User login
Award program to drive more community-based rheumatology research
Practice makes perfect. It also makes the perfect setting for real-world research in rheumatology. Traditionally, however, rheumatologists in day-to-day private practice settings have been hampered by limited opportunities, time constraints, and competition from larger academic medical centers to conduct cutting edge research.
That could soon change. The Norman B. Gaylis, MD, Research Award for Rheumatologists in Community Practice is being relaunched to offer rheumatologists research grants from $50,000-$200,000 per year, for up to 2 years, to drive the field forward. The program stems from a generous $1 million commitment from Dr. Gaylis, a rheumatologist in private practice in Aventura, Fla., in partnership with the Rheumatology Research Foundation.
“Clinicians are very busy with their day-to-day practices,” Dr. Gaylis said. “I really want to support this kind of research for clinicians with ideas but who didn’t have the resources or the time to develop their ideas.” During his nearly 4 decades in rheumatology practice, Dr. Gaylis has performed “a lot of clinical research, including research being driven purely by my own ideas.” This award program is his way of paying it forward.
Investigator-driven initiatives
In addition to financial support, the program will help community rheumatologists with viable ideas, including clinicians with less research experience, to refine their hypothesis and methodology as appropriate. “For example, if someone submits a proposal to study the effect of diet on gout, we, as part of the application process, will help them develop the application so it meets the quality expectations of the review committee,” Dr. Gaylis said. “We want it to be their idea, uniquely, the idea of the application. We can guide them so it will be a quality application,” Dr. Gaylis said. “Then it’s up to them.”
Support from the Foundation will remain available and periodic reports will be required to ensure the research is progressing on schedule. “We don’t expect them to get this turned around in 6 months,” Dr. Gaylis said. “It could be a 2-year study ... or even longer.”
“Understanding their priorities and research interests are very different from their colleagues in academia, the Foundation wants to encourage rheumatologists in a clinical setting to explore their own, independent research ideas,” said Shelley A. Malcolm, director of marketing and communication at the Rheumatology Research Foundation.
“The application process and award terms are tailored for rheumatology health professionals who may not have experience in writing grant proposals, or have time to draft applications similar to those required for NIH funding, because their priority lies in patient care and practice management,” Ms. Malcolm said. The Foundation will begin accepting proposals in March 2018 and up until the July 1, 2018 deadline.
Smart but not academic
Dr. Gaylis and the Rheumatology Research Foundation worked together to streamline the process with busy clinicians in mind.
This award is really for the rheumatologist in practice … who is not affiliated with academic institutions. They can be attached as a clinical professor, but they’re not really supported by an institution,” Dr. Gaylis said. “Effectively, this should really allow them to have the flexibility to do the research they feel needs to be done without having to go through the whole administrative process you would normally find in an academic institution.”
Recipients will not be competing with academic medical centers that have “the reputation, the manpower, and the capabilities that in general can swallow up all the research awards available.” This recognizes what the practicing clinician brings to the table without making them feel like they’re wasting their time by applying, Dr. Gaylis added.
“This is not saying that academia doesn’t have its role.” But the award program “levels the playing field.”
Keeping it real
Clinical practice “is really a real-world environment. Whether one is trying to understand the possibilities in using treatments differently, approaching patients differently, or seeing outcomes you’re seeing that are different from the standard, controlled, double-blind placebo study that is the norm in academic research,” Dr. Gaylis said.
“This is much more focused on the patient who walks into your office,” he continued. “I believe there are many, many more rheumatologists like me who could embrace this opportunity.” He added, “If I was allowed to, I would apply for it myself.”
The research award program can serve as a platform not only for making new discoveries but also taking drugs that are on the marketplace and using them in different forms or fashions in a successful way, Dr. Gaylis said. “And it doesn’t just have to be medications; it could be behavior mechanisms – understanding which patients might be more responsive to therapies, for example.”
The purpose is to initiate research, including but not limited to, health services research or outcome studies, practice supply and demand, and/or patient communications, Ms. Malcolm said. “The goal of the award is to provide independent investigators with the funding they need to pursue ideas that could lead to important breakthroughs in discovering new treatments and, one day, a cure.”
“Clinical practice is an incredible petri dish for research,” Dr. Gaylis said. “We end up losing a lot of opportunities by pigeonholing most research in academic centers. So if we can show the value and validity and identify clinicians who have the aptitude for this kind of clinical research, I think not only will this award program become more exciting, it will become more valuable.”
Maintain career-long clinical curiosity
Clinical practice is a very important point in the journey of being a rheumatologist, Dr. Gaylis said, but research shouldn’t end when you complete your fellowship. “It should continue for your whole career. One should be putting into effect the principles of investigation, the principles of observation, and the principle of generating ideas that are instilled in everyone during their education, but they get diluted as time goes on. We’re trying to prevent that.”
Rheumatologists, or rheumatology health professionals, with an idea or discovery they want to explore are encouraged to reach out to the Foundation staff with any questions or concerns at (404) 365-1373 or [email protected]. Foundation staff will provide assistance, including connecting applicants with a mentor to help simplify the process.
Practice makes perfect. It also makes the perfect setting for real-world research in rheumatology. Traditionally, however, rheumatologists in day-to-day private practice settings have been hampered by limited opportunities, time constraints, and competition from larger academic medical centers to conduct cutting edge research.
That could soon change. The Norman B. Gaylis, MD, Research Award for Rheumatologists in Community Practice is being relaunched to offer rheumatologists research grants from $50,000-$200,000 per year, for up to 2 years, to drive the field forward. The program stems from a generous $1 million commitment from Dr. Gaylis, a rheumatologist in private practice in Aventura, Fla., in partnership with the Rheumatology Research Foundation.
“Clinicians are very busy with their day-to-day practices,” Dr. Gaylis said. “I really want to support this kind of research for clinicians with ideas but who didn’t have the resources or the time to develop their ideas.” During his nearly 4 decades in rheumatology practice, Dr. Gaylis has performed “a lot of clinical research, including research being driven purely by my own ideas.” This award program is his way of paying it forward.
Investigator-driven initiatives
In addition to financial support, the program will help community rheumatologists with viable ideas, including clinicians with less research experience, to refine their hypothesis and methodology as appropriate. “For example, if someone submits a proposal to study the effect of diet on gout, we, as part of the application process, will help them develop the application so it meets the quality expectations of the review committee,” Dr. Gaylis said. “We want it to be their idea, uniquely, the idea of the application. We can guide them so it will be a quality application,” Dr. Gaylis said. “Then it’s up to them.”
Support from the Foundation will remain available and periodic reports will be required to ensure the research is progressing on schedule. “We don’t expect them to get this turned around in 6 months,” Dr. Gaylis said. “It could be a 2-year study ... or even longer.”
“Understanding their priorities and research interests are very different from their colleagues in academia, the Foundation wants to encourage rheumatologists in a clinical setting to explore their own, independent research ideas,” said Shelley A. Malcolm, director of marketing and communication at the Rheumatology Research Foundation.
“The application process and award terms are tailored for rheumatology health professionals who may not have experience in writing grant proposals, or have time to draft applications similar to those required for NIH funding, because their priority lies in patient care and practice management,” Ms. Malcolm said. The Foundation will begin accepting proposals in March 2018 and up until the July 1, 2018 deadline.
Smart but not academic
Dr. Gaylis and the Rheumatology Research Foundation worked together to streamline the process with busy clinicians in mind.
This award is really for the rheumatologist in practice … who is not affiliated with academic institutions. They can be attached as a clinical professor, but they’re not really supported by an institution,” Dr. Gaylis said. “Effectively, this should really allow them to have the flexibility to do the research they feel needs to be done without having to go through the whole administrative process you would normally find in an academic institution.”
Recipients will not be competing with academic medical centers that have “the reputation, the manpower, and the capabilities that in general can swallow up all the research awards available.” This recognizes what the practicing clinician brings to the table without making them feel like they’re wasting their time by applying, Dr. Gaylis added.
“This is not saying that academia doesn’t have its role.” But the award program “levels the playing field.”
Keeping it real
Clinical practice “is really a real-world environment. Whether one is trying to understand the possibilities in using treatments differently, approaching patients differently, or seeing outcomes you’re seeing that are different from the standard, controlled, double-blind placebo study that is the norm in academic research,” Dr. Gaylis said.
“This is much more focused on the patient who walks into your office,” he continued. “I believe there are many, many more rheumatologists like me who could embrace this opportunity.” He added, “If I was allowed to, I would apply for it myself.”
The research award program can serve as a platform not only for making new discoveries but also taking drugs that are on the marketplace and using them in different forms or fashions in a successful way, Dr. Gaylis said. “And it doesn’t just have to be medications; it could be behavior mechanisms – understanding which patients might be more responsive to therapies, for example.”
The purpose is to initiate research, including but not limited to, health services research or outcome studies, practice supply and demand, and/or patient communications, Ms. Malcolm said. “The goal of the award is to provide independent investigators with the funding they need to pursue ideas that could lead to important breakthroughs in discovering new treatments and, one day, a cure.”
“Clinical practice is an incredible petri dish for research,” Dr. Gaylis said. “We end up losing a lot of opportunities by pigeonholing most research in academic centers. So if we can show the value and validity and identify clinicians who have the aptitude for this kind of clinical research, I think not only will this award program become more exciting, it will become more valuable.”
Maintain career-long clinical curiosity
Clinical practice is a very important point in the journey of being a rheumatologist, Dr. Gaylis said, but research shouldn’t end when you complete your fellowship. “It should continue for your whole career. One should be putting into effect the principles of investigation, the principles of observation, and the principle of generating ideas that are instilled in everyone during their education, but they get diluted as time goes on. We’re trying to prevent that.”
