User login
The Journal of Clinical Outcomes Management® is an independent, peer-reviewed journal offering evidence-based, practical information for improving the quality, safety, and value of health care.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
AAP approves 2023 child and adolescent immunization schedule
The American Academy of Pediatrics said it supports the Recommended Childhood and Adolescent Immunization Schedule: United States, 2023.
In a policy statement published online in the journal Pediatrics, the AAP said the updated recommendations do not include major changes from those released in 2022 by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention.
In one small shift, COVID-19 is now addressed in the main text instead of being relegated to the notes section.
“And a new vaccine – Priorix [GlaxoSmithKline] – has been added for MMR [measles, mumps, rubella], so now there are two available,” Sean T. O’Leary, MD, MPH, chair of the AAP’s Committee on Infectious Diseases, told this news organization. “There’s also a second pneumococcal conjugate vaccine listed, PCV15, and this and PCV13 can essentially be used interchangeably.”
Minor updates to the schedule, reflected on the cover page, relate to vaccines for COVID-19, dengue fever, and pneumococcal disease, added Dr. O’Leary, a professor of pediatrics at the University of Colorado Anschutz Medical Campus and Children’s Hospital Colorado, Aurora.
The committee also changed layouts to improve the usability of the schedule. Updated annually, the guidance provides a table on recommended pediatric immunizations from birth to age 18 years, and catch-up recommendations for children aged 4 months to 18 years who start their vaccinations late or are more than 1 month behind the recommended age for vaccine administration.
“We hope this annual update will encourage clinicians to make sure all their patients are up to date on their routine vaccinations,” Dr. O’Leary said. “It’s an opportunity to develop strategies to improve vaccination rates.”
The 2023 schedule follows news from the CDC that kindergarten vaccination rates declined during the 2021-2022 school year. Only 93% of kindergarteners obtained full vaccinations, representing a drop of 1 percentage point from the year before and 2 percentage points from the 2019-2020 school year.
The dip in coverage has been attributed to disruptions caused by the COVID-19 pandemic. AAP advises health care professionals to urge families to make sure their child’s vaccines are current.
Among other additions:
In Table 1
- MMR: Second vaccine added (Priorix, GlaxoSmithKline Biologicals)
- Pneumococcal disease: second conjugate vaccine, PCV15, added (Vaxneuvance, Merck Sharp & Dohme).
- COVID-19: New row added.
- Dengue: Text changed from “Seropositive in endemic areas only” to “Seropositive in endemic dengue areas.”
- Inactivated polio vaccine: “See Notes” added to the column for children aged 18 years.
In Table 2
- PCV: Dose 3 to dose 4 interval revised to align with ACIP’s recommendation for dose 4. This dose is necessary only for children ages 12-59 months regardless of risk, or age 60-71 months with any risk who received three doses before age 12 months.
A parent-friendly vaccine schedule for children and adolescents is available on the CDC’s website.
“Vaccines are essential for the health of our whole society, including children and adolescents,” Dr. O’Leary said in a press release from AAP. “These schedules provide a road map [that] parents and pediatricians can follow to help children get the vaccines they need so their immune systems will be ready to recognize and resist diseases.”
As previously, the 2023 schedule was adjusted to ensure consistency between the formats of the childhood/adolescent and adult immunization guidance. A meeting of stakeholder organizations in October 2022 harmonized the two formats.
A version of this article first appeared on Medscape.com.
The American Academy of Pediatrics said it supports the Recommended Childhood and Adolescent Immunization Schedule: United States, 2023.
In a policy statement published online in the journal Pediatrics, the AAP said the updated recommendations do not include major changes from those released in 2022 by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention.
In one small shift, COVID-19 is now addressed in the main text instead of being relegated to the notes section.
“And a new vaccine – Priorix [GlaxoSmithKline] – has been added for MMR [measles, mumps, rubella], so now there are two available,” Sean T. O’Leary, MD, MPH, chair of the AAP’s Committee on Infectious Diseases, told this news organization. “There’s also a second pneumococcal conjugate vaccine listed, PCV15, and this and PCV13 can essentially be used interchangeably.”
Minor updates to the schedule, reflected on the cover page, relate to vaccines for COVID-19, dengue fever, and pneumococcal disease, added Dr. O’Leary, a professor of pediatrics at the University of Colorado Anschutz Medical Campus and Children’s Hospital Colorado, Aurora.
The committee also changed layouts to improve the usability of the schedule. Updated annually, the guidance provides a table on recommended pediatric immunizations from birth to age 18 years, and catch-up recommendations for children aged 4 months to 18 years who start their vaccinations late or are more than 1 month behind the recommended age for vaccine administration.
“We hope this annual update will encourage clinicians to make sure all their patients are up to date on their routine vaccinations,” Dr. O’Leary said. “It’s an opportunity to develop strategies to improve vaccination rates.”
The 2023 schedule follows news from the CDC that kindergarten vaccination rates declined during the 2021-2022 school year. Only 93% of kindergarteners obtained full vaccinations, representing a drop of 1 percentage point from the year before and 2 percentage points from the 2019-2020 school year.
The dip in coverage has been attributed to disruptions caused by the COVID-19 pandemic. AAP advises health care professionals to urge families to make sure their child’s vaccines are current.
Among other additions:
In Table 1
- MMR: Second vaccine added (Priorix, GlaxoSmithKline Biologicals)
- Pneumococcal disease: second conjugate vaccine, PCV15, added (Vaxneuvance, Merck Sharp & Dohme).
- COVID-19: New row added.
- Dengue: Text changed from “Seropositive in endemic areas only” to “Seropositive in endemic dengue areas.”
- Inactivated polio vaccine: “See Notes” added to the column for children aged 18 years.
In Table 2
- PCV: Dose 3 to dose 4 interval revised to align with ACIP’s recommendation for dose 4. This dose is necessary only for children ages 12-59 months regardless of risk, or age 60-71 months with any risk who received three doses before age 12 months.
A parent-friendly vaccine schedule for children and adolescents is available on the CDC’s website.
“Vaccines are essential for the health of our whole society, including children and adolescents,” Dr. O’Leary said in a press release from AAP. “These schedules provide a road map [that] parents and pediatricians can follow to help children get the vaccines they need so their immune systems will be ready to recognize and resist diseases.”
As previously, the 2023 schedule was adjusted to ensure consistency between the formats of the childhood/adolescent and adult immunization guidance. A meeting of stakeholder organizations in October 2022 harmonized the two formats.
A version of this article first appeared on Medscape.com.
The American Academy of Pediatrics said it supports the Recommended Childhood and Adolescent Immunization Schedule: United States, 2023.
In a policy statement published online in the journal Pediatrics, the AAP said the updated recommendations do not include major changes from those released in 2022 by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention.
In one small shift, COVID-19 is now addressed in the main text instead of being relegated to the notes section.
“And a new vaccine – Priorix [GlaxoSmithKline] – has been added for MMR [measles, mumps, rubella], so now there are two available,” Sean T. O’Leary, MD, MPH, chair of the AAP’s Committee on Infectious Diseases, told this news organization. “There’s also a second pneumococcal conjugate vaccine listed, PCV15, and this and PCV13 can essentially be used interchangeably.”
Minor updates to the schedule, reflected on the cover page, relate to vaccines for COVID-19, dengue fever, and pneumococcal disease, added Dr. O’Leary, a professor of pediatrics at the University of Colorado Anschutz Medical Campus and Children’s Hospital Colorado, Aurora.
The committee also changed layouts to improve the usability of the schedule. Updated annually, the guidance provides a table on recommended pediatric immunizations from birth to age 18 years, and catch-up recommendations for children aged 4 months to 18 years who start their vaccinations late or are more than 1 month behind the recommended age for vaccine administration.
“We hope this annual update will encourage clinicians to make sure all their patients are up to date on their routine vaccinations,” Dr. O’Leary said. “It’s an opportunity to develop strategies to improve vaccination rates.”
The 2023 schedule follows news from the CDC that kindergarten vaccination rates declined during the 2021-2022 school year. Only 93% of kindergarteners obtained full vaccinations, representing a drop of 1 percentage point from the year before and 2 percentage points from the 2019-2020 school year.
The dip in coverage has been attributed to disruptions caused by the COVID-19 pandemic. AAP advises health care professionals to urge families to make sure their child’s vaccines are current.
Among other additions:
In Table 1
- MMR: Second vaccine added (Priorix, GlaxoSmithKline Biologicals)
- Pneumococcal disease: second conjugate vaccine, PCV15, added (Vaxneuvance, Merck Sharp & Dohme).
- COVID-19: New row added.
- Dengue: Text changed from “Seropositive in endemic areas only” to “Seropositive in endemic dengue areas.”
- Inactivated polio vaccine: “See Notes” added to the column for children aged 18 years.
In Table 2
- PCV: Dose 3 to dose 4 interval revised to align with ACIP’s recommendation for dose 4. This dose is necessary only for children ages 12-59 months regardless of risk, or age 60-71 months with any risk who received three doses before age 12 months.
A parent-friendly vaccine schedule for children and adolescents is available on the CDC’s website.
“Vaccines are essential for the health of our whole society, including children and adolescents,” Dr. O’Leary said in a press release from AAP. “These schedules provide a road map [that] parents and pediatricians can follow to help children get the vaccines they need so their immune systems will be ready to recognize and resist diseases.”
As previously, the 2023 schedule was adjusted to ensure consistency between the formats of the childhood/adolescent and adult immunization guidance. A meeting of stakeholder organizations in October 2022 harmonized the two formats.
A version of this article first appeared on Medscape.com.
FROM PEDIATRICS
Nature, not nurture, the culprit in OCD
new research suggests.
This finding from a large, register-based study is particularly surprising because results from previous studies of major depression and anxiety disorder have shown a significant effect of parenting and a child’s home environment on the risk for these disorders, the investigators noted.
While the results likely won’t change patient treatment, one expert said it could alleviate concerns of some parents with OCD who fear that witnessing their obsessive behaviors might put their children at higher risk for the disorder.
“The evidence is consistent with the idea that the psychological transmission of OCD from parent to child, if it exists, is really pretty weak,” lead author Kenneth S. Kendler, MD, professor of psychiatry and director of the Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, said in an interview.
The findings were published online in JAMA Psychiatry.
Family analysis
The study is the first to include adoptive parents in an analysis of OCD transmission, which allowed investigators to answer the nature versus nurture question that is often difficult to decipher.
Working with Swedish population registries, researchers identified more than 2.4 million offspring. Of these, 27,141 individuals (1.1%) had a lifetime diagnosis of OCD.
Families were divided into four types: intact families, with kids who lived at home with their biological parents from birth to at least age 15 years; families with kids who never lived with their biological father; families with children who did not live with their biological fathers between birth and age 15 years but who lived with a stepfather for at least 10 of those years; and families with children who were adopted before the age of 5 by people with no biological connection to the child.
After analyzing data from all parent-child relationships, researchers found that genes plus rearing (odds ratio, 3.94; 95% confidence interval, 3.58-4.33) and genes only (OR, 3.34; 95% CI, 2.27-4.93) were significantly more likely to be correlated to transmission of OCD from parent to offspring than rearing alone. Rearing only (OR, 1.4; 95% CI, 0.45-4.39) was not significantly correlated with OCD transmission
“It appears from our data that the only substantial transmission that occurs is in the genes parents transmit, not by the modeling of behavior,” Dr. Kendler said.
“There’s an idea that you can learn some things from your parents from psychopathology, but we didn’t see that kids picked that up much in the case of OCD,” he added.
However, there was one outlier: Children raised by stepparents or adoptive parents with an anxiety disorder had a greater risk of developing OCD.
Given the lack of evidence of a strong rearing effect in other analyses, Dr. Kendler noted that this rogue finding could be caused by an underpowered sample; the researchers plan to study the data further.
“Psychiatric disorders, like many other conditions, are often correlated with neighboring conditions,” he said. “Our study would suggest that some of the molecular genetic variants between OCD and generalized anxiety disorder or other anxiety disorders would be shared, but some would be unique.”
Answers an old question
In a comment, Jon Grant, JD, MD, MPH, professor of psychiatry and director of the Addictive, Compulsive, and Impulsive Disorders Research Lab at the University of Chicago, said the findings fill an important gap in what is known about OCD.
“I think the findings are really answering this old question of: ‘Is OCD due to the rearing patterns in a family versus genetics?’ This was able to get at that information showing that it’s virtually all due to genetics within families, and that’s really good to know,” said Dr. Grant, who was not a part of the study.
He was also struck by the finding of a strong genetic relationship between OCD and generalized anxiety disorder (GAD).
While identifying that OCD and GAD are genetically linked likely won’t change clinical care, “I think it at least allows clinicians to know when we see that comorbidity that it may be much more genetically linked in the case of GAD,” Dr. Grant said.
The study was funded by the Swedish Research Council, as well as Avtal om Läkarutbildning och Forskning funding from Region Skåne. Dr. Kendler and Dr. Grant reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
This finding from a large, register-based study is particularly surprising because results from previous studies of major depression and anxiety disorder have shown a significant effect of parenting and a child’s home environment on the risk for these disorders, the investigators noted.
While the results likely won’t change patient treatment, one expert said it could alleviate concerns of some parents with OCD who fear that witnessing their obsessive behaviors might put their children at higher risk for the disorder.
“The evidence is consistent with the idea that the psychological transmission of OCD from parent to child, if it exists, is really pretty weak,” lead author Kenneth S. Kendler, MD, professor of psychiatry and director of the Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, said in an interview.
The findings were published online in JAMA Psychiatry.
Family analysis
The study is the first to include adoptive parents in an analysis of OCD transmission, which allowed investigators to answer the nature versus nurture question that is often difficult to decipher.
Working with Swedish population registries, researchers identified more than 2.4 million offspring. Of these, 27,141 individuals (1.1%) had a lifetime diagnosis of OCD.
Families were divided into four types: intact families, with kids who lived at home with their biological parents from birth to at least age 15 years; families with kids who never lived with their biological father; families with children who did not live with their biological fathers between birth and age 15 years but who lived with a stepfather for at least 10 of those years; and families with children who were adopted before the age of 5 by people with no biological connection to the child.
After analyzing data from all parent-child relationships, researchers found that genes plus rearing (odds ratio, 3.94; 95% confidence interval, 3.58-4.33) and genes only (OR, 3.34; 95% CI, 2.27-4.93) were significantly more likely to be correlated to transmission of OCD from parent to offspring than rearing alone. Rearing only (OR, 1.4; 95% CI, 0.45-4.39) was not significantly correlated with OCD transmission
“It appears from our data that the only substantial transmission that occurs is in the genes parents transmit, not by the modeling of behavior,” Dr. Kendler said.
“There’s an idea that you can learn some things from your parents from psychopathology, but we didn’t see that kids picked that up much in the case of OCD,” he added.
However, there was one outlier: Children raised by stepparents or adoptive parents with an anxiety disorder had a greater risk of developing OCD.
Given the lack of evidence of a strong rearing effect in other analyses, Dr. Kendler noted that this rogue finding could be caused by an underpowered sample; the researchers plan to study the data further.
“Psychiatric disorders, like many other conditions, are often correlated with neighboring conditions,” he said. “Our study would suggest that some of the molecular genetic variants between OCD and generalized anxiety disorder or other anxiety disorders would be shared, but some would be unique.”
Answers an old question
In a comment, Jon Grant, JD, MD, MPH, professor of psychiatry and director of the Addictive, Compulsive, and Impulsive Disorders Research Lab at the University of Chicago, said the findings fill an important gap in what is known about OCD.
“I think the findings are really answering this old question of: ‘Is OCD due to the rearing patterns in a family versus genetics?’ This was able to get at that information showing that it’s virtually all due to genetics within families, and that’s really good to know,” said Dr. Grant, who was not a part of the study.
He was also struck by the finding of a strong genetic relationship between OCD and generalized anxiety disorder (GAD).
While identifying that OCD and GAD are genetically linked likely won’t change clinical care, “I think it at least allows clinicians to know when we see that comorbidity that it may be much more genetically linked in the case of GAD,” Dr. Grant said.
The study was funded by the Swedish Research Council, as well as Avtal om Läkarutbildning och Forskning funding from Region Skåne. Dr. Kendler and Dr. Grant reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
This finding from a large, register-based study is particularly surprising because results from previous studies of major depression and anxiety disorder have shown a significant effect of parenting and a child’s home environment on the risk for these disorders, the investigators noted.
While the results likely won’t change patient treatment, one expert said it could alleviate concerns of some parents with OCD who fear that witnessing their obsessive behaviors might put their children at higher risk for the disorder.
“The evidence is consistent with the idea that the psychological transmission of OCD from parent to child, if it exists, is really pretty weak,” lead author Kenneth S. Kendler, MD, professor of psychiatry and director of the Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, said in an interview.
