User login
Telephone calls improve long-term follow-up after hernia repair
Follow-up telephone calls can significantly improve the collection of long-term patient-reported outcomes following ventral hernia repair, according to a study published online in the Oct. 20 edition of the Journal of the American College of Surgeons.
Nishant Ganesh Kumar, a medical student, and his colleagues at Vanderbilt University, Nashville, Tenn., wrote that while ventral hernia repair is one of the most common surgical procedures in the world, reliable long-term, prospective data on outcomes has been extremely difficult to collect.
In this Plan-Do-Study-Act (PDSA) prospective study, 99 patients who had undergone ventral hernia repair were followed up by telephone, in addition to the usual email communication, 1 year after their procedure. The calls were initially made between 1:00 p.m. and 3:00 p.m. in the first phase of the study, then changed to after 3:00 p.m. in the second phase.
Compared to the long-term completion rate of 16.3% prior to the intervention – where follow-up was largely through physical clinical visits – researchers saw a completion rate of 35.7% with the telephone calls between 1:00 p.m. and 3:00 p.m., and a 55.1% completion rate after changing the call time to after 3:00 p.m. The mean participation rate was 45.4%.
Once contact was made, all the patients completed the full patient-reported outcomes assessment, although the researchers did note that some seem to experience fatigue during questioning that required the interviewers to gently steer them back to the questions.
“The advantage of making phone calls was severalfold, including clarification of survey questions to help patients with providing more insightful responses, allaying concerns of patients, and personalizing long-term follow-up, a crucial aspect missing through automated surveys,” the authors wrote.
In addition to changing the time in which the calls were made, the researchers also changed how the survey was introduced to the patients, such as referring to the survey as “follow-up,” which seemed to improve patient participation.
“Further, it was observed that during conversations with the patient, highlighting relevant features of their medical and surgical history, such as the date of the surgery, the surgeon who operated on them, and their disease progression since surgery helped in developing a rapport with the patient and increased the chances of their participation,” they reported. “With these approaches, the participation rate after the second PDSA cycle increased to 55.1%.”
The data analyses in the study were supported by the Americas Hernia Society Quality Collaborative. There were no disclosures relevant to the study.
Follow-up telephone calls can significantly improve the collection of long-term patient-reported outcomes following ventral hernia repair, according to a study published online in the Oct. 20 edition of the Journal of the American College of Surgeons.
Nishant Ganesh Kumar, a medical student, and his colleagues at Vanderbilt University, Nashville, Tenn., wrote that while ventral hernia repair is one of the most common surgical procedures in the world, reliable long-term, prospective data on outcomes has been extremely difficult to collect.
In this Plan-Do-Study-Act (PDSA) prospective study, 99 patients who had undergone ventral hernia repair were followed up by telephone, in addition to the usual email communication, 1 year after their procedure. The calls were initially made between 1:00 p.m. and 3:00 p.m. in the first phase of the study, then changed to after 3:00 p.m. in the second phase.
Compared to the long-term completion rate of 16.3% prior to the intervention – where follow-up was largely through physical clinical visits – researchers saw a completion rate of 35.7% with the telephone calls between 1:00 p.m. and 3:00 p.m., and a 55.1% completion rate after changing the call time to after 3:00 p.m. The mean participation rate was 45.4%.
Once contact was made, all the patients completed the full patient-reported outcomes assessment, although the researchers did note that some seem to experience fatigue during questioning that required the interviewers to gently steer them back to the questions.
“The advantage of making phone calls was severalfold, including clarification of survey questions to help patients with providing more insightful responses, allaying concerns of patients, and personalizing long-term follow-up, a crucial aspect missing through automated surveys,” the authors wrote.
In addition to changing the time in which the calls were made, the researchers also changed how the survey was introduced to the patients, such as referring to the survey as “follow-up,” which seemed to improve patient participation.
“Further, it was observed that during conversations with the patient, highlighting relevant features of their medical and surgical history, such as the date of the surgery, the surgeon who operated on them, and their disease progression since surgery helped in developing a rapport with the patient and increased the chances of their participation,” they reported. “With these approaches, the participation rate after the second PDSA cycle increased to 55.1%.”
