User login
Pembrolizumab could change treatment paradigm, team says
The anti-PD-1 therapy pembrolizumab could change the treatment paradigm of relapsed or refractory classic Hodgkin lymphoma (cHL), according to researchers.
In a phase 2 trial, pembrolizumab produced an overall response rate (ORR) of 69% and a complete response (CR) rate of 22% in adults with cHL who had failed treatment with brentuximab vedotin (BV), autologous hematopoietic stem cell transplant (auto-HSCT), or both.
The researchers said the safety profile of pembrolizumab was “acceptable” and largely consistent with safety in previous studies of the drug.
Twelve percent of patients temporarily stopped taking pembrolizumab due to treatment-related adverse events (AEs), and 4% stopped taking the drug entirely as a result of AEs.
Craig H. Moskowitz, MD, of Memorial Sloan Kettering Cancer Center in New York, New York, and his colleagues reported these results, from the KEYNOTE-087 trial, in the Journal of Clinical Oncology.
The trial was sponsored by Merck, the company that markets pembrolizumab as Keytruda.
In KEYNOTE-087, the researchers evaluated pembrolizumab (a 200 mg fixed dose every 3 weeks) in patients with relapsed or refractory cHL across 3 cohorts:
Cohort 1: Patients who progressed after auto-HSCT and subsequent treatment with BV
Cohort 2: Patients who failed salvage chemotherapy, were ineligible for a transplant, and progressed after BV
Cohort 3: Patients who progressed after auto-HSCT and did not receive BV after transplant.
Efficacy
Across all 210 enrolled patients, the ORR was 69.0%, and the CR rate was 22.4%.
In Cohort 1 (n=69), the ORR was 73.9%. The CR rate was 21.7%, the partial response (PR) rate was 52.2%, 15.9% of patients had stable disease (SD), and 7.2% progressed. In 82.2% of responders, the response lasted 6 months or more.
In Cohort 2 (n=81), the ORR was 64.2%. The CR rate was 24.7%, the PR rate was 39.5%, 12.3% of patients had SD, and 21.0% progressed. In 70.0% of responders, the response lasted 6 months or more.
In Cohort 3 (n=60), the ORR was 70.0%. Twenty percent of patients had a CR, 50.0% had a PR, 16.7% had SD, and 13.3% progressed. In 75.6% of responders, the response lasted 6 months or more.
Results also included an analysis of patients with primary refractory disease (n=73), which was defined as failure to achieve CR or PR with first-line treatment. In this patient population, the ORR was 79.5%.
An ORR of 67.8% was reported in patients who relapsed after 3 or more lines of prior therapy (99/146).
For the entire study cohort, the median duration of response was not reached, and the median overall survival was not reached. At 9 months, the overall survival rate was 97.5%, and the progression-free survival rate was 63.4%.
Safety
The most common AEs related to pembrolizumab were hypothyroidism (12.4%), pyrexia (10.5%), fatigue (9.0%), rash (7.6%), diarrhea (7.1%), headache (6.2%), nausea (5.7%), cough (5.7%), and neutropenia (5.2%).
The most common grade 3/4 treatment-related AEs were neutropenia (2.4%), diarrhea (1.0%), and dyspnea (1.0%). Immune-mediated AEs included pneumonitis (2.9%), hyperthyroidism (2.9%), colitis (1.0%), and myositis (1.0%).
Nine patients (4.3%) stopped taking pembrolizumab due to treatment-related AEs, including myocarditis, myelitis, myositis, pneumonitis, infusion-related reactions, and cytokine release syndrome.
Twenty-six patients (12.4%) had treatment interruptions due to pembrolizumab-related AEs.
Two patients died during follow-up, but neither death was considered related to pembrolizumab. One patient died of septic shock and the other of acute graft-versus-host disease. ![]()
The anti-PD-1 therapy pembrolizumab could change the treatment paradigm of relapsed or refractory classic Hodgkin lymphoma (cHL), according to researchers.
In a phase 2 trial, pembrolizumab produced an overall response rate (ORR) of 69% and a complete response (CR) rate of 22% in adults with cHL who had failed treatment with brentuximab vedotin (BV), autologous hematopoietic stem cell transplant (auto-HSCT), or both.
The researchers said the safety profile of pembrolizumab was “acceptable” and largely consistent with safety in previous studies of the drug.
Twelve percent of patients temporarily stopped taking pembrolizumab due to treatment-related adverse events (AEs), and 4% stopped taking the drug entirely as a result of AEs.
Craig H. Moskowitz, MD, of Memorial Sloan Kettering Cancer Center in New York, New York, and his colleagues reported these results, from the KEYNOTE-087 trial, in the Journal of Clinical Oncology.
The trial was sponsored by Merck, the company that markets pembrolizumab as Keytruda.
In KEYNOTE-087, the researchers evaluated pembrolizumab (a 200 mg fixed dose every 3 weeks) in patients with relapsed or refractory cHL across 3 cohorts:
Cohort 1: Patients who progressed after auto-HSCT and subsequent treatment with BV
Cohort 2: Patients who failed salvage chemotherapy, were ineligible for a transplant, and progressed after BV
Cohort 3: Patients who progressed after auto-HSCT and did not receive BV after transplant.
Efficacy
Across all 210 enrolled patients, the ORR was 69.0%, and the CR rate was 22.4%.
In Cohort 1 (n=69), the ORR was 73.9%. The CR rate was 21.7%, the partial response (PR) rate was 52.2%, 15.9% of patients had stable disease (SD), and 7.2% progressed. In 82.2% of responders, the response lasted 6 months or more.
In Cohort 2 (n=81), the ORR was 64.2%. The CR rate was 24.7%, the PR rate was 39.5%, 12.3% of patients had SD, and 21.0% progressed. In 70.0% of responders, the response lasted 6 months or more.
In Cohort 3 (n=60), the ORR was 70.0%. Twenty percent of patients had a CR, 50.0% had a PR, 16.7% had SD, and 13.3% progressed. In 75.6% of responders, the response lasted 6 months or more.
Results also included an analysis of patients with primary refractory disease (n=73), which was defined as failure to achieve CR or PR with first-line treatment. In this patient population, the ORR was 79.5%.
An ORR of 67.8% was reported in patients who relapsed after 3 or more lines of prior therapy (99/146).
For the entire study cohort, the median duration of response was not reached, and the median overall survival was not reached. At 9 months, the overall survival rate was 97.5%, and the progression-free survival rate was 63.4%.
Safety
The most common AEs related to pembrolizumab were hypothyroidism (12.4%), pyrexia (10.5%), fatigue (9.0%), rash (7.6%), diarrhea (7.1%), headache (6.2%), nausea (5.7%), cough (5.7%), and neutropenia (5.2%).
The most common grade 3/4 treatment-related AEs were neutropenia (2.4%), diarrhea (1.0%), and dyspnea (1.0%). Immune-mediated AEs included pneumonitis (2.9%), hyperthyroidism (2.9%), colitis (1.0%), and myositis (1.0%).
Nine patients (4.3%) stopped taking pembrolizumab due to treatment-related AEs, including myocarditis, myelitis, myositis, pneumonitis, infusion-related reactions, and cytokine release syndrome.
Twenty-six patients (12.4%) had treatment interruptions due to pembrolizumab-related AEs.
Two patients died during follow-up, but neither death was considered related to pembrolizumab. One patient died of septic shock and the other of acute graft-versus-host disease. ![]()
The anti-PD-1 therapy pembrolizumab could change the treatment paradigm of relapsed or refractory classic Hodgkin lymphoma (cHL), according to researchers.
In a phase 2 trial, pembrolizumab produced an overall response rate (ORR) of 69% and a complete response (CR) rate of 22% in adults with cHL who had failed treatment with brentuximab vedotin (BV), autologous hematopoietic stem cell transplant (auto-HSCT), or both.
The researchers said the safety profile of pembrolizumab was “acceptable” and largely consistent with safety in previous studies of the drug.
Twelve percent of patients temporarily stopped taking pembrolizumab due to treatment-related adverse events (AEs), and 4% stopped taking the drug entirely as a result of AEs.
Craig H. Moskowitz, MD, of Memorial Sloan Kettering Cancer Center in New York, New York, and his colleagues reported these results, from the KEYNOTE-087 trial, in the Journal of Clinical Oncology.
The trial was sponsored by Merck, the company that markets pembrolizumab as Keytruda.
In KEYNOTE-087, the researchers evaluated pembrolizumab (a 200 mg fixed dose every 3 weeks) in patients with relapsed or refractory cHL across 3 cohorts:
Cohort 1: Patients who progressed after auto-HSCT and subsequent treatment with BV
Cohort 2: Patients who failed salvage chemotherapy, were ineligible for a transplant, and progressed after BV
Cohort 3: Patients who progressed after auto-HSCT and did not receive BV after transplant.
Efficacy
Across all 210 enrolled patients, the ORR was 69.0%, and the CR rate was 22.4%.
In Cohort 1 (n=69), the ORR was 73.9%. The CR rate was 21.7%, the partial response (PR) rate was 52.2%, 15.9% of patients had stable disease (SD), and 7.2% progressed. In 82.2% of responders, the response lasted 6 months or more.
In Cohort 2 (n=81), the ORR was 64.2%. The CR rate was 24.7%, the PR rate was 39.5%, 12.3% of patients had SD, and 21.0% progressed. In 70.0% of responders, the response lasted 6 months or more.
In Cohort 3 (n=60), the ORR was 70.0%. Twenty percent of patients had a CR, 50.0% had a PR, 16.7% had SD, and 13.3% progressed. In 75.6% of responders, the response lasted 6 months or more.
Results also included an analysis of patients with primary refractory disease (n=73), which was defined as failure to achieve CR or PR with first-line treatment. In this patient population, the ORR was 79.5%.
An ORR of 67.8% was reported in patients who relapsed after 3 or more lines of prior therapy (99/146).
For the entire study cohort, the median duration of response was not reached, and the median overall survival was not reached. At 9 months, the overall survival rate was 97.5%, and the progression-free survival rate was 63.4%.
Safety
The most common AEs related to pembrolizumab were hypothyroidism (12.4%), pyrexia (10.5%), fatigue (9.0%), rash (7.6%), diarrhea (7.1%), headache (6.2%), nausea (5.7%), cough (5.7%), and neutropenia (5.2%).
The most common grade 3/4 treatment-related AEs were neutropenia (2.4%), diarrhea (1.0%), and dyspnea (1.0%). Immune-mediated AEs included pneumonitis (2.9%), hyperthyroidism (2.9%), colitis (1.0%), and myositis (1.0%).
