User login
Ultrasound aids treat-to-target approach for gout
AMSTERDAM – Results from the longitudinal NOR-GOUT study show that ultrasound can help visualize decreasing levels of uric acid deposits that occur during a treat-to-target approach with urate-lowering therapy.
“Gout is a really painful disease when there are flares,” said Dr. Hammer, a senior consultant in the rheumatology department at Diakonhjemmet Hospital in Oslo. Ultrasound has been shown to be a sensitive method to detect uric monosodium urate (MSU) deposition and its use is included in the classification criteria for gout.
“MSU depositions are found in many different regions with some predilection sites,” Dr. Hammer noted. This led the OMERACT (Outcome Measures in Rheumatology) Ultrasound Group to develop three key definitions for MSU lesions: the “double contour sign” (DC), which occurs when urate crystals form on the surface of cartilage; tophus, which is where there is a larger, hypoechoic aggregation of crystals that are usually well delineated; and “aggregates,” which are small, hyperechoic deposits.
“There are, up until now, only a few smaller studies that have explored the decrease of depositions during uric acid–lowering treatment,” Dr. Hammer observed.
NOR-GOUT was a prospective, observational study of 161 consecutively-recruited patients with urate crystal–proven gout who needed treatment with urate-lowering therapy. Patients were included if they had a recent gout flare and had serum urate levels of more than 360 micromol/L (6.0 mg/dL) and had no contraindication to urate-lowering therapy.
“We used a treat-to-target approach with the medication,” Dr. Hammer explained. The aim was to get uric acid levels to 360 micromol/L or lower, or to less than 300 micromol/L (5.0 mg/dL) if clinical tophi were present. “The medication was optimized by monthly follow-up by a study nurse until the treatment target was met,” she added.
Patients underwent an extensive ultrasound assessment at study entry and again after 3, 6, and 12 months of urate-lowering therapy. This included bilateral assessment of all relevant joints and the presence of crystals semiquantitatively scored from 0 to 3, the latter signifying many deposits. The sum of scores for the three key OMERACT definitions were calculated each time the patients were assessed, with a total score for all three also calculated.
Mean serum urate levels dropped from a baseline of 487 to 312 micromol/L (from 8.2 to 5.3 mg/dL) at 12 months (P less than .001), Dr. Hammer reported. The percentage of patients achieving a urate target of less than 360 micromol/L increased from 71% at 3 months to 81% at 6 months and to 84% at 12 months, she said.
Ultrasound scores decreased with decreasing urate levels at 3, 6, and 12 months, with the highest numeric difference from baseline seen at 12 months for DC (3.1, 2.3, and 1.2; all P less than .001 vs. baseline of 4.2). The respective values for tophi were 6.3, 5.4, and 4.2 versus a baseline of 6.5; for aggregates, the values were 8.8, 7.9, and 6.7 versus a baseline of 9.1.
Standardized Response Mean values from baseline to 3, 6, and 12 months showed that DC was the most sensitive for change, with a respective 0.73, 1.02, and 1.26 in ultrasound scores. Values for tophi were 0.06, 0.57, and 0.91, and 0.20, 0.51 and 0.66 for aggregates.
“Not all patients had reached 12 months of follow-up when we made these calculations,” Dr. Hammer said, noting the limitations of the study. Nevertheless, these interim findings suggest that ultrasound is a valuable tool that can help see how patients fare on a treat-to-target approach, she concluded.
Dr. Hammer had no conflicts of interest to disclose.
SOURCE: Hammer HB et al. Ann Rheum Dis. 2018;77(Suppl 2):154-5. Abstract OP0211.
AMSTERDAM – Results from the longitudinal NOR-GOUT study show that ultrasound can help visualize decreasing levels of uric acid deposits that occur during a treat-to-target approach with urate-lowering therapy.
“Gout is a really painful disease when there are flares,” said Dr. Hammer, a senior consultant in the rheumatology department at Diakonhjemmet Hospital in Oslo. Ultrasound has been shown to be a sensitive method to detect uric monosodium urate (MSU) deposition and its use is included in the classification criteria for gout.
“MSU depositions are found in many different regions with some predilection sites,” Dr. Hammer noted. This led the OMERACT (Outcome Measures in Rheumatology) Ultrasound Group to develop three key definitions for MSU lesions: the “double contour sign” (DC), which occurs when urate crystals form on the surface of cartilage; tophus, which is where there is a larger, hypoechoic aggregation of crystals that are usually well delineated; and “aggregates,” which are small, hyperechoic deposits.
“There are, up until now, only a few smaller studies that have explored the decrease of depositions during uric acid–lowering treatment,” Dr. Hammer observed.
NOR-GOUT was a prospective, observational study of 161 consecutively-recruited patients with urate crystal–proven gout who needed treatment with urate-lowering therapy. Patients were included if they had a recent gout flare and had serum urate levels of more than 360 micromol/L (6.0 mg/dL) and had no contraindication to urate-lowering therapy.
“We used a treat-to-target approach with the medication,” Dr. Hammer explained. The aim was to get uric acid levels to 360 micromol/L or lower, or to less than 300 micromol/L (5.0 mg/dL) if clinical tophi were present. “The medication was optimized by monthly follow-up by a study nurse until the treatment target was met,” she added.
Patients underwent an extensive ultrasound assessment at study entry and again after 3, 6, and 12 months of urate-lowering therapy. This included bilateral assessment of all relevant joints and the presence of crystals semiquantitatively scored from 0 to 3, the latter signifying many deposits. The sum of scores for the three key OMERACT definitions were calculated each time the patients were assessed, with a total score for all three also calculated.
Mean serum urate levels dropped from a baseline of 487 to 312 micromol/L (from 8.2 to 5.3 mg/dL) at 12 months (P less than .001), Dr. Hammer reported. The percentage of patients achieving a urate target of less than 360 micromol/L increased from 71% at 3 months to 81% at 6 months and to 84% at 12 months, she said.
Ultrasound scores decreased with decreasing urate levels at 3, 6, and 12 months, with the highest numeric difference from baseline seen at 12 months for DC (3.1, 2.3, and 1.2; all P less than .001 vs. baseline of 4.2). The respective values for tophi were 6.3, 5.4, and 4.2 versus a baseline of 6.5; for aggregates, the values were 8.8, 7.9, and 6.7 versus a baseline of 9.1.
Standardized Response Mean values from baseline to 3, 6, and 12 months showed that DC was the most sensitive for change, with a respective 0.73, 1.02, and 1.26 in ultrasound scores. Values for tophi were 0.06, 0.57, and 0.91, and 0.20, 0.51 and 0.66 for aggregates.
“Not all patients had reached 12 months of follow-up when we made these calculations,” Dr. Hammer said, noting the limitations of the study. Nevertheless, these interim findings suggest that ultrasound is a valuable tool that can help see how patients fare on a treat-to-target approach, she concluded.
Dr. Hammer had no conflicts of interest to disclose.
SOURCE: Hammer HB et al. Ann Rheum Dis. 2018;77(Suppl 2):154-5. Abstract OP0211.
AMSTERDAM – Results from the longitudinal NOR-GOUT study show that ultrasound can help visualize decreasing levels of uric acid deposits that occur during a treat-to-target approach with urate-lowering therapy.
“Gout is a really painful disease when there are flares,” said Dr. Hammer, a senior consultant in the rheumatology department at Diakonhjemmet Hospital in Oslo. Ultrasound has been shown to be a sensitive method to detect uric monosodium urate (MSU) deposition and its use is included in the classification criteria for gout.
“MSU depositions are found in many different regions with some predilection sites,” Dr. Hammer noted. This led the OMERACT (Outcome Measures in Rheumatology) Ultrasound Group to develop three key definitions for MSU lesions: the “double contour sign” (DC), which occurs when urate crystals form on the surface of cartilage; tophus, which is where there is a larger, hypoechoic aggregation of crystals that are usually well delineated; and “aggregates,” which are small, hyperechoic deposits.
“There are, up until now, only a few smaller studies that have explored the decrease of depositions during uric acid–lowering treatment,” Dr. Hammer observed.
NOR-GOUT was a prospective, observational study of 161 consecutively-recruited patients with urate crystal–proven gout who needed treatment with urate-lowering therapy. Patients were included if they had a recent gout flare and had serum urate levels of more than 360 micromol/L (6.0 mg/dL) and had no contraindication to urate-lowering therapy.
“We used a treat-to-target approach with the medication,” Dr. Hammer explained. The aim was to get uric acid levels to 360 micromol/L or lower, or to less than 300 micromol/L (5.0 mg/dL) if clinical tophi were present. “The medication was optimized by monthly follow-up by a study nurse until the treatment target was met,” she added.
Patients underwent an extensive ultrasound assessment at study entry and again after 3, 6, and 12 months of urate-lowering therapy. This included bilateral assessment of all relevant joints and the presence of crystals semiquantitatively scored from 0 to 3, the latter signifying many deposits. The sum of scores for the three key OMERACT definitions were calculated each time the patients were assessed, with a total score for all three also calculated.
Mean serum urate levels dropped from a baseline of 487 to 312 micromol/L (from 8.2 to 5.3 mg/dL) at 12 months (P less than .001), Dr. Hammer reported. The percentage of patients achieving a urate target of less than 360 micromol/L increased from 71% at 3 months to 81% at 6 months and to 84% at 12 months, she said.
Ultrasound scores decreased with decreasing urate levels at 3, 6, and 12 months, with the highest numeric difference from baseline seen at 12 months for DC (3.1, 2.3, and 1.2; all P less than .001 vs. baseline of 4.2). The respective values for tophi were 6.3, 5.4, and 4.2 versus a baseline of 6.5; for aggregates, the values were 8.8, 7.9, and 6.7 versus a baseline of 9.1.
Standardized Response Mean values from baseline to 3, 6, and 12 months showed that DC was the most sensitive for change, with a respective 0.73, 1.02, and 1.26 in ultrasound scores. Values for tophi were 0.06, 0.57, and 0.91, and 0.20, 0.51 and 0.66 for aggregates.
“Not all patients had reached 12 months of follow-up when we made these calculations,” Dr. Hammer said, noting the limitations of the study. Nevertheless, these interim findings suggest that ultrasound is a valuable tool that can help see how patients fare on a treat-to-target approach, she concluded.
Dr. Hammer had no conflicts of interest to disclose.
SOURCE: Hammer HB et al. Ann Rheum Dis. 2018;77(Suppl 2):154-5. Abstract OP0211.
REPORTING FROM THE EULAR 2018 CONGRESS
Key clinical point: Deceasing uric acid load during a treat-to-target approach can be seen on ultrasound.
Major finding: Ultrasound scores decreased with decreasing urate levels at 3, 6 and 12 month, with the highest numeric difference from baseline seen at 12 months for double contour sign (3.1, 2.3, and 1.2; all P less than .001 vs. baseline of 4.2).
Study details: A prospective, observational study of 161 patients with urate crystal–proven gout treated with urate-lowering therapy.
Disclosures: Dr. Hammer had no conflicts of interest to disclose.
Sources: Hammer HB et al. Ann Rheum Dis. 2018;77(Suppl 2):154-5. Abstract OP0211.
Hydroxyurea well tolerated in longitudinal European study
WASHINGTON – European patients with sickle cell disease (SCD) are tolerating hydroxyurea treatment well, 9 years into a 10-year prospective cohort study.
ESCORT-HU (European Sickle Cell Disease Cohort – Hydroxyurea) is slated to enroll 2,000 children and adults over the study period to assess the long-term safety and efficacy of hydroxyurea (HU) as a treatment for SCD.
“Hydroxyurea is still underused in sickle cell disease” both in Europe and the United States, said Bernard Dauvergne, PharmD, executive director of Addmedica, which markets hydroxyurea as Siklos. In part, fears about toxicity and side effects contribute to this underuse, Dr. Dauvergne said at a top abstracts session of the annual meeting of the Foundation for Sickle Cell Disease Research.
ESCORT-HU was designed as a purely observational, noninterventional study of patients treated with HU. It was initiated as part of the European Medicines Agency risk management plan, conceived at the time of the drug’s approval for SCD, explained Dr. Dauvergne.
“This prospective cohort study could enable the identification of delayed rare adverse events in real life, occurring in between 1 in 10,000 and 1 in 1,000 patients,” Dr. Dauvergne said. However, “no new safety information has been detected ... and no secondary cancer has been reported.”
At the last data analysis cutpoint of June 2017, 1,921 patients had been enrolled. Patients have come from 63 centers in France, Germany, Greece, and Italy, Dr. Dauvergne reported.
Of the 1,829 patients with data available for analysis, 804 were under the age of 18. The pediatric patients were a mean 9 years of age, and the adult patients were a mean 33 years old at enrollment. Most enrollees (84%) have the HbSS genotype.
At baseline, the pediatric patients were dosed at a mean 17.2 mg/kg per day of HU; for adult patients, the figure was 15.54 mg/kg per day. More than one-third (35.4%) of pediatric patients had been on HU at the time of study enrollment, for a mean of 4.5 years. In contrast, more than half (60.4%) of adults had been taking hydroxyurea for a mean of 6.25 years at enrollment.
The 1,002 adult patients with recently reported safety data were on a mean HU dose of 20.2 mg/kg per day. About 40% of adults reported at least one adverse event (AE), and a total of 334 AEs in 16.3% of adult patients were judged to be related to HU.
Skin and subcutaneous tissue reactions occurred in about 1 in 10 patients, with 153 reported incidences of skin dryness, skin reactions, alopecia, or changes in skin pigmentation. The next most common adverse events were blood and lymphatic system disorders, mostly neutropenia or thrombocytopenia, occurring in 9.6% of patients.
Discontinuation rates have been low, with an overall dropout rate of 3.8%.
The ESCORT-HU data “confirm that HU is an efficient and well-tolerated drug in both children and adults,” Dr. Dauvergne said. Over the short term, adverse events are related to the expected dose dependent myelosuppression that’s key to the drug’s mechanism of action. This makes sense given the narrow therapeutic index, with a tight range between an efficacious dose and a cytotoxic one, he said. “And the lower the [patient] weight is, the more sensitive the dose variations become,” Dr. Dauvergne said.
Being flexible about fine-tuning doses is key to finding the balance between tolerability and efficacy, “and consequently, for compliance,” he said.
Data collection for the study will end in 2018, with safety and efficacy data expected in 2019.
