User login
Faciobrachial dystonic seizures require urgent immunotherapy
SAN DIEGO – The sooner immunotherapy is started for faciobrachial dystonic seizures, the better, according to a retrospective review presented at the American Neurological Association annual meeting.
Only recently described, patients with faciobrachial dystonic seizures (FBDS) have frequent episodes – sometimes hundreds a day – of abrupt, involuntary, stereotypical movements lasting 1-5 seconds and typically involving one half of their face and the arm on the same side, such as a left-sided grimace and arm flex. It’s closely associated with antibodies against leucine-rich glioma, inactivated 1 (LGI-1), a protein that plays a role in synaptic transmission and myelination.
“This is an autoimmune condition. It’s important to get onto it early; you’ve got to treat these seizures with immunotherapy and treat them fast,” she said.
A lot of the time, FBDS is probably mistaken for a movement disorder or tic, but tics aren’t typically dystonic, plus FBDS patients can’t suppress their movements and they don’t feel the buildup of tension, then release typical of tics. “If something doesn’t add up, test for the antibodies,” Dr. Thompson said.
Her team reviewed 103 cases culled from South Korea, Great Britain, Australia, and the United States, the largest cohort assembled to date. The median age was 64 years old; most patients were white, and 62% were men. There were no associations with tumors, and none of the seasonal variation typical of viral causes.
FBDS showed “a striking time-dependent response to immunotherapy. Prompt immunotherapy” stops the seizures and prevents brain damage, “maybe via inhibiting IgG1-mediated complement deposition,” Dr. Thompson said.
Antiepileptic drugs didn’t help much, but immunotherapy did; among patients who had immunotherapy, seizures stopped within 30 days in over half, and in 88% after 3 months. Only one patient with seizure cessation went on to develop cognitive impairment. For every day that immunotherapy was delayed, there was a 0.69% reduction in the probability of stopping the seizures. The window of opportunity appears to be short: among patients whose seizures weren’t terminated within 3 months, 56% progressed to cognitive impairment.
Immunotherapy varied greatly across the study centers, and included intravenous immunoglobulin, azathioprine, and mycophenolate, among other options that were generally given on a background of steroids.
“It became quite obvious that immunotherapy was the key,” but there weren’t enough patients to determine the optimal approach. Dr. Thompson and her colleagues are working to figure that out, as well as what triggers FBDS and its pathophysiology, she said.
Patients who just had seizures had almost exclusively LGI-1 IgG4 antibodies; those who had progressed to cognitive impairment had LGI-1 IgG1 antibodies. It’s unclear at this point what causes the subclass switch as patients progress.
Medial temporal lobe T2-hyperintensities and temporal and frontal lobe ictal EEG changes, as well as serum hyponatremia, were also found almost exclusively in patients with cognitive impairment.
Much remains to be learned about the condition.
There was no industry funding for the work, and Dr. Thompson didn’t have any disclosures.
SAN DIEGO – The sooner immunotherapy is started for faciobrachial dystonic seizures, the better, according to a retrospective review presented at the American Neurological Association annual meeting.
Only recently described, patients with faciobrachial dystonic seizures (FBDS) have frequent episodes – sometimes hundreds a day – of abrupt, involuntary, stereotypical movements lasting 1-5 seconds and typically involving one half of their face and the arm on the same side, such as a left-sided grimace and arm flex. It’s closely associated with antibodies against leucine-rich glioma, inactivated 1 (LGI-1), a protein that plays a role in synaptic transmission and myelination.
“This is an autoimmune condition. It’s important to get onto it early; you’ve got to treat these seizures with immunotherapy and treat them fast,” she said.
A lot of the time, FBDS is probably mistaken for a movement disorder or tic, but tics aren’t typically dystonic, plus FBDS patients can’t suppress their movements and they don’t feel the buildup of tension, then release typical of tics. “If something doesn’t add up, test for the antibodies,” Dr. Thompson said.
Her team reviewed 103 cases culled from South Korea, Great Britain, Australia, and the United States, the largest cohort assembled to date. The median age was 64 years old; most patients were white, and 62% were men. There were no associations with tumors, and none of the seasonal variation typical of viral causes.
FBDS showed “a striking time-dependent response to immunotherapy. Prompt immunotherapy” stops the seizures and prevents brain damage, “maybe via inhibiting IgG1-mediated complement deposition,” Dr. Thompson said.
Antiepileptic drugs didn’t help much, but immunotherapy did; among patients who had immunotherapy, seizures stopped within 30 days in over half, and in 88% after 3 months. Only one patient with seizure cessation went on to develop cognitive impairment. For every day that immunotherapy was delayed, there was a 0.69% reduction in the probability of stopping the seizures. The window of opportunity appears to be short: among patients whose seizures weren’t terminated within 3 months, 56% progressed to cognitive impairment.
Immunotherapy varied greatly across the study centers, and included intravenous immunoglobulin, azathioprine, and mycophenolate, among other options that were generally given on a background of steroids.
“It became quite obvious that immunotherapy was the key,” but there weren’t enough patients to determine the optimal approach. Dr. Thompson and her colleagues are working to figure that out, as well as what triggers FBDS and its pathophysiology, she said.
Patients who just had seizures had almost exclusively LGI-1 IgG4 antibodies; those who had progressed to cognitive impairment had LGI-1 IgG1 antibodies. It’s unclear at this point what causes the subclass switch as patients progress.
Medial temporal lobe T2-hyperintensities and temporal and frontal lobe ictal EEG changes, as well as serum hyponatremia, were also found almost exclusively in patients with cognitive impairment.
Much remains to be learned about the condition.
There was no industry funding for the work, and Dr. Thompson didn’t have any disclosures.
SAN DIEGO – The sooner immunotherapy is started for faciobrachial dystonic seizures, the better, according to a retrospective review presented at the American Neurological Association annual meeting.
Only recently described, patients with faciobrachial dystonic seizures (FBDS) have frequent episodes – sometimes hundreds a day – of abrupt, involuntary, stereotypical movements lasting 1-5 seconds and typically involving one half of their face and the arm on the same side, such as a left-sided grimace and arm flex. It’s closely associated with antibodies against leucine-rich glioma, inactivated 1 (LGI-1), a protein that plays a role in synaptic transmission and myelination.
“This is an autoimmune condition. It’s important to get onto it early; you’ve got to treat these seizures with immunotherapy and treat them fast,” she said.
A lot of the time, FBDS is probably mistaken for a movement disorder or tic, but tics aren’t typically dystonic, plus FBDS patients can’t suppress their movements and they don’t feel the buildup of tension, then release typical of tics. “If something doesn’t add up, test for the antibodies,” Dr. Thompson said.
Her team reviewed 103 cases culled from South Korea, Great Britain, Australia, and the United States, the largest cohort assembled to date. The median age was 64 years old; most patients were white, and 62% were men. There were no associations with tumors, and none of the seasonal variation typical of viral causes.
FBDS showed “a striking time-dependent response to immunotherapy. Prompt immunotherapy” stops the seizures and prevents brain damage, “maybe via inhibiting IgG1-mediated complement deposition,” Dr. Thompson said.
Antiepileptic drugs didn’t help much, but immunotherapy did; among patients who had immunotherapy, seizures stopped within 30 days in over half, and in 88% after 3 months. Only one patient with seizure cessation went on to develop cognitive impairment. For every day that immunotherapy was delayed, there was a 0.69% reduction in the probability of stopping the seizures. The window of opportunity appears to be short: among patients whose seizures weren’t terminated within 3 months, 56% progressed to cognitive impairment.
Immunotherapy varied greatly across the study centers, and included intravenous immunoglobulin, azathioprine, and mycophenolate, among other options that were generally given on a background of steroids.
“It became quite obvious that immunotherapy was the key,” but there weren’t enough patients to determine the optimal approach. Dr. Thompson and her colleagues are working to figure that out, as well as what triggers FBDS and its pathophysiology, she said.
Patients who just had seizures had almost exclusively LGI-1 IgG4 antibodies; those who had progressed to cognitive impairment had LGI-1 IgG1 antibodies. It’s unclear at this point what causes the subclass switch as patients progress.
Medial temporal lobe T2-hyperintensities and temporal and frontal lobe ictal EEG changes, as well as serum hyponatremia, were also found almost exclusively in patients with cognitive impairment.
Much remains to be learned about the condition.
There was no industry funding for the work, and Dr. Thompson didn’t have any disclosures.
AT ANA 2017
Key clinical point:
Major finding: For every day that immunotherapy was delayed, there was a 0.69% reduction in the probability of stopping the seizures and progression to limbic encephalitis and permanent disability.
Data source: Review of 103 patients, the largest cohort assembled to date.
Disclosures: There was no industry funding for the work, and the lead investigator had no disclosures.
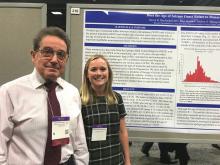
Analysis strengthens association between epilepsy onset, menarche
WASHINGTON – The high rate of new onset epilepsy during the period surrounding menarche has been strengthened in a data analysis that suggests surging hormones may be a treatable trigger of epileptogenic activity, according to a new analysis of the Epilepsy Birth Control Registry (EBCR) presented at the annual meeting of the American Epilepsy Society.
“The evidence connecting neuroactive sexual maturation hormones with the onset of epilepsy and seizure activity is becoming strong enough that we can at least conceptualize how hormonal interventions might be used for prevention or treatment,” reported Andrew G. Herzog, MD, director of the neuroendocrine unit at Beth Israel Deaconess Hospital, Boston.
Confirming previous observations, new onset epilepsy was more likely to occur in the year of menarche than in any other year, and the rate, 8.3%, was approximately four times greater than an expected rate of 2.1% (P less than .0001), Dr. Herzog reported. However, the association was even stronger when a cluster analysis was performed to widen the window in which sexual maturation hormones begin to surge.
“Menarche is a single event along a continuum of sexual maturation that involves hormonal surges that begin much earlier,” Dr. Herzog explained. He suggested that adrenarche is a better term to capture the relationship between increasing hormone levels and risk of new onset epilepsy. Adrenarche describes a period in which sex steroids released by the adrenal cortex drive puberty and secondary sexual characteristics, such as growth of pubic hair.
In the cluster analysis, the most common period of new onset epilepsy occurred in a span stemming from 2 years before the onset of menarche to 6 year after onset. Almost half of new onset epilepsy in the EBCR occurred in this 8-year period, and it was more than double the rate that would have been expected if new onset epilepsy were distributed evenly by age (49.3% vs. 18.9%; P less than .0001).
“This implicates the onset of puberty and the massive increase in neuroactive steroids that modulate neurohormonal activity and seizures,” said Dr. Herzog, who noted that some neuroactive steroids increase 10-fold during this period. He suggested that the fact that there is also an increased rate of new onset epilepsy in males during the same period does not weaken this association but is likely related to the same phenomenon of neuroactive steroid release.
These data are consistent with a wide variety of other evidence from the EBCR that has linked hormones involved in sexual maturation with change in epilepsy risk, according to Dr. Herzog. He noted, for example, that his group has shown that the release of unopposed estrogen in anovulatory cycles experienced by adolescent girls in the early years of menstruation produces a higher rate of seizures than does ovulatory cycles in which both estrogen and progesterone are released. This is consistent with evidence that estrogen is associated with increased and progesterone with reduced risk of seizure activity.
The relationship between steroid release and risk of new onset epilepsy or seizure activity in patients who already have epilepsy is becoming sufficiently strong that Dr. Herzog believes that efforts should now turn to considering how this information might lead to new interventions. Although clinical trials are not near, he suggested that it might make sense to pursue medications that inhibit neuroactive hormones to prevent seizures in girls at high risk for new onset epilepsy or treat seizures suspected of being hormone related.
Dr. Herzog reports no potential conflicts of interest related to this topic. The study was partially funded by Lundbeck.
WASHINGTON – The high rate of new onset epilepsy during the period surrounding menarche has been strengthened in a data analysis that suggests surging hormones may be a treatable trigger of epileptogenic activity, according to a new analysis of the Epilepsy Birth Control Registry (EBCR) presented at the annual meeting of the American Epilepsy Society.
“The evidence connecting neuroactive sexual maturation hormones with the onset of epilepsy and seizure activity is becoming strong enough that we can at least conceptualize how hormonal interventions might be used for prevention or treatment,” reported Andrew G. Herzog, MD, director of the neuroendocrine unit at Beth Israel Deaconess Hospital, Boston.
Confirming previous observations, new onset epilepsy was more likely to occur in the year of menarche than in any other year, and the rate, 8.3%, was approximately four times greater than an expected rate of 2.1% (P less than .0001), Dr. Herzog reported. However, the association was even stronger when a cluster analysis was performed to widen the window in which sexual maturation hormones begin to surge.
“Menarche is a single event along a continuum of sexual maturation that involves hormonal surges that begin much earlier,” Dr. Herzog explained. He suggested that adrenarche is a better term to capture the relationship between increasing hormone levels and risk of new onset epilepsy. Adrenarche describes a period in which sex steroids released by the adrenal cortex drive puberty and secondary sexual characteristics, such as growth of pubic hair.
In the cluster analysis, the most common period of new onset epilepsy occurred in a span stemming from 2 years before the onset of menarche to 6 year after onset. Almost half of new onset epilepsy in the EBCR occurred in this 8-year period, and it was more than double the rate that would have been expected if new onset epilepsy were distributed evenly by age (49.3% vs. 18.9%; P less than .0001).
“This implicates the onset of puberty and the massive increase in neuroactive steroids that modulate neurohormonal activity and seizures,” said Dr. Herzog, who noted that some neuroactive steroids increase 10-fold during this period. He suggested that the fact that there is also an increased rate of new onset epilepsy in males during the same period does not weaken this association but is likely related to the same phenomenon of neuroactive steroid release.
These data are consistent with a wide variety of other evidence from the EBCR that has linked hormones involved in sexual maturation with change in epilepsy risk, according to Dr. Herzog. He noted, for example, that his group has shown that the release of unopposed estrogen in anovulatory cycles experienced by adolescent girls in the early years of menstruation produces a higher rate of seizures than does ovulatory cycles in which both estrogen and progesterone are released. This is consistent with evidence that estrogen is associated with increased and progesterone with reduced risk of seizure activity.