Nine patients (4.3%) stopped taking pembrolizumab due to treatment-related AEs, including myocarditis, myelitis, myositis, pneumonitis, infusion-related reactions, and cytokine release syndrome.
Twenty-six patients (12.4%) had treatment interruptions due to pembrolizumab-related AEs.
Two patients died during follow-up, but neither death was considered related to pembrolizumab. One patient died of septic shock and the other of acute graft-versus-host disease. ![]()
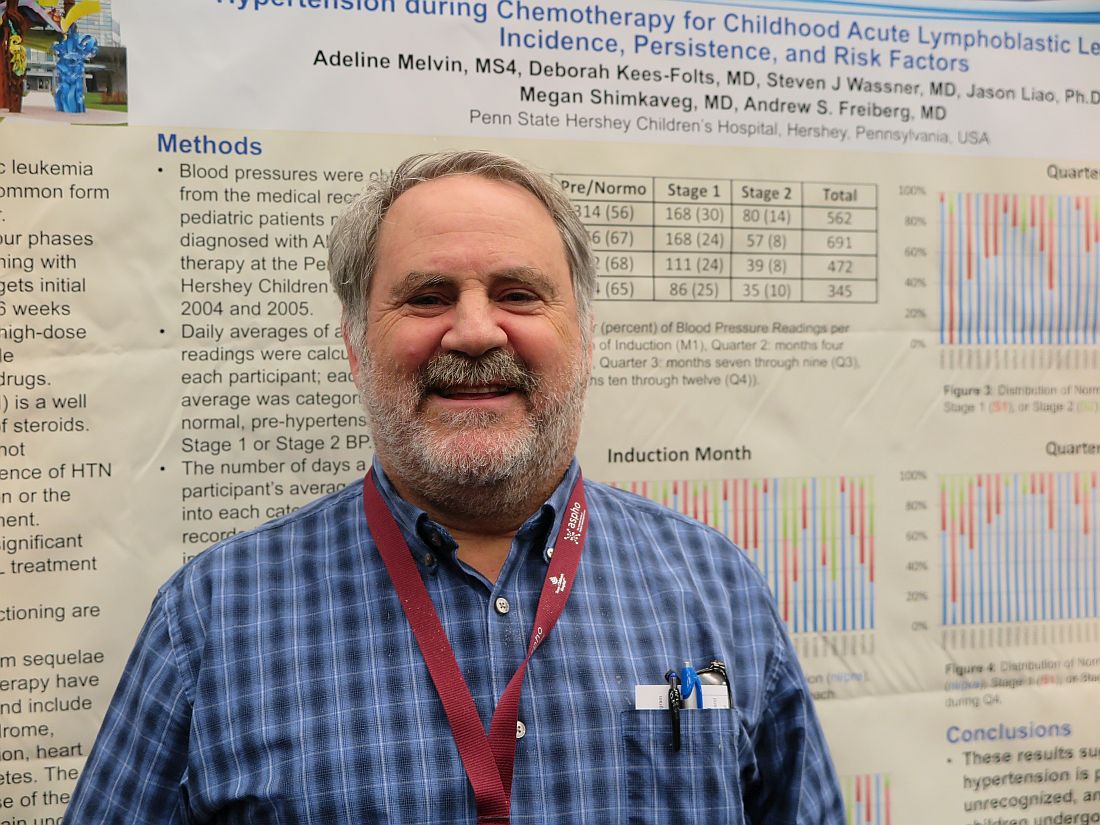
Medicaid acceptance up among cardiologists
Medicaid acceptance was 77% among cardiologists in the 2017 edition of an ongoing survey conducted in 15 large cities by physician recruitment firm Merritt Hawkins.
That was up from 61% in the previous survey, conducted in 2014, and higher than the average of 72% for cardiologists in 15 midsized cities that were included for the first time in 2017, the company reported.
There were four large cities with Medicaid acceptance rates of 100% – Boston, Detroit, Minneapolis (up from just 7% in 2014), and Portland, Ore. – along with four midsized cities – Cedar Rapids, Iowa; Evansville, Ind.; Fargo, N.D.; and Yakima, Wash. The lowest rate among the large cities was in Dallas (15%), with the midsized basement occupied by Lafayette, La., at 13%, Merritt Hawkins said.
Investigators called 259 randomly selected cardiologists in the large cities and 87 cardiologists in the midsized cities in January and February. It was the fourth such survey the company has conducted since 2004.
The survey also included four other specialties – dermatology, family medicine, ob.gyn., and orthopedic surgery. The Medicaid acceptance rate for all 1,414 physicians in all five specialties in the 15 large cities was 53%, and the average rate for all specialties in the midsized cities was 60% for the 494 offices surveyed, the company said. Cardiology had the highest rates by specialty and dermatology the lowest in both the large and midsized cities.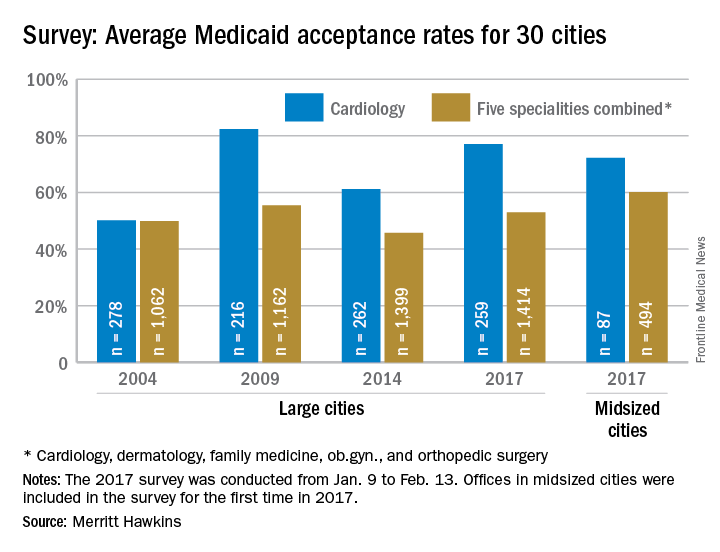
Medicaid acceptance was 77% among cardiologists in the 2017 edition of an ongoing survey conducted in 15 large cities by physician recruitment firm Merritt Hawkins.
That was up from 61% in the previous survey, conducted in 2014, and higher than the average of 72% for cardiologists in 15 midsized cities that were included for the first time in 2017, the company reported.
There were four large cities with Medicaid acceptance rates of 100% – Boston, Detroit, Minneapolis (up from just 7% in 2014), and Portland, Ore. – along with four midsized cities – Cedar Rapids, Iowa; Evansville, Ind.; Fargo, N.D.; and Yakima, Wash. The lowest rate among the large cities was in Dallas (15%), with the midsized basement occupied by Lafayette, La., at 13%, Merritt Hawkins said.
Investigators called 259 randomly selected cardiologists in the large cities and 87 cardiologists in the midsized cities in January and February. It was the fourth such survey the company has conducted since 2004.
The survey also included four other specialties – dermatology, family medicine, ob.gyn., and orthopedic surgery. The Medicaid acceptance rate for all 1,414 physicians in all five specialties in the 15 large cities was 53%, and the average rate for all specialties in the midsized cities was 60% for the 494 offices surveyed, the company said. Cardiology had the highest rates by specialty and dermatology the lowest in both the large and midsized cities.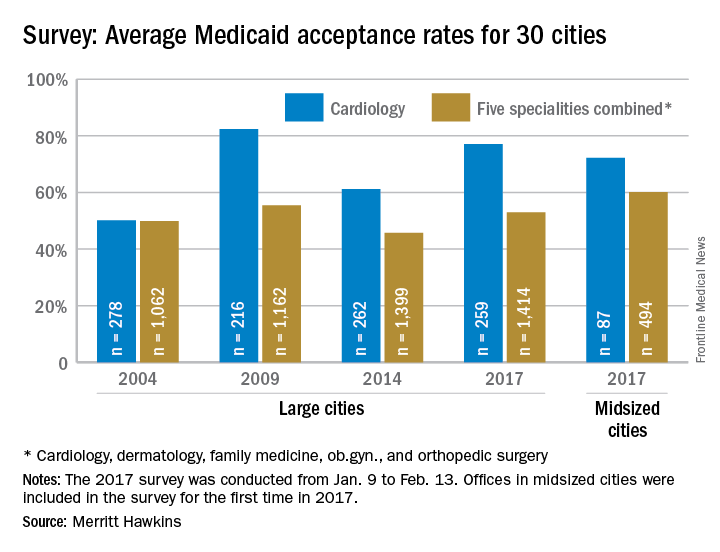
Medicaid acceptance was 77% among cardiologists in the 2017 edition of an ongoing survey conducted in 15 large cities by physician recruitment firm Merritt Hawkins.
That was up from 61% in the previous survey, conducted in 2014, and higher than the average of 72% for cardiologists in 15 midsized cities that were included for the first time in 2017, the company reported.
There were four large cities with Medicaid acceptance rates of 100% – Boston, Detroit, Minneapolis (up from just 7% in 2014), and Portland, Ore. – along with four midsized cities – Cedar Rapids, Iowa; Evansville, Ind.; Fargo, N.D.; and Yakima, Wash. The lowest rate among the large cities was in Dallas (15%), with the midsized basement occupied by Lafayette, La., at 13%, Merritt Hawkins said.
Investigators called 259 randomly selected cardiologists in the large cities and 87 cardiologists in the midsized cities in January and February. It was the fourth such survey the company has conducted since 2004.
The survey also included four other specialties – dermatology, family medicine, ob.gyn., and orthopedic surgery. The Medicaid acceptance rate for all 1,414 physicians in all five specialties in the 15 large cities was 53%, and the average rate for all specialties in the midsized cities was 60% for the 494 offices surveyed, the company said. Cardiology had the highest rates by specialty and dermatology the lowest in both the large and midsized cities.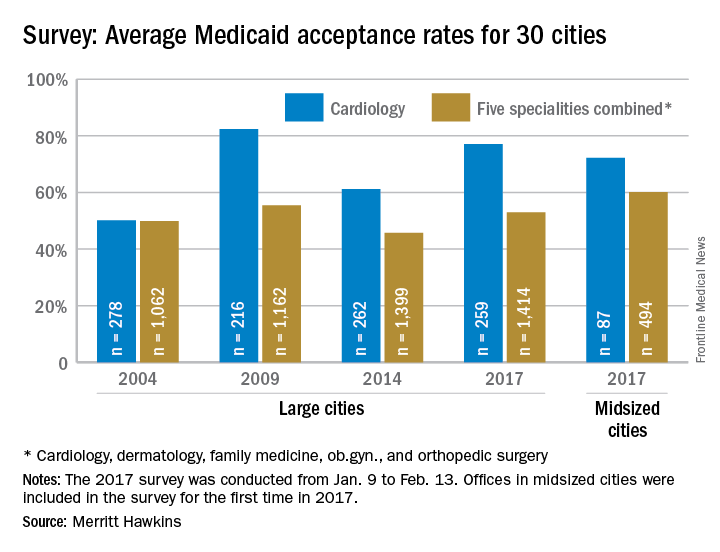
VIDEO: Surgery use declines for non–small cell lung cancer
BOSTON – The use of surgical therapy for early stage lung cancer in the United States has declined as other nonsurgical treatment options have become available, according to a study reported at the annual meeting of the American Association for Thoracic Surgery.