Rheumatologists, or rheumatology health professionals, with an idea or discovery they want to explore are encouraged to reach out to the Foundation staff with any questions or concerns at (404) 365-1373 or [email protected]. Foundation staff will provide assistance, including connecting applicants with a mentor to help simplify the process.
Practice makes perfect. It also makes the perfect setting for real-world research in rheumatology. Traditionally, however, rheumatologists in day-to-day private practice settings have been hampered by limited opportunities, time constraints, and competition from larger academic medical centers to conduct cutting edge research.
That could soon change. The Norman B. Gaylis, MD, Research Award for Rheumatologists in Community Practice is being relaunched to offer rheumatologists research grants from $50,000-$200,000 per year, for up to 2 years, to drive the field forward. The program stems from a generous $1 million commitment from Dr. Gaylis, a rheumatologist in private practice in Aventura, Fla., in partnership with the Rheumatology Research Foundation.
“Clinicians are very busy with their day-to-day practices,” Dr. Gaylis said. “I really want to support this kind of research for clinicians with ideas but who didn’t have the resources or the time to develop their ideas.” During his nearly 4 decades in rheumatology practice, Dr. Gaylis has performed “a lot of clinical research, including research being driven purely by my own ideas.” This award program is his way of paying it forward.
Investigator-driven initiatives
In addition to financial support, the program will help community rheumatologists with viable ideas, including clinicians with less research experience, to refine their hypothesis and methodology as appropriate. “For example, if someone submits a proposal to study the effect of diet on gout, we, as part of the application process, will help them develop the application so it meets the quality expectations of the review committee,” Dr. Gaylis said. “We want it to be their idea, uniquely, the idea of the application. We can guide them so it will be a quality application,” Dr. Gaylis said. “Then it’s up to them.”
Support from the Foundation will remain available and periodic reports will be required to ensure the research is progressing on schedule. “We don’t expect them to get this turned around in 6 months,” Dr. Gaylis said. “It could be a 2-year study ... or even longer.”
“Understanding their priorities and research interests are very different from their colleagues in academia, the Foundation wants to encourage rheumatologists in a clinical setting to explore their own, independent research ideas,” said Shelley A. Malcolm, director of marketing and communication at the Rheumatology Research Foundation.
“The application process and award terms are tailored for rheumatology health professionals who may not have experience in writing grant proposals, or have time to draft applications similar to those required for NIH funding, because their priority lies in patient care and practice management,” Ms. Malcolm said. The Foundation will begin accepting proposals in March 2018 and up until the July 1, 2018 deadline.
Smart but not academic
Dr. Gaylis and the Rheumatology Research Foundation worked together to streamline the process with busy clinicians in mind.
This award is really for the rheumatologist in practice … who is not affiliated with academic institutions. They can be attached as a clinical professor, but they’re not really supported by an institution,” Dr. Gaylis said. “Effectively, this should really allow them to have the flexibility to do the research they feel needs to be done without having to go through the whole administrative process you would normally find in an academic institution.”
Recipients will not be competing with academic medical centers that have “the reputation, the manpower, and the capabilities that in general can swallow up all the research awards available.” This recognizes what the practicing clinician brings to the table without making them feel like they’re wasting their time by applying, Dr. Gaylis added.
“This is not saying that academia doesn’t have its role.” But the award program “levels the playing field.”
Keeping it real
Clinical practice “is really a real-world environment. Whether one is trying to understand the possibilities in using treatments differently, approaching patients differently, or seeing outcomes you’re seeing that are different from the standard, controlled, double-blind placebo study that is the norm in academic research,” Dr. Gaylis said.
“This is much more focused on the patient who walks into your office,” he continued. “I believe there are many, many more rheumatologists like me who could embrace this opportunity.” He added, “If I was allowed to, I would apply for it myself.”
The research award program can serve as a platform not only for making new discoveries but also taking drugs that are on the marketplace and using them in different forms or fashions in a successful way, Dr. Gaylis said. “And it doesn’t just have to be medications; it could be behavior mechanisms – understanding which patients might be more responsive to therapies, for example.”
The purpose is to initiate research, including but not limited to, health services research or outcome studies, practice supply and demand, and/or patient communications, Ms. Malcolm said. “The goal of the award is to provide independent investigators with the funding they need to pursue ideas that could lead to important breakthroughs in discovering new treatments and, one day, a cure.”
“Clinical practice is an incredible petri dish for research,” Dr. Gaylis said. “We end up losing a lot of opportunities by pigeonholing most research in academic centers. So if we can show the value and validity and identify clinicians who have the aptitude for this kind of clinical research, I think not only will this award program become more exciting, it will become more valuable.”
Maintain career-long clinical curiosity
Clinical practice is a very important point in the journey of being a rheumatologist, Dr. Gaylis said, but research shouldn’t end when you complete your fellowship. “It should continue for your whole career. One should be putting into effect the principles of investigation, the principles of observation, and the principle of generating ideas that are instilled in everyone during their education, but they get diluted as time goes on. We’re trying to prevent that.”
Rheumatologists, or rheumatology health professionals, with an idea or discovery they want to explore are encouraged to reach out to the Foundation staff with any questions or concerns at (404) 365-1373 or [email protected]. Foundation staff will provide assistance, including connecting applicants with a mentor to help simplify the process.
Thread lifts: A face-lift alternative? Or not?
The rise of noninvasive procedures has shifted the aesthetic culture. Patients now are asking for less invasive, less painful, less expensive procedures with short recovery times. Thread-lifts are one of the newest approaches to nonsurgical facial tightening. However, are they of value? Where, and for whom?
The thread-lifts initially came onto the market in the late 1990s but were difficult to use. The nonabsorbable threads had to be anchored into the scalp, temple, and brow region. The anchoring knots were carefully tied and were permanent. The newest technology threads – NovaThreads and the Silhouette Instalift – have recently received Food and Drug Administration clearance and grown in popularity because of their “lunchtime” appeal and their ease of use. Primarily marketed for the neck, jowls, and lower face, these threads – available in various sizes, lengths, and diameters – can be used almost anywhere. The sutures dissolve over time and do not need any anchoring, making it a very simple in-office procedure.
Side effects include mild procedural pain, edema, erythema, bruising, and rarely, suture granuloma formation; and they may need to be replaced. If not done properly, buckling of the skin can occur and superficially placed sutures can be visible.
Similar to fillers that provide a “liquid face-lift,” the down time is minimal. Common side effects include bruising, and patients should refrain from heavy exercise and opening their mouth wide with chewing for 5-7 days (such as eating a large apple). Soreness, particularly in or near the hairline or jaw line, can occur and can last up to 2 weeks. Dimpling in the skin can occur and usually resolves on its own; however, if threads are placed incorrectly, dimpling can cause some disfigurement.
Results can vary based on the tissue laxity, and the type, amount, and location of the threads used. While results have been reported to last 18 months to 2 years, the procedure is not a replacement for fillers. Facial aging is caused by a combination of skeletal, soft tissue, and skin changes that lead to soft tissue laxity and volume loss. Fillers are essential in restoring lost volume in the aging face and are particularly helpful in combination with tissue tightening lasers, face-lifts and the thread-lift procedures. Fillers used in combination with thread-lifts also increase the longevity of the thread-lift because of additional collagen stimulation.
As the procedure is not indicated for severe laxity, thread-lifts also do not replace the traditional face-lift. Tissue is not released from its underlying attachments, and skin contraction and gravitational pull limit its extent of improvement and its longevity.
Long-term success of the thread-lift procedure for facial rejuvenation was evaluated in a retrospective review of 33 patients who underwent the traditional thread-lift procedure alone or in combination with other facial rejuvenation procedures to the brow, mid-face, jowl, and neck published in 2009.1 The study compared results in 10 patients who had a thread-lift alone, 23 who had thread-lifts combined with other procedures, and controls, who were 10 ten patients who had non–thread-lift rejuvenation procedures, which included lipotransfer, chemical peels, and rhytidectomies. Independent, blinded, board-certified facial plastic surgeons evaluated pre- and postoperative photos. Patients were followed-up for a mean of 21 months.
While thread-lifts are a beneficial addition to our armamentarium of noninvasive aesthetic procedures, they have better outcomes and higher patient satisfaction when used in combination with fillers, radiofrequency, and fractional lasers and neuromodulators.
Reference
1. Abraham RF et al. Arch Facial Plast Surg. 2009 May-Jun;11(3):178-83.
Dr. Talakoub and Dr. Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
The rise of noninvasive procedures has shifted the aesthetic culture. Patients now are asking for less invasive, less painful, less expensive procedures with short recovery times. Thread-lifts are one of the newest approaches to nonsurgical facial tightening. However, are they of value? Where, and for whom?
The thread-lifts initially came onto the market in the late 1990s but were difficult to use. The nonabsorbable threads had to be anchored into the scalp, temple, and brow region. The anchoring knots were carefully tied and were permanent. The newest technology threads – NovaThreads and the Silhouette Instalift – have recently received Food and Drug Administration clearance and grown in popularity because of their “lunchtime” appeal and their ease of use. Primarily marketed for the neck, jowls, and lower face, these threads – available in various sizes, lengths, and diameters – can be used almost anywhere. The sutures dissolve over time and do not need any anchoring, making it a very simple in-office procedure.
Side effects include mild procedural pain, edema, erythema, bruising, and rarely, suture granuloma formation; and they may need to be replaced. If not done properly, buckling of the skin can occur and superficially placed sutures can be visible.
Similar to fillers that provide a “liquid face-lift,” the down time is minimal. Common side effects include bruising, and patients should refrain from heavy exercise and opening their mouth wide with chewing for 5-7 days (such as eating a large apple). Soreness, particularly in or near the hairline or jaw line, can occur and can last up to 2 weeks. Dimpling in the skin can occur and usually resolves on its own; however, if threads are placed incorrectly, dimpling can cause some disfigurement.
