User login
Reducing the Expenditures and Workload Associated With VA Partial-Fill Prescription Processing
According to the US Department of Veterans Affairs (VA) Pharmacy Benefits Management Service, about 80% of all outpatient prescriptions filled by the VA are sent to veterans by mail order, using the Centralized Mail Order Pharmacy (CMOP) network of highly automated pharmacies around the country.1 During fiscal year (FY) 2016, the 7 VA CMOP facilities throughout the US processed 119.7 million outpatient prescriptions. Each day, these CMOPs process nearly 470,000 prescriptions, an evidence of the efficiency provided through this mail-order service.1 The use of CMOP results in lower processing costs and increased convenience for veterans compared with filling prescriptions at pharmacies at individual VA facilities. Notably, VA CMOP has been rated “among the best” mail-order pharmacies in customer satisfaction according to the 2017 J.D. Power US Pharmacy Study.2
Background
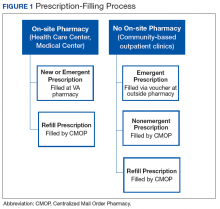
Within the Fayetteville VA Medical Center (FVAMC) system in North Carolina, on-site patients receive a new prescription where an on-site pharmacy is available (at health care centers [HCC] and the medical center). For veterans seen at community-based outpatient clinics (CBOCs), emergent new prescriptions are filled through vouchers at contract community pharmacies, and nonemergent new prescriptions are filled by the CMOP (Figure 1).
The appropriate use of the VA CMOP for refills is intended to allow on-site pharmacy staff to focus on providing customer service for veterans requesting medication counseling from a clinical pharmacist, as well as those with new, changing, or urgent prescription needs. Filling prescriptions through the CMOP also can help control the VA facility pharmacy budget.
Despite the established mail-order process, FVAMC staff noted a high volume of medication refill and partial-fill prescriptions being requested at the on-site pharmacy. When a veteran presented to a pharmacy requesting a medication refill, pharmacy staff members ordered a refill to be filled by the CMOP and provided a limited quantity, otherwise known as a partial fill, to serve as an emergency supply to supplement the veteran until the full quantity of the prescription arrived by mail. Partial fills also were completed for new prescriptions that veterans requested to pick up at the on-site pharmacy. For new 90-day supply prescriptions, pharmacy staff often filled a 30-day supply in addition to submitting the entire 90-day prescription through the CMOP, which led to an unnecessary increase in material expenditures and workload.Preliminary data noted the most frequently used partial-fill days’ supply to be 10 days. Due to the lack of partial-fill criteria, prescriptions of all classes, quantities, and days’ supplies were provided as partial fills. Prior to the implementation of this quality improvement (QI) project, there was no standard approach for how to handle these requests.
Partial fills do not provide copay reimbursement to the facility filling the prescription. In an effort to steward the funds provided to the FVAMC pharmacy department wisely, an evaluation was performed with reference to partial fills. During FY 2016, about $350,000 was spent on medications, materials, and workload associated with the partial filling of FVAMC prescriptions. With respect to unique individuals who were provided care over the course of FY 2015 and 2016, the number of unique patients served by local comparator hospitals increased by only 2%, while the number of unique patients served by FVAMC increased by 12%. This substantial growth in the number of veterans served places further emphasis on the necessity of stewarding the allotted pharmacy budget. Moreover, the excessive number of medication refill and partial-fill prescriptions filled at on-site VA pharmacies can contribute to increased wait times for veterans with urgent prescription needs.
In November 2016, FVAMC implemented an updated partial-fill guidance. Partial-fill process and refill education was provided for VA staff and veterans in an effort to allow all parties involved to use pharmacy services efficiently. This analysis reviewed the reduction in partial-fill expenditures with a secondary focus on workload expenditures following the execution of this education.
Methods
This project was deemed to be a QI project and did not require institutional review board approval. Implementation for this QI project began in November 2016. Baseline raw drug cost, number, and class of prescriptions partialed were retrospectively collected for a 90-day period prior to implementation using all available data. Postintervention data were collected for 90 days following the implementation phase to compare partial-fill expenditures and workload expenditures with baseline data.
Calculations
Materials included in the partial-fill expenditure calculation were prescription vials, prescription vial caps, and prescription labeling. Material cost per partial fill was determined by using the facility’s wholesaler acquisition unit costs to estimate a summed cost for an individual prescription vial and prescription vial cap. The estimated acquisition price of 7 prescription-labeling pages was used in the material calculation, as this was the average number of pages used when performing test partial fills.
The following equation was used to calculate total partial-fill expenditures for any specified time frame:
Total partial-fill expenditure = total raw drug cost + (material cost × number of partial fills)
In addition, the average personnel cost per partial-fill prescription was determined. Average workload expenditure per partial fill was calculated by filling a subset of 10 test prescriptions and multiplying the average time spent by an average of the general station (GS) rate for pharmacists and technicians. The average hourly rate of a GS-12 pharmacist was calculated based on an average of the 10 available pay grades within the GS-12 ranking. The average hourly rate of a GS-6 pharmacy technician was calculated based on an average of the 10 available pay grades within the GS-6 ranking.3 The average workload expenditures were calculated using the following equations:
Average pharmacist workload expenditure per partial fill = time (in hours) × average hourly rate.
Average technician workload expenditure per partial fill = time (in hours) × average hourly rate.
Partial-Fill Guidance
Updated partial-fill guidance was drafted designating acceptable prescriptions to be limited to those responsible for preventing hospitalization and treatment of acute illness. This guidance provided generalized examples of medication classes that could be acceptable for partial filling, though it was not intended to be an all-inclusive list. The guidance also noted examples of classes or groups that should not be partial filled for nonemergent reasons (vitamins, nonprescription items, antilipemics), as well as controlled substances. The refill-process education was reiterated throughout the entirety of the guidance. Specifically, if a pharmacy staff member was to perform a partial fill, a review explaining the appropriate refill process to the veteran also must be provided. If the medication was determined to be of emergent need and not yet transmitted for filling via the CMOP, the directive recommended to fill the entire quantity locally as a onetime fill.
If a onetime on-site fill was determined infeasible, partial-fill quantities were recommended to be limited to only a 7-day supply, and the full quantity filled through the CMOP. Anticipated mail wait time for CMOP prescription delivery was estimated to be less than 7 days based on experience, local pending queues, and guidance from the regional CMOP; however, time could vary among VA and CMOP facilities. Original prescriptions were to be filled for the entire quantity for the first fill at the on-site pharmacy if requested by the veteran. If the pharmacy had an insufficient quantity for an entire initial supply, it could then be partial filled for a 7-day supply and then filled through the CMOP.
The final portion of the partial-fill guidance pertained to the use of partial-fill justification codes. Prior to the execution of the partial-fill guidance, free text was entered into the comments field when processing a partial-fill prescription, as the prescription-processing system used requires a comment to proceed with the partial fill. The use of these codes served to streamline data collection in the postintervention phase and helped identify areas for further education following the close of this project.
Education
Education to the pharmacy staff was disseminated by various modalities, including in-person sessions and written and electronic correspondences. This written guidance was distributed to pharmacy staff by e-mail, the pharmacy newsletter (Rx-tra), signage posted throughout the outpatient pharmacies, and on the facility’s pharmacy Microsoft SharePoint (Redmond, WA) site. In-services provided during pharmacy staff meetings detailed information on the updated partial-fill guidance. A FVAMC Talent Management System (TMS) training module was developed and assigned to all pharmacy service staff to reiterate key points regarding this QI initiative (eAppendix).
Nonpharmacy staff were educated through staff and in-service meetings and e-mail correspondences. These in-services emphasized how nurses, medical support assistants, and health care providers (HCPs) could assist veterans by knowing the correct refill process, ensuring sufficient refills remained until the next appointment, and providing continual refill-process education.
Following implementation, all veterans receiving prescriptions through the on-site pharmacies in the FVAMC were provided a copy of the refill-process handout with each trip to the pharmacy. Nonpharmacy staff and HCPs also were provided this handout to distribute to patients. The intent of this handout was to clearly detail the various ways in which refills could be ordered and the time frame in which they should be ordered. The pharmacy became involved in new patient orientation classes for all veterans new to FVAMC. Digital signage and messaging was created and circulated throughout several of the FVAMC facilities.
Results
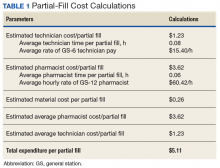
The results of calculations for material cost, personnel time spent, hourly employee rates, and average workload expenditure per partial fill are summarized in Table 1.
Following the implementation of partial-fill and refill-process education, there was a 54.3% decrease in the total number of partial fills from 5,596 in the 90 days prior to implementation, to 2,555 partials completed over the 90 days postimplementation. Regarding the primary objective, total partial-fill expenditures decreased from $52,015.44 to $44,063.01 (-15.3%). When dissecting the individual components of partial-fill expenditures, material expenditures decreased from $1,454.96 to $664.28 (-54.3%), and raw drug cost expenditures decreased from $50,596.48 to $43,398.73 (-14.3%). Workload expenditures also decreased from $27,140.60 to $12,391.75 (-54.3%).
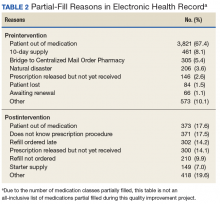
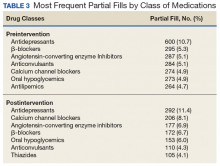
Several points of descriptive information also were collected. The average days’ supply trended down from a mode of 10 days to 7 days. This reduction in days’ supply likely was seen because staff became more aware of the customary amount required to bridge the veteran until the CMOP supply arrived by mail. Postintervention data showed a 70% utilization of partial-fill reasoning codes. The reasons for partial filling of prescriptions are summarized in Table 2.
Discussion
Following the implementation of the updated partial-fill guidance and provision of education to the FVAMC veterans and staff, a noteworthy cost savings was observed with respect to both material and workload expenditures. This large reduction in expenditure likely was not related to a reduction in the total prescription volume, as the number of total prescriptions filled by the CMOP and at FVAMC were similar in both the preliminary and postintervention periods. When the results of this 3-month QI project were extrapolated, the annual projected cost avoidance was $91,949.12.
Of note, there was no established process for adjudicating appeals to the partial-fill guidance. Any extenuating circumstances that fell outside the guidance were addressed by the outpatient pharmacy supervisor. There was no formal documentation for these disputed cases. Since there was no prespecified supervisory override code, the most appropriate partial-fill code was entered into the comments field for these scenarios. As such, there is no way to distinguish precisely how many of these partial fills were escalated to a supervisory level for a decision.
The positive fiscal impact noted from the implementation of this project should not be viewed as the only utility for such guidance. Though not directly measured within the confines of this project, a reduction in pharmacy staff time spent on partial-fill prescriptions will likely result in shorter pharmacy wait times, line lengths, and streamlining of pharmacy workflow. When the pharmacy staff is free to work on pressing issues rather than on continually educating veterans on the partial-fill or refill process, many will benefit. Veteran satisfaction was not directly measured during this project but could be an interesting topic to review as a future study.
