User login
More cost compression coming
In mid-March, the President released his FY2020 budget proposal. Traditionally, the White House budget has little relation to the ultimate budget since Congress actually creates the final iteration (assuming the government can pass a budget at all). This budget cuts funding for the NIH, Medicare, Medicaid, and most agencies not related to defense, border security, or the TSA. No matter what the final version looks like, the federal deficit will balloon as a result of last year’s tax cuts that were combined with relentless increases in entitlement program spending. The message for health care leaders is clear: Since we are responsible for an enormous percentage of committed federal and state spending, we will be in the cross-hairs of cost compression.
As we enter the 2020 election cycle in earnest, politicians will argue about “Medicare for All” versus government overreach. We will wrestle with competing philosophies of States’ Rights versus Federalism. As physicians, we must advocate for a system of funds flow and regulatory power that we believe best serves our patients within a financially sustainable framework.
On to this month’s issue – there are two stories on early-age colon cancer. A page one story adds to our understanding of the molecular pathways involved (microsatellite instability) and tumor location. Another story points out that younger CRC patients often go undiagnosed or are misdiagnosed. The AGA has published important clinical guidance about pregnancy and IBD and switching from biologic medications to biosimilars. Finally, an enormously important study, published in The Lancet, confirmed that hepatitis C treatment with direct-acting antiviral medications reduces mortality and cancer risk – something we suspected but needed confirmed.
I hope to see everyone at DDW next month.
John I. Allen, MD, MBA, AGAF
Editor in Chief
In mid-March, the President released his FY2020 budget proposal. Traditionally, the White House budget has little relation to the ultimate budget since Congress actually creates the final iteration (assuming the government can pass a budget at all). This budget cuts funding for the NIH, Medicare, Medicaid, and most agencies not related to defense, border security, or the TSA. No matter what the final version looks like, the federal deficit will balloon as a result of last year’s tax cuts that were combined with relentless increases in entitlement program spending. The message for health care leaders is clear: Since we are responsible for an enormous percentage of committed federal and state spending, we will be in the cross-hairs of cost compression.
As we enter the 2020 election cycle in earnest, politicians will argue about “Medicare for All” versus government overreach. We will wrestle with competing philosophies of States’ Rights versus Federalism. As physicians, we must advocate for a system of funds flow and regulatory power that we believe best serves our patients within a financially sustainable framework.
On to this month’s issue – there are two stories on early-age colon cancer. A page one story adds to our understanding of the molecular pathways involved (microsatellite instability) and tumor location. Another story points out that younger CRC patients often go undiagnosed or are misdiagnosed. The AGA has published important clinical guidance about pregnancy and IBD and switching from biologic medications to biosimilars. Finally, an enormously important study, published in The Lancet, confirmed that hepatitis C treatment with direct-acting antiviral medications reduces mortality and cancer risk – something we suspected but needed confirmed.
I hope to see everyone at DDW next month.
John I. Allen, MD, MBA, AGAF
Editor in Chief
In mid-March, the President released his FY2020 budget proposal. Traditionally, the White House budget has little relation to the ultimate budget since Congress actually creates the final iteration (assuming the government can pass a budget at all). This budget cuts funding for the NIH, Medicare, Medicaid, and most agencies not related to defense, border security, or the TSA. No matter what the final version looks like, the federal deficit will balloon as a result of last year’s tax cuts that were combined with relentless increases in entitlement program spending. The message for health care leaders is clear: Since we are responsible for an enormous percentage of committed federal and state spending, we will be in the cross-hairs of cost compression.
As we enter the 2020 election cycle in earnest, politicians will argue about “Medicare for All” versus government overreach. We will wrestle with competing philosophies of States’ Rights versus Federalism. As physicians, we must advocate for a system of funds flow and regulatory power that we believe best serves our patients within a financially sustainable framework.
On to this month’s issue – there are two stories on early-age colon cancer. A page one story adds to our understanding of the molecular pathways involved (microsatellite instability) and tumor location. Another story points out that younger CRC patients often go undiagnosed or are misdiagnosed. The AGA has published important clinical guidance about pregnancy and IBD and switching from biologic medications to biosimilars. Finally, an enormously important study, published in The Lancet, confirmed that hepatitis C treatment with direct-acting antiviral medications reduces mortality and cancer risk – something we suspected but needed confirmed.
I hope to see everyone at DDW next month.
John I. Allen, MD, MBA, AGAF
Editor in Chief
Postpartum psychosis: Protecting mother and infant
A new mother drowned her 6-month-old daughter in the bathtub. The married woman, who had a history of schizoaffective disorder, had been high functioning and worked in a managerial role prior to giving birth. However, within a day of delivery, her mental state deteriorated. She quickly became convinced that her daughter had a genetic disorder such as achondroplasia. Physical examinations, genetic testing, and x-rays all failed to alleviate her concerns. Examination of her computer revealed thousands of searches for various medical conditions and surgical treatments. After the baby’s death, the mother was admitted to a psychiatric hospital. She eventually pled guilty to manslaughter.1
Mothers with postpartum psychosis (PPP) typically present fulminantly within days to weeks of giving birth. Symptoms of PPP may include not only psychosis, but also confusion and dysphoric mania. These symptoms often wax and wane, which can make it challenging to establish the diagnosis. In addition, many mothers hide their symptoms due to poor insight, delusions, or fear of loss of custody of their infant. In the vast majority of cases, psychiatric hospitalization is required to protect both mother and baby; untreated, there is an elevated risk of both maternal suicide and infanticide. This article discusses the presentation of PPP, its differential diagnosis, risk factors for developing PPP, suicide and infanticide risk assessment, treatment (including during breastfeeding), and prevention.
The bipolar connection
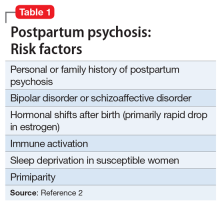
While multiple factors may increase the risk of PPP (Table 12), women with bipolar disorder have a particularly elevated risk. After experiencing incipient postpartum affective psychosis, a woman has a 50% to 80% chance of having another psychiatric episode, usually within the bipolar spectrum.2 Of all women with PPP, 70% to 90% have bipolar illness or schizoaffective disorder, while approximately 12% have schizophrenia.3,4Women with bipolar disorder are more likely to experience a postpartum psychiatric admission than mothers with any other psychiatric diagnosis5 and have an increased risk of PPP by a factor of 100 over the general population.2
For women with bipolar disorder, PPP should be understood as a recurrence of the chronic disease. Recent evidence does suggest, however, that a significant minority of women progress to experience mood and psychotic symptoms only in the postpartum period.6,7 It is hypothesized that this subgroup of women has a biologic vulnerability to affective psychosis that is limited to the postpartum period. Clinically, understanding a woman’s disease course is important because it may guide decision-making about prophylactic medications during or after pregnancy.
A rapid, delirium-like presentation
Postpartum psychosis is a rare disorder, with a prevalence of 1 to 2 cases per 1,000 childbirths.3 While symptoms may begin days to weeks postpartum, the typical time of onset is between 3 to 10 days after birth, occurring after a woman has been discharged from the hospital and during a time of change and uncertainty. This can make the presentation of PPP a confusing and distressing experience for both the new mother and the family, resulting in delays in seeking care.
Subtle prodromal symptoms may include insomnia, mood fluctuation, and irritability. As symptoms progress, PPP is notable for a rapid onset and a delirium-like appearance that may include waxing and waning cognitive symptoms such as disorientation and confusion.8 Grossly disorganized behaviors and rapid mood fluctuations are typical. Distinct from mood episodes outside the peripartum period, women with PPP often experience mood-incongruent delusions and obsessive thoughts, often focused on their child.9 Women with PPP appear less likely to experience thought insertion or withdrawal or auditory hallucinations that give a running commentary.2
Differential diagnosis includes depression, OCD
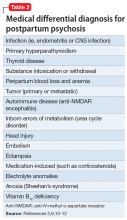
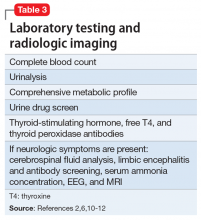
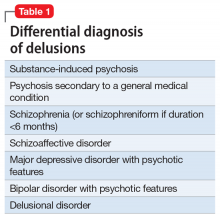
When evaluating a woman with possible postpartum psychotic symptoms or delirium, it is important to include a thorough history, physical examination, and relevant laboratory and/or imaging investigations to assess for organic causes or contributors (Table 22,6,10-12 and Table 32,6,10-12). A detailed psychiatric history should establish whether the patient is presenting with new-onset psychosis or has had previous mood or psychotic episodes that may have gone undetected. Important perinatal psychiatric differential diagnoses should include “baby blues,” postpartum depression (PPD), and obsessive-compulsive disorder (OCD).
Continue to: PPP vs "baby blues."
PPP vs “baby blues.” “Baby blues” is not an official DSM-5 diagnosis but rather a normative postpartum experience that affects 50% to 80% of postpartum women. A woman with the “baby blues” may feel weepy or have mild mood lability, irritability, or anxiety; however, these symptoms do not significantly impair function. Peak symptoms typically occur between 2 to 5 days postpartum and generally resolve within 2 weeks. Women who have the “baby blues” are at an increased risk for PPD and should be monitored over time.13,14
PPP vs PPD. Postpartum depression affects approximately 10% to 15% of new mothers.15 Women with PPD may experience feelings of persistent and severe sadness, feelings of detachment, insomnia, and fatigue. Symptoms of PPD can interfere with a mother’s interest in caring for her baby and present a barrier to maternal bonding.16,17
As the awareness of PPD has increased in recent years, screening for depressive symptoms during and after pregnancy has increasingly become the standard of care.18 When evaluating a postpartum woman for PPD, it is important to consider PPP in the differential. Women with severe or persistent depressive symptoms may also develop psychotic symptoms. Furthermore, suicidal thoughts or thoughts of harming the infant may be present in either PPD or PPP. One study found that 41% of mothers with depression endorsed thoughts of harming their infants.19
PPP vs postpartum OCD. Postpartum obsessive-compulsive symptoms commonly occur comorbidly with PPD,9 and OCD often presents for the first time in the postpartum period.20 Obsessive-compulsive disorder affects between 2% to 9% of new mothers.21,22 It is critical to properly differentiate PPP from postpartum OCD. Clinical questions should be posed with a non-judgmental stance. Just as delusions in PPP are often focused on the infant, for women with OCD, obsessive thoughts may center on worries about the infant’s safety. Distressing obsessions about violence are common in OCD.23 Mothers with OCD may experience intrusive thinking about accidentally or purposefully harming their infant. For example, they may intrusively worry that they will accidentally put the baby in the microwave or oven, leave the baby in a hot car, or throw the baby down the stairs. However, a postpartum woman with OCD may be reluctant to share her ego-dystonic thoughts of infant harm. Mothers with OCD are not out of touch with reality; instead, their intrusive thoughts are ego-dystonic and distressing. These are thoughts and fears that they focus on and try to avoid, rather than plan. The psychiatrist must carefully differentiate between ego-syntonic and ego-dystonic thoughts. These patients often avoid seeking treatment because of their shame and guilt.23 Clinicians often under-recognize OCD and risk inappropriate hospitalization, treatment, and inappropriate referral to Child Protective Services (CPS).23
Perinatal psychiatric risk assessment
When a mother develops PPP, consider the risks of suicide, child harm, and infanticide. Although suicide risk is generally lower in the postpartum period, suicide is the cause of 20% of postpartum deaths.24,25 When PPP is untreated, suicide risk is elevated. A careful suicide risk assessment should be completed.
Continue to: Particularly in PPP...
Particularly in PPP, a mother may be at risk of child neglect or abuse due to her confused or delusional thinking and mood state.26 For example, one mother heated empty bottles and gave them to her baby, and then became frustrated when the baby continued to cry.
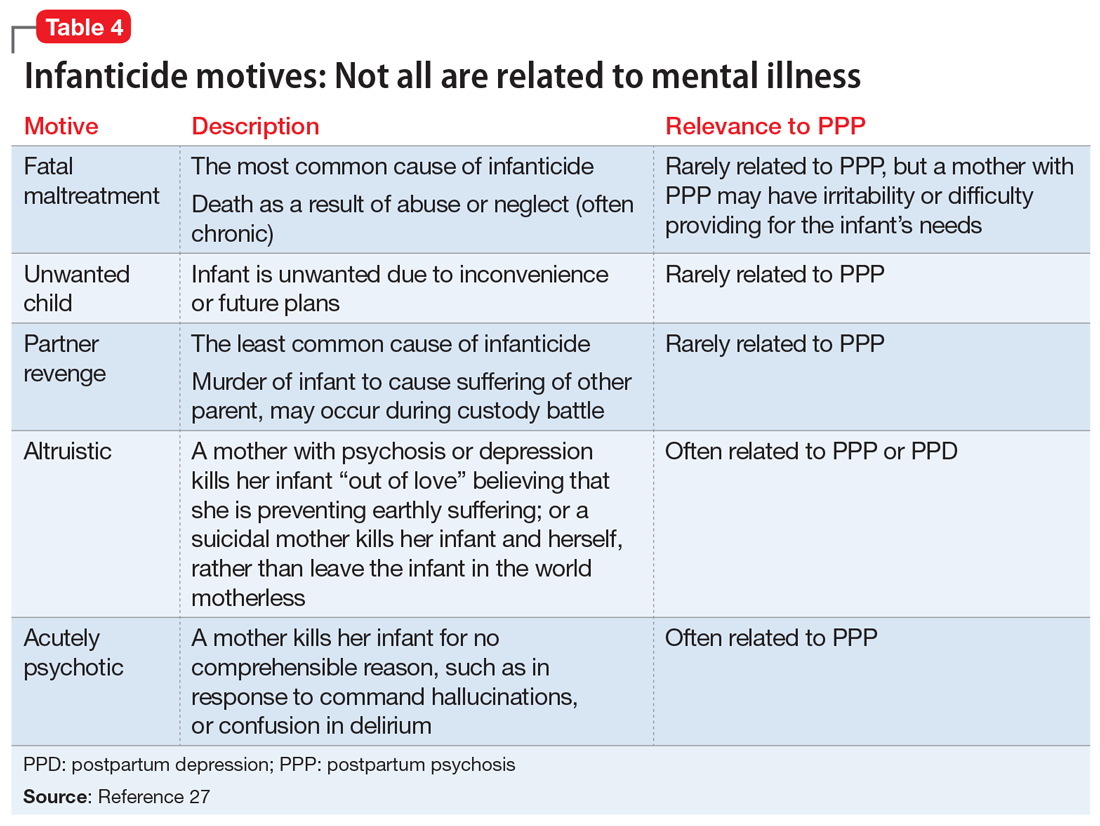
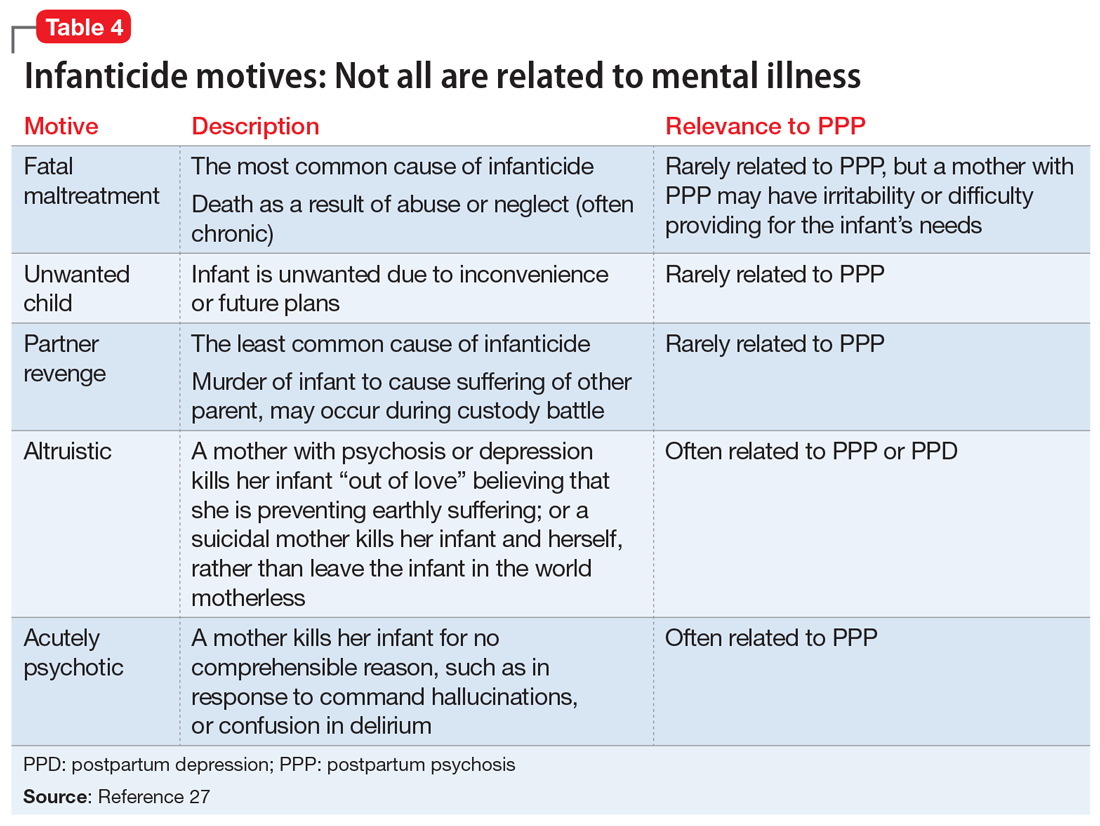
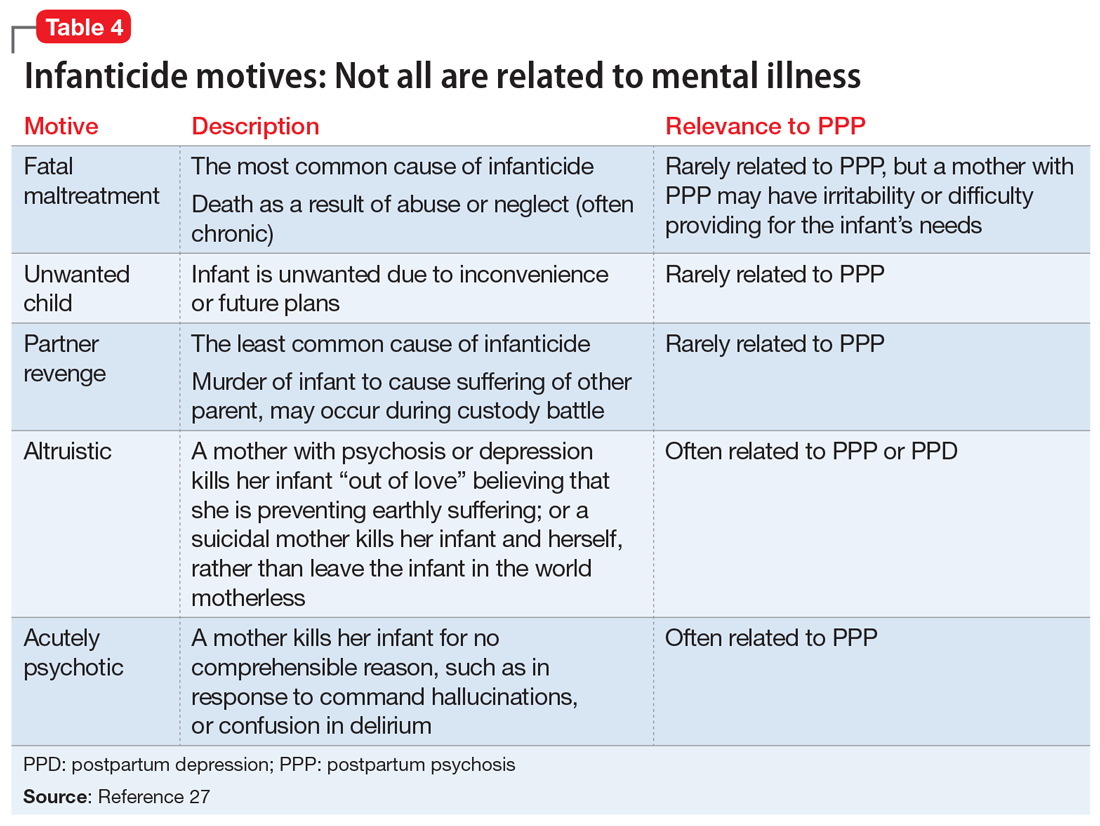
The risk of infanticide is also elevated in untreated PPP, with approximately 4% of these women committing infanticide.9 There are 5 motives for infanticide (Table 427). Altruistic and acutely psychotic motives are more likely to be related to PPP, while fatal maltreatment, unwanted child, and partner revenge motives are less likely to be related to PPP. Among mothers who kill both their child and themselves (filicide-suicide), altruistic motives were the most common.28 Mothers in psychiatric samples who kill their children have often experienced psychosis, suicidality, depression, and significant life stresses.27 Both infanticidal ideas and behaviors have been associated with psychotic thinking about the infant,29 so it is critical to ascertain whether the mother’s delusions or hallucinations involve the infant.30 In contrast, neonaticide (murder in the first day of life) is rarely related to PPP because PPP typically has a later onset.31
Treating acute PPP
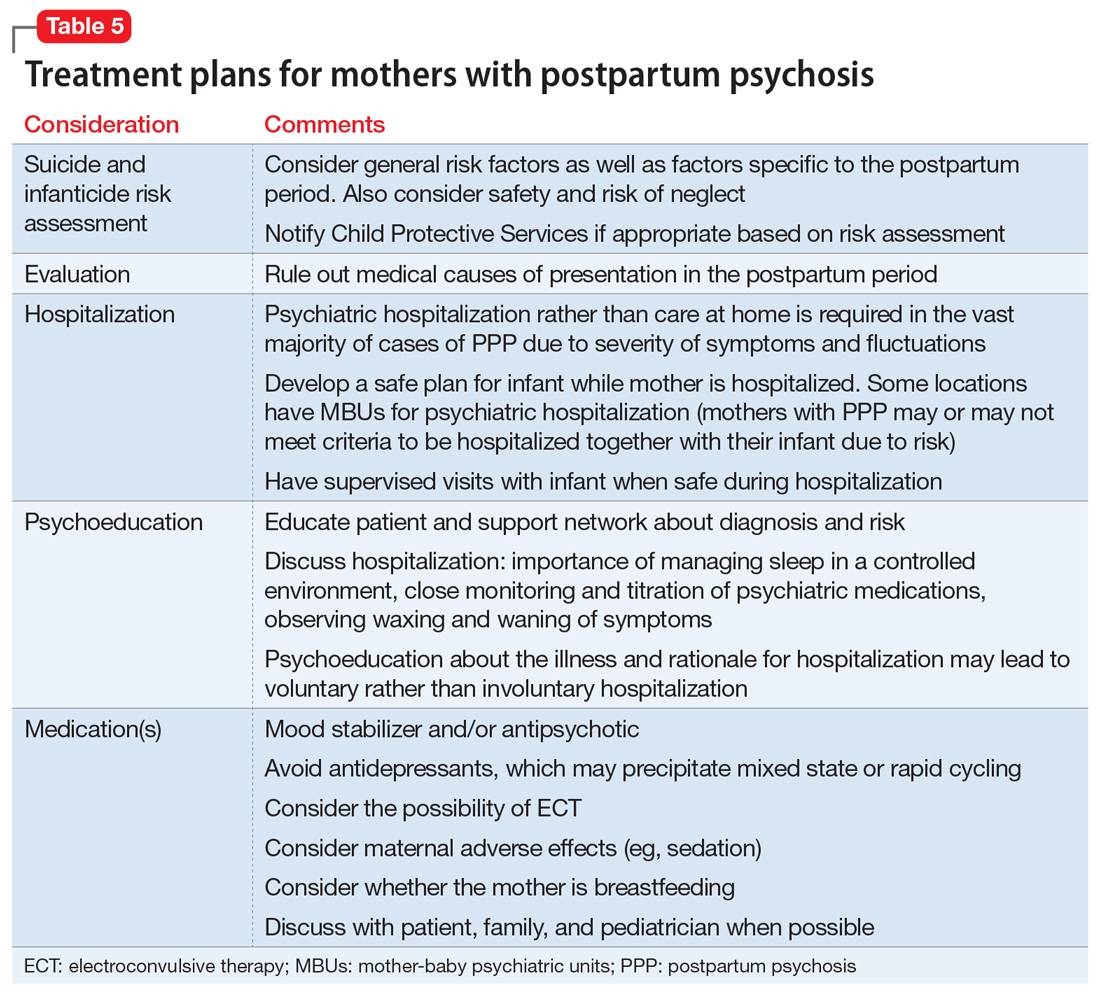
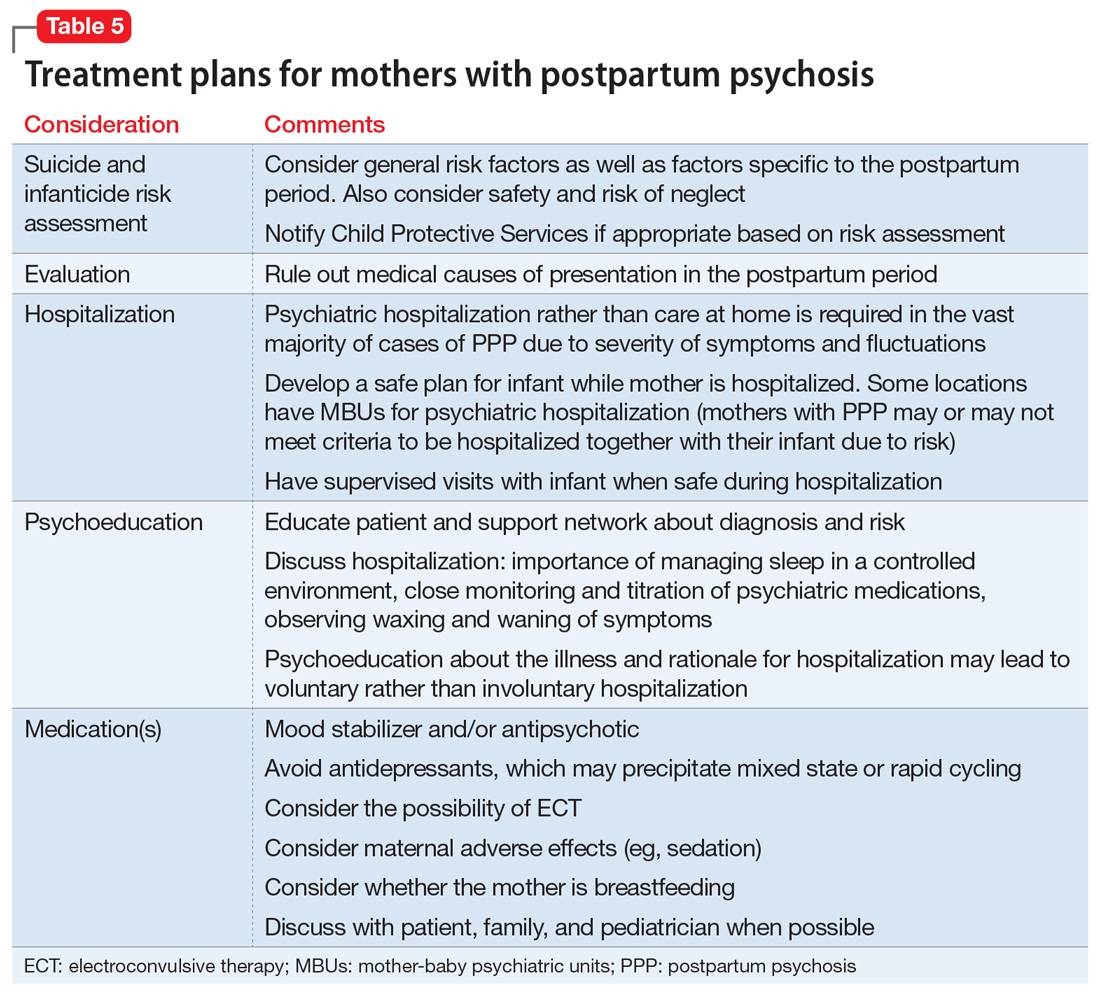
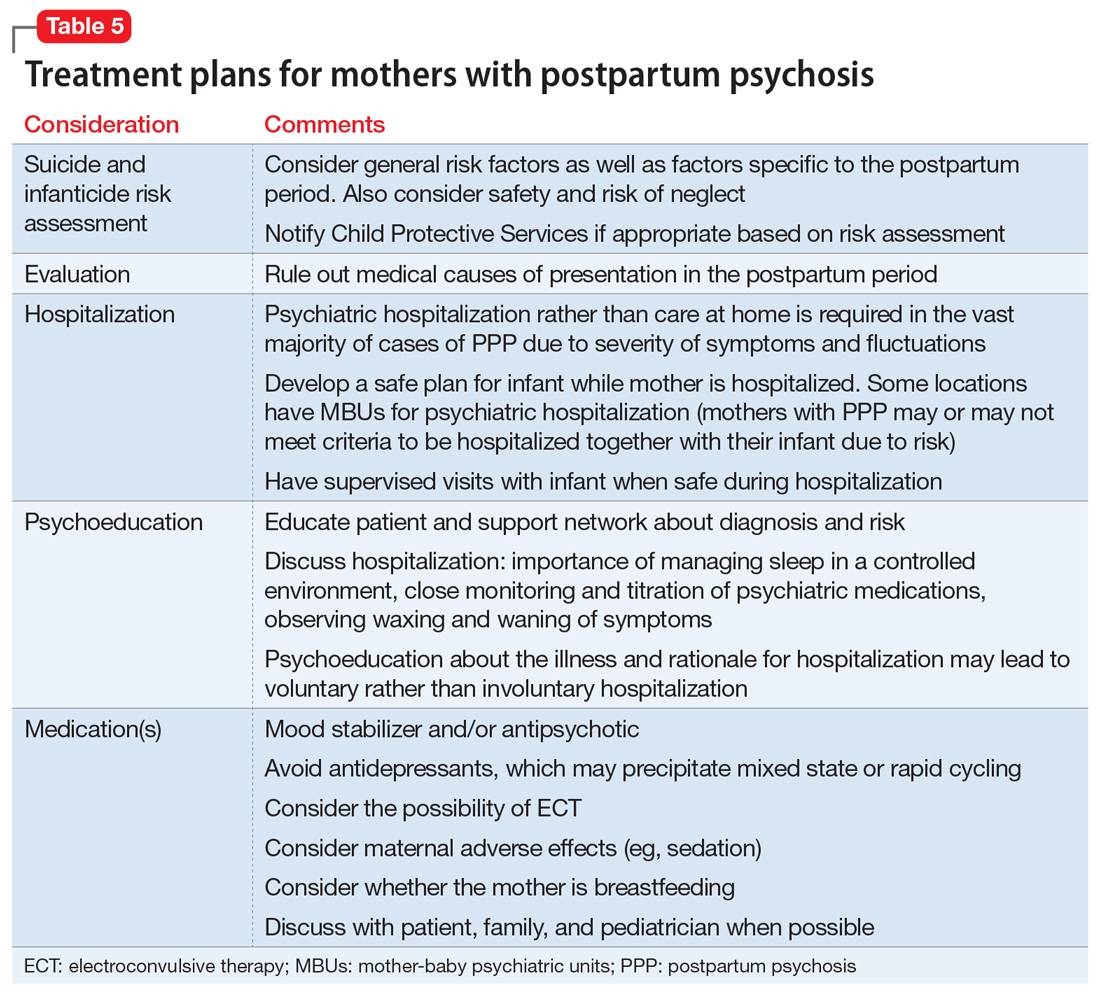
The fulminant nature of PPP can make its treatment difficult. Thinking through the case in an organized fashion is critical (Table 5).
Hospitalization. Postpartum psychosis is a psychiatric emergency with a rapid onset of symptoms. Hospitalization is required in almost all cases for diagnostic evaluation, assessment and management of safety, and initiation of treatment. While maternal-infant bonding in the perinatal period is important, infant safety is critical and usually requires maternal psychiatric hospitalization.
The specialized mother-baby psychiatric unit (MBU) is a model of care first developed in the United Kingdom and is now available in many European countries as well as in New Zealand and Australia. Mother-baby psychiatric units admit the mother and the baby together and provide dyadic treatment to allow for enhanced bonding and parenting support, and often to encourage breastfeeding.30 In the United States, there has been growing interest in specialized inpatient settings that acknowledge the importance of maternal-infant attachment in the treatment of perinatal disorders and provide care with a dyadic focus; however, differences in the health care payer system have been a barrier to full-scale MBUs. The Perinatal Psychiatry Inpatient Unit at University of North Carolina-Chapel Hill is among the first of such a model in the United States.32
Continue to: Although this specialized treatment setting...
Although this specialized treatment setting is unlikely to be available in most American cities, treatment should still consider the maternal role. When possible, the infant should stay with the father or family members during the mother’s hospitalization, and supervised visits should be arranged when appropriate. If the mother is breastfeeding, or plans to breastfeed after the hospitalization, the treatment team may consider providing supervised use of a breast pump and making arrangements for breast milk storage. During the mother’s hospitalization, staff should provide psychoeducation and convey hopefulness and support.
Medication management. Mood stabilizers and second-generation antipsychotics (SGAs) are often used for acute management of PPP. The choice of medication is determined by individual symptoms, severity of presentation, previous response to medication, and maternal adverse effects.30 In a naturalistic study of 64 women admitted for new-onset PPP, sequential administration of benzodiazepines, antipsychotics, and lithium was found to be effective in achieving remission for 99% of patients, with 80% sustaining remission at 9 months postpartum.6 Second-generation antipsychotics such as
Breastfeeding. It is important to discuss breastfeeding with the mother and her partner or family. The patient’s preference, the maternal and infant benefits of breastfeeding, the potential for sleep disruption, and the safety profile of needed medications should all be considered. Because sleep loss is a modifiable risk factor in PPP, the benefits of breastfeeding may be outweighed by the risks for some patients.9 For others, breastfeeding during the day and bottle-feeding at night may be preferred.
What to consider during discharge planning
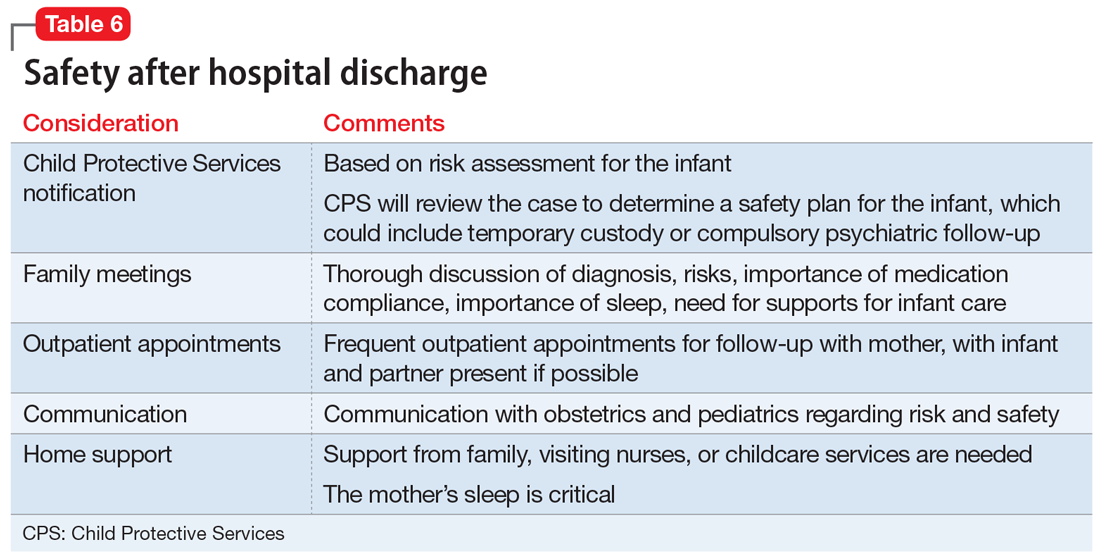
Discharge arrangements require careful consideration (Table 6). Meet with the family prior to discharge to provide psychoeducation and to underscore the importance of family involvement with both mother and infant. It is important to ensure adequate support at home, including at night, since sleep is critical to improved stability. Encourage the patient and her family to monitor for early warning signs of relapse, which might include refractory insomnia, mood instability, poor judgment, or hypomanic symptoms.35 She should be followed closely as an outpatient. Having her partner (or another close family member) and infant present during appointments can help in obtaining collateral information and assessing mother-infant bonding. The clinician should also consider whether it is necessary to contact CPS. Many mothers with mental illness appropriately parent their child, but CPS should be alerted when there is a reasonable concern about safe parenting—abuse, neglect, or significant risk.36
Take steps for prevention
An important part of managing PPP is prevention. This involves providing preconception counseling to the woman and her partner.30 Preconception advice should be individualized and include discussion of:
- risks of relapse in pregnancy and the postpartum period
- optimal physical and mental health
- potential risks and benefits of medication options in pregnancy
- potential effects of untreated illness for the fetus, infant, and family
- a strategy outlining whether medication is continued in pregnancy or started in the postpartum period.
Continue to: For women at risk of PPP...
For women at risk of PPP, the risks of medications need to be balanced with the risks of untreated illness. To reduce the risk of PPP relapse, guidelines recommend a robust antenatal care plan that should include37,38:
- close monitoring of a woman’s mental state for early warning signs of PPP, with active participation from the woman’s partner and family
- ongoing discussion of the risks and benefits of pharmacotherapy (and, for women who prefer to not take medication in the first trimester, a plan for when medications will be restarted)
- collaboration with other professionals involved in care during pregnancy and postpartum (eg, obstetricians, midwives, family practitioners, pediatricians)
- planning to minimize risk factors associated with relapse (eg, sleep deprivation, lack of social supports, domestic violence, and substance abuse).
Evidence clearly suggests that women with bipolar disorder are at increased risk for illness recurrence without continued maintenance medication.39 A subgroup of women with PPP go on to have psychosis limited to the postpartum period, and reinstating prophylactic medication in late pregnancy (preferably) or immediately after birth should be discussed.2 The choice of prophylactic medication should be determined by the woman’s previous response.
