User login
The revenge of the ‘late COVID adopters’
The COVID-19 pandemic has stressed all aspects of the world’s health care systems. The sheer volume of pandemic-related research produced over the past year has been challenging to process. This is as it should be, given its unprecedented spread and related morbidity and mortality. However, such rapid production and application leaves little time for proper vetting. Large numbers of providers adopted suggested, but largely unproven, practices that deviated from pre–COVID-19 guidelines. These “early adopters” theorized that COVID-19–related disease processes were different, necessitating a modification to existing practices.
Other equally prominent researchers countered this argument. Martin Tobin drew on physiology, while Arthur Slutsky and Niall Ferguson used emerging data to make their case. Tobin and colleagues cautioned against early intubation for anyone who could be maintained using noninvasive support. In August 2020 (well into the pandemic and after more data were available), Slutsky and colleagues argued that ARDS caused by COVID-19 wasn’t much different from lung injury due to other causes.
Two more recent studies published online recently are relevant to the debate over COVID-19 ARDS. One was a prospective study and the other a retrospective study; both had comparison groups, and both came to the same conclusions. Overall, COVID-19 ARDS isn’t much different from ARDS due to other causes. These studies were comprehensive in their comparisons and measures of outcomes, but they were both rather small and included patients from one and two hospitals, respectively. The discussions of both provide a nice review of the existing literature on COVID-19 ARDS.
A second controversial, but unproven, COVID-19 practice is aggressive anticoagulation. Early reports of a high prevalence of venous thromboembolism (VTE) in patients with COVID-19 pushed many to recommend empirically increasing prophylaxis. Most of the data guiding this approach were from retrospective, observational studies that suffered from selection bias. Early on, many of the studies were from China, where baseline VTE prophylaxis rates were low. Despite these limitations, many physicians acted on the basis of these data. An arbitrarily defined “intermediate” or treatment dose for prophylaxis was used, with some measuring D-dimer to guide their approach. An evidence-based argument against this practice, published in the New England Journal of Medicine, failed to sway readers. (Look at the poll at the end of the article and you’ll see how readers answered.)
Two articles recently published online in CHEST attempted to bring clarity to the debate over COVID-19 and VTE prophylaxis. The first study evaluated critically ill patients in France, and researchers found that higher doses of anticoagulation reduced thrombotic complications without an associated increase in bleeding events. The study is well done but certainly has its flaws. It is observational and retrospective, and it essentially uses a before-after comparison technique. Such an approach is particularly prone to bias during COVID-19, given that practice patterns change quickly.
The second paper is a systematic review looking at VTE and bleeding rates among patients hospitalized with COVID-19. The authors found high rates of VTE (17.0% overall), with screening, admission to the ICU, and the prospective study design all being associated with increased rates. Of importance, unlike the retrospective trial cited in the previous paragraph, the authors of the systematic review found treatment-dose anticoagulation was associated with higher bleeding rates.
I admit, the title of this piece is a bit of a misnomer. The “late adopters” would truly have their revenge if deviation from guidelines for COVID-19–related ARDS and VTE prophylaxis proves to be harmful. It’s not clear that’s the case, and at least for VTE prophylaxis, results from several randomized, controlled trials (REMAP-CAP, ATTACC, and ACTIV-4a) will be released soon. These are sure to provide more definitive answers. If nothing else, the COVID-19–related ARDS and VTE data reinforce how difficult it is to obtain high-quality data that yield clear results. Until something more definitive is published and released, I will remain a “late adopter.” Standard non–COVID-19 guidelines for ARDS and VTE prophylaxis are good enough for me.
Dr. Holley is program director of the Pulmonary and Critical Care Medical Fellowship at Walter Reed National Military Medical Center, Bethesda, Md.
A version of this article first appeared on Medscape.com.
The COVID-19 pandemic has stressed all aspects of the world’s health care systems. The sheer volume of pandemic-related research produced over the past year has been challenging to process. This is as it should be, given its unprecedented spread and related morbidity and mortality. However, such rapid production and application leaves little time for proper vetting. Large numbers of providers adopted suggested, but largely unproven, practices that deviated from pre–COVID-19 guidelines. These “early adopters” theorized that COVID-19–related disease processes were different, necessitating a modification to existing practices.
Other equally prominent researchers countered this argument. Martin Tobin drew on physiology, while Arthur Slutsky and Niall Ferguson used emerging data to make their case. Tobin and colleagues cautioned against early intubation for anyone who could be maintained using noninvasive support. In August 2020 (well into the pandemic and after more data were available), Slutsky and colleagues argued that ARDS caused by COVID-19 wasn’t much different from lung injury due to other causes.
Two more recent studies published online recently are relevant to the debate over COVID-19 ARDS. One was a prospective study and the other a retrospective study; both had comparison groups, and both came to the same conclusions. Overall, COVID-19 ARDS isn’t much different from ARDS due to other causes. These studies were comprehensive in their comparisons and measures of outcomes, but they were both rather small and included patients from one and two hospitals, respectively. The discussions of both provide a nice review of the existing literature on COVID-19 ARDS.
A second controversial, but unproven, COVID-19 practice is aggressive anticoagulation. Early reports of a high prevalence of venous thromboembolism (VTE) in patients with COVID-19 pushed many to recommend empirically increasing prophylaxis. Most of the data guiding this approach were from retrospective, observational studies that suffered from selection bias. Early on, many of the studies were from China, where baseline VTE prophylaxis rates were low. Despite these limitations, many physicians acted on the basis of these data. An arbitrarily defined “intermediate” or treatment dose for prophylaxis was used, with some measuring D-dimer to guide their approach. An evidence-based argument against this practice, published in the New England Journal of Medicine, failed to sway readers. (Look at the poll at the end of the article and you’ll see how readers answered.)
Two articles recently published online in CHEST attempted to bring clarity to the debate over COVID-19 and VTE prophylaxis. The first study evaluated critically ill patients in France, and researchers found that higher doses of anticoagulation reduced thrombotic complications without an associated increase in bleeding events. The study is well done but certainly has its flaws. It is observational and retrospective, and it essentially uses a before-after comparison technique. Such an approach is particularly prone to bias during COVID-19, given that practice patterns change quickly.
The second paper is a systematic review looking at VTE and bleeding rates among patients hospitalized with COVID-19. The authors found high rates of VTE (17.0% overall), with screening, admission to the ICU, and the prospective study design all being associated with increased rates. Of importance, unlike the retrospective trial cited in the previous paragraph, the authors of the systematic review found treatment-dose anticoagulation was associated with higher bleeding rates.
I admit, the title of this piece is a bit of a misnomer. The “late adopters” would truly have their revenge if deviation from guidelines for COVID-19–related ARDS and VTE prophylaxis proves to be harmful. It’s not clear that’s the case, and at least for VTE prophylaxis, results from several randomized, controlled trials (REMAP-CAP, ATTACC, and ACTIV-4a) will be released soon. These are sure to provide more definitive answers. If nothing else, the COVID-19–related ARDS and VTE data reinforce how difficult it is to obtain high-quality data that yield clear results. Until something more definitive is published and released, I will remain a “late adopter.” Standard non–COVID-19 guidelines for ARDS and VTE prophylaxis are good enough for me.
Dr. Holley is program director of the Pulmonary and Critical Care Medical Fellowship at Walter Reed National Military Medical Center, Bethesda, Md.
A version of this article first appeared on Medscape.com.
The COVID-19 pandemic has stressed all aspects of the world’s health care systems. The sheer volume of pandemic-related research produced over the past year has been challenging to process. This is as it should be, given its unprecedented spread and related morbidity and mortality. However, such rapid production and application leaves little time for proper vetting. Large numbers of providers adopted suggested, but largely unproven, practices that deviated from pre–COVID-19 guidelines. These “early adopters” theorized that COVID-19–related disease processes were different, necessitating a modification to existing practices.
Other equally prominent researchers countered this argument. Martin Tobin drew on physiology, while Arthur Slutsky and Niall Ferguson used emerging data to make their case. Tobin and colleagues cautioned against early intubation for anyone who could be maintained using noninvasive support. In August 2020 (well into the pandemic and after more data were available), Slutsky and colleagues argued that ARDS caused by COVID-19 wasn’t much different from lung injury due to other causes.
Two more recent studies published online recently are relevant to the debate over COVID-19 ARDS. One was a prospective study and the other a retrospective study; both had comparison groups, and both came to the same conclusions. Overall, COVID-19 ARDS isn’t much different from ARDS due to other causes. These studies were comprehensive in their comparisons and measures of outcomes, but they were both rather small and included patients from one and two hospitals, respectively. The discussions of both provide a nice review of the existing literature on COVID-19 ARDS.
A second controversial, but unproven, COVID-19 practice is aggressive anticoagulation. Early reports of a high prevalence of venous thromboembolism (VTE) in patients with COVID-19 pushed many to recommend empirically increasing prophylaxis. Most of the data guiding this approach were from retrospective, observational studies that suffered from selection bias. Early on, many of the studies were from China, where baseline VTE prophylaxis rates were low. Despite these limitations, many physicians acted on the basis of these data. An arbitrarily defined “intermediate” or treatment dose for prophylaxis was used, with some measuring D-dimer to guide their approach. An evidence-based argument against this practice, published in the New England Journal of Medicine, failed to sway readers. (Look at the poll at the end of the article and you’ll see how readers answered.)
Two articles recently published online in CHEST attempted to bring clarity to the debate over COVID-19 and VTE prophylaxis. The first study evaluated critically ill patients in France, and researchers found that higher doses of anticoagulation reduced thrombotic complications without an associated increase in bleeding events. The study is well done but certainly has its flaws. It is observational and retrospective, and it essentially uses a before-after comparison technique. Such an approach is particularly prone to bias during COVID-19, given that practice patterns change quickly.
The second paper is a systematic review looking at VTE and bleeding rates among patients hospitalized with COVID-19. The authors found high rates of VTE (17.0% overall), with screening, admission to the ICU, and the prospective study design all being associated with increased rates. Of importance, unlike the retrospective trial cited in the previous paragraph, the authors of the systematic review found treatment-dose anticoagulation was associated with higher bleeding rates.
I admit, the title of this piece is a bit of a misnomer. The “late adopters” would truly have their revenge if deviation from guidelines for COVID-19–related ARDS and VTE prophylaxis proves to be harmful. It’s not clear that’s the case, and at least for VTE prophylaxis, results from several randomized, controlled trials (REMAP-CAP, ATTACC, and ACTIV-4a) will be released soon. These are sure to provide more definitive answers. If nothing else, the COVID-19–related ARDS and VTE data reinforce how difficult it is to obtain high-quality data that yield clear results. Until something more definitive is published and released, I will remain a “late adopter.” Standard non–COVID-19 guidelines for ARDS and VTE prophylaxis are good enough for me.
Dr. Holley is program director of the Pulmonary and Critical Care Medical Fellowship at Walter Reed National Military Medical Center, Bethesda, Md.
A version of this article first appeared on Medscape.com.
Time is of the essence: DST up for debate again
Seasonal time change is now up for consideration in the U.S. Congress, prompting sleep medicine specialists to weigh in on the health impact of a major policy change.
As lawmakers in Washington propose an end to seasonal time changes by permanently establishing daylight saving time (DST), the American Academy of Sleep Medicine (AASM) is pushing for a Congressional hearing so scientists can present evidence in favor of converse legislation – to make standard time the new norm.
According to the AASM, ; however, the switch from standard time to DST incurs more risk.
“Current evidence best supports the adoption of year-round standard time, which aligns best with human circadian biology and provides distinct benefits for public health and safety,” the AASM noted in a 2020 position statement on DST.
The statement cites a number of studies that have reported associations between the switch to DST and acute, negative health outcomes, including higher rates of hospital admission, cardiovascular morbidity, atrial fibrillation, and stroke. The time shift has been associated with a spectrum of cellular, metabolic, and circadian derangements, from increased production of inflammatory markers, to higher blood pressure, and loss of sleep. These biological effects may have far-reaching consequences, including increased rates of fatal motor accidents in the days following the time change, and even increased volatility in the stock market, which may stem from cognitive deficits.
U.S. Senator Marco Rubio (R-Fla.) and others in the U.S. Congress have reintroduced the 2019 Sunshine Protection Act, legislation that would make DST permanent across the country. According to a statement on Sen. Rubio’s website, “The bill reflects the Florida legislature’s 2018 enactment of year-round DST; however, for Florida’s change to apply, a change in the federal statute is required. Fifteen other states – Arkansas, Alabama, California, Delaware, Georgia, Idaho, Louisiana, Maine, Ohio, Oregon, South Carolina, Tennessee, Utah, Washington, and Wyoming – have passed similar laws, resolutions, or voter initiatives, and dozens more are looking. The legislation, if enacted, would apply to those states [that] currently participate in DST, which most states observe for eight months out of the year.”
A stitch in time
“The sudden change in clock time disrupts sleep/wake patterns, decreasing total sleep time and sleep quality, leading to decrements in daytime cognition,” said Kannan Ramar, MBBS, MD, president of the AASM and a sleep medicine specialist at Mayo Clinic, Rochester, Minn.
Emphasizing this point, Dr. Ramar noted a recent study that reported an 18% increase in “patient safety-related incidents associated with human error” among health care workers within a week of the spring time change.
“Irregular bedtimes and wake times disrupt the timing of our circadian rhythms, which can lead to symptoms of insomnia or long-term, excessive daytime sleepiness. Lack of sleep can lead to numerous adverse effects on our minds, including decreased cognitive function, trouble concentrating, and general moodiness,” Dr. Ramar said.
He noted that these impacts may be more significant among certain individuals.
“The daylight saving time changes can be especially problematic for any populations that already experience chronic insufficient sleep or other sleep difficulties,” Dr. Ramar said. “Populations at greatest risk include teenagers, who tend to experience chronic sleep restriction during the school week, and night shift workers, who often struggle to sleep well during daytime hours.”
While fewer studies have evaluated the long-term effects of seasonal time changes, the AASM position statement cited evidence that “the body clock does not adjust to daylight saving time after several months,” possibly because “daylight saving time is less well-aligned with intrinsic human circadian physiology, and it disrupts the natural seasonal adjustment of the human clock due to the effect of late-evening light on the circadian rhythm.”
According to the AASM, permanent DST, as proposed by Sen. Rubio and colleagues, could “result in permanent phase delay, a condition that can also lead to a perpetual discrepancy between the innate biological clock and the extrinsic environmental clock, as well as chronic sleep loss due to early morning social demands that truncate the opportunity to sleep.” This mismatch between sleep/wake cycles and social demands, known as “social jet lag,” has been associated with chronic health risks, including metabolic syndrome, obesity, depression, and cardiovascular disease.
Cardiac impacts of seasonal time change
Muhammad Adeel Rishi, MD, a sleep specialist at Mayo Clinic, Eau Claire, Wis., and lead author of the AASM position statement, highlighted cardiovascular risks in a written statement for this article, noting increased rates of heart attack following the spring time change, and a higher risk of atrial fibrillation.
“Mayo Clinic has not taken a position on this issue,” Dr. Rishi noted. Still, he advocated for permanent standard time as the author of the AASM position statement and vice chair of the AASM public safety committee.
Jay Chudow, MD, and Andrew K. Krumerman, MD, of Montefiore Medical Center, New York, lead author and principal author, respectively, of a recent study that reported increased rates of atrial fibrillation admissions after DST transitions, had the same stance.
“We support elimination of seasonal time changes from a health perspective,” they wrote in a joint comment. “There is mounting evidence of a negative health impact with these seasonal time changes related to effects on sleep and circadian rhythm. Our work found the spring change was associated with more admissions for atrial fibrillation. This added to prior evidence of increased cardiovascular events related to these time changes. If physicians counsel patients on reducing risk factors for disease, shouldn’t we do the same as a society?”
Pros and cons
Not all sleep experts are convinced. Mary Jo Farmer, MD, PhD, FCCP, a sleep specialist and director of pulmonary hypertension services at Baystate Medical Center, and assistant professor of medicine at the University of Massachusetts, Springfield, considers perspectives from both sides of the issue.
