User login
Nonablative laser improved PIH in patients with darker skin
Yoon‐Soo Cindy Bae, MD, and colleagues reported.
Among patients treated with the nonablative fractional 1,927 nm laser, there was a mean improvement of about 43% in hyperpigmented areas, and no side effects were reported, wrote Dr. Bae, of the department of dermatology at New York University and the Laser & Skin Surgery Center of New York, and coauthors in Lasers in Surgery and Medicine.
Lasers have not been the first choice for hyperpigmentation in Fitzpatrick skin types IV, V, and VI, they pointed out. More commonly used treatments are hydroquinone and chemical peels that use glycolic acid or salicylic acid. But these are not always ideal options, Dr. Bae said in an interview.
“There are side effects to medical therapy. The drawbacks of medical therapy include compliance issues, risk of skin irritation from the product ... and a risk of hyperpigmentation specifically for hydroquinone. There are also risks to laser therapy, including dyspigmentation and scarring,” she added. “However, the laser we used is a low energy, nonablative type of laser, so the risk of scarring is extremely rare and the dyspigmentation is actually what we are aiming to treat.”
The retrospective study comprised 61 patients with PIH who had received more than one treatment with the low energy fractionated 1,927 nm diode laser between 2013 and 2016. Most were Fitzpatrick type IV (73.8%). The remainder were Type V (16.4%) and Type VI (9.8%). The most common treatment site was the face or cheeks (68.9%), followed by legs (13%), the rest of the cases were unspecified.
Patients had received treatment with the laser with fixed fluence at 5 mJ, fixed spot size of 140 micrometers, depth of 170 micrometers, and 5% coverage. They required several treatments: 15 had two, 14 had three, 16 had four, and the remainder had five or more. Topical treatment data were not collected. Photographs taken before treatment and before the last treatment were evaluated by dermatologists who had not treated the patients. Based on those evaluations, the mean improvement was a statistically significant 43.2%.
There did not, however, appear to be much difference between the treatment groups. The mean improvement among patients with two treatments was 44.5%; three treatments, 44.29%; four treatments, 40.63%; five or more treatments, 43.75%.
Although those with darker skin types tended to have better results, there were no statistically significant differences between the skin-type groups. Among those with Fitzpatrick skin type IV, the mean improvement was 40.39%; skin type V, 47.25%; and skin type VI, 57.92%.
“The fact that there was no correlation between Fitzpatrick skin type … and average percent improvement demonstrates that this laser is a viable treatment option for patients with very dark skin,” the authors wrote. “There were also no significant differences between the average percent improvements for people receiving different numbers of treatments. A trend was observed that favored treating patients with darker skin type; however, this lacked statistical significance. This may have been due to an underpowered study.”
Limitations of the study included the retrospective design and nonstandardization of photographs; “further studies with prospective controlled designs are needed to confirm our findings,” they added.
No funding or disclosure information was provided.
[email protected]
SOURCE: Bae YS et al. Lasers Surg Med. 2019 Oct 29. doi: 10.1002/lsm.23173.
Yoon‐Soo Cindy Bae, MD, and colleagues reported.
Among patients treated with the nonablative fractional 1,927 nm laser, there was a mean improvement of about 43% in hyperpigmented areas, and no side effects were reported, wrote Dr. Bae, of the department of dermatology at New York University and the Laser & Skin Surgery Center of New York, and coauthors in Lasers in Surgery and Medicine.
Lasers have not been the first choice for hyperpigmentation in Fitzpatrick skin types IV, V, and VI, they pointed out. More commonly used treatments are hydroquinone and chemical peels that use glycolic acid or salicylic acid. But these are not always ideal options, Dr. Bae said in an interview.
“There are side effects to medical therapy. The drawbacks of medical therapy include compliance issues, risk of skin irritation from the product ... and a risk of hyperpigmentation specifically for hydroquinone. There are also risks to laser therapy, including dyspigmentation and scarring,” she added. “However, the laser we used is a low energy, nonablative type of laser, so the risk of scarring is extremely rare and the dyspigmentation is actually what we are aiming to treat.”
The retrospective study comprised 61 patients with PIH who had received more than one treatment with the low energy fractionated 1,927 nm diode laser between 2013 and 2016. Most were Fitzpatrick type IV (73.8%). The remainder were Type V (16.4%) and Type VI (9.8%). The most common treatment site was the face or cheeks (68.9%), followed by legs (13%), the rest of the cases were unspecified.
Patients had received treatment with the laser with fixed fluence at 5 mJ, fixed spot size of 140 micrometers, depth of 170 micrometers, and 5% coverage. They required several treatments: 15 had two, 14 had three, 16 had four, and the remainder had five or more. Topical treatment data were not collected. Photographs taken before treatment and before the last treatment were evaluated by dermatologists who had not treated the patients. Based on those evaluations, the mean improvement was a statistically significant 43.2%.
There did not, however, appear to be much difference between the treatment groups. The mean improvement among patients with two treatments was 44.5%; three treatments, 44.29%; four treatments, 40.63%; five or more treatments, 43.75%.
Although those with darker skin types tended to have better results, there were no statistically significant differences between the skin-type groups. Among those with Fitzpatrick skin type IV, the mean improvement was 40.39%; skin type V, 47.25%; and skin type VI, 57.92%.
“The fact that there was no correlation between Fitzpatrick skin type … and average percent improvement demonstrates that this laser is a viable treatment option for patients with very dark skin,” the authors wrote. “There were also no significant differences between the average percent improvements for people receiving different numbers of treatments. A trend was observed that favored treating patients with darker skin type; however, this lacked statistical significance. This may have been due to an underpowered study.”
Limitations of the study included the retrospective design and nonstandardization of photographs; “further studies with prospective controlled designs are needed to confirm our findings,” they added.
No funding or disclosure information was provided.
[email protected]
SOURCE: Bae YS et al. Lasers Surg Med. 2019 Oct 29. doi: 10.1002/lsm.23173.
Yoon‐Soo Cindy Bae, MD, and colleagues reported.
Among patients treated with the nonablative fractional 1,927 nm laser, there was a mean improvement of about 43% in hyperpigmented areas, and no side effects were reported, wrote Dr. Bae, of the department of dermatology at New York University and the Laser & Skin Surgery Center of New York, and coauthors in Lasers in Surgery and Medicine.
Lasers have not been the first choice for hyperpigmentation in Fitzpatrick skin types IV, V, and VI, they pointed out. More commonly used treatments are hydroquinone and chemical peels that use glycolic acid or salicylic acid. But these are not always ideal options, Dr. Bae said in an interview.
“There are side effects to medical therapy. The drawbacks of medical therapy include compliance issues, risk of skin irritation from the product ... and a risk of hyperpigmentation specifically for hydroquinone. There are also risks to laser therapy, including dyspigmentation and scarring,” she added. “However, the laser we used is a low energy, nonablative type of laser, so the risk of scarring is extremely rare and the dyspigmentation is actually what we are aiming to treat.”
The retrospective study comprised 61 patients with PIH who had received more than one treatment with the low energy fractionated 1,927 nm diode laser between 2013 and 2016. Most were Fitzpatrick type IV (73.8%). The remainder were Type V (16.4%) and Type VI (9.8%). The most common treatment site was the face or cheeks (68.9%), followed by legs (13%), the rest of the cases were unspecified.
Patients had received treatment with the laser with fixed fluence at 5 mJ, fixed spot size of 140 micrometers, depth of 170 micrometers, and 5% coverage. They required several treatments: 15 had two, 14 had three, 16 had four, and the remainder had five or more. Topical treatment data were not collected. Photographs taken before treatment and before the last treatment were evaluated by dermatologists who had not treated the patients. Based on those evaluations, the mean improvement was a statistically significant 43.2%.
There did not, however, appear to be much difference between the treatment groups. The mean improvement among patients with two treatments was 44.5%; three treatments, 44.29%; four treatments, 40.63%; five or more treatments, 43.75%.
Although those with darker skin types tended to have better results, there were no statistically significant differences between the skin-type groups. Among those with Fitzpatrick skin type IV, the mean improvement was 40.39%; skin type V, 47.25%; and skin type VI, 57.92%.
“The fact that there was no correlation between Fitzpatrick skin type … and average percent improvement demonstrates that this laser is a viable treatment option for patients with very dark skin,” the authors wrote. “There were also no significant differences between the average percent improvements for people receiving different numbers of treatments. A trend was observed that favored treating patients with darker skin type; however, this lacked statistical significance. This may have been due to an underpowered study.”
Limitations of the study included the retrospective design and nonstandardization of photographs; “further studies with prospective controlled designs are needed to confirm our findings,” they added.
No funding or disclosure information was provided.
[email protected]
SOURCE: Bae YS et al. Lasers Surg Med. 2019 Oct 29. doi: 10.1002/lsm.23173.
FROM LASERS IN SURGERY AND MEDICINE
Bilateral mastectomy reduces second breast cancer risk, but not deaths
Bilateral mastectomy significantly decreases the risk for a second contralateral breast cancer, but does not decrease the risk of death, compared with breast-conserving therapy, results of a large retrospective study indicate.
Among 245,418 patients followed for a median of 6.7 years, the risk of death from breast cancer was similar for those who had undergone either breast-conserving therapy or bilateral mastectomy (BLM) but was 20% higher among women who had undergone unilateral mastectomy (ULM) when compared with breast-conserving therapy, reported Allison W. Kurian, MD, MSc, from Stanford (Calif.) University, and colleagues.
“Second breast cancers are rare, and their reduction should be weighed against the harms associated with BLM,” they wrote in a study published online in Cancer.
The investigators extracted data from the Surveillance, Epidemiology, and End Results program on all women diagnosed with American Joint Committee on Cancer stage 0 to stage III unilateral breast cancer in California from 1998 to 2015 who were treated with either BLM versus breast-conserving therapy, including surgery and radiation or unilateral mastectomy.
They calculated the absolute excess risk of contralateral breast cancer as the observed minus expected number of breast cancers in the general population divided by 10,000 person-years at risk.
Of 421,643 women with a first diagnosis of primary breast cancer during the study period, 245,418 met the study criteria. Of this cohort, 7,784 (3.2%) developed a contralateral second breast cancer more than 6 months after diagnosis of the first, after a median 6.7 years of follow-up.
Slightly more than half of the cohort (52.1%) had undergone breast-conserving therapy, 37.5% underwent unilateral mastectomy, and 7.6% had bilateral mastectomy. An additional 2.9% of patients were women aged 70 years and older with stage I hormone receptor–positive, HER2-negative disease who underwent breast-conserving surgery without radiation (percentages exceed 100% because of rounding).
A multivariate-adjusted model showed that, as might be expected, patients who underwent bilateral mastectomy had a 90% reduction in risk of contralateral cancer (hazard ratio, 0.10; P less than .001), compared with breast-conserving therapy. In contrast, patients who underwent unilateral mastectomy had a slight but significant increase in risk for a second contralateral breast cancer (HR, 1.07; P = .008).
The absolute excess risk for second contralateral breast cancer was 5 per 10,000 person-years with breast-conserving therapy, 13.6 per 10,000 person-years with unilateral mastectomy, and –28.6 per 10,000 person-years with bilateral mastectomy.
When they looked at risk for death, however they found that, compared with breast-conserving therapy, breast-conserving surgery alone (HR, 1.36; P = .0001) and unilateral mastectomy (HR, 1.21; P less than .001), but not bilateral mastectomy (HR, 1.03; P = .35) were significantly associated with increased risk for breast cancer death.
The authors noted that their estimates of absolute risk of second contralateral breast cancer jibe with those of earlier studies, and can help clinicians frame the discussion of the benefits versus risks for individual patients.
“What one patient might consider to be a negligible benefit of BLM, weighed against its potential harms of greater pain, recovery time, and impact on body image and employment, might appear worthwhile to another,” they wrote.
The study was funded by the National Cancer Institute, National Institutes of Health, Department of Health & Human Services, Suzanne Pride Bryan Fund for Breast Cancer Research, Jan Weimer Faculty Chair for Breast Oncology, and the BRCA Foundation. Dr. Kurian disclosed institutional research funding from Myriad Genetics.
SOURCE: Kurin AW et al. Cancer. 2019 Nov 21. doi: 10.1002/cncr.32618.
Bilateral mastectomy significantly decreases the risk for a second contralateral breast cancer, but does not decrease the risk of death, compared with breast-conserving therapy, results of a large retrospective study indicate.
Among 245,418 patients followed for a median of 6.7 years, the risk of death from breast cancer was similar for those who had undergone either breast-conserving therapy or bilateral mastectomy (BLM) but was 20% higher among women who had undergone unilateral mastectomy (ULM) when compared with breast-conserving therapy, reported Allison W. Kurian, MD, MSc, from Stanford (Calif.) University, and colleagues.
“Second breast cancers are rare, and their reduction should be weighed against the harms associated with BLM,” they wrote in a study published online in Cancer.
The investigators extracted data from the Surveillance, Epidemiology, and End Results program on all women diagnosed with American Joint Committee on Cancer stage 0 to stage III unilateral breast cancer in California from 1998 to 2015 who were treated with either BLM versus breast-conserving therapy, including surgery and radiation or unilateral mastectomy.
They calculated the absolute excess risk of contralateral breast cancer as the observed minus expected number of breast cancers in the general population divided by 10,000 person-years at risk.
Of 421,643 women with a first diagnosis of primary breast cancer during the study period, 245,418 met the study criteria. Of this cohort, 7,784 (3.2%) developed a contralateral second breast cancer more than 6 months after diagnosis of the first, after a median 6.7 years of follow-up.
Slightly more than half of the cohort (52.1%) had undergone breast-conserving therapy, 37.5% underwent unilateral mastectomy, and 7.6% had bilateral mastectomy. An additional 2.9% of patients were women aged 70 years and older with stage I hormone receptor–positive, HER2-negative disease who underwent breast-conserving surgery without radiation (percentages exceed 100% because of rounding).
A multivariate-adjusted model showed that, as might be expected, patients who underwent bilateral mastectomy had a 90% reduction in risk of contralateral cancer (hazard ratio, 0.10; P less than .001), compared with breast-conserving therapy. In contrast, patients who underwent unilateral mastectomy had a slight but significant increase in risk for a second contralateral breast cancer (HR, 1.07; P = .008).
The absolute excess risk for second contralateral breast cancer was 5 per 10,000 person-years with breast-conserving therapy, 13.6 per 10,000 person-years with unilateral mastectomy, and –28.6 per 10,000 person-years with bilateral mastectomy.
When they looked at risk for death, however they found that, compared with breast-conserving therapy, breast-conserving surgery alone (HR, 1.36; P = .0001) and unilateral mastectomy (HR, 1.21; P less than .001), but not bilateral mastectomy (HR, 1.03; P = .35) were significantly associated with increased risk for breast cancer death.
The authors noted that their estimates of absolute risk of second contralateral breast cancer jibe with those of earlier studies, and can help clinicians frame the discussion of the benefits versus risks for individual patients.
“What one patient might consider to be a negligible benefit of BLM, weighed against its potential harms of greater pain, recovery time, and impact on body image and employment, might appear worthwhile to another,” they wrote.
The study was funded by the National Cancer Institute, National Institutes of Health, Department of Health & Human Services, Suzanne Pride Bryan Fund for Breast Cancer Research, Jan Weimer Faculty Chair for Breast Oncology, and the BRCA Foundation. Dr. Kurian disclosed institutional research funding from Myriad Genetics.
SOURCE: Kurin AW et al. Cancer. 2019 Nov 21. doi: 10.1002/cncr.32618.
Bilateral mastectomy significantly decreases the risk for a second contralateral breast cancer, but does not decrease the risk of death, compared with breast-conserving therapy, results of a large retrospective study indicate.
Among 245,418 patients followed for a median of 6.7 years, the risk of death from breast cancer was similar for those who had undergone either breast-conserving therapy or bilateral mastectomy (BLM) but was 20% higher among women who had undergone unilateral mastectomy (ULM) when compared with breast-conserving therapy, reported Allison W. Kurian, MD, MSc, from Stanford (Calif.) University, and colleagues.
“Second breast cancers are rare, and their reduction should be weighed against the harms associated with BLM,” they wrote in a study published online in Cancer.
The investigators extracted data from the Surveillance, Epidemiology, and End Results program on all women diagnosed with American Joint Committee on Cancer stage 0 to stage III unilateral breast cancer in California from 1998 to 2015 who were treated with either BLM versus breast-conserving therapy, including surgery and radiation or unilateral mastectomy.
They calculated the absolute excess risk of contralateral breast cancer as the observed minus expected number of breast cancers in the general population divided by 10,000 person-years at risk.
Of 421,643 women with a first diagnosis of primary breast cancer during the study period, 245,418 met the study criteria. Of this cohort, 7,784 (3.2%) developed a contralateral second breast cancer more than 6 months after diagnosis of the first, after a median 6.7 years of follow-up.
Slightly more than half of the cohort (52.1%) had undergone breast-conserving therapy, 37.5% underwent unilateral mastectomy, and 7.6% had bilateral mastectomy. An additional 2.9% of patients were women aged 70 years and older with stage I hormone receptor–positive, HER2-negative disease who underwent breast-conserving surgery without radiation (percentages exceed 100% because of rounding).
A multivariate-adjusted model showed that, as might be expected, patients who underwent bilateral mastectomy had a 90% reduction in risk of contralateral cancer (hazard ratio, 0.10; P less than .001), compared with breast-conserving therapy. In contrast, patients who underwent unilateral mastectomy had a slight but significant increase in risk for a second contralateral breast cancer (HR, 1.07; P = .008).
The absolute excess risk for second contralateral breast cancer was 5 per 10,000 person-years with breast-conserving therapy, 13.6 per 10,000 person-years with unilateral mastectomy, and –28.6 per 10,000 person-years with bilateral mastectomy.
When they looked at risk for death, however they found that, compared with breast-conserving therapy, breast-conserving surgery alone (HR, 1.36; P = .0001) and unilateral mastectomy (HR, 1.21; P less than .001), but not bilateral mastectomy (HR, 1.03; P = .35) were significantly associated with increased risk for breast cancer death.
The authors noted that their estimates of absolute risk of second contralateral breast cancer jibe with those of earlier studies, and can help clinicians frame the discussion of the benefits versus risks for individual patients.
“What one patient might consider to be a negligible benefit of BLM, weighed against its potential harms of greater pain, recovery time, and impact on body image and employment, might appear worthwhile to another,” they wrote.
The study was funded by the National Cancer Institute, National Institutes of Health, Department of Health & Human Services, Suzanne Pride Bryan Fund for Breast Cancer Research, Jan Weimer Faculty Chair for Breast Oncology, and the BRCA Foundation. Dr. Kurian disclosed institutional research funding from Myriad Genetics.
SOURCE: Kurin AW et al. Cancer. 2019 Nov 21. doi: 10.1002/cncr.32618.
FROM CANCER
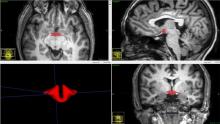
Reward, decision-making brain regions altered in teens with obesity
CHICAGO – according to a Brazilian study that used MRI to detect these changes.
Brain changes were significantly correlated with increased levels of insulin, leptin, and other appetite- and diet-related hormones and neurohormones, as well as with inflammatory markers.
In an interview at the annual meeting of the Radiological Society of North America, Pamela Bertolazzi, a PhD student at the University of São Paulo, explained that childhood obesity in Brazil is estimated to have climbed by up to 40% in recent years, with almost one-third of Brazilian children and adolescents experiencing obesity. Epidemiologists estimate that there’s the potential for 2.6 million premature deaths from this level of overweight and obesity, she said. Brazil has over 211 million residents.
Previous studies have established diffusion tensor imaging as an MRI technique to assess white-matter integrity and architecture. Fractional anisotropy (FA) is a measure of brain tract integrity, and decreased FA can indicate demyelination or axonal degeneration.
Ms. Bertolazzi and colleagues compared 60 healthy weight adolescents with 57 adolescents with obesity to see how cerebral connectivity differed, and further correlated MRI findings with a serum assay of 57 analytes including inflammatory markers, neuropeptides, and hormones.
Adolescents aged 12-16 years were included if they met World Health Organization criteria for obesity or for healthy weight. The z score for the participants with obesity was 2.74, and 0.25 for the healthy-weight participants (P less than .001). Individuals who were underweight or overweight (but not obese) were excluded. Those with known significant psychiatric diagnoses or prior traumatic brain injury or neurosurgery also were excluded.
The mean age of participants was 14 years, and 29 of the 57 (51%) participants with obesity were female, as were 33 of 60 (55%) healthy weight participants. There was no significant difference in socioeconomic status between the two groups.
When participants’ brain MRI results were reviewed, Ms. Bertolazzi and associates saw several regions that had decreased FA only in the adolescents with obesity. In general terms, these brain areas are known to be concerned with appetite and reward.
Decreased FA – indicating demyelination or axonal degeneration – was seen particularly on the left-hand side of the corpus callosum, “the largest association pathway in the human brain,” said Ms. Bertolazzi. Looking at the interaction between decreased FA in this area and levels of various analytes, leptin, insulin, C-peptide, and total glucagonlike peptide–1 levels all were negatively associated with FA levels. A ratio of leptin to the anti-inflammatory cytokine interleukin-10 also had a negative correlation with FA levels. All of these associations were statistically significant.
Decreased FA also was seen in the orbitofrontal gyrus, an area of the prefrontal cortex that links decision making with emotions and reward. Here, significant negative associations were seen with C-peptide, amylin, and the ratios of several other inflammatory markers to IL-10.
“Obesity was associated with a reduction of cerebral integrity in obese adolescents,” said Ms. Bertolazzi. The clinical significance of these findings is not yet known. However, she said that the disruption in regulation of reward and appetite circuitry her study found may set up adolescents with excess body mass for a maladaptive positive feedback loop: elevated insulin, leptin, and inflammatory cytokine levels may be contributing to disrupted appetite, which in turn contributes to ongoing increases in body mass index.
She and her colleagues are planning to enroll adolescents with obesity and their families in nutritional education and exercise programs, hoping to interrupt the cycle. They plan to obtain a baseline serum assay and MRI scan with diffusion tensor imaging and FA, and to repeat the studies about 3 months into an intensive intervention, to test the hypothesis that increased exercise and improved diet will result in reversal of the brain changes they found in this exploratory study. In particular, said Ms. Bertolazzi, they hope that encouraging physical activity will boost levels of HDL cholesterol, which may have a neuroprotective effect.
Ms. Bertolazzi reported no outside sources of funding and no conflicts of interest.
CHICAGO – according to a Brazilian study that used MRI to detect these changes.