Regarding prophylaxis, the most evidence exists for lithium.6 Lithium use during the first trimester carries a risk of Ebstein’s anomaly. However, a recent systematic review and meta-analysis have concluded that the teratogenic risks of lithium have been overestimated.40,41
Lamotrigine is an alternative mood stabilizer with a favorable safety profile in pregnancy. In a small naturalistic study in which lamotrigine was continued in pregnancy in women with bipolar disorder, the medication was effective in preventing relapse in pregnancy and postpartum.42 A small population-based cohort study found lamotrigine was as effective as lithium in preventing severe postpartum relapse in women with bipolar disorder,43 although this study was limited by its observational design. Recently published studies have found no significant association between
Box
It is essential to consider the patient’s individual symptoms and treatment history when making pharmacologic recommendations during pregnancy. Discussion with the patient about the risks and benefits of lithium is recommended. For women who continue to use lithium during pregnancy, ongoing pharmacokinetic changes warrant more frequent monitoring (some experts advise monthly monitoring throughout pregnancy, moving to more frequent monitoring at 36 weeks).47 During labor, the team might consider temporary cessation of lithium and particular attention to hydration status.30 In the postpartum period, there is a quick return to baseline glomerular filtration rate and a rapid decrease in vascular volume, so it is advisable to restart the patient at her pre-pregnancy lithium dosage. It is recommended to check lithium levels within 24 hours of delivery.47 While lithium is not an absolute contraindication to breastfeeding, there is particular concern in situations of prematurity or neonatal dehydration. Collaboration with and close monitoring by the pediatrician is essential to determine an infant monitoring plan.48
If lamotrigine is used during pregnancy, be aware that pregnancy-related pharmacokinetic changes result in increased lamotrigine clearance, which will vary in magnitude among individuals. Faster clearance may necessitate dose increases during pregnancy and a taper back to pre-pregnancy dose in the postpartum period. Dosing should always take clinical symptoms into account.
Pharmacotherapy can reduce relapse risk
To prevent relapse in the postpartum period, consider initiating treatment with mood stabilizers and/or SGAs, particularly for women with bipolar disorder who do not take medication during pregnancy. A recent meta-analysis found a high postpartum relapse rate (66%) in women with bipolar disorder who did not take prophylactic medication, compared with a relapse rate of 23% for women who did take such medication. In women with psychosis limited to the postpartum period, prophylaxis with lithium or antipsychotics in the immediate postpartum can prevent relapse.39 The SGAs olanzapine and quetiapine are often used to manage acute symptoms because they are considered acceptable during breastfeeding.33 The use of lithium when breastfeeding is complex to manage48 and may require advice to not breastfeed, which can be an important consideration for patients and their families.
Bottom Line
Postpartum psychosis (PPP) typically presents with a rapid onset of hallucinations, delusions, confusion, and mood swings within days to weeks of giving birth. Mothers with PPP almost always require hospitalization for the safety of their infants and themselves. Mood stabilizers and second-generation antipsychotics are used for acute management.
Related Resources
- Clark CT, Wisner KL. Treatment of peripartum bipolar disorder. Obstet Gynecol Clin N Am. 2018;45:403-417.
- Massachusetts General Hospital Center for Women’s Mental Health. https://womensmentalhealth.org/. 2018.
- Postpartum Support International. Postpartum psychosis. http://www.postpartum.net/learn-more/postpartumpsychosis/. 2019.
Drug Brand Names
Bromocriptine • Cycloset, Parlodel
Cabergoline • Dostinex
Lamotrigine • Lamictal
Lithium • Eskalith, Lithobid
Olanzapine • Zyprexa
Quetiapine • Seroquel
1. Hall L. Mother who killed baby believing she was a dwarf should not be jailed, court told. The Sydney Morning Herald. https://www.smh.com.au/national/nsw/mother-who-killed-baby-believing-she-was-a-dwarf-should-not-be-jailed-court-told-20170428-gvud4d.html. Published April 28, 2017. Accessed March 12, 2019.
2. Bergink V, Rasgon N, Wisner KL. Postpartum psychosis: madness, mania, and melancholia in motherhood. Am J Psychiatry. 2016;173(12):1179-1188.
3. Sit D, Rothschild AJ, Wisner KL. A review of postpartum psychosis. J Womens Health (Larchmt). 2006;15(4):352-368.
4. Kendell RE, Chalmers JC, Platz C. Epidemiology of puerperal psychoses. Br J Psychiatry. 1987;150(5):662-673.
5. Munk-Olsen T, Laursen TM, Mendelson T, et al. Risks and predictors of readmission for a mental disorder during the postpartum period. Arch Gen Psychiatry. 2009;66(2):189-195.
6. Bergink V, Burgerhout KM, Koorengevel KM, et al. Treatment of psychosis and mania in the postpartum period. Am J Psychiatry. 2015;172(2):115-123.
7. Wesseloo R, Kamperman AM, Munk-Olsen T, et al. Risk of postpartum relapse in bipolar disorder and postpartum psychosis: a systematic review and meta-analysis. Am J Psychiatry. 2015;173(2):117-127.
8. Wisner KL, Peindl K, Hanusa BH. Symptomatology of affective and psychotic illnesses related to childbearing. J Affect Disord. 1994;30(2):77-87.
9. Spinelli MG. Postpartum psychosis: detection of risk and management. Am J Psychiatry. 2009;166(4):405-408.
10. Fassier T, Guffon N, Acquaviva C, et al. Misdiagnosed postpartum psychosis revealing a late-onset urea cycle disorder. Am J Psychiatry. 2011;168(6):576-580.
11. Yu AYX, Moore FG. Paraneoplastic encephalitis presenting as postpartum psychosis. Psychosomatics. 2011;52(6):568-570.
12. Patil NJ, Yadav SS, Gokhale YA, et al. Primary hypoparathyroidism: psychosis in postpartum period. J Assoc Physicians India. 2010;58:506-508.
13. O’Hara MW, Schlechte JA, Lewis DA, et al. Prospective study of postpartum blues: biologic and psychosocial factors. Arch Gen Psychiatry. 1991;48(9):801-806.
14. Burt VK, Hendrick VC. Clinical manual of women’s mental health. Washington, DC. American Psychiatric Association Publishing; 2007:79-80.
15. Melzer-Brody S. Postpartum depression: what to tell patients who breast-feed. Current Psychiatry. 2008;7(5):87-95.
16. Alhusen JL, Gross D, Hayat MJ, et al. The role of mental health on maternal‐fetal attachment in low‐income women. J Obstet Gynecol Neonatal Nurs. 2012;41(6):E71-E81.
17. McLearn KT, Minkovitz CS, Strobino DM, et al. Maternal depressive symptoms at 2 to 4 months postpartum and early parenting practices. Arch Pediatr Adolesc Med. 2006;160(3):279-284.
18. Committee on Obstetric Practice. The American College of Obstetricians and Gynecologists Committee Opinion no. 630. Screening for perinatal depression. Obstet Gynecol. 2015;125(5):1268-1271.
19. Jennings KD, Ross S, Popper S. Thoughts of harming infants in depressed and nondepressed mothers. J Affect Disord. 1999;54(1-2):21-28.
20. Miller ES, Hoxha D, Wisner KL, et al. Obsessions and compulsions in postpartum women without obsessive compulsive disorder. J Womens Health. 2015;24(10):825-830.
21. Russell EJ, Fawcett JM, Mazmanian D. Risk of obsessive-compulsive disorder in pregnant and postpartum women: a meta-analysis. J Clin Psychiatry. 2013;74(4):377-385.
22. Zambaldi CF, Cantilino A, Montenegro AC, et al. Postpartum obsessive-compulsive disorder: prevalence and clinical characteristics. Compr Psychiatry. 2009;50(6):503-509.
23. Booth BD, Friedman SH, Curry S, et al. Obsessions of child murder: underrecognized manifestations of obsessive-compulsive disorder. J Am Acad Psychiatry Law. 2014;42(1):66-74.
24. Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health. 2005;8(2):77-87.
25. Samandari G, Martin SL, Kupper LL, et al. Are pregnant and postpartum women: at increased risk for violent death? Suicide and homicide findings from North Carolina. Matern Child Health J. 2011;15(5):660-669.
26. Friedman SH, Sorrentino R. Commentary: postpartum psychosis, infanticide, and insanity—implications for forensic psychiatry. J Am Acad Psychiatry Law. 2012;40(3):326-332.
27. Friedman SH, Resnick PJ. Child murder by mothers: patterns and prevention. World Psychiatry. 2007;6(3):137-141.
28. Friedman SH, Hrouda DR, Holden CE, et al. Filicide-suicide: common factors in parents who kill their children and themselves. J Am Acad Psychiatry Law. 2005;33(4):496-504.
29. Chandra PS, Venkatasubramanian G, Thomas T. Infanticidal ideas and infanticidal behavior in Indian women with severe postpartum psychiatric disorders. J Nerv Ment Dis. 2002;190(7):457-461.
30. Jones I, Chandra PS, Dazzan P, et al. Bipolar disorder, affective psychosis, and schizophrenia in pregnancy and the post-partum period. Lancet. 2014;384(9956):1789-1799.
31. Friedman SH. Neonaticide. In: Friedman SH. Family murder: pathologies of love and hate. Washington, DC: American Psychiatric Association Publishing; 2018:53-67.
32. Meltzer-Brody S, Brandon AR, Pearson B, et al. Evaluating the clinical effectiveness of a specialized perinatal psychiatry inpatient unit. Arch Womens Ment Health. 2014;17(2):107-113.
33. Klinger G, Stahl B, Fusar-Poli P, et al. Antipsychotic drugs and breastfeeding. Pediatri Endocrinol Rev. 2013;10(3):308-317.
34. Focht A, Kellner CH. Electroconvulsive therapy (ECT) in the treatment of postpartum psychosis. J ECT. 2012;28(1):31-33.
35. Heron J, McGuinness M, Blackmore ER, et al. Early postpartum symptoms in puerperal psychosis. BJOG. 2008;115(3):348-353.
36. McEwan M, Friedman SH. Violence by parents against their children: reporting of maltreatment suspicions, child protection, and risk in mental illness. Psychiatr Clin North Am. 2016;39(4):691-700.
37. Centre of Perinatal Excellence. National Perinatal Mental Health Guideline. http://cope.org.au/about/review-of-new-perinatal-mental-health-guidelines/. Published October 27, 2017. Accessed November 22, 2018.
38. National Institute for Health and Care Excellence. Antenatal and postnatal mental health overview. https://pathways.nice.org.uk/pathways/antenatal-and-postnatal-mental-health. 2017. Accessed November 22, 2018.
39. Wesseloo R, Kamperman AM, Olsen TM, et al. Risk of postpartum relapse in bipolar disorder and postpartum psychosis: a systematic review and meta-analysis. Am J Psychiatry. 2016;173(2):117-127.
40. McKnight RF, Adida M, Budge K, et al. Lithium toxicity profile: a systematic review and meta-analysis. Lancet. 2012;379(9817):721-728.
41. Munk-Olsen T, Liu X, Viktorin A, et al. Maternal and infant outcomes associated with lithium use in pregnancy: an international collaborative meta-analysis of six cohort studies. Lancet Psychiatry. 2018;5(8):644-652.
42. Prakash C, Friedman SH, Moller-Olsen C, et al. Maternal and fetal outcomes after lamotrigine use in pregnancy: a retrospective analysis from an urban maternal mental health centre in New Zealand. Psychopharmacology Bull. 2016;46(2):63-69.
43. Wesseloo R, Liu X, Clark CT, et al. Risk of postpartum episodes in women with bipolar disorder after lamotrigine or lithium use in pregnancy: a population-based cohort study. J Affect Disord. 2017;218:394-397.
44. Dolk H, Wang H, Loane M, et al. Lamotrigine use in pregnancy and risk of orofacial cleft and other congenital anomalies. Neurology. 2016;86(18):1716-1725.
45. Diav-Citrin O, Shechtman S, Zvi N, et al. Is it safe to use lamotrigine during pregnancy? A prospective comparative observational study. Birth Defects Res. 2017;109(15):1196-1203.
46. Kong L, Zhou T, Wang B, et al. The risks associated with the use of lamotrigine during pregnancy. Int J Psychiatry Clin Pract. 2018;22(1):2-5.
47. Deligiannidis KM, Byatt N, Freeman MP. Pharmacotherapy for mood disorders in pregnancy: a review of pharmacokinetic changes and clinical recommendations for therapeutic drug monitoring. J Clin Psychopharmacol. 2014;34(2):244.
48. Bogen DL, Sit D, Genovese A, et al. Three cases of lithium exposure and exclusive breastfeeding. Arch Womens Ment Health. 2012;15(1):69-72.
A new mother drowned her 6-month-old daughter in the bathtub. The married woman, who had a history of schizoaffective disorder, had been high functioning and worked in a managerial role prior to giving birth. However, within a day of delivery, her mental state deteriorated. She quickly became convinced that her daughter had a genetic disorder such as achondroplasia. Physical examinations, genetic testing, and x-rays all failed to alleviate her concerns. Examination of her computer revealed thousands of searches for various medical conditions and surgical treatments. After the baby’s death, the mother was admitted to a psychiatric hospital. She eventually pled guilty to manslaughter.1
Mothers with postpartum psychosis (PPP) typically present fulminantly within days to weeks of giving birth. Symptoms of PPP may include not only psychosis, but also confusion and dysphoric mania. These symptoms often wax and wane, which can make it challenging to establish the diagnosis. In addition, many mothers hide their symptoms due to poor insight, delusions, or fear of loss of custody of their infant. In the vast majority of cases, psychiatric hospitalization is required to protect both mother and baby; untreated, there is an elevated risk of both maternal suicide and infanticide. This article discusses the presentation of PPP, its differential diagnosis, risk factors for developing PPP, suicide and infanticide risk assessment, treatment (including during breastfeeding), and prevention.
The bipolar connection
While multiple factors may increase the risk of PPP (Table 12), women with bipolar disorder have a particularly elevated risk. After experiencing incipient postpartum affective psychosis, a woman has a 50% to 80% chance of having another psychiatric episode, usually within the bipolar spectrum.2 Of all women with PPP, 70% to 90% have bipolar illness or schizoaffective disorder, while approximately 12% have schizophrenia.3,4Women with bipolar disorder are more likely to experience a postpartum psychiatric admission than mothers with any other psychiatric diagnosis5 and have an increased risk of PPP by a factor of 100 over the general population.2
For women with bipolar disorder, PPP should be understood as a recurrence of the chronic disease. Recent evidence does suggest, however, that a significant minority of women progress to experience mood and psychotic symptoms only in the postpartum period.6,7 It is hypothesized that this subgroup of women has a biologic vulnerability to affective psychosis that is limited to the postpartum period. Clinically, understanding a woman’s disease course is important because it may guide decision-making about prophylactic medications during or after pregnancy.
A rapid, delirium-like presentation
Postpartum psychosis is a rare disorder, with a prevalence of 1 to 2 cases per 1,000 childbirths.3 While symptoms may begin days to weeks postpartum, the typical time of onset is between 3 to 10 days after birth, occurring after a woman has been discharged from the hospital and during a time of change and uncertainty. This can make the presentation of PPP a confusing and distressing experience for both the new mother and the family, resulting in delays in seeking care.
Subtle prodromal symptoms may include insomnia, mood fluctuation, and irritability. As symptoms progress, PPP is notable for a rapid onset and a delirium-like appearance that may include waxing and waning cognitive symptoms such as disorientation and confusion.8 Grossly disorganized behaviors and rapid mood fluctuations are typical. Distinct from mood episodes outside the peripartum period, women with PPP often experience mood-incongruent delusions and obsessive thoughts, often focused on their child.9 Women with PPP appear less likely to experience thought insertion or withdrawal or auditory hallucinations that give a running commentary.2
Differential diagnosis includes depression, OCD
When evaluating a woman with possible postpartum psychotic symptoms or delirium, it is important to include a thorough history, physical examination, and relevant laboratory and/or imaging investigations to assess for organic causes or contributors (Table 22,6,10-12 and Table 32,6,10-12). A detailed psychiatric history should establish whether the patient is presenting with new-onset psychosis or has had previous mood or psychotic episodes that may have gone undetected. Important perinatal psychiatric differential diagnoses should include “baby blues,” postpartum depression (PPD), and obsessive-compulsive disorder (OCD).
Continue to: PPP vs "baby blues."
PPP vs “baby blues.” “Baby blues” is not an official DSM-5 diagnosis but rather a normative postpartum experience that affects 50% to 80% of postpartum women. A woman with the “baby blues” may feel weepy or have mild mood lability, irritability, or anxiety; however, these symptoms do not significantly impair function. Peak symptoms typically occur between 2 to 5 days postpartum and generally resolve within 2 weeks. Women who have the “baby blues” are at an increased risk for PPD and should be monitored over time.13,14
PPP vs PPD. Postpartum depression affects approximately 10% to 15% of new mothers.15 Women with PPD may experience feelings of persistent and severe sadness, feelings of detachment, insomnia, and fatigue. Symptoms of PPD can interfere with a mother’s interest in caring for her baby and present a barrier to maternal bonding.16,17
As the awareness of PPD has increased in recent years, screening for depressive symptoms during and after pregnancy has increasingly become the standard of care.18 When evaluating a postpartum woman for PPD, it is important to consider PPP in the differential. Women with severe or persistent depressive symptoms may also develop psychotic symptoms. Furthermore, suicidal thoughts or thoughts of harming the infant may be present in either PPD or PPP. One study found that 41% of mothers with depression endorsed thoughts of harming their infants.19
PPP vs postpartum OCD. Postpartum obsessive-compulsive symptoms commonly occur comorbidly with PPD,9 and OCD often presents for the first time in the postpartum period.20 Obsessive-compulsive disorder affects between 2% to 9% of new mothers.21,22 It is critical to properly differentiate PPP from postpartum OCD. Clinical questions should be posed with a non-judgmental stance. Just as delusions in PPP are often focused on the infant, for women with OCD, obsessive thoughts may center on worries about the infant’s safety. Distressing obsessions about violence are common in OCD.23 Mothers with OCD may experience intrusive thinking about accidentally or purposefully harming their infant. For example, they may intrusively worry that they will accidentally put the baby in the microwave or oven, leave the baby in a hot car, or throw the baby down the stairs. However, a postpartum woman with OCD may be reluctant to share her ego-dystonic thoughts of infant harm. Mothers with OCD are not out of touch with reality; instead, their intrusive thoughts are ego-dystonic and distressing. These are thoughts and fears that they focus on and try to avoid, rather than plan. The psychiatrist must carefully differentiate between ego-syntonic and ego-dystonic thoughts. These patients often avoid seeking treatment because of their shame and guilt.23 Clinicians often under-recognize OCD and risk inappropriate hospitalization, treatment, and inappropriate referral to Child Protective Services (CPS).23
Perinatal psychiatric risk assessment
When a mother develops PPP, consider the risks of suicide, child harm, and infanticide. Although suicide risk is generally lower in the postpartum period, suicide is the cause of 20% of postpartum deaths.24,25 When PPP is untreated, suicide risk is elevated. A careful suicide risk assessment should be completed.
Continue to: Particularly in PPP...
Particularly in PPP, a mother may be at risk of child neglect or abuse due to her confused or delusional thinking and mood state.26 For example, one mother heated empty bottles and gave them to her baby, and then became frustrated when the baby continued to cry.
The risk of infanticide is also elevated in untreated PPP, with approximately 4% of these women committing infanticide.9 There are 5 motives for infanticide (Table 427). Altruistic and acutely psychotic motives are more likely to be related to PPP, while fatal maltreatment, unwanted child, and partner revenge motives are less likely to be related to PPP. Among mothers who kill both their child and themselves (filicide-suicide), altruistic motives were the most common.28 Mothers in psychiatric samples who kill their children have often experienced psychosis, suicidality, depression, and significant life stresses.27 Both infanticidal ideas and behaviors have been associated with psychotic thinking about the infant,29 so it is critical to ascertain whether the mother’s delusions or hallucinations involve the infant.30 In contrast, neonaticide (murder in the first day of life) is rarely related to PPP because PPP typically has a later onset.31
Treating acute PPP
The fulminant nature of PPP can make its treatment difficult. Thinking through the case in an organized fashion is critical (Table 5).
Hospitalization. Postpartum psychosis is a psychiatric emergency with a rapid onset of symptoms. Hospitalization is required in almost all cases for diagnostic evaluation, assessment and management of safety, and initiation of treatment. While maternal-infant bonding in the perinatal period is important, infant safety is critical and usually requires maternal psychiatric hospitalization.
The specialized mother-baby psychiatric unit (MBU) is a model of care first developed in the United Kingdom and is now available in many European countries as well as in New Zealand and Australia. Mother-baby psychiatric units admit the mother and the baby together and provide dyadic treatment to allow for enhanced bonding and parenting support, and often to encourage breastfeeding.30 In the United States, there has been growing interest in specialized inpatient settings that acknowledge the importance of maternal-infant attachment in the treatment of perinatal disorders and provide care with a dyadic focus; however, differences in the health care payer system have been a barrier to full-scale MBUs. The Perinatal Psychiatry Inpatient Unit at University of North Carolina-Chapel Hill is among the first of such a model in the United States.32
Continue to: Although this specialized treatment setting...
Although this specialized treatment setting is unlikely to be available in most American cities, treatment should still consider the maternal role. When possible, the infant should stay with the father or family members during the mother’s hospitalization, and supervised visits should be arranged when appropriate. If the mother is breastfeeding, or plans to breastfeed after the hospitalization, the treatment team may consider providing supervised use of a breast pump and making arrangements for breast milk storage. During the mother’s hospitalization, staff should provide psychoeducation and convey hopefulness and support.
Medication management. Mood stabilizers and second-generation antipsychotics (SGAs) are often used for acute management of PPP. The choice of medication is determined by individual symptoms, severity of presentation, previous response to medication, and maternal adverse effects.30 In a naturalistic study of 64 women admitted for new-onset PPP, sequential administration of benzodiazepines, antipsychotics, and lithium was found to be effective in achieving remission for 99% of patients, with 80% sustaining remission at 9 months postpartum.6 Second-generation antipsychotics such as
Breastfeeding. It is important to discuss breastfeeding with the mother and her partner or family. The patient’s preference, the maternal and infant benefits of breastfeeding, the potential for sleep disruption, and the safety profile of needed medications should all be considered. Because sleep loss is a modifiable risk factor in PPP, the benefits of breastfeeding may be outweighed by the risks for some patients.9 For others, breastfeeding during the day and bottle-feeding at night may be preferred.
What to consider during discharge planning
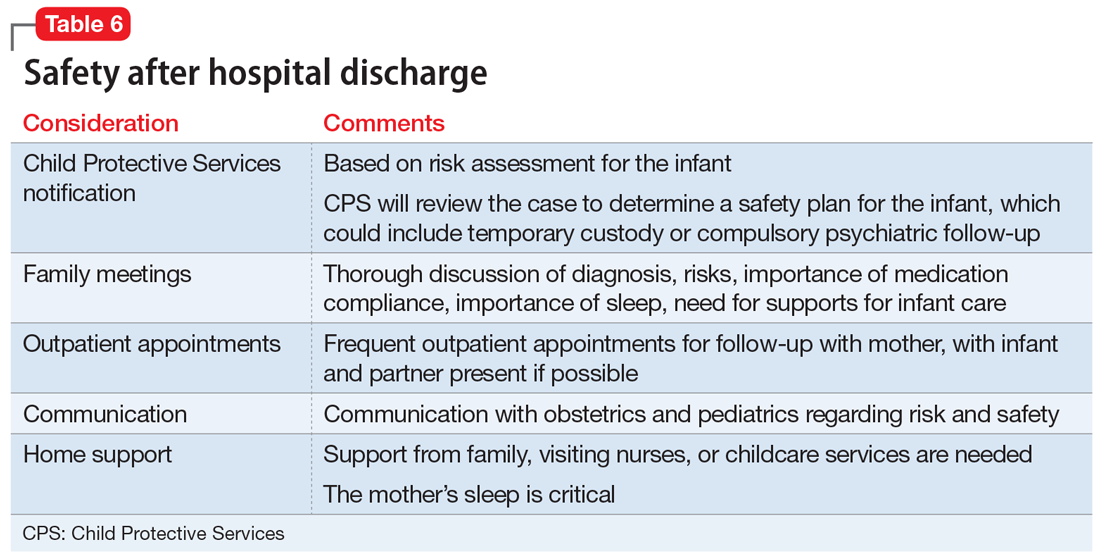
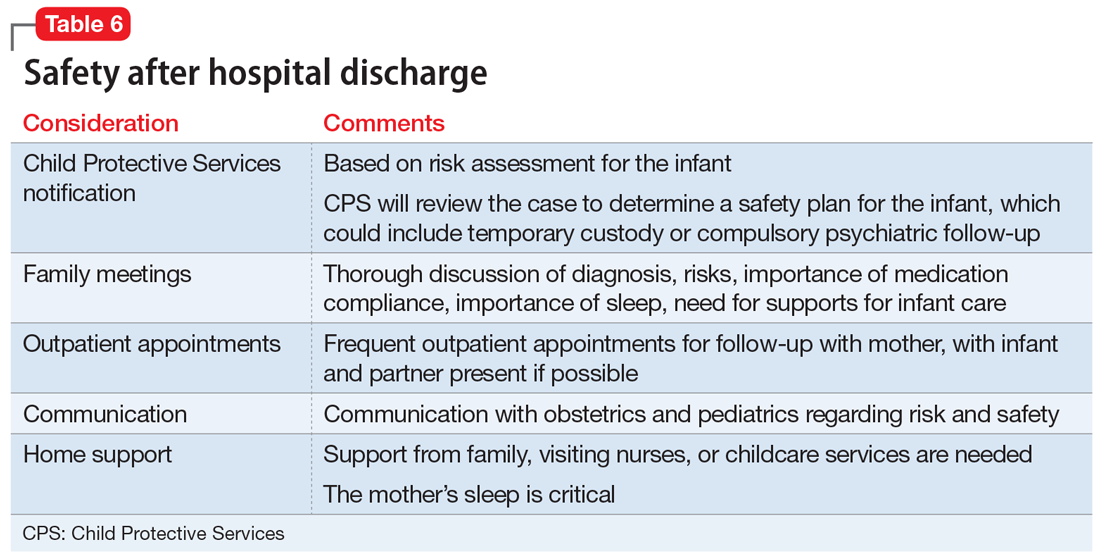
Discharge arrangements require careful consideration (Table 6). Meet with the family prior to discharge to provide psychoeducation and to underscore the importance of family involvement with both mother and infant. It is important to ensure adequate support at home, including at night, since sleep is critical to improved stability. Encourage the patient and her family to monitor for early warning signs of relapse, which might include refractory insomnia, mood instability, poor judgment, or hypomanic symptoms.35 She should be followed closely as an outpatient. Having her partner (or another close family member) and infant present during appointments can help in obtaining collateral information and assessing mother-infant bonding. The clinician should also consider whether it is necessary to contact CPS. Many mothers with mental illness appropriately parent their child, but CPS should be alerted when there is a reasonable concern about safe parenting—abuse, neglect, or significant risk.36
Take steps for prevention
An important part of managing PPP is prevention. This involves providing preconception counseling to the woman and her partner.30 Preconception advice should be individualized and include discussion of:
- risks of relapse in pregnancy and the postpartum period
- optimal physical and mental health
- potential risks and benefits of medication options in pregnancy
- potential effects of untreated illness for the fetus, infant, and family
- a strategy outlining whether medication is continued in pregnancy or started in the postpartum period.
Continue to: For women at risk of PPP...
For women at risk of PPP, the risks of medications need to be balanced with the risks of untreated illness. To reduce the risk of PPP relapse, guidelines recommend a robust antenatal care plan that should include37,38:
- close monitoring of a woman’s mental state for early warning signs of PPP, with active participation from the woman’s partner and family
- ongoing discussion of the risks and benefits of pharmacotherapy (and, for women who prefer to not take medication in the first trimester, a plan for when medications will be restarted)
- collaboration with other professionals involved in care during pregnancy and postpartum (eg, obstetricians, midwives, family practitioners, pediatricians)
- planning to minimize risk factors associated with relapse (eg, sleep deprivation, lack of social supports, domestic violence, and substance abuse).
Evidence clearly suggests that women with bipolar disorder are at increased risk for illness recurrence without continued maintenance medication.39 A subgroup of women with PPP go on to have psychosis limited to the postpartum period, and reinstating prophylactic medication in late pregnancy (preferably) or immediately after birth should be discussed.2 The choice of prophylactic medication should be determined by the woman’s previous response.
Regarding prophylaxis, the most evidence exists for lithium.6 Lithium use during the first trimester carries a risk of Ebstein’s anomaly. However, a recent systematic review and meta-analysis have concluded that the teratogenic risks of lithium have been overestimated.40,41
Lamotrigine is an alternative mood stabilizer with a favorable safety profile in pregnancy. In a small naturalistic study in which lamotrigine was continued in pregnancy in women with bipolar disorder, the medication was effective in preventing relapse in pregnancy and postpartum.42 A small population-based cohort study found lamotrigine was as effective as lithium in preventing severe postpartum relapse in women with bipolar disorder,43 although this study was limited by its observational design. Recently published studies have found no significant association between
Box
It is essential to consider the patient’s individual symptoms and treatment history when making pharmacologic recommendations during pregnancy. Discussion with the patient about the risks and benefits of lithium is recommended. For women who continue to use lithium during pregnancy, ongoing pharmacokinetic changes warrant more frequent monitoring (some experts advise monthly monitoring throughout pregnancy, moving to more frequent monitoring at 36 weeks).47 During labor, the team might consider temporary cessation of lithium and particular attention to hydration status.30 In the postpartum period, there is a quick return to baseline glomerular filtration rate and a rapid decrease in vascular volume, so it is advisable to restart the patient at her pre-pregnancy lithium dosage. It is recommended to check lithium levels within 24 hours of delivery.47 While lithium is not an absolute contraindication to breastfeeding, there is particular concern in situations of prematurity or neonatal dehydration. Collaboration with and close monitoring by the pediatrician is essential to determine an infant monitoring plan.48
If lamotrigine is used during pregnancy, be aware that pregnancy-related pharmacokinetic changes result in increased lamotrigine clearance, which will vary in magnitude among individuals. Faster clearance may necessitate dose increases during pregnancy and a taper back to pre-pregnancy dose in the postpartum period. Dosing should always take clinical symptoms into account.
Pharmacotherapy can reduce relapse risk
To prevent relapse in the postpartum period, consider initiating treatment with mood stabilizers and/or SGAs, particularly for women with bipolar disorder who do not take medication during pregnancy. A recent meta-analysis found a high postpartum relapse rate (66%) in women with bipolar disorder who did not take prophylactic medication, compared with a relapse rate of 23% for women who did take such medication. In women with psychosis limited to the postpartum period, prophylaxis with lithium or antipsychotics in the immediate postpartum can prevent relapse.39 The SGAs olanzapine and quetiapine are often used to manage acute symptoms because they are considered acceptable during breastfeeding.33 The use of lithium when breastfeeding is complex to manage48 and may require advice to not breastfeed, which can be an important consideration for patients and their families.
Bottom Line
Postpartum psychosis (PPP) typically presents with a rapid onset of hallucinations, delusions, confusion, and mood swings within days to weeks of giving birth. Mothers with PPP almost always require hospitalization for the safety of their infants and themselves. Mood stabilizers and second-generation antipsychotics are used for acute management.
Related Resources
- Clark CT, Wisner KL. Treatment of peripartum bipolar disorder. Obstet Gynecol Clin N Am. 2018;45:403-417.
- Massachusetts General Hospital Center for Women’s Mental Health. https://womensmentalhealth.org/. 2018.
- Postpartum Support International. Postpartum psychosis. http://www.postpartum.net/learn-more/postpartumpsychosis/. 2019.
Drug Brand Names
Bromocriptine • Cycloset, Parlodel
Cabergoline • Dostinex
Lamotrigine • Lamictal
Lithium • Eskalith, Lithobid
Olanzapine • Zyprexa
Quetiapine • Seroquel
A new mother drowned her 6-month-old daughter in the bathtub. The married woman, who had a history of schizoaffective disorder, had been high functioning and worked in a managerial role prior to giving birth. However, within a day of delivery, her mental state deteriorated. She quickly became convinced that her daughter had a genetic disorder such as achondroplasia. Physical examinations, genetic testing, and x-rays all failed to alleviate her concerns. Examination of her computer revealed thousands of searches for various medical conditions and surgical treatments. After the baby’s death, the mother was admitted to a psychiatric hospital. She eventually pled guilty to manslaughter.1
Mothers with postpartum psychosis (PPP) typically present fulminantly within days to weeks of giving birth. Symptoms of PPP may include not only psychosis, but also confusion and dysphoric mania. These symptoms often wax and wane, which can make it challenging to establish the diagnosis. In addition, many mothers hide their symptoms due to poor insight, delusions, or fear of loss of custody of their infant. In the vast majority of cases, psychiatric hospitalization is required to protect both mother and baby; untreated, there is an elevated risk of both maternal suicide and infanticide. This article discusses the presentation of PPP, its differential diagnosis, risk factors for developing PPP, suicide and infanticide risk assessment, treatment (including during breastfeeding), and prevention.
The bipolar connection
While multiple factors may increase the risk of PPP (Table 12), women with bipolar disorder have a particularly elevated risk. After experiencing incipient postpartum affective psychosis, a woman has a 50% to 80% chance of having another psychiatric episode, usually within the bipolar spectrum.2 Of all women with PPP, 70% to 90% have bipolar illness or schizoaffective disorder, while approximately 12% have schizophrenia.3,4Women with bipolar disorder are more likely to experience a postpartum psychiatric admission than mothers with any other psychiatric diagnosis5 and have an increased risk of PPP by a factor of 100 over the general population.2
For women with bipolar disorder, PPP should be understood as a recurrence of the chronic disease. Recent evidence does suggest, however, that a significant minority of women progress to experience mood and psychotic symptoms only in the postpartum period.6,7 It is hypothesized that this subgroup of women has a biologic vulnerability to affective psychosis that is limited to the postpartum period. Clinically, understanding a woman’s disease course is important because it may guide decision-making about prophylactic medications during or after pregnancy.
A rapid, delirium-like presentation
Postpartum psychosis is a rare disorder, with a prevalence of 1 to 2 cases per 1,000 childbirths.3 While symptoms may begin days to weeks postpartum, the typical time of onset is between 3 to 10 days after birth, occurring after a woman has been discharged from the hospital and during a time of change and uncertainty. This can make the presentation of PPP a confusing and distressing experience for both the new mother and the family, resulting in delays in seeking care.
Subtle prodromal symptoms may include insomnia, mood fluctuation, and irritability. As symptoms progress, PPP is notable for a rapid onset and a delirium-like appearance that may include waxing and waning cognitive symptoms such as disorientation and confusion.8 Grossly disorganized behaviors and rapid mood fluctuations are typical. Distinct from mood episodes outside the peripartum period, women with PPP often experience mood-incongruent delusions and obsessive thoughts, often focused on their child.9 Women with PPP appear less likely to experience thought insertion or withdrawal or auditory hallucinations that give a running commentary.2
Differential diagnosis includes depression, OCD
When evaluating a woman with possible postpartum psychotic symptoms or delirium, it is important to include a thorough history, physical examination, and relevant laboratory and/or imaging investigations to assess for organic causes or contributors (Table 22,6,10-12 and Table 32,6,10-12). A detailed psychiatric history should establish whether the patient is presenting with new-onset psychosis or has had previous mood or psychotic episodes that may have gone undetected. Important perinatal psychiatric differential diagnoses should include “baby blues,” postpartum depression (PPD), and obsessive-compulsive disorder (OCD).
Continue to: PPP vs "baby blues."
PPP vs “baby blues.” “Baby blues” is not an official DSM-5 diagnosis but rather a normative postpartum experience that affects 50% to 80% of postpartum women. A woman with the “baby blues” may feel weepy or have mild mood lability, irritability, or anxiety; however, these symptoms do not significantly impair function. Peak symptoms typically occur between 2 to 5 days postpartum and generally resolve within 2 weeks. Women who have the “baby blues” are at an increased risk for PPD and should be monitored over time.13,14
PPP vs PPD. Postpartum depression affects approximately 10% to 15% of new mothers.15 Women with PPD may experience feelings of persistent and severe sadness, feelings of detachment, insomnia, and fatigue. Symptoms of PPD can interfere with a mother’s interest in caring for her baby and present a barrier to maternal bonding.16,17
As the awareness of PPD has increased in recent years, screening for depressive symptoms during and after pregnancy has increasingly become the standard of care.18 When evaluating a postpartum woman for PPD, it is important to consider PPP in the differential. Women with severe or persistent depressive symptoms may also develop psychotic symptoms. Furthermore, suicidal thoughts or thoughts of harming the infant may be present in either PPD or PPP. One study found that 41% of mothers with depression endorsed thoughts of harming their infants.19
PPP vs postpartum OCD. Postpartum obsessive-compulsive symptoms commonly occur comorbidly with PPD,9 and OCD often presents for the first time in the postpartum period.20 Obsessive-compulsive disorder affects between 2% to 9% of new mothers.21,22 It is critical to properly differentiate PPP from postpartum OCD. Clinical questions should be posed with a non-judgmental stance. Just as delusions in PPP are often focused on the infant, for women with OCD, obsessive thoughts may center on worries about the infant’s safety. Distressing obsessions about violence are common in OCD.23 Mothers with OCD may experience intrusive thinking about accidentally or purposefully harming their infant. For example, they may intrusively worry that they will accidentally put the baby in the microwave or oven, leave the baby in a hot car, or throw the baby down the stairs. However, a postpartum woman with OCD may be reluctant to share her ego-dystonic thoughts of infant harm. Mothers with OCD are not out of touch with reality; instead, their intrusive thoughts are ego-dystonic and distressing. These are thoughts and fears that they focus on and try to avoid, rather than plan. The psychiatrist must carefully differentiate between ego-syntonic and ego-dystonic thoughts. These patients often avoid seeking treatment because of their shame and guilt.23 Clinicians often under-recognize OCD and risk inappropriate hospitalization, treatment, and inappropriate referral to Child Protective Services (CPS).23
Perinatal psychiatric risk assessment
When a mother develops PPP, consider the risks of suicide, child harm, and infanticide. Although suicide risk is generally lower in the postpartum period, suicide is the cause of 20% of postpartum deaths.24,25 When PPP is untreated, suicide risk is elevated. A careful suicide risk assessment should be completed.
Continue to: Particularly in PPP...
Particularly in PPP, a mother may be at risk of child neglect or abuse due to her confused or delusional thinking and mood state.26 For example, one mother heated empty bottles and gave them to her baby, and then became frustrated when the baby continued to cry.
The risk of infanticide is also elevated in untreated PPP, with approximately 4% of these women committing infanticide.9 There are 5 motives for infanticide (Table 427). Altruistic and acutely psychotic motives are more likely to be related to PPP, while fatal maltreatment, unwanted child, and partner revenge motives are less likely to be related to PPP. Among mothers who kill both their child and themselves (filicide-suicide), altruistic motives were the most common.28 Mothers in psychiatric samples who kill their children have often experienced psychosis, suicidality, depression, and significant life stresses.27 Both infanticidal ideas and behaviors have been associated with psychotic thinking about the infant,29 so it is critical to ascertain whether the mother’s delusions or hallucinations involve the infant.30 In contrast, neonaticide (murder in the first day of life) is rarely related to PPP because PPP typically has a later onset.31
Treating acute PPP
The fulminant nature of PPP can make its treatment difficult. Thinking through the case in an organized fashion is critical (Table 5).
Hospitalization. Postpartum psychosis is a psychiatric emergency with a rapid onset of symptoms. Hospitalization is required in almost all cases for diagnostic evaluation, assessment and management of safety, and initiation of treatment. While maternal-infant bonding in the perinatal period is important, infant safety is critical and usually requires maternal psychiatric hospitalization.