“Daylight saving time promotes active lifestyles as people engage in more outdoor activities after work and school, [and] daylight saving time produces economic and safety benefits to society as retail revenues are higher and crimes are lower,” Dr. Farmer said. “Alternatively, moving the clocks forward is a cost burden to the U.S. economy when health issues, decreased productivity, and workplace injuries are considered.”
If one time system is permanently established, Dr. Farmer anticipates divided opinions from patients with sleep issues, regardless of which system is chosen.
“I can tell you, I have a cohort of sleep patients who prefer more evening light and look forward to the spring time change to daylight saving time,” she said. “However, they would not want the sun coming up at 9:00 a.m. in the winter months if we stayed on daylight saving time year-round. Similarly, patients would not want the sun coming up at 4:00 a.m. on the longest day of the year if we stayed on standard time all year round.”
Dr. Farmer called for more research before a decision is made.
“I suggest we need more information about the dangers of staying on daylight saving or standard time year-round because perhaps the current strategy of keeping morning light consistent is not so bad,” she said.
Time for a Congressional hearing?
According to Dr. Ramar, the time is now for a Congressional hearing, as lawmakers and the public need to be adequately informed when considering new legislation.
“There are public misconceptions about daylight saving time and standard time,” Dr. Ramar said. “People often like the idea of daylight saving time because they think it provides more light, and they dislike the concept of standard time because they think it provides more darkness. The reality is that neither time system provides more light or darkness than the other; it is only the timing that changes.”
Until new legislation is introduced, Dr. Ramar offered some practical advice for navigating seasonal time shifts.
“Beginning 2-3 days before the time change, it can be helpful to gradually adjust sleep and wake times, as well as other daily routines such as meal times,” he said. “After the time change, going outside for some morning light can help adjust the timing of your internal body clock.”
The investigators reported no conflicts of interest.
Seasonal time change is now up for consideration in the U.S. Congress, prompting sleep medicine specialists to weigh in on the health impact of a major policy change.
As lawmakers in Washington propose an end to seasonal time changes by permanently establishing daylight saving time (DST), the American Academy of Sleep Medicine (AASM) is pushing for a Congressional hearing so scientists can present evidence in favor of converse legislation – to make standard time the new norm.
According to the AASM, ; however, the switch from standard time to DST incurs more risk.
“Current evidence best supports the adoption of year-round standard time, which aligns best with human circadian biology and provides distinct benefits for public health and safety,” the AASM noted in a 2020 position statement on DST.
The statement cites a number of studies that have reported associations between the switch to DST and acute, negative health outcomes, including higher rates of hospital admission, cardiovascular morbidity, atrial fibrillation, and stroke. The time shift has been associated with a spectrum of cellular, metabolic, and circadian derangements, from increased production of inflammatory markers, to higher blood pressure, and loss of sleep. These biological effects may have far-reaching consequences, including increased rates of fatal motor accidents in the days following the time change, and even increased volatility in the stock market, which may stem from cognitive deficits.
U.S. Senator Marco Rubio (R-Fla.) and others in the U.S. Congress have reintroduced the 2019 Sunshine Protection Act, legislation that would make DST permanent across the country. According to a statement on Sen. Rubio’s website, “The bill reflects the Florida legislature’s 2018 enactment of year-round DST; however, for Florida’s change to apply, a change in the federal statute is required. Fifteen other states – Arkansas, Alabama, California, Delaware, Georgia, Idaho, Louisiana, Maine, Ohio, Oregon, South Carolina, Tennessee, Utah, Washington, and Wyoming – have passed similar laws, resolutions, or voter initiatives, and dozens more are looking. The legislation, if enacted, would apply to those states [that] currently participate in DST, which most states observe for eight months out of the year.”
A stitch in time
“The sudden change in clock time disrupts sleep/wake patterns, decreasing total sleep time and sleep quality, leading to decrements in daytime cognition,” said Kannan Ramar, MBBS, MD, president of the AASM and a sleep medicine specialist at Mayo Clinic, Rochester, Minn.
Emphasizing this point, Dr. Ramar noted a recent study that reported an 18% increase in “patient safety-related incidents associated with human error” among health care workers within a week of the spring time change.
“Irregular bedtimes and wake times disrupt the timing of our circadian rhythms, which can lead to symptoms of insomnia or long-term, excessive daytime sleepiness. Lack of sleep can lead to numerous adverse effects on our minds, including decreased cognitive function, trouble concentrating, and general moodiness,” Dr. Ramar said.
He noted that these impacts may be more significant among certain individuals.
“The daylight saving time changes can be especially problematic for any populations that already experience chronic insufficient sleep or other sleep difficulties,” Dr. Ramar said. “Populations at greatest risk include teenagers, who tend to experience chronic sleep restriction during the school week, and night shift workers, who often struggle to sleep well during daytime hours.”
While fewer studies have evaluated the long-term effects of seasonal time changes, the AASM position statement cited evidence that “the body clock does not adjust to daylight saving time after several months,” possibly because “daylight saving time is less well-aligned with intrinsic human circadian physiology, and it disrupts the natural seasonal adjustment of the human clock due to the effect of late-evening light on the circadian rhythm.”
According to the AASM, permanent DST, as proposed by Sen. Rubio and colleagues, could “result in permanent phase delay, a condition that can also lead to a perpetual discrepancy between the innate biological clock and the extrinsic environmental clock, as well as chronic sleep loss due to early morning social demands that truncate the opportunity to sleep.” This mismatch between sleep/wake cycles and social demands, known as “social jet lag,” has been associated with chronic health risks, including metabolic syndrome, obesity, depression, and cardiovascular disease.
Cardiac impacts of seasonal time change
Muhammad Adeel Rishi, MD, a sleep specialist at Mayo Clinic, Eau Claire, Wis., and lead author of the AASM position statement, highlighted cardiovascular risks in a written statement for this article, noting increased rates of heart attack following the spring time change, and a higher risk of atrial fibrillation.
“Mayo Clinic has not taken a position on this issue,” Dr. Rishi noted. Still, he advocated for permanent standard time as the author of the AASM position statement and vice chair of the AASM public safety committee.
Jay Chudow, MD, and Andrew K. Krumerman, MD, of Montefiore Medical Center, New York, lead author and principal author, respectively, of a recent study that reported increased rates of atrial fibrillation admissions after DST transitions, had the same stance.
“We support elimination of seasonal time changes from a health perspective,” they wrote in a joint comment. “There is mounting evidence of a negative health impact with these seasonal time changes related to effects on sleep and circadian rhythm. Our work found the spring change was associated with more admissions for atrial fibrillation. This added to prior evidence of increased cardiovascular events related to these time changes. If physicians counsel patients on reducing risk factors for disease, shouldn’t we do the same as a society?”
Pros and cons
Not all sleep experts are convinced. Mary Jo Farmer, MD, PhD, FCCP, a sleep specialist and director of pulmonary hypertension services at Baystate Medical Center, and assistant professor of medicine at the University of Massachusetts, Springfield, considers perspectives from both sides of the issue.
“Daylight saving time promotes active lifestyles as people engage in more outdoor activities after work and school, [and] daylight saving time produces economic and safety benefits to society as retail revenues are higher and crimes are lower,” Dr. Farmer said. “Alternatively, moving the clocks forward is a cost burden to the U.S. economy when health issues, decreased productivity, and workplace injuries are considered.”
If one time system is permanently established, Dr. Farmer anticipates divided opinions from patients with sleep issues, regardless of which system is chosen.
“I can tell you, I have a cohort of sleep patients who prefer more evening light and look forward to the spring time change to daylight saving time,” she said. “However, they would not want the sun coming up at 9:00 a.m. in the winter months if we stayed on daylight saving time year-round. Similarly, patients would not want the sun coming up at 4:00 a.m. on the longest day of the year if we stayed on standard time all year round.”
Dr. Farmer called for more research before a decision is made.
“I suggest we need more information about the dangers of staying on daylight saving or standard time year-round because perhaps the current strategy of keeping morning light consistent is not so bad,” she said.
Time for a Congressional hearing?
According to Dr. Ramar, the time is now for a Congressional hearing, as lawmakers and the public need to be adequately informed when considering new legislation.
“There are public misconceptions about daylight saving time and standard time,” Dr. Ramar said. “People often like the idea of daylight saving time because they think it provides more light, and they dislike the concept of standard time because they think it provides more darkness. The reality is that neither time system provides more light or darkness than the other; it is only the timing that changes.”
Until new legislation is introduced, Dr. Ramar offered some practical advice for navigating seasonal time shifts.
“Beginning 2-3 days before the time change, it can be helpful to gradually adjust sleep and wake times, as well as other daily routines such as meal times,” he said. “After the time change, going outside for some morning light can help adjust the timing of your internal body clock.”
The investigators reported no conflicts of interest.
Seasonal time change is now up for consideration in the U.S. Congress, prompting sleep medicine specialists to weigh in on the health impact of a major policy change.
As lawmakers in Washington propose an end to seasonal time changes by permanently establishing daylight saving time (DST), the American Academy of Sleep Medicine (AASM) is pushing for a Congressional hearing so scientists can present evidence in favor of converse legislation – to make standard time the new norm.
According to the AASM, ; however, the switch from standard time to DST incurs more risk.
“Current evidence best supports the adoption of year-round standard time, which aligns best with human circadian biology and provides distinct benefits for public health and safety,” the AASM noted in a 2020 position statement on DST.
The statement cites a number of studies that have reported associations between the switch to DST and acute, negative health outcomes, including higher rates of hospital admission, cardiovascular morbidity, atrial fibrillation, and stroke. The time shift has been associated with a spectrum of cellular, metabolic, and circadian derangements, from increased production of inflammatory markers, to higher blood pressure, and loss of sleep. These biological effects may have far-reaching consequences, including increased rates of fatal motor accidents in the days following the time change, and even increased volatility in the stock market, which may stem from cognitive deficits.
U.S. Senator Marco Rubio (R-Fla.) and others in the U.S. Congress have reintroduced the 2019 Sunshine Protection Act, legislation that would make DST permanent across the country. According to a statement on Sen. Rubio’s website, “The bill reflects the Florida legislature’s 2018 enactment of year-round DST; however, for Florida’s change to apply, a change in the federal statute is required. Fifteen other states – Arkansas, Alabama, California, Delaware, Georgia, Idaho, Louisiana, Maine, Ohio, Oregon, South Carolina, Tennessee, Utah, Washington, and Wyoming – have passed similar laws, resolutions, or voter initiatives, and dozens more are looking. The legislation, if enacted, would apply to those states [that] currently participate in DST, which most states observe for eight months out of the year.”
A stitch in time
“The sudden change in clock time disrupts sleep/wake patterns, decreasing total sleep time and sleep quality, leading to decrements in daytime cognition,” said Kannan Ramar, MBBS, MD, president of the AASM and a sleep medicine specialist at Mayo Clinic, Rochester, Minn.
Emphasizing this point, Dr. Ramar noted a recent study that reported an 18% increase in “patient safety-related incidents associated with human error” among health care workers within a week of the spring time change.
“Irregular bedtimes and wake times disrupt the timing of our circadian rhythms, which can lead to symptoms of insomnia or long-term, excessive daytime sleepiness. Lack of sleep can lead to numerous adverse effects on our minds, including decreased cognitive function, trouble concentrating, and general moodiness,” Dr. Ramar said.
He noted that these impacts may be more significant among certain individuals.
“The daylight saving time changes can be especially problematic for any populations that already experience chronic insufficient sleep or other sleep difficulties,” Dr. Ramar said. “Populations at greatest risk include teenagers, who tend to experience chronic sleep restriction during the school week, and night shift workers, who often struggle to sleep well during daytime hours.”
While fewer studies have evaluated the long-term effects of seasonal time changes, the AASM position statement cited evidence that “the body clock does not adjust to daylight saving time after several months,” possibly because “daylight saving time is less well-aligned with intrinsic human circadian physiology, and it disrupts the natural seasonal adjustment of the human clock due to the effect of late-evening light on the circadian rhythm.”
According to the AASM, permanent DST, as proposed by Sen. Rubio and colleagues, could “result in permanent phase delay, a condition that can also lead to a perpetual discrepancy between the innate biological clock and the extrinsic environmental clock, as well as chronic sleep loss due to early morning social demands that truncate the opportunity to sleep.” This mismatch between sleep/wake cycles and social demands, known as “social jet lag,” has been associated with chronic health risks, including metabolic syndrome, obesity, depression, and cardiovascular disease.
Cardiac impacts of seasonal time change
Muhammad Adeel Rishi, MD, a sleep specialist at Mayo Clinic, Eau Claire, Wis., and lead author of the AASM position statement, highlighted cardiovascular risks in a written statement for this article, noting increased rates of heart attack following the spring time change, and a higher risk of atrial fibrillation.
“Mayo Clinic has not taken a position on this issue,” Dr. Rishi noted. Still, he advocated for permanent standard time as the author of the AASM position statement and vice chair of the AASM public safety committee.
Jay Chudow, MD, and Andrew K. Krumerman, MD, of Montefiore Medical Center, New York, lead author and principal author, respectively, of a recent study that reported increased rates of atrial fibrillation admissions after DST transitions, had the same stance.
“We support elimination of seasonal time changes from a health perspective,” they wrote in a joint comment. “There is mounting evidence of a negative health impact with these seasonal time changes related to effects on sleep and circadian rhythm. Our work found the spring change was associated with more admissions for atrial fibrillation. This added to prior evidence of increased cardiovascular events related to these time changes. If physicians counsel patients on reducing risk factors for disease, shouldn’t we do the same as a society?”
Pros and cons
Not all sleep experts are convinced. Mary Jo Farmer, MD, PhD, FCCP, a sleep specialist and director of pulmonary hypertension services at Baystate Medical Center, and assistant professor of medicine at the University of Massachusetts, Springfield, considers perspectives from both sides of the issue.
“Daylight saving time promotes active lifestyles as people engage in more outdoor activities after work and school, [and] daylight saving time produces economic and safety benefits to society as retail revenues are higher and crimes are lower,” Dr. Farmer said. “Alternatively, moving the clocks forward is a cost burden to the U.S. economy when health issues, decreased productivity, and workplace injuries are considered.”
If one time system is permanently established, Dr. Farmer anticipates divided opinions from patients with sleep issues, regardless of which system is chosen.
“I can tell you, I have a cohort of sleep patients who prefer more evening light and look forward to the spring time change to daylight saving time,” she said. “However, they would not want the sun coming up at 9:00 a.m. in the winter months if we stayed on daylight saving time year-round. Similarly, patients would not want the sun coming up at 4:00 a.m. on the longest day of the year if we stayed on standard time all year round.”
Dr. Farmer called for more research before a decision is made.
“I suggest we need more information about the dangers of staying on daylight saving or standard time year-round because perhaps the current strategy of keeping morning light consistent is not so bad,” she said.
Time for a Congressional hearing?
According to Dr. Ramar, the time is now for a Congressional hearing, as lawmakers and the public need to be adequately informed when considering new legislation.
“There are public misconceptions about daylight saving time and standard time,” Dr. Ramar said. “People often like the idea of daylight saving time because they think it provides more light, and they dislike the concept of standard time because they think it provides more darkness. The reality is that neither time system provides more light or darkness than the other; it is only the timing that changes.”
Until new legislation is introduced, Dr. Ramar offered some practical advice for navigating seasonal time shifts.
“Beginning 2-3 days before the time change, it can be helpful to gradually adjust sleep and wake times, as well as other daily routines such as meal times,” he said. “After the time change, going outside for some morning light can help adjust the timing of your internal body clock.”
The investigators reported no conflicts of interest.
COVID-19 can cause atypical thyroid inflammation
Individuals who experience inflammation of the thyroid gland during acute COVID-19 illness may still have subacute thyroiditis months later, even if thyroid function has normalized, new research suggests.