Results can vary based on the tissue laxity, and the type, amount, and location of the threads used. While results have been reported to last 18 months to 2 years, the procedure is not a replacement for fillers. Facial aging is caused by a combination of skeletal, soft tissue, and skin changes that lead to soft tissue laxity and volume loss. Fillers are essential in restoring lost volume in the aging face and are particularly helpful in combination with tissue tightening lasers, face-lifts and the thread-lift procedures. Fillers used in combination with thread-lifts also increase the longevity of the thread-lift because of additional collagen stimulation.
As the procedure is not indicated for severe laxity, thread-lifts also do not replace the traditional face-lift. Tissue is not released from its underlying attachments, and skin contraction and gravitational pull limit its extent of improvement and its longevity.
Long-term success of the thread-lift procedure for facial rejuvenation was evaluated in a retrospective review of 33 patients who underwent the traditional thread-lift procedure alone or in combination with other facial rejuvenation procedures to the brow, mid-face, jowl, and neck published in 2009.1 The study compared results in 10 patients who had a thread-lift alone, 23 who had thread-lifts combined with other procedures, and controls, who were 10 ten patients who had non–thread-lift rejuvenation procedures, which included lipotransfer, chemical peels, and rhytidectomies. Independent, blinded, board-certified facial plastic surgeons evaluated pre- and postoperative photos. Patients were followed-up for a mean of 21 months.
While thread-lifts are a beneficial addition to our armamentarium of noninvasive aesthetic procedures, they have better outcomes and higher patient satisfaction when used in combination with fillers, radiofrequency, and fractional lasers and neuromodulators.
Reference
1. Abraham RF et al. Arch Facial Plast Surg. 2009 May-Jun;11(3):178-83.
Dr. Talakoub and Dr. Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
The rise of noninvasive procedures has shifted the aesthetic culture. Patients now are asking for less invasive, less painful, less expensive procedures with short recovery times. Thread-lifts are one of the newest approaches to nonsurgical facial tightening. However, are they of value? Where, and for whom?
The thread-lifts initially came onto the market in the late 1990s but were difficult to use. The nonabsorbable threads had to be anchored into the scalp, temple, and brow region. The anchoring knots were carefully tied and were permanent. The newest technology threads – NovaThreads and the Silhouette Instalift – have recently received Food and Drug Administration clearance and grown in popularity because of their “lunchtime” appeal and their ease of use. Primarily marketed for the neck, jowls, and lower face, these threads – available in various sizes, lengths, and diameters – can be used almost anywhere. The sutures dissolve over time and do not need any anchoring, making it a very simple in-office procedure.
Side effects include mild procedural pain, edema, erythema, bruising, and rarely, suture granuloma formation; and they may need to be replaced. If not done properly, buckling of the skin can occur and superficially placed sutures can be visible.
Similar to fillers that provide a “liquid face-lift,” the down time is minimal. Common side effects include bruising, and patients should refrain from heavy exercise and opening their mouth wide with chewing for 5-7 days (such as eating a large apple). Soreness, particularly in or near the hairline or jaw line, can occur and can last up to 2 weeks. Dimpling in the skin can occur and usually resolves on its own; however, if threads are placed incorrectly, dimpling can cause some disfigurement.
Results can vary based on the tissue laxity, and the type, amount, and location of the threads used. While results have been reported to last 18 months to 2 years, the procedure is not a replacement for fillers. Facial aging is caused by a combination of skeletal, soft tissue, and skin changes that lead to soft tissue laxity and volume loss. Fillers are essential in restoring lost volume in the aging face and are particularly helpful in combination with tissue tightening lasers, face-lifts and the thread-lift procedures. Fillers used in combination with thread-lifts also increase the longevity of the thread-lift because of additional collagen stimulation.
As the procedure is not indicated for severe laxity, thread-lifts also do not replace the traditional face-lift. Tissue is not released from its underlying attachments, and skin contraction and gravitational pull limit its extent of improvement and its longevity.
Long-term success of the thread-lift procedure for facial rejuvenation was evaluated in a retrospective review of 33 patients who underwent the traditional thread-lift procedure alone or in combination with other facial rejuvenation procedures to the brow, mid-face, jowl, and neck published in 2009.1 The study compared results in 10 patients who had a thread-lift alone, 23 who had thread-lifts combined with other procedures, and controls, who were 10 ten patients who had non–thread-lift rejuvenation procedures, which included lipotransfer, chemical peels, and rhytidectomies. Independent, blinded, board-certified facial plastic surgeons evaluated pre- and postoperative photos. Patients were followed-up for a mean of 21 months.
While thread-lifts are a beneficial addition to our armamentarium of noninvasive aesthetic procedures, they have better outcomes and higher patient satisfaction when used in combination with fillers, radiofrequency, and fractional lasers and neuromodulators.
Reference
1. Abraham RF et al. Arch Facial Plast Surg. 2009 May-Jun;11(3):178-83.
Dr. Talakoub and Dr. Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
VIDEO: SABCS 2017 roundtable with Dr. Hope S. Rugo and Dr. William J. Gradishar
SAN ANTONIO – Dr. William A. Gradishar and Dr. Hope S. Rugo reflect on some familiar questions at the conclusion of the San Antonio Breast Cancer Symposium: Should young, high-risk women receive ovarian suppression? What is the optimal duration for trastuzumab therapy? What about extended aromatase inhibitor therapy? But new questions were considered as well, based on results presented at the 40th annual symposium.
Will combining a checkpoint inhibitor with trastuzumab help overcome trastuzumab resistance?
Are CDK 4/6 inhibitors here to stay?
Does acupuncture relieve joint pain in women on adjuvant aromatase inhibitor treatment?
The potential approval of a few novel agents in 2018 – an antibody-drug conjugate and a new PARP inhibitor – were also discussed in the video roundtable.
Dr. William A. Gradishar is the Betsy Bramsen Professor of Breast Oncology at Northwestern University, Chicago. He had no disclosures to report. Dr. Hope S. Rugo is professor of medicine at the University of California, San Francisco. She disclosed that she receives research funding (institutional) from Plexxikon, Macrogenics, OBI Pharma, Eisai, Pfizer, Novartis, Lilly, Genentech, and Merck.
SAN ANTONIO – Dr. William A. Gradishar and Dr. Hope S. Rugo reflect on some familiar questions at the conclusion of the San Antonio Breast Cancer Symposium: Should young, high-risk women receive ovarian suppression? What is the optimal duration for trastuzumab therapy? What about extended aromatase inhibitor therapy? But new questions were considered as well, based on results presented at the 40th annual symposium.
Will combining a checkpoint inhibitor with trastuzumab help overcome trastuzumab resistance?
Are CDK 4/6 inhibitors here to stay?
Does acupuncture relieve joint pain in women on adjuvant aromatase inhibitor treatment?
The potential approval of a few novel agents in 2018 – an antibody-drug conjugate and a new PARP inhibitor – were also discussed in the video roundtable.
Dr. William A. Gradishar is the Betsy Bramsen Professor of Breast Oncology at Northwestern University, Chicago. He had no disclosures to report. Dr. Hope S. Rugo is professor of medicine at the University of California, San Francisco. She disclosed that she receives research funding (institutional) from Plexxikon, Macrogenics, OBI Pharma, Eisai, Pfizer, Novartis, Lilly, Genentech, and Merck.
SAN ANTONIO – Dr. William A. Gradishar and Dr. Hope S. Rugo reflect on some familiar questions at the conclusion of the San Antonio Breast Cancer Symposium: Should young, high-risk women receive ovarian suppression? What is the optimal duration for trastuzumab therapy? What about extended aromatase inhibitor therapy? But new questions were considered as well, based on results presented at the 40th annual symposium.
Will combining a checkpoint inhibitor with trastuzumab help overcome trastuzumab resistance?
Are CDK 4/6 inhibitors here to stay?
Does acupuncture relieve joint pain in women on adjuvant aromatase inhibitor treatment?
The potential approval of a few novel agents in 2018 – an antibody-drug conjugate and a new PARP inhibitor – were also discussed in the video roundtable.
Dr. William A. Gradishar is the Betsy Bramsen Professor of Breast Oncology at Northwestern University, Chicago. He had no disclosures to report. Dr. Hope S. Rugo is professor of medicine at the University of California, San Francisco. She disclosed that she receives research funding (institutional) from Plexxikon, Macrogenics, OBI Pharma, Eisai, Pfizer, Novartis, Lilly, Genentech, and Merck.
