User login
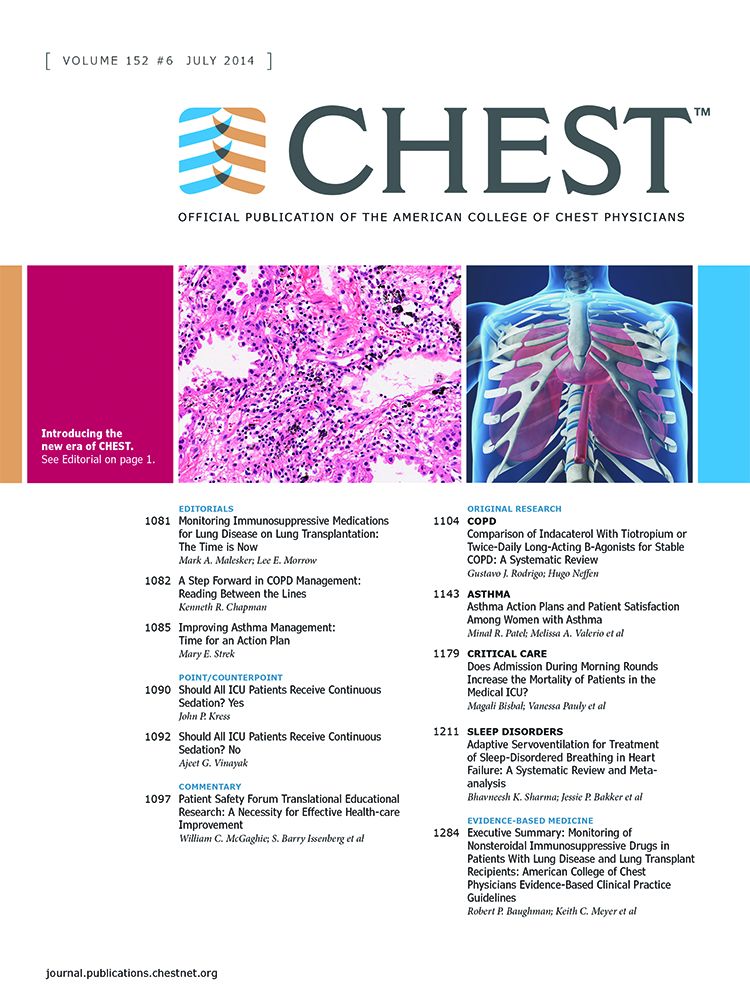
This month in CHEST Editor’s picks
Original Research
Pharmacotherapy for Non-Cystic Fibrosis Bronchiectasis: Results From an NTM Info and Research Patient Survey and the Bronchiectasis and NTM Research Registry.
By Dr. E. Henkle, et al.
By Dr. A. Lautenbach, et al.
Commentary
Crotalaria (Monocrotaline) Pulmonary Hypertension: The Fiftieth Anniversary.
By Dr. J. Kay.
Original Research
Pharmacotherapy for Non-Cystic Fibrosis Bronchiectasis: Results From an NTM Info and Research Patient Survey and the Bronchiectasis and NTM Research Registry.
By Dr. E. Henkle, et al.
By Dr. A. Lautenbach, et al.
Commentary
Crotalaria (Monocrotaline) Pulmonary Hypertension: The Fiftieth Anniversary.
By Dr. J. Kay.
Original Research
Pharmacotherapy for Non-Cystic Fibrosis Bronchiectasis: Results From an NTM Info and Research Patient Survey and the Bronchiectasis and NTM Research Registry.
By Dr. E. Henkle, et al.
By Dr. A. Lautenbach, et al.
Commentary
Crotalaria (Monocrotaline) Pulmonary Hypertension: The Fiftieth Anniversary.
By Dr. J. Kay.
NAMDRC Report
In mid-September, NAMDRC, along with the American Thoracic Society, the American Association for Respiratory Care, the COPD Foundation, the American Lung Association, and others met to discuss the components of a legislative agenda for the coming years. The primary purpose behind the meeting was the premise that IF the current Republican majority would shift in either the House or Senate after the 2018 election, the community should be prepared to move an already agreed upon legislative agenda. CHEST was involved in the preliminary discussions, as well as follow-up, but was not in attendance at the meeting due to a scheduling conflict. There was also tacit agreement that as these policies are fleshed out and crafted into specific legislative language, the community would re-evaluate the current political climate to determine the value of pushing an agreed upon agenda prior to the 2018 elections.
Various patient groups were also invited to participate, but scheduling conflicts precluded some societies from participating but signaled their desire to work with the broad pulmonary medicine community to pursue common goals.
Each society brought its legislative priorities to the table, and there was active discussion on issues ranging from funding for NIH/NHLBI, to CDC and its COPD Action Plan, to a range of Medicare-related issues.
NAMDRC brought three specific Medicare coverage and payment issues to the discussion: home mechanical ventilation, payment for high flow oxygen therapy, and site of service/Section 603 issues.
Home mechanical ventilation is admittedly a complex issue, but it is moving forward in at least two political directions. First, Senator Bill Cassidy (R-LA) and a physician by training, has signaled his desire to move this issue forward, either legislatively or giving CMS one last chance to move forward through the regulatory structure. He agrees that a payment system that inhibits access to appropriate bi-level mechanical ventilators and encourages access to more complex life-sustaining ventilators, regardless of documented medical need, is appropriate. While CMS does have the authority to act, it has chosen to ignore repeated requests for action over the past 4 years.
Ironically, the House Energy and Commerce Committee, which shares jurisdiction on the House of Representatives with the Ways and Means Committee on Medicare issues, has sent a request to the Congressional Budget Office to provide a cost estimate (a “score” in Washington vernacular) of likely savings from a legislative solution to this matter. In the current political climate, a legislative proposal that actually saves $$$ is politically attractive, and we are working both the regulatory and legislative pathway to seek a workable solution.
On the oxygen therapy issue, there is growing evidence that, for a small group of Medicare beneficiaries who need high flow oxygen therapy as their disease progresses (pulmonary fibrosis, end-stage COPD, etc), there are no oxygen systems readily available to meet that need outside the home. At home, numerous concentrators can meet that need, but outside the home, the ideal solution, liquid systems, is not readily available because of the payment system tied to competitive bidding. CMS payment data indicate that a very low percentage of oxygen users need more than 4 liters per minute, and current law would make a payment adjustment unique to certain patients a very difficult hurdle, particularly in the era of competitive bidding, a legislative change is the best solution facing the community. The challenge is to craft legislative language that addresses the need but would preclude abuse by suppliers who might jump at the chance for higher payment for liquid, well above current payment levels. And because liquid systems fit into a “delivery model” business plan, contrary to portable oxygen concentrators and transfill systems, the solution is not as easy as a payment bump to make provision of liquid systems more attractive.
Site of service regulations are hitting pulmonary rehabilitation particularly hard, and CMS concedes that the only solution is a legislative one. Under current policy, a pulmonary rehab program that is located off campus but needs to expand or move from its current location (losing a lease, for example), if the expanded program is NOT within 250 yards of the main hospital campus, the program is then reimbursed at the physician fee schedule rate, a rate cut of approximately 50%. Needless to say, hospitals are not pursuing that approach. Likewise, a hospital that chooses to open a NEW program is also constrained, needing to locate within 250 yards of the main campus or face the dramatic cut in payment.
As these issues evolve and the political climate perhaps opens unique opportunities, we can expect the broad pulmonary community to pursue these and other issues.
In mid-September, NAMDRC, along with the American Thoracic Society, the American Association for Respiratory Care, the COPD Foundation, the American Lung Association, and others met to discuss the components of a legislative agenda for the coming years. The primary purpose behind the meeting was the premise that IF the current Republican majority would shift in either the House or Senate after the 2018 election, the community should be prepared to move an already agreed upon legislative agenda. CHEST was involved in the preliminary discussions, as well as follow-up, but was not in attendance at the meeting due to a scheduling conflict. There was also tacit agreement that as these policies are fleshed out and crafted into specific legislative language, the community would re-evaluate the current political climate to determine the value of pushing an agreed upon agenda prior to the 2018 elections.
Various patient groups were also invited to participate, but scheduling conflicts precluded some societies from participating but signaled their desire to work with the broad pulmonary medicine community to pursue common goals.
Each society brought its legislative priorities to the table, and there was active discussion on issues ranging from funding for NIH/NHLBI, to CDC and its COPD Action Plan, to a range of Medicare-related issues.
NAMDRC brought three specific Medicare coverage and payment issues to the discussion: home mechanical ventilation, payment for high flow oxygen therapy, and site of service/Section 603 issues.
Home mechanical ventilation is admittedly a complex issue, but it is moving forward in at least two political directions. First, Senator Bill Cassidy (R-LA) and a physician by training, has signaled his desire to move this issue forward, either legislatively or giving CMS one last chance to move forward through the regulatory structure. He agrees that a payment system that inhibits access to appropriate bi-level mechanical ventilators and encourages access to more complex life-sustaining ventilators, regardless of documented medical need, is appropriate. While CMS does have the authority to act, it has chosen to ignore repeated requests for action over the past 4 years.
Ironically, the House Energy and Commerce Committee, which shares jurisdiction on the House of Representatives with the Ways and Means Committee on Medicare issues, has sent a request to the Congressional Budget Office to provide a cost estimate (a “score” in Washington vernacular) of likely savings from a legislative solution to this matter. In the current political climate, a legislative proposal that actually saves $$$ is politically attractive, and we are working both the regulatory and legislative pathway to seek a workable solution.
On the oxygen therapy issue, there is growing evidence that, for a small group of Medicare beneficiaries who need high flow oxygen therapy as their disease progresses (pulmonary fibrosis, end-stage COPD, etc), there are no oxygen systems readily available to meet that need outside the home. At home, numerous concentrators can meet that need, but outside the home, the ideal solution, liquid systems, is not readily available because of the payment system tied to competitive bidding. CMS payment data indicate that a very low percentage of oxygen users need more than 4 liters per minute, and current law would make a payment adjustment unique to certain patients a very difficult hurdle, particularly in the era of competitive bidding, a legislative change is the best solution facing the community. The challenge is to craft legislative language that addresses the need but would preclude abuse by suppliers who might jump at the chance for higher payment for liquid, well above current payment levels. And because liquid systems fit into a “delivery model” business plan, contrary to portable oxygen concentrators and transfill systems, the solution is not as easy as a payment bump to make provision of liquid systems more attractive.
Site of service regulations are hitting pulmonary rehabilitation particularly hard, and CMS concedes that the only solution is a legislative one. Under current policy, a pulmonary rehab program that is located off campus but needs to expand or move from its current location (losing a lease, for example), if the expanded program is NOT within 250 yards of the main hospital campus, the program is then reimbursed at the physician fee schedule rate, a rate cut of approximately 50%. Needless to say, hospitals are not pursuing that approach. Likewise, a hospital that chooses to open a NEW program is also constrained, needing to locate within 250 yards of the main campus or face the dramatic cut in payment.
As these issues evolve and the political climate perhaps opens unique opportunities, we can expect the broad pulmonary community to pursue these and other issues.
In mid-September, NAMDRC, along with the American Thoracic Society, the American Association for Respiratory Care, the COPD Foundation, the American Lung Association, and others met to discuss the components of a legislative agenda for the coming years. The primary purpose behind the meeting was the premise that IF the current Republican majority would shift in either the House or Senate after the 2018 election, the community should be prepared to move an already agreed upon legislative agenda. CHEST was involved in the preliminary discussions, as well as follow-up, but was not in attendance at the meeting due to a scheduling conflict. There was also tacit agreement that as these policies are fleshed out and crafted into specific legislative language, the community would re-evaluate the current political climate to determine the value of pushing an agreed upon agenda prior to the 2018 elections.
Various patient groups were also invited to participate, but scheduling conflicts precluded some societies from participating but signaled their desire to work with the broad pulmonary medicine community to pursue common goals.
Each society brought its legislative priorities to the table, and there was active discussion on issues ranging from funding for NIH/NHLBI, to CDC and its COPD Action Plan, to a range of Medicare-related issues.
NAMDRC brought three specific Medicare coverage and payment issues to the discussion: home mechanical ventilation, payment for high flow oxygen therapy, and site of service/Section 603 issues.