Furthermore, the thyroiditis seems to be different from thyroid inflammation caused by other viruses, said Ilaria Muller, MD, PhD, when presenting her findings March 21 at the virtual ENDO 2021 meeting.
“SARS-CoV-2 seems to have multifactorial action on thyroid function,” said Dr. Muller, of the University of Milan, Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Italy.
In July 2020, Dr. Muller and colleagues described patients hospitalized at their institution with severe COVID-19, 15% of whom had thyrotoxicosis due to atypical subacute thyroiditis, compared with just 1% of a comparison group hospitalized in the same subintensive care units during the spring of 2019, as reported by this news organization.
The “atypical” thyroiditis that occurred in the patients with COVID-19 was not associated with neck pain and affected more men than women. Moreover, it was associated with low TSH and free-triiodothyronine (T3) levels, and normal or elevated levels of free-thyroxine (T4), which is a very different presentation to classic nonthyroidal illness syndrome (NTIS) usually seen in critically ill patients, she explained.
Although transient T4 elevations can occur in acute illness, that phenomenon is not associated with low TSH. This newly described scenario appears to be a combination of thyrotoxicosis and NTIS, Dr. Muller and colleagues had speculated last summer.
Follow patients with COVID-19 and thyroid dysfunction for a year
Now, in an assessment of 51 patients 3 months after hospitalization for moderate-to-severe COVID-19 reported by Dr. Muller at ENDO 2021, both inflammatory markers and thyroid function had normalized, yet on imaging, a third of patients still exhibited focal hypoechoic areas suggestive of thyroiditis.
Of those, two-thirds had reduced uptake on thyroid scintigraphy, but few had antithyroid autoantibodies.
“The thyroid dysfunction induced by COVID-19 seems not mediated by autoimmunity. It is important to continue to follow these patients since they might develop thyroid dysfunction during the following months,” Dr. Muller emphasized.
Asked to comment, session moderator Robert W. Lash, MD, the Endocrine Society’s chief professional & clinical affairs officer, told this news organization: “When you’re ICU-level sick, it’s not unusual to have weird thyroid tests. Some viruses cause thyroid problems as well ... What makes this different is that while a lot of thyroid inflammation is caused by antibodies, this was not.”
“It looks like this was [SARS-CoV-2] causing damage to the thyroid gland, which is interesting,” he noted, adding that the thyroid gland expresses high levels of angiotensin-converting enzyme 2 (ACE2) and transmembrane protease serine 2 (TMPRSS2), which allow SARS-CoV-2 to infect human cells.
“This is probably part of that same story,” Dr. Lash said.
For patients who had thyroid abnormalities during acute COVID-19 illness or develop symptoms that might be thyroid-related afterward, he advises: “You should keep an eye on thyroid tests. It just raises your awareness ... You might check their thyroid tests every 6 months for a year.”
Signs of focal thyroiditis despite normalized thyroid function
The 51 patients (33 men and 18 women) hospitalized with moderate-to-severe COVID-19 had no history of thyroid disease and had not been taking thyroid medications, amiodarone, or steroids before baseline TSH was measured.
From baseline to 3 months, TSH rose from 1.2 to 1.6 mIU/L, while serum concentrations of T4, T3, C-reactive protein, and full blood counts had all normalized (all P < 0.01 vs. baseline).
Thyroid ultrasound at 3 months in 49 patients showed signs of focal thyroiditis in 16 (33%).
Among 14 patients of those who further underwent thyroid 99mTc or I123 uptake scans, four (29%) were normal, eight (57%) had focally reduced uptake, and two (14%) had diffusely reduced uptake.
Of the 16 patients with focal thyroiditis, only three were positive for autoantibodies to thyroglobulin (TgAb) or thyroid peroxidase (TPOAb). All were negative for autoantibodies to the TSH receptor.
“Importantly, of the two with diffusely reduced uptake, only one was positive for TPOAb or TgAb,” Dr. Muller noted, adding, “SARS-CoV-2 disease seems to trigger some dysfunction which very likely has complex and multifactorial mechanisms.”
In response to a question about a possible role for biopsies and thyroid cytology, Dr. Muller replied: “That’s definitely the key ... So far we’re just making guesses, so the key will be cytological or histological studies to see what is really going on in the thyroid.”
“What we know is that [unlike] classical thyroiditis that has been described after viral diseases including SARS-CoV-2, these patients have a different scenario ... Probably something is going on within the thyroid with a different mechanism, so surely cytology and histology studies are what we need,” she concluded.
The study was funded by Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milan, and by a COVID-19 research grant from the European Society of Endocrinology. Dr. Muller and Dr. Lash have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Individuals who experience inflammation of the thyroid gland during acute COVID-19 illness may still have subacute thyroiditis months later, even if thyroid function has normalized, new research suggests.
Furthermore, the thyroiditis seems to be different from thyroid inflammation caused by other viruses, said Ilaria Muller, MD, PhD, when presenting her findings March 21 at the virtual ENDO 2021 meeting.
“SARS-CoV-2 seems to have multifactorial action on thyroid function,” said Dr. Muller, of the University of Milan, Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Italy.
In July 2020, Dr. Muller and colleagues described patients hospitalized at their institution with severe COVID-19, 15% of whom had thyrotoxicosis due to atypical subacute thyroiditis, compared with just 1% of a comparison group hospitalized in the same subintensive care units during the spring of 2019, as reported by this news organization.
The “atypical” thyroiditis that occurred in the patients with COVID-19 was not associated with neck pain and affected more men than women. Moreover, it was associated with low TSH and free-triiodothyronine (T3) levels, and normal or elevated levels of free-thyroxine (T4), which is a very different presentation to classic nonthyroidal illness syndrome (NTIS) usually seen in critically ill patients, she explained.
Although transient T4 elevations can occur in acute illness, that phenomenon is not associated with low TSH. This newly described scenario appears to be a combination of thyrotoxicosis and NTIS, Dr. Muller and colleagues had speculated last summer.
Follow patients with COVID-19 and thyroid dysfunction for a year
Now, in an assessment of 51 patients 3 months after hospitalization for moderate-to-severe COVID-19 reported by Dr. Muller at ENDO 2021, both inflammatory markers and thyroid function had normalized, yet on imaging, a third of patients still exhibited focal hypoechoic areas suggestive of thyroiditis.
Of those, two-thirds had reduced uptake on thyroid scintigraphy, but few had antithyroid autoantibodies.
“The thyroid dysfunction induced by COVID-19 seems not mediated by autoimmunity. It is important to continue to follow these patients since they might develop thyroid dysfunction during the following months,” Dr. Muller emphasized.
Asked to comment, session moderator Robert W. Lash, MD, the Endocrine Society’s chief professional & clinical affairs officer, told this news organization: “When you’re ICU-level sick, it’s not unusual to have weird thyroid tests. Some viruses cause thyroid problems as well ... What makes this different is that while a lot of thyroid inflammation is caused by antibodies, this was not.”
“It looks like this was [SARS-CoV-2] causing damage to the thyroid gland, which is interesting,” he noted, adding that the thyroid gland expresses high levels of angiotensin-converting enzyme 2 (ACE2) and transmembrane protease serine 2 (TMPRSS2), which allow SARS-CoV-2 to infect human cells.
“This is probably part of that same story,” Dr. Lash said.
For patients who had thyroid abnormalities during acute COVID-19 illness or develop symptoms that might be thyroid-related afterward, he advises: “You should keep an eye on thyroid tests. It just raises your awareness ... You might check their thyroid tests every 6 months for a year.”
Signs of focal thyroiditis despite normalized thyroid function
The 51 patients (33 men and 18 women) hospitalized with moderate-to-severe COVID-19 had no history of thyroid disease and had not been taking thyroid medications, amiodarone, or steroids before baseline TSH was measured.
From baseline to 3 months, TSH rose from 1.2 to 1.6 mIU/L, while serum concentrations of T4, T3, C-reactive protein, and full blood counts had all normalized (all P < 0.01 vs. baseline).
Thyroid ultrasound at 3 months in 49 patients showed signs of focal thyroiditis in 16 (33%).
Among 14 patients of those who further underwent thyroid 99mTc or I123 uptake scans, four (29%) were normal, eight (57%) had focally reduced uptake, and two (14%) had diffusely reduced uptake.
Of the 16 patients with focal thyroiditis, only three were positive for autoantibodies to thyroglobulin (TgAb) or thyroid peroxidase (TPOAb). All were negative for autoantibodies to the TSH receptor.
“Importantly, of the two with diffusely reduced uptake, only one was positive for TPOAb or TgAb,” Dr. Muller noted, adding, “SARS-CoV-2 disease seems to trigger some dysfunction which very likely has complex and multifactorial mechanisms.”
In response to a question about a possible role for biopsies and thyroid cytology, Dr. Muller replied: “That’s definitely the key ... So far we’re just making guesses, so the key will be cytological or histological studies to see what is really going on in the thyroid.”
“What we know is that [unlike] classical thyroiditis that has been described after viral diseases including SARS-CoV-2, these patients have a different scenario ... Probably something is going on within the thyroid with a different mechanism, so surely cytology and histology studies are what we need,” she concluded.
The study was funded by Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milan, and by a COVID-19 research grant from the European Society of Endocrinology. Dr. Muller and Dr. Lash have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Individuals who experience inflammation of the thyroid gland during acute COVID-19 illness may still have subacute thyroiditis months later, even if thyroid function has normalized, new research suggests.
Furthermore, the thyroiditis seems to be different from thyroid inflammation caused by other viruses, said Ilaria Muller, MD, PhD, when presenting her findings March 21 at the virtual ENDO 2021 meeting.
“SARS-CoV-2 seems to have multifactorial action on thyroid function,” said Dr. Muller, of the University of Milan, Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Italy.
In July 2020, Dr. Muller and colleagues described patients hospitalized at their institution with severe COVID-19, 15% of whom had thyrotoxicosis due to atypical subacute thyroiditis, compared with just 1% of a comparison group hospitalized in the same subintensive care units during the spring of 2019, as reported by this news organization.
The “atypical” thyroiditis that occurred in the patients with COVID-19 was not associated with neck pain and affected more men than women. Moreover, it was associated with low TSH and free-triiodothyronine (T3) levels, and normal or elevated levels of free-thyroxine (T4), which is a very different presentation to classic nonthyroidal illness syndrome (NTIS) usually seen in critically ill patients, she explained.
Although transient T4 elevations can occur in acute illness, that phenomenon is not associated with low TSH. This newly described scenario appears to be a combination of thyrotoxicosis and NTIS, Dr. Muller and colleagues had speculated last summer.
Follow patients with COVID-19 and thyroid dysfunction for a year
Now, in an assessment of 51 patients 3 months after hospitalization for moderate-to-severe COVID-19 reported by Dr. Muller at ENDO 2021, both inflammatory markers and thyroid function had normalized, yet on imaging, a third of patients still exhibited focal hypoechoic areas suggestive of thyroiditis.
Of those, two-thirds had reduced uptake on thyroid scintigraphy, but few had antithyroid autoantibodies.
“The thyroid dysfunction induced by COVID-19 seems not mediated by autoimmunity. It is important to continue to follow these patients since they might develop thyroid dysfunction during the following months,” Dr. Muller emphasized.
Asked to comment, session moderator Robert W. Lash, MD, the Endocrine Society’s chief professional & clinical affairs officer, told this news organization: “When you’re ICU-level sick, it’s not unusual to have weird thyroid tests. Some viruses cause thyroid problems as well ... What makes this different is that while a lot of thyroid inflammation is caused by antibodies, this was not.”
“It looks like this was [SARS-CoV-2] causing damage to the thyroid gland, which is interesting,” he noted, adding that the thyroid gland expresses high levels of angiotensin-converting enzyme 2 (ACE2) and transmembrane protease serine 2 (TMPRSS2), which allow SARS-CoV-2 to infect human cells.
“This is probably part of that same story,” Dr. Lash said.
For patients who had thyroid abnormalities during acute COVID-19 illness or develop symptoms that might be thyroid-related afterward, he advises: “You should keep an eye on thyroid tests. It just raises your awareness ... You might check their thyroid tests every 6 months for a year.”
Signs of focal thyroiditis despite normalized thyroid function
The 51 patients (33 men and 18 women) hospitalized with moderate-to-severe COVID-19 had no history of thyroid disease and had not been taking thyroid medications, amiodarone, or steroids before baseline TSH was measured.
From baseline to 3 months, TSH rose from 1.2 to 1.6 mIU/L, while serum concentrations of T4, T3, C-reactive protein, and full blood counts had all normalized (all P < 0.01 vs. baseline).
Thyroid ultrasound at 3 months in 49 patients showed signs of focal thyroiditis in 16 (33%).
Among 14 patients of those who further underwent thyroid 99mTc or I123 uptake scans, four (29%) were normal, eight (57%) had focally reduced uptake, and two (14%) had diffusely reduced uptake.
Of the 16 patients with focal thyroiditis, only three were positive for autoantibodies to thyroglobulin (TgAb) or thyroid peroxidase (TPOAb). All were negative for autoantibodies to the TSH receptor.
“Importantly, of the two with diffusely reduced uptake, only one was positive for TPOAb or TgAb,” Dr. Muller noted, adding, “SARS-CoV-2 disease seems to trigger some dysfunction which very likely has complex and multifactorial mechanisms.”
In response to a question about a possible role for biopsies and thyroid cytology, Dr. Muller replied: “That’s definitely the key ... So far we’re just making guesses, so the key will be cytological or histological studies to see what is really going on in the thyroid.”
“What we know is that [unlike] classical thyroiditis that has been described after viral diseases including SARS-CoV-2, these patients have a different scenario ... Probably something is going on within the thyroid with a different mechanism, so surely cytology and histology studies are what we need,” she concluded.
The study was funded by Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milan, and by a COVID-19 research grant from the European Society of Endocrinology. Dr. Muller and Dr. Lash have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Less sleep, more burnout linked to higher COVID-19 risk, study shows
among health care workers considered to be at high risk for exposure to patients with COVID-19, new evidence reveals.
For each additional hour of sleep at night, for example, risk for COVID-19 dropped by 12% in a study of 2844 frontline health care workers.
Furthermore, those who reported experiencing work-related burnout every day were 2.6 times more likely to report having COVID-19, to report having COVID-19 for a longer time, and to experience COVID-19 of more severity.
“This study underscores the importance of non–hygiene-related risk factors for COVID-19 and supports a holistic approach to health – including optimal sleep and job stress reduction to protect our health care workers from this and future pandemics,” senior author Sara B. Seidelmann, MD, said in an interview.
“Our findings add to the literature that sleep duration at night, sleep problems, and burnout may be risk factors for viral illnesses like COVID-19,” wrote Dr. Seidelmann and colleagues.
This is the first study to link COVID-19 risk to sleep habits – including number of hours of sleep at night, daytime napping hours, and severe sleep problems – among health care workers across multiple countries.
The study was published online March 22 in BMJ Nutrition, Prevention, and Health.
The researchers surveyed health care professionals in specialties considered to place personnel at high risk for exposure to SARS-CoV-2: critical care, emergency care, and internal medicine.
The association between sleep and burnout risk factors and COVID-19 did not vary significantly by specialty. “We didn’t detect any significant interactions between age, sex, specialty, or country,” said Dr. Seidelmann, assistant professor of clinical medicine at Columbia University College of Physicians and Surgeons, New York, and an internist at Stamford (Conn.) Hospital.
In addition to the 12% lower risk associated with each additional hour of sleep at night, each 1 additional hour of daytime napping was linked with a 6% increased risk for COVID-19 in an adjusted analysis (odds ratio [OR], 1.06; 95% confidence interval [CI], 1.01-1.12).
Daytime napping slightly increased risk for COVID-19 in five of the six countries included in the study: France, Germany, Italy, the United Kingdom, and the United States. In contrast, in Spain, napping had a nonsignificant protective effect.
The survey asked health care workers to recall nighttime sleep duration, sleep disorders, and burnout in the year prior to onset of the COVID-19 pandemic.
‘Significant, close contact’ with COVID-19?