WASHINGTON – European patients with sickle cell disease (SCD) are tolerating hydroxyurea treatment well, 9 years into a 10-year prospective cohort study.
ESCORT-HU (European Sickle Cell Disease Cohort – Hydroxyurea) is slated to enroll 2,000 children and adults over the study period to assess the long-term safety and efficacy of hydroxyurea (HU) as a treatment for SCD.
“Hydroxyurea is still underused in sickle cell disease” both in Europe and the United States, said Bernard Dauvergne, PharmD, executive director of Addmedica, which markets hydroxyurea as Siklos. In part, fears about toxicity and side effects contribute to this underuse, Dr. Dauvergne said at a top abstracts session of the annual meeting of the Foundation for Sickle Cell Disease Research.
ESCORT-HU was designed as a purely observational, noninterventional study of patients treated with HU. It was initiated as part of the European Medicines Agency risk management plan, conceived at the time of the drug’s approval for SCD, explained Dr. Dauvergne.
“This prospective cohort study could enable the identification of delayed rare adverse events in real life, occurring in between 1 in 10,000 and 1 in 1,000 patients,” Dr. Dauvergne said. However, “no new safety information has been detected ... and no secondary cancer has been reported.”
At the last data analysis cutpoint of June 2017, 1,921 patients had been enrolled. Patients have come from 63 centers in France, Germany, Greece, and Italy, Dr. Dauvergne reported.
Of the 1,829 patients with data available for analysis, 804 were under the age of 18. The pediatric patients were a mean 9 years of age, and the adult patients were a mean 33 years old at enrollment. Most enrollees (84%) have the HbSS genotype.
At baseline, the pediatric patients were dosed at a mean 17.2 mg/kg per day of HU; for adult patients, the figure was 15.54 mg/kg per day. More than one-third (35.4%) of pediatric patients had been on HU at the time of study enrollment, for a mean of 4.5 years. In contrast, more than half (60.4%) of adults had been taking hydroxyurea for a mean of 6.25 years at enrollment.
The 1,002 adult patients with recently reported safety data were on a mean HU dose of 20.2 mg/kg per day. About 40% of adults reported at least one adverse event (AE), and a total of 334 AEs in 16.3% of adult patients were judged to be related to HU.
Skin and subcutaneous tissue reactions occurred in about 1 in 10 patients, with 153 reported incidences of skin dryness, skin reactions, alopecia, or changes in skin pigmentation. The next most common adverse events were blood and lymphatic system disorders, mostly neutropenia or thrombocytopenia, occurring in 9.6% of patients.
Discontinuation rates have been low, with an overall dropout rate of 3.8%.
The ESCORT-HU data “confirm that HU is an efficient and well-tolerated drug in both children and adults,” Dr. Dauvergne said. Over the short term, adverse events are related to the expected dose dependent myelosuppression that’s key to the drug’s mechanism of action. This makes sense given the narrow therapeutic index, with a tight range between an efficacious dose and a cytotoxic one, he said. “And the lower the [patient] weight is, the more sensitive the dose variations become,” Dr. Dauvergne said.
Being flexible about fine-tuning doses is key to finding the balance between tolerability and efficacy, “and consequently, for compliance,” he said.
Data collection for the study will end in 2018, with safety and efficacy data expected in 2019.
WASHINGTON – European patients with sickle cell disease (SCD) are tolerating hydroxyurea treatment well, 9 years into a 10-year prospective cohort study.
ESCORT-HU (European Sickle Cell Disease Cohort – Hydroxyurea) is slated to enroll 2,000 children and adults over the study period to assess the long-term safety and efficacy of hydroxyurea (HU) as a treatment for SCD.
“Hydroxyurea is still underused in sickle cell disease” both in Europe and the United States, said Bernard Dauvergne, PharmD, executive director of Addmedica, which markets hydroxyurea as Siklos. In part, fears about toxicity and side effects contribute to this underuse, Dr. Dauvergne said at a top abstracts session of the annual meeting of the Foundation for Sickle Cell Disease Research.
ESCORT-HU was designed as a purely observational, noninterventional study of patients treated with HU. It was initiated as part of the European Medicines Agency risk management plan, conceived at the time of the drug’s approval for SCD, explained Dr. Dauvergne.
“This prospective cohort study could enable the identification of delayed rare adverse events in real life, occurring in between 1 in 10,000 and 1 in 1,000 patients,” Dr. Dauvergne said. However, “no new safety information has been detected ... and no secondary cancer has been reported.”
At the last data analysis cutpoint of June 2017, 1,921 patients had been enrolled. Patients have come from 63 centers in France, Germany, Greece, and Italy, Dr. Dauvergne reported.
Of the 1,829 patients with data available for analysis, 804 were under the age of 18. The pediatric patients were a mean 9 years of age, and the adult patients were a mean 33 years old at enrollment. Most enrollees (84%) have the HbSS genotype.
At baseline, the pediatric patients were dosed at a mean 17.2 mg/kg per day of HU; for adult patients, the figure was 15.54 mg/kg per day. More than one-third (35.4%) of pediatric patients had been on HU at the time of study enrollment, for a mean of 4.5 years. In contrast, more than half (60.4%) of adults had been taking hydroxyurea for a mean of 6.25 years at enrollment.
The 1,002 adult patients with recently reported safety data were on a mean HU dose of 20.2 mg/kg per day. About 40% of adults reported at least one adverse event (AE), and a total of 334 AEs in 16.3% of adult patients were judged to be related to HU.
Skin and subcutaneous tissue reactions occurred in about 1 in 10 patients, with 153 reported incidences of skin dryness, skin reactions, alopecia, or changes in skin pigmentation. The next most common adverse events were blood and lymphatic system disorders, mostly neutropenia or thrombocytopenia, occurring in 9.6% of patients.
Discontinuation rates have been low, with an overall dropout rate of 3.8%.
The ESCORT-HU data “confirm that HU is an efficient and well-tolerated drug in both children and adults,” Dr. Dauvergne said. Over the short term, adverse events are related to the expected dose dependent myelosuppression that’s key to the drug’s mechanism of action. This makes sense given the narrow therapeutic index, with a tight range between an efficacious dose and a cytotoxic one, he said. “And the lower the [patient] weight is, the more sensitive the dose variations become,” Dr. Dauvergne said.
Being flexible about fine-tuning doses is key to finding the balance between tolerability and efficacy, “and consequently, for compliance,” he said.
Data collection for the study will end in 2018, with safety and efficacy data expected in 2019.
REPORTING FROM FSCDR 2018
Key clinical point:
Major finding: Of adult participants, 16.9% have experienced hydroxyurea-related adverse events.
Study details: Observational 10-year study of 2,000 adults and children with SCD who were taking hydroxyurea.
Disclosures: The study was sponsored by Addmedica, which markets hydroxyurea as Siklos. Dr. Dauvergne is employed by Addmedica.
Source: Dauvergne B et al. FSCDR 2018, presentation JSCDH-D-18-00052.
PET-driven chemo strategy helps reduce toxicity in Hodgkin lymphoma
CHICAGO – Positron emission tomography (PET) performed after two cycles of BEACOPP could help identify a subset of advanced-stage Hodgkin lymphoma patients who can receive de-escalated treatment without compromising disease control, results of a phase 3 randomized trial show.
Five-year progression-free survival (PFS) exceeded 85% not only for patients receiving six cycles of escalated BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone) but also for patients who were de-escalated to ABVD (doxorubicin, bleomycin, vinblastine, dacarbazine) chemotherapy based on negative PET results, according to the final analysis of the AHL2011 LYSA study, presented at the annual meeting of the American Society of Clinical Oncology.
“This approach allows us to significantly reduce the treatment-related toxicity in most patients, and provides similar patient outcomes compared to standard BEACOPP escalated treatment,” said Olivier Casasnovas, MD, of the University Hospital Le Bocage and Inserm, Dijon, France.
Previous studies have shown that BEACOPP may improve PFS, compared with ABVD, but is more toxic and associated with a higher risk of infertility and myelodysplasia or acute leukemia. Dr. Casasnovas and his colleagues sought to evaluate whether upfront BEACOPP followed by de-escalation to ABVD, when warranted by negative PET results, would improve outcomes without compromising efficacy.
The AHL2011 LYSA study included 823 patients (median age, 30 years; 63% male) with previously untreated advanced classical Hodgkin lymphoma. All patients received PET at baseline, after cycle two of chemotherapy, and again after cycle four.
Patients were randomized either to six cycles of escalated BEACOPP, or to an experimental arm in which patients started with BEACOPP but were de-escalated to ABVD if PET results were negative after two or four cycles of treatment.
PET results after cycle two were negative for 87% of patients in the experimental arm, so on an intent-to-treat basis, 84% of them received two cycles of BEACOPP and four cycles of ABVD, Dr. Casasnovas reported.
PFS, with a median follow-up of 50.4 months, was not significantly different for the standard versus the experimental arm (hazard ratio, 1.084; 95% confidence interval, 0.73-1.59; P = .68). Five-year PFS was 85.7% in the experimental treatment de-escalation arm, compared with 86.2% in the standard arm.
Overall survival was likewise similar between arms, with 5-year overall survival exceeding 95% in both groups, Dr. Casasnovas said.
Although there was no significant difference overall in the incidence of adverse events, there was significantly less anemia, febrile neutropenia, thrombocytopenia, and sepsis in the PET-driven de-escalation arm. Overall, 27% of patients in the standard chemotherapy arm experienced at least one serious adverse event, compared with 17% in the PET-driven arm (P less than .002).
The incidence of second primary malignancies was numerically lower in the experimental arm (1.2% vs. 2.4%), though that finding did not reach statistical significance.
On multivariate analysis, interim PET positivity after cycle two was associated with increased risk of disease progression for patients in this study (HR, 3.316). Risk of progression was even higher for patients with PET positivity after four cycles (HR, 12.968), identifying a subset of patients with “particularly poor outcome” who could benefit from development of new treatment options, Dr. Casasnovas said.
Dr. Casasnovas reported financial ties to AbbVie, Bristol-Myers Squibb, Celgene, Gilead Sciences, Janssen, Merck, Roche/Genentech, Sanofi, and Takeda.
SOURCE: Casasnovas O et al. ASCO 2018, Abstract 7503.
CHICAGO – Positron emission tomography (PET) performed after two cycles of BEACOPP could help identify a subset of advanced-stage Hodgkin lymphoma patients who can receive de-escalated treatment without compromising disease control, results of a phase 3 randomized trial show.
Five-year progression-free survival (PFS) exceeded 85% not only for patients receiving six cycles of escalated BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone) but also for patients who were de-escalated to ABVD (doxorubicin, bleomycin, vinblastine, dacarbazine) chemotherapy based on negative PET results, according to the final analysis of the AHL2011 LYSA study, presented at the annual meeting of the American Society of Clinical Oncology.
“This approach allows us to significantly reduce the treatment-related toxicity in most patients, and provides similar patient outcomes compared to standard BEACOPP escalated treatment,” said Olivier Casasnovas, MD, of the University Hospital Le Bocage and Inserm, Dijon, France.
Previous studies have shown that BEACOPP may improve PFS, compared with ABVD, but is more toxic and associated with a higher risk of infertility and myelodysplasia or acute leukemia. Dr. Casasnovas and his colleagues sought to evaluate whether upfront BEACOPP followed by de-escalation to ABVD, when warranted by negative PET results, would improve outcomes without compromising efficacy.
The AHL2011 LYSA study included 823 patients (median age, 30 years; 63% male) with previously untreated advanced classical Hodgkin lymphoma. All patients received PET at baseline, after cycle two of chemotherapy, and again after cycle four.
Patients were randomized either to six cycles of escalated BEACOPP, or to an experimental arm in which patients started with BEACOPP but were de-escalated to ABVD if PET results were negative after two or four cycles of treatment.
PET results after cycle two were negative for 87% of patients in the experimental arm, so on an intent-to-treat basis, 84% of them received two cycles of BEACOPP and four cycles of ABVD, Dr. Casasnovas reported.
PFS, with a median follow-up of 50.4 months, was not significantly different for the standard versus the experimental arm (hazard ratio, 1.084; 95% confidence interval, 0.73-1.59; P = .68). Five-year PFS was 85.7% in the experimental treatment de-escalation arm, compared with 86.2% in the standard arm.
Overall survival was likewise similar between arms, with 5-year overall survival exceeding 95% in both groups, Dr. Casasnovas said.
Although there was no significant difference overall in the incidence of adverse events, there was significantly less anemia, febrile neutropenia, thrombocytopenia, and sepsis in the PET-driven de-escalation arm. Overall, 27% of patients in the standard chemotherapy arm experienced at least one serious adverse event, compared with 17% in the PET-driven arm (P less than .002).
The incidence of second primary malignancies was numerically lower in the experimental arm (1.2% vs. 2.4%), though that finding did not reach statistical significance.
On multivariate analysis, interim PET positivity after cycle two was associated with increased risk of disease progression for patients in this study (HR, 3.316). Risk of progression was even higher for patients with PET positivity after four cycles (HR, 12.968), identifying a subset of patients with “particularly poor outcome” who could benefit from development of new treatment options, Dr. Casasnovas said.
Dr. Casasnovas reported financial ties to AbbVie, Bristol-Myers Squibb, Celgene, Gilead Sciences, Janssen, Merck, Roche/Genentech, Sanofi, and Takeda.
SOURCE: Casasnovas O et al. ASCO 2018, Abstract 7503.
CHICAGO – Positron emission tomography (PET) performed after two cycles of BEACOPP could help identify a subset of advanced-stage Hodgkin lymphoma patients who can receive de-escalated treatment without compromising disease control, results of a phase 3 randomized trial show.
Five-year progression-free survival (PFS) exceeded 85% not only for patients receiving six cycles of escalated BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone) but also for patients who were de-escalated to ABVD (doxorubicin, bleomycin, vinblastine, dacarbazine) chemotherapy based on negative PET results, according to the final analysis of the AHL2011 LYSA study, presented at the annual meeting of the American Society of Clinical Oncology.
“This approach allows us to significantly reduce the treatment-related toxicity in most patients, and provides similar patient outcomes compared to standard BEACOPP escalated treatment,” said Olivier Casasnovas, MD, of the University Hospital Le Bocage and Inserm, Dijon, France.
