User login
Introduction: Challenges and advances in cardiovascular disease
In cardiovascular medicine, advances in our understanding of disease processes, medical management, and interventional and surgical techniques have gone a long way toward improving the health of patients. But we face challenges and opportunities in how best to apply these discoveries to improve the quality of care we provide and do so without driving up costs or wasting resources.
This Cleveland Clinic Journal of Medicine supplement on cardiovascular disease aims to illuminate some of the challenges and advances in the management of cardiac amyloidosis, coronary artery chronic total occlusion, venous thromboembolism, implantable device infection, and lung transplant. In so doing, my colleagues present insights into which advances will benefit which patients to improve quality and contain cost.
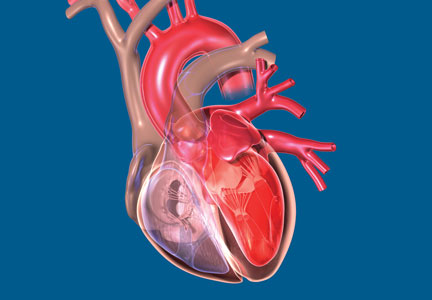
Cardiac amyloidosis, sometimes called stiff heart syndrome, is the most common restrictive cardiomyopathy. Amyloid deposits in the heart muscle can affect conduction of electrical signals leading to arrhythmias and heart block. Joseph P. Donnelly, MD, and Mazen Hanna, MD, present a comprehensive review of cardiac amyloidosis and share exciting advances in the detection and treatment of this condition and clues to identify patients who may be affected by this often overlooked condition.
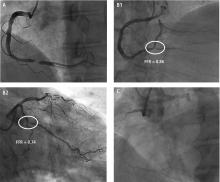
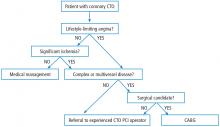
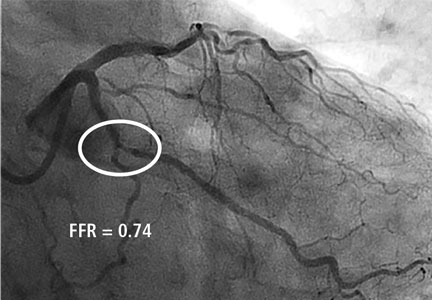
Also in this supplement, Jaikirshan Khatri, MD, and colleagues review the use of percutaneous coronary intervention (PCI) for patients with coronary artery chronic total occlusion (CTO). Though CTO is often considered benign, the affected myocardium is ischemic and patients with significant ischemic burden may benefit clinically from CTO PCI. A technically demanding procedure, CTO PCI success rates are highly operator-dependent.
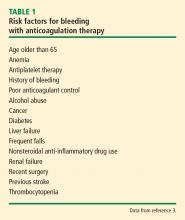
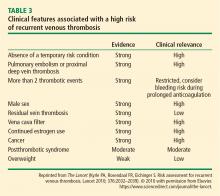
John R. Bartholomew, MD, presents information about the management of venous thromboembolism (VTE) including recent changes to treatment guidelines. Patients with VTE require immediate treatment with anticoagulation therapy. Recent changes to treatment guidelines now recommend direct oral anticoagulants for patients with VTE and no cancer. Direct oral anticoagulants are an important new option for patients and further study would be beneficial to strengthen the level of evidence regarding which anticoagulation therapy is best for which patients.
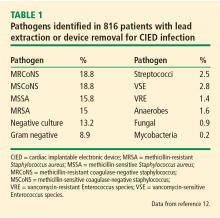
Cardiac implantable electronic devices (CIEDs) improve quality of life and longevity for increasing numbers of patients with cardiac disease. Cameron T. Lambert, MD, and Khaldoun G. Tarakji, MD, MPH, discuss the types of CIED infections that occur in about 1% of patients receiving a first CIED. Prompt diagnosis improves the success of antibiotic therapy, device removal, and resolution of the infection.
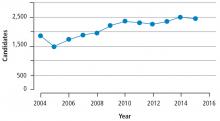
Finally, Kenneth R. McCurry, MD, and Marie M. Budev, DO, MPH, discuss lung transplant for patients with end-stage lung disease. Lung transplant may be an option to extend survival and improve the quality of life for some patients. In this article, the authors review the selection criteria for lung transplant candidates, including when physicians should refer patients to lung transplant centers for evaluation and placement on the lung transplant waiting list.
We hope this supplement is a useful review of some of the challenges and advances in cardiovascular medicine and is beneficial to you and your clinical practice.
In cardiovascular medicine, advances in our understanding of disease processes, medical management, and interventional and surgical techniques have gone a long way toward improving the health of patients. But we face challenges and opportunities in how best to apply these discoveries to improve the quality of care we provide and do so without driving up costs or wasting resources.
This Cleveland Clinic Journal of Medicine supplement on cardiovascular disease aims to illuminate some of the challenges and advances in the management of cardiac amyloidosis, coronary artery chronic total occlusion, venous thromboembolism, implantable device infection, and lung transplant. In so doing, my colleagues present insights into which advances will benefit which patients to improve quality and contain cost.
Cardiac amyloidosis, sometimes called stiff heart syndrome, is the most common restrictive cardiomyopathy. Amyloid deposits in the heart muscle can affect conduction of electrical signals leading to arrhythmias and heart block. Joseph P. Donnelly, MD, and Mazen Hanna, MD, present a comprehensive review of cardiac amyloidosis and share exciting advances in the detection and treatment of this condition and clues to identify patients who may be affected by this often overlooked condition.
Also in this supplement, Jaikirshan Khatri, MD, and colleagues review the use of percutaneous coronary intervention (PCI) for patients with coronary artery chronic total occlusion (CTO). Though CTO is often considered benign, the affected myocardium is ischemic and patients with significant ischemic burden may benefit clinically from CTO PCI. A technically demanding procedure, CTO PCI success rates are highly operator-dependent.
John R. Bartholomew, MD, presents information about the management of venous thromboembolism (VTE) including recent changes to treatment guidelines. Patients with VTE require immediate treatment with anticoagulation therapy. Recent changes to treatment guidelines now recommend direct oral anticoagulants for patients with VTE and no cancer. Direct oral anticoagulants are an important new option for patients and further study would be beneficial to strengthen the level of evidence regarding which anticoagulation therapy is best for which patients.
Cardiac implantable electronic devices (CIEDs) improve quality of life and longevity for increasing numbers of patients with cardiac disease. Cameron T. Lambert, MD, and Khaldoun G. Tarakji, MD, MPH, discuss the types of CIED infections that occur in about 1% of patients receiving a first CIED. Prompt diagnosis improves the success of antibiotic therapy, device removal, and resolution of the infection.
Finally, Kenneth R. McCurry, MD, and Marie M. Budev, DO, MPH, discuss lung transplant for patients with end-stage lung disease. Lung transplant may be an option to extend survival and improve the quality of life for some patients. In this article, the authors review the selection criteria for lung transplant candidates, including when physicians should refer patients to lung transplant centers for evaluation and placement on the lung transplant waiting list.
We hope this supplement is a useful review of some of the challenges and advances in cardiovascular medicine and is beneficial to you and your clinical practice.
In cardiovascular medicine, advances in our understanding of disease processes, medical management, and interventional and surgical techniques have gone a long way toward improving the health of patients. But we face challenges and opportunities in how best to apply these discoveries to improve the quality of care we provide and do so without driving up costs or wasting resources.
This Cleveland Clinic Journal of Medicine supplement on cardiovascular disease aims to illuminate some of the challenges and advances in the management of cardiac amyloidosis, coronary artery chronic total occlusion, venous thromboembolism, implantable device infection, and lung transplant. In so doing, my colleagues present insights into which advances will benefit which patients to improve quality and contain cost.
Cardiac amyloidosis, sometimes called stiff heart syndrome, is the most common restrictive cardiomyopathy. Amyloid deposits in the heart muscle can affect conduction of electrical signals leading to arrhythmias and heart block. Joseph P. Donnelly, MD, and Mazen Hanna, MD, present a comprehensive review of cardiac amyloidosis and share exciting advances in the detection and treatment of this condition and clues to identify patients who may be affected by this often overlooked condition.
Also in this supplement, Jaikirshan Khatri, MD, and colleagues review the use of percutaneous coronary intervention (PCI) for patients with coronary artery chronic total occlusion (CTO). Though CTO is often considered benign, the affected myocardium is ischemic and patients with significant ischemic burden may benefit clinically from CTO PCI. A technically demanding procedure, CTO PCI success rates are highly operator-dependent.
John R. Bartholomew, MD, presents information about the management of venous thromboembolism (VTE) including recent changes to treatment guidelines. Patients with VTE require immediate treatment with anticoagulation therapy. Recent changes to treatment guidelines now recommend direct oral anticoagulants for patients with VTE and no cancer. Direct oral anticoagulants are an important new option for patients and further study would be beneficial to strengthen the level of evidence regarding which anticoagulation therapy is best for which patients.
Cardiac implantable electronic devices (CIEDs) improve quality of life and longevity for increasing numbers of patients with cardiac disease. Cameron T. Lambert, MD, and Khaldoun G. Tarakji, MD, MPH, discuss the types of CIED infections that occur in about 1% of patients receiving a first CIED. Prompt diagnosis improves the success of antibiotic therapy, device removal, and resolution of the infection.
Finally, Kenneth R. McCurry, MD, and Marie M. Budev, DO, MPH, discuss lung transplant for patients with end-stage lung disease. Lung transplant may be an option to extend survival and improve the quality of life for some patients. In this article, the authors review the selection criteria for lung transplant candidates, including when physicians should refer patients to lung transplant centers for evaluation and placement on the lung transplant waiting list.
We hope this supplement is a useful review of some of the challenges and advances in cardiovascular medicine and is beneficial to you and your clinical practice.
Cardiac amyloidosis: An update on diagnosis and treatment
WHAT IS AMYLOIDOSIS?
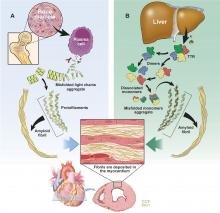
Amyloidosis is a protein deposition disease in which a specific precursor protein pathologically misfolds from its physiologic tertiary structure into a more linear shape dominated by beta-pleated sheets. The misfolded protein aggregates into oligomers, eventually forming insoluble amyloid fibrils that deposit extracellularly in tissues. Both the circulating oligomers, which are cytotoxic, and the fibrils, which cause distortion of the tissue architecture, lead to organ dysfunction. Amyloid fibrils are rigid, nonbranching structures, 7 to 10 nanometers in diameter, with a characteristic appearance on electron microscopy. Affinity for Congo red staining, which binds to the beta-pleated sheets, produces the pathognomonic “apple-green” birefringence when visualized under polarized light microscopy. Universal to all amyloid fibrils are chaperone proteins such as serum amyloid P (SAP) and glycosaminoglycans, as well as calcium. There are more than 30 different precursor proteins implicated in various amyloid diseases, arising as hereditary or nonhereditary, localized or systemic, with different organ involvement and prognosis.1–3
TWO MAIN TYPES OF CARDIAC AMYLOIDOSIS
Light chain amyloidosis (AL)
AL, formerly called primary amyloidosis, is a clonal plasma cell disorder due to the overproduction and misfolding of antibody light chain fragments. It is a rare disease with about 3,000 new cases per year in the United States.5 The median age at diagnosis is 63, although it can present in patients in their 30s and 40s.5,6 It is a systemic disease that often affects the heart, but it can affect several other organs, most commonly the kidneys, gastrointestinal (GI) tract, and nervous system.7
AL is a more aggressive disease than ATTR, with a median untreated survival of less than 6 months in patients who present with heart failure.8 Early diagnosis is crucial as mortality is high without prompt treatment.
Transthyretin amyloidosis (ATTR)
ATTR is due to misfolding of the liver-derived precursor protein transthyretin (TTR) (previously called prealbumin), either as an acquired wild-type variant (ATTRwt) or as a hereditary mutant variant (ATTRm). ATTRwt, known previously as senile CA, typically affects older males and presents as a late onset hypertrophic restrictive cardiomyopathy, often preceded by carpal tunnel syndrome or spinal stenosis or both. The ATTRm variant, caused by one of many different point mutations in the TTR gene, can manifest as a polyneuropathy, cardiomyopathy, or a mixed phenotype that varies according to the specific mutation.
While ATTR portends a better prognosis than AL, it is still a progressive disorder with significantly reduced survival and quality of life. The median survival of patients with the ATTRwt variant is about 4 years and for patients with the ATTRm variant, survival depends on the mutation.9 TTR is a protein tetramer composed of 4 identical 127-amino acid monomers noncovalently bound at a dimer-dimer interface (Figure 1). It is a transport protein for thyroxine and retinol binding protein. The dissociation of the tetramer is the rate-limiting step for amyloid fibrillogenesis. Differentiating the ATTRwt variant and the ATTRm variant is done by testing the TTR gene for a mutation.1,3
How common is the ATTRwt variant? The ATTRwt variant is often an unrecognized cause of diastolic heart failure in the elderly, with up to 25% of patients 85 and older showing ATTRwt amyloid deposits on autopsy studies.10 A recent study showed that 13% of patients 60 and older hospitalized with heart failure with preserved ejection fraction had grade 2 to 3 uptake on 99mtechnetium-pyrophosphate (99mTcPYP) scintigraphy, which is consistent with ATTR-CA.11 In 43 consecutive patients undergoing transcatheter aortic valve replacement, 11.6% were found to have significant uptake on 99mTcPYP scan.12 It is clear given the aging population that the ATTRwt variant will become the most common form of amyloidosis. It is much more common in white males, with a median age at diagnosis of 75.13 Carpal tunnel syndrome (almost always bilateral) and spinal stenosis are present in about 50% of patients diagnosed with ATTRwt-CA and often precede clinical presentation of heart failure by 5 to 15 years.14–17
How common is the ATTRm variant? There are more than 100 point mutations in the TTR gene that lead to various familial TTR-related amyloid syndromes, either neuropathic (familial amyloid polyneuropathy [FAP]) or cardiomyopathic (familial amyloid cardiomyopathy).18 The most common mutation in the United States is V122I in which there is an isoleucine substitution for valine at the 122nd amino acid position. This mutation is seen in African Americans, 3% to 4% of whom are heterozygote carriers.19 Although the true penetrance is unknown, this mutation can lead to a late-onset restrictive cardiomyopathy with minimal neuropathy and is frequently misdiagnosed as hypertensive heart disease or diastolic heart failure. The median survival for V122I ATTRm-CA is about 2 years but likely depends on the stage at the time of diagnosis.20 The second most common mutation in the United States, T60A, is seen in patients of Irish descent and causes a mixed neuropathy and cardiomyopathy.17
PATHOLOGY AND PATHOPHYSIOLOGY OF CA
The atria are universally involved with interatrial septal thickening, which can lead to poor atrial function and increased rates of atrial fibrillation (ATTR more so than AL).21,29 The conduction system can be affected causing varying degrees of heart block, as well as bundle branch block (ATTR more so than AL).30 The valves are usually thickened, often associated with mild to moderate regurgitation. Pericardial involvement can lead to small pericardial effusions (large effusions are rare), and coronary involvement (classically, small intramural vessels) can lead to ischemia and angina with normal epicardial coronaries (AL more so than ATTR).31–33
Thickened left and right ventricular walls result in a nondilated ventricle that is stiff and poorly compliant, resulting in progressive diastolic filling abnormalities. Systolic dysfunction can be seen in severe and advanced disease. Importantly, ejection fraction measured by echocardiography is misleading in CA, as reduced end-diastolic volume produces a low stroke volume. For example, an ejection fraction of 50%, when starting at a significantly reduced end-diastolic volume (for example, 70 mL), leads to a significantly reduced stroke volume (35 mL) and, thus, cardiac output. This explains why patients with CA cannot usually tolerate reduced heart rates, as their cardiac output is dependent on heart rate.34–36
CLINICAL PRESENTATION
Patients with CA typically exhibit heart failure with preserved ejection fraction (otherwise known as diastolic heart failure). Dyspnea on exertion is common; however, some patients can present with more right-sided heart failure symptoms such as lower-extremity edema and ascites. Fatigue and weakness are related to low cardiac output and often attributed to nonspecific symptoms of aging. Because of the thickened ventricles, patients can often be misdiagnosed as having HCM with or without obstruction.7,34 The first manifestation of CA may be atrial fibrillation, most commonly in ATTRwt-CA, or cardioembolic stroke. Atrial fibrillation can be present for years before CA is considered. Bundle branch block and complete heart block (more common in ATTR-CA than AL-CA) may lead to pacemaker implantation.30 Angina with normal coronaries can occur, and a rare presentation may be cardiogenic shock due to diffuse ischemia.31–33 Elderly patients with CA can present with low-flow, low-gradient aortic stenosis.37
DIAGNOSIS
ECG
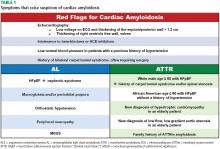
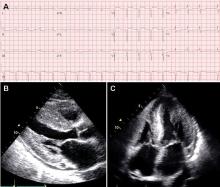
As opposed to that seen in true left ventricular hypertrophy (LVH), which leads to increased voltage on ECG, amyloid infiltration of the myocardium leads to lower voltage. Thus, what is indicative of LVH on echocardiogram combined with low voltage on the ECG is a classic finding for CA. However, only about 50% of patients with AL-CA and about 30% of patients with ATTR-CA meet true low-voltage criteria (QRS amplitude less than 5 mm in limb leads or less than 10 mm in precordial leads).30,38 Hence, the absence of low-voltage criteria does not exclude the diagnosis of CA. Approximately 10% of patients with CA confirmed by biopsy met ECG criteria for LVH.38 The key point is to consider the overall degree of voltage on the ECG relative to the degree of LV thickening on the echocardiogram, recognizing that lower voltage than what would be expected may indicate possible infiltrative disease such as CA. The other main finding on the ECG in patients with CA is a pseudoinfarct pattern with Q waves in the early precordial leads mimicking a prior anteroseptal myocardial infarction.38,39 This finding is seen in about 50% of patients (Figure 3).39 Wide QRS complexes are more frequent in ATTR-CA and lower limb voltages are more frequent in AL-CA.30
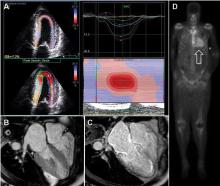
Echocardiogram
The echocardiographic finding of LVH in patients with CA is misleading in that the LV thickening is due to infiltrating amyloid fibrils and not to myocyte hypertrophy. That said, the terms LVH and LV thickening are used interchangeably when describing the echocardiographic phenotype. LV wall thickness greater than 12 mm (6 mm to 10 mm is normal) in the absence of hypertension should prompt suspicion for CA.34 LV thickening most often appears symmetric; however, occasionally it may exhibit asymmetric septal hypertrophy, particularly in ATTRwt-CA. In some cases, there may be a smaller subset that can actually have dynamic LV outflow obstruction similar to that seen in hypertrophic obstructive cardiomyopathy.22–24 An important echocardiographic clue that can differentiate CA from other diseases is thickening of both the LV and right ventricle (Figure 3). Septal wall thickness and LV mass index are greater in ATTR-CA compared with AL-CA.30 On average, the LV septum is around 15 mm in AL-CA and around 18 mm in ATTRwt-CA.40 Historically, the characteristic myocardial “granular sparking” or “speckling” pattern has low sensitivity and specificity.16 The left ventricle is not dilated; rather, the ventricular dimensions are usually smaller than normal. Although ejection fraction is usually preserved, cardiac output is low due to decreased ventricular volume.37 Systolic dysfunction occurs late in the disease.16 Diastolic dysfunction is universal, with a mitral inflow pattern that can range from stage I (abnormal relaxation) in early disease to stage III (restrictive filling pattern) in more advanced disease. Septal and lateral tissue Doppler velocities are very low in amyloid heart disease.41 Another echocardiographic clue to diagnosis is thickening of the heart valves, which is not seen in hypertensive heart disease or hypertrophic cardiomyopathy. Biatrial dilation is common, and there can be thickening of the interatrial septum.
Laboratory testing
N-terminal pro-b-type natriuretic peptide (NT-proBNP) is universally elevated in CA and is typically higher in AL-CA than in ATTR-CA. Troponin T or troponin I or both may be chronically elevated in CA and likely signify small-vessel ischemia. In the appropriate clinical context of a thickened ventricle and heart failure, an elevated troponin value (outside of an acute coronary syndrome) should trigger suspicion for CA. Workup for a monoclonal protein process should always be done when considering CA to rule out AL. Serum and urine protein electrophoresis are insensitive tests to detect AL and should not be relied upon as a screening test. The serum free light chain (sFLC) assay, which measures free kappa and lambda light chain levels and reports the ratio, is a sensitive test that should be measured routinely along with immunofixation of the serum and urine. In AL, sFLC will reveal an abnormal kappa-lambda ratio. An abnormally low ratio (less than 0.26) suggests a monoclonal lambda light chain process, while an abnormally high ratio (greater than 1.65) suggests a monoclonal kappa light chain process. Immunofixation will reveal an M-protein. Because light chains are excreted by the kidney, the serum levels of both kappa and lambda will be elevated in renal dysfunction, but the ratio should remain normal.16,31,34,40,42–47
Advanced noninvasive diagnostic tools for CA
Over the past decade, the ability to diagnose CA noninvasively has dramatically improved with strain imaging using 2D speckle tracking echocardiography, cardiac magnetic resonance imaging (MRI), and nuclear bone scintigraphy. These diagnostic tools have given clinicians options to pursue the diagnosis of CA without directly proceeding to endomyocardial biopsy.
Cardiac MRI. Cardiac MRI is useful for the diagnosis of CA (Figure 4B, 4C). Imaging after administration of gadolinium contrast shows a characteristic late gadolinium enhancement (LGE) pattern that is diffuse and subendocardial, and does not follow any particular coronary distribution.49 LGE can also be seen in the right ventricle and the atrial walls, and can be transmural and patchy in ATTRwt-CA. This pattern is highly sensitive (93%) and specific (70%) for CA with an overall negative predictive accuracy of 84%.50
One of the main limitations of cardiac MRI for the diagnosis of CA is the inability to give contrast in patients with reduced glomerular filtration rate. However, native T1-myocardial mapping techniques that do not require contrast show significantly increased native T1 times in CA and offer a promising alternative. Cardiac MRI parameters such as LGE, the difference in inversion time between the LV cavity and myocardium, native T1 mapping, and extracellular volume offer prognostic information. A greater than fivefold mortality increase is seen in CA patients with transmural LGE compared with those without LGE.49,50
99mTcPYP scintigraphy. 99mTcPYP, a radiotracer used in bone scans, was initially used in cardiology to quantify myocardial infarction due to its ability to localize calcium.51 Its potential utility in CA came in 1982 when diffuse myocardial 99mTcPYP uptake on cardiac radionucleotide imaging was noted in 10 patients with tissue-proven amyloidosis.52 Several subsequent studies reproduced and expanded upon this observation and revealed its diagnostic value, specifically showing that there is significant uptake in ATTR-CA and no to mild uptake in AL-CA. This offers a significant advantage over other noninvasive modalities in that it not only confirms the diagnosis of CA but differentiates ATTR-CA.16
99mTcPYP myocardial radiotracer uptake is graded by the semiquantitative visual score of cardiac retention, where grade 0 = no cardiac uptake, grade 1 = mild uptake less than bone, grade 2 = moderate uptake equal to bone, and grade 3 = high uptake greater than bone (Figure 4D).42 Additionally, quantitative analysis of heart retention can be calculated drawing circular regions of interest over the heart and mirrored on the contralateral chest wall. A heart-to-contralateral ratio greater than 1.5 is consistent with the diagnosis of ATTR-CA.53,54 In 2016, a multicenter study showed that grade 2 or 3 myocardial radiotracer uptake on bone scintigraphy in the absence of evidence of a monoclonal gammopathy was diagnostic for ATTR-CA, providing a cost-effective and non-invasive technique with a specificity and positive predictive value of 100% (confidence interval, 99.0–100%).42
Endomyocardial biopsy, right heart catheterization, and fat biopsy
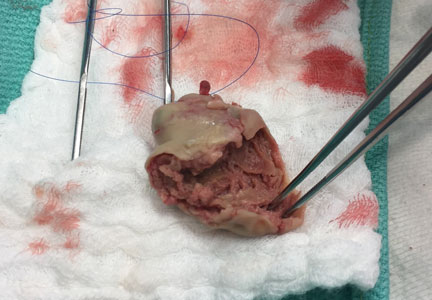
Endomyocardial biopsy is essentially 100% sensitive for the diagnosis of CA.25 The main risk of pursuing endomyocardial biopsy is about a 1% risk of right ventricular perforation leading to cardiac tamponade.55 The other limitation to this approach is that not all centers are equipped to perform this procedure. Birefringence under polarized light microscopy is histopathologically diagnostic of CA; however, further subtyping by the pathologist to determine if it is AL or ATTR is absolutely crucial. Subtyping can be performed by immunohistochemistry with caution taken for misinterpretation. If there is any question of accuracy, the specimen should be sent for laser microdissection and mass spectroscopy for accurate identification of the precursor protein type (some centers routinely perform mass spectroscopy on all myocardial specimens).16,31
Right heart catheterization is nonspecific and shows restrictive hemodynamics. The right atrial waveform shows rapid x and y descents and the right ventriclular tracing may show a dip-and-plateau pattern typical of restrictive cardiomyopathy. Cardiac output can be preserved but more commonly is low.16,31
Fat pad biopsy is 60% to 80% sensitive in AL, 65% to 85% sensitive in ATTRm, and only 14% sensitive in ATTRwt, with the accuracy dependent on the operator, pathologist, and how much tissue is removed (fat pad aspirate vs biopsy specimen).56–58 Fat pad biopsy has diagnostic limitations, and a negative fat pad biopsy does not rule out amyloidosis.
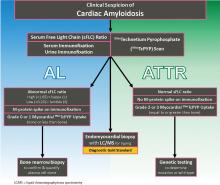
DIAGNOSTIC ALGORITHM FOR CARDIAC AMYLOIDOSIS
In conjunction with laboratory tests, 99mTcPYP scan of the heart can be ordered to investigate the possibility of ATTR-CA. Grade 2 to 3 myocardial uptake in the absence of a monoclonal plasma cell process is consistent with the diagnosis of ATTR-CA. Grade 0 or 1 myocardial uptake on 99mTcPYP scan with an abnormal sFLC ratio or positive M protein on immunofixation suggests AL-CA and a bone marrow biopsy should be performed. If the patient has an abnormal sFLC ratio and grade 2 to 3 uptake on 99mTcPYP scan, the diagnosis of ATTR-CA with unrelated monoclonal gammopathy of undetermined significance should be considered. However, this would need to be reconciled by pursuing endomyocardial biopsy and accurate tissue typing. If the 99mTcPYP scan is negative, and the sFLC ratio is normal, and immunofixation is negative, a diagnosis of CA is very unlikely.16,31,40,42–47
If the diagnosis of ATTR-CA is made, genetic testing can determine the presence or absence of a mutation to differentiate ATTRm or ATTRwt, respectively. If the diagnosis of AL-CA is suggested, a bone marrow biopsy is necessary to identify and quantify the plasma cell clone.16,31,40,42–47
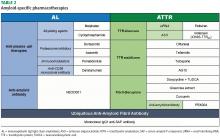
TREATMENT
Management of heart failure in cardiac amyloidosis
The main treatment of heart failure revolves around sodium restriction and diuretics to relieve congestion. This can prove challenging in many patients due to the narrow window between too high or too low filling pressures. A combination of loop diuretics and an aldosterone antagonist is most effective.31,34,44,45 Torsemide is preferred over furosemide due to its superior bioavailability and longer duration of action, particularly since these patients have issues with gut edema and GI absorption. Due to dependence of the cardiac output on heart rate and the tendency for orthostatic hypotension, traditional neurohormonal antagonists including beta blockers and angiotensin-converting enzyme inhibitors are neither effective nor well tolerated.60 However, in patients with atrial fibrillation, beta blockers may need to be used for rate control. Nondihydropyridine calcium channel blockers bind avidly to amyloid fibrils and are contraindicated due to risk of profound hypotension and syncope.30,31,34,44,45 Digoxin is usually avoided in CA due to concerns of increased risk of toxicity; however, it may be used with caution for rate control in atrial fibrillation given its lack of negative inotropy.61 Maintenance of normal sinus rhythm is preferable due to the importance of atrial contribution to cardiac output.
Anticoagulation in patients with atrial fibrillation and even in patients with normal sinus rhythm and poor atrial function is important due to the high risk of thromboembolic complications.62 Pacemakers are indicated for heart block or symptomatic bradycardia.63 The role of intracardiac defibrillators is controversial, but may be warranted in selected patients with AL-CA.64,65
AL treatment
Risk stratification and prognostication for AL. The most important determinant of clinical outcome in AL is the extent of cardiac involvement, as congestive heart failure and sudden cardiac death are the most common causes of death. The level of NT-proBNP and the level of either troponin T or troponin I have strong prognostic value and form the basis for the staging system in AL. Various iterations have evolved over the years, but the most widely adopted is the 4-stage system developed and validated by Mayo Clinic. This system uses a cutoff value at diagnosis for NT-proBNP greater than 1,800 ng/mL, troponin T greater than 0.025 μg/L, and the difference between kappa and lambda free light chain levels greater than 180 mg/L. Stage level increases by the number of cutoff values exceeded, with stage IV carrying a median survival of 6 months.47 Additionally, the troponin T level can help risk-stratify patients being considered for autologous stem cell transplant. In a retrospective study, troponin T greater than 0.06 μg/L was associated with increased mortality following stem cell transplant.66 Ultimately, prognosis in AL-CA is related to the hematologic response to chemotherapy.
Current treatment strategies for AL. The survival of patients with AL has improved over the years with the advent of more effective chemotherapeutic regimens that kill the underlying plasma cell clone producing the unstable light chains. The goal of treatment is to achieve a complete hematologic response with normalization of the affected light chain and sFLC ratio as well as elimination of the M protein on immunofixation.
The development of the proteasome inhibitor bortezomib has improved efficacy and survival in AL causing a faster and more complete hematologic response than prior regimens.43,67,68
The most commonly used first-line treatment consists of a 3-drug combination with the alkylating agent cyclophosphamide, the proteasome inhibitor bortezomib, and the steroid dexamethasone, which is given weekly.43 A retrospective study by Sperry et al8 showed that patients receiving an alkylating agent, bortezomib, and a steroid had the best outcomes compared with other regimens.
For patients with refractory or relapsed disease, the CD38 monoclonal antibody daratumumab can be used if patients meet myeloma criteria and has been found to be effective thus far.68,69 Newer proteasome inhibitors such as ixazomib, which is taken orally, are being studied in alternative combination regimens.70 High-dose chemotherapy with autologous stem cell transplant can be considered in patients with an acceptable cardiac risk profile and may offer more complete and durable remission than chemotherapy, although this is controversial.43,71
The cardiologist’s role in AL-CA. The hematologist directs the chemotherapy for AL but works closely with the cardiologist when there is cardiac involvement. The main role of the cardiologist is to manage volume status with diuretics, monitor for arrhythmia, and evaluate the cardiac response to treatment.43,71 Cardiac response was traditionally measured by echocardiographic changes of wall thickness, diastolic function, and ejection fraction, as well as changes in New York Heart Association (NYHA) functional class.67 However, it is uncommon to see reduction in LV wall thickness or significant improvement in ejection fraction and if it does occur, it is a slow process that usually takes more than 1 year. With the advent of longitudinal myocardial strain imaging, improvements in strain can be seen despite the lack of structural changes on echocardiogram.72 In 2012, consensus criteria defined a cardiac response as a greater than 30% reduction in NT-proBNP.73 Misfolded light chains are toxic to cardiomyocytes by causing increased oxidative stress and impairing contractility. Thus, reduction in light chain levels can lead to clinical improvement and significant reductions in NT-proBNP without changing amyloid fibril burden in the heart.
Heart transplant for patients with AL-CA. For patients who have a good hematologic response to initial chemotherapy but have limited predicted survival due to severe heart failure, heart transplant followed by autologous stem cell transplant, is a treatment strategy that can be considered. The patient must have clinically isolated severe cardiac disease, minimal amyloid burden in other organs, and a plasma cell clone that is responsive to therapy. Initial reports of heart transplant showed poor survival rates due to recurrent amyloid in the transplanted heart and progressive amyloid deposition in other organs. However, due to improved anti-plasma-cell-directed therapy and refinement in patient selection, outcomes have improved. Contemporary series of patients undergoing heart transplant followed by stem cell transplant showed that outcomes are almost comparable to heart transplant for other indications, with a 5-year survival rate of approximately 65%.74
Future therapies for AL. There is an AL amyloid-directed monoclonal antibody designed to remove amyloid fibrils from affected organs and is currently undergoing clinical trials. NEOD001, a humanized murine monoclonal antibody that targets an epitope exposed during light chain misfolding, binds to the light chain amyloid fibril and signals an immune response to clear the deposits. This agent has completed phase 1 and 2 clinical trials of 27 patients previously treated with at least 1 plasma cell-directed therapy. It showed good tolerability and achieved both renal and cardiac responses in most patients.75
A phase 2b clinical trial (NCT02632786) of patients with AL with a previous hematologic response to treatment and persistent heart dysfunction is underway and expected to be completed in January 2018. A phase 3 clinical trial (NCT02312206) of NEOD001 as an adjunct to chemotherapy is also ongoing and results are expected in February 2019.
ATTR treatment
Liver transplant for ATTRm amyloidosis for the V30M mutation that causes FAP was first described in 1990, but it has not been well validated in other mutations and is not a solution for ATTRwt.76 Significant progress has been made over the past 2 decades in the understanding of the pathophysiologyy of ATTR, paving the way for promising advancements in pharmacotherapy. Presently, there are 3 classes of pharmacologic agents, grouped by the point of disease process each strategy targets:
- Block TTR synthesis at the translational level in hepatocytes
- Stabilize the TTR tetramer to inhibit the rate-determining step of amyloidogenesis
- Disrupt and clear the ATTR amyloid fibril.77
Block TTR synthesis. TTR messenger RNA (mRNA) can be targeted by “silencers” preventing translation, thereby reducing the production TTR protein by hepatocytes. The resultant sustained reduction of plasma TTR should decrease or halt amyloid deposition by making less TTR available to dissociate and deposit in the heart and nerves. There are 2 approaches to silencing TTR mRNA translation: small interfering RNA (siRNA) and antisense oligonucleotide (ASO).77
An siRNA, packaged in a lipid nanoparticle to ensure delivery to the liver, has been designed to bind to a conserved region of TTR mRNA, degrading the mRNA and reducing TTR protein expression. One siRNA, patisiran, completed the phase 3 APOLLO clinical trial (NCT01960348) in August 2017. It is an intravenous medication that requires premedication. The APOLLO trial studied patients with neuropathic variants of ATTRm, with a primary end point of neuropathy progression over 18 months. Patisrian met the primary end point and will likely be approved by the US Food and Drug Administration (FDA) by the third quarter of 2018. Given its target of a conserved 3’ untranslated region of TTR mRNA, patisiran should theoretically yield benefits not just in FAP but to both ATTRm-CA and ATTRwt-CA.68,77
ASOs are single-stranded oligonucleotides, typically 20 nucleotides in length, that bind to mRNA and elicit enzymatic mRNA degradation and reduced protein expression. Inotersen (IONIS-TTRRx) is an ASO drug that targets a conserved region of TTR mRNA. Inotersen is administered by weekly subcutaneous injection. A phase 2/3 clinical trial (NCT01737398) completed in October 2017 studied the drug's efficacy in treating FAP, with a primary end point of neuropathy progression over 65 weeks. It met the primary end point and a subset of patients actually improved. Like patisiran, inotersen is likely to be approved by the FDA for a neuropathy indication by the third quarter of 2018 and may benefit patients with ATTRm-CA and ATTRwt-CA. More studies are needed in the ATTR cardiac population.68,77
Stabilize the TTR tetramer. The TTR tetramer has 2 thyroxine binding pockets that stabilize the structure when bound preventing dissociation. Dissociation of the tetramer, the rate limiting step for ATTR fibrillogenesis, can be reduced using pharmacologic agents that bind to the thyroxine binding pockets. Both new and repurposed agents have been found to stabilize the TTR tetramer, including diflunisal, tafamidis, tolcapone, and AG10.68,77
Diflunisal (Dolobid) is a nonacetylated salicylate nonsteroidal anti-inflammatory drug used for over 3 decades to treat arthritis and musculoskeletal pain. Unrelated to its anti-inflammatory properties, it interacts with TTR’s thyroxine binding pocket to increase the stability of the tetramer. A 2013 randomized, placebo-controlled, international multicenter trial of 130 patients with FAP demonstrated a statistically significant slowing of polyneuropathy progression; however, 67 patients (diflunisal n = 27, placebo n = 40) did not complete the study.78 A small study revealed diflunisal to be reasonably well-tolerated in ATTR-CA, and to date it is the only readily available pharmacotherapy for ATTR supported by a randomized, placebo-controlled trial.79,80 Diflunisal may be considered for off-label use in patients with ATTR-CA with relatively preserved kidney function and no increased bleeding risk, taken under the supervision of a cardiologist who will monitor for fluid retention and changes in renal function.77
Tafamidis (Vyndaqel), like diflunisal, interacts with TTR’s thyroxine binding pocket and increases tetrameric stability. A phase 2 open-label clinical trial studied the efficacy and tolerance of tafamidis in 31 patients with ATTRwt and NYHA functional class 1 and 2 followed for 1 year. Twenty-eight patients completed the study and 2 patients died. TTR stabilization at 6 weeks was achieved in 30 of 31 patients (96.8%), and success at 1 year in 25 of 28 patients (89.3%). No clinical progression occurred in 16 of 31 patients (51.5%), and tafamidis was generally well-tolerated, with diarrhea the most common side effect in 7 of 31 patients (22.6% ).81,82
A phase 3 clinical trial (NCT01994889) is studying tafamidis vs placebo in patients with ATTRm-CA or ATTRwt-CA (excluding NYHA functional class 4) with the primary outcome measure of all-cause mortality and heart failure-related hospitalizations over 30 months. This is a large trial that enrolled 446 patients and data collection is expected to be completed in February 2018.
Tolcapone, approved by the FDA for Parkinson disease, has been found to be a potent TTR stabilizer by binding both thyroxine binding pockets of the TTR tetramer simultaneously. However, tolcapone has an FDA “black box” warning due to the risk of potentially fatal acute fulminant liver failure and is not currently used in ATTR therapy.68 Nonetheless, it will likely undergo further study for ATTR.
Recruiting is underway for a phase 1 clinical trial of AG10, a potent selective TTR stabilizer (NCT03294707).68
Disruption and clearance of the ATTR amyloid fibril. Even though treatment directed at blocking TTR synthesis or stabilizing the tetramer may be effective at preventing further deposition, the residual amyloid deposits persist and continue to affect organ function. With that need in mind, several agents that disrupt the amyloid formation process further downstream have been evaluated at a basic science level and in a few small nonrandomized open-label studies.77
Doxycycline is a tetracycline antibiotic with demonstrated effectiveness in disrupting mature amyloid fibrils in mouse models.83 Tauroursodeoxycholic acid is a bile acid with the ability to disrupt prefibrillar amyloid components. This combination has been studied in patients with ATTR-CA in 2 small open-label trials, with only 1 having results published. There was no progression in NT-proBNP or wall thickness in a cohort of 7 patients who completed 12 months of treatment.84 These data are nonrandomized and hypothesis-generating, as adequate studies would need to be performed to evaluate this hypothesis further. Because there are currently no FDA-approved therapies for ATTR, patients may be offered this combination fully informed that the data are limited. (Note: ursodiol is substituted for tauroursodeoxycholic acid, which is not available in the United States.)68
Green tea extract contains the polyphenol epigallocatechin-3-gallate, which has shown the ability for fibril disruption as well as TTR stabilization, importantly using a binding site separate from the thyroxine binding pocket (utilized in diflunisal and tafamidis). A small open-label study of 19 patients with ATTR-CA of whom 14 took green tea extract for 1 year reported a reduction in intraventricular septal wall thickness at 1 year, and in 9 patients a reduction of 12.5% in LV mass measured by cardiac MRI.85
Curcumin, the active ingredient in the household spice turmeric, has displayed in vitro promise as a TTR stabilizer by binding to the thyroxine binding pocket, and as an amyloid fibril disruptor by increasing macrophage degradation activity. Although there have only been preliminary animal studies, this supplement may be promising for further study in humans with ATTR-CA.68
PRX004 is a synthetic antibody designed to bind to non-native misfolded forms of TTR with the goal of potentially preventing deposition and promoting clearance of TTR aggregates.86 A phase 1 open-label escalation trial (NCT03336580) in 36 patients with ATTRm is planned and, hopefully, will pave the way for further study.
Heart transplant for patients with ATTR-CA. Patients with ATTRwt-CA who are young enough to undergo heart transplant have displayed favorable outcomes given that it causes clinically isolated heart disease and is an indolent process that should not affect the transplanted heart over the average life span of the allograft. Patients with the ATTRm mutation V122I have been treated with heart transplant alone, with the thought process that again, due to the indolent nature of amyloid deposition, concomitant liver transplant may not be needed.74 Thus far, 6 patients with this mutation have undergone successful transplant at our institution with heart alone, 1 of whom is 9 years posttransplant without any recurrent amyloid in the allograft. Patients with the T60A mutation that causes both polyneuropathy and cardiomyopathy require combined heart and liver transplant.74
Are there other therapies being studied to clear amyloid deposits and reverse organ dysfunction?
Extracellular deposits of amyloid fibrils, regardless of precursor protein, contain common elements such as calcium, glycosaminoglycans, and an SAP component. SAP stabilizes amyloid fibrils and makes them resistant to degradation. A monoclonal immunoglobulin G1 anti-SAP antibody has been designed to target the ubiquitous SAP component, signaling an immune response that leads to macrophage mediated clearance of amyloid fibrils, regardless of the type. Treatment with this approach was studied in a pilot trial of 16 patients mostly with AL, and within a 6-week period some of the patients had dramatic reversal of liver amyloid deposition.2 This has paved the way for a phase 2 open-label trial to be performed in patients with AL-CA and ATTR-CA (NCT03044353) and plans for a randomized phase 3 trial in CA are in discussion. There is optimism that this therapy may achieve the holy grail of removing amyloid rather than just preventing further deposition.
CONCLUSION
The diagnosis of CA requires a high index of suspicion. The diagnostic tools have improved due to the availability of modern imaging techniques, and the advent of measuring the sFLC assay along with immunofixation of the serum and urine. The prognosis for patients with AL-CA used to be dismal, with very poor survival rates. The current treatment strategies that include proteasome inhibitors have significantly improved survival, emphasizing the importance of early diagnosis and prompt initiation of therapy. Monoclonal antibodies against plasma cells (daratumumab) and light chain amyloid deposits (NEOD001) have the potential to further improve outcomes. The diagnosis of ATTR-CA used to be a futile academic pursuit given the lack of available therapies. However, there are several new FDA-approved agents on the horizon, including TTR gene silencers and stabilizers. CA is no longer considered to be rare and hopeless. Rather, it is more common than previously recognized and even more treatable.
- Merlini G, Bellotti V. Molecular mechanisms of amyloidosis. N Engl J Med 2003; 349:583–596.
- Richards DB, Cookson LM, Berges AC, et al. Therapeutic clearance of amyloid by antibodies to serum amyloid P component. N Engl J Med 2015; 373:1106–1114.
- Sipe JD, Benson MD, Buxbaum JN, et al. Nomenclature 2014: amyloid fibril proteins and clinical classification of the amyloidosis. Amyloid 2014; 21:221–224.
- Maleszewski JJ. Cardiac amyloidosis: pathology, nomenclature, and typing. Cardiovasc Pathol 2015; 24:343–350.
- Kyle RA, Linos A, Beard CM, et al. Incidence and natural history of primary systemic amyloidosis in Olmsted County, Minnesota, 1950 through 1989. Blood 1992; 79:1817–1822.
- Krsnik I, Cabero M, Morillo D, et al. Light chain amyloidosis: Experience in a tertiary hospital: 2005-2013. Rev Clin Esp 2015; 215:1–8.
- Dubrey SW, Cha K, Anderson J, et al. The clinical features of immunoglobulin light-chain (AL) amyloidosis with heart involvement. QJM 1998; 91:141–157.
- Sperry BW, Ikram A, Hachamovitch R, et al. Efficacy of chemotherapy for light-chain amyloidosis in patients presenting with symptomatic heart failure. J Am Coll Cardiol 2016; 67:2941–2948.
- Gillmore JD, Damy T, Fontana M, et al. A new staging system for cardiac transthyretin amyloidosis. Eur Heart J 2017; Oct 18. [Epub ahead of print] doi:10.1093/eurheartj/ehx589.
- Tanskanen M, Peuralinna T, Polvikoski T, et al. Senile systemic amyloidosis affects 25% of the very aged and associates with genetic variation in alpha2-macroglobulin and tau: a population-based autopsy study. Ann Med 2008; 40:232–239.
- González-López E, Gallego-Delgado M, Guzzo-Merello G, et al. Wild-type transthyretin amyloidosis as a cause of heart failure with preserved ejection fraction. Eur Heart J 2015; 36:2585–2594.
- Longhi S, Lorenzini M, Gagliardi C, et al. Coexistence of degenerative aortic stenosis and wild-type transthyretin-related cardiac amyloidosis. JACC Cardiovasc Imaging 2016;9:325–327.
- Grogan M, Scott CG, Kyle RA, et al. Natural history of wild-type transthyretin cardiac amyloidosis and risk stratification using a novel staging system. J Am Coll Cardiol 2016; 68:1014–1020.
- Gioeva Z, Urban P, Meliss RR, et al. ATTR amyloid in the carpal tunnel ligament is frequently of wildtype transthyretin origin. Amyloid 2013; 20:1–6.
- Yanagisawa A, Ueda M, Sueyoshi T, et al. Amyloid deposits derived from transthyretin in the ligamentum flavum as related to lumbar spinal canal stenosis. Mod Pathol 2015; 28:201–207.
- Siddiqi OK, Ruberg FL. Cardiac amyloidosis: an update on pathophysiology, diagnosis, and treatment. Trends Cardiovasc Med 2017; Jul 13. [Epub ahead of print] doi:10.1016/j.tcm.2017.07.004.
- Nakagawa M, Sekijima Y, Yazaki M, et al. Carpal tunnel syndrome: A common initial symptom of systemic wild-type ATTR (ATTRwt) amyloidosis. Amyloid 2016; 23:58–63.
- Sekijima Y, Yoshida K, Tokuda T, Ikeda S-I. Familial Transthyretin Amyloidosis. In: Adam MP, Ardinger HH, Pagon RA, et al, eds. Seattle, WA: University of Washington, Seattle; 1993–2017. Available at: https://www-ncbi-nlm-nih-gov.ccmain.ohionet.org/books/NBK1194. Updated January 26, 2012. Accessed November 16, 2017.
- Buxbaum J, Jacobson DR, Tagoe C, et al. Transthyretin V122I in African Americans with congestive heart failure. J Am Coll Cardiol 2006; 47:1724–1725.
- Ruberg FL, Maurer MS, Judge DP, et al. Prospective evaluation of the morbidity and mortality of wild-type and V122I mutant transthyretin amyloid cardiomyopathy: The Transthyretin Amyloidosis Cardiac Study (TRACS). Am Heart J 2012; 164:222–228.e1.
- Wright JR, Calkins E. Amyloid in the aged heart: frequency and clinical significance. J Am Geriatr Soc 1975; 23:97–103.
- Vermeer AMC, Janssen A, Boorsma PC, Mannens MMAM, Wilde AAM, Christiaans I. Transthyretin amyloidosis: a phenocopy of hypertrophic cardiomyopathy. Amyloid 2017; 24:87–91.
- Velazquez-Ceceña JL, Lubell DL, Nagajothi N, Al-Masri H, Siddiqui M, Khosla S. Syncope cardiomyopathy in a patient with primary AL-type amyloid heart disease. Tex Heart Inst J 2009; 36:50–54.
- Stegman BM, Kwon D, Rodriguez ER, Hanna M, Cho L. Left ventricular hypertrophy in a runner: things are not always what they seem. Circulation 2014; 130:590–592.
- Ardehali H, Qasim A, Cappola T, et al. Endomyocardial biopsy plays a role in diagnosing patients with unexplained cardiomyopathy. Am Heart J 2004; 147:919–923.
- Berghoff M, Kathpal M, Khan F, Skinner M, Falk R, Freeman R. Endothelial dysfunction precedes C-fiber abnormalities in primary (AL) amyloidosis. Ann Neurol 2003; 53:725–730.
- Khan MF, Falk RH. Amyloidosis. Postgrad Med J 2001; 77:686–693.
- Martinez-Naharro A, Treibel TA, Abdel-Gadir A, et al. Magnetic resonance in transthyretin cardiac amyloidosis. J Am Coll Cardiol 2017; 70:466–477.
- Longhi S, Quarta CC, Milandri A, et al. Atrial fibrillation in amyloidotic cardiomyopathy: prevalence, incidence, risk factors and prognostic role. Amyloid 2015; 22:147–155.
- Sperry BW, Vranian MN, Hachamovitch R, et al. Are classic predictors of voltage valid in cardiac amyloidosis? A contemporary analysis of electrocardiographic findings. Int J Cardiol 2016; 214:477–481.
- Falk RH. Diagnosis and management of the cardiac amyloidoses. Circulation 2005; 112:2047–2060.
- Berk JL, Keane J, Seldin DC, et al. Persistent pleural effusions in primary systemic amyloidosis: etiology and prognosis. Chest 2003; 124:969–977.
- Miani D, Rocco M, Alberti E, Spedicato L, Fioretti PM. Amyloidosis of epicardial and intramural coronary arteries as an unusual cause of myocardial infarction and refractory angina pectoris. Ital Heart J 2002; 3:479–482.
- Mesquita ET, Jorge AJL, Souza CV Junior, Andrade TR. Cardiac amyloidosis and its new clinical phenotype: heart failure with preserved ejection fraction. Arg Bras Cardiol 2017; 109:71–80.
- Swanton RH, Brooksby IAB, Davies MJ, Coltart DJ, Jenkins BS, Webb-Peploe MM. Systolic and diastolic ventricular function in cardiac amyloidosis: studies in six cases diagnosed with endomyocardial biopsy. Am J Cardiol 1977; 39:658–664.
- Tyberg TI, Goodyer AVN, Hurst VW 3rd, Alexander J, Langou RA. Left ventricular filling in differentiating restrictive amyloid cardiomyopathy and constrictive pericarditis. Am J Cardiol 1981; 47:791–796.
- Sperry BW, Jones BM, Vranian MN, Hanna M, Jaber WA. Recognizing transthyretin cardiac amyloidosis in patients with aortic stenosis: impact on prognosis. JACC Cardiovasc Imaging 2016; 9:904–906.
- Cyrille NB, Goldsmith J, Alvarez J, Maurer MS. Prevalence and prognostic significance of low QRS voltage among the three main types of cardiac amyloidosis. Am J Cardiol 2014; 114:1089–1093.
- Hongo M, Yamamoto H, Kohda T, et al. Comparison of electrocardiographic findings in patients with AL (primary) amyloidosis and in familial amyloid polyneuropathy and anginal pain and their relation to histopathologic findings. Am J Cardiol 2000; 85:849–853.
- Maurer MS, Elliott P, Comenzo R, Semigran M, Rapezzi C. Addressing common questions encountered in the diagnosis and management of cardiac amyloidosis. Circulation 2017; 135:1357–1377.
- Abdalla I, Murray RD, Lee JC, Stewart WJ, Tajik AJ, Klein AL. Duration of pulmonary venous atrial reversal flow velocity and mitral inflow a wave: new measure of severity of cardiac amyloidosis. J Am Soc Echocardiogr 1998; 11:1125–1133.
- Gillmore JD, Maurer MS, Falk RH, et al. Nonbiopsy diagnosis of cardiac transthyretin amyloidosis. Circulation 2016; 133:2404–2412.
- Gertz MA. Immunoglobulin light chain amyloidosis: 2016 update on diagnosis, prognosis, and treatment. Am J Hematol 2016; 91:947–956.
- Patel KS, Hawkins PN. Cardiac amyloidosis: where are we today? J Intern Med 2015; 278:126–144.
- Ritts AJ, Cornell RF, Swiger K, Singh J, Goodman S, Lenihan DJ. Current concepts of cardiac amyloidosis: diagnosis, clinical management, and the need for collaboration. Heart Fail Clin 2017; 13:409–416.
- Sperry BW, Vranian MN, Hachamovitch R, et al. Subtype-specific interactions and prognosis in cardiac amyloidosis. J Am Heart Assoc 2016; 5:e002877.
- Kumar S, Dispenzieri A, Lacy MQ, et al. Revised prognostic staging system for light chain amyloidosis incorporating cardiac biomarkers and serum free light chain measurements. J Clin Oncol 2012; 30:989–995.
- Phelan D, Collier P, Thavendiranathan P, et al. Relative apical sparing of longitudinal strain using two-dimensional speckle-tracking echocardiography is both sensitive and specific for the diagnosis of cardiac amyloidosis. Heart 2012; 98:1442–1448.
- Patel AR, Kramer CM. Role of cardiac magnetic resonance in the diagnosis and prognosis of nonischemic cardiomyopathy. JACC Cardiovasc Imaging 2017; 10(10 Pt A):1180–1193.
- White JA, Kim HW, Shah D, et al. CMR imaging with rapid visual T1 assessment predicts mortality in patients suspected of cardiac amyloidosis. JACC Cardiovasc Imaging 2014; 7:143–156.
- Parkey RW, Bonte FJ, Meyer SL, et al. A new method for radionuclide imaging of acute myocardial infarction in humans. Circulation 1974; 50:540–546.
- Wizenberg TA, Muz J, Sohn YH, Samlowski W, Weissler AM. Value of positive myocardial technetium-99m-pyrophosphate scintigraphy in the noninvasive diagnosis of cardiac amyloidosis. Am Heart J 1982; 103(4 Pt 1):468–473.
- Bokhari S, Castaño A, Pozniakoff T, Deslisle S, Latif F, Maurer MS. 99mTc-Pyrophosphate scintigraphy for differentiating light-chain cardiac amyloidosis from the transthyretin-related familial and senile cardiac amyloidoses. Circ Cardiovasc Imaging 2013; 6:195–201.
- Vranian MN, Sperry BW, Hanna M, et al. Technetium pyrophosphate uptake in transthyretin cardiac amyloidosis: associations with echocardiographic disease severity and outcomes. J Nucl Cardiol 2017; Jan 3. [Epub ahead of print] doi: 10.1007/s12350-016-0768-9.
- Bennett MK, Gilotra NA, Harrington C, et al. Evaluation of the role of endomyocardial biopsy in 851 patients with unexplained heart failure from 2000-2009. Circ Heart Fail 2013; 6:676–684.
- Garcia Y, Collins AB, Stone JR. Abdominal fat pad excisional biopsy for the diagnosis and typing of systemic amyloidosis. Hum Pathol 2017; Nov 10. [Epub ahead of print] doi:10.1016/j.humpath.2017.11.001.
- Quarta CC, Gonzalez-Lopez E, Gilbertson JA, et al. Diagnostic sensitivity of abdominal fat aspiration in cardiac amyloidosis. Eur Heart J 2017; 38:1905–1908.
- Fine NM, Arruda-Olson AM, Dispenzieri A, et al. Yield of noncardiac biopsy for the diagnosis of transthyretin cardiac amyloidosis. Am J Cardiol 2014; 113:1723–1727.
- Katzmann JA, Abraham RS, Dispenzieri A, Lust JA, Kyle RA. Diagnostic performance of quantitative kappa and lambda free light chain assays in clinical practice. Clin Chem 2005; 51:878–781.
- Malha L, Mann SJ. Loop diuretics in the treatment of hypertension. Curr Hypertens Rep 2016; 18:27.
- Rubinow A, Skinner M, Cohen AS. Digoxin sensitivity in amyloid cardiomyopathy. Circulation 1981; 63:1285–1288.
- Feng D, Syed IS, Martinez M, et al. Intracardiac thrombosis and anticoagulation therapy in cardiac amyloidosis. Circulation 2009; 119:2490–2497.
- Castaño A, Drachman BM, Judge D, Maurer MS. Natural history and therapy of TTR-cardiac amyloidosis: emerging disease-modifying therapies from organ transplantation to stabilizer and silencer drugs. Heart Fail Rev 2015; 20:163–178.
- Hamon D, Algalarrondo V, Gandjbakhch E, et al. Outcome and incidence of appropriate implantable cardioverter-defibrillator therapy in patients with cardiac amyloidosis. Int J Cardiol 2016; 222:562–568.
- Patel KS, Hawkins PN, Whelan CJ, Gillmore JD. Life-saving implantable cardioverter defibrillator therapy in cardiac AL amyloidosis. BMJ Case Rep 2014; Dec 22. doi:10.1136/bcr-2014-206600.
- Gertz M, Lacy M, Dispenzieri A, et al. Troponin T level as an exclusion criterion for stem cell transplantation in light-chain amyloidosis. Leuk Lymphoma 2008; 49:36–41.
- Vranian MN, Sperry BW, Valent J, Hanna M. Emerging advances in the management of cardiac amyloidosis. Curr Cardiol Rep 2015; 17:100.
- Alexander KM, Singh A, Falk RH. Novel pharmacotherapies for cardiac amyloidosis. Pharmacol Ther 2017; 180:129–138.
- Sher T, Fenton B, Akhtar A, Gertz MA. First report of safety and efficacy of daratumumab in 2 cases of advanced immunoglobulin light chain amyloidosis. Blood 2016; 128:1987–1989.
- Sanchorawala V, Palladini G, Kukreti V, et al. A phase 1/2 study of the oral proteasome inhibitor ixazomib in relapsed or refractory AL amyloidosis. Blood 2017; 130:597–605.
- Zumbo G, Sadeghi-Alavijeh O, Hawkins PN, Fontana M. New and developing therapies for AL amyloidosis. Expert Opin Pharmacother 2017; 18:139–149.
- Koyama J, Falk RH. Prognostic significance of strain Doppler imaging in light-chain amyloidosis. JACC Cardiovasc Imaging 2010; 3:333–342.
- Palladini G, Dispenzieri A, Gertz MA, et al. New criteria for response to treatment in immunoglobulin light chain amyloidosis based on free light chain measurement and cardiac biomarkers: impact on survival outcomes. J Clin Oncol 2012; 30:4541–4549.
- Sousa M, Monohan G, Rajagopalan N, Grigorian A. Heart transplantation in cardiac amyloidosis. Heart Fail Rev 2017; 22:317–327.
- Gertz MA, Landau H, Comenzo RL, et al. First-in-human phase I/II study of NEOD001 in patients with light chain amyloidosis and persistent organ dysfunction. J Clin Oncol 2016; 34:1097–1103.
- Holmgren G, Steen L, Ekstedt J, et al. Biochemical effect of liver transplantation in two Swedish patients with familial amyloidotic polyneuropathy (FAP-met30). Clin Genet 1991; 40:242–246.
- Hanna M. Novel drugs targeting transthyretin amyloidosis. Curr Heart Fail Rep 2014; 11:50–57.
- Berk JL, Suhr OB, Obici L, et al; Diflunisal Trial Consortium. Repurposing diflunisal for familial amyloid polyneuropathy: a randomized clinical trial. JAMA 2013; 310:2658–2667.
- Castaño A, Helmke S, Alvarez J, Delisle S, Maurer MS. Diflunisal for ATTR cardiac amyloidosis. Congest Heart Fail 2012; 18:315–319.
- Sekijima Y, Tojo K, Morita H, Koyama J, Ikeda S-I. Safety and efficacy of long-term diflunisal administration in hereditary transthyretin (ATTR) amyloidosis. Amyloid 2015; 22:79–83.
- Coelho T, Maia LF, Martins da Silva A, et al. Tafamidis for transthyretin familial amyloid polyneuropathy: a randomized, controlled trial. Neurology 2012; 79:785–792.
- Maurer MS, Grogan DR, Judge DP, et al. Tafamidis in transthyretin amyloid cardiomyopathy: effects on transthyretin stabilization and clinical outcomes. Circ Heart Fail 2015; 8:519–526.
- Cardoso I, Martins D, Ribeiro T, Merlini G, Saraiva MJ. Synergy of combined doxycycline/TUDCA treatment in lowering transthyretin deposition and associated biomarkers: studies in FAP mouse models. J Transl Med 2010; 8:74.
- Obici L, Cortese A, Lozza A, et al. Doxycycline plus tauroursodeoxycholic acid for transthyretin amyloidosis: A phase II study. Amyloid 2012; 19(suppl 1):34–36.
- Kristen AV, Lehrke S, Buss S, et al. Green tea halts progression of cardiac transthyretin amyloidosis: An observational report. Clin Res Cardiol 2012; 101:805–813.
- Higaki JN, Chakrabartty A, Galant NJ, et al. Novel conformation-specific monoclonal antibodies against amyloidogenic forms of forms of transthyretin. Amyloid 2016; 23:86–97.
WHAT IS AMYLOIDOSIS?
Amyloidosis is a protein deposition disease in which a specific precursor protein pathologically misfolds from its physiologic tertiary structure into a more linear shape dominated by beta-pleated sheets. The misfolded protein aggregates into oligomers, eventually forming insoluble amyloid fibrils that deposit extracellularly in tissues. Both the circulating oligomers, which are cytotoxic, and the fibrils, which cause distortion of the tissue architecture, lead to organ dysfunction. Amyloid fibrils are rigid, nonbranching structures, 7 to 10 nanometers in diameter, with a characteristic appearance on electron microscopy. Affinity for Congo red staining, which binds to the beta-pleated sheets, produces the pathognomonic “apple-green” birefringence when visualized under polarized light microscopy. Universal to all amyloid fibrils are chaperone proteins such as serum amyloid P (SAP) and glycosaminoglycans, as well as calcium. There are more than 30 different precursor proteins implicated in various amyloid diseases, arising as hereditary or nonhereditary, localized or systemic, with different organ involvement and prognosis.1–3
TWO MAIN TYPES OF CARDIAC AMYLOIDOSIS
Light chain amyloidosis (AL)
AL, formerly called primary amyloidosis, is a clonal plasma cell disorder due to the overproduction and misfolding of antibody light chain fragments. It is a rare disease with about 3,000 new cases per year in the United States.5 The median age at diagnosis is 63, although it can present in patients in their 30s and 40s.5,6 It is a systemic disease that often affects the heart, but it can affect several other organs, most commonly the kidneys, gastrointestinal (GI) tract, and nervous system.7
AL is a more aggressive disease than ATTR, with a median untreated survival of less than 6 months in patients who present with heart failure.8 Early diagnosis is crucial as mortality is high without prompt treatment.
Transthyretin amyloidosis (ATTR)
ATTR is due to misfolding of the liver-derived precursor protein transthyretin (TTR) (previously called prealbumin), either as an acquired wild-type variant (ATTRwt) or as a hereditary mutant variant (ATTRm). ATTRwt, known previously as senile CA, typically affects older males and presents as a late onset hypertrophic restrictive cardiomyopathy, often preceded by carpal tunnel syndrome or spinal stenosis or both. The ATTRm variant, caused by one of many different point mutations in the TTR gene, can manifest as a polyneuropathy, cardiomyopathy, or a mixed phenotype that varies according to the specific mutation.
While ATTR portends a better prognosis than AL, it is still a progressive disorder with significantly reduced survival and quality of life. The median survival of patients with the ATTRwt variant is about 4 years and for patients with the ATTRm variant, survival depends on the mutation.9 TTR is a protein tetramer composed of 4 identical 127-amino acid monomers noncovalently bound at a dimer-dimer interface (Figure 1). It is a transport protein for thyroxine and retinol binding protein. The dissociation of the tetramer is the rate-limiting step for amyloid fibrillogenesis. Differentiating the ATTRwt variant and the ATTRm variant is done by testing the TTR gene for a mutation.1,3
How common is the ATTRwt variant? The ATTRwt variant is often an unrecognized cause of diastolic heart failure in the elderly, with up to 25% of patients 85 and older showing ATTRwt amyloid deposits on autopsy studies.10 A recent study showed that 13% of patients 60 and older hospitalized with heart failure with preserved ejection fraction had grade 2 to 3 uptake on 99mtechnetium-pyrophosphate (99mTcPYP) scintigraphy, which is consistent with ATTR-CA.11 In 43 consecutive patients undergoing transcatheter aortic valve replacement, 11.6% were found to have significant uptake on 99mTcPYP scan.12 It is clear given the aging population that the ATTRwt variant will become the most common form of amyloidosis. It is much more common in white males, with a median age at diagnosis of 75.13 Carpal tunnel syndrome (almost always bilateral) and spinal stenosis are present in about 50% of patients diagnosed with ATTRwt-CA and often precede clinical presentation of heart failure by 5 to 15 years.14–17
How common is the ATTRm variant? There are more than 100 point mutations in the TTR gene that lead to various familial TTR-related amyloid syndromes, either neuropathic (familial amyloid polyneuropathy [FAP]) or cardiomyopathic (familial amyloid cardiomyopathy).18 The most common mutation in the United States is V122I in which there is an isoleucine substitution for valine at the 122nd amino acid position. This mutation is seen in African Americans, 3% to 4% of whom are heterozygote carriers.19 Although the true penetrance is unknown, this mutation can lead to a late-onset restrictive cardiomyopathy with minimal neuropathy and is frequently misdiagnosed as hypertensive heart disease or diastolic heart failure. The median survival for V122I ATTRm-CA is about 2 years but likely depends on the stage at the time of diagnosis.20 The second most common mutation in the United States, T60A, is seen in patients of Irish descent and causes a mixed neuropathy and cardiomyopathy.17
PATHOLOGY AND PATHOPHYSIOLOGY OF CA
The atria are universally involved with interatrial septal thickening, which can lead to poor atrial function and increased rates of atrial fibrillation (ATTR more so than AL).21,29 The conduction system can be affected causing varying degrees of heart block, as well as bundle branch block (ATTR more so than AL).30 The valves are usually thickened, often associated with mild to moderate regurgitation. Pericardial involvement can lead to small pericardial effusions (large effusions are rare), and coronary involvement (classically, small intramural vessels) can lead to ischemia and angina with normal epicardial coronaries (AL more so than ATTR).31–33
Thickened left and right ventricular walls result in a nondilated ventricle that is stiff and poorly compliant, resulting in progressive diastolic filling abnormalities. Systolic dysfunction can be seen in severe and advanced disease. Importantly, ejection fraction measured by echocardiography is misleading in CA, as reduced end-diastolic volume produces a low stroke volume. For example, an ejection fraction of 50%, when starting at a significantly reduced end-diastolic volume (for example, 70 mL), leads to a significantly reduced stroke volume (35 mL) and, thus, cardiac output. This explains why patients with CA cannot usually tolerate reduced heart rates, as their cardiac output is dependent on heart rate.34–36
CLINICAL PRESENTATION
Patients with CA typically exhibit heart failure with preserved ejection fraction (otherwise known as diastolic heart failure). Dyspnea on exertion is common; however, some patients can present with more right-sided heart failure symptoms such as lower-extremity edema and ascites. Fatigue and weakness are related to low cardiac output and often attributed to nonspecific symptoms of aging. Because of the thickened ventricles, patients can often be misdiagnosed as having HCM with or without obstruction.7,34 The first manifestation of CA may be atrial fibrillation, most commonly in ATTRwt-CA, or cardioembolic stroke. Atrial fibrillation can be present for years before CA is considered. Bundle branch block and complete heart block (more common in ATTR-CA than AL-CA) may lead to pacemaker implantation.30 Angina with normal coronaries can occur, and a rare presentation may be cardiogenic shock due to diffuse ischemia.31–33 Elderly patients with CA can present with low-flow, low-gradient aortic stenosis.37
DIAGNOSIS
ECG
As opposed to that seen in true left ventricular hypertrophy (LVH), which leads to increased voltage on ECG, amyloid infiltration of the myocardium leads to lower voltage. Thus, what is indicative of LVH on echocardiogram combined with low voltage on the ECG is a classic finding for CA. However, only about 50% of patients with AL-CA and about 30% of patients with ATTR-CA meet true low-voltage criteria (QRS amplitude less than 5 mm in limb leads or less than 10 mm in precordial leads).30,38 Hence, the absence of low-voltage criteria does not exclude the diagnosis of CA. Approximately 10% of patients with CA confirmed by biopsy met ECG criteria for LVH.38 The key point is to consider the overall degree of voltage on the ECG relative to the degree of LV thickening on the echocardiogram, recognizing that lower voltage than what would be expected may indicate possible infiltrative disease such as CA. The other main finding on the ECG in patients with CA is a pseudoinfarct pattern with Q waves in the early precordial leads mimicking a prior anteroseptal myocardial infarction.38,39 This finding is seen in about 50% of patients (Figure 3).39 Wide QRS complexes are more frequent in ATTR-CA and lower limb voltages are more frequent in AL-CA.30
Echocardiogram
The echocardiographic finding of LVH in patients with CA is misleading in that the LV thickening is due to infiltrating amyloid fibrils and not to myocyte hypertrophy. That said, the terms LVH and LV thickening are used interchangeably when describing the echocardiographic phenotype. LV wall thickness greater than 12 mm (6 mm to 10 mm is normal) in the absence of hypertension should prompt suspicion for CA.34 LV thickening most often appears symmetric; however, occasionally it may exhibit asymmetric septal hypertrophy, particularly in ATTRwt-CA. In some cases, there may be a smaller subset that can actually have dynamic LV outflow obstruction similar to that seen in hypertrophic obstructive cardiomyopathy.22–24 An important echocardiographic clue that can differentiate CA from other diseases is thickening of both the LV and right ventricle (Figure 3). Septal wall thickness and LV mass index are greater in ATTR-CA compared with AL-CA.30 On average, the LV septum is around 15 mm in AL-CA and around 18 mm in ATTRwt-CA.40 Historically, the characteristic myocardial “granular sparking” or “speckling” pattern has low sensitivity and specificity.16 The left ventricle is not dilated; rather, the ventricular dimensions are usually smaller than normal. Although ejection fraction is usually preserved, cardiac output is low due to decreased ventricular volume.37 Systolic dysfunction occurs late in the disease.16 Diastolic dysfunction is universal, with a mitral inflow pattern that can range from stage I (abnormal relaxation) in early disease to stage III (restrictive filling pattern) in more advanced disease. Septal and lateral tissue Doppler velocities are very low in amyloid heart disease.41 Another echocardiographic clue to diagnosis is thickening of the heart valves, which is not seen in hypertensive heart disease or hypertrophic cardiomyopathy. Biatrial dilation is common, and there can be thickening of the interatrial septum.