Lead author Hyunju Kim, NP, Dr. Seidelmann, and colleagues conducted the population-based, case-control study from July 17 to Sept. 25, 2020. They identified health care workers from the SurveyHealthcareGlobus (SHG) network.
Of the respondents, 72% were men. The mean age of the participants was 48 years, and the study population was 77% White, 12% Asian, 6% mixed background, 2% Black, and 1% other. (The remainder preferred not to say).
The 568 health care workers considered to have COVID-19 were classified on the basis of self-reported symptoms. Control participants had no symptoms associated with COVID-19.
All 2,844 participants answered yes to a question about having “significant close contact” with COVID-19 patients in their workplace.
Compared to reporting no sleep problems, having three such problems – difficulty sleeping at night, poor sleep continuity, and frequent use of sleeping pills – was associated with 88% greater odds of COVID-19 (OR, 1.88; 95% CI, 1.17–3.01).
Having one sleep problem was not associated with COVID-19.
More burnout, greater risk
The health care workers reported the severity of any work-related burnout. “There was a significant dose-response relationship between frequency of burnout and COVID-19,” the researchers noted.
Those who reported having burnout rarely or weekly had a 1.3-1.4 greater chance of reporting COVID-19 compared to those who reported having no burnout, for example.
In addition, reporting a high level of burnout was linked to about three times the risk for having COVID-19 of longer duration and of greater severity.
What drives the association between sleep problems, burnout, and higher risk for COVID-19 and severe COVID-19 remains unknown.
“The mechanism underlying these associations isn’t clear, but suboptimal sleep, sleep disorders, and stress may result in immune system dysregulation, increased inflammation, and alterations in hormones such as cortisol and melatonin that may increase vulnerability to viral infections,” Dr. Seidelmann said.
Strengths and limitations
Using a large network of health care workers in the early phase of the pandemic is a strength of the study. How generalizable the findings are outside the SHG database of 1.5 million health care workers remains unknown.
Another limitation was reliance on self-reporting of COVID-19 patient exposure, outcomes, and covariates, which could have introduced bias.
“However,” the researchers noted, “health care workers are likely a reliable source of information.”
Insomnia a common challenge
A 2020 meta-analysis examined the effect of insomnia and psychological factors on COVID-19 risk among health care workers. Lead author Kavita Batra, PhD, of the University of Nevada, Las Vegas (UNLV), and colleagues found that the pooled prevalence of insomnia was almost 28%.
“The recent six-country study by Kim and colleagues also underscores this relationship between lack of sleep and having higher odds of COVID-19 infection,” Manoj Sharma, MBBS, PhD, professor of social and behavioral health in the UNLV department of environmental and occupational health, and one of the study authors, said in an interview.
More research is warranted to learn the direction of the association, he said. Does reduced sleep lower immunity and make a health care worker more susceptible to SARS-CoV-2 infection, or does the anxiety associated with COVID-19 contribute to insomnia?
“Practicing sleep hygiene is a must not only for health workers but also for everyone,” Dr. Sharma added. Recommendations include having fixed hours of going to bed, fixed hours of waking up, not overdoing naps, having at least 30 minutes of winding down before sleeping, having a dark bedroom devoid of all electronics and other disturbances, avoiding smoking, alcohol, and stimulants (such as caffeine) before sleeping, and practicing relaxation right before sleeping, he said.
“It is hard for some health care workers, especially those who work night shifts, but it must be a priority to follow as many sleep hygiene measures as possible,” Dr. Sharma said. “After all, if you do not take care of yourself how can you take care of others?”
Dr. Seidelmann, Dr. Batra, and Dr. Sharma have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
among health care workers considered to be at high risk for exposure to patients with COVID-19, new evidence reveals.
For each additional hour of sleep at night, for example, risk for COVID-19 dropped by 12% in a study of 2844 frontline health care workers.
Furthermore, those who reported experiencing work-related burnout every day were 2.6 times more likely to report having COVID-19, to report having COVID-19 for a longer time, and to experience COVID-19 of more severity.
“This study underscores the importance of non–hygiene-related risk factors for COVID-19 and supports a holistic approach to health – including optimal sleep and job stress reduction to protect our health care workers from this and future pandemics,” senior author Sara B. Seidelmann, MD, said in an interview.
“Our findings add to the literature that sleep duration at night, sleep problems, and burnout may be risk factors for viral illnesses like COVID-19,” wrote Dr. Seidelmann and colleagues.
This is the first study to link COVID-19 risk to sleep habits – including number of hours of sleep at night, daytime napping hours, and severe sleep problems – among health care workers across multiple countries.
The study was published online March 22 in BMJ Nutrition, Prevention, and Health.
The researchers surveyed health care professionals in specialties considered to place personnel at high risk for exposure to SARS-CoV-2: critical care, emergency care, and internal medicine.
The association between sleep and burnout risk factors and COVID-19 did not vary significantly by specialty. “We didn’t detect any significant interactions between age, sex, specialty, or country,” said Dr. Seidelmann, assistant professor of clinical medicine at Columbia University College of Physicians and Surgeons, New York, and an internist at Stamford (Conn.) Hospital.
In addition to the 12% lower risk associated with each additional hour of sleep at night, each 1 additional hour of daytime napping was linked with a 6% increased risk for COVID-19 in an adjusted analysis (odds ratio [OR], 1.06; 95% confidence interval [CI], 1.01-1.12).
Daytime napping slightly increased risk for COVID-19 in five of the six countries included in the study: France, Germany, Italy, the United Kingdom, and the United States. In contrast, in Spain, napping had a nonsignificant protective effect.
The survey asked health care workers to recall nighttime sleep duration, sleep disorders, and burnout in the year prior to onset of the COVID-19 pandemic.
‘Significant, close contact’ with COVID-19?
Lead author Hyunju Kim, NP, Dr. Seidelmann, and colleagues conducted the population-based, case-control study from July 17 to Sept. 25, 2020. They identified health care workers from the SurveyHealthcareGlobus (SHG) network.
Of the respondents, 72% were men. The mean age of the participants was 48 years, and the study population was 77% White, 12% Asian, 6% mixed background, 2% Black, and 1% other. (The remainder preferred not to say).
The 568 health care workers considered to have COVID-19 were classified on the basis of self-reported symptoms. Control participants had no symptoms associated with COVID-19.
All 2,844 participants answered yes to a question about having “significant close contact” with COVID-19 patients in their workplace.
Compared to reporting no sleep problems, having three such problems – difficulty sleeping at night, poor sleep continuity, and frequent use of sleeping pills – was associated with 88% greater odds of COVID-19 (OR, 1.88; 95% CI, 1.17–3.01).
Having one sleep problem was not associated with COVID-19.
More burnout, greater risk
The health care workers reported the severity of any work-related burnout. “There was a significant dose-response relationship between frequency of burnout and COVID-19,” the researchers noted.
Those who reported having burnout rarely or weekly had a 1.3-1.4 greater chance of reporting COVID-19 compared to those who reported having no burnout, for example.
In addition, reporting a high level of burnout was linked to about three times the risk for having COVID-19 of longer duration and of greater severity.
What drives the association between sleep problems, burnout, and higher risk for COVID-19 and severe COVID-19 remains unknown.
“The mechanism underlying these associations isn’t clear, but suboptimal sleep, sleep disorders, and stress may result in immune system dysregulation, increased inflammation, and alterations in hormones such as cortisol and melatonin that may increase vulnerability to viral infections,” Dr. Seidelmann said.
Strengths and limitations
Using a large network of health care workers in the early phase of the pandemic is a strength of the study. How generalizable the findings are outside the SHG database of 1.5 million health care workers remains unknown.
Another limitation was reliance on self-reporting of COVID-19 patient exposure, outcomes, and covariates, which could have introduced bias.
“However,” the researchers noted, “health care workers are likely a reliable source of information.”
Insomnia a common challenge
A 2020 meta-analysis examined the effect of insomnia and psychological factors on COVID-19 risk among health care workers. Lead author Kavita Batra, PhD, of the University of Nevada, Las Vegas (UNLV), and colleagues found that the pooled prevalence of insomnia was almost 28%.
“The recent six-country study by Kim and colleagues also underscores this relationship between lack of sleep and having higher odds of COVID-19 infection,” Manoj Sharma, MBBS, PhD, professor of social and behavioral health in the UNLV department of environmental and occupational health, and one of the study authors, said in an interview.
More research is warranted to learn the direction of the association, he said. Does reduced sleep lower immunity and make a health care worker more susceptible to SARS-CoV-2 infection, or does the anxiety associated with COVID-19 contribute to insomnia?
“Practicing sleep hygiene is a must not only for health workers but also for everyone,” Dr. Sharma added. Recommendations include having fixed hours of going to bed, fixed hours of waking up, not overdoing naps, having at least 30 minutes of winding down before sleeping, having a dark bedroom devoid of all electronics and other disturbances, avoiding smoking, alcohol, and stimulants (such as caffeine) before sleeping, and practicing relaxation right before sleeping, he said.
“It is hard for some health care workers, especially those who work night shifts, but it must be a priority to follow as many sleep hygiene measures as possible,” Dr. Sharma said. “After all, if you do not take care of yourself how can you take care of others?”
Dr. Seidelmann, Dr. Batra, and Dr. Sharma have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
among health care workers considered to be at high risk for exposure to patients with COVID-19, new evidence reveals.
For each additional hour of sleep at night, for example, risk for COVID-19 dropped by 12% in a study of 2844 frontline health care workers.
Furthermore, those who reported experiencing work-related burnout every day were 2.6 times more likely to report having COVID-19, to report having COVID-19 for a longer time, and to experience COVID-19 of more severity.
“This study underscores the importance of non–hygiene-related risk factors for COVID-19 and supports a holistic approach to health – including optimal sleep and job stress reduction to protect our health care workers from this and future pandemics,” senior author Sara B. Seidelmann, MD, said in an interview.
“Our findings add to the literature that sleep duration at night, sleep problems, and burnout may be risk factors for viral illnesses like COVID-19,” wrote Dr. Seidelmann and colleagues.
This is the first study to link COVID-19 risk to sleep habits – including number of hours of sleep at night, daytime napping hours, and severe sleep problems – among health care workers across multiple countries.
The study was published online March 22 in BMJ Nutrition, Prevention, and Health.
The researchers surveyed health care professionals in specialties considered to place personnel at high risk for exposure to SARS-CoV-2: critical care, emergency care, and internal medicine.
The association between sleep and burnout risk factors and COVID-19 did not vary significantly by specialty. “We didn’t detect any significant interactions between age, sex, specialty, or country,” said Dr. Seidelmann, assistant professor of clinical medicine at Columbia University College of Physicians and Surgeons, New York, and an internist at Stamford (Conn.) Hospital.
In addition to the 12% lower risk associated with each additional hour of sleep at night, each 1 additional hour of daytime napping was linked with a 6% increased risk for COVID-19 in an adjusted analysis (odds ratio [OR], 1.06; 95% confidence interval [CI], 1.01-1.12).
Daytime napping slightly increased risk for COVID-19 in five of the six countries included in the study: France, Germany, Italy, the United Kingdom, and the United States. In contrast, in Spain, napping had a nonsignificant protective effect.
The survey asked health care workers to recall nighttime sleep duration, sleep disorders, and burnout in the year prior to onset of the COVID-19 pandemic.
‘Significant, close contact’ with COVID-19?
Lead author Hyunju Kim, NP, Dr. Seidelmann, and colleagues conducted the population-based, case-control study from July 17 to Sept. 25, 2020. They identified health care workers from the SurveyHealthcareGlobus (SHG) network.
Of the respondents, 72% were men. The mean age of the participants was 48 years, and the study population was 77% White, 12% Asian, 6% mixed background, 2% Black, and 1% other. (The remainder preferred not to say).
The 568 health care workers considered to have COVID-19 were classified on the basis of self-reported symptoms. Control participants had no symptoms associated with COVID-19.
All 2,844 participants answered yes to a question about having “significant close contact” with COVID-19 patients in their workplace.
Compared to reporting no sleep problems, having three such problems – difficulty sleeping at night, poor sleep continuity, and frequent use of sleeping pills – was associated with 88% greater odds of COVID-19 (OR, 1.88; 95% CI, 1.17–3.01).
Having one sleep problem was not associated with COVID-19.
More burnout, greater risk
The health care workers reported the severity of any work-related burnout. “There was a significant dose-response relationship between frequency of burnout and COVID-19,” the researchers noted.
Those who reported having burnout rarely or weekly had a 1.3-1.4 greater chance of reporting COVID-19 compared to those who reported having no burnout, for example.
In addition, reporting a high level of burnout was linked to about three times the risk for having COVID-19 of longer duration and of greater severity.
What drives the association between sleep problems, burnout, and higher risk for COVID-19 and severe COVID-19 remains unknown.
“The mechanism underlying these associations isn’t clear, but suboptimal sleep, sleep disorders, and stress may result in immune system dysregulation, increased inflammation, and alterations in hormones such as cortisol and melatonin that may increase vulnerability to viral infections,” Dr. Seidelmann said.
Strengths and limitations
Using a large network of health care workers in the early phase of the pandemic is a strength of the study. How generalizable the findings are outside the SHG database of 1.5 million health care workers remains unknown.
Another limitation was reliance on self-reporting of COVID-19 patient exposure, outcomes, and covariates, which could have introduced bias.
“However,” the researchers noted, “health care workers are likely a reliable source of information.”
Insomnia a common challenge
A 2020 meta-analysis examined the effect of insomnia and psychological factors on COVID-19 risk among health care workers. Lead author Kavita Batra, PhD, of the University of Nevada, Las Vegas (UNLV), and colleagues found that the pooled prevalence of insomnia was almost 28%.
“The recent six-country study by Kim and colleagues also underscores this relationship between lack of sleep and having higher odds of COVID-19 infection,” Manoj Sharma, MBBS, PhD, professor of social and behavioral health in the UNLV department of environmental and occupational health, and one of the study authors, said in an interview.
More research is warranted to learn the direction of the association, he said. Does reduced sleep lower immunity and make a health care worker more susceptible to SARS-CoV-2 infection, or does the anxiety associated with COVID-19 contribute to insomnia?
“Practicing sleep hygiene is a must not only for health workers but also for everyone,” Dr. Sharma added. Recommendations include having fixed hours of going to bed, fixed hours of waking up, not overdoing naps, having at least 30 minutes of winding down before sleeping, having a dark bedroom devoid of all electronics and other disturbances, avoiding smoking, alcohol, and stimulants (such as caffeine) before sleeping, and practicing relaxation right before sleeping, he said.
“It is hard for some health care workers, especially those who work night shifts, but it must be a priority to follow as many sleep hygiene measures as possible,” Dr. Sharma said. “After all, if you do not take care of yourself how can you take care of others?”
Dr. Seidelmann, Dr. Batra, and Dr. Sharma have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Combo thyroid hormones as good as levothyroxine for hypothyroidism
Patients with hypothyroidism treated with the three most common pharmacologic strategies of levothyroxine (LT4) alone, LT4 in combination with triiodothyronine (T3), or desiccated thyroid extract showed no differences in thyroid symptoms or secondary outcomes in a double-blind, randomized study.
“There are now proven good treatment options for the more than 1 in 10 patients with hypothyroidism who continue to experience symptoms of fatigue, mental fogginess, weight gain, and other symptoms despite taking levothyroxine,” first author Thanh Duc Hoang, DO, an endocrinologist at the Walter Reed National Military Medical Center, in Bethesda, Md., said in a press statement.
The findings were presented at the annual meeting of the Endocrine Society.
Commenting on the study, Alan P. Farwell, MD, said these new results are a valuable contribution to the understanding of treatment effects. “I think this is an interesting and important study and further studies are needed to clarify the optimal way to treat hypothyroidism,” said Dr. Farwell, who is director of endocrine clinics at Boston University.
Importantly, “the findings are different than studies where the patients are aware of what medication they are receiving,” he stressed in an interview, underscoring the importance of the double-blind design of the trial.