The relationship between steroid release and risk of new onset epilepsy or seizure activity in patients who already have epilepsy is becoming sufficiently strong that Dr. Herzog believes that efforts should now turn to considering how this information might lead to new interventions. Although clinical trials are not near, he suggested that it might make sense to pursue medications that inhibit neuroactive hormones to prevent seizures in girls at high risk for new onset epilepsy or treat seizures suspected of being hormone related.
Dr. Herzog reports no potential conflicts of interest related to this topic. The study was partially funded by Lundbeck.
WASHINGTON – The high rate of new onset epilepsy during the period surrounding menarche has been strengthened in a data analysis that suggests surging hormones may be a treatable trigger of epileptogenic activity, according to a new analysis of the Epilepsy Birth Control Registry (EBCR) presented at the annual meeting of the American Epilepsy Society.
“The evidence connecting neuroactive sexual maturation hormones with the onset of epilepsy and seizure activity is becoming strong enough that we can at least conceptualize how hormonal interventions might be used for prevention or treatment,” reported Andrew G. Herzog, MD, director of the neuroendocrine unit at Beth Israel Deaconess Hospital, Boston.
Confirming previous observations, new onset epilepsy was more likely to occur in the year of menarche than in any other year, and the rate, 8.3%, was approximately four times greater than an expected rate of 2.1% (P less than .0001), Dr. Herzog reported. However, the association was even stronger when a cluster analysis was performed to widen the window in which sexual maturation hormones begin to surge.
“Menarche is a single event along a continuum of sexual maturation that involves hormonal surges that begin much earlier,” Dr. Herzog explained. He suggested that adrenarche is a better term to capture the relationship between increasing hormone levels and risk of new onset epilepsy. Adrenarche describes a period in which sex steroids released by the adrenal cortex drive puberty and secondary sexual characteristics, such as growth of pubic hair.
In the cluster analysis, the most common period of new onset epilepsy occurred in a span stemming from 2 years before the onset of menarche to 6 year after onset. Almost half of new onset epilepsy in the EBCR occurred in this 8-year period, and it was more than double the rate that would have been expected if new onset epilepsy were distributed evenly by age (49.3% vs. 18.9%; P less than .0001).
“This implicates the onset of puberty and the massive increase in neuroactive steroids that modulate neurohormonal activity and seizures,” said Dr. Herzog, who noted that some neuroactive steroids increase 10-fold during this period. He suggested that the fact that there is also an increased rate of new onset epilepsy in males during the same period does not weaken this association but is likely related to the same phenomenon of neuroactive steroid release.
These data are consistent with a wide variety of other evidence from the EBCR that has linked hormones involved in sexual maturation with change in epilepsy risk, according to Dr. Herzog. He noted, for example, that his group has shown that the release of unopposed estrogen in anovulatory cycles experienced by adolescent girls in the early years of menstruation produces a higher rate of seizures than does ovulatory cycles in which both estrogen and progesterone are released. This is consistent with evidence that estrogen is associated with increased and progesterone with reduced risk of seizure activity.
The relationship between steroid release and risk of new onset epilepsy or seizure activity in patients who already have epilepsy is becoming sufficiently strong that Dr. Herzog believes that efforts should now turn to considering how this information might lead to new interventions. Although clinical trials are not near, he suggested that it might make sense to pursue medications that inhibit neuroactive hormones to prevent seizures in girls at high risk for new onset epilepsy or treat seizures suspected of being hormone related.
Dr. Herzog reports no potential conflicts of interest related to this topic. The study was partially funded by Lundbeck.
AT AES 2017
Key clinical point:
Major finding: In an 8-year period surrounding menarche, the rate of new onset epilepsy is more than double that expected (49.3% vs. 18.9%; P less than .0001).
Data source: Retrospective study of participants in the Epilepsy Birth Control Registry.
Disclosures: Dr. Herzog reports no potential conflicts of interest related to this topic. The study was partially funded by Lundbeck.
EXCEL: Quality of life better after PCI than CABG
DENVER – Several key validated measures of health status were significantly more favorable a full year after percutaneous coronary intervention using an everolimus-eluting stent than with coronary artery bypass surgery in patients with unprotected left main CAD in the prespecified quality-of-life analysis of the landmark EXCEL trial.
By 3 years of follow-up, there was no longer a difference between the PCI and CABG groups in terms of the various quality-of-life measures, Suzanne J. Baron, MD, reported at the Transcatheter Cardiovascular Therapeutics annual educational meeting. Nor as previously reported was there any significant difference in the primary composite endpoint comprised of all-cause mortality, stroke, or MI.
“My take away from this is that these results provide an ideal opportunity to give patients a choice about which choice they would want: An earlier recovery with angioplasty versus really similar outcomes long-term with either procedure. For me, these EXCEL results make me feel that angioplasty for less complex coronary disease is really probably the preferred option,” said John A. Spertus, MD, director of health outcomes research at Saint Luke’s Mid America Heart Institute and professor of medicine at the University of Missouri-Kansas City.
“The faster recovery with PCI, the similar angina relief after 3 years, and also the less depression with PCI, which is an important finding, I think – all this goes in favor of PCI for left main disease,” commented Evald H. Christiansen, MD, a cardiologist at Aarhus (Denmark) University and senior investigator in the NOBLE trial (Lancet. 2016 Dec 3;388[10061]:2743-52), which randomized patients to CABG or a stent that’s no longer marketed.
The previously published clinical outcomes of EXCEL (N Engl J Med. 2016 Dec 8;375[23]:2223-35) were based upon a median 3 years of follow-up. Dr. Baron presented updated outcomes in which all study participants had completed the full 3 years of follow-up. The results were little changed: The primary composite endpoint of all-cause mortality, stroke, or MI occurred in 15.2% of the group treated with the everolimus-eluting Xience stent and was closely similar at 14.7% of the CABG patients, while the 12.5% repeat revascularization rate in the PCI arm was significantly greater than the 7.4% rate with CABG.
But the prespecified EXCEL quality-of-life substudy with assessments at baseline, 1 month, 1 year, and 3 years in 1,788 participants is all new information. Among the highlights: The proportion of patients with clinically significant depression as defined by a Patient Health Questionnaire 8 (PHQ-8) score of 10 or more was 21% at baseline in both groups; 8% in the PCI group, compared with 19% in the CABG arm at 1 month; and 8% in the PCI arm versus 12% with CABG at 12 months of follow-up, with the differences at both time points being significant. By 3 years, the rate was 8%-9% in both groups, reported Dr. Baron of Saint Luke’s Mid America Health Institute and the University of Missouri-Kansas City.
“We now have a new treatment for depression: PCI,” quipped session moderator Gregg W. Stone, MD, professor of medicine at Columbia University in New York, who was lead investigator in EXCEL.
Also, scores on the SF-12 physical summary scale improved sharply from a baseline of 39 points in the PCI group during the first month of follow-up while worsening in the CABG group, such that at 1 month the between-group difference averaged 8.2 points. The gap narrowed over the next 11 months, and by 1 year the CABG patients had caught up.
Scores on the Seattle Angina Questionnaire and the Rose Dyspnea Scale were significantly better in the PCI group than the CABG arm at 1 month, but at 12 and 36 months the two groups were indistinguishable in these domains.
Dr. Spertus, who is credited with inventing both the Seattle Angina Questionnaire and the Kansas City Cardiomyopathy Questionnaire, said that in the context of EXCEL he puts more stock in the SF-12 and PHQ-8 results than the angina and dyspnea measures.
Jonathan Hill, MD, an interventional cardiologist at King’s College London, said the EXCEL quality-of-life substudy provides a valuable picture of the real-life impact of sternotomy.
“We mustn’t underplay that, the months and even up to a year of your life for recovery from the revascularization procedure, compared with days of recovery time with PCI. Patients want the option of PCI if it’s available. This data really vindicates that decision making,” he said.
“I think we minimize the recovery period from CABG. People talk a lot about outcomes at 3 years and 5 years, but look at this prolonged recovery. I think that’s very, very important,” said Dr. Grines, chair of cardiology at Hofstra University, Hempstead, N.Y.
The updated full 3-year data show a trend, albeit not statistically significant, for higher all-cause mortality in the PCI group, by a margin of 8% versus 5.8% with CABG. When asked about it, Dr. Baron said she and her coinvestigators took a closer look and determined that the cardiovascular death rate was virtually identical in the two groups.
“You have to wonder if this was just a random signal regarding the non-cardiovascular-associated deaths,” she added.
The EXCEL trial was supported by Abbott Vascular. Dr. Baron reported serving as a consultant to Edwards Lifesciences and St. Jude Medical.
DENVER – Several key validated measures of health status were significantly more favorable a full year after percutaneous coronary intervention using an everolimus-eluting stent than with coronary artery bypass surgery in patients with unprotected left main CAD in the prespecified quality-of-life analysis of the landmark EXCEL trial.
By 3 years of follow-up, there was no longer a difference between the PCI and CABG groups in terms of the various quality-of-life measures, Suzanne J. Baron, MD, reported at the Transcatheter Cardiovascular Therapeutics annual educational meeting. Nor as previously reported was there any significant difference in the primary composite endpoint comprised of all-cause mortality, stroke, or MI.
“My take away from this is that these results provide an ideal opportunity to give patients a choice about which choice they would want: An earlier recovery with angioplasty versus really similar outcomes long-term with either procedure. For me, these EXCEL results make me feel that angioplasty for less complex coronary disease is really probably the preferred option,” said John A. Spertus, MD, director of health outcomes research at Saint Luke’s Mid America Heart Institute and professor of medicine at the University of Missouri-Kansas City.
“The faster recovery with PCI, the similar angina relief after 3 years, and also the less depression with PCI, which is an important finding, I think – all this goes in favor of PCI for left main disease,” commented Evald H. Christiansen, MD, a cardiologist at Aarhus (Denmark) University and senior investigator in the NOBLE trial (Lancet. 2016 Dec 3;388[10061]:2743-52), which randomized patients to CABG or a stent that’s no longer marketed.
The previously published clinical outcomes of EXCEL (N Engl J Med. 2016 Dec 8;375[23]:2223-35) were based upon a median 3 years of follow-up. Dr. Baron presented updated outcomes in which all study participants had completed the full 3 years of follow-up. The results were little changed: The primary composite endpoint of all-cause mortality, stroke, or MI occurred in 15.2% of the group treated with the everolimus-eluting Xience stent and was closely similar at 14.7% of the CABG patients, while the 12.5% repeat revascularization rate in the PCI arm was significantly greater than the 7.4% rate with CABG.
But the prespecified EXCEL quality-of-life substudy with assessments at baseline, 1 month, 1 year, and 3 years in 1,788 participants is all new information. Among the highlights: The proportion of patients with clinically significant depression as defined by a Patient Health Questionnaire 8 (PHQ-8) score of 10 or more was 21% at baseline in both groups; 8% in the PCI group, compared with 19% in the CABG arm at 1 month; and 8% in the PCI arm versus 12% with CABG at 12 months of follow-up, with the differences at both time points being significant. By 3 years, the rate was 8%-9% in both groups, reported Dr. Baron of Saint Luke’s Mid America Health Institute and the University of Missouri-Kansas City.
“We now have a new treatment for depression: PCI,” quipped session moderator Gregg W. Stone, MD, professor of medicine at Columbia University in New York, who was lead investigator in EXCEL.
Also, scores on the SF-12 physical summary scale improved sharply from a baseline of 39 points in the PCI group during the first month of follow-up while worsening in the CABG group, such that at 1 month the between-group difference averaged 8.2 points. The gap narrowed over the next 11 months, and by 1 year the CABG patients had caught up.
Scores on the Seattle Angina Questionnaire and the Rose Dyspnea Scale were significantly better in the PCI group than the CABG arm at 1 month, but at 12 and 36 months the two groups were indistinguishable in these domains.
Dr. Spertus, who is credited with inventing both the Seattle Angina Questionnaire and the Kansas City Cardiomyopathy Questionnaire, said that in the context of EXCEL he puts more stock in the SF-12 and PHQ-8 results than the angina and dyspnea measures.
Jonathan Hill, MD, an interventional cardiologist at King’s College London, said the EXCEL quality-of-life substudy provides a valuable picture of the real-life impact of sternotomy.
“We mustn’t underplay that, the months and even up to a year of your life for recovery from the revascularization procedure, compared with days of recovery time with PCI. Patients want the option of PCI if it’s available. This data really vindicates that decision making,” he said.
“I think we minimize the recovery period from CABG. People talk a lot about outcomes at 3 years and 5 years, but look at this prolonged recovery. I think that’s very, very important,” said Dr. Grines, chair of cardiology at Hofstra University, Hempstead, N.Y.
The updated full 3-year data show a trend, albeit not statistically significant, for higher all-cause mortality in the PCI group, by a margin of 8% versus 5.8% with CABG. When asked about it, Dr. Baron said she and her coinvestigators took a closer look and determined that the cardiovascular death rate was virtually identical in the two groups.
“You have to wonder if this was just a random signal regarding the non-cardiovascular-associated deaths,” she added.
The EXCEL trial was supported by Abbott Vascular. Dr. Baron reported serving as a consultant to Edwards Lifesciences and St. Jude Medical.
DENVER – Several key validated measures of health status were significantly more favorable a full year after percutaneous coronary intervention using an everolimus-eluting stent than with coronary artery bypass surgery in patients with unprotected left main CAD in the prespecified quality-of-life analysis of the landmark EXCEL trial.
By 3 years of follow-up, there was no longer a difference between the PCI and CABG groups in terms of the various quality-of-life measures, Suzanne J. Baron, MD, reported at the Transcatheter Cardiovascular Therapeutics annual educational meeting. Nor as previously reported was there any significant difference in the primary composite endpoint comprised of all-cause mortality, stroke, or MI.
“My take away from this is that these results provide an ideal opportunity to give patients a choice about which choice they would want: An earlier recovery with angioplasty versus really similar outcomes long-term with either procedure. For me, these EXCEL results make me feel that angioplasty for less complex coronary disease is really probably the preferred option,” said John A. Spertus, MD, director of health outcomes research at Saint Luke’s Mid America Heart Institute and professor of medicine at the University of Missouri-Kansas City.
