User login
Rivaroxaban versus heparin at preventing recurrent, cancer-related VTE
Clinical question: Is an oral direct factor Xa inhibitor an effective alternative to low-molecular-weight heparin (LMWH) in treating cancer related venous thromboembolism (VTE)?
Background: LMWH has been the standard of care for treatment in patients with VTE and cancer. A newer class of drug, the direct factor Xa inhibitors, have been shown to be noninferior to vitamin K antagonists (VKAs) in treatment of VTE in noncancer patients, but little is known about their use in patients with cancer.
Study Design: Randomized, open-label, multicenter pilot trial.
Setting: United Kingdom; patients were recruited through the Clinical Trials Unit at the University of Warwick, Coventry.
Synopsis: The authors randomly assigned 406 cancer patients with diagnosed VTE either to the LMWH group or to the oral direct factor Xa inhibitor group to evaluate the primary endpoint of VTE reoccurrence and secondary endpoints of major bleeding or clinically relevant but not major bleeding (CRNMB). Rivaroxaban was noninferior to dalteparin in preventing VTE reoccurrence, with a 6-month VTE reoccurrence rate for dalteparin of 11% (95% confidence interval, 7%-16%) and a reoccurrence rate of 6% for rivaroxaban (95% CI, 2%-9%). Rates of major bleeding events were similar, although patients with esophageal or gastroesophageal cancers tended to experience more major bleeds with rivaroxaban than with dalteparin (4 of 11 vs. 1 of 19). CRNMB was 4% for dalteparin and 13% for rivaroxaban (hazard ratio, 3.76; 95% CI, 1.64-8.69). Limitations include slow recruitment, high mortality rate, and the treatment length being only 6 months.
Bottom line: In this small study, rivaroxaban was equally effective at reducing the rate of reoccurrence of cancer related VTE at 6 months but had higher rates of CRNMB. Patients with GI cancers may be at higher risk for major GI bleeding with rivaroxaban.
Citation: Young AM et al. Comparison of an oral factor Xa inhibitor with low molecular weight heparin in patients with cancer with venous thromboembolism: Results of a randomized trial (SELECT-D). J Clin Oncol. 2018 Jul 10. 36(20):2017-23.
Dr. Marten is an assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta.
Clinical question: Is an oral direct factor Xa inhibitor an effective alternative to low-molecular-weight heparin (LMWH) in treating cancer related venous thromboembolism (VTE)?
Background: LMWH has been the standard of care for treatment in patients with VTE and cancer. A newer class of drug, the direct factor Xa inhibitors, have been shown to be noninferior to vitamin K antagonists (VKAs) in treatment of VTE in noncancer patients, but little is known about their use in patients with cancer.
Study Design: Randomized, open-label, multicenter pilot trial.
Setting: United Kingdom; patients were recruited through the Clinical Trials Unit at the University of Warwick, Coventry.
Synopsis: The authors randomly assigned 406 cancer patients with diagnosed VTE either to the LMWH group or to the oral direct factor Xa inhibitor group to evaluate the primary endpoint of VTE reoccurrence and secondary endpoints of major bleeding or clinically relevant but not major bleeding (CRNMB). Rivaroxaban was noninferior to dalteparin in preventing VTE reoccurrence, with a 6-month VTE reoccurrence rate for dalteparin of 11% (95% confidence interval, 7%-16%) and a reoccurrence rate of 6% for rivaroxaban (95% CI, 2%-9%). Rates of major bleeding events were similar, although patients with esophageal or gastroesophageal cancers tended to experience more major bleeds with rivaroxaban than with dalteparin (4 of 11 vs. 1 of 19). CRNMB was 4% for dalteparin and 13% for rivaroxaban (hazard ratio, 3.76; 95% CI, 1.64-8.69). Limitations include slow recruitment, high mortality rate, and the treatment length being only 6 months.
Bottom line: In this small study, rivaroxaban was equally effective at reducing the rate of reoccurrence of cancer related VTE at 6 months but had higher rates of CRNMB. Patients with GI cancers may be at higher risk for major GI bleeding with rivaroxaban.
Citation: Young AM et al. Comparison of an oral factor Xa inhibitor with low molecular weight heparin in patients with cancer with venous thromboembolism: Results of a randomized trial (SELECT-D). J Clin Oncol. 2018 Jul 10. 36(20):2017-23.
Dr. Marten is an assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta.
Clinical question: Is an oral direct factor Xa inhibitor an effective alternative to low-molecular-weight heparin (LMWH) in treating cancer related venous thromboembolism (VTE)?
Background: LMWH has been the standard of care for treatment in patients with VTE and cancer. A newer class of drug, the direct factor Xa inhibitors, have been shown to be noninferior to vitamin K antagonists (VKAs) in treatment of VTE in noncancer patients, but little is known about their use in patients with cancer.
Study Design: Randomized, open-label, multicenter pilot trial.
Setting: United Kingdom; patients were recruited through the Clinical Trials Unit at the University of Warwick, Coventry.
Synopsis: The authors randomly assigned 406 cancer patients with diagnosed VTE either to the LMWH group or to the oral direct factor Xa inhibitor group to evaluate the primary endpoint of VTE reoccurrence and secondary endpoints of major bleeding or clinically relevant but not major bleeding (CRNMB). Rivaroxaban was noninferior to dalteparin in preventing VTE reoccurrence, with a 6-month VTE reoccurrence rate for dalteparin of 11% (95% confidence interval, 7%-16%) and a reoccurrence rate of 6% for rivaroxaban (95% CI, 2%-9%). Rates of major bleeding events were similar, although patients with esophageal or gastroesophageal cancers tended to experience more major bleeds with rivaroxaban than with dalteparin (4 of 11 vs. 1 of 19). CRNMB was 4% for dalteparin and 13% for rivaroxaban (hazard ratio, 3.76; 95% CI, 1.64-8.69). Limitations include slow recruitment, high mortality rate, and the treatment length being only 6 months.
Bottom line: In this small study, rivaroxaban was equally effective at reducing the rate of reoccurrence of cancer related VTE at 6 months but had higher rates of CRNMB. Patients with GI cancers may be at higher risk for major GI bleeding with rivaroxaban.
Citation: Young AM et al. Comparison of an oral factor Xa inhibitor with low molecular weight heparin in patients with cancer with venous thromboembolism: Results of a randomized trial (SELECT-D). J Clin Oncol. 2018 Jul 10. 36(20):2017-23.
Dr. Marten is an assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta.
Rate of objects ingested by young children increased over last two decades
– from an estimated 9 cases per 10,000 children to 18 cases per 10,000 (R2 = 0.90; P less than .001) – according to an analysis in Pediatrics.
The analysis was conducted by Danielle Orsagh-Yentis, MD, of Vanderbilt University, Nashville, Tenn., and her colleagues. They estimated that, during the study period, 759,074 children younger than 6 years of age were evaluated in U.S. EDs for suspected or confirmed foreign-body ingestions. These estimates were based on data for 29,893 actual cases taken from the National Electronic Injury Surveillance System (NEISS), which represents about 100 hospitals. Each case in this system is given a sample weight by the Consumer Product Safety Commission using a validated method, and the estimates are based on this weighting.
The analysis showed that children aged 1 year (21%) and boys (53%) were the most likely to ingest foreign bodies. Coins were the most frequently ingested objects, at 62%. Among cases which had the location noted (59%), most ingestions occurred in the home (97%).
The authors noted that, although batteries and magnets represented only 7% and 2% of all cases, respectively, “they can both enact considerable damage when ingested.” For example, despite being only the fourth mostly likely object to be ingested, batteries were the second mostly likely to be implicated among hospitalized patients.
The authors noted that the NEISS captures patients in the ED only; the total number of foreign-body ingestions, then, was likely underestimated. Despite this, the authors felt the long study period and large sample were strengths of their analysis.
Dr. Orsagh-Yentis and her associates disclosed no potential conflicts of interest.
SOURCE: Orsagh-Yentis D et al. Pediatrics. 2019 Apr 12. doi: 10.1542/peds.2018-1988.
– from an estimated 9 cases per 10,000 children to 18 cases per 10,000 (R2 = 0.90; P less than .001) – according to an analysis in Pediatrics.
The analysis was conducted by Danielle Orsagh-Yentis, MD, of Vanderbilt University, Nashville, Tenn., and her colleagues. They estimated that, during the study period, 759,074 children younger than 6 years of age were evaluated in U.S. EDs for suspected or confirmed foreign-body ingestions. These estimates were based on data for 29,893 actual cases taken from the National Electronic Injury Surveillance System (NEISS), which represents about 100 hospitals. Each case in this system is given a sample weight by the Consumer Product Safety Commission using a validated method, and the estimates are based on this weighting.
The analysis showed that children aged 1 year (21%) and boys (53%) were the most likely to ingest foreign bodies. Coins were the most frequently ingested objects, at 62%. Among cases which had the location noted (59%), most ingestions occurred in the home (97%).
The authors noted that, although batteries and magnets represented only 7% and 2% of all cases, respectively, “they can both enact considerable damage when ingested.” For example, despite being only the fourth mostly likely object to be ingested, batteries were the second mostly likely to be implicated among hospitalized patients.
The authors noted that the NEISS captures patients in the ED only; the total number of foreign-body ingestions, then, was likely underestimated. Despite this, the authors felt the long study period and large sample were strengths of their analysis.
Dr. Orsagh-Yentis and her associates disclosed no potential conflicts of interest.
SOURCE: Orsagh-Yentis D et al. Pediatrics. 2019 Apr 12. doi: 10.1542/peds.2018-1988.
– from an estimated 9 cases per 10,000 children to 18 cases per 10,000 (R2 = 0.90; P less than .001) – according to an analysis in Pediatrics.
The analysis was conducted by Danielle Orsagh-Yentis, MD, of Vanderbilt University, Nashville, Tenn., and her colleagues. They estimated that, during the study period, 759,074 children younger than 6 years of age were evaluated in U.S. EDs for suspected or confirmed foreign-body ingestions. These estimates were based on data for 29,893 actual cases taken from the National Electronic Injury Surveillance System (NEISS), which represents about 100 hospitals. Each case in this system is given a sample weight by the Consumer Product Safety Commission using a validated method, and the estimates are based on this weighting.
The analysis showed that children aged 1 year (21%) and boys (53%) were the most likely to ingest foreign bodies. Coins were the most frequently ingested objects, at 62%. Among cases which had the location noted (59%), most ingestions occurred in the home (97%).
The authors noted that, although batteries and magnets represented only 7% and 2% of all cases, respectively, “they can both enact considerable damage when ingested.” For example, despite being only the fourth mostly likely object to be ingested, batteries were the second mostly likely to be implicated among hospitalized patients.
The authors noted that the NEISS captures patients in the ED only; the total number of foreign-body ingestions, then, was likely underestimated. Despite this, the authors felt the long study period and large sample were strengths of their analysis.
Dr. Orsagh-Yentis and her associates disclosed no potential conflicts of interest.
SOURCE: Orsagh-Yentis D et al. Pediatrics. 2019 Apr 12. doi: 10.1542/peds.2018-1988.
FROM PEDIATRICS
Dr. Douglas Paauw: Consider rechallenging patients with penicillin allergy
PHILADELPHIA – As fluoroquinolone warnings stack up, internists seeking treatment alternatives should consider rechallenging patients with penicillin allergy or referring those patients for testing, said Douglas S. Paauw, MD, during a presentation.
This was one of the pieces of advice provided by Dr. Paauw, professor of medicine in the division of general internal medicine at the University of Washington, Seattle, at the annual meeting of the American College of Physicians.
“The FDA [Food and Drug Administration] has been just killing trees, sending us letters over the last 5-10 years, with fluoroquinolone warnings,” said Dr. Paauw, referencing previous warnings describing risks of tendon rupture, peripheral neuropathy, hypoglycemia, mental health side effects, and more.
“I think the buzz in 2019 is that we should not overreact to a history of penicillin allergy,” he said.
As many as 98% of patients who have reported penicillin allergy don’t have true allergy and can safely receive penicillin, he explained.
“If they don’t have an allergy, make sure you get it out of the electronic record,” Dr. Paauw also advised.
The latest warning on fluoroquinolones from the FDA, issued in Dec. 20, 2018, said that clinicians should avoid prescribing these antibiotics in patients who have, or are at risk of, aortic aneurysm. This comprises a very large proportion of patients in an internist’s practice, Dr. Paauw noted. The warning specifically singled out elderly patients as being in the at-risk population, along with patients who have peripheral atherosclerotic vascular diseases, hypertension, or genetic conditions such as Marfan syndrome or Ehlers-Danlos syndrome, he added.
Dr. Paauw further supported his suggestions by describing two relevant studies.
In one of those studies, which was published this year in an allergy and asthma journal, 20 subjects with a history of penicillin allergy agreed to direct oral amoxicillin rechallenge by an allergist, he said. None of those 20 patients were observed to have developed immediate or delayed hypersensitivity reactions, investigators reported. That study included a total of 50 adults with a penicillin allergy label, of whom 24 (48%) had the label removed from their medical records.
In another recent and reassuring study, penicillin allergy testing was conducted in 100 children with parent-reported penicillin allergy that was considered low risk based on reported symptoms, Dr. Paauw said. Of that group, all 100 children were found to be negative for true penicillin allergy.
Dr. Paauw had no relevant disclosures.
SOURCE: Paauw DS. Annual Meeting of the American College of Physicians, Presentation MTP 013.
PHILADELPHIA – As fluoroquinolone warnings stack up, internists seeking treatment alternatives should consider rechallenging patients with penicillin allergy or referring those patients for testing, said Douglas S. Paauw, MD, during a presentation.
This was one of the pieces of advice provided by Dr. Paauw, professor of medicine in the division of general internal medicine at the University of Washington, Seattle, at the annual meeting of the American College of Physicians.
“The FDA [Food and Drug Administration] has been just killing trees, sending us letters over the last 5-10 years, with fluoroquinolone warnings,” said Dr. Paauw, referencing previous warnings describing risks of tendon rupture, peripheral neuropathy, hypoglycemia, mental health side effects, and more.
“I think the buzz in 2019 is that we should not overreact to a history of penicillin allergy,” he said.
As many as 98% of patients who have reported penicillin allergy don’t have true allergy and can safely receive penicillin, he explained.
“If they don’t have an allergy, make sure you get it out of the electronic record,” Dr. Paauw also advised.
The latest warning on fluoroquinolones from the FDA, issued in Dec. 20, 2018, said that clinicians should avoid prescribing these antibiotics in patients who have, or are at risk of, aortic aneurysm. This comprises a very large proportion of patients in an internist’s practice, Dr. Paauw noted. The warning specifically singled out elderly patients as being in the at-risk population, along with patients who have peripheral atherosclerotic vascular diseases, hypertension, or genetic conditions such as Marfan syndrome or Ehlers-Danlos syndrome, he added.
Dr. Paauw further supported his suggestions by describing two relevant studies.
In one of those studies, which was published this year in an allergy and asthma journal, 20 subjects with a history of penicillin allergy agreed to direct oral amoxicillin rechallenge by an allergist, he said. None of those 20 patients were observed to have developed immediate or delayed hypersensitivity reactions, investigators reported. That study included a total of 50 adults with a penicillin allergy label, of whom 24 (48%) had the label removed from their medical records.
In another recent and reassuring study, penicillin allergy testing was conducted in 100 children with parent-reported penicillin allergy that was considered low risk based on reported symptoms, Dr. Paauw said. Of that group, all 100 children were found to be negative for true penicillin allergy.
Dr. Paauw had no relevant disclosures.
SOURCE: Paauw DS. Annual Meeting of the American College of Physicians, Presentation MTP 013.
PHILADELPHIA – As fluoroquinolone warnings stack up, internists seeking treatment alternatives should consider rechallenging patients with penicillin allergy or referring those patients for testing, said Douglas S. Paauw, MD, during a presentation.
This was one of the pieces of advice provided by Dr. Paauw, professor of medicine in the division of general internal medicine at the University of Washington, Seattle, at the annual meeting of the American College of Physicians.
“The FDA [Food and Drug Administration] has been just killing trees, sending us letters over the last 5-10 years, with fluoroquinolone warnings,” said Dr. Paauw, referencing previous warnings describing risks of tendon rupture, peripheral neuropathy, hypoglycemia, mental health side effects, and more.
“I think the buzz in 2019 is that we should not overreact to a history of penicillin allergy,” he said.
As many as 98% of patients who have reported penicillin allergy don’t have true allergy and can safely receive penicillin, he explained.
“If they don’t have an allergy, make sure you get it out of the electronic record,” Dr. Paauw also advised.
The latest warning on fluoroquinolones from the FDA, issued in Dec. 20, 2018, said that clinicians should avoid prescribing these antibiotics in patients who have, or are at risk of, aortic aneurysm. This comprises a very large proportion of patients in an internist’s practice, Dr. Paauw noted. The warning specifically singled out elderly patients as being in the at-risk population, along with patients who have peripheral atherosclerotic vascular diseases, hypertension, or genetic conditions such as Marfan syndrome or Ehlers-Danlos syndrome, he added.
Dr. Paauw further supported his suggestions by describing two relevant studies.
In one of those studies, which was published this year in an allergy and asthma journal, 20 subjects with a history of penicillin allergy agreed to direct oral amoxicillin rechallenge by an allergist, he said. None of those 20 patients were observed to have developed immediate or delayed hypersensitivity reactions, investigators reported. That study included a total of 50 adults with a penicillin allergy label, of whom 24 (48%) had the label removed from their medical records.
In another recent and reassuring study, penicillin allergy testing was conducted in 100 children with parent-reported penicillin allergy that was considered low risk based on reported symptoms, Dr. Paauw said. Of that group, all 100 children were found to be negative for true penicillin allergy.
Dr. Paauw had no relevant disclosures.
SOURCE: Paauw DS. Annual Meeting of the American College of Physicians, Presentation MTP 013.
REPORTING FROM INTERNAL MEDICINE 2019
FDA modifies safety label for Addyi
The Food and Drug Administration has issued a safety labeling change for flibanserin (Addyi), a treatment for premenopausal women with acquired, generalized hypoactive sexual desire disorder, according to a press release issued April 11 by the agency. Previously, the warning said women should abstain from alcohol entirely.
According to the release, the manufacturer, Sprout, had hoped the FDA would remove the boxed warning and contraindication entirely. However, based on a review of two postmarket research studies, the agency chose to order these modifications to the warnings instead.
The first postmarket study was missing information related to participants’ blood pressure, which FDA officials thought was critical in determining risk; it appeared that this resulted from safety precautions built into the trial. The concern was that not only did this absent information provide further evidence of an interaction but that women at home would not have the benefit of these safety precautions and could suffer serious outcomes, including falls, accidents, and bodily harm. The other postmarketing trial showed that delaying administration of flibanserin until at least 2 hours after consuming alcohol reduced the risk of serious hypotension and syncope.
It is recommended that flibanserin be taken at bedtime because of risks associated with hypotension and syncope, as well as risks associated with central nervous system depression (such as sleepiness). Furthermore, patients are encouraged to discontinue treatment with flibanserin if their hypoactive sexual desire disorder does not improve after 8 weeks. The most common adverse reactions include dizziness, sleepiness, nausea, fatigue, insomnia, and dry mouth.
Full prescribing information is available on the FDA website, as is the full release regarding these safety label modifications.
