User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Home telemonitoring for heart failure cuts mortality
MUNICH – A comprehensive home telemonitoring program paid off big for selected patients with heart failure in a large, German nationwide masked randomization trial.
First, TIM-HF2 didn’t rely on passive monitoring of the patients’ daily electronically submitted home data. Instead, the data went straight to a central telemonitoring center staffed 24/7 by physicians and nurses with heart failure expertise. There, the information was immediately analyzed using proprietary telemedical analytic software known as the Fontane system. The software employs individually tailored, self-adapting algorithms in order to alert staff when trouble is brewing.
But the telemonitoring intervention doesn’t merely detect early clinical deterioration. It’s also a vehicle for ongoing patient education, outpatient adjustment of drugs, management of major comorbid conditions, and hospital admissions as needed. The patient’s local primary care physician was also plugged into the remote monitoring system and kept abreast of the patient’s condition.
Second, TIM-HF2 focused on a carefully selected subgroup of heart failure patients whom prior studies suggested were particularly likely to benefit from home telemedical management. All participants were NYHA class II or III with a left ventricular ejection fraction of 45% or less, a hospitalization for heart failure within 12 months prior to randomization, and free of moderate or severe depression as evidenced by a baseline Patient Health Questionnaire-9 score of 9 or less, explained Dr. Koehler, head of the center for cardiovascular telemedicine at Charite University in Berlin.
Why exclude patients with depression?
“In this concept, with wholistic remote patient management, we need an active patient who is able to measure every day, who is able to communicate with the telemedical center, and who is able to communicate in this network created between the telemedical center and local caregivers. If someone is really depressed, unable to act, lying in bed saying it makes no sense to take drugs or do anything, then we cannot help. That is for us, I think, the most important thing. We’ve seen it now in two trials,” according to the cardiologist.
The all-cause mortality rate was 7.86 per 100 person-years in the home-telemonitoring group versus 11.34 in usual-care controls. Patients in the active intervention arm lost a mean of 17.8 days per year because of unplanned cardiovascular hospital admissions, compared with 24.2 days per year in controls.
Importantly, outcomes were equally good in the remote patient-management group regardless of whether patients were among the 40% of participants living in urban Germany or the 60% in rural areas. Thus, the telemonitoring intervention eliminated the geographic disparity in health care outcomes which is a prominent issue in Germany, as well as the United States.
A formal cost-benefit analysis of the TIM-HF2 results is in the works, Dr. Koehler said.
Simultaneous with his presentation in Munich, the TIM-HF2 study was published online in the Lancet.
In an accompanying editorial, two prominent heart failure experts – John F.G. Cleland, MD, of the University of Glasgow and Robin A. Clark, MD, of Flinders University in Adelaide – hailed TIM-HF2 as a major advance and indicated in sharp terms that it’s time for guideline writers to sit up and take notice.
“Despite much clinical skepticism and feeble support from most guidelines, in our view the growing weight of evidence suggests that home telemonitoring does reduce mortality for patients with heart failure, and this effect might be substantial. These and other trials also show that the emphasis placed on hospital admission for heart failure might be misplaced, at least from a patient’s perspective, because the proportion of days lost due to hospital admission is small, compared with those lost to death,” the physicians wrote in the editorial.
They also noted that, even though the between-group difference in the number of days during which patients were hospitalized for cardiovascular causes was relatively small, it’s clear that home telemonitoring triggered some potentially life-saving hospitalizations. “Home telemonitoring puts the patient back in the center of health care, ensuring that they know what the health professional is trying to achieve and that they agree with those aims. Ultimately, patients and their families are a large and relatively untapped health care resource,” they wrote.
The TIM-HF 2 trial was funded by the German Federal Ministry of Education and Research. Dr. Koehler reported receiving speaking and/or consultant fees from Novartis, Abbott, and Medtronic.
[email protected]
SOURCE: Koehler F et al. ESC Congress 2018. Lancet. 2018 Sep 22;392(10152):1047-57.
MUNICH – A comprehensive home telemonitoring program paid off big for selected patients with heart failure in a large, German nationwide masked randomization trial.
First, TIM-HF2 didn’t rely on passive monitoring of the patients’ daily electronically submitted home data. Instead, the data went straight to a central telemonitoring center staffed 24/7 by physicians and nurses with heart failure expertise. There, the information was immediately analyzed using proprietary telemedical analytic software known as the Fontane system. The software employs individually tailored, self-adapting algorithms in order to alert staff when trouble is brewing.
But the telemonitoring intervention doesn’t merely detect early clinical deterioration. It’s also a vehicle for ongoing patient education, outpatient adjustment of drugs, management of major comorbid conditions, and hospital admissions as needed. The patient’s local primary care physician was also plugged into the remote monitoring system and kept abreast of the patient’s condition.
Second, TIM-HF2 focused on a carefully selected subgroup of heart failure patients whom prior studies suggested were particularly likely to benefit from home telemedical management. All participants were NYHA class II or III with a left ventricular ejection fraction of 45% or less, a hospitalization for heart failure within 12 months prior to randomization, and free of moderate or severe depression as evidenced by a baseline Patient Health Questionnaire-9 score of 9 or less, explained Dr. Koehler, head of the center for cardiovascular telemedicine at Charite University in Berlin.
Why exclude patients with depression?
“In this concept, with wholistic remote patient management, we need an active patient who is able to measure every day, who is able to communicate with the telemedical center, and who is able to communicate in this network created between the telemedical center and local caregivers. If someone is really depressed, unable to act, lying in bed saying it makes no sense to take drugs or do anything, then we cannot help. That is for us, I think, the most important thing. We’ve seen it now in two trials,” according to the cardiologist.
The all-cause mortality rate was 7.86 per 100 person-years in the home-telemonitoring group versus 11.34 in usual-care controls. Patients in the active intervention arm lost a mean of 17.8 days per year because of unplanned cardiovascular hospital admissions, compared with 24.2 days per year in controls.
Importantly, outcomes were equally good in the remote patient-management group regardless of whether patients were among the 40% of participants living in urban Germany or the 60% in rural areas. Thus, the telemonitoring intervention eliminated the geographic disparity in health care outcomes which is a prominent issue in Germany, as well as the United States.
A formal cost-benefit analysis of the TIM-HF2 results is in the works, Dr. Koehler said.
Simultaneous with his presentation in Munich, the TIM-HF2 study was published online in the Lancet.
In an accompanying editorial, two prominent heart failure experts – John F.G. Cleland, MD, of the University of Glasgow and Robin A. Clark, MD, of Flinders University in Adelaide – hailed TIM-HF2 as a major advance and indicated in sharp terms that it’s time for guideline writers to sit up and take notice.
“Despite much clinical skepticism and feeble support from most guidelines, in our view the growing weight of evidence suggests that home telemonitoring does reduce mortality for patients with heart failure, and this effect might be substantial. These and other trials also show that the emphasis placed on hospital admission for heart failure might be misplaced, at least from a patient’s perspective, because the proportion of days lost due to hospital admission is small, compared with those lost to death,” the physicians wrote in the editorial.
They also noted that, even though the between-group difference in the number of days during which patients were hospitalized for cardiovascular causes was relatively small, it’s clear that home telemonitoring triggered some potentially life-saving hospitalizations. “Home telemonitoring puts the patient back in the center of health care, ensuring that they know what the health professional is trying to achieve and that they agree with those aims. Ultimately, patients and their families are a large and relatively untapped health care resource,” they wrote.
The TIM-HF 2 trial was funded by the German Federal Ministry of Education and Research. Dr. Koehler reported receiving speaking and/or consultant fees from Novartis, Abbott, and Medtronic.
[email protected]
SOURCE: Koehler F et al. ESC Congress 2018. Lancet. 2018 Sep 22;392(10152):1047-57.
MUNICH – A comprehensive home telemonitoring program paid off big for selected patients with heart failure in a large, German nationwide masked randomization trial.
First, TIM-HF2 didn’t rely on passive monitoring of the patients’ daily electronically submitted home data. Instead, the data went straight to a central telemonitoring center staffed 24/7 by physicians and nurses with heart failure expertise. There, the information was immediately analyzed using proprietary telemedical analytic software known as the Fontane system. The software employs individually tailored, self-adapting algorithms in order to alert staff when trouble is brewing.
But the telemonitoring intervention doesn’t merely detect early clinical deterioration. It’s also a vehicle for ongoing patient education, outpatient adjustment of drugs, management of major comorbid conditions, and hospital admissions as needed. The patient’s local primary care physician was also plugged into the remote monitoring system and kept abreast of the patient’s condition.
Second, TIM-HF2 focused on a carefully selected subgroup of heart failure patients whom prior studies suggested were particularly likely to benefit from home telemedical management. All participants were NYHA class II or III with a left ventricular ejection fraction of 45% or less, a hospitalization for heart failure within 12 months prior to randomization, and free of moderate or severe depression as evidenced by a baseline Patient Health Questionnaire-9 score of 9 or less, explained Dr. Koehler, head of the center for cardiovascular telemedicine at Charite University in Berlin.
Why exclude patients with depression?
“In this concept, with wholistic remote patient management, we need an active patient who is able to measure every day, who is able to communicate with the telemedical center, and who is able to communicate in this network created between the telemedical center and local caregivers. If someone is really depressed, unable to act, lying in bed saying it makes no sense to take drugs or do anything, then we cannot help. That is for us, I think, the most important thing. We’ve seen it now in two trials,” according to the cardiologist.
The all-cause mortality rate was 7.86 per 100 person-years in the home-telemonitoring group versus 11.34 in usual-care controls. Patients in the active intervention arm lost a mean of 17.8 days per year because of unplanned cardiovascular hospital admissions, compared with 24.2 days per year in controls.
Importantly, outcomes were equally good in the remote patient-management group regardless of whether patients were among the 40% of participants living in urban Germany or the 60% in rural areas. Thus, the telemonitoring intervention eliminated the geographic disparity in health care outcomes which is a prominent issue in Germany, as well as the United States.
A formal cost-benefit analysis of the TIM-HF2 results is in the works, Dr. Koehler said.
Simultaneous with his presentation in Munich, the TIM-HF2 study was published online in the Lancet.
In an accompanying editorial, two prominent heart failure experts – John F.G. Cleland, MD, of the University of Glasgow and Robin A. Clark, MD, of Flinders University in Adelaide – hailed TIM-HF2 as a major advance and indicated in sharp terms that it’s time for guideline writers to sit up and take notice.
“Despite much clinical skepticism and feeble support from most guidelines, in our view the growing weight of evidence suggests that home telemonitoring does reduce mortality for patients with heart failure, and this effect might be substantial. These and other trials also show that the emphasis placed on hospital admission for heart failure might be misplaced, at least from a patient’s perspective, because the proportion of days lost due to hospital admission is small, compared with those lost to death,” the physicians wrote in the editorial.
They also noted that, even though the between-group difference in the number of days during which patients were hospitalized for cardiovascular causes was relatively small, it’s clear that home telemonitoring triggered some potentially life-saving hospitalizations. “Home telemonitoring puts the patient back in the center of health care, ensuring that they know what the health professional is trying to achieve and that they agree with those aims. Ultimately, patients and their families are a large and relatively untapped health care resource,” they wrote.
The TIM-HF 2 trial was funded by the German Federal Ministry of Education and Research. Dr. Koehler reported receiving speaking and/or consultant fees from Novartis, Abbott, and Medtronic.
[email protected]
SOURCE: Koehler F et al. ESC Congress 2018. Lancet. 2018 Sep 22;392(10152):1047-57.
REPORTING FROM THE ESC CONGRESS 2018
Key clinical point: Comprehensive home-telemonitoring program for heart failure saves lives.
Major finding: All-cause mortality was reduced by 30% at 1 year with a comprehensive home-telemonitoring program.
Study details: This prospective, masked randomization study included 1,538 German heart failure patients.
Disclosures: The TIM-HF2 trial was funded by the German Federal Ministry of Education and Research.
Source: Koehler F. ESC Congress 2018. Lancet. 2018 Sep 22;392(10152):1047-57.
Admission eosinopenia predicted severe CDI outcomes
For patients with even in the absence of hypotension and tachycardia, researchers wrote in JAMA Surgery.
“In animal models, peripheral eosinopenia is a biologically plausible predictive factor for adverse outcomes, and human data from this study indicate that this frequent addition to an admission complete blood cell count is an inexpensive, widely available risk index in the treatment of C. difficile infection,” wrote Audrey S. Kulaylat, MD, of Penn State University, Hershey, and her associates.
In their cohort study of 2,065 patients admitted to two tertiary referral centers with C. difficile infection, undetectable eosinophil counts at hospital admission were associated with significantly increased odds of in-hospital mortality in both a training dataset (odds ratio, 2.01; 95% confidence interval, 1.08-3.73; P = .03) and a validation dataset (OR, 2.26; 95% CI, 1.33-3.83; P = .002). Undetectable eosinophil counts also were associated with elevated odds of severe disease requiring intensive care, vasopressor use, and emergency total colectomy. Besides eosinopenia, significant predictors of mortality included having more comorbidities and lower systolic blood pressure at admission. Strikingly, when patients had no initial hypotension or tachycardia, an undetectable eosinophil count was the only identifiable predictor of in-hospital death (OR, 5.76; 95% CI, 1.99-16.64). An elevated white blood cell count was not a significant predictor of mortality in this subgroup.
Dr. Kulaylat and her associates are studying the microbiome in C. difficile infection. Their work has identified a host immune reaction marked by an “exaggerated inflammasome response” and peripheral eosinopenia, they explained. Two recent murine models have produced similar results.
Admission eosinophil counts “allow for an immediate assessment of mortality risk at admission that is inexpensive and part of a differential for a standard complete blood count available at any hospital,” they concluded. They are now prospectively evaluating a prognostic score for C. difficile infection that includes eosinopenia and other easily discernible admission factors. The National Institutes of Health supported the work. The researchers reported having no conflicts of interest.
SOURCE: Kulaylat AS et al. JAMA Surg. 2018 Sep 12. doi: 10.1001/jamasurg.2018.3174.
For patients with even in the absence of hypotension and tachycardia, researchers wrote in JAMA Surgery.
“In animal models, peripheral eosinopenia is a biologically plausible predictive factor for adverse outcomes, and human data from this study indicate that this frequent addition to an admission complete blood cell count is an inexpensive, widely available risk index in the treatment of C. difficile infection,” wrote Audrey S. Kulaylat, MD, of Penn State University, Hershey, and her associates.
In their cohort study of 2,065 patients admitted to two tertiary referral centers with C. difficile infection, undetectable eosinophil counts at hospital admission were associated with significantly increased odds of in-hospital mortality in both a training dataset (odds ratio, 2.01; 95% confidence interval, 1.08-3.73; P = .03) and a validation dataset (OR, 2.26; 95% CI, 1.33-3.83; P = .002). Undetectable eosinophil counts also were associated with elevated odds of severe disease requiring intensive care, vasopressor use, and emergency total colectomy. Besides eosinopenia, significant predictors of mortality included having more comorbidities and lower systolic blood pressure at admission. Strikingly, when patients had no initial hypotension or tachycardia, an undetectable eosinophil count was the only identifiable predictor of in-hospital death (OR, 5.76; 95% CI, 1.99-16.64). An elevated white blood cell count was not a significant predictor of mortality in this subgroup.
Dr. Kulaylat and her associates are studying the microbiome in C. difficile infection. Their work has identified a host immune reaction marked by an “exaggerated inflammasome response” and peripheral eosinopenia, they explained. Two recent murine models have produced similar results.
