User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Transporting stroke patients directly to thrombectomy boosts outcomes
LOS ANGELES – Evidence continues to mount that in the new era of thrombectomy treatment for selected acute ischemic stroke patients outcomes are better when patients go directly to the closest comprehensive stroke center that offers intravascular procedures rather than first being taken to a closer hospital and then needing transfer.
Nils H. Mueller-Kronast, MD, presented a modeled analysis of data collected in a registry on 236 real-world U.S. patients who underwent mechanical thrombectomy for an acute, large-vessel occlusion stroke following transfer from a hospital that could perform thrombolysis but couldn’t offer thrombectomy. The analysis showed that if the patients had instead gone directly to the closest thrombectomy center the result would have been a 16-percentage-point increase in patients with a modified Rankin Scale (mRS) score of 0-1 after 90 days, and a 9-percentage-point increase in mRS 0-2 outcomes, Dr. Mueller-Kronast said at the International Stroke Conference, sponsored by the American Heart Association.
The analysis he presented used data from the Systematic Evaluation of Patients Treated With Stroke Devices for Acute Ischemic Stroke (STRATIS) registry, which included 984 acute ischemic stroke patients who underwent mechanical thrombectomy at any one of 55 participating U.S. sites (Stroke. 2017 Oct;48[10]:2760-8). A previously-reported analysis of the STRATIS data showed that the 55% of patients taken directly to a center that performed thrombectomy had a 60% rate of mRS score 0-2 after 90 days, compared with 52% of patients taken first to a hospital unable to perform thrombectomy and then transferred (Circulation. 2017 Dec 12;136[24]:2311-21).
The current analysis focused on 236 of the transferred patients with complete information on their location at the time of their stroke and subsequent time intervals during their transport and treatment, including 117 patients with ground transfer from their first hospital to the thrombectomy site, 114 with air transfer, and 5 with an unreported means of transport.
Dr. Mueller-Kronast and his associates calculated the time it would have taken each of the 117 ground transported patients to have gone directly to the closest thrombectomy center (adjusted by traffic conditions at the time of the stroke), and modeled the likely outcomes of these patients based on the data collected in the registry. This projected a 47% rate of mRS scores 0-1 (good outcomes) after 90 days, and a 60% rate of mRS 0-2 scores with a direct-to-thrombectomy strategy, compared with actual rates of 31% and 51%, respectively, among the patients who were transferred from their initial hospital.
“Bypass to an endovascular-capable center may be an option to improve rapid access to mechanical thrombectomy,” he concluded.
The STRATIS registry is sponsored by Medtronic. Dr. Mueller-Kronast has been a consultant to Medtronic.
SOURCE: Mueller-Kronast N et al. Abstract LB12.
LOS ANGELES – Evidence continues to mount that in the new era of thrombectomy treatment for selected acute ischemic stroke patients outcomes are better when patients go directly to the closest comprehensive stroke center that offers intravascular procedures rather than first being taken to a closer hospital and then needing transfer.
Nils H. Mueller-Kronast, MD, presented a modeled analysis of data collected in a registry on 236 real-world U.S. patients who underwent mechanical thrombectomy for an acute, large-vessel occlusion stroke following transfer from a hospital that could perform thrombolysis but couldn’t offer thrombectomy. The analysis showed that if the patients had instead gone directly to the closest thrombectomy center the result would have been a 16-percentage-point increase in patients with a modified Rankin Scale (mRS) score of 0-1 after 90 days, and a 9-percentage-point increase in mRS 0-2 outcomes, Dr. Mueller-Kronast said at the International Stroke Conference, sponsored by the American Heart Association.
The analysis he presented used data from the Systematic Evaluation of Patients Treated With Stroke Devices for Acute Ischemic Stroke (STRATIS) registry, which included 984 acute ischemic stroke patients who underwent mechanical thrombectomy at any one of 55 participating U.S. sites (Stroke. 2017 Oct;48[10]:2760-8). A previously-reported analysis of the STRATIS data showed that the 55% of patients taken directly to a center that performed thrombectomy had a 60% rate of mRS score 0-2 after 90 days, compared with 52% of patients taken first to a hospital unable to perform thrombectomy and then transferred (Circulation. 2017 Dec 12;136[24]:2311-21).
The current analysis focused on 236 of the transferred patients with complete information on their location at the time of their stroke and subsequent time intervals during their transport and treatment, including 117 patients with ground transfer from their first hospital to the thrombectomy site, 114 with air transfer, and 5 with an unreported means of transport.
Dr. Mueller-Kronast and his associates calculated the time it would have taken each of the 117 ground transported patients to have gone directly to the closest thrombectomy center (adjusted by traffic conditions at the time of the stroke), and modeled the likely outcomes of these patients based on the data collected in the registry. This projected a 47% rate of mRS scores 0-1 (good outcomes) after 90 days, and a 60% rate of mRS 0-2 scores with a direct-to-thrombectomy strategy, compared with actual rates of 31% and 51%, respectively, among the patients who were transferred from their initial hospital.
“Bypass to an endovascular-capable center may be an option to improve rapid access to mechanical thrombectomy,” he concluded.
The STRATIS registry is sponsored by Medtronic. Dr. Mueller-Kronast has been a consultant to Medtronic.
SOURCE: Mueller-Kronast N et al. Abstract LB12.
LOS ANGELES – Evidence continues to mount that in the new era of thrombectomy treatment for selected acute ischemic stroke patients outcomes are better when patients go directly to the closest comprehensive stroke center that offers intravascular procedures rather than first being taken to a closer hospital and then needing transfer.
Nils H. Mueller-Kronast, MD, presented a modeled analysis of data collected in a registry on 236 real-world U.S. patients who underwent mechanical thrombectomy for an acute, large-vessel occlusion stroke following transfer from a hospital that could perform thrombolysis but couldn’t offer thrombectomy. The analysis showed that if the patients had instead gone directly to the closest thrombectomy center the result would have been a 16-percentage-point increase in patients with a modified Rankin Scale (mRS) score of 0-1 after 90 days, and a 9-percentage-point increase in mRS 0-2 outcomes, Dr. Mueller-Kronast said at the International Stroke Conference, sponsored by the American Heart Association.
The analysis he presented used data from the Systematic Evaluation of Patients Treated With Stroke Devices for Acute Ischemic Stroke (STRATIS) registry, which included 984 acute ischemic stroke patients who underwent mechanical thrombectomy at any one of 55 participating U.S. sites (Stroke. 2017 Oct;48[10]:2760-8). A previously-reported analysis of the STRATIS data showed that the 55% of patients taken directly to a center that performed thrombectomy had a 60% rate of mRS score 0-2 after 90 days, compared with 52% of patients taken first to a hospital unable to perform thrombectomy and then transferred (Circulation. 2017 Dec 12;136[24]:2311-21).
The current analysis focused on 236 of the transferred patients with complete information on their location at the time of their stroke and subsequent time intervals during their transport and treatment, including 117 patients with ground transfer from their first hospital to the thrombectomy site, 114 with air transfer, and 5 with an unreported means of transport.
Dr. Mueller-Kronast and his associates calculated the time it would have taken each of the 117 ground transported patients to have gone directly to the closest thrombectomy center (adjusted by traffic conditions at the time of the stroke), and modeled the likely outcomes of these patients based on the data collected in the registry. This projected a 47% rate of mRS scores 0-1 (good outcomes) after 90 days, and a 60% rate of mRS 0-2 scores with a direct-to-thrombectomy strategy, compared with actual rates of 31% and 51%, respectively, among the patients who were transferred from their initial hospital.
“Bypass to an endovascular-capable center may be an option to improve rapid access to mechanical thrombectomy,” he concluded.
The STRATIS registry is sponsored by Medtronic. Dr. Mueller-Kronast has been a consultant to Medtronic.
SOURCE: Mueller-Kronast N et al. Abstract LB12.
REPORTING FROM ISC 2018
Key clinical point: A direct-to-thrombectomy strategy maximizes good stroke outcomes.
Major finding: Modeling showed a 47% rate of good 90-day outcomes by taking patients to the closest thrombectomy center, compared with an actual 31% rate with transfers.
Study details: A simulation-model analysis of data collected by the STRATIS registry of acute stroke thrombectomies.
Disclosures: The STRATIS registry is sponsored by Medtronic. Dr. Mueller-Kronast has been a consultant to Medtronic.
Source: Mueller-Kronast N et al. Abstract LB12.
VIDEO: Dabigatran effective for myocardial injury after noncardiac surgery
ORLANDO – Treating patients who developed myocardial injury after noncardiac surgery with the anticoagulant dabigatran significantly cut the rate of subsequent major vascular complications in a randomized, multicenter trial with 1,754 patients, a result that gives surgeons and physicians the first evidence-based intervention for treating a common postsurgical condition.
“Because we have not systematically followed noncardiac surgery patients, it’s easy to presume that everyone is okay, but all the epidemiology data show that these patients [who develop myocardial injury after noncardiac surgery] don’t do okay. We need to be aggressive with secondary prophylaxis,” P.J. Devereaux, MD, said at the annual meeting of the American College of Cardiology. “The unfortunate thing is that right now, we don’t do much for these patients,” said Dr. Devereaux, professor of medicine and director of cardiology at McMaster University in Hamilton, Ont.
Results from prior epidemiology studies have shown that, among the roughly 200 million patients who undergo noncardiac surgery worldwide each year, 8% will develop MINS (myocardial injury after noncardiac surgery) (Anesthesiology. 2014 March;120[3]:564-78). The myocardial injury that defines MINS is identified by either an overt MI that meets the universal definition, or an otherwise unexplained rise in serum troponin levels from baseline in the first couple of days after surgery. In the new study, Dr. Devereaux and his associates identified 80% of MINS by a troponin rise and 20% by a diagnosed MI.
The challenge in diagnosing MINS and then administering dabigatran will be implementation of this strategy into routine practice, commented Erin A. Bohula May, MD, a cardiologist at Brigham and Women’s Hospital in Boston. “The problem is, troponin is not routinely measured in postoperative patients. It will be hard to change practice,” she noted.
Dr. Devereaux agreed that a significant barrier is convincing clinicians, especially surgeons, to routinely measure a patient’s troponin levels just before and immediately after surgery. “People are lulled into a false sense of security because patients [who develop MINS] usually don’t have chest pain,” he said in a video interview. “When we first showed that patients with MINS have bad outcomes, that convinced some [surgeons] to measure troponin after surgery. “Showing we can do something about it” is another important step toward fostering more awareness of and interest in diagnosing and treating MINS.
The Management of Myocardial Injury After Noncardiac Surgery Trial (MANAGE) enrolled 1,754 patients at 82 centers in 19 countries. Researchers randomized patients to treatment with either 110 mg dabigatran b.i.d. or placebo. A majority of patients in both arms also received aspirin and a statin, treatments that Dr. Devereaux should be used along with dabigatran in routine practice, based on observational findings, although the efficacy of these drugs for MINS patients has not been tested in randomized studies. The study’s primary endpoint was the incidence of major vascular complications, a composite that included vascular mortality, nonfatal MI, nonfatal and nonhemorrhagic stroke, peripheral arterial thrombosis, amputation, or symptomatic venous thromboembolism.
After an average follow-up of 16 months, the primary endpoint occurred in 11% of the dabigatran-treated patients and in 15% of controls, which represented a 28% risk reduction that was statistically significant. The study’s primary safety endpoint was a composite of life-threatening, major, and critical organ bleeds, which occurred in 3% of the dabigatran-treated patients and in 4% of controls, a nonsignificant difference. The dabigatran-treated patients showed a significant excess of both minor bleeds – 15% compared with 10% in controls – and “nonsignificant” lower gastrointestinal bleeds, 4% with dabigatran and 1% in the controls. The dabigatran-treated patients also had a significantly higher incidence of dyspepsia.
MANAGE was funded by the Population Health Research Institute and had no commercial funding. Dr. Devereaux has received research support from Abbott Diagnostics, Boehringer Ingelheim, Philips Healthcare, and Roche Diagnostics. Dr. May has been a consultant to Daiichi Sankyo, Merck, and Servier and has received research funding from Eisai.
SOURCE: Devereaux P et al. ACC 18.
Dr. Devereaux and his associates are to be congratulated on identifying a new disease entity, MINS (myocardial injury after noncardiac surgery), and now giving us a way to treat it. MINS is extremely common and quite morbid, and there had never before been a trial that studied its treatment. Identifying patients with MINS is extremely important. These are very-high-risk patients, and they are very hard to find. The results from MANAGE give us a way to do something about MINS and an opportunity to improve patient outcomes.
Pamela S. Douglas, MD , is a cardiologist and professor of medicine at Duke University in Durham, N.C. She had no disclosures. She made these comments as a discussant for MANAGE and in an interview.
Dr. Devereaux and his associates are to be congratulated on identifying a new disease entity, MINS (myocardial injury after noncardiac surgery), and now giving us a way to treat it. MINS is extremely common and quite morbid, and there had never before been a trial that studied its treatment. Identifying patients with MINS is extremely important. These are very-high-risk patients, and they are very hard to find. The results from MANAGE give us a way to do something about MINS and an opportunity to improve patient outcomes.
Pamela S. Douglas, MD , is a cardiologist and professor of medicine at Duke University in Durham, N.C. She had no disclosures. She made these comments as a discussant for MANAGE and in an interview.
