User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Stroke risk in new-onset atrial fib goes up with greater alcohol intake
There’s abundant evidence linking higher alcohol intake levels to greater stroke risk and, separately, increasing risk for new-onset atrial fibrillation (AFib). Less settled is whether moderate to heavy drinking worsens the risk for stroke in patients already in AFib and whether giving up alcohol can attenuate that risk. A new observational study suggests the answer to both questions is yes.
The risk for ischemic stroke was only around 1% over about 5 years in a Korean nationwide cohort of almost 98,000 patients with new-onset AFib. About half the patients followed were nondrinkers, as they had been before the study, 13% became abstinent soon after their AFib diagnosis, and 36% were currently drinkers.
But stroke risk went up about 30% with “moderate” current alcohol intake, compared with no intake, and by more than 40% for current drinkers reporting “heavy” alcohol intake, researchers found in an adjusted analysis.
However, abstainers who had mild to moderate alcohol-intake levels before their AFib diagnosis “had a similar risk of ischemic stroke as nondrinkers,” write the authors, led by So-Ryoung Lee, MD, PhD, and colleagues, Seoul National University Hospital, Republic of Korea, in their report published June 7 in the European Heart Journal. In a secondary analysis, binge drinking was also independently associated with risk for ischemic stroke.
The findings suggest that “alcohol abstinence after the diagnosis of AFib could reduce the risk of ischemic stroke,” they conclude. “Lifestyle interventions, including attention to alcohol consumption, should be encouraged as part of a comprehensive approach in the management of patients with a new diagnosis of AFib” for lowering the risk for stroke and other clinical outcomes.
“These results are pretty comparable to those obtained in the more general population,” David Conen, MD, MPH, not connected to the analysis, told this news organization.
In the study’s population with new-onset AFib, there is an alcohol-dependent risk for stroke “that goes up with increasing alcohol intake, which is more or less similar to that found without atrial fibrillation in previous studies,” said Dr. Conen, from the Population Health Research Institute, McMaster University, Hamilton, Ont.
The study, “which overall I think is very well done,” he said, is noteworthy for also suggesting that binge drinking, which was scrutinized in a secondary analysis, appeared independently to worsen the risk for stroke in its AFib population.
Dr. Conen said the observed 1% overall risk for stroke was very similar to the rate he and his colleagues saw in a recent combined analysis of two European cohorts with AFib that was usually longer standing; the median was 3 years. That analysis, in contrast, showed no significant association between increasing levels of alcohol intake and risk for stroke or systemic embolism.
However, “our confidence limits did not exclude the possibility of a small to moderate association,” he said. Given that, and the current study from Korea, there might indeed be “a weak association between alcohol consumption and stroke” in patients with AFib.
“Their results are just more precise because of the larger sample size. That’s why they were able to show those associations,” said Dr. Conen, who was senior author on the earlier report, which covered a pooled analysis of 3,852 patients with AFib in the BEAT-AF and SWISS-AF cohort studies. It was published January 25 in CMAJ, with lead author Philipp Reddiess, MD, Cardiovascular Research Institute Basel, Switzerland.
The two published studies contrast in other ways that are worth noting and together suggest the stroke rate might have been 1% in both by chance, Dr. Conen said. “The populations were pretty different.”
In the earlier study, for example, the overwhelmingly European patients had more comorbidities and had been in AFib for much longer; their mean age was 71 years; and 84% were on oral anticoagulation (OAC).
In contrast, the Korean cohort averaged 61 years in age and only about 24% were taking oral anticoagulants. Given their distribution of CHA2DS2-VASc scores and mean score of 2.3, more than twice as many should have been on OAC, Dr. Conen speculated. “Even if you take into account that some patients may have contraindications, this is clearly an underanticoagulated population.”
The European cohort might have been “a little bit more representative because atrial fibrillation is a disease of the elderly,” Dr. Conen said, but “the Korean paper has the advantage of being a population-based study.”
It involved 97,869 patients from a Korean national data base who were newly diagnosed with AFib from 2010 to 2016. Of the total, 49,781 (51%) were continuously nondrinkers before and after their diagnosis; 12,789 (13%) abstained from alcohol only after their AFib diagnosis; and 35,299 (36%) were drinkers during the follow-up, either because they continued to drink or newly started after their diagnosis.
Of the cohort, 3,120 were diagnosed with new ischemic stroke over a follow-up of 310,926 person-years, for a rate of 1 per 100 person-years.
The adjusted hazard ratio (HR) for ischemic stroke over a 5-year follow-up, compared with nondrinkers, was:
- 1.127 (95% confidence interval, 1.003-1.266) among abstainers
- 1.280 (95% CI, 1.166-1.405) for current drinkers
The corresponding HR, compared with current drinkers, was:
- 0.781 (95% CI, 0.712-0.858) for nondrinkers
- 0.880 (95% CI, 0.782-0.990) among abstainers
No significant interactions with ischemic stroke risk were observed in groups by sex, age, CHA2DS2-VASc score, or smoking status. The risk rose consistently with current drinking levels.
The overall stroke rate of 1% per year is “very low,” and “the absolute differences are small, even though there is a clear significant trend from nondrinking to drinking,” Dr. Conen said.
However, “the difference becomes more sizable when you compare heavy drinking to abstinence.”
Dr. Lee reports no conflicts of interest; disclosures for the other authors are in their report. Dr. Conen reports receiving speaker fees from Servier Canada; disclosures for the other authors are in their report.
A version of this article first appeared on Medscape.com.
There’s abundant evidence linking higher alcohol intake levels to greater stroke risk and, separately, increasing risk for new-onset atrial fibrillation (AFib). Less settled is whether moderate to heavy drinking worsens the risk for stroke in patients already in AFib and whether giving up alcohol can attenuate that risk. A new observational study suggests the answer to both questions is yes.
The risk for ischemic stroke was only around 1% over about 5 years in a Korean nationwide cohort of almost 98,000 patients with new-onset AFib. About half the patients followed were nondrinkers, as they had been before the study, 13% became abstinent soon after their AFib diagnosis, and 36% were currently drinkers.
But stroke risk went up about 30% with “moderate” current alcohol intake, compared with no intake, and by more than 40% for current drinkers reporting “heavy” alcohol intake, researchers found in an adjusted analysis.
However, abstainers who had mild to moderate alcohol-intake levels before their AFib diagnosis “had a similar risk of ischemic stroke as nondrinkers,” write the authors, led by So-Ryoung Lee, MD, PhD, and colleagues, Seoul National University Hospital, Republic of Korea, in their report published June 7 in the European Heart Journal. In a secondary analysis, binge drinking was also independently associated with risk for ischemic stroke.
The findings suggest that “alcohol abstinence after the diagnosis of AFib could reduce the risk of ischemic stroke,” they conclude. “Lifestyle interventions, including attention to alcohol consumption, should be encouraged as part of a comprehensive approach in the management of patients with a new diagnosis of AFib” for lowering the risk for stroke and other clinical outcomes.
“These results are pretty comparable to those obtained in the more general population,” David Conen, MD, MPH, not connected to the analysis, told this news organization.
In the study’s population with new-onset AFib, there is an alcohol-dependent risk for stroke “that goes up with increasing alcohol intake, which is more or less similar to that found without atrial fibrillation in previous studies,” said Dr. Conen, from the Population Health Research Institute, McMaster University, Hamilton, Ont.
The study, “which overall I think is very well done,” he said, is noteworthy for also suggesting that binge drinking, which was scrutinized in a secondary analysis, appeared independently to worsen the risk for stroke in its AFib population.
Dr. Conen said the observed 1% overall risk for stroke was very similar to the rate he and his colleagues saw in a recent combined analysis of two European cohorts with AFib that was usually longer standing; the median was 3 years. That analysis, in contrast, showed no significant association between increasing levels of alcohol intake and risk for stroke or systemic embolism.
However, “our confidence limits did not exclude the possibility of a small to moderate association,” he said. Given that, and the current study from Korea, there might indeed be “a weak association between alcohol consumption and stroke” in patients with AFib.
“Their results are just more precise because of the larger sample size. That’s why they were able to show those associations,” said Dr. Conen, who was senior author on the earlier report, which covered a pooled analysis of 3,852 patients with AFib in the BEAT-AF and SWISS-AF cohort studies. It was published January 25 in CMAJ, with lead author Philipp Reddiess, MD, Cardiovascular Research Institute Basel, Switzerland.
The two published studies contrast in other ways that are worth noting and together suggest the stroke rate might have been 1% in both by chance, Dr. Conen said. “The populations were pretty different.”
In the earlier study, for example, the overwhelmingly European patients had more comorbidities and had been in AFib for much longer; their mean age was 71 years; and 84% were on oral anticoagulation (OAC).
In contrast, the Korean cohort averaged 61 years in age and only about 24% were taking oral anticoagulants. Given their distribution of CHA2DS2-VASc scores and mean score of 2.3, more than twice as many should have been on OAC, Dr. Conen speculated. “Even if you take into account that some patients may have contraindications, this is clearly an underanticoagulated population.”
The European cohort might have been “a little bit more representative because atrial fibrillation is a disease of the elderly,” Dr. Conen said, but “the Korean paper has the advantage of being a population-based study.”
It involved 97,869 patients from a Korean national data base who were newly diagnosed with AFib from 2010 to 2016. Of the total, 49,781 (51%) were continuously nondrinkers before and after their diagnosis; 12,789 (13%) abstained from alcohol only after their AFib diagnosis; and 35,299 (36%) were drinkers during the follow-up, either because they continued to drink or newly started after their diagnosis.
Of the cohort, 3,120 were diagnosed with new ischemic stroke over a follow-up of 310,926 person-years, for a rate of 1 per 100 person-years.
The adjusted hazard ratio (HR) for ischemic stroke over a 5-year follow-up, compared with nondrinkers, was:
- 1.127 (95% confidence interval, 1.003-1.266) among abstainers
- 1.280 (95% CI, 1.166-1.405) for current drinkers
The corresponding HR, compared with current drinkers, was:
- 0.781 (95% CI, 0.712-0.858) for nondrinkers
- 0.880 (95% CI, 0.782-0.990) among abstainers
No significant interactions with ischemic stroke risk were observed in groups by sex, age, CHA2DS2-VASc score, or smoking status. The risk rose consistently with current drinking levels.
The overall stroke rate of 1% per year is “very low,” and “the absolute differences are small, even though there is a clear significant trend from nondrinking to drinking,” Dr. Conen said.
However, “the difference becomes more sizable when you compare heavy drinking to abstinence.”
Dr. Lee reports no conflicts of interest; disclosures for the other authors are in their report. Dr. Conen reports receiving speaker fees from Servier Canada; disclosures for the other authors are in their report.
A version of this article first appeared on Medscape.com.
There’s abundant evidence linking higher alcohol intake levels to greater stroke risk and, separately, increasing risk for new-onset atrial fibrillation (AFib). Less settled is whether moderate to heavy drinking worsens the risk for stroke in patients already in AFib and whether giving up alcohol can attenuate that risk. A new observational study suggests the answer to both questions is yes.
The risk for ischemic stroke was only around 1% over about 5 years in a Korean nationwide cohort of almost 98,000 patients with new-onset AFib. About half the patients followed were nondrinkers, as they had been before the study, 13% became abstinent soon after their AFib diagnosis, and 36% were currently drinkers.
But stroke risk went up about 30% with “moderate” current alcohol intake, compared with no intake, and by more than 40% for current drinkers reporting “heavy” alcohol intake, researchers found in an adjusted analysis.
However, abstainers who had mild to moderate alcohol-intake levels before their AFib diagnosis “had a similar risk of ischemic stroke as nondrinkers,” write the authors, led by So-Ryoung Lee, MD, PhD, and colleagues, Seoul National University Hospital, Republic of Korea, in their report published June 7 in the European Heart Journal. In a secondary analysis, binge drinking was also independently associated with risk for ischemic stroke.
The findings suggest that “alcohol abstinence after the diagnosis of AFib could reduce the risk of ischemic stroke,” they conclude. “Lifestyle interventions, including attention to alcohol consumption, should be encouraged as part of a comprehensive approach in the management of patients with a new diagnosis of AFib” for lowering the risk for stroke and other clinical outcomes.
“These results are pretty comparable to those obtained in the more general population,” David Conen, MD, MPH, not connected to the analysis, told this news organization.
In the study’s population with new-onset AFib, there is an alcohol-dependent risk for stroke “that goes up with increasing alcohol intake, which is more or less similar to that found without atrial fibrillation in previous studies,” said Dr. Conen, from the Population Health Research Institute, McMaster University, Hamilton, Ont.
The study, “which overall I think is very well done,” he said, is noteworthy for also suggesting that binge drinking, which was scrutinized in a secondary analysis, appeared independently to worsen the risk for stroke in its AFib population.
Dr. Conen said the observed 1% overall risk for stroke was very similar to the rate he and his colleagues saw in a recent combined analysis of two European cohorts with AFib that was usually longer standing; the median was 3 years. That analysis, in contrast, showed no significant association between increasing levels of alcohol intake and risk for stroke or systemic embolism.
However, “our confidence limits did not exclude the possibility of a small to moderate association,” he said. Given that, and the current study from Korea, there might indeed be “a weak association between alcohol consumption and stroke” in patients with AFib.
“Their results are just more precise because of the larger sample size. That’s why they were able to show those associations,” said Dr. Conen, who was senior author on the earlier report, which covered a pooled analysis of 3,852 patients with AFib in the BEAT-AF and SWISS-AF cohort studies. It was published January 25 in CMAJ, with lead author Philipp Reddiess, MD, Cardiovascular Research Institute Basel, Switzerland.
The two published studies contrast in other ways that are worth noting and together suggest the stroke rate might have been 1% in both by chance, Dr. Conen said. “The populations were pretty different.”
In the earlier study, for example, the overwhelmingly European patients had more comorbidities and had been in AFib for much longer; their mean age was 71 years; and 84% were on oral anticoagulation (OAC).
In contrast, the Korean cohort averaged 61 years in age and only about 24% were taking oral anticoagulants. Given their distribution of CHA2DS2-VASc scores and mean score of 2.3, more than twice as many should have been on OAC, Dr. Conen speculated. “Even if you take into account that some patients may have contraindications, this is clearly an underanticoagulated population.”
The European cohort might have been “a little bit more representative because atrial fibrillation is a disease of the elderly,” Dr. Conen said, but “the Korean paper has the advantage of being a population-based study.”
It involved 97,869 patients from a Korean national data base who were newly diagnosed with AFib from 2010 to 2016. Of the total, 49,781 (51%) were continuously nondrinkers before and after their diagnosis; 12,789 (13%) abstained from alcohol only after their AFib diagnosis; and 35,299 (36%) were drinkers during the follow-up, either because they continued to drink or newly started after their diagnosis.
Of the cohort, 3,120 were diagnosed with new ischemic stroke over a follow-up of 310,926 person-years, for a rate of 1 per 100 person-years.
The adjusted hazard ratio (HR) for ischemic stroke over a 5-year follow-up, compared with nondrinkers, was:
- 1.127 (95% confidence interval, 1.003-1.266) among abstainers
- 1.280 (95% CI, 1.166-1.405) for current drinkers
The corresponding HR, compared with current drinkers, was:
- 0.781 (95% CI, 0.712-0.858) for nondrinkers
- 0.880 (95% CI, 0.782-0.990) among abstainers
No significant interactions with ischemic stroke risk were observed in groups by sex, age, CHA2DS2-VASc score, or smoking status. The risk rose consistently with current drinking levels.
The overall stroke rate of 1% per year is “very low,” and “the absolute differences are small, even though there is a clear significant trend from nondrinking to drinking,” Dr. Conen said.
However, “the difference becomes more sizable when you compare heavy drinking to abstinence.”
Dr. Lee reports no conflicts of interest; disclosures for the other authors are in their report. Dr. Conen reports receiving speaker fees from Servier Canada; disclosures for the other authors are in their report.
A version of this article first appeared on Medscape.com.
New data on COVID-19’s cognitive fallout
Investigators found cognitive changes, depression, and PTSD in infected patients, both in the subacute phase and 10 months after hospital discharge.
“We showed that cognitive and behavioral alterations are associated with COVID-19 infection within 2 months from hospital discharge and that they partially persist in the post-COVID phase,” study investigator Elisa Canu, PhD, neuroimaging research unit, division of neuroscience, IRCCS San Raffaele Scientific Institute, Milan, told a press briefing.
The findings were presented at the annual congress of the European Academy of Neurology.
Executive dysfunction
Previous research suggests about 30% of COVID-19 survivors have cognitive disturbances and 30%-40% have psychopathological disorders including anxiety and depression, said Dr. Canu.
These disturbances have been associated with the severity of acute-phase respiratory symptoms, infection-triggered neuroinflammation, cerebrovascular alterations, and/or neurodegeneration.
However, it’s unclear whether these disturbances persist in the post-COVID phase.
To investigate, the researchers explored cognitive and psychopathological features in 49 patients with confirmed COVID-19 admitted to a hospital ED. They examined these factors at 2 months (subacute phase) and at 10 months (post-COVID phase).
Participants had an average age of 61 years (age range, 40-75 years) and 73% were men. Most had at least one cardiovascular risk factor such as hypertension (55%), smoking (22%), and dyslipidemia (18%).
At hospital admission, 71% had an abnormal neurologic exam, 59% had hypogeusia (reduced sense of taste), 45% hyposmia (reduced sense of smell), 39% headache, and 20% confusion or drowsiness. During hospitalization, 27% had noninvasive ventilation.
In addition to cognitive and neurologic assessments, participants underwent MRI 2 months after hospital discharge. Researchers obtained data on gray matter, white matter, and total brain volume.
At 2 months post discharge, 53% of patients presented with at least one cognitive deficit. Many deficits related to executive function including difficulty planning, attention, and problem solving (16%).
