User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Noncardiac surgery has 7% covert stroke rate in elderly
HONOLULU – Covert strokes are relatively common in elderly patients who undergo noncardiac surgery, with a 7% incidence among a group of prospectively followed but generally unselected patients in a multicenter, international study.
By definition, these covert strokes were acutely asymptomatic, but showed evidence of clinical effects during the subsequent year. Twelve months after surgery, patients with acute, perioperative covert strokes found by systematic collection of postoperative MRI brain scans had a twofold increased rate of cognitive decline and a greater than twofold increased rate of delirium, compared with the patients who did not have evidence of a covert stroke, Marko Mrkobrada, MD, said at the International Stroke Conference sponsored by the American Heart Association.
The message from these findings is that, when elderly patients exhibit confusion or delirium after noncardiac surgery, their physicians should have a high index of suspicion that a covert stroke may have occurred, Dr. Mrkobrada said in a video interview. It’s possible that typical stroke symptoms do not appear in many of the covert stroke patients because they are masked in the immediate postoperative period, he added.
Right now, the only way to screen for a covert stroke is with a brain MR, a test that generally costs several hundred dollars, which is too expensive for routine screening. Dr. Mrkobrada said that his team hopes further study will identify a biomarker that can flag patients with a covert stroke at a lower cost. For example, colleagues of Dr. Mrkobrada have successfully used high-sensitivity troponin T, a biomarker of myocardial injury, to identify patients who have myocardial injury after noncardiac surgery (MINS; JAMA. 2017 April 25;371[16]:1642-51). Study results also established that treating MINS patients with dabigatran improved their long-term clinical outcomes (Lancet. 2018 June 9;391[10137]:2325-34).
Covert stroke after noncardiac surgery “is the same concept” as MINS, said Dr. Mrkobrada, a researcher at the London Health Sciences Centre in Canada. “We find strokes that do not get picked up after noncardiac surgery just like MIs that are not picked up,” he said. It’s also possible that certain interventions may improve outcomes in patients with covert strokes, just as they have helped MINS patients, he suggested. Potentially helpful interventions could include aspirin, a statin, and improved blood pressure control. A major goal for his research group is finding a biomarker that makes diagnosing covert stroke as easy as using high sensitivity troponin T to diagnose MINS.
The NeuroVISION (Detection and Neurological Impact of Cerebrovascular Events In Noncardiac Surgery Patients: A Cohort EvaluatioN) study enrolled and tested 1,114 people aged 65 years or older scheduled for elective noncardiac surgery anticipated to keep them hospitalized for at least 2 days at any of 12 participating centers in nine countries. Patients underwent cognitive function testing before surgery and had a brain MR scan 2-9 days after surgery, and they were excluded if they developed an overt stroke prior to the scan. Patients underwent a second round of cognitive testing a year after surgery. Patients averaged 73 years old.
The screening MR scans identified covert strokes in 78 of the study subjects (7%). The 1-year cognitive tests showed measurable drops in cognitive function in 42% of those who had experience covert strokes and in 29% of everyone else. Those rates translated to a doubled odds ratio for cognitive decline after covert stroke, compared with people without covert stroke after adjustment for baseline between-group differences, a highly statistically significant between-group difference for the study’s primary endpoint. Delirium occurred 2.2-fold more often in the covert stroke patients after adjustment, and overt strokes during 1-year follow-up were 4.1-fold more common patients who’d experienced a covert stroke, compared with everyone else, after adjustment, Dr. Mrkobrada reported. NeuroVISION is the first large-scale study to assess the incidence and associations of covert strokes after noncardiac surgery, he noted.
SOURCE: Mrkobrada M. ISC 2019, Late-Breaking Abstract LB18.
HONOLULU – Covert strokes are relatively common in elderly patients who undergo noncardiac surgery, with a 7% incidence among a group of prospectively followed but generally unselected patients in a multicenter, international study.
By definition, these covert strokes were acutely asymptomatic, but showed evidence of clinical effects during the subsequent year. Twelve months after surgery, patients with acute, perioperative covert strokes found by systematic collection of postoperative MRI brain scans had a twofold increased rate of cognitive decline and a greater than twofold increased rate of delirium, compared with the patients who did not have evidence of a covert stroke, Marko Mrkobrada, MD, said at the International Stroke Conference sponsored by the American Heart Association.
The message from these findings is that, when elderly patients exhibit confusion or delirium after noncardiac surgery, their physicians should have a high index of suspicion that a covert stroke may have occurred, Dr. Mrkobrada said in a video interview. It’s possible that typical stroke symptoms do not appear in many of the covert stroke patients because they are masked in the immediate postoperative period, he added.
Right now, the only way to screen for a covert stroke is with a brain MR, a test that generally costs several hundred dollars, which is too expensive for routine screening. Dr. Mrkobrada said that his team hopes further study will identify a biomarker that can flag patients with a covert stroke at a lower cost. For example, colleagues of Dr. Mrkobrada have successfully used high-sensitivity troponin T, a biomarker of myocardial injury, to identify patients who have myocardial injury after noncardiac surgery (MINS; JAMA. 2017 April 25;371[16]:1642-51). Study results also established that treating MINS patients with dabigatran improved their long-term clinical outcomes (Lancet. 2018 June 9;391[10137]:2325-34).
Covert stroke after noncardiac surgery “is the same concept” as MINS, said Dr. Mrkobrada, a researcher at the London Health Sciences Centre in Canada. “We find strokes that do not get picked up after noncardiac surgery just like MIs that are not picked up,” he said. It’s also possible that certain interventions may improve outcomes in patients with covert strokes, just as they have helped MINS patients, he suggested. Potentially helpful interventions could include aspirin, a statin, and improved blood pressure control. A major goal for his research group is finding a biomarker that makes diagnosing covert stroke as easy as using high sensitivity troponin T to diagnose MINS.
The NeuroVISION (Detection and Neurological Impact of Cerebrovascular Events In Noncardiac Surgery Patients: A Cohort EvaluatioN) study enrolled and tested 1,114 people aged 65 years or older scheduled for elective noncardiac surgery anticipated to keep them hospitalized for at least 2 days at any of 12 participating centers in nine countries. Patients underwent cognitive function testing before surgery and had a brain MR scan 2-9 days after surgery, and they were excluded if they developed an overt stroke prior to the scan. Patients underwent a second round of cognitive testing a year after surgery. Patients averaged 73 years old.
The screening MR scans identified covert strokes in 78 of the study subjects (7%). The 1-year cognitive tests showed measurable drops in cognitive function in 42% of those who had experience covert strokes and in 29% of everyone else. Those rates translated to a doubled odds ratio for cognitive decline after covert stroke, compared with people without covert stroke after adjustment for baseline between-group differences, a highly statistically significant between-group difference for the study’s primary endpoint. Delirium occurred 2.2-fold more often in the covert stroke patients after adjustment, and overt strokes during 1-year follow-up were 4.1-fold more common patients who’d experienced a covert stroke, compared with everyone else, after adjustment, Dr. Mrkobrada reported. NeuroVISION is the first large-scale study to assess the incidence and associations of covert strokes after noncardiac surgery, he noted.
SOURCE: Mrkobrada M. ISC 2019, Late-Breaking Abstract LB18.
HONOLULU – Covert strokes are relatively common in elderly patients who undergo noncardiac surgery, with a 7% incidence among a group of prospectively followed but generally unselected patients in a multicenter, international study.
By definition, these covert strokes were acutely asymptomatic, but showed evidence of clinical effects during the subsequent year. Twelve months after surgery, patients with acute, perioperative covert strokes found by systematic collection of postoperative MRI brain scans had a twofold increased rate of cognitive decline and a greater than twofold increased rate of delirium, compared with the patients who did not have evidence of a covert stroke, Marko Mrkobrada, MD, said at the International Stroke Conference sponsored by the American Heart Association.
The message from these findings is that, when elderly patients exhibit confusion or delirium after noncardiac surgery, their physicians should have a high index of suspicion that a covert stroke may have occurred, Dr. Mrkobrada said in a video interview. It’s possible that typical stroke symptoms do not appear in many of the covert stroke patients because they are masked in the immediate postoperative period, he added.
Right now, the only way to screen for a covert stroke is with a brain MR, a test that generally costs several hundred dollars, which is too expensive for routine screening. Dr. Mrkobrada said that his team hopes further study will identify a biomarker that can flag patients with a covert stroke at a lower cost. For example, colleagues of Dr. Mrkobrada have successfully used high-sensitivity troponin T, a biomarker of myocardial injury, to identify patients who have myocardial injury after noncardiac surgery (MINS; JAMA. 2017 April 25;371[16]:1642-51). Study results also established that treating MINS patients with dabigatran improved their long-term clinical outcomes (Lancet. 2018 June 9;391[10137]:2325-34).
Covert stroke after noncardiac surgery “is the same concept” as MINS, said Dr. Mrkobrada, a researcher at the London Health Sciences Centre in Canada. “We find strokes that do not get picked up after noncardiac surgery just like MIs that are not picked up,” he said. It’s also possible that certain interventions may improve outcomes in patients with covert strokes, just as they have helped MINS patients, he suggested. Potentially helpful interventions could include aspirin, a statin, and improved blood pressure control. A major goal for his research group is finding a biomarker that makes diagnosing covert stroke as easy as using high sensitivity troponin T to diagnose MINS.
The NeuroVISION (Detection and Neurological Impact of Cerebrovascular Events In Noncardiac Surgery Patients: A Cohort EvaluatioN) study enrolled and tested 1,114 people aged 65 years or older scheduled for elective noncardiac surgery anticipated to keep them hospitalized for at least 2 days at any of 12 participating centers in nine countries. Patients underwent cognitive function testing before surgery and had a brain MR scan 2-9 days after surgery, and they were excluded if they developed an overt stroke prior to the scan. Patients underwent a second round of cognitive testing a year after surgery. Patients averaged 73 years old.
The screening MR scans identified covert strokes in 78 of the study subjects (7%). The 1-year cognitive tests showed measurable drops in cognitive function in 42% of those who had experience covert strokes and in 29% of everyone else. Those rates translated to a doubled odds ratio for cognitive decline after covert stroke, compared with people without covert stroke after adjustment for baseline between-group differences, a highly statistically significant between-group difference for the study’s primary endpoint. Delirium occurred 2.2-fold more often in the covert stroke patients after adjustment, and overt strokes during 1-year follow-up were 4.1-fold more common patients who’d experienced a covert stroke, compared with everyone else, after adjustment, Dr. Mrkobrada reported. NeuroVISION is the first large-scale study to assess the incidence and associations of covert strokes after noncardiac surgery, he noted.
SOURCE: Mrkobrada M. ISC 2019, Late-Breaking Abstract LB18.
REPORTING FROM ISC 2019
Key clinical point:
Major finding: Elderly patients who underwent noncardiac surgery had a 7% incidence of covert stroke.
Study details: NeuroVISION, a prospective, multicenter, observational study with 1,114 patients.
Disclosures: NeuroVISION did not receive commercial funding. Dr. Mrkobrada had no disclosures.
Source: Mrkobrada M. ISC 2019, Late-Breaking Abstract LB18.
Shaping the future of hospital medicine
Dr. Therese Franco leads SHM’s Pacific Northwest chapter
Therese Franco, MD, SFHM, a hospitalist at the Virginia Mason Medical Center in Seattle, is the current president of SHM’s Pacific Northwest chapter.
The Hospitalist recently sat down with her to learn about her background and discuss some of the initiatives that the Pacific Northwest chapter has been working on.
Can you tell us about your education and training on the way to becoming a hospitalist?
My undergraduate degree is in engineering from Michigan State University. I then went to the University of Michigan in Ann Arbor and did one degree at the School of Public Health in environmental and industrial health, and another degree in the College of Engineering in industrial and operations engineering. In my work with the safety department at an automotive company, I found I was spending a lot of time looking at data, and not talking to people. I got into a conversation with one of the occupational medicine physicians there, and he said, “You ought to try this.” I spoke with a good friend, who was a medical student, and she agreed.
So then I went to medical school thinking that I would practice occupational medicine. I went to medical school at Wayne State University in Detroit and did a couple of rotations in occupational medicine. I wasn’t sure that was the right fit, so I then went off to residency in internal medicine at the University of Connecticut and really enjoyed my wards experience. I liked the pace, I liked the variety, and just really liked all of hospital medicine. So that’s what I decided to do.
What are your areas of research interest?
This year I’m doing a research fellowship through the Center for Healthcare Improvement Science, at Virginia Mason. Through SHM’s mentored implementation program, I have done a lot of work on diabetes and glycemic control but never really published much of it. I think it is so important to share what you learn, so I’m working on publishing some of our results from the diabetes work.
Another area of interest is advanced-practice providers in hospital medicine, which I think is very important, given all the issues that health care is facing. I think that medicine has gotten more complex and that we’re going to have to look at working in a collaborative, inter-professional, multidisciplinary way. I think that advanced practice can really improve the care of hospitalized patients, if we practice appropriate skill-task alignment, develop a culture of mutual respect, and find the best ways to deploy our advanced-practice providers and our physicians.
That can be challenging. Some people, I think, are worried about losing their jobs, and some people feel like they want to “own” all of the patient, because it’s such a part of the culture of medicine. So it’s a really complicated issue, and I think that doctors are going to have to get used to delegating tasks that they used to perform.
So a collaborative practice requires both a professional and a cultural shift?
I think so. I was our inaugural program director for an advanced-practice fellowship in hospital medicine, and in that role, I attended conferences and learning events for program development. I think that many institutions are facing some of the same challenges. For the most part, I’m optimistic about things. I think we’re on the right track, and help is on the way – we just have to figure out how to use it.
Has your institution made any changes along these lines?
We’re primarily using the fellowship as a tool to recruit and retain some of the brightest and best. We’ve got three fellows that matriculated from our program and are currently working in the section of hospital medicine. Everyone’s been really flexible and open to the idea that the job description is emerging. I think my colleagues are very appreciative of our advanced-practice providers. We’ve got two nurse practitioners and one physician assistant who is also a PhD-trained pharmacist. They’ve been great additions to our team.
What are some of the other issues that the Pacific Northwest chapter members are concerned about?
One of our most successful meetings was around telemedicine. There’s a lot of interest in that, and it’s very financially and technically complex. Some hospitals in the area are really doing novel things. One of the most interesting things is an addiction medicine teleconsult.
That’s out of Swedish Medical Center, Seattle. Of course there’s telestroke, which I think is picking up in popularity. We had speakers from Virginia Mason who presented on telestroke. Some institutions are even doing admissions this way. The University of Washington is doing some good antimicrobial stewardship work. They present cases and they teleconference and have an infectious disease consultant. It’s not a program directed at revenue generation, but is focused instead on sharing and spreading expertise.
Our chapter also hosted a presentation on burnout that was pretty well attended. And then, unfortunately, we did lose a hospitalist to suicide over the summer. That was the inspiration for offering the screening of the movie, “Do No Harm: Exposing the Hippocratic Hoax.”
What was the program that you put together around the screening?
We had the filmmaker come for the screening, and we organized a panel discussion with a wellness officer from a local clinic and a psychiatrist who used to be on the board of the Physician Health Program. John Nelson, MD, MHM, one of SHM’s cofounders and a local hospitalist here, also participated as a panelist.
Overall, the event was well received. There were some things that I didn’t really expect. I’m not sure that the film resonated with too many people in the room. It is very much directed at the educational process – med students and residents – and at times the dialogue is a little inflammatory.
I learned a few important things from the film. I did not realize that the tragedy of physician suicide is not unique to the United States – it’s an international issue. And we sometimes use the term “pimping” to talk about questioning interns or residents on rounds. Apparently, that stands for “put in my place,” which is very condescending and unacceptable. I will not use the term again.
I think future conversations need to come from thoughtful, rational, respectful leaders who are willing to work with regulatory agencies, hospitals, and administrators. If we want to move forward, physicians, administrators, and the public need to come together in the best interest of the patient and of public health. And I don’t know who leads that conversation.
Will your chapter have another event around that subject?
We will do what our membership wants and needs. We meet quarterly, and once a year we hold a people’s choice meeting and I solicit topics. If members want to keep the conversation moving, I’m going to do what I can to support them.
What are some other issues that stand out as important to your chapter?
One key topic is the financial side of hospitalist practice, and dealing with issues that seem to create inefficiencies – regulatory issues, documentation issues, things that are important because we want to tell the story of what we’re doing. We certainly want to be reimbursed for the value-added work that we’re doing, but a lot of value-added work creates inefficiencies of practice, and I hear a lot of dissatisfaction around documentation, coding, billing, and other issues related to reimbursement. While people are concerned about these problems, nobody wants to talk about them. They just want somebody to fix it. So I’m not sure what to do with that, because I think if I had a meeting about coding and billing, I would have three attendees.
But our annual poster meeting is always well attended. We always do it at the end of the year, to kick off the holiday season. It’s a nice opportunity to connect socially with colleagues because you mix and you mingle and look at the posters. We had some really great posters, and our top three prize winners were medical students, which is inspirational. They make you feel good about the future.