EXPERT ANALYSIS FROM SABCS 2017
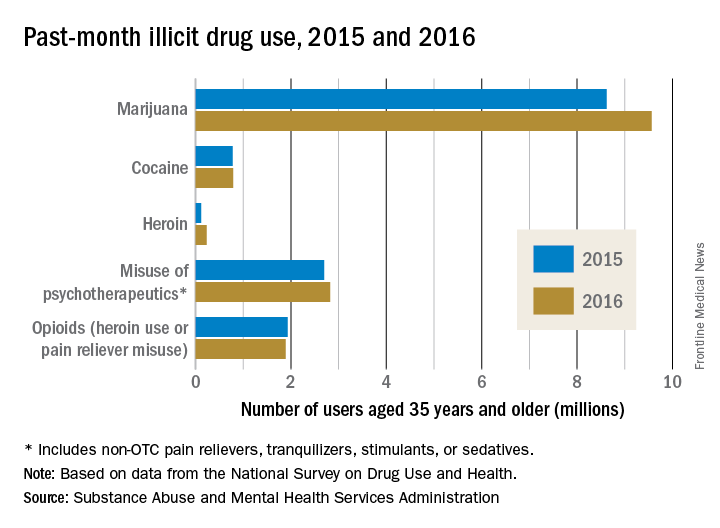
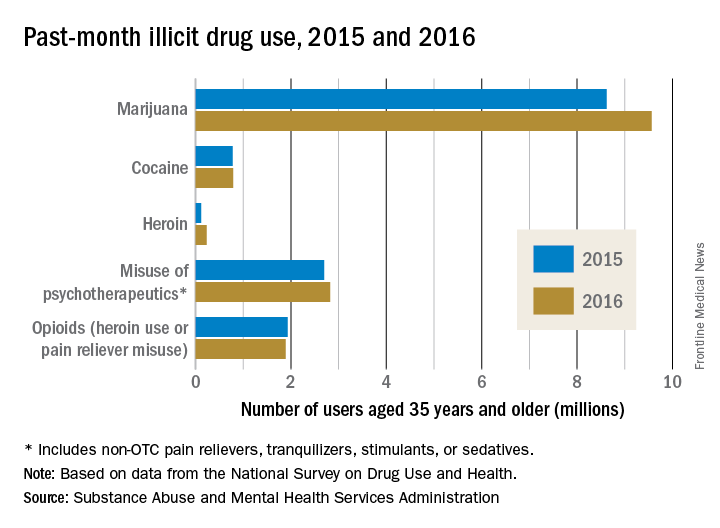
Helping patients with addictions get, stay clean
Roughly 6 months ago, a primary care physician referred a patient to our clinic for an assessment for opioid use disorder and a recommendation for treatment. The patient estimated, likely underestimated, his daily heroin use to five bags and dropped positive, in addition to heroin, for benzodiazepines, amphetamines, and cannabis. He was in a profession in which public safety was a critical concern, and he refused to notify his employer’s employee assistance program. He also declined to voluntarily admit himself for detox and treatment at the local, fully accredited addiction program, which was affiliated with a major university medical center. Instead, after an Internet search, the patient opted for an opioid treatment center featuring massage therapy, acupuncture, a stable, a sweat lodge – and a magnificent view of the Pacific Ocean.
Mental health professionals and lay people alike are aware of the “opioid crisis” – the derailment of lives, the devastation to communities, the death toll. But despite proposals to increase research funding, policies aimed at tightening the prescribing of opioids, and pledges to ramp up interdiction of heroin traffic, there is often an ignorance and confusion regarding the best, evidence-based approaches to getting patients with substance use disorders clean and keeping them clean.
Unfortunately, as with any crisis, there will be opportunists preying on vulnerable patients and their families. And this travesty has reportedly escalated, as outpatient treatment centers take advantage of laws guaranteeing mental health parity and insurance companies paying out tens of thousands of dollars for residential and outpatient opioid treatment. The potential for significant profit is plainly illustrated by the influx of private equity firms, such as Bain Capital, that are investing heavily in treatment centers.
Reports of malfeasance and misconduct, by owners, operators, staff, and others connected with the industry are beginning to get the attention of authorities. There have been reports of outpatient treatment centers that spend lavishly on furnishing, on BMWs and signed art, yet are understaffed, leading to inadequate one-on-one counseling and even sexual transgressions between residents. There are centers that have been investigated for insurance fraud, such as illegally waiving a copay or a deductible or for charging up to $5,000 for a simple urine five drug screen, often multiple times a day. And there is evidence of “junkie hunters” who cruise for people with addictions and brokers who provide such people with fake addresses in order to qualify for insurance plans with excellent benefits for addiction treatment.
Probably the best means to find a suitable outpatient treatment center is by way of a local, experienced, and respected chemical dependency counselor or physician certified in addiction medicine. If people with substance use disorders and their families want to independently conduct a search, as a good rule of thumb, they should be advised to consider programs affiliated with major medical centers and hospitals or outpatient treatment centers that have been established in good standing for years, in contrast to the rash of pop-up, for-profit programs. Of equal, or even greater importance, is that the prospective center ought to be accredited by a national organization, for example, The Joint Commission, and its staff ought to be licensed and credentialed as well.
In addition, there is merit if the staff has been educated, trained, and supervised under the direction of a respected institution. Needless to add, an outpatient treatment center must use evidence-based practices as the bedrock of treatment; this includes pharmacotherapies such as Suboxone and naltrexone (Vivitrol), and behavioral therapies such as cognitive-behavioral therapy, contingency management, and motivational enhancement. To date, massage and essential oils might be relaxing and pleasurable, but they are not considered accepted standard of care.
It is crucial, too, that an outpatient treatment center have both the resources to reliably handle acute medical detox, which can be a potentially life-threatening emergency, and the medical personnel who can assess and treat such medical conditions as hypertension as well as psychiatric illnesses such as bipolar and generalized anxiety disorders. A prospective patient also should inquire whether any of the staff has been the subject of disciplinary action by a licensing board or whether the center has been investigated by the state or a national accrediting organization.
Because addiction so often has facets rooted in the family system, and recovery so often depends on family support, an outpatient treatment center should provide a structured family program integrated into the patient’s treatment and emphasize the importance of continued family involvement after discharge.
Lastly, the best treatment centers often regularly update a patient’s local therapist and physician, spell out the elements of successful aftercare (12-step programs, and so on), and provide amenities, such as calls to a recently discharged patient and an alumni support network.
Dr. Marseille is a psychiatrist who works on the staff of a clinic in Wheaton, Ill. His special interests include adolescent and addiction medicine, eating disorders, trauma, bipolar disorder, and the psychiatric manifestations of acute and chronic medical conditions.
This article was updated 12/15/17.
Roughly 6 months ago, a primary care physician referred a patient to our clinic for an assessment for opioid use disorder and a recommendation for treatment. The patient estimated, likely underestimated, his daily heroin use to five bags and dropped positive, in addition to heroin, for benzodiazepines, amphetamines, and cannabis. He was in a profession in which public safety was a critical concern, and he refused to notify his employer’s employee assistance program. He also declined to voluntarily admit himself for detox and treatment at the local, fully accredited addiction program, which was affiliated with a major university medical center. Instead, after an Internet search, the patient opted for an opioid treatment center featuring massage therapy, acupuncture, a stable, a sweat lodge – and a magnificent view of the Pacific Ocean.
Mental health professionals and lay people alike are aware of the “opioid crisis” – the derailment of lives, the devastation to communities, the death toll. But despite proposals to increase research funding, policies aimed at tightening the prescribing of opioids, and pledges to ramp up interdiction of heroin traffic, there is often an ignorance and confusion regarding the best, evidence-based approaches to getting patients with substance use disorders clean and keeping them clean.
Unfortunately, as with any crisis, there will be opportunists preying on vulnerable patients and their families. And this travesty has reportedly escalated, as outpatient treatment centers take advantage of laws guaranteeing mental health parity and insurance companies paying out tens of thousands of dollars for residential and outpatient opioid treatment. The potential for significant profit is plainly illustrated by the influx of private equity firms, such as Bain Capital, that are investing heavily in treatment centers.
Reports of malfeasance and misconduct, by owners, operators, staff, and others connected with the industry are beginning to get the attention of authorities. There have been reports of outpatient treatment centers that spend lavishly on furnishing, on BMWs and signed art, yet are understaffed, leading to inadequate one-on-one counseling and even sexual transgressions between residents. There are centers that have been investigated for insurance fraud, such as illegally waiving a copay or a deductible or for charging up to $5,000 for a simple urine five drug screen, often multiple times a day. And there is evidence of “junkie hunters” who cruise for people with addictions and brokers who provide such people with fake addresses in order to qualify for insurance plans with excellent benefits for addiction treatment.
Probably the best means to find a suitable outpatient treatment center is by way of a local, experienced, and respected chemical dependency counselor or physician certified in addiction medicine. If people with substance use disorders and their families want to independently conduct a search, as a good rule of thumb, they should be advised to consider programs affiliated with major medical centers and hospitals or outpatient treatment centers that have been established in good standing for years, in contrast to the rash of pop-up, for-profit programs. Of equal, or even greater importance, is that the prospective center ought to be accredited by a national organization, for example, The Joint Commission, and its staff ought to be licensed and credentialed as well.
In addition, there is merit if the staff has been educated, trained, and supervised under the direction of a respected institution. Needless to add, an outpatient treatment center must use evidence-based practices as the bedrock of treatment; this includes pharmacotherapies such as Suboxone and naltrexone (Vivitrol), and behavioral therapies such as cognitive-behavioral therapy, contingency management, and motivational enhancement. To date, massage and essential oils might be relaxing and pleasurable, but they are not considered accepted standard of care.
It is crucial, too, that an outpatient treatment center have both the resources to reliably handle acute medical detox, which can be a potentially life-threatening emergency, and the medical personnel who can assess and treat such medical conditions as hypertension as well as psychiatric illnesses such as bipolar and generalized anxiety disorders. A prospective patient also should inquire whether any of the staff has been the subject of disciplinary action by a licensing board or whether the center has been investigated by the state or a national accrediting organization.
Because addiction so often has facets rooted in the family system, and recovery so often depends on family support, an outpatient treatment center should provide a structured family program integrated into the patient’s treatment and emphasize the importance of continued family involvement after discharge.
Lastly, the best treatment centers often regularly update a patient’s local therapist and physician, spell out the elements of successful aftercare (12-step programs, and so on), and provide amenities, such as calls to a recently discharged patient and an alumni support network.
Dr. Marseille is a psychiatrist who works on the staff of a clinic in Wheaton, Ill. His special interests include adolescent and addiction medicine, eating disorders, trauma, bipolar disorder, and the psychiatric manifestations of acute and chronic medical conditions.
This article was updated 12/15/17.
