User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Population study supports migraine–dementia link
Preliminary results from a population-based cohort study support previous reports that migraine is a midlife risk factor for dementia later in life, but further determined that according to results from a Danish registry presented at the virtual annual meeting of the American Headache Society.
“The findings of this study emphasize the need for studies in the migraine-dementia pathophysiology, in particular in migraine cases with aura,” said Sabrina Islamoska, MSc, PhD, a postdoctoral researcher in the department of public health at the University of Copenhagen. “This study highlights the importance of monitoring severe migraine to potentially prevent dementia.”
A national register-based study
The study used Danish national register–based data from 1988 to 2017 of 1.66 million individuals born between 1935 and 1956, retrieving exposure information until age 59 years and following individuals for dementia after age 60. The matched analysis included 18,135 people registered with migraine before age 59 and 1.38 million without migraine. The matched study population was 62,578.
A diagnosis of dementia or use of dementia medications after age 60 years was the main outcome. Covariates included socioeconomic factors, psychiatric comorbidities and other headache diagnoses.
“To the best of our knowledge, no previous national register–based studies have investigated the risk of dementia among individuals who suffer from migraine with aura,” Dr. Islamoska said.
The preliminary findings revealed that the median age at diagnosis was 49 years and about 70% of the migraine population were women. “There was a 50% higher dementia rate in individuals who had any migraine diagnosis,” Dr. Islamoska said.
“We also found a 20% higher but nonsignificant dementia rate in individuals who had migraine without aura,” she said. However, when the migraine-with-aura population was evaluated, it was found to have a dementia rate two times higher than people with no migraine. “The dementia rate was higher if individuals had more frequent hospital contacts with migraine.”
The findings support the hypothesis that migraine is a midlife risk factor for dementia later in life, she said.
“The findings underline the value of investigating the effect of migraine medications in dementia risk to assess the impact of mild to moderate migraines,” Dr. Islamoska said. “Therefore, the next step is to investigate the risk of dementia among users of migraine medications who are not diagnosed with migraines at hospitals.”
Strengths of the study, Dr. Islamoska noted, were its size and national nature of its population, that it included all migraine diagnoses at hospitals over a 29-year period, that it made adjustments for confounding of well-established dementia risk factors, and that it validated dementia diagnoses after age 60 years.
One limitation was that the study only included hospital-based diagnoses of dementia while 60% of cases in Denmark are undiagnosed, “thus our results only apply to migraine that is severe enough to require a hospital contact,” Dr. Islamoska said, while most migraine cases are treated in the primary care setting.
Also, the young study population may have a lower dementia risk. “We also know that age of migraine registration may not corresponded with the actual onset, since migraine is a complex disorder with individual variation in patient’s burden and course of disease,” Dr. Islamoska said.
“Future studies are needed to understand the pathological mechanisms underlying the relationship between migraine and dementia and to investigate whether proper prophylactic treatment of migraine can potentially prevent dementia,” Dr. Islamoska said. “In addition, when investigating the association between these two prevalent neurological disorders, the timing of migraine diagnosis and dementia onset is important to ensure temporality. We took this into account in our study to strengthen the validity of our results.”
‘Surprising’ findings
Andrew Charles, MD, director of the Goldberg Migraine Program at the University of California, Los Angeles, said the Danish study makes an important contribution to the literature on dementia risk factors. “Vanishingly small amounts of attention have been paid to migraine as a potential risk factor,” he said. However, he called the results “surprising” based on his own clinical experience. “I actually had a sense that migraine was somehow protective against Alzheimer’s or other kinds of dementias.”
He questioned if the migraine-dementia link could be a “reporting artifact” of migraine sufferers merely going to the neurologist, raising the likelihood of a positive migraine diagnosis. Nonetheless, the results are “intriguing” and raise important questions about migraine therapy and dementia risk.
“If it holds up, it really is something that behooves us to understand whether intervening in terms of therapy for migraine has even more consequences beyond just the immediate relief of symptoms,” Dr. Charles said. “It’s something we should be thinking about in terms of preventing longer-term consequences of this disorder.”
Dr. Islamoska disclosed that Veluxfondent funded the study as part of her PhD project. Dr. Charles disclosed he is a consultant to Amgen, Biohaven Pharmaceuticals, Eli Lilly, Lundbeck, and Novartis.
SOURCE: Islamoska S et al. AHS 2020, Submission 846214.
Preliminary results from a population-based cohort study support previous reports that migraine is a midlife risk factor for dementia later in life, but further determined that according to results from a Danish registry presented at the virtual annual meeting of the American Headache Society.
“The findings of this study emphasize the need for studies in the migraine-dementia pathophysiology, in particular in migraine cases with aura,” said Sabrina Islamoska, MSc, PhD, a postdoctoral researcher in the department of public health at the University of Copenhagen. “This study highlights the importance of monitoring severe migraine to potentially prevent dementia.”
A national register-based study
The study used Danish national register–based data from 1988 to 2017 of 1.66 million individuals born between 1935 and 1956, retrieving exposure information until age 59 years and following individuals for dementia after age 60. The matched analysis included 18,135 people registered with migraine before age 59 and 1.38 million without migraine. The matched study population was 62,578.
A diagnosis of dementia or use of dementia medications after age 60 years was the main outcome. Covariates included socioeconomic factors, psychiatric comorbidities and other headache diagnoses.
“To the best of our knowledge, no previous national register–based studies have investigated the risk of dementia among individuals who suffer from migraine with aura,” Dr. Islamoska said.
The preliminary findings revealed that the median age at diagnosis was 49 years and about 70% of the migraine population were women. “There was a 50% higher dementia rate in individuals who had any migraine diagnosis,” Dr. Islamoska said.
“We also found a 20% higher but nonsignificant dementia rate in individuals who had migraine without aura,” she said. However, when the migraine-with-aura population was evaluated, it was found to have a dementia rate two times higher than people with no migraine. “The dementia rate was higher if individuals had more frequent hospital contacts with migraine.”
The findings support the hypothesis that migraine is a midlife risk factor for dementia later in life, she said.
“The findings underline the value of investigating the effect of migraine medications in dementia risk to assess the impact of mild to moderate migraines,” Dr. Islamoska said. “Therefore, the next step is to investigate the risk of dementia among users of migraine medications who are not diagnosed with migraines at hospitals.”
Strengths of the study, Dr. Islamoska noted, were its size and national nature of its population, that it included all migraine diagnoses at hospitals over a 29-year period, that it made adjustments for confounding of well-established dementia risk factors, and that it validated dementia diagnoses after age 60 years.
One limitation was that the study only included hospital-based diagnoses of dementia while 60% of cases in Denmark are undiagnosed, “thus our results only apply to migraine that is severe enough to require a hospital contact,” Dr. Islamoska said, while most migraine cases are treated in the primary care setting.
Also, the young study population may have a lower dementia risk. “We also know that age of migraine registration may not corresponded with the actual onset, since migraine is a complex disorder with individual variation in patient’s burden and course of disease,” Dr. Islamoska said.
“Future studies are needed to understand the pathological mechanisms underlying the relationship between migraine and dementia and to investigate whether proper prophylactic treatment of migraine can potentially prevent dementia,” Dr. Islamoska said. “In addition, when investigating the association between these two prevalent neurological disorders, the timing of migraine diagnosis and dementia onset is important to ensure temporality. We took this into account in our study to strengthen the validity of our results.”
‘Surprising’ findings
Andrew Charles, MD, director of the Goldberg Migraine Program at the University of California, Los Angeles, said the Danish study makes an important contribution to the literature on dementia risk factors. “Vanishingly small amounts of attention have been paid to migraine as a potential risk factor,” he said. However, he called the results “surprising” based on his own clinical experience. “I actually had a sense that migraine was somehow protective against Alzheimer’s or other kinds of dementias.”
He questioned if the migraine-dementia link could be a “reporting artifact” of migraine sufferers merely going to the neurologist, raising the likelihood of a positive migraine diagnosis. Nonetheless, the results are “intriguing” and raise important questions about migraine therapy and dementia risk.
“If it holds up, it really is something that behooves us to understand whether intervening in terms of therapy for migraine has even more consequences beyond just the immediate relief of symptoms,” Dr. Charles said. “It’s something we should be thinking about in terms of preventing longer-term consequences of this disorder.”
Dr. Islamoska disclosed that Veluxfondent funded the study as part of her PhD project. Dr. Charles disclosed he is a consultant to Amgen, Biohaven Pharmaceuticals, Eli Lilly, Lundbeck, and Novartis.
SOURCE: Islamoska S et al. AHS 2020, Submission 846214.
Preliminary results from a population-based cohort study support previous reports that migraine is a midlife risk factor for dementia later in life, but further determined that according to results from a Danish registry presented at the virtual annual meeting of the American Headache Society.
“The findings of this study emphasize the need for studies in the migraine-dementia pathophysiology, in particular in migraine cases with aura,” said Sabrina Islamoska, MSc, PhD, a postdoctoral researcher in the department of public health at the University of Copenhagen. “This study highlights the importance of monitoring severe migraine to potentially prevent dementia.”
A national register-based study
The study used Danish national register–based data from 1988 to 2017 of 1.66 million individuals born between 1935 and 1956, retrieving exposure information until age 59 years and following individuals for dementia after age 60. The matched analysis included 18,135 people registered with migraine before age 59 and 1.38 million without migraine. The matched study population was 62,578.
A diagnosis of dementia or use of dementia medications after age 60 years was the main outcome. Covariates included socioeconomic factors, psychiatric comorbidities and other headache diagnoses.
“To the best of our knowledge, no previous national register–based studies have investigated the risk of dementia among individuals who suffer from migraine with aura,” Dr. Islamoska said.
The preliminary findings revealed that the median age at diagnosis was 49 years and about 70% of the migraine population were women. “There was a 50% higher dementia rate in individuals who had any migraine diagnosis,” Dr. Islamoska said.
“We also found a 20% higher but nonsignificant dementia rate in individuals who had migraine without aura,” she said. However, when the migraine-with-aura population was evaluated, it was found to have a dementia rate two times higher than people with no migraine. “The dementia rate was higher if individuals had more frequent hospital contacts with migraine.”
The findings support the hypothesis that migraine is a midlife risk factor for dementia later in life, she said.
“The findings underline the value of investigating the effect of migraine medications in dementia risk to assess the impact of mild to moderate migraines,” Dr. Islamoska said. “Therefore, the next step is to investigate the risk of dementia among users of migraine medications who are not diagnosed with migraines at hospitals.”
Strengths of the study, Dr. Islamoska noted, were its size and national nature of its population, that it included all migraine diagnoses at hospitals over a 29-year period, that it made adjustments for confounding of well-established dementia risk factors, and that it validated dementia diagnoses after age 60 years.
One limitation was that the study only included hospital-based diagnoses of dementia while 60% of cases in Denmark are undiagnosed, “thus our results only apply to migraine that is severe enough to require a hospital contact,” Dr. Islamoska said, while most migraine cases are treated in the primary care setting.
Also, the young study population may have a lower dementia risk. “We also know that age of migraine registration may not corresponded with the actual onset, since migraine is a complex disorder with individual variation in patient’s burden and course of disease,” Dr. Islamoska said.
“Future studies are needed to understand the pathological mechanisms underlying the relationship between migraine and dementia and to investigate whether proper prophylactic treatment of migraine can potentially prevent dementia,” Dr. Islamoska said. “In addition, when investigating the association between these two prevalent neurological disorders, the timing of migraine diagnosis and dementia onset is important to ensure temporality. We took this into account in our study to strengthen the validity of our results.”
‘Surprising’ findings
Andrew Charles, MD, director of the Goldberg Migraine Program at the University of California, Los Angeles, said the Danish study makes an important contribution to the literature on dementia risk factors. “Vanishingly small amounts of attention have been paid to migraine as a potential risk factor,” he said. However, he called the results “surprising” based on his own clinical experience. “I actually had a sense that migraine was somehow protective against Alzheimer’s or other kinds of dementias.”
He questioned if the migraine-dementia link could be a “reporting artifact” of migraine sufferers merely going to the neurologist, raising the likelihood of a positive migraine diagnosis. Nonetheless, the results are “intriguing” and raise important questions about migraine therapy and dementia risk.
“If it holds up, it really is something that behooves us to understand whether intervening in terms of therapy for migraine has even more consequences beyond just the immediate relief of symptoms,” Dr. Charles said. “It’s something we should be thinking about in terms of preventing longer-term consequences of this disorder.”
Dr. Islamoska disclosed that Veluxfondent funded the study as part of her PhD project. Dr. Charles disclosed he is a consultant to Amgen, Biohaven Pharmaceuticals, Eli Lilly, Lundbeck, and Novartis.
SOURCE: Islamoska S et al. AHS 2020, Submission 846214.
FROM AHS 2020
Health experts link rise in Arizona COVID cases to end of stay-at-home order
With new daily coronavirus cases rising in at least two dozen states,
Arizona has emerged as one of the country’s newest coronavirus hot spots, with the weekly average of daily cases more than doubling from 2 weeks ago. The total number of people hospitalized is climbing, too.
Over the past week, Arizona has seen an average of more than 1,300 new COVID-19 cases each day.
After the state’s largest hospital system warned about a shortage of ICU beds, Arizona Gov. Doug Ducey, a Republican, pushed back on claims that the health care system could soon be overwhelmed.
“The entire time we’ve been focused on a possible worst-case scenario with surge capacity for hospital beds, ICU beds and ventilators,” Ducey told reporters on Thursday. “Those are not needed or necessary right now.”
While he acknowledged a spike in positive cases, Ducey said a second stay-at-home order was “not under discussion.”
“We put the stay-at-home order there so we could prepare for what we are going through,” he said.
Some states have reopened more slowly with a set of specific benchmarks for different regions, but Arizona took a more aggressive approach.
The state began easing restrictions on businesses in early May and lifted its statewide lockdown order after May 15. Under Arizona’s reopening plan, businesses are advised to follow federal guidance on social distancing.
There is also no requirement for everyone to wear masks in public.
Public health experts agree: The timing of this spike reflects the state’s reopening.
“Perhaps, Arizona will be a warning sign to other areas,” said Katherine Ellingson, an epidemiologist at the University of Arizona. “We never had that consistent downward trend that would signal it’s time to reopen and we have everything in place to do it safely.”
Before Arizona lifted its stay-at-home order, only about 5% of COVID-19 tests registered as positive. On Monday, that number was around 16%.
A slower reopening gives public health agencies time to identify whether cases are rising and then respond with contact tracing and isolating those who are infected.
“With a fast, rapid reopening, we don’t have the time to mobilize those resources,” said Ellingson.
Maricopa County, home to about 60% of the state’s population, has ramped up contact tracing in recent weeks, but it may not have enough capacity if the surge in cases continues.
Dr. Peter Hotez said the spike in Arizona, as well as in parts of Texas such as Houston, Dallas and Austin, is the consequence of removing restrictions too quickly and without a public health system that can keep pace.
“It was just ‘open it up’ and then more or less business as usual, with a little bit of window dressing,” said Hotez, the dean for the National School of Tropical Medicine at Baylor College of Medicine in Houston. “This is not an abstract number of cases. We’re seeing people pile into intensive care units.”
Arizona’s governor has also faced criticism from the mayors of Arizona’s two biggest cities for not putting in place more stringent requirements.
“There is a pandemic and it’s spreading uncontrollably,” said Tucson Mayor Regina Romero, a Democrat. Ducey, she said, “is just putting up his hands and saying ‘the spread is happening and we just have to go about our business.’”
And the governor’s executive order forbids local governments from implementing their own extra measures, which adds to Romero’s frustration. Texas has a similar measure.
“What he did was pretty much tie the hands of mayors and public health officials,” Romero said.