However, some participants had memory issues (6%) or visuospatial disturbances (6%). Almost a quarter (23%) presented with a combination of symptoms related to executive dysfunction.
Low oxygen tied to more cognitive deficits
More than one-third of patients experienced symptoms of depression (16%) or PTSD (18%).
Patients younger than 50 years had more executive dysfunction, with these symptoms affecting 75% of younger patients. “Our explanation for that is that younger people had a milder clinical profile regarding COVID, so they were cared for at home,” said Dr. Canu.
While in hospital, patients may be on “continued alert” and receive structured interventions for cognitive and behavioral issues, she said.
More severe respiratory symptoms at hospital admission were significantly associated with deficits during the subacute phase (P = .002 for information processing).
“Low levels of oxygen in the brain could lead to confusion, headache, and brain fog, and cause the cognitive disturbances that we see,” said Dr. Canu.
White-matter hyperintensities were linked to cognitive deficits during this phase (P < .001 for verbal memory and delayed recall).
“These white-matter lesions are probably preexisting due to cardiovascular risk factors that were present in our population and may have amplified the memory disturbances we saw,” commented Dr. Canu.
The investigators did not find a significant relationship between cognitive performance and brain volume. Dr. Canu noted that cognitive and psychopathological disturbances are linked. For instance, she said, a patient with PTSD or depression may also have problems with attention or memory.
In the post-COVID phase, cognitive symptoms were reduced from 53% to 36%; again, the most common deficit was combined executive dysfunction symptoms. Depression persisted in 15% of patients and PTSD in 18%.
“We still don’t know if these alterations are a consequence of the infection,” said Dr. Canu. “And we don’t know whether the deficits are reversible or are part of a neurodegenerative process.”
The researchers plan to follow these patients further. “We definitely need longer follow-up and bigger populations, if possible, to see if these cognitive and psychopathological disturbances can improve in some way,” said Dr. Canu.
The study results underline the need for neuropsychological and neurologic monitoring in COVID patients. Cognitive stimulation training and physical activity, preferably outdoors, could be beneficial, Dr. Canu added.
A version of this article first appeared on Medscape.com.
Investigators found cognitive changes, depression, and PTSD in infected patients, both in the subacute phase and 10 months after hospital discharge.
“We showed that cognitive and behavioral alterations are associated with COVID-19 infection within 2 months from hospital discharge and that they partially persist in the post-COVID phase,” study investigator Elisa Canu, PhD, neuroimaging research unit, division of neuroscience, IRCCS San Raffaele Scientific Institute, Milan, told a press briefing.
The findings were presented at the annual congress of the European Academy of Neurology.
Executive dysfunction
Previous research suggests about 30% of COVID-19 survivors have cognitive disturbances and 30%-40% have psychopathological disorders including anxiety and depression, said Dr. Canu.
These disturbances have been associated with the severity of acute-phase respiratory symptoms, infection-triggered neuroinflammation, cerebrovascular alterations, and/or neurodegeneration.
However, it’s unclear whether these disturbances persist in the post-COVID phase.
To investigate, the researchers explored cognitive and psychopathological features in 49 patients with confirmed COVID-19 admitted to a hospital ED. They examined these factors at 2 months (subacute phase) and at 10 months (post-COVID phase).
Participants had an average age of 61 years (age range, 40-75 years) and 73% were men. Most had at least one cardiovascular risk factor such as hypertension (55%), smoking (22%), and dyslipidemia (18%).
At hospital admission, 71% had an abnormal neurologic exam, 59% had hypogeusia (reduced sense of taste), 45% hyposmia (reduced sense of smell), 39% headache, and 20% confusion or drowsiness. During hospitalization, 27% had noninvasive ventilation.
In addition to cognitive and neurologic assessments, participants underwent MRI 2 months after hospital discharge. Researchers obtained data on gray matter, white matter, and total brain volume.
At 2 months post discharge, 53% of patients presented with at least one cognitive deficit. Many deficits related to executive function including difficulty planning, attention, and problem solving (16%).
However, some participants had memory issues (6%) or visuospatial disturbances (6%). Almost a quarter (23%) presented with a combination of symptoms related to executive dysfunction.
Low oxygen tied to more cognitive deficits
More than one-third of patients experienced symptoms of depression (16%) or PTSD (18%).
Patients younger than 50 years had more executive dysfunction, with these symptoms affecting 75% of younger patients. “Our explanation for that is that younger people had a milder clinical profile regarding COVID, so they were cared for at home,” said Dr. Canu.
While in hospital, patients may be on “continued alert” and receive structured interventions for cognitive and behavioral issues, she said.
More severe respiratory symptoms at hospital admission were significantly associated with deficits during the subacute phase (P = .002 for information processing).
“Low levels of oxygen in the brain could lead to confusion, headache, and brain fog, and cause the cognitive disturbances that we see,” said Dr. Canu.
White-matter hyperintensities were linked to cognitive deficits during this phase (P < .001 for verbal memory and delayed recall).
“These white-matter lesions are probably preexisting due to cardiovascular risk factors that were present in our population and may have amplified the memory disturbances we saw,” commented Dr. Canu.
The investigators did not find a significant relationship between cognitive performance and brain volume. Dr. Canu noted that cognitive and psychopathological disturbances are linked. For instance, she said, a patient with PTSD or depression may also have problems with attention or memory.
In the post-COVID phase, cognitive symptoms were reduced from 53% to 36%; again, the most common deficit was combined executive dysfunction symptoms. Depression persisted in 15% of patients and PTSD in 18%.
“We still don’t know if these alterations are a consequence of the infection,” said Dr. Canu. “And we don’t know whether the deficits are reversible or are part of a neurodegenerative process.”
The researchers plan to follow these patients further. “We definitely need longer follow-up and bigger populations, if possible, to see if these cognitive and psychopathological disturbances can improve in some way,” said Dr. Canu.
The study results underline the need for neuropsychological and neurologic monitoring in COVID patients. Cognitive stimulation training and physical activity, preferably outdoors, could be beneficial, Dr. Canu added.
A version of this article first appeared on Medscape.com.
Investigators found cognitive changes, depression, and PTSD in infected patients, both in the subacute phase and 10 months after hospital discharge.
“We showed that cognitive and behavioral alterations are associated with COVID-19 infection within 2 months from hospital discharge and that they partially persist in the post-COVID phase,” study investigator Elisa Canu, PhD, neuroimaging research unit, division of neuroscience, IRCCS San Raffaele Scientific Institute, Milan, told a press briefing.
The findings were presented at the annual congress of the European Academy of Neurology.
Executive dysfunction
Previous research suggests about 30% of COVID-19 survivors have cognitive disturbances and 30%-40% have psychopathological disorders including anxiety and depression, said Dr. Canu.
These disturbances have been associated with the severity of acute-phase respiratory symptoms, infection-triggered neuroinflammation, cerebrovascular alterations, and/or neurodegeneration.
However, it’s unclear whether these disturbances persist in the post-COVID phase.
To investigate, the researchers explored cognitive and psychopathological features in 49 patients with confirmed COVID-19 admitted to a hospital ED. They examined these factors at 2 months (subacute phase) and at 10 months (post-COVID phase).
Participants had an average age of 61 years (age range, 40-75 years) and 73% were men. Most had at least one cardiovascular risk factor such as hypertension (55%), smoking (22%), and dyslipidemia (18%).
At hospital admission, 71% had an abnormal neurologic exam, 59% had hypogeusia (reduced sense of taste), 45% hyposmia (reduced sense of smell), 39% headache, and 20% confusion or drowsiness. During hospitalization, 27% had noninvasive ventilation.
In addition to cognitive and neurologic assessments, participants underwent MRI 2 months after hospital discharge. Researchers obtained data on gray matter, white matter, and total brain volume.
At 2 months post discharge, 53% of patients presented with at least one cognitive deficit. Many deficits related to executive function including difficulty planning, attention, and problem solving (16%).
However, some participants had memory issues (6%) or visuospatial disturbances (6%). Almost a quarter (23%) presented with a combination of symptoms related to executive dysfunction.
Low oxygen tied to more cognitive deficits
More than one-third of patients experienced symptoms of depression (16%) or PTSD (18%).
Patients younger than 50 years had more executive dysfunction, with these symptoms affecting 75% of younger patients. “Our explanation for that is that younger people had a milder clinical profile regarding COVID, so they were cared for at home,” said Dr. Canu.
While in hospital, patients may be on “continued alert” and receive structured interventions for cognitive and behavioral issues, she said.
More severe respiratory symptoms at hospital admission were significantly associated with deficits during the subacute phase (P = .002 for information processing).
“Low levels of oxygen in the brain could lead to confusion, headache, and brain fog, and cause the cognitive disturbances that we see,” said Dr. Canu.
White-matter hyperintensities were linked to cognitive deficits during this phase (P < .001 for verbal memory and delayed recall).
“These white-matter lesions are probably preexisting due to cardiovascular risk factors that were present in our population and may have amplified the memory disturbances we saw,” commented Dr. Canu.
The investigators did not find a significant relationship between cognitive performance and brain volume. Dr. Canu noted that cognitive and psychopathological disturbances are linked. For instance, she said, a patient with PTSD or depression may also have problems with attention or memory.
In the post-COVID phase, cognitive symptoms were reduced from 53% to 36%; again, the most common deficit was combined executive dysfunction symptoms. Depression persisted in 15% of patients and PTSD in 18%.
“We still don’t know if these alterations are a consequence of the infection,” said Dr. Canu. “And we don’t know whether the deficits are reversible or are part of a neurodegenerative process.”
The researchers plan to follow these patients further. “We definitely need longer follow-up and bigger populations, if possible, to see if these cognitive and psychopathological disturbances can improve in some way,” said Dr. Canu.
The study results underline the need for neuropsychological and neurologic monitoring in COVID patients. Cognitive stimulation training and physical activity, preferably outdoors, could be beneficial, Dr. Canu added.
A version of this article first appeared on Medscape.com.
COVID-19 vaccines are safe and effective for patients with migraine
according to a presentation at the American Headache Society’s 2021 annual meeting.
Amy Gelfand, MD, director of pediatric headache at University of California, San Francisco, reviewed common concerns migraine patients or their clinicians might have related any of the three vaccines, starting with a review of how the vaccines work – by targeting the spike protein of the SARS-CoV-2 virus.
“The vaccines induce response to that protein, but only that protein, so there’s no reason to think they’re going to cause the body to produce neutralizing antibodies against any of our migraine therapeutics,” Dr. Gelfand said. She added that the phase 3 clinical trials included participants from a wide range of ages and comorbidities, so there were likely many people in the trials who have migraine, though no subgroup analyses have been performed for this group or are likely to be performed.
Common questions
The two treatments people have the most questions about concerning the COVID-19 vaccine are onabotulinumtoxinA and CGRP pathway monoclonal antibodies (mAbs), likely because both of these are injections, as is the vaccine, Dr. Gelfand said. First, she reminded attendees that onabotulinumtoxinA is not a dermal filler, since some reports following administration of the Moderna vaccine suggested that some people with dermal fillers had swelling in those areas after vaccination.
In addition, “there’s no reason to think the onabotulinumtoxinA would influence our body’s immune response to any vaccine, so there’s no need to retime the onabotulinumtoxinA injections around COVID-19 vaccine administration,” Dr. Gelfand said.
Regarding mAbs, she acknowledged that some white blood cells have CGRP receptors, which may have a pro- or anti-inflammatory role, but clinical trials of mAbs did not show any evidence of being immunosuppressive or myelosuppressive.
“The monoclonal antibodies themselves have undergone engineering so that they are just going after their one target,” Dr. Gelfand said. “They’re not going to be expected to bind to anything else outside of their targets, so I don’t think there’s anything there to make us retime the monoclonal antibody administration relative to the COVID-19 vaccine.”
She did note that patients who choose to get mAbs injections in their arm instead of their thigh or abdomen may want to receive it in the opposite arm than they one they have gotten or will get the vaccine in since the vaccine can cause discomfort.
The other common question patients may have is whether taking any NSAIDs or acetaminophen before getting the COVID-19 vaccine will reduce their immune response to the vaccination. This concern arises because of past evidence showing that some infants tended to have lower immunologic responses when they received acetaminophen after their primary vaccines’ series, but the clinical significance of those reduced responses is not clear since they still had strong responses. Further, this effect was not seen with booster shots, suggesting it’s an age-dependent effect.
During the clinical trials of the AstraZeneca vaccine, several sites gave prophylactic paracetamol without any apparent detrimental effect on antibody response, Dr. Gelfand said. Further, the mRNA and adenovirus-vectored vaccines appear to induce antibodies far above what many believe is needed for protection.
“Even if there were a slight decrease, it’s not clear that that would have any kind of clinical significance for that person in terms of their level of protection against COVID-19,” she said. “Bottom line, it’s fine for patients to use either of these after administration of the COVID-19 vaccine.” The Centers for Disease Control and Prevention doesn’t recommend it prophylactically beforehand, but it’s fine to take it for a fever, aches or headache after getting the vaccine.
Migraine or vaccine reaction?
Dr. Gelfand then addressed whether it should affect physicians’ headache differential if seeing a patient who recently received an adenovirus-vectored vaccine, such as the Johnson & Johnson or AstraZeneca vaccines. The question relates to the discovery of a very rare potential adverse event from these vaccines: cerebral venous sinus thrombosis (CVST) with thrombocytopenia and thromboses in other major vessels, together called thrombosis thrombocytopenia syndrome (TTS). No TTS cases have been reported following mRNA vaccines.
TTS’s mechanism appears similar to autoimmune heparin-induced thrombocytopenia, where the body produces platelet-activating antibodies. TTS currently has three diagnostic criteria: new-onset thrombocytopenia (<150,000/microliter) without evidence of platelet clumping, venous or arterial thrombosis, and absence of prior exposure to heparin.
So far, TTS has been limited only to the vaccines that use an adenovirus vector. One male clinical trial participant experienced CVST with thrombocytopenia in Johnson & Johnson phase 3 trials, and 12 cases out of approximately 8 million Johnson & Johnson doses were reported to the Vaccine Adverse Event Reporting System between March 2 and April 21, 2021. Three TTS more cases followed these, resulting in 15 TTS events per 8 million doses.
In terms of clinical features, all 15 cases were females under age 60, mostly white, and all 11 who were tested were positive for the heparin-platelet factor 4 antibody test. TTS occurred 6-15 days after vaccination for these cases, and all but one had a headache. Their platelet count was 9,000-127,000. None were pregnant or postpartum.
“For us, as headache clinicians, the epidemiology of TTS overlaps with the epidemiology of migraine – they’re happening to the same group of patients,” Dr. Gelfand said. Most of the cases occurred in women aged 30-39 years, while the estimated incidence in women aged 50 or older is 0.9 cases per million doses.
The CDC has proceeded with the Johnson & Johnson vaccine because a risk-benefit analysis revealed that use of the vaccine will result in fewer hospitalization and deaths from COVID-19, compared with adverse events from the vaccine, Dr. Gelfand explained. However, the CDC notes that “women younger than 50 years old should be made aware of a rare risk of blood clots with low platelets following vaccination and the availability of other COVID-19 vaccines where this risk has not been observed.”
For clinicians, the existence of TTS raises a question when patients with a history of migraine call after having received the Johnson & Johnson vaccine, Dr. Gelfand said: “How do we know if this is a spontaneous attack, if it’s a headache provoked by receiving the vaccine, or they have one of these rare cases of [TTS]?”
Three things help with this differential, she said: timing, epidemiology, and headache phenotype. Headache after a vaccine is very common, but it usually happens within the first couple of hours or days after the vaccine. By day 4 after vaccination, few people had headaches in the clinical trials. Since TTS requires production of antibodies, a headache within a few hours of vaccination should not raise concerns about TTS. It should be considered, however, for patients who experience a headache within a week or 2 after vaccination.
Then consider the epidemiology: If it’s a woman between ages 18 and49 calling, the risk is higher than if it’s a male over age 50. Then consider whether there are any unusual headache features, positionality, encephalopathy, or clinical features that could suggest clots in other parts of the body, such as abdominal pain, shortness of breath, or pain in the legs.
“At the end of the day, if it’s a person who’s in this epidemiological window and they’re calling a week or 2 out from the Johnson & Johnson vaccine, we may just need to work it up and see,” Dr. Gelfand said. Work-up involves a CBC, a platelet count to see if they’re thrombocytopenic, and perhaps imaging, preferentially using MRI/MRV over CT since it’s a younger population. Treatment for CVST with thrombocytopenia is a nonheparin anticoagulant, and platelet transfusion should not occur before consulting with hematology.
Continue to vaccinate
“The big take home is that we should continue to vaccinate patients with migraine and that your current therapies do not interfere with the vaccine working and that the vaccine does not interact with our therapies,” Brian D. Loftus, MD, BSChE, immediate past president of the Southern Headache Society and a neurologist at Bellaire (Pa.) Neurology, said of the presentation. He also felt it was helpful to know that NSAIDs likely have no impact on the vaccines’ effectiveness as well.
“The most important new information for me was that the median onset of the CSVT was 8 days post vaccine,” Dr. Loftus said. “Typically, postvaccine headache is seen much sooner, within 1-2 days, so this is a useful clinical feature to separate out who needs to closer follow-up and possible neuroimaging.”
Given the epidemiology of those most likely to have TTS, Dr. Loftus said he would advise his female patients younger than 60 to simply get the Pfizer or Moderna vaccine since they appear safer for this demographic.
Dr. Gelfand is editor of the journal Headache but has no industry disclosures. Her spouse has received clinical trial grant support from Genentech and honoraria for editorial work from Dynamed Plus. Dr. Loftus has received grants or fees from Teva, Amgen, Abbvie, and Biohaven.
according to a presentation at the American Headache Society’s 2021 annual meeting.