Each VA facility is unique, with its own challenges for implementation of a project such as this. Nevertheless, the incorporation of a formal guidance and education process, perhaps adapted to the indi vidual facility’s needs may be considered for overall pharmacy operations QI.
Limitations
During the preliminary data collection period, FVAMC and its catchment area were impacted by a natural disaster, Hurricane Matthew. Based on a review of the text entered into the comments field for all partial fills, about 4% of the partial fills completed in the preliminary phase can be attributed to the hurricane. The effects of this hurricane may have potentially increased the number of partial fills completed in the preliminary phase compared with that in the postintervention phase, due to the number of veterans who were temporarily or permanently displaced from their homes. This increase in partial fills and associated expenses preintervention likely caused a slightly higher cost savings to be reflected in the postimplementation phase than what would have traditionally been observed without extenuating factors.
Several other limitations must be considered for this QI project. The implementation phase, during which all education and training was completed, was only 1 month. A longer implementation period and more opportunities to educate veterans and staff might have created a greater impact on the results. Additionally, because there were no data collected on New Patient Orientation attendance for this project, it is unclear exactly how many veterans received refill-process education through this outlet.
Though all staff members were trained on the appropriate process, it was discovered during interim analysis that several pharmacists were not following the partial-fill guidance, potentially negatively impacting the results. It is likely that staff would have benefited from continual reeducation of the process throughout the entirety of the project, as the restriction of partial filling was a novel concept to many. In addition to continual reeducation of current employees, any new hires would likely need this information as part of initial training.
Cost variance in the type of partial fills completed between the preliminary and postintervention phases also may have negatively impacted the results. The postintervention phase contained 2 high-cost classes of drugs (antivirals and immunoglobulins) that received multiple partial fills but were not partialed in the preliminary phase, which increased the raw drug cost in the postintervention phase.
Conclusion
The implementation of partial-fill and process education to FVAMC staff and veterans proved beneficial in reducing the expenditures and workload associated with partial-fill prescription processing. The continued use of the updated partial-fill guidance will provide a standardized approach for pharmacy staff when completing partial-fill prescriptions.
Facilities may consider annual reeducation on their guidance through a local TMS module, as well as occasional process reminders during staff meetings to improve staff adherence to the guidance. Moreover, the sustained incorporation of improved refill process education to new patients and with every prescription pickup could help guide the FVAMC veteran population to use pharmacy services more effectively. The adoption of such procedures may be useful for VA facilities’ health care system looking to maximize the use of funding provided for prescription services as well as improve veterans’ understanding of how to appropriately order prescription refills.
1. US Department of Veterans Affairs. Pharmacy benefits management services. https://www.pbm.va.gov/PBM/CMOP/VA_Mail_Order_Pharmacy.asp. Updated July 14, 2017. Accessed on February 26, 2018.
2. J.D. Power. Decline in pharmacy customer satisfaction driven by prescription drug costs, J. D. Power finds. [press release]. http://www.jdpower.com/press-releases/jd-power-2017-us-pharmacy-study. Published September 5, 2017. Accessed February 26, 2018.
3. US Office of Personnel Management. Pay and leave. https://www.opm.gov/policy-data-oversight/pay-leave/salaries-wages/. Accessed February 26, 2018.
4. Aragon BR, Pierce RA, Jones WN. VA CMOPs: producing a pattern of quality and efficiency in government. J Am Pharm Assoc (2003). 2012;52(6):810-815.
According to the US Department of Veterans Affairs (VA) Pharmacy Benefits Management Service, about 80% of all outpatient prescriptions filled by the VA are sent to veterans by mail order, using the Centralized Mail Order Pharmacy (CMOP) network of highly automated pharmacies around the country.1 During fiscal year (FY) 2016, the 7 VA CMOP facilities throughout the US processed 119.7 million outpatient prescriptions. Each day, these CMOPs process nearly 470,000 prescriptions, an evidence of the efficiency provided through this mail-order service.1 The use of CMOP results in lower processing costs and increased convenience for veterans compared with filling prescriptions at pharmacies at individual VA facilities. Notably, VA CMOP has been rated “among the best” mail-order pharmacies in customer satisfaction according to the 2017 J.D. Power US Pharmacy Study.2
Background
Within the Fayetteville VA Medical Center (FVAMC) system in North Carolina, on-site patients receive a new prescription where an on-site pharmacy is available (at health care centers [HCC] and the medical center). For veterans seen at community-based outpatient clinics (CBOCs), emergent new prescriptions are filled through vouchers at contract community pharmacies, and nonemergent new prescriptions are filled by the CMOP (Figure 1).
The appropriate use of the VA CMOP for refills is intended to allow on-site pharmacy staff to focus on providing customer service for veterans requesting medication counseling from a clinical pharmacist, as well as those with new, changing, or urgent prescription needs. Filling prescriptions through the CMOP also can help control the VA facility pharmacy budget.
Despite the established mail-order process, FVAMC staff noted a high volume of medication refill and partial-fill prescriptions being requested at the on-site pharmacy. When a veteran presented to a pharmacy requesting a medication refill, pharmacy staff members ordered a refill to be filled by the CMOP and provided a limited quantity, otherwise known as a partial fill, to serve as an emergency supply to supplement the veteran until the full quantity of the prescription arrived by mail. Partial fills also were completed for new prescriptions that veterans requested to pick up at the on-site pharmacy. For new 90-day supply prescriptions, pharmacy staff often filled a 30-day supply in addition to submitting the entire 90-day prescription through the CMOP, which led to an unnecessary increase in material expenditures and workload.Preliminary data noted the most frequently used partial-fill days’ supply to be 10 days. Due to the lack of partial-fill criteria, prescriptions of all classes, quantities, and days’ supplies were provided as partial fills. Prior to the implementation of this quality improvement (QI) project, there was no standard approach for how to handle these requests.
Partial fills do not provide copay reimbursement to the facility filling the prescription. In an effort to steward the funds provided to the FVAMC pharmacy department wisely, an evaluation was performed with reference to partial fills. During FY 2016, about $350,000 was spent on medications, materials, and workload associated with the partial filling of FVAMC prescriptions. With respect to unique individuals who were provided care over the course of FY 2015 and 2016, the number of unique patients served by local comparator hospitals increased by only 2%, while the number of unique patients served by FVAMC increased by 12%. This substantial growth in the number of veterans served places further emphasis on the necessity of stewarding the allotted pharmacy budget. Moreover, the excessive number of medication refill and partial-fill prescriptions filled at on-site VA pharmacies can contribute to increased wait times for veterans with urgent prescription needs.
In November 2016, FVAMC implemented an updated partial-fill guidance. Partial-fill process and refill education was provided for VA staff and veterans in an effort to allow all parties involved to use pharmacy services efficiently. This analysis reviewed the reduction in partial-fill expenditures with a secondary focus on workload expenditures following the execution of this education.
Methods
This project was deemed to be a QI project and did not require institutional review board approval. Implementation for this QI project began in November 2016. Baseline raw drug cost, number, and class of prescriptions partialed were retrospectively collected for a 90-day period prior to implementation using all available data. Postintervention data were collected for 90 days following the implementation phase to compare partial-fill expenditures and workload expenditures with baseline data.
Calculations
Materials included in the partial-fill expenditure calculation were prescription vials, prescription vial caps, and prescription labeling. Material cost per partial fill was determined by using the facility’s wholesaler acquisition unit costs to estimate a summed cost for an individual prescription vial and prescription vial cap. The estimated acquisition price of 7 prescription-labeling pages was used in the material calculation, as this was the average number of pages used when performing test partial fills.
The following equation was used to calculate total partial-fill expenditures for any specified time frame:
Total partial-fill expenditure = total raw drug cost + (material cost × number of partial fills)
In addition, the average personnel cost per partial-fill prescription was determined. Average workload expenditure per partial fill was calculated by filling a subset of 10 test prescriptions and multiplying the average time spent by an average of the general station (GS) rate for pharmacists and technicians. The average hourly rate of a GS-12 pharmacist was calculated based on an average of the 10 available pay grades within the GS-12 ranking. The average hourly rate of a GS-6 pharmacy technician was calculated based on an average of the 10 available pay grades within the GS-6 ranking.3 The average workload expenditures were calculated using the following equations:
Average pharmacist workload expenditure per partial fill = time (in hours) × average hourly rate.
Average technician workload expenditure per partial fill = time (in hours) × average hourly rate.
Partial-Fill Guidance
Updated partial-fill guidance was drafted designating acceptable prescriptions to be limited to those responsible for preventing hospitalization and treatment of acute illness. This guidance provided generalized examples of medication classes that could be acceptable for partial filling, though it was not intended to be an all-inclusive list. The guidance also noted examples of classes or groups that should not be partial filled for nonemergent reasons (vitamins, nonprescription items, antilipemics), as well as controlled substances. The refill-process education was reiterated throughout the entirety of the guidance. Specifically, if a pharmacy staff member was to perform a partial fill, a review explaining the appropriate refill process to the veteran also must be provided. If the medication was determined to be of emergent need and not yet transmitted for filling via the CMOP, the directive recommended to fill the entire quantity locally as a onetime fill.
If a onetime on-site fill was determined infeasible, partial-fill quantities were recommended to be limited to only a 7-day supply, and the full quantity filled through the CMOP. Anticipated mail wait time for CMOP prescription delivery was estimated to be less than 7 days based on experience, local pending queues, and guidance from the regional CMOP; however, time could vary among VA and CMOP facilities. Original prescriptions were to be filled for the entire quantity for the first fill at the on-site pharmacy if requested by the veteran. If the pharmacy had an insufficient quantity for an entire initial supply, it could then be partial filled for a 7-day supply and then filled through the CMOP.
The final portion of the partial-fill guidance pertained to the use of partial-fill justification codes. Prior to the execution of the partial-fill guidance, free text was entered into the comments field when processing a partial-fill prescription, as the prescription-processing system used requires a comment to proceed with the partial fill. The use of these codes served to streamline data collection in the postintervention phase and helped identify areas for further education following the close of this project.
Education
Education to the pharmacy staff was disseminated by various modalities, including in-person sessions and written and electronic correspondences. This written guidance was distributed to pharmacy staff by e-mail, the pharmacy newsletter (Rx-tra), signage posted throughout the outpatient pharmacies, and on the facility’s pharmacy Microsoft SharePoint (Redmond, WA) site. In-services provided during pharmacy staff meetings detailed information on the updated partial-fill guidance. A FVAMC Talent Management System (TMS) training module was developed and assigned to all pharmacy service staff to reiterate key points regarding this QI initiative (eAppendix).
