User login
AHA: Chagas disease and its heart effects have come to the U.S.
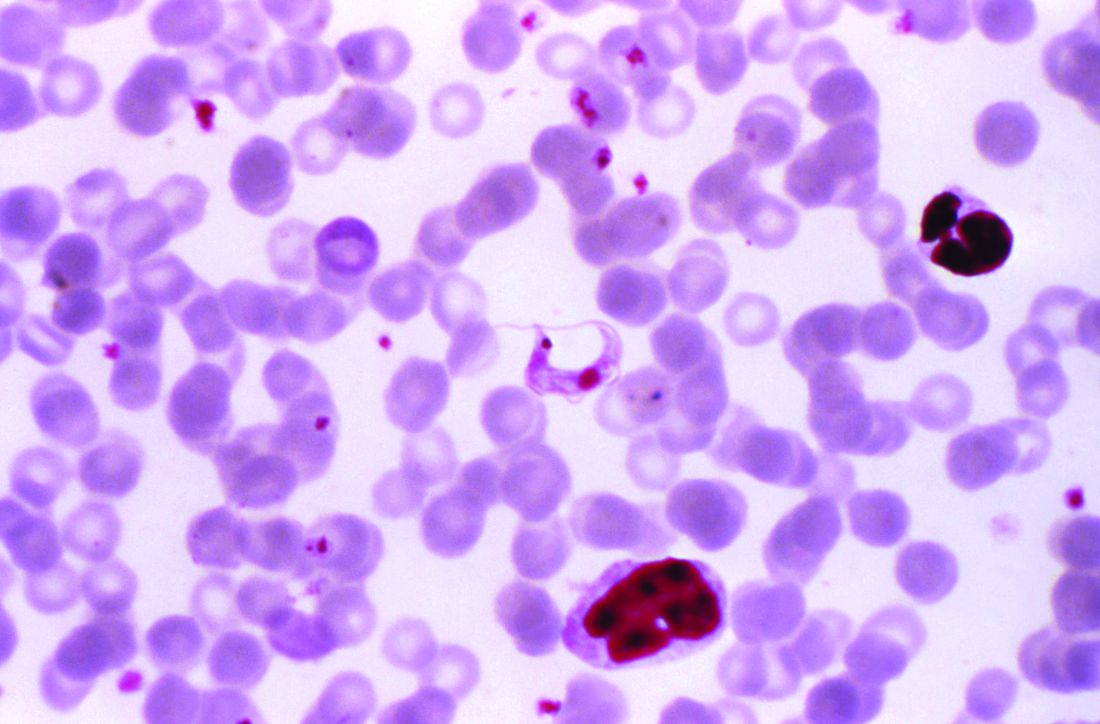
Chagas disease, a cause of serious cardiovascular problems and sudden death, was previously localized mainly in the tropics, but now affects at least 300,000 people in the United States and is growing in prevalence in other traditionally nonendemic areas, including Europe, Australia, and Japan. The American Heart Association and the Inter-American Society of Cardiology have released a statement to “increase global awareness among providers who may encounter patients with Chagas disease outside of traditionally endemic environments.”
The document summarizes the most up-to-date information on diagnosis, screening, and treatment of Trypanosoma cruzi (the protozoan cause of Chagas) infection, focusing primarily on its cardiovascular aspects, and was developed by Maria Carmo Pereira Nunes, MD, chair, and her colleagues on the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Disease Committee.
Chagas disease is transmitted by a blood-sucking insect vector Triatoma infestans and, less frequently, from mother to fetus or by contaminated food or drink, and about one third of infected individuals develop chronic heart disease.
Although 60%-70% of people infected with T. cruzi never develop any symptoms, those who do can develop heart disease, including heart failure, stroke, life threatening ventricular arrhythmias, and cardiac arrest, according to the statement published in Circulation.
Chronic Chagas-related heart disease develops after several decades of the indeterminate, or subclinical, form of the disease following the initial acute infection. Potential risk factors for progression to the chronic stage include African ancestry, age, severity of acute infection, nutritional status, alcoholism, and their concomitant diseases.
In most studies, sudden death is the most common overall cause of death in patients with Chagas-related cardiomyopathy (55%-60%), followed by heart failure (25%-30%) and embolic events (10%-15%), according to the authors.
Benznidazole and nifurtimox are the only drugs with proven efficacy against Chagas disease, with benznidazole as the first-line treatment because it has better tolerance, is more widely available, and has more published data published on its efficacy. Furthermore, it is available in the United States, after the Food and Drug Administration granted fast-track approved 2017 for treatment of Chagas disease. Use of nifurtimox in the United States entails consultation with the Centers for Disease Control and prevention, according to the statement.
“More data are needed on the best practices for the treatment of Chagas cardiomyopathy. Because no specific clinical trials have been conducted, care for
patients with Chagas-induced ventricular dysfunction is extrapolated from general heart failure recommendations with unclear efficacy (and potential harm),” Dr. Pereira Nunes and her colleagues concluded.
One author disclosed receiving a research grant from Merck and speakers’ bureau and/or honoraria from Bayer; Biotronik, and Medtronic. The others had no relevant disclosures.
SOURCE: Nunes, MCP, et al., Circulation. 2018 Aug 20; doi: 10.1161/CIR.0000000000000599.
Chagas disease, a cause of serious cardiovascular problems and sudden death, was previously localized mainly in the tropics, but now affects at least 300,000 people in the United States and is growing in prevalence in other traditionally nonendemic areas, including Europe, Australia, and Japan. The American Heart Association and the Inter-American Society of Cardiology have released a statement to “increase global awareness among providers who may encounter patients with Chagas disease outside of traditionally endemic environments.”
The document summarizes the most up-to-date information on diagnosis, screening, and treatment of Trypanosoma cruzi (the protozoan cause of Chagas) infection, focusing primarily on its cardiovascular aspects, and was developed by Maria Carmo Pereira Nunes, MD, chair, and her colleagues on the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Disease Committee.
Chagas disease is transmitted by a blood-sucking insect vector Triatoma infestans and, less frequently, from mother to fetus or by contaminated food or drink, and about one third of infected individuals develop chronic heart disease.
Although 60%-70% of people infected with T. cruzi never develop any symptoms, those who do can develop heart disease, including heart failure, stroke, life threatening ventricular arrhythmias, and cardiac arrest, according to the statement published in Circulation.
Chronic Chagas-related heart disease develops after several decades of the indeterminate, or subclinical, form of the disease following the initial acute infection. Potential risk factors for progression to the chronic stage include African ancestry, age, severity of acute infection, nutritional status, alcoholism, and their concomitant diseases.
In most studies, sudden death is the most common overall cause of death in patients with Chagas-related cardiomyopathy (55%-60%), followed by heart failure (25%-30%) and embolic events (10%-15%), according to the authors.
Benznidazole and nifurtimox are the only drugs with proven efficacy against Chagas disease, with benznidazole as the first-line treatment because it has better tolerance, is more widely available, and has more published data published on its efficacy. Furthermore, it is available in the United States, after the Food and Drug Administration granted fast-track approved 2017 for treatment of Chagas disease. Use of nifurtimox in the United States entails consultation with the Centers for Disease Control and prevention, according to the statement.
“More data are needed on the best practices for the treatment of Chagas cardiomyopathy. Because no specific clinical trials have been conducted, care for
patients with Chagas-induced ventricular dysfunction is extrapolated from general heart failure recommendations with unclear efficacy (and potential harm),” Dr. Pereira Nunes and her colleagues concluded.
One author disclosed receiving a research grant from Merck and speakers’ bureau and/or honoraria from Bayer; Biotronik, and Medtronic. The others had no relevant disclosures.
SOURCE: Nunes, MCP, et al., Circulation. 2018 Aug 20; doi: 10.1161/CIR.0000000000000599.
Chagas disease, a cause of serious cardiovascular problems and sudden death, was previously localized mainly in the tropics, but now affects at least 300,000 people in the United States and is growing in prevalence in other traditionally nonendemic areas, including Europe, Australia, and Japan. The American Heart Association and the Inter-American Society of Cardiology have released a statement to “increase global awareness among providers who may encounter patients with Chagas disease outside of traditionally endemic environments.”
The document summarizes the most up-to-date information on diagnosis, screening, and treatment of Trypanosoma cruzi (the protozoan cause of Chagas) infection, focusing primarily on its cardiovascular aspects, and was developed by Maria Carmo Pereira Nunes, MD, chair, and her colleagues on the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Disease Committee.
Chagas disease is transmitted by a blood-sucking insect vector Triatoma infestans and, less frequently, from mother to fetus or by contaminated food or drink, and about one third of infected individuals develop chronic heart disease.
Although 60%-70% of people infected with T. cruzi never develop any symptoms, those who do can develop heart disease, including heart failure, stroke, life threatening ventricular arrhythmias, and cardiac arrest, according to the statement published in Circulation.
Chronic Chagas-related heart disease develops after several decades of the indeterminate, or subclinical, form of the disease following the initial acute infection. Potential risk factors for progression to the chronic stage include African ancestry, age, severity of acute infection, nutritional status, alcoholism, and their concomitant diseases.
In most studies, sudden death is the most common overall cause of death in patients with Chagas-related cardiomyopathy (55%-60%), followed by heart failure (25%-30%) and embolic events (10%-15%), according to the authors.
Benznidazole and nifurtimox are the only drugs with proven efficacy against Chagas disease, with benznidazole as the first-line treatment because it has better tolerance, is more widely available, and has more published data published on its efficacy. Furthermore, it is available in the United States, after the Food and Drug Administration granted fast-track approved 2017 for treatment of Chagas disease. Use of nifurtimox in the United States entails consultation with the Centers for Disease Control and prevention, according to the statement.
“More data are needed on the best practices for the treatment of Chagas cardiomyopathy. Because no specific clinical trials have been conducted, care for
patients with Chagas-induced ventricular dysfunction is extrapolated from general heart failure recommendations with unclear efficacy (and potential harm),” Dr. Pereira Nunes and her colleagues concluded.
One author disclosed receiving a research grant from Merck and speakers’ bureau and/or honoraria from Bayer; Biotronik, and Medtronic. The others had no relevant disclosures.
SOURCE: Nunes, MCP, et al., Circulation. 2018 Aug 20; doi: 10.1161/CIR.0000000000000599.
FROM CIRCULATION
Access to care drives disparity between urban, rural cancer patients
New research suggests that better access to quality care may reduce disparities in survival between cancer patients living in rural areas of the US and those living in urban areas.
The study showed that urban and rural cancer patients had similar survival outcomes when they were enrolled in clinical trials.
These results, published in JAMA Network Open, cast new light on decades of research showing that cancer patients living in rural areas don’t live as long as urban cancer patients.
“These findings were a surprise, since we thought we might find the same disparities others had found,” said study author Joseph Unger, PhD, of Fred Hutchinson Cancer Research Center in Seattle, Washington.
“But clinical trials are a key difference here. In trials, patients are uniformly assessed, treated, and followed under a strict, guideline-driven protocol. This suggests that giving people with cancer access to uniform treatment strategies could help resolve the disparities in outcomes that we see between rural and urban patients.”
Dr Unger and his colleagues studied data on 36,995 patients who were enrolled in 44 phase 3 or phase 2/3 SWOG trials from 1986 through 2012. All 50 states were represented.
Patients had 17 different cancer types, including acute myeloid leukemia (AML), non-Hodgkin lymphoma (NHL), and multiple myeloma (MM).
Using US Department of Agriculture population classifications known as Rural-Urban Continuum Codes, the researchers categorized the patients as either rural or urban and analyzed their outcomes.
A minority of patients (19.4%, n=7184) were from rural locations. They were significantly more likely than urban patients to be 65 or older (P<0.001) and significantly less likely to be black (vs all other races; P<0.001).
However, there was no significant between-group difference in sex (P=0.53), and all major US geographic regions (West, Midwest, South, and Northeast) were represented.
Results
The researchers limited their analysis of survival to the first 5 years after trial enrollment to emphasize outcomes related to cancer and its treatment. They looked at overall survival (OS) as well as cancer-specific survival.
The team found no meaningful difference in OS or cancer-specific survival between rural and urban patients for 16 of the 17 cancer types.
The exception was estrogen receptor-negative, progesterone receptor-negative breast cancer. Rural patients with this cancer didn’t live as long as their urban counterparts. The hazard ratio (HR) was 1.27 (95% CI, 1.06-1.51; P=0.008) for OS and 1.26 (95% CI, 1.04-1.52; P=0.02) for cancer-specific survival.
The researchers believe this finding could be attributed to a few factors, including timely access to follow-up chemotherapy after patients’ first round of cancer treatment.
Although there were no significant survival differences for patients with hematologic malignancies, rural patients had slightly better OS if they had advanced indolent NHL or AML but slightly worse OS if they had MM or advanced aggressive NHL. The HRs were as follows:
- Advanced indolent NHL—HR=0.91 (95% CI, 0.64-1.29; P=0.60)
- AML—HR=0.94 (95% CI, 0.83-1.06; P=0.29)
- MM—HR=1.05 (95% CI, 0.93-1.18, P=0.46)
- Advanced aggressive NHL—HR=1.05 (95% CI, 0.87-1.27; P=0.60).
Rural patients had slightly better cancer-specific survival if they had advanced indolent NHL but slightly worse cancer-specific survival if they had AML, MM, or advanced aggressive NHL. The HRs were as follows:
- Advanced indolent NHL—HR=0.98 (95% CI, 0.66-1.45; P=0.90)
- AML—HR=1.01 (95% CI, 0.86-1.20; P=0.87)
- MM—HR=1.04 (95% CI, 0.90-1.20; P=0.60)
- Advanced aggressive NHL—HR=1.08 (95% CI, 0.87-1.34; P=0.50).
The researchers said these findings suggest it is access to care, and not other characteristics, that drive the survival disparities typically observed between urban and rural cancer patients.
“If people diagnosed with cancer, regardless of where they live, receive similar care and have similar outcomes, then a reasonable inference is that the best way to improve outcomes for rural patients is to improve their access to quality care,” Dr Unger said.
This research was supported by the National Cancer Institute and the HOPE Foundation. The researchers reported financial relationships with various pharmaceutical companies.
New research suggests that better access to quality care may reduce disparities in survival between cancer patients living in rural areas of the US and those living in urban areas.
The study showed that urban and rural cancer patients had similar survival outcomes when they were enrolled in clinical trials.
These results, published in JAMA Network Open, cast new light on decades of research showing that cancer patients living in rural areas don’t live as long as urban cancer patients.
“These findings were a surprise, since we thought we might find the same disparities others had found,” said study author Joseph Unger, PhD, of Fred Hutchinson Cancer Research Center in Seattle, Washington.
“But clinical trials are a key difference here. In trials, patients are uniformly assessed, treated, and followed under a strict, guideline-driven protocol. This suggests that giving people with cancer access to uniform treatment strategies could help resolve the disparities in outcomes that we see between rural and urban patients.”