Dr. Devereaux and his associates are to be congratulated on identifying a new disease entity, MINS (myocardial injury after noncardiac surgery), and now giving us a way to treat it. MINS is extremely common and quite morbid, and there had never before been a trial that studied its treatment. Identifying patients with MINS is extremely important. These are very-high-risk patients, and they are very hard to find. The results from MANAGE give us a way to do something about MINS and an opportunity to improve patient outcomes.
Pamela S. Douglas, MD , is a cardiologist and professor of medicine at Duke University in Durham, N.C. She had no disclosures. She made these comments as a discussant for MANAGE and in an interview.
ORLANDO – Treating patients who developed myocardial injury after noncardiac surgery with the anticoagulant dabigatran significantly cut the rate of subsequent major vascular complications in a randomized, multicenter trial with 1,754 patients, a result that gives surgeons and physicians the first evidence-based intervention for treating a common postsurgical condition.
“Because we have not systematically followed noncardiac surgery patients, it’s easy to presume that everyone is okay, but all the epidemiology data show that these patients [who develop myocardial injury after noncardiac surgery] don’t do okay. We need to be aggressive with secondary prophylaxis,” P.J. Devereaux, MD, said at the annual meeting of the American College of Cardiology. “The unfortunate thing is that right now, we don’t do much for these patients,” said Dr. Devereaux, professor of medicine and director of cardiology at McMaster University in Hamilton, Ont.
Results from prior epidemiology studies have shown that, among the roughly 200 million patients who undergo noncardiac surgery worldwide each year, 8% will develop MINS (myocardial injury after noncardiac surgery) (Anesthesiology. 2014 March;120[3]:564-78). The myocardial injury that defines MINS is identified by either an overt MI that meets the universal definition, or an otherwise unexplained rise in serum troponin levels from baseline in the first couple of days after surgery. In the new study, Dr. Devereaux and his associates identified 80% of MINS by a troponin rise and 20% by a diagnosed MI.
The challenge in diagnosing MINS and then administering dabigatran will be implementation of this strategy into routine practice, commented Erin A. Bohula May, MD, a cardiologist at Brigham and Women’s Hospital in Boston. “The problem is, troponin is not routinely measured in postoperative patients. It will be hard to change practice,” she noted.
Dr. Devereaux agreed that a significant barrier is convincing clinicians, especially surgeons, to routinely measure a patient’s troponin levels just before and immediately after surgery. “People are lulled into a false sense of security because patients [who develop MINS] usually don’t have chest pain,” he said in a video interview. “When we first showed that patients with MINS have bad outcomes, that convinced some [surgeons] to measure troponin after surgery. “Showing we can do something about it” is another important step toward fostering more awareness of and interest in diagnosing and treating MINS.
The Management of Myocardial Injury After Noncardiac Surgery Trial (MANAGE) enrolled 1,754 patients at 82 centers in 19 countries. Researchers randomized patients to treatment with either 110 mg dabigatran b.i.d. or placebo. A majority of patients in both arms also received aspirin and a statin, treatments that Dr. Devereaux should be used along with dabigatran in routine practice, based on observational findings, although the efficacy of these drugs for MINS patients has not been tested in randomized studies. The study’s primary endpoint was the incidence of major vascular complications, a composite that included vascular mortality, nonfatal MI, nonfatal and nonhemorrhagic stroke, peripheral arterial thrombosis, amputation, or symptomatic venous thromboembolism.
After an average follow-up of 16 months, the primary endpoint occurred in 11% of the dabigatran-treated patients and in 15% of controls, which represented a 28% risk reduction that was statistically significant. The study’s primary safety endpoint was a composite of life-threatening, major, and critical organ bleeds, which occurred in 3% of the dabigatran-treated patients and in 4% of controls, a nonsignificant difference. The dabigatran-treated patients showed a significant excess of both minor bleeds – 15% compared with 10% in controls – and “nonsignificant” lower gastrointestinal bleeds, 4% with dabigatran and 1% in the controls. The dabigatran-treated patients also had a significantly higher incidence of dyspepsia.
MANAGE was funded by the Population Health Research Institute and had no commercial funding. Dr. Devereaux has received research support from Abbott Diagnostics, Boehringer Ingelheim, Philips Healthcare, and Roche Diagnostics. Dr. May has been a consultant to Daiichi Sankyo, Merck, and Servier and has received research funding from Eisai.
SOURCE: Devereaux P et al. ACC 18.
ORLANDO – Treating patients who developed myocardial injury after noncardiac surgery with the anticoagulant dabigatran significantly cut the rate of subsequent major vascular complications in a randomized, multicenter trial with 1,754 patients, a result that gives surgeons and physicians the first evidence-based intervention for treating a common postsurgical condition.
“Because we have not systematically followed noncardiac surgery patients, it’s easy to presume that everyone is okay, but all the epidemiology data show that these patients [who develop myocardial injury after noncardiac surgery] don’t do okay. We need to be aggressive with secondary prophylaxis,” P.J. Devereaux, MD, said at the annual meeting of the American College of Cardiology. “The unfortunate thing is that right now, we don’t do much for these patients,” said Dr. Devereaux, professor of medicine and director of cardiology at McMaster University in Hamilton, Ont.
Results from prior epidemiology studies have shown that, among the roughly 200 million patients who undergo noncardiac surgery worldwide each year, 8% will develop MINS (myocardial injury after noncardiac surgery) (Anesthesiology. 2014 March;120[3]:564-78). The myocardial injury that defines MINS is identified by either an overt MI that meets the universal definition, or an otherwise unexplained rise in serum troponin levels from baseline in the first couple of days after surgery. In the new study, Dr. Devereaux and his associates identified 80% of MINS by a troponin rise and 20% by a diagnosed MI.
The challenge in diagnosing MINS and then administering dabigatran will be implementation of this strategy into routine practice, commented Erin A. Bohula May, MD, a cardiologist at Brigham and Women’s Hospital in Boston. “The problem is, troponin is not routinely measured in postoperative patients. It will be hard to change practice,” she noted.
Dr. Devereaux agreed that a significant barrier is convincing clinicians, especially surgeons, to routinely measure a patient’s troponin levels just before and immediately after surgery. “People are lulled into a false sense of security because patients [who develop MINS] usually don’t have chest pain,” he said in a video interview. “When we first showed that patients with MINS have bad outcomes, that convinced some [surgeons] to measure troponin after surgery. “Showing we can do something about it” is another important step toward fostering more awareness of and interest in diagnosing and treating MINS.
The Management of Myocardial Injury After Noncardiac Surgery Trial (MANAGE) enrolled 1,754 patients at 82 centers in 19 countries. Researchers randomized patients to treatment with either 110 mg dabigatran b.i.d. or placebo. A majority of patients in both arms also received aspirin and a statin, treatments that Dr. Devereaux should be used along with dabigatran in routine practice, based on observational findings, although the efficacy of these drugs for MINS patients has not been tested in randomized studies. The study’s primary endpoint was the incidence of major vascular complications, a composite that included vascular mortality, nonfatal MI, nonfatal and nonhemorrhagic stroke, peripheral arterial thrombosis, amputation, or symptomatic venous thromboembolism.
After an average follow-up of 16 months, the primary endpoint occurred in 11% of the dabigatran-treated patients and in 15% of controls, which represented a 28% risk reduction that was statistically significant. The study’s primary safety endpoint was a composite of life-threatening, major, and critical organ bleeds, which occurred in 3% of the dabigatran-treated patients and in 4% of controls, a nonsignificant difference. The dabigatran-treated patients showed a significant excess of both minor bleeds – 15% compared with 10% in controls – and “nonsignificant” lower gastrointestinal bleeds, 4% with dabigatran and 1% in the controls. The dabigatran-treated patients also had a significantly higher incidence of dyspepsia.
MANAGE was funded by the Population Health Research Institute and had no commercial funding. Dr. Devereaux has received research support from Abbott Diagnostics, Boehringer Ingelheim, Philips Healthcare, and Roche Diagnostics. Dr. May has been a consultant to Daiichi Sankyo, Merck, and Servier and has received research funding from Eisai.
SOURCE: Devereaux P et al. ACC 18.
REPORTING FROM ACC 18
Key clinical point: Dabigatran is the first intervention proven to benefit patients with MINS.
Major finding: Major vascular complications occurred in 11% of patients on dabigatran and 15% on placebo.
Study details: MANAGE, a multicenter, randomized trial with 1,754 patients.
Disclosures: MANAGE was funded by the Population Health Research Institute and had no commercial funding. Dr. Devereaux has received research support from Abbott Diagnostics, Boehringer Ingelheim, Philips Healthcare, and Roche Diagnostics. Dr. May has been a consultant to Daiichi Sankyo, Merck, and Servier and has received research funding from Eisai.
Source: Devereaux P et al. ACC 18.
Teleconference is effective in assessing penicillin allergy
ORLANDO – and resulted in almost every patient having their allergy label removed, researchers reported.
In what the researchers said was the first study showing the utility of telemedicine in evaluating patient-reported penicillin allergies, allergy and immunology physicians did a secure telemedicine consultation with patients after they underwent penicillin skin testing with a physician assistant; an approach which, on average, took 123 minutes fewer each time than if the physician had done the consultation face-to-face. The teleconference can be done on a laptop or smartphone.
She said the approach is sensible and effective, and it is a good alternative to the traditional way of doing these tests. “What this takes out of that is the travel part. Someone else is doing the travel and the technique of testing,” added that people often are labeled in childhood after getting a rash that was thought to be related to penicillin, but actually was just a coincidence that was unrelated. Then the false allergy label is attached to them for life.
“This is so overlabeled,” Dr. Ramsey said. “Ten percent of the population thinks they’re allergic to penicillin, and 90% of them are not.”
A stark difference was found in the types of medicines administered before and after the evaluations, with aminopenicillin therapy jumping from 0 days of use to 188 days, and vancomycin – a more potent, but more costly alternative – dropping from 130 days of use to 16 days (P less than .05 for both).
Dr. Ramsey noted that, in part because of the time-consuming nature of the penicillin skin tests, they often are simply not done, so the false allergy labels are not caught, leading to pointless costs and exposure to more potent and potentially harmful forms of antibiotic therapy.
“Some hospitals don’t have allergists who will come in to do testing,” she said. “Sometimes patients are on medications that may interfere. And then a lot of times it’s just underrecognized – the implications of a penicillin allergy label. That is a very hot topic in our field and also in infectious disease.”
She hopes the telemedicine approach catches on more widely, which would help minimize the multitude of problems linked to penicillin allergy labels.
“Patients that avoid penicillin, they’re on more costly second-line antibiotics that are, in general, less effective, depending on which infection you’re talking about,” Dr. Ramsey said. “The [second-line antibiotics] have more side effects. And there’s data to show that patients with [a] penicillin allergy label have longer hospital stays, more costly hospital stays, are at risk for more resistant infections. And it breeds antimicrobial resistance in the long-term.”
Dr. Ramsey had no relevant financial disclosures.
SOURCE: Ramsey AC et al. AAAAI/WAO Joint Congress, Abstract 104.
ORLANDO – and resulted in almost every patient having their allergy label removed, researchers reported.
In what the researchers said was the first study showing the utility of telemedicine in evaluating patient-reported penicillin allergies, allergy and immunology physicians did a secure telemedicine consultation with patients after they underwent penicillin skin testing with a physician assistant; an approach which, on average, took 123 minutes fewer each time than if the physician had done the consultation face-to-face. The teleconference can be done on a laptop or smartphone.
She said the approach is sensible and effective, and it is a good alternative to the traditional way of doing these tests. “What this takes out of that is the travel part. Someone else is doing the travel and the technique of testing,” added that people often are labeled in childhood after getting a rash that was thought to be related to penicillin, but actually was just a coincidence that was unrelated. Then the false allergy label is attached to them for life.
“This is so overlabeled,” Dr. Ramsey said. “Ten percent of the population thinks they’re allergic to penicillin, and 90% of them are not.”
A stark difference was found in the types of medicines administered before and after the evaluations, with aminopenicillin therapy jumping from 0 days of use to 188 days, and vancomycin – a more potent, but more costly alternative – dropping from 130 days of use to 16 days (P less than .05 for both).
Dr. Ramsey noted that, in part because of the time-consuming nature of the penicillin skin tests, they often are simply not done, so the false allergy labels are not caught, leading to pointless costs and exposure to more potent and potentially harmful forms of antibiotic therapy.
“Some hospitals don’t have allergists who will come in to do testing,” she said. “Sometimes patients are on medications that may interfere. And then a lot of times it’s just underrecognized – the implications of a penicillin allergy label. That is a very hot topic in our field and also in infectious disease.”
She hopes the telemedicine approach catches on more widely, which would help minimize the multitude of problems linked to penicillin allergy labels.
“Patients that avoid penicillin, they’re on more costly second-line antibiotics that are, in general, less effective, depending on which infection you’re talking about,” Dr. Ramsey said. “The [second-line antibiotics] have more side effects. And there’s data to show that patients with [a] penicillin allergy label have longer hospital stays, more costly hospital stays, are at risk for more resistant infections. And it breeds antimicrobial resistance in the long-term.”
Dr. Ramsey had no relevant financial disclosures.
SOURCE: Ramsey AC et al. AAAAI/WAO Joint Congress, Abstract 104.
ORLANDO – and resulted in almost every patient having their allergy label removed, researchers reported.