Nonpharmacy staff were educated through staff and in-service meetings and e-mail correspondences. These in-services emphasized how nurses, medical support assistants, and health care providers (HCPs) could assist veterans by knowing the correct refill process, ensuring sufficient refills remained until the next appointment, and providing continual refill-process education.
Following implementation, all veterans receiving prescriptions through the on-site pharmacies in the FVAMC were provided a copy of the refill-process handout with each trip to the pharmacy. Nonpharmacy staff and HCPs also were provided this handout to distribute to patients. The intent of this handout was to clearly detail the various ways in which refills could be ordered and the time frame in which they should be ordered. The pharmacy became involved in new patient orientation classes for all veterans new to FVAMC. Digital signage and messaging was created and circulated throughout several of the FVAMC facilities.
Results
The results of calculations for material cost, personnel time spent, hourly employee rates, and average workload expenditure per partial fill are summarized in Table 1.
Following the implementation of partial-fill and refill-process education, there was a 54.3% decrease in the total number of partial fills from 5,596 in the 90 days prior to implementation, to 2,555 partials completed over the 90 days postimplementation. Regarding the primary objective, total partial-fill expenditures decreased from $52,015.44 to $44,063.01 (-15.3%). When dissecting the individual components of partial-fill expenditures, material expenditures decreased from $1,454.96 to $664.28 (-54.3%), and raw drug cost expenditures decreased from $50,596.48 to $43,398.73 (-14.3%). Workload expenditures also decreased from $27,140.60 to $12,391.75 (-54.3%).
Several points of descriptive information also were collected. The average days’ supply trended down from a mode of 10 days to 7 days. This reduction in days’ supply likely was seen because staff became more aware of the customary amount required to bridge the veteran until the CMOP supply arrived by mail. Postintervention data showed a 70% utilization of partial-fill reasoning codes. The reasons for partial filling of prescriptions are summarized in Table 2.
Discussion
Following the implementation of the updated partial-fill guidance and provision of education to the FVAMC veterans and staff, a noteworthy cost savings was observed with respect to both material and workload expenditures. This large reduction in expenditure likely was not related to a reduction in the total prescription volume, as the number of total prescriptions filled by the CMOP and at FVAMC were similar in both the preliminary and postintervention periods. When the results of this 3-month QI project were extrapolated, the annual projected cost avoidance was $91,949.12.
Of note, there was no established process for adjudicating appeals to the partial-fill guidance. Any extenuating circumstances that fell outside the guidance were addressed by the outpatient pharmacy supervisor. There was no formal documentation for these disputed cases. Since there was no prespecified supervisory override code, the most appropriate partial-fill code was entered into the comments field for these scenarios. As such, there is no way to distinguish precisely how many of these partial fills were escalated to a supervisory level for a decision.
The positive fiscal impact noted from the implementation of this project should not be viewed as the only utility for such guidance. Though not directly measured within the confines of this project, a reduction in pharmacy staff time spent on partial-fill prescriptions will likely result in shorter pharmacy wait times, line lengths, and streamlining of pharmacy workflow. When the pharmacy staff is free to work on pressing issues rather than on continually educating veterans on the partial-fill or refill process, many will benefit. Veteran satisfaction was not directly measured during this project but could be an interesting topic to review as a future study.
Each VA facility is unique, with its own challenges for implementation of a project such as this. Nevertheless, the incorporation of a formal guidance and education process, perhaps adapted to the indi vidual facility’s needs may be considered for overall pharmacy operations QI.
Limitations
During the preliminary data collection period, FVAMC and its catchment area were impacted by a natural disaster, Hurricane Matthew. Based on a review of the text entered into the comments field for all partial fills, about 4% of the partial fills completed in the preliminary phase can be attributed to the hurricane. The effects of this hurricane may have potentially increased the number of partial fills completed in the preliminary phase compared with that in the postintervention phase, due to the number of veterans who were temporarily or permanently displaced from their homes. This increase in partial fills and associated expenses preintervention likely caused a slightly higher cost savings to be reflected in the postimplementation phase than what would have traditionally been observed without extenuating factors.
Several other limitations must be considered for this QI project. The implementation phase, during which all education and training was completed, was only 1 month. A longer implementation period and more opportunities to educate veterans and staff might have created a greater impact on the results. Additionally, because there were no data collected on New Patient Orientation attendance for this project, it is unclear exactly how many veterans received refill-process education through this outlet.
Though all staff members were trained on the appropriate process, it was discovered during interim analysis that several pharmacists were not following the partial-fill guidance, potentially negatively impacting the results. It is likely that staff would have benefited from continual reeducation of the process throughout the entirety of the project, as the restriction of partial filling was a novel concept to many. In addition to continual reeducation of current employees, any new hires would likely need this information as part of initial training.
Cost variance in the type of partial fills completed between the preliminary and postintervention phases also may have negatively impacted the results. The postintervention phase contained 2 high-cost classes of drugs (antivirals and immunoglobulins) that received multiple partial fills but were not partialed in the preliminary phase, which increased the raw drug cost in the postintervention phase.
Conclusion
The implementation of partial-fill and process education to FVAMC staff and veterans proved beneficial in reducing the expenditures and workload associated with partial-fill prescription processing. The continued use of the updated partial-fill guidance will provide a standardized approach for pharmacy staff when completing partial-fill prescriptions.
Facilities may consider annual reeducation on their guidance through a local TMS module, as well as occasional process reminders during staff meetings to improve staff adherence to the guidance. Moreover, the sustained incorporation of improved refill process education to new patients and with every prescription pickup could help guide the FVAMC veteran population to use pharmacy services more effectively. The adoption of such procedures may be useful for VA facilities’ health care system looking to maximize the use of funding provided for prescription services as well as improve veterans’ understanding of how to appropriately order prescription refills.
According to the US Department of Veterans Affairs (VA) Pharmacy Benefits Management Service, about 80% of all outpatient prescriptions filled by the VA are sent to veterans by mail order, using the Centralized Mail Order Pharmacy (CMOP) network of highly automated pharmacies around the country.1 During fiscal year (FY) 2016, the 7 VA CMOP facilities throughout the US processed 119.7 million outpatient prescriptions. Each day, these CMOPs process nearly 470,000 prescriptions, an evidence of the efficiency provided through this mail-order service.1 The use of CMOP results in lower processing costs and increased convenience for veterans compared with filling prescriptions at pharmacies at individual VA facilities. Notably, VA CMOP has been rated “among the best” mail-order pharmacies in customer satisfaction according to the 2017 J.D. Power US Pharmacy Study.2
Background
Within the Fayetteville VA Medical Center (FVAMC) system in North Carolina, on-site patients receive a new prescription where an on-site pharmacy is available (at health care centers [HCC] and the medical center). For veterans seen at community-based outpatient clinics (CBOCs), emergent new prescriptions are filled through vouchers at contract community pharmacies, and nonemergent new prescriptions are filled by the CMOP (Figure 1).
The appropriate use of the VA CMOP for refills is intended to allow on-site pharmacy staff to focus on providing customer service for veterans requesting medication counseling from a clinical pharmacist, as well as those with new, changing, or urgent prescription needs. Filling prescriptions through the CMOP also can help control the VA facility pharmacy budget.
Despite the established mail-order process, FVAMC staff noted a high volume of medication refill and partial-fill prescriptions being requested at the on-site pharmacy. When a veteran presented to a pharmacy requesting a medication refill, pharmacy staff members ordered a refill to be filled by the CMOP and provided a limited quantity, otherwise known as a partial fill, to serve as an emergency supply to supplement the veteran until the full quantity of the prescription arrived by mail. Partial fills also were completed for new prescriptions that veterans requested to pick up at the on-site pharmacy. For new 90-day supply prescriptions, pharmacy staff often filled a 30-day supply in addition to submitting the entire 90-day prescription through the CMOP, which led to an unnecessary increase in material expenditures and workload.Preliminary data noted the most frequently used partial-fill days’ supply to be 10 days. Due to the lack of partial-fill criteria, prescriptions of all classes, quantities, and days’ supplies were provided as partial fills. Prior to the implementation of this quality improvement (QI) project, there was no standard approach for how to handle these requests.
Partial fills do not provide copay reimbursement to the facility filling the prescription. In an effort to steward the funds provided to the FVAMC pharmacy department wisely, an evaluation was performed with reference to partial fills. During FY 2016, about $350,000 was spent on medications, materials, and workload associated with the partial filling of FVAMC prescriptions. With respect to unique individuals who were provided care over the course of FY 2015 and 2016, the number of unique patients served by local comparator hospitals increased by only 2%, while the number of unique patients served by FVAMC increased by 12%. This substantial growth in the number of veterans served places further emphasis on the necessity of stewarding the allotted pharmacy budget. Moreover, the excessive number of medication refill and partial-fill prescriptions filled at on-site VA pharmacies can contribute to increased wait times for veterans with urgent prescription needs.
In November 2016, FVAMC implemented an updated partial-fill guidance. Partial-fill process and refill education was provided for VA staff and veterans in an effort to allow all parties involved to use pharmacy services efficiently. This analysis reviewed the reduction in partial-fill expenditures with a secondary focus on workload expenditures following the execution of this education.
Methods
This project was deemed to be a QI project and did not require institutional review board approval. Implementation for this QI project began in November 2016. Baseline raw drug cost, number, and class of prescriptions partialed were retrospectively collected for a 90-day period prior to implementation using all available data. Postintervention data were collected for 90 days following the implementation phase to compare partial-fill expenditures and workload expenditures with baseline data.
Calculations
Materials included in the partial-fill expenditure calculation were prescription vials, prescription vial caps, and prescription labeling. Material cost per partial fill was determined by using the facility’s wholesaler acquisition unit costs to estimate a summed cost for an individual prescription vial and prescription vial cap. The estimated acquisition price of 7 prescription-labeling pages was used in the material calculation, as this was the average number of pages used when performing test partial fills.
The following equation was used to calculate total partial-fill expenditures for any specified time frame:
Total partial-fill expenditure = total raw drug cost + (material cost × number of partial fills)
In addition, the average personnel cost per partial-fill prescription was determined. Average workload expenditure per partial fill was calculated by filling a subset of 10 test prescriptions and multiplying the average time spent by an average of the general station (GS) rate for pharmacists and technicians. The average hourly rate of a GS-12 pharmacist was calculated based on an average of the 10 available pay grades within the GS-12 ranking. The average hourly rate of a GS-6 pharmacy technician was calculated based on an average of the 10 available pay grades within the GS-6 ranking.3 The average workload expenditures were calculated using the following equations:
Average pharmacist workload expenditure per partial fill = time (in hours) × average hourly rate.
Average technician workload expenditure per partial fill = time (in hours) × average hourly rate.