Brain changes were significantly correlated with increased levels of insulin, leptin, and other appetite- and diet-related hormones and neurohormones, as well as with inflammatory markers.
In an interview at the annual meeting of the Radiological Society of North America, Pamela Bertolazzi, a PhD student at the University of São Paulo, explained that childhood obesity in Brazil is estimated to have climbed by up to 40% in recent years, with almost one-third of Brazilian children and adolescents experiencing obesity. Epidemiologists estimate that there’s the potential for 2.6 million premature deaths from this level of overweight and obesity, she said. Brazil has over 211 million residents.
Previous studies have established diffusion tensor imaging as an MRI technique to assess white-matter integrity and architecture. Fractional anisotropy (FA) is a measure of brain tract integrity, and decreased FA can indicate demyelination or axonal degeneration.
Ms. Bertolazzi and colleagues compared 60 healthy weight adolescents with 57 adolescents with obesity to see how cerebral connectivity differed, and further correlated MRI findings with a serum assay of 57 analytes including inflammatory markers, neuropeptides, and hormones.
Adolescents aged 12-16 years were included if they met World Health Organization criteria for obesity or for healthy weight. The z score for the participants with obesity was 2.74, and 0.25 for the healthy-weight participants (P less than .001). Individuals who were underweight or overweight (but not obese) were excluded. Those with known significant psychiatric diagnoses or prior traumatic brain injury or neurosurgery also were excluded.
The mean age of participants was 14 years, and 29 of the 57 (51%) participants with obesity were female, as were 33 of 60 (55%) healthy weight participants. There was no significant difference in socioeconomic status between the two groups.
When participants’ brain MRI results were reviewed, Ms. Bertolazzi and associates saw several regions that had decreased FA only in the adolescents with obesity. In general terms, these brain areas are known to be concerned with appetite and reward.
Decreased FA – indicating demyelination or axonal degeneration – was seen particularly on the left-hand side of the corpus callosum, “the largest association pathway in the human brain,” said Ms. Bertolazzi. Looking at the interaction between decreased FA in this area and levels of various analytes, leptin, insulin, C-peptide, and total glucagonlike peptide–1 levels all were negatively associated with FA levels. A ratio of leptin to the anti-inflammatory cytokine interleukin-10 also had a negative correlation with FA levels. All of these associations were statistically significant.
Decreased FA also was seen in the orbitofrontal gyrus, an area of the prefrontal cortex that links decision making with emotions and reward. Here, significant negative associations were seen with C-peptide, amylin, and the ratios of several other inflammatory markers to IL-10.
“Obesity was associated with a reduction of cerebral integrity in obese adolescents,” said Ms. Bertolazzi. The clinical significance of these findings is not yet known. However, she said that the disruption in regulation of reward and appetite circuitry her study found may set up adolescents with excess body mass for a maladaptive positive feedback loop: elevated insulin, leptin, and inflammatory cytokine levels may be contributing to disrupted appetite, which in turn contributes to ongoing increases in body mass index.
She and her colleagues are planning to enroll adolescents with obesity and their families in nutritional education and exercise programs, hoping to interrupt the cycle. They plan to obtain a baseline serum assay and MRI scan with diffusion tensor imaging and FA, and to repeat the studies about 3 months into an intensive intervention, to test the hypothesis that increased exercise and improved diet will result in reversal of the brain changes they found in this exploratory study. In particular, said Ms. Bertolazzi, they hope that encouraging physical activity will boost levels of HDL cholesterol, which may have a neuroprotective effect.
Ms. Bertolazzi reported no outside sources of funding and no conflicts of interest.
CHICAGO – according to a Brazilian study that used MRI to detect these changes.
Brain changes were significantly correlated with increased levels of insulin, leptin, and other appetite- and diet-related hormones and neurohormones, as well as with inflammatory markers.
In an interview at the annual meeting of the Radiological Society of North America, Pamela Bertolazzi, a PhD student at the University of São Paulo, explained that childhood obesity in Brazil is estimated to have climbed by up to 40% in recent years, with almost one-third of Brazilian children and adolescents experiencing obesity. Epidemiologists estimate that there’s the potential for 2.6 million premature deaths from this level of overweight and obesity, she said. Brazil has over 211 million residents.
Previous studies have established diffusion tensor imaging as an MRI technique to assess white-matter integrity and architecture. Fractional anisotropy (FA) is a measure of brain tract integrity, and decreased FA can indicate demyelination or axonal degeneration.
Ms. Bertolazzi and colleagues compared 60 healthy weight adolescents with 57 adolescents with obesity to see how cerebral connectivity differed, and further correlated MRI findings with a serum assay of 57 analytes including inflammatory markers, neuropeptides, and hormones.
Adolescents aged 12-16 years were included if they met World Health Organization criteria for obesity or for healthy weight. The z score for the participants with obesity was 2.74, and 0.25 for the healthy-weight participants (P less than .001). Individuals who were underweight or overweight (but not obese) were excluded. Those with known significant psychiatric diagnoses or prior traumatic brain injury or neurosurgery also were excluded.
The mean age of participants was 14 years, and 29 of the 57 (51%) participants with obesity were female, as were 33 of 60 (55%) healthy weight participants. There was no significant difference in socioeconomic status between the two groups.
When participants’ brain MRI results were reviewed, Ms. Bertolazzi and associates saw several regions that had decreased FA only in the adolescents with obesity. In general terms, these brain areas are known to be concerned with appetite and reward.
Decreased FA – indicating demyelination or axonal degeneration – was seen particularly on the left-hand side of the corpus callosum, “the largest association pathway in the human brain,” said Ms. Bertolazzi. Looking at the interaction between decreased FA in this area and levels of various analytes, leptin, insulin, C-peptide, and total glucagonlike peptide–1 levels all were negatively associated with FA levels. A ratio of leptin to the anti-inflammatory cytokine interleukin-10 also had a negative correlation with FA levels. All of these associations were statistically significant.
Decreased FA also was seen in the orbitofrontal gyrus, an area of the prefrontal cortex that links decision making with emotions and reward. Here, significant negative associations were seen with C-peptide, amylin, and the ratios of several other inflammatory markers to IL-10.
“Obesity was associated with a reduction of cerebral integrity in obese adolescents,” said Ms. Bertolazzi. The clinical significance of these findings is not yet known. However, she said that the disruption in regulation of reward and appetite circuitry her study found may set up adolescents with excess body mass for a maladaptive positive feedback loop: elevated insulin, leptin, and inflammatory cytokine levels may be contributing to disrupted appetite, which in turn contributes to ongoing increases in body mass index.
She and her colleagues are planning to enroll adolescents with obesity and their families in nutritional education and exercise programs, hoping to interrupt the cycle. They plan to obtain a baseline serum assay and MRI scan with diffusion tensor imaging and FA, and to repeat the studies about 3 months into an intensive intervention, to test the hypothesis that increased exercise and improved diet will result in reversal of the brain changes they found in this exploratory study. In particular, said Ms. Bertolazzi, they hope that encouraging physical activity will boost levels of HDL cholesterol, which may have a neuroprotective effect.
Ms. Bertolazzi reported no outside sources of funding and no conflicts of interest.
REPORTING FROM RSNA 2019
The clinical impact of new approvals in sickle cell, MCL
In this edition of “How I Will Treat My Next Patient,” I highlight two recent drug approvals by the Food and Drug Administration – crizanlizumab for sickle cell patients with painful crises and zanubrutinib for mantle cell lymphoma (MCL) patients in relapse.
Crizanlizumab
P-selectin is an adhesion molecule expressed on activated vascular endothelial cells and platelets. It is a key molecule in the initiation of leukocyte rolling on vessel walls and promotes firm attachment and extravasation to underlying tissues during inflammation. Up-regulation of P-selectin on endothelial cells and platelets contributes to the cell-cell interactions involved in the pathogenesis of sickle cell pain crises.
The SUSTAIN study was a multisite, placebo-controlled, randomized phase 2 trial of two different dosage levels of intravenous crizanlizumab (2.5 mg/kg or 5 mg/kg for 52 weeks), a humanized anti–P-selectin antibody, examining its effect on pain crises in patients with sickle cell disease. The primary endpoint was the annual rate of sickle cell pain crises, with a variety of clinically relevant secondary endpoints. The target population had 2-10 pain crises in the 12 months before enrollment. Patients on a stable dose of hydroxyurea for at least the most recent 3 months were allowed to enter, but if patients were not receiving hydroxyurea, it could not be initiated during the trial. Patients who were undergoing chronic red-cell transfusion therapy were excluded.
Among 198 enrolled patients, 35% did not complete the 52 weeks of treatment. Discontinuations were equally balanced among patients assigned to the high-dose, low-dose, and placebo cohorts. Adverse events associated with crizanlizumab included back pain, nausea, pyrexia, and arthralgia. Serious adverse events occurred in 55 patients, with 5 deaths, all of which were unrelated to treatment. Crizanlizumab did not augment hemolysis or bacterial infections.
In the efficacy analysis, patients receiving high-dose crizanlizumab had a median annual rate of 1.63 health care visits for sickle cell pain crises, compared with 2.98 visits for placebo patients (P = .01). In comparison with placebo, high-dose crizanlizumab also delayed the first pain crisis after starting treatment (4.1 months vs. 1.4 months), delayed the median time to a second pain crisis, and decreased the median number of pain crises annually.
More than twice as many high-dose crizanlizumab patients had no pain crisis episodes, compared with placebo patients. In general, differences were more striking in patients who were not taking hydroxyurea and who had non–hemoglobin SS disease. Differences in the primary endpoint between low-dose crizanlizumab and placebo were numerically, but not statistically, different.
How these results influence practice
It has been over 20 years since a new agent (hydroxyurea) was approved for sickle cell patients and, despite its use, sickle cell pain crises remain a frequent problem. Pain crises are associated with worse quality of life and increased risk of death. A promising advance is badly needed, especially in an era in which sensitivity to providers’ role in the opioid addiction crisis is highly scrutinized and may contribute to future undertreatment of pain episodes. This is especially true for patients from areas with high levels of opioid misuse.
The SUSTAIN trial was international, multi-institutional, placebo-controlled, and inclusive. These attributes enhance the likelihood that crizanlizumab will enhance patient care in routine practice. As an intravenous agent, monitoring adherence and toxicity are less challenging than with hydroxyurea. Despite these factors, however, there are some concerns. Crizanlizumab was not free of toxicity, quality of life via the Brief Pain Inventory used in the trial was not improved, and changes in the pain-severity and pain-interference domains were small. Treatment in SUSTAIN ensued for 52 weeks, so the emergence of late neutralizing antibodies and late toxicities with longer-term therapy will require careful postmarketing assessment.
These concerns notwithstanding, anyone who has cared for sickle cell patients would be excited about the potential benefits crizanlizumab could bring to patient care.
Zanubrutinib
The FDA has approved zanubrutinib for the treatment of MCL in adult patients who have received at least one prior therapy. The approval is based on the results of two studies in which overall response rate was the primary endpoint.
BGB-3111-206 (NCT03206970) was a phase 2, open-label, multicenter, single-arm trial of 86 patients with MCL who received at least one prior therapy. Zanubrutinib was given orally at 160 mg twice daily until disease progression or unacceptable toxicity. BGB-3111-AU-003 (NCT 02343120) was a phase 1/2, open-label, dose-escalation trial of B-cell malignancies, including 32 previously treated MCL patients treated with zanubrutinib at 160 mg twice daily or 320 mg once daily.
In the phase 2 trial, 18fluorodeoxyglucose (FDG)–PET scans were required and the ORR was 84% (95% confidence interval, 74%-91%), with a complete response rate of 59% (95% CI, 48%-70%) and a median response duration of 19.5 months (95% CI, 16.6% to not estimable). In the phase 1/2 dose-escalation trial, FDG-PET scans were not required and the ORR was 84% (95% CI, 67%-95%), with a complete response rate of 22% (95% CI, 9%-40%) and a median response duration of 18.5 months (95% CI, 12.6% to not estimable). In both trials, median follow-up on study was about 18 months.
The most common adverse reactions were cytopenias, upper respiratory tract infection, rash, bruising, diarrhea, and cough. The most common serious adverse reactions were pneumonia in 11% and hemorrhage in 5% of patients. Of 118 MCL patients, 8 stopped therapy because of an adverse event, most frequently pneumonia (3.4%).
How these results influence practice
Unfortunately, the therapy of recurrent MCL is noncurative, because of the rapid development of treatment resistance. There are multiple single-and multiagent chemotherapy regimens that may be tried, many incorporating immunotherapy options such as anti-CD20- or Bruton tyrosine kinase (BTK)–targeted agents. Given the limited efficacy of these agents, temporary nature of remissions, and paucity of data comparing these various treatment options, participation in clinical trials is encouraged whenever possible.
Outside of a clinical trial, zanubrutinib joins ibrutinib and acalabrutinib as approved single-agent BTK inhibitors for adult MCL patients in relapse. The impressive ORR and response duration reported for zanubrutinib are similar to the results achieved with the other agents, but the toxicity pattern may be slightly different.
As in the treatment of hormonally sensitive breast cancer, clinicians and patients benefit when they have multiple similar, equally efficacious oral agents with slightly different toxicity patterns so that quality of life can be improved and treatment duration maximized before treatment resistance develops and a more toxic and/or inconvenient therapy needs to be employed.
Whether zanubrutinib has benefits beyond those for MCL patients in relapse will depend on the results of confirmatory trials and patient-reported outcome data.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers and in expanding access to clinical trials to medically underserved populations.
In this edition of “How I Will Treat My Next Patient,” I highlight two recent drug approvals by the Food and Drug Administration – crizanlizumab for sickle cell patients with painful crises and zanubrutinib for mantle cell lymphoma (MCL) patients in relapse.
Crizanlizumab
P-selectin is an adhesion molecule expressed on activated vascular endothelial cells and platelets. It is a key molecule in the initiation of leukocyte rolling on vessel walls and promotes firm attachment and extravasation to underlying tissues during inflammation. Up-regulation of P-selectin on endothelial cells and platelets contributes to the cell-cell interactions involved in the pathogenesis of sickle cell pain crises.
The SUSTAIN study was a multisite, placebo-controlled, randomized phase 2 trial of two different dosage levels of intravenous crizanlizumab (2.5 mg/kg or 5 mg/kg for 52 weeks), a humanized anti–P-selectin antibody, examining its effect on pain crises in patients with sickle cell disease. The primary endpoint was the annual rate of sickle cell pain crises, with a variety of clinically relevant secondary endpoints. The target population had 2-10 pain crises in the 12 months before enrollment. Patients on a stable dose of hydroxyurea for at least the most recent 3 months were allowed to enter, but if patients were not receiving hydroxyurea, it could not be initiated during the trial. Patients who were undergoing chronic red-cell transfusion therapy were excluded.
Among 198 enrolled patients, 35% did not complete the 52 weeks of treatment. Discontinuations were equally balanced among patients assigned to the high-dose, low-dose, and placebo cohorts. Adverse events associated with crizanlizumab included back pain, nausea, pyrexia, and arthralgia. Serious adverse events occurred in 55 patients, with 5 deaths, all of which were unrelated to treatment. Crizanlizumab did not augment hemolysis or bacterial infections.
In the efficacy analysis, patients receiving high-dose crizanlizumab had a median annual rate of 1.63 health care visits for sickle cell pain crises, compared with 2.98 visits for placebo patients (P = .01). In comparison with placebo, high-dose crizanlizumab also delayed the first pain crisis after starting treatment (4.1 months vs. 1.4 months), delayed the median time to a second pain crisis, and decreased the median number of pain crises annually.
More than twice as many high-dose crizanlizumab patients had no pain crisis episodes, compared with placebo patients. In general, differences were more striking in patients who were not taking hydroxyurea and who had non–hemoglobin SS disease. Differences in the primary endpoint between low-dose crizanlizumab and placebo were numerically, but not statistically, different.
How these results influence practice
It has been over 20 years since a new agent (hydroxyurea) was approved for sickle cell patients and, despite its use, sickle cell pain crises remain a frequent problem. Pain crises are associated with worse quality of life and increased risk of death. A promising advance is badly needed, especially in an era in which sensitivity to providers’ role in the opioid addiction crisis is highly scrutinized and may contribute to future undertreatment of pain episodes. This is especially true for patients from areas with high levels of opioid misuse.
The SUSTAIN trial was international, multi-institutional, placebo-controlled, and inclusive. These attributes enhance the likelihood that crizanlizumab will enhance patient care in routine practice. As an intravenous agent, monitoring adherence and toxicity are less challenging than with hydroxyurea. Despite these factors, however, there are some concerns. Crizanlizumab was not free of toxicity, quality of life via the Brief Pain Inventory used in the trial was not improved, and changes in the pain-severity and pain-interference domains were small. Treatment in SUSTAIN ensued for 52 weeks, so the emergence of late neutralizing antibodies and late toxicities with longer-term therapy will require careful postmarketing assessment.
These concerns notwithstanding, anyone who has cared for sickle cell patients would be excited about the potential benefits crizanlizumab could bring to patient care.
Zanubrutinib
The FDA has approved zanubrutinib for the treatment of MCL in adult patients who have received at least one prior therapy. The approval is based on the results of two studies in which overall response rate was the primary endpoint.
BGB-3111-206 (NCT03206970) was a phase 2, open-label, multicenter, single-arm trial of 86 patients with MCL who received at least one prior therapy. Zanubrutinib was given orally at 160 mg twice daily until disease progression or unacceptable toxicity. BGB-3111-AU-003 (NCT 02343120) was a phase 1/2, open-label, dose-escalation trial of B-cell malignancies, including 32 previously treated MCL patients treated with zanubrutinib at 160 mg twice daily or 320 mg once daily.
In the phase 2 trial, 18fluorodeoxyglucose (FDG)–PET scans were required and the ORR was 84% (95% confidence interval, 74%-91%), with a complete response rate of 59% (95% CI, 48%-70%) and a median response duration of 19.5 months (95% CI, 16.6% to not estimable). In the phase 1/2 dose-escalation trial, FDG-PET scans were not required and the ORR was 84% (95% CI, 67%-95%), with a complete response rate of 22% (95% CI, 9%-40%) and a median response duration of 18.5 months (95% CI, 12.6% to not estimable). In both trials, median follow-up on study was about 18 months.
The most common adverse reactions were cytopenias, upper respiratory tract infection, rash, bruising, diarrhea, and cough. The most common serious adverse reactions were pneumonia in 11% and hemorrhage in 5% of patients. Of 118 MCL patients, 8 stopped therapy because of an adverse event, most frequently pneumonia (3.4%).
How these results influence practice
Unfortunately, the therapy of recurrent MCL is noncurative, because of the rapid development of treatment resistance. There are multiple single-and multiagent chemotherapy regimens that may be tried, many incorporating immunotherapy options such as anti-CD20- or Bruton tyrosine kinase (BTK)–targeted agents. Given the limited efficacy of these agents, temporary nature of remissions, and paucity of data comparing these various treatment options, participation in clinical trials is encouraged whenever possible.
Outside of a clinical trial, zanubrutinib joins ibrutinib and acalabrutinib as approved single-agent BTK inhibitors for adult MCL patients in relapse. The impressive ORR and response duration reported for zanubrutinib are similar to the results achieved with the other agents, but the toxicity pattern may be slightly different.
As in the treatment of hormonally sensitive breast cancer, clinicians and patients benefit when they have multiple similar, equally efficacious oral agents with slightly different toxicity patterns so that quality of life can be improved and treatment duration maximized before treatment resistance develops and a more toxic and/or inconvenient therapy needs to be employed.
Whether zanubrutinib has benefits beyond those for MCL patients in relapse will depend on the results of confirmatory trials and patient-reported outcome data.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers and in expanding access to clinical trials to medically underserved populations.
In this edition of “How I Will Treat My Next Patient,” I highlight two recent drug approvals by the Food and Drug Administration – crizanlizumab for sickle cell patients with painful crises and zanubrutinib for mantle cell lymphoma (MCL) patients in relapse.
Crizanlizumab
P-selectin is an adhesion molecule expressed on activated vascular endothelial cells and platelets. It is a key molecule in the initiation of leukocyte rolling on vessel walls and promotes firm attachment and extravasation to underlying tissues during inflammation. Up-regulation of P-selectin on endothelial cells and platelets contributes to the cell-cell interactions involved in the pathogenesis of sickle cell pain crises.
The SUSTAIN study was a multisite, placebo-controlled, randomized phase 2 trial of two different dosage levels of intravenous crizanlizumab (2.5 mg/kg or 5 mg/kg for 52 weeks), a humanized anti–P-selectin antibody, examining its effect on pain crises in patients with sickle cell disease. The primary endpoint was the annual rate of sickle cell pain crises, with a variety of clinically relevant secondary endpoints. The target population had 2-10 pain crises in the 12 months before enrollment. Patients on a stable dose of hydroxyurea for at least the most recent 3 months were allowed to enter, but if patients were not receiving hydroxyurea, it could not be initiated during the trial. Patients who were undergoing chronic red-cell transfusion therapy were excluded.
Among 198 enrolled patients, 35% did not complete the 52 weeks of treatment. Discontinuations were equally balanced among patients assigned to the high-dose, low-dose, and placebo cohorts. Adverse events associated with crizanlizumab included back pain, nausea, pyrexia, and arthralgia. Serious adverse events occurred in 55 patients, with 5 deaths, all of which were unrelated to treatment. Crizanlizumab did not augment hemolysis or bacterial infections.
In the efficacy analysis, patients receiving high-dose crizanlizumab had a median annual rate of 1.63 health care visits for sickle cell pain crises, compared with 2.98 visits for placebo patients (P = .01). In comparison with placebo, high-dose crizanlizumab also delayed the first pain crisis after starting treatment (4.1 months vs. 1.4 months), delayed the median time to a second pain crisis, and decreased the median number of pain crises annually.
More than twice as many high-dose crizanlizumab patients had no pain crisis episodes, compared with placebo patients. In general, differences were more striking in patients who were not taking hydroxyurea and who had non–hemoglobin SS disease. Differences in the primary endpoint between low-dose crizanlizumab and placebo were numerically, but not statistically, different.
How these results influence practice
It has been over 20 years since a new agent (hydroxyurea) was approved for sickle cell patients and, despite its use, sickle cell pain crises remain a frequent problem. Pain crises are associated with worse quality of life and increased risk of death. A promising advance is badly needed, especially in an era in which sensitivity to providers’ role in the opioid addiction crisis is highly scrutinized and may contribute to future undertreatment of pain episodes. This is especially true for patients from areas with high levels of opioid misuse.
