of their own accord to support things like response teams that might go into heavily affected areas to assist, for instance.”
WHO Director-General Dr. Tedros Adhanom Ghebreyesus stressed that cooperation among countries is key during the PHEIC.
“We can only stop it together,” he said during the press conference. “This is the time for facts, not fear. This is the time for science, not rumors. This is the time for solidarity, not stigma.”
This is the sixth PHEIC declared by WHO in the last 10 years. Such declarations were made for the 2009 H1NI influenza pandemic, the 2014 polio resurgence, the 2014 Ebola outbreak in West Africa, the 2016 Zika virus, and the 2019 Kivu Ebola outbreak in the Democratic Republic of Congo.
Amid the rising spread of the 2019 Novel Coronavirus (2019-nCoV),
The declaration was made during a press briefing on Jan. 30 after a week of growing concern and pressure on WHO to designate the virus at a higher emergency level. WHO’s Emergency Committee made the nearly unanimous decision after considering the increasing number of coronavirus cases in China, the rising infections outside of China, and the questionable measures some countries are taking regarding travel, said committee chair Didier Houssin, MD, said during the press conference.
As of Jan. 30, there were 8,236 confirmed cases of the coronavirus in China and 171 deaths, with another 112 cases identified outside of China in 21 other countries.
“Declaring a Public Health Emergency of International Concern is likely to facilitate [WHO’s] leadership role for public health measures, holding countries to account concerning additional measures they may take regarding travel, trade, quarantine or screening, research efforts, global coordination and anticipation of economic impact [and] support to vulnerable states,” Dr. Houssin said during the press conference. “Declaring a PHEIC should certainly not be seen as manifestation of distrust in the Chinese authorities and people which are doing tremendous efforts on the frontlines of this outbreak, with transparency, and let us hope, with success.”
What happens next?
Once a PHEIC is declared, WHO launches a series of steps, including the release of temporary recommendations for the affected country on health measures to implement and guidance for other countries on preventing and reducing the international spread of the disease, WHO spokesman Tarik Jasarevic said in an interview.
“The purpose of declaring a PHEIC is to advise the world on what measures need to be taken to enhance global health security by preventing international transmission of an infectious hazard,” he said.
Following the Jan. 30 press conference, WHO released temporary guidance for China and for other countries regarding identifying, managing, containing, and preventing the virus. China is advised to continue updating the population about the outbreak, continue enhancing its public health measures for containment and surveillance of cases, and to continue collaboration with WHO and other partners to investigate the epidemiology and evolution of the outbreak and share data on all human cases.
Other countries should be prepared for containment, including the active surveillance, early detection, isolation, case management, and prevention of virus transmission and to share full data with WHO, according to the recommendations.
Under the International Health Regulations (IHR), countries are required to share information and data with WHO. Additionally, WHO leaders advised the global community to support low- and middle-income countries with their response to the coronavirus and to facilitate diagnostics, potential vaccines, and therapeutics in these areas.
The IHR requires that countries implementing health measures that go beyond what WHO recommends must send to WHO the public health rationale and justification within 48 hours of their implementation for WHO review, Mr. Jasarevic noted.
“WHO is obliged to share the information about measures and the justification received with other countries involved,” he said.
PHEIC travel and resource impact
Declaration of a PHEIC means WHO will now oversee any travel restrictions made by other countries in response to 2019-nCoV. The agency recommends that countries conduct a risk and cost-benefit analysis before enacting travel restrictions and other countries are required to inform WHO about any travel measures taken.
“Countries will be asked to provide public health justification for any travel or trade measures that are not scientifically based, such as refusal of entry of suspect cases or unaffected persons to affected areas,” Mr. Jasarevic said in an interview.
As far as resources, the PHEIC mechanism is not a fundraising mechanism, but some donors might consider a PHEIC declaration as a trigger for releasing additional funding to respond to the health threat, he said.
Allison T. Chamberlain, PhD, acting director for the Emory Center for Public Health Preparedness and Research at the Emory Rollins School of Public Health in Atlanta, said national governments and nongovernmental aid organizations are among the most affected by a PHEIC because they are looked at to provide assistance to the most heavily affected areas and to bolster public health preparedness within their own borders.
“In terms of resources that are deployed, a Public Health Emergency of International Concern raises levels of international support and commitment to stopping the emergency,” Dr. Chamberlain said in an interview. “By doing so, it gives countries the needed flexibility to release financial resources of their own accord to support things like response teams that might go into heavily affected areas to assist, for instance.”
WHO Director-General Dr. Tedros Adhanom Ghebreyesus stressed that cooperation among countries is key during the PHEIC.
“We can only stop it together,” he said during the press conference. “This is the time for facts, not fear. This is the time for science, not rumors. This is the time for solidarity, not stigma.”
This is the sixth PHEIC declared by WHO in the last 10 years. Such declarations were made for the 2009 H1NI influenza pandemic, the 2014 polio resurgence, the 2014 Ebola outbreak in West Africa, the 2016 Zika virus, and the 2019 Kivu Ebola outbreak in the Democratic Republic of Congo.
Amid the rising spread of the 2019 Novel Coronavirus (2019-nCoV),
The declaration was made during a press briefing on Jan. 30 after a week of growing concern and pressure on WHO to designate the virus at a higher emergency level. WHO’s Emergency Committee made the nearly unanimous decision after considering the increasing number of coronavirus cases in China, the rising infections outside of China, and the questionable measures some countries are taking regarding travel, said committee chair Didier Houssin, MD, said during the press conference.
As of Jan. 30, there were 8,236 confirmed cases of the coronavirus in China and 171 deaths, with another 112 cases identified outside of China in 21 other countries.
“Declaring a Public Health Emergency of International Concern is likely to facilitate [WHO’s] leadership role for public health measures, holding countries to account concerning additional measures they may take regarding travel, trade, quarantine or screening, research efforts, global coordination and anticipation of economic impact [and] support to vulnerable states,” Dr. Houssin said during the press conference. “Declaring a PHEIC should certainly not be seen as manifestation of distrust in the Chinese authorities and people which are doing tremendous efforts on the frontlines of this outbreak, with transparency, and let us hope, with success.”
What happens next?
Once a PHEIC is declared, WHO launches a series of steps, including the release of temporary recommendations for the affected country on health measures to implement and guidance for other countries on preventing and reducing the international spread of the disease, WHO spokesman Tarik Jasarevic said in an interview.
“The purpose of declaring a PHEIC is to advise the world on what measures need to be taken to enhance global health security by preventing international transmission of an infectious hazard,” he said.
Following the Jan. 30 press conference, WHO released temporary guidance for China and for other countries regarding identifying, managing, containing, and preventing the virus. China is advised to continue updating the population about the outbreak, continue enhancing its public health measures for containment and surveillance of cases, and to continue collaboration with WHO and other partners to investigate the epidemiology and evolution of the outbreak and share data on all human cases.
Other countries should be prepared for containment, including the active surveillance, early detection, isolation, case management, and prevention of virus transmission and to share full data with WHO, according to the recommendations.
Under the International Health Regulations (IHR), countries are required to share information and data with WHO. Additionally, WHO leaders advised the global community to support low- and middle-income countries with their response to the coronavirus and to facilitate diagnostics, potential vaccines, and therapeutics in these areas.
The IHR requires that countries implementing health measures that go beyond what WHO recommends must send to WHO the public health rationale and justification within 48 hours of their implementation for WHO review, Mr. Jasarevic noted.
“WHO is obliged to share the information about measures and the justification received with other countries involved,” he said.
PHEIC travel and resource impact
Declaration of a PHEIC means WHO will now oversee any travel restrictions made by other countries in response to 2019-nCoV. The agency recommends that countries conduct a risk and cost-benefit analysis before enacting travel restrictions and other countries are required to inform WHO about any travel measures taken.
“Countries will be asked to provide public health justification for any travel or trade measures that are not scientifically based, such as refusal of entry of suspect cases or unaffected persons to affected areas,” Mr. Jasarevic said in an interview.
As far as resources, the PHEIC mechanism is not a fundraising mechanism, but some donors might consider a PHEIC declaration as a trigger for releasing additional funding to respond to the health threat, he said.
Allison T. Chamberlain, PhD, acting director for the Emory Center for Public Health Preparedness and Research at the Emory Rollins School of Public Health in Atlanta, said national governments and nongovernmental aid organizations are among the most affected by a PHEIC because they are looked at to provide assistance to the most heavily affected areas and to bolster public health preparedness within their own borders.
“In terms of resources that are deployed, a Public Health Emergency of International Concern raises levels of international support and commitment to stopping the emergency,” Dr. Chamberlain said in an interview. “By doing so, it gives countries the needed flexibility to release financial resources of their own accord to support things like response teams that might go into heavily affected areas to assist, for instance.”
WHO Director-General Dr. Tedros Adhanom Ghebreyesus stressed that cooperation among countries is key during the PHEIC.
“We can only stop it together,” he said during the press conference. “This is the time for facts, not fear. This is the time for science, not rumors. This is the time for solidarity, not stigma.”
This is the sixth PHEIC declared by WHO in the last 10 years. Such declarations were made for the 2009 H1NI influenza pandemic, the 2014 polio resurgence, the 2014 Ebola outbreak in West Africa, the 2016 Zika virus, and the 2019 Kivu Ebola outbreak in the Democratic Republic of Congo.
2019 Novel Coronavirus: Frequently asked questions for clinicians
The 2019 Novel Coronavirus (2019-nCoV) outbreak has unfolded so rapidly that many clinicians are scrambling to stay on top of it. Here are the answers to some frequently asked questions about how to prepare your clinic to respond to this outbreak.
Keep in mind that the outbreak is moving rapidly. Though scientific and epidemiologic knowledge has increased at unprecedented speed, there is much we don’t know, and some of what we think we know will change. Follow the links for the most up-to-date information.
What should our clinic do first?
Plan ahead with the following:
- Develop a plan for office staff to take travel histories from anyone with a respiratory illness and provide training for those who need it. Travel history at present should include asking about travel to China in the past 14 days, specifically Wuhan city or Hubei province.
- Review up-to-date infection control practices with all office staff and provide training for those who need it.
- Take an inventory of supplies of personal protective equipment (PPE), such as gowns, gloves, masks, eye protection, and N95 respirators or powered air-purifying respirators (PAPRs), and order items that are missing or low in stock.
- Fit-test users of N95 masks for maximal effectiveness.
- Plan where a potential patient would be isolated while obtaining expert advice.
- Know whom to contact at the state or local health department if you have a patient with the appropriate travel history.
The Centers for Disease Control and Prevention has prepared a toolkit to help frontline health care professionals prepare for this virus. Providers need to stay up to date on the latest recommendations, as the situation is changing rapidly.
When should I suspect 2019-nCoV illness, and what should I do?
Take the following steps to assess the concern and respond:
- If a patient with respiratory illness has traveled to China in the past 14 days, immediately put a mask on the patient and move the individual to a private room. Use a negative-pressure room if available.
- Put on appropriate PPE (including gloves, gown, eye protection, and mask) for contact, droplet, and airborne precautions. CDC recommends an N95 respirator mask if available, although we don’t know yet if there is true airborne spread.
- Obtain an accurate travel history, including dates and cities. (Tip: Get the correct spelling, as the English spelling of cities in China can cause confusion.)
- If the patient meets the current CDC definition of “person under investigation” or PUI, or if you need guidance on how to proceed, notify infection control (if you are in a facility that has it) and call your state or local health department immediately.
- Contact public health authorities who can help decide whether the patient should be admitted to airborne isolation or monitored at home with appropriate precautions.
What is the definition of a PUI?
The current definition of a PUI is a person who has fever and symptoms of a respiratory infection (cough, shortness of breath) AND who has EITHER been in Wuhan city or Hubei province in the past 14 days OR had close contact with a person either under investigation for 2019-nCoV infection or with confirmed infection. The definition of a PUI will change over time, so check this link.
How can I test for 2019-nCoV?
As of Jan. 30, 2020, testing is by polymerase chain reaction (PCR) and is available in the United States only through the CDC in Atlanta. Testing should soon be available in state health department laboratories. If public health authorities decide that your patient should be tested, they will instruct you on which samples to obtain.
The full sequence of 2019-nCoV has been shared, so some reference laboratories may develop and validate tests, ideally with assistance from CDC. If testing becomes available, make certain that it is a reputable lab that has carefully validated the test.
Should I test for other viruses?
Because the symptoms of 2019-nCoV infection overlap with those of influenza and other respiratory viruses, PCR testing for other viruses should be considered if it will change management (i.e., change the decision to provide influenza antivirals). Use appropriate PPE while collecting specimens, including eye protection. If 2019-nCoV is a consideration, you may want to send the specimen to a hospital lab for testing, where the sample will be processed under a biosafety hood, rather than doing point-of-care testing in the office.
How dangerous is 2019-nCoV?
The current estimated mortality rate is 2%-3%. That is probably an overestimate, as those with severe disease and those who die are more likely to be tested and reported early in an epidemic.
Our current knowledge is based on preliminary reports from hospitalized patients and will probably change. From the speed of spread and a single family cluster, it seems likely that there are milder cases and perhaps asymptomatic infection.
What else do I need to know about coronaviruses?
Coronaviruses are a large and diverse group of viruses, many of which are animal viruses. Before the discovery of the 2019-nCoV, six coronaviruses were known to infect humans. Four of these (HKU1, NL63, OC43, and 229E) predominantly caused mild to moderate upper respiratory illness, and they are thought to be responsible for 10%-30% of colds. They occasionally cause viral pneumonia and can be detected by some commercial multiplex panels.