The specialized mother-baby psychiatric unit (MBU) is a model of care first developed in the United Kingdom and is now available in many European countries as well as in New Zealand and Australia. Mother-baby psychiatric units admit the mother and the baby together and provide dyadic treatment to allow for enhanced bonding and parenting support, and often to encourage breastfeeding.30 In the United States, there has been growing interest in specialized inpatient settings that acknowledge the importance of maternal-infant attachment in the treatment of perinatal disorders and provide care with a dyadic focus; however, differences in the health care payer system have been a barrier to full-scale MBUs. The Perinatal Psychiatry Inpatient Unit at University of North Carolina-Chapel Hill is among the first of such a model in the United States.32
Continue to: Although this specialized treatment setting...
Although this specialized treatment setting is unlikely to be available in most American cities, treatment should still consider the maternal role. When possible, the infant should stay with the father or family members during the mother’s hospitalization, and supervised visits should be arranged when appropriate. If the mother is breastfeeding, or plans to breastfeed after the hospitalization, the treatment team may consider providing supervised use of a breast pump and making arrangements for breast milk storage. During the mother’s hospitalization, staff should provide psychoeducation and convey hopefulness and support.
Medication management. Mood stabilizers and second-generation antipsychotics (SGAs) are often used for acute management of PPP. The choice of medication is determined by individual symptoms, severity of presentation, previous response to medication, and maternal adverse effects.30 In a naturalistic study of 64 women admitted for new-onset PPP, sequential administration of benzodiazepines, antipsychotics, and lithium was found to be effective in achieving remission for 99% of patients, with 80% sustaining remission at 9 months postpartum.6 Second-generation antipsychotics such as
Breastfeeding. It is important to discuss breastfeeding with the mother and her partner or family. The patient’s preference, the maternal and infant benefits of breastfeeding, the potential for sleep disruption, and the safety profile of needed medications should all be considered. Because sleep loss is a modifiable risk factor in PPP, the benefits of breastfeeding may be outweighed by the risks for some patients.9 For others, breastfeeding during the day and bottle-feeding at night may be preferred.
What to consider during discharge planning
Discharge arrangements require careful consideration (Table 6). Meet with the family prior to discharge to provide psychoeducation and to underscore the importance of family involvement with both mother and infant. It is important to ensure adequate support at home, including at night, since sleep is critical to improved stability. Encourage the patient and her family to monitor for early warning signs of relapse, which might include refractory insomnia, mood instability, poor judgment, or hypomanic symptoms.35 She should be followed closely as an outpatient. Having her partner (or another close family member) and infant present during appointments can help in obtaining collateral information and assessing mother-infant bonding. The clinician should also consider whether it is necessary to contact CPS. Many mothers with mental illness appropriately parent their child, but CPS should be alerted when there is a reasonable concern about safe parenting—abuse, neglect, or significant risk.36
Take steps for prevention
An important part of managing PPP is prevention. This involves providing preconception counseling to the woman and her partner.30 Preconception advice should be individualized and include discussion of:
- risks of relapse in pregnancy and the postpartum period
- optimal physical and mental health
- potential risks and benefits of medication options in pregnancy
- potential effects of untreated illness for the fetus, infant, and family
- a strategy outlining whether medication is continued in pregnancy or started in the postpartum period.
Continue to: For women at risk of PPP...
For women at risk of PPP, the risks of medications need to be balanced with the risks of untreated illness. To reduce the risk of PPP relapse, guidelines recommend a robust antenatal care plan that should include37,38:
- close monitoring of a woman’s mental state for early warning signs of PPP, with active participation from the woman’s partner and family
- ongoing discussion of the risks and benefits of pharmacotherapy (and, for women who prefer to not take medication in the first trimester, a plan for when medications will be restarted)
- collaboration with other professionals involved in care during pregnancy and postpartum (eg, obstetricians, midwives, family practitioners, pediatricians)
- planning to minimize risk factors associated with relapse (eg, sleep deprivation, lack of social supports, domestic violence, and substance abuse).
Evidence clearly suggests that women with bipolar disorder are at increased risk for illness recurrence without continued maintenance medication.39 A subgroup of women with PPP go on to have psychosis limited to the postpartum period, and reinstating prophylactic medication in late pregnancy (preferably) or immediately after birth should be discussed.2 The choice of prophylactic medication should be determined by the woman’s previous response.
Regarding prophylaxis, the most evidence exists for lithium.6 Lithium use during the first trimester carries a risk of Ebstein’s anomaly. However, a recent systematic review and meta-analysis have concluded that the teratogenic risks of lithium have been overestimated.40,41
Lamotrigine is an alternative mood stabilizer with a favorable safety profile in pregnancy. In a small naturalistic study in which lamotrigine was continued in pregnancy in women with bipolar disorder, the medication was effective in preventing relapse in pregnancy and postpartum.42 A small population-based cohort study found lamotrigine was as effective as lithium in preventing severe postpartum relapse in women with bipolar disorder,43 although this study was limited by its observational design. Recently published studies have found no significant association between
Box
It is essential to consider the patient’s individual symptoms and treatment history when making pharmacologic recommendations during pregnancy. Discussion with the patient about the risks and benefits of lithium is recommended. For women who continue to use lithium during pregnancy, ongoing pharmacokinetic changes warrant more frequent monitoring (some experts advise monthly monitoring throughout pregnancy, moving to more frequent monitoring at 36 weeks).47 During labor, the team might consider temporary cessation of lithium and particular attention to hydration status.30 In the postpartum period, there is a quick return to baseline glomerular filtration rate and a rapid decrease in vascular volume, so it is advisable to restart the patient at her pre-pregnancy lithium dosage. It is recommended to check lithium levels within 24 hours of delivery.47 While lithium is not an absolute contraindication to breastfeeding, there is particular concern in situations of prematurity or neonatal dehydration. Collaboration with and close monitoring by the pediatrician is essential to determine an infant monitoring plan.48
If lamotrigine is used during pregnancy, be aware that pregnancy-related pharmacokinetic changes result in increased lamotrigine clearance, which will vary in magnitude among individuals. Faster clearance may necessitate dose increases during pregnancy and a taper back to pre-pregnancy dose in the postpartum period. Dosing should always take clinical symptoms into account.
Pharmacotherapy can reduce relapse risk
To prevent relapse in the postpartum period, consider initiating treatment with mood stabilizers and/or SGAs, particularly for women with bipolar disorder who do not take medication during pregnancy. A recent meta-analysis found a high postpartum relapse rate (66%) in women with bipolar disorder who did not take prophylactic medication, compared with a relapse rate of 23% for women who did take such medication. In women with psychosis limited to the postpartum period, prophylaxis with lithium or antipsychotics in the immediate postpartum can prevent relapse.39 The SGAs olanzapine and quetiapine are often used to manage acute symptoms because they are considered acceptable during breastfeeding.33 The use of lithium when breastfeeding is complex to manage48 and may require advice to not breastfeed, which can be an important consideration for patients and their families.
Bottom Line
Postpartum psychosis (PPP) typically presents with a rapid onset of hallucinations, delusions, confusion, and mood swings within days to weeks of giving birth. Mothers with PPP almost always require hospitalization for the safety of their infants and themselves. Mood stabilizers and second-generation antipsychotics are used for acute management.
Related Resources
- Clark CT, Wisner KL. Treatment of peripartum bipolar disorder. Obstet Gynecol Clin N Am. 2018;45:403-417.
- Massachusetts General Hospital Center for Women’s Mental Health. https://womensmentalhealth.org/. 2018.
- Postpartum Support International. Postpartum psychosis. http://www.postpartum.net/learn-more/postpartumpsychosis/. 2019.
Drug Brand Names
Bromocriptine • Cycloset, Parlodel
Cabergoline • Dostinex
Lamotrigine • Lamictal
Lithium • Eskalith, Lithobid
Olanzapine • Zyprexa
Quetiapine • Seroquel
1. Hall L. Mother who killed baby believing she was a dwarf should not be jailed, court told. The Sydney Morning Herald. https://www.smh.com.au/national/nsw/mother-who-killed-baby-believing-she-was-a-dwarf-should-not-be-jailed-court-told-20170428-gvud4d.html. Published April 28, 2017. Accessed March 12, 2019.
2. Bergink V, Rasgon N, Wisner KL. Postpartum psychosis: madness, mania, and melancholia in motherhood. Am J Psychiatry. 2016;173(12):1179-1188.
3. Sit D, Rothschild AJ, Wisner KL. A review of postpartum psychosis. J Womens Health (Larchmt). 2006;15(4):352-368.
4. Kendell RE, Chalmers JC, Platz C. Epidemiology of puerperal psychoses. Br J Psychiatry. 1987;150(5):662-673.
5. Munk-Olsen T, Laursen TM, Mendelson T, et al. Risks and predictors of readmission for a mental disorder during the postpartum period. Arch Gen Psychiatry. 2009;66(2):189-195.
6. Bergink V, Burgerhout KM, Koorengevel KM, et al. Treatment of psychosis and mania in the postpartum period. Am J Psychiatry. 2015;172(2):115-123.
7. Wesseloo R, Kamperman AM, Munk-Olsen T, et al. Risk of postpartum relapse in bipolar disorder and postpartum psychosis: a systematic review and meta-analysis. Am J Psychiatry. 2015;173(2):117-127.
8. Wisner KL, Peindl K, Hanusa BH. Symptomatology of affective and psychotic illnesses related to childbearing. J Affect Disord. 1994;30(2):77-87.
9. Spinelli MG. Postpartum psychosis: detection of risk and management. Am J Psychiatry. 2009;166(4):405-408.
10. Fassier T, Guffon N, Acquaviva C, et al. Misdiagnosed postpartum psychosis revealing a late-onset urea cycle disorder. Am J Psychiatry. 2011;168(6):576-580.
11. Yu AYX, Moore FG. Paraneoplastic encephalitis presenting as postpartum psychosis. Psychosomatics. 2011;52(6):568-570.
12. Patil NJ, Yadav SS, Gokhale YA, et al. Primary hypoparathyroidism: psychosis in postpartum period. J Assoc Physicians India. 2010;58:506-508.
13. O’Hara MW, Schlechte JA, Lewis DA, et al. Prospective study of postpartum blues: biologic and psychosocial factors. Arch Gen Psychiatry. 1991;48(9):801-806.
14. Burt VK, Hendrick VC. Clinical manual of women’s mental health. Washington, DC. American Psychiatric Association Publishing; 2007:79-80.
15. Melzer-Brody S. Postpartum depression: what to tell patients who breast-feed. Current Psychiatry. 2008;7(5):87-95.
16. Alhusen JL, Gross D, Hayat MJ, et al. The role of mental health on maternal‐fetal attachment in low‐income women. J Obstet Gynecol Neonatal Nurs. 2012;41(6):E71-E81.
17. McLearn KT, Minkovitz CS, Strobino DM, et al. Maternal depressive symptoms at 2 to 4 months postpartum and early parenting practices. Arch Pediatr Adolesc Med. 2006;160(3):279-284.
18. Committee on Obstetric Practice. The American College of Obstetricians and Gynecologists Committee Opinion no. 630. Screening for perinatal depression. Obstet Gynecol. 2015;125(5):1268-1271.
19. Jennings KD, Ross S, Popper S. Thoughts of harming infants in depressed and nondepressed mothers. J Affect Disord. 1999;54(1-2):21-28.
20. Miller ES, Hoxha D, Wisner KL, et al. Obsessions and compulsions in postpartum women without obsessive compulsive disorder. J Womens Health. 2015;24(10):825-830.
21. Russell EJ, Fawcett JM, Mazmanian D. Risk of obsessive-compulsive disorder in pregnant and postpartum women: a meta-analysis. J Clin Psychiatry. 2013;74(4):377-385.
22. Zambaldi CF, Cantilino A, Montenegro AC, et al. Postpartum obsessive-compulsive disorder: prevalence and clinical characteristics. Compr Psychiatry. 2009;50(6):503-509.
23. Booth BD, Friedman SH, Curry S, et al. Obsessions of child murder: underrecognized manifestations of obsessive-compulsive disorder. J Am Acad Psychiatry Law. 2014;42(1):66-74.
24. Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health. 2005;8(2):77-87.
25. Samandari G, Martin SL, Kupper LL, et al. Are pregnant and postpartum women: at increased risk for violent death? Suicide and homicide findings from North Carolina. Matern Child Health J. 2011;15(5):660-669.
26. Friedman SH, Sorrentino R. Commentary: postpartum psychosis, infanticide, and insanity—implications for forensic psychiatry. J Am Acad Psychiatry Law. 2012;40(3):326-332.
27. Friedman SH, Resnick PJ. Child murder by mothers: patterns and prevention. World Psychiatry. 2007;6(3):137-141.
28. Friedman SH, Hrouda DR, Holden CE, et al. Filicide-suicide: common factors in parents who kill their children and themselves. J Am Acad Psychiatry Law. 2005;33(4):496-504.
29. Chandra PS, Venkatasubramanian G, Thomas T. Infanticidal ideas and infanticidal behavior in Indian women with severe postpartum psychiatric disorders. J Nerv Ment Dis. 2002;190(7):457-461.
30. Jones I, Chandra PS, Dazzan P, et al. Bipolar disorder, affective psychosis, and schizophrenia in pregnancy and the post-partum period. Lancet. 2014;384(9956):1789-1799.
31. Friedman SH. Neonaticide. In: Friedman SH. Family murder: pathologies of love and hate. Washington, DC: American Psychiatric Association Publishing; 2018:53-67.
32. Meltzer-Brody S, Brandon AR, Pearson B, et al. Evaluating the clinical effectiveness of a specialized perinatal psychiatry inpatient unit. Arch Womens Ment Health. 2014;17(2):107-113.
33. Klinger G, Stahl B, Fusar-Poli P, et al. Antipsychotic drugs and breastfeeding. Pediatri Endocrinol Rev. 2013;10(3):308-317.
34. Focht A, Kellner CH. Electroconvulsive therapy (ECT) in the treatment of postpartum psychosis. J ECT. 2012;28(1):31-33.
35. Heron J, McGuinness M, Blackmore ER, et al. Early postpartum symptoms in puerperal psychosis. BJOG. 2008;115(3):348-353.
36. McEwan M, Friedman SH. Violence by parents against their children: reporting of maltreatment suspicions, child protection, and risk in mental illness. Psychiatr Clin North Am. 2016;39(4):691-700.
37. Centre of Perinatal Excellence. National Perinatal Mental Health Guideline. http://cope.org.au/about/review-of-new-perinatal-mental-health-guidelines/. Published October 27, 2017. Accessed November 22, 2018.
38. National Institute for Health and Care Excellence. Antenatal and postnatal mental health overview. https://pathways.nice.org.uk/pathways/antenatal-and-postnatal-mental-health. 2017. Accessed November 22, 2018.
39. Wesseloo R, Kamperman AM, Olsen TM, et al. Risk of postpartum relapse in bipolar disorder and postpartum psychosis: a systematic review and meta-analysis. Am J Psychiatry. 2016;173(2):117-127.
40. McKnight RF, Adida M, Budge K, et al. Lithium toxicity profile: a systematic review and meta-analysis. Lancet. 2012;379(9817):721-728.
41. Munk-Olsen T, Liu X, Viktorin A, et al. Maternal and infant outcomes associated with lithium use in pregnancy: an international collaborative meta-analysis of six cohort studies. Lancet Psychiatry. 2018;5(8):644-652.
42. Prakash C, Friedman SH, Moller-Olsen C, et al. Maternal and fetal outcomes after lamotrigine use in pregnancy: a retrospective analysis from an urban maternal mental health centre in New Zealand. Psychopharmacology Bull. 2016;46(2):63-69.
43. Wesseloo R, Liu X, Clark CT, et al. Risk of postpartum episodes in women with bipolar disorder after lamotrigine or lithium use in pregnancy: a population-based cohort study. J Affect Disord. 2017;218:394-397.
44. Dolk H, Wang H, Loane M, et al. Lamotrigine use in pregnancy and risk of orofacial cleft and other congenital anomalies. Neurology. 2016;86(18):1716-1725.
45. Diav-Citrin O, Shechtman S, Zvi N, et al. Is it safe to use lamotrigine during pregnancy? A prospective comparative observational study. Birth Defects Res. 2017;109(15):1196-1203.
46. Kong L, Zhou T, Wang B, et al. The risks associated with the use of lamotrigine during pregnancy. Int J Psychiatry Clin Pract. 2018;22(1):2-5.
47. Deligiannidis KM, Byatt N, Freeman MP. Pharmacotherapy for mood disorders in pregnancy: a review of pharmacokinetic changes and clinical recommendations for therapeutic drug monitoring. J Clin Psychopharmacol. 2014;34(2):244.
48. Bogen DL, Sit D, Genovese A, et al. Three cases of lithium exposure and exclusive breastfeeding. Arch Womens Ment Health. 2012;15(1):69-72.
1. Hall L. Mother who killed baby believing she was a dwarf should not be jailed, court told. The Sydney Morning Herald. https://www.smh.com.au/national/nsw/mother-who-killed-baby-believing-she-was-a-dwarf-should-not-be-jailed-court-told-20170428-gvud4d.html. Published April 28, 2017. Accessed March 12, 2019.
2. Bergink V, Rasgon N, Wisner KL. Postpartum psychosis: madness, mania, and melancholia in motherhood. Am J Psychiatry. 2016;173(12):1179-1188.
3. Sit D, Rothschild AJ, Wisner KL. A review of postpartum psychosis. J Womens Health (Larchmt). 2006;15(4):352-368.
4. Kendell RE, Chalmers JC, Platz C. Epidemiology of puerperal psychoses. Br J Psychiatry. 1987;150(5):662-673.
5. Munk-Olsen T, Laursen TM, Mendelson T, et al. Risks and predictors of readmission for a mental disorder during the postpartum period. Arch Gen Psychiatry. 2009;66(2):189-195.
6. Bergink V, Burgerhout KM, Koorengevel KM, et al. Treatment of psychosis and mania in the postpartum period. Am J Psychiatry. 2015;172(2):115-123.
7. Wesseloo R, Kamperman AM, Munk-Olsen T, et al. Risk of postpartum relapse in bipolar disorder and postpartum psychosis: a systematic review and meta-analysis. Am J Psychiatry. 2015;173(2):117-127.
8. Wisner KL, Peindl K, Hanusa BH. Symptomatology of affective and psychotic illnesses related to childbearing. J Affect Disord. 1994;30(2):77-87.
9. Spinelli MG. Postpartum psychosis: detection of risk and management. Am J Psychiatry. 2009;166(4):405-408.
10. Fassier T, Guffon N, Acquaviva C, et al. Misdiagnosed postpartum psychosis revealing a late-onset urea cycle disorder. Am J Psychiatry. 2011;168(6):576-580.
11. Yu AYX, Moore FG. Paraneoplastic encephalitis presenting as postpartum psychosis. Psychosomatics. 2011;52(6):568-570.
12. Patil NJ, Yadav SS, Gokhale YA, et al. Primary hypoparathyroidism: psychosis in postpartum period. J Assoc Physicians India. 2010;58:506-508.
13. O’Hara MW, Schlechte JA, Lewis DA, et al. Prospective study of postpartum blues: biologic and psychosocial factors. Arch Gen Psychiatry. 1991;48(9):801-806.
14. Burt VK, Hendrick VC. Clinical manual of women’s mental health. Washington, DC. American Psychiatric Association Publishing; 2007:79-80.
15. Melzer-Brody S. Postpartum depression: what to tell patients who breast-feed. Current Psychiatry. 2008;7(5):87-95.
16. Alhusen JL, Gross D, Hayat MJ, et al. The role of mental health on maternal‐fetal attachment in low‐income women. J Obstet Gynecol Neonatal Nurs. 2012;41(6):E71-E81.
17. McLearn KT, Minkovitz CS, Strobino DM, et al. Maternal depressive symptoms at 2 to 4 months postpartum and early parenting practices. Arch Pediatr Adolesc Med. 2006;160(3):279-284.
18. Committee on Obstetric Practice. The American College of Obstetricians and Gynecologists Committee Opinion no. 630. Screening for perinatal depression. Obstet Gynecol. 2015;125(5):1268-1271.
19. Jennings KD, Ross S, Popper S. Thoughts of harming infants in depressed and nondepressed mothers. J Affect Disord. 1999;54(1-2):21-28.
20. Miller ES, Hoxha D, Wisner KL, et al. Obsessions and compulsions in postpartum women without obsessive compulsive disorder. J Womens Health. 2015;24(10):825-830.
21. Russell EJ, Fawcett JM, Mazmanian D. Risk of obsessive-compulsive disorder in pregnant and postpartum women: a meta-analysis. J Clin Psychiatry. 2013;74(4):377-385.
22. Zambaldi CF, Cantilino A, Montenegro AC, et al. Postpartum obsessive-compulsive disorder: prevalence and clinical characteristics. Compr Psychiatry. 2009;50(6):503-509.
23. Booth BD, Friedman SH, Curry S, et al. Obsessions of child murder: underrecognized manifestations of obsessive-compulsive disorder. J Am Acad Psychiatry Law. 2014;42(1):66-74.
24. Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health. 2005;8(2):77-87.
25. Samandari G, Martin SL, Kupper LL, et al. Are pregnant and postpartum women: at increased risk for violent death? Suicide and homicide findings from North Carolina. Matern Child Health J. 2011;15(5):660-669.
26. Friedman SH, Sorrentino R. Commentary: postpartum psychosis, infanticide, and insanity—implications for forensic psychiatry. J Am Acad Psychiatry Law. 2012;40(3):326-332.
27. Friedman SH, Resnick PJ. Child murder by mothers: patterns and prevention. World Psychiatry. 2007;6(3):137-141.
28. Friedman SH, Hrouda DR, Holden CE, et al. Filicide-suicide: common factors in parents who kill their children and themselves. J Am Acad Psychiatry Law. 2005;33(4):496-504.
29. Chandra PS, Venkatasubramanian G, Thomas T. Infanticidal ideas and infanticidal behavior in Indian women with severe postpartum psychiatric disorders. J Nerv Ment Dis. 2002;190(7):457-461.
30. Jones I, Chandra PS, Dazzan P, et al. Bipolar disorder, affective psychosis, and schizophrenia in pregnancy and the post-partum period. Lancet. 2014;384(9956):1789-1799.
31. Friedman SH. Neonaticide. In: Friedman SH. Family murder: pathologies of love and hate. Washington, DC: American Psychiatric Association Publishing; 2018:53-67.
32. Meltzer-Brody S, Brandon AR, Pearson B, et al. Evaluating the clinical effectiveness of a specialized perinatal psychiatry inpatient unit. Arch Womens Ment Health. 2014;17(2):107-113.
33. Klinger G, Stahl B, Fusar-Poli P, et al. Antipsychotic drugs and breastfeeding. Pediatri Endocrinol Rev. 2013;10(3):308-317.
34. Focht A, Kellner CH. Electroconvulsive therapy (ECT) in the treatment of postpartum psychosis. J ECT. 2012;28(1):31-33.
35. Heron J, McGuinness M, Blackmore ER, et al. Early postpartum symptoms in puerperal psychosis. BJOG. 2008;115(3):348-353.
36. McEwan M, Friedman SH. Violence by parents against their children: reporting of maltreatment suspicions, child protection, and risk in mental illness. Psychiatr Clin North Am. 2016;39(4):691-700.
37. Centre of Perinatal Excellence. National Perinatal Mental Health Guideline. http://cope.org.au/about/review-of-new-perinatal-mental-health-guidelines/. Published October 27, 2017. Accessed November 22, 2018.
38. National Institute for Health and Care Excellence. Antenatal and postnatal mental health overview. https://pathways.nice.org.uk/pathways/antenatal-and-postnatal-mental-health. 2017. Accessed November 22, 2018.
39. Wesseloo R, Kamperman AM, Olsen TM, et al. Risk of postpartum relapse in bipolar disorder and postpartum psychosis: a systematic review and meta-analysis. Am J Psychiatry. 2016;173(2):117-127.
40. McKnight RF, Adida M, Budge K, et al. Lithium toxicity profile: a systematic review and meta-analysis. Lancet. 2012;379(9817):721-728.
41. Munk-Olsen T, Liu X, Viktorin A, et al. Maternal and infant outcomes associated with lithium use in pregnancy: an international collaborative meta-analysis of six cohort studies. Lancet Psychiatry. 2018;5(8):644-652.
42. Prakash C, Friedman SH, Moller-Olsen C, et al. Maternal and fetal outcomes after lamotrigine use in pregnancy: a retrospective analysis from an urban maternal mental health centre in New Zealand. Psychopharmacology Bull. 2016;46(2):63-69.
43. Wesseloo R, Liu X, Clark CT, et al. Risk of postpartum episodes in women with bipolar disorder after lamotrigine or lithium use in pregnancy: a population-based cohort study. J Affect Disord. 2017;218:394-397.
44. Dolk H, Wang H, Loane M, et al. Lamotrigine use in pregnancy and risk of orofacial cleft and other congenital anomalies. Neurology. 2016;86(18):1716-1725.
45. Diav-Citrin O, Shechtman S, Zvi N, et al. Is it safe to use lamotrigine during pregnancy? A prospective comparative observational study. Birth Defects Res. 2017;109(15):1196-1203.
46. Kong L, Zhou T, Wang B, et al. The risks associated with the use of lamotrigine during pregnancy. Int J Psychiatry Clin Pract. 2018;22(1):2-5.
47. Deligiannidis KM, Byatt N, Freeman MP. Pharmacotherapy for mood disorders in pregnancy: a review of pharmacokinetic changes and clinical recommendations for therapeutic drug monitoring. J Clin Psychopharmacol. 2014;34(2):244.
48. Bogen DL, Sit D, Genovese A, et al. Three cases of lithium exposure and exclusive breastfeeding. Arch Womens Ment Health. 2012;15(1):69-72.
Organizing the P in a SOAP note
The Subjective, Objective, Assessment, Plan (SOAP) format of the progress note is widely recognized by clinicians in many specialties, including p
The Plan section should be organized in a way that is systematic and relevant across many psychiatric settings, including outpatient, inpatient, emergency room, jail, pediatric, geriatric, addiction, and consultation-liaison. To best accomplish this, I have designed a format for this section that consists of 6 categories:
1. Safety: Which safety issues need to be addressed?
Examples: If your patient is an inpatient, what precautions are required? If outpatient, Tarasoff? Involuntary hold? Police presence? Child or Adult Protective Services? Access to a firearm?
2. Collateral: Would it be helpful to obtain collateral information from any source?
Examples: Family? Friend? Caregiver? Teacher? Primary care clinician? Therapist? Past medical or psychiatric records?
3. Medical: Are there any medical tests or resources to consider?
Continue to: Examples...
Examples: Laboratory studies or imaging? Consult with a specialist from another field? Nursing orders?
4. Nonpharmacologic: What interventions or assessments would be helpful?
Examples: Psychotherapy? Cognitive testing? Social work? Case manager? Housing assistance? Job coach?
5. Pharmacologic: What interventions or assessments would be helpful? (I placed this category fifth to slow myself down and consider other strategies before quickly jumping to prescribe a medication.)
Examples: Medication? Long-acting injectable? Check pill count? Prescription drug monitoring program?
Continue to: 6. Disposition/follow-up...
6. Disposition/follow-up: What is the disposition/follow-up plan?
Examples: If outpatient, what is the time frame? If inpatient or an emergency room, when should the patient be discharged?
Using these 6 categories in the P section of my SOAP notes has helped me stay organized and think holistically about each patient I assess and treat. I hope other clinicians find this format helpful.
1. Pearce PF, Ferguson LA, George GS, et al. The essential SOAP note in an EHR age. Nurse Pract. 2016;41(2):29-36.
2. Foreman T, Dickstein LJ, Garakani A, et al (eds). A resident’s guide to surviving psychiatric training, 3rd ed. Washington, DC: American Psychiatric Association; 2015.
3. Aftab A, Latorre S, Nagle-Yang S. Effective note-writing: a primer for psychiatry residents. Psychiatric Times. http://www.psychiatrictimes.com/couch-crisis/effective-note-writing-primer-psychiatry-residents. Published January 13, 2017. Accessed August 20, 2018.
The Subjective, Objective, Assessment, Plan (SOAP) format of the progress note is widely recognized by clinicians in many specialties, including p
The Plan section should be organized in a way that is systematic and relevant across many psychiatric settings, including outpatient, inpatient, emergency room, jail, pediatric, geriatric, addiction, and consultation-liaison. To best accomplish this, I have designed a format for this section that consists of 6 categories:
1. Safety: Which safety issues need to be addressed?
Examples: If your patient is an inpatient, what precautions are required? If outpatient, Tarasoff? Involuntary hold? Police presence? Child or Adult Protective Services? Access to a firearm?
2. Collateral: Would it be helpful to obtain collateral information from any source?
Examples: Family? Friend? Caregiver? Teacher? Primary care clinician? Therapist? Past medical or psychiatric records?
3. Medical: Are there any medical tests or resources to consider?
Continue to: Examples...
Examples: Laboratory studies or imaging? Consult with a specialist from another field? Nursing orders?
4. Nonpharmacologic: What interventions or assessments would be helpful?
Examples: Psychotherapy? Cognitive testing? Social work? Case manager? Housing assistance? Job coach?
5. Pharmacologic: What interventions or assessments would be helpful? (I placed this category fifth to slow myself down and consider other strategies before quickly jumping to prescribe a medication.)
Examples: Medication? Long-acting injectable? Check pill count? Prescription drug monitoring program?
Continue to: 6. Disposition/follow-up...
6. Disposition/follow-up: What is the disposition/follow-up plan?
Examples: If outpatient, what is the time frame? If inpatient or an emergency room, when should the patient be discharged?
Using these 6 categories in the P section of my SOAP notes has helped me stay organized and think holistically about each patient I assess and treat. I hope other clinicians find this format helpful.
The Subjective, Objective, Assessment, Plan (SOAP) format of the progress note is widely recognized by clinicians in many specialties, including p
The Plan section should be organized in a way that is systematic and relevant across many psychiatric settings, including outpatient, inpatient, emergency room, jail, pediatric, geriatric, addiction, and consultation-liaison. To best accomplish this, I have designed a format for this section that consists of 6 categories:
1. Safety: Which safety issues need to be addressed?
Examples: If your patient is an inpatient, what precautions are required? If outpatient, Tarasoff? Involuntary hold? Police presence? Child or Adult Protective Services? Access to a firearm?
2. Collateral: Would it be helpful to obtain collateral information from any source?
Examples: Family? Friend? Caregiver? Teacher? Primary care clinician? Therapist? Past medical or psychiatric records?
3. Medical: Are there any medical tests or resources to consider?
Continue to: Examples...
Examples: Laboratory studies or imaging? Consult with a specialist from another field? Nursing orders?
4. Nonpharmacologic: What interventions or assessments would be helpful?
Examples: Psychotherapy? Cognitive testing? Social work? Case manager? Housing assistance? Job coach?
5. Pharmacologic: What interventions or assessments would be helpful? (I placed this category fifth to slow myself down and consider other strategies before quickly jumping to prescribe a medication.)
Examples: Medication? Long-acting injectable? Check pill count? Prescription drug monitoring program?
Continue to: 6. Disposition/follow-up...
6. Disposition/follow-up: What is the disposition/follow-up plan?
Examples: If outpatient, what is the time frame? If inpatient or an emergency room, when should the patient be discharged?
Using these 6 categories in the P section of my SOAP notes has helped me stay organized and think holistically about each patient I assess and treat. I hope other clinicians find this format helpful.
1. Pearce PF, Ferguson LA, George GS, et al. The essential SOAP note in an EHR age. Nurse Pract. 2016;41(2):29-36.
2. Foreman T, Dickstein LJ, Garakani A, et al (eds). A resident’s guide to surviving psychiatric training, 3rd ed. Washington, DC: American Psychiatric Association; 2015.
3. Aftab A, Latorre S, Nagle-Yang S. Effective note-writing: a primer for psychiatry residents. Psychiatric Times. http://www.psychiatrictimes.com/couch-crisis/effective-note-writing-primer-psychiatry-residents. Published January 13, 2017. Accessed August 20, 2018.
1. Pearce PF, Ferguson LA, George GS, et al. The essential SOAP note in an EHR age. Nurse Pract. 2016;41(2):29-36.
2. Foreman T, Dickstein LJ, Garakani A, et al (eds). A resident’s guide to surviving psychiatric training, 3rd ed. Washington, DC: American Psychiatric Association; 2015.
3. Aftab A, Latorre S, Nagle-Yang S. Effective note-writing: a primer for psychiatry residents. Psychiatric Times. http://www.psychiatrictimes.com/couch-crisis/effective-note-writing-primer-psychiatry-residents. Published January 13, 2017. Accessed August 20, 2018.
COMBS: Feeling positive about negative symptoms of schizophrenia
Negative symptoms of schizophrenia—such as social withdrawal, avolition, avoidance, lack of spontaneity, anhedonia, poverty of speech, and blunted affect—often persist after successful treatment of positive symptoms, such as hallucinations and delusions.1 Negative symptoms can be debilitating and are associated with poor social and occupational outcomes, as well as cognitive dysfunction. Currently, treatments for negative symptoms are not nearly as effective as treatments for positive symptoms. The mnemonic COMBS can be used to easily recall 3 treatment modalities often used to address negative symptoms.
COgnitive-behavioral therapy
Cognitive-behavioral therapy (CBT) and other psychosocial therapies derived from it, such as social skills training, recovery-oriented cognitive therapy, motivation and enhancement therapy, and cognitive-behavioral social skills training (CBSST), have shown to be effective for treating negative symptoms.2 In a study of 149 patients with schizophrenia, CBSST reduced symptoms of avolition and apathy and improved functioning outcomes.2
Medications
Antipsychotics. Although second-generation antipsychotics (SGAs) were initially promising, accumulating clinical experience and research have shown that these agents have limited efficacy for treating negative symptoms.1 Unlike first-generation antipsychotics, SGAs do not cause affective blunting, and are effective at treating depressive symptoms; however, depressive symptoms can sometimes be difficult to distinguish from negative symptoms. Improvement of depressive symptoms observed with SGA treatment could be mistakenly interpreted as alleviation of negative symptoms; however, clinical trials that focused specifically on treating negative symptoms have found no specific efficacy of SGAs.1
Antidepressants. Although clinical trials and meta-analyses have had mixed results,1 antidepressants appear to be safe add-on treatments with small efficacy for negative symptoms.
Anticonvulsants have long been used as augmentation to antipsychotics for patients with treatment-resistant schizophrenia; however, there is no evidence that these medications can improve negative symptoms.1
Stimulants. There is no strong evidence that stimulants could be an efficacious treatment for negative symptoms.1
Other pharmacologic agents,1 such as acetylcholine-related medications, oxytocin, and medications with a mechanism of action that is related to an inflammatory response and immunologic pathways (ie, minocycline), are being evaluated for treating negative symptoms. Research into the efficacy of glutamate-related agents also appears to be continuing.1
Continue to: Brain Stimulation therapies
Brain Stimulation therapies
Transcranial magnetic stimulation (TMS), transdirect current stimulation (tDCS), vagus nerve stimulation, and deep brain stimulation have been evaluated for treating negative symptoms. A recent meta-analysis of randomized controlled trials comparing the effects of brain stimulation with sham interventions in patients with schizophrenia found that TMS and tDCS that targeted the left dorsolateral prefrontal cortex effectively reduced the severity of negative symptoms.3
The Table1-3 summarizes available treatments for negative symptoms of schizophrenia and their efficacies. Although research investigating the improvement of negative symptoms is currently insufficient, CBT-related therapies and antidepressants appear to be helpful. For more information, see “Treating negative symptoms of schizophrenia” (C
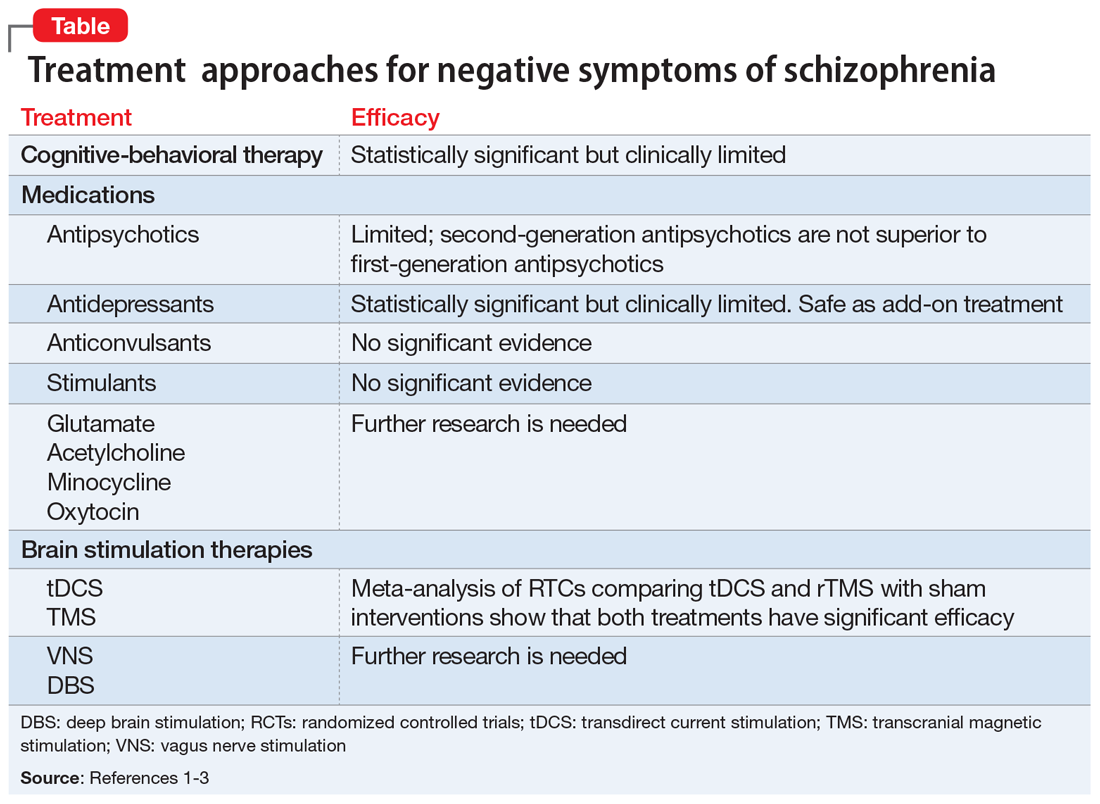
1. Remington G, Foussias G, Fervaha G, et al. Treating negative symptoms in schizophrenia: an update. Curr Treat Options Psychiatry. 2016;3:133-150.
2. Granholm E, Holden J, Worley M. Improvement in negative symptoms and functioning in cognitive-behavioral social skills training for schizophrenia: mediation by defeatist performance attitudes and asocial beliefs. Schizophr Bull. 2018;44(3):653-661.