Admission eosinophil counts “allow for an immediate assessment of mortality risk at admission that is inexpensive and part of a differential for a standard complete blood count available at any hospital,” they concluded. They are now prospectively evaluating a prognostic score for C. difficile infection that includes eosinopenia and other easily discernible admission factors. The National Institutes of Health supported the work. The researchers reported having no conflicts of interest.
SOURCE: Kulaylat AS et al. JAMA Surg. 2018 Sep 12. doi: 10.1001/jamasurg.2018.3174.
For patients with even in the absence of hypotension and tachycardia, researchers wrote in JAMA Surgery.
“In animal models, peripheral eosinopenia is a biologically plausible predictive factor for adverse outcomes, and human data from this study indicate that this frequent addition to an admission complete blood cell count is an inexpensive, widely available risk index in the treatment of C. difficile infection,” wrote Audrey S. Kulaylat, MD, of Penn State University, Hershey, and her associates.
In their cohort study of 2,065 patients admitted to two tertiary referral centers with C. difficile infection, undetectable eosinophil counts at hospital admission were associated with significantly increased odds of in-hospital mortality in both a training dataset (odds ratio, 2.01; 95% confidence interval, 1.08-3.73; P = .03) and a validation dataset (OR, 2.26; 95% CI, 1.33-3.83; P = .002). Undetectable eosinophil counts also were associated with elevated odds of severe disease requiring intensive care, vasopressor use, and emergency total colectomy. Besides eosinopenia, significant predictors of mortality included having more comorbidities and lower systolic blood pressure at admission. Strikingly, when patients had no initial hypotension or tachycardia, an undetectable eosinophil count was the only identifiable predictor of in-hospital death (OR, 5.76; 95% CI, 1.99-16.64). An elevated white blood cell count was not a significant predictor of mortality in this subgroup.
Dr. Kulaylat and her associates are studying the microbiome in C. difficile infection. Their work has identified a host immune reaction marked by an “exaggerated inflammasome response” and peripheral eosinopenia, they explained. Two recent murine models have produced similar results.
Admission eosinophil counts “allow for an immediate assessment of mortality risk at admission that is inexpensive and part of a differential for a standard complete blood count available at any hospital,” they concluded. They are now prospectively evaluating a prognostic score for C. difficile infection that includes eosinopenia and other easily discernible admission factors. The National Institutes of Health supported the work. The researchers reported having no conflicts of interest.
SOURCE: Kulaylat AS et al. JAMA Surg. 2018 Sep 12. doi: 10.1001/jamasurg.2018.3174.
FROM JAMA SURGERY
Key clinical point: Undetectable peripheral eosinophils predicted severe outcomes in patients admitted with Clostridium difficile infection.
Major finding: In the training and validation datasets, odds of in-hospital mortality were 2.01 (95% CI, 1.08-3.73) and 2.26 (95% CI, 1.33-3.83), respectively.
Study details: Two-hospital cohort study of 2,065 patients admitted with C. difficile infection.
Disclosures: The National Institutes of Health supported the work. The researchers reported having no conflicts of interest.
Source: Kulaylat A et al. JAMA Surg. 2018 Sep 12. doi: 10.1001/jamasurg.2018.3174.
Treating cannabinoid hyperemesis syndrome
Incidence may increase as marijuana use rises
Case
WS is a 54-year-old African American male with a medical history of diabetes mellitus type 2, hypertension, obstructive sleep apnea, and gastroparesis. He has multiple admissions for intractable nausea, vomiting, and abdominal pain believed to be from diabetic gastroparesis despite a normal gastric-emptying study. Endoscopy done in prior admission showed duodenitis, gastritis, and esophagitis, and colonoscopy revealed diverticulosis. He had a negative gastric-emptying study of 6% retention at 4 hrs. His last hemoglobin A1c was 5 and his glucose has been well controlled. He is hospitalized again for intractable abdominal pain, nausea, and vomiting. His examination was unremarkable except for dry mucosa and epigastric tenderness. His labs were also insignificant except for prerenal azotemia. Upon further questioning he admitted to significant marijuana use, and his symptoms transiently improved with a hot shower in the hospital. He was diagnosed with cannabinoid hyperemesis syndrome (CHS) and admitted for further management.
Background
In the United States, 9 states and the District of Columbia have legalized recreational marijuana use, and 29 states and DC have legalized medical marijuana. Marijuana use is likely to rise, and with it may arise an increasing incidence of CHS.
The exact prevalence of CHS is not known. Diagnosis is often delayed as there is no reliable diagnostic test. A high index of suspicion is needed for prompt diagnosis.
CHS was first described in 2004 in South Australia and since then many case reports have been published. Marijuana has both proemetic and antiemetic effects. Unlike its antiemetic effect, the pathophysiology of the proemetic effect of marijuana is not well understood.
Key clinical features
CHS typically has three phases. Initially patients present with prodromal symptoms of abdominal discomfort and nausea. There is no emesis at this early phase. Patients are still able to tolerate a liquid diet in this prodromal phase.
This is followed by a more active phase of intractable vomiting, which is relieved by hot showers or baths. Most patients take compulsively long hot showers or baths many times a day. Also, they develop diaphoresis, restlessness, agitation, and weight loss.
The active phase is followed by a recovery phase when symptoms resolve and patients return to baseline, only to have it recur if marijuana use continues.
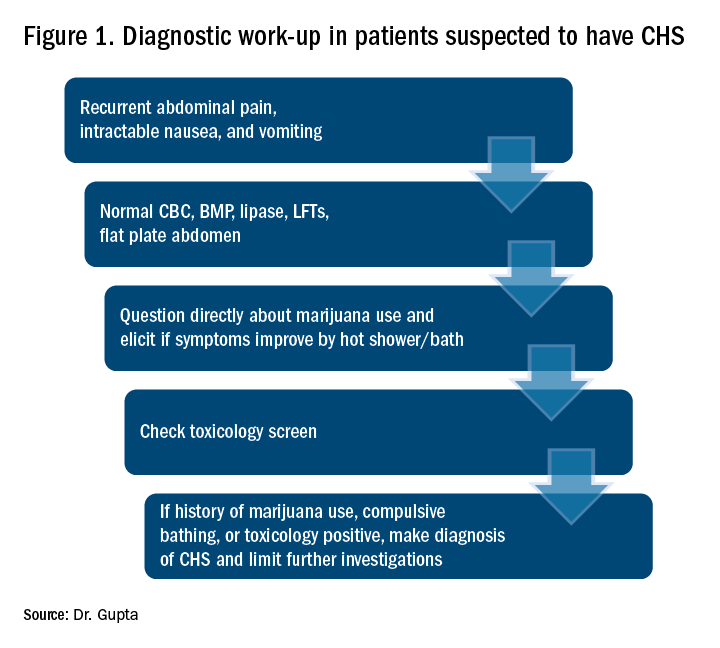
Diagnostic approach and management
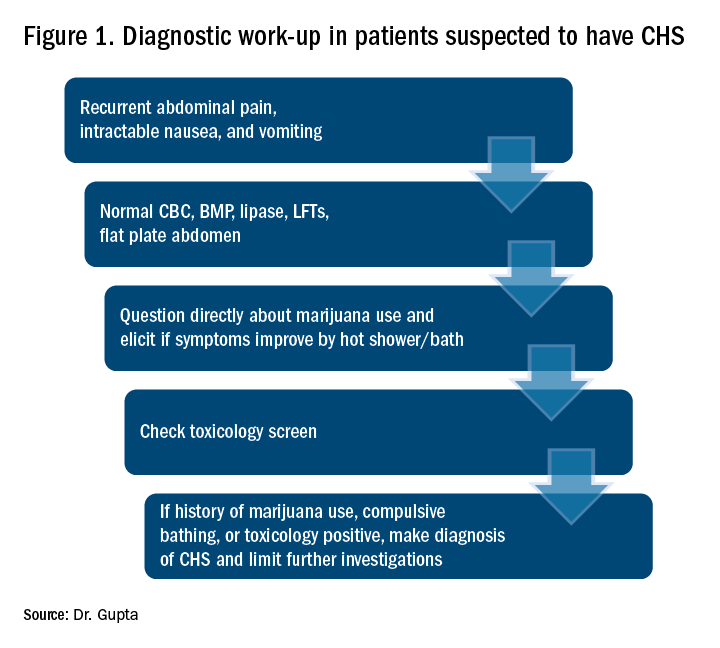
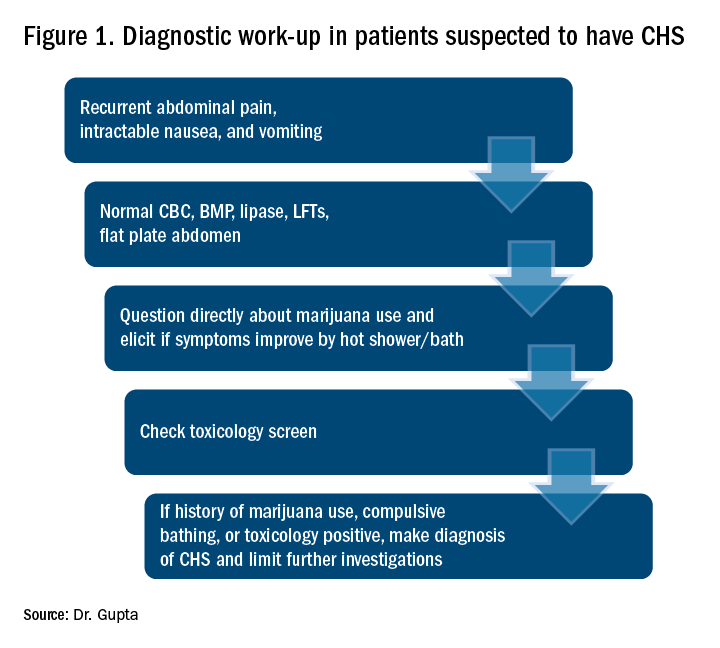
CHS should be suspected in patients coming in with recurrent symptoms of abdominal pain, nausea and vomiting, and who have normal CBC, basic metabolic panel, lipase, and liver function tests. Patients should be directly questioned about marijuana use and whether symptoms are relieved with hot showers. A toxicology screen should be done. For patients with marijuana use and compulsive hot showers, further work up of their symptoms (e.g., upper endoscopy, abdominal ultrasound, and/or nuclear medicine emptying study) should be avoided. Figure 1 shows the suggested work-up.
The differential diagnosis for recurrent abdominal pain, nausea, and vomiting is chronic pancreatitis, gastroparesis, severe gastritis, medication adverse effects (especially GLP1 receptor agonists), cyclic vomiting syndrome, psychogenic vomiting, and (with the rise of narcotic abuse) narcotic bowel syndrome.
Our patient had a history of diabetes with an HbA1c at goal and a normal nuclear medicine gastric-emptying study (6% retention at 4 hours). He was also on liraglutide, but his symptoms predated this medicine use.
The mainstay of treatment for CHS is supportive therapy with intravenous fluids and antiemetics like 5-HT3-receptor antagonists (ondansetron); D2-receptor antagonists (metoclopramide); and H1-receptor antagonists (diphenhydramine). The effectiveness of these agents is limited, which is also a clue for the diagnosis of CHS. If traditional agents fail in controlling the symptoms, haloperidol can be tried, but it has been used with limited success. Our patient did not respond to traditional antiemetics, but responded well to a small dose of lorazepam. Even though a benzodiazepine is not the mainstay of treatment, it may be tried if other agents fail. Acid-suppression therapy with a proton pump inhibitor should be used as esophagogastroduodenoscopy (EGD) usually reveals mild gastritis and esophagitis, as in our patient. Narcotic use should be avoided for management of abdominal pain.
Patients should be counseled against marijuana use. This may be difficult if marijuana is being used as an appetite stimulant or for treatment of chemotherapy-induced nausea and vomiting. If willing, patients should be referred to a substance abuse rehabilitation center.
Back to the case
In this case, after a diagnosis of CHS was made, the patient was counseled against marijuana use. His abdominal pain and intractable vomiting did not improve with conservative management of n.p.o status, prochlorperazine, metoclopramide, and ondansetron. He was given a trial of low-dose lorazepam with significant improvement in his symptoms. He was counseled extensively against marijuana use and discharged. A follow-up phone call at 3 months showed continued abstinence and no recurrence of symptoms.
Dr. Gupta is a hospitalist at Yale New Haven Health and Bridgeport (Conn.) Hospital.
References
1. Bajgoric S et al. Cannabinoid hyperemesis syndrome: A guide for the practising clinician. BMJ Case Rep. 2015. doi: 10.1136/bcr-2015-210246.
2. Batke M et al. The cannabis hyperemesis syndrome characterized by persistent nausea and vomiting, abdominal pain, and compulsive bathing associated with chronic marijuana use: A report of eight cases in the united states. Dig Dis Sci. 2010 Nov;55(11):3113-9.
3. Iacopetti CL et al. Cannabinoid hyperemesis syndrome: a case report and review of pathophysiology. Clin Med Res. 2014 Sep;12(1-2):65-7.
4. Hickey JL et al. Haloperidol for treatment of cannabinoid hyperemesis syndrome. Am J Emerg Med. 2013 Jun. 31(6):1003.e5-6. Epub 2013 Apr 10.
Key points
Suspect CHS for patients with recurrent abdominal pain, nausea, and vomiting with negative initial work-up.
- Ask directly about marijuana use.
- Ask whether symptoms are relieved with hot shower/ bath.
- Send a toxicology screen.
- Make a diagnosis of CHS if:
1. Positive marijuana use.
2. Symptom improvement with hot baths or
3. Toxicology positive for marijuana.
- Manage conservatively with hydration and antiemetics.
- Suspect CHS if traditional antiemetics are not providing relief .
- If traditional antiemetics fail, trial of haloperidol or low-dose benzodiazepines.
- Avoid narcotics.
- Avoid unnecessary investigations.
- Counsel patients against marijuana use and refer to substance abuse center if patient agrees.
Incidence may increase as marijuana use rises
Incidence may increase as marijuana use rises
Case
WS is a 54-year-old African American male with a medical history of diabetes mellitus type 2, hypertension, obstructive sleep apnea, and gastroparesis. He has multiple admissions for intractable nausea, vomiting, and abdominal pain believed to be from diabetic gastroparesis despite a normal gastric-emptying study. Endoscopy done in prior admission showed duodenitis, gastritis, and esophagitis, and colonoscopy revealed diverticulosis. He had a negative gastric-emptying study of 6% retention at 4 hrs. His last hemoglobin A1c was 5 and his glucose has been well controlled. He is hospitalized again for intractable abdominal pain, nausea, and vomiting. His examination was unremarkable except for dry mucosa and epigastric tenderness. His labs were also insignificant except for prerenal azotemia. Upon further questioning he admitted to significant marijuana use, and his symptoms transiently improved with a hot shower in the hospital. He was diagnosed with cannabinoid hyperemesis syndrome (CHS) and admitted for further management.
Background
In the United States, 9 states and the District of Columbia have legalized recreational marijuana use, and 29 states and DC have legalized medical marijuana. Marijuana use is likely to rise, and with it may arise an increasing incidence of CHS.
The exact prevalence of CHS is not known. Diagnosis is often delayed as there is no reliable diagnostic test. A high index of suspicion is needed for prompt diagnosis.
CHS was first described in 2004 in South Australia and since then many case reports have been published. Marijuana has both proemetic and antiemetic effects. Unlike its antiemetic effect, the pathophysiology of the proemetic effect of marijuana is not well understood.
Key clinical features
CHS typically has three phases. Initially patients present with prodromal symptoms of abdominal discomfort and nausea. There is no emesis at this early phase. Patients are still able to tolerate a liquid diet in this prodromal phase.
This is followed by a more active phase of intractable vomiting, which is relieved by hot showers or baths. Most patients take compulsively long hot showers or baths many times a day. Also, they develop diaphoresis, restlessness, agitation, and weight loss.