Arizona’s hospital industry has tried to tamp down fears that it’s on the verge of a crisis. Hospitals are still performing elective surgeries.
“It’s very unfortunate because hospitals right now in Arizona are quite busy with elective procedures,” said Saskia Popescu, a Phoenix-based epidemiologist with George Mason University. “You throw in increasing cases of COVID, and that’s going to very much stress your hospital systems.”
Phoenix’s triple-digit summer temperatures actually may fuel the spread of the virus. People forgo outdoor activities and retreat to air-conditioned indoor spaces, where the risk of transmitting the virus goes up significantly.
“My concern is we’re going to see a lot more people in close quarters for prolonged periods of time,” Popescu said.
Since the stay-at-home order was lifted, Popescu and others say they’ve seen people returning to a pre-pandemic mindset, neglecting to wear masks or maintain social distance. Videos of crowded bars have only propelled these fears.
On Thursday, however, Arizona’s top doctor stressed there were also dangers to keeping the state on lockdown, including the mental health effects of loneliness and isolation.
“We know that it’s in the community. We are not going to be able to stop the spread. And so we can’t stop living as well,” said Dr. Cara Christ, health director for the Arizona Department of Health Services.
But Dr. Quinn Snyder, an emergency medicine physician in Mesa, Arizona, said there needs to be more consistent messaging on public health measures like wearing masks.
“Frankly, I just think a wholesale reevaluation of where we’re at is critical right now, but I can tell you that we’re not doing nearly enough,” said Snyder, who has seen the uptick in seriously ill COVID-19 patients firsthand.
“If we continue to head down this path, the virus will press our health care facilities beyond capacity, where we’re going to have to be making tough decisions like who gets a ventilator and who doesn’t.”
A version of this article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
With new daily coronavirus cases rising in at least two dozen states,
Arizona has emerged as one of the country’s newest coronavirus hot spots, with the weekly average of daily cases more than doubling from 2 weeks ago. The total number of people hospitalized is climbing, too.
Over the past week, Arizona has seen an average of more than 1,300 new COVID-19 cases each day.
After the state’s largest hospital system warned about a shortage of ICU beds, Arizona Gov. Doug Ducey, a Republican, pushed back on claims that the health care system could soon be overwhelmed.
“The entire time we’ve been focused on a possible worst-case scenario with surge capacity for hospital beds, ICU beds and ventilators,” Ducey told reporters on Thursday. “Those are not needed or necessary right now.”
While he acknowledged a spike in positive cases, Ducey said a second stay-at-home order was “not under discussion.”
“We put the stay-at-home order there so we could prepare for what we are going through,” he said.
Some states have reopened more slowly with a set of specific benchmarks for different regions, but Arizona took a more aggressive approach.
The state began easing restrictions on businesses in early May and lifted its statewide lockdown order after May 15. Under Arizona’s reopening plan, businesses are advised to follow federal guidance on social distancing.
There is also no requirement for everyone to wear masks in public.
Public health experts agree: The timing of this spike reflects the state’s reopening.
“Perhaps, Arizona will be a warning sign to other areas,” said Katherine Ellingson, an epidemiologist at the University of Arizona. “We never had that consistent downward trend that would signal it’s time to reopen and we have everything in place to do it safely.”
Before Arizona lifted its stay-at-home order, only about 5% of COVID-19 tests registered as positive. On Monday, that number was around 16%.
A slower reopening gives public health agencies time to identify whether cases are rising and then respond with contact tracing and isolating those who are infected.
“With a fast, rapid reopening, we don’t have the time to mobilize those resources,” said Ellingson.
Maricopa County, home to about 60% of the state’s population, has ramped up contact tracing in recent weeks, but it may not have enough capacity if the surge in cases continues.
Dr. Peter Hotez said the spike in Arizona, as well as in parts of Texas such as Houston, Dallas and Austin, is the consequence of removing restrictions too quickly and without a public health system that can keep pace.
“It was just ‘open it up’ and then more or less business as usual, with a little bit of window dressing,” said Hotez, the dean for the National School of Tropical Medicine at Baylor College of Medicine in Houston. “This is not an abstract number of cases. We’re seeing people pile into intensive care units.”
Arizona’s governor has also faced criticism from the mayors of Arizona’s two biggest cities for not putting in place more stringent requirements.
“There is a pandemic and it’s spreading uncontrollably,” said Tucson Mayor Regina Romero, a Democrat. Ducey, she said, “is just putting up his hands and saying ‘the spread is happening and we just have to go about our business.’”
And the governor’s executive order forbids local governments from implementing their own extra measures, which adds to Romero’s frustration. Texas has a similar measure.
“What he did was pretty much tie the hands of mayors and public health officials,” Romero said.
Arizona’s hospital industry has tried to tamp down fears that it’s on the verge of a crisis. Hospitals are still performing elective surgeries.
“It’s very unfortunate because hospitals right now in Arizona are quite busy with elective procedures,” said Saskia Popescu, a Phoenix-based epidemiologist with George Mason University. “You throw in increasing cases of COVID, and that’s going to very much stress your hospital systems.”
Phoenix’s triple-digit summer temperatures actually may fuel the spread of the virus. People forgo outdoor activities and retreat to air-conditioned indoor spaces, where the risk of transmitting the virus goes up significantly.
“My concern is we’re going to see a lot more people in close quarters for prolonged periods of time,” Popescu said.
Since the stay-at-home order was lifted, Popescu and others say they’ve seen people returning to a pre-pandemic mindset, neglecting to wear masks or maintain social distance. Videos of crowded bars have only propelled these fears.
On Thursday, however, Arizona’s top doctor stressed there were also dangers to keeping the state on lockdown, including the mental health effects of loneliness and isolation.
“We know that it’s in the community. We are not going to be able to stop the spread. And so we can’t stop living as well,” said Dr. Cara Christ, health director for the Arizona Department of Health Services.
But Dr. Quinn Snyder, an emergency medicine physician in Mesa, Arizona, said there needs to be more consistent messaging on public health measures like wearing masks.
“Frankly, I just think a wholesale reevaluation of where we’re at is critical right now, but I can tell you that we’re not doing nearly enough,” said Snyder, who has seen the uptick in seriously ill COVID-19 patients firsthand.
“If we continue to head down this path, the virus will press our health care facilities beyond capacity, where we’re going to have to be making tough decisions like who gets a ventilator and who doesn’t.”
A version of this article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
With new daily coronavirus cases rising in at least two dozen states,
Arizona has emerged as one of the country’s newest coronavirus hot spots, with the weekly average of daily cases more than doubling from 2 weeks ago. The total number of people hospitalized is climbing, too.
Over the past week, Arizona has seen an average of more than 1,300 new COVID-19 cases each day.
After the state’s largest hospital system warned about a shortage of ICU beds, Arizona Gov. Doug Ducey, a Republican, pushed back on claims that the health care system could soon be overwhelmed.
“The entire time we’ve been focused on a possible worst-case scenario with surge capacity for hospital beds, ICU beds and ventilators,” Ducey told reporters on Thursday. “Those are not needed or necessary right now.”
While he acknowledged a spike in positive cases, Ducey said a second stay-at-home order was “not under discussion.”
“We put the stay-at-home order there so we could prepare for what we are going through,” he said.
Some states have reopened more slowly with a set of specific benchmarks for different regions, but Arizona took a more aggressive approach.
The state began easing restrictions on businesses in early May and lifted its statewide lockdown order after May 15. Under Arizona’s reopening plan, businesses are advised to follow federal guidance on social distancing.
There is also no requirement for everyone to wear masks in public.
Public health experts agree: The timing of this spike reflects the state’s reopening.
“Perhaps, Arizona will be a warning sign to other areas,” said Katherine Ellingson, an epidemiologist at the University of Arizona. “We never had that consistent downward trend that would signal it’s time to reopen and we have everything in place to do it safely.”
Before Arizona lifted its stay-at-home order, only about 5% of COVID-19 tests registered as positive. On Monday, that number was around 16%.
A slower reopening gives public health agencies time to identify whether cases are rising and then respond with contact tracing and isolating those who are infected.
“With a fast, rapid reopening, we don’t have the time to mobilize those resources,” said Ellingson.
Maricopa County, home to about 60% of the state’s population, has ramped up contact tracing in recent weeks, but it may not have enough capacity if the surge in cases continues.
Dr. Peter Hotez said the spike in Arizona, as well as in parts of Texas such as Houston, Dallas and Austin, is the consequence of removing restrictions too quickly and without a public health system that can keep pace.
“It was just ‘open it up’ and then more or less business as usual, with a little bit of window dressing,” said Hotez, the dean for the National School of Tropical Medicine at Baylor College of Medicine in Houston. “This is not an abstract number of cases. We’re seeing people pile into intensive care units.”
Arizona’s governor has also faced criticism from the mayors of Arizona’s two biggest cities for not putting in place more stringent requirements.
“There is a pandemic and it’s spreading uncontrollably,” said Tucson Mayor Regina Romero, a Democrat. Ducey, she said, “is just putting up his hands and saying ‘the spread is happening and we just have to go about our business.’”
And the governor’s executive order forbids local governments from implementing their own extra measures, which adds to Romero’s frustration. Texas has a similar measure.
“What he did was pretty much tie the hands of mayors and public health officials,” Romero said.
Arizona’s hospital industry has tried to tamp down fears that it’s on the verge of a crisis. Hospitals are still performing elective surgeries.
“It’s very unfortunate because hospitals right now in Arizona are quite busy with elective procedures,” said Saskia Popescu, a Phoenix-based epidemiologist with George Mason University. “You throw in increasing cases of COVID, and that’s going to very much stress your hospital systems.”
Phoenix’s triple-digit summer temperatures actually may fuel the spread of the virus. People forgo outdoor activities and retreat to air-conditioned indoor spaces, where the risk of transmitting the virus goes up significantly.
“My concern is we’re going to see a lot more people in close quarters for prolonged periods of time,” Popescu said.
Since the stay-at-home order was lifted, Popescu and others say they’ve seen people returning to a pre-pandemic mindset, neglecting to wear masks or maintain social distance. Videos of crowded bars have only propelled these fears.
On Thursday, however, Arizona’s top doctor stressed there were also dangers to keeping the state on lockdown, including the mental health effects of loneliness and isolation.
“We know that it’s in the community. We are not going to be able to stop the spread. And so we can’t stop living as well,” said Dr. Cara Christ, health director for the Arizona Department of Health Services.
But Dr. Quinn Snyder, an emergency medicine physician in Mesa, Arizona, said there needs to be more consistent messaging on public health measures like wearing masks.
“Frankly, I just think a wholesale reevaluation of where we’re at is critical right now, but I can tell you that we’re not doing nearly enough,” said Snyder, who has seen the uptick in seriously ill COVID-19 patients firsthand.
“If we continue to head down this path, the virus will press our health care facilities beyond capacity, where we’re going to have to be making tough decisions like who gets a ventilator and who doesn’t.”
A version of this article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Relapsing, progressive MS classifications should be abandoned
Most disability accumulation in relapsing multiple sclerosis (MS) is not associated with overt relapses, challenging the current clinical distinction of relapsing and progressive forms of the disease, a new analysis shows. “We have to abandon the distinction between relapsing and progressive MS being different populations,” said lead author Ludwig Kappos, MD, University of Basel (Switzerland). “The disease appears to be more of a continuum of disability progression, which is sometimes also accompanied by relapses.”
The analysis was published online June 8 in JAMA Neurology.
Assessing disability progression
Noting that there are mounting data to suggest patients with relapsing MS frequently experience worsening disability over time – even when relapse activity appears well controlled – the researchers aimed to investigate the relative contributions of progression independent of relapse activity and relapse-associated worsening to overall accumulating disability in patients with relapsing multiple sclerosis. To do this, they analyzed data from two identical randomized clinical trials (OPERA I and OPERA II) conducted between 2011 and 2015, which compared treatment with the new B-cell–depleting therapy ocrelizumab with interferon beta-1a in 1,656 patients with relapsing MS.
Confirmed disability accumulation was defined by an increase in 1 or more of 3 measures (Expanded Disability Status Scale, timed 25-ft walk, or 9-hole peg test), confirmed after 3 or 6 months, and was classified as being related to a clinical relapse or occurring in the absence of a relapse.
Results showed that after 96 weeks (1.8 years) of treatment, 12-week composite confirmed disability accumulation had occurred in 29.6% of patients receiving interferon beta-1a and 21.1% of those given ocrelizumab; 24-week composite confirmed disability accumulation occurred in 22.7% of interferon beta-1a patients and 16.2% of the ocrelizumab group.
In both treatment groups, the vast majority of events contributing to disability accumulation occurred independently of relapse activity. In the interferon group, 78% of events contributing to 12-week confirmed disability accumulation and 80.6% of events contributing to 24-week confirmed disability accumulation occurred in the absence of clinical relapses, with the corresponding figures in the ocrelizumab group being 88.0% (12 weeks) and 89.1% (24 weeks).
Only a minority of patients (about 17% in both groups) had confirmed disability accumulation accompanied by clinical relapses. Very few patients with confirmed disability accumulation (4% to 5%) experienced disability worsening both associated and independent of relapses. Ocrelizumab was associated with a reduced risk of both relapse-associated and relapse-independent confirmed disability accumulation, compared with interferon beta-1a.
“We found that there was progression of disability in both groups, and the really astonishing finding was that although all patients were classified as having relapsing remitting MS, actually most of the disability progression occurred without preceding relapses,” Dr. Kappos commented. He noted that there have been two previous observational studies that have shown a high rate of disability progressions without temporal association to relapses in relapsing remitting patients, but this is the first time that this progression of disability independent of relapses has been shown in the controlled setting of two prospective, randomized clinical trials over a 2-year period.
“While we expected to see some disability progression independent of relapses, we were surprised to see that the disability progression occurring in both studies was almost exclusively happening without temporal relation to relapses. That was certainly an unexpected finding,” Dr. Kappos said. “These observations make it difficult to keep the current definitions of ‘relapsing remitting’ and ‘secondary progressive’ MS, [ones] that suggest a clear-cut distinction marked by the presence or absence of relapses. This can no longer be justified,” he stressed.
“We are not saying that relapses do not contribute to disability progression. There are a lot of data to support the fact that they do. But I think what we might be seeing is that the drug therapy is quite effective in reducing disability due to relapses but only partially effective in reducing progression independent of relapses,” Dr. Kappos explained.
Although there have been many advances in reducing relapses with drug therapy, focus now needs to shift to the other more continuous process of disability progression independent of relapses, Dr. Kappos said. “There is still a lot of room for improvement here.”
“If continuous progression independent of relapses is already present in the early phases of MS, it is reasonable to study the effects of intervention on steady progression already in this early phase,” he noted. “This might help to capture patients at earlier stages who better respond to treatment aimed at halting progression.”
Dr. Kappos also called for more subtle measurements of disability than the EDSS alone, including measures such as the 9-hole peg test and the 25-ft walk as they did in this analysis. But other measures could also be added that would characterize continuous disease activity and progression, such as laboratory values (e.g., neurofilament light chain) and advanced, more tissue-specific quantitative MRI techniques and digital biomarkers to detect subtle changes in neurologic function.
An artificial distinction?
Commenting on the study, Jeffrey Cohen, MD, director of the experimental therapeutics program at the Mellen Center for Multiple Sclerosis Treatment and Research, Cleveland Clinic, said he too sees very little distinction between relapsing remitting and progressive forms of the disease.
“This study confirms what has been suspected for quite a few years –that if one looks sufficiently and carefully, there is gradual worsening of some aspects of the disease in many patients from the earliest stages,” Dr. Cohen said. “Conversely, some patients with progressive MS have superimposed relapses or MRI lesion activity.
“Thus, the distinction between relapsing-remitting and progressive MS subtypes appears artificial,” he concluded.