Our chapter is trying to diversify geographically and clinically. We were fortunate to receive a development funds grant to use technology to do streaming meetings. Our hope is that we can host streaming meetings and eventually transition hosting to rotate around the state. Once there’s large enough attendance, the different delegates can develop their own leadership teams and, eventually, their own chapter. We’re hoping to grow the organization that way.
What else is on the horizon for hospitalists in the Pacific Northwest?
I’d like to see more frequent meetings and a greater variety of meetings. I think there’s interest in adding some kind of service element to the chapter. Maybe we can do a blood pressure screening at a sporting event.
I think we’ll also be focusing on students and residents and trying to create support for them. We held a student event around financial planning, and that was very well attended. I think we would like to do something around mentorship. Of course it’s hard to find mentors, because everybody is so busy.
Our chapter really needs to leverage our technology if we want to have the reach that I’m talking about. I’m looking forward to piloting the streaming meeting concept, and I hope to do some live polling of our meeting attendees to get them engaged. I hope we continue to grow and keep the dialogue going about what matters in hospital medicine, and do our part to shape the future in the way we want it.
Dr. Therese Franco leads SHM’s Pacific Northwest chapter
Dr. Therese Franco leads SHM’s Pacific Northwest chapter
Therese Franco, MD, SFHM, a hospitalist at the Virginia Mason Medical Center in Seattle, is the current president of SHM’s Pacific Northwest chapter.
The Hospitalist recently sat down with her to learn about her background and discuss some of the initiatives that the Pacific Northwest chapter has been working on.
Can you tell us about your education and training on the way to becoming a hospitalist?
My undergraduate degree is in engineering from Michigan State University. I then went to the University of Michigan in Ann Arbor and did one degree at the School of Public Health in environmental and industrial health, and another degree in the College of Engineering in industrial and operations engineering. In my work with the safety department at an automotive company, I found I was spending a lot of time looking at data, and not talking to people. I got into a conversation with one of the occupational medicine physicians there, and he said, “You ought to try this.” I spoke with a good friend, who was a medical student, and she agreed.
So then I went to medical school thinking that I would practice occupational medicine. I went to medical school at Wayne State University in Detroit and did a couple of rotations in occupational medicine. I wasn’t sure that was the right fit, so I then went off to residency in internal medicine at the University of Connecticut and really enjoyed my wards experience. I liked the pace, I liked the variety, and just really liked all of hospital medicine. So that’s what I decided to do.
What are your areas of research interest?
This year I’m doing a research fellowship through the Center for Healthcare Improvement Science, at Virginia Mason. Through SHM’s mentored implementation program, I have done a lot of work on diabetes and glycemic control but never really published much of it. I think it is so important to share what you learn, so I’m working on publishing some of our results from the diabetes work.
Another area of interest is advanced-practice providers in hospital medicine, which I think is very important, given all the issues that health care is facing. I think that medicine has gotten more complex and that we’re going to have to look at working in a collaborative, inter-professional, multidisciplinary way. I think that advanced practice can really improve the care of hospitalized patients, if we practice appropriate skill-task alignment, develop a culture of mutual respect, and find the best ways to deploy our advanced-practice providers and our physicians.
That can be challenging. Some people, I think, are worried about losing their jobs, and some people feel like they want to “own” all of the patient, because it’s such a part of the culture of medicine. So it’s a really complicated issue, and I think that doctors are going to have to get used to delegating tasks that they used to perform.
So a collaborative practice requires both a professional and a cultural shift?
I think so. I was our inaugural program director for an advanced-practice fellowship in hospital medicine, and in that role, I attended conferences and learning events for program development. I think that many institutions are facing some of the same challenges. For the most part, I’m optimistic about things. I think we’re on the right track, and help is on the way – we just have to figure out how to use it.
Has your institution made any changes along these lines?
We’re primarily using the fellowship as a tool to recruit and retain some of the brightest and best. We’ve got three fellows that matriculated from our program and are currently working in the section of hospital medicine. Everyone’s been really flexible and open to the idea that the job description is emerging. I think my colleagues are very appreciative of our advanced-practice providers. We’ve got two nurse practitioners and one physician assistant who is also a PhD-trained pharmacist. They’ve been great additions to our team.
What are some of the other issues that the Pacific Northwest chapter members are concerned about?
One of our most successful meetings was around telemedicine. There’s a lot of interest in that, and it’s very financially and technically complex. Some hospitals in the area are really doing novel things. One of the most interesting things is an addiction medicine teleconsult.
That’s out of Swedish Medical Center, Seattle. Of course there’s telestroke, which I think is picking up in popularity. We had speakers from Virginia Mason who presented on telestroke. Some institutions are even doing admissions this way. The University of Washington is doing some good antimicrobial stewardship work. They present cases and they teleconference and have an infectious disease consultant. It’s not a program directed at revenue generation, but is focused instead on sharing and spreading expertise.
Our chapter also hosted a presentation on burnout that was pretty well attended. And then, unfortunately, we did lose a hospitalist to suicide over the summer. That was the inspiration for offering the screening of the movie, “Do No Harm: Exposing the Hippocratic Hoax.”
What was the program that you put together around the screening?
We had the filmmaker come for the screening, and we organized a panel discussion with a wellness officer from a local clinic and a psychiatrist who used to be on the board of the Physician Health Program. John Nelson, MD, MHM, one of SHM’s cofounders and a local hospitalist here, also participated as a panelist.
Overall, the event was well received. There were some things that I didn’t really expect. I’m not sure that the film resonated with too many people in the room. It is very much directed at the educational process – med students and residents – and at times the dialogue is a little inflammatory.
I learned a few important things from the film. I did not realize that the tragedy of physician suicide is not unique to the United States – it’s an international issue. And we sometimes use the term “pimping” to talk about questioning interns or residents on rounds. Apparently, that stands for “put in my place,” which is very condescending and unacceptable. I will not use the term again.
I think future conversations need to come from thoughtful, rational, respectful leaders who are willing to work with regulatory agencies, hospitals, and administrators. If we want to move forward, physicians, administrators, and the public need to come together in the best interest of the patient and of public health. And I don’t know who leads that conversation.
Will your chapter have another event around that subject?
We will do what our membership wants and needs. We meet quarterly, and once a year we hold a people’s choice meeting and I solicit topics. If members want to keep the conversation moving, I’m going to do what I can to support them.
What are some other issues that stand out as important to your chapter?
One key topic is the financial side of hospitalist practice, and dealing with issues that seem to create inefficiencies – regulatory issues, documentation issues, things that are important because we want to tell the story of what we’re doing. We certainly want to be reimbursed for the value-added work that we’re doing, but a lot of value-added work creates inefficiencies of practice, and I hear a lot of dissatisfaction around documentation, coding, billing, and other issues related to reimbursement. While people are concerned about these problems, nobody wants to talk about them. They just want somebody to fix it. So I’m not sure what to do with that, because I think if I had a meeting about coding and billing, I would have three attendees.
But our annual poster meeting is always well attended. We always do it at the end of the year, to kick off the holiday season. It’s a nice opportunity to connect socially with colleagues because you mix and you mingle and look at the posters. We had some really great posters, and our top three prize winners were medical students, which is inspirational. They make you feel good about the future.
Our chapter is trying to diversify geographically and clinically. We were fortunate to receive a development funds grant to use technology to do streaming meetings. Our hope is that we can host streaming meetings and eventually transition hosting to rotate around the state. Once there’s large enough attendance, the different delegates can develop their own leadership teams and, eventually, their own chapter. We’re hoping to grow the organization that way.
What else is on the horizon for hospitalists in the Pacific Northwest?
I’d like to see more frequent meetings and a greater variety of meetings. I think there’s interest in adding some kind of service element to the chapter. Maybe we can do a blood pressure screening at a sporting event.
I think we’ll also be focusing on students and residents and trying to create support for them. We held a student event around financial planning, and that was very well attended. I think we would like to do something around mentorship. Of course it’s hard to find mentors, because everybody is so busy.
Our chapter really needs to leverage our technology if we want to have the reach that I’m talking about. I’m looking forward to piloting the streaming meeting concept, and I hope to do some live polling of our meeting attendees to get them engaged. I hope we continue to grow and keep the dialogue going about what matters in hospital medicine, and do our part to shape the future in the way we want it.
Therese Franco, MD, SFHM, a hospitalist at the Virginia Mason Medical Center in Seattle, is the current president of SHM’s Pacific Northwest chapter.
The Hospitalist recently sat down with her to learn about her background and discuss some of the initiatives that the Pacific Northwest chapter has been working on.
Can you tell us about your education and training on the way to becoming a hospitalist?
My undergraduate degree is in engineering from Michigan State University. I then went to the University of Michigan in Ann Arbor and did one degree at the School of Public Health in environmental and industrial health, and another degree in the College of Engineering in industrial and operations engineering. In my work with the safety department at an automotive company, I found I was spending a lot of time looking at data, and not talking to people. I got into a conversation with one of the occupational medicine physicians there, and he said, “You ought to try this.” I spoke with a good friend, who was a medical student, and she agreed.
So then I went to medical school thinking that I would practice occupational medicine. I went to medical school at Wayne State University in Detroit and did a couple of rotations in occupational medicine. I wasn’t sure that was the right fit, so I then went off to residency in internal medicine at the University of Connecticut and really enjoyed my wards experience. I liked the pace, I liked the variety, and just really liked all of hospital medicine. So that’s what I decided to do.
What are your areas of research interest?
This year I’m doing a research fellowship through the Center for Healthcare Improvement Science, at Virginia Mason. Through SHM’s mentored implementation program, I have done a lot of work on diabetes and glycemic control but never really published much of it. I think it is so important to share what you learn, so I’m working on publishing some of our results from the diabetes work.
Another area of interest is advanced-practice providers in hospital medicine, which I think is very important, given all the issues that health care is facing. I think that medicine has gotten more complex and that we’re going to have to look at working in a collaborative, inter-professional, multidisciplinary way. I think that advanced practice can really improve the care of hospitalized patients, if we practice appropriate skill-task alignment, develop a culture of mutual respect, and find the best ways to deploy our advanced-practice providers and our physicians.
That can be challenging. Some people, I think, are worried about losing their jobs, and some people feel like they want to “own” all of the patient, because it’s such a part of the culture of medicine. So it’s a really complicated issue, and I think that doctors are going to have to get used to delegating tasks that they used to perform.
So a collaborative practice requires both a professional and a cultural shift?
I think so. I was our inaugural program director for an advanced-practice fellowship in hospital medicine, and in that role, I attended conferences and learning events for program development. I think that many institutions are facing some of the same challenges. For the most part, I’m optimistic about things. I think we’re on the right track, and help is on the way – we just have to figure out how to use it.
Has your institution made any changes along these lines?
We’re primarily using the fellowship as a tool to recruit and retain some of the brightest and best. We’ve got three fellows that matriculated from our program and are currently working in the section of hospital medicine. Everyone’s been really flexible and open to the idea that the job description is emerging. I think my colleagues are very appreciative of our advanced-practice providers. We’ve got two nurse practitioners and one physician assistant who is also a PhD-trained pharmacist. They’ve been great additions to our team.
What are some of the other issues that the Pacific Northwest chapter members are concerned about?
One of our most successful meetings was around telemedicine. There’s a lot of interest in that, and it’s very financially and technically complex. Some hospitals in the area are really doing novel things. One of the most interesting things is an addiction medicine teleconsult.
That’s out of Swedish Medical Center, Seattle. Of course there’s telestroke, which I think is picking up in popularity. We had speakers from Virginia Mason who presented on telestroke. Some institutions are even doing admissions this way. The University of Washington is doing some good antimicrobial stewardship work. They present cases and they teleconference and have an infectious disease consultant. It’s not a program directed at revenue generation, but is focused instead on sharing and spreading expertise.
Our chapter also hosted a presentation on burnout that was pretty well attended. And then, unfortunately, we did lose a hospitalist to suicide over the summer. That was the inspiration for offering the screening of the movie, “Do No Harm: Exposing the Hippocratic Hoax.”
What was the program that you put together around the screening?
We had the filmmaker come for the screening, and we organized a panel discussion with a wellness officer from a local clinic and a psychiatrist who used to be on the board of the Physician Health Program. John Nelson, MD, MHM, one of SHM’s cofounders and a local hospitalist here, also participated as a panelist.
Overall, the event was well received. There were some things that I didn’t really expect. I’m not sure that the film resonated with too many people in the room. It is very much directed at the educational process – med students and residents – and at times the dialogue is a little inflammatory.
I learned a few important things from the film. I did not realize that the tragedy of physician suicide is not unique to the United States – it’s an international issue. And we sometimes use the term “pimping” to talk about questioning interns or residents on rounds. Apparently, that stands for “put in my place,” which is very condescending and unacceptable. I will not use the term again.
I think future conversations need to come from thoughtful, rational, respectful leaders who are willing to work with regulatory agencies, hospitals, and administrators. If we want to move forward, physicians, administrators, and the public need to come together in the best interest of the patient and of public health. And I don’t know who leads that conversation.
Will your chapter have another event around that subject?
We will do what our membership wants and needs. We meet quarterly, and once a year we hold a people’s choice meeting and I solicit topics. If members want to keep the conversation moving, I’m going to do what I can to support them.
What are some other issues that stand out as important to your chapter?
One key topic is the financial side of hospitalist practice, and dealing with issues that seem to create inefficiencies – regulatory issues, documentation issues, things that are important because we want to tell the story of what we’re doing. We certainly want to be reimbursed for the value-added work that we’re doing, but a lot of value-added work creates inefficiencies of practice, and I hear a lot of dissatisfaction around documentation, coding, billing, and other issues related to reimbursement. While people are concerned about these problems, nobody wants to talk about them. They just want somebody to fix it. So I’m not sure what to do with that, because I think if I had a meeting about coding and billing, I would have three attendees.
But our annual poster meeting is always well attended. We always do it at the end of the year, to kick off the holiday season. It’s a nice opportunity to connect socially with colleagues because you mix and you mingle and look at the posters. We had some really great posters, and our top three prize winners were medical students, which is inspirational. They make you feel good about the future.
Our chapter is trying to diversify geographically and clinically. We were fortunate to receive a development funds grant to use technology to do streaming meetings. Our hope is that we can host streaming meetings and eventually transition hosting to rotate around the state. Once there’s large enough attendance, the different delegates can develop their own leadership teams and, eventually, their own chapter. We’re hoping to grow the organization that way.
What else is on the horizon for hospitalists in the Pacific Northwest?
I’d like to see more frequent meetings and a greater variety of meetings. I think there’s interest in adding some kind of service element to the chapter. Maybe we can do a blood pressure screening at a sporting event.
I think we’ll also be focusing on students and residents and trying to create support for them. We held a student event around financial planning, and that was very well attended. I think we would like to do something around mentorship. Of course it’s hard to find mentors, because everybody is so busy.
Our chapter really needs to leverage our technology if we want to have the reach that I’m talking about. I’m looking forward to piloting the streaming meeting concept, and I hope to do some live polling of our meeting attendees to get them engaged. I hope we continue to grow and keep the dialogue going about what matters in hospital medicine, and do our part to shape the future in the way we want it.
Bag-mask ventilation during intubation reduces severe hypoxemia
, according to data presented at the Critical Care Congress, sponsored by the Society of Critical Care Medicine.

A multicenter study, published simultaneously in the Feb. 18 issue of the New England Journal of Medicine, randomized 401 critically-ill patients in the ICU who were undergoing tracheal intubation to receive either ventilation with a bag-mask device during induction for intubation or no ventilation.
The median lowest oxygen saturation between induction and 2 minutes after intubation was 96% in the bag-mask ventilated patients and 93% in the no-ventilation group, representing a 4.7% difference after adjusting for prespecified covariates (P = .01).
In a post-hoc analysis that adjusted for other factors such as the provision of preoxygenation, the preoxygenation device, pneumonia, and gastrointestinal bleeding, there was a 5.2% difference between the two groups in median lowest oxygen saturation, favoring the bag-mask group.
Bag-mask ventilation was also associated with almost a halving in the incidence of severe hypoxemia – defined as an oxygen saturation below 80% – compared with no-ventilation (10.9% vs. 22.8%; relative risk = 0.48). There was also a lower incidence of patients with an oxygen saturation below 90% and below 70% in the bag-mask ventilation group, compared with the no-ventilation group.
Overall, the median decrease in oxygen saturation from induction to the lowest point was 1% in the bag-mask group, and 5% in the no-ventilation group.
The study saw no effects of factors such as body-mass index, operator experience, or Acute Physiology and Chronic Health Evaluation (APACHE II) score. The patients had a median age of 60 years, about half had sepsis or septic shock, and close to 60% had hypoxemic respiratory failure as an indication for tracheal intubation.
Jonathan D. Casey, MD, of Vanderbilt University, Nashville, Tenn., and his coauthors wrote that their results suggested for every nine critically ill patients undergoing tracheal intubation, bag-mask ventilation would prevent severe hypoxemia in one patient.
“These findings are important because oxygen saturation is an established endpoint in airway management trials and is a contributing factor to periprocedural cardiac arrest and death,” they wrote.
They noted that there are conflicting guidelines on the use of bag-mask ventilation during tracheal intubation, with some recommending its use for all patients – even those who are not hypoxemic – and others advising their use only for patients with hypoxemia. This study excluded patients who were identified as hypoxemic or in whom bag-mask ventilation was contraindicated.