The active phase is followed by a recovery phase when symptoms resolve and patients return to baseline, only to have it recur if marijuana use continues.
Diagnostic approach and management
CHS should be suspected in patients coming in with recurrent symptoms of abdominal pain, nausea and vomiting, and who have normal CBC, basic metabolic panel, lipase, and liver function tests. Patients should be directly questioned about marijuana use and whether symptoms are relieved with hot showers. A toxicology screen should be done. For patients with marijuana use and compulsive hot showers, further work up of their symptoms (e.g., upper endoscopy, abdominal ultrasound, and/or nuclear medicine emptying study) should be avoided. Figure 1 shows the suggested work-up.
The differential diagnosis for recurrent abdominal pain, nausea, and vomiting is chronic pancreatitis, gastroparesis, severe gastritis, medication adverse effects (especially GLP1 receptor agonists), cyclic vomiting syndrome, psychogenic vomiting, and (with the rise of narcotic abuse) narcotic bowel syndrome.
Our patient had a history of diabetes with an HbA1c at goal and a normal nuclear medicine gastric-emptying study (6% retention at 4 hours). He was also on liraglutide, but his symptoms predated this medicine use.
The mainstay of treatment for CHS is supportive therapy with intravenous fluids and antiemetics like 5-HT3-receptor antagonists (ondansetron); D2-receptor antagonists (metoclopramide); and H1-receptor antagonists (diphenhydramine). The effectiveness of these agents is limited, which is also a clue for the diagnosis of CHS. If traditional agents fail in controlling the symptoms, haloperidol can be tried, but it has been used with limited success. Our patient did not respond to traditional antiemetics, but responded well to a small dose of lorazepam. Even though a benzodiazepine is not the mainstay of treatment, it may be tried if other agents fail. Acid-suppression therapy with a proton pump inhibitor should be used as esophagogastroduodenoscopy (EGD) usually reveals mild gastritis and esophagitis, as in our patient. Narcotic use should be avoided for management of abdominal pain.
Patients should be counseled against marijuana use. This may be difficult if marijuana is being used as an appetite stimulant or for treatment of chemotherapy-induced nausea and vomiting. If willing, patients should be referred to a substance abuse rehabilitation center.
Back to the case
In this case, after a diagnosis of CHS was made, the patient was counseled against marijuana use. His abdominal pain and intractable vomiting did not improve with conservative management of n.p.o status, prochlorperazine, metoclopramide, and ondansetron. He was given a trial of low-dose lorazepam with significant improvement in his symptoms. He was counseled extensively against marijuana use and discharged. A follow-up phone call at 3 months showed continued abstinence and no recurrence of symptoms.
Dr. Gupta is a hospitalist at Yale New Haven Health and Bridgeport (Conn.) Hospital.
References
1. Bajgoric S et al. Cannabinoid hyperemesis syndrome: A guide for the practising clinician. BMJ Case Rep. 2015. doi: 10.1136/bcr-2015-210246.
2. Batke M et al. The cannabis hyperemesis syndrome characterized by persistent nausea and vomiting, abdominal pain, and compulsive bathing associated with chronic marijuana use: A report of eight cases in the united states. Dig Dis Sci. 2010 Nov;55(11):3113-9.
3. Iacopetti CL et al. Cannabinoid hyperemesis syndrome: a case report and review of pathophysiology. Clin Med Res. 2014 Sep;12(1-2):65-7.
4. Hickey JL et al. Haloperidol for treatment of cannabinoid hyperemesis syndrome. Am J Emerg Med. 2013 Jun. 31(6):1003.e5-6. Epub 2013 Apr 10.
Key points
Suspect CHS for patients with recurrent abdominal pain, nausea, and vomiting with negative initial work-up.
- Ask directly about marijuana use.
- Ask whether symptoms are relieved with hot shower/ bath.
- Send a toxicology screen.
- Make a diagnosis of CHS if:
1. Positive marijuana use.
2. Symptom improvement with hot baths or
3. Toxicology positive for marijuana.
- Manage conservatively with hydration and antiemetics.
- Suspect CHS if traditional antiemetics are not providing relief .
- If traditional antiemetics fail, trial of haloperidol or low-dose benzodiazepines.
- Avoid narcotics.
- Avoid unnecessary investigations.
- Counsel patients against marijuana use and refer to substance abuse center if patient agrees.
Case
WS is a 54-year-old African American male with a medical history of diabetes mellitus type 2, hypertension, obstructive sleep apnea, and gastroparesis. He has multiple admissions for intractable nausea, vomiting, and abdominal pain believed to be from diabetic gastroparesis despite a normal gastric-emptying study. Endoscopy done in prior admission showed duodenitis, gastritis, and esophagitis, and colonoscopy revealed diverticulosis. He had a negative gastric-emptying study of 6% retention at 4 hrs. His last hemoglobin A1c was 5 and his glucose has been well controlled. He is hospitalized again for intractable abdominal pain, nausea, and vomiting. His examination was unremarkable except for dry mucosa and epigastric tenderness. His labs were also insignificant except for prerenal azotemia. Upon further questioning he admitted to significant marijuana use, and his symptoms transiently improved with a hot shower in the hospital. He was diagnosed with cannabinoid hyperemesis syndrome (CHS) and admitted for further management.
Background
In the United States, 9 states and the District of Columbia have legalized recreational marijuana use, and 29 states and DC have legalized medical marijuana. Marijuana use is likely to rise, and with it may arise an increasing incidence of CHS.
The exact prevalence of CHS is not known. Diagnosis is often delayed as there is no reliable diagnostic test. A high index of suspicion is needed for prompt diagnosis.
CHS was first described in 2004 in South Australia and since then many case reports have been published. Marijuana has both proemetic and antiemetic effects. Unlike its antiemetic effect, the pathophysiology of the proemetic effect of marijuana is not well understood.
Key clinical features
CHS typically has three phases. Initially patients present with prodromal symptoms of abdominal discomfort and nausea. There is no emesis at this early phase. Patients are still able to tolerate a liquid diet in this prodromal phase.
This is followed by a more active phase of intractable vomiting, which is relieved by hot showers or baths. Most patients take compulsively long hot showers or baths many times a day. Also, they develop diaphoresis, restlessness, agitation, and weight loss.
The active phase is followed by a recovery phase when symptoms resolve and patients return to baseline, only to have it recur if marijuana use continues.
Diagnostic approach and management
CHS should be suspected in patients coming in with recurrent symptoms of abdominal pain, nausea and vomiting, and who have normal CBC, basic metabolic panel, lipase, and liver function tests. Patients should be directly questioned about marijuana use and whether symptoms are relieved with hot showers. A toxicology screen should be done. For patients with marijuana use and compulsive hot showers, further work up of their symptoms (e.g., upper endoscopy, abdominal ultrasound, and/or nuclear medicine emptying study) should be avoided. Figure 1 shows the suggested work-up.
The differential diagnosis for recurrent abdominal pain, nausea, and vomiting is chronic pancreatitis, gastroparesis, severe gastritis, medication adverse effects (especially GLP1 receptor agonists), cyclic vomiting syndrome, psychogenic vomiting, and (with the rise of narcotic abuse) narcotic bowel syndrome.
Our patient had a history of diabetes with an HbA1c at goal and a normal nuclear medicine gastric-emptying study (6% retention at 4 hours). He was also on liraglutide, but his symptoms predated this medicine use.
The mainstay of treatment for CHS is supportive therapy with intravenous fluids and antiemetics like 5-HT3-receptor antagonists (ondansetron); D2-receptor antagonists (metoclopramide); and H1-receptor antagonists (diphenhydramine). The effectiveness of these agents is limited, which is also a clue for the diagnosis of CHS. If traditional agents fail in controlling the symptoms, haloperidol can be tried, but it has been used with limited success. Our patient did not respond to traditional antiemetics, but responded well to a small dose of lorazepam. Even though a benzodiazepine is not the mainstay of treatment, it may be tried if other agents fail. Acid-suppression therapy with a proton pump inhibitor should be used as esophagogastroduodenoscopy (EGD) usually reveals mild gastritis and esophagitis, as in our patient. Narcotic use should be avoided for management of abdominal pain.
Patients should be counseled against marijuana use. This may be difficult if marijuana is being used as an appetite stimulant or for treatment of chemotherapy-induced nausea and vomiting. If willing, patients should be referred to a substance abuse rehabilitation center.
Back to the case
In this case, after a diagnosis of CHS was made, the patient was counseled against marijuana use. His abdominal pain and intractable vomiting did not improve with conservative management of n.p.o status, prochlorperazine, metoclopramide, and ondansetron. He was given a trial of low-dose lorazepam with significant improvement in his symptoms. He was counseled extensively against marijuana use and discharged. A follow-up phone call at 3 months showed continued abstinence and no recurrence of symptoms.
Dr. Gupta is a hospitalist at Yale New Haven Health and Bridgeport (Conn.) Hospital.
References
1. Bajgoric S et al. Cannabinoid hyperemesis syndrome: A guide for the practising clinician. BMJ Case Rep. 2015. doi: 10.1136/bcr-2015-210246.
2. Batke M et al. The cannabis hyperemesis syndrome characterized by persistent nausea and vomiting, abdominal pain, and compulsive bathing associated with chronic marijuana use: A report of eight cases in the united states. Dig Dis Sci. 2010 Nov;55(11):3113-9.
3. Iacopetti CL et al. Cannabinoid hyperemesis syndrome: a case report and review of pathophysiology. Clin Med Res. 2014 Sep;12(1-2):65-7.
4. Hickey JL et al. Haloperidol for treatment of cannabinoid hyperemesis syndrome. Am J Emerg Med. 2013 Jun. 31(6):1003.e5-6. Epub 2013 Apr 10.
Key points
Suspect CHS for patients with recurrent abdominal pain, nausea, and vomiting with negative initial work-up.
- Ask directly about marijuana use.
- Ask whether symptoms are relieved with hot shower/ bath.
- Send a toxicology screen.
- Make a diagnosis of CHS if:
1. Positive marijuana use.
2. Symptom improvement with hot baths or
3. Toxicology positive for marijuana.
- Manage conservatively with hydration and antiemetics.
- Suspect CHS if traditional antiemetics are not providing relief .
- If traditional antiemetics fail, trial of haloperidol or low-dose benzodiazepines.
- Avoid narcotics.
- Avoid unnecessary investigations.
- Counsel patients against marijuana use and refer to substance abuse center if patient agrees.
Point-of-care test for respiratory viruses lowers antibiotic use
Routine testing in the ED is advocated
PARIS – Using a point-of-care test for viral pathogens, hospital admissions were avoided in about a third of emergency department patients with suspected respiratory infection when other clinical signs also suggested a low risk of a bacterial pathogen, according to a single-center experience presented at the annual congress of the European Respiratory Society.
“We found that when patients had point-of-care respiratory viral testing soon after they were admitted to the emergency department, we were able to reduce unnecessary admission and improve bed flow in our center,” reported Kay Roy, MBBS, consultant physician in respiratory medicine, West Hertfordshire (England) Hospital NHS Trust.
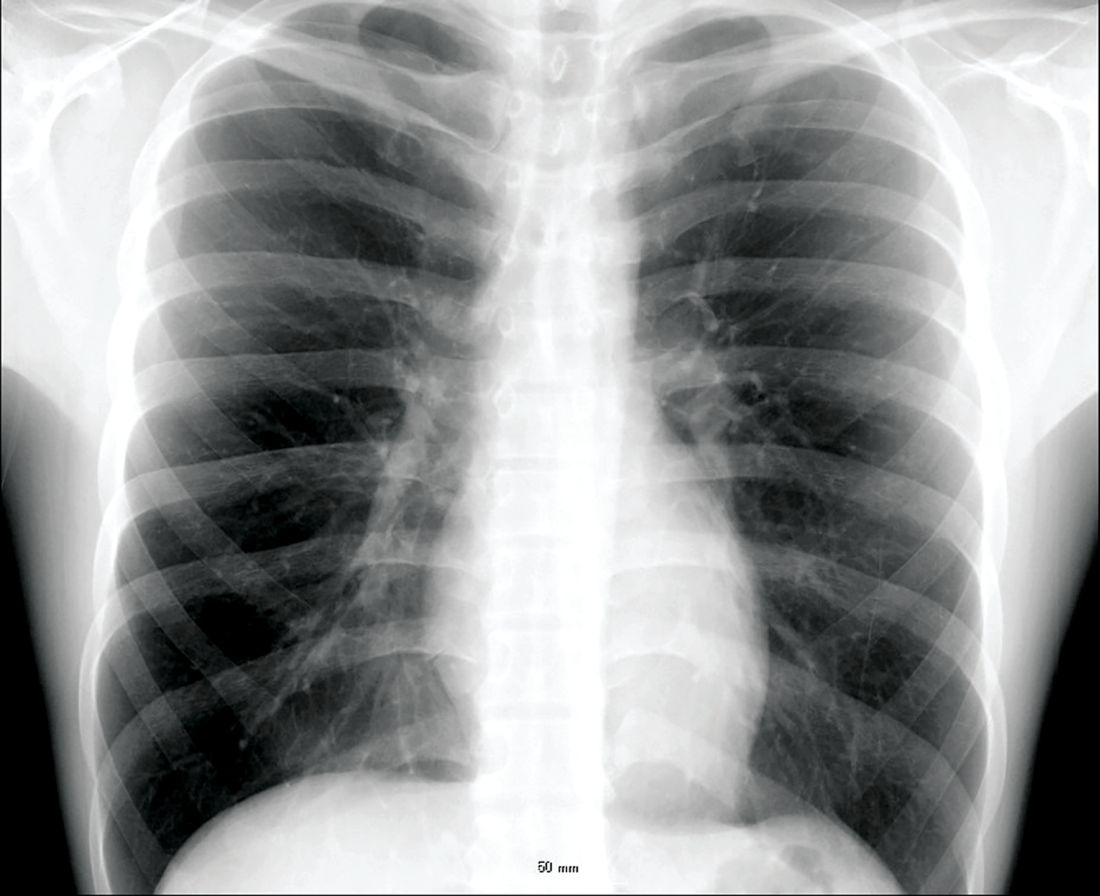
In a protocol that was launched at Dr. Kay’s institution in January 2018, the point-of-care viral test was combined with other clinical factors, particularly chest x-rays and elevated C-reactive protein (CRP), to determine whether patients had a viral pathogen and whether they could be discharged without antibiotics.
“Clinical judgment will always be required in individual patient decisions regarding antibiotic avoidance and early discharge,” Dr. Roy maintained. “But the point-of-care viral assay can be integrated into a strategy that permits more informed and rapid decision-making.”
This assertion is supported by the experience using a protocol anchored with the point-of-care viral test over a 4-month period. During this time, 901 patients with respiratory symptoms suspected of having a viral etiology were evaluated with the proprietary point-of-care device called FilmArray (bioMérieux).
From a sample taken with a nasopharyngeal swab, the test can identify a broad array of viruses using polymerase chain reaction technology in less than 45 minutes. However, the ED protocol for considering discharge without antibiotics requires additional evidence that the pathogen is viral, including a normal chest x-ray and a CRP less than 50 mg/L.
Of the 901 patients tested, a substantial proportion of whom had chronic obstructive pulmonary disease (COPD) or asthma, 507 (56%) tested positive for at least one virus, including influenza, rhinoviruses, coronaviruses, and adenovirus. Of these, 239 had normal chest x-rays and CRPs less than 50 mg/L. Because of the severity of symptoms or other clinical considerations, 154 patients were admitted, but 85 (36% of those meeting protocol criteria) were discharged without an antibiotic prescription.