Two other coronaviruses have caused outbreaks of severe respiratory illness in people: SARS, which emerged in Southern China in 2002, and MERS in the Middle East, in 2012. Unlike SARS, sporadic cases of MERS continue to occur.
The current outbreak is caused by 2019-nCoV, a previously unknown beta coronavirus. It is most closely related (~96%) to a bat virus and shares about 80% sequence homology with SARS CoV.
Andrew T. Pavia, MD, is the George and Esther Gross Presidential Professor and chief of the division of pediatric infectious disease in the department of pediatrics at the University of Utah, Salt Lake City. He is also director of hospital epidemiology and associate director of antimicrobial stewardship at Primary Children’s Hospital, Salt Lake City. Dr. Pavia has disclosed that he has served as a consultant for Genentech, Merck, and Seqirus and that he has served as associate editor for The Sanford Guide.
This article first appeared on Medscape.com.
The 2019 Novel Coronavirus (2019-nCoV) outbreak has unfolded so rapidly that many clinicians are scrambling to stay on top of it. Here are the answers to some frequently asked questions about how to prepare your clinic to respond to this outbreak.
Keep in mind that the outbreak is moving rapidly. Though scientific and epidemiologic knowledge has increased at unprecedented speed, there is much we don’t know, and some of what we think we know will change. Follow the links for the most up-to-date information.
What should our clinic do first?
Plan ahead with the following:
- Develop a plan for office staff to take travel histories from anyone with a respiratory illness and provide training for those who need it. Travel history at present should include asking about travel to China in the past 14 days, specifically Wuhan city or Hubei province.
- Review up-to-date infection control practices with all office staff and provide training for those who need it.
- Take an inventory of supplies of personal protective equipment (PPE), such as gowns, gloves, masks, eye protection, and N95 respirators or powered air-purifying respirators (PAPRs), and order items that are missing or low in stock.
- Fit-test users of N95 masks for maximal effectiveness.
- Plan where a potential patient would be isolated while obtaining expert advice.
- Know whom to contact at the state or local health department if you have a patient with the appropriate travel history.
The Centers for Disease Control and Prevention has prepared a toolkit to help frontline health care professionals prepare for this virus. Providers need to stay up to date on the latest recommendations, as the situation is changing rapidly.
When should I suspect 2019-nCoV illness, and what should I do?
Take the following steps to assess the concern and respond:
- If a patient with respiratory illness has traveled to China in the past 14 days, immediately put a mask on the patient and move the individual to a private room. Use a negative-pressure room if available.
- Put on appropriate PPE (including gloves, gown, eye protection, and mask) for contact, droplet, and airborne precautions. CDC recommends an N95 respirator mask if available, although we don’t know yet if there is true airborne spread.
- Obtain an accurate travel history, including dates and cities. (Tip: Get the correct spelling, as the English spelling of cities in China can cause confusion.)
- If the patient meets the current CDC definition of “person under investigation” or PUI, or if you need guidance on how to proceed, notify infection control (if you are in a facility that has it) and call your state or local health department immediately.
- Contact public health authorities who can help decide whether the patient should be admitted to airborne isolation or monitored at home with appropriate precautions.
What is the definition of a PUI?
The current definition of a PUI is a person who has fever and symptoms of a respiratory infection (cough, shortness of breath) AND who has EITHER been in Wuhan city or Hubei province in the past 14 days OR had close contact with a person either under investigation for 2019-nCoV infection or with confirmed infection. The definition of a PUI will change over time, so check this link.
How can I test for 2019-nCoV?
As of Jan. 30, 2020, testing is by polymerase chain reaction (PCR) and is available in the United States only through the CDC in Atlanta. Testing should soon be available in state health department laboratories. If public health authorities decide that your patient should be tested, they will instruct you on which samples to obtain.
The full sequence of 2019-nCoV has been shared, so some reference laboratories may develop and validate tests, ideally with assistance from CDC. If testing becomes available, make certain that it is a reputable lab that has carefully validated the test.
Should I test for other viruses?
Because the symptoms of 2019-nCoV infection overlap with those of influenza and other respiratory viruses, PCR testing for other viruses should be considered if it will change management (i.e., change the decision to provide influenza antivirals). Use appropriate PPE while collecting specimens, including eye protection. If 2019-nCoV is a consideration, you may want to send the specimen to a hospital lab for testing, where the sample will be processed under a biosafety hood, rather than doing point-of-care testing in the office.
How dangerous is 2019-nCoV?
The current estimated mortality rate is 2%-3%. That is probably an overestimate, as those with severe disease and those who die are more likely to be tested and reported early in an epidemic.
Our current knowledge is based on preliminary reports from hospitalized patients and will probably change. From the speed of spread and a single family cluster, it seems likely that there are milder cases and perhaps asymptomatic infection.
What else do I need to know about coronaviruses?
Coronaviruses are a large and diverse group of viruses, many of which are animal viruses. Before the discovery of the 2019-nCoV, six coronaviruses were known to infect humans. Four of these (HKU1, NL63, OC43, and 229E) predominantly caused mild to moderate upper respiratory illness, and they are thought to be responsible for 10%-30% of colds. They occasionally cause viral pneumonia and can be detected by some commercial multiplex panels.
Two other coronaviruses have caused outbreaks of severe respiratory illness in people: SARS, which emerged in Southern China in 2002, and MERS in the Middle East, in 2012. Unlike SARS, sporadic cases of MERS continue to occur.
The current outbreak is caused by 2019-nCoV, a previously unknown beta coronavirus. It is most closely related (~96%) to a bat virus and shares about 80% sequence homology with SARS CoV.
Andrew T. Pavia, MD, is the George and Esther Gross Presidential Professor and chief of the division of pediatric infectious disease in the department of pediatrics at the University of Utah, Salt Lake City. He is also director of hospital epidemiology and associate director of antimicrobial stewardship at Primary Children’s Hospital, Salt Lake City. Dr. Pavia has disclosed that he has served as a consultant for Genentech, Merck, and Seqirus and that he has served as associate editor for The Sanford Guide.
This article first appeared on Medscape.com.
The 2019 Novel Coronavirus (2019-nCoV) outbreak has unfolded so rapidly that many clinicians are scrambling to stay on top of it. Here are the answers to some frequently asked questions about how to prepare your clinic to respond to this outbreak.
Keep in mind that the outbreak is moving rapidly. Though scientific and epidemiologic knowledge has increased at unprecedented speed, there is much we don’t know, and some of what we think we know will change. Follow the links for the most up-to-date information.
What should our clinic do first?
Plan ahead with the following:
- Develop a plan for office staff to take travel histories from anyone with a respiratory illness and provide training for those who need it. Travel history at present should include asking about travel to China in the past 14 days, specifically Wuhan city or Hubei province.
- Review up-to-date infection control practices with all office staff and provide training for those who need it.
- Take an inventory of supplies of personal protective equipment (PPE), such as gowns, gloves, masks, eye protection, and N95 respirators or powered air-purifying respirators (PAPRs), and order items that are missing or low in stock.
- Fit-test users of N95 masks for maximal effectiveness.
- Plan where a potential patient would be isolated while obtaining expert advice.
- Know whom to contact at the state or local health department if you have a patient with the appropriate travel history.
The Centers for Disease Control and Prevention has prepared a toolkit to help frontline health care professionals prepare for this virus. Providers need to stay up to date on the latest recommendations, as the situation is changing rapidly.
When should I suspect 2019-nCoV illness, and what should I do?
Take the following steps to assess the concern and respond:
- If a patient with respiratory illness has traveled to China in the past 14 days, immediately put a mask on the patient and move the individual to a private room. Use a negative-pressure room if available.
- Put on appropriate PPE (including gloves, gown, eye protection, and mask) for contact, droplet, and airborne precautions. CDC recommends an N95 respirator mask if available, although we don’t know yet if there is true airborne spread.
- Obtain an accurate travel history, including dates and cities. (Tip: Get the correct spelling, as the English spelling of cities in China can cause confusion.)
- If the patient meets the current CDC definition of “person under investigation” or PUI, or if you need guidance on how to proceed, notify infection control (if you are in a facility that has it) and call your state or local health department immediately.
- Contact public health authorities who can help decide whether the patient should be admitted to airborne isolation or monitored at home with appropriate precautions.
What is the definition of a PUI?
The current definition of a PUI is a person who has fever and symptoms of a respiratory infection (cough, shortness of breath) AND who has EITHER been in Wuhan city or Hubei province in the past 14 days OR had close contact with a person either under investigation for 2019-nCoV infection or with confirmed infection. The definition of a PUI will change over time, so check this link.
How can I test for 2019-nCoV?
As of Jan. 30, 2020, testing is by polymerase chain reaction (PCR) and is available in the United States only through the CDC in Atlanta. Testing should soon be available in state health department laboratories. If public health authorities decide that your patient should be tested, they will instruct you on which samples to obtain.
The full sequence of 2019-nCoV has been shared, so some reference laboratories may develop and validate tests, ideally with assistance from CDC. If testing becomes available, make certain that it is a reputable lab that has carefully validated the test.
Should I test for other viruses?
Because the symptoms of 2019-nCoV infection overlap with those of influenza and other respiratory viruses, PCR testing for other viruses should be considered if it will change management (i.e., change the decision to provide influenza antivirals). Use appropriate PPE while collecting specimens, including eye protection. If 2019-nCoV is a consideration, you may want to send the specimen to a hospital lab for testing, where the sample will be processed under a biosafety hood, rather than doing point-of-care testing in the office.
How dangerous is 2019-nCoV?
The current estimated mortality rate is 2%-3%. That is probably an overestimate, as those with severe disease and those who die are more likely to be tested and reported early in an epidemic.
Our current knowledge is based on preliminary reports from hospitalized patients and will probably change. From the speed of spread and a single family cluster, it seems likely that there are milder cases and perhaps asymptomatic infection.
What else do I need to know about coronaviruses?
Coronaviruses are a large and diverse group of viruses, many of which are animal viruses. Before the discovery of the 2019-nCoV, six coronaviruses were known to infect humans. Four of these (HKU1, NL63, OC43, and 229E) predominantly caused mild to moderate upper respiratory illness, and they are thought to be responsible for 10%-30% of colds. They occasionally cause viral pneumonia and can be detected by some commercial multiplex panels.
Two other coronaviruses have caused outbreaks of severe respiratory illness in people: SARS, which emerged in Southern China in 2002, and MERS in the Middle East, in 2012. Unlike SARS, sporadic cases of MERS continue to occur.
The current outbreak is caused by 2019-nCoV, a previously unknown beta coronavirus. It is most closely related (~96%) to a bat virus and shares about 80% sequence homology with SARS CoV.
Andrew T. Pavia, MD, is the George and Esther Gross Presidential Professor and chief of the division of pediatric infectious disease in the department of pediatrics at the University of Utah, Salt Lake City. He is also director of hospital epidemiology and associate director of antimicrobial stewardship at Primary Children’s Hospital, Salt Lake City. Dr. Pavia has disclosed that he has served as a consultant for Genentech, Merck, and Seqirus and that he has served as associate editor for The Sanford Guide.
This article first appeared on Medscape.com.
CDC: First person-to-person spread of novel coronavirus in U.S.
A Chicago woman in her 60s who tested positive for the 2019 Novel Coronavirus (2019-nCoV) after returning from Wuhan, China, earlier this month has infected her husband, becoming the first known instance of person-to-person transmission of the 2019-nCoV in the United States.
“Limited person-to-person spread of this new virus outside of China has already been seen in nine close contacts, where travelers were infected and transmitted the virus to someone else,” Robert R. Redfield, MD, director of the Centers for Disease Control and Prevention, said during a press briefing on Jan. 30, 2020. “However, the full picture of how easy and how sustainable this virus can spread is unclear. Today’s news underscores the important risk-dependent exposure. The vast majority of Americans have not had recent travel to China, where sustained human-to-human transmission is occurring. Individuals who are close personal contacts of cases, though, could have a risk.”
The affected man, also in his 60s, is the spouse of the first confirmed travel-associated case of 2019-nCoV to be reported in the state of Illinois, according to Ngozi O. Ezike, MD, director of the Illinois Department of Public Health. The man had no history of recent travel to China. “This person-to-person spread was between two very close contacts: a wife and husband,” said Dr. Ezike, who added that 21 individuals in the state are under investigation for 2019-nCoV. “The virus is not spreading widely across the community. At this time, we are not recommending that people in the general public take additional precautions such as canceling activities or avoiding going out. While there is concern with this second case, public health officials are actively monitoring close contacts, including health care workers, and we believe that people in Illinois are at low risk.”
Jennifer Layden, MD, state epidemiologist at the Illinois Department of Public Health, said that the infected Chicago woman returned from Wuhan, China on Jan. 13, 2020. She is hospitalized in stable condition “and continues to do well,” Dr. Layden said. “Public health officials have been actively and closely monitoring individuals who had contacts with her, including her husband, who had close contact for symptoms. He recently began reporting symptoms and was immediately admitted to the hospital and placed in an isolation room, where he is in stable condition. We are actively monitoring individuals such as health care workers, household contacts, and others who were in contact with either of the confirmed cases in the goal to contain and reduce the risk of additional transmission.”