Roughly 6 months ago, a primary care physician referred a patient to our clinic for an assessment for opioid use disorder and a recommendation for treatment. The patient estimated, likely underestimated, his daily heroin use to five bags and dropped positive, in addition to heroin, for benzodiazepines, amphetamines, and cannabis. He was in a profession in which public safety was a critical concern, and he refused to notify his employer’s employee assistance program. He also declined to voluntarily admit himself for detox and treatment at the local, fully accredited addiction program, which was affiliated with a major university medical center. Instead, after an Internet search, the patient opted for an opioid treatment center featuring massage therapy, acupuncture, a stable, a sweat lodge – and a magnificent view of the Pacific Ocean.
Mental health professionals and lay people alike are aware of the “opioid crisis” – the derailment of lives, the devastation to communities, the death toll. But despite proposals to increase research funding, policies aimed at tightening the prescribing of opioids, and pledges to ramp up interdiction of heroin traffic, there is often an ignorance and confusion regarding the best, evidence-based approaches to getting patients with substance use disorders clean and keeping them clean.
Unfortunately, as with any crisis, there will be opportunists preying on vulnerable patients and their families. And this travesty has reportedly escalated, as outpatient treatment centers take advantage of laws guaranteeing mental health parity and insurance companies paying out tens of thousands of dollars for residential and outpatient opioid treatment. The potential for significant profit is plainly illustrated by the influx of private equity firms, such as Bain Capital, that are investing heavily in treatment centers.
Reports of malfeasance and misconduct, by owners, operators, staff, and others connected with the industry are beginning to get the attention of authorities. There have been reports of outpatient treatment centers that spend lavishly on furnishing, on BMWs and signed art, yet are understaffed, leading to inadequate one-on-one counseling and even sexual transgressions between residents. There are centers that have been investigated for insurance fraud, such as illegally waiving a copay or a deductible or for charging up to $5,000 for a simple urine five drug screen, often multiple times a day. And there is evidence of “junkie hunters” who cruise for people with addictions and brokers who provide such people with fake addresses in order to qualify for insurance plans with excellent benefits for addiction treatment.
Probably the best means to find a suitable outpatient treatment center is by way of a local, experienced, and respected chemical dependency counselor or physician certified in addiction medicine. If people with substance use disorders and their families want to independently conduct a search, as a good rule of thumb, they should be advised to consider programs affiliated with major medical centers and hospitals or outpatient treatment centers that have been established in good standing for years, in contrast to the rash of pop-up, for-profit programs. Of equal, or even greater importance, is that the prospective center ought to be accredited by a national organization, for example, The Joint Commission, and its staff ought to be licensed and credentialed as well.
In addition, there is merit if the staff has been educated, trained, and supervised under the direction of a respected institution. Needless to add, an outpatient treatment center must use evidence-based practices as the bedrock of treatment; this includes pharmacotherapies such as Suboxone and naltrexone (Vivitrol), and behavioral therapies such as cognitive-behavioral therapy, contingency management, and motivational enhancement. To date, massage and essential oils might be relaxing and pleasurable, but they are not considered accepted standard of care.
It is crucial, too, that an outpatient treatment center have both the resources to reliably handle acute medical detox, which can be a potentially life-threatening emergency, and the medical personnel who can assess and treat such medical conditions as hypertension as well as psychiatric illnesses such as bipolar and generalized anxiety disorders. A prospective patient also should inquire whether any of the staff has been the subject of disciplinary action by a licensing board or whether the center has been investigated by the state or a national accrediting organization.
Because addiction so often has facets rooted in the family system, and recovery so often depends on family support, an outpatient treatment center should provide a structured family program integrated into the patient’s treatment and emphasize the importance of continued family involvement after discharge.
Lastly, the best treatment centers often regularly update a patient’s local therapist and physician, spell out the elements of successful aftercare (12-step programs, and so on), and provide amenities, such as calls to a recently discharged patient and an alumni support network.
Dr. Marseille is a psychiatrist who works on the staff of a clinic in Wheaton, Ill. His special interests include adolescent and addiction medicine, eating disorders, trauma, bipolar disorder, and the psychiatric manifestations of acute and chronic medical conditions.
This article was updated 12/15/17.
FDA approves premixed, low-volume colon-cleansing solution
in adults preparing to undergo colonoscopy, according to Ferring Pharmaceuticals.
The sodium picosulfate, magnesium oxide, and anhydrous citric acid oral solution is a relatively low-volume, premixed, cranberry-flavored solution, making it easier to use and more palatable for patients.
The oral solution is approved with two dosing options: split dose, one dose the evening prior and one dose the morning of the procedure, or the day before dose, which involves taking both doses the day prior to the procedure. Day before dosing is an alternative and should be used when split dosing is not appropriate. After each dose of sodium picosulfate, magnesium oxide, and anhydrous citric acid oral solution, clear liquids should be consumed based on the dosing recommendation. The American College of Gastroenterology recommends the split-dose regimen because of its improved cleansing quality of the colon and better tolerability of the liquid volume by patients.
Patients with impaired renal function should exercise caution if using sodium picosulfate, magnesium oxide, and anhydrous citric acid oral solution as it may effect renal function. A more comprehensive list of safety information is available at www.clenpiq.com.
in adults preparing to undergo colonoscopy, according to Ferring Pharmaceuticals.
The sodium picosulfate, magnesium oxide, and anhydrous citric acid oral solution is a relatively low-volume, premixed, cranberry-flavored solution, making it easier to use and more palatable for patients.
The oral solution is approved with two dosing options: split dose, one dose the evening prior and one dose the morning of the procedure, or the day before dose, which involves taking both doses the day prior to the procedure. Day before dosing is an alternative and should be used when split dosing is not appropriate. After each dose of sodium picosulfate, magnesium oxide, and anhydrous citric acid oral solution, clear liquids should be consumed based on the dosing recommendation. The American College of Gastroenterology recommends the split-dose regimen because of its improved cleansing quality of the colon and better tolerability of the liquid volume by patients.
Patients with impaired renal function should exercise caution if using sodium picosulfate, magnesium oxide, and anhydrous citric acid oral solution as it may effect renal function. A more comprehensive list of safety information is available at www.clenpiq.com.
in adults preparing to undergo colonoscopy, according to Ferring Pharmaceuticals.
The sodium picosulfate, magnesium oxide, and anhydrous citric acid oral solution is a relatively low-volume, premixed, cranberry-flavored solution, making it easier to use and more palatable for patients.
The oral solution is approved with two dosing options: split dose, one dose the evening prior and one dose the morning of the procedure, or the day before dose, which involves taking both doses the day prior to the procedure. Day before dosing is an alternative and should be used when split dosing is not appropriate. After each dose of sodium picosulfate, magnesium oxide, and anhydrous citric acid oral solution, clear liquids should be consumed based on the dosing recommendation. The American College of Gastroenterology recommends the split-dose regimen because of its improved cleansing quality of the colon and better tolerability of the liquid volume by patients.
Patients with impaired renal function should exercise caution if using sodium picosulfate, magnesium oxide, and anhydrous citric acid oral solution as it may effect renal function. A more comprehensive list of safety information is available at www.clenpiq.com.
Sprifermin shows cartilage-building potential in knee OA patients
in the initial 2-year results of the ongoing FORWARD trial.
“Sprifermin appears to be the first investigational medicinal product to show dose-dependent prevention of cartilage loss and an increase in cartilage thickness, not only in the total tibiofemoral joint [TFJ] but also in both the medial and lateral compartments, including the central medial femorotibial region,” said Marc H. Hochberg, MD, primary investigator in the trial and division head of rheumatology and clinical immunology at the University of Maryland, Baltimore. “The recommendation is that these findings should be further evaluated in phase 3 clinical trials.”
He and his colleagues randomized 549 osteoarthritis (OA) patients to double-blind treatment with one of four different dosing regimens of sprifermin or placebo. These patients were aged 40-85 with symptomatic radiographic primary femorotibial knee OA measuring grade 2 or 3 on the Kellgren-Lawrence scale and a medial minimum joint space width (mJSW) 2.5 mm or greater.
At 2 years, researchers observed a significant dose-dependent relationship between the amount of sprifermin given and the increase in total TFJ cartilage thickness. Patients who received three 100-mcg intra-articular injections of sprifermin every 6 months (group 1) showed a gain in TFJ cartilage thickness of 0.03 mm as seen on MRI, while those who received three 100-mcg injections of sprifermin every 12 months (group 2) had a gain of 0.02 mm, Dr. Hochberg said during a late-breaking abstract session at the annual meeting of the American College of Rheumatology. By contrast, those who received placebo had a loss in TFJ cartilage thickness of 0.02 mm (P less than .001). The other two groups received 30 mcg of sprifermin in three weekly injections every 6 months (group 3) or every 12 months (group 4), and these had TFJ cartilage thickness losses of about 0.01 mm or less.
Similar dose-dependent relationships were observed for some of the secondary endpoints, which included changes in cartilage thickness seen in the medial and lateral compartments, changes in cartilage thickness in the compartments’ subregions, and changes in mJSW. Significant differences in cartilage thickness were observed between sprifermin treatment groups and placebo in the medial (group 1, gain of 0.02 mm vs. loss of 0.03 mm; P less than .001) and lateral (groups 1 and 2, gain of 0.04 mm vs. loss of 0.01 mm; P less than .001) TFJ compartments, and in central medial and lateral TFJ subregions.
Changes in mJSW as seen on x-ray between those in group 1 and those on placebo were significant for the lateral compartment, with an increase in mJSW at the higher doses and a decline in the placebo group, but not for the medial compartment.
There were no significant differences in Western Ontario and McMaster Universities Arthritis Index (WOMAC) scores among the treatment groups. Dr. Hochberg noted that patients were permitted to take pain medications during the study, which could have affected this result.