This study was sponsored by F. Hoffmann–La Roche. Dr. Kappos has received research support from the company.
This article first appeared on Medscape.com.
Most disability accumulation in relapsing multiple sclerosis (MS) is not associated with overt relapses, challenging the current clinical distinction of relapsing and progressive forms of the disease, a new analysis shows. “We have to abandon the distinction between relapsing and progressive MS being different populations,” said lead author Ludwig Kappos, MD, University of Basel (Switzerland). “The disease appears to be more of a continuum of disability progression, which is sometimes also accompanied by relapses.”
The analysis was published online June 8 in JAMA Neurology.
Assessing disability progression
Noting that there are mounting data to suggest patients with relapsing MS frequently experience worsening disability over time – even when relapse activity appears well controlled – the researchers aimed to investigate the relative contributions of progression independent of relapse activity and relapse-associated worsening to overall accumulating disability in patients with relapsing multiple sclerosis. To do this, they analyzed data from two identical randomized clinical trials (OPERA I and OPERA II) conducted between 2011 and 2015, which compared treatment with the new B-cell–depleting therapy ocrelizumab with interferon beta-1a in 1,656 patients with relapsing MS.
Confirmed disability accumulation was defined by an increase in 1 or more of 3 measures (Expanded Disability Status Scale, timed 25-ft walk, or 9-hole peg test), confirmed after 3 or 6 months, and was classified as being related to a clinical relapse or occurring in the absence of a relapse.
Results showed that after 96 weeks (1.8 years) of treatment, 12-week composite confirmed disability accumulation had occurred in 29.6% of patients receiving interferon beta-1a and 21.1% of those given ocrelizumab; 24-week composite confirmed disability accumulation occurred in 22.7% of interferon beta-1a patients and 16.2% of the ocrelizumab group.
In both treatment groups, the vast majority of events contributing to disability accumulation occurred independently of relapse activity. In the interferon group, 78% of events contributing to 12-week confirmed disability accumulation and 80.6% of events contributing to 24-week confirmed disability accumulation occurred in the absence of clinical relapses, with the corresponding figures in the ocrelizumab group being 88.0% (12 weeks) and 89.1% (24 weeks).
Only a minority of patients (about 17% in both groups) had confirmed disability accumulation accompanied by clinical relapses. Very few patients with confirmed disability accumulation (4% to 5%) experienced disability worsening both associated and independent of relapses. Ocrelizumab was associated with a reduced risk of both relapse-associated and relapse-independent confirmed disability accumulation, compared with interferon beta-1a.
“We found that there was progression of disability in both groups, and the really astonishing finding was that although all patients were classified as having relapsing remitting MS, actually most of the disability progression occurred without preceding relapses,” Dr. Kappos commented. He noted that there have been two previous observational studies that have shown a high rate of disability progressions without temporal association to relapses in relapsing remitting patients, but this is the first time that this progression of disability independent of relapses has been shown in the controlled setting of two prospective, randomized clinical trials over a 2-year period.
“While we expected to see some disability progression independent of relapses, we were surprised to see that the disability progression occurring in both studies was almost exclusively happening without temporal relation to relapses. That was certainly an unexpected finding,” Dr. Kappos said. “These observations make it difficult to keep the current definitions of ‘relapsing remitting’ and ‘secondary progressive’ MS, [ones] that suggest a clear-cut distinction marked by the presence or absence of relapses. This can no longer be justified,” he stressed.
“We are not saying that relapses do not contribute to disability progression. There are a lot of data to support the fact that they do. But I think what we might be seeing is that the drug therapy is quite effective in reducing disability due to relapses but only partially effective in reducing progression independent of relapses,” Dr. Kappos explained.
Although there have been many advances in reducing relapses with drug therapy, focus now needs to shift to the other more continuous process of disability progression independent of relapses, Dr. Kappos said. “There is still a lot of room for improvement here.”
“If continuous progression independent of relapses is already present in the early phases of MS, it is reasonable to study the effects of intervention on steady progression already in this early phase,” he noted. “This might help to capture patients at earlier stages who better respond to treatment aimed at halting progression.”
Dr. Kappos also called for more subtle measurements of disability than the EDSS alone, including measures such as the 9-hole peg test and the 25-ft walk as they did in this analysis. But other measures could also be added that would characterize continuous disease activity and progression, such as laboratory values (e.g., neurofilament light chain) and advanced, more tissue-specific quantitative MRI techniques and digital biomarkers to detect subtle changes in neurologic function.
An artificial distinction?
Commenting on the study, Jeffrey Cohen, MD, director of the experimental therapeutics program at the Mellen Center for Multiple Sclerosis Treatment and Research, Cleveland Clinic, said he too sees very little distinction between relapsing remitting and progressive forms of the disease.
“This study confirms what has been suspected for quite a few years –that if one looks sufficiently and carefully, there is gradual worsening of some aspects of the disease in many patients from the earliest stages,” Dr. Cohen said. “Conversely, some patients with progressive MS have superimposed relapses or MRI lesion activity.
“Thus, the distinction between relapsing-remitting and progressive MS subtypes appears artificial,” he concluded.
This study was sponsored by F. Hoffmann–La Roche. Dr. Kappos has received research support from the company.
This article first appeared on Medscape.com.
Most disability accumulation in relapsing multiple sclerosis (MS) is not associated with overt relapses, challenging the current clinical distinction of relapsing and progressive forms of the disease, a new analysis shows. “We have to abandon the distinction between relapsing and progressive MS being different populations,” said lead author Ludwig Kappos, MD, University of Basel (Switzerland). “The disease appears to be more of a continuum of disability progression, which is sometimes also accompanied by relapses.”
The analysis was published online June 8 in JAMA Neurology.
Assessing disability progression
Noting that there are mounting data to suggest patients with relapsing MS frequently experience worsening disability over time – even when relapse activity appears well controlled – the researchers aimed to investigate the relative contributions of progression independent of relapse activity and relapse-associated worsening to overall accumulating disability in patients with relapsing multiple sclerosis. To do this, they analyzed data from two identical randomized clinical trials (OPERA I and OPERA II) conducted between 2011 and 2015, which compared treatment with the new B-cell–depleting therapy ocrelizumab with interferon beta-1a in 1,656 patients with relapsing MS.
Confirmed disability accumulation was defined by an increase in 1 or more of 3 measures (Expanded Disability Status Scale, timed 25-ft walk, or 9-hole peg test), confirmed after 3 or 6 months, and was classified as being related to a clinical relapse or occurring in the absence of a relapse.
Results showed that after 96 weeks (1.8 years) of treatment, 12-week composite confirmed disability accumulation had occurred in 29.6% of patients receiving interferon beta-1a and 21.1% of those given ocrelizumab; 24-week composite confirmed disability accumulation occurred in 22.7% of interferon beta-1a patients and 16.2% of the ocrelizumab group.
In both treatment groups, the vast majority of events contributing to disability accumulation occurred independently of relapse activity. In the interferon group, 78% of events contributing to 12-week confirmed disability accumulation and 80.6% of events contributing to 24-week confirmed disability accumulation occurred in the absence of clinical relapses, with the corresponding figures in the ocrelizumab group being 88.0% (12 weeks) and 89.1% (24 weeks).
Only a minority of patients (about 17% in both groups) had confirmed disability accumulation accompanied by clinical relapses. Very few patients with confirmed disability accumulation (4% to 5%) experienced disability worsening both associated and independent of relapses. Ocrelizumab was associated with a reduced risk of both relapse-associated and relapse-independent confirmed disability accumulation, compared with interferon beta-1a.
“We found that there was progression of disability in both groups, and the really astonishing finding was that although all patients were classified as having relapsing remitting MS, actually most of the disability progression occurred without preceding relapses,” Dr. Kappos commented. He noted that there have been two previous observational studies that have shown a high rate of disability progressions without temporal association to relapses in relapsing remitting patients, but this is the first time that this progression of disability independent of relapses has been shown in the controlled setting of two prospective, randomized clinical trials over a 2-year period.
“While we expected to see some disability progression independent of relapses, we were surprised to see that the disability progression occurring in both studies was almost exclusively happening without temporal relation to relapses. That was certainly an unexpected finding,” Dr. Kappos said. “These observations make it difficult to keep the current definitions of ‘relapsing remitting’ and ‘secondary progressive’ MS, [ones] that suggest a clear-cut distinction marked by the presence or absence of relapses. This can no longer be justified,” he stressed.
“We are not saying that relapses do not contribute to disability progression. There are a lot of data to support the fact that they do. But I think what we might be seeing is that the drug therapy is quite effective in reducing disability due to relapses but only partially effective in reducing progression independent of relapses,” Dr. Kappos explained.
Although there have been many advances in reducing relapses with drug therapy, focus now needs to shift to the other more continuous process of disability progression independent of relapses, Dr. Kappos said. “There is still a lot of room for improvement here.”
“If continuous progression independent of relapses is already present in the early phases of MS, it is reasonable to study the effects of intervention on steady progression already in this early phase,” he noted. “This might help to capture patients at earlier stages who better respond to treatment aimed at halting progression.”
Dr. Kappos also called for more subtle measurements of disability than the EDSS alone, including measures such as the 9-hole peg test and the 25-ft walk as they did in this analysis. But other measures could also be added that would characterize continuous disease activity and progression, such as laboratory values (e.g., neurofilament light chain) and advanced, more tissue-specific quantitative MRI techniques and digital biomarkers to detect subtle changes in neurologic function.
An artificial distinction?
Commenting on the study, Jeffrey Cohen, MD, director of the experimental therapeutics program at the Mellen Center for Multiple Sclerosis Treatment and Research, Cleveland Clinic, said he too sees very little distinction between relapsing remitting and progressive forms of the disease.
“This study confirms what has been suspected for quite a few years –that if one looks sufficiently and carefully, there is gradual worsening of some aspects of the disease in many patients from the earliest stages,” Dr. Cohen said. “Conversely, some patients with progressive MS have superimposed relapses or MRI lesion activity.
“Thus, the distinction between relapsing-remitting and progressive MS subtypes appears artificial,” he concluded.
This study was sponsored by F. Hoffmann–La Roche. Dr. Kappos has received research support from the company.
This article first appeared on Medscape.com.
FDA revokes emergency use of hydroxychloroquine
The U.S. Food and Drug Administration revoked its decision from March 28 allowing use of hydroxychloroquine and chloroquine to treat people hospitalized with COVID-19 under an emergency use authorization (EUA).
“Based on its ongoing analysis of the EUA and emerging scientific data, the FDA determined that chloroquine and hydroxychloroquine are unlikely to be effective in treating COVID-19 for the authorized uses in the EUA,” the agency announced in a June 15 statement.
The FDA also warned today that the use of hydroxychloroquine or chloroquine may have a potential drug interaction with the investigational antiviral drug remdesivir that limits its effectiveness against COVID-19.
Remdesivir was granted emergency use authorization by the FDA on May 1.
“Based on a recently completed nonclinical laboratory study, the FDA is revising the fact sheet for healthcare providers that accompanies the drug to state that coadministration of remdesivir and chloroquine phosphate or hydroxychloroquine sulfate is not recommended as it may result in reduced antiviral activity of remdesivir. The agency is not aware of instances of this reduced activity occurring in the clinical setting but is continuing to evaluate all data related to remdesivir,” the FDA said in a news release.
Controversy over hydroxychloroquine
Even with such federal permission, since late March the use of these two agents has been mired in controversy.
President Donald J. Trump promoted the use of hydroxychloroquine and chloroquine to treat Americans with COVID-19, while scientific studies raised questions about their safety and effectiveness. Recent research, for example, pointed to elevated cardiovascular risks, as reported by Medscape Medical News.
The FDA acknowledged this recent evidence. “Additionally, in light of ongoing serious cardiac adverse events and other potential serious side effects, the known and potential benefits of chloroquine and hydroxychloroquine no longer outweigh the known and potential risks for the authorized use.”
The full suspension of the EUA follows a warning the agency issued on April 24. The FDA’s Safety Communication cautioned against use of the two agents outside of a hospital setting, citing an increase in outpatient prescriptions and “reports of serious heart rhythm problems.”
“While additional clinical trials continue to evaluate the potential benefit of these drugs in treating or preventing COVID-19, we determined the emergency use authorization was no longer appropriate,” based on a rigorous assessment by scientists in our Center for Drug Evaluation and Research,” Patrizia Cavazzoni, MD, acting director of CDER, noted in the FDA statement.
This article first appeared on Medscape.com.
The U.S. Food and Drug Administration revoked its decision from March 28 allowing use of hydroxychloroquine and chloroquine to treat people hospitalized with COVID-19 under an emergency use authorization (EUA).
“Based on its ongoing analysis of the EUA and emerging scientific data, the FDA determined that chloroquine and hydroxychloroquine are unlikely to be effective in treating COVID-19 for the authorized uses in the EUA,” the agency announced in a June 15 statement.
The FDA also warned today that the use of hydroxychloroquine or chloroquine may have a potential drug interaction with the investigational antiviral drug remdesivir that limits its effectiveness against COVID-19.
Remdesivir was granted emergency use authorization by the FDA on May 1.
“Based on a recently completed nonclinical laboratory study, the FDA is revising the fact sheet for healthcare providers that accompanies the drug to state that coadministration of remdesivir and chloroquine phosphate or hydroxychloroquine sulfate is not recommended as it may result in reduced antiviral activity of remdesivir. The agency is not aware of instances of this reduced activity occurring in the clinical setting but is continuing to evaluate all data related to remdesivir,” the FDA said in a news release.
Controversy over hydroxychloroquine
Even with such federal permission, since late March the use of these two agents has been mired in controversy.
President Donald J. Trump promoted the use of hydroxychloroquine and chloroquine to treat Americans with COVID-19, while scientific studies raised questions about their safety and effectiveness. Recent research, for example, pointed to elevated cardiovascular risks, as reported by Medscape Medical News.
The FDA acknowledged this recent evidence. “Additionally, in light of ongoing serious cardiac adverse events and other potential serious side effects, the known and potential benefits of chloroquine and hydroxychloroquine no longer outweigh the known and potential risks for the authorized use.”
The full suspension of the EUA follows a warning the agency issued on April 24. The FDA’s Safety Communication cautioned against use of the two agents outside of a hospital setting, citing an increase in outpatient prescriptions and “reports of serious heart rhythm problems.”
“While additional clinical trials continue to evaluate the potential benefit of these drugs in treating or preventing COVID-19, we determined the emergency use authorization was no longer appropriate,” based on a rigorous assessment by scientists in our Center for Drug Evaluation and Research,” Patrizia Cavazzoni, MD, acting director of CDER, noted in the FDA statement.
This article first appeared on Medscape.com.
The U.S. Food and Drug Administration revoked its decision from March 28 allowing use of hydroxychloroquine and chloroquine to treat people hospitalized with COVID-19 under an emergency use authorization (EUA).
“Based on its ongoing analysis of the EUA and emerging scientific data, the FDA determined that chloroquine and hydroxychloroquine are unlikely to be effective in treating COVID-19 for the authorized uses in the EUA,” the agency announced in a June 15 statement.
The FDA also warned today that the use of hydroxychloroquine or chloroquine may have a potential drug interaction with the investigational antiviral drug remdesivir that limits its effectiveness against COVID-19.
Remdesivir was granted emergency use authorization by the FDA on May 1.
“Based on a recently completed nonclinical laboratory study, the FDA is revising the fact sheet for healthcare providers that accompanies the drug to state that coadministration of remdesivir and chloroquine phosphate or hydroxychloroquine sulfate is not recommended as it may result in reduced antiviral activity of remdesivir. The agency is not aware of instances of this reduced activity occurring in the clinical setting but is continuing to evaluate all data related to remdesivir,” the FDA said in a news release.