Nancy Messonnier, MD, director, National Center for Immunization and Respiratory Diseases, expects that more cases of 2019-nCoV will transpire in the United States.
“More cases means the potential for more person-to-person spread,” Dr. Messonnier said. “We’re trying to strike a balance in our response right now. We want to be aggressive, but we want our actions to be evidence-based and appropriate for the current circumstance. For example, CDC does not currently recommend use of face masks for the general public. The virus is not spreading in the general community.”
A Chicago woman in her 60s who tested positive for the 2019 Novel Coronavirus (2019-nCoV) after returning from Wuhan, China, earlier this month has infected her husband, becoming the first known instance of person-to-person transmission of the 2019-nCoV in the United States.
“Limited person-to-person spread of this new virus outside of China has already been seen in nine close contacts, where travelers were infected and transmitted the virus to someone else,” Robert R. Redfield, MD, director of the Centers for Disease Control and Prevention, said during a press briefing on Jan. 30, 2020. “However, the full picture of how easy and how sustainable this virus can spread is unclear. Today’s news underscores the important risk-dependent exposure. The vast majority of Americans have not had recent travel to China, where sustained human-to-human transmission is occurring. Individuals who are close personal contacts of cases, though, could have a risk.”
The affected man, also in his 60s, is the spouse of the first confirmed travel-associated case of 2019-nCoV to be reported in the state of Illinois, according to Ngozi O. Ezike, MD, director of the Illinois Department of Public Health. The man had no history of recent travel to China. “This person-to-person spread was between two very close contacts: a wife and husband,” said Dr. Ezike, who added that 21 individuals in the state are under investigation for 2019-nCoV. “The virus is not spreading widely across the community. At this time, we are not recommending that people in the general public take additional precautions such as canceling activities or avoiding going out. While there is concern with this second case, public health officials are actively monitoring close contacts, including health care workers, and we believe that people in Illinois are at low risk.”
Jennifer Layden, MD, state epidemiologist at the Illinois Department of Public Health, said that the infected Chicago woman returned from Wuhan, China on Jan. 13, 2020. She is hospitalized in stable condition “and continues to do well,” Dr. Layden said. “Public health officials have been actively and closely monitoring individuals who had contacts with her, including her husband, who had close contact for symptoms. He recently began reporting symptoms and was immediately admitted to the hospital and placed in an isolation room, where he is in stable condition. We are actively monitoring individuals such as health care workers, household contacts, and others who were in contact with either of the confirmed cases in the goal to contain and reduce the risk of additional transmission.”
Nancy Messonnier, MD, director, National Center for Immunization and Respiratory Diseases, expects that more cases of 2019-nCoV will transpire in the United States.
“More cases means the potential for more person-to-person spread,” Dr. Messonnier said. “We’re trying to strike a balance in our response right now. We want to be aggressive, but we want our actions to be evidence-based and appropriate for the current circumstance. For example, CDC does not currently recommend use of face masks for the general public. The virus is not spreading in the general community.”
A Chicago woman in her 60s who tested positive for the 2019 Novel Coronavirus (2019-nCoV) after returning from Wuhan, China, earlier this month has infected her husband, becoming the first known instance of person-to-person transmission of the 2019-nCoV in the United States.
“Limited person-to-person spread of this new virus outside of China has already been seen in nine close contacts, where travelers were infected and transmitted the virus to someone else,” Robert R. Redfield, MD, director of the Centers for Disease Control and Prevention, said during a press briefing on Jan. 30, 2020. “However, the full picture of how easy and how sustainable this virus can spread is unclear. Today’s news underscores the important risk-dependent exposure. The vast majority of Americans have not had recent travel to China, where sustained human-to-human transmission is occurring. Individuals who are close personal contacts of cases, though, could have a risk.”
The affected man, also in his 60s, is the spouse of the first confirmed travel-associated case of 2019-nCoV to be reported in the state of Illinois, according to Ngozi O. Ezike, MD, director of the Illinois Department of Public Health. The man had no history of recent travel to China. “This person-to-person spread was between two very close contacts: a wife and husband,” said Dr. Ezike, who added that 21 individuals in the state are under investigation for 2019-nCoV. “The virus is not spreading widely across the community. At this time, we are not recommending that people in the general public take additional precautions such as canceling activities or avoiding going out. While there is concern with this second case, public health officials are actively monitoring close contacts, including health care workers, and we believe that people in Illinois are at low risk.”
Jennifer Layden, MD, state epidemiologist at the Illinois Department of Public Health, said that the infected Chicago woman returned from Wuhan, China on Jan. 13, 2020. She is hospitalized in stable condition “and continues to do well,” Dr. Layden said. “Public health officials have been actively and closely monitoring individuals who had contacts with her, including her husband, who had close contact for symptoms. He recently began reporting symptoms and was immediately admitted to the hospital and placed in an isolation room, where he is in stable condition. We are actively monitoring individuals such as health care workers, household contacts, and others who were in contact with either of the confirmed cases in the goal to contain and reduce the risk of additional transmission.”
Nancy Messonnier, MD, director, National Center for Immunization and Respiratory Diseases, expects that more cases of 2019-nCoV will transpire in the United States.
“More cases means the potential for more person-to-person spread,” Dr. Messonnier said. “We’re trying to strike a balance in our response right now. We want to be aggressive, but we want our actions to be evidence-based and appropriate for the current circumstance. For example, CDC does not currently recommend use of face masks for the general public. The virus is not spreading in the general community.”
Introduction to population management
Defining the key terms
Traditionally, U.S. health care has operated under a fee-for-service payment model, in which health care providers (such as physicians, hospitals, and health care systems) receive a fee for services such as office visits, hospital stays, procedures, and tests. However, reimbursement discussions are increasingly moving from fee-for-service to value-based, in which payments are tied to managing population health and total cost of care.
Because these changes will impact the entire system all the way down to individual providers, in the upcoming Population Management article series in The Hospitalist, we will discuss the nuances and implications that physicians, executives, and hospitals should be aware of. In this first article, we will examine the impetus for the shift toward population management and introduce common terminology to lay the foundation for the future content.
The traditional model: Fee for service
Under the traditional fee-for-service payment system, health care providers are paid per unit of service. For example, hospitals receive diagnosis-related group (DRG) payments for inpatient stays, and physicians are paid per patient visit. The more services that hospitals or physicians provide, the more money both get paid, without financial consequences for quality outcomes or total cost of care. Total cost of care includes clinic visits, outpatient procedures and tests, hospital and ED visits, home health, skilled nursing facilities, durable medical equipment, and sometimes drugs during an episode of care (for example, a hospital stay plus 90 days after discharge) or over a period of time (for example, a month or a year).
As a result of the fee-for-service payment system, the United States spends more money on health care than other wealthy countries, yet it lags behind other countries on many quality measures, such as disease burden, overall mortality, premature death, and preventable death.1,2
In 2007, the Institute for Healthcare Improvement (IHI) developed the Triple Aim framework that focused on the following:
- Improving the patient experience of care (including quality and satisfaction).
- Improving the health of populations.
- Reducing per capita cost of care.
Both public payers like Medicare and Medicaid, as well as private payers, embraced the Triple Aim to reform how health care is delivered and paid for. As such, health care delivery focus and financial incentives are shifting from managing discrete patient encounters for acute illness to managing population health and total cost of care.
A new approach: Population management
Before diving into population management, it is important to first understand the terms “population” and “population health.” A population can be defined geographically or may include employees of an organization, members of a health plan, or patients receiving care from a specific physician group or health care system. David A. Kindig, MD, PhD, professor emeritus of population health sciences at the University of Wisconsin–Madison, defined population health as “the health outcomes of a group of individuals, including the distribution of such outcomes within the group.”3 Dr. Kindig noted that population health outcomes have many determinants, such as the following:4
- Health care (access, cost, quantity, and quality of health care services).
- Individual behavior (including diet, exercise, and substance abuse).
- Genetics.
- The social environment (education, income, occupation, class, and social support).
- Physical environment (air and water quality, lead exposure, and the design of neighborhoods).
IHI operationally defines population health by measures such as life expectancy, mortality rates, health and functional status, the incidence and/or prevalence of chronic disease, and behavioral and physiological factors such as smoking, physical activity, diet, blood pressure, body mass index, and cholesterol.5
On the other hand, population management is primarily concerned with health care determinants of health and, according to IHI, should be clearly distinguished from population health, which focuses on the broader determinants of health.5
According to Ron Greeno, MD, MHM, one of the founding members and a past-president of the Society of Hospital Medicine, population management is a “global approach of caring for an entire patient population to deliver safe and equitable care and to more intelligently allocate resources to keep people well.”
Population management requires understanding the patient population, which includes risk stratification and redesigning and delivering services that are guided by integrated clinical and administrative data and enabled by information technology.
Cost-sharing payment models
The cornerstone of population management is provider accountability for the cost of care, which can be accomplished through shared-risk models or population-based payments. Let’s take a closer look at each.
Under shared-risk models, providers receive payment based on their performance against cost targets. The goal is to generate cost savings by improving care coordination, engaging patients in shared decision making based on their health goals, and reducing utilization of care that provides little to no value for patients (for example, preventable hospital admissions or unnecessary imaging or procedures).
Cost targets and actual spending are reconciled retrospectively. If providers beat cost targets, they are eligible to keep a share of generated savings based on their performance on selected quality measures. However, if providers’ actual spending exceeds cost targets, they will compensate payers for a portion of the losses. Under one-sided risk models, providers are eligible for shared savings but not financially responsible for losses. Under two-sided risk models, providers are accountable for both savings and losses.
With prospective population-based payments, also known as capitation, providers receive in advance a fixed amount of money per patient per unit of time (for example, per month) that creates a budget to cover the cost of agreed-upon health care services. The prospective payments are risk adjusted and typically tied to performance on selected quality, effectiveness, and patient experience measures.
Professional services capitation arrangements between physician groups and payers cover the cost of physician services including primary care, specialty care, and related laboratory and radiology services. Under global capitation or global payment arrangements, health care systems receive payments that cover the total cost of care for the patient population for a defined period.
Population-based payments create incentives to provide high-quality and efficient care within a set budget.6 If actual cost of delivering services to the defined patient population comes under the budget, the providers will realize savings, but otherwise will encounter losses.
What is next?
Now that we have explained the impetus for population management and the terminology, in the next article in this series we will discuss the current state of population management. We will also delve into a hospitalist’s role and participation so you can be aware of impending changes and ensure you are set up for success, no matter how the payment models evolve.
Dr. Farah is a hospitalist, physician adviser, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. Source: https://www.healthsystemtracker.org/chart-collection/health-spending-u-s-compare-countries/#item-start
2. Source: https://www.healthsystemtracker.org/brief/on-several-indicators-of-healthcare-quality the-u-s-falls-short/
3. Kindig D, Asada Y, Booske B. (2008). A Population Health Framework for Setting National and State Health Goals. JAMA, 299, 2081-2083.
4. Source: https://improvingpopulationhealth.typepad.com/blog/what-are-health-factorsdeterminants.html
5. Source: http://www.ihi.org/communities/blogs/population-health-population-management-terminology-in-us-health-care
6. Source: http://hcp-lan.org/workproducts/apm-refresh-whitepaper-final.pdf
Defining the key terms
Defining the key terms
Traditionally, U.S. health care has operated under a fee-for-service payment model, in which health care providers (such as physicians, hospitals, and health care systems) receive a fee for services such as office visits, hospital stays, procedures, and tests. However, reimbursement discussions are increasingly moving from fee-for-service to value-based, in which payments are tied to managing population health and total cost of care.
Because these changes will impact the entire system all the way down to individual providers, in the upcoming Population Management article series in The Hospitalist, we will discuss the nuances and implications that physicians, executives, and hospitals should be aware of. In this first article, we will examine the impetus for the shift toward population management and introduce common terminology to lay the foundation for the future content.
The traditional model: Fee for service
Under the traditional fee-for-service payment system, health care providers are paid per unit of service. For example, hospitals receive diagnosis-related group (DRG) payments for inpatient stays, and physicians are paid per patient visit. The more services that hospitals or physicians provide, the more money both get paid, without financial consequences for quality outcomes or total cost of care. Total cost of care includes clinic visits, outpatient procedures and tests, hospital and ED visits, home health, skilled nursing facilities, durable medical equipment, and sometimes drugs during an episode of care (for example, a hospital stay plus 90 days after discharge) or over a period of time (for example, a month or a year).
As a result of the fee-for-service payment system, the United States spends more money on health care than other wealthy countries, yet it lags behind other countries on many quality measures, such as disease burden, overall mortality, premature death, and preventable death.1,2
In 2007, the Institute for Healthcare Improvement (IHI) developed the Triple Aim framework that focused on the following:
- Improving the patient experience of care (including quality and satisfaction).
- Improving the health of populations.
- Reducing per capita cost of care.
Both public payers like Medicare and Medicaid, as well as private payers, embraced the Triple Aim to reform how health care is delivered and paid for. As such, health care delivery focus and financial incentives are shifting from managing discrete patient encounters for acute illness to managing population health and total cost of care.
A new approach: Population management
Before diving into population management, it is important to first understand the terms “population” and “population health.” A population can be defined geographically or may include employees of an organization, members of a health plan, or patients receiving care from a specific physician group or health care system. David A. Kindig, MD, PhD, professor emeritus of population health sciences at the University of Wisconsin–Madison, defined population health as “the health outcomes of a group of individuals, including the distribution of such outcomes within the group.”3 Dr. Kindig noted that population health outcomes have many determinants, such as the following:4
- Health care (access, cost, quantity, and quality of health care services).
