User login
Why do people act that way?
You can try all you want, but you never really figure people out.
Take Brendan. He spent a good few minutes chewing out my front desk staffer Linda. “You’re incompetent!” he shouted at her.
Linda tried to explain. “We can’t administer the Botox for your sweating today,” she said, “because it hasn’t come in yet.”
No, Brendan certainly didn’t want to hear that. Nor did he want to hear that we had called in advance to ask him to actually wait until we let him know that the Botox was in. But here he was, hyperinflating his lungs.
“You’re just damned useless!” he explained.
OK, we all have unreasonable patients from time to time. But what I’m describing is behavior that’s not just aggressive and unpleasant but incomprehensible. Would you like to know why I call it incomprehensible?
Because Brendan has been coming in for axillary Botox injections every 6 months for 5 years! He knows the drill. He knows the staff. He’s always pleasant as punch. Just not today. Why? Who knows?
What’s true for patients can of course also be true for employees. Model workers, superb team players, reliable folks who show up in snowstorms, who come right back to work after major surgery, who deliver heartfelt speeches at holiday parties about their good luck in overcoming adversity to be able to work. Contributors who share their pleasant disposition and can-do energy year after year ...
Until one day that they don’t show up, send a text to say they quit, no warning or explanation, then apply for Workmen’s Compensation, and at the magistrate’s hearing to which they’ve dragged my staff and our HR attorney, lie right to the face of the manager who was their best friend and confidante until the day before yesterday.
Get it? I don’t. Never will.
Two pieces of advice: 1) Don’t ever take things like that personally; and 2) Hire a good human resources attorney.
**********************
On the other hand ...
Jeralyn is 27 years old. She lists her chief complaint as “dark spots on my back.”
“How did you notice these?” I ask. “Did you see them, or did you doctor point them out?”
“It was when I tried on my wedding dress,” she says.
I understand, or think I do. Her dress exposed her back, her mother noticed the spots ...
“When is the wedding?” I ask.
“The wedding? Oh, the wedding already was. A year and a half ago.”
“You saw the spots when you tried on your wedding dress, and you’re coming in a year and half later?” I ask, trying not to sound incredulous. I’ve met enough nervous brides – and brides’ mothers – to find her account astonishing. “You must be a very patient person,” I say.
“Well,” says Jeralyn, “the spots didn’t spread or get any worse. And I am patient. I teach kindergarten. You have to be patient with little ones.”
“If you decide to have children, they’ll benefit from that,” I reply.
“That’s actually why I’m here,” says Jeralyn. “My husband and I want to start a family, and we want to be sure my skin condition wouldn’t affect that.”
A bride so unconcerned with herself that she wears a wedding dress that reveals a rash she doesn’t go running to a doctor to fix? Who comes only when the rash might affect someone else?
What is the matter with Jeralyn? Doesn’t she know she’s a millennial?
**********************
Kidding aside, wouldn’t it be nice if everyone acted like Jeralyn, and acted in a measured manner, appropriate to the concerns and circumstances? Wouldn’t it be nice if no one acted like Brendan?
That’s not how it is, though, is it? As professionals who deal with the public (as patients, coworkers, employees), we take all comers and roll with them: tolerate the annoyances and celebrate the (much larger, if less individually memorable) group who are pleasant, often delightful, sometimes inspiring.
And every once in a while, someone like Jeralyn comes along, upending all those negative expectations and reminding us that even if you can never really figure people out, it’s still worth the effort to keep trying.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at [email protected].
You can try all you want, but you never really figure people out.
Take Brendan. He spent a good few minutes chewing out my front desk staffer Linda. “You’re incompetent!” he shouted at her.
Linda tried to explain. “We can’t administer the Botox for your sweating today,” she said, “because it hasn’t come in yet.”
No, Brendan certainly didn’t want to hear that. Nor did he want to hear that we had called in advance to ask him to actually wait until we let him know that the Botox was in. But here he was, hyperinflating his lungs.
“You’re just damned useless!” he explained.
OK, we all have unreasonable patients from time to time. But what I’m describing is behavior that’s not just aggressive and unpleasant but incomprehensible. Would you like to know why I call it incomprehensible?
Because Brendan has been coming in for axillary Botox injections every 6 months for 5 years! He knows the drill. He knows the staff. He’s always pleasant as punch. Just not today. Why? Who knows?
What’s true for patients can of course also be true for employees. Model workers, superb team players, reliable folks who show up in snowstorms, who come right back to work after major surgery, who deliver heartfelt speeches at holiday parties about their good luck in overcoming adversity to be able to work. Contributors who share their pleasant disposition and can-do energy year after year ...
Until one day that they don’t show up, send a text to say they quit, no warning or explanation, then apply for Workmen’s Compensation, and at the magistrate’s hearing to which they’ve dragged my staff and our HR attorney, lie right to the face of the manager who was their best friend and confidante until the day before yesterday.
Get it? I don’t. Never will.
Two pieces of advice: 1) Don’t ever take things like that personally; and 2) Hire a good human resources attorney.
**********************
On the other hand ...
Jeralyn is 27 years old. She lists her chief complaint as “dark spots on my back.”
“How did you notice these?” I ask. “Did you see them, or did you doctor point them out?”
“It was when I tried on my wedding dress,” she says.
I understand, or think I do. Her dress exposed her back, her mother noticed the spots ...
“When is the wedding?” I ask.
“The wedding? Oh, the wedding already was. A year and a half ago.”
“You saw the spots when you tried on your wedding dress, and you’re coming in a year and half later?” I ask, trying not to sound incredulous. I’ve met enough nervous brides – and brides’ mothers – to find her account astonishing. “You must be a very patient person,” I say.
“Well,” says Jeralyn, “the spots didn’t spread or get any worse. And I am patient. I teach kindergarten. You have to be patient with little ones.”
“If you decide to have children, they’ll benefit from that,” I reply.
“That’s actually why I’m here,” says Jeralyn. “My husband and I want to start a family, and we want to be sure my skin condition wouldn’t affect that.”
A bride so unconcerned with herself that she wears a wedding dress that reveals a rash she doesn’t go running to a doctor to fix? Who comes only when the rash might affect someone else?
What is the matter with Jeralyn? Doesn’t she know she’s a millennial?
**********************
Kidding aside, wouldn’t it be nice if everyone acted like Jeralyn, and acted in a measured manner, appropriate to the concerns and circumstances? Wouldn’t it be nice if no one acted like Brendan?
That’s not how it is, though, is it? As professionals who deal with the public (as patients, coworkers, employees), we take all comers and roll with them: tolerate the annoyances and celebrate the (much larger, if less individually memorable) group who are pleasant, often delightful, sometimes inspiring.
And every once in a while, someone like Jeralyn comes along, upending all those negative expectations and reminding us that even if you can never really figure people out, it’s still worth the effort to keep trying.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at [email protected].
You can try all you want, but you never really figure people out.
Take Brendan. He spent a good few minutes chewing out my front desk staffer Linda. “You’re incompetent!” he shouted at her.
Linda tried to explain. “We can’t administer the Botox for your sweating today,” she said, “because it hasn’t come in yet.”
No, Brendan certainly didn’t want to hear that. Nor did he want to hear that we had called in advance to ask him to actually wait until we let him know that the Botox was in. But here he was, hyperinflating his lungs.
“You’re just damned useless!” he explained.
OK, we all have unreasonable patients from time to time. But what I’m describing is behavior that’s not just aggressive and unpleasant but incomprehensible. Would you like to know why I call it incomprehensible?
Because Brendan has been coming in for axillary Botox injections every 6 months for 5 years! He knows the drill. He knows the staff. He’s always pleasant as punch. Just not today. Why? Who knows?
What’s true for patients can of course also be true for employees. Model workers, superb team players, reliable folks who show up in snowstorms, who come right back to work after major surgery, who deliver heartfelt speeches at holiday parties about their good luck in overcoming adversity to be able to work. Contributors who share their pleasant disposition and can-do energy year after year ...
Until one day that they don’t show up, send a text to say they quit, no warning or explanation, then apply for Workmen’s Compensation, and at the magistrate’s hearing to which they’ve dragged my staff and our HR attorney, lie right to the face of the manager who was their best friend and confidante until the day before yesterday.
Get it? I don’t. Never will.
Two pieces of advice: 1) Don’t ever take things like that personally; and 2) Hire a good human resources attorney.
**********************
On the other hand ...
Jeralyn is 27 years old. She lists her chief complaint as “dark spots on my back.”
“How did you notice these?” I ask. “Did you see them, or did you doctor point them out?”
“It was when I tried on my wedding dress,” she says.
I understand, or think I do. Her dress exposed her back, her mother noticed the spots ...
“When is the wedding?” I ask.
“The wedding? Oh, the wedding already was. A year and a half ago.”
“You saw the spots when you tried on your wedding dress, and you’re coming in a year and half later?” I ask, trying not to sound incredulous. I’ve met enough nervous brides – and brides’ mothers – to find her account astonishing. “You must be a very patient person,” I say.
“Well,” says Jeralyn, “the spots didn’t spread or get any worse. And I am patient. I teach kindergarten. You have to be patient with little ones.”
“If you decide to have children, they’ll benefit from that,” I reply.
“That’s actually why I’m here,” says Jeralyn. “My husband and I want to start a family, and we want to be sure my skin condition wouldn’t affect that.”
A bride so unconcerned with herself that she wears a wedding dress that reveals a rash she doesn’t go running to a doctor to fix? Who comes only when the rash might affect someone else?
What is the matter with Jeralyn? Doesn’t she know she’s a millennial?
**********************
Kidding aside, wouldn’t it be nice if everyone acted like Jeralyn, and acted in a measured manner, appropriate to the concerns and circumstances? Wouldn’t it be nice if no one acted like Brendan?
That’s not how it is, though, is it? As professionals who deal with the public (as patients, coworkers, employees), we take all comers and roll with them: tolerate the annoyances and celebrate the (much larger, if less individually memorable) group who are pleasant, often delightful, sometimes inspiring.
And every once in a while, someone like Jeralyn comes along, upending all those negative expectations and reminding us that even if you can never really figure people out, it’s still worth the effort to keep trying.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at [email protected].
Treating female-to-male transgender adolescents with acne presents unique concerns with depression
according to the results of a case series.
“Acne is a foreseeable adverse effect of testosterone treatment in transgender adolescents, and it may be advisable that, once such treatment has begun, they be monitored for the appearance of acne,” Lucia Campos-Munoz, MD, of the Hospital Clinico San Carlos in Madrid wrote in Pediatric Dermatology. “Even if only mild, treatment should be provided.”
Dr. Campos-Munoz and her colleagues examined five female-to-male transgender patients who were admitted to their clinic from 2016-2017. All five patients presented with testosterone-associated acne. Two patients with severe acne were treated with 20 mg/day of isotretinoin. While one patient tolerated this well and discontinued treatment after 4 months, another patient stopped treatment because of a bout of depression at 3 months. The remaining patients received other treatments, including doxycycline, 0.05 topical tretinoin, and 3% benzoyl peroxide.
This case study highlights the unique role that dermatologists and primary care providers play in treating acne in female-to-male transgender patients. Using the proper pronouns and recognizing that physical examinations of the chest and thorax may be especially embarrassing for these patients are important considerations, according to Dr. Campos-Munoz and her colleagues. Also, neither antiandrogenic agents nor contraceptives can be given because “this would conflict with the masculinization sought.”
Apart from being aware of the patients’ feelings, there are real medical concerns associated with dermatologic treatment of acne in female-to-male transgender patients. One of these risks is depression, which several studies have shown to be associated with severe acne. This is compounded by higher rates of depression and suicidal ideation in transgender adolescents, they said.
An additional concern is the teratogenic effects of isotretinoin in patients with natal female internal genitalia. While these patients may not think they can get pregnant because of testosterone-associated amenorrhea, the potential is still present and pregnancy should be avoided, Dr. Campos-Munoz and her colleagues warned.
No funding or conflicts of interest were disclosed.
SOURCE: Campos-Munoz L et al. Pediatr Dermatol. 2018 Mar 25. doi: 10.1111/pde.13448.
according to the results of a case series.
“Acne is a foreseeable adverse effect of testosterone treatment in transgender adolescents, and it may be advisable that, once such treatment has begun, they be monitored for the appearance of acne,” Lucia Campos-Munoz, MD, of the Hospital Clinico San Carlos in Madrid wrote in Pediatric Dermatology. “Even if only mild, treatment should be provided.”