The findings were published online in JAMA Psychiatry.
Family analysis
The study is the first to include adoptive parents in an analysis of OCD transmission, which allowed investigators to answer the nature versus nurture question that is often difficult to decipher.
Working with Swedish population registries, researchers identified more than 2.4 million offspring. Of these, 27,141 individuals (1.1%) had a lifetime diagnosis of OCD.
Families were divided into four types: intact families, with kids who lived at home with their biological parents from birth to at least age 15 years; families with kids who never lived with their biological father; families with children who did not live with their biological fathers between birth and age 15 years but who lived with a stepfather for at least 10 of those years; and families with children who were adopted before the age of 5 by people with no biological connection to the child.
After analyzing data from all parent-child relationships, researchers found that genes plus rearing (odds ratio, 3.94; 95% confidence interval, 3.58-4.33) and genes only (OR, 3.34; 95% CI, 2.27-4.93) were significantly more likely to be correlated to transmission of OCD from parent to offspring than rearing alone. Rearing only (OR, 1.4; 95% CI, 0.45-4.39) was not significantly correlated with OCD transmission
“It appears from our data that the only substantial transmission that occurs is in the genes parents transmit, not by the modeling of behavior,” Dr. Kendler said.
“There’s an idea that you can learn some things from your parents from psychopathology, but we didn’t see that kids picked that up much in the case of OCD,” he added.
However, there was one outlier: Children raised by stepparents or adoptive parents with an anxiety disorder had a greater risk of developing OCD.
Given the lack of evidence of a strong rearing effect in other analyses, Dr. Kendler noted that this rogue finding could be caused by an underpowered sample; the researchers plan to study the data further.
“Psychiatric disorders, like many other conditions, are often correlated with neighboring conditions,” he said. “Our study would suggest that some of the molecular genetic variants between OCD and generalized anxiety disorder or other anxiety disorders would be shared, but some would be unique.”
Answers an old question
In a comment, Jon Grant, JD, MD, MPH, professor of psychiatry and director of the Addictive, Compulsive, and Impulsive Disorders Research Lab at the University of Chicago, said the findings fill an important gap in what is known about OCD.
“I think the findings are really answering this old question of: ‘Is OCD due to the rearing patterns in a family versus genetics?’ This was able to get at that information showing that it’s virtually all due to genetics within families, and that’s really good to know,” said Dr. Grant, who was not a part of the study.
He was also struck by the finding of a strong genetic relationship between OCD and generalized anxiety disorder (GAD).
While identifying that OCD and GAD are genetically linked likely won’t change clinical care, “I think it at least allows clinicians to know when we see that comorbidity that it may be much more genetically linked in the case of GAD,” Dr. Grant said.
The study was funded by the Swedish Research Council, as well as Avtal om Läkarutbildning och Forskning funding from Region Skåne. Dr. Kendler and Dr. Grant reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
A new (old) drug joins the COVID fray, and guess what? It works
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
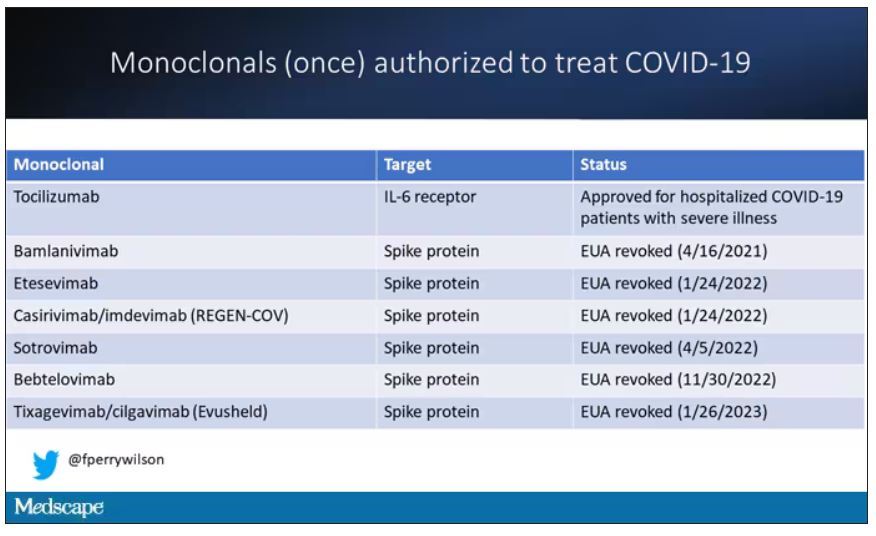
At this point, with the monoclonals found to be essentially useless, we are left with remdesivir with its modest efficacy and Paxlovid, which, for some reason, people don’t seem to be taking.
Part of the reason the monoclonals have failed lately is because of their specificity; they are homogeneous antibodies targeted toward a very specific epitope that may change from variant to variant. We need a broader therapeutic, one that has activity across all variants — maybe even one that has activity against all viruses? We’ve got one. Interferon.
The first mention of interferon as a potential COVID therapy was at the very start of the pandemic, so I’m sort of surprised that the first large, randomized trial is only being reported now in the New England Journal of Medicine.
Before we dig into the results, let’s talk mechanism. This is a trial of interferon-lambda, also known as interleukin-29.
The lambda interferons were only discovered in 2003. They differ from the more familiar interferons only in their cellular receptors; the downstream effects seem quite similar. As opposed to the cellular receptors for interferon alfa, which are widely expressed, the receptors for lambda are restricted to epithelial tissues. This makes it a good choice as a COVID treatment, since the virus also preferentially targets those epithelial cells.
In this study, 1,951 participants from Brazil and Canada, but mostly Brazil, with new COVID infections who were not yet hospitalized were randomized to receive 180 mcg of interferon lambda or placebo.
This was a relatively current COVID trial, as you can see from the participant characteristics. The majority had been vaccinated, and nearly half of the infections were during the Omicron phase of the pandemic.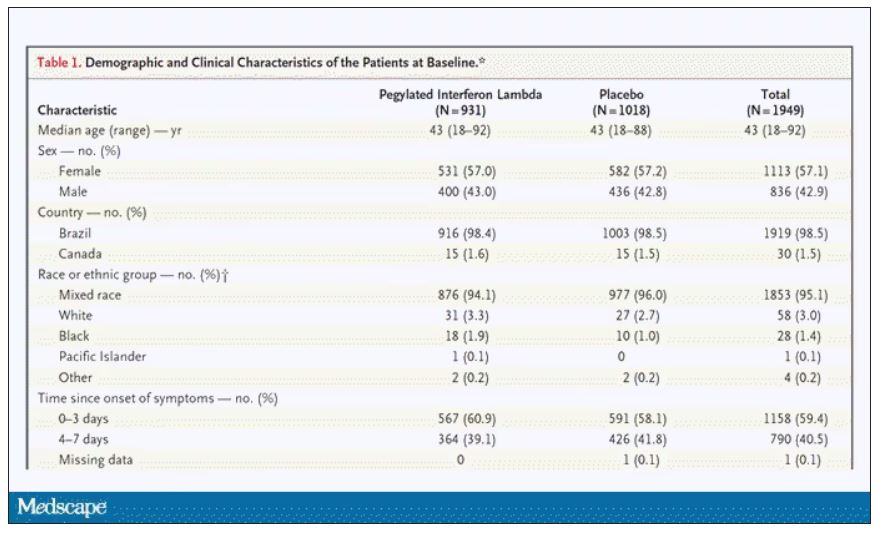
If you just want to cut to the chase, interferon worked.
The primary outcome – hospitalization or a prolonged emergency room visit for COVID – was 50% lower in the interferon group.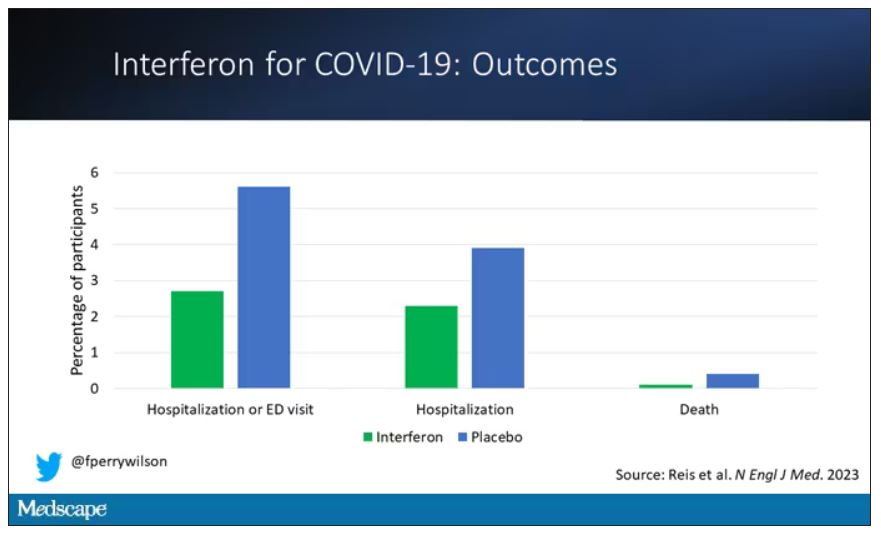
Key secondary outcomes, including death from COVID, were lower in the interferon group as well. These effects persisted across most of the subgroups I was looking out for.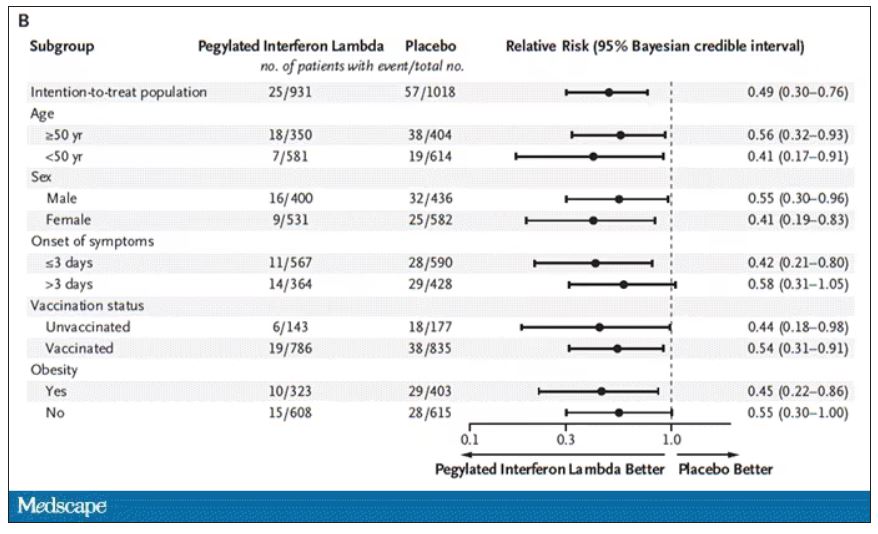
Interferon seemed to help those who were already vaccinated and those who were unvaccinated. There’s a hint that it works better within the first few days of symptoms, which isn’t surprising; we’ve seen this for many of the therapeutics, including Paxlovid. Time is of the essence. Encouragingly, the effect was a bit more pronounced among those infected with Omicron.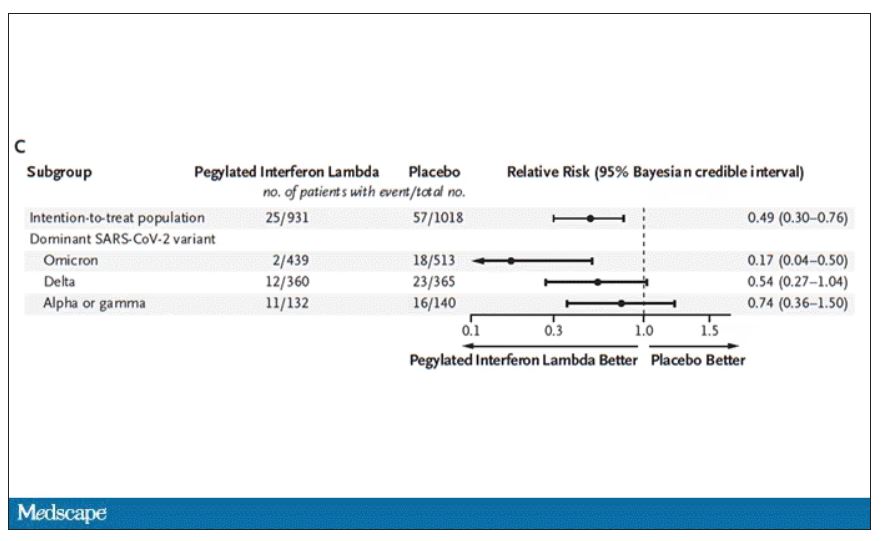
Of course, if you have any experience with interferon, you know that the side effects can be pretty rough. In the bad old days when we treated hepatitis C infection with interferon, patients would get their injections on Friday in anticipation of being essentially out of commission with flu-like symptoms through the weekend. But we don’t see much evidence of adverse events in this trial, maybe due to the greater specificity of interferon lambda.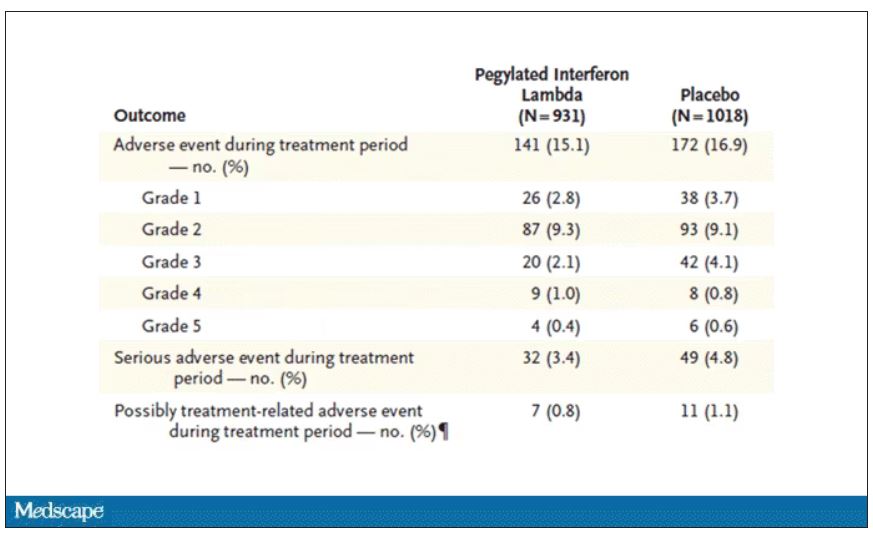
Putting it all together, the state of play for interferons in COVID may be changing. To date, the FDA has not recommended the use of interferon alfa or -beta for COVID-19, citing some data that they are ineffective or even harmful in hospitalized patients with COVID. Interferon lambda is not FDA approved and thus not even available in the United States. But the reason it has not been approved is that there has not been a large, well-conducted interferon lambda trial. Now there is. Will this study be enough to prompt an emergency use authorization? The elephant in the room, of course, is Paxlovid, which at this point has a longer safety track record and, importantly, is oral. I’d love to see a head-to-head trial. Short of that, I tend to be in favor of having more options on the table.
Dr. Perry Wilson is associate professor, department of medicine, and director, Clinical and Translational Research Accelerator, at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
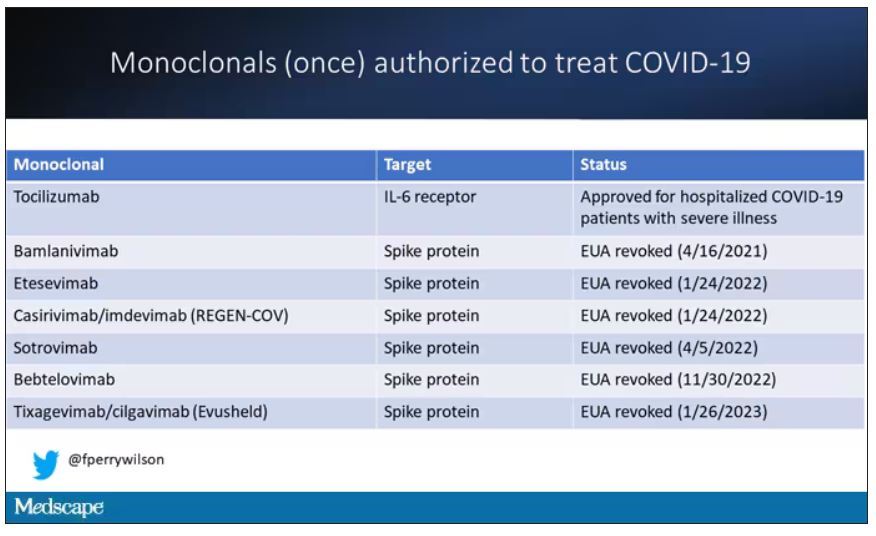
At this point, with the monoclonals found to be essentially useless, we are left with remdesivir with its modest efficacy and Paxlovid, which, for some reason, people don’t seem to be taking.