Dr Unger and his colleagues studied data on 36,995 patients who were enrolled in 44 phase 3 or phase 2/3 SWOG trials from 1986 through 2012. All 50 states were represented.
Patients had 17 different cancer types, including acute myeloid leukemia (AML), non-Hodgkin lymphoma (NHL), and multiple myeloma (MM).
Using US Department of Agriculture population classifications known as Rural-Urban Continuum Codes, the researchers categorized the patients as either rural or urban and analyzed their outcomes.
A minority of patients (19.4%, n=7184) were from rural locations. They were significantly more likely than urban patients to be 65 or older (P<0.001) and significantly less likely to be black (vs all other races; P<0.001).
However, there was no significant between-group difference in sex (P=0.53), and all major US geographic regions (West, Midwest, South, and Northeast) were represented.
Results
The researchers limited their analysis of survival to the first 5 years after trial enrollment to emphasize outcomes related to cancer and its treatment. They looked at overall survival (OS) as well as cancer-specific survival.
The team found no meaningful difference in OS or cancer-specific survival between rural and urban patients for 16 of the 17 cancer types.
The exception was estrogen receptor-negative, progesterone receptor-negative breast cancer. Rural patients with this cancer didn’t live as long as their urban counterparts. The hazard ratio (HR) was 1.27 (95% CI, 1.06-1.51; P=0.008) for OS and 1.26 (95% CI, 1.04-1.52; P=0.02) for cancer-specific survival.
The researchers believe this finding could be attributed to a few factors, including timely access to follow-up chemotherapy after patients’ first round of cancer treatment.
Although there were no significant survival differences for patients with hematologic malignancies, rural patients had slightly better OS if they had advanced indolent NHL or AML but slightly worse OS if they had MM or advanced aggressive NHL. The HRs were as follows:
- Advanced indolent NHL—HR=0.91 (95% CI, 0.64-1.29; P=0.60)
- AML—HR=0.94 (95% CI, 0.83-1.06; P=0.29)
- MM—HR=1.05 (95% CI, 0.93-1.18, P=0.46)
- Advanced aggressive NHL—HR=1.05 (95% CI, 0.87-1.27; P=0.60).
Rural patients had slightly better cancer-specific survival if they had advanced indolent NHL but slightly worse cancer-specific survival if they had AML, MM, or advanced aggressive NHL. The HRs were as follows:
- Advanced indolent NHL—HR=0.98 (95% CI, 0.66-1.45; P=0.90)
- AML—HR=1.01 (95% CI, 0.86-1.20; P=0.87)
- MM—HR=1.04 (95% CI, 0.90-1.20; P=0.60)
- Advanced aggressive NHL—HR=1.08 (95% CI, 0.87-1.34; P=0.50).
The researchers said these findings suggest it is access to care, and not other characteristics, that drive the survival disparities typically observed between urban and rural cancer patients.
“If people diagnosed with cancer, regardless of where they live, receive similar care and have similar outcomes, then a reasonable inference is that the best way to improve outcomes for rural patients is to improve their access to quality care,” Dr Unger said.
This research was supported by the National Cancer Institute and the HOPE Foundation. The researchers reported financial relationships with various pharmaceutical companies.
New research suggests that better access to quality care may reduce disparities in survival between cancer patients living in rural areas of the US and those living in urban areas.
The study showed that urban and rural cancer patients had similar survival outcomes when they were enrolled in clinical trials.
These results, published in JAMA Network Open, cast new light on decades of research showing that cancer patients living in rural areas don’t live as long as urban cancer patients.
“These findings were a surprise, since we thought we might find the same disparities others had found,” said study author Joseph Unger, PhD, of Fred Hutchinson Cancer Research Center in Seattle, Washington.
“But clinical trials are a key difference here. In trials, patients are uniformly assessed, treated, and followed under a strict, guideline-driven protocol. This suggests that giving people with cancer access to uniform treatment strategies could help resolve the disparities in outcomes that we see between rural and urban patients.”
Dr Unger and his colleagues studied data on 36,995 patients who were enrolled in 44 phase 3 or phase 2/3 SWOG trials from 1986 through 2012. All 50 states were represented.
Patients had 17 different cancer types, including acute myeloid leukemia (AML), non-Hodgkin lymphoma (NHL), and multiple myeloma (MM).
Using US Department of Agriculture population classifications known as Rural-Urban Continuum Codes, the researchers categorized the patients as either rural or urban and analyzed their outcomes.
A minority of patients (19.4%, n=7184) were from rural locations. They were significantly more likely than urban patients to be 65 or older (P<0.001) and significantly less likely to be black (vs all other races; P<0.001).
However, there was no significant between-group difference in sex (P=0.53), and all major US geographic regions (West, Midwest, South, and Northeast) were represented.
Results
The researchers limited their analysis of survival to the first 5 years after trial enrollment to emphasize outcomes related to cancer and its treatment. They looked at overall survival (OS) as well as cancer-specific survival.
The team found no meaningful difference in OS or cancer-specific survival between rural and urban patients for 16 of the 17 cancer types.
The exception was estrogen receptor-negative, progesterone receptor-negative breast cancer. Rural patients with this cancer didn’t live as long as their urban counterparts. The hazard ratio (HR) was 1.27 (95% CI, 1.06-1.51; P=0.008) for OS and 1.26 (95% CI, 1.04-1.52; P=0.02) for cancer-specific survival.
The researchers believe this finding could be attributed to a few factors, including timely access to follow-up chemotherapy after patients’ first round of cancer treatment.
Although there were no significant survival differences for patients with hematologic malignancies, rural patients had slightly better OS if they had advanced indolent NHL or AML but slightly worse OS if they had MM or advanced aggressive NHL. The HRs were as follows:
- Advanced indolent NHL—HR=0.91 (95% CI, 0.64-1.29; P=0.60)
- AML—HR=0.94 (95% CI, 0.83-1.06; P=0.29)
- MM—HR=1.05 (95% CI, 0.93-1.18, P=0.46)
- Advanced aggressive NHL—HR=1.05 (95% CI, 0.87-1.27; P=0.60).
Rural patients had slightly better cancer-specific survival if they had advanced indolent NHL but slightly worse cancer-specific survival if they had AML, MM, or advanced aggressive NHL. The HRs were as follows:
- Advanced indolent NHL—HR=0.98 (95% CI, 0.66-1.45; P=0.90)
- AML—HR=1.01 (95% CI, 0.86-1.20; P=0.87)
- MM—HR=1.04 (95% CI, 0.90-1.20; P=0.60)
- Advanced aggressive NHL—HR=1.08 (95% CI, 0.87-1.34; P=0.50).
The researchers said these findings suggest it is access to care, and not other characteristics, that drive the survival disparities typically observed between urban and rural cancer patients.
“If people diagnosed with cancer, regardless of where they live, receive similar care and have similar outcomes, then a reasonable inference is that the best way to improve outcomes for rural patients is to improve their access to quality care,” Dr Unger said.
This research was supported by the National Cancer Institute and the HOPE Foundation. The researchers reported financial relationships with various pharmaceutical companies.
The emotionally exhausted physician
CASE ‘I’m stuck’
Dr. D, age 48, an internist practicing general medicine who is a married mother of 2 teenagers, presents with emotional exhaustion. Her medical history is unremarkable other than hyperlipidemia controlled by diet. She describes an episode of reactive depressive symptoms and anxiety when in college, which was related to the stress of final exams, finances, and the dissolution of a long-standing relationship. Regardless, she functioned well and graduated summa cum laude. She says her current feelings of being “stuck” have gradually increased during the past 3 to 4 years. Although she describes being mildly anxious and dysphoric, she also said she feels like her “wheels are spinning” and that she doesn’t even seem to care. Dr. D had been a high achiever, yet says she feels like she isn’t getting anywhere at work or at home.
[polldaddy:10064977]
The authors’ observations
As psychiatrists in the business of diagnosis and treatment, we immediately considered common diagnoses, such as major depressive disorder and persistent depressive disorder. However, despite our training in pathology, we believe patients should be considered well until proven sick. This paradigm shift is in line with the definition of mental health per the World Health Organization: “A state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community.”1
In Dr. D’s case, there was not enough information yet to fully support any of the diagnoses. She did not exhibit enough depressive symptoms to support a diagnosis of a depressive disorder. She said that she didn’t feel like she was getting anywhere at work or home. Yet there was no objective information that suggested impairment in functioning, which would preclude a diagnosis of adjustment disorder. At this point, we would support the “V code” diagnosis of phase of life problem, or even what is rarely seen in a psychiatric evaluation: “no diagnosis.”
EVALUATION Is work the problem?
We diligently conduct a thorough review of systems with Dr. D and confirm there is not enough information to diagnose a depressive disorder, anxiety disorder, or other psychiatric disorder. Collateral history suggests her teenagers are well-adjusted and doing well in high school, and she is well-respected at work with reportedly excellent performance ratings. We identify strongly with her and her situation.
Dr. D admits she is an idealist and half-jokingly says she entered into medicine “to save the world.” Yet she laments the long hours and finding herself mired in paperwork. She is barely making it to her kids’ school events and says she can’t believe her first child will be graduating within a year. She has had some particularly challenging patients recently, and although she is still diligent about their care, she is shocked she doesn’t seem to care as much about “solving the medical puzzle.” This came to light for her when a longtime patient observed that Dr. D didn’t seem herself and asked, “Are you all right, Doc?”
Dr. D is professionally dressed and has excellent grooming and hygiene. She looks tired, yet has a full affect, a witty conversational style, and responds appropriately to humor.
[polldaddy:10064980]
The authors’ observations
It can be difficult to know what to do next when there isn’t an established “playbook” for a problem without a diagnosis. We realized Dr. D was describing burnout, a syndrome of depersonalization (detached and not caring, to the point of viewing people as objects), emotional exhaustion, and low personal accomplishment that leads to decreased effectiveness at work.2 DSM-5 does not include “burnout” as a diagnosis3; however, if symptoms evolve to the point where they affect occupational or social functioning, burnout can be similar to adjustment disorder. Treatment with an antidepressant medication is not appropriate. It is possible that CBT might be helpful for many patients, yet there is no evidence that Dr. D has any cognitive distortions. Although we already had some collateral information, it is never wrong to gather additional collateral. However, because burnout is common, we may not need additional information. We could reassure her and send her on her way, but we want to add therapeutic value. We advocated exploring issues in her life and work related to meaning.
Continue to: Physician burnout
Physician burnout
Burnout is an alarmingly common problem among physicians that affects approximately half of psychiatrists. In 2014, 54.4% of physicians, and slightly less than 50% of psychiatrists, had at least 1 symptom of burnout.4 This was up from the 45.5% of physicians and a little more than 40% of psychiatrists who reported burnout in 2011,4 which suggests that as medicine continues to change, doctors may increasingly feel the brunt of this change. The rate of burnout is highest in front-line specialties (family medicine, general internal medicine, and emergency medicine) and lowest in preventive medicine.5 Physician burnout leads to real-world occupational issues, such as medical errors, poor relationships with coworkers and patients, decreased patient satisfaction, and medical malpractice suits.6,7
Even though burnout is clearly a concern for our colleagues, don’t expect them to proactively line up outside our offices. In a survey of 7,197 surgeons, 86.6% of respondents answered it was not important that “I have regular meetings with a psychologist/psychiatrist to discuss stress.”8 At the same time, the idea of meeting with a psychologist/psychiatrist was rated more highly by surgeons who were burnt out and found to be a factor independently associated with burnout.8 Perhaps we have some work to do in marketing our services in a way that welcomes our colleagues.
Although physician burnout has been a focus of recent studies, burnout in general has been studied for decades in other working populations. There are 2 useful models describing burnout:
- The job demand-control(-support) model suggests that individuals experience strain and subsequent ill effects when the demands of their job exceed the control they have,9 and social support from supervisors and colleagues can buffer the harmful effects of job strain.10
- The effort-reward imbalance model suggests that high-effort, low-reward occupational conditions are particularly stressful.11
Both models are simple, intuitive, and suggest solutions.
When engaging your physician colleagues about their burnout, remember that physicians are people, too, and have the same difficulties that everyone else does in successfully practicing healthy behaviors. As physicians, we have significant demands on our time that make it difficult to control our ability to eat, sleep, and exercise. In general, the food available where we work is not nutritious,12 half of us are overweight or obese,13 and working more than 40 hours per week increases the likelihood we’ll have a higher body mass index.14 We don’t sleep well, either—we get less sleep than the general population,15 and more sleep equates to less burnout.16 Regarding exercise, doctors who cannot prioritize exercise tend to have more burnout.17
Continue to: When evaluating a physician colleague for symptoms of burnout...
When evaluating a physician colleague for symptoms of burnout, start by assessing the basics: eating, sleeping, and moving. In Dr. D’s case, this also included taking a quick inventory of what demands were on her proverbial plate. Taking inventory of these demands (ie, demand-control[-support] model) may lead to new insights about what she can control. Prioritization is important to determine where efforts go (ie, effort-reward imbalance model). This is where your skills as a psychiatrist can especially help, as you explore values and bring trade-offs to light.
EVALUATION Permission not to be perfect
As we interview Dr. D, we realize she has some obsessive-compulsive personality traits that are mostly self-serving. She places a high value on being thorough and having elegant clinical notes. Yet this value competes with her desire to be efficient and get home on time to see her kids’ school events. You point this out to her and see if she can come up with some solutions. You also discuss with Dr. D the tension everyone feels between valuing career and valuing family and friends. You normalize her situation, and give her permission to pick something about which she will allow herself not to be perfect.
[polldaddy:10064981]
The authors’ observations
Since perfectionism is a common trait among physicians,18 failure doesn’t seem to be compatible with their DNA. We encourage other physicians to be scientific about their own lives, just as they are in the profession they have chosen. Physicians can delude themselves into thinking they can have it all, not recognizing that every choice has its cost. For example, a physician who decides that it’s okay to publish one fewer research paper this year might have more time to enjoy spending time with his or her children. In our work with physicians, we strive to normalize their experiences, helping them reframe their perfectionistic viewpoint to recognize that everyone struggles with work-life balance issues. We validate that physicians have difficult choices to make in finding what works for them, and we challenge and support them in exploring these choices.
Choosing where to put one’s efforts is also contingent upon the expected rewards. Sometime before the daily grind of our careers in medicine started, we had strong visions of what such careers would mean to us. We visualized the ideal of helping people and making a difference. Then, at some point, many of us took this for granted and forgot about the intrinsic rewards of our work. In a 2014-2015 survey of U.S. physicians across all specialties, only 64.6% of respondents who were highly burned out said they found their work personally rewarding. This is a sharp contrast to the 97.5% of respondents who were not burned out who reported that they found their work personally rewarding.19
As psychiatrists, we can challenge our physician colleagues to dare to dream again. We can help them rediscover the rewarding aspects of their work (ie, per effort-reward imbalance model) that drew them into medicine in the first place. This may include exploring their future legacy. How do they want to be remembered at retirement? Such consideration is linked to mental simulation and meaning in their lives.20 We guide our colleagues to reframe their current situation to see the myriad of choices they have based upon their own specific value system. If family and friends are currently taking priority over work, it also helps to reframe that working allows us to make a good living so we can fully enjoy that time spent with family and friends.
