User login
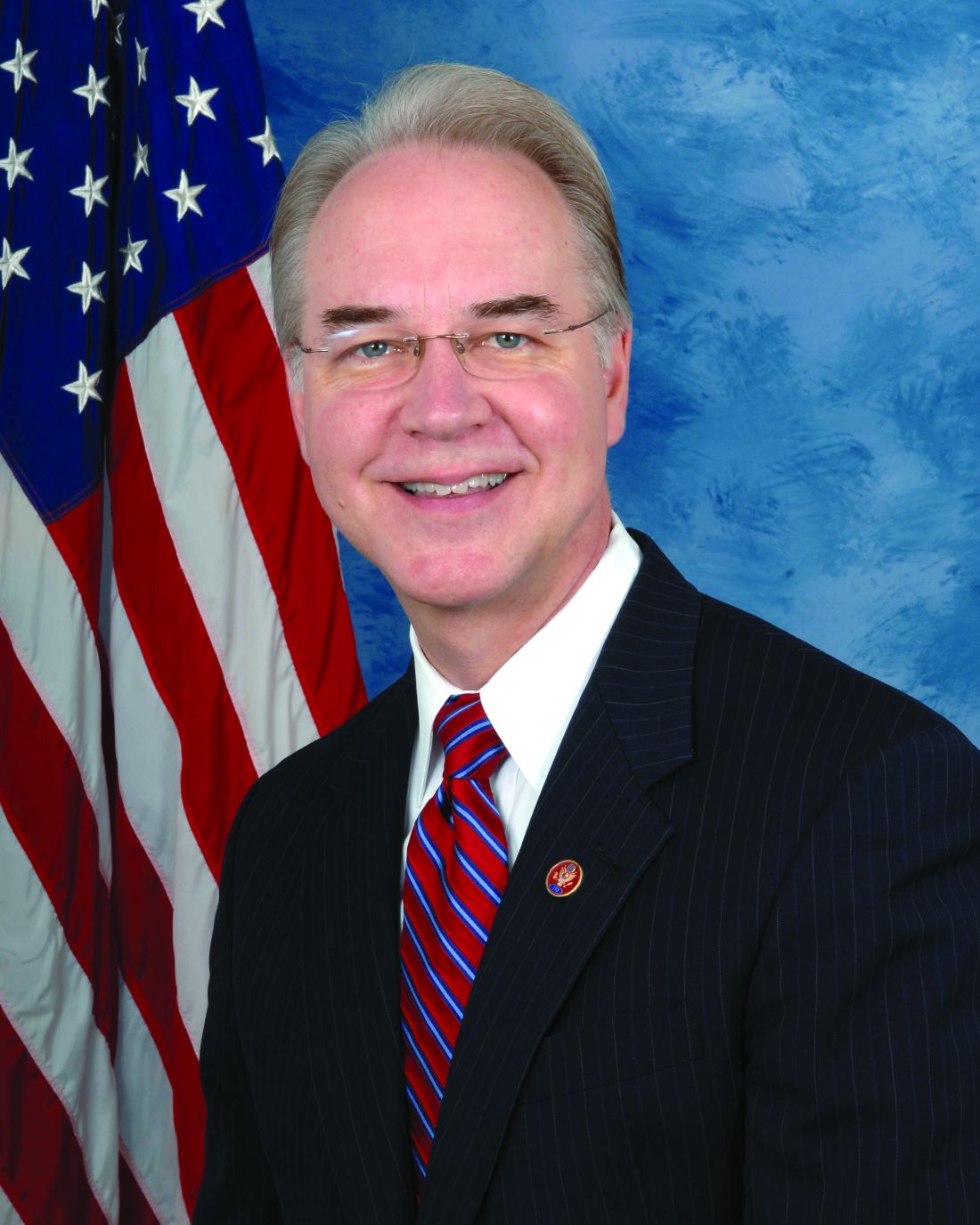
Five quick ways HHS Secretary Tom Price could change the course of health policy
After a bruising confirmation process, the Senate confirmed Rep. Tom Price, R-Ga., to head up the Department of Health and Human Services, by a 52-47 vote.
As secretary, Price will have significant authority to rewrite the rules for the Affordable Care Act, some of which are reportedly nearly ready to be issued.
But there is much more now within Price’s purview, as head of an agency with a budget of more than $1 trillion for the current fiscal year. He can interpret laws in different ways than his predecessors and rewrite regulations and guidance, which is how many important policies are actually carried out.
“Virtually everything people do every day is impacted by the way the Department of Health and Human Services is run,” said Matt Myers, president of the Campaign for Tobacco-Free Kids. HHS responsibilities include food and drug safety, biomedical research, disease prevention and control, as well as oversight over everything from medical laboratories to nursing homes.
Price, a Georgia physician who opposes the Affordable Care Act, abortion, and funding for Planned Parenthood, among other things, could have a rapid impact without even a presidential order or an act of Congress.
Some advocates are excited by that possibility. “With Dr. Price taking the helm of American health policy, doctors and patients alike have sound reasons to hope for a welcome and long-overdue change,” Robert Moffit, a senior fellow at the conservative Heritage Foundation, said in a statement when Price’s nomination was announced.
Others are less enthusiastic. Asked about what policies Price might enact, Topher Spiro of the liberal Center for American Progress said at that time: “I don’t know if I want to brainstorm bad ideas for him to do.”
Here are five actions the new HHS secretary might take, according to advocates on both sides, that would disrupt health policies currently in force:
Birth control coverage: Under the ACA, most insurance plans must provide women with any form of contraception approved by the Food and Drug Administration at no additional cost. This has been particularly controversial in regards to religious employers who object to artificial contraception, leading to alterations in the rules, and resulting in two separate Supreme Court rulings, one about private firms’ rights to make religious objections, and one about nonprofit religious hospitals and schools.
As secretary, Price would have two main options. He could expand the “accommodation” that already exempts some houses of worship from the requirement to any employer with a religious objection. Or, because the specific inclusion of birth control came via a regulation rather than the law itself, he could simply eliminate no-copay birth control coverage from the benefits insurance plans must offer. (This assumes continuing existence of the health law, at least for the short term.)
Medicare payment changes: The health law created an agency within Medicare, called the Center for Medicare and Medicaid Innovation, that was tasked with exploring new ways to pay doctors and hospitals that would reduce costs while maintaining quality. The HHS secretary has the authority to require doctors and hospitals to participate in the experiments and new payment models. Some have proved unpopular with physician and hospital groups, in particular the idea of paying providers so-called bundled payments for packages of care, rather than allowing them to bill item-by-item; one such package covers hip and knee replacements, from the time of surgery through postsurgical rehabilitation. Price, as a former orthopedic surgeon himself, would likely act to scale back, delay, or cancel that project, since he “has been a critic in the past,” said Dan Mendelson, CEO of Avalere Health, a Washington-based consulting firm.
Planned Parenthood funding: Republicans have been agitating to separate Planned Parenthood from its federal funding literally for decades. Congress would have to change Medicaid law to permanently defund the women’s health group, which also performs abortions (with non-federal funds) at many of its sites. But an HHS secretary has many tools at his disposal to make life miserable for the organization.
For example, during the Reagan and George H.W. Bush administrations, rules were put in place, and eventually upheld by the Supreme Court, that would have banned staff in federally funded family planning clinics from counseling or referring for abortion women with unintended pregnancies. The subsequent Clinton administration repealed the rules, but they could make a comeback under the new secretary’s leadership.
Price could also throw the weight of the department into a probe into Planned Parenthood’s ties to firms allegedly selling fetal tissue for profit, which has also been investigated by a House committee.
Tobacco regulation: After years of discord, Congress finally agreed to give the Food and Drug Administration (limited) authority to regulate tobacco products in 2009. “The core authority is statutory,” said Matt Myers of the Campaign for Tobacco-Free Kids, who advocated for the law. That means Congress would have to act to eliminate many of its changes. But a secretary who opposes the law (Price voted against it at the time) could weaken enforcement, says Myers. Or he could rewrite and water down some rules, including recent ones affecting cigars and e-cigarettes.
“The secretary has very broad discretionary authority not to vigorously enforce or implement the statute in an aggressive manner,” Myers said.
Conscience protections: At the very end of the George W. Bush administration, HHS issued rules intended to clarify that health care professionals did not have to participate in performing abortions, sterilizations, or other procedures that violated a “religious belief or moral conviction.”
Opponents of the rules complained, however, that they were so vague and sweeping that they could apply not just to opponents of abortion, but also to those who don’t want to provide birth control to unmarried women, or HIV treatment to homosexuals.
The Obama administration revised the rules dramatically, much to the continuing consternation of conservatives. They were among the few health-related items included in the health section of Trump’s website before he was inaugurated and the page was taken down. “The Administration will act to protect individual conscience in health care,” it said. Many expect the rules to be reinstated in their original form.
This is an updated version of a story that initially ran Dec. 9, 2016. It was updated Feb. 10, 2017 to reflect that Tom Price had been confirmed by the Senate.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
After a bruising confirmation process, the Senate confirmed Rep. Tom Price, R-Ga., to head up the Department of Health and Human Services, by a 52-47 vote.
As secretary, Price will have significant authority to rewrite the rules for the Affordable Care Act, some of which are reportedly nearly ready to be issued.
But there is much more now within Price’s purview, as head of an agency with a budget of more than $1 trillion for the current fiscal year. He can interpret laws in different ways than his predecessors and rewrite regulations and guidance, which is how many important policies are actually carried out.
“Virtually everything people do every day is impacted by the way the Department of Health and Human Services is run,” said Matt Myers, president of the Campaign for Tobacco-Free Kids. HHS responsibilities include food and drug safety, biomedical research, disease prevention and control, as well as oversight over everything from medical laboratories to nursing homes.
Price, a Georgia physician who opposes the Affordable Care Act, abortion, and funding for Planned Parenthood, among other things, could have a rapid impact without even a presidential order or an act of Congress.
Some advocates are excited by that possibility. “With Dr. Price taking the helm of American health policy, doctors and patients alike have sound reasons to hope for a welcome and long-overdue change,” Robert Moffit, a senior fellow at the conservative Heritage Foundation, said in a statement when Price’s nomination was announced.
Others are less enthusiastic. Asked about what policies Price might enact, Topher Spiro of the liberal Center for American Progress said at that time: “I don’t know if I want to brainstorm bad ideas for him to do.”
Here are five actions the new HHS secretary might take, according to advocates on both sides, that would disrupt health policies currently in force:
Birth control coverage: Under the ACA, most insurance plans must provide women with any form of contraception approved by the Food and Drug Administration at no additional cost. This has been particularly controversial in regards to religious employers who object to artificial contraception, leading to alterations in the rules, and resulting in two separate Supreme Court rulings, one about private firms’ rights to make religious objections, and one about nonprofit religious hospitals and schools.
As secretary, Price would have two main options. He could expand the “accommodation” that already exempts some houses of worship from the requirement to any employer with a religious objection. Or, because the specific inclusion of birth control came via a regulation rather than the law itself, he could simply eliminate no-copay birth control coverage from the benefits insurance plans must offer. (This assumes continuing existence of the health law, at least for the short term.)
Medicare payment changes: The health law created an agency within Medicare, called the Center for Medicare and Medicaid Innovation, that was tasked with exploring new ways to pay doctors and hospitals that would reduce costs while maintaining quality. The HHS secretary has the authority to require doctors and hospitals to participate in the experiments and new payment models. Some have proved unpopular with physician and hospital groups, in particular the idea of paying providers so-called bundled payments for packages of care, rather than allowing them to bill item-by-item; one such package covers hip and knee replacements, from the time of surgery through postsurgical rehabilitation. Price, as a former orthopedic surgeon himself, would likely act to scale back, delay, or cancel that project, since he “has been a critic in the past,” said Dan Mendelson, CEO of Avalere Health, a Washington-based consulting firm.
Planned Parenthood funding: Republicans have been agitating to separate Planned Parenthood from its federal funding literally for decades. Congress would have to change Medicaid law to permanently defund the women’s health group, which also performs abortions (with non-federal funds) at many of its sites. But an HHS secretary has many tools at his disposal to make life miserable for the organization.
For example, during the Reagan and George H.W. Bush administrations, rules were put in place, and eventually upheld by the Supreme Court, that would have banned staff in federally funded family planning clinics from counseling or referring for abortion women with unintended pregnancies. The subsequent Clinton administration repealed the rules, but they could make a comeback under the new secretary’s leadership.
Price could also throw the weight of the department into a probe into Planned Parenthood’s ties to firms allegedly selling fetal tissue for profit, which has also been investigated by a House committee.
Tobacco regulation: After years of discord, Congress finally agreed to give the Food and Drug Administration (limited) authority to regulate tobacco products in 2009. “The core authority is statutory,” said Matt Myers of the Campaign for Tobacco-Free Kids, who advocated for the law. That means Congress would have to act to eliminate many of its changes. But a secretary who opposes the law (Price voted against it at the time) could weaken enforcement, says Myers. Or he could rewrite and water down some rules, including recent ones affecting cigars and e-cigarettes.
“The secretary has very broad discretionary authority not to vigorously enforce or implement the statute in an aggressive manner,” Myers said.
Conscience protections: At the very end of the George W. Bush administration, HHS issued rules intended to clarify that health care professionals did not have to participate in performing abortions, sterilizations, or other procedures that violated a “religious belief or moral conviction.”
Opponents of the rules complained, however, that they were so vague and sweeping that they could apply not just to opponents of abortion, but also to those who don’t want to provide birth control to unmarried women, or HIV treatment to homosexuals.
The Obama administration revised the rules dramatically, much to the continuing consternation of conservatives. They were among the few health-related items included in the health section of Trump’s website before he was inaugurated and the page was taken down. “The Administration will act to protect individual conscience in health care,” it said. Many expect the rules to be reinstated in their original form.
This is an updated version of a story that initially ran Dec. 9, 2016. It was updated Feb. 10, 2017 to reflect that Tom Price had been confirmed by the Senate.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
After a bruising confirmation process, the Senate confirmed Rep. Tom Price, R-Ga., to head up the Department of Health and Human Services, by a 52-47 vote.
As secretary, Price will have significant authority to rewrite the rules for the Affordable Care Act, some of which are reportedly nearly ready to be issued.
But there is much more now within Price’s purview, as head of an agency with a budget of more than $1 trillion for the current fiscal year. He can interpret laws in different ways than his predecessors and rewrite regulations and guidance, which is how many important policies are actually carried out.
“Virtually everything people do every day is impacted by the way the Department of Health and Human Services is run,” said Matt Myers, president of the Campaign for Tobacco-Free Kids. HHS responsibilities include food and drug safety, biomedical research, disease prevention and control, as well as oversight over everything from medical laboratories to nursing homes.
Price, a Georgia physician who opposes the Affordable Care Act, abortion, and funding for Planned Parenthood, among other things, could have a rapid impact without even a presidential order or an act of Congress.
Some advocates are excited by that possibility. “With Dr. Price taking the helm of American health policy, doctors and patients alike have sound reasons to hope for a welcome and long-overdue change,” Robert Moffit, a senior fellow at the conservative Heritage Foundation, said in a statement when Price’s nomination was announced.
Others are less enthusiastic. Asked about what policies Price might enact, Topher Spiro of the liberal Center for American Progress said at that time: “I don’t know if I want to brainstorm bad ideas for him to do.”
Here are five actions the new HHS secretary might take, according to advocates on both sides, that would disrupt health policies currently in force:
Birth control coverage: Under the ACA, most insurance plans must provide women with any form of contraception approved by the Food and Drug Administration at no additional cost. This has been particularly controversial in regards to religious employers who object to artificial contraception, leading to alterations in the rules, and resulting in two separate Supreme Court rulings, one about private firms’ rights to make religious objections, and one about nonprofit religious hospitals and schools.
As secretary, Price would have two main options. He could expand the “accommodation” that already exempts some houses of worship from the requirement to any employer with a religious objection. Or, because the specific inclusion of birth control came via a regulation rather than the law itself, he could simply eliminate no-copay birth control coverage from the benefits insurance plans must offer. (This assumes continuing existence of the health law, at least for the short term.)