Part of the reason the monoclonals have failed lately is because of their specificity; they are homogeneous antibodies targeted toward a very specific epitope that may change from variant to variant. We need a broader therapeutic, one that has activity across all variants — maybe even one that has activity against all viruses? We’ve got one. Interferon.
The first mention of interferon as a potential COVID therapy was at the very start of the pandemic, so I’m sort of surprised that the first large, randomized trial is only being reported now in the New England Journal of Medicine.
Before we dig into the results, let’s talk mechanism. This is a trial of interferon-lambda, also known as interleukin-29.
The lambda interferons were only discovered in 2003. They differ from the more familiar interferons only in their cellular receptors; the downstream effects seem quite similar. As opposed to the cellular receptors for interferon alfa, which are widely expressed, the receptors for lambda are restricted to epithelial tissues. This makes it a good choice as a COVID treatment, since the virus also preferentially targets those epithelial cells.
In this study, 1,951 participants from Brazil and Canada, but mostly Brazil, with new COVID infections who were not yet hospitalized were randomized to receive 180 mcg of interferon lambda or placebo.
This was a relatively current COVID trial, as you can see from the participant characteristics. The majority had been vaccinated, and nearly half of the infections were during the Omicron phase of the pandemic.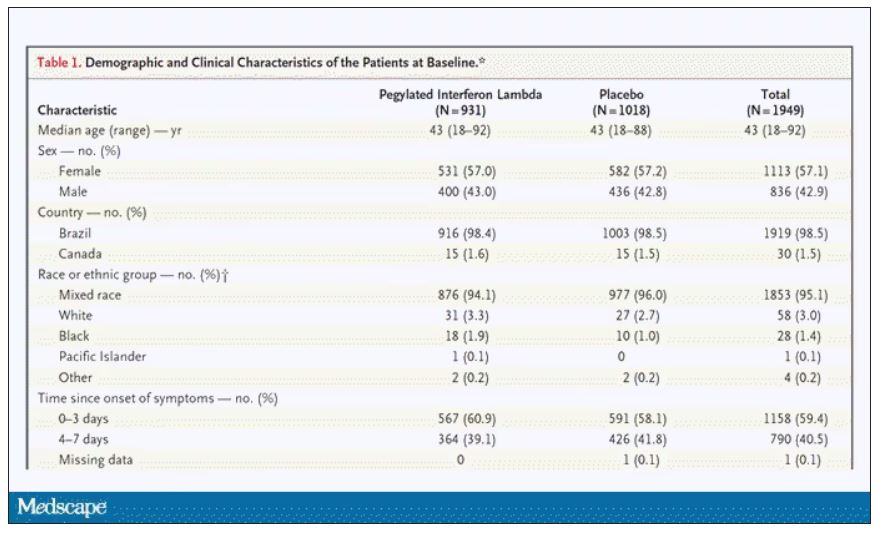
If you just want to cut to the chase, interferon worked.
The primary outcome – hospitalization or a prolonged emergency room visit for COVID – was 50% lower in the interferon group.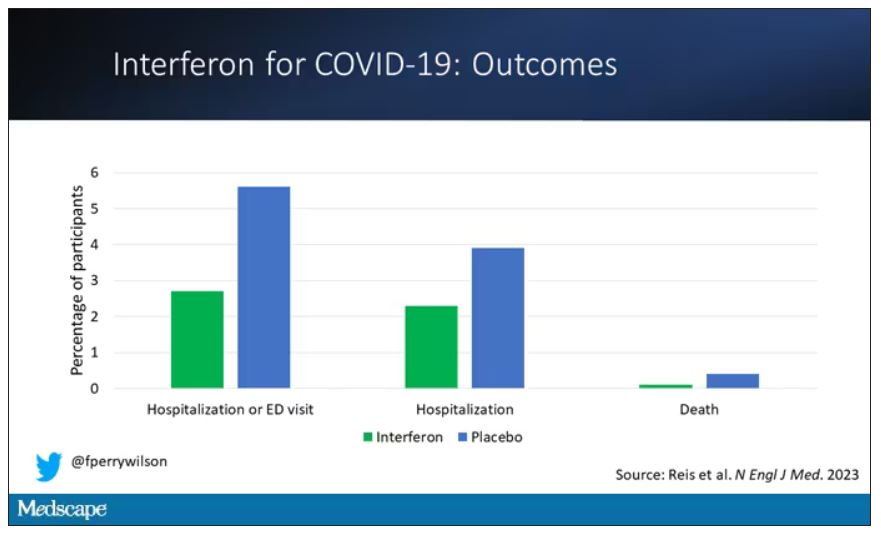
Key secondary outcomes, including death from COVID, were lower in the interferon group as well. These effects persisted across most of the subgroups I was looking out for.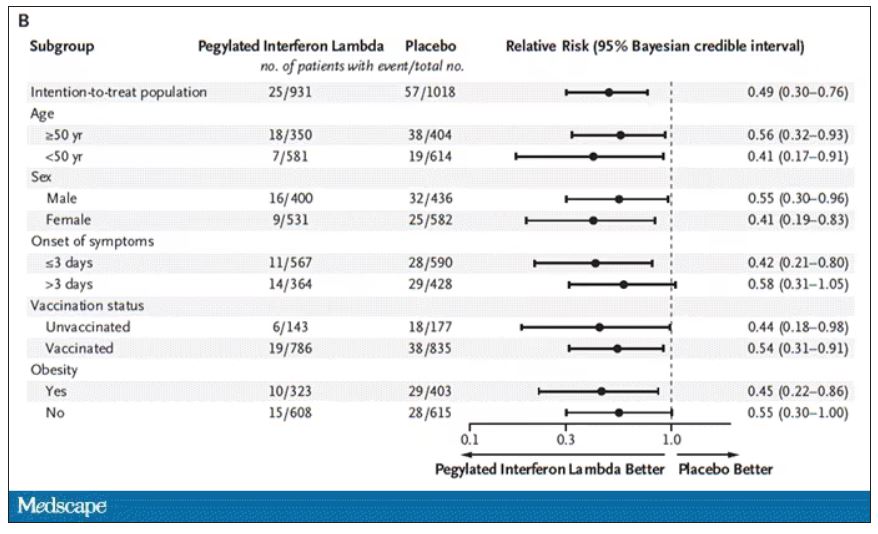
Interferon seemed to help those who were already vaccinated and those who were unvaccinated. There’s a hint that it works better within the first few days of symptoms, which isn’t surprising; we’ve seen this for many of the therapeutics, including Paxlovid. Time is of the essence. Encouragingly, the effect was a bit more pronounced among those infected with Omicron.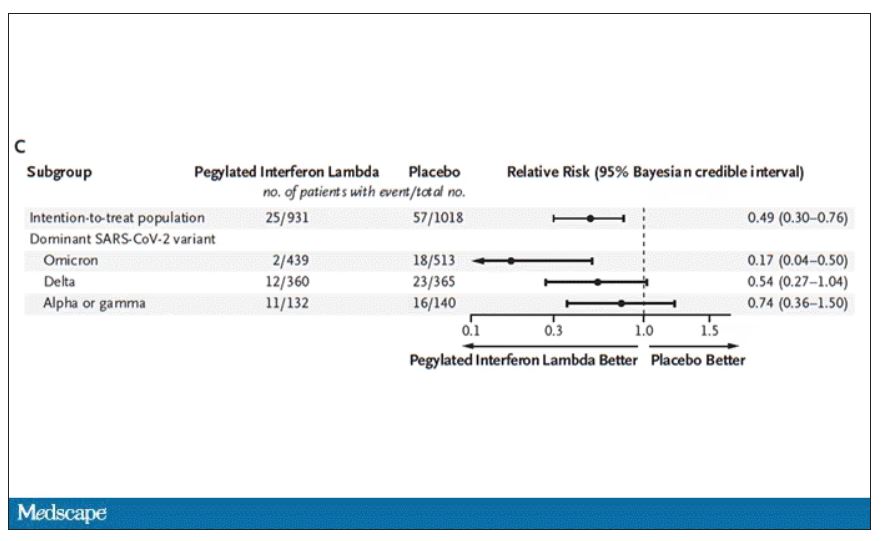
Of course, if you have any experience with interferon, you know that the side effects can be pretty rough. In the bad old days when we treated hepatitis C infection with interferon, patients would get their injections on Friday in anticipation of being essentially out of commission with flu-like symptoms through the weekend. But we don’t see much evidence of adverse events in this trial, maybe due to the greater specificity of interferon lambda.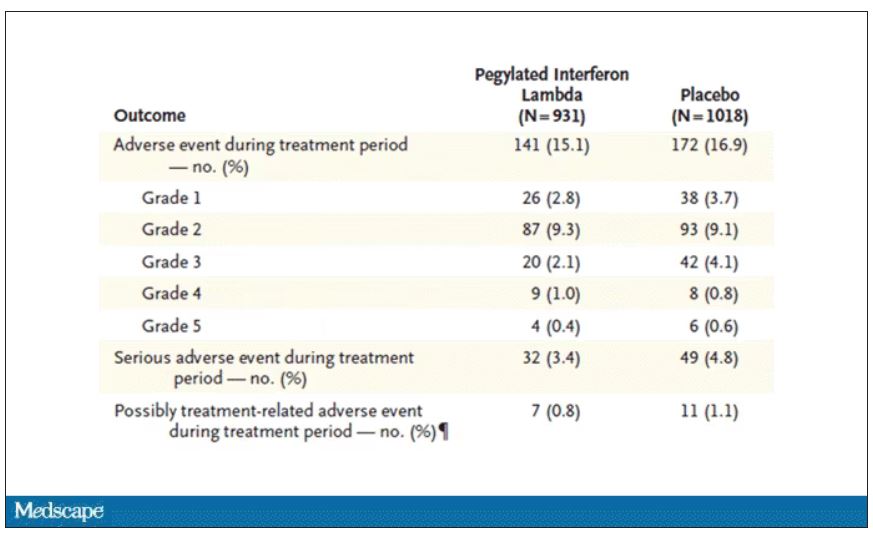
Putting it all together, the state of play for interferons in COVID may be changing. To date, the FDA has not recommended the use of interferon alfa or -beta for COVID-19, citing some data that they are ineffective or even harmful in hospitalized patients with COVID. Interferon lambda is not FDA approved and thus not even available in the United States. But the reason it has not been approved is that there has not been a large, well-conducted interferon lambda trial. Now there is. Will this study be enough to prompt an emergency use authorization? The elephant in the room, of course, is Paxlovid, which at this point has a longer safety track record and, importantly, is oral. I’d love to see a head-to-head trial. Short of that, I tend to be in favor of having more options on the table.
Dr. Perry Wilson is associate professor, department of medicine, and director, Clinical and Translational Research Accelerator, at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
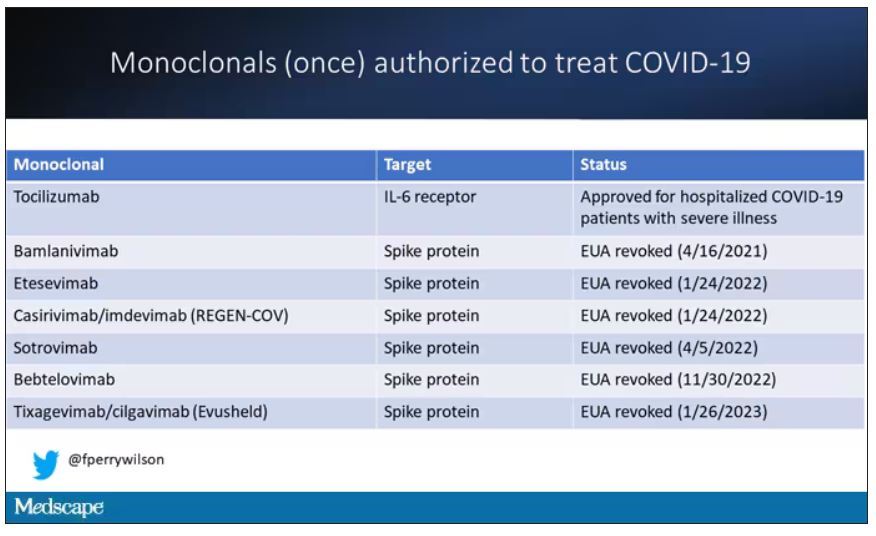
At this point, with the monoclonals found to be essentially useless, we are left with remdesivir with its modest efficacy and Paxlovid, which, for some reason, people don’t seem to be taking.
Part of the reason the monoclonals have failed lately is because of their specificity; they are homogeneous antibodies targeted toward a very specific epitope that may change from variant to variant. We need a broader therapeutic, one that has activity across all variants — maybe even one that has activity against all viruses? We’ve got one. Interferon.
The first mention of interferon as a potential COVID therapy was at the very start of the pandemic, so I’m sort of surprised that the first large, randomized trial is only being reported now in the New England Journal of Medicine.
Before we dig into the results, let’s talk mechanism. This is a trial of interferon-lambda, also known as interleukin-29.
The lambda interferons were only discovered in 2003. They differ from the more familiar interferons only in their cellular receptors; the downstream effects seem quite similar. As opposed to the cellular receptors for interferon alfa, which are widely expressed, the receptors for lambda are restricted to epithelial tissues. This makes it a good choice as a COVID treatment, since the virus also preferentially targets those epithelial cells.
In this study, 1,951 participants from Brazil and Canada, but mostly Brazil, with new COVID infections who were not yet hospitalized were randomized to receive 180 mcg of interferon lambda or placebo.
This was a relatively current COVID trial, as you can see from the participant characteristics. The majority had been vaccinated, and nearly half of the infections were during the Omicron phase of the pandemic.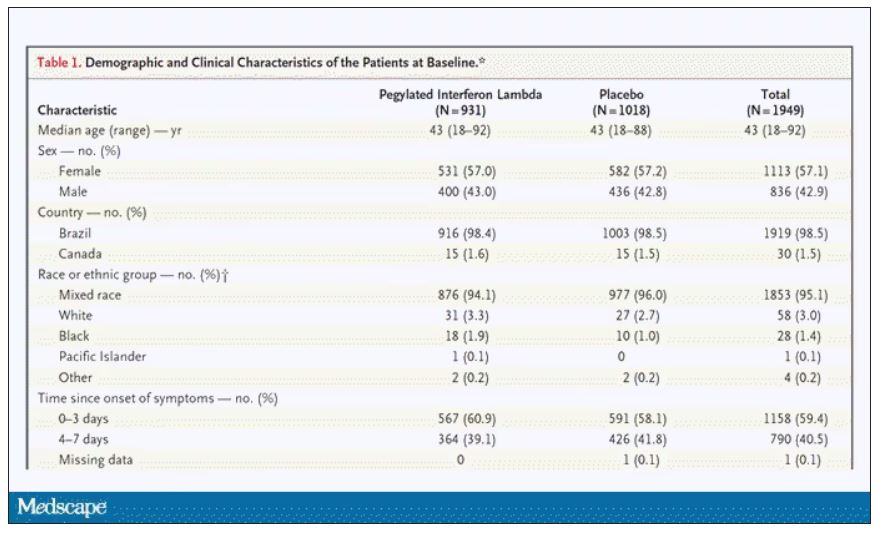
If you just want to cut to the chase, interferon worked.