The data analyses in the study were supported by the Americas Hernia Society Quality Collaborative. There were no disclosures relevant to the study.
Follow-up telephone calls can significantly improve the collection of long-term patient-reported outcomes following ventral hernia repair, according to a study published online in the Oct. 20 edition of the Journal of the American College of Surgeons.
Nishant Ganesh Kumar, a medical student, and his colleagues at Vanderbilt University, Nashville, Tenn., wrote that while ventral hernia repair is one of the most common surgical procedures in the world, reliable long-term, prospective data on outcomes has been extremely difficult to collect.
In this Plan-Do-Study-Act (PDSA) prospective study, 99 patients who had undergone ventral hernia repair were followed up by telephone, in addition to the usual email communication, 1 year after their procedure. The calls were initially made between 1:00 p.m. and 3:00 p.m. in the first phase of the study, then changed to after 3:00 p.m. in the second phase.
Compared to the long-term completion rate of 16.3% prior to the intervention – where follow-up was largely through physical clinical visits – researchers saw a completion rate of 35.7% with the telephone calls between 1:00 p.m. and 3:00 p.m., and a 55.1% completion rate after changing the call time to after 3:00 p.m. The mean participation rate was 45.4%.
Once contact was made, all the patients completed the full patient-reported outcomes assessment, although the researchers did note that some seem to experience fatigue during questioning that required the interviewers to gently steer them back to the questions.
“The advantage of making phone calls was severalfold, including clarification of survey questions to help patients with providing more insightful responses, allaying concerns of patients, and personalizing long-term follow-up, a crucial aspect missing through automated surveys,” the authors wrote.
In addition to changing the time in which the calls were made, the researchers also changed how the survey was introduced to the patients, such as referring to the survey as “follow-up,” which seemed to improve patient participation.
“Further, it was observed that during conversations with the patient, highlighting relevant features of their medical and surgical history, such as the date of the surgery, the surgeon who operated on them, and their disease progression since surgery helped in developing a rapport with the patient and increased the chances of their participation,” they reported. “With these approaches, the participation rate after the second PDSA cycle increased to 55.1%.”
The data analyses in the study were supported by the Americas Hernia Society Quality Collaborative. There were no disclosures relevant to the study.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: Follow-up telephone calls can significantly improve the collection of long-term patient-reported outcomes following ventral hernia repair.
Major finding: Compared to the long-term completion rate of 16.3% prior to the intervention, a telephone call follow-up increased the mean participation rate to 45.4%.
Data source: Prospective cohort study of 99 patients who underwent ventral hernia repair.
Disclosures: The data analyses in the study were supported by the Americas Hernia Society Quality Collaborative. There were no disclosures relevant to the study.
Lenalidomide improves PFS after 1st and 2nd line CLL therapy
SAN DIEGO – Lenalidomide, a mainstay of maintenance therapy for multiple myeloma, is now making inroads into maintenance therapy following first- and second-line therapy for chronic lymphocytic leukemia (CLL), investigators reported in two phase III studies.
Among patients with previously untreated CLL who were at high risk for early disease progression following standard chemotherapy, lenalidomide (Revlimid) maintenance therapy was associated with an 80% reduction in the relative risk for disease progression compared with placebo, reported Anna Fink, MD, of the University of Cologne, Germany, and her colleagues in the German CLL Study Group.
Similarly, lenalidomide maintenance significantly improved progression-free survival (PFS) compared with placebo among patients with CLL who had at least partial responses to second-line therapy, reported Anna Schuh, MD, of the University of Oxford, England, and her colleagues in the CONTINUUM trial.
“Lenalidomide maintenance therapy significantly improved progression-free survival, from just about 9 months to almost 40 months when given to patients with CLL who responded to second-line therapy,” Dr. Schuh said at the American Society of Hematology annual meeting.
Both studies were unblinded because of the superiority of lenalidomide after prespecified analyses, on the recommendation of the respective data safety monitoring boards (DSMBs).
The PFS advantage with lenalidomide seen in each study did not translate into differences in overall survival in either study, however.