Continue to: If we do our jobs well...
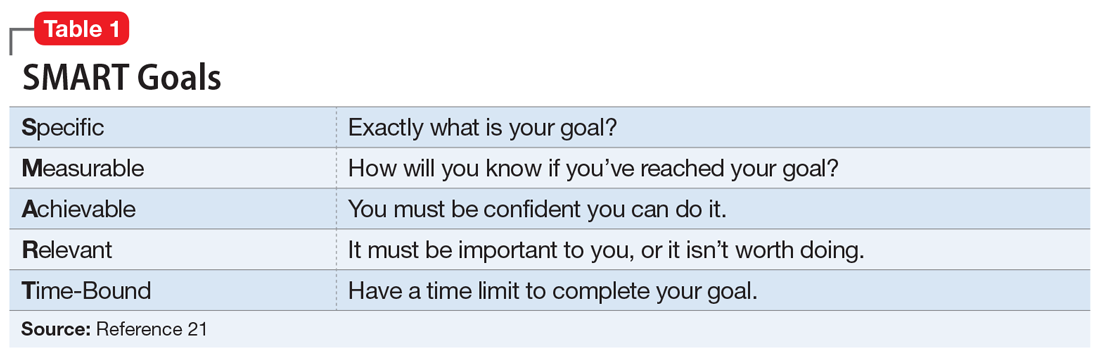
If we do our jobs well, the next part is easy. We have them set specific short- and long-term goals related to their situation. This is something we do every day in our practices. It may help to make sure we’re using SMART (Specific, Measurable, Achievable, Relevant, Time-Bound), a well-known mnemonic used for goals (Table 121), and brush up on our motivational interviewing skills (see Related Resources). It is especially important to make sure our colleagues have goals that are relevant—the “R” in the SMART mnemonic—to their situation.
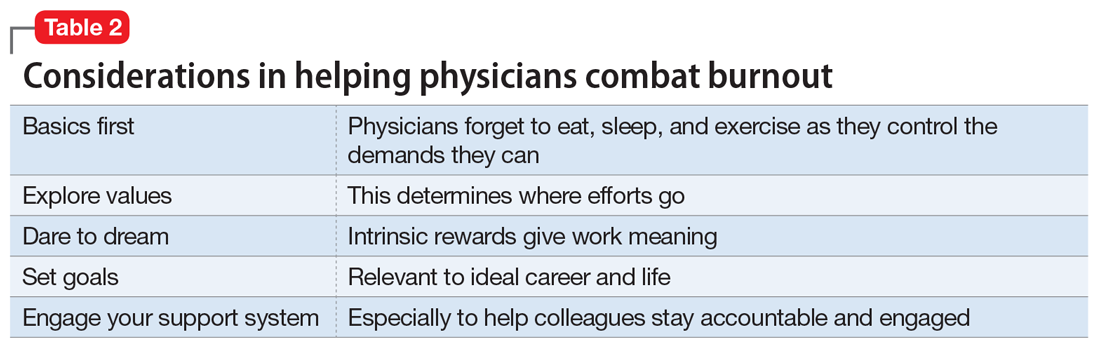
Finally, we do a better job of reaching our goals and engaging more at work and at home when we have good social support. For physicians, co-worker support has been found to be directly related to our well-being as well as buffering the negative effects of work demands.22 Furthermore, our colleagues are the most acceptable sources of support when we are faced with stressful situations.23 Thus, as psychiatrists, we can doubly help our physician patients by providing collegial support and doing our usual job of holding them accountable to their goals (Table 2).
OUTCOME Goal-setting, priorities, accountability
As we’re exploring goals with Dr. D, she makes a conscious decision to spend less time on documentation and start focusing on being present with her patients. She returns in 1 month to tell you time management is still a struggle, but her visit with you was instrumental in making her realize how important it was to get home on time for her kids’ activities. She says it greatly helped that you kept her accountable, yet also validated her struggles and gave her permission to design her life within the constraints of her situation and without the burden of having to be perfect at everything.
Bottom Line
We can best help our physician colleagues who are experiencing burnout by shifting our paradigm to a wellness model that focuses on helping them reach their potential and balance their professional and personal lives.
Related Resources
- Balch CM, Shanafelt TD. Combating stress and burnout in surgical practice: a review. Thorac Surg Clin. 2011;21(3):417-430.
- Miller WR, Rollnick S. Motivational interviewing: preparing people for change, 2nd ed. New York, NY: The Guilford Press; 2002.
- Stanford Medicine WellMD. Stress & Burnout. https://wellmd.stanford.edu.
1. World Health Organization. Mental health: a state of well-being. http://www.who.int/features/factfiles/mental_health/en/. Updated August 2014. Accessed March 17, 2017.
2. Maslach C, Jackson S, Leiter M. Maslach burnout inventory manual, 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996.
3. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
4. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600-1613.
5. Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377-1385.
6. Shanafelt TD, Sloan JA, Habermann TM. The well-being of physicians. Am J Med. 2003;114(6):513-519.
7. Balch CM, Shanafelt TD. Combating stress and burnout in surgical practice: a review. Adv Surg. 2010;44:29-47.
8. Shanafelt TD, Oreskovich MR, Dyrbye LN, et al. Avoiding burnout: the personal health habits and wellness practices of US Surgeons. Ann Surg. 2012;255(4):625-633.
9. Karasek RA Jr. Job demands, job decision latitude, and mental strain: implications for job redesign. Adm Sci Q. 1979;24(2):285-308.
10. Johnson JV. Collective control: strategies for survival in the workplace. Int J Health Serv. 1989;19(3):469-480.
11. Siegrist J. Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol. 1996;1(1):27-41.
12. Lesser LI, Cohen DA, Brook RH. Changing eating habits for the medical profession. JAMA. 2012;308(10):983-984.
13. Bleich SN, Bennett WL, Gudzune KA, et al. Impact of physician BMI on obesity care and beliefs. Obesity (Silver Spring). 2012;20(5):999-1005.
14. Stanford FC, Durkin MW, Blair SN, et al. Determining levels of physical activity in attending physicians, resident and fellow physicians, and medical students in the USA. Br J Sports Med. 2012;46(5):360-364.
15. Tucker P, Bejerot E, Kecklund G, et al. Stress Research Institute at Stockholm University. Stress Research Report-doctors’ work hours in Sweden: their impact on sleep, health, work-family balance, patient care and thoughts about work. https://www.stressforskning.su.se/polopoly_fs/1.233341.1429526778!/menu/standard/file/sfr325.pdf. Accessed March 17, 2017.
16. Wisetborisut A, Angkurawaranon C, Jiraporncharoen W, et al. Shift work and burnout among health care workers. Occup Med (Lond). 2014;64(4):279-286.
17. Eckleberry-Hunt J, Lick D, Boura J, et al. An exploratory study of resident burnout and wellness. Acad Med. 2009;84(2):269-277.
18. Peters M, King J. Perfectionism in doctors. BMJ. 2012;344:e1674. doi: https://doi.org/10.1136/bmj.e1674.
19. Jager AJ, Tutty MA, Kao AC. Association between physician burnout and identification with medicine as a calling. Mayo Clin Proc. 2017;92(3):415-422.
20. Waytz A, Hershfield HE, Tamir DI. Neural and behavioral evidence for the role of mental simulation in meaning in life. J Pers Soc Psychol. 2015;108(2):336-355.
21. SMART Criteria. https://en.wikipedia.org/wiki/SMART_criteria. Accessed March 17, 2017.
22. Hu YY, Fix ML, Hevelone ND, et al. Physicians’ needs in coping with emotional stressors: the case for peer support. Arch Surg. 2012;147(3):212-217.
23. Wallace JE, Lemaire J. On physician well being–you’ll get by with a little help from your friends. Soc Sci Med. 2007;64(12):2565-2577.
CASE ‘I’m stuck’
Dr. D, age 48, an internist practicing general medicine who is a married mother of 2 teenagers, presents with emotional exhaustion. Her medical history is unremarkable other than hyperlipidemia controlled by diet. She describes an episode of reactive depressive symptoms and anxiety when in college, which was related to the stress of final exams, finances, and the dissolution of a long-standing relationship. Regardless, she functioned well and graduated summa cum laude. She says her current feelings of being “stuck” have gradually increased during the past 3 to 4 years. Although she describes being mildly anxious and dysphoric, she also said she feels like her “wheels are spinning” and that she doesn’t even seem to care. Dr. D had been a high achiever, yet says she feels like she isn’t getting anywhere at work or at home.
[polldaddy:10064977]
The authors’ observations
As psychiatrists in the business of diagnosis and treatment, we immediately considered common diagnoses, such as major depressive disorder and persistent depressive disorder. However, despite our training in pathology, we believe patients should be considered well until proven sick. This paradigm shift is in line with the definition of mental health per the World Health Organization: “A state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community.”1
In Dr. D’s case, there was not enough information yet to fully support any of the diagnoses. She did not exhibit enough depressive symptoms to support a diagnosis of a depressive disorder. She said that she didn’t feel like she was getting anywhere at work or home. Yet there was no objective information that suggested impairment in functioning, which would preclude a diagnosis of adjustment disorder. At this point, we would support the “V code” diagnosis of phase of life problem, or even what is rarely seen in a psychiatric evaluation: “no diagnosis.”
EVALUATION Is work the problem?
We diligently conduct a thorough review of systems with Dr. D and confirm there is not enough information to diagnose a depressive disorder, anxiety disorder, or other psychiatric disorder. Collateral history suggests her teenagers are well-adjusted and doing well in high school, and she is well-respected at work with reportedly excellent performance ratings. We identify strongly with her and her situation.
Dr. D admits she is an idealist and half-jokingly says she entered into medicine “to save the world.” Yet she laments the long hours and finding herself mired in paperwork. She is barely making it to her kids’ school events and says she can’t believe her first child will be graduating within a year. She has had some particularly challenging patients recently, and although she is still diligent about their care, she is shocked she doesn’t seem to care as much about “solving the medical puzzle.” This came to light for her when a longtime patient observed that Dr. D didn’t seem herself and asked, “Are you all right, Doc?”
Dr. D is professionally dressed and has excellent grooming and hygiene. She looks tired, yet has a full affect, a witty conversational style, and responds appropriately to humor.
[polldaddy:10064980]
The authors’ observations
It can be difficult to know what to do next when there isn’t an established “playbook” for a problem without a diagnosis. We realized Dr. D was describing burnout, a syndrome of depersonalization (detached and not caring, to the point of viewing people as objects), emotional exhaustion, and low personal accomplishment that leads to decreased effectiveness at work.2 DSM-5 does not include “burnout” as a diagnosis3; however, if symptoms evolve to the point where they affect occupational or social functioning, burnout can be similar to adjustment disorder. Treatment with an antidepressant medication is not appropriate. It is possible that CBT might be helpful for many patients, yet there is no evidence that Dr. D has any cognitive distortions. Although we already had some collateral information, it is never wrong to gather additional collateral. However, because burnout is common, we may not need additional information. We could reassure her and send her on her way, but we want to add therapeutic value. We advocated exploring issues in her life and work related to meaning.
Continue to: Physician burnout
Physician burnout
Burnout is an alarmingly common problem among physicians that affects approximately half of psychiatrists. In 2014, 54.4% of physicians, and slightly less than 50% of psychiatrists, had at least 1 symptom of burnout.4 This was up from the 45.5% of physicians and a little more than 40% of psychiatrists who reported burnout in 2011,4 which suggests that as medicine continues to change, doctors may increasingly feel the brunt of this change. The rate of burnout is highest in front-line specialties (family medicine, general internal medicine, and emergency medicine) and lowest in preventive medicine.5 Physician burnout leads to real-world occupational issues, such as medical errors, poor relationships with coworkers and patients, decreased patient satisfaction, and medical malpractice suits.6,7
Even though burnout is clearly a concern for our colleagues, don’t expect them to proactively line up outside our offices. In a survey of 7,197 surgeons, 86.6% of respondents answered it was not important that “I have regular meetings with a psychologist/psychiatrist to discuss stress.”8 At the same time, the idea of meeting with a psychologist/psychiatrist was rated more highly by surgeons who were burnt out and found to be a factor independently associated with burnout.8 Perhaps we have some work to do in marketing our services in a way that welcomes our colleagues.
Although physician burnout has been a focus of recent studies, burnout in general has been studied for decades in other working populations. There are 2 useful models describing burnout:
- The job demand-control(-support) model suggests that individuals experience strain and subsequent ill effects when the demands of their job exceed the control they have,9 and social support from supervisors and colleagues can buffer the harmful effects of job strain.10
- The effort-reward imbalance model suggests that high-effort, low-reward occupational conditions are particularly stressful.11
Both models are simple, intuitive, and suggest solutions.
When engaging your physician colleagues about their burnout, remember that physicians are people, too, and have the same difficulties that everyone else does in successfully practicing healthy behaviors. As physicians, we have significant demands on our time that make it difficult to control our ability to eat, sleep, and exercise. In general, the food available where we work is not nutritious,12 half of us are overweight or obese,13 and working more than 40 hours per week increases the likelihood we’ll have a higher body mass index.14 We don’t sleep well, either—we get less sleep than the general population,15 and more sleep equates to less burnout.16 Regarding exercise, doctors who cannot prioritize exercise tend to have more burnout.17
Continue to: When evaluating a physician colleague for symptoms of burnout...
When evaluating a physician colleague for symptoms of burnout, start by assessing the basics: eating, sleeping, and moving. In Dr. D’s case, this also included taking a quick inventory of what demands were on her proverbial plate. Taking inventory of these demands (ie, demand-control[-support] model) may lead to new insights about what she can control. Prioritization is important to determine where efforts go (ie, effort-reward imbalance model). This is where your skills as a psychiatrist can especially help, as you explore values and bring trade-offs to light.
EVALUATION Permission not to be perfect
As we interview Dr. D, we realize she has some obsessive-compulsive personality traits that are mostly self-serving. She places a high value on being thorough and having elegant clinical notes. Yet this value competes with her desire to be efficient and get home on time to see her kids’ school events. You point this out to her and see if she can come up with some solutions. You also discuss with Dr. D the tension everyone feels between valuing career and valuing family and friends. You normalize her situation, and give her permission to pick something about which she will allow herself not to be perfect.
[polldaddy:10064981]
The authors’ observations
Since perfectionism is a common trait among physicians,18 failure doesn’t seem to be compatible with their DNA. We encourage other physicians to be scientific about their own lives, just as they are in the profession they have chosen. Physicians can delude themselves into thinking they can have it all, not recognizing that every choice has its cost. For example, a physician who decides that it’s okay to publish one fewer research paper this year might have more time to enjoy spending time with his or her children. In our work with physicians, we strive to normalize their experiences, helping them reframe their perfectionistic viewpoint to recognize that everyone struggles with work-life balance issues. We validate that physicians have difficult choices to make in finding what works for them, and we challenge and support them in exploring these choices.