Previous studies have shown that BEACOPP may improve PFS, compared with ABVD, but is more toxic and associated with a higher risk of infertility and myelodysplasia or acute leukemia. Dr. Casasnovas and his colleagues sought to evaluate whether upfront BEACOPP followed by de-escalation to ABVD, when warranted by negative PET results, would improve outcomes without compromising efficacy.
The AHL2011 LYSA study included 823 patients (median age, 30 years; 63% male) with previously untreated advanced classical Hodgkin lymphoma. All patients received PET at baseline, after cycle two of chemotherapy, and again after cycle four.
Patients were randomized either to six cycles of escalated BEACOPP, or to an experimental arm in which patients started with BEACOPP but were de-escalated to ABVD if PET results were negative after two or four cycles of treatment.
PET results after cycle two were negative for 87% of patients in the experimental arm, so on an intent-to-treat basis, 84% of them received two cycles of BEACOPP and four cycles of ABVD, Dr. Casasnovas reported.
PFS, with a median follow-up of 50.4 months, was not significantly different for the standard versus the experimental arm (hazard ratio, 1.084; 95% confidence interval, 0.73-1.59; P = .68). Five-year PFS was 85.7% in the experimental treatment de-escalation arm, compared with 86.2% in the standard arm.
Overall survival was likewise similar between arms, with 5-year overall survival exceeding 95% in both groups, Dr. Casasnovas said.
Although there was no significant difference overall in the incidence of adverse events, there was significantly less anemia, febrile neutropenia, thrombocytopenia, and sepsis in the PET-driven de-escalation arm. Overall, 27% of patients in the standard chemotherapy arm experienced at least one serious adverse event, compared with 17% in the PET-driven arm (P less than .002).
The incidence of second primary malignancies was numerically lower in the experimental arm (1.2% vs. 2.4%), though that finding did not reach statistical significance.
On multivariate analysis, interim PET positivity after cycle two was associated with increased risk of disease progression for patients in this study (HR, 3.316). Risk of progression was even higher for patients with PET positivity after four cycles (HR, 12.968), identifying a subset of patients with “particularly poor outcome” who could benefit from development of new treatment options, Dr. Casasnovas said.
Dr. Casasnovas reported financial ties to AbbVie, Bristol-Myers Squibb, Celgene, Gilead Sciences, Janssen, Merck, Roche/Genentech, Sanofi, and Takeda.
SOURCE: Casasnovas O et al. ASCO 2018, Abstract 7503.
REPORTING FROM ASCO 2018
Key clinical point:
Major finding: With a median follow-up of 50.4 months, PFS was not significantly different for escalated BEACOPP vs. the experimental arm (HR, 1.084; 95% CI, 0.73-1.59; P = .68).
Study details: Final analysis of AHL2011 LYSA, a randomized phase 3 study including 823 patients with advanced-stage Hodgkin lymphoma.
Disclosures: Dr. Casasnovas reported financial ties to AbbVie, Bristol-Myers Squibb, Celgene, Gilead Sciences, Janssen, Merck, Roche/Genentech, Sanofi, and Takeda.
Source: Casasnovas O et al. ASCO 2018, Abstract 7503.
EUS and MRCP as complementary studies in the etiologic diagnosis of idiopathic acute pancreatitis
Background: Approximately 10%-30% of patients with acute pancreatitis do not have an established etiology after routine investigation with imaging. These patients are classified as IAP. Less invasive tests, such as EUS, MRCP, and secretin stimulation MRCP (S-MRCP) have been used to further explore IAP, but their comparison in the etiologic diagnosis of idiopathic acute pancreatitis is lacking.
Study design: Meta-analysis involving 34 studies that investigated the etiology of IAP with MRCP and/or S-MRCP and/or EUS.
Setting: Brazil, Canada, China, France, Hong Kong, India, Italy, Korea, Spain, the United Kingdom, and the United States.
Synopsis: When EUS was compared with MRCP, the diagnostic yield of EUS (153/239 patients; 64%) was higher than that of MRCP (82/238 patients; 34%; P less than .01). Specifically, EUS seemed to have a significant benefit in detecting biliary disease, compared with MRCP. In the subgroup analysis, the diagnostic yield of EUS was higher than that of MRCP for detecting parenchymal changes suggestive of chronic pancreatitis (10% vs. 1%). S-MRCP was superior to EUS and MRCP (12% vs. 2% vs. 2%, respectively) in diagnosing pancreatic divisum, a congenital anomaly that is prevalent in 5%-14% of the population and an etiology of IAP.
A limitation in this meta-analysis was that EUS was used in seven times as many studies as was MRCP, which may have influenced the overall results.
Bottom line: Less invasive modalities, such as EUS and S-MRCP, used together could improve the diagnostic yield in evaluating the etiology of AIP.
Citation: Wang J et al. Comparison of EUS with MRCP in idiopathic acute pancreatitis: A systemic review and meta-analysis. Gastrointest Endosc. 2017 Dec 7. doi: 10.1016/j.gie.2017.11.028.
Dr. Farkhondehpour is a hospitalist at UC San Diego Health and an assistant clinical professor at the University of California, San Diego.
Background: Approximately 10%-30% of patients with acute pancreatitis do not have an established etiology after routine investigation with imaging. These patients are classified as IAP. Less invasive tests, such as EUS, MRCP, and secretin stimulation MRCP (S-MRCP) have been used to further explore IAP, but their comparison in the etiologic diagnosis of idiopathic acute pancreatitis is lacking.
Study design: Meta-analysis involving 34 studies that investigated the etiology of IAP with MRCP and/or S-MRCP and/or EUS.
Setting: Brazil, Canada, China, France, Hong Kong, India, Italy, Korea, Spain, the United Kingdom, and the United States.
Synopsis: When EUS was compared with MRCP, the diagnostic yield of EUS (153/239 patients; 64%) was higher than that of MRCP (82/238 patients; 34%; P less than .01). Specifically, EUS seemed to have a significant benefit in detecting biliary disease, compared with MRCP. In the subgroup analysis, the diagnostic yield of EUS was higher than that of MRCP for detecting parenchymal changes suggestive of chronic pancreatitis (10% vs. 1%). S-MRCP was superior to EUS and MRCP (12% vs. 2% vs. 2%, respectively) in diagnosing pancreatic divisum, a congenital anomaly that is prevalent in 5%-14% of the population and an etiology of IAP.
A limitation in this meta-analysis was that EUS was used in seven times as many studies as was MRCP, which may have influenced the overall results.
Bottom line: Less invasive modalities, such as EUS and S-MRCP, used together could improve the diagnostic yield in evaluating the etiology of AIP.
Citation: Wang J et al. Comparison of EUS with MRCP in idiopathic acute pancreatitis: A systemic review and meta-analysis. Gastrointest Endosc. 2017 Dec 7. doi: 10.1016/j.gie.2017.11.028.
Dr. Farkhondehpour is a hospitalist at UC San Diego Health and an assistant clinical professor at the University of California, San Diego.
Background: Approximately 10%-30% of patients with acute pancreatitis do not have an established etiology after routine investigation with imaging. These patients are classified as IAP. Less invasive tests, such as EUS, MRCP, and secretin stimulation MRCP (S-MRCP) have been used to further explore IAP, but their comparison in the etiologic diagnosis of idiopathic acute pancreatitis is lacking.
Study design: Meta-analysis involving 34 studies that investigated the etiology of IAP with MRCP and/or S-MRCP and/or EUS.
Setting: Brazil, Canada, China, France, Hong Kong, India, Italy, Korea, Spain, the United Kingdom, and the United States.
Synopsis: When EUS was compared with MRCP, the diagnostic yield of EUS (153/239 patients; 64%) was higher than that of MRCP (82/238 patients; 34%; P less than .01). Specifically, EUS seemed to have a significant benefit in detecting biliary disease, compared with MRCP. In the subgroup analysis, the diagnostic yield of EUS was higher than that of MRCP for detecting parenchymal changes suggestive of chronic pancreatitis (10% vs. 1%). S-MRCP was superior to EUS and MRCP (12% vs. 2% vs. 2%, respectively) in diagnosing pancreatic divisum, a congenital anomaly that is prevalent in 5%-14% of the population and an etiology of IAP.
A limitation in this meta-analysis was that EUS was used in seven times as many studies as was MRCP, which may have influenced the overall results.
Bottom line: Less invasive modalities, such as EUS and S-MRCP, used together could improve the diagnostic yield in evaluating the etiology of AIP.
Citation: Wang J et al. Comparison of EUS with MRCP in idiopathic acute pancreatitis: A systemic review and meta-analysis. Gastrointest Endosc. 2017 Dec 7. doi: 10.1016/j.gie.2017.11.028.
Dr. Farkhondehpour is a hospitalist at UC San Diego Health and an assistant clinical professor at the University of California, San Diego.
Patients With Concussions Aren’t Getting Enough Follow-Up
Many patients with traumatic brain injury (TBI) may not be receiving follow-up care, according to findings from Transforming Research and Clinical Knowledge in Traumatic Brain Injury (TRACK-TBI), a long-term NIH-funded study.
Of 831 patients who completed questionnaires 2 weeks and 3 months after sustaining TBI, 44% reported seeing a health care provider within 3 months. Of those, 15% visited a clinic that specialized in head injury. Approximately half saw a general practitioner; close to a third reported seeing ≥ 1 type of doctor.
Among the 279 patients with ≥ 3 symptoms of moderate to severe postconcussion, 41% had not had a follow-up visit at 3 months. Moreover, half of the patients were discharged without TBI educational materials.
Rates and components of follow-up care varied widely from institution to institution even among patients with the same initial degree of injury.
Many patients with traumatic brain injury (TBI) may not be receiving follow-up care, according to findings from Transforming Research and Clinical Knowledge in Traumatic Brain Injury (TRACK-TBI), a long-term NIH-funded study.
Of 831 patients who completed questionnaires 2 weeks and 3 months after sustaining TBI, 44% reported seeing a health care provider within 3 months. Of those, 15% visited a clinic that specialized in head injury. Approximately half saw a general practitioner; close to a third reported seeing ≥ 1 type of doctor.
Among the 279 patients with ≥ 3 symptoms of moderate to severe postconcussion, 41% had not had a follow-up visit at 3 months. Moreover, half of the patients were discharged without TBI educational materials.
Rates and components of follow-up care varied widely from institution to institution even among patients with the same initial degree of injury.
Many patients with traumatic brain injury (TBI) may not be receiving follow-up care, according to findings from Transforming Research and Clinical Knowledge in Traumatic Brain Injury (TRACK-TBI), a long-term NIH-funded study.
Of 831 patients who completed questionnaires 2 weeks and 3 months after sustaining TBI, 44% reported seeing a health care provider within 3 months. Of those, 15% visited a clinic that specialized in head injury. Approximately half saw a general practitioner; close to a third reported seeing ≥ 1 type of doctor.
Among the 279 patients with ≥ 3 symptoms of moderate to severe postconcussion, 41% had not had a follow-up visit at 3 months. Moreover, half of the patients were discharged without TBI educational materials.
Rates and components of follow-up care varied widely from institution to institution even among patients with the same initial degree of injury.
Talk Therapy—Without Words
Many forms of therapy rely on the patient being able to verbally communicate thoughts and feelings. Arts-based therapies, however, can help people explore sensitive and controversial topics that might be hard to talk about.
Body mapping, which has been in use for more than 30 years, is an interesting, revealing, and productive way of using art to help patients “talk” about their thoughts and feelings. Several studies have used body maps as therapy for patients with HIV/AIDS, but researchers from University of New South Wales, Sydney, theorized that it could be particularly helpful for patients with cognitive disability who have complex support needs as well as those who are socially marginalized.
In body-mapping sessions, participants trace outlines of their bodies and then “populate” the outlines with drawings, magazine photos, symbols, words, and other visual representations of the experience they are investigating. It is a form of storytelling that allows the participant to engage physically, visually, verbally, and relationally (through dialogue and interaction with the researcher).
The researchers used body mapping in 2 studies, first with 29 adults with cognitive disability and complex support needs, such as mental illness and sensory impairment, to explore experiences of support planning. In the second study, one of the researchers used body mapping with 13 teens and young adults with complex support needs (eg, drug and alcohol misuse) to explore support they received during a life transition.
The body-mapping technique, the researchers say, shifts the power balance between researcher and participant, because the patient is in control of the images used and where they are placed on the map. Patients could decide not only how they spoke about the topic, but also which topic they spoke about. The researchers say, “we were often taken to surprising places” that might not have come up in an interview, as when participants used images to reveal aspects of cultural heritage and sexual orientation that had not come up in conversation. For example, a transsexual woman in the second study was uncomfortable with the process until she covered her incorrectly gendered body with another piece of paper on which she could redraw her body as she wished.
Body mapping does not suit everyone, the researchers acknowledge. Participants need to be able to engage in a level of abstraction and reflection about personal experiences. It is important to have other methods available for those who do not want to take part. The researchers say one way they protected patients was by recruiting through service providers so support could be “embedded in existing relationships.” The potential vulnerabilities of the patients mean researchers need to be flexible, they add, and allow the method to evolve, much like the patients’ personal stories.
Source:
Dew A, Smith L, Collings S, Savage ID. FQS. 2018;19(2).
doi: http://dx.doi.org/10.17169/fqs-19.2.2929.
Many forms of therapy rely on the patient being able to verbally communicate thoughts and feelings. Arts-based therapies, however, can help people explore sensitive and controversial topics that might be hard to talk about.
Body mapping, which has been in use for more than 30 years, is an interesting, revealing, and productive way of using art to help patients “talk” about their thoughts and feelings. Several studies have used body maps as therapy for patients with HIV/AIDS, but researchers from University of New South Wales, Sydney, theorized that it could be particularly helpful for patients with cognitive disability who have complex support needs as well as those who are socially marginalized.
In body-mapping sessions, participants trace outlines of their bodies and then “populate” the outlines with drawings, magazine photos, symbols, words, and other visual representations of the experience they are investigating. It is a form of storytelling that allows the participant to engage physically, visually, verbally, and relationally (through dialogue and interaction with the researcher).
The researchers used body mapping in 2 studies, first with 29 adults with cognitive disability and complex support needs, such as mental illness and sensory impairment, to explore experiences of support planning. In the second study, one of the researchers used body mapping with 13 teens and young adults with complex support needs (eg, drug and alcohol misuse) to explore support they received during a life transition.