Maintenance after first-line therapy
In the CLLM1 trial, Dr. Fink and her colleagues enrolled physically fit, previously untreated patients with CLL and delivered chemoimmunotherapy at the investigator’s choice: either FCR (fludarabine, cyclophosphamide, and rituximab), FR (fludarabine and rituximab), FC (fludarabine and cyclophosphamide), or BR (bendamustine and rituximab).
Patients who had at least a partial response after a minimum of four cycles were identified as being at high risk for progression if they had minimal residual disease (MRD) levels of at least 10-2 cells, or MRD levels from 10-4 to less than 10-2 combined with either an unmutated IGHV gene status, del(17p) or TP53 mutation at baseline.
Of 468 screened patients, 89 were deemed to have high risk disease, and these patients were randomly assigned on a 2:1 basis to maintenance with lenalidomide given 5 mg orally for the first cycle and escalated to a target dose of 15 mg by the seventh cycle, or to placebo.
Additional dose escalations could be performed based on MRD assessments every 6 months, with the drug continued until progression or unacceptable toxicity. Patients also were assigned to daily low-dose aspirin or to an anticoagulation agent depending on their individual risk for thromboembolic events.
The study was stopped and unblinded after a planned interim analysis showed that the difference in PFS met the stopping boundary for efficacy.
Ultimately, 56 patients assigned to lenalidomide received study treatment, as did 29 assigned to placebo.
At a median follow-up of 17.5 months, the median PFS according to independent review was not reached for lenalidomide, vs. 13.3 months for placebo. Lenalidomide was associated with a hazard ratio (HR) for progression of 0.148 (P less than .00001), and a relative risk reduction of 80%.
Lenalidomide was also significantly better for PFS in analysis by MRD at baseline, with a PFS of 19.4 months for placebo vs. not reached among patients with less than 10-2 but more than 10-4 cells (HR, 0.125) and 3.7 vs. 32.3 months, respectively, for patients with MRD greater than 10-2 (HR 0.165).
There were three deaths (two in patients on placebo), and at the last analysis there was no difference in overall survival. In all, 42.9% of patients on lenalidomide discontinued because of adverse events, compared with 72.4% of those on placebo.
Maintenance after second-line therapy
In CONTINUUM, patients with at least a partial response after two prior lines of therapy and an Eastern Cooperative Oncology Group performance score of 0-2 were enrolled and randomized to receive either lenalidomide (160 patients) at a starting dose of 2.5 mg/day for the first 28-day cycle, 5 mg/day from cycle 2, and, if well tolerated, up to 10 mg/day from cycle 7 on, or to placebo (154 patients).
This study, as noted before, was also unblinded at the time of the primary analysis as recommended by the DSMB, after a prespecified number of events had occurred.
At a median follow-up of 31.5 months, the median PFS, a co-primary endpoint with OS, was 33.9 months in the lenalidomide arm, compared with 9.2 months in the placebo arm, translating into a HR for lenalidomide of 0.40 (P less than .001).
The lenalidomide advantage also was seen in a subgroup analysis by age, prior response to chemotherapy, and number of factors for poor prognosis. Of note, among patients older than age 70, the PFS with lenalidomide was 52.5 months, compared with 7.3 months for placebo (HR 0.34, P = .005).
In a second PFS analysis conducted after 71 months of follow-up, lenalidomide remained superior, with a median PFS of 57.5 months vs. 32.7 months in the placebo arm. As noted, there was no difference in overall survival in this study.
Grade 3 or greater adverse events occurring more frequently with lenalidomide were neutropenia, thrombocytopenia, diarrhea, pneumonia, fatigue, hypokalemia, pulmonary embolism, and sepsis. There was no difference in the incidence of second primary malignancies, however.
CLLM1 was sponsored by the German CLL Study Group with support from Celgene. CONTINUUM was supported by Celgene. Dr. Fink disclosed research funding from the company, and travel grants and honoraria from others. Dr. Schuh disclosed honoraria from and consulting with Celgene and other companies.