The primary outcome – hospitalization or a prolonged emergency room visit for COVID – was 50% lower in the interferon group.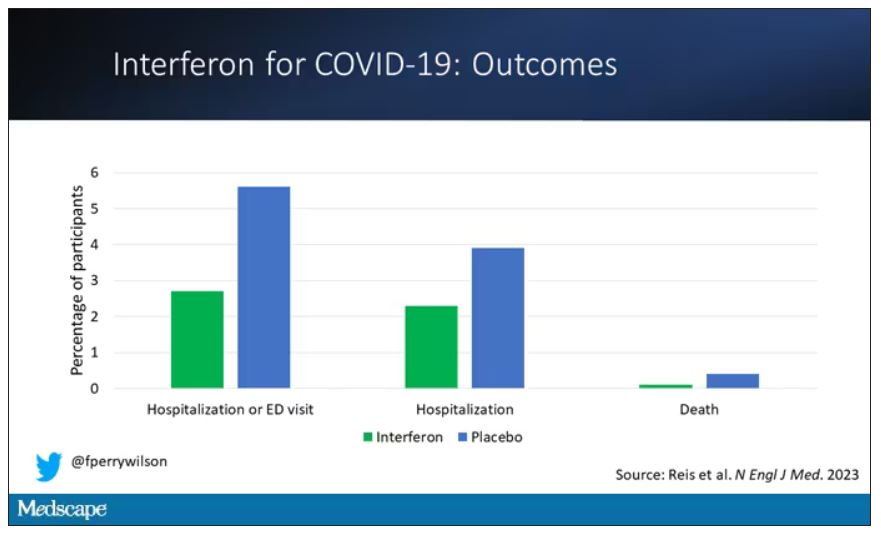
Key secondary outcomes, including death from COVID, were lower in the interferon group as well. These effects persisted across most of the subgroups I was looking out for.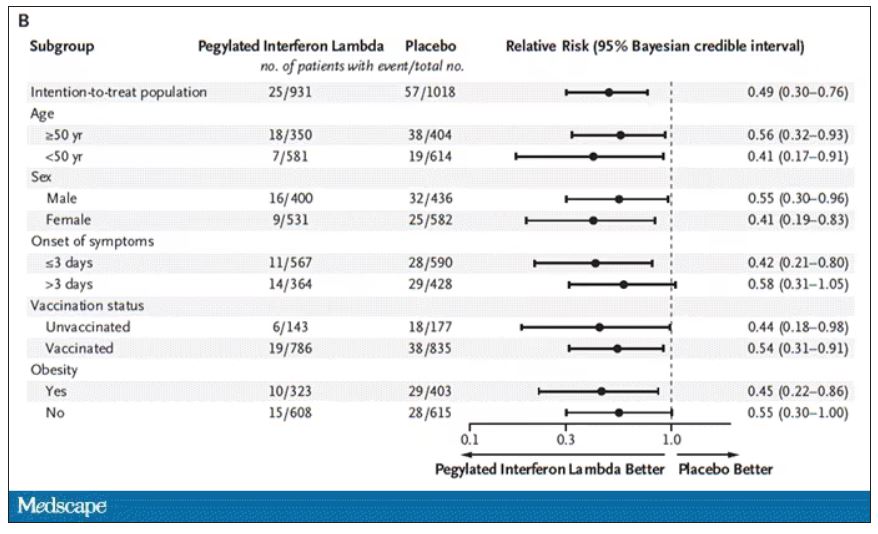
Interferon seemed to help those who were already vaccinated and those who were unvaccinated. There’s a hint that it works better within the first few days of symptoms, which isn’t surprising; we’ve seen this for many of the therapeutics, including Paxlovid. Time is of the essence. Encouragingly, the effect was a bit more pronounced among those infected with Omicron.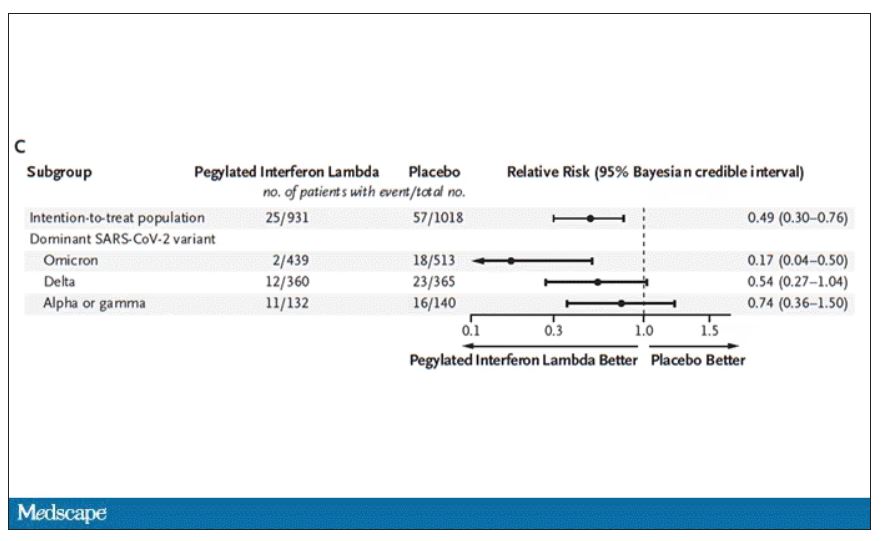
Of course, if you have any experience with interferon, you know that the side effects can be pretty rough. In the bad old days when we treated hepatitis C infection with interferon, patients would get their injections on Friday in anticipation of being essentially out of commission with flu-like symptoms through the weekend. But we don’t see much evidence of adverse events in this trial, maybe due to the greater specificity of interferon lambda.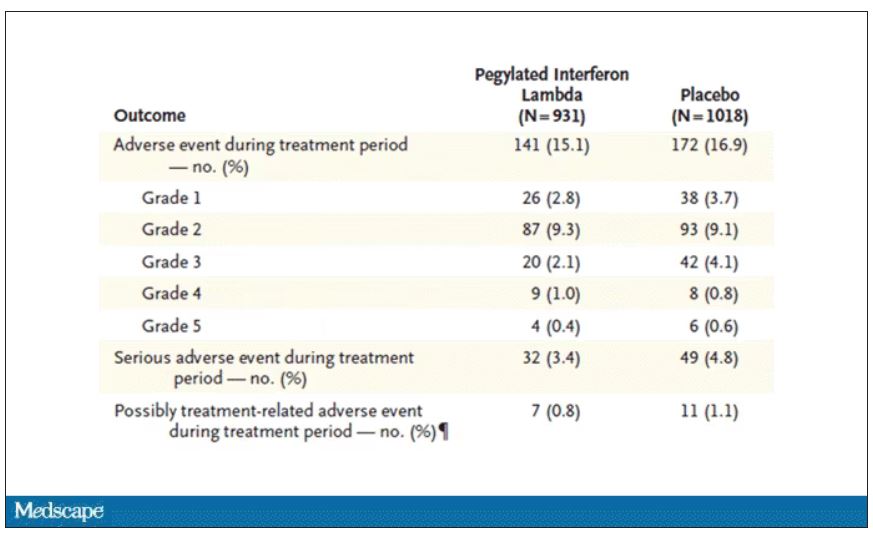
Putting it all together, the state of play for interferons in COVID may be changing. To date, the FDA has not recommended the use of interferon alfa or -beta for COVID-19, citing some data that they are ineffective or even harmful in hospitalized patients with COVID. Interferon lambda is not FDA approved and thus not even available in the United States. But the reason it has not been approved is that there has not been a large, well-conducted interferon lambda trial. Now there is. Will this study be enough to prompt an emergency use authorization? The elephant in the room, of course, is Paxlovid, which at this point has a longer safety track record and, importantly, is oral. I’d love to see a head-to-head trial. Short of that, I tend to be in favor of having more options on the table.
Dr. Perry Wilson is associate professor, department of medicine, and director, Clinical and Translational Research Accelerator, at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Maternal COVID-19 vaccine curbs infant infection
a new study shows.
Previous research has confirmed that COVID-19 neutralizing antibodies following maternal vaccination or maternal COVID-19 infection are present in umbilical cord blood, breast milk, and infant serum specimens, wrote Sarah C.J. Jorgensen, PharmD, MPH, of the University of Toronto, and colleagues in their article published in The BMJ.
In the study, the researchers identified maternal and newborn pairs using administrative databases from Canada. The study population included 8,809 infants aged younger than 6 months who were born between May 7, 2021, and March 31, 2022, and who underwent testing for COVID-19 between May 7, 2021, and September 5, 2022.
Maternal vaccination with the primary COVID-19 mRNA monovalent vaccine series was defined as two vaccine doses administered up to 14 days before delivery, with at least one of the doses after the conception date.
Maternal vaccination with the primary series plus one booster was defined as three doses administered up to 14 days before delivery, with at least one of these doses after the conception date.
The primary outcome was the presence of delta or omicron COVID-19 infection or hospital admission of the infants.
The study population included 99 COVID-19 cases with the delta variant (with 4,365 controls) and 1,501 cases with the omicron variant (with 4,847 controls).
Overall, the vaccine effectiveness of maternal doses was 95% against delta infection and 45% against omicron.
The effectiveness against hospital admission in cases of delta and omicron variants were 97% and 53%, respectively.
The effectiveness of three doses was 73% against omicron infant infection and 80% against omicron-related infant hospitalization. Data were not available for the effectiveness of three doses against the delta variant.
The effectiveness of two doses of vaccine against infant omicron infection was highest when mothers received the second dose during the third trimester of pregnancy, compared with during the first trimester or second trimester (53% vs. 47% and 53% vs. 37%, respectively).
Vaccine effectiveness with two doses against infant infection from omicron was highest in the first 8 weeks of life (57%), then decreased to 40% among infants after 16 weeks of age.
Although the study was not designed to assess the mechanism of action of the impact of maternal vaccination on infants, the current study results were consistent with other recent studies showing a reduction in infections and hospitalizations among infants whose mothers received COVID-19 vaccines during pregnancy, the researchers wrote in their discussion.
The findings were limited by several factors including the potential unmeasured confounders not available in databases, such as whether infants were breastfed, the researchers noted. Other limitations included a lack of data on home test results and the inability to assess the waning impact of the vaccine effectiveness against the delta variant because of the small number of delta cases, they said. However, the results suggest that the mRNA COVID-19 vaccine during pregnancy was moderately to highly effective for protection against omicron and delta infection and infection-related hospitalization – especially during the first 8 weeks of life.
Effectiveness is encouraging, but updates are needed
The effectiveness of maternal vaccination to prevent COVID-19 infection and related hospitalizations in infants is promising, especially since those younger than 6 months have no other source of vaccine protection against COVID-19 infection, wrote Dana Danino, MD, of Soroka University Medical Center, Israel, and Ilan Youngster, MD, of Shamir Medical Center, Israel, in an accompanying editorial also published in The BMJ.
They also noted that maternal vaccination during pregnancy is an established method of protecting infants from infections such as influenza and pertussis.
Data from previous studies show that most infants whose mothers were vaccinated against COVID-19 during pregnancy retained maternal antibodies at 6 months, “but evidence for protection against neonatal COVID-19 infection has been deficient,” they said.
The current study findings support the value of vaccination during pregnancy, and the findings were strengthened by the large study population, the editorialists wrote. However, whether the same effectiveness holds for other COVID-19 strains such as BQ.1, BQ.1.1, BF.7, XBB, and XBB.1 remains unknown, they said.
Other areas in need of exploration include the optimal timing of vaccination during pregnancy, the protective effects of a bivalent mRNA vaccine (vs. the primary monovalent vaccine in the current study), and the potential benefits of additional boosters, they added.
“Although Jorgenson and colleagues’ study reinforces the value of maternal vaccination against COVID-19 during pregnancy, more studies are needed to better inform vaccination recommendations in an evolving landscape of new SARS-CoV-2 strains and novel vaccines,” the editorialists concluded.
The study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and the Ministry of Long-term Care; the study also received funding from the Canadian Immunization Research Network and the Public Health Agency of Canada. Dr. Jorgensen and the editorialists had no financial conflicts to disclose.
*This article was updated on 3/2/2023.
a new study shows.
Previous research has confirmed that COVID-19 neutralizing antibodies following maternal vaccination or maternal COVID-19 infection are present in umbilical cord blood, breast milk, and infant serum specimens, wrote Sarah C.J. Jorgensen, PharmD, MPH, of the University of Toronto, and colleagues in their article published in The BMJ.
In the study, the researchers identified maternal and newborn pairs using administrative databases from Canada. The study population included 8,809 infants aged younger than 6 months who were born between May 7, 2021, and March 31, 2022, and who underwent testing for COVID-19 between May 7, 2021, and September 5, 2022.
Maternal vaccination with the primary COVID-19 mRNA monovalent vaccine series was defined as two vaccine doses administered up to 14 days before delivery, with at least one of the doses after the conception date.
Maternal vaccination with the primary series plus one booster was defined as three doses administered up to 14 days before delivery, with at least one of these doses after the conception date.
The primary outcome was the presence of delta or omicron COVID-19 infection or hospital admission of the infants.
The study population included 99 COVID-19 cases with the delta variant (with 4,365 controls) and 1,501 cases with the omicron variant (with 4,847 controls).
Overall, the vaccine effectiveness of maternal doses was 95% against delta infection and 45% against omicron.
The effectiveness against hospital admission in cases of delta and omicron variants were 97% and 53%, respectively.
The effectiveness of three doses was 73% against omicron infant infection and 80% against omicron-related infant hospitalization. Data were not available for the effectiveness of three doses against the delta variant.
The effectiveness of two doses of vaccine against infant omicron infection was highest when mothers received the second dose during the third trimester of pregnancy, compared with during the first trimester or second trimester (53% vs. 47% and 53% vs. 37%, respectively).
Vaccine effectiveness with two doses against infant infection from omicron was highest in the first 8 weeks of life (57%), then decreased to 40% among infants after 16 weeks of age.
Although the study was not designed to assess the mechanism of action of the impact of maternal vaccination on infants, the current study results were consistent with other recent studies showing a reduction in infections and hospitalizations among infants whose mothers received COVID-19 vaccines during pregnancy, the researchers wrote in their discussion.
The findings were limited by several factors including the potential unmeasured confounders not available in databases, such as whether infants were breastfed, the researchers noted. Other limitations included a lack of data on home test results and the inability to assess the waning impact of the vaccine effectiveness against the delta variant because of the small number of delta cases, they said. However, the results suggest that the mRNA COVID-19 vaccine during pregnancy was moderately to highly effective for protection against omicron and delta infection and infection-related hospitalization – especially during the first 8 weeks of life.
Effectiveness is encouraging, but updates are needed
The effectiveness of maternal vaccination to prevent COVID-19 infection and related hospitalizations in infants is promising, especially since those younger than 6 months have no other source of vaccine protection against COVID-19 infection, wrote Dana Danino, MD, of Soroka University Medical Center, Israel, and Ilan Youngster, MD, of Shamir Medical Center, Israel, in an accompanying editorial also published in The BMJ.
They also noted that maternal vaccination during pregnancy is an established method of protecting infants from infections such as influenza and pertussis.
Data from previous studies show that most infants whose mothers were vaccinated against COVID-19 during pregnancy retained maternal antibodies at 6 months, “but evidence for protection against neonatal COVID-19 infection has been deficient,” they said.
The current study findings support the value of vaccination during pregnancy, and the findings were strengthened by the large study population, the editorialists wrote. However, whether the same effectiveness holds for other COVID-19 strains such as BQ.1, BQ.1.1, BF.7, XBB, and XBB.1 remains unknown, they said.
Other areas in need of exploration include the optimal timing of vaccination during pregnancy, the protective effects of a bivalent mRNA vaccine (vs. the primary monovalent vaccine in the current study), and the potential benefits of additional boosters, they added.
“Although Jorgenson and colleagues’ study reinforces the value of maternal vaccination against COVID-19 during pregnancy, more studies are needed to better inform vaccination recommendations in an evolving landscape of new SARS-CoV-2 strains and novel vaccines,” the editorialists concluded.
The study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and the Ministry of Long-term Care; the study also received funding from the Canadian Immunization Research Network and the Public Health Agency of Canada. Dr. Jorgensen and the editorialists had no financial conflicts to disclose.
*This article was updated on 3/2/2023.
a new study shows.
Previous research has confirmed that COVID-19 neutralizing antibodies following maternal vaccination or maternal COVID-19 infection are present in umbilical cord blood, breast milk, and infant serum specimens, wrote Sarah C.J. Jorgensen, PharmD, MPH, of the University of Toronto, and colleagues in their article published in The BMJ.
In the study, the researchers identified maternal and newborn pairs using administrative databases from Canada. The study population included 8,809 infants aged younger than 6 months who were born between May 7, 2021, and March 31, 2022, and who underwent testing for COVID-19 between May 7, 2021, and September 5, 2022.
Maternal vaccination with the primary COVID-19 mRNA monovalent vaccine series was defined as two vaccine doses administered up to 14 days before delivery, with at least one of the doses after the conception date.
Maternal vaccination with the primary series plus one booster was defined as three doses administered up to 14 days before delivery, with at least one of these doses after the conception date.
The primary outcome was the presence of delta or omicron COVID-19 infection or hospital admission of the infants.
The study population included 99 COVID-19 cases with the delta variant (with 4,365 controls) and 1,501 cases with the omicron variant (with 4,847 controls).
Overall, the vaccine effectiveness of maternal doses was 95% against delta infection and 45% against omicron.
The effectiveness against hospital admission in cases of delta and omicron variants were 97% and 53%, respectively.
The effectiveness of three doses was 73% against omicron infant infection and 80% against omicron-related infant hospitalization. Data were not available for the effectiveness of three doses against the delta variant.
The effectiveness of two doses of vaccine against infant omicron infection was highest when mothers received the second dose during the third trimester of pregnancy, compared with during the first trimester or second trimester (53% vs. 47% and 53% vs. 37%, respectively).