But Anne Cappola, MD, of the University of Pennsylvania, Philadelphia, pointed out that “the study was small and unlikely to have the statistical power to detect differences that could have been clinically important.”
Nevertheless, she too agreed that the double-blind study design is key: “My experience with patients is [the effects] are affected by patients’ perceptions about their thyroid medication. That is why studies designed so that patients do not know which treatment they are receiving are so important in this area.”
Randomized, double-blind comparison
Prior to the widespread availability of the current gold standard hypothyroidism treatment of LT4, the condition was typically treated with desiccated (animal) thyroid extract. And with many patients continuing to have a preference for this therapeutic approach, it is still commonly used.
Additionally, some patients treated with LT4 alone report greater improvements in symptoms with the addition of T3 – despite studies showing no benefits from the two together – leading to many clinicians commonly trying the combination approach.
To compare the efficacy of the three approaches in a prospective, double-blind, cross-over fashion, 75 patients received three therapeutic approaches each for 3 months: desiccated thyroid extract, an LT4/T3 combination, or LT4 alone.
After each 3-month treatment, patients completed a 36-point thyroid symptom questionnaire.
There was no significant differences in symptom relief, the primary outcome, between the three treatments (P = .32).
Overall, 45% of patients indicated they preferred desiccated thyroid as their first choice of treatment, 32% preferred LT4/T3 as their first choice, and 23% preferred LT4 alone.
For the secondary endpoints of weight, general health, depression (assessed using the Beck Depression Inventory), memory (Wechsler Memory Scale), lipids, and thyroid function, again, there were no significant differences between groups in any of the measures.
When switched to desiccated thyroid, many felt ‘much better’
A further exploratory analysis revealed that those who experienced symptoms while taking LT4 alone reported greater alleviation of symptoms with the other two treatments.
“As a whole group, there was no significant difference between the three treatment arms,” Dr. Hoang explained in an interview.
“However, with the subgroup analysis based on the scores of symptom questionnaires, we found that symptomatic patients on LT4 improved while being treated with LT4/T3 or desiccated thyroid,” he said.
Reports of improvements in switching to desiccated thyroid were notable, Dr. Hoang added. “Many patients when switched from LT4 to desiccated thyroid extract said they felt much better, [with] more energy, less mental fogginess, a better outlook, less flair of lupus symptoms, easier to lose weight, etc.”
The study also showed more patients with Hashimoto’s disease preferred desiccated thyroid extract and LT4/T3, compared with LT4 alone, however, the differences were not significant.
Treatment adjustments a helpful first step
Dr. Farwell noted that his approach when patients are still reporting symptoms despite LT4 treatment is to first try tweaking the dose.
“In my own practice, I prefer to adjust LT4 dosing first, and on occasion add T3, with a goal of getting both hormone levels in the upper half of the normal range,” he said. “I find that to be a better approach than desiccated thyroid extract. T3 should be taken twice a day due to its half-life.”
The approach is generally successful, he added. “Even those that come in asking for desiccated thyroid extract whom I am able to convince to try LT4/T3 end up being happy with their treatment in the end.
“The key is that you need to spend time discussing the options with patients and come to a consensus as to the therapy that will best resolve their symptoms and that they are most comfortable with,” he concluded.
In response to mounting evidence of different hypothyroidism treatment responses according to various subgroups of patients, experts recently called for the initiation of more thorough clinical trials on the issue of combination therapy, as recently reported by this news organization.
Dr. Hoang reported being a speaker for Acella Pharmaceuticals. Dr. Farwell and Dr. Cappola reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients with hypothyroidism treated with the three most common pharmacologic strategies of levothyroxine (LT4) alone, LT4 in combination with triiodothyronine (T3), or desiccated thyroid extract showed no differences in thyroid symptoms or secondary outcomes in a double-blind, randomized study.
“There are now proven good treatment options for the more than 1 in 10 patients with hypothyroidism who continue to experience symptoms of fatigue, mental fogginess, weight gain, and other symptoms despite taking levothyroxine,” first author Thanh Duc Hoang, DO, an endocrinologist at the Walter Reed National Military Medical Center, in Bethesda, Md., said in a press statement.
The findings were presented at the annual meeting of the Endocrine Society.
Commenting on the study, Alan P. Farwell, MD, said these new results are a valuable contribution to the understanding of treatment effects. “I think this is an interesting and important study and further studies are needed to clarify the optimal way to treat hypothyroidism,” said Dr. Farwell, who is director of endocrine clinics at Boston University.
Importantly, “the findings are different than studies where the patients are aware of what medication they are receiving,” he stressed in an interview, underscoring the importance of the double-blind design of the trial.
But Anne Cappola, MD, of the University of Pennsylvania, Philadelphia, pointed out that “the study was small and unlikely to have the statistical power to detect differences that could have been clinically important.”
Nevertheless, she too agreed that the double-blind study design is key: “My experience with patients is [the effects] are affected by patients’ perceptions about their thyroid medication. That is why studies designed so that patients do not know which treatment they are receiving are so important in this area.”
Randomized, double-blind comparison
Prior to the widespread availability of the current gold standard hypothyroidism treatment of LT4, the condition was typically treated with desiccated (animal) thyroid extract. And with many patients continuing to have a preference for this therapeutic approach, it is still commonly used.
Additionally, some patients treated with LT4 alone report greater improvements in symptoms with the addition of T3 – despite studies showing no benefits from the two together – leading to many clinicians commonly trying the combination approach.
To compare the efficacy of the three approaches in a prospective, double-blind, cross-over fashion, 75 patients received three therapeutic approaches each for 3 months: desiccated thyroid extract, an LT4/T3 combination, or LT4 alone.
After each 3-month treatment, patients completed a 36-point thyroid symptom questionnaire.
There was no significant differences in symptom relief, the primary outcome, between the three treatments (P = .32).
Overall, 45% of patients indicated they preferred desiccated thyroid as their first choice of treatment, 32% preferred LT4/T3 as their first choice, and 23% preferred LT4 alone.
For the secondary endpoints of weight, general health, depression (assessed using the Beck Depression Inventory), memory (Wechsler Memory Scale), lipids, and thyroid function, again, there were no significant differences between groups in any of the measures.
When switched to desiccated thyroid, many felt ‘much better’
A further exploratory analysis revealed that those who experienced symptoms while taking LT4 alone reported greater alleviation of symptoms with the other two treatments.
“As a whole group, there was no significant difference between the three treatment arms,” Dr. Hoang explained in an interview.
“However, with the subgroup analysis based on the scores of symptom questionnaires, we found that symptomatic patients on LT4 improved while being treated with LT4/T3 or desiccated thyroid,” he said.
Reports of improvements in switching to desiccated thyroid were notable, Dr. Hoang added. “Many patients when switched from LT4 to desiccated thyroid extract said they felt much better, [with] more energy, less mental fogginess, a better outlook, less flair of lupus symptoms, easier to lose weight, etc.”
The study also showed more patients with Hashimoto’s disease preferred desiccated thyroid extract and LT4/T3, compared with LT4 alone, however, the differences were not significant.
Treatment adjustments a helpful first step
Dr. Farwell noted that his approach when patients are still reporting symptoms despite LT4 treatment is to first try tweaking the dose.
“In my own practice, I prefer to adjust LT4 dosing first, and on occasion add T3, with a goal of getting both hormone levels in the upper half of the normal range,” he said. “I find that to be a better approach than desiccated thyroid extract. T3 should be taken twice a day due to its half-life.”
The approach is generally successful, he added. “Even those that come in asking for desiccated thyroid extract whom I am able to convince to try LT4/T3 end up being happy with their treatment in the end.
“The key is that you need to spend time discussing the options with patients and come to a consensus as to the therapy that will best resolve their symptoms and that they are most comfortable with,” he concluded.
In response to mounting evidence of different hypothyroidism treatment responses according to various subgroups of patients, experts recently called for the initiation of more thorough clinical trials on the issue of combination therapy, as recently reported by this news organization.
Dr. Hoang reported being a speaker for Acella Pharmaceuticals. Dr. Farwell and Dr. Cappola reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients with hypothyroidism treated with the three most common pharmacologic strategies of levothyroxine (LT4) alone, LT4 in combination with triiodothyronine (T3), or desiccated thyroid extract showed no differences in thyroid symptoms or secondary outcomes in a double-blind, randomized study.
“There are now proven good treatment options for the more than 1 in 10 patients with hypothyroidism who continue to experience symptoms of fatigue, mental fogginess, weight gain, and other symptoms despite taking levothyroxine,” first author Thanh Duc Hoang, DO, an endocrinologist at the Walter Reed National Military Medical Center, in Bethesda, Md., said in a press statement.
The findings were presented at the annual meeting of the Endocrine Society.
Commenting on the study, Alan P. Farwell, MD, said these new results are a valuable contribution to the understanding of treatment effects. “I think this is an interesting and important study and further studies are needed to clarify the optimal way to treat hypothyroidism,” said Dr. Farwell, who is director of endocrine clinics at Boston University.
Importantly, “the findings are different than studies where the patients are aware of what medication they are receiving,” he stressed in an interview, underscoring the importance of the double-blind design of the trial.
But Anne Cappola, MD, of the University of Pennsylvania, Philadelphia, pointed out that “the study was small and unlikely to have the statistical power to detect differences that could have been clinically important.”
Nevertheless, she too agreed that the double-blind study design is key: “My experience with patients is [the effects] are affected by patients’ perceptions about their thyroid medication. That is why studies designed so that patients do not know which treatment they are receiving are so important in this area.”
Randomized, double-blind comparison
Prior to the widespread availability of the current gold standard hypothyroidism treatment of LT4, the condition was typically treated with desiccated (animal) thyroid extract. And with many patients continuing to have a preference for this therapeutic approach, it is still commonly used.
Additionally, some patients treated with LT4 alone report greater improvements in symptoms with the addition of T3 – despite studies showing no benefits from the two together – leading to many clinicians commonly trying the combination approach.
To compare the efficacy of the three approaches in a prospective, double-blind, cross-over fashion, 75 patients received three therapeutic approaches each for 3 months: desiccated thyroid extract, an LT4/T3 combination, or LT4 alone.
After each 3-month treatment, patients completed a 36-point thyroid symptom questionnaire.
There was no significant differences in symptom relief, the primary outcome, between the three treatments (P = .32).
Overall, 45% of patients indicated they preferred desiccated thyroid as their first choice of treatment, 32% preferred LT4/T3 as their first choice, and 23% preferred LT4 alone.
For the secondary endpoints of weight, general health, depression (assessed using the Beck Depression Inventory), memory (Wechsler Memory Scale), lipids, and thyroid function, again, there were no significant differences between groups in any of the measures.
When switched to desiccated thyroid, many felt ‘much better’
A further exploratory analysis revealed that those who experienced symptoms while taking LT4 alone reported greater alleviation of symptoms with the other two treatments.
“As a whole group, there was no significant difference between the three treatment arms,” Dr. Hoang explained in an interview.
“However, with the subgroup analysis based on the scores of symptom questionnaires, we found that symptomatic patients on LT4 improved while being treated with LT4/T3 or desiccated thyroid,” he said.
Reports of improvements in switching to desiccated thyroid were notable, Dr. Hoang added. “Many patients when switched from LT4 to desiccated thyroid extract said they felt much better, [with] more energy, less mental fogginess, a better outlook, less flair of lupus symptoms, easier to lose weight, etc.”
The study also showed more patients with Hashimoto’s disease preferred desiccated thyroid extract and LT4/T3, compared with LT4 alone, however, the differences were not significant.
Treatment adjustments a helpful first step
Dr. Farwell noted that his approach when patients are still reporting symptoms despite LT4 treatment is to first try tweaking the dose.
“In my own practice, I prefer to adjust LT4 dosing first, and on occasion add T3, with a goal of getting both hormone levels in the upper half of the normal range,” he said. “I find that to be a better approach than desiccated thyroid extract. T3 should be taken twice a day due to its half-life.”
The approach is generally successful, he added. “Even those that come in asking for desiccated thyroid extract whom I am able to convince to try LT4/T3 end up being happy with their treatment in the end.
“The key is that you need to spend time discussing the options with patients and come to a consensus as to the therapy that will best resolve their symptoms and that they are most comfortable with,” he concluded.
In response to mounting evidence of different hypothyroidism treatment responses according to various subgroups of patients, experts recently called for the initiation of more thorough clinical trials on the issue of combination therapy, as recently reported by this news organization.
Dr. Hoang reported being a speaker for Acella Pharmaceuticals. Dr. Farwell and Dr. Cappola reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Family-involved interventions reduce postoperative delirium
Background: Postoperative delirium is common in older patients undergoing surgery and often leads to complications including longer length of stay (LOS), increased mortality, functional decline, and dementia. The volunteer-based Hospital Elder Life Program (HELP) is one of the most widely implemented prevention tools to reduce POD; however, different cultures may not use volunteers in their hospital systems.
Study design: Randomized clinical trial.
Setting: West China Hospital in Chengdu.
Synopsis: This Chinese-based clinical trial evaluated 281 patients aged 70 years or older who underwent elective surgery and were randomized to either t-HELP units or usual-care units. t-HELP patients received three universal protocols that included family-driven interventions of orientation, therapeutic activities, and early mobilization protocols, as well as targeted protocols based on delirium risk factors, while control participants received usual nursing care. The incidence of POD was significantly reduced in the t-HELP group, compared with the control group (2.6% vs. 19.4%), which was also associated with a shorter LOS. Patients were also noted to have less cognitive and functional decline that was sustained after discharge.
Bottom line: For hospitals that do not use volunteers in delirium prevention, involving family appears to be effective in reducing POD and maintaining physical and cognitive function post operatively.
Citation: Wang YY et al. Effect of the Tailored, Family-Involved Hospital Elder Life Program on postoperative delirium and function in older adults: A randomized clinical trial. JAMA Intern Med. 2019 Oct 21. doi: 10.1001/jamainternmed.2019.4446.
Dr. Ciarkowski is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
Background: Postoperative delirium is common in older patients undergoing surgery and often leads to complications including longer length of stay (LOS), increased mortality, functional decline, and dementia. The volunteer-based Hospital Elder Life Program (HELP) is one of the most widely implemented prevention tools to reduce POD; however, different cultures may not use volunteers in their hospital systems.
Study design: Randomized clinical trial.
Setting: West China Hospital in Chengdu.
Synopsis: This Chinese-based clinical trial evaluated 281 patients aged 70 years or older who underwent elective surgery and were randomized to either t-HELP units or usual-care units. t-HELP patients received three universal protocols that included family-driven interventions of orientation, therapeutic activities, and early mobilization protocols, as well as targeted protocols based on delirium risk factors, while control participants received usual nursing care. The incidence of POD was significantly reduced in the t-HELP group, compared with the control group (2.6% vs. 19.4%), which was also associated with a shorter LOS. Patients were also noted to have less cognitive and functional decline that was sustained after discharge.
Bottom line: For hospitals that do not use volunteers in delirium prevention, involving family appears to be effective in reducing POD and maintaining physical and cognitive function post operatively.
Citation: Wang YY et al. Effect of the Tailored, Family-Involved Hospital Elder Life Program on postoperative delirium and function in older adults: A randomized clinical trial. JAMA Intern Med. 2019 Oct 21. doi: 10.1001/jamainternmed.2019.4446.
Dr. Ciarkowski is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
Background: Postoperative delirium is common in older patients undergoing surgery and often leads to complications including longer length of stay (LOS), increased mortality, functional decline, and dementia. The volunteer-based Hospital Elder Life Program (HELP) is one of the most widely implemented prevention tools to reduce POD; however, different cultures may not use volunteers in their hospital systems.
Study design: Randomized clinical trial.
Setting: West China Hospital in Chengdu.
Synopsis: This Chinese-based clinical trial evaluated 281 patients aged 70 years or older who underwent elective surgery and were randomized to either t-HELP units or usual-care units. t-HELP patients received three universal protocols that included family-driven interventions of orientation, therapeutic activities, and early mobilization protocols, as well as targeted protocols based on delirium risk factors, while control participants received usual nursing care. The incidence of POD was significantly reduced in the t-HELP group, compared with the control group (2.6% vs. 19.4%), which was also associated with a shorter LOS. Patients were also noted to have less cognitive and functional decline that was sustained after discharge.