Dr. Campos-Munoz and her colleagues examined five female-to-male transgender patients who were admitted to their clinic from 2016-2017. All five patients presented with testosterone-associated acne. Two patients with severe acne were treated with 20 mg/day of isotretinoin. While one patient tolerated this well and discontinued treatment after 4 months, another patient stopped treatment because of a bout of depression at 3 months. The remaining patients received other treatments, including doxycycline, 0.05 topical tretinoin, and 3% benzoyl peroxide.
This case study highlights the unique role that dermatologists and primary care providers play in treating acne in female-to-male transgender patients. Using the proper pronouns and recognizing that physical examinations of the chest and thorax may be especially embarrassing for these patients are important considerations, according to Dr. Campos-Munoz and her colleagues. Also, neither antiandrogenic agents nor contraceptives can be given because “this would conflict with the masculinization sought.”
Apart from being aware of the patients’ feelings, there are real medical concerns associated with dermatologic treatment of acne in female-to-male transgender patients. One of these risks is depression, which several studies have shown to be associated with severe acne. This is compounded by higher rates of depression and suicidal ideation in transgender adolescents, they said.
An additional concern is the teratogenic effects of isotretinoin in patients with natal female internal genitalia. While these patients may not think they can get pregnant because of testosterone-associated amenorrhea, the potential is still present and pregnancy should be avoided, Dr. Campos-Munoz and her colleagues warned.
No funding or conflicts of interest were disclosed.
SOURCE: Campos-Munoz L et al. Pediatr Dermatol. 2018 Mar 25. doi: 10.1111/pde.13448.
according to the results of a case series.
“Acne is a foreseeable adverse effect of testosterone treatment in transgender adolescents, and it may be advisable that, once such treatment has begun, they be monitored for the appearance of acne,” Lucia Campos-Munoz, MD, of the Hospital Clinico San Carlos in Madrid wrote in Pediatric Dermatology. “Even if only mild, treatment should be provided.”
Dr. Campos-Munoz and her colleagues examined five female-to-male transgender patients who were admitted to their clinic from 2016-2017. All five patients presented with testosterone-associated acne. Two patients with severe acne were treated with 20 mg/day of isotretinoin. While one patient tolerated this well and discontinued treatment after 4 months, another patient stopped treatment because of a bout of depression at 3 months. The remaining patients received other treatments, including doxycycline, 0.05 topical tretinoin, and 3% benzoyl peroxide.
This case study highlights the unique role that dermatologists and primary care providers play in treating acne in female-to-male transgender patients. Using the proper pronouns and recognizing that physical examinations of the chest and thorax may be especially embarrassing for these patients are important considerations, according to Dr. Campos-Munoz and her colleagues. Also, neither antiandrogenic agents nor contraceptives can be given because “this would conflict with the masculinization sought.”
Apart from being aware of the patients’ feelings, there are real medical concerns associated with dermatologic treatment of acne in female-to-male transgender patients. One of these risks is depression, which several studies have shown to be associated with severe acne. This is compounded by higher rates of depression and suicidal ideation in transgender adolescents, they said.
An additional concern is the teratogenic effects of isotretinoin in patients with natal female internal genitalia. While these patients may not think they can get pregnant because of testosterone-associated amenorrhea, the potential is still present and pregnancy should be avoided, Dr. Campos-Munoz and her colleagues warned.
No funding or conflicts of interest were disclosed.
SOURCE: Campos-Munoz L et al. Pediatr Dermatol. 2018 Mar 25. doi: 10.1111/pde.13448.
FROM PEDIATRIC DERMATOLOGY
Key clinical point: Being transgender and severe acne both are related to higher rates of depression and suicide.
Major finding: In the case study, one of the five patients discontinued use of isotretinoin because of a bout of depression.
Study details: A 2016-2017 case series of five female-to-male transgender adolescents (aged 16-18 years) who had testosterone-associated acne.
Disclosures: No funding or conflicts of interest were disclosed.
Source: Campos-Munoz L et al. Pediatr Dermatol. 2018 Mar 25. doi: 10.1111/pde.13448.
Winners chosen at the SHM Clinical Vignettes competition
ORLANDO – Researchers presenting a case of starving ketoacidosis in a woman who was on a “Paleo” diet while breastfeeding won the Clinical Vignettes competition held Monday at HM18. The announcement capped a flurry of presenting and judging of posters on single cases that were captivating in both the stories they told and the lessons they taught.
The trainee award winner in the competition were presenters of a case of licorice-induced hypokalemia that, clinicians learned, was brought about by the drinking of an obscure kind of tea. The two others that made it into the final round of judging were on cases of syphilitic hepatitis and cardiac amyloidosis.
By chance, both of the winners highlighted dietary triggers, said Stephanie Sherman, MD, chair of the annual meeting’s clinical vignettes committee.
“The common themes in both of these were the importance of dietary history when interviewing patients,” Dr. Sherman said. “And then both had a beautiful review of the physiology that’s normal and how it gets broken in these situations.”
The Clinical Vignettes portion of the RIV competition, which also includes research and innovations categories, was separate this year because of space constraints, Dr. Sherman said.
Judges said they looked not only at how interesting and applicable each case was, but also the quality of the oral presentation and the poster’s visual appeal and clarity.
The ketoacidosis case, presented by Timothy Judson, MD, a resident at University of California, San Francisco, involved a 40-year-old woman who was previously healthy and had given birth 9 weeks earlier. Since the birth, the woman had been on a Paleo diet, a low-carbohydrate, ketogenic diet. She also was breastfeeding her newborn and continuing to breastfeed her 2-year-old son.
She presented with nonbilious, nonbloody emesis. On physical exam, she was found to be tachycardic, with diffuse tenderness of the abdomen. She was positive for ketones and had an elevated acetone level and elevated osmolar gap, the difference between the measured and calculated solutes in the serum.
Clinicians identified that low carbohydrate intake, high fat intake, and a high metabolic state, such as that brought on by breastfeeding, can contribute to ketoacidosis. She was treated with IV glucose-containing fluids, bicarbonate, fomepizole, and thiamine.
The case shows that patients should be warned about ketoacidosis risk when they start an ultra-low carbohydrate diet, especially if they are breastfeeding or lactating, Dr. Hudson said.
“Usually they’re safe, but they may not be if you’re in a high metabolic state,” he told judges.
“We take care of so many patients on a daily basis and we rarely get to tell their stories,” he said. “To be able to tell the story of the patients and give the learning points that we took away to others, I think is very rewarding.”
The winner of the trainee award, Maxwell Bressman, MD, a resident at Montefiore Medical Center in New York, presented the case of a 62-year-old woman with hypertension who had profound generalized weakness and an inability to walk.
“She actually came to the hospital because she couldn’t lift a cup of tea,” Dr. Bressman told judges.
Clinicians traced her problem to that very tea – a licorice-containing brew – after an ECG indicated hypokalemia. A breakdown product of licorice, glycyrrhizic acid, can prevent the breakdown of cortisol into cortisone, causing increased absorption of sodium in exchange for potassium, he explained.
“I really like interesting cases – it’s something I’ve thought about throughout medical school,” Dr. Bressman said. “It’s been incredibly fun. We have great cases at Montefiore. ... It’s taught me to think very broadly and with an expansive differential.”
ORLANDO – Researchers presenting a case of starving ketoacidosis in a woman who was on a “Paleo” diet while breastfeeding won the Clinical Vignettes competition held Monday at HM18. The announcement capped a flurry of presenting and judging of posters on single cases that were captivating in both the stories they told and the lessons they taught.
The trainee award winner in the competition were presenters of a case of licorice-induced hypokalemia that, clinicians learned, was brought about by the drinking of an obscure kind of tea. The two others that made it into the final round of judging were on cases of syphilitic hepatitis and cardiac amyloidosis.
By chance, both of the winners highlighted dietary triggers, said Stephanie Sherman, MD, chair of the annual meeting’s clinical vignettes committee.
“The common themes in both of these were the importance of dietary history when interviewing patients,” Dr. Sherman said. “And then both had a beautiful review of the physiology that’s normal and how it gets broken in these situations.”
The Clinical Vignettes portion of the RIV competition, which also includes research and innovations categories, was separate this year because of space constraints, Dr. Sherman said.
Judges said they looked not only at how interesting and applicable each case was, but also the quality of the oral presentation and the poster’s visual appeal and clarity.
The ketoacidosis case, presented by Timothy Judson, MD, a resident at University of California, San Francisco, involved a 40-year-old woman who was previously healthy and had given birth 9 weeks earlier. Since the birth, the woman had been on a Paleo diet, a low-carbohydrate, ketogenic diet. She also was breastfeeding her newborn and continuing to breastfeed her 2-year-old son.
She presented with nonbilious, nonbloody emesis. On physical exam, she was found to be tachycardic, with diffuse tenderness of the abdomen. She was positive for ketones and had an elevated acetone level and elevated osmolar gap, the difference between the measured and calculated solutes in the serum.
Clinicians identified that low carbohydrate intake, high fat intake, and a high metabolic state, such as that brought on by breastfeeding, can contribute to ketoacidosis. She was treated with IV glucose-containing fluids, bicarbonate, fomepizole, and thiamine.
The case shows that patients should be warned about ketoacidosis risk when they start an ultra-low carbohydrate diet, especially if they are breastfeeding or lactating, Dr. Hudson said.
“Usually they’re safe, but they may not be if you’re in a high metabolic state,” he told judges.
“We take care of so many patients on a daily basis and we rarely get to tell their stories,” he said. “To be able to tell the story of the patients and give the learning points that we took away to others, I think is very rewarding.”
The winner of the trainee award, Maxwell Bressman, MD, a resident at Montefiore Medical Center in New York, presented the case of a 62-year-old woman with hypertension who had profound generalized weakness and an inability to walk.
“She actually came to the hospital because she couldn’t lift a cup of tea,” Dr. Bressman told judges.
Clinicians traced her problem to that very tea – a licorice-containing brew – after an ECG indicated hypokalemia. A breakdown product of licorice, glycyrrhizic acid, can prevent the breakdown of cortisol into cortisone, causing increased absorption of sodium in exchange for potassium, he explained.
“I really like interesting cases – it’s something I’ve thought about throughout medical school,” Dr. Bressman said. “It’s been incredibly fun. We have great cases at Montefiore. ... It’s taught me to think very broadly and with an expansive differential.”
ORLANDO – Researchers presenting a case of starving ketoacidosis in a woman who was on a “Paleo” diet while breastfeeding won the Clinical Vignettes competition held Monday at HM18. The announcement capped a flurry of presenting and judging of posters on single cases that were captivating in both the stories they told and the lessons they taught.
The trainee award winner in the competition were presenters of a case of licorice-induced hypokalemia that, clinicians learned, was brought about by the drinking of an obscure kind of tea. The two others that made it into the final round of judging were on cases of syphilitic hepatitis and cardiac amyloidosis.
By chance, both of the winners highlighted dietary triggers, said Stephanie Sherman, MD, chair of the annual meeting’s clinical vignettes committee.
“The common themes in both of these were the importance of dietary history when interviewing patients,” Dr. Sherman said. “And then both had a beautiful review of the physiology that’s normal and how it gets broken in these situations.”
The Clinical Vignettes portion of the RIV competition, which also includes research and innovations categories, was separate this year because of space constraints, Dr. Sherman said.
Judges said they looked not only at how interesting and applicable each case was, but also the quality of the oral presentation and the poster’s visual appeal and clarity.
The ketoacidosis case, presented by Timothy Judson, MD, a resident at University of California, San Francisco, involved a 40-year-old woman who was previously healthy and had given birth 9 weeks earlier. Since the birth, the woman had been on a Paleo diet, a low-carbohydrate, ketogenic diet. She also was breastfeeding her newborn and continuing to breastfeed her 2-year-old son.
She presented with nonbilious, nonbloody emesis. On physical exam, she was found to be tachycardic, with diffuse tenderness of the abdomen. She was positive for ketones and had an elevated acetone level and elevated osmolar gap, the difference between the measured and calculated solutes in the serum.
Clinicians identified that low carbohydrate intake, high fat intake, and a high metabolic state, such as that brought on by breastfeeding, can contribute to ketoacidosis. She was treated with IV glucose-containing fluids, bicarbonate, fomepizole, and thiamine.
The case shows that patients should be warned about ketoacidosis risk when they start an ultra-low carbohydrate diet, especially if they are breastfeeding or lactating, Dr. Hudson said.
“Usually they’re safe, but they may not be if you’re in a high metabolic state,” he told judges.
“We take care of so many patients on a daily basis and we rarely get to tell their stories,” he said. “To be able to tell the story of the patients and give the learning points that we took away to others, I think is very rewarding.”