In what the researchers said was the first study showing the utility of telemedicine in evaluating patient-reported penicillin allergies, allergy and immunology physicians did a secure telemedicine consultation with patients after they underwent penicillin skin testing with a physician assistant; an approach which, on average, took 123 minutes fewer each time than if the physician had done the consultation face-to-face. The teleconference can be done on a laptop or smartphone.
She said the approach is sensible and effective, and it is a good alternative to the traditional way of doing these tests. “What this takes out of that is the travel part. Someone else is doing the travel and the technique of testing,” added that people often are labeled in childhood after getting a rash that was thought to be related to penicillin, but actually was just a coincidence that was unrelated. Then the false allergy label is attached to them for life.
“This is so overlabeled,” Dr. Ramsey said. “Ten percent of the population thinks they’re allergic to penicillin, and 90% of them are not.”
A stark difference was found in the types of medicines administered before and after the evaluations, with aminopenicillin therapy jumping from 0 days of use to 188 days, and vancomycin – a more potent, but more costly alternative – dropping from 130 days of use to 16 days (P less than .05 for both).
Dr. Ramsey noted that, in part because of the time-consuming nature of the penicillin skin tests, they often are simply not done, so the false allergy labels are not caught, leading to pointless costs and exposure to more potent and potentially harmful forms of antibiotic therapy.
“Some hospitals don’t have allergists who will come in to do testing,” she said. “Sometimes patients are on medications that may interfere. And then a lot of times it’s just underrecognized – the implications of a penicillin allergy label. That is a very hot topic in our field and also in infectious disease.”
She hopes the telemedicine approach catches on more widely, which would help minimize the multitude of problems linked to penicillin allergy labels.
“Patients that avoid penicillin, they’re on more costly second-line antibiotics that are, in general, less effective, depending on which infection you’re talking about,” Dr. Ramsey said. “The [second-line antibiotics] have more side effects. And there’s data to show that patients with [a] penicillin allergy label have longer hospital stays, more costly hospital stays, are at risk for more resistant infections. And it breeds antimicrobial resistance in the long-term.”
Dr. Ramsey had no relevant financial disclosures.
SOURCE: Ramsey AC et al. AAAAI/WAO Joint Congress, Abstract 104.
REPORTING FROM AAAAI/WAO JOINT CONGRESS
Key clinical point: Teleconferencing to assess patient-reported penicillin allergies saves time and results in 9 out of 10 patients being delabeled.
Major finding: Of 50 patients prospectively assessed with this approach over a 4-month period last year, 46 were delabeled, with $23,000 in direct antibiotic cost savings, or $360 per patient.
Study details: A prospective study conducted over 4 months in 2017.
Disclosures: Dr. Ramsey had no relevant financial disclosures.
Source: Ramsey AC et al. AAAAI/WAO Joint Congress, Abstract 104.
Career development: One of many new focal points at HM 2018
Editor’s note: Each month, the Society of Hospital Medicine puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Kathleen Finn, MD, M. Phil, FACP, FHM, the inpatient associate program director of the internal medicine residency program at Massachusetts General Hospital and an assistant professor of medicine at Harvard Medical School, both in Boston. Dr. Finn has been a member of the Society of Hospital Medicine’s Annual Conference Committee for the past 8 years and is the course director for Hospital Medicine 2018 (HM18), to be held April 8-11 in Orlando.
When did you become a member of SHM, and how did you initially become involved with the Annual Conference Committee?
I became involved with the Annual Conference Committee 8 years ago because of my interest in education. Being a founding member of the SHM Boston Chapter, I gained experience planning the quarterly local chapter meetings. As a clinical educator and hospitalist, I was involved in planning conferences for faculty at my hospital. I found I really enjoyed developing educational conferences and curriculum, so when I heard about the Annual Conference Committee, I thought it would be a perfect fit.
It’s been a great experience getting to know committee members from all over the country and hearing their thoughts about the annual conference. It’s always exciting to brainstorm topic ideas and think about what would interest conference attendees.
Describe your role as course director.
My job as course director is to challenge committee members to be as creative as possible and help focus the discussion around the needs of SHM members while keeping to a schedule. I led a team of 23 amazing committee members through the planning stages for HM18 this past summer. With the help of Brittany Evans, SHM’s Education and Meetings Project Manager, and Dustin Smith, MD, FHM, the cocourse director, the committee reviewed prior conference agendas and feedback from attendees and from other SHM committees. Using that information, we discussed, brainstormed, voted on, and planned this year’s clinical content talks, workshops, and many of the specialty tracks.
What are you most looking forward to at HM18?
I am looking forward to the entire meeting! First, the location is exciting since this is our first time in Orlando. I’m curious to see what the facility is like, and I am hoping attendees use the location as a reason to bring their families and visit the theme parks. In recognition of our Orlando location, the committee got creative with titles for the conference. For example, geriatrics became “The Tale as Old as Time.” I hope some of the titles put a smile on the attendees’ faces.
I am also eagerly anticipating the nationally recognized speakers. We invited the best speakers we know from both subspecialty backgrounds and fellow hospitalists, and given the Orlando location, we tried to feature the best speakers from the Southeast. Finally, I am looking forward to the diversity of topics. The committee really thought broadly about relevant topics to today’s practicing hospitalists.
What will be new and different for attendees at HM18 in comparison to previous annual conferences?
There are many new things this year. Given the field of hospital medicine is now more than 20 years old, the committee thought it was important to focus on career development – not just for new hospitalists, but midcareer hospitalists as well. How do you make hospital medicine a lifelong, enjoyable, and engaging career? To explore and answer these questions, the Annual Conference Committee created several new tracks for HM18.
We created a Seasoning Your Career track that offers ideas on how to change your role midcareer – how to advance to a leadership position, how to use emotional intelligence to achieve success, how to prevent burnout, and, best of all, how to consider and change your hospitalist group’s work schedule, which rules our lives and our families’ lives. We also added financial planning advice to help you prepare for retirement.
Another new track at HM18 is the Career Development Workshops track, which includes a diversity of workshops meant to help build leadership skills, develop presentation/communication skills, encourage peers to give each other feedback, promote women in hospital medicine, prevent burnout, and turn ideas into clinical research. The Medical Education track also has a session on how to break into educational roles, especially if you want to expand your career into a leadership position in medical education.
In addition to Seasoning Your Career and Career Development Workshops, we have three other new tracks: Palliative Care, NP/PA, and The Great Debate. The Great Debate track uses the popular format of the perioperative debate given every year at the annual conference to tackle topics in infectious disease and pulmonary medicine. We ask very talented, opinionated, and humorous speakers to debate with each other over clinical content; it will be a great “smack down!”
Other new things for HM18 include:
- An interventional radiologist will speak about the latest procedures and when to refer your patients.
- A few surgeons will talk about managing surgical patients on your service and about decubitus ulcers.
- An oncologist will discuss the complications of the latest advanced agents on the wards.
- A rheumatologist will discuss the complications of new biologic agents.
- A rehab specialist will discuss the benefits and limitations of physical/occupational therapists and physiatrists.
- A speaker will discussing vulnerable populations, focusing on the social determinants of health, which last year’s HM17 plenary speaker Karen DeSalvo, MD, MPH, MSc raised as an important issue.
- There will be an “Updates in Addiction Medicine” lecture.
- There will be a new cardiology precourse and an expanded infectious disease precourse, which will also focus on sepsis.
How has the committee worked to ensure the course content is refreshed and current?
The reason the Annual Conference Committee is large is to ensure that there is a diversity of voices and talents from all over the country. There are both academic and community hospitalists on the committee; its members represent internal medicine, family medicine, pediatrics, and subspecialists, as well as administrators and hospitalist leaders. The annual meetings are planned over 3-4 months via weekly calls. In between calls, committee members are encouraged to discuss topics with their colleagues at home for opinions and advice.
The best ideas from the committee come from the group discussion and brainstorming. Someone mentions a topic, which leads someone else to add to it, and so on. Within the hour, we have some fantastic suggestions that the committee can run with. We also rely on input from SHM members: For example, many of the workshops’ topics are chosen from hundreds of submissions from members; speaker and content suggestions are submitted by hospitalist leaders from around the country and thereby provide insight into current topics. Combined, these offer a richness of ideas, which allows the committee to stay up to date and refresh old ideas.
What advice can you offer to early career hospitalists looking to get involved with the Annual Conference Committee or other conference planning roles?
My advice for early career hospitalists is to start locally. Join your local SHM chapter, or start one. In trying to plan local conferences, you begin to figure out which content areas interest hospitalists and how they can best be delivered. You might offer to give a talk at your local chapter or at your hospital and develop presentation skills. Developing a network of fellow hospitalists through your local chapter is important. The more local hospitalists you connect with, the more likely it is that they will think of you when they are planning a conference. At the national level, consider submitting a workshop or submitting an idea for content. Workshops are a great way to get recognized at the national level.
The Annual Conference Committee takes applications every year. Once you have some experience planning conferences or coordinating speakers, it would definitely be worth applying. You may not be selected your first year, but do not let that discourage you! Demonstrating interest and perseverance goes a long way. There are also many other national SHM committees to join and other ways to get involved. Your willingness to provide some of your time makes the society – and the specialty – what it is.
Ms. Steele is the marketing communications specialist at the Society of Hospital Medicine.
Editor’s note: Each month, the Society of Hospital Medicine puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Kathleen Finn, MD, M. Phil, FACP, FHM, the inpatient associate program director of the internal medicine residency program at Massachusetts General Hospital and an assistant professor of medicine at Harvard Medical School, both in Boston. Dr. Finn has been a member of the Society of Hospital Medicine’s Annual Conference Committee for the past 8 years and is the course director for Hospital Medicine 2018 (HM18), to be held April 8-11 in Orlando.
When did you become a member of SHM, and how did you initially become involved with the Annual Conference Committee?
I became involved with the Annual Conference Committee 8 years ago because of my interest in education. Being a founding member of the SHM Boston Chapter, I gained experience planning the quarterly local chapter meetings. As a clinical educator and hospitalist, I was involved in planning conferences for faculty at my hospital. I found I really enjoyed developing educational conferences and curriculum, so when I heard about the Annual Conference Committee, I thought it would be a perfect fit.
It’s been a great experience getting to know committee members from all over the country and hearing their thoughts about the annual conference. It’s always exciting to brainstorm topic ideas and think about what would interest conference attendees.
Describe your role as course director.
My job as course director is to challenge committee members to be as creative as possible and help focus the discussion around the needs of SHM members while keeping to a schedule. I led a team of 23 amazing committee members through the planning stages for HM18 this past summer. With the help of Brittany Evans, SHM’s Education and Meetings Project Manager, and Dustin Smith, MD, FHM, the cocourse director, the committee reviewed prior conference agendas and feedback from attendees and from other SHM committees. Using that information, we discussed, brainstormed, voted on, and planned this year’s clinical content talks, workshops, and many of the specialty tracks.
What are you most looking forward to at HM18?
I am looking forward to the entire meeting! First, the location is exciting since this is our first time in Orlando. I’m curious to see what the facility is like, and I am hoping attendees use the location as a reason to bring their families and visit the theme parks. In recognition of our Orlando location, the committee got creative with titles for the conference. For example, geriatrics became “The Tale as Old as Time.” I hope some of the titles put a smile on the attendees’ faces.
I am also eagerly anticipating the nationally recognized speakers. We invited the best speakers we know from both subspecialty backgrounds and fellow hospitalists, and given the Orlando location, we tried to feature the best speakers from the Southeast. Finally, I am looking forward to the diversity of topics. The committee really thought broadly about relevant topics to today’s practicing hospitalists.
What will be new and different for attendees at HM18 in comparison to previous annual conferences?
There are many new things this year. Given the field of hospital medicine is now more than 20 years old, the committee thought it was important to focus on career development – not just for new hospitalists, but midcareer hospitalists as well. How do you make hospital medicine a lifelong, enjoyable, and engaging career? To explore and answer these questions, the Annual Conference Committee created several new tracks for HM18.
We created a Seasoning Your Career track that offers ideas on how to change your role midcareer – how to advance to a leadership position, how to use emotional intelligence to achieve success, how to prevent burnout, and, best of all, how to consider and change your hospitalist group’s work schedule, which rules our lives and our families’ lives. We also added financial planning advice to help you prepare for retirement.
Another new track at HM18 is the Career Development Workshops track, which includes a diversity of workshops meant to help build leadership skills, develop presentation/communication skills, encourage peers to give each other feedback, promote women in hospital medicine, prevent burnout, and turn ideas into clinical research. The Medical Education track also has a session on how to break into educational roles, especially if you want to expand your career into a leadership position in medical education.
In addition to Seasoning Your Career and Career Development Workshops, we have three other new tracks: Palliative Care, NP/PA, and The Great Debate. The Great Debate track uses the popular format of the perioperative debate given every year at the annual conference to tackle topics in infectious disease and pulmonary medicine. We ask very talented, opinionated, and humorous speakers to debate with each other over clinical content; it will be a great “smack down!”
Other new things for HM18 include:
- An interventional radiologist will speak about the latest procedures and when to refer your patients.
- A few surgeons will talk about managing surgical patients on your service and about decubitus ulcers.
- An oncologist will discuss the complications of the latest advanced agents on the wards.
- A rheumatologist will discuss the complications of new biologic agents.
- A rehab specialist will discuss the benefits and limitations of physical/occupational therapists and physiatrists.