Controversy over hydroxychloroquine
Even with such federal permission, since late March the use of these two agents has been mired in controversy.
President Donald J. Trump promoted the use of hydroxychloroquine and chloroquine to treat Americans with COVID-19, while scientific studies raised questions about their safety and effectiveness. Recent research, for example, pointed to elevated cardiovascular risks, as reported by Medscape Medical News.
The FDA acknowledged this recent evidence. “Additionally, in light of ongoing serious cardiac adverse events and other potential serious side effects, the known and potential benefits of chloroquine and hydroxychloroquine no longer outweigh the known and potential risks for the authorized use.”
The full suspension of the EUA follows a warning the agency issued on April 24. The FDA’s Safety Communication cautioned against use of the two agents outside of a hospital setting, citing an increase in outpatient prescriptions and “reports of serious heart rhythm problems.”
“While additional clinical trials continue to evaluate the potential benefit of these drugs in treating or preventing COVID-19, we determined the emergency use authorization was no longer appropriate,” based on a rigorous assessment by scientists in our Center for Drug Evaluation and Research,” Patrizia Cavazzoni, MD, acting director of CDER, noted in the FDA statement.
This article first appeared on Medscape.com.
Perfect storm of SARS-CoV-2 during flu season
COVID-19 now. The urban phase of the U.S. pandemic is leveling somewhat, while the rural phase is accelerating – in part because of food processing and handling industries. The pediatric burden has been surprisingly small, with the multisystem inflammatory disease (MIS-c) in children noted in several hundred cases now being seen across the country.
Next wave? Given ongoing COVID-19 disease, controversy rages about when and how to re-open the country. Regardless how more reopening occurs over the next months, we should expect a next or ongoing COVID-19 wave, particularly given loss of social distancing during social justice protests. A sawtooth disease prevalence pattern is predicted by many experts: a drop in prevalence leading to reopening, leading to scattered prevalence increases and regional if not local restriction tightening, followed by another drop in prevalence. Then “rinse and repeat” until 70% of the population is immune either by disease experience or vaccine-induced immunity, likely sometime in 2021.
Influenza too. A COVID-19 up-cycle is likely during influenza season, although influenza season’s onset could be altered because of whatever social distancing rules are in place in November and December. That said, we need to consider the worst. We have seen what happens if we fail to prepare and then react only after a prevalent respiratory infection has surged into the overall population. Best estimates are that at most 20% of the U.S. population is currently immune to SARS-CoV-2. Given that at least some of that 20% of individuals currently immune to SARS-CoV-2 will lose their neutralizing antibody over the next 4-6 months, we can still expect 70%-80% of the U.S. population to be susceptible to SARS-CoV-2 infection in the fall of 2020.
Pediatric preparedness. As pediatric providers, we have struggled with lower patient loads and dramatic income losses/declines. Many clinics/offices’ attendance remain less than 50% of pre–COVID-19 levels, with necessary furloughs of personnel and spotty office hours. But influenza is coming, and SARS-CoV-2 will not be gone yet. How do we prepare for concurrent influenza and COVID-19?
The annual purchase/administration of influenza vaccine in summer/fall is expensive, time consuming, and logistically difficult even in the best times. Given the loss of income, likely reluctance of patients to come to clinics/offices if COVID-19 is still circulating, and likely need for some form of social distancing during late summer and early fall, how will providers, health departments, and hospitals implement influenza vaccine administration this year?
Minimize double whammy infections. It is easy to understand why we should maximize influenza protection in SARS-CoV-2 vulnerables (elderly or persons with existing comorbidities). But is it as critical for otherwise healthy children? My answer is yes.
Children are not currently known as SARS-CoV-2 vectors, but children are excellent influenza vectors, shedding higher titers for longer than other age groups. As with SARS-CoV-2, influenza exposure is cumulative, i.e., the more intense and more frequently a person is exposed, the more likely that infection/disease will result. So, the fewer who get and can transmit influenza during the COVID-19 pandemic, the fewer people are likely to get a double whammy of SARS-CoV-2 concurrent or in tandem with influenza. Double whammy infections likely would further increase the medical care burden and return us to March-April crisis mode.
One alarming new question is whether recent influenza could make children vulnerable to SARS-CoV-2 and trigger hospitalizations. A surge in pediatric plus adult COVID-19 disease plus a surge in all-ages influenza disease would likely break the medical care system, at least in some areas.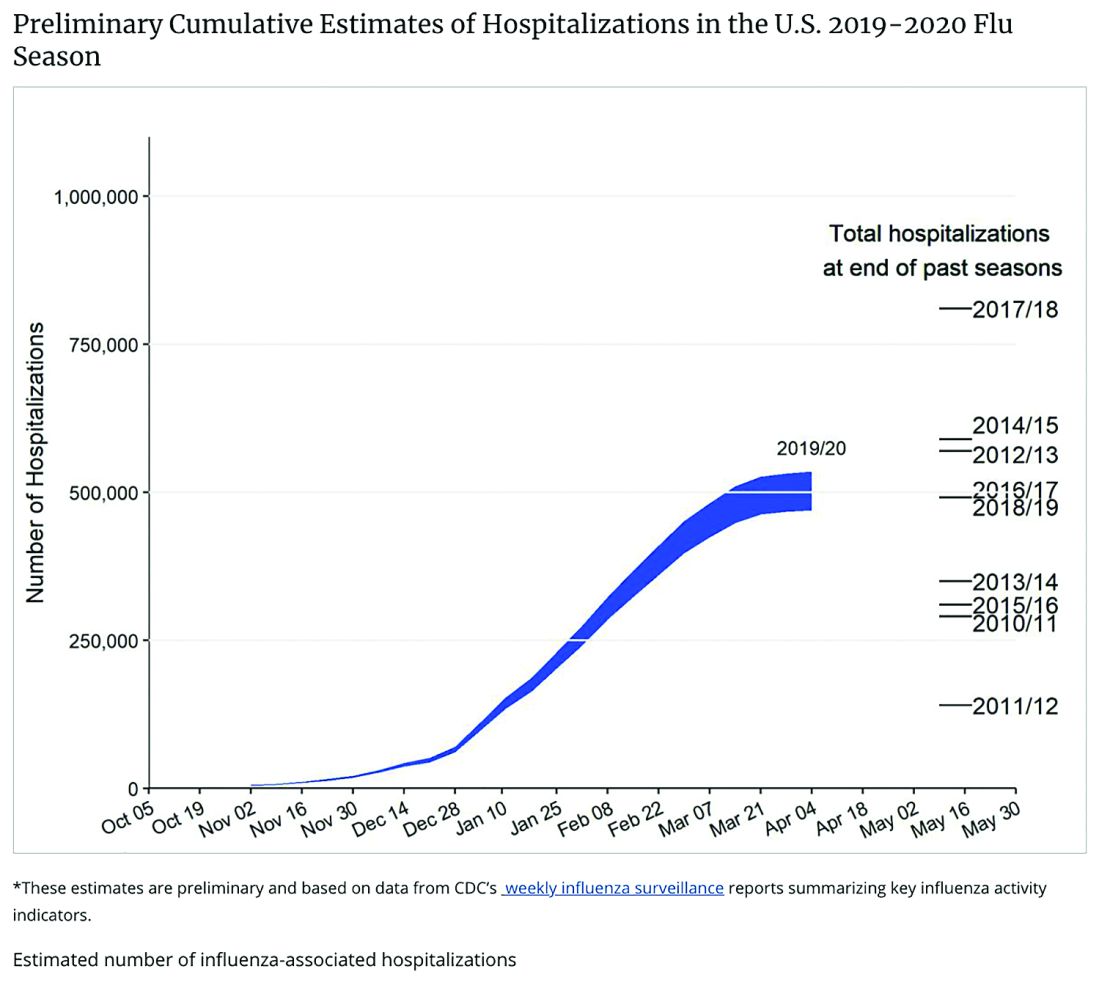
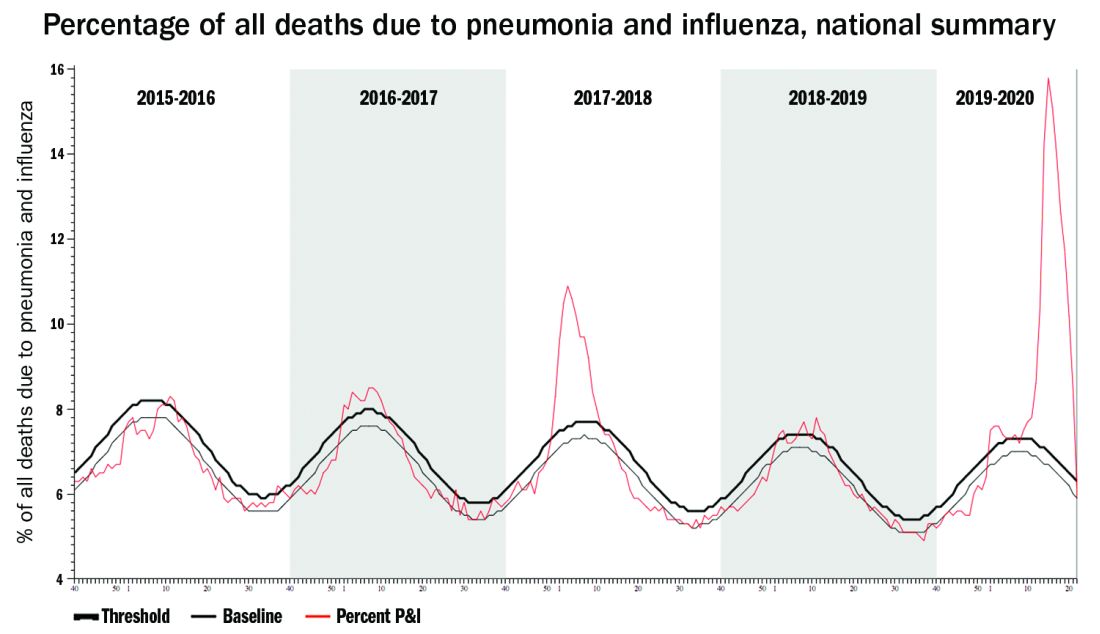
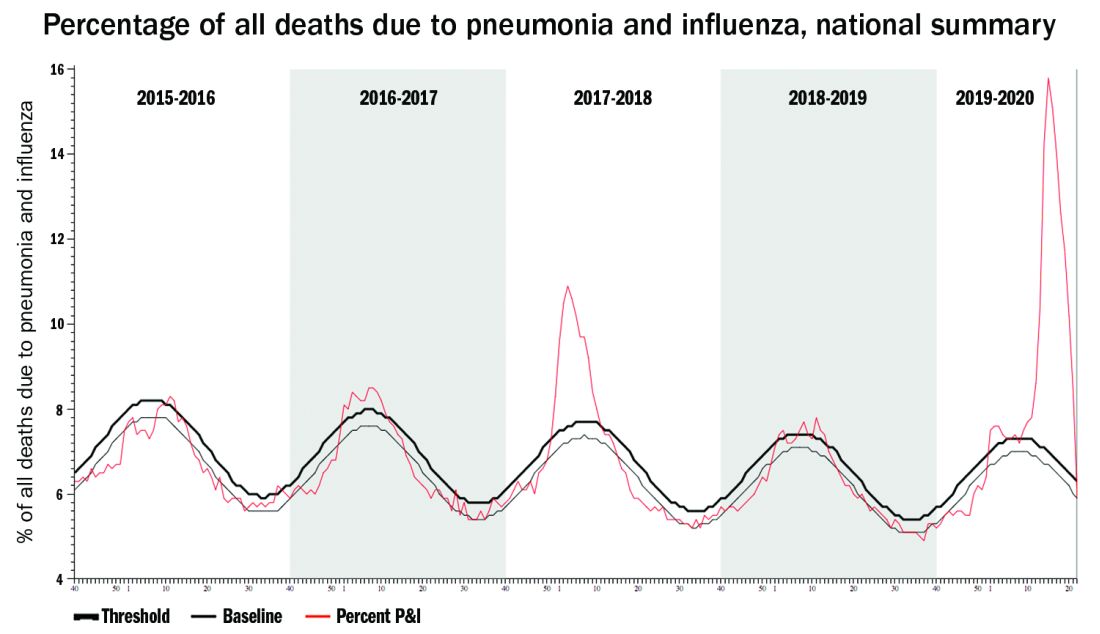
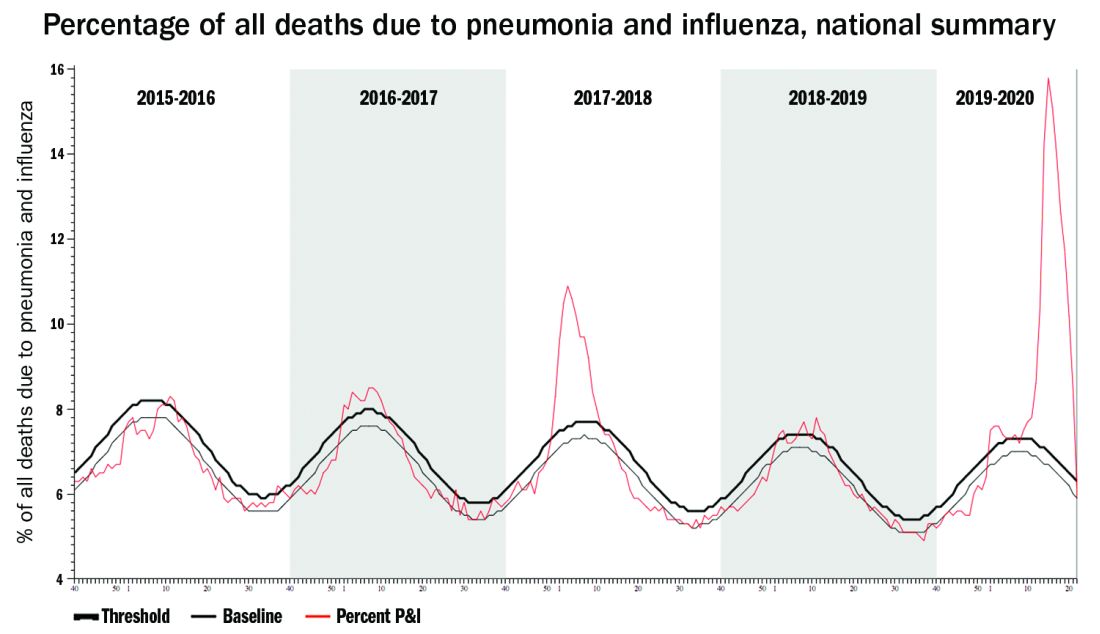
Staggering COVID-19 burden. As of June 8, we have had approximately 2 million SARS-CoV-2 cases with 500,000 hospitalizations and 120,000 deaths. Over the past 10 years, total annual U.S. influenza hospitalizations ranged from 180,000 (2011-2012) to 825,000 (2017-2018). The interquartile range for hospitalization length of stay for influenza is 4-6 days1 vs. 15-23 days2 for SARS-CoV-2. One COVID-19 hospitalization uses hospital resources roughly equal to four influenza hospitalizations. To date COVID-19 hospitalizations have used resources equal to an estimated 1.9 million influenza hospitalizations – over twice the worst influenza season in this century – and we are still on the rise. We are likely not even halfway to truly controlling the U.S. pandemic, so expect another 500,000 hospitalizations – equal to another 1.9 million influenza hospitalizations. Further, pneumonia deaths have skyrocketed this year when COVID-19 was superimposed on the last third of influenza season. One hope is that widespread use of antivirals (for example, new antivirals, convalescent plasma, or other interventions) can reduce length of stay by 30% for COVID-19 hospitalizations, yet even with that the numbers remain grim.