Medicare payment changes: The health law created an agency within Medicare, called the Center for Medicare and Medicaid Innovation, that was tasked with exploring new ways to pay doctors and hospitals that would reduce costs while maintaining quality. The HHS secretary has the authority to require doctors and hospitals to participate in the experiments and new payment models. Some have proved unpopular with physician and hospital groups, in particular the idea of paying providers so-called bundled payments for packages of care, rather than allowing them to bill item-by-item; one such package covers hip and knee replacements, from the time of surgery through postsurgical rehabilitation. Price, as a former orthopedic surgeon himself, would likely act to scale back, delay, or cancel that project, since he “has been a critic in the past,” said Dan Mendelson, CEO of Avalere Health, a Washington-based consulting firm.
Planned Parenthood funding: Republicans have been agitating to separate Planned Parenthood from its federal funding literally for decades. Congress would have to change Medicaid law to permanently defund the women’s health group, which also performs abortions (with non-federal funds) at many of its sites. But an HHS secretary has many tools at his disposal to make life miserable for the organization.
For example, during the Reagan and George H.W. Bush administrations, rules were put in place, and eventually upheld by the Supreme Court, that would have banned staff in federally funded family planning clinics from counseling or referring for abortion women with unintended pregnancies. The subsequent Clinton administration repealed the rules, but they could make a comeback under the new secretary’s leadership.
Price could also throw the weight of the department into a probe into Planned Parenthood’s ties to firms allegedly selling fetal tissue for profit, which has also been investigated by a House committee.
Tobacco regulation: After years of discord, Congress finally agreed to give the Food and Drug Administration (limited) authority to regulate tobacco products in 2009. “The core authority is statutory,” said Matt Myers of the Campaign for Tobacco-Free Kids, who advocated for the law. That means Congress would have to act to eliminate many of its changes. But a secretary who opposes the law (Price voted against it at the time) could weaken enforcement, says Myers. Or he could rewrite and water down some rules, including recent ones affecting cigars and e-cigarettes.
“The secretary has very broad discretionary authority not to vigorously enforce or implement the statute in an aggressive manner,” Myers said.
Conscience protections: At the very end of the George W. Bush administration, HHS issued rules intended to clarify that health care professionals did not have to participate in performing abortions, sterilizations, or other procedures that violated a “religious belief or moral conviction.”
Opponents of the rules complained, however, that they were so vague and sweeping that they could apply not just to opponents of abortion, but also to those who don’t want to provide birth control to unmarried women, or HIV treatment to homosexuals.
The Obama administration revised the rules dramatically, much to the continuing consternation of conservatives. They were among the few health-related items included in the health section of Trump’s website before he was inaugurated and the page was taken down. “The Administration will act to protect individual conscience in health care,” it said. Many expect the rules to be reinstated in their original form.
This is an updated version of a story that initially ran Dec. 9, 2016. It was updated Feb. 10, 2017 to reflect that Tom Price had been confirmed by the Senate.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Why like attracts like in malaria

Photo courtesy of CDC
Past research has shown that malaria-carrying mosquitoes prefer to feed on humans who are already infected with malaria.
Now, researchers believe they have discovered why.
The
team identified a naturally occurring compound, known as HMBPP, that is derived from the malaria parasite Plasmodium falciparum and
triggers the release of mosquito-attracting chemicals, making a human
host more enticing to the insects.
“The malaria parasite produces a molecule, HMBPP, which stimulates the human red blood cells to release more carbon dioxide and volatile compounds with an irresistible smell to malaria mosquitoes,” explained study author Ingrid Faye, of Stockholm University in Sweden.
She and her colleagues described this discovery in Science.
To determine if HMBPP could influence mosquitoes’ blood-meal-seeking and feeding behaviors, the researchers devised a “dual choice attraction” test for Anopheles gambiae mosquitoes.
Specifically, the team evaluated the mosquitoes’ preference to land on and feed off of an artificial membrane containing HMBPP-supplemented red blood cells (hmbRBCs) or normal red blood cells (RBCs).
More than 95% of the mosquitoes tested chose hmbRBCs over RBCs, and the mosquitoes consumed hmbRBCs more intensively and for longer periods of time than they did RBCs.
The researchers also found that blood spiked with HMBPP activated the expression of Plasmodium-specific genes involved in protecting the mosquitoes’ vital functions while also improving receptivity to infection and amplifying the likelihood of parasite transmission.
“This seems to be a well-functioning system, developed over millions of years, which means that the malaria parasite can survive and spread to more people without killing the host,” Faye said.
She and her colleagues believe the discovery of HMBPP as a driver of mosquito attraction exposes a weakness in Plasmodium that could be exploited to better pinpoint disease-carrying Anopheles gambiae mosquitoes and possibly prevent the spread of malaria. ![]()

Photo courtesy of CDC
Past research has shown that malaria-carrying mosquitoes prefer to feed on humans who are already infected with malaria.
Now, researchers believe they have discovered why.
The
team identified a naturally occurring compound, known as HMBPP, that is derived from the malaria parasite Plasmodium falciparum and
triggers the release of mosquito-attracting chemicals, making a human
host more enticing to the insects.
“The malaria parasite produces a molecule, HMBPP, which stimulates the human red blood cells to release more carbon dioxide and volatile compounds with an irresistible smell to malaria mosquitoes,” explained study author Ingrid Faye, of Stockholm University in Sweden.
She and her colleagues described this discovery in Science.
To determine if HMBPP could influence mosquitoes’ blood-meal-seeking and feeding behaviors, the researchers devised a “dual choice attraction” test for Anopheles gambiae mosquitoes.
Specifically, the team evaluated the mosquitoes’ preference to land on and feed off of an artificial membrane containing HMBPP-supplemented red blood cells (hmbRBCs) or normal red blood cells (RBCs).
More than 95% of the mosquitoes tested chose hmbRBCs over RBCs, and the mosquitoes consumed hmbRBCs more intensively and for longer periods of time than they did RBCs.
The researchers also found that blood spiked with HMBPP activated the expression of Plasmodium-specific genes involved in protecting the mosquitoes’ vital functions while also improving receptivity to infection and amplifying the likelihood of parasite transmission.
“This seems to be a well-functioning system, developed over millions of years, which means that the malaria parasite can survive and spread to more people without killing the host,” Faye said.
She and her colleagues believe the discovery of HMBPP as a driver of mosquito attraction exposes a weakness in Plasmodium that could be exploited to better pinpoint disease-carrying Anopheles gambiae mosquitoes and possibly prevent the spread of malaria. ![]()

Photo courtesy of CDC
Past research has shown that malaria-carrying mosquitoes prefer to feed on humans who are already infected with malaria.
Now, researchers believe they have discovered why.
The
team identified a naturally occurring compound, known as HMBPP, that is derived from the malaria parasite Plasmodium falciparum and
triggers the release of mosquito-attracting chemicals, making a human
host more enticing to the insects.
“The malaria parasite produces a molecule, HMBPP, which stimulates the human red blood cells to release more carbon dioxide and volatile compounds with an irresistible smell to malaria mosquitoes,” explained study author Ingrid Faye, of Stockholm University in Sweden.
She and her colleagues described this discovery in Science.
To determine if HMBPP could influence mosquitoes’ blood-meal-seeking and feeding behaviors, the researchers devised a “dual choice attraction” test for Anopheles gambiae mosquitoes.
Specifically, the team evaluated the mosquitoes’ preference to land on and feed off of an artificial membrane containing HMBPP-supplemented red blood cells (hmbRBCs) or normal red blood cells (RBCs).
More than 95% of the mosquitoes tested chose hmbRBCs over RBCs, and the mosquitoes consumed hmbRBCs more intensively and for longer periods of time than they did RBCs.
The researchers also found that blood spiked with HMBPP activated the expression of Plasmodium-specific genes involved in protecting the mosquitoes’ vital functions while also improving receptivity to infection and amplifying the likelihood of parasite transmission.
“This seems to be a well-functioning system, developed over millions of years, which means that the malaria parasite can survive and spread to more people without killing the host,” Faye said.
She and her colleagues believe the discovery of HMBPP as a driver of mosquito attraction exposes a weakness in Plasmodium that could be exploited to better pinpoint disease-carrying Anopheles gambiae mosquitoes and possibly prevent the spread of malaria. ![]()
Emergency department visits from adverse drug events
Clinical question: The purpose of this study was to describe emergency department (ED) visits for adverse drug events in year 2013-2014 compared to year 2005-2006 to learn changing patterns of ADEs and to help advance medication safety initiatives in outpatient settings.
Background: Adverse drug events (ADEs) are the most common cause of iatrogenic harm to patients and there have been significant national-level initiatives to prevent them as a part of patient safety. In the outpatient setting, where 90% of prescription drug expenditures occur, preventing ADEs remains a patient safety challenge because patients can have complex medication regimens, at times prescribed by multiple clinicians, with far less monitoring compared with hospitalized patients.
Setting and study design: Active, public health surveillance in 58 EDs in the United States that participate in the National Electronic Injury Surveillance System–Cooperative Adverse Drug Event Surveillance Project (NEISS-CADES). Trained data abstractors at each hospital reviewed each ED visit to identify any clinician-diagnosed ADEs that were the reason for the ED visit. Reports were coded by CDC and analyzed.
Synopsis: Based on 42,585 cases, 4.0 (95% CI, 3.1-5) ED visits for ADEs per 1,000 individuals occurred annually in the United States in 2013-2014 and 27.3% (22.2%-32.4%) of ED visits for ADEs resulted in hospitalization.
An estimated 34.5 % (95% CI, 30.3-38.8) of ED visits for ADEs occurred among adults aged 65 or older in 2013 compared with an estimated 25.6% (95% CI, 21-30) in 2005-2006. The population rate for adults older than 65 years was 9.7 visits per 1,000 individuals, compared with 3.1 visits per 1,000 individuals for those younger than 65 years. Older adults experienced higher hospitalization rates 43.6% (95% CI, 36.6-50.5). When adjusted for the U.S. population, the hospitalization rate for ADEs among older individuals was seven times higher compared with younger patients.
A single medication was implicated in most ED visits for ADEs (83.8%; 95% CI, 81.5-86.1). Supratherapeutic effects of ingestion of excess dose was the most common type of ADE (37.2%; 95% CI, 34.7-39.6). Medication errors were documented in 1 of 10 ED visits for ADEs (10.5%; 95% CI, 8.9-12.2).
The most commonly implicated drug classes were anticoagulants (17.6%), systemic antibiotics (16.1%), diabetes agents (13.3%), opioid analgesics (6.8%), antiplatelets (6.6%), renin-angiotensin system inhibitors (3.5%), antineoplastic agents (3%) and sedative/hypnotics (3%). Since 2005-2006, the proportions of ED visits for ADEs involving anticoagulants, antiplatelets, and diabetic agents have increased, whereas proportions involving antibiotics have decreased.
In children aged 5 years or younger, antibiotics were the most common drug class (56.4; 95% CI, 51.8-61). Among children and adolescents aged 6-19 years, antibiotics also were the most common class (31.8%; 95% CI, 28.7-34.9), followed by antipsychotics (4.5%; 95% CI, 3.3-5.6).
Among older adults, three drug classes recently targeted by federal patient safety initiatives (anticoagulants, diabetes agents, and opioid analgesics) were implicated in an estimated 59.9% (95% CI, 56.8-62.9) of ED visits. Four anticoagulants (warfarin, rivaroxaban, dabigatran, and enoxaparin) and five diabetes agents (insulin and four oral agents) were among the 15 most common drugs implicated. Medications to always avoid in older adults according to Beers criteria were implicated in 1.8% (95% CI, 1.5-2.1) of ED visits for adverse drug events.
Summary: The most common drug classes implicated in ED visits for ADEs in the United States are the same ones identified a decade ago – anticoagulants, antibiotics, diabetes agents, and opioid analgesics. The proportion of ED visits for ADEs involving anticoagulants has increased during the last decade with increased anticoagulant use. The prevalence of potentially inappropriate medication use in older patients also remains high.
Citation: JAMA. 2016;316(20):2115-25. doi: 10.1001/jama.2016.16201.
Dr. Patel is a hospitalist in the division of hospital medicine and assistant professor of medicine at Cooper Medical School of Rowan University, Camden, N.J. He is CMSRU’s associate residency program director and serves as codirector of the Foundation of Medical Practice curriculum.
Clinical question: The purpose of this study was to describe emergency department (ED) visits for adverse drug events in year 2013-2014 compared to year 2005-2006 to learn changing patterns of ADEs and to help advance medication safety initiatives in outpatient settings.
Background: Adverse drug events (ADEs) are the most common cause of iatrogenic harm to patients and there have been significant national-level initiatives to prevent them as a part of patient safety. In the outpatient setting, where 90% of prescription drug expenditures occur, preventing ADEs remains a patient safety challenge because patients can have complex medication regimens, at times prescribed by multiple clinicians, with far less monitoring compared with hospitalized patients.
Setting and study design: Active, public health surveillance in 58 EDs in the United States that participate in the National Electronic Injury Surveillance System–Cooperative Adverse Drug Event Surveillance Project (NEISS-CADES). Trained data abstractors at each hospital reviewed each ED visit to identify any clinician-diagnosed ADEs that were the reason for the ED visit. Reports were coded by CDC and analyzed.
Synopsis: Based on 42,585 cases, 4.0 (95% CI, 3.1-5) ED visits for ADEs per 1,000 individuals occurred annually in the United States in 2013-2014 and 27.3% (22.2%-32.4%) of ED visits for ADEs resulted in hospitalization.
An estimated 34.5 % (95% CI, 30.3-38.8) of ED visits for ADEs occurred among adults aged 65 or older in 2013 compared with an estimated 25.6% (95% CI, 21-30) in 2005-2006. The population rate for adults older than 65 years was 9.7 visits per 1,000 individuals, compared with 3.1 visits per 1,000 individuals for those younger than 65 years. Older adults experienced higher hospitalization rates 43.6% (95% CI, 36.6-50.5). When adjusted for the U.S. population, the hospitalization rate for ADEs among older individuals was seven times higher compared with younger patients.
A single medication was implicated in most ED visits for ADEs (83.8%; 95% CI, 81.5-86.1). Supratherapeutic effects of ingestion of excess dose was the most common type of ADE (37.2%; 95% CI, 34.7-39.6). Medication errors were documented in 1 of 10 ED visits for ADEs (10.5%; 95% CI, 8.9-12.2).
The most commonly implicated drug classes were anticoagulants (17.6%), systemic antibiotics (16.1%), diabetes agents (13.3%), opioid analgesics (6.8%), antiplatelets (6.6%), renin-angiotensin system inhibitors (3.5%), antineoplastic agents (3%) and sedative/hypnotics (3%). Since 2005-2006, the proportions of ED visits for ADEs involving anticoagulants, antiplatelets, and diabetic agents have increased, whereas proportions involving antibiotics have decreased.
In children aged 5 years or younger, antibiotics were the most common drug class (56.4; 95% CI, 51.8-61). Among children and adolescents aged 6-19 years, antibiotics also were the most common class (31.8%; 95% CI, 28.7-34.9), followed by antipsychotics (4.5%; 95% CI, 3.3-5.6).
Among older adults, three drug classes recently targeted by federal patient safety initiatives (anticoagulants, diabetes agents, and opioid analgesics) were implicated in an estimated 59.9% (95% CI, 56.8-62.9) of ED visits. Four anticoagulants (warfarin, rivaroxaban, dabigatran, and enoxaparin) and five diabetes agents (insulin and four oral agents) were among the 15 most common drugs implicated. Medications to always avoid in older adults according to Beers criteria were implicated in 1.8% (95% CI, 1.5-2.1) of ED visits for adverse drug events.
Summary: The most common drug classes implicated in ED visits for ADEs in the United States are the same ones identified a decade ago – anticoagulants, antibiotics, diabetes agents, and opioid analgesics. The proportion of ED visits for ADEs involving anticoagulants has increased during the last decade with increased anticoagulant use. The prevalence of potentially inappropriate medication use in older patients also remains high.
Citation: JAMA. 2016;316(20):2115-25. doi: 10.1001/jama.2016.16201.
Dr. Patel is a hospitalist in the division of hospital medicine and assistant professor of medicine at Cooper Medical School of Rowan University, Camden, N.J. He is CMSRU’s associate residency program director and serves as codirector of the Foundation of Medical Practice curriculum.