- A speaker will discussing vulnerable populations, focusing on the social determinants of health, which last year’s HM17 plenary speaker Karen DeSalvo, MD, MPH, MSc raised as an important issue.
- There will be an “Updates in Addiction Medicine” lecture.
- There will be a new cardiology precourse and an expanded infectious disease precourse, which will also focus on sepsis.
How has the committee worked to ensure the course content is refreshed and current?
The reason the Annual Conference Committee is large is to ensure that there is a diversity of voices and talents from all over the country. There are both academic and community hospitalists on the committee; its members represent internal medicine, family medicine, pediatrics, and subspecialists, as well as administrators and hospitalist leaders. The annual meetings are planned over 3-4 months via weekly calls. In between calls, committee members are encouraged to discuss topics with their colleagues at home for opinions and advice.
The best ideas from the committee come from the group discussion and brainstorming. Someone mentions a topic, which leads someone else to add to it, and so on. Within the hour, we have some fantastic suggestions that the committee can run with. We also rely on input from SHM members: For example, many of the workshops’ topics are chosen from hundreds of submissions from members; speaker and content suggestions are submitted by hospitalist leaders from around the country and thereby provide insight into current topics. Combined, these offer a richness of ideas, which allows the committee to stay up to date and refresh old ideas.
What advice can you offer to early career hospitalists looking to get involved with the Annual Conference Committee or other conference planning roles?
My advice for early career hospitalists is to start locally. Join your local SHM chapter, or start one. In trying to plan local conferences, you begin to figure out which content areas interest hospitalists and how they can best be delivered. You might offer to give a talk at your local chapter or at your hospital and develop presentation skills. Developing a network of fellow hospitalists through your local chapter is important. The more local hospitalists you connect with, the more likely it is that they will think of you when they are planning a conference. At the national level, consider submitting a workshop or submitting an idea for content. Workshops are a great way to get recognized at the national level.
The Annual Conference Committee takes applications every year. Once you have some experience planning conferences or coordinating speakers, it would definitely be worth applying. You may not be selected your first year, but do not let that discourage you! Demonstrating interest and perseverance goes a long way. There are also many other national SHM committees to join and other ways to get involved. Your willingness to provide some of your time makes the society – and the specialty – what it is.
Ms. Steele is the marketing communications specialist at the Society of Hospital Medicine.
Editor’s note: Each month, the Society of Hospital Medicine puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org for more information on how you can lend your expertise to help SHM improve the care of hospitalized patients.
This month, The Hospitalist spotlights Kathleen Finn, MD, M. Phil, FACP, FHM, the inpatient associate program director of the internal medicine residency program at Massachusetts General Hospital and an assistant professor of medicine at Harvard Medical School, both in Boston. Dr. Finn has been a member of the Society of Hospital Medicine’s Annual Conference Committee for the past 8 years and is the course director for Hospital Medicine 2018 (HM18), to be held April 8-11 in Orlando.
When did you become a member of SHM, and how did you initially become involved with the Annual Conference Committee?
I became involved with the Annual Conference Committee 8 years ago because of my interest in education. Being a founding member of the SHM Boston Chapter, I gained experience planning the quarterly local chapter meetings. As a clinical educator and hospitalist, I was involved in planning conferences for faculty at my hospital. I found I really enjoyed developing educational conferences and curriculum, so when I heard about the Annual Conference Committee, I thought it would be a perfect fit.
It’s been a great experience getting to know committee members from all over the country and hearing their thoughts about the annual conference. It’s always exciting to brainstorm topic ideas and think about what would interest conference attendees.
Describe your role as course director.
My job as course director is to challenge committee members to be as creative as possible and help focus the discussion around the needs of SHM members while keeping to a schedule. I led a team of 23 amazing committee members through the planning stages for HM18 this past summer. With the help of Brittany Evans, SHM’s Education and Meetings Project Manager, and Dustin Smith, MD, FHM, the cocourse director, the committee reviewed prior conference agendas and feedback from attendees and from other SHM committees. Using that information, we discussed, brainstormed, voted on, and planned this year’s clinical content talks, workshops, and many of the specialty tracks.
What are you most looking forward to at HM18?
I am looking forward to the entire meeting! First, the location is exciting since this is our first time in Orlando. I’m curious to see what the facility is like, and I am hoping attendees use the location as a reason to bring their families and visit the theme parks. In recognition of our Orlando location, the committee got creative with titles for the conference. For example, geriatrics became “The Tale as Old as Time.” I hope some of the titles put a smile on the attendees’ faces.
I am also eagerly anticipating the nationally recognized speakers. We invited the best speakers we know from both subspecialty backgrounds and fellow hospitalists, and given the Orlando location, we tried to feature the best speakers from the Southeast. Finally, I am looking forward to the diversity of topics. The committee really thought broadly about relevant topics to today’s practicing hospitalists.
What will be new and different for attendees at HM18 in comparison to previous annual conferences?
There are many new things this year. Given the field of hospital medicine is now more than 20 years old, the committee thought it was important to focus on career development – not just for new hospitalists, but midcareer hospitalists as well. How do you make hospital medicine a lifelong, enjoyable, and engaging career? To explore and answer these questions, the Annual Conference Committee created several new tracks for HM18.
We created a Seasoning Your Career track that offers ideas on how to change your role midcareer – how to advance to a leadership position, how to use emotional intelligence to achieve success, how to prevent burnout, and, best of all, how to consider and change your hospitalist group’s work schedule, which rules our lives and our families’ lives. We also added financial planning advice to help you prepare for retirement.
Another new track at HM18 is the Career Development Workshops track, which includes a diversity of workshops meant to help build leadership skills, develop presentation/communication skills, encourage peers to give each other feedback, promote women in hospital medicine, prevent burnout, and turn ideas into clinical research. The Medical Education track also has a session on how to break into educational roles, especially if you want to expand your career into a leadership position in medical education.
In addition to Seasoning Your Career and Career Development Workshops, we have three other new tracks: Palliative Care, NP/PA, and The Great Debate. The Great Debate track uses the popular format of the perioperative debate given every year at the annual conference to tackle topics in infectious disease and pulmonary medicine. We ask very talented, opinionated, and humorous speakers to debate with each other over clinical content; it will be a great “smack down!”
Other new things for HM18 include:
- An interventional radiologist will speak about the latest procedures and when to refer your patients.
- A few surgeons will talk about managing surgical patients on your service and about decubitus ulcers.
- An oncologist will discuss the complications of the latest advanced agents on the wards.
- A rheumatologist will discuss the complications of new biologic agents.
- A rehab specialist will discuss the benefits and limitations of physical/occupational therapists and physiatrists.
- A speaker will discussing vulnerable populations, focusing on the social determinants of health, which last year’s HM17 plenary speaker Karen DeSalvo, MD, MPH, MSc raised as an important issue.
- There will be an “Updates in Addiction Medicine” lecture.
- There will be a new cardiology precourse and an expanded infectious disease precourse, which will also focus on sepsis.
How has the committee worked to ensure the course content is refreshed and current?
The reason the Annual Conference Committee is large is to ensure that there is a diversity of voices and talents from all over the country. There are both academic and community hospitalists on the committee; its members represent internal medicine, family medicine, pediatrics, and subspecialists, as well as administrators and hospitalist leaders. The annual meetings are planned over 3-4 months via weekly calls. In between calls, committee members are encouraged to discuss topics with their colleagues at home for opinions and advice.
The best ideas from the committee come from the group discussion and brainstorming. Someone mentions a topic, which leads someone else to add to it, and so on. Within the hour, we have some fantastic suggestions that the committee can run with. We also rely on input from SHM members: For example, many of the workshops’ topics are chosen from hundreds of submissions from members; speaker and content suggestions are submitted by hospitalist leaders from around the country and thereby provide insight into current topics. Combined, these offer a richness of ideas, which allows the committee to stay up to date and refresh old ideas.
What advice can you offer to early career hospitalists looking to get involved with the Annual Conference Committee or other conference planning roles?
My advice for early career hospitalists is to start locally. Join your local SHM chapter, or start one. In trying to plan local conferences, you begin to figure out which content areas interest hospitalists and how they can best be delivered. You might offer to give a talk at your local chapter or at your hospital and develop presentation skills. Developing a network of fellow hospitalists through your local chapter is important. The more local hospitalists you connect with, the more likely it is that they will think of you when they are planning a conference. At the national level, consider submitting a workshop or submitting an idea for content. Workshops are a great way to get recognized at the national level.
The Annual Conference Committee takes applications every year. Once you have some experience planning conferences or coordinating speakers, it would definitely be worth applying. You may not be selected your first year, but do not let that discourage you! Demonstrating interest and perseverance goes a long way. There are also many other national SHM committees to join and other ways to get involved. Your willingness to provide some of your time makes the society – and the specialty – what it is.
Ms. Steele is the marketing communications specialist at the Society of Hospital Medicine.
Hospital urine screening reduces TB deaths in HIV+ adults
BOSTON – Urine-based screening for tuberculosis added to standard sputum-based screening can reduce the risk of TB-associated deaths among hospitalized patients with advanced HIV compared with sputum-based screening alone, results of a randomized trial indicate.
Among 2,574 hospitalized HIV-positive patients, the rate of death at 56 days, the primary endpoint, was 21.1% for patients screened with standard-of-care sputum testing using the Xpert MTB/RIF assay, compared with 18.3% for patients screened with sputum testing and urine-sample testing by the Xpert MTB/RIF and the Determine TB-LAM urine dipstick test, reported Ankur Gupta-Wright, MBBS, MRCP, from the London School of Hygiene and Tropical Medicine.
“For every 100 patients who are HIV-positive admitted to hospital, with screening for TB using new urine-based testing in addition to sputum testing we can diagnose approximately seven extra TB case, and save approximately three lives,” he said at a briefing following his presentation of the data in a late-breaking oral abstract session.
“The findings our trial support the use of urine-based TB screening, and we hope to change how we screen for TB in HIV-positive admissions in the hospital in places with high burden of HIV and TB,” he said, speaking on behalf of colleagues in the STAMP Study.
HIV-related TB caused an estimated 400,000 deaths worldwide in 2016, and is responsible for between 32% and 67% of deaths in HIV-positive adults admit to hospitals in Africa. Yet half of all of those cases of TB are undiagnosed at the time of death, he said.
Urine based screens are easily obtained and have good diagnostic yield for disseminated TB, which is common in patients with advanced HIV, he said.
To see whether adding urine screening could increase TB diagnosis and treatment and reduce TB deaths among hospitalized HIV+ patients, the investigators enrolled 2,600 unselected HIV+ adults admitted to hospitals in South Africa and Malawi. Patients less than 18 years of age, those who had been treated for TB with the last 12 months or had received TB prophylaxis with isoniazid within the last 6 months were excluded, leaving a sample size of 2,574.
The patients were randomly assigned to standard-of-care Xpert MTB/RIF sputum screening either alone or with the addition of the two urine-based screens already described.
The overall absolute difference in risk of death at 56 days was -2.8% favoring urine screening (P = .074). As noted, this difference was only significant among patients with CD4 counts below 100/uL. Among these patients, mortality rates for nonurine screened versus screened were 35.7% vs. 28.8%, respectively (P = .036).
Baseline hemoglobin below 8 g/dl and TB suspected at admission were also predictive of better outcomes with the addition of urine-based screening.
An analysis of time to death stratified by baseline CD4 cell count also showed the advantage of urine screening for the sickest patients, with an adjusted hazard ratio for patients with CD4 counts below 100 of 0.77 (P = .047).
The urine-based screening also lead to significantly more microbiologically confirmed and clinically diagnosed TB, and more TB treatment (P less than .001 for each).
A separate cost analysis, presented in a scientific poster (CROI 2018 Abstract 1117LB), showed that the incremental cost-effectiveness ratios for the urine-based intervention were $490 per year of life save in Malawi, and $850 per year of life saved in South Africa.
The study was funded by UK AID, the UK Medical Research Council, and the Wellcome Trust. Dr. Gupta-Wright reported having no conflicts of interest to disclose.
SOURCE: Gupta-Wright, A et al. CROI 2018, Abstract 38LB.
BOSTON – Urine-based screening for tuberculosis added to standard sputum-based screening can reduce the risk of TB-associated deaths among hospitalized patients with advanced HIV compared with sputum-based screening alone, results of a randomized trial indicate.
Among 2,574 hospitalized HIV-positive patients, the rate of death at 56 days, the primary endpoint, was 21.1% for patients screened with standard-of-care sputum testing using the Xpert MTB/RIF assay, compared with 18.3% for patients screened with sputum testing and urine-sample testing by the Xpert MTB/RIF and the Determine TB-LAM urine dipstick test, reported Ankur Gupta-Wright, MBBS, MRCP, from the London School of Hygiene and Tropical Medicine.
“For every 100 patients who are HIV-positive admitted to hospital, with screening for TB using new urine-based testing in addition to sputum testing we can diagnose approximately seven extra TB case, and save approximately three lives,” he said at a briefing following his presentation of the data in a late-breaking oral abstract session.
“The findings our trial support the use of urine-based TB screening, and we hope to change how we screen for TB in HIV-positive admissions in the hospital in places with high burden of HIV and TB,” he said, speaking on behalf of colleagues in the STAMP Study.