The SUSTAIN trial was international, multi-institutional, placebo-controlled, and inclusive. These attributes enhance the likelihood that crizanlizumab will enhance patient care in routine practice. As an intravenous agent, monitoring adherence and toxicity are less challenging than with hydroxyurea. Despite these factors, however, there are some concerns. Crizanlizumab was not free of toxicity, quality of life via the Brief Pain Inventory used in the trial was not improved, and changes in the pain-severity and pain-interference domains were small. Treatment in SUSTAIN ensued for 52 weeks, so the emergence of late neutralizing antibodies and late toxicities with longer-term therapy will require careful postmarketing assessment.
These concerns notwithstanding, anyone who has cared for sickle cell patients would be excited about the potential benefits crizanlizumab could bring to patient care.
Zanubrutinib
The FDA has approved zanubrutinib for the treatment of MCL in adult patients who have received at least one prior therapy. The approval is based on the results of two studies in which overall response rate was the primary endpoint.
BGB-3111-206 (NCT03206970) was a phase 2, open-label, multicenter, single-arm trial of 86 patients with MCL who received at least one prior therapy. Zanubrutinib was given orally at 160 mg twice daily until disease progression or unacceptable toxicity. BGB-3111-AU-003 (NCT 02343120) was a phase 1/2, open-label, dose-escalation trial of B-cell malignancies, including 32 previously treated MCL patients treated with zanubrutinib at 160 mg twice daily or 320 mg once daily.
In the phase 2 trial, 18fluorodeoxyglucose (FDG)–PET scans were required and the ORR was 84% (95% confidence interval, 74%-91%), with a complete response rate of 59% (95% CI, 48%-70%) and a median response duration of 19.5 months (95% CI, 16.6% to not estimable). In the phase 1/2 dose-escalation trial, FDG-PET scans were not required and the ORR was 84% (95% CI, 67%-95%), with a complete response rate of 22% (95% CI, 9%-40%) and a median response duration of 18.5 months (95% CI, 12.6% to not estimable). In both trials, median follow-up on study was about 18 months.
The most common adverse reactions were cytopenias, upper respiratory tract infection, rash, bruising, diarrhea, and cough. The most common serious adverse reactions were pneumonia in 11% and hemorrhage in 5% of patients. Of 118 MCL patients, 8 stopped therapy because of an adverse event, most frequently pneumonia (3.4%).
How these results influence practice
Unfortunately, the therapy of recurrent MCL is noncurative, because of the rapid development of treatment resistance. There are multiple single-and multiagent chemotherapy regimens that may be tried, many incorporating immunotherapy options such as anti-CD20- or Bruton tyrosine kinase (BTK)–targeted agents. Given the limited efficacy of these agents, temporary nature of remissions, and paucity of data comparing these various treatment options, participation in clinical trials is encouraged whenever possible.
Outside of a clinical trial, zanubrutinib joins ibrutinib and acalabrutinib as approved single-agent BTK inhibitors for adult MCL patients in relapse. The impressive ORR and response duration reported for zanubrutinib are similar to the results achieved with the other agents, but the toxicity pattern may be slightly different.
As in the treatment of hormonally sensitive breast cancer, clinicians and patients benefit when they have multiple similar, equally efficacious oral agents with slightly different toxicity patterns so that quality of life can be improved and treatment duration maximized before treatment resistance develops and a more toxic and/or inconvenient therapy needs to be employed.
Whether zanubrutinib has benefits beyond those for MCL patients in relapse will depend on the results of confirmatory trials and patient-reported outcome data.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers and in expanding access to clinical trials to medically underserved populations.
Positive functional results reported for aducanumab in a pooled, post hoc analysis
SAN DIEGO – Positive findings from a post hoc subanalysis of two unsuccessful studies represent “a major step forward in Alzheimer’s disease research” and could set the antiamyloid antibody up as a “foothold” in slowing disease progression, study investigators said at the Clinical Trials on Alzheimer’s Disease conference.
After full follow-up of 78 weeks, patients with mild Alzheimer’s disease (AD) who took the highest 10-mg/kg dose for a full 14 doses experienced up to a 53% slowing of functional decline on the Clinical Dementia Rating–Sum of Boxes (CDR-SB) in one study and a 48% slowing in the other study – relative to placebo – a result that might give them “an extra year or 2” of independence; they might perhaps retain the ability to drive and even stay employed, said Sharon Cohen, MD, a panelist at the meeting’s aducanumab presentation session and a clinical investigator in EMERGE, one of two phase 3 studies from which the data were derived.
Samantha Budd Haeberlein, PhD, Biogen’s vice president and head of late-stage clinical development in Alzheimer’s disease, presented the new data. They “are complex” and require much more study before investigators, clinicians, and federal regulators can fully embrace them, said the panelists who discussed the results. Nevertheless, Biogen, which is codeveloping the antibody with partner Eisai, said in October it will put aducanumab forward to the Food and Drug Administration in a new drug application for the first-ever AD disease-modifying agent. FDA regulators have said they will review the data.
The new subanalysis comprised 570 of 3,285 patients in two identical studies with negative primary endpoint results. One, ENGAGE, failed to reach both its primary and secondary endpoints; the other, EMERGE, was halted last spring after a futility analysis determined that aducanumab was unlikely to confer significant benefit. The post hoc subanalysis looked at a combined subset of those who received the highest 10-mg/kg dose for the full 78 weeks of each trial. The statistically significant functional endpoints occurred in this group, comprised largely of apolipoprotein E epsilon-4 (APOE4) allele carriers.
“The futility analysis of EMERGE was highly unfortunate,” said panelist Paul Aisen, MD, founding director of the Alzheimer’s Therapeutic Research Institute at the University of Southern California, Los Angeles. “Clearly in the final analysis, EMERGE was positive in the primary endpoints, and now the secondary analysis of both studies is positive and consistent.” The diverging trajectory of placebo and treatment groups continued to the end of follow-up in both studies, a finding that at least suggests continuing improvement, he added.
Biogen undertook the pooled analysis after ENGAGE’s futility analysis. Early in the development program, concern about amyloid-related imaging abnormalities (ARIA) in APOE4 carriers led Biogen to stratify doses in that group.
“When we started [creating aducanumab trials], we stratified the dose so that e4 carriers had the lowest dose, but in PRIME [the phase 1b study], we saw the best result from the 10-mg/kg dose, so we believed that was important for efficacy. However, we didn’t have sufficient evidence to believe that it was safe to put carriers on that dose. In EMERGE, we saw that carriers could safely take it until the end of the study.”
Since the trials were running almost synchronously, a new version of randomization ensued. This allowed more e4 carriers to go forward on the 10-mg/kg dose.
“I would not normally recommend changing dose in the middle of a phase 3 trial, but it did have a real impact in the high-dose group,” Dr. Haeberlein said. Additionally, by the time of data lock after the futility analysis, more patients had completed the entire 78 weeks at the 10-mg/kg dose. Cumulative dosing ended up being quite different in the APOE4 carriers after this new version ensued. Before, the median cumulative dose for both carriers and noncarriers was 116 mg/kg. After the change, the median cumulative dose was 153 mg/kg. And before the alteration, 21% in EMERGE and 15% in ENGAGE received the full 14 possible 10-mg/kg doses. After the change, 51% in EMERGE and 47% in ENGAGE received the full 14 doses of 10 mg/kg.
The pooled analysis comprised this combined group, which was then largely composed of APOE4 carriers.
Imaging confirmed such dose-driven reductions in both brain amyloid plaques and phosphorylated tau. Although amyloid reduction has never been tied to cognitive or functional benefits, tau reduction has been associated with nonsignificant cognitive benefits in prior studies.
In the primary analysis of ENGAGE, aducanumab conferred no cognitive or functional benefit. In EMERGE, there were significant cognitive improvements on both the Mini Mental State Exam score (an 18% slowing of decline relative to placebo) and the Alzheimer’s Disease Assessment Scale cognitive portion (a 27% slowing).
However, the functional improvements seen in the pooled post hoc data “are a big deal,” and probably more meaningful to patients and families than the memory improvements, Dr. Cohen said.
“Those of us who know this disease well know what it means to lose yourself slice by slice, and anything you can hang onto is a triumph,” said Dr. Cohen, medical director and principal investigator of the Toronto Memory Program, an independent medical facility for dementia care and research. “I am pleased with a 27% slowing of cognitive decline, but a 40% slowing of functional decline is what will be really meaningful to patients. This is a long, slow disease, and if we can slow it at all, we’re winning out.”
Safety endpoints, especially ARIA, were not unexpected considering past studies. ARIA occurred in 41% of patients treated with the high aducanumab dose in EMERGE and in 40% in ENGAGE. It was largely asymptomatic (80% in EMERGE and 71% in ENGAGE). Headache was the next most common adverse event, followed by dizziness, visual disturbance, and nausea and vomiting. ARIA generally resolved within 4-6 weeks, and most patients continued their 10-mg/kg dose.
Biogen intends to begin a new study, an open-label nonrandomized trial that will offer the 10-mg/kg dose to all patients in both trials, including those who took placebo. This may provide interesting data regarding redosing patients who were off their successful 10-mg/kg dose for an extended period of time, said Laurie Ryan, PhD, chief of the Dementias of Aging Branch in the Division of Neuroscience at the National Institute on Aging.
“If those in the high-dose group had a regression of their improvements and then improved again when restarted, that would certainly tell us something,” she said in an interview. Likewise, researchers will be carefully looking at any placebo group response. “But we have to remember that this will not be a randomized study,” and will bring with it all the issues that such a study typically carries.
“I agree it’s unfortunate that they had to stop the EMERGE trial,” she said. “It really did complicate the results, even though they are certainly trending in the right way. But we have had a number of post hoc analyses that show APOE4-positive benefiting, or e4-negative benefiting, and these haven’t panned out.”
SAN DIEGO – Positive findings from a post hoc subanalysis of two unsuccessful studies represent “a major step forward in Alzheimer’s disease research” and could set the antiamyloid antibody up as a “foothold” in slowing disease progression, study investigators said at the Clinical Trials on Alzheimer’s Disease conference.
After full follow-up of 78 weeks, patients with mild Alzheimer’s disease (AD) who took the highest 10-mg/kg dose for a full 14 doses experienced up to a 53% slowing of functional decline on the Clinical Dementia Rating–Sum of Boxes (CDR-SB) in one study and a 48% slowing in the other study – relative to placebo – a result that might give them “an extra year or 2” of independence; they might perhaps retain the ability to drive and even stay employed, said Sharon Cohen, MD, a panelist at the meeting’s aducanumab presentation session and a clinical investigator in EMERGE, one of two phase 3 studies from which the data were derived.
Samantha Budd Haeberlein, PhD, Biogen’s vice president and head of late-stage clinical development in Alzheimer’s disease, presented the new data. They “are complex” and require much more study before investigators, clinicians, and federal regulators can fully embrace them, said the panelists who discussed the results. Nevertheless, Biogen, which is codeveloping the antibody with partner Eisai, said in October it will put aducanumab forward to the Food and Drug Administration in a new drug application for the first-ever AD disease-modifying agent. FDA regulators have said they will review the data.
The new subanalysis comprised 570 of 3,285 patients in two identical studies with negative primary endpoint results. One, ENGAGE, failed to reach both its primary and secondary endpoints; the other, EMERGE, was halted last spring after a futility analysis determined that aducanumab was unlikely to confer significant benefit. The post hoc subanalysis looked at a combined subset of those who received the highest 10-mg/kg dose for the full 78 weeks of each trial. The statistically significant functional endpoints occurred in this group, comprised largely of apolipoprotein E epsilon-4 (APOE4) allele carriers.
“The futility analysis of EMERGE was highly unfortunate,” said panelist Paul Aisen, MD, founding director of the Alzheimer’s Therapeutic Research Institute at the University of Southern California, Los Angeles. “Clearly in the final analysis, EMERGE was positive in the primary endpoints, and now the secondary analysis of both studies is positive and consistent.” The diverging trajectory of placebo and treatment groups continued to the end of follow-up in both studies, a finding that at least suggests continuing improvement, he added.
Biogen undertook the pooled analysis after ENGAGE’s futility analysis. Early in the development program, concern about amyloid-related imaging abnormalities (ARIA) in APOE4 carriers led Biogen to stratify doses in that group.
“When we started [creating aducanumab trials], we stratified the dose so that e4 carriers had the lowest dose, but in PRIME [the phase 1b study], we saw the best result from the 10-mg/kg dose, so we believed that was important for efficacy. However, we didn’t have sufficient evidence to believe that it was safe to put carriers on that dose. In EMERGE, we saw that carriers could safely take it until the end of the study.”
Since the trials were running almost synchronously, a new version of randomization ensued. This allowed more e4 carriers to go forward on the 10-mg/kg dose.
“I would not normally recommend changing dose in the middle of a phase 3 trial, but it did have a real impact in the high-dose group,” Dr. Haeberlein said. Additionally, by the time of data lock after the futility analysis, more patients had completed the entire 78 weeks at the 10-mg/kg dose. Cumulative dosing ended up being quite different in the APOE4 carriers after this new version ensued. Before, the median cumulative dose for both carriers and noncarriers was 116 mg/kg. After the change, the median cumulative dose was 153 mg/kg. And before the alteration, 21% in EMERGE and 15% in ENGAGE received the full 14 possible 10-mg/kg doses. After the change, 51% in EMERGE and 47% in ENGAGE received the full 14 doses of 10 mg/kg.
The pooled analysis comprised this combined group, which was then largely composed of APOE4 carriers.
Imaging confirmed such dose-driven reductions in both brain amyloid plaques and phosphorylated tau. Although amyloid reduction has never been tied to cognitive or functional benefits, tau reduction has been associated with nonsignificant cognitive benefits in prior studies.
In the primary analysis of ENGAGE, aducanumab conferred no cognitive or functional benefit. In EMERGE, there were significant cognitive improvements on both the Mini Mental State Exam score (an 18% slowing of decline relative to placebo) and the Alzheimer’s Disease Assessment Scale cognitive portion (a 27% slowing).
However, the functional improvements seen in the pooled post hoc data “are a big deal,” and probably more meaningful to patients and families than the memory improvements, Dr. Cohen said.
“Those of us who know this disease well know what it means to lose yourself slice by slice, and anything you can hang onto is a triumph,” said Dr. Cohen, medical director and principal investigator of the Toronto Memory Program, an independent medical facility for dementia care and research. “I am pleased with a 27% slowing of cognitive decline, but a 40% slowing of functional decline is what will be really meaningful to patients. This is a long, slow disease, and if we can slow it at all, we’re winning out.”
Safety endpoints, especially ARIA, were not unexpected considering past studies. ARIA occurred in 41% of patients treated with the high aducanumab dose in EMERGE and in 40% in ENGAGE. It was largely asymptomatic (80% in EMERGE and 71% in ENGAGE). Headache was the next most common adverse event, followed by dizziness, visual disturbance, and nausea and vomiting. ARIA generally resolved within 4-6 weeks, and most patients continued their 10-mg/kg dose.
Biogen intends to begin a new study, an open-label nonrandomized trial that will offer the 10-mg/kg dose to all patients in both trials, including those who took placebo. This may provide interesting data regarding redosing patients who were off their successful 10-mg/kg dose for an extended period of time, said Laurie Ryan, PhD, chief of the Dementias of Aging Branch in the Division of Neuroscience at the National Institute on Aging.
“If those in the high-dose group had a regression of their improvements and then improved again when restarted, that would certainly tell us something,” she said in an interview. Likewise, researchers will be carefully looking at any placebo group response. “But we have to remember that this will not be a randomized study,” and will bring with it all the issues that such a study typically carries.
“I agree it’s unfortunate that they had to stop the EMERGE trial,” she said. “It really did complicate the results, even though they are certainly trending in the right way. But we have had a number of post hoc analyses that show APOE4-positive benefiting, or e4-negative benefiting, and these haven’t panned out.”
SAN DIEGO – Positive findings from a post hoc subanalysis of two unsuccessful studies represent “a major step forward in Alzheimer’s disease research” and could set the antiamyloid antibody up as a “foothold” in slowing disease progression, study investigators said at the Clinical Trials on Alzheimer’s Disease conference.
After full follow-up of 78 weeks, patients with mild Alzheimer’s disease (AD) who took the highest 10-mg/kg dose for a full 14 doses experienced up to a 53% slowing of functional decline on the Clinical Dementia Rating–Sum of Boxes (CDR-SB) in one study and a 48% slowing in the other study – relative to placebo – a result that might give them “an extra year or 2” of independence; they might perhaps retain the ability to drive and even stay employed, said Sharon Cohen, MD, a panelist at the meeting’s aducanumab presentation session and a clinical investigator in EMERGE, one of two phase 3 studies from which the data were derived.
Samantha Budd Haeberlein, PhD, Biogen’s vice president and head of late-stage clinical development in Alzheimer’s disease, presented the new data. They “are complex” and require much more study before investigators, clinicians, and federal regulators can fully embrace them, said the panelists who discussed the results. Nevertheless, Biogen, which is codeveloping the antibody with partner Eisai, said in October it will put aducanumab forward to the Food and Drug Administration in a new drug application for the first-ever AD disease-modifying agent. FDA regulators have said they will review the data.
The new subanalysis comprised 570 of 3,285 patients in two identical studies with negative primary endpoint results. One, ENGAGE, failed to reach both its primary and secondary endpoints; the other, EMERGE, was halted last spring after a futility analysis determined that aducanumab was unlikely to confer significant benefit. The post hoc subanalysis looked at a combined subset of those who received the highest 10-mg/kg dose for the full 78 weeks of each trial. The statistically significant functional endpoints occurred in this group, comprised largely of apolipoprotein E epsilon-4 (APOE4) allele carriers.
“The futility analysis of EMERGE was highly unfortunate,” said panelist Paul Aisen, MD, founding director of the Alzheimer’s Therapeutic Research Institute at the University of Southern California, Los Angeles. “Clearly in the final analysis, EMERGE was positive in the primary endpoints, and now the secondary analysis of both studies is positive and consistent.” The diverging trajectory of placebo and treatment groups continued to the end of follow-up in both studies, a finding that at least suggests continuing improvement, he added.
Biogen undertook the pooled analysis after ENGAGE’s futility analysis. Early in the development program, concern about amyloid-related imaging abnormalities (ARIA) in APOE4 carriers led Biogen to stratify doses in that group.
“When we started [creating aducanumab trials], we stratified the dose so that e4 carriers had the lowest dose, but in PRIME [the phase 1b study], we saw the best result from the 10-mg/kg dose, so we believed that was important for efficacy. However, we didn’t have sufficient evidence to believe that it was safe to put carriers on that dose. In EMERGE, we saw that carriers could safely take it until the end of the study.”
Since the trials were running almost synchronously, a new version of randomization ensued. This allowed more e4 carriers to go forward on the 10-mg/kg dose.
“I would not normally recommend changing dose in the middle of a phase 3 trial, but it did have a real impact in the high-dose group,” Dr. Haeberlein said. Additionally, by the time of data lock after the futility analysis, more patients had completed the entire 78 weeks at the 10-mg/kg dose. Cumulative dosing ended up being quite different in the APOE4 carriers after this new version ensued. Before, the median cumulative dose for both carriers and noncarriers was 116 mg/kg. After the change, the median cumulative dose was 153 mg/kg. And before the alteration, 21% in EMERGE and 15% in ENGAGE received the full 14 possible 10-mg/kg doses. After the change, 51% in EMERGE and 47% in ENGAGE received the full 14 doses of 10 mg/kg.
The pooled analysis comprised this combined group, which was then largely composed of APOE4 carriers.
Imaging confirmed such dose-driven reductions in both brain amyloid plaques and phosphorylated tau. Although amyloid reduction has never been tied to cognitive or functional benefits, tau reduction has been associated with nonsignificant cognitive benefits in prior studies.
In the primary analysis of ENGAGE, aducanumab conferred no cognitive or functional benefit. In EMERGE, there were significant cognitive improvements on both the Mini Mental State Exam score (an 18% slowing of decline relative to placebo) and the Alzheimer’s Disease Assessment Scale cognitive portion (a 27% slowing).
However, the functional improvements seen in the pooled post hoc data “are a big deal,” and probably more meaningful to patients and families than the memory improvements, Dr. Cohen said.
“Those of us who know this disease well know what it means to lose yourself slice by slice, and anything you can hang onto is a triumph,” said Dr. Cohen, medical director and principal investigator of the Toronto Memory Program, an independent medical facility for dementia care and research. “I am pleased with a 27% slowing of cognitive decline, but a 40% slowing of functional decline is what will be really meaningful to patients. This is a long, slow disease, and if we can slow it at all, we’re winning out.”
Safety endpoints, especially ARIA, were not unexpected considering past studies. ARIA occurred in 41% of patients treated with the high aducanumab dose in EMERGE and in 40% in ENGAGE. It was largely asymptomatic (80% in EMERGE and 71% in ENGAGE). Headache was the next most common adverse event, followed by dizziness, visual disturbance, and nausea and vomiting. ARIA generally resolved within 4-6 weeks, and most patients continued their 10-mg/kg dose.
Biogen intends to begin a new study, an open-label nonrandomized trial that will offer the 10-mg/kg dose to all patients in both trials, including those who took placebo. This may provide interesting data regarding redosing patients who were off their successful 10-mg/kg dose for an extended period of time, said Laurie Ryan, PhD, chief of the Dementias of Aging Branch in the Division of Neuroscience at the National Institute on Aging.
“If those in the high-dose group had a regression of their improvements and then improved again when restarted, that would certainly tell us something,” she said in an interview. Likewise, researchers will be carefully looking at any placebo group response. “But we have to remember that this will not be a randomized study,” and will bring with it all the issues that such a study typically carries.
“I agree it’s unfortunate that they had to stop the EMERGE trial,” she said. “It really did complicate the results, even though they are certainly trending in the right way. But we have had a number of post hoc analyses that show APOE4-positive benefiting, or e4-negative benefiting, and these haven’t panned out.”
REPORTING FROM CTAD 2019
Key clinical point: A pooled posthoc subanalysis of two unsuccessful phase 3 trials, found that the antiamyloid antibody aducanumab conferred significant functional benefits in patients with mild Alzheimer’s disease who took the highest 10-mg/kg dose for a full 78 weeks.
Major finding: Aducanumab conferred a 53% slowing of functional decline on the Clinical Dementia Rating–Sum of Boxes (CDR-SB) in one study, ENGAGE, and a 48% slowing in the other, EMERGE, relative to placebo.
Study details: The pooled group comprised 570 of 3,285 patients in the two identical ENGAGE and EMERGE studies.
Disclosures: Biogen and Eisai sponsored the studies and are codeveloping aducanumab.