3. Kennedy NI, Lee WH. Efficacy of non-invasive brain stimulation on the symptom dimensions of schizophrenia: a meta-analysis of randomized controlled trials. Eur Psychiatry. 2018;49:69-77.
Negative symptoms of schizophrenia—such as social withdrawal, avolition, avoidance, lack of spontaneity, anhedonia, poverty of speech, and blunted affect—often persist after successful treatment of positive symptoms, such as hallucinations and delusions.1 Negative symptoms can be debilitating and are associated with poor social and occupational outcomes, as well as cognitive dysfunction. Currently, treatments for negative symptoms are not nearly as effective as treatments for positive symptoms. The mnemonic COMBS can be used to easily recall 3 treatment modalities often used to address negative symptoms.
COgnitive-behavioral therapy
Cognitive-behavioral therapy (CBT) and other psychosocial therapies derived from it, such as social skills training, recovery-oriented cognitive therapy, motivation and enhancement therapy, and cognitive-behavioral social skills training (CBSST), have shown to be effective for treating negative symptoms.2 In a study of 149 patients with schizophrenia, CBSST reduced symptoms of avolition and apathy and improved functioning outcomes.2
Medications
Antipsychotics. Although second-generation antipsychotics (SGAs) were initially promising, accumulating clinical experience and research have shown that these agents have limited efficacy for treating negative symptoms.1 Unlike first-generation antipsychotics, SGAs do not cause affective blunting, and are effective at treating depressive symptoms; however, depressive symptoms can sometimes be difficult to distinguish from negative symptoms. Improvement of depressive symptoms observed with SGA treatment could be mistakenly interpreted as alleviation of negative symptoms; however, clinical trials that focused specifically on treating negative symptoms have found no specific efficacy of SGAs.1
Antidepressants. Although clinical trials and meta-analyses have had mixed results,1 antidepressants appear to be safe add-on treatments with small efficacy for negative symptoms.
Anticonvulsants have long been used as augmentation to antipsychotics for patients with treatment-resistant schizophrenia; however, there is no evidence that these medications can improve negative symptoms.1
Stimulants. There is no strong evidence that stimulants could be an efficacious treatment for negative symptoms.1
Other pharmacologic agents,1 such as acetylcholine-related medications, oxytocin, and medications with a mechanism of action that is related to an inflammatory response and immunologic pathways (ie, minocycline), are being evaluated for treating negative symptoms. Research into the efficacy of glutamate-related agents also appears to be continuing.1
Continue to: Brain Stimulation therapies
Brain Stimulation therapies
Transcranial magnetic stimulation (TMS), transdirect current stimulation (tDCS), vagus nerve stimulation, and deep brain stimulation have been evaluated for treating negative symptoms. A recent meta-analysis of randomized controlled trials comparing the effects of brain stimulation with sham interventions in patients with schizophrenia found that TMS and tDCS that targeted the left dorsolateral prefrontal cortex effectively reduced the severity of negative symptoms.3
The Table1-3 summarizes available treatments for negative symptoms of schizophrenia and their efficacies. Although research investigating the improvement of negative symptoms is currently insufficient, CBT-related therapies and antidepressants appear to be helpful. For more information, see “Treating negative symptoms of schizophrenia” (C
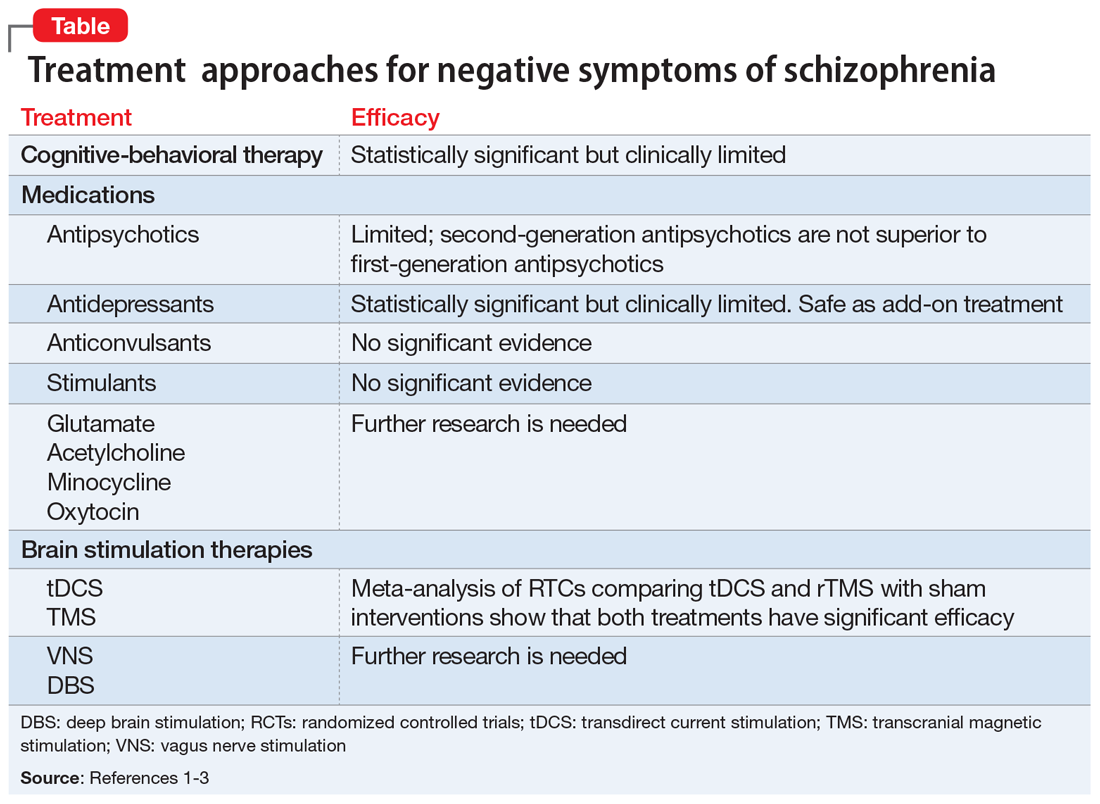
Negative symptoms of schizophrenia—such as social withdrawal, avolition, avoidance, lack of spontaneity, anhedonia, poverty of speech, and blunted affect—often persist after successful treatment of positive symptoms, such as hallucinations and delusions.1 Negative symptoms can be debilitating and are associated with poor social and occupational outcomes, as well as cognitive dysfunction. Currently, treatments for negative symptoms are not nearly as effective as treatments for positive symptoms. The mnemonic COMBS can be used to easily recall 3 treatment modalities often used to address negative symptoms.
COgnitive-behavioral therapy
Cognitive-behavioral therapy (CBT) and other psychosocial therapies derived from it, such as social skills training, recovery-oriented cognitive therapy, motivation and enhancement therapy, and cognitive-behavioral social skills training (CBSST), have shown to be effective for treating negative symptoms.2 In a study of 149 patients with schizophrenia, CBSST reduced symptoms of avolition and apathy and improved functioning outcomes.2
Medications
Antipsychotics. Although second-generation antipsychotics (SGAs) were initially promising, accumulating clinical experience and research have shown that these agents have limited efficacy for treating negative symptoms.1 Unlike first-generation antipsychotics, SGAs do not cause affective blunting, and are effective at treating depressive symptoms; however, depressive symptoms can sometimes be difficult to distinguish from negative symptoms. Improvement of depressive symptoms observed with SGA treatment could be mistakenly interpreted as alleviation of negative symptoms; however, clinical trials that focused specifically on treating negative symptoms have found no specific efficacy of SGAs.1
Antidepressants. Although clinical trials and meta-analyses have had mixed results,1 antidepressants appear to be safe add-on treatments with small efficacy for negative symptoms.
Anticonvulsants have long been used as augmentation to antipsychotics for patients with treatment-resistant schizophrenia; however, there is no evidence that these medications can improve negative symptoms.1
Stimulants. There is no strong evidence that stimulants could be an efficacious treatment for negative symptoms.1
Other pharmacologic agents,1 such as acetylcholine-related medications, oxytocin, and medications with a mechanism of action that is related to an inflammatory response and immunologic pathways (ie, minocycline), are being evaluated for treating negative symptoms. Research into the efficacy of glutamate-related agents also appears to be continuing.1
Continue to: Brain Stimulation therapies
Brain Stimulation therapies
Transcranial magnetic stimulation (TMS), transdirect current stimulation (tDCS), vagus nerve stimulation, and deep brain stimulation have been evaluated for treating negative symptoms. A recent meta-analysis of randomized controlled trials comparing the effects of brain stimulation with sham interventions in patients with schizophrenia found that TMS and tDCS that targeted the left dorsolateral prefrontal cortex effectively reduced the severity of negative symptoms.3
The Table1-3 summarizes available treatments for negative symptoms of schizophrenia and their efficacies. Although research investigating the improvement of negative symptoms is currently insufficient, CBT-related therapies and antidepressants appear to be helpful. For more information, see “Treating negative symptoms of schizophrenia” (C
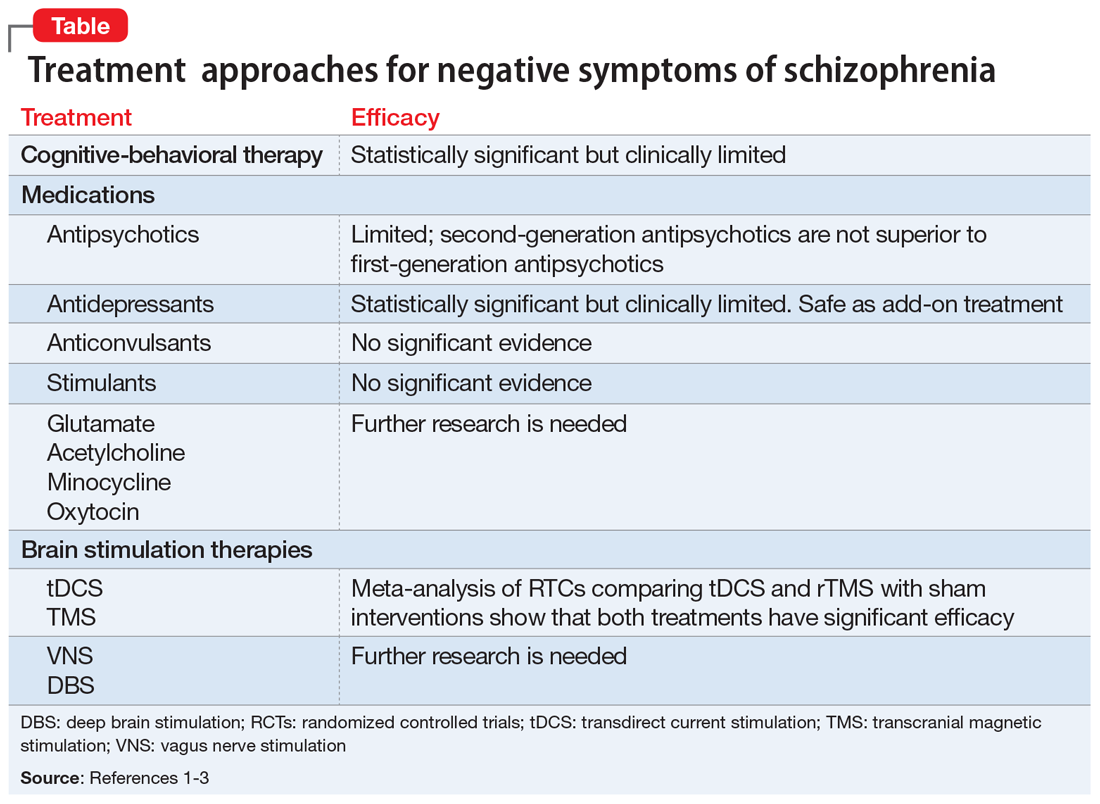
1. Remington G, Foussias G, Fervaha G, et al. Treating negative symptoms in schizophrenia: an update. Curr Treat Options Psychiatry. 2016;3:133-150.
2. Granholm E, Holden J, Worley M. Improvement in negative symptoms and functioning in cognitive-behavioral social skills training for schizophrenia: mediation by defeatist performance attitudes and asocial beliefs. Schizophr Bull. 2018;44(3):653-661.
3. Kennedy NI, Lee WH. Efficacy of non-invasive brain stimulation on the symptom dimensions of schizophrenia: a meta-analysis of randomized controlled trials. Eur Psychiatry. 2018;49:69-77.
1. Remington G, Foussias G, Fervaha G, et al. Treating negative symptoms in schizophrenia: an update. Curr Treat Options Psychiatry. 2016;3:133-150.
2. Granholm E, Holden J, Worley M. Improvement in negative symptoms and functioning in cognitive-behavioral social skills training for schizophrenia: mediation by defeatist performance attitudes and asocial beliefs. Schizophr Bull. 2018;44(3):653-661.
3. Kennedy NI, Lee WH. Efficacy of non-invasive brain stimulation on the symptom dimensions of schizophrenia: a meta-analysis of randomized controlled trials. Eur Psychiatry. 2018;49:69-77.
The angry disciple
CASE Disorganized thoughts and grandiose delusions
Mr. J, age 54, presents to the psychiatric emergency department (ED) with agitation and disruptive behavior. He claims that he is “the son of Jesus Christ” and has to travel to the Middle East to be baptized. Mr. J is irritable, shouting, and threatening staff members. He receives
The next day, he is calm and cooperative, but continues to express the same religious delusions. Mr. J is admitted to the psychiatric inpatient unit for further evaluation.
On the unit, Mr. J is pleasant and cooperative, but tangential in thought process. He reports he was “saved” by God 4 years ago, and that God communicates with him through music. Despite this, he denies having auditory or visual hallucinations.
Approximately 3 months earlier, Mr. J had stopped working and left his home and family in another state to pursue his “mission” of being baptized in the Middle East. Mr. J has been homeless since then. Despite that, he reports that his mood is “great” and denies any recent changes in mood, sleep, appetite, energy level, or psychomotor agitation. Although no formal cognitive testing is performed, Mr. J is alert and oriented to person, place, and time with intact remote and recent memory, no language deficits, and no lapses in concentration or attention throughout interview.
Mr. J says he has been drinking alcohol regularly throughout his adult life, often a few times per week, up to “a case and a half” of beer at times. He claims he’s had multiple periods of sobriety but denies having experienced withdrawal symptoms during those times. Mr. J reports 1 prior psychiatric hospitalization 25 years ago after attempting suicide by overdose following the loss of a loved one. At that time, he was diagnosed with posttraumatic stress disorder (PTSD). During this admission, he denies having any symptoms of PTSD or periods of mania or depression, and he has not undergone psychiatric treatment since he had been diagnosed with PTSD. He denies any family history of psychiatric illness as well as any medical comorbidities or medication use.
[polldaddy:10279202]
The authors’ observations
Mr. J’s presentation had a wide differential diagnosis (Table 1). The initial agitation Mr. J displayed in the psychiatric ED was likely secondary to acute alcohol intoxication, given that he was subsequently pleasant, calm, and cooperative after the alcohol was metabolized. Despite this, Mr. J continued to demonstrate delusions of a religious and somewhat grandiose nature with tangential thought processes, which made substance-induced psychosis less likely to be the sole diagnosis. Although it is possible to develop psychotic symptoms due to severe alcohol withdrawal (alcoholic hallucinosis), Mr. J’s vital signs remained stable, and he demonstrated no other signs or symptoms of withdrawal throughout his hospitalization. His presentation also did not fit that of delirium tremens because he was not confused or disoriented, and did not demonstrate perceptual disturbance.
While delusions were the most prominent feature of Mr. J’s apparent psychosis, the presence of disorganized thought processes and impaired functioning, as evidenced by Mr. J’s unemployment and recent homelessness, were more consistent with a primary psychotic disorder than a delusional disorder.1
Continue to: Mr. J began to exhibit...
Mr. J began to exhibit these psychotic symptoms in his early 50s; because the average age of onset of schizophrenia for males is approximately age 20 to 25, the likelihood of his presentation being the result of a primary psychotic disorder was low.1 Although less common, it was possible that Mr. J had developed late-onset schizophrenia, where the first episode typically occurs after approximately age 40 to 45. Mr. J also described that he was in a “great” mood but had grandiose delusions and had made recent impulsive decisions, which suggests there was a possible mood component to his presentation and a potential diagnosis of schizoaffective disorder or bipolar disorder with psychotic symptoms. However, before any of these diagnoses could be made, a medical or neurologic condition that could cause his symptoms needed to be investigated and ruled out. Further collateral information regarding Mr. J’s history and timeline of symptoms was required.
EVALUATION Family history reveals clues
All laboratory studies completed during Mr. J’s hospitalization are unremarkable, including complete blood count, basic metabolic panel, hepatic function panel, gamma-glutamyl transferase test, magnesium, phosphate, thyroid-stimulating hormone, vitamin B12, thiamine, folate, urinalysis, and urine drug screen. Mr. J does not undergo any head imaging.
Mr. J has not been in touch with his family since leaving his home approximately 3 months before he presented to the ED, and he gives consent for the inpatient team to attempt to contact them. One week into hospitalization, Mr. J’s sibling informs the team of a family history of genetically confirmed Huntington’s disease (HD), with psychiatric symptoms preceding the onset of motor symptoms in multiple first-degree relatives. His family says that before Mr. J first developed delusions 4 years ago, he had not exhibited any psychotic symptoms during periods of alcohol use or sobriety.
Mr. J does not demonstrate any overt movement symptoms on the unit and denies noting any rigidity, change in gait, or abnormal/uncontrolled movements. The inpatient psychiatric team consults neurology and a full neurologic evaluation is performed. The results are unremarkable outside of his psychiatric symptoms; specifically, Mr. J does not demonstrate even subtle motor signs or cognitive impairment. Given Mr. J’s family history, unremarkable lab findings, and age at presentation, the neurology team and inpatient psychiatry team suspect that his psychosis is likely an early presentation of HD.
[polldaddy:10279212]
The authors’ observations
Genetics of Huntington’s disease
Huntington’s disease is an autosomal dominant neurodegenerative disorder caused by expansion of cytosine-adenine-guanine (CAG) trinucleotide repeats within the Huntingtin (HTT) gene on chromosome 4, which codes for the huntingtin protein.2,3 While the function of “normal” huntingtin protein is not fully understood, it is known that CAG repeat expansion in the HTT gene of >35 repeats codes for a mutant huntingtin protein.2,3 The mutant huntingtin protein causes progressive neuronal loss in the basal ganglia and striatum, resulting in the clinical Huntington’s phenotype.3 Notably, the patient’s age at disease onset is inversely correlated with the number of repeats. For example, expansions of approximately 40 to 50 CAG repeats often result in adult-onset HD, while expansions of >60 repeats are typically associated with juvenile-onset HD (before age 20). CAG repeat lengths of approximately 36 to 39 demonstrate reduced penetrance, with some individuals developing symptomatic HD while others do not.2 Instability of the CAG repeat expansion can result in genetic “anticipation,” wherein repeat length increases between generations, causing earlier age of onset in affected offspring. Genetic anticipation in HD occurs more frequently in paternal transmission—approximately 80% to 90% of juvenile HD cases are inherited paternally, at times with the number of CAG repeats exceeding 200.3
Continue to: Psychiatric manifestations of Huntington's disease
Psychiatric manifestations of Huntington’s disease
Huntington’s disease is characterized by motor, cognitive, and behavioral disturbances (Table 22,4). Motor symptoms include a characteristic and well-recognized chorea, often predominating earlier in HD, that progresses to rigidity, spasticity, and bradykinesia later in the disease course.2 Cognitive impairments develop in a similar progressive manner and can often precede the onset of motor symptoms, beginning with early executive dysfunction. Thinking often becomes more rigid and less efficient, causing difficulty with multi-tasking and concentration, and often progressing to subcortical dementia.2
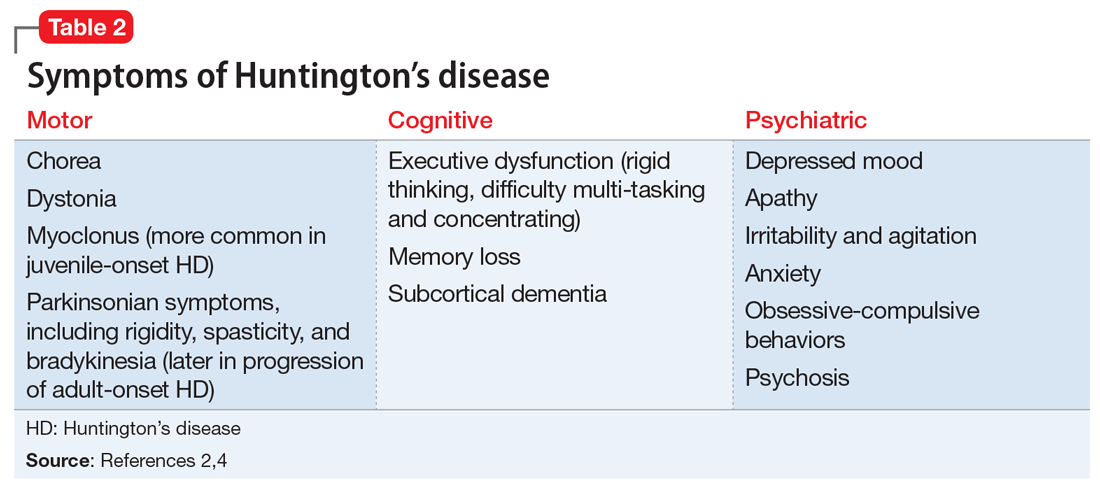
Psychiatric symptoms have long been recognized as a feature of HD; the estimated lifetime prevalence in patients with HD ranges from approximately 33% to 76%.4 Depressed mood, anxiety, irritability, and apathy are the most commonly reported symptoms, while a smaller percentage of patients with HD can experience obsessive-compulsive disorder (10% to 52%) or psychotic symptoms (3% to 11%).4 A more specific schizophrenia-like psychosis occurs in approximately 3% to 6% of patients, and often is a paranoid type.5,6 Positive psychotic symptoms, such as hallucinations and delusions, typically become less overt as HD progresses and cognitive impairments worsen.7
Although the onset of motor symptoms leads to diagnosis in the majority of patients with HD, many patients present with psychiatric symptoms—most commonly depression—prior to motor symptoms.8 An increasing body of literature details instances of psychosis preceding motor symptom onset by up to 10 years.6,9-12 In many of these cases, the patient has a family history of HD-associated psychosis. Family history is a major risk factor for HD-associated psychosis, as is early-onset HD.7,9
TREATMENT Antipsychotics result in some improvement
On Day 1 or 2, Mr. J is started on risperidone, 1 mg twice daily, to manage his symptoms. He shows incremental improvement in thought organization. Although his religious and grandiose delusions persist, they become less fixed, and he is able to take the team’s suggestion that he reconnect with his family.
Mr. J is aware of his family history of HD and acknowledges that multiple relatives had early psychiatric manifestations of HD. Despite this, he still has difficulty recognizing any connection between other family members’ presentation and his own. The psychiatry and neurology teams discuss the process, ethics, and implications of genetic testing for HD with Mr. J; however, he is ambivalent regarding genetic testing, and states he would consider it after discussing it with his family.
Continue to: The neurology team recommends...
The neurology team recommends against imaging for Mr. J because HD-related changes are not typically seen until later in the disease progression. On Day 9, they recommend changing from risperidone to quetiapine (50 mg every night at bedtime) due to evidence of its effectiveness specifically for treating behavioral symptoms of HD.13
While receiving quetiapine, Mr. J experiences significant drowsiness. Because he had experienced improvement in thought organization while he was receiving risperidone, he is switched back to risperidone.
[polldaddy:10279220]
The authors’ observations
Currently, no treatments are available to prevent the development or progression of HD. However, symptomatic treatment of motor and behavioral disturbances can lead to functional improvement and improved quality of life for individuals affected by HD.
There are no extensive clinical trials to date, but multiple case reports and studies have shown second-generation antipsychotics (SGAs), including quetiapine, olanzapine,
OUTCOME Discharge despite persistent delusions
Mr. J’s religious and grandiose delusions continue throughout hospitalization despite treatment with antipsychotics. However, because he remains calm and cooperative and demonstrates improvement in thought organization, he is deemed safe for discharge and instructed to continue risperidone. The team coordinates with Mr. J’s family to arrange transportation home and outpatient neurology follow-up.
Bottom Line
Psychiatric manifestations, including psychosis, are prominent symptoms of Huntington’s disease (HD) and may precede the onset of more readily recognized motor symptoms. This poses a diagnostic challenge, and clinicians should remain cognizant of this possibility, especially in patients with a family history of HD-associated psychosis.
Related Resources
- Huntington’s Disease Society of America. http://hdsa.org.
- National Institute of Neurological Disorders and Stroke. Huntington’s disease information page: What research is being done? https://www.ninds.nih.gov/Disorders/All-Disorders/Huntingtons-Disease-Information-Page.
- Scher LM. How to target psychiatric symptoms of Huntington’s disease. Current Psychiatry. 2012;11(9):34-39.
Drug Brand Names
Aripiprazole • Abilify
Clozapine • Clozaril
Haloperidol • Haldol
Olanzapine • Zyprexa
Quetiapine • Seroquel
Risperidone • Risperdal
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
2. Novak MJ, Tabrizi SJ. Huntington’s disease: clinical presentation and treatment. Int Rev Neurobiol. 2011;98:297-323.
3. Reiner A, Dragatsis I, Dietrich P. Genetics and neuropathology of Huntington’s disease. Int Rev Neurobiol. 2011;98:325-372.
4. van Duijn E, Kingma EM, Van der mast RC. Psychopathology in verified Huntington’s disease gene carriers. J Neuropsychiatry Clin Neurosci. 2007;19(4):441-448.
5. Naarding P, Kremer HP, Zitman FG. Huntington’s disease: a review of the literature on prevalence and treatment of neuropsychiatric phenomena. Eur Psychiatry. 2001;16(8):439-445.
6. Xu C, Yogaratnam J, Tan N, et al. Psychosis, treatment emergent extrapyramidal events, and subsequent onset of Huntington’s disease: a case report and review of the literature. Clin Psychopharmacol Neurosci. 2016;14(3):302-304.
7. Mendez MF. Huntington’s disease: update and review of neuropsychiatric aspects. Int J Psychiatry Med. 1994;24(3):189-208.
8. Di Maio L, Squitieri F, Napolitano G, et al. Onset symptoms in 510 patients with Huntington’s disease. J Med Genet. 1993;30(4):289-292.
9. Jauhar S, Ritchie S. Psychiatric and behavioural manifestations of Huntington’s disease. Adv Psychiatr Treat. 2010;16(3):168-175.
10. Nagel M, Rumpf HJ, Kasten M. Acute psychosis in a verified Huntington disease gene carrier with subtle motor signs: psychiatric criteria should be considered for the diagnosis. Gen Hosp Psychiatry. 2014;36(3):361.e3-e4. doi: 10.1016/j.genhosppsych.2014.01.008.
11. Corrêa BB, Xavier M, Guimarães J. Association of Huntington’s disease and schizophrenia-like psychosis in a Huntington’s disease pedigree. Clin Pract Epidemiol Ment Health. 2006;2:1.
12. Ding J, Gadit AM. Psychosis with Huntington’s disease: role of antipsychotic medications. BMJ Case Rep. 2014: bcr2013202625. doi: 10.1136/bcr-2013-202625.
13. Alpay M, Koroshetz WJ. Quetiapine in the treatment of behavioral disturbances in patients with Huntington’s disease. Psychosomatics. 2006;47(1):70-72.
14. Duff K, Beglinger LJ, O’Rourke ME, et al. Risperidone and the treatment of psychiatric, motor, and cognitive symptoms in Huntington’s disease. Ann Clin Psychiatry. 2008;20(1):1-3.
15. Paleacu D, Anca M, Giladi N. Olanzapine in Huntington’s disease. Acta Neurol Scand. 2002;105(6):441-444.
16. Lin W, Chou Y. Aripiprazole effects on psychosis and chorea in a patient with Huntington’s disease. Am J Psychiatry. 2008;165(9):1207-1208.
17. van Vugt JP, Siesling S, Vergeer M, et al. Clozapine versus placebo in Huntington’s disease: a double blind randomized comparative study. J Neurol Neurosurg Psychiatr. 1997;63(1):35-39.
CASE Disorganized thoughts and grandiose delusions
Mr. J, age 54, presents to the psychiatric emergency department (ED) with agitation and disruptive behavior. He claims that he is “the son of Jesus Christ” and has to travel to the Middle East to be baptized. Mr. J is irritable, shouting, and threatening staff members. He receives
The next day, he is calm and cooperative, but continues to express the same religious delusions. Mr. J is admitted to the psychiatric inpatient unit for further evaluation.
On the unit, Mr. J is pleasant and cooperative, but tangential in thought process. He reports he was “saved” by God 4 years ago, and that God communicates with him through music. Despite this, he denies having auditory or visual hallucinations.
Approximately 3 months earlier, Mr. J had stopped working and left his home and family in another state to pursue his “mission” of being baptized in the Middle East. Mr. J has been homeless since then. Despite that, he reports that his mood is “great” and denies any recent changes in mood, sleep, appetite, energy level, or psychomotor agitation. Although no formal cognitive testing is performed, Mr. J is alert and oriented to person, place, and time with intact remote and recent memory, no language deficits, and no lapses in concentration or attention throughout interview.
Mr. J says he has been drinking alcohol regularly throughout his adult life, often a few times per week, up to “a case and a half” of beer at times. He claims he’s had multiple periods of sobriety but denies having experienced withdrawal symptoms during those times. Mr. J reports 1 prior psychiatric hospitalization 25 years ago after attempting suicide by overdose following the loss of a loved one. At that time, he was diagnosed with posttraumatic stress disorder (PTSD). During this admission, he denies having any symptoms of PTSD or periods of mania or depression, and he has not undergone psychiatric treatment since he had been diagnosed with PTSD. He denies any family history of psychiatric illness as well as any medical comorbidities or medication use.
[polldaddy:10279202]
The authors’ observations
Mr. J’s presentation had a wide differential diagnosis (Table 1). The initial agitation Mr. J displayed in the psychiatric ED was likely secondary to acute alcohol intoxication, given that he was subsequently pleasant, calm, and cooperative after the alcohol was metabolized. Despite this, Mr. J continued to demonstrate delusions of a religious and somewhat grandiose nature with tangential thought processes, which made substance-induced psychosis less likely to be the sole diagnosis. Although it is possible to develop psychotic symptoms due to severe alcohol withdrawal (alcoholic hallucinosis), Mr. J’s vital signs remained stable, and he demonstrated no other signs or symptoms of withdrawal throughout his hospitalization. His presentation also did not fit that of delirium tremens because he was not confused or disoriented, and did not demonstrate perceptual disturbance.
While delusions were the most prominent feature of Mr. J’s apparent psychosis, the presence of disorganized thought processes and impaired functioning, as evidenced by Mr. J’s unemployment and recent homelessness, were more consistent with a primary psychotic disorder than a delusional disorder.1
Continue to: Mr. J began to exhibit...
Mr. J began to exhibit these psychotic symptoms in his early 50s; because the average age of onset of schizophrenia for males is approximately age 20 to 25, the likelihood of his presentation being the result of a primary psychotic disorder was low.1 Although less common, it was possible that Mr. J had developed late-onset schizophrenia, where the first episode typically occurs after approximately age 40 to 45. Mr. J also described that he was in a “great” mood but had grandiose delusions and had made recent impulsive decisions, which suggests there was a possible mood component to his presentation and a potential diagnosis of schizoaffective disorder or bipolar disorder with psychotic symptoms. However, before any of these diagnoses could be made, a medical or neurologic condition that could cause his symptoms needed to be investigated and ruled out. Further collateral information regarding Mr. J’s history and timeline of symptoms was required.
EVALUATION Family history reveals clues
All laboratory studies completed during Mr. J’s hospitalization are unremarkable, including complete blood count, basic metabolic panel, hepatic function panel, gamma-glutamyl transferase test, magnesium, phosphate, thyroid-stimulating hormone, vitamin B12, thiamine, folate, urinalysis, and urine drug screen. Mr. J does not undergo any head imaging.
Mr. J has not been in touch with his family since leaving his home approximately 3 months before he presented to the ED, and he gives consent for the inpatient team to attempt to contact them. One week into hospitalization, Mr. J’s sibling informs the team of a family history of genetically confirmed Huntington’s disease (HD), with psychiatric symptoms preceding the onset of motor symptoms in multiple first-degree relatives. His family says that before Mr. J first developed delusions 4 years ago, he had not exhibited any psychotic symptoms during periods of alcohol use or sobriety.
Mr. J does not demonstrate any overt movement symptoms on the unit and denies noting any rigidity, change in gait, or abnormal/uncontrolled movements. The inpatient psychiatric team consults neurology and a full neurologic evaluation is performed. The results are unremarkable outside of his psychiatric symptoms; specifically, Mr. J does not demonstrate even subtle motor signs or cognitive impairment. Given Mr. J’s family history, unremarkable lab findings, and age at presentation, the neurology team and inpatient psychiatry team suspect that his psychosis is likely an early presentation of HD.
[polldaddy:10279212]
The authors’ observations
Genetics of Huntington’s disease
Huntington’s disease is an autosomal dominant neurodegenerative disorder caused by expansion of cytosine-adenine-guanine (CAG) trinucleotide repeats within the Huntingtin (HTT) gene on chromosome 4, which codes for the huntingtin protein.2,3 While the function of “normal” huntingtin protein is not fully understood, it is known that CAG repeat expansion in the HTT gene of >35 repeats codes for a mutant huntingtin protein.2,3 The mutant huntingtin protein causes progressive neuronal loss in the basal ganglia and striatum, resulting in the clinical Huntington’s phenotype.3 Notably, the patient’s age at disease onset is inversely correlated with the number of repeats. For example, expansions of approximately 40 to 50 CAG repeats often result in adult-onset HD, while expansions of >60 repeats are typically associated with juvenile-onset HD (before age 20). CAG repeat lengths of approximately 36 to 39 demonstrate reduced penetrance, with some individuals developing symptomatic HD while others do not.2 Instability of the CAG repeat expansion can result in genetic “anticipation,” wherein repeat length increases between generations, causing earlier age of onset in affected offspring. Genetic anticipation in HD occurs more frequently in paternal transmission—approximately 80% to 90% of juvenile HD cases are inherited paternally, at times with the number of CAG repeats exceeding 200.3
Continue to: Psychiatric manifestations of Huntington's disease
Psychiatric manifestations of Huntington’s disease
Huntington’s disease is characterized by motor, cognitive, and behavioral disturbances (Table 22,4). Motor symptoms include a characteristic and well-recognized chorea, often predominating earlier in HD, that progresses to rigidity, spasticity, and bradykinesia later in the disease course.2 Cognitive impairments develop in a similar progressive manner and can often precede the onset of motor symptoms, beginning with early executive dysfunction. Thinking often becomes more rigid and less efficient, causing difficulty with multi-tasking and concentration, and often progressing to subcortical dementia.2
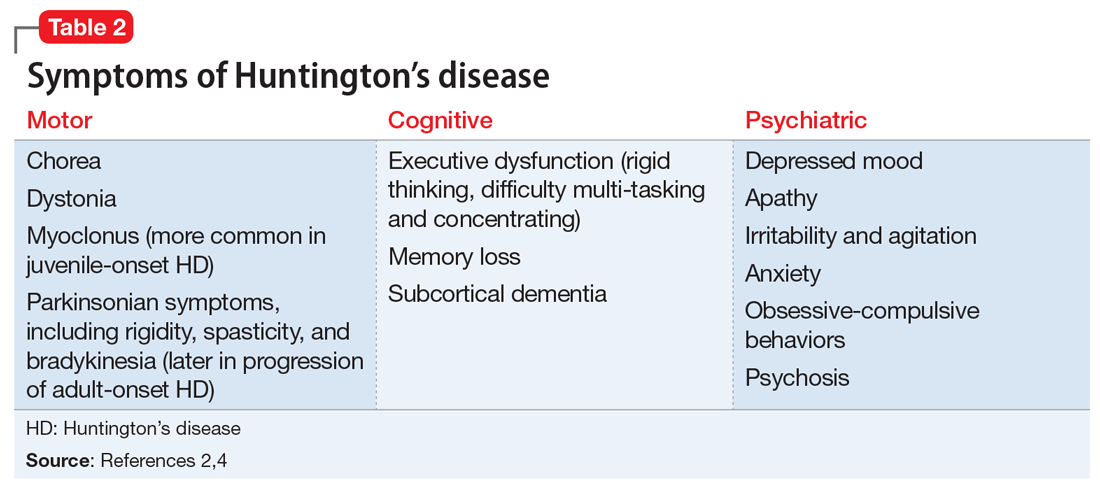
Psychiatric symptoms have long been recognized as a feature of HD; the estimated lifetime prevalence in patients with HD ranges from approximately 33% to 76%.4 Depressed mood, anxiety, irritability, and apathy are the most commonly reported symptoms, while a smaller percentage of patients with HD can experience obsessive-compulsive disorder (10% to 52%) or psychotic symptoms (3% to 11%).4 A more specific schizophrenia-like psychosis occurs in approximately 3% to 6% of patients, and often is a paranoid type.5,6 Positive psychotic symptoms, such as hallucinations and delusions, typically become less overt as HD progresses and cognitive impairments worsen.7
Although the onset of motor symptoms leads to diagnosis in the majority of patients with HD, many patients present with psychiatric symptoms—most commonly depression—prior to motor symptoms.8 An increasing body of literature details instances of psychosis preceding motor symptom onset by up to 10 years.6,9-12 In many of these cases, the patient has a family history of HD-associated psychosis. Family history is a major risk factor for HD-associated psychosis, as is early-onset HD.7,9
TREATMENT Antipsychotics result in some improvement
On Day 1 or 2, Mr. J is started on risperidone, 1 mg twice daily, to manage his symptoms. He shows incremental improvement in thought organization. Although his religious and grandiose delusions persist, they become less fixed, and he is able to take the team’s suggestion that he reconnect with his family.
Mr. J is aware of his family history of HD and acknowledges that multiple relatives had early psychiatric manifestations of HD. Despite this, he still has difficulty recognizing any connection between other family members’ presentation and his own. The psychiatry and neurology teams discuss the process, ethics, and implications of genetic testing for HD with Mr. J; however, he is ambivalent regarding genetic testing, and states he would consider it after discussing it with his family.
Continue to: The neurology team recommends...
The neurology team recommends against imaging for Mr. J because HD-related changes are not typically seen until later in the disease progression. On Day 9, they recommend changing from risperidone to quetiapine (50 mg every night at bedtime) due to evidence of its effectiveness specifically for treating behavioral symptoms of HD.13
While receiving quetiapine, Mr. J experiences significant drowsiness. Because he had experienced improvement in thought organization while he was receiving risperidone, he is switched back to risperidone.
[polldaddy:10279220]
The authors’ observations
Currently, no treatments are available to prevent the development or progression of HD. However, symptomatic treatment of motor and behavioral disturbances can lead to functional improvement and improved quality of life for individuals affected by HD.