- Individual behavior (including diet, exercise, and substance abuse).
- Genetics.
- The social environment (education, income, occupation, class, and social support).
- Physical environment (air and water quality, lead exposure, and the design of neighborhoods).
IHI operationally defines population health by measures such as life expectancy, mortality rates, health and functional status, the incidence and/or prevalence of chronic disease, and behavioral and physiological factors such as smoking, physical activity, diet, blood pressure, body mass index, and cholesterol.5
On the other hand, population management is primarily concerned with health care determinants of health and, according to IHI, should be clearly distinguished from population health, which focuses on the broader determinants of health.5
According to Ron Greeno, MD, MHM, one of the founding members and a past-president of the Society of Hospital Medicine, population management is a “global approach of caring for an entire patient population to deliver safe and equitable care and to more intelligently allocate resources to keep people well.”
Population management requires understanding the patient population, which includes risk stratification and redesigning and delivering services that are guided by integrated clinical and administrative data and enabled by information technology.
Cost-sharing payment models
The cornerstone of population management is provider accountability for the cost of care, which can be accomplished through shared-risk models or population-based payments. Let’s take a closer look at each.
Under shared-risk models, providers receive payment based on their performance against cost targets. The goal is to generate cost savings by improving care coordination, engaging patients in shared decision making based on their health goals, and reducing utilization of care that provides little to no value for patients (for example, preventable hospital admissions or unnecessary imaging or procedures).
Cost targets and actual spending are reconciled retrospectively. If providers beat cost targets, they are eligible to keep a share of generated savings based on their performance on selected quality measures. However, if providers’ actual spending exceeds cost targets, they will compensate payers for a portion of the losses. Under one-sided risk models, providers are eligible for shared savings but not financially responsible for losses. Under two-sided risk models, providers are accountable for both savings and losses.
With prospective population-based payments, also known as capitation, providers receive in advance a fixed amount of money per patient per unit of time (for example, per month) that creates a budget to cover the cost of agreed-upon health care services. The prospective payments are risk adjusted and typically tied to performance on selected quality, effectiveness, and patient experience measures.
Professional services capitation arrangements between physician groups and payers cover the cost of physician services including primary care, specialty care, and related laboratory and radiology services. Under global capitation or global payment arrangements, health care systems receive payments that cover the total cost of care for the patient population for a defined period.
Population-based payments create incentives to provide high-quality and efficient care within a set budget.6 If actual cost of delivering services to the defined patient population comes under the budget, the providers will realize savings, but otherwise will encounter losses.
What is next?
Now that we have explained the impetus for population management and the terminology, in the next article in this series we will discuss the current state of population management. We will also delve into a hospitalist’s role and participation so you can be aware of impending changes and ensure you are set up for success, no matter how the payment models evolve.
Dr. Farah is a hospitalist, physician adviser, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. Source: https://www.healthsystemtracker.org/chart-collection/health-spending-u-s-compare-countries/#item-start
2. Source: https://www.healthsystemtracker.org/brief/on-several-indicators-of-healthcare-quality the-u-s-falls-short/
3. Kindig D, Asada Y, Booske B. (2008). A Population Health Framework for Setting National and State Health Goals. JAMA, 299, 2081-2083.
4. Source: https://improvingpopulationhealth.typepad.com/blog/what-are-health-factorsdeterminants.html
5. Source: http://www.ihi.org/communities/blogs/population-health-population-management-terminology-in-us-health-care
6. Source: http://hcp-lan.org/workproducts/apm-refresh-whitepaper-final.pdf
Traditionally, U.S. health care has operated under a fee-for-service payment model, in which health care providers (such as physicians, hospitals, and health care systems) receive a fee for services such as office visits, hospital stays, procedures, and tests. However, reimbursement discussions are increasingly moving from fee-for-service to value-based, in which payments are tied to managing population health and total cost of care.
Because these changes will impact the entire system all the way down to individual providers, in the upcoming Population Management article series in The Hospitalist, we will discuss the nuances and implications that physicians, executives, and hospitals should be aware of. In this first article, we will examine the impetus for the shift toward population management and introduce common terminology to lay the foundation for the future content.
The traditional model: Fee for service
Under the traditional fee-for-service payment system, health care providers are paid per unit of service. For example, hospitals receive diagnosis-related group (DRG) payments for inpatient stays, and physicians are paid per patient visit. The more services that hospitals or physicians provide, the more money both get paid, without financial consequences for quality outcomes or total cost of care. Total cost of care includes clinic visits, outpatient procedures and tests, hospital and ED visits, home health, skilled nursing facilities, durable medical equipment, and sometimes drugs during an episode of care (for example, a hospital stay plus 90 days after discharge) or over a period of time (for example, a month or a year).
As a result of the fee-for-service payment system, the United States spends more money on health care than other wealthy countries, yet it lags behind other countries on many quality measures, such as disease burden, overall mortality, premature death, and preventable death.1,2
In 2007, the Institute for Healthcare Improvement (IHI) developed the Triple Aim framework that focused on the following:
- Improving the patient experience of care (including quality and satisfaction).
- Improving the health of populations.
- Reducing per capita cost of care.
Both public payers like Medicare and Medicaid, as well as private payers, embraced the Triple Aim to reform how health care is delivered and paid for. As such, health care delivery focus and financial incentives are shifting from managing discrete patient encounters for acute illness to managing population health and total cost of care.
A new approach: Population management
Before diving into population management, it is important to first understand the terms “population” and “population health.” A population can be defined geographically or may include employees of an organization, members of a health plan, or patients receiving care from a specific physician group or health care system. David A. Kindig, MD, PhD, professor emeritus of population health sciences at the University of Wisconsin–Madison, defined population health as “the health outcomes of a group of individuals, including the distribution of such outcomes within the group.”3 Dr. Kindig noted that population health outcomes have many determinants, such as the following:4
- Health care (access, cost, quantity, and quality of health care services).
- Individual behavior (including diet, exercise, and substance abuse).
- Genetics.
- The social environment (education, income, occupation, class, and social support).
- Physical environment (air and water quality, lead exposure, and the design of neighborhoods).
IHI operationally defines population health by measures such as life expectancy, mortality rates, health and functional status, the incidence and/or prevalence of chronic disease, and behavioral and physiological factors such as smoking, physical activity, diet, blood pressure, body mass index, and cholesterol.5
On the other hand, population management is primarily concerned with health care determinants of health and, according to IHI, should be clearly distinguished from population health, which focuses on the broader determinants of health.5
According to Ron Greeno, MD, MHM, one of the founding members and a past-president of the Society of Hospital Medicine, population management is a “global approach of caring for an entire patient population to deliver safe and equitable care and to more intelligently allocate resources to keep people well.”
Population management requires understanding the patient population, which includes risk stratification and redesigning and delivering services that are guided by integrated clinical and administrative data and enabled by information technology.
Cost-sharing payment models
The cornerstone of population management is provider accountability for the cost of care, which can be accomplished through shared-risk models or population-based payments. Let’s take a closer look at each.
Under shared-risk models, providers receive payment based on their performance against cost targets. The goal is to generate cost savings by improving care coordination, engaging patients in shared decision making based on their health goals, and reducing utilization of care that provides little to no value for patients (for example, preventable hospital admissions or unnecessary imaging or procedures).
Cost targets and actual spending are reconciled retrospectively. If providers beat cost targets, they are eligible to keep a share of generated savings based on their performance on selected quality measures. However, if providers’ actual spending exceeds cost targets, they will compensate payers for a portion of the losses. Under one-sided risk models, providers are eligible for shared savings but not financially responsible for losses. Under two-sided risk models, providers are accountable for both savings and losses.
With prospective population-based payments, also known as capitation, providers receive in advance a fixed amount of money per patient per unit of time (for example, per month) that creates a budget to cover the cost of agreed-upon health care services. The prospective payments are risk adjusted and typically tied to performance on selected quality, effectiveness, and patient experience measures.
Professional services capitation arrangements between physician groups and payers cover the cost of physician services including primary care, specialty care, and related laboratory and radiology services. Under global capitation or global payment arrangements, health care systems receive payments that cover the total cost of care for the patient population for a defined period.
Population-based payments create incentives to provide high-quality and efficient care within a set budget.6 If actual cost of delivering services to the defined patient population comes under the budget, the providers will realize savings, but otherwise will encounter losses.
What is next?
Now that we have explained the impetus for population management and the terminology, in the next article in this series we will discuss the current state of population management. We will also delve into a hospitalist’s role and participation so you can be aware of impending changes and ensure you are set up for success, no matter how the payment models evolve.
Dr. Farah is a hospitalist, physician adviser, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of The Hospitalist’s editorial advisory board.
References
1. Source: https://www.healthsystemtracker.org/chart-collection/health-spending-u-s-compare-countries/#item-start
2. Source: https://www.healthsystemtracker.org/brief/on-several-indicators-of-healthcare-quality the-u-s-falls-short/
3. Kindig D, Asada Y, Booske B. (2008). A Population Health Framework for Setting National and State Health Goals. JAMA, 299, 2081-2083.
4. Source: https://improvingpopulationhealth.typepad.com/blog/what-are-health-factorsdeterminants.html
5. Source: http://www.ihi.org/communities/blogs/population-health-population-management-terminology-in-us-health-care
6. Source: http://hcp-lan.org/workproducts/apm-refresh-whitepaper-final.pdf
CDC: Risk in U.S. from 2019-nCoV remains low
A total of 165 persons in the United States are under investigation for infection with the 2019 Novel Coronavirus (2019-nCoV), with 68 testing negative and only 5 confirming positive, according to data presented Jan. 29 during a Centers for Disease Control and Prevention (CDC) briefing.
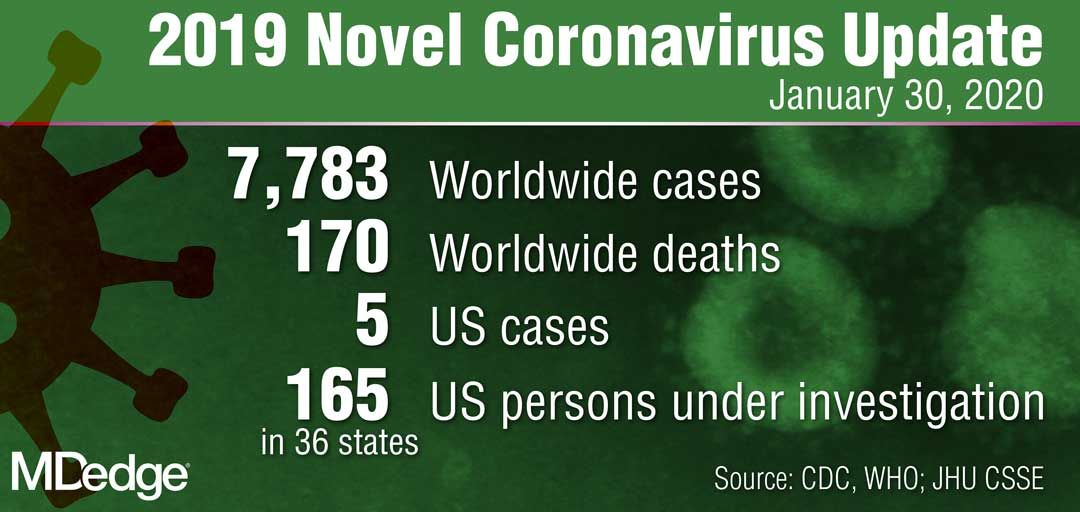
The remaining samples are in transit or are being processed at the CDC for testing, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during the briefing.
“The genetic sequence for all five viruses detected in the United States to date has been uploaded to the CDC website,” she said. “We are working quickly through the process to get the CDC-developed test into the hands of public health partners in the U.S. and internationally.”
Dr. Messonnier reported that the CDC is expanding screening efforts to U.S. ports of entry that house CDC quarantine stations. Also, in collaboration with U.S. Customs and Border Protection, the agency is expanding distribution of travel health education materials to all travelers from China.
“The good news here is that, despite an aggressive public health investigation to find new cases [of 2019-nCoV], we have not,” she said. “The situation in China is concerning, however, we are looking hard here in the U.S. We will continue to be proactive. I still expect that we will find additional cases.”
In another development, the federal government facilitated the return of a plane full of U.S. citizens living in Wuhan, China, to March Air Reserve Force Base in Riverside County, Calif. “We have taken every precaution to ensure their safety while also continuing to protect the health of our nation and the people around them,” Dr. Messonnier said.
All 195 passengers have been screened, monitored, and evaluated by medical personnel “every step of the way,” including before takeoff, during the flight, during a refueling stop in Alaska, and again upon landing at March Air Reserve Force Base on Jan. 28. “All 195 patients are without the symptoms of the novel coronavirus, and all have been assigned living quarters at the Air Force base,” Dr. Messonnier said.
The CDC has launched a second stage of further screening and information gathering from the passengers, who will be offered testing as part of a thorough risk assessment.
“I understand that many people in the U.S. are worried about this virus and whether it will affect them,” Dr. Messonnier said. “Outbreaks like this are always concerning, particularly when a new virus is emerging. But we are well prepared and working closely with federal, state, and local partners to protect our communities and others nationwide from this public health threat. At this time, we continue to believe that the immediate health risk from this new virus to the general American public is low.”