Laboratory testing
N-terminal pro-b-type natriuretic peptide (NT-proBNP) is universally elevated in CA and is typically higher in AL-CA than in ATTR-CA. Troponin T or troponin I or both may be chronically elevated in CA and likely signify small-vessel ischemia. In the appropriate clinical context of a thickened ventricle and heart failure, an elevated troponin value (outside of an acute coronary syndrome) should trigger suspicion for CA. Workup for a monoclonal protein process should always be done when considering CA to rule out AL. Serum and urine protein electrophoresis are insensitive tests to detect AL and should not be relied upon as a screening test. The serum free light chain (sFLC) assay, which measures free kappa and lambda light chain levels and reports the ratio, is a sensitive test that should be measured routinely along with immunofixation of the serum and urine. In AL, sFLC will reveal an abnormal kappa-lambda ratio. An abnormally low ratio (less than 0.26) suggests a monoclonal lambda light chain process, while an abnormally high ratio (greater than 1.65) suggests a monoclonal kappa light chain process. Immunofixation will reveal an M-protein. Because light chains are excreted by the kidney, the serum levels of both kappa and lambda will be elevated in renal dysfunction, but the ratio should remain normal.16,31,34,40,42–47
Advanced noninvasive diagnostic tools for CA
Over the past decade, the ability to diagnose CA noninvasively has dramatically improved with strain imaging using 2D speckle tracking echocardiography, cardiac magnetic resonance imaging (MRI), and nuclear bone scintigraphy. These diagnostic tools have given clinicians options to pursue the diagnosis of CA without directly proceeding to endomyocardial biopsy.
Cardiac MRI. Cardiac MRI is useful for the diagnosis of CA (Figure 4B, 4C). Imaging after administration of gadolinium contrast shows a characteristic late gadolinium enhancement (LGE) pattern that is diffuse and subendocardial, and does not follow any particular coronary distribution.49 LGE can also be seen in the right ventricle and the atrial walls, and can be transmural and patchy in ATTRwt-CA. This pattern is highly sensitive (93%) and specific (70%) for CA with an overall negative predictive accuracy of 84%.50
One of the main limitations of cardiac MRI for the diagnosis of CA is the inability to give contrast in patients with reduced glomerular filtration rate. However, native T1-myocardial mapping techniques that do not require contrast show significantly increased native T1 times in CA and offer a promising alternative. Cardiac MRI parameters such as LGE, the difference in inversion time between the LV cavity and myocardium, native T1 mapping, and extracellular volume offer prognostic information. A greater than fivefold mortality increase is seen in CA patients with transmural LGE compared with those without LGE.49,50
99mTcPYP scintigraphy. 99mTcPYP, a radiotracer used in bone scans, was initially used in cardiology to quantify myocardial infarction due to its ability to localize calcium.51 Its potential utility in CA came in 1982 when diffuse myocardial 99mTcPYP uptake on cardiac radionucleotide imaging was noted in 10 patients with tissue-proven amyloidosis.52 Several subsequent studies reproduced and expanded upon this observation and revealed its diagnostic value, specifically showing that there is significant uptake in ATTR-CA and no to mild uptake in AL-CA. This offers a significant advantage over other noninvasive modalities in that it not only confirms the diagnosis of CA but differentiates ATTR-CA.16
99mTcPYP myocardial radiotracer uptake is graded by the semiquantitative visual score of cardiac retention, where grade 0 = no cardiac uptake, grade 1 = mild uptake less than bone, grade 2 = moderate uptake equal to bone, and grade 3 = high uptake greater than bone (Figure 4D).42 Additionally, quantitative analysis of heart retention can be calculated drawing circular regions of interest over the heart and mirrored on the contralateral chest wall. A heart-to-contralateral ratio greater than 1.5 is consistent with the diagnosis of ATTR-CA.53,54 In 2016, a multicenter study showed that grade 2 or 3 myocardial radiotracer uptake on bone scintigraphy in the absence of evidence of a monoclonal gammopathy was diagnostic for ATTR-CA, providing a cost-effective and non-invasive technique with a specificity and positive predictive value of 100% (confidence interval, 99.0–100%).42
Endomyocardial biopsy, right heart catheterization, and fat biopsy
Endomyocardial biopsy is essentially 100% sensitive for the diagnosis of CA.25 The main risk of pursuing endomyocardial biopsy is about a 1% risk of right ventricular perforation leading to cardiac tamponade.55 The other limitation to this approach is that not all centers are equipped to perform this procedure. Birefringence under polarized light microscopy is histopathologically diagnostic of CA; however, further subtyping by the pathologist to determine if it is AL or ATTR is absolutely crucial. Subtyping can be performed by immunohistochemistry with caution taken for misinterpretation. If there is any question of accuracy, the specimen should be sent for laser microdissection and mass spectroscopy for accurate identification of the precursor protein type (some centers routinely perform mass spectroscopy on all myocardial specimens).16,31
Right heart catheterization is nonspecific and shows restrictive hemodynamics. The right atrial waveform shows rapid x and y descents and the right ventriclular tracing may show a dip-and-plateau pattern typical of restrictive cardiomyopathy. Cardiac output can be preserved but more commonly is low.16,31
Fat pad biopsy is 60% to 80% sensitive in AL, 65% to 85% sensitive in ATTRm, and only 14% sensitive in ATTRwt, with the accuracy dependent on the operator, pathologist, and how much tissue is removed (fat pad aspirate vs biopsy specimen).56–58 Fat pad biopsy has diagnostic limitations, and a negative fat pad biopsy does not rule out amyloidosis.
DIAGNOSTIC ALGORITHM FOR CARDIAC AMYLOIDOSIS
In conjunction with laboratory tests, 99mTcPYP scan of the heart can be ordered to investigate the possibility of ATTR-CA. Grade 2 to 3 myocardial uptake in the absence of a monoclonal plasma cell process is consistent with the diagnosis of ATTR-CA. Grade 0 or 1 myocardial uptake on 99mTcPYP scan with an abnormal sFLC ratio or positive M protein on immunofixation suggests AL-CA and a bone marrow biopsy should be performed. If the patient has an abnormal sFLC ratio and grade 2 to 3 uptake on 99mTcPYP scan, the diagnosis of ATTR-CA with unrelated monoclonal gammopathy of undetermined significance should be considered. However, this would need to be reconciled by pursuing endomyocardial biopsy and accurate tissue typing. If the 99mTcPYP scan is negative, and the sFLC ratio is normal, and immunofixation is negative, a diagnosis of CA is very unlikely.16,31,40,42–47
If the diagnosis of ATTR-CA is made, genetic testing can determine the presence or absence of a mutation to differentiate ATTRm or ATTRwt, respectively. If the diagnosis of AL-CA is suggested, a bone marrow biopsy is necessary to identify and quantify the plasma cell clone.16,31,40,42–47
TREATMENT
Management of heart failure in cardiac amyloidosis
The main treatment of heart failure revolves around sodium restriction and diuretics to relieve congestion. This can prove challenging in many patients due to the narrow window between too high or too low filling pressures. A combination of loop diuretics and an aldosterone antagonist is most effective.31,34,44,45 Torsemide is preferred over furosemide due to its superior bioavailability and longer duration of action, particularly since these patients have issues with gut edema and GI absorption. Due to dependence of the cardiac output on heart rate and the tendency for orthostatic hypotension, traditional neurohormonal antagonists including beta blockers and angiotensin-converting enzyme inhibitors are neither effective nor well tolerated.60 However, in patients with atrial fibrillation, beta blockers may need to be used for rate control. Nondihydropyridine calcium channel blockers bind avidly to amyloid fibrils and are contraindicated due to risk of profound hypotension and syncope.30,31,34,44,45 Digoxin is usually avoided in CA due to concerns of increased risk of toxicity; however, it may be used with caution for rate control in atrial fibrillation given its lack of negative inotropy.61 Maintenance of normal sinus rhythm is preferable due to the importance of atrial contribution to cardiac output.
Anticoagulation in patients with atrial fibrillation and even in patients with normal sinus rhythm and poor atrial function is important due to the high risk of thromboembolic complications.62 Pacemakers are indicated for heart block or symptomatic bradycardia.63 The role of intracardiac defibrillators is controversial, but may be warranted in selected patients with AL-CA.64,65
AL treatment
Risk stratification and prognostication for AL. The most important determinant of clinical outcome in AL is the extent of cardiac involvement, as congestive heart failure and sudden cardiac death are the most common causes of death. The level of NT-proBNP and the level of either troponin T or troponin I have strong prognostic value and form the basis for the staging system in AL. Various iterations have evolved over the years, but the most widely adopted is the 4-stage system developed and validated by Mayo Clinic. This system uses a cutoff value at diagnosis for NT-proBNP greater than 1,800 ng/mL, troponin T greater than 0.025 μg/L, and the difference between kappa and lambda free light chain levels greater than 180 mg/L. Stage level increases by the number of cutoff values exceeded, with stage IV carrying a median survival of 6 months.47 Additionally, the troponin T level can help risk-stratify patients being considered for autologous stem cell transplant. In a retrospective study, troponin T greater than 0.06 μg/L was associated with increased mortality following stem cell transplant.66 Ultimately, prognosis in AL-CA is related to the hematologic response to chemotherapy.
Current treatment strategies for AL. The survival of patients with AL has improved over the years with the advent of more effective chemotherapeutic regimens that kill the underlying plasma cell clone producing the unstable light chains. The goal of treatment is to achieve a complete hematologic response with normalization of the affected light chain and sFLC ratio as well as elimination of the M protein on immunofixation.
The development of the proteasome inhibitor bortezomib has improved efficacy and survival in AL causing a faster and more complete hematologic response than prior regimens.43,67,68
The most commonly used first-line treatment consists of a 3-drug combination with the alkylating agent cyclophosphamide, the proteasome inhibitor bortezomib, and the steroid dexamethasone, which is given weekly.43 A retrospective study by Sperry et al8 showed that patients receiving an alkylating agent, bortezomib, and a steroid had the best outcomes compared with other regimens.
For patients with refractory or relapsed disease, the CD38 monoclonal antibody daratumumab can be used if patients meet myeloma criteria and has been found to be effective thus far.68,69 Newer proteasome inhibitors such as ixazomib, which is taken orally, are being studied in alternative combination regimens.70 High-dose chemotherapy with autologous stem cell transplant can be considered in patients with an acceptable cardiac risk profile and may offer more complete and durable remission than chemotherapy, although this is controversial.43,71
The cardiologist’s role in AL-CA. The hematologist directs the chemotherapy for AL but works closely with the cardiologist when there is cardiac involvement. The main role of the cardiologist is to manage volume status with diuretics, monitor for arrhythmia, and evaluate the cardiac response to treatment.43,71 Cardiac response was traditionally measured by echocardiographic changes of wall thickness, diastolic function, and ejection fraction, as well as changes in New York Heart Association (NYHA) functional class.67 However, it is uncommon to see reduction in LV wall thickness or significant improvement in ejection fraction and if it does occur, it is a slow process that usually takes more than 1 year. With the advent of longitudinal myocardial strain imaging, improvements in strain can be seen despite the lack of structural changes on echocardiogram.72 In 2012, consensus criteria defined a cardiac response as a greater than 30% reduction in NT-proBNP.73 Misfolded light chains are toxic to cardiomyocytes by causing increased oxidative stress and impairing contractility. Thus, reduction in light chain levels can lead to clinical improvement and significant reductions in NT-proBNP without changing amyloid fibril burden in the heart.
Heart transplant for patients with AL-CA. For patients who have a good hematologic response to initial chemotherapy but have limited predicted survival due to severe heart failure, heart transplant followed by autologous stem cell transplant, is a treatment strategy that can be considered. The patient must have clinically isolated severe cardiac disease, minimal amyloid burden in other organs, and a plasma cell clone that is responsive to therapy. Initial reports of heart transplant showed poor survival rates due to recurrent amyloid in the transplanted heart and progressive amyloid deposition in other organs. However, due to improved anti-plasma-cell-directed therapy and refinement in patient selection, outcomes have improved. Contemporary series of patients undergoing heart transplant followed by stem cell transplant showed that outcomes are almost comparable to heart transplant for other indications, with a 5-year survival rate of approximately 65%.74
Future therapies for AL. There is an AL amyloid-directed monoclonal antibody designed to remove amyloid fibrils from affected organs and is currently undergoing clinical trials. NEOD001, a humanized murine monoclonal antibody that targets an epitope exposed during light chain misfolding, binds to the light chain amyloid fibril and signals an immune response to clear the deposits. This agent has completed phase 1 and 2 clinical trials of 27 patients previously treated with at least 1 plasma cell-directed therapy. It showed good tolerability and achieved both renal and cardiac responses in most patients.75
A phase 2b clinical trial (NCT02632786) of patients with AL with a previous hematologic response to treatment and persistent heart dysfunction is underway and expected to be completed in January 2018. A phase 3 clinical trial (NCT02312206) of NEOD001 as an adjunct to chemotherapy is also ongoing and results are expected in February 2019.
ATTR treatment
Liver transplant for ATTRm amyloidosis for the V30M mutation that causes FAP was first described in 1990, but it has not been well validated in other mutations and is not a solution for ATTRwt.76 Significant progress has been made over the past 2 decades in the understanding of the pathophysiologyy of ATTR, paving the way for promising advancements in pharmacotherapy. Presently, there are 3 classes of pharmacologic agents, grouped by the point of disease process each strategy targets:
- Block TTR synthesis at the translational level in hepatocytes
- Stabilize the TTR tetramer to inhibit the rate-determining step of amyloidogenesis
- Disrupt and clear the ATTR amyloid fibril.77
Block TTR synthesis. TTR messenger RNA (mRNA) can be targeted by “silencers” preventing translation, thereby reducing the production TTR protein by hepatocytes. The resultant sustained reduction of plasma TTR should decrease or halt amyloid deposition by making less TTR available to dissociate and deposit in the heart and nerves. There are 2 approaches to silencing TTR mRNA translation: small interfering RNA (siRNA) and antisense oligonucleotide (ASO).77
An siRNA, packaged in a lipid nanoparticle to ensure delivery to the liver, has been designed to bind to a conserved region of TTR mRNA, degrading the mRNA and reducing TTR protein expression. One siRNA, patisiran, completed the phase 3 APOLLO clinical trial (NCT01960348) in August 2017. It is an intravenous medication that requires premedication. The APOLLO trial studied patients with neuropathic variants of ATTRm, with a primary end point of neuropathy progression over 18 months. Patisrian met the primary end point and will likely be approved by the US Food and Drug Administration (FDA) by the third quarter of 2018. Given its target of a conserved 3’ untranslated region of TTR mRNA, patisiran should theoretically yield benefits not just in FAP but to both ATTRm-CA and ATTRwt-CA.68,77
ASOs are single-stranded oligonucleotides, typically 20 nucleotides in length, that bind to mRNA and elicit enzymatic mRNA degradation and reduced protein expression. Inotersen (IONIS-TTRRx) is an ASO drug that targets a conserved region of TTR mRNA. Inotersen is administered by weekly subcutaneous injection. A phase 2/3 clinical trial (NCT01737398) completed in October 2017 studied the drug's efficacy in treating FAP, with a primary end point of neuropathy progression over 65 weeks. It met the primary end point and a subset of patients actually improved. Like patisiran, inotersen is likely to be approved by the FDA for a neuropathy indication by the third quarter of 2018 and may benefit patients with ATTRm-CA and ATTRwt-CA. More studies are needed in the ATTR cardiac population.68,77
Stabilize the TTR tetramer. The TTR tetramer has 2 thyroxine binding pockets that stabilize the structure when bound preventing dissociation. Dissociation of the tetramer, the rate limiting step for ATTR fibrillogenesis, can be reduced using pharmacologic agents that bind to the thyroxine binding pockets. Both new and repurposed agents have been found to stabilize the TTR tetramer, including diflunisal, tafamidis, tolcapone, and AG10.68,77
Diflunisal (Dolobid) is a nonacetylated salicylate nonsteroidal anti-inflammatory drug used for over 3 decades to treat arthritis and musculoskeletal pain. Unrelated to its anti-inflammatory properties, it interacts with TTR’s thyroxine binding pocket to increase the stability of the tetramer. A 2013 randomized, placebo-controlled, international multicenter trial of 130 patients with FAP demonstrated a statistically significant slowing of polyneuropathy progression; however, 67 patients (diflunisal n = 27, placebo n = 40) did not complete the study.78 A small study revealed diflunisal to be reasonably well-tolerated in ATTR-CA, and to date it is the only readily available pharmacotherapy for ATTR supported by a randomized, placebo-controlled trial.79,80 Diflunisal may be considered for off-label use in patients with ATTR-CA with relatively preserved kidney function and no increased bleeding risk, taken under the supervision of a cardiologist who will monitor for fluid retention and changes in renal function.77
Tafamidis (Vyndaqel), like diflunisal, interacts with TTR’s thyroxine binding pocket and increases tetrameric stability. A phase 2 open-label clinical trial studied the efficacy and tolerance of tafamidis in 31 patients with ATTRwt and NYHA functional class 1 and 2 followed for 1 year. Twenty-eight patients completed the study and 2 patients died. TTR stabilization at 6 weeks was achieved in 30 of 31 patients (96.8%), and success at 1 year in 25 of 28 patients (89.3%). No clinical progression occurred in 16 of 31 patients (51.5%), and tafamidis was generally well-tolerated, with diarrhea the most common side effect in 7 of 31 patients (22.6% ).81,82
A phase 3 clinical trial (NCT01994889) is studying tafamidis vs placebo in patients with ATTRm-CA or ATTRwt-CA (excluding NYHA functional class 4) with the primary outcome measure of all-cause mortality and heart failure-related hospitalizations over 30 months. This is a large trial that enrolled 446 patients and data collection is expected to be completed in February 2018.
Tolcapone, approved by the FDA for Parkinson disease, has been found to be a potent TTR stabilizer by binding both thyroxine binding pockets of the TTR tetramer simultaneously. However, tolcapone has an FDA “black box” warning due to the risk of potentially fatal acute fulminant liver failure and is not currently used in ATTR therapy.68 Nonetheless, it will likely undergo further study for ATTR.
Recruiting is underway for a phase 1 clinical trial of AG10, a potent selective TTR stabilizer (NCT03294707).68
Disruption and clearance of the ATTR amyloid fibril. Even though treatment directed at blocking TTR synthesis or stabilizing the tetramer may be effective at preventing further deposition, the residual amyloid deposits persist and continue to affect organ function. With that need in mind, several agents that disrupt the amyloid formation process further downstream have been evaluated at a basic science level and in a few small nonrandomized open-label studies.77
Doxycycline is a tetracycline antibiotic with demonstrated effectiveness in disrupting mature amyloid fibrils in mouse models.83 Tauroursodeoxycholic acid is a bile acid with the ability to disrupt prefibrillar amyloid components. This combination has been studied in patients with ATTR-CA in 2 small open-label trials, with only 1 having results published. There was no progression in NT-proBNP or wall thickness in a cohort of 7 patients who completed 12 months of treatment.84 These data are nonrandomized and hypothesis-generating, as adequate studies would need to be performed to evaluate this hypothesis further. Because there are currently no FDA-approved therapies for ATTR, patients may be offered this combination fully informed that the data are limited. (Note: ursodiol is substituted for tauroursodeoxycholic acid, which is not available in the United States.)68
Green tea extract contains the polyphenol epigallocatechin-3-gallate, which has shown the ability for fibril disruption as well as TTR stabilization, importantly using a binding site separate from the thyroxine binding pocket (utilized in diflunisal and tafamidis). A small open-label study of 19 patients with ATTR-CA of whom 14 took green tea extract for 1 year reported a reduction in intraventricular septal wall thickness at 1 year, and in 9 patients a reduction of 12.5% in LV mass measured by cardiac MRI.85
Curcumin, the active ingredient in the household spice turmeric, has displayed in vitro promise as a TTR stabilizer by binding to the thyroxine binding pocket, and as an amyloid fibril disruptor by increasing macrophage degradation activity. Although there have only been preliminary animal studies, this supplement may be promising for further study in humans with ATTR-CA.68
PRX004 is a synthetic antibody designed to bind to non-native misfolded forms of TTR with the goal of potentially preventing deposition and promoting clearance of TTR aggregates.86 A phase 1 open-label escalation trial (NCT03336580) in 36 patients with ATTRm is planned and, hopefully, will pave the way for further study.
Heart transplant for patients with ATTR-CA. Patients with ATTRwt-CA who are young enough to undergo heart transplant have displayed favorable outcomes given that it causes clinically isolated heart disease and is an indolent process that should not affect the transplanted heart over the average life span of the allograft. Patients with the ATTRm mutation V122I have been treated with heart transplant alone, with the thought process that again, due to the indolent nature of amyloid deposition, concomitant liver transplant may not be needed.74 Thus far, 6 patients with this mutation have undergone successful transplant at our institution with heart alone, 1 of whom is 9 years posttransplant without any recurrent amyloid in the allograft. Patients with the T60A mutation that causes both polyneuropathy and cardiomyopathy require combined heart and liver transplant.74
Are there other therapies being studied to clear amyloid deposits and reverse organ dysfunction?
Extracellular deposits of amyloid fibrils, regardless of precursor protein, contain common elements such as calcium, glycosaminoglycans, and an SAP component. SAP stabilizes amyloid fibrils and makes them resistant to degradation. A monoclonal immunoglobulin G1 anti-SAP antibody has been designed to target the ubiquitous SAP component, signaling an immune response that leads to macrophage mediated clearance of amyloid fibrils, regardless of the type. Treatment with this approach was studied in a pilot trial of 16 patients mostly with AL, and within a 6-week period some of the patients had dramatic reversal of liver amyloid deposition.2 This has paved the way for a phase 2 open-label trial to be performed in patients with AL-CA and ATTR-CA (NCT03044353) and plans for a randomized phase 3 trial in CA are in discussion. There is optimism that this therapy may achieve the holy grail of removing amyloid rather than just preventing further deposition.
CONCLUSION
The diagnosis of CA requires a high index of suspicion. The diagnostic tools have improved due to the availability of modern imaging techniques, and the advent of measuring the sFLC assay along with immunofixation of the serum and urine. The prognosis for patients with AL-CA used to be dismal, with very poor survival rates. The current treatment strategies that include proteasome inhibitors have significantly improved survival, emphasizing the importance of early diagnosis and prompt initiation of therapy. Monoclonal antibodies against plasma cells (daratumumab) and light chain amyloid deposits (NEOD001) have the potential to further improve outcomes. The diagnosis of ATTR-CA used to be a futile academic pursuit given the lack of available therapies. However, there are several new FDA-approved agents on the horizon, including TTR gene silencers and stabilizers. CA is no longer considered to be rare and hopeless. Rather, it is more common than previously recognized and even more treatable.
WHAT IS AMYLOIDOSIS?
Amyloidosis is a protein deposition disease in which a specific precursor protein pathologically misfolds from its physiologic tertiary structure into a more linear shape dominated by beta-pleated sheets. The misfolded protein aggregates into oligomers, eventually forming insoluble amyloid fibrils that deposit extracellularly in tissues. Both the circulating oligomers, which are cytotoxic, and the fibrils, which cause distortion of the tissue architecture, lead to organ dysfunction. Amyloid fibrils are rigid, nonbranching structures, 7 to 10 nanometers in diameter, with a characteristic appearance on electron microscopy. Affinity for Congo red staining, which binds to the beta-pleated sheets, produces the pathognomonic “apple-green” birefringence when visualized under polarized light microscopy. Universal to all amyloid fibrils are chaperone proteins such as serum amyloid P (SAP) and glycosaminoglycans, as well as calcium. There are more than 30 different precursor proteins implicated in various amyloid diseases, arising as hereditary or nonhereditary, localized or systemic, with different organ involvement and prognosis.1–3
TWO MAIN TYPES OF CARDIAC AMYLOIDOSIS
Light chain amyloidosis (AL)
AL, formerly called primary amyloidosis, is a clonal plasma cell disorder due to the overproduction and misfolding of antibody light chain fragments. It is a rare disease with about 3,000 new cases per year in the United States.5 The median age at diagnosis is 63, although it can present in patients in their 30s and 40s.5,6 It is a systemic disease that often affects the heart, but it can affect several other organs, most commonly the kidneys, gastrointestinal (GI) tract, and nervous system.7
AL is a more aggressive disease than ATTR, with a median untreated survival of less than 6 months in patients who present with heart failure.8 Early diagnosis is crucial as mortality is high without prompt treatment.
Transthyretin amyloidosis (ATTR)
ATTR is due to misfolding of the liver-derived precursor protein transthyretin (TTR) (previously called prealbumin), either as an acquired wild-type variant (ATTRwt) or as a hereditary mutant variant (ATTRm). ATTRwt, known previously as senile CA, typically affects older males and presents as a late onset hypertrophic restrictive cardiomyopathy, often preceded by carpal tunnel syndrome or spinal stenosis or both. The ATTRm variant, caused by one of many different point mutations in the TTR gene, can manifest as a polyneuropathy, cardiomyopathy, or a mixed phenotype that varies according to the specific mutation.
While ATTR portends a better prognosis than AL, it is still a progressive disorder with significantly reduced survival and quality of life. The median survival of patients with the ATTRwt variant is about 4 years and for patients with the ATTRm variant, survival depends on the mutation.9 TTR is a protein tetramer composed of 4 identical 127-amino acid monomers noncovalently bound at a dimer-dimer interface (Figure 1). It is a transport protein for thyroxine and retinol binding protein. The dissociation of the tetramer is the rate-limiting step for amyloid fibrillogenesis. Differentiating the ATTRwt variant and the ATTRm variant is done by testing the TTR gene for a mutation.1,3
How common is the ATTRwt variant? The ATTRwt variant is often an unrecognized cause of diastolic heart failure in the elderly, with up to 25% of patients 85 and older showing ATTRwt amyloid deposits on autopsy studies.10 A recent study showed that 13% of patients 60 and older hospitalized with heart failure with preserved ejection fraction had grade 2 to 3 uptake on 99mtechnetium-pyrophosphate (99mTcPYP) scintigraphy, which is consistent with ATTR-CA.11 In 43 consecutive patients undergoing transcatheter aortic valve replacement, 11.6% were found to have significant uptake on 99mTcPYP scan.12 It is clear given the aging population that the ATTRwt variant will become the most common form of amyloidosis. It is much more common in white males, with a median age at diagnosis of 75.13 Carpal tunnel syndrome (almost always bilateral) and spinal stenosis are present in about 50% of patients diagnosed with ATTRwt-CA and often precede clinical presentation of heart failure by 5 to 15 years.14–17
How common is the ATTRm variant? There are more than 100 point mutations in the TTR gene that lead to various familial TTR-related amyloid syndromes, either neuropathic (familial amyloid polyneuropathy [FAP]) or cardiomyopathic (familial amyloid cardiomyopathy).18 The most common mutation in the United States is V122I in which there is an isoleucine substitution for valine at the 122nd amino acid position. This mutation is seen in African Americans, 3% to 4% of whom are heterozygote carriers.19 Although the true penetrance is unknown, this mutation can lead to a late-onset restrictive cardiomyopathy with minimal neuropathy and is frequently misdiagnosed as hypertensive heart disease or diastolic heart failure. The median survival for V122I ATTRm-CA is about 2 years but likely depends on the stage at the time of diagnosis.20 The second most common mutation in the United States, T60A, is seen in patients of Irish descent and causes a mixed neuropathy and cardiomyopathy.17
PATHOLOGY AND PATHOPHYSIOLOGY OF CA
The atria are universally involved with interatrial septal thickening, which can lead to poor atrial function and increased rates of atrial fibrillation (ATTR more so than AL).21,29 The conduction system can be affected causing varying degrees of heart block, as well as bundle branch block (ATTR more so than AL).30 The valves are usually thickened, often associated with mild to moderate regurgitation. Pericardial involvement can lead to small pericardial effusions (large effusions are rare), and coronary involvement (classically, small intramural vessels) can lead to ischemia and angina with normal epicardial coronaries (AL more so than ATTR).31–33
Thickened left and right ventricular walls result in a nondilated ventricle that is stiff and poorly compliant, resulting in progressive diastolic filling abnormalities. Systolic dysfunction can be seen in severe and advanced disease. Importantly, ejection fraction measured by echocardiography is misleading in CA, as reduced end-diastolic volume produces a low stroke volume. For example, an ejection fraction of 50%, when starting at a significantly reduced end-diastolic volume (for example, 70 mL), leads to a significantly reduced stroke volume (35 mL) and, thus, cardiac output. This explains why patients with CA cannot usually tolerate reduced heart rates, as their cardiac output is dependent on heart rate.34–36
CLINICAL PRESENTATION
Patients with CA typically exhibit heart failure with preserved ejection fraction (otherwise known as diastolic heart failure). Dyspnea on exertion is common; however, some patients can present with more right-sided heart failure symptoms such as lower-extremity edema and ascites. Fatigue and weakness are related to low cardiac output and often attributed to nonspecific symptoms of aging. Because of the thickened ventricles, patients can often be misdiagnosed as having HCM with or without obstruction.7,34 The first manifestation of CA may be atrial fibrillation, most commonly in ATTRwt-CA, or cardioembolic stroke. Atrial fibrillation can be present for years before CA is considered. Bundle branch block and complete heart block (more common in ATTR-CA than AL-CA) may lead to pacemaker implantation.30 Angina with normal coronaries can occur, and a rare presentation may be cardiogenic shock due to diffuse ischemia.31–33 Elderly patients with CA can present with low-flow, low-gradient aortic stenosis.37
DIAGNOSIS
ECG
As opposed to that seen in true left ventricular hypertrophy (LVH), which leads to increased voltage on ECG, amyloid infiltration of the myocardium leads to lower voltage. Thus, what is indicative of LVH on echocardiogram combined with low voltage on the ECG is a classic finding for CA. However, only about 50% of patients with AL-CA and about 30% of patients with ATTR-CA meet true low-voltage criteria (QRS amplitude less than 5 mm in limb leads or less than 10 mm in precordial leads).30,38 Hence, the absence of low-voltage criteria does not exclude the diagnosis of CA. Approximately 10% of patients with CA confirmed by biopsy met ECG criteria for LVH.38 The key point is to consider the overall degree of voltage on the ECG relative to the degree of LV thickening on the echocardiogram, recognizing that lower voltage than what would be expected may indicate possible infiltrative disease such as CA. The other main finding on the ECG in patients with CA is a pseudoinfarct pattern with Q waves in the early precordial leads mimicking a prior anteroseptal myocardial infarction.38,39 This finding is seen in about 50% of patients (Figure 3).39 Wide QRS complexes are more frequent in ATTR-CA and lower limb voltages are more frequent in AL-CA.30
Echocardiogram
The echocardiographic finding of LVH in patients with CA is misleading in that the LV thickening is due to infiltrating amyloid fibrils and not to myocyte hypertrophy. That said, the terms LVH and LV thickening are used interchangeably when describing the echocardiographic phenotype. LV wall thickness greater than 12 mm (6 mm to 10 mm is normal) in the absence of hypertension should prompt suspicion for CA.34 LV thickening most often appears symmetric; however, occasionally it may exhibit asymmetric septal hypertrophy, particularly in ATTRwt-CA. In some cases, there may be a smaller subset that can actually have dynamic LV outflow obstruction similar to that seen in hypertrophic obstructive cardiomyopathy.22–24 An important echocardiographic clue that can differentiate CA from other diseases is thickening of both the LV and right ventricle (Figure 3). Septal wall thickness and LV mass index are greater in ATTR-CA compared with AL-CA.30 On average, the LV septum is around 15 mm in AL-CA and around 18 mm in ATTRwt-CA.40 Historically, the characteristic myocardial “granular sparking” or “speckling” pattern has low sensitivity and specificity.16 The left ventricle is not dilated; rather, the ventricular dimensions are usually smaller than normal. Although ejection fraction is usually preserved, cardiac output is low due to decreased ventricular volume.37 Systolic dysfunction occurs late in the disease.16 Diastolic dysfunction is universal, with a mitral inflow pattern that can range from stage I (abnormal relaxation) in early disease to stage III (restrictive filling pattern) in more advanced disease. Septal and lateral tissue Doppler velocities are very low in amyloid heart disease.41 Another echocardiographic clue to diagnosis is thickening of the heart valves, which is not seen in hypertensive heart disease or hypertrophic cardiomyopathy. Biatrial dilation is common, and there can be thickening of the interatrial septum.
Laboratory testing
N-terminal pro-b-type natriuretic peptide (NT-proBNP) is universally elevated in CA and is typically higher in AL-CA than in ATTR-CA. Troponin T or troponin I or both may be chronically elevated in CA and likely signify small-vessel ischemia. In the appropriate clinical context of a thickened ventricle and heart failure, an elevated troponin value (outside of an acute coronary syndrome) should trigger suspicion for CA. Workup for a monoclonal protein process should always be done when considering CA to rule out AL. Serum and urine protein electrophoresis are insensitive tests to detect AL and should not be relied upon as a screening test. The serum free light chain (sFLC) assay, which measures free kappa and lambda light chain levels and reports the ratio, is a sensitive test that should be measured routinely along with immunofixation of the serum and urine. In AL, sFLC will reveal an abnormal kappa-lambda ratio. An abnormally low ratio (less than 0.26) suggests a monoclonal lambda light chain process, while an abnormally high ratio (greater than 1.65) suggests a monoclonal kappa light chain process. Immunofixation will reveal an M-protein. Because light chains are excreted by the kidney, the serum levels of both kappa and lambda will be elevated in renal dysfunction, but the ratio should remain normal.16,31,34,40,42–47
Advanced noninvasive diagnostic tools for CA
Over the past decade, the ability to diagnose CA noninvasively has dramatically improved with strain imaging using 2D speckle tracking echocardiography, cardiac magnetic resonance imaging (MRI), and nuclear bone scintigraphy. These diagnostic tools have given clinicians options to pursue the diagnosis of CA without directly proceeding to endomyocardial biopsy.
Cardiac MRI. Cardiac MRI is useful for the diagnosis of CA (Figure 4B, 4C). Imaging after administration of gadolinium contrast shows a characteristic late gadolinium enhancement (LGE) pattern that is diffuse and subendocardial, and does not follow any particular coronary distribution.49 LGE can also be seen in the right ventricle and the atrial walls, and can be transmural and patchy in ATTRwt-CA. This pattern is highly sensitive (93%) and specific (70%) for CA with an overall negative predictive accuracy of 84%.50
One of the main limitations of cardiac MRI for the diagnosis of CA is the inability to give contrast in patients with reduced glomerular filtration rate. However, native T1-myocardial mapping techniques that do not require contrast show significantly increased native T1 times in CA and offer a promising alternative. Cardiac MRI parameters such as LGE, the difference in inversion time between the LV cavity and myocardium, native T1 mapping, and extracellular volume offer prognostic information. A greater than fivefold mortality increase is seen in CA patients with transmural LGE compared with those without LGE.49,50
99mTcPYP scintigraphy. 99mTcPYP, a radiotracer used in bone scans, was initially used in cardiology to quantify myocardial infarction due to its ability to localize calcium.51 Its potential utility in CA came in 1982 when diffuse myocardial 99mTcPYP uptake on cardiac radionucleotide imaging was noted in 10 patients with tissue-proven amyloidosis.52 Several subsequent studies reproduced and expanded upon this observation and revealed its diagnostic value, specifically showing that there is significant uptake in ATTR-CA and no to mild uptake in AL-CA. This offers a significant advantage over other noninvasive modalities in that it not only confirms the diagnosis of CA but differentiates ATTR-CA.16
99mTcPYP myocardial radiotracer uptake is graded by the semiquantitative visual score of cardiac retention, where grade 0 = no cardiac uptake, grade 1 = mild uptake less than bone, grade 2 = moderate uptake equal to bone, and grade 3 = high uptake greater than bone (Figure 4D).42 Additionally, quantitative analysis of heart retention can be calculated drawing circular regions of interest over the heart and mirrored on the contralateral chest wall. A heart-to-contralateral ratio greater than 1.5 is consistent with the diagnosis of ATTR-CA.53,54 In 2016, a multicenter study showed that grade 2 or 3 myocardial radiotracer uptake on bone scintigraphy in the absence of evidence of a monoclonal gammopathy was diagnostic for ATTR-CA, providing a cost-effective and non-invasive technique with a specificity and positive predictive value of 100% (confidence interval, 99.0–100%).42
Endomyocardial biopsy, right heart catheterization, and fat biopsy
Endomyocardial biopsy is essentially 100% sensitive for the diagnosis of CA.25 The main risk of pursuing endomyocardial biopsy is about a 1% risk of right ventricular perforation leading to cardiac tamponade.55 The other limitation to this approach is that not all centers are equipped to perform this procedure. Birefringence under polarized light microscopy is histopathologically diagnostic of CA; however, further subtyping by the pathologist to determine if it is AL or ATTR is absolutely crucial. Subtyping can be performed by immunohistochemistry with caution taken for misinterpretation. If there is any question of accuracy, the specimen should be sent for laser microdissection and mass spectroscopy for accurate identification of the precursor protein type (some centers routinely perform mass spectroscopy on all myocardial specimens).16,31
Right heart catheterization is nonspecific and shows restrictive hemodynamics. The right atrial waveform shows rapid x and y descents and the right ventriclular tracing may show a dip-and-plateau pattern typical of restrictive cardiomyopathy. Cardiac output can be preserved but more commonly is low.16,31
Fat pad biopsy is 60% to 80% sensitive in AL, 65% to 85% sensitive in ATTRm, and only 14% sensitive in ATTRwt, with the accuracy dependent on the operator, pathologist, and how much tissue is removed (fat pad aspirate vs biopsy specimen).56–58 Fat pad biopsy has diagnostic limitations, and a negative fat pad biopsy does not rule out amyloidosis.
DIAGNOSTIC ALGORITHM FOR CARDIAC AMYLOIDOSIS
In conjunction with laboratory tests, 99mTcPYP scan of the heart can be ordered to investigate the possibility of ATTR-CA. Grade 2 to 3 myocardial uptake in the absence of a monoclonal plasma cell process is consistent with the diagnosis of ATTR-CA. Grade 0 or 1 myocardial uptake on 99mTcPYP scan with an abnormal sFLC ratio or positive M protein on immunofixation suggests AL-CA and a bone marrow biopsy should be performed. If the patient has an abnormal sFLC ratio and grade 2 to 3 uptake on 99mTcPYP scan, the diagnosis of ATTR-CA with unrelated monoclonal gammopathy of undetermined significance should be considered. However, this would need to be reconciled by pursuing endomyocardial biopsy and accurate tissue typing. If the 99mTcPYP scan is negative, and the sFLC ratio is normal, and immunofixation is negative, a diagnosis of CA is very unlikely.16,31,40,42–47
If the diagnosis of ATTR-CA is made, genetic testing can determine the presence or absence of a mutation to differentiate ATTRm or ATTRwt, respectively. If the diagnosis of AL-CA is suggested, a bone marrow biopsy is necessary to identify and quantify the plasma cell clone.16,31,40,42–47
TREATMENT
Management of heart failure in cardiac amyloidosis
The main treatment of heart failure revolves around sodium restriction and diuretics to relieve congestion. This can prove challenging in many patients due to the narrow window between too high or too low filling pressures. A combination of loop diuretics and an aldosterone antagonist is most effective.31,34,44,45 Torsemide is preferred over furosemide due to its superior bioavailability and longer duration of action, particularly since these patients have issues with gut edema and GI absorption. Due to dependence of the cardiac output on heart rate and the tendency for orthostatic hypotension, traditional neurohormonal antagonists including beta blockers and angiotensin-converting enzyme inhibitors are neither effective nor well tolerated.60 However, in patients with atrial fibrillation, beta blockers may need to be used for rate control. Nondihydropyridine calcium channel blockers bind avidly to amyloid fibrils and are contraindicated due to risk of profound hypotension and syncope.30,31,34,44,45 Digoxin is usually avoided in CA due to concerns of increased risk of toxicity; however, it may be used with caution for rate control in atrial fibrillation given its lack of negative inotropy.61 Maintenance of normal sinus rhythm is preferable due to the importance of atrial contribution to cardiac output.
Anticoagulation in patients with atrial fibrillation and even in patients with normal sinus rhythm and poor atrial function is important due to the high risk of thromboembolic complications.62 Pacemakers are indicated for heart block or symptomatic bradycardia.63 The role of intracardiac defibrillators is controversial, but may be warranted in selected patients with AL-CA.64,65
AL treatment
Risk stratification and prognostication for AL. The most important determinant of clinical outcome in AL is the extent of cardiac involvement, as congestive heart failure and sudden cardiac death are the most common causes of death. The level of NT-proBNP and the level of either troponin T or troponin I have strong prognostic value and form the basis for the staging system in AL. Various iterations have evolved over the years, but the most widely adopted is the 4-stage system developed and validated by Mayo Clinic. This system uses a cutoff value at diagnosis for NT-proBNP greater than 1,800 ng/mL, troponin T greater than 0.025 μg/L, and the difference between kappa and lambda free light chain levels greater than 180 mg/L. Stage level increases by the number of cutoff values exceeded, with stage IV carrying a median survival of 6 months.47 Additionally, the troponin T level can help risk-stratify patients being considered for autologous stem cell transplant. In a retrospective study, troponin T greater than 0.06 μg/L was associated with increased mortality following stem cell transplant.66 Ultimately, prognosis in AL-CA is related to the hematologic response to chemotherapy.
Current treatment strategies for AL. The survival of patients with AL has improved over the years with the advent of more effective chemotherapeutic regimens that kill the underlying plasma cell clone producing the unstable light chains. The goal of treatment is to achieve a complete hematologic response with normalization of the affected light chain and sFLC ratio as well as elimination of the M protein on immunofixation.
The development of the proteasome inhibitor bortezomib has improved efficacy and survival in AL causing a faster and more complete hematologic response than prior regimens.43,67,68
The most commonly used first-line treatment consists of a 3-drug combination with the alkylating agent cyclophosphamide, the proteasome inhibitor bortezomib, and the steroid dexamethasone, which is given weekly.43 A retrospective study by Sperry et al8 showed that patients receiving an alkylating agent, bortezomib, and a steroid had the best outcomes compared with other regimens.
For patients with refractory or relapsed disease, the CD38 monoclonal antibody daratumumab can be used if patients meet myeloma criteria and has been found to be effective thus far.68,69 Newer proteasome inhibitors such as ixazomib, which is taken orally, are being studied in alternative combination regimens.70 High-dose chemotherapy with autologous stem cell transplant can be considered in patients with an acceptable cardiac risk profile and may offer more complete and durable remission than chemotherapy, although this is controversial.43,71
The cardiologist’s role in AL-CA. The hematologist directs the chemotherapy for AL but works closely with the cardiologist when there is cardiac involvement. The main role of the cardiologist is to manage volume status with diuretics, monitor for arrhythmia, and evaluate the cardiac response to treatment.43,71 Cardiac response was traditionally measured by echocardiographic changes of wall thickness, diastolic function, and ejection fraction, as well as changes in New York Heart Association (NYHA) functional class.67 However, it is uncommon to see reduction in LV wall thickness or significant improvement in ejection fraction and if it does occur, it is a slow process that usually takes more than 1 year. With the advent of longitudinal myocardial strain imaging, improvements in strain can be seen despite the lack of structural changes on echocardiogram.72 In 2012, consensus criteria defined a cardiac response as a greater than 30% reduction in NT-proBNP.73 Misfolded light chains are toxic to cardiomyocytes by causing increased oxidative stress and impairing contractility. Thus, reduction in light chain levels can lead to clinical improvement and significant reductions in NT-proBNP without changing amyloid fibril burden in the heart.
Heart transplant for patients with AL-CA. For patients who have a good hematologic response to initial chemotherapy but have limited predicted survival due to severe heart failure, heart transplant followed by autologous stem cell transplant, is a treatment strategy that can be considered. The patient must have clinically isolated severe cardiac disease, minimal amyloid burden in other organs, and a plasma cell clone that is responsive to therapy. Initial reports of heart transplant showed poor survival rates due to recurrent amyloid in the transplanted heart and progressive amyloid deposition in other organs. However, due to improved anti-plasma-cell-directed therapy and refinement in patient selection, outcomes have improved. Contemporary series of patients undergoing heart transplant followed by stem cell transplant showed that outcomes are almost comparable to heart transplant for other indications, with a 5-year survival rate of approximately 65%.74
Future therapies for AL. There is an AL amyloid-directed monoclonal antibody designed to remove amyloid fibrils from affected organs and is currently undergoing clinical trials. NEOD001, a humanized murine monoclonal antibody that targets an epitope exposed during light chain misfolding, binds to the light chain amyloid fibril and signals an immune response to clear the deposits. This agent has completed phase 1 and 2 clinical trials of 27 patients previously treated with at least 1 plasma cell-directed therapy. It showed good tolerability and achieved both renal and cardiac responses in most patients.75
A phase 2b clinical trial (NCT02632786) of patients with AL with a previous hematologic response to treatment and persistent heart dysfunction is underway and expected to be completed in January 2018. A phase 3 clinical trial (NCT02312206) of NEOD001 as an adjunct to chemotherapy is also ongoing and results are expected in February 2019.
ATTR treatment
Liver transplant for ATTRm amyloidosis for the V30M mutation that causes FAP was first described in 1990, but it has not been well validated in other mutations and is not a solution for ATTRwt.76 Significant progress has been made over the past 2 decades in the understanding of the pathophysiologyy of ATTR, paving the way for promising advancements in pharmacotherapy. Presently, there are 3 classes of pharmacologic agents, grouped by the point of disease process each strategy targets:
- Block TTR synthesis at the translational level in hepatocytes
- Stabilize the TTR tetramer to inhibit the rate-determining step of amyloidogenesis
- Disrupt and clear the ATTR amyloid fibril.77
Block TTR synthesis. TTR messenger RNA (mRNA) can be targeted by “silencers” preventing translation, thereby reducing the production TTR protein by hepatocytes. The resultant sustained reduction of plasma TTR should decrease or halt amyloid deposition by making less TTR available to dissociate and deposit in the heart and nerves. There are 2 approaches to silencing TTR mRNA translation: small interfering RNA (siRNA) and antisense oligonucleotide (ASO).77
An siRNA, packaged in a lipid nanoparticle to ensure delivery to the liver, has been designed to bind to a conserved region of TTR mRNA, degrading the mRNA and reducing TTR protein expression. One siRNA, patisiran, completed the phase 3 APOLLO clinical trial (NCT01960348) in August 2017. It is an intravenous medication that requires premedication. The APOLLO trial studied patients with neuropathic variants of ATTRm, with a primary end point of neuropathy progression over 18 months. Patisrian met the primary end point and will likely be approved by the US Food and Drug Administration (FDA) by the third quarter of 2018. Given its target of a conserved 3’ untranslated region of TTR mRNA, patisiran should theoretically yield benefits not just in FAP but to both ATTRm-CA and ATTRwt-CA.68,77
ASOs are single-stranded oligonucleotides, typically 20 nucleotides in length, that bind to mRNA and elicit enzymatic mRNA degradation and reduced protein expression. Inotersen (IONIS-TTRRx) is an ASO drug that targets a conserved region of TTR mRNA. Inotersen is administered by weekly subcutaneous injection. A phase 2/3 clinical trial (NCT01737398) completed in October 2017 studied the drug's efficacy in treating FAP, with a primary end point of neuropathy progression over 65 weeks. It met the primary end point and a subset of patients actually improved. Like patisiran, inotersen is likely to be approved by the FDA for a neuropathy indication by the third quarter of 2018 and may benefit patients with ATTRm-CA and ATTRwt-CA. More studies are needed in the ATTR cardiac population.68,77
Stabilize the TTR tetramer. The TTR tetramer has 2 thyroxine binding pockets that stabilize the structure when bound preventing dissociation. Dissociation of the tetramer, the rate limiting step for ATTR fibrillogenesis, can be reduced using pharmacologic agents that bind to the thyroxine binding pockets. Both new and repurposed agents have been found to stabilize the TTR tetramer, including diflunisal, tafamidis, tolcapone, and AG10.68,77
Diflunisal (Dolobid) is a nonacetylated salicylate nonsteroidal anti-inflammatory drug used for over 3 decades to treat arthritis and musculoskeletal pain. Unrelated to its anti-inflammatory properties, it interacts with TTR’s thyroxine binding pocket to increase the stability of the tetramer. A 2013 randomized, placebo-controlled, international multicenter trial of 130 patients with FAP demonstrated a statistically significant slowing of polyneuropathy progression; however, 67 patients (diflunisal n = 27, placebo n = 40) did not complete the study.78 A small study revealed diflunisal to be reasonably well-tolerated in ATTR-CA, and to date it is the only readily available pharmacotherapy for ATTR supported by a randomized, placebo-controlled trial.79,80 Diflunisal may be considered for off-label use in patients with ATTR-CA with relatively preserved kidney function and no increased bleeding risk, taken under the supervision of a cardiologist who will monitor for fluid retention and changes in renal function.77
Tafamidis (Vyndaqel), like diflunisal, interacts with TTR’s thyroxine binding pocket and increases tetrameric stability. A phase 2 open-label clinical trial studied the efficacy and tolerance of tafamidis in 31 patients with ATTRwt and NYHA functional class 1 and 2 followed for 1 year. Twenty-eight patients completed the study and 2 patients died. TTR stabilization at 6 weeks was achieved in 30 of 31 patients (96.8%), and success at 1 year in 25 of 28 patients (89.3%). No clinical progression occurred in 16 of 31 patients (51.5%), and tafamidis was generally well-tolerated, with diarrhea the most common side effect in 7 of 31 patients (22.6% ).81,82
A phase 3 clinical trial (NCT01994889) is studying tafamidis vs placebo in patients with ATTRm-CA or ATTRwt-CA (excluding NYHA functional class 4) with the primary outcome measure of all-cause mortality and heart failure-related hospitalizations over 30 months. This is a large trial that enrolled 446 patients and data collection is expected to be completed in February 2018.
Tolcapone, approved by the FDA for Parkinson disease, has been found to be a potent TTR stabilizer by binding both thyroxine binding pockets of the TTR tetramer simultaneously. However, tolcapone has an FDA “black box” warning due to the risk of potentially fatal acute fulminant liver failure and is not currently used in ATTR therapy.68 Nonetheless, it will likely undergo further study for ATTR.
Recruiting is underway for a phase 1 clinical trial of AG10, a potent selective TTR stabilizer (NCT03294707).68
Disruption and clearance of the ATTR amyloid fibril. Even though treatment directed at blocking TTR synthesis or stabilizing the tetramer may be effective at preventing further deposition, the residual amyloid deposits persist and continue to affect organ function. With that need in mind, several agents that disrupt the amyloid formation process further downstream have been evaluated at a basic science level and in a few small nonrandomized open-label studies.77
Doxycycline is a tetracycline antibiotic with demonstrated effectiveness in disrupting mature amyloid fibrils in mouse models.83 Tauroursodeoxycholic acid is a bile acid with the ability to disrupt prefibrillar amyloid components. This combination has been studied in patients with ATTR-CA in 2 small open-label trials, with only 1 having results published. There was no progression in NT-proBNP or wall thickness in a cohort of 7 patients who completed 12 months of treatment.84 These data are nonrandomized and hypothesis-generating, as adequate studies would need to be performed to evaluate this hypothesis further. Because there are currently no FDA-approved therapies for ATTR, patients may be offered this combination fully informed that the data are limited. (Note: ursodiol is substituted for tauroursodeoxycholic acid, which is not available in the United States.)68
Green tea extract contains the polyphenol epigallocatechin-3-gallate, which has shown the ability for fibril disruption as well as TTR stabilization, importantly using a binding site separate from the thyroxine binding pocket (utilized in diflunisal and tafamidis). A small open-label study of 19 patients with ATTR-CA of whom 14 took green tea extract for 1 year reported a reduction in intraventricular septal wall thickness at 1 year, and in 9 patients a reduction of 12.5% in LV mass measured by cardiac MRI.85
Curcumin, the active ingredient in the household spice turmeric, has displayed in vitro promise as a TTR stabilizer by binding to the thyroxine binding pocket, and as an amyloid fibril disruptor by increasing macrophage degradation activity. Although there have only been preliminary animal studies, this supplement may be promising for further study in humans with ATTR-CA.68
PRX004 is a synthetic antibody designed to bind to non-native misfolded forms of TTR with the goal of potentially preventing deposition and promoting clearance of TTR aggregates.86 A phase 1 open-label escalation trial (NCT03336580) in 36 patients with ATTRm is planned and, hopefully, will pave the way for further study.
Heart transplant for patients with ATTR-CA. Patients with ATTRwt-CA who are young enough to undergo heart transplant have displayed favorable outcomes given that it causes clinically isolated heart disease and is an indolent process that should not affect the transplanted heart over the average life span of the allograft. Patients with the ATTRm mutation V122I have been treated with heart transplant alone, with the thought process that again, due to the indolent nature of amyloid deposition, concomitant liver transplant may not be needed.74 Thus far, 6 patients with this mutation have undergone successful transplant at our institution with heart alone, 1 of whom is 9 years posttransplant without any recurrent amyloid in the allograft. Patients with the T60A mutation that causes both polyneuropathy and cardiomyopathy require combined heart and liver transplant.74
Are there other therapies being studied to clear amyloid deposits and reverse organ dysfunction?
Extracellular deposits of amyloid fibrils, regardless of precursor protein, contain common elements such as calcium, glycosaminoglycans, and an SAP component. SAP stabilizes amyloid fibrils and makes them resistant to degradation. A monoclonal immunoglobulin G1 anti-SAP antibody has been designed to target the ubiquitous SAP component, signaling an immune response that leads to macrophage mediated clearance of amyloid fibrils, regardless of the type. Treatment with this approach was studied in a pilot trial of 16 patients mostly with AL, and within a 6-week period some of the patients had dramatic reversal of liver amyloid deposition.2 This has paved the way for a phase 2 open-label trial to be performed in patients with AL-CA and ATTR-CA (NCT03044353) and plans for a randomized phase 3 trial in CA are in discussion. There is optimism that this therapy may achieve the holy grail of removing amyloid rather than just preventing further deposition.
CONCLUSION
The diagnosis of CA requires a high index of suspicion. The diagnostic tools have improved due to the availability of modern imaging techniques, and the advent of measuring the sFLC assay along with immunofixation of the serum and urine. The prognosis for patients with AL-CA used to be dismal, with very poor survival rates. The current treatment strategies that include proteasome inhibitors have significantly improved survival, emphasizing the importance of early diagnosis and prompt initiation of therapy. Monoclonal antibodies against plasma cells (daratumumab) and light chain amyloid deposits (NEOD001) have the potential to further improve outcomes. The diagnosis of ATTR-CA used to be a futile academic pursuit given the lack of available therapies. However, there are several new FDA-approved agents on the horizon, including TTR gene silencers and stabilizers. CA is no longer considered to be rare and hopeless. Rather, it is more common than previously recognized and even more treatable.
- Merlini G, Bellotti V. Molecular mechanisms of amyloidosis. N Engl J Med 2003; 349:583–596.
- Richards DB, Cookson LM, Berges AC, et al. Therapeutic clearance of amyloid by antibodies to serum amyloid P component. N Engl J Med 2015; 373:1106–1114.
- Sipe JD, Benson MD, Buxbaum JN, et al. Nomenclature 2014: amyloid fibril proteins and clinical classification of the amyloidosis. Amyloid 2014; 21:221–224.
- Maleszewski JJ. Cardiac amyloidosis: pathology, nomenclature, and typing. Cardiovasc Pathol 2015; 24:343–350.
- Kyle RA, Linos A, Beard CM, et al. Incidence and natural history of primary systemic amyloidosis in Olmsted County, Minnesota, 1950 through 1989. Blood 1992; 79:1817–1822.
- Krsnik I, Cabero M, Morillo D, et al. Light chain amyloidosis: Experience in a tertiary hospital: 2005-2013. Rev Clin Esp 2015; 215:1–8.
- Dubrey SW, Cha K, Anderson J, et al. The clinical features of immunoglobulin light-chain (AL) amyloidosis with heart involvement. QJM 1998; 91:141–157.
- Sperry BW, Ikram A, Hachamovitch R, et al. Efficacy of chemotherapy for light-chain amyloidosis in patients presenting with symptomatic heart failure. J Am Coll Cardiol 2016; 67:2941–2948.
- Gillmore JD, Damy T, Fontana M, et al. A new staging system for cardiac transthyretin amyloidosis. Eur Heart J 2017; Oct 18. [Epub ahead of print] doi:10.1093/eurheartj/ehx589.
- Tanskanen M, Peuralinna T, Polvikoski T, et al. Senile systemic amyloidosis affects 25% of the very aged and associates with genetic variation in alpha2-macroglobulin and tau: a population-based autopsy study. Ann Med 2008; 40:232–239.
- González-López E, Gallego-Delgado M, Guzzo-Merello G, et al. Wild-type transthyretin amyloidosis as a cause of heart failure with preserved ejection fraction. Eur Heart J 2015; 36:2585–2594.
- Longhi S, Lorenzini M, Gagliardi C, et al. Coexistence of degenerative aortic stenosis and wild-type transthyretin-related cardiac amyloidosis. JACC Cardiovasc Imaging 2016;9:325–327.
- Grogan M, Scott CG, Kyle RA, et al. Natural history of wild-type transthyretin cardiac amyloidosis and risk stratification using a novel staging system. J Am Coll Cardiol 2016; 68:1014–1020.
- Gioeva Z, Urban P, Meliss RR, et al. ATTR amyloid in the carpal tunnel ligament is frequently of wildtype transthyretin origin. Amyloid 2013; 20:1–6.
- Yanagisawa A, Ueda M, Sueyoshi T, et al. Amyloid deposits derived from transthyretin in the ligamentum flavum as related to lumbar spinal canal stenosis. Mod Pathol 2015; 28:201–207.
- Siddiqi OK, Ruberg FL. Cardiac amyloidosis: an update on pathophysiology, diagnosis, and treatment. Trends Cardiovasc Med 2017; Jul 13. [Epub ahead of print] doi:10.1016/j.tcm.2017.07.004.
- Nakagawa M, Sekijima Y, Yazaki M, et al. Carpal tunnel syndrome: A common initial symptom of systemic wild-type ATTR (ATTRwt) amyloidosis. Amyloid 2016; 23:58–63.
- Sekijima Y, Yoshida K, Tokuda T, Ikeda S-I. Familial Transthyretin Amyloidosis. In: Adam MP, Ardinger HH, Pagon RA, et al, eds. Seattle, WA: University of Washington, Seattle; 1993–2017. Available at: https://www-ncbi-nlm-nih-gov.ccmain.ohionet.org/books/NBK1194. Updated January 26, 2012. Accessed November 16, 2017.
- Buxbaum J, Jacobson DR, Tagoe C, et al. Transthyretin V122I in African Americans with congestive heart failure. J Am Coll Cardiol 2006; 47:1724–1725.
- Ruberg FL, Maurer MS, Judge DP, et al. Prospective evaluation of the morbidity and mortality of wild-type and V122I mutant transthyretin amyloid cardiomyopathy: The Transthyretin Amyloidosis Cardiac Study (TRACS). Am Heart J 2012; 164:222–228.e1.
- Wright JR, Calkins E. Amyloid in the aged heart: frequency and clinical significance. J Am Geriatr Soc 1975; 23:97–103.
- Vermeer AMC, Janssen A, Boorsma PC, Mannens MMAM, Wilde AAM, Christiaans I. Transthyretin amyloidosis: a phenocopy of hypertrophic cardiomyopathy. Amyloid 2017; 24:87–91.
- Velazquez-Ceceña JL, Lubell DL, Nagajothi N, Al-Masri H, Siddiqui M, Khosla S. Syncope cardiomyopathy in a patient with primary AL-type amyloid heart disease. Tex Heart Inst J 2009; 36:50–54.
- Stegman BM, Kwon D, Rodriguez ER, Hanna M, Cho L. Left ventricular hypertrophy in a runner: things are not always what they seem. Circulation 2014; 130:590–592.
- Ardehali H, Qasim A, Cappola T, et al. Endomyocardial biopsy plays a role in diagnosing patients with unexplained cardiomyopathy. Am Heart J 2004; 147:919–923.
- Berghoff M, Kathpal M, Khan F, Skinner M, Falk R, Freeman R. Endothelial dysfunction precedes C-fiber abnormalities in primary (AL) amyloidosis. Ann Neurol 2003; 53:725–730.
- Khan MF, Falk RH. Amyloidosis. Postgrad Med J 2001; 77:686–693.
- Martinez-Naharro A, Treibel TA, Abdel-Gadir A, et al. Magnetic resonance in transthyretin cardiac amyloidosis. J Am Coll Cardiol 2017; 70:466–477.
- Longhi S, Quarta CC, Milandri A, et al. Atrial fibrillation in amyloidotic cardiomyopathy: prevalence, incidence, risk factors and prognostic role. Amyloid 2015; 22:147–155.
- Sperry BW, Vranian MN, Hachamovitch R, et al. Are classic predictors of voltage valid in cardiac amyloidosis? A contemporary analysis of electrocardiographic findings. Int J Cardiol 2016; 214:477–481.
- Falk RH. Diagnosis and management of the cardiac amyloidoses. Circulation 2005; 112:2047–2060.
- Berk JL, Keane J, Seldin DC, et al. Persistent pleural effusions in primary systemic amyloidosis: etiology and prognosis. Chest 2003; 124:969–977.
- Miani D, Rocco M, Alberti E, Spedicato L, Fioretti PM. Amyloidosis of epicardial and intramural coronary arteries as an unusual cause of myocardial infarction and refractory angina pectoris. Ital Heart J 2002; 3:479–482.
- Mesquita ET, Jorge AJL, Souza CV Junior, Andrade TR. Cardiac amyloidosis and its new clinical phenotype: heart failure with preserved ejection fraction. Arg Bras Cardiol 2017; 109:71–80.
- Swanton RH, Brooksby IAB, Davies MJ, Coltart DJ, Jenkins BS, Webb-Peploe MM. Systolic and diastolic ventricular function in cardiac amyloidosis: studies in six cases diagnosed with endomyocardial biopsy. Am J Cardiol 1977; 39:658–664.
- Tyberg TI, Goodyer AVN, Hurst VW 3rd, Alexander J, Langou RA. Left ventricular filling in differentiating restrictive amyloid cardiomyopathy and constrictive pericarditis. Am J Cardiol 1981; 47:791–796.
- Sperry BW, Jones BM, Vranian MN, Hanna M, Jaber WA. Recognizing transthyretin cardiac amyloidosis in patients with aortic stenosis: impact on prognosis. JACC Cardiovasc Imaging 2016; 9:904–906.
- Cyrille NB, Goldsmith J, Alvarez J, Maurer MS. Prevalence and prognostic significance of low QRS voltage among the three main types of cardiac amyloidosis. Am J Cardiol 2014; 114:1089–1093.
- Hongo M, Yamamoto H, Kohda T, et al. Comparison of electrocardiographic findings in patients with AL (primary) amyloidosis and in familial amyloid polyneuropathy and anginal pain and their relation to histopathologic findings. Am J Cardiol 2000; 85:849–853.
- Maurer MS, Elliott P, Comenzo R, Semigran M, Rapezzi C. Addressing common questions encountered in the diagnosis and management of cardiac amyloidosis. Circulation 2017; 135:1357–1377.
- Abdalla I, Murray RD, Lee JC, Stewart WJ, Tajik AJ, Klein AL. Duration of pulmonary venous atrial reversal flow velocity and mitral inflow a wave: new measure of severity of cardiac amyloidosis. J Am Soc Echocardiogr 1998; 11:1125–1133.
- Gillmore JD, Maurer MS, Falk RH, et al. Nonbiopsy diagnosis of cardiac transthyretin amyloidosis. Circulation 2016; 133:2404–2412.
- Gertz MA. Immunoglobulin light chain amyloidosis: 2016 update on diagnosis, prognosis, and treatment. Am J Hematol 2016; 91:947–956.
- Patel KS, Hawkins PN. Cardiac amyloidosis: where are we today? J Intern Med 2015; 278:126–144.
- Ritts AJ, Cornell RF, Swiger K, Singh J, Goodman S, Lenihan DJ. Current concepts of cardiac amyloidosis: diagnosis, clinical management, and the need for collaboration. Heart Fail Clin 2017; 13:409–416.
- Sperry BW, Vranian MN, Hachamovitch R, et al. Subtype-specific interactions and prognosis in cardiac amyloidosis. J Am Heart Assoc 2016; 5:e002877.
- Kumar S, Dispenzieri A, Lacy MQ, et al. Revised prognostic staging system for light chain amyloidosis incorporating cardiac biomarkers and serum free light chain measurements. J Clin Oncol 2012; 30:989–995.
- Phelan D, Collier P, Thavendiranathan P, et al. Relative apical sparing of longitudinal strain using two-dimensional speckle-tracking echocardiography is both sensitive and specific for the diagnosis of cardiac amyloidosis. Heart 2012; 98:1442–1448.
- Patel AR, Kramer CM. Role of cardiac magnetic resonance in the diagnosis and prognosis of nonischemic cardiomyopathy. JACC Cardiovasc Imaging 2017; 10(10 Pt A):1180–1193.
- White JA, Kim HW, Shah D, et al. CMR imaging with rapid visual T1 assessment predicts mortality in patients suspected of cardiac amyloidosis. JACC Cardiovasc Imaging 2014; 7:143–156.
- Parkey RW, Bonte FJ, Meyer SL, et al. A new method for radionuclide imaging of acute myocardial infarction in humans. Circulation 1974; 50:540–546.
- Wizenberg TA, Muz J, Sohn YH, Samlowski W, Weissler AM. Value of positive myocardial technetium-99m-pyrophosphate scintigraphy in the noninvasive diagnosis of cardiac amyloidosis. Am Heart J 1982; 103(4 Pt 1):468–473.
- Bokhari S, Castaño A, Pozniakoff T, Deslisle S, Latif F, Maurer MS. 99mTc-Pyrophosphate scintigraphy for differentiating light-chain cardiac amyloidosis from the transthyretin-related familial and senile cardiac amyloidoses. Circ Cardiovasc Imaging 2013; 6:195–201.
- Vranian MN, Sperry BW, Hanna M, et al. Technetium pyrophosphate uptake in transthyretin cardiac amyloidosis: associations with echocardiographic disease severity and outcomes. J Nucl Cardiol 2017; Jan 3. [Epub ahead of print] doi: 10.1007/s12350-016-0768-9.
- Bennett MK, Gilotra NA, Harrington C, et al. Evaluation of the role of endomyocardial biopsy in 851 patients with unexplained heart failure from 2000-2009. Circ Heart Fail 2013; 6:676–684.
- Garcia Y, Collins AB, Stone JR. Abdominal fat pad excisional biopsy for the diagnosis and typing of systemic amyloidosis. Hum Pathol 2017; Nov 10. [Epub ahead of print] doi:10.1016/j.humpath.2017.11.001.
- Quarta CC, Gonzalez-Lopez E, Gilbertson JA, et al. Diagnostic sensitivity of abdominal fat aspiration in cardiac amyloidosis. Eur Heart J 2017; 38:1905–1908.
- Fine NM, Arruda-Olson AM, Dispenzieri A, et al. Yield of noncardiac biopsy for the diagnosis of transthyretin cardiac amyloidosis. Am J Cardiol 2014; 113:1723–1727.
- Katzmann JA, Abraham RS, Dispenzieri A, Lust JA, Kyle RA. Diagnostic performance of quantitative kappa and lambda free light chain assays in clinical practice. Clin Chem 2005; 51:878–781.
- Malha L, Mann SJ. Loop diuretics in the treatment of hypertension. Curr Hypertens Rep 2016; 18:27.
- Rubinow A, Skinner M, Cohen AS. Digoxin sensitivity in amyloid cardiomyopathy. Circulation 1981; 63:1285–1288.
- Feng D, Syed IS, Martinez M, et al. Intracardiac thrombosis and anticoagulation therapy in cardiac amyloidosis. Circulation 2009; 119:2490–2497.
- Castaño A, Drachman BM, Judge D, Maurer MS. Natural history and therapy of TTR-cardiac amyloidosis: emerging disease-modifying therapies from organ transplantation to stabilizer and silencer drugs. Heart Fail Rev 2015; 20:163–178.
- Hamon D, Algalarrondo V, Gandjbakhch E, et al. Outcome and incidence of appropriate implantable cardioverter-defibrillator therapy in patients with cardiac amyloidosis. Int J Cardiol 2016; 222:562–568.
- Patel KS, Hawkins PN, Whelan CJ, Gillmore JD. Life-saving implantable cardioverter defibrillator therapy in cardiac AL amyloidosis. BMJ Case Rep 2014; Dec 22. doi:10.1136/bcr-2014-206600.
- Gertz M, Lacy M, Dispenzieri A, et al. Troponin T level as an exclusion criterion for stem cell transplantation in light-chain amyloidosis. Leuk Lymphoma 2008; 49:36–41.
- Vranian MN, Sperry BW, Valent J, Hanna M. Emerging advances in the management of cardiac amyloidosis. Curr Cardiol Rep 2015; 17:100.
- Alexander KM, Singh A, Falk RH. Novel pharmacotherapies for cardiac amyloidosis. Pharmacol Ther 2017; 180:129–138.
- Sher T, Fenton B, Akhtar A, Gertz MA. First report of safety and efficacy of daratumumab in 2 cases of advanced immunoglobulin light chain amyloidosis. Blood 2016; 128:1987–1989.
- Sanchorawala V, Palladini G, Kukreti V, et al. A phase 1/2 study of the oral proteasome inhibitor ixazomib in relapsed or refractory AL amyloidosis. Blood 2017; 130:597–605.
- Zumbo G, Sadeghi-Alavijeh O, Hawkins PN, Fontana M. New and developing therapies for AL amyloidosis. Expert Opin Pharmacother 2017; 18:139–149.
- Koyama J, Falk RH. Prognostic significance of strain Doppler imaging in light-chain amyloidosis. JACC Cardiovasc Imaging 2010; 3:333–342.
- Palladini G, Dispenzieri A, Gertz MA, et al. New criteria for response to treatment in immunoglobulin light chain amyloidosis based on free light chain measurement and cardiac biomarkers: impact on survival outcomes. J Clin Oncol 2012; 30:4541–4549.
- Sousa M, Monohan G, Rajagopalan N, Grigorian A. Heart transplantation in cardiac amyloidosis. Heart Fail Rev 2017; 22:317–327.
- Gertz MA, Landau H, Comenzo RL, et al. First-in-human phase I/II study of NEOD001 in patients with light chain amyloidosis and persistent organ dysfunction. J Clin Oncol 2016; 34:1097–1103.