The body-mapping technique, the researchers say, shifts the power balance between researcher and participant, because the patient is in control of the images used and where they are placed on the map. Patients could decide not only how they spoke about the topic, but also which topic they spoke about. The researchers say, “we were often taken to surprising places” that might not have come up in an interview, as when participants used images to reveal aspects of cultural heritage and sexual orientation that had not come up in conversation. For example, a transsexual woman in the second study was uncomfortable with the process until she covered her incorrectly gendered body with another piece of paper on which she could redraw her body as she wished.
Body mapping does not suit everyone, the researchers acknowledge. Participants need to be able to engage in a level of abstraction and reflection about personal experiences. It is important to have other methods available for those who do not want to take part. The researchers say one way they protected patients was by recruiting through service providers so support could be “embedded in existing relationships.” The potential vulnerabilities of the patients mean researchers need to be flexible, they add, and allow the method to evolve, much like the patients’ personal stories.
Source:
Dew A, Smith L, Collings S, Savage ID. FQS. 2018;19(2).
doi: http://dx.doi.org/10.17169/fqs-19.2.2929.
Many forms of therapy rely on the patient being able to verbally communicate thoughts and feelings. Arts-based therapies, however, can help people explore sensitive and controversial topics that might be hard to talk about.
Body mapping, which has been in use for more than 30 years, is an interesting, revealing, and productive way of using art to help patients “talk” about their thoughts and feelings. Several studies have used body maps as therapy for patients with HIV/AIDS, but researchers from University of New South Wales, Sydney, theorized that it could be particularly helpful for patients with cognitive disability who have complex support needs as well as those who are socially marginalized.
In body-mapping sessions, participants trace outlines of their bodies and then “populate” the outlines with drawings, magazine photos, symbols, words, and other visual representations of the experience they are investigating. It is a form of storytelling that allows the participant to engage physically, visually, verbally, and relationally (through dialogue and interaction with the researcher).
The researchers used body mapping in 2 studies, first with 29 adults with cognitive disability and complex support needs, such as mental illness and sensory impairment, to explore experiences of support planning. In the second study, one of the researchers used body mapping with 13 teens and young adults with complex support needs (eg, drug and alcohol misuse) to explore support they received during a life transition.
The body-mapping technique, the researchers say, shifts the power balance between researcher and participant, because the patient is in control of the images used and where they are placed on the map. Patients could decide not only how they spoke about the topic, but also which topic they spoke about. The researchers say, “we were often taken to surprising places” that might not have come up in an interview, as when participants used images to reveal aspects of cultural heritage and sexual orientation that had not come up in conversation. For example, a transsexual woman in the second study was uncomfortable with the process until she covered her incorrectly gendered body with another piece of paper on which she could redraw her body as she wished.
Body mapping does not suit everyone, the researchers acknowledge. Participants need to be able to engage in a level of abstraction and reflection about personal experiences. It is important to have other methods available for those who do not want to take part. The researchers say one way they protected patients was by recruiting through service providers so support could be “embedded in existing relationships.” The potential vulnerabilities of the patients mean researchers need to be flexible, they add, and allow the method to evolve, much like the patients’ personal stories.
Source:
Dew A, Smith L, Collings S, Savage ID. FQS. 2018;19(2).
doi: http://dx.doi.org/10.17169/fqs-19.2.2929.
EC approves new use, formulation of dasatinib
The European Commission (EC) has expanded the marketing authorization for dasatinib (Sprycel).
The drug is now approved to treat patients ages 1 to 18 with Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in chronic phase (CP).
The EC has also approved a new formulation of dasatinib—a powder for oral suspension (PFOS) intended for patients who cannot swallow tablets whole or who weigh 10 kg or less.
Dasatinib is also EC-approved to treat adults with:
- Newly diagnosed Ph+ CML-CP
- Chronic, accelerated, or blast phase CML with resistance or intolerance to prior therapy, including imatinib
- Ph+ acute lymphoblastic leukemia and lymphoid blast CML with resistance or intolerance to prior therapy.
The EC’s latest approval of dasatinib is supported by results from a phase 2 trial (NCT00777036), which were published in the Journal of Clinical Oncology in March.
The trial included 29 patients with imatinib-resistant/intolerant CML-CP and 84 patients with newly diagnosed CML-CP.
The previously treated patients received dasatinib tablets. Newly diagnosed patients were treated with dasatinib tablets (n=51) or PFOS (n=33).
Patients who started on PFOS could switch to tablets after receiving PFOS for at least 1 year. Sixty-seven percent of patients on PFOS switched to tablets due to patient preference.
The average daily dose of dasatinib was 58.18 mg/m2 in the previously treated patients and 59.84 mg/m2 in the newly diagnosed patients (for both tablets and PFOS). The median duration of treatment was 49.91 months (range, 1.9 to 90.2) and 42.30 months (range, 0.1 to 75.2), respectively.
Rates of confirmed complete hematologic response (CHR) at any time were 93% in the previously treated patients and 96% in the newly diagnosed patients.
At 12 months, previously treated patients had a major molecular response (MMR) rate of 41% and a complete molecular response (CMR) rate of 7%. In newly diagnosed patients, MMR was 52%, and CMR was 8%.
At 24 months, previously treated patients had an MMR rate of 55% and a CMR rate of 17%. In the newly diagnosed patients, MMR was 70%, and CMR was 21%.
The rate of major cytogenetic response (MCyR) at any time was 89.7% in all previously treated patients and 90% when the researchers excluded patients with MCyR or unknown cytogenetic status at baseline.
The rate of complete cytogenetic response (CCyR) at any time was 94% in all newly diagnosed patients and 93.9% when the researchers excluded patients with CCyR or unknown cytogenetic status at baseline.
The median progression-free survival and overall survival had not been reached at last follow-up.
The estimated 48-month progression-free survival was 78% in the previously treated patients and 93% in the newly diagnosed patients. The estimated 48-month overall survival was 96% and 100%, respectively.
Dasatinib-related adverse events (AEs) occurring in at least 10% of the previously treated patients included nausea/vomiting (31%), myalgia/arthralgia (17%), fatigue (14%), rash (14%), diarrhea (14%), hemorrhage (10%), bone growth and development events (10%), and shortness of breath (10%).
Dasatinib-related AEs occurring in at least 10% of the newly diagnosed patients included nausea/vomiting (20%), myalgia/arthralgia (10%), fatigue (11%), rash (19%), diarrhea (18%), and hemorrhage (10%).
The European Commission (EC) has expanded the marketing authorization for dasatinib (Sprycel).
The drug is now approved to treat patients ages 1 to 18 with Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in chronic phase (CP).
The EC has also approved a new formulation of dasatinib—a powder for oral suspension (PFOS) intended for patients who cannot swallow tablets whole or who weigh 10 kg or less.
Dasatinib is also EC-approved to treat adults with:
- Newly diagnosed Ph+ CML-CP
- Chronic, accelerated, or blast phase CML with resistance or intolerance to prior therapy, including imatinib
- Ph+ acute lymphoblastic leukemia and lymphoid blast CML with resistance or intolerance to prior therapy.
The EC’s latest approval of dasatinib is supported by results from a phase 2 trial (NCT00777036), which were published in the Journal of Clinical Oncology in March.
The trial included 29 patients with imatinib-resistant/intolerant CML-CP and 84 patients with newly diagnosed CML-CP.
The previously treated patients received dasatinib tablets. Newly diagnosed patients were treated with dasatinib tablets (n=51) or PFOS (n=33).
Patients who started on PFOS could switch to tablets after receiving PFOS for at least 1 year. Sixty-seven percent of patients on PFOS switched to tablets due to patient preference.
The average daily dose of dasatinib was 58.18 mg/m2 in the previously treated patients and 59.84 mg/m2 in the newly diagnosed patients (for both tablets and PFOS). The median duration of treatment was 49.91 months (range, 1.9 to 90.2) and 42.30 months (range, 0.1 to 75.2), respectively.
Rates of confirmed complete hematologic response (CHR) at any time were 93% in the previously treated patients and 96% in the newly diagnosed patients.
At 12 months, previously treated patients had a major molecular response (MMR) rate of 41% and a complete molecular response (CMR) rate of 7%. In newly diagnosed patients, MMR was 52%, and CMR was 8%.
At 24 months, previously treated patients had an MMR rate of 55% and a CMR rate of 17%. In the newly diagnosed patients, MMR was 70%, and CMR was 21%.
The rate of major cytogenetic response (MCyR) at any time was 89.7% in all previously treated patients and 90% when the researchers excluded patients with MCyR or unknown cytogenetic status at baseline.
The rate of complete cytogenetic response (CCyR) at any time was 94% in all newly diagnosed patients and 93.9% when the researchers excluded patients with CCyR or unknown cytogenetic status at baseline.
The median progression-free survival and overall survival had not been reached at last follow-up.
The estimated 48-month progression-free survival was 78% in the previously treated patients and 93% in the newly diagnosed patients. The estimated 48-month overall survival was 96% and 100%, respectively.
Dasatinib-related adverse events (AEs) occurring in at least 10% of the previously treated patients included nausea/vomiting (31%), myalgia/arthralgia (17%), fatigue (14%), rash (14%), diarrhea (14%), hemorrhage (10%), bone growth and development events (10%), and shortness of breath (10%).
Dasatinib-related AEs occurring in at least 10% of the newly diagnosed patients included nausea/vomiting (20%), myalgia/arthralgia (10%), fatigue (11%), rash (19%), diarrhea (18%), and hemorrhage (10%).
The European Commission (EC) has expanded the marketing authorization for dasatinib (Sprycel).
The drug is now approved to treat patients ages 1 to 18 with Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in chronic phase (CP).
The EC has also approved a new formulation of dasatinib—a powder for oral suspension (PFOS) intended for patients who cannot swallow tablets whole or who weigh 10 kg or less.
Dasatinib is also EC-approved to treat adults with:
- Newly diagnosed Ph+ CML-CP
- Chronic, accelerated, or blast phase CML with resistance or intolerance to prior therapy, including imatinib
- Ph+ acute lymphoblastic leukemia and lymphoid blast CML with resistance or intolerance to prior therapy.
The EC’s latest approval of dasatinib is supported by results from a phase 2 trial (NCT00777036), which were published in the Journal of Clinical Oncology in March.
The trial included 29 patients with imatinib-resistant/intolerant CML-CP and 84 patients with newly diagnosed CML-CP.
The previously treated patients received dasatinib tablets. Newly diagnosed patients were treated with dasatinib tablets (n=51) or PFOS (n=33).
Patients who started on PFOS could switch to tablets after receiving PFOS for at least 1 year. Sixty-seven percent of patients on PFOS switched to tablets due to patient preference.
The average daily dose of dasatinib was 58.18 mg/m2 in the previously treated patients and 59.84 mg/m2 in the newly diagnosed patients (for both tablets and PFOS). The median duration of treatment was 49.91 months (range, 1.9 to 90.2) and 42.30 months (range, 0.1 to 75.2), respectively.
Rates of confirmed complete hematologic response (CHR) at any time were 93% in the previously treated patients and 96% in the newly diagnosed patients.
At 12 months, previously treated patients had a major molecular response (MMR) rate of 41% and a complete molecular response (CMR) rate of 7%. In newly diagnosed patients, MMR was 52%, and CMR was 8%.
At 24 months, previously treated patients had an MMR rate of 55% and a CMR rate of 17%. In the newly diagnosed patients, MMR was 70%, and CMR was 21%.
The rate of major cytogenetic response (MCyR) at any time was 89.7% in all previously treated patients and 90% when the researchers excluded patients with MCyR or unknown cytogenetic status at baseline.
The rate of complete cytogenetic response (CCyR) at any time was 94% in all newly diagnosed patients and 93.9% when the researchers excluded patients with CCyR or unknown cytogenetic status at baseline.
The median progression-free survival and overall survival had not been reached at last follow-up.
The estimated 48-month progression-free survival was 78% in the previously treated patients and 93% in the newly diagnosed patients. The estimated 48-month overall survival was 96% and 100%, respectively.
Dasatinib-related adverse events (AEs) occurring in at least 10% of the previously treated patients included nausea/vomiting (31%), myalgia/arthralgia (17%), fatigue (14%), rash (14%), diarrhea (14%), hemorrhage (10%), bone growth and development events (10%), and shortness of breath (10%).
Dasatinib-related AEs occurring in at least 10% of the newly diagnosed patients included nausea/vomiting (20%), myalgia/arthralgia (10%), fatigue (11%), rash (19%), diarrhea (18%), and hemorrhage (10%).
Transplant strategy not viable for aggressive B-NHL
Transplant with radioimmunotherapy (RIT)-based conditioning is a viable treatment option for patients with indolent—but not aggressive—B-cell non-Hodgkin lymphomas (NHLs), according to researchers.
Long-term follow-up data showed “excellent” outcomes in patients with indolent B-NHL who received conditioning with 90Y-ibritumomab tiuxetan plus fludarabine and low-dose total body irradiation (TBI) prior to HLA-matched hematopoietic stem cell transplant (HSCT).
However, long-term outcomes were inferior in patients with diffuse large B-cell lymphoma (DLBCL) and mantle cell lymphoma (MCL).
Camille E. Puronen, MD, of the University of Washington in Seattle, and her colleagues reported these results in Biology of Blood and Marrow Transplantation.
The study enrolled 40 patients with high-risk B-NHL. This included DLBCL (n=14), chronic lymphocytic leukemia (CLL; n=10), MCL (n=8), follicular lymphoma (FL; n=6); hairy cell leukemia (HCL; n=1), and marginal zone lymphoma (MZL; n=1).
Patients were treated with 0.4 mCi/kg 90Y-ibritumomab tiuxetan, given 2 weeks prior to HSCT, to a maximum dose of 32 mCi.
Patients also received fludarabine at 30 mg/m2 on day 5, 6, and 7 prior to HSCT and 2 Gy TBI given on the day of transplant.
In an earlier report, the objective response rate (ORR) was 60%, and 35% of patients had a complete response (CR) or unconfirmed CR.
The researchers said early responses were not associated with disease bulk or chemoresistance, as the ORR was 59% in patients with bulky or chemoresistant disease.
However, responses were associated with histology, as the ORR was 38% in patients with DLBCL, 50% in those with MCL, 83% in those with FL, and 90% in those with CLL.