A total of 165 persons in the United States are under investigation for infection with the 2019 Novel Coronavirus (2019-nCoV), with 68 testing negative and only 5 confirming positive, according to data presented Jan. 29 during a Centers for Disease Control and Prevention (CDC) briefing.
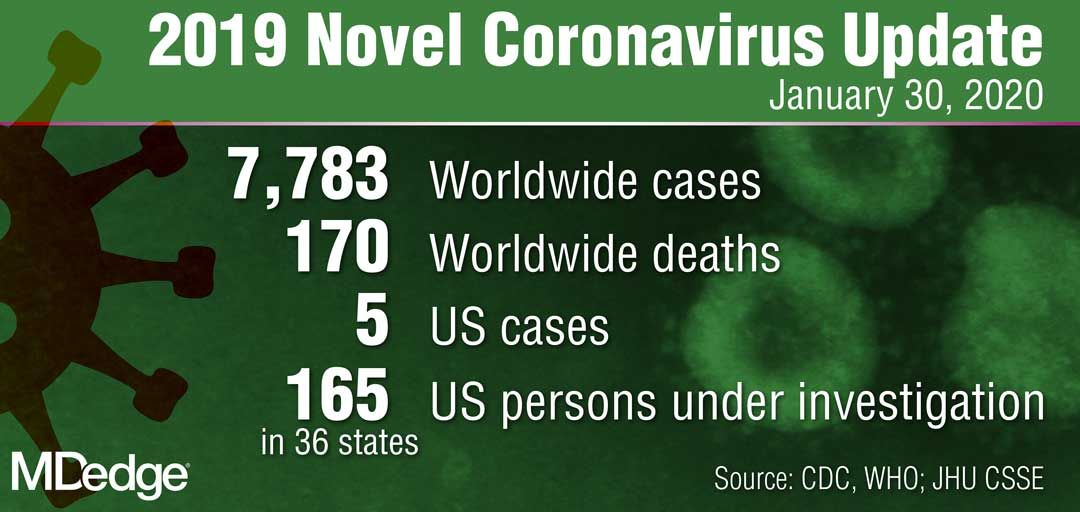
The remaining samples are in transit or are being processed at the CDC for testing, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during the briefing.
“The genetic sequence for all five viruses detected in the United States to date has been uploaded to the CDC website,” she said. “We are working quickly through the process to get the CDC-developed test into the hands of public health partners in the U.S. and internationally.”
Dr. Messonnier reported that the CDC is expanding screening efforts to U.S. ports of entry that house CDC quarantine stations. Also, in collaboration with U.S. Customs and Border Protection, the agency is expanding distribution of travel health education materials to all travelers from China.
“The good news here is that, despite an aggressive public health investigation to find new cases [of 2019-nCoV], we have not,” she said. “The situation in China is concerning, however, we are looking hard here in the U.S. We will continue to be proactive. I still expect that we will find additional cases.”
In another development, the federal government facilitated the return of a plane full of U.S. citizens living in Wuhan, China, to March Air Reserve Force Base in Riverside County, Calif. “We have taken every precaution to ensure their safety while also continuing to protect the health of our nation and the people around them,” Dr. Messonnier said.
All 195 passengers have been screened, monitored, and evaluated by medical personnel “every step of the way,” including before takeoff, during the flight, during a refueling stop in Alaska, and again upon landing at March Air Reserve Force Base on Jan. 28. “All 195 patients are without the symptoms of the novel coronavirus, and all have been assigned living quarters at the Air Force base,” Dr. Messonnier said.
The CDC has launched a second stage of further screening and information gathering from the passengers, who will be offered testing as part of a thorough risk assessment.
“I understand that many people in the U.S. are worried about this virus and whether it will affect them,” Dr. Messonnier said. “Outbreaks like this are always concerning, particularly when a new virus is emerging. But we are well prepared and working closely with federal, state, and local partners to protect our communities and others nationwide from this public health threat. At this time, we continue to believe that the immediate health risk from this new virus to the general American public is low.”
A total of 165 persons in the United States are under investigation for infection with the 2019 Novel Coronavirus (2019-nCoV), with 68 testing negative and only 5 confirming positive, according to data presented Jan. 29 during a Centers for Disease Control and Prevention (CDC) briefing.
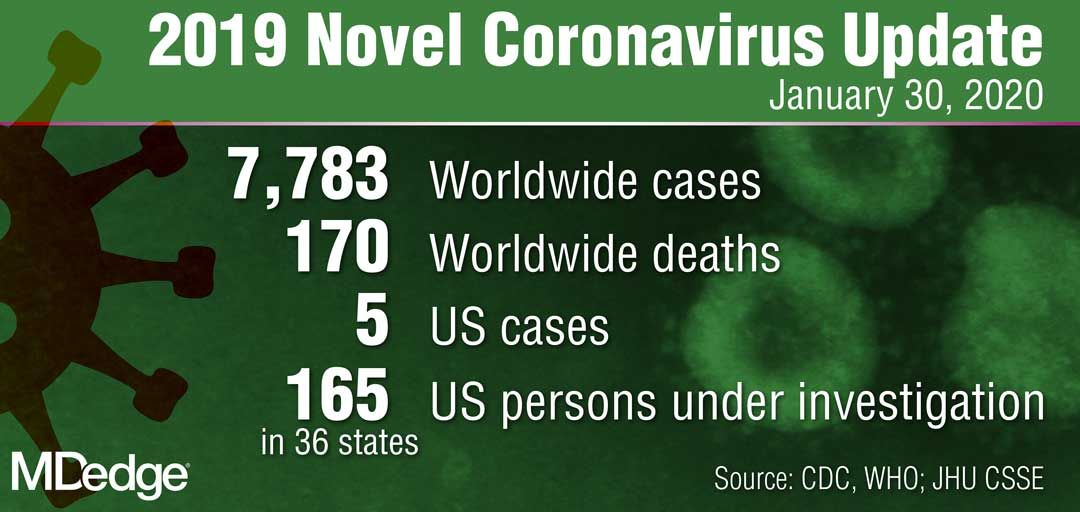
The remaining samples are in transit or are being processed at the CDC for testing, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during the briefing.
“The genetic sequence for all five viruses detected in the United States to date has been uploaded to the CDC website,” she said. “We are working quickly through the process to get the CDC-developed test into the hands of public health partners in the U.S. and internationally.”
Dr. Messonnier reported that the CDC is expanding screening efforts to U.S. ports of entry that house CDC quarantine stations. Also, in collaboration with U.S. Customs and Border Protection, the agency is expanding distribution of travel health education materials to all travelers from China.
“The good news here is that, despite an aggressive public health investigation to find new cases [of 2019-nCoV], we have not,” she said. “The situation in China is concerning, however, we are looking hard here in the U.S. We will continue to be proactive. I still expect that we will find additional cases.”
In another development, the federal government facilitated the return of a plane full of U.S. citizens living in Wuhan, China, to March Air Reserve Force Base in Riverside County, Calif. “We have taken every precaution to ensure their safety while also continuing to protect the health of our nation and the people around them,” Dr. Messonnier said.
All 195 passengers have been screened, monitored, and evaluated by medical personnel “every step of the way,” including before takeoff, during the flight, during a refueling stop in Alaska, and again upon landing at March Air Reserve Force Base on Jan. 28. “All 195 patients are without the symptoms of the novel coronavirus, and all have been assigned living quarters at the Air Force base,” Dr. Messonnier said.
The CDC has launched a second stage of further screening and information gathering from the passengers, who will be offered testing as part of a thorough risk assessment.
“I understand that many people in the U.S. are worried about this virus and whether it will affect them,” Dr. Messonnier said. “Outbreaks like this are always concerning, particularly when a new virus is emerging. But we are well prepared and working closely with federal, state, and local partners to protect our communities and others nationwide from this public health threat. At this time, we continue to believe that the immediate health risk from this new virus to the general American public is low.”
Quick Byte: EHRs and clinician wellness
Concerns abound regarding the workload created by electronic health records (EHRs), but little attention has been paid to the relationship between physicians’ well-being and the volume and sources of in-basket messages they receive.
According to a recent paper in Health Affairs, “in a survey, 36 percent of the physicians reported burnout symptoms, and 29 percent intended to reduce their clinical work time in the upcoming year. Receiving more than the average number of system-generated in-basket messages was associated with 40 percent higher probability of burnout and 38 percent higher probability of intending to reduce clinical work time.”
Reference
1. Tai-Seale M, Dillon EC, Yang Y, et al. Physicians’ Well-Being Linked To In-Basket Messages Generated By Algorithms In Electronic Health Records. Health Aff. 2019 Jul. doi: 10.1377/hlthaff.2018.05509.
Concerns abound regarding the workload created by electronic health records (EHRs), but little attention has been paid to the relationship between physicians’ well-being and the volume and sources of in-basket messages they receive.
According to a recent paper in Health Affairs, “in a survey, 36 percent of the physicians reported burnout symptoms, and 29 percent intended to reduce their clinical work time in the upcoming year. Receiving more than the average number of system-generated in-basket messages was associated with 40 percent higher probability of burnout and 38 percent higher probability of intending to reduce clinical work time.”
Reference
1. Tai-Seale M, Dillon EC, Yang Y, et al. Physicians’ Well-Being Linked To In-Basket Messages Generated By Algorithms In Electronic Health Records. Health Aff. 2019 Jul. doi: 10.1377/hlthaff.2018.05509.
Concerns abound regarding the workload created by electronic health records (EHRs), but little attention has been paid to the relationship between physicians’ well-being and the volume and sources of in-basket messages they receive.
According to a recent paper in Health Affairs, “in a survey, 36 percent of the physicians reported burnout symptoms, and 29 percent intended to reduce their clinical work time in the upcoming year. Receiving more than the average number of system-generated in-basket messages was associated with 40 percent higher probability of burnout and 38 percent higher probability of intending to reduce clinical work time.”
Reference
1. Tai-Seale M, Dillon EC, Yang Y, et al. Physicians’ Well-Being Linked To In-Basket Messages Generated By Algorithms In Electronic Health Records. Health Aff. 2019 Jul. doi: 10.1377/hlthaff.2018.05509.
What 2019’s top five CAD trials tell us
SNOWMASS, COLO. – A repeated theme threading through much of one prominent interventional cardiologist’s personal list of the top five coronary artery disease (CAD) trials of the past year is that aspirin is very often more trouble than it’s worth.
“For some years I’ve been concerned that the only thing that aspirin does [in patients after percutaneous coronary intervention] is increase your risk of bleeding. It doesn’t really provide any additional ischemic protection,” Malcolm R. Bell, MBBS, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
“I’ll remind you that, when we go back to the early stent days, observed Dr. Bell, professor of medicine and vice chair of the department of cardiovascular medicine at the Mayo Clinic in Rochester, Minn.
Here are the key takeaway messages from his five most important randomized trials in CAD during the last year.
AUGUSTUS
For years, cardiologists have grappled with how to best manage high-cardiovascular-risk patients with atrial fibrillation who seem like they might benefit from triple-antithrombotic therapy. AUGUSTUS supplied the answer: Don’t do it. Skip the aspirin and turn instead to a P2Y12 inhibitor plus a non–vitamin K antagonist oral anticoagulant (NOAC), rather than warfarin.
“I would like you to think of triple therapy as a triple threat. That’s really what triple therapy is all about”– a three-pronged threat to patient safety, Dr. Bell commented.
In AUGUSTUS, 4,614 patients with atrial fibrillation and CAD with an acute coronary syndrome (ACS) and/or percutaneous coronary intervention (PCI) in 33 countries were placed on a P2Y12 inhibitor – most often clopidogrel – and randomized double blind to either apixaban (Eliquis) or warfarin, and further to aspirin or placebo, for 6 months of antithrombotic therapy. The strategy of a P2Y12 inhibitor and apixaban without aspirin was the clear winner, resulting in significantly less major bleeding, mortality, and hospitalizations than treatment with a P2Y12 inhibitor and warfarin, with or without aspirin. Most importantly, ischemic event rates didn’t differ between the apixaban and warfarin groups. And patients randomized to aspirin had rates of ischemic events and death or hospitalization similar to placebo-treated controls, meaning aspirin accomplished nothing (N Engl J Med. 2019 Apr 18;380[16]:1509-24).
Dr. Bell noted that a meta-analysis of AUGUSTUS and three smaller randomized trials including more than 10,000 AUGUSTUS-type patients with atrial fibrillation concluded that a treatment strategy utilizing a NOAC and a P2Y12 inhibitor resulted in less bleeding than warfarin plus DAPT, and at no cost in terms of excess ischemic events. Moreover, regimens without aspirin resulted in less intracranial and other major bleeding without any difference in major adverse cardiovascular events (JAMA Cardiol. 2019 Jun 19. doi: 10.1001/jamacardio.2019.1880).
A key message of these four trials is that a NOAC is preferable to warfarin, so much so that, in high-risk patients who are already on warfarin, it’s worth considering a switch to a NOAC.
“And we should really be avoiding DAPT,” Dr. Bell added.
How soon after an ACS and/or PCI should patients with atrial fibrillation stop taking aspirin?
“In AUGUSTUS, randomization occurred at a median of 6 days, so we know that half the patients stopped their aspirin by then. In our own practice, we’re just dropping the aspirin for the most part before the patient leaves the hospital. I think if you leave them with instructions to stop the aspirin in a week’s time or a month’s time it just leads to confusion. And we should also remember that half of the major bleeding after PCI or ACS happens in the first 30 days, so it doesn’t make a lot of sense to say that we should continue it for a month and then drop it,” according to the cardiologist.