“The faster recovery with PCI, the similar angina relief after 3 years, and also the less depression with PCI, which is an important finding, I think – all this goes in favor of PCI for left main disease,” commented Evald H. Christiansen, MD, a cardiologist at Aarhus (Denmark) University and senior investigator in the NOBLE trial (Lancet. 2016 Dec 3;388[10061]:2743-52), which randomized patients to CABG or a stent that’s no longer marketed.
The previously published clinical outcomes of EXCEL (N Engl J Med. 2016 Dec 8;375[23]:2223-35) were based upon a median 3 years of follow-up. Dr. Baron presented updated outcomes in which all study participants had completed the full 3 years of follow-up. The results were little changed: The primary composite endpoint of all-cause mortality, stroke, or MI occurred in 15.2% of the group treated with the everolimus-eluting Xience stent and was closely similar at 14.7% of the CABG patients, while the 12.5% repeat revascularization rate in the PCI arm was significantly greater than the 7.4% rate with CABG.
But the prespecified EXCEL quality-of-life substudy with assessments at baseline, 1 month, 1 year, and 3 years in 1,788 participants is all new information. Among the highlights: The proportion of patients with clinically significant depression as defined by a Patient Health Questionnaire 8 (PHQ-8) score of 10 or more was 21% at baseline in both groups; 8% in the PCI group, compared with 19% in the CABG arm at 1 month; and 8% in the PCI arm versus 12% with CABG at 12 months of follow-up, with the differences at both time points being significant. By 3 years, the rate was 8%-9% in both groups, reported Dr. Baron of Saint Luke’s Mid America Health Institute and the University of Missouri-Kansas City.
“We now have a new treatment for depression: PCI,” quipped session moderator Gregg W. Stone, MD, professor of medicine at Columbia University in New York, who was lead investigator in EXCEL.
Also, scores on the SF-12 physical summary scale improved sharply from a baseline of 39 points in the PCI group during the first month of follow-up while worsening in the CABG group, such that at 1 month the between-group difference averaged 8.2 points. The gap narrowed over the next 11 months, and by 1 year the CABG patients had caught up.
Scores on the Seattle Angina Questionnaire and the Rose Dyspnea Scale were significantly better in the PCI group than the CABG arm at 1 month, but at 12 and 36 months the two groups were indistinguishable in these domains.
Dr. Spertus, who is credited with inventing both the Seattle Angina Questionnaire and the Kansas City Cardiomyopathy Questionnaire, said that in the context of EXCEL he puts more stock in the SF-12 and PHQ-8 results than the angina and dyspnea measures.
Jonathan Hill, MD, an interventional cardiologist at King’s College London, said the EXCEL quality-of-life substudy provides a valuable picture of the real-life impact of sternotomy.
“We mustn’t underplay that, the months and even up to a year of your life for recovery from the revascularization procedure, compared with days of recovery time with PCI. Patients want the option of PCI if it’s available. This data really vindicates that decision making,” he said.
“I think we minimize the recovery period from CABG. People talk a lot about outcomes at 3 years and 5 years, but look at this prolonged recovery. I think that’s very, very important,” said Dr. Grines, chair of cardiology at Hofstra University, Hempstead, N.Y.
The updated full 3-year data show a trend, albeit not statistically significant, for higher all-cause mortality in the PCI group, by a margin of 8% versus 5.8% with CABG. When asked about it, Dr. Baron said she and her coinvestigators took a closer look and determined that the cardiovascular death rate was virtually identical in the two groups.
“You have to wonder if this was just a random signal regarding the non-cardiovascular-associated deaths,” she added.
The EXCEL trial was supported by Abbott Vascular. Dr. Baron reported serving as a consultant to Edwards Lifesciences and St. Jude Medical.
AT TCT 2017
Key clinical point:
Major finding: The rate of clinically significant depression 1 year after revascularization of unprotected left main CAD via PCI using an everolimus-eluting stent was 8%, significantly lower than the 12% rate in CABG patients.
Data source: This was a prespecified prospective quality-of-life substudy featuring 3 years of follow-up in 1,788 patients randomized to PCI or CABG.
Disclosures: The EXCEL trial was supported by Abbott Vascular. The presenter reported serving as a consultant to Edwards Lifesciences and St. Jude Medical.
Panel votes against universal blood donor screens for Zika virus
SILVER SPRING, MD – Universal testing of individual blood donations for the presence of Zika virus was unanimously rejected by voting members of the Food and Drug Administration’s Blood Products Advisory Committee at a December 1 meeting.
Universal individual donor testing, while comprehensive, is resource intensive and places a burden on the blood system that is not outweighed by the benefits, 10 of the 11 committee members concluded. The other committee member could not be reached by phone for this vote.
The committee instead recommended by a vote of 10 to 1 that mini-pool nucleic acid testing (MP-NAT) be performed in all states and territories with known cases of Zika virus infection and the presence of A. aegypti mosquitoes, as well as in states and territories with a high number of travelers from areas with Zika virus infections. Also, the committee members agreed that a trigger needs to be defined for when to undertake universal individual donor nucleic acid testing (ID-NAT) in those areas.
Additionally, the committee agreed that it was not necessary to maintain a Zika virus-negative blood inventory for at-risk patients, such as pregnant women and newborns. Zika virus, a vector-borne disease carried by the Aedes aegypti and Aedes albopictus mosquitoes, has also been transmitted via sexual contact and blood transfusion. Infection has been linked to fetal loss and microcephaly in the offspring of infected pregnant women. Other neurological disorders, including Guillain-Barré Syndrome, also have been linked to Zika virus infection.
Noting the complexity of managing an inventory of tested and non-tested blood, the committee rejected the separate inventory approach by a vote of 9 to 2.*
The panel was clearly divided on the possibility of eliminating all Zika virus testing in some states and territories; 5 members supported this measure, 4 opposed it, and 2 abstained from voting.
The panel unanimously rejected using screening questionnaires to determine whether to selectively test individual at-risk donors in areas with active vector-borne Zika virus infections. This option was considered particularly troublesome, they agreed, because it relies on the use of nonspecific, insensitive, and error-prone questionnaires.
Some level of Zika virus testing is needed to safeguard blood products, the committee said. Eliminating all Zika virus testing of blood products would open the door for infections via transfusion and would diminish preparedness against a potential epidemic, they unanimously determined.
Prior to voting, the committee listened to presentations on the epidemiology of Zika virus infections, the effectiveness of screening tests, and the risk for transmission via transfusion.
Carolyn Gould, MD, of the Centers for Disease Control and Prevention, Atlanta, reported that the number of laboratory-confirmed Zika virus infections in 2016 was 4,830 for travelers to endemic areas and 224 for locally-acquired cases. In 2017, those numbers dropped to 344 confirmed cases for travelers and 2 for locally-acquired cases.
More than 4 million blood donations in the United States and Puerto Rico have been screened for Zika virus RNA using the cobas assay, which is now FDA approved. The overall confirmed positive rate of Zika virus is 0.0007% in donations from the continental United States (29 positive results in 4,341,770 donations) and 0.326% in donations from Puerto Rico (356 out of 111,808 donations) based on data obtained from May 23, 2016 to October 7, 2017, according to Tony Hardiman, Blood Screening, Life Cycle Leader at Roche Molecular Systems.
Of the Zika virus-positive donors who were available for follow up, 23 of 27 had traveled to Zika-active areas, including 3 cases associated with domestic travel to Florida. “I was surprised that 4 of the 29 were from Cuba, but it does seem, as we just saw, (that) an increasing number are coming out from Cuba, from travel to Cuba,” Mr. Hardiman said during his presentation to the committee.
Findings concerning viral RNA duration in blood and other body fluids were presented by Michael Busch, MD of the University of California, San Francisco, who spoke during the public hearing portion of the meeting.**
According to Dr. Busch, blood is likely not infectious to others once donors develop Zika virus-neutralizing antibodies and their viral load levels become very low.
Based on his review of various studies, Dr. Busch concluded that mini-pool testing options with triggers for individual testing are appropriate and effective for detecting Zika virus in endemic areas.
“In Puerto Rico, within a day of picking up a mini-pool positive [result}, we would have ID-NAT in place,” Dr. Busch said. “The mini-pool testing is picking up 90% of those at highest risk.”
The committee recommendations serve as guidance to the FDA, which is not obligated to follow the committee’s recommendations.
*Correction 12/14/17: An earlier version of this story misstated the vote on maintaining a Zika virus-negative blood inventory for at-risk patients. The advisory committee voted against that approach.
**Correction 12/14/17: Dr. Michael Busch's name was misstated in an earlier version of this article.
SILVER SPRING, MD – Universal testing of individual blood donations for the presence of Zika virus was unanimously rejected by voting members of the Food and Drug Administration’s Blood Products Advisory Committee at a December 1 meeting.
Universal individual donor testing, while comprehensive, is resource intensive and places a burden on the blood system that is not outweighed by the benefits, 10 of the 11 committee members concluded. The other committee member could not be reached by phone for this vote.
The committee instead recommended by a vote of 10 to 1 that mini-pool nucleic acid testing (MP-NAT) be performed in all states and territories with known cases of Zika virus infection and the presence of A. aegypti mosquitoes, as well as in states and territories with a high number of travelers from areas with Zika virus infections. Also, the committee members agreed that a trigger needs to be defined for when to undertake universal individual donor nucleic acid testing (ID-NAT) in those areas.
Additionally, the committee agreed that it was not necessary to maintain a Zika virus-negative blood inventory for at-risk patients, such as pregnant women and newborns. Zika virus, a vector-borne disease carried by the Aedes aegypti and Aedes albopictus mosquitoes, has also been transmitted via sexual contact and blood transfusion. Infection has been linked to fetal loss and microcephaly in the offspring of infected pregnant women. Other neurological disorders, including Guillain-Barré Syndrome, also have been linked to Zika virus infection.
Noting the complexity of managing an inventory of tested and non-tested blood, the committee rejected the separate inventory approach by a vote of 9 to 2.*
The panel was clearly divided on the possibility of eliminating all Zika virus testing in some states and territories; 5 members supported this measure, 4 opposed it, and 2 abstained from voting.
The panel unanimously rejected using screening questionnaires to determine whether to selectively test individual at-risk donors in areas with active vector-borne Zika virus infections. This option was considered particularly troublesome, they agreed, because it relies on the use of nonspecific, insensitive, and error-prone questionnaires.
Some level of Zika virus testing is needed to safeguard blood products, the committee said. Eliminating all Zika virus testing of blood products would open the door for infections via transfusion and would diminish preparedness against a potential epidemic, they unanimously determined.
Prior to voting, the committee listened to presentations on the epidemiology of Zika virus infections, the effectiveness of screening tests, and the risk for transmission via transfusion.
Carolyn Gould, MD, of the Centers for Disease Control and Prevention, Atlanta, reported that the number of laboratory-confirmed Zika virus infections in 2016 was 4,830 for travelers to endemic areas and 224 for locally-acquired cases. In 2017, those numbers dropped to 344 confirmed cases for travelers and 2 for locally-acquired cases.
More than 4 million blood donations in the United States and Puerto Rico have been screened for Zika virus RNA using the cobas assay, which is now FDA approved. The overall confirmed positive rate of Zika virus is 0.0007% in donations from the continental United States (29 positive results in 4,341,770 donations) and 0.326% in donations from Puerto Rico (356 out of 111,808 donations) based on data obtained from May 23, 2016 to October 7, 2017, according to Tony Hardiman, Blood Screening, Life Cycle Leader at Roche Molecular Systems.
Of the Zika virus-positive donors who were available for follow up, 23 of 27 had traveled to Zika-active areas, including 3 cases associated with domestic travel to Florida. “I was surprised that 4 of the 29 were from Cuba, but it does seem, as we just saw, (that) an increasing number are coming out from Cuba, from travel to Cuba,” Mr. Hardiman said during his presentation to the committee.
Findings concerning viral RNA duration in blood and other body fluids were presented by Michael Busch, MD of the University of California, San Francisco, who spoke during the public hearing portion of the meeting.**
According to Dr. Busch, blood is likely not infectious to others once donors develop Zika virus-neutralizing antibodies and their viral load levels become very low.
Based on his review of various studies, Dr. Busch concluded that mini-pool testing options with triggers for individual testing are appropriate and effective for detecting Zika virus in endemic areas.
“In Puerto Rico, within a day of picking up a mini-pool positive [result}, we would have ID-NAT in place,” Dr. Busch said. “The mini-pool testing is picking up 90% of those at highest risk.”
The committee recommendations serve as guidance to the FDA, which is not obligated to follow the committee’s recommendations.
*Correction 12/14/17: An earlier version of this story misstated the vote on maintaining a Zika virus-negative blood inventory for at-risk patients. The advisory committee voted against that approach.
**Correction 12/14/17: Dr. Michael Busch's name was misstated in an earlier version of this article.
SILVER SPRING, MD – Universal testing of individual blood donations for the presence of Zika virus was unanimously rejected by voting members of the Food and Drug Administration’s Blood Products Advisory Committee at a December 1 meeting.
Universal individual donor testing, while comprehensive, is resource intensive and places a burden on the blood system that is not outweighed by the benefits, 10 of the 11 committee members concluded. The other committee member could not be reached by phone for this vote.
The committee instead recommended by a vote of 10 to 1 that mini-pool nucleic acid testing (MP-NAT) be performed in all states and territories with known cases of Zika virus infection and the presence of A. aegypti mosquitoes, as well as in states and territories with a high number of travelers from areas with Zika virus infections. Also, the committee members agreed that a trigger needs to be defined for when to undertake universal individual donor nucleic acid testing (ID-NAT) in those areas.
Additionally, the committee agreed that it was not necessary to maintain a Zika virus-negative blood inventory for at-risk patients, such as pregnant women and newborns. Zika virus, a vector-borne disease carried by the Aedes aegypti and Aedes albopictus mosquitoes, has also been transmitted via sexual contact and blood transfusion. Infection has been linked to fetal loss and microcephaly in the offspring of infected pregnant women. Other neurological disorders, including Guillain-Barré Syndrome, also have been linked to Zika virus infection.