Vaccine effectiveness with two doses against infant infection from omicron was highest in the first 8 weeks of life (57%), then decreased to 40% among infants after 16 weeks of age.
Although the study was not designed to assess the mechanism of action of the impact of maternal vaccination on infants, the current study results were consistent with other recent studies showing a reduction in infections and hospitalizations among infants whose mothers received COVID-19 vaccines during pregnancy, the researchers wrote in their discussion.
The findings were limited by several factors including the potential unmeasured confounders not available in databases, such as whether infants were breastfed, the researchers noted. Other limitations included a lack of data on home test results and the inability to assess the waning impact of the vaccine effectiveness against the delta variant because of the small number of delta cases, they said. However, the results suggest that the mRNA COVID-19 vaccine during pregnancy was moderately to highly effective for protection against omicron and delta infection and infection-related hospitalization – especially during the first 8 weeks of life.
Effectiveness is encouraging, but updates are needed
The effectiveness of maternal vaccination to prevent COVID-19 infection and related hospitalizations in infants is promising, especially since those younger than 6 months have no other source of vaccine protection against COVID-19 infection, wrote Dana Danino, MD, of Soroka University Medical Center, Israel, and Ilan Youngster, MD, of Shamir Medical Center, Israel, in an accompanying editorial also published in The BMJ.
They also noted that maternal vaccination during pregnancy is an established method of protecting infants from infections such as influenza and pertussis.
Data from previous studies show that most infants whose mothers were vaccinated against COVID-19 during pregnancy retained maternal antibodies at 6 months, “but evidence for protection against neonatal COVID-19 infection has been deficient,” they said.
The current study findings support the value of vaccination during pregnancy, and the findings were strengthened by the large study population, the editorialists wrote. However, whether the same effectiveness holds for other COVID-19 strains such as BQ.1, BQ.1.1, BF.7, XBB, and XBB.1 remains unknown, they said.
Other areas in need of exploration include the optimal timing of vaccination during pregnancy, the protective effects of a bivalent mRNA vaccine (vs. the primary monovalent vaccine in the current study), and the potential benefits of additional boosters, they added.
“Although Jorgenson and colleagues’ study reinforces the value of maternal vaccination against COVID-19 during pregnancy, more studies are needed to better inform vaccination recommendations in an evolving landscape of new SARS-CoV-2 strains and novel vaccines,” the editorialists concluded.
The study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and the Ministry of Long-term Care; the study also received funding from the Canadian Immunization Research Network and the Public Health Agency of Canada. Dr. Jorgensen and the editorialists had no financial conflicts to disclose.
*This article was updated on 3/2/2023.
FROM THE BMJ
Drinking tea can keep your heart healthy as you age
according to the Heart Foundation and researchers from Edith Cowan University, Perth, Australia.
What to know
- Elderly women who drank black tea on a regular basis or consumed a high level of flavonoids in their diet were found to be far less likely to develop extensive AAC.
- AAC is calcification of the large artery that supplies oxygenated blood from the heart to the abdominal organs and lower limbs. It is associated with cardiovascular disorders, such as heart attack and stroke, as well as late-life dementia.
- Flavonoids are naturally occurring substances that regulate cellular activity. They are found in many common foods and beverages, such as black tea, green tea, apples, nuts, citrus fruit, berries, red wine, dark chocolate, and others.
- Study participants who had a higher intake of total flavonoids, flavan-3-ols, and flavonols were almost 40% less likely to have extensive AAC, while those who drank two to six cups of black tea per day had up to 42% less chance of experiencing extensive AAC.
- People who do not drink tea can still benefit by including foods rich in flavonoids in their diet, which protects against extensive calcification of the arteries.
This is a summary of the article, “Higher Habitual Dietary Flavonoid Intake Associates With Less Extensive Abdominal Aortic Calcification in a Cohort of Older Women,” published in Arteriosclerosis, Thrombosis, and Vascular Biology on Nov. 2, 2022. The full article can be found on ahajournals.org. A version of this article originally appeared on Medscape.com.
according to the Heart Foundation and researchers from Edith Cowan University, Perth, Australia.
What to know
- Elderly women who drank black tea on a regular basis or consumed a high level of flavonoids in their diet were found to be far less likely to develop extensive AAC.
- AAC is calcification of the large artery that supplies oxygenated blood from the heart to the abdominal organs and lower limbs. It is associated with cardiovascular disorders, such as heart attack and stroke, as well as late-life dementia.
- Flavonoids are naturally occurring substances that regulate cellular activity. They are found in many common foods and beverages, such as black tea, green tea, apples, nuts, citrus fruit, berries, red wine, dark chocolate, and others.
- Study participants who had a higher intake of total flavonoids, flavan-3-ols, and flavonols were almost 40% less likely to have extensive AAC, while those who drank two to six cups of black tea per day had up to 42% less chance of experiencing extensive AAC.
- People who do not drink tea can still benefit by including foods rich in flavonoids in their diet, which protects against extensive calcification of the arteries.
This is a summary of the article, “Higher Habitual Dietary Flavonoid Intake Associates With Less Extensive Abdominal Aortic Calcification in a Cohort of Older Women,” published in Arteriosclerosis, Thrombosis, and Vascular Biology on Nov. 2, 2022. The full article can be found on ahajournals.org. A version of this article originally appeared on Medscape.com.
according to the Heart Foundation and researchers from Edith Cowan University, Perth, Australia.
What to know
- Elderly women who drank black tea on a regular basis or consumed a high level of flavonoids in their diet were found to be far less likely to develop extensive AAC.
- AAC is calcification of the large artery that supplies oxygenated blood from the heart to the abdominal organs and lower limbs. It is associated with cardiovascular disorders, such as heart attack and stroke, as well as late-life dementia.
- Flavonoids are naturally occurring substances that regulate cellular activity. They are found in many common foods and beverages, such as black tea, green tea, apples, nuts, citrus fruit, berries, red wine, dark chocolate, and others.
- Study participants who had a higher intake of total flavonoids, flavan-3-ols, and flavonols were almost 40% less likely to have extensive AAC, while those who drank two to six cups of black tea per day had up to 42% less chance of experiencing extensive AAC.
- People who do not drink tea can still benefit by including foods rich in flavonoids in their diet, which protects against extensive calcification of the arteries.
This is a summary of the article, “Higher Habitual Dietary Flavonoid Intake Associates With Less Extensive Abdominal Aortic Calcification in a Cohort of Older Women,” published in Arteriosclerosis, Thrombosis, and Vascular Biology on Nov. 2, 2022. The full article can be found on ahajournals.org. A version of this article originally appeared on Medscape.com.
No spike in overdose deaths from relaxed buprenorphine regulations
Researchers say the data add weight to the argument for permanently adopting the pandemic-era prescribing regulations for buprenorphine, a treatment for opioid use disorder.
“We saw no evidence that increased availability of buprenorphine through the loosening of rules around prescribing and dispensing of buprenorphine during the pandemic increased overdose deaths,” investigator Wilson Compton, MD, deputy director of the National Institute on Drug Abuse, told this news organization.
“This is reassuring that, even when we opened up the doors to easier access to buprenorphine, we didn’t see that most serious consequence,” Dr. Compton said.
The findings were published online in JAMA Network Open .
Cause and effect
Federal agencies relaxed prescribing regulations for buprenorphine in March 2020 to make it easier for clinicians to prescribe the drug via telemedicine and for patients to take the medication at home.
The number of buprenorphine prescriptions has increased since that change, with more than 1 million people receiving the medication in 2021 from retail pharmacies in the United States.
However, questions remained about whether increased access would lead to an increase in buprenorphine-involved overdose.
Researchers with NIDA and the Centers for Disease Control and Prevention analyzed data from the State Unintentional Drug Overdose Reporting System, a CDC database that combines medical examiner and coroner reports and postmortem toxicology testing.
The study included information about overdose deaths from July 2019 to June 2021 in 46 states and the District of Columbia.
Between July 2019 and June 2021, there were 1,955 buprenorphine-involved overdose deaths, which accounted for 2.2% of all drug overdose deaths and 2.6% of opioid-involved overdose deaths.
However, researchers went beyond overall numbers and evaluated details from coroner’s and medical examiner reports, something they had not done before.
“For the first time we looked at the characteristics of decedents from buprenorphine because this has not been studied in this type of detail with a near-national sample,” Dr. Compton said.
“That allowed us to look at patterns of use of other substances as well as the circumstances that are recorded at the death scene that are in the data set,” he added.
Important insights
Reports from nearly all buprenorphine-involved deaths included the presence of at least one other drug, compared with opioid overdose deaths that typically involved only one drug.
“This is consistent with the pharmacology of buprenorphine being a partial agonist, so it may not be as fatal all by itself as some of the other opioids,” Dr. Compton said.
Deaths involving buprenorphine were less likely to include illicitly manufactured fentanyls, and other prescription medications were more often found on the scene, such as antidepressants.
Compared with opioid decedents, buprenorphine decedents were more likely to be women, age 35-44, White, and receiving treatment for mental health conditions, including for substance use disorder (SUD).
These kinds of characteristics provide important insights about potential ways to improve safety and clinical outcomes, Dr. Compton noted.
“When we see things like a little higher rate of SUD treatment and this evidence of other prescription drugs on the scene, and some higher rates of antidepressants in these decedents than I might have expected, I’m very curious about their use of other medical services outside of substance use treatment, because that might be a place where some interventions could be implemented,” he said.
A similar study showed pandemic-era policy changes that allowed methadone to be taken at home was followed by a decrease in methadone-related overdose deaths.
The new findings are consistent with those results, Dr. Compton said.
‘Chipping away’ at stigma
Commenting on the study, O. Trent Hall, DO, assistant professor of addiction medicine, Department of Psychiatry and Behavioral Health, Ohio State University Wexner Medical Center, Columbus, said that, although he welcomed the findings, they aren’t unexpected.
“Buprenorphine is well established as a safe and effective medication for opioid use disorder and as a physician who routinely cares for patients in the hospital after opioid overdose, I am not at all surprised by these results,” said Dr. Hall, who was not involved with the research.
“When my patients leave the hospital with a buprenorphine prescription, they are much less likely to return with another overdose or serious opioid-related medical problem,” he added.
U.S. drug overdose deaths topped 100,000 for the first time in 2021, and most were opioid-related. Although the latest data from the CDC shows drug overdose deaths have been declining slowly since early 2022, the numbers remain high.
Buprenorphine is one of only two drugs known to reduce the risk of opioid overdose. While prescriptions have increased since 2020, the medication remains underutilized, despite its known effectiveness in treating opioid use disorder.
Dr. Hall noted that research such as the new study could help increase buprenorphine’s use.
“Studies like this one chip away at the stigma that has been misapplied to buprenorphine,” he said. “I hope this article will encourage more providers to offer buprenorphine to patients with opioid use disorder.”
The study was funded internally by NIDA and the CDC. Dr. Compton reported owning stock in General Electric, 3M, and Pfizer outside the submitted work. Dr. Hall has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers say the data add weight to the argument for permanently adopting the pandemic-era prescribing regulations for buprenorphine, a treatment for opioid use disorder.
“We saw no evidence that increased availability of buprenorphine through the loosening of rules around prescribing and dispensing of buprenorphine during the pandemic increased overdose deaths,” investigator Wilson Compton, MD, deputy director of the National Institute on Drug Abuse, told this news organization.
“This is reassuring that, even when we opened up the doors to easier access to buprenorphine, we didn’t see that most serious consequence,” Dr. Compton said.
The findings were published online in JAMA Network Open .
Cause and effect
Federal agencies relaxed prescribing regulations for buprenorphine in March 2020 to make it easier for clinicians to prescribe the drug via telemedicine and for patients to take the medication at home.
The number of buprenorphine prescriptions has increased since that change, with more than 1 million people receiving the medication in 2021 from retail pharmacies in the United States.
However, questions remained about whether increased access would lead to an increase in buprenorphine-involved overdose.
Researchers with NIDA and the Centers for Disease Control and Prevention analyzed data from the State Unintentional Drug Overdose Reporting System, a CDC database that combines medical examiner and coroner reports and postmortem toxicology testing.
The study included information about overdose deaths from July 2019 to June 2021 in 46 states and the District of Columbia.
Between July 2019 and June 2021, there were 1,955 buprenorphine-involved overdose deaths, which accounted for 2.2% of all drug overdose deaths and 2.6% of opioid-involved overdose deaths.
However, researchers went beyond overall numbers and evaluated details from coroner’s and medical examiner reports, something they had not done before.
“For the first time we looked at the characteristics of decedents from buprenorphine because this has not been studied in this type of detail with a near-national sample,” Dr. Compton said.
“That allowed us to look at patterns of use of other substances as well as the circumstances that are recorded at the death scene that are in the data set,” he added.
Important insights
Reports from nearly all buprenorphine-involved deaths included the presence of at least one other drug, compared with opioid overdose deaths that typically involved only one drug.
“This is consistent with the pharmacology of buprenorphine being a partial agonist, so it may not be as fatal all by itself as some of the other opioids,” Dr. Compton said.
Deaths involving buprenorphine were less likely to include illicitly manufactured fentanyls, and other prescription medications were more often found on the scene, such as antidepressants.
Compared with opioid decedents, buprenorphine decedents were more likely to be women, age 35-44, White, and receiving treatment for mental health conditions, including for substance use disorder (SUD).
These kinds of characteristics provide important insights about potential ways to improve safety and clinical outcomes, Dr. Compton noted.
“When we see things like a little higher rate of SUD treatment and this evidence of other prescription drugs on the scene, and some higher rates of antidepressants in these decedents than I might have expected, I’m very curious about their use of other medical services outside of substance use treatment, because that might be a place where some interventions could be implemented,” he said.
A similar study showed pandemic-era policy changes that allowed methadone to be taken at home was followed by a decrease in methadone-related overdose deaths.
The new findings are consistent with those results, Dr. Compton said.
‘Chipping away’ at stigma
Commenting on the study, O. Trent Hall, DO, assistant professor of addiction medicine, Department of Psychiatry and Behavioral Health, Ohio State University Wexner Medical Center, Columbus, said that, although he welcomed the findings, they aren’t unexpected.
“Buprenorphine is well established as a safe and effective medication for opioid use disorder and as a physician who routinely cares for patients in the hospital after opioid overdose, I am not at all surprised by these results,” said Dr. Hall, who was not involved with the research.
“When my patients leave the hospital with a buprenorphine prescription, they are much less likely to return with another overdose or serious opioid-related medical problem,” he added.
U.S. drug overdose deaths topped 100,000 for the first time in 2021, and most were opioid-related. Although the latest data from the CDC shows drug overdose deaths have been declining slowly since early 2022, the numbers remain high.
Buprenorphine is one of only two drugs known to reduce the risk of opioid overdose. While prescriptions have increased since 2020, the medication remains underutilized, despite its known effectiveness in treating opioid use disorder.
Dr. Hall noted that research such as the new study could help increase buprenorphine’s use.
“Studies like this one chip away at the stigma that has been misapplied to buprenorphine,” he said. “I hope this article will encourage more providers to offer buprenorphine to patients with opioid use disorder.”
The study was funded internally by NIDA and the CDC. Dr. Compton reported owning stock in General Electric, 3M, and Pfizer outside the submitted work. Dr. Hall has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers say the data add weight to the argument for permanently adopting the pandemic-era prescribing regulations for buprenorphine, a treatment for opioid use disorder.
“We saw no evidence that increased availability of buprenorphine through the loosening of rules around prescribing and dispensing of buprenorphine during the pandemic increased overdose deaths,” investigator Wilson Compton, MD, deputy director of the National Institute on Drug Abuse, told this news organization.
“This is reassuring that, even when we opened up the doors to easier access to buprenorphine, we didn’t see that most serious consequence,” Dr. Compton said.
The findings were published online in JAMA Network Open .
Cause and effect
Federal agencies relaxed prescribing regulations for buprenorphine in March 2020 to make it easier for clinicians to prescribe the drug via telemedicine and for patients to take the medication at home.
The number of buprenorphine prescriptions has increased since that change, with more than 1 million people receiving the medication in 2021 from retail pharmacies in the United States.
However, questions remained about whether increased access would lead to an increase in buprenorphine-involved overdose.
Researchers with NIDA and the Centers for Disease Control and Prevention analyzed data from the State Unintentional Drug Overdose Reporting System, a CDC database that combines medical examiner and coroner reports and postmortem toxicology testing.
The study included information about overdose deaths from July 2019 to June 2021 in 46 states and the District of Columbia.
Between July 2019 and June 2021, there were 1,955 buprenorphine-involved overdose deaths, which accounted for 2.2% of all drug overdose deaths and 2.6% of opioid-involved overdose deaths.