The Food and Drug Administration has issued a safety labeling change for flibanserin (Addyi), a treatment for premenopausal women with acquired, generalized hypoactive sexual desire disorder, according to a press release issued April 11 by the agency. Previously, the warning said women should abstain from alcohol entirely.
According to the release, the manufacturer, Sprout, had hoped the FDA would remove the boxed warning and contraindication entirely. However, based on a review of two postmarket research studies, the agency chose to order these modifications to the warnings instead.
The first postmarket study was missing information related to participants’ blood pressure, which FDA officials thought was critical in determining risk; it appeared that this resulted from safety precautions built into the trial. The concern was that not only did this absent information provide further evidence of an interaction but that women at home would not have the benefit of these safety precautions and could suffer serious outcomes, including falls, accidents, and bodily harm. The other postmarketing trial showed that delaying administration of flibanserin until at least 2 hours after consuming alcohol reduced the risk of serious hypotension and syncope.
It is recommended that flibanserin be taken at bedtime because of risks associated with hypotension and syncope, as well as risks associated with central nervous system depression (such as sleepiness). Furthermore, patients are encouraged to discontinue treatment with flibanserin if their hypoactive sexual desire disorder does not improve after 8 weeks. The most common adverse reactions include dizziness, sleepiness, nausea, fatigue, insomnia, and dry mouth.
Full prescribing information is available on the FDA website, as is the full release regarding these safety label modifications.
The Food and Drug Administration has issued a safety labeling change for flibanserin (Addyi), a treatment for premenopausal women with acquired, generalized hypoactive sexual desire disorder, according to a press release issued April 11 by the agency. Previously, the warning said women should abstain from alcohol entirely.
According to the release, the manufacturer, Sprout, had hoped the FDA would remove the boxed warning and contraindication entirely. However, based on a review of two postmarket research studies, the agency chose to order these modifications to the warnings instead.
The first postmarket study was missing information related to participants’ blood pressure, which FDA officials thought was critical in determining risk; it appeared that this resulted from safety precautions built into the trial. The concern was that not only did this absent information provide further evidence of an interaction but that women at home would not have the benefit of these safety precautions and could suffer serious outcomes, including falls, accidents, and bodily harm. The other postmarketing trial showed that delaying administration of flibanserin until at least 2 hours after consuming alcohol reduced the risk of serious hypotension and syncope.
It is recommended that flibanserin be taken at bedtime because of risks associated with hypotension and syncope, as well as risks associated with central nervous system depression (such as sleepiness). Furthermore, patients are encouraged to discontinue treatment with flibanserin if their hypoactive sexual desire disorder does not improve after 8 weeks. The most common adverse reactions include dizziness, sleepiness, nausea, fatigue, insomnia, and dry mouth.
Full prescribing information is available on the FDA website, as is the full release regarding these safety label modifications.
As Sanders officially revives Medicare-for-all, Plan B for Democrats gains traction
On April 10, Sen. Bernie Sanders (I-Vt.) reaffirmed his stance by reintroducing a Medicare-for-all bill, the idea that fueled his 2016 presidential run.
As with its previous iterations, Sen. Sanders’s latest bill would establish a national single-payer Medicare system with vastly expanded benefits, prohibit private plans from competing with Medicare, and eliminate cost sharing. New in this version is a universal provision for long-term care in home and community settings (but Medicaid would continue to cover institutional care).
Already, it has an impressive list of Senate cosponsors – including Sen. Sanders’s rivals for the Democratic presidential nomination, Cory Booker (D-N.J.), Kirsten Gillibrand (D-N.Y.), Kamala Harris (D-Calif.), and Elizabeth Warren (D-Mass.).
But many of the candidates – even official Medicare-for-all cosponsors – are at the same time edging toward a more incremental approach, called “Medicare for America.” Proponents argue it could deliver better health care to Americans while avoiding political, budgetary, and legal objections.
It comes as politicians tread carefully over the political land mines a Medicare-for-all endorsement could unleash, while seeking to capitalize on a growing appetite for health reform.
During the 2018 midterm election campaigns, some congressional candidates talked about allowing people older than 55 years to join Medicare, or allowing people younger than 65 years to buy into it if they choose (the “public option”). Many aren’t eager to face the industry opposition that a full-on Medicare expansion would surely trigger.
From the consumer perspective, sweeping reform poses a risk. Despite Medicare’s popularity with its beneficiaries, the majority of Americans express satisfaction with their health care, and many are nervous about giving up private options. Also, many analysts are worried that a generous Medicare-for-all plan that promises everything would break the bank without any patient payments.
That tension is pushing a number of candidates toward the emerging Medicare for America option. The bill was introduced last December to little fanfare by two Democrats, Rep. Rosa DeLauro of Connecticut and Rep. Jan Schakowsky of Illinois. It hasn’t been reintroduced in the new Congress.
This proposed system would guarantee universal coverage, but leaves job-based insurance available for those who want it. Unlike Medicare-for-all, though, it preserves premiums and deductibles, so beneficiaries would still have to pay some out-of-pocket costs. It allows private insurers to operate Medicare plans as well, a system called Medicare Advantage that covers about a third of the program’s beneficiaries currently, and which would be outlawed under Medicare-for-all.
“Before policies get defined, what you see is people endorsing a plan that is a little, perhaps, less subject to early attack,” said Celinda Lake, a Democratic pollster. “A lot of candidates feel if they endorse a plan that leaves some private insurance, they get more time to say what their ideas are about.”
Medicare for America got its first high-profile endorsement from former Texas Rep. Beto O’Rourke, who launched his own 2020 bid in mid-March. Other candidates – including Sen. Warren, Sen. Gillibrand, and Pete Buttigieg, the mayor of South Bend, Ind. – have tiptoed toward it without making any endorsements, suggesting they back Medicare-for-all in theory but also support a system that retains private insurance, at least temporarily.
Such an approach is perhaps unsurprising. Polling indicates voters want strong health reform. Candidates, election experts say, need something powerful to deliver.
Improving the Affordable Care Act, an idea backed by Sen. Amy Klobuchar (D-Minn.) who is running in the presidential primary’s moderate lane, may not suffice.
“The ACA is popular at the 50% level, but it’s not energetic. It doesn’t get people who really like it,” said Bob Blendon, a political analyst at the Harvard T.H. Chan School of Public Health. “What they’re looking for is something that is exciting but isn’t threatening.”
Both Medicare-for-all and Medicare for America, experts noted, offer something that presidential candidates can campaign on and a health alternative that at first blush sounds appealing to many. But the latter could skirt some potential obstacles.
Approval for Medicare-for-all drops when people learn that, under such a program, they would likely lose their current health plan (even if the government-offered plan could theoretically provide more generous coverage).
The cost-sharing element of Medicare for America, meanwhile, would ostensibly quiet some of the concerns about paying for Medicare’s expansion, though critics on the left worry it would mean some people would still be unable to afford care.
This also tracks with recent polling suggesting that, while Medicare-for-all support can be swayed, voters of all political stripes favor some sort of way to extend optional Medicare coverage, without necessarily eliminating the private industry altogether.
Employers would have to offer plans that were at least as generous as the government program, or direct employees to Medicare. Employers who stop offering health benefits would have to pay a Medicare payroll tax.
For now, most candidates are still avoiding a concrete stance on Medicare for America. Despite signs of interest, the campaigns of Mr. Buttigieg, Sen. Gillibrand, and Sen. Warren all declined to directly answer questions about whether they endorse Medicare for America. The campaigns of other Democratic candidates in the race – Sen. Harris, Sen. Klobuchar, Sen. Booker, and former Housing and Urban Development Secretary Julian Castro and Washington Gov. Jay Inslee – similarly declined to comment.
Reading between the lines, though, their promises to achieve universal health care by expanding Medicare – while retaining private insurance – leaves them few options besides something like Medicare for America, argued one of its main architects.
“There are variations besides this particular plan, but once you start to actually dig into this, if you want universal coverage you’re going to have to do the kinds of things” spelled out in Medicare for America, argued Jacob Hacker, a political scientist at Yale University, who played a lead role in devising this proposal.
Still, though, it has prompted objections from both the left and the right.
On the far left, the cost sharing is a dominant concern. (Under Medicare for America, an individual would have a $3,500 out-of-pocket limit; a family would have a $5,000 limit. Premiums would be capped at almost 10% of a household’s income.) Those critics also say the plan’s accommodations to private insurance limit the government’s ability to negotiate lower prices.
Conservatives repeat many of the arguments levied against Medicare-for-all – too expensive and too disruptive.
Hospitals, insurance, drugmakers, and doctors, who have already mobilized against Medicare-for-all, also can be expected to make just as strong a showing against Medicare for America, political analysts said. More Medicare means less revenue for the medical industry.
Said David Blumenthal of the Commonwealth Fund: “The fact of expanded Medicare will be the focus of attacks.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
On April 10, Sen. Bernie Sanders (I-Vt.) reaffirmed his stance by reintroducing a Medicare-for-all bill, the idea that fueled his 2016 presidential run.
As with its previous iterations, Sen. Sanders’s latest bill would establish a national single-payer Medicare system with vastly expanded benefits, prohibit private plans from competing with Medicare, and eliminate cost sharing. New in this version is a universal provision for long-term care in home and community settings (but Medicaid would continue to cover institutional care).
Already, it has an impressive list of Senate cosponsors – including Sen. Sanders’s rivals for the Democratic presidential nomination, Cory Booker (D-N.J.), Kirsten Gillibrand (D-N.Y.), Kamala Harris (D-Calif.), and Elizabeth Warren (D-Mass.).
But many of the candidates – even official Medicare-for-all cosponsors – are at the same time edging toward a more incremental approach, called “Medicare for America.” Proponents argue it could deliver better health care to Americans while avoiding political, budgetary, and legal objections.
It comes as politicians tread carefully over the political land mines a Medicare-for-all endorsement could unleash, while seeking to capitalize on a growing appetite for health reform.
During the 2018 midterm election campaigns, some congressional candidates talked about allowing people older than 55 years to join Medicare, or allowing people younger than 65 years to buy into it if they choose (the “public option”). Many aren’t eager to face the industry opposition that a full-on Medicare expansion would surely trigger.
From the consumer perspective, sweeping reform poses a risk. Despite Medicare’s popularity with its beneficiaries, the majority of Americans express satisfaction with their health care, and many are nervous about giving up private options. Also, many analysts are worried that a generous Medicare-for-all plan that promises everything would break the bank without any patient payments.
That tension is pushing a number of candidates toward the emerging Medicare for America option. The bill was introduced last December to little fanfare by two Democrats, Rep. Rosa DeLauro of Connecticut and Rep. Jan Schakowsky of Illinois. It hasn’t been reintroduced in the new Congress.
This proposed system would guarantee universal coverage, but leaves job-based insurance available for those who want it. Unlike Medicare-for-all, though, it preserves premiums and deductibles, so beneficiaries would still have to pay some out-of-pocket costs. It allows private insurers to operate Medicare plans as well, a system called Medicare Advantage that covers about a third of the program’s beneficiaries currently, and which would be outlawed under Medicare-for-all.
“Before policies get defined, what you see is people endorsing a plan that is a little, perhaps, less subject to early attack,” said Celinda Lake, a Democratic pollster. “A lot of candidates feel if they endorse a plan that leaves some private insurance, they get more time to say what their ideas are about.”
Medicare for America got its first high-profile endorsement from former Texas Rep. Beto O’Rourke, who launched his own 2020 bid in mid-March. Other candidates – including Sen. Warren, Sen. Gillibrand, and Pete Buttigieg, the mayor of South Bend, Ind. – have tiptoed toward it without making any endorsements, suggesting they back Medicare-for-all in theory but also support a system that retains private insurance, at least temporarily.
Such an approach is perhaps unsurprising. Polling indicates voters want strong health reform. Candidates, election experts say, need something powerful to deliver.
Improving the Affordable Care Act, an idea backed by Sen. Amy Klobuchar (D-Minn.) who is running in the presidential primary’s moderate lane, may not suffice.
“The ACA is popular at the 50% level, but it’s not energetic. It doesn’t get people who really like it,” said Bob Blendon, a political analyst at the Harvard T.H. Chan School of Public Health. “What they’re looking for is something that is exciting but isn’t threatening.”
Both Medicare-for-all and Medicare for America, experts noted, offer something that presidential candidates can campaign on and a health alternative that at first blush sounds appealing to many. But the latter could skirt some potential obstacles.
Approval for Medicare-for-all drops when people learn that, under such a program, they would likely lose their current health plan (even if the government-offered plan could theoretically provide more generous coverage).
The cost-sharing element of Medicare for America, meanwhile, would ostensibly quiet some of the concerns about paying for Medicare’s expansion, though critics on the left worry it would mean some people would still be unable to afford care.
This also tracks with recent polling suggesting that, while Medicare-for-all support can be swayed, voters of all political stripes favor some sort of way to extend optional Medicare coverage, without necessarily eliminating the private industry altogether.
Employers would have to offer plans that were at least as generous as the government program, or direct employees to Medicare. Employers who stop offering health benefits would have to pay a Medicare payroll tax.
For now, most candidates are still avoiding a concrete stance on Medicare for America. Despite signs of interest, the campaigns of Mr. Buttigieg, Sen. Gillibrand, and Sen. Warren all declined to directly answer questions about whether they endorse Medicare for America. The campaigns of other Democratic candidates in the race – Sen. Harris, Sen. Klobuchar, Sen. Booker, and former Housing and Urban Development Secretary Julian Castro and Washington Gov. Jay Inslee – similarly declined to comment.
Reading between the lines, though, their promises to achieve universal health care by expanding Medicare – while retaining private insurance – leaves them few options besides something like Medicare for America, argued one of its main architects.
“There are variations besides this particular plan, but once you start to actually dig into this, if you want universal coverage you’re going to have to do the kinds of things” spelled out in Medicare for America, argued Jacob Hacker, a political scientist at Yale University, who played a lead role in devising this proposal.
Still, though, it has prompted objections from both the left and the right.
On the far left, the cost sharing is a dominant concern. (Under Medicare for America, an individual would have a $3,500 out-of-pocket limit; a family would have a $5,000 limit. Premiums would be capped at almost 10% of a household’s income.) Those critics also say the plan’s accommodations to private insurance limit the government’s ability to negotiate lower prices.
Conservatives repeat many of the arguments levied against Medicare-for-all – too expensive and too disruptive.
Hospitals, insurance, drugmakers, and doctors, who have already mobilized against Medicare-for-all, also can be expected to make just as strong a showing against Medicare for America, political analysts said. More Medicare means less revenue for the medical industry.
Said David Blumenthal of the Commonwealth Fund: “The fact of expanded Medicare will be the focus of attacks.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
On April 10, Sen. Bernie Sanders (I-Vt.) reaffirmed his stance by reintroducing a Medicare-for-all bill, the idea that fueled his 2016 presidential run.
As with its previous iterations, Sen. Sanders’s latest bill would establish a national single-payer Medicare system with vastly expanded benefits, prohibit private plans from competing with Medicare, and eliminate cost sharing. New in this version is a universal provision for long-term care in home and community settings (but Medicaid would continue to cover institutional care).
Already, it has an impressive list of Senate cosponsors – including Sen. Sanders’s rivals for the Democratic presidential nomination, Cory Booker (D-N.J.), Kirsten Gillibrand (D-N.Y.), Kamala Harris (D-Calif.), and Elizabeth Warren (D-Mass.).
But many of the candidates – even official Medicare-for-all cosponsors – are at the same time edging toward a more incremental approach, called “Medicare for America.” Proponents argue it could deliver better health care to Americans while avoiding political, budgetary, and legal objections.
It comes as politicians tread carefully over the political land mines a Medicare-for-all endorsement could unleash, while seeking to capitalize on a growing appetite for health reform.
During the 2018 midterm election campaigns, some congressional candidates talked about allowing people older than 55 years to join Medicare, or allowing people younger than 65 years to buy into it if they choose (the “public option”). Many aren’t eager to face the industry opposition that a full-on Medicare expansion would surely trigger.
From the consumer perspective, sweeping reform poses a risk. Despite Medicare’s popularity with its beneficiaries, the majority of Americans express satisfaction with their health care, and many are nervous about giving up private options. Also, many analysts are worried that a generous Medicare-for-all plan that promises everything would break the bank without any patient payments.
That tension is pushing a number of candidates toward the emerging Medicare for America option. The bill was introduced last December to little fanfare by two Democrats, Rep. Rosa DeLauro of Connecticut and Rep. Jan Schakowsky of Illinois. It hasn’t been reintroduced in the new Congress.
This proposed system would guarantee universal coverage, but leaves job-based insurance available for those who want it. Unlike Medicare-for-all, though, it preserves premiums and deductibles, so beneficiaries would still have to pay some out-of-pocket costs. It allows private insurers to operate Medicare plans as well, a system called Medicare Advantage that covers about a third of the program’s beneficiaries currently, and which would be outlawed under Medicare-for-all.
“Before policies get defined, what you see is people endorsing a plan that is a little, perhaps, less subject to early attack,” said Celinda Lake, a Democratic pollster. “A lot of candidates feel if they endorse a plan that leaves some private insurance, they get more time to say what their ideas are about.”
Medicare for America got its first high-profile endorsement from former Texas Rep. Beto O’Rourke, who launched his own 2020 bid in mid-March. Other candidates – including Sen. Warren, Sen. Gillibrand, and Pete Buttigieg, the mayor of South Bend, Ind. – have tiptoed toward it without making any endorsements, suggesting they back Medicare-for-all in theory but also support a system that retains private insurance, at least temporarily.
Such an approach is perhaps unsurprising. Polling indicates voters want strong health reform. Candidates, election experts say, need something powerful to deliver.
Improving the Affordable Care Act, an idea backed by Sen. Amy Klobuchar (D-Minn.) who is running in the presidential primary’s moderate lane, may not suffice.
“The ACA is popular at the 50% level, but it’s not energetic. It doesn’t get people who really like it,” said Bob Blendon, a political analyst at the Harvard T.H. Chan School of Public Health. “What they’re looking for is something that is exciting but isn’t threatening.”
Both Medicare-for-all and Medicare for America, experts noted, offer something that presidential candidates can campaign on and a health alternative that at first blush sounds appealing to many. But the latter could skirt some potential obstacles.
Approval for Medicare-for-all drops when people learn that, under such a program, they would likely lose their current health plan (even if the government-offered plan could theoretically provide more generous coverage).
The cost-sharing element of Medicare for America, meanwhile, would ostensibly quiet some of the concerns about paying for Medicare’s expansion, though critics on the left worry it would mean some people would still be unable to afford care.
This also tracks with recent polling suggesting that, while Medicare-for-all support can be swayed, voters of all political stripes favor some sort of way to extend optional Medicare coverage, without necessarily eliminating the private industry altogether.
Employers would have to offer plans that were at least as generous as the government program, or direct employees to Medicare. Employers who stop offering health benefits would have to pay a Medicare payroll tax.
For now, most candidates are still avoiding a concrete stance on Medicare for America. Despite signs of interest, the campaigns of Mr. Buttigieg, Sen. Gillibrand, and Sen. Warren all declined to directly answer questions about whether they endorse Medicare for America. The campaigns of other Democratic candidates in the race – Sen. Harris, Sen. Klobuchar, Sen. Booker, and former Housing and Urban Development Secretary Julian Castro and Washington Gov. Jay Inslee – similarly declined to comment.