Noting the complexity of managing an inventory of tested and non-tested blood, the committee rejected the separate inventory approach by a vote of 9 to 2.*
The panel was clearly divided on the possibility of eliminating all Zika virus testing in some states and territories; 5 members supported this measure, 4 opposed it, and 2 abstained from voting.
The panel unanimously rejected using screening questionnaires to determine whether to selectively test individual at-risk donors in areas with active vector-borne Zika virus infections. This option was considered particularly troublesome, they agreed, because it relies on the use of nonspecific, insensitive, and error-prone questionnaires.
Some level of Zika virus testing is needed to safeguard blood products, the committee said. Eliminating all Zika virus testing of blood products would open the door for infections via transfusion and would diminish preparedness against a potential epidemic, they unanimously determined.
Prior to voting, the committee listened to presentations on the epidemiology of Zika virus infections, the effectiveness of screening tests, and the risk for transmission via transfusion.
Carolyn Gould, MD, of the Centers for Disease Control and Prevention, Atlanta, reported that the number of laboratory-confirmed Zika virus infections in 2016 was 4,830 for travelers to endemic areas and 224 for locally-acquired cases. In 2017, those numbers dropped to 344 confirmed cases for travelers and 2 for locally-acquired cases.
More than 4 million blood donations in the United States and Puerto Rico have been screened for Zika virus RNA using the cobas assay, which is now FDA approved. The overall confirmed positive rate of Zika virus is 0.0007% in donations from the continental United States (29 positive results in 4,341,770 donations) and 0.326% in donations from Puerto Rico (356 out of 111,808 donations) based on data obtained from May 23, 2016 to October 7, 2017, according to Tony Hardiman, Blood Screening, Life Cycle Leader at Roche Molecular Systems.
Of the Zika virus-positive donors who were available for follow up, 23 of 27 had traveled to Zika-active areas, including 3 cases associated with domestic travel to Florida. “I was surprised that 4 of the 29 were from Cuba, but it does seem, as we just saw, (that) an increasing number are coming out from Cuba, from travel to Cuba,” Mr. Hardiman said during his presentation to the committee.
Findings concerning viral RNA duration in blood and other body fluids were presented by Michael Busch, MD of the University of California, San Francisco, who spoke during the public hearing portion of the meeting.**
According to Dr. Busch, blood is likely not infectious to others once donors develop Zika virus-neutralizing antibodies and their viral load levels become very low.
Based on his review of various studies, Dr. Busch concluded that mini-pool testing options with triggers for individual testing are appropriate and effective for detecting Zika virus in endemic areas.
“In Puerto Rico, within a day of picking up a mini-pool positive [result}, we would have ID-NAT in place,” Dr. Busch said. “The mini-pool testing is picking up 90% of those at highest risk.”
The committee recommendations serve as guidance to the FDA, which is not obligated to follow the committee’s recommendations.
*Correction 12/14/17: An earlier version of this story misstated the vote on maintaining a Zika virus-negative blood inventory for at-risk patients. The advisory committee voted against that approach.
**Correction 12/14/17: Dr. Michael Busch's name was misstated in an earlier version of this article.
AT AN FDA ADVISORY COMMITTEE MEETING
Walking has beneficial cognitive effects in amyloid-positive older adults
BOSTON – Walking appears to moderate cognitive decline in people with elevated brain amyloid, a 4-year observational study has determined.
Among a group of cognitively normal older adults with beta-amyloid brain plaques, those who walked the most experienced significantly less decline in memory and thinking than those who didn’t walk much, Dylan Kirn reported at the Clinical Trials on Alzheimer’s Disease conference. Walking didn’t affect any of the hallmark biomarkers of Alzheimer’s disease, such as brain glucose utilization, amyloid accumulation, or hippocampal volume, but it was associated with significantly better cognitive scores on a composite measure of memory over time.
“We should be careful in interpreting these data, because this is an observational cohort and we can’t make claims regarding causality or the mechanism by which physical activity may be influencing cognitive decline,” said Mr. Kirn of the Athinoula A. Martinos Center for Biomedical Imaging at Massachusetts General Hospital, Boston. “But I find these results interesting and novel, and I think they support further investigation.”
The walking study comprised 255 subjects with a mean age of 73 years. They were highly educated, with a mean of 16 years’ schooling. About 24% were amyloid-positive by PET imaging. All were cognitively normal, with a Clinical Dementia Rating scale score of 0. Activity was established at baseline with a pedometer, which was worn for 7 consecutive days; only those who walked at least 100 steps per day were included in the analysis.
In addition to amyloid PET imaging, subjects also underwent a 18F-fluorodeoxyglucose (FDG) PET scan to assess brain glucose utilization, and MRI to measure hippocampal volume changes and assess white matter hyperintensities (WMHs). Changes in all of these biomarkers can herald the onset of Alzheimer’s.
The primary outcome was the relationship between physical activity as measured by number of walking steps per day and changes on the Preclinical Alzheimer’s Cognitive Composite (PACC) test. This relatively new cognitive scale is an increasingly popular item in clinical trials. The PACC is a composite of the Digit Symbol Substitution Test score from the Wechsler Adult Intelligence Scale–Revised, the Mini Mental State Exam, the Total Recall score from the Free and Cued Selective Reminding Test, and the Delayed Recall score on the Logical Memory IIa sub-test from the Wechsler Memory Scale. It correlates well with amyloid accumulation in the brain, Mr. Kirn said.
The cohort was followed for up to 6 years (median of 4), and PACC scores were calculated annually. The investigators looked at the relationship between walking at baseline and PACC decline over the study period in two multivariate models: One controlling for age, sex, and years of education, and the second for those variables plus the biomarkers of cortical WMHs, bilateral hippocampal volume (HV), and FDG-PET in brain regions typically affected by Alzheimer’s.
Physical activity was divided into tertiles by the average number of steps per day over the 7-day measuring period: Mean (5,616 steps), one standard deviation above mean (high; 8,482 steps), and one standard deviation below mean (low, 2,751 steps). Amyloid-positive patients were further divided into those with high brain amyloid load and those with low amyloid brain load.
There were no significant relationships between any of the biomarkers and any level of physical activity in either of the analyses, Mr. Kirn said. However, when looking at the time-linked changes in the PACC, significant differences did emerge. Subjects who walked at least the mean number of steps per day were much more likely to maintain a stable cognitive score, while those who walked the fewest steps declined about a quarter of a point on the PACC. The difference in decline between the high activity and low activity subjects was statistically significant, even when the investigators controlled for amyloid burden and the other hallmark Alzheimer’s biomarkers.
The level of physical activity at baseline was a particularly strong predictor of cognitive health among amyloid-positive subjects. Those in the high-activity group maintained a steady score on the PACC. Those in the mean activity group declined slightly, and those in the low activity group showed a sharp decline, losing almost a full point on the PACC by the end of follow-up.
In the amyloid-negative group, there was no association between cognition and activity. All the groups improved their PACC scores over the study period, probably reflecting a practice effect, Mr. Kirn said.
Finally, he split the amyloid-positive group into subjects with low and high brain amyloid levels. “We observed that physical activity was significantly predictive of cognitive decline in high-amyloid participants, but not in low-amyloid participants,” he said. “Individuals with high amyloid and low physical activity at baseline had the steepest decline in cognition over time. But in those with high amyloid and high physical activity at baseline, we didn’t see a tremendous amount of decline.”
The study suggests that pedometers may have a place in stratifying patients for clinical trials, or assessing cognitive risk in elderly subjects. “Most studies that have looked at physical activity and dementia use a self-reported activity level, so the results have been varied,” Mr. Kirn said. “These findings support consideration of objectively measured physical activity in clinical research, and perhaps in stratification for risk of cognitive decline.”
He had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
BOSTON – Walking appears to moderate cognitive decline in people with elevated brain amyloid, a 4-year observational study has determined.
Among a group of cognitively normal older adults with beta-amyloid brain plaques, those who walked the most experienced significantly less decline in memory and thinking than those who didn’t walk much, Dylan Kirn reported at the Clinical Trials on Alzheimer’s Disease conference. Walking didn’t affect any of the hallmark biomarkers of Alzheimer’s disease, such as brain glucose utilization, amyloid accumulation, or hippocampal volume, but it was associated with significantly better cognitive scores on a composite measure of memory over time.
“We should be careful in interpreting these data, because this is an observational cohort and we can’t make claims regarding causality or the mechanism by which physical activity may be influencing cognitive decline,” said Mr. Kirn of the Athinoula A. Martinos Center for Biomedical Imaging at Massachusetts General Hospital, Boston. “But I find these results interesting and novel, and I think they support further investigation.”
The walking study comprised 255 subjects with a mean age of 73 years. They were highly educated, with a mean of 16 years’ schooling. About 24% were amyloid-positive by PET imaging. All were cognitively normal, with a Clinical Dementia Rating scale score of 0. Activity was established at baseline with a pedometer, which was worn for 7 consecutive days; only those who walked at least 100 steps per day were included in the analysis.
In addition to amyloid PET imaging, subjects also underwent a 18F-fluorodeoxyglucose (FDG) PET scan to assess brain glucose utilization, and MRI to measure hippocampal volume changes and assess white matter hyperintensities (WMHs). Changes in all of these biomarkers can herald the onset of Alzheimer’s.
The primary outcome was the relationship between physical activity as measured by number of walking steps per day and changes on the Preclinical Alzheimer’s Cognitive Composite (PACC) test. This relatively new cognitive scale is an increasingly popular item in clinical trials. The PACC is a composite of the Digit Symbol Substitution Test score from the Wechsler Adult Intelligence Scale–Revised, the Mini Mental State Exam, the Total Recall score from the Free and Cued Selective Reminding Test, and the Delayed Recall score on the Logical Memory IIa sub-test from the Wechsler Memory Scale. It correlates well with amyloid accumulation in the brain, Mr. Kirn said.
The cohort was followed for up to 6 years (median of 4), and PACC scores were calculated annually. The investigators looked at the relationship between walking at baseline and PACC decline over the study period in two multivariate models: One controlling for age, sex, and years of education, and the second for those variables plus the biomarkers of cortical WMHs, bilateral hippocampal volume (HV), and FDG-PET in brain regions typically affected by Alzheimer’s.
Physical activity was divided into tertiles by the average number of steps per day over the 7-day measuring period: Mean (5,616 steps), one standard deviation above mean (high; 8,482 steps), and one standard deviation below mean (low, 2,751 steps). Amyloid-positive patients were further divided into those with high brain amyloid load and those with low amyloid brain load.
There were no significant relationships between any of the biomarkers and any level of physical activity in either of the analyses, Mr. Kirn said. However, when looking at the time-linked changes in the PACC, significant differences did emerge. Subjects who walked at least the mean number of steps per day were much more likely to maintain a stable cognitive score, while those who walked the fewest steps declined about a quarter of a point on the PACC. The difference in decline between the high activity and low activity subjects was statistically significant, even when the investigators controlled for amyloid burden and the other hallmark Alzheimer’s biomarkers.
The level of physical activity at baseline was a particularly strong predictor of cognitive health among amyloid-positive subjects. Those in the high-activity group maintained a steady score on the PACC. Those in the mean activity group declined slightly, and those in the low activity group showed a sharp decline, losing almost a full point on the PACC by the end of follow-up.
In the amyloid-negative group, there was no association between cognition and activity. All the groups improved their PACC scores over the study period, probably reflecting a practice effect, Mr. Kirn said.
Finally, he split the amyloid-positive group into subjects with low and high brain amyloid levels. “We observed that physical activity was significantly predictive of cognitive decline in high-amyloid participants, but not in low-amyloid participants,” he said. “Individuals with high amyloid and low physical activity at baseline had the steepest decline in cognition over time. But in those with high amyloid and high physical activity at baseline, we didn’t see a tremendous amount of decline.”
The study suggests that pedometers may have a place in stratifying patients for clinical trials, or assessing cognitive risk in elderly subjects. “Most studies that have looked at physical activity and dementia use a self-reported activity level, so the results have been varied,” Mr. Kirn said. “These findings support consideration of objectively measured physical activity in clinical research, and perhaps in stratification for risk of cognitive decline.”
He had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
BOSTON – Walking appears to moderate cognitive decline in people with elevated brain amyloid, a 4-year observational study has determined.
Among a group of cognitively normal older adults with beta-amyloid brain plaques, those who walked the most experienced significantly less decline in memory and thinking than those who didn’t walk much, Dylan Kirn reported at the Clinical Trials on Alzheimer’s Disease conference. Walking didn’t affect any of the hallmark biomarkers of Alzheimer’s disease, such as brain glucose utilization, amyloid accumulation, or hippocampal volume, but it was associated with significantly better cognitive scores on a composite measure of memory over time.
“We should be careful in interpreting these data, because this is an observational cohort and we can’t make claims regarding causality or the mechanism by which physical activity may be influencing cognitive decline,” said Mr. Kirn of the Athinoula A. Martinos Center for Biomedical Imaging at Massachusetts General Hospital, Boston. “But I find these results interesting and novel, and I think they support further investigation.”
The walking study comprised 255 subjects with a mean age of 73 years. They were highly educated, with a mean of 16 years’ schooling. About 24% were amyloid-positive by PET imaging. All were cognitively normal, with a Clinical Dementia Rating scale score of 0. Activity was established at baseline with a pedometer, which was worn for 7 consecutive days; only those who walked at least 100 steps per day were included in the analysis.
In addition to amyloid PET imaging, subjects also underwent a 18F-fluorodeoxyglucose (FDG) PET scan to assess brain glucose utilization, and MRI to measure hippocampal volume changes and assess white matter hyperintensities (WMHs). Changes in all of these biomarkers can herald the onset of Alzheimer’s.
The primary outcome was the relationship between physical activity as measured by number of walking steps per day and changes on the Preclinical Alzheimer’s Cognitive Composite (PACC) test. This relatively new cognitive scale is an increasingly popular item in clinical trials. The PACC is a composite of the Digit Symbol Substitution Test score from the Wechsler Adult Intelligence Scale–Revised, the Mini Mental State Exam, the Total Recall score from the Free and Cued Selective Reminding Test, and the Delayed Recall score on the Logical Memory IIa sub-test from the Wechsler Memory Scale. It correlates well with amyloid accumulation in the brain, Mr. Kirn said.