Amy Gelfand, MD, director of pediatric headache at University of California, San Francisco, reviewed common concerns migraine patients or their clinicians might have related any of the three vaccines, starting with a review of how the vaccines work – by targeting the spike protein of the SARS-CoV-2 virus.
“The vaccines induce response to that protein, but only that protein, so there’s no reason to think they’re going to cause the body to produce neutralizing antibodies against any of our migraine therapeutics,” Dr. Gelfand said. She added that the phase 3 clinical trials included participants from a wide range of ages and comorbidities, so there were likely many people in the trials who have migraine, though no subgroup analyses have been performed for this group or are likely to be performed.
Common questions
The two treatments people have the most questions about concerning the COVID-19 vaccine are onabotulinumtoxinA and CGRP pathway monoclonal antibodies (mAbs), likely because both of these are injections, as is the vaccine, Dr. Gelfand said. First, she reminded attendees that onabotulinumtoxinA is not a dermal filler, since some reports following administration of the Moderna vaccine suggested that some people with dermal fillers had swelling in those areas after vaccination.
In addition, “there’s no reason to think the onabotulinumtoxinA would influence our body’s immune response to any vaccine, so there’s no need to retime the onabotulinumtoxinA injections around COVID-19 vaccine administration,” Dr. Gelfand said.
Regarding mAbs, she acknowledged that some white blood cells have CGRP receptors, which may have a pro- or anti-inflammatory role, but clinical trials of mAbs did not show any evidence of being immunosuppressive or myelosuppressive.
“The monoclonal antibodies themselves have undergone engineering so that they are just going after their one target,” Dr. Gelfand said. “They’re not going to be expected to bind to anything else outside of their targets, so I don’t think there’s anything there to make us retime the monoclonal antibody administration relative to the COVID-19 vaccine.”
She did note that patients who choose to get mAbs injections in their arm instead of their thigh or abdomen may want to receive it in the opposite arm than they one they have gotten or will get the vaccine in since the vaccine can cause discomfort.
The other common question patients may have is whether taking any NSAIDs or acetaminophen before getting the COVID-19 vaccine will reduce their immune response to the vaccination. This concern arises because of past evidence showing that some infants tended to have lower immunologic responses when they received acetaminophen after their primary vaccines’ series, but the clinical significance of those reduced responses is not clear since they still had strong responses. Further, this effect was not seen with booster shots, suggesting it’s an age-dependent effect.
During the clinical trials of the AstraZeneca vaccine, several sites gave prophylactic paracetamol without any apparent detrimental effect on antibody response, Dr. Gelfand said. Further, the mRNA and adenovirus-vectored vaccines appear to induce antibodies far above what many believe is needed for protection.
“Even if there were a slight decrease, it’s not clear that that would have any kind of clinical significance for that person in terms of their level of protection against COVID-19,” she said. “Bottom line, it’s fine for patients to use either of these after administration of the COVID-19 vaccine.” The Centers for Disease Control and Prevention doesn’t recommend it prophylactically beforehand, but it’s fine to take it for a fever, aches or headache after getting the vaccine.
Migraine or vaccine reaction?
Dr. Gelfand then addressed whether it should affect physicians’ headache differential if seeing a patient who recently received an adenovirus-vectored vaccine, such as the Johnson & Johnson or AstraZeneca vaccines. The question relates to the discovery of a very rare potential adverse event from these vaccines: cerebral venous sinus thrombosis (CVST) with thrombocytopenia and thromboses in other major vessels, together called thrombosis thrombocytopenia syndrome (TTS). No TTS cases have been reported following mRNA vaccines.
TTS’s mechanism appears similar to autoimmune heparin-induced thrombocytopenia, where the body produces platelet-activating antibodies. TTS currently has three diagnostic criteria: new-onset thrombocytopenia (<150,000/microliter) without evidence of platelet clumping, venous or arterial thrombosis, and absence of prior exposure to heparin.
So far, TTS has been limited only to the vaccines that use an adenovirus vector. One male clinical trial participant experienced CVST with thrombocytopenia in Johnson & Johnson phase 3 trials, and 12 cases out of approximately 8 million Johnson & Johnson doses were reported to the Vaccine Adverse Event Reporting System between March 2 and April 21, 2021. Three TTS more cases followed these, resulting in 15 TTS events per 8 million doses.
In terms of clinical features, all 15 cases were females under age 60, mostly white, and all 11 who were tested were positive for the heparin-platelet factor 4 antibody test. TTS occurred 6-15 days after vaccination for these cases, and all but one had a headache. Their platelet count was 9,000-127,000. None were pregnant or postpartum.
“For us, as headache clinicians, the epidemiology of TTS overlaps with the epidemiology of migraine – they’re happening to the same group of patients,” Dr. Gelfand said. Most of the cases occurred in women aged 30-39 years, while the estimated incidence in women aged 50 or older is 0.9 cases per million doses.
The CDC has proceeded with the Johnson & Johnson vaccine because a risk-benefit analysis revealed that use of the vaccine will result in fewer hospitalization and deaths from COVID-19, compared with adverse events from the vaccine, Dr. Gelfand explained. However, the CDC notes that “women younger than 50 years old should be made aware of a rare risk of blood clots with low platelets following vaccination and the availability of other COVID-19 vaccines where this risk has not been observed.”
For clinicians, the existence of TTS raises a question when patients with a history of migraine call after having received the Johnson & Johnson vaccine, Dr. Gelfand said: “How do we know if this is a spontaneous attack, if it’s a headache provoked by receiving the vaccine, or they have one of these rare cases of [TTS]?”
Three things help with this differential, she said: timing, epidemiology, and headache phenotype. Headache after a vaccine is very common, but it usually happens within the first couple of hours or days after the vaccine. By day 4 after vaccination, few people had headaches in the clinical trials. Since TTS requires production of antibodies, a headache within a few hours of vaccination should not raise concerns about TTS. It should be considered, however, for patients who experience a headache within a week or 2 after vaccination.
Then consider the epidemiology: If it’s a woman between ages 18 and49 calling, the risk is higher than if it’s a male over age 50. Then consider whether there are any unusual headache features, positionality, encephalopathy, or clinical features that could suggest clots in other parts of the body, such as abdominal pain, shortness of breath, or pain in the legs.
“At the end of the day, if it’s a person who’s in this epidemiological window and they’re calling a week or 2 out from the Johnson & Johnson vaccine, we may just need to work it up and see,” Dr. Gelfand said. Work-up involves a CBC, a platelet count to see if they’re thrombocytopenic, and perhaps imaging, preferentially using MRI/MRV over CT since it’s a younger population. Treatment for CVST with thrombocytopenia is a nonheparin anticoagulant, and platelet transfusion should not occur before consulting with hematology.
Continue to vaccinate
“The big take home is that we should continue to vaccinate patients with migraine and that your current therapies do not interfere with the vaccine working and that the vaccine does not interact with our therapies,” Brian D. Loftus, MD, BSChE, immediate past president of the Southern Headache Society and a neurologist at Bellaire (Pa.) Neurology, said of the presentation. He also felt it was helpful to know that NSAIDs likely have no impact on the vaccines’ effectiveness as well.
“The most important new information for me was that the median onset of the CSVT was 8 days post vaccine,” Dr. Loftus said. “Typically, postvaccine headache is seen much sooner, within 1-2 days, so this is a useful clinical feature to separate out who needs to closer follow-up and possible neuroimaging.”
Given the epidemiology of those most likely to have TTS, Dr. Loftus said he would advise his female patients younger than 60 to simply get the Pfizer or Moderna vaccine since they appear safer for this demographic.
Dr. Gelfand is editor of the journal Headache but has no industry disclosures. Her spouse has received clinical trial grant support from Genentech and honoraria for editorial work from Dynamed Plus. Dr. Loftus has received grants or fees from Teva, Amgen, Abbvie, and Biohaven.
according to a presentation at the American Headache Society’s 2021 annual meeting.
Amy Gelfand, MD, director of pediatric headache at University of California, San Francisco, reviewed common concerns migraine patients or their clinicians might have related any of the three vaccines, starting with a review of how the vaccines work – by targeting the spike protein of the SARS-CoV-2 virus.
“The vaccines induce response to that protein, but only that protein, so there’s no reason to think they’re going to cause the body to produce neutralizing antibodies against any of our migraine therapeutics,” Dr. Gelfand said. She added that the phase 3 clinical trials included participants from a wide range of ages and comorbidities, so there were likely many people in the trials who have migraine, though no subgroup analyses have been performed for this group or are likely to be performed.
Common questions
The two treatments people have the most questions about concerning the COVID-19 vaccine are onabotulinumtoxinA and CGRP pathway monoclonal antibodies (mAbs), likely because both of these are injections, as is the vaccine, Dr. Gelfand said. First, she reminded attendees that onabotulinumtoxinA is not a dermal filler, since some reports following administration of the Moderna vaccine suggested that some people with dermal fillers had swelling in those areas after vaccination.
In addition, “there’s no reason to think the onabotulinumtoxinA would influence our body’s immune response to any vaccine, so there’s no need to retime the onabotulinumtoxinA injections around COVID-19 vaccine administration,” Dr. Gelfand said.
Regarding mAbs, she acknowledged that some white blood cells have CGRP receptors, which may have a pro- or anti-inflammatory role, but clinical trials of mAbs did not show any evidence of being immunosuppressive or myelosuppressive.
“The monoclonal antibodies themselves have undergone engineering so that they are just going after their one target,” Dr. Gelfand said. “They’re not going to be expected to bind to anything else outside of their targets, so I don’t think there’s anything there to make us retime the monoclonal antibody administration relative to the COVID-19 vaccine.”
She did note that patients who choose to get mAbs injections in their arm instead of their thigh or abdomen may want to receive it in the opposite arm than they one they have gotten or will get the vaccine in since the vaccine can cause discomfort.
The other common question patients may have is whether taking any NSAIDs or acetaminophen before getting the COVID-19 vaccine will reduce their immune response to the vaccination. This concern arises because of past evidence showing that some infants tended to have lower immunologic responses when they received acetaminophen after their primary vaccines’ series, but the clinical significance of those reduced responses is not clear since they still had strong responses. Further, this effect was not seen with booster shots, suggesting it’s an age-dependent effect.
During the clinical trials of the AstraZeneca vaccine, several sites gave prophylactic paracetamol without any apparent detrimental effect on antibody response, Dr. Gelfand said. Further, the mRNA and adenovirus-vectored vaccines appear to induce antibodies far above what many believe is needed for protection.
“Even if there were a slight decrease, it’s not clear that that would have any kind of clinical significance for that person in terms of their level of protection against COVID-19,” she said. “Bottom line, it’s fine for patients to use either of these after administration of the COVID-19 vaccine.” The Centers for Disease Control and Prevention doesn’t recommend it prophylactically beforehand, but it’s fine to take it for a fever, aches or headache after getting the vaccine.
Migraine or vaccine reaction?
Dr. Gelfand then addressed whether it should affect physicians’ headache differential if seeing a patient who recently received an adenovirus-vectored vaccine, such as the Johnson & Johnson or AstraZeneca vaccines. The question relates to the discovery of a very rare potential adverse event from these vaccines: cerebral venous sinus thrombosis (CVST) with thrombocytopenia and thromboses in other major vessels, together called thrombosis thrombocytopenia syndrome (TTS). No TTS cases have been reported following mRNA vaccines.
TTS’s mechanism appears similar to autoimmune heparin-induced thrombocytopenia, where the body produces platelet-activating antibodies. TTS currently has three diagnostic criteria: new-onset thrombocytopenia (<150,000/microliter) without evidence of platelet clumping, venous or arterial thrombosis, and absence of prior exposure to heparin.
So far, TTS has been limited only to the vaccines that use an adenovirus vector. One male clinical trial participant experienced CVST with thrombocytopenia in Johnson & Johnson phase 3 trials, and 12 cases out of approximately 8 million Johnson & Johnson doses were reported to the Vaccine Adverse Event Reporting System between March 2 and April 21, 2021. Three TTS more cases followed these, resulting in 15 TTS events per 8 million doses.
In terms of clinical features, all 15 cases were females under age 60, mostly white, and all 11 who were tested were positive for the heparin-platelet factor 4 antibody test. TTS occurred 6-15 days after vaccination for these cases, and all but one had a headache. Their platelet count was 9,000-127,000. None were pregnant or postpartum.
“For us, as headache clinicians, the epidemiology of TTS overlaps with the epidemiology of migraine – they’re happening to the same group of patients,” Dr. Gelfand said. Most of the cases occurred in women aged 30-39 years, while the estimated incidence in women aged 50 or older is 0.9 cases per million doses.
The CDC has proceeded with the Johnson & Johnson vaccine because a risk-benefit analysis revealed that use of the vaccine will result in fewer hospitalization and deaths from COVID-19, compared with adverse events from the vaccine, Dr. Gelfand explained. However, the CDC notes that “women younger than 50 years old should be made aware of a rare risk of blood clots with low platelets following vaccination and the availability of other COVID-19 vaccines where this risk has not been observed.”
For clinicians, the existence of TTS raises a question when patients with a history of migraine call after having received the Johnson & Johnson vaccine, Dr. Gelfand said: “How do we know if this is a spontaneous attack, if it’s a headache provoked by receiving the vaccine, or they have one of these rare cases of [TTS]?”
Three things help with this differential, she said: timing, epidemiology, and headache phenotype. Headache after a vaccine is very common, but it usually happens within the first couple of hours or days after the vaccine. By day 4 after vaccination, few people had headaches in the clinical trials. Since TTS requires production of antibodies, a headache within a few hours of vaccination should not raise concerns about TTS. It should be considered, however, for patients who experience a headache within a week or 2 after vaccination.
Then consider the epidemiology: If it’s a woman between ages 18 and49 calling, the risk is higher than if it’s a male over age 50. Then consider whether there are any unusual headache features, positionality, encephalopathy, or clinical features that could suggest clots in other parts of the body, such as abdominal pain, shortness of breath, or pain in the legs.
“At the end of the day, if it’s a person who’s in this epidemiological window and they’re calling a week or 2 out from the Johnson & Johnson vaccine, we may just need to work it up and see,” Dr. Gelfand said. Work-up involves a CBC, a platelet count to see if they’re thrombocytopenic, and perhaps imaging, preferentially using MRI/MRV over CT since it’s a younger population. Treatment for CVST with thrombocytopenia is a nonheparin anticoagulant, and platelet transfusion should not occur before consulting with hematology.
Continue to vaccinate
“The big take home is that we should continue to vaccinate patients with migraine and that your current therapies do not interfere with the vaccine working and that the vaccine does not interact with our therapies,” Brian D. Loftus, MD, BSChE, immediate past president of the Southern Headache Society and a neurologist at Bellaire (Pa.) Neurology, said of the presentation. He also felt it was helpful to know that NSAIDs likely have no impact on the vaccines’ effectiveness as well.
“The most important new information for me was that the median onset of the CSVT was 8 days post vaccine,” Dr. Loftus said. “Typically, postvaccine headache is seen much sooner, within 1-2 days, so this is a useful clinical feature to separate out who needs to closer follow-up and possible neuroimaging.”
Given the epidemiology of those most likely to have TTS, Dr. Loftus said he would advise his female patients younger than 60 to simply get the Pfizer or Moderna vaccine since they appear safer for this demographic.
Dr. Gelfand is editor of the journal Headache but has no industry disclosures. Her spouse has received clinical trial grant support from Genentech and honoraria for editorial work from Dynamed Plus. Dr. Loftus has received grants or fees from Teva, Amgen, Abbvie, and Biohaven.
FROM AHS 2021
High rates of work-related trauma, PTSD in intern physicians
Work-related posttraumatic stress disorder is three times higher in interns than the general population, new research shows.
Investigators assessed PTSD in more than 1,100 physicians at the end of their internship year and found that a little over half reported work-related trauma exposure, and of these, 20% screened positive for PTSD.
Overall, 10% of participants screened positive for PTSD by the end of the internship year, compared with a 12-month PTSD prevalence of 3.6% in the general population.
“Work-related trauma exposure and PTSD are common and underdiscussed phenomena among intern physicians,” lead author Mary Vance, MD, assistant professor of psychiatry, Uniformed Services University of the Health Sciences, Bethesda, Md., said in an interview.
“I urge medical educators and policy makers to include this topic in their discussions about physician well-being and to implement effective interventions to mitigate the impact of work-related trauma and PTSD among physician trainees,” she said.
The study was published online June 8 in JAMA Network Open.
Burnout, depression, suicide
“Burnout, depression, and suicide are increasingly recognized as occupational mental health hazards among health care professionals, including physicians,” Dr. Vance said.
“However, in my professional experience as a physician and educator, despite observing anecdotal evidence among my peers and trainees that this is also an issue,” she added.
This gap prompted her “to investigate rates of work-related trauma exposure and PTSD among physicians.”
The researchers sent emails to 4,350 individuals during academic year 2018-2019, 2 months prior to starting internships. Of these, 2,129 agreed to participate and 1,134 (58.6% female, 61.6% non-Hispanic White; mean age, 27.52) completed the study.
Prior to beginning internship, participants completed a baseline survey that assessed demographic characteristics as well as medical education and psychological and psychosocial factors.
Participants completed follow-up surveys sent by email at 3, 6, 9, and 12 months of the internship year. The surveys assessed stressful life events, concern over perceived medical errors in the past 3 months, and number of hours worked over the past week.
At month 12, current PTSD and symptoms of depression and anxiety were also assessed using the Primary Care PTSD Screen for DSM-5, the 9-item Patient Health Questionnaire, and the Generalized Anxiety Disorder 7-item scale, respectively.
Participants were asked to self-report whether they ever had an episode of depression and to complete the Risky Families Questionnaire to assess if they had experienced childhood abuse, neglect, and family conflict. Additionally, they completed an 11-item scale developed specifically for the study regarding recent stressful events.