The most frequently reported adverse events were musculoskeletal and connective tissue disorders, specifically arthralgias and back pain, Dr. Hochberg said. The incidence of acute inflammatory reactions was higher with sprifermin, compared with placebo, but the increase was only significant after the first injection cycle, he said.
Merck KGaA and the EMD Serono Research Institute funded the study. Dr. Hochberg reported receiving consulting fees from numerous companies that market or are developing OA drugs, including EMD Serono.
in the initial 2-year results of the ongoing FORWARD trial.
“Sprifermin appears to be the first investigational medicinal product to show dose-dependent prevention of cartilage loss and an increase in cartilage thickness, not only in the total tibiofemoral joint [TFJ] but also in both the medial and lateral compartments, including the central medial femorotibial region,” said Marc H. Hochberg, MD, primary investigator in the trial and division head of rheumatology and clinical immunology at the University of Maryland, Baltimore. “The recommendation is that these findings should be further evaluated in phase 3 clinical trials.”
He and his colleagues randomized 549 osteoarthritis (OA) patients to double-blind treatment with one of four different dosing regimens of sprifermin or placebo. These patients were aged 40-85 with symptomatic radiographic primary femorotibial knee OA measuring grade 2 or 3 on the Kellgren-Lawrence scale and a medial minimum joint space width (mJSW) 2.5 mm or greater.
At 2 years, researchers observed a significant dose-dependent relationship between the amount of sprifermin given and the increase in total TFJ cartilage thickness. Patients who received three 100-mcg intra-articular injections of sprifermin every 6 months (group 1) showed a gain in TFJ cartilage thickness of 0.03 mm as seen on MRI, while those who received three 100-mcg injections of sprifermin every 12 months (group 2) had a gain of 0.02 mm, Dr. Hochberg said during a late-breaking abstract session at the annual meeting of the American College of Rheumatology. By contrast, those who received placebo had a loss in TFJ cartilage thickness of 0.02 mm (P less than .001). The other two groups received 30 mcg of sprifermin in three weekly injections every 6 months (group 3) or every 12 months (group 4), and these had TFJ cartilage thickness losses of about 0.01 mm or less.
Similar dose-dependent relationships were observed for some of the secondary endpoints, which included changes in cartilage thickness seen in the medial and lateral compartments, changes in cartilage thickness in the compartments’ subregions, and changes in mJSW. Significant differences in cartilage thickness were observed between sprifermin treatment groups and placebo in the medial (group 1, gain of 0.02 mm vs. loss of 0.03 mm; P less than .001) and lateral (groups 1 and 2, gain of 0.04 mm vs. loss of 0.01 mm; P less than .001) TFJ compartments, and in central medial and lateral TFJ subregions.
Changes in mJSW as seen on x-ray between those in group 1 and those on placebo were significant for the lateral compartment, with an increase in mJSW at the higher doses and a decline in the placebo group, but not for the medial compartment.
There were no significant differences in Western Ontario and McMaster Universities Arthritis Index (WOMAC) scores among the treatment groups. Dr. Hochberg noted that patients were permitted to take pain medications during the study, which could have affected this result.
The most frequently reported adverse events were musculoskeletal and connective tissue disorders, specifically arthralgias and back pain, Dr. Hochberg said. The incidence of acute inflammatory reactions was higher with sprifermin, compared with placebo, but the increase was only significant after the first injection cycle, he said.
Merck KGaA and the EMD Serono Research Institute funded the study. Dr. Hochberg reported receiving consulting fees from numerous companies that market or are developing OA drugs, including EMD Serono.
in the initial 2-year results of the ongoing FORWARD trial.
“Sprifermin appears to be the first investigational medicinal product to show dose-dependent prevention of cartilage loss and an increase in cartilage thickness, not only in the total tibiofemoral joint [TFJ] but also in both the medial and lateral compartments, including the central medial femorotibial region,” said Marc H. Hochberg, MD, primary investigator in the trial and division head of rheumatology and clinical immunology at the University of Maryland, Baltimore. “The recommendation is that these findings should be further evaluated in phase 3 clinical trials.”
He and his colleagues randomized 549 osteoarthritis (OA) patients to double-blind treatment with one of four different dosing regimens of sprifermin or placebo. These patients were aged 40-85 with symptomatic radiographic primary femorotibial knee OA measuring grade 2 or 3 on the Kellgren-Lawrence scale and a medial minimum joint space width (mJSW) 2.5 mm or greater.
At 2 years, researchers observed a significant dose-dependent relationship between the amount of sprifermin given and the increase in total TFJ cartilage thickness. Patients who received three 100-mcg intra-articular injections of sprifermin every 6 months (group 1) showed a gain in TFJ cartilage thickness of 0.03 mm as seen on MRI, while those who received three 100-mcg injections of sprifermin every 12 months (group 2) had a gain of 0.02 mm, Dr. Hochberg said during a late-breaking abstract session at the annual meeting of the American College of Rheumatology. By contrast, those who received placebo had a loss in TFJ cartilage thickness of 0.02 mm (P less than .001). The other two groups received 30 mcg of sprifermin in three weekly injections every 6 months (group 3) or every 12 months (group 4), and these had TFJ cartilage thickness losses of about 0.01 mm or less.
Similar dose-dependent relationships were observed for some of the secondary endpoints, which included changes in cartilage thickness seen in the medial and lateral compartments, changes in cartilage thickness in the compartments’ subregions, and changes in mJSW. Significant differences in cartilage thickness were observed between sprifermin treatment groups and placebo in the medial (group 1, gain of 0.02 mm vs. loss of 0.03 mm; P less than .001) and lateral (groups 1 and 2, gain of 0.04 mm vs. loss of 0.01 mm; P less than .001) TFJ compartments, and in central medial and lateral TFJ subregions.
Changes in mJSW as seen on x-ray between those in group 1 and those on placebo were significant for the lateral compartment, with an increase in mJSW at the higher doses and a decline in the placebo group, but not for the medial compartment.
There were no significant differences in Western Ontario and McMaster Universities Arthritis Index (WOMAC) scores among the treatment groups. Dr. Hochberg noted that patients were permitted to take pain medications during the study, which could have affected this result.
The most frequently reported adverse events were musculoskeletal and connective tissue disorders, specifically arthralgias and back pain, Dr. Hochberg said. The incidence of acute inflammatory reactions was higher with sprifermin, compared with placebo, but the increase was only significant after the first injection cycle, he said.
Merck KGaA and the EMD Serono Research Institute funded the study. Dr. Hochberg reported receiving consulting fees from numerous companies that market or are developing OA drugs, including EMD Serono.
REPORTING FROM ACR 2017
Key clinical point: Sprifermin may help build knee joint cartilage in patients with OA.
Major finding: Patients taking sprifermin 100 mcg three times a week every 6 months or every 12 months had gains in tibiofemoral joint cartilage thickness of 0.03 mm and 0.02 mm, respectively, over a 2-year period.
Study details: A study of 549 patients with symptomatic knee OA randomized to receive either 30 mcg or 100 mcg of sprifermin three times a week every 6 or every 12 months, or placebo.
Disclosures: Merck KGaA and the EMD Serono Research Institute funded the study. The presenter reported receiving consulting fees from numerous companies that market or are developing OA drugs, including EMD Serono.
Source: Hochberg M et al. ACR 2017 abstract 1L.
New HIV vaccine trial launched in Africa
The National Institutes of Health has partnered with Janssen Vaccines & Prevention B.V. to conduct the phase 2b proof-of-concept “Imbokodo” study of a quadrivalent HIV vaccine regimen using “mosaic” immunogens, which means the vaccine components are designed to trigger an immune response against a variety of HIV strains.
Preclinical studies in monkeys suggest this approach can protect against HIV infection, and two early-stage clinical trials in humans showed the vaccine was well tolerated and generated immune responses against HIV in healthy individuals.
The four doses of the vaccine will be spread out over a year, and the final two doses will be given together with doses of an HIV protein, clade C gp140, and an aluminum phosphate adjuvant to boost immune responses. The study has already begun to immunize some of the 2,600 HIV-negative sub-Saharan African women to be recruited for the study.
The study is sponsored by Janssen Vaccines & Prevention B.V. and cofunded by the Bill & Melinda Gates Foundation and the NIH.
SOURCE: National Institute of Allergy and Infectious Diseases News Releases Nov. 30, 2017.
The National Institutes of Health has partnered with Janssen Vaccines & Prevention B.V. to conduct the phase 2b proof-of-concept “Imbokodo” study of a quadrivalent HIV vaccine regimen using “mosaic” immunogens, which means the vaccine components are designed to trigger an immune response against a variety of HIV strains.
Preclinical studies in monkeys suggest this approach can protect against HIV infection, and two early-stage clinical trials in humans showed the vaccine was well tolerated and generated immune responses against HIV in healthy individuals.
The four doses of the vaccine will be spread out over a year, and the final two doses will be given together with doses of an HIV protein, clade C gp140, and an aluminum phosphate adjuvant to boost immune responses. The study has already begun to immunize some of the 2,600 HIV-negative sub-Saharan African women to be recruited for the study.
The study is sponsored by Janssen Vaccines & Prevention B.V. and cofunded by the Bill & Melinda Gates Foundation and the NIH.
SOURCE: National Institute of Allergy and Infectious Diseases News Releases Nov. 30, 2017.
The National Institutes of Health has partnered with Janssen Vaccines & Prevention B.V. to conduct the phase 2b proof-of-concept “Imbokodo” study of a quadrivalent HIV vaccine regimen using “mosaic” immunogens, which means the vaccine components are designed to trigger an immune response against a variety of HIV strains.