The winner of the trainee award, Maxwell Bressman, MD, a resident at Montefiore Medical Center in New York, presented the case of a 62-year-old woman with hypertension who had profound generalized weakness and an inability to walk.
“She actually came to the hospital because she couldn’t lift a cup of tea,” Dr. Bressman told judges.
Clinicians traced her problem to that very tea – a licorice-containing brew – after an ECG indicated hypokalemia. A breakdown product of licorice, glycyrrhizic acid, can prevent the breakdown of cortisol into cortisone, causing increased absorption of sodium in exchange for potassium, he explained.
“I really like interesting cases – it’s something I’ve thought about throughout medical school,” Dr. Bressman said. “It’s been incredibly fun. We have great cases at Montefiore. ... It’s taught me to think very broadly and with an expansive differential.”
REPORTING FROM HOSPITAL MEDICINE 2018
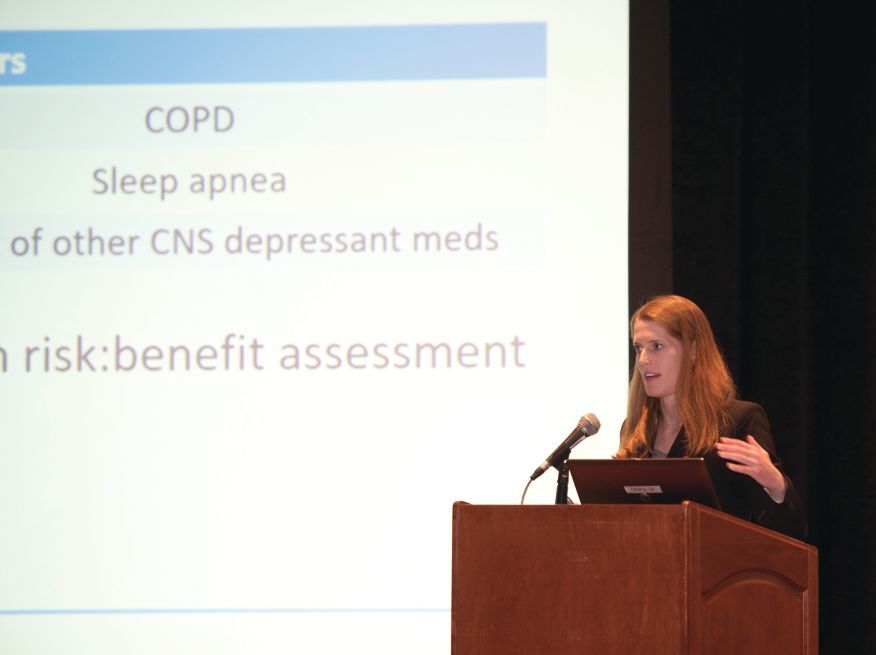
New guidance for inpatient opioid prescribing
ORLANDO – A new guidance statement for opioid prescribing for hospitalized adults who have acute noncancer pain has been issued by the Society for Hospital Medicine.
The statement comes after an exhaustive systematic review that found just four existing guidelines met inclusion criteria, though none focused specifically on acute pain in hospitalized adults.
Among the key issues taken from the existing guidelines and addressed in the new SHM guidance statement are deciding when opioids – or a nonopioid alternative – should be used, as well as selection of appropriate dose, route, and duration of administration. The guidance statement advises that clinicians prescribe the lowest effective opioid dose for the shortest duration possible.
Best practices for screening and monitoring before and during opioid initiation is another major focus, as is minimizing opioid-related adverse events, both by careful patient selection and by judicious prescribing.
Finally, the statement acknowledges that, when a discharge medication list includes an opioid prescription, there is potential risk for misuse or diversion. Accordingly, the recommendation is to limit the duration of outpatient prescribing to 7 days of medication, with consideration of a 3-5 day prescription.
An interactive session at the 2018 SHM annual meeting presenting the guidance statement focused less on marching through the guidance’s 16 specific statements, and more on teasing out the why, when, how – and how long – of inpatient opioid prescribing.
The well-attended session, led by two of the guideline authors, Shoshana Herzig, MD, MPH, and Teryl K. Nuckols, MD, FHM, began with Dr. Herzig, director of hospital medicine research at Beth Israel Deaconess Medical Center, Boston, making a compelling case for why guidance is needed for inpatient opioid prescribing for acute pain.
“Few would disagree that, at the end of the day, we are the final common pathway” for hospitalized patients who receive opioids, said Dr. Herzig. And there’s ample evidence that troublesome opioid prescribing is widespread, she said, adding that associated problems aren’t limited to such inpatient adverse events as falls, respiratory arrest, and acute kidney injury; plenty of opioid-exposed patients who leave the hospital continue to use opioids in problematic ways after discharge.
Of patients who were opioid naive and filled outpatient opioid prescriptions on discharge, “Almost half of patients were still using opioids 90 days later,” Dr. Herzig said. “Hospitals contribute to opioid initiation in millions of patients each year, so our prescribing patterns in the hospital do matter.”
“We tend to prescribe high doses,” said Dr. Herzig – an average of a 68-mg oral morphine equivalent (OME) dose on days that opioids were received, according to a 2014 study she coauthored. Overall, Dr. Herzig and her colleagues found that about 40% of patients who received opioids had a daily dose of at least 50 mg OME, and about a quarter received a daily dose at or exceeding 100 mg OME (Herzig et al. J Hosp Med. 2014 Feb;9[2]:73-81).
Further, she said, “We tend to prescribe a bit haphazardly.” The same study found wide variation in regional inpatient opioid-prescribing practices, with inpatients in the U.S. Midwest, South, and West seeing adjusted relative rates of exposure to opioids of 1.26, 1.33, and 1.37, compared with the Northeast, she said.
Among the more concerning findings, she said, was that “hospitals that prescribe opioids more frequently appear to do so less safely.” In hospitals that fell into the top quartile for inpatient opioid exposure, the overall rate of opioid-related adverse events was 0.39%, compared with 0.21% for hospitals in the bottom quartile of opioid prescribing, for an overall adjusted relative risk of 1.23 in opioid-exposed patients in the hospitals with the highest prescribing, said Dr. Herzig.
Dr. Nuckols, director of the division of general internal medicine at Cedars-Sinai Medical Center, Los Angeles, engaged attendees to identify challenges in acute pain management among hospitalized adults.
The audience was quick and prolific with answers, which included varying physician standards for opioid prescribing; patient expectations for pain management – and sometimes denial that opioid use has become a disorder; varying expectations for pain management among care team members who may be reluctant to let go of pain as “the fifth vital sign;” difficulty accessing and being reimbursed for nonpharmacologic strategies; and, acknowledged by all, patient satisfaction scores.
To this last point, Dr. Nuckols said that there have been “a few recent changes for the better.” The Joint Commission is revising its standards to move away from pain as a vital sign, toward a focused assessment of pain that considers how patients are responding to pain, as well as functional status. However, she said, “There aren’t any validated measures yet for how we’re going to do this.”
Similar shifts are underway with pain-related HCAHPS (the Hospital Consumer Assessment of Healthcare Providers and Systems) questions, which have undergone a “big pullback” from an emphasis on complete control of pain, and now put more focus on whether caregivers asked about pain and talked with inpatients about ways to treat pain, said Dr. Nuckols.
Speaking to the process of developing the guidance statement, Dr. Nuckols said that “I think it’s important to note that the empirical literature about managing pain for inpatients … is almost nonexistent.” Of the four criteria that met inclusion criteria – “and we were tough raters when it comes to the guidelines” – most were based on expert consensus, she said, and most had primarily an outpatient focus.
Themes that emerged from the review process included consideration of a nonopioid strategy before initiating an opioid. These might include pharmacologic interventions such as acetaminophen or a nonsteroidal anti-inflammatory for nociceptive pain, pregabalin, gabapentin, or other medication to manage neuropathic pain, or nonpharmacologic interventions such as heat, ice, or distraction. All of these should also be considered as adjuncts to minimize opioid dosing as well, said Dr. Nuckols, citing well-documented synergy with multiple modalities of pain treatment.
Careful patient selection is also key, said Dr. Nuckols. She noted that she asks herself, “How likely is this patient to get into trouble?” with inpatient opioid administration. A concept that goes hand-in-hand, she said, is choosing the appropriate dose and route.
Dr. Herzig picked up this theme, noting that route of administration matters. A speedy route, such as intravenous administration, has been shown to reinforce the potentially addictive effect of opioids. There are times when IV is the route to use, such as when the patient can’t take medication by mouth or when immediate pain control truly is needed. However, oral medication is just as effective, albeit slightly slower acting, she said.
Conversion from IV to oral opioids is a potential time for trouble, said Dr. Herzig. “Always use an opioid conversion chart,” she said. Cross-tolerance can be incomplete between opioids, so safe practice is to begin with about 50% of the OME dose with the new medication and titrate up. And don’t use a long-acting opioid for acute pain, she said, noting that not only will there be a long half-life and washout period if the dose is too high, but patient risk for later opioid use disorder is also upped with this strategy. “You can always add more, but it’s hard to take away,” said Dr. Herzig.
On discharge, consider whether an opioid should be prescribed at all, said Dr. Herzig. The guidance statement advises generally prescribing less than a 7-day supply, with the rationale that, if posthospitalization acute pain is severe enough to require an opioid at that point, the patient should have outpatient follow-up.
This approach doesn’t undertreat outpatient pain, said Dr. Herzig, pointing to studies that show that, at discharge, “the majority of opioids that patients are getting, they are not taking – which tells us that by definition we are overprescribing.”
The authors of the guidance statement wanted to address two important topics that were not sufficiently evidence backed, Dr. Herzig said. They had hoped to give clear guidance about best practices for communication and follow-up with outpatient providers after hospital discharge. Though they didn’t find clear guidance in this area, “We do believe that outpatient providers need to be kept in the loop.”
A second area, currently a hot button topic both in the medical community and in the lay press, is whether a naloxone prescription should accompany an opioid prescription at discharge. “There just aren’t studies for this,” said Dr. Herzig.
The full text of the guidance statement may be found here: https://www.journalofhospitalmedicine.com/jhospmed/article/161927/hospital-medicine/improving-safety-opioid-use-acute-noncancer-pain.
ORLANDO – A new guidance statement for opioid prescribing for hospitalized adults who have acute noncancer pain has been issued by the Society for Hospital Medicine.
The statement comes after an exhaustive systematic review that found just four existing guidelines met inclusion criteria, though none focused specifically on acute pain in hospitalized adults.
Among the key issues taken from the existing guidelines and addressed in the new SHM guidance statement are deciding when opioids – or a nonopioid alternative – should be used, as well as selection of appropriate dose, route, and duration of administration. The guidance statement advises that clinicians prescribe the lowest effective opioid dose for the shortest duration possible.
Best practices for screening and monitoring before and during opioid initiation is another major focus, as is minimizing opioid-related adverse events, both by careful patient selection and by judicious prescribing.
Finally, the statement acknowledges that, when a discharge medication list includes an opioid prescription, there is potential risk for misuse or diversion. Accordingly, the recommendation is to limit the duration of outpatient prescribing to 7 days of medication, with consideration of a 3-5 day prescription.
An interactive session at the 2018 SHM annual meeting presenting the guidance statement focused less on marching through the guidance’s 16 specific statements, and more on teasing out the why, when, how – and how long – of inpatient opioid prescribing.
The well-attended session, led by two of the guideline authors, Shoshana Herzig, MD, MPH, and Teryl K. Nuckols, MD, FHM, began with Dr. Herzig, director of hospital medicine research at Beth Israel Deaconess Medical Center, Boston, making a compelling case for why guidance is needed for inpatient opioid prescribing for acute pain.
“Few would disagree that, at the end of the day, we are the final common pathway” for hospitalized patients who receive opioids, said Dr. Herzig. And there’s ample evidence that troublesome opioid prescribing is widespread, she said, adding that associated problems aren’t limited to such inpatient adverse events as falls, respiratory arrest, and acute kidney injury; plenty of opioid-exposed patients who leave the hospital continue to use opioids in problematic ways after discharge.
Of patients who were opioid naive and filled outpatient opioid prescriptions on discharge, “Almost half of patients were still using opioids 90 days later,” Dr. Herzig said. “Hospitals contribute to opioid initiation in millions of patients each year, so our prescribing patterns in the hospital do matter.”
“We tend to prescribe high doses,” said Dr. Herzig – an average of a 68-mg oral morphine equivalent (OME) dose on days that opioids were received, according to a 2014 study she coauthored. Overall, Dr. Herzig and her colleagues found that about 40% of patients who received opioids had a daily dose of at least 50 mg OME, and about a quarter received a daily dose at or exceeding 100 mg OME (Herzig et al. J Hosp Med. 2014 Feb;9[2]:73-81).