Bottom line: For hospitals that do not use volunteers in delirium prevention, involving family appears to be effective in reducing POD and maintaining physical and cognitive function post operatively.
Citation: Wang YY et al. Effect of the Tailored, Family-Involved Hospital Elder Life Program on postoperative delirium and function in older adults: A randomized clinical trial. JAMA Intern Med. 2019 Oct 21. doi: 10.1001/jamainternmed.2019.4446.
Dr. Ciarkowski is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
COVID-19’s impact on lupus inpatients examined in study
Severe COVID-19 infection was more likely in hospitalized patients with systemic lupus erythematosus (SLE) who had comorbidities and risk factors associated with severe infection in the general population, notably older age, male gender, and hypertension, based on data from a nationwide epidemiologic study of inpatients in France.
“Recently, anti-interferon antibodies have been implicated in severe SARS-CoV-2 infection while it has been known for decades that patients with SLE may produce such autoantibodies,” but large-scale data on the risk of severe COVID-19 infection in SLE patients are limited, Arthur Mageau, MD, of Bichat–Claude Bernard Hospital in Paris, and colleagues wrote.
In a research letter published in Annals of the Rheumatic Diseases, the researchers used the French health care database Programme de Médicalisation des Systèmes d’Information to identify 11,055 adult SLE patients who had at least one hospital stay between March 1, 2020, and Oct.31, 2020. Of these, 1,411 (12.8%) also were diagnosed with COVID-19, and these patients had a total of 1,721 hospital stays.
Overall, in-hospital mortality was approximately four times higher among SLE patients with COVID-19 infection, compared with SLE patients without COVID-19 infection (9.5% vs. 2.4%, P < .001), and 293 (17%) of the COVID-19 hospital stays involved an intensive care unit. In the ICU, 78 (26.7%) of the COVID-19 patients required invasive ventilation, and 71 (24.7%) required noninvasive mechanical ventilation.
The SLE patients with COVID-19 who died were significantly more likely than the SLE patients with COVID-19 who recovered to be older and male, and to have conditions including chronic kidney disease, high blood pressure, chronic pulmonary disease, and a history of cardiovascular events or lupus nephritis. The study findings were limited by the focus on hospitalized patients only, so the results cannot be generalized to all lupus patients, the researchers said.
“Interestingly, while the overall mortality rate was lower in SLE/COVID-19–positive inpatients as compared with the total population admitted for SARS-CoV-2 infection in France during the same period (9.5% vs 15.7%, P < .0001), the mortality rate at a younger age tended to be higher in patients with SLE,” the researchers wrote, but the difference for these younger patients was not statistically significant. This disparity may be caused by the reduced need for immunosuppressive drugs in SLE patients as they age, and the observed increased mortality in younger SLE patients, compared with the general population, suggests that SLE may promote poor outcomes from COVID-19 infection.
Dr. Mageau received PhD fellowship support from the Agence Nationale pour la recherche. He and the other researchers had no financial conflicts to disclose. The study received no outside funding.
Severe COVID-19 infection was more likely in hospitalized patients with systemic lupus erythematosus (SLE) who had comorbidities and risk factors associated with severe infection in the general population, notably older age, male gender, and hypertension, based on data from a nationwide epidemiologic study of inpatients in France.
“Recently, anti-interferon antibodies have been implicated in severe SARS-CoV-2 infection while it has been known for decades that patients with SLE may produce such autoantibodies,” but large-scale data on the risk of severe COVID-19 infection in SLE patients are limited, Arthur Mageau, MD, of Bichat–Claude Bernard Hospital in Paris, and colleagues wrote.
In a research letter published in Annals of the Rheumatic Diseases, the researchers used the French health care database Programme de Médicalisation des Systèmes d’Information to identify 11,055 adult SLE patients who had at least one hospital stay between March 1, 2020, and Oct.31, 2020. Of these, 1,411 (12.8%) also were diagnosed with COVID-19, and these patients had a total of 1,721 hospital stays.
Overall, in-hospital mortality was approximately four times higher among SLE patients with COVID-19 infection, compared with SLE patients without COVID-19 infection (9.5% vs. 2.4%, P < .001), and 293 (17%) of the COVID-19 hospital stays involved an intensive care unit. In the ICU, 78 (26.7%) of the COVID-19 patients required invasive ventilation, and 71 (24.7%) required noninvasive mechanical ventilation.
The SLE patients with COVID-19 who died were significantly more likely than the SLE patients with COVID-19 who recovered to be older and male, and to have conditions including chronic kidney disease, high blood pressure, chronic pulmonary disease, and a history of cardiovascular events or lupus nephritis. The study findings were limited by the focus on hospitalized patients only, so the results cannot be generalized to all lupus patients, the researchers said.
“Interestingly, while the overall mortality rate was lower in SLE/COVID-19–positive inpatients as compared with the total population admitted for SARS-CoV-2 infection in France during the same period (9.5% vs 15.7%, P < .0001), the mortality rate at a younger age tended to be higher in patients with SLE,” the researchers wrote, but the difference for these younger patients was not statistically significant. This disparity may be caused by the reduced need for immunosuppressive drugs in SLE patients as they age, and the observed increased mortality in younger SLE patients, compared with the general population, suggests that SLE may promote poor outcomes from COVID-19 infection.
Dr. Mageau received PhD fellowship support from the Agence Nationale pour la recherche. He and the other researchers had no financial conflicts to disclose. The study received no outside funding.
Severe COVID-19 infection was more likely in hospitalized patients with systemic lupus erythematosus (SLE) who had comorbidities and risk factors associated with severe infection in the general population, notably older age, male gender, and hypertension, based on data from a nationwide epidemiologic study of inpatients in France.
“Recently, anti-interferon antibodies have been implicated in severe SARS-CoV-2 infection while it has been known for decades that patients with SLE may produce such autoantibodies,” but large-scale data on the risk of severe COVID-19 infection in SLE patients are limited, Arthur Mageau, MD, of Bichat–Claude Bernard Hospital in Paris, and colleagues wrote.
In a research letter published in Annals of the Rheumatic Diseases, the researchers used the French health care database Programme de Médicalisation des Systèmes d’Information to identify 11,055 adult SLE patients who had at least one hospital stay between March 1, 2020, and Oct.31, 2020. Of these, 1,411 (12.8%) also were diagnosed with COVID-19, and these patients had a total of 1,721 hospital stays.
Overall, in-hospital mortality was approximately four times higher among SLE patients with COVID-19 infection, compared with SLE patients without COVID-19 infection (9.5% vs. 2.4%, P < .001), and 293 (17%) of the COVID-19 hospital stays involved an intensive care unit. In the ICU, 78 (26.7%) of the COVID-19 patients required invasive ventilation, and 71 (24.7%) required noninvasive mechanical ventilation.
The SLE patients with COVID-19 who died were significantly more likely than the SLE patients with COVID-19 who recovered to be older and male, and to have conditions including chronic kidney disease, high blood pressure, chronic pulmonary disease, and a history of cardiovascular events or lupus nephritis. The study findings were limited by the focus on hospitalized patients only, so the results cannot be generalized to all lupus patients, the researchers said.
“Interestingly, while the overall mortality rate was lower in SLE/COVID-19–positive inpatients as compared with the total population admitted for SARS-CoV-2 infection in France during the same period (9.5% vs 15.7%, P < .0001), the mortality rate at a younger age tended to be higher in patients with SLE,” the researchers wrote, but the difference for these younger patients was not statistically significant. This disparity may be caused by the reduced need for immunosuppressive drugs in SLE patients as they age, and the observed increased mortality in younger SLE patients, compared with the general population, suggests that SLE may promote poor outcomes from COVID-19 infection.
Dr. Mageau received PhD fellowship support from the Agence Nationale pour la recherche. He and the other researchers had no financial conflicts to disclose. The study received no outside funding.
FROM ANNALS OF THE RHEUMATIC DISEASES
How long is the second stage of labor in women delivering twins?
, researchers say.
Although the analysis found statistically significant differences in second-stage labor lengths for twin and singleton deliveries, “ultimately I think the value in this is seeing that it is not much different,” said Nathan Fox, MD, a maternal-fetal medicine specialist who has studied twin pregnancies and delivery of twins.
Knowledge gap
While most twin births occur by cesarean delivery, vaginal delivery is a preferred method for diamniotic twins with the first twin in vertex presentation, wrote study author Gabriel Levin, MD, and colleagues. Prior studies, however, have not clearly established the duration of the second stage of labor in twin deliveries – that is, the time from 10-cm dilation until delivery of the first twin, they said.
Knowing “the parameters of the normal second stage of labor” for twin deliveries may help guide clinical practice and possibly avoid unnecessary operative deliveries, the researchers wrote.
To establish normal ranges for the second stage of labor in twin deliveries, Dr. Levin, of the department of obstetrics and gynecology at Hadassah-Hebrew University Medical Center, Jerusalem, and coauthors conducted a retrospective cohort study. They analyzed data from three large academic hospitals in Israel between 2011 and June 2020 and assessed the length of the second stage of labor by obstetric history and clinical characteristics.
The researchers included data from women who delivered the first of diamniotic twins spontaneously or delivered a singleton spontaneously. The researchers excluded twin pregnancies with fetal demise of one or both twins, structural anomaly or chromosomal abnormality, monochorionic complications, and first twin in a nonvertex presentation. They did not consider the delivery mode of the second twin.
The study included 2,009 twin deliveries and 135,217 singleton deliveries. Of the women with twin deliveries, 32.6% were nulliparous (that is, no previous vaginal deliveries), 61.5% were parous (one to four previous vaginal deliveries, and no cesarean deliveries), and 5.9% were grand multiparous (at least five previous deliveries).
Of the women with singleton deliveries, 29% were nulliparous.
For nulliparous women delivering twins, the median length of the second stage was 1 hour 27 minutes (interquartile range, 40-147 minutes), and the 95th percentile was 3 hours 51 minutes.
For parous women delivering twins, the median length of the second stage was 18 minutes (interquartile range, 8-36 minutes), and the 95th percentile was 1 hour 56 minutes.
For grand multiparous women, the median length of the second stage was 10 minutes.
In a multivariable analysis, epidural anesthesia and induction of labor were independently associated with increased length of the second stage of labor.
Second-stage labor longer than the 95th percentile based on parity and epidural status was associated with approximately twice the risk of admission to the neonatal intensive care unit (35.4% vs. 16.4%) and need for phototherapy, the researchers reported.
Compared with singleton deliveries, the second stage was longer in twin deliveries. Among nulliparous patients, the median length of the second stage of labor was 1 hour 18 minutes for singleton deliveries, versus 1 hour 30 minutes for twin deliveries. Among parous patients, the median length of the second stage was 19 minutes for twin deliveries, compared with 10 minutes for singleton deliveries.
The study was conducted in Israel, which may limit its generalizability, the authors noted. In addition, the researchers lacked data about maternal morbidity and had limited data about neonatal morbidity. “The exact time that the woman became 10-cm dilated cannot be known, a problem inherent to all such studies,” and cases where doctors artificially ended labor with operative delivery were not included, the researchers added. “More research is needed to determine at what point, if any, intervention is warranted to shorten the second stage in patients delivering twins,” Dr. Levin and colleagues wrote.
Providing a framework
“We always get more concerned if the labor process is happening in a way that is unusual,” and this study provides data that can provide a framework for that thought process, said Dr. Fox, who was not involved in the study.
The results demonstrate that the second stage of labor for twin deliveries may take a long time and “that is not necessarily a bad thing,” said Dr. Fox, clinical professor of obstetrics and gynecology and maternal and fetal medicine at the Icahn School of Medicine at Mount Sinai in New York.
For women having their first child, the second stage of labor tends to take much longer than it does for women who have had children. “That is well known for singletons, and everyone assumes it is the same for twins,” but this study quantifies the durations for twins, he said. “That is valuable, and it is also helpful for women to know what to expect.”
A study coauthor disclosed financial ties to PregnanTech and Anthem AI, and money paid to their institution from New Sight. Dr. Fox works at Maternal Fetal Medicine Associates and Carnegie Imaging for Women in New York and is the creator and host of the Healthful Woman Podcast. He had no relevant financial disclosures.
, researchers say.
Although the analysis found statistically significant differences in second-stage labor lengths for twin and singleton deliveries, “ultimately I think the value in this is seeing that it is not much different,” said Nathan Fox, MD, a maternal-fetal medicine specialist who has studied twin pregnancies and delivery of twins.
Knowledge gap
While most twin births occur by cesarean delivery, vaginal delivery is a preferred method for diamniotic twins with the first twin in vertex presentation, wrote study author Gabriel Levin, MD, and colleagues. Prior studies, however, have not clearly established the duration of the second stage of labor in twin deliveries – that is, the time from 10-cm dilation until delivery of the first twin, they said.
Knowing “the parameters of the normal second stage of labor” for twin deliveries may help guide clinical practice and possibly avoid unnecessary operative deliveries, the researchers wrote.
To establish normal ranges for the second stage of labor in twin deliveries, Dr. Levin, of the department of obstetrics and gynecology at Hadassah-Hebrew University Medical Center, Jerusalem, and coauthors conducted a retrospective cohort study. They analyzed data from three large academic hospitals in Israel between 2011 and June 2020 and assessed the length of the second stage of labor by obstetric history and clinical characteristics.
The researchers included data from women who delivered the first of diamniotic twins spontaneously or delivered a singleton spontaneously. The researchers excluded twin pregnancies with fetal demise of one or both twins, structural anomaly or chromosomal abnormality, monochorionic complications, and first twin in a nonvertex presentation. They did not consider the delivery mode of the second twin.
The study included 2,009 twin deliveries and 135,217 singleton deliveries. Of the women with twin deliveries, 32.6% were nulliparous (that is, no previous vaginal deliveries), 61.5% were parous (one to four previous vaginal deliveries, and no cesarean deliveries), and 5.9% were grand multiparous (at least five previous deliveries).
Of the women with singleton deliveries, 29% were nulliparous.
For nulliparous women delivering twins, the median length of the second stage was 1 hour 27 minutes (interquartile range, 40-147 minutes), and the 95th percentile was 3 hours 51 minutes.
For parous women delivering twins, the median length of the second stage was 18 minutes (interquartile range, 8-36 minutes), and the 95th percentile was 1 hour 56 minutes.
For grand multiparous women, the median length of the second stage was 10 minutes.
In a multivariable analysis, epidural anesthesia and induction of labor were independently associated with increased length of the second stage of labor.
Second-stage labor longer than the 95th percentile based on parity and epidural status was associated with approximately twice the risk of admission to the neonatal intensive care unit (35.4% vs. 16.4%) and need for phototherapy, the researchers reported.
Compared with singleton deliveries, the second stage was longer in twin deliveries. Among nulliparous patients, the median length of the second stage of labor was 1 hour 18 minutes for singleton deliveries, versus 1 hour 30 minutes for twin deliveries. Among parous patients, the median length of the second stage was 19 minutes for twin deliveries, compared with 10 minutes for singleton deliveries.
The study was conducted in Israel, which may limit its generalizability, the authors noted. In addition, the researchers lacked data about maternal morbidity and had limited data about neonatal morbidity. “The exact time that the woman became 10-cm dilated cannot be known, a problem inherent to all such studies,” and cases where doctors artificially ended labor with operative delivery were not included, the researchers added. “More research is needed to determine at what point, if any, intervention is warranted to shorten the second stage in patients delivering twins,” Dr. Levin and colleagues wrote.
Providing a framework
“We always get more concerned if the labor process is happening in a way that is unusual,” and this study provides data that can provide a framework for that thought process, said Dr. Fox, who was not involved in the study.
The results demonstrate that the second stage of labor for twin deliveries may take a long time and “that is not necessarily a bad thing,” said Dr. Fox, clinical professor of obstetrics and gynecology and maternal and fetal medicine at the Icahn School of Medicine at Mount Sinai in New York.