Preclinical studies in monkeys suggest this approach can protect against HIV infection, and two early-stage clinical trials in humans showed the vaccine was well tolerated and generated immune responses against HIV in healthy individuals.
The four doses of the vaccine will be spread out over a year, and the final two doses will be given together with doses of an HIV protein, clade C gp140, and an aluminum phosphate adjuvant to boost immune responses. The study has already begun to immunize some of the 2,600 HIV-negative sub-Saharan African women to be recruited for the study.
The study is sponsored by Janssen Vaccines & Prevention B.V. and cofunded by the Bill & Melinda Gates Foundation and the NIH.
SOURCE: National Institute of Allergy and Infectious Diseases News Releases Nov. 30, 2017.
VIDEO: Ibrutinib PFS is nearly 3 years in MCL patients who had one prior therapy
ATLANTA – Ibrutinib yielded a median progression-free survival (PFS) of nearly 3 years for patients with relapsed or refractory mantle cell lymphoma (MCL) treated with the agent after just one prior line of therapy, according to pooled long-term follow-up data presented at the annual meeting of the American Society of Hematology.
With a 3.5-year median follow-up, a median PFS of 33.6 months was reported for MCL patients with one prior line of therapy, compared to 8.4 months for patients who had two or more prior lines of therapy, reported lead study author Simon Rule, MD, of Plymouth (England) University Medical School.
“I think the take-home message from the ibrutinib data is the earlier you use the drug in the relapse setting, the better the outcomes you’re going to get,” Dr. Rule said in an interview. “It is quite dramatic, the difference between one prior line of therapy and subsequent lines of therapy.”
Response rates were also higher in MCL patients who had only one prior line of therapy, Dr. Rule said.
The overall and complete response rates for that group were 77.8% and 36.4%, respectively, according to data Dr. Rule presented in an oral presentation. For patients receiving more than one line of therapy prior to ibrutinib, overall and complete response rates were 66.8% and 22.9%.
The pooled analysis presented by Dr. Rule included 370 patients enrolled in ibrutinib trials between 2011 and 2013. Patients in those trials received oral ibrutinib 560 mg daily until progressive disease or unacceptable toxicity.
Patients achieving a CR had an “extraordinary” PFS of nearly 4 years and a median duration of response of 55 months, Dr. Rule said.
Atrial fibrillation (AF) rates were reported to be 5.7% (21/370 patients). A total of 53 patients in the analysis had ongoing controlled AF/arrhythmia or had a history of it. Over the course of follow-up, 70% of them (37 patients) had no recurrences, according to Dr. Rule and his colleagues.
No patients discontinued ibrutinib because of grade 3-4 AF, they reported. Moreover, less than 2% of the 370 patients discontinued or reduced dose of ibrutinib because of grade 3-4 bleeding or AF.
New onset grade 3-4 adverse events were more common in the first year of treatment and generally were less frequent over time, Dr. Rule said.
Patients with only one prior line of therapy were less likely to have grade 3-4 adverse events, suggesting again that “the earlier you use [ibrutinib], the fewer side effects you get, particularly with hematologic toxicity,” Dr. Rule said.
Sponsorship for the research came from Janssen, and funding for writing assistance came from Janssen Global Services. Dr. Rule reported financial relationships with Janssen and several other companies.
SOURCE: Rule S et al. ASH 2017 Abstract 151.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ATLANTA – Ibrutinib yielded a median progression-free survival (PFS) of nearly 3 years for patients with relapsed or refractory mantle cell lymphoma (MCL) treated with the agent after just one prior line of therapy, according to pooled long-term follow-up data presented at the annual meeting of the American Society of Hematology.
With a 3.5-year median follow-up, a median PFS of 33.6 months was reported for MCL patients with one prior line of therapy, compared to 8.4 months for patients who had two or more prior lines of therapy, reported lead study author Simon Rule, MD, of Plymouth (England) University Medical School.
“I think the take-home message from the ibrutinib data is the earlier you use the drug in the relapse setting, the better the outcomes you’re going to get,” Dr. Rule said in an interview. “It is quite dramatic, the difference between one prior line of therapy and subsequent lines of therapy.”
Response rates were also higher in MCL patients who had only one prior line of therapy, Dr. Rule said.
The overall and complete response rates for that group were 77.8% and 36.4%, respectively, according to data Dr. Rule presented in an oral presentation. For patients receiving more than one line of therapy prior to ibrutinib, overall and complete response rates were 66.8% and 22.9%.
The pooled analysis presented by Dr. Rule included 370 patients enrolled in ibrutinib trials between 2011 and 2013. Patients in those trials received oral ibrutinib 560 mg daily until progressive disease or unacceptable toxicity.
Patients achieving a CR had an “extraordinary” PFS of nearly 4 years and a median duration of response of 55 months, Dr. Rule said.
Atrial fibrillation (AF) rates were reported to be 5.7% (21/370 patients). A total of 53 patients in the analysis had ongoing controlled AF/arrhythmia or had a history of it. Over the course of follow-up, 70% of them (37 patients) had no recurrences, according to Dr. Rule and his colleagues.
No patients discontinued ibrutinib because of grade 3-4 AF, they reported. Moreover, less than 2% of the 370 patients discontinued or reduced dose of ibrutinib because of grade 3-4 bleeding or AF.
New onset grade 3-4 adverse events were more common in the first year of treatment and generally were less frequent over time, Dr. Rule said.
Patients with only one prior line of therapy were less likely to have grade 3-4 adverse events, suggesting again that “the earlier you use [ibrutinib], the fewer side effects you get, particularly with hematologic toxicity,” Dr. Rule said.
Sponsorship for the research came from Janssen, and funding for writing assistance came from Janssen Global Services. Dr. Rule reported financial relationships with Janssen and several other companies.
SOURCE: Rule S et al. ASH 2017 Abstract 151.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ATLANTA – Ibrutinib yielded a median progression-free survival (PFS) of nearly 3 years for patients with relapsed or refractory mantle cell lymphoma (MCL) treated with the agent after just one prior line of therapy, according to pooled long-term follow-up data presented at the annual meeting of the American Society of Hematology.
With a 3.5-year median follow-up, a median PFS of 33.6 months was reported for MCL patients with one prior line of therapy, compared to 8.4 months for patients who had two or more prior lines of therapy, reported lead study author Simon Rule, MD, of Plymouth (England) University Medical School.
“I think the take-home message from the ibrutinib data is the earlier you use the drug in the relapse setting, the better the outcomes you’re going to get,” Dr. Rule said in an interview. “It is quite dramatic, the difference between one prior line of therapy and subsequent lines of therapy.”
Response rates were also higher in MCL patients who had only one prior line of therapy, Dr. Rule said.
The overall and complete response rates for that group were 77.8% and 36.4%, respectively, according to data Dr. Rule presented in an oral presentation. For patients receiving more than one line of therapy prior to ibrutinib, overall and complete response rates were 66.8% and 22.9%.
The pooled analysis presented by Dr. Rule included 370 patients enrolled in ibrutinib trials between 2011 and 2013. Patients in those trials received oral ibrutinib 560 mg daily until progressive disease or unacceptable toxicity.
Patients achieving a CR had an “extraordinary” PFS of nearly 4 years and a median duration of response of 55 months, Dr. Rule said.
Atrial fibrillation (AF) rates were reported to be 5.7% (21/370 patients). A total of 53 patients in the analysis had ongoing controlled AF/arrhythmia or had a history of it. Over the course of follow-up, 70% of them (37 patients) had no recurrences, according to Dr. Rule and his colleagues.
No patients discontinued ibrutinib because of grade 3-4 AF, they reported. Moreover, less than 2% of the 370 patients discontinued or reduced dose of ibrutinib because of grade 3-4 bleeding or AF.
New onset grade 3-4 adverse events were more common in the first year of treatment and generally were less frequent over time, Dr. Rule said.
Patients with only one prior line of therapy were less likely to have grade 3-4 adverse events, suggesting again that “the earlier you use [ibrutinib], the fewer side effects you get, particularly with hematologic toxicity,” Dr. Rule said.
Sponsorship for the research came from Janssen, and funding for writing assistance came from Janssen Global Services. Dr. Rule reported financial relationships with Janssen and several other companies.
SOURCE: Rule S et al. ASH 2017 Abstract 151.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
REPORTING FROM ASH 2017
Key clinical point:
Major finding: Median PFS was 33.6 months for MCL patients with one prior line of therapy, versus 8.4 months for patients who had two or more prior lines of therapy.
Study details: A pooled analysis of 370 patients enrolled in ibrutinib clinical trials with a median 3.5-year follow-up.
Disclosures: Janssen sponsored the research and Janssen Global Services funded writing assistance. Lead author Simon Rule, MD, reported financial relationships with Janssen and several other companies.
Source: Rule S et al. ASH 2017 Abstract 151.
Intrauterine exposure to methylphenidate tied to increased cardiac risk
The use of methylphenidate by pregnant women is associated with a small increased risk of congenital cardiac malformations in newborns. However, a comparable increased risk is not found with intrauterine exposure to stimulants, according to a population-based cohort study published Dec. 13.
Krista F. Huybrechts, PhD, and her associates analyzed data from more than 1 million pregnancies in the United States. They found that the overall incidence of congenital malformations among the 1,813,894 pregnancies was 35 per 1,000 control infants, compared with 45.9 per 1,000 infants whose mothers used methylphenidate and 45.4 per 1,000 infants whose mothers used amphetamines.
For the subset of infants with cardiac malformations, the risk per 1,000 infants was 12.7 for controls, 18.8 for methylphenidate exposure, and 15.4 for amphetamine exposure. The researchers identified an adjusted relative risk of 1.11 for overall congenital abnormalities and 1.28 for cardiac abnormalities with methylphenidate exposure, compared with a relative risk of 1.05 for overall congenital abnormalities and 0.96 for cardiac abnormalities with stimulant exposure.