“Antibiotics were continued in 90% of the patients who had an abnormal chest x-ray and abnormal CRP,” Dr. Roy reported. However, an objective strategy that permits clinicians to discharge patients at very low risk of a bacterial infection has many advantages even if it applies to a relatively modest proportion of those tested, according to Dr. Roy.
“Each respiratory admission can cost around [2,000 pounds] at our center,” reported Dr. Kay, referring to a figure equivalent to more than $2,600. In addition, she said that avoiding hospitalization frees up hospital beds and facilitates improved antimicrobial stewardship, which is vital to stem resistance.
Avoiding antibiotic use in patients with viral respiratory infections also is relevant to improved antibiotic stewardship in the community. For this reason, a randomized trial with a similar protocol involving the point-of-care viral test is planned in the outpatient setting. According to Dr. Roy, this will involve a community hub to which patients can be referred for testing and clinical evaluation.
“We hope that the quality of care can be improved with the point-of-care test for respiratory viruses as well as helping to reduce antibiotic resistance,” Dr. Roy said.
This approach is promising, according to Tobias Welte, MD, of the department of respiratory medicine at Hannover (Germany) Medical School, but he cautioned that it is not a standard approach.
“The protocol described by Dr. Roy will have to be compared to guidelines and recommended best clinical practice to confirm its usefulness,” he said, while conceding that any strategy that reduces unnecessary hospitalizations deserves further evaluation.
Routine testing in the ED is advocated
Routine testing in the ED is advocated
PARIS – Using a point-of-care test for viral pathogens, hospital admissions were avoided in about a third of emergency department patients with suspected respiratory infection when other clinical signs also suggested a low risk of a bacterial pathogen, according to a single-center experience presented at the annual congress of the European Respiratory Society.
“We found that when patients had point-of-care respiratory viral testing soon after they were admitted to the emergency department, we were able to reduce unnecessary admission and improve bed flow in our center,” reported Kay Roy, MBBS, consultant physician in respiratory medicine, West Hertfordshire (England) Hospital NHS Trust.
In a protocol that was launched at Dr. Kay’s institution in January 2018, the point-of-care viral test was combined with other clinical factors, particularly chest x-rays and elevated C-reactive protein (CRP), to determine whether patients had a viral pathogen and whether they could be discharged without antibiotics.
“Clinical judgment will always be required in individual patient decisions regarding antibiotic avoidance and early discharge,” Dr. Roy maintained. “But the point-of-care viral assay can be integrated into a strategy that permits more informed and rapid decision-making.”
This assertion is supported by the experience using a protocol anchored with the point-of-care viral test over a 4-month period. During this time, 901 patients with respiratory symptoms suspected of having a viral etiology were evaluated with the proprietary point-of-care device called FilmArray (bioMérieux).
From a sample taken with a nasopharyngeal swab, the test can identify a broad array of viruses using polymerase chain reaction technology in less than 45 minutes. However, the ED protocol for considering discharge without antibiotics requires additional evidence that the pathogen is viral, including a normal chest x-ray and a CRP less than 50 mg/L.
Of the 901 patients tested, a substantial proportion of whom had chronic obstructive pulmonary disease (COPD) or asthma, 507 (56%) tested positive for at least one virus, including influenza, rhinoviruses, coronaviruses, and adenovirus. Of these, 239 had normal chest x-rays and CRPs less than 50 mg/L. Because of the severity of symptoms or other clinical considerations, 154 patients were admitted, but 85 (36% of those meeting protocol criteria) were discharged without an antibiotic prescription.
“Antibiotics were continued in 90% of the patients who had an abnormal chest x-ray and abnormal CRP,” Dr. Roy reported. However, an objective strategy that permits clinicians to discharge patients at very low risk of a bacterial infection has many advantages even if it applies to a relatively modest proportion of those tested, according to Dr. Roy.
“Each respiratory admission can cost around [2,000 pounds] at our center,” reported Dr. Kay, referring to a figure equivalent to more than $2,600. In addition, she said that avoiding hospitalization frees up hospital beds and facilitates improved antimicrobial stewardship, which is vital to stem resistance.
Avoiding antibiotic use in patients with viral respiratory infections also is relevant to improved antibiotic stewardship in the community. For this reason, a randomized trial with a similar protocol involving the point-of-care viral test is planned in the outpatient setting. According to Dr. Roy, this will involve a community hub to which patients can be referred for testing and clinical evaluation.
“We hope that the quality of care can be improved with the point-of-care test for respiratory viruses as well as helping to reduce antibiotic resistance,” Dr. Roy said.
This approach is promising, according to Tobias Welte, MD, of the department of respiratory medicine at Hannover (Germany) Medical School, but he cautioned that it is not a standard approach.
“The protocol described by Dr. Roy will have to be compared to guidelines and recommended best clinical practice to confirm its usefulness,” he said, while conceding that any strategy that reduces unnecessary hospitalizations deserves further evaluation.
PARIS – Using a point-of-care test for viral pathogens, hospital admissions were avoided in about a third of emergency department patients with suspected respiratory infection when other clinical signs also suggested a low risk of a bacterial pathogen, according to a single-center experience presented at the annual congress of the European Respiratory Society.
“We found that when patients had point-of-care respiratory viral testing soon after they were admitted to the emergency department, we were able to reduce unnecessary admission and improve bed flow in our center,” reported Kay Roy, MBBS, consultant physician in respiratory medicine, West Hertfordshire (England) Hospital NHS Trust.
In a protocol that was launched at Dr. Kay’s institution in January 2018, the point-of-care viral test was combined with other clinical factors, particularly chest x-rays and elevated C-reactive protein (CRP), to determine whether patients had a viral pathogen and whether they could be discharged without antibiotics.
“Clinical judgment will always be required in individual patient decisions regarding antibiotic avoidance and early discharge,” Dr. Roy maintained. “But the point-of-care viral assay can be integrated into a strategy that permits more informed and rapid decision-making.”
This assertion is supported by the experience using a protocol anchored with the point-of-care viral test over a 4-month period. During this time, 901 patients with respiratory symptoms suspected of having a viral etiology were evaluated with the proprietary point-of-care device called FilmArray (bioMérieux).
From a sample taken with a nasopharyngeal swab, the test can identify a broad array of viruses using polymerase chain reaction technology in less than 45 minutes. However, the ED protocol for considering discharge without antibiotics requires additional evidence that the pathogen is viral, including a normal chest x-ray and a CRP less than 50 mg/L.
Of the 901 patients tested, a substantial proportion of whom had chronic obstructive pulmonary disease (COPD) or asthma, 507 (56%) tested positive for at least one virus, including influenza, rhinoviruses, coronaviruses, and adenovirus. Of these, 239 had normal chest x-rays and CRPs less than 50 mg/L. Because of the severity of symptoms or other clinical considerations, 154 patients were admitted, but 85 (36% of those meeting protocol criteria) were discharged without an antibiotic prescription.
“Antibiotics were continued in 90% of the patients who had an abnormal chest x-ray and abnormal CRP,” Dr. Roy reported. However, an objective strategy that permits clinicians to discharge patients at very low risk of a bacterial infection has many advantages even if it applies to a relatively modest proportion of those tested, according to Dr. Roy.
“Each respiratory admission can cost around [2,000 pounds] at our center,” reported Dr. Kay, referring to a figure equivalent to more than $2,600. In addition, she said that avoiding hospitalization frees up hospital beds and facilitates improved antimicrobial stewardship, which is vital to stem resistance.
Avoiding antibiotic use in patients with viral respiratory infections also is relevant to improved antibiotic stewardship in the community. For this reason, a randomized trial with a similar protocol involving the point-of-care viral test is planned in the outpatient setting. According to Dr. Roy, this will involve a community hub to which patients can be referred for testing and clinical evaluation.
“We hope that the quality of care can be improved with the point-of-care test for respiratory viruses as well as helping to reduce antibiotic resistance,” Dr. Roy said.
This approach is promising, according to Tobias Welte, MD, of the department of respiratory medicine at Hannover (Germany) Medical School, but he cautioned that it is not a standard approach.
“The protocol described by Dr. Roy will have to be compared to guidelines and recommended best clinical practice to confirm its usefulness,” he said, while conceding that any strategy that reduces unnecessary hospitalizations deserves further evaluation.
REPORTING FROM THE ERS CONGRESS 2018
Key clinical point:
Major finding: Of patients with a negative chest x-ray and low CRP level, 36% avoided hospital admission due to a positive test for a virus.
Study details: A case series.
Disclosures: Dr. Roy reports no financial relationships relevant to this study.
Coagulopathy outbreak underscores danger of synthetic cannabinoids
Synthetic cannabinoids laced with superwarfarin were behind a recent outbreak of severe coagulopathy in Illinois.
In most cases, vitamin K replacement therapy alleviated symptoms, but four patients died after developing intracranial bleeding, said Amar H. Kelkar, MD, of the University of Illinois at Peoria.
Experts continue to look for how and why superwarfarin ended up in synthetic cannabinoids, whose street names include spice and K2, wrote Dr. Kelkar and his associates. Their report is in the New England Journal of Medicine.
Starting in March 2018, more than 150 patients across Illinois presented to hospitals with bleeding diathesis that involved persistent coagulopathy, the investigators explained. Early inquiries revealed that patients had consumed synthetic cannabinoids. Serum tests identified vitamin K antagonists, including brodifacoum, bromadiolone, and difenacoum. During arrests of suspected distributors, police confiscated synthetic cannabinoids that also tested positive for brodifacoum.
To help characterize the outbreak, the investigators reviewed admissions to Saint Francis Medical Center in Peoria, Ill., between March 28 and April 21, 2018. They identified 34 cases in which patients with vitamin K–dependent factor coagulopathy reported recent exposure to synthetic cannabinoids.
Fifteen of these patients underwent confirmatory anticoagulant testing, which universally confirmed superwarfarin poisoning. Brodifacoum was detected in all patients, difenacoum in five patients, bromadiolone in two patients, and warfarin in one patient.
Common presenting symptoms included gross hematuria (56% of patients) and abdominal pain (47%). Computed tomography identified renal abnormalities in 12 patients.
All patients received oral vitamin K1 (phytonadione). Red cell transfusions, fresh-frozen plasma infusions, and 4-factor prothrombin complex concentrate, or a combination of these treatments, were also used in some patients.
Among the four confirmed deaths in this outbreak, one occurred in a patient in this case series. The patient, a 37-year-old woman presenting to the emergency department with markedly reduced consciousness, was reported by her friends to have recently used synthetic cannabinoids and methamphetamine. She had no personal or family history of coagulopathy.
Computed tomography of the head without contrast material revealed severe acute intraparenchymal hemorrhage of the right basal nuclei and insula with intraventricular extension, a 10-mm left-sided midline shift, and herniation.
She met criteria for brain death 15 hours after hospital admission despite treatment with 10 mg of intravenous vitamin K1, four units of fresh frozen plasma, and 2,300 units of Kcentra.
Treating these patients after hospital discharge was difficult because of a lack of consensus guidelines and access to follow-up care, Dr. Kelkar and his associates noted. Some patients were quoted $24,000 to $34,000 per month for oral vitamin K1 therapy, which also made caring for them difficult and highlighted the need for confirmatory laboratory testing of suspected cases of superwarfarin poisoning.
Dr. Kelkar reported having no conflicts of interest. Two coinvestigators reported relationships outside the submitted work with Shire, CSL Behring, HEMA Biologics, and other companies.
SOURCE: Kelkar AH et al. N Engl J Med. 2018;379:1216-23.
Treating patients who are exposed to synthetic cannabinoid and a superwarfarin such as brodifacoum “requires more than the usual ‘treat ’em and street ’em’ approach,” wrote Jean M. Connors, MD.
“Brodifacoum is a successful rodenticide because of its extremely long half-life (approximately 16-36 days in humans),” Dr. Connors noted.
The drug also is lipophilic, causing tissue sequestration. Once exposed, patients often develop coagulopathy lasting 9 months or longer, she said.
Compared with warfarin poisoning, brodifacoum therefore requires substantially higher-dose and longer-term vitamin K1 therapy. Among the patients in this case series, the maximum outpatient dose was 50 mg, three times daily, and one patient was prescribed 25 mg, twice daily for 270 days, Dr. Connors noted.
“[Dr. Kelkar and his associates] highlight the resources and coordination needed for dealing with a public health crisis that has a prolonged duration of effect,” she added. “Because the synthetic cannabinoid market is lucrative, new products with new toxicity profiles are likely to crop up.”
Dr. Connors is with Brigham and Women’s Hospital, Dana-Farber Cancer Institute, and Harvard Medical School, all in Boston. She reported personal fees from Bristol-Myers Squibb, Portola, Dova Pharmaceuticals, and Unum Therapeutics outside the submitted work. These comments are from her accompanying editorial (N Engl J Med. 2018;379:1275-7).
Treating patients who are exposed to synthetic cannabinoid and a superwarfarin such as brodifacoum “requires more than the usual ‘treat ’em and street ’em’ approach,” wrote Jean M. Connors, MD.
“Brodifacoum is a successful rodenticide because of its extremely long half-life (approximately 16-36 days in humans),” Dr. Connors noted.
The drug also is lipophilic, causing tissue sequestration. Once exposed, patients often develop coagulopathy lasting 9 months or longer, she said.
Compared with warfarin poisoning, brodifacoum therefore requires substantially higher-dose and longer-term vitamin K1 therapy. Among the patients in this case series, the maximum outpatient dose was 50 mg, three times daily, and one patient was prescribed 25 mg, twice daily for 270 days, Dr. Connors noted.
“[Dr. Kelkar and his associates] highlight the resources and coordination needed for dealing with a public health crisis that has a prolonged duration of effect,” she added. “Because the synthetic cannabinoid market is lucrative, new products with new toxicity profiles are likely to crop up.”
Dr. Connors is with Brigham and Women’s Hospital, Dana-Farber Cancer Institute, and Harvard Medical School, all in Boston. She reported personal fees from Bristol-Myers Squibb, Portola, Dova Pharmaceuticals, and Unum Therapeutics outside the submitted work. These comments are from her accompanying editorial (N Engl J Med. 2018;379:1275-7).
Treating patients who are exposed to synthetic cannabinoid and a superwarfarin such as brodifacoum “requires more than the usual ‘treat ’em and street ’em’ approach,” wrote Jean M. Connors, MD.
“Brodifacoum is a successful rodenticide because of its extremely long half-life (approximately 16-36 days in humans),” Dr. Connors noted.
The drug also is lipophilic, causing tissue sequestration. Once exposed, patients often develop coagulopathy lasting 9 months or longer, she said.
Compared with warfarin poisoning, brodifacoum therefore requires substantially higher-dose and longer-term vitamin K1 therapy. Among the patients in this case series, the maximum outpatient dose was 50 mg, three times daily, and one patient was prescribed 25 mg, twice daily for 270 days, Dr. Connors noted.
“[Dr. Kelkar and his associates] highlight the resources and coordination needed for dealing with a public health crisis that has a prolonged duration of effect,” she added. “Because the synthetic cannabinoid market is lucrative, new products with new toxicity profiles are likely to crop up.”
Dr. Connors is with Brigham and Women’s Hospital, Dana-Farber Cancer Institute, and Harvard Medical School, all in Boston. She reported personal fees from Bristol-Myers Squibb, Portola, Dova Pharmaceuticals, and Unum Therapeutics outside the submitted work. These comments are from her accompanying editorial (N Engl J Med. 2018;379:1275-7).
Synthetic cannabinoids laced with superwarfarin were behind a recent outbreak of severe coagulopathy in Illinois.
In most cases, vitamin K replacement therapy alleviated symptoms, but four patients died after developing intracranial bleeding, said Amar H. Kelkar, MD, of the University of Illinois at Peoria.