SMART-CHOICE and STOPDAPT-2
These two large multicenter studies demonstrate that DAPT can safely be stopped early if needed. SMART-CHOICE from South Korea and STOPDAPT-2 from Japan each randomized roughly 3,000 patients undergoing PCI to 12 months of DAPT or to DAPT for only 3 months or 1 month, respectively, at which point the aspirin was dropped and patients in the abbreviated DAPT arm continued on P2Y12 inhibitor monotherapy, mostly clopidogrel, for the remainder of the 12 months. In the Japanese STOPDAPT-2 trial, 1 month of DAPT proved superior to 12 months of DAPT for the primary composite endpoint of cardiovascular death, MI, stroke, definite stent thrombosis, or major or minor bleeding at 12 months (JAMA. 2019 Jun 25;321[24]:2414-27). In the South Korean SMART-CHOICE trial, 3 months of DAPT was noninferior to 12 months for major adverse cardiac and cerebrovascular events, and superior in terms of bleeding risk (JAMA. 2019 Jun 25;321[24]:2428-37). Of note, roughly half of patients in the two trials were lower-risk individuals undergoing PCI for stable angina.
Dr. Bell noted that, while the TWILIGHT trial (Ticagrelor With or Without Aspirin in High-Risk Patients After PCI) didn’t make his top-five list, it certainly fits well with the two East Asian studies. The TWILIGHT investigators randomized more than 7,000 patients to 12 months of DAPT or discontinuation of aspirin after 3 months. The result: a lower incidence of clinically relevant bleeding with ticagrelor monotherapy, and with no increased risk of death, MI, or stroke, compared with 12 months of DAPT (N Engl J Med. 2019 Nov 21;381[21]:2032-42).
“Again, I would just question what the added value of aspirin is here,” Dr. Bell commented. “Many interventional cardiologists are absolutely terrified of their patients having stent thrombosis, but with second-generation drug-eluting stents – the stents we’re putting in day in and day out – the risk of stent thrombosis is less than 1%. And in these two trials it was less than 0.5%. There’s more risk of having major bleeding events than there is of ischemia, so I think the balance is in favor of preventing bleeding. We know that major bleeding predicts short- and long-term mortality.”
COLCOT
This double-blind trial randomized 4,745 patients within 30 days post MI to low-dose colchicine or placebo on top of excellent rates of background guideline-directed medical therapy. The goal was to see if this anti-inflammatory agent could reduce cardiovascular events independent of any lipid-lowering effect, as was earlier seen with canakinumab in the CANTOS trial. It did so to a statistically significant but relatively modest degree, with a 5.5% rate of the composite cardiovascular events endpoint in the colchicine group and 7.1% in placebo-treated controls (N Engl J Med. 2019 Dec 26;381[26]:2497-505). But Dr. Bell was unimpressed.
“All-cause mortality was identical at 1.8% in both groups. So colchicine is not saving lives. In fact, the only real differences were in stroke – but the study wasn’t powered to look at stroke – and in urgent hospitalization for angina leading to revascularization, which is a soft endpoint,” he observed.
Plus, 2.5% of patients were lost to follow-up, which Dr. Bell considers “a little concerning” in a trial conducted in the current era.
“In my opinion, the evidence that colchicine is effective is weak, and I don’t think really supports the drug’s routine use post MI. We already send these patients out on numerous medications. We have to think about cost/benefit, and if a patient asks me: ‘Is this going to prevent another heart attack or make me live longer?’ I think the unequivocal answer is no,” he said.
These days colchicine is no longer an inexpensive drug, either, at an average cost of $300-$400 per month, the cardiologist added.
COMPLETE
This study randomized more than 4,000 patients with ST-segment elevation MI (STEMI) and multivessel disease to primary PCI of the culprit lesion only or to staged complete revascularization via PCI of all angiographically significant nonculprit lesions. Complete revascularization proved to be the superior strategy, with a 26% reduction in the risk of the composite of cardiovascular death or MI at a median of 3 years (N Engl J Med. 2019 Oct 10;381[15]:1411-21).
The optimal timing of the staged procedure remains unclear, since the study didn’t specify a protocol.
“I’m still a bit uncomfortable doing multivessel PCI at 2 o’clock in the morning in the setting of STEMI in someone I’ve never met before. I don’t think there’s a rush to do anything then. Often in this middle-of-the-night stuff, we miss things or we overinterpret things. I think it’s better to let the patient cool down, get to know them,” according to Dr. Bell.
EXCEL
Publication of the 5-year outcomes of the largest-ever randomized trial of PCI versus coronary artery bypass grafting (CABG) for left main coronary disease has led to furious controversy, with a few of the surgeons involved in the study opting to publically broadcast allegations of misbehavior on the part of the interventional cardiologist study leadership, charges that have been strongly denied.
The actual results are in line with findings reported from smaller randomized trials. At 5 years in EXCEL, there was no significant difference between the PCI and CABG groups in the primary composite endpoint of death, cerebrovascular accident, or MI (N Engl J Med. 2019 Nov 7;381[19]:1820-30). The all-cause mortality rate was 13% in the PCI arm and 9.9% with CABG, but this finding comes with a caveat.
“I’ll emphasize this trial was never powered to look at mortality. Neither were any of the other randomized trials. On the other hand, I don’t think you can necessarily ignore the finding of an absolute 3.1% difference,” Dr. Bell said.
PCI and CABG are both very good, mature therapies for left main disease, in his view. In the setting of more-complex coronary disease in younger patients, he often views the complete revascularization offered by surgery as the preferred option. On the other hand, in an 80-year-old with severe comorbidities, clearly PCI is attractive.
He considers the highly public nature of this interspecialty spat a regrettable black eye for the entire field of cardiovascular medicine. And he predicted that an ongoing outside neutral-party review of the study data and procedures will conclude, as he has, “there was no malfeasance at all in the trial.”
Dr. Bell reported having no financial conflicts regarding his presentation.
SNOWMASS, COLO. – A repeated theme threading through much of one prominent interventional cardiologist’s personal list of the top five coronary artery disease (CAD) trials of the past year is that aspirin is very often more trouble than it’s worth.
“For some years I’ve been concerned that the only thing that aspirin does [in patients after percutaneous coronary intervention] is increase your risk of bleeding. It doesn’t really provide any additional ischemic protection,” Malcolm R. Bell, MBBS, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
“I’ll remind you that, when we go back to the early stent days, observed Dr. Bell, professor of medicine and vice chair of the department of cardiovascular medicine at the Mayo Clinic in Rochester, Minn.
Here are the key takeaway messages from his five most important randomized trials in CAD during the last year.
AUGUSTUS
For years, cardiologists have grappled with how to best manage high-cardiovascular-risk patients with atrial fibrillation who seem like they might benefit from triple-antithrombotic therapy. AUGUSTUS supplied the answer: Don’t do it. Skip the aspirin and turn instead to a P2Y12 inhibitor plus a non–vitamin K antagonist oral anticoagulant (NOAC), rather than warfarin.
“I would like you to think of triple therapy as a triple threat. That’s really what triple therapy is all about”– a three-pronged threat to patient safety, Dr. Bell commented.
In AUGUSTUS, 4,614 patients with atrial fibrillation and CAD with an acute coronary syndrome (ACS) and/or percutaneous coronary intervention (PCI) in 33 countries were placed on a P2Y12 inhibitor – most often clopidogrel – and randomized double blind to either apixaban (Eliquis) or warfarin, and further to aspirin or placebo, for 6 months of antithrombotic therapy. The strategy of a P2Y12 inhibitor and apixaban without aspirin was the clear winner, resulting in significantly less major bleeding, mortality, and hospitalizations than treatment with a P2Y12 inhibitor and warfarin, with or without aspirin. Most importantly, ischemic event rates didn’t differ between the apixaban and warfarin groups. And patients randomized to aspirin had rates of ischemic events and death or hospitalization similar to placebo-treated controls, meaning aspirin accomplished nothing (N Engl J Med. 2019 Apr 18;380[16]:1509-24).
Dr. Bell noted that a meta-analysis of AUGUSTUS and three smaller randomized trials including more than 10,000 AUGUSTUS-type patients with atrial fibrillation concluded that a treatment strategy utilizing a NOAC and a P2Y12 inhibitor resulted in less bleeding than warfarin plus DAPT, and at no cost in terms of excess ischemic events. Moreover, regimens without aspirin resulted in less intracranial and other major bleeding without any difference in major adverse cardiovascular events (JAMA Cardiol. 2019 Jun 19. doi: 10.1001/jamacardio.2019.1880).
A key message of these four trials is that a NOAC is preferable to warfarin, so much so that, in high-risk patients who are already on warfarin, it’s worth considering a switch to a NOAC.
“And we should really be avoiding DAPT,” Dr. Bell added.
How soon after an ACS and/or PCI should patients with atrial fibrillation stop taking aspirin?
“In AUGUSTUS, randomization occurred at a median of 6 days, so we know that half the patients stopped their aspirin by then. In our own practice, we’re just dropping the aspirin for the most part before the patient leaves the hospital. I think if you leave them with instructions to stop the aspirin in a week’s time or a month’s time it just leads to confusion. And we should also remember that half of the major bleeding after PCI or ACS happens in the first 30 days, so it doesn’t make a lot of sense to say that we should continue it for a month and then drop it,” according to the cardiologist.
SMART-CHOICE and STOPDAPT-2
These two large multicenter studies demonstrate that DAPT can safely be stopped early if needed. SMART-CHOICE from South Korea and STOPDAPT-2 from Japan each randomized roughly 3,000 patients undergoing PCI to 12 months of DAPT or to DAPT for only 3 months or 1 month, respectively, at which point the aspirin was dropped and patients in the abbreviated DAPT arm continued on P2Y12 inhibitor monotherapy, mostly clopidogrel, for the remainder of the 12 months. In the Japanese STOPDAPT-2 trial, 1 month of DAPT proved superior to 12 months of DAPT for the primary composite endpoint of cardiovascular death, MI, stroke, definite stent thrombosis, or major or minor bleeding at 12 months (JAMA. 2019 Jun 25;321[24]:2414-27). In the South Korean SMART-CHOICE trial, 3 months of DAPT was noninferior to 12 months for major adverse cardiac and cerebrovascular events, and superior in terms of bleeding risk (JAMA. 2019 Jun 25;321[24]:2428-37). Of note, roughly half of patients in the two trials were lower-risk individuals undergoing PCI for stable angina.
Dr. Bell noted that, while the TWILIGHT trial (Ticagrelor With or Without Aspirin in High-Risk Patients After PCI) didn’t make his top-five list, it certainly fits well with the two East Asian studies. The TWILIGHT investigators randomized more than 7,000 patients to 12 months of DAPT or discontinuation of aspirin after 3 months. The result: a lower incidence of clinically relevant bleeding with ticagrelor monotherapy, and with no increased risk of death, MI, or stroke, compared with 12 months of DAPT (N Engl J Med. 2019 Nov 21;381[21]:2032-42).
“Again, I would just question what the added value of aspirin is here,” Dr. Bell commented. “Many interventional cardiologists are absolutely terrified of their patients having stent thrombosis, but with second-generation drug-eluting stents – the stents we’re putting in day in and day out – the risk of stent thrombosis is less than 1%. And in these two trials it was less than 0.5%. There’s more risk of having major bleeding events than there is of ischemia, so I think the balance is in favor of preventing bleeding. We know that major bleeding predicts short- and long-term mortality.”
COLCOT
This double-blind trial randomized 4,745 patients within 30 days post MI to low-dose colchicine or placebo on top of excellent rates of background guideline-directed medical therapy. The goal was to see if this anti-inflammatory agent could reduce cardiovascular events independent of any lipid-lowering effect, as was earlier seen with canakinumab in the CANTOS trial. It did so to a statistically significant but relatively modest degree, with a 5.5% rate of the composite cardiovascular events endpoint in the colchicine group and 7.1% in placebo-treated controls (N Engl J Med. 2019 Dec 26;381[26]:2497-505). But Dr. Bell was unimpressed.
“All-cause mortality was identical at 1.8% in both groups. So colchicine is not saving lives. In fact, the only real differences were in stroke – but the study wasn’t powered to look at stroke – and in urgent hospitalization for angina leading to revascularization, which is a soft endpoint,” he observed.
Plus, 2.5% of patients were lost to follow-up, which Dr. Bell considers “a little concerning” in a trial conducted in the current era.
“In my opinion, the evidence that colchicine is effective is weak, and I don’t think really supports the drug’s routine use post MI. We already send these patients out on numerous medications. We have to think about cost/benefit, and if a patient asks me: ‘Is this going to prevent another heart attack or make me live longer?’ I think the unequivocal answer is no,” he said.
These days colchicine is no longer an inexpensive drug, either, at an average cost of $300-$400 per month, the cardiologist added.
COMPLETE
This study randomized more than 4,000 patients with ST-segment elevation MI (STEMI) and multivessel disease to primary PCI of the culprit lesion only or to staged complete revascularization via PCI of all angiographically significant nonculprit lesions. Complete revascularization proved to be the superior strategy, with a 26% reduction in the risk of the composite of cardiovascular death or MI at a median of 3 years (N Engl J Med. 2019 Oct 10;381[15]:1411-21).