Home mechanical ventilation is admittedly a complex issue, but it is moving forward in at least two political directions. First, Senator Bill Cassidy (R-LA) and a physician by training, has signaled his desire to move this issue forward, either legislatively or giving CMS one last chance to move forward through the regulatory structure. He agrees that a payment system that inhibits access to appropriate bi-level mechanical ventilators and encourages access to more complex life-sustaining ventilators, regardless of documented medical need, is appropriate. While CMS does have the authority to act, it has chosen to ignore repeated requests for action over the past 4 years.
Ironically, the House Energy and Commerce Committee, which shares jurisdiction on the House of Representatives with the Ways and Means Committee on Medicare issues, has sent a request to the Congressional Budget Office to provide a cost estimate (a “score” in Washington vernacular) of likely savings from a legislative solution to this matter. In the current political climate, a legislative proposal that actually saves $$$ is politically attractive, and we are working both the regulatory and legislative pathway to seek a workable solution.
On the oxygen therapy issue, there is growing evidence that, for a small group of Medicare beneficiaries who need high flow oxygen therapy as their disease progresses (pulmonary fibrosis, end-stage COPD, etc), there are no oxygen systems readily available to meet that need outside the home. At home, numerous concentrators can meet that need, but outside the home, the ideal solution, liquid systems, is not readily available because of the payment system tied to competitive bidding. CMS payment data indicate that a very low percentage of oxygen users need more than 4 liters per minute, and current law would make a payment adjustment unique to certain patients a very difficult hurdle, particularly in the era of competitive bidding, a legislative change is the best solution facing the community. The challenge is to craft legislative language that addresses the need but would preclude abuse by suppliers who might jump at the chance for higher payment for liquid, well above current payment levels. And because liquid systems fit into a “delivery model” business plan, contrary to portable oxygen concentrators and transfill systems, the solution is not as easy as a payment bump to make provision of liquid systems more attractive.
Site of service regulations are hitting pulmonary rehabilitation particularly hard, and CMS concedes that the only solution is a legislative one. Under current policy, a pulmonary rehab program that is located off campus but needs to expand or move from its current location (losing a lease, for example), if the expanded program is NOT within 250 yards of the main hospital campus, the program is then reimbursed at the physician fee schedule rate, a rate cut of approximately 50%. Needless to say, hospitals are not pursuing that approach. Likewise, a hospital that chooses to open a NEW program is also constrained, needing to locate within 250 yards of the main campus or face the dramatic cut in payment.
As these issues evolve and the political climate perhaps opens unique opportunities, we can expect the broad pulmonary community to pursue these and other issues.
CHEST Foundation Champions
Champion…. You ARE A CHAMPION for your patients, and as a CHEST Foundation supporter, you are a Champion for Lung Health! These words are now staples in our foundation mission. To champion lung health through clinical research and community service grants, patient education, and community service, the impact your support can have is quite profound. You are a part of an elite group to be called “champions,” and you should be celebrated for all the ways that you have championed lung health in 2017.
- YOU funded more than a half-million dollars in community service grants awarded to the next generation of CHEST leaders.
- YOU educated MILLIONS by supporting nationwide disease awareness campaigns for COPD, asthma, sarcoidosis, and lung cancer.
- YOU brought the Lung Health Experience to communities where over 1,000 people received COPD and asthma education, as well as spirometry screening.
- YOU created awareness in rare disease spaces and raised crucial support by partnering with family foundations, such as the Irv Family Foundation.
- The reach of these activities in 2017 has been astounding, and YOU, as a champion for lung health, have generated a great impact on the chest medicine community and the patients we serve.
- Now, the CHEST Foundation asks YOU to join us and support our efforts for 2018 by giving to the CHEST Foundation Annual Fund today. We ask you to help:
- Meet our fundraising goal of $700,000 for new clinical research and community service grants.
- Support NEW lung health disease awareness campaigns.
- Expand family foundation partnerships to create NEW patient resources.
- Provide NEW e-learning modules to aide patients and caregivers in managing health.
Your support today makes possible tomorrow’s advances in lung health and chest medicine. YOU believe in patient outcomes and, for that commitment, we graciously thank you. YOU save lives by supporting clinical research, patient education, and community service.
Be THE Champion for Lung Health that patients and families count on, and make an impact today. YOU can be a champion and DONATE today through a new gift to the CHEST Foundation. We cannot meet our goals for the health professionals, patients, families, and caregivers we serve without you.
Thank you for your essential continued support!
Champion…. You ARE A CHAMPION for your patients, and as a CHEST Foundation supporter, you are a Champion for Lung Health! These words are now staples in our foundation mission. To champion lung health through clinical research and community service grants, patient education, and community service, the impact your support can have is quite profound. You are a part of an elite group to be called “champions,” and you should be celebrated for all the ways that you have championed lung health in 2017.
- YOU funded more than a half-million dollars in community service grants awarded to the next generation of CHEST leaders.
- YOU educated MILLIONS by supporting nationwide disease awareness campaigns for COPD, asthma, sarcoidosis, and lung cancer.
- YOU brought the Lung Health Experience to communities where over 1,000 people received COPD and asthma education, as well as spirometry screening.
- YOU created awareness in rare disease spaces and raised crucial support by partnering with family foundations, such as the Irv Family Foundation.
- The reach of these activities in 2017 has been astounding, and YOU, as a champion for lung health, have generated a great impact on the chest medicine community and the patients we serve.
- Now, the CHEST Foundation asks YOU to join us and support our efforts for 2018 by giving to the CHEST Foundation Annual Fund today. We ask you to help:
- Meet our fundraising goal of $700,000 for new clinical research and community service grants.
- Support NEW lung health disease awareness campaigns.
- Expand family foundation partnerships to create NEW patient resources.
- Provide NEW e-learning modules to aide patients and caregivers in managing health.
Your support today makes possible tomorrow’s advances in lung health and chest medicine. YOU believe in patient outcomes and, for that commitment, we graciously thank you. YOU save lives by supporting clinical research, patient education, and community service.
Be THE Champion for Lung Health that patients and families count on, and make an impact today. YOU can be a champion and DONATE today through a new gift to the CHEST Foundation. We cannot meet our goals for the health professionals, patients, families, and caregivers we serve without you.
Thank you for your essential continued support!
Champion…. You ARE A CHAMPION for your patients, and as a CHEST Foundation supporter, you are a Champion for Lung Health! These words are now staples in our foundation mission. To champion lung health through clinical research and community service grants, patient education, and community service, the impact your support can have is quite profound. You are a part of an elite group to be called “champions,” and you should be celebrated for all the ways that you have championed lung health in 2017.
- YOU funded more than a half-million dollars in community service grants awarded to the next generation of CHEST leaders.
- YOU educated MILLIONS by supporting nationwide disease awareness campaigns for COPD, asthma, sarcoidosis, and lung cancer.
- YOU brought the Lung Health Experience to communities where over 1,000 people received COPD and asthma education, as well as spirometry screening.
- YOU created awareness in rare disease spaces and raised crucial support by partnering with family foundations, such as the Irv Family Foundation.
- The reach of these activities in 2017 has been astounding, and YOU, as a champion for lung health, have generated a great impact on the chest medicine community and the patients we serve.
- Now, the CHEST Foundation asks YOU to join us and support our efforts for 2018 by giving to the CHEST Foundation Annual Fund today. We ask you to help:
- Meet our fundraising goal of $700,000 for new clinical research and community service grants.
- Support NEW lung health disease awareness campaigns.
- Expand family foundation partnerships to create NEW patient resources.
- Provide NEW e-learning modules to aide patients and caregivers in managing health.
Your support today makes possible tomorrow’s advances in lung health and chest medicine. YOU believe in patient outcomes and, for that commitment, we graciously thank you. YOU save lives by supporting clinical research, patient education, and community service.
Be THE Champion for Lung Health that patients and families count on, and make an impact today. YOU can be a champion and DONATE today through a new gift to the CHEST Foundation. We cannot meet our goals for the health professionals, patients, families, and caregivers we serve without you.
Thank you for your essential continued support!
The rise and fall of treatment trials in group 3 pulmonary hypertension: Where do we go from here?
Treatment of fibrotic interstitial lung disease (ILD) is often dissatisfying to clinicians and patients. Despite significant advances in the field, particularly the validation of the efficacy of the antifibrotic drugs nintedanib (Richeldi L, et al. N Engl J Med. 2014;370[22]:2071) and pirfenidone (King TE Jr, et al. N Engl J Med. 2014;370[(22]:2083) in slowing the progression of idiopathic pulmonary fibrosis (IPF), we are still left with a paucity of therapeutic options to modulate the course of disease and improve functional outcomes. Given the difficulties in addressing the progression of parenchymal fibrosis, the pulmonary community has looked for alternative ways to approach treatment of ILD. One potential therapeutic inroad that has garnered substantial interest is the treatment of concurrent pulmonary hypertension (PH) or group 3 PH (Seeger W, et al. J Am Coll Cardiol. 2013;62 (25 Suppl):D109).
Group 3 PH – The rationale to treat
Group 3 PH has an indisputable association with adverse outcomes, including decreased functional status, increased need for supplemental oxygen, and decreased survival (King CS, Nathan SD. Pulmonary Hypertension and Interstitial Lung Disease. Ed 2. Ch 4.2017;67-84). In fact, PH is such a powerful predictor of survival in fibrotic ILD, the International Society of Heart and Lung Transplant (ISHLT) guidelines on candidate selection for lung transplantation cite development of PH as an indication for transplant listing (Weill D, et al. J Heart Lung Transplant. 2015;34:1). When one considers the strong association between group 3 PH and adverse outcomes, the numerous pulmonary vasodilator agents available to treat pulmonary arterial hypertension (PAH), and the success achieved in treating PAH, it is easy to see why group 3 PH is such a tempting therapeutic target.
Previous studies of pulmonary vasodilator therapy for group 3 PH
Over 20 studies assessing the effectiveness of pulmonary vasodilator therapy in ILD have been published (King CS, Nathan SD. Pulmonary Hypertension and Interstitial Lung Disease. Ed 2. Ch 4. 2017;67) The majority was small and unblinded with inherent limitations. To date, no randomized controlled trial (RCT) of therapy for group 3 PH has demonstrated efficacy. Several studies amongst the RCTs deserve highlighting. The most encouraging RCT of therapy for group 3 PH was STEP-IPF. This study compared sildenafil with placebo in 180 patients with advanced IPF. Though the study failed to demonstrate a difference in the primary endpoint of ≥ 20% increase in 6-minute walk test (6MWT) distance, it did show improvement in several secondary endpoints, including arterial oxygen saturation and quality of life measures (Zisman DA, et al. N Engl J Med. 2010;363[7]:620).
The BUILD-3 study compared bosentan with placebo in 617 patients with IPF. Enrolled patients were not required to have PH. While bosentan was well tolerated, it failed to improve the primary endpoint of time to disease progression or death or secondary endpoints regarding quality of life or dyspnea (King TE Jr, et al. Am J Respir Crit Care Med. 2011; 184[1]:92). A smaller study comparing bosentan with placebo in 60 patients with fibrotic ILD with right-sided heart catheterization (RHC) confirmed PH failed to demonstrate any difference in pulmonary vascular hemodynamics, functional status, or symptoms (Corte TJ, et al. Am J Respir Crit Care Med. 2014;190[2]:208). Studies of the newer endothelin receptor antagonists, macitentan (Raghu, et al. Eur Respir J. 2013;42[6]:1622) and ambrisentan (Raghu, et al. Ann Int Med. 2013;158[9]:641), were conducted and failed to demonstrate improvements in outcomes, as well. Overall, the results of the available RCTs of pulmonary vasodilator therapy in group 3 PH have been disappointing, failing to conclusively improve the primary outcome in any of the studies performed.
Hot off the presses – RISE-IIP
The latest letdown in group 3 PH is “Riociguat for the Treatment of Pulmonary Hypertension in Idiopathic Interstitial Pneumonia (RISE-IIP). The results of the study were recently presented at the European Respiratory Society meeting in Milan, Italy, by my colleague from Inova Fairfax Hospital (Falls Church, VA), Dr. Steven Nathan. Riociguat is a soluble guanylate cyclase stimulator approved for use in PAH and chronic thromboembolic pulmonary hypertension. The rationale for the study was that riociguat would improve pulmonary hemodynamics leading to improved functional status. Additionally, several preclinical models have demonstrated antifibrotic effects of the drug (Geschka S, et al. PLoS One. 2011;6:e21853). Justification for the study was also bolstered by promising results from a pilot study conducted in 22 patients with RHC-confirmed PH with a mean pulmonary artery pressure (mPAP) > 30 and fibrotic lung disease. In this study, patients treated with riociguat had improved pulmonary vascular resistance, cardiac output, and 6MWT distance.