SAN DIEGO – Lenalidomide, a mainstay of maintenance therapy for multiple myeloma, is now making inroads into maintenance therapy following first- and second-line therapy for chronic lymphocytic leukemia (CLL), investigators reported in two phase III studies.
Among patients with previously untreated CLL who were at high risk for early disease progression following standard chemotherapy, lenalidomide (Revlimid) maintenance therapy was associated with an 80% reduction in the relative risk for disease progression compared with placebo, reported Anna Fink, MD, of the University of Cologne, Germany, and her colleagues in the German CLL Study Group.
Similarly, lenalidomide maintenance significantly improved progression-free survival (PFS) compared with placebo among patients with CLL who had at least partial responses to second-line therapy, reported Anna Schuh, MD, of the University of Oxford, England, and her colleagues in the CONTINUUM trial.
“Lenalidomide maintenance therapy significantly improved progression-free survival, from just about 9 months to almost 40 months when given to patients with CLL who responded to second-line therapy,” Dr. Schuh said at the American Society of Hematology annual meeting.
Both studies were unblinded because of the superiority of lenalidomide after prespecified analyses, on the recommendation of the respective data safety monitoring boards (DSMBs).
The PFS advantage with lenalidomide seen in each study did not translate into differences in overall survival in either study, however.
Maintenance after first-line therapy
In the CLLM1 trial, Dr. Fink and her colleagues enrolled physically fit, previously untreated patients with CLL and delivered chemoimmunotherapy at the investigator’s choice: either FCR (fludarabine, cyclophosphamide, and rituximab), FR (fludarabine and rituximab), FC (fludarabine and cyclophosphamide), or BR (bendamustine and rituximab).
Patients who had at least a partial response after a minimum of four cycles were identified as being at high risk for progression if they had minimal residual disease (MRD) levels of at least 10-2 cells, or MRD levels from 10-4 to less than 10-2 combined with either an unmutated IGHV gene status, del(17p) or TP53 mutation at baseline.
Of 468 screened patients, 89 were deemed to have high risk disease, and these patients were randomly assigned on a 2:1 basis to maintenance with lenalidomide given 5 mg orally for the first cycle and escalated to a target dose of 15 mg by the seventh cycle, or to placebo.
Additional dose escalations could be performed based on MRD assessments every 6 months, with the drug continued until progression or unacceptable toxicity. Patients also were assigned to daily low-dose aspirin or to an anticoagulation agent depending on their individual risk for thromboembolic events.
The study was stopped and unblinded after a planned interim analysis showed that the difference in PFS met the stopping boundary for efficacy.
Ultimately, 56 patients assigned to lenalidomide received study treatment, as did 29 assigned to placebo.
At a median follow-up of 17.5 months, the median PFS according to independent review was not reached for lenalidomide, vs. 13.3 months for placebo. Lenalidomide was associated with a hazard ratio (HR) for progression of 0.148 (P less than .00001), and a relative risk reduction of 80%.
Lenalidomide was also significantly better for PFS in analysis by MRD at baseline, with a PFS of 19.4 months for placebo vs. not reached among patients with less than 10-2 but more than 10-4 cells (HR, 0.125) and 3.7 vs. 32.3 months, respectively, for patients with MRD greater than 10-2 (HR 0.165).
There were three deaths (two in patients on placebo), and at the last analysis there was no difference in overall survival. In all, 42.9% of patients on lenalidomide discontinued because of adverse events, compared with 72.4% of those on placebo.
Maintenance after second-line therapy
In CONTINUUM, patients with at least a partial response after two prior lines of therapy and an Eastern Cooperative Oncology Group performance score of 0-2 were enrolled and randomized to receive either lenalidomide (160 patients) at a starting dose of 2.5 mg/day for the first 28-day cycle, 5 mg/day from cycle 2, and, if well tolerated, up to 10 mg/day from cycle 7 on, or to placebo (154 patients).
This study, as noted before, was also unblinded at the time of the primary analysis as recommended by the DSMB, after a prespecified number of events had occurred.
At a median follow-up of 31.5 months, the median PFS, a co-primary endpoint with OS, was 33.9 months in the lenalidomide arm, compared with 9.2 months in the placebo arm, translating into a HR for lenalidomide of 0.40 (P less than .001).