The cohort was followed for up to 6 years (median of 4), and PACC scores were calculated annually. The investigators looked at the relationship between walking at baseline and PACC decline over the study period in two multivariate models: One controlling for age, sex, and years of education, and the second for those variables plus the biomarkers of cortical WMHs, bilateral hippocampal volume (HV), and FDG-PET in brain regions typically affected by Alzheimer’s.
Physical activity was divided into tertiles by the average number of steps per day over the 7-day measuring period: Mean (5,616 steps), one standard deviation above mean (high; 8,482 steps), and one standard deviation below mean (low, 2,751 steps). Amyloid-positive patients were further divided into those with high brain amyloid load and those with low amyloid brain load.
There were no significant relationships between any of the biomarkers and any level of physical activity in either of the analyses, Mr. Kirn said. However, when looking at the time-linked changes in the PACC, significant differences did emerge. Subjects who walked at least the mean number of steps per day were much more likely to maintain a stable cognitive score, while those who walked the fewest steps declined about a quarter of a point on the PACC. The difference in decline between the high activity and low activity subjects was statistically significant, even when the investigators controlled for amyloid burden and the other hallmark Alzheimer’s biomarkers.
The level of physical activity at baseline was a particularly strong predictor of cognitive health among amyloid-positive subjects. Those in the high-activity group maintained a steady score on the PACC. Those in the mean activity group declined slightly, and those in the low activity group showed a sharp decline, losing almost a full point on the PACC by the end of follow-up.
In the amyloid-negative group, there was no association between cognition and activity. All the groups improved their PACC scores over the study period, probably reflecting a practice effect, Mr. Kirn said.
Finally, he split the amyloid-positive group into subjects with low and high brain amyloid levels. “We observed that physical activity was significantly predictive of cognitive decline in high-amyloid participants, but not in low-amyloid participants,” he said. “Individuals with high amyloid and low physical activity at baseline had the steepest decline in cognition over time. But in those with high amyloid and high physical activity at baseline, we didn’t see a tremendous amount of decline.”
The study suggests that pedometers may have a place in stratifying patients for clinical trials, or assessing cognitive risk in elderly subjects. “Most studies that have looked at physical activity and dementia use a self-reported activity level, so the results have been varied,” Mr. Kirn said. “These findings support consideration of objectively measured physical activity in clinical research, and perhaps in stratification for risk of cognitive decline.”
He had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
AT CTAD
Key clinical point:
Major finding: Subjects with high amyloid burden who walked the least declined by almost 1 point on the PACC score; high-amyloid subjects who walked the most stayed at their baseline score.
Data source: A prospective, observational study comprising 255 elderly subjects with normal cognition.
Disclosures: The presenter had no financial disclosures.
Benefit of dabigatran over warfarin persists in AF patient subgroups undergoing PCI
ANAHEIM, CALIF. – The benefit of dabigatran dual therapy versus warfarin triple therapy after percutaneous coronary intervention in patients with atrial fibrillation was consistent whether patients had drug-eluting or bare-metal stents, concomitant treatment with ticagrelor or clopidogrel, or acute coronary syndrome or stable disease as the indication for PCI, according to a subgroup analysis of the RE-DUAL PCI trial.
The trial, presented at the American Heart Association scientific sessions, randomized 2,725 patients to triple therapy with warfarin plus a P2Y12 inhibitor (clopidogrel or ticagrelor) and aspirin – the triple therapy group – or dabigatran 110 mg or 150 mg twice daily plus clopidogrel or ticagrelor – the dual therapy groups (N Engl J Med. 2017 Oct 19;377[16]:1513-24).
After a mean follow-up 14 months, the incidence of the major or clinically relevant nonmajor bleeding was 15.4% in the 110-mg dual-therapy group (hazard ratio, 0.52; 95% CI, 0.42-0.63; P less than .001) and 20.2% in the 150-mg dual-therapy group (HR, 0.72; 95% CI, 0.58-0.88; P less than .001), versus about 26% with triple-therapy.
The incidence of the composite efficacy endpoint – death, unplanned revascularization, myocardial infarction, stroke, or systemic embolism – was 13.7% in the two dual-therapy groups versus 13.4% with triple-therapy (HR, 1.04; 95% CI, 0.84-1.29; P = .005).
The investigators found consistent results when they analyzed their prespecified subgroups.
Drug-eluting stents were placed in 83% of patients; the rest had bare metal stents (BMS). The groups were well-balanced, except BMS patients were again more likely to be new to oral anticoagulation. Bleeding, thromboembolic events, and mortality were consistent with the main results regardless of the stent type, Most of the subjects were on clopidogrel, with just 12% on ticagrelor in both the dabigatran and warfarin groups. Ticagrelor patients were more likely to have ACS as their PCI indication and be new to oral anticoagulation. Ticagrelor patients were also more clinically complex, with a higher bleeding risk. Even so, they had relative bleeding risk reduction and efficacy results with dabigatran that were consistent with the overall finding, Dr. Oldgren said.
Patients were eligible for RE-DUAL PCI (Evaluation of Dual Therapy with Dabigatran vs. Triple Therapy with Warfarin in Patients with AF That Undergo a PCI with Stenting) if they had nonvalvular atrial fibrillation and a successful PCI within 120 hours. Those with bioprosthetic or mechanical heart valves, severe renal insufficiency, or other major comorbidities were excluded.
The trial was funded by Boehringer Ingelheim, the maker of dabigatran. Several investigators were employees. Dr. Oldgren is an adviser to Boehringer Ingelheim. Other authors reported financial ties to the company as well.
ANAHEIM, CALIF. – The benefit of dabigatran dual therapy versus warfarin triple therapy after percutaneous coronary intervention in patients with atrial fibrillation was consistent whether patients had drug-eluting or bare-metal stents, concomitant treatment with ticagrelor or clopidogrel, or acute coronary syndrome or stable disease as the indication for PCI, according to a subgroup analysis of the RE-DUAL PCI trial.
The trial, presented at the American Heart Association scientific sessions, randomized 2,725 patients to triple therapy with warfarin plus a P2Y12 inhibitor (clopidogrel or ticagrelor) and aspirin – the triple therapy group – or dabigatran 110 mg or 150 mg twice daily plus clopidogrel or ticagrelor – the dual therapy groups (N Engl J Med. 2017 Oct 19;377[16]:1513-24).
After a mean follow-up 14 months, the incidence of the major or clinically relevant nonmajor bleeding was 15.4% in the 110-mg dual-therapy group (hazard ratio, 0.52; 95% CI, 0.42-0.63; P less than .001) and 20.2% in the 150-mg dual-therapy group (HR, 0.72; 95% CI, 0.58-0.88; P less than .001), versus about 26% with triple-therapy.
The incidence of the composite efficacy endpoint – death, unplanned revascularization, myocardial infarction, stroke, or systemic embolism – was 13.7% in the two dual-therapy groups versus 13.4% with triple-therapy (HR, 1.04; 95% CI, 0.84-1.29; P = .005).
The investigators found consistent results when they analyzed their prespecified subgroups.
Drug-eluting stents were placed in 83% of patients; the rest had bare metal stents (BMS). The groups were well-balanced, except BMS patients were again more likely to be new to oral anticoagulation. Bleeding, thromboembolic events, and mortality were consistent with the main results regardless of the stent type, Most of the subjects were on clopidogrel, with just 12% on ticagrelor in both the dabigatran and warfarin groups. Ticagrelor patients were more likely to have ACS as their PCI indication and be new to oral anticoagulation. Ticagrelor patients were also more clinically complex, with a higher bleeding risk. Even so, they had relative bleeding risk reduction and efficacy results with dabigatran that were consistent with the overall finding, Dr. Oldgren said.
Patients were eligible for RE-DUAL PCI (Evaluation of Dual Therapy with Dabigatran vs. Triple Therapy with Warfarin in Patients with AF That Undergo a PCI with Stenting) if they had nonvalvular atrial fibrillation and a successful PCI within 120 hours. Those with bioprosthetic or mechanical heart valves, severe renal insufficiency, or other major comorbidities were excluded.
The trial was funded by Boehringer Ingelheim, the maker of dabigatran. Several investigators were employees. Dr. Oldgren is an adviser to Boehringer Ingelheim. Other authors reported financial ties to the company as well.
ANAHEIM, CALIF. – The benefit of dabigatran dual therapy versus warfarin triple therapy after percutaneous coronary intervention in patients with atrial fibrillation was consistent whether patients had drug-eluting or bare-metal stents, concomitant treatment with ticagrelor or clopidogrel, or acute coronary syndrome or stable disease as the indication for PCI, according to a subgroup analysis of the RE-DUAL PCI trial.
The trial, presented at the American Heart Association scientific sessions, randomized 2,725 patients to triple therapy with warfarin plus a P2Y12 inhibitor (clopidogrel or ticagrelor) and aspirin – the triple therapy group – or dabigatran 110 mg or 150 mg twice daily plus clopidogrel or ticagrelor – the dual therapy groups (N Engl J Med. 2017 Oct 19;377[16]:1513-24).
After a mean follow-up 14 months, the incidence of the major or clinically relevant nonmajor bleeding was 15.4% in the 110-mg dual-therapy group (hazard ratio, 0.52; 95% CI, 0.42-0.63; P less than .001) and 20.2% in the 150-mg dual-therapy group (HR, 0.72; 95% CI, 0.58-0.88; P less than .001), versus about 26% with triple-therapy.
The incidence of the composite efficacy endpoint – death, unplanned revascularization, myocardial infarction, stroke, or systemic embolism – was 13.7% in the two dual-therapy groups versus 13.4% with triple-therapy (HR, 1.04; 95% CI, 0.84-1.29; P = .005).
The investigators found consistent results when they analyzed their prespecified subgroups.
Drug-eluting stents were placed in 83% of patients; the rest had bare metal stents (BMS). The groups were well-balanced, except BMS patients were again more likely to be new to oral anticoagulation. Bleeding, thromboembolic events, and mortality were consistent with the main results regardless of the stent type, Most of the subjects were on clopidogrel, with just 12% on ticagrelor in both the dabigatran and warfarin groups. Ticagrelor patients were more likely to have ACS as their PCI indication and be new to oral anticoagulation. Ticagrelor patients were also more clinically complex, with a higher bleeding risk. Even so, they had relative bleeding risk reduction and efficacy results with dabigatran that were consistent with the overall finding, Dr. Oldgren said.
Patients were eligible for RE-DUAL PCI (Evaluation of Dual Therapy with Dabigatran vs. Triple Therapy with Warfarin in Patients with AF That Undergo a PCI with Stenting) if they had nonvalvular atrial fibrillation and a successful PCI within 120 hours. Those with bioprosthetic or mechanical heart valves, severe renal insufficiency, or other major comorbidities were excluded.
The trial was funded by Boehringer Ingelheim, the maker of dabigatran. Several investigators were employees. Dr. Oldgren is an adviser to Boehringer Ingelheim. Other authors reported financial ties to the company as well.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: After a mean follow-up of 14 months, the incidence of major or clinically relevant nonmajor bleeding was 15.4% in the 110-mg dual-therapy group (HR, 0.52; 95% CI, 0.42-0.63, P less than .001) and 20.2% in the 150-mg dual-therapy group (HR, 0.72; 95% CI, 0.58-0.88; P less than .001), versus about 26% with triple-therapy.
Data source: Subgroup analysis of RE-DUAL PCI trial
Disclosures: The trial was funded by Boehringer Ingelheim, the maker of dabigatran. Several investigators were employees. Authors disclosed various financial ties to the company.
Plek2 may be therapeutic target in MPNs
New research suggests plecktrin-2 (Plek2) may be a therapeutic target for myeloproliferative neoplasms (MPNs).
Plek2 was previously shown to be involved in red blood cell production.
Now, researchers have found Plek2 is upregulated in patients with JAK2V617F-positive MPNs.
And loss of Plek2 ameliorated JAK2V617F-induced myeloproliferative phenotypes in a mouse model.
Peng Ji, MD, PhD, of Northwestern University in Chicago, Illinois, and his colleagues conducted this research and reported the results in The Journal of Clinical Investigation.
The researchers found that Plek2 was significantly upregulated in patients with JAK2V617F-positive MPNs, including myelofibrosis, essential thrombocythemia, and polycythemia vera.
Plek2 was also upregulated in myeloid, lymphoid, and erythroid cells in a JAK2V617F hematopoietic-specific knock-in mouse model that mimics the pathogenesis of MPNs.
The researchers assessed the effects of turning off Plek2 in this model and found that loss of Plek2 significantly reverted neutrophilia and thrombocytosis, partially reverted reticulocytosis, mildly reduced red blood cell count, significantly reduced megakaryocyte numbers and clusters, and reduced spleen size.
Loss of Plek2 also reduced red blood cell mass, which was the main contributing factor in the reversion of vascular occlusions, according to the researchers. The team detected “widespread vascular occlusions” in mice with Plek2, but mice without Plek2 had “relatively clear vasculature.”
“The risk of thrombosis was not completely cured because there are other factors aside from pleckstrin-2, but we saw a very dramatic amelioration in blood clotting,” Dr Ji said.
Finally, loss of Plek2 improved survival. All mice with Plek2 died at around 30 weeks, but more than 80% of the mice without Plek2 survived beyond 40 weeks.
Dr Ji and his colleagues hope to build upon these findings by developing a Plek2 inhibitor.
“We are looking for a molecule that can bind with pleckstrin-2 and block its functions,” Dr Ji said. “We’ve already screened compounds, and we have about 40 we are testing right now.”
“Mice with pleckstrin-2 deactivated experienced fewer side effects compared to mice without JAK2, so we believe the pleckstrin-2 inhibitor will generate fewer side effects as well.” ![]()
New research suggests plecktrin-2 (Plek2) may be a therapeutic target for myeloproliferative neoplasms (MPNs).
Plek2 was previously shown to be involved in red blood cell production.
Now, researchers have found Plek2 is upregulated in patients with JAK2V617F-positive MPNs.
And loss of Plek2 ameliorated JAK2V617F-induced myeloproliferative phenotypes in a mouse model.
Peng Ji, MD, PhD, of Northwestern University in Chicago, Illinois, and his colleagues conducted this research and reported the results in The Journal of Clinical Investigation.