- Holmgren G, Steen L, Ekstedt J, et al. Biochemical effect of liver transplantation in two Swedish patients with familial amyloidotic polyneuropathy (FAP-met30). Clin Genet 1991; 40:242–246.
- Hanna M. Novel drugs targeting transthyretin amyloidosis. Curr Heart Fail Rep 2014; 11:50–57.
- Berk JL, Suhr OB, Obici L, et al; Diflunisal Trial Consortium. Repurposing diflunisal for familial amyloid polyneuropathy: a randomized clinical trial. JAMA 2013; 310:2658–2667.
- Castaño A, Helmke S, Alvarez J, Delisle S, Maurer MS. Diflunisal for ATTR cardiac amyloidosis. Congest Heart Fail 2012; 18:315–319.
- Sekijima Y, Tojo K, Morita H, Koyama J, Ikeda S-I. Safety and efficacy of long-term diflunisal administration in hereditary transthyretin (ATTR) amyloidosis. Amyloid 2015; 22:79–83.
- Coelho T, Maia LF, Martins da Silva A, et al. Tafamidis for transthyretin familial amyloid polyneuropathy: a randomized, controlled trial. Neurology 2012; 79:785–792.
- Maurer MS, Grogan DR, Judge DP, et al. Tafamidis in transthyretin amyloid cardiomyopathy: effects on transthyretin stabilization and clinical outcomes. Circ Heart Fail 2015; 8:519–526.
- Cardoso I, Martins D, Ribeiro T, Merlini G, Saraiva MJ. Synergy of combined doxycycline/TUDCA treatment in lowering transthyretin deposition and associated biomarkers: studies in FAP mouse models. J Transl Med 2010; 8:74.
- Obici L, Cortese A, Lozza A, et al. Doxycycline plus tauroursodeoxycholic acid for transthyretin amyloidosis: A phase II study. Amyloid 2012; 19(suppl 1):34–36.
- Kristen AV, Lehrke S, Buss S, et al. Green tea halts progression of cardiac transthyretin amyloidosis: An observational report. Clin Res Cardiol 2012; 101:805–813.
- Higaki JN, Chakrabartty A, Galant NJ, et al. Novel conformation-specific monoclonal antibodies against amyloidogenic forms of forms of transthyretin. Amyloid 2016; 23:86–97.
- Merlini G, Bellotti V. Molecular mechanisms of amyloidosis. N Engl J Med 2003; 349:583–596.
- Richards DB, Cookson LM, Berges AC, et al. Therapeutic clearance of amyloid by antibodies to serum amyloid P component. N Engl J Med 2015; 373:1106–1114.
- Sipe JD, Benson MD, Buxbaum JN, et al. Nomenclature 2014: amyloid fibril proteins and clinical classification of the amyloidosis. Amyloid 2014; 21:221–224.
- Maleszewski JJ. Cardiac amyloidosis: pathology, nomenclature, and typing. Cardiovasc Pathol 2015; 24:343–350.
- Kyle RA, Linos A, Beard CM, et al. Incidence and natural history of primary systemic amyloidosis in Olmsted County, Minnesota, 1950 through 1989. Blood 1992; 79:1817–1822.
- Krsnik I, Cabero M, Morillo D, et al. Light chain amyloidosis: Experience in a tertiary hospital: 2005-2013. Rev Clin Esp 2015; 215:1–8.
- Dubrey SW, Cha K, Anderson J, et al. The clinical features of immunoglobulin light-chain (AL) amyloidosis with heart involvement. QJM 1998; 91:141–157.
- Sperry BW, Ikram A, Hachamovitch R, et al. Efficacy of chemotherapy for light-chain amyloidosis in patients presenting with symptomatic heart failure. J Am Coll Cardiol 2016; 67:2941–2948.
- Gillmore JD, Damy T, Fontana M, et al. A new staging system for cardiac transthyretin amyloidosis. Eur Heart J 2017; Oct 18. [Epub ahead of print] doi:10.1093/eurheartj/ehx589.
- Tanskanen M, Peuralinna T, Polvikoski T, et al. Senile systemic amyloidosis affects 25% of the very aged and associates with genetic variation in alpha2-macroglobulin and tau: a population-based autopsy study. Ann Med 2008; 40:232–239.
- González-López E, Gallego-Delgado M, Guzzo-Merello G, et al. Wild-type transthyretin amyloidosis as a cause of heart failure with preserved ejection fraction. Eur Heart J 2015; 36:2585–2594.
- Longhi S, Lorenzini M, Gagliardi C, et al. Coexistence of degenerative aortic stenosis and wild-type transthyretin-related cardiac amyloidosis. JACC Cardiovasc Imaging 2016;9:325–327.
- Grogan M, Scott CG, Kyle RA, et al. Natural history of wild-type transthyretin cardiac amyloidosis and risk stratification using a novel staging system. J Am Coll Cardiol 2016; 68:1014–1020.
- Gioeva Z, Urban P, Meliss RR, et al. ATTR amyloid in the carpal tunnel ligament is frequently of wildtype transthyretin origin. Amyloid 2013; 20:1–6.
- Yanagisawa A, Ueda M, Sueyoshi T, et al. Amyloid deposits derived from transthyretin in the ligamentum flavum as related to lumbar spinal canal stenosis. Mod Pathol 2015; 28:201–207.
- Siddiqi OK, Ruberg FL. Cardiac amyloidosis: an update on pathophysiology, diagnosis, and treatment. Trends Cardiovasc Med 2017; Jul 13. [Epub ahead of print] doi:10.1016/j.tcm.2017.07.004.
- Nakagawa M, Sekijima Y, Yazaki M, et al. Carpal tunnel syndrome: A common initial symptom of systemic wild-type ATTR (ATTRwt) amyloidosis. Amyloid 2016; 23:58–63.
- Sekijima Y, Yoshida K, Tokuda T, Ikeda S-I. Familial Transthyretin Amyloidosis. In: Adam MP, Ardinger HH, Pagon RA, et al, eds. Seattle, WA: University of Washington, Seattle; 1993–2017. Available at: https://www-ncbi-nlm-nih-gov.ccmain.ohionet.org/books/NBK1194. Updated January 26, 2012. Accessed November 16, 2017.
- Buxbaum J, Jacobson DR, Tagoe C, et al. Transthyretin V122I in African Americans with congestive heart failure. J Am Coll Cardiol 2006; 47:1724–1725.
- Ruberg FL, Maurer MS, Judge DP, et al. Prospective evaluation of the morbidity and mortality of wild-type and V122I mutant transthyretin amyloid cardiomyopathy: The Transthyretin Amyloidosis Cardiac Study (TRACS). Am Heart J 2012; 164:222–228.e1.
- Wright JR, Calkins E. Amyloid in the aged heart: frequency and clinical significance. J Am Geriatr Soc 1975; 23:97–103.
- Vermeer AMC, Janssen A, Boorsma PC, Mannens MMAM, Wilde AAM, Christiaans I. Transthyretin amyloidosis: a phenocopy of hypertrophic cardiomyopathy. Amyloid 2017; 24:87–91.
- Velazquez-Ceceña JL, Lubell DL, Nagajothi N, Al-Masri H, Siddiqui M, Khosla S. Syncope cardiomyopathy in a patient with primary AL-type amyloid heart disease. Tex Heart Inst J 2009; 36:50–54.
- Stegman BM, Kwon D, Rodriguez ER, Hanna M, Cho L. Left ventricular hypertrophy in a runner: things are not always what they seem. Circulation 2014; 130:590–592.
- Ardehali H, Qasim A, Cappola T, et al. Endomyocardial biopsy plays a role in diagnosing patients with unexplained cardiomyopathy. Am Heart J 2004; 147:919–923.
- Berghoff M, Kathpal M, Khan F, Skinner M, Falk R, Freeman R. Endothelial dysfunction precedes C-fiber abnormalities in primary (AL) amyloidosis. Ann Neurol 2003; 53:725–730.
- Khan MF, Falk RH. Amyloidosis. Postgrad Med J 2001; 77:686–693.
- Martinez-Naharro A, Treibel TA, Abdel-Gadir A, et al. Magnetic resonance in transthyretin cardiac amyloidosis. J Am Coll Cardiol 2017; 70:466–477.
- Longhi S, Quarta CC, Milandri A, et al. Atrial fibrillation in amyloidotic cardiomyopathy: prevalence, incidence, risk factors and prognostic role. Amyloid 2015; 22:147–155.
- Sperry BW, Vranian MN, Hachamovitch R, et al. Are classic predictors of voltage valid in cardiac amyloidosis? A contemporary analysis of electrocardiographic findings. Int J Cardiol 2016; 214:477–481.
- Falk RH. Diagnosis and management of the cardiac amyloidoses. Circulation 2005; 112:2047–2060.
- Berk JL, Keane J, Seldin DC, et al. Persistent pleural effusions in primary systemic amyloidosis: etiology and prognosis. Chest 2003; 124:969–977.
- Miani D, Rocco M, Alberti E, Spedicato L, Fioretti PM. Amyloidosis of epicardial and intramural coronary arteries as an unusual cause of myocardial infarction and refractory angina pectoris. Ital Heart J 2002; 3:479–482.
- Mesquita ET, Jorge AJL, Souza CV Junior, Andrade TR. Cardiac amyloidosis and its new clinical phenotype: heart failure with preserved ejection fraction. Arg Bras Cardiol 2017; 109:71–80.
- Swanton RH, Brooksby IAB, Davies MJ, Coltart DJ, Jenkins BS, Webb-Peploe MM. Systolic and diastolic ventricular function in cardiac amyloidosis: studies in six cases diagnosed with endomyocardial biopsy. Am J Cardiol 1977; 39:658–664.
- Tyberg TI, Goodyer AVN, Hurst VW 3rd, Alexander J, Langou RA. Left ventricular filling in differentiating restrictive amyloid cardiomyopathy and constrictive pericarditis. Am J Cardiol 1981; 47:791–796.
- Sperry BW, Jones BM, Vranian MN, Hanna M, Jaber WA. Recognizing transthyretin cardiac amyloidosis in patients with aortic stenosis: impact on prognosis. JACC Cardiovasc Imaging 2016; 9:904–906.
- Cyrille NB, Goldsmith J, Alvarez J, Maurer MS. Prevalence and prognostic significance of low QRS voltage among the three main types of cardiac amyloidosis. Am J Cardiol 2014; 114:1089–1093.
- Hongo M, Yamamoto H, Kohda T, et al. Comparison of electrocardiographic findings in patients with AL (primary) amyloidosis and in familial amyloid polyneuropathy and anginal pain and their relation to histopathologic findings. Am J Cardiol 2000; 85:849–853.
- Maurer MS, Elliott P, Comenzo R, Semigran M, Rapezzi C. Addressing common questions encountered in the diagnosis and management of cardiac amyloidosis. Circulation 2017; 135:1357–1377.
- Abdalla I, Murray RD, Lee JC, Stewart WJ, Tajik AJ, Klein AL. Duration of pulmonary venous atrial reversal flow velocity and mitral inflow a wave: new measure of severity of cardiac amyloidosis. J Am Soc Echocardiogr 1998; 11:1125–1133.
- Gillmore JD, Maurer MS, Falk RH, et al. Nonbiopsy diagnosis of cardiac transthyretin amyloidosis. Circulation 2016; 133:2404–2412.
- Gertz MA. Immunoglobulin light chain amyloidosis: 2016 update on diagnosis, prognosis, and treatment. Am J Hematol 2016; 91:947–956.
- Patel KS, Hawkins PN. Cardiac amyloidosis: where are we today? J Intern Med 2015; 278:126–144.
- Ritts AJ, Cornell RF, Swiger K, Singh J, Goodman S, Lenihan DJ. Current concepts of cardiac amyloidosis: diagnosis, clinical management, and the need for collaboration. Heart Fail Clin 2017; 13:409–416.
- Sperry BW, Vranian MN, Hachamovitch R, et al. Subtype-specific interactions and prognosis in cardiac amyloidosis. J Am Heart Assoc 2016; 5:e002877.
- Kumar S, Dispenzieri A, Lacy MQ, et al. Revised prognostic staging system for light chain amyloidosis incorporating cardiac biomarkers and serum free light chain measurements. J Clin Oncol 2012; 30:989–995.
- Phelan D, Collier P, Thavendiranathan P, et al. Relative apical sparing of longitudinal strain using two-dimensional speckle-tracking echocardiography is both sensitive and specific for the diagnosis of cardiac amyloidosis. Heart 2012; 98:1442–1448.
- Patel AR, Kramer CM. Role of cardiac magnetic resonance in the diagnosis and prognosis of nonischemic cardiomyopathy. JACC Cardiovasc Imaging 2017; 10(10 Pt A):1180–1193.
- White JA, Kim HW, Shah D, et al. CMR imaging with rapid visual T1 assessment predicts mortality in patients suspected of cardiac amyloidosis. JACC Cardiovasc Imaging 2014; 7:143–156.
- Parkey RW, Bonte FJ, Meyer SL, et al. A new method for radionuclide imaging of acute myocardial infarction in humans. Circulation 1974; 50:540–546.
- Wizenberg TA, Muz J, Sohn YH, Samlowski W, Weissler AM. Value of positive myocardial technetium-99m-pyrophosphate scintigraphy in the noninvasive diagnosis of cardiac amyloidosis. Am Heart J 1982; 103(4 Pt 1):468–473.
- Bokhari S, Castaño A, Pozniakoff T, Deslisle S, Latif F, Maurer MS. 99mTc-Pyrophosphate scintigraphy for differentiating light-chain cardiac amyloidosis from the transthyretin-related familial and senile cardiac amyloidoses. Circ Cardiovasc Imaging 2013; 6:195–201.
- Vranian MN, Sperry BW, Hanna M, et al. Technetium pyrophosphate uptake in transthyretin cardiac amyloidosis: associations with echocardiographic disease severity and outcomes. J Nucl Cardiol 2017; Jan 3. [Epub ahead of print] doi: 10.1007/s12350-016-0768-9.
- Bennett MK, Gilotra NA, Harrington C, et al. Evaluation of the role of endomyocardial biopsy in 851 patients with unexplained heart failure from 2000-2009. Circ Heart Fail 2013; 6:676–684.
- Garcia Y, Collins AB, Stone JR. Abdominal fat pad excisional biopsy for the diagnosis and typing of systemic amyloidosis. Hum Pathol 2017; Nov 10. [Epub ahead of print] doi:10.1016/j.humpath.2017.11.001.
- Quarta CC, Gonzalez-Lopez E, Gilbertson JA, et al. Diagnostic sensitivity of abdominal fat aspiration in cardiac amyloidosis. Eur Heart J 2017; 38:1905–1908.
- Fine NM, Arruda-Olson AM, Dispenzieri A, et al. Yield of noncardiac biopsy for the diagnosis of transthyretin cardiac amyloidosis. Am J Cardiol 2014; 113:1723–1727.
- Katzmann JA, Abraham RS, Dispenzieri A, Lust JA, Kyle RA. Diagnostic performance of quantitative kappa and lambda free light chain assays in clinical practice. Clin Chem 2005; 51:878–781.
- Malha L, Mann SJ. Loop diuretics in the treatment of hypertension. Curr Hypertens Rep 2016; 18:27.
- Rubinow A, Skinner M, Cohen AS. Digoxin sensitivity in amyloid cardiomyopathy. Circulation 1981; 63:1285–1288.
- Feng D, Syed IS, Martinez M, et al. Intracardiac thrombosis and anticoagulation therapy in cardiac amyloidosis. Circulation 2009; 119:2490–2497.
- Castaño A, Drachman BM, Judge D, Maurer MS. Natural history and therapy of TTR-cardiac amyloidosis: emerging disease-modifying therapies from organ transplantation to stabilizer and silencer drugs. Heart Fail Rev 2015; 20:163–178.
- Hamon D, Algalarrondo V, Gandjbakhch E, et al. Outcome and incidence of appropriate implantable cardioverter-defibrillator therapy in patients with cardiac amyloidosis. Int J Cardiol 2016; 222:562–568.
- Patel KS, Hawkins PN, Whelan CJ, Gillmore JD. Life-saving implantable cardioverter defibrillator therapy in cardiac AL amyloidosis. BMJ Case Rep 2014; Dec 22. doi:10.1136/bcr-2014-206600.
- Gertz M, Lacy M, Dispenzieri A, et al. Troponin T level as an exclusion criterion for stem cell transplantation in light-chain amyloidosis. Leuk Lymphoma 2008; 49:36–41.
- Vranian MN, Sperry BW, Valent J, Hanna M. Emerging advances in the management of cardiac amyloidosis. Curr Cardiol Rep 2015; 17:100.
- Alexander KM, Singh A, Falk RH. Novel pharmacotherapies for cardiac amyloidosis. Pharmacol Ther 2017; 180:129–138.
- Sher T, Fenton B, Akhtar A, Gertz MA. First report of safety and efficacy of daratumumab in 2 cases of advanced immunoglobulin light chain amyloidosis. Blood 2016; 128:1987–1989.
- Sanchorawala V, Palladini G, Kukreti V, et al. A phase 1/2 study of the oral proteasome inhibitor ixazomib in relapsed or refractory AL amyloidosis. Blood 2017; 130:597–605.
- Zumbo G, Sadeghi-Alavijeh O, Hawkins PN, Fontana M. New and developing therapies for AL amyloidosis. Expert Opin Pharmacother 2017; 18:139–149.
- Koyama J, Falk RH. Prognostic significance of strain Doppler imaging in light-chain amyloidosis. JACC Cardiovasc Imaging 2010; 3:333–342.
- Palladini G, Dispenzieri A, Gertz MA, et al. New criteria for response to treatment in immunoglobulin light chain amyloidosis based on free light chain measurement and cardiac biomarkers: impact on survival outcomes. J Clin Oncol 2012; 30:4541–4549.
- Sousa M, Monohan G, Rajagopalan N, Grigorian A. Heart transplantation in cardiac amyloidosis. Heart Fail Rev 2017; 22:317–327.
- Gertz MA, Landau H, Comenzo RL, et al. First-in-human phase I/II study of NEOD001 in patients with light chain amyloidosis and persistent organ dysfunction. J Clin Oncol 2016; 34:1097–1103.
- Holmgren G, Steen L, Ekstedt J, et al. Biochemical effect of liver transplantation in two Swedish patients with familial amyloidotic polyneuropathy (FAP-met30). Clin Genet 1991; 40:242–246.
- Hanna M. Novel drugs targeting transthyretin amyloidosis. Curr Heart Fail Rep 2014; 11:50–57.
- Berk JL, Suhr OB, Obici L, et al; Diflunisal Trial Consortium. Repurposing diflunisal for familial amyloid polyneuropathy: a randomized clinical trial. JAMA 2013; 310:2658–2667.
- Castaño A, Helmke S, Alvarez J, Delisle S, Maurer MS. Diflunisal for ATTR cardiac amyloidosis. Congest Heart Fail 2012; 18:315–319.
- Sekijima Y, Tojo K, Morita H, Koyama J, Ikeda S-I. Safety and efficacy of long-term diflunisal administration in hereditary transthyretin (ATTR) amyloidosis. Amyloid 2015; 22:79–83.
- Coelho T, Maia LF, Martins da Silva A, et al. Tafamidis for transthyretin familial amyloid polyneuropathy: a randomized, controlled trial. Neurology 2012; 79:785–792.
- Maurer MS, Grogan DR, Judge DP, et al. Tafamidis in transthyretin amyloid cardiomyopathy: effects on transthyretin stabilization and clinical outcomes. Circ Heart Fail 2015; 8:519–526.
- Cardoso I, Martins D, Ribeiro T, Merlini G, Saraiva MJ. Synergy of combined doxycycline/TUDCA treatment in lowering transthyretin deposition and associated biomarkers: studies in FAP mouse models. J Transl Med 2010; 8:74.
- Obici L, Cortese A, Lozza A, et al. Doxycycline plus tauroursodeoxycholic acid for transthyretin amyloidosis: A phase II study. Amyloid 2012; 19(suppl 1):34–36.
- Kristen AV, Lehrke S, Buss S, et al. Green tea halts progression of cardiac transthyretin amyloidosis: An observational report. Clin Res Cardiol 2012; 101:805–813.
- Higaki JN, Chakrabartty A, Galant NJ, et al. Novel conformation-specific monoclonal antibodies against amyloidogenic forms of forms of transthyretin. Amyloid 2016; 23:86–97.
KEY POINTS
- AL and ATTR are the 2 main types of amyloidosis that affect the heart.
- Serum and urine protein electrophoresis are inadequate laboratory tests to screen for AL given low sensitivity, and should be replaced by the serum free light chain assay as well as immunofixation of the serum and urine.
- AL cardiac amyloidosis (AL-CA) requires timely diagnosis and referral to hematology due to high mortality without prompt treatment.
- 99mTechnetium pyrophosphate bone scintigraphy is an affordable, noninvasive tool that has revolutionized the diagnosis of ATTR cardiac amyloidosis (ATTR-CA).
- The US Food and Drug Administration will likely approve new therapies for ATTR in late 2018.
Management of coronary chronic total occlusion
In patients with stable coronary artery disease (CAD), the cornerstone of treatment is medical management to control symptoms such as angina and dyspnea on exertion. But in a select group of patients, percutaneous coronary intervention (PCI) is indicated in addition to medical management. Invasive and noninvasive hemodynamic assessments of coronary artery stenosis in conjunction with anatomic considerations play a role in decision-making and in advising patients on revascularization vs medical management. However, in the case of coronary artery chronic total occlusion (CTO), the decision-making process remains challenging due to limited evidence supporting clinical efficacy of CTO PCI, as well as practical considerations including lower success rates and higher complication rates in comparison with patent-vessel PCI.
CLINICAL VIGNETTE
A 42-year-old man, an avid runner with hyperlipidemia and a strong family history of premature CAD, presents with several months of declining exercise tolerance. His physical examination and electrocardiogram are unremarkable. Myocardial perfusion imaging shows stress-induced ischemia affecting about 20% of the inferolateral myocardium. He is then referred for coronary angiography.
- Panel A: Discrete, high-grade stenosis of the mid-right coronary artery
- Panel B: Diffuse, multivessel disease involving the distal right coronary artery (B1) and the proximal left circumflex coronary artery (B2)
- Panel C: Total occlusion of the proximal right coronary artery with extensive left-to-right collaterals.
Treatment based on angiographic findings
In panel A, there is little to debate. The patient is likely to benefit from percutaneous revascularization of the right coronary artery to treat symptoms.
In panels B1 and B2, there is abundant evidence that the hemodynamic assessment of stenosis is superior to a visual estimate in directing PCI.1,2 Hemodynamic assessments including fractional flow reserve (FFR) inform the risk-benefit analysis of percutaneous vs medical treatment of coronary stenosis. In the case of FFR, 0.8 represents an inflection point. The lower FFR values are below 0.8, the greater the benefit of PCI as opposed to medical therapy. Conversely, the greater FFR values are above 0.8, the greater the benefit of medical therapy as opposed to PCI.
However, in panel C, there is significant variability in the data supporting the best treatment strategy for symptomatic patients with CTO.
CORONARY CTO
Coronary CTO is defined as TIMI 0 flow for more than 3 months in an epicardial coronary artery. CTO is not uncommon, seen on 30% of routine coronary angiograms. In the United States, attempt rates of PCI for CTO remain low and have been static at around 12.4%, representing less than 5% of total PCI volume.3 In addition, success rates of CTO PCI are disappointingly low at 59% compared with success rates of patent-vessel PCI at 96%.3 The most frequently cited barriers to CTO PCI are incomplete evidence for efficacy and concerns about safety. Because of the ongoing controversy about the risks and benefits of CTO PCI, it remains a class IIa indication in current American and European practice guidelines.4,5 In addition, these procedures remain technically challenging, and thus variability in local expertise can influence the decision to manage patients medically or refer for CTO PCI.
Patients are often advised that CTO is benign. However, the myocardium affected by a CTO is ischemic. Collateral vessels do not provide adequate flow reserve. FFR data collected from CTOs that were successfully crossed and subsequently interrogated with a pressure wire prior to stenting show that the myocardium supplied by the reconstituted distal bed remains ischemic. This ischemic burden appears to be independent of the size and quality of collaterals.6,7 In addition, a moderate stenosis in a donor coronary artery supplying collateral vessels to a CTO may result in an ischemic FFR as a consequence of coronary “steal” from the donor artery to the collateral vessels. The ischemic FFR in the donor artery can be corrected by treating the recipient CTO vessel.8
Similar to FFR, noninvasive assessment using myocardial perfusion imaging can define ischemic burden and a threshold for benefit of percutaneous vs medical management of CAD. Ischemia greater than 10% on myocardial perfusion imaging is associated with a high risk of major adverse cardiac events (MACE).9 Similar findings were noted in the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy, which showed superior reduction in angina and MACE in patients with greater than 10% ischemia on myocardial perfusion imaging treated with PCI vs medical therapy.10 In the case of coronary CTO, ischemia greater than 12.5% is predictive of significant improvement in symptoms after intervention.11
PROGNOSIS AND DISEASE BURDEN
CTO is associated with adverse prognosis, implying the importance of incomplete revascularization. The Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery (SYNTAX) trial used a scoring system to direct surgical vs percutaneous revascularization strategies in patients with complex or multivessel CAD. A post hoc analysis of the SYNTAX trial showed that incomplete revascularization was associated with significantly higher rates of 4-year mortality and MACE.12 This was likely from the ischemic burden remaining from incomplete revascularization. The presence of CTO was the strongest independent predictor of incomplete revascularization in the SYNTAX PCI arm. Similarly, the negative prognostic impact of having a CTO has been observed in a large population of patients followed prospectively after undergoing coronary angiography.13 Furthermore, the presence of CTO in a non-infarct-related artery at the time of ST-elevation myocardial infarction appears to be an independent predictor of death at 30 days, with a persistent negative prognostic impact lasting for up to 36 months of follow-up.14
CLINICAL BENEFITS OF CTO PCI
In patients with significant ischemic burden, CTO PCI has multiple clinical benefits. Symptomatic relief based on the Seattle Angina Questionnaire appears to be similar to that obtained with coronary artery bypass grafting (CABG) at 1-month follow up.15 Successful CTO PCI can have a positive impact on the risk of mortality in prospective13 and retrospective observational studies.16
CTO intervention may also have beneficial effects on left ventricular systolic function in patients with viable myocardium in the corresponding coronary territory.17 This improvement in systolic function appears to be sustained at 3 years of follow-up.18 Meta-analysis of observational data in symptomatic and ischemic patients who underwent successful CTO PCI shows reduced rates of all-cause mortality and MACE and a reduced need for subsequent CABG.19 This is in contrast to the frequently cited Occluded Artery Trial (OAT) trial, which showed no clinical benefit of PCI for a subacutely occluded infarct-related artery.20
EVIDENCE-BASED BENEFITS
Evidence of the merits of CTO PCI from randomized clinical trials is mixed. The only published study to date, the Evaluating Xience and Left Ventricular Function in Percutaneous Coronary Intervention on Occlusions After ST-Segment Elevation (EXPLORE) trial, showed no difference in left ventricular systolic function 4 months after ST-elevation myocardial infarction in patients undergoing staged CTO PCI of a non-infarct-related artery vs optimal medical therapy.21 Two larger trials presented at scientific meetings in 2017 remain unpublished. One trial showed noninferiority of optimal medical therapy vs successful CTO PCI in reducing the composite end point of all-cause mortality, myocardial infarction, stroke, and repeat revascularization; the other trial showed significant improvement in quality of life measures using the Seattle Angina Questionnaire score and Canadian Cardiovascular Society angina classification in patients who underwent successful CTO PCI compared with medical management.
High-volume CTO PCI centers now report procedural success rates as high as 92.9%22 and a correlation between the CTO PCI volume and CTO PCI success rates.3 The dramatic improvement in success rates achieved by high-volume operators globally can be attributed to a combination of operator experience, improved technology, and widespread adoption of the hybrid algorithm, which has helped to improve efficiency and standardize treatment in CTO PCI based on angiographic criteria.23 CTO PCI remains a highly specialized procedure, unique from patent-vessel PCI and with little correlation between total PCI volume and CTO PCI success rate. Despite recent advances, CTO PCI success remains heavily dependent on operator expertises, with a steep and long learning curve. In addition, the unique technical aspects of CTO PCI such as a retrograde and subintimal guidewire tracking that have accelerated procedural success are associated with higher rates of MACE compared with traditional antegrade and intraluminal guidewire tracking.24,25 Therefore, CTO PCI requires unique considerations beyond standard PCI in terms of potential complications. Uncommon but potentially life-threatening complications such as donor artery thrombosis, collateral vessel trauma, gear entrapment, and radiation skin injury demand a specialized informed consent process for the patient.26
In light of incomplete evidence based on extensive observational data and limited randomized clinical trials, the decision to refer patients for CTO PCI requires a comprehensive clinical evaluation. We know from data derived from patients with patent but stenotic coronary arteries that physiologically rather than angiographically driven decisions to revascularize can produce superior clinical results. There is an ischemic burden threshold beyond which revascularization is superior to optimal medical therapy. In this context, we know that CTO is not benign and is associated with ischemic burden. Consequently, patients with symptoms related to CTO represent a subset of patients with incomplete revascularization.
CONCLUSION
Despite recent advances, CTO PCI procedures remain technically demanding, and success with a low complication rate is heavily dependent on operator expertise. Therefore, CTO PCI should be used judiciously in patients with angina refractory to optimal medical therapy. It is an important tool to be used in conjunction with non-CTO PCI, CABG, and optimal medical therapy to produce favorable outcomes in patients with CAD.
- De Bruyne B, Pijls NHJ, Kalesan B, et al; FAME 2 Trial Investigators. Fractional flow reserve–guided PCI versus medical therapy in stable coronary disease. N Engl J Med 2012; 367:991–1001.
- Tonino PAL, De Bruyne B, Pijls NHJ, et al; FAME Study Investigators. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009; 360:213–224.
- Brilakis ES, Banerjee S, Karmpaliotis D, et al. Procedural outcomes of chronic total occlusion percutaneous coronary intervention: a report from the NCDR (National Cardiovascular Data Registry). JACC Cardiovasc Interv 2015; 8:245–253.
- Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol 2011; 58:e44–e122.
- Author/Task Force members; Windeker S, Kolh P, Alfonso R, et al. 2014 ESC/EACTS guidelines on myocardial revascularization: the task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 2014; 35:2541–2619.
- Sachdeva R, Agrawal M, Flynn SE, Werner GS, Uretsky BF. The myocardium supplied by a chronic total occlusion is a persistently ischemic zone. Catheter Cardiovasc Interv 2014; 83:9–16.
- Werner GS, Surber R, Ferrari M, Fritzenwanger M, Figulla HR. The functional reserve of collaterals supplying long-term chronic total coronary occlusions in patients without prior myocardial infarction. Eur Heart J 2006; 27:2406–2412.
- Sachdeva R, Agrawal M, Flynn SE, Werner GS, Uretsky BF. Reversal of ischemia of donor artery myocardium after recanalization of a chronic total occlusion. Catheter Cardiovasc Interv 2013; 82:E453–E458.
- Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation 2003; 107:2900–2907.
- Shaw LJ, Berman DS, Maron DJ, et al; COURAGE Investigators. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation 2008; 117:1283–1291.
- Safley DM, Koshy S, Grantham JA, et al. Changes in myocardial ischemic burden following percutaneous coronary intervention of chronic total occlusions. Catheter Cardiovasc Interv 2011; 78:337–343.
- Farooq V, Serruys PW, Garcia-Garcia HM, et al. The negative impact of incomplete angiographic revascularization on clinical outcomes and its association with total occlusions: the SYNTAX (Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) trial. J Am Coll Cardiol 2013; 61:282–294.
- Råmunddal T, Hoebers LP, Henriques JP, et al. Prognostic impact of chronic total occlusions: a report from SCAAR (Swedish Coronary Angiography and Angioplasty Registry). JACC Cardiovasc Interv 2016; 9:1535–1544.
- Claessen BE, Dangas GD, Weisz G, et al. Prognostic impact of a chronic total occlusion in a non-infarct-related artery in patients with ST-segment elevation myocardial infarction: 3-year results from the HORIZONS-AMI trial. Eur Heart J 2012; 33:768–775.
- Grantham JA, Jones PG, Cannon L, Spertus JA. Quantifying the early health status benefits of successful chronic total occlusion recanalization: Results from the FlowCardia’s Approach to Chronic Total Occlusion Recanalization (FACTOR) Trial. Circ Cardiovasc Qual Outcomes 2010; 3:284–290.
- Yang ZK, Zhang RY, Hu J, Zhang Q, Ding FH, Shen WF. Impact of successful staged revascularization of a chronic total occlusion in the non-infarct-related artery on long-term outcome in patients with acute ST-segment elevation myocardial infarction. Int J Cardiol 2013; 165:76–79.
- Baks T, van Geuns R-J, Duncker DJ, et al. Prediction of left ventricular function after drug-eluting stent implantation for chronic total coronary occlusions. J Am Coll Cardiol 2006; 47:721–725.
- Kirschbaum SW, Baks T, van den Ent M, et al. Evaluation of left ventricular function three years after percutaneous recanalization of chronic total coronary occlusions. Am J Cardiol 2008; 101:179–185.
- Khan MF, Wendel CS, Thai HM, Movahed MR. Effects of percutaneous revascularization of chronic total occlusions on clinical outcomes: a meta-analysis comparing successful versus failed percutaneous intervention for chronic total occlusion. Catheter Cardiovasc Interv 2013; 82:95–107.
- Hochman JS, Lamas GA, Buller CE, et al; Occluded Artery Trial Investigators. Coronary intervention for persistent occlusion after myocardial infarction. N Engl J Med 2006; 355:2395–2407.
- Henriques JP, Hoebers LP, Råmunddal T, et al; EXPLORE Trial Investigators. Percutaneous intervention for concurrent chronic total occlusions in patients with STEMI: The EXPLORE trial. J Am Coll Cardiol 2016; 68:1622–1632.
- Christopoulos G, Kandzari DE, Yeh RW, et al. Development and validation of a novel scoring system for predicting technical success of chronic total occlusion percutaneous coronary interventions: The PROGRESS CTO (Prospective Global Registry for the Study of Chronic Total Occlusion Intervention) score. JACC Cardiovasc Interv 2016; 9:1–9.
- Brilakis ES, Grantham JA, Rinfret S, et al. A percutaneous treatment algorithm for crossing coronary chronic total occlusions. JACC Cardiovasc Interv 2012; 5:367–379.
- Karmpaliotis D, Karatasakis A, Alaswad K, et al. Outcomes with the use of the retrograde approach for coronary chronic total occlusion interventions in a contemporary multicenter US registry. Circ Cardiovasc Interv 2016; 9. pii: e003434. doi:10.1161/CIRCINTERVENTIONS.115.003434.
- Song L, Maehara A, Finn MT, et al. Intravascular ultrasound analysis of intraplaque versus subintimal tracking in percutaneous intervention for coronary chronic total occlusions and association with procedural outcomes. JACC Cardiovasc Interv 2017; 10:1011–1021.
- Patel VG, Brayton KM, Tamayo A, et al. Angiographic success and procedural complications in patients undergoing percutaneous coronary chronic total occlusion interventions: a weighted meta-analysis of 18,061 patients from 65 studies. JACC Cardiovasc Interv 2013; 6:128–136.
In patients with stable coronary artery disease (CAD), the cornerstone of treatment is medical management to control symptoms such as angina and dyspnea on exertion. But in a select group of patients, percutaneous coronary intervention (PCI) is indicated in addition to medical management. Invasive and noninvasive hemodynamic assessments of coronary artery stenosis in conjunction with anatomic considerations play a role in decision-making and in advising patients on revascularization vs medical management. However, in the case of coronary artery chronic total occlusion (CTO), the decision-making process remains challenging due to limited evidence supporting clinical efficacy of CTO PCI, as well as practical considerations including lower success rates and higher complication rates in comparison with patent-vessel PCI.
CLINICAL VIGNETTE
A 42-year-old man, an avid runner with hyperlipidemia and a strong family history of premature CAD, presents with several months of declining exercise tolerance. His physical examination and electrocardiogram are unremarkable. Myocardial perfusion imaging shows stress-induced ischemia affecting about 20% of the inferolateral myocardium. He is then referred for coronary angiography.
- Panel A: Discrete, high-grade stenosis of the mid-right coronary artery
- Panel B: Diffuse, multivessel disease involving the distal right coronary artery (B1) and the proximal left circumflex coronary artery (B2)
- Panel C: Total occlusion of the proximal right coronary artery with extensive left-to-right collaterals.
Treatment based on angiographic findings
In panel A, there is little to debate. The patient is likely to benefit from percutaneous revascularization of the right coronary artery to treat symptoms.
In panels B1 and B2, there is abundant evidence that the hemodynamic assessment of stenosis is superior to a visual estimate in directing PCI.1,2 Hemodynamic assessments including fractional flow reserve (FFR) inform the risk-benefit analysis of percutaneous vs medical treatment of coronary stenosis. In the case of FFR, 0.8 represents an inflection point. The lower FFR values are below 0.8, the greater the benefit of PCI as opposed to medical therapy. Conversely, the greater FFR values are above 0.8, the greater the benefit of medical therapy as opposed to PCI.
However, in panel C, there is significant variability in the data supporting the best treatment strategy for symptomatic patients with CTO.
CORONARY CTO
Coronary CTO is defined as TIMI 0 flow for more than 3 months in an epicardial coronary artery. CTO is not uncommon, seen on 30% of routine coronary angiograms. In the United States, attempt rates of PCI for CTO remain low and have been static at around 12.4%, representing less than 5% of total PCI volume.3 In addition, success rates of CTO PCI are disappointingly low at 59% compared with success rates of patent-vessel PCI at 96%.3 The most frequently cited barriers to CTO PCI are incomplete evidence for efficacy and concerns about safety. Because of the ongoing controversy about the risks and benefits of CTO PCI, it remains a class IIa indication in current American and European practice guidelines.4,5 In addition, these procedures remain technically challenging, and thus variability in local expertise can influence the decision to manage patients medically or refer for CTO PCI.
Patients are often advised that CTO is benign. However, the myocardium affected by a CTO is ischemic. Collateral vessels do not provide adequate flow reserve. FFR data collected from CTOs that were successfully crossed and subsequently interrogated with a pressure wire prior to stenting show that the myocardium supplied by the reconstituted distal bed remains ischemic. This ischemic burden appears to be independent of the size and quality of collaterals.6,7 In addition, a moderate stenosis in a donor coronary artery supplying collateral vessels to a CTO may result in an ischemic FFR as a consequence of coronary “steal” from the donor artery to the collateral vessels. The ischemic FFR in the donor artery can be corrected by treating the recipient CTO vessel.8
Similar to FFR, noninvasive assessment using myocardial perfusion imaging can define ischemic burden and a threshold for benefit of percutaneous vs medical management of CAD. Ischemia greater than 10% on myocardial perfusion imaging is associated with a high risk of major adverse cardiac events (MACE).9 Similar findings were noted in the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy, which showed superior reduction in angina and MACE in patients with greater than 10% ischemia on myocardial perfusion imaging treated with PCI vs medical therapy.10 In the case of coronary CTO, ischemia greater than 12.5% is predictive of significant improvement in symptoms after intervention.11
PROGNOSIS AND DISEASE BURDEN
CTO is associated with adverse prognosis, implying the importance of incomplete revascularization. The Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery (SYNTAX) trial used a scoring system to direct surgical vs percutaneous revascularization strategies in patients with complex or multivessel CAD. A post hoc analysis of the SYNTAX trial showed that incomplete revascularization was associated with significantly higher rates of 4-year mortality and MACE.12 This was likely from the ischemic burden remaining from incomplete revascularization. The presence of CTO was the strongest independent predictor of incomplete revascularization in the SYNTAX PCI arm. Similarly, the negative prognostic impact of having a CTO has been observed in a large population of patients followed prospectively after undergoing coronary angiography.13 Furthermore, the presence of CTO in a non-infarct-related artery at the time of ST-elevation myocardial infarction appears to be an independent predictor of death at 30 days, with a persistent negative prognostic impact lasting for up to 36 months of follow-up.14
CLINICAL BENEFITS OF CTO PCI
In patients with significant ischemic burden, CTO PCI has multiple clinical benefits. Symptomatic relief based on the Seattle Angina Questionnaire appears to be similar to that obtained with coronary artery bypass grafting (CABG) at 1-month follow up.15 Successful CTO PCI can have a positive impact on the risk of mortality in prospective13 and retrospective observational studies.16
CTO intervention may also have beneficial effects on left ventricular systolic function in patients with viable myocardium in the corresponding coronary territory.17 This improvement in systolic function appears to be sustained at 3 years of follow-up.18 Meta-analysis of observational data in symptomatic and ischemic patients who underwent successful CTO PCI shows reduced rates of all-cause mortality and MACE and a reduced need for subsequent CABG.19 This is in contrast to the frequently cited Occluded Artery Trial (OAT) trial, which showed no clinical benefit of PCI for a subacutely occluded infarct-related artery.20
EVIDENCE-BASED BENEFITS
Evidence of the merits of CTO PCI from randomized clinical trials is mixed. The only published study to date, the Evaluating Xience and Left Ventricular Function in Percutaneous Coronary Intervention on Occlusions After ST-Segment Elevation (EXPLORE) trial, showed no difference in left ventricular systolic function 4 months after ST-elevation myocardial infarction in patients undergoing staged CTO PCI of a non-infarct-related artery vs optimal medical therapy.21 Two larger trials presented at scientific meetings in 2017 remain unpublished. One trial showed noninferiority of optimal medical therapy vs successful CTO PCI in reducing the composite end point of all-cause mortality, myocardial infarction, stroke, and repeat revascularization; the other trial showed significant improvement in quality of life measures using the Seattle Angina Questionnaire score and Canadian Cardiovascular Society angina classification in patients who underwent successful CTO PCI compared with medical management.
High-volume CTO PCI centers now report procedural success rates as high as 92.9%22 and a correlation between the CTO PCI volume and CTO PCI success rates.3 The dramatic improvement in success rates achieved by high-volume operators globally can be attributed to a combination of operator experience, improved technology, and widespread adoption of the hybrid algorithm, which has helped to improve efficiency and standardize treatment in CTO PCI based on angiographic criteria.23 CTO PCI remains a highly specialized procedure, unique from patent-vessel PCI and with little correlation between total PCI volume and CTO PCI success rate. Despite recent advances, CTO PCI success remains heavily dependent on operator expertises, with a steep and long learning curve. In addition, the unique technical aspects of CTO PCI such as a retrograde and subintimal guidewire tracking that have accelerated procedural success are associated with higher rates of MACE compared with traditional antegrade and intraluminal guidewire tracking.24,25 Therefore, CTO PCI requires unique considerations beyond standard PCI in terms of potential complications. Uncommon but potentially life-threatening complications such as donor artery thrombosis, collateral vessel trauma, gear entrapment, and radiation skin injury demand a specialized informed consent process for the patient.26
In light of incomplete evidence based on extensive observational data and limited randomized clinical trials, the decision to refer patients for CTO PCI requires a comprehensive clinical evaluation. We know from data derived from patients with patent but stenotic coronary arteries that physiologically rather than angiographically driven decisions to revascularize can produce superior clinical results. There is an ischemic burden threshold beyond which revascularization is superior to optimal medical therapy. In this context, we know that CTO is not benign and is associated with ischemic burden. Consequently, patients with symptoms related to CTO represent a subset of patients with incomplete revascularization.
CONCLUSION
Despite recent advances, CTO PCI procedures remain technically demanding, and success with a low complication rate is heavily dependent on operator expertise. Therefore, CTO PCI should be used judiciously in patients with angina refractory to optimal medical therapy. It is an important tool to be used in conjunction with non-CTO PCI, CABG, and optimal medical therapy to produce favorable outcomes in patients with CAD.
In patients with stable coronary artery disease (CAD), the cornerstone of treatment is medical management to control symptoms such as angina and dyspnea on exertion. But in a select group of patients, percutaneous coronary intervention (PCI) is indicated in addition to medical management. Invasive and noninvasive hemodynamic assessments of coronary artery stenosis in conjunction with anatomic considerations play a role in decision-making and in advising patients on revascularization vs medical management. However, in the case of coronary artery chronic total occlusion (CTO), the decision-making process remains challenging due to limited evidence supporting clinical efficacy of CTO PCI, as well as practical considerations including lower success rates and higher complication rates in comparison with patent-vessel PCI.
CLINICAL VIGNETTE
A 42-year-old man, an avid runner with hyperlipidemia and a strong family history of premature CAD, presents with several months of declining exercise tolerance. His physical examination and electrocardiogram are unremarkable. Myocardial perfusion imaging shows stress-induced ischemia affecting about 20% of the inferolateral myocardium. He is then referred for coronary angiography.
- Panel A: Discrete, high-grade stenosis of the mid-right coronary artery
- Panel B: Diffuse, multivessel disease involving the distal right coronary artery (B1) and the proximal left circumflex coronary artery (B2)
- Panel C: Total occlusion of the proximal right coronary artery with extensive left-to-right collaterals.
Treatment based on angiographic findings
In panel A, there is little to debate. The patient is likely to benefit from percutaneous revascularization of the right coronary artery to treat symptoms.
In panels B1 and B2, there is abundant evidence that the hemodynamic assessment of stenosis is superior to a visual estimate in directing PCI.1,2 Hemodynamic assessments including fractional flow reserve (FFR) inform the risk-benefit analysis of percutaneous vs medical treatment of coronary stenosis. In the case of FFR, 0.8 represents an inflection point. The lower FFR values are below 0.8, the greater the benefit of PCI as opposed to medical therapy. Conversely, the greater FFR values are above 0.8, the greater the benefit of medical therapy as opposed to PCI.
However, in panel C, there is significant variability in the data supporting the best treatment strategy for symptomatic patients with CTO.
CORONARY CTO
Coronary CTO is defined as TIMI 0 flow for more than 3 months in an epicardial coronary artery. CTO is not uncommon, seen on 30% of routine coronary angiograms. In the United States, attempt rates of PCI for CTO remain low and have been static at around 12.4%, representing less than 5% of total PCI volume.3 In addition, success rates of CTO PCI are disappointingly low at 59% compared with success rates of patent-vessel PCI at 96%.3 The most frequently cited barriers to CTO PCI are incomplete evidence for efficacy and concerns about safety. Because of the ongoing controversy about the risks and benefits of CTO PCI, it remains a class IIa indication in current American and European practice guidelines.4,5 In addition, these procedures remain technically challenging, and thus variability in local expertise can influence the decision to manage patients medically or refer for CTO PCI.
Patients are often advised that CTO is benign. However, the myocardium affected by a CTO is ischemic. Collateral vessels do not provide adequate flow reserve. FFR data collected from CTOs that were successfully crossed and subsequently interrogated with a pressure wire prior to stenting show that the myocardium supplied by the reconstituted distal bed remains ischemic. This ischemic burden appears to be independent of the size and quality of collaterals.6,7 In addition, a moderate stenosis in a donor coronary artery supplying collateral vessels to a CTO may result in an ischemic FFR as a consequence of coronary “steal” from the donor artery to the collateral vessels. The ischemic FFR in the donor artery can be corrected by treating the recipient CTO vessel.8
Similar to FFR, noninvasive assessment using myocardial perfusion imaging can define ischemic burden and a threshold for benefit of percutaneous vs medical management of CAD. Ischemia greater than 10% on myocardial perfusion imaging is associated with a high risk of major adverse cardiac events (MACE).9 Similar findings were noted in the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy, which showed superior reduction in angina and MACE in patients with greater than 10% ischemia on myocardial perfusion imaging treated with PCI vs medical therapy.10 In the case of coronary CTO, ischemia greater than 12.5% is predictive of significant improvement in symptoms after intervention.11
PROGNOSIS AND DISEASE BURDEN
CTO is associated with adverse prognosis, implying the importance of incomplete revascularization. The Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery (SYNTAX) trial used a scoring system to direct surgical vs percutaneous revascularization strategies in patients with complex or multivessel CAD. A post hoc analysis of the SYNTAX trial showed that incomplete revascularization was associated with significantly higher rates of 4-year mortality and MACE.12 This was likely from the ischemic burden remaining from incomplete revascularization. The presence of CTO was the strongest independent predictor of incomplete revascularization in the SYNTAX PCI arm. Similarly, the negative prognostic impact of having a CTO has been observed in a large population of patients followed prospectively after undergoing coronary angiography.13 Furthermore, the presence of CTO in a non-infarct-related artery at the time of ST-elevation myocardial infarction appears to be an independent predictor of death at 30 days, with a persistent negative prognostic impact lasting for up to 36 months of follow-up.14
CLINICAL BENEFITS OF CTO PCI
In patients with significant ischemic burden, CTO PCI has multiple clinical benefits. Symptomatic relief based on the Seattle Angina Questionnaire appears to be similar to that obtained with coronary artery bypass grafting (CABG) at 1-month follow up.15 Successful CTO PCI can have a positive impact on the risk of mortality in prospective13 and retrospective observational studies.16
CTO intervention may also have beneficial effects on left ventricular systolic function in patients with viable myocardium in the corresponding coronary territory.17 This improvement in systolic function appears to be sustained at 3 years of follow-up.18 Meta-analysis of observational data in symptomatic and ischemic patients who underwent successful CTO PCI shows reduced rates of all-cause mortality and MACE and a reduced need for subsequent CABG.19 This is in contrast to the frequently cited Occluded Artery Trial (OAT) trial, which showed no clinical benefit of PCI for a subacutely occluded infarct-related artery.20
EVIDENCE-BASED BENEFITS
Evidence of the merits of CTO PCI from randomized clinical trials is mixed. The only published study to date, the Evaluating Xience and Left Ventricular Function in Percutaneous Coronary Intervention on Occlusions After ST-Segment Elevation (EXPLORE) trial, showed no difference in left ventricular systolic function 4 months after ST-elevation myocardial infarction in patients undergoing staged CTO PCI of a non-infarct-related artery vs optimal medical therapy.21 Two larger trials presented at scientific meetings in 2017 remain unpublished. One trial showed noninferiority of optimal medical therapy vs successful CTO PCI in reducing the composite end point of all-cause mortality, myocardial infarction, stroke, and repeat revascularization; the other trial showed significant improvement in quality of life measures using the Seattle Angina Questionnaire score and Canadian Cardiovascular Society angina classification in patients who underwent successful CTO PCI compared with medical management.
High-volume CTO PCI centers now report procedural success rates as high as 92.9%22 and a correlation between the CTO PCI volume and CTO PCI success rates.3 The dramatic improvement in success rates achieved by high-volume operators globally can be attributed to a combination of operator experience, improved technology, and widespread adoption of the hybrid algorithm, which has helped to improve efficiency and standardize treatment in CTO PCI based on angiographic criteria.23 CTO PCI remains a highly specialized procedure, unique from patent-vessel PCI and with little correlation between total PCI volume and CTO PCI success rate. Despite recent advances, CTO PCI success remains heavily dependent on operator expertises, with a steep and long learning curve. In addition, the unique technical aspects of CTO PCI such as a retrograde and subintimal guidewire tracking that have accelerated procedural success are associated with higher rates of MACE compared with traditional antegrade and intraluminal guidewire tracking.24,25 Therefore, CTO PCI requires unique considerations beyond standard PCI in terms of potential complications. Uncommon but potentially life-threatening complications such as donor artery thrombosis, collateral vessel trauma, gear entrapment, and radiation skin injury demand a specialized informed consent process for the patient.26
In light of incomplete evidence based on extensive observational data and limited randomized clinical trials, the decision to refer patients for CTO PCI requires a comprehensive clinical evaluation. We know from data derived from patients with patent but stenotic coronary arteries that physiologically rather than angiographically driven decisions to revascularize can produce superior clinical results. There is an ischemic burden threshold beyond which revascularization is superior to optimal medical therapy. In this context, we know that CTO is not benign and is associated with ischemic burden. Consequently, patients with symptoms related to CTO represent a subset of patients with incomplete revascularization.
CONCLUSION
Despite recent advances, CTO PCI procedures remain technically demanding, and success with a low complication rate is heavily dependent on operator expertise. Therefore, CTO PCI should be used judiciously in patients with angina refractory to optimal medical therapy. It is an important tool to be used in conjunction with non-CTO PCI, CABG, and optimal medical therapy to produce favorable outcomes in patients with CAD.
- De Bruyne B, Pijls NHJ, Kalesan B, et al; FAME 2 Trial Investigators. Fractional flow reserve–guided PCI versus medical therapy in stable coronary disease. N Engl J Med 2012; 367:991–1001.
- Tonino PAL, De Bruyne B, Pijls NHJ, et al; FAME Study Investigators. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009; 360:213–224.
- Brilakis ES, Banerjee S, Karmpaliotis D, et al. Procedural outcomes of chronic total occlusion percutaneous coronary intervention: a report from the NCDR (National Cardiovascular Data Registry). JACC Cardiovasc Interv 2015; 8:245–253.
- Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol 2011; 58:e44–e122.
- Author/Task Force members; Windeker S, Kolh P, Alfonso R, et al. 2014 ESC/EACTS guidelines on myocardial revascularization: the task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 2014; 35:2541–2619.
- Sachdeva R, Agrawal M, Flynn SE, Werner GS, Uretsky BF. The myocardium supplied by a chronic total occlusion is a persistently ischemic zone. Catheter Cardiovasc Interv 2014; 83:9–16.
- Werner GS, Surber R, Ferrari M, Fritzenwanger M, Figulla HR. The functional reserve of collaterals supplying long-term chronic total coronary occlusions in patients without prior myocardial infarction. Eur Heart J 2006; 27:2406–2412.
- Sachdeva R, Agrawal M, Flynn SE, Werner GS, Uretsky BF. Reversal of ischemia of donor artery myocardium after recanalization of a chronic total occlusion. Catheter Cardiovasc Interv 2013; 82:E453–E458.
- Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation 2003; 107:2900–2907.
- Shaw LJ, Berman DS, Maron DJ, et al; COURAGE Investigators. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation 2008; 117:1283–1291.
- Safley DM, Koshy S, Grantham JA, et al. Changes in myocardial ischemic burden following percutaneous coronary intervention of chronic total occlusions. Catheter Cardiovasc Interv 2011; 78:337–343.
- Farooq V, Serruys PW, Garcia-Garcia HM, et al. The negative impact of incomplete angiographic revascularization on clinical outcomes and its association with total occlusions: the SYNTAX (Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) trial. J Am Coll Cardiol 2013; 61:282–294.
- Råmunddal T, Hoebers LP, Henriques JP, et al. Prognostic impact of chronic total occlusions: a report from SCAAR (Swedish Coronary Angiography and Angioplasty Registry). JACC Cardiovasc Interv 2016; 9:1535–1544.
- Claessen BE, Dangas GD, Weisz G, et al. Prognostic impact of a chronic total occlusion in a non-infarct-related artery in patients with ST-segment elevation myocardial infarction: 3-year results from the HORIZONS-AMI trial. Eur Heart J 2012; 33:768–775.
- Grantham JA, Jones PG, Cannon L, Spertus JA. Quantifying the early health status benefits of successful chronic total occlusion recanalization: Results from the FlowCardia’s Approach to Chronic Total Occlusion Recanalization (FACTOR) Trial. Circ Cardiovasc Qual Outcomes 2010; 3:284–290.
- Yang ZK, Zhang RY, Hu J, Zhang Q, Ding FH, Shen WF. Impact of successful staged revascularization of a chronic total occlusion in the non-infarct-related artery on long-term outcome in patients with acute ST-segment elevation myocardial infarction. Int J Cardiol 2013; 165:76–79.
- Baks T, van Geuns R-J, Duncker DJ, et al. Prediction of left ventricular function after drug-eluting stent implantation for chronic total coronary occlusions. J Am Coll Cardiol 2006; 47:721–725.
- Kirschbaum SW, Baks T, van den Ent M, et al. Evaluation of left ventricular function three years after percutaneous recanalization of chronic total coronary occlusions. Am J Cardiol 2008; 101:179–185.
- Khan MF, Wendel CS, Thai HM, Movahed MR. Effects of percutaneous revascularization of chronic total occlusions on clinical outcomes: a meta-analysis comparing successful versus failed percutaneous intervention for chronic total occlusion. Catheter Cardiovasc Interv 2013; 82:95–107.
- Hochman JS, Lamas GA, Buller CE, et al; Occluded Artery Trial Investigators. Coronary intervention for persistent occlusion after myocardial infarction. N Engl J Med 2006; 355:2395–2407.
- Henriques JP, Hoebers LP, Råmunddal T, et al; EXPLORE Trial Investigators. Percutaneous intervention for concurrent chronic total occlusions in patients with STEMI: The EXPLORE trial. J Am Coll Cardiol 2016; 68:1622–1632.
- Christopoulos G, Kandzari DE, Yeh RW, et al. Development and validation of a novel scoring system for predicting technical success of chronic total occlusion percutaneous coronary interventions: The PROGRESS CTO (Prospective Global Registry for the Study of Chronic Total Occlusion Intervention) score. JACC Cardiovasc Interv 2016; 9:1–9.
- Brilakis ES, Grantham JA, Rinfret S, et al. A percutaneous treatment algorithm for crossing coronary chronic total occlusions. JACC Cardiovasc Interv 2012; 5:367–379.
- Karmpaliotis D, Karatasakis A, Alaswad K, et al. Outcomes with the use of the retrograde approach for coronary chronic total occlusion interventions in a contemporary multicenter US registry. Circ Cardiovasc Interv 2016; 9. pii: e003434. doi:10.1161/CIRCINTERVENTIONS.115.003434.
- Song L, Maehara A, Finn MT, et al. Intravascular ultrasound analysis of intraplaque versus subintimal tracking in percutaneous intervention for coronary chronic total occlusions and association with procedural outcomes. JACC Cardiovasc Interv 2017; 10:1011–1021.
- Patel VG, Brayton KM, Tamayo A, et al. Angiographic success and procedural complications in patients undergoing percutaneous coronary chronic total occlusion interventions: a weighted meta-analysis of 18,061 patients from 65 studies. JACC Cardiovasc Interv 2013; 6:128–136.
- De Bruyne B, Pijls NHJ, Kalesan B, et al; FAME 2 Trial Investigators. Fractional flow reserve–guided PCI versus medical therapy in stable coronary disease. N Engl J Med 2012; 367:991–1001.
- Tonino PAL, De Bruyne B, Pijls NHJ, et al; FAME Study Investigators. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009; 360:213–224.
- Brilakis ES, Banerjee S, Karmpaliotis D, et al. Procedural outcomes of chronic total occlusion percutaneous coronary intervention: a report from the NCDR (National Cardiovascular Data Registry). JACC Cardiovasc Interv 2015; 8:245–253.
- Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol 2011; 58:e44–e122.
- Author/Task Force members; Windeker S, Kolh P, Alfonso R, et al. 2014 ESC/EACTS guidelines on myocardial revascularization: the task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 2014; 35:2541–2619.
- Sachdeva R, Agrawal M, Flynn SE, Werner GS, Uretsky BF. The myocardium supplied by a chronic total occlusion is a persistently ischemic zone. Catheter Cardiovasc Interv 2014; 83:9–16.
- Werner GS, Surber R, Ferrari M, Fritzenwanger M, Figulla HR. The functional reserve of collaterals supplying long-term chronic total coronary occlusions in patients without prior myocardial infarction. Eur Heart J 2006; 27:2406–2412.
- Sachdeva R, Agrawal M, Flynn SE, Werner GS, Uretsky BF. Reversal of ischemia of donor artery myocardium after recanalization of a chronic total occlusion. Catheter Cardiovasc Interv 2013; 82:E453–E458.
- Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation 2003; 107:2900–2907.
- Shaw LJ, Berman DS, Maron DJ, et al; COURAGE Investigators. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation 2008; 117:1283–1291.
- Safley DM, Koshy S, Grantham JA, et al. Changes in myocardial ischemic burden following percutaneous coronary intervention of chronic total occlusions. Catheter Cardiovasc Interv 2011; 78:337–343.
- Farooq V, Serruys PW, Garcia-Garcia HM, et al. The negative impact of incomplete angiographic revascularization on clinical outcomes and its association with total occlusions: the SYNTAX (Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) trial. J Am Coll Cardiol 2013; 61:282–294.
- Råmunddal T, Hoebers LP, Henriques JP, et al. Prognostic impact of chronic total occlusions: a report from SCAAR (Swedish Coronary Angiography and Angioplasty Registry). JACC Cardiovasc Interv 2016; 9:1535–1544.
- Claessen BE, Dangas GD, Weisz G, et al. Prognostic impact of a chronic total occlusion in a non-infarct-related artery in patients with ST-segment elevation myocardial infarction: 3-year results from the HORIZONS-AMI trial. Eur Heart J 2012; 33:768–775.
- Grantham JA, Jones PG, Cannon L, Spertus JA. Quantifying the early health status benefits of successful chronic total occlusion recanalization: Results from the FlowCardia’s Approach to Chronic Total Occlusion Recanalization (FACTOR) Trial. Circ Cardiovasc Qual Outcomes 2010; 3:284–290.
- Yang ZK, Zhang RY, Hu J, Zhang Q, Ding FH, Shen WF. Impact of successful staged revascularization of a chronic total occlusion in the non-infarct-related artery on long-term outcome in patients with acute ST-segment elevation myocardial infarction. Int J Cardiol 2013; 165:76–79.
- Baks T, van Geuns R-J, Duncker DJ, et al. Prediction of left ventricular function after drug-eluting stent implantation for chronic total coronary occlusions. J Am Coll Cardiol 2006; 47:721–725.
- Kirschbaum SW, Baks T, van den Ent M, et al. Evaluation of left ventricular function three years after percutaneous recanalization of chronic total coronary occlusions. Am J Cardiol 2008; 101:179–185.
- Khan MF, Wendel CS, Thai HM, Movahed MR. Effects of percutaneous revascularization of chronic total occlusions on clinical outcomes: a meta-analysis comparing successful versus failed percutaneous intervention for chronic total occlusion. Catheter Cardiovasc Interv 2013; 82:95–107.
- Hochman JS, Lamas GA, Buller CE, et al; Occluded Artery Trial Investigators. Coronary intervention for persistent occlusion after myocardial infarction. N Engl J Med 2006; 355:2395–2407.
- Henriques JP, Hoebers LP, Råmunddal T, et al; EXPLORE Trial Investigators. Percutaneous intervention for concurrent chronic total occlusions in patients with STEMI: The EXPLORE trial. J Am Coll Cardiol 2016; 68:1622–1632.
- Christopoulos G, Kandzari DE, Yeh RW, et al. Development and validation of a novel scoring system for predicting technical success of chronic total occlusion percutaneous coronary interventions: The PROGRESS CTO (Prospective Global Registry for the Study of Chronic Total Occlusion Intervention) score. JACC Cardiovasc Interv 2016; 9:1–9.
- Brilakis ES, Grantham JA, Rinfret S, et al. A percutaneous treatment algorithm for crossing coronary chronic total occlusions. JACC Cardiovasc Interv 2012; 5:367–379.
- Karmpaliotis D, Karatasakis A, Alaswad K, et al. Outcomes with the use of the retrograde approach for coronary chronic total occlusion interventions in a contemporary multicenter US registry. Circ Cardiovasc Interv 2016; 9. pii: e003434. doi:10.1161/CIRCINTERVENTIONS.115.003434.
- Song L, Maehara A, Finn MT, et al. Intravascular ultrasound analysis of intraplaque versus subintimal tracking in percutaneous intervention for coronary chronic total occlusions and association with procedural outcomes. JACC Cardiovasc Interv 2017; 10:1011–1021.
- Patel VG, Brayton KM, Tamayo A, et al. Angiographic success and procedural complications in patients undergoing percutaneous coronary chronic total occlusion interventions: a weighted meta-analysis of 18,061 patients from 65 studies. JACC Cardiovasc Interv 2013; 6:128–136.
KEY POINTS
- Coronary CTO is not benign and is associated with ischemic burden.
- There is a threshold of ischemic burden at which revascularization is superior to optimal medical therapy.
- Revascularization based on physiology rather than angiography can produce superior clinical results.
- CTO PCI procedures are technically demanding and heavily operator-dependent in order to achieve high success rates at an acceptably low complication rate.
Update on the management of venous thromboembolism
Venous thromboembolism (VTE) includes both deep vein thrombosis (DVT) and pulmonary embolism (PE). Although the exact incidence of VTE is unknown, an estimated 1 million people in the United States are affected each year, with about a third experiencing a recurrence within 10 years.1 VTE affects hospitalized and nonhospitalized patients, is often overlooked, and results in long-term complications including postthrombotic syndrome (PTS) for DVT, postpulmonary embolism syndrome and chronic thromboembolic pulmonary hypertension for PE, and death.2
TREATMENT
Treatment for VTE should be initiated in the following cases:
- Proximal DVT of the lower extremity
- Symptomatic distal (calf vein) DVT
- Symptomatic upper extremity DVT (axillary-subclavian veins)
- PE
- Subsegmental PE in a patient at risk for recurrence
- Surveillance for subsegmental PE in a patient with no proximal DVT and a low risk of recurrence.
In addition to anticoagulants, other more aggressive therapies for VTE may be appropriate, such as systemic thrombolysis in the case of PE or catheter-directed thrombolytic or pharmacomechnical therapies for DVT or PE, surgical intervention (acute pulmonary embolectomy), or placement of an inferior vena cava (IVC) filter.
This article reviews the management of VTE, highlighting the recent changes in treatment and prevention guidelines from the American College of Chest Physicians (ACCP).3
Risk of bleeding
In assessing a patient’s risk of bleeding for anticoagulation therapy (Table 1), the absence of risk factors is considered low risk for bleeding, the presence of 1 risk factor is considered intermediate risk, and 2 or more risk factors is considered high risk. Compared with low-risk patients, moderate-risk patients have a twofold increased risk of major bleeding and high-risk patients have an eightfold increased risk of major bleeding. This equates to an annualized risk of major bleeding of 0.8% for low-risk patients, 1.6% for moderate-risk patients, and greater than 6.5% for high-risk patients.3
Anticoagulants
Deciding on which anticoagulant to use depends on the indication, the patient’s underlying condition, the patient’s preference, and the patient’s risk of bleeding. Heparin, the LMWHs, fondaparinux and the DOACs (rivaroxaban and apixaban) are the only agents approved by the US Food and Drug Administration (FDA) recommended for the acute treatment phase, while the DOACs and warfarin are anticoagulation options for the long-term and extended treatment phases. The LMWHs should be used for the patient with cancer and during pregnancy.
Unfractionated heparin. UFH is administered parenterally and can be used for the prevention and treatment of VTE. Heparin remains an option for initial treatment of patients with acute VTE and is generally preferred over LMWH for patients who may require advanced therapies, such as for hemodynamically unstable PE or iliofemoral DVT. It is also recommended for patients with renal failure.3 Weight-based dosing (80 U/kg bolus followed by 18 U/kg/hour intravenous infusion) is recommended, targeting an antifactor activated clotting factor (anti-Xa) assay level of 0.3 IU/mL to 0.7 IU/mL. Heparin may also be given subcutaneously in an outpatient setting using an initial bolus of 333 U/kg followed by a subcutaneous dose of 17,500 U twice daily.5
Low-molecular-weight heparin. LMWHs are administered as weight-based subcutaneous injections and have indications for patients with acute VTE and for VTE prophylaxis. LMWHs are used for transitioning to warfarin, dabigatran, or edoxaban for long-term anticoagulation and are recommended over warfarin and DOACs for treatment of VTE in patients with cancer and in pregnant women.3
Enoxaparin (Lovenox), the most commonly used agent in the United States, is given either as a once-daily injection (1.5 mg/kg/day) or a twice-daily injection (1 mg/kg every 12 hours). It is also approved for VTE prophylaxis in patients undergoing hip or knee replacement surgery or abdominal surgery, or in patients with severely restricted mobility during acute illness. LMWH can also be given in patients with renal insufficiency (creatinine clearance [CrCL] < 30 mL/minute) after dose adjustment. No monitoring is required, although it is advised in pediatric patients, pregnant women, obese patients, and patients with renal insufficiency. If monitoring is required, an anti-Xa assay using LMWH as a reference standard should be done 4 hours after subcutaneous injection. The therapeutic range for enoxaparin is 0.5 IU/mL to 1.0 IU/mL for the 12-hour regimen and greater than 1.0 IU/mL for the once-daily dose. Other LMWHs available in the United States include dalteparin (Fragmin) and tinzaparin (Innohep). Each has its own specific indications.
Fondaparinux. Fondaparinux is an indirect factor Xa inhibitor, chemically related to LMWH. It is approved for treatment of patients with acute VTE when used in combination with a VKA (warfarin) or dabigatran or edoxaban. It also has approval for VTE prophylaxis in patients undergoing hip fracture, hip or knee replacement, and abdominal surgery. Fondaparinux is administered as a once-daily subcutaneous injection of 2.5 mg for DVT prophylaxis and a body weight-based dose for the treatment of VTE (5 mg < 50 kg; 7.5 mg 50 to 100 kg; 10 mg > 100 kg).6 Fondaparinux is contraindicated in patients with severe renal impairment (CrCL les 30 mL/min) and bacterial endocarditis.6
Warfarin. Warfarin, a VKA, was the mainstay of therapy for long-term and extended treatment of VTE until the advent of the DOACs. Warfarin must be coadministered with heparin, LMWH, or fondaparinux initially and continued as overlap therapy for a minimum of 5 days until the international normalized ratio [INR] is at least 2.0 for 24 hours.4 Early initiation of a VKA on the first day of parenteral therapy is advised.
Warfarin remains the best option for patients on long-term or extended anticoagulation with liver dysfunction (elevated serum transaminases exceeding twice the upper limits of normal or active liver disease) or renal disease (CrCL < 30 mL/min), as well as patients unable to afford DOACs. Additionally, select patient populations may still be best served by warfarin as these groups were underrepresented or not included in DOAC trials, including pediatric patients, individuals with body weight less than 50 kg or greater than 150 kg, and patients with select types of thrombophilia (eg, antiphospholipid syndrome). Warfarin is also advised for patients with poor compliance, as international normalized ratio of prothrombin time (PT/INR) monitoring is required using a point-of-care testing device or during a visit to an anticoagulation clinic. DOACs do not require monitoring, and noncompliance will not be readily apparent.