Long-term survival
In the current report, 11 of 40 patients were still alive at a median follow up of 9 years (range, 5.3 to 10.2). Fourteen patients died of disease progression, and 14 died from complications of HSCT.
The 5-year overall survival (OS) was 40%, and the 5-year progression-free survival (PFS) was 28%.
The best survival rates were in patients with indolent histology. The 5-year PFS was 44% in these patients, and the 5-year OS was 67%.
The researchers said early CR was not associated with long-term survival. However, patients who had at least stable disease (SD) at earlier time points did have the opportunity to achieve long-term survival. All patients who progressed before day 84 were dead by the 1-year mark.
Of the 11 patients who were still alive at a median follow up of 9 years, 4 had a CR or unconfirmed CR at day 84 (FL: 1; CLL: 2; MCL: 1); 6 were in partial response (CLL: 3; FL: 1; MCL: 1; MZL: 1); and 1 patient with FL had SD.
Among the 18 patients with indolent NHL, long-term PFS was observed in 5 of the 7 patients who achieved early CR and 8 of the 11 patients who did not achieve early CR.
Two of the 4 MCL patients who achieved an early CR had long-term PFS, but none of the MCL patients without an early CR had long-term PFS.
Among DLBCL patients, 1 of the 4 who achieved early CR had long-term PFS, but none of the patients without an early CR had long-term PFS. Only 1 DLBCL patient survived beyond 5 years. None survived beyond 8 years.
The researchers said the favorable outcomes in patients with indolent B-NHL are consistent with the known efficacy of RIT and the graft-versus-leukemia effect in these patients.
The team also noted that, since this trial began, several novel agents have been approved for the treatment of indolent B-NHL, which means allogeneic HSCT is often moved to later in the disease course.
The researchers concluded that 90Y-ibritumomab tiuxetan-based conditioning could “continue to play an important role in these settings,” but “improved strategies are needed” for patients with MCL and DLBCL.
Transplant with radioimmunotherapy (RIT)-based conditioning is a viable treatment option for patients with indolent—but not aggressive—B-cell non-Hodgkin lymphomas (NHLs), according to researchers.
Long-term follow-up data showed “excellent” outcomes in patients with indolent B-NHL who received conditioning with 90Y-ibritumomab tiuxetan plus fludarabine and low-dose total body irradiation (TBI) prior to HLA-matched hematopoietic stem cell transplant (HSCT).
However, long-term outcomes were inferior in patients with diffuse large B-cell lymphoma (DLBCL) and mantle cell lymphoma (MCL).
Camille E. Puronen, MD, of the University of Washington in Seattle, and her colleagues reported these results in Biology of Blood and Marrow Transplantation.
The study enrolled 40 patients with high-risk B-NHL. This included DLBCL (n=14), chronic lymphocytic leukemia (CLL; n=10), MCL (n=8), follicular lymphoma (FL; n=6); hairy cell leukemia (HCL; n=1), and marginal zone lymphoma (MZL; n=1).
Patients were treated with 0.4 mCi/kg 90Y-ibritumomab tiuxetan, given 2 weeks prior to HSCT, to a maximum dose of 32 mCi.
Patients also received fludarabine at 30 mg/m2 on day 5, 6, and 7 prior to HSCT and 2 Gy TBI given on the day of transplant.
In an earlier report, the objective response rate (ORR) was 60%, and 35% of patients had a complete response (CR) or unconfirmed CR.
The researchers said early responses were not associated with disease bulk or chemoresistance, as the ORR was 59% in patients with bulky or chemoresistant disease.
However, responses were associated with histology, as the ORR was 38% in patients with DLBCL, 50% in those with MCL, 83% in those with FL, and 90% in those with CLL.
Long-term survival
In the current report, 11 of 40 patients were still alive at a median follow up of 9 years (range, 5.3 to 10.2). Fourteen patients died of disease progression, and 14 died from complications of HSCT.
The 5-year overall survival (OS) was 40%, and the 5-year progression-free survival (PFS) was 28%.
The best survival rates were in patients with indolent histology. The 5-year PFS was 44% in these patients, and the 5-year OS was 67%.
The researchers said early CR was not associated with long-term survival. However, patients who had at least stable disease (SD) at earlier time points did have the opportunity to achieve long-term survival. All patients who progressed before day 84 were dead by the 1-year mark.
Of the 11 patients who were still alive at a median follow up of 9 years, 4 had a CR or unconfirmed CR at day 84 (FL: 1; CLL: 2; MCL: 1); 6 were in partial response (CLL: 3; FL: 1; MCL: 1; MZL: 1); and 1 patient with FL had SD.
Among the 18 patients with indolent NHL, long-term PFS was observed in 5 of the 7 patients who achieved early CR and 8 of the 11 patients who did not achieve early CR.
Two of the 4 MCL patients who achieved an early CR had long-term PFS, but none of the MCL patients without an early CR had long-term PFS.
Among DLBCL patients, 1 of the 4 who achieved early CR had long-term PFS, but none of the patients without an early CR had long-term PFS. Only 1 DLBCL patient survived beyond 5 years. None survived beyond 8 years.
The researchers said the favorable outcomes in patients with indolent B-NHL are consistent with the known efficacy of RIT and the graft-versus-leukemia effect in these patients.
The team also noted that, since this trial began, several novel agents have been approved for the treatment of indolent B-NHL, which means allogeneic HSCT is often moved to later in the disease course.
The researchers concluded that 90Y-ibritumomab tiuxetan-based conditioning could “continue to play an important role in these settings,” but “improved strategies are needed” for patients with MCL and DLBCL.
Transplant with radioimmunotherapy (RIT)-based conditioning is a viable treatment option for patients with indolent—but not aggressive—B-cell non-Hodgkin lymphomas (NHLs), according to researchers.
Long-term follow-up data showed “excellent” outcomes in patients with indolent B-NHL who received conditioning with 90Y-ibritumomab tiuxetan plus fludarabine and low-dose total body irradiation (TBI) prior to HLA-matched hematopoietic stem cell transplant (HSCT).
However, long-term outcomes were inferior in patients with diffuse large B-cell lymphoma (DLBCL) and mantle cell lymphoma (MCL).
Camille E. Puronen, MD, of the University of Washington in Seattle, and her colleagues reported these results in Biology of Blood and Marrow Transplantation.
The study enrolled 40 patients with high-risk B-NHL. This included DLBCL (n=14), chronic lymphocytic leukemia (CLL; n=10), MCL (n=8), follicular lymphoma (FL; n=6); hairy cell leukemia (HCL; n=1), and marginal zone lymphoma (MZL; n=1).
Patients were treated with 0.4 mCi/kg 90Y-ibritumomab tiuxetan, given 2 weeks prior to HSCT, to a maximum dose of 32 mCi.
Patients also received fludarabine at 30 mg/m2 on day 5, 6, and 7 prior to HSCT and 2 Gy TBI given on the day of transplant.
In an earlier report, the objective response rate (ORR) was 60%, and 35% of patients had a complete response (CR) or unconfirmed CR.
The researchers said early responses were not associated with disease bulk or chemoresistance, as the ORR was 59% in patients with bulky or chemoresistant disease.
However, responses were associated with histology, as the ORR was 38% in patients with DLBCL, 50% in those with MCL, 83% in those with FL, and 90% in those with CLL.
Long-term survival
In the current report, 11 of 40 patients were still alive at a median follow up of 9 years (range, 5.3 to 10.2). Fourteen patients died of disease progression, and 14 died from complications of HSCT.
The 5-year overall survival (OS) was 40%, and the 5-year progression-free survival (PFS) was 28%.
The best survival rates were in patients with indolent histology. The 5-year PFS was 44% in these patients, and the 5-year OS was 67%.
The researchers said early CR was not associated with long-term survival. However, patients who had at least stable disease (SD) at earlier time points did have the opportunity to achieve long-term survival. All patients who progressed before day 84 were dead by the 1-year mark.
Of the 11 patients who were still alive at a median follow up of 9 years, 4 had a CR or unconfirmed CR at day 84 (FL: 1; CLL: 2; MCL: 1); 6 were in partial response (CLL: 3; FL: 1; MCL: 1; MZL: 1); and 1 patient with FL had SD.
Among the 18 patients with indolent NHL, long-term PFS was observed in 5 of the 7 patients who achieved early CR and 8 of the 11 patients who did not achieve early CR.
Two of the 4 MCL patients who achieved an early CR had long-term PFS, but none of the MCL patients without an early CR had long-term PFS.
Among DLBCL patients, 1 of the 4 who achieved early CR had long-term PFS, but none of the patients without an early CR had long-term PFS. Only 1 DLBCL patient survived beyond 5 years. None survived beyond 8 years.
The researchers said the favorable outcomes in patients with indolent B-NHL are consistent with the known efficacy of RIT and the graft-versus-leukemia effect in these patients.
The team also noted that, since this trial began, several novel agents have been approved for the treatment of indolent B-NHL, which means allogeneic HSCT is often moved to later in the disease course.
The researchers concluded that 90Y-ibritumomab tiuxetan-based conditioning could “continue to play an important role in these settings,” but “improved strategies are needed” for patients with MCL and DLBCL.
Drug proves active in resistant MM
STOCKHOLM—The alkylating peptide melflufen has demonstrated activity in patients with treatment-resistant multiple myeloma (MM).
In a phase 2 trial, melflufen plus dexamethasone produced an overall response rate (ORR) of 32.1% in MM patients who were refractory to pomalidomide and/or daratumumab and had failed treatment with immunomodulatory drugs (IMiDs) and proteasome inhibitors (PIs).
Nearly all patients experienced an adverse event (AE) related to study treatment, and most of these were hematologic events.
These results, from the ongoing HORIZON trial, were presented at the 23rd Congress of the European Hematology Association (EHA) as abstract PF581.
The research was sponsored by Oncopeptides AB, the company developing melflufen.
“With an increasing number of patients with highly resistant myeloma, there is a real need for additional treatment options based on new mechanisms of action,” said study investigator Paul Richardson, MD, of the Dana-Farber Cancer Institute in Boston, Massachusetts.
“[Melflufen], a peptidase-enhanced compound, with its potent activity, manageable tolerability, and lack of shared resistance mechanisms with other modalities, is a promising molecule that is making encouraging progress in clinical development.”
Patients and treatment
The data presented at EHA include 62 patients. The data cut-off was May 10, 2018.
The patients had a median age of 62.5 (range, 41-82), 54% had high-risk cytogenetics, and 46% were ISS stage III. The patients had a median of 5.5 prior lines of therapy, and their median time since initial diagnosis was 6.1 years.
All patients were refractory to pomalidomide or daratumumab, 56% were refractory to both drugs, and 89% were double-refractory to IMiDs and PIs. Ninety-eight percent of patients had disease progression on or within 60 days of completing their last therapy.
Patients received melflufen at 40 mg (intravenously over 30 minutes) on day 1 of each 28-day cycle. They also received dexamethasone at 40 mg weekly. Patients were treated until disease progression, unacceptable toxicity, or withdrawal of consent.
At the data cutoff, 49 patients (79%) had completed at least 2 cycles of melflufen. The median number of cycles was 2 (range, 1-11).
Twenty-one patients (34%) were still receiving study treatment at the data cutoff. Reasons for discontinuation included disease progression (47%), AEs (15%), and physician decision (3%). One discontinuation was due to patient request.
Results
Fifty-six patients received at least 1 dose of melflufen and were evaluable for response.
The ORR was 32.1%, and the clinical benefit rate was 39.3%. ORR was defined as partial response (PR) or better, and clinical benefit rate was defined as minor response or better.
Two percent of patients had a complete response, 9% had a very good PR, 21% had a PR, and 7% had a minor response. Forty-five percent of patients had stable disease, and 16% progressed.
Subgroup analyses showed that response didn’t vary across refractory subsets, but it did vary according to the underlying disease and health status of the patient.
Treatment-related AEs occurred in 97% of all patients (60/62), and grade 3/4 treatment-related AEs occurred in 77% (n=48).
Grade 3/4 treatment-related AEs included neutropenia (60%), thrombocytopenia (60%), anemia (31%), leukopenia (6%), lymphopenia (6%), febrile neutropenia (6%), and infections (6%).
Twenty-one percent of patients had at least 1 treatment-related serious AE. The most frequent were febrile neutropenia (6%) and pneumonia (3%).
There were no treatment-related deaths.
STOCKHOLM—The alkylating peptide melflufen has demonstrated activity in patients with treatment-resistant multiple myeloma (MM).
In a phase 2 trial, melflufen plus dexamethasone produced an overall response rate (ORR) of 32.1% in MM patients who were refractory to pomalidomide and/or daratumumab and had failed treatment with immunomodulatory drugs (IMiDs) and proteasome inhibitors (PIs).
Nearly all patients experienced an adverse event (AE) related to study treatment, and most of these were hematologic events.
These results, from the ongoing HORIZON trial, were presented at the 23rd Congress of the European Hematology Association (EHA) as abstract PF581.
The research was sponsored by Oncopeptides AB, the company developing melflufen.
“With an increasing number of patients with highly resistant myeloma, there is a real need for additional treatment options based on new mechanisms of action,” said study investigator Paul Richardson, MD, of the Dana-Farber Cancer Institute in Boston, Massachusetts.
“[Melflufen], a peptidase-enhanced compound, with its potent activity, manageable tolerability, and lack of shared resistance mechanisms with other modalities, is a promising molecule that is making encouraging progress in clinical development.”
Patients and treatment
The data presented at EHA include 62 patients. The data cut-off was May 10, 2018.
The patients had a median age of 62.5 (range, 41-82), 54% had high-risk cytogenetics, and 46% were ISS stage III. The patients had a median of 5.5 prior lines of therapy, and their median time since initial diagnosis was 6.1 years.
All patients were refractory to pomalidomide or daratumumab, 56% were refractory to both drugs, and 89% were double-refractory to IMiDs and PIs. Ninety-eight percent of patients had disease progression on or within 60 days of completing their last therapy.
Patients received melflufen at 40 mg (intravenously over 30 minutes) on day 1 of each 28-day cycle. They also received dexamethasone at 40 mg weekly. Patients were treated until disease progression, unacceptable toxicity, or withdrawal of consent.
At the data cutoff, 49 patients (79%) had completed at least 2 cycles of melflufen. The median number of cycles was 2 (range, 1-11).
Twenty-one patients (34%) were still receiving study treatment at the data cutoff. Reasons for discontinuation included disease progression (47%), AEs (15%), and physician decision (3%). One discontinuation was due to patient request.