Choosing where to put one’s efforts is also contingent upon the expected rewards. Sometime before the daily grind of our careers in medicine started, we had strong visions of what such careers would mean to us. We visualized the ideal of helping people and making a difference. Then, at some point, many of us took this for granted and forgot about the intrinsic rewards of our work. In a 2014-2015 survey of U.S. physicians across all specialties, only 64.6% of respondents who were highly burned out said they found their work personally rewarding. This is a sharp contrast to the 97.5% of respondents who were not burned out who reported that they found their work personally rewarding.19
As psychiatrists, we can challenge our physician colleagues to dare to dream again. We can help them rediscover the rewarding aspects of their work (ie, per effort-reward imbalance model) that drew them into medicine in the first place. This may include exploring their future legacy. How do they want to be remembered at retirement? Such consideration is linked to mental simulation and meaning in their lives.20 We guide our colleagues to reframe their current situation to see the myriad of choices they have based upon their own specific value system. If family and friends are currently taking priority over work, it also helps to reframe that working allows us to make a good living so we can fully enjoy that time spent with family and friends.
Continue to: If we do our jobs well...
If we do our jobs well, the next part is easy. We have them set specific short- and long-term goals related to their situation. This is something we do every day in our practices. It may help to make sure we’re using SMART (Specific, Measurable, Achievable, Relevant, Time-Bound), a well-known mnemonic used for goals (Table 121), and brush up on our motivational interviewing skills (see Related Resources). It is especially important to make sure our colleagues have goals that are relevant—the “R” in the SMART mnemonic—to their situation.
Finally, we do a better job of reaching our goals and engaging more at work and at home when we have good social support. For physicians, co-worker support has been found to be directly related to our well-being as well as buffering the negative effects of work demands.22 Furthermore, our colleagues are the most acceptable sources of support when we are faced with stressful situations.23 Thus, as psychiatrists, we can doubly help our physician patients by providing collegial support and doing our usual job of holding them accountable to their goals (Table 2).
OUTCOME Goal-setting, priorities, accountability
As we’re exploring goals with Dr. D, she makes a conscious decision to spend less time on documentation and start focusing on being present with her patients. She returns in 1 month to tell you time management is still a struggle, but her visit with you was instrumental in making her realize how important it was to get home on time for her kids’ activities. She says it greatly helped that you kept her accountable, yet also validated her struggles and gave her permission to design her life within the constraints of her situation and without the burden of having to be perfect at everything.
Bottom Line
We can best help our physician colleagues who are experiencing burnout by shifting our paradigm to a wellness model that focuses on helping them reach their potential and balance their professional and personal lives.
Related Resources
- Balch CM, Shanafelt TD. Combating stress and burnout in surgical practice: a review. Thorac Surg Clin. 2011;21(3):417-430.
- Miller WR, Rollnick S. Motivational interviewing: preparing people for change, 2nd ed. New York, NY: The Guilford Press; 2002.
- Stanford Medicine WellMD. Stress & Burnout. https://wellmd.stanford.edu.
CASE ‘I’m stuck’
Dr. D, age 48, an internist practicing general medicine who is a married mother of 2 teenagers, presents with emotional exhaustion. Her medical history is unremarkable other than hyperlipidemia controlled by diet. She describes an episode of reactive depressive symptoms and anxiety when in college, which was related to the stress of final exams, finances, and the dissolution of a long-standing relationship. Regardless, she functioned well and graduated summa cum laude. She says her current feelings of being “stuck” have gradually increased during the past 3 to 4 years. Although she describes being mildly anxious and dysphoric, she also said she feels like her “wheels are spinning” and that she doesn’t even seem to care. Dr. D had been a high achiever, yet says she feels like she isn’t getting anywhere at work or at home.
[polldaddy:10064977]
The authors’ observations
As psychiatrists in the business of diagnosis and treatment, we immediately considered common diagnoses, such as major depressive disorder and persistent depressive disorder. However, despite our training in pathology, we believe patients should be considered well until proven sick. This paradigm shift is in line with the definition of mental health per the World Health Organization: “A state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community.”1
In Dr. D’s case, there was not enough information yet to fully support any of the diagnoses. She did not exhibit enough depressive symptoms to support a diagnosis of a depressive disorder. She said that she didn’t feel like she was getting anywhere at work or home. Yet there was no objective information that suggested impairment in functioning, which would preclude a diagnosis of adjustment disorder. At this point, we would support the “V code” diagnosis of phase of life problem, or even what is rarely seen in a psychiatric evaluation: “no diagnosis.”
EVALUATION Is work the problem?
We diligently conduct a thorough review of systems with Dr. D and confirm there is not enough information to diagnose a depressive disorder, anxiety disorder, or other psychiatric disorder. Collateral history suggests her teenagers are well-adjusted and doing well in high school, and she is well-respected at work with reportedly excellent performance ratings. We identify strongly with her and her situation.
Dr. D admits she is an idealist and half-jokingly says she entered into medicine “to save the world.” Yet she laments the long hours and finding herself mired in paperwork. She is barely making it to her kids’ school events and says she can’t believe her first child will be graduating within a year. She has had some particularly challenging patients recently, and although she is still diligent about their care, she is shocked she doesn’t seem to care as much about “solving the medical puzzle.” This came to light for her when a longtime patient observed that Dr. D didn’t seem herself and asked, “Are you all right, Doc?”
Dr. D is professionally dressed and has excellent grooming and hygiene. She looks tired, yet has a full affect, a witty conversational style, and responds appropriately to humor.
[polldaddy:10064980]
The authors’ observations
It can be difficult to know what to do next when there isn’t an established “playbook” for a problem without a diagnosis. We realized Dr. D was describing burnout, a syndrome of depersonalization (detached and not caring, to the point of viewing people as objects), emotional exhaustion, and low personal accomplishment that leads to decreased effectiveness at work.2 DSM-5 does not include “burnout” as a diagnosis3; however, if symptoms evolve to the point where they affect occupational or social functioning, burnout can be similar to adjustment disorder. Treatment with an antidepressant medication is not appropriate. It is possible that CBT might be helpful for many patients, yet there is no evidence that Dr. D has any cognitive distortions. Although we already had some collateral information, it is never wrong to gather additional collateral. However, because burnout is common, we may not need additional information. We could reassure her and send her on her way, but we want to add therapeutic value. We advocated exploring issues in her life and work related to meaning.
Continue to: Physician burnout
Physician burnout
Burnout is an alarmingly common problem among physicians that affects approximately half of psychiatrists. In 2014, 54.4% of physicians, and slightly less than 50% of psychiatrists, had at least 1 symptom of burnout.4 This was up from the 45.5% of physicians and a little more than 40% of psychiatrists who reported burnout in 2011,4 which suggests that as medicine continues to change, doctors may increasingly feel the brunt of this change. The rate of burnout is highest in front-line specialties (family medicine, general internal medicine, and emergency medicine) and lowest in preventive medicine.5 Physician burnout leads to real-world occupational issues, such as medical errors, poor relationships with coworkers and patients, decreased patient satisfaction, and medical malpractice suits.6,7
Even though burnout is clearly a concern for our colleagues, don’t expect them to proactively line up outside our offices. In a survey of 7,197 surgeons, 86.6% of respondents answered it was not important that “I have regular meetings with a psychologist/psychiatrist to discuss stress.”8 At the same time, the idea of meeting with a psychologist/psychiatrist was rated more highly by surgeons who were burnt out and found to be a factor independently associated with burnout.8 Perhaps we have some work to do in marketing our services in a way that welcomes our colleagues.
Although physician burnout has been a focus of recent studies, burnout in general has been studied for decades in other working populations. There are 2 useful models describing burnout:
- The job demand-control(-support) model suggests that individuals experience strain and subsequent ill effects when the demands of their job exceed the control they have,9 and social support from supervisors and colleagues can buffer the harmful effects of job strain.10
- The effort-reward imbalance model suggests that high-effort, low-reward occupational conditions are particularly stressful.11
Both models are simple, intuitive, and suggest solutions.
When engaging your physician colleagues about their burnout, remember that physicians are people, too, and have the same difficulties that everyone else does in successfully practicing healthy behaviors. As physicians, we have significant demands on our time that make it difficult to control our ability to eat, sleep, and exercise. In general, the food available where we work is not nutritious,12 half of us are overweight or obese,13 and working more than 40 hours per week increases the likelihood we’ll have a higher body mass index.14 We don’t sleep well, either—we get less sleep than the general population,15 and more sleep equates to less burnout.16 Regarding exercise, doctors who cannot prioritize exercise tend to have more burnout.17
Continue to: When evaluating a physician colleague for symptoms of burnout...
When evaluating a physician colleague for symptoms of burnout, start by assessing the basics: eating, sleeping, and moving. In Dr. D’s case, this also included taking a quick inventory of what demands were on her proverbial plate. Taking inventory of these demands (ie, demand-control[-support] model) may lead to new insights about what she can control. Prioritization is important to determine where efforts go (ie, effort-reward imbalance model). This is where your skills as a psychiatrist can especially help, as you explore values and bring trade-offs to light.
EVALUATION Permission not to be perfect
As we interview Dr. D, we realize she has some obsessive-compulsive personality traits that are mostly self-serving. She places a high value on being thorough and having elegant clinical notes. Yet this value competes with her desire to be efficient and get home on time to see her kids’ school events. You point this out to her and see if she can come up with some solutions. You also discuss with Dr. D the tension everyone feels between valuing career and valuing family and friends. You normalize her situation, and give her permission to pick something about which she will allow herself not to be perfect.
[polldaddy:10064981]
The authors’ observations
Since perfectionism is a common trait among physicians,18 failure doesn’t seem to be compatible with their DNA. We encourage other physicians to be scientific about their own lives, just as they are in the profession they have chosen. Physicians can delude themselves into thinking they can have it all, not recognizing that every choice has its cost. For example, a physician who decides that it’s okay to publish one fewer research paper this year might have more time to enjoy spending time with his or her children. In our work with physicians, we strive to normalize their experiences, helping them reframe their perfectionistic viewpoint to recognize that everyone struggles with work-life balance issues. We validate that physicians have difficult choices to make in finding what works for them, and we challenge and support them in exploring these choices.
Choosing where to put one’s efforts is also contingent upon the expected rewards. Sometime before the daily grind of our careers in medicine started, we had strong visions of what such careers would mean to us. We visualized the ideal of helping people and making a difference. Then, at some point, many of us took this for granted and forgot about the intrinsic rewards of our work. In a 2014-2015 survey of U.S. physicians across all specialties, only 64.6% of respondents who were highly burned out said they found their work personally rewarding. This is a sharp contrast to the 97.5% of respondents who were not burned out who reported that they found their work personally rewarding.19
As psychiatrists, we can challenge our physician colleagues to dare to dream again. We can help them rediscover the rewarding aspects of their work (ie, per effort-reward imbalance model) that drew them into medicine in the first place. This may include exploring their future legacy. How do they want to be remembered at retirement? Such consideration is linked to mental simulation and meaning in their lives.20 We guide our colleagues to reframe their current situation to see the myriad of choices they have based upon their own specific value system. If family and friends are currently taking priority over work, it also helps to reframe that working allows us to make a good living so we can fully enjoy that time spent with family and friends.
Continue to: If we do our jobs well...
If we do our jobs well, the next part is easy. We have them set specific short- and long-term goals related to their situation. This is something we do every day in our practices. It may help to make sure we’re using SMART (Specific, Measurable, Achievable, Relevant, Time-Bound), a well-known mnemonic used for goals (Table 121), and brush up on our motivational interviewing skills (see Related Resources). It is especially important to make sure our colleagues have goals that are relevant—the “R” in the SMART mnemonic—to their situation.
Finally, we do a better job of reaching our goals and engaging more at work and at home when we have good social support. For physicians, co-worker support has been found to be directly related to our well-being as well as buffering the negative effects of work demands.22 Furthermore, our colleagues are the most acceptable sources of support when we are faced with stressful situations.23 Thus, as psychiatrists, we can doubly help our physician patients by providing collegial support and doing our usual job of holding them accountable to their goals (Table 2).
OUTCOME Goal-setting, priorities, accountability
As we’re exploring goals with Dr. D, she makes a conscious decision to spend less time on documentation and start focusing on being present with her patients. She returns in 1 month to tell you time management is still a struggle, but her visit with you was instrumental in making her realize how important it was to get home on time for her kids’ activities. She says it greatly helped that you kept her accountable, yet also validated her struggles and gave her permission to design her life within the constraints of her situation and without the burden of having to be perfect at everything.
Bottom Line
We can best help our physician colleagues who are experiencing burnout by shifting our paradigm to a wellness model that focuses on helping them reach their potential and balance their professional and personal lives.
Related Resources
- Balch CM, Shanafelt TD. Combating stress and burnout in surgical practice: a review. Thorac Surg Clin. 2011;21(3):417-430.
- Miller WR, Rollnick S. Motivational interviewing: preparing people for change, 2nd ed. New York, NY: The Guilford Press; 2002.
- Stanford Medicine WellMD. Stress & Burnout. https://wellmd.stanford.edu.
1. World Health Organization. Mental health: a state of well-being. http://www.who.int/features/factfiles/mental_health/en/. Updated August 2014. Accessed March 17, 2017.
2. Maslach C, Jackson S, Leiter M. Maslach burnout inventory manual, 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996.
3. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
4. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600-1613.
5. Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377-1385.
6. Shanafelt TD, Sloan JA, Habermann TM. The well-being of physicians. Am J Med. 2003;114(6):513-519.
7. Balch CM, Shanafelt TD. Combating stress and burnout in surgical practice: a review. Adv Surg. 2010;44:29-47.
8. Shanafelt TD, Oreskovich MR, Dyrbye LN, et al. Avoiding burnout: the personal health habits and wellness practices of US Surgeons. Ann Surg. 2012;255(4):625-633.
9. Karasek RA Jr. Job demands, job decision latitude, and mental strain: implications for job redesign. Adm Sci Q. 1979;24(2):285-308.
10. Johnson JV. Collective control: strategies for survival in the workplace. Int J Health Serv. 1989;19(3):469-480.
11. Siegrist J. Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol. 1996;1(1):27-41.
12. Lesser LI, Cohen DA, Brook RH. Changing eating habits for the medical profession. JAMA. 2012;308(10):983-984.
13. Bleich SN, Bennett WL, Gudzune KA, et al. Impact of physician BMI on obesity care and beliefs. Obesity (Silver Spring). 2012;20(5):999-1005.
14. Stanford FC, Durkin MW, Blair SN, et al. Determining levels of physical activity in attending physicians, resident and fellow physicians, and medical students in the USA. Br J Sports Med. 2012;46(5):360-364.