Clinical question: The purpose of this study was to describe emergency department (ED) visits for adverse drug events in year 2013-2014 compared to year 2005-2006 to learn changing patterns of ADEs and to help advance medication safety initiatives in outpatient settings.
Background: Adverse drug events (ADEs) are the most common cause of iatrogenic harm to patients and there have been significant national-level initiatives to prevent them as a part of patient safety. In the outpatient setting, where 90% of prescription drug expenditures occur, preventing ADEs remains a patient safety challenge because patients can have complex medication regimens, at times prescribed by multiple clinicians, with far less monitoring compared with hospitalized patients.
Setting and study design: Active, public health surveillance in 58 EDs in the United States that participate in the National Electronic Injury Surveillance System–Cooperative Adverse Drug Event Surveillance Project (NEISS-CADES). Trained data abstractors at each hospital reviewed each ED visit to identify any clinician-diagnosed ADEs that were the reason for the ED visit. Reports were coded by CDC and analyzed.
Synopsis: Based on 42,585 cases, 4.0 (95% CI, 3.1-5) ED visits for ADEs per 1,000 individuals occurred annually in the United States in 2013-2014 and 27.3% (22.2%-32.4%) of ED visits for ADEs resulted in hospitalization.
An estimated 34.5 % (95% CI, 30.3-38.8) of ED visits for ADEs occurred among adults aged 65 or older in 2013 compared with an estimated 25.6% (95% CI, 21-30) in 2005-2006. The population rate for adults older than 65 years was 9.7 visits per 1,000 individuals, compared with 3.1 visits per 1,000 individuals for those younger than 65 years. Older adults experienced higher hospitalization rates 43.6% (95% CI, 36.6-50.5). When adjusted for the U.S. population, the hospitalization rate for ADEs among older individuals was seven times higher compared with younger patients.
A single medication was implicated in most ED visits for ADEs (83.8%; 95% CI, 81.5-86.1). Supratherapeutic effects of ingestion of excess dose was the most common type of ADE (37.2%; 95% CI, 34.7-39.6). Medication errors were documented in 1 of 10 ED visits for ADEs (10.5%; 95% CI, 8.9-12.2).
The most commonly implicated drug classes were anticoagulants (17.6%), systemic antibiotics (16.1%), diabetes agents (13.3%), opioid analgesics (6.8%), antiplatelets (6.6%), renin-angiotensin system inhibitors (3.5%), antineoplastic agents (3%) and sedative/hypnotics (3%). Since 2005-2006, the proportions of ED visits for ADEs involving anticoagulants, antiplatelets, and diabetic agents have increased, whereas proportions involving antibiotics have decreased.
In children aged 5 years or younger, antibiotics were the most common drug class (56.4; 95% CI, 51.8-61). Among children and adolescents aged 6-19 years, antibiotics also were the most common class (31.8%; 95% CI, 28.7-34.9), followed by antipsychotics (4.5%; 95% CI, 3.3-5.6).
Among older adults, three drug classes recently targeted by federal patient safety initiatives (anticoagulants, diabetes agents, and opioid analgesics) were implicated in an estimated 59.9% (95% CI, 56.8-62.9) of ED visits. Four anticoagulants (warfarin, rivaroxaban, dabigatran, and enoxaparin) and five diabetes agents (insulin and four oral agents) were among the 15 most common drugs implicated. Medications to always avoid in older adults according to Beers criteria were implicated in 1.8% (95% CI, 1.5-2.1) of ED visits for adverse drug events.
Summary: The most common drug classes implicated in ED visits for ADEs in the United States are the same ones identified a decade ago – anticoagulants, antibiotics, diabetes agents, and opioid analgesics. The proportion of ED visits for ADEs involving anticoagulants has increased during the last decade with increased anticoagulant use. The prevalence of potentially inappropriate medication use in older patients also remains high.
Citation: JAMA. 2016;316(20):2115-25. doi: 10.1001/jama.2016.16201.
Dr. Patel is a hospitalist in the division of hospital medicine and assistant professor of medicine at Cooper Medical School of Rowan University, Camden, N.J. He is CMSRU’s associate residency program director and serves as codirector of the Foundation of Medical Practice curriculum.
Staying the course after first progression yields better mRCC survival
AMSTERDAM – Patients with metastatic renal cell carcinoma (mRCC) who experience disease progression in one or more metastatic sites while on treatment with a targeted therapy may still benefit from staying on the same drug rather than switching to another following locoregional treatment, results of a retrospective study suggest.
Among 55 patients with RCC, those who continued on the same targeted therapy after locoregional treatment of a site of progression had significantly longer post–first oligoprogression overall survival (PFOPOS) than patients who had been switched to another targeted agent, reported Della De Lisi, MD, from the University of Rome and colleagues.
“Locoregional treatments represent an option for oligometastatic mRCC treated with targeted therapy. Continuing the same systemic treatment after radical locoregional treatment in one or more metastatic site[s] appear[s] to be an independent predictive factor of better outcome in this subset of patients. Bone oligoprogressive mRCC showed similar better outcome[s].” they wrote in a poster presented at an annual congress sponsored by the European Cancer Organisation.
One option for patients with mRCC with slow or limited metastatic progression is locoregional therapy with radical intent, with the goal of achieving a complete response. When a patient’s disease progresses while on a targeted agent such as sorafenib (Nexavar) or sunitinib(Sutent), he or she may be switched to a different agent, but there is a lack of data on outcomes with this strategy, the authors said.
To see whether sticking with the same therapy or switching to another could be the wiser course, they took a retrospective look at outcomes for 55 patients with mRCC who had disease progression after at least 6 months of a first-line therapy in one or more sites treated radically with locoregional therapy.
The majority of patients (52 of 55; 94.5%) had clear-cell histology tumors. Slightly more than half (31 patients, 56.4%) had good risk disease according to the Memorial Sloan Kettering Cancer Center kidney cancer risk prediction tool, and 23 (41.8%) had intermediate risk. The risk category was not calculable for the one remaining patient.
In all, 36 patients (65.5%) did not have evidence of metastasis at diagnosis. All patients had oligoprogression in a single site. The most common metastatic sites were to lung in 15 patients, bone in 10, kidney in 8, brain in 4, and liver in 4 (other sites not listed).
Forty-eight patients received sunitinib in the first line, five received pazopanib (Votrient), and two received sorafenib. Locoregional therapy at the site of progression was radiotherapy in 25 patients (45.5%), surgery in 25, and cryoablation or thermoablation in 5.
The majority of patients (48; 83.6%) remained on the same tyrosine kinase inhibitor (TKI) after locoregional therapy, while 7 were switched to another agent. Of this latter group, four patients were switched to a different TKI, and three were started on a mammalian target of rapamycin (mTOR) inhibitor.
For all patients, the median PFOPOS was 37 months. However, comparing patients who continued the same therapy after locoregional treatment with those who switched, the investigators found a significant survival advantage to sticking with the same therapy, with a median PFOPOS of 39 months, compared with 11 months for patients who were switched to another agent (P = .014)
Other factors contributing to improved survival were good vs. intermediate risk score (39 vs. 29 months; P = .036), metastases to bone vs. viscera (median PFOPOS not reached, vs. 31 months; P = .045), and Fuhrman grade 1 and 2 vs. grade 3 and 4 (57 vs. 37 months; P = .021).
Switching therapies after first progression was an independent risk factor for poor prognosis in a multivariate analysis (hazard ratio 6.280, P = .007).
An analysis of progression-free survival (PFS) after first oligoprogression showed an overall PFS of 14 months. There were no statistically significant differences in terms of post-progression PFS between patients who stayed on the same therapy or were switched, however (15 vs. 7 months, P = .207).
The study was sponsored by participating institutions. The authors reported no conflicts of interest.
AMSTERDAM – Patients with metastatic renal cell carcinoma (mRCC) who experience disease progression in one or more metastatic sites while on treatment with a targeted therapy may still benefit from staying on the same drug rather than switching to another following locoregional treatment, results of a retrospective study suggest.
Among 55 patients with RCC, those who continued on the same targeted therapy after locoregional treatment of a site of progression had significantly longer post–first oligoprogression overall survival (PFOPOS) than patients who had been switched to another targeted agent, reported Della De Lisi, MD, from the University of Rome and colleagues.
“Locoregional treatments represent an option for oligometastatic mRCC treated with targeted therapy. Continuing the same systemic treatment after radical locoregional treatment in one or more metastatic site[s] appear[s] to be an independent predictive factor of better outcome in this subset of patients. Bone oligoprogressive mRCC showed similar better outcome[s].” they wrote in a poster presented at an annual congress sponsored by the European Cancer Organisation.
One option for patients with mRCC with slow or limited metastatic progression is locoregional therapy with radical intent, with the goal of achieving a complete response. When a patient’s disease progresses while on a targeted agent such as sorafenib (Nexavar) or sunitinib(Sutent), he or she may be switched to a different agent, but there is a lack of data on outcomes with this strategy, the authors said.
To see whether sticking with the same therapy or switching to another could be the wiser course, they took a retrospective look at outcomes for 55 patients with mRCC who had disease progression after at least 6 months of a first-line therapy in one or more sites treated radically with locoregional therapy.
The majority of patients (52 of 55; 94.5%) had clear-cell histology tumors. Slightly more than half (31 patients, 56.4%) had good risk disease according to the Memorial Sloan Kettering Cancer Center kidney cancer risk prediction tool, and 23 (41.8%) had intermediate risk. The risk category was not calculable for the one remaining patient.
In all, 36 patients (65.5%) did not have evidence of metastasis at diagnosis. All patients had oligoprogression in a single site. The most common metastatic sites were to lung in 15 patients, bone in 10, kidney in 8, brain in 4, and liver in 4 (other sites not listed).
Forty-eight patients received sunitinib in the first line, five received pazopanib (Votrient), and two received sorafenib. Locoregional therapy at the site of progression was radiotherapy in 25 patients (45.5%), surgery in 25, and cryoablation or thermoablation in 5.
The majority of patients (48; 83.6%) remained on the same tyrosine kinase inhibitor (TKI) after locoregional therapy, while 7 were switched to another agent. Of this latter group, four patients were switched to a different TKI, and three were started on a mammalian target of rapamycin (mTOR) inhibitor.
For all patients, the median PFOPOS was 37 months. However, comparing patients who continued the same therapy after locoregional treatment with those who switched, the investigators found a significant survival advantage to sticking with the same therapy, with a median PFOPOS of 39 months, compared with 11 months for patients who were switched to another agent (P = .014)
Other factors contributing to improved survival were good vs. intermediate risk score (39 vs. 29 months; P = .036), metastases to bone vs. viscera (median PFOPOS not reached, vs. 31 months; P = .045), and Fuhrman grade 1 and 2 vs. grade 3 and 4 (57 vs. 37 months; P = .021).
Switching therapies after first progression was an independent risk factor for poor prognosis in a multivariate analysis (hazard ratio 6.280, P = .007).
An analysis of progression-free survival (PFS) after first oligoprogression showed an overall PFS of 14 months. There were no statistically significant differences in terms of post-progression PFS between patients who stayed on the same therapy or were switched, however (15 vs. 7 months, P = .207).
The study was sponsored by participating institutions. The authors reported no conflicts of interest.
AMSTERDAM – Patients with metastatic renal cell carcinoma (mRCC) who experience disease progression in one or more metastatic sites while on treatment with a targeted therapy may still benefit from staying on the same drug rather than switching to another following locoregional treatment, results of a retrospective study suggest.
Among 55 patients with RCC, those who continued on the same targeted therapy after locoregional treatment of a site of progression had significantly longer post–first oligoprogression overall survival (PFOPOS) than patients who had been switched to another targeted agent, reported Della De Lisi, MD, from the University of Rome and colleagues.
“Locoregional treatments represent an option for oligometastatic mRCC treated with targeted therapy. Continuing the same systemic treatment after radical locoregional treatment in one or more metastatic site[s] appear[s] to be an independent predictive factor of better outcome in this subset of patients. Bone oligoprogressive mRCC showed similar better outcome[s].” they wrote in a poster presented at an annual congress sponsored by the European Cancer Organisation.
One option for patients with mRCC with slow or limited metastatic progression is locoregional therapy with radical intent, with the goal of achieving a complete response. When a patient’s disease progresses while on a targeted agent such as sorafenib (Nexavar) or sunitinib(Sutent), he or she may be switched to a different agent, but there is a lack of data on outcomes with this strategy, the authors said.
To see whether sticking with the same therapy or switching to another could be the wiser course, they took a retrospective look at outcomes for 55 patients with mRCC who had disease progression after at least 6 months of a first-line therapy in one or more sites treated radically with locoregional therapy.
The majority of patients (52 of 55; 94.5%) had clear-cell histology tumors. Slightly more than half (31 patients, 56.4%) had good risk disease according to the Memorial Sloan Kettering Cancer Center kidney cancer risk prediction tool, and 23 (41.8%) had intermediate risk. The risk category was not calculable for the one remaining patient.
In all, 36 patients (65.5%) did not have evidence of metastasis at diagnosis. All patients had oligoprogression in a single site. The most common metastatic sites were to lung in 15 patients, bone in 10, kidney in 8, brain in 4, and liver in 4 (other sites not listed).
Forty-eight patients received sunitinib in the first line, five received pazopanib (Votrient), and two received sorafenib. Locoregional therapy at the site of progression was radiotherapy in 25 patients (45.5%), surgery in 25, and cryoablation or thermoablation in 5.
The majority of patients (48; 83.6%) remained on the same tyrosine kinase inhibitor (TKI) after locoregional therapy, while 7 were switched to another agent. Of this latter group, four patients were switched to a different TKI, and three were started on a mammalian target of rapamycin (mTOR) inhibitor.
For all patients, the median PFOPOS was 37 months. However, comparing patients who continued the same therapy after locoregional treatment with those who switched, the investigators found a significant survival advantage to sticking with the same therapy, with a median PFOPOS of 39 months, compared with 11 months for patients who were switched to another agent (P = .014)
Other factors contributing to improved survival were good vs. intermediate risk score (39 vs. 29 months; P = .036), metastases to bone vs. viscera (median PFOPOS not reached, vs. 31 months; P = .045), and Fuhrman grade 1 and 2 vs. grade 3 and 4 (57 vs. 37 months; P = .021).
Switching therapies after first progression was an independent risk factor for poor prognosis in a multivariate analysis (hazard ratio 6.280, P = .007).
An analysis of progression-free survival (PFS) after first oligoprogression showed an overall PFS of 14 months. There were no statistically significant differences in terms of post-progression PFS between patients who stayed on the same therapy or were switched, however (15 vs. 7 months, P = .207).
The study was sponsored by participating institutions. The authors reported no conflicts of interest.
AT ECCO 2017
Key clinical point: Patients with metastatic renal cell carcinoma (mRCC) who stayed on the same targeted therapy following locoregional treatment after first progression had better overall survival than those who were switched to another drug.
Major finding: Median post–first oligoprogression overall survival was 39 months for patients who stayed on the same drug, compared with 11 months for patients who were switched (P = .014).
Data source: Retrospective review of outcomes for 55 patients with mRCC treated with targeted therapy and locoregional treatment of metastases.
Disclosures: The study was sponsored by participating institutions. The authors reported no conflicts of interest.
Familial and sporadic ankylosing spondylitis differ in small ways
While differences do exist between familial and sporadic ankylosing spondylitis, key similarities suggest that the two conditions can be treated the same way, according to a new study presented at the annual meeting of the Canadian Rheumatology Association.
“AS [ankylosing spondylitis] patients with a family history of AS are not very different from patients without any family history,” Nigil Haroon, MD, of the University Health Network in Toronto, explained in an interview. “They have similar disease activity as measured by markers of inflammation [and] similar disease severity as assessed by radiographic scoring for spinal damage.”
Dr. Haroon, along with his coinvestigators – including Bruce Sheng, MD,of the same institution, who presented the study at the meeting – prospectively followed AS patients satisfying the New York criteria for a period of 15 years, collecting data on 888 eligible subjects who were eventually included in the study. Of the subjects included, 74% were male, the average age was 45.6 years (standard deviation, 13.7 years), and average disease duration was 15 years (SD, 11.5 years).