Most notably, the study finds that surgery for early stage non–small cell lung cancer decreased by 12% from 2004 to 2013.
In a video interview, Keith Naunheim, MD, a professor of surgery at Saint Louis University, discusses the study findings and the potential reasons behind declining surgery use for lung cancer. Dr. Naunheim also addresses why physicians should keep an open mind about alternative therapy options for lung cancer, while ensuring that the treatments are safe and effective for patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @legal_med
BOSTON – The use of surgical therapy for early stage lung cancer in the United States has declined as other nonsurgical treatment options have become available, according to a study reported at the annual meeting of the American Association for Thoracic Surgery.
Most notably, the study finds that surgery for early stage non–small cell lung cancer decreased by 12% from 2004 to 2013.
In a video interview, Keith Naunheim, MD, a professor of surgery at Saint Louis University, discusses the study findings and the potential reasons behind declining surgery use for lung cancer. Dr. Naunheim also addresses why physicians should keep an open mind about alternative therapy options for lung cancer, while ensuring that the treatments are safe and effective for patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @legal_med
BOSTON – The use of surgical therapy for early stage lung cancer in the United States has declined as other nonsurgical treatment options have become available, according to a study reported at the annual meeting of the American Association for Thoracic Surgery.
Most notably, the study finds that surgery for early stage non–small cell lung cancer decreased by 12% from 2004 to 2013.
In a video interview, Keith Naunheim, MD, a professor of surgery at Saint Louis University, discusses the study findings and the potential reasons behind declining surgery use for lung cancer. Dr. Naunheim also addresses why physicians should keep an open mind about alternative therapy options for lung cancer, while ensuring that the treatments are safe and effective for patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @legal_med
AT THE AATS ANNUAL MEETING
Preeclampsia/eclampsia rate highest in black women
The rate of preeclampsia and eclampsia for black women is 61% higher than it is for white women and 50% higher than for women overall, according to the Agency for Healthcare Research and Quality.
In 2014, black women experienced preeclampsia/eclampsia in 69.8 of every 1,000 deliveries, compared with 43.3 per 1,000 deliveries in white women and 46.6 per 1,000 for all women. Hispanic women were just above the overall rate at 46.8 per 1,000 deliveries, and Asian/Pacific Islander women were 38% lower than the overall rate at 28.8 per 1,000 deliveries, AHRQ said in its report. The overall rate was up 21% over the 38.4 per 1,000 reported in 2005.
Looking at degree of severity, 1.7% of all preeclampsia/eclampsia births in black women were eclampsia, compared with 1.4% for white and Hispanic women and 0.9% for Asian/Pacific Islanders. Severe preeclampsia was most common in Asian/Pacific Islanders – 40.4% of those diagnosed – with Hispanics at 40.3%, blacks at 38.5%, and whites at 34.3%. Mild or unspecified preeclampsia was diagnosed in 52% of preeclamptic/eclamptic white women, 46% of Hispanic women, 45% of Asians/Pacific Islanders, and 37% of black women, the AHRQ said in its analysis of data from the National Inpatient Sample.
Altogether, there were almost 177,000 delivery hospitalizations with preeclampsia/eclampsia in 2014, representing 4.7% of all deliveries and making it the most common hypertension-related diagnosis, followed by gestational hypertension (3.8%) and preexisting hypertension (1.7%). Compared with hospital stays for all other deliveries, those complicated by preeclampsia/eclampsia were 70% longer (mean, 4.4 vs. 2.6 days) and 70% more expensive (mean, $7,500 vs. $4,400), according to the report. 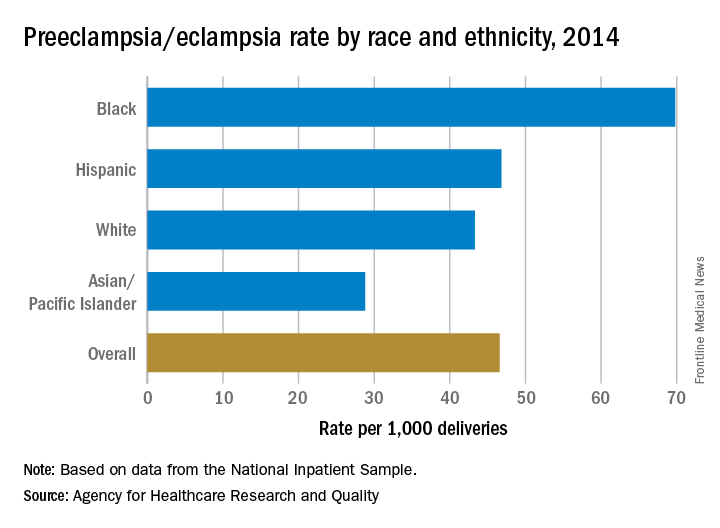
The rate of preeclampsia and eclampsia for black women is 61% higher than it is for white women and 50% higher than for women overall, according to the Agency for Healthcare Research and Quality.
In 2014, black women experienced preeclampsia/eclampsia in 69.8 of every 1,000 deliveries, compared with 43.3 per 1,000 deliveries in white women and 46.6 per 1,000 for all women. Hispanic women were just above the overall rate at 46.8 per 1,000 deliveries, and Asian/Pacific Islander women were 38% lower than the overall rate at 28.8 per 1,000 deliveries, AHRQ said in its report. The overall rate was up 21% over the 38.4 per 1,000 reported in 2005.
Looking at degree of severity, 1.7% of all preeclampsia/eclampsia births in black women were eclampsia, compared with 1.4% for white and Hispanic women and 0.9% for Asian/Pacific Islanders. Severe preeclampsia was most common in Asian/Pacific Islanders – 40.4% of those diagnosed – with Hispanics at 40.3%, blacks at 38.5%, and whites at 34.3%. Mild or unspecified preeclampsia was diagnosed in 52% of preeclamptic/eclamptic white women, 46% of Hispanic women, 45% of Asians/Pacific Islanders, and 37% of black women, the AHRQ said in its analysis of data from the National Inpatient Sample.
Altogether, there were almost 177,000 delivery hospitalizations with preeclampsia/eclampsia in 2014, representing 4.7% of all deliveries and making it the most common hypertension-related diagnosis, followed by gestational hypertension (3.8%) and preexisting hypertension (1.7%). Compared with hospital stays for all other deliveries, those complicated by preeclampsia/eclampsia were 70% longer (mean, 4.4 vs. 2.6 days) and 70% more expensive (mean, $7,500 vs. $4,400), according to the report. 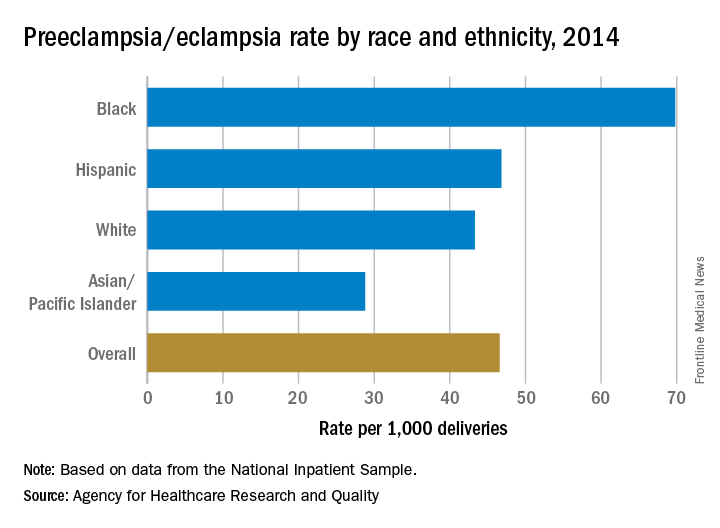
The rate of preeclampsia and eclampsia for black women is 61% higher than it is for white women and 50% higher than for women overall, according to the Agency for Healthcare Research and Quality.
In 2014, black women experienced preeclampsia/eclampsia in 69.8 of every 1,000 deliveries, compared with 43.3 per 1,000 deliveries in white women and 46.6 per 1,000 for all women. Hispanic women were just above the overall rate at 46.8 per 1,000 deliveries, and Asian/Pacific Islander women were 38% lower than the overall rate at 28.8 per 1,000 deliveries, AHRQ said in its report. The overall rate was up 21% over the 38.4 per 1,000 reported in 2005.
Looking at degree of severity, 1.7% of all preeclampsia/eclampsia births in black women were eclampsia, compared with 1.4% for white and Hispanic women and 0.9% for Asian/Pacific Islanders. Severe preeclampsia was most common in Asian/Pacific Islanders – 40.4% of those diagnosed – with Hispanics at 40.3%, blacks at 38.5%, and whites at 34.3%. Mild or unspecified preeclampsia was diagnosed in 52% of preeclamptic/eclamptic white women, 46% of Hispanic women, 45% of Asians/Pacific Islanders, and 37% of black women, the AHRQ said in its analysis of data from the National Inpatient Sample.