Source: Budd SH et al. CTAD 2019, OC 1-4.
Colchicine pre-PCI improves biomarkers, not injury risk
PHILADELPHIA – Giving patients a single shot of colchicine before percutaneous coronary intervention was found to favorably impact inflammatory biomarkers linked to vascular injury, but not to lower the risk of procedure-related myocardial injury, according to results of the COLCHICINE-PCI randomized trial reported at the American Heart Association scientific sessions.
This is the first study to evaluate pre-PCI colchicine versus placebo on markers of myocardial injury and inflammation, said Binita Shah, MD, of Veterans Affairs New York Harbor Healthcare System and New York University.
“More work is needed to determine the optimal dosing and timing regimen of colchicine administration in patients undergoing PCI,” Dr. Shah said in an interview. “In this study, we saw inflammatory markers decrease around the 24-hour time point post PCI, so an earlier start to preprocedural colchicine regimen warrants further investigation.” The study found that pre-PCI colchicine attenuated increases in interleukin-6 and high-sensitivity C-reactive protein (CRP) concentrations at 24 hours post PCI, Dr. Shah said.
The results followed by a day the presentation of results from the COLCOT trial (Colchicine Cardiovascular Outcomes Trial) that showed a 23% reduction in cardiovascular events in patients with coronary disease on colchicine 0.5 mg daily vs. placebo (N Engl J Med. 2019 Nov 16. doi: 10.1056/NEJMoa1912388), as Subodh Verma, MD, PhD, of the University of Toronto noted in his discussant comments. COLCHICINE-PCI “has important implications, since patients with acute coronary syndrome often have variable biomarker responses, as biomarkers often function as acute-phase reactants in that setting.”
The COLCHICINE-PCI study of 400 patients investigated oral 1.8 mg colchicine given 1-2 hours before the patient went to the cath lab. The drug was given in a 1.2-mg dose followed an hour later by an 0.6-mg dose. Patients received placebo at the same intervals. An inflammatory biomarker substudy of 280 patients evaluated differences in plasma interleukin-6 levels at baseline and 1 hour post PCI, as well as other key biomarkers at longer intervals.
The primary outcome of PCI-related myocardial injury showed no statistically significant difference between the two groups, Dr. Shah said: 57.3% for colchicine and 64.2% for placebo (P = 0.19). The same was true of 30-day major adverse cardiovascular events, she said: 11.7% and 12.9% for the treatment and placebo groups, respectively (P = 0.82). Rates of PCI-related MI were also similar between the two groups.
However, the biomarker substudy told a different story. IL-6 levels in the treatment group were stable at 1 and 6-8 hours post PCI. “However, at 22-24 hours we see a significant attenuation in the rise of IL-6 with colchicine,” she said.
While IL-beta levels showed no deviation after PCI, the colchicine group showed a noticeable attenuation in the rise of high-sensitivity CRP levels at 22-24 hours.
“This is the first study to demonstrate that an oral load of colchicine prevents a rise of inflammatory markers in an acute-injury setting,” Dr. Shah said.
While results of the COLCOT trial affirmed a “resounding yes” for the use of colchicine in patients who’ve had a recent MI, Dr. Verma said the COLCHICINE-PCI results did not give as clear an answer.
“What about pre- or peri-PCI?” he said. “I don’t think we’re there yet, but I do think that more studies are needed that target residual inflammatory risk and potentially couple an acute loading dose with a chronic, ongoing treatment.” Results from higher-risk primary prevention studies, such as the CLEAR SYNERGY (OASIS 9) of a colchicine-spironolactone combination in patients with STEMI having PCI, are needed, he said.
Dr. Shah disclosed financial relationships with Phillips Volcano and Radux. The VA Office of Research and Development and AHA provided grant funding and Takeda Pharmaceuticals provided the drug.
SOURCE: Shah B. AHA 2019, Late Breaking Science session IV.
PHILADELPHIA – Giving patients a single shot of colchicine before percutaneous coronary intervention was found to favorably impact inflammatory biomarkers linked to vascular injury, but not to lower the risk of procedure-related myocardial injury, according to results of the COLCHICINE-PCI randomized trial reported at the American Heart Association scientific sessions.
This is the first study to evaluate pre-PCI colchicine versus placebo on markers of myocardial injury and inflammation, said Binita Shah, MD, of Veterans Affairs New York Harbor Healthcare System and New York University.
“More work is needed to determine the optimal dosing and timing regimen of colchicine administration in patients undergoing PCI,” Dr. Shah said in an interview. “In this study, we saw inflammatory markers decrease around the 24-hour time point post PCI, so an earlier start to preprocedural colchicine regimen warrants further investigation.” The study found that pre-PCI colchicine attenuated increases in interleukin-6 and high-sensitivity C-reactive protein (CRP) concentrations at 24 hours post PCI, Dr. Shah said.
The results followed by a day the presentation of results from the COLCOT trial (Colchicine Cardiovascular Outcomes Trial) that showed a 23% reduction in cardiovascular events in patients with coronary disease on colchicine 0.5 mg daily vs. placebo (N Engl J Med. 2019 Nov 16. doi: 10.1056/NEJMoa1912388), as Subodh Verma, MD, PhD, of the University of Toronto noted in his discussant comments. COLCHICINE-PCI “has important implications, since patients with acute coronary syndrome often have variable biomarker responses, as biomarkers often function as acute-phase reactants in that setting.”
The COLCHICINE-PCI study of 400 patients investigated oral 1.8 mg colchicine given 1-2 hours before the patient went to the cath lab. The drug was given in a 1.2-mg dose followed an hour later by an 0.6-mg dose. Patients received placebo at the same intervals. An inflammatory biomarker substudy of 280 patients evaluated differences in plasma interleukin-6 levels at baseline and 1 hour post PCI, as well as other key biomarkers at longer intervals.
The primary outcome of PCI-related myocardial injury showed no statistically significant difference between the two groups, Dr. Shah said: 57.3% for colchicine and 64.2% for placebo (P = 0.19). The same was true of 30-day major adverse cardiovascular events, she said: 11.7% and 12.9% for the treatment and placebo groups, respectively (P = 0.82). Rates of PCI-related MI were also similar between the two groups.
However, the biomarker substudy told a different story. IL-6 levels in the treatment group were stable at 1 and 6-8 hours post PCI. “However, at 22-24 hours we see a significant attenuation in the rise of IL-6 with colchicine,” she said.
While IL-beta levels showed no deviation after PCI, the colchicine group showed a noticeable attenuation in the rise of high-sensitivity CRP levels at 22-24 hours.
“This is the first study to demonstrate that an oral load of colchicine prevents a rise of inflammatory markers in an acute-injury setting,” Dr. Shah said.
While results of the COLCOT trial affirmed a “resounding yes” for the use of colchicine in patients who’ve had a recent MI, Dr. Verma said the COLCHICINE-PCI results did not give as clear an answer.
“What about pre- or peri-PCI?” he said. “I don’t think we’re there yet, but I do think that more studies are needed that target residual inflammatory risk and potentially couple an acute loading dose with a chronic, ongoing treatment.” Results from higher-risk primary prevention studies, such as the CLEAR SYNERGY (OASIS 9) of a colchicine-spironolactone combination in patients with STEMI having PCI, are needed, he said.
Dr. Shah disclosed financial relationships with Phillips Volcano and Radux. The VA Office of Research and Development and AHA provided grant funding and Takeda Pharmaceuticals provided the drug.
SOURCE: Shah B. AHA 2019, Late Breaking Science session IV.
PHILADELPHIA – Giving patients a single shot of colchicine before percutaneous coronary intervention was found to favorably impact inflammatory biomarkers linked to vascular injury, but not to lower the risk of procedure-related myocardial injury, according to results of the COLCHICINE-PCI randomized trial reported at the American Heart Association scientific sessions.
This is the first study to evaluate pre-PCI colchicine versus placebo on markers of myocardial injury and inflammation, said Binita Shah, MD, of Veterans Affairs New York Harbor Healthcare System and New York University.
“More work is needed to determine the optimal dosing and timing regimen of colchicine administration in patients undergoing PCI,” Dr. Shah said in an interview. “In this study, we saw inflammatory markers decrease around the 24-hour time point post PCI, so an earlier start to preprocedural colchicine regimen warrants further investigation.” The study found that pre-PCI colchicine attenuated increases in interleukin-6 and high-sensitivity C-reactive protein (CRP) concentrations at 24 hours post PCI, Dr. Shah said.
The results followed by a day the presentation of results from the COLCOT trial (Colchicine Cardiovascular Outcomes Trial) that showed a 23% reduction in cardiovascular events in patients with coronary disease on colchicine 0.5 mg daily vs. placebo (N Engl J Med. 2019 Nov 16. doi: 10.1056/NEJMoa1912388), as Subodh Verma, MD, PhD, of the University of Toronto noted in his discussant comments. COLCHICINE-PCI “has important implications, since patients with acute coronary syndrome often have variable biomarker responses, as biomarkers often function as acute-phase reactants in that setting.”
The COLCHICINE-PCI study of 400 patients investigated oral 1.8 mg colchicine given 1-2 hours before the patient went to the cath lab. The drug was given in a 1.2-mg dose followed an hour later by an 0.6-mg dose. Patients received placebo at the same intervals. An inflammatory biomarker substudy of 280 patients evaluated differences in plasma interleukin-6 levels at baseline and 1 hour post PCI, as well as other key biomarkers at longer intervals.
The primary outcome of PCI-related myocardial injury showed no statistically significant difference between the two groups, Dr. Shah said: 57.3% for colchicine and 64.2% for placebo (P = 0.19). The same was true of 30-day major adverse cardiovascular events, she said: 11.7% and 12.9% for the treatment and placebo groups, respectively (P = 0.82). Rates of PCI-related MI were also similar between the two groups.
However, the biomarker substudy told a different story. IL-6 levels in the treatment group were stable at 1 and 6-8 hours post PCI. “However, at 22-24 hours we see a significant attenuation in the rise of IL-6 with colchicine,” she said.
While IL-beta levels showed no deviation after PCI, the colchicine group showed a noticeable attenuation in the rise of high-sensitivity CRP levels at 22-24 hours.
“This is the first study to demonstrate that an oral load of colchicine prevents a rise of inflammatory markers in an acute-injury setting,” Dr. Shah said.
While results of the COLCOT trial affirmed a “resounding yes” for the use of colchicine in patients who’ve had a recent MI, Dr. Verma said the COLCHICINE-PCI results did not give as clear an answer.
“What about pre- or peri-PCI?” he said. “I don’t think we’re there yet, but I do think that more studies are needed that target residual inflammatory risk and potentially couple an acute loading dose with a chronic, ongoing treatment.” Results from higher-risk primary prevention studies, such as the CLEAR SYNERGY (OASIS 9) of a colchicine-spironolactone combination in patients with STEMI having PCI, are needed, he said.
Dr. Shah disclosed financial relationships with Phillips Volcano and Radux. The VA Office of Research and Development and AHA provided grant funding and Takeda Pharmaceuticals provided the drug.
SOURCE: Shah B. AHA 2019, Late Breaking Science session IV.
REPORTING FROM AHA 2019
TULIP trials show clinical benefit of anifrolumab for SLE
ATLANTA –
In TULIP-1, which compared intravenous anifrolumab at doses of 300 or 150 mg and placebo given every 4 weeks for 48 weeks, the primary endpoint of SLE Responder Index (SRI) in the 300 mg versus the placebo group was not met, but in post hoc analyses, numeric improvements at thresholds associated with clinical benefit were observed for several secondary outcomes, Richard A. Furie, MD, a professor of medicine at the Hofstra University/Northwell, Hempstead, N.Y., reported during a plenary session at the annual meeting of the American College of Rheumatology.
The findings were published online Nov. 11 in Lancet Rheumatology.
TULIP-2 compared IV anifrolumab at a dose of 300 mg versus placebo every 4 weeks for 48 weeks and demonstrated the superiority of anifrolumab for multiple efficacy endpoints, including the primary study endpoint of British Isles Lupus Assessment Group (BILAG)-based Composite Lupus Assessment (BICLA), Eric F. Morand, MD, PhD, reported during a late-breaking abstract session at the meeting.
The double-blind, phase 3 TULIP trials each enrolled seropositive SLE patients with moderate to severe active disease despite standard-of-care therapy (SOC). All patients met ACR criteria, had a SLE Disease Activity Index (SLEDAI)-2K of 6 or greater, and BILAG index scoring showing one or more organ systems with grade A involvement or two or more with grade B. Both trials required stable SOC therapy throughout the study except for mandatory attempts at oral corticosteroid (OCS) tapering for patients who were receiving 10 mg/day or more of prednisone or its equivalent at study entry.
The trials followed a phase 2 trial, reported by Dr. Furie at the 2015 ACR meeting and published in Arthritis & Rheumatology in 2017, which showed “very robust” efficacy of anifrolumab in this setting.
“The burning question for the last 20 years has been, ‘Can type 1 interferon inhibitors actually reduce lupus clinical activity?’ ” Dr. Furie said. “The problem here [is that] you can inhibit interferon-alpha, but there are four other subtypes capable of binding to the interferon receptor.”
Anifrolumab, which was first studied in scleroderma, inhibits the interferon (IFN) receptor, thereby providing broader inhibition than strategies that specifically target interferon-alpha, he explained.
In the phase 2 trial, the primary composite endpoint of SRI response at day 169 and sustained reduction of OCS dose between days 85 and 169 was met by 51.5% of patients receiving 300 mg of anifrolumab versus 26.6% of those receiving placebo.
TULIP-1
The TULIP-1 trial, however, failed to show a significant difference in the primary endpoint of week 52 SRI, although initial analyses showed some numeric benefit with respect to BICLA, OCS dose reductions, and other organ-specific endpoints.
The percentage of SRI responders at week 52 in the double-blind trial was 36.2% in 180 patients who received 300 mg anifrolumab vs. 40.4% in 184 who received placebo (nominal P value = .41), and in a subgroup of patients who had high IFN gene signature (IFNGS) test results, the rates were 35.9% and 39.3% (nominal P value = 0.55), respectively.
Sustained OCS reduction to 7.5 mg/day or less occurred in 41% of anifrolumab and 32.1% of placebo group patients, and a 50% or greater reduction in Cutaneous Lupus Erythematosus Disease Activity Severity Index (CLASI) activity from baseline to week 12 occurred in 41.9% and 24.9%, respectively. The annualized flare rate to week 52 was 0.72 for anifrolumab and 0.60 for placebo.
BICLA response at week 52 was 37.1% with anifrolumab versus 27% with placebo, and a 50% or greater reduction in active joints from baseline to week 52 occurred in 47% versus 32.5% of patients in the groups, respectively.
The 150-mg dose, which was included to provide dose-response data, did not show efficacy in secondary outcomes.
“We see a delta of about 10 percentage points [for BICLA], and about a 15-percentage point change [in swollen and tender joint count] in favor of anifrolumab,” Dr. Furie said. “So why the big difference between phase 2 results and phase 3 results? Well, that led to a year-long interrogation of all the data ... [which revealed that] about 8% of patients were misclassified as nonresponders for [NSAID] use.”
The medication rules in the study automatically required any patient who used a restricted drug, including NSAIDs, to be classified as a nonresponder. That means a patient who took an NSAID for a headache at the beginning of the study, for example, would have been considered a nonresponder regardless of their outcome, he explained.
“This led to a review of all the restricted medication classification rules, and after unblinding, a meeting was convened with SLE experts and the sponsors to actually revise the medication rules just to make them clinically more appropriate. The key analyses were repeated post hoc,” he said.
The difference between the treatment and placebo groups in terms of the week 52 SRI didn’t change much in the post hoc analysis (46.9% vs. 43% of treatment and placebo patients, respectively, met the endpoint). Similarly, SRI rates in the IFNGS test–high subgroup were 48.2% and 41.8%, respectively.
However, more pronounced “shifts to the right,” indicating larger differences favoring anifrolumab over placebo, were seen for OCS dose reduction (48.8% vs. 32.1%), CLASI response (43.6% vs. 24.9%), and BICLA response (48.1% vs. 29.8%).
“For BICLA response, we see a fairly significant change ... with what appears to be a clinically significant delta (about 16 percentage points), and as far as the change in active joints, also very significant in my eyes,” he said.
Also of note, the time to BICLA response sustained to week 52 was improved with anifrolumab (hazard ratio, 1.93), and CLASI response differences emerged early, at about 12 weeks, he said.
The type 1 IFNGS was reduced by a median of 88% to 90% in the anifrolumab groups vs. with placebo, and modest changes in serologies were also noted.
Serious adverse events occurred in 13.9% and 10.8% of patients in the anifrolumab 300- and 150-mg arms, compared with 16.3% in the placebo arm. Herpes zoster was more common in the anifrolumab groups (5.6% for 300 mg and 5.4% for 150 mg vs. 1.6% for placebo).
“But other than that, no major standouts as far as the safety profile,” Dr. Furie said.
The findings, particularly after the medication rules were amended, suggest efficacy of anifrolumab for corticosteroid reductions, skin activity, BICLA, and joint scores, he said, noting that corticosteroid dose reductions are very important for patients, and that BICLA is “actually a very rigorous composite.”
Importantly, the findings also underscore the importance and impact of medication rules, and the critical role that endpoint selection plays in SLE trials.
“We’ve been seeing discordance lately between the SRI and BICLA ... so [there is] still a lot to learn,” he said. “And I think it’s important in evaluating the drug effect to look at the totality of the data.”
TULIP-2
BICLA response, the primary endpoint of TULIP-2, was achieved by 47.8% of 180 patients who received anifrolumab, compared with 31.5% of 182 who received placebo, said Dr. Morand, professor and head of the School of Clinical Sciences at Monash University, Melbourne.
“The effect size was 16.3 percentage points with an adjusted p value of 0.001. Therefore, the primary outcome of this trial was attained,” said Dr. Morand, who also is head of the Monash Health Rheumatology Unit. “Separation between the treatment arms occurred early and was maintained across the progression of the trial.”
Anifrolumab was also superior to placebo for key secondary endpoints, including OCS dose reduction to 7.5 mg/day or less (51.5% vs. 30.2%) and CLASI response (49.0% vs. 25.0%).
“Joint responses did not show a significant difference between the anifrolumab and placebo arms,” he said, adding that the annualized flare rate also did not differ significantly between the groups, but was numerically lower in anifrolumab-treated patients (0.43 vs. 0.64; rate ratio, 0.67; P = .081).
Numeric differences also favored anifrolumab for multiple secondary endpoints, including SRI responses, time to onset of BICLA-sustained response, and time to first flare, he noted.
Further, in patients with high baseline IFNGS, anifrolumab induced neutralization of IFNGS by week 12, with a median suppression of 88.0%, which persisted for the duration of the study; no such effect was seen in the placebo arm.
Serum anti–double stranded DNA also trended toward normalization with anifrolumab.
The safety profile of anifrolumab was similar to that seen in previous trials, including TULIP-1, with herpes zoster occurring more often in those receiving anifrolumab (7.2% vs. 1.1% in the placebo group), Dr. Morand said, noting that “all herpes zoster episodes were cutaneous, all responded to antiviral therapy, and none required [treatment] discontinuation.”
Serious adverse events, including pneumonia and SLE worsening, occurred less frequently in the anifrolumab arm (8.3% vs. 17.0%, respectively), as did adverse events leading to treatment discontinuation (2.8% and 7.1%). One death occurred in the anifrolumab group from community-acquired pneumonia, and few patients (0.6%) developed antidrug antibodies.
No new safety signals were identified, he said, noting that “the findings add to cumulative evidence identifying anifrolumab as a potential new treatment option for SLE.”
“In conclusion, TULIP-2 was a positive phase 3 trial in lupus, and there aren’t many times that that sentence has been spoken,” he said.
The TULIP-1 and -2 trials were sponsored by AstraZeneca. Dr. Furie And Dr. Morand both reported grant/research support and consulting fees from AstraZeneca, as well as speaker’s bureau participation for AstraZeneca.
SOURCES: Furie RA et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract 1763; Morand EF et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract L17.
ATLANTA –
In TULIP-1, which compared intravenous anifrolumab at doses of 300 or 150 mg and placebo given every 4 weeks for 48 weeks, the primary endpoint of SLE Responder Index (SRI) in the 300 mg versus the placebo group was not met, but in post hoc analyses, numeric improvements at thresholds associated with clinical benefit were observed for several secondary outcomes, Richard A. Furie, MD, a professor of medicine at the Hofstra University/Northwell, Hempstead, N.Y., reported during a plenary session at the annual meeting of the American College of Rheumatology.
The findings were published online Nov. 11 in Lancet Rheumatology.
TULIP-2 compared IV anifrolumab at a dose of 300 mg versus placebo every 4 weeks for 48 weeks and demonstrated the superiority of anifrolumab for multiple efficacy endpoints, including the primary study endpoint of British Isles Lupus Assessment Group (BILAG)-based Composite Lupus Assessment (BICLA), Eric F. Morand, MD, PhD, reported during a late-breaking abstract session at the meeting.
The double-blind, phase 3 TULIP trials each enrolled seropositive SLE patients with moderate to severe active disease despite standard-of-care therapy (SOC). All patients met ACR criteria, had a SLE Disease Activity Index (SLEDAI)-2K of 6 or greater, and BILAG index scoring showing one or more organ systems with grade A involvement or two or more with grade B. Both trials required stable SOC therapy throughout the study except for mandatory attempts at oral corticosteroid (OCS) tapering for patients who were receiving 10 mg/day or more of prednisone or its equivalent at study entry.
The trials followed a phase 2 trial, reported by Dr. Furie at the 2015 ACR meeting and published in Arthritis & Rheumatology in 2017, which showed “very robust” efficacy of anifrolumab in this setting.
“The burning question for the last 20 years has been, ‘Can type 1 interferon inhibitors actually reduce lupus clinical activity?’ ” Dr. Furie said. “The problem here [is that] you can inhibit interferon-alpha, but there are four other subtypes capable of binding to the interferon receptor.”
Anifrolumab, which was first studied in scleroderma, inhibits the interferon (IFN) receptor, thereby providing broader inhibition than strategies that specifically target interferon-alpha, he explained.
In the phase 2 trial, the primary composite endpoint of SRI response at day 169 and sustained reduction of OCS dose between days 85 and 169 was met by 51.5% of patients receiving 300 mg of anifrolumab versus 26.6% of those receiving placebo.
TULIP-1
The TULIP-1 trial, however, failed to show a significant difference in the primary endpoint of week 52 SRI, although initial analyses showed some numeric benefit with respect to BICLA, OCS dose reductions, and other organ-specific endpoints.