Further, she said, “We tend to prescribe a bit haphazardly.” The same study found wide variation in regional inpatient opioid-prescribing practices, with inpatients in the U.S. Midwest, South, and West seeing adjusted relative rates of exposure to opioids of 1.26, 1.33, and 1.37, compared with the Northeast, she said.
Among the more concerning findings, she said, was that “hospitals that prescribe opioids more frequently appear to do so less safely.” In hospitals that fell into the top quartile for inpatient opioid exposure, the overall rate of opioid-related adverse events was 0.39%, compared with 0.21% for hospitals in the bottom quartile of opioid prescribing, for an overall adjusted relative risk of 1.23 in opioid-exposed patients in the hospitals with the highest prescribing, said Dr. Herzig.
Dr. Nuckols, director of the division of general internal medicine at Cedars-Sinai Medical Center, Los Angeles, engaged attendees to identify challenges in acute pain management among hospitalized adults.
The audience was quick and prolific with answers, which included varying physician standards for opioid prescribing; patient expectations for pain management – and sometimes denial that opioid use has become a disorder; varying expectations for pain management among care team members who may be reluctant to let go of pain as “the fifth vital sign;” difficulty accessing and being reimbursed for nonpharmacologic strategies; and, acknowledged by all, patient satisfaction scores.
To this last point, Dr. Nuckols said that there have been “a few recent changes for the better.” The Joint Commission is revising its standards to move away from pain as a vital sign, toward a focused assessment of pain that considers how patients are responding to pain, as well as functional status. However, she said, “There aren’t any validated measures yet for how we’re going to do this.”
Similar shifts are underway with pain-related HCAHPS (the Hospital Consumer Assessment of Healthcare Providers and Systems) questions, which have undergone a “big pullback” from an emphasis on complete control of pain, and now put more focus on whether caregivers asked about pain and talked with inpatients about ways to treat pain, said Dr. Nuckols.
Speaking to the process of developing the guidance statement, Dr. Nuckols said that “I think it’s important to note that the empirical literature about managing pain for inpatients … is almost nonexistent.” Of the four criteria that met inclusion criteria – “and we were tough raters when it comes to the guidelines” – most were based on expert consensus, she said, and most had primarily an outpatient focus.
Themes that emerged from the review process included consideration of a nonopioid strategy before initiating an opioid. These might include pharmacologic interventions such as acetaminophen or a nonsteroidal anti-inflammatory for nociceptive pain, pregabalin, gabapentin, or other medication to manage neuropathic pain, or nonpharmacologic interventions such as heat, ice, or distraction. All of these should also be considered as adjuncts to minimize opioid dosing as well, said Dr. Nuckols, citing well-documented synergy with multiple modalities of pain treatment.
Careful patient selection is also key, said Dr. Nuckols. She noted that she asks herself, “How likely is this patient to get into trouble?” with inpatient opioid administration. A concept that goes hand-in-hand, she said, is choosing the appropriate dose and route.
Dr. Herzig picked up this theme, noting that route of administration matters. A speedy route, such as intravenous administration, has been shown to reinforce the potentially addictive effect of opioids. There are times when IV is the route to use, such as when the patient can’t take medication by mouth or when immediate pain control truly is needed. However, oral medication is just as effective, albeit slightly slower acting, she said.
Conversion from IV to oral opioids is a potential time for trouble, said Dr. Herzig. “Always use an opioid conversion chart,” she said. Cross-tolerance can be incomplete between opioids, so safe practice is to begin with about 50% of the OME dose with the new medication and titrate up. And don’t use a long-acting opioid for acute pain, she said, noting that not only will there be a long half-life and washout period if the dose is too high, but patient risk for later opioid use disorder is also upped with this strategy. “You can always add more, but it’s hard to take away,” said Dr. Herzig.
On discharge, consider whether an opioid should be prescribed at all, said Dr. Herzig. The guidance statement advises generally prescribing less than a 7-day supply, with the rationale that, if posthospitalization acute pain is severe enough to require an opioid at that point, the patient should have outpatient follow-up.
This approach doesn’t undertreat outpatient pain, said Dr. Herzig, pointing to studies that show that, at discharge, “the majority of opioids that patients are getting, they are not taking – which tells us that by definition we are overprescribing.”
The authors of the guidance statement wanted to address two important topics that were not sufficiently evidence backed, Dr. Herzig said. They had hoped to give clear guidance about best practices for communication and follow-up with outpatient providers after hospital discharge. Though they didn’t find clear guidance in this area, “We do believe that outpatient providers need to be kept in the loop.”
A second area, currently a hot button topic both in the medical community and in the lay press, is whether a naloxone prescription should accompany an opioid prescription at discharge. “There just aren’t studies for this,” said Dr. Herzig.
The full text of the guidance statement may be found here: https://www.journalofhospitalmedicine.com/jhospmed/article/161927/hospital-medicine/improving-safety-opioid-use-acute-noncancer-pain.
ORLANDO – A new guidance statement for opioid prescribing for hospitalized adults who have acute noncancer pain has been issued by the Society for Hospital Medicine.
The statement comes after an exhaustive systematic review that found just four existing guidelines met inclusion criteria, though none focused specifically on acute pain in hospitalized adults.
Among the key issues taken from the existing guidelines and addressed in the new SHM guidance statement are deciding when opioids – or a nonopioid alternative – should be used, as well as selection of appropriate dose, route, and duration of administration. The guidance statement advises that clinicians prescribe the lowest effective opioid dose for the shortest duration possible.
Best practices for screening and monitoring before and during opioid initiation is another major focus, as is minimizing opioid-related adverse events, both by careful patient selection and by judicious prescribing.
Finally, the statement acknowledges that, when a discharge medication list includes an opioid prescription, there is potential risk for misuse or diversion. Accordingly, the recommendation is to limit the duration of outpatient prescribing to 7 days of medication, with consideration of a 3-5 day prescription.
An interactive session at the 2018 SHM annual meeting presenting the guidance statement focused less on marching through the guidance’s 16 specific statements, and more on teasing out the why, when, how – and how long – of inpatient opioid prescribing.
The well-attended session, led by two of the guideline authors, Shoshana Herzig, MD, MPH, and Teryl K. Nuckols, MD, FHM, began with Dr. Herzig, director of hospital medicine research at Beth Israel Deaconess Medical Center, Boston, making a compelling case for why guidance is needed for inpatient opioid prescribing for acute pain.
“Few would disagree that, at the end of the day, we are the final common pathway” for hospitalized patients who receive opioids, said Dr. Herzig. And there’s ample evidence that troublesome opioid prescribing is widespread, she said, adding that associated problems aren’t limited to such inpatient adverse events as falls, respiratory arrest, and acute kidney injury; plenty of opioid-exposed patients who leave the hospital continue to use opioids in problematic ways after discharge.
Of patients who were opioid naive and filled outpatient opioid prescriptions on discharge, “Almost half of patients were still using opioids 90 days later,” Dr. Herzig said. “Hospitals contribute to opioid initiation in millions of patients each year, so our prescribing patterns in the hospital do matter.”
“We tend to prescribe high doses,” said Dr. Herzig – an average of a 68-mg oral morphine equivalent (OME) dose on days that opioids were received, according to a 2014 study she coauthored. Overall, Dr. Herzig and her colleagues found that about 40% of patients who received opioids had a daily dose of at least 50 mg OME, and about a quarter received a daily dose at or exceeding 100 mg OME (Herzig et al. J Hosp Med. 2014 Feb;9[2]:73-81).
Further, she said, “We tend to prescribe a bit haphazardly.” The same study found wide variation in regional inpatient opioid-prescribing practices, with inpatients in the U.S. Midwest, South, and West seeing adjusted relative rates of exposure to opioids of 1.26, 1.33, and 1.37, compared with the Northeast, she said.
Among the more concerning findings, she said, was that “hospitals that prescribe opioids more frequently appear to do so less safely.” In hospitals that fell into the top quartile for inpatient opioid exposure, the overall rate of opioid-related adverse events was 0.39%, compared with 0.21% for hospitals in the bottom quartile of opioid prescribing, for an overall adjusted relative risk of 1.23 in opioid-exposed patients in the hospitals with the highest prescribing, said Dr. Herzig.
Dr. Nuckols, director of the division of general internal medicine at Cedars-Sinai Medical Center, Los Angeles, engaged attendees to identify challenges in acute pain management among hospitalized adults.
The audience was quick and prolific with answers, which included varying physician standards for opioid prescribing; patient expectations for pain management – and sometimes denial that opioid use has become a disorder; varying expectations for pain management among care team members who may be reluctant to let go of pain as “the fifth vital sign;” difficulty accessing and being reimbursed for nonpharmacologic strategies; and, acknowledged by all, patient satisfaction scores.
To this last point, Dr. Nuckols said that there have been “a few recent changes for the better.” The Joint Commission is revising its standards to move away from pain as a vital sign, toward a focused assessment of pain that considers how patients are responding to pain, as well as functional status. However, she said, “There aren’t any validated measures yet for how we’re going to do this.”
Similar shifts are underway with pain-related HCAHPS (the Hospital Consumer Assessment of Healthcare Providers and Systems) questions, which have undergone a “big pullback” from an emphasis on complete control of pain, and now put more focus on whether caregivers asked about pain and talked with inpatients about ways to treat pain, said Dr. Nuckols.
Speaking to the process of developing the guidance statement, Dr. Nuckols said that “I think it’s important to note that the empirical literature about managing pain for inpatients … is almost nonexistent.” Of the four criteria that met inclusion criteria – “and we were tough raters when it comes to the guidelines” – most were based on expert consensus, she said, and most had primarily an outpatient focus.
Themes that emerged from the review process included consideration of a nonopioid strategy before initiating an opioid. These might include pharmacologic interventions such as acetaminophen or a nonsteroidal anti-inflammatory for nociceptive pain, pregabalin, gabapentin, or other medication to manage neuropathic pain, or nonpharmacologic interventions such as heat, ice, or distraction. All of these should also be considered as adjuncts to minimize opioid dosing as well, said Dr. Nuckols, citing well-documented synergy with multiple modalities of pain treatment.
Careful patient selection is also key, said Dr. Nuckols. She noted that she asks herself, “How likely is this patient to get into trouble?” with inpatient opioid administration. A concept that goes hand-in-hand, she said, is choosing the appropriate dose and route.
Dr. Herzig picked up this theme, noting that route of administration matters. A speedy route, such as intravenous administration, has been shown to reinforce the potentially addictive effect of opioids. There are times when IV is the route to use, such as when the patient can’t take medication by mouth or when immediate pain control truly is needed. However, oral medication is just as effective, albeit slightly slower acting, she said.
Conversion from IV to oral opioids is a potential time for trouble, said Dr. Herzig. “Always use an opioid conversion chart,” she said. Cross-tolerance can be incomplete between opioids, so safe practice is to begin with about 50% of the OME dose with the new medication and titrate up. And don’t use a long-acting opioid for acute pain, she said, noting that not only will there be a long half-life and washout period if the dose is too high, but patient risk for later opioid use disorder is also upped with this strategy. “You can always add more, but it’s hard to take away,” said Dr. Herzig.
On discharge, consider whether an opioid should be prescribed at all, said Dr. Herzig. The guidance statement advises generally prescribing less than a 7-day supply, with the rationale that, if posthospitalization acute pain is severe enough to require an opioid at that point, the patient should have outpatient follow-up.
This approach doesn’t undertreat outpatient pain, said Dr. Herzig, pointing to studies that show that, at discharge, “the majority of opioids that patients are getting, they are not taking – which tells us that by definition we are overprescribing.”
The authors of the guidance statement wanted to address two important topics that were not sufficiently evidence backed, Dr. Herzig said. They had hoped to give clear guidance about best practices for communication and follow-up with outpatient providers after hospital discharge. Though they didn’t find clear guidance in this area, “We do believe that outpatient providers need to be kept in the loop.”
A second area, currently a hot button topic both in the medical community and in the lay press, is whether a naloxone prescription should accompany an opioid prescription at discharge. “There just aren’t studies for this,” said Dr. Herzig.
The full text of the guidance statement may be found here: https://www.journalofhospitalmedicine.com/jhospmed/article/161927/hospital-medicine/improving-safety-opioid-use-acute-noncancer-pain.