Despite concerns about bag-mask ventilation increasing the risk the aspiration, the study showed no significant difference between the two groups in the incidence of operator-reported aspiration or the presence of a new opacity on chest radiograph in the 48 hours after intubation.
The authors acknowledged that, given the low incidence of operator-reported aspiration during tracheal intubation, a much larger study would be needed to show whether bag-mask ventilation did increase the risk of aspiration.
“However, our trial provides some reassurance, since the incidence of operator-reported aspiration was numerically lower in the bag-mask ventilation group than in the no-ventilation group,” they wrote.
There were also no significant differences between the two groups in oxygen saturation, fraction of inspired oxygen or positive end-expiratory pressure in the 24 hours after intubation. Bag-mask ventilation was also associated with similar rates of in-hospital mortality, number of ventilator-free days, and days out of the ICU as no-ventilation.
The authors noted that their trial focused on critically-ill patients in the ICU, so the results may not be generalizable to patients in the emergency department or in a prehospital setting.
The study and some authors were supported by the National Institutes of Health. Two authors declared personal fees from the pharmaceutical industry unrelated to the study, and no other conflicts of interest were declared.
SOURCE: Casey J et al. N Engl J Med. 2019 Feb 18. doi: 10.1056/NEJMoa1812405
Debate around the question of whether to use bag-mask ventilation in critically-ill patients has been limited by the lack of high-quality evidence on the risk of aspiration or on the benefits of this approach. This study found no evidence of an increase in the incidence of aspiration, despite using multiple measures to detect it, which provide some reassurance that manual ventilation during tracheal intubation is not likely to cause significant harm.
One significant limitation of this trial, however, is that it did not standardize the preoxygenation strategy across the two groups, so significantly more patients in the bag-mask group received bag-mask ventilation before induction. Median oxygen saturation before induction was the same in the two groups, but this does not rule out the possibility of differences in the arterial pressure of oxygen.
This study may not settle the question of whether to use bag-mask ventilation during tracheal intubation, but it provides strong suggestion that the practice is not harmful.
Patricia A. Kritek, MD, and Andrew M. Luks, MD, are with the division of pulmonary, critical care, and sleep medicine at the University of Washington in Seattle. These comments are adapted from their editorial accompanying the paper by Casey et al. (N Engl J Med. 2019 Feb 18. doi: 10.1056/NEJMe1900708). Dr. Luks declared personal fees from private industry outside the submitted work. Dr. Kritek reported having nothing to disclose.
Debate around the question of whether to use bag-mask ventilation in critically-ill patients has been limited by the lack of high-quality evidence on the risk of aspiration or on the benefits of this approach. This study found no evidence of an increase in the incidence of aspiration, despite using multiple measures to detect it, which provide some reassurance that manual ventilation during tracheal intubation is not likely to cause significant harm.
One significant limitation of this trial, however, is that it did not standardize the preoxygenation strategy across the two groups, so significantly more patients in the bag-mask group received bag-mask ventilation before induction. Median oxygen saturation before induction was the same in the two groups, but this does not rule out the possibility of differences in the arterial pressure of oxygen.
This study may not settle the question of whether to use bag-mask ventilation during tracheal intubation, but it provides strong suggestion that the practice is not harmful.
Patricia A. Kritek, MD, and Andrew M. Luks, MD, are with the division of pulmonary, critical care, and sleep medicine at the University of Washington in Seattle. These comments are adapted from their editorial accompanying the paper by Casey et al. (N Engl J Med. 2019 Feb 18. doi: 10.1056/NEJMe1900708). Dr. Luks declared personal fees from private industry outside the submitted work. Dr. Kritek reported having nothing to disclose.
Debate around the question of whether to use bag-mask ventilation in critically-ill patients has been limited by the lack of high-quality evidence on the risk of aspiration or on the benefits of this approach. This study found no evidence of an increase in the incidence of aspiration, despite using multiple measures to detect it, which provide some reassurance that manual ventilation during tracheal intubation is not likely to cause significant harm.
One significant limitation of this trial, however, is that it did not standardize the preoxygenation strategy across the two groups, so significantly more patients in the bag-mask group received bag-mask ventilation before induction. Median oxygen saturation before induction was the same in the two groups, but this does not rule out the possibility of differences in the arterial pressure of oxygen.
This study may not settle the question of whether to use bag-mask ventilation during tracheal intubation, but it provides strong suggestion that the practice is not harmful.
Patricia A. Kritek, MD, and Andrew M. Luks, MD, are with the division of pulmonary, critical care, and sleep medicine at the University of Washington in Seattle. These comments are adapted from their editorial accompanying the paper by Casey et al. (N Engl J Med. 2019 Feb 18. doi: 10.1056/NEJMe1900708). Dr. Luks declared personal fees from private industry outside the submitted work. Dr. Kritek reported having nothing to disclose.
, according to data presented at the Critical Care Congress, sponsored by the Society of Critical Care Medicine.

A multicenter study, published simultaneously in the Feb. 18 issue of the New England Journal of Medicine, randomized 401 critically-ill patients in the ICU who were undergoing tracheal intubation to receive either ventilation with a bag-mask device during induction for intubation or no ventilation.
The median lowest oxygen saturation between induction and 2 minutes after intubation was 96% in the bag-mask ventilated patients and 93% in the no-ventilation group, representing a 4.7% difference after adjusting for prespecified covariates (P = .01).
In a post-hoc analysis that adjusted for other factors such as the provision of preoxygenation, the preoxygenation device, pneumonia, and gastrointestinal bleeding, there was a 5.2% difference between the two groups in median lowest oxygen saturation, favoring the bag-mask group.
Bag-mask ventilation was also associated with almost a halving in the incidence of severe hypoxemia – defined as an oxygen saturation below 80% – compared with no-ventilation (10.9% vs. 22.8%; relative risk = 0.48). There was also a lower incidence of patients with an oxygen saturation below 90% and below 70% in the bag-mask ventilation group, compared with the no-ventilation group.
Overall, the median decrease in oxygen saturation from induction to the lowest point was 1% in the bag-mask group, and 5% in the no-ventilation group.
The study saw no effects of factors such as body-mass index, operator experience, or Acute Physiology and Chronic Health Evaluation (APACHE II) score. The patients had a median age of 60 years, about half had sepsis or septic shock, and close to 60% had hypoxemic respiratory failure as an indication for tracheal intubation.
Jonathan D. Casey, MD, of Vanderbilt University, Nashville, Tenn., and his coauthors wrote that their results suggested for every nine critically ill patients undergoing tracheal intubation, bag-mask ventilation would prevent severe hypoxemia in one patient.
“These findings are important because oxygen saturation is an established endpoint in airway management trials and is a contributing factor to periprocedural cardiac arrest and death,” they wrote.
They noted that there are conflicting guidelines on the use of bag-mask ventilation during tracheal intubation, with some recommending its use for all patients – even those who are not hypoxemic – and others advising their use only for patients with hypoxemia. This study excluded patients who were identified as hypoxemic or in whom bag-mask ventilation was contraindicated.
Despite concerns about bag-mask ventilation increasing the risk the aspiration, the study showed no significant difference between the two groups in the incidence of operator-reported aspiration or the presence of a new opacity on chest radiograph in the 48 hours after intubation.
The authors acknowledged that, given the low incidence of operator-reported aspiration during tracheal intubation, a much larger study would be needed to show whether bag-mask ventilation did increase the risk of aspiration.
“However, our trial provides some reassurance, since the incidence of operator-reported aspiration was numerically lower in the bag-mask ventilation group than in the no-ventilation group,” they wrote.
There were also no significant differences between the two groups in oxygen saturation, fraction of inspired oxygen or positive end-expiratory pressure in the 24 hours after intubation. Bag-mask ventilation was also associated with similar rates of in-hospital mortality, number of ventilator-free days, and days out of the ICU as no-ventilation.
The authors noted that their trial focused on critically-ill patients in the ICU, so the results may not be generalizable to patients in the emergency department or in a prehospital setting.
The study and some authors were supported by the National Institutes of Health. Two authors declared personal fees from the pharmaceutical industry unrelated to the study, and no other conflicts of interest were declared.
SOURCE: Casey J et al. N Engl J Med. 2019 Feb 18. doi: 10.1056/NEJMoa1812405
, according to data presented at the Critical Care Congress, sponsored by the Society of Critical Care Medicine.

A multicenter study, published simultaneously in the Feb. 18 issue of the New England Journal of Medicine, randomized 401 critically-ill patients in the ICU who were undergoing tracheal intubation to receive either ventilation with a bag-mask device during induction for intubation or no ventilation.
The median lowest oxygen saturation between induction and 2 minutes after intubation was 96% in the bag-mask ventilated patients and 93% in the no-ventilation group, representing a 4.7% difference after adjusting for prespecified covariates (P = .01).
In a post-hoc analysis that adjusted for other factors such as the provision of preoxygenation, the preoxygenation device, pneumonia, and gastrointestinal bleeding, there was a 5.2% difference between the two groups in median lowest oxygen saturation, favoring the bag-mask group.
Bag-mask ventilation was also associated with almost a halving in the incidence of severe hypoxemia – defined as an oxygen saturation below 80% – compared with no-ventilation (10.9% vs. 22.8%; relative risk = 0.48). There was also a lower incidence of patients with an oxygen saturation below 90% and below 70% in the bag-mask ventilation group, compared with the no-ventilation group.
Overall, the median decrease in oxygen saturation from induction to the lowest point was 1% in the bag-mask group, and 5% in the no-ventilation group.
The study saw no effects of factors such as body-mass index, operator experience, or Acute Physiology and Chronic Health Evaluation (APACHE II) score. The patients had a median age of 60 years, about half had sepsis or septic shock, and close to 60% had hypoxemic respiratory failure as an indication for tracheal intubation.
Jonathan D. Casey, MD, of Vanderbilt University, Nashville, Tenn., and his coauthors wrote that their results suggested for every nine critically ill patients undergoing tracheal intubation, bag-mask ventilation would prevent severe hypoxemia in one patient.
“These findings are important because oxygen saturation is an established endpoint in airway management trials and is a contributing factor to periprocedural cardiac arrest and death,” they wrote.
They noted that there are conflicting guidelines on the use of bag-mask ventilation during tracheal intubation, with some recommending its use for all patients – even those who are not hypoxemic – and others advising their use only for patients with hypoxemia. This study excluded patients who were identified as hypoxemic or in whom bag-mask ventilation was contraindicated.
Despite concerns about bag-mask ventilation increasing the risk the aspiration, the study showed no significant difference between the two groups in the incidence of operator-reported aspiration or the presence of a new opacity on chest radiograph in the 48 hours after intubation.
The authors acknowledged that, given the low incidence of operator-reported aspiration during tracheal intubation, a much larger study would be needed to show whether bag-mask ventilation did increase the risk of aspiration.
“However, our trial provides some reassurance, since the incidence of operator-reported aspiration was numerically lower in the bag-mask ventilation group than in the no-ventilation group,” they wrote.
There were also no significant differences between the two groups in oxygen saturation, fraction of inspired oxygen or positive end-expiratory pressure in the 24 hours after intubation. Bag-mask ventilation was also associated with similar rates of in-hospital mortality, number of ventilator-free days, and days out of the ICU as no-ventilation.
The authors noted that their trial focused on critically-ill patients in the ICU, so the results may not be generalizable to patients in the emergency department or in a prehospital setting.
The study and some authors were supported by the National Institutes of Health. Two authors declared personal fees from the pharmaceutical industry unrelated to the study, and no other conflicts of interest were declared.
SOURCE: Casey J et al. N Engl J Med. 2019 Feb 18. doi: 10.1056/NEJMoa1812405
FROM CCC48
Key clinical point: Bag-mask ventilation during tracheal intubation reduces the risk of severe hypoxemia.
Major finding: For every nine patients who receive bag-mask ventilation during tracheal intubation, one case of severe hypoxemia is avoided.
Study details: Randomized, controlled trial in 401 critically-ill patients undergoing tracheal intubation.
Disclosures: The study and some authors were supported by the National Institutes of Health. Two authors declared personal fees from the pharmaceutical industry unrelated to the study.
Source: Casey J et al. N Engl J Med. 2019 Feb 18. doi: 10.1056/NEJMoa1812405
Culture change needed to improve gender inequalities in medicine
LONDON –
“Gender equality is everyone’s business,” Sarah Hawkes, MBBS, PhD, a professor of global public health at University College London (England), said at the event.
“We’re not talking about women taking over the shop, but women being given an equal opportunity to run the shop. It doesn’t matter where we place ourselves on the gender spectrum as far as advancing equality in science is concerned. What matters is that we all, irrespective of gender, call ourselves feminists.”
For years, women have been “underrepresented in positions of power and leadership, undervalued, and experience discrimination and gender-based violence in scientific and health disciplines across the world,” according to an editorial in the British-based journal (Lancet. 2019;393:493). Such inequalities are compounded and hard to separate from other inequalities, including ethnicity, disability, class, geography, and sexuality.
Despite efforts to readdress the predominantly male culture of medicine, the problem of gender inequality remains “stubbornly persistent,” the editorial said.
“We have spent years being told that the problem lies with us as individuals and that we just need to be better, stronger, more vocal, as women,” Dr. Hawkes observed. “But what really needs to happen is for change to happen in places that hold power.” She further argued: “We don’t need any more individual change; we need organizational and institutional norm change.”
Gender inequality has a long history, and not just in medicine, said British journalist Caroline Criado-Perez OBE, who gave a keynote speech. Ms. Criado-Perez, who is a well-respected feminist campaigner, noted that the world was largely “modeled to fit men.” From architecture to transport, and even crash-test dummies, everything was largely modeled on, or to accommodate, the male rather than the female body.
“I don’t need to tell you that women are 50% more likely to be misdiagnosed following a heart attack” than men. There is no more urgent need to challenge gender inequality than in medicine, Women are dying because of the gender data gap in medicine,” she asserted. “In medical research, in medical education, in medical practice, it needs to be closed as a matter of urgency.”
Original data published in the Advancing Women in Science, Medicine and Global Health special edition of The Lancet found that only 31% of biomedical research papers published in 2016 reported outcomes for both men and women (Lancet. 2019;393:550-9). Reporting of sex differences was somewhat better in clinical or public health-related research papers, at 67% and 69%, respectively. Sex-differences were more likely to be reported if a woman was one of the key authors, Cassidy R. Sugimoto, PhD, associate professor of informatics at Indiana University in Bloomington, and associates, observed in their paper.
That said, women often have to fight to be included as an author on a paper, even when they have done the majority of the work, the event participants highlighted. Women were still less likely than men to be named as the first or last author on a paper, as well as be less likely to receive research funding to enable them to do the work in the first place (Lancet. 2018;393:531-40).
“Was it really you?” was a question sometimes asked of a woman named as a lead or first author, noted Sonia Gandhi, MD, PhD, group leader of the Neurodegeneration Biology Laboratory at the Francis Crick Institute in Cambridge (England). Women network differently to men, Dr. Gandhi observed, and not necessarily in networks that forward careers. Women were also often questioned about their productivity, and regardless of any training on unconscious bias, women were still at a disadvantage if they took a career break to have children.
Women’s credentials and capabilities were often felt to be less respected by male colleagues, and there was talk of being met with microaggressions in the workplace, as in one example given by Nana Odom, MSc, a clinical engineer at the Royal United Hospital Bath (England). She was told “you’re not an engineer, because I have not got a set of screwdrivers and sit at a computer and program.” Such comments can deeply affect a person, Dr. Odom said. “Sometimes I feel that if I don’t go into the workshop and open up a bit of kit that I am not an engineer, but it’s so unconscious, it carries on with you.” These types of stories need to be told so then they can be properly addressed when they do happen, she said.
Female representation is so important, said F. Gigi Osler, MD, head of otolaryngology-head and neck surgery at St. Boniface Hospital in Winnipeg. Dr. Osler is the 2018-2019 president of the Canadian Medical Association, the eighth woman to hold this prestigious position in the organization’s 151 years of operation. She also happens to be the first female surgeon and the first woman of color in the role. “When I stepped into the presidency last August, I thought very long and very hard about how I was going to use my voice and this platform,” Dr. Osler said. “It became very clear to me after I started how important representation was. I can’t tell you how many women, young women, and women of color...have come up to me to say, ‘I’m so excited to have you in this position. I’ve never seen someone who looks like me in that type of leadership position,’ ” she observed.
“As leaders, I think we can advocate for structures and processes,” Dr. Osler added, “I think we set the culture.” Leaders have the responsibility for creating and nurturing and fostering a professional, respectful, and inclusive environment, she said.
“We need more strong leaders, we need more diversity in leadership.” Dr. Osler was keen to point out that greater diversity does not mean only women, but other groups as well. “Look around the room. Who is not here? How can I make it easier for them to get here?”
Another strong female role model at the event was Dame Sally Davies, the Chief Medical Officer for England, a hematologist by training. Not only is she the first female in that role, she will also become the first female Master of Trinity College Cambridge starting in October 2019, a role dominated by men for more than 500 years.
All people, women and men, need to be given fair opportunity, Dame Sally said. Addressing structural issues can help, she said. “We need role models, mentors, and champions,” she said, noting that there were differences between the three. “Mentors give you advice, they get to know you, and they help you think through your issue. Champions may not have time for that, but they know you are good,” and they are putting you forward for opportunities.