Results
Fifty-six patients received at least 1 dose of melflufen and were evaluable for response.
The ORR was 32.1%, and the clinical benefit rate was 39.3%. ORR was defined as partial response (PR) or better, and clinical benefit rate was defined as minor response or better.
Two percent of patients had a complete response, 9% had a very good PR, 21% had a PR, and 7% had a minor response. Forty-five percent of patients had stable disease, and 16% progressed.
Subgroup analyses showed that response didn’t vary across refractory subsets, but it did vary according to the underlying disease and health status of the patient.
Treatment-related AEs occurred in 97% of all patients (60/62), and grade 3/4 treatment-related AEs occurred in 77% (n=48).
Grade 3/4 treatment-related AEs included neutropenia (60%), thrombocytopenia (60%), anemia (31%), leukopenia (6%), lymphopenia (6%), febrile neutropenia (6%), and infections (6%).
Twenty-one percent of patients had at least 1 treatment-related serious AE. The most frequent were febrile neutropenia (6%) and pneumonia (3%).
There were no treatment-related deaths.
STOCKHOLM—The alkylating peptide melflufen has demonstrated activity in patients with treatment-resistant multiple myeloma (MM).
In a phase 2 trial, melflufen plus dexamethasone produced an overall response rate (ORR) of 32.1% in MM patients who were refractory to pomalidomide and/or daratumumab and had failed treatment with immunomodulatory drugs (IMiDs) and proteasome inhibitors (PIs).
Nearly all patients experienced an adverse event (AE) related to study treatment, and most of these were hematologic events.
These results, from the ongoing HORIZON trial, were presented at the 23rd Congress of the European Hematology Association (EHA) as abstract PF581.
The research was sponsored by Oncopeptides AB, the company developing melflufen.
“With an increasing number of patients with highly resistant myeloma, there is a real need for additional treatment options based on new mechanisms of action,” said study investigator Paul Richardson, MD, of the Dana-Farber Cancer Institute in Boston, Massachusetts.
“[Melflufen], a peptidase-enhanced compound, with its potent activity, manageable tolerability, and lack of shared resistance mechanisms with other modalities, is a promising molecule that is making encouraging progress in clinical development.”
Patients and treatment
The data presented at EHA include 62 patients. The data cut-off was May 10, 2018.
The patients had a median age of 62.5 (range, 41-82), 54% had high-risk cytogenetics, and 46% were ISS stage III. The patients had a median of 5.5 prior lines of therapy, and their median time since initial diagnosis was 6.1 years.
All patients were refractory to pomalidomide or daratumumab, 56% were refractory to both drugs, and 89% were double-refractory to IMiDs and PIs. Ninety-eight percent of patients had disease progression on or within 60 days of completing their last therapy.
Patients received melflufen at 40 mg (intravenously over 30 minutes) on day 1 of each 28-day cycle. They also received dexamethasone at 40 mg weekly. Patients were treated until disease progression, unacceptable toxicity, or withdrawal of consent.
At the data cutoff, 49 patients (79%) had completed at least 2 cycles of melflufen. The median number of cycles was 2 (range, 1-11).
Twenty-one patients (34%) were still receiving study treatment at the data cutoff. Reasons for discontinuation included disease progression (47%), AEs (15%), and physician decision (3%). One discontinuation was due to patient request.
Results
Fifty-six patients received at least 1 dose of melflufen and were evaluable for response.
The ORR was 32.1%, and the clinical benefit rate was 39.3%. ORR was defined as partial response (PR) or better, and clinical benefit rate was defined as minor response or better.
Two percent of patients had a complete response, 9% had a very good PR, 21% had a PR, and 7% had a minor response. Forty-five percent of patients had stable disease, and 16% progressed.
Subgroup analyses showed that response didn’t vary across refractory subsets, but it did vary according to the underlying disease and health status of the patient.
Treatment-related AEs occurred in 97% of all patients (60/62), and grade 3/4 treatment-related AEs occurred in 77% (n=48).
Grade 3/4 treatment-related AEs included neutropenia (60%), thrombocytopenia (60%), anemia (31%), leukopenia (6%), lymphopenia (6%), febrile neutropenia (6%), and infections (6%).
Twenty-one percent of patients had at least 1 treatment-related serious AE. The most frequent were febrile neutropenia (6%) and pneumonia (3%).
There were no treatment-related deaths.
How the IHS Reduced Kidney Disease in the Highest-risk Population
Alaska is a vast state—larger than Texas, Montana, and California combined. It is also home to the highest percentage of American Indian (AI) and Alaska Native (AN) persons in the United States. These two populations—collectively referred to as Native Americans—have been served by the Indian Health Services (IHS) since it was established through the Snyder Act of 1921, in response to the dismal health conditions of the indigenous tribes in this country.1 Across the US (not only in Alaska), the IHS has partnered with AI/AN peoples to decrease health disparities in a culturally acceptable manner that honors and protects their traditions and values.
The IHS—which in 2016 comprised 2,500 nurses, 750 physicians, 700 pharmacists, 200 PAs and NPs, and 280 dentists, as well as nutritionists, diabetes educators, administrators, and other professionals—has made huge advances in decreasing health disparities in their populations. Among them: decreased rates of tuberculosis and of maternal and infant deaths.
However, life expectancy among Native Americans remains four years shorter than that of the rest of the US population. This disparity can be traced to three recalcitrant factors: unintentional injuries, liver disease, and diabetes.
The IHS practitioners decided to tackle diabetes with a multipronged approach. And what they achieved is astonishing.
WHAT THEY DID
Worldwide, diabetes is the most common cause of kidney failure; identifying patients with diabetes and early-stage chronic kidney disease allows for aggressive treatment that can slow progression to kidney failure and dialysis.
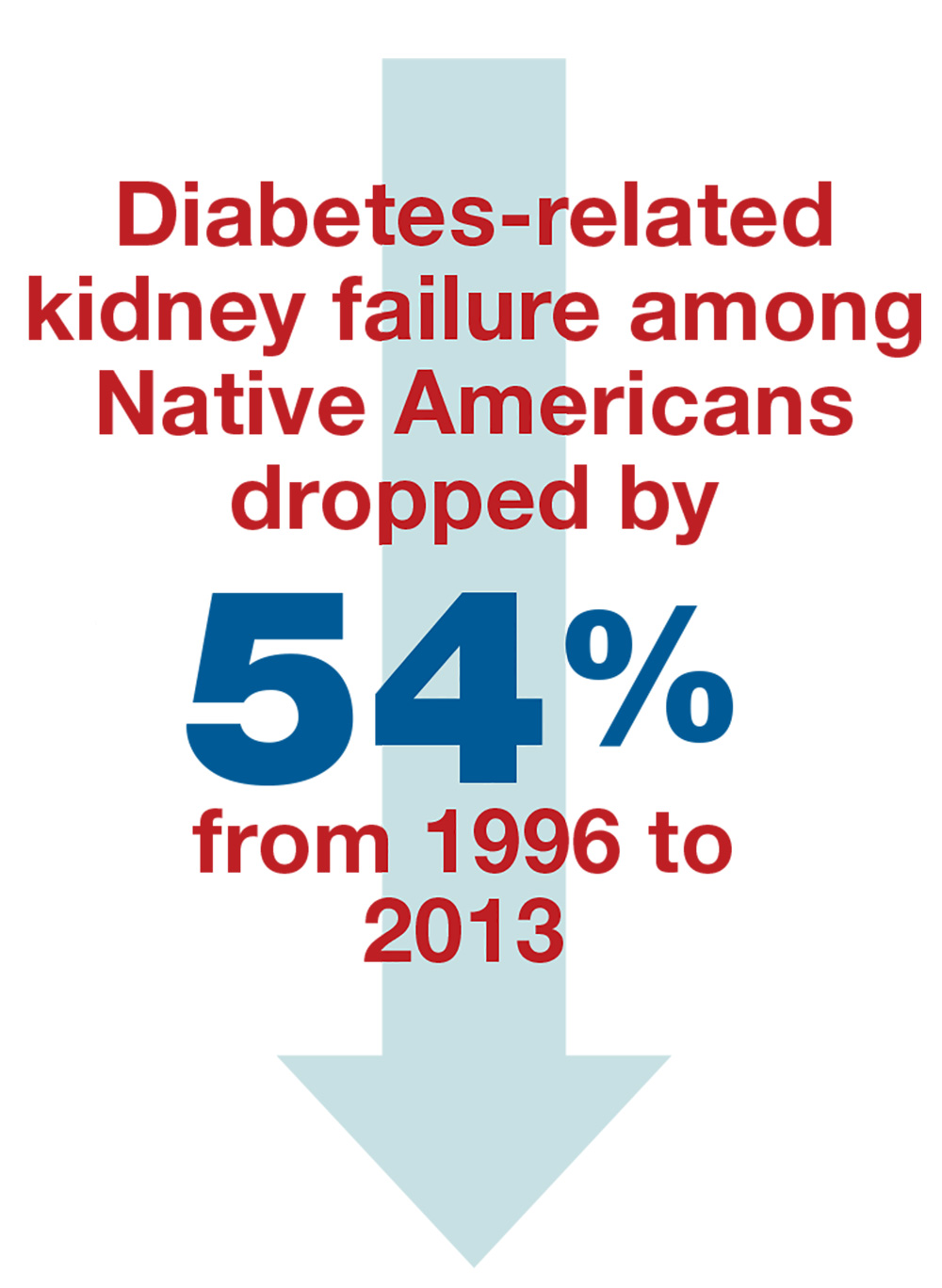
The IHS providers knew when they decided to tackle the problem of diabetes in the AI/AN population that the incidence was 16%—and the rate of diabetes leading to kidney failure in this population was the highest for any ethnic group in the US.2,3 And yet …
From 1996 to 2013, the rate of diabetes-related kidney failure among Native Americans dropped by 54%.3 Yes—the group of patients with the highest percentage of diabetes diagnoses has had the greatest improvement in prevention of kidney failure.4
Continue to: Some of the clinical achievements that contributed to...
Some of the clinical achievements that contributed to this significant change include
- Increased use of ACE inhibitors or angiotensin receptor blockers (ARBs) (from 42% to 74% over a five-year period)
- Reduced average blood pressure among hypertensive patients (to 133/76 mm Hg)
- Improved blood glucose control (by 10%)
- Increased testing for kidney disease among older patients (50% higher than the rest of the Medicare diabetes population).3
HOW THEY DID IT
This is not rocket science. The IHS staff integrated both population- and team-based approaches to achieve a more impressive decrease than ever could have been expected. In retrospect, perhaps this success should not come as such a surprise—many religious beliefs held by Native Americans focus around society, communal harmony, kinship, and cooperation.
The population health approach focused on promoting the wellness of the entire community and connecting people to local resources, including healthy food, transportation, housing, and mental health care. In the team approach, IHS medical experts implemented strategies to improve patient education, community outreach, care coordination, health outcome tracking, and access to a wide variety of health care providers.3,5
In a place like Alaska—where the northernmost city, Barrow, is more than 700 miles (two hours by plane) from Anchorage, and the southeastern Annette Island is more than 1,000 miles (six hours by plane) from the capital—this can be an especially challenging prospect. To reduce travel burden for rural patients, the IHS sponsors a diabetes team that travels from village to village. Nephrology services are not included in these field visits, however, so the kidney team relies heavily on telehealth. This requires extensive clinic staff coordination, as well as equipment and knowledgeable information systems support teams.
Other challenges require educational and logistical solutions. As noted, the use of ACE inhibitors and ARBs increased through the IHS’s efforts—and contributed to the delayed progression of diabetic kidney disease—but those additional prescriptions necessitate patient education. Understanding of these medications can be limited; many rural patients trust that when the bottle is empty, their practitioner has treated and cured their disease—mistakenly believing that no refills are needed. And even when the need to continue the prescription is understood, rural clinics may have difficulty tracking appointments and prescriptions written by providers at specialty clinics in Anchorage, making ongoing refills an issue.
Continue to: The necessary dietary changes can also be...
The necessary dietary changes can also be difficult for AI/AN populations. For example, in rural Alaska, tap water may not be safe to drink, and soda costs less than bottled water. Fresh produce is expensive and has often begun to spoil by the time it reaches local stores. The Native villagers often prefer their usual diets of gathered berries, fish, and red meat from subsistence hunting, making implementation of dietary changes difficult.
However, as the success of the IHS initiative shows, challenges can be met and overcome by practitioners who see a need, formulate a solution individualized to the circumstance, and think outside the box. One of the keys is developing a trusting relationship with patients. Another is to recognize informational needs and utilize available resources to educate patients. For example, visual representations of kidney function tend to be helpful in explaining the nature and course of disease; the National Kidney Disease Education Program uses an illustration similar to a gas gauge to demonstrate glomerular filtration rate (which would otherwise seem abstract and hard to understand for some patients; see below).6 When you understand your patient population and their needs, it makes addressing the challenging aspects of health care and prevention easier.