Direct oral anticoagulants. The DOACs, which include the factor Xa inhibitors rivaroxaban (Xarelto), apixaban (Eliquis), and edoxaban (Savaysa) and the direct thrombin inhibitor dabigatran (Pradaxa), been studied extensively and shown to be noninferior to VKAs for treatment of VTE.7 DOACs are currently recommended by the ACCP for long-term treatment of VTE, and several have extended treatment recommendations for VTE over the VKAs.3
The advantages of DOACs include no need for PT/INR monitoring, a fixed dosage, shorter half-life, rapid onset of action (for monotherapy), and in most cases, no need for bridging for interventional or surgical procedures. Additional advantages may include a decreased burden of care for the physician and improved quality of life for the patient. DOACs are also the agents of choice for patients who prefer oral therapy (avoiding parenteral therapy), have limited access to an anticoagulation clinic (home bound or geographic inaccessibility for PT/INR monitoring), or have food or drug-drug interactions. Patients at risk of gastrointestinal bleeding or dyspepsia should avoid dabigatran, while apixaban may be preferred if there is a history of gastrointestinal bleeding.8
Rivaroxaban or apixaban can be used as monotherapy for the initial treatment of VTE, while a 5-day course of heparin, LMWH, or fondaparinux is necessary with dabigatran or edoxaban. Rivaroxaban has been approved by the FDA for use in the prevention and treatment of VTE.9,10 For VTE prophylaxis, rivaroxaban is given orally at 10 mg once daily for 35 days for patients undergoing total hip replacement surgery and for 12 days for patients undergoing knee replacement surgery. For the treatment of VTE, rivaroxaban is given orally at 15 mg twice a day for the initial 21 days of treatment, followed by once daily at 20 mg per day for long-term treatment. It is also approved for extended-duration therapy in both 10-mg and 20-mg doses. In a recently published randomized double-blind trial of rivaroxaban compared with aspirin, the risk of a recurrent event was lower with either dose of rivaroxaban compared with aspirin without an increase in bleeding.11 Rivaroxaban is contraindicated in patients with renal insufficiency (CrCL < 30 mL/min). Both the 15-mg and 20-mg tablets must be taken with food.
Apixaban is also approved for monotherapy of VTE and was found to be noninferior to standard therapy of LMWH and warfarin with less bleeding.12 Apixaban is used for VTE prophylaxis in patients undergoing hip or knee replacement surgery, given at 2.5 mg twice daily beginning 12 to 24 hours postoperatively for 35 days (hip) or 12 days (knee). The acute-phase dosage is 10 mg twice daily for 7 days followed by 5 mg twice daily for long-term treatment of VTE. The recommended dose should be reduced to 2.5 mg twice daily in patients that meet 2 of the following criteria: age 80 or older; body weight of 60 kg or less; or with a serum creatinine 1.5 mg/dL or greater. Apixaban is also approved for extended treatment of VTE. In a randomized, double-blind study of 2 doses (2.5 mg and 5 mg, twice daily) of apixaban compared with placebo, apixaban reduced the risk of recurrent VTE without increasing the risk of bleeding.13
Both dabigatran and edoxaban require an initial 5-day overlap with a parenteral anticoagulant.14,15 Dabigatran is given at 150 mg orally twice daily if the CrCL is greater than 30 mL/min for the long-term treatment of VTE. Edoxaban is given orally at 60 mg once daily but reduced to 30 mg once daily if the CrCL is 30 mL/min to 50 mL/min, if body weight is 60 kg or less, or with use of certain P-glycoprotein inhibitors. Dabigatran has been evaluated in 2 double-blind, randomized controlled trials comparing the extended use of dabigatran with warfarin or placebo in patients with VTE.16 Dabigatran carried a lower risk of major or clinically relevant bleeding than warfarin but a higher risk than placebo. Dabigatran was noninferior to warfarin but significantly reduced the rate of recurrence in the placebo group.16
The major side effect observed with all DOACs is bleeding, but they have been proven safer particularly in the terms of major bleeding compared with the standard heparin-LMWH-VKA regimen for treatment of VTE.17–19 The risk of major bleeding, and in particular intracranial bleeding, has been shown to be less with DOACs compared with VKAs in 2 meta-analysis trials.17,18 Of the 4 new DOACs, only dabigatran currently has an anticoagulant-reversing agent (idarucizumab), although an antidote for the other 3 agents is awaiting FDA approval.20
Subsegmental pulmonary embolism
There is debate as to the need for treatment of patients with subsegmental PE. The most recent guidelines advise clinical surveillance over anticoagulation for patients with a low risk for recurrent VTE and no evidence for a proximal DVT.3 However, individuals who are hospitalized, have reduced mobility, have active cancer or are being treated with chemotherapy, or have a low cardiopulmonary reserve should be considered for anticoagulation unless they have a high bleeding risk.
Thrombolytic therapy
Thrombolytic therapy may be beneficial in select patients with VTE and can be delivered systemically or locally per catheter-directed therapy (CDT). Both routes carry an increased risk of hemorrhage compared with standard anticoagulation. The Catheter-Directed-Venous Thrombolysis (CaVenT) trial and Thrombus Obliteration by Rapid Percutaneous Endovenous Intervention in Deep Venous Occlusion (TORPEDO) trial compared CDT with standard therapy.21,22 In CaVEnT, CDT resulted in increased clinical benefit during the 5-year follow-up but did not result in improved quality of life.21 In the TORPEDO trial, patients with proximal DVT receiving percutaneous endovenous intervention and anticoagulation compared with anticoagulation alone demonstrated superiority in the reduction of PTS at greater than 2 years.22 Early results of the Acute Venous Thrombosis: Thrombus Removal With Adjunctive Catheter-directed Thrombolysis (ATTRACT) trial show that most patients with DVT did not have a long-term benefit from CDT, buy they did have reduced leg pain and swelling and some had reduced risk of moderate-to-severe PTS.23
The 2012 and 2016 ACCP guidelines advise anticoagulant therapy over CDT for patients with acute DVT of the leg but suggest patients who may benefit are those with iliofemoral DVT with symptoms for less than 14 days, good functional status, a life expectancy greater than 1 year, and a low risk of bleeding.3,4 This is in contrast to the 2008 CHEST guidelines that recommended patients who have extensive proximal DVT, who have a high risk of limb gangrene, who are at low risk of bleeding, and who otherwise have good functional status be given CDT if the expertise and resources are available.24 It has been suggested that CDT promotes early recanalization and minimizes the incidence of PTS.
Thrombolytic therapy for acute PE remains controversial because there is no clearly established short-term mortality benefit. In the Pulmonary Embolism Thrombolysis (PEITHO) trial, thrombolysis prevented hemodynamic decompensation but increased the risk of major hemorrhage and stroke.25 A lower dose (50 mg) of thrombolytic therapy was studied in the Moderate Pulmonary Embolism Treated With Thrombolysis (MOPPET) trial and was found to be safe and effective in the treatment of moderate PE.26
CDT has also been shown to be effective in the treatment of PE. The Ultrasound Acceleration Thrombolysis of Pulmonary Embolism (ULTIMA) trial demonstrated that catheter-directed thrombolysis with ultrasonographic guidance in patients with acute intermediate-risk PE was superior in reversing right ventricular dilatation without an increase in bleeding complications compared with UFH.27 The Ultrasound-Facilitated, Catheter-Directed, Low-Dose Fibrinolysis for Acute Massive and Submassive Pulmonary Embolism (SEATTLE II) study found that this approach decreased right ventricular dilation, decreased pulmonary hypertension, decreased anatomic burden, and minimized the risk of intracranial hemorrhage in patients with massive and submassive PE.28
Alteplase (Activase) is a recombinant tissue-type plasminogen activator approved by the FDA for treatment of acute PE. Alteplase is administered as a 100-mg infusion over 2 hours. Because of favorable outcomes with prompt recognition and anticoagulation for PE, the ACCP guidelines recommend systemic thrombolysis for hemodynamically unstable patients (systolic blood pressure < 90 mm Hg) with acute PE and a low risk of bleeding using a peripheral vein.3 These guidelines also recommend thrombolysis for the patient whose condition deteriorates after starting anticoagulant therapy but who have yet to develop hypotension.
If the appropriate expertise is available, CDT is suggested for patients with acute PE if they have hypotension and a high bleeding risk, have failed systemic thrombolysis, or are in shock that is likely to cause death before systemic thrombolysis can take effect.3 An area of ongoing debate is whether there is a benefit for thrombolytic therapy in patients with submassive PE who are hemodynamically stable but have evidence of right ventricular dysfunction on echocardiography or computed tomographic angiography. Bleeding remains the most serious complication of thrombolytic therapy.4
Surgical interventions: Pulmonary embolectomy and IVC filters
Pulmonary embolectomy. According to ACCP guidelines, surgical pulmonary embolectomy for the initial treatment of PE is reserved for patients with massive PE (documented angiographically, if possible), shock despite heparin and resuscitation efforts, and failure of thrombolytic therapy or a contraindication to its use.4 To date, there have been no randomized trials evaluating this procedure. Pooled data published by Stein et al29 reported a 20% operative mortality rate in patients undergoing pulmonary embolectomy between 1985 and 2005 compared with 32% in patients undergoing the procedure before 1985. A more recent retrospective review of 214 patients undergoing surgical embolectomy for massive and submassive PE reported an in-hospital mortality rate of 11.7%, with the highest death rate (32.1%) in patients who had a preoperative cardiac arrest.30 The use of surgical embolectomy has also been reported in patients with intermediate-risk to high-risk conditions (defined as elevated biomarkers and evidence of right heart strain on computed tomographic angiography or echocardiography).19
IVC filters. Current guidelines recommend against routine use of IVC filters for patients with DVT or PE who are able to be treated with anticoagulants.3 Absolute indications for the placement of IVC filters include a contraindication to anticoagulation, complications of anticoagulation, and recurrent thromboembolism despite adequate anticoagulant therapy.4 Relative indications for IVC filters are massive PE, iliocaval DVT, free-floating proximal DVT, cardiac or pulmonary insufficiency, high risk of complications from anticoagulation (frequent falls, ataxia), and poor compliance.
Retrievable filters may be considered for situations in which anticoagulation is temporarily contraindicated or there is a short duration of PE risk.31 The current consensus guidelines advise that indications for placing a retrievable IVC filter are the same as for placing a permanent device.31 An IVC filter alone is not effective therapy for VTE, and resumption of anticoagulation is recommended as soon as possible after placement.
DURATION OF TREATMENT
Current guidelines recommend 3 months of anticoagulation (long-term) for patients with an episode of acute proximal or isolated distal DVT of the leg or PE resulting from surgery or a nonsurgical transient cause.3 Patients who have the antiphospholipid syndrome, who are homozygous for factor V Leiden, or who are doubly heterozygous for factor V Leiden and prothrombin gene mutation should be considered for longer (extended) anticoagulation. Extended anticoagulation is also recommended in patients with active cancer and in patients who have unexplained recurrent VTE (Table 2).3
The duration of treatment for unprovoked VTE remains controversial. In the most recent ACCP guidelines, indefinite or extended anticoagulation is indicated for patients with a low or moderate risk of bleeding for a first (and second) unprovoked VTE.4 Patients with a high risk of bleeding with a first (or second) unprovoked VTE that is a proximal DVT of the leg or PE be treated for 3 months.3,4 Three DOACs (rivaroxaban, apixaban, and dabigatran) have extended-duration indications. The 2016 ACCP guidelines suggest aspirin over no treatment for the patient who has decided to stop anticoagulation therapy, although the guidelines do not consider aspirin a reasonable alternative to anticoagulation.34,35 Use of markers such as residual venous obstruction and D-dimer level in conjunction with the DASH score have been studied in an effort to predict the risk of recurrence and thus the duration of anticoagulation.36,37 Residual venous obstruction appears to be less useful than the D-dimer level as an indicator for recurrence. The D-dimer used in conjunction with the DASH prediction score may help to calculate recurrence risk based on the following predictors: abnormal D-dimer 3 weeks after stopping anticoagulation, age under 50, male sex, and hormone use at the time of the VTE.38 DASH score assessment may help physicians decide whether to continue anticoagulation therapy but it has not been shown to be helpful in men.4 A more recent study confirmed the validity of the DASH score with better prediction in patients under age 65. The recurrence rate was higher in the older population, suggesting that this population should be considered for prolonged treatment if the bleeding risk is acceptable.39 Other prediction tools include the Vienna prediction model and the clinical decision rule “Men continue and HER DOO2”—ie, HER = hyperpigmentation, edema, redness; DOO = D-dimer ≥ 250 μg/L, obesity body mass index ≥ 30 kg/m2, old age (≥ 65); 2 = high risk if more than 2 of these factors.40,41
SCREENING AND PREVENTION
Nearly 60% of all VTE events occur in hospitals and nursing homes.42 Yet anticoagulant prophylaxis is used in only 16% to 33% of at-risk hospitalized medical patients compared with 90% of at-risk hospitalized surgical patients.43 Adequate prophylaxis can reduce the incidence of VTE as demonstrated in a meta-analysis involving 19,958 patients, which revealed a 64% reduction in relative risk (RR) of a fatal PE, 58% reduction in RR of a symptomic PE, and a 53% reduction in RR of a symptomatic DVT.43
The consequences of VTE include symptomatic DVT and PE, fatal PE, the cost of investigating symptomatic patients, the risk and cost of treatment (bleeding), PTS, and chronic thromboembolic pulmonary hypertension. Heparin, enoxaparin, and fondaparinux are approved agents for prophylactic but each agent has specific indications. Factor Xa inhibitors, rivaroxaban, and apixaban are approved for use in patients undergoing total knee or hip replacement. More recently, the factor Xa inhibitor, betrixaban, has been approved for VTE prophylaxis for up to 42 days in adult patients hospitalized for acute medical illness.44 For patients with increased bleeding risk who are unable to receive pharmacologic prophylaxis, intermittent pneumatic compression devices or graduated compression stockings should be used.
Compression stockings
Current ACCP guidelines advise against routine use of compression stockings to prevent PTS in patients who have had a DVT.3 While current evidence suggests compression stockings do not prevent PTS, they reduce symptoms of acute or chronic DVT for some patients.
- Centers for Disease Control and Prevention. Venous thromboembolism (blood clots). https://www.cdc.gov/ncbddd/dvt/data.html. Updated June 22, 2015. Reviewed April 6, 2017. Accessed October 24, 2017.
- Klok FA, van der Hulle T, den Exter PL, Lankeit M, Huisman MV, Konstantinides S. The post-PE syndrome: A new concept for chronic complications of pulmonary embolism. Blood Rev 2014; 28:221–226.
- Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest 2016; 149:315–352.
- Kearon C, Akl EA, Comerota AJ, et al. Antithrombotic therapy for VTE disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2012; 141(suppl 2):e419S–494S.
- Kearon C, Ginsberg JS, Julian JA, et al; Fixed-Dose Heparin (FIDO) Investigators. Comparison of fixed-dose weight-adjusted unfractionated heparin and low-molecular-weight heparin for acute treatment of venous thromboembolism. JAMA 2006; 296:935–942.
- Arixtra [package insert]. Research Triangle Park, NC: GlaxoSmithKline; 2010. https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/021345s023lbl.pdf. Accessed October 24, 2017.
- Adam SS, McDuffie JR, Ortel TL, Williams Jr JW. Comparative effectiveness of warfarin and new oral anticoagulants for the management of atrial fibrillation and venous thromboembolism: a systematic review. Ann Intern Med 2012; 157:796–807.
- Yeh CH, Gross PL, Weitz JI. Evolving use of new oral anticoagulants for treatment of venous thromboembolism. Blood 2014; 124:1020–1028.
- EINSTEIN–PE Investigators; Büller HR, Prins MH, Lensin AW, et al. Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med 2012; 366:1287–1297.
- EINSTEIN Investigators; Bauersachs R, Berkowitz SD, Brenner B, et al. Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med 2010; 363:2499–2510.
- Weitz JI, Lensing AWA, Prins MH, et al; EINSTEIN CHOICE Investigators. Rivaroxaban or aspirin for extended treatment of venous thromboembolism. N Engl J Med 2017; 376:1211–1222.
- Agnelli G, Buller HR, Cohen A, et al; AMPLIFY Investigators. Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med 2013; 369:799–808.
- Agnelli G, Buller HR, Cohen A, et al; AMPLIFY-EXT Investigators. Apixaban for extended treatment of venous thromboembolism. N Engl J Med 2013; 368:699–708.
- Schulman S, Kearon C, Kakkar AK, et al; RE-COVER Study Group. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med 2009; 361:2342–2352.
- The Hokusai-VTE Investigators; Büller HR, Décousus H, Grosso MA, et al. Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. N Engl J Med 2013; 369:1406–1415.
- Schulman S, Kearon C, Kakkar AK, et al; RE-MEDY Trial Investigators; RE-SONATE Trial Investigators. Extended use of dabigatran, warfarin, or placebo in venous thromboembolism. N Engl J Med 2013; 368:709–718.
- van Es N, Coppens M, Schulman S, Middeldorp S, Büller HR. Direct oral anticoagulants compared with vitamin K antagonists for acute venous thromboembolism: evidence from phase 3 trials. Blood 2014; 124:1968–1975.
- Chai-Adisaksopha C, Crowther M, Isayama T, Lim W. The impact of bleeding complications in patients receiving target-specific oral anticoagulants: a systematic review and meta-analysis. Blood 2014; 124:2450–2458.
- Konstantinides SV, Torbicki A, Agnelli G, et al; Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J 2014; 35:3033–3069, 3069a–3069k.
- Pollack CV Jr, Reilly PA, Eikelboom J, et al. Idarucizumab for dabigatran reversal. N Engl J Med 2015; 373:511–520.
- Haig Y, Enden T, Grøtta O, et al; CaVenT Study Group. Post-thrombotic syndrome after catheter-directed thrombolysis for deep vein thrombosis (CaVenT): 5-year follow-up results of an open-label, randomised controlled trial. Lancet Haematol 2016; 3:e64–e71.
- Sharifi M, Bay C, Mehdipour M, Sharifi J; TORPEDO Investigators. Thrombus obliteration by rapid percutaneous endovenous intervention in deep venous occlusion (TORPEDO) trial: midterm results. J Endovasc Ther 2012; 19:273–280.
- Society of Interventional Radiology. Pivotal study of minimally invasive therapy improves the care of patients with deep vein thrombosis [news release]. https://www.sirweb.org/advocacy-and-outreach/media/news-release-archive/news-release-ATTRACT-Trial. Published March 6, 2017. Accessed November 28, 2017.
- Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians evidence-based clinical practice guidelines (8th ed). Chest 2008; 133(suppl 6):454S–545S.
- Meyer G, Vicaut E, Danays T, et al; PEITHO Investigators. Fibrinolysis for patients with intermediate-risk pulmonary embolism. N Engl J Med 2014; 370:1402–1411.
- Sharifi M, Bay C, Skrocki L, Rahimi F, Mehdipour M; “MOPETT” Investigators. Moderate pulmonary embolism treated with thrombolysis (from the “MOPETT” Trial). Am J Cardiol 2013; 111:273–277.
- Kucher N, Boekstegers P, Müller OJ, et al. Randomized, controlled trial of ultrasound-assisted catheter-directed thrombolysis for acute intermediate-risk pulmonary embolism. Circulation 2014; 129:479–486.
- Piazza G, Hohlfelder B, Jaff MR, et al; SEATTLE II Investigators. A prospective, single-arm, multicenter trial of ultrasound-facilitated, catheter-directed, low-dose fibrinolysis for acute massive and submassive pulmonary embolism: the SEATTLE II study. JACC Cardiovasc Interv 2015; 8:1382–1392.
- Stein PD, Alnas M, Beemath A, Patel NR. Outcome of pulmonary embolectomy. Am J Cardiol 2007; 99:421–423.
- Keeling WB, Sundt T, Leacche M, et al; SPEAR Working Group. Outcomes after surgical pulmonary embolectomy for acute pulmonary embolus: a multi-institutional study. Ann Thorac Surg 2016; 102:1498–1502.
- Kaufman JA, Kinney TB, Streiff MB, et al. Guidelines for the use of retrievable and convertible vena cava filters: report from the Society of Interventional Radiology multidisciplinary consensus conference. J Vasc Interv Radiol 2006; 17:449–459.
- Kyrle PA, Rosendaal FR, Eichinger S. Risk assessment for recurrent venous thrombosis. Lancet 2010; 376:2032–2039.
- Heit JA. Predicting the risk of venous thromboembolism recurrence. Am J Hematol 2012; 87(suppl 1):S63–S67.
- Becattini C, Agnelli G, Schenone A, et al; WARFASA Investigators. Aspirin for preventing the recurrence of venous thromboembolism. N Engl J Med 2012; 366:1959–1967.
- Brighton TA, Eikelboom JW, Mann K, et al; ASPIRE Investigators. Low-dose aspirin for preventing recurrent venous thromboembolism. N Engl J Med 2012; 367:1979–1987.
- Carrier M, Rodger MA, Wells PS, Righini M, LE Gal G. Residual vein obstruction to predict the risk of recurrent venous thromboembolism in patients with deep vein thrombosis: a systematic review and meta-analysis. J Thromb Haemost 2011; 9:1119–1125.
- Siragusa S, Malato A, Saccullo G, et al. Residual vein thrombosis for assessing duration of anticoagulation after unprovoked deep vein thrombosis of the lower limbs: the extended DACUS study. Am J Hematol 2011; 86:914–917.
- Tosetto A, Iorio A, Marcucci M, et al. Predicting disease recurrence in patients with previous unprovoked venous thromboembolism: a proposed prediction score (DASH). J Thromb Haemost 2012; 10:1019–1025.
- Tosetto A, Testa S, Martinelli I, et al. External validation of the DASH prediction rule: a retrospective cohort study. J Thromb Haemost 2017; 15:1963–1970.
- Rodger MA, Kahn SR, Wells PS, et al. Identifying unprovoked thromboembolism patients at low risk for recurrence who can discontinue anticoagulant therapy. CMAJ 2008; 179:417–426.
- Eichinger S, Heinze G, Jandeck LM, Kyrle PA. Risk assessment of recurrence in patients with unprovoked deep vein thrombosis or pulmonary embolism: the Vienna prediction model. Circulation 2010; 121:1630–1636.
- Heit JA, O’Fallon WM, Petterson TM, et al. Relative impact of risk factors for deep vein thrombosis and pulmonary embolism: a population-based study. Arch Intern Med 2002; 162:1245–1248.
- Dentali F, Douketis JD, Gianni M, Lim W, Crowther MA. Meta-analysis: anticoagulant prophylaxis to prevent symptomatic venous thromboembolism in hospitalized medical patients. Ann Intern Med 2007; 146:278–288.
- Cohen AT, Harrington RA, Goldhaber SZ, et al; APEX Investigators. Extended thromboprophylaxis with betrixaban in acutely ill medical patients. N Engl J Med 2016; 375:534–544.
Venous thromboembolism (VTE) includes both deep vein thrombosis (DVT) and pulmonary embolism (PE). Although the exact incidence of VTE is unknown, an estimated 1 million people in the United States are affected each year, with about a third experiencing a recurrence within 10 years.1 VTE affects hospitalized and nonhospitalized patients, is often overlooked, and results in long-term complications including postthrombotic syndrome (PTS) for DVT, postpulmonary embolism syndrome and chronic thromboembolic pulmonary hypertension for PE, and death.2
TREATMENT
Treatment for VTE should be initiated in the following cases:
- Proximal DVT of the lower extremity
- Symptomatic distal (calf vein) DVT
- Symptomatic upper extremity DVT (axillary-subclavian veins)
- PE
- Subsegmental PE in a patient at risk for recurrence
- Surveillance for subsegmental PE in a patient with no proximal DVT and a low risk of recurrence.
In addition to anticoagulants, other more aggressive therapies for VTE may be appropriate, such as systemic thrombolysis in the case of PE or catheter-directed thrombolytic or pharmacomechnical therapies for DVT or PE, surgical intervention (acute pulmonary embolectomy), or placement of an inferior vena cava (IVC) filter.
This article reviews the management of VTE, highlighting the recent changes in treatment and prevention guidelines from the American College of Chest Physicians (ACCP).3
Risk of bleeding
In assessing a patient’s risk of bleeding for anticoagulation therapy (Table 1), the absence of risk factors is considered low risk for bleeding, the presence of 1 risk factor is considered intermediate risk, and 2 or more risk factors is considered high risk. Compared with low-risk patients, moderate-risk patients have a twofold increased risk of major bleeding and high-risk patients have an eightfold increased risk of major bleeding. This equates to an annualized risk of major bleeding of 0.8% for low-risk patients, 1.6% for moderate-risk patients, and greater than 6.5% for high-risk patients.3
Anticoagulants
Deciding on which anticoagulant to use depends on the indication, the patient’s underlying condition, the patient’s preference, and the patient’s risk of bleeding. Heparin, the LMWHs, fondaparinux and the DOACs (rivaroxaban and apixaban) are the only agents approved by the US Food and Drug Administration (FDA) recommended for the acute treatment phase, while the DOACs and warfarin are anticoagulation options for the long-term and extended treatment phases. The LMWHs should be used for the patient with cancer and during pregnancy.
Unfractionated heparin. UFH is administered parenterally and can be used for the prevention and treatment of VTE. Heparin remains an option for initial treatment of patients with acute VTE and is generally preferred over LMWH for patients who may require advanced therapies, such as for hemodynamically unstable PE or iliofemoral DVT. It is also recommended for patients with renal failure.3 Weight-based dosing (80 U/kg bolus followed by 18 U/kg/hour intravenous infusion) is recommended, targeting an antifactor activated clotting factor (anti-Xa) assay level of 0.3 IU/mL to 0.7 IU/mL. Heparin may also be given subcutaneously in an outpatient setting using an initial bolus of 333 U/kg followed by a subcutaneous dose of 17,500 U twice daily.5
Low-molecular-weight heparin. LMWHs are administered as weight-based subcutaneous injections and have indications for patients with acute VTE and for VTE prophylaxis. LMWHs are used for transitioning to warfarin, dabigatran, or edoxaban for long-term anticoagulation and are recommended over warfarin and DOACs for treatment of VTE in patients with cancer and in pregnant women.3
Enoxaparin (Lovenox), the most commonly used agent in the United States, is given either as a once-daily injection (1.5 mg/kg/day) or a twice-daily injection (1 mg/kg every 12 hours). It is also approved for VTE prophylaxis in patients undergoing hip or knee replacement surgery or abdominal surgery, or in patients with severely restricted mobility during acute illness. LMWH can also be given in patients with renal insufficiency (creatinine clearance [CrCL] < 30 mL/minute) after dose adjustment. No monitoring is required, although it is advised in pediatric patients, pregnant women, obese patients, and patients with renal insufficiency. If monitoring is required, an anti-Xa assay using LMWH as a reference standard should be done 4 hours after subcutaneous injection. The therapeutic range for enoxaparin is 0.5 IU/mL to 1.0 IU/mL for the 12-hour regimen and greater than 1.0 IU/mL for the once-daily dose. Other LMWHs available in the United States include dalteparin (Fragmin) and tinzaparin (Innohep). Each has its own specific indications.
Fondaparinux. Fondaparinux is an indirect factor Xa inhibitor, chemically related to LMWH. It is approved for treatment of patients with acute VTE when used in combination with a VKA (warfarin) or dabigatran or edoxaban. It also has approval for VTE prophylaxis in patients undergoing hip fracture, hip or knee replacement, and abdominal surgery. Fondaparinux is administered as a once-daily subcutaneous injection of 2.5 mg for DVT prophylaxis and a body weight-based dose for the treatment of VTE (5 mg < 50 kg; 7.5 mg 50 to 100 kg; 10 mg > 100 kg).6 Fondaparinux is contraindicated in patients with severe renal impairment (CrCL les 30 mL/min) and bacterial endocarditis.6
Warfarin. Warfarin, a VKA, was the mainstay of therapy for long-term and extended treatment of VTE until the advent of the DOACs. Warfarin must be coadministered with heparin, LMWH, or fondaparinux initially and continued as overlap therapy for a minimum of 5 days until the international normalized ratio [INR] is at least 2.0 for 24 hours.4 Early initiation of a VKA on the first day of parenteral therapy is advised.
Warfarin remains the best option for patients on long-term or extended anticoagulation with liver dysfunction (elevated serum transaminases exceeding twice the upper limits of normal or active liver disease) or renal disease (CrCL < 30 mL/min), as well as patients unable to afford DOACs. Additionally, select patient populations may still be best served by warfarin as these groups were underrepresented or not included in DOAC trials, including pediatric patients, individuals with body weight less than 50 kg or greater than 150 kg, and patients with select types of thrombophilia (eg, antiphospholipid syndrome). Warfarin is also advised for patients with poor compliance, as international normalized ratio of prothrombin time (PT/INR) monitoring is required using a point-of-care testing device or during a visit to an anticoagulation clinic. DOACs do not require monitoring, and noncompliance will not be readily apparent.
Direct oral anticoagulants. The DOACs, which include the factor Xa inhibitors rivaroxaban (Xarelto), apixaban (Eliquis), and edoxaban (Savaysa) and the direct thrombin inhibitor dabigatran (Pradaxa), been studied extensively and shown to be noninferior to VKAs for treatment of VTE.7 DOACs are currently recommended by the ACCP for long-term treatment of VTE, and several have extended treatment recommendations for VTE over the VKAs.3
The advantages of DOACs include no need for PT/INR monitoring, a fixed dosage, shorter half-life, rapid onset of action (for monotherapy), and in most cases, no need for bridging for interventional or surgical procedures. Additional advantages may include a decreased burden of care for the physician and improved quality of life for the patient. DOACs are also the agents of choice for patients who prefer oral therapy (avoiding parenteral therapy), have limited access to an anticoagulation clinic (home bound or geographic inaccessibility for PT/INR monitoring), or have food or drug-drug interactions. Patients at risk of gastrointestinal bleeding or dyspepsia should avoid dabigatran, while apixaban may be preferred if there is a history of gastrointestinal bleeding.8
Rivaroxaban or apixaban can be used as monotherapy for the initial treatment of VTE, while a 5-day course of heparin, LMWH, or fondaparinux is necessary with dabigatran or edoxaban. Rivaroxaban has been approved by the FDA for use in the prevention and treatment of VTE.9,10 For VTE prophylaxis, rivaroxaban is given orally at 10 mg once daily for 35 days for patients undergoing total hip replacement surgery and for 12 days for patients undergoing knee replacement surgery. For the treatment of VTE, rivaroxaban is given orally at 15 mg twice a day for the initial 21 days of treatment, followed by once daily at 20 mg per day for long-term treatment. It is also approved for extended-duration therapy in both 10-mg and 20-mg doses. In a recently published randomized double-blind trial of rivaroxaban compared with aspirin, the risk of a recurrent event was lower with either dose of rivaroxaban compared with aspirin without an increase in bleeding.11 Rivaroxaban is contraindicated in patients with renal insufficiency (CrCL < 30 mL/min). Both the 15-mg and 20-mg tablets must be taken with food.
Apixaban is also approved for monotherapy of VTE and was found to be noninferior to standard therapy of LMWH and warfarin with less bleeding.12 Apixaban is used for VTE prophylaxis in patients undergoing hip or knee replacement surgery, given at 2.5 mg twice daily beginning 12 to 24 hours postoperatively for 35 days (hip) or 12 days (knee). The acute-phase dosage is 10 mg twice daily for 7 days followed by 5 mg twice daily for long-term treatment of VTE. The recommended dose should be reduced to 2.5 mg twice daily in patients that meet 2 of the following criteria: age 80 or older; body weight of 60 kg or less; or with a serum creatinine 1.5 mg/dL or greater. Apixaban is also approved for extended treatment of VTE. In a randomized, double-blind study of 2 doses (2.5 mg and 5 mg, twice daily) of apixaban compared with placebo, apixaban reduced the risk of recurrent VTE without increasing the risk of bleeding.13
Both dabigatran and edoxaban require an initial 5-day overlap with a parenteral anticoagulant.14,15 Dabigatran is given at 150 mg orally twice daily if the CrCL is greater than 30 mL/min for the long-term treatment of VTE. Edoxaban is given orally at 60 mg once daily but reduced to 30 mg once daily if the CrCL is 30 mL/min to 50 mL/min, if body weight is 60 kg or less, or with use of certain P-glycoprotein inhibitors. Dabigatran has been evaluated in 2 double-blind, randomized controlled trials comparing the extended use of dabigatran with warfarin or placebo in patients with VTE.16 Dabigatran carried a lower risk of major or clinically relevant bleeding than warfarin but a higher risk than placebo. Dabigatran was noninferior to warfarin but significantly reduced the rate of recurrence in the placebo group.16
The major side effect observed with all DOACs is bleeding, but they have been proven safer particularly in the terms of major bleeding compared with the standard heparin-LMWH-VKA regimen for treatment of VTE.17–19 The risk of major bleeding, and in particular intracranial bleeding, has been shown to be less with DOACs compared with VKAs in 2 meta-analysis trials.17,18 Of the 4 new DOACs, only dabigatran currently has an anticoagulant-reversing agent (idarucizumab), although an antidote for the other 3 agents is awaiting FDA approval.20
Subsegmental pulmonary embolism
There is debate as to the need for treatment of patients with subsegmental PE. The most recent guidelines advise clinical surveillance over anticoagulation for patients with a low risk for recurrent VTE and no evidence for a proximal DVT.3 However, individuals who are hospitalized, have reduced mobility, have active cancer or are being treated with chemotherapy, or have a low cardiopulmonary reserve should be considered for anticoagulation unless they have a high bleeding risk.
Thrombolytic therapy
Thrombolytic therapy may be beneficial in select patients with VTE and can be delivered systemically or locally per catheter-directed therapy (CDT). Both routes carry an increased risk of hemorrhage compared with standard anticoagulation. The Catheter-Directed-Venous Thrombolysis (CaVenT) trial and Thrombus Obliteration by Rapid Percutaneous Endovenous Intervention in Deep Venous Occlusion (TORPEDO) trial compared CDT with standard therapy.21,22 In CaVEnT, CDT resulted in increased clinical benefit during the 5-year follow-up but did not result in improved quality of life.21 In the TORPEDO trial, patients with proximal DVT receiving percutaneous endovenous intervention and anticoagulation compared with anticoagulation alone demonstrated superiority in the reduction of PTS at greater than 2 years.22 Early results of the Acute Venous Thrombosis: Thrombus Removal With Adjunctive Catheter-directed Thrombolysis (ATTRACT) trial show that most patients with DVT did not have a long-term benefit from CDT, buy they did have reduced leg pain and swelling and some had reduced risk of moderate-to-severe PTS.23
The 2012 and 2016 ACCP guidelines advise anticoagulant therapy over CDT for patients with acute DVT of the leg but suggest patients who may benefit are those with iliofemoral DVT with symptoms for less than 14 days, good functional status, a life expectancy greater than 1 year, and a low risk of bleeding.3,4 This is in contrast to the 2008 CHEST guidelines that recommended patients who have extensive proximal DVT, who have a high risk of limb gangrene, who are at low risk of bleeding, and who otherwise have good functional status be given CDT if the expertise and resources are available.24 It has been suggested that CDT promotes early recanalization and minimizes the incidence of PTS.
Thrombolytic therapy for acute PE remains controversial because there is no clearly established short-term mortality benefit. In the Pulmonary Embolism Thrombolysis (PEITHO) trial, thrombolysis prevented hemodynamic decompensation but increased the risk of major hemorrhage and stroke.25 A lower dose (50 mg) of thrombolytic therapy was studied in the Moderate Pulmonary Embolism Treated With Thrombolysis (MOPPET) trial and was found to be safe and effective in the treatment of moderate PE.26
CDT has also been shown to be effective in the treatment of PE. The Ultrasound Acceleration Thrombolysis of Pulmonary Embolism (ULTIMA) trial demonstrated that catheter-directed thrombolysis with ultrasonographic guidance in patients with acute intermediate-risk PE was superior in reversing right ventricular dilatation without an increase in bleeding complications compared with UFH.27 The Ultrasound-Facilitated, Catheter-Directed, Low-Dose Fibrinolysis for Acute Massive and Submassive Pulmonary Embolism (SEATTLE II) study found that this approach decreased right ventricular dilation, decreased pulmonary hypertension, decreased anatomic burden, and minimized the risk of intracranial hemorrhage in patients with massive and submassive PE.28
Alteplase (Activase) is a recombinant tissue-type plasminogen activator approved by the FDA for treatment of acute PE. Alteplase is administered as a 100-mg infusion over 2 hours. Because of favorable outcomes with prompt recognition and anticoagulation for PE, the ACCP guidelines recommend systemic thrombolysis for hemodynamically unstable patients (systolic blood pressure < 90 mm Hg) with acute PE and a low risk of bleeding using a peripheral vein.3 These guidelines also recommend thrombolysis for the patient whose condition deteriorates after starting anticoagulant therapy but who have yet to develop hypotension.
If the appropriate expertise is available, CDT is suggested for patients with acute PE if they have hypotension and a high bleeding risk, have failed systemic thrombolysis, or are in shock that is likely to cause death before systemic thrombolysis can take effect.3 An area of ongoing debate is whether there is a benefit for thrombolytic therapy in patients with submassive PE who are hemodynamically stable but have evidence of right ventricular dysfunction on echocardiography or computed tomographic angiography. Bleeding remains the most serious complication of thrombolytic therapy.4
Surgical interventions: Pulmonary embolectomy and IVC filters
Pulmonary embolectomy. According to ACCP guidelines, surgical pulmonary embolectomy for the initial treatment of PE is reserved for patients with massive PE (documented angiographically, if possible), shock despite heparin and resuscitation efforts, and failure of thrombolytic therapy or a contraindication to its use.4 To date, there have been no randomized trials evaluating this procedure. Pooled data published by Stein et al29 reported a 20% operative mortality rate in patients undergoing pulmonary embolectomy between 1985 and 2005 compared with 32% in patients undergoing the procedure before 1985. A more recent retrospective review of 214 patients undergoing surgical embolectomy for massive and submassive PE reported an in-hospital mortality rate of 11.7%, with the highest death rate (32.1%) in patients who had a preoperative cardiac arrest.30 The use of surgical embolectomy has also been reported in patients with intermediate-risk to high-risk conditions (defined as elevated biomarkers and evidence of right heart strain on computed tomographic angiography or echocardiography).19
IVC filters. Current guidelines recommend against routine use of IVC filters for patients with DVT or PE who are able to be treated with anticoagulants.3 Absolute indications for the placement of IVC filters include a contraindication to anticoagulation, complications of anticoagulation, and recurrent thromboembolism despite adequate anticoagulant therapy.4 Relative indications for IVC filters are massive PE, iliocaval DVT, free-floating proximal DVT, cardiac or pulmonary insufficiency, high risk of complications from anticoagulation (frequent falls, ataxia), and poor compliance.
Retrievable filters may be considered for situations in which anticoagulation is temporarily contraindicated or there is a short duration of PE risk.31 The current consensus guidelines advise that indications for placing a retrievable IVC filter are the same as for placing a permanent device.31 An IVC filter alone is not effective therapy for VTE, and resumption of anticoagulation is recommended as soon as possible after placement.
DURATION OF TREATMENT
Current guidelines recommend 3 months of anticoagulation (long-term) for patients with an episode of acute proximal or isolated distal DVT of the leg or PE resulting from surgery or a nonsurgical transient cause.3 Patients who have the antiphospholipid syndrome, who are homozygous for factor V Leiden, or who are doubly heterozygous for factor V Leiden and prothrombin gene mutation should be considered for longer (extended) anticoagulation. Extended anticoagulation is also recommended in patients with active cancer and in patients who have unexplained recurrent VTE (Table 2).3
The duration of treatment for unprovoked VTE remains controversial. In the most recent ACCP guidelines, indefinite or extended anticoagulation is indicated for patients with a low or moderate risk of bleeding for a first (and second) unprovoked VTE.4 Patients with a high risk of bleeding with a first (or second) unprovoked VTE that is a proximal DVT of the leg or PE be treated for 3 months.3,4 Three DOACs (rivaroxaban, apixaban, and dabigatran) have extended-duration indications. The 2016 ACCP guidelines suggest aspirin over no treatment for the patient who has decided to stop anticoagulation therapy, although the guidelines do not consider aspirin a reasonable alternative to anticoagulation.34,35 Use of markers such as residual venous obstruction and D-dimer level in conjunction with the DASH score have been studied in an effort to predict the risk of recurrence and thus the duration of anticoagulation.36,37 Residual venous obstruction appears to be less useful than the D-dimer level as an indicator for recurrence. The D-dimer used in conjunction with the DASH prediction score may help to calculate recurrence risk based on the following predictors: abnormal D-dimer 3 weeks after stopping anticoagulation, age under 50, male sex, and hormone use at the time of the VTE.38 DASH score assessment may help physicians decide whether to continue anticoagulation therapy but it has not been shown to be helpful in men.4 A more recent study confirmed the validity of the DASH score with better prediction in patients under age 65. The recurrence rate was higher in the older population, suggesting that this population should be considered for prolonged treatment if the bleeding risk is acceptable.39 Other prediction tools include the Vienna prediction model and the clinical decision rule “Men continue and HER DOO2”—ie, HER = hyperpigmentation, edema, redness; DOO = D-dimer ≥ 250 μg/L, obesity body mass index ≥ 30 kg/m2, old age (≥ 65); 2 = high risk if more than 2 of these factors.40,41
SCREENING AND PREVENTION
Nearly 60% of all VTE events occur in hospitals and nursing homes.42 Yet anticoagulant prophylaxis is used in only 16% to 33% of at-risk hospitalized medical patients compared with 90% of at-risk hospitalized surgical patients.43 Adequate prophylaxis can reduce the incidence of VTE as demonstrated in a meta-analysis involving 19,958 patients, which revealed a 64% reduction in relative risk (RR) of a fatal PE, 58% reduction in RR of a symptomic PE, and a 53% reduction in RR of a symptomatic DVT.43
The consequences of VTE include symptomatic DVT and PE, fatal PE, the cost of investigating symptomatic patients, the risk and cost of treatment (bleeding), PTS, and chronic thromboembolic pulmonary hypertension. Heparin, enoxaparin, and fondaparinux are approved agents for prophylactic but each agent has specific indications. Factor Xa inhibitors, rivaroxaban, and apixaban are approved for use in patients undergoing total knee or hip replacement. More recently, the factor Xa inhibitor, betrixaban, has been approved for VTE prophylaxis for up to 42 days in adult patients hospitalized for acute medical illness.44 For patients with increased bleeding risk who are unable to receive pharmacologic prophylaxis, intermittent pneumatic compression devices or graduated compression stockings should be used.
Compression stockings
Current ACCP guidelines advise against routine use of compression stockings to prevent PTS in patients who have had a DVT.3 While current evidence suggests compression stockings do not prevent PTS, they reduce symptoms of acute or chronic DVT for some patients.
Venous thromboembolism (VTE) includes both deep vein thrombosis (DVT) and pulmonary embolism (PE). Although the exact incidence of VTE is unknown, an estimated 1 million people in the United States are affected each year, with about a third experiencing a recurrence within 10 years.1 VTE affects hospitalized and nonhospitalized patients, is often overlooked, and results in long-term complications including postthrombotic syndrome (PTS) for DVT, postpulmonary embolism syndrome and chronic thromboembolic pulmonary hypertension for PE, and death.2
TREATMENT
Treatment for VTE should be initiated in the following cases:
- Proximal DVT of the lower extremity
- Symptomatic distal (calf vein) DVT
- Symptomatic upper extremity DVT (axillary-subclavian veins)
- PE
- Subsegmental PE in a patient at risk for recurrence
- Surveillance for subsegmental PE in a patient with no proximal DVT and a low risk of recurrence.
In addition to anticoagulants, other more aggressive therapies for VTE may be appropriate, such as systemic thrombolysis in the case of PE or catheter-directed thrombolytic or pharmacomechnical therapies for DVT or PE, surgical intervention (acute pulmonary embolectomy), or placement of an inferior vena cava (IVC) filter.
This article reviews the management of VTE, highlighting the recent changes in treatment and prevention guidelines from the American College of Chest Physicians (ACCP).3
Risk of bleeding
In assessing a patient’s risk of bleeding for anticoagulation therapy (Table 1), the absence of risk factors is considered low risk for bleeding, the presence of 1 risk factor is considered intermediate risk, and 2 or more risk factors is considered high risk. Compared with low-risk patients, moderate-risk patients have a twofold increased risk of major bleeding and high-risk patients have an eightfold increased risk of major bleeding. This equates to an annualized risk of major bleeding of 0.8% for low-risk patients, 1.6% for moderate-risk patients, and greater than 6.5% for high-risk patients.3
Anticoagulants
Deciding on which anticoagulant to use depends on the indication, the patient’s underlying condition, the patient’s preference, and the patient’s risk of bleeding. Heparin, the LMWHs, fondaparinux and the DOACs (rivaroxaban and apixaban) are the only agents approved by the US Food and Drug Administration (FDA) recommended for the acute treatment phase, while the DOACs and warfarin are anticoagulation options for the long-term and extended treatment phases. The LMWHs should be used for the patient with cancer and during pregnancy.
Unfractionated heparin. UFH is administered parenterally and can be used for the prevention and treatment of VTE. Heparin remains an option for initial treatment of patients with acute VTE and is generally preferred over LMWH for patients who may require advanced therapies, such as for hemodynamically unstable PE or iliofemoral DVT. It is also recommended for patients with renal failure.3 Weight-based dosing (80 U/kg bolus followed by 18 U/kg/hour intravenous infusion) is recommended, targeting an antifactor activated clotting factor (anti-Xa) assay level of 0.3 IU/mL to 0.7 IU/mL. Heparin may also be given subcutaneously in an outpatient setting using an initial bolus of 333 U/kg followed by a subcutaneous dose of 17,500 U twice daily.5
Low-molecular-weight heparin. LMWHs are administered as weight-based subcutaneous injections and have indications for patients with acute VTE and for VTE prophylaxis. LMWHs are used for transitioning to warfarin, dabigatran, or edoxaban for long-term anticoagulation and are recommended over warfarin and DOACs for treatment of VTE in patients with cancer and in pregnant women.3
Enoxaparin (Lovenox), the most commonly used agent in the United States, is given either as a once-daily injection (1.5 mg/kg/day) or a twice-daily injection (1 mg/kg every 12 hours). It is also approved for VTE prophylaxis in patients undergoing hip or knee replacement surgery or abdominal surgery, or in patients with severely restricted mobility during acute illness. LMWH can also be given in patients with renal insufficiency (creatinine clearance [CrCL] < 30 mL/minute) after dose adjustment. No monitoring is required, although it is advised in pediatric patients, pregnant women, obese patients, and patients with renal insufficiency. If monitoring is required, an anti-Xa assay using LMWH as a reference standard should be done 4 hours after subcutaneous injection. The therapeutic range for enoxaparin is 0.5 IU/mL to 1.0 IU/mL for the 12-hour regimen and greater than 1.0 IU/mL for the once-daily dose. Other LMWHs available in the United States include dalteparin (Fragmin) and tinzaparin (Innohep). Each has its own specific indications.
Fondaparinux. Fondaparinux is an indirect factor Xa inhibitor, chemically related to LMWH. It is approved for treatment of patients with acute VTE when used in combination with a VKA (warfarin) or dabigatran or edoxaban. It also has approval for VTE prophylaxis in patients undergoing hip fracture, hip or knee replacement, and abdominal surgery. Fondaparinux is administered as a once-daily subcutaneous injection of 2.5 mg for DVT prophylaxis and a body weight-based dose for the treatment of VTE (5 mg < 50 kg; 7.5 mg 50 to 100 kg; 10 mg > 100 kg).6 Fondaparinux is contraindicated in patients with severe renal impairment (CrCL les 30 mL/min) and bacterial endocarditis.6
Warfarin. Warfarin, a VKA, was the mainstay of therapy for long-term and extended treatment of VTE until the advent of the DOACs. Warfarin must be coadministered with heparin, LMWH, or fondaparinux initially and continued as overlap therapy for a minimum of 5 days until the international normalized ratio [INR] is at least 2.0 for 24 hours.4 Early initiation of a VKA on the first day of parenteral therapy is advised.
Warfarin remains the best option for patients on long-term or extended anticoagulation with liver dysfunction (elevated serum transaminases exceeding twice the upper limits of normal or active liver disease) or renal disease (CrCL < 30 mL/min), as well as patients unable to afford DOACs. Additionally, select patient populations may still be best served by warfarin as these groups were underrepresented or not included in DOAC trials, including pediatric patients, individuals with body weight less than 50 kg or greater than 150 kg, and patients with select types of thrombophilia (eg, antiphospholipid syndrome). Warfarin is also advised for patients with poor compliance, as international normalized ratio of prothrombin time (PT/INR) monitoring is required using a point-of-care testing device or during a visit to an anticoagulation clinic. DOACs do not require monitoring, and noncompliance will not be readily apparent.
Direct oral anticoagulants. The DOACs, which include the factor Xa inhibitors rivaroxaban (Xarelto), apixaban (Eliquis), and edoxaban (Savaysa) and the direct thrombin inhibitor dabigatran (Pradaxa), been studied extensively and shown to be noninferior to VKAs for treatment of VTE.7 DOACs are currently recommended by the ACCP for long-term treatment of VTE, and several have extended treatment recommendations for VTE over the VKAs.3
The advantages of DOACs include no need for PT/INR monitoring, a fixed dosage, shorter half-life, rapid onset of action (for monotherapy), and in most cases, no need for bridging for interventional or surgical procedures. Additional advantages may include a decreased burden of care for the physician and improved quality of life for the patient. DOACs are also the agents of choice for patients who prefer oral therapy (avoiding parenteral therapy), have limited access to an anticoagulation clinic (home bound or geographic inaccessibility for PT/INR monitoring), or have food or drug-drug interactions. Patients at risk of gastrointestinal bleeding or dyspepsia should avoid dabigatran, while apixaban may be preferred if there is a history of gastrointestinal bleeding.8
Rivaroxaban or apixaban can be used as monotherapy for the initial treatment of VTE, while a 5-day course of heparin, LMWH, or fondaparinux is necessary with dabigatran or edoxaban. Rivaroxaban has been approved by the FDA for use in the prevention and treatment of VTE.9,10 For VTE prophylaxis, rivaroxaban is given orally at 10 mg once daily for 35 days for patients undergoing total hip replacement surgery and for 12 days for patients undergoing knee replacement surgery. For the treatment of VTE, rivaroxaban is given orally at 15 mg twice a day for the initial 21 days of treatment, followed by once daily at 20 mg per day for long-term treatment. It is also approved for extended-duration therapy in both 10-mg and 20-mg doses. In a recently published randomized double-blind trial of rivaroxaban compared with aspirin, the risk of a recurrent event was lower with either dose of rivaroxaban compared with aspirin without an increase in bleeding.11 Rivaroxaban is contraindicated in patients with renal insufficiency (CrCL < 30 mL/min). Both the 15-mg and 20-mg tablets must be taken with food.
Apixaban is also approved for monotherapy of VTE and was found to be noninferior to standard therapy of LMWH and warfarin with less bleeding.12 Apixaban is used for VTE prophylaxis in patients undergoing hip or knee replacement surgery, given at 2.5 mg twice daily beginning 12 to 24 hours postoperatively for 35 days (hip) or 12 days (knee). The acute-phase dosage is 10 mg twice daily for 7 days followed by 5 mg twice daily for long-term treatment of VTE. The recommended dose should be reduced to 2.5 mg twice daily in patients that meet 2 of the following criteria: age 80 or older; body weight of 60 kg or less; or with a serum creatinine 1.5 mg/dL or greater. Apixaban is also approved for extended treatment of VTE. In a randomized, double-blind study of 2 doses (2.5 mg and 5 mg, twice daily) of apixaban compared with placebo, apixaban reduced the risk of recurrent VTE without increasing the risk of bleeding.13
Both dabigatran and edoxaban require an initial 5-day overlap with a parenteral anticoagulant.14,15 Dabigatran is given at 150 mg orally twice daily if the CrCL is greater than 30 mL/min for the long-term treatment of VTE. Edoxaban is given orally at 60 mg once daily but reduced to 30 mg once daily if the CrCL is 30 mL/min to 50 mL/min, if body weight is 60 kg or less, or with use of certain P-glycoprotein inhibitors. Dabigatran has been evaluated in 2 double-blind, randomized controlled trials comparing the extended use of dabigatran with warfarin or placebo in patients with VTE.16 Dabigatran carried a lower risk of major or clinically relevant bleeding than warfarin but a higher risk than placebo. Dabigatran was noninferior to warfarin but significantly reduced the rate of recurrence in the placebo group.16
The major side effect observed with all DOACs is bleeding, but they have been proven safer particularly in the terms of major bleeding compared with the standard heparin-LMWH-VKA regimen for treatment of VTE.17–19 The risk of major bleeding, and in particular intracranial bleeding, has been shown to be less with DOACs compared with VKAs in 2 meta-analysis trials.17,18 Of the 4 new DOACs, only dabigatran currently has an anticoagulant-reversing agent (idarucizumab), although an antidote for the other 3 agents is awaiting FDA approval.20
Subsegmental pulmonary embolism
There is debate as to the need for treatment of patients with subsegmental PE. The most recent guidelines advise clinical surveillance over anticoagulation for patients with a low risk for recurrent VTE and no evidence for a proximal DVT.3 However, individuals who are hospitalized, have reduced mobility, have active cancer or are being treated with chemotherapy, or have a low cardiopulmonary reserve should be considered for anticoagulation unless they have a high bleeding risk.
Thrombolytic therapy
Thrombolytic therapy may be beneficial in select patients with VTE and can be delivered systemically or locally per catheter-directed therapy (CDT). Both routes carry an increased risk of hemorrhage compared with standard anticoagulation. The Catheter-Directed-Venous Thrombolysis (CaVenT) trial and Thrombus Obliteration by Rapid Percutaneous Endovenous Intervention in Deep Venous Occlusion (TORPEDO) trial compared CDT with standard therapy.21,22 In CaVEnT, CDT resulted in increased clinical benefit during the 5-year follow-up but did not result in improved quality of life.21 In the TORPEDO trial, patients with proximal DVT receiving percutaneous endovenous intervention and anticoagulation compared with anticoagulation alone demonstrated superiority in the reduction of PTS at greater than 2 years.22 Early results of the Acute Venous Thrombosis: Thrombus Removal With Adjunctive Catheter-directed Thrombolysis (ATTRACT) trial show that most patients with DVT did not have a long-term benefit from CDT, buy they did have reduced leg pain and swelling and some had reduced risk of moderate-to-severe PTS.23
The 2012 and 2016 ACCP guidelines advise anticoagulant therapy over CDT for patients with acute DVT of the leg but suggest patients who may benefit are those with iliofemoral DVT with symptoms for less than 14 days, good functional status, a life expectancy greater than 1 year, and a low risk of bleeding.3,4 This is in contrast to the 2008 CHEST guidelines that recommended patients who have extensive proximal DVT, who have a high risk of limb gangrene, who are at low risk of bleeding, and who otherwise have good functional status be given CDT if the expertise and resources are available.24 It has been suggested that CDT promotes early recanalization and minimizes the incidence of PTS.
Thrombolytic therapy for acute PE remains controversial because there is no clearly established short-term mortality benefit. In the Pulmonary Embolism Thrombolysis (PEITHO) trial, thrombolysis prevented hemodynamic decompensation but increased the risk of major hemorrhage and stroke.25 A lower dose (50 mg) of thrombolytic therapy was studied in the Moderate Pulmonary Embolism Treated With Thrombolysis (MOPPET) trial and was found to be safe and effective in the treatment of moderate PE.26
CDT has also been shown to be effective in the treatment of PE. The Ultrasound Acceleration Thrombolysis of Pulmonary Embolism (ULTIMA) trial demonstrated that catheter-directed thrombolysis with ultrasonographic guidance in patients with acute intermediate-risk PE was superior in reversing right ventricular dilatation without an increase in bleeding complications compared with UFH.27 The Ultrasound-Facilitated, Catheter-Directed, Low-Dose Fibrinolysis for Acute Massive and Submassive Pulmonary Embolism (SEATTLE II) study found that this approach decreased right ventricular dilation, decreased pulmonary hypertension, decreased anatomic burden, and minimized the risk of intracranial hemorrhage in patients with massive and submassive PE.28
Alteplase (Activase) is a recombinant tissue-type plasminogen activator approved by the FDA for treatment of acute PE. Alteplase is administered as a 100-mg infusion over 2 hours. Because of favorable outcomes with prompt recognition and anticoagulation for PE, the ACCP guidelines recommend systemic thrombolysis for hemodynamically unstable patients (systolic blood pressure < 90 mm Hg) with acute PE and a low risk of bleeding using a peripheral vein.3 These guidelines also recommend thrombolysis for the patient whose condition deteriorates after starting anticoagulant therapy but who have yet to develop hypotension.
If the appropriate expertise is available, CDT is suggested for patients with acute PE if they have hypotension and a high bleeding risk, have failed systemic thrombolysis, or are in shock that is likely to cause death before systemic thrombolysis can take effect.3 An area of ongoing debate is whether there is a benefit for thrombolytic therapy in patients with submassive PE who are hemodynamically stable but have evidence of right ventricular dysfunction on echocardiography or computed tomographic angiography. Bleeding remains the most serious complication of thrombolytic therapy.4
Surgical interventions: Pulmonary embolectomy and IVC filters
Pulmonary embolectomy. According to ACCP guidelines, surgical pulmonary embolectomy for the initial treatment of PE is reserved for patients with massive PE (documented angiographically, if possible), shock despite heparin and resuscitation efforts, and failure of thrombolytic therapy or a contraindication to its use.4 To date, there have been no randomized trials evaluating this procedure. Pooled data published by Stein et al29 reported a 20% operative mortality rate in patients undergoing pulmonary embolectomy between 1985 and 2005 compared with 32% in patients undergoing the procedure before 1985. A more recent retrospective review of 214 patients undergoing surgical embolectomy for massive and submassive PE reported an in-hospital mortality rate of 11.7%, with the highest death rate (32.1%) in patients who had a preoperative cardiac arrest.30 The use of surgical embolectomy has also been reported in patients with intermediate-risk to high-risk conditions (defined as elevated biomarkers and evidence of right heart strain on computed tomographic angiography or echocardiography).19
IVC filters. Current guidelines recommend against routine use of IVC filters for patients with DVT or PE who are able to be treated with anticoagulants.3 Absolute indications for the placement of IVC filters include a contraindication to anticoagulation, complications of anticoagulation, and recurrent thromboembolism despite adequate anticoagulant therapy.4 Relative indications for IVC filters are massive PE, iliocaval DVT, free-floating proximal DVT, cardiac or pulmonary insufficiency, high risk of complications from anticoagulation (frequent falls, ataxia), and poor compliance.
Retrievable filters may be considered for situations in which anticoagulation is temporarily contraindicated or there is a short duration of PE risk.31 The current consensus guidelines advise that indications for placing a retrievable IVC filter are the same as for placing a permanent device.31 An IVC filter alone is not effective therapy for VTE, and resumption of anticoagulation is recommended as soon as possible after placement.
DURATION OF TREATMENT
Current guidelines recommend 3 months of anticoagulation (long-term) for patients with an episode of acute proximal or isolated distal DVT of the leg or PE resulting from surgery or a nonsurgical transient cause.3 Patients who have the antiphospholipid syndrome, who are homozygous for factor V Leiden, or who are doubly heterozygous for factor V Leiden and prothrombin gene mutation should be considered for longer (extended) anticoagulation. Extended anticoagulation is also recommended in patients with active cancer and in patients who have unexplained recurrent VTE (Table 2).3
The duration of treatment for unprovoked VTE remains controversial. In the most recent ACCP guidelines, indefinite or extended anticoagulation is indicated for patients with a low or moderate risk of bleeding for a first (and second) unprovoked VTE.4 Patients with a high risk of bleeding with a first (or second) unprovoked VTE that is a proximal DVT of the leg or PE be treated for 3 months.3,4 Three DOACs (rivaroxaban, apixaban, and dabigatran) have extended-duration indications. The 2016 ACCP guidelines suggest aspirin over no treatment for the patient who has decided to stop anticoagulation therapy, although the guidelines do not consider aspirin a reasonable alternative to anticoagulation.34,35 Use of markers such as residual venous obstruction and D-dimer level in conjunction with the DASH score have been studied in an effort to predict the risk of recurrence and thus the duration of anticoagulation.36,37 Residual venous obstruction appears to be less useful than the D-dimer level as an indicator for recurrence. The D-dimer used in conjunction with the DASH prediction score may help to calculate recurrence risk based on the following predictors: abnormal D-dimer 3 weeks after stopping anticoagulation, age under 50, male sex, and hormone use at the time of the VTE.38 DASH score assessment may help physicians decide whether to continue anticoagulation therapy but it has not been shown to be helpful in men.4 A more recent study confirmed the validity of the DASH score with better prediction in patients under age 65. The recurrence rate was higher in the older population, suggesting that this population should be considered for prolonged treatment if the bleeding risk is acceptable.39 Other prediction tools include the Vienna prediction model and the clinical decision rule “Men continue and HER DOO2”—ie, HER = hyperpigmentation, edema, redness; DOO = D-dimer ≥ 250 μg/L, obesity body mass index ≥ 30 kg/m2, old age (≥ 65); 2 = high risk if more than 2 of these factors.40,41
SCREENING AND PREVENTION
Nearly 60% of all VTE events occur in hospitals and nursing homes.42 Yet anticoagulant prophylaxis is used in only 16% to 33% of at-risk hospitalized medical patients compared with 90% of at-risk hospitalized surgical patients.43 Adequate prophylaxis can reduce the incidence of VTE as demonstrated in a meta-analysis involving 19,958 patients, which revealed a 64% reduction in relative risk (RR) of a fatal PE, 58% reduction in RR of a symptomic PE, and a 53% reduction in RR of a symptomatic DVT.43
The consequences of VTE include symptomatic DVT and PE, fatal PE, the cost of investigating symptomatic patients, the risk and cost of treatment (bleeding), PTS, and chronic thromboembolic pulmonary hypertension. Heparin, enoxaparin, and fondaparinux are approved agents for prophylactic but each agent has specific indications. Factor Xa inhibitors, rivaroxaban, and apixaban are approved for use in patients undergoing total knee or hip replacement. More recently, the factor Xa inhibitor, betrixaban, has been approved for VTE prophylaxis for up to 42 days in adult patients hospitalized for acute medical illness.44 For patients with increased bleeding risk who are unable to receive pharmacologic prophylaxis, intermittent pneumatic compression devices or graduated compression stockings should be used.
Compression stockings
Current ACCP guidelines advise against routine use of compression stockings to prevent PTS in patients who have had a DVT.3 While current evidence suggests compression stockings do not prevent PTS, they reduce symptoms of acute or chronic DVT for some patients.
- Centers for Disease Control and Prevention. Venous thromboembolism (blood clots). https://www.cdc.gov/ncbddd/dvt/data.html. Updated June 22, 2015. Reviewed April 6, 2017. Accessed October 24, 2017.
- Klok FA, van der Hulle T, den Exter PL, Lankeit M, Huisman MV, Konstantinides S. The post-PE syndrome: A new concept for chronic complications of pulmonary embolism. Blood Rev 2014; 28:221–226.
- Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest 2016; 149:315–352.
- Kearon C, Akl EA, Comerota AJ, et al. Antithrombotic therapy for VTE disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2012; 141(suppl 2):e419S–494S.
- Kearon C, Ginsberg JS, Julian JA, et al; Fixed-Dose Heparin (FIDO) Investigators. Comparison of fixed-dose weight-adjusted unfractionated heparin and low-molecular-weight heparin for acute treatment of venous thromboembolism. JAMA 2006; 296:935–942.
- Arixtra [package insert]. Research Triangle Park, NC: GlaxoSmithKline; 2010. https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/021345s023lbl.pdf. Accessed October 24, 2017.
- Adam SS, McDuffie JR, Ortel TL, Williams Jr JW. Comparative effectiveness of warfarin and new oral anticoagulants for the management of atrial fibrillation and venous thromboembolism: a systematic review. Ann Intern Med 2012; 157:796–807.
- Yeh CH, Gross PL, Weitz JI. Evolving use of new oral anticoagulants for treatment of venous thromboembolism. Blood 2014; 124:1020–1028.
- EINSTEIN–PE Investigators; Büller HR, Prins MH, Lensin AW, et al. Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med 2012; 366:1287–1297.
- EINSTEIN Investigators; Bauersachs R, Berkowitz SD, Brenner B, et al. Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med 2010; 363:2499–2510.
- Weitz JI, Lensing AWA, Prins MH, et al; EINSTEIN CHOICE Investigators. Rivaroxaban or aspirin for extended treatment of venous thromboembolism. N Engl J Med 2017; 376:1211–1222.
- Agnelli G, Buller HR, Cohen A, et al; AMPLIFY Investigators. Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med 2013; 369:799–808.
- Agnelli G, Buller HR, Cohen A, et al; AMPLIFY-EXT Investigators. Apixaban for extended treatment of venous thromboembolism. N Engl J Med 2013; 368:699–708.
- Schulman S, Kearon C, Kakkar AK, et al; RE-COVER Study Group. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med 2009; 361:2342–2352.
- The Hokusai-VTE Investigators; Büller HR, Décousus H, Grosso MA, et al. Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. N Engl J Med 2013; 369:1406–1415.
- Schulman S, Kearon C, Kakkar AK, et al; RE-MEDY Trial Investigators; RE-SONATE Trial Investigators. Extended use of dabigatran, warfarin, or placebo in venous thromboembolism. N Engl J Med 2013; 368:709–718.
- van Es N, Coppens M, Schulman S, Middeldorp S, Büller HR. Direct oral anticoagulants compared with vitamin K antagonists for acute venous thromboembolism: evidence from phase 3 trials. Blood 2014; 124:1968–1975.
- Chai-Adisaksopha C, Crowther M, Isayama T, Lim W. The impact of bleeding complications in patients receiving target-specific oral anticoagulants: a systematic review and meta-analysis. Blood 2014; 124:2450–2458.
- Konstantinides SV, Torbicki A, Agnelli G, et al; Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J 2014; 35:3033–3069, 3069a–3069k.
- Pollack CV Jr, Reilly PA, Eikelboom J, et al. Idarucizumab for dabigatran reversal. N Engl J Med 2015; 373:511–520.
- Haig Y, Enden T, Grøtta O, et al; CaVenT Study Group. Post-thrombotic syndrome after catheter-directed thrombolysis for deep vein thrombosis (CaVenT): 5-year follow-up results of an open-label, randomised controlled trial. Lancet Haematol 2016; 3:e64–e71.
- Sharifi M, Bay C, Mehdipour M, Sharifi J; TORPEDO Investigators. Thrombus obliteration by rapid percutaneous endovenous intervention in deep venous occlusion (TORPEDO) trial: midterm results. J Endovasc Ther 2012; 19:273–280.
- Society of Interventional Radiology. Pivotal study of minimally invasive therapy improves the care of patients with deep vein thrombosis [news release]. https://www.sirweb.org/advocacy-and-outreach/media/news-release-archive/news-release-ATTRACT-Trial. Published March 6, 2017. Accessed November 28, 2017.
- Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians evidence-based clinical practice guidelines (8th ed). Chest 2008; 133(suppl 6):454S–545S.
- Meyer G, Vicaut E, Danays T, et al; PEITHO Investigators. Fibrinolysis for patients with intermediate-risk pulmonary embolism. N Engl J Med 2014; 370:1402–1411.
- Sharifi M, Bay C, Skrocki L, Rahimi F, Mehdipour M; “MOPETT” Investigators. Moderate pulmonary embolism treated with thrombolysis (from the “MOPETT” Trial). Am J Cardiol 2013; 111:273–277.
- Kucher N, Boekstegers P, Müller OJ, et al. Randomized, controlled trial of ultrasound-assisted catheter-directed thrombolysis for acute intermediate-risk pulmonary embolism. Circulation 2014; 129:479–486.
- Piazza G, Hohlfelder B, Jaff MR, et al; SEATTLE II Investigators. A prospective, single-arm, multicenter trial of ultrasound-facilitated, catheter-directed, low-dose fibrinolysis for acute massive and submassive pulmonary embolism: the SEATTLE II study. JACC Cardiovasc Interv 2015; 8:1382–1392.
- Stein PD, Alnas M, Beemath A, Patel NR. Outcome of pulmonary embolectomy. Am J Cardiol 2007; 99:421–423.
- Keeling WB, Sundt T, Leacche M, et al; SPEAR Working Group. Outcomes after surgical pulmonary embolectomy for acute pulmonary embolus: a multi-institutional study. Ann Thorac Surg 2016; 102:1498–1502.
- Kaufman JA, Kinney TB, Streiff MB, et al. Guidelines for the use of retrievable and convertible vena cava filters: report from the Society of Interventional Radiology multidisciplinary consensus conference. J Vasc Interv Radiol 2006; 17:449–459.
- Kyrle PA, Rosendaal FR, Eichinger S. Risk assessment for recurrent venous thrombosis. Lancet 2010; 376:2032–2039.
- Heit JA. Predicting the risk of venous thromboembolism recurrence. Am J Hematol 2012; 87(suppl 1):S63–S67.
- Becattini C, Agnelli G, Schenone A, et al; WARFASA Investigators. Aspirin for preventing the recurrence of venous thromboembolism. N Engl J Med 2012; 366:1959–1967.
- Brighton TA, Eikelboom JW, Mann K, et al; ASPIRE Investigators. Low-dose aspirin for preventing recurrent venous thromboembolism. N Engl J Med 2012; 367:1979–1987.
- Carrier M, Rodger MA, Wells PS, Righini M, LE Gal G. Residual vein obstruction to predict the risk of recurrent venous thromboembolism in patients with deep vein thrombosis: a systematic review and meta-analysis. J Thromb Haemost 2011; 9:1119–1125.
- Siragusa S, Malato A, Saccullo G, et al. Residual vein thrombosis for assessing duration of anticoagulation after unprovoked deep vein thrombosis of the lower limbs: the extended DACUS study. Am J Hematol 2011; 86:914–917.
- Tosetto A, Iorio A, Marcucci M, et al. Predicting disease recurrence in patients with previous unprovoked venous thromboembolism: a proposed prediction score (DASH). J Thromb Haemost 2012; 10:1019–1025.
- Tosetto A, Testa S, Martinelli I, et al. External validation of the DASH prediction rule: a retrospective cohort study. J Thromb Haemost 2017; 15:1963–1970.
- Rodger MA, Kahn SR, Wells PS, et al. Identifying unprovoked thromboembolism patients at low risk for recurrence who can discontinue anticoagulant therapy. CMAJ 2008; 179:417–426.
- Eichinger S, Heinze G, Jandeck LM, Kyrle PA. Risk assessment of recurrence in patients with unprovoked deep vein thrombosis or pulmonary embolism: the Vienna prediction model. Circulation 2010; 121:1630–1636.
- Heit JA, O’Fallon WM, Petterson TM, et al. Relative impact of risk factors for deep vein thrombosis and pulmonary embolism: a population-based study. Arch Intern Med 2002; 162:1245–1248.