“If the system isn’t right, or we are treated badly, we need to call it out,” Dame Sally said. “I do think that we often let things pass that we shouldn’t.” A classic situation is where a woman may suggest something at a meeting and it is ignored, but when a man says the same thing it is taken on board. That kind of behavior needs to stop and be addressed when it happens, by everyone at the table, she said.
Dr. Hawkes observed in her summing up of the day: “Throughout the history of health, change comes about not just through action at the top, but also from action from the bottom up.” She added: “The question is how do we make that change happen?” That’s where the next phase of research needs to take place, she suggested, “we need to actually see, in a very evidence-informed way, what actually works to make and sustain change.”
No financial disclosures were reported by any of the speakers quoted.
SOURCE: Lancet. 2019;393:493–610, e6-e28
LONDON –
“Gender equality is everyone’s business,” Sarah Hawkes, MBBS, PhD, a professor of global public health at University College London (England), said at the event.
“We’re not talking about women taking over the shop, but women being given an equal opportunity to run the shop. It doesn’t matter where we place ourselves on the gender spectrum as far as advancing equality in science is concerned. What matters is that we all, irrespective of gender, call ourselves feminists.”
For years, women have been “underrepresented in positions of power and leadership, undervalued, and experience discrimination and gender-based violence in scientific and health disciplines across the world,” according to an editorial in the British-based journal (Lancet. 2019;393:493). Such inequalities are compounded and hard to separate from other inequalities, including ethnicity, disability, class, geography, and sexuality.
Despite efforts to readdress the predominantly male culture of medicine, the problem of gender inequality remains “stubbornly persistent,” the editorial said.
“We have spent years being told that the problem lies with us as individuals and that we just need to be better, stronger, more vocal, as women,” Dr. Hawkes observed. “But what really needs to happen is for change to happen in places that hold power.” She further argued: “We don’t need any more individual change; we need organizational and institutional norm change.”
Gender inequality has a long history, and not just in medicine, said British journalist Caroline Criado-Perez OBE, who gave a keynote speech. Ms. Criado-Perez, who is a well-respected feminist campaigner, noted that the world was largely “modeled to fit men.” From architecture to transport, and even crash-test dummies, everything was largely modeled on, or to accommodate, the male rather than the female body.
“I don’t need to tell you that women are 50% more likely to be misdiagnosed following a heart attack” than men. There is no more urgent need to challenge gender inequality than in medicine, Women are dying because of the gender data gap in medicine,” she asserted. “In medical research, in medical education, in medical practice, it needs to be closed as a matter of urgency.”
Original data published in the Advancing Women in Science, Medicine and Global Health special edition of The Lancet found that only 31% of biomedical research papers published in 2016 reported outcomes for both men and women (Lancet. 2019;393:550-9). Reporting of sex differences was somewhat better in clinical or public health-related research papers, at 67% and 69%, respectively. Sex-differences were more likely to be reported if a woman was one of the key authors, Cassidy R. Sugimoto, PhD, associate professor of informatics at Indiana University in Bloomington, and associates, observed in their paper.
That said, women often have to fight to be included as an author on a paper, even when they have done the majority of the work, the event participants highlighted. Women were still less likely than men to be named as the first or last author on a paper, as well as be less likely to receive research funding to enable them to do the work in the first place (Lancet. 2018;393:531-40).
“Was it really you?” was a question sometimes asked of a woman named as a lead or first author, noted Sonia Gandhi, MD, PhD, group leader of the Neurodegeneration Biology Laboratory at the Francis Crick Institute in Cambridge (England). Women network differently to men, Dr. Gandhi observed, and not necessarily in networks that forward careers. Women were also often questioned about their productivity, and regardless of any training on unconscious bias, women were still at a disadvantage if they took a career break to have children.
Women’s credentials and capabilities were often felt to be less respected by male colleagues, and there was talk of being met with microaggressions in the workplace, as in one example given by Nana Odom, MSc, a clinical engineer at the Royal United Hospital Bath (England). She was told “you’re not an engineer, because I have not got a set of screwdrivers and sit at a computer and program.” Such comments can deeply affect a person, Dr. Odom said. “Sometimes I feel that if I don’t go into the workshop and open up a bit of kit that I am not an engineer, but it’s so unconscious, it carries on with you.” These types of stories need to be told so then they can be properly addressed when they do happen, she said.
Female representation is so important, said F. Gigi Osler, MD, head of otolaryngology-head and neck surgery at St. Boniface Hospital in Winnipeg. Dr. Osler is the 2018-2019 president of the Canadian Medical Association, the eighth woman to hold this prestigious position in the organization’s 151 years of operation. She also happens to be the first female surgeon and the first woman of color in the role. “When I stepped into the presidency last August, I thought very long and very hard about how I was going to use my voice and this platform,” Dr. Osler said. “It became very clear to me after I started how important representation was. I can’t tell you how many women, young women, and women of color...have come up to me to say, ‘I’m so excited to have you in this position. I’ve never seen someone who looks like me in that type of leadership position,’ ” she observed.
“As leaders, I think we can advocate for structures and processes,” Dr. Osler added, “I think we set the culture.” Leaders have the responsibility for creating and nurturing and fostering a professional, respectful, and inclusive environment, she said.
“We need more strong leaders, we need more diversity in leadership.” Dr. Osler was keen to point out that greater diversity does not mean only women, but other groups as well. “Look around the room. Who is not here? How can I make it easier for them to get here?”
Another strong female role model at the event was Dame Sally Davies, the Chief Medical Officer for England, a hematologist by training. Not only is she the first female in that role, she will also become the first female Master of Trinity College Cambridge starting in October 2019, a role dominated by men for more than 500 years.
All people, women and men, need to be given fair opportunity, Dame Sally said. Addressing structural issues can help, she said. “We need role models, mentors, and champions,” she said, noting that there were differences between the three. “Mentors give you advice, they get to know you, and they help you think through your issue. Champions may not have time for that, but they know you are good,” and they are putting you forward for opportunities.
“If the system isn’t right, or we are treated badly, we need to call it out,” Dame Sally said. “I do think that we often let things pass that we shouldn’t.” A classic situation is where a woman may suggest something at a meeting and it is ignored, but when a man says the same thing it is taken on board. That kind of behavior needs to stop and be addressed when it happens, by everyone at the table, she said.
Dr. Hawkes observed in her summing up of the day: “Throughout the history of health, change comes about not just through action at the top, but also from action from the bottom up.” She added: “The question is how do we make that change happen?” That’s where the next phase of research needs to take place, she suggested, “we need to actually see, in a very evidence-informed way, what actually works to make and sustain change.”
No financial disclosures were reported by any of the speakers quoted.
SOURCE: Lancet. 2019;393:493–610, e6-e28
LONDON –
“Gender equality is everyone’s business,” Sarah Hawkes, MBBS, PhD, a professor of global public health at University College London (England), said at the event.
“We’re not talking about women taking over the shop, but women being given an equal opportunity to run the shop. It doesn’t matter where we place ourselves on the gender spectrum as far as advancing equality in science is concerned. What matters is that we all, irrespective of gender, call ourselves feminists.”
For years, women have been “underrepresented in positions of power and leadership, undervalued, and experience discrimination and gender-based violence in scientific and health disciplines across the world,” according to an editorial in the British-based journal (Lancet. 2019;393:493). Such inequalities are compounded and hard to separate from other inequalities, including ethnicity, disability, class, geography, and sexuality.
Despite efforts to readdress the predominantly male culture of medicine, the problem of gender inequality remains “stubbornly persistent,” the editorial said.
“We have spent years being told that the problem lies with us as individuals and that we just need to be better, stronger, more vocal, as women,” Dr. Hawkes observed. “But what really needs to happen is for change to happen in places that hold power.” She further argued: “We don’t need any more individual change; we need organizational and institutional norm change.”
Gender inequality has a long history, and not just in medicine, said British journalist Caroline Criado-Perez OBE, who gave a keynote speech. Ms. Criado-Perez, who is a well-respected feminist campaigner, noted that the world was largely “modeled to fit men.” From architecture to transport, and even crash-test dummies, everything was largely modeled on, or to accommodate, the male rather than the female body.
“I don’t need to tell you that women are 50% more likely to be misdiagnosed following a heart attack” than men. There is no more urgent need to challenge gender inequality than in medicine, Women are dying because of the gender data gap in medicine,” she asserted. “In medical research, in medical education, in medical practice, it needs to be closed as a matter of urgency.”
Original data published in the Advancing Women in Science, Medicine and Global Health special edition of The Lancet found that only 31% of biomedical research papers published in 2016 reported outcomes for both men and women (Lancet. 2019;393:550-9). Reporting of sex differences was somewhat better in clinical or public health-related research papers, at 67% and 69%, respectively. Sex-differences were more likely to be reported if a woman was one of the key authors, Cassidy R. Sugimoto, PhD, associate professor of informatics at Indiana University in Bloomington, and associates, observed in their paper.
That said, women often have to fight to be included as an author on a paper, even when they have done the majority of the work, the event participants highlighted. Women were still less likely than men to be named as the first or last author on a paper, as well as be less likely to receive research funding to enable them to do the work in the first place (Lancet. 2018;393:531-40).
“Was it really you?” was a question sometimes asked of a woman named as a lead or first author, noted Sonia Gandhi, MD, PhD, group leader of the Neurodegeneration Biology Laboratory at the Francis Crick Institute in Cambridge (England). Women network differently to men, Dr. Gandhi observed, and not necessarily in networks that forward careers. Women were also often questioned about their productivity, and regardless of any training on unconscious bias, women were still at a disadvantage if they took a career break to have children.
Women’s credentials and capabilities were often felt to be less respected by male colleagues, and there was talk of being met with microaggressions in the workplace, as in one example given by Nana Odom, MSc, a clinical engineer at the Royal United Hospital Bath (England). She was told “you’re not an engineer, because I have not got a set of screwdrivers and sit at a computer and program.” Such comments can deeply affect a person, Dr. Odom said. “Sometimes I feel that if I don’t go into the workshop and open up a bit of kit that I am not an engineer, but it’s so unconscious, it carries on with you.” These types of stories need to be told so then they can be properly addressed when they do happen, she said.
Female representation is so important, said F. Gigi Osler, MD, head of otolaryngology-head and neck surgery at St. Boniface Hospital in Winnipeg. Dr. Osler is the 2018-2019 president of the Canadian Medical Association, the eighth woman to hold this prestigious position in the organization’s 151 years of operation. She also happens to be the first female surgeon and the first woman of color in the role. “When I stepped into the presidency last August, I thought very long and very hard about how I was going to use my voice and this platform,” Dr. Osler said. “It became very clear to me after I started how important representation was. I can’t tell you how many women, young women, and women of color...have come up to me to say, ‘I’m so excited to have you in this position. I’ve never seen someone who looks like me in that type of leadership position,’ ” she observed.
“As leaders, I think we can advocate for structures and processes,” Dr. Osler added, “I think we set the culture.” Leaders have the responsibility for creating and nurturing and fostering a professional, respectful, and inclusive environment, she said.
“We need more strong leaders, we need more diversity in leadership.” Dr. Osler was keen to point out that greater diversity does not mean only women, but other groups as well. “Look around the room. Who is not here? How can I make it easier for them to get here?”
Another strong female role model at the event was Dame Sally Davies, the Chief Medical Officer for England, a hematologist by training. Not only is she the first female in that role, she will also become the first female Master of Trinity College Cambridge starting in October 2019, a role dominated by men for more than 500 years.
All people, women and men, need to be given fair opportunity, Dame Sally said. Addressing structural issues can help, she said. “We need role models, mentors, and champions,” she said, noting that there were differences between the three. “Mentors give you advice, they get to know you, and they help you think through your issue. Champions may not have time for that, but they know you are good,” and they are putting you forward for opportunities.
“If the system isn’t right, or we are treated badly, we need to call it out,” Dame Sally said. “I do think that we often let things pass that we shouldn’t.” A classic situation is where a woman may suggest something at a meeting and it is ignored, but when a man says the same thing it is taken on board. That kind of behavior needs to stop and be addressed when it happens, by everyone at the table, she said.
Dr. Hawkes observed in her summing up of the day: “Throughout the history of health, change comes about not just through action at the top, but also from action from the bottom up.” She added: “The question is how do we make that change happen?” That’s where the next phase of research needs to take place, she suggested, “we need to actually see, in a very evidence-informed way, what actually works to make and sustain change.”
No financial disclosures were reported by any of the speakers quoted.
SOURCE: Lancet. 2019;393:493–610, e6-e28
FROM A LAUNCH EVENT HELD BY THE LANCET
Flu season showing its staying power
Like an unwelcome guest, the 2018-2019 flu season seems to be settling in for a lengthy stay as three more states have reached the highest level of influenza-like illness (ILI) activity, according to the Centers for Disease Control and Prevention.
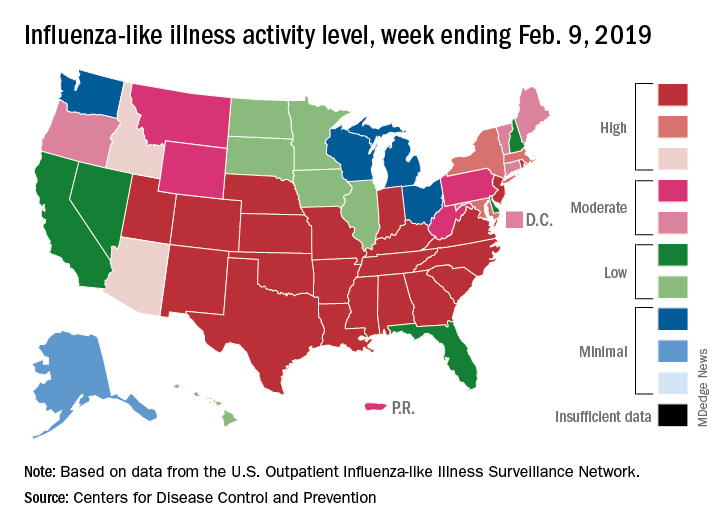
There are now 21 states at level 10 on the CDC’s 1-10 scale, with the South showing up almost solidly red on the flu activity map for the week ending Feb. 9. Another five states are at levels 8 and 9, bringing the total in the high range to 26 for the week, compared with 24 the previous week, the CDC’s influenza division reported Feb. 15.
National activity, reflected in the proportion of outpatient visits involving ILI, took a step up from 4.3% the week before to 4.8% for the week ending Feb. 9. The national baseline rate is 2.2% for ILI, which the CDC defines “as fever (temperature of 100°F [37.8°C] or greater) and cough and/or sore throat.”
Two flu-related pediatric deaths occurred during the week ending Feb. 9, and another four were reported from earlier weeks, which brings the total for the 2018-2019 season to 34, the CDC said. At the same point in last year’s flu season, there had been 84 flu-related deaths in children.
In a separate report, the CDC said that, based on data collected from Nov. 23, 2018 to Feb. 2, 2019, “the influenza vaccine has been 47% effective in preventing medically attended acute respiratory virus infection across all age groups and specifically was 46% effective in preventing medical visits associated with influenza A(H1N1)pdm09.” The effectiveness of the vaccine was 61% for children aged 6 months to 17 years, the CDC said (MMWR. 2019 Feb 15;68[6];135-9).
Flu vaccination during the 2017-2018 season prevented 7.1 million illnesses, 3.7 million medical visits, 109,000 hospitalizations, and 8,000 flu-related deaths, the CDC said, adding that “vaccination has been found to reduce deaths, intensive care unit admissions and length of stay, and overall duration of hospitalization among hospitalized influenza patients.”
Forecasts for the rest of the 2018-2019 season “predict that elevated influenza activity in parts of the United States will continue for several more weeks,” the CDC said.
Like an unwelcome guest, the 2018-2019 flu season seems to be settling in for a lengthy stay as three more states have reached the highest level of influenza-like illness (ILI) activity, according to the Centers for Disease Control and Prevention.
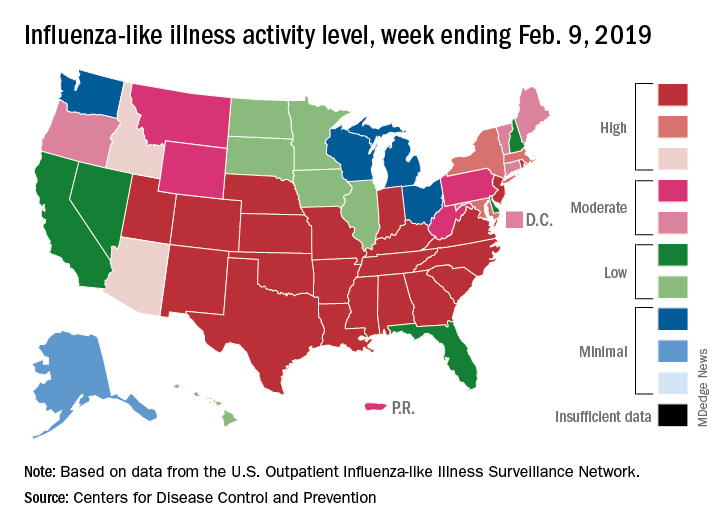
There are now 21 states at level 10 on the CDC’s 1-10 scale, with the South showing up almost solidly red on the flu activity map for the week ending Feb. 9. Another five states are at levels 8 and 9, bringing the total in the high range to 26 for the week, compared with 24 the previous week, the CDC’s influenza division reported Feb. 15.