Partial-Fill Guidance
Updated partial-fill guidance was drafted designating acceptable prescriptions to be limited to those responsible for preventing hospitalization and treatment of acute illness. This guidance provided generalized examples of medication classes that could be acceptable for partial filling, though it was not intended to be an all-inclusive list. The guidance also noted examples of classes or groups that should not be partial filled for nonemergent reasons (vitamins, nonprescription items, antilipemics), as well as controlled substances. The refill-process education was reiterated throughout the entirety of the guidance. Specifically, if a pharmacy staff member was to perform a partial fill, a review explaining the appropriate refill process to the veteran also must be provided. If the medication was determined to be of emergent need and not yet transmitted for filling via the CMOP, the directive recommended to fill the entire quantity locally as a onetime fill.
If a onetime on-site fill was determined infeasible, partial-fill quantities were recommended to be limited to only a 7-day supply, and the full quantity filled through the CMOP. Anticipated mail wait time for CMOP prescription delivery was estimated to be less than 7 days based on experience, local pending queues, and guidance from the regional CMOP; however, time could vary among VA and CMOP facilities. Original prescriptions were to be filled for the entire quantity for the first fill at the on-site pharmacy if requested by the veteran. If the pharmacy had an insufficient quantity for an entire initial supply, it could then be partial filled for a 7-day supply and then filled through the CMOP.
The final portion of the partial-fill guidance pertained to the use of partial-fill justification codes. Prior to the execution of the partial-fill guidance, free text was entered into the comments field when processing a partial-fill prescription, as the prescription-processing system used requires a comment to proceed with the partial fill. The use of these codes served to streamline data collection in the postintervention phase and helped identify areas for further education following the close of this project.
Education
Education to the pharmacy staff was disseminated by various modalities, including in-person sessions and written and electronic correspondences. This written guidance was distributed to pharmacy staff by e-mail, the pharmacy newsletter (Rx-tra), signage posted throughout the outpatient pharmacies, and on the facility’s pharmacy Microsoft SharePoint (Redmond, WA) site. In-services provided during pharmacy staff meetings detailed information on the updated partial-fill guidance. A FVAMC Talent Management System (TMS) training module was developed and assigned to all pharmacy service staff to reiterate key points regarding this QI initiative (eAppendix).
Nonpharmacy staff were educated through staff and in-service meetings and e-mail correspondences. These in-services emphasized how nurses, medical support assistants, and health care providers (HCPs) could assist veterans by knowing the correct refill process, ensuring sufficient refills remained until the next appointment, and providing continual refill-process education.
Following implementation, all veterans receiving prescriptions through the on-site pharmacies in the FVAMC were provided a copy of the refill-process handout with each trip to the pharmacy. Nonpharmacy staff and HCPs also were provided this handout to distribute to patients. The intent of this handout was to clearly detail the various ways in which refills could be ordered and the time frame in which they should be ordered. The pharmacy became involved in new patient orientation classes for all veterans new to FVAMC. Digital signage and messaging was created and circulated throughout several of the FVAMC facilities.
Results
The results of calculations for material cost, personnel time spent, hourly employee rates, and average workload expenditure per partial fill are summarized in Table 1.
Following the implementation of partial-fill and refill-process education, there was a 54.3% decrease in the total number of partial fills from 5,596 in the 90 days prior to implementation, to 2,555 partials completed over the 90 days postimplementation. Regarding the primary objective, total partial-fill expenditures decreased from $52,015.44 to $44,063.01 (-15.3%). When dissecting the individual components of partial-fill expenditures, material expenditures decreased from $1,454.96 to $664.28 (-54.3%), and raw drug cost expenditures decreased from $50,596.48 to $43,398.73 (-14.3%). Workload expenditures also decreased from $27,140.60 to $12,391.75 (-54.3%).
Several points of descriptive information also were collected. The average days’ supply trended down from a mode of 10 days to 7 days. This reduction in days’ supply likely was seen because staff became more aware of the customary amount required to bridge the veteran until the CMOP supply arrived by mail. Postintervention data showed a 70% utilization of partial-fill reasoning codes. The reasons for partial filling of prescriptions are summarized in Table 2.
Discussion
Following the implementation of the updated partial-fill guidance and provision of education to the FVAMC veterans and staff, a noteworthy cost savings was observed with respect to both material and workload expenditures. This large reduction in expenditure likely was not related to a reduction in the total prescription volume, as the number of total prescriptions filled by the CMOP and at FVAMC were similar in both the preliminary and postintervention periods. When the results of this 3-month QI project were extrapolated, the annual projected cost avoidance was $91,949.12.
Of note, there was no established process for adjudicating appeals to the partial-fill guidance. Any extenuating circumstances that fell outside the guidance were addressed by the outpatient pharmacy supervisor. There was no formal documentation for these disputed cases. Since there was no prespecified supervisory override code, the most appropriate partial-fill code was entered into the comments field for these scenarios. As such, there is no way to distinguish precisely how many of these partial fills were escalated to a supervisory level for a decision.
The positive fiscal impact noted from the implementation of this project should not be viewed as the only utility for such guidance. Though not directly measured within the confines of this project, a reduction in pharmacy staff time spent on partial-fill prescriptions will likely result in shorter pharmacy wait times, line lengths, and streamlining of pharmacy workflow. When the pharmacy staff is free to work on pressing issues rather than on continually educating veterans on the partial-fill or refill process, many will benefit. Veteran satisfaction was not directly measured during this project but could be an interesting topic to review as a future study.
Each VA facility is unique, with its own challenges for implementation of a project such as this. Nevertheless, the incorporation of a formal guidance and education process, perhaps adapted to the indi vidual facility’s needs may be considered for overall pharmacy operations QI.
Limitations
During the preliminary data collection period, FVAMC and its catchment area were impacted by a natural disaster, Hurricane Matthew. Based on a review of the text entered into the comments field for all partial fills, about 4% of the partial fills completed in the preliminary phase can be attributed to the hurricane. The effects of this hurricane may have potentially increased the number of partial fills completed in the preliminary phase compared with that in the postintervention phase, due to the number of veterans who were temporarily or permanently displaced from their homes. This increase in partial fills and associated expenses preintervention likely caused a slightly higher cost savings to be reflected in the postimplementation phase than what would have traditionally been observed without extenuating factors.
Several other limitations must be considered for this QI project. The implementation phase, during which all education and training was completed, was only 1 month. A longer implementation period and more opportunities to educate veterans and staff might have created a greater impact on the results. Additionally, because there were no data collected on New Patient Orientation attendance for this project, it is unclear exactly how many veterans received refill-process education through this outlet.
Though all staff members were trained on the appropriate process, it was discovered during interim analysis that several pharmacists were not following the partial-fill guidance, potentially negatively impacting the results. It is likely that staff would have benefited from continual reeducation of the process throughout the entirety of the project, as the restriction of partial filling was a novel concept to many. In addition to continual reeducation of current employees, any new hires would likely need this information as part of initial training.
Cost variance in the type of partial fills completed between the preliminary and postintervention phases also may have negatively impacted the results. The postintervention phase contained 2 high-cost classes of drugs (antivirals and immunoglobulins) that received multiple partial fills but were not partialed in the preliminary phase, which increased the raw drug cost in the postintervention phase.
Conclusion
The implementation of partial-fill and process education to FVAMC staff and veterans proved beneficial in reducing the expenditures and workload associated with partial-fill prescription processing. The continued use of the updated partial-fill guidance will provide a standardized approach for pharmacy staff when completing partial-fill prescriptions.
Facilities may consider annual reeducation on their guidance through a local TMS module, as well as occasional process reminders during staff meetings to improve staff adherence to the guidance. Moreover, the sustained incorporation of improved refill process education to new patients and with every prescription pickup could help guide the FVAMC veteran population to use pharmacy services more effectively. The adoption of such procedures may be useful for VA facilities’ health care system looking to maximize the use of funding provided for prescription services as well as improve veterans’ understanding of how to appropriately order prescription refills.
1. US Department of Veterans Affairs. Pharmacy benefits management services. https://www.pbm.va.gov/PBM/CMOP/VA_Mail_Order_Pharmacy.asp. Updated July 14, 2017. Accessed on February 26, 2018.
2. J.D. Power. Decline in pharmacy customer satisfaction driven by prescription drug costs, J. D. Power finds. [press release]. http://www.jdpower.com/press-releases/jd-power-2017-us-pharmacy-study. Published September 5, 2017. Accessed February 26, 2018.
3. US Office of Personnel Management. Pay and leave. https://www.opm.gov/policy-data-oversight/pay-leave/salaries-wages/. Accessed February 26, 2018.
4. Aragon BR, Pierce RA, Jones WN. VA CMOPs: producing a pattern of quality and efficiency in government. J Am Pharm Assoc (2003). 2012;52(6):810-815.
1. US Department of Veterans Affairs. Pharmacy benefits management services. https://www.pbm.va.gov/PBM/CMOP/VA_Mail_Order_Pharmacy.asp. Updated July 14, 2017. Accessed on February 26, 2018.
2. J.D. Power. Decline in pharmacy customer satisfaction driven by prescription drug costs, J. D. Power finds. [press release]. http://www.jdpower.com/press-releases/jd-power-2017-us-pharmacy-study. Published September 5, 2017. Accessed February 26, 2018.
3. US Office of Personnel Management. Pay and leave. https://www.opm.gov/policy-data-oversight/pay-leave/salaries-wages/. Accessed February 26, 2018.
4. Aragon BR, Pierce RA, Jones WN. VA CMOPs: producing a pattern of quality and efficiency in government. J Am Pharm Assoc (2003). 2012;52(6):810-815.
Physical activity led to lower risk of CV events – regardless of genetic risk
Exercise might help compensate for a high genetic risk of cardiovascular disease, according to the findings of a large prospective observational cohort study.
High-risk individuals in the top cardiorespiratory fitness tertile had a 49% lower risk of coronary heart disease (hazard ratio, 0.51; 95% confidence interval, 0.38-0.69) and a 60% lower risk of atrial fibrillation (HR, 0.40; 95% CI, 0.30-0.55) compared with those in the bottom fitness tertile, reported Emmi Tikkanen, PhD, of Stanford (Calif.) University, and her associates. The study was published in Circulation.
Little is known about whether exercise offsets genetic risk for cardiovascular disease. For the study, the researchers measured grip strength, cardiorespiratory fitness (based on net oxygen consumption while riding a stationary bicycle), cardiovascular events, and mortality among 482,702 participants in the UK Biobank longitudinal cohort study. More than half of individuals were women and none had baseline evidence of heart disease. The researchers stratified cases of coronary artery disease (CHD) and atrial fibrillation (AF) by whether individuals were at high, intermediate, or low genetic risk based on genome-wide association data.
Over a median follow-up period of 6.1 years (interquartile range, 5.4 to 6.8 years), there were nearly 21,000 cardiovascular events, including more than 8,000 cases of CHD and nearly 10,000 cases of AF. For all risk groups, increased grip strength and cardiorespiratory fitness were associated with a significantly lower risk of CHD and AF (P less than .001), even after adjustment for demographic factors, diabetes, smoking, systolic blood pressure, body mass index, and use of lipid-lowering medications.