The percentage of SRI responders at week 52 in the double-blind trial was 36.2% in 180 patients who received 300 mg anifrolumab vs. 40.4% in 184 who received placebo (nominal P value = .41), and in a subgroup of patients who had high IFN gene signature (IFNGS) test results, the rates were 35.9% and 39.3% (nominal P value = 0.55), respectively.
Sustained OCS reduction to 7.5 mg/day or less occurred in 41% of anifrolumab and 32.1% of placebo group patients, and a 50% or greater reduction in Cutaneous Lupus Erythematosus Disease Activity Severity Index (CLASI) activity from baseline to week 12 occurred in 41.9% and 24.9%, respectively. The annualized flare rate to week 52 was 0.72 for anifrolumab and 0.60 for placebo.
BICLA response at week 52 was 37.1% with anifrolumab versus 27% with placebo, and a 50% or greater reduction in active joints from baseline to week 52 occurred in 47% versus 32.5% of patients in the groups, respectively.
The 150-mg dose, which was included to provide dose-response data, did not show efficacy in secondary outcomes.
“We see a delta of about 10 percentage points [for BICLA], and about a 15-percentage point change [in swollen and tender joint count] in favor of anifrolumab,” Dr. Furie said. “So why the big difference between phase 2 results and phase 3 results? Well, that led to a year-long interrogation of all the data ... [which revealed that] about 8% of patients were misclassified as nonresponders for [NSAID] use.”
The medication rules in the study automatically required any patient who used a restricted drug, including NSAIDs, to be classified as a nonresponder. That means a patient who took an NSAID for a headache at the beginning of the study, for example, would have been considered a nonresponder regardless of their outcome, he explained.
“This led to a review of all the restricted medication classification rules, and after unblinding, a meeting was convened with SLE experts and the sponsors to actually revise the medication rules just to make them clinically more appropriate. The key analyses were repeated post hoc,” he said.
The difference between the treatment and placebo groups in terms of the week 52 SRI didn’t change much in the post hoc analysis (46.9% vs. 43% of treatment and placebo patients, respectively, met the endpoint). Similarly, SRI rates in the IFNGS test–high subgroup were 48.2% and 41.8%, respectively.
However, more pronounced “shifts to the right,” indicating larger differences favoring anifrolumab over placebo, were seen for OCS dose reduction (48.8% vs. 32.1%), CLASI response (43.6% vs. 24.9%), and BICLA response (48.1% vs. 29.8%).
“For BICLA response, we see a fairly significant change ... with what appears to be a clinically significant delta (about 16 percentage points), and as far as the change in active joints, also very significant in my eyes,” he said.
Also of note, the time to BICLA response sustained to week 52 was improved with anifrolumab (hazard ratio, 1.93), and CLASI response differences emerged early, at about 12 weeks, he said.
The type 1 IFNGS was reduced by a median of 88% to 90% in the anifrolumab groups vs. with placebo, and modest changes in serologies were also noted.
Serious adverse events occurred in 13.9% and 10.8% of patients in the anifrolumab 300- and 150-mg arms, compared with 16.3% in the placebo arm. Herpes zoster was more common in the anifrolumab groups (5.6% for 300 mg and 5.4% for 150 mg vs. 1.6% for placebo).
“But other than that, no major standouts as far as the safety profile,” Dr. Furie said.
The findings, particularly after the medication rules were amended, suggest efficacy of anifrolumab for corticosteroid reductions, skin activity, BICLA, and joint scores, he said, noting that corticosteroid dose reductions are very important for patients, and that BICLA is “actually a very rigorous composite.”
Importantly, the findings also underscore the importance and impact of medication rules, and the critical role that endpoint selection plays in SLE trials.
“We’ve been seeing discordance lately between the SRI and BICLA ... so [there is] still a lot to learn,” he said. “And I think it’s important in evaluating the drug effect to look at the totality of the data.”
TULIP-2
BICLA response, the primary endpoint of TULIP-2, was achieved by 47.8% of 180 patients who received anifrolumab, compared with 31.5% of 182 who received placebo, said Dr. Morand, professor and head of the School of Clinical Sciences at Monash University, Melbourne.
“The effect size was 16.3 percentage points with an adjusted p value of 0.001. Therefore, the primary outcome of this trial was attained,” said Dr. Morand, who also is head of the Monash Health Rheumatology Unit. “Separation between the treatment arms occurred early and was maintained across the progression of the trial.”
Anifrolumab was also superior to placebo for key secondary endpoints, including OCS dose reduction to 7.5 mg/day or less (51.5% vs. 30.2%) and CLASI response (49.0% vs. 25.0%).
“Joint responses did not show a significant difference between the anifrolumab and placebo arms,” he said, adding that the annualized flare rate also did not differ significantly between the groups, but was numerically lower in anifrolumab-treated patients (0.43 vs. 0.64; rate ratio, 0.67; P = .081).
Numeric differences also favored anifrolumab for multiple secondary endpoints, including SRI responses, time to onset of BICLA-sustained response, and time to first flare, he noted.
Further, in patients with high baseline IFNGS, anifrolumab induced neutralization of IFNGS by week 12, with a median suppression of 88.0%, which persisted for the duration of the study; no such effect was seen in the placebo arm.
Serum anti–double stranded DNA also trended toward normalization with anifrolumab.
The safety profile of anifrolumab was similar to that seen in previous trials, including TULIP-1, with herpes zoster occurring more often in those receiving anifrolumab (7.2% vs. 1.1% in the placebo group), Dr. Morand said, noting that “all herpes zoster episodes were cutaneous, all responded to antiviral therapy, and none required [treatment] discontinuation.”
Serious adverse events, including pneumonia and SLE worsening, occurred less frequently in the anifrolumab arm (8.3% vs. 17.0%, respectively), as did adverse events leading to treatment discontinuation (2.8% and 7.1%). One death occurred in the anifrolumab group from community-acquired pneumonia, and few patients (0.6%) developed antidrug antibodies.
No new safety signals were identified, he said, noting that “the findings add to cumulative evidence identifying anifrolumab as a potential new treatment option for SLE.”
“In conclusion, TULIP-2 was a positive phase 3 trial in lupus, and there aren’t many times that that sentence has been spoken,” he said.
The TULIP-1 and -2 trials were sponsored by AstraZeneca. Dr. Furie And Dr. Morand both reported grant/research support and consulting fees from AstraZeneca, as well as speaker’s bureau participation for AstraZeneca.
SOURCES: Furie RA et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract 1763; Morand EF et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract L17.
ATLANTA –
In TULIP-1, which compared intravenous anifrolumab at doses of 300 or 150 mg and placebo given every 4 weeks for 48 weeks, the primary endpoint of SLE Responder Index (SRI) in the 300 mg versus the placebo group was not met, but in post hoc analyses, numeric improvements at thresholds associated with clinical benefit were observed for several secondary outcomes, Richard A. Furie, MD, a professor of medicine at the Hofstra University/Northwell, Hempstead, N.Y., reported during a plenary session at the annual meeting of the American College of Rheumatology.
The findings were published online Nov. 11 in Lancet Rheumatology.
TULIP-2 compared IV anifrolumab at a dose of 300 mg versus placebo every 4 weeks for 48 weeks and demonstrated the superiority of anifrolumab for multiple efficacy endpoints, including the primary study endpoint of British Isles Lupus Assessment Group (BILAG)-based Composite Lupus Assessment (BICLA), Eric F. Morand, MD, PhD, reported during a late-breaking abstract session at the meeting.
The double-blind, phase 3 TULIP trials each enrolled seropositive SLE patients with moderate to severe active disease despite standard-of-care therapy (SOC). All patients met ACR criteria, had a SLE Disease Activity Index (SLEDAI)-2K of 6 or greater, and BILAG index scoring showing one or more organ systems with grade A involvement or two or more with grade B. Both trials required stable SOC therapy throughout the study except for mandatory attempts at oral corticosteroid (OCS) tapering for patients who were receiving 10 mg/day or more of prednisone or its equivalent at study entry.
The trials followed a phase 2 trial, reported by Dr. Furie at the 2015 ACR meeting and published in Arthritis & Rheumatology in 2017, which showed “very robust” efficacy of anifrolumab in this setting.
“The burning question for the last 20 years has been, ‘Can type 1 interferon inhibitors actually reduce lupus clinical activity?’ ” Dr. Furie said. “The problem here [is that] you can inhibit interferon-alpha, but there are four other subtypes capable of binding to the interferon receptor.”
Anifrolumab, which was first studied in scleroderma, inhibits the interferon (IFN) receptor, thereby providing broader inhibition than strategies that specifically target interferon-alpha, he explained.
In the phase 2 trial, the primary composite endpoint of SRI response at day 169 and sustained reduction of OCS dose between days 85 and 169 was met by 51.5% of patients receiving 300 mg of anifrolumab versus 26.6% of those receiving placebo.
TULIP-1
The TULIP-1 trial, however, failed to show a significant difference in the primary endpoint of week 52 SRI, although initial analyses showed some numeric benefit with respect to BICLA, OCS dose reductions, and other organ-specific endpoints.
The percentage of SRI responders at week 52 in the double-blind trial was 36.2% in 180 patients who received 300 mg anifrolumab vs. 40.4% in 184 who received placebo (nominal P value = .41), and in a subgroup of patients who had high IFN gene signature (IFNGS) test results, the rates were 35.9% and 39.3% (nominal P value = 0.55), respectively.
Sustained OCS reduction to 7.5 mg/day or less occurred in 41% of anifrolumab and 32.1% of placebo group patients, and a 50% or greater reduction in Cutaneous Lupus Erythematosus Disease Activity Severity Index (CLASI) activity from baseline to week 12 occurred in 41.9% and 24.9%, respectively. The annualized flare rate to week 52 was 0.72 for anifrolumab and 0.60 for placebo.
BICLA response at week 52 was 37.1% with anifrolumab versus 27% with placebo, and a 50% or greater reduction in active joints from baseline to week 52 occurred in 47% versus 32.5% of patients in the groups, respectively.
The 150-mg dose, which was included to provide dose-response data, did not show efficacy in secondary outcomes.
“We see a delta of about 10 percentage points [for BICLA], and about a 15-percentage point change [in swollen and tender joint count] in favor of anifrolumab,” Dr. Furie said. “So why the big difference between phase 2 results and phase 3 results? Well, that led to a year-long interrogation of all the data ... [which revealed that] about 8% of patients were misclassified as nonresponders for [NSAID] use.”
The medication rules in the study automatically required any patient who used a restricted drug, including NSAIDs, to be classified as a nonresponder. That means a patient who took an NSAID for a headache at the beginning of the study, for example, would have been considered a nonresponder regardless of their outcome, he explained.
“This led to a review of all the restricted medication classification rules, and after unblinding, a meeting was convened with SLE experts and the sponsors to actually revise the medication rules just to make them clinically more appropriate. The key analyses were repeated post hoc,” he said.
The difference between the treatment and placebo groups in terms of the week 52 SRI didn’t change much in the post hoc analysis (46.9% vs. 43% of treatment and placebo patients, respectively, met the endpoint). Similarly, SRI rates in the IFNGS test–high subgroup were 48.2% and 41.8%, respectively.
However, more pronounced “shifts to the right,” indicating larger differences favoring anifrolumab over placebo, were seen for OCS dose reduction (48.8% vs. 32.1%), CLASI response (43.6% vs. 24.9%), and BICLA response (48.1% vs. 29.8%).
“For BICLA response, we see a fairly significant change ... with what appears to be a clinically significant delta (about 16 percentage points), and as far as the change in active joints, also very significant in my eyes,” he said.
Also of note, the time to BICLA response sustained to week 52 was improved with anifrolumab (hazard ratio, 1.93), and CLASI response differences emerged early, at about 12 weeks, he said.
The type 1 IFNGS was reduced by a median of 88% to 90% in the anifrolumab groups vs. with placebo, and modest changes in serologies were also noted.
Serious adverse events occurred in 13.9% and 10.8% of patients in the anifrolumab 300- and 150-mg arms, compared with 16.3% in the placebo arm. Herpes zoster was more common in the anifrolumab groups (5.6% for 300 mg and 5.4% for 150 mg vs. 1.6% for placebo).
“But other than that, no major standouts as far as the safety profile,” Dr. Furie said.
The findings, particularly after the medication rules were amended, suggest efficacy of anifrolumab for corticosteroid reductions, skin activity, BICLA, and joint scores, he said, noting that corticosteroid dose reductions are very important for patients, and that BICLA is “actually a very rigorous composite.”
Importantly, the findings also underscore the importance and impact of medication rules, and the critical role that endpoint selection plays in SLE trials.
“We’ve been seeing discordance lately between the SRI and BICLA ... so [there is] still a lot to learn,” he said. “And I think it’s important in evaluating the drug effect to look at the totality of the data.”
TULIP-2
BICLA response, the primary endpoint of TULIP-2, was achieved by 47.8% of 180 patients who received anifrolumab, compared with 31.5% of 182 who received placebo, said Dr. Morand, professor and head of the School of Clinical Sciences at Monash University, Melbourne.
“The effect size was 16.3 percentage points with an adjusted p value of 0.001. Therefore, the primary outcome of this trial was attained,” said Dr. Morand, who also is head of the Monash Health Rheumatology Unit. “Separation between the treatment arms occurred early and was maintained across the progression of the trial.”
Anifrolumab was also superior to placebo for key secondary endpoints, including OCS dose reduction to 7.5 mg/day or less (51.5% vs. 30.2%) and CLASI response (49.0% vs. 25.0%).
“Joint responses did not show a significant difference between the anifrolumab and placebo arms,” he said, adding that the annualized flare rate also did not differ significantly between the groups, but was numerically lower in anifrolumab-treated patients (0.43 vs. 0.64; rate ratio, 0.67; P = .081).
Numeric differences also favored anifrolumab for multiple secondary endpoints, including SRI responses, time to onset of BICLA-sustained response, and time to first flare, he noted.
Further, in patients with high baseline IFNGS, anifrolumab induced neutralization of IFNGS by week 12, with a median suppression of 88.0%, which persisted for the duration of the study; no such effect was seen in the placebo arm.
Serum anti–double stranded DNA also trended toward normalization with anifrolumab.
The safety profile of anifrolumab was similar to that seen in previous trials, including TULIP-1, with herpes zoster occurring more often in those receiving anifrolumab (7.2% vs. 1.1% in the placebo group), Dr. Morand said, noting that “all herpes zoster episodes were cutaneous, all responded to antiviral therapy, and none required [treatment] discontinuation.”
Serious adverse events, including pneumonia and SLE worsening, occurred less frequently in the anifrolumab arm (8.3% vs. 17.0%, respectively), as did adverse events leading to treatment discontinuation (2.8% and 7.1%). One death occurred in the anifrolumab group from community-acquired pneumonia, and few patients (0.6%) developed antidrug antibodies.
No new safety signals were identified, he said, noting that “the findings add to cumulative evidence identifying anifrolumab as a potential new treatment option for SLE.”
“In conclusion, TULIP-2 was a positive phase 3 trial in lupus, and there aren’t many times that that sentence has been spoken,” he said.
The TULIP-1 and -2 trials were sponsored by AstraZeneca. Dr. Furie And Dr. Morand both reported grant/research support and consulting fees from AstraZeneca, as well as speaker’s bureau participation for AstraZeneca.
SOURCES: Furie RA et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract 1763; Morand EF et al. Arthritis Rheumatol. 2019;71(suppl 10), Abstract L17.
REPORTING FROM ACR 2019
Health care: More uninsured as insurance costs grow faster
WASHINGTON – The number of uninsured grew in 2018 as the rate of health care spending grew, according to data from the Centers for Medicare & Medicaid Services.
A total of 30.7 million people in the United States were uninsured in 2018 – up 1 million from 2017. It was the second year in a row that the number of uninsured grew by that amount.
The newly uninsured came from the private insurance sector, which saw the number of insured decrease to 200.5 million in 2018 from 202.1 million in the previous year, partially offset by increases in Americans covered by Medicare and Medicaid.
The increase in uninsured people comes as the growth rate in health care spending rose to 4.6% in 2018 from 4.2% in 2017, though much of that growth in the rate of spending was attributed to the application of a health insurance tax in 2018 that Congress put a moratorium on in the previous year. The tax was part of the Affordable Care Act and was enacted in 2014.
“We see that health care spending reached $3.6 trillion, or $11,172 per person, and spending was faster,” Micah Hartman, statistician in the National Health Statistics Group in the CMS Office of the Actuary, said during a press conference to review the national health expenditure results. “The main reason for the acceleration was faster growth in the net cost of insurance, and that was particularly the case for private health insurance and also for Medicare.”
The net cost of insurance includes nonmedical expenses such as administration, taxes, and fees, as well as gains or losses for private health insurers. The ACA’s health insurance tax generated $14.3 billion in spending, according to Internal Revenue Service data.
Also contributing to the rise in the rate of growth was faster growth in medical prices, “and that was due to underlying economy-wide inflation, as well as the impacts of the tax,” Mr. Hartman said.
Despite this growth in the rate of spending, health care spending as a percentage of GDP fell slightly from 17.9% in 2017 in 17.7%, as the GDP grew faster than health care spending in 2018.
The faster growth in prices more than offset the slightly slower growth in the use and intensity of medical services, CMS reported.
The growth rate on spending on physician and clinical services slowed to 4.1% in 2018 from 4.7% in 2017. Overall spending on physician and clinical services in 2018 reached $725.6 billion and accounted for 20% of overall health care spending.
Spending on hospital services also slowed, but only slightly, dropping to a growth rate of 4.5% from 4.7% during this period. Hospital spending in 2018, at $1.2 trillion, accounted for 33% of overall health care spending.
On a personal level, overall growth in personal health care spending held steady with growth rate of 4.1% in 2018, the same as 2017, though individual components that feed into the figure varied. For example, growth rate in the spending on retail pharmaceuticals rose to 2.5% from 1.4% during this period. Spending on retail pharmaceuticals reached $335 billion and accounted for 9% of overall health care spending.
Another factor in the rising growth rate in spending came from employer-sponsored insurance.
“Growth in health spending by private business was due to faster growth in employer contributions to private health insurance premiums,” Anne B. Martin, economist in the National Health Statistics Group, said during the press conference. There also was faster growth in spending by the federal government, “driven mainly by faster growth in the federally funded portions of Medicare and Medicaid.”
Spending by private health insurance grew at a rate of 5.8% and reached $1.2 trillion in 2018. Medicare spending grew by 6.4% and reached $750.2 billion, while Medicaid spending grew 3.0%, reaching $597.4 billion.
SOURCE: Hartman M et al. Health Affairs. 2019. doi: 10.1377/hlthaff.2019.00451
WASHINGTON – The number of uninsured grew in 2018 as the rate of health care spending grew, according to data from the Centers for Medicare & Medicaid Services.
A total of 30.7 million people in the United States were uninsured in 2018 – up 1 million from 2017. It was the second year in a row that the number of uninsured grew by that amount.
The newly uninsured came from the private insurance sector, which saw the number of insured decrease to 200.5 million in 2018 from 202.1 million in the previous year, partially offset by increases in Americans covered by Medicare and Medicaid.
The increase in uninsured people comes as the growth rate in health care spending rose to 4.6% in 2018 from 4.2% in 2017, though much of that growth in the rate of spending was attributed to the application of a health insurance tax in 2018 that Congress put a moratorium on in the previous year. The tax was part of the Affordable Care Act and was enacted in 2014.
“We see that health care spending reached $3.6 trillion, or $11,172 per person, and spending was faster,” Micah Hartman, statistician in the National Health Statistics Group in the CMS Office of the Actuary, said during a press conference to review the national health expenditure results. “The main reason for the acceleration was faster growth in the net cost of insurance, and that was particularly the case for private health insurance and also for Medicare.”
The net cost of insurance includes nonmedical expenses such as administration, taxes, and fees, as well as gains or losses for private health insurers. The ACA’s health insurance tax generated $14.3 billion in spending, according to Internal Revenue Service data.
Also contributing to the rise in the rate of growth was faster growth in medical prices, “and that was due to underlying economy-wide inflation, as well as the impacts of the tax,” Mr. Hartman said.
Despite this growth in the rate of spending, health care spending as a percentage of GDP fell slightly from 17.9% in 2017 in 17.7%, as the GDP grew faster than health care spending in 2018.
The faster growth in prices more than offset the slightly slower growth in the use and intensity of medical services, CMS reported.
The growth rate on spending on physician and clinical services slowed to 4.1% in 2018 from 4.7% in 2017. Overall spending on physician and clinical services in 2018 reached $725.6 billion and accounted for 20% of overall health care spending.
Spending on hospital services also slowed, but only slightly, dropping to a growth rate of 4.5% from 4.7% during this period. Hospital spending in 2018, at $1.2 trillion, accounted for 33% of overall health care spending.
On a personal level, overall growth in personal health care spending held steady with growth rate of 4.1% in 2018, the same as 2017, though individual components that feed into the figure varied. For example, growth rate in the spending on retail pharmaceuticals rose to 2.5% from 1.4% during this period. Spending on retail pharmaceuticals reached $335 billion and accounted for 9% of overall health care spending.
Another factor in the rising growth rate in spending came from employer-sponsored insurance.
“Growth in health spending by private business was due to faster growth in employer contributions to private health insurance premiums,” Anne B. Martin, economist in the National Health Statistics Group, said during the press conference. There also was faster growth in spending by the federal government, “driven mainly by faster growth in the federally funded portions of Medicare and Medicaid.”
Spending by private health insurance grew at a rate of 5.8% and reached $1.2 trillion in 2018. Medicare spending grew by 6.4% and reached $750.2 billion, while Medicaid spending grew 3.0%, reaching $597.4 billion.
SOURCE: Hartman M et al. Health Affairs. 2019. doi: 10.1377/hlthaff.2019.00451
WASHINGTON – The number of uninsured grew in 2018 as the rate of health care spending grew, according to data from the Centers for Medicare & Medicaid Services.
A total of 30.7 million people in the United States were uninsured in 2018 – up 1 million from 2017. It was the second year in a row that the number of uninsured grew by that amount.
The newly uninsured came from the private insurance sector, which saw the number of insured decrease to 200.5 million in 2018 from 202.1 million in the previous year, partially offset by increases in Americans covered by Medicare and Medicaid.
The increase in uninsured people comes as the growth rate in health care spending rose to 4.6% in 2018 from 4.2% in 2017, though much of that growth in the rate of spending was attributed to the application of a health insurance tax in 2018 that Congress put a moratorium on in the previous year. The tax was part of the Affordable Care Act and was enacted in 2014.