The researchers found that Plek2 was significantly upregulated in patients with JAK2V617F-positive MPNs, including myelofibrosis, essential thrombocythemia, and polycythemia vera.
Plek2 was also upregulated in myeloid, lymphoid, and erythroid cells in a JAK2V617F hematopoietic-specific knock-in mouse model that mimics the pathogenesis of MPNs.
The researchers assessed the effects of turning off Plek2 in this model and found that loss of Plek2 significantly reverted neutrophilia and thrombocytosis, partially reverted reticulocytosis, mildly reduced red blood cell count, significantly reduced megakaryocyte numbers and clusters, and reduced spleen size.
Loss of Plek2 also reduced red blood cell mass, which was the main contributing factor in the reversion of vascular occlusions, according to the researchers. The team detected “widespread vascular occlusions” in mice with Plek2, but mice without Plek2 had “relatively clear vasculature.”
“The risk of thrombosis was not completely cured because there are other factors aside from pleckstrin-2, but we saw a very dramatic amelioration in blood clotting,” Dr Ji said.
Finally, loss of Plek2 improved survival. All mice with Plek2 died at around 30 weeks, but more than 80% of the mice without Plek2 survived beyond 40 weeks.
Dr Ji and his colleagues hope to build upon these findings by developing a Plek2 inhibitor.
“We are looking for a molecule that can bind with pleckstrin-2 and block its functions,” Dr Ji said. “We’ve already screened compounds, and we have about 40 we are testing right now.”
“Mice with pleckstrin-2 deactivated experienced fewer side effects compared to mice without JAK2, so we believe the pleckstrin-2 inhibitor will generate fewer side effects as well.” ![]()
New research suggests plecktrin-2 (Plek2) may be a therapeutic target for myeloproliferative neoplasms (MPNs).
Plek2 was previously shown to be involved in red blood cell production.
Now, researchers have found Plek2 is upregulated in patients with JAK2V617F-positive MPNs.
And loss of Plek2 ameliorated JAK2V617F-induced myeloproliferative phenotypes in a mouse model.
Peng Ji, MD, PhD, of Northwestern University in Chicago, Illinois, and his colleagues conducted this research and reported the results in The Journal of Clinical Investigation.
The researchers found that Plek2 was significantly upregulated in patients with JAK2V617F-positive MPNs, including myelofibrosis, essential thrombocythemia, and polycythemia vera.
Plek2 was also upregulated in myeloid, lymphoid, and erythroid cells in a JAK2V617F hematopoietic-specific knock-in mouse model that mimics the pathogenesis of MPNs.
The researchers assessed the effects of turning off Plek2 in this model and found that loss of Plek2 significantly reverted neutrophilia and thrombocytosis, partially reverted reticulocytosis, mildly reduced red blood cell count, significantly reduced megakaryocyte numbers and clusters, and reduced spleen size.
Loss of Plek2 also reduced red blood cell mass, which was the main contributing factor in the reversion of vascular occlusions, according to the researchers. The team detected “widespread vascular occlusions” in mice with Plek2, but mice without Plek2 had “relatively clear vasculature.”
“The risk of thrombosis was not completely cured because there are other factors aside from pleckstrin-2, but we saw a very dramatic amelioration in blood clotting,” Dr Ji said.
Finally, loss of Plek2 improved survival. All mice with Plek2 died at around 30 weeks, but more than 80% of the mice without Plek2 survived beyond 40 weeks.
Dr Ji and his colleagues hope to build upon these findings by developing a Plek2 inhibitor.
“We are looking for a molecule that can bind with pleckstrin-2 and block its functions,” Dr Ji said. “We’ve already screened compounds, and we have about 40 we are testing right now.”
“Mice with pleckstrin-2 deactivated experienced fewer side effects compared to mice without JAK2, so we believe the pleckstrin-2 inhibitor will generate fewer side effects as well.” ![]()
Which Is Junk: The Aspartame, or the Science?
A DIETARY DIAGNOSIS
I’m a hospital CEO and came across an NP colleague’s issue of Clinician Reviews; your September editorial on aspartame (2017;27[9]:6-7) caught my eye. While mine is another “n = 1” experience with the effects of aspartame, it was life-changing.
About 10 years ago, my former wife’s seizures suddenly increased in frequency after a fairly lengthy period without them. The problem was severe enough that she was faced with losing her ability to drive a car.
I had a good business relationship with the Massachusetts General Hospital and sought help from a prominent neurologist there. He asked us to keep a dietary journal before the appointment.
Though he ordered routine diagnostic tests, the journal told him all he needed to know: He told her to eliminate aspartame from her diet. It felt like a miracle when the seizures disappeared—no longer did I need to maintain bumpers on every sharp edge in the house!
Since this experience, I read every article that I can about this chemical additive and was interested to learn of your experiences.
Doug Jones
Ellsworth, ME
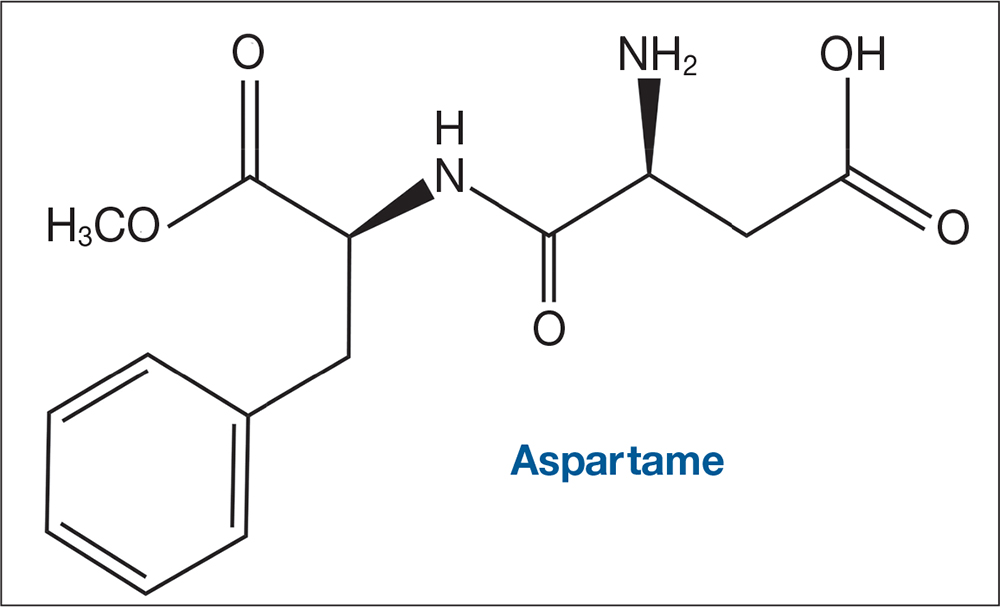
THE SCIENCE IS JUNK
I had to write because I can’t believe they allowed you to publish such a ridiculous article based on junk science. Anecdotal reports have no place in medicine. Aspartame is one of the most studied food items around. Many of these claims about the alleged danger of aspartame have been debunked by real scientists.
I am very disappointed.
Darlene Elliott, MSN, RN, CNP
Albuquerque, NM
STOP IGNORING THE BODY OF KNOWLEDGE
Thank you for addressing an issue that I believe to be of great importance. There is a huge body of knowledge that the medical community is ignoring regarding the correlation between diet and health in general, in particular the diabetes epidemic. As NPs, we are in a great position to lead.
I encourage you to read Jason Fung’s book, The Obesity Code. The entire book is eye popping, but chapter 15 (“The Diet Soda Delusion”) is particularly pertinent. He has the most thorough understanding of carbohydrate metabolism of all the authors I have read. However, Gary Taubes and Eric Westman have also published valuable resources; their books have changed my life, and I believe their knowledge could apply to many of our patients. If doctors will not embrace science, perhaps NPs will.
Martha DelGiudice, CNM
Smithtown, NY
MAYBE IT'S US …
Every time the “fasten seat belt” sign comes on, the ride gets very bumpy—so from now on, I’m going to ignore it. Aspartame “tricks our brain,” does it? What about agency? Or are we just passive leaves in the air blown about by gusts of aspartame?
Robert Pearlman, PA
Providence, RI
FAST TRACK FROM SWEET TO SOUR
Thank you for shedding light on the dangers of aspartame! My personal experience with it has not been good: One night, after drinking a large quantity of artificially sweetened powdered iced tea, I began to feel numb and experienced strange nerve sensations. I quickly learned that it is a migraine trigger for me. I now avoid aspartame and all other artificial sweeteners.
As a clinical dietitian (and NP), I’ve realized that fake food just doesn’t cut it for the body. Another issue in the dietary realm is that of folic acid. Yes, fortification has done wonders for preventing neural tube defects. But did you know that the folic acid put in our grains is a chemical that our bodies have to methylate to folinic acid, and that more than half of us do not do that well? This means excess synthetic folic acid is floating around in our bodies and brains, attributing to seizures, ADD, ADHD, migraines, miscarriages, etc.
I try to avoid eating foods with added folic acid. Talk about difficult! It means eating a lot of organic grains, whole grains, and natural vitamins with natural methylfolate to prevent anemia. Our bodies are designed to eat natural foods; the more processed something is, the more likely it is to be harmful to us.
Caroline Conneen, C-FNP, RD, IBCLC
Fredericksburg, VA
FAKE FOOD, NOT OUR FRIEND
My husband was habitually drinking flavored seltzer sweetened with aspartame when he became anxious, irritable, and developed insomnia. As soon as he stopped consuming it, the adverse effects dissipated. Since then, he has been astute about reading labels, and we do not support the use of any artificial sweeteners.
I believe aspartame should be taken off the market. The Internet is full of articles that report adverse effects from it. It seems more people are trying to avoid it. As an FNP and PMHNP, I educate my clients about aspartame and how it can exacerbate preexisting problems and contribute to insomnia, mood disorders, and panic/anxiety disorders.
I appreciate your scientific information about aspartame. We need to talk more about this chemical food additive; it is not our friend.
SUCRALOSE, ASPARTAME … ARE THE EFFECTS ONE AND THE SAME?
I have had negative thoughts concerning artificial sweeteners, including sucralose, which seems to be commonly used these days. I do not like the way I feel after ingesting these substances; it’s hard to describe—I just don’t feel right. I wonder if one answer lies in genomics and an individual’s inability to metabolize it? And to think of the byproducts you describe. Thank you for bringing this topic to light.
Anna Simon, CRNP
Allentown, PA
A DIETARY DIAGNOSIS
I’m a hospital CEO and came across an NP colleague’s issue of Clinician Reviews; your September editorial on aspartame (2017;27[9]:6-7) caught my eye. While mine is another “n = 1” experience with the effects of aspartame, it was life-changing.
About 10 years ago, my former wife’s seizures suddenly increased in frequency after a fairly lengthy period without them. The problem was severe enough that she was faced with losing her ability to drive a car.
I had a good business relationship with the Massachusetts General Hospital and sought help from a prominent neurologist there. He asked us to keep a dietary journal before the appointment.
Though he ordered routine diagnostic tests, the journal told him all he needed to know: He told her to eliminate aspartame from her diet. It felt like a miracle when the seizures disappeared—no longer did I need to maintain bumpers on every sharp edge in the house!
Since this experience, I read every article that I can about this chemical additive and was interested to learn of your experiences.
Doug Jones
Ellsworth, ME
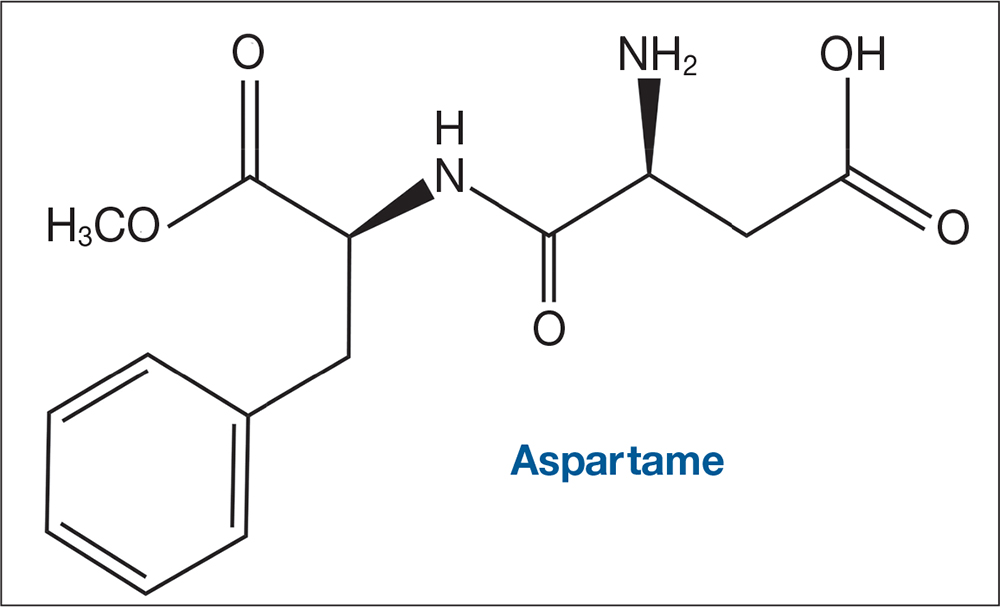
THE SCIENCE IS JUNK
I had to write because I can’t believe they allowed you to publish such a ridiculous article based on junk science. Anecdotal reports have no place in medicine. Aspartame is one of the most studied food items around. Many of these claims about the alleged danger of aspartame have been debunked by real scientists.
I am very disappointed.
Darlene Elliott, MSN, RN, CNP
Albuquerque, NM
STOP IGNORING THE BODY OF KNOWLEDGE
Thank you for addressing an issue that I believe to be of great importance. There is a huge body of knowledge that the medical community is ignoring regarding the correlation between diet and health in general, in particular the diabetes epidemic. As NPs, we are in a great position to lead.
I encourage you to read Jason Fung’s book, The Obesity Code. The entire book is eye popping, but chapter 15 (“The Diet Soda Delusion”) is particularly pertinent. He has the most thorough understanding of carbohydrate metabolism of all the authors I have read. However, Gary Taubes and Eric Westman have also published valuable resources; their books have changed my life, and I believe their knowledge could apply to many of our patients. If doctors will not embrace science, perhaps NPs will.