The researchers did not look closely at types or durations of exercise. “Future studies evaluating the effects of strength versus aerobic training on subclinical or clinical cardiovascular outcomes could help to tailor exercise programs for individuals with elevated genetic risk for these diseases,” they wrote.
Funders included the National Institutes of Health, Knut and Alice Wallenberg Foundation, Finnish Cultural Foundation, Finnish Foundation for Cardiovascular Research, and Emil Aaltonen Foundation. Coauthor Erik Ingelsson, MD, disclosed advisory relationships with Precision Wellness and Olink Proteomics. The other authors reported having no conflicts of interest.
SOURCE: Tikkanen E et al. Circulation. 2018 Apr 9. doi: 10.1161/CIRCULATIONAHA.117.032432.
Exercise might help compensate for a high genetic risk of cardiovascular disease, according to the findings of a large prospective observational cohort study.
High-risk individuals in the top cardiorespiratory fitness tertile had a 49% lower risk of coronary heart disease (hazard ratio, 0.51; 95% confidence interval, 0.38-0.69) and a 60% lower risk of atrial fibrillation (HR, 0.40; 95% CI, 0.30-0.55) compared with those in the bottom fitness tertile, reported Emmi Tikkanen, PhD, of Stanford (Calif.) University, and her associates. The study was published in Circulation.
Little is known about whether exercise offsets genetic risk for cardiovascular disease. For the study, the researchers measured grip strength, cardiorespiratory fitness (based on net oxygen consumption while riding a stationary bicycle), cardiovascular events, and mortality among 482,702 participants in the UK Biobank longitudinal cohort study. More than half of individuals were women and none had baseline evidence of heart disease. The researchers stratified cases of coronary artery disease (CHD) and atrial fibrillation (AF) by whether individuals were at high, intermediate, or low genetic risk based on genome-wide association data.
Over a median follow-up period of 6.1 years (interquartile range, 5.4 to 6.8 years), there were nearly 21,000 cardiovascular events, including more than 8,000 cases of CHD and nearly 10,000 cases of AF. For all risk groups, increased grip strength and cardiorespiratory fitness were associated with a significantly lower risk of CHD and AF (P less than .001), even after adjustment for demographic factors, diabetes, smoking, systolic blood pressure, body mass index, and use of lipid-lowering medications.
The researchers did not look closely at types or durations of exercise. “Future studies evaluating the effects of strength versus aerobic training on subclinical or clinical cardiovascular outcomes could help to tailor exercise programs for individuals with elevated genetic risk for these diseases,” they wrote.
Funders included the National Institutes of Health, Knut and Alice Wallenberg Foundation, Finnish Cultural Foundation, Finnish Foundation for Cardiovascular Research, and Emil Aaltonen Foundation. Coauthor Erik Ingelsson, MD, disclosed advisory relationships with Precision Wellness and Olink Proteomics. The other authors reported having no conflicts of interest.
SOURCE: Tikkanen E et al. Circulation. 2018 Apr 9. doi: 10.1161/CIRCULATIONAHA.117.032432.
Exercise might help compensate for a high genetic risk of cardiovascular disease, according to the findings of a large prospective observational cohort study.
High-risk individuals in the top cardiorespiratory fitness tertile had a 49% lower risk of coronary heart disease (hazard ratio, 0.51; 95% confidence interval, 0.38-0.69) and a 60% lower risk of atrial fibrillation (HR, 0.40; 95% CI, 0.30-0.55) compared with those in the bottom fitness tertile, reported Emmi Tikkanen, PhD, of Stanford (Calif.) University, and her associates. The study was published in Circulation.
Little is known about whether exercise offsets genetic risk for cardiovascular disease. For the study, the researchers measured grip strength, cardiorespiratory fitness (based on net oxygen consumption while riding a stationary bicycle), cardiovascular events, and mortality among 482,702 participants in the UK Biobank longitudinal cohort study. More than half of individuals were women and none had baseline evidence of heart disease. The researchers stratified cases of coronary artery disease (CHD) and atrial fibrillation (AF) by whether individuals were at high, intermediate, or low genetic risk based on genome-wide association data.
Over a median follow-up period of 6.1 years (interquartile range, 5.4 to 6.8 years), there were nearly 21,000 cardiovascular events, including more than 8,000 cases of CHD and nearly 10,000 cases of AF. For all risk groups, increased grip strength and cardiorespiratory fitness were associated with a significantly lower risk of CHD and AF (P less than .001), even after adjustment for demographic factors, diabetes, smoking, systolic blood pressure, body mass index, and use of lipid-lowering medications.
The researchers did not look closely at types or durations of exercise. “Future studies evaluating the effects of strength versus aerobic training on subclinical or clinical cardiovascular outcomes could help to tailor exercise programs for individuals with elevated genetic risk for these diseases,” they wrote.
Funders included the National Institutes of Health, Knut and Alice Wallenberg Foundation, Finnish Cultural Foundation, Finnish Foundation for Cardiovascular Research, and Emil Aaltonen Foundation. Coauthor Erik Ingelsson, MD, disclosed advisory relationships with Precision Wellness and Olink Proteomics. The other authors reported having no conflicts of interest.
SOURCE: Tikkanen E et al. Circulation. 2018 Apr 9. doi: 10.1161/CIRCULATIONAHA.117.032432.
FROM CIRCULATION
Key clinical point: Exercise may offset a high genetic risk of cardiovascular disease.
Major finding: High levels of cardiovascular fitness were associated with a 49% lower risk of coronary heart disease and a 60% lower risk of atrial fibrillation among genetically high-risk individuals.
Study details: Prospective observational cohort study of 482,702 persons (median follow-up, 6.1 years).
Disclosures: Funders included the National Institutes of Health, Knut and Alice Wallenberg Foundation, Finnish Cultural Foundation, Finnish Foundation for Cardiovascular Research, and Emil Aaltonen Foundation. Coauthor Erik Ingelsson, MD, disclosed advisory relationships with Precision Wellness and Olink Proteomics. The other authors reported having no conflicts of interest.
Source: Tikkanen E et al. Circulation. 2018 Apr 9. doi: 10.1161/CIRCULATIONAHA.117.032432.
Team maps genetic evolution of T-ALL subtype
Single-cell analysis has revealed key genetic events in a type of T-cell acute lymphoblastic leukemia (T-ALL), according to researchers.
The team tracked the branching pattern of evolution in STIL-TAL1-positive T-ALL and identified mutations that may trigger development of the disease.
The researchers believe their findings could be used in minimal residual disease assessments as well as for the development of new targeted drugs.
Caroline Furness, MD, of Institute of Cancer Research in London, UK, and her colleagues described this research in Leukemia.
To determine the sequence of mutational events in STIL-TAL1-positive T-ALL, the researchers examined individual leukemia cells from 19 children and young adults with the disease, as well as 1 cell line with the STIL-TAL1 rearrangement (RPMI 8402).
The team found the STIL-TAL1 gene fusion and inactivation of the CDKN2A gene occurred very early in leukemia development.
The researchers said it was difficult to tell whether STIL-TAL1 fusion or CDKN2A loss are initiating events in this disease, and it isn’t clear which mutational event occurs first.
However, the team believes the STIL-TAL1 fusion is likely a founder or truncal event for this type of leukemia, so targeting the TAL1 regulatory complex could be an effective way to treat the disease.
The researchers also identified mutations in NOTCH1 and PTEN as secondary subclonal events.
Half of the samples examined had errors affecting PTEN, which suggests these events are key to maintaining leukemia growth and survival in STIL-TAL1-positive T-ALL, according to the researchers.
“We need to understand how cancers evolve and unpick which mutations are key to triggering cancer development and which are important for driving its growth and spread,” Dr Furness said.
“Our study uncovered these crucial mutations in a type of leukemia that accounts for around a quarter of cases of T-cell leukemia in children and young adults. This will help us to develop more effective treatments, especially in those children who relapse, and kinder treatments that won’t cause life-long side effects.”
Single-cell analysis has revealed key genetic events in a type of T-cell acute lymphoblastic leukemia (T-ALL), according to researchers.
The team tracked the branching pattern of evolution in STIL-TAL1-positive T-ALL and identified mutations that may trigger development of the disease.
The researchers believe their findings could be used in minimal residual disease assessments as well as for the development of new targeted drugs.
Caroline Furness, MD, of Institute of Cancer Research in London, UK, and her colleagues described this research in Leukemia.
To determine the sequence of mutational events in STIL-TAL1-positive T-ALL, the researchers examined individual leukemia cells from 19 children and young adults with the disease, as well as 1 cell line with the STIL-TAL1 rearrangement (RPMI 8402).
The team found the STIL-TAL1 gene fusion and inactivation of the CDKN2A gene occurred very early in leukemia development.
The researchers said it was difficult to tell whether STIL-TAL1 fusion or CDKN2A loss are initiating events in this disease, and it isn’t clear which mutational event occurs first.
However, the team believes the STIL-TAL1 fusion is likely a founder or truncal event for this type of leukemia, so targeting the TAL1 regulatory complex could be an effective way to treat the disease.
The researchers also identified mutations in NOTCH1 and PTEN as secondary subclonal events.
Half of the samples examined had errors affecting PTEN, which suggests these events are key to maintaining leukemia growth and survival in STIL-TAL1-positive T-ALL, according to the researchers.
“We need to understand how cancers evolve and unpick which mutations are key to triggering cancer development and which are important for driving its growth and spread,” Dr Furness said.
“Our study uncovered these crucial mutations in a type of leukemia that accounts for around a quarter of cases of T-cell leukemia in children and young adults. This will help us to develop more effective treatments, especially in those children who relapse, and kinder treatments that won’t cause life-long side effects.”
Single-cell analysis has revealed key genetic events in a type of T-cell acute lymphoblastic leukemia (T-ALL), according to researchers.
The team tracked the branching pattern of evolution in STIL-TAL1-positive T-ALL and identified mutations that may trigger development of the disease.
The researchers believe their findings could be used in minimal residual disease assessments as well as for the development of new targeted drugs.
Caroline Furness, MD, of Institute of Cancer Research in London, UK, and her colleagues described this research in Leukemia.
To determine the sequence of mutational events in STIL-TAL1-positive T-ALL, the researchers examined individual leukemia cells from 19 children and young adults with the disease, as well as 1 cell line with the STIL-TAL1 rearrangement (RPMI 8402).
The team found the STIL-TAL1 gene fusion and inactivation of the CDKN2A gene occurred very early in leukemia development.
The researchers said it was difficult to tell whether STIL-TAL1 fusion or CDKN2A loss are initiating events in this disease, and it isn’t clear which mutational event occurs first.
However, the team believes the STIL-TAL1 fusion is likely a founder or truncal event for this type of leukemia, so targeting the TAL1 regulatory complex could be an effective way to treat the disease.