Experts continue to look for how and why superwarfarin ended up in synthetic cannabinoids, whose street names include spice and K2, wrote Dr. Kelkar and his associates. Their report is in the New England Journal of Medicine.
Starting in March 2018, more than 150 patients across Illinois presented to hospitals with bleeding diathesis that involved persistent coagulopathy, the investigators explained. Early inquiries revealed that patients had consumed synthetic cannabinoids. Serum tests identified vitamin K antagonists, including brodifacoum, bromadiolone, and difenacoum. During arrests of suspected distributors, police confiscated synthetic cannabinoids that also tested positive for brodifacoum.
To help characterize the outbreak, the investigators reviewed admissions to Saint Francis Medical Center in Peoria, Ill., between March 28 and April 21, 2018. They identified 34 cases in which patients with vitamin K–dependent factor coagulopathy reported recent exposure to synthetic cannabinoids.
Fifteen of these patients underwent confirmatory anticoagulant testing, which universally confirmed superwarfarin poisoning. Brodifacoum was detected in all patients, difenacoum in five patients, bromadiolone in two patients, and warfarin in one patient.
Common presenting symptoms included gross hematuria (56% of patients) and abdominal pain (47%). Computed tomography identified renal abnormalities in 12 patients.
All patients received oral vitamin K1 (phytonadione). Red cell transfusions, fresh-frozen plasma infusions, and 4-factor prothrombin complex concentrate, or a combination of these treatments, were also used in some patients.
Among the four confirmed deaths in this outbreak, one occurred in a patient in this case series. The patient, a 37-year-old woman presenting to the emergency department with markedly reduced consciousness, was reported by her friends to have recently used synthetic cannabinoids and methamphetamine. She had no personal or family history of coagulopathy.
Computed tomography of the head without contrast material revealed severe acute intraparenchymal hemorrhage of the right basal nuclei and insula with intraventricular extension, a 10-mm left-sided midline shift, and herniation.
She met criteria for brain death 15 hours after hospital admission despite treatment with 10 mg of intravenous vitamin K1, four units of fresh frozen plasma, and 2,300 units of Kcentra.
Treating these patients after hospital discharge was difficult because of a lack of consensus guidelines and access to follow-up care, Dr. Kelkar and his associates noted. Some patients were quoted $24,000 to $34,000 per month for oral vitamin K1 therapy, which also made caring for them difficult and highlighted the need for confirmatory laboratory testing of suspected cases of superwarfarin poisoning.
Dr. Kelkar reported having no conflicts of interest. Two coinvestigators reported relationships outside the submitted work with Shire, CSL Behring, HEMA Biologics, and other companies.
SOURCE: Kelkar AH et al. N Engl J Med. 2018;379:1216-23.
Synthetic cannabinoids laced with superwarfarin were behind a recent outbreak of severe coagulopathy in Illinois.
In most cases, vitamin K replacement therapy alleviated symptoms, but four patients died after developing intracranial bleeding, said Amar H. Kelkar, MD, of the University of Illinois at Peoria.
Experts continue to look for how and why superwarfarin ended up in synthetic cannabinoids, whose street names include spice and K2, wrote Dr. Kelkar and his associates. Their report is in the New England Journal of Medicine.
Starting in March 2018, more than 150 patients across Illinois presented to hospitals with bleeding diathesis that involved persistent coagulopathy, the investigators explained. Early inquiries revealed that patients had consumed synthetic cannabinoids. Serum tests identified vitamin K antagonists, including brodifacoum, bromadiolone, and difenacoum. During arrests of suspected distributors, police confiscated synthetic cannabinoids that also tested positive for brodifacoum.
To help characterize the outbreak, the investigators reviewed admissions to Saint Francis Medical Center in Peoria, Ill., between March 28 and April 21, 2018. They identified 34 cases in which patients with vitamin K–dependent factor coagulopathy reported recent exposure to synthetic cannabinoids.
Fifteen of these patients underwent confirmatory anticoagulant testing, which universally confirmed superwarfarin poisoning. Brodifacoum was detected in all patients, difenacoum in five patients, bromadiolone in two patients, and warfarin in one patient.
Common presenting symptoms included gross hematuria (56% of patients) and abdominal pain (47%). Computed tomography identified renal abnormalities in 12 patients.
All patients received oral vitamin K1 (phytonadione). Red cell transfusions, fresh-frozen plasma infusions, and 4-factor prothrombin complex concentrate, or a combination of these treatments, were also used in some patients.
Among the four confirmed deaths in this outbreak, one occurred in a patient in this case series. The patient, a 37-year-old woman presenting to the emergency department with markedly reduced consciousness, was reported by her friends to have recently used synthetic cannabinoids and methamphetamine. She had no personal or family history of coagulopathy.
Computed tomography of the head without contrast material revealed severe acute intraparenchymal hemorrhage of the right basal nuclei and insula with intraventricular extension, a 10-mm left-sided midline shift, and herniation.
She met criteria for brain death 15 hours after hospital admission despite treatment with 10 mg of intravenous vitamin K1, four units of fresh frozen plasma, and 2,300 units of Kcentra.
Treating these patients after hospital discharge was difficult because of a lack of consensus guidelines and access to follow-up care, Dr. Kelkar and his associates noted. Some patients were quoted $24,000 to $34,000 per month for oral vitamin K1 therapy, which also made caring for them difficult and highlighted the need for confirmatory laboratory testing of suspected cases of superwarfarin poisoning.
Dr. Kelkar reported having no conflicts of interest. Two coinvestigators reported relationships outside the submitted work with Shire, CSL Behring, HEMA Biologics, and other companies.
SOURCE: Kelkar AH et al. N Engl J Med. 2018;379:1216-23.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: There were more than 150 cases in Illinois with four deaths among patients who developed spontaneous intracranial bleeding.
Study details: A single-institution case series of 15 patients.
Disclosures: Dr. Kelkar reported having no conflicts of interest. Two coinvestigators reported relationships outside the submitted work with Shire, CSL Behring, HEMA Biologics, and other companies.
Source: Kelkar AH et al. N Engl J Med. 2018;379:1216-23.
Atrial fib guidelines may fall short on oral anticoagulation
Anticoagulation thresholds based on CHA2DS2-VASc risk score varied from population to population, researchers reported in the Annals of Internal Medicine.
After accounting for differing rates of stroke in published studies, the benefit of warfarin anticoagulation varied nearly fourfold, said Sachin J. Shah, MD, of the University of California San Francisco and his associates. They called for guidelines that “better reflect the uncertainty in current thresholds of stroke risk score for recommending anticoagulation.”
Oral anticoagulation markedly reduces risk of ischemic stroke in patients with atrial fibrillation but increases the risk of major bleeding, including intracranial hemorrhage, which often is fatal. Therefore, when deciding whether to recommend oral anticoagulation, physicians must estimate clinical net benefit by quantifying the difference between reduction in stroke risk and increase in major bleeding risk, weighted by the severity of each outcome.
Guidelines on nonvalvular atrial fibrillation from the European Society of Cardiology and joint guidelines from the American Heart Association, American College of Cardiology, and Heart Rhythm Society (AHA/ACC/HRS) recommend oral anticoagulation when CHA2DS2-VASc (congestive heart failure, hypertension, age, diabetes, stroke, and vascular disease) risk score is 2 or greater. These guidelines implicitly assume that a particular CHA2DS2-VASc score denotes the same amount of risk across populations, even though a recent meta-analysis found otherwise, as the researchers noted.
To further test this assumption, they applied an existing Markov model to data from more than 33,000 members of the ATRIA-CVRN cohort. All patients had nonvalvular atrial fibrillation, were members of Kaiser Permanente Northern California, and were diagnosed during 1996-1997. About 81% had a CHA2DS2-VASc score of at least 2. For each patient, the researchers produced four estimates of the net clinical benefit of oral anticoagulation based on ischemic stroke rates from ATRIA, the Swedish AF cohort study, the SPORTIF study, and the Danish National Patient Registry.
Optimal anticoagulation thresholds were a CHA2DS2-VASc score of 3 or more using stroke rates from ATRIA, 2 or more based on Swedish AF rates, 1 or more based on SPORTIF rates, and 0 or more using rates from the Danish National Patient Registry. Oral anticoagulation thresholds were lower but still varied widely after accounting for the lower rates of intracranial hemorrhage associated with non–vitamin K antagonist therapy.
Therefore, current guidelines based on CHA2DS2-VASc score may need revising “in favor of more accurate, individualized assessments of risk for both ischemic stroke and major bleeding,” the investigators wrote. “Until such time, guidelines should better reflect the uncertainty of the current approach in which a patient’s CHA2DS2-VASc score is used as the primary basis for recommending oral anticoagulation.”
The study had no primary funding source. Dr. Shah reported having no conflicts of interest. Three coinvestigators disclosed research support from relevant pharmaceutical or device companies.
SOURCE: Shah SJ et al. Ann Intern Med. 2018 Sep 25. doi: 10.7326/M17-2762
Based on this study, the CHA2DS2-VASc score threshold for anticoagulation might not be a “one-size-fits all approach but rather a starting point for a more tailored assessment,” wrote Jennifer M. Wright, MD, and Craig T. January, MD, PhD, in an editorial accompanying the report.
The CHA2DS2-VASc algorithm uses fixed whole integers and therefore might lack the sensitivity and flexibility needed to accurately reflect the effects of its components, the experts wrote. “For example, female sex now seems to be a risk modifier, and its intensity depends on other risk factors.”
However, CHA2DS2-VASc remains the main way to assess net clinical benefit of oral anticoagulation for patients with anticoagulation, they conceded. “When it comes to the conversation about the risks and benefits of anticoagulation for our patients with atrial fibrillation, we must remember that each patient is an individual and has his or her own ‘score.’ ”
The editorialists are with the University of Wisconsin in Madison. They reported having no relevant conflicts of interest. These comments are based on their editorial (Ann Intern Med. 2018 Sep 25. doi: 10.7326/M18-2355).
Based on this study, the CHA2DS2-VASc score threshold for anticoagulation might not be a “one-size-fits all approach but rather a starting point for a more tailored assessment,” wrote Jennifer M. Wright, MD, and Craig T. January, MD, PhD, in an editorial accompanying the report.
The CHA2DS2-VASc algorithm uses fixed whole integers and therefore might lack the sensitivity and flexibility needed to accurately reflect the effects of its components, the experts wrote. “For example, female sex now seems to be a risk modifier, and its intensity depends on other risk factors.”
However, CHA2DS2-VASc remains the main way to assess net clinical benefit of oral anticoagulation for patients with anticoagulation, they conceded. “When it comes to the conversation about the risks and benefits of anticoagulation for our patients with atrial fibrillation, we must remember that each patient is an individual and has his or her own ‘score.’ ”
The editorialists are with the University of Wisconsin in Madison. They reported having no relevant conflicts of interest. These comments are based on their editorial (Ann Intern Med. 2018 Sep 25. doi: 10.7326/M18-2355).
Based on this study, the CHA2DS2-VASc score threshold for anticoagulation might not be a “one-size-fits all approach but rather a starting point for a more tailored assessment,” wrote Jennifer M. Wright, MD, and Craig T. January, MD, PhD, in an editorial accompanying the report.
The CHA2DS2-VASc algorithm uses fixed whole integers and therefore might lack the sensitivity and flexibility needed to accurately reflect the effects of its components, the experts wrote. “For example, female sex now seems to be a risk modifier, and its intensity depends on other risk factors.”
However, CHA2DS2-VASc remains the main way to assess net clinical benefit of oral anticoagulation for patients with anticoagulation, they conceded. “When it comes to the conversation about the risks and benefits of anticoagulation for our patients with atrial fibrillation, we must remember that each patient is an individual and has his or her own ‘score.’ ”
The editorialists are with the University of Wisconsin in Madison. They reported having no relevant conflicts of interest. These comments are based on their editorial (Ann Intern Med. 2018 Sep 25. doi: 10.7326/M18-2355).
Anticoagulation thresholds based on CHA2DS2-VASc risk score varied from population to population, researchers reported in the Annals of Internal Medicine.
After accounting for differing rates of stroke in published studies, the benefit of warfarin anticoagulation varied nearly fourfold, said Sachin J. Shah, MD, of the University of California San Francisco and his associates. They called for guidelines that “better reflect the uncertainty in current thresholds of stroke risk score for recommending anticoagulation.”
Oral anticoagulation markedly reduces risk of ischemic stroke in patients with atrial fibrillation but increases the risk of major bleeding, including intracranial hemorrhage, which often is fatal. Therefore, when deciding whether to recommend oral anticoagulation, physicians must estimate clinical net benefit by quantifying the difference between reduction in stroke risk and increase in major bleeding risk, weighted by the severity of each outcome.
Guidelines on nonvalvular atrial fibrillation from the European Society of Cardiology and joint guidelines from the American Heart Association, American College of Cardiology, and Heart Rhythm Society (AHA/ACC/HRS) recommend oral anticoagulation when CHA2DS2-VASc (congestive heart failure, hypertension, age, diabetes, stroke, and vascular disease) risk score is 2 or greater. These guidelines implicitly assume that a particular CHA2DS2-VASc score denotes the same amount of risk across populations, even though a recent meta-analysis found otherwise, as the researchers noted.
To further test this assumption, they applied an existing Markov model to data from more than 33,000 members of the ATRIA-CVRN cohort. All patients had nonvalvular atrial fibrillation, were members of Kaiser Permanente Northern California, and were diagnosed during 1996-1997. About 81% had a CHA2DS2-VASc score of at least 2. For each patient, the researchers produced four estimates of the net clinical benefit of oral anticoagulation based on ischemic stroke rates from ATRIA, the Swedish AF cohort study, the SPORTIF study, and the Danish National Patient Registry.
Optimal anticoagulation thresholds were a CHA2DS2-VASc score of 3 or more using stroke rates from ATRIA, 2 or more based on Swedish AF rates, 1 or more based on SPORTIF rates, and 0 or more using rates from the Danish National Patient Registry. Oral anticoagulation thresholds were lower but still varied widely after accounting for the lower rates of intracranial hemorrhage associated with non–vitamin K antagonist therapy.
Therefore, current guidelines based on CHA2DS2-VASc score may need revising “in favor of more accurate, individualized assessments of risk for both ischemic stroke and major bleeding,” the investigators wrote. “Until such time, guidelines should better reflect the uncertainty of the current approach in which a patient’s CHA2DS2-VASc score is used as the primary basis for recommending oral anticoagulation.”
The study had no primary funding source. Dr. Shah reported having no conflicts of interest. Three coinvestigators disclosed research support from relevant pharmaceutical or device companies.
SOURCE: Shah SJ et al. Ann Intern Med. 2018 Sep 25. doi: 10.7326/M17-2762
Anticoagulation thresholds based on CHA2DS2-VASc risk score varied from population to population, researchers reported in the Annals of Internal Medicine.
After accounting for differing rates of stroke in published studies, the benefit of warfarin anticoagulation varied nearly fourfold, said Sachin J. Shah, MD, of the University of California San Francisco and his associates. They called for guidelines that “better reflect the uncertainty in current thresholds of stroke risk score for recommending anticoagulation.”
Oral anticoagulation markedly reduces risk of ischemic stroke in patients with atrial fibrillation but increases the risk of major bleeding, including intracranial hemorrhage, which often is fatal. Therefore, when deciding whether to recommend oral anticoagulation, physicians must estimate clinical net benefit by quantifying the difference between reduction in stroke risk and increase in major bleeding risk, weighted by the severity of each outcome.