HIV-related TB caused an estimated 400,000 deaths worldwide in 2016, and is responsible for between 32% and 67% of deaths in HIV-positive adults admit to hospitals in Africa. Yet half of all of those cases of TB are undiagnosed at the time of death, he said.
Urine based screens are easily obtained and have good diagnostic yield for disseminated TB, which is common in patients with advanced HIV, he said.
To see whether adding urine screening could increase TB diagnosis and treatment and reduce TB deaths among hospitalized HIV+ patients, the investigators enrolled 2,600 unselected HIV+ adults admitted to hospitals in South Africa and Malawi. Patients less than 18 years of age, those who had been treated for TB with the last 12 months or had received TB prophylaxis with isoniazid within the last 6 months were excluded, leaving a sample size of 2,574.
The patients were randomly assigned to standard-of-care Xpert MTB/RIF sputum screening either alone or with the addition of the two urine-based screens already described.
The overall absolute difference in risk of death at 56 days was -2.8% favoring urine screening (P = .074). As noted, this difference was only significant among patients with CD4 counts below 100/uL. Among these patients, mortality rates for nonurine screened versus screened were 35.7% vs. 28.8%, respectively (P = .036).
Baseline hemoglobin below 8 g/dl and TB suspected at admission were also predictive of better outcomes with the addition of urine-based screening.
An analysis of time to death stratified by baseline CD4 cell count also showed the advantage of urine screening for the sickest patients, with an adjusted hazard ratio for patients with CD4 counts below 100 of 0.77 (P = .047).
The urine-based screening also lead to significantly more microbiologically confirmed and clinically diagnosed TB, and more TB treatment (P less than .001 for each).
A separate cost analysis, presented in a scientific poster (CROI 2018 Abstract 1117LB), showed that the incremental cost-effectiveness ratios for the urine-based intervention were $490 per year of life save in Malawi, and $850 per year of life saved in South Africa.
The study was funded by UK AID, the UK Medical Research Council, and the Wellcome Trust. Dr. Gupta-Wright reported having no conflicts of interest to disclose.
SOURCE: Gupta-Wright, A et al. CROI 2018, Abstract 38LB.
BOSTON – Urine-based screening for tuberculosis added to standard sputum-based screening can reduce the risk of TB-associated deaths among hospitalized patients with advanced HIV compared with sputum-based screening alone, results of a randomized trial indicate.
Among 2,574 hospitalized HIV-positive patients, the rate of death at 56 days, the primary endpoint, was 21.1% for patients screened with standard-of-care sputum testing using the Xpert MTB/RIF assay, compared with 18.3% for patients screened with sputum testing and urine-sample testing by the Xpert MTB/RIF and the Determine TB-LAM urine dipstick test, reported Ankur Gupta-Wright, MBBS, MRCP, from the London School of Hygiene and Tropical Medicine.
“For every 100 patients who are HIV-positive admitted to hospital, with screening for TB using new urine-based testing in addition to sputum testing we can diagnose approximately seven extra TB case, and save approximately three lives,” he said at a briefing following his presentation of the data in a late-breaking oral abstract session.
“The findings our trial support the use of urine-based TB screening, and we hope to change how we screen for TB in HIV-positive admissions in the hospital in places with high burden of HIV and TB,” he said, speaking on behalf of colleagues in the STAMP Study.
HIV-related TB caused an estimated 400,000 deaths worldwide in 2016, and is responsible for between 32% and 67% of deaths in HIV-positive adults admit to hospitals in Africa. Yet half of all of those cases of TB are undiagnosed at the time of death, he said.
Urine based screens are easily obtained and have good diagnostic yield for disseminated TB, which is common in patients with advanced HIV, he said.
To see whether adding urine screening could increase TB diagnosis and treatment and reduce TB deaths among hospitalized HIV+ patients, the investigators enrolled 2,600 unselected HIV+ adults admitted to hospitals in South Africa and Malawi. Patients less than 18 years of age, those who had been treated for TB with the last 12 months or had received TB prophylaxis with isoniazid within the last 6 months were excluded, leaving a sample size of 2,574.
The patients were randomly assigned to standard-of-care Xpert MTB/RIF sputum screening either alone or with the addition of the two urine-based screens already described.
The overall absolute difference in risk of death at 56 days was -2.8% favoring urine screening (P = .074). As noted, this difference was only significant among patients with CD4 counts below 100/uL. Among these patients, mortality rates for nonurine screened versus screened were 35.7% vs. 28.8%, respectively (P = .036).
Baseline hemoglobin below 8 g/dl and TB suspected at admission were also predictive of better outcomes with the addition of urine-based screening.
An analysis of time to death stratified by baseline CD4 cell count also showed the advantage of urine screening for the sickest patients, with an adjusted hazard ratio for patients with CD4 counts below 100 of 0.77 (P = .047).
The urine-based screening also lead to significantly more microbiologically confirmed and clinically diagnosed TB, and more TB treatment (P less than .001 for each).
A separate cost analysis, presented in a scientific poster (CROI 2018 Abstract 1117LB), showed that the incremental cost-effectiveness ratios for the urine-based intervention were $490 per year of life save in Malawi, and $850 per year of life saved in South Africa.
The study was funded by UK AID, the UK Medical Research Council, and the Wellcome Trust. Dr. Gupta-Wright reported having no conflicts of interest to disclose.
SOURCE: Gupta-Wright, A et al. CROI 2018, Abstract 38LB.
REPORTING FROM CROI
Key clinical point: Adding urine screening for TB to sputum screening in hospitalized HIV+ patients can reduce risk for death from TB.
Major finding: Among patients with CD4 counts below 100/uL, the 56-day mortality rates was of 35.7% with sputum screening alone vs. 28.8% for combined urine and sputum screening.
Data source: Randomized pragmatic trial in 2,574 HIV+ hospitalized adults in Malawi and South Africa.
Disclosures: The study was funded by UK AID, the UK Medical Research Council, and the Wellcome Trust. Dr. Gupta-Wright reported having no conflicts of interest to disclose.
Source: Gupta-Wright A et al. CROI 2018, Abstract 38LB.
Ticagrelor noninferior to clopidogrel in terms of major bleeds in STEMI
For patients under age 75 years with ST-segment elevation myocardial infarction, switching from clopidogrel to ticagrelor was noninferior to continuing clopidogrel in terms of 30-day rates of major bleeding, investigators reported at the annual meeting of the American College of Cardiology.
Rates of thrombolysis in myocardial infarction (TIMI) major bleeding through 30 days were 0.73% in the ticagrelor group and 0.69% in the clopidogrel group, for an absolute difference of 0.04% (95% confidence interval, −0.49% to 0.58%; P less than .001 for noninferiority). “However, minor bleeding was increased with ticagrelor, and there was no benefit on efficacy outcomes,” Otavio Berwanger, MD, PhD, wrote simultaneously in JAMA Cardiology, on behalf of the writing committee for the randomized, phase 3, open-label TREAT trial.
Abundant, robust data support prompt revascularization in ST-elevation myocardial infarction (STEMI), but the real world doesn’t always meet this standard, and lytics remain in wide use in many countries, noted Dr. Berwanger, Director of the Research Institute at the Heart Hospital of Sao Paulo (Brazil). In the early 2000s, two large trials showed that dual antiplatelet therapy with aspirin and clopidogrel reduced major adverse cardiovascular events in patients receiving fibrinolytics for STEMI. More recently, the Platelet Inhibition and Patient Outcomes (PLATO) study favored ticagrelor over clopidogrel for reducing cardiovascular or stroke-related death, with no increase in the risk of major bleeding, despite ticagrelor’s boxed warning.
However, PLATO excluded patients who received fibrinolytics in the 24 hours before treatment because of concerns that ticagrelor might contribute to serious or fatal bleeding. To assess this risk, Dr. Berwanger and his associates from 10 countries randomly assigned 3,799 patients with STEMI to receive either ticagrelor (180-mg loading dose; 90 mg twice daily thereafter) or clopidogrel (300-mg to 600-mg loading dose; 75 mg daily thereafter) a median of 11.4 hours after fibrinolysis. Patients averaged 58 years in age (standard deviation, 9.5 years), 77% were men, and 57% were white.
Because about 90% of patients had been pretreated with clopidogrel, the study primarily compared the effect of staying on clopidogrel with switching to ticagrelor, the investigators noted. “Our trial was an investigator- initiated trial with limited funding that did not allow a double-dummy design,” they added. “We attempted to minimize the risk of bias associated with the open-label nature of the study by performing blinded outcome adjudication.”
In terms of secondary endpoints, 23 patients (1.2%) on ticagrelor developed major bleeding according to PLATO criteria and Bleeding Academic Research Consortium (BARC) criteria, as did 26 patients (1.4%) on clopidogrel at 30-day follow-up (absolute difference, −0.18%; 95% CI, −0.89% to 0.54; P = .001 for noninferiority). Ticagrelor and clopidogrel also resembled each other in terms of fatal bleeds (0.16% versus 0.11%, respectively; P = .67) and intracranial bleeds (0.42% versus 0.37%; P = .82).
However, minimal PLATO bleeding was significantly more common with ticagrelor (3.2%) than with clopidogrel (2%; P = .02), the researchers reported. Clinically significant TIMI bleeding requiring medical attention occurred in 2% of the ticagrelor group and 1.2% of the clopidogrel group (P = .06), and ticagrelor was no more effective than clopidogrel in terms of preventing death from vascular causes, myocardial infarction, or stroke, with a composite rate of 4% in each arm and a statistically insignificant hazard ratio of (0.91; 95% CI, 0.67 to 1.25; P = .57).
Additionally, while similar proportions of patients stopped treatment because of adverse events, dyspnea was more common with ticagrelor (13.9%) than clopidogrel (7.6%). “Based on our findings, patients with STEMI younger than 75 years who initially received clopidogrel can be safely switched to ticagrelor in the first 24 hours after fibrinolysis,” the researchers wrote. “Whether this strategy will result in fewer cardiovascular events in the long term remains to be determined.”
AstraZeneca makes ticagrelor and funded the trial. Dr. Berwanger disclosed grants and personal fees from AstraZeneca and several other pharmaceutical companies.
Source: JAMA Cardiol. doi:10.1001/jamacardio.2018.0612
The TREAT trial “answers some questions, but critical others remain,” Clyde W. Yancy, MD, MSc, and Robert A. Harrington, MD, write in a brief accompanying editorial in JAMA Cardiology.
Perhaps most notably, the trial does not answer the “crucial” question on concomitant ticagrelor-lytic therapy for acute revascularization, they write. “Given the worldwide burden of acute coronary syndromes and the recognized exigencies which preclude the ubiquitous availability of PCI, we believe this question needs urgent attention. We await future trials.”
Dr. Yancy is at Feinberg School of Medicine, Northwestern University, Chicago. Dr. Harrington is at the department of medicine, Stanford University, Stanford, Calif. Dr. Harrington disclosed ties to Astra, Amgen, Bayer, Bristol-Myers Squibb, and several other pharmaceutical companies, and reported having served on the board of directors of the American Heart Association and Stanford Health Care. Dr. Yancy had no disclosures.
The TREAT trial “answers some questions, but critical others remain,” Clyde W. Yancy, MD, MSc, and Robert A. Harrington, MD, write in a brief accompanying editorial in JAMA Cardiology.
Perhaps most notably, the trial does not answer the “crucial” question on concomitant ticagrelor-lytic therapy for acute revascularization, they write. “Given the worldwide burden of acute coronary syndromes and the recognized exigencies which preclude the ubiquitous availability of PCI, we believe this question needs urgent attention. We await future trials.”
Dr. Yancy is at Feinberg School of Medicine, Northwestern University, Chicago. Dr. Harrington is at the department of medicine, Stanford University, Stanford, Calif. Dr. Harrington disclosed ties to Astra, Amgen, Bayer, Bristol-Myers Squibb, and several other pharmaceutical companies, and reported having served on the board of directors of the American Heart Association and Stanford Health Care. Dr. Yancy had no disclosures.
The TREAT trial “answers some questions, but critical others remain,” Clyde W. Yancy, MD, MSc, and Robert A. Harrington, MD, write in a brief accompanying editorial in JAMA Cardiology.
Perhaps most notably, the trial does not answer the “crucial” question on concomitant ticagrelor-lytic therapy for acute revascularization, they write. “Given the worldwide burden of acute coronary syndromes and the recognized exigencies which preclude the ubiquitous availability of PCI, we believe this question needs urgent attention. We await future trials.”
Dr. Yancy is at Feinberg School of Medicine, Northwestern University, Chicago. Dr. Harrington is at the department of medicine, Stanford University, Stanford, Calif. Dr. Harrington disclosed ties to Astra, Amgen, Bayer, Bristol-Myers Squibb, and several other pharmaceutical companies, and reported having served on the board of directors of the American Heart Association and Stanford Health Care. Dr. Yancy had no disclosures.
For patients under age 75 years with ST-segment elevation myocardial infarction, switching from clopidogrel to ticagrelor was noninferior to continuing clopidogrel in terms of 30-day rates of major bleeding, investigators reported at the annual meeting of the American College of Cardiology.
Rates of thrombolysis in myocardial infarction (TIMI) major bleeding through 30 days were 0.73% in the ticagrelor group and 0.69% in the clopidogrel group, for an absolute difference of 0.04% (95% confidence interval, −0.49% to 0.58%; P less than .001 for noninferiority). “However, minor bleeding was increased with ticagrelor, and there was no benefit on efficacy outcomes,” Otavio Berwanger, MD, PhD, wrote simultaneously in JAMA Cardiology, on behalf of the writing committee for the randomized, phase 3, open-label TREAT trial.