National activity, reflected in the proportion of outpatient visits involving ILI, took a step up from 4.3% the week before to 4.8% for the week ending Feb. 9. The national baseline rate is 2.2% for ILI, which the CDC defines “as fever (temperature of 100°F [37.8°C] or greater) and cough and/or sore throat.”
Two flu-related pediatric deaths occurred during the week ending Feb. 9, and another four were reported from earlier weeks, which brings the total for the 2018-2019 season to 34, the CDC said. At the same point in last year’s flu season, there had been 84 flu-related deaths in children.
In a separate report, the CDC said that, based on data collected from Nov. 23, 2018 to Feb. 2, 2019, “the influenza vaccine has been 47% effective in preventing medically attended acute respiratory virus infection across all age groups and specifically was 46% effective in preventing medical visits associated with influenza A(H1N1)pdm09.” The effectiveness of the vaccine was 61% for children aged 6 months to 17 years, the CDC said (MMWR. 2019 Feb 15;68[6];135-9).
Flu vaccination during the 2017-2018 season prevented 7.1 million illnesses, 3.7 million medical visits, 109,000 hospitalizations, and 8,000 flu-related deaths, the CDC said, adding that “vaccination has been found to reduce deaths, intensive care unit admissions and length of stay, and overall duration of hospitalization among hospitalized influenza patients.”
Forecasts for the rest of the 2018-2019 season “predict that elevated influenza activity in parts of the United States will continue for several more weeks,” the CDC said.
Like an unwelcome guest, the 2018-2019 flu season seems to be settling in for a lengthy stay as three more states have reached the highest level of influenza-like illness (ILI) activity, according to the Centers for Disease Control and Prevention.
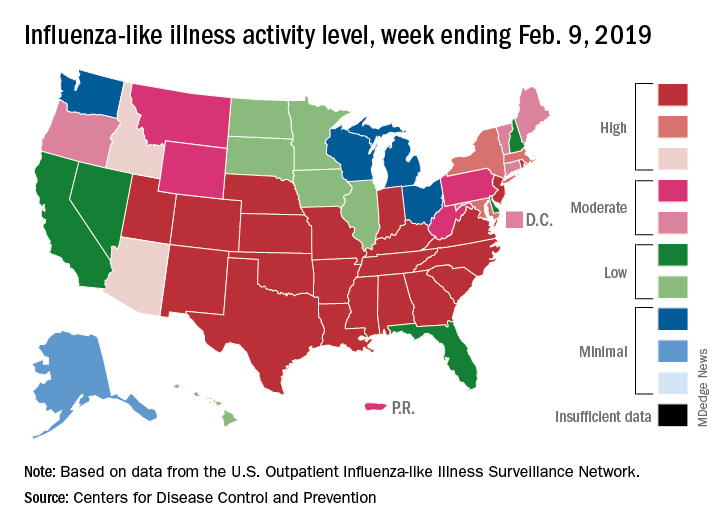
There are now 21 states at level 10 on the CDC’s 1-10 scale, with the South showing up almost solidly red on the flu activity map for the week ending Feb. 9. Another five states are at levels 8 and 9, bringing the total in the high range to 26 for the week, compared with 24 the previous week, the CDC’s influenza division reported Feb. 15.
National activity, reflected in the proportion of outpatient visits involving ILI, took a step up from 4.3% the week before to 4.8% for the week ending Feb. 9. The national baseline rate is 2.2% for ILI, which the CDC defines “as fever (temperature of 100°F [37.8°C] or greater) and cough and/or sore throat.”
Two flu-related pediatric deaths occurred during the week ending Feb. 9, and another four were reported from earlier weeks, which brings the total for the 2018-2019 season to 34, the CDC said. At the same point in last year’s flu season, there had been 84 flu-related deaths in children.
In a separate report, the CDC said that, based on data collected from Nov. 23, 2018 to Feb. 2, 2019, “the influenza vaccine has been 47% effective in preventing medically attended acute respiratory virus infection across all age groups and specifically was 46% effective in preventing medical visits associated with influenza A(H1N1)pdm09.” The effectiveness of the vaccine was 61% for children aged 6 months to 17 years, the CDC said (MMWR. 2019 Feb 15;68[6];135-9).
Flu vaccination during the 2017-2018 season prevented 7.1 million illnesses, 3.7 million medical visits, 109,000 hospitalizations, and 8,000 flu-related deaths, the CDC said, adding that “vaccination has been found to reduce deaths, intensive care unit admissions and length of stay, and overall duration of hospitalization among hospitalized influenza patients.”
Forecasts for the rest of the 2018-2019 season “predict that elevated influenza activity in parts of the United States will continue for several more weeks,” the CDC said.
The amazing work we get to do
Serving people, connecting, and improving care
Stories are told of the first meeting, 20 years ago, where a hat was passed to collect donations to develop a fledgling organization of inpatient physicians. Today, 90% of hospitals with 200+ beds operate with a hospitalist model. Today, we are the Society of Hospital Medicine.
In the early 1900s, health care in many ways was simple. It was a doctor with a shingle hung. It was house calls. Remedies were limited. In the 1940s, companies developed insurance benefits to lure workers during World War II; this third party, the payer, added complexity. Meanwhile, treatment options began to diversify. Then, in the 1960s, Medicare was passed, and the government came into the mix, further increasing this complexity. Diagnostic and treatment options continued to diversify, seemingly exponentially. Some would say it took 30 years for our country to recognize that it had created the most advanced and expensive, as well as one of the least quality-controlled, health systems in the world. Thus, as hospital medicine was conceived in the 1990s, our national health system was awakening to the need – the creative niche – that hospitalists would fill.
When I began my career, I was unaware that I was a hospitalist. The title didn’t exist. Yes, I was working solely in the hospital. I was developing programs to improve care delivery. I was rounding, teaching, collaborating, connecting – everything that we now call hospital medicine. That first job has evolved into my career, one that I find both honorable and enjoyable.
As health care changes with the passing years, being a hospitalist continues to be about serving people, connecting, and improving care. Being a hospitalist is being innovative, willing, and even daring. Dare to try, dare to fail, dare to redesign and try again. Hospital medicine is thinking outside of the box while knowing how to color between the lines. In the coming decades, health care will continue to evolve, and hospital medicine will too. We now encompass surgical comanagement and perioperative care, palliative care, postacute care, and transitions of care services. In corners, hospital medicine is already experimenting with telecare, virtual health, and hospital at home. Our hospital medicine workforce is innovative, diverse, tech savvy and poised for leading.
We are ready and willing to face the pressures affecting health care in the United States today: the recognition of an overwhelming expense to society, the relative underperformance with regard to quality, the increasing complexity of illness and treatment options, the worsening health of the average American citizen, the aging population, the role of medical error in patient harm, the increasing engagement of people in their own care, and the desire to make care better. What our country is facing is actually a phenomenal opportunity, no matter what side of the political aisle you live on. Being in hospital medicine today is being at the center front of this evolutionary stage.
Since joining the SHM board of directors, I continue to find examples of the stellar work of our staff and our members across the country. Having the privilege as a board member to join several Chapter meetings, I have witnessed firsthand the camaraderie, the compassion, the team that makes our Society work. From Houston to San Francisco and from St. Louis to Seattle, I have been honored to work with SHM members that create and nurture local and regional networks with the support of SHM’s Chapters program – a program that now houses more than 50 chapters and has launched regional districts to further support networking and growth. SHM’s chapter venues allow our larger hospital medicine team – yes, the national one – to connect and collaborate.
Take the Pacific Northwest Chapter. In its early years hospitalists from various and competing health systems would convene at a restaurant and just talk. They spoke of how to staff, how to pay, and how to negotiate with hospital leadership. As I have joined chapter meetings in recent years, meetings continue to be the place to share ideas – how to develop new programs; what is the most recent approach to glycemic control, sepsis care, or antibiotic stewardship; how best to approach diagnosis without “anchoring”; and even how to care for each other in the time of loss of a colleague to suicide. It is here in our community that we share experiences, knowledge, new ideas – and this sharing makes us all stronger.
Our hospital medicine community also comes together through areas of shared interest. There are 18 Special Interest Groups (SIGs), focused on specific topic areas. I have been privileged as a board member to work with our Perioperative/Comanagement SIG as it launched in 2017 and has grown rapidly. Currently, the community hosts a “case of the month” hospital medicine discussion as well as a regular journal club webinar that allows participants to review recent literature and interact directly with the authors. As this SIG has grown, shared resources and ideas have allowed for diffusion of knowledge, providing our nation with infrastructure for improving perioperative care. It is networks like this that support our national hospital medicine team to build strength through sharing.
It is our society, our people, that have taken us from the passing of a hat to developing our national community and network. This March, we get to celebrate our field in a new way – Thursday, March 7, 2019, marks the inaugural National Hospitalist Day. Then, March 24-27, our annual conference, Hospital Medicine 2019, will bring thousands of our national team to National Harbor, Maryland. Join your colleagues. Find your niche and your community. Be a part of the change you want to see. While you are there, come introduce yourself to me and let me thank you for the amazing work you are doing.
We are all a part of this movement transforming patient care both on a local and national level. As we move to the future, our innovative, diverse, and connected network of hospital medicine will continue to create and guide health care advances in our country.
Dr. Thompson is professor and chief of the section of hospital medicine at University of Nebraska Medical Center, and medical director of clinical care transitions at Nebraska Medicine, Omaha.
Serving people, connecting, and improving care
Serving people, connecting, and improving care
Stories are told of the first meeting, 20 years ago, where a hat was passed to collect donations to develop a fledgling organization of inpatient physicians. Today, 90% of hospitals with 200+ beds operate with a hospitalist model. Today, we are the Society of Hospital Medicine.
In the early 1900s, health care in many ways was simple. It was a doctor with a shingle hung. It was house calls. Remedies were limited. In the 1940s, companies developed insurance benefits to lure workers during World War II; this third party, the payer, added complexity. Meanwhile, treatment options began to diversify. Then, in the 1960s, Medicare was passed, and the government came into the mix, further increasing this complexity. Diagnostic and treatment options continued to diversify, seemingly exponentially. Some would say it took 30 years for our country to recognize that it had created the most advanced and expensive, as well as one of the least quality-controlled, health systems in the world. Thus, as hospital medicine was conceived in the 1990s, our national health system was awakening to the need – the creative niche – that hospitalists would fill.
When I began my career, I was unaware that I was a hospitalist. The title didn’t exist. Yes, I was working solely in the hospital. I was developing programs to improve care delivery. I was rounding, teaching, collaborating, connecting – everything that we now call hospital medicine. That first job has evolved into my career, one that I find both honorable and enjoyable.
As health care changes with the passing years, being a hospitalist continues to be about serving people, connecting, and improving care. Being a hospitalist is being innovative, willing, and even daring. Dare to try, dare to fail, dare to redesign and try again. Hospital medicine is thinking outside of the box while knowing how to color between the lines. In the coming decades, health care will continue to evolve, and hospital medicine will too. We now encompass surgical comanagement and perioperative care, palliative care, postacute care, and transitions of care services. In corners, hospital medicine is already experimenting with telecare, virtual health, and hospital at home. Our hospital medicine workforce is innovative, diverse, tech savvy and poised for leading.
We are ready and willing to face the pressures affecting health care in the United States today: the recognition of an overwhelming expense to society, the relative underperformance with regard to quality, the increasing complexity of illness and treatment options, the worsening health of the average American citizen, the aging population, the role of medical error in patient harm, the increasing engagement of people in their own care, and the desire to make care better. What our country is facing is actually a phenomenal opportunity, no matter what side of the political aisle you live on. Being in hospital medicine today is being at the center front of this evolutionary stage.
Since joining the SHM board of directors, I continue to find examples of the stellar work of our staff and our members across the country. Having the privilege as a board member to join several Chapter meetings, I have witnessed firsthand the camaraderie, the compassion, the team that makes our Society work. From Houston to San Francisco and from St. Louis to Seattle, I have been honored to work with SHM members that create and nurture local and regional networks with the support of SHM’s Chapters program – a program that now houses more than 50 chapters and has launched regional districts to further support networking and growth. SHM’s chapter venues allow our larger hospital medicine team – yes, the national one – to connect and collaborate.
Take the Pacific Northwest Chapter. In its early years hospitalists from various and competing health systems would convene at a restaurant and just talk. They spoke of how to staff, how to pay, and how to negotiate with hospital leadership. As I have joined chapter meetings in recent years, meetings continue to be the place to share ideas – how to develop new programs; what is the most recent approach to glycemic control, sepsis care, or antibiotic stewardship; how best to approach diagnosis without “anchoring”; and even how to care for each other in the time of loss of a colleague to suicide. It is here in our community that we share experiences, knowledge, new ideas – and this sharing makes us all stronger.
Our hospital medicine community also comes together through areas of shared interest. There are 18 Special Interest Groups (SIGs), focused on specific topic areas. I have been privileged as a board member to work with our Perioperative/Comanagement SIG as it launched in 2017 and has grown rapidly. Currently, the community hosts a “case of the month” hospital medicine discussion as well as a regular journal club webinar that allows participants to review recent literature and interact directly with the authors. As this SIG has grown, shared resources and ideas have allowed for diffusion of knowledge, providing our nation with infrastructure for improving perioperative care. It is networks like this that support our national hospital medicine team to build strength through sharing.
It is our society, our people, that have taken us from the passing of a hat to developing our national community and network. This March, we get to celebrate our field in a new way – Thursday, March 7, 2019, marks the inaugural National Hospitalist Day. Then, March 24-27, our annual conference, Hospital Medicine 2019, will bring thousands of our national team to National Harbor, Maryland. Join your colleagues. Find your niche and your community. Be a part of the change you want to see. While you are there, come introduce yourself to me and let me thank you for the amazing work you are doing.
We are all a part of this movement transforming patient care both on a local and national level. As we move to the future, our innovative, diverse, and connected network of hospital medicine will continue to create and guide health care advances in our country.
Dr. Thompson is professor and chief of the section of hospital medicine at University of Nebraska Medical Center, and medical director of clinical care transitions at Nebraska Medicine, Omaha.
Stories are told of the first meeting, 20 years ago, where a hat was passed to collect donations to develop a fledgling organization of inpatient physicians. Today, 90% of hospitals with 200+ beds operate with a hospitalist model. Today, we are the Society of Hospital Medicine.
In the early 1900s, health care in many ways was simple. It was a doctor with a shingle hung. It was house calls. Remedies were limited. In the 1940s, companies developed insurance benefits to lure workers during World War II; this third party, the payer, added complexity. Meanwhile, treatment options began to diversify. Then, in the 1960s, Medicare was passed, and the government came into the mix, further increasing this complexity. Diagnostic and treatment options continued to diversify, seemingly exponentially. Some would say it took 30 years for our country to recognize that it had created the most advanced and expensive, as well as one of the least quality-controlled, health systems in the world. Thus, as hospital medicine was conceived in the 1990s, our national health system was awakening to the need – the creative niche – that hospitalists would fill.
When I began my career, I was unaware that I was a hospitalist. The title didn’t exist. Yes, I was working solely in the hospital. I was developing programs to improve care delivery. I was rounding, teaching, collaborating, connecting – everything that we now call hospital medicine. That first job has evolved into my career, one that I find both honorable and enjoyable.
As health care changes with the passing years, being a hospitalist continues to be about serving people, connecting, and improving care. Being a hospitalist is being innovative, willing, and even daring. Dare to try, dare to fail, dare to redesign and try again. Hospital medicine is thinking outside of the box while knowing how to color between the lines. In the coming decades, health care will continue to evolve, and hospital medicine will too. We now encompass surgical comanagement and perioperative care, palliative care, postacute care, and transitions of care services. In corners, hospital medicine is already experimenting with telecare, virtual health, and hospital at home. Our hospital medicine workforce is innovative, diverse, tech savvy and poised for leading.
We are ready and willing to face the pressures affecting health care in the United States today: the recognition of an overwhelming expense to society, the relative underperformance with regard to quality, the increasing complexity of illness and treatment options, the worsening health of the average American citizen, the aging population, the role of medical error in patient harm, the increasing engagement of people in their own care, and the desire to make care better. What our country is facing is actually a phenomenal opportunity, no matter what side of the political aisle you live on. Being in hospital medicine today is being at the center front of this evolutionary stage.
Since joining the SHM board of directors, I continue to find examples of the stellar work of our staff and our members across the country. Having the privilege as a board member to join several Chapter meetings, I have witnessed firsthand the camaraderie, the compassion, the team that makes our Society work. From Houston to San Francisco and from St. Louis to Seattle, I have been honored to work with SHM members that create and nurture local and regional networks with the support of SHM’s Chapters program – a program that now houses more than 50 chapters and has launched regional districts to further support networking and growth. SHM’s chapter venues allow our larger hospital medicine team – yes, the national one – to connect and collaborate.