Reading between the lines, though, their promises to achieve universal health care by expanding Medicare – while retaining private insurance – leaves them few options besides something like Medicare for America, argued one of its main architects.
“There are variations besides this particular plan, but once you start to actually dig into this, if you want universal coverage you’re going to have to do the kinds of things” spelled out in Medicare for America, argued Jacob Hacker, a political scientist at Yale University, who played a lead role in devising this proposal.
Still, though, it has prompted objections from both the left and the right.
On the far left, the cost sharing is a dominant concern. (Under Medicare for America, an individual would have a $3,500 out-of-pocket limit; a family would have a $5,000 limit. Premiums would be capped at almost 10% of a household’s income.) Those critics also say the plan’s accommodations to private insurance limit the government’s ability to negotiate lower prices.
Conservatives repeat many of the arguments levied against Medicare-for-all – too expensive and too disruptive.
Hospitals, insurance, drugmakers, and doctors, who have already mobilized against Medicare-for-all, also can be expected to make just as strong a showing against Medicare for America, political analysts said. More Medicare means less revenue for the medical industry.
Said David Blumenthal of the Commonwealth Fund: “The fact of expanded Medicare will be the focus of attacks.”
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
A blood biomarker for MS: Coming to clinics soon?
DALLAS – Neurologists soon may use a blood biomarker of axonal damage to monitor patients with multiple sclerosis (MS) and guide treatment decisions, according to a lecture delivered at ACTRIMS Forum 2019.
said David Leppert, MD, senior research associate in the department of neurology at University Hopsital Basel (Switzerland).
Among patients with MS, blood NfL levels predict disability, brain volume loss, and spinal cord atrophy. In addition, studies have found that blood NfL decreases in response to disease-modifying therapy (DMT) and that second-line DMTs may decrease blood NfL more than first-line DMTs do.
The establishment of normative databases and reference biomarkers may allow neurologists to use NfL in their care of individual patients, Dr. Leppert predicted at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “I am very positive that we will make a breakthrough in the next 2 or 3 years for an individual use of neurofilaments,” he said.
Response to DMT
An analysis of blood NfL levels from patients with MS and from healthy controls in two phase 3 trials of fingolimod, FREEDOMS and TRANSFORMS, provides insights into NfL’s response to DMT (Neurology. 2019 Mar 5;92[10]:e1007-15). In FREEDOMS, which compared fingolimod with placebo, “fingolimod leads to a rapid decrease of neurofilament levels, close to normality, while placebo patients continue to have high levels,” said Dr. Leppert, a coauthor of the study.
TRANSFORMS compared interferon-beta and fingolimod. “The clinical experience that fingolimod is a more potent compound than interferon is actually reflected here by the NfL results,” Dr. Leppert said. “Both compounds lead to a decrease of neurofilaments – so, a decrease of neuronal damage – but one drug is more potent than the other one.”
Similarly, data from the observational EPIC study indicate that patients who do not receive DMT have a consistent increase in NfL levels, whereas those who receive platform therapies have a slight decrease in NfL and those who receive second-line therapies have a greater decrease, Dr. Leppert said.
Decades of research
For about 20 years, researchers have studied neurofilaments in cerebrospinal fluid (CSF) as a potential biomarker for MS and other diseases, including Alzheimer’s disease, amyotrophic lateral sclerosis, Parkinson’s disease, and head trauma.
“What prevented the emergence of NfL to clinical practice was the inability to measure it in blood because levels are 50-100 times lower [in blood] than in CSF,” Dr. Leppert said.
The development of single molecule array (SIMOA) technology enabled researchers to show a proper correlation between levels of NfL in CSF and those in blood, Dr. Leppert said. “That is now allowing repetitive testing in an accessible fluid compartment, meaning serum or plasma,” he said.
Compared with brain MRI, NfL may provide novel insights into MS disease activity. “MRI is measuring a structural deficit of the past,” Dr. Leppert said. “NfL is measuring online, real time what axonal damage is occurring.”
Correlation with outcomes
At the group level, patients with MS have higher levels of NfL, compared with controls, and levels are higher in patients with progressive forms of MS versus relapsing forms. “Levels increase dramatically in the wake of relapse,” he said.
Barro et al. found that patients with higher serum levels of NfL are more likely to experience Expanded Disability Status Scale (EDSS) worsening (Brain. 2018 Aug 1;141[8]:2382-91). Furthermore, MRI lesions are independently associated with serum NfL, and patients with higher levels of serum NfL have significantly greater average loss in brain volume and spinal cord volume over 5 years.
A treatment algorithm
NfL someday could be incorporated into MS treatment algorithms, Dr. Leppert suggested. For instance, if a patient has high levels of disease activity based on MRI or clinical grounds, then prescribe a high-efficacy therapy. If not, measure NfL. “If the levels are low, then you can be assured to use platform therapies or continue what the patient has. But if NfL levels are high, then you should choose high efficacious therapies or switch to high-efficacious therapies in the long run,” he said.
Limitations and next steps
Although NfL is a specific marker of neuronal damage, it is not specific for the cause of the damage. Further studies are needed to better understand NfL metabolism and confounding factors such as age. Reference biomarkers likely will be needed “to conceptualize whether the signal of NfL is due to acute disease or chronic disease,” Dr. Leppert said.
“We need to optimize the assay and come to a worldwide agreement on the platform. We need to have prospective studies, mainly to achieve regulatory acceptance. And we need to have a normative database” to determine which NfL values are pathologic at a particular age, he said.
Despite the biomarker’s potential, blood NfL levels will not replace clinical expertise. “Biomarkers cannot be of value without a clinical backing and a clinical evaluation,” Dr. Leppert said. “The idea that this will replace us or any other person who makes a clinical judgment is a big error. NfL will prevail as a biomarker. ... But interpretation of the clinical background is germane.”
Dr. Leppert has been an employee of pharmaceutical companies, most recently Novartis.
DALLAS – Neurologists soon may use a blood biomarker of axonal damage to monitor patients with multiple sclerosis (MS) and guide treatment decisions, according to a lecture delivered at ACTRIMS Forum 2019.
said David Leppert, MD, senior research associate in the department of neurology at University Hopsital Basel (Switzerland).
Among patients with MS, blood NfL levels predict disability, brain volume loss, and spinal cord atrophy. In addition, studies have found that blood NfL decreases in response to disease-modifying therapy (DMT) and that second-line DMTs may decrease blood NfL more than first-line DMTs do.
The establishment of normative databases and reference biomarkers may allow neurologists to use NfL in their care of individual patients, Dr. Leppert predicted at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “I am very positive that we will make a breakthrough in the next 2 or 3 years for an individual use of neurofilaments,” he said.
Response to DMT
An analysis of blood NfL levels from patients with MS and from healthy controls in two phase 3 trials of fingolimod, FREEDOMS and TRANSFORMS, provides insights into NfL’s response to DMT (Neurology. 2019 Mar 5;92[10]:e1007-15). In FREEDOMS, which compared fingolimod with placebo, “fingolimod leads to a rapid decrease of neurofilament levels, close to normality, while placebo patients continue to have high levels,” said Dr. Leppert, a coauthor of the study.
TRANSFORMS compared interferon-beta and fingolimod. “The clinical experience that fingolimod is a more potent compound than interferon is actually reflected here by the NfL results,” Dr. Leppert said. “Both compounds lead to a decrease of neurofilaments – so, a decrease of neuronal damage – but one drug is more potent than the other one.”
Similarly, data from the observational EPIC study indicate that patients who do not receive DMT have a consistent increase in NfL levels, whereas those who receive platform therapies have a slight decrease in NfL and those who receive second-line therapies have a greater decrease, Dr. Leppert said.
Decades of research
For about 20 years, researchers have studied neurofilaments in cerebrospinal fluid (CSF) as a potential biomarker for MS and other diseases, including Alzheimer’s disease, amyotrophic lateral sclerosis, Parkinson’s disease, and head trauma.
“What prevented the emergence of NfL to clinical practice was the inability to measure it in blood because levels are 50-100 times lower [in blood] than in CSF,” Dr. Leppert said.
The development of single molecule array (SIMOA) technology enabled researchers to show a proper correlation between levels of NfL in CSF and those in blood, Dr. Leppert said. “That is now allowing repetitive testing in an accessible fluid compartment, meaning serum or plasma,” he said.
Compared with brain MRI, NfL may provide novel insights into MS disease activity. “MRI is measuring a structural deficit of the past,” Dr. Leppert said. “NfL is measuring online, real time what axonal damage is occurring.”
Correlation with outcomes
At the group level, patients with MS have higher levels of NfL, compared with controls, and levels are higher in patients with progressive forms of MS versus relapsing forms. “Levels increase dramatically in the wake of relapse,” he said.
Barro et al. found that patients with higher serum levels of NfL are more likely to experience Expanded Disability Status Scale (EDSS) worsening (Brain. 2018 Aug 1;141[8]:2382-91). Furthermore, MRI lesions are independently associated with serum NfL, and patients with higher levels of serum NfL have significantly greater average loss in brain volume and spinal cord volume over 5 years.
A treatment algorithm
NfL someday could be incorporated into MS treatment algorithms, Dr. Leppert suggested. For instance, if a patient has high levels of disease activity based on MRI or clinical grounds, then prescribe a high-efficacy therapy. If not, measure NfL. “If the levels are low, then you can be assured to use platform therapies or continue what the patient has. But if NfL levels are high, then you should choose high efficacious therapies or switch to high-efficacious therapies in the long run,” he said.
Limitations and next steps
Although NfL is a specific marker of neuronal damage, it is not specific for the cause of the damage. Further studies are needed to better understand NfL metabolism and confounding factors such as age. Reference biomarkers likely will be needed “to conceptualize whether the signal of NfL is due to acute disease or chronic disease,” Dr. Leppert said.
“We need to optimize the assay and come to a worldwide agreement on the platform. We need to have prospective studies, mainly to achieve regulatory acceptance. And we need to have a normative database” to determine which NfL values are pathologic at a particular age, he said.
Despite the biomarker’s potential, blood NfL levels will not replace clinical expertise. “Biomarkers cannot be of value without a clinical backing and a clinical evaluation,” Dr. Leppert said. “The idea that this will replace us or any other person who makes a clinical judgment is a big error. NfL will prevail as a biomarker. ... But interpretation of the clinical background is germane.”
Dr. Leppert has been an employee of pharmaceutical companies, most recently Novartis.
DALLAS – Neurologists soon may use a blood biomarker of axonal damage to monitor patients with multiple sclerosis (MS) and guide treatment decisions, according to a lecture delivered at ACTRIMS Forum 2019.
said David Leppert, MD, senior research associate in the department of neurology at University Hopsital Basel (Switzerland).
Among patients with MS, blood NfL levels predict disability, brain volume loss, and spinal cord atrophy. In addition, studies have found that blood NfL decreases in response to disease-modifying therapy (DMT) and that second-line DMTs may decrease blood NfL more than first-line DMTs do.
The establishment of normative databases and reference biomarkers may allow neurologists to use NfL in their care of individual patients, Dr. Leppert predicted at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “I am very positive that we will make a breakthrough in the next 2 or 3 years for an individual use of neurofilaments,” he said.
Response to DMT
An analysis of blood NfL levels from patients with MS and from healthy controls in two phase 3 trials of fingolimod, FREEDOMS and TRANSFORMS, provides insights into NfL’s response to DMT (Neurology. 2019 Mar 5;92[10]:e1007-15). In FREEDOMS, which compared fingolimod with placebo, “fingolimod leads to a rapid decrease of neurofilament levels, close to normality, while placebo patients continue to have high levels,” said Dr. Leppert, a coauthor of the study.
TRANSFORMS compared interferon-beta and fingolimod. “The clinical experience that fingolimod is a more potent compound than interferon is actually reflected here by the NfL results,” Dr. Leppert said. “Both compounds lead to a decrease of neurofilaments – so, a decrease of neuronal damage – but one drug is more potent than the other one.”
Similarly, data from the observational EPIC study indicate that patients who do not receive DMT have a consistent increase in NfL levels, whereas those who receive platform therapies have a slight decrease in NfL and those who receive second-line therapies have a greater decrease, Dr. Leppert said.
Decades of research
For about 20 years, researchers have studied neurofilaments in cerebrospinal fluid (CSF) as a potential biomarker for MS and other diseases, including Alzheimer’s disease, amyotrophic lateral sclerosis, Parkinson’s disease, and head trauma.
“What prevented the emergence of NfL to clinical practice was the inability to measure it in blood because levels are 50-100 times lower [in blood] than in CSF,” Dr. Leppert said.
The development of single molecule array (SIMOA) technology enabled researchers to show a proper correlation between levels of NfL in CSF and those in blood, Dr. Leppert said. “That is now allowing repetitive testing in an accessible fluid compartment, meaning serum or plasma,” he said.
Compared with brain MRI, NfL may provide novel insights into MS disease activity. “MRI is measuring a structural deficit of the past,” Dr. Leppert said. “NfL is measuring online, real time what axonal damage is occurring.”
Correlation with outcomes
At the group level, patients with MS have higher levels of NfL, compared with controls, and levels are higher in patients with progressive forms of MS versus relapsing forms. “Levels increase dramatically in the wake of relapse,” he said.
Barro et al. found that patients with higher serum levels of NfL are more likely to experience Expanded Disability Status Scale (EDSS) worsening (Brain. 2018 Aug 1;141[8]:2382-91). Furthermore, MRI lesions are independently associated with serum NfL, and patients with higher levels of serum NfL have significantly greater average loss in brain volume and spinal cord volume over 5 years.
A treatment algorithm
NfL someday could be incorporated into MS treatment algorithms, Dr. Leppert suggested. For instance, if a patient has high levels of disease activity based on MRI or clinical grounds, then prescribe a high-efficacy therapy. If not, measure NfL. “If the levels are low, then you can be assured to use platform therapies or continue what the patient has. But if NfL levels are high, then you should choose high efficacious therapies or switch to high-efficacious therapies in the long run,” he said.
Limitations and next steps
Although NfL is a specific marker of neuronal damage, it is not specific for the cause of the damage. Further studies are needed to better understand NfL metabolism and confounding factors such as age. Reference biomarkers likely will be needed “to conceptualize whether the signal of NfL is due to acute disease or chronic disease,” Dr. Leppert said.
“We need to optimize the assay and come to a worldwide agreement on the platform. We need to have prospective studies, mainly to achieve regulatory acceptance. And we need to have a normative database” to determine which NfL values are pathologic at a particular age, he said.
Despite the biomarker’s potential, blood NfL levels will not replace clinical expertise. “Biomarkers cannot be of value without a clinical backing and a clinical evaluation,” Dr. Leppert said. “The idea that this will replace us or any other person who makes a clinical judgment is a big error. NfL will prevail as a biomarker. ... But interpretation of the clinical background is germane.”
Dr. Leppert has been an employee of pharmaceutical companies, most recently Novartis.
EXPERT ANALYSIS FROM ACTRIMS FORUM 2019
Dr. Louis Weiner: AACR presentations highlight new “transformative strategies”
ATLANTA – Several studies featured during a press briefing at the annual meeting of the American Association for Cancer Research highlight the types of “transformative strategies” currently being developed and implemented, according to Louis Weiner, MD.
“Had this been the AACR [meeting] 20 years ago ... each one of them would have been a main plenary presentation and would have been the talk of the meeting,” Dr. Weiner, director of the Georgetown Lombardi Cancer Center at Georgetown University, Washington, and press briefing moderator, said of the findings.
While they are well accepted as being high quality presentations of great value, they don’t cause the same amount of stir, he said, adding: “I wouldn’t say we’re jaded, but we’ve come to the point where we almost expect great results at these meetings, and isn’t that wonderful?”
In this video interview he discussed the findings of two of the studies, including the phase 2 UNITY-NHL study and a preclinical Lynch syndrome mouse model used to develop a potential cancer preventive vaccine.
The Lynch syndrome data “suggest the strong possibility that we might be able to immunize people and combine that treatment with standard nonsteroidal anti-inflammatory agents such as naproxen to delay or reduce the impact of Lynch syndrome.”
“This set of findings ... opens the door to investigators in many different areas of cancer research to explore whether or not there are common frameshift mutations that might create novel neoantigens that we can go after with vaccines – be they for therapeutic benefit or for prevention,” he said.
The UNITY-NHL study, which showed that umbralisib is active and well tolerated as single-agent therapy in patients with relapsed or refractory marginal zone lymphoma, suggests “it’s quite possible that [the phosphoinositide 3-kinase delta inhibitor] is going to become a very important element in the treatment of patients with marginal zone lymphomas, and obviously it can be then used in earlier stages of diseases since it’s well tolerated, and it may well have useful activity in other B-cell malignancies,” he said.
Dr. Weiner reported having no relevant disclosures.
ATLANTA – Several studies featured during a press briefing at the annual meeting of the American Association for Cancer Research highlight the types of “transformative strategies” currently being developed and implemented, according to Louis Weiner, MD.
“Had this been the AACR [meeting] 20 years ago ... each one of them would have been a main plenary presentation and would have been the talk of the meeting,” Dr. Weiner, director of the Georgetown Lombardi Cancer Center at Georgetown University, Washington, and press briefing moderator, said of the findings.
While they are well accepted as being high quality presentations of great value, they don’t cause the same amount of stir, he said, adding: “I wouldn’t say we’re jaded, but we’ve come to the point where we almost expect great results at these meetings, and isn’t that wonderful?”
In this video interview he discussed the findings of two of the studies, including the phase 2 UNITY-NHL study and a preclinical Lynch syndrome mouse model used to develop a potential cancer preventive vaccine.
The Lynch syndrome data “suggest the strong possibility that we might be able to immunize people and combine that treatment with standard nonsteroidal anti-inflammatory agents such as naproxen to delay or reduce the impact of Lynch syndrome.”
“This set of findings ... opens the door to investigators in many different areas of cancer research to explore whether or not there are common frameshift mutations that might create novel neoantigens that we can go after with vaccines – be they for therapeutic benefit or for prevention,” he said.
The UNITY-NHL study, which showed that umbralisib is active and well tolerated as single-agent therapy in patients with relapsed or refractory marginal zone lymphoma, suggests “it’s quite possible that [the phosphoinositide 3-kinase delta inhibitor] is going to become a very important element in the treatment of patients with marginal zone lymphomas, and obviously it can be then used in earlier stages of diseases since it’s well tolerated, and it may well have useful activity in other B-cell malignancies,” he said.
Dr. Weiner reported having no relevant disclosures.
ATLANTA – Several studies featured during a press briefing at the annual meeting of the American Association for Cancer Research highlight the types of “transformative strategies” currently being developed and implemented, according to Louis Weiner, MD.
“Had this been the AACR [meeting] 20 years ago ... each one of them would have been a main plenary presentation and would have been the talk of the meeting,” Dr. Weiner, director of the Georgetown Lombardi Cancer Center at Georgetown University, Washington, and press briefing moderator, said of the findings.
While they are well accepted as being high quality presentations of great value, they don’t cause the same amount of stir, he said, adding: “I wouldn’t say we’re jaded, but we’ve come to the point where we almost expect great results at these meetings, and isn’t that wonderful?”