The lenalidomide advantage also was seen in a subgroup analysis by age, prior response to chemotherapy, and number of factors for poor prognosis. Of note, among patients older than age 70, the PFS with lenalidomide was 52.5 months, compared with 7.3 months for placebo (HR 0.34, P = .005).
In a second PFS analysis conducted after 71 months of follow-up, lenalidomide remained superior, with a median PFS of 57.5 months vs. 32.7 months in the placebo arm. As noted, there was no difference in overall survival in this study.
Grade 3 or greater adverse events occurring more frequently with lenalidomide were neutropenia, thrombocytopenia, diarrhea, pneumonia, fatigue, hypokalemia, pulmonary embolism, and sepsis. There was no difference in the incidence of second primary malignancies, however.
CLLM1 was sponsored by the German CLL Study Group with support from Celgene. CONTINUUM was supported by Celgene. Dr. Fink disclosed research funding from the company, and travel grants and honoraria from others. Dr. Schuh disclosed honoraria from and consulting with Celgene and other companies.
SAN DIEGO – Lenalidomide, a mainstay of maintenance therapy for multiple myeloma, is now making inroads into maintenance therapy following first- and second-line therapy for chronic lymphocytic leukemia (CLL), investigators reported in two phase III studies.
Among patients with previously untreated CLL who were at high risk for early disease progression following standard chemotherapy, lenalidomide (Revlimid) maintenance therapy was associated with an 80% reduction in the relative risk for disease progression compared with placebo, reported Anna Fink, MD, of the University of Cologne, Germany, and her colleagues in the German CLL Study Group.
Similarly, lenalidomide maintenance significantly improved progression-free survival (PFS) compared with placebo among patients with CLL who had at least partial responses to second-line therapy, reported Anna Schuh, MD, of the University of Oxford, England, and her colleagues in the CONTINUUM trial.
“Lenalidomide maintenance therapy significantly improved progression-free survival, from just about 9 months to almost 40 months when given to patients with CLL who responded to second-line therapy,” Dr. Schuh said at the American Society of Hematology annual meeting.
Both studies were unblinded because of the superiority of lenalidomide after prespecified analyses, on the recommendation of the respective data safety monitoring boards (DSMBs).
The PFS advantage with lenalidomide seen in each study did not translate into differences in overall survival in either study, however.
Maintenance after first-line therapy
In the CLLM1 trial, Dr. Fink and her colleagues enrolled physically fit, previously untreated patients with CLL and delivered chemoimmunotherapy at the investigator’s choice: either FCR (fludarabine, cyclophosphamide, and rituximab), FR (fludarabine and rituximab), FC (fludarabine and cyclophosphamide), or BR (bendamustine and rituximab).
Patients who had at least a partial response after a minimum of four cycles were identified as being at high risk for progression if they had minimal residual disease (MRD) levels of at least 10-2 cells, or MRD levels from 10-4 to less than 10-2 combined with either an unmutated IGHV gene status, del(17p) or TP53 mutation at baseline.
Of 468 screened patients, 89 were deemed to have high risk disease, and these patients were randomly assigned on a 2:1 basis to maintenance with lenalidomide given 5 mg orally for the first cycle and escalated to a target dose of 15 mg by the seventh cycle, or to placebo.
Additional dose escalations could be performed based on MRD assessments every 6 months, with the drug continued until progression or unacceptable toxicity. Patients also were assigned to daily low-dose aspirin or to an anticoagulation agent depending on their individual risk for thromboembolic events.
The study was stopped and unblinded after a planned interim analysis showed that the difference in PFS met the stopping boundary for efficacy.
Ultimately, 56 patients assigned to lenalidomide received study treatment, as did 29 assigned to placebo.
At a median follow-up of 17.5 months, the median PFS according to independent review was not reached for lenalidomide, vs. 13.3 months for placebo. Lenalidomide was associated with a hazard ratio (HR) for progression of 0.148 (P less than .00001), and a relative risk reduction of 80%.