There are no extensive clinical trials to date, but multiple case reports and studies have shown second-generation antipsychotics (SGAs), including quetiapine, olanzapine,
OUTCOME Discharge despite persistent delusions
Mr. J’s religious and grandiose delusions continue throughout hospitalization despite treatment with antipsychotics. However, because he remains calm and cooperative and demonstrates improvement in thought organization, he is deemed safe for discharge and instructed to continue risperidone. The team coordinates with Mr. J’s family to arrange transportation home and outpatient neurology follow-up.
Bottom Line
Psychiatric manifestations, including psychosis, are prominent symptoms of Huntington’s disease (HD) and may precede the onset of more readily recognized motor symptoms. This poses a diagnostic challenge, and clinicians should remain cognizant of this possibility, especially in patients with a family history of HD-associated psychosis.
Related Resources
- Huntington’s Disease Society of America. http://hdsa.org.
- National Institute of Neurological Disorders and Stroke. Huntington’s disease information page: What research is being done? https://www.ninds.nih.gov/Disorders/All-Disorders/Huntingtons-Disease-Information-Page.
- Scher LM. How to target psychiatric symptoms of Huntington’s disease. Current Psychiatry. 2012;11(9):34-39.
Drug Brand Names
Aripiprazole • Abilify
Clozapine • Clozaril
Haloperidol • Haldol
Olanzapine • Zyprexa
Quetiapine • Seroquel
Risperidone • Risperdal
CASE Disorganized thoughts and grandiose delusions
Mr. J, age 54, presents to the psychiatric emergency department (ED) with agitation and disruptive behavior. He claims that he is “the son of Jesus Christ” and has to travel to the Middle East to be baptized. Mr. J is irritable, shouting, and threatening staff members. He receives
The next day, he is calm and cooperative, but continues to express the same religious delusions. Mr. J is admitted to the psychiatric inpatient unit for further evaluation.
On the unit, Mr. J is pleasant and cooperative, but tangential in thought process. He reports he was “saved” by God 4 years ago, and that God communicates with him through music. Despite this, he denies having auditory or visual hallucinations.
Approximately 3 months earlier, Mr. J had stopped working and left his home and family in another state to pursue his “mission” of being baptized in the Middle East. Mr. J has been homeless since then. Despite that, he reports that his mood is “great” and denies any recent changes in mood, sleep, appetite, energy level, or psychomotor agitation. Although no formal cognitive testing is performed, Mr. J is alert and oriented to person, place, and time with intact remote and recent memory, no language deficits, and no lapses in concentration or attention throughout interview.
Mr. J says he has been drinking alcohol regularly throughout his adult life, often a few times per week, up to “a case and a half” of beer at times. He claims he’s had multiple periods of sobriety but denies having experienced withdrawal symptoms during those times. Mr. J reports 1 prior psychiatric hospitalization 25 years ago after attempting suicide by overdose following the loss of a loved one. At that time, he was diagnosed with posttraumatic stress disorder (PTSD). During this admission, he denies having any symptoms of PTSD or periods of mania or depression, and he has not undergone psychiatric treatment since he had been diagnosed with PTSD. He denies any family history of psychiatric illness as well as any medical comorbidities or medication use.
[polldaddy:10279202]
The authors’ observations
Mr. J’s presentation had a wide differential diagnosis (Table 1). The initial agitation Mr. J displayed in the psychiatric ED was likely secondary to acute alcohol intoxication, given that he was subsequently pleasant, calm, and cooperative after the alcohol was metabolized. Despite this, Mr. J continued to demonstrate delusions of a religious and somewhat grandiose nature with tangential thought processes, which made substance-induced psychosis less likely to be the sole diagnosis. Although it is possible to develop psychotic symptoms due to severe alcohol withdrawal (alcoholic hallucinosis), Mr. J’s vital signs remained stable, and he demonstrated no other signs or symptoms of withdrawal throughout his hospitalization. His presentation also did not fit that of delirium tremens because he was not confused or disoriented, and did not demonstrate perceptual disturbance.
While delusions were the most prominent feature of Mr. J’s apparent psychosis, the presence of disorganized thought processes and impaired functioning, as evidenced by Mr. J’s unemployment and recent homelessness, were more consistent with a primary psychotic disorder than a delusional disorder.1
Continue to: Mr. J began to exhibit...
Mr. J began to exhibit these psychotic symptoms in his early 50s; because the average age of onset of schizophrenia for males is approximately age 20 to 25, the likelihood of his presentation being the result of a primary psychotic disorder was low.1 Although less common, it was possible that Mr. J had developed late-onset schizophrenia, where the first episode typically occurs after approximately age 40 to 45. Mr. J also described that he was in a “great” mood but had grandiose delusions and had made recent impulsive decisions, which suggests there was a possible mood component to his presentation and a potential diagnosis of schizoaffective disorder or bipolar disorder with psychotic symptoms. However, before any of these diagnoses could be made, a medical or neurologic condition that could cause his symptoms needed to be investigated and ruled out. Further collateral information regarding Mr. J’s history and timeline of symptoms was required.
EVALUATION Family history reveals clues
All laboratory studies completed during Mr. J’s hospitalization are unremarkable, including complete blood count, basic metabolic panel, hepatic function panel, gamma-glutamyl transferase test, magnesium, phosphate, thyroid-stimulating hormone, vitamin B12, thiamine, folate, urinalysis, and urine drug screen. Mr. J does not undergo any head imaging.
Mr. J has not been in touch with his family since leaving his home approximately 3 months before he presented to the ED, and he gives consent for the inpatient team to attempt to contact them. One week into hospitalization, Mr. J’s sibling informs the team of a family history of genetically confirmed Huntington’s disease (HD), with psychiatric symptoms preceding the onset of motor symptoms in multiple first-degree relatives. His family says that before Mr. J first developed delusions 4 years ago, he had not exhibited any psychotic symptoms during periods of alcohol use or sobriety.
Mr. J does not demonstrate any overt movement symptoms on the unit and denies noting any rigidity, change in gait, or abnormal/uncontrolled movements. The inpatient psychiatric team consults neurology and a full neurologic evaluation is performed. The results are unremarkable outside of his psychiatric symptoms; specifically, Mr. J does not demonstrate even subtle motor signs or cognitive impairment. Given Mr. J’s family history, unremarkable lab findings, and age at presentation, the neurology team and inpatient psychiatry team suspect that his psychosis is likely an early presentation of HD.
[polldaddy:10279212]
The authors’ observations
Genetics of Huntington’s disease
Huntington’s disease is an autosomal dominant neurodegenerative disorder caused by expansion of cytosine-adenine-guanine (CAG) trinucleotide repeats within the Huntingtin (HTT) gene on chromosome 4, which codes for the huntingtin protein.2,3 While the function of “normal” huntingtin protein is not fully understood, it is known that CAG repeat expansion in the HTT gene of >35 repeats codes for a mutant huntingtin protein.2,3 The mutant huntingtin protein causes progressive neuronal loss in the basal ganglia and striatum, resulting in the clinical Huntington’s phenotype.3 Notably, the patient’s age at disease onset is inversely correlated with the number of repeats. For example, expansions of approximately 40 to 50 CAG repeats often result in adult-onset HD, while expansions of >60 repeats are typically associated with juvenile-onset HD (before age 20). CAG repeat lengths of approximately 36 to 39 demonstrate reduced penetrance, with some individuals developing symptomatic HD while others do not.2 Instability of the CAG repeat expansion can result in genetic “anticipation,” wherein repeat length increases between generations, causing earlier age of onset in affected offspring. Genetic anticipation in HD occurs more frequently in paternal transmission—approximately 80% to 90% of juvenile HD cases are inherited paternally, at times with the number of CAG repeats exceeding 200.3
Continue to: Psychiatric manifestations of Huntington's disease
Psychiatric manifestations of Huntington’s disease
Huntington’s disease is characterized by motor, cognitive, and behavioral disturbances (Table 22,4). Motor symptoms include a characteristic and well-recognized chorea, often predominating earlier in HD, that progresses to rigidity, spasticity, and bradykinesia later in the disease course.2 Cognitive impairments develop in a similar progressive manner and can often precede the onset of motor symptoms, beginning with early executive dysfunction. Thinking often becomes more rigid and less efficient, causing difficulty with multi-tasking and concentration, and often progressing to subcortical dementia.2
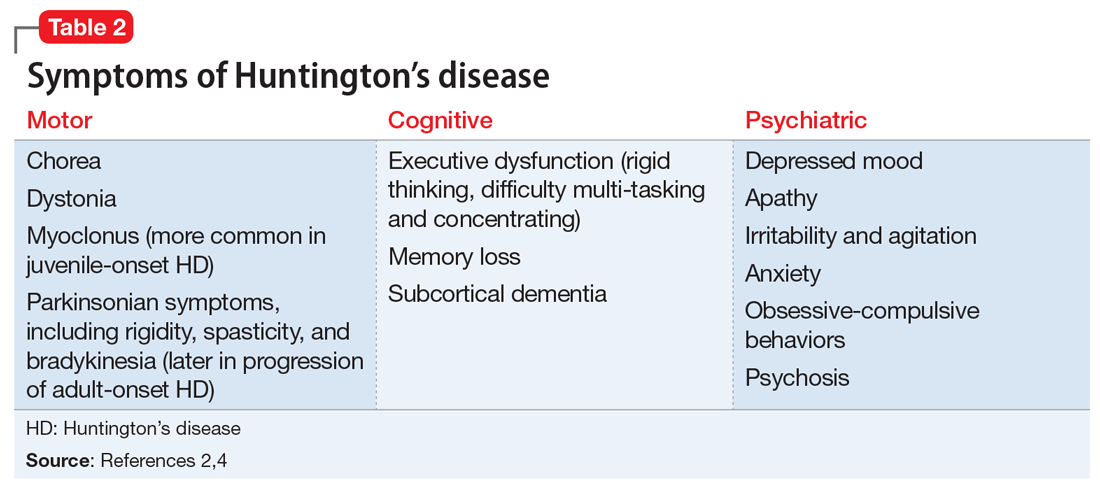
Psychiatric symptoms have long been recognized as a feature of HD; the estimated lifetime prevalence in patients with HD ranges from approximately 33% to 76%.4 Depressed mood, anxiety, irritability, and apathy are the most commonly reported symptoms, while a smaller percentage of patients with HD can experience obsessive-compulsive disorder (10% to 52%) or psychotic symptoms (3% to 11%).4 A more specific schizophrenia-like psychosis occurs in approximately 3% to 6% of patients, and often is a paranoid type.5,6 Positive psychotic symptoms, such as hallucinations and delusions, typically become less overt as HD progresses and cognitive impairments worsen.7
Although the onset of motor symptoms leads to diagnosis in the majority of patients with HD, many patients present with psychiatric symptoms—most commonly depression—prior to motor symptoms.8 An increasing body of literature details instances of psychosis preceding motor symptom onset by up to 10 years.6,9-12 In many of these cases, the patient has a family history of HD-associated psychosis. Family history is a major risk factor for HD-associated psychosis, as is early-onset HD.7,9
TREATMENT Antipsychotics result in some improvement
On Day 1 or 2, Mr. J is started on risperidone, 1 mg twice daily, to manage his symptoms. He shows incremental improvement in thought organization. Although his religious and grandiose delusions persist, they become less fixed, and he is able to take the team’s suggestion that he reconnect with his family.
Mr. J is aware of his family history of HD and acknowledges that multiple relatives had early psychiatric manifestations of HD. Despite this, he still has difficulty recognizing any connection between other family members’ presentation and his own. The psychiatry and neurology teams discuss the process, ethics, and implications of genetic testing for HD with Mr. J; however, he is ambivalent regarding genetic testing, and states he would consider it after discussing it with his family.
Continue to: The neurology team recommends...
The neurology team recommends against imaging for Mr. J because HD-related changes are not typically seen until later in the disease progression. On Day 9, they recommend changing from risperidone to quetiapine (50 mg every night at bedtime) due to evidence of its effectiveness specifically for treating behavioral symptoms of HD.13
While receiving quetiapine, Mr. J experiences significant drowsiness. Because he had experienced improvement in thought organization while he was receiving risperidone, he is switched back to risperidone.
[polldaddy:10279220]
The authors’ observations
Currently, no treatments are available to prevent the development or progression of HD. However, symptomatic treatment of motor and behavioral disturbances can lead to functional improvement and improved quality of life for individuals affected by HD.
There are no extensive clinical trials to date, but multiple case reports and studies have shown second-generation antipsychotics (SGAs), including quetiapine, olanzapine,
OUTCOME Discharge despite persistent delusions
Mr. J’s religious and grandiose delusions continue throughout hospitalization despite treatment with antipsychotics. However, because he remains calm and cooperative and demonstrates improvement in thought organization, he is deemed safe for discharge and instructed to continue risperidone. The team coordinates with Mr. J’s family to arrange transportation home and outpatient neurology follow-up.
Bottom Line
Psychiatric manifestations, including psychosis, are prominent symptoms of Huntington’s disease (HD) and may precede the onset of more readily recognized motor symptoms. This poses a diagnostic challenge, and clinicians should remain cognizant of this possibility, especially in patients with a family history of HD-associated psychosis.
Related Resources
- Huntington’s Disease Society of America. http://hdsa.org.
- National Institute of Neurological Disorders and Stroke. Huntington’s disease information page: What research is being done? https://www.ninds.nih.gov/Disorders/All-Disorders/Huntingtons-Disease-Information-Page.
- Scher LM. How to target psychiatric symptoms of Huntington’s disease. Current Psychiatry. 2012;11(9):34-39.
Drug Brand Names
Aripiprazole • Abilify
Clozapine • Clozaril
Haloperidol • Haldol
Olanzapine • Zyprexa
Quetiapine • Seroquel
Risperidone • Risperdal
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
2. Novak MJ, Tabrizi SJ. Huntington’s disease: clinical presentation and treatment. Int Rev Neurobiol. 2011;98:297-323.
3. Reiner A, Dragatsis I, Dietrich P. Genetics and neuropathology of Huntington’s disease. Int Rev Neurobiol. 2011;98:325-372.
4. van Duijn E, Kingma EM, Van der mast RC. Psychopathology in verified Huntington’s disease gene carriers. J Neuropsychiatry Clin Neurosci. 2007;19(4):441-448.
5. Naarding P, Kremer HP, Zitman FG. Huntington’s disease: a review of the literature on prevalence and treatment of neuropsychiatric phenomena. Eur Psychiatry. 2001;16(8):439-445.
6. Xu C, Yogaratnam J, Tan N, et al. Psychosis, treatment emergent extrapyramidal events, and subsequent onset of Huntington’s disease: a case report and review of the literature. Clin Psychopharmacol Neurosci. 2016;14(3):302-304.
7. Mendez MF. Huntington’s disease: update and review of neuropsychiatric aspects. Int J Psychiatry Med. 1994;24(3):189-208.
8. Di Maio L, Squitieri F, Napolitano G, et al. Onset symptoms in 510 patients with Huntington’s disease. J Med Genet. 1993;30(4):289-292.
9. Jauhar S, Ritchie S. Psychiatric and behavioural manifestations of Huntington’s disease. Adv Psychiatr Treat. 2010;16(3):168-175.
10. Nagel M, Rumpf HJ, Kasten M. Acute psychosis in a verified Huntington disease gene carrier with subtle motor signs: psychiatric criteria should be considered for the diagnosis. Gen Hosp Psychiatry. 2014;36(3):361.e3-e4. doi: 10.1016/j.genhosppsych.2014.01.008.
11. Corrêa BB, Xavier M, Guimarães J. Association of Huntington’s disease and schizophrenia-like psychosis in a Huntington’s disease pedigree. Clin Pract Epidemiol Ment Health. 2006;2:1.
12. Ding J, Gadit AM. Psychosis with Huntington’s disease: role of antipsychotic medications. BMJ Case Rep. 2014: bcr2013202625. doi: 10.1136/bcr-2013-202625.
13. Alpay M, Koroshetz WJ. Quetiapine in the treatment of behavioral disturbances in patients with Huntington’s disease. Psychosomatics. 2006;47(1):70-72.
14. Duff K, Beglinger LJ, O’Rourke ME, et al. Risperidone and the treatment of psychiatric, motor, and cognitive symptoms in Huntington’s disease. Ann Clin Psychiatry. 2008;20(1):1-3.
15. Paleacu D, Anca M, Giladi N. Olanzapine in Huntington’s disease. Acta Neurol Scand. 2002;105(6):441-444.
16. Lin W, Chou Y. Aripiprazole effects on psychosis and chorea in a patient with Huntington’s disease. Am J Psychiatry. 2008;165(9):1207-1208.
17. van Vugt JP, Siesling S, Vergeer M, et al. Clozapine versus placebo in Huntington’s disease: a double blind randomized comparative study. J Neurol Neurosurg Psychiatr. 1997;63(1):35-39.
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
2. Novak MJ, Tabrizi SJ. Huntington’s disease: clinical presentation and treatment. Int Rev Neurobiol. 2011;98:297-323.
3. Reiner A, Dragatsis I, Dietrich P. Genetics and neuropathology of Huntington’s disease. Int Rev Neurobiol. 2011;98:325-372.
4. van Duijn E, Kingma EM, Van der mast RC. Psychopathology in verified Huntington’s disease gene carriers. J Neuropsychiatry Clin Neurosci. 2007;19(4):441-448.
5. Naarding P, Kremer HP, Zitman FG. Huntington’s disease: a review of the literature on prevalence and treatment of neuropsychiatric phenomena. Eur Psychiatry. 2001;16(8):439-445.
6. Xu C, Yogaratnam J, Tan N, et al. Psychosis, treatment emergent extrapyramidal events, and subsequent onset of Huntington’s disease: a case report and review of the literature. Clin Psychopharmacol Neurosci. 2016;14(3):302-304.
7. Mendez MF. Huntington’s disease: update and review of neuropsychiatric aspects. Int J Psychiatry Med. 1994;24(3):189-208.
8. Di Maio L, Squitieri F, Napolitano G, et al. Onset symptoms in 510 patients with Huntington’s disease. J Med Genet. 1993;30(4):289-292.
9. Jauhar S, Ritchie S. Psychiatric and behavioural manifestations of Huntington’s disease. Adv Psychiatr Treat. 2010;16(3):168-175.
10. Nagel M, Rumpf HJ, Kasten M. Acute psychosis in a verified Huntington disease gene carrier with subtle motor signs: psychiatric criteria should be considered for the diagnosis. Gen Hosp Psychiatry. 2014;36(3):361.e3-e4. doi: 10.1016/j.genhosppsych.2014.01.008.
11. Corrêa BB, Xavier M, Guimarães J. Association of Huntington’s disease and schizophrenia-like psychosis in a Huntington’s disease pedigree. Clin Pract Epidemiol Ment Health. 2006;2:1.
12. Ding J, Gadit AM. Psychosis with Huntington’s disease: role of antipsychotic medications. BMJ Case Rep. 2014: bcr2013202625. doi: 10.1136/bcr-2013-202625.
13. Alpay M, Koroshetz WJ. Quetiapine in the treatment of behavioral disturbances in patients with Huntington’s disease. Psychosomatics. 2006;47(1):70-72.
14. Duff K, Beglinger LJ, O’Rourke ME, et al. Risperidone and the treatment of psychiatric, motor, and cognitive symptoms in Huntington’s disease. Ann Clin Psychiatry. 2008;20(1):1-3.
15. Paleacu D, Anca M, Giladi N. Olanzapine in Huntington’s disease. Acta Neurol Scand. 2002;105(6):441-444.
16. Lin W, Chou Y. Aripiprazole effects on psychosis and chorea in a patient with Huntington’s disease. Am J Psychiatry. 2008;165(9):1207-1208.
17. van Vugt JP, Siesling S, Vergeer M, et al. Clozapine versus placebo in Huntington’s disease: a double blind randomized comparative study. J Neurol Neurosurg Psychiatr. 1997;63(1):35-39.
Pharmacogenomics testing: What the FDA says
Mr. R, age 30, is referred to you by his primary care physician, who diagnosed him with depression approximately 2 years ago. When he was first diagnosed, Mr. R was prescribed
Mr. R says that based on his primary care physician’s recommendation, he had undergone pharmacogenomics testing to help guide therapy. He presents the results to you, and you notice that he has the cytochrome P450 (CYP) 2C19 *2/*3 genotype and a CYP2D6*4/*5 genotype. Both are associated with a poor metabolism phenotype. Should you use these findings to determine which medication Mr. R should be treated with next?
While the field of pharmacogenomics is not new, within the last few years this science has begun to transition into clinical practice. A recent meta-analysis found support for using pharmacogenomics testing results in clinical practice.1 This study included more than 1,700 patients who took part in 5 controlled trials that randomized participants to either pharmacogenetics-guided or unguided (ie, standard) treatment. Each participant was assessed using the Hamilton Depression Rating Scale-17 (HDRS-17) a minimum of 3 times over a minimum of 8 weeks.1 While the exact inclusion and exclusion criteria for each trial differed, they all defined remission of depression as achieving an HDRS-17 score ≤7. Overall, the authors concluded that based on the random-effects pooled risk ratio, there was a significant association between pharmacogenetics-guided prescribing and remission (relative risk = 1.71, 95% confidence interval [CI], 1.17 to 2.48; P = .005). The results of this meta-analysis are controversial, however, because all 5 studies were industry-funded, and interpretation of the testing results was based on proprietary algorithms.
Experts in the field and professional societies, such as the International Society of Psychiatric Genetics (ISPG), have issued policy statements on genetic testing within psychiatry.2,3 While the ISPG did not necessarily endorse use of pharmacogenomics in practice, they recommended that clinicians follow good medical practice and stay current on changes to drug labeling and adverse event reports.3 The ISPG also noted that useful but not exhaustive lists of pharmacogenetic tests are maintained by the Clinical Pharmacogenetics Implementation Consortium (CPIC) and the US FDA.3
Laboratory developed vs direct-to-consumer tests
In a previous Savvy Psychopharmacology article,4 we had discussed the role of CPIC, but not the role of the FDA. This issue is key because there is a lack of clarity regarding pharmacogenomics tests and whether they are considered Class II devices by the FDA, which would require their review and approval. Until recently, the FDA was fairly quiet regarding pharmacogenomics tests because most of these tests were considered laboratory developed tests, which were regulated under the Clinic Laboratory Improvements Amendments program. The critical distinction of a laboratory developed test is that it is developed and performed in a single laboratory and is offered to patients only when prescribed by a clinician. Due to this distinction, laboratory developed pharmacogenomics tests did not need FDA 510(k) clearance, which is a premarket submission common for medical devices.
Direct-to-consumer pharmacogenomics tests are different in that the FDA has classified these platforms as medical devices; however, they are reviewed by the FDA only if they are being used for moderate- to high-risk medical purposes, or if the results of the testing may have a higher impact on medical care. As part of its review, the FDA examines test accuracy and reliably measures to determine if the measurement is predictive of a certain state of health and supported by what the company claims about the test and how well it works. Additionally, the FDA examines the company-provided descriptive information to ensure that consumers can easily understand it without the help of a clinician.5
Conflicting FDA statements
Recently the FDA issued 2 statements—one a policy statement and the other a safety communication—about laboratory developed tests and direct-to-consumer tests. The statements appear to contradict themselves, despite focusing on using pharmacogenomics testing in practice.
Continue to: The FDA's first statement
The FDA’s first statement. On October 31, 2018, the FDA released a policy statement that they had “permitted marketing, with special controls,” of the Personal Genome Service Pharmacogenetic Reports test through 23andMe (a direct-to-consumer genetic testing company) for 33 different variants within specific pharmacogenomic genes (CYP2C19, CYP2C9, CYP3A5, UGT1A1, DPYD, TPMT, SLC01B1, and CYP2D6) that may impact drug metabolism or response.6 As part of its review of this Personal Genome Service Pharmacogenetic Reports test, the FDA found that the company-provided data showed that the test is accurate and can correctly identify the 33 specific genetic variants. The FDA review also showed that the testing results were reproducible, and the test instructions and reports could be understood by consumers.
While the specific reports related to this testing are not yet available within 23andMe, this approval allows for greater oversight by the FDA with regard to the pharmacogenomics information provided through this company’s Personal Genome Service Pharmacogenetic Reports test. The FDA noted that this approval was only for adults age >185 and that consumers “should not use the test results to stop or change any medication.”6 Further, the FDA stated that the results of the direct-to-consumer test should be confirmed with independent pharmacogenomics testing before making any medical decision. Unfortunately, the FDA did not offer guidance on what would be an appropriate independent pharmacogenomics test, but it did provide a link to a list of FDA-approved nucleic acid–based tests, on which 23andMe’s Personal Genome Service Pharmacogenetic Reports test is included.7
The FDA’s second statement. On November 1, 2018, the FDA issued a separate safety communication that cautioned clinicians and patients that most of the current commercially available testing platforms for pharmacogenomics have not been FDA-reviewed, meaning that they may lack clinical evidence supporting their use.8 Further, the FDA safety communication stated, “Changing drug treatment based on the results from such a genetic test could lead to inappropriate treatment decisions and potentially serious health consequences for the patient.”8
Taken together, these FDA statements appear to support pharmacogenomics testing with approval of the 23andMe’s Personal Genome Service Pharmacogenetic Reports test but warn that the testing results should not be used to make treatment decisions, and that they should be verified. However, the FDA does not offer any guidance on what an appropriate testing platform would be
What the FDA advises
The FDA has provided some guidance to clinicians and patients regarding next steps for patients who are interested in having pharmacogenomics testing or who have already undergone testing. The FDA’s first point is that both clinicians and patients need to be aware that pharmacogenomics testing is not FDA-reviewed, that patients should discuss the results of their testing with their clinicians, and that they should not stop their medication based on the results of the testing. Additionally, the FDA recommends that clinicians and patients should be aware that any claims made by the testing companies regarding the specific effect of a medication may not be supported by evidence. Furthermore, the FDA strongly recommends that clinicians consult the FDA-approved drug label, or the label of the FDA-cleared or FDA-approved genetic test, for information regarding how genetic information should be used in making treatment decisions. The FDA recommends reviewing the Warning section, as well as the Indications and Usage, Dosage and Administration, or Use in Specific Populations sections of the FDA-approved drug labeling.
Continue to: Unfortunately, this information...
Unfortunately, this information might be difficult to locate due to the lack of consistency regarding where it is placed in the FDA-approved drug labeling. The Pharmacogenomics Knowledgebase (https://www.pharmgkb.org/) can help clinicians quickly identify information regarding medications, their metabolic pathways, CPIC dosing guidelines, and the FDA-approved drug labeling information.9 By searching for specific medications within the Pharmacogenomic Knowledge Base, information regarding the FDA-approved drug labeling can be easily found, which is important because currently >120 medications contain pharmacogenomics information in their FDA-approved drug labeling.10
CASE CONTINUED
Overall Mr. R’s pharmacogenomics testing results indicate that he has 2 genotypes that are associated with poor metabolism phenotypes and could result in reduced metabolism of medications that are metabolized by these CYP enzymes, leading to higher blood levels and an increased risk of adverse effects. The Table11 lists pharmacogenomics information from the FDA-approved drug labeling and from the Pharmacogenomics Knowledgebase for both the medications Mr. R has previously been prescribed and for several potential medications to consider.
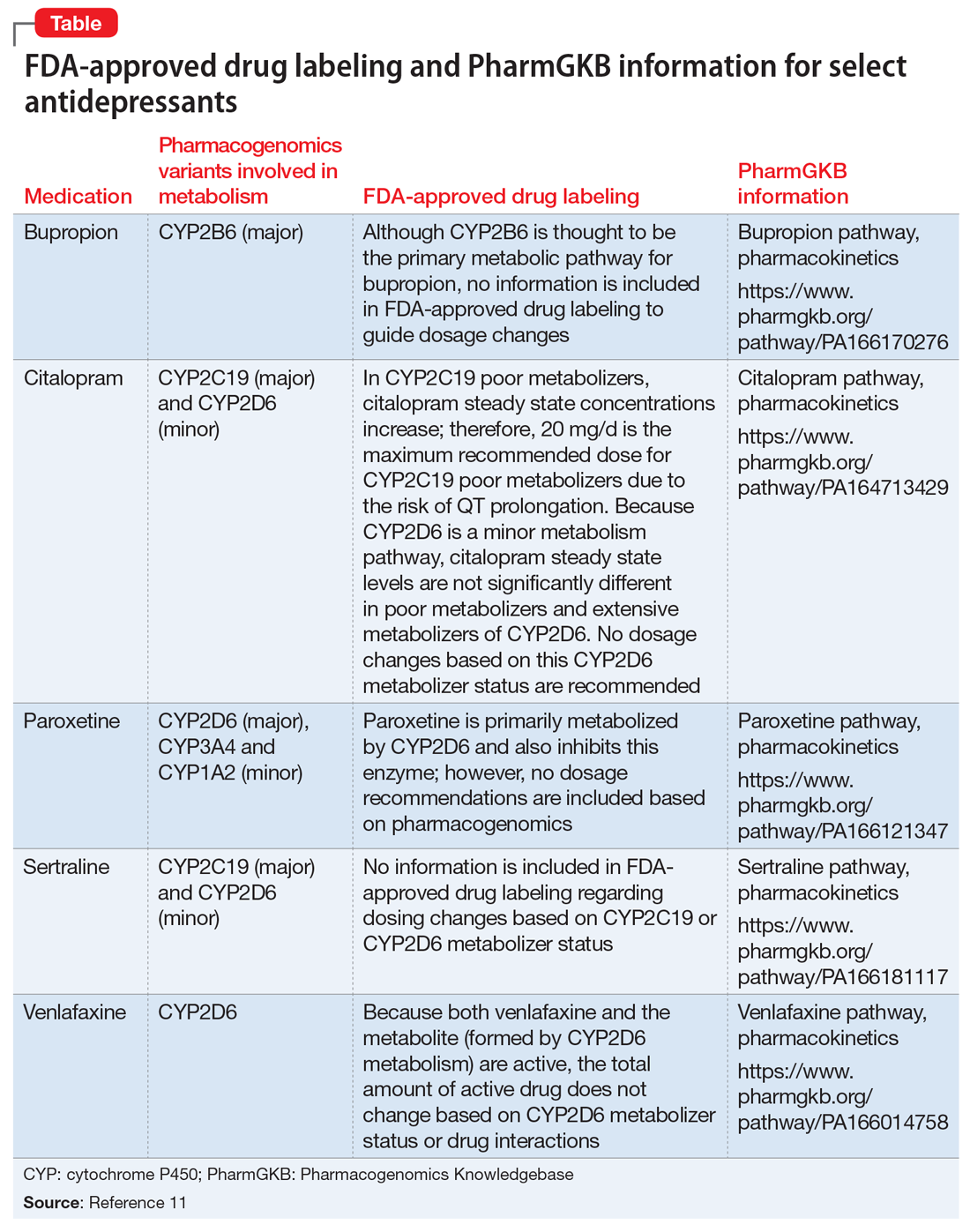
It would be prudent to first discuss with Mr. R the FDA’s recent policy statement and safety communication. While you could recommend that he pursue additional pharmacogenomics testing, it is unclear which specific laboratory is available to conduct this confirmatory analysis.
Because Mr. R has had unsuccessful trials of several medications that primarily fall in the selective serotonin reuptake inhibitors class, it might be time to consider a medication from a different class. A quick review of the FDA-approved drug labeling for
Related Resources
- Gammal RS, Gardner KN, Burghardt KJ. Where to find guidance on using pharmacogenomics in psychiatric practice. Current Psychiatry. 2016;15(9):93-94.
- Clinical Pharmacogenomics Implementation Consortium. What is CPIC? https://www.pharmgkb.org/page/cpic.
Drug Brand Names
Bupropion • Wellbutrin, Zyban
Citalopram • Celexa
Paroxetine • Paxil
Sertraline • Zoloft
Venlafaxine • Effexor
1. Bousman CA, Arandjelovic K, Mancuso SG, et al. Pharmacogenetic tests and depressive symptom remission: a meta-analysis of randomized controlled trials. Pharmacogenomics. 2019;20(1):37-47.
2. Zubenko GS, Sommer BR, Cohen BM. Pharmacogenetics in psychiatry: a companion, rather than competitor, to protocol-based care-reply. JAMA Psychiatry. 2018;75(10):1090-1091.
3. International Society for Psychiatric Genetics. Genetic testing statement: genetic testing and psychiatric disorders: a statement from the International Society of Psychiatric Genetics. https://ispg.net/genetic-testing-statement/. Revised January 26, 2017. Accessed January 1, 2019.
4. Ellingrod VL, Ward KM. Using pharmacogenetics guidelines when prescribing: what’s available. Current Psychiatry. 2018;17(1):43-46.
5. U.S. Food and Drug Administration. Medical devices: direct-to-consumer tests. https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/InVitroDiagnostics/ucm624726.htm. Published November 1, 2018. Accessed January 1, 2019.
6. U.S. Food and Drug Administration. FDA news releases: FDA authorizes first direct-to consumer test for detecting variants that may be associated with medication metabolism. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm624753.htm. Published October 31, 2018. Accessed January 1, 2019.
7. U.S. Food and Drug Administration. Medical devices: nucleic acid based tests. https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/InVitroDiagnostics/ucm330711.htm. Published February 5, 2019. Accessed March 1, 2019.
8. U.S. Food and Drug Administration. Medical devices. The FDA warns against the use of many genetic tests with unapproved claims to predict patient response to specific medications: FDA Safety Communications. https://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm624725.htm. Published November 1, 2018. Accessed January 1, 2019.
9. Whirl-Carrillo EM, McDonagh JM, Hebert L, et al. Pharmacogenomics knowledge for personalized medicine. Clin Pharmacol Ther. 2012;92(4):414-417.
10. U.S. Food and Drug Administration. Drugs. Table of pharmacogenomic biomarkers in drug labeling. https://www.fda.gov/Drugs/ScienceResearch/ucm572698.htm. Published August 3, 2018. Accessed January 1, 2019.
11. U.S. Food and Drug Administration. Drugs@FDA: FDA approved drug products. https://www.accessdata.fda.gov/scripts/cder/daf. Accessed March 4, 2019.
Mr. R, age 30, is referred to you by his primary care physician, who diagnosed him with depression approximately 2 years ago. When he was first diagnosed, Mr. R was prescribed
Mr. R says that based on his primary care physician’s recommendation, he had undergone pharmacogenomics testing to help guide therapy. He presents the results to you, and you notice that he has the cytochrome P450 (CYP) 2C19 *2/*3 genotype and a CYP2D6*4/*5 genotype. Both are associated with a poor metabolism phenotype. Should you use these findings to determine which medication Mr. R should be treated with next?
While the field of pharmacogenomics is not new, within the last few years this science has begun to transition into clinical practice. A recent meta-analysis found support for using pharmacogenomics testing results in clinical practice.1 This study included more than 1,700 patients who took part in 5 controlled trials that randomized participants to either pharmacogenetics-guided or unguided (ie, standard) treatment. Each participant was assessed using the Hamilton Depression Rating Scale-17 (HDRS-17) a minimum of 3 times over a minimum of 8 weeks.1 While the exact inclusion and exclusion criteria for each trial differed, they all defined remission of depression as achieving an HDRS-17 score ≤7. Overall, the authors concluded that based on the random-effects pooled risk ratio, there was a significant association between pharmacogenetics-guided prescribing and remission (relative risk = 1.71, 95% confidence interval [CI], 1.17 to 2.48; P = .005). The results of this meta-analysis are controversial, however, because all 5 studies were industry-funded, and interpretation of the testing results was based on proprietary algorithms.
Experts in the field and professional societies, such as the International Society of Psychiatric Genetics (ISPG), have issued policy statements on genetic testing within psychiatry.2,3 While the ISPG did not necessarily endorse use of pharmacogenomics in practice, they recommended that clinicians follow good medical practice and stay current on changes to drug labeling and adverse event reports.3 The ISPG also noted that useful but not exhaustive lists of pharmacogenetic tests are maintained by the Clinical Pharmacogenetics Implementation Consortium (CPIC) and the US FDA.3
Laboratory developed vs direct-to-consumer tests
In a previous Savvy Psychopharmacology article,4 we had discussed the role of CPIC, but not the role of the FDA. This issue is key because there is a lack of clarity regarding pharmacogenomics tests and whether they are considered Class II devices by the FDA, which would require their review and approval. Until recently, the FDA was fairly quiet regarding pharmacogenomics tests because most of these tests were considered laboratory developed tests, which were regulated under the Clinic Laboratory Improvements Amendments program. The critical distinction of a laboratory developed test is that it is developed and performed in a single laboratory and is offered to patients only when prescribed by a clinician. Due to this distinction, laboratory developed pharmacogenomics tests did not need FDA 510(k) clearance, which is a premarket submission common for medical devices.
Direct-to-consumer pharmacogenomics tests are different in that the FDA has classified these platforms as medical devices; however, they are reviewed by the FDA only if they are being used for moderate- to high-risk medical purposes, or if the results of the testing may have a higher impact on medical care. As part of its review, the FDA examines test accuracy and reliably measures to determine if the measurement is predictive of a certain state of health and supported by what the company claims about the test and how well it works. Additionally, the FDA examines the company-provided descriptive information to ensure that consumers can easily understand it without the help of a clinician.5
Conflicting FDA statements
Recently the FDA issued 2 statements—one a policy statement and the other a safety communication—about laboratory developed tests and direct-to-consumer tests. The statements appear to contradict themselves, despite focusing on using pharmacogenomics testing in practice.
Continue to: The FDA's first statement
The FDA’s first statement. On October 31, 2018, the FDA released a policy statement that they had “permitted marketing, with special controls,” of the Personal Genome Service Pharmacogenetic Reports test through 23andMe (a direct-to-consumer genetic testing company) for 33 different variants within specific pharmacogenomic genes (CYP2C19, CYP2C9, CYP3A5, UGT1A1, DPYD, TPMT, SLC01B1, and CYP2D6) that may impact drug metabolism or response.6 As part of its review of this Personal Genome Service Pharmacogenetic Reports test, the FDA found that the company-provided data showed that the test is accurate and can correctly identify the 33 specific genetic variants. The FDA review also showed that the testing results were reproducible, and the test instructions and reports could be understood by consumers.