The researchers also identified mutations in NOTCH1 and PTEN as secondary subclonal events.
Half of the samples examined had errors affecting PTEN, which suggests these events are key to maintaining leukemia growth and survival in STIL-TAL1-positive T-ALL, according to the researchers.
“We need to understand how cancers evolve and unpick which mutations are key to triggering cancer development and which are important for driving its growth and spread,” Dr Furness said.
“Our study uncovered these crucial mutations in a type of leukemia that accounts for around a quarter of cases of T-cell leukemia in children and young adults. This will help us to develop more effective treatments, especially in those children who relapse, and kinder treatments that won’t cause life-long side effects.”
Language difficulties persist until age 13 for very preterm infants
Children born very preterm continue to display language difficulties compared with term controls at 13 years of age, with no evidence of developmental “catch up.”
Given the functional implications associated with language deficits, early language-based interventions should be considered for children born VP, investigators wrote in Pediatrics.
“Difficulties in language functioning in this cohort of children born VP remained stable from 2 to 13 years of age. Although generalized language deficits were observed, the VP group had marked difficulties on expressive components of language,” wrote Thi-Nhu-Ngoc Nguyen, BSc, of Monash University, Melbourne, and her associates.
Read the full story here.
Children born very preterm continue to display language difficulties compared with term controls at 13 years of age, with no evidence of developmental “catch up.”
Given the functional implications associated with language deficits, early language-based interventions should be considered for children born VP, investigators wrote in Pediatrics.
“Difficulties in language functioning in this cohort of children born VP remained stable from 2 to 13 years of age. Although generalized language deficits were observed, the VP group had marked difficulties on expressive components of language,” wrote Thi-Nhu-Ngoc Nguyen, BSc, of Monash University, Melbourne, and her associates.
Read the full story here.
Children born very preterm continue to display language difficulties compared with term controls at 13 years of age, with no evidence of developmental “catch up.”
Given the functional implications associated with language deficits, early language-based interventions should be considered for children born VP, investigators wrote in Pediatrics.
“Difficulties in language functioning in this cohort of children born VP remained stable from 2 to 13 years of age. Although generalized language deficits were observed, the VP group had marked difficulties on expressive components of language,” wrote Thi-Nhu-Ngoc Nguyen, BSc, of Monash University, Melbourne, and her associates.
Read the full story here.
FROM PEDIATRICS
From Local Bar to Police Car

ANSWER
The radiograph demonstrates no acute injury to the wrist. There is, however, a subtle nondisplaced fracture of the distal fifth metacarpal joint. The patient was given a wrist splint for symptomatic relief, and orthopedic follow-up was coordinated.

ANSWER
The radiograph demonstrates no acute injury to the wrist. There is, however, a subtle nondisplaced fracture of the distal fifth metacarpal joint. The patient was given a wrist splint for symptomatic relief, and orthopedic follow-up was coordinated.

ANSWER
The radiograph demonstrates no acute injury to the wrist. There is, however, a subtle nondisplaced fracture of the distal fifth metacarpal joint. The patient was given a wrist splint for symptomatic relief, and orthopedic follow-up was coordinated.

A 31-year-old man is brought to your facility by local law enforcement for evaluation of left wrist pain following an altercation. The patient was reportedly at a local bar; as he was leaving, he started arguing with some other patrons. A fight ensued.
The patient believes he was struck by something on his left wrist. He denies any other injuries or complaints. His medical history is unremarkable, and vital signs are stable.
Physical examination of his left wrist shows no obvious deformity. There is some mild swelling over the dorsal aspect of his wrist. Range of motion is painful and limited. Good capillary refill is noted in the fingers, and sensation is intact. Good pulses are present.
Radiograph of the left wrist is obtained. What is your impression?
Use of a risk score may be able to identify high-risk patients presenting with acute heart failure
Clinical question: Can we use readily available data to risk stratify patients who present to the emergency department in acute heart failure (AHF)?
Background: Although cardiac biomarkers such as troponin and B-natriuretic peptide have general prognostic value in patients with AHF presenting to the emergency department, these values do not reliably aid in determining patients’ risk for unfavorable outcomes at the time of clinical decision making. Currently available published scores for risk-stratifying patients with AHF in the ED have limited applicability.
Setting: The registry included patients from 34 different hospitals in Spain.
Synopsis: This study analyzed clinical variables from a cohort of 4,897 AHF patients to determine predictors of patient outcomes. Thirteen clinical variables were identified as independent predictors of 30-day mortality and were incorporated into a risk score calculator (MEESSI-AHF). The risk score includes variables such as vital signs, age, labs values, and performance status. A second cohort of 3,229 patients were used to validate the risk score. The risk score effectively discriminates patients into low-, intermediate-, and high-risk patients. One important limitation is a high number of missing values in derivation cohort that required advanced statistics to overcome. The generalizability of the population studies (Spanish population) to other countries is still unclear. A risk score that can reasonably identify low-risk patients may be the most clinically useful in order to identify patients that either can be treated effectively in the emergency department and may not warrant inpatient admission.
Bottom line: The MEESSI-AHF risk score may be a helpful tool in identifying the risk of 30-day mortality in patients who present to the ED with AHF, but it is currently unclear if the score can be generalized to other populations.
Citation: Miro O et al. Predicting 30-day mortality for patients with acute heart failure in the emergency department: A cohort study. Ann Intern Med. 2017 Nov 21;167(10):698-705.
Dr. Maleque is assistant professor of medicine in the division of hospital medicine, Emory University, Atlanta.
Clinical question: Can we use readily available data to risk stratify patients who present to the emergency department in acute heart failure (AHF)?
Background: Although cardiac biomarkers such as troponin and B-natriuretic peptide have general prognostic value in patients with AHF presenting to the emergency department, these values do not reliably aid in determining patients’ risk for unfavorable outcomes at the time of clinical decision making. Currently available published scores for risk-stratifying patients with AHF in the ED have limited applicability.
Setting: The registry included patients from 34 different hospitals in Spain.
Synopsis: This study analyzed clinical variables from a cohort of 4,897 AHF patients to determine predictors of patient outcomes. Thirteen clinical variables were identified as independent predictors of 30-day mortality and were incorporated into a risk score calculator (MEESSI-AHF). The risk score includes variables such as vital signs, age, labs values, and performance status. A second cohort of 3,229 patients were used to validate the risk score. The risk score effectively discriminates patients into low-, intermediate-, and high-risk patients. One important limitation is a high number of missing values in derivation cohort that required advanced statistics to overcome. The generalizability of the population studies (Spanish population) to other countries is still unclear. A risk score that can reasonably identify low-risk patients may be the most clinically useful in order to identify patients that either can be treated effectively in the emergency department and may not warrant inpatient admission.
Bottom line: The MEESSI-AHF risk score may be a helpful tool in identifying the risk of 30-day mortality in patients who present to the ED with AHF, but it is currently unclear if the score can be generalized to other populations.
Citation: Miro O et al. Predicting 30-day mortality for patients with acute heart failure in the emergency department: A cohort study. Ann Intern Med. 2017 Nov 21;167(10):698-705.
Dr. Maleque is assistant professor of medicine in the division of hospital medicine, Emory University, Atlanta.
Clinical question: Can we use readily available data to risk stratify patients who present to the emergency department in acute heart failure (AHF)?
Background: Although cardiac biomarkers such as troponin and B-natriuretic peptide have general prognostic value in patients with AHF presenting to the emergency department, these values do not reliably aid in determining patients’ risk for unfavorable outcomes at the time of clinical decision making. Currently available published scores for risk-stratifying patients with AHF in the ED have limited applicability.
Setting: The registry included patients from 34 different hospitals in Spain.
Synopsis: This study analyzed clinical variables from a cohort of 4,897 AHF patients to determine predictors of patient outcomes. Thirteen clinical variables were identified as independent predictors of 30-day mortality and were incorporated into a risk score calculator (MEESSI-AHF). The risk score includes variables such as vital signs, age, labs values, and performance status. A second cohort of 3,229 patients were used to validate the risk score. The risk score effectively discriminates patients into low-, intermediate-, and high-risk patients. One important limitation is a high number of missing values in derivation cohort that required advanced statistics to overcome. The generalizability of the population studies (Spanish population) to other countries is still unclear. A risk score that can reasonably identify low-risk patients may be the most clinically useful in order to identify patients that either can be treated effectively in the emergency department and may not warrant inpatient admission.
Bottom line: The MEESSI-AHF risk score may be a helpful tool in identifying the risk of 30-day mortality in patients who present to the ED with AHF, but it is currently unclear if the score can be generalized to other populations.
Citation: Miro O et al. Predicting 30-day mortality for patients with acute heart failure in the emergency department: A cohort study. Ann Intern Med. 2017 Nov 21;167(10):698-705.
Dr. Maleque is assistant professor of medicine in the division of hospital medicine, Emory University, Atlanta.
Video: SHM President Nasim Afsar seeks an “unrelenting focus on delivering value”
ORLANDO – In a video interview, Nasim Afsar, MD, SFHM, details the career road that led her to the “tremendous honor” of becoming president of the Society of Hospital Medicine.
Having been on the board of directors for 6 years was a profound experience, according to Dr. Afsar, and now as president she looks to take what she has learned and focus on the future of the field.
When asked about her overall vision for the coming year for the Society, Dr. Afsar said that she is committed to “an unrelenting focus on delivering value to our patients, our institutions, and society, and the way we do that is through population health management.”
ORLANDO – In a video interview, Nasim Afsar, MD, SFHM, details the career road that led her to the “tremendous honor” of becoming president of the Society of Hospital Medicine.
Having been on the board of directors for 6 years was a profound experience, according to Dr. Afsar, and now as president she looks to take what she has learned and focus on the future of the field.
When asked about her overall vision for the coming year for the Society, Dr. Afsar said that she is committed to “an unrelenting focus on delivering value to our patients, our institutions, and society, and the way we do that is through population health management.”
ORLANDO – In a video interview, Nasim Afsar, MD, SFHM, details the career road that led her to the “tremendous honor” of becoming president of the Society of Hospital Medicine.
Having been on the board of directors for 6 years was a profound experience, according to Dr. Afsar, and now as president she looks to take what she has learned and focus on the future of the field.
When asked about her overall vision for the coming year for the Society, Dr. Afsar said that she is committed to “an unrelenting focus on delivering value to our patients, our institutions, and society, and the way we do that is through population health management.”
REPORTING FROM HOSPITAL MEDICINE 2018
Two scoring systems helpful in diagnosing heparin-induced thrombocytopenia
SAN DIEGO – Both the 4Ts Score and the HIT Expert Probability (HEP) Score are useful in clinical practice for the diagnosis of heparin-induced thrombocytopenia, but the HEP score may have better operative characteristics in ICU patients, results from a “real world” analysis showed.