To be included in RISE-IIP, patients were required to have an idiopathic interstitial pneumonia, PH confirmed by RHC with a mPAP ≥ 25 mm Hg, World Health Organization Functional Class 2-4 symptoms, and a forced vital capacity (FVC) ≥ 45% predicted. Pertinent exclusion criteria included significant left-sided heart disease and extent of emphysema greater than fibrosis on HRCT. Patients with connective tissue disease, chronic hypersensitivity pneumonitis, occupational lung disease, and sarcoidosis were ineligible to participate. The placebo-controlled portion of the study lasted 26 weeks then crossed into an open label extension trial.
The study enrolled 147 total patients, with 73 receiving riociguat and 74 in the placebo arm. There was no significant improvement in the primary outcome of change in 6MWT distance or the secondary combined endpoint assessing clinical worsening. The study was terminated early for safety due to an increased number of deaths and adverse events in the treatment group. During the blinded phase of the study, eight deaths (11%) occurred in the riociguat arm as compared with three deaths (4%) in the placebo arm. Seventy patients entered the open label extension phase of the trial, and 9 of these patients died. Eight of these deaths occurred in the patients previously receiving placebo who were switched to riociguat. The authors of the study found no conclusive potential etiology to explain the increased mortality seen.
RISE’ing from the ashes – Where do we go from here?
So, what should we take away from the negative results of the RISE-IIP trial? Some may argue that treatment of group 3 PH is a flawed premise and should be abandoned. Perhaps development of group 3 PH is an adaptive response to worsening fibrotic lung disease, and treatment of the PH is unlikely to alter outcomes and introduces the possibility of harm through worsening hypoxemia due to increased ventilation/perfusion mismatch with nonselective pulmonary vasodilation. I suspect the truth is somewhat more nuanced. I believe there is a select population with severe or “out-of-proportion” PH that may still benefit from vasodilator therapy. Trials targeting patients with a higher mPAP or low cardiac index could test this hypothesis but will be difficult to enroll. Another possibility is that our mechanism of drug delivery in prior trials has been suboptimal. Inhaled pulmonary vasodilator therapy should minimize the risk of worsening ventilation/perfusion mismatch. An RCT assessing the response to inhaled treprostinil in group 3 PH (NCT02630316) is currently enrolling at 96 centers across the United States. Until data supporting positive effects from treating group 3 PH emerge, I would recommend against off-label treatment and encourage referral to clinical trials. Given the potential for harm, riociguat should be avoided in group 3 PH. If off-label therapy is being entertained in a patient with severe PH that is out of proportion to the extent of fibrotic lung disease, it should be initiated cautiously at a center experienced in treating PH. Finally, clinicians should refer appropriate candidates with ILD and group 3 PH for lung transplantation evaluation.
The great inventor Thomas Edison is credited with saying “I have not failed. I’ve just found 10,000 ways that won’t work.” While disappointing, negative studies are to be expected as we search for improved therapies for our patients. It’s essential that we reflect upon these studies, so we can improve future trial design.
Treatment of fibrotic interstitial lung disease (ILD) is often dissatisfying to clinicians and patients. Despite significant advances in the field, particularly the validation of the efficacy of the antifibrotic drugs nintedanib (Richeldi L, et al. N Engl J Med. 2014;370[22]:2071) and pirfenidone (King TE Jr, et al. N Engl J Med. 2014;370[(22]:2083) in slowing the progression of idiopathic pulmonary fibrosis (IPF), we are still left with a paucity of therapeutic options to modulate the course of disease and improve functional outcomes. Given the difficulties in addressing the progression of parenchymal fibrosis, the pulmonary community has looked for alternative ways to approach treatment of ILD. One potential therapeutic inroad that has garnered substantial interest is the treatment of concurrent pulmonary hypertension (PH) or group 3 PH (Seeger W, et al. J Am Coll Cardiol. 2013;62 (25 Suppl):D109).
Group 3 PH – The rationale to treat
Group 3 PH has an indisputable association with adverse outcomes, including decreased functional status, increased need for supplemental oxygen, and decreased survival (King CS, Nathan SD. Pulmonary Hypertension and Interstitial Lung Disease. Ed 2. Ch 4.2017;67-84). In fact, PH is such a powerful predictor of survival in fibrotic ILD, the International Society of Heart and Lung Transplant (ISHLT) guidelines on candidate selection for lung transplantation cite development of PH as an indication for transplant listing (Weill D, et al. J Heart Lung Transplant. 2015;34:1). When one considers the strong association between group 3 PH and adverse outcomes, the numerous pulmonary vasodilator agents available to treat pulmonary arterial hypertension (PAH), and the success achieved in treating PAH, it is easy to see why group 3 PH is such a tempting therapeutic target.
Previous studies of pulmonary vasodilator therapy for group 3 PH
Over 20 studies assessing the effectiveness of pulmonary vasodilator therapy in ILD have been published (King CS, Nathan SD. Pulmonary Hypertension and Interstitial Lung Disease. Ed 2. Ch 4. 2017;67) The majority was small and unblinded with inherent limitations. To date, no randomized controlled trial (RCT) of therapy for group 3 PH has demonstrated efficacy. Several studies amongst the RCTs deserve highlighting. The most encouraging RCT of therapy for group 3 PH was STEP-IPF. This study compared sildenafil with placebo in 180 patients with advanced IPF. Though the study failed to demonstrate a difference in the primary endpoint of ≥ 20% increase in 6-minute walk test (6MWT) distance, it did show improvement in several secondary endpoints, including arterial oxygen saturation and quality of life measures (Zisman DA, et al. N Engl J Med. 2010;363[7]:620).
The BUILD-3 study compared bosentan with placebo in 617 patients with IPF. Enrolled patients were not required to have PH. While bosentan was well tolerated, it failed to improve the primary endpoint of time to disease progression or death or secondary endpoints regarding quality of life or dyspnea (King TE Jr, et al. Am J Respir Crit Care Med. 2011; 184[1]:92). A smaller study comparing bosentan with placebo in 60 patients with fibrotic ILD with right-sided heart catheterization (RHC) confirmed PH failed to demonstrate any difference in pulmonary vascular hemodynamics, functional status, or symptoms (Corte TJ, et al. Am J Respir Crit Care Med. 2014;190[2]:208). Studies of the newer endothelin receptor antagonists, macitentan (Raghu, et al. Eur Respir J. 2013;42[6]:1622) and ambrisentan (Raghu, et al. Ann Int Med. 2013;158[9]:641), were conducted and failed to demonstrate improvements in outcomes, as well. Overall, the results of the available RCTs of pulmonary vasodilator therapy in group 3 PH have been disappointing, failing to conclusively improve the primary outcome in any of the studies performed.
Hot off the presses – RISE-IIP
The latest letdown in group 3 PH is “Riociguat for the Treatment of Pulmonary Hypertension in Idiopathic Interstitial Pneumonia (RISE-IIP). The results of the study were recently presented at the European Respiratory Society meeting in Milan, Italy, by my colleague from Inova Fairfax Hospital (Falls Church, VA), Dr. Steven Nathan. Riociguat is a soluble guanylate cyclase stimulator approved for use in PAH and chronic thromboembolic pulmonary hypertension. The rationale for the study was that riociguat would improve pulmonary hemodynamics leading to improved functional status. Additionally, several preclinical models have demonstrated antifibrotic effects of the drug (Geschka S, et al. PLoS One. 2011;6:e21853). Justification for the study was also bolstered by promising results from a pilot study conducted in 22 patients with RHC-confirmed PH with a mean pulmonary artery pressure (mPAP) > 30 and fibrotic lung disease. In this study, patients treated with riociguat had improved pulmonary vascular resistance, cardiac output, and 6MWT distance.
To be included in RISE-IIP, patients were required to have an idiopathic interstitial pneumonia, PH confirmed by RHC with a mPAP ≥ 25 mm Hg, World Health Organization Functional Class 2-4 symptoms, and a forced vital capacity (FVC) ≥ 45% predicted. Pertinent exclusion criteria included significant left-sided heart disease and extent of emphysema greater than fibrosis on HRCT. Patients with connective tissue disease, chronic hypersensitivity pneumonitis, occupational lung disease, and sarcoidosis were ineligible to participate. The placebo-controlled portion of the study lasted 26 weeks then crossed into an open label extension trial.
The study enrolled 147 total patients, with 73 receiving riociguat and 74 in the placebo arm. There was no significant improvement in the primary outcome of change in 6MWT distance or the secondary combined endpoint assessing clinical worsening. The study was terminated early for safety due to an increased number of deaths and adverse events in the treatment group. During the blinded phase of the study, eight deaths (11%) occurred in the riociguat arm as compared with three deaths (4%) in the placebo arm. Seventy patients entered the open label extension phase of the trial, and 9 of these patients died. Eight of these deaths occurred in the patients previously receiving placebo who were switched to riociguat. The authors of the study found no conclusive potential etiology to explain the increased mortality seen.
RISE’ing from the ashes – Where do we go from here?
So, what should we take away from the negative results of the RISE-IIP trial? Some may argue that treatment of group 3 PH is a flawed premise and should be abandoned. Perhaps development of group 3 PH is an adaptive response to worsening fibrotic lung disease, and treatment of the PH is unlikely to alter outcomes and introduces the possibility of harm through worsening hypoxemia due to increased ventilation/perfusion mismatch with nonselective pulmonary vasodilation. I suspect the truth is somewhat more nuanced. I believe there is a select population with severe or “out-of-proportion” PH that may still benefit from vasodilator therapy. Trials targeting patients with a higher mPAP or low cardiac index could test this hypothesis but will be difficult to enroll. Another possibility is that our mechanism of drug delivery in prior trials has been suboptimal. Inhaled pulmonary vasodilator therapy should minimize the risk of worsening ventilation/perfusion mismatch. An RCT assessing the response to inhaled treprostinil in group 3 PH (NCT02630316) is currently enrolling at 96 centers across the United States. Until data supporting positive effects from treating group 3 PH emerge, I would recommend against off-label treatment and encourage referral to clinical trials. Given the potential for harm, riociguat should be avoided in group 3 PH. If off-label therapy is being entertained in a patient with severe PH that is out of proportion to the extent of fibrotic lung disease, it should be initiated cautiously at a center experienced in treating PH. Finally, clinicians should refer appropriate candidates with ILD and group 3 PH for lung transplantation evaluation.
The great inventor Thomas Edison is credited with saying “I have not failed. I’ve just found 10,000 ways that won’t work.” While disappointing, negative studies are to be expected as we search for improved therapies for our patients. It’s essential that we reflect upon these studies, so we can improve future trial design.
Treatment of fibrotic interstitial lung disease (ILD) is often dissatisfying to clinicians and patients. Despite significant advances in the field, particularly the validation of the efficacy of the antifibrotic drugs nintedanib (Richeldi L, et al. N Engl J Med. 2014;370[22]:2071) and pirfenidone (King TE Jr, et al. N Engl J Med. 2014;370[(22]:2083) in slowing the progression of idiopathic pulmonary fibrosis (IPF), we are still left with a paucity of therapeutic options to modulate the course of disease and improve functional outcomes. Given the difficulties in addressing the progression of parenchymal fibrosis, the pulmonary community has looked for alternative ways to approach treatment of ILD. One potential therapeutic inroad that has garnered substantial interest is the treatment of concurrent pulmonary hypertension (PH) or group 3 PH (Seeger W, et al. J Am Coll Cardiol. 2013;62 (25 Suppl):D109).