Altogether, there were almost 177,000 delivery hospitalizations with preeclampsia/eclampsia in 2014, representing 4.7% of all deliveries and making it the most common hypertension-related diagnosis, followed by gestational hypertension (3.8%) and preexisting hypertension (1.7%). Compared with hospital stays for all other deliveries, those complicated by preeclampsia/eclampsia were 70% longer (mean, 4.4 vs. 2.6 days) and 70% more expensive (mean, $7,500 vs. $4,400), according to the report. 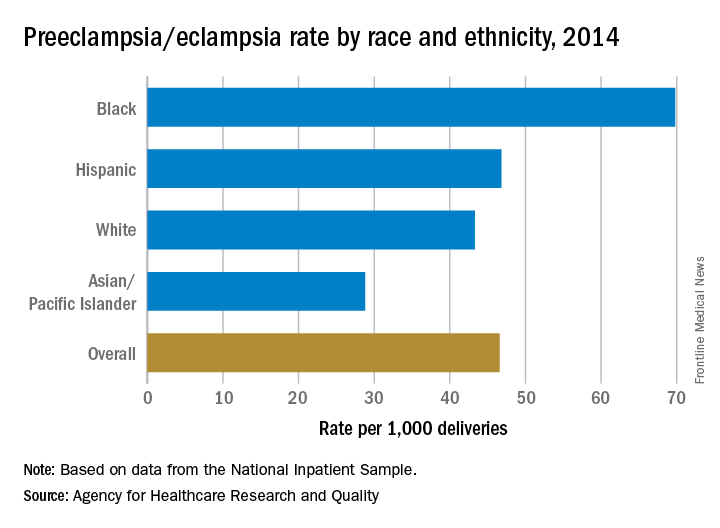
VIDEO: Setbacks of serelaxin, ularitide prompt rethinking acute heart failure strategies
PARIS – Serelaxin’s failure to meet its primary endpoints in an acute heart failure trial with more than 6,500 patients, coupled with a similar failure by ularitide in the same patient population in pivotal trial results first reported in November 2016, led some experts to rethink their conception of potential interventions for patients hospitalized for acute heart failure decompensations.
“We learned in TRUE-AHF that giving a drug very early [in acute heart failure] does not prevent [long-term] death. It means that early is not early enough,” Alexandre Mebazaa, MD, said in a video interview at a meeting held by the Heart Failure Association of the European Society of Cardiology.
In terms of finding new management strategies for patients who develop acute decompensations, “we need to better understand acute heart failure and the best subset of patients who might benefit” from existing or new drugs, he said.
The RELAX-AHF-2 trial enrolled and analyzed 6,545 patients hospitalized with an acute heart failure decompensation at more than 500 sites in 34 countries. The study compared the impact of a 48-hour IV infusion of serelaxin with placebo when begun within 16 hours of hospitalization for acute heart failure and added to standard treatment.
These findings closely matched the performance of ularitide in a similar study design, TRUE-AHF (New Engl J Med. 2017 Apr 12. doi: 10.1056/NEJMoa1601895).
At the 2016 meeting of the Heart Failure Association of the ESC, the organization released revised guidelines for diagnosing and managing heart failure that stressed the importance of rapid response to acute heart failure, including possible treatment with vasodilator drugs. The guidelines acknowledged that while “Vasodilators are the second most often used agents in acute heart failure for symptomatic relief; however, there is no robust evidence confirming their beneficial effects” (Eur Heart J. 2016 Jul 14;37[27]:2129-200).
Both ularitide and serelaxin are potent IV vasodilators, and their failure to meet their efficacy endpoints in these two trials put vasodilation and rapid decongestion into question as strategies to improve midterm prognosis in heart failure patients following acute decompensation episodes.
Serelaxin has been developed by Novartis, and ularitide has been developed by Cardiorentis. Dr. Mebazaa has received honoraria from Novartis and Cardiorentis, as well as from several other companies. Dr. Metra has been a consultant to Novartis. She has also served as consultant or spokesperson for Abbott Vascular, Amgen, AstraZeneca, Fresenius, Relypsa, and Servier.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @mitchelzoler
PARIS – Serelaxin’s failure to meet its primary endpoints in an acute heart failure trial with more than 6,500 patients, coupled with a similar failure by ularitide in the same patient population in pivotal trial results first reported in November 2016, led some experts to rethink their conception of potential interventions for patients hospitalized for acute heart failure decompensations.
“We learned in TRUE-AHF that giving a drug very early [in acute heart failure] does not prevent [long-term] death. It means that early is not early enough,” Alexandre Mebazaa, MD, said in a video interview at a meeting held by the Heart Failure Association of the European Society of Cardiology.
In terms of finding new management strategies for patients who develop acute decompensations, “we need to better understand acute heart failure and the best subset of patients who might benefit” from existing or new drugs, he said.
The RELAX-AHF-2 trial enrolled and analyzed 6,545 patients hospitalized with an acute heart failure decompensation at more than 500 sites in 34 countries. The study compared the impact of a 48-hour IV infusion of serelaxin with placebo when begun within 16 hours of hospitalization for acute heart failure and added to standard treatment.
These findings closely matched the performance of ularitide in a similar study design, TRUE-AHF (New Engl J Med. 2017 Apr 12. doi: 10.1056/NEJMoa1601895).
At the 2016 meeting of the Heart Failure Association of the ESC, the organization released revised guidelines for diagnosing and managing heart failure that stressed the importance of rapid response to acute heart failure, including possible treatment with vasodilator drugs. The guidelines acknowledged that while “Vasodilators are the second most often used agents in acute heart failure for symptomatic relief; however, there is no robust evidence confirming their beneficial effects” (Eur Heart J. 2016 Jul 14;37[27]:2129-200).
Both ularitide and serelaxin are potent IV vasodilators, and their failure to meet their efficacy endpoints in these two trials put vasodilation and rapid decongestion into question as strategies to improve midterm prognosis in heart failure patients following acute decompensation episodes.
Serelaxin has been developed by Novartis, and ularitide has been developed by Cardiorentis. Dr. Mebazaa has received honoraria from Novartis and Cardiorentis, as well as from several other companies. Dr. Metra has been a consultant to Novartis. She has also served as consultant or spokesperson for Abbott Vascular, Amgen, AstraZeneca, Fresenius, Relypsa, and Servier.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @mitchelzoler
PARIS – Serelaxin’s failure to meet its primary endpoints in an acute heart failure trial with more than 6,500 patients, coupled with a similar failure by ularitide in the same patient population in pivotal trial results first reported in November 2016, led some experts to rethink their conception of potential interventions for patients hospitalized for acute heart failure decompensations.
“We learned in TRUE-AHF that giving a drug very early [in acute heart failure] does not prevent [long-term] death. It means that early is not early enough,” Alexandre Mebazaa, MD, said in a video interview at a meeting held by the Heart Failure Association of the European Society of Cardiology.
In terms of finding new management strategies for patients who develop acute decompensations, “we need to better understand acute heart failure and the best subset of patients who might benefit” from existing or new drugs, he said.
The RELAX-AHF-2 trial enrolled and analyzed 6,545 patients hospitalized with an acute heart failure decompensation at more than 500 sites in 34 countries. The study compared the impact of a 48-hour IV infusion of serelaxin with placebo when begun within 16 hours of hospitalization for acute heart failure and added to standard treatment.
These findings closely matched the performance of ularitide in a similar study design, TRUE-AHF (New Engl J Med. 2017 Apr 12. doi: 10.1056/NEJMoa1601895).
At the 2016 meeting of the Heart Failure Association of the ESC, the organization released revised guidelines for diagnosing and managing heart failure that stressed the importance of rapid response to acute heart failure, including possible treatment with vasodilator drugs. The guidelines acknowledged that while “Vasodilators are the second most often used agents in acute heart failure for symptomatic relief; however, there is no robust evidence confirming their beneficial effects” (Eur Heart J. 2016 Jul 14;37[27]:2129-200).
Both ularitide and serelaxin are potent IV vasodilators, and their failure to meet their efficacy endpoints in these two trials put vasodilation and rapid decongestion into question as strategies to improve midterm prognosis in heart failure patients following acute decompensation episodes.
Serelaxin has been developed by Novartis, and ularitide has been developed by Cardiorentis. Dr. Mebazaa has received honoraria from Novartis and Cardiorentis, as well as from several other companies. Dr. Metra has been a consultant to Novartis. She has also served as consultant or spokesperson for Abbott Vascular, Amgen, AstraZeneca, Fresenius, Relypsa, and Servier.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM HEART FAILURE 2017
Acne, rosacea prescriptions cost more when prescribed by dermatologists
PORTLAND, ORE. – Dermatologists have plenty of room to improve when it comes to choosing cost-effective medications for acne or rosacea, based on the results of a large retrospective analysis of Medicare claims data.
Patients with acne or rosacea consistently paid more for topical retinoids, topical antibiotics, and oral tetracyclines when the prescriber was a dermatologist instead of a family or internal medicine physician, Myron Zhang reported at the annual meeting of the Society for Investigative Dermatology.
“There is a large potential for reducing expenditures on health care for patients with acne and rosacea by choosing more generics and less expensive options within drug classes,” said Mr. Zhang, a medical student at the Ohio State University, Columbus, who conducted the study with colleagues there and at Northwestern University in Chicago.
Treating acne and rosacea falls under the purview of both primary and specialty outpatient care, but, researchers had not broken down costs of prescriptions for these conditions by provider type. To help fill that gap, Mr. Zhang and his colleagues retrospectively analyzed all Medicare drug claims for topical retinoids, topical antibiotics, isotretinoin, and oral tetracycline-class antibiotics used to treat acne and rosacea in the United States in 2008 and 2010.
Medicare claims for these prescriptions added up to $65 million in 2008 and $74 million in 2004, Mr. Zhang said. Although most generics either dropped in cost or rose by small amounts in that 2-year span, many brand name prescriptions rose by between 30% and 70%. “Specialist prescriptions were associated with higher brand name usage, a greater variety of medications, and higher costs,” Mr. Zhang said.
Patients paid an average of about $2-$3 more for a topical retinoid, $3-$4 more for oral tetracycline, and $1 more for a topical antibiotic prescribed by a specialist instead of a primary care physician.
This finding might indicate that dermatologists are more comfortable prescribing a greater variety of medications for acne and rosacea, such as tazarotene, azelaic acid, and sulfacetamide, while primary care physicians might stick to a narrower range of medicines, Mr. Zhang said. However, the prescribing behavior of dermatologists could also reflect “external factors,” such as increased contact with representatives from pharmaceutical companies, he added.
“As always, prescription costs need to be weighed against patient preference, compliance, and quality of care,” he said. “More outcomes research is needed to understand the comparative efficacy of generic and brand name treatments.”
The study included both rosacea and acne so that the researchers could capture the total costs of medications such as tretinoin, which is used to treat both conditions. Approximately 80% of topical retinoid prescriptions were for tretinoin, about 50% of topical antibiotic prescriptions were for metronidazole, while about 27% were for clindamycin. About half of oral antibiotic prescriptions were for tetracycline, while about 40% were for minocycline.
Mr. Zhang reported having no conflicts of interest.