The investigators found some similarities between the 177 (20%) patients with familial AS who had at least one first- or second-generation relative with the disease and the 711 with sporadic AS. Anti–tumor necrosis factor (anti-TNF) treatment failed in 23.1% of familial AS patients and 23.6% of sporadic disease patients based on the lack of a “sustained clinical effect” for more than 1 year. There were also no differences found between the groups in clinical and radiographic severity of disease.
However, patients with familial AS did record earlier onset of disease (22.5 years vs. 24.3 years; P = .016), longer disease duration (17.4 years vs. 14.3 years; P = .003), and higher HLA-B27 positivity (90% vs. 65%; P less than .001), along with higher rates of uveitis, psoriatic arthritis, and inflammatory bowel disease.
“Some of the findings are expected, including the higher prevalence of HLA-B27 due to gene sharing in the family. ... The higher B27 sharing may also affect the uveitis prevalence as well in familial AS,” Dr. Haroon explained. “The similar radiographic progression rates and treatment responses are interesting findings.”
In terms of the ramifications of these findings, Dr. Haroon stated that clinicians should reevaluate how they prescribe drugs to their AS patients.
“The high likelihood of uveitis in familial AS patients – 43% versus 29% – may affect the choice of treatment as all drugs are not equally effective in uveitis,” he said. “As the family history of extra-articular manifestations is high in familial AS, it remains to be seen if a lower threshold for investigating symptoms suggestive of IBD/uveitis will decrease delays in diagnosis of these conditions in individuals with a family history of AS.”
Moving forward from here, Dr. Haroon called for family studies, especially those including families with multiple individuals affected with AS, as these can help identify genetic risk factors that may be contribute to the development of AS.
“There is paucity of data on familial AS,” Dr. Haroon said. “The strength of this study is the large dataset.”
The study was funded by the Canadian Rheumatology Association’s Summer Research Program, which supported Dr. Sheng. Dr. Sheng and Dr. Haroon did not report any other relevant financial disclosures.
While differences do exist between familial and sporadic ankylosing spondylitis, key similarities suggest that the two conditions can be treated the same way, according to a new study presented at the annual meeting of the Canadian Rheumatology Association.
“AS [ankylosing spondylitis] patients with a family history of AS are not very different from patients without any family history,” Nigil Haroon, MD, of the University Health Network in Toronto, explained in an interview. “They have similar disease activity as measured by markers of inflammation [and] similar disease severity as assessed by radiographic scoring for spinal damage.”
Dr. Haroon, along with his coinvestigators – including Bruce Sheng, MD,of the same institution, who presented the study at the meeting – prospectively followed AS patients satisfying the New York criteria for a period of 15 years, collecting data on 888 eligible subjects who were eventually included in the study. Of the subjects included, 74% were male, the average age was 45.6 years (standard deviation, 13.7 years), and average disease duration was 15 years (SD, 11.5 years).
The investigators found some similarities between the 177 (20%) patients with familial AS who had at least one first- or second-generation relative with the disease and the 711 with sporadic AS. Anti–tumor necrosis factor (anti-TNF) treatment failed in 23.1% of familial AS patients and 23.6% of sporadic disease patients based on the lack of a “sustained clinical effect” for more than 1 year. There were also no differences found between the groups in clinical and radiographic severity of disease.
However, patients with familial AS did record earlier onset of disease (22.5 years vs. 24.3 years; P = .016), longer disease duration (17.4 years vs. 14.3 years; P = .003), and higher HLA-B27 positivity (90% vs. 65%; P less than .001), along with higher rates of uveitis, psoriatic arthritis, and inflammatory bowel disease.
“Some of the findings are expected, including the higher prevalence of HLA-B27 due to gene sharing in the family. ... The higher B27 sharing may also affect the uveitis prevalence as well in familial AS,” Dr. Haroon explained. “The similar radiographic progression rates and treatment responses are interesting findings.”
In terms of the ramifications of these findings, Dr. Haroon stated that clinicians should reevaluate how they prescribe drugs to their AS patients.
“The high likelihood of uveitis in familial AS patients – 43% versus 29% – may affect the choice of treatment as all drugs are not equally effective in uveitis,” he said. “As the family history of extra-articular manifestations is high in familial AS, it remains to be seen if a lower threshold for investigating symptoms suggestive of IBD/uveitis will decrease delays in diagnosis of these conditions in individuals with a family history of AS.”
Moving forward from here, Dr. Haroon called for family studies, especially those including families with multiple individuals affected with AS, as these can help identify genetic risk factors that may be contribute to the development of AS.
“There is paucity of data on familial AS,” Dr. Haroon said. “The strength of this study is the large dataset.”
The study was funded by the Canadian Rheumatology Association’s Summer Research Program, which supported Dr. Sheng. Dr. Sheng and Dr. Haroon did not report any other relevant financial disclosures.
While differences do exist between familial and sporadic ankylosing spondylitis, key similarities suggest that the two conditions can be treated the same way, according to a new study presented at the annual meeting of the Canadian Rheumatology Association.
“AS [ankylosing spondylitis] patients with a family history of AS are not very different from patients without any family history,” Nigil Haroon, MD, of the University Health Network in Toronto, explained in an interview. “They have similar disease activity as measured by markers of inflammation [and] similar disease severity as assessed by radiographic scoring for spinal damage.”
Dr. Haroon, along with his coinvestigators – including Bruce Sheng, MD,of the same institution, who presented the study at the meeting – prospectively followed AS patients satisfying the New York criteria for a period of 15 years, collecting data on 888 eligible subjects who were eventually included in the study. Of the subjects included, 74% were male, the average age was 45.6 years (standard deviation, 13.7 years), and average disease duration was 15 years (SD, 11.5 years).
The investigators found some similarities between the 177 (20%) patients with familial AS who had at least one first- or second-generation relative with the disease and the 711 with sporadic AS. Anti–tumor necrosis factor (anti-TNF) treatment failed in 23.1% of familial AS patients and 23.6% of sporadic disease patients based on the lack of a “sustained clinical effect” for more than 1 year. There were also no differences found between the groups in clinical and radiographic severity of disease.
However, patients with familial AS did record earlier onset of disease (22.5 years vs. 24.3 years; P = .016), longer disease duration (17.4 years vs. 14.3 years; P = .003), and higher HLA-B27 positivity (90% vs. 65%; P less than .001), along with higher rates of uveitis, psoriatic arthritis, and inflammatory bowel disease.
“Some of the findings are expected, including the higher prevalence of HLA-B27 due to gene sharing in the family. ... The higher B27 sharing may also affect the uveitis prevalence as well in familial AS,” Dr. Haroon explained. “The similar radiographic progression rates and treatment responses are interesting findings.”
In terms of the ramifications of these findings, Dr. Haroon stated that clinicians should reevaluate how they prescribe drugs to their AS patients.
“The high likelihood of uveitis in familial AS patients – 43% versus 29% – may affect the choice of treatment as all drugs are not equally effective in uveitis,” he said. “As the family history of extra-articular manifestations is high in familial AS, it remains to be seen if a lower threshold for investigating symptoms suggestive of IBD/uveitis will decrease delays in diagnosis of these conditions in individuals with a family history of AS.”
Moving forward from here, Dr. Haroon called for family studies, especially those including families with multiple individuals affected with AS, as these can help identify genetic risk factors that may be contribute to the development of AS.
“There is paucity of data on familial AS,” Dr. Haroon said. “The strength of this study is the large dataset.”
The study was funded by the Canadian Rheumatology Association’s Summer Research Program, which supported Dr. Sheng. Dr. Sheng and Dr. Haroon did not report any other relevant financial disclosures.
FROM THE CRA SCIENTIFIC CONFERENCE
Key clinical point:
Major finding: Anti-TNF treatment failed in 23.1% of familial AS patients and 23.6% of sporadic disease patients based on the lack of a “sustained clinical effect” for more than 1 year.
Data source: Prospective cohort study of 888 patients with AS over 15 years.
Disclosures: Funded by the Canadian Rheumatology Association’s Summer Research Program. No other relevant disclosures were reported.
Strategies for preventing and detecting false-negatives in urine drug screens
Urine drug screening (UDS) is an important tool in emergency settings and substance abuse or pain management clinics. According to the 2015 National Survey on Drug Use and Health, 9.2% of individuals age ≥12 used an illicit drug other than marijuana within the previous year.1
There are 2 types of UDS: gas chromatography–mass spectroscopy (GC-MS) and enzymatic immunoassay (EIA). A GC-MS uses a 2-step mechanisms to detect chemical compounds. First the GC separate the illicit substance into molecules, which is then introduced to the MS, which then separates compounds depending on their mass and charge using magnetic fields.2,3 Although GC-MS is a more definitive means to confirm the presence of a specific drug, it rarely is used in clinical settings because it is expensive and time-consuming.
EIA is an anti-drug antibody added to the patient’s urine that causes a positive indicator reaction that can be measured.2,3 It is a rapid, accurate, and cost-effective way of detecting illicit substances.4 However, there are limitations to EIAs used in most hospital laboratories.
Limitations of EIAs
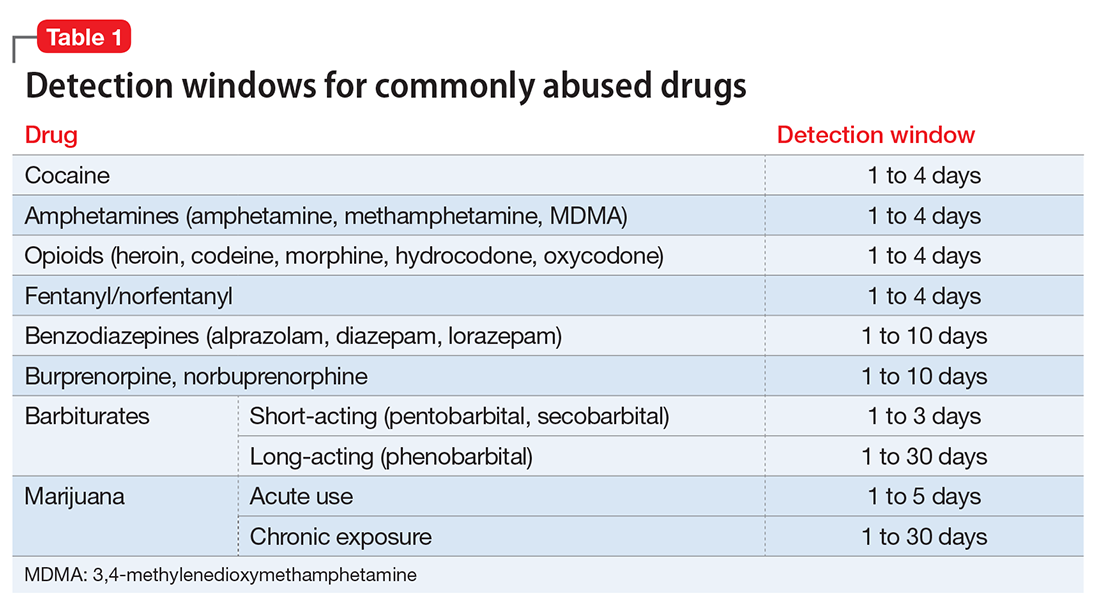
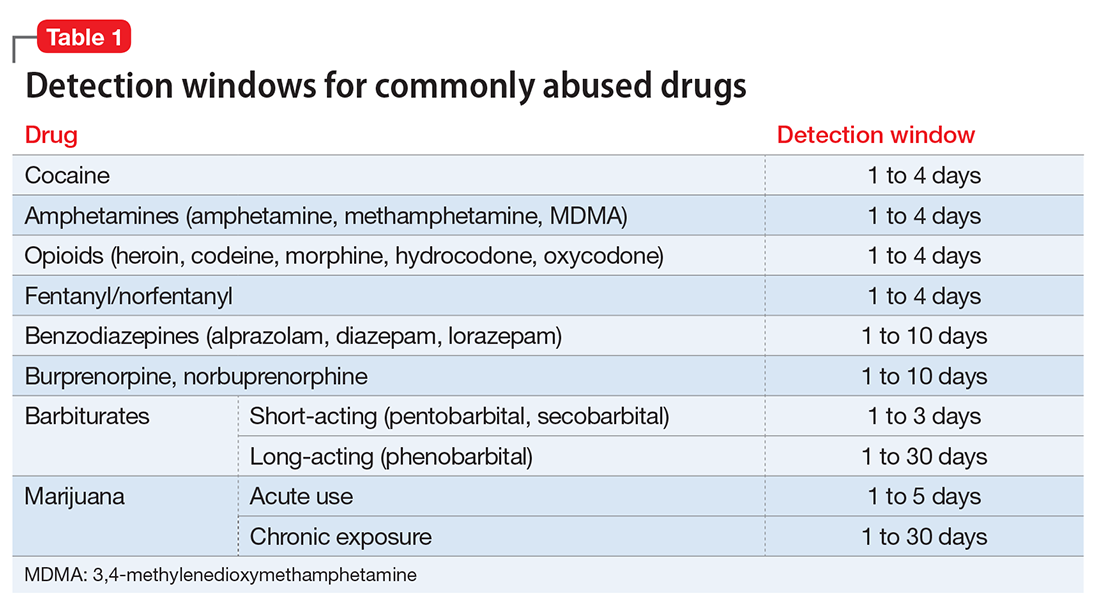
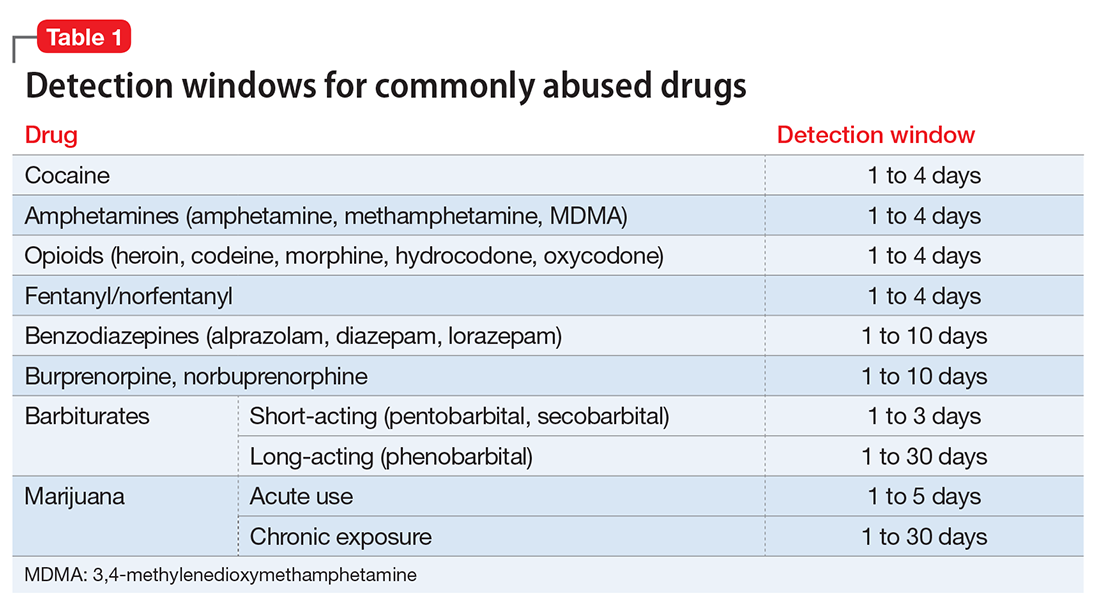
Timing. Results of the drug screen depend on the time and frequency of drug use (Table 1).5
Sensitivity. The immunoassay methods used vary in their ability to detect substances and depend on the test’s sensitivity; however, most of these versions have high sensitivity for detecting many illicit substances.4
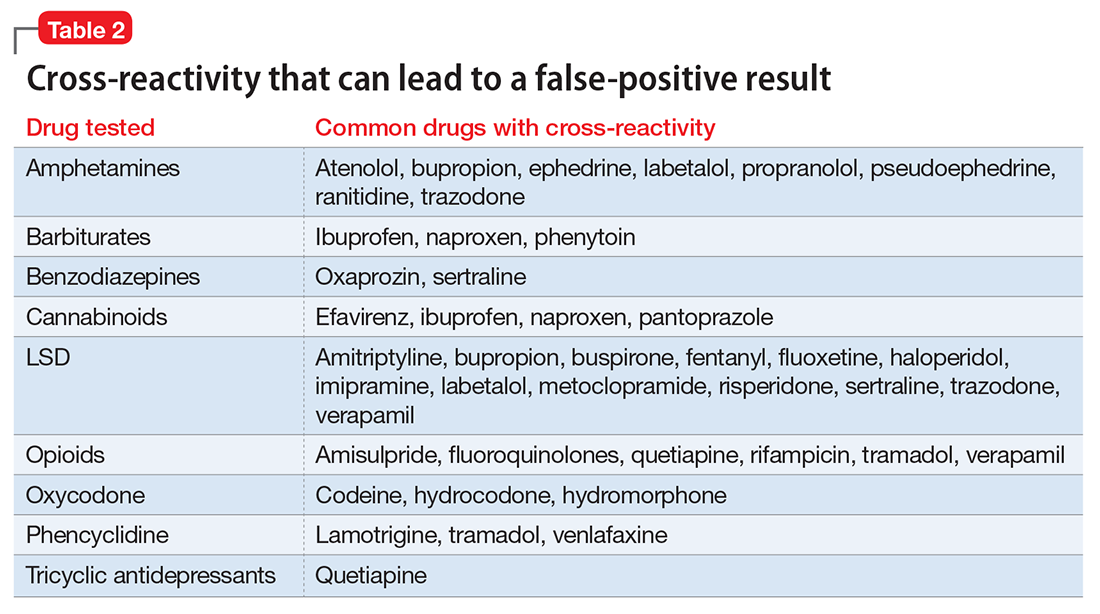
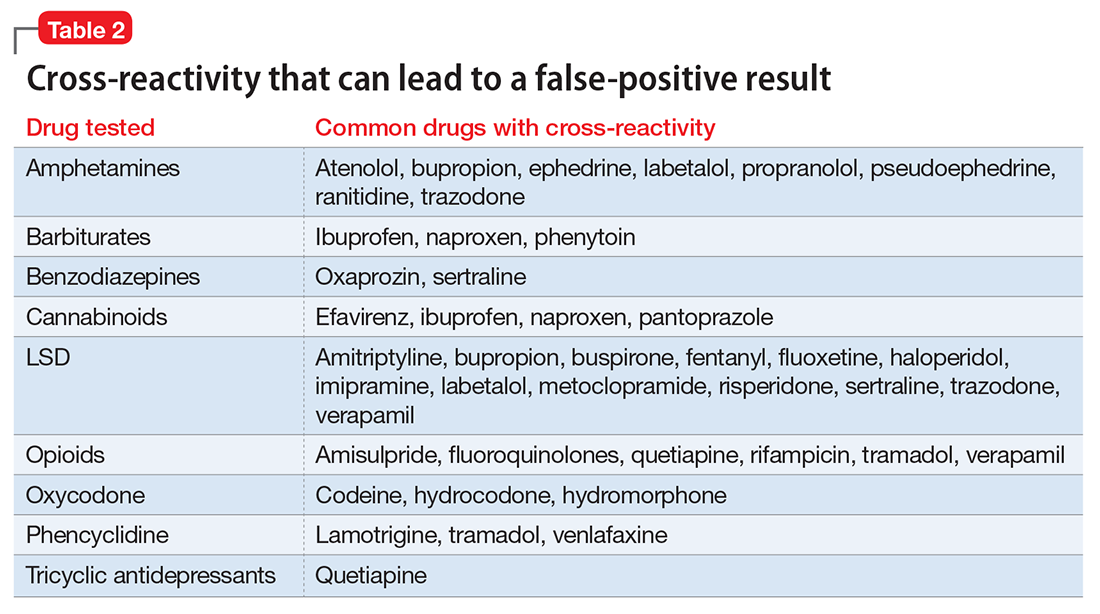
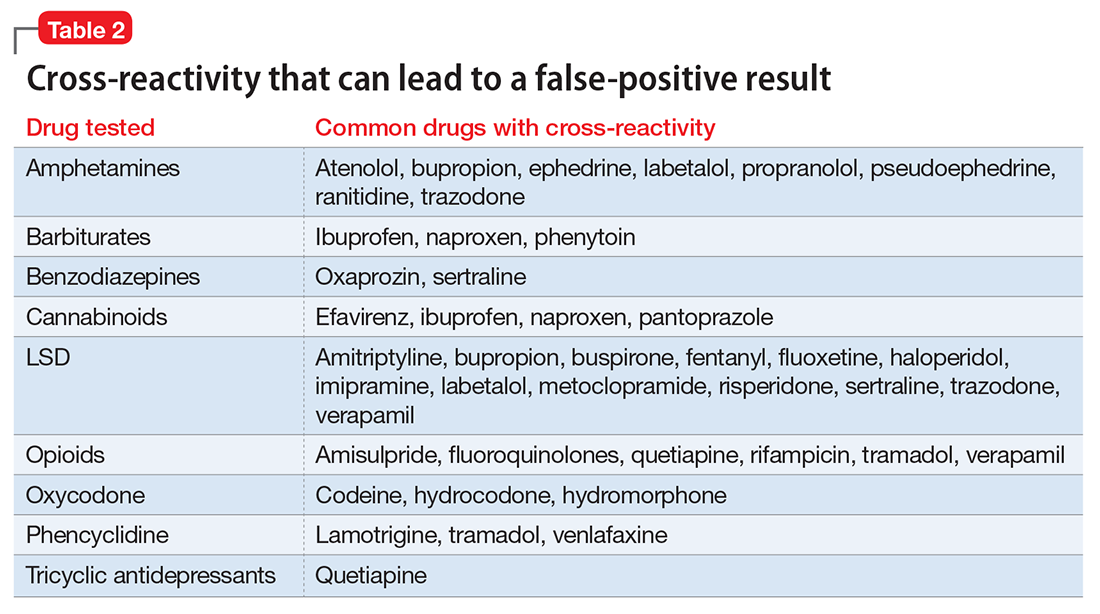
Specificity and cross-reactivity. Unfortunately, many drugs, such as opioids, amphetamines, and commonly prescribed medications, exhibit cross-reactivity that can produce false-positive results (Table 2).5,6
Synthetic cannabinoids, such as “spice” and cathinones, also known as “bath salts,” cannot be detected with standard UDS. However, some newer EIA kits can detect synthetic cannabinoids but do not detect newer designer drugs.7 Detection of specific cathinones by EIA is not yet available.7