Group 3 PH – The rationale to treat
Group 3 PH has an indisputable association with adverse outcomes, including decreased functional status, increased need for supplemental oxygen, and decreased survival (King CS, Nathan SD. Pulmonary Hypertension and Interstitial Lung Disease. Ed 2. Ch 4.2017;67-84). In fact, PH is such a powerful predictor of survival in fibrotic ILD, the International Society of Heart and Lung Transplant (ISHLT) guidelines on candidate selection for lung transplantation cite development of PH as an indication for transplant listing (Weill D, et al. J Heart Lung Transplant. 2015;34:1). When one considers the strong association between group 3 PH and adverse outcomes, the numerous pulmonary vasodilator agents available to treat pulmonary arterial hypertension (PAH), and the success achieved in treating PAH, it is easy to see why group 3 PH is such a tempting therapeutic target.
Previous studies of pulmonary vasodilator therapy for group 3 PH
Over 20 studies assessing the effectiveness of pulmonary vasodilator therapy in ILD have been published (King CS, Nathan SD. Pulmonary Hypertension and Interstitial Lung Disease. Ed 2. Ch 4. 2017;67) The majority was small and unblinded with inherent limitations. To date, no randomized controlled trial (RCT) of therapy for group 3 PH has demonstrated efficacy. Several studies amongst the RCTs deserve highlighting. The most encouraging RCT of therapy for group 3 PH was STEP-IPF. This study compared sildenafil with placebo in 180 patients with advanced IPF. Though the study failed to demonstrate a difference in the primary endpoint of ≥ 20% increase in 6-minute walk test (6MWT) distance, it did show improvement in several secondary endpoints, including arterial oxygen saturation and quality of life measures (Zisman DA, et al. N Engl J Med. 2010;363[7]:620).
The BUILD-3 study compared bosentan with placebo in 617 patients with IPF. Enrolled patients were not required to have PH. While bosentan was well tolerated, it failed to improve the primary endpoint of time to disease progression or death or secondary endpoints regarding quality of life or dyspnea (King TE Jr, et al. Am J Respir Crit Care Med. 2011; 184[1]:92). A smaller study comparing bosentan with placebo in 60 patients with fibrotic ILD with right-sided heart catheterization (RHC) confirmed PH failed to demonstrate any difference in pulmonary vascular hemodynamics, functional status, or symptoms (Corte TJ, et al. Am J Respir Crit Care Med. 2014;190[2]:208). Studies of the newer endothelin receptor antagonists, macitentan (Raghu, et al. Eur Respir J. 2013;42[6]:1622) and ambrisentan (Raghu, et al. Ann Int Med. 2013;158[9]:641), were conducted and failed to demonstrate improvements in outcomes, as well. Overall, the results of the available RCTs of pulmonary vasodilator therapy in group 3 PH have been disappointing, failing to conclusively improve the primary outcome in any of the studies performed.
Hot off the presses – RISE-IIP
The latest letdown in group 3 PH is “Riociguat for the Treatment of Pulmonary Hypertension in Idiopathic Interstitial Pneumonia (RISE-IIP). The results of the study were recently presented at the European Respiratory Society meeting in Milan, Italy, by my colleague from Inova Fairfax Hospital (Falls Church, VA), Dr. Steven Nathan. Riociguat is a soluble guanylate cyclase stimulator approved for use in PAH and chronic thromboembolic pulmonary hypertension. The rationale for the study was that riociguat would improve pulmonary hemodynamics leading to improved functional status. Additionally, several preclinical models have demonstrated antifibrotic effects of the drug (Geschka S, et al. PLoS One. 2011;6:e21853). Justification for the study was also bolstered by promising results from a pilot study conducted in 22 patients with RHC-confirmed PH with a mean pulmonary artery pressure (mPAP) > 30 and fibrotic lung disease. In this study, patients treated with riociguat had improved pulmonary vascular resistance, cardiac output, and 6MWT distance.
To be included in RISE-IIP, patients were required to have an idiopathic interstitial pneumonia, PH confirmed by RHC with a mPAP ≥ 25 mm Hg, World Health Organization Functional Class 2-4 symptoms, and a forced vital capacity (FVC) ≥ 45% predicted. Pertinent exclusion criteria included significant left-sided heart disease and extent of emphysema greater than fibrosis on HRCT. Patients with connective tissue disease, chronic hypersensitivity pneumonitis, occupational lung disease, and sarcoidosis were ineligible to participate. The placebo-controlled portion of the study lasted 26 weeks then crossed into an open label extension trial.
The study enrolled 147 total patients, with 73 receiving riociguat and 74 in the placebo arm. There was no significant improvement in the primary outcome of change in 6MWT distance or the secondary combined endpoint assessing clinical worsening. The study was terminated early for safety due to an increased number of deaths and adverse events in the treatment group. During the blinded phase of the study, eight deaths (11%) occurred in the riociguat arm as compared with three deaths (4%) in the placebo arm. Seventy patients entered the open label extension phase of the trial, and 9 of these patients died. Eight of these deaths occurred in the patients previously receiving placebo who were switched to riociguat. The authors of the study found no conclusive potential etiology to explain the increased mortality seen.
RISE’ing from the ashes – Where do we go from here?
So, what should we take away from the negative results of the RISE-IIP trial? Some may argue that treatment of group 3 PH is a flawed premise and should be abandoned. Perhaps development of group 3 PH is an adaptive response to worsening fibrotic lung disease, and treatment of the PH is unlikely to alter outcomes and introduces the possibility of harm through worsening hypoxemia due to increased ventilation/perfusion mismatch with nonselective pulmonary vasodilation. I suspect the truth is somewhat more nuanced. I believe there is a select population with severe or “out-of-proportion” PH that may still benefit from vasodilator therapy. Trials targeting patients with a higher mPAP or low cardiac index could test this hypothesis but will be difficult to enroll. Another possibility is that our mechanism of drug delivery in prior trials has been suboptimal. Inhaled pulmonary vasodilator therapy should minimize the risk of worsening ventilation/perfusion mismatch. An RCT assessing the response to inhaled treprostinil in group 3 PH (NCT02630316) is currently enrolling at 96 centers across the United States. Until data supporting positive effects from treating group 3 PH emerge, I would recommend against off-label treatment and encourage referral to clinical trials. Given the potential for harm, riociguat should be avoided in group 3 PH. If off-label therapy is being entertained in a patient with severe PH that is out of proportion to the extent of fibrotic lung disease, it should be initiated cautiously at a center experienced in treating PH. Finally, clinicians should refer appropriate candidates with ILD and group 3 PH for lung transplantation evaluation.
The great inventor Thomas Edison is credited with saying “I have not failed. I’ve just found 10,000 ways that won’t work.” While disappointing, negative studies are to be expected as we search for improved therapies for our patients. It’s essential that we reflect upon these studies, so we can improve future trial design.
ABIM to allow do-overs for all subspecialties with Knowledge Check-In
ABIM previously announced that, beginning in 2018, physicians taking the Knowledge Check-In in 2018 would get another chance to take it in 2 years if they were unsuccessful, even if they were due to pass the maintenance of certification (MOC) exam later that year. In 2018, Knowledge Check-Ins will be offered in internal medicine and nephrology.
“Based on feedback ABIM has received from the physician community, we are happy to let you know that we are extending this policy to include all other internal medicine subspecialties in the future,” ABIM said in a Dec. 4 announcement on its website. “This means that if a physician takes the Knowledge Check-In in the first year it is offered in their subspecialty and is unsuccessful, they will get at least one additional opportunity to take and pass it 2 years later.”
The Knowledge Check-In is an alternative to the traditional MOC process, and is administered every 2 years rather than the standard decade between MOC exams. ABIM noted that a single failure on a Knowledge Check-In will not result in a status change to a physician’s certification status.
Separately, ABIM also announced that it will continue to make practice assessment activities (part IV of the MOC program) a part of the portfolio of options that can be used to satisfy MOC requirements.
“Our intent is to support physicians completing MOC activities that are most meaningful to their practice, including those that enhance and improve medical knowledge, as well as many existing quality improvement activities, and those that blend both,” ABIM said in its announcement.
ABIM previously announced that, beginning in 2018, physicians taking the Knowledge Check-In in 2018 would get another chance to take it in 2 years if they were unsuccessful, even if they were due to pass the maintenance of certification (MOC) exam later that year. In 2018, Knowledge Check-Ins will be offered in internal medicine and nephrology.
“Based on feedback ABIM has received from the physician community, we are happy to let you know that we are extending this policy to include all other internal medicine subspecialties in the future,” ABIM said in a Dec. 4 announcement on its website. “This means that if a physician takes the Knowledge Check-In in the first year it is offered in their subspecialty and is unsuccessful, they will get at least one additional opportunity to take and pass it 2 years later.”
The Knowledge Check-In is an alternative to the traditional MOC process, and is administered every 2 years rather than the standard decade between MOC exams. ABIM noted that a single failure on a Knowledge Check-In will not result in a status change to a physician’s certification status.
Separately, ABIM also announced that it will continue to make practice assessment activities (part IV of the MOC program) a part of the portfolio of options that can be used to satisfy MOC requirements.
“Our intent is to support physicians completing MOC activities that are most meaningful to their practice, including those that enhance and improve medical knowledge, as well as many existing quality improvement activities, and those that blend both,” ABIM said in its announcement.
ABIM previously announced that, beginning in 2018, physicians taking the Knowledge Check-In in 2018 would get another chance to take it in 2 years if they were unsuccessful, even if they were due to pass the maintenance of certification (MOC) exam later that year. In 2018, Knowledge Check-Ins will be offered in internal medicine and nephrology.
“Based on feedback ABIM has received from the physician community, we are happy to let you know that we are extending this policy to include all other internal medicine subspecialties in the future,” ABIM said in a Dec. 4 announcement on its website. “This means that if a physician takes the Knowledge Check-In in the first year it is offered in their subspecialty and is unsuccessful, they will get at least one additional opportunity to take and pass it 2 years later.”
The Knowledge Check-In is an alternative to the traditional MOC process, and is administered every 2 years rather than the standard decade between MOC exams. ABIM noted that a single failure on a Knowledge Check-In will not result in a status change to a physician’s certification status.
Separately, ABIM also announced that it will continue to make practice assessment activities (part IV of the MOC program) a part of the portfolio of options that can be used to satisfy MOC requirements.
“Our intent is to support physicians completing MOC activities that are most meaningful to their practice, including those that enhance and improve medical knowledge, as well as many existing quality improvement activities, and those that blend both,” ABIM said in its announcement.
Intranasal insulin, ketogenic diet may benefit Alzheimer’s patients
LOS ANGELES – Growing evidence from basic science and preclinical studies demonstrates that
In addition, brain insulin resistance in Alzheimer’s disease (AD) is associated with increased cerebral hyperglycemia, reduced cerebral glucose utilization, reduced blood flow, and reduced accumulation of amyloid and tau.
When that process goes awry, several pathologic processes linking insulin resistance (IR) and Alzheimer’s disease occur, including impaired proteostasis (oligomeric beta amyloid, microtubule-associated tau, and oligomeric insulin); hyperglycemia-induced toxicity and reduced glucose utilization; mitochondrial dysfunction; and vascular dysfunction, Dr. Craft continued.
In the past 5 years, researchers have developed ways to measure expression levels of insulin resistance markers like insulin receptor substrate 1 (IRS-1) pSer–positive neurons, Dr. Craft said. Others have found that increased IRS-1 pSer is associated with paired helical filaments (PHFs) tau in mild cognitive impairment (MCI) and AD, and that increased IRS-1 pSer in neutrally derived plasma exomes increased in AD years before onset and in type 2 diabetes. “We can look at the neurons themselves and what we see is that this IR marker colocalizes with tau,” Dr. Craft said. “It’s not very common in normal folks, but as you progress through the stages of MCI to AD, it becomes more common. So there’s a progressive increase in IR markers that associates with neurons in tau.” Other imaging studies have shown that homeostatic model assessment IR predicts gray matter atrophy, reduced blood flow, and amyloid deposition in middle-aged adults.
One way to overcome IR in AD is to increase insulin availability in the brain. Intranasal administration of insulin is a novel method being tested by Dr. Craft and her associates. “This is not inhaled insulin; it does not target the lungs,” she explained. “It’s insulin administered with a very specialized device that targets the olfactory cleft in the upper nasal passages. Virtually none of the insulin is deposited in the lungs or nasopharyngeally.” The approach is modeled on the notion that there are pathways from the olfactory perivascular spaces to the brain by which peptides can travel readily by bulk flow. “They reach the brain within minutes,” she said. “It’s a way of delivering peptides to the brain that bypasses the blood-brain barrier.”