Guidelines on nonvalvular atrial fibrillation from the European Society of Cardiology and joint guidelines from the American Heart Association, American College of Cardiology, and Heart Rhythm Society (AHA/ACC/HRS) recommend oral anticoagulation when CHA2DS2-VASc (congestive heart failure, hypertension, age, diabetes, stroke, and vascular disease) risk score is 2 or greater. These guidelines implicitly assume that a particular CHA2DS2-VASc score denotes the same amount of risk across populations, even though a recent meta-analysis found otherwise, as the researchers noted.
To further test this assumption, they applied an existing Markov model to data from more than 33,000 members of the ATRIA-CVRN cohort. All patients had nonvalvular atrial fibrillation, were members of Kaiser Permanente Northern California, and were diagnosed during 1996-1997. About 81% had a CHA2DS2-VASc score of at least 2. For each patient, the researchers produced four estimates of the net clinical benefit of oral anticoagulation based on ischemic stroke rates from ATRIA, the Swedish AF cohort study, the SPORTIF study, and the Danish National Patient Registry.
Optimal anticoagulation thresholds were a CHA2DS2-VASc score of 3 or more using stroke rates from ATRIA, 2 or more based on Swedish AF rates, 1 or more based on SPORTIF rates, and 0 or more using rates from the Danish National Patient Registry. Oral anticoagulation thresholds were lower but still varied widely after accounting for the lower rates of intracranial hemorrhage associated with non–vitamin K antagonist therapy.
Therefore, current guidelines based on CHA2DS2-VASc score may need revising “in favor of more accurate, individualized assessments of risk for both ischemic stroke and major bleeding,” the investigators wrote. “Until such time, guidelines should better reflect the uncertainty of the current approach in which a patient’s CHA2DS2-VASc score is used as the primary basis for recommending oral anticoagulation.”
The study had no primary funding source. Dr. Shah reported having no conflicts of interest. Three coinvestigators disclosed research support from relevant pharmaceutical or device companies.
SOURCE: Shah SJ et al. Ann Intern Med. 2018 Sep 25. doi: 10.7326/M17-2762
FROM THE ANNALS OF INTERNAL MEDICINE
Key clinical point:
Major finding: After accounting for differing rates of stroke in published studies, the benefit of warfarin anticoagulation varied nearly fourfold. Anticoagulation thresholds were lower but still varied widely in a model of non–vitamin K antagonist therapy.
Study details: Markov state-transition model of 33,434 patients with nonvalvular atrial fibrillation.
Disclosures: The study had no primary funding source. Dr. Shah reported having no conflicts of interest. Three coinvestigators disclosed research support from relevant pharmaceutical or device companies.
Source: Shah SJ et al. Ann Intern Med. 2018 Sep 25. doi: 10.7326/M17-2762.
Five mistakes to avoid when starting a locum tenens position
Beware inefficient placement systems
For the last 8 years I have worked as a locum tenens hospitalist. I began on this path when it was the least popular option upon graduation from residency.
I did countless hours of research trying to find accurate information about locum tenens companies, but never found anything written by physicians, only by the companies themselves. So, I stepped into this field blindfolded and learned the hard way. Since than, I have worked with over 16 locum tenens companies, 14 hospitals, and eight electronic medical record systems.
Through these experiences I’ve realized that, unfortunately, some locum tenens companies do not act with the professionalism and efficiency that both physicians and hospital systems would expect. This can lead to more stress than an actual employed position for physicians, and poor coverage with enormous costs for hospitals.
I decided to take matters into my own hands because I wanted to make the locum tenens system easier to navigate. I believe that the system can play a role in decreasing physician burnout, and I deeply understand the need that hospitals have to serve their patients with a shortage of doctors. As locum tenens physicians, we serve a need and shouldn’t have to deal with inefficient placement systems.
Here are five mistakes to avoid for physicians that are first entering into the locum tenens world:
1. Beware choosing a “factory mill” locum tenens company. Bigger companies have higher overhead, which usually means that they take more of a margin from physicians. Generally speaking, larger locum tenens companies pay their recruiters a lower percentage commission, so each recruiter has more physicians. This can lead to mistakes which can cause stress for both physicians and hospitals.
2. Beware long travel. Hourly rates that are $5-$10 dollars more per hour in remote locations are attractive. However, the amount of travel needed to get to these locations may not be worth it. When negotiating a rate, make sure not to lose sight of the amount of time it will take to travel to the hospital or outpatient location.
3. Beware short-term placements. There are a lot of hospitals that just need one or two weeks covered. Even if it’s at a much higher rate, the amount of paper work and credentialing hassle may not be worth the amount of time you work there. The greater number of cumulative hospitals worked, the longer credentialing will take in future locum tenens placements.
4. Beware using multiple travel services. Stick to one airline, one rental car company, and one hotel chain. This way when you are not working, you may be able to use the points earned during your work days for future vacations.
5. Beware companies that are not organized. If you find that a locum tenens company is asking you to do all of the paperwork to get credentialed, move on. This can be a red flag and may mean they lack credentialing staff. You should never have to fill out your own paperwork; rather you should be the one that simply reviews and corrects it.
Dr. Arora works as a liaison between hospitals, physicians, and locum tenens companies and is a member of The Hospitalist’s editorial advisory board. She negotiates rates and expectations with multiple locum tenens companies on behalf of physicians in all fields of practice and does not own or endorse a locum tenens company. You can contact her at www.doctorsliaison.com.
Beware inefficient placement systems
Beware inefficient placement systems
For the last 8 years I have worked as a locum tenens hospitalist. I began on this path when it was the least popular option upon graduation from residency.
I did countless hours of research trying to find accurate information about locum tenens companies, but never found anything written by physicians, only by the companies themselves. So, I stepped into this field blindfolded and learned the hard way. Since than, I have worked with over 16 locum tenens companies, 14 hospitals, and eight electronic medical record systems.
Through these experiences I’ve realized that, unfortunately, some locum tenens companies do not act with the professionalism and efficiency that both physicians and hospital systems would expect. This can lead to more stress than an actual employed position for physicians, and poor coverage with enormous costs for hospitals.
I decided to take matters into my own hands because I wanted to make the locum tenens system easier to navigate. I believe that the system can play a role in decreasing physician burnout, and I deeply understand the need that hospitals have to serve their patients with a shortage of doctors. As locum tenens physicians, we serve a need and shouldn’t have to deal with inefficient placement systems.
Here are five mistakes to avoid for physicians that are first entering into the locum tenens world:
1. Beware choosing a “factory mill” locum tenens company. Bigger companies have higher overhead, which usually means that they take more of a margin from physicians. Generally speaking, larger locum tenens companies pay their recruiters a lower percentage commission, so each recruiter has more physicians. This can lead to mistakes which can cause stress for both physicians and hospitals.
2. Beware long travel. Hourly rates that are $5-$10 dollars more per hour in remote locations are attractive. However, the amount of travel needed to get to these locations may not be worth it. When negotiating a rate, make sure not to lose sight of the amount of time it will take to travel to the hospital or outpatient location.
3. Beware short-term placements. There are a lot of hospitals that just need one or two weeks covered. Even if it’s at a much higher rate, the amount of paper work and credentialing hassle may not be worth the amount of time you work there. The greater number of cumulative hospitals worked, the longer credentialing will take in future locum tenens placements.
4. Beware using multiple travel services. Stick to one airline, one rental car company, and one hotel chain. This way when you are not working, you may be able to use the points earned during your work days for future vacations.
5. Beware companies that are not organized. If you find that a locum tenens company is asking you to do all of the paperwork to get credentialed, move on. This can be a red flag and may mean they lack credentialing staff. You should never have to fill out your own paperwork; rather you should be the one that simply reviews and corrects it.
Dr. Arora works as a liaison between hospitals, physicians, and locum tenens companies and is a member of The Hospitalist’s editorial advisory board. She negotiates rates and expectations with multiple locum tenens companies on behalf of physicians in all fields of practice and does not own or endorse a locum tenens company. You can contact her at www.doctorsliaison.com.
For the last 8 years I have worked as a locum tenens hospitalist. I began on this path when it was the least popular option upon graduation from residency.
I did countless hours of research trying to find accurate information about locum tenens companies, but never found anything written by physicians, only by the companies themselves. So, I stepped into this field blindfolded and learned the hard way. Since than, I have worked with over 16 locum tenens companies, 14 hospitals, and eight electronic medical record systems.
Through these experiences I’ve realized that, unfortunately, some locum tenens companies do not act with the professionalism and efficiency that both physicians and hospital systems would expect. This can lead to more stress than an actual employed position for physicians, and poor coverage with enormous costs for hospitals.
I decided to take matters into my own hands because I wanted to make the locum tenens system easier to navigate. I believe that the system can play a role in decreasing physician burnout, and I deeply understand the need that hospitals have to serve their patients with a shortage of doctors. As locum tenens physicians, we serve a need and shouldn’t have to deal with inefficient placement systems.
Here are five mistakes to avoid for physicians that are first entering into the locum tenens world:
1. Beware choosing a “factory mill” locum tenens company. Bigger companies have higher overhead, which usually means that they take more of a margin from physicians. Generally speaking, larger locum tenens companies pay their recruiters a lower percentage commission, so each recruiter has more physicians. This can lead to mistakes which can cause stress for both physicians and hospitals.
2. Beware long travel. Hourly rates that are $5-$10 dollars more per hour in remote locations are attractive. However, the amount of travel needed to get to these locations may not be worth it. When negotiating a rate, make sure not to lose sight of the amount of time it will take to travel to the hospital or outpatient location.
3. Beware short-term placements. There are a lot of hospitals that just need one or two weeks covered. Even if it’s at a much higher rate, the amount of paper work and credentialing hassle may not be worth the amount of time you work there. The greater number of cumulative hospitals worked, the longer credentialing will take in future locum tenens placements.
4. Beware using multiple travel services. Stick to one airline, one rental car company, and one hotel chain. This way when you are not working, you may be able to use the points earned during your work days for future vacations.
5. Beware companies that are not organized. If you find that a locum tenens company is asking you to do all of the paperwork to get credentialed, move on. This can be a red flag and may mean they lack credentialing staff. You should never have to fill out your own paperwork; rather you should be the one that simply reviews and corrects it.
Dr. Arora works as a liaison between hospitals, physicians, and locum tenens companies and is a member of The Hospitalist’s editorial advisory board. She negotiates rates and expectations with multiple locum tenens companies on behalf of physicians in all fields of practice and does not own or endorse a locum tenens company. You can contact her at www.doctorsliaison.com.
Five-year follow-up confirms safety of antibiotics for uncomplicated appendicitis
Longer-term outcomes of treating uncomplicated acute appendicitis with antibiotics suggest it is a feasible alternative to appendectomy.
Researchers have presented the 5-year follow-up data from the Appendicitis Acuta (APPAC) multicenter randomized clinical trial comparing appendectomy with antibiotic therapy in 530 patients.
They found that 39.1% (100) of the 257 patients randomized to antibiotic therapy – 3 days of intravenous ertapenem followed by 7 days of oral levofloxacin and metronidazole – experienced a recurrence of appendicitis within 5 years and subsequently had surgery.
However the authors noted that seven of these patients were later found not to have appendicitis, so the true success rate for antibiotic treatment was actually 63.7%.
Seventy of the patients who experienced a recurrence underwent surgery in the first year after randomization, 17 in the second year, 3 in the third year, 5 in the fourth year, and the remaining 5 patients in the fifth year, the authors wrote in an article published in JAMA.
However the overall complication rate was similar in patients who were randomized to undergo appendectomy and in those who were initially randomized to the antibiotic group but later experienced a recurrence and underwent surgery.
“No patient initially treated with antibiotics, who ultimately developed recurrent appendicitis, had any complications related to the delay in surgery,” wrote Paulina Salminen, MD, from Turku (Finland) University Hospital and coauthors. “Nearly two-thirds of all patients who initially presented with uncomplicated appendicitis were successfully treated with antibiotics alone, and those who ultimately developed recurrent disease did not experience any adverse outcomes related to the delay in appendectomy.”
Of the 100 patients randomized to antibiotics who underwent appendectomy after a recurrence, 15 were operated on when they were first hospitalized at study admission.
The authors commented that the study design allowed for surgeons to exercise their clinical judgment in choosing when to perform an appendectomy on patients in the antibiotic group, because antibiotics alone was not considered acceptable treatment for appendicitis.
“This led to some patients undergoing appendectomy who did not have appendicitis or who might have been successfully treated with antibiotics or an another course of antibiotics,” they wrote. “Future studies should investigate protocols for further imaging or antibiotic treatment for patients who develop recurrent appendicitis after they were initially treated with antibiotics.”
In the recurrence group, the majority were found to have uncomplicated appendicitis, but complicated appendicitis was seen in two patients between 2 and 5 years after the index admission.
There was a significant 17.9% higher complication rate in the appendectomy group, compared with the antibiotic group – 24.4% versus 6.5% – at 5 years and two patients in the appendectomy group had severe complications requiring reoperation.
They suggested that the higher complication rate with surgery, which was mostly attributable to infections, could be reduced by the use of laparoscopic appendectomy, which is also associated with faster recovery.
The median length of hospital stay was 3 days for both the appendectomy group and the antibiotics-only group, but patients randomized to appendectomy took a median of 22 days of sick leave, compared with 11 days for those randomized to antibiotics (P less than .001).
In the absence of standard protocol on treating appendicitis with antibiotics, the authors noted that they took a conservative approach, using broad-spectrum antibiotics and keeping patients in hospital for 3 days for observation.
“The success of antibiotic treatment for appendicitis calls into question prior beliefs that appendicitis inevitably results in serious intra-abdominal infection if appendectomy is not performed.”
The study was supported by the Mary and Georg C. Ehrnrooth Foundation, the EVO Foundation, and Turku University. One author declared lecture fees from three pharmaceutical companies but no other conflicts of interest were declared.
SOURCE: Salminen P et al. JAMA 2018;320:1259-65. doi: 10.1001/jama.2018.13201.
“When the earlier results of the APPAC trial were published, showing that 73% of patients with uncomplicated acute appendicitis did not require surgery at 1 year of follow-up, critics raised concerns that many more of these patients would eventually require surgery,” wrote Edward H. Livingston, MD, deputy editor of JAMA in an accompanying editorial (JAMA 2018;320:1245-46).Surgeons have since been waiting until longer-term outcomes were known. These 5-year results are supportive of the antibiotics approach. “They show no increase in major complications in patients who experienced a recurrence and underwent appendectomy after initially being randomized to antibiotic therapy. They challenge the notion that uncomplicated acute appendicitis is a surgical emergency and show that nonsurgical treatment is a reasonable option,” Dr Livingston wrote.
He declared no conflicts of interest.
“When the earlier results of the APPAC trial were published, showing that 73% of patients with uncomplicated acute appendicitis did not require surgery at 1 year of follow-up, critics raised concerns that many more of these patients would eventually require surgery,” wrote Edward H. Livingston, MD, deputy editor of JAMA in an accompanying editorial (JAMA 2018;320:1245-46).Surgeons have since been waiting until longer-term outcomes were known. These 5-year results are supportive of the antibiotics approach. “They show no increase in major complications in patients who experienced a recurrence and underwent appendectomy after initially being randomized to antibiotic therapy. They challenge the notion that uncomplicated acute appendicitis is a surgical emergency and show that nonsurgical treatment is a reasonable option,” Dr Livingston wrote.
He declared no conflicts of interest.
“When the earlier results of the APPAC trial were published, showing that 73% of patients with uncomplicated acute appendicitis did not require surgery at 1 year of follow-up, critics raised concerns that many more of these patients would eventually require surgery,” wrote Edward H. Livingston, MD, deputy editor of JAMA in an accompanying editorial (JAMA 2018;320:1245-46).Surgeons have since been waiting until longer-term outcomes were known. These 5-year results are supportive of the antibiotics approach. “They show no increase in major complications in patients who experienced a recurrence and underwent appendectomy after initially being randomized to antibiotic therapy. They challenge the notion that uncomplicated acute appendicitis is a surgical emergency and show that nonsurgical treatment is a reasonable option,” Dr Livingston wrote.