However, researchers went beyond overall numbers and evaluated details from coroner’s and medical examiner reports, something they had not done before.
“For the first time we looked at the characteristics of decedents from buprenorphine because this has not been studied in this type of detail with a near-national sample,” Dr. Compton said.
“That allowed us to look at patterns of use of other substances as well as the circumstances that are recorded at the death scene that are in the data set,” he added.
Important insights
Reports from nearly all buprenorphine-involved deaths included the presence of at least one other drug, compared with opioid overdose deaths that typically involved only one drug.
“This is consistent with the pharmacology of buprenorphine being a partial agonist, so it may not be as fatal all by itself as some of the other opioids,” Dr. Compton said.
Deaths involving buprenorphine were less likely to include illicitly manufactured fentanyls, and other prescription medications were more often found on the scene, such as antidepressants.
Compared with opioid decedents, buprenorphine decedents were more likely to be women, age 35-44, White, and receiving treatment for mental health conditions, including for substance use disorder (SUD).
These kinds of characteristics provide important insights about potential ways to improve safety and clinical outcomes, Dr. Compton noted.
“When we see things like a little higher rate of SUD treatment and this evidence of other prescription drugs on the scene, and some higher rates of antidepressants in these decedents than I might have expected, I’m very curious about their use of other medical services outside of substance use treatment, because that might be a place where some interventions could be implemented,” he said.
A similar study showed pandemic-era policy changes that allowed methadone to be taken at home was followed by a decrease in methadone-related overdose deaths.
The new findings are consistent with those results, Dr. Compton said.
‘Chipping away’ at stigma
Commenting on the study, O. Trent Hall, DO, assistant professor of addiction medicine, Department of Psychiatry and Behavioral Health, Ohio State University Wexner Medical Center, Columbus, said that, although he welcomed the findings, they aren’t unexpected.
“Buprenorphine is well established as a safe and effective medication for opioid use disorder and as a physician who routinely cares for patients in the hospital after opioid overdose, I am not at all surprised by these results,” said Dr. Hall, who was not involved with the research.
“When my patients leave the hospital with a buprenorphine prescription, they are much less likely to return with another overdose or serious opioid-related medical problem,” he added.
U.S. drug overdose deaths topped 100,000 for the first time in 2021, and most were opioid-related. Although the latest data from the CDC shows drug overdose deaths have been declining slowly since early 2022, the numbers remain high.
Buprenorphine is one of only two drugs known to reduce the risk of opioid overdose. While prescriptions have increased since 2020, the medication remains underutilized, despite its known effectiveness in treating opioid use disorder.
Dr. Hall noted that research such as the new study could help increase buprenorphine’s use.
“Studies like this one chip away at the stigma that has been misapplied to buprenorphine,” he said. “I hope this article will encourage more providers to offer buprenorphine to patients with opioid use disorder.”
The study was funded internally by NIDA and the CDC. Dr. Compton reported owning stock in General Electric, 3M, and Pfizer outside the submitted work. Dr. Hall has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Keeping physician stress in check
Fahri Saatcioglu, PhD, and colleagues, whose report was published in the Journal of Clinical Oncology, described it as a “dire situation” with resolutions needed “urgently” to “mitigate the negative consequences of physician burnout.” Both individual and whole-system approaches are needed, wrote Dr. Saatcioglu, a researcher with Oslo University Hospital in Norway who reviewed well-being interventions designed to mitigate physician stress.
When burnout sets in it is marked by emotional exhaustion, depersonalization, and a lack of confidence in one’s ability to do his or her job effectively (often because of lack of support or organizational constraints). It can lead to reduced work efficacy, medical errors, job dissatisfaction, and turnover, Fay J. Hlubocky, PhD, and colleagues, wrote in a report published in the Journal of Clinical Oncology.
During the COVID-19 pandemic, patients postponed doctor visits and procedures. Telemedicine was adopted in place of in-person visits, surgeries were delayed, and oral chemotherapy was prescribed over intravenous therapies, wrote Dr. Hlubocky and colleagues, who addressed the heightened sense of burnout oncologists experienced during the COVID-19 pandemic.
But before the pandemic, oncologists were already overburdened by a system unable to meet the demand for services. And now, because patients delayed doctor visits, more patients are being diagnosed with advanced malignancies.
According to the American Society of Clinical Oncology, the demand for cancer-related services is expected to grow by 40% over the next 6 years. And, by 2025, there will be a shortage of more than 2,200 oncologists in the United States.
Addressing physician burnout can affect the bottom line. According to a report published in Annals of Internal Medicine, physician turnover and reduced clinical hours due to burnout costs the United States $4.6 billion each year.
“It is estimated that 30%-50% of physicians either have burnout symptoms or they experience burnout. A recent study on oncologists in Canada found that symptoms of burnout may reach 73%,” wrote Dr. Saatcioglu and colleagues. “It is clear, for example, that an appropriate workload, resource sufficiency, positive work culture and values, and sufficient social and community support are all very critical for a sustainable and successful health care organization. All of these are also required for the professional satisfaction and well-being of physicians.”
Physician stress has become so serious, that Dr. Saatcioglu and colleagues recommend that hospital administrators “firmly establish the culture of wellness at the workplace” by including physician wellness under the institutional initiatives umbrella. Hospital leadership, they wrote, should strive to mitigate burnout at all levels by addressing issues and adopting strategies for physicians as a workforce and as individuals.
“There is a distinct need to approach the personal needs of the physician as an individual who is experiencing chronic stress that can trigger psychologic symptoms, which further affects not only their own health, family life, etc., but also their clinical performance, quality of the resulting health care, patient satisfaction, and finally the health economy,” the authors wrote.
Some health care organizations have adopted programs and made institutional changes designed to reduce burnout for health care workers. These include online wellness programs both free and paid, but there is little data on the efficacy of these programs.
The review by Dr. Saatcioglu and coauthors included the Online Breath and Meditation Program, a Sudarshan Kriya Yoga (SKY) program of three 90-minute sessions on yoga, effective breathing techniques, and cognitive coping and stressor evaluation strategies that have been effective in helping war veterans, prisoners, patients, and students. The ultimate goal would be to have participants adopt a daily yoga routine. Among 803 health care workers who participated in the program and completed a survey, 85% said they benefited from the program and 94% reported experiencing less stress. And, 81% felt the program would help improve their job performance.
“In the future, we believe that the best place for the individual approaches to physician wellness would be to have them as an integral part of the organizational measures, and ideally, implemented as part of the daily work routine of the physician where the organizational and individual responsibilities would merge,” the authors wrote.
Freelance writer Lorraine L. Janeczko, MPH, contributed to this article.
Fahri Saatcioglu, PhD, and colleagues, whose report was published in the Journal of Clinical Oncology, described it as a “dire situation” with resolutions needed “urgently” to “mitigate the negative consequences of physician burnout.” Both individual and whole-system approaches are needed, wrote Dr. Saatcioglu, a researcher with Oslo University Hospital in Norway who reviewed well-being interventions designed to mitigate physician stress.
When burnout sets in it is marked by emotional exhaustion, depersonalization, and a lack of confidence in one’s ability to do his or her job effectively (often because of lack of support or organizational constraints). It can lead to reduced work efficacy, medical errors, job dissatisfaction, and turnover, Fay J. Hlubocky, PhD, and colleagues, wrote in a report published in the Journal of Clinical Oncology.
During the COVID-19 pandemic, patients postponed doctor visits and procedures. Telemedicine was adopted in place of in-person visits, surgeries were delayed, and oral chemotherapy was prescribed over intravenous therapies, wrote Dr. Hlubocky and colleagues, who addressed the heightened sense of burnout oncologists experienced during the COVID-19 pandemic.
But before the pandemic, oncologists were already overburdened by a system unable to meet the demand for services. And now, because patients delayed doctor visits, more patients are being diagnosed with advanced malignancies.
According to the American Society of Clinical Oncology, the demand for cancer-related services is expected to grow by 40% over the next 6 years. And, by 2025, there will be a shortage of more than 2,200 oncologists in the United States.
Addressing physician burnout can affect the bottom line. According to a report published in Annals of Internal Medicine, physician turnover and reduced clinical hours due to burnout costs the United States $4.6 billion each year.
“It is estimated that 30%-50% of physicians either have burnout symptoms or they experience burnout. A recent study on oncologists in Canada found that symptoms of burnout may reach 73%,” wrote Dr. Saatcioglu and colleagues. “It is clear, for example, that an appropriate workload, resource sufficiency, positive work culture and values, and sufficient social and community support are all very critical for a sustainable and successful health care organization. All of these are also required for the professional satisfaction and well-being of physicians.”
Physician stress has become so serious, that Dr. Saatcioglu and colleagues recommend that hospital administrators “firmly establish the culture of wellness at the workplace” by including physician wellness under the institutional initiatives umbrella. Hospital leadership, they wrote, should strive to mitigate burnout at all levels by addressing issues and adopting strategies for physicians as a workforce and as individuals.
“There is a distinct need to approach the personal needs of the physician as an individual who is experiencing chronic stress that can trigger psychologic symptoms, which further affects not only their own health, family life, etc., but also their clinical performance, quality of the resulting health care, patient satisfaction, and finally the health economy,” the authors wrote.
Some health care organizations have adopted programs and made institutional changes designed to reduce burnout for health care workers. These include online wellness programs both free and paid, but there is little data on the efficacy of these programs.
The review by Dr. Saatcioglu and coauthors included the Online Breath and Meditation Program, a Sudarshan Kriya Yoga (SKY) program of three 90-minute sessions on yoga, effective breathing techniques, and cognitive coping and stressor evaluation strategies that have been effective in helping war veterans, prisoners, patients, and students. The ultimate goal would be to have participants adopt a daily yoga routine. Among 803 health care workers who participated in the program and completed a survey, 85% said they benefited from the program and 94% reported experiencing less stress. And, 81% felt the program would help improve their job performance.
“In the future, we believe that the best place for the individual approaches to physician wellness would be to have them as an integral part of the organizational measures, and ideally, implemented as part of the daily work routine of the physician where the organizational and individual responsibilities would merge,” the authors wrote.
Freelance writer Lorraine L. Janeczko, MPH, contributed to this article.
Fahri Saatcioglu, PhD, and colleagues, whose report was published in the Journal of Clinical Oncology, described it as a “dire situation” with resolutions needed “urgently” to “mitigate the negative consequences of physician burnout.” Both individual and whole-system approaches are needed, wrote Dr. Saatcioglu, a researcher with Oslo University Hospital in Norway who reviewed well-being interventions designed to mitigate physician stress.
When burnout sets in it is marked by emotional exhaustion, depersonalization, and a lack of confidence in one’s ability to do his or her job effectively (often because of lack of support or organizational constraints). It can lead to reduced work efficacy, medical errors, job dissatisfaction, and turnover, Fay J. Hlubocky, PhD, and colleagues, wrote in a report published in the Journal of Clinical Oncology.
During the COVID-19 pandemic, patients postponed doctor visits and procedures. Telemedicine was adopted in place of in-person visits, surgeries were delayed, and oral chemotherapy was prescribed over intravenous therapies, wrote Dr. Hlubocky and colleagues, who addressed the heightened sense of burnout oncologists experienced during the COVID-19 pandemic.
But before the pandemic, oncologists were already overburdened by a system unable to meet the demand for services. And now, because patients delayed doctor visits, more patients are being diagnosed with advanced malignancies.
According to the American Society of Clinical Oncology, the demand for cancer-related services is expected to grow by 40% over the next 6 years. And, by 2025, there will be a shortage of more than 2,200 oncologists in the United States.
Addressing physician burnout can affect the bottom line. According to a report published in Annals of Internal Medicine, physician turnover and reduced clinical hours due to burnout costs the United States $4.6 billion each year.
“It is estimated that 30%-50% of physicians either have burnout symptoms or they experience burnout. A recent study on oncologists in Canada found that symptoms of burnout may reach 73%,” wrote Dr. Saatcioglu and colleagues. “It is clear, for example, that an appropriate workload, resource sufficiency, positive work culture and values, and sufficient social and community support are all very critical for a sustainable and successful health care organization. All of these are also required for the professional satisfaction and well-being of physicians.”
Physician stress has become so serious, that Dr. Saatcioglu and colleagues recommend that hospital administrators “firmly establish the culture of wellness at the workplace” by including physician wellness under the institutional initiatives umbrella. Hospital leadership, they wrote, should strive to mitigate burnout at all levels by addressing issues and adopting strategies for physicians as a workforce and as individuals.
“There is a distinct need to approach the personal needs of the physician as an individual who is experiencing chronic stress that can trigger psychologic symptoms, which further affects not only their own health, family life, etc., but also their clinical performance, quality of the resulting health care, patient satisfaction, and finally the health economy,” the authors wrote.
Some health care organizations have adopted programs and made institutional changes designed to reduce burnout for health care workers. These include online wellness programs both free and paid, but there is little data on the efficacy of these programs.
The review by Dr. Saatcioglu and coauthors included the Online Breath and Meditation Program, a Sudarshan Kriya Yoga (SKY) program of three 90-minute sessions on yoga, effective breathing techniques, and cognitive coping and stressor evaluation strategies that have been effective in helping war veterans, prisoners, patients, and students. The ultimate goal would be to have participants adopt a daily yoga routine. Among 803 health care workers who participated in the program and completed a survey, 85% said they benefited from the program and 94% reported experiencing less stress. And, 81% felt the program would help improve their job performance.
“In the future, we believe that the best place for the individual approaches to physician wellness would be to have them as an integral part of the organizational measures, and ideally, implemented as part of the daily work routine of the physician where the organizational and individual responsibilities would merge,” the authors wrote.
Freelance writer Lorraine L. Janeczko, MPH, contributed to this article.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Acute cardiac events common during COVID hospitalization
particularly among those with underlying heart disease, and are associated with more severe disease outcomes, a new study suggests.
“We expected to see acute cardiac events occurring among adults hospitalized with COVID-19 but were surprised by how frequently they occurred,” Rebecca C. Woodruff, PhD, MPH, of the U.S. Centers for Disease Control and Prevention, Atlanta, told this news organization.
Overall, she said, “about 1 in 10 adults experienced an acute cardiac event – including heart attacks and acute heart failure – while hospitalized with COVID-19, and this included people with no preexisting heart disease.”
However, she added, “about a quarter of those with underlying heart disease had an acute cardiac event. These patients tended to experience more severe disease outcomes relative to patients hospitalized with COVID-19 who did not experience an acute cardiac event.”
The findings might be relevant to hospitalizations for other viral diseases, “though we can’t say for sure,” she noted. “This study was modeled off a previous study conducted before the COVID-19 pandemic among adults hospitalized with influenza. About 11.7% of [those] adults experienced an acute cardiac event, which was a similar percentage as what we found among patients hospitalized with COVID-19.”
The study was published online in the Journal of the American College of Cardiology.
Underlying cardiac disease key
Dr. Woodruff and colleagues analyzed medical records on a probability sample of 8,460 adults hospitalized with SARS-CoV-2 infection identified from 99 U.S. counties in 14 U.S. states (about 10% of the United States population) from January to November 2021.
Among participants, 11.4% had an acute cardiac event during their hospitalization. The median age was 69 years; 56.5% were men; 48.7%, non-Hispanic White; 33.6%, non-Hispanic Black; 7.4%, Hispanic; and 7.1%, non-Hispanic Asian or Pacific Islander.
As indicated, the prevalence was higher among those with underlying cardiac disease (23.4%), compared with those without (6.2%).
Acute ischemic heart disease (5.5%) and acute heart failure (5.4%) were the most prevalent events; 0.3% of participants had acute myocarditis or pericarditis.
Risk factors varied, depending on underlying cardiac disease status. Those who experienced one or more acute cardiac events had a greater risk for intensive care unit admission (adjusted risk ratio,1.9) and in-hospital death (aRR, 1.7) versus those who did not.
In multivariable analyses, the risk of experiencing acute heart failure was significantly greater among men (aRR, 1.5) and among those with a history of congestive heart failure (aRR, 13.5), atrial fibrillation (aRR, 1.6) or hypertension (aRR,1.3).
Among patients who experienced one or more acute cardiac events, 39.2% required an intensive care unit stay for a median of 5 days. Approximately 22.4% required invasive mechanical ventilation or extracorporeal membrane oxygenation, and 21.1% died while hospitalized.
“Persons at greater risk for experiencing acute cardiac events during COVID-19–associated hospitalizations might benefit from more intensive clinical evaluation and monitoring during hospitalization,” the authors conclude.
The team currently is taking a closer look at acute myocarditis among patients hospitalized with COVID-19, Dr. Woodruff said. Preliminary results were presented at the 2022 annual scientific sessions of the American Heart Association and a paper is forthcoming.