While the specific reports related to this testing are not yet available within 23andMe, this approval allows for greater oversight by the FDA with regard to the pharmacogenomics information provided through this company’s Personal Genome Service Pharmacogenetic Reports test. The FDA noted that this approval was only for adults age >185 and that consumers “should not use the test results to stop or change any medication.”6 Further, the FDA stated that the results of the direct-to-consumer test should be confirmed with independent pharmacogenomics testing before making any medical decision. Unfortunately, the FDA did not offer guidance on what would be an appropriate independent pharmacogenomics test, but it did provide a link to a list of FDA-approved nucleic acid–based tests, on which 23andMe’s Personal Genome Service Pharmacogenetic Reports test is included.7
The FDA’s second statement. On November 1, 2018, the FDA issued a separate safety communication that cautioned clinicians and patients that most of the current commercially available testing platforms for pharmacogenomics have not been FDA-reviewed, meaning that they may lack clinical evidence supporting their use.8 Further, the FDA safety communication stated, “Changing drug treatment based on the results from such a genetic test could lead to inappropriate treatment decisions and potentially serious health consequences for the patient.”8
Taken together, these FDA statements appear to support pharmacogenomics testing with approval of the 23andMe’s Personal Genome Service Pharmacogenetic Reports test but warn that the testing results should not be used to make treatment decisions, and that they should be verified. However, the FDA does not offer any guidance on what an appropriate testing platform would be
What the FDA advises
The FDA has provided some guidance to clinicians and patients regarding next steps for patients who are interested in having pharmacogenomics testing or who have already undergone testing. The FDA’s first point is that both clinicians and patients need to be aware that pharmacogenomics testing is not FDA-reviewed, that patients should discuss the results of their testing with their clinicians, and that they should not stop their medication based on the results of the testing. Additionally, the FDA recommends that clinicians and patients should be aware that any claims made by the testing companies regarding the specific effect of a medication may not be supported by evidence. Furthermore, the FDA strongly recommends that clinicians consult the FDA-approved drug label, or the label of the FDA-cleared or FDA-approved genetic test, for information regarding how genetic information should be used in making treatment decisions. The FDA recommends reviewing the Warning section, as well as the Indications and Usage, Dosage and Administration, or Use in Specific Populations sections of the FDA-approved drug labeling.
Continue to: Unfortunately, this information...
Unfortunately, this information might be difficult to locate due to the lack of consistency regarding where it is placed in the FDA-approved drug labeling. The Pharmacogenomics Knowledgebase (https://www.pharmgkb.org/) can help clinicians quickly identify information regarding medications, their metabolic pathways, CPIC dosing guidelines, and the FDA-approved drug labeling information.9 By searching for specific medications within the Pharmacogenomic Knowledge Base, information regarding the FDA-approved drug labeling can be easily found, which is important because currently >120 medications contain pharmacogenomics information in their FDA-approved drug labeling.10
CASE CONTINUED
Overall Mr. R’s pharmacogenomics testing results indicate that he has 2 genotypes that are associated with poor metabolism phenotypes and could result in reduced metabolism of medications that are metabolized by these CYP enzymes, leading to higher blood levels and an increased risk of adverse effects. The Table11 lists pharmacogenomics information from the FDA-approved drug labeling and from the Pharmacogenomics Knowledgebase for both the medications Mr. R has previously been prescribed and for several potential medications to consider.
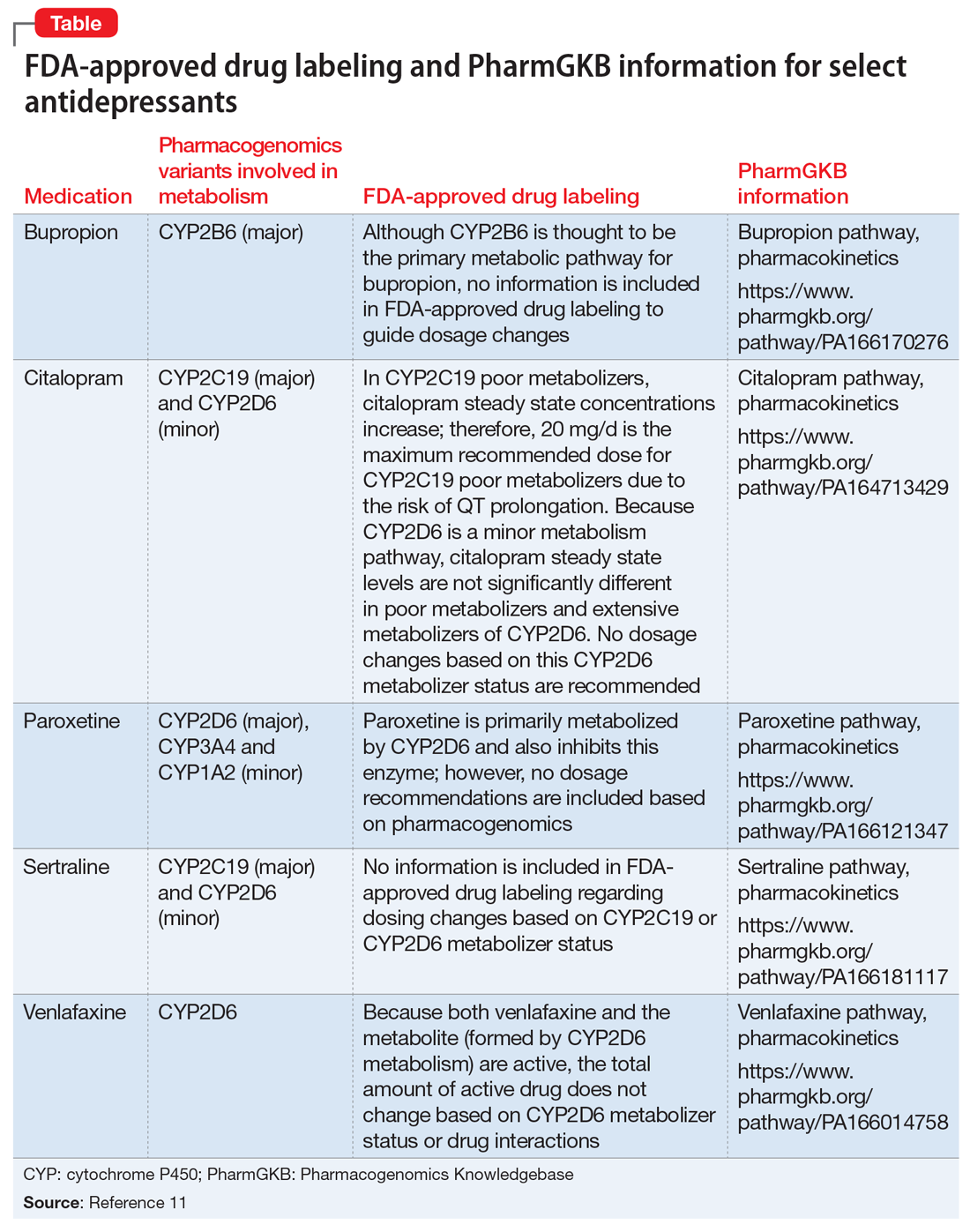
It would be prudent to first discuss with Mr. R the FDA’s recent policy statement and safety communication. While you could recommend that he pursue additional pharmacogenomics testing, it is unclear which specific laboratory is available to conduct this confirmatory analysis.
Because Mr. R has had unsuccessful trials of several medications that primarily fall in the selective serotonin reuptake inhibitors class, it might be time to consider a medication from a different class. A quick review of the FDA-approved drug labeling for
Related Resources
- Gammal RS, Gardner KN, Burghardt KJ. Where to find guidance on using pharmacogenomics in psychiatric practice. Current Psychiatry. 2016;15(9):93-94.
- Clinical Pharmacogenomics Implementation Consortium. What is CPIC? https://www.pharmgkb.org/page/cpic.
Drug Brand Names
Bupropion • Wellbutrin, Zyban
Citalopram • Celexa
Paroxetine • Paxil
Sertraline • Zoloft
Venlafaxine • Effexor
Mr. R, age 30, is referred to you by his primary care physician, who diagnosed him with depression approximately 2 years ago. When he was first diagnosed, Mr. R was prescribed
Mr. R says that based on his primary care physician’s recommendation, he had undergone pharmacogenomics testing to help guide therapy. He presents the results to you, and you notice that he has the cytochrome P450 (CYP) 2C19 *2/*3 genotype and a CYP2D6*4/*5 genotype. Both are associated with a poor metabolism phenotype. Should you use these findings to determine which medication Mr. R should be treated with next?
While the field of pharmacogenomics is not new, within the last few years this science has begun to transition into clinical practice. A recent meta-analysis found support for using pharmacogenomics testing results in clinical practice.1 This study included more than 1,700 patients who took part in 5 controlled trials that randomized participants to either pharmacogenetics-guided or unguided (ie, standard) treatment. Each participant was assessed using the Hamilton Depression Rating Scale-17 (HDRS-17) a minimum of 3 times over a minimum of 8 weeks.1 While the exact inclusion and exclusion criteria for each trial differed, they all defined remission of depression as achieving an HDRS-17 score ≤7. Overall, the authors concluded that based on the random-effects pooled risk ratio, there was a significant association between pharmacogenetics-guided prescribing and remission (relative risk = 1.71, 95% confidence interval [CI], 1.17 to 2.48; P = .005). The results of this meta-analysis are controversial, however, because all 5 studies were industry-funded, and interpretation of the testing results was based on proprietary algorithms.
Experts in the field and professional societies, such as the International Society of Psychiatric Genetics (ISPG), have issued policy statements on genetic testing within psychiatry.2,3 While the ISPG did not necessarily endorse use of pharmacogenomics in practice, they recommended that clinicians follow good medical practice and stay current on changes to drug labeling and adverse event reports.3 The ISPG also noted that useful but not exhaustive lists of pharmacogenetic tests are maintained by the Clinical Pharmacogenetics Implementation Consortium (CPIC) and the US FDA.3
Laboratory developed vs direct-to-consumer tests
In a previous Savvy Psychopharmacology article,4 we had discussed the role of CPIC, but not the role of the FDA. This issue is key because there is a lack of clarity regarding pharmacogenomics tests and whether they are considered Class II devices by the FDA, which would require their review and approval. Until recently, the FDA was fairly quiet regarding pharmacogenomics tests because most of these tests were considered laboratory developed tests, which were regulated under the Clinic Laboratory Improvements Amendments program. The critical distinction of a laboratory developed test is that it is developed and performed in a single laboratory and is offered to patients only when prescribed by a clinician. Due to this distinction, laboratory developed pharmacogenomics tests did not need FDA 510(k) clearance, which is a premarket submission common for medical devices.
Direct-to-consumer pharmacogenomics tests are different in that the FDA has classified these platforms as medical devices; however, they are reviewed by the FDA only if they are being used for moderate- to high-risk medical purposes, or if the results of the testing may have a higher impact on medical care. As part of its review, the FDA examines test accuracy and reliably measures to determine if the measurement is predictive of a certain state of health and supported by what the company claims about the test and how well it works. Additionally, the FDA examines the company-provided descriptive information to ensure that consumers can easily understand it without the help of a clinician.5
Conflicting FDA statements
Recently the FDA issued 2 statements—one a policy statement and the other a safety communication—about laboratory developed tests and direct-to-consumer tests. The statements appear to contradict themselves, despite focusing on using pharmacogenomics testing in practice.
Continue to: The FDA's first statement
The FDA’s first statement. On October 31, 2018, the FDA released a policy statement that they had “permitted marketing, with special controls,” of the Personal Genome Service Pharmacogenetic Reports test through 23andMe (a direct-to-consumer genetic testing company) for 33 different variants within specific pharmacogenomic genes (CYP2C19, CYP2C9, CYP3A5, UGT1A1, DPYD, TPMT, SLC01B1, and CYP2D6) that may impact drug metabolism or response.6 As part of its review of this Personal Genome Service Pharmacogenetic Reports test, the FDA found that the company-provided data showed that the test is accurate and can correctly identify the 33 specific genetic variants. The FDA review also showed that the testing results were reproducible, and the test instructions and reports could be understood by consumers.
While the specific reports related to this testing are not yet available within 23andMe, this approval allows for greater oversight by the FDA with regard to the pharmacogenomics information provided through this company’s Personal Genome Service Pharmacogenetic Reports test. The FDA noted that this approval was only for adults age >185 and that consumers “should not use the test results to stop or change any medication.”6 Further, the FDA stated that the results of the direct-to-consumer test should be confirmed with independent pharmacogenomics testing before making any medical decision. Unfortunately, the FDA did not offer guidance on what would be an appropriate independent pharmacogenomics test, but it did provide a link to a list of FDA-approved nucleic acid–based tests, on which 23andMe’s Personal Genome Service Pharmacogenetic Reports test is included.7
The FDA’s second statement. On November 1, 2018, the FDA issued a separate safety communication that cautioned clinicians and patients that most of the current commercially available testing platforms for pharmacogenomics have not been FDA-reviewed, meaning that they may lack clinical evidence supporting their use.8 Further, the FDA safety communication stated, “Changing drug treatment based on the results from such a genetic test could lead to inappropriate treatment decisions and potentially serious health consequences for the patient.”8
Taken together, these FDA statements appear to support pharmacogenomics testing with approval of the 23andMe’s Personal Genome Service Pharmacogenetic Reports test but warn that the testing results should not be used to make treatment decisions, and that they should be verified. However, the FDA does not offer any guidance on what an appropriate testing platform would be
What the FDA advises
The FDA has provided some guidance to clinicians and patients regarding next steps for patients who are interested in having pharmacogenomics testing or who have already undergone testing. The FDA’s first point is that both clinicians and patients need to be aware that pharmacogenomics testing is not FDA-reviewed, that patients should discuss the results of their testing with their clinicians, and that they should not stop their medication based on the results of the testing. Additionally, the FDA recommends that clinicians and patients should be aware that any claims made by the testing companies regarding the specific effect of a medication may not be supported by evidence. Furthermore, the FDA strongly recommends that clinicians consult the FDA-approved drug label, or the label of the FDA-cleared or FDA-approved genetic test, for information regarding how genetic information should be used in making treatment decisions. The FDA recommends reviewing the Warning section, as well as the Indications and Usage, Dosage and Administration, or Use in Specific Populations sections of the FDA-approved drug labeling.
Continue to: Unfortunately, this information...
Unfortunately, this information might be difficult to locate due to the lack of consistency regarding where it is placed in the FDA-approved drug labeling. The Pharmacogenomics Knowledgebase (https://www.pharmgkb.org/) can help clinicians quickly identify information regarding medications, their metabolic pathways, CPIC dosing guidelines, and the FDA-approved drug labeling information.9 By searching for specific medications within the Pharmacogenomic Knowledge Base, information regarding the FDA-approved drug labeling can be easily found, which is important because currently >120 medications contain pharmacogenomics information in their FDA-approved drug labeling.10
CASE CONTINUED
Overall Mr. R’s pharmacogenomics testing results indicate that he has 2 genotypes that are associated with poor metabolism phenotypes and could result in reduced metabolism of medications that are metabolized by these CYP enzymes, leading to higher blood levels and an increased risk of adverse effects. The Table11 lists pharmacogenomics information from the FDA-approved drug labeling and from the Pharmacogenomics Knowledgebase for both the medications Mr. R has previously been prescribed and for several potential medications to consider.
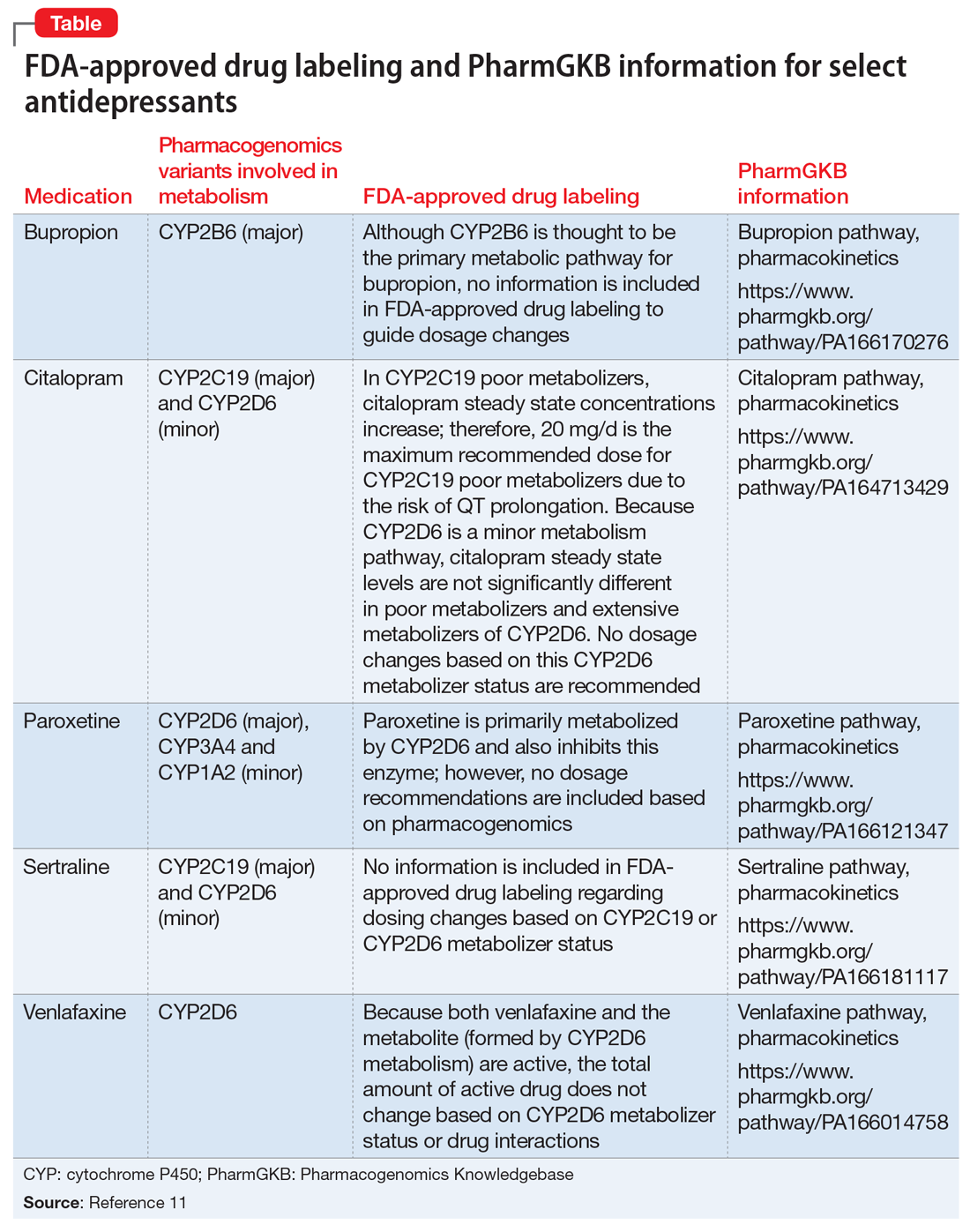
It would be prudent to first discuss with Mr. R the FDA’s recent policy statement and safety communication. While you could recommend that he pursue additional pharmacogenomics testing, it is unclear which specific laboratory is available to conduct this confirmatory analysis.
Because Mr. R has had unsuccessful trials of several medications that primarily fall in the selective serotonin reuptake inhibitors class, it might be time to consider a medication from a different class. A quick review of the FDA-approved drug labeling for
Related Resources
- Gammal RS, Gardner KN, Burghardt KJ. Where to find guidance on using pharmacogenomics in psychiatric practice. Current Psychiatry. 2016;15(9):93-94.
- Clinical Pharmacogenomics Implementation Consortium. What is CPIC? https://www.pharmgkb.org/page/cpic.
Drug Brand Names
Bupropion • Wellbutrin, Zyban
Citalopram • Celexa
Paroxetine • Paxil
Sertraline • Zoloft
Venlafaxine • Effexor
1. Bousman CA, Arandjelovic K, Mancuso SG, et al. Pharmacogenetic tests and depressive symptom remission: a meta-analysis of randomized controlled trials. Pharmacogenomics. 2019;20(1):37-47.
2. Zubenko GS, Sommer BR, Cohen BM. Pharmacogenetics in psychiatry: a companion, rather than competitor, to protocol-based care-reply. JAMA Psychiatry. 2018;75(10):1090-1091.
3. International Society for Psychiatric Genetics. Genetic testing statement: genetic testing and psychiatric disorders: a statement from the International Society of Psychiatric Genetics. https://ispg.net/genetic-testing-statement/. Revised January 26, 2017. Accessed January 1, 2019.
4. Ellingrod VL, Ward KM. Using pharmacogenetics guidelines when prescribing: what’s available. Current Psychiatry. 2018;17(1):43-46.
5. U.S. Food and Drug Administration. Medical devices: direct-to-consumer tests. https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/InVitroDiagnostics/ucm624726.htm. Published November 1, 2018. Accessed January 1, 2019.
6. U.S. Food and Drug Administration. FDA news releases: FDA authorizes first direct-to consumer test for detecting variants that may be associated with medication metabolism. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm624753.htm. Published October 31, 2018. Accessed January 1, 2019.
7. U.S. Food and Drug Administration. Medical devices: nucleic acid based tests. https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/InVitroDiagnostics/ucm330711.htm. Published February 5, 2019. Accessed March 1, 2019.
8. U.S. Food and Drug Administration. Medical devices. The FDA warns against the use of many genetic tests with unapproved claims to predict patient response to specific medications: FDA Safety Communications. https://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm624725.htm. Published November 1, 2018. Accessed January 1, 2019.
9. Whirl-Carrillo EM, McDonagh JM, Hebert L, et al. Pharmacogenomics knowledge for personalized medicine. Clin Pharmacol Ther. 2012;92(4):414-417.
10. U.S. Food and Drug Administration. Drugs. Table of pharmacogenomic biomarkers in drug labeling. https://www.fda.gov/Drugs/ScienceResearch/ucm572698.htm. Published August 3, 2018. Accessed January 1, 2019.
11. U.S. Food and Drug Administration. Drugs@FDA: FDA approved drug products. https://www.accessdata.fda.gov/scripts/cder/daf. Accessed March 4, 2019.
1. Bousman CA, Arandjelovic K, Mancuso SG, et al. Pharmacogenetic tests and depressive symptom remission: a meta-analysis of randomized controlled trials. Pharmacogenomics. 2019;20(1):37-47.
2. Zubenko GS, Sommer BR, Cohen BM. Pharmacogenetics in psychiatry: a companion, rather than competitor, to protocol-based care-reply. JAMA Psychiatry. 2018;75(10):1090-1091.
3. International Society for Psychiatric Genetics. Genetic testing statement: genetic testing and psychiatric disorders: a statement from the International Society of Psychiatric Genetics. https://ispg.net/genetic-testing-statement/. Revised January 26, 2017. Accessed January 1, 2019.
4. Ellingrod VL, Ward KM. Using pharmacogenetics guidelines when prescribing: what’s available. Current Psychiatry. 2018;17(1):43-46.
5. U.S. Food and Drug Administration. Medical devices: direct-to-consumer tests. https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/InVitroDiagnostics/ucm624726.htm. Published November 1, 2018. Accessed January 1, 2019.
6. U.S. Food and Drug Administration. FDA news releases: FDA authorizes first direct-to consumer test for detecting variants that may be associated with medication metabolism. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm624753.htm. Published October 31, 2018. Accessed January 1, 2019.
7. U.S. Food and Drug Administration. Medical devices: nucleic acid based tests. https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/InVitroDiagnostics/ucm330711.htm. Published February 5, 2019. Accessed March 1, 2019.
8. U.S. Food and Drug Administration. Medical devices. The FDA warns against the use of many genetic tests with unapproved claims to predict patient response to specific medications: FDA Safety Communications. https://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm624725.htm. Published November 1, 2018. Accessed January 1, 2019.
9. Whirl-Carrillo EM, McDonagh JM, Hebert L, et al. Pharmacogenomics knowledge for personalized medicine. Clin Pharmacol Ther. 2012;92(4):414-417.
10. U.S. Food and Drug Administration. Drugs. Table of pharmacogenomic biomarkers in drug labeling. https://www.fda.gov/Drugs/ScienceResearch/ucm572698.htm. Published August 3, 2018. Accessed January 1, 2019.
11. U.S. Food and Drug Administration. Drugs@FDA: FDA approved drug products. https://www.accessdata.fda.gov/scripts/cder/daf. Accessed March 4, 2019.
Pimavanserin: A potentially safer alternative to clozapine for refractory hallucinations and delusions
Up to 30% of patients with schizophrenia do not respond to dopamine antagonists, which include all first- and second-generation antipsychotics. They are labeled as “treatment-resistant” if they have a partial response, or “treatment-refractory” if their hallucinations and/or delusions do not improve at all despite multiple trials of antipsychotics.
That’s why clozapine is considered a “lifesaver” for such patients, a last-resort medication that unshackles patients with refractory psychotic symptoms from the tyranny of auditory and/or visual hallucinations and the reality distortion of fixed false beliefs such as paranoid delusions.
Many long-suffering patients with refractory psychosis recover and return to their baseline, thanks to clozapine. In a past editorial, I discussed how one of my patients, Bethany, who had dropped out of college and became homeless for 4 years with refractory delusions and hallucinations, recovered completely when she received clozapine.1 She then returned to college, graduated with honors, and authored a book about her journey of recovery.2 She and I later established a nonprofit foundation we called CURESZ (Comprehensive Understanding via Research and Education in Schizophrenia), and assembled a panel of 80 clozapine experts across the country to provide access to clozapine for the hundreds of thousands of individuals with refractory psychosis who never received a trial of clozapine from their psychiatrists or psychiatric nurse practitioners. (Visit CURESZ.org for details.)
Bethany was very lucky to respond and recover completely, because only 40% of patients with refractory psychosis respond to clozapine. She does not mind having her blood drawn every week to measure her white blood cell count for early detection of potentially fatal agranulocytosis. Many refractory, often homeless patients with chronic schizophrenia refuse to have weekly phlebotomy and therefore are not treated with clozapine. Bethany was also fortunate to experience only 1 adverse effect of clozapine: extreme sedation that forced her to sleep up to 15 hours a day (this was reduced to 9 to 10 hours a day with adjunctive modafinil). Fortunately, she was spared the multiple other serious adverse effects of clozapine, which include excessive salivation, extreme weight gain, diabetes, hyperlipidemia, cardiomyopathy, pancreatitis, seizures, and ileus.3 Clozapine is also associated with sudden death more than any other antipsychotic agent.4
So, what can be done for patients with refractory hallucinations and delusions who are among the 60% who fail to respond to clozapine, or who experience intolerable adverse effects or safety problems, or who refuse to take clozapine and have their blood drawn every week? This is a desperately ill and seriously disabled group of patients who are deemed to be beyond the reach of medical intervention by psychiatry. They are often treated with various off-label medications as adjunctive therapy to clozapine, to which they failed to respond. This includes adding lamotrigine5 or benzoate,6 but none have been approved as an efficacious and safe monotherapy alternative to clozapine. So, what can be done for patients with refractory illness?
Enter pimavanserin. This new medication is an inverse agonist of serotonin 5-HT2A receptors and (to a lesser extent) serotonin 5-HT2C receptors. It was recently FDA-approved for treating the hallucinations and delusions of Parkinson’s disease psychosis,7 which is estimated to develop in up to 50% of individuals with Parkinson’s disease. It does not have any affinity to any dopamine receptors, which makes it an ideal antipsychotic for Parkinson’s disease, where any dopamine antagonism can worsen the motor symptoms (rigidity, hypokinesia, and tremors) associated with that movement disorder. Thus, pimavanserin became the first ever non-dopaminergic antipsychotic in the world and is indicated only for Parkinson’s disease psychosis.
Our clinical team made a serendipitous discovery about the efficacy of pimavanserin in patients with schizophrenia who failed to respond to clozapine therapy after several months at clinically adequate doses. Our findings were published online last month in the highly respected journal Schizophrenia Research.8 We reported the successful treatment with pimavanserin in 2 groups:
- patients who had not responded to clozapine received pimavanserin as an add-on to clozapine in doses of 34 mg/d, the same dose recommended for patients with Parkinson’s disease hallucinations and/or delusions.
- patients who had hallucinations and delusions that failed to respond to several non-clozapine antipsychotics received pimavanserin monotherapy instead of clozapine to avoid blood draws and serious adverse effects.
Continue to: Pimavanserin successfully treated...
Pimavanserin successfully treated the hallucinations and delusions of all 10 patients in both groups. Remission occurred within 1 month in most cases, and after 2 months in 1 patient. Those patients no longer required hospitalization as they did prior to taking pimavanserin, and they maintained their response for several months of follow-up. We were also pleased to note that most patients became more sociable and affable, with improved mood and affect, after their hallucinations and delusions disappeared with pimavanserin. We did have a few patients who did not respond to 34 mg/d of pimavanserin, and some who responded for several months but then showed signs of recurrence. We are considering increasing the dose to 68 mg/d in such patients because it is possible that a higher dose may be needed in some patients with refractory illness, who may vary in symptom severity or biology.
We are now planning to apply for a research grant to conduct a controlled trial to confirm our very encouraging clinical findings, and we hope other investigators will also conduct clinical trials in patients with refractory psychosis comparing pimavanserin with placebo or pimavanserin with clozapine in double-blind studies.
As a disclosure, our clinical findings were obtained without any knowledge of, or funding from, the company that makes pimavanserin (Acadia Pharmaceuticals Inc.). The company was informed of our findings only after our article was accepted for publication.
I hope this important finding of a potentially safer alternative to clozapine may address a major unmet need in psychiatry, involving the treatment of hundreds of thousands of patients with treatment-resistant or treatment-refractory psychosis, which includes patients with schizophrenia, schizoaffective disorder, or psychotic bipolar disorder.
To comment on this editorial or other topics of interest: [email protected].
1. Nasrallah HA. Clozapine is a vastly underutilized, unique agent with multiple applications. Current Psychiatry. 2014;13(10):21, 24-25.
2. Yeiser B. Mind estranged: my journey from schizophrenia and homelessness to recovery. Seattle, WA: Amazon; 2014.
3. Raja M, Raja S. Clozapine safety, 40 years later. Curr Drug Saf. 2014;9(3):163-195.
4. Manu P, Kane JM, Corell CU. Sudden deaths in psychiatric patients. J Clin Psychiatry. 2011;72(7):936-941.
5. Tiihonen J, Wahlbeck K, Kiviniemi V. The efficacy of lamotrigine in clozapine-resistant schizophrenia: a systematic review and meta-analysis. Schizophrenia Research. 2009;109(1-3):10-14.
6. Lin CH, Lin CH, Chang YC, et al. Sodium benzoate, a D-amino acid oxidase inhibitor, added to clozapine for the treatment of schizophrenia: a randomized, double-blind, placebo-controlled trial. Biol Psychiatry. 2017;84(6):422-432.
7. Ballard C, Banister C, Khan Z, et al; ADP Investigators. Evaluation of the safety, tolerability, and efficacy of pimavanserin versus placebo in p atients with Alzheimer’s disease psychosis: a phase 2, randomised, placebo-controlled, double-blind study. Lancet Neurol. 2018;17(3):213-222.
8. Nasrallah HA, Fedora R, Morton R. Successful treatment of clozapine-nonresponsive refractory hallucinations and delusions with pimavanserin, a serotonin 5HT-2A receptor inverse agonist [Epub ahead of print March 2, 2019]. Schizophrenia Res. 2019. doi: 10.1016/j.schres.2019.02.018.
Up to 30% of patients with schizophrenia do not respond to dopamine antagonists, which include all first- and second-generation antipsychotics. They are labeled as “treatment-resistant” if they have a partial response, or “treatment-refractory” if their hallucinations and/or delusions do not improve at all despite multiple trials of antipsychotics.
That’s why clozapine is considered a “lifesaver” for such patients, a last-resort medication that unshackles patients with refractory psychotic symptoms from the tyranny of auditory and/or visual hallucinations and the reality distortion of fixed false beliefs such as paranoid delusions.
Many long-suffering patients with refractory psychosis recover and return to their baseline, thanks to clozapine. In a past editorial, I discussed how one of my patients, Bethany, who had dropped out of college and became homeless for 4 years with refractory delusions and hallucinations, recovered completely when she received clozapine.1 She then returned to college, graduated with honors, and authored a book about her journey of recovery.2 She and I later established a nonprofit foundation we called CURESZ (Comprehensive Understanding via Research and Education in Schizophrenia), and assembled a panel of 80 clozapine experts across the country to provide access to clozapine for the hundreds of thousands of individuals with refractory psychosis who never received a trial of clozapine from their psychiatrists or psychiatric nurse practitioners. (Visit CURESZ.org for details.)
Bethany was very lucky to respond and recover completely, because only 40% of patients with refractory psychosis respond to clozapine. She does not mind having her blood drawn every week to measure her white blood cell count for early detection of potentially fatal agranulocytosis. Many refractory, often homeless patients with chronic schizophrenia refuse to have weekly phlebotomy and therefore are not treated with clozapine. Bethany was also fortunate to experience only 1 adverse effect of clozapine: extreme sedation that forced her to sleep up to 15 hours a day (this was reduced to 9 to 10 hours a day with adjunctive modafinil). Fortunately, she was spared the multiple other serious adverse effects of clozapine, which include excessive salivation, extreme weight gain, diabetes, hyperlipidemia, cardiomyopathy, pancreatitis, seizures, and ileus.3 Clozapine is also associated with sudden death more than any other antipsychotic agent.4
So, what can be done for patients with refractory hallucinations and delusions who are among the 60% who fail to respond to clozapine, or who experience intolerable adverse effects or safety problems, or who refuse to take clozapine and have their blood drawn every week? This is a desperately ill and seriously disabled group of patients who are deemed to be beyond the reach of medical intervention by psychiatry. They are often treated with various off-label medications as adjunctive therapy to clozapine, to which they failed to respond. This includes adding lamotrigine5 or benzoate,6 but none have been approved as an efficacious and safe monotherapy alternative to clozapine. So, what can be done for patients with refractory illness?
Enter pimavanserin. This new medication is an inverse agonist of serotonin 5-HT2A receptors and (to a lesser extent) serotonin 5-HT2C receptors. It was recently FDA-approved for treating the hallucinations and delusions of Parkinson’s disease psychosis,7 which is estimated to develop in up to 50% of individuals with Parkinson’s disease. It does not have any affinity to any dopamine receptors, which makes it an ideal antipsychotic for Parkinson’s disease, where any dopamine antagonism can worsen the motor symptoms (rigidity, hypokinesia, and tremors) associated with that movement disorder. Thus, pimavanserin became the first ever non-dopaminergic antipsychotic in the world and is indicated only for Parkinson’s disease psychosis.
Our clinical team made a serendipitous discovery about the efficacy of pimavanserin in patients with schizophrenia who failed to respond to clozapine therapy after several months at clinically adequate doses. Our findings were published online last month in the highly respected journal Schizophrenia Research.8 We reported the successful treatment with pimavanserin in 2 groups:
- patients who had not responded to clozapine received pimavanserin as an add-on to clozapine in doses of 34 mg/d, the same dose recommended for patients with Parkinson’s disease hallucinations and/or delusions.
- patients who had hallucinations and delusions that failed to respond to several non-clozapine antipsychotics received pimavanserin monotherapy instead of clozapine to avoid blood draws and serious adverse effects.
Continue to: Pimavanserin successfully treated...
Pimavanserin successfully treated the hallucinations and delusions of all 10 patients in both groups. Remission occurred within 1 month in most cases, and after 2 months in 1 patient. Those patients no longer required hospitalization as they did prior to taking pimavanserin, and they maintained their response for several months of follow-up. We were also pleased to note that most patients became more sociable and affable, with improved mood and affect, after their hallucinations and delusions disappeared with pimavanserin. We did have a few patients who did not respond to 34 mg/d of pimavanserin, and some who responded for several months but then showed signs of recurrence. We are considering increasing the dose to 68 mg/d in such patients because it is possible that a higher dose may be needed in some patients with refractory illness, who may vary in symptom severity or biology.
We are now planning to apply for a research grant to conduct a controlled trial to confirm our very encouraging clinical findings, and we hope other investigators will also conduct clinical trials in patients with refractory psychosis comparing pimavanserin with placebo or pimavanserin with clozapine in double-blind studies.
As a disclosure, our clinical findings were obtained without any knowledge of, or funding from, the company that makes pimavanserin (Acadia Pharmaceuticals Inc.). The company was informed of our findings only after our article was accepted for publication.
I hope this important finding of a potentially safer alternative to clozapine may address a major unmet need in psychiatry, involving the treatment of hundreds of thousands of patients with treatment-resistant or treatment-refractory psychosis, which includes patients with schizophrenia, schizoaffective disorder, or psychotic bipolar disorder.
To comment on this editorial or other topics of interest: [email protected].
Up to 30% of patients with schizophrenia do not respond to dopamine antagonists, which include all first- and second-generation antipsychotics. They are labeled as “treatment-resistant” if they have a partial response, or “treatment-refractory” if their hallucinations and/or delusions do not improve at all despite multiple trials of antipsychotics.
That’s why clozapine is considered a “lifesaver” for such patients, a last-resort medication that unshackles patients with refractory psychotic symptoms from the tyranny of auditory and/or visual hallucinations and the reality distortion of fixed false beliefs such as paranoid delusions.
Many long-suffering patients with refractory psychosis recover and return to their baseline, thanks to clozapine. In a past editorial, I discussed how one of my patients, Bethany, who had dropped out of college and became homeless for 4 years with refractory delusions and hallucinations, recovered completely when she received clozapine.1 She then returned to college, graduated with honors, and authored a book about her journey of recovery.2 She and I later established a nonprofit foundation we called CURESZ (Comprehensive Understanding via Research and Education in Schizophrenia), and assembled a panel of 80 clozapine experts across the country to provide access to clozapine for the hundreds of thousands of individuals with refractory psychosis who never received a trial of clozapine from their psychiatrists or psychiatric nurse practitioners. (Visit CURESZ.org for details.)
Bethany was very lucky to respond and recover completely, because only 40% of patients with refractory psychosis respond to clozapine. She does not mind having her blood drawn every week to measure her white blood cell count for early detection of potentially fatal agranulocytosis. Many refractory, often homeless patients with chronic schizophrenia refuse to have weekly phlebotomy and therefore are not treated with clozapine. Bethany was also fortunate to experience only 1 adverse effect of clozapine: extreme sedation that forced her to sleep up to 15 hours a day (this was reduced to 9 to 10 hours a day with adjunctive modafinil). Fortunately, she was spared the multiple other serious adverse effects of clozapine, which include excessive salivation, extreme weight gain, diabetes, hyperlipidemia, cardiomyopathy, pancreatitis, seizures, and ileus.3 Clozapine is also associated with sudden death more than any other antipsychotic agent.4
So, what can be done for patients with refractory hallucinations and delusions who are among the 60% who fail to respond to clozapine, or who experience intolerable adverse effects or safety problems, or who refuse to take clozapine and have their blood drawn every week? This is a desperately ill and seriously disabled group of patients who are deemed to be beyond the reach of medical intervention by psychiatry. They are often treated with various off-label medications as adjunctive therapy to clozapine, to which they failed to respond. This includes adding lamotrigine5 or benzoate,6 but none have been approved as an efficacious and safe monotherapy alternative to clozapine. So, what can be done for patients with refractory illness?
Enter pimavanserin. This new medication is an inverse agonist of serotonin 5-HT2A receptors and (to a lesser extent) serotonin 5-HT2C receptors. It was recently FDA-approved for treating the hallucinations and delusions of Parkinson’s disease psychosis,7 which is estimated to develop in up to 50% of individuals with Parkinson’s disease. It does not have any affinity to any dopamine receptors, which makes it an ideal antipsychotic for Parkinson’s disease, where any dopamine antagonism can worsen the motor symptoms (rigidity, hypokinesia, and tremors) associated with that movement disorder. Thus, pimavanserin became the first ever non-dopaminergic antipsychotic in the world and is indicated only for Parkinson’s disease psychosis.