Less influenza disease can free up medical resources. Planning ahead could prevent a bad influenza season (for example, up to 850,000 hospitalizations just for influenza). Can we preemptively use vaccine to reduce influenza hospitalizations below 2011-2012 levels – less than 150,000 hospitalizations? Perhaps, if we start by reducing pediatric influenza.
1. Aim to exceed 75% influenza vaccine uptake in your patients.
a. It is ambitious, but if there was ever a year that needed influenza herd immunity, it is 2020-2021.
2. Review practice/group/institution plans for vaccine purchase and ensure adequate personnel to administer vaccine.
3. Plan safe and efficient processes to vaccinate large numbers in August through November.
a. Consider that routine and influenza vaccines can be given concurrently with the annual uptick in school and sports physical examinations.
b. What social distancing and masking rules will be needed?
i. Will patients need to bring their own masks, or will you supply them?
c. What extra supplies and efforts are needed, e.g. hand sanitizer, new signage, 6-foot interval markings on floors or sidewalks, families calling from parking lot to announce their arrivals, etc.?
d. Remember younger patients need two doses before Dec 1, 2020.
e. Be creative, for example, are parking-lot tents for influenza vaccination feasible?
f. Can we partner with other providers to implement influenza vaccine–specific mass clinics?
Ramping up to give seasonal influenza vaccine in 2020 is daunting. But if we do not prepare, it will be even more difficult. Let’s make this the mildest influenza season in memory by vaccinating more than any time in memory – and by doing so, we can hope to blunt medical care burdens despite ongoing COVID-19 disease.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Kansas City (Mo.). Children’s Mercy receives funding from GlaxoSmithKline, Merck, and Pfizer for vaccine research studies on which Dr. Harrison is an investigator. Email him at [email protected].
References
1.. HCUP Statistical Brief #253. 2019 Oct.
2. medrxiv. 2020 Apr 10. doi: 10.1101/2020.04.07.20057299.
COVID-19 now. The urban phase of the U.S. pandemic is leveling somewhat, while the rural phase is accelerating – in part because of food processing and handling industries. The pediatric burden has been surprisingly small, with the multisystem inflammatory disease (MIS-c) in children noted in several hundred cases now being seen across the country.
Next wave? Given ongoing COVID-19 disease, controversy rages about when and how to re-open the country. Regardless how more reopening occurs over the next months, we should expect a next or ongoing COVID-19 wave, particularly given loss of social distancing during social justice protests. A sawtooth disease prevalence pattern is predicted by many experts: a drop in prevalence leading to reopening, leading to scattered prevalence increases and regional if not local restriction tightening, followed by another drop in prevalence. Then “rinse and repeat” until 70% of the population is immune either by disease experience or vaccine-induced immunity, likely sometime in 2021.
Influenza too. A COVID-19 up-cycle is likely during influenza season, although influenza season’s onset could be altered because of whatever social distancing rules are in place in November and December. That said, we need to consider the worst. We have seen what happens if we fail to prepare and then react only after a prevalent respiratory infection has surged into the overall population. Best estimates are that at most 20% of the U.S. population is currently immune to SARS-CoV-2. Given that at least some of that 20% of individuals currently immune to SARS-CoV-2 will lose their neutralizing antibody over the next 4-6 months, we can still expect 70%-80% of the U.S. population to be susceptible to SARS-CoV-2 infection in the fall of 2020.
Pediatric preparedness. As pediatric providers, we have struggled with lower patient loads and dramatic income losses/declines. Many clinics/offices’ attendance remain less than 50% of pre–COVID-19 levels, with necessary furloughs of personnel and spotty office hours. But influenza is coming, and SARS-CoV-2 will not be gone yet. How do we prepare for concurrent influenza and COVID-19?
The annual purchase/administration of influenza vaccine in summer/fall is expensive, time consuming, and logistically difficult even in the best times. Given the loss of income, likely reluctance of patients to come to clinics/offices if COVID-19 is still circulating, and likely need for some form of social distancing during late summer and early fall, how will providers, health departments, and hospitals implement influenza vaccine administration this year?
Minimize double whammy infections. It is easy to understand why we should maximize influenza protection in SARS-CoV-2 vulnerables (elderly or persons with existing comorbidities). But is it as critical for otherwise healthy children? My answer is yes.
Children are not currently known as SARS-CoV-2 vectors, but children are excellent influenza vectors, shedding higher titers for longer than other age groups. As with SARS-CoV-2, influenza exposure is cumulative, i.e., the more intense and more frequently a person is exposed, the more likely that infection/disease will result. So, the fewer who get and can transmit influenza during the COVID-19 pandemic, the fewer people are likely to get a double whammy of SARS-CoV-2 concurrent or in tandem with influenza. Double whammy infections likely would further increase the medical care burden and return us to March-April crisis mode.
One alarming new question is whether recent influenza could make children vulnerable to SARS-CoV-2 and trigger hospitalizations. A surge in pediatric plus adult COVID-19 disease plus a surge in all-ages influenza disease would likely break the medical care system, at least in some areas.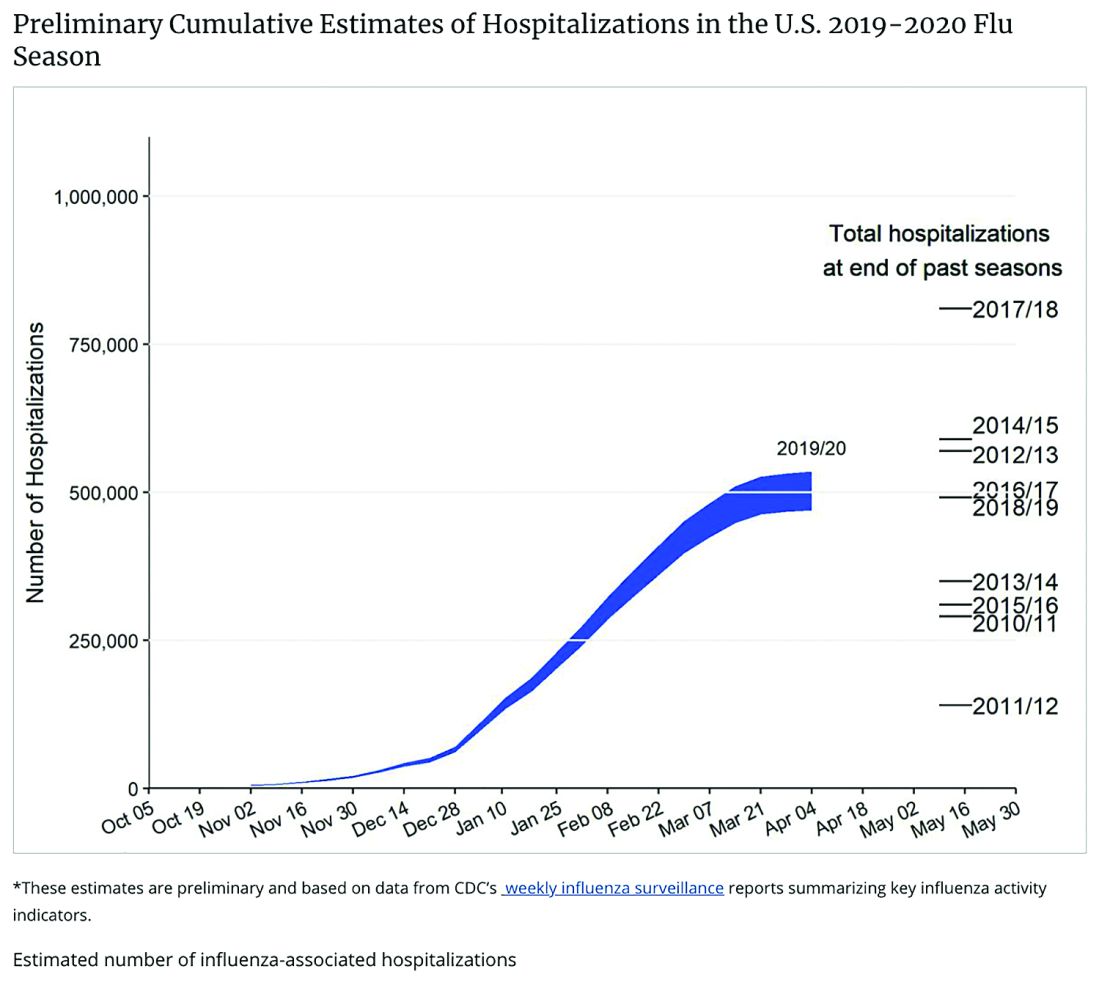
Staggering COVID-19 burden. As of June 8, we have had approximately 2 million SARS-CoV-2 cases with 500,000 hospitalizations and 120,000 deaths. Over the past 10 years, total annual U.S. influenza hospitalizations ranged from 180,000 (2011-2012) to 825,000 (2017-2018). The interquartile range for hospitalization length of stay for influenza is 4-6 days1 vs. 15-23 days2 for SARS-CoV-2. One COVID-19 hospitalization uses hospital resources roughly equal to four influenza hospitalizations. To date COVID-19 hospitalizations have used resources equal to an estimated 1.9 million influenza hospitalizations – over twice the worst influenza season in this century – and we are still on the rise. We are likely not even halfway to truly controlling the U.S. pandemic, so expect another 500,000 hospitalizations – equal to another 1.9 million influenza hospitalizations. Further, pneumonia deaths have skyrocketed this year when COVID-19 was superimposed on the last third of influenza season. One hope is that widespread use of antivirals (for example, new antivirals, convalescent plasma, or other interventions) can reduce length of stay by 30% for COVID-19 hospitalizations, yet even with that the numbers remain grim.
Less influenza disease can free up medical resources. Planning ahead could prevent a bad influenza season (for example, up to 850,000 hospitalizations just for influenza). Can we preemptively use vaccine to reduce influenza hospitalizations below 2011-2012 levels – less than 150,000 hospitalizations? Perhaps, if we start by reducing pediatric influenza.
1. Aim to exceed 75% influenza vaccine uptake in your patients.
a. It is ambitious, but if there was ever a year that needed influenza herd immunity, it is 2020-2021.
2. Review practice/group/institution plans for vaccine purchase and ensure adequate personnel to administer vaccine.
3. Plan safe and efficient processes to vaccinate large numbers in August through November.
a. Consider that routine and influenza vaccines can be given concurrently with the annual uptick in school and sports physical examinations.
b. What social distancing and masking rules will be needed?
i. Will patients need to bring their own masks, or will you supply them?
c. What extra supplies and efforts are needed, e.g. hand sanitizer, new signage, 6-foot interval markings on floors or sidewalks, families calling from parking lot to announce their arrivals, etc.?
d. Remember younger patients need two doses before Dec 1, 2020.
e. Be creative, for example, are parking-lot tents for influenza vaccination feasible?
f. Can we partner with other providers to implement influenza vaccine–specific mass clinics?
Ramping up to give seasonal influenza vaccine in 2020 is daunting. But if we do not prepare, it will be even more difficult. Let’s make this the mildest influenza season in memory by vaccinating more than any time in memory – and by doing so, we can hope to blunt medical care burdens despite ongoing COVID-19 disease.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Kansas City (Mo.). Children’s Mercy receives funding from GlaxoSmithKline, Merck, and Pfizer for vaccine research studies on which Dr. Harrison is an investigator. Email him at [email protected].
References
1.. HCUP Statistical Brief #253. 2019 Oct.
2. medrxiv. 2020 Apr 10. doi: 10.1101/2020.04.07.20057299.
COVID-19 now. The urban phase of the U.S. pandemic is leveling somewhat, while the rural phase is accelerating – in part because of food processing and handling industries. The pediatric burden has been surprisingly small, with the multisystem inflammatory disease (MIS-c) in children noted in several hundred cases now being seen across the country.
Next wave? Given ongoing COVID-19 disease, controversy rages about when and how to re-open the country. Regardless how more reopening occurs over the next months, we should expect a next or ongoing COVID-19 wave, particularly given loss of social distancing during social justice protests. A sawtooth disease prevalence pattern is predicted by many experts: a drop in prevalence leading to reopening, leading to scattered prevalence increases and regional if not local restriction tightening, followed by another drop in prevalence. Then “rinse and repeat” until 70% of the population is immune either by disease experience or vaccine-induced immunity, likely sometime in 2021.
Influenza too. A COVID-19 up-cycle is likely during influenza season, although influenza season’s onset could be altered because of whatever social distancing rules are in place in November and December. That said, we need to consider the worst. We have seen what happens if we fail to prepare and then react only after a prevalent respiratory infection has surged into the overall population. Best estimates are that at most 20% of the U.S. population is currently immune to SARS-CoV-2. Given that at least some of that 20% of individuals currently immune to SARS-CoV-2 will lose their neutralizing antibody over the next 4-6 months, we can still expect 70%-80% of the U.S. population to be susceptible to SARS-CoV-2 infection in the fall of 2020.
Pediatric preparedness. As pediatric providers, we have struggled with lower patient loads and dramatic income losses/declines. Many clinics/offices’ attendance remain less than 50% of pre–COVID-19 levels, with necessary furloughs of personnel and spotty office hours. But influenza is coming, and SARS-CoV-2 will not be gone yet. How do we prepare for concurrent influenza and COVID-19?
The annual purchase/administration of influenza vaccine in summer/fall is expensive, time consuming, and logistically difficult even in the best times. Given the loss of income, likely reluctance of patients to come to clinics/offices if COVID-19 is still circulating, and likely need for some form of social distancing during late summer and early fall, how will providers, health departments, and hospitals implement influenza vaccine administration this year?
Minimize double whammy infections. It is easy to understand why we should maximize influenza protection in SARS-CoV-2 vulnerables (elderly or persons with existing comorbidities). But is it as critical for otherwise healthy children? My answer is yes.
Children are not currently known as SARS-CoV-2 vectors, but children are excellent influenza vectors, shedding higher titers for longer than other age groups. As with SARS-CoV-2, influenza exposure is cumulative, i.e., the more intense and more frequently a person is exposed, the more likely that infection/disease will result. So, the fewer who get and can transmit influenza during the COVID-19 pandemic, the fewer people are likely to get a double whammy of SARS-CoV-2 concurrent or in tandem with influenza. Double whammy infections likely would further increase the medical care burden and return us to March-April crisis mode.