Abundant, robust data support prompt revascularization in ST-elevation myocardial infarction (STEMI), but the real world doesn’t always meet this standard, and lytics remain in wide use in many countries, noted Dr. Berwanger, Director of the Research Institute at the Heart Hospital of Sao Paulo (Brazil). In the early 2000s, two large trials showed that dual antiplatelet therapy with aspirin and clopidogrel reduced major adverse cardiovascular events in patients receiving fibrinolytics for STEMI. More recently, the Platelet Inhibition and Patient Outcomes (PLATO) study favored ticagrelor over clopidogrel for reducing cardiovascular or stroke-related death, with no increase in the risk of major bleeding, despite ticagrelor’s boxed warning.
However, PLATO excluded patients who received fibrinolytics in the 24 hours before treatment because of concerns that ticagrelor might contribute to serious or fatal bleeding. To assess this risk, Dr. Berwanger and his associates from 10 countries randomly assigned 3,799 patients with STEMI to receive either ticagrelor (180-mg loading dose; 90 mg twice daily thereafter) or clopidogrel (300-mg to 600-mg loading dose; 75 mg daily thereafter) a median of 11.4 hours after fibrinolysis. Patients averaged 58 years in age (standard deviation, 9.5 years), 77% were men, and 57% were white.
Because about 90% of patients had been pretreated with clopidogrel, the study primarily compared the effect of staying on clopidogrel with switching to ticagrelor, the investigators noted. “Our trial was an investigator- initiated trial with limited funding that did not allow a double-dummy design,” they added. “We attempted to minimize the risk of bias associated with the open-label nature of the study by performing blinded outcome adjudication.”
In terms of secondary endpoints, 23 patients (1.2%) on ticagrelor developed major bleeding according to PLATO criteria and Bleeding Academic Research Consortium (BARC) criteria, as did 26 patients (1.4%) on clopidogrel at 30-day follow-up (absolute difference, −0.18%; 95% CI, −0.89% to 0.54; P = .001 for noninferiority). Ticagrelor and clopidogrel also resembled each other in terms of fatal bleeds (0.16% versus 0.11%, respectively; P = .67) and intracranial bleeds (0.42% versus 0.37%; P = .82).
However, minimal PLATO bleeding was significantly more common with ticagrelor (3.2%) than with clopidogrel (2%; P = .02), the researchers reported. Clinically significant TIMI bleeding requiring medical attention occurred in 2% of the ticagrelor group and 1.2% of the clopidogrel group (P = .06), and ticagrelor was no more effective than clopidogrel in terms of preventing death from vascular causes, myocardial infarction, or stroke, with a composite rate of 4% in each arm and a statistically insignificant hazard ratio of (0.91; 95% CI, 0.67 to 1.25; P = .57).
Additionally, while similar proportions of patients stopped treatment because of adverse events, dyspnea was more common with ticagrelor (13.9%) than clopidogrel (7.6%). “Based on our findings, patients with STEMI younger than 75 years who initially received clopidogrel can be safely switched to ticagrelor in the first 24 hours after fibrinolysis,” the researchers wrote. “Whether this strategy will result in fewer cardiovascular events in the long term remains to be determined.”
AstraZeneca makes ticagrelor and funded the trial. Dr. Berwanger disclosed grants and personal fees from AstraZeneca and several other pharmaceutical companies.
Source: JAMA Cardiol. doi:10.1001/jamacardio.2018.0612
For patients under age 75 years with ST-segment elevation myocardial infarction, switching from clopidogrel to ticagrelor was noninferior to continuing clopidogrel in terms of 30-day rates of major bleeding, investigators reported at the annual meeting of the American College of Cardiology.
Rates of thrombolysis in myocardial infarction (TIMI) major bleeding through 30 days were 0.73% in the ticagrelor group and 0.69% in the clopidogrel group, for an absolute difference of 0.04% (95% confidence interval, −0.49% to 0.58%; P less than .001 for noninferiority). “However, minor bleeding was increased with ticagrelor, and there was no benefit on efficacy outcomes,” Otavio Berwanger, MD, PhD, wrote simultaneously in JAMA Cardiology, on behalf of the writing committee for the randomized, phase 3, open-label TREAT trial.
Abundant, robust data support prompt revascularization in ST-elevation myocardial infarction (STEMI), but the real world doesn’t always meet this standard, and lytics remain in wide use in many countries, noted Dr. Berwanger, Director of the Research Institute at the Heart Hospital of Sao Paulo (Brazil). In the early 2000s, two large trials showed that dual antiplatelet therapy with aspirin and clopidogrel reduced major adverse cardiovascular events in patients receiving fibrinolytics for STEMI. More recently, the Platelet Inhibition and Patient Outcomes (PLATO) study favored ticagrelor over clopidogrel for reducing cardiovascular or stroke-related death, with no increase in the risk of major bleeding, despite ticagrelor’s boxed warning.
However, PLATO excluded patients who received fibrinolytics in the 24 hours before treatment because of concerns that ticagrelor might contribute to serious or fatal bleeding. To assess this risk, Dr. Berwanger and his associates from 10 countries randomly assigned 3,799 patients with STEMI to receive either ticagrelor (180-mg loading dose; 90 mg twice daily thereafter) or clopidogrel (300-mg to 600-mg loading dose; 75 mg daily thereafter) a median of 11.4 hours after fibrinolysis. Patients averaged 58 years in age (standard deviation, 9.5 years), 77% were men, and 57% were white.
Because about 90% of patients had been pretreated with clopidogrel, the study primarily compared the effect of staying on clopidogrel with switching to ticagrelor, the investigators noted. “Our trial was an investigator- initiated trial with limited funding that did not allow a double-dummy design,” they added. “We attempted to minimize the risk of bias associated with the open-label nature of the study by performing blinded outcome adjudication.”
In terms of secondary endpoints, 23 patients (1.2%) on ticagrelor developed major bleeding according to PLATO criteria and Bleeding Academic Research Consortium (BARC) criteria, as did 26 patients (1.4%) on clopidogrel at 30-day follow-up (absolute difference, −0.18%; 95% CI, −0.89% to 0.54; P = .001 for noninferiority). Ticagrelor and clopidogrel also resembled each other in terms of fatal bleeds (0.16% versus 0.11%, respectively; P = .67) and intracranial bleeds (0.42% versus 0.37%; P = .82).
However, minimal PLATO bleeding was significantly more common with ticagrelor (3.2%) than with clopidogrel (2%; P = .02), the researchers reported. Clinically significant TIMI bleeding requiring medical attention occurred in 2% of the ticagrelor group and 1.2% of the clopidogrel group (P = .06), and ticagrelor was no more effective than clopidogrel in terms of preventing death from vascular causes, myocardial infarction, or stroke, with a composite rate of 4% in each arm and a statistically insignificant hazard ratio of (0.91; 95% CI, 0.67 to 1.25; P = .57).
Additionally, while similar proportions of patients stopped treatment because of adverse events, dyspnea was more common with ticagrelor (13.9%) than clopidogrel (7.6%). “Based on our findings, patients with STEMI younger than 75 years who initially received clopidogrel can be safely switched to ticagrelor in the first 24 hours after fibrinolysis,” the researchers wrote. “Whether this strategy will result in fewer cardiovascular events in the long term remains to be determined.”
AstraZeneca makes ticagrelor and funded the trial. Dr. Berwanger disclosed grants and personal fees from AstraZeneca and several other pharmaceutical companies.
Source: JAMA Cardiol. doi:10.1001/jamacardio.2018.0612
FROM ACC 2018
Key clinical point: Ticagrelor was noninferior to clopidogrel after fibrinolytic therapy in patients with ST-elevation myocardial infarction.
Major finding: Rates of thrombolysis in myocardial infarction (TIMI) major bleeding through 30 days were 0.73% and 0.69%, respectively (absolute difference, 0.04%; 95% confidence interval, −0.49% to 0.58%; P less than .001 for noninferiority).
Data source: A phase 3, international, randomized, open-label trial with blinded outcomes assessments of 3,799 patients with ST-elevation myocardial infarction (TREAT).
Disclosures: AstraZeneca makes ticagrelor and funded the trial. Dr. Berwanger disclosed grants and personal fees from AstraZeneca and several other pharmaceutical companies.
Source: JAMA Cardiol. doi:10.1001/jamacardio.2018.0612
ODYSSEY Outcomes trial redefines secondary cardiovascular prevention
ORLANDO – In what was hailed as a major advance in preventive cardiology, the ODYSSEY Outcomes trial has shown that adding the PCSK9 inhibitor alirocumab on top of intensive statin therapy reduced major adverse cardiovascular events and all-cause mortality significantly more than placebo plus intensive statin therapy in patients with a recent acute coronary syndrome and an elevated on-statin LDL cholesterol level.
ODYSSEY Outcomes was a double-blind trial in which 18,924 patients at 1,315 sites in 57 countries were randomized to alirocumab (Praluent) or placebo plus background high-intensity statin therapy starting a median of 2.5 months after an acute coronary syndrome. All participants had to have a baseline LDL cholesterol level of 70 mg/dL or higher despite intensive statin therapy. Alirocumab was titrated to maintain a target LDL of 25-50 mg/dL. An LDL of 15-25 mg/dL was deemed acceptable, but if the level dropped below 15 mg/dL on two consecutive measurements the patient was blindly switched to placebo, as occurred in 7.7% of the alirocumab group.
The primary study endpoint was a composite outcome comprised of CHD (coronary heart disease) death, nonfatal MI, ischemic stroke, or unstable angina requiring hospitalization. During a median 2.8 years of follow-up, this outcome occurred in 9.5% of the overall population randomized to alirocumab and 11.1% of those on placebo, for a statistically significant and clinically meaningful 15% reduction in relative risk. The CHD death rates in the two study arms were similar; however, the other three components of the primary endpoint occurred significantly less often in the alirocumab group: The risk of nonfatal MI was 14% less (6.6% vs. 7.6%), ischemic stroke was 27% less (1.2 vs. 1.6%), and unstable angina was 39% less (0.4% vs. 0.6%).
All-cause mortality occurred in 3.5% of patients receiving alirocumab and 4.1% on placebo, once again for a statistically significant 15% reduction in risk. This was a major achievement, since even statins haven’t shown a mortality benefit in the post-ACS setting, observed Dr. Steg, cochair of the study.
The greatest benefits were seen in the 5,629 participants with a baseline LDL of 100 mg/dL or more on high-intensity statin therapy. In this large subgroup at highest baseline risk, alirocumab resulted in an absolute 3.4% risk reduction and a 24% reduction in relative risk of MACE. All-cause mortality decreased by an absolute 1.7%, translating to a 29% relative risk reduction. The number-needed-to-treat (NNT) for the duration of the study in order to prevent one additional MACE event in this group was 29, with an NNT to prevent one additional death of 60, added Dr. Steg, professor of cardiology at the University of Paris and chief of cardiology at Bichat Hospital.
“The risk/benefit for alirocumab is extraordinarily favorable. There was almost no risk over the course of the trial. There was no increase in neurocognitive disorders, new-onset or worsening diabetes, cataracts, or hemorrhagic stroke,” the cardiologist said.
Indeed, the sole adverse event that occurred more frequently in the alirocumab group was mild local injection site reactions, which occurred in 3.8% of the alirocumab group and 2.1% of controls.
There was a tendency for LDL to creep upward in both the alirocumab and placebo arms over the course of follow-up. Dr. Steg attributed this to down-titration or cessation of alirocumab as per protocol along with the inability of a substantial proportion of patients to tolerate intensive statin therapy. Most study participants had never been on a statin until their ACS.
A year ago at ACC 2017, other investigators presented the results of FOURIER, a large clinical outcomes trial of evolocumab (Repatha), another PCSK9 (proprotein convertase subtilisin/kexin type 9) inhibitor. FOURIER also showed a 15% relative risk reduction in major adverse cardiovascular events, but unlike in ODYSSEY Outcomes, there was no significant impact upon mortality. Dr. Steg attributed this to several key differences between the two trials.
The post-ACS population of ODYSSEY Outcomes was on average higher-risk than FOURIER participants, who had stable atherosclerotic cardiovascular disease. The background statin therapy was more intensive in ODYSSEY, and the average follow-up was close to 8 months longer, too.
The study population is representative of an enormous number of patients seen in clinical practice, added Dr. Fuster, professor of medicine and physician-in-chief at Mount Sinai Hospital in New York. He estimated that one-third of patients who experience ACS can’t subsequently get their LDL down to the 70 mg/dL range on statin therapy, generally because of drug intolerance.
He voiced a concern: “Up until now, the feasibility and affordability of using this type of drug has been extremely difficult. I hope this particular study is a trigger – a catalyzer – for making this drug much more available to people who need it.”
The study met with an enthusiastic audience reception. Prior to presentation of the results at the meeting’s opening session, 79% of the audience of more than 4,000 in the main arena indicated they either don’t prescribe PCSK9 inhibitors or do so only a handful of times per year.
Immediately after seeing the data, 62% of the audience said their practice will change as a result of the study findings.
ODYSSEY Outcomes was funded by Sanofi and Regeneron Pharmaceuticals. Dr. Steg reported serving as a consultant to and receiving research grants from those pharmaceutical companies and numerous others.