‘Crucible’ year
A total of 56.4% of respondents reported work-related trauma exposure, and among these, 19.0% screened positive for PTSD. One-tenth (10.8%) of the entire sample screened positive for PTSD by the end of internship year, which is three times higher than the 12-month prevalence of PTSD in the general population (3.6%), the authors noted.
Trauma exposure differed by specialty, ranging from 43.1% in anesthesiology to 72.4% in emergency medicine. Of the respondents in internal medicine, surgery, and medicine/pediatrics, 56.6%, 63.3%, and 71%, respectively, reported work-related trauma exposure.
Work-related PTSD also differed by specialty, ranging from 7.5% in ob.gyn. to 30.0% in pediatrics. Of respondents in internal medicine and family practice, 23.9% and 25.9%, respectively, reported work-related PTSD.
Dr. Vance called the intern year “a crucible, during which newly minted doctors receive intensive on-the-job training at the front lines of patient care [and] work long hours in rapidly shifting environments, often caring for critically ill patients.”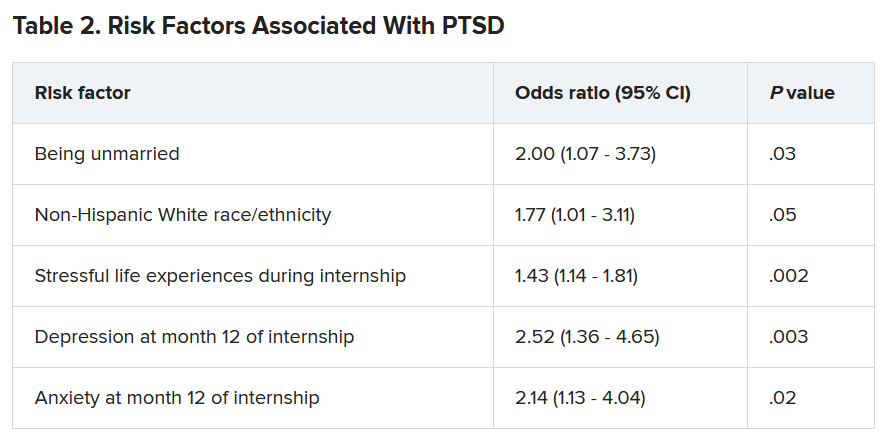
Work-related trauma exposure “is more likely to occur during this high-stress internship year than during the same year in the general population,” she said.
She noted that the “issue of workplace trauma and PTSD among health care workers became even more salient during the height of COVID,” adding that she expects it “to remain a pressure issue for healthcare workers in the post-COVID era.”
Call to action
Commenting on the study David A. Marcus, MD, chair, GME Physician Well-Being Committee, Northwell Health, New Hyde Park, N.Y., noted the study’s “relatively low response rate” is a “significant limitation” of the study.
An additional limitation is the lack of a baseline PTSD assessment, said Dr. Marcus, an assistant professor at Hofstra University, Hempstead, N.Y., who was not involved in the research.
Nevertheless, the “overall prevalence [of work-related PTSD] should serve as a call to action for physician leaders and for leaders in academic medicine,” he said.
Additionally, the study “reminds us that trauma-informed care should be an essential part of mental health support services provided to trainees and to physicians in general,” Dr. Marcus stated.
Also commenting on the study, Lotte N. Dyrbye, MD, professor of medicine and medical education, Mayo Clinic, Rochester, Minn., agreed.
“Organizational strategies should include system-level interventions to reduce the risk of frightening, horrible, or traumatic events from occurring in the workplace in the first place, as well as faculty development efforts to upskill teaching faculty in their ability to support trainees when such events do occur,” she said.
These approaches “should coincide with organizational efforts to support individual trainees by providing adequate time off after traumatic events, ensuring trainees can access affordable mental healthcare, and reducing other barriers to appropriate help-seeking, such as stigma, and efforts to build a culture of well-being,” suggested Dr. Dyrbye, who is codirector of the Mayo Clinic Program on Physician Wellbeing and was not involved in the study.
The study was supported by grants from the Blue Cross Blue Shield Foundation of Michigan and National Institutes of Health. Dr. Vance and coauthors, Dr. Marcus, and Dr. Dyrbye reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Work-related posttraumatic stress disorder is three times higher in interns than the general population, new research shows.
Investigators assessed PTSD in more than 1,100 physicians at the end of their internship year and found that a little over half reported work-related trauma exposure, and of these, 20% screened positive for PTSD.
Overall, 10% of participants screened positive for PTSD by the end of the internship year, compared with a 12-month PTSD prevalence of 3.6% in the general population.
“Work-related trauma exposure and PTSD are common and underdiscussed phenomena among intern physicians,” lead author Mary Vance, MD, assistant professor of psychiatry, Uniformed Services University of the Health Sciences, Bethesda, Md., said in an interview.
“I urge medical educators and policy makers to include this topic in their discussions about physician well-being and to implement effective interventions to mitigate the impact of work-related trauma and PTSD among physician trainees,” she said.
The study was published online June 8 in JAMA Network Open.
Burnout, depression, suicide
“Burnout, depression, and suicide are increasingly recognized as occupational mental health hazards among health care professionals, including physicians,” Dr. Vance said.
“However, in my professional experience as a physician and educator, despite observing anecdotal evidence among my peers and trainees that this is also an issue,” she added.
This gap prompted her “to investigate rates of work-related trauma exposure and PTSD among physicians.”
The researchers sent emails to 4,350 individuals during academic year 2018-2019, 2 months prior to starting internships. Of these, 2,129 agreed to participate and 1,134 (58.6% female, 61.6% non-Hispanic White; mean age, 27.52) completed the study.
Prior to beginning internship, participants completed a baseline survey that assessed demographic characteristics as well as medical education and psychological and psychosocial factors.
Participants completed follow-up surveys sent by email at 3, 6, 9, and 12 months of the internship year. The surveys assessed stressful life events, concern over perceived medical errors in the past 3 months, and number of hours worked over the past week.
At month 12, current PTSD and symptoms of depression and anxiety were also assessed using the Primary Care PTSD Screen for DSM-5, the 9-item Patient Health Questionnaire, and the Generalized Anxiety Disorder 7-item scale, respectively.
Participants were asked to self-report whether they ever had an episode of depression and to complete the Risky Families Questionnaire to assess if they had experienced childhood abuse, neglect, and family conflict. Additionally, they completed an 11-item scale developed specifically for the study regarding recent stressful events.
‘Crucible’ year
A total of 56.4% of respondents reported work-related trauma exposure, and among these, 19.0% screened positive for PTSD. One-tenth (10.8%) of the entire sample screened positive for PTSD by the end of internship year, which is three times higher than the 12-month prevalence of PTSD in the general population (3.6%), the authors noted.
Trauma exposure differed by specialty, ranging from 43.1% in anesthesiology to 72.4% in emergency medicine. Of the respondents in internal medicine, surgery, and medicine/pediatrics, 56.6%, 63.3%, and 71%, respectively, reported work-related trauma exposure.
Work-related PTSD also differed by specialty, ranging from 7.5% in ob.gyn. to 30.0% in pediatrics. Of respondents in internal medicine and family practice, 23.9% and 25.9%, respectively, reported work-related PTSD.
Dr. Vance called the intern year “a crucible, during which newly minted doctors receive intensive on-the-job training at the front lines of patient care [and] work long hours in rapidly shifting environments, often caring for critically ill patients.”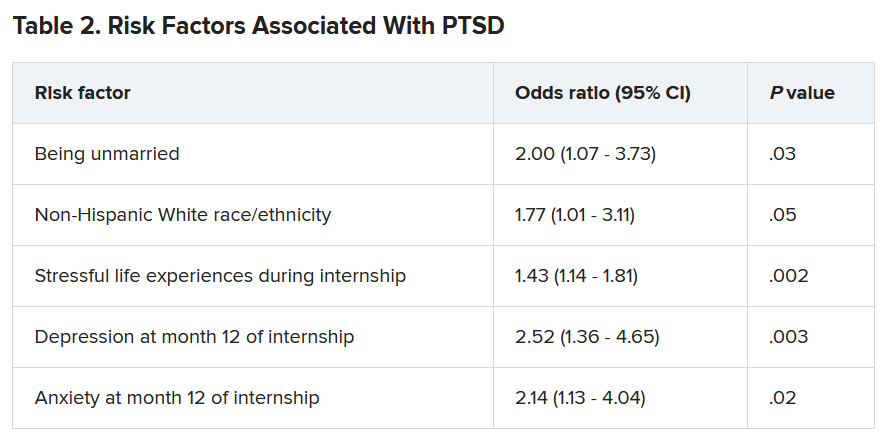
Work-related trauma exposure “is more likely to occur during this high-stress internship year than during the same year in the general population,” she said.
She noted that the “issue of workplace trauma and PTSD among health care workers became even more salient during the height of COVID,” adding that she expects it “to remain a pressure issue for healthcare workers in the post-COVID era.”
Call to action
Commenting on the study David A. Marcus, MD, chair, GME Physician Well-Being Committee, Northwell Health, New Hyde Park, N.Y., noted the study’s “relatively low response rate” is a “significant limitation” of the study.
An additional limitation is the lack of a baseline PTSD assessment, said Dr. Marcus, an assistant professor at Hofstra University, Hempstead, N.Y., who was not involved in the research.
Nevertheless, the “overall prevalence [of work-related PTSD] should serve as a call to action for physician leaders and for leaders in academic medicine,” he said.
Additionally, the study “reminds us that trauma-informed care should be an essential part of mental health support services provided to trainees and to physicians in general,” Dr. Marcus stated.
Also commenting on the study, Lotte N. Dyrbye, MD, professor of medicine and medical education, Mayo Clinic, Rochester, Minn., agreed.
“Organizational strategies should include system-level interventions to reduce the risk of frightening, horrible, or traumatic events from occurring in the workplace in the first place, as well as faculty development efforts to upskill teaching faculty in their ability to support trainees when such events do occur,” she said.
These approaches “should coincide with organizational efforts to support individual trainees by providing adequate time off after traumatic events, ensuring trainees can access affordable mental healthcare, and reducing other barriers to appropriate help-seeking, such as stigma, and efforts to build a culture of well-being,” suggested Dr. Dyrbye, who is codirector of the Mayo Clinic Program on Physician Wellbeing and was not involved in the study.
The study was supported by grants from the Blue Cross Blue Shield Foundation of Michigan and National Institutes of Health. Dr. Vance and coauthors, Dr. Marcus, and Dr. Dyrbye reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Work-related posttraumatic stress disorder is three times higher in interns than the general population, new research shows.
Investigators assessed PTSD in more than 1,100 physicians at the end of their internship year and found that a little over half reported work-related trauma exposure, and of these, 20% screened positive for PTSD.
Overall, 10% of participants screened positive for PTSD by the end of the internship year, compared with a 12-month PTSD prevalence of 3.6% in the general population.
“Work-related trauma exposure and PTSD are common and underdiscussed phenomena among intern physicians,” lead author Mary Vance, MD, assistant professor of psychiatry, Uniformed Services University of the Health Sciences, Bethesda, Md., said in an interview.
“I urge medical educators and policy makers to include this topic in their discussions about physician well-being and to implement effective interventions to mitigate the impact of work-related trauma and PTSD among physician trainees,” she said.
The study was published online June 8 in JAMA Network Open.
Burnout, depression, suicide
“Burnout, depression, and suicide are increasingly recognized as occupational mental health hazards among health care professionals, including physicians,” Dr. Vance said.
“However, in my professional experience as a physician and educator, despite observing anecdotal evidence among my peers and trainees that this is also an issue,” she added.
This gap prompted her “to investigate rates of work-related trauma exposure and PTSD among physicians.”
The researchers sent emails to 4,350 individuals during academic year 2018-2019, 2 months prior to starting internships. Of these, 2,129 agreed to participate and 1,134 (58.6% female, 61.6% non-Hispanic White; mean age, 27.52) completed the study.
Prior to beginning internship, participants completed a baseline survey that assessed demographic characteristics as well as medical education and psychological and psychosocial factors.
Participants completed follow-up surveys sent by email at 3, 6, 9, and 12 months of the internship year. The surveys assessed stressful life events, concern over perceived medical errors in the past 3 months, and number of hours worked over the past week.
At month 12, current PTSD and symptoms of depression and anxiety were also assessed using the Primary Care PTSD Screen for DSM-5, the 9-item Patient Health Questionnaire, and the Generalized Anxiety Disorder 7-item scale, respectively.
Participants were asked to self-report whether they ever had an episode of depression and to complete the Risky Families Questionnaire to assess if they had experienced childhood abuse, neglect, and family conflict. Additionally, they completed an 11-item scale developed specifically for the study regarding recent stressful events.
‘Crucible’ year
A total of 56.4% of respondents reported work-related trauma exposure, and among these, 19.0% screened positive for PTSD. One-tenth (10.8%) of the entire sample screened positive for PTSD by the end of internship year, which is three times higher than the 12-month prevalence of PTSD in the general population (3.6%), the authors noted.
Trauma exposure differed by specialty, ranging from 43.1% in anesthesiology to 72.4% in emergency medicine. Of the respondents in internal medicine, surgery, and medicine/pediatrics, 56.6%, 63.3%, and 71%, respectively, reported work-related trauma exposure.
Work-related PTSD also differed by specialty, ranging from 7.5% in ob.gyn. to 30.0% in pediatrics. Of respondents in internal medicine and family practice, 23.9% and 25.9%, respectively, reported work-related PTSD.
Dr. Vance called the intern year “a crucible, during which newly minted doctors receive intensive on-the-job training at the front lines of patient care [and] work long hours in rapidly shifting environments, often caring for critically ill patients.”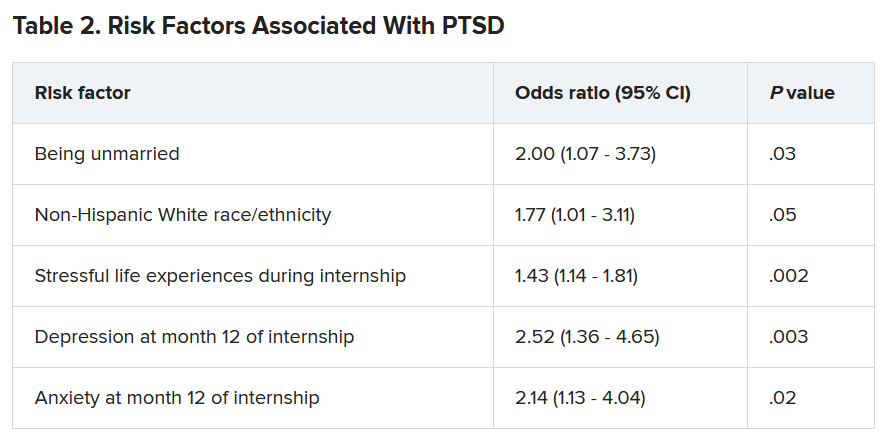
Work-related trauma exposure “is more likely to occur during this high-stress internship year than during the same year in the general population,” she said.
She noted that the “issue of workplace trauma and PTSD among health care workers became even more salient during the height of COVID,” adding that she expects it “to remain a pressure issue for healthcare workers in the post-COVID era.”
Call to action
Commenting on the study David A. Marcus, MD, chair, GME Physician Well-Being Committee, Northwell Health, New Hyde Park, N.Y., noted the study’s “relatively low response rate” is a “significant limitation” of the study.
An additional limitation is the lack of a baseline PTSD assessment, said Dr. Marcus, an assistant professor at Hofstra University, Hempstead, N.Y., who was not involved in the research.
Nevertheless, the “overall prevalence [of work-related PTSD] should serve as a call to action for physician leaders and for leaders in academic medicine,” he said.
Additionally, the study “reminds us that trauma-informed care should be an essential part of mental health support services provided to trainees and to physicians in general,” Dr. Marcus stated.
Also commenting on the study, Lotte N. Dyrbye, MD, professor of medicine and medical education, Mayo Clinic, Rochester, Minn., agreed.
“Organizational strategies should include system-level interventions to reduce the risk of frightening, horrible, or traumatic events from occurring in the workplace in the first place, as well as faculty development efforts to upskill teaching faculty in their ability to support trainees when such events do occur,” she said.
These approaches “should coincide with organizational efforts to support individual trainees by providing adequate time off after traumatic events, ensuring trainees can access affordable mental healthcare, and reducing other barriers to appropriate help-seeking, such as stigma, and efforts to build a culture of well-being,” suggested Dr. Dyrbye, who is codirector of the Mayo Clinic Program on Physician Wellbeing and was not involved in the study.
The study was supported by grants from the Blue Cross Blue Shield Foundation of Michigan and National Institutes of Health. Dr. Vance and coauthors, Dr. Marcus, and Dr. Dyrbye reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Ten killer steps to writing a great medical thriller
For many physicians and other professionals, aspirations of crafting a work of fiction are not uncommon — and with good reason. We are, after all, a generally well-disciplined bunch capable of completing complex tasks, and there is certainly no shortage of excitement and drama in medicine and surgery — ample fodder for thrilling stories. Nonetheless, writing a novel is a major commitment, and it requires persistence, patience, and dedicated time, especially for one with a busy medical career.
Getting started is not easy. Writing workshops are helpful, and in my case, I tried to mentor with some of the best. Before writing my novel, I attended workshops for aspiring novelists, given by noted physician authors Tess Gerritsen (Body Double, The Surgeon) and the late Michael Palmer (The Society, The Fifth Vial).
Writers are often advised to “write about what you know.” In my case, I combined my knowledge of medicine and my experience with the thoroughbred racing world to craft a thriller that one reviewer described as “Dick Francis meets Robin Cook.” For those who have never read the Dick Francis series, he was a renowned crime writer whose novels centered on horse racing in England. Having been an avid reader of both authors, that comparison was the ultimate compliment.