“We see that health care spending reached $3.6 trillion, or $11,172 per person, and spending was faster,” Micah Hartman, statistician in the National Health Statistics Group in the CMS Office of the Actuary, said during a press conference to review the national health expenditure results. “The main reason for the acceleration was faster growth in the net cost of insurance, and that was particularly the case for private health insurance and also for Medicare.”
The net cost of insurance includes nonmedical expenses such as administration, taxes, and fees, as well as gains or losses for private health insurers. The ACA’s health insurance tax generated $14.3 billion in spending, according to Internal Revenue Service data.
Also contributing to the rise in the rate of growth was faster growth in medical prices, “and that was due to underlying economy-wide inflation, as well as the impacts of the tax,” Mr. Hartman said.
Despite this growth in the rate of spending, health care spending as a percentage of GDP fell slightly from 17.9% in 2017 in 17.7%, as the GDP grew faster than health care spending in 2018.
The faster growth in prices more than offset the slightly slower growth in the use and intensity of medical services, CMS reported.
The growth rate on spending on physician and clinical services slowed to 4.1% in 2018 from 4.7% in 2017. Overall spending on physician and clinical services in 2018 reached $725.6 billion and accounted for 20% of overall health care spending.
Spending on hospital services also slowed, but only slightly, dropping to a growth rate of 4.5% from 4.7% during this period. Hospital spending in 2018, at $1.2 trillion, accounted for 33% of overall health care spending.
On a personal level, overall growth in personal health care spending held steady with growth rate of 4.1% in 2018, the same as 2017, though individual components that feed into the figure varied. For example, growth rate in the spending on retail pharmaceuticals rose to 2.5% from 1.4% during this period. Spending on retail pharmaceuticals reached $335 billion and accounted for 9% of overall health care spending.
Another factor in the rising growth rate in spending came from employer-sponsored insurance.
“Growth in health spending by private business was due to faster growth in employer contributions to private health insurance premiums,” Anne B. Martin, economist in the National Health Statistics Group, said during the press conference. There also was faster growth in spending by the federal government, “driven mainly by faster growth in the federally funded portions of Medicare and Medicaid.”
Spending by private health insurance grew at a rate of 5.8% and reached $1.2 trillion in 2018. Medicare spending grew by 6.4% and reached $750.2 billion, while Medicaid spending grew 3.0%, reaching $597.4 billion.
SOURCE: Hartman M et al. Health Affairs. 2019. doi: 10.1377/hlthaff.2019.00451
Oral contraceptive use associated with smaller hypothalamic and pituitary volumes
CHICAGO – Women taking oral contraceptives had, on average, a hypothalamus that was 6% smaller than those who didn’t, in a small study that used magnetic resonance imaging. Pituitary volume was also smaller.
Though the sample size was relatively small, 50 women in total, it’s the only study to date that looks at the relationship between hypothalamic volume and oral contraceptive (OC) use, and the largest examining pituitary volume, according to Ke Xun (Kevin) Chen, MD, who presented the findings at the annual meeting of the Radiological Society of North America.
Using MRI, Dr. Chen and his colleagues found that hypothalamic volume was significantly smaller in women taking oral contraceptives than those who were naturally cycling (b value = –64.1; P = .006). The pituitary gland also was significantly smaller in those taking OCs (b = –92.8; P = .007).
“I was quite surprised [at the finding], because the magnitude of the effect is not small,” especially in the context of changes in volume of other brain structures, senior author Michael L. Lipton, MD, PhD, said in an interview. In Alzheimer’s disease, for example, a volume loss of 4% annually can be expected.
However, “it’s not shocking to me in a negative way at all. I can’t tell you what it means in terms of how it’s going to affect people,” since this is a cross-sectional study that only detected a correlation and can’t say anything about a causative relationship, he added. “We don’t even know that [OCs] cause this effect. ... It’s plausible that this is just a plasticity-related change that’s simply showing us the effect of the drug.
“We’re going to be much more careful to consider oral contraceptive use as a covariate in future research studies; that’s for sure,” he said.
Although OCs have been available since their 1960 Food and Drug Administration approval, and their effects in some areas of physiology and health have been well studied, there’s still not much known about how oral contraceptives affect brain function, said Dr. Lipton, professor of neuroradiology and psychiatry and behavioral sciences at Albert Einstein College of Medicine, in the Montefiore medical system, New York.
The spark for this study came from one of Dr. Lipton’s main areas of research – sex differences in susceptibility to and recovery from traumatic brain injury. “Women are more likely to exhibit changes in their brain [after injury] – and changes in their brain function – than men,” he said.
In the present study, “we went at this trying to understand the effect to which the hormone effect might be doing something in regular, healthy people that we need to consider as part of the bigger picture,” he said.
Dr. Lipton, Dr. Chen (then a radiology resident at Albert Einstein College of Medicine), and their coauthors constructed the study to look for differences in brain structure between women who were experiencing natural menstrual cycles and those who were taking exogenous hormones, to begin to learn how oral contraceptive use might modify risk and susceptibility for neurologic disease and injury.
It had already been established that global brain volume didn’t differ between naturally cycling women and those using OCs. However, some studies had shown differences in volume of some specific brain regions, and one study had shown smaller pituitary volume in OC users, according to the presentation by Dr. Chen, who is now a radiology fellow at Brigham and Women’s Hospital, Boston. Accurately measuring hypothalamic volume represents a technical challenge, and the effect of OCs on the structure’s volume hadn’t previously been studied.
Sex hormones, said Dr. Lipton, have known trophic effects on brain tissue and ovarian sex hormones cross the blood brain barrier, so the idea that there would be some plasticity in the brains of those taking OCs wasn’t completely surprising, especially since there are hormone receptors that lie within the central nervous system. However, he said he was “very surprised” by the effect size seen in the study.
The study included 21 healthy women taking combined oral contraceptives, and 29 naturally cycling women. Participants’ mean age was 23 years for the OC users, and 21 for the naturally cycling women. Body mass index and smoking history didn’t differ between groups. Women on OCs were significantly more likely to use alcohol and to drink more frequently than those not taking OCs (P = .001). Participants were included only if they were taking a combined estrogen-progestin pill; those on noncyclical contraceptives such as implants and hormone-emitting intrauterine devices were excluded, as were naturally cycling women with very long or irregular menstrual cycles.
After multivariable statistical analysis, the only two significant predictors of hypothalamic volume were total intracranial volume and OC use. For pituitary volume, body mass index and OC use remained significant.
In addition to the MRI scans, participants also completed neurobehavioral testing to assess mood and cognition. An exploratory analysis showed no correlation between hypothalamic volume and the cognitive testing battery results, which included assessments for verbal learning and memory, executive function, and working memory.
However, a moderate positive association was seen between hypothalamic volume and anger scores (r = 0.34; P = .02). The investigators found a “strong positive correlation of hypothalamic volume with depression,” said Dr. Chen (r = 0.25; P = .09).
The investigators found no menstrual cycle-related changes in hypothalamic and pituitary volume among naturally cycling women.
Hypothalamic volume was obtained using manual segmentation of the MRIs; a combined automated-manual approach was used to obtain pituitary volume. Reliability was tested by having 5 raters each assess volumes for a randomly selected subset of the scans; inter-rater reliability fell between 0.78 and 0.86, values considered to indicate “good” reliability.
In addition to the small sample size, Dr. Chen acknowledged several limitations to the study. These included the lack of accounting for details of OC use including duration, exact type of OC, and whether women were taking the placebo phase of their pill packs at the time of scanning. Additionally, women who were naturally cycling were not asked about prior history of OC use.
Also, women’s menstrual phase was estimated from the self-reported date of the last menstrual period, rather than obtained by direct measurement via serum hormone levels.
Dr. Lipton’s perspective adds a strong note of caution to avoid overinterpretation from the study. Dr. Chen and Dr. Lipton agreed, however, that OC use should be accounted for when brain structure and function are studied in female participants.
Dr. Chen, Dr. Lipton, and their coauthors reported that they had no conflicts of interest. The authors reported no outside sources of funding.
SOURCE: Chen K et al. RSNA 2019. Presentation SSM-1904.
CHICAGO – Women taking oral contraceptives had, on average, a hypothalamus that was 6% smaller than those who didn’t, in a small study that used magnetic resonance imaging. Pituitary volume was also smaller.
Though the sample size was relatively small, 50 women in total, it’s the only study to date that looks at the relationship between hypothalamic volume and oral contraceptive (OC) use, and the largest examining pituitary volume, according to Ke Xun (Kevin) Chen, MD, who presented the findings at the annual meeting of the Radiological Society of North America.
Using MRI, Dr. Chen and his colleagues found that hypothalamic volume was significantly smaller in women taking oral contraceptives than those who were naturally cycling (b value = –64.1; P = .006). The pituitary gland also was significantly smaller in those taking OCs (b = –92.8; P = .007).
“I was quite surprised [at the finding], because the magnitude of the effect is not small,” especially in the context of changes in volume of other brain structures, senior author Michael L. Lipton, MD, PhD, said in an interview. In Alzheimer’s disease, for example, a volume loss of 4% annually can be expected.
However, “it’s not shocking to me in a negative way at all. I can’t tell you what it means in terms of how it’s going to affect people,” since this is a cross-sectional study that only detected a correlation and can’t say anything about a causative relationship, he added. “We don’t even know that [OCs] cause this effect. ... It’s plausible that this is just a plasticity-related change that’s simply showing us the effect of the drug.
“We’re going to be much more careful to consider oral contraceptive use as a covariate in future research studies; that’s for sure,” he said.
Although OCs have been available since their 1960 Food and Drug Administration approval, and their effects in some areas of physiology and health have been well studied, there’s still not much known about how oral contraceptives affect brain function, said Dr. Lipton, professor of neuroradiology and psychiatry and behavioral sciences at Albert Einstein College of Medicine, in the Montefiore medical system, New York.
The spark for this study came from one of Dr. Lipton’s main areas of research – sex differences in susceptibility to and recovery from traumatic brain injury. “Women are more likely to exhibit changes in their brain [after injury] – and changes in their brain function – than men,” he said.
In the present study, “we went at this trying to understand the effect to which the hormone effect might be doing something in regular, healthy people that we need to consider as part of the bigger picture,” he said.
Dr. Lipton, Dr. Chen (then a radiology resident at Albert Einstein College of Medicine), and their coauthors constructed the study to look for differences in brain structure between women who were experiencing natural menstrual cycles and those who were taking exogenous hormones, to begin to learn how oral contraceptive use might modify risk and susceptibility for neurologic disease and injury.
It had already been established that global brain volume didn’t differ between naturally cycling women and those using OCs. However, some studies had shown differences in volume of some specific brain regions, and one study had shown smaller pituitary volume in OC users, according to the presentation by Dr. Chen, who is now a radiology fellow at Brigham and Women’s Hospital, Boston. Accurately measuring hypothalamic volume represents a technical challenge, and the effect of OCs on the structure’s volume hadn’t previously been studied.
Sex hormones, said Dr. Lipton, have known trophic effects on brain tissue and ovarian sex hormones cross the blood brain barrier, so the idea that there would be some plasticity in the brains of those taking OCs wasn’t completely surprising, especially since there are hormone receptors that lie within the central nervous system. However, he said he was “very surprised” by the effect size seen in the study.
The study included 21 healthy women taking combined oral contraceptives, and 29 naturally cycling women. Participants’ mean age was 23 years for the OC users, and 21 for the naturally cycling women. Body mass index and smoking history didn’t differ between groups. Women on OCs were significantly more likely to use alcohol and to drink more frequently than those not taking OCs (P = .001). Participants were included only if they were taking a combined estrogen-progestin pill; those on noncyclical contraceptives such as implants and hormone-emitting intrauterine devices were excluded, as were naturally cycling women with very long or irregular menstrual cycles.
After multivariable statistical analysis, the only two significant predictors of hypothalamic volume were total intracranial volume and OC use. For pituitary volume, body mass index and OC use remained significant.
In addition to the MRI scans, participants also completed neurobehavioral testing to assess mood and cognition. An exploratory analysis showed no correlation between hypothalamic volume and the cognitive testing battery results, which included assessments for verbal learning and memory, executive function, and working memory.
However, a moderate positive association was seen between hypothalamic volume and anger scores (r = 0.34; P = .02). The investigators found a “strong positive correlation of hypothalamic volume with depression,” said Dr. Chen (r = 0.25; P = .09).
The investigators found no menstrual cycle-related changes in hypothalamic and pituitary volume among naturally cycling women.
Hypothalamic volume was obtained using manual segmentation of the MRIs; a combined automated-manual approach was used to obtain pituitary volume. Reliability was tested by having 5 raters each assess volumes for a randomly selected subset of the scans; inter-rater reliability fell between 0.78 and 0.86, values considered to indicate “good” reliability.
In addition to the small sample size, Dr. Chen acknowledged several limitations to the study. These included the lack of accounting for details of OC use including duration, exact type of OC, and whether women were taking the placebo phase of their pill packs at the time of scanning. Additionally, women who were naturally cycling were not asked about prior history of OC use.
Also, women’s menstrual phase was estimated from the self-reported date of the last menstrual period, rather than obtained by direct measurement via serum hormone levels.
Dr. Lipton’s perspective adds a strong note of caution to avoid overinterpretation from the study. Dr. Chen and Dr. Lipton agreed, however, that OC use should be accounted for when brain structure and function are studied in female participants.
Dr. Chen, Dr. Lipton, and their coauthors reported that they had no conflicts of interest. The authors reported no outside sources of funding.
SOURCE: Chen K et al. RSNA 2019. Presentation SSM-1904.
CHICAGO – Women taking oral contraceptives had, on average, a hypothalamus that was 6% smaller than those who didn’t, in a small study that used magnetic resonance imaging. Pituitary volume was also smaller.
Though the sample size was relatively small, 50 women in total, it’s the only study to date that looks at the relationship between hypothalamic volume and oral contraceptive (OC) use, and the largest examining pituitary volume, according to Ke Xun (Kevin) Chen, MD, who presented the findings at the annual meeting of the Radiological Society of North America.
Using MRI, Dr. Chen and his colleagues found that hypothalamic volume was significantly smaller in women taking oral contraceptives than those who were naturally cycling (b value = –64.1; P = .006). The pituitary gland also was significantly smaller in those taking OCs (b = –92.8; P = .007).
“I was quite surprised [at the finding], because the magnitude of the effect is not small,” especially in the context of changes in volume of other brain structures, senior author Michael L. Lipton, MD, PhD, said in an interview. In Alzheimer’s disease, for example, a volume loss of 4% annually can be expected.
However, “it’s not shocking to me in a negative way at all. I can’t tell you what it means in terms of how it’s going to affect people,” since this is a cross-sectional study that only detected a correlation and can’t say anything about a causative relationship, he added. “We don’t even know that [OCs] cause this effect. ... It’s plausible that this is just a plasticity-related change that’s simply showing us the effect of the drug.
“We’re going to be much more careful to consider oral contraceptive use as a covariate in future research studies; that’s for sure,” he said.
Although OCs have been available since their 1960 Food and Drug Administration approval, and their effects in some areas of physiology and health have been well studied, there’s still not much known about how oral contraceptives affect brain function, said Dr. Lipton, professor of neuroradiology and psychiatry and behavioral sciences at Albert Einstein College of Medicine, in the Montefiore medical system, New York.
The spark for this study came from one of Dr. Lipton’s main areas of research – sex differences in susceptibility to and recovery from traumatic brain injury. “Women are more likely to exhibit changes in their brain [after injury] – and changes in their brain function – than men,” he said.
In the present study, “we went at this trying to understand the effect to which the hormone effect might be doing something in regular, healthy people that we need to consider as part of the bigger picture,” he said.
Dr. Lipton, Dr. Chen (then a radiology resident at Albert Einstein College of Medicine), and their coauthors constructed the study to look for differences in brain structure between women who were experiencing natural menstrual cycles and those who were taking exogenous hormones, to begin to learn how oral contraceptive use might modify risk and susceptibility for neurologic disease and injury.
It had already been established that global brain volume didn’t differ between naturally cycling women and those using OCs. However, some studies had shown differences in volume of some specific brain regions, and one study had shown smaller pituitary volume in OC users, according to the presentation by Dr. Chen, who is now a radiology fellow at Brigham and Women’s Hospital, Boston. Accurately measuring hypothalamic volume represents a technical challenge, and the effect of OCs on the structure’s volume hadn’t previously been studied.
Sex hormones, said Dr. Lipton, have known trophic effects on brain tissue and ovarian sex hormones cross the blood brain barrier, so the idea that there would be some plasticity in the brains of those taking OCs wasn’t completely surprising, especially since there are hormone receptors that lie within the central nervous system. However, he said he was “very surprised” by the effect size seen in the study.
The study included 21 healthy women taking combined oral contraceptives, and 29 naturally cycling women. Participants’ mean age was 23 years for the OC users, and 21 for the naturally cycling women. Body mass index and smoking history didn’t differ between groups. Women on OCs were significantly more likely to use alcohol and to drink more frequently than those not taking OCs (P = .001). Participants were included only if they were taking a combined estrogen-progestin pill; those on noncyclical contraceptives such as implants and hormone-emitting intrauterine devices were excluded, as were naturally cycling women with very long or irregular menstrual cycles.
After multivariable statistical analysis, the only two significant predictors of hypothalamic volume were total intracranial volume and OC use. For pituitary volume, body mass index and OC use remained significant.
In addition to the MRI scans, participants also completed neurobehavioral testing to assess mood and cognition. An exploratory analysis showed no correlation between hypothalamic volume and the cognitive testing battery results, which included assessments for verbal learning and memory, executive function, and working memory.
However, a moderate positive association was seen between hypothalamic volume and anger scores (r = 0.34; P = .02). The investigators found a “strong positive correlation of hypothalamic volume with depression,” said Dr. Chen (r = 0.25; P = .09).
The investigators found no menstrual cycle-related changes in hypothalamic and pituitary volume among naturally cycling women.
Hypothalamic volume was obtained using manual segmentation of the MRIs; a combined automated-manual approach was used to obtain pituitary volume. Reliability was tested by having 5 raters each assess volumes for a randomly selected subset of the scans; inter-rater reliability fell between 0.78 and 0.86, values considered to indicate “good” reliability.
In addition to the small sample size, Dr. Chen acknowledged several limitations to the study. These included the lack of accounting for details of OC use including duration, exact type of OC, and whether women were taking the placebo phase of their pill packs at the time of scanning. Additionally, women who were naturally cycling were not asked about prior history of OC use.
Also, women’s menstrual phase was estimated from the self-reported date of the last menstrual period, rather than obtained by direct measurement via serum hormone levels.
Dr. Lipton’s perspective adds a strong note of caution to avoid overinterpretation from the study. Dr. Chen and Dr. Lipton agreed, however, that OC use should be accounted for when brain structure and function are studied in female participants.
Dr. Chen, Dr. Lipton, and their coauthors reported that they had no conflicts of interest. The authors reported no outside sources of funding.
SOURCE: Chen K et al. RSNA 2019. Presentation SSM-1904.
REPORTING FROM RSNA 2019
2019 Update on bone health
Prior to last year, this column was titled “Update on osteoporosis.” My observation, however, is that too many ObGyn providers simply measure bone mass (known as bone mineral density, or BMD), label a patient as normal, osteopenic, or osteoporotic, and then consider pharmacotherapy. The FRAX fracture prediction algorithm, which incorporates age, weight, height, history of any previous fracture, family history of hip fracture, current smoking, use of glucocorticoid medications, and any history of rheumatoid arthritis, has refined the screening process somewhat, if and when it is utilized. As clinicians, we should never lose sight of our goal: to prevent fragility fractures. Having osteoporosis increases that risk, but not having osteoporosis does not eliminate it.
In this Update, I highlight various ways in which work published this past year may help us to improve our patients’ bone health and reduce fragility fractures.
Updated ISCD guidance emphasizes appropriate BMD testing, use of the
Z-score, and terminology
International Society for Clinical Densitometry. 2019 ISCD Official Positions-Adult. June 2019. https://www.iscd.org/official-positions/2019-ISCD-official-positions-adult.
Continue to: Indications for BMD testing...
Indications for BMD testing
The ISCD's indications for BMD testing remain for women age 65 and older. For postmenopausal women younger than age 65, a BMD test is indicated if they have a risk factor for low bone mass, such as 1) low body weight, 2) prior fracture, 3) high-risk medication use, or 4) a disease or condition associated with bone loss. A BMD test also is indicated for women during the menopausal transition with clinical risk factors for fracture, such as low body weight, prior fracture, or high-risk medication use. Interestingly, the ISCD recommendation for men is similar but uses age 70 for this group.
In addition, the ISCD recommends BMD testing in adults with a fragility fracture, with a disease or condition associated with low bone mass, or taking medications associated with low bone mass, as well as for anyone being considered for pharmacologic therapy, being treated (to monitor treatment effect), not receiving therapy in whom evidence of bone loss would lead to treatment, and in women discontinuing estrogen who should be considered for BMD testing according to the indications already mentioned.
Sites to assess for osteoporosis. The World Health Organization international reference standard for osteoporosis diagnosis is a T-score of -2.5 or less at the femoral neck. The reference standard, from which the T-score is calculated, is for white women aged 20 to 29 years of age from the database of the Third National Health and Nutrition Examination Survey. Osteoporosis also may be diagnosed in postmenopausal women if the T-score of the lumbar spine, total hip, or femoral neck is -2.5 or less. In certain circumstances, the 33% radius (also called the one-third radius) may be utilized. Other hip regions of interest, including Ward's area and the greater trochanter, should not be used for diagnosis.
The skeletal sites at which to measure BMD include the anteroposterior of the spine and hip in all patients. In terms of the spine, use L1-L4 for spine BMD measurement. However, exclude vertebrae that are affected by local structural changes or artifact. Use 3 vertebrae if 4 cannot be used, and 2 if 3 cannot be used. BMD-based diagnostic classification should not be made using a single vertebra. Anatomically abnormal vertebrae may be excluded from analysis if they are clearly abnormal and nonassessable within the resolution of the system, or if there is more than a 1.0 T-score difference between the vertebra in question and adjacent vertebrae. When vertebrae are excluded, the BMD of the remaining vertebrae are used to derive the T-score.
For BMD measurement at the hip, the femoral neck or total proximal femur—whichever is lowest—should be used. Either hip may be measured. Data are insufficient on whether mean T-scores for bilateral hip BMD should be used for diagnosis.
Terminology. While the ISCD retains the term osteopenia, the term low bone mass or low bone density is preferred. People with low bone mass or density are not necessarily at high fracture risk.