Take the Pacific Northwest Chapter. In its early years hospitalists from various and competing health systems would convene at a restaurant and just talk. They spoke of how to staff, how to pay, and how to negotiate with hospital leadership. As I have joined chapter meetings in recent years, meetings continue to be the place to share ideas – how to develop new programs; what is the most recent approach to glycemic control, sepsis care, or antibiotic stewardship; how best to approach diagnosis without “anchoring”; and even how to care for each other in the time of loss of a colleague to suicide. It is here in our community that we share experiences, knowledge, new ideas – and this sharing makes us all stronger.
Our hospital medicine community also comes together through areas of shared interest. There are 18 Special Interest Groups (SIGs), focused on specific topic areas. I have been privileged as a board member to work with our Perioperative/Comanagement SIG as it launched in 2017 and has grown rapidly. Currently, the community hosts a “case of the month” hospital medicine discussion as well as a regular journal club webinar that allows participants to review recent literature and interact directly with the authors. As this SIG has grown, shared resources and ideas have allowed for diffusion of knowledge, providing our nation with infrastructure for improving perioperative care. It is networks like this that support our national hospital medicine team to build strength through sharing.
It is our society, our people, that have taken us from the passing of a hat to developing our national community and network. This March, we get to celebrate our field in a new way – Thursday, March 7, 2019, marks the inaugural National Hospitalist Day. Then, March 24-27, our annual conference, Hospital Medicine 2019, will bring thousands of our national team to National Harbor, Maryland. Join your colleagues. Find your niche and your community. Be a part of the change you want to see. While you are there, come introduce yourself to me and let me thank you for the amazing work you are doing.
We are all a part of this movement transforming patient care both on a local and national level. As we move to the future, our innovative, diverse, and connected network of hospital medicine will continue to create and guide health care advances in our country.
Dr. Thompson is professor and chief of the section of hospital medicine at University of Nebraska Medical Center, and medical director of clinical care transitions at Nebraska Medicine, Omaha.
Deferoxamine does not improve 90-day outcomes after ICH
HONOLULU – (ICH), according to trial results described at the International Stroke Conference sponsored by the American Heart Association. However, the drug is safe and well tolerated and data suggest that it may improve outcomes at 180 days.
Animal studies indicate that iron, which is released from hemolyzed red blood cells, accumulates in the brain after ICH and is associated with secondary neuronal injury and death. Researchers have found that deferoxamine, an iron chelator, provides neuroprotection and improves recovery after experimental ICH. The drug also has anti-inflammatory, antiapoptotic, and BP-lowering effects. Deferoxamine has been approved since the 1960s.
Magdy H. Selim, MD, PhD, a neurologist at Beth Israel Deaconess Medical Center in Boston, and colleagues hypothesized that treatment with deferoxamine could improve outcomes in patients with ICH. The researchers conducted a phase 2 clinical trial to evaluate whether deferoxamine should be studied in a phase 3 efficacy trial. In their multicenter, double-blind study, Dr. Selim and his colleagues randomized patients with spontaneous supratentorial ICH in equal groups to 32 mg/kg per day of deferoxamine or saline placebo. Treatments were administered as intravenous infusions for 3 consecutive days, and therapy was initiated within 24 hours after ICH onset. The follow-up period was 6 months.
Eligible participants had an National Institutes of Health Stroke Scale score of 6 or higher, a Glasgow Coma Scale score greater than 6, and had been functionally independent before the hemorrhage. The researchers excluded patients with a secondary cause for ICH or coagulopathy.
The primary endpoint in the futility analysis was the proportion of participants with a good clinical outcome – defined as a modified Rankin Scale (mRS) score of 0-2 – at 90 days and 180 days. The secondary endpoint was good outcome, defined as an mRS score of 0-3, at 90 days. Safety endpoints included all deferoxamine-related adverse events until day 7 or discharge (whichever was earlier) and serious adverse events through day 90.
Dr. Selim and his colleagues enrolled 294 participants in their trial, 3 of whom did not receive treatment. Of these included participants, 147 (50.5%) were randomized to placebo and 144 (49.5%) were randomized to deferoxamine. Participants’ mean age was 60.3 years, and 38.5% of the population was female.
Overall, the two study arms did not differ significantly according to demographic and clinical characteristics, however, there were more nonwhite patients in the deferoxamine arm than in the placebo arm, however. In addition, thalamic hemorrhage and intraventricular hemorrhage were more common in the placebo-treated group and hemorrhages in the putamen and basal ganglia were more common in the deferoxamine-treated group.
The rates of adverse events were comparable between the two study arms. Dr. Selim and his colleagues found no unexpected safety issues. Mortality was low, and the 90-day and 180-day mortality rates were comparable between the two treatment arms.
Approximately 34% of deferoxamine-treated patients and 33% of placebo-treated patients had an mRS score of 0-2 at 90 days. The adjusted absolute risk difference between arms was 0.6%; this result did not surpass the predefined futility threshold. The risk difference between groups for mRS score of 0-2 at 180 days was 8.6% in favor of deferoxamine, which did surpass the futility threshold.
The risk difference for meeting the secondary endpoint was 6.2% in favor of deferoxamine; this result did not surpass the futility threshold. Patients in both treatment groups improved between day 90 and day 180. The likelihood of good outcome was approximately 10% higher in the deferoxamine group at day 90 and 26% higher in the deferoxamine group at day 180.
“It is futile to conduct a phase 3 trial with the anticipation that treatment with deferoxamine would improve outcome, defined as mRS score of 0-2 at 90 days,” said Dr. Selim. “These data, together with the data from MISTIE and CLEAR, suggest that ICH trials need to have a longer follow-up period to capture the full extent of recovery after ICH. Several of our secondary analyses tended to favor deferoxamine over the placebo arm and leave open the possibility that deferoxamine might lead to improved outcome at 180 days.”
The researchers received support from the NIH and the National Institute of Neurological Disorders and Stroke.
SOURCE: Selim MH et al. ISC 2019, Abstract LB22.
HONOLULU – (ICH), according to trial results described at the International Stroke Conference sponsored by the American Heart Association. However, the drug is safe and well tolerated and data suggest that it may improve outcomes at 180 days.
Animal studies indicate that iron, which is released from hemolyzed red blood cells, accumulates in the brain after ICH and is associated with secondary neuronal injury and death. Researchers have found that deferoxamine, an iron chelator, provides neuroprotection and improves recovery after experimental ICH. The drug also has anti-inflammatory, antiapoptotic, and BP-lowering effects. Deferoxamine has been approved since the 1960s.
Magdy H. Selim, MD, PhD, a neurologist at Beth Israel Deaconess Medical Center in Boston, and colleagues hypothesized that treatment with deferoxamine could improve outcomes in patients with ICH. The researchers conducted a phase 2 clinical trial to evaluate whether deferoxamine should be studied in a phase 3 efficacy trial. In their multicenter, double-blind study, Dr. Selim and his colleagues randomized patients with spontaneous supratentorial ICH in equal groups to 32 mg/kg per day of deferoxamine or saline placebo. Treatments were administered as intravenous infusions for 3 consecutive days, and therapy was initiated within 24 hours after ICH onset. The follow-up period was 6 months.
Eligible participants had an National Institutes of Health Stroke Scale score of 6 or higher, a Glasgow Coma Scale score greater than 6, and had been functionally independent before the hemorrhage. The researchers excluded patients with a secondary cause for ICH or coagulopathy.
The primary endpoint in the futility analysis was the proportion of participants with a good clinical outcome – defined as a modified Rankin Scale (mRS) score of 0-2 – at 90 days and 180 days. The secondary endpoint was good outcome, defined as an mRS score of 0-3, at 90 days. Safety endpoints included all deferoxamine-related adverse events until day 7 or discharge (whichever was earlier) and serious adverse events through day 90.
Dr. Selim and his colleagues enrolled 294 participants in their trial, 3 of whom did not receive treatment. Of these included participants, 147 (50.5%) were randomized to placebo and 144 (49.5%) were randomized to deferoxamine. Participants’ mean age was 60.3 years, and 38.5% of the population was female.
Overall, the two study arms did not differ significantly according to demographic and clinical characteristics, however, there were more nonwhite patients in the deferoxamine arm than in the placebo arm, however. In addition, thalamic hemorrhage and intraventricular hemorrhage were more common in the placebo-treated group and hemorrhages in the putamen and basal ganglia were more common in the deferoxamine-treated group.
The rates of adverse events were comparable between the two study arms. Dr. Selim and his colleagues found no unexpected safety issues. Mortality was low, and the 90-day and 180-day mortality rates were comparable between the two treatment arms.
Approximately 34% of deferoxamine-treated patients and 33% of placebo-treated patients had an mRS score of 0-2 at 90 days. The adjusted absolute risk difference between arms was 0.6%; this result did not surpass the predefined futility threshold. The risk difference between groups for mRS score of 0-2 at 180 days was 8.6% in favor of deferoxamine, which did surpass the futility threshold.
The risk difference for meeting the secondary endpoint was 6.2% in favor of deferoxamine; this result did not surpass the futility threshold. Patients in both treatment groups improved between day 90 and day 180. The likelihood of good outcome was approximately 10% higher in the deferoxamine group at day 90 and 26% higher in the deferoxamine group at day 180.
“It is futile to conduct a phase 3 trial with the anticipation that treatment with deferoxamine would improve outcome, defined as mRS score of 0-2 at 90 days,” said Dr. Selim. “These data, together with the data from MISTIE and CLEAR, suggest that ICH trials need to have a longer follow-up period to capture the full extent of recovery after ICH. Several of our secondary analyses tended to favor deferoxamine over the placebo arm and leave open the possibility that deferoxamine might lead to improved outcome at 180 days.”
The researchers received support from the NIH and the National Institute of Neurological Disorders and Stroke.
SOURCE: Selim MH et al. ISC 2019, Abstract LB22.
HONOLULU – (ICH), according to trial results described at the International Stroke Conference sponsored by the American Heart Association. However, the drug is safe and well tolerated and data suggest that it may improve outcomes at 180 days.
Animal studies indicate that iron, which is released from hemolyzed red blood cells, accumulates in the brain after ICH and is associated with secondary neuronal injury and death. Researchers have found that deferoxamine, an iron chelator, provides neuroprotection and improves recovery after experimental ICH. The drug also has anti-inflammatory, antiapoptotic, and BP-lowering effects. Deferoxamine has been approved since the 1960s.
Magdy H. Selim, MD, PhD, a neurologist at Beth Israel Deaconess Medical Center in Boston, and colleagues hypothesized that treatment with deferoxamine could improve outcomes in patients with ICH. The researchers conducted a phase 2 clinical trial to evaluate whether deferoxamine should be studied in a phase 3 efficacy trial. In their multicenter, double-blind study, Dr. Selim and his colleagues randomized patients with spontaneous supratentorial ICH in equal groups to 32 mg/kg per day of deferoxamine or saline placebo. Treatments were administered as intravenous infusions for 3 consecutive days, and therapy was initiated within 24 hours after ICH onset. The follow-up period was 6 months.
Eligible participants had an National Institutes of Health Stroke Scale score of 6 or higher, a Glasgow Coma Scale score greater than 6, and had been functionally independent before the hemorrhage. The researchers excluded patients with a secondary cause for ICH or coagulopathy.
The primary endpoint in the futility analysis was the proportion of participants with a good clinical outcome – defined as a modified Rankin Scale (mRS) score of 0-2 – at 90 days and 180 days. The secondary endpoint was good outcome, defined as an mRS score of 0-3, at 90 days. Safety endpoints included all deferoxamine-related adverse events until day 7 or discharge (whichever was earlier) and serious adverse events through day 90.
Dr. Selim and his colleagues enrolled 294 participants in their trial, 3 of whom did not receive treatment. Of these included participants, 147 (50.5%) were randomized to placebo and 144 (49.5%) were randomized to deferoxamine. Participants’ mean age was 60.3 years, and 38.5% of the population was female.
Overall, the two study arms did not differ significantly according to demographic and clinical characteristics, however, there were more nonwhite patients in the deferoxamine arm than in the placebo arm, however. In addition, thalamic hemorrhage and intraventricular hemorrhage were more common in the placebo-treated group and hemorrhages in the putamen and basal ganglia were more common in the deferoxamine-treated group.
The rates of adverse events were comparable between the two study arms. Dr. Selim and his colleagues found no unexpected safety issues. Mortality was low, and the 90-day and 180-day mortality rates were comparable between the two treatment arms.
Approximately 34% of deferoxamine-treated patients and 33% of placebo-treated patients had an mRS score of 0-2 at 90 days. The adjusted absolute risk difference between arms was 0.6%; this result did not surpass the predefined futility threshold. The risk difference between groups for mRS score of 0-2 at 180 days was 8.6% in favor of deferoxamine, which did surpass the futility threshold.
The risk difference for meeting the secondary endpoint was 6.2% in favor of deferoxamine; this result did not surpass the futility threshold. Patients in both treatment groups improved between day 90 and day 180. The likelihood of good outcome was approximately 10% higher in the deferoxamine group at day 90 and 26% higher in the deferoxamine group at day 180.
“It is futile to conduct a phase 3 trial with the anticipation that treatment with deferoxamine would improve outcome, defined as mRS score of 0-2 at 90 days,” said Dr. Selim. “These data, together with the data from MISTIE and CLEAR, suggest that ICH trials need to have a longer follow-up period to capture the full extent of recovery after ICH. Several of our secondary analyses tended to favor deferoxamine over the placebo arm and leave open the possibility that deferoxamine might lead to improved outcome at 180 days.”
The researchers received support from the NIH and the National Institute of Neurological Disorders and Stroke.
SOURCE: Selim MH et al. ISC 2019, Abstract LB22.
REPORTING FROM ISC 2019
Key clinical point: Deferoxamine does not improve disability at 90 days after intracranial hemorrhage.
Major finding: Approximately one-third of patients in both treatment groups had a good outcome.
Study details: A multicenter, randomized, double-blind study of 294 participants with intracranial hemorrhage.
Disclosures: The National Institutes of Health and National Institute of Neurological Disorders and Stroke supported this study.
Source: Selim MH et al. ISC 2019, Abstract LB22.
An unplanned career
A focus on health system transformation
I have to admit that I am not sure I am a legacy in hospital medicine, and the term legacy throws me off a bit. I came to medical school after working at McKinsey & Co. consulting, and I chose pediatrics because of my love of working with children and families, as well as a vague notion that I wanted to work on “system” issues, and therefore, more generalist-type training seemed applicable.
I met Chris Landrigan, MD, MPH, and Vinny Chiang, MD, and learned what a hospitalist was, as an intern in 2002. We had a research elective and I was able to publish a couple of papers in Pediatrics on pediatric hospital medicine with Chris and Raj Srivastava, MD, MPH. In 2004, I went to my first Society of Hospital Medicine meeting and met Larry Wellikson, MD, MHM, and others. From there, I went to the Robert Wood Johnson Clinical Scholars Program, with Ron Keren, MD, MPH, and others, and along with faculty from the Cincinnati Children’s in hospital medicine.
In 2007, I applied for a White House Fellowship and told my wife that I didn’t think there was a chance that I would get it, so we should keep building our new home in Cincinnati. We were both surprised when I was selected. I served Michael Leavitt, the then-Secretary of the Department of Health & Human Services, as his White House fellow during the Bush administration, and then served as his chief medical officer. Exposure to health policy and leadership at that level was career shaping. Cincinnati Children’s was searching for a leader for the conversion of pediatric hospital medicine into a full division in 2009. So I returned to Cincinnati to take on leading pediatric hospital medicine, and a role leading quality measurement and improvement efforts for the entire health system. I loved the work and thought I would remain in that role, and our family would be in Cincinnati for a long time. Best laid plans …
In early 2011, Don Berwick, MD, who was then the administrator of the Centers for Medicare & Medicaid Services called and asked whether I “would come talk with him in D.C.” That talk quickly became a series of interviews, and he offered me the opportunity to be chief medical officer of CMS. He said “this platform is like no other to drive change.” He was right. I have been fortunate to have a few step-change opportunities in my life, and that was one.
On my first day at CMS, I looked around the table of senior executives reporting to me and realized they had more than 200 years of CMS experience. I was a bit scared. Together, we led the implementation of Hospital Value-Based Purchasing, the Compare websites, and numerous quality measurement and improvement programs. Partnership for Patients works on patient safety and was associated with preventing more than 3 million infections and adverse events, over 125,000 lives saved, and more than $26 billion in savings.
In early 2013, I was asked to lead the CMS Innovation Center (CMMI). The goal was to launch new payment and service delivery models to improve quality and lower costs. We launched Accountable Care Organizations, Bundled Payment programs, primary care medical homes, state-based innovation, and so much more. Medicare went from zero dollars in alternative payment models, where providers are accountable for quality and total cost of care, to more than 30% of Medicare payments, representing over $200 billion through agreements with more than 200,000 providers in these alternative payment models. It was the biggest shift in U.S. history in how CMS paid for care. Later, I became principal deputy administrator and acting administrator of CMS, leading an agency that spends over $1 trillion per year, or more than $2.5 billion per day and insures over 130 million Americans. We also improved from being bottom quintile in employee engagement and satisfaction across the federal government to No. 2.