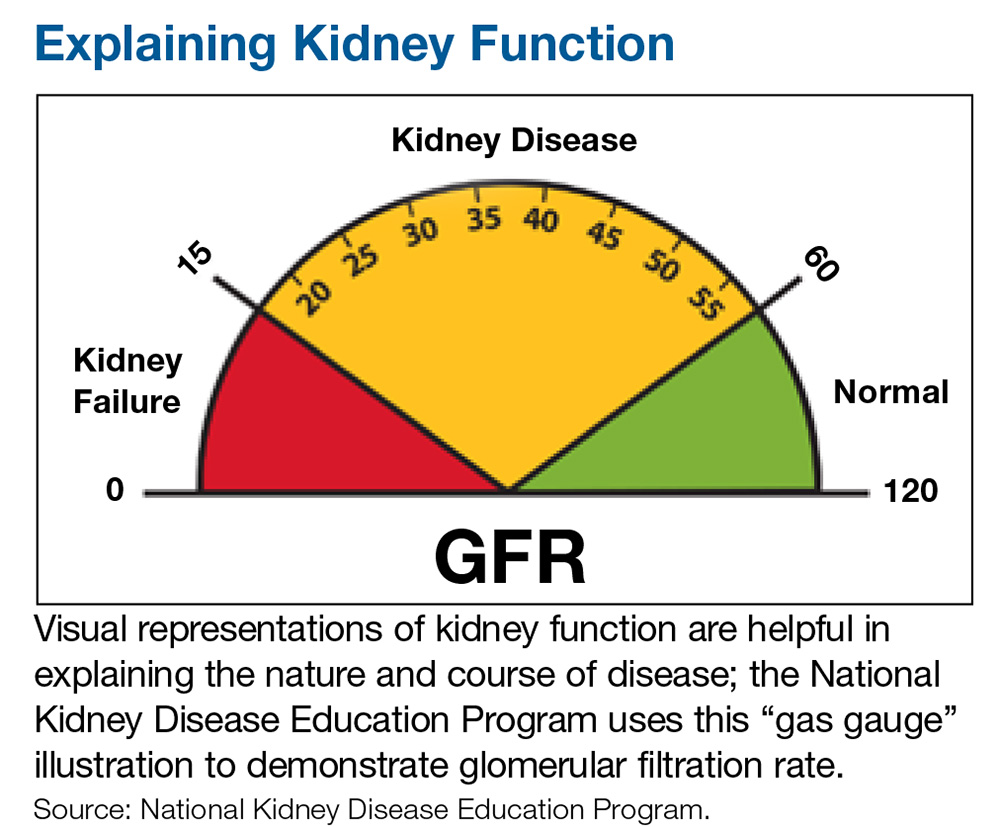
CONCLUSION
The results that the IHS achieved should serve as an example for all Americans with diabetes and their health care providers. We must be open to delivery of care via different approaches and practitioners in order to successfully help patients of different backgrounds and circumstances. This is the individualization of care that we hear so much about.
In 2016, the costs of caring for the kidney failure population were greater than the entire budget of the NIH. By aggressively identifying and treating patients at risk for kidney failure, we can slow disease progression—saving society money, but more importantly allowing our patients many more years of life free from the constraints of dialysis. —MET, RB
Mandy E. Thompson, PA-C
Kidney Center of Denver Health
Robin Bassett, DNP
Nephrology and Hypertension Associates, Anchorage
Adjunct Professor, NP program, University of Alaska, Anchorage
1. Indian Health Service. Legislation. www.ihs.gov/aboutihs/legislation. Accessed June 13, 2018.
2. National Health Interview Survey and Indian Health Service, 2010-2012.
3. CDC. Native Americans with diabetes. www.cdc.gov/vitalsigns/aian-diabetes/. Accessed June 13, 2018.
4. United States Renal Data System. Figure 1.5: Trends in adjusted* ESRD incidence rate (per million/year), by race, in the U.S. population, 1996-2014. In: 2016 USRDS annual data report: Epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2016.
5. Indian Health Service. Special diabetes program for Indians. www.ihs.gov/newsroom/factsheets/diabetes. Accessed June 13, 2018.
6. National Kidney Disease Education Program. How well are your kidneys working? Explaining your kidney test results. www.niddk.nih.gov/health-information/professionals/clinical-tools-patient-education-outreach/explain-kidney-test-results. Accessed June 13, 2018.
Alaska is a vast state—larger than Texas, Montana, and California combined. It is also home to the highest percentage of American Indian (AI) and Alaska Native (AN) persons in the United States. These two populations—collectively referred to as Native Americans—have been served by the Indian Health Services (IHS) since it was established through the Snyder Act of 1921, in response to the dismal health conditions of the indigenous tribes in this country.1 Across the US (not only in Alaska), the IHS has partnered with AI/AN peoples to decrease health disparities in a culturally acceptable manner that honors and protects their traditions and values.
The IHS—which in 2016 comprised 2,500 nurses, 750 physicians, 700 pharmacists, 200 PAs and NPs, and 280 dentists, as well as nutritionists, diabetes educators, administrators, and other professionals—has made huge advances in decreasing health disparities in their populations. Among them: decreased rates of tuberculosis and of maternal and infant deaths.
However, life expectancy among Native Americans remains four years shorter than that of the rest of the US population. This disparity can be traced to three recalcitrant factors: unintentional injuries, liver disease, and diabetes.
The IHS practitioners decided to tackle diabetes with a multipronged approach. And what they achieved is astonishing.
WHAT THEY DID
Worldwide, diabetes is the most common cause of kidney failure; identifying patients with diabetes and early-stage chronic kidney disease allows for aggressive treatment that can slow progression to kidney failure and dialysis.
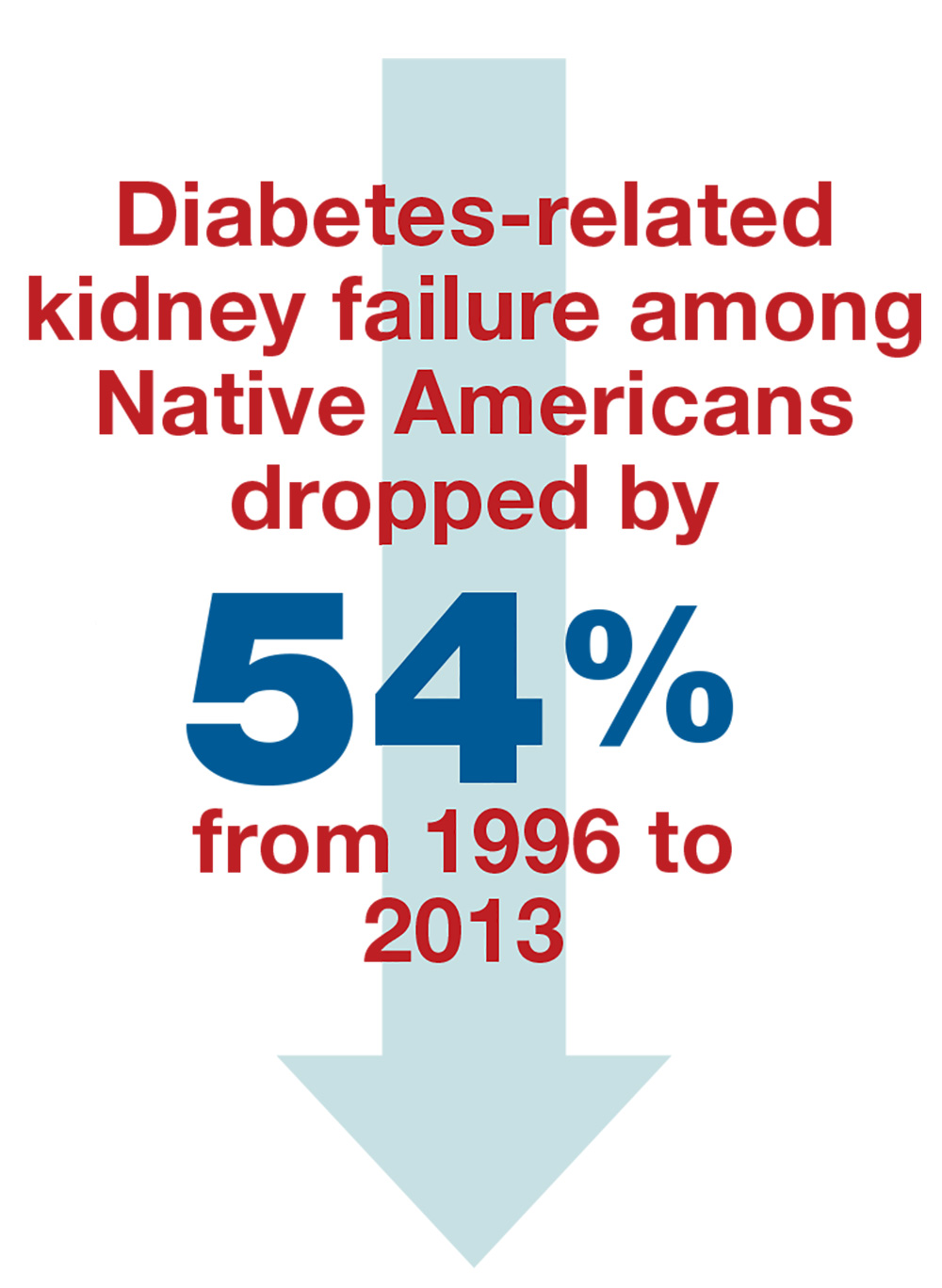
The IHS providers knew when they decided to tackle the problem of diabetes in the AI/AN population that the incidence was 16%—and the rate of diabetes leading to kidney failure in this population was the highest for any ethnic group in the US.2,3 And yet …
From 1996 to 2013, the rate of diabetes-related kidney failure among Native Americans dropped by 54%.3 Yes—the group of patients with the highest percentage of diabetes diagnoses has had the greatest improvement in prevention of kidney failure.4
Continue to: Some of the clinical achievements that contributed to...
Some of the clinical achievements that contributed to this significant change include
- Increased use of ACE inhibitors or angiotensin receptor blockers (ARBs) (from 42% to 74% over a five-year period)
- Reduced average blood pressure among hypertensive patients (to 133/76 mm Hg)
- Improved blood glucose control (by 10%)
- Increased testing for kidney disease among older patients (50% higher than the rest of the Medicare diabetes population).3
HOW THEY DID IT
This is not rocket science. The IHS staff integrated both population- and team-based approaches to achieve a more impressive decrease than ever could have been expected. In retrospect, perhaps this success should not come as such a surprise—many religious beliefs held by Native Americans focus around society, communal harmony, kinship, and cooperation.
The population health approach focused on promoting the wellness of the entire community and connecting people to local resources, including healthy food, transportation, housing, and mental health care. In the team approach, IHS medical experts implemented strategies to improve patient education, community outreach, care coordination, health outcome tracking, and access to a wide variety of health care providers.3,5
In a place like Alaska—where the northernmost city, Barrow, is more than 700 miles (two hours by plane) from Anchorage, and the southeastern Annette Island is more than 1,000 miles (six hours by plane) from the capital—this can be an especially challenging prospect. To reduce travel burden for rural patients, the IHS sponsors a diabetes team that travels from village to village. Nephrology services are not included in these field visits, however, so the kidney team relies heavily on telehealth. This requires extensive clinic staff coordination, as well as equipment and knowledgeable information systems support teams.
Other challenges require educational and logistical solutions. As noted, the use of ACE inhibitors and ARBs increased through the IHS’s efforts—and contributed to the delayed progression of diabetic kidney disease—but those additional prescriptions necessitate patient education. Understanding of these medications can be limited; many rural patients trust that when the bottle is empty, their practitioner has treated and cured their disease—mistakenly believing that no refills are needed. And even when the need to continue the prescription is understood, rural clinics may have difficulty tracking appointments and prescriptions written by providers at specialty clinics in Anchorage, making ongoing refills an issue.
Continue to: The necessary dietary changes can also be...
The necessary dietary changes can also be difficult for AI/AN populations. For example, in rural Alaska, tap water may not be safe to drink, and soda costs less than bottled water. Fresh produce is expensive and has often begun to spoil by the time it reaches local stores. The Native villagers often prefer their usual diets of gathered berries, fish, and red meat from subsistence hunting, making implementation of dietary changes difficult.
However, as the success of the IHS initiative shows, challenges can be met and overcome by practitioners who see a need, formulate a solution individualized to the circumstance, and think outside the box. One of the keys is developing a trusting relationship with patients. Another is to recognize informational needs and utilize available resources to educate patients. For example, visual representations of kidney function tend to be helpful in explaining the nature and course of disease; the National Kidney Disease Education Program uses an illustration similar to a gas gauge to demonstrate glomerular filtration rate (which would otherwise seem abstract and hard to understand for some patients; see below).6 When you understand your patient population and their needs, it makes addressing the challenging aspects of health care and prevention easier.
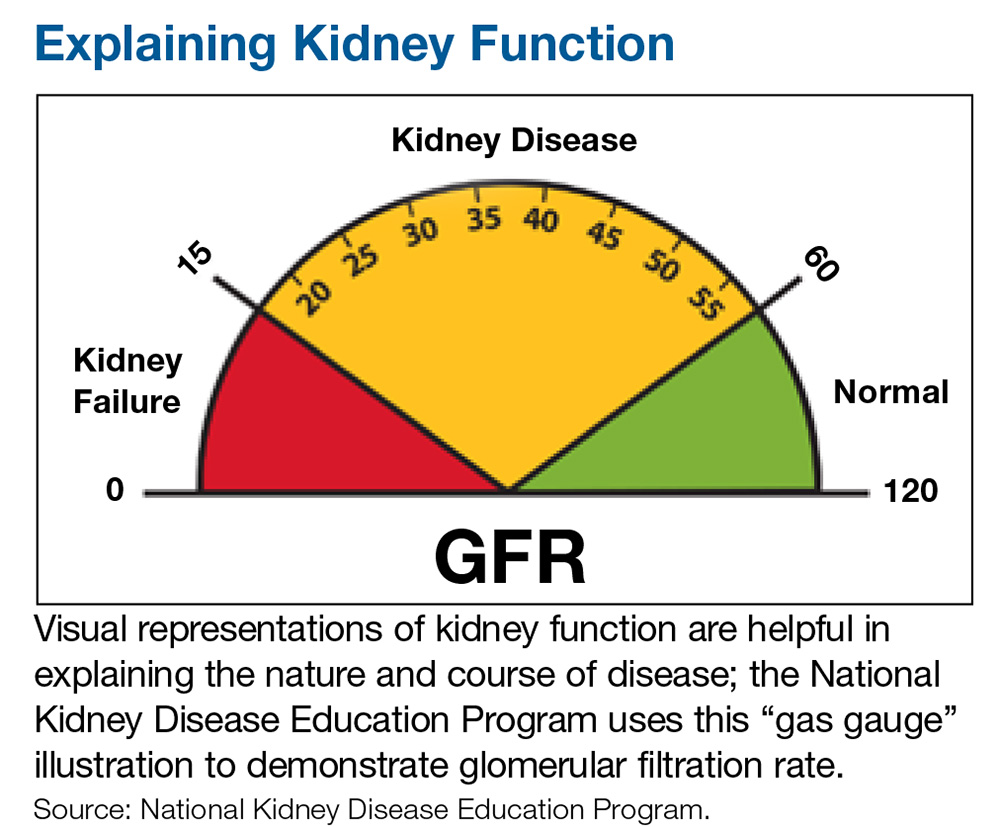
CONCLUSION
The results that the IHS achieved should serve as an example for all Americans with diabetes and their health care providers. We must be open to delivery of care via different approaches and practitioners in order to successfully help patients of different backgrounds and circumstances. This is the individualization of care that we hear so much about.