So against that backdrop, the novel Shedrow, along with some shared wisdom from a few legendary writers.
1. Start with the big “what if.” Any great story starts with that simple “what if” question. What if a series of high-profile executives in the managed care industry are serially murdered (Michael Palmer’s The Society)? What if a multimillion-dollar stallion dies suddenly under very mysterious circumstances on a supposedly secure farm in Kentucky (Dean DeLuke’s Shedrow)?
2. Put a MacGuffin to work in your story. Popularized by Alfred Hitchcock, the MacGuffin is that essential plot element that drives virtually all characters in the story, although it may be rather vague and meaningless to the story itself. In the iconic movie Pulp Fiction, the MacGuffin is the briefcase — everyone wants it, and we never do find out what’s in it.
3. Pacing is critical. Plot out the timeline of emotional highs and lows in a story. It should look like a rolling pattern of highs and lows that crescendo upward to the ultimate crisis. Take advantage of the fact that following any of those emotional peaks, you probably have the reader’s undivided attention. That would be a good time to provide backstory or fill in needed information for the reader – information that may be critical but perhaps not as exciting as what just transpired.
4. Torture your protagonists. Just when the reader thinks that the hero is finally home free, throw in another obstacle. Readers will empathize with the character and be drawn in by the unexpected hurdle.
5. Be original and surprise your readers. Create twists and turns that are totally unexpected, yet believable. This is easier said than done but will go a long way toward making your novel original, gripping, and unpredictable.
6. As a general rule, consider short sentences and short chapters. This is strictly a personal preference, but who can argue with James Patterson’s short chapters or with Robert Parker’s short and engaging sentences? Sentence length can be varied for effect, too, with shorter sentences serving to heighten action or increase tension.
7. Avoid the passive voice. Your readers want action. This is an important rule in almost any type of writing.
8. Keep descriptions brief. Long, drawn-out descriptions of the way characters look, or even setting descriptions, are easily overdone in a thriller. The thriller genre is very different from literary fiction in this regard. Stephen King advises writers to “just say what they see, then get on with the story.”
9. Sustain the reader’s interest throughout. Assess each chapter ending and determine whether the reader has been given enough reason to want to continue reading. Pose a question, end with a minor cliffhanger, or at least ensure that there is enough accumulated tension in the story.
10. Edit aggressively and cut out the fluff. Ernest Hemingway once confided to F. Scott Fitzgerald, “I write one page of masterpiece to 91 pages of shit. I try to put the shit in the wastebasket.”
Dr. DeLuke is professor emeritus of oral and facial surgery at Virginia Commonwealth University and author of the novel Shedrow.
A version of this article first appeared on Medscape.com.
For many physicians and other professionals, aspirations of crafting a work of fiction are not uncommon — and with good reason. We are, after all, a generally well-disciplined bunch capable of completing complex tasks, and there is certainly no shortage of excitement and drama in medicine and surgery — ample fodder for thrilling stories. Nonetheless, writing a novel is a major commitment, and it requires persistence, patience, and dedicated time, especially for one with a busy medical career.
Getting started is not easy. Writing workshops are helpful, and in my case, I tried to mentor with some of the best. Before writing my novel, I attended workshops for aspiring novelists, given by noted physician authors Tess Gerritsen (Body Double, The Surgeon) and the late Michael Palmer (The Society, The Fifth Vial).
Writers are often advised to “write about what you know.” In my case, I combined my knowledge of medicine and my experience with the thoroughbred racing world to craft a thriller that one reviewer described as “Dick Francis meets Robin Cook.” For those who have never read the Dick Francis series, he was a renowned crime writer whose novels centered on horse racing in England. Having been an avid reader of both authors, that comparison was the ultimate compliment.
So against that backdrop, the novel Shedrow, along with some shared wisdom from a few legendary writers.
1. Start with the big “what if.” Any great story starts with that simple “what if” question. What if a series of high-profile executives in the managed care industry are serially murdered (Michael Palmer’s The Society)? What if a multimillion-dollar stallion dies suddenly under very mysterious circumstances on a supposedly secure farm in Kentucky (Dean DeLuke’s Shedrow)?
2. Put a MacGuffin to work in your story. Popularized by Alfred Hitchcock, the MacGuffin is that essential plot element that drives virtually all characters in the story, although it may be rather vague and meaningless to the story itself. In the iconic movie Pulp Fiction, the MacGuffin is the briefcase — everyone wants it, and we never do find out what’s in it.
3. Pacing is critical. Plot out the timeline of emotional highs and lows in a story. It should look like a rolling pattern of highs and lows that crescendo upward to the ultimate crisis. Take advantage of the fact that following any of those emotional peaks, you probably have the reader’s undivided attention. That would be a good time to provide backstory or fill in needed information for the reader – information that may be critical but perhaps not as exciting as what just transpired.
4. Torture your protagonists. Just when the reader thinks that the hero is finally home free, throw in another obstacle. Readers will empathize with the character and be drawn in by the unexpected hurdle.
5. Be original and surprise your readers. Create twists and turns that are totally unexpected, yet believable. This is easier said than done but will go a long way toward making your novel original, gripping, and unpredictable.
6. As a general rule, consider short sentences and short chapters. This is strictly a personal preference, but who can argue with James Patterson’s short chapters or with Robert Parker’s short and engaging sentences? Sentence length can be varied for effect, too, with shorter sentences serving to heighten action or increase tension.
7. Avoid the passive voice. Your readers want action. This is an important rule in almost any type of writing.
8. Keep descriptions brief. Long, drawn-out descriptions of the way characters look, or even setting descriptions, are easily overdone in a thriller. The thriller genre is very different from literary fiction in this regard. Stephen King advises writers to “just say what they see, then get on with the story.”
9. Sustain the reader’s interest throughout. Assess each chapter ending and determine whether the reader has been given enough reason to want to continue reading. Pose a question, end with a minor cliffhanger, or at least ensure that there is enough accumulated tension in the story.
10. Edit aggressively and cut out the fluff. Ernest Hemingway once confided to F. Scott Fitzgerald, “I write one page of masterpiece to 91 pages of shit. I try to put the shit in the wastebasket.”
Dr. DeLuke is professor emeritus of oral and facial surgery at Virginia Commonwealth University and author of the novel Shedrow.
A version of this article first appeared on Medscape.com.
For many physicians and other professionals, aspirations of crafting a work of fiction are not uncommon — and with good reason. We are, after all, a generally well-disciplined bunch capable of completing complex tasks, and there is certainly no shortage of excitement and drama in medicine and surgery — ample fodder for thrilling stories. Nonetheless, writing a novel is a major commitment, and it requires persistence, patience, and dedicated time, especially for one with a busy medical career.
Getting started is not easy. Writing workshops are helpful, and in my case, I tried to mentor with some of the best. Before writing my novel, I attended workshops for aspiring novelists, given by noted physician authors Tess Gerritsen (Body Double, The Surgeon) and the late Michael Palmer (The Society, The Fifth Vial).
Writers are often advised to “write about what you know.” In my case, I combined my knowledge of medicine and my experience with the thoroughbred racing world to craft a thriller that one reviewer described as “Dick Francis meets Robin Cook.” For those who have never read the Dick Francis series, he was a renowned crime writer whose novels centered on horse racing in England. Having been an avid reader of both authors, that comparison was the ultimate compliment.
So against that backdrop, the novel Shedrow, along with some shared wisdom from a few legendary writers.
1. Start with the big “what if.” Any great story starts with that simple “what if” question. What if a series of high-profile executives in the managed care industry are serially murdered (Michael Palmer’s The Society)? What if a multimillion-dollar stallion dies suddenly under very mysterious circumstances on a supposedly secure farm in Kentucky (Dean DeLuke’s Shedrow)?
2. Put a MacGuffin to work in your story. Popularized by Alfred Hitchcock, the MacGuffin is that essential plot element that drives virtually all characters in the story, although it may be rather vague and meaningless to the story itself. In the iconic movie Pulp Fiction, the MacGuffin is the briefcase — everyone wants it, and we never do find out what’s in it.
3. Pacing is critical. Plot out the timeline of emotional highs and lows in a story. It should look like a rolling pattern of highs and lows that crescendo upward to the ultimate crisis. Take advantage of the fact that following any of those emotional peaks, you probably have the reader’s undivided attention. That would be a good time to provide backstory or fill in needed information for the reader – information that may be critical but perhaps not as exciting as what just transpired.
4. Torture your protagonists. Just when the reader thinks that the hero is finally home free, throw in another obstacle. Readers will empathize with the character and be drawn in by the unexpected hurdle.
5. Be original and surprise your readers. Create twists and turns that are totally unexpected, yet believable. This is easier said than done but will go a long way toward making your novel original, gripping, and unpredictable.
6. As a general rule, consider short sentences and short chapters. This is strictly a personal preference, but who can argue with James Patterson’s short chapters or with Robert Parker’s short and engaging sentences? Sentence length can be varied for effect, too, with shorter sentences serving to heighten action or increase tension.
7. Avoid the passive voice. Your readers want action. This is an important rule in almost any type of writing.
8. Keep descriptions brief. Long, drawn-out descriptions of the way characters look, or even setting descriptions, are easily overdone in a thriller. The thriller genre is very different from literary fiction in this regard. Stephen King advises writers to “just say what they see, then get on with the story.”
9. Sustain the reader’s interest throughout. Assess each chapter ending and determine whether the reader has been given enough reason to want to continue reading. Pose a question, end with a minor cliffhanger, or at least ensure that there is enough accumulated tension in the story.
10. Edit aggressively and cut out the fluff. Ernest Hemingway once confided to F. Scott Fitzgerald, “I write one page of masterpiece to 91 pages of shit. I try to put the shit in the wastebasket.”
Dr. DeLuke is professor emeritus of oral and facial surgery at Virginia Commonwealth University and author of the novel Shedrow.
A version of this article first appeared on Medscape.com.
Treating sleep apnea lowers MI and stroke risk
particularly for patients with moderate to severe OSA and those who are more adherent to CPAP therapy, a new study suggests.
“Most clinical trials on the effect of CPAP on CV diseases to date have focused on secondary CV prevention. This study contributes another piece of evidence about the role of CPAP therapy to prevent CV diseases,” said Diego R. Mazzotti, PhD, an assistant professor at the University of Kansas Medical Center, Kansas City.
“Our study, while observational, suggests that clinical trials focused on understanding how to sustain long-term CPAP adherence in obstructive sleep apnea patients are necessary and could be critical for optimizing comorbidity risk reduction,” Dr. Mazzotti said.
The study was presented at the virtual annual meeting of the Associated Professional Sleep Societies.
Good adherence important
The researchers analyzed the electronic health records of adults referred for a sleep study through the Kaiser Permanente Southern California health system. The sample included 11,145 adults without OSA, 13,898 with OSA who used CPAP, and 20,884 adults with OSA who did not use CPAP. None of them had CV disease at baseline. Median follow-up was 262 days.
The primary outcome was first occurrence of myocardial infarction, stroke, unstable angina, heart failure, or death caused by CV disease.
In adjusted models, adults with moderate to severe OSA (apnea-hypopnea index ≥15) who did not use CPAP were 71% more likely than those without OSA to have a first CV event (hazard ratio, 1.71; 95% CI, 1.11-2.64). However, the risk for a CV event during follow-up was 32% lower among OSA patients with any CPAP use (HR, 0.68; 95% CI, 0.50-0.93; P = .016).
The effect was mostly driven by those who used CPAP for at least 4 hours per night (HR, 0.60; 95% CI, 0.39-0.95). This association was stronger for those with moderate to severe OSA (HR, 0.56; 95% CI, 0.39-0.81).
“This study highlights the importance of long-term management of CPAP therapy in patients with moderate-severe OSA,” Dr. Mazzotti said in an interview.
“It suggests that maintaining good CPAP adherence might be beneficial for cardiovascular health, besides the already established benefits on quality of life, sleepiness, and other cardiometabolic functions,” he said.
Dr. Mazzotti said several mechanisms might explain the association between CPAP use and lower risk for CV events. “CPAP treats OSA by preventing respiratory pauses that occur during sleep, therefore preventing arousals, sleep fragmentation, and decreases in blood oxygen. These improved cardiorespiratory functions can be beneficial to avoid certain molecular changes that are known to contribute to cardiovascular risk, such as oxidative stress and inflammation,” he explained.
“However, specific studies fully understanding these mechanisms are necessary,” Dr. Mazzotti added.
In a comment, Nitun Verma, MD, a spokesperson for the American Academy of Sleep Medicine, said that “the frequent decreases in oxygen levels and fragmented sleep from apnea are associated with cardiovascular disorders. We know this from multiple studies. This, however, was a large study and strengthens the association between improving apnea and reduced serious cardiovascular events.”
Funding for the study was provided by the American Academy of Sleep Medicine Foundation and the American Heart Association. Dr. Mazzotti and Dr. Verma disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
particularly for patients with moderate to severe OSA and those who are more adherent to CPAP therapy, a new study suggests.
“Most clinical trials on the effect of CPAP on CV diseases to date have focused on secondary CV prevention. This study contributes another piece of evidence about the role of CPAP therapy to prevent CV diseases,” said Diego R. Mazzotti, PhD, an assistant professor at the University of Kansas Medical Center, Kansas City.
“Our study, while observational, suggests that clinical trials focused on understanding how to sustain long-term CPAP adherence in obstructive sleep apnea patients are necessary and could be critical for optimizing comorbidity risk reduction,” Dr. Mazzotti said.
The study was presented at the virtual annual meeting of the Associated Professional Sleep Societies.
Good adherence important
The researchers analyzed the electronic health records of adults referred for a sleep study through the Kaiser Permanente Southern California health system. The sample included 11,145 adults without OSA, 13,898 with OSA who used CPAP, and 20,884 adults with OSA who did not use CPAP. None of them had CV disease at baseline. Median follow-up was 262 days.
The primary outcome was first occurrence of myocardial infarction, stroke, unstable angina, heart failure, or death caused by CV disease.
In adjusted models, adults with moderate to severe OSA (apnea-hypopnea index ≥15) who did not use CPAP were 71% more likely than those without OSA to have a first CV event (hazard ratio, 1.71; 95% CI, 1.11-2.64). However, the risk for a CV event during follow-up was 32% lower among OSA patients with any CPAP use (HR, 0.68; 95% CI, 0.50-0.93; P = .016).
The effect was mostly driven by those who used CPAP for at least 4 hours per night (HR, 0.60; 95% CI, 0.39-0.95). This association was stronger for those with moderate to severe OSA (HR, 0.56; 95% CI, 0.39-0.81).
“This study highlights the importance of long-term management of CPAP therapy in patients with moderate-severe OSA,” Dr. Mazzotti said in an interview.
“It suggests that maintaining good CPAP adherence might be beneficial for cardiovascular health, besides the already established benefits on quality of life, sleepiness, and other cardiometabolic functions,” he said.
Dr. Mazzotti said several mechanisms might explain the association between CPAP use and lower risk for CV events. “CPAP treats OSA by preventing respiratory pauses that occur during sleep, therefore preventing arousals, sleep fragmentation, and decreases in blood oxygen. These improved cardiorespiratory functions can be beneficial to avoid certain molecular changes that are known to contribute to cardiovascular risk, such as oxidative stress and inflammation,” he explained.
“However, specific studies fully understanding these mechanisms are necessary,” Dr. Mazzotti added.
In a comment, Nitun Verma, MD, a spokesperson for the American Academy of Sleep Medicine, said that “the frequent decreases in oxygen levels and fragmented sleep from apnea are associated with cardiovascular disorders. We know this from multiple studies. This, however, was a large study and strengthens the association between improving apnea and reduced serious cardiovascular events.”
Funding for the study was provided by the American Academy of Sleep Medicine Foundation and the American Heart Association. Dr. Mazzotti and Dr. Verma disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
particularly for patients with moderate to severe OSA and those who are more adherent to CPAP therapy, a new study suggests.
“Most clinical trials on the effect of CPAP on CV diseases to date have focused on secondary CV prevention. This study contributes another piece of evidence about the role of CPAP therapy to prevent CV diseases,” said Diego R. Mazzotti, PhD, an assistant professor at the University of Kansas Medical Center, Kansas City.
“Our study, while observational, suggests that clinical trials focused on understanding how to sustain long-term CPAP adherence in obstructive sleep apnea patients are necessary and could be critical for optimizing comorbidity risk reduction,” Dr. Mazzotti said.
The study was presented at the virtual annual meeting of the Associated Professional Sleep Societies.
Good adherence important
The researchers analyzed the electronic health records of adults referred for a sleep study through the Kaiser Permanente Southern California health system. The sample included 11,145 adults without OSA, 13,898 with OSA who used CPAP, and 20,884 adults with OSA who did not use CPAP. None of them had CV disease at baseline. Median follow-up was 262 days.
The primary outcome was first occurrence of myocardial infarction, stroke, unstable angina, heart failure, or death caused by CV disease.
In adjusted models, adults with moderate to severe OSA (apnea-hypopnea index ≥15) who did not use CPAP were 71% more likely than those without OSA to have a first CV event (hazard ratio, 1.71; 95% CI, 1.11-2.64). However, the risk for a CV event during follow-up was 32% lower among OSA patients with any CPAP use (HR, 0.68; 95% CI, 0.50-0.93; P = .016).
The effect was mostly driven by those who used CPAP for at least 4 hours per night (HR, 0.60; 95% CI, 0.39-0.95). This association was stronger for those with moderate to severe OSA (HR, 0.56; 95% CI, 0.39-0.81).
“This study highlights the importance of long-term management of CPAP therapy in patients with moderate-severe OSA,” Dr. Mazzotti said in an interview.
“It suggests that maintaining good CPAP adherence might be beneficial for cardiovascular health, besides the already established benefits on quality of life, sleepiness, and other cardiometabolic functions,” he said.