The optimal timing of the staged procedure remains unclear, since the study didn’t specify a protocol.
“I’m still a bit uncomfortable doing multivessel PCI at 2 o’clock in the morning in the setting of STEMI in someone I’ve never met before. I don’t think there’s a rush to do anything then. Often in this middle-of-the-night stuff, we miss things or we overinterpret things. I think it’s better to let the patient cool down, get to know them,” according to Dr. Bell.
EXCEL
Publication of the 5-year outcomes of the largest-ever randomized trial of PCI versus coronary artery bypass grafting (CABG) for left main coronary disease has led to furious controversy, with a few of the surgeons involved in the study opting to publically broadcast allegations of misbehavior on the part of the interventional cardiologist study leadership, charges that have been strongly denied.
The actual results are in line with findings reported from smaller randomized trials. At 5 years in EXCEL, there was no significant difference between the PCI and CABG groups in the primary composite endpoint of death, cerebrovascular accident, or MI (N Engl J Med. 2019 Nov 7;381[19]:1820-30). The all-cause mortality rate was 13% in the PCI arm and 9.9% with CABG, but this finding comes with a caveat.
“I’ll emphasize this trial was never powered to look at mortality. Neither were any of the other randomized trials. On the other hand, I don’t think you can necessarily ignore the finding of an absolute 3.1% difference,” Dr. Bell said.
PCI and CABG are both very good, mature therapies for left main disease, in his view. In the setting of more-complex coronary disease in younger patients, he often views the complete revascularization offered by surgery as the preferred option. On the other hand, in an 80-year-old with severe comorbidities, clearly PCI is attractive.
He considers the highly public nature of this interspecialty spat a regrettable black eye for the entire field of cardiovascular medicine. And he predicted that an ongoing outside neutral-party review of the study data and procedures will conclude, as he has, “there was no malfeasance at all in the trial.”
Dr. Bell reported having no financial conflicts regarding his presentation.
SNOWMASS, COLO. – A repeated theme threading through much of one prominent interventional cardiologist’s personal list of the top five coronary artery disease (CAD) trials of the past year is that aspirin is very often more trouble than it’s worth.
“For some years I’ve been concerned that the only thing that aspirin does [in patients after percutaneous coronary intervention] is increase your risk of bleeding. It doesn’t really provide any additional ischemic protection,” Malcolm R. Bell, MBBS, said at the annual Cardiovascular Conference at Snowmass sponsored by the American College of Cardiology.
“I’ll remind you that, when we go back to the early stent days, observed Dr. Bell, professor of medicine and vice chair of the department of cardiovascular medicine at the Mayo Clinic in Rochester, Minn.
Here are the key takeaway messages from his five most important randomized trials in CAD during the last year.
AUGUSTUS
For years, cardiologists have grappled with how to best manage high-cardiovascular-risk patients with atrial fibrillation who seem like they might benefit from triple-antithrombotic therapy. AUGUSTUS supplied the answer: Don’t do it. Skip the aspirin and turn instead to a P2Y12 inhibitor plus a non–vitamin K antagonist oral anticoagulant (NOAC), rather than warfarin.
“I would like you to think of triple therapy as a triple threat. That’s really what triple therapy is all about”– a three-pronged threat to patient safety, Dr. Bell commented.
In AUGUSTUS, 4,614 patients with atrial fibrillation and CAD with an acute coronary syndrome (ACS) and/or percutaneous coronary intervention (PCI) in 33 countries were placed on a P2Y12 inhibitor – most often clopidogrel – and randomized double blind to either apixaban (Eliquis) or warfarin, and further to aspirin or placebo, for 6 months of antithrombotic therapy. The strategy of a P2Y12 inhibitor and apixaban without aspirin was the clear winner, resulting in significantly less major bleeding, mortality, and hospitalizations than treatment with a P2Y12 inhibitor and warfarin, with or without aspirin. Most importantly, ischemic event rates didn’t differ between the apixaban and warfarin groups. And patients randomized to aspirin had rates of ischemic events and death or hospitalization similar to placebo-treated controls, meaning aspirin accomplished nothing (N Engl J Med. 2019 Apr 18;380[16]:1509-24).
Dr. Bell noted that a meta-analysis of AUGUSTUS and three smaller randomized trials including more than 10,000 AUGUSTUS-type patients with atrial fibrillation concluded that a treatment strategy utilizing a NOAC and a P2Y12 inhibitor resulted in less bleeding than warfarin plus DAPT, and at no cost in terms of excess ischemic events. Moreover, regimens without aspirin resulted in less intracranial and other major bleeding without any difference in major adverse cardiovascular events (JAMA Cardiol. 2019 Jun 19. doi: 10.1001/jamacardio.2019.1880).
A key message of these four trials is that a NOAC is preferable to warfarin, so much so that, in high-risk patients who are already on warfarin, it’s worth considering a switch to a NOAC.
“And we should really be avoiding DAPT,” Dr. Bell added.
How soon after an ACS and/or PCI should patients with atrial fibrillation stop taking aspirin?
“In AUGUSTUS, randomization occurred at a median of 6 days, so we know that half the patients stopped their aspirin by then. In our own practice, we’re just dropping the aspirin for the most part before the patient leaves the hospital. I think if you leave them with instructions to stop the aspirin in a week’s time or a month’s time it just leads to confusion. And we should also remember that half of the major bleeding after PCI or ACS happens in the first 30 days, so it doesn’t make a lot of sense to say that we should continue it for a month and then drop it,” according to the cardiologist.
SMART-CHOICE and STOPDAPT-2
These two large multicenter studies demonstrate that DAPT can safely be stopped early if needed. SMART-CHOICE from South Korea and STOPDAPT-2 from Japan each randomized roughly 3,000 patients undergoing PCI to 12 months of DAPT or to DAPT for only 3 months or 1 month, respectively, at which point the aspirin was dropped and patients in the abbreviated DAPT arm continued on P2Y12 inhibitor monotherapy, mostly clopidogrel, for the remainder of the 12 months. In the Japanese STOPDAPT-2 trial, 1 month of DAPT proved superior to 12 months of DAPT for the primary composite endpoint of cardiovascular death, MI, stroke, definite stent thrombosis, or major or minor bleeding at 12 months (JAMA. 2019 Jun 25;321[24]:2414-27). In the South Korean SMART-CHOICE trial, 3 months of DAPT was noninferior to 12 months for major adverse cardiac and cerebrovascular events, and superior in terms of bleeding risk (JAMA. 2019 Jun 25;321[24]:2428-37). Of note, roughly half of patients in the two trials were lower-risk individuals undergoing PCI for stable angina.
Dr. Bell noted that, while the TWILIGHT trial (Ticagrelor With or Without Aspirin in High-Risk Patients After PCI) didn’t make his top-five list, it certainly fits well with the two East Asian studies. The TWILIGHT investigators randomized more than 7,000 patients to 12 months of DAPT or discontinuation of aspirin after 3 months. The result: a lower incidence of clinically relevant bleeding with ticagrelor monotherapy, and with no increased risk of death, MI, or stroke, compared with 12 months of DAPT (N Engl J Med. 2019 Nov 21;381[21]:2032-42).
“Again, I would just question what the added value of aspirin is here,” Dr. Bell commented. “Many interventional cardiologists are absolutely terrified of their patients having stent thrombosis, but with second-generation drug-eluting stents – the stents we’re putting in day in and day out – the risk of stent thrombosis is less than 1%. And in these two trials it was less than 0.5%. There’s more risk of having major bleeding events than there is of ischemia, so I think the balance is in favor of preventing bleeding. We know that major bleeding predicts short- and long-term mortality.”
COLCOT
This double-blind trial randomized 4,745 patients within 30 days post MI to low-dose colchicine or placebo on top of excellent rates of background guideline-directed medical therapy. The goal was to see if this anti-inflammatory agent could reduce cardiovascular events independent of any lipid-lowering effect, as was earlier seen with canakinumab in the CANTOS trial. It did so to a statistically significant but relatively modest degree, with a 5.5% rate of the composite cardiovascular events endpoint in the colchicine group and 7.1% in placebo-treated controls (N Engl J Med. 2019 Dec 26;381[26]:2497-505). But Dr. Bell was unimpressed.
“All-cause mortality was identical at 1.8% in both groups. So colchicine is not saving lives. In fact, the only real differences were in stroke – but the study wasn’t powered to look at stroke – and in urgent hospitalization for angina leading to revascularization, which is a soft endpoint,” he observed.
Plus, 2.5% of patients were lost to follow-up, which Dr. Bell considers “a little concerning” in a trial conducted in the current era.
“In my opinion, the evidence that colchicine is effective is weak, and I don’t think really supports the drug’s routine use post MI. We already send these patients out on numerous medications. We have to think about cost/benefit, and if a patient asks me: ‘Is this going to prevent another heart attack or make me live longer?’ I think the unequivocal answer is no,” he said.
These days colchicine is no longer an inexpensive drug, either, at an average cost of $300-$400 per month, the cardiologist added.
COMPLETE
This study randomized more than 4,000 patients with ST-segment elevation MI (STEMI) and multivessel disease to primary PCI of the culprit lesion only or to staged complete revascularization via PCI of all angiographically significant nonculprit lesions. Complete revascularization proved to be the superior strategy, with a 26% reduction in the risk of the composite of cardiovascular death or MI at a median of 3 years (N Engl J Med. 2019 Oct 10;381[15]:1411-21).
The optimal timing of the staged procedure remains unclear, since the study didn’t specify a protocol.
“I’m still a bit uncomfortable doing multivessel PCI at 2 o’clock in the morning in the setting of STEMI in someone I’ve never met before. I don’t think there’s a rush to do anything then. Often in this middle-of-the-night stuff, we miss things or we overinterpret things. I think it’s better to let the patient cool down, get to know them,” according to Dr. Bell.
EXCEL
Publication of the 5-year outcomes of the largest-ever randomized trial of PCI versus coronary artery bypass grafting (CABG) for left main coronary disease has led to furious controversy, with a few of the surgeons involved in the study opting to publically broadcast allegations of misbehavior on the part of the interventional cardiologist study leadership, charges that have been strongly denied.
The actual results are in line with findings reported from smaller randomized trials. At 5 years in EXCEL, there was no significant difference between the PCI and CABG groups in the primary composite endpoint of death, cerebrovascular accident, or MI (N Engl J Med. 2019 Nov 7;381[19]:1820-30). The all-cause mortality rate was 13% in the PCI arm and 9.9% with CABG, but this finding comes with a caveat.
“I’ll emphasize this trial was never powered to look at mortality. Neither were any of the other randomized trials. On the other hand, I don’t think you can necessarily ignore the finding of an absolute 3.1% difference,” Dr. Bell said.
PCI and CABG are both very good, mature therapies for left main disease, in his view. In the setting of more-complex coronary disease in younger patients, he often views the complete revascularization offered by surgery as the preferred option. On the other hand, in an 80-year-old with severe comorbidities, clearly PCI is attractive.
He considers the highly public nature of this interspecialty spat a regrettable black eye for the entire field of cardiovascular medicine. And he predicted that an ongoing outside neutral-party review of the study data and procedures will conclude, as he has, “there was no malfeasance at all in the trial.”
Dr. Bell reported having no financial conflicts regarding his presentation.
REPORTING FROM ACC SNOWMASS 2020
HHS: Coronavirus risk low in U.S., vaccine development underway
U.S. public health officials attempted to stymie concerns about the coronavirus during a press conference on Tuesday,
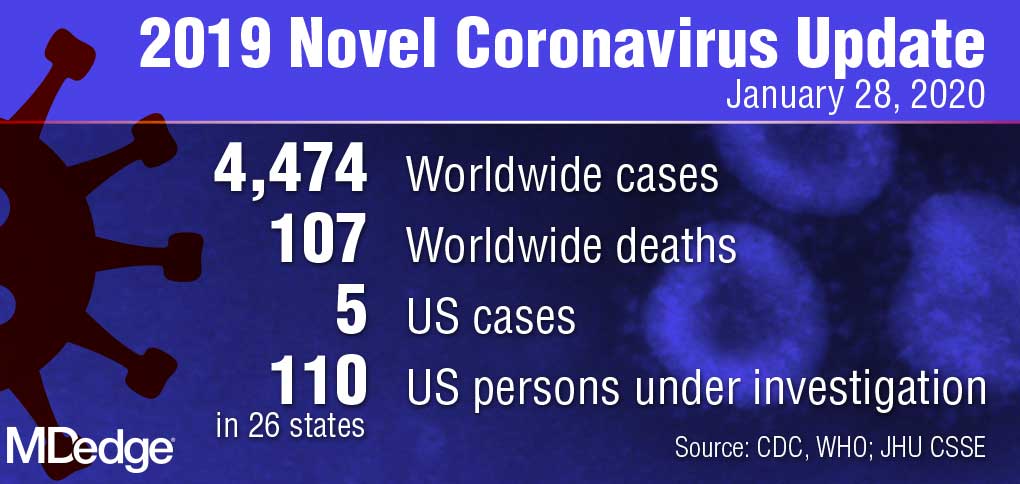
“Right now, there is no spread of this virus in our communities here at home,” Centers for Disease Control and Prevention director Robert Redfield, MD, said during the Jan. 28 press conference. “This is why our current assessment is that the immediate health risk of this new virus to the general public is low in our nation. The coming days and weeks are likely to bring more confirmed cases here and around the world, including the possibility of some person-to-person spreading, but our goal of the ongoing U.S. public health response is to contain this outbreak and prevent sustained spread of the virus in our country.”