Lenalidomide was also significantly better for PFS in analysis by MRD at baseline, with a PFS of 19.4 months for placebo vs. not reached among patients with less than 10-2 but more than 10-4 cells (HR, 0.125) and 3.7 vs. 32.3 months, respectively, for patients with MRD greater than 10-2 (HR 0.165).
There were three deaths (two in patients on placebo), and at the last analysis there was no difference in overall survival. In all, 42.9% of patients on lenalidomide discontinued because of adverse events, compared with 72.4% of those on placebo.
Maintenance after second-line therapy
In CONTINUUM, patients with at least a partial response after two prior lines of therapy and an Eastern Cooperative Oncology Group performance score of 0-2 were enrolled and randomized to receive either lenalidomide (160 patients) at a starting dose of 2.5 mg/day for the first 28-day cycle, 5 mg/day from cycle 2, and, if well tolerated, up to 10 mg/day from cycle 7 on, or to placebo (154 patients).
This study, as noted before, was also unblinded at the time of the primary analysis as recommended by the DSMB, after a prespecified number of events had occurred.
At a median follow-up of 31.5 months, the median PFS, a co-primary endpoint with OS, was 33.9 months in the lenalidomide arm, compared with 9.2 months in the placebo arm, translating into a HR for lenalidomide of 0.40 (P less than .001).
The lenalidomide advantage also was seen in a subgroup analysis by age, prior response to chemotherapy, and number of factors for poor prognosis. Of note, among patients older than age 70, the PFS with lenalidomide was 52.5 months, compared with 7.3 months for placebo (HR 0.34, P = .005).
In a second PFS analysis conducted after 71 months of follow-up, lenalidomide remained superior, with a median PFS of 57.5 months vs. 32.7 months in the placebo arm. As noted, there was no difference in overall survival in this study.
Grade 3 or greater adverse events occurring more frequently with lenalidomide were neutropenia, thrombocytopenia, diarrhea, pneumonia, fatigue, hypokalemia, pulmonary embolism, and sepsis. There was no difference in the incidence of second primary malignancies, however.
CLLM1 was sponsored by the German CLL Study Group with support from Celgene. CONTINUUM was supported by Celgene. Dr. Fink disclosed research funding from the company, and travel grants and honoraria from others. Dr. Schuh disclosed honoraria from and consulting with Celgene and other companies.
AT ASH 2016
Key clinical point: Lenalidomide (Revlimid) maintenance improves progression free survival following first- and second-line therapies for chronic lymphocytic leukemia.
Major finding: Median PFS vs. placebo was not reached vs. 13.3 months in CLLM1, and 33.9 vs. 9.2 months in CONTINUUM.
Data source: Phase III randomized studies of lenalidomide maintenance following first-line therapy (CLLM1) and second-line therapy (CONTINUUM).
Disclosures: CLLM1 was sponsored by the German CLL Study Group with support from Celgene. CONTINUUM was supported by Celgene. Dr. Fink disclosed research funding from Celgene, and travel grants and honoraria from other drug companies. Dr. Schuh disclosed honoraria from and consulting with Celgene and other companies.
Adding respiratory rate to triage criteria improves accurate staging of chest trauma patients
WASHINGTON – Adding respiratory rate and suspected blunt chest injury to a trauma assessment in the field significantly improved the appropriate triaging of level III trauma patients.
When the assessment specifically evaluated for tachypnea in the setting of blunt chest injury, undertriaging improved by 1.2%, John Yonge, MD, said at the annual clinical congress of the American College of Surgeons.
“When we applied this new criteria to our 10-year study, we identified 661 patients who should have been activated as a level I or level II,” but instead were assessed as less critically injured, Dr. Yonge said in an interview. This initial misstep significantly extended the time before patients could have critical surgical procedures and was related to higher mortality among them.
Dr. Yonge, a surgical fellow at Oregon Health & Science University, Portland, and his mentor Martin Schreiber, MD, conducted the retrospective study of 7,880 trauma patients admitted at level III activation from 2004 to 2014. The OHSU trauma system has three activation levels.
• Level I activations are reserved for the most critically injured patients; attending trauma surgeon and anesthesiologist presence is mandatory.