Dr. Mazzotti said several mechanisms might explain the association between CPAP use and lower risk for CV events. “CPAP treats OSA by preventing respiratory pauses that occur during sleep, therefore preventing arousals, sleep fragmentation, and decreases in blood oxygen. These improved cardiorespiratory functions can be beneficial to avoid certain molecular changes that are known to contribute to cardiovascular risk, such as oxidative stress and inflammation,” he explained.
“However, specific studies fully understanding these mechanisms are necessary,” Dr. Mazzotti added.
In a comment, Nitun Verma, MD, a spokesperson for the American Academy of Sleep Medicine, said that “the frequent decreases in oxygen levels and fragmented sleep from apnea are associated with cardiovascular disorders. We know this from multiple studies. This, however, was a large study and strengthens the association between improving apnea and reduced serious cardiovascular events.”
Funding for the study was provided by the American Academy of Sleep Medicine Foundation and the American Heart Association. Dr. Mazzotti and Dr. Verma disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM SLEEP 2021
Memory benefit seen with antihypertensives crossing blood-brain barrier
Over a 3-year period, cognitively normal older adults taking BBB-crossing antihypertensives demonstrated superior verbal memory, compared with similar individuals receiving non–BBB-crossing antihypertensives, reported lead author Jean K. Ho, PhD, of the Institute for Memory Impairments and Neurological Disorders at the University of California, Irvine, and colleagues.
According to the investigators, the findings add color to a known link between hypertension and neurologic degeneration, and may aid the search for new therapeutic targets.
“Hypertension is a well-established risk factor for cognitive decline and dementia, possibly through its effects on both cerebrovascular disease and Alzheimer’s disease,” Dr. Ho and colleagues wrote in Hypertension. “Studies of antihypertensive treatments have reported possible salutary effects on cognition and cerebrovascular disease, as well as Alzheimer’s disease neuropathology.”
In a previous study, individuals younger than 75 years exposed to antihypertensives had an 8% decreased risk of dementia per year of use, while another trial showed that intensive blood pressure–lowering therapy reduced mild cognitive impairment by 19%.
“Despite these encouraging findings ... larger meta-analytic studies have been hampered by the fact that pharmacokinetic properties are typically not considered in existing studies or routine clinical practice,” wrote Dr. Ho and colleagues. “The present study sought to fill this gap [in that it was] a large and longitudinal meta-analytic study of existing data recoded to assess the effects of BBB-crossing potential in renin-angiotensin system [RAS] treatments among hypertensive adults.”
Methods and results
The meta-analysis included randomized clinical trials, prospective cohort studies, and retrospective observational studies. The researchers assessed data on 12,849 individuals from 14 cohorts that received either BBB-crossing or non–BBB-crossing antihypertensives.
The BBB-crossing properties of RAS treatments were identified by a literature review. Of ACE inhibitors, captopril, fosinopril, lisinopril, perindopril, ramipril, and trandolapril were classified as BBB crossing, and benazepril, enalapril, moexipril, and quinapril were classified as non–BBB-crossing. Of ARBs, telmisartan and candesartan were considered BBB-crossing, and olmesartan, eprosartan, irbesartan, and losartan were tagged as non–BBB-crossing.
Cognition was assessed via the following seven domains: executive function, attention, verbal memory learning, language, mental status, recall, and processing speed.
Compared with individuals taking non–BBB-crossing antihypertensives, those taking BBB-crossing agents had significantly superior verbal memory (recall), with a maximum effect size of 0.07 (P = .03).
According to the investigators, this finding was particularly noteworthy, as the BBB-crossing group had relatively higher vascular risk burden and lower mean education level.
“These differences make it all the more remarkable that the BBB-crossing group displayed better memory ability over time despite these cognitive disadvantages,” the investigators wrote.
Still, not all the findings favored BBB-crossing agents. Individuals in the BBB-crossing group had relatively inferior attention ability, with a minimum effect size of –0.17 (P = .02).
The other cognitive measures were not significantly different between groups.
Clinicians may consider findings after accounting for other factors
Principal investigator Daniel A. Nation, PhD, associate professor of psychological science and a faculty member of the Institute for Memory Impairments and Neurological Disorders at the University of California, Irvine, suggested that the small difference in verbal memory between groups could be clinically significant over a longer period of time.
“Although the overall effect size was pretty small, if you look at how long it would take for someone [with dementia] to progress over many years of decline, it would actually end up being a pretty big effect,” Dr. Nation said in an interview. “Small effect sizes could actually end up preventing a lot of cases of dementia,” he added.
The conflicting results in the BBB-crossing group – better verbal memory but worse attention ability – were “surprising,” he noted.
“I sort of didn’t believe it at first,” Dr. Nation said, “because the memory finding is sort of replication – we’d observed the same exact effect on memory in a smaller sample in another study. ... The attention [finding], going another way, was a new thing.”
Dr. Nation suggested that the intergroup differences in attention ability may stem from idiosyncrasies of the tests used to measure that domain, which can be impacted by cardiovascular or brain vascular disease. Or it could be caused by something else entirely, he said, noting that further investigation is needed.
He added that the improvements in verbal memory within the BBB-crossing group could be caused by direct effects on the brain. He pointed out that certain ACE polymorphisms have been linked with Alzheimer’s disease risk, and those same polymorphisms, in animal models, lead to neurodegeneration, with reversal possible through administration of ACE inhibitors.
“It could be that what we’re observing has nothing really to do with blood pressure,” Dr. Nation explained. “This could be a neuronal effect on learning memory systems.”
He went on to suggest that clinicians may consider these findings when selecting antihypertensive agents for their patients, with the caveat that all other prescribing factors have already been taking to account.
“In the event that you’re going to give an ACE inhibitor or an angiotensin receptor blocker anyway, and it ends up being a somewhat arbitrary decision in terms of which specific drug you’re going to give, then perhaps this is a piece of information you would take into account – that one gets in the brain and one doesn’t – in somebody at risk for cognitive decline,” Dr. Nation said.
Exact mechanisms of action unknown
Hélène Girouard, PhD, assistant professor of pharmacology and physiology at the University of Montreal, said in an interview that the findings are “of considerable importance, knowing that brain alterations could begin as much as 30 years before manifestation of dementia.”
Since 2003, Dr. Girouard has been studying the cognitive effects of antihypertensive medications. She noted that previous studies involving rodents “have shown beneficial effects [of BBB-crossing antihypertensive drugs] on cognition independent of their effects on blood pressure.”
The drugs’ exact mechanisms of action, however, remain elusive, according to Dr. Girouard, who offered several possible explanations, including amelioration of BBB disruption, brain inflammation, cerebral blood flow dysregulation, cholinergic dysfunction, and neurologic deficits. “Whether these mechanisms may explain Ho and colleagues’ observations remains to be established,” she added.
Andrea L. Schneider, MD, PhD, assistant professor of neurology at the University of Pennsylvania, Philadelphia, applauded the study, but ultimately suggested that more research is needed to impact clinical decision-making.
“The results of this important and well-done study suggest that further investigation into targeted mechanism-based approaches to selecting hypertension treatment agents, with a specific focus on cognitive outcomes, is warranted,” Dr. Schneider said in an interview. “Before changing clinical practice, further work is necessary to disentangle contributions of medication mechanism, comorbid vascular risk factors, and achieved blood pressure reduction, among others.”
The investigators disclosed support from the National Institutes of Health, the Alzheimer’s Association, the Waksman Foundation of Japan, and others. The interviewees reported no relevant conflicts of interest.
Over a 3-year period, cognitively normal older adults taking BBB-crossing antihypertensives demonstrated superior verbal memory, compared with similar individuals receiving non–BBB-crossing antihypertensives, reported lead author Jean K. Ho, PhD, of the Institute for Memory Impairments and Neurological Disorders at the University of California, Irvine, and colleagues.
According to the investigators, the findings add color to a known link between hypertension and neurologic degeneration, and may aid the search for new therapeutic targets.
“Hypertension is a well-established risk factor for cognitive decline and dementia, possibly through its effects on both cerebrovascular disease and Alzheimer’s disease,” Dr. Ho and colleagues wrote in Hypertension. “Studies of antihypertensive treatments have reported possible salutary effects on cognition and cerebrovascular disease, as well as Alzheimer’s disease neuropathology.”
In a previous study, individuals younger than 75 years exposed to antihypertensives had an 8% decreased risk of dementia per year of use, while another trial showed that intensive blood pressure–lowering therapy reduced mild cognitive impairment by 19%.
“Despite these encouraging findings ... larger meta-analytic studies have been hampered by the fact that pharmacokinetic properties are typically not considered in existing studies or routine clinical practice,” wrote Dr. Ho and colleagues. “The present study sought to fill this gap [in that it was] a large and longitudinal meta-analytic study of existing data recoded to assess the effects of BBB-crossing potential in renin-angiotensin system [RAS] treatments among hypertensive adults.”
Methods and results
The meta-analysis included randomized clinical trials, prospective cohort studies, and retrospective observational studies. The researchers assessed data on 12,849 individuals from 14 cohorts that received either BBB-crossing or non–BBB-crossing antihypertensives.
The BBB-crossing properties of RAS treatments were identified by a literature review. Of ACE inhibitors, captopril, fosinopril, lisinopril, perindopril, ramipril, and trandolapril were classified as BBB crossing, and benazepril, enalapril, moexipril, and quinapril were classified as non–BBB-crossing. Of ARBs, telmisartan and candesartan were considered BBB-crossing, and olmesartan, eprosartan, irbesartan, and losartan were tagged as non–BBB-crossing.
Cognition was assessed via the following seven domains: executive function, attention, verbal memory learning, language, mental status, recall, and processing speed.
Compared with individuals taking non–BBB-crossing antihypertensives, those taking BBB-crossing agents had significantly superior verbal memory (recall), with a maximum effect size of 0.07 (P = .03).
According to the investigators, this finding was particularly noteworthy, as the BBB-crossing group had relatively higher vascular risk burden and lower mean education level.
“These differences make it all the more remarkable that the BBB-crossing group displayed better memory ability over time despite these cognitive disadvantages,” the investigators wrote.
Still, not all the findings favored BBB-crossing agents. Individuals in the BBB-crossing group had relatively inferior attention ability, with a minimum effect size of –0.17 (P = .02).
The other cognitive measures were not significantly different between groups.
Clinicians may consider findings after accounting for other factors
Principal investigator Daniel A. Nation, PhD, associate professor of psychological science and a faculty member of the Institute for Memory Impairments and Neurological Disorders at the University of California, Irvine, suggested that the small difference in verbal memory between groups could be clinically significant over a longer period of time.
“Although the overall effect size was pretty small, if you look at how long it would take for someone [with dementia] to progress over many years of decline, it would actually end up being a pretty big effect,” Dr. Nation said in an interview. “Small effect sizes could actually end up preventing a lot of cases of dementia,” he added.
The conflicting results in the BBB-crossing group – better verbal memory but worse attention ability – were “surprising,” he noted.
“I sort of didn’t believe it at first,” Dr. Nation said, “because the memory finding is sort of replication – we’d observed the same exact effect on memory in a smaller sample in another study. ... The attention [finding], going another way, was a new thing.”
Dr. Nation suggested that the intergroup differences in attention ability may stem from idiosyncrasies of the tests used to measure that domain, which can be impacted by cardiovascular or brain vascular disease. Or it could be caused by something else entirely, he said, noting that further investigation is needed.
He added that the improvements in verbal memory within the BBB-crossing group could be caused by direct effects on the brain. He pointed out that certain ACE polymorphisms have been linked with Alzheimer’s disease risk, and those same polymorphisms, in animal models, lead to neurodegeneration, with reversal possible through administration of ACE inhibitors.
“It could be that what we’re observing has nothing really to do with blood pressure,” Dr. Nation explained. “This could be a neuronal effect on learning memory systems.”
He went on to suggest that clinicians may consider these findings when selecting antihypertensive agents for their patients, with the caveat that all other prescribing factors have already been taking to account.
“In the event that you’re going to give an ACE inhibitor or an angiotensin receptor blocker anyway, and it ends up being a somewhat arbitrary decision in terms of which specific drug you’re going to give, then perhaps this is a piece of information you would take into account – that one gets in the brain and one doesn’t – in somebody at risk for cognitive decline,” Dr. Nation said.
Exact mechanisms of action unknown
Hélène Girouard, PhD, assistant professor of pharmacology and physiology at the University of Montreal, said in an interview that the findings are “of considerable importance, knowing that brain alterations could begin as much as 30 years before manifestation of dementia.”
Since 2003, Dr. Girouard has been studying the cognitive effects of antihypertensive medications. She noted that previous studies involving rodents “have shown beneficial effects [of BBB-crossing antihypertensive drugs] on cognition independent of their effects on blood pressure.”
The drugs’ exact mechanisms of action, however, remain elusive, according to Dr. Girouard, who offered several possible explanations, including amelioration of BBB disruption, brain inflammation, cerebral blood flow dysregulation, cholinergic dysfunction, and neurologic deficits. “Whether these mechanisms may explain Ho and colleagues’ observations remains to be established,” she added.
Andrea L. Schneider, MD, PhD, assistant professor of neurology at the University of Pennsylvania, Philadelphia, applauded the study, but ultimately suggested that more research is needed to impact clinical decision-making.
“The results of this important and well-done study suggest that further investigation into targeted mechanism-based approaches to selecting hypertension treatment agents, with a specific focus on cognitive outcomes, is warranted,” Dr. Schneider said in an interview. “Before changing clinical practice, further work is necessary to disentangle contributions of medication mechanism, comorbid vascular risk factors, and achieved blood pressure reduction, among others.”
The investigators disclosed support from the National Institutes of Health, the Alzheimer’s Association, the Waksman Foundation of Japan, and others. The interviewees reported no relevant conflicts of interest.
Over a 3-year period, cognitively normal older adults taking BBB-crossing antihypertensives demonstrated superior verbal memory, compared with similar individuals receiving non–BBB-crossing antihypertensives, reported lead author Jean K. Ho, PhD, of the Institute for Memory Impairments and Neurological Disorders at the University of California, Irvine, and colleagues.
According to the investigators, the findings add color to a known link between hypertension and neurologic degeneration, and may aid the search for new therapeutic targets.
“Hypertension is a well-established risk factor for cognitive decline and dementia, possibly through its effects on both cerebrovascular disease and Alzheimer’s disease,” Dr. Ho and colleagues wrote in Hypertension. “Studies of antihypertensive treatments have reported possible salutary effects on cognition and cerebrovascular disease, as well as Alzheimer’s disease neuropathology.”
In a previous study, individuals younger than 75 years exposed to antihypertensives had an 8% decreased risk of dementia per year of use, while another trial showed that intensive blood pressure–lowering therapy reduced mild cognitive impairment by 19%.
“Despite these encouraging findings ... larger meta-analytic studies have been hampered by the fact that pharmacokinetic properties are typically not considered in existing studies or routine clinical practice,” wrote Dr. Ho and colleagues. “The present study sought to fill this gap [in that it was] a large and longitudinal meta-analytic study of existing data recoded to assess the effects of BBB-crossing potential in renin-angiotensin system [RAS] treatments among hypertensive adults.”
Methods and results
The meta-analysis included randomized clinical trials, prospective cohort studies, and retrospective observational studies. The researchers assessed data on 12,849 individuals from 14 cohorts that received either BBB-crossing or non–BBB-crossing antihypertensives.
The BBB-crossing properties of RAS treatments were identified by a literature review. Of ACE inhibitors, captopril, fosinopril, lisinopril, perindopril, ramipril, and trandolapril were classified as BBB crossing, and benazepril, enalapril, moexipril, and quinapril were classified as non–BBB-crossing. Of ARBs, telmisartan and candesartan were considered BBB-crossing, and olmesartan, eprosartan, irbesartan, and losartan were tagged as non–BBB-crossing.
Cognition was assessed via the following seven domains: executive function, attention, verbal memory learning, language, mental status, recall, and processing speed.
Compared with individuals taking non–BBB-crossing antihypertensives, those taking BBB-crossing agents had significantly superior verbal memory (recall), with a maximum effect size of 0.07 (P = .03).
According to the investigators, this finding was particularly noteworthy, as the BBB-crossing group had relatively higher vascular risk burden and lower mean education level.
“These differences make it all the more remarkable that the BBB-crossing group displayed better memory ability over time despite these cognitive disadvantages,” the investigators wrote.
Still, not all the findings favored BBB-crossing agents. Individuals in the BBB-crossing group had relatively inferior attention ability, with a minimum effect size of –0.17 (P = .02).
The other cognitive measures were not significantly different between groups.
Clinicians may consider findings after accounting for other factors
Principal investigator Daniel A. Nation, PhD, associate professor of psychological science and a faculty member of the Institute for Memory Impairments and Neurological Disorders at the University of California, Irvine, suggested that the small difference in verbal memory between groups could be clinically significant over a longer period of time.
“Although the overall effect size was pretty small, if you look at how long it would take for someone [with dementia] to progress over many years of decline, it would actually end up being a pretty big effect,” Dr. Nation said in an interview. “Small effect sizes could actually end up preventing a lot of cases of dementia,” he added.
The conflicting results in the BBB-crossing group – better verbal memory but worse attention ability – were “surprising,” he noted.
“I sort of didn’t believe it at first,” Dr. Nation said, “because the memory finding is sort of replication – we’d observed the same exact effect on memory in a smaller sample in another study. ... The attention [finding], going another way, was a new thing.”
Dr. Nation suggested that the intergroup differences in attention ability may stem from idiosyncrasies of the tests used to measure that domain, which can be impacted by cardiovascular or brain vascular disease. Or it could be caused by something else entirely, he said, noting that further investigation is needed.