[email protected]
SOURCE: Steg GP.
ORLANDO – In what was hailed as a major advance in preventive cardiology, the ODYSSEY Outcomes trial has shown that adding the PCSK9 inhibitor alirocumab on top of intensive statin therapy reduced major adverse cardiovascular events and all-cause mortality significantly more than placebo plus intensive statin therapy in patients with a recent acute coronary syndrome and an elevated on-statin LDL cholesterol level.
ODYSSEY Outcomes was a double-blind trial in which 18,924 patients at 1,315 sites in 57 countries were randomized to alirocumab (Praluent) or placebo plus background high-intensity statin therapy starting a median of 2.5 months after an acute coronary syndrome. All participants had to have a baseline LDL cholesterol level of 70 mg/dL or higher despite intensive statin therapy. Alirocumab was titrated to maintain a target LDL of 25-50 mg/dL. An LDL of 15-25 mg/dL was deemed acceptable, but if the level dropped below 15 mg/dL on two consecutive measurements the patient was blindly switched to placebo, as occurred in 7.7% of the alirocumab group.
The primary study endpoint was a composite outcome comprised of CHD (coronary heart disease) death, nonfatal MI, ischemic stroke, or unstable angina requiring hospitalization. During a median 2.8 years of follow-up, this outcome occurred in 9.5% of the overall population randomized to alirocumab and 11.1% of those on placebo, for a statistically significant and clinically meaningful 15% reduction in relative risk. The CHD death rates in the two study arms were similar; however, the other three components of the primary endpoint occurred significantly less often in the alirocumab group: The risk of nonfatal MI was 14% less (6.6% vs. 7.6%), ischemic stroke was 27% less (1.2 vs. 1.6%), and unstable angina was 39% less (0.4% vs. 0.6%).
All-cause mortality occurred in 3.5% of patients receiving alirocumab and 4.1% on placebo, once again for a statistically significant 15% reduction in risk. This was a major achievement, since even statins haven’t shown a mortality benefit in the post-ACS setting, observed Dr. Steg, cochair of the study.
The greatest benefits were seen in the 5,629 participants with a baseline LDL of 100 mg/dL or more on high-intensity statin therapy. In this large subgroup at highest baseline risk, alirocumab resulted in an absolute 3.4% risk reduction and a 24% reduction in relative risk of MACE. All-cause mortality decreased by an absolute 1.7%, translating to a 29% relative risk reduction. The number-needed-to-treat (NNT) for the duration of the study in order to prevent one additional MACE event in this group was 29, with an NNT to prevent one additional death of 60, added Dr. Steg, professor of cardiology at the University of Paris and chief of cardiology at Bichat Hospital.
“The risk/benefit for alirocumab is extraordinarily favorable. There was almost no risk over the course of the trial. There was no increase in neurocognitive disorders, new-onset or worsening diabetes, cataracts, or hemorrhagic stroke,” the cardiologist said.
Indeed, the sole adverse event that occurred more frequently in the alirocumab group was mild local injection site reactions, which occurred in 3.8% of the alirocumab group and 2.1% of controls.
There was a tendency for LDL to creep upward in both the alirocumab and placebo arms over the course of follow-up. Dr. Steg attributed this to down-titration or cessation of alirocumab as per protocol along with the inability of a substantial proportion of patients to tolerate intensive statin therapy. Most study participants had never been on a statin until their ACS.
A year ago at ACC 2017, other investigators presented the results of FOURIER, a large clinical outcomes trial of evolocumab (Repatha), another PCSK9 (proprotein convertase subtilisin/kexin type 9) inhibitor. FOURIER also showed a 15% relative risk reduction in major adverse cardiovascular events, but unlike in ODYSSEY Outcomes, there was no significant impact upon mortality. Dr. Steg attributed this to several key differences between the two trials.
The post-ACS population of ODYSSEY Outcomes was on average higher-risk than FOURIER participants, who had stable atherosclerotic cardiovascular disease. The background statin therapy was more intensive in ODYSSEY, and the average follow-up was close to 8 months longer, too.
The study population is representative of an enormous number of patients seen in clinical practice, added Dr. Fuster, professor of medicine and physician-in-chief at Mount Sinai Hospital in New York. He estimated that one-third of patients who experience ACS can’t subsequently get their LDL down to the 70 mg/dL range on statin therapy, generally because of drug intolerance.
He voiced a concern: “Up until now, the feasibility and affordability of using this type of drug has been extremely difficult. I hope this particular study is a trigger – a catalyzer – for making this drug much more available to people who need it.”
The study met with an enthusiastic audience reception. Prior to presentation of the results at the meeting’s opening session, 79% of the audience of more than 4,000 in the main arena indicated they either don’t prescribe PCSK9 inhibitors or do so only a handful of times per year.
Immediately after seeing the data, 62% of the audience said their practice will change as a result of the study findings.
ODYSSEY Outcomes was funded by Sanofi and Regeneron Pharmaceuticals. Dr. Steg reported serving as a consultant to and receiving research grants from those pharmaceutical companies and numerous others.
[email protected]
SOURCE: Steg GP.
ORLANDO – In what was hailed as a major advance in preventive cardiology, the ODYSSEY Outcomes trial has shown that adding the PCSK9 inhibitor alirocumab on top of intensive statin therapy reduced major adverse cardiovascular events and all-cause mortality significantly more than placebo plus intensive statin therapy in patients with a recent acute coronary syndrome and an elevated on-statin LDL cholesterol level.
ODYSSEY Outcomes was a double-blind trial in which 18,924 patients at 1,315 sites in 57 countries were randomized to alirocumab (Praluent) or placebo plus background high-intensity statin therapy starting a median of 2.5 months after an acute coronary syndrome. All participants had to have a baseline LDL cholesterol level of 70 mg/dL or higher despite intensive statin therapy. Alirocumab was titrated to maintain a target LDL of 25-50 mg/dL. An LDL of 15-25 mg/dL was deemed acceptable, but if the level dropped below 15 mg/dL on two consecutive measurements the patient was blindly switched to placebo, as occurred in 7.7% of the alirocumab group.
The primary study endpoint was a composite outcome comprised of CHD (coronary heart disease) death, nonfatal MI, ischemic stroke, or unstable angina requiring hospitalization. During a median 2.8 years of follow-up, this outcome occurred in 9.5% of the overall population randomized to alirocumab and 11.1% of those on placebo, for a statistically significant and clinically meaningful 15% reduction in relative risk. The CHD death rates in the two study arms were similar; however, the other three components of the primary endpoint occurred significantly less often in the alirocumab group: The risk of nonfatal MI was 14% less (6.6% vs. 7.6%), ischemic stroke was 27% less (1.2 vs. 1.6%), and unstable angina was 39% less (0.4% vs. 0.6%).
All-cause mortality occurred in 3.5% of patients receiving alirocumab and 4.1% on placebo, once again for a statistically significant 15% reduction in risk. This was a major achievement, since even statins haven’t shown a mortality benefit in the post-ACS setting, observed Dr. Steg, cochair of the study.
The greatest benefits were seen in the 5,629 participants with a baseline LDL of 100 mg/dL or more on high-intensity statin therapy. In this large subgroup at highest baseline risk, alirocumab resulted in an absolute 3.4% risk reduction and a 24% reduction in relative risk of MACE. All-cause mortality decreased by an absolute 1.7%, translating to a 29% relative risk reduction. The number-needed-to-treat (NNT) for the duration of the study in order to prevent one additional MACE event in this group was 29, with an NNT to prevent one additional death of 60, added Dr. Steg, professor of cardiology at the University of Paris and chief of cardiology at Bichat Hospital.
“The risk/benefit for alirocumab is extraordinarily favorable. There was almost no risk over the course of the trial. There was no increase in neurocognitive disorders, new-onset or worsening diabetes, cataracts, or hemorrhagic stroke,” the cardiologist said.
Indeed, the sole adverse event that occurred more frequently in the alirocumab group was mild local injection site reactions, which occurred in 3.8% of the alirocumab group and 2.1% of controls.
There was a tendency for LDL to creep upward in both the alirocumab and placebo arms over the course of follow-up. Dr. Steg attributed this to down-titration or cessation of alirocumab as per protocol along with the inability of a substantial proportion of patients to tolerate intensive statin therapy. Most study participants had never been on a statin until their ACS.
A year ago at ACC 2017, other investigators presented the results of FOURIER, a large clinical outcomes trial of evolocumab (Repatha), another PCSK9 (proprotein convertase subtilisin/kexin type 9) inhibitor. FOURIER also showed a 15% relative risk reduction in major adverse cardiovascular events, but unlike in ODYSSEY Outcomes, there was no significant impact upon mortality. Dr. Steg attributed this to several key differences between the two trials.
The post-ACS population of ODYSSEY Outcomes was on average higher-risk than FOURIER participants, who had stable atherosclerotic cardiovascular disease. The background statin therapy was more intensive in ODYSSEY, and the average follow-up was close to 8 months longer, too.
The study population is representative of an enormous number of patients seen in clinical practice, added Dr. Fuster, professor of medicine and physician-in-chief at Mount Sinai Hospital in New York. He estimated that one-third of patients who experience ACS can’t subsequently get their LDL down to the 70 mg/dL range on statin therapy, generally because of drug intolerance.
He voiced a concern: “Up until now, the feasibility and affordability of using this type of drug has been extremely difficult. I hope this particular study is a trigger – a catalyzer – for making this drug much more available to people who need it.”
The study met with an enthusiastic audience reception. Prior to presentation of the results at the meeting’s opening session, 79% of the audience of more than 4,000 in the main arena indicated they either don’t prescribe PCSK9 inhibitors or do so only a handful of times per year.
Immediately after seeing the data, 62% of the audience said their practice will change as a result of the study findings.
ODYSSEY Outcomes was funded by Sanofi and Regeneron Pharmaceuticals. Dr. Steg reported serving as a consultant to and receiving research grants from those pharmaceutical companies and numerous others.
[email protected]
SOURCE: Steg GP.
REPORTING FROM ACC 2018
Key clinical point: Alirocumab reduced both all-cause mortality and major adverse cardiovascular events in high-risk patients with a recent acute coronary syndrome.
Major finding: Alirocumab reduced MACE by 15% and all-cause mortality by an equal margin compared with placebo in patients with a recent acute coronary syndrome and elevated LDL cholesterol despite intensive statin therapy alone.
Study details: The ODYSSEY Outcomes trial was a double-blind, randomized trial of nearly 19,000 patients with a recent acute coronary syndrome and an LDL cholesterol of 70 mg/dL or more despite intensive statin therapy.
Disclosures: ODYSSEY Outcomes was funded by Sanofi and Regeneron Pharmaceuticals. The presenter reported serving as a consultant to and receiving research grants from those pharmaceutical companies and numerous others.
Source: Steig, GP.
Post-ACS death lowered in ODYSSEY Outcomes
ORLANDO – should set the stage for broader use of the PCSK9-inhibitor in certain high-risk patients, Gabriel Steg, MD, said in a video interview at the annual meeting of the American College of Cardiology.
The findings from the 3-year trial are threefold: First, the trial met its primary goal, significantly lower major adverse cardiovascular events and 15% lower mortality in alirocumab-treated patients compared with those on placebo; second, the effect was greater in patients who started with an LDL level above 100 mg/dL; and third, alirocumab was remarkably safe, said Dr. Steg, director of the coronary care unit of Bichat Hospital in Paris.
“We now have good reason to target a lower LDL range of at least less than 50 mg/dL, and possibly even lower, using PCSK9 inhibitors to get the benefits we’re seeing in the trial applied to broader groups of patients,” he added.
SOURCE: Steg G ACC 18.
ORLANDO – should set the stage for broader use of the PCSK9-inhibitor in certain high-risk patients, Gabriel Steg, MD, said in a video interview at the annual meeting of the American College of Cardiology.
The findings from the 3-year trial are threefold: First, the trial met its primary goal, significantly lower major adverse cardiovascular events and 15% lower mortality in alirocumab-treated patients compared with those on placebo; second, the effect was greater in patients who started with an LDL level above 100 mg/dL; and third, alirocumab was remarkably safe, said Dr. Steg, director of the coronary care unit of Bichat Hospital in Paris.
“We now have good reason to target a lower LDL range of at least less than 50 mg/dL, and possibly even lower, using PCSK9 inhibitors to get the benefits we’re seeing in the trial applied to broader groups of patients,” he added.
SOURCE: Steg G ACC 18.
ORLANDO – should set the stage for broader use of the PCSK9-inhibitor in certain high-risk patients, Gabriel Steg, MD, said in a video interview at the annual meeting of the American College of Cardiology.
The findings from the 3-year trial are threefold: First, the trial met its primary goal, significantly lower major adverse cardiovascular events and 15% lower mortality in alirocumab-treated patients compared with those on placebo; second, the effect was greater in patients who started with an LDL level above 100 mg/dL; and third, alirocumab was remarkably safe, said Dr. Steg, director of the coronary care unit of Bichat Hospital in Paris.
“We now have good reason to target a lower LDL range of at least less than 50 mg/dL, and possibly even lower, using PCSK9 inhibitors to get the benefits we’re seeing in the trial applied to broader groups of patients,” he added.
SOURCE: Steg G ACC 18.
REPORTING FROM ACC 18
Flu activity continues to decline
The 2017-2018 flu season continued to loosen its grip on the country as both outpatient activity and pediatric deaths dropped during the week ending March 3, according to the Centers for Disease Control and Prevention.