One alarming new question is whether recent influenza could make children vulnerable to SARS-CoV-2 and trigger hospitalizations. A surge in pediatric plus adult COVID-19 disease plus a surge in all-ages influenza disease would likely break the medical care system, at least in some areas.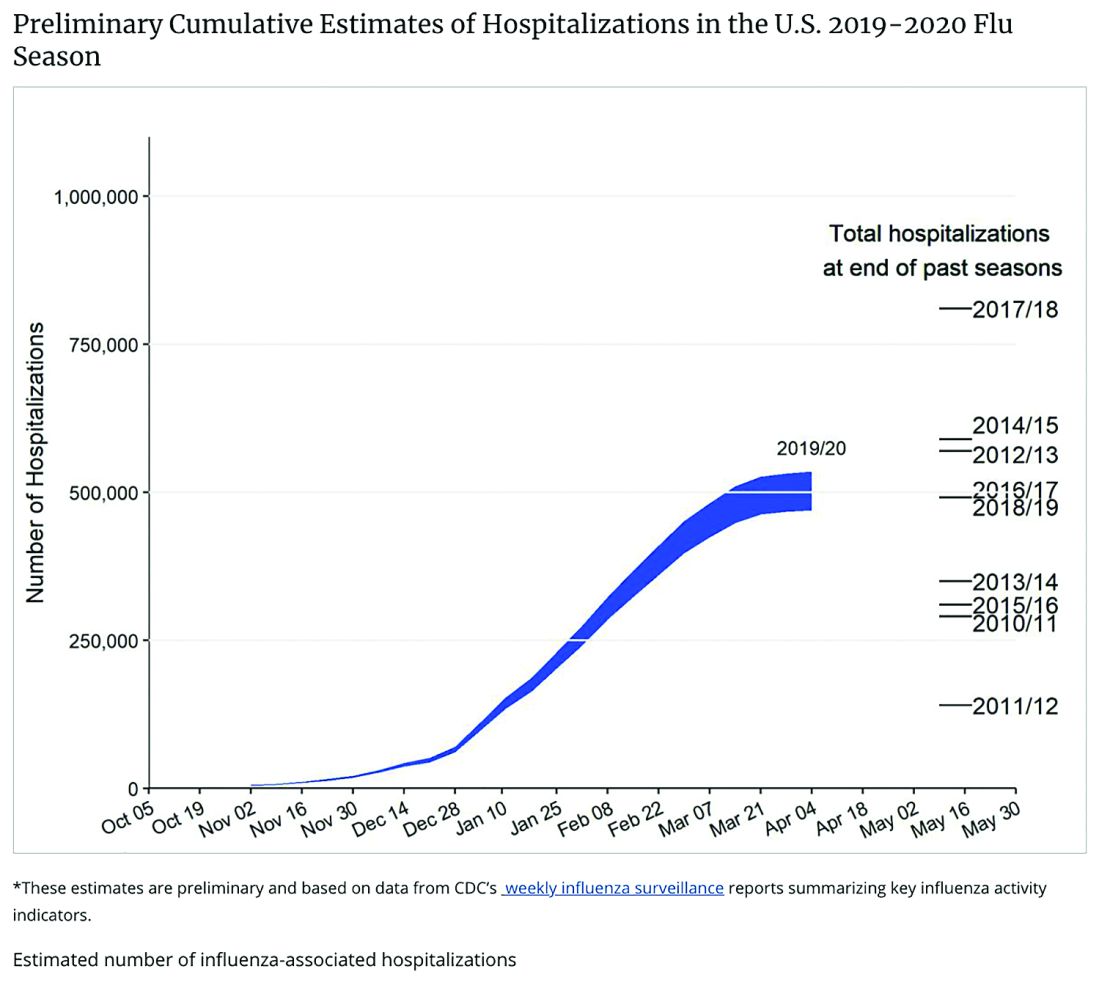
Staggering COVID-19 burden. As of June 8, we have had approximately 2 million SARS-CoV-2 cases with 500,000 hospitalizations and 120,000 deaths. Over the past 10 years, total annual U.S. influenza hospitalizations ranged from 180,000 (2011-2012) to 825,000 (2017-2018). The interquartile range for hospitalization length of stay for influenza is 4-6 days1 vs. 15-23 days2 for SARS-CoV-2. One COVID-19 hospitalization uses hospital resources roughly equal to four influenza hospitalizations. To date COVID-19 hospitalizations have used resources equal to an estimated 1.9 million influenza hospitalizations – over twice the worst influenza season in this century – and we are still on the rise. We are likely not even halfway to truly controlling the U.S. pandemic, so expect another 500,000 hospitalizations – equal to another 1.9 million influenza hospitalizations. Further, pneumonia deaths have skyrocketed this year when COVID-19 was superimposed on the last third of influenza season. One hope is that widespread use of antivirals (for example, new antivirals, convalescent plasma, or other interventions) can reduce length of stay by 30% for COVID-19 hospitalizations, yet even with that the numbers remain grim.
Less influenza disease can free up medical resources. Planning ahead could prevent a bad influenza season (for example, up to 850,000 hospitalizations just for influenza). Can we preemptively use vaccine to reduce influenza hospitalizations below 2011-2012 levels – less than 150,000 hospitalizations? Perhaps, if we start by reducing pediatric influenza.
1. Aim to exceed 75% influenza vaccine uptake in your patients.
a. It is ambitious, but if there was ever a year that needed influenza herd immunity, it is 2020-2021.
2. Review practice/group/institution plans for vaccine purchase and ensure adequate personnel to administer vaccine.
3. Plan safe and efficient processes to vaccinate large numbers in August through November.
a. Consider that routine and influenza vaccines can be given concurrently with the annual uptick in school and sports physical examinations.
b. What social distancing and masking rules will be needed?
i. Will patients need to bring their own masks, or will you supply them?
c. What extra supplies and efforts are needed, e.g. hand sanitizer, new signage, 6-foot interval markings on floors or sidewalks, families calling from parking lot to announce their arrivals, etc.?
d. Remember younger patients need two doses before Dec 1, 2020.
e. Be creative, for example, are parking-lot tents for influenza vaccination feasible?
f. Can we partner with other providers to implement influenza vaccine–specific mass clinics?
Ramping up to give seasonal influenza vaccine in 2020 is daunting. But if we do not prepare, it will be even more difficult. Let’s make this the mildest influenza season in memory by vaccinating more than any time in memory – and by doing so, we can hope to blunt medical care burdens despite ongoing COVID-19 disease.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Kansas City (Mo.). Children’s Mercy receives funding from GlaxoSmithKline, Merck, and Pfizer for vaccine research studies on which Dr. Harrison is an investigator. Email him at [email protected].
References
1.. HCUP Statistical Brief #253. 2019 Oct.
2. medrxiv. 2020 Apr 10. doi: 10.1101/2020.04.07.20057299.
Learning the ICU
Although deployment of hospitalists into ICUs during the COVID-19 crisis varies widely, in that sense it reflects the pre-COVID hospital landscape of variable involvement, in which many hospitalists pressed into this role expressed discomfort practicing critical care beyond their scope of training, according to a survey published in the Journal of Hospital Medicine in 2018.1 “Hospitalists frequently deliver critical care services without adequate training or support, most prevalently in rural hospitals,” the authors concluded.
A Critical Care for the Hospitalist Series of resources and lectures developed by Eric Siegal, MD, a pulmonologist in Milwaukee, Wisc., and David Aymond, MD, a hospitalist in Alexandria, La., is available on the SHM website. They recommend that hospitalists trying to get oriented to working in the ICU start with the online courses on fluid resuscitation, mechanical ventilation, and noninvasive ventilation.
“Ninety-five percent of management of COVID-19 patients is nothing other than practicing sound critical care medicine,” Dr. Siegal said. “If you want to take effective care of sick COVID patients, you need to develop good foundational critical care skills and knowledge. Without them, you’re doing stuff without understand it.”
Dr. Aymond also encourages hospitalists to develop a stronger understanding of key physiological concepts by reviewing the critical care clinical topics compiled at SHM’s website.
References
1. Sweigart JR et al. Characterizing hospitalist practice and perceptions of critical care delivery. J Hosp Med. 2018 Jan;13(1):6-12.
Although deployment of hospitalists into ICUs during the COVID-19 crisis varies widely, in that sense it reflects the pre-COVID hospital landscape of variable involvement, in which many hospitalists pressed into this role expressed discomfort practicing critical care beyond their scope of training, according to a survey published in the Journal of Hospital Medicine in 2018.1 “Hospitalists frequently deliver critical care services without adequate training or support, most prevalently in rural hospitals,” the authors concluded.
A Critical Care for the Hospitalist Series of resources and lectures developed by Eric Siegal, MD, a pulmonologist in Milwaukee, Wisc., and David Aymond, MD, a hospitalist in Alexandria, La., is available on the SHM website. They recommend that hospitalists trying to get oriented to working in the ICU start with the online courses on fluid resuscitation, mechanical ventilation, and noninvasive ventilation.
“Ninety-five percent of management of COVID-19 patients is nothing other than practicing sound critical care medicine,” Dr. Siegal said. “If you want to take effective care of sick COVID patients, you need to develop good foundational critical care skills and knowledge. Without them, you’re doing stuff without understand it.”
Dr. Aymond also encourages hospitalists to develop a stronger understanding of key physiological concepts by reviewing the critical care clinical topics compiled at SHM’s website.
References
1. Sweigart JR et al. Characterizing hospitalist practice and perceptions of critical care delivery. J Hosp Med. 2018 Jan;13(1):6-12.
Although deployment of hospitalists into ICUs during the COVID-19 crisis varies widely, in that sense it reflects the pre-COVID hospital landscape of variable involvement, in which many hospitalists pressed into this role expressed discomfort practicing critical care beyond their scope of training, according to a survey published in the Journal of Hospital Medicine in 2018.1 “Hospitalists frequently deliver critical care services without adequate training or support, most prevalently in rural hospitals,” the authors concluded.
A Critical Care for the Hospitalist Series of resources and lectures developed by Eric Siegal, MD, a pulmonologist in Milwaukee, Wisc., and David Aymond, MD, a hospitalist in Alexandria, La., is available on the SHM website. They recommend that hospitalists trying to get oriented to working in the ICU start with the online courses on fluid resuscitation, mechanical ventilation, and noninvasive ventilation.
“Ninety-five percent of management of COVID-19 patients is nothing other than practicing sound critical care medicine,” Dr. Siegal said. “If you want to take effective care of sick COVID patients, you need to develop good foundational critical care skills and knowledge. Without them, you’re doing stuff without understand it.”
Dr. Aymond also encourages hospitalists to develop a stronger understanding of key physiological concepts by reviewing the critical care clinical topics compiled at SHM’s website.
References
1. Sweigart JR et al. Characterizing hospitalist practice and perceptions of critical care delivery. J Hosp Med. 2018 Jan;13(1):6-12.
Daily Recap: FDA revokes emergency use of hydroxychloroquine; Hardest hit specialties ranked in financial report
Here are the stories our MDedge editors across specialties think you need to know about today:
It’s official: COVID-19 is bad for your health care business
For the months of March and April 2020, use of medical professional services dropped by 65% and 68%, respectively, compared with last year, and estimated revenue fell by 45% and 48%, FAIR Health, a nonprofit organization that manages a database of 31 billion claim records, said in a new report.
Of the seven specialties included in the study, oral surgery was hit the hardest, followed by gastroenterology, cardiology, orthopedics, dermatology, adult primary care, and pediatric primary care, FAIR Health said.
“Even when medical practices have continued to function via telehealth, many have experienced lower reimbursements for telehealth visits than for in-person visits and more time educating patients on how to use the technology,” according to the report. Read more.
FDA revokes emergency use of hydroxychloroquine
The FDA revoked its decision from March 28 allowing use of hydroxychloroquine and chloroquine to treat people hospitalized with COVID-19 under an emergency use authorization (EUA).
"Based on its ongoing analysis of the EUA and emerging scientific data, the FDA determined that chloroquine and hydroxychloroquine are unlikely to be effective in treating COVID-19," the agency announced in a June 15 statement.
"In light of ongoing serious cardiac adverse events and other potential serious side effects, the known and potential benefits of chloroquine and hydroxychloroquine no longer outweigh the known and potential risks for the authorized use," noted the FDA. Read more.
Secondary infections common in COVID-19, implications unclear
Secondary respiratory infections appear to be highly prevalent among patients with severe COVID-19, but at this point, most physicians aren’t sure what to make of this understudied phenomenon.
“We really do not understand the implications of secondary infections on outcomes in COVID-19 patients,” David L. Bowton, MD, FCCP, said in an interview. “In most early reports the incidence of secondary infections was much higher in patients dying from COVID-19, compared to survivors, but it isn’t clear whether this indicates that the secondary infection itself led to excess mortality or was more a marker of the severity of the COVID-19 infection."
An early retrospective cohort study including 191 COVID-19 patients in Wuhan, China found that of the 54 who died in hospital, half had secondary bacterial lung infections (Lancet. 2020 Mar 28;395[10229]:1054-62). That comes as no surprise to U.S. physicians, who learned in training that many deaths during the so-called Spanish influenza epidemic were actually caused by secondary pneumonia involving Staphylococcus aureus, commented Daniel L. Ouellette, MD, FCCP. Read more.
Automated insulin delivery system ‘getting better and better’
Medtronic’s next-generation automated insulin delivery system offers significant improvements over the currently available model, particularly in young people with type 1 diabetes, new data suggest.
Data from three trials of such systems using Medtronic’s advanced hybrid closed-loop (AHCL) algorithm (trade name SmartGuard) were presented during the virtual American Diabetes Association (ADA) 80th Scientific Sessions.
Taken together, the data from the three trials showed that the AHCL-based system improved glycemic time-in-range with no increased risk for hypoglycemia, including in children and teenagers, with high patient-reported satisfaction.
“None of these devices is perfect, but they are a substantial improvement over what we’ve had ... They might make the quality of [patient] lives better. That’s really underappreciated,” session moderator Timothy S. Bailey, MD, commented. Read more.
Access more top news from the ADA virtual meeting.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
It’s official: COVID-19 is bad for your health care business
For the months of March and April 2020, use of medical professional services dropped by 65% and 68%, respectively, compared with last year, and estimated revenue fell by 45% and 48%, FAIR Health, a nonprofit organization that manages a database of 31 billion claim records, said in a new report.
Of the seven specialties included in the study, oral surgery was hit the hardest, followed by gastroenterology, cardiology, orthopedics, dermatology, adult primary care, and pediatric primary care, FAIR Health said.
“Even when medical practices have continued to function via telehealth, many have experienced lower reimbursements for telehealth visits than for in-person visits and more time educating patients on how to use the technology,” according to the report. Read more.
FDA revokes emergency use of hydroxychloroquine
The FDA revoked its decision from March 28 allowing use of hydroxychloroquine and chloroquine to treat people hospitalized with COVID-19 under an emergency use authorization (EUA).
"Based on its ongoing analysis of the EUA and emerging scientific data, the FDA determined that chloroquine and hydroxychloroquine are unlikely to be effective in treating COVID-19," the agency announced in a June 15 statement.
"In light of ongoing serious cardiac adverse events and other potential serious side effects, the known and potential benefits of chloroquine and hydroxychloroquine no longer outweigh the known and potential risks for the authorized use," noted the FDA. Read more.
Secondary infections common in COVID-19, implications unclear
Secondary respiratory infections appear to be highly prevalent among patients with severe COVID-19, but at this point, most physicians aren’t sure what to make of this understudied phenomenon.
“We really do not understand the implications of secondary infections on outcomes in COVID-19 patients,” David L. Bowton, MD, FCCP, said in an interview. “In most early reports the incidence of secondary infections was much higher in patients dying from COVID-19, compared to survivors, but it isn’t clear whether this indicates that the secondary infection itself led to excess mortality or was more a marker of the severity of the COVID-19 infection."
An early retrospective cohort study including 191 COVID-19 patients in Wuhan, China found that of the 54 who died in hospital, half had secondary bacterial lung infections (Lancet. 2020 Mar 28;395[10229]:1054-62). That comes as no surprise to U.S. physicians, who learned in training that many deaths during the so-called Spanish influenza epidemic were actually caused by secondary pneumonia involving Staphylococcus aureus, commented Daniel L. Ouellette, MD, FCCP. Read more.
Automated insulin delivery system ‘getting better and better’
Medtronic’s next-generation automated insulin delivery system offers significant improvements over the currently available model, particularly in young people with type 1 diabetes, new data suggest.
Data from three trials of such systems using Medtronic’s advanced hybrid closed-loop (AHCL) algorithm (trade name SmartGuard) were presented during the virtual American Diabetes Association (ADA) 80th Scientific Sessions.
Taken together, the data from the three trials showed that the AHCL-based system improved glycemic time-in-range with no increased risk for hypoglycemia, including in children and teenagers, with high patient-reported satisfaction.
“None of these devices is perfect, but they are a substantial improvement over what we’ve had ... They might make the quality of [patient] lives better. That’s really underappreciated,” session moderator Timothy S. Bailey, MD, commented. Read more.