Concerning BMD reporting in women prior to menopause, Z-scores, not T-scores, are preferred. A Z-score of -2.0 or lower is defined as "below the expected range for age"; a Z-score above -2.0 is "within the expected range for age."
Use of serial BMD testing
Finally, regarding serial BMD measurements, such testing in combination with clinical assessment of fracture risk can be used to determine whether treatment should be initiated in untreated patients. Furthermore, serial BMD testing can monitor a patient's response to therapy by finding an increase or stability of bone density. It should be used to monitor individuals following cessation of osteoporosis drug therapy. Serial BMD testing can detect loss of bone density, indicating the need to assess treatment adherence, evaluate possible secondary causes of osteoporosis, and possibly re-evaluate therapeutic options.
Intervals between BMD testing should be determined according to each patient's clinical status. Typically, 1 year after initiating or changing therapy is appropriate, with longer intervals once therapeutic effect is established.
Patients commonly ask for BMD testing and ObGyn providers commonly order it. Understanding appropriate use of BMD testing in terms of who to scan, what sites to evaluate, when there may be spurious results of vertebrae due to artifacts, avoiding T-scores in premenopausal women in favor of Z-scores, understanding that low bone mass is a preferred term to osteopenia, and knowing how to order and use serial BMD testing will likely improve our role as the frontline providers to improving bone health in our patients.
Continue to: Dyspareunia drug has positive effects on bone...
Dyspareunia drug has positive effects on bone
de Villiers TJ, Altomare C, Particco M, et al. Effects of ospemifene on bone in postmenopausal women. Climacteric. 2019;22:442-447.
Previously, ospemifene effectively reduced bone loss in ovariectomized rats, with activity comparable to that of estradiol and raloxifene.3 Clinical data from 3 phase 1 or 2 clinical trials found that ospemifene 60 mg/day had a positive effect on biochemical markers for bone turnover in healthy postmenopausal women, with significant improvements relative to placebo and effects comparable to those of raloxifene.4
Effects on bone formation/resorption biomarkers
In a recent study, de Villiers and colleagues reported the first phase 3 trial that looked at markers of bone formation and bone resorption.5 A total of 316 women were randomly assigned to receive ospemifene, and 315 received placebo.
Demographic and baseline characteristics were similar between treatment groups. Participants' mean age was approximately 60 years, mean body mass index (BMI) was 27.2 kg/m2, and mean duration of VVA was 8 to 9 years. Serum levels of 9 bone biomarkers were similar between groups at baseline.
At week 12, all 5 markers of bone resorption improved with ospemifene treatment, and 3 of the 5 (NTX, CTX, and TRACP-5b) did so in a statistically significant fashion compared with placebo (P≤.02). In addition, at week 12, all 4 markers of bone formation improved with ospemifene treatment compared with placebo (P≤.008). Furthermore, lower bone resorption markers with ospemifene were observed regardless of time since menopause (≤ 5 years or
> 5 years) or baseline BMD, whether normal, osteopenic, or osteoporotic.
Interpret results cautiously
The authors caution that the data are limited to biochemical markers rather than fracture or BMD. It is known that there is good correlation between biochemical markers for bone turnover and the occurrence of fracture.6
Ospemifene is an oral SERM approved for the treatment of moderate to severe dyspareunia as well as dryness from VVA due to menopause. The preclinical animal data and human markers of bone turnover all support the antiresorptive action of ospemifene on bones. Thus, one may safely surmise that ospemifene's direction of activity in bone is virtually indisputable. The magnitude of that activity is, however, unstudied. Therefore, when choosing an agent to treat women with dyspareunia or vaginal dryness from VVA of menopause, determining any potential add-on benefit in bone may be appropriate for that particular patient, although one would not use it as a stand-alone agent for bone only.
Continue to: Sarcopenia adds to osteoporotic risk for fractures...
Sarcopenia adds to osteoporotic risk for fractures
Lima RM, de Oliveira RJ, Raposo R, et al. Stages of sarcopenia, bone mineral density, and the prevalence of osteoporosis in older women. Arch Osteoporos. 2019;14:38.
In 1989, the term sarcopenia was introduced to refer to the age-related decline in skeletal muscle mass.8 Currently, sarcopenia is defined as a progressive decline in muscle mass, strength, and physical function, thus increasing the risk for various adverse outcomes, including osteoporosis.9 Although muscle and bone tissues differ morphologically, their functioning is closely interconnected.
The sarcopenia-osteoporosis connection
Lima and colleagues sought to investigate the relationship between sarcopenia and osteoporosis.10 They measured women's fat free mass with dual-energy x-ray absorptiometry (DXA) scanning, muscle strength using a dynamometer to measure knee extension torque while participants were seated, and functional performance using the timed "up and go test" in which participants were timed as they got up from a chair, walked 3 meters around a cone, and returned to sit in the chair.10,11
The authors used definitions from the European Working Group on Sarcopenia in Older People (EWGSOP). Participants who had normal results in all 3 domains were considered nonsarcopenic. Presarcopenia was defined as having low fat free mass on DXA scanning but normal strength and function. Participants who had low fat free mass and either low strength or low function were labeled as having sarcopenia. Severe sarcopenia was defined as abnormal results in all 3 domains.
Two hundred thirty-four women (mean age, 68.3 years; range, 60-80) underwent BMD testing and were evaluated according to the 3 domains of possible sarcopenia. All were community dwelling and did not have cognitive impairment or functional dependency.
The rates of osteoporosis were 15.8%, 19.2%, 35.3%, and 46.2% for nonsarcopenia, presarcopenia, sarcopenia, and severe sarcopenia, respectively (P=.002). Whole-body and femoral neck BMD values were significantly lower among all sarcopenia stages when compared with nonsarcopenia (P<.05). The severe sarcopenia group showed the lowest lumbar spine T-scores (P<.05). When clustered, sarcopenia and severe sarcopenia presented a significantly higher risk for osteoporosis (odds ratio, 3.4; 95% confidence interval [CI], 1.5-7.8).
Consider sarcopenia a risk factor
The authors concluded that these "results provide support for the concept that a dose-response relationship exists between sarcopenia stages, BMD, and the presence of osteoporosis. These findings strengthen the clinical significance of the EWGSOP sarcopenia definitions and indicate that severe sarcopenia should be viewed with attention by healthcare professionals."
Osteoporotic fractures are defined as fragility fractures. While "frailty" has been a risk factor for such fractures in the past, increasing evidence now suggests that what we previously called frailty includes a significant component of loss of muscle mass, strength, and function—referred to as sarcopenia. While it is not likely that many ObGyns will perform objective testing for sarcopenia, conducting even a subjective assessment of such status should be considered in addition to BMD determinations in making decisions about pharmacotherapy.
Continue to: Certain characteristics may offset fracture risk in aromatase inhibitor users...
Certain characteristics may offset fracture risk in aromatase inhibitor users
Leslie WD, Morin SN, Lix LM, et al. Fracture risk in women with breast cancer initiating aromatase inhibitor therapy: a registry-based cohort study. Oncologist. 2019;24:1432-1438.
The use of AIs increases bone turnover and induces bone loss at trabecular-rich bone sites at an average rate of 1% to 3% per year, with reports of up to a threefold increased fracture incidence.13 By contrast, a large nationwide population-based cohort study using US Medicare data identified minimal fracture risk from AI use compared with tamoxifen use (11% higher for nonvertebral fractures, not significantly increased for hip fractures).14
An article published previously in this column reported that women on AIs treated with intravenous zoledronic acid had improvements in BMD, while women treated with denosumab had statistically significant fewer fractures compared with those receiving placebo, whether they had normal bone mass, osteopenia, or osteoporosis at
baseline.15-17
Data derived from a population-based BMD registry
In a recent cohort study, Leslie and colleagues offer the opinion that "observations in the clinical trial setting may differ from routine clinical practice."18 The authors examined fracture outcomes using a large clinical registry of BMD results from women in Manitoba, Canada. They identified women at least 40 years of age initiating AI therapy for breast cancer (n = 1,775), women with breast cancer not receiving AI therapy (n = 1,016), and women from the general population without breast cancer (n = 34,205).
Fracture outcomes were assessed after a mean of 6.2 years for the AI users, all of whom had at least 12 months of AI exposure. At baseline, AI users had higher BMI, higher BMD, lower osteoporosis prevalence, and fewer prior fractures than women from the general population or women with breast cancer without AI use (all P<.001). After adjusting for all covariates, AI users were not at significantly greater risk for major osteoporotic fractures (hazard ratio [HR], 1.15; 95% CI, 0.93-1.42), hip fracture (HR, 0.90; 95% CI, 0.56-1.43), or any fracture (HR, 1.06; 95% CI, 0.88-1.28) compared with the general population.
Results challenge prevailing view
Thus, the authors concluded that higher baseline BMI, BMD, and lower prevalence of prior fracture at baseline may offset the adverse effects of AI exposure. Although confirmatory data from large cohort studies are required, the authors stated that their findings challenge the view that all women with breast cancer initiating AI therapy should be considered at high risk for fracture.
It is well known that women with estrogen receptor-positive breast cancers tend to be more obese than noncancer patients and have higher levels of circulating estrogens. The study by Leslie and colleagues shows that such patients will have fewer previous fractures and better baseline bone mass values than the general population. This may prompt us to rethink whether all women initiating AI therapy need to be treated for fracture prevention, as some previous studies have suggested. Clearly, further study is necessary.
- International Society for Clinical Densitometry. 2019 ISCD Official Positions-Adult. June 2019. https://www.iscd.org/official-positions/2019-iscd-official-positions-adult. Accessed November 22, 2019.
- Goldstein SR, Neven P, Cummings S, et al. Postmenopausal evaluation and risk reduction with lasofoxifene (PEARL) trial: 5-year gynecological outcomes. Menopause. 2011;18:17-22.
- Kangas L, Unkila M. Tissue selectivity of ospemifene: pharmacologic profile and clinical implications. Steroids. 2013;78:1273-1280.
- Constantine GD, Kagan R, Miller PD. Effects of ospemifene on bone parameters including clinical biomarkers in postmenopausal women. Menopause. 2016;23:638-644.
- de Villiers TJ, Altomare C, Particco M, et al. Effects of ospemifene on bone in postmenopausal women. Climacteric. 2019;22:442-447.
- Gerdhem P, Ivaska KK, Alatalo SL, et al. Biochemical markers of bone metabolism and prediction of fracture in elderly women. J Bone Miner Res. 2004;19:386-393.
- Siris ES, Adler R, Bilezikian J, et al. The clinical diagnosis of osteoporosis: a position statement from the National Bone Health Alliance Working Group. Osteoporos Int. 2014;25:1439-1443.
- Epidemiologic and methodologic problems in determining nutritional status of older persons. Proceedings of a conference. Albuquerque, New Mexico, October 19-21, 1988. Am J Clin Nutr. 1989;50(5 suppl):1121-1235.
- Drey M, Sieber CC, Bertsch T, et al. Osteosarcopenia is more than sarcopenia and osteopenia alone. Aging Clin Exp Res. 2016;28:895-899.
- Lima RM, de Oliveira RJ, Raposo R, et al. Stages of sarcopenia, bone mineral density, and the prevalence of osteoporosis in older women. Arch Osteoporos. 2019;14:38.
- Mathias S, Nayak U, Isaacs B. Balance in elderly patients: the "get-up and go" test. Arch Phys Med Rehabil. 1986;67:387-389.
- Burstein HJ, Temin S, Anderson H, et al. Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: American Society of Clinical Oncology clinical practice guideline focused update. J Clin Oncol. 2014;32:2255-2269.
- Schmidt N, Jacob L, Coleman R, et al. The impact of treatment compliance on fracture risk in women with breast cancer treated with aromatase inhibitors in the United Kingdom. Breast Cancer Res Treat. 2016;155:151-157.
- Neuner JM, Shi Y, Kong AL, et al. Fractures in a nationwide population-based cohort of users of breast cancer hormonal therapy. J Cancer Surviv. 2018;12:268-275.
- Goldstein SR. 2015 Update on osteoporosis. OBG Manag. 2015;27:31-39.
- Majithia N, Atherton PJ, Lafky JM, et al. Zoledronic acid for treatment of osteopenia and osteoporosis in women with primary breast cancer undergoing adjuvant aromatase inhibitor therapy: a 5-year follow-up. Support Care Cancer. 2016;24:1219-1226.
- Gnant M, Pfeiler G, Dubsky PC, et al; Austrian Breast and Colorectal Cancer Study Group. Adjuvant denosumab in breast cancer (ABCSG-18): a multicenter, randomized, double-blind, placebo-controlled trial. Lancet. 2015;386:433-443.
- Leslie WD, Morin SN, Lix LM, et al. Fracture risk in women with breast cancer initiating aromatase inhibitor therapy: a registry-based cohort study. Oncologist. 2019;24:1432-1438.
Prior to last year, this column was titled “Update on osteoporosis.” My observation, however, is that too many ObGyn providers simply measure bone mass (known as bone mineral density, or BMD), label a patient as normal, osteopenic, or osteoporotic, and then consider pharmacotherapy. The FRAX fracture prediction algorithm, which incorporates age, weight, height, history of any previous fracture, family history of hip fracture, current smoking, use of glucocorticoid medications, and any history of rheumatoid arthritis, has refined the screening process somewhat, if and when it is utilized. As clinicians, we should never lose sight of our goal: to prevent fragility fractures. Having osteoporosis increases that risk, but not having osteoporosis does not eliminate it.
In this Update, I highlight various ways in which work published this past year may help us to improve our patients’ bone health and reduce fragility fractures.
Updated ISCD guidance emphasizes appropriate BMD testing, use of the
Z-score, and terminology
International Society for Clinical Densitometry. 2019 ISCD Official Positions-Adult. June 2019. https://www.iscd.org/official-positions/2019-ISCD-official-positions-adult.
Continue to: Indications for BMD testing...
Indications for BMD testing
The ISCD's indications for BMD testing remain for women age 65 and older. For postmenopausal women younger than age 65, a BMD test is indicated if they have a risk factor for low bone mass, such as 1) low body weight, 2) prior fracture, 3) high-risk medication use, or 4) a disease or condition associated with bone loss. A BMD test also is indicated for women during the menopausal transition with clinical risk factors for fracture, such as low body weight, prior fracture, or high-risk medication use. Interestingly, the ISCD recommendation for men is similar but uses age 70 for this group.
In addition, the ISCD recommends BMD testing in adults with a fragility fracture, with a disease or condition associated with low bone mass, or taking medications associated with low bone mass, as well as for anyone being considered for pharmacologic therapy, being treated (to monitor treatment effect), not receiving therapy in whom evidence of bone loss would lead to treatment, and in women discontinuing estrogen who should be considered for BMD testing according to the indications already mentioned.
Sites to assess for osteoporosis. The World Health Organization international reference standard for osteoporosis diagnosis is a T-score of -2.5 or less at the femoral neck. The reference standard, from which the T-score is calculated, is for white women aged 20 to 29 years of age from the database of the Third National Health and Nutrition Examination Survey. Osteoporosis also may be diagnosed in postmenopausal women if the T-score of the lumbar spine, total hip, or femoral neck is -2.5 or less. In certain circumstances, the 33% radius (also called the one-third radius) may be utilized. Other hip regions of interest, including Ward's area and the greater trochanter, should not be used for diagnosis.
The skeletal sites at which to measure BMD include the anteroposterior of the spine and hip in all patients. In terms of the spine, use L1-L4 for spine BMD measurement. However, exclude vertebrae that are affected by local structural changes or artifact. Use 3 vertebrae if 4 cannot be used, and 2 if 3 cannot be used. BMD-based diagnostic classification should not be made using a single vertebra. Anatomically abnormal vertebrae may be excluded from analysis if they are clearly abnormal and nonassessable within the resolution of the system, or if there is more than a 1.0 T-score difference between the vertebra in question and adjacent vertebrae. When vertebrae are excluded, the BMD of the remaining vertebrae are used to derive the T-score.
For BMD measurement at the hip, the femoral neck or total proximal femur—whichever is lowest—should be used. Either hip may be measured. Data are insufficient on whether mean T-scores for bilateral hip BMD should be used for diagnosis.
Terminology. While the ISCD retains the term osteopenia, the term low bone mass or low bone density is preferred. People with low bone mass or density are not necessarily at high fracture risk.
Concerning BMD reporting in women prior to menopause, Z-scores, not T-scores, are preferred. A Z-score of -2.0 or lower is defined as "below the expected range for age"; a Z-score above -2.0 is "within the expected range for age."
Use of serial BMD testing
Finally, regarding serial BMD measurements, such testing in combination with clinical assessment of fracture risk can be used to determine whether treatment should be initiated in untreated patients. Furthermore, serial BMD testing can monitor a patient's response to therapy by finding an increase or stability of bone density. It should be used to monitor individuals following cessation of osteoporosis drug therapy. Serial BMD testing can detect loss of bone density, indicating the need to assess treatment adherence, evaluate possible secondary causes of osteoporosis, and possibly re-evaluate therapeutic options.
Intervals between BMD testing should be determined according to each patient's clinical status. Typically, 1 year after initiating or changing therapy is appropriate, with longer intervals once therapeutic effect is established.
Patients commonly ask for BMD testing and ObGyn providers commonly order it. Understanding appropriate use of BMD testing in terms of who to scan, what sites to evaluate, when there may be spurious results of vertebrae due to artifacts, avoiding T-scores in premenopausal women in favor of Z-scores, understanding that low bone mass is a preferred term to osteopenia, and knowing how to order and use serial BMD testing will likely improve our role as the frontline providers to improving bone health in our patients.
Continue to: Dyspareunia drug has positive effects on bone...
Dyspareunia drug has positive effects on bone
de Villiers TJ, Altomare C, Particco M, et al. Effects of ospemifene on bone in postmenopausal women. Climacteric. 2019;22:442-447.
Previously, ospemifene effectively reduced bone loss in ovariectomized rats, with activity comparable to that of estradiol and raloxifene.3 Clinical data from 3 phase 1 or 2 clinical trials found that ospemifene 60 mg/day had a positive effect on biochemical markers for bone turnover in healthy postmenopausal women, with significant improvements relative to placebo and effects comparable to those of raloxifene.4
Effects on bone formation/resorption biomarkers
In a recent study, de Villiers and colleagues reported the first phase 3 trial that looked at markers of bone formation and bone resorption.5 A total of 316 women were randomly assigned to receive ospemifene, and 315 received placebo.
Demographic and baseline characteristics were similar between treatment groups. Participants' mean age was approximately 60 years, mean body mass index (BMI) was 27.2 kg/m2, and mean duration of VVA was 8 to 9 years. Serum levels of 9 bone biomarkers were similar between groups at baseline.
At week 12, all 5 markers of bone resorption improved with ospemifene treatment, and 3 of the 5 (NTX, CTX, and TRACP-5b) did so in a statistically significant fashion compared with placebo (P≤.02). In addition, at week 12, all 4 markers of bone formation improved with ospemifene treatment compared with placebo (P≤.008). Furthermore, lower bone resorption markers with ospemifene were observed regardless of time since menopause (≤ 5 years or
> 5 years) or baseline BMD, whether normal, osteopenic, or osteoporotic.
Interpret results cautiously
The authors caution that the data are limited to biochemical markers rather than fracture or BMD. It is known that there is good correlation between biochemical markers for bone turnover and the occurrence of fracture.6
Ospemifene is an oral SERM approved for the treatment of moderate to severe dyspareunia as well as dryness from VVA due to menopause. The preclinical animal data and human markers of bone turnover all support the antiresorptive action of ospemifene on bones. Thus, one may safely surmise that ospemifene's direction of activity in bone is virtually indisputable. The magnitude of that activity is, however, unstudied. Therefore, when choosing an agent to treat women with dyspareunia or vaginal dryness from VVA of menopause, determining any potential add-on benefit in bone may be appropriate for that particular patient, although one would not use it as a stand-alone agent for bone only.
Continue to: Sarcopenia adds to osteoporotic risk for fractures...
Sarcopenia adds to osteoporotic risk for fractures
Lima RM, de Oliveira RJ, Raposo R, et al. Stages of sarcopenia, bone mineral density, and the prevalence of osteoporosis in older women. Arch Osteoporos. 2019;14:38.
In 1989, the term sarcopenia was introduced to refer to the age-related decline in skeletal muscle mass.8 Currently, sarcopenia is defined as a progressive decline in muscle mass, strength, and physical function, thus increasing the risk for various adverse outcomes, including osteoporosis.9 Although muscle and bone tissues differ morphologically, their functioning is closely interconnected.
The sarcopenia-osteoporosis connection
Lima and colleagues sought to investigate the relationship between sarcopenia and osteoporosis.10 They measured women's fat free mass with dual-energy x-ray absorptiometry (DXA) scanning, muscle strength using a dynamometer to measure knee extension torque while participants were seated, and functional performance using the timed "up and go test" in which participants were timed as they got up from a chair, walked 3 meters around a cone, and returned to sit in the chair.10,11
The authors used definitions from the European Working Group on Sarcopenia in Older People (EWGSOP). Participants who had normal results in all 3 domains were considered nonsarcopenic. Presarcopenia was defined as having low fat free mass on DXA scanning but normal strength and function. Participants who had low fat free mass and either low strength or low function were labeled as having sarcopenia. Severe sarcopenia was defined as abnormal results in all 3 domains.
Two hundred thirty-four women (mean age, 68.3 years; range, 60-80) underwent BMD testing and were evaluated according to the 3 domains of possible sarcopenia. All were community dwelling and did not have cognitive impairment or functional dependency.
The rates of osteoporosis were 15.8%, 19.2%, 35.3%, and 46.2% for nonsarcopenia, presarcopenia, sarcopenia, and severe sarcopenia, respectively (P=.002). Whole-body and femoral neck BMD values were significantly lower among all sarcopenia stages when compared with nonsarcopenia (P<.05). The severe sarcopenia group showed the lowest lumbar spine T-scores (P<.05). When clustered, sarcopenia and severe sarcopenia presented a significantly higher risk for osteoporosis (odds ratio, 3.4; 95% confidence interval [CI], 1.5-7.8).
Consider sarcopenia a risk factor
The authors concluded that these "results provide support for the concept that a dose-response relationship exists between sarcopenia stages, BMD, and the presence of osteoporosis. These findings strengthen the clinical significance of the EWGSOP sarcopenia definitions and indicate that severe sarcopenia should be viewed with attention by healthcare professionals."