I had assumed that, after working at CMS, I would return to a hospital/health system leadership role. But then, a recruiter called about the CEO role at Blue Cross Blue Shield of North Carolina. It is one of the largest not-for-profit health plans in the country and insures most of the people in North Carolina, many for most of their lives. I met a 75-year-old woman the other day that we have insured every day of her life. I am almost a year into the role and it is a mission-driven organization that drives positive change. I love it so far.
We are going to partner with providers, so that more than half of our payments will be in advanced alternative payment models. No payer in the United States has done that yet. This allows us to innovate and decrease friction in the system (e.g., turn off prior authorization) and be jointly accountable with providers for quality and total cost of care. We insure people through the ACA [Affordable Care Act], commercial, and Medicare markets, and are competing to serve Medicaid as well. We have invested more than $50 million to address social determinants of health across the state. We are making major investments in primary care, and mental and behavioral health. Our goal is to be a Model Blue – or a Model of Health Transformation for our state and nation – and achieve better health outcomes, lower costs, and best-in-class experience for all people we serve. I have learned that no physician leads a health plan of this size, and apparently, no practicing physician has ever led a health plan of this size.
What are some lessons learned over my career? I have had five criteria for all my career decisions: 1) family; 2) impact – better care and outcomes, lower costs, and exceptional experience for populations of patients; 3) people – mentors and colleagues; 4) learning; and 5) joy in work. If someone gives you a chance to lead people in your career as a physician, jump at the chance. We do a relatively poor job of providing this type of opportunity to those early in their careers in medicine, and learning how to manage people and money allows you to progress as a leader and manager.
Don’t listen to the people who say “you must do X before Y” or “you must take this path.” They are usually wrong. Take chances. I applied for many roles for which I was a long shot, and I didn’t always succeed. That’s life and learning. Hospital medicine is a great career. I worked in the hospital on a recent weekend and was able to help families through everything from palliative care decisions and new diagnoses, to recovering from illness. It is an honor to serve and help families in their time of need. Hospitalists have been – and should continue to be – primary drivers of the shift in our health system to value-based care.
As I look back on my career (and I hope I am only halfway done), I could not have predicted more than 90% of it. I was blessed with many opportunities, mentors, and teachers along the way. I try to pass this on by mentoring and teaching others. How did my career happen? I am not sure, but it has been a fun ride! And hopefully I have helped improve the health system some, along the way.
Dr. Conway is president and CEO of Blue Cross and Blue Shield of North Carolina. He is a hospitalist and former deputy administrator for innovation and quality at the Centers for Medicare and Medicaid Services.
A focus on health system transformation
A focus on health system transformation
I have to admit that I am not sure I am a legacy in hospital medicine, and the term legacy throws me off a bit. I came to medical school after working at McKinsey & Co. consulting, and I chose pediatrics because of my love of working with children and families, as well as a vague notion that I wanted to work on “system” issues, and therefore, more generalist-type training seemed applicable.
I met Chris Landrigan, MD, MPH, and Vinny Chiang, MD, and learned what a hospitalist was, as an intern in 2002. We had a research elective and I was able to publish a couple of papers in Pediatrics on pediatric hospital medicine with Chris and Raj Srivastava, MD, MPH. In 2004, I went to my first Society of Hospital Medicine meeting and met Larry Wellikson, MD, MHM, and others. From there, I went to the Robert Wood Johnson Clinical Scholars Program, with Ron Keren, MD, MPH, and others, and along with faculty from the Cincinnati Children’s in hospital medicine.
In 2007, I applied for a White House Fellowship and told my wife that I didn’t think there was a chance that I would get it, so we should keep building our new home in Cincinnati. We were both surprised when I was selected. I served Michael Leavitt, the then-Secretary of the Department of Health & Human Services, as his White House fellow during the Bush administration, and then served as his chief medical officer. Exposure to health policy and leadership at that level was career shaping. Cincinnati Children’s was searching for a leader for the conversion of pediatric hospital medicine into a full division in 2009. So I returned to Cincinnati to take on leading pediatric hospital medicine, and a role leading quality measurement and improvement efforts for the entire health system. I loved the work and thought I would remain in that role, and our family would be in Cincinnati for a long time. Best laid plans …
In early 2011, Don Berwick, MD, who was then the administrator of the Centers for Medicare & Medicaid Services called and asked whether I “would come talk with him in D.C.” That talk quickly became a series of interviews, and he offered me the opportunity to be chief medical officer of CMS. He said “this platform is like no other to drive change.” He was right. I have been fortunate to have a few step-change opportunities in my life, and that was one.
On my first day at CMS, I looked around the table of senior executives reporting to me and realized they had more than 200 years of CMS experience. I was a bit scared. Together, we led the implementation of Hospital Value-Based Purchasing, the Compare websites, and numerous quality measurement and improvement programs. Partnership for Patients works on patient safety and was associated with preventing more than 3 million infections and adverse events, over 125,000 lives saved, and more than $26 billion in savings.
In early 2013, I was asked to lead the CMS Innovation Center (CMMI). The goal was to launch new payment and service delivery models to improve quality and lower costs. We launched Accountable Care Organizations, Bundled Payment programs, primary care medical homes, state-based innovation, and so much more. Medicare went from zero dollars in alternative payment models, where providers are accountable for quality and total cost of care, to more than 30% of Medicare payments, representing over $200 billion through agreements with more than 200,000 providers in these alternative payment models. It was the biggest shift in U.S. history in how CMS paid for care. Later, I became principal deputy administrator and acting administrator of CMS, leading an agency that spends over $1 trillion per year, or more than $2.5 billion per day and insures over 130 million Americans. We also improved from being bottom quintile in employee engagement and satisfaction across the federal government to No. 2.
I had assumed that, after working at CMS, I would return to a hospital/health system leadership role. But then, a recruiter called about the CEO role at Blue Cross Blue Shield of North Carolina. It is one of the largest not-for-profit health plans in the country and insures most of the people in North Carolina, many for most of their lives. I met a 75-year-old woman the other day that we have insured every day of her life. I am almost a year into the role and it is a mission-driven organization that drives positive change. I love it so far.
We are going to partner with providers, so that more than half of our payments will be in advanced alternative payment models. No payer in the United States has done that yet. This allows us to innovate and decrease friction in the system (e.g., turn off prior authorization) and be jointly accountable with providers for quality and total cost of care. We insure people through the ACA [Affordable Care Act], commercial, and Medicare markets, and are competing to serve Medicaid as well. We have invested more than $50 million to address social determinants of health across the state. We are making major investments in primary care, and mental and behavioral health. Our goal is to be a Model Blue – or a Model of Health Transformation for our state and nation – and achieve better health outcomes, lower costs, and best-in-class experience for all people we serve. I have learned that no physician leads a health plan of this size, and apparently, no practicing physician has ever led a health plan of this size.
What are some lessons learned over my career? I have had five criteria for all my career decisions: 1) family; 2) impact – better care and outcomes, lower costs, and exceptional experience for populations of patients; 3) people – mentors and colleagues; 4) learning; and 5) joy in work. If someone gives you a chance to lead people in your career as a physician, jump at the chance. We do a relatively poor job of providing this type of opportunity to those early in their careers in medicine, and learning how to manage people and money allows you to progress as a leader and manager.
Don’t listen to the people who say “you must do X before Y” or “you must take this path.” They are usually wrong. Take chances. I applied for many roles for which I was a long shot, and I didn’t always succeed. That’s life and learning. Hospital medicine is a great career. I worked in the hospital on a recent weekend and was able to help families through everything from palliative care decisions and new diagnoses, to recovering from illness. It is an honor to serve and help families in their time of need. Hospitalists have been – and should continue to be – primary drivers of the shift in our health system to value-based care.
As I look back on my career (and I hope I am only halfway done), I could not have predicted more than 90% of it. I was blessed with many opportunities, mentors, and teachers along the way. I try to pass this on by mentoring and teaching others. How did my career happen? I am not sure, but it has been a fun ride! And hopefully I have helped improve the health system some, along the way.
Dr. Conway is president and CEO of Blue Cross and Blue Shield of North Carolina. He is a hospitalist and former deputy administrator for innovation and quality at the Centers for Medicare and Medicaid Services.
I have to admit that I am not sure I am a legacy in hospital medicine, and the term legacy throws me off a bit. I came to medical school after working at McKinsey & Co. consulting, and I chose pediatrics because of my love of working with children and families, as well as a vague notion that I wanted to work on “system” issues, and therefore, more generalist-type training seemed applicable.
I met Chris Landrigan, MD, MPH, and Vinny Chiang, MD, and learned what a hospitalist was, as an intern in 2002. We had a research elective and I was able to publish a couple of papers in Pediatrics on pediatric hospital medicine with Chris and Raj Srivastava, MD, MPH. In 2004, I went to my first Society of Hospital Medicine meeting and met Larry Wellikson, MD, MHM, and others. From there, I went to the Robert Wood Johnson Clinical Scholars Program, with Ron Keren, MD, MPH, and others, and along with faculty from the Cincinnati Children’s in hospital medicine.
In 2007, I applied for a White House Fellowship and told my wife that I didn’t think there was a chance that I would get it, so we should keep building our new home in Cincinnati. We were both surprised when I was selected. I served Michael Leavitt, the then-Secretary of the Department of Health & Human Services, as his White House fellow during the Bush administration, and then served as his chief medical officer. Exposure to health policy and leadership at that level was career shaping. Cincinnati Children’s was searching for a leader for the conversion of pediatric hospital medicine into a full division in 2009. So I returned to Cincinnati to take on leading pediatric hospital medicine, and a role leading quality measurement and improvement efforts for the entire health system. I loved the work and thought I would remain in that role, and our family would be in Cincinnati for a long time. Best laid plans …
In early 2011, Don Berwick, MD, who was then the administrator of the Centers for Medicare & Medicaid Services called and asked whether I “would come talk with him in D.C.” That talk quickly became a series of interviews, and he offered me the opportunity to be chief medical officer of CMS. He said “this platform is like no other to drive change.” He was right. I have been fortunate to have a few step-change opportunities in my life, and that was one.
On my first day at CMS, I looked around the table of senior executives reporting to me and realized they had more than 200 years of CMS experience. I was a bit scared. Together, we led the implementation of Hospital Value-Based Purchasing, the Compare websites, and numerous quality measurement and improvement programs. Partnership for Patients works on patient safety and was associated with preventing more than 3 million infections and adverse events, over 125,000 lives saved, and more than $26 billion in savings.
In early 2013, I was asked to lead the CMS Innovation Center (CMMI). The goal was to launch new payment and service delivery models to improve quality and lower costs. We launched Accountable Care Organizations, Bundled Payment programs, primary care medical homes, state-based innovation, and so much more. Medicare went from zero dollars in alternative payment models, where providers are accountable for quality and total cost of care, to more than 30% of Medicare payments, representing over $200 billion through agreements with more than 200,000 providers in these alternative payment models. It was the biggest shift in U.S. history in how CMS paid for care. Later, I became principal deputy administrator and acting administrator of CMS, leading an agency that spends over $1 trillion per year, or more than $2.5 billion per day and insures over 130 million Americans. We also improved from being bottom quintile in employee engagement and satisfaction across the federal government to No. 2.
I had assumed that, after working at CMS, I would return to a hospital/health system leadership role. But then, a recruiter called about the CEO role at Blue Cross Blue Shield of North Carolina. It is one of the largest not-for-profit health plans in the country and insures most of the people in North Carolina, many for most of their lives. I met a 75-year-old woman the other day that we have insured every day of her life. I am almost a year into the role and it is a mission-driven organization that drives positive change. I love it so far.
We are going to partner with providers, so that more than half of our payments will be in advanced alternative payment models. No payer in the United States has done that yet. This allows us to innovate and decrease friction in the system (e.g., turn off prior authorization) and be jointly accountable with providers for quality and total cost of care. We insure people through the ACA [Affordable Care Act], commercial, and Medicare markets, and are competing to serve Medicaid as well. We have invested more than $50 million to address social determinants of health across the state. We are making major investments in primary care, and mental and behavioral health. Our goal is to be a Model Blue – or a Model of Health Transformation for our state and nation – and achieve better health outcomes, lower costs, and best-in-class experience for all people we serve. I have learned that no physician leads a health plan of this size, and apparently, no practicing physician has ever led a health plan of this size.
What are some lessons learned over my career? I have had five criteria for all my career decisions: 1) family; 2) impact – better care and outcomes, lower costs, and exceptional experience for populations of patients; 3) people – mentors and colleagues; 4) learning; and 5) joy in work. If someone gives you a chance to lead people in your career as a physician, jump at the chance. We do a relatively poor job of providing this type of opportunity to those early in their careers in medicine, and learning how to manage people and money allows you to progress as a leader and manager.
Don’t listen to the people who say “you must do X before Y” or “you must take this path.” They are usually wrong. Take chances. I applied for many roles for which I was a long shot, and I didn’t always succeed. That’s life and learning. Hospital medicine is a great career. I worked in the hospital on a recent weekend and was able to help families through everything from palliative care decisions and new diagnoses, to recovering from illness. It is an honor to serve and help families in their time of need. Hospitalists have been – and should continue to be – primary drivers of the shift in our health system to value-based care.
As I look back on my career (and I hope I am only halfway done), I could not have predicted more than 90% of it. I was blessed with many opportunities, mentors, and teachers along the way. I try to pass this on by mentoring and teaching others. How did my career happen? I am not sure, but it has been a fun ride! And hopefully I have helped improve the health system some, along the way.
Dr. Conway is president and CEO of Blue Cross and Blue Shield of North Carolina. He is a hospitalist and former deputy administrator for innovation and quality at the Centers for Medicare and Medicaid Services.
ONC aims to help docs, patients with information sharing in proposed rule
The Office of the National Coordinator of Health Information Technology is looking to adopt standardized application programming interfaces (APIs) in an effort to boost interoperability of health data.
The Department of Health & Human Services office posted a proposed rule Feb. 11, 2019, that would, according to an agency press release, “help allow individuals to securely and easily access structured and unstructured EHI [electronic health information] formats using smartphones and other mobile devices.”
“We think our rule is going to help reduce burden and improve care,” Michael Lipinski, director of the Regulatory Affairs Division in the ONC Office of Policy, said in an interview. “It is going to do that through technology. With the APIs, you should be able to get to your information easier and have it readily available. Whether that is from another health care provider or using other health care products through the API to improve care, you will have that ability between the certified API and the information blocking policies to use third party developers and their products.”
The proposed rule also included a requirement that EHRs certified by ONC be able to easily export information contained within the EHR and make the format used to extract and export the data contained within the EHR publicly available.
“Another third party developer can build to that and offer competing services to pull that information out,” Mr. Lipinski said. “That would obviously help if you were choosing to switch [EHRs] if you didn’t like the features you were getting from your EHR. ... That functionality should help if you want to do that.”
The standardizing of APIs to help the delivery of data will go hand in hand with information blocking aspects of the proposed rule, which defines the few exceptions where an activity would not be considered information blocking, such as when engaging in practices will prevent patient harm; engaging in consistent, nondiscriminatory practices to protect patient privacy; and implementing practices to promote the security of health information.
Mr. Lipinski said these changes will help prevent providers from hiding behind HIPAA rules as the excuse to not share patient information, which will help with care coordination. “From a provider’s perspective, this should help them get more access to information, more access in a structured way and then easily get and share that information.”
Ultimately, Mr. Lipinski said, the goal is “to increase competition and lower cost while still improving the quality of care for patients.”
The Office of the National Coordinator of Health Information Technology is looking to adopt standardized application programming interfaces (APIs) in an effort to boost interoperability of health data.
The Department of Health & Human Services office posted a proposed rule Feb. 11, 2019, that would, according to an agency press release, “help allow individuals to securely and easily access structured and unstructured EHI [electronic health information] formats using smartphones and other mobile devices.”
“We think our rule is going to help reduce burden and improve care,” Michael Lipinski, director of the Regulatory Affairs Division in the ONC Office of Policy, said in an interview. “It is going to do that through technology. With the APIs, you should be able to get to your information easier and have it readily available. Whether that is from another health care provider or using other health care products through the API to improve care, you will have that ability between the certified API and the information blocking policies to use third party developers and their products.”
The proposed rule also included a requirement that EHRs certified by ONC be able to easily export information contained within the EHR and make the format used to extract and export the data contained within the EHR publicly available.
“Another third party developer can build to that and offer competing services to pull that information out,” Mr. Lipinski said. “That would obviously help if you were choosing to switch [EHRs] if you didn’t like the features you were getting from your EHR. ... That functionality should help if you want to do that.”
The standardizing of APIs to help the delivery of data will go hand in hand with information blocking aspects of the proposed rule, which defines the few exceptions where an activity would not be considered information blocking, such as when engaging in practices will prevent patient harm; engaging in consistent, nondiscriminatory practices to protect patient privacy; and implementing practices to promote the security of health information.
Mr. Lipinski said these changes will help prevent providers from hiding behind HIPAA rules as the excuse to not share patient information, which will help with care coordination. “From a provider’s perspective, this should help them get more access to information, more access in a structured way and then easily get and share that information.”
Ultimately, Mr. Lipinski said, the goal is “to increase competition and lower cost while still improving the quality of care for patients.”