In a published study, she and her associates randomized 104 adults with MCI or AD to receive 20 IU insulin, 40 IU insulin, or placebo twice daily for 4 months (Arch Neurol. 2012;61[1]:29-38). Tests performed at baseline and at 4 months included cognitive evaluation based on story recall and the ADAS-Cog (Alzheimer’s Disease Assessment Scale–Cognitive subscale); function based on the Dementia Rating Severity Scale, FDG-PET (positron emission tomography with 18fluorodeoxyglucose), and cerebrospinal fluid biomarkers. “We showed that the 20-IU dose of intranasal insulin improved memory quite substantially (P less than .05),” Dr. Craft said. “It also improved glucose utilization as assessed by FDG-PET. We also saw changes in spinal fluid biomarkers of amyloid in a favorable direction. Most recently, we looked at the exosomal indicator of IR (IRS-1 pSer), and what we saw quite remarkably was a reduction in the same condition that the memory improved. This gives us hope that we have a marker of whether or not we’re having a positive impact.”
She and her research team recently finished a phase 2 pilot study of regular insulin vs. long-acting insulin detemir, to determine if a longer-acting agent with longer exposure would have greater efficacy (J Alzheimers Dis. 2017;57[4]:1325–34). In all, 36 participants were randomized to receive placebo, 40 IU of insulin detemir, or 40 IU of regular insulin daily for 4 months, administered with a nasal delivery device. The investigators found that only the group treated with 40 IU regular insulin had better memory after 2 and 4 months, compared with placebo (P less than .03). Regular insulin treatment was also associated with preserved volume on MRI. “The normal pattern is for AD patients to lose brain volume rather rapidly,” Dr. Craft commented. “We see that abolished by the insulin treatment, which suggests to us that we’re able to stave off this disease-related mechanism.” She and her associates are currently conducting a phase 3 clinical trial with regular insulin and a phase 3 trial with rapid-acting insulin that are expected to be completed in the summer of 2018.
Dr. Craft spent the last few minutes of her presentation discussing the ketogenic diet as a nonpharmacologic approach to preventing or treating brain insulin resistance and AD. “I think the power of diet is underestimated, both in terms of causing disease and potentially modulating it,” she said. Her research team just completed a study of 87 middle-aged adults who were randomized to a Western diet or a healthy diet. The Western diet was high in saturated fat, sugar, and salt. The healthy diet was low in saturated fat, sugar, and salt, but the macronutrient composition of both diets was the same. “It was a eucaloric diet with normal calorie intake; no weight change, so trying to understand the integrated effect of the Western diet,” she said. “All food was prepared by us and delivered to the patients two times per week.” Patients with type 2 diabetes, patients with hypertension, and those who were on statins were excluded from the study.
The researchers observed pronounced diet-induced changes in cerebral blood flow, all which favored the healthy diet group. “The Western diet reduced blood flow, and the healthy diet increased blood blow in the hippocampus, which is critical for memory, as in some other regions that are known to be affected in AD,” Dr. Craft said. “We saw an effect on memory as well, with the healthy diet improving memory and the Western diet reducing it. Both of these effects were significant, so 4 weeks on a diet such as this is sufficient to modulate key aspects of brain function.”
More recently, Dr. Craft and her colleagues have been evaluating the effects of what they term the modified Mediterranean ketogenic diet (MMKD). “It does allow for higher carbohydrate consumption, compared with a traditional ketogenic diet, but they still have to stay under 10% a day,” she said. “We have an emphasis on healthy fats. We send everybody home with extra virgin olive oil. We think it gives us extra compliance and the potential for long-term nutrition.” She explained that the diet increases plasma and CNS ketone bodies, beta-hydroxybutyrate, acetoacetate, and acetone, which serves as preferred alternative fuel for the brain. “If the brain has a choice between glucose and ketones, it will choose ketones,” Dr. Craft said. “It can use them more easily.”
Ketone bodies are derived from hepatic fatty acid oxidation and readily diffuse across the blood-brain barrier into the brain. They are also synthesized in the brain by astrocytes, and they appear to have direct neuroprotective effects. “Ketone bodies may be beneficial because they may correct the hyperglycemic state and reduce glucose utilization in the brain in AD years prior to symptom onset,” Dr. Craft said. “They may correct neuronal hyperexcitability and preclinical seizures in presymptomatic and early stages of AD; they restore the balance between inhibitory and excitatory neurotransmitters like GABA [gamma-aminobutyric acid] and glutamate.”
In an unpublished, 16-week study, Dr. Craft and her associates randomized 16 patients to a Mediterranean ketogenic diet or to an American Heart Association low-fat diet. Lumbar punctures and brain imaging were performed before and after diet intervention. By the end of 6 weeks, they observed significant increases in ketones and in HDL cholesterol level in the MMKD group, compared with the AHA diet group, as well as significant decreases in trigylcerides and HbA1c level. “I would say that we improved the peripheral metabolic profile with the ketogenic diet,” Dr. Craft said. They also observed significant improvements from baseline in memory, spinal fluid AD biomarkers, and mitochondrial respiration.
“One of the things we’re appreciating is the role of insulin in a host of activities in the brain,” she concluded. “Disrupting those activities can have dire consequences on brain function that may lead to a neurological milieu that lends itself to pathological aging conditions like Alzheimer’s. Several large ongoing trials are poised to validate results of smaller studies, elucidate underlying mechanisms, and provide new therapeutic targets. It’s an exciting time.”
Dr. Craft’s research is supported by the National Institute on Aging and the Alzheimer’s Association Zenith Program. Intranasal delivery devices were provided by Kurve Technology.
LOS ANGELES – Growing evidence from basic science and preclinical studies demonstrates that
In addition, brain insulin resistance in Alzheimer’s disease (AD) is associated with increased cerebral hyperglycemia, reduced cerebral glucose utilization, reduced blood flow, and reduced accumulation of amyloid and tau.
When that process goes awry, several pathologic processes linking insulin resistance (IR) and Alzheimer’s disease occur, including impaired proteostasis (oligomeric beta amyloid, microtubule-associated tau, and oligomeric insulin); hyperglycemia-induced toxicity and reduced glucose utilization; mitochondrial dysfunction; and vascular dysfunction, Dr. Craft continued.
In the past 5 years, researchers have developed ways to measure expression levels of insulin resistance markers like insulin receptor substrate 1 (IRS-1) pSer–positive neurons, Dr. Craft said. Others have found that increased IRS-1 pSer is associated with paired helical filaments (PHFs) tau in mild cognitive impairment (MCI) and AD, and that increased IRS-1 pSer in neutrally derived plasma exomes increased in AD years before onset and in type 2 diabetes. “We can look at the neurons themselves and what we see is that this IR marker colocalizes with tau,” Dr. Craft said. “It’s not very common in normal folks, but as you progress through the stages of MCI to AD, it becomes more common. So there’s a progressive increase in IR markers that associates with neurons in tau.” Other imaging studies have shown that homeostatic model assessment IR predicts gray matter atrophy, reduced blood flow, and amyloid deposition in middle-aged adults.
One way to overcome IR in AD is to increase insulin availability in the brain. Intranasal administration of insulin is a novel method being tested by Dr. Craft and her associates. “This is not inhaled insulin; it does not target the lungs,” she explained. “It’s insulin administered with a very specialized device that targets the olfactory cleft in the upper nasal passages. Virtually none of the insulin is deposited in the lungs or nasopharyngeally.” The approach is modeled on the notion that there are pathways from the olfactory perivascular spaces to the brain by which peptides can travel readily by bulk flow. “They reach the brain within minutes,” she said. “It’s a way of delivering peptides to the brain that bypasses the blood-brain barrier.”
In a published study, she and her associates randomized 104 adults with MCI or AD to receive 20 IU insulin, 40 IU insulin, or placebo twice daily for 4 months (Arch Neurol. 2012;61[1]:29-38). Tests performed at baseline and at 4 months included cognitive evaluation based on story recall and the ADAS-Cog (Alzheimer’s Disease Assessment Scale–Cognitive subscale); function based on the Dementia Rating Severity Scale, FDG-PET (positron emission tomography with 18fluorodeoxyglucose), and cerebrospinal fluid biomarkers. “We showed that the 20-IU dose of intranasal insulin improved memory quite substantially (P less than .05),” Dr. Craft said. “It also improved glucose utilization as assessed by FDG-PET. We also saw changes in spinal fluid biomarkers of amyloid in a favorable direction. Most recently, we looked at the exosomal indicator of IR (IRS-1 pSer), and what we saw quite remarkably was a reduction in the same condition that the memory improved. This gives us hope that we have a marker of whether or not we’re having a positive impact.”
She and her research team recently finished a phase 2 pilot study of regular insulin vs. long-acting insulin detemir, to determine if a longer-acting agent with longer exposure would have greater efficacy (J Alzheimers Dis. 2017;57[4]:1325–34). In all, 36 participants were randomized to receive placebo, 40 IU of insulin detemir, or 40 IU of regular insulin daily for 4 months, administered with a nasal delivery device. The investigators found that only the group treated with 40 IU regular insulin had better memory after 2 and 4 months, compared with placebo (P less than .03). Regular insulin treatment was also associated with preserved volume on MRI. “The normal pattern is for AD patients to lose brain volume rather rapidly,” Dr. Craft commented. “We see that abolished by the insulin treatment, which suggests to us that we’re able to stave off this disease-related mechanism.” She and her associates are currently conducting a phase 3 clinical trial with regular insulin and a phase 3 trial with rapid-acting insulin that are expected to be completed in the summer of 2018.
Dr. Craft spent the last few minutes of her presentation discussing the ketogenic diet as a nonpharmacologic approach to preventing or treating brain insulin resistance and AD. “I think the power of diet is underestimated, both in terms of causing disease and potentially modulating it,” she said. Her research team just completed a study of 87 middle-aged adults who were randomized to a Western diet or a healthy diet. The Western diet was high in saturated fat, sugar, and salt. The healthy diet was low in saturated fat, sugar, and salt, but the macronutrient composition of both diets was the same. “It was a eucaloric diet with normal calorie intake; no weight change, so trying to understand the integrated effect of the Western diet,” she said. “All food was prepared by us and delivered to the patients two times per week.” Patients with type 2 diabetes, patients with hypertension, and those who were on statins were excluded from the study.
The researchers observed pronounced diet-induced changes in cerebral blood flow, all which favored the healthy diet group. “The Western diet reduced blood flow, and the healthy diet increased blood blow in the hippocampus, which is critical for memory, as in some other regions that are known to be affected in AD,” Dr. Craft said. “We saw an effect on memory as well, with the healthy diet improving memory and the Western diet reducing it. Both of these effects were significant, so 4 weeks on a diet such as this is sufficient to modulate key aspects of brain function.”
More recently, Dr. Craft and her colleagues have been evaluating the effects of what they term the modified Mediterranean ketogenic diet (MMKD). “It does allow for higher carbohydrate consumption, compared with a traditional ketogenic diet, but they still have to stay under 10% a day,” she said. “We have an emphasis on healthy fats. We send everybody home with extra virgin olive oil. We think it gives us extra compliance and the potential for long-term nutrition.” She explained that the diet increases plasma and CNS ketone bodies, beta-hydroxybutyrate, acetoacetate, and acetone, which serves as preferred alternative fuel for the brain. “If the brain has a choice between glucose and ketones, it will choose ketones,” Dr. Craft said. “It can use them more easily.”
Ketone bodies are derived from hepatic fatty acid oxidation and readily diffuse across the blood-brain barrier into the brain. They are also synthesized in the brain by astrocytes, and they appear to have direct neuroprotective effects. “Ketone bodies may be beneficial because they may correct the hyperglycemic state and reduce glucose utilization in the brain in AD years prior to symptom onset,” Dr. Craft said. “They may correct neuronal hyperexcitability and preclinical seizures in presymptomatic and early stages of AD; they restore the balance between inhibitory and excitatory neurotransmitters like GABA [gamma-aminobutyric acid] and glutamate.”
In an unpublished, 16-week study, Dr. Craft and her associates randomized 16 patients to a Mediterranean ketogenic diet or to an American Heart Association low-fat diet. Lumbar punctures and brain imaging were performed before and after diet intervention. By the end of 6 weeks, they observed significant increases in ketones and in HDL cholesterol level in the MMKD group, compared with the AHA diet group, as well as significant decreases in trigylcerides and HbA1c level. “I would say that we improved the peripheral metabolic profile with the ketogenic diet,” Dr. Craft said. They also observed significant improvements from baseline in memory, spinal fluid AD biomarkers, and mitochondrial respiration.