REPORTING FROM HM18
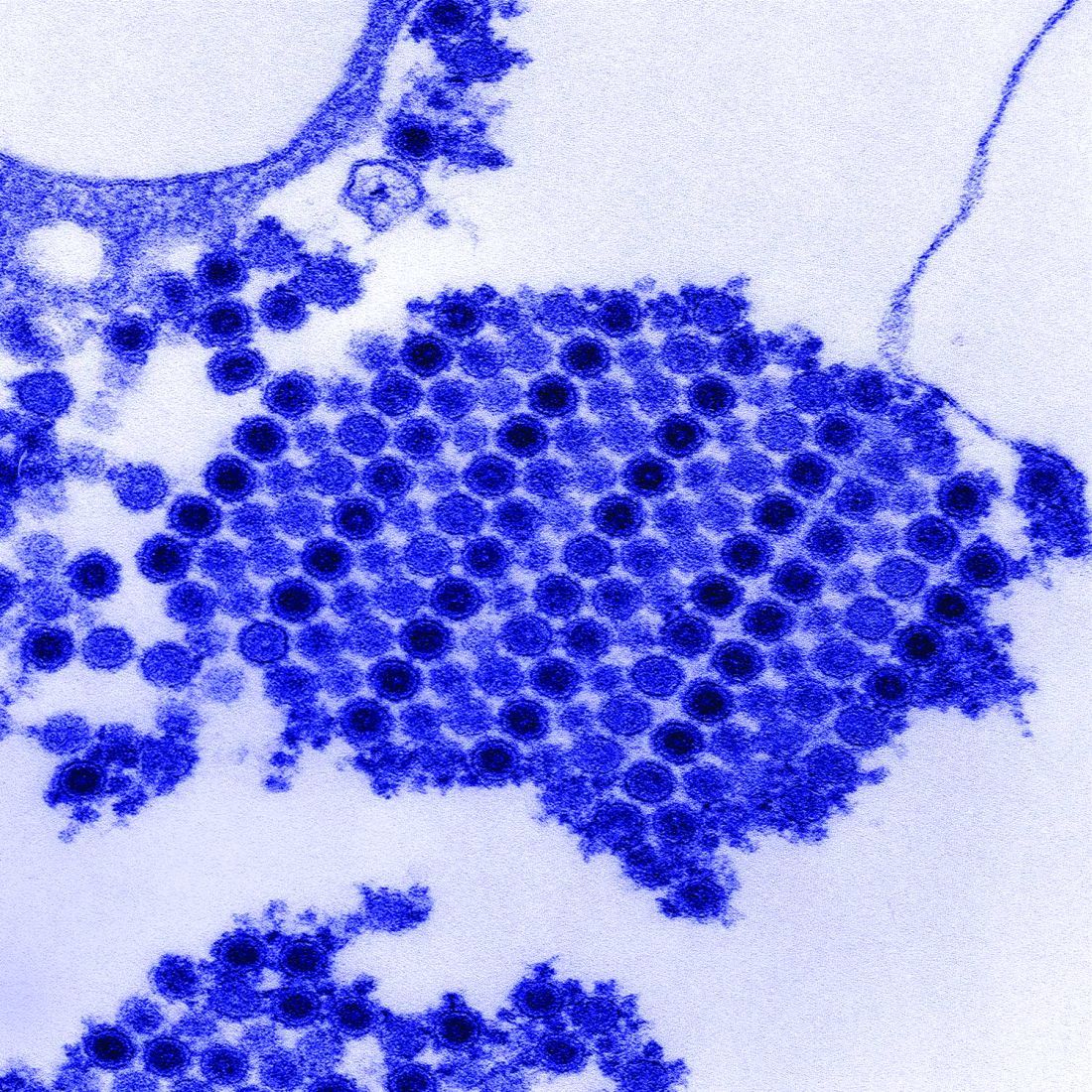
Chikungunya infection in children masquerades as SJS-TEN
Chikungunya infections in young children resemble skin symptoms characteristic of Stevens-Johnson syndrome and toxic epidermal necrolysis, (SJS-TEN), according to data from a case series of 21 children seen during a chikungunya outbreak in India in August and September 2016.
The researchers described their observations of 13 boys and eight girls aged 1-36 months in Pediatric Dermatology. All 21 children presented with vesiculobullous and necrotic lesions and mild to moderate fever; 16 children (76%) had large erosions, purpuric macules, and necrosis. Most of the lesions occurred on the extremities.
The time from the onset of illness to presentation ranged from 1 to 9 days, and the skin lesions resolved in 5-7 days. The lesions resolved with no sequelae in 11 patients, with hyperpigmentation in seven (33%) , and with hypopigmentation in three patients (14%).
In addition, three patients (14%) developed minor oral erosions, and four (19%) developed palmoplantar erythema, which also may be associated with SJS-TEN. However, none of the patients experienced the severe mucositis and ocular and genital involvement common to SJS-TEN, Dr. Garg and associates noted. A total of seven children tested positive for chikungunya based on enzyme-linked immunosorbent assay results.
Severity of illness can be helpful to distinguish chikungunya from SJS-TEN, the researchers said. Based on the Nelson severity index, 11 children in this series met the criteria for “not sick,” nine were “moderately sick,” and one was “very sick.”
It is key “to be aware of SJS-TEN–like presentation of chikungunya and not to misinterpret it as true SJS-TEN, which will lead to unnecessary intervention and management,” Dr. Garg and associates said.
The researchers had no financial conflicts to disclose.
SOURCE: Garg T et al. Pediatr Dermatol. 2018 Mar 24. doi: 10.1111/pde.13450.
Chikungunya infections in young children resemble skin symptoms characteristic of Stevens-Johnson syndrome and toxic epidermal necrolysis, (SJS-TEN), according to data from a case series of 21 children seen during a chikungunya outbreak in India in August and September 2016.
The researchers described their observations of 13 boys and eight girls aged 1-36 months in Pediatric Dermatology. All 21 children presented with vesiculobullous and necrotic lesions and mild to moderate fever; 16 children (76%) had large erosions, purpuric macules, and necrosis. Most of the lesions occurred on the extremities.
The time from the onset of illness to presentation ranged from 1 to 9 days, and the skin lesions resolved in 5-7 days. The lesions resolved with no sequelae in 11 patients, with hyperpigmentation in seven (33%) , and with hypopigmentation in three patients (14%).
In addition, three patients (14%) developed minor oral erosions, and four (19%) developed palmoplantar erythema, which also may be associated with SJS-TEN. However, none of the patients experienced the severe mucositis and ocular and genital involvement common to SJS-TEN, Dr. Garg and associates noted. A total of seven children tested positive for chikungunya based on enzyme-linked immunosorbent assay results.
Severity of illness can be helpful to distinguish chikungunya from SJS-TEN, the researchers said. Based on the Nelson severity index, 11 children in this series met the criteria for “not sick,” nine were “moderately sick,” and one was “very sick.”
It is key “to be aware of SJS-TEN–like presentation of chikungunya and not to misinterpret it as true SJS-TEN, which will lead to unnecessary intervention and management,” Dr. Garg and associates said.
The researchers had no financial conflicts to disclose.
SOURCE: Garg T et al. Pediatr Dermatol. 2018 Mar 24. doi: 10.1111/pde.13450.
Chikungunya infections in young children resemble skin symptoms characteristic of Stevens-Johnson syndrome and toxic epidermal necrolysis, (SJS-TEN), according to data from a case series of 21 children seen during a chikungunya outbreak in India in August and September 2016.
The researchers described their observations of 13 boys and eight girls aged 1-36 months in Pediatric Dermatology. All 21 children presented with vesiculobullous and necrotic lesions and mild to moderate fever; 16 children (76%) had large erosions, purpuric macules, and necrosis. Most of the lesions occurred on the extremities.
The time from the onset of illness to presentation ranged from 1 to 9 days, and the skin lesions resolved in 5-7 days. The lesions resolved with no sequelae in 11 patients, with hyperpigmentation in seven (33%) , and with hypopigmentation in three patients (14%).
In addition, three patients (14%) developed minor oral erosions, and four (19%) developed palmoplantar erythema, which also may be associated with SJS-TEN. However, none of the patients experienced the severe mucositis and ocular and genital involvement common to SJS-TEN, Dr. Garg and associates noted. A total of seven children tested positive for chikungunya based on enzyme-linked immunosorbent assay results.
Severity of illness can be helpful to distinguish chikungunya from SJS-TEN, the researchers said. Based on the Nelson severity index, 11 children in this series met the criteria for “not sick,” nine were “moderately sick,” and one was “very sick.”
It is key “to be aware of SJS-TEN–like presentation of chikungunya and not to misinterpret it as true SJS-TEN, which will lead to unnecessary intervention and management,” Dr. Garg and associates said.
The researchers had no financial conflicts to disclose.
SOURCE: Garg T et al. Pediatr Dermatol. 2018 Mar 24. doi: 10.1111/pde.13450.
FROM PEDIATRIC DERMATOLOGY
Key clinical point:
Major finding: Of 21 children with chikungunya, 76% had developed vesicles and bullae with purpuric macules and necrosis.
Study details: A case series of 21 children with chikungunya fever in India.
Disclosures: The researchers had no financial conflicts to disclose.
Source: Garg T et al. Pediatr Dermatol. 2018 Mar 24. doi: 10.1111/pde.13450.
Video : The SHM Research Committee: Expanding the role and footprint of research in hospital medicine
ORLANDO – In a video interview, Stephanie Mueller, MD, SFHM, of Brigham and Women’s Hospital, Boston, discusses the scope and importance of the SHM Research Committee.
One of its most important roles is overseeing the yearly Scientific Abstract and Poster Competition, known as the Research, Innovations and Clinical Vignettes (RIV) portion of the annual conference, which brings the best of current research in hospital medicine, especially in the increasingly important area of value in patient care, to the members.
In discussing the work of the committee, Dr. Mueller – who is in her third year as a member – adds that they “are working to expand the research footprint within the Society of Hospital Medicine,” including implementing initiatives such as the VIP program, which is a visiting professorship in which junior and mid-level faculty can do an exchange program between institutions.
ORLANDO – In a video interview, Stephanie Mueller, MD, SFHM, of Brigham and Women’s Hospital, Boston, discusses the scope and importance of the SHM Research Committee.
One of its most important roles is overseeing the yearly Scientific Abstract and Poster Competition, known as the Research, Innovations and Clinical Vignettes (RIV) portion of the annual conference, which brings the best of current research in hospital medicine, especially in the increasingly important area of value in patient care, to the members.
In discussing the work of the committee, Dr. Mueller – who is in her third year as a member – adds that they “are working to expand the research footprint within the Society of Hospital Medicine,” including implementing initiatives such as the VIP program, which is a visiting professorship in which junior and mid-level faculty can do an exchange program between institutions.
ORLANDO – In a video interview, Stephanie Mueller, MD, SFHM, of Brigham and Women’s Hospital, Boston, discusses the scope and importance of the SHM Research Committee.
One of its most important roles is overseeing the yearly Scientific Abstract and Poster Competition, known as the Research, Innovations and Clinical Vignettes (RIV) portion of the annual conference, which brings the best of current research in hospital medicine, especially in the increasingly important area of value in patient care, to the members.
In discussing the work of the committee, Dr. Mueller – who is in her third year as a member – adds that they “are working to expand the research footprint within the Society of Hospital Medicine,” including implementing initiatives such as the VIP program, which is a visiting professorship in which junior and mid-level faculty can do an exchange program between institutions.
REPORTING FROM HOSPITAL MEDICINE 2018
FDA orders new restrictions on sale, distribution of Essure
The Food and Drug Administration has restricted the sale and distribution of Bayer’s Essure permanent contraception device to only health care providers and facilities that provide patients with information about the risks and benefits of the device.
In an order issued April 9, the FDA’s Center for Devices and Radiological Health informed Bayer of the restrictions, citing a need to “provide reasonable assurance of the safety and effectiveness of the device.”
Bayer must implement the restrictions immediately and must ensure health care provider compliance.
“The FDA is taking this step after becoming aware that some women were not being adequately informed of Essure’s risks before getting the device implanted, despite previous significant efforts to educate patients and doctors about the risks associated with this device,” the agency said in a press release, adding that it “plans to enforce these requirements and will take appropriate action for a failure to comply, including applicable criminal and civil penalties.”
Essure, which is the only permanently implanted birth control device for women on the market that does not require a surgical incision, was approved in 2002 and has been associated with adverse events including perforation of the uterus and/or fallopian tubes, device migration into the abdomen or pelvis, persistent pain, and suspected allergic reactions or hypersensitivity. Some women have also reported headache, fatigue, weight changes, hair loss, and mood changes.
In 2016, based on product safety monitoring by the FDA, a postmarketing study was ordered, as was a boxed warning and a more comprehensive patient decision checklist to inform patients about the risk of adverse events.