Preventing false-negatives
Substance abusing individuals could try to avoid detection of illicit drug use by using the following techniques:
- In vivo methods, such as drinking a large amount of water or using herbal products, can lead to false-negative results because of dilution.8
- In vitro adulterants are substances added to urine samples after urination to avoid drug detection. Active ingredients include glutaraldehyde (Clean-X), sodium or potassium nitrate (Klear, Whizzies), pyridinium chlorochromate (Urine Luck), andj (Stealth).9
- Other methods used to avoid drug detection include substituting a urine sample with someone else’s clean urine or adding household products, such as bleach, vinegar, or pipe cleaner.
You can spot and prevent false-negatives by:
Directly observing the patient, which helps to prevent individuals from adding foreign materials or substituting the urine sample.
Visually inspecting the urine helps identify sample tampering. Adding household adulterants can produce unusually bubbly, cloudy, clear, or dark sample.
On-site analyses and laboratory analyses of samples. Commercially sold kits can detect adulterants by on-site analysis, such as Intect 7 and AdultaCheck 4 test strips.9 Simple on-site methods can help discover tampering, such as measuring the urine’s temperature and using pigmented toilet water. The U.S. Substance Abuse and Mental Health Services Administration recommends validity checks during laboratory analysis for all urine samples, including temperature, creatinine, specific gravity, pH, and tests for oxidizing adulterants.10
Considerations
The results of UDS should not be interpreted as absolute. Knowing the sensitivity and specificity of the UDS that your institution uses and the patient’s current medication regimen is valuable in distinguishing between true results and false-positives. False-positives can strain the relationship between patient and provider, thus compromising care. When EIA is positive and patient denies substance use, confirming the result with GC-MS may be a good clinical practice.3 Ordering a GC-MS test can be helpful in situations requiring greater precision, such as in methadone or pain management clinics, to verify if the patient is taking a prescribed medication properly or to rule out illicit exposures with greater certainty.
Acknowledgment
The authors would like to thank Steven Lippmann, MD, for his mentorship, encouragement, and editorial support.
1. Substance Abuse and Mental Health Services Administration. Results from the National Survey on Drug Use and Health: detailed tables. Prevalence estimates, standard errors, P values, and sample sizes. https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015.pdf. Published September 8, 2016. Accessed February 7, 2017.
2. Schweitzer BN. An assessment of lateral flow immunoassay testing and gas chromatography mass spectrometry as methods for the detection of five drugs of abuse in forensic bloodstains. https://open.bu.edu/bitstream/handle/2144/19477/Schweitzer_bu_0017N_12357.pdf?sequence=1. Published 2016. Accessed February 7, 2017.
3. Pawlowski J, Ellingrod VL. Urine drug screens: when might a test result be false-positive? Current Psychiatry. 2015;14(10):17,22-24.
4. Tenore PL. Advanced urine toxicology testing. J Addict Dis. 2010;29(4):436-448.
5. AIT Laboratories. Physician’s reference for urine and blood drug testing and interpretation. http://web.archive.org/web/20160312195526/http://aitlabs.com/uploadedfiles/services/pocket_guide_smr086.pdf. Published 2011. Accessed February 7, 2017.
6. Saitman A, Park HD, Fitzgerald RL. False-positive interferences of common urine drug screen immunoassays: a review. J Anal Toxicol. 2014;38(7):387-396.
7. Namera A, Kawamura M, Nakamoto A, et al. Comprehensive review of the detection methods for synthetic cannabinoids and cathinones. Forensic Toxicol. 2015;33(2):175-194.
8. Cone EJ, Lange R, Darwin WD. In vivo adulteration: excess fluid ingestion causes false-negative marijuana and cocaine urine test results. J Anal Toxicol. 1998;22(6):460-473.
9. Jaffee WB, Trucco E, Levy S, et al. Is this urine really negative? A systematic review of tampering methods in urine drug screening and testing. J Subst Abuse Treat. 2007;33(1):33-42.
10. Substance Abuse and Mental Health Services Administration. Mandatory guidelines for federal workplace drug testing programs. Federal Register. 2004;69:19644-19673.
Urine drug screening (UDS) is an important tool in emergency settings and substance abuse or pain management clinics. According to the 2015 National Survey on Drug Use and Health, 9.2% of individuals age ≥12 used an illicit drug other than marijuana within the previous year.1
There are 2 types of UDS: gas chromatography–mass spectroscopy (GC-MS) and enzymatic immunoassay (EIA). A GC-MS uses a 2-step mechanisms to detect chemical compounds. First the GC separate the illicit substance into molecules, which is then introduced to the MS, which then separates compounds depending on their mass and charge using magnetic fields.2,3 Although GC-MS is a more definitive means to confirm the presence of a specific drug, it rarely is used in clinical settings because it is expensive and time-consuming.
EIA is an anti-drug antibody added to the patient’s urine that causes a positive indicator reaction that can be measured.2,3 It is a rapid, accurate, and cost-effective way of detecting illicit substances.4 However, there are limitations to EIAs used in most hospital laboratories.
Limitations of EIAs
Timing. Results of the drug screen depend on the time and frequency of drug use (Table 1).5
Sensitivity. The immunoassay methods used vary in their ability to detect substances and depend on the test’s sensitivity; however, most of these versions have high sensitivity for detecting many illicit substances.4
Specificity and cross-reactivity. Unfortunately, many drugs, such as opioids, amphetamines, and commonly prescribed medications, exhibit cross-reactivity that can produce false-positive results (Table 2).5,6
Synthetic cannabinoids, such as “spice” and cathinones, also known as “bath salts,” cannot be detected with standard UDS. However, some newer EIA kits can detect synthetic cannabinoids but do not detect newer designer drugs.7 Detection of specific cathinones by EIA is not yet available.7
Preventing false-negatives
Substance abusing individuals could try to avoid detection of illicit drug use by using the following techniques:
- In vivo methods, such as drinking a large amount of water or using herbal products, can lead to false-negative results because of dilution.8
- In vitro adulterants are substances added to urine samples after urination to avoid drug detection. Active ingredients include glutaraldehyde (Clean-X), sodium or potassium nitrate (Klear, Whizzies), pyridinium chlorochromate (Urine Luck), andj (Stealth).9
- Other methods used to avoid drug detection include substituting a urine sample with someone else’s clean urine or adding household products, such as bleach, vinegar, or pipe cleaner.
You can spot and prevent false-negatives by:
Directly observing the patient, which helps to prevent individuals from adding foreign materials or substituting the urine sample.
Visually inspecting the urine helps identify sample tampering. Adding household adulterants can produce unusually bubbly, cloudy, clear, or dark sample.
On-site analyses and laboratory analyses of samples. Commercially sold kits can detect adulterants by on-site analysis, such as Intect 7 and AdultaCheck 4 test strips.9 Simple on-site methods can help discover tampering, such as measuring the urine’s temperature and using pigmented toilet water. The U.S. Substance Abuse and Mental Health Services Administration recommends validity checks during laboratory analysis for all urine samples, including temperature, creatinine, specific gravity, pH, and tests for oxidizing adulterants.10
Considerations
The results of UDS should not be interpreted as absolute. Knowing the sensitivity and specificity of the UDS that your institution uses and the patient’s current medication regimen is valuable in distinguishing between true results and false-positives. False-positives can strain the relationship between patient and provider, thus compromising care. When EIA is positive and patient denies substance use, confirming the result with GC-MS may be a good clinical practice.3 Ordering a GC-MS test can be helpful in situations requiring greater precision, such as in methadone or pain management clinics, to verify if the patient is taking a prescribed medication properly or to rule out illicit exposures with greater certainty.
Acknowledgment
The authors would like to thank Steven Lippmann, MD, for his mentorship, encouragement, and editorial support.
Urine drug screening (UDS) is an important tool in emergency settings and substance abuse or pain management clinics. According to the 2015 National Survey on Drug Use and Health, 9.2% of individuals age ≥12 used an illicit drug other than marijuana within the previous year.1
There are 2 types of UDS: gas chromatography–mass spectroscopy (GC-MS) and enzymatic immunoassay (EIA). A GC-MS uses a 2-step mechanisms to detect chemical compounds. First the GC separate the illicit substance into molecules, which is then introduced to the MS, which then separates compounds depending on their mass and charge using magnetic fields.2,3 Although GC-MS is a more definitive means to confirm the presence of a specific drug, it rarely is used in clinical settings because it is expensive and time-consuming.
EIA is an anti-drug antibody added to the patient’s urine that causes a positive indicator reaction that can be measured.2,3 It is a rapid, accurate, and cost-effective way of detecting illicit substances.4 However, there are limitations to EIAs used in most hospital laboratories.
Limitations of EIAs
Timing. Results of the drug screen depend on the time and frequency of drug use (Table 1).5
Sensitivity. The immunoassay methods used vary in their ability to detect substances and depend on the test’s sensitivity; however, most of these versions have high sensitivity for detecting many illicit substances.4
Specificity and cross-reactivity. Unfortunately, many drugs, such as opioids, amphetamines, and commonly prescribed medications, exhibit cross-reactivity that can produce false-positive results (Table 2).5,6
Synthetic cannabinoids, such as “spice” and cathinones, also known as “bath salts,” cannot be detected with standard UDS. However, some newer EIA kits can detect synthetic cannabinoids but do not detect newer designer drugs.7 Detection of specific cathinones by EIA is not yet available.7
Preventing false-negatives
Substance abusing individuals could try to avoid detection of illicit drug use by using the following techniques:
- In vivo methods, such as drinking a large amount of water or using herbal products, can lead to false-negative results because of dilution.8
- In vitro adulterants are substances added to urine samples after urination to avoid drug detection. Active ingredients include glutaraldehyde (Clean-X), sodium or potassium nitrate (Klear, Whizzies), pyridinium chlorochromate (Urine Luck), andj (Stealth).9
- Other methods used to avoid drug detection include substituting a urine sample with someone else’s clean urine or adding household products, such as bleach, vinegar, or pipe cleaner.
You can spot and prevent false-negatives by:
Directly observing the patient, which helps to prevent individuals from adding foreign materials or substituting the urine sample.
Visually inspecting the urine helps identify sample tampering. Adding household adulterants can produce unusually bubbly, cloudy, clear, or dark sample.