Martha DelGiudice, CNM
Smithtown, NY
MAYBE IT'S US …
Every time the “fasten seat belt” sign comes on, the ride gets very bumpy—so from now on, I’m going to ignore it. Aspartame “tricks our brain,” does it? What about agency? Or are we just passive leaves in the air blown about by gusts of aspartame?
Robert Pearlman, PA
Providence, RI
FAST TRACK FROM SWEET TO SOUR
Thank you for shedding light on the dangers of aspartame! My personal experience with it has not been good: One night, after drinking a large quantity of artificially sweetened powdered iced tea, I began to feel numb and experienced strange nerve sensations. I quickly learned that it is a migraine trigger for me. I now avoid aspartame and all other artificial sweeteners.
As a clinical dietitian (and NP), I’ve realized that fake food just doesn’t cut it for the body. Another issue in the dietary realm is that of folic acid. Yes, fortification has done wonders for preventing neural tube defects. But did you know that the folic acid put in our grains is a chemical that our bodies have to methylate to folinic acid, and that more than half of us do not do that well? This means excess synthetic folic acid is floating around in our bodies and brains, attributing to seizures, ADD, ADHD, migraines, miscarriages, etc.
I try to avoid eating foods with added folic acid. Talk about difficult! It means eating a lot of organic grains, whole grains, and natural vitamins with natural methylfolate to prevent anemia. Our bodies are designed to eat natural foods; the more processed something is, the more likely it is to be harmful to us.
Caroline Conneen, C-FNP, RD, IBCLC
Fredericksburg, VA
FAKE FOOD, NOT OUR FRIEND
My husband was habitually drinking flavored seltzer sweetened with aspartame when he became anxious, irritable, and developed insomnia. As soon as he stopped consuming it, the adverse effects dissipated. Since then, he has been astute about reading labels, and we do not support the use of any artificial sweeteners.
I believe aspartame should be taken off the market. The Internet is full of articles that report adverse effects from it. It seems more people are trying to avoid it. As an FNP and PMHNP, I educate my clients about aspartame and how it can exacerbate preexisting problems and contribute to insomnia, mood disorders, and panic/anxiety disorders.
I appreciate your scientific information about aspartame. We need to talk more about this chemical food additive; it is not our friend.
SUCRALOSE, ASPARTAME … ARE THE EFFECTS ONE AND THE SAME?
I have had negative thoughts concerning artificial sweeteners, including sucralose, which seems to be commonly used these days. I do not like the way I feel after ingesting these substances; it’s hard to describe—I just don’t feel right. I wonder if one answer lies in genomics and an individual’s inability to metabolize it? And to think of the byproducts you describe. Thank you for bringing this topic to light.
Anna Simon, CRNP
Allentown, PA
A DIETARY DIAGNOSIS
I’m a hospital CEO and came across an NP colleague’s issue of Clinician Reviews; your September editorial on aspartame (2017;27[9]:6-7) caught my eye. While mine is another “n = 1” experience with the effects of aspartame, it was life-changing.
About 10 years ago, my former wife’s seizures suddenly increased in frequency after a fairly lengthy period without them. The problem was severe enough that she was faced with losing her ability to drive a car.
I had a good business relationship with the Massachusetts General Hospital and sought help from a prominent neurologist there. He asked us to keep a dietary journal before the appointment.
Though he ordered routine diagnostic tests, the journal told him all he needed to know: He told her to eliminate aspartame from her diet. It felt like a miracle when the seizures disappeared—no longer did I need to maintain bumpers on every sharp edge in the house!
Since this experience, I read every article that I can about this chemical additive and was interested to learn of your experiences.
Doug Jones
Ellsworth, ME
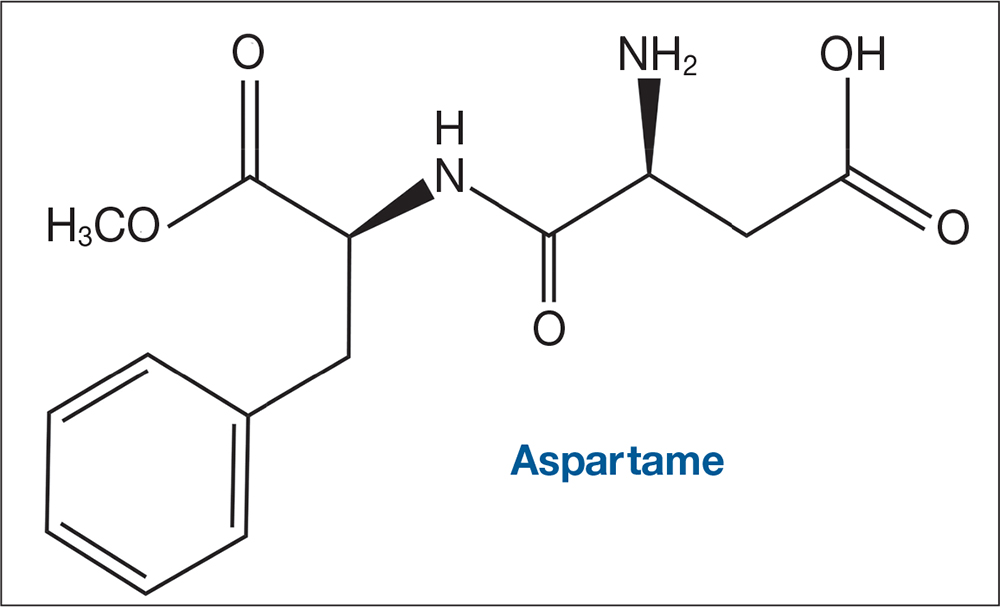
THE SCIENCE IS JUNK
I had to write because I can’t believe they allowed you to publish such a ridiculous article based on junk science. Anecdotal reports have no place in medicine. Aspartame is one of the most studied food items around. Many of these claims about the alleged danger of aspartame have been debunked by real scientists.
I am very disappointed.
Darlene Elliott, MSN, RN, CNP
Albuquerque, NM
STOP IGNORING THE BODY OF KNOWLEDGE
Thank you for addressing an issue that I believe to be of great importance. There is a huge body of knowledge that the medical community is ignoring regarding the correlation between diet and health in general, in particular the diabetes epidemic. As NPs, we are in a great position to lead.
I encourage you to read Jason Fung’s book, The Obesity Code. The entire book is eye popping, but chapter 15 (“The Diet Soda Delusion”) is particularly pertinent. He has the most thorough understanding of carbohydrate metabolism of all the authors I have read. However, Gary Taubes and Eric Westman have also published valuable resources; their books have changed my life, and I believe their knowledge could apply to many of our patients. If doctors will not embrace science, perhaps NPs will.
Martha DelGiudice, CNM
Smithtown, NY
MAYBE IT'S US …
Every time the “fasten seat belt” sign comes on, the ride gets very bumpy—so from now on, I’m going to ignore it. Aspartame “tricks our brain,” does it? What about agency? Or are we just passive leaves in the air blown about by gusts of aspartame?
Robert Pearlman, PA
Providence, RI
FAST TRACK FROM SWEET TO SOUR
Thank you for shedding light on the dangers of aspartame! My personal experience with it has not been good: One night, after drinking a large quantity of artificially sweetened powdered iced tea, I began to feel numb and experienced strange nerve sensations. I quickly learned that it is a migraine trigger for me. I now avoid aspartame and all other artificial sweeteners.
As a clinical dietitian (and NP), I’ve realized that fake food just doesn’t cut it for the body. Another issue in the dietary realm is that of folic acid. Yes, fortification has done wonders for preventing neural tube defects. But did you know that the folic acid put in our grains is a chemical that our bodies have to methylate to folinic acid, and that more than half of us do not do that well? This means excess synthetic folic acid is floating around in our bodies and brains, attributing to seizures, ADD, ADHD, migraines, miscarriages, etc.
I try to avoid eating foods with added folic acid. Talk about difficult! It means eating a lot of organic grains, whole grains, and natural vitamins with natural methylfolate to prevent anemia. Our bodies are designed to eat natural foods; the more processed something is, the more likely it is to be harmful to us.
Caroline Conneen, C-FNP, RD, IBCLC
Fredericksburg, VA
FAKE FOOD, NOT OUR FRIEND
My husband was habitually drinking flavored seltzer sweetened with aspartame when he became anxious, irritable, and developed insomnia. As soon as he stopped consuming it, the adverse effects dissipated. Since then, he has been astute about reading labels, and we do not support the use of any artificial sweeteners.
I believe aspartame should be taken off the market. The Internet is full of articles that report adverse effects from it. It seems more people are trying to avoid it. As an FNP and PMHNP, I educate my clients about aspartame and how it can exacerbate preexisting problems and contribute to insomnia, mood disorders, and panic/anxiety disorders.
I appreciate your scientific information about aspartame. We need to talk more about this chemical food additive; it is not our friend.
SUCRALOSE, ASPARTAME … ARE THE EFFECTS ONE AND THE SAME?
I have had negative thoughts concerning artificial sweeteners, including sucralose, which seems to be commonly used these days. I do not like the way I feel after ingesting these substances; it’s hard to describe—I just don’t feel right. I wonder if one answer lies in genomics and an individual’s inability to metabolize it? And to think of the byproducts you describe. Thank you for bringing this topic to light.
Anna Simon, CRNP
Allentown, PA
Sleep apnea treatment may reduce risk of epileptic seizures
WASHINGTON – In patients with epilepsy, treatment of obstructive sleep apnea with continuous positive airway pressure may lead to substantial and sustained reductions in seizure activity, according to data presented at the annual meeting of the American Epilepsy Society.
The reduction in seizure activity with continuous positive airway pressure (cPAP) in patients with epilepsy contributes to other evidence that poor sleep quality is an important but preventable risk factor for seizures, according to Thapanee Somboon, MD, a research fellow at the Sleep Disorders Center at the Cleveland Clinic in Ohio.
In this study, which was characterized as the largest yet to evaluate the effect of cPAP on seizure activity, all 197 patients had epilepsy but only 122 had obstructive sleep apnea (OSA). Of those with OSA, 73 were treated with cPAP and 49 were not. An additional 75 patients with epilepsy but no OSA were also treated with cPAP. Seizure activity in all groups was evaluated over a period of 1 year.
Treatment success, defined as no seizure activity or at least a 50% reduction from baseline in seizure activity, was achieved in 85% of those with OSA treated with cPAP, 55% of those with OSA that did not receive cPAP, and 65% of those who were treated with cPAP but did not have OSA.
The difference was even greater among those with seizure activity in the 6 months prior to cPAP use. In these, a 50% or greater reduction in seizure activity was achieved in 63% of those with OSA treated with cPAP but in only 14% of those with OSA that did not receive cPAP. In the group without OSA, 44% achieved a 50% or greater reduction in seizure activity from baseline on cPAP.
“Epilepsy patients without OSA also appeared to benefit from cPAP, although prospective data are needed to further explore this observation,” Dr. Somboon said.
All patients remained on antiepileptic drugs over the course of study, and the drug levels were not different between groups, according to Dr. Somboon. About half of all three groups were seizure free in the 6 months prior to cPAP. Those with OSA who received cPAP had a higher body mass index than did those who were not treated (34.6 vs. 31.1; P less than .001), but they were of similar age (47.6 vs. 47.9 years). Those without OSA who were treated with cPAP had a lower BMI (27.5; P less than .001) and were 10 years younger than were those with OSA (37.7 years; P less than .001). About two-thirds of all three groups had a history of focal seizures.
When expressed as odds ratios (OR), those treated for OSA had almost 10 times the likelihood of treatment success at 1 year (OR, 9.58; P less than .001), although being seizure free in the 6 months prior to cPAP had a 20-fold increased likelihood of treatment success (OR, 20.88; P less than .001).
Sleep disturbances and OSA are more common in patients with epilepsy than age-matched controls, according to Dr. Somboon, who cited published studies substantiating these statements. She noted that there are also previously published studies associating improved sleep hygiene, including improved sleep hygiene achieved with cPAP, with a reduced risk of seizure activity in epilepsy patients. However, at present there are no guideline recommendations for screening patients with epilepsy for OSA or other causes of impaired sleep, according to Dr. Somboon.
Although Dr. Somboon acknowledged that the data collected in this study cannot provide a definitive link between cPAP treatment, improved sleep, and reduced risk of seizure activity, this study does support these associations in the context of other evidence.
“We think clinicians should routinely screen patients with epilepsy for OSA and consider cPAP as a strategy to reduce seizure risk,” she said.
Dr. Somboon reported no financial relationships relevant to the study.
WASHINGTON – In patients with epilepsy, treatment of obstructive sleep apnea with continuous positive airway pressure may lead to substantial and sustained reductions in seizure activity, according to data presented at the annual meeting of the American Epilepsy Society.
The reduction in seizure activity with continuous positive airway pressure (cPAP) in patients with epilepsy contributes to other evidence that poor sleep quality is an important but preventable risk factor for seizures, according to Thapanee Somboon, MD, a research fellow at the Sleep Disorders Center at the Cleveland Clinic in Ohio.
In this study, which was characterized as the largest yet to evaluate the effect of cPAP on seizure activity, all 197 patients had epilepsy but only 122 had obstructive sleep apnea (OSA). Of those with OSA, 73 were treated with cPAP and 49 were not. An additional 75 patients with epilepsy but no OSA were also treated with cPAP. Seizure activity in all groups was evaluated over a period of 1 year.
Treatment success, defined as no seizure activity or at least a 50% reduction from baseline in seizure activity, was achieved in 85% of those with OSA treated with cPAP, 55% of those with OSA that did not receive cPAP, and 65% of those who were treated with cPAP but did not have OSA.
The difference was even greater among those with seizure activity in the 6 months prior to cPAP use. In these, a 50% or greater reduction in seizure activity was achieved in 63% of those with OSA treated with cPAP but in only 14% of those with OSA that did not receive cPAP. In the group without OSA, 44% achieved a 50% or greater reduction in seizure activity from baseline on cPAP.
“Epilepsy patients without OSA also appeared to benefit from cPAP, although prospective data are needed to further explore this observation,” Dr. Somboon said.