“One of the things we’re appreciating is the role of insulin in a host of activities in the brain,” she concluded. “Disrupting those activities can have dire consequences on brain function that may lead to a neurological milieu that lends itself to pathological aging conditions like Alzheimer’s. Several large ongoing trials are poised to validate results of smaller studies, elucidate underlying mechanisms, and provide new therapeutic targets. It’s an exciting time.”
Dr. Craft’s research is supported by the National Institute on Aging and the Alzheimer’s Association Zenith Program. Intranasal delivery devices were provided by Kurve Technology.
LOS ANGELES – Growing evidence from basic science and preclinical studies demonstrates that
In addition, brain insulin resistance in Alzheimer’s disease (AD) is associated with increased cerebral hyperglycemia, reduced cerebral glucose utilization, reduced blood flow, and reduced accumulation of amyloid and tau.
When that process goes awry, several pathologic processes linking insulin resistance (IR) and Alzheimer’s disease occur, including impaired proteostasis (oligomeric beta amyloid, microtubule-associated tau, and oligomeric insulin); hyperglycemia-induced toxicity and reduced glucose utilization; mitochondrial dysfunction; and vascular dysfunction, Dr. Craft continued.
In the past 5 years, researchers have developed ways to measure expression levels of insulin resistance markers like insulin receptor substrate 1 (IRS-1) pSer–positive neurons, Dr. Craft said. Others have found that increased IRS-1 pSer is associated with paired helical filaments (PHFs) tau in mild cognitive impairment (MCI) and AD, and that increased IRS-1 pSer in neutrally derived plasma exomes increased in AD years before onset and in type 2 diabetes. “We can look at the neurons themselves and what we see is that this IR marker colocalizes with tau,” Dr. Craft said. “It’s not very common in normal folks, but as you progress through the stages of MCI to AD, it becomes more common. So there’s a progressive increase in IR markers that associates with neurons in tau.” Other imaging studies have shown that homeostatic model assessment IR predicts gray matter atrophy, reduced blood flow, and amyloid deposition in middle-aged adults.
One way to overcome IR in AD is to increase insulin availability in the brain. Intranasal administration of insulin is a novel method being tested by Dr. Craft and her associates. “This is not inhaled insulin; it does not target the lungs,” she explained. “It’s insulin administered with a very specialized device that targets the olfactory cleft in the upper nasal passages. Virtually none of the insulin is deposited in the lungs or nasopharyngeally.” The approach is modeled on the notion that there are pathways from the olfactory perivascular spaces to the brain by which peptides can travel readily by bulk flow. “They reach the brain within minutes,” she said. “It’s a way of delivering peptides to the brain that bypasses the blood-brain barrier.”
In a published study, she and her associates randomized 104 adults with MCI or AD to receive 20 IU insulin, 40 IU insulin, or placebo twice daily for 4 months (Arch Neurol. 2012;61[1]:29-38). Tests performed at baseline and at 4 months included cognitive evaluation based on story recall and the ADAS-Cog (Alzheimer’s Disease Assessment Scale–Cognitive subscale); function based on the Dementia Rating Severity Scale, FDG-PET (positron emission tomography with 18fluorodeoxyglucose), and cerebrospinal fluid biomarkers. “We showed that the 20-IU dose of intranasal insulin improved memory quite substantially (P less than .05),” Dr. Craft said. “It also improved glucose utilization as assessed by FDG-PET. We also saw changes in spinal fluid biomarkers of amyloid in a favorable direction. Most recently, we looked at the exosomal indicator of IR (IRS-1 pSer), and what we saw quite remarkably was a reduction in the same condition that the memory improved. This gives us hope that we have a marker of whether or not we’re having a positive impact.”
She and her research team recently finished a phase 2 pilot study of regular insulin vs. long-acting insulin detemir, to determine if a longer-acting agent with longer exposure would have greater efficacy (J Alzheimers Dis. 2017;57[4]:1325–34). In all, 36 participants were randomized to receive placebo, 40 IU of insulin detemir, or 40 IU of regular insulin daily for 4 months, administered with a nasal delivery device. The investigators found that only the group treated with 40 IU regular insulin had better memory after 2 and 4 months, compared with placebo (P less than .03). Regular insulin treatment was also associated with preserved volume on MRI. “The normal pattern is for AD patients to lose brain volume rather rapidly,” Dr. Craft commented. “We see that abolished by the insulin treatment, which suggests to us that we’re able to stave off this disease-related mechanism.” She and her associates are currently conducting a phase 3 clinical trial with regular insulin and a phase 3 trial with rapid-acting insulin that are expected to be completed in the summer of 2018.
Dr. Craft spent the last few minutes of her presentation discussing the ketogenic diet as a nonpharmacologic approach to preventing or treating brain insulin resistance and AD. “I think the power of diet is underestimated, both in terms of causing disease and potentially modulating it,” she said. Her research team just completed a study of 87 middle-aged adults who were randomized to a Western diet or a healthy diet. The Western diet was high in saturated fat, sugar, and salt. The healthy diet was low in saturated fat, sugar, and salt, but the macronutrient composition of both diets was the same. “It was a eucaloric diet with normal calorie intake; no weight change, so trying to understand the integrated effect of the Western diet,” she said. “All food was prepared by us and delivered to the patients two times per week.” Patients with type 2 diabetes, patients with hypertension, and those who were on statins were excluded from the study.
The researchers observed pronounced diet-induced changes in cerebral blood flow, all which favored the healthy diet group. “The Western diet reduced blood flow, and the healthy diet increased blood blow in the hippocampus, which is critical for memory, as in some other regions that are known to be affected in AD,” Dr. Craft said. “We saw an effect on memory as well, with the healthy diet improving memory and the Western diet reducing it. Both of these effects were significant, so 4 weeks on a diet such as this is sufficient to modulate key aspects of brain function.”
More recently, Dr. Craft and her colleagues have been evaluating the effects of what they term the modified Mediterranean ketogenic diet (MMKD). “It does allow for higher carbohydrate consumption, compared with a traditional ketogenic diet, but they still have to stay under 10% a day,” she said. “We have an emphasis on healthy fats. We send everybody home with extra virgin olive oil. We think it gives us extra compliance and the potential for long-term nutrition.” She explained that the diet increases plasma and CNS ketone bodies, beta-hydroxybutyrate, acetoacetate, and acetone, which serves as preferred alternative fuel for the brain. “If the brain has a choice between glucose and ketones, it will choose ketones,” Dr. Craft said. “It can use them more easily.”
Ketone bodies are derived from hepatic fatty acid oxidation and readily diffuse across the blood-brain barrier into the brain. They are also synthesized in the brain by astrocytes, and they appear to have direct neuroprotective effects. “Ketone bodies may be beneficial because they may correct the hyperglycemic state and reduce glucose utilization in the brain in AD years prior to symptom onset,” Dr. Craft said. “They may correct neuronal hyperexcitability and preclinical seizures in presymptomatic and early stages of AD; they restore the balance between inhibitory and excitatory neurotransmitters like GABA [gamma-aminobutyric acid] and glutamate.”
In an unpublished, 16-week study, Dr. Craft and her associates randomized 16 patients to a Mediterranean ketogenic diet or to an American Heart Association low-fat diet. Lumbar punctures and brain imaging were performed before and after diet intervention. By the end of 6 weeks, they observed significant increases in ketones and in HDL cholesterol level in the MMKD group, compared with the AHA diet group, as well as significant decreases in trigylcerides and HbA1c level. “I would say that we improved the peripheral metabolic profile with the ketogenic diet,” Dr. Craft said. They also observed significant improvements from baseline in memory, spinal fluid AD biomarkers, and mitochondrial respiration.
“One of the things we’re appreciating is the role of insulin in a host of activities in the brain,” she concluded. “Disrupting those activities can have dire consequences on brain function that may lead to a neurological milieu that lends itself to pathological aging conditions like Alzheimer’s. Several large ongoing trials are poised to validate results of smaller studies, elucidate underlying mechanisms, and provide new therapeutic targets. It’s an exciting time.”
Dr. Craft’s research is supported by the National Institute on Aging and the Alzheimer’s Association Zenith Program. Intranasal delivery devices were provided by Kurve Technology.
AT WCIRDC 2017
Edaravone: Costs versus benefits
On May 5, 2017, the Food and Drug Administration approved edaravone (Radicava) for the treatment of patients with amyotrophic lateral sclerosis (ALS). Developed by Mitsubishi Tanabe Pharma Corporation, edaravone is the first FDA-approved treatment for ALS since the approval of riluzole (Rilutek) in 1995. Edaravone was originally developed as an acute stroke treatment and then later studied in two separate trials in Japan to assess its efficacy in treating ALS.
Edaravone is administered intravenously and the standard dose of 60 mg takes about 1 hour to complete. The initial treatment cycle consists of once-daily dosing for 2 weeks, followed by a 2-week drug-free period. After the initial cycle, subsequent cycles consist of once-daily dosing for 10 days out of the next 2 weeks, followed by a 2-week drug-free period. The question of how long patients should take edaravone has not been resolved. The FDA did not define a limit to the duration of treatment. Some insurance companies have limited authorization to 6 months as that was the duration of treatment that showed benefit in the study. However, an open-label, 24-week extension of the second study showed that the change in ALSFRS-R was linear throughout the study. This suggests that the treatment benefit in patients with short duration of illness may continue for an additional 24 weeks. Thus, patients who have duration of illness of less than 2 years at presentation may benefit from 12 months of treatment.
The rigorous treatment schedule and IV administration of edaravone create additional concerns for ALS patients. Many patients will need to have a port placed. Patients with impaired mobility will need assistance with transportation to an infusion center. The time involved with taking all of these IV infusions will be considerable. Our experience at the Mayo Clinic reflects differing patient opinions. Some ALS patients with short duration of illness who clearly meet the criteria are not willing to commit to this form of therapy even if insurance will cover it. In contrast, some patients with advanced disease who do not meet the eligibility criteria have expressed the wish to try it.
To have access to edaravone in the United States, ALS patients must first complete an enrollment form and register with a Mitsubishi Tanabe subsidiary called Searchlight. Searchlight creates a Searchlight patient ID and conducts a benefit investigation to determine if the patient’s insurance will cover edaravone treatment. If the patient’s insurance approves edaravone, arrangements are made to ship the drug to the site or company that will perform the infusions. Insurance companies have taken different approaches to the approval of edaravone for ALS patients. Some insurers require that the patient meets the eligibility requirements of the Japanese study that showed benefit (duration of illness less than 2 years from symptom onset and forced vital capacity of at least 80% predicted). These strict criteria will exclude many patients. Other insurers have required only the diagnosis of ALS and the physician’s order. The cost of edaravone is estimated to be around $145,500 per year. The actual out-of-pocket cost to patients will vary depending on their specific insurance plans. In-home infusion of edaravone is another option patients can consider. Patients can pay the separate charges for in-home infusion if their insurance plans do not cover this.
The costs of edaravone are substantial. Beyond the expenses for the medication and infusion services, the patient faces the burden of committing time to frequent IV infusions and potential complications associated with having a port placed. Many ALS patients have decided against pursuing edaravone, suggesting that the perceived costs exceed the perceived benefits. Many ALS patients have started edaravone treatment with the belief that slowing of progression is worth the costs. It is too soon to know if those who have started edaravone will remain committed to the treatment for 6-12 months. Despite the differing approaches to edaravone treatment, it can be agreed upon that it is good to have a new treatment for ALS and that we must continue working to find therapies effective in substantially slowing or stopping the progression of ALS.
Ms. Chang is a research intern, and Dr. Ross is a professor of neurology and director of the ALS Clinic, at Mayo Clinic Arizona in Scottsdale. Dr. Ross reported serving as the Mayo Clinic Arizona site primary investigator for the ALS investigational drug NP001.
On May 5, 2017, the Food and Drug Administration approved edaravone (Radicava) for the treatment of patients with amyotrophic lateral sclerosis (ALS). Developed by Mitsubishi Tanabe Pharma Corporation, edaravone is the first FDA-approved treatment for ALS since the approval of riluzole (Rilutek) in 1995. Edaravone was originally developed as an acute stroke treatment and then later studied in two separate trials in Japan to assess its efficacy in treating ALS.