PORTLAND, ORE. – Dermatologists have plenty of room to improve when it comes to choosing cost-effective medications for acne or rosacea, based on the results of a large retrospective analysis of Medicare claims data.
Patients with acne or rosacea consistently paid more for topical retinoids, topical antibiotics, and oral tetracyclines when the prescriber was a dermatologist instead of a family or internal medicine physician, Myron Zhang reported at the annual meeting of the Society for Investigative Dermatology.
“There is a large potential for reducing expenditures on health care for patients with acne and rosacea by choosing more generics and less expensive options within drug classes,” said Mr. Zhang, a medical student at the Ohio State University, Columbus, who conducted the study with colleagues there and at Northwestern University in Chicago.
Treating acne and rosacea falls under the purview of both primary and specialty outpatient care, but, researchers had not broken down costs of prescriptions for these conditions by provider type. To help fill that gap, Mr. Zhang and his colleagues retrospectively analyzed all Medicare drug claims for topical retinoids, topical antibiotics, isotretinoin, and oral tetracycline-class antibiotics used to treat acne and rosacea in the United States in 2008 and 2010.
Medicare claims for these prescriptions added up to $65 million in 2008 and $74 million in 2004, Mr. Zhang said. Although most generics either dropped in cost or rose by small amounts in that 2-year span, many brand name prescriptions rose by between 30% and 70%. “Specialist prescriptions were associated with higher brand name usage, a greater variety of medications, and higher costs,” Mr. Zhang said.
Patients paid an average of about $2-$3 more for a topical retinoid, $3-$4 more for oral tetracycline, and $1 more for a topical antibiotic prescribed by a specialist instead of a primary care physician.
This finding might indicate that dermatologists are more comfortable prescribing a greater variety of medications for acne and rosacea, such as tazarotene, azelaic acid, and sulfacetamide, while primary care physicians might stick to a narrower range of medicines, Mr. Zhang said. However, the prescribing behavior of dermatologists could also reflect “external factors,” such as increased contact with representatives from pharmaceutical companies, he added.
“As always, prescription costs need to be weighed against patient preference, compliance, and quality of care,” he said. “More outcomes research is needed to understand the comparative efficacy of generic and brand name treatments.”
The study included both rosacea and acne so that the researchers could capture the total costs of medications such as tretinoin, which is used to treat both conditions. Approximately 80% of topical retinoid prescriptions were for tretinoin, about 50% of topical antibiotic prescriptions were for metronidazole, while about 27% were for clindamycin. About half of oral antibiotic prescriptions were for tetracycline, while about 40% were for minocycline.
Mr. Zhang reported having no conflicts of interest.
PORTLAND, ORE. – Dermatologists have plenty of room to improve when it comes to choosing cost-effective medications for acne or rosacea, based on the results of a large retrospective analysis of Medicare claims data.
Patients with acne or rosacea consistently paid more for topical retinoids, topical antibiotics, and oral tetracyclines when the prescriber was a dermatologist instead of a family or internal medicine physician, Myron Zhang reported at the annual meeting of the Society for Investigative Dermatology.
“There is a large potential for reducing expenditures on health care for patients with acne and rosacea by choosing more generics and less expensive options within drug classes,” said Mr. Zhang, a medical student at the Ohio State University, Columbus, who conducted the study with colleagues there and at Northwestern University in Chicago.
Treating acne and rosacea falls under the purview of both primary and specialty outpatient care, but, researchers had not broken down costs of prescriptions for these conditions by provider type. To help fill that gap, Mr. Zhang and his colleagues retrospectively analyzed all Medicare drug claims for topical retinoids, topical antibiotics, isotretinoin, and oral tetracycline-class antibiotics used to treat acne and rosacea in the United States in 2008 and 2010.
Medicare claims for these prescriptions added up to $65 million in 2008 and $74 million in 2004, Mr. Zhang said. Although most generics either dropped in cost or rose by small amounts in that 2-year span, many brand name prescriptions rose by between 30% and 70%. “Specialist prescriptions were associated with higher brand name usage, a greater variety of medications, and higher costs,” Mr. Zhang said.
Patients paid an average of about $2-$3 more for a topical retinoid, $3-$4 more for oral tetracycline, and $1 more for a topical antibiotic prescribed by a specialist instead of a primary care physician.
This finding might indicate that dermatologists are more comfortable prescribing a greater variety of medications for acne and rosacea, such as tazarotene, azelaic acid, and sulfacetamide, while primary care physicians might stick to a narrower range of medicines, Mr. Zhang said. However, the prescribing behavior of dermatologists could also reflect “external factors,” such as increased contact with representatives from pharmaceutical companies, he added.
“As always, prescription costs need to be weighed against patient preference, compliance, and quality of care,” he said. “More outcomes research is needed to understand the comparative efficacy of generic and brand name treatments.”
The study included both rosacea and acne so that the researchers could capture the total costs of medications such as tretinoin, which is used to treat both conditions. Approximately 80% of topical retinoid prescriptions were for tretinoin, about 50% of topical antibiotic prescriptions were for metronidazole, while about 27% were for clindamycin. About half of oral antibiotic prescriptions were for tetracycline, while about 40% were for minocycline.
Mr. Zhang reported having no conflicts of interest.
At SID 2017
Key clinical point:
Major finding: Patients paid an average of $2-$3 more for a topical retinoid, $3-$4 more for an oral tetracycline-class antibiotic, and $1 more for a topical antibiotic prescribed by a dermatologist, compared with prescriptions from a primary care physician.
Data source: A retrospective analysis of Medicare prescription claims for oral antibiotics, topical antibiotics, and topical retinoids for acne and rosacea in 2008 and 2010.
Disclosures: Mr. Zhang reported having no conflicts of interest.
Treatment-related hypertension, kidney injury are undertreated in kids with leukemia
MONTREAL – Hypertension is a frequent, but underrecognized and undertreated, complication of chemotherapy for acute lymphoblastic leukemia (ALL), the most common childhood malignancy, investigators in a single-center U.S. study reported.
Additionally, there is a “concerningly high” incidence of acute kidney injury among children and young adults who undergo multiagent chemotherapy for acute myeloid leukemia (AML), said the authors of a study conducted in Canada.
Both studies were reported in a scientific poster session at the annual meeting of the American Society for Pediatric Hematology/Oncology.
Hypertension in ALL
Although standard induction regimens for childhood ALL contain high-dose steroids, which are known to be associated with increased risk for hypertension, the incidence of hypertension throughout induction, consolidation, and maintenance for ALL in children has not been adequately evaluated, according to Andrew S. Freiberg, MD, and his colleagues at Penn State Children’s Hospital in Hershey, Penn.
“The incidence of hypertension was much higher than the under 5% expected for a healthy pediatric population,” the investigators found.
Of 562 total readings taken during induction, 56% were in the normo- or prehypertensive range, but 30% were classified as stage 1 and 14% as stage II hypertension.
The combined percentage of stage 1 and 2 readings declined slightly over the year from 44% during induction to 35% during Q4 “but remained well above expected for the pediatric population,” the investigators reported.
Despite the high incidence, “I was surprised at how few of the patients with hypertension we actually treated,” Dr. Freiberg said in an interview.
Just 3 of the 36 patients studied received treatment for hypertension, he said, possibly because clinicians assumed that the effect was steroid related and transient.
“Now that we’re paying attention, however, we’re treating more of these patients,” Dr. Freiberg said.
The electronic record system used at his institution now alerts clinicians to hypertensive episodes during treatment, he added.
Kidney injury in AML
Like Dr. Freiberg and his colleagues, Liezl du Plessis, MBChB, from the British Columbia Children’s Hospital in Vancouver, Canada, and her colleagues were similarly taken aback when they looked into the incidence of acute kidney injury (AKI) in children and adolescents undergoing multidrug chemotherapy for AML.
“Chemotherapy agents that are used in acute myeloid leukemia are not considered to be nephrotoxic, so it was quite alarming to us to see that there is such a high rate of kidney injury in these patients,” Dr. du Plessis said in an interview.
They found that 34 of the 53 patients (64%) had AKI, with 11 patients having stage 1 (rise in serum creatinine of 1.5 or more times the baseline level), 11 having stage 2 (SCr 2 or more times baseline), and 12 having stage 3 AKI (SCr 3 or more times baseline or the need for dialysis).
Creatinine changes were counted only if they occurred within 7 days from nadir to peak.
AKI occurred in all chemotherapy cycles, with severe injury having the highest frequency in cycle 1.
In a logistical regression model, factors significantly associated with risk for AKI were male sex (odds ratio, 0.2; P = .03) and age 10 years or older (OR, 17.3; P less than .01). Neither sepsis nor aminoglycoside or vancomycin use for more than 3 days was significantly associated with risk for AKI, however.
“I think people need to realize that many of these injuries are happening on the oncology ward, and some of these kids may not even look acutely unwell, so people need to take note.” Dr. du Plessis said.
She recommended curtailing use of nephrotoxic agents whenever possible, and emphasized that clinicians need to document AKI in the medical record.
“A big portion of our AML population goes on to bone marrow transplant, and that is known to be a high risk for further kidney injury. So, I think it would be important to know that before your patient goes for his transplant that he already has certain toxicities and organ injury, so that you can limit things like fluids and get the nephrology team on board to help with the management of these patients,” she said.
The study by Dr. Freiberg was supported by the Four Diamonds Fund. The study by Dr. du Plessis was internally funded. The investigators for each study reported having no relevant financial disclosures.
MONTREAL – Hypertension is a frequent, but underrecognized and undertreated, complication of chemotherapy for acute lymphoblastic leukemia (ALL), the most common childhood malignancy, investigators in a single-center U.S. study reported.
Additionally, there is a “concerningly high” incidence of acute kidney injury among children and young adults who undergo multiagent chemotherapy for acute myeloid leukemia (AML), said the authors of a study conducted in Canada.
Both studies were reported in a scientific poster session at the annual meeting of the American Society for Pediatric Hematology/Oncology.
Hypertension in ALL
Although standard induction regimens for childhood ALL contain high-dose steroids, which are known to be associated with increased risk for hypertension, the incidence of hypertension throughout induction, consolidation, and maintenance for ALL in children has not been adequately evaluated, according to Andrew S. Freiberg, MD, and his colleagues at Penn State Children’s Hospital in Hershey, Penn.
“The incidence of hypertension was much higher than the under 5% expected for a healthy pediatric population,” the investigators found.
Of 562 total readings taken during induction, 56% were in the normo- or prehypertensive range, but 30% were classified as stage 1 and 14% as stage II hypertension.