He added that the improvements in verbal memory within the BBB-crossing group could be caused by direct effects on the brain. He pointed out that certain ACE polymorphisms have been linked with Alzheimer’s disease risk, and those same polymorphisms, in animal models, lead to neurodegeneration, with reversal possible through administration of ACE inhibitors.
“It could be that what we’re observing has nothing really to do with blood pressure,” Dr. Nation explained. “This could be a neuronal effect on learning memory systems.”
He went on to suggest that clinicians may consider these findings when selecting antihypertensive agents for their patients, with the caveat that all other prescribing factors have already been taking to account.
“In the event that you’re going to give an ACE inhibitor or an angiotensin receptor blocker anyway, and it ends up being a somewhat arbitrary decision in terms of which specific drug you’re going to give, then perhaps this is a piece of information you would take into account – that one gets in the brain and one doesn’t – in somebody at risk for cognitive decline,” Dr. Nation said.
Exact mechanisms of action unknown
Hélène Girouard, PhD, assistant professor of pharmacology and physiology at the University of Montreal, said in an interview that the findings are “of considerable importance, knowing that brain alterations could begin as much as 30 years before manifestation of dementia.”
Since 2003, Dr. Girouard has been studying the cognitive effects of antihypertensive medications. She noted that previous studies involving rodents “have shown beneficial effects [of BBB-crossing antihypertensive drugs] on cognition independent of their effects on blood pressure.”
The drugs’ exact mechanisms of action, however, remain elusive, according to Dr. Girouard, who offered several possible explanations, including amelioration of BBB disruption, brain inflammation, cerebral blood flow dysregulation, cholinergic dysfunction, and neurologic deficits. “Whether these mechanisms may explain Ho and colleagues’ observations remains to be established,” she added.
Andrea L. Schneider, MD, PhD, assistant professor of neurology at the University of Pennsylvania, Philadelphia, applauded the study, but ultimately suggested that more research is needed to impact clinical decision-making.
“The results of this important and well-done study suggest that further investigation into targeted mechanism-based approaches to selecting hypertension treatment agents, with a specific focus on cognitive outcomes, is warranted,” Dr. Schneider said in an interview. “Before changing clinical practice, further work is necessary to disentangle contributions of medication mechanism, comorbid vascular risk factors, and achieved blood pressure reduction, among others.”
The investigators disclosed support from the National Institutes of Health, the Alzheimer’s Association, the Waksman Foundation of Japan, and others. The interviewees reported no relevant conflicts of interest.
FROM HYPERTENSION
Potential first-in-class, targeted therapy for myasthenia gravis
(gMG), new research suggests. Results from the phase 3, randomized, placebo-controlled ADAPT trial showed that reduction in disease burden and improvement in strength and quality of life in patients with gMG were consistent across four MG-specific scales for those receiving the novel treatment. In addition, these benefits were observed early and were reproducible and durable, the researchers noted.
Efgartigimod is a “very rapidly acting drug relative to other treatments that may take 4, 6, sometimes 10 months before they start to work, and the side effect profile is much like placebo,” said principal investigator James Howard, Jr., MD, Distinguished Professor of Neuromuscular Disease, department of neurology, University of North Carolina at Chapel Hill.
The ADAPT results are “important for the MG community, and I am hopeful efgartigimod will provide a first-in-class targeted therapy that can be dosed in an individual way for people living with this chronic autoimmune disease,” Dr. Howard added in a news release.
The findings were published online June 17 in Lancet Neurology.
Targeted molecular therapy
The rare and chronic autoimmune neuromuscular disorder of gMG causes debilitating and potentially life-threatening muscle weakness and significantly impaired independence and quality of life. Most patients with gMG have immunoglobulin G (IgG) antibodies, which are most often directed against skeletal muscle nicotinic acetylcholine receptors.
Efgartigimod is an investigational antibody fragment designed to reduce pathogenic IgG antibodies and block the IgG recycling process in patients with gMG.
The novel agent binds to the neonatal Fc receptor (FcRn), which is widely expressed throughout the body and plays a central role in rescuing IgG antibodies from degradation. Blocking FcRn reduces IgG antibody levels.
The ADAPT trial was conducted at 56 neuromuscular academic and community centers in 15 countries in North America, Europe, and Japan. The study included 167 adults with gMG, regardless of acetylcholine receptor antibody status. All had a Myasthenia Gravis Activities of Daily Living (MG-ADL) score of at least 5 (greater than 50% non-ocular) on a background of a stable dose of at least one MG drug.
For 26 weeks, 84 patients were randomly assigned to receive efgartigimod 10 mg/kg and 83 to receive matching placebo. Both treatments were administered as four infusions per cycle at one infusion per week. The process was repeated as needed depending on clinical response no sooner than 8 weeks after initiation of the previous cycle.
ADAPT was designed to allow an individualized treatment approach with an initial treatment cycle followed by a variable number of subsequent treatment cycles, the investigators noted.
Primary endpoint met
The primary efficacy endpoint was number of acetylcholine receptor antibody-positive (AChR-Ab+) patients who achieved a clinically meaningful response on the MG-ADL score. This was defined as at least a 2-point improvement from baseline for 4 or more consecutive weeks. Forty-four (68%) of 65 AChR-Ab+ patients treated with efgartigimod met this endpoint versus 19 (30%) of 64 patients treated with placebo (odds ratio, 4.95; 95% confidence interval, 2.21-11.53; P < .0001).
Many of the patients treated with efgartigimod showed improvement “beyond the clinically meaningful threshold, achieving up to 9-point reductions in MG-ADL,” the investigators reported. In addition, 40% of the efgartigimod group attained an MG-ADL score of 0 or 1 (minimal symptom expression) in cycle 1 versus 11% of the placebo group (P < .0001).
Nearly two-thirds (63%) of AChR-Ab+ patients responded to the first cycle of efgartigimod, and most of these patients (83%) responded to treatment within the first 2 weeks. Among the AChR-Ab+ participants who responded to efgartigimod in cycle 1, the duration of responder status was 6 to 7 weeks in 32% of patients, 8 to 11 weeks in 23% of patients, and 12 weeks or more in 34% of patients.
Safety profile
“Some patients never required retreatment over the 26-week period that they were under observation,” Dr. Howard said. “Patients want to be individuals. They don’t want to be assigned to a regimented therapy, and I think these results show that this therapy can be tailored to the individual patient, rather than simply giving it to them in a cookbook fashion,” he added.
The safety profile of efgartigimod was comparable to placebo. Most adverse events were mild or moderate in severity. The most commonly reported adverse events were headache, nasopharyngitis, nausea, diarrhea, upper respiratory tract infection, and urinary tract infection.
Four (5%) efgartigimod-treated patients had a serious adverse event, which included thrombocytosis, rectal adenocarcinoma, worsening MG, and depression.
The novel agent is currently under review with the U.S. Food and Drug Administration for the treatment of gMG, with a Prescription Drug User Fee Act target action date of Dec. 17. If approved, it would become the first FDA-approved FcRn antagonist.
Expanding therapeutic landscape
In a linked commentary, Shigeaki Suzuki, MD, PhD, department of neurology, Keio University School of Medicine, Tokyo, noted that the therapeutic landscape for patients with MG is “expanding year by year,” with several additional complement inhibitors and FcRn antagonists now in phase 3 testing.
“Biological drugs should be preferentially used as the treatment for patients with refractory myasthenia gravis, although the definition of refractory myasthenia gravis is different depending on the criteria used,” Dr. Suzuki wrote.
He noted that when “cost-effectiveness is not taken into account, targeted molecular therapy might be used widely” in patients with MG.
“Risks of myasthenic exacerbation and crises should be substantially decreased, particularly in patients with refractory myasthenia gravis,” Dr. Suzuki added.
The ADAPT study was supported by argenx. Dr. Howard has reported receiving research support from argenx, Alexion Pharmaceuticals, the Centers for Disease Control and Prevention, the Muscular Dystrophy Association, the National Institutes of Health, Patient-Centered Outcomes Research Institute, and Ra Pharmaceuticals; honoraria from argenx, Alexion, Immunovant, Ra, Regeneron Pharmaceuticals, and Viela Bio; and nonfinancial support from argenx, Alexion, Ra, and Toleranzia. Disclosures for the other investigators are listed in the original article. Dr. Suzuki has reported relationships with Alexion Pharmaceuticals, Japan Blood Products Organization, and Asahi Kasei Medical.
A version of this article first appeared on Medscape.com.
(gMG), new research suggests. Results from the phase 3, randomized, placebo-controlled ADAPT trial showed that reduction in disease burden and improvement in strength and quality of life in patients with gMG were consistent across four MG-specific scales for those receiving the novel treatment. In addition, these benefits were observed early and were reproducible and durable, the researchers noted.
Efgartigimod is a “very rapidly acting drug relative to other treatments that may take 4, 6, sometimes 10 months before they start to work, and the side effect profile is much like placebo,” said principal investigator James Howard, Jr., MD, Distinguished Professor of Neuromuscular Disease, department of neurology, University of North Carolina at Chapel Hill.
The ADAPT results are “important for the MG community, and I am hopeful efgartigimod will provide a first-in-class targeted therapy that can be dosed in an individual way for people living with this chronic autoimmune disease,” Dr. Howard added in a news release.
The findings were published online June 17 in Lancet Neurology.
Targeted molecular therapy
The rare and chronic autoimmune neuromuscular disorder of gMG causes debilitating and potentially life-threatening muscle weakness and significantly impaired independence and quality of life. Most patients with gMG have immunoglobulin G (IgG) antibodies, which are most often directed against skeletal muscle nicotinic acetylcholine receptors.
Efgartigimod is an investigational antibody fragment designed to reduce pathogenic IgG antibodies and block the IgG recycling process in patients with gMG.
The novel agent binds to the neonatal Fc receptor (FcRn), which is widely expressed throughout the body and plays a central role in rescuing IgG antibodies from degradation. Blocking FcRn reduces IgG antibody levels.
The ADAPT trial was conducted at 56 neuromuscular academic and community centers in 15 countries in North America, Europe, and Japan. The study included 167 adults with gMG, regardless of acetylcholine receptor antibody status. All had a Myasthenia Gravis Activities of Daily Living (MG-ADL) score of at least 5 (greater than 50% non-ocular) on a background of a stable dose of at least one MG drug.
For 26 weeks, 84 patients were randomly assigned to receive efgartigimod 10 mg/kg and 83 to receive matching placebo. Both treatments were administered as four infusions per cycle at one infusion per week. The process was repeated as needed depending on clinical response no sooner than 8 weeks after initiation of the previous cycle.
ADAPT was designed to allow an individualized treatment approach with an initial treatment cycle followed by a variable number of subsequent treatment cycles, the investigators noted.
Primary endpoint met
The primary efficacy endpoint was number of acetylcholine receptor antibody-positive (AChR-Ab+) patients who achieved a clinically meaningful response on the MG-ADL score. This was defined as at least a 2-point improvement from baseline for 4 or more consecutive weeks. Forty-four (68%) of 65 AChR-Ab+ patients treated with efgartigimod met this endpoint versus 19 (30%) of 64 patients treated with placebo (odds ratio, 4.95; 95% confidence interval, 2.21-11.53; P < .0001).
Many of the patients treated with efgartigimod showed improvement “beyond the clinically meaningful threshold, achieving up to 9-point reductions in MG-ADL,” the investigators reported. In addition, 40% of the efgartigimod group attained an MG-ADL score of 0 or 1 (minimal symptom expression) in cycle 1 versus 11% of the placebo group (P < .0001).
Nearly two-thirds (63%) of AChR-Ab+ patients responded to the first cycle of efgartigimod, and most of these patients (83%) responded to treatment within the first 2 weeks. Among the AChR-Ab+ participants who responded to efgartigimod in cycle 1, the duration of responder status was 6 to 7 weeks in 32% of patients, 8 to 11 weeks in 23% of patients, and 12 weeks or more in 34% of patients.
Safety profile
“Some patients never required retreatment over the 26-week period that they were under observation,” Dr. Howard said. “Patients want to be individuals. They don’t want to be assigned to a regimented therapy, and I think these results show that this therapy can be tailored to the individual patient, rather than simply giving it to them in a cookbook fashion,” he added.
The safety profile of efgartigimod was comparable to placebo. Most adverse events were mild or moderate in severity. The most commonly reported adverse events were headache, nasopharyngitis, nausea, diarrhea, upper respiratory tract infection, and urinary tract infection.
Four (5%) efgartigimod-treated patients had a serious adverse event, which included thrombocytosis, rectal adenocarcinoma, worsening MG, and depression.
The novel agent is currently under review with the U.S. Food and Drug Administration for the treatment of gMG, with a Prescription Drug User Fee Act target action date of Dec. 17. If approved, it would become the first FDA-approved FcRn antagonist.
Expanding therapeutic landscape
In a linked commentary, Shigeaki Suzuki, MD, PhD, department of neurology, Keio University School of Medicine, Tokyo, noted that the therapeutic landscape for patients with MG is “expanding year by year,” with several additional complement inhibitors and FcRn antagonists now in phase 3 testing.
“Biological drugs should be preferentially used as the treatment for patients with refractory myasthenia gravis, although the definition of refractory myasthenia gravis is different depending on the criteria used,” Dr. Suzuki wrote.
He noted that when “cost-effectiveness is not taken into account, targeted molecular therapy might be used widely” in patients with MG.
“Risks of myasthenic exacerbation and crises should be substantially decreased, particularly in patients with refractory myasthenia gravis,” Dr. Suzuki added.
The ADAPT study was supported by argenx. Dr. Howard has reported receiving research support from argenx, Alexion Pharmaceuticals, the Centers for Disease Control and Prevention, the Muscular Dystrophy Association, the National Institutes of Health, Patient-Centered Outcomes Research Institute, and Ra Pharmaceuticals; honoraria from argenx, Alexion, Immunovant, Ra, Regeneron Pharmaceuticals, and Viela Bio; and nonfinancial support from argenx, Alexion, Ra, and Toleranzia. Disclosures for the other investigators are listed in the original article. Dr. Suzuki has reported relationships with Alexion Pharmaceuticals, Japan Blood Products Organization, and Asahi Kasei Medical.
A version of this article first appeared on Medscape.com.
(gMG), new research suggests. Results from the phase 3, randomized, placebo-controlled ADAPT trial showed that reduction in disease burden and improvement in strength and quality of life in patients with gMG were consistent across four MG-specific scales for those receiving the novel treatment. In addition, these benefits were observed early and were reproducible and durable, the researchers noted.
Efgartigimod is a “very rapidly acting drug relative to other treatments that may take 4, 6, sometimes 10 months before they start to work, and the side effect profile is much like placebo,” said principal investigator James Howard, Jr., MD, Distinguished Professor of Neuromuscular Disease, department of neurology, University of North Carolina at Chapel Hill.
The ADAPT results are “important for the MG community, and I am hopeful efgartigimod will provide a first-in-class targeted therapy that can be dosed in an individual way for people living with this chronic autoimmune disease,” Dr. Howard added in a news release.
The findings were published online June 17 in Lancet Neurology.
Targeted molecular therapy
The rare and chronic autoimmune neuromuscular disorder of gMG causes debilitating and potentially life-threatening muscle weakness and significantly impaired independence and quality of life. Most patients with gMG have immunoglobulin G (IgG) antibodies, which are most often directed against skeletal muscle nicotinic acetylcholine receptors.
Efgartigimod is an investigational antibody fragment designed to reduce pathogenic IgG antibodies and block the IgG recycling process in patients with gMG.
The novel agent binds to the neonatal Fc receptor (FcRn), which is widely expressed throughout the body and plays a central role in rescuing IgG antibodies from degradation. Blocking FcRn reduces IgG antibody levels.
The ADAPT trial was conducted at 56 neuromuscular academic and community centers in 15 countries in North America, Europe, and Japan. The study included 167 adults with gMG, regardless of acetylcholine receptor antibody status. All had a Myasthenia Gravis Activities of Daily Living (MG-ADL) score of at least 5 (greater than 50% non-ocular) on a background of a stable dose of at least one MG drug.
For 26 weeks, 84 patients were randomly assigned to receive efgartigimod 10 mg/kg and 83 to receive matching placebo. Both treatments were administered as four infusions per cycle at one infusion per week. The process was repeated as needed depending on clinical response no sooner than 8 weeks after initiation of the previous cycle.
ADAPT was designed to allow an individualized treatment approach with an initial treatment cycle followed by a variable number of subsequent treatment cycles, the investigators noted.
Primary endpoint met
The primary efficacy endpoint was number of acetylcholine receptor antibody-positive (AChR-Ab+) patients who achieved a clinically meaningful response on the MG-ADL score. This was defined as at least a 2-point improvement from baseline for 4 or more consecutive weeks. Forty-four (68%) of 65 AChR-Ab+ patients treated with efgartigimod met this endpoint versus 19 (30%) of 64 patients treated with placebo (odds ratio, 4.95; 95% confidence interval, 2.21-11.53; P < .0001).
Many of the patients treated with efgartigimod showed improvement “beyond the clinically meaningful threshold, achieving up to 9-point reductions in MG-ADL,” the investigators reported. In addition, 40% of the efgartigimod group attained an MG-ADL score of 0 or 1 (minimal symptom expression) in cycle 1 versus 11% of the placebo group (P < .0001).
Nearly two-thirds (63%) of AChR-Ab+ patients responded to the first cycle of efgartigimod, and most of these patients (83%) responded to treatment within the first 2 weeks. Among the AChR-Ab+ participants who responded to efgartigimod in cycle 1, the duration of responder status was 6 to 7 weeks in 32% of patients, 8 to 11 weeks in 23% of patients, and 12 weeks or more in 34% of patients.
Safety profile
“Some patients never required retreatment over the 26-week period that they were under observation,” Dr. Howard said. “Patients want to be individuals. They don’t want to be assigned to a regimented therapy, and I think these results show that this therapy can be tailored to the individual patient, rather than simply giving it to them in a cookbook fashion,” he added.