In 2016, the costs of caring for the kidney failure population were greater than the entire budget of the NIH. By aggressively identifying and treating patients at risk for kidney failure, we can slow disease progression—saving society money, but more importantly allowing our patients many more years of life free from the constraints of dialysis. —MET, RB
Mandy E. Thompson, PA-C
Kidney Center of Denver Health
Robin Bassett, DNP
Nephrology and Hypertension Associates, Anchorage
Adjunct Professor, NP program, University of Alaska, Anchorage
Alaska is a vast state—larger than Texas, Montana, and California combined. It is also home to the highest percentage of American Indian (AI) and Alaska Native (AN) persons in the United States. These two populations—collectively referred to as Native Americans—have been served by the Indian Health Services (IHS) since it was established through the Snyder Act of 1921, in response to the dismal health conditions of the indigenous tribes in this country.1 Across the US (not only in Alaska), the IHS has partnered with AI/AN peoples to decrease health disparities in a culturally acceptable manner that honors and protects their traditions and values.
The IHS—which in 2016 comprised 2,500 nurses, 750 physicians, 700 pharmacists, 200 PAs and NPs, and 280 dentists, as well as nutritionists, diabetes educators, administrators, and other professionals—has made huge advances in decreasing health disparities in their populations. Among them: decreased rates of tuberculosis and of maternal and infant deaths.
However, life expectancy among Native Americans remains four years shorter than that of the rest of the US population. This disparity can be traced to three recalcitrant factors: unintentional injuries, liver disease, and diabetes.
The IHS practitioners decided to tackle diabetes with a multipronged approach. And what they achieved is astonishing.
WHAT THEY DID
Worldwide, diabetes is the most common cause of kidney failure; identifying patients with diabetes and early-stage chronic kidney disease allows for aggressive treatment that can slow progression to kidney failure and dialysis.
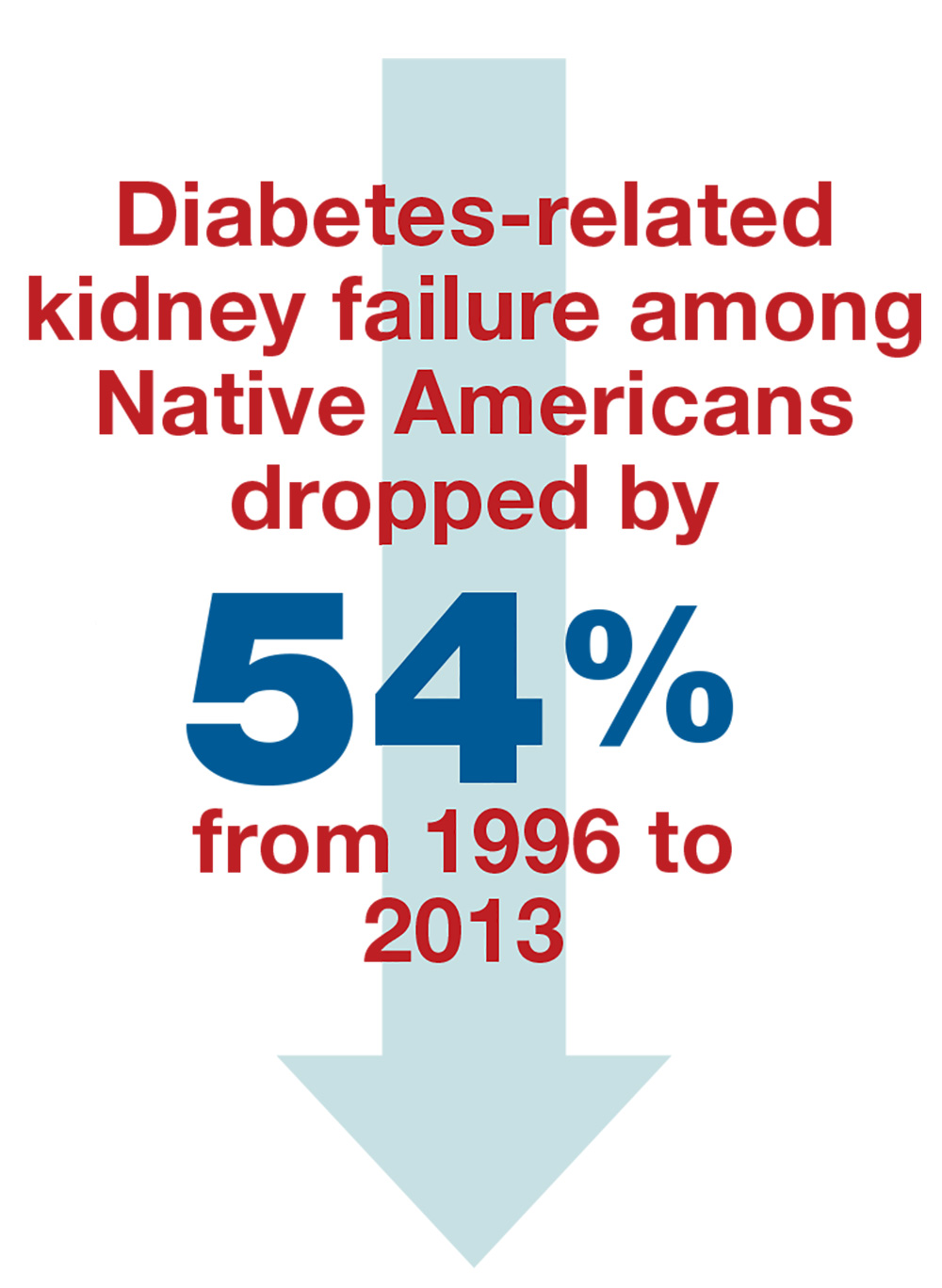
The IHS providers knew when they decided to tackle the problem of diabetes in the AI/AN population that the incidence was 16%—and the rate of diabetes leading to kidney failure in this population was the highest for any ethnic group in the US.2,3 And yet …
From 1996 to 2013, the rate of diabetes-related kidney failure among Native Americans dropped by 54%.3 Yes—the group of patients with the highest percentage of diabetes diagnoses has had the greatest improvement in prevention of kidney failure.4
Continue to: Some of the clinical achievements that contributed to...
Some of the clinical achievements that contributed to this significant change include
- Increased use of ACE inhibitors or angiotensin receptor blockers (ARBs) (from 42% to 74% over a five-year period)
- Reduced average blood pressure among hypertensive patients (to 133/76 mm Hg)
- Improved blood glucose control (by 10%)
- Increased testing for kidney disease among older patients (50% higher than the rest of the Medicare diabetes population).3
HOW THEY DID IT
This is not rocket science. The IHS staff integrated both population- and team-based approaches to achieve a more impressive decrease than ever could have been expected. In retrospect, perhaps this success should not come as such a surprise—many religious beliefs held by Native Americans focus around society, communal harmony, kinship, and cooperation.
The population health approach focused on promoting the wellness of the entire community and connecting people to local resources, including healthy food, transportation, housing, and mental health care. In the team approach, IHS medical experts implemented strategies to improve patient education, community outreach, care coordination, health outcome tracking, and access to a wide variety of health care providers.3,5
In a place like Alaska—where the northernmost city, Barrow, is more than 700 miles (two hours by plane) from Anchorage, and the southeastern Annette Island is more than 1,000 miles (six hours by plane) from the capital—this can be an especially challenging prospect. To reduce travel burden for rural patients, the IHS sponsors a diabetes team that travels from village to village. Nephrology services are not included in these field visits, however, so the kidney team relies heavily on telehealth. This requires extensive clinic staff coordination, as well as equipment and knowledgeable information systems support teams.
Other challenges require educational and logistical solutions. As noted, the use of ACE inhibitors and ARBs increased through the IHS’s efforts—and contributed to the delayed progression of diabetic kidney disease—but those additional prescriptions necessitate patient education. Understanding of these medications can be limited; many rural patients trust that when the bottle is empty, their practitioner has treated and cured their disease—mistakenly believing that no refills are needed. And even when the need to continue the prescription is understood, rural clinics may have difficulty tracking appointments and prescriptions written by providers at specialty clinics in Anchorage, making ongoing refills an issue.
Continue to: The necessary dietary changes can also be...
The necessary dietary changes can also be difficult for AI/AN populations. For example, in rural Alaska, tap water may not be safe to drink, and soda costs less than bottled water. Fresh produce is expensive and has often begun to spoil by the time it reaches local stores. The Native villagers often prefer their usual diets of gathered berries, fish, and red meat from subsistence hunting, making implementation of dietary changes difficult.
However, as the success of the IHS initiative shows, challenges can be met and overcome by practitioners who see a need, formulate a solution individualized to the circumstance, and think outside the box. One of the keys is developing a trusting relationship with patients. Another is to recognize informational needs and utilize available resources to educate patients. For example, visual representations of kidney function tend to be helpful in explaining the nature and course of disease; the National Kidney Disease Education Program uses an illustration similar to a gas gauge to demonstrate glomerular filtration rate (which would otherwise seem abstract and hard to understand for some patients; see below).6 When you understand your patient population and their needs, it makes addressing the challenging aspects of health care and prevention easier.
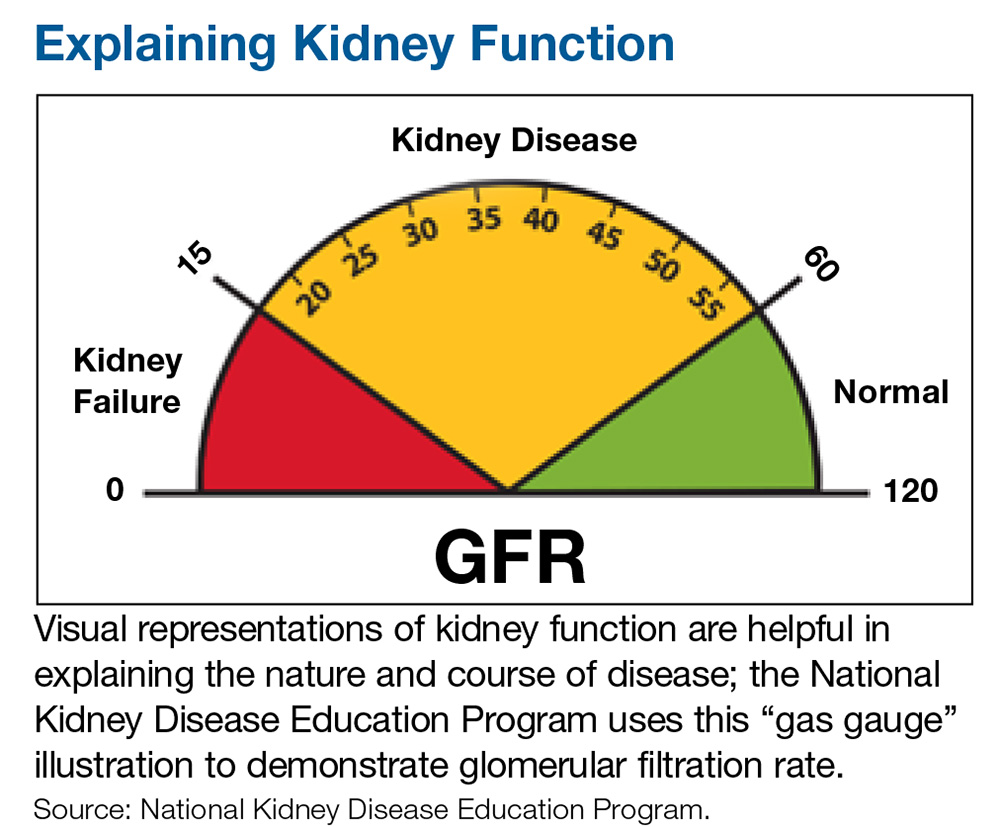
CONCLUSION
The results that the IHS achieved should serve as an example for all Americans with diabetes and their health care providers. We must be open to delivery of care via different approaches and practitioners in order to successfully help patients of different backgrounds and circumstances. This is the individualization of care that we hear so much about.
In 2016, the costs of caring for the kidney failure population were greater than the entire budget of the NIH. By aggressively identifying and treating patients at risk for kidney failure, we can slow disease progression—saving society money, but more importantly allowing our patients many more years of life free from the constraints of dialysis. —MET, RB
Mandy E. Thompson, PA-C
Kidney Center of Denver Health
Robin Bassett, DNP
Nephrology and Hypertension Associates, Anchorage
Adjunct Professor, NP program, University of Alaska, Anchorage
1. Indian Health Service. Legislation. www.ihs.gov/aboutihs/legislation. Accessed June 13, 2018.
2. National Health Interview Survey and Indian Health Service, 2010-2012.
3. CDC. Native Americans with diabetes. www.cdc.gov/vitalsigns/aian-diabetes/. Accessed June 13, 2018.
4. United States Renal Data System. Figure 1.5: Trends in adjusted* ESRD incidence rate (per million/year), by race, in the U.S. population, 1996-2014. In: 2016 USRDS annual data report: Epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2016.
5. Indian Health Service. Special diabetes program for Indians. www.ihs.gov/newsroom/factsheets/diabetes. Accessed June 13, 2018.
6. National Kidney Disease Education Program. How well are your kidneys working? Explaining your kidney test results. www.niddk.nih.gov/health-information/professionals/clinical-tools-patient-education-outreach/explain-kidney-test-results. Accessed June 13, 2018.
1. Indian Health Service. Legislation. www.ihs.gov/aboutihs/legislation. Accessed June 13, 2018.
2. National Health Interview Survey and Indian Health Service, 2010-2012.
3. CDC. Native Americans with diabetes. www.cdc.gov/vitalsigns/aian-diabetes/. Accessed June 13, 2018.
4. United States Renal Data System. Figure 1.5: Trends in adjusted* ESRD incidence rate (per million/year), by race, in the U.S. population, 1996-2014. In: 2016 USRDS annual data report: Epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2016.
5. Indian Health Service. Special diabetes program for Indians. www.ihs.gov/newsroom/factsheets/diabetes. Accessed June 13, 2018.
6. National Kidney Disease Education Program. How well are your kidneys working? Explaining your kidney test results. www.niddk.nih.gov/health-information/professionals/clinical-tools-patient-education-outreach/explain-kidney-test-results. Accessed June 13, 2018.