The combined percentage of stage 1 and 2 readings declined slightly over the year from 44% during induction to 35% during Q4 “but remained well above expected for the pediatric population,” the investigators reported.
Despite the high incidence, “I was surprised at how few of the patients with hypertension we actually treated,” Dr. Freiberg said in an interview.
Just 3 of the 36 patients studied received treatment for hypertension, he said, possibly because clinicians assumed that the effect was steroid related and transient.
“Now that we’re paying attention, however, we’re treating more of these patients,” Dr. Freiberg said.
The electronic record system used at his institution now alerts clinicians to hypertensive episodes during treatment, he added.
Kidney injury in AML
Like Dr. Freiberg and his colleagues, Liezl du Plessis, MBChB, from the British Columbia Children’s Hospital in Vancouver, Canada, and her colleagues were similarly taken aback when they looked into the incidence of acute kidney injury (AKI) in children and adolescents undergoing multidrug chemotherapy for AML.
“Chemotherapy agents that are used in acute myeloid leukemia are not considered to be nephrotoxic, so it was quite alarming to us to see that there is such a high rate of kidney injury in these patients,” Dr. du Plessis said in an interview.
They found that 34 of the 53 patients (64%) had AKI, with 11 patients having stage 1 (rise in serum creatinine of 1.5 or more times the baseline level), 11 having stage 2 (SCr 2 or more times baseline), and 12 having stage 3 AKI (SCr 3 or more times baseline or the need for dialysis).
Creatinine changes were counted only if they occurred within 7 days from nadir to peak.
AKI occurred in all chemotherapy cycles, with severe injury having the highest frequency in cycle 1.
In a logistical regression model, factors significantly associated with risk for AKI were male sex (odds ratio, 0.2; P = .03) and age 10 years or older (OR, 17.3; P less than .01). Neither sepsis nor aminoglycoside or vancomycin use for more than 3 days was significantly associated with risk for AKI, however.
“I think people need to realize that many of these injuries are happening on the oncology ward, and some of these kids may not even look acutely unwell, so people need to take note.” Dr. du Plessis said.
She recommended curtailing use of nephrotoxic agents whenever possible, and emphasized that clinicians need to document AKI in the medical record.
“A big portion of our AML population goes on to bone marrow transplant, and that is known to be a high risk for further kidney injury. So, I think it would be important to know that before your patient goes for his transplant that he already has certain toxicities and organ injury, so that you can limit things like fluids and get the nephrology team on board to help with the management of these patients,” she said.
The study by Dr. Freiberg was supported by the Four Diamonds Fund. The study by Dr. du Plessis was internally funded. The investigators for each study reported having no relevant financial disclosures.
MONTREAL – Hypertension is a frequent, but underrecognized and undertreated, complication of chemotherapy for acute lymphoblastic leukemia (ALL), the most common childhood malignancy, investigators in a single-center U.S. study reported.
Additionally, there is a “concerningly high” incidence of acute kidney injury among children and young adults who undergo multiagent chemotherapy for acute myeloid leukemia (AML), said the authors of a study conducted in Canada.
Both studies were reported in a scientific poster session at the annual meeting of the American Society for Pediatric Hematology/Oncology.
Hypertension in ALL
Although standard induction regimens for childhood ALL contain high-dose steroids, which are known to be associated with increased risk for hypertension, the incidence of hypertension throughout induction, consolidation, and maintenance for ALL in children has not been adequately evaluated, according to Andrew S. Freiberg, MD, and his colleagues at Penn State Children’s Hospital in Hershey, Penn.
“The incidence of hypertension was much higher than the under 5% expected for a healthy pediatric population,” the investigators found.
Of 562 total readings taken during induction, 56% were in the normo- or prehypertensive range, but 30% were classified as stage 1 and 14% as stage II hypertension.
The combined percentage of stage 1 and 2 readings declined slightly over the year from 44% during induction to 35% during Q4 “but remained well above expected for the pediatric population,” the investigators reported.
Despite the high incidence, “I was surprised at how few of the patients with hypertension we actually treated,” Dr. Freiberg said in an interview.
Just 3 of the 36 patients studied received treatment for hypertension, he said, possibly because clinicians assumed that the effect was steroid related and transient.
“Now that we’re paying attention, however, we’re treating more of these patients,” Dr. Freiberg said.
The electronic record system used at his institution now alerts clinicians to hypertensive episodes during treatment, he added.
Kidney injury in AML
Like Dr. Freiberg and his colleagues, Liezl du Plessis, MBChB, from the British Columbia Children’s Hospital in Vancouver, Canada, and her colleagues were similarly taken aback when they looked into the incidence of acute kidney injury (AKI) in children and adolescents undergoing multidrug chemotherapy for AML.
“Chemotherapy agents that are used in acute myeloid leukemia are not considered to be nephrotoxic, so it was quite alarming to us to see that there is such a high rate of kidney injury in these patients,” Dr. du Plessis said in an interview.
They found that 34 of the 53 patients (64%) had AKI, with 11 patients having stage 1 (rise in serum creatinine of 1.5 or more times the baseline level), 11 having stage 2 (SCr 2 or more times baseline), and 12 having stage 3 AKI (SCr 3 or more times baseline or the need for dialysis).
Creatinine changes were counted only if they occurred within 7 days from nadir to peak.
AKI occurred in all chemotherapy cycles, with severe injury having the highest frequency in cycle 1.
In a logistical regression model, factors significantly associated with risk for AKI were male sex (odds ratio, 0.2; P = .03) and age 10 years or older (OR, 17.3; P less than .01). Neither sepsis nor aminoglycoside or vancomycin use for more than 3 days was significantly associated with risk for AKI, however.
“I think people need to realize that many of these injuries are happening on the oncology ward, and some of these kids may not even look acutely unwell, so people need to take note.” Dr. du Plessis said.
She recommended curtailing use of nephrotoxic agents whenever possible, and emphasized that clinicians need to document AKI in the medical record.
“A big portion of our AML population goes on to bone marrow transplant, and that is known to be a high risk for further kidney injury. So, I think it would be important to know that before your patient goes for his transplant that he already has certain toxicities and organ injury, so that you can limit things like fluids and get the nephrology team on board to help with the management of these patients,” she said.
The study by Dr. Freiberg was supported by the Four Diamonds Fund. The study by Dr. du Plessis was internally funded. The investigators for each study reported having no relevant financial disclosures.
At ASPHO 2017
Key clinical point:
Major finding: The combined incidence of stage 1 or 2 hypertension in children during induction therapy for acute lymphoblastic leukemia was 44%.
Data source: Two retrospective institutional studies.
Disclosures: The study by Dr. Freiberg was supported by the Four Diamonds Fund. The study by Dr. du Plessis was internally funded. The investigators for each study reported having no relevant financial disclosures.
Don’t rely on MRI findings after DCIS needle biopsy
LAS VEGAS – MRI results after percutaneous biopsy for ductal carcinoma in situ (DCIS) are often unreliable, overestimating the extent of disease and leading to over treatment, investigators from the Mayo Clinic in Phoenix concluded after reviewing 54 cases.
Of the 54 women, 7 (13%) had mastectomies driven by postbiopsy MRI findings that were not indicated on final pathology, Barbara Pockaj, MD, senior investigator and surgical oncologist at the Mayo Clinic in Phoenix, reported at the annual meeting of the American Society of Breast Surgeons.
Dr. Pockaj and the Mayo radiologists had a hunch that there was a problem and were uncomfortable interpreting MRI findings after needle biopsy, but there was nothing in the literature about it. The goal of the study was to quantify the problem and “bring this issue to light,” she said.
“I feel better, now that we have this data in hand, as I counsel patients,” who are sometimes so alarmed by MRI findings after needle biopsy that they opt for mastectomies. Now, Dr. Pockaj can tell them with certainty that MRI “may overestimate the extent of disease, so we have to take MRI findings with a grain of salt,” she said.
“Surgeons should be aware that, in patients with a postbiopsy MRI, tumor size may be different than anticipated” and may adversely “affect surgical decision-making and potentially cosmetic results. Percutaneous biopsy significantly limits the ability to accurately interpret the extent of DCIS on preoperative breast MRI by overestimating extent of disease,” the investigators concluded.
Postbiopsy MRIs were performed in 38 of the 54 women (70%), and 14 women (26%) had bigger surgeries because of their MRI results.
Three women had larger lumpectomies, and 11 had mastectomies. “Three really needed it, and one maybe half way,” but the remaining seven turned out on pathology to have only needed lumpectomies, Dr. Pockaj said.
Mean lesion size on preoperative MRI was 3.6 cm while mean lesion size on pathologic specimen was 1.6 cm. Postbiopsy MRI did not significantly correlate with the actual size of the tumor specimen (r = 0.028; P = 0.921).
If the core needle biopsy shows DCIS, in many cases, “I think you can go right to surgery,” Dr. Pockaj said. MRI might still be indicted for very large lesions, suspicions of invasive disease, or very dense breasts, but, even so, the results need to be put into context with the postbiopsy changes, she said.
Women in the study were a mean of 59 years old. Most had high- or intermediate-grade DCIS. Women upgraded to invasive disease at surgery were excluded from the analysis.
There was no industry funding for the work, and the investigators reported having no relevant financial disclosures.
LAS VEGAS – MRI results after percutaneous biopsy for ductal carcinoma in situ (DCIS) are often unreliable, overestimating the extent of disease and leading to over treatment, investigators from the Mayo Clinic in Phoenix concluded after reviewing 54 cases.
Of the 54 women, 7 (13%) had mastectomies driven by postbiopsy MRI findings that were not indicated on final pathology, Barbara Pockaj, MD, senior investigator and surgical oncologist at the Mayo Clinic in Phoenix, reported at the annual meeting of the American Society of Breast Surgeons.
Dr. Pockaj and the Mayo radiologists had a hunch that there was a problem and were uncomfortable interpreting MRI findings after needle biopsy, but there was nothing in the literature about it. The goal of the study was to quantify the problem and “bring this issue to light,” she said.
“I feel better, now that we have this data in hand, as I counsel patients,” who are sometimes so alarmed by MRI findings after needle biopsy that they opt for mastectomies. Now, Dr. Pockaj can tell them with certainty that MRI “may overestimate the extent of disease, so we have to take MRI findings with a grain of salt,” she said.
“Surgeons should be aware that, in patients with a postbiopsy MRI, tumor size may be different than anticipated” and may adversely “affect surgical decision-making and potentially cosmetic results. Percutaneous biopsy significantly limits the ability to accurately interpret the extent of DCIS on preoperative breast MRI by overestimating extent of disease,” the investigators concluded.