Our clinical team made a serendipitous discovery about the efficacy of pimavanserin in patients with schizophrenia who failed to respond to clozapine therapy after several months at clinically adequate doses. Our findings were published online last month in the highly respected journal Schizophrenia Research.8 We reported the successful treatment with pimavanserin in 2 groups:
- patients who had not responded to clozapine received pimavanserin as an add-on to clozapine in doses of 34 mg/d, the same dose recommended for patients with Parkinson’s disease hallucinations and/or delusions.
- patients who had hallucinations and delusions that failed to respond to several non-clozapine antipsychotics received pimavanserin monotherapy instead of clozapine to avoid blood draws and serious adverse effects.
Continue to: Pimavanserin successfully treated...
Pimavanserin successfully treated the hallucinations and delusions of all 10 patients in both groups. Remission occurred within 1 month in most cases, and after 2 months in 1 patient. Those patients no longer required hospitalization as they did prior to taking pimavanserin, and they maintained their response for several months of follow-up. We were also pleased to note that most patients became more sociable and affable, with improved mood and affect, after their hallucinations and delusions disappeared with pimavanserin. We did have a few patients who did not respond to 34 mg/d of pimavanserin, and some who responded for several months but then showed signs of recurrence. We are considering increasing the dose to 68 mg/d in such patients because it is possible that a higher dose may be needed in some patients with refractory illness, who may vary in symptom severity or biology.
We are now planning to apply for a research grant to conduct a controlled trial to confirm our very encouraging clinical findings, and we hope other investigators will also conduct clinical trials in patients with refractory psychosis comparing pimavanserin with placebo or pimavanserin with clozapine in double-blind studies.
As a disclosure, our clinical findings were obtained without any knowledge of, or funding from, the company that makes pimavanserin (Acadia Pharmaceuticals Inc.). The company was informed of our findings only after our article was accepted for publication.
I hope this important finding of a potentially safer alternative to clozapine may address a major unmet need in psychiatry, involving the treatment of hundreds of thousands of patients with treatment-resistant or treatment-refractory psychosis, which includes patients with schizophrenia, schizoaffective disorder, or psychotic bipolar disorder.
To comment on this editorial or other topics of interest: [email protected].
1. Nasrallah HA. Clozapine is a vastly underutilized, unique agent with multiple applications. Current Psychiatry. 2014;13(10):21, 24-25.
2. Yeiser B. Mind estranged: my journey from schizophrenia and homelessness to recovery. Seattle, WA: Amazon; 2014.
3. Raja M, Raja S. Clozapine safety, 40 years later. Curr Drug Saf. 2014;9(3):163-195.
4. Manu P, Kane JM, Corell CU. Sudden deaths in psychiatric patients. J Clin Psychiatry. 2011;72(7):936-941.
5. Tiihonen J, Wahlbeck K, Kiviniemi V. The efficacy of lamotrigine in clozapine-resistant schizophrenia: a systematic review and meta-analysis. Schizophrenia Research. 2009;109(1-3):10-14.
6. Lin CH, Lin CH, Chang YC, et al. Sodium benzoate, a D-amino acid oxidase inhibitor, added to clozapine for the treatment of schizophrenia: a randomized, double-blind, placebo-controlled trial. Biol Psychiatry. 2017;84(6):422-432.
7. Ballard C, Banister C, Khan Z, et al; ADP Investigators. Evaluation of the safety, tolerability, and efficacy of pimavanserin versus placebo in p atients with Alzheimer’s disease psychosis: a phase 2, randomised, placebo-controlled, double-blind study. Lancet Neurol. 2018;17(3):213-222.
8. Nasrallah HA, Fedora R, Morton R. Successful treatment of clozapine-nonresponsive refractory hallucinations and delusions with pimavanserin, a serotonin 5HT-2A receptor inverse agonist [Epub ahead of print March 2, 2019]. Schizophrenia Res. 2019. doi: 10.1016/j.schres.2019.02.018.
1. Nasrallah HA. Clozapine is a vastly underutilized, unique agent with multiple applications. Current Psychiatry. 2014;13(10):21, 24-25.
2. Yeiser B. Mind estranged: my journey from schizophrenia and homelessness to recovery. Seattle, WA: Amazon; 2014.
3. Raja M, Raja S. Clozapine safety, 40 years later. Curr Drug Saf. 2014;9(3):163-195.
4. Manu P, Kane JM, Corell CU. Sudden deaths in psychiatric patients. J Clin Psychiatry. 2011;72(7):936-941.
5. Tiihonen J, Wahlbeck K, Kiviniemi V. The efficacy of lamotrigine in clozapine-resistant schizophrenia: a systematic review and meta-analysis. Schizophrenia Research. 2009;109(1-3):10-14.
6. Lin CH, Lin CH, Chang YC, et al. Sodium benzoate, a D-amino acid oxidase inhibitor, added to clozapine for the treatment of schizophrenia: a randomized, double-blind, placebo-controlled trial. Biol Psychiatry. 2017;84(6):422-432.
7. Ballard C, Banister C, Khan Z, et al; ADP Investigators. Evaluation of the safety, tolerability, and efficacy of pimavanserin versus placebo in p atients with Alzheimer’s disease psychosis: a phase 2, randomised, placebo-controlled, double-blind study. Lancet Neurol. 2018;17(3):213-222.
8. Nasrallah HA, Fedora R, Morton R. Successful treatment of clozapine-nonresponsive refractory hallucinations and delusions with pimavanserin, a serotonin 5HT-2A receptor inverse agonist [Epub ahead of print March 2, 2019]. Schizophrenia Res. 2019. doi: 10.1016/j.schres.2019.02.018.
Treating military members, veterans, and their families
I had the unique opportunity to attend a civilian medical school followed by residency and fellowship training along civilian providers, and I often was asked about my military experience. The more time I spent with civilian providers, the more I realized how unaware they are about the intricacies of military lifestyle and culture.
Of course, this makes sense. During the draft era, almost every family had a member who served, and more people were exposed to the uniqueness of military culture.1 However, with the shift to an all-volunteer military came a decrease in the number of both active duty members and veterans.2 Consequently, today’s society is generally less aware of the realities of the military lifestyle. This is especially true among people born after the Vietnam War, whose knowledge about military life is frequently limited to movies and video games. These movies and games are as accurate a reflection of military life as watching TV series such as ER or The Resident are for learning what it’s like to be a physician. To add to the problem, most medical schools and residency training curricula include little information about military culture.3 As a result, psychiatrists, like many other physicians, often feel unequipped to provide care for veterans, current military personnel, and their loved ones.4 At the very least, most psychiatrists are unaware of the differences between military and civilian cultures.
Veterans, current military members, and their families who seek mental health services outside the Veterans Affairs (VA) and military treatment facilities are more likely to encounter a clinician who does not feel comfortable with the nuances of the military lifestyle and its challenges.3 Facing a physician with limited familiarity with their experiences, and out of fear of being misunderstood, patients may not feel comfortable disclosing pertinent details.
The US military has its own culture, lingo, customs, rules, and regulations. Its structure is hierarchical and mission-oriented. The moment a person joins the military, he or she falls under a set of legal guidelines of the Uniform Code of Military Justice (UCMJ).5 For example, extra-marital sexual conduct, fistfighting (not in combat), disrespecting superior officers, and insubordination are all punishable under UCMJ.5,6 Active duty military members are also prohibited from suing the federal government for injuries.7 The Health Insurance Portability and Accountability Act (HIPAA) permits protected health information of Armed Forces personnel to be disclosed under special circumstances. These include fitness for duty determinations, fitness to perform a particular assignment, or other activities necessary for the military mission.8 A mental health provider’s understanding of the unique aspects of military culture can positively influence the patient-provider relationship whether the patient is still serving, has left the military, or is a family member of a current or former military member.
Not all military veterans qualify for VA health care. For example, those who didn’t serve the required time on active duty, those whose injury existed prior to joining the military and was not worsened by their military service, and those discharged under other-than-honorable, bad conduct, or dishonorable conditions are unlikely to qualify.9 Other veterans simply prefer to be privately treated outside the VA. However, despite where a veteran receives treatment, the clinician’s knowledge of important military concepts can facilitate rapport-building and providing a safe space for disclosure of pertinent history. Obtaining a military history that includes (for example) years of service, number and location of deployments, combat experience, and number of transfers can help with understanding the biopsychosocial factors contributing to the diagnosis and important treatment needs.
While military dependents (spouses and children) don’t wear uniforms, they are also affected by the service and sacrifices of the military member. Spouses have to deal with adjusting to the military lifestyle, searching for new housing and jobs, finding schools for children, and separation and reconnection with a military member. Military children are not spared, either. They, too, have to leave their friends and find new ones, and adjust to new places, routines, and schools, knowing that in 2 to 3 years they likely will have to move again.
As a military member, mother, and spouse of a former military member, I know how life-changing military service can be for the entire family. I encourage all physicians to start routinely asking if their patient or his or her loved ones have ever been in the military, because a positive answer could help you to better understand the patient and provide the most appropriate, person-centered, culturally-informed treatment.
1. Pew Research Center. The military-civilian gap: War and sacrifice in the post-9/11 era. http://www.pewsocialtrends.org/2011/10/05/war-and-sacrifice-in-the-post-911-era. Published October 5, 2011. Accessed March 12, 2019.
2. Bialik K. The changing face of America’s veteran population. http://www.pewresearch.org/fact-tank/2017/11/10/the-changing-face-of-americas-veteran-population. Published November 10, 2017. Accessed March 12, 2019.
3. Meyer EG, Writer BW, Brim W. The importance of military cultural competence. Curr Psychiatry Rep. 2016;18(3):26.
4. Tanielian T, Farris C, Epley C, et al; RAND Corporation. Ready to serve: community-based provider capacity to deliver culturally competent, quality mental health care to veterans and their families. https://www.rand.org/content/dam/rand/pubs/research_reports/RR800/RR806/RAND_RR806.pdf. Accessed December 10, 2018.
5. The Uniform Code of Military Justice. http://www.ucmj.us. Accessed March 4, 2019.
6. Myers M. Here’s what you need to know about the biggest update to UCMJ in decades. Military Times. https://www.militarytimes.com/news/your-army/2019/01/15/heres-what-you-need-to-know-about-the-biggest-update-to-ucmj-in-decades/. Published Jan 15, 2019. Accessed March 12, 2019.
7. Information Institute. Feres Doctrine. https://www.law.cornell.edu/wex/feres_doctrine. Accessed March 12, 2019.
8. Defense Health Agency Privacy and Civil Liberties Office. The military command exception and disclosing PHI of armed forces personnel. https://health.mil/Reference-Center/Fact-Sheets/2015/05/13/Info-Paper-Military-Command-Exception-and-Disclosing-PHI-of-Armed-Forces-Personnel. Published May 13, 2015. Accessed March 12, 2019.
9. Veterans Benefits Administration. Applying for benefits and your character of discharge. https://www.benefits.va.gov/benefits/character_of_discharge.asp. Updated May 19, 2015. Accessed March 12, 2019.
I had the unique opportunity to attend a civilian medical school followed by residency and fellowship training along civilian providers, and I often was asked about my military experience. The more time I spent with civilian providers, the more I realized how unaware they are about the intricacies of military lifestyle and culture.
Of course, this makes sense. During the draft era, almost every family had a member who served, and more people were exposed to the uniqueness of military culture.1 However, with the shift to an all-volunteer military came a decrease in the number of both active duty members and veterans.2 Consequently, today’s society is generally less aware of the realities of the military lifestyle. This is especially true among people born after the Vietnam War, whose knowledge about military life is frequently limited to movies and video games. These movies and games are as accurate a reflection of military life as watching TV series such as ER or The Resident are for learning what it’s like to be a physician. To add to the problem, most medical schools and residency training curricula include little information about military culture.3 As a result, psychiatrists, like many other physicians, often feel unequipped to provide care for veterans, current military personnel, and their loved ones.4 At the very least, most psychiatrists are unaware of the differences between military and civilian cultures.
Veterans, current military members, and their families who seek mental health services outside the Veterans Affairs (VA) and military treatment facilities are more likely to encounter a clinician who does not feel comfortable with the nuances of the military lifestyle and its challenges.3 Facing a physician with limited familiarity with their experiences, and out of fear of being misunderstood, patients may not feel comfortable disclosing pertinent details.
The US military has its own culture, lingo, customs, rules, and regulations. Its structure is hierarchical and mission-oriented. The moment a person joins the military, he or she falls under a set of legal guidelines of the Uniform Code of Military Justice (UCMJ).5 For example, extra-marital sexual conduct, fistfighting (not in combat), disrespecting superior officers, and insubordination are all punishable under UCMJ.5,6 Active duty military members are also prohibited from suing the federal government for injuries.7 The Health Insurance Portability and Accountability Act (HIPAA) permits protected health information of Armed Forces personnel to be disclosed under special circumstances. These include fitness for duty determinations, fitness to perform a particular assignment, or other activities necessary for the military mission.8 A mental health provider’s understanding of the unique aspects of military culture can positively influence the patient-provider relationship whether the patient is still serving, has left the military, or is a family member of a current or former military member.
Not all military veterans qualify for VA health care. For example, those who didn’t serve the required time on active duty, those whose injury existed prior to joining the military and was not worsened by their military service, and those discharged under other-than-honorable, bad conduct, or dishonorable conditions are unlikely to qualify.9 Other veterans simply prefer to be privately treated outside the VA. However, despite where a veteran receives treatment, the clinician’s knowledge of important military concepts can facilitate rapport-building and providing a safe space for disclosure of pertinent history. Obtaining a military history that includes (for example) years of service, number and location of deployments, combat experience, and number of transfers can help with understanding the biopsychosocial factors contributing to the diagnosis and important treatment needs.
While military dependents (spouses and children) don’t wear uniforms, they are also affected by the service and sacrifices of the military member. Spouses have to deal with adjusting to the military lifestyle, searching for new housing and jobs, finding schools for children, and separation and reconnection with a military member. Military children are not spared, either. They, too, have to leave their friends and find new ones, and adjust to new places, routines, and schools, knowing that in 2 to 3 years they likely will have to move again.
As a military member, mother, and spouse of a former military member, I know how life-changing military service can be for the entire family. I encourage all physicians to start routinely asking if their patient or his or her loved ones have ever been in the military, because a positive answer could help you to better understand the patient and provide the most appropriate, person-centered, culturally-informed treatment.
I had the unique opportunity to attend a civilian medical school followed by residency and fellowship training along civilian providers, and I often was asked about my military experience. The more time I spent with civilian providers, the more I realized how unaware they are about the intricacies of military lifestyle and culture.
Of course, this makes sense. During the draft era, almost every family had a member who served, and more people were exposed to the uniqueness of military culture.1 However, with the shift to an all-volunteer military came a decrease in the number of both active duty members and veterans.2 Consequently, today’s society is generally less aware of the realities of the military lifestyle. This is especially true among people born after the Vietnam War, whose knowledge about military life is frequently limited to movies and video games. These movies and games are as accurate a reflection of military life as watching TV series such as ER or The Resident are for learning what it’s like to be a physician. To add to the problem, most medical schools and residency training curricula include little information about military culture.3 As a result, psychiatrists, like many other physicians, often feel unequipped to provide care for veterans, current military personnel, and their loved ones.4 At the very least, most psychiatrists are unaware of the differences between military and civilian cultures.
Veterans, current military members, and their families who seek mental health services outside the Veterans Affairs (VA) and military treatment facilities are more likely to encounter a clinician who does not feel comfortable with the nuances of the military lifestyle and its challenges.3 Facing a physician with limited familiarity with their experiences, and out of fear of being misunderstood, patients may not feel comfortable disclosing pertinent details.
The US military has its own culture, lingo, customs, rules, and regulations. Its structure is hierarchical and mission-oriented. The moment a person joins the military, he or she falls under a set of legal guidelines of the Uniform Code of Military Justice (UCMJ).5 For example, extra-marital sexual conduct, fistfighting (not in combat), disrespecting superior officers, and insubordination are all punishable under UCMJ.5,6 Active duty military members are also prohibited from suing the federal government for injuries.7 The Health Insurance Portability and Accountability Act (HIPAA) permits protected health information of Armed Forces personnel to be disclosed under special circumstances. These include fitness for duty determinations, fitness to perform a particular assignment, or other activities necessary for the military mission.8 A mental health provider’s understanding of the unique aspects of military culture can positively influence the patient-provider relationship whether the patient is still serving, has left the military, or is a family member of a current or former military member.
Not all military veterans qualify for VA health care. For example, those who didn’t serve the required time on active duty, those whose injury existed prior to joining the military and was not worsened by their military service, and those discharged under other-than-honorable, bad conduct, or dishonorable conditions are unlikely to qualify.9 Other veterans simply prefer to be privately treated outside the VA. However, despite where a veteran receives treatment, the clinician’s knowledge of important military concepts can facilitate rapport-building and providing a safe space for disclosure of pertinent history. Obtaining a military history that includes (for example) years of service, number and location of deployments, combat experience, and number of transfers can help with understanding the biopsychosocial factors contributing to the diagnosis and important treatment needs.
While military dependents (spouses and children) don’t wear uniforms, they are also affected by the service and sacrifices of the military member. Spouses have to deal with adjusting to the military lifestyle, searching for new housing and jobs, finding schools for children, and separation and reconnection with a military member. Military children are not spared, either. They, too, have to leave their friends and find new ones, and adjust to new places, routines, and schools, knowing that in 2 to 3 years they likely will have to move again.
As a military member, mother, and spouse of a former military member, I know how life-changing military service can be for the entire family. I encourage all physicians to start routinely asking if their patient or his or her loved ones have ever been in the military, because a positive answer could help you to better understand the patient and provide the most appropriate, person-centered, culturally-informed treatment.
1. Pew Research Center. The military-civilian gap: War and sacrifice in the post-9/11 era. http://www.pewsocialtrends.org/2011/10/05/war-and-sacrifice-in-the-post-911-era. Published October 5, 2011. Accessed March 12, 2019.
2. Bialik K. The changing face of America’s veteran population. http://www.pewresearch.org/fact-tank/2017/11/10/the-changing-face-of-americas-veteran-population. Published November 10, 2017. Accessed March 12, 2019.
3. Meyer EG, Writer BW, Brim W. The importance of military cultural competence. Curr Psychiatry Rep. 2016;18(3):26.
4. Tanielian T, Farris C, Epley C, et al; RAND Corporation. Ready to serve: community-based provider capacity to deliver culturally competent, quality mental health care to veterans and their families. https://www.rand.org/content/dam/rand/pubs/research_reports/RR800/RR806/RAND_RR806.pdf. Accessed December 10, 2018.
5. The Uniform Code of Military Justice. http://www.ucmj.us. Accessed March 4, 2019.
6. Myers M. Here’s what you need to know about the biggest update to UCMJ in decades. Military Times. https://www.militarytimes.com/news/your-army/2019/01/15/heres-what-you-need-to-know-about-the-biggest-update-to-ucmj-in-decades/. Published Jan 15, 2019. Accessed March 12, 2019.
7. Information Institute. Feres Doctrine. https://www.law.cornell.edu/wex/feres_doctrine. Accessed March 12, 2019.
8. Defense Health Agency Privacy and Civil Liberties Office. The military command exception and disclosing PHI of armed forces personnel. https://health.mil/Reference-Center/Fact-Sheets/2015/05/13/Info-Paper-Military-Command-Exception-and-Disclosing-PHI-of-Armed-Forces-Personnel. Published May 13, 2015. Accessed March 12, 2019.
9. Veterans Benefits Administration. Applying for benefits and your character of discharge. https://www.benefits.va.gov/benefits/character_of_discharge.asp. Updated May 19, 2015. Accessed March 12, 2019.
1. Pew Research Center. The military-civilian gap: War and sacrifice in the post-9/11 era. http://www.pewsocialtrends.org/2011/10/05/war-and-sacrifice-in-the-post-911-era. Published October 5, 2011. Accessed March 12, 2019.
2. Bialik K. The changing face of America’s veteran population. http://www.pewresearch.org/fact-tank/2017/11/10/the-changing-face-of-americas-veteran-population. Published November 10, 2017. Accessed March 12, 2019.
3. Meyer EG, Writer BW, Brim W. The importance of military cultural competence. Curr Psychiatry Rep. 2016;18(3):26.
4. Tanielian T, Farris C, Epley C, et al; RAND Corporation. Ready to serve: community-based provider capacity to deliver culturally competent, quality mental health care to veterans and their families. https://www.rand.org/content/dam/rand/pubs/research_reports/RR800/RR806/RAND_RR806.pdf. Accessed December 10, 2018.
5. The Uniform Code of Military Justice. http://www.ucmj.us. Accessed March 4, 2019.
6. Myers M. Here’s what you need to know about the biggest update to UCMJ in decades. Military Times. https://www.militarytimes.com/news/your-army/2019/01/15/heres-what-you-need-to-know-about-the-biggest-update-to-ucmj-in-decades/. Published Jan 15, 2019. Accessed March 12, 2019.
7. Information Institute. Feres Doctrine. https://www.law.cornell.edu/wex/feres_doctrine. Accessed March 12, 2019.
8. Defense Health Agency Privacy and Civil Liberties Office. The military command exception and disclosing PHI of armed forces personnel. https://health.mil/Reference-Center/Fact-Sheets/2015/05/13/Info-Paper-Military-Command-Exception-and-Disclosing-PHI-of-Armed-Forces-Personnel. Published May 13, 2015. Accessed March 12, 2019.
9. Veterans Benefits Administration. Applying for benefits and your character of discharge. https://www.benefits.va.gov/benefits/character_of_discharge.asp. Updated May 19, 2015. Accessed March 12, 2019.
Paraphilic disorders: A better understanding
In my role as the Director of The Johns Hopkins Sex and Gender Clinic, I have had the opportunity to provide care to 3 broad categories of patients: patients with sexual dysfunctions, patients experiencing gender dysphoria, and patients manifesting a paraphilic disorder. This article will not address sexual dysfunctions or gender dysphoria, but these terms are defined in the Box1-3 to clearly distinguish them from paraphilic disorders.
Box
Individuals with a sexual dysfunction (eg, erectile dysfunction or anorgasmia) generally experience conventional sexual feelings, but they may have difficulty performing sexually.1 Although ordinarily capable of adequate sexual performance, persons with a paraphilic disorder experience atypical erotic cravings.2 Such cravings can either be for an atypical or unacceptable category of potential partner (eg, animals or children), or for an atypical or unacceptable type of behavior (eg, crossdressing or public exhibitionism). Individuals with gender dysphoria frequently experience distress because their internal sense of feeling either male or female is not congruent with their external physical anatomy.3 The primary concerns of individuals experiencing gender dysphoria relate to feelings of gender identity, as opposed to problems involving erotic arousal.
Persons with paraphilic disorders (predominantly males) experience recurrent atypical sexual fantasies and urges that cause clinically significant impairment or distress.1 Those atypical fantasies and urges may be directed towards unacceptable partners such as animals or children, or towards unacceptable behaviors such as public exhibitionism. Table 11 lists the paraphilic disorders identified in DSM-5. This article focuses primarily, though not exclusively, upon pedophilic disorder, and its pharmacologic treatment. However, the rationale underlying such treatment is applicable across the paraphilic spectrum. Before providing such treatment, it is important for clinicians to have a clear conceptual understanding of paraphilic disorders.
When is a difference a disorder?
Cancer and respiration are 2 different biologic phenomenon. Cancer causes suffering and impairment, and as a consequence, we label it a disorder. We do so in the hope of learning more about it, and being able to successfully treat it. We do not classify respiration as a disorder because we do not consider it to be harmful.
The spectrum of human sexuality is quite broad, and psychiatry is generally not concerned with private sexual thoughts and behaviors involving consenting adults that do not cause suffering or impairment. When adults choose to engage in “kinky sex” that causes neither harm nor distress, so be it.
Some individuals may be privately aware of experiencing either an exclusive or nonexclusive sexual attraction to children. Some of these individuals may not be distressed by experiencing such attractions, and may be fully capable of resisting the temptation to enact them. In such an instance, even though an individual may be experiencing sexual attractions that are different from the norm, there may not be a sufficient basis for diagnosing pedophilic disorder. However, that difference in sexual phenomenology (ie, mental experience) could rise to the level of a diagnosable disorder if the individual in question expresses distress about experiencing such attractions, and/or if his capacity to resist acting upon them is impaired.4 Under such circumstances, treatment would be warranted.
Patients with paraphilic disorders deserve treatment
Prior to establishment of the Betty Ford Clinic in 1982, individuals who were drug- or alcohol-dependent were often portrayed in a negative light and referred to by derogatory pejoratives such as “bum” or “pothead.”5 Over time, society came to appreciate that good people, deserving of treatment, can become dependent upon substances, and in recent years there has been considerable support for related research initiatives and humane care. However, there has not been analogous support for individuals who manifest paraphilic disorders, especially those with pedophilic disorder. Instead, such individuals are often perceived as undeserving of mental health care and resources. This has been the case, even though successful treatment of a pedophilic disorder could help prevent the serious consequences of child molestation from occurring.
In contemporary society, the term pedophilia, which is a psychiatric specifier intended to guide research and treatment, has been hijacked by the nonmedical community and turned into a demeaning pejorative. In the collective consciousness of the public, the term pedophilia is routinely and mistakenly equated with the behavior of child molestation. Just as all alcoholics are not drunk drivers, all individuals with pedophilic disorder are not “child molesters.” Conversely, not all “child molesters” have pedophilic disorder.
Continue to: Individuals with other types...
Individuals with other types of paraphilic disorders are frequently similarly maligned and referred to as “perverts” or “deviants.” Public service announcements are frequently aired to reach out to individuals who are depressed, or drug- or alcohol-dependent, or suffering with other forms of mental disorders. When does one hear a public service announcement that encourages young people who may be experiencing disturbing or unacceptable sexual feelings to seek psychiatric treatment? There is a support group on the internet called Virtuous Pedophiles.6 That organization is unequivocally opposed to child molestation, while supporting efforts to improve the mental well-being of individuals who, through no fault of their own, experience unwanted pedophilic feelings.
Causes and noncauses
In attempting to elucidate etiology, researchers typically investigate nature (biology) and/or nurture (life experiences). In terms of the development of pedophilic disorder, there is evidence that both nature and nurture can play a role. Researchers have found that boys who are sexually abused are at increased risk for developing pedophilic disorder, and evidence of temporal lobe disturbances has also been documented in some instances.7,8
From clinical, societal, and forensic perspectives, it may be equally important to identify noncausal factors. Paraphilic disorders, including pedophilic disorder, do not develop as a consequence of volitional choice.9 For example, none of us decide which category, or categories, of potential partners are going to attract us sexually. Rather, in maturing we discover the nature of our own sexuality. Children do not ponder their options, somehow deciding while growing up to be attracted to the opposite sex (heterosexuality), the same sex (homosexuality), or both sexes (bisexuality). Similarly, in maturing into adulthood, individuals do not decide to become sexually attracted to prepubescent children. Who would decide to do that? Instead, unlike most of us, some individuals discover this about themselves; this often is a deeply disturbing insight.
It is not an individual’s fault that he or she has a paraphilic disorder. It is, however, his or her responsibility to do something about it. This may require accessing appropriate psychiatric care.
Why treatment may be needed
Sex is a powerful, biologically based appetite that recurrently craves satiation. God or nature has put that drive into all of us to ensure the survival of humanity. Even when that powerful biologic drive becomes misdirected (for example, towards children, or towards a desire to engage in public exhibitionism), it still recurrently craves satisfaction. It does not require mental health expertise to appreciate what a problematic situation this could become.
Continue to: Some individuals need help...
Some individuals need help in overcoming cravings related to nonsexual appetites. For example, Americans spend millions of dollars each year trying to diet; they often require some form of assistance in order to succeed. Individuals who crave drugs or alcohol often require mental health interventions to abstain because they are unable to consistently resist through willpower alone the powerful biologic urges that drive their actions.
The fundamental mental characteristic of any paraphilic disorder is the presence of intense, recurrent, sexual urges of an atypical nature. In the case of a pedophilic disorder, those urges involve sexual feelings about children.2 In the case of an exhibitionistic disorder, the afflicted individual experiences intense, recurrent sexual fantasies/urges related to exposing his genitals in public.1 Clearly, most men do not have to recurrently fight off the urge to act in such a fashion. Given the driven nature of intense erotic cravings, individuals who experience such cravings will frequently require access to competent mental health care.
Pharmacologic treatment of paraphilic disorders
In the future, we may develop a scientifically based understanding of the biologic factors that underlie qualitative differences in sexuality. At that point, it may become possible to intervene pharmacologically, changing the qualitative nature of a sexual urge with pharmacologic interventions. This cannot yet be done. H
In 1939, a Nobel Prize in Chemistry was awarded for the identification and isolation of the hormone testosterone, which energizes sexual drive.10 If an individual is hungering sexually to expose himself, to view child pornography, or to engage in sexual acts with children, the intensity of such hungers can be significantly reduced by lowering testosterone, thereby enhancing the capacity for successful sexual self-control.
A large body of scientific data has documented a marked decrease in sexually motivated behaviors when testosterone levels are significantly diminished.11 There is also evidence that recidivism rates of sexually motivated crimes can be significantly reduced when testosterone-lowering interventions are used.12
Continue to: Historically, removal of the testes...
Historically, removal of the testes (surgical castration) had been the only effective way to reliably lower testosterone. Today, this can be achieved pharmacologically. Use of a sex drive–lowering medication should be considered when either the clinician or the patient is concerned that a nonpharmacologic approach may be inadequate. In all instances, a patient with a paraphilic disorder should be informed that pharmacologic treatment is an option. A protocol for the pharmacologic treatment of paraphilic disorders that is based on my clinical experience is summarized in Table 2.
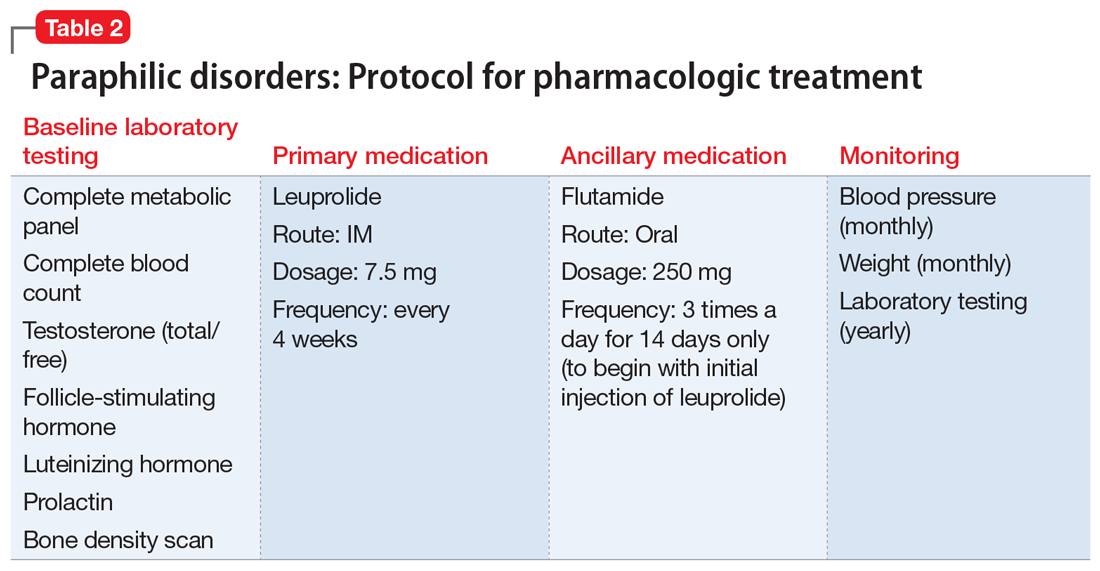
Leuprolide. A depot form of leuprolide is the most commonly employed agent to pharmacologically lower testosterone to treat a paraphilic disorder.13 When injected into muscle, leuprolide binds to it before gradually being released into the bloodstream. Previously, a depot medroxyprogesterone (a form of progesterone) had been used to treat paraphilic disorders.14 However, that had required weekly rather than monthly injections, and carried an increased risk of thrombotic emboli.
Prescribing leuprolide to treat a paraphilic disorder falls under FDA guidelines regarding the use of an approved drug for an “off-label” indication, and therefore is not considered investigational. For treating a paraphilic disorder, an effective dosage of leuprolide is 7.5 mg IM every 4 weeks. Long-term treatment is generally required, analogous to the management of diabetes. Because the initial injection of the series can cause a transient increase in testosterone (prior to its sustained decline), flutamide, a testosterone receptor blocking agent, is ordinarily prescribed for the first 14 days only, following initiation of treatment with depot leuprolide.15 Using flutamide in this fashion prevents the transient increase in testosterone from transiently increasing sexual drive. Flutamide should be discontinued after 14 days because long-term use can result in liver toxicity.
Some clinicians have been hesitant to prescribe leuprolide because of negative connotations associated with the term “chemical castration.” Unlike surgical castration, use of leuprolide is not a physically irreversible intervention, and does not result in sterility (although there may be an increase of atypical sperm and a decrease in total sperm production). The dosage can sometimes be titrated without a loss of efficacy.
In general, leuprolide’s safety protocol is well within the range associated with psychotropic medications.13 Low-risk adverse effects, such as hot flashes or cold sweats, may occur, especially during the period when hormone levels are in transition. There are no absolute contraindications to the use of leuprolide.
Continue to: Other medications
Other medications. Some researchers have suggested treating paraphilic disorders with psychotropic medications known to lower libido, such as selective serotonin reuptake inhibitors (SSRIs).16 However, leuprolide is far more reliable in consistently lowering testosterone and lowering the frequency and intensity of sexual urges. Although psychiatrists unfamiliar with treating paraphilic disorders may feel more comfortable initiating treatment with an SSRI, in my clinical experience, SSRIs have often proven inadequate for this purpose. When it comes to those paraphilic disorders in which treatment failure can result in significant harm (eg, pedophilic disorder), in my judgment, leuprolide should be the pharmacologic treatment of choice.
The opioid antagonist naltrexone has been used clinically to reduce cravings, primarily cravings for alcohol or drugs.17 However, I have not seen convincing evidence that it can be reliably beneficial in treating paraphilic disorders.
Tests to order before starting leuprolide
Long-term use of leuprolide can increase the risk of osteoporosis. Therefore, a baseline bone density scan should be performed before starting a patient on leuprolide. Baseline levels of testosterone, follicle-stimulating hormone, and luteinizing hormone also should be obtained. Patients should have yearly physical examinations, with accompanying laboratory testing. Hematocrit levels are often marginally low after beginning treatment, but not in a clinically significant way. Patients should also undergo routine monitoring for possible weight gain and the potential for associated hypertension. Treatment is predicated upon the known testosterone-suppressing effects of leuprolide, not upon routine monitoring of blood androgen levels.
Pharmacologic treatment of a paraphilic disorder should ordinarily occur in conjunction with nonpharmacologic modalities. One such modality would be group therapy, similar to the type frequently used to treat other craving disorders, such as drug or alcohol dependency.
In recent years, I have seen increasing numbers of patients presenting with a history of accessing and viewing child pornography. Once they have become more aware of the serious consequences of this behavior, most patients have been able to discontinue doing so without pharmacologic treatment. However, for patients in whom that behavior has seemed more driven (suggestive of a variant of voyeuristic disorder), prescription of leuprolide has been beneficial. Under such circumstances, I have diagnosed the patient’s condition as “other specified paraphilic disorder” with elements of pedophilia and voyeurism—the associated behaviors restricted to the voyeuristic viewing of child pornography.18
Continue to: Can treated patients still be sexual?
Can treated patients still be sexual?
If pharmacologic treatment of a paraphilic disorder results in erectile dysfunction, prescription of a medication such as sildenafil can be considered for patients who are in a consenting adult relationship, generally with the knowledge of their partner. Sildenafil can facilitate erectile capacity without increasing sexual drive. It can be helpful to explain to a patient that the purpose of pharmacologic treatment is not to prevent the enjoyment of sexual feelings within the context of a healthy, consenting, adult relationship, but instead to lower the intensity of problematic sexual urges, thereby facilitating sexual self-control. Just as lowering the appetite for food can make it easier to diet but not impossible to eat, lowering sexual appetite can facilitate successful self-control without necessarily interfering with erotic feelings experienced during sexual intimacy.
Bottom Line
Paraphilic disorders are not manifestations of a character flaw, but manifestations of unchosen qualitative differences in the nature of one’s sexual cravings. Not enough is yet known about the biology of sex to be able to pharmacologically alter its qualitative nature. However, pharmacologically lowering the intensity of a patient’s sexual drive can facilitate successful sexual self-regulation.
Related Resources
- LeVay S. Gay, straight and the reason why: the science of sexual orientation. London, UK: Oxford University Press; 2011.
- Rosler A, Witztum E. Treatment of men with paraphilia with a long-acting analogue of gonadotropin-releasing hormone. N Engl J Med. 1998;338(7):416-422.
- Brown GR. Overview of paraphilic disorders (paraphilias). https://www.merckmanuals.com/professional/psychiatricdisorders/sexuality,-gender-dysphoria,-and-paraphilias/overview-of-paraphilic-disorders.
Drug Brand Names
Flutamide • Eulexin
Leuprolide injection •
Eligard, Lupron Depot
Medroxyprogesterone •
Provera
Naltrexone • Revia, Vivitrol
Progesterone • Prometrium
Sildenafil • Viagra
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:423-450.
2. Berlin FS. Pedophilia: criminal mind-set or mental disorder? A conceptual review. American Journal of Forensic Psychiatry. 2001;32(2):3-25.
3. Berlin FS. A conceptual overview and commentary on gender dysphoria. J Am Acad Psychiatry Law. 2016;44(2):246-252
4. Berlin FS. Pedophilia: when is a difference a disorder: Peer commentaries on Green (2002) and Schmidt (2002). Arch Sex Behav. 2002;31:1-2.
5. Ford B, Chase C. Betty: a glad awakening. New York, NY: Doubleday; 1987.
6. Virtuous Pedophiles. https://www.virped.org/. Accessed September 28, 2018.
7. Freund K, Kuban M. The basis of the abused abuser theory of pedophilia: A further elaboration of an earlier study. Arch Sex Behav. 1994;23(5):553-563.
8. Mendes MF, Chow T, Ringman T, et al. Pedophilia and temporal lobe disturbances. J Neuropsychiatry Clin Neurosci. 2000;12(1):71-76.
9. Money J. Love and love sickness: The science of sex, gender differences, and pair bonding. Baltimore, MD: Johns Hopkins University Press; 1980.
10. The Nobel Prize in Chemistry 1939. https://www.nobelprize.org/prizes/chemistry/1939/summary/. Accessed September 29, 2018.
11. Berlin FS. Commentary: The impact of surgical castration on sexual recidivism risk among civilly committed sex offenders. J Am Acad Psychiatry Law. 2005;33(1):37-41.