After five consecutive weeks of double-digit pediatric deaths related to influenza-like illness (ILI), five deaths were reported for the week ending March 3, four of which occurred in previous weeks. The total for the 2017-2018 season is now 119, the CDC said in its weekly surveillance report.
The proportion of outpatient visits for ILI was 3.7% for the week, which is down from 4.9% the week before and less than half of the seasonal high of 7.5% that was recorded for the week of Feb. 3, CDC data show. The national baseline level of outpatient activity is 2.2%.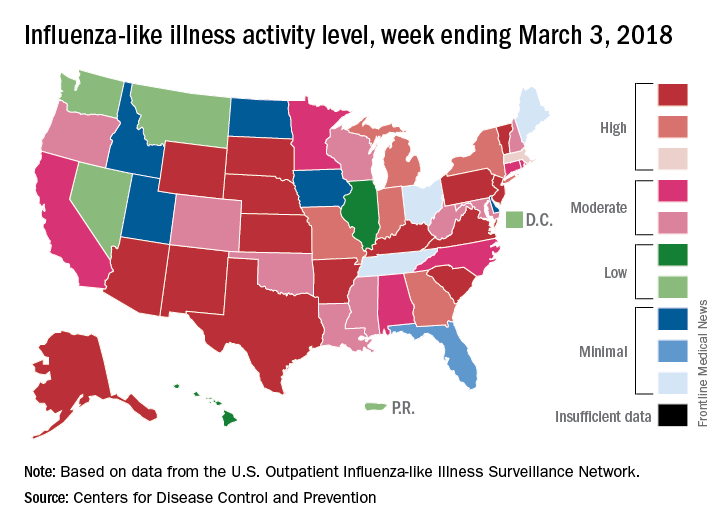
The cumulative hospitalization rate for the 2017-2018 flu season climbed from 84.2 the previous week to 86.3 per 100,000 population – well above the rate of 57.2 per 100,000 that was recorded for the corresponding week of the hospitalization-record-setting 2014-2015 season, FluView data show.
The 2017-2018 flu season continued to loosen its grip on the country as both outpatient activity and pediatric deaths dropped during the week ending March 3, according to the Centers for Disease Control and Prevention.
After five consecutive weeks of double-digit pediatric deaths related to influenza-like illness (ILI), five deaths were reported for the week ending March 3, four of which occurred in previous weeks. The total for the 2017-2018 season is now 119, the CDC said in its weekly surveillance report.
The proportion of outpatient visits for ILI was 3.7% for the week, which is down from 4.9% the week before and less than half of the seasonal high of 7.5% that was recorded for the week of Feb. 3, CDC data show. The national baseline level of outpatient activity is 2.2%.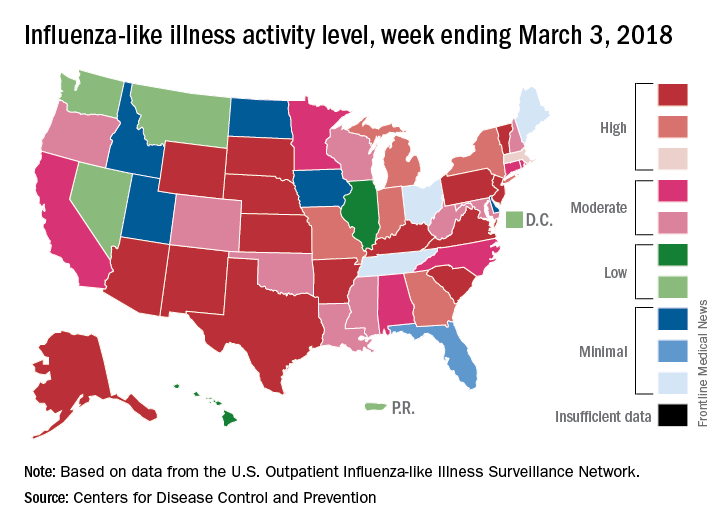
The cumulative hospitalization rate for the 2017-2018 flu season climbed from 84.2 the previous week to 86.3 per 100,000 population – well above the rate of 57.2 per 100,000 that was recorded for the corresponding week of the hospitalization-record-setting 2014-2015 season, FluView data show.
The 2017-2018 flu season continued to loosen its grip on the country as both outpatient activity and pediatric deaths dropped during the week ending March 3, according to the Centers for Disease Control and Prevention.
After five consecutive weeks of double-digit pediatric deaths related to influenza-like illness (ILI), five deaths were reported for the week ending March 3, four of which occurred in previous weeks. The total for the 2017-2018 season is now 119, the CDC said in its weekly surveillance report.
The proportion of outpatient visits for ILI was 3.7% for the week, which is down from 4.9% the week before and less than half of the seasonal high of 7.5% that was recorded for the week of Feb. 3, CDC data show. The national baseline level of outpatient activity is 2.2%.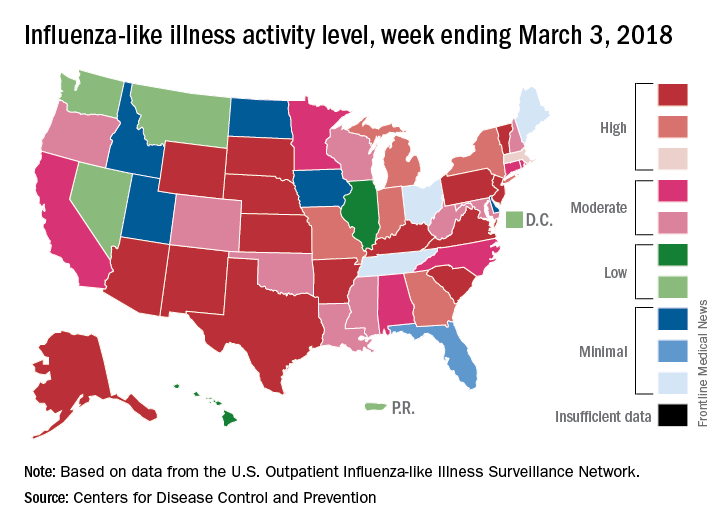
The cumulative hospitalization rate for the 2017-2018 flu season climbed from 84.2 the previous week to 86.3 per 100,000 population – well above the rate of 57.2 per 100,000 that was recorded for the corresponding week of the hospitalization-record-setting 2014-2015 season, FluView data show.
Peanut is most prevalent culprit in anaphylaxis PICU admits
ORLANDO – Food was found to be the most commonly identified trigger, with peanuts the most prevalent food cause, in what researchers say is the largest comprehensive review of anaphylaxis episodes in North America that led to pediatric intensive-care unit stays.
Researchers examined the Virtual Pediatrics Systems database, an international database of pediatric intensive care unit (PICU) information, said Carla M. Davis, MD, a pediatrician at Baylor College of Medicine, Houston. During 2010-2015, there were 1,989 pediatric anaphylaxis admissions to these units in North America, she reported at the joint congress of the American Academy of Allergy, Asthma and Immunology and the World Asthma Organization.
“Because anaphylaxis is one of the most severe consequences of allergic disease, we decided that this study needed to be done to see really what the landscape was in the most critically ill children,” she said.
Peanuts accounted for 45% of the food triggers, followed by tree nuts and seeds at 19%, and milk at 10%.
Common causes aside from food included drug, blood products, and venom, Dr. Davis said.
Anaphylaxis accounted for 0.3% of all PICU admissions over the 5-year period, researchers found. Dr. Davis said this was “higher than what we anticipated.”
The overall mortality rate was 1%, and researchers found that peanuts and dairy were main causes of death of all the food-induced cases.
Anaphylaxis occurred more often in children ages 6-18 years than in kids of other ages and was least common among those aged 2-5 years. Asian children were disproportionately represented among the PICU anaphylaxis patients, but the mortality rate didn’t vary by any demographic factors.
Admissions were most likely to happen in the fall and were more common in the Northeast and Western regions of the United States, Dr. Davis reported.
She said the deep look at the causes of these severe cases should help drive home the importance of counseling patients and families about prevention.
“For patients that have had a history of an allergic reaction to food or medication, but specifically food, I think really stressing avoidance measures will be something that will be very helpful, as well as counseling about epinephrine injectors and carrying them is going to help,” she said. “I think having a little more knowledge, pediatricians should be able to counsel and refer to allergists when they don’t feel they have all the necessary skills.”
Dr. Davis reports financial relationships with Aimmune Therapeutics and DBV Technologies.
SOURCE: Davis CM et al. 2018 AAAAI/WAO Joint Congress Abstract 775.
ORLANDO – Food was found to be the most commonly identified trigger, with peanuts the most prevalent food cause, in what researchers say is the largest comprehensive review of anaphylaxis episodes in North America that led to pediatric intensive-care unit stays.
Researchers examined the Virtual Pediatrics Systems database, an international database of pediatric intensive care unit (PICU) information, said Carla M. Davis, MD, a pediatrician at Baylor College of Medicine, Houston. During 2010-2015, there were 1,989 pediatric anaphylaxis admissions to these units in North America, she reported at the joint congress of the American Academy of Allergy, Asthma and Immunology and the World Asthma Organization.
“Because anaphylaxis is one of the most severe consequences of allergic disease, we decided that this study needed to be done to see really what the landscape was in the most critically ill children,” she said.
Peanuts accounted for 45% of the food triggers, followed by tree nuts and seeds at 19%, and milk at 10%.
Common causes aside from food included drug, blood products, and venom, Dr. Davis said.
Anaphylaxis accounted for 0.3% of all PICU admissions over the 5-year period, researchers found. Dr. Davis said this was “higher than what we anticipated.”
The overall mortality rate was 1%, and researchers found that peanuts and dairy were main causes of death of all the food-induced cases.
Anaphylaxis occurred more often in children ages 6-18 years than in kids of other ages and was least common among those aged 2-5 years. Asian children were disproportionately represented among the PICU anaphylaxis patients, but the mortality rate didn’t vary by any demographic factors.
Admissions were most likely to happen in the fall and were more common in the Northeast and Western regions of the United States, Dr. Davis reported.
She said the deep look at the causes of these severe cases should help drive home the importance of counseling patients and families about prevention.
“For patients that have had a history of an allergic reaction to food or medication, but specifically food, I think really stressing avoidance measures will be something that will be very helpful, as well as counseling about epinephrine injectors and carrying them is going to help,” she said. “I think having a little more knowledge, pediatricians should be able to counsel and refer to allergists when they don’t feel they have all the necessary skills.”
Dr. Davis reports financial relationships with Aimmune Therapeutics and DBV Technologies.
SOURCE: Davis CM et al. 2018 AAAAI/WAO Joint Congress Abstract 775.
ORLANDO – Food was found to be the most commonly identified trigger, with peanuts the most prevalent food cause, in what researchers say is the largest comprehensive review of anaphylaxis episodes in North America that led to pediatric intensive-care unit stays.
Researchers examined the Virtual Pediatrics Systems database, an international database of pediatric intensive care unit (PICU) information, said Carla M. Davis, MD, a pediatrician at Baylor College of Medicine, Houston. During 2010-2015, there were 1,989 pediatric anaphylaxis admissions to these units in North America, she reported at the joint congress of the American Academy of Allergy, Asthma and Immunology and the World Asthma Organization.
“Because anaphylaxis is one of the most severe consequences of allergic disease, we decided that this study needed to be done to see really what the landscape was in the most critically ill children,” she said.
Peanuts accounted for 45% of the food triggers, followed by tree nuts and seeds at 19%, and milk at 10%.
Common causes aside from food included drug, blood products, and venom, Dr. Davis said.
Anaphylaxis accounted for 0.3% of all PICU admissions over the 5-year period, researchers found. Dr. Davis said this was “higher than what we anticipated.”
The overall mortality rate was 1%, and researchers found that peanuts and dairy were main causes of death of all the food-induced cases.
Anaphylaxis occurred more often in children ages 6-18 years than in kids of other ages and was least common among those aged 2-5 years. Asian children were disproportionately represented among the PICU anaphylaxis patients, but the mortality rate didn’t vary by any demographic factors.
Admissions were most likely to happen in the fall and were more common in the Northeast and Western regions of the United States, Dr. Davis reported.
She said the deep look at the causes of these severe cases should help drive home the importance of counseling patients and families about prevention.
“For patients that have had a history of an allergic reaction to food or medication, but specifically food, I think really stressing avoidance measures will be something that will be very helpful, as well as counseling about epinephrine injectors and carrying them is going to help,” she said. “I think having a little more knowledge, pediatricians should be able to counsel and refer to allergists when they don’t feel they have all the necessary skills.”
Dr. Davis reports financial relationships with Aimmune Therapeutics and DBV Technologies.
SOURCE: Davis CM et al. 2018 AAAAI/WAO Joint Congress Abstract 775.
REPORTING FROM AAAAI/WAO JOINT CONGRESS
Key clinical point:
Major finding: Researchers found that 45% of these PICU stays from food were caused by reactions to peanuts.
Study details: A review of 1,989 cases during 2010-2015 in the Virtual Pediatrics Systems database, which collects international PICU information.
Disclosures: Dr. Davis reports financial relationships with Aimmune Therapeutics and DBV Technologies.
Source: Davis CM et al. 2018 AAAAI/WAO Joint Congress, Abstract 775.


