Osteoporotic fractures are defined as fragility fractures. While "frailty" has been a risk factor for such fractures in the past, increasing evidence now suggests that what we previously called frailty includes a significant component of loss of muscle mass, strength, and function—referred to as sarcopenia. While it is not likely that many ObGyns will perform objective testing for sarcopenia, conducting even a subjective assessment of such status should be considered in addition to BMD determinations in making decisions about pharmacotherapy.
Continue to: Certain characteristics may offset fracture risk in aromatase inhibitor users...
Certain characteristics may offset fracture risk in aromatase inhibitor users
Leslie WD, Morin SN, Lix LM, et al. Fracture risk in women with breast cancer initiating aromatase inhibitor therapy: a registry-based cohort study. Oncologist. 2019;24:1432-1438.
The use of AIs increases bone turnover and induces bone loss at trabecular-rich bone sites at an average rate of 1% to 3% per year, with reports of up to a threefold increased fracture incidence.13 By contrast, a large nationwide population-based cohort study using US Medicare data identified minimal fracture risk from AI use compared with tamoxifen use (11% higher for nonvertebral fractures, not significantly increased for hip fractures).14
An article published previously in this column reported that women on AIs treated with intravenous zoledronic acid had improvements in BMD, while women treated with denosumab had statistically significant fewer fractures compared with those receiving placebo, whether they had normal bone mass, osteopenia, or osteoporosis at
baseline.15-17
Data derived from a population-based BMD registry
In a recent cohort study, Leslie and colleagues offer the opinion that "observations in the clinical trial setting may differ from routine clinical practice."18 The authors examined fracture outcomes using a large clinical registry of BMD results from women in Manitoba, Canada. They identified women at least 40 years of age initiating AI therapy for breast cancer (n = 1,775), women with breast cancer not receiving AI therapy (n = 1,016), and women from the general population without breast cancer (n = 34,205).
Fracture outcomes were assessed after a mean of 6.2 years for the AI users, all of whom had at least 12 months of AI exposure. At baseline, AI users had higher BMI, higher BMD, lower osteoporosis prevalence, and fewer prior fractures than women from the general population or women with breast cancer without AI use (all P<.001). After adjusting for all covariates, AI users were not at significantly greater risk for major osteoporotic fractures (hazard ratio [HR], 1.15; 95% CI, 0.93-1.42), hip fracture (HR, 0.90; 95% CI, 0.56-1.43), or any fracture (HR, 1.06; 95% CI, 0.88-1.28) compared with the general population.
Results challenge prevailing view
Thus, the authors concluded that higher baseline BMI, BMD, and lower prevalence of prior fracture at baseline may offset the adverse effects of AI exposure. Although confirmatory data from large cohort studies are required, the authors stated that their findings challenge the view that all women with breast cancer initiating AI therapy should be considered at high risk for fracture.
It is well known that women with estrogen receptor-positive breast cancers tend to be more obese than noncancer patients and have higher levels of circulating estrogens. The study by Leslie and colleagues shows that such patients will have fewer previous fractures and better baseline bone mass values than the general population. This may prompt us to rethink whether all women initiating AI therapy need to be treated for fracture prevention, as some previous studies have suggested. Clearly, further study is necessary.
Prior to last year, this column was titled “Update on osteoporosis.” My observation, however, is that too many ObGyn providers simply measure bone mass (known as bone mineral density, or BMD), label a patient as normal, osteopenic, or osteoporotic, and then consider pharmacotherapy. The FRAX fracture prediction algorithm, which incorporates age, weight, height, history of any previous fracture, family history of hip fracture, current smoking, use of glucocorticoid medications, and any history of rheumatoid arthritis, has refined the screening process somewhat, if and when it is utilized. As clinicians, we should never lose sight of our goal: to prevent fragility fractures. Having osteoporosis increases that risk, but not having osteoporosis does not eliminate it.
In this Update, I highlight various ways in which work published this past year may help us to improve our patients’ bone health and reduce fragility fractures.
Updated ISCD guidance emphasizes appropriate BMD testing, use of the
Z-score, and terminology
International Society for Clinical Densitometry. 2019 ISCD Official Positions-Adult. June 2019. https://www.iscd.org/official-positions/2019-ISCD-official-positions-adult.
Continue to: Indications for BMD testing...
Indications for BMD testing
The ISCD's indications for BMD testing remain for women age 65 and older. For postmenopausal women younger than age 65, a BMD test is indicated if they have a risk factor for low bone mass, such as 1) low body weight, 2) prior fracture, 3) high-risk medication use, or 4) a disease or condition associated with bone loss. A BMD test also is indicated for women during the menopausal transition with clinical risk factors for fracture, such as low body weight, prior fracture, or high-risk medication use. Interestingly, the ISCD recommendation for men is similar but uses age 70 for this group.
In addition, the ISCD recommends BMD testing in adults with a fragility fracture, with a disease or condition associated with low bone mass, or taking medications associated with low bone mass, as well as for anyone being considered for pharmacologic therapy, being treated (to monitor treatment effect), not receiving therapy in whom evidence of bone loss would lead to treatment, and in women discontinuing estrogen who should be considered for BMD testing according to the indications already mentioned.
Sites to assess for osteoporosis. The World Health Organization international reference standard for osteoporosis diagnosis is a T-score of -2.5 or less at the femoral neck. The reference standard, from which the T-score is calculated, is for white women aged 20 to 29 years of age from the database of the Third National Health and Nutrition Examination Survey. Osteoporosis also may be diagnosed in postmenopausal women if the T-score of the lumbar spine, total hip, or femoral neck is -2.5 or less. In certain circumstances, the 33% radius (also called the one-third radius) may be utilized. Other hip regions of interest, including Ward's area and the greater trochanter, should not be used for diagnosis.
The skeletal sites at which to measure BMD include the anteroposterior of the spine and hip in all patients. In terms of the spine, use L1-L4 for spine BMD measurement. However, exclude vertebrae that are affected by local structural changes or artifact. Use 3 vertebrae if 4 cannot be used, and 2 if 3 cannot be used. BMD-based diagnostic classification should not be made using a single vertebra. Anatomically abnormal vertebrae may be excluded from analysis if they are clearly abnormal and nonassessable within the resolution of the system, or if there is more than a 1.0 T-score difference between the vertebra in question and adjacent vertebrae. When vertebrae are excluded, the BMD of the remaining vertebrae are used to derive the T-score.
For BMD measurement at the hip, the femoral neck or total proximal femur—whichever is lowest—should be used. Either hip may be measured. Data are insufficient on whether mean T-scores for bilateral hip BMD should be used for diagnosis.
Terminology. While the ISCD retains the term osteopenia, the term low bone mass or low bone density is preferred. People with low bone mass or density are not necessarily at high fracture risk.
Concerning BMD reporting in women prior to menopause, Z-scores, not T-scores, are preferred. A Z-score of -2.0 or lower is defined as "below the expected range for age"; a Z-score above -2.0 is "within the expected range for age."
Use of serial BMD testing
Finally, regarding serial BMD measurements, such testing in combination with clinical assessment of fracture risk can be used to determine whether treatment should be initiated in untreated patients. Furthermore, serial BMD testing can monitor a patient's response to therapy by finding an increase or stability of bone density. It should be used to monitor individuals following cessation of osteoporosis drug therapy. Serial BMD testing can detect loss of bone density, indicating the need to assess treatment adherence, evaluate possible secondary causes of osteoporosis, and possibly re-evaluate therapeutic options.
Intervals between BMD testing should be determined according to each patient's clinical status. Typically, 1 year after initiating or changing therapy is appropriate, with longer intervals once therapeutic effect is established.
Patients commonly ask for BMD testing and ObGyn providers commonly order it. Understanding appropriate use of BMD testing in terms of who to scan, what sites to evaluate, when there may be spurious results of vertebrae due to artifacts, avoiding T-scores in premenopausal women in favor of Z-scores, understanding that low bone mass is a preferred term to osteopenia, and knowing how to order and use serial BMD testing will likely improve our role as the frontline providers to improving bone health in our patients.
Continue to: Dyspareunia drug has positive effects on bone...
Dyspareunia drug has positive effects on bone
de Villiers TJ, Altomare C, Particco M, et al. Effects of ospemifene on bone in postmenopausal women. Climacteric. 2019;22:442-447.
Previously, ospemifene effectively reduced bone loss in ovariectomized rats, with activity comparable to that of estradiol and raloxifene.3 Clinical data from 3 phase 1 or 2 clinical trials found that ospemifene 60 mg/day had a positive effect on biochemical markers for bone turnover in healthy postmenopausal women, with significant improvements relative to placebo and effects comparable to those of raloxifene.4
Effects on bone formation/resorption biomarkers
In a recent study, de Villiers and colleagues reported the first phase 3 trial that looked at markers of bone formation and bone resorption.5 A total of 316 women were randomly assigned to receive ospemifene, and 315 received placebo.
Demographic and baseline characteristics were similar between treatment groups. Participants' mean age was approximately 60 years, mean body mass index (BMI) was 27.2 kg/m2, and mean duration of VVA was 8 to 9 years. Serum levels of 9 bone biomarkers were similar between groups at baseline.
At week 12, all 5 markers of bone resorption improved with ospemifene treatment, and 3 of the 5 (NTX, CTX, and TRACP-5b) did so in a statistically significant fashion compared with placebo (P≤.02). In addition, at week 12, all 4 markers of bone formation improved with ospemifene treatment compared with placebo (P≤.008). Furthermore, lower bone resorption markers with ospemifene were observed regardless of time since menopause (≤ 5 years or
> 5 years) or baseline BMD, whether normal, osteopenic, or osteoporotic.
Interpret results cautiously
The authors caution that the data are limited to biochemical markers rather than fracture or BMD. It is known that there is good correlation between biochemical markers for bone turnover and the occurrence of fracture.6
Ospemifene is an oral SERM approved for the treatment of moderate to severe dyspareunia as well as dryness from VVA due to menopause. The preclinical animal data and human markers of bone turnover all support the antiresorptive action of ospemifene on bones. Thus, one may safely surmise that ospemifene's direction of activity in bone is virtually indisputable. The magnitude of that activity is, however, unstudied. Therefore, when choosing an agent to treat women with dyspareunia or vaginal dryness from VVA of menopause, determining any potential add-on benefit in bone may be appropriate for that particular patient, although one would not use it as a stand-alone agent for bone only.
Continue to: Sarcopenia adds to osteoporotic risk for fractures...
Sarcopenia adds to osteoporotic risk for fractures
Lima RM, de Oliveira RJ, Raposo R, et al. Stages of sarcopenia, bone mineral density, and the prevalence of osteoporosis in older women. Arch Osteoporos. 2019;14:38.
In 1989, the term sarcopenia was introduced to refer to the age-related decline in skeletal muscle mass.8 Currently, sarcopenia is defined as a progressive decline in muscle mass, strength, and physical function, thus increasing the risk for various adverse outcomes, including osteoporosis.9 Although muscle and bone tissues differ morphologically, their functioning is closely interconnected.
The sarcopenia-osteoporosis connection
Lima and colleagues sought to investigate the relationship between sarcopenia and osteoporosis.10 They measured women's fat free mass with dual-energy x-ray absorptiometry (DXA) scanning, muscle strength using a dynamometer to measure knee extension torque while participants were seated, and functional performance using the timed "up and go test" in which participants were timed as they got up from a chair, walked 3 meters around a cone, and returned to sit in the chair.10,11
The authors used definitions from the European Working Group on Sarcopenia in Older People (EWGSOP). Participants who had normal results in all 3 domains were considered nonsarcopenic. Presarcopenia was defined as having low fat free mass on DXA scanning but normal strength and function. Participants who had low fat free mass and either low strength or low function were labeled as having sarcopenia. Severe sarcopenia was defined as abnormal results in all 3 domains.
Two hundred thirty-four women (mean age, 68.3 years; range, 60-80) underwent BMD testing and were evaluated according to the 3 domains of possible sarcopenia. All were community dwelling and did not have cognitive impairment or functional dependency.
The rates of osteoporosis were 15.8%, 19.2%, 35.3%, and 46.2% for nonsarcopenia, presarcopenia, sarcopenia, and severe sarcopenia, respectively (P=.002). Whole-body and femoral neck BMD values were significantly lower among all sarcopenia stages when compared with nonsarcopenia (P<.05). The severe sarcopenia group showed the lowest lumbar spine T-scores (P<.05). When clustered, sarcopenia and severe sarcopenia presented a significantly higher risk for osteoporosis (odds ratio, 3.4; 95% confidence interval [CI], 1.5-7.8).
Consider sarcopenia a risk factor
The authors concluded that these "results provide support for the concept that a dose-response relationship exists between sarcopenia stages, BMD, and the presence of osteoporosis. These findings strengthen the clinical significance of the EWGSOP sarcopenia definitions and indicate that severe sarcopenia should be viewed with attention by healthcare professionals."
Osteoporotic fractures are defined as fragility fractures. While "frailty" has been a risk factor for such fractures in the past, increasing evidence now suggests that what we previously called frailty includes a significant component of loss of muscle mass, strength, and function—referred to as sarcopenia. While it is not likely that many ObGyns will perform objective testing for sarcopenia, conducting even a subjective assessment of such status should be considered in addition to BMD determinations in making decisions about pharmacotherapy.
Continue to: Certain characteristics may offset fracture risk in aromatase inhibitor users...
Certain characteristics may offset fracture risk in aromatase inhibitor users
Leslie WD, Morin SN, Lix LM, et al. Fracture risk in women with breast cancer initiating aromatase inhibitor therapy: a registry-based cohort study. Oncologist. 2019;24:1432-1438.
The use of AIs increases bone turnover and induces bone loss at trabecular-rich bone sites at an average rate of 1% to 3% per year, with reports of up to a threefold increased fracture incidence.13 By contrast, a large nationwide population-based cohort study using US Medicare data identified minimal fracture risk from AI use compared with tamoxifen use (11% higher for nonvertebral fractures, not significantly increased for hip fractures).14
An article published previously in this column reported that women on AIs treated with intravenous zoledronic acid had improvements in BMD, while women treated with denosumab had statistically significant fewer fractures compared with those receiving placebo, whether they had normal bone mass, osteopenia, or osteoporosis at
baseline.15-17
Data derived from a population-based BMD registry
In a recent cohort study, Leslie and colleagues offer the opinion that "observations in the clinical trial setting may differ from routine clinical practice."18 The authors examined fracture outcomes using a large clinical registry of BMD results from women in Manitoba, Canada. They identified women at least 40 years of age initiating AI therapy for breast cancer (n = 1,775), women with breast cancer not receiving AI therapy (n = 1,016), and women from the general population without breast cancer (n = 34,205).
Fracture outcomes were assessed after a mean of 6.2 years for the AI users, all of whom had at least 12 months of AI exposure. At baseline, AI users had higher BMI, higher BMD, lower osteoporosis prevalence, and fewer prior fractures than women from the general population or women with breast cancer without AI use (all P<.001). After adjusting for all covariates, AI users were not at significantly greater risk for major osteoporotic fractures (hazard ratio [HR], 1.15; 95% CI, 0.93-1.42), hip fracture (HR, 0.90; 95% CI, 0.56-1.43), or any fracture (HR, 1.06; 95% CI, 0.88-1.28) compared with the general population.
Results challenge prevailing view
Thus, the authors concluded that higher baseline BMI, BMD, and lower prevalence of prior fracture at baseline may offset the adverse effects of AI exposure. Although confirmatory data from large cohort studies are required, the authors stated that their findings challenge the view that all women with breast cancer initiating AI therapy should be considered at high risk for fracture.
It is well known that women with estrogen receptor-positive breast cancers tend to be more obese than noncancer patients and have higher levels of circulating estrogens. The study by Leslie and colleagues shows that such patients will have fewer previous fractures and better baseline bone mass values than the general population. This may prompt us to rethink whether all women initiating AI therapy need to be treated for fracture prevention, as some previous studies have suggested. Clearly, further study is necessary.
- International Society for Clinical Densitometry. 2019 ISCD Official Positions-Adult. June 2019. https://www.iscd.org/official-positions/2019-iscd-official-positions-adult. Accessed November 22, 2019.
- Goldstein SR, Neven P, Cummings S, et al. Postmenopausal evaluation and risk reduction with lasofoxifene (PEARL) trial: 5-year gynecological outcomes. Menopause. 2011;18:17-22.
- Kangas L, Unkila M. Tissue selectivity of ospemifene: pharmacologic profile and clinical implications. Steroids. 2013;78:1273-1280.
- Constantine GD, Kagan R, Miller PD. Effects of ospemifene on bone parameters including clinical biomarkers in postmenopausal women. Menopause. 2016;23:638-644.
- de Villiers TJ, Altomare C, Particco M, et al. Effects of ospemifene on bone in postmenopausal women. Climacteric. 2019;22:442-447.
- Gerdhem P, Ivaska KK, Alatalo SL, et al. Biochemical markers of bone metabolism and prediction of fracture in elderly women. J Bone Miner Res. 2004;19:386-393.
- Siris ES, Adler R, Bilezikian J, et al. The clinical diagnosis of osteoporosis: a position statement from the National Bone Health Alliance Working Group. Osteoporos Int. 2014;25:1439-1443.
- Epidemiologic and methodologic problems in determining nutritional status of older persons. Proceedings of a conference. Albuquerque, New Mexico, October 19-21, 1988. Am J Clin Nutr. 1989;50(5 suppl):1121-1235.
- Drey M, Sieber CC, Bertsch T, et al. Osteosarcopenia is more than sarcopenia and osteopenia alone. Aging Clin Exp Res. 2016;28:895-899.
- Lima RM, de Oliveira RJ, Raposo R, et al. Stages of sarcopenia, bone mineral density, and the prevalence of osteoporosis in older women. Arch Osteoporos. 2019;14:38.
- Mathias S, Nayak U, Isaacs B. Balance in elderly patients: the "get-up and go" test. Arch Phys Med Rehabil. 1986;67:387-389.
- Burstein HJ, Temin S, Anderson H, et al. Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: American Society of Clinical Oncology clinical practice guideline focused update. J Clin Oncol. 2014;32:2255-2269.
- Schmidt N, Jacob L, Coleman R, et al. The impact of treatment compliance on fracture risk in women with breast cancer treated with aromatase inhibitors in the United Kingdom. Breast Cancer Res Treat. 2016;155:151-157.
- Neuner JM, Shi Y, Kong AL, et al. Fractures in a nationwide population-based cohort of users of breast cancer hormonal therapy. J Cancer Surviv. 2018;12:268-275.
- Goldstein SR. 2015 Update on osteoporosis. OBG Manag. 2015;27:31-39.
- Majithia N, Atherton PJ, Lafky JM, et al. Zoledronic acid for treatment of osteopenia and osteoporosis in women with primary breast cancer undergoing adjuvant aromatase inhibitor therapy: a 5-year follow-up. Support Care Cancer. 2016;24:1219-1226.
- Gnant M, Pfeiler G, Dubsky PC, et al; Austrian Breast and Colorectal Cancer Study Group. Adjuvant denosumab in breast cancer (ABCSG-18): a multicenter, randomized, double-blind, placebo-controlled trial. Lancet. 2015;386:433-443.
- Leslie WD, Morin SN, Lix LM, et al. Fracture risk in women with breast cancer initiating aromatase inhibitor therapy: a registry-based cohort study. Oncologist. 2019;24:1432-1438.
- International Society for Clinical Densitometry. 2019 ISCD Official Positions-Adult. June 2019. https://www.iscd.org/official-positions/2019-iscd-official-positions-adult. Accessed November 22, 2019.
- Goldstein SR, Neven P, Cummings S, et al. Postmenopausal evaluation and risk reduction with lasofoxifene (PEARL) trial: 5-year gynecological outcomes. Menopause. 2011;18:17-22.
- Kangas L, Unkila M. Tissue selectivity of ospemifene: pharmacologic profile and clinical implications. Steroids. 2013;78:1273-1280.
- Constantine GD, Kagan R, Miller PD. Effects of ospemifene on bone parameters including clinical biomarkers in postmenopausal women. Menopause. 2016;23:638-644.
- de Villiers TJ, Altomare C, Particco M, et al. Effects of ospemifene on bone in postmenopausal women. Climacteric. 2019;22:442-447.
- Gerdhem P, Ivaska KK, Alatalo SL, et al. Biochemical markers of bone metabolism and prediction of fracture in elderly women. J Bone Miner Res. 2004;19:386-393.
- Siris ES, Adler R, Bilezikian J, et al. The clinical diagnosis of osteoporosis: a position statement from the National Bone Health Alliance Working Group. Osteoporos Int. 2014;25:1439-1443.
- Epidemiologic and methodologic problems in determining nutritional status of older persons. Proceedings of a conference. Albuquerque, New Mexico, October 19-21, 1988. Am J Clin Nutr. 1989;50(5 suppl):1121-1235.
- Drey M, Sieber CC, Bertsch T, et al. Osteosarcopenia is more than sarcopenia and osteopenia alone. Aging Clin Exp Res. 2016;28:895-899.
- Lima RM, de Oliveira RJ, Raposo R, et al. Stages of sarcopenia, bone mineral density, and the prevalence of osteoporosis in older women. Arch Osteoporos. 2019;14:38.
- Mathias S, Nayak U, Isaacs B. Balance in elderly patients: the "get-up and go" test. Arch Phys Med Rehabil. 1986;67:387-389.
- Burstein HJ, Temin S, Anderson H, et al. Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: American Society of Clinical Oncology clinical practice guideline focused update. J Clin Oncol. 2014;32:2255-2269.
- Schmidt N, Jacob L, Coleman R, et al. The impact of treatment compliance on fracture risk in women with breast cancer treated with aromatase inhibitors in the United Kingdom. Breast Cancer Res Treat. 2016;155:151-157.
- Neuner JM, Shi Y, Kong AL, et al. Fractures in a nationwide population-based cohort of users of breast cancer hormonal therapy. J Cancer Surviv. 2018;12:268-275.
- Goldstein SR. 2015 Update on osteoporosis. OBG Manag. 2015;27:31-39.
- Majithia N, Atherton PJ, Lafky JM, et al. Zoledronic acid for treatment of osteopenia and osteoporosis in women with primary breast cancer undergoing adjuvant aromatase inhibitor therapy: a 5-year follow-up. Support Care Cancer. 2016;24:1219-1226.
- Gnant M, Pfeiler G, Dubsky PC, et al; Austrian Breast and Colorectal Cancer Study Group. Adjuvant denosumab in breast cancer (ABCSG-18): a multicenter, randomized, double-blind, placebo-controlled trial. Lancet. 2015;386:433-443.
- Leslie WD, Morin SN, Lix LM, et al. Fracture risk in women with breast cancer initiating aromatase inhibitor therapy: a registry-based cohort study. Oncologist. 2019;24:1432-1438.