The Office of the National Coordinator of Health Information Technology is looking to adopt standardized application programming interfaces (APIs) in an effort to boost interoperability of health data.
The Department of Health & Human Services office posted a proposed rule Feb. 11, 2019, that would, according to an agency press release, “help allow individuals to securely and easily access structured and unstructured EHI [electronic health information] formats using smartphones and other mobile devices.”
“We think our rule is going to help reduce burden and improve care,” Michael Lipinski, director of the Regulatory Affairs Division in the ONC Office of Policy, said in an interview. “It is going to do that through technology. With the APIs, you should be able to get to your information easier and have it readily available. Whether that is from another health care provider or using other health care products through the API to improve care, you will have that ability between the certified API and the information blocking policies to use third party developers and their products.”
The proposed rule also included a requirement that EHRs certified by ONC be able to easily export information contained within the EHR and make the format used to extract and export the data contained within the EHR publicly available.
“Another third party developer can build to that and offer competing services to pull that information out,” Mr. Lipinski said. “That would obviously help if you were choosing to switch [EHRs] if you didn’t like the features you were getting from your EHR. ... That functionality should help if you want to do that.”
The standardizing of APIs to help the delivery of data will go hand in hand with information blocking aspects of the proposed rule, which defines the few exceptions where an activity would not be considered information blocking, such as when engaging in practices will prevent patient harm; engaging in consistent, nondiscriminatory practices to protect patient privacy; and implementing practices to promote the security of health information.
Mr. Lipinski said these changes will help prevent providers from hiding behind HIPAA rules as the excuse to not share patient information, which will help with care coordination. “From a provider’s perspective, this should help them get more access to information, more access in a structured way and then easily get and share that information.”
Ultimately, Mr. Lipinski said, the goal is “to increase competition and lower cost while still improving the quality of care for patients.”
Fund projects, not people to address gender bias in research funding
LONDON – Female investigators are less likely to secure research funding than male investigators, not because their proposed project is of lesser scientific merit, but simply because they are women, according to research published in The Lancet.
Women had a 30% lower chance of success in getting funding for a project than did their male counterparts when the caliber of the principal investigator was considered as an explicit part of the grant application process, with an 8.8% probability of getting funded versus 12.7%, respectively. If the application was considered solely on a project basis, however, the gender bias was less (12.1% vs. 12.9%).
The overall success of grant applications was 15.8% in the analysis, which considered almost 24,000 grant applications from more than 7,000 principal investigators submitted to the Canadian Institutes of Health Research (CIHR) between 2011 and 2016.
“I see our study as basically one good thwack in a long game of whack-a-mole,” lead study author Holly O. Witteman, PhD, said during an event to launch a special edition of The Lancet focusing on advancing women in science, medicine, and global health.
Dr. Witteman’s research is one of three original articles included in the thematic issue that brings together female authors and commentators to look at gender equity and what needs to be done to address imbalances. The issue is the result of a call for papers that led to more than 300 submissions from more than 40 countries and, according to an editorial from The Lancet, highlights that gender equity in medicine “is not only a matter of justice and rights, it is crucial for producing the best research and providing the best care to patients.”
That there are discrepancies in research funding awarded to female and male investigators has been known for years, Dr. Witteman, associate professor of family and emergency medicine at Laval University, Quebec City, said at the London press conference. To learn how and why, a “quasiexperimental” approach was used to find out what factors might be influencing the gender gap.
“Women are scored lower for competence compared to men with the same publication record,” she said. It’s not that they publish less or do easier research, or that the quality is lower, they are just viewed less favorably overall throughout their careers. Even when you control for confounding factors, “they still don’t advance as quickly,” she said.
“It had been documented for a while that, overall, women tend to get less grant funding and there hasn’t been any evidence to show either way if maybe women’s grant applications weren’t as good,” Dr. Witteman explained.
In 2014, the CIHR changed the way it funded research projects, creating a “natural experiment.” Two new grant application programs were put in place which largely differed by whether or not an explicit review of the principal investigator and their ability to conduct the research was included.
Adjusting for age and type of research, Dr. Witteman and her coauthors found that there was little difference in the success of women in securing research funding when their grant applications were judged solely on a scientific basis; however, when the focus was placed on the principal investigator, women were disadvantaged.
Dr. Witteman said that “this provides robust evidence in support of the idea that women write equally good grant applications but aren’t evaluated as being equally good scientists.”
So how to redress the balance? Dr. Witteman suggested that one way was for funders to collect robust evidence on the success of grant applications and be transparent who is getting funded and how much funding is being awarded. Institutions should invest in and support young investigators, distributing power and flattening traditionally male-led hierarchies. Salaries should be aligned and research support evened out, she said.
Investigators themselves also have a role to play to do the best possible work and try to change the system. “Advocate for others,” she said. That included advocating for others in groups that you may not be part of – which can be easier in some respects than advocating for a group that you are in.
“Funders should evaluate projects, not people,” Jennifer L. Raymond, PhD, and Miriam B. Goodman, PhD, both professors at Stanford (Calif.) University wrote in a comment in The Lancet special issue. They suggested that people-based funding had been gaining popularity but that funders would be better off funding by project to achieve scientific and clinical goals. “Assess the investigator only after double-blind review of the proposed research is complete,” they suggested. “Reduce the assessment of the investigator to a binary judgment of whether or not the investigator has the expertise and resources needed do the proposed research.”
During a panel discussion at The Lancet event, Cassidy R. Sugimoto, PhD, associate professor of informatics at Indiana University in Bloomington and a program director for the Science and Innovation Policy Program at the National Science Foundation (NSF) observed that data on gender equality in research funding were already being collected and will be used to determine how best to adjust funding policies.
“Looking from the 1980s to the present, women make up shy of 20% of the funds given by the National Science Foundation,” Dr. Sugimoto said. “That’s improved over time, and it’s at 28% currently, which is less than their authorship.”
Tammy Clifford, PhD, vice president of research programs at the CIHR observed that data collection was “a critically important step, but of course that’s not the only step,” she said. “We need to look at and analyze the data regularly, and then when you see things that are not on track, you make changes.”
One of the changes the CIHR has made is to train people who are reviewing grant applications on factors that may unconsciously affect their decisions. “There are things to be done, and I don’t think we are quite there yet, but we are committed to continually looking at those data, to making the changes that are required.”
Representing the Wellcome Trust, Ed Whiting, director of policy and chief of staff, said that the funding of projects led by female investigators was moving in the right direction. He noted that there was still a lower rate of applications from women for senior award levels, but that the panels that decide upon the funding were moving toward equal gender representation. The aim was to get to a 50/50 female to male ratio on the panels by 2020, he said; it is was at 46%-52% in 2018.
Dr. Witteman and all other commentators had no financial disclosures.
SOURCE: Witteman HO et al. Lancet. 2019. doi: 10.1016/S0140-6736(18)32611-4
LONDON – Female investigators are less likely to secure research funding than male investigators, not because their proposed project is of lesser scientific merit, but simply because they are women, according to research published in The Lancet.
Women had a 30% lower chance of success in getting funding for a project than did their male counterparts when the caliber of the principal investigator was considered as an explicit part of the grant application process, with an 8.8% probability of getting funded versus 12.7%, respectively. If the application was considered solely on a project basis, however, the gender bias was less (12.1% vs. 12.9%).
The overall success of grant applications was 15.8% in the analysis, which considered almost 24,000 grant applications from more than 7,000 principal investigators submitted to the Canadian Institutes of Health Research (CIHR) between 2011 and 2016.
“I see our study as basically one good thwack in a long game of whack-a-mole,” lead study author Holly O. Witteman, PhD, said during an event to launch a special edition of The Lancet focusing on advancing women in science, medicine, and global health.
Dr. Witteman’s research is one of three original articles included in the thematic issue that brings together female authors and commentators to look at gender equity and what needs to be done to address imbalances. The issue is the result of a call for papers that led to more than 300 submissions from more than 40 countries and, according to an editorial from The Lancet, highlights that gender equity in medicine “is not only a matter of justice and rights, it is crucial for producing the best research and providing the best care to patients.”
That there are discrepancies in research funding awarded to female and male investigators has been known for years, Dr. Witteman, associate professor of family and emergency medicine at Laval University, Quebec City, said at the London press conference. To learn how and why, a “quasiexperimental” approach was used to find out what factors might be influencing the gender gap.
“Women are scored lower for competence compared to men with the same publication record,” she said. It’s not that they publish less or do easier research, or that the quality is lower, they are just viewed less favorably overall throughout their careers. Even when you control for confounding factors, “they still don’t advance as quickly,” she said.
“It had been documented for a while that, overall, women tend to get less grant funding and there hasn’t been any evidence to show either way if maybe women’s grant applications weren’t as good,” Dr. Witteman explained.
In 2014, the CIHR changed the way it funded research projects, creating a “natural experiment.” Two new grant application programs were put in place which largely differed by whether or not an explicit review of the principal investigator and their ability to conduct the research was included.
Adjusting for age and type of research, Dr. Witteman and her coauthors found that there was little difference in the success of women in securing research funding when their grant applications were judged solely on a scientific basis; however, when the focus was placed on the principal investigator, women were disadvantaged.
Dr. Witteman said that “this provides robust evidence in support of the idea that women write equally good grant applications but aren’t evaluated as being equally good scientists.”
So how to redress the balance? Dr. Witteman suggested that one way was for funders to collect robust evidence on the success of grant applications and be transparent who is getting funded and how much funding is being awarded. Institutions should invest in and support young investigators, distributing power and flattening traditionally male-led hierarchies. Salaries should be aligned and research support evened out, she said.
Investigators themselves also have a role to play to do the best possible work and try to change the system. “Advocate for others,” she said. That included advocating for others in groups that you may not be part of – which can be easier in some respects than advocating for a group that you are in.
“Funders should evaluate projects, not people,” Jennifer L. Raymond, PhD, and Miriam B. Goodman, PhD, both professors at Stanford (Calif.) University wrote in a comment in The Lancet special issue. They suggested that people-based funding had been gaining popularity but that funders would be better off funding by project to achieve scientific and clinical goals. “Assess the investigator only after double-blind review of the proposed research is complete,” they suggested. “Reduce the assessment of the investigator to a binary judgment of whether or not the investigator has the expertise and resources needed do the proposed research.”
During a panel discussion at The Lancet event, Cassidy R. Sugimoto, PhD, associate professor of informatics at Indiana University in Bloomington and a program director for the Science and Innovation Policy Program at the National Science Foundation (NSF) observed that data on gender equality in research funding were already being collected and will be used to determine how best to adjust funding policies.
“Looking from the 1980s to the present, women make up shy of 20% of the funds given by the National Science Foundation,” Dr. Sugimoto said. “That’s improved over time, and it’s at 28% currently, which is less than their authorship.”
Tammy Clifford, PhD, vice president of research programs at the CIHR observed that data collection was “a critically important step, but of course that’s not the only step,” she said. “We need to look at and analyze the data regularly, and then when you see things that are not on track, you make changes.”
One of the changes the CIHR has made is to train people who are reviewing grant applications on factors that may unconsciously affect their decisions. “There are things to be done, and I don’t think we are quite there yet, but we are committed to continually looking at those data, to making the changes that are required.”
Representing the Wellcome Trust, Ed Whiting, director of policy and chief of staff, said that the funding of projects led by female investigators was moving in the right direction. He noted that there was still a lower rate of applications from women for senior award levels, but that the panels that decide upon the funding were moving toward equal gender representation. The aim was to get to a 50/50 female to male ratio on the panels by 2020, he said; it is was at 46%-52% in 2018.
Dr. Witteman and all other commentators had no financial disclosures.
SOURCE: Witteman HO et al. Lancet. 2019. doi: 10.1016/S0140-6736(18)32611-4
LONDON – Female investigators are less likely to secure research funding than male investigators, not because their proposed project is of lesser scientific merit, but simply because they are women, according to research published in The Lancet.
Women had a 30% lower chance of success in getting funding for a project than did their male counterparts when the caliber of the principal investigator was considered as an explicit part of the grant application process, with an 8.8% probability of getting funded versus 12.7%, respectively. If the application was considered solely on a project basis, however, the gender bias was less (12.1% vs. 12.9%).
The overall success of grant applications was 15.8% in the analysis, which considered almost 24,000 grant applications from more than 7,000 principal investigators submitted to the Canadian Institutes of Health Research (CIHR) between 2011 and 2016.
“I see our study as basically one good thwack in a long game of whack-a-mole,” lead study author Holly O. Witteman, PhD, said during an event to launch a special edition of The Lancet focusing on advancing women in science, medicine, and global health.
Dr. Witteman’s research is one of three original articles included in the thematic issue that brings together female authors and commentators to look at gender equity and what needs to be done to address imbalances. The issue is the result of a call for papers that led to more than 300 submissions from more than 40 countries and, according to an editorial from The Lancet, highlights that gender equity in medicine “is not only a matter of justice and rights, it is crucial for producing the best research and providing the best care to patients.”
That there are discrepancies in research funding awarded to female and male investigators has been known for years, Dr. Witteman, associate professor of family and emergency medicine at Laval University, Quebec City, said at the London press conference. To learn how and why, a “quasiexperimental” approach was used to find out what factors might be influencing the gender gap.
“Women are scored lower for competence compared to men with the same publication record,” she said. It’s not that they publish less or do easier research, or that the quality is lower, they are just viewed less favorably overall throughout their careers. Even when you control for confounding factors, “they still don’t advance as quickly,” she said.
“It had been documented for a while that, overall, women tend to get less grant funding and there hasn’t been any evidence to show either way if maybe women’s grant applications weren’t as good,” Dr. Witteman explained.
In 2014, the CIHR changed the way it funded research projects, creating a “natural experiment.” Two new grant application programs were put in place which largely differed by whether or not an explicit review of the principal investigator and their ability to conduct the research was included.
Adjusting for age and type of research, Dr. Witteman and her coauthors found that there was little difference in the success of women in securing research funding when their grant applications were judged solely on a scientific basis; however, when the focus was placed on the principal investigator, women were disadvantaged.
Dr. Witteman said that “this provides robust evidence in support of the idea that women write equally good grant applications but aren’t evaluated as being equally good scientists.”
So how to redress the balance? Dr. Witteman suggested that one way was for funders to collect robust evidence on the success of grant applications and be transparent who is getting funded and how much funding is being awarded. Institutions should invest in and support young investigators, distributing power and flattening traditionally male-led hierarchies. Salaries should be aligned and research support evened out, she said.
Investigators themselves also have a role to play to do the best possible work and try to change the system. “Advocate for others,” she said. That included advocating for others in groups that you may not be part of – which can be easier in some respects than advocating for a group that you are in.
“Funders should evaluate projects, not people,” Jennifer L. Raymond, PhD, and Miriam B. Goodman, PhD, both professors at Stanford (Calif.) University wrote in a comment in The Lancet special issue. They suggested that people-based funding had been gaining popularity but that funders would be better off funding by project to achieve scientific and clinical goals. “Assess the investigator only after double-blind review of the proposed research is complete,” they suggested. “Reduce the assessment of the investigator to a binary judgment of whether or not the investigator has the expertise and resources needed do the proposed research.”
During a panel discussion at The Lancet event, Cassidy R. Sugimoto, PhD, associate professor of informatics at Indiana University in Bloomington and a program director for the Science and Innovation Policy Program at the National Science Foundation (NSF) observed that data on gender equality in research funding were already being collected and will be used to determine how best to adjust funding policies.
“Looking from the 1980s to the present, women make up shy of 20% of the funds given by the National Science Foundation,” Dr. Sugimoto said. “That’s improved over time, and it’s at 28% currently, which is less than their authorship.”
Tammy Clifford, PhD, vice president of research programs at the CIHR observed that data collection was “a critically important step, but of course that’s not the only step,” she said. “We need to look at and analyze the data regularly, and then when you see things that are not on track, you make changes.”
One of the changes the CIHR has made is to train people who are reviewing grant applications on factors that may unconsciously affect their decisions. “There are things to be done, and I don’t think we are quite there yet, but we are committed to continually looking at those data, to making the changes that are required.”
Representing the Wellcome Trust, Ed Whiting, director of policy and chief of staff, said that the funding of projects led by female investigators was moving in the right direction. He noted that there was still a lower rate of applications from women for senior award levels, but that the panels that decide upon the funding were moving toward equal gender representation. The aim was to get to a 50/50 female to male ratio on the panels by 2020, he said; it is was at 46%-52% in 2018.
Dr. Witteman and all other commentators had no financial disclosures.
SOURCE: Witteman HO et al. Lancet. 2019. doi: 10.1016/S0140-6736(18)32611-4
FROM A LAUNCH EVENT HELD BY THE LANCET
Key clinical point: Funding bodies should focus on the science of a research project not on who is conducting the research.
Major finding: Between 2011 and 2016, 8.8% of projects proposed by female researchers and 12.7% of those proposed by male researchers were funded.
Study details: Analysis of nearly 24,000 grant applications from more than 7,000 principal investigators submitted to the Canadian Institutes of Health Research during 2011-2016.
Disclosures: The research was unfunded. Dr. Witteman and all other commentators had no financial disclosures.
Source: Witteman HO et al. Lancet. 2019. doi: 10.1016/S0140-6736(18)32611-4.