On-site analyses and laboratory analyses of samples. Commercially sold kits can detect adulterants by on-site analysis, such as Intect 7 and AdultaCheck 4 test strips.9 Simple on-site methods can help discover tampering, such as measuring the urine’s temperature and using pigmented toilet water. The U.S. Substance Abuse and Mental Health Services Administration recommends validity checks during laboratory analysis for all urine samples, including temperature, creatinine, specific gravity, pH, and tests for oxidizing adulterants.10
Considerations
The results of UDS should not be interpreted as absolute. Knowing the sensitivity and specificity of the UDS that your institution uses and the patient’s current medication regimen is valuable in distinguishing between true results and false-positives. False-positives can strain the relationship between patient and provider, thus compromising care. When EIA is positive and patient denies substance use, confirming the result with GC-MS may be a good clinical practice.3 Ordering a GC-MS test can be helpful in situations requiring greater precision, such as in methadone or pain management clinics, to verify if the patient is taking a prescribed medication properly or to rule out illicit exposures with greater certainty.
Acknowledgment
The authors would like to thank Steven Lippmann, MD, for his mentorship, encouragement, and editorial support.
1. Substance Abuse and Mental Health Services Administration. Results from the National Survey on Drug Use and Health: detailed tables. Prevalence estimates, standard errors, P values, and sample sizes. https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015.pdf. Published September 8, 2016. Accessed February 7, 2017.
2. Schweitzer BN. An assessment of lateral flow immunoassay testing and gas chromatography mass spectrometry as methods for the detection of five drugs of abuse in forensic bloodstains. https://open.bu.edu/bitstream/handle/2144/19477/Schweitzer_bu_0017N_12357.pdf?sequence=1. Published 2016. Accessed February 7, 2017.
3. Pawlowski J, Ellingrod VL. Urine drug screens: when might a test result be false-positive? Current Psychiatry. 2015;14(10):17,22-24.
4. Tenore PL. Advanced urine toxicology testing. J Addict Dis. 2010;29(4):436-448.
5. AIT Laboratories. Physician’s reference for urine and blood drug testing and interpretation. http://web.archive.org/web/20160312195526/http://aitlabs.com/uploadedfiles/services/pocket_guide_smr086.pdf. Published 2011. Accessed February 7, 2017.
6. Saitman A, Park HD, Fitzgerald RL. False-positive interferences of common urine drug screen immunoassays: a review. J Anal Toxicol. 2014;38(7):387-396.
7. Namera A, Kawamura M, Nakamoto A, et al. Comprehensive review of the detection methods for synthetic cannabinoids and cathinones. Forensic Toxicol. 2015;33(2):175-194.
8. Cone EJ, Lange R, Darwin WD. In vivo adulteration: excess fluid ingestion causes false-negative marijuana and cocaine urine test results. J Anal Toxicol. 1998;22(6):460-473.
9. Jaffee WB, Trucco E, Levy S, et al. Is this urine really negative? A systematic review of tampering methods in urine drug screening and testing. J Subst Abuse Treat. 2007;33(1):33-42.
10. Substance Abuse and Mental Health Services Administration. Mandatory guidelines for federal workplace drug testing programs. Federal Register. 2004;69:19644-19673.
1. Substance Abuse and Mental Health Services Administration. Results from the National Survey on Drug Use and Health: detailed tables. Prevalence estimates, standard errors, P values, and sample sizes. https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015.pdf. Published September 8, 2016. Accessed February 7, 2017.
2. Schweitzer BN. An assessment of lateral flow immunoassay testing and gas chromatography mass spectrometry as methods for the detection of five drugs of abuse in forensic bloodstains. https://open.bu.edu/bitstream/handle/2144/19477/Schweitzer_bu_0017N_12357.pdf?sequence=1. Published 2016. Accessed February 7, 2017.
3. Pawlowski J, Ellingrod VL. Urine drug screens: when might a test result be false-positive? Current Psychiatry. 2015;14(10):17,22-24.
4. Tenore PL. Advanced urine toxicology testing. J Addict Dis. 2010;29(4):436-448.
5. AIT Laboratories. Physician’s reference for urine and blood drug testing and interpretation. http://web.archive.org/web/20160312195526/http://aitlabs.com/uploadedfiles/services/pocket_guide_smr086.pdf. Published 2011. Accessed February 7, 2017.
6. Saitman A, Park HD, Fitzgerald RL. False-positive interferences of common urine drug screen immunoassays: a review. J Anal Toxicol. 2014;38(7):387-396.
7. Namera A, Kawamura M, Nakamoto A, et al. Comprehensive review of the detection methods for synthetic cannabinoids and cathinones. Forensic Toxicol. 2015;33(2):175-194.
8. Cone EJ, Lange R, Darwin WD. In vivo adulteration: excess fluid ingestion causes false-negative marijuana and cocaine urine test results. J Anal Toxicol. 1998;22(6):460-473.
9. Jaffee WB, Trucco E, Levy S, et al. Is this urine really negative? A systematic review of tampering methods in urine drug screening and testing. J Subst Abuse Treat. 2007;33(1):33-42.
10. Substance Abuse and Mental Health Services Administration. Mandatory guidelines for federal workplace drug testing programs. Federal Register. 2004;69:19644-19673.
Doctors, drug reps, and free speech
Question: The First Amendment guarantees the right of free speech, but the U.S. Supreme Court has held that under a strict scrutiny standard, the government may regulate:
A. Obscenity.
B. Fighting words.
C. Professional speech.
D. A and B.
E. A, B, and C.
Answer: D. The First Amendment forbids the government from “abridging the freedom of speech,” which extends to certain nonverbal conduct, such as flag burning. At the same time, the U.S. Supreme Court has also ruled that certain categories of speech such as obscenity and fighting words can be regulated under a strict scrutiny standard. However, it remains unsettled whether and to what extent professional speech – such as in the context of the doctor-patient relationship – may be curtailed.
Two recent cases grapple with this issue of free speech – with rather unexpected results.
The first, overturning a decades-old prohibition of the off-label detailing of drugs, surprisingly was decided against the government. The second challenges a Florida statute censoring the discussion of firearms safety between a doctor and a patient. An early decision, under reconsideration, in fact supported the state’s regulation of physicians’ freedom of speech under the circumstances.
Because the FDA has no jurisdiction over physician conduct, it has no power to regulate the off-label use of an otherwise approved drug, which explains why such off-label prescriptions are widespread, especially in the oncology field.
In U.S. v. Caronia, the defendant, a pharmaceutical sales representative, was criminally prosecuted and found guilty of conspiracy in a New York court for introducing a misbranded drug into interstate commerce.1 Specifically, Alfred Caronia promoted the drug Xyrem for use in a manner not approved by the FDA.
Orphan Medical, now known as Jazz Pharmaceuticals, is the manufacturer of Xyrem, a powerful central nervous system depressant. Xyrem’s active ingredient is gamma-hydroxybutyrate, which has been federally classified as the “date rape drug” for its use in the commission of sexual assaults. The FDA had approved Xyrem for two conditions: to treat narcolepsy patients who experience cataplexy, a condition associated with weak or paralyzed muscles; and to treat those with excessive daytime sleepiness.
Caronia was found to provide off-label detailing of the drug to doctors for unapproved indications such as chronic fatigue, fibromyalgia, restless leg syndrome, and Parkinson’s disease.
Caronia argued that in promoting an FDA-approved drug, albeit for off-label use, he was within his right of free speech under the First Amendment. In overturning his conviction, a three-judge panel of the U.S. Second Circuit Court of Appeals agreed, noting the overly broad FDA regulations and specifically that nothing Caronia did constituted conspiracy to put a false or misleading or deficient label on a drug product.
The court concluded: “The government cannot prosecute pharmaceutical manufacturers and their representatives under the FDCA [Federal Food, Drug, and Cosmetic Act] for speech promoting the lawful, off-label use of an FDA-approved drug.”
In 2011, the U.S. Supreme Court had used a First Amendment argument to invalidate a Vermont law that prohibited the practice of pharmaceutical data mining – purchasing information about prescribers from pharmacies and others.2
Taken together, the FDA now appears resigned to the free speech argument.3 For example, it has decided not to appeal a judge’s ruling that the First Amendment protects Amarin from promoting its fish-oil capsules for unapproved uses. Just recently, the FDA published a draft proposal in tacit acceptance of this new policy position, merely recommending the disclosure of relevant information including limitations and unfavorable or inconsistent findings surrounding the off-label use of a drug.
The next issue concerns professional speech. It is well documented that the presence of a gun in the home increases the risk of death especially by suicide, and this serves as the impetus for the long-established recommendation that physicians discuss firearm safety with their patients.
The medical profession was therefore aghast when Florida enacted its law on “Privacy of Firearm Owners.”4 Codified on June 2, 2011, it provides that a licensed practitioner or facility may not record firearm ownership information in a patient’s medical record, and that unless information is relevant to the patient’s medical care or safety or safety of others, inquiries regarding firearm ownership or possession should not be made. A practitioner is also forbidden from unnecessarily harassing a patient about firearm ownership during an examination.
Violation can result in disciplinary action; the original intent was to make this a third-degree felony with penalties of up to $5 million in fines and 5 years of imprisonment, but the final bill was stripped of criminal penalties.
In July 2015, a panel of three judges of the U.S. 11th Circuit Court of Appeals, in a split 2-1 decision, found that the inquiry, record-keeping, and harassment provisions of the act specifically regulate professional speech, which is subject to an intermediate level of scrutiny. Under this level of scrutiny, the court found that the act was precisely tailored to directly advance the state’s substantial interests in protecting the public and patient privacy rights.
Holding that the act was not so overly broad as to violate the First Amendment, the court ruled that laws regulating speech that occurs in the course of the physician-patient relationship are constitutional if they directly advance a substantial state interest.5
Predictably, several medical societies, including the AMA, have filed briefs arguing that the law is unconstitutional and intrudes on the practice of medicine. Effective medical care is believed to require “unfettered communications” between physicians and their patients. Besides, the law is at odds with the AMA’s longstanding policy that encourages members to inquire into the presence of firearms in households and to promote the use of safety locks on guns in an effort to reduce injuries to children.
On June 21, 2016, the full 11th Circuit Court of Appeals (sitting “en banc”) heard arguments, and the profession eagerly awaits its final opinion.
Meanwhile, commentators have expressed concerns that such laws threaten the sanctity of the physician-patient relationship, which relies on truthful communication to freely counsel patients.
This infringement may be gathering force. Missouri and Montana already have similar gun privacy laws, while other states have required physicians to keep confidential any information regarding chemicals used in fracking, or mandate the provision of various birth-related information prior to a woman’s decision to have an abortion.6
References
1. U.S. v. Caronia, 703 F.3d 149 (2d Cir. 2012).
2. Sorrell v. IMS Health, 131 S. Ct. 2653 (2011).
3. N Engl J Med. 2013 Jan 10;368(2):103-5.
4. Fla. St. 381.026, 456.072, 790.338.
5. Wollschlaeger v. Governor of Florida, 797 F.3d 859 (11th Cir. 2015).
6. N Engl J Med. 2016 Jun 16;374(24):2304-7.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Question: The First Amendment guarantees the right of free speech, but the U.S. Supreme Court has held that under a strict scrutiny standard, the government may regulate:
A. Obscenity.
B. Fighting words.
C. Professional speech.
D. A and B.
E. A, B, and C.
Answer: D. The First Amendment forbids the government from “abridging the freedom of speech,” which extends to certain nonverbal conduct, such as flag burning. At the same time, the U.S. Supreme Court has also ruled that certain categories of speech such as obscenity and fighting words can be regulated under a strict scrutiny standard. However, it remains unsettled whether and to what extent professional speech – such as in the context of the doctor-patient relationship – may be curtailed.
Two recent cases grapple with this issue of free speech – with rather unexpected results.
The first, overturning a decades-old prohibition of the off-label detailing of drugs, surprisingly was decided against the government. The second challenges a Florida statute censoring the discussion of firearms safety between a doctor and a patient. An early decision, under reconsideration, in fact supported the state’s regulation of physicians’ freedom of speech under the circumstances.
Because the FDA has no jurisdiction over physician conduct, it has no power to regulate the off-label use of an otherwise approved drug, which explains why such off-label prescriptions are widespread, especially in the oncology field.
In U.S. v. Caronia, the defendant, a pharmaceutical sales representative, was criminally prosecuted and found guilty of conspiracy in a New York court for introducing a misbranded drug into interstate commerce.1 Specifically, Alfred Caronia promoted the drug Xyrem for use in a manner not approved by the FDA.
Orphan Medical, now known as Jazz Pharmaceuticals, is the manufacturer of Xyrem, a powerful central nervous system depressant. Xyrem’s active ingredient is gamma-hydroxybutyrate, which has been federally classified as the “date rape drug” for its use in the commission of sexual assaults. The FDA had approved Xyrem for two conditions: to treat narcolepsy patients who experience cataplexy, a condition associated with weak or paralyzed muscles; and to treat those with excessive daytime sleepiness.
Caronia was found to provide off-label detailing of the drug to doctors for unapproved indications such as chronic fatigue, fibromyalgia, restless leg syndrome, and Parkinson’s disease.
Caronia argued that in promoting an FDA-approved drug, albeit for off-label use, he was within his right of free speech under the First Amendment. In overturning his conviction, a three-judge panel of the U.S. Second Circuit Court of Appeals agreed, noting the overly broad FDA regulations and specifically that nothing Caronia did constituted conspiracy to put a false or misleading or deficient label on a drug product.
The court concluded: “The government cannot prosecute pharmaceutical manufacturers and their representatives under the FDCA [Federal Food, Drug, and Cosmetic Act] for speech promoting the lawful, off-label use of an FDA-approved drug.”
In 2011, the U.S. Supreme Court had used a First Amendment argument to invalidate a Vermont law that prohibited the practice of pharmaceutical data mining – purchasing information about prescribers from pharmacies and others.2
Taken together, the FDA now appears resigned to the free speech argument.3 For example, it has decided not to appeal a judge’s ruling that the First Amendment protects Amarin from promoting its fish-oil capsules for unapproved uses. Just recently, the FDA published a draft proposal in tacit acceptance of this new policy position, merely recommending the disclosure of relevant information including limitations and unfavorable or inconsistent findings surrounding the off-label use of a drug.
The next issue concerns professional speech. It is well documented that the presence of a gun in the home increases the risk of death especially by suicide, and this serves as the impetus for the long-established recommendation that physicians discuss firearm safety with their patients.
The medical profession was therefore aghast when Florida enacted its law on “Privacy of Firearm Owners.”4 Codified on June 2, 2011, it provides that a licensed practitioner or facility may not record firearm ownership information in a patient’s medical record, and that unless information is relevant to the patient’s medical care or safety or safety of others, inquiries regarding firearm ownership or possession should not be made. A practitioner is also forbidden from unnecessarily harassing a patient about firearm ownership during an examination.
Violation can result in disciplinary action; the original intent was to make this a third-degree felony with penalties of up to $5 million in fines and 5 years of imprisonment, but the final bill was stripped of criminal penalties.
In July 2015, a panel of three judges of the U.S. 11th Circuit Court of Appeals, in a split 2-1 decision, found that the inquiry, record-keeping, and harassment provisions of the act specifically regulate professional speech, which is subject to an intermediate level of scrutiny. Under this level of scrutiny, the court found that the act was precisely tailored to directly advance the state’s substantial interests in protecting the public and patient privacy rights.
Holding that the act was not so overly broad as to violate the First Amendment, the court ruled that laws regulating speech that occurs in the course of the physician-patient relationship are constitutional if they directly advance a substantial state interest.5
Predictably, several medical societies, including the AMA, have filed briefs arguing that the law is unconstitutional and intrudes on the practice of medicine. Effective medical care is believed to require “unfettered communications” between physicians and their patients. Besides, the law is at odds with the AMA’s longstanding policy that encourages members to inquire into the presence of firearms in households and to promote the use of safety locks on guns in an effort to reduce injuries to children.
On June 21, 2016, the full 11th Circuit Court of Appeals (sitting “en banc”) heard arguments, and the profession eagerly awaits its final opinion.
Meanwhile, commentators have expressed concerns that such laws threaten the sanctity of the physician-patient relationship, which relies on truthful communication to freely counsel patients.