“We’ve been closely evaluating new information on the use of Essure, and based on our review of a growing body of evidence, we believe this product requires additional, meaningful safeguards to ensure women are able to make informed decisions about risk when considering this option,” FDA commissioner Scott Gottlieb, MD, said in the press release, adding that it is unacceptable that some women were not being adequately informed.
“Every single woman receiving this device should fully understand the associated risks,” he said.
Terri Cornelison, MD, assistant director for the health of women in the Center for Devices and Radiological Health added that ensuring informed decision making is just one important step in ongoing efforts to monitor the Essure device.
“We remain committed to carefully and throughly considering all new data and evidence and will continue to work with patients affected by this device as part of our process,” she said. “While some women may continue to choose Essure as their birth control option based on current information, as new information becomes available, the FDA will continue to keep the public informed of the agency’s evaluation and findings and consider regulatory options that appropriately balance benefits and risks for Essure.”
The Food and Drug Administration has restricted the sale and distribution of Bayer’s Essure permanent contraception device to only health care providers and facilities that provide patients with information about the risks and benefits of the device.
In an order issued April 9, the FDA’s Center for Devices and Radiological Health informed Bayer of the restrictions, citing a need to “provide reasonable assurance of the safety and effectiveness of the device.”
Bayer must implement the restrictions immediately and must ensure health care provider compliance.
“The FDA is taking this step after becoming aware that some women were not being adequately informed of Essure’s risks before getting the device implanted, despite previous significant efforts to educate patients and doctors about the risks associated with this device,” the agency said in a press release, adding that it “plans to enforce these requirements and will take appropriate action for a failure to comply, including applicable criminal and civil penalties.”
Essure, which is the only permanently implanted birth control device for women on the market that does not require a surgical incision, was approved in 2002 and has been associated with adverse events including perforation of the uterus and/or fallopian tubes, device migration into the abdomen or pelvis, persistent pain, and suspected allergic reactions or hypersensitivity. Some women have also reported headache, fatigue, weight changes, hair loss, and mood changes.
In 2016, based on product safety monitoring by the FDA, a postmarketing study was ordered, as was a boxed warning and a more comprehensive patient decision checklist to inform patients about the risk of adverse events.
“We’ve been closely evaluating new information on the use of Essure, and based on our review of a growing body of evidence, we believe this product requires additional, meaningful safeguards to ensure women are able to make informed decisions about risk when considering this option,” FDA commissioner Scott Gottlieb, MD, said in the press release, adding that it is unacceptable that some women were not being adequately informed.
“Every single woman receiving this device should fully understand the associated risks,” he said.
Terri Cornelison, MD, assistant director for the health of women in the Center for Devices and Radiological Health added that ensuring informed decision making is just one important step in ongoing efforts to monitor the Essure device.
“We remain committed to carefully and throughly considering all new data and evidence and will continue to work with patients affected by this device as part of our process,” she said. “While some women may continue to choose Essure as their birth control option based on current information, as new information becomes available, the FDA will continue to keep the public informed of the agency’s evaluation and findings and consider regulatory options that appropriately balance benefits and risks for Essure.”
The Food and Drug Administration has restricted the sale and distribution of Bayer’s Essure permanent contraception device to only health care providers and facilities that provide patients with information about the risks and benefits of the device.
In an order issued April 9, the FDA’s Center for Devices and Radiological Health informed Bayer of the restrictions, citing a need to “provide reasonable assurance of the safety and effectiveness of the device.”
Bayer must implement the restrictions immediately and must ensure health care provider compliance.
“The FDA is taking this step after becoming aware that some women were not being adequately informed of Essure’s risks before getting the device implanted, despite previous significant efforts to educate patients and doctors about the risks associated with this device,” the agency said in a press release, adding that it “plans to enforce these requirements and will take appropriate action for a failure to comply, including applicable criminal and civil penalties.”
Essure, which is the only permanently implanted birth control device for women on the market that does not require a surgical incision, was approved in 2002 and has been associated with adverse events including perforation of the uterus and/or fallopian tubes, device migration into the abdomen or pelvis, persistent pain, and suspected allergic reactions or hypersensitivity. Some women have also reported headache, fatigue, weight changes, hair loss, and mood changes.
In 2016, based on product safety monitoring by the FDA, a postmarketing study was ordered, as was a boxed warning and a more comprehensive patient decision checklist to inform patients about the risk of adverse events.
“We’ve been closely evaluating new information on the use of Essure, and based on our review of a growing body of evidence, we believe this product requires additional, meaningful safeguards to ensure women are able to make informed decisions about risk when considering this option,” FDA commissioner Scott Gottlieb, MD, said in the press release, adding that it is unacceptable that some women were not being adequately informed.
“Every single woman receiving this device should fully understand the associated risks,” he said.
Terri Cornelison, MD, assistant director for the health of women in the Center for Devices and Radiological Health added that ensuring informed decision making is just one important step in ongoing efforts to monitor the Essure device.
“We remain committed to carefully and throughly considering all new data and evidence and will continue to work with patients affected by this device as part of our process,” she said. “While some women may continue to choose Essure as their birth control option based on current information, as new information becomes available, the FDA will continue to keep the public informed of the agency’s evaluation and findings and consider regulatory options that appropriately balance benefits and risks for Essure.”
SHM presidents: Innovate and avoid complacency
ORLANDO – In a time of tumult in American health care, hospital medicine can expect to see a reimagined – but not reduced – role, said the outgoing and current presidents of the Society of Hospital Medicine at Monday’s HM18 opening plenary.
Despite the many successes of the relatively young field of hospital medicine, there’s no room for complacency, said SHM’s immediate past president Ron Greeno, MD, MHM.
Dr. Greeno drew on his 25-year career in hospital medicine to frame past successes and upcoming challenges for hospital medicine in the 21st century.
As the profession defined itself and grew from the 1980s onward, “the model was challenged, and challenged significantly, mostly by our physician colleagues,” who either feared or didn’t understand the model, he said. All along, though, pioneers in hospital medicine were just trying “to figure out a way to take better care of patients in the hospital.”
The result, said Dr. Greeno, is that hospital medicine stands unique among physician specialties. “We as a specialty are in a very enviable position as we move into the post–health care reform era. More than any other specialty in the history of medicine, we are not expected to p
“Colleagues honor us by trusting us with their patients’ care … but we need to be aware that they are watching us and judging whether we are living up to our promises,” Dr. Greeno said. “So we need to be asking ourselves some tough questions. Perhaps we’re becoming too self-satisfied. Perhaps we are starting to believe our own press.”
Without an appetite for innovation as well as hard work, hospitalists could risk becoming “highly paid worker bees,” said Dr. Greeno.
“There are people who think this is happening. I know because I have talked to them while traveling around the country” as SHM president, he said. “I am not among that group. I think the best is yet to come … that we will become more integrated and have ever more impact and influence in the redesign of the U.S. health care system.”
More than anything, Dr. Greeno’s faith in the profession’s future is grounded in its human capital. Addressing the plenary attendees, he said, “You come here just to become better, to try to make things better. I see all of you who refuse to let the urgent get in the way of the important.”
In her first address as the new SHM president, Nasim Afsar, MD, SFHM, agreed that the people really do make the profession. “We will prevail because of our perseverance and our passion to be part of the solution for challenges in health care,” she said.
Dr. Afsar is chief ambulatory officer and chief medical officer for ACOs at UC Irvine Health. She said that earlier this year, she’d never felt more sure of her job security. Serving on the inpatient hospitalist service during the height of this year’s surging influenza season, Dr. Afsar saw a packed emergency department and a completely full house for her hospital. “We had to create a new hospitalist service” just to handle the volume, she said.
A sobering experience later that month, though, had her rethinking things. At a meeting of chief executive officers of health care systems, leaders spoke of hospitals transitioning from profit centers to cost centers. Some of the proposed innovations were startling: “When I heard talk of hospitals at home, and of virtual hospitals, I got a very different sense of our specialty,” said Dr. Afsar.
Still, she said, she’s confident there will be jobs for hospitalists in the future. “We can’t ignore the significant, irrefutable fact that has emerged: Value will prevail. And the only way to deliver that is population health management,” meaning the delivery of high value care at fair cost across the entire human lifespan, she said.
This call can be answered in two ways, said Dr. Afsar. “First, we have to define and deliver value for hospitalized patients every single day. Second, we have to look at what population health management means for our specialty.”
“I encourage us not to be confined by our names,” Dr. Afsar said. Rather, hospitalists will be defined by the attributes that they’ve become known for over the years: “Innovators. Problem solvers. Collaborators. Patient advocates.”
ORLANDO – In a time of tumult in American health care, hospital medicine can expect to see a reimagined – but not reduced – role, said the outgoing and current presidents of the Society of Hospital Medicine at Monday’s HM18 opening plenary.
Despite the many successes of the relatively young field of hospital medicine, there’s no room for complacency, said SHM’s immediate past president Ron Greeno, MD, MHM.
Dr. Greeno drew on his 25-year career in hospital medicine to frame past successes and upcoming challenges for hospital medicine in the 21st century.
As the profession defined itself and grew from the 1980s onward, “the model was challenged, and challenged significantly, mostly by our physician colleagues,” who either feared or didn’t understand the model, he said. All along, though, pioneers in hospital medicine were just trying “to figure out a way to take better care of patients in the hospital.”
The result, said Dr. Greeno, is that hospital medicine stands unique among physician specialties. “We as a specialty are in a very enviable position as we move into the post–health care reform era. More than any other specialty in the history of medicine, we are not expected to p
“Colleagues honor us by trusting us with their patients’ care … but we need to be aware that they are watching us and judging whether we are living up to our promises,” Dr. Greeno said. “So we need to be asking ourselves some tough questions. Perhaps we’re becoming too self-satisfied. Perhaps we are starting to believe our own press.”
Without an appetite for innovation as well as hard work, hospitalists could risk becoming “highly paid worker bees,” said Dr. Greeno.
“There are people who think this is happening. I know because I have talked to them while traveling around the country” as SHM president, he said. “I am not among that group. I think the best is yet to come … that we will become more integrated and have ever more impact and influence in the redesign of the U.S. health care system.”
More than anything, Dr. Greeno’s faith in the profession’s future is grounded in its human capital. Addressing the plenary attendees, he said, “You come here just to become better, to try to make things better. I see all of you who refuse to let the urgent get in the way of the important.”
In her first address as the new SHM president, Nasim Afsar, MD, SFHM, agreed that the people really do make the profession. “We will prevail because of our perseverance and our passion to be part of the solution for challenges in health care,” she said.
Dr. Afsar is chief ambulatory officer and chief medical officer for ACOs at UC Irvine Health. She said that earlier this year, she’d never felt more sure of her job security. Serving on the inpatient hospitalist service during the height of this year’s surging influenza season, Dr. Afsar saw a packed emergency department and a completely full house for her hospital. “We had to create a new hospitalist service” just to handle the volume, she said.
A sobering experience later that month, though, had her rethinking things. At a meeting of chief executive officers of health care systems, leaders spoke of hospitals transitioning from profit centers to cost centers. Some of the proposed innovations were startling: “When I heard talk of hospitals at home, and of virtual hospitals, I got a very different sense of our specialty,” said Dr. Afsar.
Still, she said, she’s confident there will be jobs for hospitalists in the future. “We can’t ignore the significant, irrefutable fact that has emerged: Value will prevail. And the only way to deliver that is population health management,” meaning the delivery of high value care at fair cost across the entire human lifespan, she said.
This call can be answered in two ways, said Dr. Afsar. “First, we have to define and deliver value for hospitalized patients every single day. Second, we have to look at what population health management means for our specialty.”
“I encourage us not to be confined by our names,” Dr. Afsar said. Rather, hospitalists will be defined by the attributes that they’ve become known for over the years: “Innovators. Problem solvers. Collaborators. Patient advocates.”
ORLANDO – In a time of tumult in American health care, hospital medicine can expect to see a reimagined – but not reduced – role, said the outgoing and current presidents of the Society of Hospital Medicine at Monday’s HM18 opening plenary.
Despite the many successes of the relatively young field of hospital medicine, there’s no room for complacency, said SHM’s immediate past president Ron Greeno, MD, MHM.
Dr. Greeno drew on his 25-year career in hospital medicine to frame past successes and upcoming challenges for hospital medicine in the 21st century.
As the profession defined itself and grew from the 1980s onward, “the model was challenged, and challenged significantly, mostly by our physician colleagues,” who either feared or didn’t understand the model, he said. All along, though, pioneers in hospital medicine were just trying “to figure out a way to take better care of patients in the hospital.”