Contemporary data needed
James A. de Lemos, MD, co-chair of the American Heart Association’s COVID-19 CVD Registry Steering Committee and professor of medicine at the University of Texas Southwestern Medical Center, Dallas, said the findings mirror his team’s clinical experience in 2020 and 2021 and echo what was seen in the AHA COVID registry: that is, a 0.3% rate of myocarditis.
“The major caveat is that [the findings] may not be generalizable to contemporary COVID infection, both due to changing viral variants and higher levels of immunity in the population,” he said.
“Rates of COVID hospitalization are markedly lower with the current dominant variants, and we would expect the cardiac risk to be lower as well. I would like to see more contemporary data with current variants, particularly focused on higher risk patients with cardiovascular disease,” Dr. de Lemos added.
In a related editorial, George A. Mensa, MD, of the National Heart, Lung, and Blood Institute in Bethesda, Md., and colleagues suggest that the broader impact of the COVID-19 pandemic on human health remains “incompletely examined.”
“The impact of COVID-19 on cardiovascular mortality, in particular, appears to have varied widely, with no large increases seen in a number of the most developed countries but marked increases in hypertensive heart disease mortality seen in the United States in 2021,” they conclude. “The potential contribution of COVID-19 to these deaths, either directly or indirectly, remains to be determined.”
No commercial funding or relevant financial relationships were reported.
A version of this article first appeared on Medscape.com.
particularly among those with underlying heart disease, and are associated with more severe disease outcomes, a new study suggests.
“We expected to see acute cardiac events occurring among adults hospitalized with COVID-19 but were surprised by how frequently they occurred,” Rebecca C. Woodruff, PhD, MPH, of the U.S. Centers for Disease Control and Prevention, Atlanta, told this news organization.
Overall, she said, “about 1 in 10 adults experienced an acute cardiac event – including heart attacks and acute heart failure – while hospitalized with COVID-19, and this included people with no preexisting heart disease.”
However, she added, “about a quarter of those with underlying heart disease had an acute cardiac event. These patients tended to experience more severe disease outcomes relative to patients hospitalized with COVID-19 who did not experience an acute cardiac event.”
The findings might be relevant to hospitalizations for other viral diseases, “though we can’t say for sure,” she noted. “This study was modeled off a previous study conducted before the COVID-19 pandemic among adults hospitalized with influenza. About 11.7% of [those] adults experienced an acute cardiac event, which was a similar percentage as what we found among patients hospitalized with COVID-19.”
The study was published online in the Journal of the American College of Cardiology.
Underlying cardiac disease key
Dr. Woodruff and colleagues analyzed medical records on a probability sample of 8,460 adults hospitalized with SARS-CoV-2 infection identified from 99 U.S. counties in 14 U.S. states (about 10% of the United States population) from January to November 2021.
Among participants, 11.4% had an acute cardiac event during their hospitalization. The median age was 69 years; 56.5% were men; 48.7%, non-Hispanic White; 33.6%, non-Hispanic Black; 7.4%, Hispanic; and 7.1%, non-Hispanic Asian or Pacific Islander.
As indicated, the prevalence was higher among those with underlying cardiac disease (23.4%), compared with those without (6.2%).
Acute ischemic heart disease (5.5%) and acute heart failure (5.4%) were the most prevalent events; 0.3% of participants had acute myocarditis or pericarditis.
Risk factors varied, depending on underlying cardiac disease status. Those who experienced one or more acute cardiac events had a greater risk for intensive care unit admission (adjusted risk ratio,1.9) and in-hospital death (aRR, 1.7) versus those who did not.
In multivariable analyses, the risk of experiencing acute heart failure was significantly greater among men (aRR, 1.5) and among those with a history of congestive heart failure (aRR, 13.5), atrial fibrillation (aRR, 1.6) or hypertension (aRR,1.3).
Among patients who experienced one or more acute cardiac events, 39.2% required an intensive care unit stay for a median of 5 days. Approximately 22.4% required invasive mechanical ventilation or extracorporeal membrane oxygenation, and 21.1% died while hospitalized.
“Persons at greater risk for experiencing acute cardiac events during COVID-19–associated hospitalizations might benefit from more intensive clinical evaluation and monitoring during hospitalization,” the authors conclude.
The team currently is taking a closer look at acute myocarditis among patients hospitalized with COVID-19, Dr. Woodruff said. Preliminary results were presented at the 2022 annual scientific sessions of the American Heart Association and a paper is forthcoming.
Contemporary data needed
James A. de Lemos, MD, co-chair of the American Heart Association’s COVID-19 CVD Registry Steering Committee and professor of medicine at the University of Texas Southwestern Medical Center, Dallas, said the findings mirror his team’s clinical experience in 2020 and 2021 and echo what was seen in the AHA COVID registry: that is, a 0.3% rate of myocarditis.
“The major caveat is that [the findings] may not be generalizable to contemporary COVID infection, both due to changing viral variants and higher levels of immunity in the population,” he said.
“Rates of COVID hospitalization are markedly lower with the current dominant variants, and we would expect the cardiac risk to be lower as well. I would like to see more contemporary data with current variants, particularly focused on higher risk patients with cardiovascular disease,” Dr. de Lemos added.
In a related editorial, George A. Mensa, MD, of the National Heart, Lung, and Blood Institute in Bethesda, Md., and colleagues suggest that the broader impact of the COVID-19 pandemic on human health remains “incompletely examined.”
“The impact of COVID-19 on cardiovascular mortality, in particular, appears to have varied widely, with no large increases seen in a number of the most developed countries but marked increases in hypertensive heart disease mortality seen in the United States in 2021,” they conclude. “The potential contribution of COVID-19 to these deaths, either directly or indirectly, remains to be determined.”
No commercial funding or relevant financial relationships were reported.
A version of this article first appeared on Medscape.com.
particularly among those with underlying heart disease, and are associated with more severe disease outcomes, a new study suggests.
“We expected to see acute cardiac events occurring among adults hospitalized with COVID-19 but were surprised by how frequently they occurred,” Rebecca C. Woodruff, PhD, MPH, of the U.S. Centers for Disease Control and Prevention, Atlanta, told this news organization.
Overall, she said, “about 1 in 10 adults experienced an acute cardiac event – including heart attacks and acute heart failure – while hospitalized with COVID-19, and this included people with no preexisting heart disease.”
However, she added, “about a quarter of those with underlying heart disease had an acute cardiac event. These patients tended to experience more severe disease outcomes relative to patients hospitalized with COVID-19 who did not experience an acute cardiac event.”
The findings might be relevant to hospitalizations for other viral diseases, “though we can’t say for sure,” she noted. “This study was modeled off a previous study conducted before the COVID-19 pandemic among adults hospitalized with influenza. About 11.7% of [those] adults experienced an acute cardiac event, which was a similar percentage as what we found among patients hospitalized with COVID-19.”
The study was published online in the Journal of the American College of Cardiology.
Underlying cardiac disease key
Dr. Woodruff and colleagues analyzed medical records on a probability sample of 8,460 adults hospitalized with SARS-CoV-2 infection identified from 99 U.S. counties in 14 U.S. states (about 10% of the United States population) from January to November 2021.
Among participants, 11.4% had an acute cardiac event during their hospitalization. The median age was 69 years; 56.5% were men; 48.7%, non-Hispanic White; 33.6%, non-Hispanic Black; 7.4%, Hispanic; and 7.1%, non-Hispanic Asian or Pacific Islander.
As indicated, the prevalence was higher among those with underlying cardiac disease (23.4%), compared with those without (6.2%).
Acute ischemic heart disease (5.5%) and acute heart failure (5.4%) were the most prevalent events; 0.3% of participants had acute myocarditis or pericarditis.
Risk factors varied, depending on underlying cardiac disease status. Those who experienced one or more acute cardiac events had a greater risk for intensive care unit admission (adjusted risk ratio,1.9) and in-hospital death (aRR, 1.7) versus those who did not.
In multivariable analyses, the risk of experiencing acute heart failure was significantly greater among men (aRR, 1.5) and among those with a history of congestive heart failure (aRR, 13.5), atrial fibrillation (aRR, 1.6) or hypertension (aRR,1.3).
Among patients who experienced one or more acute cardiac events, 39.2% required an intensive care unit stay for a median of 5 days. Approximately 22.4% required invasive mechanical ventilation or extracorporeal membrane oxygenation, and 21.1% died while hospitalized.
“Persons at greater risk for experiencing acute cardiac events during COVID-19–associated hospitalizations might benefit from more intensive clinical evaluation and monitoring during hospitalization,” the authors conclude.
The team currently is taking a closer look at acute myocarditis among patients hospitalized with COVID-19, Dr. Woodruff said. Preliminary results were presented at the 2022 annual scientific sessions of the American Heart Association and a paper is forthcoming.
Contemporary data needed
James A. de Lemos, MD, co-chair of the American Heart Association’s COVID-19 CVD Registry Steering Committee and professor of medicine at the University of Texas Southwestern Medical Center, Dallas, said the findings mirror his team’s clinical experience in 2020 and 2021 and echo what was seen in the AHA COVID registry: that is, a 0.3% rate of myocarditis.
“The major caveat is that [the findings] may not be generalizable to contemporary COVID infection, both due to changing viral variants and higher levels of immunity in the population,” he said.
“Rates of COVID hospitalization are markedly lower with the current dominant variants, and we would expect the cardiac risk to be lower as well. I would like to see more contemporary data with current variants, particularly focused on higher risk patients with cardiovascular disease,” Dr. de Lemos added.
In a related editorial, George A. Mensa, MD, of the National Heart, Lung, and Blood Institute in Bethesda, Md., and colleagues suggest that the broader impact of the COVID-19 pandemic on human health remains “incompletely examined.”
“The impact of COVID-19 on cardiovascular mortality, in particular, appears to have varied widely, with no large increases seen in a number of the most developed countries but marked increases in hypertensive heart disease mortality seen in the United States in 2021,” they conclude. “The potential contribution of COVID-19 to these deaths, either directly or indirectly, remains to be determined.”
No commercial funding or relevant financial relationships were reported.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Physician opinions vary on surveillance colonoscopies in older adults with prior adenomas, survey finds
Physician recommendations for surveillance colonoscopies in older adults with prior adenomas vary based on several factors, including patient age, health, adenoma risk, and physician specialty, according to a national survey.
In general, physicians were more likely to recommend surveillance for patients at a younger age, with better health, and with prior high-risk adenomas. Additionally, a large proportion of physicians reported uncertainty about whether the benefits of continued surveillance outweighed the risk of harm in older adults.
“There are no existing surveillance colonoscopy guidelines that integrate patient age, health, and adenoma risk, and physicians report significant decisional uncertainty,” Nancy Schoenborn, MD, MHS, associate professor of medicine at Johns Hopkins University, Baltimore, and colleagues wrote.
“Developing the evidence base to evaluate the risks and benefits of surveillance colonoscopy in older adults and decisional support tools that help physicians and patients incorporate available data and weigh risks and benefits are needed to address current gaps in care for older adults with prior adenomas,” the authors wrote.
The study was published online in the American Journal of Gastroenterology.
Surveying physicians
National guidelines recommend surveillance colonoscopy after adenoma removal at more frequent intervals than screening colonoscopy because of a higher risk of colorectal cancer among patients with adenomas. The high quality of screening colonoscopies coupled with an aging population means that many older adults have a history of adenomas and continue to undergo surveillance colonoscopies, the authors wrote.
they wrote.
Dr. Schoenborn and colleagues conducted a national cross-sectional survey of 1,800 primary care physicians and 600 gastroenterologists between April and November 2021. The primary care group included internal medicine, family medicine, general practice, and geriatric medicine physicians.
The research team asked whether physicians would recommend surveillance colonoscopy in a series of 12 vignettes that varied by patient age (75 or 85), patient health (good, medium, or poor), and prior adenoma risk (low or high).
Good health was described as well-controlled hypertension and living independently, whereas moderate health was described as moderate heart failure and has difficulty walking, and poor health was described as severe chronic obstructive pulmonary disease on oxygenand requires help with self-care.
For prior adenomas, high risk involved five tubular adenomas, one of which was 15 mm, and low risk involved two tubular adenomas, both of which were less than 10 mm. The survey also noted that the recommended surveillance intervals were 3 years in the high-risk scenario and 7 years in the low-risk scenario.
Researchers mailed 2,400 surveys and received 1,040 responses. They included 874 in the analysis because the physician respondents provided care to patients ages 65 and older and spent time seeing patients in clinic. Decisions about surveillance colonoscopies for adenomas in the absence of symptoms almost always occur in the outpatient setting, rather than acute or urgent care, the authors wrote.
Large variations found
Overall, physicians were less likely to recommend surveillance colonoscopies if the patient was older, had poor health, and had lower-risk adenomas. Patient age and health had larger effects on decision-making than adenoma risk, with health status having the largest effect.
About 20.6% of physicians recommended surveillance if the patient was 85, compared with 49.8% if the patient was 75. In addition, 7.1% of physicians recommended surveillance if the patient was in poor health, compared with 28.8% for those in moderate health, and 67.7% for patients in good health.
If the prior adenoma was low risk, 29.7% of physicians recommended surveillance, compared with 41.6% if the prior adenoma was high risk.
In general, family medicine and general practice physicians were most likely to recommend surveillance, at 40%, and gastroenterologists were least likely to recommend surveillance, at 30.9%. Patient age and health had larger effects among gastroenterologists than among primary care physicians, and adenoma risk had similar effects between the two groups.
“The importance of patient age and health status found in our study mirrors study results on physician decision-making regarding screening colonoscopies in older adults and makes intuitive sense,” the authors wrote. “Whether the priorities reflected in our findings are supported by evidence is not clear, and our results highlight important knowledge gaps in the field that warrant future research.”
Physician uncertainty
Additional guidance would be helpful, the authors wrote. In the survey, about 52.3% of primary care physicians and 35.4% of gastroenterologists reported uncertainty about the benefit–harm balance of surveillance in older adults.
“Current guidelines on surveillance colonoscopies are solely based on prior adenoma characteristics,” the authors wrote. “Guidelines need to incorporate guidance that considers patient age and health status, as well as adenoma risk, and explicitly considers when surveillance should stop in older adults.”
In addition, most physicians in the survey – 85.9% of primary care physicians and 77% of gastroenterologists – said they would find a decision support tool helpful. At the same time, 32.8% of primary care physicians and 71.5% of gastroenterologists perceived it as the gastroenterologist’s role to decide about surveillance colonoscopies.
“Developing patient-facing materials, communication tools for clinicians, and tools to support shared decision-making about surveillance colonoscopies that engage both physicians and patients are all important next steps,” the authors wrote. “To our knowledge, there is no existing patient decision aid about surveillance colonoscopies; developing such a tool may be valuable.”
The study was supported by Dr. Schoenborn’s career development award from the National Institute on Aging. The authors reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Physician recommendations for surveillance colonoscopies in older adults with prior adenomas vary based on several factors, including patient age, health, adenoma risk, and physician specialty, according to a national survey.
In general, physicians were more likely to recommend surveillance for patients at a younger age, with better health, and with prior high-risk adenomas. Additionally, a large proportion of physicians reported uncertainty about whether the benefits of continued surveillance outweighed the risk of harm in older adults.
“There are no existing surveillance colonoscopy guidelines that integrate patient age, health, and adenoma risk, and physicians report significant decisional uncertainty,” Nancy Schoenborn, MD, MHS, associate professor of medicine at Johns Hopkins University, Baltimore, and colleagues wrote.
“Developing the evidence base to evaluate the risks and benefits of surveillance colonoscopy in older adults and decisional support tools that help physicians and patients incorporate available data and weigh risks and benefits are needed to address current gaps in care for older adults with prior adenomas,” the authors wrote.
The study was published online in the American Journal of Gastroenterology.
Surveying physicians
National guidelines recommend surveillance colonoscopy after adenoma removal at more frequent intervals than screening colonoscopy because of a higher risk of colorectal cancer among patients with adenomas. The high quality of screening colonoscopies coupled with an aging population means that many older adults have a history of adenomas and continue to undergo surveillance colonoscopies, the authors wrote.
they wrote.
Dr. Schoenborn and colleagues conducted a national cross-sectional survey of 1,800 primary care physicians and 600 gastroenterologists between April and November 2021. The primary care group included internal medicine, family medicine, general practice, and geriatric medicine physicians.
The research team asked whether physicians would recommend surveillance colonoscopy in a series of 12 vignettes that varied by patient age (75 or 85), patient health (good, medium, or poor), and prior adenoma risk (low or high).
Good health was described as well-controlled hypertension and living independently, whereas moderate health was described as moderate heart failure and has difficulty walking, and poor health was described as severe chronic obstructive pulmonary disease on oxygenand requires help with self-care.