For women having their first child, the second stage of labor tends to take much longer than it does for women who have had children. “That is well known for singletons, and everyone assumes it is the same for twins,” but this study quantifies the durations for twins, he said. “That is valuable, and it is also helpful for women to know what to expect.”
A study coauthor disclosed financial ties to PregnanTech and Anthem AI, and money paid to their institution from New Sight. Dr. Fox works at Maternal Fetal Medicine Associates and Carnegie Imaging for Women in New York and is the creator and host of the Healthful Woman Podcast. He had no relevant financial disclosures.
, researchers say.
Although the analysis found statistically significant differences in second-stage labor lengths for twin and singleton deliveries, “ultimately I think the value in this is seeing that it is not much different,” said Nathan Fox, MD, a maternal-fetal medicine specialist who has studied twin pregnancies and delivery of twins.
Knowledge gap
While most twin births occur by cesarean delivery, vaginal delivery is a preferred method for diamniotic twins with the first twin in vertex presentation, wrote study author Gabriel Levin, MD, and colleagues. Prior studies, however, have not clearly established the duration of the second stage of labor in twin deliveries – that is, the time from 10-cm dilation until delivery of the first twin, they said.
Knowing “the parameters of the normal second stage of labor” for twin deliveries may help guide clinical practice and possibly avoid unnecessary operative deliveries, the researchers wrote.
To establish normal ranges for the second stage of labor in twin deliveries, Dr. Levin, of the department of obstetrics and gynecology at Hadassah-Hebrew University Medical Center, Jerusalem, and coauthors conducted a retrospective cohort study. They analyzed data from three large academic hospitals in Israel between 2011 and June 2020 and assessed the length of the second stage of labor by obstetric history and clinical characteristics.
The researchers included data from women who delivered the first of diamniotic twins spontaneously or delivered a singleton spontaneously. The researchers excluded twin pregnancies with fetal demise of one or both twins, structural anomaly or chromosomal abnormality, monochorionic complications, and first twin in a nonvertex presentation. They did not consider the delivery mode of the second twin.
The study included 2,009 twin deliveries and 135,217 singleton deliveries. Of the women with twin deliveries, 32.6% were nulliparous (that is, no previous vaginal deliveries), 61.5% were parous (one to four previous vaginal deliveries, and no cesarean deliveries), and 5.9% were grand multiparous (at least five previous deliveries).
Of the women with singleton deliveries, 29% were nulliparous.
For nulliparous women delivering twins, the median length of the second stage was 1 hour 27 minutes (interquartile range, 40-147 minutes), and the 95th percentile was 3 hours 51 minutes.
For parous women delivering twins, the median length of the second stage was 18 minutes (interquartile range, 8-36 minutes), and the 95th percentile was 1 hour 56 minutes.
For grand multiparous women, the median length of the second stage was 10 minutes.
In a multivariable analysis, epidural anesthesia and induction of labor were independently associated with increased length of the second stage of labor.
Second-stage labor longer than the 95th percentile based on parity and epidural status was associated with approximately twice the risk of admission to the neonatal intensive care unit (35.4% vs. 16.4%) and need for phototherapy, the researchers reported.
Compared with singleton deliveries, the second stage was longer in twin deliveries. Among nulliparous patients, the median length of the second stage of labor was 1 hour 18 minutes for singleton deliveries, versus 1 hour 30 minutes for twin deliveries. Among parous patients, the median length of the second stage was 19 minutes for twin deliveries, compared with 10 minutes for singleton deliveries.
The study was conducted in Israel, which may limit its generalizability, the authors noted. In addition, the researchers lacked data about maternal morbidity and had limited data about neonatal morbidity. “The exact time that the woman became 10-cm dilated cannot be known, a problem inherent to all such studies,” and cases where doctors artificially ended labor with operative delivery were not included, the researchers added. “More research is needed to determine at what point, if any, intervention is warranted to shorten the second stage in patients delivering twins,” Dr. Levin and colleagues wrote.
Providing a framework
“We always get more concerned if the labor process is happening in a way that is unusual,” and this study provides data that can provide a framework for that thought process, said Dr. Fox, who was not involved in the study.
The results demonstrate that the second stage of labor for twin deliveries may take a long time and “that is not necessarily a bad thing,” said Dr. Fox, clinical professor of obstetrics and gynecology and maternal and fetal medicine at the Icahn School of Medicine at Mount Sinai in New York.
For women having their first child, the second stage of labor tends to take much longer than it does for women who have had children. “That is well known for singletons, and everyone assumes it is the same for twins,” but this study quantifies the durations for twins, he said. “That is valuable, and it is also helpful for women to know what to expect.”
A study coauthor disclosed financial ties to PregnanTech and Anthem AI, and money paid to their institution from New Sight. Dr. Fox works at Maternal Fetal Medicine Associates and Carnegie Imaging for Women in New York and is the creator and host of the Healthful Woman Podcast. He had no relevant financial disclosures.
FROM OBSTETRICS AND GYNECOLOGY
Match Day 2021: Interest in ob.gyn. outpaced growth
In a record year for the Match, ob.gyn. residencies filled 99.8% of their available positions in 2021, according to the National Resident Matching Program.
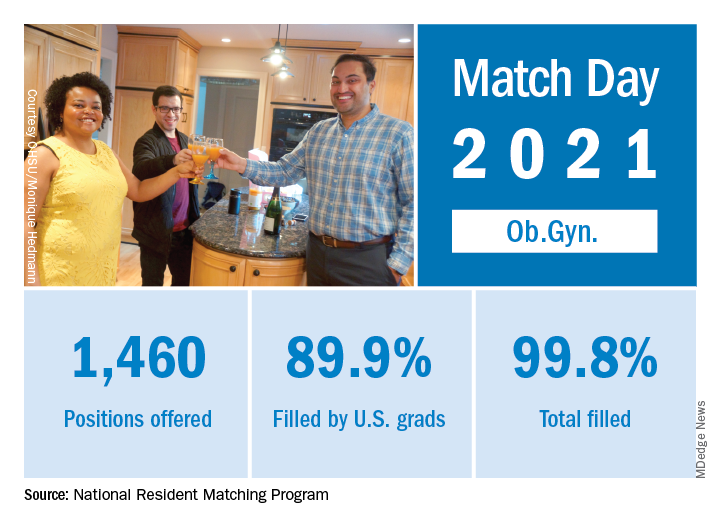
“Rather than faltering in these uncertain times, program fill rates increased across the board,” the NRMP said in a written statement. Overall, the 2021 Main Residency Match offered (35,194) and filled (33,353) more first-year (PGY-1) slots than ever before, for a fill rate of 94.8%, compared with 94.6% the year before.
The fill rate for obstetrics and gynecology was an even higher 99.8%, with 1,460 positions offered and 1,457 filled – each up 1.2% over 2020. Nearly 90% (1,313) of the available slots were given to U.S. seniors (MDs and DOs), while 6% went to international medical graduates (IMGs). The corresponding PGY-1 numbers for the Match as a whole were 70.4% U.S. and 21.1% international medical graduates, based on NRMP data.
Over the longer term, the number of positions offered in ob.gyn. residencies has increased by 172 (13.4%) since 2017, but that growth lags behind the Match as a whole, which has seen a 22% increase in available slots over the last 5 years, the NRMP said in the report.
“Concerns about the impact of virtual recruitment on applicants’ matching into PGY-1 positions were not realized,” the NRMP noted, as “growth in registration was seen in every applicant group.” Compared with 2020, submissions of rank-order lists of programs were up by 2.8% for U.S. MD seniors, 7.9% for U.S. DO seniors, 2.5% among U.S.-citizen IMGs, and 15.0% for non–U.S.-citizen IMGs.
“The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” said Donna L. Lamb, DHSc, MBA, BSN, president and CEO of the NRMP.
In a record year for the Match, ob.gyn. residencies filled 99.8% of their available positions in 2021, according to the National Resident Matching Program.
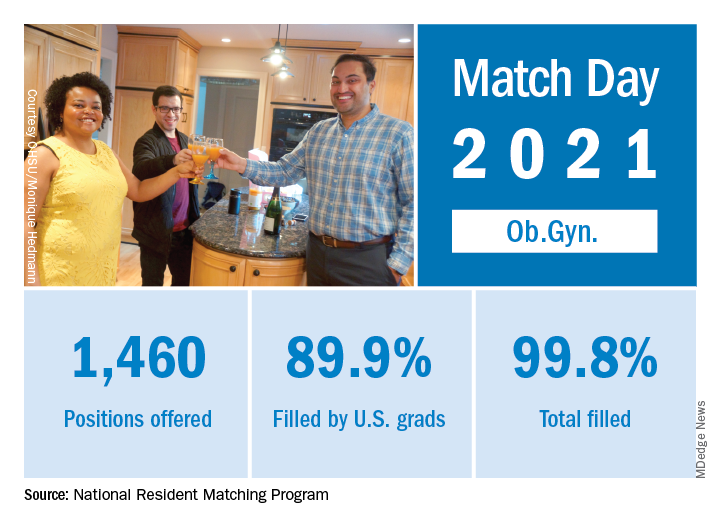
“Rather than faltering in these uncertain times, program fill rates increased across the board,” the NRMP said in a written statement. Overall, the 2021 Main Residency Match offered (35,194) and filled (33,353) more first-year (PGY-1) slots than ever before, for a fill rate of 94.8%, compared with 94.6% the year before.
The fill rate for obstetrics and gynecology was an even higher 99.8%, with 1,460 positions offered and 1,457 filled – each up 1.2% over 2020. Nearly 90% (1,313) of the available slots were given to U.S. seniors (MDs and DOs), while 6% went to international medical graduates (IMGs). The corresponding PGY-1 numbers for the Match as a whole were 70.4% U.S. and 21.1% international medical graduates, based on NRMP data.
Over the longer term, the number of positions offered in ob.gyn. residencies has increased by 172 (13.4%) since 2017, but that growth lags behind the Match as a whole, which has seen a 22% increase in available slots over the last 5 years, the NRMP said in the report.
“Concerns about the impact of virtual recruitment on applicants’ matching into PGY-1 positions were not realized,” the NRMP noted, as “growth in registration was seen in every applicant group.” Compared with 2020, submissions of rank-order lists of programs were up by 2.8% for U.S. MD seniors, 7.9% for U.S. DO seniors, 2.5% among U.S.-citizen IMGs, and 15.0% for non–U.S.-citizen IMGs.
“The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” said Donna L. Lamb, DHSc, MBA, BSN, president and CEO of the NRMP.
In a record year for the Match, ob.gyn. residencies filled 99.8% of their available positions in 2021, according to the National Resident Matching Program.
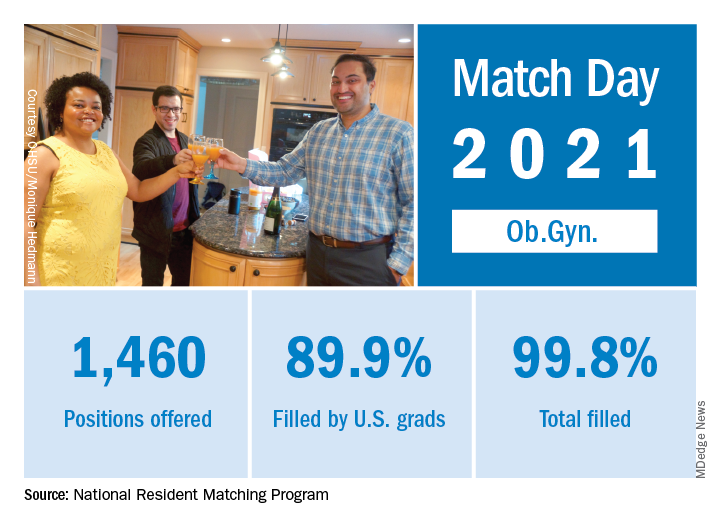
“Rather than faltering in these uncertain times, program fill rates increased across the board,” the NRMP said in a written statement. Overall, the 2021 Main Residency Match offered (35,194) and filled (33,353) more first-year (PGY-1) slots than ever before, for a fill rate of 94.8%, compared with 94.6% the year before.
The fill rate for obstetrics and gynecology was an even higher 99.8%, with 1,460 positions offered and 1,457 filled – each up 1.2% over 2020. Nearly 90% (1,313) of the available slots were given to U.S. seniors (MDs and DOs), while 6% went to international medical graduates (IMGs). The corresponding PGY-1 numbers for the Match as a whole were 70.4% U.S. and 21.1% international medical graduates, based on NRMP data.
Over the longer term, the number of positions offered in ob.gyn. residencies has increased by 172 (13.4%) since 2017, but that growth lags behind the Match as a whole, which has seen a 22% increase in available slots over the last 5 years, the NRMP said in the report.
“Concerns about the impact of virtual recruitment on applicants’ matching into PGY-1 positions were not realized,” the NRMP noted, as “growth in registration was seen in every applicant group.” Compared with 2020, submissions of rank-order lists of programs were up by 2.8% for U.S. MD seniors, 7.9% for U.S. DO seniors, 2.5% among U.S.-citizen IMGs, and 15.0% for non–U.S.-citizen IMGs.
“The application and recruitment cycle was upended as a result of the pandemic, yet the results of the Match continue to demonstrate strong and consistent outcomes for participants,” said Donna L. Lamb, DHSc, MBA, BSN, president and CEO of the NRMP.
ApoB may better predict mortality risk in statin-treated patients
A new study shows apolipoprotein B (apoB) and non-HDL cholesterol – but not LDL cholesterol – are associated with increased risk for all-cause mortality and myocardial infarction in patients taking statins.
Moreover, apoB was a more accurate marker of all-cause mortality risk than non-HDL or LDL cholesterol and was more accurate at identifying MI risk than LDL cholesterol.
“Any patient that comes to a doctor for evaluation, if statin treatment is sufficient, the doctor should look not only at LDL cholesterol but HDL cholesterol and apoB, if its available – that is the take-home message,” senior author Børge Grønne Nordestgaard, MD, DMSC, University of Copenhagen, said in an interview.
The findings are very relevant to clinical practice because international guidelines focus on LDL cholesterol and “many doctors are brainwashed that that is the only thing they should look at, just to keep LDL cholesterol down,” he said. “I’ve worked for years with triglyceride lipoproteins, what I call remnant cholesterol, and I think that the risk is very high also when you have high remnant cholesterol.”
Previous work has shown that apoB and non-HDL cholesterol better reflect atherosclerotic cardiovascular disease risk than LDL cholesterol. This is the first study, however, to show that elevated apoB and non-HDL cholesterol are associated with a higher risk for all-cause death in statin-treated patients with low LDL cholesterol, Dr. Nordestgaard noted.
The investigators compared outcomes among 13,015 statin-treated participants in the Copenhagen General Population Study using median baseline values of 92 mg/dL for apoB, 3.1 mmol/L (120 mg/dL) for non-HDL cholesterol, and 2.3 mmol/L (89 mg/dL) for LDL cholesterol. Over a median follow-up of 8 years, there were 2,499 deaths and 537 MIs.
As reported in the Journal of the American College of Cardiology, discordant apoB above the median with LDL cholesterol below was associated with a 21% increased risk for all-cause mortality (hazard ratio, 1.21; 95% confidence interval, 1.07-1.36) and 49% increased risk for MI (HR, 1.49; 95% CI, 1.15-1.92), compared with concordant apoB and LDL cholesterol below the medians.
Similar results were found for discordant non-HDL cholesterol above the median with low LDL cholesterol for all-cause mortality (HR, 1.18; 95% CI, 1.02-1.36) and MI (1.78; 95% CI, 1.35-2.34).
No such associations with mortality or MI were observed when LDL cholesterol was above the median and apoB or non-HDL below.
Additional analyses showed that high apoB with low non-HDL cholesterol was associated with a higher risk for all-cause mortality (HR, 1.21; 95% CI, 1.03-1.41), whereas high non-HDL cholesterol with low apoB was associated with a lower risk (HR, 0.75; 95% CI, 0.62-0.92).