In this video interview he discussed the findings of two of the studies, including the phase 2 UNITY-NHL study and a preclinical Lynch syndrome mouse model used to develop a potential cancer preventive vaccine.
The Lynch syndrome data “suggest the strong possibility that we might be able to immunize people and combine that treatment with standard nonsteroidal anti-inflammatory agents such as naproxen to delay or reduce the impact of Lynch syndrome.”
“This set of findings ... opens the door to investigators in many different areas of cancer research to explore whether or not there are common frameshift mutations that might create novel neoantigens that we can go after with vaccines – be they for therapeutic benefit or for prevention,” he said.
The UNITY-NHL study, which showed that umbralisib is active and well tolerated as single-agent therapy in patients with relapsed or refractory marginal zone lymphoma, suggests “it’s quite possible that [the phosphoinositide 3-kinase delta inhibitor] is going to become a very important element in the treatment of patients with marginal zone lymphomas, and obviously it can be then used in earlier stages of diseases since it’s well tolerated, and it may well have useful activity in other B-cell malignancies,” he said.
Dr. Weiner reported having no relevant disclosures.
REPORTING FROM AACR
Seniors in long-term care face higher suicide risks
Seniors who move into and live in long-term care facilities are at increased risk of suicide, according to reporting by the PBS NewsHour and Kaiser Health News. The report focused on the story of Roland K. Tiedemann, a senior who, in his younger days, was an outdoorsman, traveled around the world, and served as a surrogate dad to his granddaughter. When his health deteriorated, he moved to a long-term care facility with his wife, who later was diagnosed with dementia. At age 89, Mr. Tiedemann, who was facing a third move into a facility that would take Medicaid, “locked his door ... and jumped to his death from his fourth floor window,” the report said. The death of Mr. Tiedemann led Julie A. Rickard, PhD, to start asking questions at his facility and working with other centers to identify the signs of depression. A few years earlier, after a “rash of suicides, mostly among young people,” Dr. Rickard had started developing the Suicide Prevention Coalition of North Central Washington. It is also important for families to ask whether suicide prevention and mental health protocols are in place at long-term care facilities. Ultimately, Dr. Rickard and Jane Davis – Mr. Tiedemann’s daughter – agree that stigma needs to be reduced so that residents feel free to talk their depression and anxiety. PBS NewsHour.
More and more people are using mental health apps, and a new study has found that few of those apps have a sound scientific basis for their claims. The researchers scoured iTunes and Google Play for 1,435 mental health apps. These were whittled to 73 of the most popular. The apps addressed common mental health disorders, including depression, anxiety, and substance abuse, as well as some less common illnesses, such as schizophrenia. Of the 73 apps, 47 claimed to be able to effectively diagnose the target condition, improve the user symptoms or mood, and bolster self-management. In about 40% of cases, the app site trotted out scientific language to buttress claims of effectiveness. However, when the researchers took a rigorous look at the science behind the apps, only one was based on a published study. Moreover, for about one-third of the apps, no supporting scientific at all could be found. Science speak did not translate into evidence-based science. The annual market for self-improvement products and apps, including those focusing on mental health, is $10 billion in the United States. Forbes.
Police officers trained in helping people with mental health problems can get positive results, a newspaper report shows. That’s what happened when Logan Elliott called Clive, Iowa, police to report that his fiancé had threatened suicide – and had had a prior attempt, according to the Des Moines Register. Mr. Elliott’s fiancé, Codii Lewis, was in a “depressive state,” was suffering from the loss of his dog, and was troubled by uncertainty regarding the cost of a procedure undertaken to confirm his gender as a transgender man; as a result, Mr. Lewis climbed onto a ledge. He streamed video of his encounter with the police on Facebook Live, and eventually, after kicking one of the officers, he was subdued and taken into custody. The training that Clive officers receive “calls for less aggressive behavior by police,” the article said. “It emphasizes de-escalation, especially when the subject may be suicidal. It doesn’t expect officers to be therapists or handle all mental health situations, but it does ask that they handle mental health situations differently” from the way they might handle other calls. People with mental illness that is untreated are 16 times more likely to be killed by law enforcement than are people without mental illness. Des Moines Register.
An exhibit now running at the Dartmouth-Hitchcock Medical Center in Lebanon, N.H., is intended to put a human face on mental illness. The 99 Faces Project: Portraits Without Labels by Boston-area artist Lynda Michaud Cutrell presents photos of people with serious mental illnesses and those who love them, the New Hampshire Union Leader reported. Portraits were taken with the help of three photographers nationwide. The long list was trimmed to 99 that mirror the ethnic makeup of the U.S. population. The roster of individuals includes 33 with schizophrenia and 33 with bipolar disorder. The remaining 33 are “chronically normal” according to Ms. Cutrell. The viewer can’t tell the difference between the mentally affected individuals and those who are not; they look like people one encounters every day. And that’s the point. Marianne Barthel, director of the Dartmouth-Hitchcock Arts Program, hopes the exhibit leads to conversations that help “normalize mental health in our society, to recognize that the people you’re looking at in these images could be you or your family member,” the article said. Ms. Barthel also hopes that the exhibit, which runs until September, will help reduce the stigma around mental illness by showing that “there are people who are living successful lives with these illnesses.” One of the 99 faces is that of actress Glenn Close, who cofounded the organization Bring Change To Mind in 2010 after her sister was diagnosed with bipolar disorder and her nephew with schizoaffective disorder. New Hampshire Union Leader.
Deliberation about the use of the death penalty for a prisoner in Kansas has implications for those with mental illness who commit crimes. As the Topeka Capital-Journal reported, James Kahler was convicted of murdering his estranged wife, her grandmother, and his two teenage daughters in 2009. Two years later, he was sentenced to death, and several years later, the Kansas Supreme Court upheld that conviction. His guilt is not in question. What is at issue is his impairment. His lawyers had earlier argued that severe depression had made his grip on reality tenuous and that he could not be executed. Now comes the news that the U.S. Supreme Court will rule whether the decision by the state of Kansas to abolish insanity as a defense was constitutional under the 8th and 14th amendments. The high court’s ruling will have profound implications for people with mental illness. In addition to those in Kansas, under state laws in Alaska, Idaho, Montana, and Utah, “a traditional insanity defense in which a person must understand the difference between right and wrong before being found guilty of a crime isn’t allowed,” the report said. An accused can cite “mental disease or defect” as a partial defense. However, in such cases, it must be proven that the person had no intention of committing a crime. In their petition to the Supreme Court, his attorneys argued that he knew he was shooting people, but that he was so disturbed at the time that he could not stop himself. “A favorable decision would make it clear that the Constitution requires that a defendant be able to understand the difference between right and wrong before being found guilty, and, in cases like Mr. Kahler’s, put to death,” his defense attorney, Meryle Carver-Allmond, told the Capital-Journal. “We’re hopeful that, in taking Mr. Kahler’s case, the United States Supreme Court has indicated a desire to find that the Constitution requires better of us in our treatment of mentally ill defendants.” The Topeka Capital-Journal.
Seniors who move into and live in long-term care facilities are at increased risk of suicide, according to reporting by the PBS NewsHour and Kaiser Health News. The report focused on the story of Roland K. Tiedemann, a senior who, in his younger days, was an outdoorsman, traveled around the world, and served as a surrogate dad to his granddaughter. When his health deteriorated, he moved to a long-term care facility with his wife, who later was diagnosed with dementia. At age 89, Mr. Tiedemann, who was facing a third move into a facility that would take Medicaid, “locked his door ... and jumped to his death from his fourth floor window,” the report said. The death of Mr. Tiedemann led Julie A. Rickard, PhD, to start asking questions at his facility and working with other centers to identify the signs of depression. A few years earlier, after a “rash of suicides, mostly among young people,” Dr. Rickard had started developing the Suicide Prevention Coalition of North Central Washington. It is also important for families to ask whether suicide prevention and mental health protocols are in place at long-term care facilities. Ultimately, Dr. Rickard and Jane Davis – Mr. Tiedemann’s daughter – agree that stigma needs to be reduced so that residents feel free to talk their depression and anxiety. PBS NewsHour.
More and more people are using mental health apps, and a new study has found that few of those apps have a sound scientific basis for their claims. The researchers scoured iTunes and Google Play for 1,435 mental health apps. These were whittled to 73 of the most popular. The apps addressed common mental health disorders, including depression, anxiety, and substance abuse, as well as some less common illnesses, such as schizophrenia. Of the 73 apps, 47 claimed to be able to effectively diagnose the target condition, improve the user symptoms or mood, and bolster self-management. In about 40% of cases, the app site trotted out scientific language to buttress claims of effectiveness. However, when the researchers took a rigorous look at the science behind the apps, only one was based on a published study. Moreover, for about one-third of the apps, no supporting scientific at all could be found. Science speak did not translate into evidence-based science. The annual market for self-improvement products and apps, including those focusing on mental health, is $10 billion in the United States. Forbes.
Police officers trained in helping people with mental health problems can get positive results, a newspaper report shows. That’s what happened when Logan Elliott called Clive, Iowa, police to report that his fiancé had threatened suicide – and had had a prior attempt, according to the Des Moines Register. Mr. Elliott’s fiancé, Codii Lewis, was in a “depressive state,” was suffering from the loss of his dog, and was troubled by uncertainty regarding the cost of a procedure undertaken to confirm his gender as a transgender man; as a result, Mr. Lewis climbed onto a ledge. He streamed video of his encounter with the police on Facebook Live, and eventually, after kicking one of the officers, he was subdued and taken into custody. The training that Clive officers receive “calls for less aggressive behavior by police,” the article said. “It emphasizes de-escalation, especially when the subject may be suicidal. It doesn’t expect officers to be therapists or handle all mental health situations, but it does ask that they handle mental health situations differently” from the way they might handle other calls. People with mental illness that is untreated are 16 times more likely to be killed by law enforcement than are people without mental illness. Des Moines Register.
An exhibit now running at the Dartmouth-Hitchcock Medical Center in Lebanon, N.H., is intended to put a human face on mental illness. The 99 Faces Project: Portraits Without Labels by Boston-area artist Lynda Michaud Cutrell presents photos of people with serious mental illnesses and those who love them, the New Hampshire Union Leader reported. Portraits were taken with the help of three photographers nationwide. The long list was trimmed to 99 that mirror the ethnic makeup of the U.S. population. The roster of individuals includes 33 with schizophrenia and 33 with bipolar disorder. The remaining 33 are “chronically normal” according to Ms. Cutrell. The viewer can’t tell the difference between the mentally affected individuals and those who are not; they look like people one encounters every day. And that’s the point. Marianne Barthel, director of the Dartmouth-Hitchcock Arts Program, hopes the exhibit leads to conversations that help “normalize mental health in our society, to recognize that the people you’re looking at in these images could be you or your family member,” the article said. Ms. Barthel also hopes that the exhibit, which runs until September, will help reduce the stigma around mental illness by showing that “there are people who are living successful lives with these illnesses.” One of the 99 faces is that of actress Glenn Close, who cofounded the organization Bring Change To Mind in 2010 after her sister was diagnosed with bipolar disorder and her nephew with schizoaffective disorder. New Hampshire Union Leader.
Deliberation about the use of the death penalty for a prisoner in Kansas has implications for those with mental illness who commit crimes. As the Topeka Capital-Journal reported, James Kahler was convicted of murdering his estranged wife, her grandmother, and his two teenage daughters in 2009. Two years later, he was sentenced to death, and several years later, the Kansas Supreme Court upheld that conviction. His guilt is not in question. What is at issue is his impairment. His lawyers had earlier argued that severe depression had made his grip on reality tenuous and that he could not be executed. Now comes the news that the U.S. Supreme Court will rule whether the decision by the state of Kansas to abolish insanity as a defense was constitutional under the 8th and 14th amendments. The high court’s ruling will have profound implications for people with mental illness. In addition to those in Kansas, under state laws in Alaska, Idaho, Montana, and Utah, “a traditional insanity defense in which a person must understand the difference between right and wrong before being found guilty of a crime isn’t allowed,” the report said. An accused can cite “mental disease or defect” as a partial defense. However, in such cases, it must be proven that the person had no intention of committing a crime. In their petition to the Supreme Court, his attorneys argued that he knew he was shooting people, but that he was so disturbed at the time that he could not stop himself. “A favorable decision would make it clear that the Constitution requires that a defendant be able to understand the difference between right and wrong before being found guilty, and, in cases like Mr. Kahler’s, put to death,” his defense attorney, Meryle Carver-Allmond, told the Capital-Journal. “We’re hopeful that, in taking Mr. Kahler’s case, the United States Supreme Court has indicated a desire to find that the Constitution requires better of us in our treatment of mentally ill defendants.” The Topeka Capital-Journal.
Seniors who move into and live in long-term care facilities are at increased risk of suicide, according to reporting by the PBS NewsHour and Kaiser Health News. The report focused on the story of Roland K. Tiedemann, a senior who, in his younger days, was an outdoorsman, traveled around the world, and served as a surrogate dad to his granddaughter. When his health deteriorated, he moved to a long-term care facility with his wife, who later was diagnosed with dementia. At age 89, Mr. Tiedemann, who was facing a third move into a facility that would take Medicaid, “locked his door ... and jumped to his death from his fourth floor window,” the report said. The death of Mr. Tiedemann led Julie A. Rickard, PhD, to start asking questions at his facility and working with other centers to identify the signs of depression. A few years earlier, after a “rash of suicides, mostly among young people,” Dr. Rickard had started developing the Suicide Prevention Coalition of North Central Washington. It is also important for families to ask whether suicide prevention and mental health protocols are in place at long-term care facilities. Ultimately, Dr. Rickard and Jane Davis – Mr. Tiedemann’s daughter – agree that stigma needs to be reduced so that residents feel free to talk their depression and anxiety. PBS NewsHour.
More and more people are using mental health apps, and a new study has found that few of those apps have a sound scientific basis for their claims. The researchers scoured iTunes and Google Play for 1,435 mental health apps. These were whittled to 73 of the most popular. The apps addressed common mental health disorders, including depression, anxiety, and substance abuse, as well as some less common illnesses, such as schizophrenia. Of the 73 apps, 47 claimed to be able to effectively diagnose the target condition, improve the user symptoms or mood, and bolster self-management. In about 40% of cases, the app site trotted out scientific language to buttress claims of effectiveness. However, when the researchers took a rigorous look at the science behind the apps, only one was based on a published study. Moreover, for about one-third of the apps, no supporting scientific at all could be found. Science speak did not translate into evidence-based science. The annual market for self-improvement products and apps, including those focusing on mental health, is $10 billion in the United States. Forbes.
Police officers trained in helping people with mental health problems can get positive results, a newspaper report shows. That’s what happened when Logan Elliott called Clive, Iowa, police to report that his fiancé had threatened suicide – and had had a prior attempt, according to the Des Moines Register. Mr. Elliott’s fiancé, Codii Lewis, was in a “depressive state,” was suffering from the loss of his dog, and was troubled by uncertainty regarding the cost of a procedure undertaken to confirm his gender as a transgender man; as a result, Mr. Lewis climbed onto a ledge. He streamed video of his encounter with the police on Facebook Live, and eventually, after kicking one of the officers, he was subdued and taken into custody. The training that Clive officers receive “calls for less aggressive behavior by police,” the article said. “It emphasizes de-escalation, especially when the subject may be suicidal. It doesn’t expect officers to be therapists or handle all mental health situations, but it does ask that they handle mental health situations differently” from the way they might handle other calls. People with mental illness that is untreated are 16 times more likely to be killed by law enforcement than are people without mental illness. Des Moines Register.
An exhibit now running at the Dartmouth-Hitchcock Medical Center in Lebanon, N.H., is intended to put a human face on mental illness. The 99 Faces Project: Portraits Without Labels by Boston-area artist Lynda Michaud Cutrell presents photos of people with serious mental illnesses and those who love them, the New Hampshire Union Leader reported. Portraits were taken with the help of three photographers nationwide. The long list was trimmed to 99 that mirror the ethnic makeup of the U.S. population. The roster of individuals includes 33 with schizophrenia and 33 with bipolar disorder. The remaining 33 are “chronically normal” according to Ms. Cutrell. The viewer can’t tell the difference between the mentally affected individuals and those who are not; they look like people one encounters every day. And that’s the point. Marianne Barthel, director of the Dartmouth-Hitchcock Arts Program, hopes the exhibit leads to conversations that help “normalize mental health in our society, to recognize that the people you’re looking at in these images could be you or your family member,” the article said. Ms. Barthel also hopes that the exhibit, which runs until September, will help reduce the stigma around mental illness by showing that “there are people who are living successful lives with these illnesses.” One of the 99 faces is that of actress Glenn Close, who cofounded the organization Bring Change To Mind in 2010 after her sister was diagnosed with bipolar disorder and her nephew with schizoaffective disorder. New Hampshire Union Leader.
Deliberation about the use of the death penalty for a prisoner in Kansas has implications for those with mental illness who commit crimes. As the Topeka Capital-Journal reported, James Kahler was convicted of murdering his estranged wife, her grandmother, and his two teenage daughters in 2009. Two years later, he was sentenced to death, and several years later, the Kansas Supreme Court upheld that conviction. His guilt is not in question. What is at issue is his impairment. His lawyers had earlier argued that severe depression had made his grip on reality tenuous and that he could not be executed. Now comes the news that the U.S. Supreme Court will rule whether the decision by the state of Kansas to abolish insanity as a defense was constitutional under the 8th and 14th amendments. The high court’s ruling will have profound implications for people with mental illness. In addition to those in Kansas, under state laws in Alaska, Idaho, Montana, and Utah, “a traditional insanity defense in which a person must understand the difference between right and wrong before being found guilty of a crime isn’t allowed,” the report said. An accused can cite “mental disease or defect” as a partial defense. However, in such cases, it must be proven that the person had no intention of committing a crime. In their petition to the Supreme Court, his attorneys argued that he knew he was shooting people, but that he was so disturbed at the time that he could not stop himself. “A favorable decision would make it clear that the Constitution requires that a defendant be able to understand the difference between right and wrong before being found guilty, and, in cases like Mr. Kahler’s, put to death,” his defense attorney, Meryle Carver-Allmond, told the Capital-Journal. “We’re hopeful that, in taking Mr. Kahler’s case, the United States Supreme Court has indicated a desire to find that the Constitution requires better of us in our treatment of mentally ill defendants.” The Topeka Capital-Journal.
New data further suggest that stress does a number on the CV system
Stress disorders triggered by life events or trauma have a marked deleterious impact on the cardiovascular system, especially in the short term, suggests a Swedish population-based cohort study of more than 1.6 million people.
Previous studies have had limited power to detect associations and have seldom explored conditions other than PTSD, noted the investigators, led by Huan Song, PhD. In addition, little is known about how genetic predisposition to cardiovascular disease may influence the association.
Results of the new study, reported online in the BMJ, showed that with a median follow-up of about 6.5 years, relative to unaffected siblings, patients who had PTSD, acute stress reaction, adjustment disorder, or another stress reaction had a 64% higher risk of developing a cardiovascular disease during the first year post diagnosis, and a 29% higher risk thereafter.
In the first year, risk was most elevated for heart failure – nearly seven times higher for the patients than for their siblings. In addition, overall risk was increased to a significantly greater extent for cardiovascular diseases with early onset, starting before age 50 years, than for those with later onset, according to Dr. Song of the Center of Public Health Sciences at the University of Iceland, Reykjavík, and the Karolinska Institutet in Stockholm. Findings were essentially the same when patients were instead compared with age- and sex-matched individuals from the general population.