For prior adenomas, high risk involved five tubular adenomas, one of which was 15 mm, and low risk involved two tubular adenomas, both of which were less than 10 mm. The survey also noted that the recommended surveillance intervals were 3 years in the high-risk scenario and 7 years in the low-risk scenario.
Researchers mailed 2,400 surveys and received 1,040 responses. They included 874 in the analysis because the physician respondents provided care to patients ages 65 and older and spent time seeing patients in clinic. Decisions about surveillance colonoscopies for adenomas in the absence of symptoms almost always occur in the outpatient setting, rather than acute or urgent care, the authors wrote.
Large variations found
Overall, physicians were less likely to recommend surveillance colonoscopies if the patient was older, had poor health, and had lower-risk adenomas. Patient age and health had larger effects on decision-making than adenoma risk, with health status having the largest effect.
About 20.6% of physicians recommended surveillance if the patient was 85, compared with 49.8% if the patient was 75. In addition, 7.1% of physicians recommended surveillance if the patient was in poor health, compared with 28.8% for those in moderate health, and 67.7% for patients in good health.
If the prior adenoma was low risk, 29.7% of physicians recommended surveillance, compared with 41.6% if the prior adenoma was high risk.
In general, family medicine and general practice physicians were most likely to recommend surveillance, at 40%, and gastroenterologists were least likely to recommend surveillance, at 30.9%. Patient age and health had larger effects among gastroenterologists than among primary care physicians, and adenoma risk had similar effects between the two groups.
“The importance of patient age and health status found in our study mirrors study results on physician decision-making regarding screening colonoscopies in older adults and makes intuitive sense,” the authors wrote. “Whether the priorities reflected in our findings are supported by evidence is not clear, and our results highlight important knowledge gaps in the field that warrant future research.”
Physician uncertainty
Additional guidance would be helpful, the authors wrote. In the survey, about 52.3% of primary care physicians and 35.4% of gastroenterologists reported uncertainty about the benefit–harm balance of surveillance in older adults.
“Current guidelines on surveillance colonoscopies are solely based on prior adenoma characteristics,” the authors wrote. “Guidelines need to incorporate guidance that considers patient age and health status, as well as adenoma risk, and explicitly considers when surveillance should stop in older adults.”
In addition, most physicians in the survey – 85.9% of primary care physicians and 77% of gastroenterologists – said they would find a decision support tool helpful. At the same time, 32.8% of primary care physicians and 71.5% of gastroenterologists perceived it as the gastroenterologist’s role to decide about surveillance colonoscopies.
“Developing patient-facing materials, communication tools for clinicians, and tools to support shared decision-making about surveillance colonoscopies that engage both physicians and patients are all important next steps,” the authors wrote. “To our knowledge, there is no existing patient decision aid about surveillance colonoscopies; developing such a tool may be valuable.”
The study was supported by Dr. Schoenborn’s career development award from the National Institute on Aging. The authors reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Physician recommendations for surveillance colonoscopies in older adults with prior adenomas vary based on several factors, including patient age, health, adenoma risk, and physician specialty, according to a national survey.
In general, physicians were more likely to recommend surveillance for patients at a younger age, with better health, and with prior high-risk adenomas. Additionally, a large proportion of physicians reported uncertainty about whether the benefits of continued surveillance outweighed the risk of harm in older adults.
“There are no existing surveillance colonoscopy guidelines that integrate patient age, health, and adenoma risk, and physicians report significant decisional uncertainty,” Nancy Schoenborn, MD, MHS, associate professor of medicine at Johns Hopkins University, Baltimore, and colleagues wrote.
“Developing the evidence base to evaluate the risks and benefits of surveillance colonoscopy in older adults and decisional support tools that help physicians and patients incorporate available data and weigh risks and benefits are needed to address current gaps in care for older adults with prior adenomas,” the authors wrote.
The study was published online in the American Journal of Gastroenterology.
Surveying physicians
National guidelines recommend surveillance colonoscopy after adenoma removal at more frequent intervals than screening colonoscopy because of a higher risk of colorectal cancer among patients with adenomas. The high quality of screening colonoscopies coupled with an aging population means that many older adults have a history of adenomas and continue to undergo surveillance colonoscopies, the authors wrote.
they wrote.
Dr. Schoenborn and colleagues conducted a national cross-sectional survey of 1,800 primary care physicians and 600 gastroenterologists between April and November 2021. The primary care group included internal medicine, family medicine, general practice, and geriatric medicine physicians.
The research team asked whether physicians would recommend surveillance colonoscopy in a series of 12 vignettes that varied by patient age (75 or 85), patient health (good, medium, or poor), and prior adenoma risk (low or high).
Good health was described as well-controlled hypertension and living independently, whereas moderate health was described as moderate heart failure and has difficulty walking, and poor health was described as severe chronic obstructive pulmonary disease on oxygenand requires help with self-care.
For prior adenomas, high risk involved five tubular adenomas, one of which was 15 mm, and low risk involved two tubular adenomas, both of which were less than 10 mm. The survey also noted that the recommended surveillance intervals were 3 years in the high-risk scenario and 7 years in the low-risk scenario.
Researchers mailed 2,400 surveys and received 1,040 responses. They included 874 in the analysis because the physician respondents provided care to patients ages 65 and older and spent time seeing patients in clinic. Decisions about surveillance colonoscopies for adenomas in the absence of symptoms almost always occur in the outpatient setting, rather than acute or urgent care, the authors wrote.
Large variations found
Overall, physicians were less likely to recommend surveillance colonoscopies if the patient was older, had poor health, and had lower-risk adenomas. Patient age and health had larger effects on decision-making than adenoma risk, with health status having the largest effect.
About 20.6% of physicians recommended surveillance if the patient was 85, compared with 49.8% if the patient was 75. In addition, 7.1% of physicians recommended surveillance if the patient was in poor health, compared with 28.8% for those in moderate health, and 67.7% for patients in good health.
If the prior adenoma was low risk, 29.7% of physicians recommended surveillance, compared with 41.6% if the prior adenoma was high risk.
In general, family medicine and general practice physicians were most likely to recommend surveillance, at 40%, and gastroenterologists were least likely to recommend surveillance, at 30.9%. Patient age and health had larger effects among gastroenterologists than among primary care physicians, and adenoma risk had similar effects between the two groups.
“The importance of patient age and health status found in our study mirrors study results on physician decision-making regarding screening colonoscopies in older adults and makes intuitive sense,” the authors wrote. “Whether the priorities reflected in our findings are supported by evidence is not clear, and our results highlight important knowledge gaps in the field that warrant future research.”
Physician uncertainty
Additional guidance would be helpful, the authors wrote. In the survey, about 52.3% of primary care physicians and 35.4% of gastroenterologists reported uncertainty about the benefit–harm balance of surveillance in older adults.
“Current guidelines on surveillance colonoscopies are solely based on prior adenoma characteristics,” the authors wrote. “Guidelines need to incorporate guidance that considers patient age and health status, as well as adenoma risk, and explicitly considers when surveillance should stop in older adults.”
In addition, most physicians in the survey – 85.9% of primary care physicians and 77% of gastroenterologists – said they would find a decision support tool helpful. At the same time, 32.8% of primary care physicians and 71.5% of gastroenterologists perceived it as the gastroenterologist’s role to decide about surveillance colonoscopies.
“Developing patient-facing materials, communication tools for clinicians, and tools to support shared decision-making about surveillance colonoscopies that engage both physicians and patients are all important next steps,” the authors wrote. “To our knowledge, there is no existing patient decision aid about surveillance colonoscopies; developing such a tool may be valuable.”
The study was supported by Dr. Schoenborn’s career development award from the National Institute on Aging. The authors reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF GASTROENTEROLOGY
Use of diagnostic mammograms is inconsistent, survey finds
Existing guidelines offer little help, according to Pavani Chalasani, MD, MPH, who presented the study at the San Antonio Breast Cancer Symposium. “They just say [do an] annual mammogram, but they don’t say, ‘Do we need to do screening? Do we need to do breast MRIs?’”
Her personal experience also reflected a general confusion. “I asked my colleagues and got different answers from seven colleagues,” said Dr. Chalasani, who is an oncologist at the University of Arizona Cancer Center, Tucson.
She noted that diagnostic mammograms are generally similar to screening mammograms, but the radiologist is viewing the images in real time and can take additional views as needed while the patient is still present. “That is the biggest difference,” said Dr. Chalasani. No studies have been conducted to determine which method produces better results.
To get a snapshot of current practice, she and her colleagues developed a survey, which the American Society of Clinical Oncology sent to 1,000 randomly selected members between Oct. 19 and Nov. 22, 2021. 244 individuals responded; 93.5% were physicians, and half identified as female. A total of 174 respondents were medical oncologists, 31 were radiation oncologists, and 20 were surgical oncologists. The imbalance among respondents is a limitation of the study. That “may or may not be reflective of our real-time practices (among surgeons), but we do think that since a lot of times patients are seen by medical oncologists, there could be overlap,” said Dr. Chalasani.
About 50% of respondents said that they use breast MRI in the diagnosis of 25% or fewer patients. Approximately 64% of respondents said they used diagnostic mammograms versus about 31% who used imaging mammograms at first imaging. About 53% said they ordered mammograms within the first 6 months after treatment.
38% of those who ordered diagnostic mammograms for surveillance used it for 3-5 years, while 29% continued it for 5 years or more. One-quarter employed additional imaging during follow-up, most commonly breast ultrasound. About 65% said they had no stop date for screening mammograms, as long as the patient remained healthy. The choice of screening or diagnostic mammography was about 50:50, though about 55% said they use screening mammography for patients 80 years of age or older.
Dr. Chalasani pointed out that both screening and diagnostic mammograms provide similar imaging quality. Screening mammograms are completely covered by insurance, while diagnostic mammograms typically require a copay. “We’re doing this [diagnostic mammography] with no guidelines, but there is this out of pocket cost, without knowing if it’s the right thing to do,” she said.
National Comprehensive Cancer Network guidelines indicate that diagnostic mammograms can be conducted for 5 years after a ductal carcinoma in situ diagnosis, but it doesn’t provide guidance for invasive cancers. Some past studies suggested that doing diagnostic mammograms for 3 years may increase diagnosis, but it isn’t clear if any such advantage would actually result in a clinical difference, according to Dr. Chalasani. “With the treatments we have, we still might cure [the cancer]. So what endpoints are we looking for? Are we changing care to add on toxicity to the patient, and stress to the patient and also for the health care system?”
She hopes that physicians will look at the results and understand that diagnostic mammograms, while they intuitively feel superior, are not supported by guidelines, and patients must incur an extra cost.
Her team also plans to conduct cost-effectiveness analysis of diagnostic mammograms.
Dr. Chalasani has no relevant financial disclosures.
Existing guidelines offer little help, according to Pavani Chalasani, MD, MPH, who presented the study at the San Antonio Breast Cancer Symposium. “They just say [do an] annual mammogram, but they don’t say, ‘Do we need to do screening? Do we need to do breast MRIs?’”
Her personal experience also reflected a general confusion. “I asked my colleagues and got different answers from seven colleagues,” said Dr. Chalasani, who is an oncologist at the University of Arizona Cancer Center, Tucson.
She noted that diagnostic mammograms are generally similar to screening mammograms, but the radiologist is viewing the images in real time and can take additional views as needed while the patient is still present. “That is the biggest difference,” said Dr. Chalasani. No studies have been conducted to determine which method produces better results.
To get a snapshot of current practice, she and her colleagues developed a survey, which the American Society of Clinical Oncology sent to 1,000 randomly selected members between Oct. 19 and Nov. 22, 2021. 244 individuals responded; 93.5% were physicians, and half identified as female. A total of 174 respondents were medical oncologists, 31 were radiation oncologists, and 20 were surgical oncologists. The imbalance among respondents is a limitation of the study. That “may or may not be reflective of our real-time practices (among surgeons), but we do think that since a lot of times patients are seen by medical oncologists, there could be overlap,” said Dr. Chalasani.
About 50% of respondents said that they use breast MRI in the diagnosis of 25% or fewer patients. Approximately 64% of respondents said they used diagnostic mammograms versus about 31% who used imaging mammograms at first imaging. About 53% said they ordered mammograms within the first 6 months after treatment.
38% of those who ordered diagnostic mammograms for surveillance used it for 3-5 years, while 29% continued it for 5 years or more. One-quarter employed additional imaging during follow-up, most commonly breast ultrasound. About 65% said they had no stop date for screening mammograms, as long as the patient remained healthy. The choice of screening or diagnostic mammography was about 50:50, though about 55% said they use screening mammography for patients 80 years of age or older.
Dr. Chalasani pointed out that both screening and diagnostic mammograms provide similar imaging quality. Screening mammograms are completely covered by insurance, while diagnostic mammograms typically require a copay. “We’re doing this [diagnostic mammography] with no guidelines, but there is this out of pocket cost, without knowing if it’s the right thing to do,” she said.
National Comprehensive Cancer Network guidelines indicate that diagnostic mammograms can be conducted for 5 years after a ductal carcinoma in situ diagnosis, but it doesn’t provide guidance for invasive cancers. Some past studies suggested that doing diagnostic mammograms for 3 years may increase diagnosis, but it isn’t clear if any such advantage would actually result in a clinical difference, according to Dr. Chalasani. “With the treatments we have, we still might cure [the cancer]. So what endpoints are we looking for? Are we changing care to add on toxicity to the patient, and stress to the patient and also for the health care system?”
She hopes that physicians will look at the results and understand that diagnostic mammograms, while they intuitively feel superior, are not supported by guidelines, and patients must incur an extra cost.
Her team also plans to conduct cost-effectiveness analysis of diagnostic mammograms.
Dr. Chalasani has no relevant financial disclosures.
Existing guidelines offer little help, according to Pavani Chalasani, MD, MPH, who presented the study at the San Antonio Breast Cancer Symposium. “They just say [do an] annual mammogram, but they don’t say, ‘Do we need to do screening? Do we need to do breast MRIs?’”
Her personal experience also reflected a general confusion. “I asked my colleagues and got different answers from seven colleagues,” said Dr. Chalasani, who is an oncologist at the University of Arizona Cancer Center, Tucson.
She noted that diagnostic mammograms are generally similar to screening mammograms, but the radiologist is viewing the images in real time and can take additional views as needed while the patient is still present. “That is the biggest difference,” said Dr. Chalasani. No studies have been conducted to determine which method produces better results.
To get a snapshot of current practice, she and her colleagues developed a survey, which the American Society of Clinical Oncology sent to 1,000 randomly selected members between Oct. 19 and Nov. 22, 2021. 244 individuals responded; 93.5% were physicians, and half identified as female. A total of 174 respondents were medical oncologists, 31 were radiation oncologists, and 20 were surgical oncologists. The imbalance among respondents is a limitation of the study. That “may or may not be reflective of our real-time practices (among surgeons), but we do think that since a lot of times patients are seen by medical oncologists, there could be overlap,” said Dr. Chalasani.
About 50% of respondents said that they use breast MRI in the diagnosis of 25% or fewer patients. Approximately 64% of respondents said they used diagnostic mammograms versus about 31% who used imaging mammograms at first imaging. About 53% said they ordered mammograms within the first 6 months after treatment.
38% of those who ordered diagnostic mammograms for surveillance used it for 3-5 years, while 29% continued it for 5 years or more. One-quarter employed additional imaging during follow-up, most commonly breast ultrasound. About 65% said they had no stop date for screening mammograms, as long as the patient remained healthy. The choice of screening or diagnostic mammography was about 50:50, though about 55% said they use screening mammography for patients 80 years of age or older.
Dr. Chalasani pointed out that both screening and diagnostic mammograms provide similar imaging quality. Screening mammograms are completely covered by insurance, while diagnostic mammograms typically require a copay. “We’re doing this [diagnostic mammography] with no guidelines, but there is this out of pocket cost, without knowing if it’s the right thing to do,” she said.
National Comprehensive Cancer Network guidelines indicate that diagnostic mammograms can be conducted for 5 years after a ductal carcinoma in situ diagnosis, but it doesn’t provide guidance for invasive cancers. Some past studies suggested that doing diagnostic mammograms for 3 years may increase diagnosis, but it isn’t clear if any such advantage would actually result in a clinical difference, according to Dr. Chalasani. “With the treatments we have, we still might cure [the cancer]. So what endpoints are we looking for? Are we changing care to add on toxicity to the patient, and stress to the patient and also for the health care system?”
She hopes that physicians will look at the results and understand that diagnostic mammograms, while they intuitively feel superior, are not supported by guidelines, and patients must incur an extra cost.
Her team also plans to conduct cost-effectiveness analysis of diagnostic mammograms.
Dr. Chalasani has no relevant financial disclosures.
FROM SABCS 2022