- Dentali F, Douketis JD, Gianni M, Lim W, Crowther MA. Meta-analysis: anticoagulant prophylaxis to prevent symptomatic venous thromboembolism in hospitalized medical patients. Ann Intern Med 2007; 146:278–288.
- Cohen AT, Harrington RA, Goldhaber SZ, et al; APEX Investigators. Extended thromboprophylaxis with betrixaban in acutely ill medical patients. N Engl J Med 2016; 375:534–544.
- Centers for Disease Control and Prevention. Venous thromboembolism (blood clots). https://www.cdc.gov/ncbddd/dvt/data.html. Updated June 22, 2015. Reviewed April 6, 2017. Accessed October 24, 2017.
- Klok FA, van der Hulle T, den Exter PL, Lankeit M, Huisman MV, Konstantinides S. The post-PE syndrome: A new concept for chronic complications of pulmonary embolism. Blood Rev 2014; 28:221–226.
- Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest 2016; 149:315–352.
- Kearon C, Akl EA, Comerota AJ, et al. Antithrombotic therapy for VTE disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2012; 141(suppl 2):e419S–494S.
- Kearon C, Ginsberg JS, Julian JA, et al; Fixed-Dose Heparin (FIDO) Investigators. Comparison of fixed-dose weight-adjusted unfractionated heparin and low-molecular-weight heparin for acute treatment of venous thromboembolism. JAMA 2006; 296:935–942.
- Arixtra [package insert]. Research Triangle Park, NC: GlaxoSmithKline; 2010. https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/021345s023lbl.pdf. Accessed October 24, 2017.
- Adam SS, McDuffie JR, Ortel TL, Williams Jr JW. Comparative effectiveness of warfarin and new oral anticoagulants for the management of atrial fibrillation and venous thromboembolism: a systematic review. Ann Intern Med 2012; 157:796–807.
- Yeh CH, Gross PL, Weitz JI. Evolving use of new oral anticoagulants for treatment of venous thromboembolism. Blood 2014; 124:1020–1028.
- EINSTEIN–PE Investigators; Büller HR, Prins MH, Lensin AW, et al. Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med 2012; 366:1287–1297.
- EINSTEIN Investigators; Bauersachs R, Berkowitz SD, Brenner B, et al. Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med 2010; 363:2499–2510.
- Weitz JI, Lensing AWA, Prins MH, et al; EINSTEIN CHOICE Investigators. Rivaroxaban or aspirin for extended treatment of venous thromboembolism. N Engl J Med 2017; 376:1211–1222.
- Agnelli G, Buller HR, Cohen A, et al; AMPLIFY Investigators. Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med 2013; 369:799–808.
- Agnelli G, Buller HR, Cohen A, et al; AMPLIFY-EXT Investigators. Apixaban for extended treatment of venous thromboembolism. N Engl J Med 2013; 368:699–708.
- Schulman S, Kearon C, Kakkar AK, et al; RE-COVER Study Group. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med 2009; 361:2342–2352.
- The Hokusai-VTE Investigators; Büller HR, Décousus H, Grosso MA, et al. Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. N Engl J Med 2013; 369:1406–1415.
- Schulman S, Kearon C, Kakkar AK, et al; RE-MEDY Trial Investigators; RE-SONATE Trial Investigators. Extended use of dabigatran, warfarin, or placebo in venous thromboembolism. N Engl J Med 2013; 368:709–718.
- van Es N, Coppens M, Schulman S, Middeldorp S, Büller HR. Direct oral anticoagulants compared with vitamin K antagonists for acute venous thromboembolism: evidence from phase 3 trials. Blood 2014; 124:1968–1975.
- Chai-Adisaksopha C, Crowther M, Isayama T, Lim W. The impact of bleeding complications in patients receiving target-specific oral anticoagulants: a systematic review and meta-analysis. Blood 2014; 124:2450–2458.
- Konstantinides SV, Torbicki A, Agnelli G, et al; Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J 2014; 35:3033–3069, 3069a–3069k.
- Pollack CV Jr, Reilly PA, Eikelboom J, et al. Idarucizumab for dabigatran reversal. N Engl J Med 2015; 373:511–520.
- Haig Y, Enden T, Grøtta O, et al; CaVenT Study Group. Post-thrombotic syndrome after catheter-directed thrombolysis for deep vein thrombosis (CaVenT): 5-year follow-up results of an open-label, randomised controlled trial. Lancet Haematol 2016; 3:e64–e71.
- Sharifi M, Bay C, Mehdipour M, Sharifi J; TORPEDO Investigators. Thrombus obliteration by rapid percutaneous endovenous intervention in deep venous occlusion (TORPEDO) trial: midterm results. J Endovasc Ther 2012; 19:273–280.
- Society of Interventional Radiology. Pivotal study of minimally invasive therapy improves the care of patients with deep vein thrombosis [news release]. https://www.sirweb.org/advocacy-and-outreach/media/news-release-archive/news-release-ATTRACT-Trial. Published March 6, 2017. Accessed November 28, 2017.
- Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians evidence-based clinical practice guidelines (8th ed). Chest 2008; 133(suppl 6):454S–545S.
- Meyer G, Vicaut E, Danays T, et al; PEITHO Investigators. Fibrinolysis for patients with intermediate-risk pulmonary embolism. N Engl J Med 2014; 370:1402–1411.
- Sharifi M, Bay C, Skrocki L, Rahimi F, Mehdipour M; “MOPETT” Investigators. Moderate pulmonary embolism treated with thrombolysis (from the “MOPETT” Trial). Am J Cardiol 2013; 111:273–277.
- Kucher N, Boekstegers P, Müller OJ, et al. Randomized, controlled trial of ultrasound-assisted catheter-directed thrombolysis for acute intermediate-risk pulmonary embolism. Circulation 2014; 129:479–486.
- Piazza G, Hohlfelder B, Jaff MR, et al; SEATTLE II Investigators. A prospective, single-arm, multicenter trial of ultrasound-facilitated, catheter-directed, low-dose fibrinolysis for acute massive and submassive pulmonary embolism: the SEATTLE II study. JACC Cardiovasc Interv 2015; 8:1382–1392.
- Stein PD, Alnas M, Beemath A, Patel NR. Outcome of pulmonary embolectomy. Am J Cardiol 2007; 99:421–423.
- Keeling WB, Sundt T, Leacche M, et al; SPEAR Working Group. Outcomes after surgical pulmonary embolectomy for acute pulmonary embolus: a multi-institutional study. Ann Thorac Surg 2016; 102:1498–1502.
- Kaufman JA, Kinney TB, Streiff MB, et al. Guidelines for the use of retrievable and convertible vena cava filters: report from the Society of Interventional Radiology multidisciplinary consensus conference. J Vasc Interv Radiol 2006; 17:449–459.
- Kyrle PA, Rosendaal FR, Eichinger S. Risk assessment for recurrent venous thrombosis. Lancet 2010; 376:2032–2039.
- Heit JA. Predicting the risk of venous thromboembolism recurrence. Am J Hematol 2012; 87(suppl 1):S63–S67.
- Becattini C, Agnelli G, Schenone A, et al; WARFASA Investigators. Aspirin for preventing the recurrence of venous thromboembolism. N Engl J Med 2012; 366:1959–1967.
- Brighton TA, Eikelboom JW, Mann K, et al; ASPIRE Investigators. Low-dose aspirin for preventing recurrent venous thromboembolism. N Engl J Med 2012; 367:1979–1987.
- Carrier M, Rodger MA, Wells PS, Righini M, LE Gal G. Residual vein obstruction to predict the risk of recurrent venous thromboembolism in patients with deep vein thrombosis: a systematic review and meta-analysis. J Thromb Haemost 2011; 9:1119–1125.
- Siragusa S, Malato A, Saccullo G, et al. Residual vein thrombosis for assessing duration of anticoagulation after unprovoked deep vein thrombosis of the lower limbs: the extended DACUS study. Am J Hematol 2011; 86:914–917.
- Tosetto A, Iorio A, Marcucci M, et al. Predicting disease recurrence in patients with previous unprovoked venous thromboembolism: a proposed prediction score (DASH). J Thromb Haemost 2012; 10:1019–1025.
- Tosetto A, Testa S, Martinelli I, et al. External validation of the DASH prediction rule: a retrospective cohort study. J Thromb Haemost 2017; 15:1963–1970.
- Rodger MA, Kahn SR, Wells PS, et al. Identifying unprovoked thromboembolism patients at low risk for recurrence who can discontinue anticoagulant therapy. CMAJ 2008; 179:417–426.
- Eichinger S, Heinze G, Jandeck LM, Kyrle PA. Risk assessment of recurrence in patients with unprovoked deep vein thrombosis or pulmonary embolism: the Vienna prediction model. Circulation 2010; 121:1630–1636.
- Heit JA, O’Fallon WM, Petterson TM, et al. Relative impact of risk factors for deep vein thrombosis and pulmonary embolism: a population-based study. Arch Intern Med 2002; 162:1245–1248.
- Dentali F, Douketis JD, Gianni M, Lim W, Crowther MA. Meta-analysis: anticoagulant prophylaxis to prevent symptomatic venous thromboembolism in hospitalized medical patients. Ann Intern Med 2007; 146:278–288.
- Cohen AT, Harrington RA, Goldhaber SZ, et al; APEX Investigators. Extended thromboprophylaxis with betrixaban in acutely ill medical patients. N Engl J Med 2016; 375:534–544.
KEY POINTS
- VTE treatment should begin immediately with heparin, low-molecular-weight heparin (LMWH), fondaparinux, or the DOACs (rivaroxaban or apixaban) in patients deemed appropriate based on a risk assessment for bleeding.
- For patients with VTE and no cancer, long-term treatment with dabigatran, rivaroxaban, apixaban, or edoxaban is recommended over the vitamin K antagonists (VKA).
- LMWH is recommended for the long-term treatment of VTE in patients with cancer.
- For extended-duration anticoagulation, the DOACs (dabigatran, rivaroxaban and apixaban) and the VKA antagonists are options.
- Compression stockings are no longer recommended for prevention of PTS in patients with acute DVT but may be beneficial symptomatically.
Cardiac implantable electronic device infection
Cardiac implantable electronic devices (CIEDs) have become common tools to improve the quality of life and longevity of patients with cardiac disease over the last few decades.1–4 CIEDs include implantable cardioverter defibrillators (ICDs), permanent pacemakers, biventricular pacemakers providing cardiac resynchronization therapy with or without a defibrillator, subcutaneous ICDs, and implantable loop recorders. With increasing approved indications, the number of CIEDs implanted each year continues to grow. This, paired with the aging population of patients receiving devices and their medical complexity, has led to a corresponding increase in device-related complications.2,3 One of the most serious complications is CIED infection, which leads to significant morbidity and death. These infections also represent a significant cost burden to the healthcare system, with treatment costs for a CIED infection estimated at over $146,000 in 2008.5
SCOPE OF THE PROBLEM
More than half a million permanent pacemakers and ICDs are implanted each year in the United States, with more than 4 million implanted between 1993 and 2008.5 The risk of infection is 0.5% to 1%, for a first-time implantation and 1% to 5% for a device replacement or upgrade.1,2,5–9 These infections can involve the generator pocket, bloodstream, or cardiac structures, leading to infective endocarditis.10 The timing of CIED infection appears to be bimodal in distribution: early infections usually occur as a result of the implantation procedure itself, whereas late infections occur in patients who are generally unwell or because of an insidious process that eventually crosses a threshold of clinical significance.3,11,12
Incidence and risk factors
Klug et al13 investigated the incidence rate and risk factors of CIED infection prospectively in a large cohort of patients from 44 centers who underwent CIED implantation. Of 6,319 procedures, 4,465 were first implants and the other 1,854 were a replacement or revision; 42 patients (0.68%) developed CIED infection by 12 months after the procedure, and the incidence of infection in replacement or revision cases was nearly twice the rate found in first implants.13 Risk factors for CIED infection included renal failure, heart failure, diabetes, and fever within last 24 hours before CIED implantation.14 The Implantable Cardiac Pulse Generator Replacement (REPLACE) registry found the 6-month incidence rate of CIED infection to be 1.4% after CIED replacement.6
Recently, there has been concern that the rate of newly infected CIEDs has outpaced the rate of newly implanted ones.5,15 Voigt et al15 reported a 12% increase in the rate of CIED implantation from 2004 to 2006 and an out-of-proportion 57% increase in the rate of CIED infection. A review from 2011 confirmed these findings, showing the annual CIED implantation incidence increased an average of 4.7% per year between 1993 and 2008.5 This was probably driven by clinical trials that broadened the indications for ICD implantation for primary prevention.16–19 Between 1993 and 2008, the rate of newly implanted devices increased by 96%, while the rate for newly infected CIEDs increased by 210%; the majority of this increase occurred after 2004.5 The study showed that comorbidities in patients receiving CIEDs increased sharply starting in 2004—alluding to the contribution of comorbid medical conditions such as renal failure, respiratory failure, heart failure, and diabetes to infection risk.5
However, a major obstacle to defining the true incidence rate of CIED infection is the lack of a clear denominator. CIED infection is not limited to the first few months after implantation. In fact, over half of these patients present more than 1 year after the last CIED intervention.12 Therefore, the number of patients at risk continues to grow each year and includes patients who underwent implantation that year or before, making it very difficult to compare infection rates. Additionally, the lack of a clear definition of CIED infection and the variations in duration of follow-up in different studies make it difficult to accurately assess the incidence of CIED infection.
PATHOGENESIS
DIAGNOSIS
Prompt and accurate diagnosis of CIED infection is critical as it allows for early management with antibiotic therapy and device removal. As the number of CIED implantations increases, providers on the front lines—emergency, family practice, and internal medicine physicians—will play an increasing role in recognizing and diagnosing CIED infection. Patients with CIED infection present with a range of signs and symptoms including fever, chills, erythema, swelling, drainage, tenderness, malaise, erosion, and warmth of the skin overlying the generator pocket.2 In 55% of cases, patients present with localized pocket infection, while the remaining patients have signs of an endovascular infection without obvious pocket involvement.12 Localized pocket infection is more common during the first year after device implantation. CIED-associated endovascular infections occur more commonly in patients with multiple comorbidities including diabetes, renal failure, prior heart valve operation, rheumatic heart disease, and prior bloodstream infection.2 Despite the theoretical divide in CIED infections (endovascular vs pocket), overlap is common: many patients with pocket infection show evidence of bacteremia and vegetations on the leads.
Diagnosing pocket infection from the physical examination can be difficult due to the often subtle manifestations of the underlying pathophysiology and because visible changes to the pocket can occur over weeks and months. Furthermore, differentiating superficial infection, hematoma, seroma, and allergic reactions from deep pocket infection can be challenging. In cases when the diagnosis is not clear and there are no systemic findings of infection, conservative management with close follow-up is reasonable. Similarly, the diagnosis of endovascular infection is sometimes delayed because the symptoms are not very specific or because of a lack of awareness of the presence of a CIED and its role in endovascular infection.
MANAGEMENT
A multidisciplinary approach involving cardiology, infectious disease, electrophysiology, and cardiothoracic surgery teams is required to optimize outcomes in patients with CIED infection. CIED infection is particularly difficult to treat with antibiotic therapy alone because it involves infection of an implanted device and an associated biofilm that is resistant to the effects of antibiotics. Once infection is confirmed, antibiotic therapy serves as an adjunct to the complete removal of the hardware. Most patients receive 2 weeks of intravenous antibiotics after removal of an infected CIED, with longer courses for patients with Staphylococcus aureus infection or documented endocarditis.21
Infectious disease consultation is paramount in order to choose the appropriate type and duration of antibiotic therapy. Conservative approaches that involve using antibiotics alone or incomplete system removal have high failure rates with high rates of morbidity and mortality.13,21–28 However, chronic antibiotic suppressive therapy may be considered as a palliative measure for patients who are not candidates for lead extraction.
DEVICE REMOVAL
Confirmation of CIED infection is a class I indication for device removal and the patient should be referred to an electrophysiologist. Transvenous lead extraction (TLE) is a percutaneous procedure performed by the electrophysiologist in the electrophysiology laboratory or hybrid operating room with cardiothoracic surgery support, and it is generally performed under general anesthesia with invasive hemodynamic monitoring. After opening and debriding the infected pocket, the generator is disconnected from the leads. After the lead tips are unscrewed from the myocardium, gentle traction is applied to determine if the leads can easily be removed. If traction is unsuccessful, additional tools (both powered or mechanical sheaths) are used to complete the lead extraction29; the goal is to lyse and free the fibrotic attachments between parallel leads and between the leads and vessel wall or the myocardium. Once the lead is freed from the adhesions it can be removed safely.
REIMPLANTATION
The need for reimplantation after removal of an infected CIED should be thought about before the extraction. In general, extracting an infected CIED should be viewed as an opportunity to reassess the need for the device. Almost one-third of patients who undergo extraction of infected CIED do not require immediate reimplantation.2 This could be due to reversal of the initial indication, emergence of new clinical conditions, patient preference, or the lack of an absolute indication. If reimplantation is necessary, the new device is typically placed on the opposite side of the chest from the previously infected pocket site after blood cultures are negative for at least 72 hours.21
CIED INFECTION MORTALITY
Despite proper management with CIED removal supported by antibiotic therapy, CIED infection carries a high risk of death. The 30-day mortality is estimated to be between 5% and 6%.33 In a large case series of 412 CIED extractions, there were 19 in-hospital deaths. Of these 19 deaths, 2 were related to the extraction itself with the other 17 related to sepsis, multiorgan failure, stroke, renal failure, or heart failure.2 The 1-year mortality rate is also increased for this population; recent data show 1-year mortality rates of 8% to 17% despite device removal and antibiotic therapy.2,34,35 This increased mortality rate was also demonstrated in a large cohort of Medicare patients undergoing CIED procedures.36 Medicare patients with CIED infection had double the risk of death at 1 year compared with patients without infection.36
Risk factors for death at 1 year include worse baseline functional status, renal failure, and type of infection; eg, endovascular infection carries a risk of death 2 times higher than pocket infection.37
PREVENTION
Because CIED infection carries significant short-term and long-term mortality rates despite optimal management, the best strategy is prevention. Preventing CIED infection begins with the decision to implant a device with careful assessment of the indication, the timing of the procedure, and the patient’s clinical status. CIED procedures are performed under strict sterile surgical techniques with great attention to the incision and proper closure. Surgical data favor the use of chlorhexidine-alcohol solutions for skin preparation compared with povidone-iodine solutions to prevent both superficial and deep surgical wound infections.38 However, recent studies showed no significant difference between the 2 preparation methods in reducing rates of CIED infection.39,40 In individuals colonized with S aureus, the risk of CIED infection can be reduced using a body wash containing chlorhexidine and a nasal spray containing mupirocin.41,42
Preoperative antibiotics
The use of preoperative antibiotics has been shown to reduce the risk of infection.43 In a large prospective cohort of patients undergoing a de novo or secondary CIED procedure, the use of perioperative antibiotics was negatively associated with the risk of CIED infection.13 This was later confirmed by a double-blind randomized trial of 1,000 patients undergoing permanent pacemaker or ICD initial implantation or generator replacement. This study was stopped prematurely as the use of antibiotics was clearly associated with a lower risk of CIED infection.44 Therefore, prophylaxis with an antibiotic active against staphylococci before the incision is made is a class I indication to prevent infection.1
Currently, no data support giving prophylactic antibiotics after the procedure; however, the Prevention of Arrhythmia Device Infection Trial (PADIT) is currently comparing the risk of infection with conventional preoperative antibiotics vs a regimen of pre- and post-procedure antibiotics (clinicaltrial.gov: NCT01628666).
Hemostasis
Adequate hemostasis is critical, since the risk of CIED infection is 7 times greater with formation of a hematoma.45 Heparin products, especially low-molecular-weight heparin, should be avoided at the time of CIED implantation. In patients at high risk for thromboembolism who are on warfarin therapy, the continuation of warfarin is associated with a lower incidence of hematoma compared with bridging with heparin in patients undergoing CIED procedures.46 Therefore, if anticoagulation can be withheld, it is better to stop the anticoagulant before the procedure. When this is not possible or when it carries significant risk (eg, a patient with a mechanical mitral valve who needs a CIED implantation), it is better to maintain the patient on warfarin therapy with a therapeutic international normalized ratio rather than bridging with heparin products.
Antibacterial envelop and new devices
CONCLUSION
CIED infection is a major complication that carries significant risk of morbidity and death. Early diagnosis and referral to a multidisciplinary treatment team is crucial to increasing the possibility of a cure. While device extraction has risks, it is nevertheless typically required for complete resolution of the infection. Large clinical trials are under way to address current knowledge gaps about CIED infection, including our understanding of the true incidence rate, risk factors, and efficacy of various implantation techniques. Future trends to minimize the risk of CIED infection include better screening, better diagnostic tools, new devices with fewer or no leads, longer battery life to minimize the need for additional procedures, and the use of supportive tools and products to minimize the risk of infection.
- Baddour LM, Epstein AE, Erickson CC, et al; American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Nursing; Council on Clinical Cardiology; and the Interdisciplinary Council on Quality of Care and Outcomes Research. Update on cardiovascular implantable electronic device infections and their management: a scientific statement from the American Heart Association. Circulation 2010; 121:458–477.
- Tarakji KG, Chan EJ, Cantillon DJ, et al. Cardiac implantable electronic device infections: presentation, management, and patient outcomes. Heart Rhythm 2010; 7:1043–1047.
- Baddour LM. Cardiac device infection—or not. Circulation 2010; 121:1686–1687.
- Kusumoto FM, Schoenfeld MH, Wilkoff BL, et al. 2017 HRS expert consensus statement on cardiovascular implantable electronic device lead management and extraction. Heart Rhythm 2017; Sept 15. pii: S1547-5271(17)31080-9. doi:10.1016/j.hrthm.2017.09.001. [Epub ahead of print]
- Greenspon AJ, Patel JD, Lau E, et al. 16-Year trends in the infection burden for pacemakers and implantable cardioverter-defibrillators in the United States: 1993 to 2008. J Am Coll Cardiol 2011; 58:1001–1006.
- Poole JE, Gleva MJ, Mela T, et al; REPLACE Registry Investigators. Complication rates associated with pacemaker or implantable cardioverter-defibrillator generator replacements and upgrade procedures: results from the REPLACE registry. Circulation 2010; 122:1553–1561.
- Mela T, McGovern BA, Garan H, et al. Long-term infection rates associated with the pectoral versus abdominal approach to cardioverter-defibrillator implants. Am J Cardiol 2001; 88:750–753.
- de Bie MK, van Rees JB, Thijssen J, et al. Cardiac device infections are associated with a significant mortality risk. Heart Rhythm 2012; 9:494–498.
- Polyzos KA, Konstantelias AA, Falagas ME. Risk factors for cardiac implantable electronic device infection: a systematic review and meta-analysis. Europace 2015; 17:767–777.
- Deharo J-C, Quatre A, Mancini J, et al. Long-term outcomes following infection of cardiac implantable electronic devices: a prospective matched cohort study. Heart 2012; 98:724–731.
- Sohail MR, Hussain S, Le KY, et al; Mayo Cardiovascular Infections Study Group. Risk factors associated with early- versus late-onset implantable cardioverter-defibrillator infections. J Interv Card Electrophysiol 2011; 31:171–183.
- Hussein AA, Baghdy Y, Wazni OM, et al. Microbiology of cardiac implantable electronic device infections. JACC Clin Electrophysiol 2016; 2:498–505.
- Klug D, Balde M, Pavin D, et al; PEOPLE Study Group. Risk factors related to infections of implanted pacemakers and cardioverter-defibrillators: results of a large prospective study. Circulation 2007; 116:1349–1355.
- Tarakji KG, Wilkoff BL. Management of cardiac implantable electronic device infections: the challenges of understanding the scope of the problem and its associated mortality. Expert Rev Cardiovasc Ther 2013; 11:607–616.
- Voigt A, Shalaby A, Saba S. Continued rise in rates of cardiovascular implantable electronic device infections in the United States: temporal trends and causative insights. Pacing Clin Electrophysiol 2010; 33:414–419.
- Bardy GH, Lee KL, Mark DB, et al; Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 2005; 352:225–237.
- Moss AJ, Zareba W, Hall WJ, et al; Multicenter Automatic Defibrillator Implantation Trial II Investigators. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 2002; 346:877–883.
- Kadish A, Dyer A, Daubert JP, et al; Defibrillators in Non-Ischemic Cardiomyopathy Treatment Evaluation (DEFINITE) Investigators. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med 2004; 350:2151–2158.
- Buxton AE, Lee KL, Fisher JD, Josephson ME, Prystowsky EN, Hafley G; Multicenter Unsustained Tachycardia Trial Investigators. A randomized study of the prevention of sudden death in patients with coronary artery disease. N Engl J Med 1999; 341:1882–1890.
- Abdulmassih R, Makadia J, Como J, Paulson M, Min Z, Bhanot N. Propionibacterium acnes: Time-to-positivity in standard bacterial culture from different anatomical sites. J Clin Med Res 2016; 8:916–918.
- Sohail MR, Uslan DZ, Khan AH, et al. Management and outcome of permanent pacemaker and implantable cardioverter-defibrillator infections. J Am Coll Cardiol 2007; 49:1851–1859.
- Cacoub P, Leprince P, Nataf P, et al. Pacemaker infective endocarditis. Am J Cardiol 1998; 82:480–484.
- Chua JD, Wilkoff BL, Lee I, Juratli N, Longworth DL, Gordon SM. Diagnosis and management of infections involving implantable electrophysiologic cardiac devices. Ann Intern Med 2000; 133:604–608.
- Bracke FA, Meijer A, van Gelder LM. Pacemaker lead complications: when is extraction appropriate and what can we learn from published data? Heart 2001; 85:254–259.
- Camus C, Leport C, Raffi F, Michelet C, Cartier F, Vilde JL. Sustained bacteremia in 26 patients with a permanent endocardial pacemaker: assessment of wire removal. Clin Infect Dis 1993; 17:46–55.
- Molina JE. Undertreatment and overtreatment of patients with infected antiarrhythmic implantable devices. Ann Thorac Surg 1997; 63:504–509.
- Viganego F, O’Donoghue S, Eldadah Z, et al. Effect of early diagnosis and treatment with percutaneous lead extraction on survival in patients with cardiac device infections. Am J Cardiol 2012; 109:1466–1471.
- Le KY, Sohail MR, Friedman PA, et al; Mayo Cardiovascular Infections Study Group. Impact of timing of device removal on mortality in patients with cardiovascular implantable electronic device infections. Heart Rhythm 2011; 8:1678–1685.
- Wazni O, Wilkoff BL. Considerations for cardiac device lead extraction. Nat Rev Cardiol 2016; 13:221–229.
- Brunner MP, Cronin EM, Duarte VE, et al. Clinical predictors of adverse patient outcomes in an experience of more than 5000 chronic endovascular pacemaker and defibrillator lead extractions. Heart Rhythm 2014; 11:799–805.
- Wazni O, Epstein LM, Carrillo RG, et al. Lead extraction in the contemporary setting: the LExICon study: an observational retrospective study of consecutive laser lead extractions. J Am Coll Cardiol 2010; 55:579–586.
- Brunner MP, Cronin EM, Wazni O, et al. Outcomes of patients requiring emergent surgical or endovascular intervention for catastrophic complications during transvenous lead extraction. Heart Rhythm 2014; 11:419–425.
- Habib A, Le KY, Baddour LM, et al; for the Mayo Cardiovascular Infections Study Group. Predictors of mortality in patients with cardiovascular implantable electronic device infections. Am J Cardiol 2013; 111:874–879.
- Baman TS, Gupta SK, Valle JA, Yamada E. Risk factors for mortality in patients with cardiac device-related infection. Circ Arrhythm Electrophysiol 2009; 2:129–134.
- Deckx S, Marynissen T, Rega F, et al. Predictors of 30-day and 1-year mortality after transvenous lead extraction: a single-centre experience. Europace 2014; 16:1218–1225.
- Sohail MR, Henrikson CA, Braid-Forbes MJ, Forbes KF, Lerner DJ. Increased long-term mortality in patients with cardiovascular implantable electronic device infections. Pacing Clin Electrophysiol 2015; 38:231–239.
- Tarakji KG, Wazni OM, Harb S, Hsu A, Saliba W, Wilkoff BL. Risk factors for 1-year mortality among patients with cardiac implantable electronic device infection undergoing transvenous lead extraction: the impact of the infection type and the presence of vegetation on survival. Europace 2014; 16:1490–1495.
- Darouiche RO, Wall MJ Jr., Itani KM, et al. Chlorhexidine—alcohol versus povidone—iodine for surgical-site antisepsis. N Engl J Med 2010; 362:18–26.
- Qintar M, Zardkoohi O, Hammadah M, et al. The impact of changing antiseptic skin preparation agent used for cardiac implantable electronic device (CIED) procedures on the risk of infection. Pacing Clin Electrophysiol 2015; 38:240–246.
- Da Costa A, Tulane C, Dauphinot V, et al. Preoperative skin antiseptics for prevention of cardiac implantable electronic device infections: a historical-controlled interventional trial comparing aqueous against alcoholic povidone-iodine solutions. Europace 2015; 17:1092–1098.
- Padfield GJ, Steinberg C, Bennett MT, et al. Preventing cardiac implantable electronic device infections. Heart Rhythm 2015; 12:2344–2356.
- Bode LGM, Kluytmans JAJW, Wertheim HFL, et al. Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med 2010; 362:9–17.
- Da Costa A, Kirkorian G, Cucherat M, et al. Antibiotic prophylaxis for permanent pacemaker implantation: a meta-analysis. Circulation 1998; 97:1796–1801.
- de Oliveira JC, Martinelli M, Nishioka SADO, et al. Efficacy of antibiotic prophylaxis before the implantation of pacemakers and cardioverter-defibrillators: results of a large, prospective, randomized, double-blinded, placebo-controlled trial. Circ Arrhythm Electrophysiol 2009; 2:29–34.
- Essebag V, Verma A, Healey JS, et al; BRUISE CONTROL Investigators. Clinically significant pocket hematoma increases long-term risk of device infection: BRUISE CONTROL INFECTION study. J Am Coll Cardiol 2016; 67:1300–1308.
- Birnie DH, Healey JS, Wells GA, et al; BRUISE CONTROL Investigators. Pacemaker or defibrillator surgery without interruption of anticoagulation. N Engl J Med 2013; 368:2084–2093.
- Henrikson CA, Sohail MR, Acosta H, et al. Antibacterial envelope is associated with low infection rates after implantable cardioverter-defibrillator and cardiac resynchronization therapy device replacement: results of the Citadel and Centurion studies. 2017 http://dx.doi.org/10.1016/j.jacep.2017.02.016
- Mittal S, Shaw RE, Michel K, et al. Cardiac implantable electronic device infections: incidence, risk factors, and the effect of the AigisRx antibacterial envelope. Heart Rhythm 2014; 11:595–601.
- Tarakji KG, Mittal S, Kennergren C, et al. Worldwide Randomized Antibiotic EnveloPe Infection PrevenTion Trial (WRAP-IT). Am Heart J 2016; 180:12–B21.
- Burke MC, Gold MR, Knight BP, et al. Safety and efficacy of the totally subcutaneous implantable defibrillator: 2-year results from a pooled analysis of the IDE study and EFFORTLESS registry. J Am Coll Cardiol 2015; 65:1605–1615.
- Reddy VY, Exner DV, Cantillon DJ, et al; LEADLESS II Study Investigators. Percutaneous implantation of an entirely intracardiac leadless pacemaker. N Engl J Med 2015; 373:1125–1135.
- Reynolds D, Duray GZ, Omar R, et al; Micra Transcatheter Pacing Study Group. A leadless intracardiac transcatheter pacing system. N Engl J Med 2016; 374:533–541.
Cardiac implantable electronic devices (CIEDs) have become common tools to improve the quality of life and longevity of patients with cardiac disease over the last few decades.1–4 CIEDs include implantable cardioverter defibrillators (ICDs), permanent pacemakers, biventricular pacemakers providing cardiac resynchronization therapy with or without a defibrillator, subcutaneous ICDs, and implantable loop recorders. With increasing approved indications, the number of CIEDs implanted each year continues to grow. This, paired with the aging population of patients receiving devices and their medical complexity, has led to a corresponding increase in device-related complications.2,3 One of the most serious complications is CIED infection, which leads to significant morbidity and death. These infections also represent a significant cost burden to the healthcare system, with treatment costs for a CIED infection estimated at over $146,000 in 2008.5
SCOPE OF THE PROBLEM
More than half a million permanent pacemakers and ICDs are implanted each year in the United States, with more than 4 million implanted between 1993 and 2008.5 The risk of infection is 0.5% to 1%, for a first-time implantation and 1% to 5% for a device replacement or upgrade.1,2,5–9 These infections can involve the generator pocket, bloodstream, or cardiac structures, leading to infective endocarditis.10 The timing of CIED infection appears to be bimodal in distribution: early infections usually occur as a result of the implantation procedure itself, whereas late infections occur in patients who are generally unwell or because of an insidious process that eventually crosses a threshold of clinical significance.3,11,12
Incidence and risk factors
Klug et al13 investigated the incidence rate and risk factors of CIED infection prospectively in a large cohort of patients from 44 centers who underwent CIED implantation. Of 6,319 procedures, 4,465 were first implants and the other 1,854 were a replacement or revision; 42 patients (0.68%) developed CIED infection by 12 months after the procedure, and the incidence of infection in replacement or revision cases was nearly twice the rate found in first implants.13 Risk factors for CIED infection included renal failure, heart failure, diabetes, and fever within last 24 hours before CIED implantation.14 The Implantable Cardiac Pulse Generator Replacement (REPLACE) registry found the 6-month incidence rate of CIED infection to be 1.4% after CIED replacement.6
Recently, there has been concern that the rate of newly infected CIEDs has outpaced the rate of newly implanted ones.5,15 Voigt et al15 reported a 12% increase in the rate of CIED implantation from 2004 to 2006 and an out-of-proportion 57% increase in the rate of CIED infection. A review from 2011 confirmed these findings, showing the annual CIED implantation incidence increased an average of 4.7% per year between 1993 and 2008.5 This was probably driven by clinical trials that broadened the indications for ICD implantation for primary prevention.16–19 Between 1993 and 2008, the rate of newly implanted devices increased by 96%, while the rate for newly infected CIEDs increased by 210%; the majority of this increase occurred after 2004.5 The study showed that comorbidities in patients receiving CIEDs increased sharply starting in 2004—alluding to the contribution of comorbid medical conditions such as renal failure, respiratory failure, heart failure, and diabetes to infection risk.5
However, a major obstacle to defining the true incidence rate of CIED infection is the lack of a clear denominator. CIED infection is not limited to the first few months after implantation. In fact, over half of these patients present more than 1 year after the last CIED intervention.12 Therefore, the number of patients at risk continues to grow each year and includes patients who underwent implantation that year or before, making it very difficult to compare infection rates. Additionally, the lack of a clear definition of CIED infection and the variations in duration of follow-up in different studies make it difficult to accurately assess the incidence of CIED infection.
PATHOGENESIS
DIAGNOSIS
Prompt and accurate diagnosis of CIED infection is critical as it allows for early management with antibiotic therapy and device removal. As the number of CIED implantations increases, providers on the front lines—emergency, family practice, and internal medicine physicians—will play an increasing role in recognizing and diagnosing CIED infection. Patients with CIED infection present with a range of signs and symptoms including fever, chills, erythema, swelling, drainage, tenderness, malaise, erosion, and warmth of the skin overlying the generator pocket.2 In 55% of cases, patients present with localized pocket infection, while the remaining patients have signs of an endovascular infection without obvious pocket involvement.12 Localized pocket infection is more common during the first year after device implantation. CIED-associated endovascular infections occur more commonly in patients with multiple comorbidities including diabetes, renal failure, prior heart valve operation, rheumatic heart disease, and prior bloodstream infection.2 Despite the theoretical divide in CIED infections (endovascular vs pocket), overlap is common: many patients with pocket infection show evidence of bacteremia and vegetations on the leads.
Diagnosing pocket infection from the physical examination can be difficult due to the often subtle manifestations of the underlying pathophysiology and because visible changes to the pocket can occur over weeks and months. Furthermore, differentiating superficial infection, hematoma, seroma, and allergic reactions from deep pocket infection can be challenging. In cases when the diagnosis is not clear and there are no systemic findings of infection, conservative management with close follow-up is reasonable. Similarly, the diagnosis of endovascular infection is sometimes delayed because the symptoms are not very specific or because of a lack of awareness of the presence of a CIED and its role in endovascular infection.
MANAGEMENT
A multidisciplinary approach involving cardiology, infectious disease, electrophysiology, and cardiothoracic surgery teams is required to optimize outcomes in patients with CIED infection. CIED infection is particularly difficult to treat with antibiotic therapy alone because it involves infection of an implanted device and an associated biofilm that is resistant to the effects of antibiotics. Once infection is confirmed, antibiotic therapy serves as an adjunct to the complete removal of the hardware. Most patients receive 2 weeks of intravenous antibiotics after removal of an infected CIED, with longer courses for patients with Staphylococcus aureus infection or documented endocarditis.21
Infectious disease consultation is paramount in order to choose the appropriate type and duration of antibiotic therapy. Conservative approaches that involve using antibiotics alone or incomplete system removal have high failure rates with high rates of morbidity and mortality.13,21–28 However, chronic antibiotic suppressive therapy may be considered as a palliative measure for patients who are not candidates for lead extraction.
DEVICE REMOVAL
Confirmation of CIED infection is a class I indication for device removal and the patient should be referred to an electrophysiologist. Transvenous lead extraction (TLE) is a percutaneous procedure performed by the electrophysiologist in the electrophysiology laboratory or hybrid operating room with cardiothoracic surgery support, and it is generally performed under general anesthesia with invasive hemodynamic monitoring. After opening and debriding the infected pocket, the generator is disconnected from the leads. After the lead tips are unscrewed from the myocardium, gentle traction is applied to determine if the leads can easily be removed. If traction is unsuccessful, additional tools (both powered or mechanical sheaths) are used to complete the lead extraction29; the goal is to lyse and free the fibrotic attachments between parallel leads and between the leads and vessel wall or the myocardium. Once the lead is freed from the adhesions it can be removed safely.
REIMPLANTATION
The need for reimplantation after removal of an infected CIED should be thought about before the extraction. In general, extracting an infected CIED should be viewed as an opportunity to reassess the need for the device. Almost one-third of patients who undergo extraction of infected CIED do not require immediate reimplantation.2 This could be due to reversal of the initial indication, emergence of new clinical conditions, patient preference, or the lack of an absolute indication. If reimplantation is necessary, the new device is typically placed on the opposite side of the chest from the previously infected pocket site after blood cultures are negative for at least 72 hours.21
CIED INFECTION MORTALITY
Despite proper management with CIED removal supported by antibiotic therapy, CIED infection carries a high risk of death. The 30-day mortality is estimated to be between 5% and 6%.33 In a large case series of 412 CIED extractions, there were 19 in-hospital deaths. Of these 19 deaths, 2 were related to the extraction itself with the other 17 related to sepsis, multiorgan failure, stroke, renal failure, or heart failure.2 The 1-year mortality rate is also increased for this population; recent data show 1-year mortality rates of 8% to 17% despite device removal and antibiotic therapy.2,34,35 This increased mortality rate was also demonstrated in a large cohort of Medicare patients undergoing CIED procedures.36 Medicare patients with CIED infection had double the risk of death at 1 year compared with patients without infection.36
Risk factors for death at 1 year include worse baseline functional status, renal failure, and type of infection; eg, endovascular infection carries a risk of death 2 times higher than pocket infection.37
PREVENTION
Because CIED infection carries significant short-term and long-term mortality rates despite optimal management, the best strategy is prevention. Preventing CIED infection begins with the decision to implant a device with careful assessment of the indication, the timing of the procedure, and the patient’s clinical status. CIED procedures are performed under strict sterile surgical techniques with great attention to the incision and proper closure. Surgical data favor the use of chlorhexidine-alcohol solutions for skin preparation compared with povidone-iodine solutions to prevent both superficial and deep surgical wound infections.38 However, recent studies showed no significant difference between the 2 preparation methods in reducing rates of CIED infection.39,40 In individuals colonized with S aureus, the risk of CIED infection can be reduced using a body wash containing chlorhexidine and a nasal spray containing mupirocin.41,42
Preoperative antibiotics
The use of preoperative antibiotics has been shown to reduce the risk of infection.43 In a large prospective cohort of patients undergoing a de novo or secondary CIED procedure, the use of perioperative antibiotics was negatively associated with the risk of CIED infection.13 This was later confirmed by a double-blind randomized trial of 1,000 patients undergoing permanent pacemaker or ICD initial implantation or generator replacement. This study was stopped prematurely as the use of antibiotics was clearly associated with a lower risk of CIED infection.44 Therefore, prophylaxis with an antibiotic active against staphylococci before the incision is made is a class I indication to prevent infection.1
Currently, no data support giving prophylactic antibiotics after the procedure; however, the Prevention of Arrhythmia Device Infection Trial (PADIT) is currently comparing the risk of infection with conventional preoperative antibiotics vs a regimen of pre- and post-procedure antibiotics (clinicaltrial.gov: NCT01628666).
Hemostasis
Adequate hemostasis is critical, since the risk of CIED infection is 7 times greater with formation of a hematoma.45 Heparin products, especially low-molecular-weight heparin, should be avoided at the time of CIED implantation. In patients at high risk for thromboembolism who are on warfarin therapy, the continuation of warfarin is associated with a lower incidence of hematoma compared with bridging with heparin in patients undergoing CIED procedures.46 Therefore, if anticoagulation can be withheld, it is better to stop the anticoagulant before the procedure. When this is not possible or when it carries significant risk (eg, a patient with a mechanical mitral valve who needs a CIED implantation), it is better to maintain the patient on warfarin therapy with a therapeutic international normalized ratio rather than bridging with heparin products.
Antibacterial envelop and new devices
CONCLUSION
CIED infection is a major complication that carries significant risk of morbidity and death. Early diagnosis and referral to a multidisciplinary treatment team is crucial to increasing the possibility of a cure. While device extraction has risks, it is nevertheless typically required for complete resolution of the infection. Large clinical trials are under way to address current knowledge gaps about CIED infection, including our understanding of the true incidence rate, risk factors, and efficacy of various implantation techniques. Future trends to minimize the risk of CIED infection include better screening, better diagnostic tools, new devices with fewer or no leads, longer battery life to minimize the need for additional procedures, and the use of supportive tools and products to minimize the risk of infection.
Cardiac implantable electronic devices (CIEDs) have become common tools to improve the quality of life and longevity of patients with cardiac disease over the last few decades.1–4 CIEDs include implantable cardioverter defibrillators (ICDs), permanent pacemakers, biventricular pacemakers providing cardiac resynchronization therapy with or without a defibrillator, subcutaneous ICDs, and implantable loop recorders. With increasing approved indications, the number of CIEDs implanted each year continues to grow. This, paired with the aging population of patients receiving devices and their medical complexity, has led to a corresponding increase in device-related complications.2,3 One of the most serious complications is CIED infection, which leads to significant morbidity and death. These infections also represent a significant cost burden to the healthcare system, with treatment costs for a CIED infection estimated at over $146,000 in 2008.5
SCOPE OF THE PROBLEM
More than half a million permanent pacemakers and ICDs are implanted each year in the United States, with more than 4 million implanted between 1993 and 2008.5 The risk of infection is 0.5% to 1%, for a first-time implantation and 1% to 5% for a device replacement or upgrade.1,2,5–9 These infections can involve the generator pocket, bloodstream, or cardiac structures, leading to infective endocarditis.10 The timing of CIED infection appears to be bimodal in distribution: early infections usually occur as a result of the implantation procedure itself, whereas late infections occur in patients who are generally unwell or because of an insidious process that eventually crosses a threshold of clinical significance.3,11,12
Incidence and risk factors
Klug et al13 investigated the incidence rate and risk factors of CIED infection prospectively in a large cohort of patients from 44 centers who underwent CIED implantation. Of 6,319 procedures, 4,465 were first implants and the other 1,854 were a replacement or revision; 42 patients (0.68%) developed CIED infection by 12 months after the procedure, and the incidence of infection in replacement or revision cases was nearly twice the rate found in first implants.13 Risk factors for CIED infection included renal failure, heart failure, diabetes, and fever within last 24 hours before CIED implantation.14 The Implantable Cardiac Pulse Generator Replacement (REPLACE) registry found the 6-month incidence rate of CIED infection to be 1.4% after CIED replacement.6
Recently, there has been concern that the rate of newly infected CIEDs has outpaced the rate of newly implanted ones.5,15 Voigt et al15 reported a 12% increase in the rate of CIED implantation from 2004 to 2006 and an out-of-proportion 57% increase in the rate of CIED infection. A review from 2011 confirmed these findings, showing the annual CIED implantation incidence increased an average of 4.7% per year between 1993 and 2008.5 This was probably driven by clinical trials that broadened the indications for ICD implantation for primary prevention.16–19 Between 1993 and 2008, the rate of newly implanted devices increased by 96%, while the rate for newly infected CIEDs increased by 210%; the majority of this increase occurred after 2004.5 The study showed that comorbidities in patients receiving CIEDs increased sharply starting in 2004—alluding to the contribution of comorbid medical conditions such as renal failure, respiratory failure, heart failure, and diabetes to infection risk.5
However, a major obstacle to defining the true incidence rate of CIED infection is the lack of a clear denominator. CIED infection is not limited to the first few months after implantation. In fact, over half of these patients present more than 1 year after the last CIED intervention.12 Therefore, the number of patients at risk continues to grow each year and includes patients who underwent implantation that year or before, making it very difficult to compare infection rates. Additionally, the lack of a clear definition of CIED infection and the variations in duration of follow-up in different studies make it difficult to accurately assess the incidence of CIED infection.
PATHOGENESIS
DIAGNOSIS
Prompt and accurate diagnosis of CIED infection is critical as it allows for early management with antibiotic therapy and device removal. As the number of CIED implantations increases, providers on the front lines—emergency, family practice, and internal medicine physicians—will play an increasing role in recognizing and diagnosing CIED infection. Patients with CIED infection present with a range of signs and symptoms including fever, chills, erythema, swelling, drainage, tenderness, malaise, erosion, and warmth of the skin overlying the generator pocket.2 In 55% of cases, patients present with localized pocket infection, while the remaining patients have signs of an endovascular infection without obvious pocket involvement.12 Localized pocket infection is more common during the first year after device implantation. CIED-associated endovascular infections occur more commonly in patients with multiple comorbidities including diabetes, renal failure, prior heart valve operation, rheumatic heart disease, and prior bloodstream infection.2 Despite the theoretical divide in CIED infections (endovascular vs pocket), overlap is common: many patients with pocket infection show evidence of bacteremia and vegetations on the leads.
Diagnosing pocket infection from the physical examination can be difficult due to the often subtle manifestations of the underlying pathophysiology and because visible changes to the pocket can occur over weeks and months. Furthermore, differentiating superficial infection, hematoma, seroma, and allergic reactions from deep pocket infection can be challenging. In cases when the diagnosis is not clear and there are no systemic findings of infection, conservative management with close follow-up is reasonable. Similarly, the diagnosis of endovascular infection is sometimes delayed because the symptoms are not very specific or because of a lack of awareness of the presence of a CIED and its role in endovascular infection.
MANAGEMENT
A multidisciplinary approach involving cardiology, infectious disease, electrophysiology, and cardiothoracic surgery teams is required to optimize outcomes in patients with CIED infection. CIED infection is particularly difficult to treat with antibiotic therapy alone because it involves infection of an implanted device and an associated biofilm that is resistant to the effects of antibiotics. Once infection is confirmed, antibiotic therapy serves as an adjunct to the complete removal of the hardware. Most patients receive 2 weeks of intravenous antibiotics after removal of an infected CIED, with longer courses for patients with Staphylococcus aureus infection or documented endocarditis.21
Infectious disease consultation is paramount in order to choose the appropriate type and duration of antibiotic therapy. Conservative approaches that involve using antibiotics alone or incomplete system removal have high failure rates with high rates of morbidity and mortality.13,21–28 However, chronic antibiotic suppressive therapy may be considered as a palliative measure for patients who are not candidates for lead extraction.
DEVICE REMOVAL
Confirmation of CIED infection is a class I indication for device removal and the patient should be referred to an electrophysiologist. Transvenous lead extraction (TLE) is a percutaneous procedure performed by the electrophysiologist in the electrophysiology laboratory or hybrid operating room with cardiothoracic surgery support, and it is generally performed under general anesthesia with invasive hemodynamic monitoring. After opening and debriding the infected pocket, the generator is disconnected from the leads. After the lead tips are unscrewed from the myocardium, gentle traction is applied to determine if the leads can easily be removed. If traction is unsuccessful, additional tools (both powered or mechanical sheaths) are used to complete the lead extraction29; the goal is to lyse and free the fibrotic attachments between parallel leads and between the leads and vessel wall or the myocardium. Once the lead is freed from the adhesions it can be removed safely.
REIMPLANTATION
The need for reimplantation after removal of an infected CIED should be thought about before the extraction. In general, extracting an infected CIED should be viewed as an opportunity to reassess the need for the device. Almost one-third of patients who undergo extraction of infected CIED do not require immediate reimplantation.2 This could be due to reversal of the initial indication, emergence of new clinical conditions, patient preference, or the lack of an absolute indication. If reimplantation is necessary, the new device is typically placed on the opposite side of the chest from the previously infected pocket site after blood cultures are negative for at least 72 hours.21
CIED INFECTION MORTALITY
Despite proper management with CIED removal supported by antibiotic therapy, CIED infection carries a high risk of death. The 30-day mortality is estimated to be between 5% and 6%.33 In a large case series of 412 CIED extractions, there were 19 in-hospital deaths. Of these 19 deaths, 2 were related to the extraction itself with the other 17 related to sepsis, multiorgan failure, stroke, renal failure, or heart failure.2 The 1-year mortality rate is also increased for this population; recent data show 1-year mortality rates of 8% to 17% despite device removal and antibiotic therapy.2,34,35 This increased mortality rate was also demonstrated in a large cohort of Medicare patients undergoing CIED procedures.36 Medicare patients with CIED infection had double the risk of death at 1 year compared with patients without infection.36
Risk factors for death at 1 year include worse baseline functional status, renal failure, and type of infection; eg, endovascular infection carries a risk of death 2 times higher than pocket infection.37
PREVENTION
Because CIED infection carries significant short-term and long-term mortality rates despite optimal management, the best strategy is prevention. Preventing CIED infection begins with the decision to implant a device with careful assessment of the indication, the timing of the procedure, and the patient’s clinical status. CIED procedures are performed under strict sterile surgical techniques with great attention to the incision and proper closure. Surgical data favor the use of chlorhexidine-alcohol solutions for skin preparation compared with povidone-iodine solutions to prevent both superficial and deep surgical wound infections.38 However, recent studies showed no significant difference between the 2 preparation methods in reducing rates of CIED infection.39,40 In individuals colonized with S aureus, the risk of CIED infection can be reduced using a body wash containing chlorhexidine and a nasal spray containing mupirocin.41,42
Preoperative antibiotics
The use of preoperative antibiotics has been shown to reduce the risk of infection.43 In a large prospective cohort of patients undergoing a de novo or secondary CIED procedure, the use of perioperative antibiotics was negatively associated with the risk of CIED infection.13 This was later confirmed by a double-blind randomized trial of 1,000 patients undergoing permanent pacemaker or ICD initial implantation or generator replacement. This study was stopped prematurely as the use of antibiotics was clearly associated with a lower risk of CIED infection.44 Therefore, prophylaxis with an antibiotic active against staphylococci before the incision is made is a class I indication to prevent infection.1
Currently, no data support giving prophylactic antibiotics after the procedure; however, the Prevention of Arrhythmia Device Infection Trial (PADIT) is currently comparing the risk of infection with conventional preoperative antibiotics vs a regimen of pre- and post-procedure antibiotics (clinicaltrial.gov: NCT01628666).
Hemostasis
Adequate hemostasis is critical, since the risk of CIED infection is 7 times greater with formation of a hematoma.45 Heparin products, especially low-molecular-weight heparin, should be avoided at the time of CIED implantation. In patients at high risk for thromboembolism who are on warfarin therapy, the continuation of warfarin is associated with a lower incidence of hematoma compared with bridging with heparin in patients undergoing CIED procedures.46 Therefore, if anticoagulation can be withheld, it is better to stop the anticoagulant before the procedure. When this is not possible or when it carries significant risk (eg, a patient with a mechanical mitral valve who needs a CIED implantation), it is better to maintain the patient on warfarin therapy with a therapeutic international normalized ratio rather than bridging with heparin products.
Antibacterial envelop and new devices
CONCLUSION
CIED infection is a major complication that carries significant risk of morbidity and death. Early diagnosis and referral to a multidisciplinary treatment team is crucial to increasing the possibility of a cure. While device extraction has risks, it is nevertheless typically required for complete resolution of the infection. Large clinical trials are under way to address current knowledge gaps about CIED infection, including our understanding of the true incidence rate, risk factors, and efficacy of various implantation techniques. Future trends to minimize the risk of CIED infection include better screening, better diagnostic tools, new devices with fewer or no leads, longer battery life to minimize the need for additional procedures, and the use of supportive tools and products to minimize the risk of infection.
- Baddour LM, Epstein AE, Erickson CC, et al; American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Nursing; Council on Clinical Cardiology; and the Interdisciplinary Council on Quality of Care and Outcomes Research. Update on cardiovascular implantable electronic device infections and their management: a scientific statement from the American Heart Association. Circulation 2010; 121:458–477.
- Tarakji KG, Chan EJ, Cantillon DJ, et al. Cardiac implantable electronic device infections: presentation, management, and patient outcomes. Heart Rhythm 2010; 7:1043–1047.
- Baddour LM. Cardiac device infection—or not. Circulation 2010; 121:1686–1687.
- Kusumoto FM, Schoenfeld MH, Wilkoff BL, et al. 2017 HRS expert consensus statement on cardiovascular implantable electronic device lead management and extraction. Heart Rhythm 2017; Sept 15. pii: S1547-5271(17)31080-9. doi:10.1016/j.hrthm.2017.09.001. [Epub ahead of print]
- Greenspon AJ, Patel JD, Lau E, et al. 16-Year trends in the infection burden for pacemakers and implantable cardioverter-defibrillators in the United States: 1993 to 2008. J Am Coll Cardiol 2011; 58:1001–1006.
- Poole JE, Gleva MJ, Mela T, et al; REPLACE Registry Investigators. Complication rates associated with pacemaker or implantable cardioverter-defibrillator generator replacements and upgrade procedures: results from the REPLACE registry. Circulation 2010; 122:1553–1561.
- Mela T, McGovern BA, Garan H, et al. Long-term infection rates associated with the pectoral versus abdominal approach to cardioverter-defibrillator implants. Am J Cardiol 2001; 88:750–753.
- de Bie MK, van Rees JB, Thijssen J, et al. Cardiac device infections are associated with a significant mortality risk. Heart Rhythm 2012; 9:494–498.
- Polyzos KA, Konstantelias AA, Falagas ME. Risk factors for cardiac implantable electronic device infection: a systematic review and meta-analysis. Europace 2015; 17:767–777.
- Deharo J-C, Quatre A, Mancini J, et al. Long-term outcomes following infection of cardiac implantable electronic devices: a prospective matched cohort study. Heart 2012; 98:724–731.
- Sohail MR, Hussain S, Le KY, et al; Mayo Cardiovascular Infections Study Group. Risk factors associated with early- versus late-onset implantable cardioverter-defibrillator infections. J Interv Card Electrophysiol 2011; 31:171–183.
- Hussein AA, Baghdy Y, Wazni OM, et al. Microbiology of cardiac implantable electronic device infections. JACC Clin Electrophysiol 2016; 2:498–505.
- Klug D, Balde M, Pavin D, et al; PEOPLE Study Group. Risk factors related to infections of implanted pacemakers and cardioverter-defibrillators: results of a large prospective study. Circulation 2007; 116:1349–1355.
- Tarakji KG, Wilkoff BL. Management of cardiac implantable electronic device infections: the challenges of understanding the scope of the problem and its associated mortality. Expert Rev Cardiovasc Ther 2013; 11:607–616.
- Voigt A, Shalaby A, Saba S. Continued rise in rates of cardiovascular implantable electronic device infections in the United States: temporal trends and causative insights. Pacing Clin Electrophysiol 2010; 33:414–419.
- Bardy GH, Lee KL, Mark DB, et al; Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 2005; 352:225–237.
- Moss AJ, Zareba W, Hall WJ, et al; Multicenter Automatic Defibrillator Implantation Trial II Investigators. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 2002; 346:877–883.
- Kadish A, Dyer A, Daubert JP, et al; Defibrillators in Non-Ischemic Cardiomyopathy Treatment Evaluation (DEFINITE) Investigators. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med 2004; 350:2151–2158.
- Buxton AE, Lee KL, Fisher JD, Josephson ME, Prystowsky EN, Hafley G; Multicenter Unsustained Tachycardia Trial Investigators. A randomized study of the prevention of sudden death in patients with coronary artery disease. N Engl J Med 1999; 341:1882–1890.
- Abdulmassih R, Makadia J, Como J, Paulson M, Min Z, Bhanot N. Propionibacterium acnes: Time-to-positivity in standard bacterial culture from different anatomical sites. J Clin Med Res 2016; 8:916–918.
- Sohail MR, Uslan DZ, Khan AH, et al. Management and outcome of permanent pacemaker and implantable cardioverter-defibrillator infections. J Am Coll Cardiol 2007; 49:1851–1859.
- Cacoub P, Leprince P, Nataf P, et al. Pacemaker infective endocarditis. Am J Cardiol 1998; 82:480–484.
- Chua JD, Wilkoff BL, Lee I, Juratli N, Longworth DL, Gordon SM. Diagnosis and management of infections involving implantable electrophysiologic cardiac devices. Ann Intern Med 2000; 133:604–608.
- Bracke FA, Meijer A, van Gelder LM. Pacemaker lead complications: when is extraction appropriate and what can we learn from published data? Heart 2001; 85:254–259.
- Camus C, Leport C, Raffi F, Michelet C, Cartier F, Vilde JL. Sustained bacteremia in 26 patients with a permanent endocardial pacemaker: assessment of wire removal. Clin Infect Dis 1993; 17:46–55.
- Molina JE. Undertreatment and overtreatment of patients with infected antiarrhythmic implantable devices. Ann Thorac Surg 1997; 63:504–509.
- Viganego F, O’Donoghue S, Eldadah Z, et al. Effect of early diagnosis and treatment with percutaneous lead extraction on survival in patients with cardiac device infections. Am J Cardiol 2012; 109:1466–1471.
- Le KY, Sohail MR, Friedman PA, et al; Mayo Cardiovascular Infections Study Group. Impact of timing of device removal on mortality in patients with cardiovascular implantable electronic device infections. Heart Rhythm 2011; 8:1678–1685.
- Wazni O, Wilkoff BL. Considerations for cardiac device lead extraction. Nat Rev Cardiol 2016; 13:221–229.
- Brunner MP, Cronin EM, Duarte VE, et al. Clinical predictors of adverse patient outcomes in an experience of more than 5000 chronic endovascular pacemaker and defibrillator lead extractions. Heart Rhythm 2014; 11:799–805.
- Wazni O, Epstein LM, Carrillo RG, et al. Lead extraction in the contemporary setting: the LExICon study: an observational retrospective study of consecutive laser lead extractions. J Am Coll Cardiol 2010; 55:579–586.
- Brunner MP, Cronin EM, Wazni O, et al. Outcomes of patients requiring emergent surgical or endovascular intervention for catastrophic complications during transvenous lead extraction. Heart Rhythm 2014; 11:419–425.
- Habib A, Le KY, Baddour LM, et al; for the Mayo Cardiovascular Infections Study Group. Predictors of mortality in patients with cardiovascular implantable electronic device infections. Am J Cardiol 2013; 111:874–879.
- Baman TS, Gupta SK, Valle JA, Yamada E. Risk factors for mortality in patients with cardiac device-related infection. Circ Arrhythm Electrophysiol 2009; 2:129–134.
- Deckx S, Marynissen T, Rega F, et al. Predictors of 30-day and 1-year mortality after transvenous lead extraction: a single-centre experience. Europace 2014; 16:1218–1225.
- Sohail MR, Henrikson CA, Braid-Forbes MJ, Forbes KF, Lerner DJ. Increased long-term mortality in patients with cardiovascular implantable electronic device infections. Pacing Clin Electrophysiol 2015; 38:231–239.
- Tarakji KG, Wazni OM, Harb S, Hsu A, Saliba W, Wilkoff BL. Risk factors for 1-year mortality among patients with cardiac implantable electronic device infection undergoing transvenous lead extraction: the impact of the infection type and the presence of vegetation on survival. Europace 2014; 16:1490–1495.
- Darouiche RO, Wall MJ Jr., Itani KM, et al. Chlorhexidine—alcohol versus povidone—iodine for surgical-site antisepsis. N Engl J Med 2010; 362:18–26.
- Qintar M, Zardkoohi O, Hammadah M, et al. The impact of changing antiseptic skin preparation agent used for cardiac implantable electronic device (CIED) procedures on the risk of infection. Pacing Clin Electrophysiol 2015; 38:240–246.
- Da Costa A, Tulane C, Dauphinot V, et al. Preoperative skin antiseptics for prevention of cardiac implantable electronic device infections: a historical-controlled interventional trial comparing aqueous against alcoholic povidone-iodine solutions. Europace 2015; 17:1092–1098.
- Padfield GJ, Steinberg C, Bennett MT, et al. Preventing cardiac implantable electronic device infections. Heart Rhythm 2015; 12:2344–2356.
- Bode LGM, Kluytmans JAJW, Wertheim HFL, et al. Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med 2010; 362:9–17.
- Da Costa A, Kirkorian G, Cucherat M, et al. Antibiotic prophylaxis for permanent pacemaker implantation: a meta-analysis. Circulation 1998; 97:1796–1801.
- de Oliveira JC, Martinelli M, Nishioka SADO, et al. Efficacy of antibiotic prophylaxis before the implantation of pacemakers and cardioverter-defibrillators: results of a large, prospective, randomized, double-blinded, placebo-controlled trial. Circ Arrhythm Electrophysiol 2009; 2:29–34.
- Essebag V, Verma A, Healey JS, et al; BRUISE CONTROL Investigators. Clinically significant pocket hematoma increases long-term risk of device infection: BRUISE CONTROL INFECTION study. J Am Coll Cardiol 2016; 67:1300–1308.
- Birnie DH, Healey JS, Wells GA, et al; BRUISE CONTROL Investigators. Pacemaker or defibrillator surgery without interruption of anticoagulation. N Engl J Med 2013; 368:2084–2093.
- Henrikson CA, Sohail MR, Acosta H, et al. Antibacterial envelope is associated with low infection rates after implantable cardioverter-defibrillator and cardiac resynchronization therapy device replacement: results of the Citadel and Centurion studies. 2017 http://dx.doi.org/10.1016/j.jacep.2017.02.016
- Mittal S, Shaw RE, Michel K, et al. Cardiac implantable electronic device infections: incidence, risk factors, and the effect of the AigisRx antibacterial envelope. Heart Rhythm 2014; 11:595–601.
- Tarakji KG, Mittal S, Kennergren C, et al. Worldwide Randomized Antibiotic EnveloPe Infection PrevenTion Trial (WRAP-IT). Am Heart J 2016; 180:12–B21.
- Burke MC, Gold MR, Knight BP, et al. Safety and efficacy of the totally subcutaneous implantable defibrillator: 2-year results from a pooled analysis of the IDE study and EFFORTLESS registry. J Am Coll Cardiol 2015; 65:1605–1615.
- Reddy VY, Exner DV, Cantillon DJ, et al; LEADLESS II Study Investigators. Percutaneous implantation of an entirely intracardiac leadless pacemaker. N Engl J Med 2015; 373:1125–1135.
- Reynolds D, Duray GZ, Omar R, et al; Micra Transcatheter Pacing Study Group. A leadless intracardiac transcatheter pacing system. N Engl J Med 2016; 374:533–541.
- Baddour LM, Epstein AE, Erickson CC, et al; American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Nursing; Council on Clinical Cardiology; and the Interdisciplinary Council on Quality of Care and Outcomes Research. Update on cardiovascular implantable electronic device infections and their management: a scientific statement from the American Heart Association. Circulation 2010; 121:458–477.
- Tarakji KG, Chan EJ, Cantillon DJ, et al. Cardiac implantable electronic device infections: presentation, management, and patient outcomes. Heart Rhythm 2010; 7:1043–1047.
- Baddour LM. Cardiac device infection—or not. Circulation 2010; 121:1686–1687.
- Kusumoto FM, Schoenfeld MH, Wilkoff BL, et al. 2017 HRS expert consensus statement on cardiovascular implantable electronic device lead management and extraction. Heart Rhythm 2017; Sept 15. pii: S1547-5271(17)31080-9. doi:10.1016/j.hrthm.2017.09.001. [Epub ahead of print]
- Greenspon AJ, Patel JD, Lau E, et al. 16-Year trends in the infection burden for pacemakers and implantable cardioverter-defibrillators in the United States: 1993 to 2008. J Am Coll Cardiol 2011; 58:1001–1006.
- Poole JE, Gleva MJ, Mela T, et al; REPLACE Registry Investigators. Complication rates associated with pacemaker or implantable cardioverter-defibrillator generator replacements and upgrade procedures: results from the REPLACE registry. Circulation 2010; 122:1553–1561.
- Mela T, McGovern BA, Garan H, et al. Long-term infection rates associated with the pectoral versus abdominal approach to cardioverter-defibrillator implants. Am J Cardiol 2001; 88:750–753.
- de Bie MK, van Rees JB, Thijssen J, et al. Cardiac device infections are associated with a significant mortality risk. Heart Rhythm 2012; 9:494–498.
- Polyzos KA, Konstantelias AA, Falagas ME. Risk factors for cardiac implantable electronic device infection: a systematic review and meta-analysis. Europace 2015; 17:767–777.
- Deharo J-C, Quatre A, Mancini J, et al. Long-term outcomes following infection of cardiac implantable electronic devices: a prospective matched cohort study. Heart 2012; 98:724–731.
- Sohail MR, Hussain S, Le KY, et al; Mayo Cardiovascular Infections Study Group. Risk factors associated with early- versus late-onset implantable cardioverter-defibrillator infections. J Interv Card Electrophysiol 2011; 31:171–183.
- Hussein AA, Baghdy Y, Wazni OM, et al. Microbiology of cardiac implantable electronic device infections. JACC Clin Electrophysiol 2016; 2:498–505.
- Klug D, Balde M, Pavin D, et al; PEOPLE Study Group. Risk factors related to infections of implanted pacemakers and cardioverter-defibrillators: results of a large prospective study. Circulation 2007; 116:1349–1355.
- Tarakji KG, Wilkoff BL. Management of cardiac implantable electronic device infections: the challenges of understanding the scope of the problem and its associated mortality. Expert Rev Cardiovasc Ther 2013; 11:607–616.
- Voigt A, Shalaby A, Saba S. Continued rise in rates of cardiovascular implantable electronic device infections in the United States: temporal trends and causative insights. Pacing Clin Electrophysiol 2010; 33:414–419.
- Bardy GH, Lee KL, Mark DB, et al; Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 2005; 352:225–237.
- Moss AJ, Zareba W, Hall WJ, et al; Multicenter Automatic Defibrillator Implantation Trial II Investigators. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 2002; 346:877–883.
- Kadish A, Dyer A, Daubert JP, et al; Defibrillators in Non-Ischemic Cardiomyopathy Treatment Evaluation (DEFINITE) Investigators. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med 2004; 350:2151–2158.
- Buxton AE, Lee KL, Fisher JD, Josephson ME, Prystowsky EN, Hafley G; Multicenter Unsustained Tachycardia Trial Investigators. A randomized study of the prevention of sudden death in patients with coronary artery disease. N Engl J Med 1999; 341:1882–1890.
- Abdulmassih R, Makadia J, Como J, Paulson M, Min Z, Bhanot N. Propionibacterium acnes: Time-to-positivity in standard bacterial culture from different anatomical sites. J Clin Med Res 2016; 8:916–918.
- Sohail MR, Uslan DZ, Khan AH, et al. Management and outcome of permanent pacemaker and implantable cardioverter-defibrillator infections. J Am Coll Cardiol 2007; 49:1851–1859.
- Cacoub P, Leprince P, Nataf P, et al. Pacemaker infective endocarditis. Am J Cardiol 1998; 82:480–484.
- Chua JD, Wilkoff BL, Lee I, Juratli N, Longworth DL, Gordon SM. Diagnosis and management of infections involving implantable electrophysiologic cardiac devices. Ann Intern Med 2000; 133:604–608.
- Bracke FA, Meijer A, van Gelder LM. Pacemaker lead complications: when is extraction appropriate and what can we learn from published data? Heart 2001; 85:254–259.
- Camus C, Leport C, Raffi F, Michelet C, Cartier F, Vilde JL. Sustained bacteremia in 26 patients with a permanent endocardial pacemaker: assessment of wire removal. Clin Infect Dis 1993; 17:46–55.
- Molina JE. Undertreatment and overtreatment of patients with infected antiarrhythmic implantable devices. Ann Thorac Surg 1997; 63:504–509.
- Viganego F, O’Donoghue S, Eldadah Z, et al. Effect of early diagnosis and treatment with percutaneous lead extraction on survival in patients with cardiac device infections. Am J Cardiol 2012; 109:1466–1471.
- Le KY, Sohail MR, Friedman PA, et al; Mayo Cardiovascular Infections Study Group. Impact of timing of device removal on mortality in patients with cardiovascular implantable electronic device infections. Heart Rhythm 2011; 8:1678–1685.
- Wazni O, Wilkoff BL. Considerations for cardiac device lead extraction. Nat Rev Cardiol 2016; 13:221–229.
- Brunner MP, Cronin EM, Duarte VE, et al. Clinical predictors of adverse patient outcomes in an experience of more than 5000 chronic endovascular pacemaker and defibrillator lead extractions. Heart Rhythm 2014; 11:799–805.
- Wazni O, Epstein LM, Carrillo RG, et al. Lead extraction in the contemporary setting: the LExICon study: an observational retrospective study of consecutive laser lead extractions. J Am Coll Cardiol 2010; 55:579–586.
- Brunner MP, Cronin EM, Wazni O, et al. Outcomes of patients requiring emergent surgical or endovascular intervention for catastrophic complications during transvenous lead extraction. Heart Rhythm 2014; 11:419–425.