“Stress-related disorders are robustly associated with multiple types of cardiovascular disease, independently of familial background, history of somatic/psychiatric diseases, and psychiatric comorbidity,” Dr. Song and her coinvestigators wrote. “These findings call for enhanced clinical awareness and, if verified, monitoring or early intervention among patients with recently diagnosed stress related disorders.”
Study details
In their population-based cohort study of the Swedish National Patient Register, the investigators identified 136,637 patients with new-onset, stress-related disorders diagnosed between 1987 and 2013. They compared these patients with 171,314 unaffected full siblings and with 1,366,370 unaffected matched people from the general population. Median follow-up was 6.2 years, 6.9 years, and 6.5 years, respectively.
Results showed that the crude incidence rate of any cardiovascular disease was 10.5 per 1,000 person years among the patients with stress-related disorders, 8.4 per 1,000 person years among their unaffected siblings, and 6.9 per 1,000 person years among the matched unaffected individuals from the general population.
Compared with unaffected siblings, patients with stress-related disorders had a 60% elevated risk for developing any cardiovascular disease during the first year after diagnosis. Risk in this window was most elevated for heart failure (hazard ratio, 6.95); cerebrovascular disease other than ischemic and hemorrhagic stroke and arachnoidal bleeding (HR, 5.64), conduction disorders (HR, 5.00), and cardiac arrest (HR, 3.37).
Risk of any cardiovascular disease associated with stress-related disorders was still elevated but to a lesser extent after the first year post diagnosis (HR, 1.29). During this period, risk was most elevated for arterial thrombosis/embolus (HR, 2.02), hemorrhagic stroke (HR, 1.56), and fatal cerebrovascular events (HR, 1.56).
In analyses looking at age of onset of the cardiovascular disease, stress-related disorders showed stronger association with early-onset disease (occurring before age 50 years) than with later-onset disease (HR, 1.40 vs. 1.24; P = .002).
Fatal cardiovascular disease was the only category for which the associations were modified by presence of psychiatric comorbidity. Here, presence of such comorbidity amplified the risk conferred by the stress-related disorder.
Findings were much the same when patients were compared with matched individuals from the general population. Risk for any cardiovascular disease was again elevated substantially in the first year post diagnosis by 71%, and to 36% thereafter.
The authors reported that they had no relevant conflicts of interest. The study was supported by the Icelandic Research Fund, an ERC Consolidator Grant, the Karolinska Institutet, and the Swedish Research Council.
SOURCE: Song H et al. BMJ. 2019 Apr 10. doi: 10.1136/bmj.l1255.
The current study cannot rule out the possibility of reverse causation, whereby cardiovascular disease, which typically manifests slowly, may predispose individuals to stress-related disorders.
In fact, the association may be bidirectional.
“[T]he ultimate test of an underlying unidirectional relation between acute stress induced psychiatric disorders and cardiovascular disease will be through intervention studies to treat these disorders,” Simon L. Bacon, PhD, maintained in an editorial. A reduction in cardiovascular risk after effective treatment of the stress disorders would provide confirmation.
“Psychiatric intervention studies have so far been disappointing in relation to reductions in cardiovascular disease events ... although some people suggest that the null findings had more to do with the limitations of the interventions than a true failure of the hypothesis,” Dr. Bacon observed. “In the future, well-designed studies evaluating more appropriate interventions ... will be critical not only to confirm the inferences of the new study but also to provide real benefits to patients.”
Dr. Bacon is a professor at the Montreal Behavioural Medicine Centre, and department of health, kinesiology, and applied physiology at Concordia University, also in Montreal.
The current study cannot rule out the possibility of reverse causation, whereby cardiovascular disease, which typically manifests slowly, may predispose individuals to stress-related disorders.
In fact, the association may be bidirectional.
“[T]he ultimate test of an underlying unidirectional relation between acute stress induced psychiatric disorders and cardiovascular disease will be through intervention studies to treat these disorders,” Simon L. Bacon, PhD, maintained in an editorial. A reduction in cardiovascular risk after effective treatment of the stress disorders would provide confirmation.
“Psychiatric intervention studies have so far been disappointing in relation to reductions in cardiovascular disease events ... although some people suggest that the null findings had more to do with the limitations of the interventions than a true failure of the hypothesis,” Dr. Bacon observed. “In the future, well-designed studies evaluating more appropriate interventions ... will be critical not only to confirm the inferences of the new study but also to provide real benefits to patients.”
Dr. Bacon is a professor at the Montreal Behavioural Medicine Centre, and department of health, kinesiology, and applied physiology at Concordia University, also in Montreal.
The current study cannot rule out the possibility of reverse causation, whereby cardiovascular disease, which typically manifests slowly, may predispose individuals to stress-related disorders.
In fact, the association may be bidirectional.
“[T]he ultimate test of an underlying unidirectional relation between acute stress induced psychiatric disorders and cardiovascular disease will be through intervention studies to treat these disorders,” Simon L. Bacon, PhD, maintained in an editorial. A reduction in cardiovascular risk after effective treatment of the stress disorders would provide confirmation.
“Psychiatric intervention studies have so far been disappointing in relation to reductions in cardiovascular disease events ... although some people suggest that the null findings had more to do with the limitations of the interventions than a true failure of the hypothesis,” Dr. Bacon observed. “In the future, well-designed studies evaluating more appropriate interventions ... will be critical not only to confirm the inferences of the new study but also to provide real benefits to patients.”
Dr. Bacon is a professor at the Montreal Behavioural Medicine Centre, and department of health, kinesiology, and applied physiology at Concordia University, also in Montreal.
Stress disorders triggered by life events or trauma have a marked deleterious impact on the cardiovascular system, especially in the short term, suggests a Swedish population-based cohort study of more than 1.6 million people.
Previous studies have had limited power to detect associations and have seldom explored conditions other than PTSD, noted the investigators, led by Huan Song, PhD. In addition, little is known about how genetic predisposition to cardiovascular disease may influence the association.
Results of the new study, reported online in the BMJ, showed that with a median follow-up of about 6.5 years, relative to unaffected siblings, patients who had PTSD, acute stress reaction, adjustment disorder, or another stress reaction had a 64% higher risk of developing a cardiovascular disease during the first year post diagnosis, and a 29% higher risk thereafter.
In the first year, risk was most elevated for heart failure – nearly seven times higher for the patients than for their siblings. In addition, overall risk was increased to a significantly greater extent for cardiovascular diseases with early onset, starting before age 50 years, than for those with later onset, according to Dr. Song of the Center of Public Health Sciences at the University of Iceland, Reykjavík, and the Karolinska Institutet in Stockholm. Findings were essentially the same when patients were instead compared with age- and sex-matched individuals from the general population.
“Stress-related disorders are robustly associated with multiple types of cardiovascular disease, independently of familial background, history of somatic/psychiatric diseases, and psychiatric comorbidity,” Dr. Song and her coinvestigators wrote. “These findings call for enhanced clinical awareness and, if verified, monitoring or early intervention among patients with recently diagnosed stress related disorders.”
Study details
In their population-based cohort study of the Swedish National Patient Register, the investigators identified 136,637 patients with new-onset, stress-related disorders diagnosed between 1987 and 2013. They compared these patients with 171,314 unaffected full siblings and with 1,366,370 unaffected matched people from the general population. Median follow-up was 6.2 years, 6.9 years, and 6.5 years, respectively.
Results showed that the crude incidence rate of any cardiovascular disease was 10.5 per 1,000 person years among the patients with stress-related disorders, 8.4 per 1,000 person years among their unaffected siblings, and 6.9 per 1,000 person years among the matched unaffected individuals from the general population.
Compared with unaffected siblings, patients with stress-related disorders had a 60% elevated risk for developing any cardiovascular disease during the first year after diagnosis. Risk in this window was most elevated for heart failure (hazard ratio, 6.95); cerebrovascular disease other than ischemic and hemorrhagic stroke and arachnoidal bleeding (HR, 5.64), conduction disorders (HR, 5.00), and cardiac arrest (HR, 3.37).
Risk of any cardiovascular disease associated with stress-related disorders was still elevated but to a lesser extent after the first year post diagnosis (HR, 1.29). During this period, risk was most elevated for arterial thrombosis/embolus (HR, 2.02), hemorrhagic stroke (HR, 1.56), and fatal cerebrovascular events (HR, 1.56).
In analyses looking at age of onset of the cardiovascular disease, stress-related disorders showed stronger association with early-onset disease (occurring before age 50 years) than with later-onset disease (HR, 1.40 vs. 1.24; P = .002).
Fatal cardiovascular disease was the only category for which the associations were modified by presence of psychiatric comorbidity. Here, presence of such comorbidity amplified the risk conferred by the stress-related disorder.
Findings were much the same when patients were compared with matched individuals from the general population. Risk for any cardiovascular disease was again elevated substantially in the first year post diagnosis by 71%, and to 36% thereafter.
The authors reported that they had no relevant conflicts of interest. The study was supported by the Icelandic Research Fund, an ERC Consolidator Grant, the Karolinska Institutet, and the Swedish Research Council.
SOURCE: Song H et al. BMJ. 2019 Apr 10. doi: 10.1136/bmj.l1255.
Stress disorders triggered by life events or trauma have a marked deleterious impact on the cardiovascular system, especially in the short term, suggests a Swedish population-based cohort study of more than 1.6 million people.
Previous studies have had limited power to detect associations and have seldom explored conditions other than PTSD, noted the investigators, led by Huan Song, PhD. In addition, little is known about how genetic predisposition to cardiovascular disease may influence the association.
Results of the new study, reported online in the BMJ, showed that with a median follow-up of about 6.5 years, relative to unaffected siblings, patients who had PTSD, acute stress reaction, adjustment disorder, or another stress reaction had a 64% higher risk of developing a cardiovascular disease during the first year post diagnosis, and a 29% higher risk thereafter.
In the first year, risk was most elevated for heart failure – nearly seven times higher for the patients than for their siblings. In addition, overall risk was increased to a significantly greater extent for cardiovascular diseases with early onset, starting before age 50 years, than for those with later onset, according to Dr. Song of the Center of Public Health Sciences at the University of Iceland, Reykjavík, and the Karolinska Institutet in Stockholm. Findings were essentially the same when patients were instead compared with age- and sex-matched individuals from the general population.
“Stress-related disorders are robustly associated with multiple types of cardiovascular disease, independently of familial background, history of somatic/psychiatric diseases, and psychiatric comorbidity,” Dr. Song and her coinvestigators wrote. “These findings call for enhanced clinical awareness and, if verified, monitoring or early intervention among patients with recently diagnosed stress related disorders.”
Study details
In their population-based cohort study of the Swedish National Patient Register, the investigators identified 136,637 patients with new-onset, stress-related disorders diagnosed between 1987 and 2013. They compared these patients with 171,314 unaffected full siblings and with 1,366,370 unaffected matched people from the general population. Median follow-up was 6.2 years, 6.9 years, and 6.5 years, respectively.
Results showed that the crude incidence rate of any cardiovascular disease was 10.5 per 1,000 person years among the patients with stress-related disorders, 8.4 per 1,000 person years among their unaffected siblings, and 6.9 per 1,000 person years among the matched unaffected individuals from the general population.
Compared with unaffected siblings, patients with stress-related disorders had a 60% elevated risk for developing any cardiovascular disease during the first year after diagnosis. Risk in this window was most elevated for heart failure (hazard ratio, 6.95); cerebrovascular disease other than ischemic and hemorrhagic stroke and arachnoidal bleeding (HR, 5.64), conduction disorders (HR, 5.00), and cardiac arrest (HR, 3.37).
Risk of any cardiovascular disease associated with stress-related disorders was still elevated but to a lesser extent after the first year post diagnosis (HR, 1.29). During this period, risk was most elevated for arterial thrombosis/embolus (HR, 2.02), hemorrhagic stroke (HR, 1.56), and fatal cerebrovascular events (HR, 1.56).
In analyses looking at age of onset of the cardiovascular disease, stress-related disorders showed stronger association with early-onset disease (occurring before age 50 years) than with later-onset disease (HR, 1.40 vs. 1.24; P = .002).
Fatal cardiovascular disease was the only category for which the associations were modified by presence of psychiatric comorbidity. Here, presence of such comorbidity amplified the risk conferred by the stress-related disorder.
Findings were much the same when patients were compared with matched individuals from the general population. Risk for any cardiovascular disease was again elevated substantially in the first year post diagnosis by 71%, and to 36% thereafter.
The authors reported that they had no relevant conflicts of interest. The study was supported by the Icelandic Research Fund, an ERC Consolidator Grant, the Karolinska Institutet, and the Swedish Research Council.
SOURCE: Song H et al. BMJ. 2019 Apr 10. doi: 10.1136/bmj.l1255.
FROM BMJ
Nail Irregularities Associated With Sézary Syndrome
Sézary syndrome (SS) is an advanced leukemic form of cutaneous T-cell lymphoma (CTCL) that is characterized by generalized erythroderma and T-cell leukemia. Skin changes can include erythroderma, keratosis pilaris–like lesions, keratoderma, ectropion, alopecia, and nail changes.1 Nail changes in SS patients frequently are overlooked and underreported; they vary greatly from patient to patient, and their incidence has not been widely evaluated in the literature.
In this retrospective study, we reviewed medical records from a previously collected CTCL clinic database at the University of Texas MD Anderson Cancer Center (Houston, Texas) and found nail abnormalities in 36 of 83 (43.4%) patients with a diagnosis of SS. Findings for 2 select cases are described in more detail; they were compared to prior case reports from the literature to establish a comprehensive list of nail irregularities that have been associated with SS.
Methods
We examined records from a previously collected CTCL clinic database at the University of Texas MD Anderson Cancer Center. This database was part of an institutional review board–approved protocol to prospectively collect data from patients with CTCL. Our search yielded 83 patients with SS who were seen between 2007 and 2014.
Results
Of the 83 cases reviewed from the CTCL database, 36 (43.4%) SS patients reported at least 1 nail abnormality on the fingernails or toenails. Patients ranged in age from 59 to 85 years and included 27 (75%) men and 9 (25%) women. Nail irregularities noted on physical examination are summarized in Table 1. More than half of the patients presented with nail thickening (58.3% [21/36]), dystrophy (55.6% [20/36]), or yellowing (55.6% [20/36]) of 1 or more nails. Other findings included 15 (41.7%) patients with subungual hyperkeratosis, 3 (8.3%) with Beau lines, and 1 (2.8%) with multiple oil spots consistent with salmon patches. Five (13.9%) patients had only 1 reported nail irregularity, and 1 (2.8%) patient had 6 irregularities. The average number of nail abnormalities per patient was 2.88 (range, 1–6). We selected 2 patients with extensive nail findings who represent the spectrum of nail findings in patients with SS.
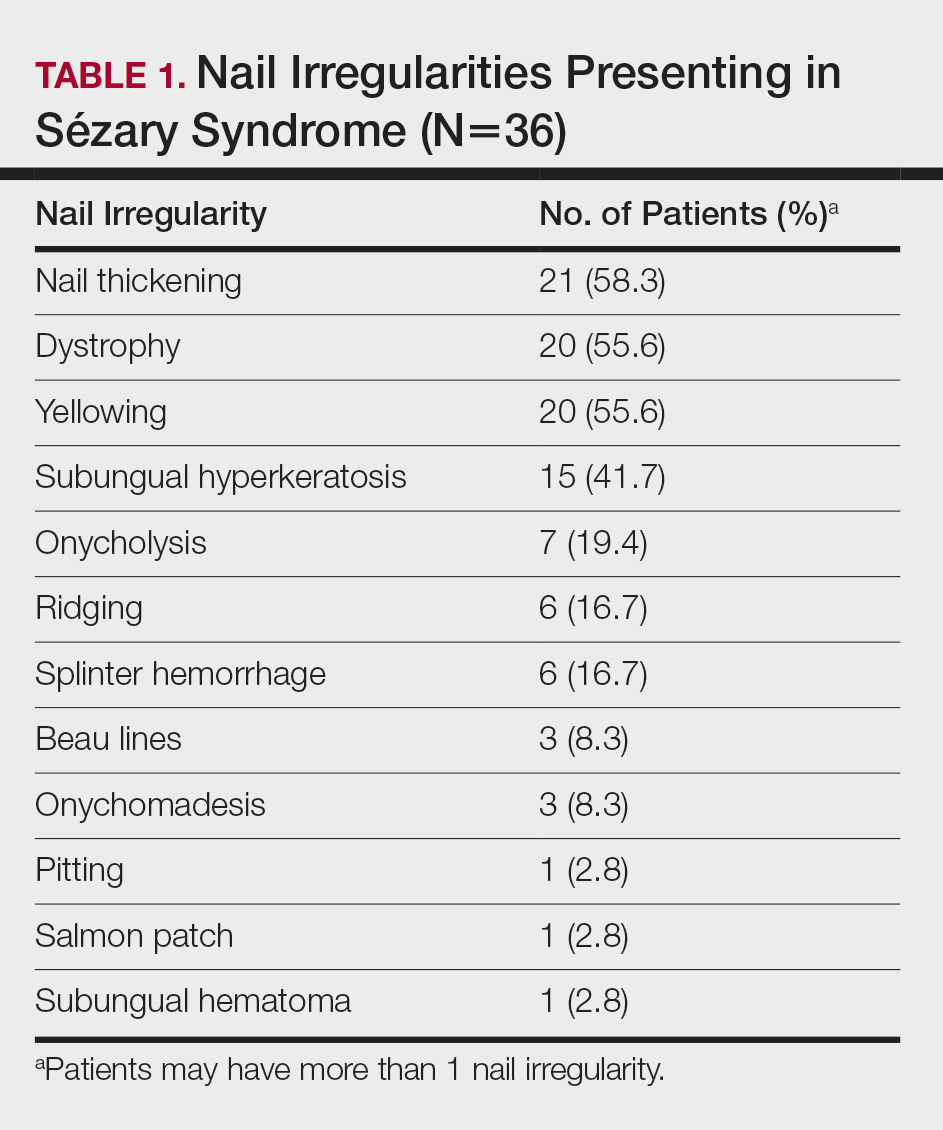
Patient 1
A 71-year-old white man presented with a papular rash of 30 years’ duration. The eruption first occurred on the soles of the feet but progressed to generalized erythroderma. He was found to be colonized with methicillin-resistant Staphylococcus aureus. Over the next 9 months, the patient was diagnosed with SS at an outside institution and was treated with cyclophosphamide, hydroxydaunorubicin, vincristine, prednisone, gemcitabine, etoposide, methylprednisolone, cytarabine, cisplatin, topical steroids, and intravenous methotrexate with no apparent improvement. At presentation to our institution, physical examination revealed pruritus; alopecia; generalized lymphadenopathy; erythroderma; and irregular nail findings, including yellowing, thickened fingernails and toenails with subungual debris, and splinter hemorrhage (Figure 1). A thick plaque with perioral distribution as well as erosions on the face and feet were noted. The total body surface area (BSA) affected was 100% (patches, 91%; plaques, 9%).