15. Tucker P, Bejerot E, Kecklund G, et al. Stress Research Institute at Stockholm University. Stress Research Report-doctors’ work hours in Sweden: their impact on sleep, health, work-family balance, patient care and thoughts about work. https://www.stressforskning.su.se/polopoly_fs/1.233341.1429526778!/menu/standard/file/sfr325.pdf. Accessed March 17, 2017.
16. Wisetborisut A, Angkurawaranon C, Jiraporncharoen W, et al. Shift work and burnout among health care workers. Occup Med (Lond). 2014;64(4):279-286.
17. Eckleberry-Hunt J, Lick D, Boura J, et al. An exploratory study of resident burnout and wellness. Acad Med. 2009;84(2):269-277.
18. Peters M, King J. Perfectionism in doctors. BMJ. 2012;344:e1674. doi: https://doi.org/10.1136/bmj.e1674.
19. Jager AJ, Tutty MA, Kao AC. Association between physician burnout and identification with medicine as a calling. Mayo Clin Proc. 2017;92(3):415-422.
20. Waytz A, Hershfield HE, Tamir DI. Neural and behavioral evidence for the role of mental simulation in meaning in life. J Pers Soc Psychol. 2015;108(2):336-355.
21. SMART Criteria. https://en.wikipedia.org/wiki/SMART_criteria. Accessed March 17, 2017.
22. Hu YY, Fix ML, Hevelone ND, et al. Physicians’ needs in coping with emotional stressors: the case for peer support. Arch Surg. 2012;147(3):212-217.
23. Wallace JE, Lemaire J. On physician well being–you’ll get by with a little help from your friends. Soc Sci Med. 2007;64(12):2565-2577.
1. World Health Organization. Mental health: a state of well-being. http://www.who.int/features/factfiles/mental_health/en/. Updated August 2014. Accessed March 17, 2017.
2. Maslach C, Jackson S, Leiter M. Maslach burnout inventory manual, 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996.
3. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
4. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600-1613.
5. Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377-1385.
6. Shanafelt TD, Sloan JA, Habermann TM. The well-being of physicians. Am J Med. 2003;114(6):513-519.
7. Balch CM, Shanafelt TD. Combating stress and burnout in surgical practice: a review. Adv Surg. 2010;44:29-47.
8. Shanafelt TD, Oreskovich MR, Dyrbye LN, et al. Avoiding burnout: the personal health habits and wellness practices of US Surgeons. Ann Surg. 2012;255(4):625-633.
9. Karasek RA Jr. Job demands, job decision latitude, and mental strain: implications for job redesign. Adm Sci Q. 1979;24(2):285-308.
10. Johnson JV. Collective control: strategies for survival in the workplace. Int J Health Serv. 1989;19(3):469-480.
11. Siegrist J. Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol. 1996;1(1):27-41.
12. Lesser LI, Cohen DA, Brook RH. Changing eating habits for the medical profession. JAMA. 2012;308(10):983-984.
13. Bleich SN, Bennett WL, Gudzune KA, et al. Impact of physician BMI on obesity care and beliefs. Obesity (Silver Spring). 2012;20(5):999-1005.
14. Stanford FC, Durkin MW, Blair SN, et al. Determining levels of physical activity in attending physicians, resident and fellow physicians, and medical students in the USA. Br J Sports Med. 2012;46(5):360-364.
15. Tucker P, Bejerot E, Kecklund G, et al. Stress Research Institute at Stockholm University. Stress Research Report-doctors’ work hours in Sweden: their impact on sleep, health, work-family balance, patient care and thoughts about work. https://www.stressforskning.su.se/polopoly_fs/1.233341.1429526778!/menu/standard/file/sfr325.pdf. Accessed March 17, 2017.
16. Wisetborisut A, Angkurawaranon C, Jiraporncharoen W, et al. Shift work and burnout among health care workers. Occup Med (Lond). 2014;64(4):279-286.
17. Eckleberry-Hunt J, Lick D, Boura J, et al. An exploratory study of resident burnout and wellness. Acad Med. 2009;84(2):269-277.
18. Peters M, King J. Perfectionism in doctors. BMJ. 2012;344:e1674. doi: https://doi.org/10.1136/bmj.e1674.
19. Jager AJ, Tutty MA, Kao AC. Association between physician burnout and identification with medicine as a calling. Mayo Clin Proc. 2017;92(3):415-422.
20. Waytz A, Hershfield HE, Tamir DI. Neural and behavioral evidence for the role of mental simulation in meaning in life. J Pers Soc Psychol. 2015;108(2):336-355.
21. SMART Criteria. https://en.wikipedia.org/wiki/SMART_criteria. Accessed March 17, 2017.
22. Hu YY, Fix ML, Hevelone ND, et al. Physicians’ needs in coping with emotional stressors: the case for peer support. Arch Surg. 2012;147(3):212-217.
23. Wallace JE, Lemaire J. On physician well being–you’ll get by with a little help from your friends. Soc Sci Med. 2007;64(12):2565-2577.
Partial hold placed on trial of drug for AML, MDS
The US Food and Drug Administration (FDA) has placed a partial clinical hold on a phase 1b/2 study of OXi4503, a vascular disrupting agent.
In this trial (NCT02576301), researchers are evaluating OXi4503, alone and in combination with cytarabine, in patients with relapsed/refractory acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS).
The partial clinical hold applies to the 12.2 mg/m2 dose of OXi4503.
The FDA is allowing the continued treatment and enrollment of patients using a dose of 9.76 mg/m2.
The agency said additional data on patients receiving OXi4503 at 9.76 mg/m2 must be evaluated before dosing at 12.2 mg/m2 can be resumed.
The partial clinical hold is a result of 2 potential dose-limiting toxicities (DLTs) observed at the 12.2 mg/m2 dose level.
One DLT was hypotension, which occurred shortly after initial treatment with OXi4503. The other DLT was acute hypoxic respiratory failure, which occurred approximately 2 weeks after receiving OXi4503 and cytarabine.
Both events were deemed “possibly related” to OXi4503, and both patients recovered following treatment.
The study protocol generally defines a DLT as any grade 3 serious adverse event where a relationship to OXi4503 cannot be ruled out.
“Although it is disappointing that we are not currently continuing with the higher dose of OXi4503, we look forward to gathering more safety and efficacy data at the previous dose level, where we observed 2 complete remissions in the 4 patients that we treated,” said William D. Schwieterman, MD, chief executive officer of Mateon Therapeutics, Inc., the company developing OXi4503.
About OXi4503
According to Mateon Therapeutics, OXi4503 has a dual mechanism of action that disrupts the shape of tumor bone marrow endothelial cells through reversible binding to tubulin at the colchicine binding site, downregulating intercellular adhesion molecules.
This alters the endothelial cell shape, releasing quiescent adherent tumor cells from bone marrow endothelial cells and activating the cell cycle, which makes the tumor cells vulnerable to chemotherapy.
OXi4503 also kills tumor cells directly via myeloperoxidase activation of an orthoquinone cytotoxic mediator.
In preclinical research, OXi4503 demonstrated activity against AML, both when given alone and in combination with bevacizumab. These results were published in Blood in 2010.
Clinical trials
In a phase 1 trial (NCT01085656), researchers evaluated OXi4503 in patients with relapsed or refractory AML or MDS. The goals were to determine the safety profile, maximum tolerated dose, and biologic activity of OXi4503.
The researchers said OXi4503 demonstrated preliminary evidence of disease response in heavily pre-treated, refractory AML and advanced MDS.
The maximum tolerated dose of OXi4503 was not identified, but adverse events attributable to the drug included hypertension, bone pain, fever, anemia, thrombocytopenia, and coagulopathies.
Results from this study were presented at the 2013 ASH Annual Meeting.
In 2015, Mateon Therapeutics initiated the phase 1b/2 study of OXi4503 (NCT02576301) that is now on partial clinical hold.
The phase 1 portion of this study was designed to assess the safety, pharmacokinetics, pharmacodynamics, and preliminary efficacy of single-agent OXi4503 in patients with relapsed/refractory AML and MDS.
The phase 1 portion was also intended to determine the safety, pharmacokinetics, and pharmacodynamics of OXi4503 plus intermediate-dose cytarabine.
The goal of the phase 2 portion is to assess the preliminary efficacy of OXi4503 and cytarabine in patients with AML and MDS.
The US Food and Drug Administration (FDA) has placed a partial clinical hold on a phase 1b/2 study of OXi4503, a vascular disrupting agent.
In this trial (NCT02576301), researchers are evaluating OXi4503, alone and in combination with cytarabine, in patients with relapsed/refractory acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS).
The partial clinical hold applies to the 12.2 mg/m2 dose of OXi4503.
The FDA is allowing the continued treatment and enrollment of patients using a dose of 9.76 mg/m2.
The agency said additional data on patients receiving OXi4503 at 9.76 mg/m2 must be evaluated before dosing at 12.2 mg/m2 can be resumed.
The partial clinical hold is a result of 2 potential dose-limiting toxicities (DLTs) observed at the 12.2 mg/m2 dose level.
One DLT was hypotension, which occurred shortly after initial treatment with OXi4503. The other DLT was acute hypoxic respiratory failure, which occurred approximately 2 weeks after receiving OXi4503 and cytarabine.
Both events were deemed “possibly related” to OXi4503, and both patients recovered following treatment.
The study protocol generally defines a DLT as any grade 3 serious adverse event where a relationship to OXi4503 cannot be ruled out.
“Although it is disappointing that we are not currently continuing with the higher dose of OXi4503, we look forward to gathering more safety and efficacy data at the previous dose level, where we observed 2 complete remissions in the 4 patients that we treated,” said William D. Schwieterman, MD, chief executive officer of Mateon Therapeutics, Inc., the company developing OXi4503.
About OXi4503
According to Mateon Therapeutics, OXi4503 has a dual mechanism of action that disrupts the shape of tumor bone marrow endothelial cells through reversible binding to tubulin at the colchicine binding site, downregulating intercellular adhesion molecules.
This alters the endothelial cell shape, releasing quiescent adherent tumor cells from bone marrow endothelial cells and activating the cell cycle, which makes the tumor cells vulnerable to chemotherapy.
OXi4503 also kills tumor cells directly via myeloperoxidase activation of an orthoquinone cytotoxic mediator.
In preclinical research, OXi4503 demonstrated activity against AML, both when given alone and in combination with bevacizumab. These results were published in Blood in 2010.
Clinical trials
In a phase 1 trial (NCT01085656), researchers evaluated OXi4503 in patients with relapsed or refractory AML or MDS. The goals were to determine the safety profile, maximum tolerated dose, and biologic activity of OXi4503.
The researchers said OXi4503 demonstrated preliminary evidence of disease response in heavily pre-treated, refractory AML and advanced MDS.
The maximum tolerated dose of OXi4503 was not identified, but adverse events attributable to the drug included hypertension, bone pain, fever, anemia, thrombocytopenia, and coagulopathies.
Results from this study were presented at the 2013 ASH Annual Meeting.
In 2015, Mateon Therapeutics initiated the phase 1b/2 study of OXi4503 (NCT02576301) that is now on partial clinical hold.
The phase 1 portion of this study was designed to assess the safety, pharmacokinetics, pharmacodynamics, and preliminary efficacy of single-agent OXi4503 in patients with relapsed/refractory AML and MDS.
The phase 1 portion was also intended to determine the safety, pharmacokinetics, and pharmacodynamics of OXi4503 plus intermediate-dose cytarabine.
The goal of the phase 2 portion is to assess the preliminary efficacy of OXi4503 and cytarabine in patients with AML and MDS.
The US Food and Drug Administration (FDA) has placed a partial clinical hold on a phase 1b/2 study of OXi4503, a vascular disrupting agent.
In this trial (NCT02576301), researchers are evaluating OXi4503, alone and in combination with cytarabine, in patients with relapsed/refractory acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS).
The partial clinical hold applies to the 12.2 mg/m2 dose of OXi4503.
The FDA is allowing the continued treatment and enrollment of patients using a dose of 9.76 mg/m2.
The agency said additional data on patients receiving OXi4503 at 9.76 mg/m2 must be evaluated before dosing at 12.2 mg/m2 can be resumed.
The partial clinical hold is a result of 2 potential dose-limiting toxicities (DLTs) observed at the 12.2 mg/m2 dose level.
One DLT was hypotension, which occurred shortly after initial treatment with OXi4503. The other DLT was acute hypoxic respiratory failure, which occurred approximately 2 weeks after receiving OXi4503 and cytarabine.
Both events were deemed “possibly related” to OXi4503, and both patients recovered following treatment.
The study protocol generally defines a DLT as any grade 3 serious adverse event where a relationship to OXi4503 cannot be ruled out.
“Although it is disappointing that we are not currently continuing with the higher dose of OXi4503, we look forward to gathering more safety and efficacy data at the previous dose level, where we observed 2 complete remissions in the 4 patients that we treated,” said William D. Schwieterman, MD, chief executive officer of Mateon Therapeutics, Inc., the company developing OXi4503.
About OXi4503
According to Mateon Therapeutics, OXi4503 has a dual mechanism of action that disrupts the shape of tumor bone marrow endothelial cells through reversible binding to tubulin at the colchicine binding site, downregulating intercellular adhesion molecules.
This alters the endothelial cell shape, releasing quiescent adherent tumor cells from bone marrow endothelial cells and activating the cell cycle, which makes the tumor cells vulnerable to chemotherapy.
OXi4503 also kills tumor cells directly via myeloperoxidase activation of an orthoquinone cytotoxic mediator.
In preclinical research, OXi4503 demonstrated activity against AML, both when given alone and in combination with bevacizumab. These results were published in Blood in 2010.
Clinical trials
In a phase 1 trial (NCT01085656), researchers evaluated OXi4503 in patients with relapsed or refractory AML or MDS. The goals were to determine the safety profile, maximum tolerated dose, and biologic activity of OXi4503.
The researchers said OXi4503 demonstrated preliminary evidence of disease response in heavily pre-treated, refractory AML and advanced MDS.
The maximum tolerated dose of OXi4503 was not identified, but adverse events attributable to the drug included hypertension, bone pain, fever, anemia, thrombocytopenia, and coagulopathies.
Results from this study were presented at the 2013 ASH Annual Meeting.
In 2015, Mateon Therapeutics initiated the phase 1b/2 study of OXi4503 (NCT02576301) that is now on partial clinical hold.
The phase 1 portion of this study was designed to assess the safety, pharmacokinetics, pharmacodynamics, and preliminary efficacy of single-agent OXi4503 in patients with relapsed/refractory AML and MDS.
The phase 1 portion was also intended to determine the safety, pharmacokinetics, and pharmacodynamics of OXi4503 plus intermediate-dose cytarabine.
The goal of the phase 2 portion is to assess the preliminary efficacy of OXi4503 and cytarabine in patients with AML and MDS.
Open AAA and peripheral bypass surgery patients among the highest users of post-acute care
in Medicare spending, according to the findings of a study that used data from the National Inpatient Sample (NIS) and the Veterans Affairs health system (VA) regarding surgical patients.