The result, said Dr. Greeno, is that hospital medicine stands unique among physician specialties. “We as a specialty are in a very enviable position as we move into the post–health care reform era. More than any other specialty in the history of medicine, we are not expected to p
“Colleagues honor us by trusting us with their patients’ care … but we need to be aware that they are watching us and judging whether we are living up to our promises,” Dr. Greeno said. “So we need to be asking ourselves some tough questions. Perhaps we’re becoming too self-satisfied. Perhaps we are starting to believe our own press.”
Without an appetite for innovation as well as hard work, hospitalists could risk becoming “highly paid worker bees,” said Dr. Greeno.
“There are people who think this is happening. I know because I have talked to them while traveling around the country” as SHM president, he said. “I am not among that group. I think the best is yet to come … that we will become more integrated and have ever more impact and influence in the redesign of the U.S. health care system.”
More than anything, Dr. Greeno’s faith in the profession’s future is grounded in its human capital. Addressing the plenary attendees, he said, “You come here just to become better, to try to make things better. I see all of you who refuse to let the urgent get in the way of the important.”
In her first address as the new SHM president, Nasim Afsar, MD, SFHM, agreed that the people really do make the profession. “We will prevail because of our perseverance and our passion to be part of the solution for challenges in health care,” she said.
Dr. Afsar is chief ambulatory officer and chief medical officer for ACOs at UC Irvine Health. She said that earlier this year, she’d never felt more sure of her job security. Serving on the inpatient hospitalist service during the height of this year’s surging influenza season, Dr. Afsar saw a packed emergency department and a completely full house for her hospital. “We had to create a new hospitalist service” just to handle the volume, she said.
A sobering experience later that month, though, had her rethinking things. At a meeting of chief executive officers of health care systems, leaders spoke of hospitals transitioning from profit centers to cost centers. Some of the proposed innovations were startling: “When I heard talk of hospitals at home, and of virtual hospitals, I got a very different sense of our specialty,” said Dr. Afsar.
Still, she said, she’s confident there will be jobs for hospitalists in the future. “We can’t ignore the significant, irrefutable fact that has emerged: Value will prevail. And the only way to deliver that is population health management,” meaning the delivery of high value care at fair cost across the entire human lifespan, she said.
This call can be answered in two ways, said Dr. Afsar. “First, we have to define and deliver value for hospitalized patients every single day. Second, we have to look at what population health management means for our specialty.”
“I encourage us not to be confined by our names,” Dr. Afsar said. Rather, hospitalists will be defined by the attributes that they’ve become known for over the years: “Innovators. Problem solvers. Collaborators. Patient advocates.”
Can cN0 and pCR limit axillary surgery in some breast cancer patients?
CHICAGO – Patients with clinically node-negative HER2-positive or triple-negative breast cancer (TNBC) who achieve a pathological complete response in the breast after neoadjuvant chemotherapy could benefit from clinical trials to evaluate the option of omitting axillary node surgery in this population, according to a retrospective analysis of more than 22,000 cases in the National Cancer Database reported at the Society of Surgical Oncology Annual Cancer Symposium.
Alison U. Barron, MD, breast surgery oncology fellow at Mayo, presented the results. “In patients with HER2+ breast cancer and TNBC who are clinically node negative (cN0) and achieve a breast pathological complete response, this data supports omitting axillary surgery in clinical trials assessing no surgery after neoadjuvant chemotherapy (NAC),” she said. “In patients who present with clinically positive node [cN1] disease with a breast pathological complete response, surgical staging of the axilla is still recommended.”
“Response rates to NAC have increased,” Dr. Barron said. She cited previous reports that showed response rates ranging from 9%-13% for anthracyclines to 19%-26% with the addition of taxanes, and to 60%-70% with the addition of trastuzumab and pertuzumab in HER2+ disease. “Furthermore, we know that tumor biology affects response rates, with TNBC and HER2+ disease having the highest rates of pathologic complete response,” she said.
“In the current era when we frequently operate on patients, we find no residual cancer in the tissue at the time of surgery,” Dr. Barron said. “The question arises as to whether we can limit surgery in patients with a pathological complete response.” While imaging has limited ability to reliably detect pCR with 100% specificity, she noted that recent trials have shown the potential of tumor-bed biopsy to identify pCR in patients after NAC (Ann Surg. Published online Oct. 23, 2017. doi: 10.1097/SLA.0000000000002573; JAMA Surg. 2017;152(7):665-70).
The National Cancer Database data the Mayo researchers analyzed yielded an overall breast pCR of 29%. “When broken down by tumor subtype, we saw significantly higher rates of breast pCR in patients with HER2+ disease (42%, n = 3,107) and TNBC (35%, n = 2,469), compared with patients with hormone-receptor positive (HR+)/HER2-negative disease (12%, n = 1,020),” she said.
When the analysis looked specifically at patients who were clinically node negative at presentation and had a pCR, the rates of positive lymph nodes at the time of surgery were 1.6% in HER2+ patients and 1.7% in TNBC disease, Dr. Barron said. “If there was residual disease in the breast, the nodal positivity rate was significantly higher, at 18% in HER2+ and 12% in TNBC,” she added. In those who were clinical N1, the breast pCR rates were similar – 41% in HER2+ and 35% in TNBC – but nodal positivity rates were significantly higher, at 13% and 14%, respectively.
The HR+/HER2- group had significantly lower rates of pCR: 12% in the cN0 and 13% in the cN1 subgroups. This subgroup also had higher nodal positivity rates – in the cN0 subgroup, 4% in those with a breast pCR and 34% in those with residual disease in the breast, and in the cN1 subgroup, 30% and 83%, respectively.
When the investigators looked at the extent of nodal burden in cN0 patients with breast pCR, they found the rate of N2 and N3 disease was near zero across all biologic subtypes. “In patients who were cN1 at presentation and achieved a breast pCR but had residual axillary disease, the majority had N1 disease with only 1.5%-4% having four or more positive lymph nodes,” Dr. Barron said.
In the discussion, session moderator Carla Fisher, MD, of Indiana University, Indianapolis, said, “While we might not be ready for prime time to not evaluate the lymph nodes of these patients, this study does speak to the importance of establishing N0 and N1 prior to NAC.” In reply to her question about how Mayo routinely evaluates node status prior to NAC, Dr. Barron noted that Mayo performs routine axillary ultrasound. However, the NCDB data does not specify what imaging was done. This is thought to vary across the centers in the NCDB, Dr. Barron said.
Noted Dr. Boughey, “The findings from this study provide data that can be used moving forward for planning future clinical trials.” She also said that these findings do not alter the current standard of care; that still calls for breast and nodal surgery after NAC. However, the ongoing NRG-BR005 phase II clinical trial is assessing the accuracy of tumor-bed biopsy in these situations (ClinicalTrials.gov Identifier: NCT03188393). “The results from that trial will help inform future trials evaluating eliminating breast surgery in patients with an excellent response to NAC,” Dr. Boughey said. “Those patients could also potentially avoid axillary surgery based on the data we have now.”
Dr. Barron and Dr. Boughey and coauthors reported having no financial disclosures.
SOURCE: Barron AU et al. Society of Surgical Oncology Annual Cancer Symposium, Abstract 48.
CHICAGO – Patients with clinically node-negative HER2-positive or triple-negative breast cancer (TNBC) who achieve a pathological complete response in the breast after neoadjuvant chemotherapy could benefit from clinical trials to evaluate the option of omitting axillary node surgery in this population, according to a retrospective analysis of more than 22,000 cases in the National Cancer Database reported at the Society of Surgical Oncology Annual Cancer Symposium.
Alison U. Barron, MD, breast surgery oncology fellow at Mayo, presented the results. “In patients with HER2+ breast cancer and TNBC who are clinically node negative (cN0) and achieve a breast pathological complete response, this data supports omitting axillary surgery in clinical trials assessing no surgery after neoadjuvant chemotherapy (NAC),” she said. “In patients who present with clinically positive node [cN1] disease with a breast pathological complete response, surgical staging of the axilla is still recommended.”
“Response rates to NAC have increased,” Dr. Barron said. She cited previous reports that showed response rates ranging from 9%-13% for anthracyclines to 19%-26% with the addition of taxanes, and to 60%-70% with the addition of trastuzumab and pertuzumab in HER2+ disease. “Furthermore, we know that tumor biology affects response rates, with TNBC and HER2+ disease having the highest rates of pathologic complete response,” she said.
“In the current era when we frequently operate on patients, we find no residual cancer in the tissue at the time of surgery,” Dr. Barron said. “The question arises as to whether we can limit surgery in patients with a pathological complete response.” While imaging has limited ability to reliably detect pCR with 100% specificity, she noted that recent trials have shown the potential of tumor-bed biopsy to identify pCR in patients after NAC (Ann Surg. Published online Oct. 23, 2017. doi: 10.1097/SLA.0000000000002573; JAMA Surg. 2017;152(7):665-70).
The National Cancer Database data the Mayo researchers analyzed yielded an overall breast pCR of 29%. “When broken down by tumor subtype, we saw significantly higher rates of breast pCR in patients with HER2+ disease (42%, n = 3,107) and TNBC (35%, n = 2,469), compared with patients with hormone-receptor positive (HR+)/HER2-negative disease (12%, n = 1,020),” she said.
When the analysis looked specifically at patients who were clinically node negative at presentation and had a pCR, the rates of positive lymph nodes at the time of surgery were 1.6% in HER2+ patients and 1.7% in TNBC disease, Dr. Barron said. “If there was residual disease in the breast, the nodal positivity rate was significantly higher, at 18% in HER2+ and 12% in TNBC,” she added. In those who were clinical N1, the breast pCR rates were similar – 41% in HER2+ and 35% in TNBC – but nodal positivity rates were significantly higher, at 13% and 14%, respectively.
The HR+/HER2- group had significantly lower rates of pCR: 12% in the cN0 and 13% in the cN1 subgroups. This subgroup also had higher nodal positivity rates – in the cN0 subgroup, 4% in those with a breast pCR and 34% in those with residual disease in the breast, and in the cN1 subgroup, 30% and 83%, respectively.
When the investigators looked at the extent of nodal burden in cN0 patients with breast pCR, they found the rate of N2 and N3 disease was near zero across all biologic subtypes. “In patients who were cN1 at presentation and achieved a breast pCR but had residual axillary disease, the majority had N1 disease with only 1.5%-4% having four or more positive lymph nodes,” Dr. Barron said.
In the discussion, session moderator Carla Fisher, MD, of Indiana University, Indianapolis, said, “While we might not be ready for prime time to not evaluate the lymph nodes of these patients, this study does speak to the importance of establishing N0 and N1 prior to NAC.” In reply to her question about how Mayo routinely evaluates node status prior to NAC, Dr. Barron noted that Mayo performs routine axillary ultrasound. However, the NCDB data does not specify what imaging was done. This is thought to vary across the centers in the NCDB, Dr. Barron said.
Noted Dr. Boughey, “The findings from this study provide data that can be used moving forward for planning future clinical trials.” She also said that these findings do not alter the current standard of care; that still calls for breast and nodal surgery after NAC. However, the ongoing NRG-BR005 phase II clinical trial is assessing the accuracy of tumor-bed biopsy in these situations (ClinicalTrials.gov Identifier: NCT03188393). “The results from that trial will help inform future trials evaluating eliminating breast surgery in patients with an excellent response to NAC,” Dr. Boughey said. “Those patients could also potentially avoid axillary surgery based on the data we have now.”
Dr. Barron and Dr. Boughey and coauthors reported having no financial disclosures.
SOURCE: Barron AU et al. Society of Surgical Oncology Annual Cancer Symposium, Abstract 48.
CHICAGO – Patients with clinically node-negative HER2-positive or triple-negative breast cancer (TNBC) who achieve a pathological complete response in the breast after neoadjuvant chemotherapy could benefit from clinical trials to evaluate the option of omitting axillary node surgery in this population, according to a retrospective analysis of more than 22,000 cases in the National Cancer Database reported at the Society of Surgical Oncology Annual Cancer Symposium.
Alison U. Barron, MD, breast surgery oncology fellow at Mayo, presented the results. “In patients with HER2+ breast cancer and TNBC who are clinically node negative (cN0) and achieve a breast pathological complete response, this data supports omitting axillary surgery in clinical trials assessing no surgery after neoadjuvant chemotherapy (NAC),” she said. “In patients who present with clinically positive node [cN1] disease with a breast pathological complete response, surgical staging of the axilla is still recommended.”