At diagnosis at our institution, the patient’s white blood cell (WBC) count was 17,800/µL (reference range, 4000–11,000/µL), with 11% Sézary cells noted. Biopsy of a lymph node from the inguinal area indicated T-cell lymphoma with clonal T-cell receptor (TCR) β gene rearrangement. Biopsy of lesional skin in the right groin area showed an atypical T-cell lymphocytic infiltrate with a CD4:CD8 ratio of 2.9:1 and partial loss of CD7 expression, consistent with mycosis fungoides (MF)/SS stage IVA. At presentation to our institution, the WBC count was 12,700/µL with a neutrophil count of 47% (reference range, 42%–66%), lymphocyte count of 36% (reference range, 24%–44%), monocyte count of 4% (reference range, 2%–7%), platelet count of 427,000/µL (reference range, 150,000–350,000/µL), hemoglobin of 9.9 g/dL (reference range, 14.0–17.5 g/dL), and lactate dehydrogenase of 733 U/L (reference range, 135–214 U/L). Lymphocytes were positive for CD2, CD3, CD4, CD5, CD25, CD52, TCRα, TCRβ, and TCR VB17; partial for CD26; and negative for CD7, CD8, and CD57. At follow-up 1 month later, the CD4+CD26− T-cell population was 56%, which was consistent with SS T-cell lymphoma.
Skin scrapings from the generalized keratoderma on the patient’s feet were positive for fungal hyphae under potassium hydroxide examination. Nail clippings showed compact keratin with periodic acid–Schiff–positive small yeast forms admixed with bacterial organisms, consistent with onychomycosis. At our institution, the patient received extracorporeal photopheresis, whirlpool therapy (a type of hydrotherapy), steroid wet wraps, and intravenous vancomycin for methicillin-resistant S aureus. He also received bexarotene, levothyroxine sodium, and fenofibrate. After antibiotics and 2 sessions of photopheresis, the total BSA improved from 100% to 33%. The feet and nails were treated with ciclopirox gel and terbinafine, but neither the keratoderma nor the nails improved.
Patient 2
An 84-year-old white man with B-cell chronic lymphocytic leukemia also was diagnosed with SS at an outside institution. One year later, he presented to our institution with mild pruritus and swelling of the lower left leg, which was diagnosed as deep vein thrombosis. There was bilateral scaling of the palms, with fissures present on the left palm. The fingernails showed dystrophy with Beau lines, and the toenails were dystrophic with onycholysis on the bilateral great toes (Figure 2). Patches were noted on most of the body, including the feet, with plaques limited to the hands; the total BSA affected was 80%. Flow cytometry showed an elevated Sézary cell count (CD4+CD26−) of 4700 cells/µL. Complete blood cell count with differential included a hemoglobin level of 11.4 g/dL, hematocrit level of 35.3% (reference range, 37%–47%), a platelet count of 217,000/µL, and a WBC count of 17,7

the bilateral great toes.
Comment
Nail changes are found in many cases of advanced-stage SS but rarely have been reported in the literature. A literature review of PubMed articles indexed for MEDLINE was conducted using the search terms Sézary, nail, onychodystrophy, cutaneous T-cell lymphoma, and CTCL. All results were reviewed for original reported cases of SS with at least 1 reported nail finding. A total of 7 reports2-8 met these requirements with a total of 43 SS patients with reported nail findings, which are summarized in Tables 2 and 3.
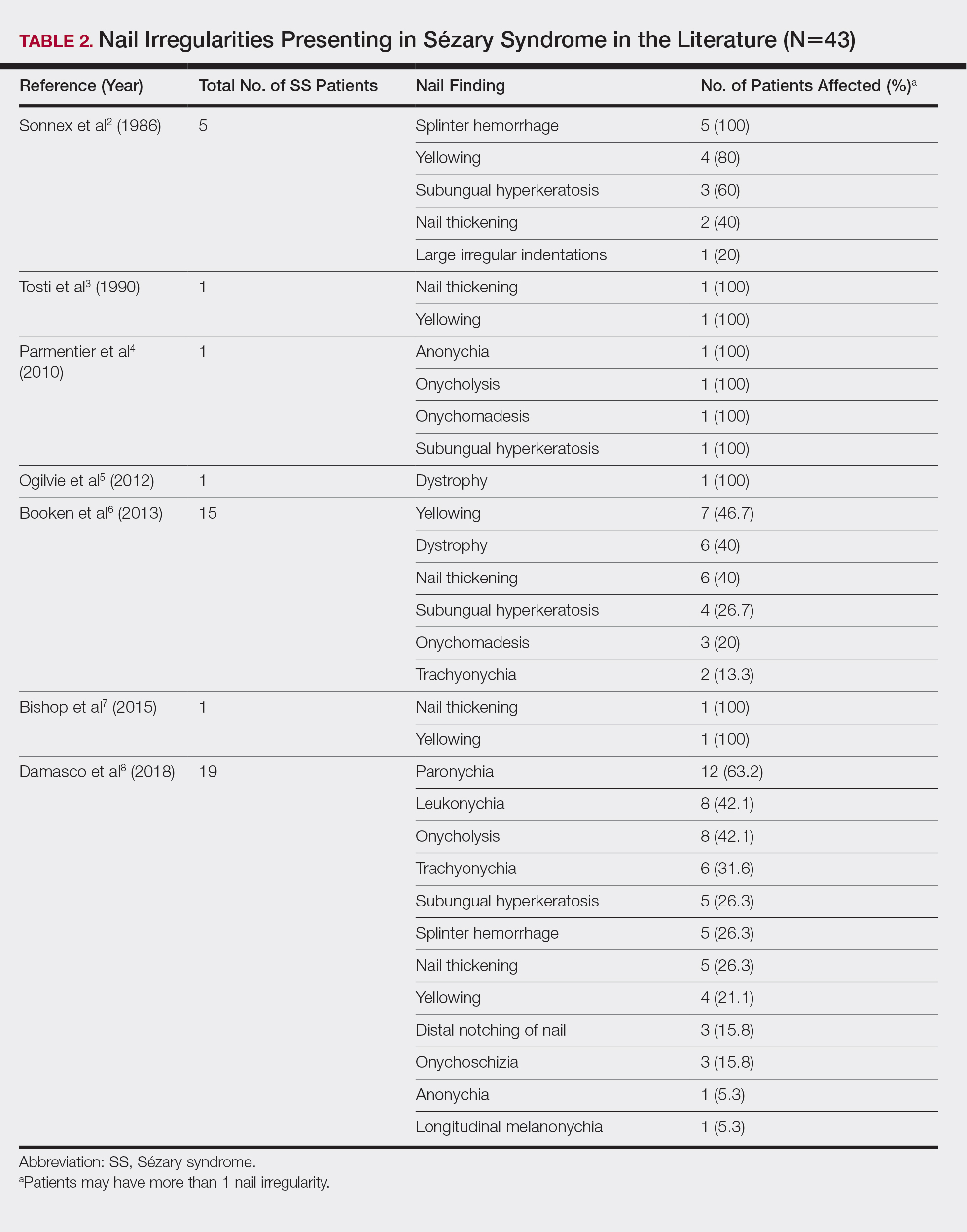

Our findings are generally consistent with those previously described in the literature. Nail thickening, yellowing, subungual hyperkeratosis, dystrophy, and onycholysis are consistently some of the most common nail findings in patients with SS. In 2012, Martin and Duvic9 found that 52.9% (45/85) of SS patients with keratoderma on physical examination were positive for dermatophyte hyphae when skin scrapings were done under potassium hydroxide examination, a considerably greater incidence than in the general population (10%–20%). The nail changes seen in our SS patients were identical to those found in dermatophyte infections, including discoloration, subungual debris, nail thickening, onycholysis, and dystrophy.10 In patient 1, nail clippings were positive for onychomycosis, a common nail condition that is especially prevalent in older or immunocompromised patients.9,10
Interestingly, findings not observed in the literature included salmon patches and Beau lines. Beau lines are horizontal depressions in the nail plate and often are indicative of temporary interruption of nail growth, such as due to an underlying disease process, severe illness, and/or chemotherapy.11,12 In our review, patient 2 had clinical findings of Beau lines. Because the average time for fingernail regrowth is 3 to 6 months,13 it is reasonable to assume that physical findings associated with fludarabine, cyclophosphamide, and rituximab chemotherapy treatment would no longer be demonstrated 11 months after completion of therapy. On the other hand, paronychia was frequently observed by Damasco et al8 (63.2% [12/19] of their cases), yet it was not found in our database or the other literature reports we reviewed. Perhaps these differences are due to differences in patient populations and/or available therapies, lack of documentation, or small sample size and limited reports in the literature.
A common question is: Are the nail irregularities caused by the physical symptoms of advanced CTCL or by the underlying disease process in response to the atypical T cells? Erythroderma has been speculated to cause many of the clinical findings of nail abnormalities found in CTCL patients.2,3 However, Fleming et al14 described an MF patient who experienced onychomadesis without erythroderma, which suggests that a different mechanism may cause these nail changes. The wide range of nail abnormalities in CTCL can cause problems with diagnosing the specific cause underlying the nail alteration.
To further complicate the issue, numerous therapies for CTCL also may cause nail changes, such as the previously described Beau lines. In 2010, Parmentier et al4 reported a patient with nail alterations that had been present for more than 1 year, with 9 of 10 fingernails demonstrating anonychia, onychomadesis, subungual distal hyperkeratosis, and onycholysis. In this case report, the authors were able to exclude phototherapy as the cause of onycholysis (visible separation of the nail plate from the nail bed) and other clinical nail findings in the SS patient based on the onset of nail changes prior to beginning psoralen plus UVA therapy and complete sparing of 1 finger.4 The findings in our patient 1, who had no history of psoralen plus UVA therapy at the time the irregular nail findings presented, supports this observation. Total skin electron beam therapy for MF also has been reported to cause temporary nail stasis and thus must be taken into account when considering nail changes in patients with MF/SS.15
A nail matrix biopsy may provide clues to the definitive cause of the clinically observed nail changes; however, this procedure typically is not performed due to patient concerns of postoperative complications including pain and nail dystrophy.16 Histopathology features were similar in reported nail biopsies of 2 SS patients.3,4 Tosti et al3 reported that longitudinal biopsy showed a dense lymphocytic infiltrate of atypical lymphocytes with involuted nuclei and notable epidermotropism. Parmentier et al4 reported a longitudinal nail biopsy in an SS patient that presented with atypical lymphocytes, epidermotropism, and Pautrier microabscess formation. Immunostaining showed CD3 positivity within the distal nail matrix, nail bed, and hyponychium. One-third of the cells stained positive for CD4, while the majority stained positive for CD8. Most notably, the skin, nails, and blood showed identical clonal rearrangement of TCRγ.4 Nail matrix biopsies in MF patients rarely have been reported in the literature, but those that are available show similar features to those seen in SS patients. Harland et al17 summarized the findings of 4 case reports of CTCL patients that included nail biopsies by stating, “[a]ll histopathologic findings from nail biopsies showed a dense subepithelial infiltrate of lymphocytes with marked epitheliotropism.” These histopathologic abnormalities are akin to skin biopsies in MF patients, thus providing an essential link to the disease state of MF and the nail abnormalities found within SS patients.
Treatment of the nail problems found within SS is challenging due to limited research. Parmentier et al4 noted an SS patient who was treated with topical mechlorethamine applied directly to the nail. In this case, topical mechlorethamine was effective at treating onychomadesis, subungual distal hyperkeratosis, and onycholysis within 6 months.4 Another SS patient, who presented with thickening and yellowing of the nail, had reported a proximal nail plate that resolved after chemotherapy. The patient did not survive long enough to note complete improvement of the nail.3 In our study, patient 1 was treated with ciclopirox gel and terbinafine, which did not result in nail improvement. Nail treatments in SS patients have yet to show much improvement and thus need more research and focus in the literature.
Conclusion
Sézary syndrome is a rare CTCL that can present with clinical features that may be mistaken for other diseases. Nail abnormalities in SS patients may be related to fungal involvement, medical therapy, or the underlying disease process of SS. We report one of the largest populations of SS patients with specific reported nail abnormalities, thus expanding the possibilities of nail changes that accompany the disease. Continued research and studies involving SS can provide a better understanding of nail involvement and successful treatment of these clinical findings.
- Willemz e R, Jaffe ES, Burg G, et al. WHO-EORTC classification for cutaneous lymphomas. Blood. 2005;105:3768-3785.
- Sonnex TS, Dawber RP, Zachary CB, et al. The nails in adult type 1 pityriasis rubra pilaris. a comparison with Sézary syndrome and psoriasis. J Am Acad Dermatol. 1986;15(5 pt 1):956-960.
- Tosti A, Fanti PA, Varotti C. Massive lymphomatous nail involvement in Sézary syndrome. Dermatologica. 1990;181:162-164.
- Parmentier L, Durr C, Vassella E, et al. Specific nail alterations in cutaneous T-cell lymphoma: successful treatment with topical mechlorethamine. Arch Dermatol. 2010;146:1287-1291.
- Ogilvie C, Jackson R, Leach M, et al. Sézary syndrome: diagnosis and management. J R Coll Physicians Edinb. 2012;42:317-321.
- Booken N, Nicolay JP, Weiss C, et al. Cutaneous tumor cell load correlates with survival in patients with Sézary syndrome. J Dtsch Dermatol Ges. 2013;11:67-79.
- Bishop BE, Wulkan A, Kerdel F, et al. Nail alterations in cutaneous T-cell lymphoma: a case series and review of nail manifestations. Skin Appendage Disord. 2015;1:82-86.
- Damasco FM, Geskin L, Akilov OE. Onychodystrophy in Sézary syndrome. J Am Acad Dermatol. 2018;79:972-973.
- Martin SJ, Duvic M. Prevalence and treatment of palmoplantar keratoderma and tinea pedis in patients with Sézary syndrome. Int J Dermatol. 2012;51:1195-1198.
- Mayo TT, Cantrell W. Putting onychomycosis under the microscope. Nurse Pract. 2014;39:8-11.
- Singh M, Kaur S. Chemotherapy-induced multiple Beau’s lines. Int J Dermatol. 1986;25:590-591.
- Tully AS, Trayes KP, Studdiford JS. Evaluation of nail abnormalities. Am Family Physician. 2012;85:779-787.
- Shirwaikar AA, Thomas T, Shirwaikar A, et al. Treatment of onychomycosis: an update. Indian J Pharm Sci. 2008;70:710-714.
- Fleming CJ, Hunt MJ, Barnetson RS. Mycosis fungoides with onychomadesis. Br J Dermatol. 1996;135:1012-1013.
- Jones GW, Kacinski BM, Wilson LD, et al. Total skin electron radiation in the management of mycosis fungoides: consensus of the European Organization for Research and Treatment of Cancer (EORTC) Cutaneous Lymphoma Project Group. J Am Acad Dermatol. 2002;47:364-370.
- Haneke E. Advanced nail surgery. J Cutan Aesthet Surg. 2011;4:167-175.
- Harland E, Dalle S, Balme B, et al. Ungueotropic T-cell lymphoma. Arch Dermatol. 2006;142:1071-1073.
Sézary syndrome (SS) is an advanced leukemic form of cutaneous T-cell lymphoma (CTCL) that is characterized by generalized erythroderma and T-cell leukemia. Skin changes can include erythroderma, keratosis pilaris–like lesions, keratoderma, ectropion, alopecia, and nail changes.1 Nail changes in SS patients frequently are overlooked and underreported; they vary greatly from patient to patient, and their incidence has not been widely evaluated in the literature.
In this retrospective study, we reviewed medical records from a previously collected CTCL clinic database at the University of Texas MD Anderson Cancer Center (Houston, Texas) and found nail abnormalities in 36 of 83 (43.4%) patients with a diagnosis of SS. Findings for 2 select cases are described in more detail; they were compared to prior case reports from the literature to establish a comprehensive list of nail irregularities that have been associated with SS.
Methods
We examined records from a previously collected CTCL clinic database at the University of Texas MD Anderson Cancer Center. This database was part of an institutional review board–approved protocol to prospectively collect data from patients with CTCL. Our search yielded 83 patients with SS who were seen between 2007 and 2014.
Results
Of the 83 cases reviewed from the CTCL database, 36 (43.4%) SS patients reported at least 1 nail abnormality on the fingernails or toenails. Patients ranged in age from 59 to 85 years and included 27 (75%) men and 9 (25%) women. Nail irregularities noted on physical examination are summarized in Table 1. More than half of the patients presented with nail thickening (58.3% [21/36]), dystrophy (55.6% [20/36]), or yellowing (55.6% [20/36]) of 1 or more nails. Other findings included 15 (41.7%) patients with subungual hyperkeratosis, 3 (8.3%) with Beau lines, and 1 (2.8%) with multiple oil spots consistent with salmon patches. Five (13.9%) patients had only 1 reported nail irregularity, and 1 (2.8%) patient had 6 irregularities. The average number of nail abnormalities per patient was 2.88 (range, 1–6). We selected 2 patients with extensive nail findings who represent the spectrum of nail findings in patients with SS.
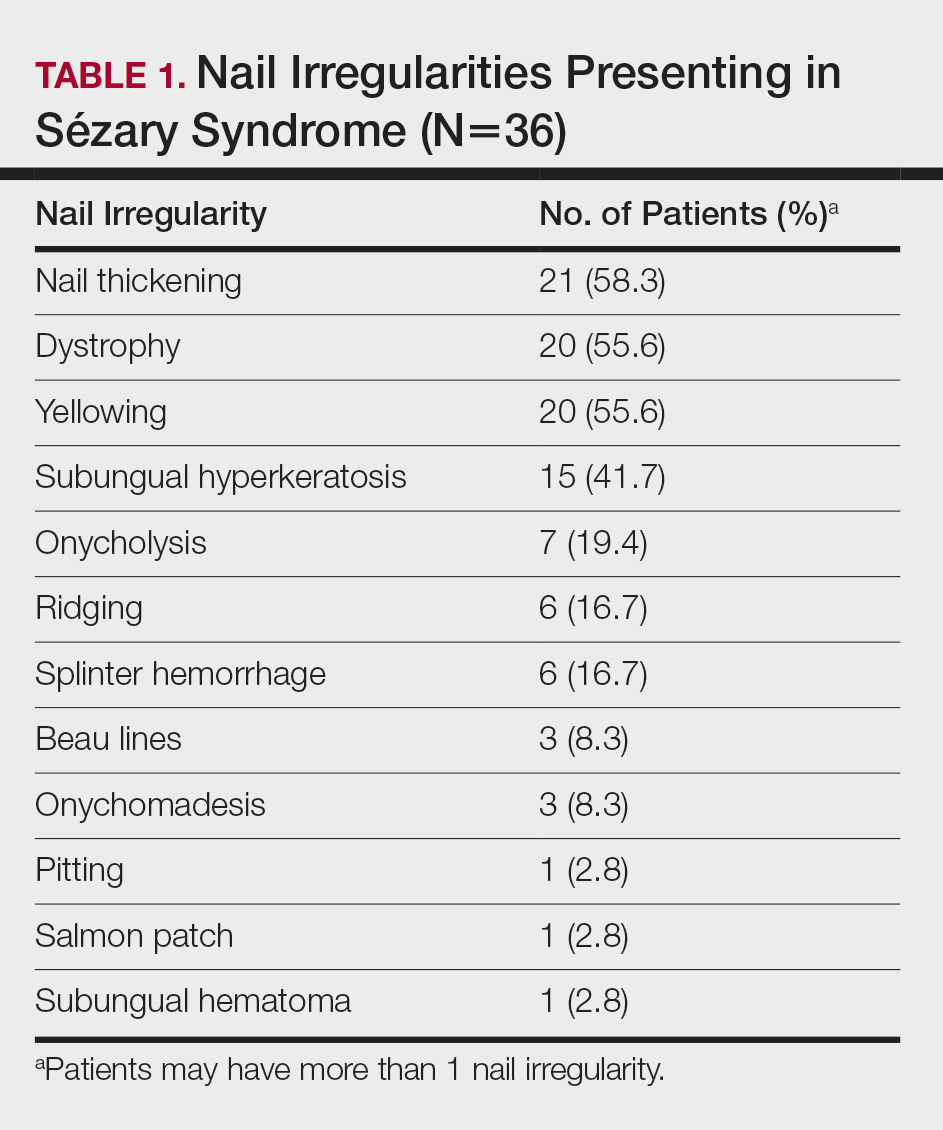
Patient 1
A 71-year-old white man presented with a papular rash of 30 years’ duration. The eruption first occurred on the soles of the feet but progressed to generalized erythroderma. He was found to be colonized with methicillin-resistant Staphylococcus aureus. Over the next 9 months, the patient was diagnosed with SS at an outside institution and was treated with cyclophosphamide, hydroxydaunorubicin, vincristine, prednisone, gemcitabine, etoposide, methylprednisolone, cytarabine, cisplatin, topical steroids, and intravenous methotrexate with no apparent improvement. At presentation to our institution, physical examination revealed pruritus; alopecia; generalized lymphadenopathy; erythroderma; and irregular nail findings, including yellowing, thickened fingernails and toenails with subungual debris, and splinter hemorrhage (Figure 1). A thick plaque with perioral distribution as well as erosions on the face and feet were noted. The total body surface area (BSA) affected was 100% (patches, 91%; plaques, 9%).