“The diagnosis of heparin-induced thrombocytopenia (HIT) is challenging,” Allyson M. Pishko, MD, one of the study authors, said at the biennial summit of the Thrombosis & Hemostasis Societies of North America. “The 4Ts Score is commonly used, but limitations include its low positive predictive value and significant interobserver variability.”
One external prospective study showed operating characteristics similar to those of 4Ts scores (Thromb Haemost 2015;113[3]:633-40).
The aim of the current study was to validate the HEP Score in a “real world” setting and to compare the performance of the HEP Score versus the 4Ts Score. The researchers enrolled 292 adults with suspected acute HIT who were hospitalized at the University of Pennsylvania or affiliated community hospitals, and who had HIT laboratory testing ordered.
The HEP Score and the 4Ts Score were calculated by a member of the clinical team and were completed prior to return of the HIT lab test result. The majority of scorers (62%) were hematology fellows, followed by attendings (35%), and residents/students (3%). All patients underwent testing with an HIT ELISA and serotonin-release assay (SRA). Patients in whom the optical density of the ELISA was less than 0.4 units were classified as not having HIT. The researchers used the Wilcoxon rank-sum test to compare HEP and 4Ts Scores in patients with and without HIT.
Of the 292 patients, 209 were HIT negative and 83 had their data reviewed by an expert panel. Of these 83 patients, 40 were found to be HIT negative and 43 were HIT positive, and their mean ages were 65 years and 63 years, respectively. Among the cases found to be positive for HIT, 93% had HIT ELISA optical density of 1 or greater and 69.7% were SRA positive. The median HEP Score in patients with and without HIT was 8 versus 5 (P less than .0001).
At the prespecified screening cut-off of 2 or more points, the HEP Score was 97.7% sensitive and 21.9% specific, with a positive predictive value of 17.7% and a negative predictive value of 98.2%. A cut-off of 5 or greater provided 90.7% sensitivity and 47.8% specificity with a positive predictive value of 23.1% and a negative predictive value of 96.8%. The mean time to calculate the HEP Score was 4.1 minutes.
The median 4Ts Score in patients with and without HIT was 5 versus 4 (P less than .0001), Dr. Pishko reported. A 4Ts Score of 4 or greater had a sensitivity of 97.7% and specificity of 32.9%, with a positive predictive value of 20.1% and a negative predictive value of 98.8%.
The area under the ROC curves for the HEP Score and 4Ts Score were similar (0.81 vs. 0.76; P = .121). Subset analysis revealed that compared with the 4Ts Score, the HEP Score had better operating characteristics in ICU patients (AUC 0.87 vs. 0.79; P= .029) and with trainee scorers (AUC 0.79 vs. 0.73; P = .032).
“Our data suggest that either the HEP Score or the 4Ts Score could be used in clinical practice,” Dr. Pishko said.
The National Institutes of Health funded the study. Dr. Pishko reported having no financial disclosures.
SOURCE: Pishko A et al. THSNA 2018.
SAN DIEGO – Both the 4Ts Score and the HIT Expert Probability (HEP) Score are useful in clinical practice for the diagnosis of heparin-induced thrombocytopenia, but the HEP score may have better operative characteristics in ICU patients, results from a “real world” analysis showed.
“The diagnosis of heparin-induced thrombocytopenia (HIT) is challenging,” Allyson M. Pishko, MD, one of the study authors, said at the biennial summit of the Thrombosis & Hemostasis Societies of North America. “The 4Ts Score is commonly used, but limitations include its low positive predictive value and significant interobserver variability.”
One external prospective study showed operating characteristics similar to those of 4Ts scores (Thromb Haemost 2015;113[3]:633-40).
The aim of the current study was to validate the HEP Score in a “real world” setting and to compare the performance of the HEP Score versus the 4Ts Score. The researchers enrolled 292 adults with suspected acute HIT who were hospitalized at the University of Pennsylvania or affiliated community hospitals, and who had HIT laboratory testing ordered.
The HEP Score and the 4Ts Score were calculated by a member of the clinical team and were completed prior to return of the HIT lab test result. The majority of scorers (62%) were hematology fellows, followed by attendings (35%), and residents/students (3%). All patients underwent testing with an HIT ELISA and serotonin-release assay (SRA). Patients in whom the optical density of the ELISA was less than 0.4 units were classified as not having HIT. The researchers used the Wilcoxon rank-sum test to compare HEP and 4Ts Scores in patients with and without HIT.
Of the 292 patients, 209 were HIT negative and 83 had their data reviewed by an expert panel. Of these 83 patients, 40 were found to be HIT negative and 43 were HIT positive, and their mean ages were 65 years and 63 years, respectively. Among the cases found to be positive for HIT, 93% had HIT ELISA optical density of 1 or greater and 69.7% were SRA positive. The median HEP Score in patients with and without HIT was 8 versus 5 (P less than .0001).
At the prespecified screening cut-off of 2 or more points, the HEP Score was 97.7% sensitive and 21.9% specific, with a positive predictive value of 17.7% and a negative predictive value of 98.2%. A cut-off of 5 or greater provided 90.7% sensitivity and 47.8% specificity with a positive predictive value of 23.1% and a negative predictive value of 96.8%. The mean time to calculate the HEP Score was 4.1 minutes.
The median 4Ts Score in patients with and without HIT was 5 versus 4 (P less than .0001), Dr. Pishko reported. A 4Ts Score of 4 or greater had a sensitivity of 97.7% and specificity of 32.9%, with a positive predictive value of 20.1% and a negative predictive value of 98.8%.
The area under the ROC curves for the HEP Score and 4Ts Score were similar (0.81 vs. 0.76; P = .121). Subset analysis revealed that compared with the 4Ts Score, the HEP Score had better operating characteristics in ICU patients (AUC 0.87 vs. 0.79; P= .029) and with trainee scorers (AUC 0.79 vs. 0.73; P = .032).
“Our data suggest that either the HEP Score or the 4Ts Score could be used in clinical practice,” Dr. Pishko said.
The National Institutes of Health funded the study. Dr. Pishko reported having no financial disclosures.
SOURCE: Pishko A et al. THSNA 2018.
SAN DIEGO – Both the 4Ts Score and the HIT Expert Probability (HEP) Score are useful in clinical practice for the diagnosis of heparin-induced thrombocytopenia, but the HEP score may have better operative characteristics in ICU patients, results from a “real world” analysis showed.
“The diagnosis of heparin-induced thrombocytopenia (HIT) is challenging,” Allyson M. Pishko, MD, one of the study authors, said at the biennial summit of the Thrombosis & Hemostasis Societies of North America. “The 4Ts Score is commonly used, but limitations include its low positive predictive value and significant interobserver variability.”
One external prospective study showed operating characteristics similar to those of 4Ts scores (Thromb Haemost 2015;113[3]:633-40).
The aim of the current study was to validate the HEP Score in a “real world” setting and to compare the performance of the HEP Score versus the 4Ts Score. The researchers enrolled 292 adults with suspected acute HIT who were hospitalized at the University of Pennsylvania or affiliated community hospitals, and who had HIT laboratory testing ordered.
The HEP Score and the 4Ts Score were calculated by a member of the clinical team and were completed prior to return of the HIT lab test result. The majority of scorers (62%) were hematology fellows, followed by attendings (35%), and residents/students (3%). All patients underwent testing with an HIT ELISA and serotonin-release assay (SRA). Patients in whom the optical density of the ELISA was less than 0.4 units were classified as not having HIT. The researchers used the Wilcoxon rank-sum test to compare HEP and 4Ts Scores in patients with and without HIT.
Of the 292 patients, 209 were HIT negative and 83 had their data reviewed by an expert panel. Of these 83 patients, 40 were found to be HIT negative and 43 were HIT positive, and their mean ages were 65 years and 63 years, respectively. Among the cases found to be positive for HIT, 93% had HIT ELISA optical density of 1 or greater and 69.7% were SRA positive. The median HEP Score in patients with and without HIT was 8 versus 5 (P less than .0001).
At the prespecified screening cut-off of 2 or more points, the HEP Score was 97.7% sensitive and 21.9% specific, with a positive predictive value of 17.7% and a negative predictive value of 98.2%. A cut-off of 5 or greater provided 90.7% sensitivity and 47.8% specificity with a positive predictive value of 23.1% and a negative predictive value of 96.8%. The mean time to calculate the HEP Score was 4.1 minutes.
The median 4Ts Score in patients with and without HIT was 5 versus 4 (P less than .0001), Dr. Pishko reported. A 4Ts Score of 4 or greater had a sensitivity of 97.7% and specificity of 32.9%, with a positive predictive value of 20.1% and a negative predictive value of 98.8%.
The area under the ROC curves for the HEP Score and 4Ts Score were similar (0.81 vs. 0.76; P = .121). Subset analysis revealed that compared with the 4Ts Score, the HEP Score had better operating characteristics in ICU patients (AUC 0.87 vs. 0.79; P= .029) and with trainee scorers (AUC 0.79 vs. 0.73; P = .032).
“Our data suggest that either the HEP Score or the 4Ts Score could be used in clinical practice,” Dr. Pishko said.
The National Institutes of Health funded the study. Dr. Pishko reported having no financial disclosures.
SOURCE: Pishko A et al. THSNA 2018.
REPORTING FROM THSNA 2018
Key clinical point:
Major finding: The area under the ROC curves for the HEP Score and 4Ts Score were similar (0.81 vs. 0.76; P = .121).
Study details: A prospective study of 292 adults with suspected acute HIT who were hospitalized at the University of Pennsylvania or affiliated community hospitals.
Disclosures: The National Institutes of Health funded the study. Dr. Pishko reported having no financial disclosures.
Source: Pishko A et al. THSNA 2018.
Boosting bedside skills in hands-on session
A low faculty-to-learner ratio helped HM18 attendees get the most from their learning experience in the Sunday pre-conference course “Bedside Procedures for the Hospitalist.”
The pre-course blended live didactic teaching and hands-on training with simulators so participants could not only learn but also review and demonstrate techniques for many common invasive procedures hospitalists encounter in practice.
“Our goal is to make the entire bedside procedures pre-course a unique experience,” course codirector Alyssa Burkhart, MD, of the Billings (Mont.) Clinic, said in an interview before the session.
“We carefully select the curriculum to create a program most relevant to the participants and their day-to-day work in patient care,” said Dr. Burkhart.
“The low faculty-to-learner ratio coupled with ample time to practice under expert guidance separates us from others. ... It’s a privilege to share our love of procedures with this year’s SHM participants,” said Dr. Burkhart, who comoderated the session with Joshua Lenchus, DO, SFHM, of the University of Miami.
An interactive focus on bedside procedures benefits novices and experienced clinicians, said Dr. Lenchus.
The simulation experience involved practice with ultrasound as well as anatomically representative training equipment.