“Response rates to NAC have increased,” Dr. Barron said. She cited previous reports that showed response rates ranging from 9%-13% for anthracyclines to 19%-26% with the addition of taxanes, and to 60%-70% with the addition of trastuzumab and pertuzumab in HER2+ disease. “Furthermore, we know that tumor biology affects response rates, with TNBC and HER2+ disease having the highest rates of pathologic complete response,” she said.
“In the current era when we frequently operate on patients, we find no residual cancer in the tissue at the time of surgery,” Dr. Barron said. “The question arises as to whether we can limit surgery in patients with a pathological complete response.” While imaging has limited ability to reliably detect pCR with 100% specificity, she noted that recent trials have shown the potential of tumor-bed biopsy to identify pCR in patients after NAC (Ann Surg. Published online Oct. 23, 2017. doi: 10.1097/SLA.0000000000002573; JAMA Surg. 2017;152(7):665-70).
The National Cancer Database data the Mayo researchers analyzed yielded an overall breast pCR of 29%. “When broken down by tumor subtype, we saw significantly higher rates of breast pCR in patients with HER2+ disease (42%, n = 3,107) and TNBC (35%, n = 2,469), compared with patients with hormone-receptor positive (HR+)/HER2-negative disease (12%, n = 1,020),” she said.
When the analysis looked specifically at patients who were clinically node negative at presentation and had a pCR, the rates of positive lymph nodes at the time of surgery were 1.6% in HER2+ patients and 1.7% in TNBC disease, Dr. Barron said. “If there was residual disease in the breast, the nodal positivity rate was significantly higher, at 18% in HER2+ and 12% in TNBC,” she added. In those who were clinical N1, the breast pCR rates were similar – 41% in HER2+ and 35% in TNBC – but nodal positivity rates were significantly higher, at 13% and 14%, respectively.
The HR+/HER2- group had significantly lower rates of pCR: 12% in the cN0 and 13% in the cN1 subgroups. This subgroup also had higher nodal positivity rates – in the cN0 subgroup, 4% in those with a breast pCR and 34% in those with residual disease in the breast, and in the cN1 subgroup, 30% and 83%, respectively.
When the investigators looked at the extent of nodal burden in cN0 patients with breast pCR, they found the rate of N2 and N3 disease was near zero across all biologic subtypes. “In patients who were cN1 at presentation and achieved a breast pCR but had residual axillary disease, the majority had N1 disease with only 1.5%-4% having four or more positive lymph nodes,” Dr. Barron said.
In the discussion, session moderator Carla Fisher, MD, of Indiana University, Indianapolis, said, “While we might not be ready for prime time to not evaluate the lymph nodes of these patients, this study does speak to the importance of establishing N0 and N1 prior to NAC.” In reply to her question about how Mayo routinely evaluates node status prior to NAC, Dr. Barron noted that Mayo performs routine axillary ultrasound. However, the NCDB data does not specify what imaging was done. This is thought to vary across the centers in the NCDB, Dr. Barron said.
Noted Dr. Boughey, “The findings from this study provide data that can be used moving forward for planning future clinical trials.” She also said that these findings do not alter the current standard of care; that still calls for breast and nodal surgery after NAC. However, the ongoing NRG-BR005 phase II clinical trial is assessing the accuracy of tumor-bed biopsy in these situations (ClinicalTrials.gov Identifier: NCT03188393). “The results from that trial will help inform future trials evaluating eliminating breast surgery in patients with an excellent response to NAC,” Dr. Boughey said. “Those patients could also potentially avoid axillary surgery based on the data we have now.”
Dr. Barron and Dr. Boughey and coauthors reported having no financial disclosures.
SOURCE: Barron AU et al. Society of Surgical Oncology Annual Cancer Symposium, Abstract 48.
REPORTING FROM SSO 2018
Key clinical point: Neoadjuvant chemotherapy for certain breast cancers achieves low rates of nodal positivity.
Major finding: In clinically node-negative HER2+ and triple-negative disease, nodal positivity after NAC in patients that had breast pathological complete response was less than 2%.
Study details: Review of 22,695 patients in NCDB with clinical T1 or T2 disease from 2010 to 2014.
Disclosure: Dr. Barron and coauthors reported having no financial disclosures.
Source: Barron AU et al. Society of Surgical Oncology Annual Cancer Symposium, Abstract 48.
Hospitalists 'perfectly poised' to drive health care reform
ORLANDO – As dizzying as the alphabet soup of payment reform might seem – with its swirl of new incentives, alignments, and models – hospitalists should already be familiar with many of its main ideas, said keynote speaker Kate Goodrich, MD, director of the Center for Clinical Standards and Quality at the Centers for Medicare and Medicaid Services.
That makes hospitalists poised to help reform a U.S. health care system with the dubious pairing of staggering costs and poor outcomes, Dr. Goodrich told a packed ballroom on Monday at the annual meeting of the Society of Hospital Medicine.
Many of the measures involved in payment reform – with its Merit-Based Incentive Payment System (MIPS), Medicare Access and CHIP Reauthorization Act (MACRA), and Advanced Payment Models (APMs) – focus on outpatient and ambulatory care, Dr. Goodrich acknowledged. But it’s also about medical systems, she said.
“What do you focus on as hospitalists? Improving systems of care,” she said. “We focus on clinical care for our individual patient, but part of our job is also to think about it in terms of how do I improve the care across my hospital system?”
One aspect of reform that is most likely to directly affect hospitalists is the facility-based measurement part of the Quality Payment Program, slated to take effect in 2019. If participating in MIPS – the payment model in which clinicians can receive an increase or decrease in payments based on performance measured by data on quality, cost, and other factors – clinicians can choose to have their hospital’s quality measures count toward their MIPS quality score. The facility measurement was developed in part after conversations between CMS and SHM, Dr. Goodrich said.
“Many stakeholders are very excited about this possibility for a couple of reasons: No. 1, there would be absolutely no quality-reporting burden for you if you chose to do that,” she said. “No. 2, it really aligns the incentives between you and the hospital that you’re working in. Because, after all, we are all in this together. And some folks have felt like they aren’t always aligned with the incentives of the hospital that they are working with, or working for.”
Dr. Goodrich didn’t try to send a message that payment reform isn’t a challenge for hospitalists or anyone else – she called the new system “complicated” and said that “we are in a stage of fairly dramatic health system transformation.”
But she said there are steps hospitalists can take to make quality change – and necessary change – happen.
“First of all, of course, continue to provide high-quality patient care, focus on the patients in front of you, and lead the teams that you need in order to provide high-quality care,” she said.
Also, Dr. Goodrich said, hospitalists should learn to work more closely with their own hospital administrators and the post-acute facilities in their local communities.
“We have to figure out ways to collaborate with them and align the incentives across all of these systems of care,” she said. “Some of that comes top down from payers, but much of that can happen at the local level as well.”
Yet, she noted that she often senses trepidation.
“I always get the question: ‘Well, how do we do this? How do we make this change? It’s not something that we’re necessarily trained for,’ ” Dr. Goodrich said. “There are people out there who are doing this well. This is actually spreading across the country. So seek out those high-performers and learn from them. There’s a lot of learning networks out there that you can access to learn how to make some of these changes.”
ORLANDO – As dizzying as the alphabet soup of payment reform might seem – with its swirl of new incentives, alignments, and models – hospitalists should already be familiar with many of its main ideas, said keynote speaker Kate Goodrich, MD, director of the Center for Clinical Standards and Quality at the Centers for Medicare and Medicaid Services.
That makes hospitalists poised to help reform a U.S. health care system with the dubious pairing of staggering costs and poor outcomes, Dr. Goodrich told a packed ballroom on Monday at the annual meeting of the Society of Hospital Medicine.
Many of the measures involved in payment reform – with its Merit-Based Incentive Payment System (MIPS), Medicare Access and CHIP Reauthorization Act (MACRA), and Advanced Payment Models (APMs) – focus on outpatient and ambulatory care, Dr. Goodrich acknowledged. But it’s also about medical systems, she said.
“What do you focus on as hospitalists? Improving systems of care,” she said. “We focus on clinical care for our individual patient, but part of our job is also to think about it in terms of how do I improve the care across my hospital system?”
One aspect of reform that is most likely to directly affect hospitalists is the facility-based measurement part of the Quality Payment Program, slated to take effect in 2019. If participating in MIPS – the payment model in which clinicians can receive an increase or decrease in payments based on performance measured by data on quality, cost, and other factors – clinicians can choose to have their hospital’s quality measures count toward their MIPS quality score. The facility measurement was developed in part after conversations between CMS and SHM, Dr. Goodrich said.
“Many stakeholders are very excited about this possibility for a couple of reasons: No. 1, there would be absolutely no quality-reporting burden for you if you chose to do that,” she said. “No. 2, it really aligns the incentives between you and the hospital that you’re working in. Because, after all, we are all in this together. And some folks have felt like they aren’t always aligned with the incentives of the hospital that they are working with, or working for.”
Dr. Goodrich didn’t try to send a message that payment reform isn’t a challenge for hospitalists or anyone else – she called the new system “complicated” and said that “we are in a stage of fairly dramatic health system transformation.”
But she said there are steps hospitalists can take to make quality change – and necessary change – happen.
“First of all, of course, continue to provide high-quality patient care, focus on the patients in front of you, and lead the teams that you need in order to provide high-quality care,” she said.
Also, Dr. Goodrich said, hospitalists should learn to work more closely with their own hospital administrators and the post-acute facilities in their local communities.
“We have to figure out ways to collaborate with them and align the incentives across all of these systems of care,” she said. “Some of that comes top down from payers, but much of that can happen at the local level as well.”
Yet, she noted that she often senses trepidation.
“I always get the question: ‘Well, how do we do this? How do we make this change? It’s not something that we’re necessarily trained for,’ ” Dr. Goodrich said. “There are people out there who are doing this well. This is actually spreading across the country. So seek out those high-performers and learn from them. There’s a lot of learning networks out there that you can access to learn how to make some of these changes.”
ORLANDO – As dizzying as the alphabet soup of payment reform might seem – with its swirl of new incentives, alignments, and models – hospitalists should already be familiar with many of its main ideas, said keynote speaker Kate Goodrich, MD, director of the Center for Clinical Standards and Quality at the Centers for Medicare and Medicaid Services.
That makes hospitalists poised to help reform a U.S. health care system with the dubious pairing of staggering costs and poor outcomes, Dr. Goodrich told a packed ballroom on Monday at the annual meeting of the Society of Hospital Medicine.
Many of the measures involved in payment reform – with its Merit-Based Incentive Payment System (MIPS), Medicare Access and CHIP Reauthorization Act (MACRA), and Advanced Payment Models (APMs) – focus on outpatient and ambulatory care, Dr. Goodrich acknowledged. But it’s also about medical systems, she said.
“What do you focus on as hospitalists? Improving systems of care,” she said. “We focus on clinical care for our individual patient, but part of our job is also to think about it in terms of how do I improve the care across my hospital system?”
One aspect of reform that is most likely to directly affect hospitalists is the facility-based measurement part of the Quality Payment Program, slated to take effect in 2019. If participating in MIPS – the payment model in which clinicians can receive an increase or decrease in payments based on performance measured by data on quality, cost, and other factors – clinicians can choose to have their hospital’s quality measures count toward their MIPS quality score. The facility measurement was developed in part after conversations between CMS and SHM, Dr. Goodrich said.
“Many stakeholders are very excited about this possibility for a couple of reasons: No. 1, there would be absolutely no quality-reporting burden for you if you chose to do that,” she said. “No. 2, it really aligns the incentives between you and the hospital that you’re working in. Because, after all, we are all in this together. And some folks have felt like they aren’t always aligned with the incentives of the hospital that they are working with, or working for.”
Dr. Goodrich didn’t try to send a message that payment reform isn’t a challenge for hospitalists or anyone else – she called the new system “complicated” and said that “we are in a stage of fairly dramatic health system transformation.”
But she said there are steps hospitalists can take to make quality change – and necessary change – happen.
“First of all, of course, continue to provide high-quality patient care, focus on the patients in front of you, and lead the teams that you need in order to provide high-quality care,” she said.
Also, Dr. Goodrich said, hospitalists should learn to work more closely with their own hospital administrators and the post-acute facilities in their local communities.
“We have to figure out ways to collaborate with them and align the incentives across all of these systems of care,” she said. “Some of that comes top down from payers, but much of that can happen at the local level as well.”
Yet, she noted that she often senses trepidation.
“I always get the question: ‘Well, how do we do this? How do we make this change? It’s not something that we’re necessarily trained for,’ ” Dr. Goodrich said. “There are people out there who are doing this well. This is actually spreading across the country. So seek out those high-performers and learn from them. There’s a lot of learning networks out there that you can access to learn how to make some of these changes.”