- Habib A, Le KY, Baddour LM, et al; for the Mayo Cardiovascular Infections Study Group. Predictors of mortality in patients with cardiovascular implantable electronic device infections. Am J Cardiol 2013; 111:874–879.
- Baman TS, Gupta SK, Valle JA, Yamada E. Risk factors for mortality in patients with cardiac device-related infection. Circ Arrhythm Electrophysiol 2009; 2:129–134.
- Deckx S, Marynissen T, Rega F, et al. Predictors of 30-day and 1-year mortality after transvenous lead extraction: a single-centre experience. Europace 2014; 16:1218–1225.
- Sohail MR, Henrikson CA, Braid-Forbes MJ, Forbes KF, Lerner DJ. Increased long-term mortality in patients with cardiovascular implantable electronic device infections. Pacing Clin Electrophysiol 2015; 38:231–239.
- Tarakji KG, Wazni OM, Harb S, Hsu A, Saliba W, Wilkoff BL. Risk factors for 1-year mortality among patients with cardiac implantable electronic device infection undergoing transvenous lead extraction: the impact of the infection type and the presence of vegetation on survival. Europace 2014; 16:1490–1495.
- Darouiche RO, Wall MJ Jr., Itani KM, et al. Chlorhexidine—alcohol versus povidone—iodine for surgical-site antisepsis. N Engl J Med 2010; 362:18–26.
- Qintar M, Zardkoohi O, Hammadah M, et al. The impact of changing antiseptic skin preparation agent used for cardiac implantable electronic device (CIED) procedures on the risk of infection. Pacing Clin Electrophysiol 2015; 38:240–246.
- Da Costa A, Tulane C, Dauphinot V, et al. Preoperative skin antiseptics for prevention of cardiac implantable electronic device infections: a historical-controlled interventional trial comparing aqueous against alcoholic povidone-iodine solutions. Europace 2015; 17:1092–1098.
- Padfield GJ, Steinberg C, Bennett MT, et al. Preventing cardiac implantable electronic device infections. Heart Rhythm 2015; 12:2344–2356.
- Bode LGM, Kluytmans JAJW, Wertheim HFL, et al. Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med 2010; 362:9–17.
- Da Costa A, Kirkorian G, Cucherat M, et al. Antibiotic prophylaxis for permanent pacemaker implantation: a meta-analysis. Circulation 1998; 97:1796–1801.
- de Oliveira JC, Martinelli M, Nishioka SADO, et al. Efficacy of antibiotic prophylaxis before the implantation of pacemakers and cardioverter-defibrillators: results of a large, prospective, randomized, double-blinded, placebo-controlled trial. Circ Arrhythm Electrophysiol 2009; 2:29–34.
- Essebag V, Verma A, Healey JS, et al; BRUISE CONTROL Investigators. Clinically significant pocket hematoma increases long-term risk of device infection: BRUISE CONTROL INFECTION study. J Am Coll Cardiol 2016; 67:1300–1308.
- Birnie DH, Healey JS, Wells GA, et al; BRUISE CONTROL Investigators. Pacemaker or defibrillator surgery without interruption of anticoagulation. N Engl J Med 2013; 368:2084–2093.
- Henrikson CA, Sohail MR, Acosta H, et al. Antibacterial envelope is associated with low infection rates after implantable cardioverter-defibrillator and cardiac resynchronization therapy device replacement: results of the Citadel and Centurion studies. 2017 http://dx.doi.org/10.1016/j.jacep.2017.02.016
- Mittal S, Shaw RE, Michel K, et al. Cardiac implantable electronic device infections: incidence, risk factors, and the effect of the AigisRx antibacterial envelope. Heart Rhythm 2014; 11:595–601.
- Tarakji KG, Mittal S, Kennergren C, et al. Worldwide Randomized Antibiotic EnveloPe Infection PrevenTion Trial (WRAP-IT). Am Heart J 2016; 180:12–B21.
- Burke MC, Gold MR, Knight BP, et al. Safety and efficacy of the totally subcutaneous implantable defibrillator: 2-year results from a pooled analysis of the IDE study and EFFORTLESS registry. J Am Coll Cardiol 2015; 65:1605–1615.
- Reddy VY, Exner DV, Cantillon DJ, et al; LEADLESS II Study Investigators. Percutaneous implantation of an entirely intracardiac leadless pacemaker. N Engl J Med 2015; 373:1125–1135.
- Reynolds D, Duray GZ, Omar R, et al; Micra Transcatheter Pacing Study Group. A leadless intracardiac transcatheter pacing system. N Engl J Med 2016; 374:533–541.
KEY POINTS
- CIED use is increasing, as are the number of CIED infections, which are associated with significant morbidity and mortality.
- Prompt diagnosis of CIED infection allows for early management with antibiotics and device removal, which is typically needed for resolution of the infection.
- Prevention of CIED infection is an important strategy, and more research is needed to inform the incidence of CIED infection, risk factors, and devices and techniques to minimize the risk of infection.
Lung transplant: Candidates for referral and the waiting list
Lung transplant is the therapy of choice for a growing number of patients with end-stage lung diseases. Patients receiving a lung transplant are faced with many challenges including drug toxicities, infections, and the risk of rejection.1 Despite these challenges, lung transplant may significantly prolong survival and improve quality of life for many patients.
CANDIDATES FOR LUNG TRANSPLANT
Identifying patients who are appropriate candidates for lung transplant is important to achieving favorable transplant outcomes and to maximizing life expectancy for each patient. The most recent edition of International Society for Heart and Lung Transplant (ISHLT) Guidelines for the Selection of Lung Transplant Candidates is an excellent guide to help physicians identify when to refer potential patients and to how to identify patients who are the most likely to benefit from lung transplant.2
Adults with end-stage lung disease are generally candidates for lung transplant if they meet the following criteria:
- A greater than 50% risk of death from lung disease within 2 years if a lung transplant is not performed
- A greater than 80% likelihood of surviving at least 90 days after the lung transplant procedure
- A greater than 80% likelihood of a 5-year survival posttransplant if graft function is preserved.2
These can only be estimated by transplant programs and not by the referring team in most cases.
Once a patient is identified as a candidate for lung transplant, early referral of patients to a lung transplant program has several advantages and is essential for positive outcomes. Early patient referral allows for timely completion of the formal evaluation of candidacy, patient and family education, as well as the opportunity for the patient and family to raise funds or use other resources to overcome financial hurdles. Listing a patient on the transplant waitlist implies that the patient has a limited life expectancy without a lung transplant and that the risk-benefit ratio favors lung transplant since all other medical options have been exhausted.1
NONCANDIDATES FOR LUNG TRANSPLANT
There are very few absolute contraindications to lung transplant. Generally, most transplant centers in the United States agree that contraindications to lung transplant include conditions associated with increased risk of mortality, including:
- A recent history of a major malignancy. Patients with a 2-year, disease-free interval combined with a low predicted risk of recurrence may be considered in certain cases of localized, non-melanoma skin cancer. A 5-year, disease-free survival is strongly suggested in patients with a history of breast, bladder, or kidney cancer as well as in cases of sarcoma, melanoma, lymphoma and certain hematologic disorders.
- The presence of significant dysfunction of another major organ systems including the heart, liver, kidney, or brain unless a combined organ transplant can be considered and performed.
- Significant coronary heart disease not amenable to revascularization or intervention prior to or at the time of lung transplant.
- The presence of an acute medical condition including but not limited to sepsis and acute liver failure.
- Active Mycobacterium tuberculosis and other highly virulent or highly resistant microbes that are poorly controlled pretransplant.
- Severe obesity with a body mass index greater than 35.
- A history of nonadherence to medical therapy, psychiatric or psychological conditions that might lead to nonadherence, poor or limited social support system, and limited functional status not amenable to rehabilitation.
- Current substance abuse or dependence, including illicit substances, alcohol, and tobacco (nicotine-containing substances). Most centers require at least 6 months’ abstinence from illicit substances prior to being added to the lung transplant waitlist.2
CANDIDATE COMORBIDITIES
Age
Many transplant centers in the US define the age cutoff for lung transplant at 65; however, some centers may consider candidates older than 65. Advanced age by itself should not be considered a contraindication to lung transplant. However, increased age is usually associated with other comorbid conditions that may increase perioperative and long-term morbidity and mortality. As mentioned previously, the number of older candidates for lung transplant has increased. In the US, 29% of the patients on the national waiting list in 2015 were over age 65.4
Past chest surgery
It is not uncommon for lung transplant candidates to have a history of chest surgery such as lung resection, pleurodesis, or coronary artery bypass grafting. The limited literature regarding the outcomes for these patients suggests they may experience higher rates of bleeding, re-exploration, and renal dysfunction.2 However, these patients should not be excluded from lung transplant and successful transplant outcomes have been achieved in this population by experienced centers.5 In candidates with a history of chronic obstructive pulmonary disease (COPD) and lung-volume reduction surgery (LVRS), early case series indicate that these patients did well after lung transplant.6 However, more recent data demonstrate that patients with prior LVRS who undergo lung transplant experience higher rates of bleeding, worse early graft dysfunction, and worse outcomes overall.7 As with lung transplant candidates with previous chest surgery, lung transplant candidates with previous LVRS are best served by experienced transplant centers.
Hepatitis and HIV
Patients with a history of infection with hepatitis B, hepatitis C, or human immunodeficiency virus (HIV) are candidates for lung transplant at centers experienced with lung transplant in patients with these infections. Most centers advocate that patients with a history of hepatitis B or C have viral infection levels that are controlled or reduced as low as possible and that there is no evidence of portal hypertension or severe cirrhosis.8,9 In the case of HIV, patients should have controlled disease with a negative or undetectable viral load and have no current acquired immunodeficiency defining illness.10 Patients colonized with particular species of Burkholderia cepacia or Mycobacterium abscessus subspecies can be considered for lung transplant only at centers with established preoperative and postoperative protocols for these infections due to the increased risk of perioperative mortality associated with these organisms.11,12
DISEASE-SPECIFIC INDICATIONS
Chronic obstructive pulmonary disease
COPD (both non- and alpha-1 antitrypsin deficiency) is the most common indication for lung transplant and accounts for almost 32% of lung transplants worldwide.13 Patients should be referred for lung transplant when medical therapies, surgical interventions (ie, LVRS) and pulmonary rehabilitation have been maximized. In COPD, the loss of lung function occurs over a long period of time but patients are often more limited by diminished quality of life as lung function slowly declines.
Patients with COPD should be referred for lung transplant if the body mass index, airflow obstruction, dyspnea, and exercise capacity (BODE) index is 5 to 6.2 The original BODE index developed by Celli et al,14 is a scoring system from 0 to 10 with a higher score indicating more severe disease and worse survival. A score of 5 to 6 indicates an estimated mortality of 60% at 4 yrs.2,14,15 Other considerations for referral for lung transplant include the presence of hypercapnia with partial pressure of carbon dioxide greater than 50 mm Hg or higher or hypoxemia with partial pressure of oxygen less than 60 mm Hg or a forced expiratory volume at 1 sec (FEV1) less than 25% predicted.
Patients with COPD should considered for listing for lung transplant if any one of the following criteria is met: BODE index of 7 or greater; FEV1 less than 15% to 20%; 3 of more severe exacerbations during the preceding year; 1 severe exacerbation with acute hypercapnic respiratory failure; or presence of moderate to severe pulmonary hypertension.2,16
Cystic fibrosis
In patients with cystic fibrosis, lung transplant should be considered in patients with an estimated 2-year survival of less than 50% and with a New York Heart Association (NYHA) Functional Classification III or IV. Referral for lung transplant is recommended for patients with a rapid decrease in FEV1 despite optimal therapy, female patients with declining weight and lung function, colonization or infection with nontuberculous mycobacterial disease, or cystic fibrosis-related diabetes. The development of pulmonary hypertension, reduction in walk distance, increasing antibiotic resistance, acute respiratory failure requiring noninvasive ventilation, worsening nutritional status, pneumothorax, and life-threatening hemoptysis despite embolization are all indications for referral for lung transplant.
Patients with cystic fibrosis with hypoxia or hypercapnia with declining lung function, needing long-term noninvasive ventilation, having more frequent exacerbations or exhibiting a decline in functional status should be listed for lung transplant.2,17–19
Restrictive lung disease
Patients with restrictive lung diseases, including interstitial pulmonary fibrosis (usual interstitial pneumonitis, nonspecific interstitial pneumonia), or interstitial lung disease, and hypersensitivity pneumonitis, should be referred for transplant evaluation at the time of diagnosis irrespective of lung function due to the unpredictable nature of these diseases.20 Some clinicians may advocate for a trial of medical therapy with antifibrotics, but this should be done in conjunction with transplant referral.
Patients should be listed for transplant if a 10% or greater decrease in FEV1 occurred in the past 6 months (of note, even a 5% decrease in FEV1 is associated with an overall poorer prognosis and warrants consideration of listing for transplant), if the diffusing capacity of the lung for carbon monoxide decreases 15% or greater during the 6-month follow-up, or if a decline of more than 50 meters is noted on the 6-minute walking test. A documented desaturation of less than 88% or a distance of less than 250 meters on the 6-minute walking test is another indication for listing. Any evidence of secondary pulmonary hypertension on right heart catheterization or on echocardiography or hospitalization for respiratory decline are also indications for listing.21 In cases of scleroderma-associated interstitial lung disease or mixed connective tissue interstitial lung disease, similar guidelines for referral and listing should be followed.2
Pulmonary arterial hypertension
Patients with pulmonary arterial hypertension should be referred for lung transplant if any 1 of the following conditions is present: rapidly progressive disease; NYHA Functional Classification III or IV symptoms during escalating therapy; use of parenteral pulmonary arterial hypertension therapy; or known or suspected pulmonary veno-occlusive disease or pulmonary capillary hemangiomatosis.2,22
Patients with pulmonary arterial hypertension should be listed for lung transplant if any of the following are present: NYHA Functional Classification III or IV symptoms despite combination therapy; right heart catheterization demonstrating a cardiac index less than 2 L/min/m2; mean right atrial pressure greater than 15 mm Hg; 6-minute walking test less than 350 meters; or development of pericardial effusion, hemoptysis, or signs of worsening right heart failure, including renal insufficiency, rising bilirubin or evidence of ascites.2,22
BRIDGE TO TRANSPLANT
Acute respiratory decompensation may occur in some candidates for lung transplant prior to listing for transplant or while on the transplant waitlist. In patients with failure of a single lung, a bridge to transplant may be necessary until a suitable organ is available. Mechanical ventilation and extracorporeal life support (ECLS) are 2 bridge strategies for lung transplant candidates. Mechanical ventilation is the most common lung transplant bridge strategy but it is less than ideal because it can lead to deconditioning and ventilator-associated infections that can negatively impact a patient’s suitability for transplant.
ECLS techniques that allow spontaneous breathing and potentially ambulation, known as awake or ambulatory ECLS, is a popular bridge therapy. Ambulatory ECLS is used as an alternative to mechanical ventilation to avoid the complications of mechanical ventilation and allow patients to avoid sedation and participate in rehabilitation.23 Irrespective of the therapy used as a bridge to transplant, patients considered for a bridge are optimally evaluated from a medical and psychosocial perspective prior to bridge therapy.
Both bridge therapies increase the risk of infection, bleeding, and neurologic events; thus, patients need to be assessed repeatedly for these risks to determine ongoing suitability for lung transplant. It is important to note that delayed referral of patients with advanced disease or patients in an acute exacerbation negatively impacts the evaluation for lung transplant, placement on the lung transplant waitlist, outcomes, and suitability for bridge transplant strategies.
CONCLUSION
To ensure good patient outcomes, the evaluation and selection of candidates for lung transplant requires communication between referring physicians and lung transplant centers. Physicians need basic knowledge of patient conditions appropriate for lung transplant and direct communication with lung transplant centers. The workup, required testing, and timing of listing for lung transplant varies among transplant centers across the country, making communication between the referring providers and transplant centers crucial to good patient care. An open, 2-way dialogue between referring providers and transplant centers facilitates listing patients for transplant in a timely manner, reduces delays, and improves outcomes.
- Kreider M, Hadjiliadis D, Kotloff R. Candidate selection, timing of listing, and choice of procedure for lung transplantation. Clin Chest Med 2011; 32:199–211.
- Weill D, Benden C, Corris P, et al. A consensus document for the selection of lung transplant candidates: 2014—An update from the Pulmonary Transplant Council of the International Society of Heart and Lung Transplantation. J Heart Lung Transplant 2015; 34:1–15.
- Tsuang WM. Contemporary issues in lung transplant allocation practices. Curr Transplant Rep 2017; 4:238–242.
- Valapour M, Skeans MA, Smith JM, et al. OPTN/SRTR 2015 annual data report: lung. Am J Transplant 2017; 17(suppl 1):357–424.
- Omara M, Okamoto T, Arafat A, Thuita L, Blackstone EH, McCurry KR. Lung transplantation in patients who have undergone prior cardiothoracic procedures. J Heart Lung Transplant 2016; 35:1462–1470.
- Senbaklavaci O, Wisser W, Ozpeker C, et al. Successful lung volume reduction surgery brings patients into better condition for later lung transplantation. Eur J Cardiothorac Surg 2002; 22:363–367.
- Shigemura N, Gilbert S, Bhama JK et al. Lung transplantation after lung volume reduction surgery. Transplantation 2013; 96:421–425.
- Sahi H, Zein NN, Mehta AC, Blazey HC, Meyer KH, Budev M. Outcomes after lung transplantation in patients with chronic hepatitis C virus infection. J Heart Lung Transplant 2007; 26:466–471.
- Kim EY, Ko HH, Yoshida EM. A concise review of hepatitis C in heart and lung transplantation. Can J Gastroenterol 2011; 25:445–448.
- Kern RM, Seethamraju H, Blanc PD, et al. The feasibility of lung transplantation in HIV-seropositive patients. Ann Am Thorac Soc 2014; 11:882–889.
- De Soyza A, Corris A, McDowell A, Archer L, et al. Burkholderia cepacia complex genomovars and pulmonary transplant outcomes in patients with cystic fibrosis. Lancet 2001; 358:1780–1781.
- De Soyza A, Meachery G, Hester HL, et al. Lung transplant for patients with cystic fibrosis and Burkholderia cepacia complex infection: a single center experience. J Heart Lung Transplant 2010; 29:1395–1404.
- Yusen RD, Edwards LB, Kucheryavaya AY, et al. The registry of the International Society for Heart and Lung Transplantation: thirty-second official adult and heart-lung transplantation report—2015; focus theme: early graft failure. J Heart Lung Transplant 2015; 34:1264–1277.
- Celli BR, Cote CG, Marin JM, et al. The body–mass index, airflow obstruction, dyspna and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 2004; 350:1005–1012.
- Marchand E. The BODE index as a tool to predict survival in COPD lung transplant candidates. Eur Respir J 2010; 36:1494–1495.
- Lahzami S, Bridevaux PO, Soccal PM, et al. Survival impact of lung transplant for COPD. Eur Respir J 2010; 36:74–80.
- Rosenbluth DB, Wilson K, Ferkol T, Schuster DP. Lung function decline in cystic fibrosis patients and timing for lung transplantation referral. Chest 2004; 126:412–419.
- Mayer-Hamblett N, Rosenfield M, Emerson J, Goss CH, Aitken ML. Developing cystic fibrosis lung transplant referral criteria using predictors of 2-year mortality. Am J Respir Crit Care Med 2002; 166:1550–1556.
- Liou TG, Adler FR, Cahill BC, et al. Survival effect of lung transplantation among patients with cystic fibrosis. JAMA 2001; 286:2683–2689.
- Raghu G, Collard HR, Egan JJ, et al; ATS/ERS/JRS/ALAT Committee on Idiopathic Pulmonary Fibrosis. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidenced-based guidelines for diagnosis and management. Am J Respir Crit Care Med 2011; 183:788–824.
- Collard HR, King TE Jr, Bartelson BB, Vourlekis JS, Schwarz MI, Brown KK. Changes in clinical and physiologic variables predict survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2003; 168:538–542.
- Edelman, JD. Navigating the road to transplantation for pulmonary arterial hypertension. Advances in Pulmonary Hypertension 2016; 15:14–18.
- Strueber M. Bridges to lung transplant. Curr Opin Organ Transplant 2011; 16:458–461.
Lung transplant is the therapy of choice for a growing number of patients with end-stage lung diseases. Patients receiving a lung transplant are faced with many challenges including drug toxicities, infections, and the risk of rejection.1 Despite these challenges, lung transplant may significantly prolong survival and improve quality of life for many patients.
CANDIDATES FOR LUNG TRANSPLANT
Identifying patients who are appropriate candidates for lung transplant is important to achieving favorable transplant outcomes and to maximizing life expectancy for each patient. The most recent edition of International Society for Heart and Lung Transplant (ISHLT) Guidelines for the Selection of Lung Transplant Candidates is an excellent guide to help physicians identify when to refer potential patients and to how to identify patients who are the most likely to benefit from lung transplant.2
Adults with end-stage lung disease are generally candidates for lung transplant if they meet the following criteria:
- A greater than 50% risk of death from lung disease within 2 years if a lung transplant is not performed
- A greater than 80% likelihood of surviving at least 90 days after the lung transplant procedure
- A greater than 80% likelihood of a 5-year survival posttransplant if graft function is preserved.2
These can only be estimated by transplant programs and not by the referring team in most cases.
Once a patient is identified as a candidate for lung transplant, early referral of patients to a lung transplant program has several advantages and is essential for positive outcomes. Early patient referral allows for timely completion of the formal evaluation of candidacy, patient and family education, as well as the opportunity for the patient and family to raise funds or use other resources to overcome financial hurdles. Listing a patient on the transplant waitlist implies that the patient has a limited life expectancy without a lung transplant and that the risk-benefit ratio favors lung transplant since all other medical options have been exhausted.1
NONCANDIDATES FOR LUNG TRANSPLANT
There are very few absolute contraindications to lung transplant. Generally, most transplant centers in the United States agree that contraindications to lung transplant include conditions associated with increased risk of mortality, including:
- A recent history of a major malignancy. Patients with a 2-year, disease-free interval combined with a low predicted risk of recurrence may be considered in certain cases of localized, non-melanoma skin cancer. A 5-year, disease-free survival is strongly suggested in patients with a history of breast, bladder, or kidney cancer as well as in cases of sarcoma, melanoma, lymphoma and certain hematologic disorders.
- The presence of significant dysfunction of another major organ systems including the heart, liver, kidney, or brain unless a combined organ transplant can be considered and performed.
- Significant coronary heart disease not amenable to revascularization or intervention prior to or at the time of lung transplant.
- The presence of an acute medical condition including but not limited to sepsis and acute liver failure.
- Active Mycobacterium tuberculosis and other highly virulent or highly resistant microbes that are poorly controlled pretransplant.
- Severe obesity with a body mass index greater than 35.
- A history of nonadherence to medical therapy, psychiatric or psychological conditions that might lead to nonadherence, poor or limited social support system, and limited functional status not amenable to rehabilitation.
- Current substance abuse or dependence, including illicit substances, alcohol, and tobacco (nicotine-containing substances). Most centers require at least 6 months’ abstinence from illicit substances prior to being added to the lung transplant waitlist.2
CANDIDATE COMORBIDITIES
Age
Many transplant centers in the US define the age cutoff for lung transplant at 65; however, some centers may consider candidates older than 65. Advanced age by itself should not be considered a contraindication to lung transplant. However, increased age is usually associated with other comorbid conditions that may increase perioperative and long-term morbidity and mortality. As mentioned previously, the number of older candidates for lung transplant has increased. In the US, 29% of the patients on the national waiting list in 2015 were over age 65.4
Past chest surgery
It is not uncommon for lung transplant candidates to have a history of chest surgery such as lung resection, pleurodesis, or coronary artery bypass grafting. The limited literature regarding the outcomes for these patients suggests they may experience higher rates of bleeding, re-exploration, and renal dysfunction.2 However, these patients should not be excluded from lung transplant and successful transplant outcomes have been achieved in this population by experienced centers.5 In candidates with a history of chronic obstructive pulmonary disease (COPD) and lung-volume reduction surgery (LVRS), early case series indicate that these patients did well after lung transplant.6 However, more recent data demonstrate that patients with prior LVRS who undergo lung transplant experience higher rates of bleeding, worse early graft dysfunction, and worse outcomes overall.7 As with lung transplant candidates with previous chest surgery, lung transplant candidates with previous LVRS are best served by experienced transplant centers.
Hepatitis and HIV
Patients with a history of infection with hepatitis B, hepatitis C, or human immunodeficiency virus (HIV) are candidates for lung transplant at centers experienced with lung transplant in patients with these infections. Most centers advocate that patients with a history of hepatitis B or C have viral infection levels that are controlled or reduced as low as possible and that there is no evidence of portal hypertension or severe cirrhosis.8,9 In the case of HIV, patients should have controlled disease with a negative or undetectable viral load and have no current acquired immunodeficiency defining illness.10 Patients colonized with particular species of Burkholderia cepacia or Mycobacterium abscessus subspecies can be considered for lung transplant only at centers with established preoperative and postoperative protocols for these infections due to the increased risk of perioperative mortality associated with these organisms.11,12
DISEASE-SPECIFIC INDICATIONS
Chronic obstructive pulmonary disease
COPD (both non- and alpha-1 antitrypsin deficiency) is the most common indication for lung transplant and accounts for almost 32% of lung transplants worldwide.13 Patients should be referred for lung transplant when medical therapies, surgical interventions (ie, LVRS) and pulmonary rehabilitation have been maximized. In COPD, the loss of lung function occurs over a long period of time but patients are often more limited by diminished quality of life as lung function slowly declines.
Patients with COPD should be referred for lung transplant if the body mass index, airflow obstruction, dyspnea, and exercise capacity (BODE) index is 5 to 6.2 The original BODE index developed by Celli et al,14 is a scoring system from 0 to 10 with a higher score indicating more severe disease and worse survival. A score of 5 to 6 indicates an estimated mortality of 60% at 4 yrs.2,14,15 Other considerations for referral for lung transplant include the presence of hypercapnia with partial pressure of carbon dioxide greater than 50 mm Hg or higher or hypoxemia with partial pressure of oxygen less than 60 mm Hg or a forced expiratory volume at 1 sec (FEV1) less than 25% predicted.
Patients with COPD should considered for listing for lung transplant if any one of the following criteria is met: BODE index of 7 or greater; FEV1 less than 15% to 20%; 3 of more severe exacerbations during the preceding year; 1 severe exacerbation with acute hypercapnic respiratory failure; or presence of moderate to severe pulmonary hypertension.2,16
Cystic fibrosis
In patients with cystic fibrosis, lung transplant should be considered in patients with an estimated 2-year survival of less than 50% and with a New York Heart Association (NYHA) Functional Classification III or IV. Referral for lung transplant is recommended for patients with a rapid decrease in FEV1 despite optimal therapy, female patients with declining weight and lung function, colonization or infection with nontuberculous mycobacterial disease, or cystic fibrosis-related diabetes. The development of pulmonary hypertension, reduction in walk distance, increasing antibiotic resistance, acute respiratory failure requiring noninvasive ventilation, worsening nutritional status, pneumothorax, and life-threatening hemoptysis despite embolization are all indications for referral for lung transplant.
Patients with cystic fibrosis with hypoxia or hypercapnia with declining lung function, needing long-term noninvasive ventilation, having more frequent exacerbations or exhibiting a decline in functional status should be listed for lung transplant.2,17–19
Restrictive lung disease
Patients with restrictive lung diseases, including interstitial pulmonary fibrosis (usual interstitial pneumonitis, nonspecific interstitial pneumonia), or interstitial lung disease, and hypersensitivity pneumonitis, should be referred for transplant evaluation at the time of diagnosis irrespective of lung function due to the unpredictable nature of these diseases.20 Some clinicians may advocate for a trial of medical therapy with antifibrotics, but this should be done in conjunction with transplant referral.
Patients should be listed for transplant if a 10% or greater decrease in FEV1 occurred in the past 6 months (of note, even a 5% decrease in FEV1 is associated with an overall poorer prognosis and warrants consideration of listing for transplant), if the diffusing capacity of the lung for carbon monoxide decreases 15% or greater during the 6-month follow-up, or if a decline of more than 50 meters is noted on the 6-minute walking test. A documented desaturation of less than 88% or a distance of less than 250 meters on the 6-minute walking test is another indication for listing. Any evidence of secondary pulmonary hypertension on right heart catheterization or on echocardiography or hospitalization for respiratory decline are also indications for listing.21 In cases of scleroderma-associated interstitial lung disease or mixed connective tissue interstitial lung disease, similar guidelines for referral and listing should be followed.2
Pulmonary arterial hypertension
Patients with pulmonary arterial hypertension should be referred for lung transplant if any 1 of the following conditions is present: rapidly progressive disease; NYHA Functional Classification III or IV symptoms during escalating therapy; use of parenteral pulmonary arterial hypertension therapy; or known or suspected pulmonary veno-occlusive disease or pulmonary capillary hemangiomatosis.2,22
Patients with pulmonary arterial hypertension should be listed for lung transplant if any of the following are present: NYHA Functional Classification III or IV symptoms despite combination therapy; right heart catheterization demonstrating a cardiac index less than 2 L/min/m2; mean right atrial pressure greater than 15 mm Hg; 6-minute walking test less than 350 meters; or development of pericardial effusion, hemoptysis, or signs of worsening right heart failure, including renal insufficiency, rising bilirubin or evidence of ascites.2,22
BRIDGE TO TRANSPLANT
Acute respiratory decompensation may occur in some candidates for lung transplant prior to listing for transplant or while on the transplant waitlist. In patients with failure of a single lung, a bridge to transplant may be necessary until a suitable organ is available. Mechanical ventilation and extracorporeal life support (ECLS) are 2 bridge strategies for lung transplant candidates. Mechanical ventilation is the most common lung transplant bridge strategy but it is less than ideal because it can lead to deconditioning and ventilator-associated infections that can negatively impact a patient’s suitability for transplant.
ECLS techniques that allow spontaneous breathing and potentially ambulation, known as awake or ambulatory ECLS, is a popular bridge therapy. Ambulatory ECLS is used as an alternative to mechanical ventilation to avoid the complications of mechanical ventilation and allow patients to avoid sedation and participate in rehabilitation.23 Irrespective of the therapy used as a bridge to transplant, patients considered for a bridge are optimally evaluated from a medical and psychosocial perspective prior to bridge therapy.
Both bridge therapies increase the risk of infection, bleeding, and neurologic events; thus, patients need to be assessed repeatedly for these risks to determine ongoing suitability for lung transplant. It is important to note that delayed referral of patients with advanced disease or patients in an acute exacerbation negatively impacts the evaluation for lung transplant, placement on the lung transplant waitlist, outcomes, and suitability for bridge transplant strategies.
CONCLUSION
To ensure good patient outcomes, the evaluation and selection of candidates for lung transplant requires communication between referring physicians and lung transplant centers. Physicians need basic knowledge of patient conditions appropriate for lung transplant and direct communication with lung transplant centers. The workup, required testing, and timing of listing for lung transplant varies among transplant centers across the country, making communication between the referring providers and transplant centers crucial to good patient care. An open, 2-way dialogue between referring providers and transplant centers facilitates listing patients for transplant in a timely manner, reduces delays, and improves outcomes.
Lung transplant is the therapy of choice for a growing number of patients with end-stage lung diseases. Patients receiving a lung transplant are faced with many challenges including drug toxicities, infections, and the risk of rejection.1 Despite these challenges, lung transplant may significantly prolong survival and improve quality of life for many patients.
CANDIDATES FOR LUNG TRANSPLANT
Identifying patients who are appropriate candidates for lung transplant is important to achieving favorable transplant outcomes and to maximizing life expectancy for each patient. The most recent edition of International Society for Heart and Lung Transplant (ISHLT) Guidelines for the Selection of Lung Transplant Candidates is an excellent guide to help physicians identify when to refer potential patients and to how to identify patients who are the most likely to benefit from lung transplant.2
Adults with end-stage lung disease are generally candidates for lung transplant if they meet the following criteria:
- A greater than 50% risk of death from lung disease within 2 years if a lung transplant is not performed
- A greater than 80% likelihood of surviving at least 90 days after the lung transplant procedure
- A greater than 80% likelihood of a 5-year survival posttransplant if graft function is preserved.2
These can only be estimated by transplant programs and not by the referring team in most cases.
Once a patient is identified as a candidate for lung transplant, early referral of patients to a lung transplant program has several advantages and is essential for positive outcomes. Early patient referral allows for timely completion of the formal evaluation of candidacy, patient and family education, as well as the opportunity for the patient and family to raise funds or use other resources to overcome financial hurdles. Listing a patient on the transplant waitlist implies that the patient has a limited life expectancy without a lung transplant and that the risk-benefit ratio favors lung transplant since all other medical options have been exhausted.1
NONCANDIDATES FOR LUNG TRANSPLANT
There are very few absolute contraindications to lung transplant. Generally, most transplant centers in the United States agree that contraindications to lung transplant include conditions associated with increased risk of mortality, including:
- A recent history of a major malignancy. Patients with a 2-year, disease-free interval combined with a low predicted risk of recurrence may be considered in certain cases of localized, non-melanoma skin cancer. A 5-year, disease-free survival is strongly suggested in patients with a history of breast, bladder, or kidney cancer as well as in cases of sarcoma, melanoma, lymphoma and certain hematologic disorders.
- The presence of significant dysfunction of another major organ systems including the heart, liver, kidney, or brain unless a combined organ transplant can be considered and performed.
- Significant coronary heart disease not amenable to revascularization or intervention prior to or at the time of lung transplant.
- The presence of an acute medical condition including but not limited to sepsis and acute liver failure.
- Active Mycobacterium tuberculosis and other highly virulent or highly resistant microbes that are poorly controlled pretransplant.
- Severe obesity with a body mass index greater than 35.
- A history of nonadherence to medical therapy, psychiatric or psychological conditions that might lead to nonadherence, poor or limited social support system, and limited functional status not amenable to rehabilitation.
- Current substance abuse or dependence, including illicit substances, alcohol, and tobacco (nicotine-containing substances). Most centers require at least 6 months’ abstinence from illicit substances prior to being added to the lung transplant waitlist.2
CANDIDATE COMORBIDITIES
Age
Many transplant centers in the US define the age cutoff for lung transplant at 65; however, some centers may consider candidates older than 65. Advanced age by itself should not be considered a contraindication to lung transplant. However, increased age is usually associated with other comorbid conditions that may increase perioperative and long-term morbidity and mortality. As mentioned previously, the number of older candidates for lung transplant has increased. In the US, 29% of the patients on the national waiting list in 2015 were over age 65.4
Past chest surgery
It is not uncommon for lung transplant candidates to have a history of chest surgery such as lung resection, pleurodesis, or coronary artery bypass grafting. The limited literature regarding the outcomes for these patients suggests they may experience higher rates of bleeding, re-exploration, and renal dysfunction.2 However, these patients should not be excluded from lung transplant and successful transplant outcomes have been achieved in this population by experienced centers.5 In candidates with a history of chronic obstructive pulmonary disease (COPD) and lung-volume reduction surgery (LVRS), early case series indicate that these patients did well after lung transplant.6 However, more recent data demonstrate that patients with prior LVRS who undergo lung transplant experience higher rates of bleeding, worse early graft dysfunction, and worse outcomes overall.7 As with lung transplant candidates with previous chest surgery, lung transplant candidates with previous LVRS are best served by experienced transplant centers.
Hepatitis and HIV
Patients with a history of infection with hepatitis B, hepatitis C, or human immunodeficiency virus (HIV) are candidates for lung transplant at centers experienced with lung transplant in patients with these infections. Most centers advocate that patients with a history of hepatitis B or C have viral infection levels that are controlled or reduced as low as possible and that there is no evidence of portal hypertension or severe cirrhosis.8,9 In the case of HIV, patients should have controlled disease with a negative or undetectable viral load and have no current acquired immunodeficiency defining illness.10 Patients colonized with particular species of Burkholderia cepacia or Mycobacterium abscessus subspecies can be considered for lung transplant only at centers with established preoperative and postoperative protocols for these infections due to the increased risk of perioperative mortality associated with these organisms.11,12
DISEASE-SPECIFIC INDICATIONS
Chronic obstructive pulmonary disease
COPD (both non- and alpha-1 antitrypsin deficiency) is the most common indication for lung transplant and accounts for almost 32% of lung transplants worldwide.13 Patients should be referred for lung transplant when medical therapies, surgical interventions (ie, LVRS) and pulmonary rehabilitation have been maximized. In COPD, the loss of lung function occurs over a long period of time but patients are often more limited by diminished quality of life as lung function slowly declines.
Patients with COPD should be referred for lung transplant if the body mass index, airflow obstruction, dyspnea, and exercise capacity (BODE) index is 5 to 6.2 The original BODE index developed by Celli et al,14 is a scoring system from 0 to 10 with a higher score indicating more severe disease and worse survival. A score of 5 to 6 indicates an estimated mortality of 60% at 4 yrs.2,14,15 Other considerations for referral for lung transplant include the presence of hypercapnia with partial pressure of carbon dioxide greater than 50 mm Hg or higher or hypoxemia with partial pressure of oxygen less than 60 mm Hg or a forced expiratory volume at 1 sec (FEV1) less than 25% predicted.
Patients with COPD should considered for listing for lung transplant if any one of the following criteria is met: BODE index of 7 or greater; FEV1 less than 15% to 20%; 3 of more severe exacerbations during the preceding year; 1 severe exacerbation with acute hypercapnic respiratory failure; or presence of moderate to severe pulmonary hypertension.2,16
Cystic fibrosis
In patients with cystic fibrosis, lung transplant should be considered in patients with an estimated 2-year survival of less than 50% and with a New York Heart Association (NYHA) Functional Classification III or IV. Referral for lung transplant is recommended for patients with a rapid decrease in FEV1 despite optimal therapy, female patients with declining weight and lung function, colonization or infection with nontuberculous mycobacterial disease, or cystic fibrosis-related diabetes. The development of pulmonary hypertension, reduction in walk distance, increasing antibiotic resistance, acute respiratory failure requiring noninvasive ventilation, worsening nutritional status, pneumothorax, and life-threatening hemoptysis despite embolization are all indications for referral for lung transplant.
Patients with cystic fibrosis with hypoxia or hypercapnia with declining lung function, needing long-term noninvasive ventilation, having more frequent exacerbations or exhibiting a decline in functional status should be listed for lung transplant.2,17–19
Restrictive lung disease
Patients with restrictive lung diseases, including interstitial pulmonary fibrosis (usual interstitial pneumonitis, nonspecific interstitial pneumonia), or interstitial lung disease, and hypersensitivity pneumonitis, should be referred for transplant evaluation at the time of diagnosis irrespective of lung function due to the unpredictable nature of these diseases.20 Some clinicians may advocate for a trial of medical therapy with antifibrotics, but this should be done in conjunction with transplant referral.
Patients should be listed for transplant if a 10% or greater decrease in FEV1 occurred in the past 6 months (of note, even a 5% decrease in FEV1 is associated with an overall poorer prognosis and warrants consideration of listing for transplant), if the diffusing capacity of the lung for carbon monoxide decreases 15% or greater during the 6-month follow-up, or if a decline of more than 50 meters is noted on the 6-minute walking test. A documented desaturation of less than 88% or a distance of less than 250 meters on the 6-minute walking test is another indication for listing. Any evidence of secondary pulmonary hypertension on right heart catheterization or on echocardiography or hospitalization for respiratory decline are also indications for listing.21 In cases of scleroderma-associated interstitial lung disease or mixed connective tissue interstitial lung disease, similar guidelines for referral and listing should be followed.2
Pulmonary arterial hypertension
Patients with pulmonary arterial hypertension should be referred for lung transplant if any 1 of the following conditions is present: rapidly progressive disease; NYHA Functional Classification III or IV symptoms during escalating therapy; use of parenteral pulmonary arterial hypertension therapy; or known or suspected pulmonary veno-occlusive disease or pulmonary capillary hemangiomatosis.2,22
Patients with pulmonary arterial hypertension should be listed for lung transplant if any of the following are present: NYHA Functional Classification III or IV symptoms despite combination therapy; right heart catheterization demonstrating a cardiac index less than 2 L/min/m2; mean right atrial pressure greater than 15 mm Hg; 6-minute walking test less than 350 meters; or development of pericardial effusion, hemoptysis, or signs of worsening right heart failure, including renal insufficiency, rising bilirubin or evidence of ascites.2,22
BRIDGE TO TRANSPLANT
Acute respiratory decompensation may occur in some candidates for lung transplant prior to listing for transplant or while on the transplant waitlist. In patients with failure of a single lung, a bridge to transplant may be necessary until a suitable organ is available. Mechanical ventilation and extracorporeal life support (ECLS) are 2 bridge strategies for lung transplant candidates. Mechanical ventilation is the most common lung transplant bridge strategy but it is less than ideal because it can lead to deconditioning and ventilator-associated infections that can negatively impact a patient’s suitability for transplant.
ECLS techniques that allow spontaneous breathing and potentially ambulation, known as awake or ambulatory ECLS, is a popular bridge therapy. Ambulatory ECLS is used as an alternative to mechanical ventilation to avoid the complications of mechanical ventilation and allow patients to avoid sedation and participate in rehabilitation.23 Irrespective of the therapy used as a bridge to transplant, patients considered for a bridge are optimally evaluated from a medical and psychosocial perspective prior to bridge therapy.
Both bridge therapies increase the risk of infection, bleeding, and neurologic events; thus, patients need to be assessed repeatedly for these risks to determine ongoing suitability for lung transplant. It is important to note that delayed referral of patients with advanced disease or patients in an acute exacerbation negatively impacts the evaluation for lung transplant, placement on the lung transplant waitlist, outcomes, and suitability for bridge transplant strategies.
CONCLUSION
To ensure good patient outcomes, the evaluation and selection of candidates for lung transplant requires communication between referring physicians and lung transplant centers. Physicians need basic knowledge of patient conditions appropriate for lung transplant and direct communication with lung transplant centers. The workup, required testing, and timing of listing for lung transplant varies among transplant centers across the country, making communication between the referring providers and transplant centers crucial to good patient care. An open, 2-way dialogue between referring providers and transplant centers facilitates listing patients for transplant in a timely manner, reduces delays, and improves outcomes.
- Kreider M, Hadjiliadis D, Kotloff R. Candidate selection, timing of listing, and choice of procedure for lung transplantation. Clin Chest Med 2011; 32:199–211.
- Weill D, Benden C, Corris P, et al. A consensus document for the selection of lung transplant candidates: 2014—An update from the Pulmonary Transplant Council of the International Society of Heart and Lung Transplantation. J Heart Lung Transplant 2015; 34:1–15.
- Tsuang WM. Contemporary issues in lung transplant allocation practices. Curr Transplant Rep 2017; 4:238–242.
- Valapour M, Skeans MA, Smith JM, et al. OPTN/SRTR 2015 annual data report: lung. Am J Transplant 2017; 17(suppl 1):357–424.
- Omara M, Okamoto T, Arafat A, Thuita L, Blackstone EH, McCurry KR. Lung transplantation in patients who have undergone prior cardiothoracic procedures. J Heart Lung Transplant 2016; 35:1462–1470.
- Senbaklavaci O, Wisser W, Ozpeker C, et al. Successful lung volume reduction surgery brings patients into better condition for later lung transplantation. Eur J Cardiothorac Surg 2002; 22:363–367.
- Shigemura N, Gilbert S, Bhama JK et al. Lung transplantation after lung volume reduction surgery. Transplantation 2013; 96:421–425.
- Sahi H, Zein NN, Mehta AC, Blazey HC, Meyer KH, Budev M. Outcomes after lung transplantation in patients with chronic hepatitis C virus infection. J Heart Lung Transplant 2007; 26:466–471.
- Kim EY, Ko HH, Yoshida EM. A concise review of hepatitis C in heart and lung transplantation. Can J Gastroenterol 2011; 25:445–448.
- Kern RM, Seethamraju H, Blanc PD, et al. The feasibility of lung transplantation in HIV-seropositive patients. Ann Am Thorac Soc 2014; 11:882–889.
- De Soyza A, Corris A, McDowell A, Archer L, et al. Burkholderia cepacia complex genomovars and pulmonary transplant outcomes in patients with cystic fibrosis. Lancet 2001; 358:1780–1781.
- De Soyza A, Meachery G, Hester HL, et al. Lung transplant for patients with cystic fibrosis and Burkholderia cepacia complex infection: a single center experience. J Heart Lung Transplant 2010; 29:1395–1404.
- Yusen RD, Edwards LB, Kucheryavaya AY, et al. The registry of the International Society for Heart and Lung Transplantation: thirty-second official adult and heart-lung transplantation report—2015; focus theme: early graft failure. J Heart Lung Transplant 2015; 34:1264–1277.
- Celli BR, Cote CG, Marin JM, et al. The body–mass index, airflow obstruction, dyspna and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 2004; 350:1005–1012.
- Marchand E. The BODE index as a tool to predict survival in COPD lung transplant candidates. Eur Respir J 2010; 36:1494–1495.
- Lahzami S, Bridevaux PO, Soccal PM, et al. Survival impact of lung transplant for COPD. Eur Respir J 2010; 36:74–80.
- Rosenbluth DB, Wilson K, Ferkol T, Schuster DP. Lung function decline in cystic fibrosis patients and timing for lung transplantation referral. Chest 2004; 126:412–419.
- Mayer-Hamblett N, Rosenfield M, Emerson J, Goss CH, Aitken ML. Developing cystic fibrosis lung transplant referral criteria using predictors of 2-year mortality. Am J Respir Crit Care Med 2002; 166:1550–1556.
- Liou TG, Adler FR, Cahill BC, et al. Survival effect of lung transplantation among patients with cystic fibrosis. JAMA 2001; 286:2683–2689.
- Raghu G, Collard HR, Egan JJ, et al; ATS/ERS/JRS/ALAT Committee on Idiopathic Pulmonary Fibrosis. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidenced-based guidelines for diagnosis and management. Am J Respir Crit Care Med 2011; 183:788–824.
- Collard HR, King TE Jr, Bartelson BB, Vourlekis JS, Schwarz MI, Brown KK. Changes in clinical and physiologic variables predict survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2003; 168:538–542.
- Edelman, JD. Navigating the road to transplantation for pulmonary arterial hypertension. Advances in Pulmonary Hypertension 2016; 15:14–18.
- Strueber M. Bridges to lung transplant. Curr Opin Organ Transplant 2011; 16:458–461.
- Kreider M, Hadjiliadis D, Kotloff R. Candidate selection, timing of listing, and choice of procedure for lung transplantation. Clin Chest Med 2011; 32:199–211.
- Weill D, Benden C, Corris P, et al. A consensus document for the selection of lung transplant candidates: 2014—An update from the Pulmonary Transplant Council of the International Society of Heart and Lung Transplantation. J Heart Lung Transplant 2015; 34:1–15.
- Tsuang WM. Contemporary issues in lung transplant allocation practices. Curr Transplant Rep 2017; 4:238–242.
- Valapour M, Skeans MA, Smith JM, et al. OPTN/SRTR 2015 annual data report: lung. Am J Transplant 2017; 17(suppl 1):357–424.
- Omara M, Okamoto T, Arafat A, Thuita L, Blackstone EH, McCurry KR. Lung transplantation in patients who have undergone prior cardiothoracic procedures. J Heart Lung Transplant 2016; 35:1462–1470.
- Senbaklavaci O, Wisser W, Ozpeker C, et al. Successful lung volume reduction surgery brings patients into better condition for later lung transplantation. Eur J Cardiothorac Surg 2002; 22:363–367.
- Shigemura N, Gilbert S, Bhama JK et al. Lung transplantation after lung volume reduction surgery. Transplantation 2013; 96:421–425.
- Sahi H, Zein NN, Mehta AC, Blazey HC, Meyer KH, Budev M. Outcomes after lung transplantation in patients with chronic hepatitis C virus infection. J Heart Lung Transplant 2007; 26:466–471.
- Kim EY, Ko HH, Yoshida EM. A concise review of hepatitis C in heart and lung transplantation. Can J Gastroenterol 2011; 25:445–448.
- Kern RM, Seethamraju H, Blanc PD, et al. The feasibility of lung transplantation in HIV-seropositive patients. Ann Am Thorac Soc 2014; 11:882–889.
- De Soyza A, Corris A, McDowell A, Archer L, et al. Burkholderia cepacia complex genomovars and pulmonary transplant outcomes in patients with cystic fibrosis. Lancet 2001; 358:1780–1781.
- De Soyza A, Meachery G, Hester HL, et al. Lung transplant for patients with cystic fibrosis and Burkholderia cepacia complex infection: a single center experience. J Heart Lung Transplant 2010; 29:1395–1404.
- Yusen RD, Edwards LB, Kucheryavaya AY, et al. The registry of the International Society for Heart and Lung Transplantation: thirty-second official adult and heart-lung transplantation report—2015; focus theme: early graft failure. J Heart Lung Transplant 2015; 34:1264–1277.
- Celli BR, Cote CG, Marin JM, et al. The body–mass index, airflow obstruction, dyspna and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 2004; 350:1005–1012.
- Marchand E. The BODE index as a tool to predict survival in COPD lung transplant candidates. Eur Respir J 2010; 36:1494–1495.
- Lahzami S, Bridevaux PO, Soccal PM, et al. Survival impact of lung transplant for COPD. Eur Respir J 2010; 36:74–80.
- Rosenbluth DB, Wilson K, Ferkol T, Schuster DP. Lung function decline in cystic fibrosis patients and timing for lung transplantation referral. Chest 2004; 126:412–419.
- Mayer-Hamblett N, Rosenfield M, Emerson J, Goss CH, Aitken ML. Developing cystic fibrosis lung transplant referral criteria using predictors of 2-year mortality. Am J Respir Crit Care Med 2002; 166:1550–1556.
- Liou TG, Adler FR, Cahill BC, et al. Survival effect of lung transplantation among patients with cystic fibrosis. JAMA 2001; 286:2683–2689.
- Raghu G, Collard HR, Egan JJ, et al; ATS/ERS/JRS/ALAT Committee on Idiopathic Pulmonary Fibrosis. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidenced-based guidelines for diagnosis and management. Am J Respir Crit Care Med 2011; 183:788–824.
- Collard HR, King TE Jr, Bartelson BB, Vourlekis JS, Schwarz MI, Brown KK. Changes in clinical and physiologic variables predict survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2003; 168:538–542.
- Edelman, JD. Navigating the road to transplantation for pulmonary arterial hypertension. Advances in Pulmonary Hypertension 2016; 15:14–18.
- Strueber M. Bridges to lung transplant. Curr Opin Organ Transplant 2011; 16:458–461.
KEY POINTS
- Lung transplant is the therapy of choice for a growing number of patients with end-stage lung disease.
- There are very few absolute contraindications to lung transplant. Potential contraindications and comorbidities can be discussed with the transplant center and vetted prior to listing for lung transplant.
- The workup for a lung transplant varies among transplant centers across the country, thus good communication between referring providers and transplant centers is crucial to quality care.
Familial essential thrombocythemia associated with JAK2 V617F mutation in siblings
Three myeloproliferative neoplasms (MPN), polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF), are associated with an abnormal somatic mutation of the JAK2 gene. Essential thrombocythemia is considered when there is a persistent increase in the peripheral blood platelet count, associated with a proliferation of atypical megakaryocytes in the bone marrow. The manifestations of PV, ET, and PMF all typically occur within the sixth or seventh decade of life. A patient may present with an abnormal blood count but be asymptomatic at the time. Over the course and progression of the disease, increases in hematocrit or platelet counts along with symptoms such as headaches, blurred vision, and plethora may occur.1 The JAK2 V617F mutation is responsible for the production of the JAK2 protein, which is continuously activated, promoting the growth and division of cells such as erythrocytes, granulocytes, and platelets. It has been reported that there is a nearly 100% incidence of the JAK2 mutation in patients with polycythemia vera, and a 50% incidence in patients with essential thrombocythemia and primary myelofibrosis.2
The discovery of the JAK2 mutation in PV, ET, and PMF was an important advancement in helping distinguish these disorders from other MPNs, including chronic myelogenous leukemia, but its presence does not explain why some individuals develop ET and others, PV or PMF.3 Although there have been familial cases proven of ET, the somatic JAK2 mutation is acquired and not inherited. In this report, we describe the unusual circumstance of JAK2 V617F mutation in a brother and a sister who were both diagnosed with essential thrombocythemia.
Case presentations and summaries
RS, a 69-year-old white man, was referred to our service in 2006 for continued care of previously diagnosed essential thrombocythemia. At the time of his initial visit to our clinic, his complete blood count was normal, the platelet count being adequately controlled by anagrelide at a daily dose of 4.0 mg. He complained of palpitations and peripheral neuropathy. A bone marrow biopsy was performed, revealing moderate hypercellularity, atypical megakaryocytosis, and a negative BCR-ABL mutation but a positive JAK2 V617F mutation. The patient is now treated with hydroxyurea 1,000 mg daily in divided doses, which better controls his counts and does not have the side effects of anagrelide.
SW, a 73-year-old woman, and brother of RS (they share the same biological mother and father), was noted to have a mild thrombocytosis in 2008. In 2013, her platelet count rose to 865,000 cells/uL (normal, 150,000-450,000 cells/uL, age and sex adjusted) and she was referred to our clinic. A bone marrow biopsy was performed, revealing borderline hypercellularity with atypical megakaryocytosis and the presence of a JAK2 V617F mutation. As with her brother, the BCR-ABL mutation was not present. She has also responded to treatment with hydroxyurea, but at a reduced dosage of 500 mg daily.
A third sibling, AS, again of the same biological mother and father, had died of multiple veno-occlusive cerebral vascular events long before the diagnoses on his younger siblings had been made. The suggestion of any underling hematologic pathology would be interesting, but speculative. Nothing is known abou
Discussion
Much research has been done to understand the pathogenesis of and find a cure for myeloproliferative disorders, but despite some progress, a cure remains elusive. However, there have been some advances that have contributed to partial cures for MPNs. One of the major breakthroughs in MPN research, about 50 years ago, was related to the “sporadic vs familial debate” around the Philadelphia chromosome.4 It led to the discovery of the reciprocal translocation between chromosomes 9 and 22, known as the BCR-ABL mutation, which is found in many CML patients. This discovery allowed researchers to focus their attention on other tyrosine kinase domains, such as the JAK2 V617F mutation, which is presented in the three other MPNs; PV, ET, and PMF. Both the JAK2 V617F and BCR-ABL mutations are active in signaling transcription, more commonly growth of cells.4
Since the discovery of the JAK2 V617F mutation in early 2005, it has become a leading diagnostic criteria for myeloproliferative diseases. The presence of the JAK2 V617F mutation and the measurement of its allele burden can be assessed by examination of either peripheral blood or bone marrow samples.5
The JAK2 V617F mutation is a result of a single change in the DNA nucleotide base pair that causes a substitution of a valine amino acid for a phenylalanine amino acid at the 617 position on exon 14 within the JAK2 kinase regulatory domain. This point mutation disrupts the regular control of the JAK2 by removing its ability to turn off, leading to uncontrolled blood cell growth.6 When the JAK2 V617F mutation cannot be demonstrated in a patient with the hallmarks of an MPN, the detection of other JAK2 and MPL proto-oncogene, thrombopoietin receptor mutations may be used as a diagnostic procedure for other MPNs.7
Other mutations incorporated in JAK2 domain can be detected in the coding portions of the DNA known as exons. One such mutation is the JAK2 exon 12, which is involved in JAK2 V617F-negative PV patients. This mutation is not detected in patients with ET or PMF and is 2%-5% present in patients with PV. There are other somatic mutations in the thrombopoietin receptors that work in accordance with thrombopoietin: MPL W515L and MPL W515K, which are found at chromosome 1p34, are identified in about 5% of PMF and 1% of ET patients, but are not present in PV patients.8.9
Pikman and colleagues reported in 2009 that the JAK2 V617F mutation is not acquired randomly.9 Their findings showed that, only in white populations, does the JAK2 V617F mutation arise preferentially on a specific constitutional JAK2 46/1 haplotype. According to the authors, the preconceived notion a of randomly acquired JAK2 V617F mutation does not account for familial MPN’s. Familial MPNs are thought to be produced by sporadic and extremely penetrant substitutions in genes that still are not identified and the 46/1 haplotype does not explain for the phenotypic diversity correlated with the JAK2 V617F gene. The 46/1 haplotype, however, correlates more frequently with different MPN subtypes. There are two hypotheses that try to explain how an acquired mutation as prevailing as the JAK2 V617F mutation can be associated with certain inherited backgrounds. The first hypothesis asserts the V617F accumulates at a faster rate than other genes because of the fundamentally unstable genetics of the 46/1 haplotype. The second theory is that all the mutated genes, including the V617F, arise at equal rates, but 46/1 may grant a selective advantage to the V617F-positive clone or interacts in some way to increase the likelihood of abnormal blood counts. A study that examined both these hypotheses concluded that the 46/1 haplotype was present more frequently in patients with myeloproliferative disorders than in their control groups and even more so in cases that were proven to be V617F-positive.10
There are very few cases that have reported familial MPN’s, especially as the pedigrees of the familial MPN’s illustrate that inheritance patterns are notably heterogeneous, indicating that there may be a range of different germline mutations driving the susceptibility. With recent data, the JAK2 V617F mutation in tandem with MPL W515L/K and inactivating TET2 mutations still continue to be the most frequently acquired mutations involved in both familial and sporadic MPN. As far as we know, there have been no cases to prove that JAK2 V617F and MPL W515L/K mutations are inherited through the germline, but there are other alleles that may pass through the germline that can be associated with hereditary thrombocytosis.11 Further cytogenetic studies will clarify the pathogenesis of these disorders and possibly lead to effective targeted therapies.
1. Murphy S, Peterson P, Iland H, Laszio J. Experience of the Polycythemia Vera Study Group with essential thrombocythemia: a final report on diagnostic criteria, survival, and leukemic transition by treatment. Semin Hematol. 1997;34:29-39.
2. Zhan H, Spivak JL. The diagnosis and management of polycythemia vera, essential thrombocythemia, and primary myelofibrosis in the JAK2 V617F era. Clin Adv Hematol Oncol. 2009;7:334-342.
3. Higgs JR, Sadek I, Neumann PE, et al. Familial essential thrombocythemia with spontaneous megakaryocyte colony formation and acquired JAK2 mutations. Leukemia. 2008;22:1551-1556.
4. Senyak Z. Eileen Wiggins – out of the blue. http://www.mpnresearchfoundation.org/White-Paper-3A-Nature-2C-Nurture-2C-or-Both-3F. Published October 2010. Accessed May 23, 2017.
5. Cankovic M, Whiteley L, Hawley RC, Zarbo RJ, Chitale D. Clinical performance of JAK2 V617F mutation detection assays in a molecular diagnostics laboratory: evaluation of screening and quantitation methods. Am J Clin Pathol. 2009;132:713-721.
6. Kralovics R, Teo SS, Li S, et al. Acquisition of the V617F mutation of JAK2 is a late genetic event in a subset of patients with myeloproliferative disorders. Blood. 2006;108:1377-1380.
7. James C. The JAK2V617F mutation in polycythemia vera and other myeloproliferative disorders: one mutation for three diseases? Hematology Am Soc Hematol Educ Program. 2008:69-75.
8. Pancrazzi A, Guglielmelli P, Ponziani V, et al. A sensitive detection method for MPLW515L or MPLW515K mutation in chronic myeloproliferative disorders with locked nucleic acid-modified probes and real-time polymerase chain reaction. J Mol Diagn. 2008;10:435-441.
9. Pikman Y, Lee BH, Mercher T, et al. MPLW515L is a novel somatic activating mutation in myelofibrosis with myeloid metaplasia. PLoS Med. 2006;3:1140-1151.
10. Jones AV, Campbell PJ, Beer PA, et al. The JAK2 46/1 haplotype predisposes to MPL-mutated myeloproliferative neoplasms. Blood. 2010;115:4517-4523.
11. Jones AV, Cross NCP. Inherited predisposition to myeloproliferative neoplasms. Ther Adv Hematol. 2013;4:237-253.
Three myeloproliferative neoplasms (MPN), polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF), are associated with an abnormal somatic mutation of the JAK2 gene. Essential thrombocythemia is considered when there is a persistent increase in the peripheral blood platelet count, associated with a proliferation of atypical megakaryocytes in the bone marrow. The manifestations of PV, ET, and PMF all typically occur within the sixth or seventh decade of life. A patient may present with an abnormal blood count but be asymptomatic at the time. Over the course and progression of the disease, increases in hematocrit or platelet counts along with symptoms such as headaches, blurred vision, and plethora may occur.1 The JAK2 V617F mutation is responsible for the production of the JAK2 protein, which is continuously activated, promoting the growth and division of cells such as erythrocytes, granulocytes, and platelets. It has been reported that there is a nearly 100% incidence of the JAK2 mutation in patients with polycythemia vera, and a 50% incidence in patients with essential thrombocythemia and primary myelofibrosis.2
The discovery of the JAK2 mutation in PV, ET, and PMF was an important advancement in helping distinguish these disorders from other MPNs, including chronic myelogenous leukemia, but its presence does not explain why some individuals develop ET and others, PV or PMF.3 Although there have been familial cases proven of ET, the somatic JAK2 mutation is acquired and not inherited. In this report, we describe the unusual circumstance of JAK2 V617F mutation in a brother and a sister who were both diagnosed with essential thrombocythemia.
Case presentations and summaries
RS, a 69-year-old white man, was referred to our service in 2006 for continued care of previously diagnosed essential thrombocythemia. At the time of his initial visit to our clinic, his complete blood count was normal, the platelet count being adequately controlled by anagrelide at a daily dose of 4.0 mg. He complained of palpitations and peripheral neuropathy. A bone marrow biopsy was performed, revealing moderate hypercellularity, atypical megakaryocytosis, and a negative BCR-ABL mutation but a positive JAK2 V617F mutation. The patient is now treated with hydroxyurea 1,000 mg daily in divided doses, which better controls his counts and does not have the side effects of anagrelide.
SW, a 73-year-old woman, and brother of RS (they share the same biological mother and father), was noted to have a mild thrombocytosis in 2008. In 2013, her platelet count rose to 865,000 cells/uL (normal, 150,000-450,000 cells/uL, age and sex adjusted) and she was referred to our clinic. A bone marrow biopsy was performed, revealing borderline hypercellularity with atypical megakaryocytosis and the presence of a JAK2 V617F mutation. As with her brother, the BCR-ABL mutation was not present. She has also responded to treatment with hydroxyurea, but at a reduced dosage of 500 mg daily.
A third sibling, AS, again of the same biological mother and father, had died of multiple veno-occlusive cerebral vascular events long before the diagnoses on his younger siblings had been made. The suggestion of any underling hematologic pathology would be interesting, but speculative. Nothing is known abou
Discussion
Much research has been done to understand the pathogenesis of and find a cure for myeloproliferative disorders, but despite some progress, a cure remains elusive. However, there have been some advances that have contributed to partial cures for MPNs. One of the major breakthroughs in MPN research, about 50 years ago, was related to the “sporadic vs familial debate” around the Philadelphia chromosome.4 It led to the discovery of the reciprocal translocation between chromosomes 9 and 22, known as the BCR-ABL mutation, which is found in many CML patients. This discovery allowed researchers to focus their attention on other tyrosine kinase domains, such as the JAK2 V617F mutation, which is presented in the three other MPNs; PV, ET, and PMF. Both the JAK2 V617F and BCR-ABL mutations are active in signaling transcription, more commonly growth of cells.4
Since the discovery of the JAK2 V617F mutation in early 2005, it has become a leading diagnostic criteria for myeloproliferative diseases. The presence of the JAK2 V617F mutation and the measurement of its allele burden can be assessed by examination of either peripheral blood or bone marrow samples.5
The JAK2 V617F mutation is a result of a single change in the DNA nucleotide base pair that causes a substitution of a valine amino acid for a phenylalanine amino acid at the 617 position on exon 14 within the JAK2 kinase regulatory domain. This point mutation disrupts the regular control of the JAK2 by removing its ability to turn off, leading to uncontrolled blood cell growth.6 When the JAK2 V617F mutation cannot be demonstrated in a patient with the hallmarks of an MPN, the detection of other JAK2 and MPL proto-oncogene, thrombopoietin receptor mutations may be used as a diagnostic procedure for other MPNs.7
Other mutations incorporated in JAK2 domain can be detected in the coding portions of the DNA known as exons. One such mutation is the JAK2 exon 12, which is involved in JAK2 V617F-negative PV patients. This mutation is not detected in patients with ET or PMF and is 2%-5% present in patients with PV. There are other somatic mutations in the thrombopoietin receptors that work in accordance with thrombopoietin: MPL W515L and MPL W515K, which are found at chromosome 1p34, are identified in about 5% of PMF and 1% of ET patients, but are not present in PV patients.8.9
Pikman and colleagues reported in 2009 that the JAK2 V617F mutation is not acquired randomly.9 Their findings showed that, only in white populations, does the JAK2 V617F mutation arise preferentially on a specific constitutional JAK2 46/1 haplotype. According to the authors, the preconceived notion a of randomly acquired JAK2 V617F mutation does not account for familial MPN’s. Familial MPNs are thought to be produced by sporadic and extremely penetrant substitutions in genes that still are not identified and the 46/1 haplotype does not explain for the phenotypic diversity correlated with the JAK2 V617F gene. The 46/1 haplotype, however, correlates more frequently with different MPN subtypes. There are two hypotheses that try to explain how an acquired mutation as prevailing as the JAK2 V617F mutation can be associated with certain inherited backgrounds. The first hypothesis asserts the V617F accumulates at a faster rate than other genes because of the fundamentally unstable genetics of the 46/1 haplotype. The second theory is that all the mutated genes, including the V617F, arise at equal rates, but 46/1 may grant a selective advantage to the V617F-positive clone or interacts in some way to increase the likelihood of abnormal blood counts. A study that examined both these hypotheses concluded that the 46/1 haplotype was present more frequently in patients with myeloproliferative disorders than in their control groups and even more so in cases that were proven to be V617F-positive.10
There are very few cases that have reported familial MPN’s, especially as the pedigrees of the familial MPN’s illustrate that inheritance patterns are notably heterogeneous, indicating that there may be a range of different germline mutations driving the susceptibility. With recent data, the JAK2 V617F mutation in tandem with MPL W515L/K and inactivating TET2 mutations still continue to be the most frequently acquired mutations involved in both familial and sporadic MPN. As far as we know, there have been no cases to prove that JAK2 V617F and MPL W515L/K mutations are inherited through the germline, but there are other alleles that may pass through the germline that can be associated with hereditary thrombocytosis.11 Further cytogenetic studies will clarify the pathogenesis of these disorders and possibly lead to effective targeted therapies.
Three myeloproliferative neoplasms (MPN), polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF), are associated with an abnormal somatic mutation of the JAK2 gene. Essential thrombocythemia is considered when there is a persistent increase in the peripheral blood platelet count, associated with a proliferation of atypical megakaryocytes in the bone marrow. The manifestations of PV, ET, and PMF all typically occur within the sixth or seventh decade of life. A patient may present with an abnormal blood count but be asymptomatic at the time. Over the course and progression of the disease, increases in hematocrit or platelet counts along with symptoms such as headaches, blurred vision, and plethora may occur.1 The JAK2 V617F mutation is responsible for the production of the JAK2 protein, which is continuously activated, promoting the growth and division of cells such as erythrocytes, granulocytes, and platelets. It has been reported that there is a nearly 100% incidence of the JAK2 mutation in patients with polycythemia vera, and a 50% incidence in patients with essential thrombocythemia and primary myelofibrosis.2
The discovery of the JAK2 mutation in PV, ET, and PMF was an important advancement in helping distinguish these disorders from other MPNs, including chronic myelogenous leukemia, but its presence does not explain why some individuals develop ET and others, PV or PMF.3 Although there have been familial cases proven of ET, the somatic JAK2 mutation is acquired and not inherited. In this report, we describe the unusual circumstance of JAK2 V617F mutation in a brother and a sister who were both diagnosed with essential thrombocythemia.
Case presentations and summaries
RS, a 69-year-old white man, was referred to our service in 2006 for continued care of previously diagnosed essential thrombocythemia. At the time of his initial visit to our clinic, his complete blood count was normal, the platelet count being adequately controlled by anagrelide at a daily dose of 4.0 mg. He complained of palpitations and peripheral neuropathy. A bone marrow biopsy was performed, revealing moderate hypercellularity, atypical megakaryocytosis, and a negative BCR-ABL mutation but a positive JAK2 V617F mutation. The patient is now treated with hydroxyurea 1,000 mg daily in divided doses, which better controls his counts and does not have the side effects of anagrelide.
SW, a 73-year-old woman, and brother of RS (they share the same biological mother and father), was noted to have a mild thrombocytosis in 2008. In 2013, her platelet count rose to 865,000 cells/uL (normal, 150,000-450,000 cells/uL, age and sex adjusted) and she was referred to our clinic. A bone marrow biopsy was performed, revealing borderline hypercellularity with atypical megakaryocytosis and the presence of a JAK2 V617F mutation. As with her brother, the BCR-ABL mutation was not present. She has also responded to treatment with hydroxyurea, but at a reduced dosage of 500 mg daily.