Edaravone is administered intravenously and the standard dose of 60 mg takes about 1 hour to complete. The initial treatment cycle consists of once-daily dosing for 2 weeks, followed by a 2-week drug-free period. After the initial cycle, subsequent cycles consist of once-daily dosing for 10 days out of the next 2 weeks, followed by a 2-week drug-free period. The question of how long patients should take edaravone has not been resolved. The FDA did not define a limit to the duration of treatment. Some insurance companies have limited authorization to 6 months as that was the duration of treatment that showed benefit in the study. However, an open-label, 24-week extension of the second study showed that the change in ALSFRS-R was linear throughout the study. This suggests that the treatment benefit in patients with short duration of illness may continue for an additional 24 weeks. Thus, patients who have duration of illness of less than 2 years at presentation may benefit from 12 months of treatment.
The rigorous treatment schedule and IV administration of edaravone create additional concerns for ALS patients. Many patients will need to have a port placed. Patients with impaired mobility will need assistance with transportation to an infusion center. The time involved with taking all of these IV infusions will be considerable. Our experience at the Mayo Clinic reflects differing patient opinions. Some ALS patients with short duration of illness who clearly meet the criteria are not willing to commit to this form of therapy even if insurance will cover it. In contrast, some patients with advanced disease who do not meet the eligibility criteria have expressed the wish to try it.
To have access to edaravone in the United States, ALS patients must first complete an enrollment form and register with a Mitsubishi Tanabe subsidiary called Searchlight. Searchlight creates a Searchlight patient ID and conducts a benefit investigation to determine if the patient’s insurance will cover edaravone treatment. If the patient’s insurance approves edaravone, arrangements are made to ship the drug to the site or company that will perform the infusions. Insurance companies have taken different approaches to the approval of edaravone for ALS patients. Some insurers require that the patient meets the eligibility requirements of the Japanese study that showed benefit (duration of illness less than 2 years from symptom onset and forced vital capacity of at least 80% predicted). These strict criteria will exclude many patients. Other insurers have required only the diagnosis of ALS and the physician’s order. The cost of edaravone is estimated to be around $145,500 per year. The actual out-of-pocket cost to patients will vary depending on their specific insurance plans. In-home infusion of edaravone is another option patients can consider. Patients can pay the separate charges for in-home infusion if their insurance plans do not cover this.
The costs of edaravone are substantial. Beyond the expenses for the medication and infusion services, the patient faces the burden of committing time to frequent IV infusions and potential complications associated with having a port placed. Many ALS patients have decided against pursuing edaravone, suggesting that the perceived costs exceed the perceived benefits. Many ALS patients have started edaravone treatment with the belief that slowing of progression is worth the costs. It is too soon to know if those who have started edaravone will remain committed to the treatment for 6-12 months. Despite the differing approaches to edaravone treatment, it can be agreed upon that it is good to have a new treatment for ALS and that we must continue working to find therapies effective in substantially slowing or stopping the progression of ALS.
Ms. Chang is a research intern, and Dr. Ross is a professor of neurology and director of the ALS Clinic, at Mayo Clinic Arizona in Scottsdale. Dr. Ross reported serving as the Mayo Clinic Arizona site primary investigator for the ALS investigational drug NP001.
On May 5, 2017, the Food and Drug Administration approved edaravone (Radicava) for the treatment of patients with amyotrophic lateral sclerosis (ALS). Developed by Mitsubishi Tanabe Pharma Corporation, edaravone is the first FDA-approved treatment for ALS since the approval of riluzole (Rilutek) in 1995. Edaravone was originally developed as an acute stroke treatment and then later studied in two separate trials in Japan to assess its efficacy in treating ALS.
Edaravone is administered intravenously and the standard dose of 60 mg takes about 1 hour to complete. The initial treatment cycle consists of once-daily dosing for 2 weeks, followed by a 2-week drug-free period. After the initial cycle, subsequent cycles consist of once-daily dosing for 10 days out of the next 2 weeks, followed by a 2-week drug-free period. The question of how long patients should take edaravone has not been resolved. The FDA did not define a limit to the duration of treatment. Some insurance companies have limited authorization to 6 months as that was the duration of treatment that showed benefit in the study. However, an open-label, 24-week extension of the second study showed that the change in ALSFRS-R was linear throughout the study. This suggests that the treatment benefit in patients with short duration of illness may continue for an additional 24 weeks. Thus, patients who have duration of illness of less than 2 years at presentation may benefit from 12 months of treatment.
The rigorous treatment schedule and IV administration of edaravone create additional concerns for ALS patients. Many patients will need to have a port placed. Patients with impaired mobility will need assistance with transportation to an infusion center. The time involved with taking all of these IV infusions will be considerable. Our experience at the Mayo Clinic reflects differing patient opinions. Some ALS patients with short duration of illness who clearly meet the criteria are not willing to commit to this form of therapy even if insurance will cover it. In contrast, some patients with advanced disease who do not meet the eligibility criteria have expressed the wish to try it.
To have access to edaravone in the United States, ALS patients must first complete an enrollment form and register with a Mitsubishi Tanabe subsidiary called Searchlight. Searchlight creates a Searchlight patient ID and conducts a benefit investigation to determine if the patient’s insurance will cover edaravone treatment. If the patient’s insurance approves edaravone, arrangements are made to ship the drug to the site or company that will perform the infusions. Insurance companies have taken different approaches to the approval of edaravone for ALS patients. Some insurers require that the patient meets the eligibility requirements of the Japanese study that showed benefit (duration of illness less than 2 years from symptom onset and forced vital capacity of at least 80% predicted). These strict criteria will exclude many patients. Other insurers have required only the diagnosis of ALS and the physician’s order. The cost of edaravone is estimated to be around $145,500 per year. The actual out-of-pocket cost to patients will vary depending on their specific insurance plans. In-home infusion of edaravone is another option patients can consider. Patients can pay the separate charges for in-home infusion if their insurance plans do not cover this.
The costs of edaravone are substantial. Beyond the expenses for the medication and infusion services, the patient faces the burden of committing time to frequent IV infusions and potential complications associated with having a port placed. Many ALS patients have decided against pursuing edaravone, suggesting that the perceived costs exceed the perceived benefits. Many ALS patients have started edaravone treatment with the belief that slowing of progression is worth the costs. It is too soon to know if those who have started edaravone will remain committed to the treatment for 6-12 months. Despite the differing approaches to edaravone treatment, it can be agreed upon that it is good to have a new treatment for ALS and that we must continue working to find therapies effective in substantially slowing or stopping the progression of ALS.
Ms. Chang is a research intern, and Dr. Ross is a professor of neurology and director of the ALS Clinic, at Mayo Clinic Arizona in Scottsdale. Dr. Ross reported serving as the Mayo Clinic Arizona site primary investigator for the ALS investigational drug NP001.
Survey reveals heavy EMR burden on surgical residents
SAN DIEGO – Surgical residents spend a large part of every working day in front of a computer screen, with first-year residents saying they spend an average of more than 13 hours a day on electronic medical records (EMRs).
“Residents are spending a lot of time sitting at a computer, and residents seem to be in agreement that this is time they could potentially be spending learning how to operate and care for patients, which is one of the fundamental purposes of residency training,” study lead author Edward S. Shipper III, MD, a PGY-3 general surgery resident at UT Health-San Antonio, said in an interview after he presented the study findings at the annual clinical congress of the American College of Surgeons.
Research into the EMR burden on residents is sparse. In 2015, researchers at the Medical College of Wisconsin, University of Wisconsin–Madison, and Northwestern University launched a study that they described as the first to examine changes in EMR use over time during surgical residency. The analysis of videos of patient-resident interactions in the exam room found that senior family medicine residents used EMRs more than junior residents (Fam Med. 2015;47[9]:722-26). The current study of surgical residents, however, showed the reverse: Senior residents used EMRs less than juniors.
Dr. Shipper and his colleagues analyzed survey results from 229 U.S. surgical residents who were reached via the Resident and Associate Society of the American College of Surgeons.
Of the 169 who reported demographic data, nearly half were women and 84.6% were training in general surgery, with the rest in subspecialties. The wide majority were in academic or academic-affiliated programs. Residents reported using EMRs exclusively for most clinical tasks, such as medication orders (90.8%), discharge summary (73.5%), and consultation requests (61.7%).
Only about half of those surveyed reported using EMRs exclusively for operative notes (which were often dictated) and signout/handoffs.
In terms of EMR workload per day, PGY-1 residents (n = 23) reported spending an average of 13.6 hours on the records. The average amount of time spent on EMRs per day fell to 10.8 hours for PGY-2 residents (n = 40) and dwindled to 4.6 among PGY-5 residents (n = 20). The researchers reported that the difference in daily EMR time between senior and junior residents is statistically significant.
“Whether or not you believe the specific numbers quoted by the residents, I think the message most people can agree upon is that residents are spending a lot of time during residency sitting in front of a computer,” Dr. Shipper said. “A parallel trend with the rise of the EMR is the rise of increased standards for, and tracking of, documentation requirements by the government and by insurance companies.”
Why are senior surgical residents spending less time on EMRs? “More senior residents generally have the primary responsibility of operating on the patients, and being in the operating room all day means less time spent in front of a computer,” he said.
Of the 63 open-ended responses about the use of EMRs in surgical education, 49% were negative and the rest were evenly divided between natural and positive. One resident described the records as essential to patient care because of their efficiency, while another said, “In this age of duty-hour limits, I spend most of my day in front of a computer interacting with the EHR. This significantly detracts from my educational experience.”
Dr. Shipper said that the study raises questions about how EMRs are affecting how surgical residents learn their craft. But Oren Sagher, MD, professor of neurosurgery at the University of Michigan, Ann Arbor, who has questioned the effect of EMRs on medical education (PLoS Med. 2009;6[5]:e1000069), isn’t impressed by the new research.
Dr. Sagher said an interview. “It’s well established that medical documentation usually falls mainly to the junior residents in surgery program. That was also true prior to EMRs. I would agree that EMRs do tend to take up more time than traditional paper charts did, but this finding is not earth shattering.”
The limit on duty hours would presumably push the burden of EMRs from residents to others, such as physician extenders, but it’s interesting that residents still report using EMRs for the bulk of their days, he added.
In the big picture, Dr. Sagher said, “EMRs are not optimized for the delivery of care. They appear to be mostly driven by billing concerns and safety optimization. Consequently, the people forced to use these systems are not very happy. I think this contributes to physician disenfranchisement and burnout.”
SAN DIEGO – Surgical residents spend a large part of every working day in front of a computer screen, with first-year residents saying they spend an average of more than 13 hours a day on electronic medical records (EMRs).
“Residents are spending a lot of time sitting at a computer, and residents seem to be in agreement that this is time they could potentially be spending learning how to operate and care for patients, which is one of the fundamental purposes of residency training,” study lead author Edward S. Shipper III, MD, a PGY-3 general surgery resident at UT Health-San Antonio, said in an interview after he presented the study findings at the annual clinical congress of the American College of Surgeons.
Research into the EMR burden on residents is sparse. In 2015, researchers at the Medical College of Wisconsin, University of Wisconsin–Madison, and Northwestern University launched a study that they described as the first to examine changes in EMR use over time during surgical residency. The analysis of videos of patient-resident interactions in the exam room found that senior family medicine residents used EMRs more than junior residents (Fam Med. 2015;47[9]:722-26). The current study of surgical residents, however, showed the reverse: Senior residents used EMRs less than juniors.
Dr. Shipper and his colleagues analyzed survey results from 229 U.S. surgical residents who were reached via the Resident and Associate Society of the American College of Surgeons.
Of the 169 who reported demographic data, nearly half were women and 84.6% were training in general surgery, with the rest in subspecialties. The wide majority were in academic or academic-affiliated programs. Residents reported using EMRs exclusively for most clinical tasks, such as medication orders (90.8%), discharge summary (73.5%), and consultation requests (61.7%).
Only about half of those surveyed reported using EMRs exclusively for operative notes (which were often dictated) and signout/handoffs.