Postbiopsy MRIs were performed in 38 of the 54 women (70%), and 14 women (26%) had bigger surgeries because of their MRI results.
Three women had larger lumpectomies, and 11 had mastectomies. “Three really needed it, and one maybe half way,” but the remaining seven turned out on pathology to have only needed lumpectomies, Dr. Pockaj said.
Mean lesion size on preoperative MRI was 3.6 cm while mean lesion size on pathologic specimen was 1.6 cm. Postbiopsy MRI did not significantly correlate with the actual size of the tumor specimen (r = 0.028; P = 0.921).
If the core needle biopsy shows DCIS, in many cases, “I think you can go right to surgery,” Dr. Pockaj said. MRI might still be indicted for very large lesions, suspicions of invasive disease, or very dense breasts, but, even so, the results need to be put into context with the postbiopsy changes, she said.
Women in the study were a mean of 59 years old. Most had high- or intermediate-grade DCIS. Women upgraded to invasive disease at surgery were excluded from the analysis.
There was no industry funding for the work, and the investigators reported having no relevant financial disclosures.
LAS VEGAS – MRI results after percutaneous biopsy for ductal carcinoma in situ (DCIS) are often unreliable, overestimating the extent of disease and leading to over treatment, investigators from the Mayo Clinic in Phoenix concluded after reviewing 54 cases.
Of the 54 women, 7 (13%) had mastectomies driven by postbiopsy MRI findings that were not indicated on final pathology, Barbara Pockaj, MD, senior investigator and surgical oncologist at the Mayo Clinic in Phoenix, reported at the annual meeting of the American Society of Breast Surgeons.
Dr. Pockaj and the Mayo radiologists had a hunch that there was a problem and were uncomfortable interpreting MRI findings after needle biopsy, but there was nothing in the literature about it. The goal of the study was to quantify the problem and “bring this issue to light,” she said.
“I feel better, now that we have this data in hand, as I counsel patients,” who are sometimes so alarmed by MRI findings after needle biopsy that they opt for mastectomies. Now, Dr. Pockaj can tell them with certainty that MRI “may overestimate the extent of disease, so we have to take MRI findings with a grain of salt,” she said.
“Surgeons should be aware that, in patients with a postbiopsy MRI, tumor size may be different than anticipated” and may adversely “affect surgical decision-making and potentially cosmetic results. Percutaneous biopsy significantly limits the ability to accurately interpret the extent of DCIS on preoperative breast MRI by overestimating extent of disease,” the investigators concluded.
Postbiopsy MRIs were performed in 38 of the 54 women (70%), and 14 women (26%) had bigger surgeries because of their MRI results.
Three women had larger lumpectomies, and 11 had mastectomies. “Three really needed it, and one maybe half way,” but the remaining seven turned out on pathology to have only needed lumpectomies, Dr. Pockaj said.
Mean lesion size on preoperative MRI was 3.6 cm while mean lesion size on pathologic specimen was 1.6 cm. Postbiopsy MRI did not significantly correlate with the actual size of the tumor specimen (r = 0.028; P = 0.921).
If the core needle biopsy shows DCIS, in many cases, “I think you can go right to surgery,” Dr. Pockaj said. MRI might still be indicted for very large lesions, suspicions of invasive disease, or very dense breasts, but, even so, the results need to be put into context with the postbiopsy changes, she said.
Women in the study were a mean of 59 years old. Most had high- or intermediate-grade DCIS. Women upgraded to invasive disease at surgery were excluded from the analysis.
There was no industry funding for the work, and the investigators reported having no relevant financial disclosures.
At ASBS 2017
Key clinical point:
Major finding: Of 54 women, 7 (13%) had mastectomies driven by postbiopsy MRI findings that were not indicated on final pathology.
Data source: Single-center review of 54 DCIS cases.
Disclosures: There was no industry funding for the work, and the investigators reported having no relevant financial disclosures.
Lumpectomy plus reconstruction outperforms mastectomy plus reconstruction
LAS VEGAS – Lumpectomy plus oncoplastic surgery has a total cost that is comparable to lumpectomy alone and that is less than mastectomy plus reconstructive surgery, according to an analysis of nearly 40,000 women.
While the complication rate was slightly higher than lumpectomy alone, the difference disappeared in the last year of data, possibly because surgical techniques had improved. The study looked at MarketScan Commercial Claims and Encounters Database data from 2000 to 2011 and confirms findings from an earlier study that looked at data from the MD Anderson Cancer Center (Ann Surg Oncol. 2016 Oct;23[10]:3190-8).
Lumpectomy plus oncoplastic surgery is increasingly being performed, but it still only represented about 2% of surgeries in women with invasive epithelial breast cancer, although this percentage had grown to 8.4% by 2011 and is likely higher now, according to Dr. Hwang, an associate professor of breast surgical oncology and surgical oncology at the University of Texas MD Anderson Cancer Center, Houston.
Candidates for lumpectomy plus oncoplastic surgery include those with large volume disease, multifocal/centric disease, poorly located tumors, or macromastia. “If oncoplastic reconstruction was not available, these patients would oftentimes be undergoing total mastectomy with reconstruction,” Dr. Hwang said.
The study included records from 39,518 women who underwent breast surgery with or without reconstruction. It excluded patients who received postmastectomy radiation or neoadjuvant chemotherapy.
A total of 40% underwent lumpectomy plus whole breast irradiation (BCT), 2% received BCT plus oncoplastic reconstruction (BCT+R), 30% had total mastectomy (TM), and 29% had total mastectomy plus reconstruction (TM+R).
After adjusting for age, race, comorbidity, chemotherapy, axillary surgery, and nodal positivity, the complication rate was lowest in the TM group (25%; relative risk compared with BCT+R, 0.71; 95% confidence interval, 0.64-0.78; P less than .001), followed by BCT (29%; RR, 0.80; 95% CI, 0.72-0.88; P less than .001), BCT+R (37%), and TM+R (54%; RR, 1.49; 95% CI, 1.35-1.64; P less than .001).
The rate of complications in BCT+R fell over time, so that, by 2011, it was only slightly higher than those of BCT alone (31.5% vs 29.4%). That trend is “probably just additional experience with the technique,” Dr. Hwang said.
Total costs for TM+R was $89,187, compared with $48,767 for TM, $66,217 for BCT, and $69,781 for BCT+R. The cost difference between BCT and TM+R was about $23,000.
The findings are encouraging, said Judy Boughey, MD, professor of surgery at the Mayo Clinic, Rochester, Minn., who moderated the session. However, she called for caution in interpreting the results because the population of interest made up just 2% of the overall sample. “I think you’re going to have the widest variability of confidence intervals around that group,” Dr. Boughey said. “It’s eye-opening, but I would just view it with caution.”
Dr. Hwang and Dr. Boughey reported having no financial disclosures.
LAS VEGAS – Lumpectomy plus oncoplastic surgery has a total cost that is comparable to lumpectomy alone and that is less than mastectomy plus reconstructive surgery, according to an analysis of nearly 40,000 women.
While the complication rate was slightly higher than lumpectomy alone, the difference disappeared in the last year of data, possibly because surgical techniques had improved. The study looked at MarketScan Commercial Claims and Encounters Database data from 2000 to 2011 and confirms findings from an earlier study that looked at data from the MD Anderson Cancer Center (Ann Surg Oncol. 2016 Oct;23[10]:3190-8).
Lumpectomy plus oncoplastic surgery is increasingly being performed, but it still only represented about 2% of surgeries in women with invasive epithelial breast cancer, although this percentage had grown to 8.4% by 2011 and is likely higher now, according to Dr. Hwang, an associate professor of breast surgical oncology and surgical oncology at the University of Texas MD Anderson Cancer Center, Houston.
Candidates for lumpectomy plus oncoplastic surgery include those with large volume disease, multifocal/centric disease, poorly located tumors, or macromastia. “If oncoplastic reconstruction was not available, these patients would oftentimes be undergoing total mastectomy with reconstruction,” Dr. Hwang said.
The study included records from 39,518 women who underwent breast surgery with or without reconstruction. It excluded patients who received postmastectomy radiation or neoadjuvant chemotherapy.
A total of 40% underwent lumpectomy plus whole breast irradiation (BCT), 2% received BCT plus oncoplastic reconstruction (BCT+R), 30% had total mastectomy (TM), and 29% had total mastectomy plus reconstruction (TM+R).
After adjusting for age, race, comorbidity, chemotherapy, axillary surgery, and nodal positivity, the complication rate was lowest in the TM group (25%; relative risk compared with BCT+R, 0.71; 95% confidence interval, 0.64-0.78; P less than .001), followed by BCT (29%; RR, 0.80; 95% CI, 0.72-0.88; P less than .001), BCT+R (37%), and TM+R (54%; RR, 1.49; 95% CI, 1.35-1.64; P less than .001).
The rate of complications in BCT+R fell over time, so that, by 2011, it was only slightly higher than those of BCT alone (31.5% vs 29.4%). That trend is “probably just additional experience with the technique,” Dr. Hwang said.
Total costs for TM+R was $89,187, compared with $48,767 for TM, $66,217 for BCT, and $69,781 for BCT+R. The cost difference between BCT and TM+R was about $23,000.
The findings are encouraging, said Judy Boughey, MD, professor of surgery at the Mayo Clinic, Rochester, Minn., who moderated the session. However, she called for caution in interpreting the results because the population of interest made up just 2% of the overall sample. “I think you’re going to have the widest variability of confidence intervals around that group,” Dr. Boughey said. “It’s eye-opening, but I would just view it with caution.”
Dr. Hwang and Dr. Boughey reported having no financial disclosures.
LAS VEGAS – Lumpectomy plus oncoplastic surgery has a total cost that is comparable to lumpectomy alone and that is less than mastectomy plus reconstructive surgery, according to an analysis of nearly 40,000 women.
While the complication rate was slightly higher than lumpectomy alone, the difference disappeared in the last year of data, possibly because surgical techniques had improved. The study looked at MarketScan Commercial Claims and Encounters Database data from 2000 to 2011 and confirms findings from an earlier study that looked at data from the MD Anderson Cancer Center (Ann Surg Oncol. 2016 Oct;23[10]:3190-8).
Lumpectomy plus oncoplastic surgery is increasingly being performed, but it still only represented about 2% of surgeries in women with invasive epithelial breast cancer, although this percentage had grown to 8.4% by 2011 and is likely higher now, according to Dr. Hwang, an associate professor of breast surgical oncology and surgical oncology at the University of Texas MD Anderson Cancer Center, Houston.