At diagnosis at our institution, the patient’s white blood cell (WBC) count was 17,800/µL (reference range, 4000–11,000/µL), with 11% Sézary cells noted. Biopsy of a lymph node from the inguinal area indicated T-cell lymphoma with clonal T-cell receptor (TCR) β gene rearrangement. Biopsy of lesional skin in the right groin area showed an atypical T-cell lymphocytic infiltrate with a CD4:CD8 ratio of 2.9:1 and partial loss of CD7 expression, consistent with mycosis fungoides (MF)/SS stage IVA. At presentation to our institution, the WBC count was 12,700/µL with a neutrophil count of 47% (reference range, 42%–66%), lymphocyte count of 36% (reference range, 24%–44%), monocyte count of 4% (reference range, 2%–7%), platelet count of 427,000/µL (reference range, 150,000–350,000/µL), hemoglobin of 9.9 g/dL (reference range, 14.0–17.5 g/dL), and lactate dehydrogenase of 733 U/L (reference range, 135–214 U/L). Lymphocytes were positive for CD2, CD3, CD4, CD5, CD25, CD52, TCRα, TCRβ, and TCR VB17; partial for CD26; and negative for CD7, CD8, and CD57. At follow-up 1 month later, the CD4+CD26− T-cell population was 56%, which was consistent with SS T-cell lymphoma.
Skin scrapings from the generalized keratoderma on the patient’s feet were positive for fungal hyphae under potassium hydroxide examination. Nail clippings showed compact keratin with periodic acid–Schiff–positive small yeast forms admixed with bacterial organisms, consistent with onychomycosis. At our institution, the patient received extracorporeal photopheresis, whirlpool therapy (a type of hydrotherapy), steroid wet wraps, and intravenous vancomycin for methicillin-resistant S aureus. He also received bexarotene, levothyroxine sodium, and fenofibrate. After antibiotics and 2 sessions of photopheresis, the total BSA improved from 100% to 33%. The feet and nails were treated with ciclopirox gel and terbinafine, but neither the keratoderma nor the nails improved.
Patient 2
An 84-year-old white man with B-cell chronic lymphocytic leukemia also was diagnosed with SS at an outside institution. One year later, he presented to our institution with mild pruritus and swelling of the lower left leg, which was diagnosed as deep vein thrombosis. There was bilateral scaling of the palms, with fissures present on the left palm. The fingernails showed dystrophy with Beau lines, and the toenails were dystrophic with onycholysis on the bilateral great toes (Figure 2). Patches were noted on most of the body, including the feet, with plaques limited to the hands; the total BSA affected was 80%. Flow cytometry showed an elevated Sézary cell count (CD4+CD26−) of 4700 cells/µL. Complete blood cell count with differential included a hemoglobin level of 11.4 g/dL, hematocrit level of 35.3% (reference range, 37%–47%), a platelet count of 217,000/µL, and a WBC count of 17,7

the bilateral great toes.
Comment
Nail changes are found in many cases of advanced-stage SS but rarely have been reported in the literature. A literature review of PubMed articles indexed for MEDLINE was conducted using the search terms Sézary, nail, onychodystrophy, cutaneous T-cell lymphoma, and CTCL. All results were reviewed for original reported cases of SS with at least 1 reported nail finding. A total of 7 reports2-8 met these requirements with a total of 43 SS patients with reported nail findings, which are summarized in Tables 2 and 3.
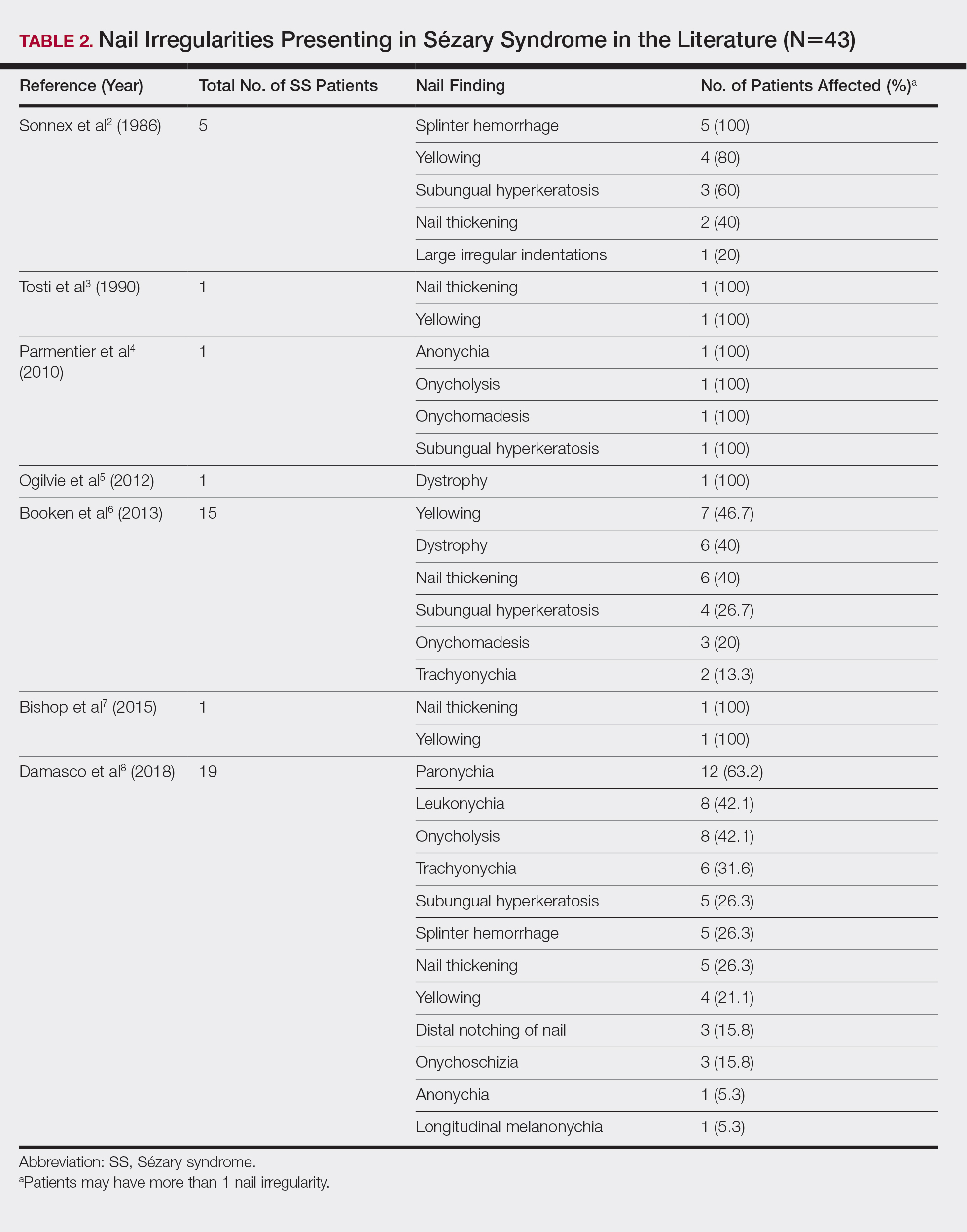

Our findings are generally consistent with those previously described in the literature. Nail thickening, yellowing, subungual hyperkeratosis, dystrophy, and onycholysis are consistently some of the most common nail findings in patients with SS. In 2012, Martin and Duvic9 found that 52.9% (45/85) of SS patients with keratoderma on physical examination were positive for dermatophyte hyphae when skin scrapings were done under potassium hydroxide examination, a considerably greater incidence than in the general population (10%–20%). The nail changes seen in our SS patients were identical to those found in dermatophyte infections, including discoloration, subungual debris, nail thickening, onycholysis, and dystrophy.10 In patient 1, nail clippings were positive for onychomycosis, a common nail condition that is especially prevalent in older or immunocompromised patients.9,10
Interestingly, findings not observed in the literature included salmon patches and Beau lines. Beau lines are horizontal depressions in the nail plate and often are indicative of temporary interruption of nail growth, such as due to an underlying disease process, severe illness, and/or chemotherapy.11,12 In our review, patient 2 had clinical findings of Beau lines. Because the average time for fingernail regrowth is 3 to 6 months,13 it is reasonable to assume that physical findings associated with fludarabine, cyclophosphamide, and rituximab chemotherapy treatment would no longer be demonstrated 11 months after completion of therapy. On the other hand, paronychia was frequently observed by Damasco et al8 (63.2% [12/19] of their cases), yet it was not found in our database or the other literature reports we reviewed. Perhaps these differences are due to differences in patient populations and/or available therapies, lack of documentation, or small sample size and limited reports in the literature.
A common question is: Are the nail irregularities caused by the physical symptoms of advanced CTCL or by the underlying disease process in response to the atypical T cells? Erythroderma has been speculated to cause many of the clinical findings of nail abnormalities found in CTCL patients.2,3 However, Fleming et al14 described an MF patient who experienced onychomadesis without erythroderma, which suggests that a different mechanism may cause these nail changes. The wide range of nail abnormalities in CTCL can cause problems with diagnosing the specific cause underlying the nail alteration.
To further complicate the issue, numerous therapies for CTCL also may cause nail changes, such as the previously described Beau lines. In 2010, Parmentier et al4 reported a patient with nail alterations that had been present for more than 1 year, with 9 of 10 fingernails demonstrating anonychia, onychomadesis, subungual distal hyperkeratosis, and onycholysis. In this case report, the authors were able to exclude phototherapy as the cause of onycholysis (visible separation of the nail plate from the nail bed) and other clinical nail findings in the SS patient based on the onset of nail changes prior to beginning psoralen plus UVA therapy and complete sparing of 1 finger.4 The findings in our patient 1, who had no history of psoralen plus UVA therapy at the time the irregular nail findings presented, supports this observation. Total skin electron beam therapy for MF also has been reported to cause temporary nail stasis and thus must be taken into account when considering nail changes in patients with MF/SS.15
A nail matrix biopsy may provide clues to the definitive cause of the clinically observed nail changes; however, this procedure typically is not performed due to patient concerns of postoperative complications including pain and nail dystrophy.16 Histopathology features were similar in reported nail biopsies of 2 SS patients.3,4 Tosti et al3 reported that longitudinal biopsy showed a dense lymphocytic infiltrate of atypical lymphocytes with involuted nuclei and notable epidermotropism. Parmentier et al4 reported a longitudinal nail biopsy in an SS patient that presented with atypical lymphocytes, epidermotropism, and Pautrier microabscess formation. Immunostaining showed CD3 positivity within the distal nail matrix, nail bed, and hyponychium. One-third of the cells stained positive for CD4, while the majority stained positive for CD8. Most notably, the skin, nails, and blood showed identical clonal rearrangement of TCRγ.4 Nail matrix biopsies in MF patients rarely have been reported in the literature, but those that are available show similar features to those seen in SS patients. Harland et al17 summarized the findings of 4 case reports of CTCL patients that included nail biopsies by stating, “[a]ll histopathologic findings from nail biopsies showed a dense subepithelial infiltrate of lymphocytes with marked epitheliotropism.” These histopathologic abnormalities are akin to skin biopsies in MF patients, thus providing an essential link to the disease state of MF and the nail abnormalities found within SS patients.
Treatment of the nail problems found within SS is challenging due to limited research. Parmentier et al4 noted an SS patient who was treated with topical mechlorethamine applied directly to the nail. In this case, topical mechlorethamine was effective at treating onychomadesis, subungual distal hyperkeratosis, and onycholysis within 6 months.4 Another SS patient, who presented with thickening and yellowing of the nail, had reported a proximal nail plate that resolved after chemotherapy. The patient did not survive long enough to note complete improvement of the nail.3 In our study, patient 1 was treated with ciclopirox gel and terbinafine, which did not result in nail improvement. Nail treatments in SS patients have yet to show much improvement and thus need more research and focus in the literature.
Conclusion
Sézary syndrome is a rare CTCL that can present with clinical features that may be mistaken for other diseases. Nail abnormalities in SS patients may be related to fungal involvement, medical therapy, or the underlying disease process of SS. We report one of the largest populations of SS patients with specific reported nail abnormalities, thus expanding the possibilities of nail changes that accompany the disease. Continued research and studies involving SS can provide a better understanding of nail involvement and successful treatment of these clinical findings.
Sézary syndrome (SS) is an advanced leukemic form of cutaneous T-cell lymphoma (CTCL) that is characterized by generalized erythroderma and T-cell leukemia. Skin changes can include erythroderma, keratosis pilaris–like lesions, keratoderma, ectropion, alopecia, and nail changes.1 Nail changes in SS patients frequently are overlooked and underreported; they vary greatly from patient to patient, and their incidence has not been widely evaluated in the literature.
In this retrospective study, we reviewed medical records from a previously collected CTCL clinic database at the University of Texas MD Anderson Cancer Center (Houston, Texas) and found nail abnormalities in 36 of 83 (43.4%) patients with a diagnosis of SS. Findings for 2 select cases are described in more detail; they were compared to prior case reports from the literature to establish a comprehensive list of nail irregularities that have been associated with SS.
Methods
We examined records from a previously collected CTCL clinic database at the University of Texas MD Anderson Cancer Center. This database was part of an institutional review board–approved protocol to prospectively collect data from patients with CTCL. Our search yielded 83 patients with SS who were seen between 2007 and 2014.
Results
Of the 83 cases reviewed from the CTCL database, 36 (43.4%) SS patients reported at least 1 nail abnormality on the fingernails or toenails. Patients ranged in age from 59 to 85 years and included 27 (75%) men and 9 (25%) women. Nail irregularities noted on physical examination are summarized in Table 1. More than half of the patients presented with nail thickening (58.3% [21/36]), dystrophy (55.6% [20/36]), or yellowing (55.6% [20/36]) of 1 or more nails. Other findings included 15 (41.7%) patients with subungual hyperkeratosis, 3 (8.3%) with Beau lines, and 1 (2.8%) with multiple oil spots consistent with salmon patches. Five (13.9%) patients had only 1 reported nail irregularity, and 1 (2.8%) patient had 6 irregularities. The average number of nail abnormalities per patient was 2.88 (range, 1–6). We selected 2 patients with extensive nail findings who represent the spectrum of nail findings in patients with SS.
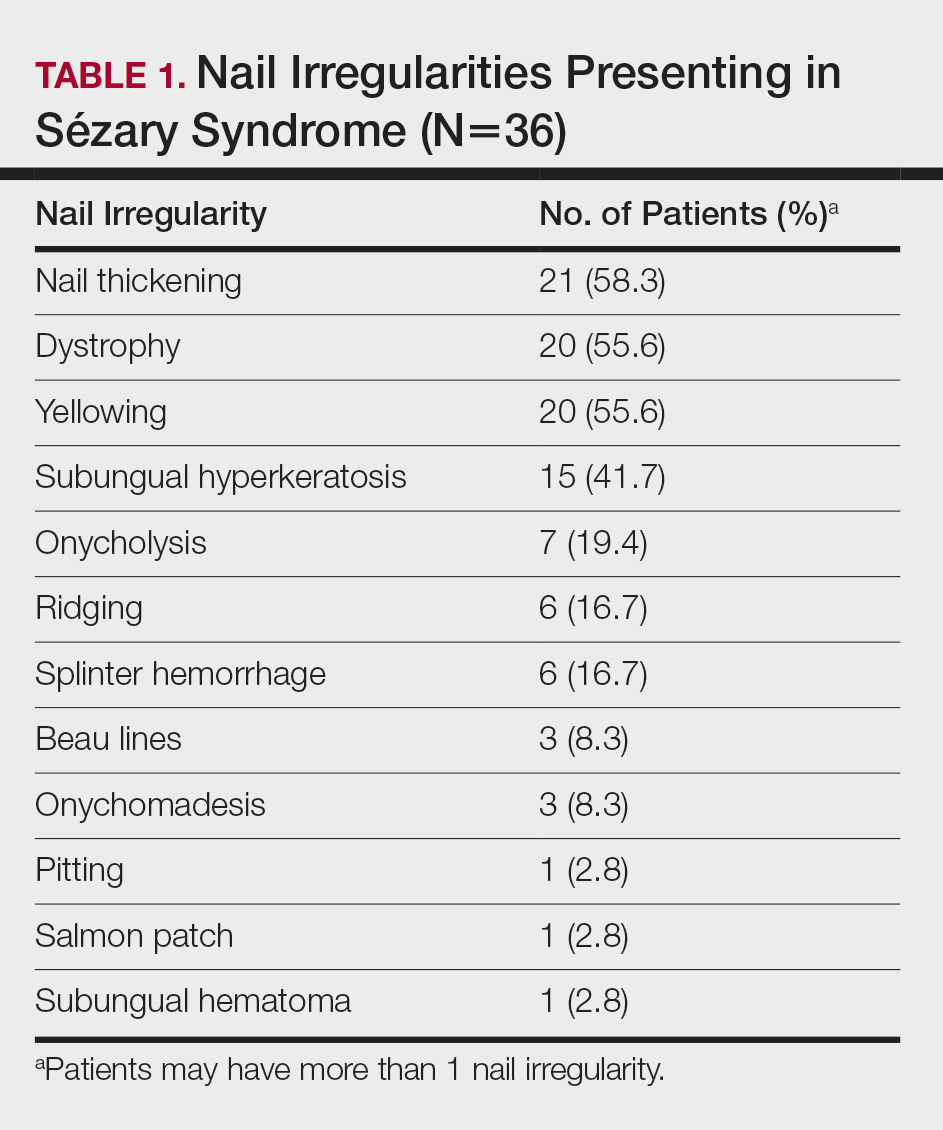
Patient 1
A 71-year-old white man presented with a papular rash of 30 years’ duration. The eruption first occurred on the soles of the feet but progressed to generalized erythroderma. He was found to be colonized with methicillin-resistant Staphylococcus aureus. Over the next 9 months, the patient was diagnosed with SS at an outside institution and was treated with cyclophosphamide, hydroxydaunorubicin, vincristine, prednisone, gemcitabine, etoposide, methylprednisolone, cytarabine, cisplatin, topical steroids, and intravenous methotrexate with no apparent improvement. At presentation to our institution, physical examination revealed pruritus; alopecia; generalized lymphadenopathy; erythroderma; and irregular nail findings, including yellowing, thickened fingernails and toenails with subungual debris, and splinter hemorrhage (Figure 1). A thick plaque with perioral distribution as well as erosions on the face and feet were noted. The total body surface area (BSA) affected was 100% (patches, 91%; plaques, 9%).