12. Hansen H. Treatment of dangerous sexual offenders. In: Seminar on Prison Health Services in Tampere, Finland. Helsinki, Finland: Ministry of Justice, Government Printing Centre; 1991:33-38.
13. Berlin FS. Risk/benefit ratio of androgen deprivation treatment for sex offenders. J Am Acad Psychiatry Law. 2009;37(1):59-62.
14. Berlin FS, Meinecke CF. Treatment of sex offenders with antiandrogenic medication: conceptualization, review of treatment modalities, and preliminary findings. Am J Psychiatry. 1981;138(5):601-607.
15. Neri R. Pharmacology and pharmacokinetics of flutamide. Urology. 1989;34(suppl 4):19-21; discussion 46-56.
16. Adi Y, Ashcroft D, Browne K, et al. Clinical effectiveness and cost consequences of selective serotonin receptor reuptake inhibitors in the treatment of sex offenders. Health Technol Assess. 2002;6(28):1-66.
17. Anton RF. Naltrexone for the management of alcohol dependence. N Engl J Med. 2008;359(7):715-721.
18. Berlin FS. Commentary on pedophilia diagnostic criteria in DSM-5. J Am Acad Psychiatry Law. 2011;39(2):242-244.
In my role as the Director of The Johns Hopkins Sex and Gender Clinic, I have had the opportunity to provide care to 3 broad categories of patients: patients with sexual dysfunctions, patients experiencing gender dysphoria, and patients manifesting a paraphilic disorder. This article will not address sexual dysfunctions or gender dysphoria, but these terms are defined in the Box1-3 to clearly distinguish them from paraphilic disorders.
Box
Individuals with a sexual dysfunction (eg, erectile dysfunction or anorgasmia) generally experience conventional sexual feelings, but they may have difficulty performing sexually.1 Although ordinarily capable of adequate sexual performance, persons with a paraphilic disorder experience atypical erotic cravings.2 Such cravings can either be for an atypical or unacceptable category of potential partner (eg, animals or children), or for an atypical or unacceptable type of behavior (eg, crossdressing or public exhibitionism). Individuals with gender dysphoria frequently experience distress because their internal sense of feeling either male or female is not congruent with their external physical anatomy.3 The primary concerns of individuals experiencing gender dysphoria relate to feelings of gender identity, as opposed to problems involving erotic arousal.
Persons with paraphilic disorders (predominantly males) experience recurrent atypical sexual fantasies and urges that cause clinically significant impairment or distress.1 Those atypical fantasies and urges may be directed towards unacceptable partners such as animals or children, or towards unacceptable behaviors such as public exhibitionism. Table 11 lists the paraphilic disorders identified in DSM-5. This article focuses primarily, though not exclusively, upon pedophilic disorder, and its pharmacologic treatment. However, the rationale underlying such treatment is applicable across the paraphilic spectrum. Before providing such treatment, it is important for clinicians to have a clear conceptual understanding of paraphilic disorders.
When is a difference a disorder?
Cancer and respiration are 2 different biologic phenomenon. Cancer causes suffering and impairment, and as a consequence, we label it a disorder. We do so in the hope of learning more about it, and being able to successfully treat it. We do not classify respiration as a disorder because we do not consider it to be harmful.
The spectrum of human sexuality is quite broad, and psychiatry is generally not concerned with private sexual thoughts and behaviors involving consenting adults that do not cause suffering or impairment. When adults choose to engage in “kinky sex” that causes neither harm nor distress, so be it.
Some individuals may be privately aware of experiencing either an exclusive or nonexclusive sexual attraction to children. Some of these individuals may not be distressed by experiencing such attractions, and may be fully capable of resisting the temptation to enact them. In such an instance, even though an individual may be experiencing sexual attractions that are different from the norm, there may not be a sufficient basis for diagnosing pedophilic disorder. However, that difference in sexual phenomenology (ie, mental experience) could rise to the level of a diagnosable disorder if the individual in question expresses distress about experiencing such attractions, and/or if his capacity to resist acting upon them is impaired.4 Under such circumstances, treatment would be warranted.
Patients with paraphilic disorders deserve treatment
Prior to establishment of the Betty Ford Clinic in 1982, individuals who were drug- or alcohol-dependent were often portrayed in a negative light and referred to by derogatory pejoratives such as “bum” or “pothead.”5 Over time, society came to appreciate that good people, deserving of treatment, can become dependent upon substances, and in recent years there has been considerable support for related research initiatives and humane care. However, there has not been analogous support for individuals who manifest paraphilic disorders, especially those with pedophilic disorder. Instead, such individuals are often perceived as undeserving of mental health care and resources. This has been the case, even though successful treatment of a pedophilic disorder could help prevent the serious consequences of child molestation from occurring.
In contemporary society, the term pedophilia, which is a psychiatric specifier intended to guide research and treatment, has been hijacked by the nonmedical community and turned into a demeaning pejorative. In the collective consciousness of the public, the term pedophilia is routinely and mistakenly equated with the behavior of child molestation. Just as all alcoholics are not drunk drivers, all individuals with pedophilic disorder are not “child molesters.” Conversely, not all “child molesters” have pedophilic disorder.
Continue to: Individuals with other types...
Individuals with other types of paraphilic disorders are frequently similarly maligned and referred to as “perverts” or “deviants.” Public service announcements are frequently aired to reach out to individuals who are depressed, or drug- or alcohol-dependent, or suffering with other forms of mental disorders. When does one hear a public service announcement that encourages young people who may be experiencing disturbing or unacceptable sexual feelings to seek psychiatric treatment? There is a support group on the internet called Virtuous Pedophiles.6 That organization is unequivocally opposed to child molestation, while supporting efforts to improve the mental well-being of individuals who, through no fault of their own, experience unwanted pedophilic feelings.
Causes and noncauses
In attempting to elucidate etiology, researchers typically investigate nature (biology) and/or nurture (life experiences). In terms of the development of pedophilic disorder, there is evidence that both nature and nurture can play a role. Researchers have found that boys who are sexually abused are at increased risk for developing pedophilic disorder, and evidence of temporal lobe disturbances has also been documented in some instances.7,8
From clinical, societal, and forensic perspectives, it may be equally important to identify noncausal factors. Paraphilic disorders, including pedophilic disorder, do not develop as a consequence of volitional choice.9 For example, none of us decide which category, or categories, of potential partners are going to attract us sexually. Rather, in maturing we discover the nature of our own sexuality. Children do not ponder their options, somehow deciding while growing up to be attracted to the opposite sex (heterosexuality), the same sex (homosexuality), or both sexes (bisexuality). Similarly, in maturing into adulthood, individuals do not decide to become sexually attracted to prepubescent children. Who would decide to do that? Instead, unlike most of us, some individuals discover this about themselves; this often is a deeply disturbing insight.
It is not an individual’s fault that he or she has a paraphilic disorder. It is, however, his or her responsibility to do something about it. This may require accessing appropriate psychiatric care.
Why treatment may be needed
Sex is a powerful, biologically based appetite that recurrently craves satiation. God or nature has put that drive into all of us to ensure the survival of humanity. Even when that powerful biologic drive becomes misdirected (for example, towards children, or towards a desire to engage in public exhibitionism), it still recurrently craves satisfaction. It does not require mental health expertise to appreciate what a problematic situation this could become.
Continue to: Some individuals need help...
Some individuals need help in overcoming cravings related to nonsexual appetites. For example, Americans spend millions of dollars each year trying to diet; they often require some form of assistance in order to succeed. Individuals who crave drugs or alcohol often require mental health interventions to abstain because they are unable to consistently resist through willpower alone the powerful biologic urges that drive their actions.
The fundamental mental characteristic of any paraphilic disorder is the presence of intense, recurrent, sexual urges of an atypical nature. In the case of a pedophilic disorder, those urges involve sexual feelings about children.2 In the case of an exhibitionistic disorder, the afflicted individual experiences intense, recurrent sexual fantasies/urges related to exposing his genitals in public.1 Clearly, most men do not have to recurrently fight off the urge to act in such a fashion. Given the driven nature of intense erotic cravings, individuals who experience such cravings will frequently require access to competent mental health care.
Pharmacologic treatment of paraphilic disorders
In the future, we may develop a scientifically based understanding of the biologic factors that underlie qualitative differences in sexuality. At that point, it may become possible to intervene pharmacologically, changing the qualitative nature of a sexual urge with pharmacologic interventions. This cannot yet be done. H
In 1939, a Nobel Prize in Chemistry was awarded for the identification and isolation of the hormone testosterone, which energizes sexual drive.10 If an individual is hungering sexually to expose himself, to view child pornography, or to engage in sexual acts with children, the intensity of such hungers can be significantly reduced by lowering testosterone, thereby enhancing the capacity for successful sexual self-control.
A large body of scientific data has documented a marked decrease in sexually motivated behaviors when testosterone levels are significantly diminished.11 There is also evidence that recidivism rates of sexually motivated crimes can be significantly reduced when testosterone-lowering interventions are used.12
Continue to: Historically, removal of the testes...
Historically, removal of the testes (surgical castration) had been the only effective way to reliably lower testosterone. Today, this can be achieved pharmacologically. Use of a sex drive–lowering medication should be considered when either the clinician or the patient is concerned that a nonpharmacologic approach may be inadequate. In all instances, a patient with a paraphilic disorder should be informed that pharmacologic treatment is an option. A protocol for the pharmacologic treatment of paraphilic disorders that is based on my clinical experience is summarized in Table 2.
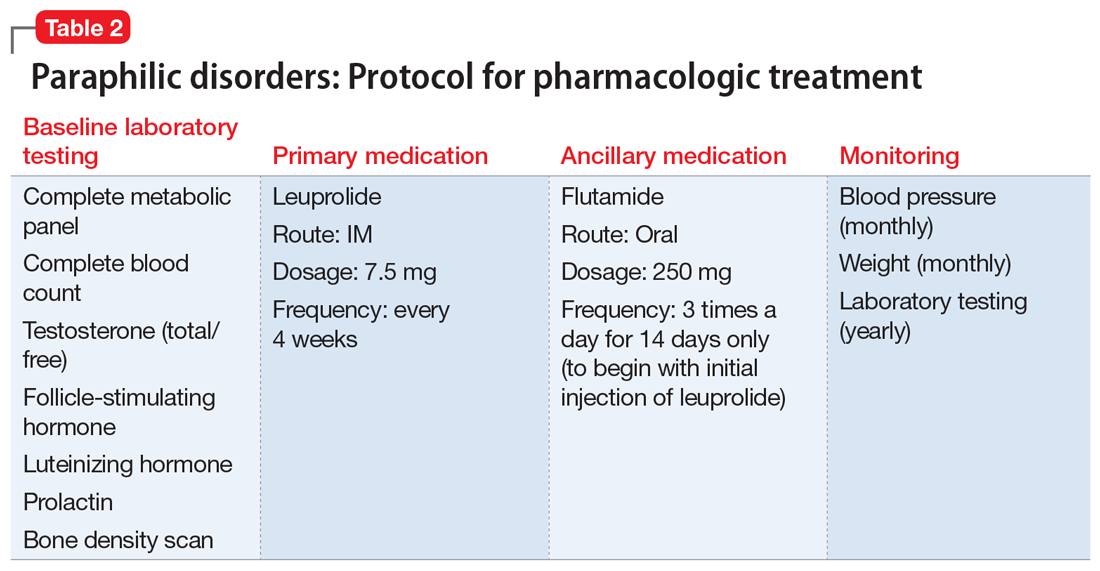
Leuprolide. A depot form of leuprolide is the most commonly employed agent to pharmacologically lower testosterone to treat a paraphilic disorder.13 When injected into muscle, leuprolide binds to it before gradually being released into the bloodstream. Previously, a depot medroxyprogesterone (a form of progesterone) had been used to treat paraphilic disorders.14 However, that had required weekly rather than monthly injections, and carried an increased risk of thrombotic emboli.
Prescribing leuprolide to treat a paraphilic disorder falls under FDA guidelines regarding the use of an approved drug for an “off-label” indication, and therefore is not considered investigational. For treating a paraphilic disorder, an effective dosage of leuprolide is 7.5 mg IM every 4 weeks. Long-term treatment is generally required, analogous to the management of diabetes. Because the initial injection of the series can cause a transient increase in testosterone (prior to its sustained decline), flutamide, a testosterone receptor blocking agent, is ordinarily prescribed for the first 14 days only, following initiation of treatment with depot leuprolide.15 Using flutamide in this fashion prevents the transient increase in testosterone from transiently increasing sexual drive. Flutamide should be discontinued after 14 days because long-term use can result in liver toxicity.
Some clinicians have been hesitant to prescribe leuprolide because of negative connotations associated with the term “chemical castration.” Unlike surgical castration, use of leuprolide is not a physically irreversible intervention, and does not result in sterility (although there may be an increase of atypical sperm and a decrease in total sperm production). The dosage can sometimes be titrated without a loss of efficacy.
In general, leuprolide’s safety protocol is well within the range associated with psychotropic medications.13 Low-risk adverse effects, such as hot flashes or cold sweats, may occur, especially during the period when hormone levels are in transition. There are no absolute contraindications to the use of leuprolide.
Continue to: Other medications
Other medications. Some researchers have suggested treating paraphilic disorders with psychotropic medications known to lower libido, such as selective serotonin reuptake inhibitors (SSRIs).16 However, leuprolide is far more reliable in consistently lowering testosterone and lowering the frequency and intensity of sexual urges. Although psychiatrists unfamiliar with treating paraphilic disorders may feel more comfortable initiating treatment with an SSRI, in my clinical experience, SSRIs have often proven inadequate for this purpose. When it comes to those paraphilic disorders in which treatment failure can result in significant harm (eg, pedophilic disorder), in my judgment, leuprolide should be the pharmacologic treatment of choice.
The opioid antagonist naltrexone has been used clinically to reduce cravings, primarily cravings for alcohol or drugs.17 However, I have not seen convincing evidence that it can be reliably beneficial in treating paraphilic disorders.
Tests to order before starting leuprolide
Long-term use of leuprolide can increase the risk of osteoporosis. Therefore, a baseline bone density scan should be performed before starting a patient on leuprolide. Baseline levels of testosterone, follicle-stimulating hormone, and luteinizing hormone also should be obtained. Patients should have yearly physical examinations, with accompanying laboratory testing. Hematocrit levels are often marginally low after beginning treatment, but not in a clinically significant way. Patients should also undergo routine monitoring for possible weight gain and the potential for associated hypertension. Treatment is predicated upon the known testosterone-suppressing effects of leuprolide, not upon routine monitoring of blood androgen levels.
Pharmacologic treatment of a paraphilic disorder should ordinarily occur in conjunction with nonpharmacologic modalities. One such modality would be group therapy, similar to the type frequently used to treat other craving disorders, such as drug or alcohol dependency.
In recent years, I have seen increasing numbers of patients presenting with a history of accessing and viewing child pornography. Once they have become more aware of the serious consequences of this behavior, most patients have been able to discontinue doing so without pharmacologic treatment. However, for patients in whom that behavior has seemed more driven (suggestive of a variant of voyeuristic disorder), prescription of leuprolide has been beneficial. Under such circumstances, I have diagnosed the patient’s condition as “other specified paraphilic disorder” with elements of pedophilia and voyeurism—the associated behaviors restricted to the voyeuristic viewing of child pornography.18
Continue to: Can treated patients still be sexual?
Can treated patients still be sexual?
If pharmacologic treatment of a paraphilic disorder results in erectile dysfunction, prescription of a medication such as sildenafil can be considered for patients who are in a consenting adult relationship, generally with the knowledge of their partner. Sildenafil can facilitate erectile capacity without increasing sexual drive. It can be helpful to explain to a patient that the purpose of pharmacologic treatment is not to prevent the enjoyment of sexual feelings within the context of a healthy, consenting, adult relationship, but instead to lower the intensity of problematic sexual urges, thereby facilitating sexual self-control. Just as lowering the appetite for food can make it easier to diet but not impossible to eat, lowering sexual appetite can facilitate successful self-control without necessarily interfering with erotic feelings experienced during sexual intimacy.
Bottom Line
Paraphilic disorders are not manifestations of a character flaw, but manifestations of unchosen qualitative differences in the nature of one’s sexual cravings. Not enough is yet known about the biology of sex to be able to pharmacologically alter its qualitative nature. However, pharmacologically lowering the intensity of a patient’s sexual drive can facilitate successful sexual self-regulation.
Related Resources
- LeVay S. Gay, straight and the reason why: the science of sexual orientation. London, UK: Oxford University Press; 2011.
- Rosler A, Witztum E. Treatment of men with paraphilia with a long-acting analogue of gonadotropin-releasing hormone. N Engl J Med. 1998;338(7):416-422.
- Brown GR. Overview of paraphilic disorders (paraphilias). https://www.merckmanuals.com/professional/psychiatricdisorders/sexuality,-gender-dysphoria,-and-paraphilias/overview-of-paraphilic-disorders.
Drug Brand Names
Flutamide • Eulexin
Leuprolide injection •
Eligard, Lupron Depot
Medroxyprogesterone •
Provera
Naltrexone • Revia, Vivitrol
Progesterone • Prometrium
Sildenafil • Viagra
In my role as the Director of The Johns Hopkins Sex and Gender Clinic, I have had the opportunity to provide care to 3 broad categories of patients: patients with sexual dysfunctions, patients experiencing gender dysphoria, and patients manifesting a paraphilic disorder. This article will not address sexual dysfunctions or gender dysphoria, but these terms are defined in the Box1-3 to clearly distinguish them from paraphilic disorders.
Box
Individuals with a sexual dysfunction (eg, erectile dysfunction or anorgasmia) generally experience conventional sexual feelings, but they may have difficulty performing sexually.1 Although ordinarily capable of adequate sexual performance, persons with a paraphilic disorder experience atypical erotic cravings.2 Such cravings can either be for an atypical or unacceptable category of potential partner (eg, animals or children), or for an atypical or unacceptable type of behavior (eg, crossdressing or public exhibitionism). Individuals with gender dysphoria frequently experience distress because their internal sense of feeling either male or female is not congruent with their external physical anatomy.3 The primary concerns of individuals experiencing gender dysphoria relate to feelings of gender identity, as opposed to problems involving erotic arousal.
Persons with paraphilic disorders (predominantly males) experience recurrent atypical sexual fantasies and urges that cause clinically significant impairment or distress.1 Those atypical fantasies and urges may be directed towards unacceptable partners such as animals or children, or towards unacceptable behaviors such as public exhibitionism. Table 11 lists the paraphilic disorders identified in DSM-5. This article focuses primarily, though not exclusively, upon pedophilic disorder, and its pharmacologic treatment. However, the rationale underlying such treatment is applicable across the paraphilic spectrum. Before providing such treatment, it is important for clinicians to have a clear conceptual understanding of paraphilic disorders.
When is a difference a disorder?
Cancer and respiration are 2 different biologic phenomenon. Cancer causes suffering and impairment, and as a consequence, we label it a disorder. We do so in the hope of learning more about it, and being able to successfully treat it. We do not classify respiration as a disorder because we do not consider it to be harmful.
The spectrum of human sexuality is quite broad, and psychiatry is generally not concerned with private sexual thoughts and behaviors involving consenting adults that do not cause suffering or impairment. When adults choose to engage in “kinky sex” that causes neither harm nor distress, so be it.
Some individuals may be privately aware of experiencing either an exclusive or nonexclusive sexual attraction to children. Some of these individuals may not be distressed by experiencing such attractions, and may be fully capable of resisting the temptation to enact them. In such an instance, even though an individual may be experiencing sexual attractions that are different from the norm, there may not be a sufficient basis for diagnosing pedophilic disorder. However, that difference in sexual phenomenology (ie, mental experience) could rise to the level of a diagnosable disorder if the individual in question expresses distress about experiencing such attractions, and/or if his capacity to resist acting upon them is impaired.4 Under such circumstances, treatment would be warranted.
Patients with paraphilic disorders deserve treatment
Prior to establishment of the Betty Ford Clinic in 1982, individuals who were drug- or alcohol-dependent were often portrayed in a negative light and referred to by derogatory pejoratives such as “bum” or “pothead.”5 Over time, society came to appreciate that good people, deserving of treatment, can become dependent upon substances, and in recent years there has been considerable support for related research initiatives and humane care. However, there has not been analogous support for individuals who manifest paraphilic disorders, especially those with pedophilic disorder. Instead, such individuals are often perceived as undeserving of mental health care and resources. This has been the case, even though successful treatment of a pedophilic disorder could help prevent the serious consequences of child molestation from occurring.
In contemporary society, the term pedophilia, which is a psychiatric specifier intended to guide research and treatment, has been hijacked by the nonmedical community and turned into a demeaning pejorative. In the collective consciousness of the public, the term pedophilia is routinely and mistakenly equated with the behavior of child molestation. Just as all alcoholics are not drunk drivers, all individuals with pedophilic disorder are not “child molesters.” Conversely, not all “child molesters” have pedophilic disorder.
Continue to: Individuals with other types...
Individuals with other types of paraphilic disorders are frequently similarly maligned and referred to as “perverts” or “deviants.” Public service announcements are frequently aired to reach out to individuals who are depressed, or drug- or alcohol-dependent, or suffering with other forms of mental disorders. When does one hear a public service announcement that encourages young people who may be experiencing disturbing or unacceptable sexual feelings to seek psychiatric treatment? There is a support group on the internet called Virtuous Pedophiles.6 That organization is unequivocally opposed to child molestation, while supporting efforts to improve the mental well-being of individuals who, through no fault of their own, experience unwanted pedophilic feelings.
Causes and noncauses
In attempting to elucidate etiology, researchers typically investigate nature (biology) and/or nurture (life experiences). In terms of the development of pedophilic disorder, there is evidence that both nature and nurture can play a role. Researchers have found that boys who are sexually abused are at increased risk for developing pedophilic disorder, and evidence of temporal lobe disturbances has also been documented in some instances.7,8
From clinical, societal, and forensic perspectives, it may be equally important to identify noncausal factors. Paraphilic disorders, including pedophilic disorder, do not develop as a consequence of volitional choice.9 For example, none of us decide which category, or categories, of potential partners are going to attract us sexually. Rather, in maturing we discover the nature of our own sexuality. Children do not ponder their options, somehow deciding while growing up to be attracted to the opposite sex (heterosexuality), the same sex (homosexuality), or both sexes (bisexuality). Similarly, in maturing into adulthood, individuals do not decide to become sexually attracted to prepubescent children. Who would decide to do that? Instead, unlike most of us, some individuals discover this about themselves; this often is a deeply disturbing insight.
It is not an individual’s fault that he or she has a paraphilic disorder. It is, however, his or her responsibility to do something about it. This may require accessing appropriate psychiatric care.
Why treatment may be needed
Sex is a powerful, biologically based appetite that recurrently craves satiation. God or nature has put that drive into all of us to ensure the survival of humanity. Even when that powerful biologic drive becomes misdirected (for example, towards children, or towards a desire to engage in public exhibitionism), it still recurrently craves satisfaction. It does not require mental health expertise to appreciate what a problematic situation this could become.
Continue to: Some individuals need help...
Some individuals need help in overcoming cravings related to nonsexual appetites. For example, Americans spend millions of dollars each year trying to diet; they often require some form of assistance in order to succeed. Individuals who crave drugs or alcohol often require mental health interventions to abstain because they are unable to consistently resist through willpower alone the powerful biologic urges that drive their actions.
The fundamental mental characteristic of any paraphilic disorder is the presence of intense, recurrent, sexual urges of an atypical nature. In the case of a pedophilic disorder, those urges involve sexual feelings about children.2 In the case of an exhibitionistic disorder, the afflicted individual experiences intense, recurrent sexual fantasies/urges related to exposing his genitals in public.1 Clearly, most men do not have to recurrently fight off the urge to act in such a fashion. Given the driven nature of intense erotic cravings, individuals who experience such cravings will frequently require access to competent mental health care.
Pharmacologic treatment of paraphilic disorders
In the future, we may develop a scientifically based understanding of the biologic factors that underlie qualitative differences in sexuality. At that point, it may become possible to intervene pharmacologically, changing the qualitative nature of a sexual urge with pharmacologic interventions. This cannot yet be done. H
In 1939, a Nobel Prize in Chemistry was awarded for the identification and isolation of the hormone testosterone, which energizes sexual drive.10 If an individual is hungering sexually to expose himself, to view child pornography, or to engage in sexual acts with children, the intensity of such hungers can be significantly reduced by lowering testosterone, thereby enhancing the capacity for successful sexual self-control.
A large body of scientific data has documented a marked decrease in sexually motivated behaviors when testosterone levels are significantly diminished.11 There is also evidence that recidivism rates of sexually motivated crimes can be significantly reduced when testosterone-lowering interventions are used.12
Continue to: Historically, removal of the testes...
Historically, removal of the testes (surgical castration) had been the only effective way to reliably lower testosterone. Today, this can be achieved pharmacologically. Use of a sex drive–lowering medication should be considered when either the clinician or the patient is concerned that a nonpharmacologic approach may be inadequate. In all instances, a patient with a paraphilic disorder should be informed that pharmacologic treatment is an option. A protocol for the pharmacologic treatment of paraphilic disorders that is based on my clinical experience is summarized in Table 2.
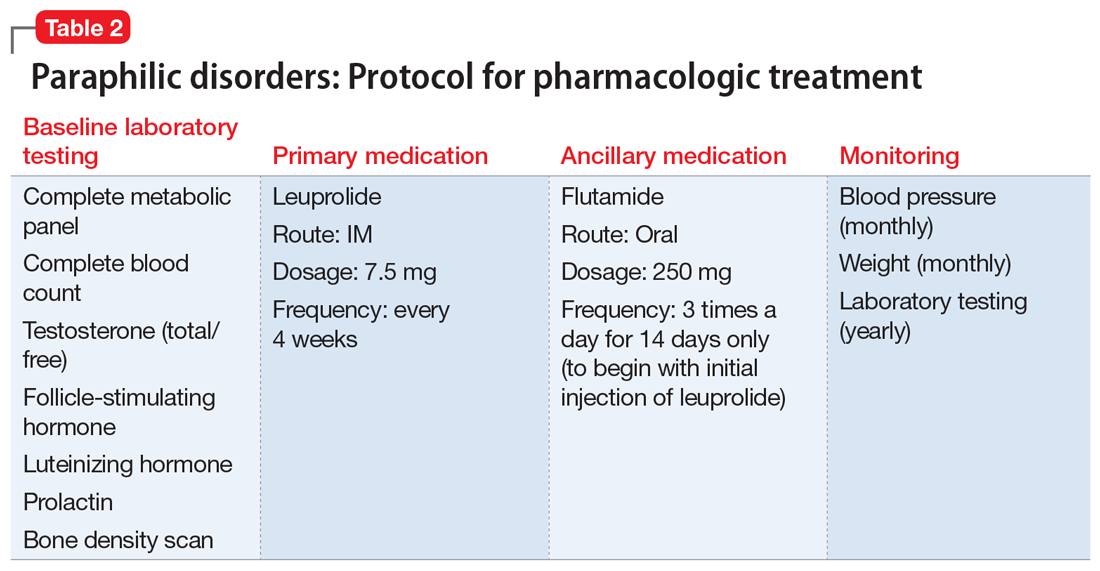
Leuprolide. A depot form of leuprolide is the most commonly employed agent to pharmacologically lower testosterone to treat a paraphilic disorder.13 When injected into muscle, leuprolide binds to it before gradually being released into the bloodstream. Previously, a depot medroxyprogesterone (a form of progesterone) had been used to treat paraphilic disorders.14 However, that had required weekly rather than monthly injections, and carried an increased risk of thrombotic emboli.
Prescribing leuprolide to treat a paraphilic disorder falls under FDA guidelines regarding the use of an approved drug for an “off-label” indication, and therefore is not considered investigational. For treating a paraphilic disorder, an effective dosage of leuprolide is 7.5 mg IM every 4 weeks. Long-term treatment is generally required, analogous to the management of diabetes. Because the initial injection of the series can cause a transient increase in testosterone (prior to its sustained decline), flutamide, a testosterone receptor blocking agent, is ordinarily prescribed for the first 14 days only, following initiation of treatment with depot leuprolide.15 Using flutamide in this fashion prevents the transient increase in testosterone from transiently increasing sexual drive. Flutamide should be discontinued after 14 days because long-term use can result in liver toxicity.
Some clinicians have been hesitant to prescribe leuprolide because of negative connotations associated with the term “chemical castration.” Unlike surgical castration, use of leuprolide is not a physically irreversible intervention, and does not result in sterility (although there may be an increase of atypical sperm and a decrease in total sperm production). The dosage can sometimes be titrated without a loss of efficacy.
In general, leuprolide’s safety protocol is well within the range associated with psychotropic medications.13 Low-risk adverse effects, such as hot flashes or cold sweats, may occur, especially during the period when hormone levels are in transition. There are no absolute contraindications to the use of leuprolide.
Continue to: Other medications
Other medications. Some researchers have suggested treating paraphilic disorders with psychotropic medications known to lower libido, such as selective serotonin reuptake inhibitors (SSRIs).16 However, leuprolide is far more reliable in consistently lowering testosterone and lowering the frequency and intensity of sexual urges. Although psychiatrists unfamiliar with treating paraphilic disorders may feel more comfortable initiating treatment with an SSRI, in my clinical experience, SSRIs have often proven inadequate for this purpose. When it comes to those paraphilic disorders in which treatment failure can result in significant harm (eg, pedophilic disorder), in my judgment, leuprolide should be the pharmacologic treatment of choice.
The opioid antagonist naltrexone has been used clinically to reduce cravings, primarily cravings for alcohol or drugs.17 However, I have not seen convincing evidence that it can be reliably beneficial in treating paraphilic disorders.
Tests to order before starting leuprolide
Long-term use of leuprolide can increase the risk of osteoporosis. Therefore, a baseline bone density scan should be performed before starting a patient on leuprolide. Baseline levels of testosterone, follicle-stimulating hormone, and luteinizing hormone also should be obtained. Patients should have yearly physical examinations, with accompanying laboratory testing. Hematocrit levels are often marginally low after beginning treatment, but not in a clinically significant way. Patients should also undergo routine monitoring for possible weight gain and the potential for associated hypertension. Treatment is predicated upon the known testosterone-suppressing effects of leuprolide, not upon routine monitoring of blood androgen levels.
Pharmacologic treatment of a paraphilic disorder should ordinarily occur in conjunction with nonpharmacologic modalities. One such modality would be group therapy, similar to the type frequently used to treat other craving disorders, such as drug or alcohol dependency.
In recent years, I have seen increasing numbers of patients presenting with a history of accessing and viewing child pornography. Once they have become more aware of the serious consequences of this behavior, most patients have been able to discontinue doing so without pharmacologic treatment. However, for patients in whom that behavior has seemed more driven (suggestive of a variant of voyeuristic disorder), prescription of leuprolide has been beneficial. Under such circumstances, I have diagnosed the patient’s condition as “other specified paraphilic disorder” with elements of pedophilia and voyeurism—the associated behaviors restricted to the voyeuristic viewing of child pornography.18
Continue to: Can treated patients still be sexual?
Can treated patients still be sexual?
If pharmacologic treatment of a paraphilic disorder results in erectile dysfunction, prescription of a medication such as sildenafil can be considered for patients who are in a consenting adult relationship, generally with the knowledge of their partner. Sildenafil can facilitate erectile capacity without increasing sexual drive. It can be helpful to explain to a patient that the purpose of pharmacologic treatment is not to prevent the enjoyment of sexual feelings within the context of a healthy, consenting, adult relationship, but instead to lower the intensity of problematic sexual urges, thereby facilitating sexual self-control. Just as lowering the appetite for food can make it easier to diet but not impossible to eat, lowering sexual appetite can facilitate successful self-control without necessarily interfering with erotic feelings experienced during sexual intimacy.
Bottom Line
Paraphilic disorders are not manifestations of a character flaw, but manifestations of unchosen qualitative differences in the nature of one’s sexual cravings. Not enough is yet known about the biology of sex to be able to pharmacologically alter its qualitative nature. However, pharmacologically lowering the intensity of a patient’s sexual drive can facilitate successful sexual self-regulation.
Related Resources
- LeVay S. Gay, straight and the reason why: the science of sexual orientation. London, UK: Oxford University Press; 2011.
- Rosler A, Witztum E. Treatment of men with paraphilia with a long-acting analogue of gonadotropin-releasing hormone. N Engl J Med. 1998;338(7):416-422.
- Brown GR. Overview of paraphilic disorders (paraphilias). https://www.merckmanuals.com/professional/psychiatricdisorders/sexuality,-gender-dysphoria,-and-paraphilias/overview-of-paraphilic-disorders.
Drug Brand Names
Flutamide • Eulexin
Leuprolide injection •
Eligard, Lupron Depot
Medroxyprogesterone •
Provera
Naltrexone • Revia, Vivitrol
Progesterone • Prometrium
Sildenafil • Viagra
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:423-450.
2. Berlin FS. Pedophilia: criminal mind-set or mental disorder? A conceptual review. American Journal of Forensic Psychiatry. 2001;32(2):3-25.
3. Berlin FS. A conceptual overview and commentary on gender dysphoria. J Am Acad Psychiatry Law. 2016;44(2):246-252
4. Berlin FS. Pedophilia: when is a difference a disorder: Peer commentaries on Green (2002) and Schmidt (2002). Arch Sex Behav. 2002;31:1-2.
5. Ford B, Chase C. Betty: a glad awakening. New York, NY: Doubleday; 1987.
6. Virtuous Pedophiles. https://www.virped.org/. Accessed September 28, 2018.
7. Freund K, Kuban M. The basis of the abused abuser theory of pedophilia: A further elaboration of an earlier study. Arch Sex Behav. 1994;23(5):553-563.
8. Mendes MF, Chow T, Ringman T, et al. Pedophilia and temporal lobe disturbances. J Neuropsychiatry Clin Neurosci. 2000;12(1):71-76.
9. Money J. Love and love sickness: The science of sex, gender differences, and pair bonding. Baltimore, MD: Johns Hopkins University Press; 1980.
10. The Nobel Prize in Chemistry 1939. https://www.nobelprize.org/prizes/chemistry/1939/summary/. Accessed September 29, 2018.
11. Berlin FS. Commentary: The impact of surgical castration on sexual recidivism risk among civilly committed sex offenders. J Am Acad Psychiatry Law. 2005;33(1):37-41.
12. Hansen H. Treatment of dangerous sexual offenders. In: Seminar on Prison Health Services in Tampere, Finland. Helsinki, Finland: Ministry of Justice, Government Printing Centre; 1991:33-38.
13. Berlin FS. Risk/benefit ratio of androgen deprivation treatment for sex offenders. J Am Acad Psychiatry Law. 2009;37(1):59-62.
14. Berlin FS, Meinecke CF. Treatment of sex offenders with antiandrogenic medication: conceptualization, review of treatment modalities, and preliminary findings. Am J Psychiatry. 1981;138(5):601-607.
15. Neri R. Pharmacology and pharmacokinetics of flutamide. Urology. 1989;34(suppl 4):19-21; discussion 46-56.
16. Adi Y, Ashcroft D, Browne K, et al. Clinical effectiveness and cost consequences of selective serotonin receptor reuptake inhibitors in the treatment of sex offenders. Health Technol Assess. 2002;6(28):1-66.
17. Anton RF. Naltrexone for the management of alcohol dependence. N Engl J Med. 2008;359(7):715-721.
18. Berlin FS. Commentary on pedophilia diagnostic criteria in DSM-5. J Am Acad Psychiatry Law. 2011;39(2):242-244.
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:423-450.
2. Berlin FS. Pedophilia: criminal mind-set or mental disorder? A conceptual review. American Journal of Forensic Psychiatry. 2001;32(2):3-25.
3. Berlin FS. A conceptual overview and commentary on gender dysphoria. J Am Acad Psychiatry Law. 2016;44(2):246-252
4. Berlin FS. Pedophilia: when is a difference a disorder: Peer commentaries on Green (2002) and Schmidt (2002). Arch Sex Behav. 2002;31:1-2.
5. Ford B, Chase C. Betty: a glad awakening. New York, NY: Doubleday; 1987.
6. Virtuous Pedophiles. https://www.virped.org/. Accessed September 28, 2018.
7. Freund K, Kuban M. The basis of the abused abuser theory of pedophilia: A further elaboration of an earlier study. Arch Sex Behav. 1994;23(5):553-563.
8. Mendes MF, Chow T, Ringman T, et al. Pedophilia and temporal lobe disturbances. J Neuropsychiatry Clin Neurosci. 2000;12(1):71-76.
9. Money J. Love and love sickness: The science of sex, gender differences, and pair bonding. Baltimore, MD: Johns Hopkins University Press; 1980.
10. The Nobel Prize in Chemistry 1939. https://www.nobelprize.org/prizes/chemistry/1939/summary/. Accessed September 29, 2018.
11. Berlin FS. Commentary: The impact of surgical castration on sexual recidivism risk among civilly committed sex offenders. J Am Acad Psychiatry Law. 2005;33(1):37-41.
12. Hansen H. Treatment of dangerous sexual offenders. In: Seminar on Prison Health Services in Tampere, Finland. Helsinki, Finland: Ministry of Justice, Government Printing Centre; 1991:33-38.
13. Berlin FS. Risk/benefit ratio of androgen deprivation treatment for sex offenders. J Am Acad Psychiatry Law. 2009;37(1):59-62.
14. Berlin FS, Meinecke CF. Treatment of sex offenders with antiandrogenic medication: conceptualization, review of treatment modalities, and preliminary findings. Am J Psychiatry. 1981;138(5):601-607.
15. Neri R. Pharmacology and pharmacokinetics of flutamide. Urology. 1989;34(suppl 4):19-21; discussion 46-56.
16. Adi Y, Ashcroft D, Browne K, et al. Clinical effectiveness and cost consequences of selective serotonin receptor reuptake inhibitors in the treatment of sex offenders. Health Technol Assess. 2002;6(28):1-66.
17. Anton RF. Naltrexone for the management of alcohol dependence. N Engl J Med. 2008;359(7):715-721.
18. Berlin FS. Commentary on pedophilia diagnostic criteria in DSM-5. J Am Acad Psychiatry Law. 2011;39(2):242-244.
Cost-Effective Treatment Option for von Willebrand Disease
Click here to read the supplement.
What can be done to provide a cost-effective treatment option for von Willebrand Disease?
Topics include:
- Review of Key Clinical Studies and Surgical Procedures
- Pharmacokinetics Comparison
- Pharmacoeconomic Comparisons
Click here to read the supplement.
Click here to read the supplement.
What can be done to provide a cost-effective treatment option for von Willebrand Disease?
Topics include:
- Review of Key Clinical Studies and Surgical Procedures
- Pharmacokinetics Comparison
- Pharmacoeconomic Comparisons
Click here to read the supplement.
Click here to read the supplement.
What can be done to provide a cost-effective treatment option for von Willebrand Disease?
Topics include:
- Review of Key Clinical Studies and Surgical Procedures
- Pharmacokinetics Comparison
- Pharmacoeconomic Comparisons