This infringement may be gathering force. Missouri and Montana already have similar gun privacy laws, while other states have required physicians to keep confidential any information regarding chemicals used in fracking, or mandate the provision of various birth-related information prior to a woman’s decision to have an abortion.6
References
1. U.S. v. Caronia, 703 F.3d 149 (2d Cir. 2012).
2. Sorrell v. IMS Health, 131 S. Ct. 2653 (2011).
3. N Engl J Med. 2013 Jan 10;368(2):103-5.
4. Fla. St. 381.026, 456.072, 790.338.
5. Wollschlaeger v. Governor of Florida, 797 F.3d 859 (11th Cir. 2015).
6. N Engl J Med. 2016 Jun 16;374(24):2304-7.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Question: The First Amendment guarantees the right of free speech, but the U.S. Supreme Court has held that under a strict scrutiny standard, the government may regulate:
A. Obscenity.
B. Fighting words.
C. Professional speech.
D. A and B.
E. A, B, and C.
Answer: D. The First Amendment forbids the government from “abridging the freedom of speech,” which extends to certain nonverbal conduct, such as flag burning. At the same time, the U.S. Supreme Court has also ruled that certain categories of speech such as obscenity and fighting words can be regulated under a strict scrutiny standard. However, it remains unsettled whether and to what extent professional speech – such as in the context of the doctor-patient relationship – may be curtailed.
Two recent cases grapple with this issue of free speech – with rather unexpected results.
The first, overturning a decades-old prohibition of the off-label detailing of drugs, surprisingly was decided against the government. The second challenges a Florida statute censoring the discussion of firearms safety between a doctor and a patient. An early decision, under reconsideration, in fact supported the state’s regulation of physicians’ freedom of speech under the circumstances.
Because the FDA has no jurisdiction over physician conduct, it has no power to regulate the off-label use of an otherwise approved drug, which explains why such off-label prescriptions are widespread, especially in the oncology field.
In U.S. v. Caronia, the defendant, a pharmaceutical sales representative, was criminally prosecuted and found guilty of conspiracy in a New York court for introducing a misbranded drug into interstate commerce.1 Specifically, Alfred Caronia promoted the drug Xyrem for use in a manner not approved by the FDA.
Orphan Medical, now known as Jazz Pharmaceuticals, is the manufacturer of Xyrem, a powerful central nervous system depressant. Xyrem’s active ingredient is gamma-hydroxybutyrate, which has been federally classified as the “date rape drug” for its use in the commission of sexual assaults. The FDA had approved Xyrem for two conditions: to treat narcolepsy patients who experience cataplexy, a condition associated with weak or paralyzed muscles; and to treat those with excessive daytime sleepiness.
Caronia was found to provide off-label detailing of the drug to doctors for unapproved indications such as chronic fatigue, fibromyalgia, restless leg syndrome, and Parkinson’s disease.
Caronia argued that in promoting an FDA-approved drug, albeit for off-label use, he was within his right of free speech under the First Amendment. In overturning his conviction, a three-judge panel of the U.S. Second Circuit Court of Appeals agreed, noting the overly broad FDA regulations and specifically that nothing Caronia did constituted conspiracy to put a false or misleading or deficient label on a drug product.
The court concluded: “The government cannot prosecute pharmaceutical manufacturers and their representatives under the FDCA [Federal Food, Drug, and Cosmetic Act] for speech promoting the lawful, off-label use of an FDA-approved drug.”
In 2011, the U.S. Supreme Court had used a First Amendment argument to invalidate a Vermont law that prohibited the practice of pharmaceutical data mining – purchasing information about prescribers from pharmacies and others.2
Taken together, the FDA now appears resigned to the free speech argument.3 For example, it has decided not to appeal a judge’s ruling that the First Amendment protects Amarin from promoting its fish-oil capsules for unapproved uses. Just recently, the FDA published a draft proposal in tacit acceptance of this new policy position, merely recommending the disclosure of relevant information including limitations and unfavorable or inconsistent findings surrounding the off-label use of a drug.
The next issue concerns professional speech. It is well documented that the presence of a gun in the home increases the risk of death especially by suicide, and this serves as the impetus for the long-established recommendation that physicians discuss firearm safety with their patients.
The medical profession was therefore aghast when Florida enacted its law on “Privacy of Firearm Owners.”4 Codified on June 2, 2011, it provides that a licensed practitioner or facility may not record firearm ownership information in a patient’s medical record, and that unless information is relevant to the patient’s medical care or safety or safety of others, inquiries regarding firearm ownership or possession should not be made. A practitioner is also forbidden from unnecessarily harassing a patient about firearm ownership during an examination.
Violation can result in disciplinary action; the original intent was to make this a third-degree felony with penalties of up to $5 million in fines and 5 years of imprisonment, but the final bill was stripped of criminal penalties.
In July 2015, a panel of three judges of the U.S. 11th Circuit Court of Appeals, in a split 2-1 decision, found that the inquiry, record-keeping, and harassment provisions of the act specifically regulate professional speech, which is subject to an intermediate level of scrutiny. Under this level of scrutiny, the court found that the act was precisely tailored to directly advance the state’s substantial interests in protecting the public and patient privacy rights.
Holding that the act was not so overly broad as to violate the First Amendment, the court ruled that laws regulating speech that occurs in the course of the physician-patient relationship are constitutional if they directly advance a substantial state interest.5
Predictably, several medical societies, including the AMA, have filed briefs arguing that the law is unconstitutional and intrudes on the practice of medicine. Effective medical care is believed to require “unfettered communications” between physicians and their patients. Besides, the law is at odds with the AMA’s longstanding policy that encourages members to inquire into the presence of firearms in households and to promote the use of safety locks on guns in an effort to reduce injuries to children.
On June 21, 2016, the full 11th Circuit Court of Appeals (sitting “en banc”) heard arguments, and the profession eagerly awaits its final opinion.
Meanwhile, commentators have expressed concerns that such laws threaten the sanctity of the physician-patient relationship, which relies on truthful communication to freely counsel patients.
This infringement may be gathering force. Missouri and Montana already have similar gun privacy laws, while other states have required physicians to keep confidential any information regarding chemicals used in fracking, or mandate the provision of various birth-related information prior to a woman’s decision to have an abortion.6
References
1. U.S. v. Caronia, 703 F.3d 149 (2d Cir. 2012).
2. Sorrell v. IMS Health, 131 S. Ct. 2653 (2011).
3. N Engl J Med. 2013 Jan 10;368(2):103-5.
4. Fla. St. 381.026, 456.072, 790.338.
5. Wollschlaeger v. Governor of Florida, 797 F.3d 859 (11th Cir. 2015).
6. N Engl J Med. 2016 Jun 16;374(24):2304-7.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Senate confirms Price as HHS secretary
The U.S. Senate voted to confirm Rep. Tom Price, MD, as secretary of the Department of Health & Human Services.
The final tally, recorded in the early hours of Feb. 10, was a strict party-line vote, with all 52 Republicans voting in favor of Rep. Price (R-Ga.) and 47 Democrats voting against. One Democrat, Sen. Claire McCaskill of Missouri, did not vote. Only a simple majority is needed to confirm cabinet members to their posts.
The confirmation comes amid ongoing concerns presented by Senate Democrats on Dr. Price’s stock purchases, particularly of Australia-based Innate Immunotherapeutics. Dr. Price was serving as a representative from Georgia at the time of his nomination, and there have been questions of possible ethics violations related to this and other securities purchases.
Democrats also rallied against the policies that Dr. Price advocated for when he was a U.S. House member, including dismantling the Affordable Care Act and pushing for block grants to fund Medicaid. He has also supported policies that would promote more extensive use of health savings accounts linked to high-deductible health plans, and high-risk pools to help ensure that those with pre-existing conditions are able to get insurance coverage without a need for guaranteed issue.
However, Democratic objections were not enough to cause any waver in support from Senate Republicans.
The American Medical Association “looks forward to working with Secretary Price to improve the health of our nation through policies that promote access to high-quality, affordable care, delivery innovation, and reduced regulatory burdens that helps patients and their physicians,” AMA President Andrew Gurman, MD, said in a statement.
The U.S. Senate voted to confirm Rep. Tom Price, MD, as secretary of the Department of Health & Human Services.
The final tally, recorded in the early hours of Feb. 10, was a strict party-line vote, with all 52 Republicans voting in favor of Rep. Price (R-Ga.) and 47 Democrats voting against. One Democrat, Sen. Claire McCaskill of Missouri, did not vote. Only a simple majority is needed to confirm cabinet members to their posts.
The confirmation comes amid ongoing concerns presented by Senate Democrats on Dr. Price’s stock purchases, particularly of Australia-based Innate Immunotherapeutics. Dr. Price was serving as a representative from Georgia at the time of his nomination, and there have been questions of possible ethics violations related to this and other securities purchases.
Democrats also rallied against the policies that Dr. Price advocated for when he was a U.S. House member, including dismantling the Affordable Care Act and pushing for block grants to fund Medicaid. He has also supported policies that would promote more extensive use of health savings accounts linked to high-deductible health plans, and high-risk pools to help ensure that those with pre-existing conditions are able to get insurance coverage without a need for guaranteed issue.
However, Democratic objections were not enough to cause any waver in support from Senate Republicans.
The American Medical Association “looks forward to working with Secretary Price to improve the health of our nation through policies that promote access to high-quality, affordable care, delivery innovation, and reduced regulatory burdens that helps patients and their physicians,” AMA President Andrew Gurman, MD, said in a statement.
The U.S. Senate voted to confirm Rep. Tom Price, MD, as secretary of the Department of Health & Human Services.
The final tally, recorded in the early hours of Feb. 10, was a strict party-line vote, with all 52 Republicans voting in favor of Rep. Price (R-Ga.) and 47 Democrats voting against. One Democrat, Sen. Claire McCaskill of Missouri, did not vote. Only a simple majority is needed to confirm cabinet members to their posts.
The confirmation comes amid ongoing concerns presented by Senate Democrats on Dr. Price’s stock purchases, particularly of Australia-based Innate Immunotherapeutics. Dr. Price was serving as a representative from Georgia at the time of his nomination, and there have been questions of possible ethics violations related to this and other securities purchases.
Democrats also rallied against the policies that Dr. Price advocated for when he was a U.S. House member, including dismantling the Affordable Care Act and pushing for block grants to fund Medicaid. He has also supported policies that would promote more extensive use of health savings accounts linked to high-deductible health plans, and high-risk pools to help ensure that those with pre-existing conditions are able to get insurance coverage without a need for guaranteed issue.
However, Democratic objections were not enough to cause any waver in support from Senate Republicans.
The American Medical Association “looks forward to working with Secretary Price to improve the health of our nation through policies that promote access to high-quality, affordable care, delivery innovation, and reduced regulatory burdens that helps patients and their physicians,” AMA President Andrew Gurman, MD, said in a statement.
Rituximab is dramatically effective in IgG4-related disease
SNOWMASS, COLO. – Glucocorticoids remain the first-line therapy in immunoglobulin G4-related disease, but it’s essential to bear in mind that their long-term efficacy in this immune-mediated fibroinflammatory disease is the exception rather than the rule, John H. Stone, MD, said at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
Dr. Stone, professor of medicine at Harvard Medical School, Boston, was a coauthor of an international expert consensus statement on the treatment of IgG4-related disease (IgG4-RD) which emphasized that point (Arthritis Rheumatol. 2015 Jul;67[7]:1688-99).
“I typically start with prednisone at 40 mg/day, and there’s a dramatic response in these patients. Then I taper them off after 2-3 months. If 2-3 months doesn’t put them into a long-term sustained remission, it’s time to go to something else,” said Dr. Stone, who also serves as director of clinical rheumatology at Massachusetts General Hospital, Boston.
“Glucocorticoids are rapidly effective, but initial reports were overoptimistic about their long-term efficacy. They don’t cure this disease any more than they cure giant cell arteritis in most of our patients, or ANCA-associated vasculitis. And since patients with IgG4-related disease are often older and may already have disease-induced damage to the pancreas and other organs, the morbidity from steroids in this population is formidable,” the rheumatologist explained.
In his series of 125 patients with biopsy-proven IgG4-RD, 83% responded to steroids initially, but 77% of steroid-treated patients failed to achieve a stable steroid-free remission after treatment discontinuation (Arthritis Rheumatol. 2015 Sep;67[9]:2466-75).
There is no evidence at all to indicate that conventional steroid-sparing drugs such as methotrexate, azathioprine, and mycophenolate mofetil are effective in IgG4-RD, the rheumatologist noted.
So what’s the next move, then, after steroids fail? Dr. Stone was a pioneer in the strikingly successful use of B cell depletion via rituximab (Rituxan) in patients with IgG4-RD. First he and his coinvestigators demonstrated that this off-label use of rituximab led to rapid clinical and histologic improvement (Ann Rheum Dis. 2015 Jun; 74[6]:1171-7), then they showed it also causes levels of circulating plasmablasts, serum IgG4, and biomarkers of fibrosis to plunge, suggesting B cell depletion may halt the destructive process of collagen deposition that characterizes this immune-related disease (Ann Rheum Dis. 2015 Dec;74[12]:2236-43). They have also reported that patients with very elevated baseline serum IgG4 levels are at more than sixfold increased risk of relapse at a median of 244 days from their first rituximab infusion (Rheumatology [Oxford]. 2016 Jun;55[6]:1000-8).
The success with rituximab is just one example of how improved understanding of the pathophysiology of IgG4-RD has opened the door to novel treatments. Dr. Stone is the lead investigator in an ongoing phase II, open-label study in which 15 patients with active IgG4-RD will receive intravenous XmAb5871 every 2 weeks for 6 months to evaluate the effect on the IgG4-RD Responder Index. XmAb5871 is a monoclonal antibody that binds to CD19 and FCgammaRIIb in order to downregulate activated B cells and plasmablasts. It is also being developed for treatment of systemic lupus erythematosus.
Dr. Stone and his coinvestigators are working on a therapeutic approach to IgG4-RD that targets antigen presentation by activated B cells to CD4+ cytotoxic T cells at sites of disease. These CD4+ cytotoxic T cells contain signaling lymphocyte activation molecule F7 (SLAMF7) as a surface marker. Elotuzumab (Empliciti), an immunostimulatory humanized monoclonal antibody targeting SLAMF7, is already on the market for treatment of multiple myeloma, he noted.
Dr. Stone reported receiving IgG4-RD-related research funding from and serving as a consultant to Genentech and Xencor, which is developing XmAb5871.
SNOWMASS, COLO. – Glucocorticoids remain the first-line therapy in immunoglobulin G4-related disease, but it’s essential to bear in mind that their long-term efficacy in this immune-mediated fibroinflammatory disease is the exception rather than the rule, John H. Stone, MD, said at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
Dr. Stone, professor of medicine at Harvard Medical School, Boston, was a coauthor of an international expert consensus statement on the treatment of IgG4-related disease (IgG4-RD) which emphasized that point (Arthritis Rheumatol. 2015 Jul;67[7]:1688-99).
“I typically start with prednisone at 40 mg/day, and there’s a dramatic response in these patients. Then I taper them off after 2-3 months. If 2-3 months doesn’t put them into a long-term sustained remission, it’s time to go to something else,” said Dr. Stone, who also serves as director of clinical rheumatology at Massachusetts General Hospital, Boston.
“Glucocorticoids are rapidly effective, but initial reports were overoptimistic about their long-term efficacy. They don’t cure this disease any more than they cure giant cell arteritis in most of our patients, or ANCA-associated vasculitis. And since patients with IgG4-related disease are often older and may already have disease-induced damage to the pancreas and other organs, the morbidity from steroids in this population is formidable,” the rheumatologist explained.
In his series of 125 patients with biopsy-proven IgG4-RD, 83% responded to steroids initially, but 77% of steroid-treated patients failed to achieve a stable steroid-free remission after treatment discontinuation (Arthritis Rheumatol. 2015 Sep;67[9]:2466-75).
There is no evidence at all to indicate that conventional steroid-sparing drugs such as methotrexate, azathioprine, and mycophenolate mofetil are effective in IgG4-RD, the rheumatologist noted.