PAC, including skilled nursing facilities and inpatient rehabilitation, accounts for 73% of regional variation in Medicare spending, and studies on hospital variation in this area have typically focused on nonsurgical patients or been limited to Medicare data. However, a high degree of variation also appears to hold for surgical patients, according to the authors of this large database study of more than 4 million patients who had aortic aneurysm repair, peripheral vascular bypass, colorectal surgery, hepatectomy, pancreatectomy, or coronary bypass.
“We found that there is significant variation in use of PAC and rates of home discharge following complex cardiac, abdominal, and vascular surgery,” Courtney J. Balentine, MD, of the University of Alabama at Birmingham and his colleagues wrote in their report in the Journal of Surgical Research.
To explore hospital variation in post-surgery PAC, they evaluated 3,487,365 patients from the NIS (39% were aged 70 years or older, and 60% were men) and 60,666 from the VA (32% were aged 70 years or older, and 98% were men) who had surgery during 2008-2011.
Within the NIS, 631,199 patients (18%) were discharged to PAC facilities, and among the 60,666 veterans, 4744 (7.8%) were discharged to PAC facilities. In addition, hospital rates of discharge to PAC facilities varied from 1% to 36% for VA hospitals and from 1% to 59% for non-VA hospitals, according to the researchers. They found that some VA hospitals were four times more likely to discharge patients to PAC facilities than would be expected from their patients’ characteristics, while others were 90% more likely to send patients home than would be expected, according to Dr. Balentine and his colleagues.
Procedure-specific rates of discharge to PAC facilities from VA hospitals ranged from 2% following endovascular aneurysm repair to 10% after pancreatectomy and peripheral vascular bypass. Among the NIS hospitals, in contrast, rates of discharge to PAC facilities ranged from 6% following hepatectomy to as high as 44% following open aneurysm repair.
“These data could be used to characterize practices that promote more effective recovery from surgery and minimize the need for PAC,” the authors wrote. “Given that skilled nursing facilities and inpatient rehabilitation cost [$5,000]-$24,000 more than treatment at home, even minor reductions in the need for PAC facilities could result in substantial cost savings,” they stated.
“Our findings suggest that there is considerable room for improvement in the use of PAC after surgery and that we still have a long way to go in terms of using PAC to help patients recover and regain their independence,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Balentine CJ et al. J Surg Res. 2018 Oct;230:61-70.
in Medicare spending, according to the findings of a study that used data from the National Inpatient Sample (NIS) and the Veterans Affairs health system (VA) regarding surgical patients.
PAC, including skilled nursing facilities and inpatient rehabilitation, accounts for 73% of regional variation in Medicare spending, and studies on hospital variation in this area have typically focused on nonsurgical patients or been limited to Medicare data. However, a high degree of variation also appears to hold for surgical patients, according to the authors of this large database study of more than 4 million patients who had aortic aneurysm repair, peripheral vascular bypass, colorectal surgery, hepatectomy, pancreatectomy, or coronary bypass.
“We found that there is significant variation in use of PAC and rates of home discharge following complex cardiac, abdominal, and vascular surgery,” Courtney J. Balentine, MD, of the University of Alabama at Birmingham and his colleagues wrote in their report in the Journal of Surgical Research.
To explore hospital variation in post-surgery PAC, they evaluated 3,487,365 patients from the NIS (39% were aged 70 years or older, and 60% were men) and 60,666 from the VA (32% were aged 70 years or older, and 98% were men) who had surgery during 2008-2011.
Within the NIS, 631,199 patients (18%) were discharged to PAC facilities, and among the 60,666 veterans, 4744 (7.8%) were discharged to PAC facilities. In addition, hospital rates of discharge to PAC facilities varied from 1% to 36% for VA hospitals and from 1% to 59% for non-VA hospitals, according to the researchers. They found that some VA hospitals were four times more likely to discharge patients to PAC facilities than would be expected from their patients’ characteristics, while others were 90% more likely to send patients home than would be expected, according to Dr. Balentine and his colleagues.
Procedure-specific rates of discharge to PAC facilities from VA hospitals ranged from 2% following endovascular aneurysm repair to 10% after pancreatectomy and peripheral vascular bypass. Among the NIS hospitals, in contrast, rates of discharge to PAC facilities ranged from 6% following hepatectomy to as high as 44% following open aneurysm repair.
“These data could be used to characterize practices that promote more effective recovery from surgery and minimize the need for PAC,” the authors wrote. “Given that skilled nursing facilities and inpatient rehabilitation cost [$5,000]-$24,000 more than treatment at home, even minor reductions in the need for PAC facilities could result in substantial cost savings,” they stated.
“Our findings suggest that there is considerable room for improvement in the use of PAC after surgery and that we still have a long way to go in terms of using PAC to help patients recover and regain their independence,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Balentine CJ et al. J Surg Res. 2018 Oct;230:61-70.
in Medicare spending, according to the findings of a study that used data from the National Inpatient Sample (NIS) and the Veterans Affairs health system (VA) regarding surgical patients.
PAC, including skilled nursing facilities and inpatient rehabilitation, accounts for 73% of regional variation in Medicare spending, and studies on hospital variation in this area have typically focused on nonsurgical patients or been limited to Medicare data. However, a high degree of variation also appears to hold for surgical patients, according to the authors of this large database study of more than 4 million patients who had aortic aneurysm repair, peripheral vascular bypass, colorectal surgery, hepatectomy, pancreatectomy, or coronary bypass.
“We found that there is significant variation in use of PAC and rates of home discharge following complex cardiac, abdominal, and vascular surgery,” Courtney J. Balentine, MD, of the University of Alabama at Birmingham and his colleagues wrote in their report in the Journal of Surgical Research.
To explore hospital variation in post-surgery PAC, they evaluated 3,487,365 patients from the NIS (39% were aged 70 years or older, and 60% were men) and 60,666 from the VA (32% were aged 70 years or older, and 98% were men) who had surgery during 2008-2011.
Within the NIS, 631,199 patients (18%) were discharged to PAC facilities, and among the 60,666 veterans, 4744 (7.8%) were discharged to PAC facilities. In addition, hospital rates of discharge to PAC facilities varied from 1% to 36% for VA hospitals and from 1% to 59% for non-VA hospitals, according to the researchers. They found that some VA hospitals were four times more likely to discharge patients to PAC facilities than would be expected from their patients’ characteristics, while others were 90% more likely to send patients home than would be expected, according to Dr. Balentine and his colleagues.
Procedure-specific rates of discharge to PAC facilities from VA hospitals ranged from 2% following endovascular aneurysm repair to 10% after pancreatectomy and peripheral vascular bypass. Among the NIS hospitals, in contrast, rates of discharge to PAC facilities ranged from 6% following hepatectomy to as high as 44% following open aneurysm repair.
“These data could be used to characterize practices that promote more effective recovery from surgery and minimize the need for PAC,” the authors wrote. “Given that skilled nursing facilities and inpatient rehabilitation cost [$5,000]-$24,000 more than treatment at home, even minor reductions in the need for PAC facilities could result in substantial cost savings,” they stated.
“Our findings suggest that there is considerable room for improvement in the use of PAC after surgery and that we still have a long way to go in terms of using PAC to help patients recover and regain their independence,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Balentine CJ et al. J Surg Res. 2018 Oct;230:61-70.
FROM THE JOURNAL OF SURGICAL RESEARCH
Key clinical point: The wide disparity among hospitals in their rates of postsurgery discharge to post-acute care (PAC) could be an area of focus for cost containment in Medicare spending.
Major finding: Rates of discharge to PAC facilities varied from 1% to 36% for VA hospitals and from 1% to 59% for non-VA hospitals.
Study details: A database analysis of 3,487,365 National Inpatient Sample patients and 60,666 VA patients who had surgery during 2008-2011.
Disclosures: The authors reported that they had no conflicts of interest.
Source: Balentine CJ et al. J Surg Res. 2018 Oct;230:61-70.
Migraine takes toll on intimate relationships
SAN FRANCISCO – Nearly 1 in 10 chronic migraine patients say they’ve delayed having children or had fewer children because of their headaches, according to a new analysis from the CaMEO study.
“I think this is the most heartbreaking of the survey responses; we asked, ‘Have you delayed having children or had fewer children because of your headaches?’ and 2.6% of patients with episodic migraine and 9.6% with chronic migraine said yes,” Dawn C. Buse, PhD, said at the annual meeting of the American Headache Society.
CaMEO (the Chronic Migraine Epidemiology and Outcomes study) is a longitudinal, prospective, Internet-based survey whose aim is to flesh out the full impact of migraine. Dr. Buse presented an analysis of 13,064 migraineur participants, which focused on the impact of migraine on intimate relationships and parenting, an aspect of the disease burden that hasn’t been closely examined. All subjects completed the in-depth Family Burden Module, which is concerned with the emotional consequences of migraine.
The bottom line is that “migraine has significant negative impact on the most important relationships in our life: with our spouses, partners, and children,” declared Dr. Buse, a clinical psychologist at the Albert Einstein College of Medicine and director of behavioral medicine for the Montefiore Headache Center in New York.
The extent to which migraineurs perceived their headaches to be a problem increased stepwise with their number of headache days per month. For example, when the 8,127 CaMEO participants in a relationship with a live-in partner were asked to respond to the statement, “If I did not have headaches, I would be a better partner,” somewhat or complete agreement was endorsed by 38% of those with low-frequency episodic migraine at a rate of up to 4 headache days per month, 68% of those with 5-9 headache days per month, 73% of those with high-frequency episodic migraine with 10-14 headache days per month, and 78% of those with chronic migraine, defined as 15 or more headache days per month.
“Not surprising, certainly, but something to keep in mind as we care for our patients; that just because someone has episodic migraine they may have a range of expressions of how much those migraines have impacted their life,” Dr. Buse observed.
Another example: The proportion of subjects who reported delaying having children or having fewer kids because of their headaches was 1.6%, 5.5%, and 6.5% in low-, moderate-, and high-frequency episodic migraineurs, respectively, before topping out at 9.6% among those with chronic migraine.
Although she and her coinvestigators broke down the data by gender, there were no significant gender differences in the impact of migraine on significant relationships. The major differences were between patients with episodic as compared with chronic migraine.
Among the more than 3,500 CaMEO participants not currently in a relationship, 37% of those with chronic migraine and 15% of those with episodic migraine indicated that their headaches had contributed to relationship problems.
Of those in a relationship but not living together, 44% of individuals with chronic migraine reported that their headaches were preventing a closer relationship, such as moving in together or getting married, as did 16% of those with episodic migraine.
About 47%of respondents with chronic migraine reported that their headaches had caused at least one previous break-up, as did 18% of those with episodic migraine.
“Health care professionals should consider the overall burden of disease when managing migraine, particularly for those with chronic migraine,” Dr. Buse concluded. “Personalized comprehensive treatment plans may include both acute and preventive pharmacologic treatments as well as behavioral treatment for the proband, marital dyad, and family members as appropriate.”
She reported receiving research support and honoraria from Allergan, the study sponsor, as well as from Avenir, Eli Lilly, and Promius.
SOURCE: Buse DC et al. AHS 2018, Abstract OR06.
SAN FRANCISCO – Nearly 1 in 10 chronic migraine patients say they’ve delayed having children or had fewer children because of their headaches, according to a new analysis from the CaMEO study.
“I think this is the most heartbreaking of the survey responses; we asked, ‘Have you delayed having children or had fewer children because of your headaches?’ and 2.6% of patients with episodic migraine and 9.6% with chronic migraine said yes,” Dawn C. Buse, PhD, said at the annual meeting of the American Headache Society.
CaMEO (the Chronic Migraine Epidemiology and Outcomes study) is a longitudinal, prospective, Internet-based survey whose aim is to flesh out the full impact of migraine. Dr. Buse presented an analysis of 13,064 migraineur participants, which focused on the impact of migraine on intimate relationships and parenting, an aspect of the disease burden that hasn’t been closely examined. All subjects completed the in-depth Family Burden Module, which is concerned with the emotional consequences of migraine.
The bottom line is that “migraine has significant negative impact on the most important relationships in our life: with our spouses, partners, and children,” declared Dr. Buse, a clinical psychologist at the Albert Einstein College of Medicine and director of behavioral medicine for the Montefiore Headache Center in New York.
The extent to which migraineurs perceived their headaches to be a problem increased stepwise with their number of headache days per month. For example, when the 8,127 CaMEO participants in a relationship with a live-in partner were asked to respond to the statement, “If I did not have headaches, I would be a better partner,” somewhat or complete agreement was endorsed by 38% of those with low-frequency episodic migraine at a rate of up to 4 headache days per month, 68% of those with 5-9 headache days per month, 73% of those with high-frequency episodic migraine with 10-14 headache days per month, and 78% of those with chronic migraine, defined as 15 or more headache days per month.
“Not surprising, certainly, but something to keep in mind as we care for our patients; that just because someone has episodic migraine they may have a range of expressions of how much those migraines have impacted their life,” Dr. Buse observed.
Another example: The proportion of subjects who reported delaying having children or having fewer kids because of their headaches was 1.6%, 5.5%, and 6.5% in low-, moderate-, and high-frequency episodic migraineurs, respectively, before topping out at 9.6% among those with chronic migraine.
Although she and her coinvestigators broke down the data by gender, there were no significant gender differences in the impact of migraine on significant relationships. The major differences were between patients with episodic as compared with chronic migraine.
Among the more than 3,500 CaMEO participants not currently in a relationship, 37% of those with chronic migraine and 15% of those with episodic migraine indicated that their headaches had contributed to relationship problems.
Of those in a relationship but not living together, 44% of individuals with chronic migraine reported that their headaches were preventing a closer relationship, such as moving in together or getting married, as did 16% of those with episodic migraine.
About 47%of respondents with chronic migraine reported that their headaches had caused at least one previous break-up, as did 18% of those with episodic migraine.
“Health care professionals should consider the overall burden of disease when managing migraine, particularly for those with chronic migraine,” Dr. Buse concluded. “Personalized comprehensive treatment plans may include both acute and preventive pharmacologic treatments as well as behavioral treatment for the proband, marital dyad, and family members as appropriate.”
She reported receiving research support and honoraria from Allergan, the study sponsor, as well as from Avenir, Eli Lilly, and Promius.
SOURCE: Buse DC et al. AHS 2018, Abstract OR06.
SAN FRANCISCO – Nearly 1 in 10 chronic migraine patients say they’ve delayed having children or had fewer children because of their headaches, according to a new analysis from the CaMEO study.
“I think this is the most heartbreaking of the survey responses; we asked, ‘Have you delayed having children or had fewer children because of your headaches?’ and 2.6% of patients with episodic migraine and 9.6% with chronic migraine said yes,” Dawn C. Buse, PhD, said at the annual meeting of the American Headache Society.
CaMEO (the Chronic Migraine Epidemiology and Outcomes study) is a longitudinal, prospective, Internet-based survey whose aim is to flesh out the full impact of migraine. Dr. Buse presented an analysis of 13,064 migraineur participants, which focused on the impact of migraine on intimate relationships and parenting, an aspect of the disease burden that hasn’t been closely examined. All subjects completed the in-depth Family Burden Module, which is concerned with the emotional consequences of migraine.