A third sibling, AS, again of the same biological mother and father, had died of multiple veno-occlusive cerebral vascular events long before the diagnoses on his younger siblings had been made. The suggestion of any underling hematologic pathology would be interesting, but speculative. Nothing is known abou
Discussion
Much research has been done to understand the pathogenesis of and find a cure for myeloproliferative disorders, but despite some progress, a cure remains elusive. However, there have been some advances that have contributed to partial cures for MPNs. One of the major breakthroughs in MPN research, about 50 years ago, was related to the “sporadic vs familial debate” around the Philadelphia chromosome.4 It led to the discovery of the reciprocal translocation between chromosomes 9 and 22, known as the BCR-ABL mutation, which is found in many CML patients. This discovery allowed researchers to focus their attention on other tyrosine kinase domains, such as the JAK2 V617F mutation, which is presented in the three other MPNs; PV, ET, and PMF. Both the JAK2 V617F and BCR-ABL mutations are active in signaling transcription, more commonly growth of cells.4
Since the discovery of the JAK2 V617F mutation in early 2005, it has become a leading diagnostic criteria for myeloproliferative diseases. The presence of the JAK2 V617F mutation and the measurement of its allele burden can be assessed by examination of either peripheral blood or bone marrow samples.5
The JAK2 V617F mutation is a result of a single change in the DNA nucleotide base pair that causes a substitution of a valine amino acid for a phenylalanine amino acid at the 617 position on exon 14 within the JAK2 kinase regulatory domain. This point mutation disrupts the regular control of the JAK2 by removing its ability to turn off, leading to uncontrolled blood cell growth.6 When the JAK2 V617F mutation cannot be demonstrated in a patient with the hallmarks of an MPN, the detection of other JAK2 and MPL proto-oncogene, thrombopoietin receptor mutations may be used as a diagnostic procedure for other MPNs.7
Other mutations incorporated in JAK2 domain can be detected in the coding portions of the DNA known as exons. One such mutation is the JAK2 exon 12, which is involved in JAK2 V617F-negative PV patients. This mutation is not detected in patients with ET or PMF and is 2%-5% present in patients with PV. There are other somatic mutations in the thrombopoietin receptors that work in accordance with thrombopoietin: MPL W515L and MPL W515K, which are found at chromosome 1p34, are identified in about 5% of PMF and 1% of ET patients, but are not present in PV patients.8.9
Pikman and colleagues reported in 2009 that the JAK2 V617F mutation is not acquired randomly.9 Their findings showed that, only in white populations, does the JAK2 V617F mutation arise preferentially on a specific constitutional JAK2 46/1 haplotype. According to the authors, the preconceived notion a of randomly acquired JAK2 V617F mutation does not account for familial MPN’s. Familial MPNs are thought to be produced by sporadic and extremely penetrant substitutions in genes that still are not identified and the 46/1 haplotype does not explain for the phenotypic diversity correlated with the JAK2 V617F gene. The 46/1 haplotype, however, correlates more frequently with different MPN subtypes. There are two hypotheses that try to explain how an acquired mutation as prevailing as the JAK2 V617F mutation can be associated with certain inherited backgrounds. The first hypothesis asserts the V617F accumulates at a faster rate than other genes because of the fundamentally unstable genetics of the 46/1 haplotype. The second theory is that all the mutated genes, including the V617F, arise at equal rates, but 46/1 may grant a selective advantage to the V617F-positive clone or interacts in some way to increase the likelihood of abnormal blood counts. A study that examined both these hypotheses concluded that the 46/1 haplotype was present more frequently in patients with myeloproliferative disorders than in their control groups and even more so in cases that were proven to be V617F-positive.10
There are very few cases that have reported familial MPN’s, especially as the pedigrees of the familial MPN’s illustrate that inheritance patterns are notably heterogeneous, indicating that there may be a range of different germline mutations driving the susceptibility. With recent data, the JAK2 V617F mutation in tandem with MPL W515L/K and inactivating TET2 mutations still continue to be the most frequently acquired mutations involved in both familial and sporadic MPN. As far as we know, there have been no cases to prove that JAK2 V617F and MPL W515L/K mutations are inherited through the germline, but there are other alleles that may pass through the germline that can be associated with hereditary thrombocytosis.11 Further cytogenetic studies will clarify the pathogenesis of these disorders and possibly lead to effective targeted therapies.
1. Murphy S, Peterson P, Iland H, Laszio J. Experience of the Polycythemia Vera Study Group with essential thrombocythemia: a final report on diagnostic criteria, survival, and leukemic transition by treatment. Semin Hematol. 1997;34:29-39.
2. Zhan H, Spivak JL. The diagnosis and management of polycythemia vera, essential thrombocythemia, and primary myelofibrosis in the JAK2 V617F era. Clin Adv Hematol Oncol. 2009;7:334-342.
3. Higgs JR, Sadek I, Neumann PE, et al. Familial essential thrombocythemia with spontaneous megakaryocyte colony formation and acquired JAK2 mutations. Leukemia. 2008;22:1551-1556.
4. Senyak Z. Eileen Wiggins – out of the blue. http://www.mpnresearchfoundation.org/White-Paper-3A-Nature-2C-Nurture-2C-or-Both-3F. Published October 2010. Accessed May 23, 2017.
5. Cankovic M, Whiteley L, Hawley RC, Zarbo RJ, Chitale D. Clinical performance of JAK2 V617F mutation detection assays in a molecular diagnostics laboratory: evaluation of screening and quantitation methods. Am J Clin Pathol. 2009;132:713-721.
6. Kralovics R, Teo SS, Li S, et al. Acquisition of the V617F mutation of JAK2 is a late genetic event in a subset of patients with myeloproliferative disorders. Blood. 2006;108:1377-1380.
7. James C. The JAK2V617F mutation in polycythemia vera and other myeloproliferative disorders: one mutation for three diseases? Hematology Am Soc Hematol Educ Program. 2008:69-75.
8. Pancrazzi A, Guglielmelli P, Ponziani V, et al. A sensitive detection method for MPLW515L or MPLW515K mutation in chronic myeloproliferative disorders with locked nucleic acid-modified probes and real-time polymerase chain reaction. J Mol Diagn. 2008;10:435-441.
9. Pikman Y, Lee BH, Mercher T, et al. MPLW515L is a novel somatic activating mutation in myelofibrosis with myeloid metaplasia. PLoS Med. 2006;3:1140-1151.
10. Jones AV, Campbell PJ, Beer PA, et al. The JAK2 46/1 haplotype predisposes to MPL-mutated myeloproliferative neoplasms. Blood. 2010;115:4517-4523.
11. Jones AV, Cross NCP. Inherited predisposition to myeloproliferative neoplasms. Ther Adv Hematol. 2013;4:237-253.
1. Murphy S, Peterson P, Iland H, Laszio J. Experience of the Polycythemia Vera Study Group with essential thrombocythemia: a final report on diagnostic criteria, survival, and leukemic transition by treatment. Semin Hematol. 1997;34:29-39.
2. Zhan H, Spivak JL. The diagnosis and management of polycythemia vera, essential thrombocythemia, and primary myelofibrosis in the JAK2 V617F era. Clin Adv Hematol Oncol. 2009;7:334-342.
3. Higgs JR, Sadek I, Neumann PE, et al. Familial essential thrombocythemia with spontaneous megakaryocyte colony formation and acquired JAK2 mutations. Leukemia. 2008;22:1551-1556.
4. Senyak Z. Eileen Wiggins – out of the blue. http://www.mpnresearchfoundation.org/White-Paper-3A-Nature-2C-Nurture-2C-or-Both-3F. Published October 2010. Accessed May 23, 2017.
5. Cankovic M, Whiteley L, Hawley RC, Zarbo RJ, Chitale D. Clinical performance of JAK2 V617F mutation detection assays in a molecular diagnostics laboratory: evaluation of screening and quantitation methods. Am J Clin Pathol. 2009;132:713-721.
6. Kralovics R, Teo SS, Li S, et al. Acquisition of the V617F mutation of JAK2 is a late genetic event in a subset of patients with myeloproliferative disorders. Blood. 2006;108:1377-1380.
7. James C. The JAK2V617F mutation in polycythemia vera and other myeloproliferative disorders: one mutation for three diseases? Hematology Am Soc Hematol Educ Program. 2008:69-75.
8. Pancrazzi A, Guglielmelli P, Ponziani V, et al. A sensitive detection method for MPLW515L or MPLW515K mutation in chronic myeloproliferative disorders with locked nucleic acid-modified probes and real-time polymerase chain reaction. J Mol Diagn. 2008;10:435-441.
9. Pikman Y, Lee BH, Mercher T, et al. MPLW515L is a novel somatic activating mutation in myelofibrosis with myeloid metaplasia. PLoS Med. 2006;3:1140-1151.
10. Jones AV, Campbell PJ, Beer PA, et al. The JAK2 46/1 haplotype predisposes to MPL-mutated myeloproliferative neoplasms. Blood. 2010;115:4517-4523.
11. Jones AV, Cross NCP. Inherited predisposition to myeloproliferative neoplasms. Ther Adv Hematol. 2013;4:237-253.
Management of tonsillar carcinoma with advanced radiation therapy and chemotherapy techniques
Tonsillar carcinoma is the most common of the oropharyngeal malignancies of the head and neck region after thyroid and laryngeal carcinoma. Squamous cell carcinoma is the most frequent histologic type of these tumors.1 Tonsillar tumors may originate in the oral cavity, oropharynx, hypopharynx, or larynx. In the United States, more than 5,000 new cases of oropharynx cancer are diagnosed annually.2 Men are affected three to four times more often than are women, and the rate of incidence increases after the 4th decade of life.3 Surveillance, Epidemiology, and End Results data from 1975-2004 show that tonsillar squamous cell carcinoma has had one of the largest increases in the male-to-female incidence rate ratios.4 The overall incidence of tonsillar carcinoma is increasing, especially in the younger population, and this may be attributed to increasing rates of human papilloma virus.5,6
Squamous cell carcinoma in the head and neck originate from subsites within the oral cavity, oropharynx, hypopharynx, larynx, and nasopharynx.7 Traditionally, alcohol consumption and tobacco use were considered the most significant risk factors for the development of tonsillar cancer.8 More recently, however, the high-risk oncogenic human papilloma virus has emerged as a clinical entity in the pathogenesis of squamous cell carcinoma in the head and neck. Other risk factors include poor oral hygiene, mechanical irritation, chewing of betel quid preparations, and a lack of vegetables and fruits in the diet.9-11 Squamous cell carcinoma of the oropharynx often presents late with lymph node involvement at the time of diagnosis. Nonspecific symptoms such as a sore throat and dysphagia can allow head and neck cancer to evade early detection. Many patients with tonsillar carcinoma present with advanced disease because early lesions are generally asymptomatic when small. This absence of symptoms is responsible for 67%-77% of patients presenting with tumors larger than 2.0 cm and often with regional nodal metastasis. At presentation, 45% of anterior tonsillar pillar lesions and 76% of tonsillar fossa lesions have clinically positive necks.12
Despite significant treatment advances, the management of advanced squamous cell carcinoma of the tonsil remains challenging. Historically, surgery was considered the standard of care for patients with tonsillar carcinoma with or without postoperative adjuvant radiotherapy. In locally advanced tonsillar carcinoma, extensive surgery with major tissue reconstruction was necessary, leading to speech dysfunction, cosmetic deformities, and difficulties in swallowing, all of which are detrimental to patient quality of life.13 Given the critical role of the oropharynx in speech and swallowing, nonsurgical therapy with organ-preserving chemoradiation has gained a greater role in the treatment of tonsil carcinoma.13 Over the past decade, innovations in radiation therapy techniques have led to the introduction of intensity-modulated radiation therapy (IMRT) and image-guided radiation therapy (IGRT) for the treatment of various cancers including tonsillar carcinoma.14,15 IMRT is an advanced mode of conformal high-precision radiotherapy that uses computer-controlled multiple small radiation beams of varying intensities to deliver precise radiation doses to the target tissues while sparing adjacent healthy tissues.14 By incorporating three-dimensional computed-tomography (CT) or positron-emission–tomography (PET) imaging technology, IMRT allows the radiation dose to conform more precisely to the three-dimensional shape of the tumor while modulating the intensity of the radiation beam and minimizing its dose to those adjacent sensitive and unaffected organs. IGRT uses a range of two-, three-, and four-dimensional imaging techniques that improve the precision and accuracy of the delivery of the radiation dose to the targeted tumor tissue while minimizing the dose to the surrounding normal tissue during the course of radiation therapy (Figure 1). In this report, we present challenging cases of advanced tonsillar carcinoma and describe our experience in managing the disease using a hyperfractionated IMRT-IGRT based three-dimensional conformal radiation therapy protocol with concurrent chemotherapy.
Case presentations and summaries
Case 1
A 52-year-old white, nonsmoking man who worked in a research chemical laboratory, presented with complaints of throat pain and difficulty in swallowing. The patient had a history of asthma and allergies and had been seen by an ear, nose, and throat (ENT) specialist prior to his visit to our oncology center. A biopsy was performed on a right tonsillar mass measuring 2.7 x 3.6 cm. A computed-tomography (CT) scan showed 2 enlarged inhomogeneous lymph nodes measuring 2.9 cm and 1.7 cm. The nodes were well defined with no soft tissue edema. Neoplasm was favored as a diagnosis and biopsy of the mass was carried out. A biopsy specimen measuring 1.0 x 0.4 x 0.3 cm revealed a moderately differentiated infiltrating squamous cell carcinoma, which extended to the edge of the biopsy specimen. The patient’s Karnofsky performance status was 90% (ie, able to carry on normal activity; minor signs or symptoms of disease).
A CT scan of the chest was clear with no evidence of malignant involvement. A subsequent CT scan of the neck revealed a primary neoplasm of the right faucial tonsil measuring 3.3 x 3.0 cm and associated with right level II, level III, and level IV pathological lymphadenopathy. Positron-emission tomography (PET) imaging of the neck revealed a right tonsillar lesion of 2.7 x 3.0 cm involving the right parapharyngeal space (Figure 2, Case 1). The standardized uptake value (SUV) of the PET scan of the primary lesion was measured at 7.3. A cluster of right level II cervical nodes measuring 3.2 x 2.5 cm had an SUV of 3.5. A 1.0-cm right level III jugular node was also seen with an SUV of 1.6, and a right level IV lymph node measuring 1.5 x 1.0 cm was seen with an SUV of 1.8. No other lesions were noted. The tumor stage was T2N2bM0, a stage IVa disease.
The patient had a percutaneous endoscopic gastrostomy (PEG) tube placement before starting radiation. He underwent a course of hyperfractionated intensity-modulated radiation therapy with image guidance (IMRT-IGRT) in 67 fractions of 120 cGy twice a day to a final tumor dose of 8,040 cGy.16 Concurrently, the patient received systemic chemotherapy with carboplatin at a dose of 240 mg weekly. To optimize the treatment, molecular profiling was performed to identify the sensitive genetic targets to systemic chemotherapy drugs.17, 18 Targets sensitive to paclitaxel and docetaxel were identified by molecular profiling of the tumor tissue, then chemotherapy with paclitaxel or docetaxel (25 mg/m2 weekly for 3 weeks and 1 week off) was also administered to the patient.
The follow-up after 41 months indicated that the patient had no evidence of recurrent disease (Figure 2, Case 1). Posttreatment magnetic-resonance imaging (MRI) of the neck also indicated no evidence of residual tonsillar cancer. The patient’s demographics, tumor characteristics, and the treatment details are summarized in the Table.
Case 2
A 49-year-old black male presented with throat pain and a mass seen initially by his family physician. The patient had a history of tobacco use (at least 1 cigar a day) periodically for about 10 years and had quit cigar smoking 15 years prior to developing his disease. An initial evaluation indicated that the patient had a hypopharyngeal mass in the left inferior pole of his tonsil with near occlusion of the hypopharyngeal airway. His larynx could not be visualized because of the obstructive mass. A neck lymph node measuring 3.0 cm in the left jugulodigastric region was also noted. The patient’s Karnofsky performance status was 90%. Subsequently, the patient underwent excision of the right tonsil and left tonsillar region.
The pathology of the right tonsil was found to be benign. Histology of the left tonsil revealed invasive squamous cell carcinoma. The resected tumor size measured 3.7 x 2.7 x 2.5 cm. The tumor was moderately differentiated involving the deep surgical margins. No lymphovascular invasion was seen. A PET scan revealed a mass arising from the left tonsillar pillar measuring 3.6 x 2.6 x 3.3 cm with deviation of the epiglottis posteriorly nearing the left vallecula. In addition, multiple large cervical nodal lesions in the left level II nodal chain were seen, with the largest measuring 3.1 x 3.0 x 4.5 cm with an SUV of 3.4. Displacement of the left submandibular gland with several further enlarged level II lymph nodes was observed. In the region of left vallecula, there was soft tissue thickening with increased activity measuring 2.7 x 1.5 cm, likely crossing the midline with an SUV of 5.5. The rest of the neck was negative for metastatic involvement (Figure 2, Case 2). The tumor stage was T3N2Mx, a stage IVa disease.
The patient had a Port-A-Cath placed, which caused a hemothorax after placement of the port and delayed initiating his treatment. A pretreatment MRI scan of the neck revealed multiple conglomerate hypodense peripherally enhancing nodular areas in the left neck posterior to the left submandibular gland deep to the parotid tail worrisome for necrotic lymphadenopathy. The patient underwent a course of hyperfractionated IMRT-IGRT in 67 fractions of 120 cGy twice daily for a total dose of 8,040 cGy to the primary tumor site.16 The patient had a port and PEG tube prior to initiating his radiation therapy. He received IMRT-IGRT with concurrent chemotherapy that was selected based on the recommendation of his genomic testing.17,18 The chemotherapy regimen used included carboplatin (300 mg weekly) and docetaxel (400 mg weekly). The patient had a treatment break because he was hospitalized for anemia and pancytopenia from his chemotherapy and he received supportive cancer care with epoetin alfa.A post therapy PET scan was negative for evidence of hypermetabolic malignancy; however, a 3.3 x 2.7 cm calcified lesion representing likely level III jugular lymph node exhibited no measurable activity at that time. The follow-up after 40 months indicated that the patient had no reported recurrence of the disease (Figure 2, Case 2). The patient’s demographics, tumor characteristics, and the treatment details are summarized in the Table.
Case 3
A 53-year-old white man, who had no smoking or tobacco history but who was exposed to chemicals including sulfuric acid, hydrogen chloride gas, and glycols at work, presented initially with a sore throat that became more painful over time. His ENT specialist referred him for a CT scan of the neck, which revealed a left-sided neck mass measuring 2.5 cm in diameter posterior to the submandibular gland and lateral to carotid sheath and anterior to the triangle (Figure 2, Case 3). The mass appeared to be encapsulated. There was a lobulated spherical mass in the left supraglottic area with formation of the airway of the pyriform sinus and additional anterior vascular involvement was noted. The mass measured 3.6 cm in transverse diameter.
A left tonsillar biopsy specimen measuring 1.4 x 0.6 x 0.2 cm was obtained, and its pathology revealed that the patient had a metastatic squamous cell carcinoma. The left neck lymph node mass aspiration also revealed the presence of squamous cell carcinoma. A PET-CT scan staging showed a dominant tonsillar fossa mass extending from the soft palate down to the pyriform sinus measuring 4.2 x 3.8 cm, with an SUV uptake of 7.3. There was a dominant left level II necrotic lymph node presence measuring 5.0 x 3.7 cm, with an SUV of 3.0. The patient’s Karnofsky performance status was 90%. The tumor stage was T4N2M0, a stage IVa disease. The patient received a course of conformal hyperfractionated IMRT-IGRT delivered to the primary tumor in 67 fractions at 120 cGy twice daily for a total dose of 8,040 cGy16 and concurrent carboplatin chemotherapy at a weekly dose of 200 mg.
After completion of his radiation therapy, chemotherapy was changed based on genomic testing from single agent to doublet with carboplatin (area under the curve (AUC) dose of 2 or 200 mg, weekly) plus docetaxel (25 mg/m2 weekly for 3 weeks and 1 week off ).17,18 A PET scan after chemoradiation therapy revealed a marked anatomical improvement in the primary neoplastic disease seen in the faucial tonsil. The tonsillar mass noted previously had almost completely resolved over the interval, with only a mild persistent asymmetrical thickening of around 1.5 cm, with a peak SUV of 2.0. A lymph node of 2.8 x 2.0 cm was present anterior to the left sternocleidomastoid muscle exhibiting SUV of only 1.8. No other abnormal lesions were noted (Figure 2, Case 3). The patient continues to do extremely well without local recurrence of the disease 46 months after radiation therapy (see Table for patient demographics, tumor characteristics, and therapy details.)
Discussion
The management of patients with primary squamous cell carcinoma of the oropharyngeal remains controversial. Traditionally, early-stage tonsillar squamous cell carcinoma was managed by a single modality treatment, either by surgery or radiation therapy, each showing similar efficacy and outcomes.19 For late-stage disease, a combined approach using surgery and radiation therapy was found to be superior to single modality treatment. However, surgery in conjugation with radiation therapy has been associated with significant toxicities compared with the radiation therapy alone.13Therefore, the use of radiation therapy without surgery is becoming more common with increasingly sophisticated radiation therapy techniques and organ preservation approach in patients with squamous cell carcinoma of the tonsil.
Findings from several studies have shown that in stage I or II oropharyngeal cancer, single modality treatment with radiation therapy achieves 80%-90% of local control of the disease, but poorer outcomes are reported for locally advanced stages III/IV with a local control rate of 63%-74%.20 These findings and others have led to a shift to evaluate the clinical benefits of radiation therapy given with concurrent chemotherapy for the primary treatment of advanced stage oropharyngeal squamous cell carcinoma.20,21 Findings from a number of studies have since reported comparable efficacy and toxicity outcomes using this regimen with concurrent chemotherapy in patients with locally advanced head and neck squamous cell cancer.22-24 Synchronous carboplatin chemotherapy was used effectively as an alternative to cisplatin with fewer potential adverse effects in the good prognosis group of patients with oropharyngeal squamous cell carcinoma.25,26 For our 3 patients, we used carboplatin-based chemotherapy with concurrent advanced hyperfractionated radiation therapy techniques to successfully manage tonsillar squamous cell carcinoma and reduce renal toxicity and neuropathy.
Advanced radiation therapy techniques such as IMRT-IGRT are used routinely at the University Cancer and Diagnostic Centers in Houston, Texas, to manage a range of malignant cancers.27 These innovative techniques have the potential to deliver highly conformal dose-intense radiation to targeted regions of disease, while sparing adjacent critical nonmalignant tissue. The improved shaping of high-dose distributions with IMRT-IGRT could mitigate treatment-related toxicities. For example, the use of advanced radiation therapy techniques has been associated with increased preservation of parotid salivary flow.28-30 The use of advanced radiation therapy techniques in head and neck squamous cell carcinoma is growing, and early evidence confirms its ability to secure excellent local and regional disease control.31,32 In this study, we have demonstrated that by using hyperfractionated conformal three-dimensional IMRT-IGRT we were able not only to manage advanced tonsillar squamous cell carcinoma and treat the malignant metastasis, but also spare adjacent critical organs that were not involved in the disease, thus reducing many of the detrimental side effects associated with hyperfractionated chemoradiation.
All 3 patients were followed for between 40 and 46 months. They continue to do extremely well without local recurrence of their disease, indicating a 100% disease control and overall survival rate. The disease control and survival outcomes for our patients with stage IVA disease compare favorably to other published reports in the literature.33,34 Findings from a study by Prestwich and colleagues33 of 41 patients with stage IV tonsillar carcinoma showed that the radiation therapy with concurrent chemotherapy achieved local and regional disease control in 91% of complete responders and an overall survival rate of 66% at 3 years. Similarly, Setton and colleagues34 reported on 442 patients – 50% with tonsillar cancer, 46% with base-of-tongue cancer – who underwent IMRT and concurrent chemotherapy and who achieved a 3-year overall survival of 84.9%. Our study findings demonstrate that hyperfractionated conformal three-dimensional IMRT-IGRT with concurrent chemotherapy can be delivered safely and effectively to patients with advanced tonsillar squamous cell carcinoma.
Acknowledgment
The authors thank Ms June Lyliston, LVN, for editing and proofreading the manuscript.
1. Stambuk HE, Karimi S, Lee N, Patel SG. Oral cavity and oropharynx tumors. Radiol Clin North Am. 2007;45(1):1-20.
2. Lin DT, Cohen SM, Coppit GL, Burkey BB. Squamous cell carcinoma of the oropharynx and hypopharynx. Otolaryngol Clin North Am. 2005;38(1):59-74, viii.
3. Golas SM. Trends in palatine tonsillar cancer incidence and mortality rates in the United States. Community Dent Oral Epidemiol. 2007;35(2):98-108.
4. Cook MB, Dawsey SM, Freedman ND, et al. Sex disparities in cancer incidence by period and age. Cancer Epidemiol Biomarkers Prev. 2009;18(4):1174-1182.
5. Enomoto LM, Bann DV, Hollenbeak CS, Goldenberg D. Trends in the Incidence of oropharyngeal cancers in the United States. Otolaryngol Head Neck Surg. 2016.
6. Shiboski CH, Schmidt BL, Jordan RC. Tongue and tonsil carcinoma: increasing trends in the U.S. population ages 20-44 years. Cancer. 2005;103(9):1843-1849.
7. Marur S, Forastiere AA. Head and neck cancer: changing epidemiology, diagnosis, and treatment. Mayo Clin Proc. 2008;83(4):489-501.
8. Hong AM, Martin A, Chatfield M, et al. Human papillomavirus, smoking status and outcomes in tonsillar squamous cell carcinoma. Int J Cancer. 2013;132(12):2748-2754.
9. Velly AM, Franco EL, Schlecht N, et al. Relationship between dental factors and risk of upper aerodigestive tract cancer. Oral Oncol. 1998;34(4):284-291.
10. Farrow DC, Vaughan TL, Berwick M, et al. Diet and nasopharyngeal cancer in a low-risk population. Int J Cancer. 1998;78(6):675-679.
11. Freedman ND, Park Y, Subar AF, et al. Fruit and vegetable intake and head and neck cancer risk in a large United States prospective cohort study. Int J Cancer. 2008;122(10):2330-2336.
12. Guay ME, Lavertu P. Tonsillar carcinoma. Eur Arch Otorhinolaryngol. 1995;252(5):259-264.
13. Parsons JT, Mendenhall WM, Stringer SP, et al. Squamous cell carcinoma of the oropharynx: surgery, radiation therapy, or both. Cancer. 2002;94(11):2967-2980.
14. Yao M, Dornfeld KJ, Buatti JM, et al. Intensity-modulated radiation treatment for head-and-neck squamous cell carcinoma--the University of Iowa experience. Int J Radiat Oncol Biol Phys. 2005;63(2):410-421.
15. Yang ES, Murphy BM, Chung CH, et al. Evolution of clinical trials in head and neck cancer. Crit Rev Oncol Hematol. 2009;71(1):29-42.
16. Beitler JJ, Zhang Q, Fu KK, et al. Final results of local-regional control and late toxicity of RTOG 9003: a randomized trial of altered fractionation radiation for locally advanced head and neck cancer. Int J Radiat Oncol Biol Phys. 2014;89(1):13-20.
17. Tomkiewicz C, Hans S, Mucchielli MH, et al. A head and neck cancer tumor response-specific gene signature for cisplatin, 5-fluorouracil induction chemotherapy fails with added taxanes. PLoS One. 2012;7(10):e47170.
18. Feldman R, Gatalica Z, Knezetic J, et al. Molecular profiling of head and neck squamous cell carcinoma. Head Neck. 2016;38 Suppl 1:E1625-1638.
19. Moose BD, Kelly MD, Levine PA, et al. Definitive radiotherapy for T1 and T2 squamous cell carcinoma of the tonsil. Head Neck. 1995;17(4):334-338.
20. Chen AY, Schrag N, Hao Y, Stewart A, Ward E. Changes in treatment of advanced oropharyngeal cancer, 1985-2001. Laryngoscope. 2007;117(1):16-21.
21. Machtay M, Rosenthal DI, Hershock D, et al. Organ preservation therapy using induction plus concurrent chemoradiation for advanced resectable oropharyngeal carcinoma: a University of Pennsylvania Phase II Trial. J Clin Oncol. 2002;20(19):3964-3971.
22. Jegannathen A, Swindell R, Yap B, et al. Can synchronous chemotherapy be added to accelerated hypofractionated radiotherapy in patients with base of tongue cancer? Clin Oncol (R Coll Radiol). 2010;22(3):185-191.
23. Budach V, Becker ET, Boehmer D, et al. Concurrent hyperfractionated accelerated radiotherapy with 5-FU and once weekly cisplatin in locally advanced head and neck cancer. The 10-year results of a prospective phase II trial. Strahlenther Onkol. 2014;190(3):250-255.
24. Tobias JS, Monson K, Gupta N, et al. Chemoradiotherapy for locally advanced head and neck cancer: 10-year follow-up of the UK Head and Neck (UKHAN1) trial. Lancet Oncol. 2010;11(1):66-74.
25. Wilkins AC, Rosenfelder N, Schick U, et al. Equivalence of cisplatin and carboplatin-based chemoradiation for locally advanced squamous cell carcinoma of the head and neck: a matched-pair analysis. Oral Oncol. 2013;49(6):615-619.
26. Benghiat H, Sanghera P, Cashmore1 J, et al. Four week hypofractionated accelerated intensity modulated radiotherapy and synchronous carboplatin or cetuximab in biologically staged oropharyngeal carcinoma. Cancer and Clinical Oncology. 2014;3:1-9.
27. D’Andrea MA, Reddy GK. Management of metastatic malignant thymoma with advanced radiation and chemotherapy techniques: report of a rare case. World J Surg Oncol. 2015;13:77.
28. Little M, Schipper M, Feng FY, et al. Reducing xerostomia after chemo-IMRT for head-and-neck cancer: beyond sparing the parotid glands. Int J Radiat Oncol Biol Phys. 2012;83(3):1007-1014.
29. Eisbruch A. Reducing xerostomia by IMRT: what may, and may not, be achieved. J Clin Oncol. 2007;25(31):4863-4864.
30. Pow EH, Kwong DL, McMillan AS, et al. Xerostomia and quality of life after intensity-modulated radiotherapy vs. conventional radiotherapy for early-stage nasopharyngeal carcinoma: initial report on a randomized controlled clinical trial. Int J Radiat Oncol Biol Phys. 2006;66(4):981-991.
31. Lee NY, de Arruda FF, Puri DR, et al. A comparison of intensity-modulated radiation therapy and concomitant boost radiotherapy in the setting of concurrent chemotherapy for locally advanced oropharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 2006;66(4):966-974.
32. Daly ME, Lieskovsky Y, Pawlicki T, et al. Evaluation of patterns of failure and subjective salivary function in patients treated with intensity modulated radiotherapy for head and neck squamous cell carcinoma. Head Neck. 2007;29(3):211-220.
33. Prestwich RJ, Kancherla K, Oksuz DC, et al. A single centre experience with sequential and concomitant chemoradiotherapy in locally advanced stage IV tonsillar cancer. Radiat Oncol. 2010;5:121.
34. Setton J, Caria N, Romanyshyn J, et al. Intensity-modulated radiotherapy in the treatment of oropharyngeal cancer: an update of the Memorial Sloan-Kettering Cancer Center experience. Int J Radiat Oncol Biol Phys. 2012;82(1):291-298.
Tonsillar carcinoma is the most common of the oropharyngeal malignancies of the head and neck region after thyroid and laryngeal carcinoma. Squamous cell carcinoma is the most frequent histologic type of these tumors.1 Tonsillar tumors may originate in the oral cavity, oropharynx, hypopharynx, or larynx. In the United States, more than 5,000 new cases of oropharynx cancer are diagnosed annually.2 Men are affected three to four times more often than are women, and the rate of incidence increases after the 4th decade of life.3 Surveillance, Epidemiology, and End Results data from 1975-2004 show that tonsillar squamous cell carcinoma has had one of the largest increases in the male-to-female incidence rate ratios.4 The overall incidence of tonsillar carcinoma is increasing, especially in the younger population, and this may be attributed to increasing rates of human papilloma virus.5,6
Squamous cell carcinoma in the head and neck originate from subsites within the oral cavity, oropharynx, hypopharynx, larynx, and nasopharynx.7 Traditionally, alcohol consumption and tobacco use were considered the most significant risk factors for the development of tonsillar cancer.8 More recently, however, the high-risk oncogenic human papilloma virus has emerged as a clinical entity in the pathogenesis of squamous cell carcinoma in the head and neck. Other risk factors include poor oral hygiene, mechanical irritation, chewing of betel quid preparations, and a lack of vegetables and fruits in the diet.9-11 Squamous cell carcinoma of the oropharynx often presents late with lymph node involvement at the time of diagnosis. Nonspecific symptoms such as a sore throat and dysphagia can allow head and neck cancer to evade early detection. Many patients with tonsillar carcinoma present with advanced disease because early lesions are generally asymptomatic when small. This absence of symptoms is responsible for 67%-77% of patients presenting with tumors larger than 2.0 cm and often with regional nodal metastasis. At presentation, 45% of anterior tonsillar pillar lesions and 76% of tonsillar fossa lesions have clinically positive necks.12
Despite significant treatment advances, the management of advanced squamous cell carcinoma of the tonsil remains challenging. Historically, surgery was considered the standard of care for patients with tonsillar carcinoma with or without postoperative adjuvant radiotherapy. In locally advanced tonsillar carcinoma, extensive surgery with major tissue reconstruction was necessary, leading to speech dysfunction, cosmetic deformities, and difficulties in swallowing, all of which are detrimental to patient quality of life.13 Given the critical role of the oropharynx in speech and swallowing, nonsurgical therapy with organ-preserving chemoradiation has gained a greater role in the treatment of tonsil carcinoma.13 Over the past decade, innovations in radiation therapy techniques have led to the introduction of intensity-modulated radiation therapy (IMRT) and image-guided radiation therapy (IGRT) for the treatment of various cancers including tonsillar carcinoma.14,15 IMRT is an advanced mode of conformal high-precision radiotherapy that uses computer-controlled multiple small radiation beams of varying intensities to deliver precise radiation doses to the target tissues while sparing adjacent healthy tissues.14 By incorporating three-dimensional computed-tomography (CT) or positron-emission–tomography (PET) imaging technology, IMRT allows the radiation dose to conform more precisely to the three-dimensional shape of the tumor while modulating the intensity of the radiation beam and minimizing its dose to those adjacent sensitive and unaffected organs. IGRT uses a range of two-, three-, and four-dimensional imaging techniques that improve the precision and accuracy of the delivery of the radiation dose to the targeted tumor tissue while minimizing the dose to the surrounding normal tissue during the course of radiation therapy (Figure 1). In this report, we present challenging cases of advanced tonsillar carcinoma and describe our experience in managing the disease using a hyperfractionated IMRT-IGRT based three-dimensional conformal radiation therapy protocol with concurrent chemotherapy.
Case presentations and summaries
Case 1
A 52-year-old white, nonsmoking man who worked in a research chemical laboratory, presented with complaints of throat pain and difficulty in swallowing. The patient had a history of asthma and allergies and had been seen by an ear, nose, and throat (ENT) specialist prior to his visit to our oncology center. A biopsy was performed on a right tonsillar mass measuring 2.7 x 3.6 cm. A computed-tomography (CT) scan showed 2 enlarged inhomogeneous lymph nodes measuring 2.9 cm and 1.7 cm. The nodes were well defined with no soft tissue edema. Neoplasm was favored as a diagnosis and biopsy of the mass was carried out. A biopsy specimen measuring 1.0 x 0.4 x 0.3 cm revealed a moderately differentiated infiltrating squamous cell carcinoma, which extended to the edge of the biopsy specimen. The patient’s Karnofsky performance status was 90% (ie, able to carry on normal activity; minor signs or symptoms of disease).
A CT scan of the chest was clear with no evidence of malignant involvement. A subsequent CT scan of the neck revealed a primary neoplasm of the right faucial tonsil measuring 3.3 x 3.0 cm and associated with right level II, level III, and level IV pathological lymphadenopathy. Positron-emission tomography (PET) imaging of the neck revealed a right tonsillar lesion of 2.7 x 3.0 cm involving the right parapharyngeal space (Figure 2, Case 1). The standardized uptake value (SUV) of the PET scan of the primary lesion was measured at 7.3. A cluster of right level II cervical nodes measuring 3.2 x 2.5 cm had an SUV of 3.5. A 1.0-cm right level III jugular node was also seen with an SUV of 1.6, and a right level IV lymph node measuring 1.5 x 1.0 cm was seen with an SUV of 1.8. No other lesions were noted. The tumor stage was T2N2bM0, a stage IVa disease.
The patient had a percutaneous endoscopic gastrostomy (PEG) tube placement before starting radiation. He underwent a course of hyperfractionated intensity-modulated radiation therapy with image guidance (IMRT-IGRT) in 67 fractions of 120 cGy twice a day to a final tumor dose of 8,040 cGy.16 Concurrently, the patient received systemic chemotherapy with carboplatin at a dose of 240 mg weekly. To optimize the treatment, molecular profiling was performed to identify the sensitive genetic targets to systemic chemotherapy drugs.17, 18 Targets sensitive to paclitaxel and docetaxel were identified by molecular profiling of the tumor tissue, then chemotherapy with paclitaxel or docetaxel (25 mg/m2 weekly for 3 weeks and 1 week off) was also administered to the patient.
The follow-up after 41 months indicated that the patient had no evidence of recurrent disease (Figure 2, Case 1). Posttreatment magnetic-resonance imaging (MRI) of the neck also indicated no evidence of residual tonsillar cancer. The patient’s demographics, tumor characteristics, and the treatment details are summarized in the Table.
Case 2
A 49-year-old black male presented with throat pain and a mass seen initially by his family physician. The patient had a history of tobacco use (at least 1 cigar a day) periodically for about 10 years and had quit cigar smoking 15 years prior to developing his disease. An initial evaluation indicated that the patient had a hypopharyngeal mass in the left inferior pole of his tonsil with near occlusion of the hypopharyngeal airway. His larynx could not be visualized because of the obstructive mass. A neck lymph node measuring 3.0 cm in the left jugulodigastric region was also noted. The patient’s Karnofsky performance status was 90%. Subsequently, the patient underwent excision of the right tonsil and left tonsillar region.
The pathology of the right tonsil was found to be benign. Histology of the left tonsil revealed invasive squamous cell carcinoma. The resected tumor size measured 3.7 x 2.7 x 2.5 cm. The tumor was moderately differentiated involving the deep surgical margins. No lymphovascular invasion was seen. A PET scan revealed a mass arising from the left tonsillar pillar measuring 3.6 x 2.6 x 3.3 cm with deviation of the epiglottis posteriorly nearing the left vallecula. In addition, multiple large cervical nodal lesions in the left level II nodal chain were seen, with the largest measuring 3.1 x 3.0 x 4.5 cm with an SUV of 3.4. Displacement of the left submandibular gland with several further enlarged level II lymph nodes was observed. In the region of left vallecula, there was soft tissue thickening with increased activity measuring 2.7 x 1.5 cm, likely crossing the midline with an SUV of 5.5. The rest of the neck was negative for metastatic involvement (Figure 2, Case 2). The tumor stage was T3N2Mx, a stage IVa disease.
The patient had a Port-A-Cath placed, which caused a hemothorax after placement of the port and delayed initiating his treatment. A pretreatment MRI scan of the neck revealed multiple conglomerate hypodense peripherally enhancing nodular areas in the left neck posterior to the left submandibular gland deep to the parotid tail worrisome for necrotic lymphadenopathy. The patient underwent a course of hyperfractionated IMRT-IGRT in 67 fractions of 120 cGy twice daily for a total dose of 8,040 cGy to the primary tumor site.16 The patient had a port and PEG tube prior to initiating his radiation therapy. He received IMRT-IGRT with concurrent chemotherapy that was selected based on the recommendation of his genomic testing.17,18 The chemotherapy regimen used included carboplatin (300 mg weekly) and docetaxel (400 mg weekly). The patient had a treatment break because he was hospitalized for anemia and pancytopenia from his chemotherapy and he received supportive cancer care with epoetin alfa.A post therapy PET scan was negative for evidence of hypermetabolic malignancy; however, a 3.3 x 2.7 cm calcified lesion representing likely level III jugular lymph node exhibited no measurable activity at that time. The follow-up after 40 months indicated that the patient had no reported recurrence of the disease (Figure 2, Case 2). The patient’s demographics, tumor characteristics, and the treatment details are summarized in the Table.
Case 3
A 53-year-old white man, who had no smoking or tobacco history but who was exposed to chemicals including sulfuric acid, hydrogen chloride gas, and glycols at work, presented initially with a sore throat that became more painful over time. His ENT specialist referred him for a CT scan of the neck, which revealed a left-sided neck mass measuring 2.5 cm in diameter posterior to the submandibular gland and lateral to carotid sheath and anterior to the triangle (Figure 2, Case 3). The mass appeared to be encapsulated. There was a lobulated spherical mass in the left supraglottic area with formation of the airway of the pyriform sinus and additional anterior vascular involvement was noted. The mass measured 3.6 cm in transverse diameter.
A left tonsillar biopsy specimen measuring 1.4 x 0.6 x 0.2 cm was obtained, and its pathology revealed that the patient had a metastatic squamous cell carcinoma. The left neck lymph node mass aspiration also revealed the presence of squamous cell carcinoma. A PET-CT scan staging showed a dominant tonsillar fossa mass extending from the soft palate down to the pyriform sinus measuring 4.2 x 3.8 cm, with an SUV uptake of 7.3. There was a dominant left level II necrotic lymph node presence measuring 5.0 x 3.7 cm, with an SUV of 3.0. The patient’s Karnofsky performance status was 90%. The tumor stage was T4N2M0, a stage IVa disease. The patient received a course of conformal hyperfractionated IMRT-IGRT delivered to the primary tumor in 67 fractions at 120 cGy twice daily for a total dose of 8,040 cGy16 and concurrent carboplatin chemotherapy at a weekly dose of 200 mg.
After completion of his radiation therapy, chemotherapy was changed based on genomic testing from single agent to doublet with carboplatin (area under the curve (AUC) dose of 2 or 200 mg, weekly) plus docetaxel (25 mg/m2 weekly for 3 weeks and 1 week off ).17,18 A PET scan after chemoradiation therapy revealed a marked anatomical improvement in the primary neoplastic disease seen in the faucial tonsil. The tonsillar mass noted previously had almost completely resolved over the interval, with only a mild persistent asymmetrical thickening of around 1.5 cm, with a peak SUV of 2.0. A lymph node of 2.8 x 2.0 cm was present anterior to the left sternocleidomastoid muscle exhibiting SUV of only 1.8. No other abnormal lesions were noted (Figure 2, Case 3). The patient continues to do extremely well without local recurrence of the disease 46 months after radiation therapy (see Table for patient demographics, tumor characteristics, and therapy details.)
Discussion
The management of patients with primary squamous cell carcinoma of the oropharyngeal remains controversial. Traditionally, early-stage tonsillar squamous cell carcinoma was managed by a single modality treatment, either by surgery or radiation therapy, each showing similar efficacy and outcomes.19 For late-stage disease, a combined approach using surgery and radiation therapy was found to be superior to single modality treatment. However, surgery in conjugation with radiation therapy has been associated with significant toxicities compared with the radiation therapy alone.13Therefore, the use of radiation therapy without surgery is becoming more common with increasingly sophisticated radiation therapy techniques and organ preservation approach in patients with squamous cell carcinoma of the tonsil.
Findings from several studies have shown that in stage I or II oropharyngeal cancer, single modality treatment with radiation therapy achieves 80%-90% of local control of the disease, but poorer outcomes are reported for locally advanced stages III/IV with a local control rate of 63%-74%.20 These findings and others have led to a shift to evaluate the clinical benefits of radiation therapy given with concurrent chemotherapy for the primary treatment of advanced stage oropharyngeal squamous cell carcinoma.20,21 Findings from a number of studies have since reported comparable efficacy and toxicity outcomes using this regimen with concurrent chemotherapy in patients with locally advanced head and neck squamous cell cancer.22-24 Synchronous carboplatin chemotherapy was used effectively as an alternative to cisplatin with fewer potential adverse effects in the good prognosis group of patients with oropharyngeal squamous cell carcinoma.25,26 For our 3 patients, we used carboplatin-based chemotherapy with concurrent advanced hyperfractionated radiation therapy techniques to successfully manage tonsillar squamous cell carcinoma and reduce renal toxicity and neuropathy.
Advanced radiation therapy techniques such as IMRT-IGRT are used routinely at the University Cancer and Diagnostic Centers in Houston, Texas, to manage a range of malignant cancers.27 These innovative techniques have the potential to deliver highly conformal dose-intense radiation to targeted regions of disease, while sparing adjacent critical nonmalignant tissue. The improved shaping of high-dose distributions with IMRT-IGRT could mitigate treatment-related toxicities. For example, the use of advanced radiation therapy techniques has been associated with increased preservation of parotid salivary flow.28-30 The use of advanced radiation therapy techniques in head and neck squamous cell carcinoma is growing, and early evidence confirms its ability to secure excellent local and regional disease control.31,32 In this study, we have demonstrated that by using hyperfractionated conformal three-dimensional IMRT-IGRT we were able not only to manage advanced tonsillar squamous cell carcinoma and treat the malignant metastasis, but also spare adjacent critical organs that were not involved in the disease, thus reducing many of the detrimental side effects associated with hyperfractionated chemoradiation.
All 3 patients were followed for between 40 and 46 months. They continue to do extremely well without local recurrence of their disease, indicating a 100% disease control and overall survival rate. The disease control and survival outcomes for our patients with stage IVA disease compare favorably to other published reports in the literature.33,34 Findings from a study by Prestwich and colleagues33 of 41 patients with stage IV tonsillar carcinoma showed that the radiation therapy with concurrent chemotherapy achieved local and regional disease control in 91% of complete responders and an overall survival rate of 66% at 3 years. Similarly, Setton and colleagues34 reported on 442 patients – 50% with tonsillar cancer, 46% with base-of-tongue cancer – who underwent IMRT and concurrent chemotherapy and who achieved a 3-year overall survival of 84.9%. Our study findings demonstrate that hyperfractionated conformal three-dimensional IMRT-IGRT with concurrent chemotherapy can be delivered safely and effectively to patients with advanced tonsillar squamous cell carcinoma.
Acknowledgment
The authors thank Ms June Lyliston, LVN, for editing and proofreading the manuscript.
Tonsillar carcinoma is the most common of the oropharyngeal malignancies of the head and neck region after thyroid and laryngeal carcinoma. Squamous cell carcinoma is the most frequent histologic type of these tumors.1 Tonsillar tumors may originate in the oral cavity, oropharynx, hypopharynx, or larynx. In the United States, more than 5,000 new cases of oropharynx cancer are diagnosed annually.2 Men are affected three to four times more often than are women, and the rate of incidence increases after the 4th decade of life.3 Surveillance, Epidemiology, and End Results data from 1975-2004 show that tonsillar squamous cell carcinoma has had one of the largest increases in the male-to-female incidence rate ratios.4 The overall incidence of tonsillar carcinoma is increasing, especially in the younger population, and this may be attributed to increasing rates of human papilloma virus.5,6
Squamous cell carcinoma in the head and neck originate from subsites within the oral cavity, oropharynx, hypopharynx, larynx, and nasopharynx.7 Traditionally, alcohol consumption and tobacco use were considered the most significant risk factors for the development of tonsillar cancer.8 More recently, however, the high-risk oncogenic human papilloma virus has emerged as a clinical entity in the pathogenesis of squamous cell carcinoma in the head and neck. Other risk factors include poor oral hygiene, mechanical irritation, chewing of betel quid preparations, and a lack of vegetables and fruits in the diet.9-11 Squamous cell carcinoma of the oropharynx often presents late with lymph node involvement at the time of diagnosis. Nonspecific symptoms such as a sore throat and dysphagia can allow head and neck cancer to evade early detection. Many patients with tonsillar carcinoma present with advanced disease because early lesions are generally asymptomatic when small. This absence of symptoms is responsible for 67%-77% of patients presenting with tumors larger than 2.0 cm and often with regional nodal metastasis. At presentation, 45% of anterior tonsillar pillar lesions and 76% of tonsillar fossa lesions have clinically positive necks.12
Despite significant treatment advances, the management of advanced squamous cell carcinoma of the tonsil remains challenging. Historically, surgery was considered the standard of care for patients with tonsillar carcinoma with or without postoperative adjuvant radiotherapy. In locally advanced tonsillar carcinoma, extensive surgery with major tissue reconstruction was necessary, leading to speech dysfunction, cosmetic deformities, and difficulties in swallowing, all of which are detrimental to patient quality of life.13 Given the critical role of the oropharynx in speech and swallowing, nonsurgical therapy with organ-preserving chemoradiation has gained a greater role in the treatment of tonsil carcinoma.13 Over the past decade, innovations in radiation therapy techniques have led to the introduction of intensity-modulated radiation therapy (IMRT) and image-guided radiation therapy (IGRT) for the treatment of various cancers including tonsillar carcinoma.14,15 IMRT is an advanced mode of conformal high-precision radiotherapy that uses computer-controlled multiple small radiation beams of varying intensities to deliver precise radiation doses to the target tissues while sparing adjacent healthy tissues.14 By incorporating three-dimensional computed-tomography (CT) or positron-emission–tomography (PET) imaging technology, IMRT allows the radiation dose to conform more precisely to the three-dimensional shape of the tumor while modulating the intensity of the radiation beam and minimizing its dose to those adjacent sensitive and unaffected organs. IGRT uses a range of two-, three-, and four-dimensional imaging techniques that improve the precision and accuracy of the delivery of the radiation dose to the targeted tumor tissue while minimizing the dose to the surrounding normal tissue during the course of radiation therapy (Figure 1). In this report, we present challenging cases of advanced tonsillar carcinoma and describe our experience in managing the disease using a hyperfractionated IMRT-IGRT based three-dimensional conformal radiation therapy protocol with concurrent chemotherapy.
Case presentations and summaries
Case 1
A 52-year-old white, nonsmoking man who worked in a research chemical laboratory, presented with complaints of throat pain and difficulty in swallowing. The patient had a history of asthma and allergies and had been seen by an ear, nose, and throat (ENT) specialist prior to his visit to our oncology center. A biopsy was performed on a right tonsillar mass measuring 2.7 x 3.6 cm. A computed-tomography (CT) scan showed 2 enlarged inhomogeneous lymph nodes measuring 2.9 cm and 1.7 cm. The nodes were well defined with no soft tissue edema. Neoplasm was favored as a diagnosis and biopsy of the mass was carried out. A biopsy specimen measuring 1.0 x 0.4 x 0.3 cm revealed a moderately differentiated infiltrating squamous cell carcinoma, which extended to the edge of the biopsy specimen. The patient’s Karnofsky performance status was 90% (ie, able to carry on normal activity; minor signs or symptoms of disease).
A CT scan of the chest was clear with no evidence of malignant involvement. A subsequent CT scan of the neck revealed a primary neoplasm of the right faucial tonsil measuring 3.3 x 3.0 cm and associated with right level II, level III, and level IV pathological lymphadenopathy. Positron-emission tomography (PET) imaging of the neck revealed a right tonsillar lesion of 2.7 x 3.0 cm involving the right parapharyngeal space (Figure 2, Case 1). The standardized uptake value (SUV) of the PET scan of the primary lesion was measured at 7.3. A cluster of right level II cervical nodes measuring 3.2 x 2.5 cm had an SUV of 3.5. A 1.0-cm right level III jugular node was also seen with an SUV of 1.6, and a right level IV lymph node measuring 1.5 x 1.0 cm was seen with an SUV of 1.8. No other lesions were noted. The tumor stage was T2N2bM0, a stage IVa disease.
The patient had a percutaneous endoscopic gastrostomy (PEG) tube placement before starting radiation. He underwent a course of hyperfractionated intensity-modulated radiation therapy with image guidance (IMRT-IGRT) in 67 fractions of 120 cGy twice a day to a final tumor dose of 8,040 cGy.16 Concurrently, the patient received systemic chemotherapy with carboplatin at a dose of 240 mg weekly. To optimize the treatment, molecular profiling was performed to identify the sensitive genetic targets to systemic chemotherapy drugs.17, 18 Targets sensitive to paclitaxel and docetaxel were identified by molecular profiling of the tumor tissue, then chemotherapy with paclitaxel or docetaxel (25 mg/m2 weekly for 3 weeks and 1 week off) was also administered to the patient.
The follow-up after 41 months indicated that the patient had no evidence of recurrent disease (Figure 2, Case 1). Posttreatment magnetic-resonance imaging (MRI) of the neck also indicated no evidence of residual tonsillar cancer. The patient’s demographics, tumor characteristics, and the treatment details are summarized in the Table.
Case 2
A 49-year-old black male presented with throat pain and a mass seen initially by his family physician. The patient had a history of tobacco use (at least 1 cigar a day) periodically for about 10 years and had quit cigar smoking 15 years prior to developing his disease. An initial evaluation indicated that the patient had a hypopharyngeal mass in the left inferior pole of his tonsil with near occlusion of the hypopharyngeal airway. His larynx could not be visualized because of the obstructive mass. A neck lymph node measuring 3.0 cm in the left jugulodigastric region was also noted. The patient’s Karnofsky performance status was 90%. Subsequently, the patient underwent excision of the right tonsil and left tonsillar region.
The pathology of the right tonsil was found to be benign. Histology of the left tonsil revealed invasive squamous cell carcinoma. The resected tumor size measured 3.7 x 2.7 x 2.5 cm. The tumor was moderately differentiated involving the deep surgical margins. No lymphovascular invasion was seen. A PET scan revealed a mass arising from the left tonsillar pillar measuring 3.6 x 2.6 x 3.3 cm with deviation of the epiglottis posteriorly nearing the left vallecula. In addition, multiple large cervical nodal lesions in the left level II nodal chain were seen, with the largest measuring 3.1 x 3.0 x 4.5 cm with an SUV of 3.4. Displacement of the left submandibular gland with several further enlarged level II lymph nodes was observed. In the region of left vallecula, there was soft tissue thickening with increased activity measuring 2.7 x 1.5 cm, likely crossing the midline with an SUV of 5.5. The rest of the neck was negative for metastatic involvement (Figure 2, Case 2). The tumor stage was T3N2Mx, a stage IVa disease.
The patient had a Port-A-Cath placed, which caused a hemothorax after placement of the port and delayed initiating his treatment. A pretreatment MRI scan of the neck revealed multiple conglomerate hypodense peripherally enhancing nodular areas in the left neck posterior to the left submandibular gland deep to the parotid tail worrisome for necrotic lymphadenopathy. The patient underwent a course of hyperfractionated IMRT-IGRT in 67 fractions of 120 cGy twice daily for a total dose of 8,040 cGy to the primary tumor site.16 The patient had a port and PEG tube prior to initiating his radiation therapy. He received IMRT-IGRT with concurrent chemotherapy that was selected based on the recommendation of his genomic testing.17,18 The chemotherapy regimen used included carboplatin (300 mg weekly) and docetaxel (400 mg weekly). The patient had a treatment break because he was hospitalized for anemia and pancytopenia from his chemotherapy and he received supportive cancer care with epoetin alfa.A post therapy PET scan was negative for evidence of hypermetabolic malignancy; however, a 3.3 x 2.7 cm calcified lesion representing likely level III jugular lymph node exhibited no measurable activity at that time. The follow-up after 40 months indicated that the patient had no reported recurrence of the disease (Figure 2, Case 2). The patient’s demographics, tumor characteristics, and the treatment details are summarized in the Table.
Case 3
A 53-year-old white man, who had no smoking or tobacco history but who was exposed to chemicals including sulfuric acid, hydrogen chloride gas, and glycols at work, presented initially with a sore throat that became more painful over time. His ENT specialist referred him for a CT scan of the neck, which revealed a left-sided neck mass measuring 2.5 cm in diameter posterior to the submandibular gland and lateral to carotid sheath and anterior to the triangle (Figure 2, Case 3). The mass appeared to be encapsulated. There was a lobulated spherical mass in the left supraglottic area with formation of the airway of the pyriform sinus and additional anterior vascular involvement was noted. The mass measured 3.6 cm in transverse diameter.
A left tonsillar biopsy specimen measuring 1.4 x 0.6 x 0.2 cm was obtained, and its pathology revealed that the patient had a metastatic squamous cell carcinoma. The left neck lymph node mass aspiration also revealed the presence of squamous cell carcinoma. A PET-CT scan staging showed a dominant tonsillar fossa mass extending from the soft palate down to the pyriform sinus measuring 4.2 x 3.8 cm, with an SUV uptake of 7.3. There was a dominant left level II necrotic lymph node presence measuring 5.0 x 3.7 cm, with an SUV of 3.0. The patient’s Karnofsky performance status was 90%. The tumor stage was T4N2M0, a stage IVa disease. The patient received a course of conformal hyperfractionated IMRT-IGRT delivered to the primary tumor in 67 fractions at 120 cGy twice daily for a total dose of 8,040 cGy16 and concurrent carboplatin chemotherapy at a weekly dose of 200 mg.
After completion of his radiation therapy, chemotherapy was changed based on genomic testing from single agent to doublet with carboplatin (area under the curve (AUC) dose of 2 or 200 mg, weekly) plus docetaxel (25 mg/m2 weekly for 3 weeks and 1 week off ).17,18 A PET scan after chemoradiation therapy revealed a marked anatomical improvement in the primary neoplastic disease seen in the faucial tonsil. The tonsillar mass noted previously had almost completely resolved over the interval, with only a mild persistent asymmetrical thickening of around 1.5 cm, with a peak SUV of 2.0. A lymph node of 2.8 x 2.0 cm was present anterior to the left sternocleidomastoid muscle exhibiting SUV of only 1.8. No other abnormal lesions were noted (Figure 2, Case 3). The patient continues to do extremely well without local recurrence of the disease 46 months after radiation therapy (see Table for patient demographics, tumor characteristics, and therapy details.)
Discussion
The management of patients with primary squamous cell carcinoma of the oropharyngeal remains controversial. Traditionally, early-stage tonsillar squamous cell carcinoma was managed by a single modality treatment, either by surgery or radiation therapy, each showing similar efficacy and outcomes.19 For late-stage disease, a combined approach using surgery and radiation therapy was found to be superior to single modality treatment. However, surgery in conjugation with radiation therapy has been associated with significant toxicities compared with the radiation therapy alone.13Therefore, the use of radiation therapy without surgery is becoming more common with increasingly sophisticated radiation therapy techniques and organ preservation approach in patients with squamous cell carcinoma of the tonsil.
Findings from several studies have shown that in stage I or II oropharyngeal cancer, single modality treatment with radiation therapy achieves 80%-90% of local control of the disease, but poorer outcomes are reported for locally advanced stages III/IV with a local control rate of 63%-74%.20 These findings and others have led to a shift to evaluate the clinical benefits of radiation therapy given with concurrent chemotherapy for the primary treatment of advanced stage oropharyngeal squamous cell carcinoma.20,21 Findings from a number of studies have since reported comparable efficacy and toxicity outcomes using this regimen with concurrent chemotherapy in patients with locally advanced head and neck squamous cell cancer.22-24 Synchronous carboplatin chemotherapy was used effectively as an alternative to cisplatin with fewer potential adverse effects in the good prognosis group of patients with oropharyngeal squamous cell carcinoma.25,26 For our 3 patients, we used carboplatin-based chemotherapy with concurrent advanced hyperfractionated radiation therapy techniques to successfully manage tonsillar squamous cell carcinoma and reduce renal toxicity and neuropathy.
Advanced radiation therapy techniques such as IMRT-IGRT are used routinely at the University Cancer and Diagnostic Centers in Houston, Texas, to manage a range of malignant cancers.27 These innovative techniques have the potential to deliver highly conformal dose-intense radiation to targeted regions of disease, while sparing adjacent critical nonmalignant tissue. The improved shaping of high-dose distributions with IMRT-IGRT could mitigate treatment-related toxicities. For example, the use of advanced radiation therapy techniques has been associated with increased preservation of parotid salivary flow.28-30 The use of advanced radiation therapy techniques in head and neck squamous cell carcinoma is growing, and early evidence confirms its ability to secure excellent local and regional disease control.31,32 In this study, we have demonstrated that by using hyperfractionated conformal three-dimensional IMRT-IGRT we were able not only to manage advanced tonsillar squamous cell carcinoma and treat the malignant metastasis, but also spare adjacent critical organs that were not involved in the disease, thus reducing many of the detrimental side effects associated with hyperfractionated chemoradiation.
All 3 patients were followed for between 40 and 46 months. They continue to do extremely well without local recurrence of their disease, indicating a 100% disease control and overall survival rate. The disease control and survival outcomes for our patients with stage IVA disease compare favorably to other published reports in the literature.33,34 Findings from a study by Prestwich and colleagues33 of 41 patients with stage IV tonsillar carcinoma showed that the radiation therapy with concurrent chemotherapy achieved local and regional disease control in 91% of complete responders and an overall survival rate of 66% at 3 years. Similarly, Setton and colleagues34 reported on 442 patients – 50% with tonsillar cancer, 46% with base-of-tongue cancer – who underwent IMRT and concurrent chemotherapy and who achieved a 3-year overall survival of 84.9%. Our study findings demonstrate that hyperfractionated conformal three-dimensional IMRT-IGRT with concurrent chemotherapy can be delivered safely and effectively to patients with advanced tonsillar squamous cell carcinoma.
Acknowledgment
The authors thank Ms June Lyliston, LVN, for editing and proofreading the manuscript.
1. Stambuk HE, Karimi S, Lee N, Patel SG. Oral cavity and oropharynx tumors. Radiol Clin North Am. 2007;45(1):1-20.
2. Lin DT, Cohen SM, Coppit GL, Burkey BB. Squamous cell carcinoma of the oropharynx and hypopharynx. Otolaryngol Clin North Am. 2005;38(1):59-74, viii.
3. Golas SM. Trends in palatine tonsillar cancer incidence and mortality rates in the United States. Community Dent Oral Epidemiol. 2007;35(2):98-108.
4. Cook MB, Dawsey SM, Freedman ND, et al. Sex disparities in cancer incidence by period and age. Cancer Epidemiol Biomarkers Prev. 2009;18(4):1174-1182.
5. Enomoto LM, Bann DV, Hollenbeak CS, Goldenberg D. Trends in the Incidence of oropharyngeal cancers in the United States. Otolaryngol Head Neck Surg. 2016.
6. Shiboski CH, Schmidt BL, Jordan RC. Tongue and tonsil carcinoma: increasing trends in the U.S. population ages 20-44 years. Cancer. 2005;103(9):1843-1849.
7. Marur S, Forastiere AA. Head and neck cancer: changing epidemiology, diagnosis, and treatment. Mayo Clin Proc. 2008;83(4):489-501.
8. Hong AM, Martin A, Chatfield M, et al. Human papillomavirus, smoking status and outcomes in tonsillar squamous cell carcinoma. Int J Cancer. 2013;132(12):2748-2754.
9. Velly AM, Franco EL, Schlecht N, et al. Relationship between dental factors and risk of upper aerodigestive tract cancer. Oral Oncol. 1998;34(4):284-291.
10. Farrow DC, Vaughan TL, Berwick M, et al. Diet and nasopharyngeal cancer in a low-risk population. Int J Cancer. 1998;78(6):675-679.
11. Freedman ND, Park Y, Subar AF, et al. Fruit and vegetable intake and head and neck cancer risk in a large United States prospective cohort study. Int J Cancer. 2008;122(10):2330-2336.
12. Guay ME, Lavertu P. Tonsillar carcinoma. Eur Arch Otorhinolaryngol. 1995;252(5):259-264.
13. Parsons JT, Mendenhall WM, Stringer SP, et al. Squamous cell carcinoma of the oropharynx: surgery, radiation therapy, or both. Cancer. 2002;94(11):2967-2980.
14. Yao M, Dornfeld KJ, Buatti JM, et al. Intensity-modulated radiation treatment for head-and-neck squamous cell carcinoma--the University of Iowa experience. Int J Radiat Oncol Biol Phys. 2005;63(2):410-421.
15. Yang ES, Murphy BM, Chung CH, et al. Evolution of clinical trials in head and neck cancer. Crit Rev Oncol Hematol. 2009;71(1):29-42.
16. Beitler JJ, Zhang Q, Fu KK, et al. Final results of local-regional control and late toxicity of RTOG 9003: a randomized trial of altered fractionation radiation for locally advanced head and neck cancer. Int J Radiat Oncol Biol Phys. 2014;89(1):13-20.
17. Tomkiewicz C, Hans S, Mucchielli MH, et al. A head and neck cancer tumor response-specific gene signature for cisplatin, 5-fluorouracil induction chemotherapy fails with added taxanes. PLoS One. 2012;7(10):e47170.
18. Feldman R, Gatalica Z, Knezetic J, et al. Molecular profiling of head and neck squamous cell carcinoma. Head Neck. 2016;38 Suppl 1:E1625-1638.
19. Moose BD, Kelly MD, Levine PA, et al. Definitive radiotherapy for T1 and T2 squamous cell carcinoma of the tonsil. Head Neck. 1995;17(4):334-338.
20. Chen AY, Schrag N, Hao Y, Stewart A, Ward E. Changes in treatment of advanced oropharyngeal cancer, 1985-2001. Laryngoscope. 2007;117(1):16-21.
21. Machtay M, Rosenthal DI, Hershock D, et al. Organ preservation therapy using induction plus concurrent chemoradiation for advanced resectable oropharyngeal carcinoma: a University of Pennsylvania Phase II Trial. J Clin Oncol. 2002;20(19):3964-3971.
22. Jegannathen A, Swindell R, Yap B, et al. Can synchronous chemotherapy be added to accelerated hypofractionated radiotherapy in patients with base of tongue cancer? Clin Oncol (R Coll Radiol). 2010;22(3):185-191.
23. Budach V, Becker ET, Boehmer D, et al. Concurrent hyperfractionated accelerated radiotherapy with 5-FU and once weekly cisplatin in locally advanced head and neck cancer. The 10-year results of a prospective phase II trial. Strahlenther Onkol. 2014;190(3):250-255.
24. Tobias JS, Monson K, Gupta N, et al. Chemoradiotherapy for locally advanced head and neck cancer: 10-year follow-up of the UK Head and Neck (UKHAN1) trial. Lancet Oncol. 2010;11(1):66-74.
25. Wilkins AC, Rosenfelder N, Schick U, et al. Equivalence of cisplatin and carboplatin-based chemoradiation for locally advanced squamous cell carcinoma of the head and neck: a matched-pair analysis. Oral Oncol. 2013;49(6):615-619.
26. Benghiat H, Sanghera P, Cashmore1 J, et al. Four week hypofractionated accelerated intensity modulated radiotherapy and synchronous carboplatin or cetuximab in biologically staged oropharyngeal carcinoma. Cancer and Clinical Oncology. 2014;3:1-9.
27. D’Andrea MA, Reddy GK. Management of metastatic malignant thymoma with advanced radiation and chemotherapy techniques: report of a rare case. World J Surg Oncol. 2015;13:77.
28. Little M, Schipper M, Feng FY, et al. Reducing xerostomia after chemo-IMRT for head-and-neck cancer: beyond sparing the parotid glands. Int J Radiat Oncol Biol Phys. 2012;83(3):1007-1014.
29. Eisbruch A. Reducing xerostomia by IMRT: what may, and may not, be achieved. J Clin Oncol. 2007;25(31):4863-4864.
30. Pow EH, Kwong DL, McMillan AS, et al. Xerostomia and quality of life after intensity-modulated radiotherapy vs. conventional radiotherapy for early-stage nasopharyngeal carcinoma: initial report on a randomized controlled clinical trial. Int J Radiat Oncol Biol Phys. 2006;66(4):981-991.
31. Lee NY, de Arruda FF, Puri DR, et al. A comparison of intensity-modulated radiation therapy and concomitant boost radiotherapy in the setting of concurrent chemotherapy for locally advanced oropharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 2006;66(4):966-974.
32. Daly ME, Lieskovsky Y, Pawlicki T, et al. Evaluation of patterns of failure and subjective salivary function in patients treated with intensity modulated radiotherapy for head and neck squamous cell carcinoma. Head Neck. 2007;29(3):211-220.
33. Prestwich RJ, Kancherla K, Oksuz DC, et al. A single centre experience with sequential and concomitant chemoradiotherapy in locally advanced stage IV tonsillar cancer. Radiat Oncol. 2010;5:121.
34. Setton J, Caria N, Romanyshyn J, et al. Intensity-modulated radiotherapy in the treatment of oropharyngeal cancer: an update of the Memorial Sloan-Kettering Cancer Center experience. Int J Radiat Oncol Biol Phys. 2012;82(1):291-298.
1. Stambuk HE, Karimi S, Lee N, Patel SG. Oral cavity and oropharynx tumors. Radiol Clin North Am. 2007;45(1):1-20.
2. Lin DT, Cohen SM, Coppit GL, Burkey BB. Squamous cell carcinoma of the oropharynx and hypopharynx. Otolaryngol Clin North Am. 2005;38(1):59-74, viii.
3. Golas SM. Trends in palatine tonsillar cancer incidence and mortality rates in the United States. Community Dent Oral Epidemiol. 2007;35(2):98-108.
4. Cook MB, Dawsey SM, Freedman ND, et al. Sex disparities in cancer incidence by period and age. Cancer Epidemiol Biomarkers Prev. 2009;18(4):1174-1182.
5. Enomoto LM, Bann DV, Hollenbeak CS, Goldenberg D. Trends in the Incidence of oropharyngeal cancers in the United States. Otolaryngol Head Neck Surg. 2016.
6. Shiboski CH, Schmidt BL, Jordan RC. Tongue and tonsil carcinoma: increasing trends in the U.S. population ages 20-44 years. Cancer. 2005;103(9):1843-1849.
7. Marur S, Forastiere AA. Head and neck cancer: changing epidemiology, diagnosis, and treatment. Mayo Clin Proc. 2008;83(4):489-501.
8. Hong AM, Martin A, Chatfield M, et al. Human papillomavirus, smoking status and outcomes in tonsillar squamous cell carcinoma. Int J Cancer. 2013;132(12):2748-2754.
9. Velly AM, Franco EL, Schlecht N, et al. Relationship between dental factors and risk of upper aerodigestive tract cancer. Oral Oncol. 1998;34(4):284-291.
10. Farrow DC, Vaughan TL, Berwick M, et al. Diet and nasopharyngeal cancer in a low-risk population. Int J Cancer. 1998;78(6):675-679.
11. Freedman ND, Park Y, Subar AF, et al. Fruit and vegetable intake and head and neck cancer risk in a large United States prospective cohort study. Int J Cancer. 2008;122(10):2330-2336.
12. Guay ME, Lavertu P. Tonsillar carcinoma. Eur Arch Otorhinolaryngol. 1995;252(5):259-264.
13. Parsons JT, Mendenhall WM, Stringer SP, et al. Squamous cell carcinoma of the oropharynx: surgery, radiation therapy, or both. Cancer. 2002;94(11):2967-2980.
14. Yao M, Dornfeld KJ, Buatti JM, et al. Intensity-modulated radiation treatment for head-and-neck squamous cell carcinoma--the University of Iowa experience. Int J Radiat Oncol Biol Phys. 2005;63(2):410-421.
15. Yang ES, Murphy BM, Chung CH, et al. Evolution of clinical trials in head and neck cancer. Crit Rev Oncol Hematol. 2009;71(1):29-42.
16. Beitler JJ, Zhang Q, Fu KK, et al. Final results of local-regional control and late toxicity of RTOG 9003: a randomized trial of altered fractionation radiation for locally advanced head and neck cancer. Int J Radiat Oncol Biol Phys. 2014;89(1):13-20.
17. Tomkiewicz C, Hans S, Mucchielli MH, et al. A head and neck cancer tumor response-specific gene signature for cisplatin, 5-fluorouracil induction chemotherapy fails with added taxanes. PLoS One. 2012;7(10):e47170.