“Our hope is that many hospitalists may once again find that spark of interest in performing more of their own procedures. The interactive sessions embedded within the pre-course are vital to the success of our program. Many other training sessions are didactics based. We strive to keep lecture time to a minimum so that small groups can learn from the expert facilitators,” Dr. Burkhart added.
“Ample hands-on practice time, interactive experience, and direct supervision separate our pre-course from other commercially available offerings,” Dr. Lenchus said.
The agenda kicked off with vascular and intraosseous access in the morning, followed by paracentesis, thoracentesis, lumbar puncture, and basic airway management, including the use of supraglottic devices.
Dr. Burkhart noted that the course included two separate practice sessions for vascular access because of the number of technical steps and potential complications. “Attendees typically wish to spend a considerable amount of time on vascular access,” she said. “The intraosseous access station and its exceptional trainers always receive very positive feedback.”
Dr. Burkhart and Dr. Lenchus had no financial conflicts to disclose.
A low faculty-to-learner ratio helped HM18 attendees get the most from their learning experience in the Sunday pre-conference course “Bedside Procedures for the Hospitalist.”
The pre-course blended live didactic teaching and hands-on training with simulators so participants could not only learn but also review and demonstrate techniques for many common invasive procedures hospitalists encounter in practice.
“Our goal is to make the entire bedside procedures pre-course a unique experience,” course codirector Alyssa Burkhart, MD, of the Billings (Mont.) Clinic, said in an interview before the session.
“We carefully select the curriculum to create a program most relevant to the participants and their day-to-day work in patient care,” said Dr. Burkhart.
“The low faculty-to-learner ratio coupled with ample time to practice under expert guidance separates us from others. ... It’s a privilege to share our love of procedures with this year’s SHM participants,” said Dr. Burkhart, who comoderated the session with Joshua Lenchus, DO, SFHM, of the University of Miami.
An interactive focus on bedside procedures benefits novices and experienced clinicians, said Dr. Lenchus.
The simulation experience involved practice with ultrasound as well as anatomically representative training equipment.
“Our hope is that many hospitalists may once again find that spark of interest in performing more of their own procedures. The interactive sessions embedded within the pre-course are vital to the success of our program. Many other training sessions are didactics based. We strive to keep lecture time to a minimum so that small groups can learn from the expert facilitators,” Dr. Burkhart added.
“Ample hands-on practice time, interactive experience, and direct supervision separate our pre-course from other commercially available offerings,” Dr. Lenchus said.
The agenda kicked off with vascular and intraosseous access in the morning, followed by paracentesis, thoracentesis, lumbar puncture, and basic airway management, including the use of supraglottic devices.
Dr. Burkhart noted that the course included two separate practice sessions for vascular access because of the number of technical steps and potential complications. “Attendees typically wish to spend a considerable amount of time on vascular access,” she said. “The intraosseous access station and its exceptional trainers always receive very positive feedback.”
Dr. Burkhart and Dr. Lenchus had no financial conflicts to disclose.
A low faculty-to-learner ratio helped HM18 attendees get the most from their learning experience in the Sunday pre-conference course “Bedside Procedures for the Hospitalist.”
The pre-course blended live didactic teaching and hands-on training with simulators so participants could not only learn but also review and demonstrate techniques for many common invasive procedures hospitalists encounter in practice.
“Our goal is to make the entire bedside procedures pre-course a unique experience,” course codirector Alyssa Burkhart, MD, of the Billings (Mont.) Clinic, said in an interview before the session.
“We carefully select the curriculum to create a program most relevant to the participants and their day-to-day work in patient care,” said Dr. Burkhart.
“The low faculty-to-learner ratio coupled with ample time to practice under expert guidance separates us from others. ... It’s a privilege to share our love of procedures with this year’s SHM participants,” said Dr. Burkhart, who comoderated the session with Joshua Lenchus, DO, SFHM, of the University of Miami.
An interactive focus on bedside procedures benefits novices and experienced clinicians, said Dr. Lenchus.
The simulation experience involved practice with ultrasound as well as anatomically representative training equipment.
“Our hope is that many hospitalists may once again find that spark of interest in performing more of their own procedures. The interactive sessions embedded within the pre-course are vital to the success of our program. Many other training sessions are didactics based. We strive to keep lecture time to a minimum so that small groups can learn from the expert facilitators,” Dr. Burkhart added.
“Ample hands-on practice time, interactive experience, and direct supervision separate our pre-course from other commercially available offerings,” Dr. Lenchus said.
The agenda kicked off with vascular and intraosseous access in the morning, followed by paracentesis, thoracentesis, lumbar puncture, and basic airway management, including the use of supraglottic devices.
Dr. Burkhart noted that the course included two separate practice sessions for vascular access because of the number of technical steps and potential complications. “Attendees typically wish to spend a considerable amount of time on vascular access,” she said. “The intraosseous access station and its exceptional trainers always receive very positive feedback.”
Dr. Burkhart and Dr. Lenchus had no financial conflicts to disclose.
Practical changes for improving practice management
An all-day HM18 pre-course – “Hospitalist Practice Management: How to Thrive in a Time of Intense Change” – for hospitalist leaders and practice administrators was all about practicality.
One of the goals of the session was to provide “quick, actionable interventions that attendees can implement right away, as well as alternatives for attendees to consider, which will require some work to employ,” said John Nelson, MD, MHM, a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif., the medical director of the Overlake Medical Center, Bellevue, Wash., and a course codirector and a faculty presenter.
Dr. Nelson pointed out that the hospitalist practice is a unique practice model. “We can’t effectively use the same approaches that other medical specialties use to ensure we have successful practices,” he said.
The pre-course, held Sunday before the official start of HM18, included more commentary and specifics than in past years about how to prosper in the rapidly changing health care landscape and how to reduce the chance of burnout.
Topics addressed included how to find, measure, and demonstrate value; how to incorporate different types of providers and clinical support staffing into a practice to support hospitalists; and how to recruit the right people and build a desirable culture.
The pre-course also covered effective roles for a variety of providers in a hospitalist group, including nurses, scribes, and coordinators, and delineated the benefits of providing telemedicine.
For group leaders and administrators in attendance, the session also shed light on how to interact with individual providers in their group and how to collaborate to build a healthy culture and practice, Ms. Flores said.
The day began with presentations that laid out valuable information and frameworks, including “A Tour of Survey Data: What It Does and Doesn’t Tell You” and “Defining and Measuring Value.” Sessions included six didactic lectures with a question-and-answer period, as well as what Dr. Nelson has dubbed “point/counterpoint” sessions in which faculty members debated particular issues, such as work scheduling models. During the last session, “Learning From Each Other,” participants shared with other attendees their own best practices in the areas covered.
Although there is no single best way to organize a hospitalist’s practice, the course provided lots of information and perspective to help listeners decide what is best for their practice.
“Even though we work in a stressful environment of constant change, hospitalists do have some control over their destiny, and there are things they can do to make hospitalist groups thrive in this challenging environment,” Ms. Flores concluded.
An all-day HM18 pre-course – “Hospitalist Practice Management: How to Thrive in a Time of Intense Change” – for hospitalist leaders and practice administrators was all about practicality.
One of the goals of the session was to provide “quick, actionable interventions that attendees can implement right away, as well as alternatives for attendees to consider, which will require some work to employ,” said John Nelson, MD, MHM, a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif., the medical director of the Overlake Medical Center, Bellevue, Wash., and a course codirector and a faculty presenter.
Dr. Nelson pointed out that the hospitalist practice is a unique practice model. “We can’t effectively use the same approaches that other medical specialties use to ensure we have successful practices,” he said.
The pre-course, held Sunday before the official start of HM18, included more commentary and specifics than in past years about how to prosper in the rapidly changing health care landscape and how to reduce the chance of burnout.
Topics addressed included how to find, measure, and demonstrate value; how to incorporate different types of providers and clinical support staffing into a practice to support hospitalists; and how to recruit the right people and build a desirable culture.
The pre-course also covered effective roles for a variety of providers in a hospitalist group, including nurses, scribes, and coordinators, and delineated the benefits of providing telemedicine.
For group leaders and administrators in attendance, the session also shed light on how to interact with individual providers in their group and how to collaborate to build a healthy culture and practice, Ms. Flores said.
The day began with presentations that laid out valuable information and frameworks, including “A Tour of Survey Data: What It Does and Doesn’t Tell You” and “Defining and Measuring Value.” Sessions included six didactic lectures with a question-and-answer period, as well as what Dr. Nelson has dubbed “point/counterpoint” sessions in which faculty members debated particular issues, such as work scheduling models. During the last session, “Learning From Each Other,” participants shared with other attendees their own best practices in the areas covered.
Although there is no single best way to organize a hospitalist’s practice, the course provided lots of information and perspective to help listeners decide what is best for their practice.
“Even though we work in a stressful environment of constant change, hospitalists do have some control over their destiny, and there are things they can do to make hospitalist groups thrive in this challenging environment,” Ms. Flores concluded.
An all-day HM18 pre-course – “Hospitalist Practice Management: How to Thrive in a Time of Intense Change” – for hospitalist leaders and practice administrators was all about practicality.
One of the goals of the session was to provide “quick, actionable interventions that attendees can implement right away, as well as alternatives for attendees to consider, which will require some work to employ,” said John Nelson, MD, MHM, a partner at Nelson Flores Hospital Medicine Consultants, La Quinta, Calif., the medical director of the Overlake Medical Center, Bellevue, Wash., and a course codirector and a faculty presenter.
Dr. Nelson pointed out that the hospitalist practice is a unique practice model. “We can’t effectively use the same approaches that other medical specialties use to ensure we have successful practices,” he said.
The pre-course, held Sunday before the official start of HM18, included more commentary and specifics than in past years about how to prosper in the rapidly changing health care landscape and how to reduce the chance of burnout.
Topics addressed included how to find, measure, and demonstrate value; how to incorporate different types of providers and clinical support staffing into a practice to support hospitalists; and how to recruit the right people and build a desirable culture.
The pre-course also covered effective roles for a variety of providers in a hospitalist group, including nurses, scribes, and coordinators, and delineated the benefits of providing telemedicine.
For group leaders and administrators in attendance, the session also shed light on how to interact with individual providers in their group and how to collaborate to build a healthy culture and practice, Ms. Flores said.
The day began with presentations that laid out valuable information and frameworks, including “A Tour of Survey Data: What It Does and Doesn’t Tell You” and “Defining and Measuring Value.” Sessions included six didactic lectures with a question-and-answer period, as well as what Dr. Nelson has dubbed “point/counterpoint” sessions in which faculty members debated particular issues, such as work scheduling models. During the last session, “Learning From Each Other,” participants shared with other attendees their own best practices in the areas covered.
Although there is no single best way to organize a hospitalist’s practice, the course provided lots of information and perspective to help listeners decide what is best for their practice.
“Even though we work in a stressful environment of constant change, hospitalists do have some control over their destiny, and there are things they can do to make hospitalist groups thrive in this challenging environment,” Ms. Flores concluded.