An analysis among 2,560,069 pregnancies in Denmark, Finland, Iceland, Norway, and Sweden yielded a similarly significant relative risk of 1.28 for cardiac malformations associated with methylphenidate exposure (JAMA Psychiatry 2017. doi: 10.1001/jamapsychiatry.2017.3644).
“We found a 28% increased prevalence of cardiac malformations after first-trimester exposure to methylphenidate,” wrote Dr. Huybrechts of Brigham and Women’s Hospital, Boston, and her associates. “Although the absolute risk is small, it is nevertheless important evidence to consider when weighing the potential risks and benefits of different treatment strategies for [attention-deficit/hyperactivity disorder] in young women of reproductive age and in pregnant women.”
The researchers had no financial conflicts to disclose. The study was supported in part by grants from the National Institutes of Mental Health, the Eunice Kennedy Shriver National Institute for Child Health & Human Development, and the Söderström König Foundation.
The use of methylphenidate by pregnant women is associated with a small increased risk of congenital cardiac malformations in newborns. However, a comparable increased risk is not found with intrauterine exposure to stimulants, according to a population-based cohort study published Dec. 13.
Krista F. Huybrechts, PhD, and her associates analyzed data from more than 1 million pregnancies in the United States. They found that the overall incidence of congenital malformations among the 1,813,894 pregnancies was 35 per 1,000 control infants, compared with 45.9 per 1,000 infants whose mothers used methylphenidate and 45.4 per 1,000 infants whose mothers used amphetamines.
For the subset of infants with cardiac malformations, the risk per 1,000 infants was 12.7 for controls, 18.8 for methylphenidate exposure, and 15.4 for amphetamine exposure. The researchers identified an adjusted relative risk of 1.11 for overall congenital abnormalities and 1.28 for cardiac abnormalities with methylphenidate exposure, compared with a relative risk of 1.05 for overall congenital abnormalities and 0.96 for cardiac abnormalities with stimulant exposure.
An analysis among 2,560,069 pregnancies in Denmark, Finland, Iceland, Norway, and Sweden yielded a similarly significant relative risk of 1.28 for cardiac malformations associated with methylphenidate exposure (JAMA Psychiatry 2017. doi: 10.1001/jamapsychiatry.2017.3644).
“We found a 28% increased prevalence of cardiac malformations after first-trimester exposure to methylphenidate,” wrote Dr. Huybrechts of Brigham and Women’s Hospital, Boston, and her associates. “Although the absolute risk is small, it is nevertheless important evidence to consider when weighing the potential risks and benefits of different treatment strategies for [attention-deficit/hyperactivity disorder] in young women of reproductive age and in pregnant women.”
The researchers had no financial conflicts to disclose. The study was supported in part by grants from the National Institutes of Mental Health, the Eunice Kennedy Shriver National Institute for Child Health & Human Development, and the Söderström König Foundation.
The use of methylphenidate by pregnant women is associated with a small increased risk of congenital cardiac malformations in newborns. However, a comparable increased risk is not found with intrauterine exposure to stimulants, according to a population-based cohort study published Dec. 13.
Krista F. Huybrechts, PhD, and her associates analyzed data from more than 1 million pregnancies in the United States. They found that the overall incidence of congenital malformations among the 1,813,894 pregnancies was 35 per 1,000 control infants, compared with 45.9 per 1,000 infants whose mothers used methylphenidate and 45.4 per 1,000 infants whose mothers used amphetamines.
For the subset of infants with cardiac malformations, the risk per 1,000 infants was 12.7 for controls, 18.8 for methylphenidate exposure, and 15.4 for amphetamine exposure. The researchers identified an adjusted relative risk of 1.11 for overall congenital abnormalities and 1.28 for cardiac abnormalities with methylphenidate exposure, compared with a relative risk of 1.05 for overall congenital abnormalities and 0.96 for cardiac abnormalities with stimulant exposure.
An analysis among 2,560,069 pregnancies in Denmark, Finland, Iceland, Norway, and Sweden yielded a similarly significant relative risk of 1.28 for cardiac malformations associated with methylphenidate exposure (JAMA Psychiatry 2017. doi: 10.1001/jamapsychiatry.2017.3644).
“We found a 28% increased prevalence of cardiac malformations after first-trimester exposure to methylphenidate,” wrote Dr. Huybrechts of Brigham and Women’s Hospital, Boston, and her associates. “Although the absolute risk is small, it is nevertheless important evidence to consider when weighing the potential risks and benefits of different treatment strategies for [attention-deficit/hyperactivity disorder] in young women of reproductive age and in pregnant women.”
The researchers had no financial conflicts to disclose. The study was supported in part by grants from the National Institutes of Mental Health, the Eunice Kennedy Shriver National Institute for Child Health & Human Development, and the Söderström König Foundation.
FROM JAMA PSYCHIATRY
Social Media Creates Anxiety for Teenagers With Acne
Adolescents with acne experience anxiety over using social media, according to a recent online survey of teenagers in the United States. The results of the survey, conducted by Harris Poll on behalf of Cutanea Life Sciences, Inc, demonstrate the negative impact of acne on body image and self-esteem.
Of 1010 teens surveyed (age range, 15–19 years), 86% said they have had acne, and a majority of respondents said that acne has a negative effect on their body image and attractiveness (71%) as well as their self-esteem (67%). Fifty-one percent of respondents who use social media said it makes having acne harder and 72% agreed most teenagers with acne are self-conscious about showing their acne on social media. As a result, 68% reported that most of their peers with acne edit or alter their photographs on social media, and 58% have offered to take a photograph to avoid being in a picture. Half of the respondents have taken at least 1 of the following actions to avoid displaying their acne on social media:
- Chose not to include a photograph on social media
- Deleted or untagged a photograph that showed their acne
- Asked someone else to take down a photograph because it showed their acne
- Altered, edited, retouched, or cropped a photograph to try and hide their acne
- Avoided having their picture taken with someone who had clearer skin
- Stayed off social media so they would not have to post or see photographs of themselves
Dermatologists should be aware of the psychosocial impact of acne in teenagers to provide effective management strategies. Although the majority of teens (61%) said they were doing everything possible to manage their acne, 1 in 3 respondents admitted to having difficulty managing their condition. To effectively treat acne, more than three-quarters said that it was at least very important to use a therapy that worked quickly (83%) and was affordable (80%) and easy to use (78%). Be sure to address the psychosocial impact of acne with your teenaged patients, especially pertaining to social media.
Adolescents with acne experience anxiety over using social media, according to a recent online survey of teenagers in the United States. The results of the survey, conducted by Harris Poll on behalf of Cutanea Life Sciences, Inc, demonstrate the negative impact of acne on body image and self-esteem.
Of 1010 teens surveyed (age range, 15–19 years), 86% said they have had acne, and a majority of respondents said that acne has a negative effect on their body image and attractiveness (71%) as well as their self-esteem (67%). Fifty-one percent of respondents who use social media said it makes having acne harder and 72% agreed most teenagers with acne are self-conscious about showing their acne on social media. As a result, 68% reported that most of their peers with acne edit or alter their photographs on social media, and 58% have offered to take a photograph to avoid being in a picture. Half of the respondents have taken at least 1 of the following actions to avoid displaying their acne on social media:
- Chose not to include a photograph on social media
- Deleted or untagged a photograph that showed their acne
- Asked someone else to take down a photograph because it showed their acne
- Altered, edited, retouched, or cropped a photograph to try and hide their acne
- Avoided having their picture taken with someone who had clearer skin
- Stayed off social media so they would not have to post or see photographs of themselves
Dermatologists should be aware of the psychosocial impact of acne in teenagers to provide effective management strategies. Although the majority of teens (61%) said they were doing everything possible to manage their acne, 1 in 3 respondents admitted to having difficulty managing their condition. To effectively treat acne, more than three-quarters said that it was at least very important to use a therapy that worked quickly (83%) and was affordable (80%) and easy to use (78%). Be sure to address the psychosocial impact of acne with your teenaged patients, especially pertaining to social media.
Adolescents with acne experience anxiety over using social media, according to a recent online survey of teenagers in the United States. The results of the survey, conducted by Harris Poll on behalf of Cutanea Life Sciences, Inc, demonstrate the negative impact of acne on body image and self-esteem.
Of 1010 teens surveyed (age range, 15–19 years), 86% said they have had acne, and a majority of respondents said that acne has a negative effect on their body image and attractiveness (71%) as well as their self-esteem (67%). Fifty-one percent of respondents who use social media said it makes having acne harder and 72% agreed most teenagers with acne are self-conscious about showing their acne on social media. As a result, 68% reported that most of their peers with acne edit or alter their photographs on social media, and 58% have offered to take a photograph to avoid being in a picture. Half of the respondents have taken at least 1 of the following actions to avoid displaying their acne on social media:
- Chose not to include a photograph on social media
- Deleted or untagged a photograph that showed their acne
- Asked someone else to take down a photograph because it showed their acne
- Altered, edited, retouched, or cropped a photograph to try and hide their acne
- Avoided having their picture taken with someone who had clearer skin
- Stayed off social media so they would not have to post or see photographs of themselves
Dermatologists should be aware of the psychosocial impact of acne in teenagers to provide effective management strategies. Although the majority of teens (61%) said they were doing everything possible to manage their acne, 1 in 3 respondents admitted to having difficulty managing their condition. To effectively treat acne, more than three-quarters said that it was at least very important to use a therapy that worked quickly (83%) and was affordable (80%) and easy to use (78%). Be sure to address the psychosocial impact of acne with your teenaged patients, especially pertaining to social media.