Access more top news from the ADA virtual meeting.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
It’s official: COVID-19 is bad for your health care business
For the months of March and April 2020, use of medical professional services dropped by 65% and 68%, respectively, compared with last year, and estimated revenue fell by 45% and 48%, FAIR Health, a nonprofit organization that manages a database of 31 billion claim records, said in a new report.
Of the seven specialties included in the study, oral surgery was hit the hardest, followed by gastroenterology, cardiology, orthopedics, dermatology, adult primary care, and pediatric primary care, FAIR Health said.
“Even when medical practices have continued to function via telehealth, many have experienced lower reimbursements for telehealth visits than for in-person visits and more time educating patients on how to use the technology,” according to the report. Read more.
FDA revokes emergency use of hydroxychloroquine
The FDA revoked its decision from March 28 allowing use of hydroxychloroquine and chloroquine to treat people hospitalized with COVID-19 under an emergency use authorization (EUA).
"Based on its ongoing analysis of the EUA and emerging scientific data, the FDA determined that chloroquine and hydroxychloroquine are unlikely to be effective in treating COVID-19," the agency announced in a June 15 statement.
"In light of ongoing serious cardiac adverse events and other potential serious side effects, the known and potential benefits of chloroquine and hydroxychloroquine no longer outweigh the known and potential risks for the authorized use," noted the FDA. Read more.
Secondary infections common in COVID-19, implications unclear
Secondary respiratory infections appear to be highly prevalent among patients with severe COVID-19, but at this point, most physicians aren’t sure what to make of this understudied phenomenon.
“We really do not understand the implications of secondary infections on outcomes in COVID-19 patients,” David L. Bowton, MD, FCCP, said in an interview. “In most early reports the incidence of secondary infections was much higher in patients dying from COVID-19, compared to survivors, but it isn’t clear whether this indicates that the secondary infection itself led to excess mortality or was more a marker of the severity of the COVID-19 infection."
An early retrospective cohort study including 191 COVID-19 patients in Wuhan, China found that of the 54 who died in hospital, half had secondary bacterial lung infections (Lancet. 2020 Mar 28;395[10229]:1054-62). That comes as no surprise to U.S. physicians, who learned in training that many deaths during the so-called Spanish influenza epidemic were actually caused by secondary pneumonia involving Staphylococcus aureus, commented Daniel L. Ouellette, MD, FCCP. Read more.
Automated insulin delivery system ‘getting better and better’
Medtronic’s next-generation automated insulin delivery system offers significant improvements over the currently available model, particularly in young people with type 1 diabetes, new data suggest.
Data from three trials of such systems using Medtronic’s advanced hybrid closed-loop (AHCL) algorithm (trade name SmartGuard) were presented during the virtual American Diabetes Association (ADA) 80th Scientific Sessions.
Taken together, the data from the three trials showed that the AHCL-based system improved glycemic time-in-range with no increased risk for hypoglycemia, including in children and teenagers, with high patient-reported satisfaction.
“None of these devices is perfect, but they are a substantial improvement over what we’ve had ... They might make the quality of [patient] lives better. That’s really underappreciated,” session moderator Timothy S. Bailey, MD, commented. Read more.
Access more top news from the ADA virtual meeting.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
FDA approves Uplizna for treatment of anti-AQP4 antibody–positive NMOSD
The Food and Drug Administration has approved Uplizna (inebilizumab-cdon) for the treatment of adult patients with neuromyelitis optica spectrum disorder (NMOSD) who are anti-AQP4 antibody positive. Uplizna is the second approved treatment for the disorder.
Approval was based on results from the global, placebo-controlled N-MOmentum trial, which included 213 anti-AQP4 antibody–positive patients and 17 anti-AQP4 antibody–negative patients who received inebilizumab-cdon or placebo. Just under 90% of patients in the positive group remained relapse free 6 months after the initial dosing, compared with 58% of patients taking placebo. People who took inebilizumab also saw a reduction in NMOSD-related hospitalizations. There was no evidence of a benefit in patients who were anti-AQP4 antibody negative.
Inebilizumab-cdon was safe and well tolerated during the trial, with the most common adverse events being urinary tract infection (20%), nasopharyngitis (13%), infusion reaction (12%), arthralgia (11%), and headache (10%). The drug is approved as twice-yearly maintenance after initial dosing. The prescribing information for Uplizna includes a warning for infusion reactions, potential depletion of certain proteins (hypogammaglobulinemia), and potential increased risk of infection—including progressive multifocal leukoencephalopathy—and potential reactivation of hepatitis B and tuberculosis.
“NMOSD is an extremely challenging disease to treat. Patients experience unpredictable attacks that can lead to permanent disability from blindness and paralysis. In addition, each subsequent attack may result in a cumulative worsening of disability,” Bruce Cree, MD, PhD, lead investigator for the N-MOmentum trial and professor of clinical neurology at the University of California, San Francisco, said in a press release. “Uplizna is an important new treatment option that provides prescribing physicians and patients living with NMOSD a therapy with proven efficacy, a favorable safety profile and a twice-a-year maintenance dosing schedule.”
The Food and Drug Administration has approved Uplizna (inebilizumab-cdon) for the treatment of adult patients with neuromyelitis optica spectrum disorder (NMOSD) who are anti-AQP4 antibody positive. Uplizna is the second approved treatment for the disorder.
Approval was based on results from the global, placebo-controlled N-MOmentum trial, which included 213 anti-AQP4 antibody–positive patients and 17 anti-AQP4 antibody–negative patients who received inebilizumab-cdon or placebo. Just under 90% of patients in the positive group remained relapse free 6 months after the initial dosing, compared with 58% of patients taking placebo. People who took inebilizumab also saw a reduction in NMOSD-related hospitalizations. There was no evidence of a benefit in patients who were anti-AQP4 antibody negative.
Inebilizumab-cdon was safe and well tolerated during the trial, with the most common adverse events being urinary tract infection (20%), nasopharyngitis (13%), infusion reaction (12%), arthralgia (11%), and headache (10%). The drug is approved as twice-yearly maintenance after initial dosing. The prescribing information for Uplizna includes a warning for infusion reactions, potential depletion of certain proteins (hypogammaglobulinemia), and potential increased risk of infection—including progressive multifocal leukoencephalopathy—and potential reactivation of hepatitis B and tuberculosis.
“NMOSD is an extremely challenging disease to treat. Patients experience unpredictable attacks that can lead to permanent disability from blindness and paralysis. In addition, each subsequent attack may result in a cumulative worsening of disability,” Bruce Cree, MD, PhD, lead investigator for the N-MOmentum trial and professor of clinical neurology at the University of California, San Francisco, said in a press release. “Uplizna is an important new treatment option that provides prescribing physicians and patients living with NMOSD a therapy with proven efficacy, a favorable safety profile and a twice-a-year maintenance dosing schedule.”
The Food and Drug Administration has approved Uplizna (inebilizumab-cdon) for the treatment of adult patients with neuromyelitis optica spectrum disorder (NMOSD) who are anti-AQP4 antibody positive. Uplizna is the second approved treatment for the disorder.
Approval was based on results from the global, placebo-controlled N-MOmentum trial, which included 213 anti-AQP4 antibody–positive patients and 17 anti-AQP4 antibody–negative patients who received inebilizumab-cdon or placebo. Just under 90% of patients in the positive group remained relapse free 6 months after the initial dosing, compared with 58% of patients taking placebo. People who took inebilizumab also saw a reduction in NMOSD-related hospitalizations. There was no evidence of a benefit in patients who were anti-AQP4 antibody negative.
Inebilizumab-cdon was safe and well tolerated during the trial, with the most common adverse events being urinary tract infection (20%), nasopharyngitis (13%), infusion reaction (12%), arthralgia (11%), and headache (10%). The drug is approved as twice-yearly maintenance after initial dosing. The prescribing information for Uplizna includes a warning for infusion reactions, potential depletion of certain proteins (hypogammaglobulinemia), and potential increased risk of infection—including progressive multifocal leukoencephalopathy—and potential reactivation of hepatitis B and tuberculosis.
“NMOSD is an extremely challenging disease to treat. Patients experience unpredictable attacks that can lead to permanent disability from blindness and paralysis. In addition, each subsequent attack may result in a cumulative worsening of disability,” Bruce Cree, MD, PhD, lead investigator for the N-MOmentum trial and professor of clinical neurology at the University of California, San Francisco, said in a press release. “Uplizna is an important new treatment option that provides prescribing physicians and patients living with NMOSD a therapy with proven efficacy, a favorable safety profile and a twice-a-year maintenance dosing schedule.”
Renal denervation response similar regardless of CV risks, comorbidities
In a new analysis of international registry data, renal denervation resulted in similar reduced blood pressure levels in patients with varying high-risk comorbidities and across a range of cardiovascular risk scores.
At 3 years, 24-hour systolic BP was reduced by an average of –8.9 mm Hg overall, with slightly higher or lower readings seen in those with higher cardiovascular risk scores (–10.4 mm Hg) and 65 years or older (–10.2 mm Hg). Similar reductions were seen in those with resistant hypertension (–8.7 mm Hg), diabetes (–8.6 mm Hg), isolated systolic hypertension (–10.1 mm Hg), chronic kidney disease (–10.1 mm Hg), or atrial fibrillation (–10.0 mm Hg).
“In the largest international registry of its kind, the efficacy of renal denervation was similar in patients with and without baseline conditions associated with increased sympathetic activity and irrespective of ASCVD [atherosclerotic cardiovascular disease] risk,” first author Felix Mahfoud, MD, said in an interview.
Dr. Mahfoud, from University Hospital of Saarland, Homburg, Germany, and colleagues published their analysis in the Journal of the American College of Cardiology.
The article reported a post hoc analysis of data from the Global SYMPLICITY Registry (GSR), an international, Medtronic-funded effort that includes 2,652 patients with uncontrolled hypertension treated with a Symplicity denervation system. Data were obtained from 196 centers in 45 countries.
“Blood pressure reductions were durable and sustained to 3 years and the rates of new-onset, end-stage renal disease and elevation in serum creatinine levels were very low in patients at high and low [cardiovascular] risk,” reported Dr. Mahfoud.
As expected, adverse event rates were higher for patients with higher baseline cardiovascular risk. “Elevated rates were also seen in patients with [atrial fibrillation] and diabetes, identifying these subgroups who might derive even greater clinical benefit from improved BP control using renal denervation,” said Dr. Mahfoud.
Asked which patients might be optimal candidates for renal denervation, Dr. Mahfoud recommended the technology for “patients with uncontrolled hypertension on medication, patients with nonadherence, unwillingness, or intolerability to medication, and patients with combined systolic and diastolic hypertension.”
Analyses limited by incomplete data
Stephen C. Textor, MD, has concerns over the amount of missing data in the GSR database and its continued use as a repository of information on renal denervation.
“I am a bit lukewarm on this paper in part because of the nature of the registry data they’re using,” he added in an interview. “The problem I see is that the registry is not terribly uniform as to what information they collect on each patient, not terribly uniform in terms of how the procedure is performed, and not terribly uniform on how they follow up patients.”
Indeed, the post hoc subgroup analyses represent only a limited subset because of incomplete data, added Dr. Textor, a nephrologist at the Cleveland Clinic in Rochester, Minn.
“Remarkably, only 504 [patients] had “matched” data for office [systolic BP] levels at the time points defined in the report,” he wrote in an editorial comment accompanying the registry report (J Am Coll Cardiol. 2020 Jun 16;75[23]:2889-91).
Similarly, the researchers were able to calculate baseline atherosclerotic cardiovascular risk scores in only 1,485 patients (56% of total), primarily because of missing cholesterol measurements.
“They simply did these paired comparison that may have included a couple hundred cases, and on average, there were no differences in response, but what I would have liked to see is a multivariate analysis, where you have all the data on everybody and look at what are the factors that impact response?” Dr. Textor said in the interview.
“They really couldn’t do that because they just, they’re just too many holes in the data,” he added.
On the bright side, Dr. Textor noted that, while the impact overall on systolic BP was “modest,” the standard deviations in some cases were large, indicating that some people had large reductions of systolic BP of more than 30-40 mm Hg.
“There is a belief out there that there are some people that really benefit from this, but how to identify them has been the question,” Dr. Textor said.
Enthusiasm for renal denervation plummeted after results from the SYMPLICITY HTN-3 showed the procedure failing to meet its efficacy endpoint in resistant hypertension. The procedure was associated with a 14–mm Hg fall in systolic BP, compared with an 11–mm Hg drop in the “sham” control group (N Engl J Med. 2014 Apr 10;370:1393-401). However, post hoc analysis of the trial revealed significant shortcomings in design and execution.
No renal denervation device is approved in the United States. The Symplicity device used in this registry is approved in the European Union.
In early 2020, the Food and Drug Administration promised a rigorous review of new renal denervation trials. Subsequently, primary results from the SPYRAL HTN-OFF MED pivotal trial were presented at the annual meeting of the American College of Cardiology in March and showed promising efficacy.
SPYRAL HTN OFF-MED was designed in collaboration with the FDA to obtain meaningful evidence of whether renal denervation performed with the Symplicity Spyral multielectrode catheter (Medtronic Vascular) could reduce BP in patients not taking antihypertensive medication.
Dr. Mahfoud reported he has received speaking honoraria from Medtronic and ReCor. Two other authors are employees of Medtronic. Dr. Textor reported no relationships relevant to the contents of this paper. The Global SYMPLICITY Registry is funded by Medtronic Vascular.
SOURCE: Mahfoud F et al. J Am Coll Cardiol. 2020 June 16;75:2879-88.
This article was updated 6/16/20.
In a new analysis of international registry data, renal denervation resulted in similar reduced blood pressure levels in patients with varying high-risk comorbidities and across a range of cardiovascular risk scores.
At 3 years, 24-hour systolic BP was reduced by an average of –8.9 mm Hg overall, with slightly higher or lower readings seen in those with higher cardiovascular risk scores (–10.4 mm Hg) and 65 years or older (–10.2 mm Hg). Similar reductions were seen in those with resistant hypertension (–8.7 mm Hg), diabetes (–8.6 mm Hg), isolated systolic hypertension (–10.1 mm Hg), chronic kidney disease (–10.1 mm Hg), or atrial fibrillation (–10.0 mm Hg).
“In the largest international registry of its kind, the efficacy of renal denervation was similar in patients with and without baseline conditions associated with increased sympathetic activity and irrespective of ASCVD [atherosclerotic cardiovascular disease] risk,” first author Felix Mahfoud, MD, said in an interview.
Dr. Mahfoud, from University Hospital of Saarland, Homburg, Germany, and colleagues published their analysis in the Journal of the American College of Cardiology.
The article reported a post hoc analysis of data from the Global SYMPLICITY Registry (GSR), an international, Medtronic-funded effort that includes 2,652 patients with uncontrolled hypertension treated with a Symplicity denervation system. Data were obtained from 196 centers in 45 countries.
“Blood pressure reductions were durable and sustained to 3 years and the rates of new-onset, end-stage renal disease and elevation in serum creatinine levels were very low in patients at high and low [cardiovascular] risk,” reported Dr. Mahfoud.
As expected, adverse event rates were higher for patients with higher baseline cardiovascular risk. “Elevated rates were also seen in patients with [atrial fibrillation] and diabetes, identifying these subgroups who might derive even greater clinical benefit from improved BP control using renal denervation,” said Dr. Mahfoud.
Asked which patients might be optimal candidates for renal denervation, Dr. Mahfoud recommended the technology for “patients with uncontrolled hypertension on medication, patients with nonadherence, unwillingness, or intolerability to medication, and patients with combined systolic and diastolic hypertension.”
Analyses limited by incomplete data
Stephen C. Textor, MD, has concerns over the amount of missing data in the GSR database and its continued use as a repository of information on renal denervation.