The bottom line is that “migraine has significant negative impact on the most important relationships in our life: with our spouses, partners, and children,” declared Dr. Buse, a clinical psychologist at the Albert Einstein College of Medicine and director of behavioral medicine for the Montefiore Headache Center in New York.
The extent to which migraineurs perceived their headaches to be a problem increased stepwise with their number of headache days per month. For example, when the 8,127 CaMEO participants in a relationship with a live-in partner were asked to respond to the statement, “If I did not have headaches, I would be a better partner,” somewhat or complete agreement was endorsed by 38% of those with low-frequency episodic migraine at a rate of up to 4 headache days per month, 68% of those with 5-9 headache days per month, 73% of those with high-frequency episodic migraine with 10-14 headache days per month, and 78% of those with chronic migraine, defined as 15 or more headache days per month.
“Not surprising, certainly, but something to keep in mind as we care for our patients; that just because someone has episodic migraine they may have a range of expressions of how much those migraines have impacted their life,” Dr. Buse observed.
Another example: The proportion of subjects who reported delaying having children or having fewer kids because of their headaches was 1.6%, 5.5%, and 6.5% in low-, moderate-, and high-frequency episodic migraineurs, respectively, before topping out at 9.6% among those with chronic migraine.
Although she and her coinvestigators broke down the data by gender, there were no significant gender differences in the impact of migraine on significant relationships. The major differences were between patients with episodic as compared with chronic migraine.
Among the more than 3,500 CaMEO participants not currently in a relationship, 37% of those with chronic migraine and 15% of those with episodic migraine indicated that their headaches had contributed to relationship problems.
Of those in a relationship but not living together, 44% of individuals with chronic migraine reported that their headaches were preventing a closer relationship, such as moving in together or getting married, as did 16% of those with episodic migraine.
About 47%of respondents with chronic migraine reported that their headaches had caused at least one previous break-up, as did 18% of those with episodic migraine.
“Health care professionals should consider the overall burden of disease when managing migraine, particularly for those with chronic migraine,” Dr. Buse concluded. “Personalized comprehensive treatment plans may include both acute and preventive pharmacologic treatments as well as behavioral treatment for the proband, marital dyad, and family members as appropriate.”
She reported receiving research support and honoraria from Allergan, the study sponsor, as well as from Avenir, Eli Lilly, and Promius.
SOURCE: Buse DC et al. AHS 2018, Abstract OR06.
REPORTING FROM THE AHS ANNUAL MEETING
Key clinical point: Migraine is a major contributor to relationship problems.
Major finding: Nearly 10% of chronic migraineurs say they’ve delayed having children or had fewer of them because of their headaches.
Study details: This analysis included more than 13,000 participants in the CaMEO study, a prospective, longitudinal, Internet-based survey.
Disclosures: The presenter reported receiving research support and honoraria from Allergan, the study sponsor, as well as from Avenir, Eli Lilly, and Promius.
Source: Buse DC et al. AHS 2018, Abstract OR06.
Exploring Link Between Sleep Disorders and Migraine
Anatomic localization (the hypothalamus as a key and early mediator in the pathophysiology of migraine), common mediating signaling molecules (such as serotonin and dopamine), and the discovery of a new central nervous system waste removal system, the glymphatic system, all point to a common pathophysiology manifesting in migraine and sleep problems, according to recent research. Patients consistently report poor sleep prior to migraine attacks and during them, identifying poor sleep as a migraine trigger. However, anecdotally, sleep is reported to serve a therapeutic role in terminating headache. Researchers reviewed studies of sleep and migraine from the last 2 decades, utilizing validated subjective and objective measures of sleep and to explore potential mechanisms underlying this complex relationship by incorporating recent advances in neuroscience. They specifically focused on:
- insomnia,
- obstructive sleep apnea,
- parasomnias,
- sleep-related movement disorders, and
- rapid eye movement (REM) sleep-related disorders and their relationship to migraine.
In addition, parts of brainstem‐cortical networks involved in sleep physiology are unintentionally being identified as important factors in the common migraine pathway.
Vgontzas A, Pavlović JM. Sleep disorders and migraine: Review of literature and potential pathophysiology mechanisms. [Published online ahead of print August 8, 2018]. Headache. doi:10.1111/head.13358.
Anatomic localization (the hypothalamus as a key and early mediator in the pathophysiology of migraine), common mediating signaling molecules (such as serotonin and dopamine), and the discovery of a new central nervous system waste removal system, the glymphatic system, all point to a common pathophysiology manifesting in migraine and sleep problems, according to recent research. Patients consistently report poor sleep prior to migraine attacks and during them, identifying poor sleep as a migraine trigger. However, anecdotally, sleep is reported to serve a therapeutic role in terminating headache. Researchers reviewed studies of sleep and migraine from the last 2 decades, utilizing validated subjective and objective measures of sleep and to explore potential mechanisms underlying this complex relationship by incorporating recent advances in neuroscience. They specifically focused on:
- insomnia,
- obstructive sleep apnea,
- parasomnias,
- sleep-related movement disorders, and
- rapid eye movement (REM) sleep-related disorders and their relationship to migraine.
In addition, parts of brainstem‐cortical networks involved in sleep physiology are unintentionally being identified as important factors in the common migraine pathway.
Vgontzas A, Pavlović JM. Sleep disorders and migraine: Review of literature and potential pathophysiology mechanisms. [Published online ahead of print August 8, 2018]. Headache. doi:10.1111/head.13358.
Anatomic localization (the hypothalamus as a key and early mediator in the pathophysiology of migraine), common mediating signaling molecules (such as serotonin and dopamine), and the discovery of a new central nervous system waste removal system, the glymphatic system, all point to a common pathophysiology manifesting in migraine and sleep problems, according to recent research. Patients consistently report poor sleep prior to migraine attacks and during them, identifying poor sleep as a migraine trigger. However, anecdotally, sleep is reported to serve a therapeutic role in terminating headache. Researchers reviewed studies of sleep and migraine from the last 2 decades, utilizing validated subjective and objective measures of sleep and to explore potential mechanisms underlying this complex relationship by incorporating recent advances in neuroscience. They specifically focused on:
- insomnia,
- obstructive sleep apnea,
- parasomnias,
- sleep-related movement disorders, and
- rapid eye movement (REM) sleep-related disorders and their relationship to migraine.
In addition, parts of brainstem‐cortical networks involved in sleep physiology are unintentionally being identified as important factors in the common migraine pathway.
Vgontzas A, Pavlović JM. Sleep disorders and migraine: Review of literature and potential pathophysiology mechanisms. [Published online ahead of print August 8, 2018]. Headache. doi:10.1111/head.13358.
Sleep Disorders and Migraine: Assessment, Treatment
The presence of a sleep disorder is associated with more frequent and severe migraine and portends a poorer headache prognosis, according to recent research that focuses on clinical assessment and treatment of sleep disorders. Interestingly, the disorders linked to migraine are quite varied, including insomnia, snoring and obstructive sleep apnea, restless legs, circadian rhythm disorders, and narcolepsy. Insomnia is by far the most common sleep disorder in headache patients. New developments in treatment have produced abbreviated and cost‐effective therapies for insomnia and obstructive sleep apnea that may reach a larger population. Recommendations include:
- behavioral sleep regulation, shown in recent controlled trials to decrease migraine frequency,
- management for sleep apnea headache, and
- cognitive behavioral therapy (CBT) for insomnia abbreviated for the physician practice setting.
There is no empirical evidence that sleep evaluation should delay or supersede usual headache care. Rather, sleep management is complimentary to standard headache practice.
Rains JC. Sleep and migraine: Assessment and treatment of comorbid sleep disorders. [Published online ahead of print August 10, 2018]. Headache. doi:10.1111/head.13357.
The presence of a sleep disorder is associated with more frequent and severe migraine and portends a poorer headache prognosis, according to recent research that focuses on clinical assessment and treatment of sleep disorders. Interestingly, the disorders linked to migraine are quite varied, including insomnia, snoring and obstructive sleep apnea, restless legs, circadian rhythm disorders, and narcolepsy. Insomnia is by far the most common sleep disorder in headache patients. New developments in treatment have produced abbreviated and cost‐effective therapies for insomnia and obstructive sleep apnea that may reach a larger population. Recommendations include:
- behavioral sleep regulation, shown in recent controlled trials to decrease migraine frequency,
- management for sleep apnea headache, and
- cognitive behavioral therapy (CBT) for insomnia abbreviated for the physician practice setting.
There is no empirical evidence that sleep evaluation should delay or supersede usual headache care. Rather, sleep management is complimentary to standard headache practice.
Rains JC. Sleep and migraine: Assessment and treatment of comorbid sleep disorders. [Published online ahead of print August 10, 2018]. Headache. doi:10.1111/head.13357.
The presence of a sleep disorder is associated with more frequent and severe migraine and portends a poorer headache prognosis, according to recent research that focuses on clinical assessment and treatment of sleep disorders. Interestingly, the disorders linked to migraine are quite varied, including insomnia, snoring and obstructive sleep apnea, restless legs, circadian rhythm disorders, and narcolepsy. Insomnia is by far the most common sleep disorder in headache patients. New developments in treatment have produced abbreviated and cost‐effective therapies for insomnia and obstructive sleep apnea that may reach a larger population. Recommendations include:
- behavioral sleep regulation, shown in recent controlled trials to decrease migraine frequency,
- management for sleep apnea headache, and
- cognitive behavioral therapy (CBT) for insomnia abbreviated for the physician practice setting.
There is no empirical evidence that sleep evaluation should delay or supersede usual headache care. Rather, sleep management is complimentary to standard headache practice.
Rains JC. Sleep and migraine: Assessment and treatment of comorbid sleep disorders. [Published online ahead of print August 10, 2018]. Headache. doi:10.1111/head.13357.
Promoting confrontation
The optimist says the glass is half-full. The pessimist says it is half-empty. An engineer says the glass is twice as large as needed to contain the specified amount of fluid. To some people, that mindset makes engineers negative people. We focus on weaknesses and inefficiencies. A chain is only as strong as its weakest link. There is no partial credit when building a bridge. 98% right is still wrong.
When I worked as an engineer, critiquing ideas was a daily activity. I am used to conflicting opinions. Industry trains people to be professional and act appropriately when disagreeing with a colleague. Tact is the art of making a point without making an enemy. Engineering has a strong culture of focusing on a problem rather than on personalities. Upper management made it clear that in any turf war, both sides will lose. Academia has a different culture. Turf wars in academia are so bitter because the stakes are so small.
Pediatrics has less confrontation and competitiveness than do other subspecialties. That makes the work environment more pleasant, as long as every other group in the hospital isn’t walking all over you. Pediatricians often view themselves as dedicated to doing what is right for the children, even to the point of martyrdom. Some early pediatric hospitalist programs got into economic trouble because they adopted tasks that benefited the children but that weren’t being performed by other physicians precisely because those tasks were neither valued nor compensated. Learning to say “No” is hard but necessary.
As a clinical ethics consultant, I was consulted when conflict had developed between providers and patients/parents or between different specialties. Ethics consults are rarely about what philosophers would call ethics. They are mostly about miscommunication, empowering voices to be heard and clarifying values. Practical skills in de-escalation and mediation are more important than either law or philosophy degrees.
There are downsides to avoiding confrontation. Truth suffers. Integrity is lost. Goals become corrupted. I will give two examples. One ED had a five-level triage system. Level 1 was reserved for life-threatening situations such as gunshot wounds and resuscitations. So I was surprised to see a “bili” baby triaged at Level 1. He was a good baby with normal vitals. Admission for phototherapy was reasonable, but the urgency of a bilirubin of 19 did not match that of a gunshot wound. A colleague warned me not to even consider challenging the practice. A powerful physician at that institution had made it policy years earlier.
I witnessed a similar dynamic many times at that institution. Residents are even better than 4-year-olds at noticing hypocritical behavior. Once they perceive that the dynamic is political power and not science, they adapt quickly. A couple days later, I asked a resident if he really thought an IV was necessary for a toddler we were admitting. He replied no, but if he hadn’t put an IV in, the hospital wouldn’t get paid for the admission. To him, that was the unspoken policy. The action didn’t even cause him moral distress. I worry about that much cynicism so early in a career. Cognitive dissonance starts small and slowly creeps its way into everything.
The art of managing conflict is particularly important in pediatric hospital medicine because of its heavy investment in reducing overdiagnosis and overtreatment. Many pediatric hospitalists are located at academic institutions and more subject to its turf wars than outpatient colleagues practicing in small groups. The recent conference for pediatric hospital medicine was held in Atlanta, a few blocks from the Center for Civil and Human Rights. That museum evokes powerful images of struggles around the world. My two takeaway lessons: Silence is a form of collaboration. Tyrannical suppression of dissent magnifies suffering.
In poorly managed academic institutions, it can be harmful to one’s career to ask questions, challenge assumptions, and seek truth. A recent report found that the Department of Veterans Affairs health system also has a culture that punishes whistle-blowers. Nationally, politics has become polarized. Splitting, once considered a dysfunctional behavior, has become normalized. So I understand the reluctance to speak up. One must choose one’s battles.
Given the personal and career risks, why confront inaccurate research, wasteful practices, and unjust policies? I believe that there is a balance and a choice each person must make. Canadian engineers wear an iron ring to remind themselves of their professional responsibilities. Doctors wear white coats. Personally, I share a memory with other engineers of my generation. In January 1986, NASA engineers could not convince their managers about a risk. The space shuttle Challenger exploded. I heard about it in the medical school’s cafeteria. So for me, disputation is part of the vocation.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
The optimist says the glass is half-full. The pessimist says it is half-empty. An engineer says the glass is twice as large as needed to contain the specified amount of fluid. To some people, that mindset makes engineers negative people. We focus on weaknesses and inefficiencies. A chain is only as strong as its weakest link. There is no partial credit when building a bridge. 98% right is still wrong.
When I worked as an engineer, critiquing ideas was a daily activity. I am used to conflicting opinions. Industry trains people to be professional and act appropriately when disagreeing with a colleague. Tact is the art of making a point without making an enemy. Engineering has a strong culture of focusing on a problem rather than on personalities. Upper management made it clear that in any turf war, both sides will lose. Academia has a different culture. Turf wars in academia are so bitter because the stakes are so small.
Pediatrics has less confrontation and competitiveness than do other subspecialties. That makes the work environment more pleasant, as long as every other group in the hospital isn’t walking all over you. Pediatricians often view themselves as dedicated to doing what is right for the children, even to the point of martyrdom. Some early pediatric hospitalist programs got into economic trouble because they adopted tasks that benefited the children but that weren’t being performed by other physicians precisely because those tasks were neither valued nor compensated. Learning to say “No” is hard but necessary.