In terms of EMR workload per day, PGY-1 residents (n = 23) reported spending an average of 13.6 hours on the records. The average amount of time spent on EMRs per day fell to 10.8 hours for PGY-2 residents (n = 40) and dwindled to 4.6 among PGY-5 residents (n = 20). The researchers reported that the difference in daily EMR time between senior and junior residents is statistically significant.
“Whether or not you believe the specific numbers quoted by the residents, I think the message most people can agree upon is that residents are spending a lot of time during residency sitting in front of a computer,” Dr. Shipper said. “A parallel trend with the rise of the EMR is the rise of increased standards for, and tracking of, documentation requirements by the government and by insurance companies.”
Why are senior surgical residents spending less time on EMRs? “More senior residents generally have the primary responsibility of operating on the patients, and being in the operating room all day means less time spent in front of a computer,” he said.
Of the 63 open-ended responses about the use of EMRs in surgical education, 49% were negative and the rest were evenly divided between natural and positive. One resident described the records as essential to patient care because of their efficiency, while another said, “In this age of duty-hour limits, I spend most of my day in front of a computer interacting with the EHR. This significantly detracts from my educational experience.”
Dr. Shipper said that the study raises questions about how EMRs are affecting how surgical residents learn their craft. But Oren Sagher, MD, professor of neurosurgery at the University of Michigan, Ann Arbor, who has questioned the effect of EMRs on medical education (PLoS Med. 2009;6[5]:e1000069), isn’t impressed by the new research.
Dr. Sagher said an interview. “It’s well established that medical documentation usually falls mainly to the junior residents in surgery program. That was also true prior to EMRs. I would agree that EMRs do tend to take up more time than traditional paper charts did, but this finding is not earth shattering.”
The limit on duty hours would presumably push the burden of EMRs from residents to others, such as physician extenders, but it’s interesting that residents still report using EMRs for the bulk of their days, he added.
In the big picture, Dr. Sagher said, “EMRs are not optimized for the delivery of care. They appear to be mostly driven by billing concerns and safety optimization. Consequently, the people forced to use these systems are not very happy. I think this contributes to physician disenfranchisement and burnout.”
SAN DIEGO – Surgical residents spend a large part of every working day in front of a computer screen, with first-year residents saying they spend an average of more than 13 hours a day on electronic medical records (EMRs).
“Residents are spending a lot of time sitting at a computer, and residents seem to be in agreement that this is time they could potentially be spending learning how to operate and care for patients, which is one of the fundamental purposes of residency training,” study lead author Edward S. Shipper III, MD, a PGY-3 general surgery resident at UT Health-San Antonio, said in an interview after he presented the study findings at the annual clinical congress of the American College of Surgeons.
Research into the EMR burden on residents is sparse. In 2015, researchers at the Medical College of Wisconsin, University of Wisconsin–Madison, and Northwestern University launched a study that they described as the first to examine changes in EMR use over time during surgical residency. The analysis of videos of patient-resident interactions in the exam room found that senior family medicine residents used EMRs more than junior residents (Fam Med. 2015;47[9]:722-26). The current study of surgical residents, however, showed the reverse: Senior residents used EMRs less than juniors.
Dr. Shipper and his colleagues analyzed survey results from 229 U.S. surgical residents who were reached via the Resident and Associate Society of the American College of Surgeons.
Of the 169 who reported demographic data, nearly half were women and 84.6% were training in general surgery, with the rest in subspecialties. The wide majority were in academic or academic-affiliated programs. Residents reported using EMRs exclusively for most clinical tasks, such as medication orders (90.8%), discharge summary (73.5%), and consultation requests (61.7%).
Only about half of those surveyed reported using EMRs exclusively for operative notes (which were often dictated) and signout/handoffs.
In terms of EMR workload per day, PGY-1 residents (n = 23) reported spending an average of 13.6 hours on the records. The average amount of time spent on EMRs per day fell to 10.8 hours for PGY-2 residents (n = 40) and dwindled to 4.6 among PGY-5 residents (n = 20). The researchers reported that the difference in daily EMR time between senior and junior residents is statistically significant.
“Whether or not you believe the specific numbers quoted by the residents, I think the message most people can agree upon is that residents are spending a lot of time during residency sitting in front of a computer,” Dr. Shipper said. “A parallel trend with the rise of the EMR is the rise of increased standards for, and tracking of, documentation requirements by the government and by insurance companies.”
Why are senior surgical residents spending less time on EMRs? “More senior residents generally have the primary responsibility of operating on the patients, and being in the operating room all day means less time spent in front of a computer,” he said.
Of the 63 open-ended responses about the use of EMRs in surgical education, 49% were negative and the rest were evenly divided between natural and positive. One resident described the records as essential to patient care because of their efficiency, while another said, “In this age of duty-hour limits, I spend most of my day in front of a computer interacting with the EHR. This significantly detracts from my educational experience.”
Dr. Shipper said that the study raises questions about how EMRs are affecting how surgical residents learn their craft. But Oren Sagher, MD, professor of neurosurgery at the University of Michigan, Ann Arbor, who has questioned the effect of EMRs on medical education (PLoS Med. 2009;6[5]:e1000069), isn’t impressed by the new research.
Dr. Sagher said an interview. “It’s well established that medical documentation usually falls mainly to the junior residents in surgery program. That was also true prior to EMRs. I would agree that EMRs do tend to take up more time than traditional paper charts did, but this finding is not earth shattering.”
The limit on duty hours would presumably push the burden of EMRs from residents to others, such as physician extenders, but it’s interesting that residents still report using EMRs for the bulk of their days, he added.
In the big picture, Dr. Sagher said, “EMRs are not optimized for the delivery of care. They appear to be mostly driven by billing concerns and safety optimization. Consequently, the people forced to use these systems are not very happy. I think this contributes to physician disenfranchisement and burnout.”
AT THE ACS CLINICAL CONGRESS
Anti-BCMA CAR T-cell therapy being fast tracked at FDA
The Food and Drug Administration has granted breakthrough therapy designation to bb2121, a chimeric antigen receptor T-cell (CAR T) therapy that targets b-cell maturation antigen (BCMA) in patients with relapsed/refractory multiple myeloma.
The therapy, being developed jointly by Celgene and bluebird bio, will be given expedited review by the FDA under the program. Meanwhile, European drug officials have granted it Priority Medicines eligibility, which also provides accelerated review.
The decision to fast track the review of bb2121 is based on preliminary data from the ongoing phase I CRB-401 trial. As of May 2017, there was 1-month clinical response data from 18 patients with multiple myeloma who were infused with bb2121. The overall response rate was 89%, but was 100% for patients who had been treated with doses of 150 × 106 CAR+ T cells or higher, according to an abstract from the annual meeting of the American Society of Hematology. Five months of follow-up data on these patients, plus initial data on additional patients, will be presented at ASH 2017 on Dec. 11.
The Food and Drug Administration has granted breakthrough therapy designation to bb2121, a chimeric antigen receptor T-cell (CAR T) therapy that targets b-cell maturation antigen (BCMA) in patients with relapsed/refractory multiple myeloma.
The therapy, being developed jointly by Celgene and bluebird bio, will be given expedited review by the FDA under the program. Meanwhile, European drug officials have granted it Priority Medicines eligibility, which also provides accelerated review.
The decision to fast track the review of bb2121 is based on preliminary data from the ongoing phase I CRB-401 trial. As of May 2017, there was 1-month clinical response data from 18 patients with multiple myeloma who were infused with bb2121. The overall response rate was 89%, but was 100% for patients who had been treated with doses of 150 × 106 CAR+ T cells or higher, according to an abstract from the annual meeting of the American Society of Hematology. Five months of follow-up data on these patients, plus initial data on additional patients, will be presented at ASH 2017 on Dec. 11.
The Food and Drug Administration has granted breakthrough therapy designation to bb2121, a chimeric antigen receptor T-cell (CAR T) therapy that targets b-cell maturation antigen (BCMA) in patients with relapsed/refractory multiple myeloma.
The therapy, being developed jointly by Celgene and bluebird bio, will be given expedited review by the FDA under the program. Meanwhile, European drug officials have granted it Priority Medicines eligibility, which also provides accelerated review.
The decision to fast track the review of bb2121 is based on preliminary data from the ongoing phase I CRB-401 trial. As of May 2017, there was 1-month clinical response data from 18 patients with multiple myeloma who were infused with bb2121. The overall response rate was 89%, but was 100% for patients who had been treated with doses of 150 × 106 CAR+ T cells or higher, according to an abstract from the annual meeting of the American Society of Hematology. Five months of follow-up data on these patients, plus initial data on additional patients, will be presented at ASH 2017 on Dec. 11.
PBC disease progression no worse for patients with concomitant NAFLD
, according to Gerald Yosel Minuk, MD, and his associates.
At baseline, the 168 patients in the PBC-only group had higher serum alkaline phosphatase and gamma-glutamyl transferase values than the 68 patients in the NAFLD/PBC group, as well as having higher FIB-4 scores. The percentage of patients with aspartate aminotransferase/platelet ratio indexes (APRI) greater than 1.5 was slightly higher in the PBC-only group, but the difference was not significant.
After follow-up periods averaging 6.7 years in the PBC-only group and 6.4 years in the NAFLD/PBC group, yearly increases in FIB-4 and prevalence of APRI greater than 1.5 were greater in the PBC-only group, though the difference did not reach significance. PBC-only patients were more likely to have developed radiologic evidence of cirrhosis during the follow-up period (42% vs. 19%, P less than .001).
“Were the results of the present study to be confirmed by others, the question arises as to why NAFLD does not adversely and may favorably impact on PBC. Here, it is tempting to speculate that because PBC livers are associated with a paucity of immunosuppressive regulator T cells (Tregs) whereas in NAFLD, Tregs are recruited to the liver in increased numbers, a restoration of the immune balance in PBC livers might explain these findings,” the investigators noted.
Find the full study in Liver International (doi: 10.1111/liv.13644).
, according to Gerald Yosel Minuk, MD, and his associates.
At baseline, the 168 patients in the PBC-only group had higher serum alkaline phosphatase and gamma-glutamyl transferase values than the 68 patients in the NAFLD/PBC group, as well as having higher FIB-4 scores. The percentage of patients with aspartate aminotransferase/platelet ratio indexes (APRI) greater than 1.5 was slightly higher in the PBC-only group, but the difference was not significant.
After follow-up periods averaging 6.7 years in the PBC-only group and 6.4 years in the NAFLD/PBC group, yearly increases in FIB-4 and prevalence of APRI greater than 1.5 were greater in the PBC-only group, though the difference did not reach significance. PBC-only patients were more likely to have developed radiologic evidence of cirrhosis during the follow-up period (42% vs. 19%, P less than .001).
“Were the results of the present study to be confirmed by others, the question arises as to why NAFLD does not adversely and may favorably impact on PBC. Here, it is tempting to speculate that because PBC livers are associated with a paucity of immunosuppressive regulator T cells (Tregs) whereas in NAFLD, Tregs are recruited to the liver in increased numbers, a restoration of the immune balance in PBC livers might explain these findings,” the investigators noted.
Find the full study in Liver International (doi: 10.1111/liv.13644).
, according to Gerald Yosel Minuk, MD, and his associates.
At baseline, the 168 patients in the PBC-only group had higher serum alkaline phosphatase and gamma-glutamyl transferase values than the 68 patients in the NAFLD/PBC group, as well as having higher FIB-4 scores. The percentage of patients with aspartate aminotransferase/platelet ratio indexes (APRI) greater than 1.5 was slightly higher in the PBC-only group, but the difference was not significant.
After follow-up periods averaging 6.7 years in the PBC-only group and 6.4 years in the NAFLD/PBC group, yearly increases in FIB-4 and prevalence of APRI greater than 1.5 were greater in the PBC-only group, though the difference did not reach significance. PBC-only patients were more likely to have developed radiologic evidence of cirrhosis during the follow-up period (42% vs. 19%, P less than .001).
“Were the results of the present study to be confirmed by others, the question arises as to why NAFLD does not adversely and may favorably impact on PBC. Here, it is tempting to speculate that because PBC livers are associated with a paucity of immunosuppressive regulator T cells (Tregs) whereas in NAFLD, Tregs are recruited to the liver in increased numbers, a restoration of the immune balance in PBC livers might explain these findings,” the investigators noted.
Find the full study in Liver International (doi: 10.1111/liv.13644).
FROM LIVER INTERNATIONAL