So what’s the next move, then, after steroids fail? Dr. Stone was a pioneer in the strikingly successful use of B cell depletion via rituximab (Rituxan) in patients with IgG4-RD. First he and his coinvestigators demonstrated that this off-label use of rituximab led to rapid clinical and histologic improvement (Ann Rheum Dis. 2015 Jun; 74[6]:1171-7), then they showed it also causes levels of circulating plasmablasts, serum IgG4, and biomarkers of fibrosis to plunge, suggesting B cell depletion may halt the destructive process of collagen deposition that characterizes this immune-related disease (Ann Rheum Dis. 2015 Dec;74[12]:2236-43). They have also reported that patients with very elevated baseline serum IgG4 levels are at more than sixfold increased risk of relapse at a median of 244 days from their first rituximab infusion (Rheumatology [Oxford]. 2016 Jun;55[6]:1000-8).
The success with rituximab is just one example of how improved understanding of the pathophysiology of IgG4-RD has opened the door to novel treatments. Dr. Stone is the lead investigator in an ongoing phase II, open-label study in which 15 patients with active IgG4-RD will receive intravenous XmAb5871 every 2 weeks for 6 months to evaluate the effect on the IgG4-RD Responder Index. XmAb5871 is a monoclonal antibody that binds to CD19 and FCgammaRIIb in order to downregulate activated B cells and plasmablasts. It is also being developed for treatment of systemic lupus erythematosus.
Dr. Stone and his coinvestigators are working on a therapeutic approach to IgG4-RD that targets antigen presentation by activated B cells to CD4+ cytotoxic T cells at sites of disease. These CD4+ cytotoxic T cells contain signaling lymphocyte activation molecule F7 (SLAMF7) as a surface marker. Elotuzumab (Empliciti), an immunostimulatory humanized monoclonal antibody targeting SLAMF7, is already on the market for treatment of multiple myeloma, he noted.
Dr. Stone reported receiving IgG4-RD-related research funding from and serving as a consultant to Genentech and Xencor, which is developing XmAb5871.
SNOWMASS, COLO. – Glucocorticoids remain the first-line therapy in immunoglobulin G4-related disease, but it’s essential to bear in mind that their long-term efficacy in this immune-mediated fibroinflammatory disease is the exception rather than the rule, John H. Stone, MD, said at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
Dr. Stone, professor of medicine at Harvard Medical School, Boston, was a coauthor of an international expert consensus statement on the treatment of IgG4-related disease (IgG4-RD) which emphasized that point (Arthritis Rheumatol. 2015 Jul;67[7]:1688-99).
“I typically start with prednisone at 40 mg/day, and there’s a dramatic response in these patients. Then I taper them off after 2-3 months. If 2-3 months doesn’t put them into a long-term sustained remission, it’s time to go to something else,” said Dr. Stone, who also serves as director of clinical rheumatology at Massachusetts General Hospital, Boston.
“Glucocorticoids are rapidly effective, but initial reports were overoptimistic about their long-term efficacy. They don’t cure this disease any more than they cure giant cell arteritis in most of our patients, or ANCA-associated vasculitis. And since patients with IgG4-related disease are often older and may already have disease-induced damage to the pancreas and other organs, the morbidity from steroids in this population is formidable,” the rheumatologist explained.
In his series of 125 patients with biopsy-proven IgG4-RD, 83% responded to steroids initially, but 77% of steroid-treated patients failed to achieve a stable steroid-free remission after treatment discontinuation (Arthritis Rheumatol. 2015 Sep;67[9]:2466-75).
There is no evidence at all to indicate that conventional steroid-sparing drugs such as methotrexate, azathioprine, and mycophenolate mofetil are effective in IgG4-RD, the rheumatologist noted.
So what’s the next move, then, after steroids fail? Dr. Stone was a pioneer in the strikingly successful use of B cell depletion via rituximab (Rituxan) in patients with IgG4-RD. First he and his coinvestigators demonstrated that this off-label use of rituximab led to rapid clinical and histologic improvement (Ann Rheum Dis. 2015 Jun; 74[6]:1171-7), then they showed it also causes levels of circulating plasmablasts, serum IgG4, and biomarkers of fibrosis to plunge, suggesting B cell depletion may halt the destructive process of collagen deposition that characterizes this immune-related disease (Ann Rheum Dis. 2015 Dec;74[12]:2236-43). They have also reported that patients with very elevated baseline serum IgG4 levels are at more than sixfold increased risk of relapse at a median of 244 days from their first rituximab infusion (Rheumatology [Oxford]. 2016 Jun;55[6]:1000-8).
The success with rituximab is just one example of how improved understanding of the pathophysiology of IgG4-RD has opened the door to novel treatments. Dr. Stone is the lead investigator in an ongoing phase II, open-label study in which 15 patients with active IgG4-RD will receive intravenous XmAb5871 every 2 weeks for 6 months to evaluate the effect on the IgG4-RD Responder Index. XmAb5871 is a monoclonal antibody that binds to CD19 and FCgammaRIIb in order to downregulate activated B cells and plasmablasts. It is also being developed for treatment of systemic lupus erythematosus.
Dr. Stone and his coinvestigators are working on a therapeutic approach to IgG4-RD that targets antigen presentation by activated B cells to CD4+ cytotoxic T cells at sites of disease. These CD4+ cytotoxic T cells contain signaling lymphocyte activation molecule F7 (SLAMF7) as a surface marker. Elotuzumab (Empliciti), an immunostimulatory humanized monoclonal antibody targeting SLAMF7, is already on the market for treatment of multiple myeloma, he noted.
Dr. Stone reported receiving IgG4-RD-related research funding from and serving as a consultant to Genentech and Xencor, which is developing XmAb5871.
EXPERT ANALYSIS FROM THE WINTER RHEUMATOLOGY SYMPOSIUM
Peripheral B cells reflect intestinal damage in celiac disease
B-cell gene expression in the peripheral blood strongly correlates with the extent of gluten-induced damage to the intestinal mucosa in patients with celiac disease, according to a report in Cellular and Molecular Gastroenterology and Hepatology.
If this finding from a single-center cohort study is validated in other patient populations, the B-cell signature may become a useful, minimally invasive tool for diagnosing celiac disease. Eventually, if biomarkers are developed from the peripheral B-cell signature, a simple blood test could be used for monitoring changes in gut inflammation over time as well as treatment response, said Mitchell E. Garber, PhD, of Alvine Pharmaceuticals, San Carlos, Calif., and the department of chemistry at Stanford University, and his associates.
However, it would be “premature but intriguing” to speculate about using this discovery to devise new, B cell–centered treatments for celiac disease, they added.
Noting that an inflammatory, gluten-induced immune response in the gut can be reflected in the peripheral blood, the investigators assessed whether a 6-week gluten challenge would induce damage to the small intestine that would show up in B-cell gene expression detected in blood samples. They assigned 73 patients at a single medical center in Finland to follow their usual gluten-free diets but to ingest an additional 6 g (20 patients), 3 g (26 patients), or 1.5 g (27 patients) of wheat gluten with a meal once per day for the study period.
The study participants (median age, 59 years; range, 23-74 years) underwent small-bowel biopsies obtained from the descending duodenum at baseline and after the gluten challenge. Damage to the intestinal mucosa was assessed by measuring the ratio of the height of the intestinal villi to the depth of the proliferative crypts at the base of the villi (villi height to crypt depth, or Vh:Cd). In celiac disease, gluten blunts the projection of the villi and causes hypertrophy or elongation of the crypts, resulting in flattened mucosa and a Vh:Cd approaching zero.
The study participants showed a wide variation in mucosal damage from the gluten exposure, with some patients showing no change and relatively healthy mucosa, and others showing extensive change and nearly flattened mucosa. The mucosal damage did not differ by gluten dose.
The largest change in Vh:Cd occurred in three patients who transitioned from relatively healthy intestinal mucosa (Vh:Cd 3.1) at baseline to nearly flat mucosa (Vh:Cd 0.2) after gluten exposure.
Patients with undamaged gut mucosa showed a relative increase in B-cell gene expression during the study period, while those who had increasing damage showed a relative decrease in B-cell expression. “The peripheral B cell therefore tracked with oral tolerance across the full spectrum of intestinal damage, from no change to a nearly flat mucosa,” Dr. Garber and his associates said (Cell Molec Gastroenterol Hepatol. 2017. doi: 10.1016/j.jcmgh.2017.01.011).
“The net increase in B-cell gene expression from baseline to 6 weeks in patients with little to no intestinal damage [suggests] that these individuals may have mounted a B-cell immune response to maintain mucosal homeostasis and circumvent inflammation,” they added.
Further study is needed to determine whether peripheral B cells are a marker that indicates tolerance to gluten but doesn’t play a functional role in the inflammatory process, or whether B cells may actually promote immune tolerance, the investigators said.
This study was funded by Alvine Pharmaceuticals, the American Recovery and Reinvestment Act, Tampere (Finland) University Hospital, the Academy of Finland Research Council for Health, and the U.S. National Institutes of Health. Dr. Garber reported ties to Alvine Pharmaceuticals, and his associates reported ties to ImmusanT, Celimmune, and ImmunogenX.
B-cell gene expression in the peripheral blood strongly correlates with the extent of gluten-induced damage to the intestinal mucosa in patients with celiac disease, according to a report in Cellular and Molecular Gastroenterology and Hepatology.
If this finding from a single-center cohort study is validated in other patient populations, the B-cell signature may become a useful, minimally invasive tool for diagnosing celiac disease. Eventually, if biomarkers are developed from the peripheral B-cell signature, a simple blood test could be used for monitoring changes in gut inflammation over time as well as treatment response, said Mitchell E. Garber, PhD, of Alvine Pharmaceuticals, San Carlos, Calif., and the department of chemistry at Stanford University, and his associates.
However, it would be “premature but intriguing” to speculate about using this discovery to devise new, B cell–centered treatments for celiac disease, they added.
Noting that an inflammatory, gluten-induced immune response in the gut can be reflected in the peripheral blood, the investigators assessed whether a 6-week gluten challenge would induce damage to the small intestine that would show up in B-cell gene expression detected in blood samples. They assigned 73 patients at a single medical center in Finland to follow their usual gluten-free diets but to ingest an additional 6 g (20 patients), 3 g (26 patients), or 1.5 g (27 patients) of wheat gluten with a meal once per day for the study period.
The study participants (median age, 59 years; range, 23-74 years) underwent small-bowel biopsies obtained from the descending duodenum at baseline and after the gluten challenge. Damage to the intestinal mucosa was assessed by measuring the ratio of the height of the intestinal villi to the depth of the proliferative crypts at the base of the villi (villi height to crypt depth, or Vh:Cd). In celiac disease, gluten blunts the projection of the villi and causes hypertrophy or elongation of the crypts, resulting in flattened mucosa and a Vh:Cd approaching zero.
The study participants showed a wide variation in mucosal damage from the gluten exposure, with some patients showing no change and relatively healthy mucosa, and others showing extensive change and nearly flattened mucosa. The mucosal damage did not differ by gluten dose.
The largest change in Vh:Cd occurred in three patients who transitioned from relatively healthy intestinal mucosa (Vh:Cd 3.1) at baseline to nearly flat mucosa (Vh:Cd 0.2) after gluten exposure.
Patients with undamaged gut mucosa showed a relative increase in B-cell gene expression during the study period, while those who had increasing damage showed a relative decrease in B-cell expression. “The peripheral B cell therefore tracked with oral tolerance across the full spectrum of intestinal damage, from no change to a nearly flat mucosa,” Dr. Garber and his associates said (Cell Molec Gastroenterol Hepatol. 2017. doi: 10.1016/j.jcmgh.2017.01.011).
“The net increase in B-cell gene expression from baseline to 6 weeks in patients with little to no intestinal damage [suggests] that these individuals may have mounted a B-cell immune response to maintain mucosal homeostasis and circumvent inflammation,” they added.
Further study is needed to determine whether peripheral B cells are a marker that indicates tolerance to gluten but doesn’t play a functional role in the inflammatory process, or whether B cells may actually promote immune tolerance, the investigators said.
This study was funded by Alvine Pharmaceuticals, the American Recovery and Reinvestment Act, Tampere (Finland) University Hospital, the Academy of Finland Research Council for Health, and the U.S. National Institutes of Health. Dr. Garber reported ties to Alvine Pharmaceuticals, and his associates reported ties to ImmusanT, Celimmune, and ImmunogenX.
B-cell gene expression in the peripheral blood strongly correlates with the extent of gluten-induced damage to the intestinal mucosa in patients with celiac disease, according to a report in Cellular and Molecular Gastroenterology and Hepatology.
If this finding from a single-center cohort study is validated in other patient populations, the B-cell signature may become a useful, minimally invasive tool for diagnosing celiac disease. Eventually, if biomarkers are developed from the peripheral B-cell signature, a simple blood test could be used for monitoring changes in gut inflammation over time as well as treatment response, said Mitchell E. Garber, PhD, of Alvine Pharmaceuticals, San Carlos, Calif., and the department of chemistry at Stanford University, and his associates.
However, it would be “premature but intriguing” to speculate about using this discovery to devise new, B cell–centered treatments for celiac disease, they added.
Noting that an inflammatory, gluten-induced immune response in the gut can be reflected in the peripheral blood, the investigators assessed whether a 6-week gluten challenge would induce damage to the small intestine that would show up in B-cell gene expression detected in blood samples. They assigned 73 patients at a single medical center in Finland to follow their usual gluten-free diets but to ingest an additional 6 g (20 patients), 3 g (26 patients), or 1.5 g (27 patients) of wheat gluten with a meal once per day for the study period.
The study participants (median age, 59 years; range, 23-74 years) underwent small-bowel biopsies obtained from the descending duodenum at baseline and after the gluten challenge. Damage to the intestinal mucosa was assessed by measuring the ratio of the height of the intestinal villi to the depth of the proliferative crypts at the base of the villi (villi height to crypt depth, or Vh:Cd). In celiac disease, gluten blunts the projection of the villi and causes hypertrophy or elongation of the crypts, resulting in flattened mucosa and a Vh:Cd approaching zero.
The study participants showed a wide variation in mucosal damage from the gluten exposure, with some patients showing no change and relatively healthy mucosa, and others showing extensive change and nearly flattened mucosa. The mucosal damage did not differ by gluten dose.
The largest change in Vh:Cd occurred in three patients who transitioned from relatively healthy intestinal mucosa (Vh:Cd 3.1) at baseline to nearly flat mucosa (Vh:Cd 0.2) after gluten exposure.
Patients with undamaged gut mucosa showed a relative increase in B-cell gene expression during the study period, while those who had increasing damage showed a relative decrease in B-cell expression. “The peripheral B cell therefore tracked with oral tolerance across the full spectrum of intestinal damage, from no change to a nearly flat mucosa,” Dr. Garber and his associates said (Cell Molec Gastroenterol Hepatol. 2017. doi: 10.1016/j.jcmgh.2017.01.011).
“The net increase in B-cell gene expression from baseline to 6 weeks in patients with little to no intestinal damage [suggests] that these individuals may have mounted a B-cell immune response to maintain mucosal homeostasis and circumvent inflammation,” they added.
Further study is needed to determine whether peripheral B cells are a marker that indicates tolerance to gluten but doesn’t play a functional role in the inflammatory process, or whether B cells may actually promote immune tolerance, the investigators said.
This study was funded by Alvine Pharmaceuticals, the American Recovery and Reinvestment Act, Tampere (Finland) University Hospital, the Academy of Finland Research Council for Health, and the U.S. National Institutes of Health. Dr. Garber reported ties to Alvine Pharmaceuticals, and his associates reported ties to ImmusanT, Celimmune, and ImmunogenX.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: B-cell gene expression in peripheral blood strongly correlates with the extent of gluten-induced intestinal damage in patients with celiac disease.
Major finding: Patients with undamaged gut mucosa showed a relative increase in B-cell gene expression during the study period, while those who had increasing damage showed a relative decrease in B-cell expression.
Data source: A single-center cohort study involving 73 adults with celiac disease who underwent a 6-week gluten challenge.
Disclosures: This study was funded by Alvine Pharmaceuticals, the American Recovery and Reinvestment Act, Tampere (Finland) University Hospital, the Academy of Finland Research Council for Health, and the U.S. National Institutes of Health. Dr. Garber reported ties to Alvine Pharmaceuticals, and his associates reported ties to ImmusanT, Celimmune, and ImmunogenX.