The safety profile of efgartigimod was comparable to placebo. Most adverse events were mild or moderate in severity. The most commonly reported adverse events were headache, nasopharyngitis, nausea, diarrhea, upper respiratory tract infection, and urinary tract infection.
Four (5%) efgartigimod-treated patients had a serious adverse event, which included thrombocytosis, rectal adenocarcinoma, worsening MG, and depression.
The novel agent is currently under review with the U.S. Food and Drug Administration for the treatment of gMG, with a Prescription Drug User Fee Act target action date of Dec. 17. If approved, it would become the first FDA-approved FcRn antagonist.
Expanding therapeutic landscape
In a linked commentary, Shigeaki Suzuki, MD, PhD, department of neurology, Keio University School of Medicine, Tokyo, noted that the therapeutic landscape for patients with MG is “expanding year by year,” with several additional complement inhibitors and FcRn antagonists now in phase 3 testing.
“Biological drugs should be preferentially used as the treatment for patients with refractory myasthenia gravis, although the definition of refractory myasthenia gravis is different depending on the criteria used,” Dr. Suzuki wrote.
He noted that when “cost-effectiveness is not taken into account, targeted molecular therapy might be used widely” in patients with MG.
“Risks of myasthenic exacerbation and crises should be substantially decreased, particularly in patients with refractory myasthenia gravis,” Dr. Suzuki added.
The ADAPT study was supported by argenx. Dr. Howard has reported receiving research support from argenx, Alexion Pharmaceuticals, the Centers for Disease Control and Prevention, the Muscular Dystrophy Association, the National Institutes of Health, Patient-Centered Outcomes Research Institute, and Ra Pharmaceuticals; honoraria from argenx, Alexion, Immunovant, Ra, Regeneron Pharmaceuticals, and Viela Bio; and nonfinancial support from argenx, Alexion, Ra, and Toleranzia. Disclosures for the other investigators are listed in the original article. Dr. Suzuki has reported relationships with Alexion Pharmaceuticals, Japan Blood Products Organization, and Asahi Kasei Medical.
A version of this article first appeared on Medscape.com.
From Lancet Neurology
How dreams might prepare you for what’s next
What you experience in your dreams might feel random and disjointed, but that chaos during sleep might serve a function, according to Erin Wamsley, PhD, an associate professor of psychology and neuroscience at Furman University in Greenville, S.C. In fact, evidence uncovered by Dr. Wamsley and associates suggests that
Previous research and anecdotal evidence have shown that dreams use fragments of past experiences, Dr. Wamsley explained. While studying dreams, her team found that the mind is using select fragments of past experiences to prepare for a known upcoming event.
“This is new evidence that dreams reflect a memory-processing function,” said Dr. Wamsley, who presented the work at the virtual annual meeting of the Associated Professional Sleep Societies.
Some high performers already use past experiences to excel in future events. For instance, Michael Phelps, the most decorated Olympic swimmer, with 28 medals, would “mentally rehearse” his swims for up to 2 hours per day, according to his coach, Bob Bowman.
Using sleep to strengthen this process is an exciting prospect that scientists have been eager to figure out, said Allison Brager, PhD, director of human performance at the U.S. Army Warrior Fitness Training Center. Deep REM sleep can lead to improved learning and memory, she said. “So, hypothetically, better dreams mean better sleep, and that equals better performance.”
For their research, Dr. Wamsley’s team hooked 48 students up to a polysomnography machine to measure sleep cycles and how often they were in a deep REM sleep. The students who took part in the study spent the night in a sleep lab.
The students were woken up multiple times during the night and asked to report what they were dreaming about.
In the morning, they were given their reports and asked to identify familiar features or potential sources for particular dreams. More than half the dreams were tied to a memory the students recalled. One-quarter of the dreams were related to specific upcoming events the students reported. And about 40% of the dreams with a future event in them also included memories of past experiences. This was more common the longer the students dreamed, the scientists explained.
And this was also more common later in the night, possibly because the dreamer is closer to waking and the anticipated event is approaching, Dr. Wamsley said.
Studying dreams is a tricky, subjective business and not always taken as seriously as other aspects of sleep and neuroscience because it involves questions of human consciousness itself, said Erik Hoel, PhD, a research assistant professor of neuroscience at Tufts University in Medford, Mass.
In a recent report published in Patterns, he suggested that our weirdest dreams help our brains process our day-to-day experiences in a way that enables deeper learning.
“This type of research is challenged by the method,” Dr. Hoel said.
In the Wamsley study, “waking people up from a deep sleep and asking them to recollect their dream content will only get you part of the experience because it fades so quickly.” That said, the value of connecting what happens as a result could be meaningful, he noted. For example, study participants could be asked whether their future event went as planned and whether they think the outcome was related to how well they “prepared” in their dreams.
Even then, it would still be a subjective analysis. But going in those directions might lead to meaningful new training, Dr. Hoel said.
And training yourself to recall only specific memories right before sleep might prepare your mind in a focused way for certain events, from giving a presentation to having a difficult conversation with someone, or maybe even winning at the Olympics.
A version of this article first appeared on WebMD.com.
What you experience in your dreams might feel random and disjointed, but that chaos during sleep might serve a function, according to Erin Wamsley, PhD, an associate professor of psychology and neuroscience at Furman University in Greenville, S.C. In fact, evidence uncovered by Dr. Wamsley and associates suggests that
Previous research and anecdotal evidence have shown that dreams use fragments of past experiences, Dr. Wamsley explained. While studying dreams, her team found that the mind is using select fragments of past experiences to prepare for a known upcoming event.
“This is new evidence that dreams reflect a memory-processing function,” said Dr. Wamsley, who presented the work at the virtual annual meeting of the Associated Professional Sleep Societies.
Some high performers already use past experiences to excel in future events. For instance, Michael Phelps, the most decorated Olympic swimmer, with 28 medals, would “mentally rehearse” his swims for up to 2 hours per day, according to his coach, Bob Bowman.
Using sleep to strengthen this process is an exciting prospect that scientists have been eager to figure out, said Allison Brager, PhD, director of human performance at the U.S. Army Warrior Fitness Training Center. Deep REM sleep can lead to improved learning and memory, she said. “So, hypothetically, better dreams mean better sleep, and that equals better performance.”
For their research, Dr. Wamsley’s team hooked 48 students up to a polysomnography machine to measure sleep cycles and how often they were in a deep REM sleep. The students who took part in the study spent the night in a sleep lab.
The students were woken up multiple times during the night and asked to report what they were dreaming about.
In the morning, they were given their reports and asked to identify familiar features or potential sources for particular dreams. More than half the dreams were tied to a memory the students recalled. One-quarter of the dreams were related to specific upcoming events the students reported. And about 40% of the dreams with a future event in them also included memories of past experiences. This was more common the longer the students dreamed, the scientists explained.
And this was also more common later in the night, possibly because the dreamer is closer to waking and the anticipated event is approaching, Dr. Wamsley said.
Studying dreams is a tricky, subjective business and not always taken as seriously as other aspects of sleep and neuroscience because it involves questions of human consciousness itself, said Erik Hoel, PhD, a research assistant professor of neuroscience at Tufts University in Medford, Mass.
In a recent report published in Patterns, he suggested that our weirdest dreams help our brains process our day-to-day experiences in a way that enables deeper learning.
“This type of research is challenged by the method,” Dr. Hoel said.
In the Wamsley study, “waking people up from a deep sleep and asking them to recollect their dream content will only get you part of the experience because it fades so quickly.” That said, the value of connecting what happens as a result could be meaningful, he noted. For example, study participants could be asked whether their future event went as planned and whether they think the outcome was related to how well they “prepared” in their dreams.
Even then, it would still be a subjective analysis. But going in those directions might lead to meaningful new training, Dr. Hoel said.
And training yourself to recall only specific memories right before sleep might prepare your mind in a focused way for certain events, from giving a presentation to having a difficult conversation with someone, or maybe even winning at the Olympics.
A version of this article first appeared on WebMD.com.
What you experience in your dreams might feel random and disjointed, but that chaos during sleep might serve a function, according to Erin Wamsley, PhD, an associate professor of psychology and neuroscience at Furman University in Greenville, S.C. In fact, evidence uncovered by Dr. Wamsley and associates suggests that
Previous research and anecdotal evidence have shown that dreams use fragments of past experiences, Dr. Wamsley explained. While studying dreams, her team found that the mind is using select fragments of past experiences to prepare for a known upcoming event.
“This is new evidence that dreams reflect a memory-processing function,” said Dr. Wamsley, who presented the work at the virtual annual meeting of the Associated Professional Sleep Societies.
Some high performers already use past experiences to excel in future events. For instance, Michael Phelps, the most decorated Olympic swimmer, with 28 medals, would “mentally rehearse” his swims for up to 2 hours per day, according to his coach, Bob Bowman.
Using sleep to strengthen this process is an exciting prospect that scientists have been eager to figure out, said Allison Brager, PhD, director of human performance at the U.S. Army Warrior Fitness Training Center. Deep REM sleep can lead to improved learning and memory, she said. “So, hypothetically, better dreams mean better sleep, and that equals better performance.”
For their research, Dr. Wamsley’s team hooked 48 students up to a polysomnography machine to measure sleep cycles and how often they were in a deep REM sleep. The students who took part in the study spent the night in a sleep lab.
The students were woken up multiple times during the night and asked to report what they were dreaming about.
In the morning, they were given their reports and asked to identify familiar features or potential sources for particular dreams. More than half the dreams were tied to a memory the students recalled. One-quarter of the dreams were related to specific upcoming events the students reported. And about 40% of the dreams with a future event in them also included memories of past experiences. This was more common the longer the students dreamed, the scientists explained.
And this was also more common later in the night, possibly because the dreamer is closer to waking and the anticipated event is approaching, Dr. Wamsley said.
Studying dreams is a tricky, subjective business and not always taken as seriously as other aspects of sleep and neuroscience because it involves questions of human consciousness itself, said Erik Hoel, PhD, a research assistant professor of neuroscience at Tufts University in Medford, Mass.
In a recent report published in Patterns, he suggested that our weirdest dreams help our brains process our day-to-day experiences in a way that enables deeper learning.
“This type of research is challenged by the method,” Dr. Hoel said.
In the Wamsley study, “waking people up from a deep sleep and asking them to recollect their dream content will only get you part of the experience because it fades so quickly.” That said, the value of connecting what happens as a result could be meaningful, he noted. For example, study participants could be asked whether their future event went as planned and whether they think the outcome was related to how well they “prepared” in their dreams.
Even then, it would still be a subjective analysis. But going in those directions might lead to meaningful new training, Dr. Hoel said.
And training yourself to recall only specific memories right before sleep might prepare your mind in a focused way for certain events, from giving a presentation to having a difficult conversation with someone, or maybe even winning at the Olympics.
A version of this article first appeared on WebMD.com.
FROM SLEEP 2021
Cortical surface changes tied to risk for movement disorders in schizophrenia
Schizophrenia patients with parkinsonism show distinctive patterns of cortical surface markers, compared with schizophrenia patients without parkinsonism and healthy controls, results of a multimodal magnetic resonance imaging study suggest.
Sensorimotor abnormalities are common in schizophrenia patients, however, “the neurobiological mechanisms underlying parkinsonism in [schizophrenia], which in treated samples represents the unity of interplay between spontaneous and antipsychotic drug-exacerbated movement disorder, are poorly understood,” wrote Robert Christian Wolf, MD, of Heidelberg (Germany) University, and colleagues.
In a study published in Schizophrenia Research (2021 May;231:54-60), the investigators examined brain imaging findings from 20 healthy controls, 38 schizophrenia patients with parkinsonism (SZ-P), and 35 schizophrenia patients without parkinsonism (SZ-nonP). Dr. Wolf and colleagues examined three cortical surface markers: cortical thickness, complexity of cortical folding, and sulcus depth.
Compared with SZ-nonP patients, the SZ-P patients showed significantly increased complexity of cortical folding in the left supplementary motor cortex (SMC) and significantly decreased left postcentral sulcus (PCS) depth. In addition, left SMC activity was higher in both SZ-P and SZ-nonP patient groups, compared with controls.
In a regression analysis, the researchers examined relationships between parkinsonism severity and brain structure. They found that parkinsonism severity was negatively associated with left middle frontal complexity of cortical folding and left anterior cingulate cortex cortical thickness.
“Overall, the data support the notion that cortical features of distinct neurodevelopmental origin, particularly cortical folding indices such as [complexity of cortical folding] and sulcus depth, contribute to the pathogenesis of parkinsonism in SZ,” the researchers wrote.
The study findings were limited by several factors, including the cross-sectional design, the potential limitations of the Simpson-Angus Scale in characterizing parkinsonism, the inability to record lifetime antibiotics exposure in the patient population, and the inability to identify changes in brain stem nuclei, the researchers noted. However, the results were strengthened by the well-matched study groups and use of multimodal MRI, they said.
Consequently, “,” and suggest a link between abnormal neurodevelopmental processes and an increased risk for movement disorders in schizophrenia, they concluded.
The study was funded by the German Research Foundation and the German Federal Ministry of Education and Research. Dr. Wolf and colleagues disclosed no conflicts.
Schizophrenia patients with parkinsonism show distinctive patterns of cortical surface markers, compared with schizophrenia patients without parkinsonism and healthy controls, results of a multimodal magnetic resonance imaging study suggest.
Sensorimotor abnormalities are common in schizophrenia patients, however, “the neurobiological mechanisms underlying parkinsonism in [schizophrenia], which in treated samples represents the unity of interplay between spontaneous and antipsychotic drug-exacerbated movement disorder, are poorly understood,” wrote Robert Christian Wolf, MD, of Heidelberg (Germany) University, and colleagues.
In a study published in Schizophrenia Research (2021 May;231:54-60), the investigators examined brain imaging findings from 20 healthy controls, 38 schizophrenia patients with parkinsonism (SZ-P), and 35 schizophrenia patients without parkinsonism (SZ-nonP). Dr. Wolf and colleagues examined three cortical surface markers: cortical thickness, complexity of cortical folding, and sulcus depth.
Compared with SZ-nonP patients, the SZ-P patients showed significantly increased complexity of cortical folding in the left supplementary motor cortex (SMC) and significantly decreased left postcentral sulcus (PCS) depth. In addition, left SMC activity was higher in both SZ-P and SZ-nonP patient groups, compared with controls.
In a regression analysis, the researchers examined relationships between parkinsonism severity and brain structure. They found that parkinsonism severity was negatively associated with left middle frontal complexity of cortical folding and left anterior cingulate cortex cortical thickness.
“Overall, the data support the notion that cortical features of distinct neurodevelopmental origin, particularly cortical folding indices such as [complexity of cortical folding] and sulcus depth, contribute to the pathogenesis of parkinsonism in SZ,” the researchers wrote.
The study findings were limited by several factors, including the cross-sectional design, the potential limitations of the Simpson-Angus Scale in characterizing parkinsonism, the inability to record lifetime antibiotics exposure in the patient population, and the inability to identify changes in brain stem nuclei, the researchers noted. However, the results were strengthened by the well-matched study groups and use of multimodal MRI, they said.
Consequently, “,” and suggest a link between abnormal neurodevelopmental processes and an increased risk for movement disorders in schizophrenia, they concluded.
The study was funded by the German Research Foundation and the German Federal Ministry of Education and Research. Dr. Wolf and colleagues disclosed no conflicts.
Schizophrenia patients with parkinsonism show distinctive patterns of cortical surface markers, compared with schizophrenia patients without parkinsonism and healthy controls, results of a multimodal magnetic resonance imaging study suggest.
Sensorimotor abnormalities are common in schizophrenia patients, however, “the neurobiological mechanisms underlying parkinsonism in [schizophrenia], which in treated samples represents the unity of interplay between spontaneous and antipsychotic drug-exacerbated movement disorder, are poorly understood,” wrote Robert Christian Wolf, MD, of Heidelberg (Germany) University, and colleagues.
In a study published in Schizophrenia Research (2021 May;231:54-60), the investigators examined brain imaging findings from 20 healthy controls, 38 schizophrenia patients with parkinsonism (SZ-P), and 35 schizophrenia patients without parkinsonism (SZ-nonP). Dr. Wolf and colleagues examined three cortical surface markers: cortical thickness, complexity of cortical folding, and sulcus depth.
Compared with SZ-nonP patients, the SZ-P patients showed significantly increased complexity of cortical folding in the left supplementary motor cortex (SMC) and significantly decreased left postcentral sulcus (PCS) depth. In addition, left SMC activity was higher in both SZ-P and SZ-nonP patient groups, compared with controls.
In a regression analysis, the researchers examined relationships between parkinsonism severity and brain structure. They found that parkinsonism severity was negatively associated with left middle frontal complexity of cortical folding and left anterior cingulate cortex cortical thickness.
“Overall, the data support the notion that cortical features of distinct neurodevelopmental origin, particularly cortical folding indices such as [complexity of cortical folding] and sulcus depth, contribute to the pathogenesis of parkinsonism in SZ,” the researchers wrote.
The study findings were limited by several factors, including the cross-sectional design, the potential limitations of the Simpson-Angus Scale in characterizing parkinsonism, the inability to record lifetime antibiotics exposure in the patient population, and the inability to identify changes in brain stem nuclei, the researchers noted. However, the results were strengthened by the well-matched study groups and use of multimodal MRI, they said.
Consequently, “,” and suggest a link between abnormal neurodevelopmental processes and an increased risk for movement disorders in schizophrenia, they concluded.
The study was funded by the German Research Foundation and the German Federal Ministry of Education and Research. Dr. Wolf and colleagues disclosed no conflicts.
FROM SCHIZOPHRENIA RESEARCH