“I am a bit lukewarm on this paper in part because of the nature of the registry data they’re using,” he added in an interview. “The problem I see is that the registry is not terribly uniform as to what information they collect on each patient, not terribly uniform in terms of how the procedure is performed, and not terribly uniform on how they follow up patients.”
Indeed, the post hoc subgroup analyses represent only a limited subset because of incomplete data, added Dr. Textor, a nephrologist at the Cleveland Clinic in Rochester, Minn.
“Remarkably, only 504 [patients] had “matched” data for office [systolic BP] levels at the time points defined in the report,” he wrote in an editorial comment accompanying the registry report (J Am Coll Cardiol. 2020 Jun 16;75[23]:2889-91).
Similarly, the researchers were able to calculate baseline atherosclerotic cardiovascular risk scores in only 1,485 patients (56% of total), primarily because of missing cholesterol measurements.
“They simply did these paired comparison that may have included a couple hundred cases, and on average, there were no differences in response, but what I would have liked to see is a multivariate analysis, where you have all the data on everybody and look at what are the factors that impact response?” Dr. Textor said in the interview.
“They really couldn’t do that because they just, they’re just too many holes in the data,” he added.
On the bright side, Dr. Textor noted that, while the impact overall on systolic BP was “modest,” the standard deviations in some cases were large, indicating that some people had large reductions of systolic BP of more than 30-40 mm Hg.
“There is a belief out there that there are some people that really benefit from this, but how to identify them has been the question,” Dr. Textor said.
Enthusiasm for renal denervation plummeted after results from the SYMPLICITY HTN-3 showed the procedure failing to meet its efficacy endpoint in resistant hypertension. The procedure was associated with a 14–mm Hg fall in systolic BP, compared with an 11–mm Hg drop in the “sham” control group (N Engl J Med. 2014 Apr 10;370:1393-401). However, post hoc analysis of the trial revealed significant shortcomings in design and execution.
No renal denervation device is approved in the United States. The Symplicity device used in this registry is approved in the European Union.
In early 2020, the Food and Drug Administration promised a rigorous review of new renal denervation trials. Subsequently, primary results from the SPYRAL HTN-OFF MED pivotal trial were presented at the annual meeting of the American College of Cardiology in March and showed promising efficacy.
SPYRAL HTN OFF-MED was designed in collaboration with the FDA to obtain meaningful evidence of whether renal denervation performed with the Symplicity Spyral multielectrode catheter (Medtronic Vascular) could reduce BP in patients not taking antihypertensive medication.
Dr. Mahfoud reported he has received speaking honoraria from Medtronic and ReCor. Two other authors are employees of Medtronic. Dr. Textor reported no relationships relevant to the contents of this paper. The Global SYMPLICITY Registry is funded by Medtronic Vascular.
SOURCE: Mahfoud F et al. J Am Coll Cardiol. 2020 June 16;75:2879-88.
This article was updated 6/16/20.
In a new analysis of international registry data, renal denervation resulted in similar reduced blood pressure levels in patients with varying high-risk comorbidities and across a range of cardiovascular risk scores.
At 3 years, 24-hour systolic BP was reduced by an average of –8.9 mm Hg overall, with slightly higher or lower readings seen in those with higher cardiovascular risk scores (–10.4 mm Hg) and 65 years or older (–10.2 mm Hg). Similar reductions were seen in those with resistant hypertension (–8.7 mm Hg), diabetes (–8.6 mm Hg), isolated systolic hypertension (–10.1 mm Hg), chronic kidney disease (–10.1 mm Hg), or atrial fibrillation (–10.0 mm Hg).
“In the largest international registry of its kind, the efficacy of renal denervation was similar in patients with and without baseline conditions associated with increased sympathetic activity and irrespective of ASCVD [atherosclerotic cardiovascular disease] risk,” first author Felix Mahfoud, MD, said in an interview.
Dr. Mahfoud, from University Hospital of Saarland, Homburg, Germany, and colleagues published their analysis in the Journal of the American College of Cardiology.
The article reported a post hoc analysis of data from the Global SYMPLICITY Registry (GSR), an international, Medtronic-funded effort that includes 2,652 patients with uncontrolled hypertension treated with a Symplicity denervation system. Data were obtained from 196 centers in 45 countries.
“Blood pressure reductions were durable and sustained to 3 years and the rates of new-onset, end-stage renal disease and elevation in serum creatinine levels were very low in patients at high and low [cardiovascular] risk,” reported Dr. Mahfoud.
As expected, adverse event rates were higher for patients with higher baseline cardiovascular risk. “Elevated rates were also seen in patients with [atrial fibrillation] and diabetes, identifying these subgroups who might derive even greater clinical benefit from improved BP control using renal denervation,” said Dr. Mahfoud.
Asked which patients might be optimal candidates for renal denervation, Dr. Mahfoud recommended the technology for “patients with uncontrolled hypertension on medication, patients with nonadherence, unwillingness, or intolerability to medication, and patients with combined systolic and diastolic hypertension.”
Analyses limited by incomplete data
Stephen C. Textor, MD, has concerns over the amount of missing data in the GSR database and its continued use as a repository of information on renal denervation.
“I am a bit lukewarm on this paper in part because of the nature of the registry data they’re using,” he added in an interview. “The problem I see is that the registry is not terribly uniform as to what information they collect on each patient, not terribly uniform in terms of how the procedure is performed, and not terribly uniform on how they follow up patients.”
Indeed, the post hoc subgroup analyses represent only a limited subset because of incomplete data, added Dr. Textor, a nephrologist at the Cleveland Clinic in Rochester, Minn.
“Remarkably, only 504 [patients] had “matched” data for office [systolic BP] levels at the time points defined in the report,” he wrote in an editorial comment accompanying the registry report (J Am Coll Cardiol. 2020 Jun 16;75[23]:2889-91).
Similarly, the researchers were able to calculate baseline atherosclerotic cardiovascular risk scores in only 1,485 patients (56% of total), primarily because of missing cholesterol measurements.
“They simply did these paired comparison that may have included a couple hundred cases, and on average, there were no differences in response, but what I would have liked to see is a multivariate analysis, where you have all the data on everybody and look at what are the factors that impact response?” Dr. Textor said in the interview.
“They really couldn’t do that because they just, they’re just too many holes in the data,” he added.
On the bright side, Dr. Textor noted that, while the impact overall on systolic BP was “modest,” the standard deviations in some cases were large, indicating that some people had large reductions of systolic BP of more than 30-40 mm Hg.
“There is a belief out there that there are some people that really benefit from this, but how to identify them has been the question,” Dr. Textor said.
Enthusiasm for renal denervation plummeted after results from the SYMPLICITY HTN-3 showed the procedure failing to meet its efficacy endpoint in resistant hypertension. The procedure was associated with a 14–mm Hg fall in systolic BP, compared with an 11–mm Hg drop in the “sham” control group (N Engl J Med. 2014 Apr 10;370:1393-401). However, post hoc analysis of the trial revealed significant shortcomings in design and execution.
No renal denervation device is approved in the United States. The Symplicity device used in this registry is approved in the European Union.
In early 2020, the Food and Drug Administration promised a rigorous review of new renal denervation trials. Subsequently, primary results from the SPYRAL HTN-OFF MED pivotal trial were presented at the annual meeting of the American College of Cardiology in March and showed promising efficacy.
SPYRAL HTN OFF-MED was designed in collaboration with the FDA to obtain meaningful evidence of whether renal denervation performed with the Symplicity Spyral multielectrode catheter (Medtronic Vascular) could reduce BP in patients not taking antihypertensive medication.
Dr. Mahfoud reported he has received speaking honoraria from Medtronic and ReCor. Two other authors are employees of Medtronic. Dr. Textor reported no relationships relevant to the contents of this paper. The Global SYMPLICITY Registry is funded by Medtronic Vascular.
SOURCE: Mahfoud F et al. J Am Coll Cardiol. 2020 June 16;75:2879-88.
This article was updated 6/16/20.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
For COVID-19 plus diabetes, glycemic control tops treatment list
Optimizing glycemic control “is the key to overall treatment in people with diabetes and COVID-19,” said Antonio Ceriello, MD, during a June 5 webinar sponsored by Harvard Medical School, Boston.
Dr. Ceriello, a research consultant with the Italian Ministry of Health, IRCCS Multi-Medica, Milan, highlighted a recent study that examined the association of blood glucose control and outcomes in COVID-19 patients with preexisting type 2 diabetes.
Among 7,000 cases of COVID-19, type 2 diabetes correlated with a higher death rate. However, those with well-controlled blood glucose (upper limit ≤10 mmol/L) had a survival rate of 98.9%, compared with just 11% among those with poorly controlled blood glucose (upper limit >10 mmol/L), a reduction in risk of 86% (adjusted hazard ratio, 0.14; Cell Metab. 2020 May 1. doi: 10.1016/j.cmet.2020.04.021).
Clinicians should also consider the possible side effects of hypoglycemic agents in the evolution of this disease. This is true of all patients, not just diabetes patients, Dr. Ceriello said. “We have data showing that ... hyperglycemia contributes directly to worsening the prognosis of COVID-19 independent of the presence of diabetes.”
One study found that the glycosylation of ACE-2 played an important role in allowing cellular entry of the virus (Am J Physiol Endocrinol Metab. 2020 Mar 31;318:E736-41). “This is something that could be related to hyperglycemia,” he added.
Another risk factor is thrombosis, a clear contributor to death rates in COVID-19. Research on thrombosis incidence in COVID-19 patients with diabetes reported higher levels of D-dimer levels in people with diabetes, especially among those who couldn’t manage their disease.
Tying all of these factors together, Dr. Ceriello discussed how ACE-2 glycosylation, in combination with other factors in SARS-CoV-2 infection, could lead to hyperglycemia, thrombosis, and subsequently multiorgan damage in diabetes patients.
Other research has associated higher HbA1c levels (mean HbA1c, 7.5%) with higher mortality risk in COVID-19 patients, said another speaker, Linong Ji, MD, director for endocrinology and metabolism at Peking University People’s Hospital, Beijing, and director of Peking University’s Diabetes Center. Proper guidance is key to ensuring early detection of hyperglycemic crisis in people with diabetes, advised Dr. Ji.
Global management of diabetes in SARS-CoV-2 patients is “quite challenging,” given that most patients don’t have their diabetes under control, said host and moderator A. Enrique Caballero, MD, an endocrinologist/investigator in the division of endocrinology, diabetes, and hypertension and division of global health equity at Brigham and Women’s Hospital, Boston. “They are not meeting treatment targets for cholesterol or glucose control. So we’re not managing optimal care. And now on top of this, we have COVID-19.”
Optimizing glycemic control “is the key to overall treatment in people with diabetes and COVID-19,” said Antonio Ceriello, MD, during a June 5 webinar sponsored by Harvard Medical School, Boston.
Dr. Ceriello, a research consultant with the Italian Ministry of Health, IRCCS Multi-Medica, Milan, highlighted a recent study that examined the association of blood glucose control and outcomes in COVID-19 patients with preexisting type 2 diabetes.
Among 7,000 cases of COVID-19, type 2 diabetes correlated with a higher death rate. However, those with well-controlled blood glucose (upper limit ≤10 mmol/L) had a survival rate of 98.9%, compared with just 11% among those with poorly controlled blood glucose (upper limit >10 mmol/L), a reduction in risk of 86% (adjusted hazard ratio, 0.14; Cell Metab. 2020 May 1. doi: 10.1016/j.cmet.2020.04.021).
Clinicians should also consider the possible side effects of hypoglycemic agents in the evolution of this disease. This is true of all patients, not just diabetes patients, Dr. Ceriello said. “We have data showing that ... hyperglycemia contributes directly to worsening the prognosis of COVID-19 independent of the presence of diabetes.”
One study found that the glycosylation of ACE-2 played an important role in allowing cellular entry of the virus (Am J Physiol Endocrinol Metab. 2020 Mar 31;318:E736-41). “This is something that could be related to hyperglycemia,” he added.
Another risk factor is thrombosis, a clear contributor to death rates in COVID-19. Research on thrombosis incidence in COVID-19 patients with diabetes reported higher levels of D-dimer levels in people with diabetes, especially among those who couldn’t manage their disease.
Tying all of these factors together, Dr. Ceriello discussed how ACE-2 glycosylation, in combination with other factors in SARS-CoV-2 infection, could lead to hyperglycemia, thrombosis, and subsequently multiorgan damage in diabetes patients.
Other research has associated higher HbA1c levels (mean HbA1c, 7.5%) with higher mortality risk in COVID-19 patients, said another speaker, Linong Ji, MD, director for endocrinology and metabolism at Peking University People’s Hospital, Beijing, and director of Peking University’s Diabetes Center. Proper guidance is key to ensuring early detection of hyperglycemic crisis in people with diabetes, advised Dr. Ji.
Global management of diabetes in SARS-CoV-2 patients is “quite challenging,” given that most patients don’t have their diabetes under control, said host and moderator A. Enrique Caballero, MD, an endocrinologist/investigator in the division of endocrinology, diabetes, and hypertension and division of global health equity at Brigham and Women’s Hospital, Boston. “They are not meeting treatment targets for cholesterol or glucose control. So we’re not managing optimal care. And now on top of this, we have COVID-19.”
Optimizing glycemic control “is the key to overall treatment in people with diabetes and COVID-19,” said Antonio Ceriello, MD, during a June 5 webinar sponsored by Harvard Medical School, Boston.
Dr. Ceriello, a research consultant with the Italian Ministry of Health, IRCCS Multi-Medica, Milan, highlighted a recent study that examined the association of blood glucose control and outcomes in COVID-19 patients with preexisting type 2 diabetes.
Among 7,000 cases of COVID-19, type 2 diabetes correlated with a higher death rate. However, those with well-controlled blood glucose (upper limit ≤10 mmol/L) had a survival rate of 98.9%, compared with just 11% among those with poorly controlled blood glucose (upper limit >10 mmol/L), a reduction in risk of 86% (adjusted hazard ratio, 0.14; Cell Metab. 2020 May 1. doi: 10.1016/j.cmet.2020.04.021).
Clinicians should also consider the possible side effects of hypoglycemic agents in the evolution of this disease. This is true of all patients, not just diabetes patients, Dr. Ceriello said. “We have data showing that ... hyperglycemia contributes directly to worsening the prognosis of COVID-19 independent of the presence of diabetes.”
One study found that the glycosylation of ACE-2 played an important role in allowing cellular entry of the virus (Am J Physiol Endocrinol Metab. 2020 Mar 31;318:E736-41). “This is something that could be related to hyperglycemia,” he added.
Another risk factor is thrombosis, a clear contributor to death rates in COVID-19. Research on thrombosis incidence in COVID-19 patients with diabetes reported higher levels of D-dimer levels in people with diabetes, especially among those who couldn’t manage their disease.
Tying all of these factors together, Dr. Ceriello discussed how ACE-2 glycosylation, in combination with other factors in SARS-CoV-2 infection, could lead to hyperglycemia, thrombosis, and subsequently multiorgan damage in diabetes patients.
Other research has associated higher HbA1c levels (mean HbA1c, 7.5%) with higher mortality risk in COVID-19 patients, said another speaker, Linong Ji, MD, director for endocrinology and metabolism at Peking University People’s Hospital, Beijing, and director of Peking University’s Diabetes Center. Proper guidance is key to ensuring early detection of hyperglycemic crisis in people with diabetes, advised Dr. Ji.
Global management of diabetes in SARS-CoV-2 patients is “quite challenging,” given that most patients don’t have their diabetes under control, said host and moderator A. Enrique Caballero, MD, an endocrinologist/investigator in the division of endocrinology, diabetes, and hypertension and division of global health equity at Brigham and Women’s Hospital, Boston. “They are not meeting treatment targets for cholesterol or glucose control. So we’re not managing optimal care. And now on top of this, we have COVID-19.”