He declared no conflicts of interest.
Longer-term outcomes of treating uncomplicated acute appendicitis with antibiotics suggest it is a feasible alternative to appendectomy.
Researchers have presented the 5-year follow-up data from the Appendicitis Acuta (APPAC) multicenter randomized clinical trial comparing appendectomy with antibiotic therapy in 530 patients.
They found that 39.1% (100) of the 257 patients randomized to antibiotic therapy – 3 days of intravenous ertapenem followed by 7 days of oral levofloxacin and metronidazole – experienced a recurrence of appendicitis within 5 years and subsequently had surgery.
However the authors noted that seven of these patients were later found not to have appendicitis, so the true success rate for antibiotic treatment was actually 63.7%.
Seventy of the patients who experienced a recurrence underwent surgery in the first year after randomization, 17 in the second year, 3 in the third year, 5 in the fourth year, and the remaining 5 patients in the fifth year, the authors wrote in an article published in JAMA.
However the overall complication rate was similar in patients who were randomized to undergo appendectomy and in those who were initially randomized to the antibiotic group but later experienced a recurrence and underwent surgery.
“No patient initially treated with antibiotics, who ultimately developed recurrent appendicitis, had any complications related to the delay in surgery,” wrote Paulina Salminen, MD, from Turku (Finland) University Hospital and coauthors. “Nearly two-thirds of all patients who initially presented with uncomplicated appendicitis were successfully treated with antibiotics alone, and those who ultimately developed recurrent disease did not experience any adverse outcomes related to the delay in appendectomy.”
Of the 100 patients randomized to antibiotics who underwent appendectomy after a recurrence, 15 were operated on when they were first hospitalized at study admission.
The authors commented that the study design allowed for surgeons to exercise their clinical judgment in choosing when to perform an appendectomy on patients in the antibiotic group, because antibiotics alone was not considered acceptable treatment for appendicitis.
“This led to some patients undergoing appendectomy who did not have appendicitis or who might have been successfully treated with antibiotics or an another course of antibiotics,” they wrote. “Future studies should investigate protocols for further imaging or antibiotic treatment for patients who develop recurrent appendicitis after they were initially treated with antibiotics.”
In the recurrence group, the majority were found to have uncomplicated appendicitis, but complicated appendicitis was seen in two patients between 2 and 5 years after the index admission.
There was a significant 17.9% higher complication rate in the appendectomy group, compared with the antibiotic group – 24.4% versus 6.5% – at 5 years and two patients in the appendectomy group had severe complications requiring reoperation.
They suggested that the higher complication rate with surgery, which was mostly attributable to infections, could be reduced by the use of laparoscopic appendectomy, which is also associated with faster recovery.
The median length of hospital stay was 3 days for both the appendectomy group and the antibiotics-only group, but patients randomized to appendectomy took a median of 22 days of sick leave, compared with 11 days for those randomized to antibiotics (P less than .001).
In the absence of standard protocol on treating appendicitis with antibiotics, the authors noted that they took a conservative approach, using broad-spectrum antibiotics and keeping patients in hospital for 3 days for observation.
“The success of antibiotic treatment for appendicitis calls into question prior beliefs that appendicitis inevitably results in serious intra-abdominal infection if appendectomy is not performed.”
The study was supported by the Mary and Georg C. Ehrnrooth Foundation, the EVO Foundation, and Turku University. One author declared lecture fees from three pharmaceutical companies but no other conflicts of interest were declared.
SOURCE: Salminen P et al. JAMA 2018;320:1259-65. doi: 10.1001/jama.2018.13201.
Longer-term outcomes of treating uncomplicated acute appendicitis with antibiotics suggest it is a feasible alternative to appendectomy.
Researchers have presented the 5-year follow-up data from the Appendicitis Acuta (APPAC) multicenter randomized clinical trial comparing appendectomy with antibiotic therapy in 530 patients.
They found that 39.1% (100) of the 257 patients randomized to antibiotic therapy – 3 days of intravenous ertapenem followed by 7 days of oral levofloxacin and metronidazole – experienced a recurrence of appendicitis within 5 years and subsequently had surgery.
However the authors noted that seven of these patients were later found not to have appendicitis, so the true success rate for antibiotic treatment was actually 63.7%.
Seventy of the patients who experienced a recurrence underwent surgery in the first year after randomization, 17 in the second year, 3 in the third year, 5 in the fourth year, and the remaining 5 patients in the fifth year, the authors wrote in an article published in JAMA.
However the overall complication rate was similar in patients who were randomized to undergo appendectomy and in those who were initially randomized to the antibiotic group but later experienced a recurrence and underwent surgery.
“No patient initially treated with antibiotics, who ultimately developed recurrent appendicitis, had any complications related to the delay in surgery,” wrote Paulina Salminen, MD, from Turku (Finland) University Hospital and coauthors. “Nearly two-thirds of all patients who initially presented with uncomplicated appendicitis were successfully treated with antibiotics alone, and those who ultimately developed recurrent disease did not experience any adverse outcomes related to the delay in appendectomy.”
Of the 100 patients randomized to antibiotics who underwent appendectomy after a recurrence, 15 were operated on when they were first hospitalized at study admission.
The authors commented that the study design allowed for surgeons to exercise their clinical judgment in choosing when to perform an appendectomy on patients in the antibiotic group, because antibiotics alone was not considered acceptable treatment for appendicitis.
“This led to some patients undergoing appendectomy who did not have appendicitis or who might have been successfully treated with antibiotics or an another course of antibiotics,” they wrote. “Future studies should investigate protocols for further imaging or antibiotic treatment for patients who develop recurrent appendicitis after they were initially treated with antibiotics.”
In the recurrence group, the majority were found to have uncomplicated appendicitis, but complicated appendicitis was seen in two patients between 2 and 5 years after the index admission.
There was a significant 17.9% higher complication rate in the appendectomy group, compared with the antibiotic group – 24.4% versus 6.5% – at 5 years and two patients in the appendectomy group had severe complications requiring reoperation.
They suggested that the higher complication rate with surgery, which was mostly attributable to infections, could be reduced by the use of laparoscopic appendectomy, which is also associated with faster recovery.
The median length of hospital stay was 3 days for both the appendectomy group and the antibiotics-only group, but patients randomized to appendectomy took a median of 22 days of sick leave, compared with 11 days for those randomized to antibiotics (P less than .001).
In the absence of standard protocol on treating appendicitis with antibiotics, the authors noted that they took a conservative approach, using broad-spectrum antibiotics and keeping patients in hospital for 3 days for observation.
“The success of antibiotic treatment for appendicitis calls into question prior beliefs that appendicitis inevitably results in serious intra-abdominal infection if appendectomy is not performed.”
The study was supported by the Mary and Georg C. Ehrnrooth Foundation, the EVO Foundation, and Turku University. One author declared lecture fees from three pharmaceutical companies but no other conflicts of interest were declared.
SOURCE: Salminen P et al. JAMA 2018;320:1259-65. doi: 10.1001/jama.2018.13201.
FROM JAMA
Key clinical point: Antibiotics could be used as an alternative to surgery for uncomplicated acute appendicitis.
Major finding: Around two-thirds of patients with acute appendicitis treated with antibiotics only did not experience a recurrence in 5 years.
Study details: Randomized controlled study in 530 patients with uncomplicated acute appendicitis.
Disclosures: The study was supported by the Mary and Georg C. Ehrnrooth Foundation, the EVO Foundation, and Turku University. One author declared lecture fees from three pharmaceutical companies but no other conflicts of interest were declared.
Source: Salminen P et al. JAMA 2018;320:1259-65. doi: 10.1001/jama.2018.13201.
Signs point to growing abuse of gabapentinoids in the U.S.
LAS VEGAS – Up to 22% of opioid abusers also abuse gabapentin, taking high doses of the antiepileptic for its psychoactive effects, or to potentiate the effect of opioids.
The drug – the 10th most commonly prescribed in the United States – is increasingly implicated in overdose deaths. In response, several states have recently reclassified the antiepileptic as a Schedule V controlled substance. Other states have declined to go that far, but have added gabapentin (Neurontin and others) to the drugs that must be reported to state prescription monitoring programs.
“Gabapentin and pregabalin [Lyrica] are versatile and important drugs that are widely prescribed and used off label for a number of conditions from seizure disorder to fibromyalgia,” said Joseph Pergolizzi Jr., MD, who discussed the issue during the annual PAINWeek. “Abuse patterns differ somewhat from abuse patterns with prescription opioids. People who misuse gabapentinoids tend to already use other drugs inappropriately. It’s rare to find a person who only takes them recreationally, but it is increasingly common to find polydrug abusers who take gabapentinoids.”
Gabapentin abuse appears to be more common in Europe than in the United States, where it’s just beginning to emerge, Dr. Pergolizzi said. And the picture is more nuanced than it might first appear: Many of those who are misusing the drug are using it as a “do-it-yourself” opioid withdrawal aid, he said in an interview.
At the meeting, he presented a literature review comprising 46 papers on pregabalin abuse and 263 on gabapentin abuse. Several important themes arose from these papers, said Dr. Pergolizzi, cofounder and chief operating officer of NEMA Research Inc., Naples, Fla.:
- Gabapentin and pregabalin are being prescribed off label for numerous conditions, including bipolar disorder, neuropathic pain, diabetic neuropathy, complex regional pain syndrome, attention deficit disorder, restless leg syndrome, trigeminal neuralgia, periodic limb movement disorder of sleep, migraine, drug and alcohol withdrawal seizures, chronic low back pain, and even menopausal symptoms.
- About a one-third of users experience withdrawal symptoms with sudden discontinuation. Symptoms include disorientation, anxiety, insomnia, heart palpitations, diaphoresis, and abdominal cramps.
- Risk factors for abuse are emerging. These include opioid use disorders, mental illnesses, and a history of taking supratherapeutic doses of the drugs. Age and sex don’t seem to be a consistent risk factor for abuse.
- Abusers can obtain nonprescription gabapentinoids more easily each year, including street sales and online orders, Dr. Pergolizzi said. “A Google search conducted in July for ‘buy gabapentin without a prescription’ yielded 4.48 million results and ‘buy pregabalin without a prescription,’ 622,000. A similar search conducted in September 2017 yielded 1.19 million and 352,000 results, respectively.”
- Few urine drug assays screen for gabapentinoids, which makes them easy to conceal in random drug testing.
Reports of gabapentin-involved drug overdoses and even deaths have recently emerged in the United States, particularly in the opioid abuse-plagued Appalachian states. An article in May in Drug and Alcohol Dependence examined the prevalence of gabapentin in postmortem toxicology in drug overdose deaths in four Appalachian states in 2015 (Drug Alcohol Depend. 2018;186:80-5). Rates were 4% in eastern Tennessee, 15% in West Virginia, 20% in North Carolina, and 41% in Kentucky.
Three states have now added gabapentin to their list of Schedule V controlled substances: Kentucky in 2017, West Virginia this May, and Tennessee in July.
Ohio, Minnesota, Virginia, and Massachusetts have taken a different tack to controlling dispensing. In those states, all pharmacies, prescribers, and wholesalers must report all dispensing and sales of gabapentin to their prescription monitoring databases.
Dr. Pergolizzi disclosed financial relationships with numerous pharmaceutical companies.
LAS VEGAS – Up to 22% of opioid abusers also abuse gabapentin, taking high doses of the antiepileptic for its psychoactive effects, or to potentiate the effect of opioids.
The drug – the 10th most commonly prescribed in the United States – is increasingly implicated in overdose deaths. In response, several states have recently reclassified the antiepileptic as a Schedule V controlled substance. Other states have declined to go that far, but have added gabapentin (Neurontin and others) to the drugs that must be reported to state prescription monitoring programs.
“Gabapentin and pregabalin [Lyrica] are versatile and important drugs that are widely prescribed and used off label for a number of conditions from seizure disorder to fibromyalgia,” said Joseph Pergolizzi Jr., MD, who discussed the issue during the annual PAINWeek. “Abuse patterns differ somewhat from abuse patterns with prescription opioids. People who misuse gabapentinoids tend to already use other drugs inappropriately. It’s rare to find a person who only takes them recreationally, but it is increasingly common to find polydrug abusers who take gabapentinoids.”
Gabapentin abuse appears to be more common in Europe than in the United States, where it’s just beginning to emerge, Dr. Pergolizzi said. And the picture is more nuanced than it might first appear: Many of those who are misusing the drug are using it as a “do-it-yourself” opioid withdrawal aid, he said in an interview.
At the meeting, he presented a literature review comprising 46 papers on pregabalin abuse and 263 on gabapentin abuse. Several important themes arose from these papers, said Dr. Pergolizzi, cofounder and chief operating officer of NEMA Research Inc., Naples, Fla.:
- Gabapentin and pregabalin are being prescribed off label for numerous conditions, including bipolar disorder, neuropathic pain, diabetic neuropathy, complex regional pain syndrome, attention deficit disorder, restless leg syndrome, trigeminal neuralgia, periodic limb movement disorder of sleep, migraine, drug and alcohol withdrawal seizures, chronic low back pain, and even menopausal symptoms.
- About a one-third of users experience withdrawal symptoms with sudden discontinuation. Symptoms include disorientation, anxiety, insomnia, heart palpitations, diaphoresis, and abdominal cramps.
- Risk factors for abuse are emerging. These include opioid use disorders, mental illnesses, and a history of taking supratherapeutic doses of the drugs. Age and sex don’t seem to be a consistent risk factor for abuse.
- Abusers can obtain nonprescription gabapentinoids more easily each year, including street sales and online orders, Dr. Pergolizzi said. “A Google search conducted in July for ‘buy gabapentin without a prescription’ yielded 4.48 million results and ‘buy pregabalin without a prescription,’ 622,000. A similar search conducted in September 2017 yielded 1.19 million and 352,000 results, respectively.”
- Few urine drug assays screen for gabapentinoids, which makes them easy to conceal in random drug testing.
Reports of gabapentin-involved drug overdoses and even deaths have recently emerged in the United States, particularly in the opioid abuse-plagued Appalachian states. An article in May in Drug and Alcohol Dependence examined the prevalence of gabapentin in postmortem toxicology in drug overdose deaths in four Appalachian states in 2015 (Drug Alcohol Depend. 2018;186:80-5). Rates were 4% in eastern Tennessee, 15% in West Virginia, 20% in North Carolina, and 41% in Kentucky.
Three states have now added gabapentin to their list of Schedule V controlled substances: Kentucky in 2017, West Virginia this May, and Tennessee in July.
Ohio, Minnesota, Virginia, and Massachusetts have taken a different tack to controlling dispensing. In those states, all pharmacies, prescribers, and wholesalers must report all dispensing and sales of gabapentin to their prescription monitoring databases.
Dr. Pergolizzi disclosed financial relationships with numerous pharmaceutical companies.
LAS VEGAS – Up to 22% of opioid abusers also abuse gabapentin, taking high doses of the antiepileptic for its psychoactive effects, or to potentiate the effect of opioids.
The drug – the 10th most commonly prescribed in the United States – is increasingly implicated in overdose deaths. In response, several states have recently reclassified the antiepileptic as a Schedule V controlled substance. Other states have declined to go that far, but have added gabapentin (Neurontin and others) to the drugs that must be reported to state prescription monitoring programs.