Current guidelines define apoB greater than 130 mg/dL as a risk modifier in patients not using statins but, the authors wrote, “based on our results, the threshold for apoB as a risk modifier in statin-treated patients should be closer to 92 mg/dL than to 130 mg/dL.”
In an accompanying editorial, Neil J. Stone, MD, and Donald Lloyd-Jones, MD, both from Northwestern University, Chicago, said that American and European guidelines acknowledge the usefulness of apoB and non-HDL cholesterol in their risk algorithms and as possible targets to indicate efficacy, but don’t give a strong recommendation for apoB to assess residual risk.
“This paper suggests that, in the next iteration, we’ve got to give a stronger thought to measuring apoB for residual risk in those with secondary prevention,” Dr. Stone, vice chair of the 2018 American Heart Association/ACC cholesterol guidelines, said in an interview.
“The whole part of the guidelines was not to focus on any one number but to focus on the clinical risk as a whole,” he said. “You can enlarge your understanding of the patient by looking at their non-HDL, which you have anyway, and in certain circumstances, for example, people with metabolic syndrome, diabetes, obesity, or high triglycerides, those people might very well benefit from an apoB to further understand their risk. This paper simply highlights that and, therefore, was very valuable.”
Dr. Stone and Dr. Lloyd-Jones, however, pointed out that statin use was self-reported and information was lacking on adherence, dose intensity, and the amount of LDL cholesterol lowering from baseline. LDL cholesterol levels were also above current recommendations for optimizing risk reduction. “If statin dosing and LDL [cholesterol] were not optimized already, then there may have been ‘room’ for non-HDL [cholesterol] and apoB to add value in understanding residual risk,” they wrote.
The editorialists suggested that sequential use, rather than regular use, of apoB and non-HDL cholesterol may be best and that incorporating this information may be particularly beneficial for patients with metabolic disorders and elevated triglycerides after statin therapy.
“Maybe this paper is a wake-up call that there are other markers out there that can tell you that you still have higher risk and need to tighten up lifestyle and maybe be more adherent,” Dr. Stone said. “I think this is a wonderful chance to say that preventive cardiology isn’t just ‘set it and forget it’.”
C. Noel Bairey Merz, MD, who coauthored the 2018 cholesterol guidelines, agreed there’s “an overexuberant focus on LDL [cholesterol] for residual risk” and highlighted a recent systematic review of statins, ezetimibe, and PCSK9 cardiovascular outcomes trials that showed very little gain from aggressively driving down LDL below 100 mg/dL, unless the patient is at extremely high risk.
“If I, as a treating cardiologist who spends a lot of time on lipids, had a patient on a high-intensity statin and they didn’t drop [their LDL cholesterol] 50% and I already had them going to cardiac rehab and they were already losing weight, would I measure apoB? Yeah, I might, to motivate them to do more or to take Vascepa,” she said.
“This study is a useful addition to a relatively important problem, which is residual risk, and really supports personalized or precision medicine,” added Bairey Merz, MD, Cedars-Sinai Medical Center, Los Angeles. “But now we have to do the work and do an intervention trial in these people and see whether these markers make a difference.”
The study was supported by Herlev and Gentofte Hospital’s Research Fund and the department of clinical biochemistry, Herlev and Gentofte Hospital, Copenhagen University Hospital. Dr. Nordestgaard has had consultancies or talks sponsored by AstraZeneca, Sanofi, Regeneron, Akcea, Amarin, Amgen, Esperion, Kowa, Novartis, Novo Nordisk, and Silence Therapeutics. All other authors, Dr. Stone, and Dr. Lloyd-Jones reported no conflicts. Dr. Merz reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
A new study shows apolipoprotein B (apoB) and non-HDL cholesterol – but not LDL cholesterol – are associated with increased risk for all-cause mortality and myocardial infarction in patients taking statins.
Moreover, apoB was a more accurate marker of all-cause mortality risk than non-HDL or LDL cholesterol and was more accurate at identifying MI risk than LDL cholesterol.
“Any patient that comes to a doctor for evaluation, if statin treatment is sufficient, the doctor should look not only at LDL cholesterol but HDL cholesterol and apoB, if its available – that is the take-home message,” senior author Børge Grønne Nordestgaard, MD, DMSC, University of Copenhagen, said in an interview.
The findings are very relevant to clinical practice because international guidelines focus on LDL cholesterol and “many doctors are brainwashed that that is the only thing they should look at, just to keep LDL cholesterol down,” he said. “I’ve worked for years with triglyceride lipoproteins, what I call remnant cholesterol, and I think that the risk is very high also when you have high remnant cholesterol.”
Previous work has shown that apoB and non-HDL cholesterol better reflect atherosclerotic cardiovascular disease risk than LDL cholesterol. This is the first study, however, to show that elevated apoB and non-HDL cholesterol are associated with a higher risk for all-cause death in statin-treated patients with low LDL cholesterol, Dr. Nordestgaard noted.
The investigators compared outcomes among 13,015 statin-treated participants in the Copenhagen General Population Study using median baseline values of 92 mg/dL for apoB, 3.1 mmol/L (120 mg/dL) for non-HDL cholesterol, and 2.3 mmol/L (89 mg/dL) for LDL cholesterol. Over a median follow-up of 8 years, there were 2,499 deaths and 537 MIs.
As reported in the Journal of the American College of Cardiology, discordant apoB above the median with LDL cholesterol below was associated with a 21% increased risk for all-cause mortality (hazard ratio, 1.21; 95% confidence interval, 1.07-1.36) and 49% increased risk for MI (HR, 1.49; 95% CI, 1.15-1.92), compared with concordant apoB and LDL cholesterol below the medians.
Similar results were found for discordant non-HDL cholesterol above the median with low LDL cholesterol for all-cause mortality (HR, 1.18; 95% CI, 1.02-1.36) and MI (1.78; 95% CI, 1.35-2.34).
No such associations with mortality or MI were observed when LDL cholesterol was above the median and apoB or non-HDL below.
Additional analyses showed that high apoB with low non-HDL cholesterol was associated with a higher risk for all-cause mortality (HR, 1.21; 95% CI, 1.03-1.41), whereas high non-HDL cholesterol with low apoB was associated with a lower risk (HR, 0.75; 95% CI, 0.62-0.92).
Current guidelines define apoB greater than 130 mg/dL as a risk modifier in patients not using statins but, the authors wrote, “based on our results, the threshold for apoB as a risk modifier in statin-treated patients should be closer to 92 mg/dL than to 130 mg/dL.”
In an accompanying editorial, Neil J. Stone, MD, and Donald Lloyd-Jones, MD, both from Northwestern University, Chicago, said that American and European guidelines acknowledge the usefulness of apoB and non-HDL cholesterol in their risk algorithms and as possible targets to indicate efficacy, but don’t give a strong recommendation for apoB to assess residual risk.
“This paper suggests that, in the next iteration, we’ve got to give a stronger thought to measuring apoB for residual risk in those with secondary prevention,” Dr. Stone, vice chair of the 2018 American Heart Association/ACC cholesterol guidelines, said in an interview.
“The whole part of the guidelines was not to focus on any one number but to focus on the clinical risk as a whole,” he said. “You can enlarge your understanding of the patient by looking at their non-HDL, which you have anyway, and in certain circumstances, for example, people with metabolic syndrome, diabetes, obesity, or high triglycerides, those people might very well benefit from an apoB to further understand their risk. This paper simply highlights that and, therefore, was very valuable.”
Dr. Stone and Dr. Lloyd-Jones, however, pointed out that statin use was self-reported and information was lacking on adherence, dose intensity, and the amount of LDL cholesterol lowering from baseline. LDL cholesterol levels were also above current recommendations for optimizing risk reduction. “If statin dosing and LDL [cholesterol] were not optimized already, then there may have been ‘room’ for non-HDL [cholesterol] and apoB to add value in understanding residual risk,” they wrote.
The editorialists suggested that sequential use, rather than regular use, of apoB and non-HDL cholesterol may be best and that incorporating this information may be particularly beneficial for patients with metabolic disorders and elevated triglycerides after statin therapy.
“Maybe this paper is a wake-up call that there are other markers out there that can tell you that you still have higher risk and need to tighten up lifestyle and maybe be more adherent,” Dr. Stone said. “I think this is a wonderful chance to say that preventive cardiology isn’t just ‘set it and forget it’.”
C. Noel Bairey Merz, MD, who coauthored the 2018 cholesterol guidelines, agreed there’s “an overexuberant focus on LDL [cholesterol] for residual risk” and highlighted a recent systematic review of statins, ezetimibe, and PCSK9 cardiovascular outcomes trials that showed very little gain from aggressively driving down LDL below 100 mg/dL, unless the patient is at extremely high risk.
“If I, as a treating cardiologist who spends a lot of time on lipids, had a patient on a high-intensity statin and they didn’t drop [their LDL cholesterol] 50% and I already had them going to cardiac rehab and they were already losing weight, would I measure apoB? Yeah, I might, to motivate them to do more or to take Vascepa,” she said.
“This study is a useful addition to a relatively important problem, which is residual risk, and really supports personalized or precision medicine,” added Bairey Merz, MD, Cedars-Sinai Medical Center, Los Angeles. “But now we have to do the work and do an intervention trial in these people and see whether these markers make a difference.”
The study was supported by Herlev and Gentofte Hospital’s Research Fund and the department of clinical biochemistry, Herlev and Gentofte Hospital, Copenhagen University Hospital. Dr. Nordestgaard has had consultancies or talks sponsored by AstraZeneca, Sanofi, Regeneron, Akcea, Amarin, Amgen, Esperion, Kowa, Novartis, Novo Nordisk, and Silence Therapeutics. All other authors, Dr. Stone, and Dr. Lloyd-Jones reported no conflicts. Dr. Merz reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
A new study shows apolipoprotein B (apoB) and non-HDL cholesterol – but not LDL cholesterol – are associated with increased risk for all-cause mortality and myocardial infarction in patients taking statins.
Moreover, apoB was a more accurate marker of all-cause mortality risk than non-HDL or LDL cholesterol and was more accurate at identifying MI risk than LDL cholesterol.
“Any patient that comes to a doctor for evaluation, if statin treatment is sufficient, the doctor should look not only at LDL cholesterol but HDL cholesterol and apoB, if its available – that is the take-home message,” senior author Børge Grønne Nordestgaard, MD, DMSC, University of Copenhagen, said in an interview.
The findings are very relevant to clinical practice because international guidelines focus on LDL cholesterol and “many doctors are brainwashed that that is the only thing they should look at, just to keep LDL cholesterol down,” he said. “I’ve worked for years with triglyceride lipoproteins, what I call remnant cholesterol, and I think that the risk is very high also when you have high remnant cholesterol.”
Previous work has shown that apoB and non-HDL cholesterol better reflect atherosclerotic cardiovascular disease risk than LDL cholesterol. This is the first study, however, to show that elevated apoB and non-HDL cholesterol are associated with a higher risk for all-cause death in statin-treated patients with low LDL cholesterol, Dr. Nordestgaard noted.
The investigators compared outcomes among 13,015 statin-treated participants in the Copenhagen General Population Study using median baseline values of 92 mg/dL for apoB, 3.1 mmol/L (120 mg/dL) for non-HDL cholesterol, and 2.3 mmol/L (89 mg/dL) for LDL cholesterol. Over a median follow-up of 8 years, there were 2,499 deaths and 537 MIs.
As reported in the Journal of the American College of Cardiology, discordant apoB above the median with LDL cholesterol below was associated with a 21% increased risk for all-cause mortality (hazard ratio, 1.21; 95% confidence interval, 1.07-1.36) and 49% increased risk for MI (HR, 1.49; 95% CI, 1.15-1.92), compared with concordant apoB and LDL cholesterol below the medians.
Similar results were found for discordant non-HDL cholesterol above the median with low LDL cholesterol for all-cause mortality (HR, 1.18; 95% CI, 1.02-1.36) and MI (1.78; 95% CI, 1.35-2.34).
No such associations with mortality or MI were observed when LDL cholesterol was above the median and apoB or non-HDL below.
Additional analyses showed that high apoB with low non-HDL cholesterol was associated with a higher risk for all-cause mortality (HR, 1.21; 95% CI, 1.03-1.41), whereas high non-HDL cholesterol with low apoB was associated with a lower risk (HR, 0.75; 95% CI, 0.62-0.92).
Current guidelines define apoB greater than 130 mg/dL as a risk modifier in patients not using statins but, the authors wrote, “based on our results, the threshold for apoB as a risk modifier in statin-treated patients should be closer to 92 mg/dL than to 130 mg/dL.”
In an accompanying editorial, Neil J. Stone, MD, and Donald Lloyd-Jones, MD, both from Northwestern University, Chicago, said that American and European guidelines acknowledge the usefulness of apoB and non-HDL cholesterol in their risk algorithms and as possible targets to indicate efficacy, but don’t give a strong recommendation for apoB to assess residual risk.
“This paper suggests that, in the next iteration, we’ve got to give a stronger thought to measuring apoB for residual risk in those with secondary prevention,” Dr. Stone, vice chair of the 2018 American Heart Association/ACC cholesterol guidelines, said in an interview.
“The whole part of the guidelines was not to focus on any one number but to focus on the clinical risk as a whole,” he said. “You can enlarge your understanding of the patient by looking at their non-HDL, which you have anyway, and in certain circumstances, for example, people with metabolic syndrome, diabetes, obesity, or high triglycerides, those people might very well benefit from an apoB to further understand their risk. This paper simply highlights that and, therefore, was very valuable.”
Dr. Stone and Dr. Lloyd-Jones, however, pointed out that statin use was self-reported and information was lacking on adherence, dose intensity, and the amount of LDL cholesterol lowering from baseline. LDL cholesterol levels were also above current recommendations for optimizing risk reduction. “If statin dosing and LDL [cholesterol] were not optimized already, then there may have been ‘room’ for non-HDL [cholesterol] and apoB to add value in understanding residual risk,” they wrote.
The editorialists suggested that sequential use, rather than regular use, of apoB and non-HDL cholesterol may be best and that incorporating this information may be particularly beneficial for patients with metabolic disorders and elevated triglycerides after statin therapy.
“Maybe this paper is a wake-up call that there are other markers out there that can tell you that you still have higher risk and need to tighten up lifestyle and maybe be more adherent,” Dr. Stone said. “I think this is a wonderful chance to say that preventive cardiology isn’t just ‘set it and forget it’.”
C. Noel Bairey Merz, MD, who coauthored the 2018 cholesterol guidelines, agreed there’s “an overexuberant focus on LDL [cholesterol] for residual risk” and highlighted a recent systematic review of statins, ezetimibe, and PCSK9 cardiovascular outcomes trials that showed very little gain from aggressively driving down LDL below 100 mg/dL, unless the patient is at extremely high risk.
“If I, as a treating cardiologist who spends a lot of time on lipids, had a patient on a high-intensity statin and they didn’t drop [their LDL cholesterol] 50% and I already had them going to cardiac rehab and they were already losing weight, would I measure apoB? Yeah, I might, to motivate them to do more or to take Vascepa,” she said.
“This study is a useful addition to a relatively important problem, which is residual risk, and really supports personalized or precision medicine,” added Bairey Merz, MD, Cedars-Sinai Medical Center, Los Angeles. “But now we have to do the work and do an intervention trial in these people and see whether these markers make a difference.”
The study was supported by Herlev and Gentofte Hospital’s Research Fund and the department of clinical biochemistry, Herlev and Gentofte Hospital, Copenhagen University Hospital. Dr. Nordestgaard has had consultancies or talks sponsored by AstraZeneca, Sanofi, Regeneron, Akcea, Amarin, Amgen, Esperion, Kowa, Novartis, Novo Nordisk, and Silence Therapeutics. All other authors, Dr. Stone, and Dr. Lloyd-Jones reported no conflicts. Dr. Merz reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
