Candidates for lumpectomy plus oncoplastic surgery include those with large volume disease, multifocal/centric disease, poorly located tumors, or macromastia. “If oncoplastic reconstruction was not available, these patients would oftentimes be undergoing total mastectomy with reconstruction,” Dr. Hwang said.
The study included records from 39,518 women who underwent breast surgery with or without reconstruction. It excluded patients who received postmastectomy radiation or neoadjuvant chemotherapy.
A total of 40% underwent lumpectomy plus whole breast irradiation (BCT), 2% received BCT plus oncoplastic reconstruction (BCT+R), 30% had total mastectomy (TM), and 29% had total mastectomy plus reconstruction (TM+R).
After adjusting for age, race, comorbidity, chemotherapy, axillary surgery, and nodal positivity, the complication rate was lowest in the TM group (25%; relative risk compared with BCT+R, 0.71; 95% confidence interval, 0.64-0.78; P less than .001), followed by BCT (29%; RR, 0.80; 95% CI, 0.72-0.88; P less than .001), BCT+R (37%), and TM+R (54%; RR, 1.49; 95% CI, 1.35-1.64; P less than .001).
The rate of complications in BCT+R fell over time, so that, by 2011, it was only slightly higher than those of BCT alone (31.5% vs 29.4%). That trend is “probably just additional experience with the technique,” Dr. Hwang said.
Total costs for TM+R was $89,187, compared with $48,767 for TM, $66,217 for BCT, and $69,781 for BCT+R. The cost difference between BCT and TM+R was about $23,000.
The findings are encouraging, said Judy Boughey, MD, professor of surgery at the Mayo Clinic, Rochester, Minn., who moderated the session. However, she called for caution in interpreting the results because the population of interest made up just 2% of the overall sample. “I think you’re going to have the widest variability of confidence intervals around that group,” Dr. Boughey said. “It’s eye-opening, but I would just view it with caution.”
Dr. Hwang and Dr. Boughey reported having no financial disclosures.
At ASBS 2017
Key clinical point:
Major finding: Mastectomy with reconstruction had a 49% higher complication rate and $20,000 higher cost, compared with lumpectomy plus reconstruction.
Data source: Nationwide retrospective analysis of 39,518 women.
Disclosures: Dr. Hwang and Dr. Boughey reported having no financial disclosures.
Schizophrenia patients’ mortality is 14.5 years shorter
SAN DIEGO – A new systematic review and meta-analysis, the first of its kind, suggests that most people with schizophrenia – especially men – do not survive past their 60s.
According to findings released at the 2017 International Congress on Schizophrenia Research, schizophrenia patients appear to die a weighted average of 14.5 years earlier than the rest of the population (95% confidence interval, 11.2-17.8).
The weighted average life expectancy for schizophrenia patients was 64.7 years (95% CI, 61.1-71.3) – 59.9 years for men (95% CI, 55.5-64.3) and 67.6 years for women (95% CI, 63.1-72.1).
“There were no indications that this is improving over time,” lead author Carsten Hjorthøj, PhD, senior researcher at the University of Copenhagen, said in an interview.
The researchers launched their paper in order to provide a wider perspective on lives lost in schizophrenia.
Previous studies had used measures like the standardized mortality ratio, which compared schizophrenia patients with a matched group from the general population, Dr. Hjorthøj said. “Saying that people with schizophrenia are, for instance, 2.5 times more likely to die at any given age may be a little difficult to understand. Identifying the actual number of years they die earlier than the rest of the population is easily understood and will probably also make the issue more obvious to policymakers.”
The researchers, whose findings were previously published in Lancet Psychiatry (2017 Apr;4[4]:295-301), examined 11 studies, mostly from Europe (n = 5) and North America (n = 3) with single studies from Africa, Asia, and Australia. (The lowest life expectancies were reported in Asia and Africa.)
One study was published in 1991, and the rest from 2001-2016. Together, the studies tracked 302,691 patients with schizophrenia.
What explains the gap between the life expectancies in men and women? “We did not investigate the reasons for this,” Dr. Hjorthøj said, “but men typically have worse adherence to treatment than women, and men typically also have poorer health-seeking behavior than women even in the general population. Given that schizophrenia is associated with a multitude of adverse somatic outcomes, this could then be aggravated by this difference in health-seeking behavior.”
In addition, he said, “It could also be the case that use of alcohol, tobacco, and illicit substances is even more skewed in schizophrenia than in the general population. Finally, it could also be attributed in part to the fact that men are more likely than women to die from suicide.”
Dr. Hjorthøj said that the findings emphasize the importance of treating physical symptoms in people with schizophrenia.
“I am aware of several cases where physical complaints were not taken seriously because they were raised by people who were known to suffer from delusions,” he said. “But, I do believe that most psychiatrists are aware of this, and the problem is perhaps more that the system in general is underfunded and that somatic and psychiatric hospitals are not good enough at communicating with each other.”
The researchers report no funding and no disclosures.
SAN DIEGO – A new systematic review and meta-analysis, the first of its kind, suggests that most people with schizophrenia – especially men – do not survive past their 60s.
According to findings released at the 2017 International Congress on Schizophrenia Research, schizophrenia patients appear to die a weighted average of 14.5 years earlier than the rest of the population (95% confidence interval, 11.2-17.8).
The weighted average life expectancy for schizophrenia patients was 64.7 years (95% CI, 61.1-71.3) – 59.9 years for men (95% CI, 55.5-64.3) and 67.6 years for women (95% CI, 63.1-72.1).
“There were no indications that this is improving over time,” lead author Carsten Hjorthøj, PhD, senior researcher at the University of Copenhagen, said in an interview.
The researchers launched their paper in order to provide a wider perspective on lives lost in schizophrenia.
Previous studies had used measures like the standardized mortality ratio, which compared schizophrenia patients with a matched group from the general population, Dr. Hjorthøj said. “Saying that people with schizophrenia are, for instance, 2.5 times more likely to die at any given age may be a little difficult to understand. Identifying the actual number of years they die earlier than the rest of the population is easily understood and will probably also make the issue more obvious to policymakers.”
The researchers, whose findings were previously published in Lancet Psychiatry (2017 Apr;4[4]:295-301), examined 11 studies, mostly from Europe (n = 5) and North America (n = 3) with single studies from Africa, Asia, and Australia. (The lowest life expectancies were reported in Asia and Africa.)
One study was published in 1991, and the rest from 2001-2016. Together, the studies tracked 302,691 patients with schizophrenia.
What explains the gap between the life expectancies in men and women? “We did not investigate the reasons for this,” Dr. Hjorthøj said, “but men typically have worse adherence to treatment than women, and men typically also have poorer health-seeking behavior than women even in the general population. Given that schizophrenia is associated with a multitude of adverse somatic outcomes, this could then be aggravated by this difference in health-seeking behavior.”
In addition, he said, “It could also be the case that use of alcohol, tobacco, and illicit substances is even more skewed in schizophrenia than in the general population. Finally, it could also be attributed in part to the fact that men are more likely than women to die from suicide.”
Dr. Hjorthøj said that the findings emphasize the importance of treating physical symptoms in people with schizophrenia.
“I am aware of several cases where physical complaints were not taken seriously because they were raised by people who were known to suffer from delusions,” he said. “But, I do believe that most psychiatrists are aware of this, and the problem is perhaps more that the system in general is underfunded and that somatic and psychiatric hospitals are not good enough at communicating with each other.”
The researchers report no funding and no disclosures.
SAN DIEGO – A new systematic review and meta-analysis, the first of its kind, suggests that most people with schizophrenia – especially men – do not survive past their 60s.
According to findings released at the 2017 International Congress on Schizophrenia Research, schizophrenia patients appear to die a weighted average of 14.5 years earlier than the rest of the population (95% confidence interval, 11.2-17.8).
The weighted average life expectancy for schizophrenia patients was 64.7 years (95% CI, 61.1-71.3) – 59.9 years for men (95% CI, 55.5-64.3) and 67.6 years for women (95% CI, 63.1-72.1).
“There were no indications that this is improving over time,” lead author Carsten Hjorthøj, PhD, senior researcher at the University of Copenhagen, said in an interview.
The researchers launched their paper in order to provide a wider perspective on lives lost in schizophrenia.
Previous studies had used measures like the standardized mortality ratio, which compared schizophrenia patients with a matched group from the general population, Dr. Hjorthøj said. “Saying that people with schizophrenia are, for instance, 2.5 times more likely to die at any given age may be a little difficult to understand. Identifying the actual number of years they die earlier than the rest of the population is easily understood and will probably also make the issue more obvious to policymakers.”
The researchers, whose findings were previously published in Lancet Psychiatry (2017 Apr;4[4]:295-301), examined 11 studies, mostly from Europe (n = 5) and North America (n = 3) with single studies from Africa, Asia, and Australia. (The lowest life expectancies were reported in Asia and Africa.)
One study was published in 1991, and the rest from 2001-2016. Together, the studies tracked 302,691 patients with schizophrenia.
What explains the gap between the life expectancies in men and women? “We did not investigate the reasons for this,” Dr. Hjorthøj said, “but men typically have worse adherence to treatment than women, and men typically also have poorer health-seeking behavior than women even in the general population. Given that schizophrenia is associated with a multitude of adverse somatic outcomes, this could then be aggravated by this difference in health-seeking behavior.”
In addition, he said, “It could also be the case that use of alcohol, tobacco, and illicit substances is even more skewed in schizophrenia than in the general population. Finally, it could also be attributed in part to the fact that men are more likely than women to die from suicide.”
Dr. Hjorthøj said that the findings emphasize the importance of treating physical symptoms in people with schizophrenia.
“I am aware of several cases where physical complaints were not taken seriously because they were raised by people who were known to suffer from delusions,” he said. “But, I do believe that most psychiatrists are aware of this, and the problem is perhaps more that the system in general is underfunded and that somatic and psychiatric hospitals are not good enough at communicating with each other.”
The researchers report no funding and no disclosures.
At the ICSR Biennial Meeting
Key clinical point:
Major finding: Schizophrenia patients die a weighted average of 14.5 years earlier than those in the general population (95% CI, 11.2-17.8), and their weighted average life expectancy is 64.7 years (95% CI, 61-71.3) – 59.9 for men (95% CI, 55.5-64.3) and 67.6 for women (95% CI, 63.1-72.1).
Data source: Review and meta-analysis of 11 studies of 302,691 schizophrenia patients.
Disclosures: No specific funding was reported, and the authors reported no disclosures.