At diagnosis at our institution, the patient’s white blood cell (WBC) count was 17,800/µL (reference range, 4000–11,000/µL), with 11% Sézary cells noted. Biopsy of a lymph node from the inguinal area indicated T-cell lymphoma with clonal T-cell receptor (TCR) β gene rearrangement. Biopsy of lesional skin in the right groin area showed an atypical T-cell lymphocytic infiltrate with a CD4:CD8 ratio of 2.9:1 and partial loss of CD7 expression, consistent with mycosis fungoides (MF)/SS stage IVA. At presentation to our institution, the WBC count was 12,700/µL with a neutrophil count of 47% (reference range, 42%–66%), lymphocyte count of 36% (reference range, 24%–44%), monocyte count of 4% (reference range, 2%–7%), platelet count of 427,000/µL (reference range, 150,000–350,000/µL), hemoglobin of 9.9 g/dL (reference range, 14.0–17.5 g/dL), and lactate dehydrogenase of 733 U/L (reference range, 135–214 U/L). Lymphocytes were positive for CD2, CD3, CD4, CD5, CD25, CD52, TCRα, TCRβ, and TCR VB17; partial for CD26; and negative for CD7, CD8, and CD57. At follow-up 1 month later, the CD4+CD26− T-cell population was 56%, which was consistent with SS T-cell lymphoma.
Skin scrapings from the generalized keratoderma on the patient’s feet were positive for fungal hyphae under potassium hydroxide examination. Nail clippings showed compact keratin with periodic acid–Schiff–positive small yeast forms admixed with bacterial organisms, consistent with onychomycosis. At our institution, the patient received extracorporeal photopheresis, whirlpool therapy (a type of hydrotherapy), steroid wet wraps, and intravenous vancomycin for methicillin-resistant S aureus. He also received bexarotene, levothyroxine sodium, and fenofibrate. After antibiotics and 2 sessions of photopheresis, the total BSA improved from 100% to 33%. The feet and nails were treated with ciclopirox gel and terbinafine, but neither the keratoderma nor the nails improved.
Patient 2
An 84-year-old white man with B-cell chronic lymphocytic leukemia also was diagnosed with SS at an outside institution. One year later, he presented to our institution with mild pruritus and swelling of the lower left leg, which was diagnosed as deep vein thrombosis. There was bilateral scaling of the palms, with fissures present on the left palm. The fingernails showed dystrophy with Beau lines, and the toenails were dystrophic with onycholysis on the bilateral great toes (Figure 2). Patches were noted on most of the body, including the feet, with plaques limited to the hands; the total BSA affected was 80%. Flow cytometry showed an elevated Sézary cell count (CD4+CD26−) of 4700 cells/µL. Complete blood cell count with differential included a hemoglobin level of 11.4 g/dL, hematocrit level of 35.3% (reference range, 37%–47%), a platelet count of 217,000/µL, and a WBC count of 17,7

the bilateral great toes.
Comment
Nail changes are found in many cases of advanced-stage SS but rarely have been reported in the literature. A literature review of PubMed articles indexed for MEDLINE was conducted using the search terms Sézary, nail, onychodystrophy, cutaneous T-cell lymphoma, and CTCL. All results were reviewed for original reported cases of SS with at least 1 reported nail finding. A total of 7 reports2-8 met these requirements with a total of 43 SS patients with reported nail findings, which are summarized in Tables 2 and 3.
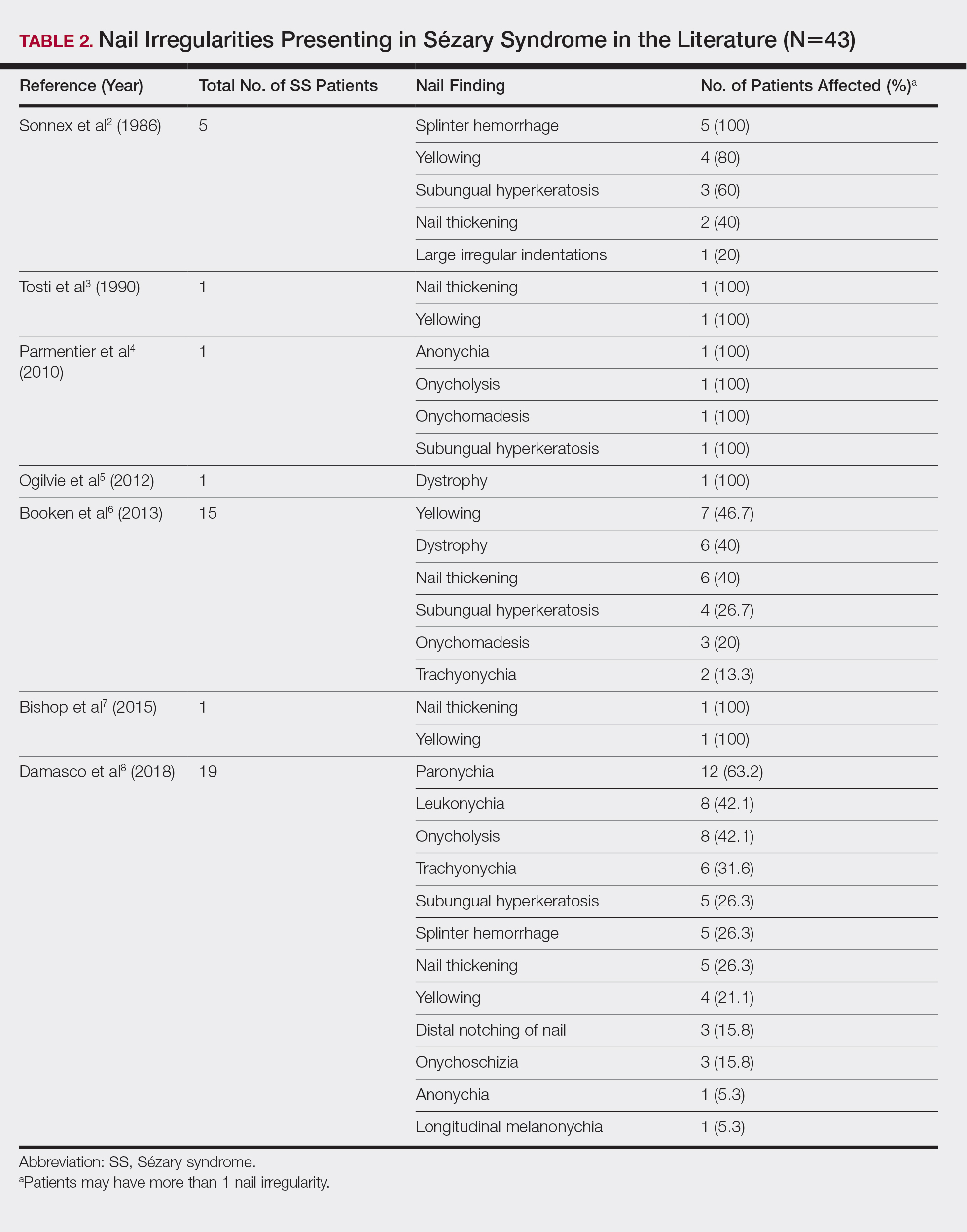

Our findings are generally consistent with those previously described in the literature. Nail thickening, yellowing, subungual hyperkeratosis, dystrophy, and onycholysis are consistently some of the most common nail findings in patients with SS. In 2012, Martin and Duvic9 found that 52.9% (45/85) of SS patients with keratoderma on physical examination were positive for dermatophyte hyphae when skin scrapings were done under potassium hydroxide examination, a considerably greater incidence than in the general population (10%–20%). The nail changes seen in our SS patients were identical to those found in dermatophyte infections, including discoloration, subungual debris, nail thickening, onycholysis, and dystrophy.10 In patient 1, nail clippings were positive for onychomycosis, a common nail condition that is especially prevalent in older or immunocompromised patients.9,10
Interestingly, findings not observed in the literature included salmon patches and Beau lines. Beau lines are horizontal depressions in the nail plate and often are indicative of temporary interruption of nail growth, such as due to an underlying disease process, severe illness, and/or chemotherapy.11,12 In our review, patient 2 had clinical findings of Beau lines. Because the average time for fingernail regrowth is 3 to 6 months,13 it is reasonable to assume that physical findings associated with fludarabine, cyclophosphamide, and rituximab chemotherapy treatment would no longer be demonstrated 11 months after completion of therapy. On the other hand, paronychia was frequently observed by Damasco et al8 (63.2% [12/19] of their cases), yet it was not found in our database or the other literature reports we reviewed. Perhaps these differences are due to differences in patient populations and/or available therapies, lack of documentation, or small sample size and limited reports in the literature.
A common question is: Are the nail irregularities caused by the physical symptoms of advanced CTCL or by the underlying disease process in response to the atypical T cells? Erythroderma has been speculated to cause many of the clinical findings of nail abnormalities found in CTCL patients.2,3 However, Fleming et al14 described an MF patient who experienced onychomadesis without erythroderma, which suggests that a different mechanism may cause these nail changes. The wide range of nail abnormalities in CTCL can cause problems with diagnosing the specific cause underlying the nail alteration.
To further complicate the issue, numerous therapies for CTCL also may cause nail changes, such as the previously described Beau lines. In 2010, Parmentier et al4 reported a patient with nail alterations that had been present for more than 1 year, with 9 of 10 fingernails demonstrating anonychia, onychomadesis, subungual distal hyperkeratosis, and onycholysis. In this case report, the authors were able to exclude phototherapy as the cause of onycholysis (visible separation of the nail plate from the nail bed) and other clinical nail findings in the SS patient based on the onset of nail changes prior to beginning psoralen plus UVA therapy and complete sparing of 1 finger.4 The findings in our patient 1, who had no history of psoralen plus UVA therapy at the time the irregular nail findings presented, supports this observation. Total skin electron beam therapy for MF also has been reported to cause temporary nail stasis and thus must be taken into account when considering nail changes in patients with MF/SS.15
A nail matrix biopsy may provide clues to the definitive cause of the clinically observed nail changes; however, this procedure typically is not performed due to patient concerns of postoperative complications including pain and nail dystrophy.16 Histopathology features were similar in reported nail biopsies of 2 SS patients.3,4 Tosti et al3 reported that longitudinal biopsy showed a dense lymphocytic infiltrate of atypical lymphocytes with involuted nuclei and notable epidermotropism. Parmentier et al4 reported a longitudinal nail biopsy in an SS patient that presented with atypical lymphocytes, epidermotropism, and Pautrier microabscess formation. Immunostaining showed CD3 positivity within the distal nail matrix, nail bed, and hyponychium. One-third of the cells stained positive for CD4, while the majority stained positive for CD8. Most notably, the skin, nails, and blood showed identical clonal rearrangement of TCRγ.4 Nail matrix biopsies in MF patients rarely have been reported in the literature, but those that are available show similar features to those seen in SS patients. Harland et al17 summarized the findings of 4 case reports of CTCL patients that included nail biopsies by stating, “[a]ll histopathologic findings from nail biopsies showed a dense subepithelial infiltrate of lymphocytes with marked epitheliotropism.” These histopathologic abnormalities are akin to skin biopsies in MF patients, thus providing an essential link to the disease state of MF and the nail abnormalities found within SS patients.
Treatment of the nail problems found within SS is challenging due to limited research. Parmentier et al4 noted an SS patient who was treated with topical mechlorethamine applied directly to the nail. In this case, topical mechlorethamine was effective at treating onychomadesis, subungual distal hyperkeratosis, and onycholysis within 6 months.4 Another SS patient, who presented with thickening and yellowing of the nail, had reported a proximal nail plate that resolved after chemotherapy. The patient did not survive long enough to note complete improvement of the nail.3 In our study, patient 1 was treated with ciclopirox gel and terbinafine, which did not result in nail improvement. Nail treatments in SS patients have yet to show much improvement and thus need more research and focus in the literature.
Conclusion
Sézary syndrome is a rare CTCL that can present with clinical features that may be mistaken for other diseases. Nail abnormalities in SS patients may be related to fungal involvement, medical therapy, or the underlying disease process of SS. We report one of the largest populations of SS patients with specific reported nail abnormalities, thus expanding the possibilities of nail changes that accompany the disease. Continued research and studies involving SS can provide a better understanding of nail involvement and successful treatment of these clinical findings.
- Willemz e R, Jaffe ES, Burg G, et al. WHO-EORTC classification for cutaneous lymphomas. Blood. 2005;105:3768-3785.
- Sonnex TS, Dawber RP, Zachary CB, et al. The nails in adult type 1 pityriasis rubra pilaris. a comparison with Sézary syndrome and psoriasis. J Am Acad Dermatol. 1986;15(5 pt 1):956-960.
- Tosti A, Fanti PA, Varotti C. Massive lymphomatous nail involvement in Sézary syndrome. Dermatologica. 1990;181:162-164.
- Parmentier L, Durr C, Vassella E, et al. Specific nail alterations in cutaneous T-cell lymphoma: successful treatment with topical mechlorethamine. Arch Dermatol. 2010;146:1287-1291.
- Ogilvie C, Jackson R, Leach M, et al. Sézary syndrome: diagnosis and management. J R Coll Physicians Edinb. 2012;42:317-321.
- Booken N, Nicolay JP, Weiss C, et al. Cutaneous tumor cell load correlates with survival in patients with Sézary syndrome. J Dtsch Dermatol Ges. 2013;11:67-79.
- Bishop BE, Wulkan A, Kerdel F, et al. Nail alterations in cutaneous T-cell lymphoma: a case series and review of nail manifestations. Skin Appendage Disord. 2015;1:82-86.
- Damasco FM, Geskin L, Akilov OE. Onychodystrophy in Sézary syndrome. J Am Acad Dermatol. 2018;79:972-973.
- Martin SJ, Duvic M. Prevalence and treatment of palmoplantar keratoderma and tinea pedis in patients with Sézary syndrome. Int J Dermatol. 2012;51:1195-1198.
- Mayo TT, Cantrell W. Putting onychomycosis under the microscope. Nurse Pract. 2014;39:8-11.
- Singh M, Kaur S. Chemotherapy-induced multiple Beau’s lines. Int J Dermatol. 1986;25:590-591.
- Tully AS, Trayes KP, Studdiford JS. Evaluation of nail abnormalities. Am Family Physician. 2012;85:779-787.
- Shirwaikar AA, Thomas T, Shirwaikar A, et al. Treatment of onychomycosis: an update. Indian J Pharm Sci. 2008;70:710-714.
- Fleming CJ, Hunt MJ, Barnetson RS. Mycosis fungoides with onychomadesis. Br J Dermatol. 1996;135:1012-1013.
- Jones GW, Kacinski BM, Wilson LD, et al. Total skin electron radiation in the management of mycosis fungoides: consensus of the European Organization for Research and Treatment of Cancer (EORTC) Cutaneous Lymphoma Project Group. J Am Acad Dermatol. 2002;47:364-370.
- Haneke E. Advanced nail surgery. J Cutan Aesthet Surg. 2011;4:167-175.
- Harland E, Dalle S, Balme B, et al. Ungueotropic T-cell lymphoma. Arch Dermatol. 2006;142:1071-1073.
- Willemz e R, Jaffe ES, Burg G, et al. WHO-EORTC classification for cutaneous lymphomas. Blood. 2005;105:3768-3785.
- Sonnex TS, Dawber RP, Zachary CB, et al. The nails in adult type 1 pityriasis rubra pilaris. a comparison with Sézary syndrome and psoriasis. J Am Acad Dermatol. 1986;15(5 pt 1):956-960.
- Tosti A, Fanti PA, Varotti C. Massive lymphomatous nail involvement in Sézary syndrome. Dermatologica. 1990;181:162-164.
- Parmentier L, Durr C, Vassella E, et al. Specific nail alterations in cutaneous T-cell lymphoma: successful treatment with topical mechlorethamine. Arch Dermatol. 2010;146:1287-1291.
- Ogilvie C, Jackson R, Leach M, et al. Sézary syndrome: diagnosis and management. J R Coll Physicians Edinb. 2012;42:317-321.
- Booken N, Nicolay JP, Weiss C, et al. Cutaneous tumor cell load correlates with survival in patients with Sézary syndrome. J Dtsch Dermatol Ges. 2013;11:67-79.
- Bishop BE, Wulkan A, Kerdel F, et al. Nail alterations in cutaneous T-cell lymphoma: a case series and review of nail manifestations. Skin Appendage Disord. 2015;1:82-86.
- Damasco FM, Geskin L, Akilov OE. Onychodystrophy in Sézary syndrome. J Am Acad Dermatol. 2018;79:972-973.
- Martin SJ, Duvic M. Prevalence and treatment of palmoplantar keratoderma and tinea pedis in patients with Sézary syndrome. Int J Dermatol. 2012;51:1195-1198.
- Mayo TT, Cantrell W. Putting onychomycosis under the microscope. Nurse Pract. 2014;39:8-11.
- Singh M, Kaur S. Chemotherapy-induced multiple Beau’s lines. Int J Dermatol. 1986;25:590-591.
- Tully AS, Trayes KP, Studdiford JS. Evaluation of nail abnormalities. Am Family Physician. 2012;85:779-787.
- Shirwaikar AA, Thomas T, Shirwaikar A, et al. Treatment of onychomycosis: an update. Indian J Pharm Sci. 2008;70:710-714.
- Fleming CJ, Hunt MJ, Barnetson RS. Mycosis fungoides with onychomadesis. Br J Dermatol. 1996;135:1012-1013.
- Jones GW, Kacinski BM, Wilson LD, et al. Total skin electron radiation in the management of mycosis fungoides: consensus of the European Organization for Research and Treatment of Cancer (EORTC) Cutaneous Lymphoma Project Group. J Am Acad Dermatol. 2002;47:364-370.
- Haneke E. Advanced nail surgery. J Cutan Aesthet Surg. 2011;4:167-175.
- Harland E, Dalle S, Balme B, et al. Ungueotropic T-cell lymphoma. Arch Dermatol. 2006;142:1071-1073.
Practice Points
- Nail changes are frequently observed in patients with Sézary syndrome.
- Nail changes in patients with cutaneous T-cell lymphoma may result from the disease process or physical symptoms of advanced disease, or they may present secondary to treatment.