As a clinical ethics consultant, I was consulted when conflict had developed between providers and patients/parents or between different specialties. Ethics consults are rarely about what philosophers would call ethics. They are mostly about miscommunication, empowering voices to be heard and clarifying values. Practical skills in de-escalation and mediation are more important than either law or philosophy degrees.
There are downsides to avoiding confrontation. Truth suffers. Integrity is lost. Goals become corrupted. I will give two examples. One ED had a five-level triage system. Level 1 was reserved for life-threatening situations such as gunshot wounds and resuscitations. So I was surprised to see a “bili” baby triaged at Level 1. He was a good baby with normal vitals. Admission for phototherapy was reasonable, but the urgency of a bilirubin of 19 did not match that of a gunshot wound. A colleague warned me not to even consider challenging the practice. A powerful physician at that institution had made it policy years earlier.
I witnessed a similar dynamic many times at that institution. Residents are even better than 4-year-olds at noticing hypocritical behavior. Once they perceive that the dynamic is political power and not science, they adapt quickly. A couple days later, I asked a resident if he really thought an IV was necessary for a toddler we were admitting. He replied no, but if he hadn’t put an IV in, the hospital wouldn’t get paid for the admission. To him, that was the unspoken policy. The action didn’t even cause him moral distress. I worry about that much cynicism so early in a career. Cognitive dissonance starts small and slowly creeps its way into everything.
The art of managing conflict is particularly important in pediatric hospital medicine because of its heavy investment in reducing overdiagnosis and overtreatment. Many pediatric hospitalists are located at academic institutions and more subject to its turf wars than outpatient colleagues practicing in small groups. The recent conference for pediatric hospital medicine was held in Atlanta, a few blocks from the Center for Civil and Human Rights. That museum evokes powerful images of struggles around the world. My two takeaway lessons: Silence is a form of collaboration. Tyrannical suppression of dissent magnifies suffering.
In poorly managed academic institutions, it can be harmful to one’s career to ask questions, challenge assumptions, and seek truth. A recent report found that the Department of Veterans Affairs health system also has a culture that punishes whistle-blowers. Nationally, politics has become polarized. Splitting, once considered a dysfunctional behavior, has become normalized. So I understand the reluctance to speak up. One must choose one’s battles.
Given the personal and career risks, why confront inaccurate research, wasteful practices, and unjust policies? I believe that there is a balance and a choice each person must make. Canadian engineers wear an iron ring to remind themselves of their professional responsibilities. Doctors wear white coats. Personally, I share a memory with other engineers of my generation. In January 1986, NASA engineers could not convince their managers about a risk. The space shuttle Challenger exploded. I heard about it in the medical school’s cafeteria. So for me, disputation is part of the vocation.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
The optimist says the glass is half-full. The pessimist says it is half-empty. An engineer says the glass is twice as large as needed to contain the specified amount of fluid. To some people, that mindset makes engineers negative people. We focus on weaknesses and inefficiencies. A chain is only as strong as its weakest link. There is no partial credit when building a bridge. 98% right is still wrong.
When I worked as an engineer, critiquing ideas was a daily activity. I am used to conflicting opinions. Industry trains people to be professional and act appropriately when disagreeing with a colleague. Tact is the art of making a point without making an enemy. Engineering has a strong culture of focusing on a problem rather than on personalities. Upper management made it clear that in any turf war, both sides will lose. Academia has a different culture. Turf wars in academia are so bitter because the stakes are so small.
Pediatrics has less confrontation and competitiveness than do other subspecialties. That makes the work environment more pleasant, as long as every other group in the hospital isn’t walking all over you. Pediatricians often view themselves as dedicated to doing what is right for the children, even to the point of martyrdom. Some early pediatric hospitalist programs got into economic trouble because they adopted tasks that benefited the children but that weren’t being performed by other physicians precisely because those tasks were neither valued nor compensated. Learning to say “No” is hard but necessary.
As a clinical ethics consultant, I was consulted when conflict had developed between providers and patients/parents or between different specialties. Ethics consults are rarely about what philosophers would call ethics. They are mostly about miscommunication, empowering voices to be heard and clarifying values. Practical skills in de-escalation and mediation are more important than either law or philosophy degrees.
There are downsides to avoiding confrontation. Truth suffers. Integrity is lost. Goals become corrupted. I will give two examples. One ED had a five-level triage system. Level 1 was reserved for life-threatening situations such as gunshot wounds and resuscitations. So I was surprised to see a “bili” baby triaged at Level 1. He was a good baby with normal vitals. Admission for phototherapy was reasonable, but the urgency of a bilirubin of 19 did not match that of a gunshot wound. A colleague warned me not to even consider challenging the practice. A powerful physician at that institution had made it policy years earlier.
I witnessed a similar dynamic many times at that institution. Residents are even better than 4-year-olds at noticing hypocritical behavior. Once they perceive that the dynamic is political power and not science, they adapt quickly. A couple days later, I asked a resident if he really thought an IV was necessary for a toddler we were admitting. He replied no, but if he hadn’t put an IV in, the hospital wouldn’t get paid for the admission. To him, that was the unspoken policy. The action didn’t even cause him moral distress. I worry about that much cynicism so early in a career. Cognitive dissonance starts small and slowly creeps its way into everything.
The art of managing conflict is particularly important in pediatric hospital medicine because of its heavy investment in reducing overdiagnosis and overtreatment. Many pediatric hospitalists are located at academic institutions and more subject to its turf wars than outpatient colleagues practicing in small groups. The recent conference for pediatric hospital medicine was held in Atlanta, a few blocks from the Center for Civil and Human Rights. That museum evokes powerful images of struggles around the world. My two takeaway lessons: Silence is a form of collaboration. Tyrannical suppression of dissent magnifies suffering.
In poorly managed academic institutions, it can be harmful to one’s career to ask questions, challenge assumptions, and seek truth. A recent report found that the Department of Veterans Affairs health system also has a culture that punishes whistle-blowers. Nationally, politics has become polarized. Splitting, once considered a dysfunctional behavior, has become normalized. So I understand the reluctance to speak up. One must choose one’s battles.
Given the personal and career risks, why confront inaccurate research, wasteful practices, and unjust policies? I believe that there is a balance and a choice each person must make. Canadian engineers wear an iron ring to remind themselves of their professional responsibilities. Doctors wear white coats. Personally, I share a memory with other engineers of my generation. In January 1986, NASA engineers could not convince their managers about a risk. The space shuttle Challenger exploded. I heard about it in the medical school’s cafeteria. So for me, disputation is part of the vocation.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
A beautiful diagnosis
Defensive medicine exists. The question is how often it happens and how large a role it plays in making medical care in the United States so costly. When Dr. Tom Price was a congressman, he was quoted as saying that defensive medicine is responsible for more than 25% of every dollar this country spends on health care. (“A Fear of Lawsuits Really Does Seem to Result in Extra Medical Tests” Margot Sanger-Katz, New York Times, July 23, 2018). Neither I nor anyone else had any data to support or refute Dr. Price’s claim in 2010, but based on 50 years of practicing and observing medicine, I don’t find his claim completely unreasonable.
Defensive medicine has been going on for so many generations of physicians that most doctors practicing today don’t realize they are doing it. A physician may order a full battery of chemistries on a patient presenting with mild anemia when only a CBC is necessary because that’s the way he was trained.
However, the evidence to support my suspicion that defensive medicine is a significant financial drain on our economy has been difficult to tease out of the tangled web of confounders that is woven into our patchwork health care system. A recent study by two economists provides a glimpse into the role of defensive medicine in the cost of health care (“Defensive Medicine: Evidence from Military Immunity” Michael D. Frakes and Jonathan Gruber, National Bureau of Economic Research, July 2018). Using the unusual combination of circumstances in which military personnel and their dependents can or cannot sue depending on where they are receiving care, the investigators found that “liability immunity reduces inpatient spending by 5% with no measurable negative effect on patient outcomes.” While that may not be as high as Dr. Price or I think it may be, 5% of three trillion dollars is serious money.
The bigger problem is that defensive medicine is ugly, artless, and intellectually unsatisfying. While the patient may not view your diagnosis of his chronic debilitating or terminal illness as a work of art, there are such things as beautiful diagnoses. One may be beautiful in its simplicity and its ability to unify a variety of previously unexplained symptoms. Another diagnosis may be the intellectually stimulating result of a carefully thought out branching decision tree to solve a puzzling array of complaints using a minimum of costly studies.
Defensive medicine decisions are made primarily to avoid mistakes and omissions. Physicians often behave as though we believe our errors will always be fatal. That may be somewhat true for surgeons, but for the rest of us errors can be an important part of learning. The unfortunate outcome of an error, particularly one of omission, can usually be avoided by following the patient closely, remaining available ... and continuing to exude an aura of caring.
With close and thoughtful follow-up, you are going to discover pretty quickly when you have missed the target. Patients understand that we aren’t going to get the correct diagnosis or prescribe the best treatment on the first try every time. What patients don’t understand and what may prompt them to sue is feeling that they are being ignored.
While practicing defensive medicine isn’t usually listed as one of the cardinal symptoms of physician burnout, it probably deserves more attention. With some introspection and a bit of courage, How many of your decisions are being made to avoid an error? Wouldn’t it be more fun to be making beautiful diagnoses you can be proud of?
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Is My Child Overtired?: The Sleep Solution for Raising Happier, Healthier Children.” Email him at [email protected].
Defensive medicine exists. The question is how often it happens and how large a role it plays in making medical care in the United States so costly. When Dr. Tom Price was a congressman, he was quoted as saying that defensive medicine is responsible for more than 25% of every dollar this country spends on health care. (“A Fear of Lawsuits Really Does Seem to Result in Extra Medical Tests” Margot Sanger-Katz, New York Times, July 23, 2018). Neither I nor anyone else had any data to support or refute Dr. Price’s claim in 2010, but based on 50 years of practicing and observing medicine, I don’t find his claim completely unreasonable.
Defensive medicine has been going on for so many generations of physicians that most doctors practicing today don’t realize they are doing it. A physician may order a full battery of chemistries on a patient presenting with mild anemia when only a CBC is necessary because that’s the way he was trained.
However, the evidence to support my suspicion that defensive medicine is a significant financial drain on our economy has been difficult to tease out of the tangled web of confounders that is woven into our patchwork health care system. A recent study by two economists provides a glimpse into the role of defensive medicine in the cost of health care (“Defensive Medicine: Evidence from Military Immunity” Michael D. Frakes and Jonathan Gruber, National Bureau of Economic Research, July 2018). Using the unusual combination of circumstances in which military personnel and their dependents can or cannot sue depending on where they are receiving care, the investigators found that “liability immunity reduces inpatient spending by 5% with no measurable negative effect on patient outcomes.” While that may not be as high as Dr. Price or I think it may be, 5% of three trillion dollars is serious money.
The bigger problem is that defensive medicine is ugly, artless, and intellectually unsatisfying. While the patient may not view your diagnosis of his chronic debilitating or terminal illness as a work of art, there are such things as beautiful diagnoses. One may be beautiful in its simplicity and its ability to unify a variety of previously unexplained symptoms. Another diagnosis may be the intellectually stimulating result of a carefully thought out branching decision tree to solve a puzzling array of complaints using a minimum of costly studies.
Defensive medicine decisions are made primarily to avoid mistakes and omissions. Physicians often behave as though we believe our errors will always be fatal. That may be somewhat true for surgeons, but for the rest of us errors can be an important part of learning. The unfortunate outcome of an error, particularly one of omission, can usually be avoided by following the patient closely, remaining available ... and continuing to exude an aura of caring.
With close and thoughtful follow-up, you are going to discover pretty quickly when you have missed the target. Patients understand that we aren’t going to get the correct diagnosis or prescribe the best treatment on the first try every time. What patients don’t understand and what may prompt them to sue is feeling that they are being ignored.
While practicing defensive medicine isn’t usually listed as one of the cardinal symptoms of physician burnout, it probably deserves more attention. With some introspection and a bit of courage, How many of your decisions are being made to avoid an error? Wouldn’t it be more fun to be making beautiful diagnoses you can be proud of?
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Is My Child Overtired?: The Sleep Solution for Raising Happier, Healthier Children.” Email him at [email protected].
Defensive medicine exists. The question is how often it happens and how large a role it plays in making medical care in the United States so costly. When Dr. Tom Price was a congressman, he was quoted as saying that defensive medicine is responsible for more than 25% of every dollar this country spends on health care. (“A Fear of Lawsuits Really Does Seem to Result in Extra Medical Tests” Margot Sanger-Katz, New York Times, July 23, 2018). Neither I nor anyone else had any data to support or refute Dr. Price’s claim in 2010, but based on 50 years of practicing and observing medicine, I don’t find his claim completely unreasonable.
Defensive medicine has been going on for so many generations of physicians that most doctors practicing today don’t realize they are doing it. A physician may order a full battery of chemistries on a patient presenting with mild anemia when only a CBC is necessary because that’s the way he was trained.
However, the evidence to support my suspicion that defensive medicine is a significant financial drain on our economy has been difficult to tease out of the tangled web of confounders that is woven into our patchwork health care system. A recent study by two economists provides a glimpse into the role of defensive medicine in the cost of health care (“Defensive Medicine: Evidence from Military Immunity” Michael D. Frakes and Jonathan Gruber, National Bureau of Economic Research, July 2018). Using the unusual combination of circumstances in which military personnel and their dependents can or cannot sue depending on where they are receiving care, the investigators found that “liability immunity reduces inpatient spending by 5% with no measurable negative effect on patient outcomes.” While that may not be as high as Dr. Price or I think it may be, 5% of three trillion dollars is serious money.
The bigger problem is that defensive medicine is ugly, artless, and intellectually unsatisfying. While the patient may not view your diagnosis of his chronic debilitating or terminal illness as a work of art, there are such things as beautiful diagnoses. One may be beautiful in its simplicity and its ability to unify a variety of previously unexplained symptoms. Another diagnosis may be the intellectually stimulating result of a carefully thought out branching decision tree to solve a puzzling array of complaints using a minimum of costly studies.
Defensive medicine decisions are made primarily to avoid mistakes and omissions. Physicians often behave as though we believe our errors will always be fatal. That may be somewhat true for surgeons, but for the rest of us errors can be an important part of learning. The unfortunate outcome of an error, particularly one of omission, can usually be avoided by following the patient closely, remaining available ... and continuing to exude an aura of caring.
With close and thoughtful follow-up, you are going to discover pretty quickly when you have missed the target. Patients understand that we aren’t going to get the correct diagnosis or prescribe the best treatment on the first try every time. What patients don’t understand and what may prompt them to sue is feeling that they are being ignored.
While practicing defensive medicine isn’t usually listed as one of the cardinal symptoms of physician burnout, it probably deserves more attention. With some introspection and a bit of courage, How many of your decisions are being made to avoid an error? Wouldn’t it be more fun to be making beautiful diagnoses you can be proud of?
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Is My Child Overtired?: The Sleep Solution for Raising Happier, Healthier Children.” Email him at [email protected].