18. Feldman R, Gatalica Z, Knezetic J, et al. Molecular profiling of head and neck squamous cell carcinoma. Head Neck. 2016;38 Suppl 1:E1625-1638.
19. Moose BD, Kelly MD, Levine PA, et al. Definitive radiotherapy for T1 and T2 squamous cell carcinoma of the tonsil. Head Neck. 1995;17(4):334-338.
20. Chen AY, Schrag N, Hao Y, Stewart A, Ward E. Changes in treatment of advanced oropharyngeal cancer, 1985-2001. Laryngoscope. 2007;117(1):16-21.
21. Machtay M, Rosenthal DI, Hershock D, et al. Organ preservation therapy using induction plus concurrent chemoradiation for advanced resectable oropharyngeal carcinoma: a University of Pennsylvania Phase II Trial. J Clin Oncol. 2002;20(19):3964-3971.
22. Jegannathen A, Swindell R, Yap B, et al. Can synchronous chemotherapy be added to accelerated hypofractionated radiotherapy in patients with base of tongue cancer? Clin Oncol (R Coll Radiol). 2010;22(3):185-191.
23. Budach V, Becker ET, Boehmer D, et al. Concurrent hyperfractionated accelerated radiotherapy with 5-FU and once weekly cisplatin in locally advanced head and neck cancer. The 10-year results of a prospective phase II trial. Strahlenther Onkol. 2014;190(3):250-255.
24. Tobias JS, Monson K, Gupta N, et al. Chemoradiotherapy for locally advanced head and neck cancer: 10-year follow-up of the UK Head and Neck (UKHAN1) trial. Lancet Oncol. 2010;11(1):66-74.
25. Wilkins AC, Rosenfelder N, Schick U, et al. Equivalence of cisplatin and carboplatin-based chemoradiation for locally advanced squamous cell carcinoma of the head and neck: a matched-pair analysis. Oral Oncol. 2013;49(6):615-619.
26. Benghiat H, Sanghera P, Cashmore1 J, et al. Four week hypofractionated accelerated intensity modulated radiotherapy and synchronous carboplatin or cetuximab in biologically staged oropharyngeal carcinoma. Cancer and Clinical Oncology. 2014;3:1-9.
27. D’Andrea MA, Reddy GK. Management of metastatic malignant thymoma with advanced radiation and chemotherapy techniques: report of a rare case. World J Surg Oncol. 2015;13:77.
28. Little M, Schipper M, Feng FY, et al. Reducing xerostomia after chemo-IMRT for head-and-neck cancer: beyond sparing the parotid glands. Int J Radiat Oncol Biol Phys. 2012;83(3):1007-1014.
29. Eisbruch A. Reducing xerostomia by IMRT: what may, and may not, be achieved. J Clin Oncol. 2007;25(31):4863-4864.
30. Pow EH, Kwong DL, McMillan AS, et al. Xerostomia and quality of life after intensity-modulated radiotherapy vs. conventional radiotherapy for early-stage nasopharyngeal carcinoma: initial report on a randomized controlled clinical trial. Int J Radiat Oncol Biol Phys. 2006;66(4):981-991.
31. Lee NY, de Arruda FF, Puri DR, et al. A comparison of intensity-modulated radiation therapy and concomitant boost radiotherapy in the setting of concurrent chemotherapy for locally advanced oropharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 2006;66(4):966-974.
32. Daly ME, Lieskovsky Y, Pawlicki T, et al. Evaluation of patterns of failure and subjective salivary function in patients treated with intensity modulated radiotherapy for head and neck squamous cell carcinoma. Head Neck. 2007;29(3):211-220.
33. Prestwich RJ, Kancherla K, Oksuz DC, et al. A single centre experience with sequential and concomitant chemoradiotherapy in locally advanced stage IV tonsillar cancer. Radiat Oncol. 2010;5:121.
34. Setton J, Caria N, Romanyshyn J, et al. Intensity-modulated radiotherapy in the treatment of oropharyngeal cancer: an update of the Memorial Sloan-Kettering Cancer Center experience. Int J Radiat Oncol Biol Phys. 2012;82(1):291-298.
AGA Clinical Practice Update: Treatment of fecal incontinence and defecatory disorders
About 25% of patients with fecal incontinence benefit from conservative treatments, which merit a “rigorous trial” before considering surgery, experts write in a Clinical Practice Update in the December issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2017.08.023).
“A stepwise approach should be followed for management of fecal incontinence. In our experience, many incontinent patients who are considered refractory to conservative therapy have not received an optimal trial of conservative therapy,” states Adil E. Bharucha, MBBS, MD, of the Mayo Clinic and the Mayo Foundation in Rochester, Minn., and his associates.
Fecal incontinence affects 7%-15% of individuals and has potentially “devastating” implications for quality of life, the experts note. They recommend starting treatment by meticulously documenting bowel habits, triggers of incontinence, and treatment history. For fecal incontinence with diarrhea, they suggest eliminating caffeine and poorly absorbed dietary sugars, such as sorbitol and fructose, and adding loperamide, starting with one 2-mg tablet taken 30 minutes before breakfast and titrating up to a maximum of 16 mg per day. Other conservative therapeutic options for diarrhea include fiber supplementation, scheduled toileting, a bowel retraining program, anticholinergic agents, clonidine, and cholestyramine or colesevelam to correct bile salt malabsorption. Patients whose fecal incontinence involves constipation should start with laxatives and anorectal testing for evacuation disorders. Rectal cleansing with a small enema or tap water can help prevent stool leakage, the experts write.
If these conservative measures fail to improve fecal incontinence, they recommend anorectal manometry to test for anal weakness, reduced or increased rectal sensation, and impaired rectal balloon expulsion, all of which can improve with biofeedback therapy to retrain the pelvic floor. If biofeedback fails, consider perianal bulking agents, such as intra-anal injection of dextranomer, the experts suggest. Sacral nerve stimulation might be indicated if moderate or severe fecal incontinence does not respond to at least 3 months of conservative treatment. However, the experts do not recommend percutaneous tibial nerve stimulation, which failed to outperform sham stimulation in a 12-week, double-blind, multicenter trial (Lancet. 2015;386:1640-8). Surgery is indicated for fecal incontinence associated with major anatomic defects, such as rectovaginal fistula, full-thickness rectal prolapse, fistula in ano, or cloaca-like deformity. Additionally, sphincteroplasty is an option for postpartum women with fecal incontinence, patients with recent sphincter injuries, and patients with sphincter damage and fecal incontinence fecal incontinence that fails to improve with conservative and biofeedback therapy, perianal bulking injection, and sacral nerve stimulation, according to the clinical practice update.
Barrier devices should be offered if fecal incontinence fails conservative treatments and surgery, or if surgery is not an option. Most anal plugs are “poorly tolerated,” with two exceptions – a Food and Drug Administration–approved device from Renew Medical and a vaginal insert and pressure-regulated pump from Pelvalon. Colostomy might be indicated if patients with severe fecal incontinence fail conservative treatment and or are not candidates for barrier devices, minimally invasive surgeries, and sphincteroplasty.
If severe fecal incontinence that is refractory to or contraindicated for all these interventions, the experts suggest considering artificial anal sphincter repair by dynamic graciloplasty. Surgery also is indicated to repair major anatomic defects such as rectovaginal fistula, full-thickness rectal prolapse, fistula in ano, or cloaca-like deformity, they noted. A magnetic anal sphincter device is a possibility for patients with medically refractory severe fecal incontinence who have failed or are not candidates for barrier devices, perianal bulking injection, sacral nerve stimulation, sphincteroplasty, or a colostomy. However, the study that led to FDA approval of a magnetic anal sphincter device included only 35 patients, and 7 (20%) had the device removed because of infection, erosion, or inefficacy. Another patient required a stoma in order to be able to defecate, and a total of 40% had moderate or severe complications when pain and bleeding were also considered, the experts noted.
Biofeedback is the preferred treatment for defecatory disorders – that is, chronic constipation or constipation-predominant irritable bowel syndrome with impaired rectal evacuation, according to the clinical practice update. The experts recommend against sacral nerve stimulation, anteretrograde colonic enemas, and stapled transanal rectal resection for patients with defecatory disorders. Surgical treatment typically is reserved for the small minority of patients with considerable pelvic organ or rectal prolapse, they note.
The National Institutes of Health Sciences provided funding. The authors reported having no conflicts of interest.
About 25% of patients with fecal incontinence benefit from conservative treatments, which merit a “rigorous trial” before considering surgery, experts write in a Clinical Practice Update in the December issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2017.08.023).
“A stepwise approach should be followed for management of fecal incontinence. In our experience, many incontinent patients who are considered refractory to conservative therapy have not received an optimal trial of conservative therapy,” states Adil E. Bharucha, MBBS, MD, of the Mayo Clinic and the Mayo Foundation in Rochester, Minn., and his associates.
Fecal incontinence affects 7%-15% of individuals and has potentially “devastating” implications for quality of life, the experts note. They recommend starting treatment by meticulously documenting bowel habits, triggers of incontinence, and treatment history. For fecal incontinence with diarrhea, they suggest eliminating caffeine and poorly absorbed dietary sugars, such as sorbitol and fructose, and adding loperamide, starting with one 2-mg tablet taken 30 minutes before breakfast and titrating up to a maximum of 16 mg per day. Other conservative therapeutic options for diarrhea include fiber supplementation, scheduled toileting, a bowel retraining program, anticholinergic agents, clonidine, and cholestyramine or colesevelam to correct bile salt malabsorption. Patients whose fecal incontinence involves constipation should start with laxatives and anorectal testing for evacuation disorders. Rectal cleansing with a small enema or tap water can help prevent stool leakage, the experts write.
If these conservative measures fail to improve fecal incontinence, they recommend anorectal manometry to test for anal weakness, reduced or increased rectal sensation, and impaired rectal balloon expulsion, all of which can improve with biofeedback therapy to retrain the pelvic floor. If biofeedback fails, consider perianal bulking agents, such as intra-anal injection of dextranomer, the experts suggest. Sacral nerve stimulation might be indicated if moderate or severe fecal incontinence does not respond to at least 3 months of conservative treatment. However, the experts do not recommend percutaneous tibial nerve stimulation, which failed to outperform sham stimulation in a 12-week, double-blind, multicenter trial (Lancet. 2015;386:1640-8). Surgery is indicated for fecal incontinence associated with major anatomic defects, such as rectovaginal fistula, full-thickness rectal prolapse, fistula in ano, or cloaca-like deformity. Additionally, sphincteroplasty is an option for postpartum women with fecal incontinence, patients with recent sphincter injuries, and patients with sphincter damage and fecal incontinence fecal incontinence that fails to improve with conservative and biofeedback therapy, perianal bulking injection, and sacral nerve stimulation, according to the clinical practice update.
Barrier devices should be offered if fecal incontinence fails conservative treatments and surgery, or if surgery is not an option. Most anal plugs are “poorly tolerated,” with two exceptions – a Food and Drug Administration–approved device from Renew Medical and a vaginal insert and pressure-regulated pump from Pelvalon. Colostomy might be indicated if patients with severe fecal incontinence fail conservative treatment and or are not candidates for barrier devices, minimally invasive surgeries, and sphincteroplasty.
If severe fecal incontinence that is refractory to or contraindicated for all these interventions, the experts suggest considering artificial anal sphincter repair by dynamic graciloplasty. Surgery also is indicated to repair major anatomic defects such as rectovaginal fistula, full-thickness rectal prolapse, fistula in ano, or cloaca-like deformity, they noted. A magnetic anal sphincter device is a possibility for patients with medically refractory severe fecal incontinence who have failed or are not candidates for barrier devices, perianal bulking injection, sacral nerve stimulation, sphincteroplasty, or a colostomy. However, the study that led to FDA approval of a magnetic anal sphincter device included only 35 patients, and 7 (20%) had the device removed because of infection, erosion, or inefficacy. Another patient required a stoma in order to be able to defecate, and a total of 40% had moderate or severe complications when pain and bleeding were also considered, the experts noted.
Biofeedback is the preferred treatment for defecatory disorders – that is, chronic constipation or constipation-predominant irritable bowel syndrome with impaired rectal evacuation, according to the clinical practice update. The experts recommend against sacral nerve stimulation, anteretrograde colonic enemas, and stapled transanal rectal resection for patients with defecatory disorders. Surgical treatment typically is reserved for the small minority of patients with considerable pelvic organ or rectal prolapse, they note.
The National Institutes of Health Sciences provided funding. The authors reported having no conflicts of interest.
About 25% of patients with fecal incontinence benefit from conservative treatments, which merit a “rigorous trial” before considering surgery, experts write in a Clinical Practice Update in the December issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2017.08.023).
“A stepwise approach should be followed for management of fecal incontinence. In our experience, many incontinent patients who are considered refractory to conservative therapy have not received an optimal trial of conservative therapy,” states Adil E. Bharucha, MBBS, MD, of the Mayo Clinic and the Mayo Foundation in Rochester, Minn., and his associates.
Fecal incontinence affects 7%-15% of individuals and has potentially “devastating” implications for quality of life, the experts note. They recommend starting treatment by meticulously documenting bowel habits, triggers of incontinence, and treatment history. For fecal incontinence with diarrhea, they suggest eliminating caffeine and poorly absorbed dietary sugars, such as sorbitol and fructose, and adding loperamide, starting with one 2-mg tablet taken 30 minutes before breakfast and titrating up to a maximum of 16 mg per day. Other conservative therapeutic options for diarrhea include fiber supplementation, scheduled toileting, a bowel retraining program, anticholinergic agents, clonidine, and cholestyramine or colesevelam to correct bile salt malabsorption. Patients whose fecal incontinence involves constipation should start with laxatives and anorectal testing for evacuation disorders. Rectal cleansing with a small enema or tap water can help prevent stool leakage, the experts write.
If these conservative measures fail to improve fecal incontinence, they recommend anorectal manometry to test for anal weakness, reduced or increased rectal sensation, and impaired rectal balloon expulsion, all of which can improve with biofeedback therapy to retrain the pelvic floor. If biofeedback fails, consider perianal bulking agents, such as intra-anal injection of dextranomer, the experts suggest. Sacral nerve stimulation might be indicated if moderate or severe fecal incontinence does not respond to at least 3 months of conservative treatment. However, the experts do not recommend percutaneous tibial nerve stimulation, which failed to outperform sham stimulation in a 12-week, double-blind, multicenter trial (Lancet. 2015;386:1640-8). Surgery is indicated for fecal incontinence associated with major anatomic defects, such as rectovaginal fistula, full-thickness rectal prolapse, fistula in ano, or cloaca-like deformity. Additionally, sphincteroplasty is an option for postpartum women with fecal incontinence, patients with recent sphincter injuries, and patients with sphincter damage and fecal incontinence fecal incontinence that fails to improve with conservative and biofeedback therapy, perianal bulking injection, and sacral nerve stimulation, according to the clinical practice update.
Barrier devices should be offered if fecal incontinence fails conservative treatments and surgery, or if surgery is not an option. Most anal plugs are “poorly tolerated,” with two exceptions – a Food and Drug Administration–approved device from Renew Medical and a vaginal insert and pressure-regulated pump from Pelvalon. Colostomy might be indicated if patients with severe fecal incontinence fail conservative treatment and or are not candidates for barrier devices, minimally invasive surgeries, and sphincteroplasty.
If severe fecal incontinence that is refractory to or contraindicated for all these interventions, the experts suggest considering artificial anal sphincter repair by dynamic graciloplasty. Surgery also is indicated to repair major anatomic defects such as rectovaginal fistula, full-thickness rectal prolapse, fistula in ano, or cloaca-like deformity, they noted. A magnetic anal sphincter device is a possibility for patients with medically refractory severe fecal incontinence who have failed or are not candidates for barrier devices, perianal bulking injection, sacral nerve stimulation, sphincteroplasty, or a colostomy. However, the study that led to FDA approval of a magnetic anal sphincter device included only 35 patients, and 7 (20%) had the device removed because of infection, erosion, or inefficacy. Another patient required a stoma in order to be able to defecate, and a total of 40% had moderate or severe complications when pain and bleeding were also considered, the experts noted.
Biofeedback is the preferred treatment for defecatory disorders – that is, chronic constipation or constipation-predominant irritable bowel syndrome with impaired rectal evacuation, according to the clinical practice update. The experts recommend against sacral nerve stimulation, anteretrograde colonic enemas, and stapled transanal rectal resection for patients with defecatory disorders. Surgical treatment typically is reserved for the small minority of patients with considerable pelvic organ or rectal prolapse, they note.
The National Institutes of Health Sciences provided funding. The authors reported having no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
A concise guide to monoamine oxidase inhibitors
Despite an abundance of evidenced-based literature supporting monoamine oxidase inhibitors (MAOIs) as an effective treatment for depression, use of these agents has decreased drastically in the past 3 decades. A lack of industry support and the ease of use of other agents are contributing factors, but the biggest impediments to routine use of MAOIs are unfamiliarity with their efficacy advantages and concerns about adverse effects, particularly the risk of hypertensive crises and serotonin syndrome. Many misconceptions regarding these medications are based on outdated data and studies that are no longer reliable.
The goal of this 2-part review is to provide clinicians with updated information regarding MAOIs. Part 1 provides a brief description of:
- the pharmacology of nonselective irreversible MAOIs
- the mechanism by which tyramine induces hypertension
- sources of clinically significant tyramine exposure
- what to tell patients about dietary restrictions and MAOIs.
Part 2 of this guide will cover the risk of serotonin syndrome when MAOIs are combined with inhibitors of serotonin reuptake, how to initiate MAOI therapy, and augmenting MAOIs with other agents.
The pharmacology of MAOIs
First used clinically in the 1950s to treat tuberculosis, MAOIs have a long and interesting history (see the Box “A brief history of monoamine oxidase inhibitors”). Table 11 lists MAOIs currently available in the United States, including the MAO-B–specific agent rasagiline, which is used for Parkinson’s disease.
Manipulation of the monoamines serotonin, norepinephrine, and dopamine is fundamental to managing major depressive disorder (MDD), yet only nonselective MAOIs directly promote neurotransmission of all 3 by inhibiting MAO-A and MAO-B.2 The Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study demonstrated that <50% of MDD patients achieve remission in monotherapy trials of selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors, mirtazapine, or bupropion, necessitating consideration of antidepressant combinations, augmentation options, and eventually irreversible, nonselective MAOIs such as phenelzine, tranylcypromine, or isocarboxazid.3,4 Nonselective MAOIs thus offer a therapeutic opportunity for patients who do not respond to single or dual-mechanism strategies; moreover, nonselective MAOIs have compelling effectiveness data for other conditions, including panic disorder and social phobia.5 Although MAOIs are among the most effective pharmacologic agents for MDD,6 they are underutilized because of an inadequate understanding of risk mechanisms and resultant fear of catastrophic outcomes. Because of the difficulties encountered in achieving clinical remission for MDD, the nonselective MAOIs deserve a second look.
Differentiation of MAO-A from MAO-B. It is essential to understand the mechanism of action of MAOIs, specifically the impact of MAO-A inhibition. Although the enzyme MAO was known in the 1950s, it wasn’t until 1968 that Johnston7 postulated the existence of >1 form. In 1971, Goridis and Neff8 used clorgyline to examine the deamination rate by MAO of tyramine and norepinephrine. They found that tyramine appeared to be a substrate of both MAO isoforms, but only 1 of the MAO types was sensitive to the inhibitory effects of clorgyline. They also discerned that norepinephrine was only a substrate for MAO-A, and that this form of MAO was sensitive to clorgyline inhibition. Thus, the forms of MAO were characterized by their preferred substrates (Table 29,10), and then later by their tissue distribution. Phenylethylamine is a naturally occurring compound found in foods, such as chocolate, and has an in vitro pharmacology similar to amphetamine but with 1 important difference: it has a short half-life of 5 to 10 minutes after oral ingestion, and therefore no appreciable CNS impact.
Within the CNS, norepinephrine and dopamine neurons possess both MAO forms, with the MAO-A content greater than MAO-B. Serotonergic neurons only contain MAO-B.11 Outside of the CNS, MAO-A predominates, with only platelets and lymphocytes possessing MAO-B activity.11 The overall relative tissue proportions of MAO-A to MAO-B activity are: brain, 25% MAO-A, 75% MAO-B; liver, 50% MAO-A, 50% MAO-B; intestine, 80% MAO-A, 20% MAO-B; and peripheral adrenergic neurons, 90% MAO-A, 10% MAO-B.
Because of its specificity for serotonin and norepinephrine, CNS MAO-A inhibition is necessary for antidepressant effects. MAO-B inhibition by itself does not appear to raise CNS dopamine levels unless exogenous dopamine is supplied.11 All MAOIs used in the United States to treat depression are irreversible, nonselective inhibitors of MAO-A and MAO-B.
Selegiline in oral form generates low plasma levels and primarily inhibits MAO-B. The transdermal form of selegiline achieves significantly greater systemic exposure, and at these higher plasma levels selegiline is a nonselective, irreversible MAOI effective for MDD (Figure 112). Administering selegiline systemically via a transdermal patch avoids clinically significant MAOI effects in the gut, so no dietary warnings exist for the lowest dose (6 mg/24 hours), although there are warnings for the higher dosages (9 mg/24 hours and 12 mg/24 hours).
Differentiation of MAOIs by chemical class. The earliest MAOI, iproniazid, was a hydrazine derivative and exhibited hepatotoxicity,13 as did certain other hydrazine MAOIs. This lead to a search for safer hydrazine and nonhydrazine alternatives. Isocarboxazid and phenelzine are the 2 hydrazine MAOIs available in the United States, while tranylcypromine and selegiline transdermal are nonhydrazines (Figure 2).
What distinguishes the nonhydrazine medication selegiline is that its metabolism generates L-amphetamine metabolites (Figure 314). This property was thought to be shared by other nonhydrazines, but recent studies indicate than neither tranylcypromine15 nor the MAO-B–selective rasagiline possess amphetamine metabolites.16 Unlike the dextro isomers, L-amphetamine structures do not inhibit dopamine reuptake or cause euphoria, but can cause stimulation (eg, sleep disturbance) by inhibiting norepinephrine reuptake, and also by interacting with the trace amine-associated receptor 1 (TAAR1), an intracellular receptor expressed within the presynaptic terminal of monoamine neurons. Activation of TAAR1 by tyramine is an important part of the hypertensive effects related to excessive tyramine exposure.17 (The importance of TAAR1 and the interaction with tyramine is discussed in the next section.) Importantly, patients taking selegiline must be warned that certain drug screens may not discriminate between levo and dextro isomers of amphetamines, and that the use of selegiline should be disclosed prior to drug testing procedures.
MAOIs and tyramine: Dietary requirements
Clinicians who are familiar with MAOIs recognize that there are dietary restrictions to minimize patients’ exposure to tyramine. As most clinicians know, significant tyramine ingestion may cause an increase in blood pressure (BP) in patients taking an MAOI, but many overestimate the prevalence of foods high in tyramine content since the original reports emerged in the early 1960s.18 In a recent monograph, one of the leading experts on MAOIs, Professor Ken Gillman, stated:
Very few foods now contain problematically high tyramine levels, that is a result of great changes in international food production methods and hygiene regulations. Cheese is the only food that, in the past, has been associated with documented fatalities resulting from hypertension. Nowadays most cheeses are quite safe, and even ‘matured’ cheeses are usually safe in healthy-sized portions. The variability of sensitivity to tyramine between individuals, and the sometimes unpredictable amount of tyramine content in foods, means a little knowledge and care are still required.19
What is tyramine? Tyramine is a biogenic amine that is virtually absent in fresh animal protein sources but is enriched after decay or fermentation.20 Modern food processing and handling methods have significantly limited the tyramine content in processed foods, with the exception of certain cheeses and sauces, as discussed below. Moreover, modern assaying techniques using high-performance liquid chromatography have generated extremely accurate assessments of the tyramine content of specific foods.21 Data published prior to 2000 are not reliable, because many of these publications employed outdated methods.17
When ingested, tyramine is metabolized by gut MAO-A, with doses up to 400 mg causing no known effects, although most people rarely ingest >25 mg during a meal.22 In addition to being a substrate for MAO-A, tyramine is also a substrate for the dopamine transporter, norepinephrine transporter (NET), the vesicular monoamine transporter 2, and TAAR1.23 Tyramine enters the cell via NET, where it interacts with TAAR1, a G protein-coupled receptor that is responsive to trace amines, such as tyramine, as well as amphetamines.20 The agonist properties at TAAR1 are the presumed site of action for the BP effects of tyramine, because binding results in potent release of norepinephrine.20,24 When tyramine is supplied to an animal in which MAO-A is inhibited, the decreased peripheral catabolism of tyramine results in markedly increased norepinephrine release by peripheral adrenergic neurons. Moreover, the absence of MAO-A activity in those neurons prevents any norepinephrine breakdown, resulting in robust synaptic norepinephrine delivery and peripheral effects.
All orally administered irreversible MAOIs potently inhibit gut and systemic MAO-A, and are susceptible to the impact of significant tyramine ingestion. The exception is selegiline transdermal (Figure 112), as appreciable gut MAO-A inhibition does not occur until doses >6 mg/24 hours are reached.22 No significant pressor response was seen in participants taking selegiline transdermal, 6 mg/24 hours for 13 days, who consumed a meal that provided 400 mg of tyramine.22 Conversely, for oral agents that produce gut MAO-A inhibition, tyramine doses as low as 8 to 10 mg (when administered as tyramine capsules) may increase systolic pressure by 30 mm Hg.25 The dietary warnings do not apply to rasagiline, which is a selective MAO-B inhibitor, although rasagiline may have an impact on resting BP; the prescribing information for rasagiline includes warnings about hypotension and hypertension.26
What to tell patients about tyramine. Although administering pure tyramine capsules can induce a measurable change in systolic BP, when ingested as food, tyramine doses <50 mg are unlikely to cause an increase in BP sufficient to warrant clinical intervention, although some individuals can be sensitive to 10 to 25 mg.19 When discussing with patients safety issues related to diet, there are a few important concepts to remember19:
- In an era when the tyramine content of foods was much higher (1960 to 1964) and MAOI users received no dietary guidance, only 14 deaths were reported among an estimated 1.5 million patients who took MAOIs.
- MAOIs do not raise BP, and their use is associated with orthostasis in some patients.
- Routine exercise or other vigorous activities (eg, weightlifting) can raise systolic pressure well above 200 mm Hg, and routine baseline systolic pressures, ranging from 180 to 220 mm Hg, do not increase the risk of subarachnoid hemorrhage.
- Hospital evaluation is needed only if a substantial amount of tyramine is ingested (eg, estimated ≥100 mg), and self-monitoring shows a systolic BP ≥220 mm Hg over a prolonged period (eg, 2 hours). Ingestion of 100 mg of tyramine would almost certainly have to be intentional, as it would require one to consume 3.5 oz of the most highly tyramine-laden cheeses.
Emphasize to patients that only a small number of highly aged cheeses, foods, and sauces contain high quantities of tyramine, and that even these foods can be enjoyed in small amounts. All patients who are prescribed an MAOI also should purchase a portable BP cuff for those rare instances when a dietary indiscretion may have occurred and the person experiences a headache within 1 to 2 hours after tyramine ingestion. Most reactions are self-limited and resolve over 2 to 4 hours.
Patients who ingest ≥100 mg of tyramine should be evaluated by a physician. Under no circumstances should a patient be given a prescription for nifedipine or other medications that can abruptly lower BP, because this may result in complications, including myocardial infarction.27,28 Counsel patients to remain calm. Some clinicians endorse the use of low doses of benzodiazepines (the equivalent of alprazolam 0.5 mg) to facilitate this, because anxiety elevates BP. A recent emergency room study of patients with an initial systolic BP ≥160 mm Hg or diastolic BP ≥100 mm Hg without end organ damage demonstrated that alprazolam, 0.5 mg, was as effective as captopril, 25 mg, in lowering BP.29
Also, tell patients that if a food is unfamiliar and highly aged or fermented, they should avoid it until they can further inquire about it. In a review, Gillman19 provides the tyramine content of an exhaustive list of cheeses, aged meats, and sauces (see Related Resources). For other products, patients often can obtain information directly from the manufacturer. In many parts of the world, assays for tyramine content are required as a demonstration of adequate product safety procedures. Even the most highly aged cheeses with a tyramine content of 1,000 g/kg can be enjoyed in small amounts (<1 oz), and most products would require heroic intake to achieve clinically significant tyramine ingestion (Table 319).
Improved education can clarify the risks
Medications such as lithium, clozapine, and MAOIs have a proven record of efficacy, yet often are underused due to fears engendered by lack of systematic training. A recent initiative in New York thus aimed to increase rates of
1. Panisset M, Chen JJ, Rhyee SH, et al. Serotonin toxicity association with concomitant antidepressants and rasagiline treatment: retrospective study (STACCATO). Pharmacotherapy. 2014;34(12):1250-1258.
2. López-Muñoz F, Alamo C. Monoaminergic neurotransmission: the history of the discovery of antidepressants from 1950s until today. Curr Pharm Des. 2009;15(14):1563-1586.
3. Nierenberg AA, Fava M, Trivedi MH, et al. A comparison of lithium and T(3) augmentation following two failed medication treatments for depression: a STAR*D report. Am J Psychiatry. 2006;163(9):1519-1530; quiz 1665.
4. Trivedi MH, Fava M, Wisniewski SR, et al; STAR*D Study Team. Medication augmentation after the failure of SSRIs for depression. New Engl J Med. 2006;354(12):1243-1252.
5. Bandelow B, Zohar J, Hollander E, et al; World Federation of Societies of Biological Psychiatry Task Force on Treatment Guidelines for Anxiety, Obsessive-Compulsive and Posttraumatic Stress Disorders. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the pharmacological treatment of anxiety, obsessive-compulsive and posttraumatic stress disorders. World J Biol Psychiatry. 2002;3(4):171-199.
6. Shulman KI, Herrmann N, Walker SE. Current place of monoamine oxidase inhibitors in the treatment of depression. CNS Drugs. 2013;27(10):789-797.
7. Johnston JP. Some observations upon a new inhibitor of monoamine oxidase in brain tissue. Biochem Pharmacol. 1968;17(7):1285-1297.
8. Goridis C, Neff NH. Monoamine oxidase in sympathetic nerves: a transmitter specific enzyme type. Br J Pharmacol. 1971;43(4):814-818.
9. Geha RM, Rebrin I, Chen K, et al. Substrate and inhibitor specificities for human monoamine oxidase A and B are influenced by a single amino acid. J Biol Chem. 2001;276(13):9877-9882.
10. O’Carroll AM, Fowler CJ, Phillips JP, et al. The deamination of dopamine by human brain monoamine oxidase. Specificity for the two enzyme forms in seven brain regions. Naunyn Schmiedebergs Arch Pharmacol. 1983;322(3):198-202.
11. Stahl SM, Felker A. Monoamine oxidase inhibitors: a modern guide to an unrequited class of antidepressants. CNS Spectr. 2008;13(10):855-780.
12. Mawhinney M, Cole D, Azzaro AJ. Daily transdermal administration of selegiline to guinea-pigs preferentially inhibits monoamine oxidase activity in brain when compared with intestinal and hepatic tissues. J Pharm Pharmacol. 2003;55(1):27-34.
13. Maille F, Duvoux C, Cherqui D, et al. Auxiliary hepatic transplantation in iproniazid-induced subfulminant hepatitis. Should iproniazid still be sold in France? [in French]. Gastroenterol Clin Biol. 1999;23(10):1083-1085.
14. Salonen JS, Nyman L, Boobis AR, et al. Comparative studies on the cytochrome p450-associated metabolism and interaction potential of selegiline between human liver-derived in vitro systems. Drug Metab Dispos. 2003;31(9):1093-1102.
15. Iwersen S, Schmoldt A. One fatal and one nonfatal intoxication with tranylcypromine. Absence of amphetamines as metabolites. J Anal Toxicol. 1996;20(5):301-304.
16. Müller T, Hoffmann JA, Dimpfel W, et al. Switch from selegiline to rasagiline is beneficial in patients with Parkinson’s disease. J Neural Transm (Vienna). 2013;120(5):761-765.
17. Lewin AH, Miller GM, Gilmour B. Trace amine-associated receptor 1 is a stereoselective binding site for compounds in the amphetamine class. Bioorg Med Chem. 2011;19(23):7044-7048.
18. Blackwell B. Hypertensive crisis due to monoamine-oxidase inhibitors. Lancet. 1963;2(7313):849-850.
19. Gillman PK. Monoamine oxidase inhibitors: a review concerning dietary tyramine and drug interactions. PsychoTropical Commentaries. 2016;16(6):1-97.
20. Pei Y, Asif-Malik A, Canales JJ. Trace amines and the trace amine-associated receptor 1: pharmacology, neurochemistry, and clinical implications. Front Neurosci. 2016;10:148.
21. Fiechter G, Sivec G, Mayer HK. Application of UHPLC for the simultaneous analysis of free amino acids and biogenic amines in ripened acid-curd cheeses. J Chromatogr B Analyt Technol Biomed Life Sci. 2013;927:191-200.
22. Blob LF, Sharoky M, Campbell BJ, et al. Effects of a tyramine-enriched meal on blood pressure response in healthy male volunteers treated with selegiline transdermal system 6 mg/24 hour. CNS Spectr. 2007;12(1):25-34.
23. Partilla JS, Dempsey AG, Nagpal AS, et al. Interaction of amphetamines and related compounds at the vesicular monoamine transporter. J Pharmacol Exp Ther. 2006;319(1):237-246.
24. Borowsky B, Adham N, Jones KA, et al. Trace amines: identification of a family of mammalian G protein-coupled receptors. Proc Natl Acad Sci U S A. 2001;98(16):8966-8971.
25. Azzaro AJ, Vandenberg CM, Blob LF, et al. Tyramine pressor sensitivity during treatment with the selegiline transdermal system 6 mg/24 h in healthy subjects. J Clin Pharmacol. 2006;46(8):933-944.
26. Azilect [package insert]. Overland Park, KS: Teva Neuroscience, Inc.; 2014.
27. Marik PE, Varon J. Hypertensive crises: challenges and management. Chest. 2007;131(6):1949-1962.
28. Burton TJ, Wilkinson IB. The dangers of immediate-release nifedipine in the emergency treatment of hypertension. J Hum Hypertens. 2008;22(4):301-302.
29. Yilmaz S, Pekdemir M, Tural U, et al. Comparison of alprazolam versus captopril in high blood pressure: a randomized controlled trial. Blood Press. 2011;20(4):239-243.
30. Carruthers J, Radigan M, Erlich MD, et al. An initiative to improve clozapine prescribing in New York State. Psychiatr Serv. 2016;67(4):369-371.
Despite an abundance of evidenced-based literature supporting monoamine oxidase inhibitors (MAOIs) as an effective treatment for depression, use of these agents has decreased drastically in the past 3 decades. A lack of industry support and the ease of use of other agents are contributing factors, but the biggest impediments to routine use of MAOIs are unfamiliarity with their efficacy advantages and concerns about adverse effects, particularly the risk of hypertensive crises and serotonin syndrome. Many misconceptions regarding these medications are based on outdated data and studies that are no longer reliable.
The goal of this 2-part review is to provide clinicians with updated information regarding MAOIs. Part 1 provides a brief description of:
- the pharmacology of nonselective irreversible MAOIs
- the mechanism by which tyramine induces hypertension
- sources of clinically significant tyramine exposure
- what to tell patients about dietary restrictions and MAOIs.
Part 2 of this guide will cover the risk of serotonin syndrome when MAOIs are combined with inhibitors of serotonin reuptake, how to initiate MAOI therapy, and augmenting MAOIs with other agents.
The pharmacology of MAOIs
First used clinically in the 1950s to treat tuberculosis, MAOIs have a long and interesting history (see the Box “A brief history of monoamine oxidase inhibitors”). Table 11 lists MAOIs currently available in the United States, including the MAO-B–specific agent rasagiline, which is used for Parkinson’s disease.
Manipulation of the monoamines serotonin, norepinephrine, and dopamine is fundamental to managing major depressive disorder (MDD), yet only nonselective MAOIs directly promote neurotransmission of all 3 by inhibiting MAO-A and MAO-B.2 The Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study demonstrated that <50% of MDD patients achieve remission in monotherapy trials of selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors, mirtazapine, or bupropion, necessitating consideration of antidepressant combinations, augmentation options, and eventually irreversible, nonselective MAOIs such as phenelzine, tranylcypromine, or isocarboxazid.3,4 Nonselective MAOIs thus offer a therapeutic opportunity for patients who do not respond to single or dual-mechanism strategies; moreover, nonselective MAOIs have compelling effectiveness data for other conditions, including panic disorder and social phobia.5 Although MAOIs are among the most effective pharmacologic agents for MDD,6 they are underutilized because of an inadequate understanding of risk mechanisms and resultant fear of catastrophic outcomes. Because of the difficulties encountered in achieving clinical remission for MDD, the nonselective MAOIs deserve a second look.
Differentiation of MAO-A from MAO-B. It is essential to understand the mechanism of action of MAOIs, specifically the impact of MAO-A inhibition. Although the enzyme MAO was known in the 1950s, it wasn’t until 1968 that Johnston7 postulated the existence of >1 form. In 1971, Goridis and Neff8 used clorgyline to examine the deamination rate by MAO of tyramine and norepinephrine. They found that tyramine appeared to be a substrate of both MAO isoforms, but only 1 of the MAO types was sensitive to the inhibitory effects of clorgyline. They also discerned that norepinephrine was only a substrate for MAO-A, and that this form of MAO was sensitive to clorgyline inhibition. Thus, the forms of MAO were characterized by their preferred substrates (Table 29,10), and then later by their tissue distribution. Phenylethylamine is a naturally occurring compound found in foods, such as chocolate, and has an in vitro pharmacology similar to amphetamine but with 1 important difference: it has a short half-life of 5 to 10 minutes after oral ingestion, and therefore no appreciable CNS impact.
Within the CNS, norepinephrine and dopamine neurons possess both MAO forms, with the MAO-A content greater than MAO-B. Serotonergic neurons only contain MAO-B.11 Outside of the CNS, MAO-A predominates, with only platelets and lymphocytes possessing MAO-B activity.11 The overall relative tissue proportions of MAO-A to MAO-B activity are: brain, 25% MAO-A, 75% MAO-B; liver, 50% MAO-A, 50% MAO-B; intestine, 80% MAO-A, 20% MAO-B; and peripheral adrenergic neurons, 90% MAO-A, 10% MAO-B.
Because of its specificity for serotonin and norepinephrine, CNS MAO-A inhibition is necessary for antidepressant effects. MAO-B inhibition by itself does not appear to raise CNS dopamine levels unless exogenous dopamine is supplied.11 All MAOIs used in the United States to treat depression are irreversible, nonselective inhibitors of MAO-A and MAO-B.
Selegiline in oral form generates low plasma levels and primarily inhibits MAO-B. The transdermal form of selegiline achieves significantly greater systemic exposure, and at these higher plasma levels selegiline is a nonselective, irreversible MAOI effective for MDD (Figure 112). Administering selegiline systemically via a transdermal patch avoids clinically significant MAOI effects in the gut, so no dietary warnings exist for the lowest dose (6 mg/24 hours), although there are warnings for the higher dosages (9 mg/24 hours and 12 mg/24 hours).
Differentiation of MAOIs by chemical class. The earliest MAOI, iproniazid, was a hydrazine derivative and exhibited hepatotoxicity,13 as did certain other hydrazine MAOIs. This lead to a search for safer hydrazine and nonhydrazine alternatives. Isocarboxazid and phenelzine are the 2 hydrazine MAOIs available in the United States, while tranylcypromine and selegiline transdermal are nonhydrazines (Figure 2).
What distinguishes the nonhydrazine medication selegiline is that its metabolism generates L-amphetamine metabolites (Figure 314). This property was thought to be shared by other nonhydrazines, but recent studies indicate than neither tranylcypromine15 nor the MAO-B–selective rasagiline possess amphetamine metabolites.16 Unlike the dextro isomers, L-amphetamine structures do not inhibit dopamine reuptake or cause euphoria, but can cause stimulation (eg, sleep disturbance) by inhibiting norepinephrine reuptake, and also by interacting with the trace amine-associated receptor 1 (TAAR1), an intracellular receptor expressed within the presynaptic terminal of monoamine neurons. Activation of TAAR1 by tyramine is an important part of the hypertensive effects related to excessive tyramine exposure.17 (The importance of TAAR1 and the interaction with tyramine is discussed in the next section.) Importantly, patients taking selegiline must be warned that certain drug screens may not discriminate between levo and dextro isomers of amphetamines, and that the use of selegiline should be disclosed prior to drug testing procedures.
MAOIs and tyramine: Dietary requirements
Clinicians who are familiar with MAOIs recognize that there are dietary restrictions to minimize patients’ exposure to tyramine. As most clinicians know, significant tyramine ingestion may cause an increase in blood pressure (BP) in patients taking an MAOI, but many overestimate the prevalence of foods high in tyramine content since the original reports emerged in the early 1960s.18 In a recent monograph, one of the leading experts on MAOIs, Professor Ken Gillman, stated:
Very few foods now contain problematically high tyramine levels, that is a result of great changes in international food production methods and hygiene regulations. Cheese is the only food that, in the past, has been associated with documented fatalities resulting from hypertension. Nowadays most cheeses are quite safe, and even ‘matured’ cheeses are usually safe in healthy-sized portions. The variability of sensitivity to tyramine between individuals, and the sometimes unpredictable amount of tyramine content in foods, means a little knowledge and care are still required.19
What is tyramine? Tyramine is a biogenic amine that is virtually absent in fresh animal protein sources but is enriched after decay or fermentation.20 Modern food processing and handling methods have significantly limited the tyramine content in processed foods, with the exception of certain cheeses and sauces, as discussed below. Moreover, modern assaying techniques using high-performance liquid chromatography have generated extremely accurate assessments of the tyramine content of specific foods.21 Data published prior to 2000 are not reliable, because many of these publications employed outdated methods.17
When ingested, tyramine is metabolized by gut MAO-A, with doses up to 400 mg causing no known effects, although most people rarely ingest >25 mg during a meal.22 In addition to being a substrate for MAO-A, tyramine is also a substrate for the dopamine transporter, norepinephrine transporter (NET), the vesicular monoamine transporter 2, and TAAR1.23 Tyramine enters the cell via NET, where it interacts with TAAR1, a G protein-coupled receptor that is responsive to trace amines, such as tyramine, as well as amphetamines.20 The agonist properties at TAAR1 are the presumed site of action for the BP effects of tyramine, because binding results in potent release of norepinephrine.20,24 When tyramine is supplied to an animal in which MAO-A is inhibited, the decreased peripheral catabolism of tyramine results in markedly increased norepinephrine release by peripheral adrenergic neurons. Moreover, the absence of MAO-A activity in those neurons prevents any norepinephrine breakdown, resulting in robust synaptic norepinephrine delivery and peripheral effects.
All orally administered irreversible MAOIs potently inhibit gut and systemic MAO-A, and are susceptible to the impact of significant tyramine ingestion. The exception is selegiline transdermal (Figure 112), as appreciable gut MAO-A inhibition does not occur until doses >6 mg/24 hours are reached.22 No significant pressor response was seen in participants taking selegiline transdermal, 6 mg/24 hours for 13 days, who consumed a meal that provided 400 mg of tyramine.22 Conversely, for oral agents that produce gut MAO-A inhibition, tyramine doses as low as 8 to 10 mg (when administered as tyramine capsules) may increase systolic pressure by 30 mm Hg.25 The dietary warnings do not apply to rasagiline, which is a selective MAO-B inhibitor, although rasagiline may have an impact on resting BP; the prescribing information for rasagiline includes warnings about hypotension and hypertension.26
What to tell patients about tyramine. Although administering pure tyramine capsules can induce a measurable change in systolic BP, when ingested as food, tyramine doses <50 mg are unlikely to cause an increase in BP sufficient to warrant clinical intervention, although some individuals can be sensitive to 10 to 25 mg.19 When discussing with patients safety issues related to diet, there are a few important concepts to remember19:
- In an era when the tyramine content of foods was much higher (1960 to 1964) and MAOI users received no dietary guidance, only 14 deaths were reported among an estimated 1.5 million patients who took MAOIs.
- MAOIs do not raise BP, and their use is associated with orthostasis in some patients.
- Routine exercise or other vigorous activities (eg, weightlifting) can raise systolic pressure well above 200 mm Hg, and routine baseline systolic pressures, ranging from 180 to 220 mm Hg, do not increase the risk of subarachnoid hemorrhage.
- Hospital evaluation is needed only if a substantial amount of tyramine is ingested (eg, estimated ≥100 mg), and self-monitoring shows a systolic BP ≥220 mm Hg over a prolonged period (eg, 2 hours). Ingestion of 100 mg of tyramine would almost certainly have to be intentional, as it would require one to consume 3.5 oz of the most highly tyramine-laden cheeses.
Emphasize to patients that only a small number of highly aged cheeses, foods, and sauces contain high quantities of tyramine, and that even these foods can be enjoyed in small amounts. All patients who are prescribed an MAOI also should purchase a portable BP cuff for those rare instances when a dietary indiscretion may have occurred and the person experiences a headache within 1 to 2 hours after tyramine ingestion. Most reactions are self-limited and resolve over 2 to 4 hours.
Patients who ingest ≥100 mg of tyramine should be evaluated by a physician. Under no circumstances should a patient be given a prescription for nifedipine or other medications that can abruptly lower BP, because this may result in complications, including myocardial infarction.27,28 Counsel patients to remain calm. Some clinicians endorse the use of low doses of benzodiazepines (the equivalent of alprazolam 0.5 mg) to facilitate this, because anxiety elevates BP. A recent emergency room study of patients with an initial systolic BP ≥160 mm Hg or diastolic BP ≥100 mm Hg without end organ damage demonstrated that alprazolam, 0.5 mg, was as effective as captopril, 25 mg, in lowering BP.29
Also, tell patients that if a food is unfamiliar and highly aged or fermented, they should avoid it until they can further inquire about it. In a review, Gillman19 provides the tyramine content of an exhaustive list of cheeses, aged meats, and sauces (see Related Resources). For other products, patients often can obtain information directly from the manufacturer. In many parts of the world, assays for tyramine content are required as a demonstration of adequate product safety procedures. Even the most highly aged cheeses with a tyramine content of 1,000 g/kg can be enjoyed in small amounts (<1 oz), and most products would require heroic intake to achieve clinically significant tyramine ingestion (Table 319).
Improved education can clarify the risks
Medications such as lithium, clozapine, and MAOIs have a proven record of efficacy, yet often are underused due to fears engendered by lack of systematic training. A recent initiative in New York thus aimed to increase rates of
Despite an abundance of evidenced-based literature supporting monoamine oxidase inhibitors (MAOIs) as an effective treatment for depression, use of these agents has decreased drastically in the past 3 decades. A lack of industry support and the ease of use of other agents are contributing factors, but the biggest impediments to routine use of MAOIs are unfamiliarity with their efficacy advantages and concerns about adverse effects, particularly the risk of hypertensive crises and serotonin syndrome. Many misconceptions regarding these medications are based on outdated data and studies that are no longer reliable.
The goal of this 2-part review is to provide clinicians with updated information regarding MAOIs. Part 1 provides a brief description of:
- the pharmacology of nonselective irreversible MAOIs
- the mechanism by which tyramine induces hypertension
- sources of clinically significant tyramine exposure
- what to tell patients about dietary restrictions and MAOIs.
Part 2 of this guide will cover the risk of serotonin syndrome when MAOIs are combined with inhibitors of serotonin reuptake, how to initiate MAOI therapy, and augmenting MAOIs with other agents.
The pharmacology of MAOIs
First used clinically in the 1950s to treat tuberculosis, MAOIs have a long and interesting history (see the Box “A brief history of monoamine oxidase inhibitors”). Table 11 lists MAOIs currently available in the United States, including the MAO-B–specific agent rasagiline, which is used for Parkinson’s disease.
Manipulation of the monoamines serotonin, norepinephrine, and dopamine is fundamental to managing major depressive disorder (MDD), yet only nonselective MAOIs directly promote neurotransmission of all 3 by inhibiting MAO-A and MAO-B.2 The Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study demonstrated that <50% of MDD patients achieve remission in monotherapy trials of selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors, mirtazapine, or bupropion, necessitating consideration of antidepressant combinations, augmentation options, and eventually irreversible, nonselective MAOIs such as phenelzine, tranylcypromine, or isocarboxazid.3,4 Nonselective MAOIs thus offer a therapeutic opportunity for patients who do not respond to single or dual-mechanism strategies; moreover, nonselective MAOIs have compelling effectiveness data for other conditions, including panic disorder and social phobia.5 Although MAOIs are among the most effective pharmacologic agents for MDD,6 they are underutilized because of an inadequate understanding of risk mechanisms and resultant fear of catastrophic outcomes. Because of the difficulties encountered in achieving clinical remission for MDD, the nonselective MAOIs deserve a second look.
Differentiation of MAO-A from MAO-B. It is essential to understand the mechanism of action of MAOIs, specifically the impact of MAO-A inhibition. Although the enzyme MAO was known in the 1950s, it wasn’t until 1968 that Johnston7 postulated the existence of >1 form. In 1971, Goridis and Neff8 used clorgyline to examine the deamination rate by MAO of tyramine and norepinephrine. They found that tyramine appeared to be a substrate of both MAO isoforms, but only 1 of the MAO types was sensitive to the inhibitory effects of clorgyline. They also discerned that norepinephrine was only a substrate for MAO-A, and that this form of MAO was sensitive to clorgyline inhibition. Thus, the forms of MAO were characterized by their preferred substrates (Table 29,10), and then later by their tissue distribution. Phenylethylamine is a naturally occurring compound found in foods, such as chocolate, and has an in vitro pharmacology similar to amphetamine but with 1 important difference: it has a short half-life of 5 to 10 minutes after oral ingestion, and therefore no appreciable CNS impact.
Within the CNS, norepinephrine and dopamine neurons possess both MAO forms, with the MAO-A content greater than MAO-B. Serotonergic neurons only contain MAO-B.11 Outside of the CNS, MAO-A predominates, with only platelets and lymphocytes possessing MAO-B activity.11 The overall relative tissue proportions of MAO-A to MAO-B activity are: brain, 25% MAO-A, 75% MAO-B; liver, 50% MAO-A, 50% MAO-B; intestine, 80% MAO-A, 20% MAO-B; and peripheral adrenergic neurons, 90% MAO-A, 10% MAO-B.
Because of its specificity for serotonin and norepinephrine, CNS MAO-A inhibition is necessary for antidepressant effects. MAO-B inhibition by itself does not appear to raise CNS dopamine levels unless exogenous dopamine is supplied.11 All MAOIs used in the United States to treat depression are irreversible, nonselective inhibitors of MAO-A and MAO-B.
Selegiline in oral form generates low plasma levels and primarily inhibits MAO-B. The transdermal form of selegiline achieves significantly greater systemic exposure, and at these higher plasma levels selegiline is a nonselective, irreversible MAOI effective for MDD (Figure 112). Administering selegiline systemically via a transdermal patch avoids clinically significant MAOI effects in the gut, so no dietary warnings exist for the lowest dose (6 mg/24 hours), although there are warnings for the higher dosages (9 mg/24 hours and 12 mg/24 hours).
Differentiation of MAOIs by chemical class. The earliest MAOI, iproniazid, was a hydrazine derivative and exhibited hepatotoxicity,13 as did certain other hydrazine MAOIs. This lead to a search for safer hydrazine and nonhydrazine alternatives. Isocarboxazid and phenelzine are the 2 hydrazine MAOIs available in the United States, while tranylcypromine and selegiline transdermal are nonhydrazines (Figure 2).
What distinguishes the nonhydrazine medication selegiline is that its metabolism generates L-amphetamine metabolites (Figure 314). This property was thought to be shared by other nonhydrazines, but recent studies indicate than neither tranylcypromine15 nor the MAO-B–selective rasagiline possess amphetamine metabolites.16 Unlike the dextro isomers, L-amphetamine structures do not inhibit dopamine reuptake or cause euphoria, but can cause stimulation (eg, sleep disturbance) by inhibiting norepinephrine reuptake, and also by interacting with the trace amine-associated receptor 1 (TAAR1), an intracellular receptor expressed within the presynaptic terminal of monoamine neurons. Activation of TAAR1 by tyramine is an important part of the hypertensive effects related to excessive tyramine exposure.17 (The importance of TAAR1 and the interaction with tyramine is discussed in the next section.) Importantly, patients taking selegiline must be warned that certain drug screens may not discriminate between levo and dextro isomers of amphetamines, and that the use of selegiline should be disclosed prior to drug testing procedures.
MAOIs and tyramine: Dietary requirements
Clinicians who are familiar with MAOIs recognize that there are dietary restrictions to minimize patients’ exposure to tyramine. As most clinicians know, significant tyramine ingestion may cause an increase in blood pressure (BP) in patients taking an MAOI, but many overestimate the prevalence of foods high in tyramine content since the original reports emerged in the early 1960s.18 In a recent monograph, one of the leading experts on MAOIs, Professor Ken Gillman, stated:
Very few foods now contain problematically high tyramine levels, that is a result of great changes in international food production methods and hygiene regulations. Cheese is the only food that, in the past, has been associated with documented fatalities resulting from hypertension. Nowadays most cheeses are quite safe, and even ‘matured’ cheeses are usually safe in healthy-sized portions. The variability of sensitivity to tyramine between individuals, and the sometimes unpredictable amount of tyramine content in foods, means a little knowledge and care are still required.19
What is tyramine? Tyramine is a biogenic amine that is virtually absent in fresh animal protein sources but is enriched after decay or fermentation.20 Modern food processing and handling methods have significantly limited the tyramine content in processed foods, with the exception of certain cheeses and sauces, as discussed below. Moreover, modern assaying techniques using high-performance liquid chromatography have generated extremely accurate assessments of the tyramine content of specific foods.21 Data published prior to 2000 are not reliable, because many of these publications employed outdated methods.17
When ingested, tyramine is metabolized by gut MAO-A, with doses up to 400 mg causing no known effects, although most people rarely ingest >25 mg during a meal.22 In addition to being a substrate for MAO-A, tyramine is also a substrate for the dopamine transporter, norepinephrine transporter (NET), the vesicular monoamine transporter 2, and TAAR1.23 Tyramine enters the cell via NET, where it interacts with TAAR1, a G protein-coupled receptor that is responsive to trace amines, such as tyramine, as well as amphetamines.20 The agonist properties at TAAR1 are the presumed site of action for the BP effects of tyramine, because binding results in potent release of norepinephrine.20,24 When tyramine is supplied to an animal in which MAO-A is inhibited, the decreased peripheral catabolism of tyramine results in markedly increased norepinephrine release by peripheral adrenergic neurons. Moreover, the absence of MAO-A activity in those neurons prevents any norepinephrine breakdown, resulting in robust synaptic norepinephrine delivery and peripheral effects.
All orally administered irreversible MAOIs potently inhibit gut and systemic MAO-A, and are susceptible to the impact of significant tyramine ingestion. The exception is selegiline transdermal (Figure 112), as appreciable gut MAO-A inhibition does not occur until doses >6 mg/24 hours are reached.22 No significant pressor response was seen in participants taking selegiline transdermal, 6 mg/24 hours for 13 days, who consumed a meal that provided 400 mg of tyramine.22 Conversely, for oral agents that produce gut MAO-A inhibition, tyramine doses as low as 8 to 10 mg (when administered as tyramine capsules) may increase systolic pressure by 30 mm Hg.25 The dietary warnings do not apply to rasagiline, which is a selective MAO-B inhibitor, although rasagiline may have an impact on resting BP; the prescribing information for rasagiline includes warnings about hypotension and hypertension.26
What to tell patients about tyramine. Although administering pure tyramine capsules can induce a measurable change in systolic BP, when ingested as food, tyramine doses <50 mg are unlikely to cause an increase in BP sufficient to warrant clinical intervention, although some individuals can be sensitive to 10 to 25 mg.19 When discussing with patients safety issues related to diet, there are a few important concepts to remember19:
- In an era when the tyramine content of foods was much higher (1960 to 1964) and MAOI users received no dietary guidance, only 14 deaths were reported among an estimated 1.5 million patients who took MAOIs.
- MAOIs do not raise BP, and their use is associated with orthostasis in some patients.
- Routine exercise or other vigorous activities (eg, weightlifting) can raise systolic pressure well above 200 mm Hg, and routine baseline systolic pressures, ranging from 180 to 220 mm Hg, do not increase the risk of subarachnoid hemorrhage.
- Hospital evaluation is needed only if a substantial amount of tyramine is ingested (eg, estimated ≥100 mg), and self-monitoring shows a systolic BP ≥220 mm Hg over a prolonged period (eg, 2 hours). Ingestion of 100 mg of tyramine would almost certainly have to be intentional, as it would require one to consume 3.5 oz of the most highly tyramine-laden cheeses.
Emphasize to patients that only a small number of highly aged cheeses, foods, and sauces contain high quantities of tyramine, and that even these foods can be enjoyed in small amounts. All patients who are prescribed an MAOI also should purchase a portable BP cuff for those rare instances when a dietary indiscretion may have occurred and the person experiences a headache within 1 to 2 hours after tyramine ingestion. Most reactions are self-limited and resolve over 2 to 4 hours.
Patients who ingest ≥100 mg of tyramine should be evaluated by a physician. Under no circumstances should a patient be given a prescription for nifedipine or other medications that can abruptly lower BP, because this may result in complications, including myocardial infarction.27,28 Counsel patients to remain calm. Some clinicians endorse the use of low doses of benzodiazepines (the equivalent of alprazolam 0.5 mg) to facilitate this, because anxiety elevates BP. A recent emergency room study of patients with an initial systolic BP ≥160 mm Hg or diastolic BP ≥100 mm Hg without end organ damage demonstrated that alprazolam, 0.5 mg, was as effective as captopril, 25 mg, in lowering BP.29
Also, tell patients that if a food is unfamiliar and highly aged or fermented, they should avoid it until they can further inquire about it. In a review, Gillman19 provides the tyramine content of an exhaustive list of cheeses, aged meats, and sauces (see Related Resources). For other products, patients often can obtain information directly from the manufacturer. In many parts of the world, assays for tyramine content are required as a demonstration of adequate product safety procedures. Even the most highly aged cheeses with a tyramine content of 1,000 g/kg can be enjoyed in small amounts (<1 oz), and most products would require heroic intake to achieve clinically significant tyramine ingestion (Table 319).
Improved education can clarify the risks
Medications such as lithium, clozapine, and MAOIs have a proven record of efficacy, yet often are underused due to fears engendered by lack of systematic training. A recent initiative in New York thus aimed to increase rates of
1. Panisset M, Chen JJ, Rhyee SH, et al. Serotonin toxicity association with concomitant antidepressants and rasagiline treatment: retrospective study (STACCATO). Pharmacotherapy. 2014;34(12):1250-1258.
2. López-Muñoz F, Alamo C. Monoaminergic neurotransmission: the history of the discovery of antidepressants from 1950s until today. Curr Pharm Des. 2009;15(14):1563-1586.
3. Nierenberg AA, Fava M, Trivedi MH, et al. A comparison of lithium and T(3) augmentation following two failed medication treatments for depression: a STAR*D report. Am J Psychiatry. 2006;163(9):1519-1530; quiz 1665.
4. Trivedi MH, Fava M, Wisniewski SR, et al; STAR*D Study Team. Medication augmentation after the failure of SSRIs for depression. New Engl J Med. 2006;354(12):1243-1252.
5. Bandelow B, Zohar J, Hollander E, et al; World Federation of Societies of Biological Psychiatry Task Force on Treatment Guidelines for Anxiety, Obsessive-Compulsive and Posttraumatic Stress Disorders. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the pharmacological treatment of anxiety, obsessive-compulsive and posttraumatic stress disorders. World J Biol Psychiatry. 2002;3(4):171-199.
6. Shulman KI, Herrmann N, Walker SE. Current place of monoamine oxidase inhibitors in the treatment of depression. CNS Drugs. 2013;27(10):789-797.
7. Johnston JP. Some observations upon a new inhibitor of monoamine oxidase in brain tissue. Biochem Pharmacol. 1968;17(7):1285-1297.
8. Goridis C, Neff NH. Monoamine oxidase in sympathetic nerves: a transmitter specific enzyme type. Br J Pharmacol. 1971;43(4):814-818.
9. Geha RM, Rebrin I, Chen K, et al. Substrate and inhibitor specificities for human monoamine oxidase A and B are influenced by a single amino acid. J Biol Chem. 2001;276(13):9877-9882.
10. O’Carroll AM, Fowler CJ, Phillips JP, et al. The deamination of dopamine by human brain monoamine oxidase. Specificity for the two enzyme forms in seven brain regions. Naunyn Schmiedebergs Arch Pharmacol. 1983;322(3):198-202.
11. Stahl SM, Felker A. Monoamine oxidase inhibitors: a modern guide to an unrequited class of antidepressants. CNS Spectr. 2008;13(10):855-780.
12. Mawhinney M, Cole D, Azzaro AJ. Daily transdermal administration of selegiline to guinea-pigs preferentially inhibits monoamine oxidase activity in brain when compared with intestinal and hepatic tissues. J Pharm Pharmacol. 2003;55(1):27-34.
13. Maille F, Duvoux C, Cherqui D, et al. Auxiliary hepatic transplantation in iproniazid-induced subfulminant hepatitis. Should iproniazid still be sold in France? [in French]. Gastroenterol Clin Biol. 1999;23(10):1083-1085.
14. Salonen JS, Nyman L, Boobis AR, et al. Comparative studies on the cytochrome p450-associated metabolism and interaction potential of selegiline between human liver-derived in vitro systems. Drug Metab Dispos. 2003;31(9):1093-1102.
15. Iwersen S, Schmoldt A. One fatal and one nonfatal intoxication with tranylcypromine. Absence of amphetamines as metabolites. J Anal Toxicol. 1996;20(5):301-304.
16. Müller T, Hoffmann JA, Dimpfel W, et al. Switch from selegiline to rasagiline is beneficial in patients with Parkinson’s disease. J Neural Transm (Vienna). 2013;120(5):761-765.
17. Lewin AH, Miller GM, Gilmour B. Trace amine-associated receptor 1 is a stereoselective binding site for compounds in the amphetamine class. Bioorg Med Chem. 2011;19(23):7044-7048.
18. Blackwell B. Hypertensive crisis due to monoamine-oxidase inhibitors. Lancet. 1963;2(7313):849-850.
19. Gillman PK. Monoamine oxidase inhibitors: a review concerning dietary tyramine and drug interactions. PsychoTropical Commentaries. 2016;16(6):1-97.
20. Pei Y, Asif-Malik A, Canales JJ. Trace amines and the trace amine-associated receptor 1: pharmacology, neurochemistry, and clinical implications. Front Neurosci. 2016;10:148.
21. Fiechter G, Sivec G, Mayer HK. Application of UHPLC for the simultaneous analysis of free amino acids and biogenic amines in ripened acid-curd cheeses. J Chromatogr B Analyt Technol Biomed Life Sci. 2013;927:191-200.
22. Blob LF, Sharoky M, Campbell BJ, et al. Effects of a tyramine-enriched meal on blood pressure response in healthy male volunteers treated with selegiline transdermal system 6 mg/24 hour. CNS Spectr. 2007;12(1):25-34.
23. Partilla JS, Dempsey AG, Nagpal AS, et al. Interaction of amphetamines and related compounds at the vesicular monoamine transporter. J Pharmacol Exp Ther. 2006;319(1):237-246.
24. Borowsky B, Adham N, Jones KA, et al. Trace amines: identification of a family of mammalian G protein-coupled receptors. Proc Natl Acad Sci U S A. 2001;98(16):8966-8971.
25. Azzaro AJ, Vandenberg CM, Blob LF, et al. Tyramine pressor sensitivity during treatment with the selegiline transdermal system 6 mg/24 h in healthy subjects. J Clin Pharmacol. 2006;46(8):933-944.
26. Azilect [package insert]. Overland Park, KS: Teva Neuroscience, Inc.; 2014.
27. Marik PE, Varon J. Hypertensive crises: challenges and management. Chest. 2007;131(6):1949-1962.
28. Burton TJ, Wilkinson IB. The dangers of immediate-release nifedipine in the emergency treatment of hypertension. J Hum Hypertens. 2008;22(4):301-302.
29. Yilmaz S, Pekdemir M, Tural U, et al. Comparison of alprazolam versus captopril in high blood pressure: a randomized controlled trial. Blood Press. 2011;20(4):239-243.
30. Carruthers J, Radigan M, Erlich MD, et al. An initiative to improve clozapine prescribing in New York State. Psychiatr Serv. 2016;67(4):369-371.
1. Panisset M, Chen JJ, Rhyee SH, et al. Serotonin toxicity association with concomitant antidepressants and rasagiline treatment: retrospective study (STACCATO). Pharmacotherapy. 2014;34(12):1250-1258.
2. López-Muñoz F, Alamo C. Monoaminergic neurotransmission: the history of the discovery of antidepressants from 1950s until today. Curr Pharm Des. 2009;15(14):1563-1586.
3. Nierenberg AA, Fava M, Trivedi MH, et al. A comparison of lithium and T(3) augmentation following two failed medication treatments for depression: a STAR*D report. Am J Psychiatry. 2006;163(9):1519-1530; quiz 1665.
4. Trivedi MH, Fava M, Wisniewski SR, et al; STAR*D Study Team. Medication augmentation after the failure of SSRIs for depression. New Engl J Med. 2006;354(12):1243-1252.
5. Bandelow B, Zohar J, Hollander E, et al; World Federation of Societies of Biological Psychiatry Task Force on Treatment Guidelines for Anxiety, Obsessive-Compulsive and Posttraumatic Stress Disorders. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the pharmacological treatment of anxiety, obsessive-compulsive and posttraumatic stress disorders. World J Biol Psychiatry. 2002;3(4):171-199.
6. Shulman KI, Herrmann N, Walker SE. Current place of monoamine oxidase inhibitors in the treatment of depression. CNS Drugs. 2013;27(10):789-797.
7. Johnston JP. Some observations upon a new inhibitor of monoamine oxidase in brain tissue. Biochem Pharmacol. 1968;17(7):1285-1297.
8. Goridis C, Neff NH. Monoamine oxidase in sympathetic nerves: a transmitter specific enzyme type. Br J Pharmacol. 1971;43(4):814-818.
9. Geha RM, Rebrin I, Chen K, et al. Substrate and inhibitor specificities for human monoamine oxidase A and B are influenced by a single amino acid. J Biol Chem. 2001;276(13):9877-9882.
10. O’Carroll AM, Fowler CJ, Phillips JP, et al. The deamination of dopamine by human brain monoamine oxidase. Specificity for the two enzyme forms in seven brain regions. Naunyn Schmiedebergs Arch Pharmacol. 1983;322(3):198-202.
11. Stahl SM, Felker A. Monoamine oxidase inhibitors: a modern guide to an unrequited class of antidepressants. CNS Spectr. 2008;13(10):855-780.
12. Mawhinney M, Cole D, Azzaro AJ. Daily transdermal administration of selegiline to guinea-pigs preferentially inhibits monoamine oxidase activity in brain when compared with intestinal and hepatic tissues. J Pharm Pharmacol. 2003;55(1):27-34.
13. Maille F, Duvoux C, Cherqui D, et al. Auxiliary hepatic transplantation in iproniazid-induced subfulminant hepatitis. Should iproniazid still be sold in France? [in French]. Gastroenterol Clin Biol. 1999;23(10):1083-1085.
14. Salonen JS, Nyman L, Boobis AR, et al. Comparative studies on the cytochrome p450-associated metabolism and interaction potential of selegiline between human liver-derived in vitro systems. Drug Metab Dispos. 2003;31(9):1093-1102.
15. Iwersen S, Schmoldt A. One fatal and one nonfatal intoxication with tranylcypromine. Absence of amphetamines as metabolites. J Anal Toxicol. 1996;20(5):301-304.
16. Müller T, Hoffmann JA, Dimpfel W, et al. Switch from selegiline to rasagiline is beneficial in patients with Parkinson’s disease. J Neural Transm (Vienna). 2013;120(5):761-765.
17. Lewin AH, Miller GM, Gilmour B. Trace amine-associated receptor 1 is a stereoselective binding site for compounds in the amphetamine class. Bioorg Med Chem. 2011;19(23):7044-7048.
18. Blackwell B. Hypertensive crisis due to monoamine-oxidase inhibitors. Lancet. 1963;2(7313):849-850.
19. Gillman PK. Monoamine oxidase inhibitors: a review concerning dietary tyramine and drug interactions. PsychoTropical Commentaries. 2016;16(6):1-97.
20. Pei Y, Asif-Malik A, Canales JJ. Trace amines and the trace amine-associated receptor 1: pharmacology, neurochemistry, and clinical implications. Front Neurosci. 2016;10:148.
21. Fiechter G, Sivec G, Mayer HK. Application of UHPLC for the simultaneous analysis of free amino acids and biogenic amines in ripened acid-curd cheeses. J Chromatogr B Analyt Technol Biomed Life Sci. 2013;927:191-200.
22. Blob LF, Sharoky M, Campbell BJ, et al. Effects of a tyramine-enriched meal on blood pressure response in healthy male volunteers treated with selegiline transdermal system 6 mg/24 hour. CNS Spectr. 2007;12(1):25-34.
23. Partilla JS, Dempsey AG, Nagpal AS, et al. Interaction of amphetamines and related compounds at the vesicular monoamine transporter. J Pharmacol Exp Ther. 2006;319(1):237-246.
24. Borowsky B, Adham N, Jones KA, et al. Trace amines: identification of a family of mammalian G protein-coupled receptors. Proc Natl Acad Sci U S A. 2001;98(16):8966-8971.
25. Azzaro AJ, Vandenberg CM, Blob LF, et al. Tyramine pressor sensitivity during treatment with the selegiline transdermal system 6 mg/24 h in healthy subjects. J Clin Pharmacol. 2006;46(8):933-944.
26. Azilect [package insert]. Overland Park, KS: Teva Neuroscience, Inc.; 2014.
27. Marik PE, Varon J. Hypertensive crises: challenges and management. Chest. 2007;131(6):1949-1962.
28. Burton TJ, Wilkinson IB. The dangers of immediate-release nifedipine in the emergency treatment of hypertension. J Hum Hypertens. 2008;22(4):301-302.
29. Yilmaz S, Pekdemir M, Tural U, et al. Comparison of alprazolam versus captopril in high blood pressure: a randomized controlled trial. Blood Press. 2011;20(4):239-243.
30. Carruthers J, Radigan M, Erlich MD, et al. An initiative to improve clozapine prescribing in New York State. Psychiatr Serv. 2016;67(4):369-371.