All patients remained on antiepileptic drugs over the course of study, and the drug levels were not different between groups, according to Dr. Somboon. About half of all three groups were seizure free in the 6 months prior to cPAP. Those with OSA who received cPAP had a higher body mass index than did those who were not treated (34.6 vs. 31.1; P less than .001), but they were of similar age (47.6 vs. 47.9 years). Those without OSA who were treated with cPAP had a lower BMI (27.5; P less than .001) and were 10 years younger than were those with OSA (37.7 years; P less than .001). About two-thirds of all three groups had a history of focal seizures.
When expressed as odds ratios (OR), those treated for OSA had almost 10 times the likelihood of treatment success at 1 year (OR, 9.58; P less than .001), although being seizure free in the 6 months prior to cPAP had a 20-fold increased likelihood of treatment success (OR, 20.88; P less than .001).
Sleep disturbances and OSA are more common in patients with epilepsy than age-matched controls, according to Dr. Somboon, who cited published studies substantiating these statements. She noted that there are also previously published studies associating improved sleep hygiene, including improved sleep hygiene achieved with cPAP, with a reduced risk of seizure activity in epilepsy patients. However, at present there are no guideline recommendations for screening patients with epilepsy for OSA or other causes of impaired sleep, according to Dr. Somboon.
Although Dr. Somboon acknowledged that the data collected in this study cannot provide a definitive link between cPAP treatment, improved sleep, and reduced risk of seizure activity, this study does support these associations in the context of other evidence.
“We think clinicians should routinely screen patients with epilepsy for OSA and consider cPAP as a strategy to reduce seizure risk,” she said.
Dr. Somboon reported no financial relationships relevant to the study.
WASHINGTON – In patients with epilepsy, treatment of obstructive sleep apnea with continuous positive airway pressure may lead to substantial and sustained reductions in seizure activity, according to data presented at the annual meeting of the American Epilepsy Society.
The reduction in seizure activity with continuous positive airway pressure (cPAP) in patients with epilepsy contributes to other evidence that poor sleep quality is an important but preventable risk factor for seizures, according to Thapanee Somboon, MD, a research fellow at the Sleep Disorders Center at the Cleveland Clinic in Ohio.
In this study, which was characterized as the largest yet to evaluate the effect of cPAP on seizure activity, all 197 patients had epilepsy but only 122 had obstructive sleep apnea (OSA). Of those with OSA, 73 were treated with cPAP and 49 were not. An additional 75 patients with epilepsy but no OSA were also treated with cPAP. Seizure activity in all groups was evaluated over a period of 1 year.
Treatment success, defined as no seizure activity or at least a 50% reduction from baseline in seizure activity, was achieved in 85% of those with OSA treated with cPAP, 55% of those with OSA that did not receive cPAP, and 65% of those who were treated with cPAP but did not have OSA.
The difference was even greater among those with seizure activity in the 6 months prior to cPAP use. In these, a 50% or greater reduction in seizure activity was achieved in 63% of those with OSA treated with cPAP but in only 14% of those with OSA that did not receive cPAP. In the group without OSA, 44% achieved a 50% or greater reduction in seizure activity from baseline on cPAP.
“Epilepsy patients without OSA also appeared to benefit from cPAP, although prospective data are needed to further explore this observation,” Dr. Somboon said.
All patients remained on antiepileptic drugs over the course of study, and the drug levels were not different between groups, according to Dr. Somboon. About half of all three groups were seizure free in the 6 months prior to cPAP. Those with OSA who received cPAP had a higher body mass index than did those who were not treated (34.6 vs. 31.1; P less than .001), but they were of similar age (47.6 vs. 47.9 years). Those without OSA who were treated with cPAP had a lower BMI (27.5; P less than .001) and were 10 years younger than were those with OSA (37.7 years; P less than .001). About two-thirds of all three groups had a history of focal seizures.
When expressed as odds ratios (OR), those treated for OSA had almost 10 times the likelihood of treatment success at 1 year (OR, 9.58; P less than .001), although being seizure free in the 6 months prior to cPAP had a 20-fold increased likelihood of treatment success (OR, 20.88; P less than .001).
Sleep disturbances and OSA are more common in patients with epilepsy than age-matched controls, according to Dr. Somboon, who cited published studies substantiating these statements. She noted that there are also previously published studies associating improved sleep hygiene, including improved sleep hygiene achieved with cPAP, with a reduced risk of seizure activity in epilepsy patients. However, at present there are no guideline recommendations for screening patients with epilepsy for OSA or other causes of impaired sleep, according to Dr. Somboon.
Although Dr. Somboon acknowledged that the data collected in this study cannot provide a definitive link between cPAP treatment, improved sleep, and reduced risk of seizure activity, this study does support these associations in the context of other evidence.
“We think clinicians should routinely screen patients with epilepsy for OSA and consider cPAP as a strategy to reduce seizure risk,” she said.
Dr. Somboon reported no financial relationships relevant to the study.
AT AES 2017
Key clinical point:
Major finding: In epilepsy patients and OSA, seizure activity was reduced by at least half in 63% of those treated with cPAP versus 14% of those who were not (P less than .001).
Data source: A retrospective study of 197 patients with epilepsy.
Disclosures: The presenter reported no financial relationships relevant to the study.
Intense urine output monitoring beneficial in ICU
Intense monitoring of urine output could be a useful tool in detecting acute kidney injury (AKI), according to a study conducted at the University of Pittsburgh.
Kui Jin, MD, of the University of Pittsburgh and his associates found that, after adjustment for baseline characteristics, intensive monitoring of urine output (UO) was associated with higher rates of AKI, with an odds ratio of 1.22. Intensive UO monitoring also was strongly associated with improved 30-day survival among patients developing AKI.
This retrospective cohort study included 15,724 adult patients admitted to the center’s ICUs during 2000-2008. All patients had either their UO or serum creatinine (SC) monitored. These patients were then divided into subcohorts that were monitored at one of two different intensities. UO intensive monitoring was defined by hourly recordings, with gaps no greater than 3 hours for the first 48 hours after ICU admission. The group receiving less intensive UO monitoring comprised patients who did not meet intensive monitoring criteria, regardless of their UO in the 7 days following ICU admission. The patients who had their SC intensively monitored had 3 calendar days of samples taken after their ICU admissions. Those who did not meet SC intensive monitoring criteria were placed into the less intensive SC monitoring group.
To understand the effect of the monitoring strategies on detecting the development of AKI, the researchers determined each patient’s baseline, admission, and reference serum creatinine levels. Baseline creatinine was defined as the lowest value in the year prior to hospital admission. Reference creatinine was the baseline creatinine, if available, or the lowest creatinine level recorded within 24 hours after ICU admission. A third method for determining reference creatinine levels was used for some patients, which involved making an estimation based on the Modification of Diet in Renal Disease equation for serum creatinine.
The crude rates of stage 2-3 AKI 7 days after admission to the ICU were similar between patients from both groups that had their UO monitored; 62.5% of intensive and 63.9% of less intensive patients displayed symptoms. After the researchers adjusted for baseline characteristics, however, intensive monitoring of UO was associated with greater rates of stage 2-3 AKI (OR, 1.22; P less than .001). Crude rates were higher in the patients who received intensive monitoring for SC, compared with patients who received less intensive monitoring for SC. Ultimately, Dr. Jin and his associates found that, when caring for patients with or without AKI, fluid management is one of the most important factors. Patients who underwent intensive UO monitoring received less fluid in their first 24 hours (3.6 L) in the ICU, compared with patients who received less intense UO monitoring (4.2 L). Patients who received intensive monitoring of their UO also were less likely to use vasopressors (29.9% vs. 43.3%; P less than .001), suggesting these patients were more hemodynamically stable. Further, the percentage of patients at or above 10% of fluid overload was lower in the group who received intensive monitoring of their UO (2.49% vs. 5.68%; P less than .001), during the first 72 hours in the ICU.
“Our results should help inform clinical decisions and ICU policy around frequency of monitoring of UO, especially for patients at high risk of AKI,” Dr. Jin and his colleagues wrote.
None of the authors had financial disclosures to report. Partial funding was provided by a research grant from C.R. Bard.
Intense monitoring of urine output could be a useful tool in detecting acute kidney injury (AKI), according to a study conducted at the University of Pittsburgh.
Kui Jin, MD, of the University of Pittsburgh and his associates found that, after adjustment for baseline characteristics, intensive monitoring of urine output (UO) was associated with higher rates of AKI, with an odds ratio of 1.22. Intensive UO monitoring also was strongly associated with improved 30-day survival among patients developing AKI.
This retrospective cohort study included 15,724 adult patients admitted to the center’s ICUs during 2000-2008. All patients had either their UO or serum creatinine (SC) monitored. These patients were then divided into subcohorts that were monitored at one of two different intensities. UO intensive monitoring was defined by hourly recordings, with gaps no greater than 3 hours for the first 48 hours after ICU admission. The group receiving less intensive UO monitoring comprised patients who did not meet intensive monitoring criteria, regardless of their UO in the 7 days following ICU admission. The patients who had their SC intensively monitored had 3 calendar days of samples taken after their ICU admissions. Those who did not meet SC intensive monitoring criteria were placed into the less intensive SC monitoring group.
To understand the effect of the monitoring strategies on detecting the development of AKI, the researchers determined each patient’s baseline, admission, and reference serum creatinine levels. Baseline creatinine was defined as the lowest value in the year prior to hospital admission. Reference creatinine was the baseline creatinine, if available, or the lowest creatinine level recorded within 24 hours after ICU admission. A third method for determining reference creatinine levels was used for some patients, which involved making an estimation based on the Modification of Diet in Renal Disease equation for serum creatinine.
The crude rates of stage 2-3 AKI 7 days after admission to the ICU were similar between patients from both groups that had their UO monitored; 62.5% of intensive and 63.9% of less intensive patients displayed symptoms. After the researchers adjusted for baseline characteristics, however, intensive monitoring of UO was associated with greater rates of stage 2-3 AKI (OR, 1.22; P less than .001). Crude rates were higher in the patients who received intensive monitoring for SC, compared with patients who received less intensive monitoring for SC. Ultimately, Dr. Jin and his associates found that, when caring for patients with or without AKI, fluid management is one of the most important factors. Patients who underwent intensive UO monitoring received less fluid in their first 24 hours (3.6 L) in the ICU, compared with patients who received less intense UO monitoring (4.2 L). Patients who received intensive monitoring of their UO also were less likely to use vasopressors (29.9% vs. 43.3%; P less than .001), suggesting these patients were more hemodynamically stable. Further, the percentage of patients at or above 10% of fluid overload was lower in the group who received intensive monitoring of their UO (2.49% vs. 5.68%; P less than .001), during the first 72 hours in the ICU.
“Our results should help inform clinical decisions and ICU policy around frequency of monitoring of UO, especially for patients at high risk of AKI,” Dr. Jin and his colleagues wrote.
None of the authors had financial disclosures to report. Partial funding was provided by a research grant from C.R. Bard.
Intense monitoring of urine output could be a useful tool in detecting acute kidney injury (AKI), according to a study conducted at the University of Pittsburgh.
Kui Jin, MD, of the University of Pittsburgh and his associates found that, after adjustment for baseline characteristics, intensive monitoring of urine output (UO) was associated with higher rates of AKI, with an odds ratio of 1.22. Intensive UO monitoring also was strongly associated with improved 30-day survival among patients developing AKI.
This retrospective cohort study included 15,724 adult patients admitted to the center’s ICUs during 2000-2008. All patients had either their UO or serum creatinine (SC) monitored. These patients were then divided into subcohorts that were monitored at one of two different intensities. UO intensive monitoring was defined by hourly recordings, with gaps no greater than 3 hours for the first 48 hours after ICU admission. The group receiving less intensive UO monitoring comprised patients who did not meet intensive monitoring criteria, regardless of their UO in the 7 days following ICU admission. The patients who had their SC intensively monitored had 3 calendar days of samples taken after their ICU admissions. Those who did not meet SC intensive monitoring criteria were placed into the less intensive SC monitoring group.
To understand the effect of the monitoring strategies on detecting the development of AKI, the researchers determined each patient’s baseline, admission, and reference serum creatinine levels. Baseline creatinine was defined as the lowest value in the year prior to hospital admission. Reference creatinine was the baseline creatinine, if available, or the lowest creatinine level recorded within 24 hours after ICU admission. A third method for determining reference creatinine levels was used for some patients, which involved making an estimation based on the Modification of Diet in Renal Disease equation for serum creatinine.
The crude rates of stage 2-3 AKI 7 days after admission to the ICU were similar between patients from both groups that had their UO monitored; 62.5% of intensive and 63.9% of less intensive patients displayed symptoms. After the researchers adjusted for baseline characteristics, however, intensive monitoring of UO was associated with greater rates of stage 2-3 AKI (OR, 1.22; P less than .001). Crude rates were higher in the patients who received intensive monitoring for SC, compared with patients who received less intensive monitoring for SC. Ultimately, Dr. Jin and his associates found that, when caring for patients with or without AKI, fluid management is one of the most important factors. Patients who underwent intensive UO monitoring received less fluid in their first 24 hours (3.6 L) in the ICU, compared with patients who received less intense UO monitoring (4.2 L). Patients who received intensive monitoring of their UO also were less likely to use vasopressors (29.9% vs. 43.3%; P less than .001), suggesting these patients were more hemodynamically stable. Further, the percentage of patients at or above 10% of fluid overload was lower in the group who received intensive monitoring of their UO (2.49% vs. 5.68%; P less than .001), during the first 72 hours in the ICU.
“Our results should help inform clinical decisions and ICU policy around frequency of monitoring of UO, especially for patients at high risk of AKI,” Dr. Jin and his colleagues wrote.
None of the authors had financial disclosures to report. Partial funding was provided by a research grant from C.R. Bard.
FROM CHEST
Key clinical point:
Major finding: AKI was more likely to be seen in patients who received intensive monitoring of their urine output (OR,1.22; P less than .001).
Data source: Retrospective cohort study at a single academic medical center of 15,724 adult patients admitted to the center’s ICUs during 2000-2008.
Disclosures: None of the authors had financial disclosures to report. Partial funding was provided by a research grant from C.R. Bard.