“Gabapentin and pregabalin [Lyrica] are versatile and important drugs that are widely prescribed and used off label for a number of conditions from seizure disorder to fibromyalgia,” said Joseph Pergolizzi Jr., MD, who discussed the issue during the annual PAINWeek. “Abuse patterns differ somewhat from abuse patterns with prescription opioids. People who misuse gabapentinoids tend to already use other drugs inappropriately. It’s rare to find a person who only takes them recreationally, but it is increasingly common to find polydrug abusers who take gabapentinoids.”
Gabapentin abuse appears to be more common in Europe than in the United States, where it’s just beginning to emerge, Dr. Pergolizzi said. And the picture is more nuanced than it might first appear: Many of those who are misusing the drug are using it as a “do-it-yourself” opioid withdrawal aid, he said in an interview.
At the meeting, he presented a literature review comprising 46 papers on pregabalin abuse and 263 on gabapentin abuse. Several important themes arose from these papers, said Dr. Pergolizzi, cofounder and chief operating officer of NEMA Research Inc., Naples, Fla.:
- Gabapentin and pregabalin are being prescribed off label for numerous conditions, including bipolar disorder, neuropathic pain, diabetic neuropathy, complex regional pain syndrome, attention deficit disorder, restless leg syndrome, trigeminal neuralgia, periodic limb movement disorder of sleep, migraine, drug and alcohol withdrawal seizures, chronic low back pain, and even menopausal symptoms.
- About a one-third of users experience withdrawal symptoms with sudden discontinuation. Symptoms include disorientation, anxiety, insomnia, heart palpitations, diaphoresis, and abdominal cramps.
- Risk factors for abuse are emerging. These include opioid use disorders, mental illnesses, and a history of taking supratherapeutic doses of the drugs. Age and sex don’t seem to be a consistent risk factor for abuse.
- Abusers can obtain nonprescription gabapentinoids more easily each year, including street sales and online orders, Dr. Pergolizzi said. “A Google search conducted in July for ‘buy gabapentin without a prescription’ yielded 4.48 million results and ‘buy pregabalin without a prescription,’ 622,000. A similar search conducted in September 2017 yielded 1.19 million and 352,000 results, respectively.”
- Few urine drug assays screen for gabapentinoids, which makes them easy to conceal in random drug testing.
Reports of gabapentin-involved drug overdoses and even deaths have recently emerged in the United States, particularly in the opioid abuse-plagued Appalachian states. An article in May in Drug and Alcohol Dependence examined the prevalence of gabapentin in postmortem toxicology in drug overdose deaths in four Appalachian states in 2015 (Drug Alcohol Depend. 2018;186:80-5). Rates were 4% in eastern Tennessee, 15% in West Virginia, 20% in North Carolina, and 41% in Kentucky.
Three states have now added gabapentin to their list of Schedule V controlled substances: Kentucky in 2017, West Virginia this May, and Tennessee in July.
Ohio, Minnesota, Virginia, and Massachusetts have taken a different tack to controlling dispensing. In those states, all pharmacies, prescribers, and wholesalers must report all dispensing and sales of gabapentin to their prescription monitoring databases.
Dr. Pergolizzi disclosed financial relationships with numerous pharmaceutical companies.
REPORTING FROM PAINWEEK 2018
Key clinical point:
Major finding: Up to 22% of opioid users are also using gabapentin.
Study details: A literature review of 46 papers on pregabalin abuse and 263 on gabapentin abuse.
Disclosures: Dr. Pergolizzi disclosed financial relationships with numerous pharmaceutical companies.
Source: Pergolizzi J et al. PAINWeek 2018, Poster 55.
Reviving rural health care
Hospitalists have an important role to play
Health care in the United States has seen tremendous change in the last 2-3 decades, stemming from a dramatic push to contain spending, a call to action to improve quality and safety, and a boom in technology and medical advancement.
While the specialty of hospital medicine in the United States matured in response to these calls to action, it mostly flourished amidst – and as a result of – market consolidation, cost containment, the rise in the underinsured, and the flight of primary care from hospitals.
Changes in the health care industry have paralleled other parts of our society. Health care organizations, like schools, churches, theaters, parks, and sports teams, are part of the social fabric of communities. They provide stability to communities as employers, educators, social supporters, and the provision of services. It is no wonder then, that smaller communities, rural areas in particular, flourish or wither when one or more of these institutions, especially health care, fail them.
Health disparities result from any number of factors but particularly when communities are destabilized. The Robert Wood Johnson Foundation has studied this across the United States. For example, in the Twin Cities of Minneapolis–St. Paul, Minn., where I live, life expectancy varies by over 10 years along the interstate highway that runs through the metro area. Similarly, this disparity is seen between urban and rural Kentucky.
To be sure, the confounding social determinants of health and the mitigating strategies for the communities are different in urban Minneapolis than in Wolfe County, Kentucky. However, much of the work around health care reform (and therefore, hospital medicine) has centered around urban populations such as Minneapolis rather than rural populations such as Wolfe County. While 80% of the U.S. population lives in urban centers, that still means that 1 in 5 people live in rural America – spread across 97% of the U.S. land mass. These rural populations are exceedingly diverse, and warrant exceedingly diverse solutions.
Eighteen years ago, when I started my career in hospital medicine, I would never have thought I would be a spokesman for rural care. I identified as an urban academic hospitalist at a safety net hospital known for serving the urban poor and diverse refugee populations. But I had not anticipated mergers involving urban and rural hospitals, nor our resulting responsibility for staffing several critical access hospitals in another state.
It was hard in the beginning to recruit hospitalists to rural areas, so I worked in those areas myself, and experienced the rich practice in nonurban centers. As our partners also joined in our efforts to staff these hospitals, they had similar experiences. Now we can’t keep physicians away. That is not to say that the challenges are over.
Since 2010, 26 states lost rural hospitals – over 80 hospitals in total. High premiums in the individual health insurance market have driven healthy people out of risk pools, pushed payers out of the market, driving premiums higher still, resulting in coverage deserts. Consolidation and alignment with urban and national health care organizations initially brought hope to cash-strapped rural hospitals. Instead of improving local access, however, referrals to urban centers drained rural hospitals of their sources of income.
Economic instability has further destabilized communities. Rural America is exceptionally diverse, and has higher rates of poverty and the working poor, a shrinking job market that still hasn’t recovered from the 2008 recession, and higher rates of disability when compared to urban America. Do I even need to mention the rural opioid epidemic? Or the rural physician crisis, with a dwindling 12% of primary care and 8% of specialty care in these communities?
There is hope. During a late-night text conversation with a millennial nocturnist who splits his time between large and small hospitals, I received this message at 11:42 p.m.: “I think I feel more appreciated/valued/respected out here. You know how it is at the smaller hospitals.”
This was a comment the young hospitalist made after he shared with me that, lately, he had been in a “funk.” Innovations such as telemedicine have brought balance to overworked rural family doctors and excitement to young, tech savvy hospitalists. Opportunities to educate rural nurses and increase the level of care, keeping patients local, have excited academic hospitalists and rural CFOs alike. For a physician in a high burnout specialty, a long peaceful drive through the country might be just what’s needed to encourage a few moments of mindfulness.
Many of our urban health systems have combined with rural ones. It’s time to embrace it. Ignoring the health disparities in rural America divides us and diminishes essential parts of our health care system. Calling the hospitals our patients are referred from “OSH” (Outside Hospitals) will only perpetuate that.
Hospitalists have an opportunity to play an important role in stabilizing rural communities, reviving rural health systems, and providing local access to health care. Let’s embrace this opportunity to make a lasting impact on this frontier in hospital medicine.
Dr. Siy is chair of the department of hospital medicine at HealthPartners in Minneapolis–St. Paul, Minn., and a member of the SHM board of directors.
Hospitalists have an important role to play
Hospitalists have an important role to play
Health care in the United States has seen tremendous change in the last 2-3 decades, stemming from a dramatic push to contain spending, a call to action to improve quality and safety, and a boom in technology and medical advancement.
While the specialty of hospital medicine in the United States matured in response to these calls to action, it mostly flourished amidst – and as a result of – market consolidation, cost containment, the rise in the underinsured, and the flight of primary care from hospitals.
Changes in the health care industry have paralleled other parts of our society. Health care organizations, like schools, churches, theaters, parks, and sports teams, are part of the social fabric of communities. They provide stability to communities as employers, educators, social supporters, and the provision of services. It is no wonder then, that smaller communities, rural areas in particular, flourish or wither when one or more of these institutions, especially health care, fail them.
Health disparities result from any number of factors but particularly when communities are destabilized. The Robert Wood Johnson Foundation has studied this across the United States. For example, in the Twin Cities of Minneapolis–St. Paul, Minn., where I live, life expectancy varies by over 10 years along the interstate highway that runs through the metro area. Similarly, this disparity is seen between urban and rural Kentucky.
To be sure, the confounding social determinants of health and the mitigating strategies for the communities are different in urban Minneapolis than in Wolfe County, Kentucky. However, much of the work around health care reform (and therefore, hospital medicine) has centered around urban populations such as Minneapolis rather than rural populations such as Wolfe County. While 80% of the U.S. population lives in urban centers, that still means that 1 in 5 people live in rural America – spread across 97% of the U.S. land mass. These rural populations are exceedingly diverse, and warrant exceedingly diverse solutions.
Eighteen years ago, when I started my career in hospital medicine, I would never have thought I would be a spokesman for rural care. I identified as an urban academic hospitalist at a safety net hospital known for serving the urban poor and diverse refugee populations. But I had not anticipated mergers involving urban and rural hospitals, nor our resulting responsibility for staffing several critical access hospitals in another state.
It was hard in the beginning to recruit hospitalists to rural areas, so I worked in those areas myself, and experienced the rich practice in nonurban centers. As our partners also joined in our efforts to staff these hospitals, they had similar experiences. Now we can’t keep physicians away. That is not to say that the challenges are over.
Since 2010, 26 states lost rural hospitals – over 80 hospitals in total. High premiums in the individual health insurance market have driven healthy people out of risk pools, pushed payers out of the market, driving premiums higher still, resulting in coverage deserts. Consolidation and alignment with urban and national health care organizations initially brought hope to cash-strapped rural hospitals. Instead of improving local access, however, referrals to urban centers drained rural hospitals of their sources of income.
Economic instability has further destabilized communities. Rural America is exceptionally diverse, and has higher rates of poverty and the working poor, a shrinking job market that still hasn’t recovered from the 2008 recession, and higher rates of disability when compared to urban America. Do I even need to mention the rural opioid epidemic? Or the rural physician crisis, with a dwindling 12% of primary care and 8% of specialty care in these communities?
There is hope. During a late-night text conversation with a millennial nocturnist who splits his time between large and small hospitals, I received this message at 11:42 p.m.: “I think I feel more appreciated/valued/respected out here. You know how it is at the smaller hospitals.”
This was a comment the young hospitalist made after he shared with me that, lately, he had been in a “funk.” Innovations such as telemedicine have brought balance to overworked rural family doctors and excitement to young, tech savvy hospitalists. Opportunities to educate rural nurses and increase the level of care, keeping patients local, have excited academic hospitalists and rural CFOs alike. For a physician in a high burnout specialty, a long peaceful drive through the country might be just what’s needed to encourage a few moments of mindfulness.
Many of our urban health systems have combined with rural ones. It’s time to embrace it. Ignoring the health disparities in rural America divides us and diminishes essential parts of our health care system. Calling the hospitals our patients are referred from “OSH” (Outside Hospitals) will only perpetuate that.
Hospitalists have an opportunity to play an important role in stabilizing rural communities, reviving rural health systems, and providing local access to health care. Let’s embrace this opportunity to make a lasting impact on this frontier in hospital medicine.
Dr. Siy is chair of the department of hospital medicine at HealthPartners in Minneapolis–St. Paul, Minn., and a member of the SHM board of directors.
Health care in the United States has seen tremendous change in the last 2-3 decades, stemming from a dramatic push to contain spending, a call to action to improve quality and safety, and a boom in technology and medical advancement.
While the specialty of hospital medicine in the United States matured in response to these calls to action, it mostly flourished amidst – and as a result of – market consolidation, cost containment, the rise in the underinsured, and the flight of primary care from hospitals.
Changes in the health care industry have paralleled other parts of our society. Health care organizations, like schools, churches, theaters, parks, and sports teams, are part of the social fabric of communities. They provide stability to communities as employers, educators, social supporters, and the provision of services. It is no wonder then, that smaller communities, rural areas in particular, flourish or wither when one or more of these institutions, especially health care, fail them.
Health disparities result from any number of factors but particularly when communities are destabilized. The Robert Wood Johnson Foundation has studied this across the United States. For example, in the Twin Cities of Minneapolis–St. Paul, Minn., where I live, life expectancy varies by over 10 years along the interstate highway that runs through the metro area. Similarly, this disparity is seen between urban and rural Kentucky.
To be sure, the confounding social determinants of health and the mitigating strategies for the communities are different in urban Minneapolis than in Wolfe County, Kentucky. However, much of the work around health care reform (and therefore, hospital medicine) has centered around urban populations such as Minneapolis rather than rural populations such as Wolfe County. While 80% of the U.S. population lives in urban centers, that still means that 1 in 5 people live in rural America – spread across 97% of the U.S. land mass. These rural populations are exceedingly diverse, and warrant exceedingly diverse solutions.
Eighteen years ago, when I started my career in hospital medicine, I would never have thought I would be a spokesman for rural care. I identified as an urban academic hospitalist at a safety net hospital known for serving the urban poor and diverse refugee populations. But I had not anticipated mergers involving urban and rural hospitals, nor our resulting responsibility for staffing several critical access hospitals in another state.
It was hard in the beginning to recruit hospitalists to rural areas, so I worked in those areas myself, and experienced the rich practice in nonurban centers. As our partners also joined in our efforts to staff these hospitals, they had similar experiences. Now we can’t keep physicians away. That is not to say that the challenges are over.
Since 2010, 26 states lost rural hospitals – over 80 hospitals in total. High premiums in the individual health insurance market have driven healthy people out of risk pools, pushed payers out of the market, driving premiums higher still, resulting in coverage deserts. Consolidation and alignment with urban and national health care organizations initially brought hope to cash-strapped rural hospitals. Instead of improving local access, however, referrals to urban centers drained rural hospitals of their sources of income.
Economic instability has further destabilized communities. Rural America is exceptionally diverse, and has higher rates of poverty and the working poor, a shrinking job market that still hasn’t recovered from the 2008 recession, and higher rates of disability when compared to urban America. Do I even need to mention the rural opioid epidemic? Or the rural physician crisis, with a dwindling 12% of primary care and 8% of specialty care in these communities?
There is hope. During a late-night text conversation with a millennial nocturnist who splits his time between large and small hospitals, I received this message at 11:42 p.m.: “I think I feel more appreciated/valued/respected out here. You know how it is at the smaller hospitals.”
This was a comment the young hospitalist made after he shared with me that, lately, he had been in a “funk.” Innovations such as telemedicine have brought balance to overworked rural family doctors and excitement to young, tech savvy hospitalists. Opportunities to educate rural nurses and increase the level of care, keeping patients local, have excited academic hospitalists and rural CFOs alike. For a physician in a high burnout specialty, a long peaceful drive through the country might be just what’s needed to encourage a few moments of mindfulness.
Many of our urban health systems have combined with rural ones. It’s time to embrace it. Ignoring the health disparities in rural America divides us and diminishes essential parts of our health care system. Calling the hospitals our patients are referred from “OSH” (Outside Hospitals) will only perpetuate that.
Hospitalists have an opportunity to play an important role in stabilizing rural communities, reviving rural health systems, and providing local access to health care. Let’s embrace this opportunity to make a lasting impact on this frontier in hospital medicine.
Dr. Siy is chair of the department of hospital medicine at HealthPartners in Minneapolis–St. Paul, Minn., and a member of the SHM board of directors.