During the press conference, Department Health & Human Services Secretary Alex M. Azar II, reiterated there have been only five confirmed U.S. cases of the coronavirus thus far and all were associated with travel to Wuhan, China, where the virus first appeared. The number of confirmed cases in China, meanwhile, has risen to more than 4,500 with about 100 associated deaths.
U.S. health providers should be on the lookout for any patient who has traveled to China recently, particularly to Hubei province, and they should pay close attention to any relevant symptoms, Secretary Azar said during the press conference.
He defended the decision not to declare a public health emergency at this time, stressing that such a move is based on standards and requirements not yet met by the coronavirus.
“It’s important to remember where we are right now; we have five cases in the United States, each of those individuals with direct contact to Wuhan and no person-to-person transmission in the United States,” Secretary Azar said. “I won’t hesitate at all to invoke any authorities that I need to ensure that we’re taking all the steps to protect the American people, but I’ll do it when it’s appropriate under the standards that we have and the authorities that I need.”
In the meantime, a number of efforts are underway by U.S. agencies to assess the nation’s emergency preparedness stockpile, to assist American families in China with evacuation, and to pursue research into diagnostics and a potential vaccine for the virus, Secretary Azar said.
With regard to countermeasures, the CDC has rapidly developed a diagnostic based on the published sequence of the virus, said Anthony Fauci, MD, director for the National Institute of Allergy and Infectious Diseases (NIAID). The National Institutes of Health and the CDC are now working on the development of next-generation diagnostics to better identify the virus in the United States and throughout the world, Dr. Fauci said during the press conference.
Currently, there are no proven therapeutics for the coronavirus infection, Dr. Fauci said. Based on experiences with SARS and MERS, however, researchers are studying certain antiviral drugs that could potentially treat the virus, he said. This includes the antiviral drug remdesivir, which was developed for the treatment of the Ebola virus, and lopinavir/ritonavir (Kaletra), a combination therapy commonly used to treat HIV. In addition, monoclonal antibodies developed during the SARS outbreak are also being studied.
“Given the somewhat close homology between SARS and the new novel coronavirus, there could be some cross reactivity there that could be utilized,” he said.
Most importantly, he said, vaccine development is underway. Since China isolated the virus and published its sequence, U.S. researchers have already analyzed the components and determined an immunogen to be used in a vaccine, Dr. Fauci said. He anticipates moving to a Phase 1 trial within the next 3 months. The trial would then move to Phase 2 after another few more months for safety data.
“What we do from that point will be determined by what has happened with the outbreak over those months,” he said. “We are proceeding as if we will have to deploy a vaccine. In other words, we’re looking at the worst scenario that this becomes a bigger outbreak.”
Federal health officials, however, stressed that more data about infected patients in China is needed for research. HHS has repeatedly offered to send a CDC team to China to help with public health efforts, research, and response, but China has so far declined the offer, Secretary Azar added.
In addition, the CDC has updated its travel advisory in response to the illness. The latest travel guidance recommends that travelers avoid all nonessential travel to all parts of China.
U.S. public health officials attempted to stymie concerns about the coronavirus during a press conference on Tuesday,
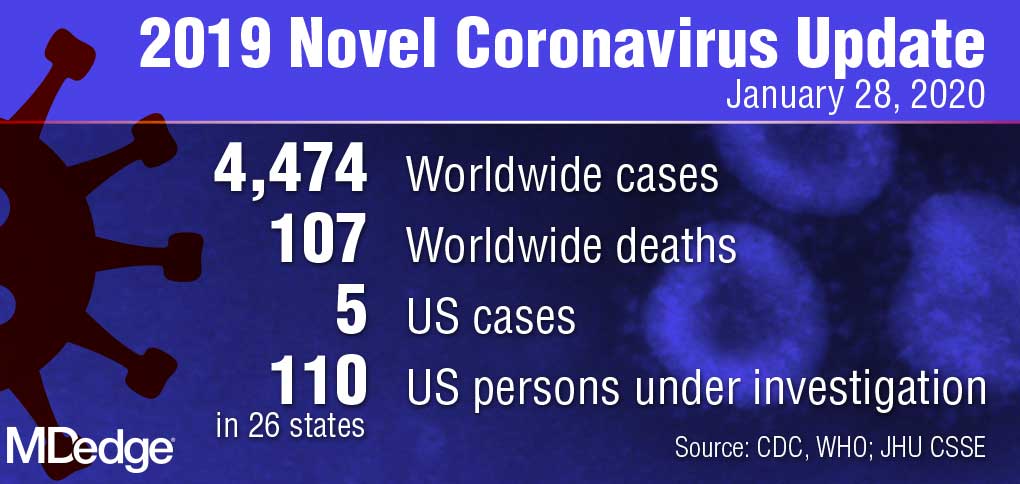
“Right now, there is no spread of this virus in our communities here at home,” Centers for Disease Control and Prevention director Robert Redfield, MD, said during the Jan. 28 press conference. “This is why our current assessment is that the immediate health risk of this new virus to the general public is low in our nation. The coming days and weeks are likely to bring more confirmed cases here and around the world, including the possibility of some person-to-person spreading, but our goal of the ongoing U.S. public health response is to contain this outbreak and prevent sustained spread of the virus in our country.”
During the press conference, Department Health & Human Services Secretary Alex M. Azar II, reiterated there have been only five confirmed U.S. cases of the coronavirus thus far and all were associated with travel to Wuhan, China, where the virus first appeared. The number of confirmed cases in China, meanwhile, has risen to more than 4,500 with about 100 associated deaths.
U.S. health providers should be on the lookout for any patient who has traveled to China recently, particularly to Hubei province, and they should pay close attention to any relevant symptoms, Secretary Azar said during the press conference.
He defended the decision not to declare a public health emergency at this time, stressing that such a move is based on standards and requirements not yet met by the coronavirus.
“It’s important to remember where we are right now; we have five cases in the United States, each of those individuals with direct contact to Wuhan and no person-to-person transmission in the United States,” Secretary Azar said. “I won’t hesitate at all to invoke any authorities that I need to ensure that we’re taking all the steps to protect the American people, but I’ll do it when it’s appropriate under the standards that we have and the authorities that I need.”
In the meantime, a number of efforts are underway by U.S. agencies to assess the nation’s emergency preparedness stockpile, to assist American families in China with evacuation, and to pursue research into diagnostics and a potential vaccine for the virus, Secretary Azar said.
With regard to countermeasures, the CDC has rapidly developed a diagnostic based on the published sequence of the virus, said Anthony Fauci, MD, director for the National Institute of Allergy and Infectious Diseases (NIAID). The National Institutes of Health and the CDC are now working on the development of next-generation diagnostics to better identify the virus in the United States and throughout the world, Dr. Fauci said during the press conference.
Currently, there are no proven therapeutics for the coronavirus infection, Dr. Fauci said. Based on experiences with SARS and MERS, however, researchers are studying certain antiviral drugs that could potentially treat the virus, he said. This includes the antiviral drug remdesivir, which was developed for the treatment of the Ebola virus, and lopinavir/ritonavir (Kaletra), a combination therapy commonly used to treat HIV. In addition, monoclonal antibodies developed during the SARS outbreak are also being studied.
“Given the somewhat close homology between SARS and the new novel coronavirus, there could be some cross reactivity there that could be utilized,” he said.
Most importantly, he said, vaccine development is underway. Since China isolated the virus and published its sequence, U.S. researchers have already analyzed the components and determined an immunogen to be used in a vaccine, Dr. Fauci said. He anticipates moving to a Phase 1 trial within the next 3 months. The trial would then move to Phase 2 after another few more months for safety data.
“What we do from that point will be determined by what has happened with the outbreak over those months,” he said. “We are proceeding as if we will have to deploy a vaccine. In other words, we’re looking at the worst scenario that this becomes a bigger outbreak.”
Federal health officials, however, stressed that more data about infected patients in China is needed for research. HHS has repeatedly offered to send a CDC team to China to help with public health efforts, research, and response, but China has so far declined the offer, Secretary Azar added.
In addition, the CDC has updated its travel advisory in response to the illness. The latest travel guidance recommends that travelers avoid all nonessential travel to all parts of China.
U.S. public health officials attempted to stymie concerns about the coronavirus during a press conference on Tuesday,
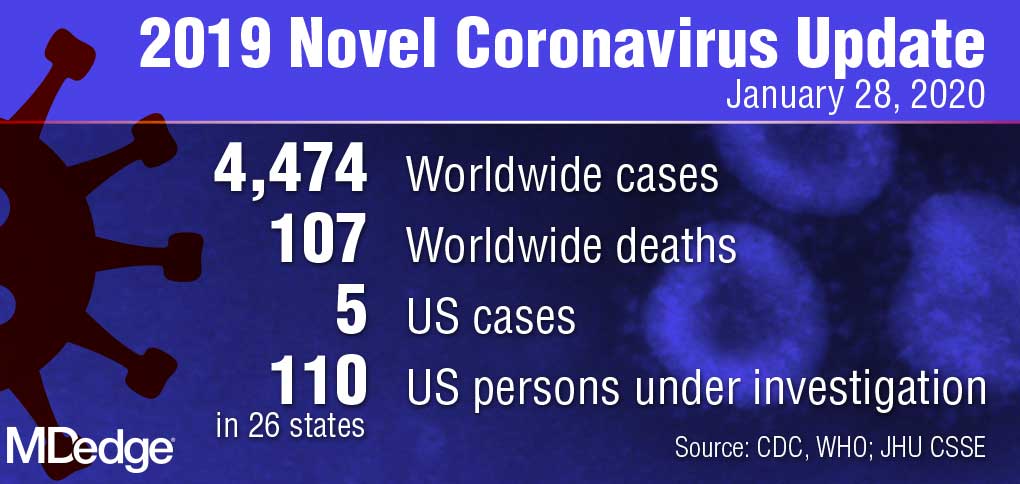
“Right now, there is no spread of this virus in our communities here at home,” Centers for Disease Control and Prevention director Robert Redfield, MD, said during the Jan. 28 press conference. “This is why our current assessment is that the immediate health risk of this new virus to the general public is low in our nation. The coming days and weeks are likely to bring more confirmed cases here and around the world, including the possibility of some person-to-person spreading, but our goal of the ongoing U.S. public health response is to contain this outbreak and prevent sustained spread of the virus in our country.”
During the press conference, Department Health & Human Services Secretary Alex M. Azar II, reiterated there have been only five confirmed U.S. cases of the coronavirus thus far and all were associated with travel to Wuhan, China, where the virus first appeared. The number of confirmed cases in China, meanwhile, has risen to more than 4,500 with about 100 associated deaths.
U.S. health providers should be on the lookout for any patient who has traveled to China recently, particularly to Hubei province, and they should pay close attention to any relevant symptoms, Secretary Azar said during the press conference.
He defended the decision not to declare a public health emergency at this time, stressing that such a move is based on standards and requirements not yet met by the coronavirus.
“It’s important to remember where we are right now; we have five cases in the United States, each of those individuals with direct contact to Wuhan and no person-to-person transmission in the United States,” Secretary Azar said. “I won’t hesitate at all to invoke any authorities that I need to ensure that we’re taking all the steps to protect the American people, but I’ll do it when it’s appropriate under the standards that we have and the authorities that I need.”
In the meantime, a number of efforts are underway by U.S. agencies to assess the nation’s emergency preparedness stockpile, to assist American families in China with evacuation, and to pursue research into diagnostics and a potential vaccine for the virus, Secretary Azar said.
With regard to countermeasures, the CDC has rapidly developed a diagnostic based on the published sequence of the virus, said Anthony Fauci, MD, director for the National Institute of Allergy and Infectious Diseases (NIAID). The National Institutes of Health and the CDC are now working on the development of next-generation diagnostics to better identify the virus in the United States and throughout the world, Dr. Fauci said during the press conference.
Currently, there are no proven therapeutics for the coronavirus infection, Dr. Fauci said. Based on experiences with SARS and MERS, however, researchers are studying certain antiviral drugs that could potentially treat the virus, he said. This includes the antiviral drug remdesivir, which was developed for the treatment of the Ebola virus, and lopinavir/ritonavir (Kaletra), a combination therapy commonly used to treat HIV. In addition, monoclonal antibodies developed during the SARS outbreak are also being studied.
“Given the somewhat close homology between SARS and the new novel coronavirus, there could be some cross reactivity there that could be utilized,” he said.
Most importantly, he said, vaccine development is underway. Since China isolated the virus and published its sequence, U.S. researchers have already analyzed the components and determined an immunogen to be used in a vaccine, Dr. Fauci said. He anticipates moving to a Phase 1 trial within the next 3 months. The trial would then move to Phase 2 after another few more months for safety data.
“What we do from that point will be determined by what has happened with the outbreak over those months,” he said. “We are proceeding as if we will have to deploy a vaccine. In other words, we’re looking at the worst scenario that this becomes a bigger outbreak.”
Federal health officials, however, stressed that more data about infected patients in China is needed for research. HHS has repeatedly offered to send a CDC team to China to help with public health efforts, research, and response, but China has so far declined the offer, Secretary Azar added.
In addition, the CDC has updated its travel advisory in response to the illness. The latest travel guidance recommends that travelers avoid all nonessential travel to all parts of China.