• Level II activations capture moderate to severe injuries; trauma surgeon and respiratory therapist presence is mandated.
• Level III activations are designed to capture patients who do not require an immediate lifesaving intervention; the presence of the trauma surgery chief resident and attending emergency medicine physician is mandatory.
Patients were considered undertriaged if they were admitted as level III activations, but then required a critical intervention (chest tube placement, intubation, needle thoracostomy, or intracranial pressure monitoring) in the emergency department or ultimately met level I or II activation criteria.
Among all the level III patients, 466 (6%) were undertriaged: 390 were undertriaged based on the existing level I or II activation criteria, and 76 were considered undertriaged based on the need for a critical intervention.
Most of the undertriaged patients (65%) met criteria for level I activation; the rest should have been triaged as level II patients. Compared with appropriately staged level III patients, mortality among the undertriaged patients was significantly higher (3.2% vs. 0.6%). Undertriaged patients also experienced longer delays before initiation of major emergency surgery: a mean of 147 minutes, compared with 106 minutes for appropriately triaged level I patients and 62 minutes for appropriately triaged level II patients.
Dr. Yonge then looked for clinical measures that would improve triage. Tachypnea (respiratory rate of more than 20 breaths per minute) in the field stood out as a significant factor. Tachypneic patients who had a suspected chest injury were 70% more likely to be undertriaged than were those with a normal respiratory rate. Tachypnea was significantly associated with a diagnosis of flail chest, emergency department intubation, and chest tube placement.
The team then constructed a new triage criterion for patients with suspected chest injury – tachypnea combined with suspected blunt thoracic injury. By applying that model to their study population of level III patients, they determined that the level III undertriage rate would be reduced by 1.2%.
Tying the physiologic marker of tachypnea to a suspected clinical diagnosis is a key factor, Dr. Yonge noted. “Just adding tachypnea doesn’t help us. In fact, it would overwhelm us, because a trauma patient could very well be tachypneic because he’s experiencing panic. But tying it to a suspected clinical diagnosis gives us a meaningful result.”
He confirmed this linkage with an additional analysis. “We looked to see how severely injured these patients were and found that 71% of them had an Abbreviated Injury Score (AIS) to the chest of 3 or more, indicating a severe chest injury. Only 29% had an AIS of 2 or less. So this proves that respiratory rate is a valid triage criterion and can be used to identify patients who need a higher level of trauma care.”
The challenge now, Dr. Yonge said, is incorporating the marker into clinical practice. “It doesn’t matter how many statistics you do, if you can’t educate the prehospital providers in this, it’s useless. They are the crux of the trauma system.”
Although national guidelines do recommend assessing respiratory rate as part of field triage, it often isn’t recorded or is only estimated, Dr. Yonge said. That’s one reason he used the 20-breaths-per-minute cutoff rate. “It doesn’t even take a full minute to assess this, but it can make a big improvement in care.”
Neither he nor Dr. Schreiber had any financial disclosures.
[email protected]
On Twitter @alz_gal
WASHINGTON – Adding respiratory rate and suspected blunt chest injury to a trauma assessment in the field significantly improved the appropriate triaging of level III trauma patients.
When the assessment specifically evaluated for tachypnea in the setting of blunt chest injury, undertriaging improved by 1.2%, John Yonge, MD, said at the annual clinical congress of the American College of Surgeons.
“When we applied this new criteria to our 10-year study, we identified 661 patients who should have been activated as a level I or level II,” but instead were assessed as less critically injured, Dr. Yonge said in an interview. This initial misstep significantly extended the time before patients could have critical surgical procedures and was related to higher mortality among them.
Dr. Yonge, a surgical fellow at Oregon Health & Science University, Portland, and his mentor Martin Schreiber, MD, conducted the retrospective study of 7,880 trauma patients admitted at level III activation from 2004 to 2014. The OHSU trauma system has three activation levels.
• Level I activations are reserved for the most critically injured patients; attending trauma surgeon and anesthesiologist presence is mandatory.
• Level II activations capture moderate to severe injuries; trauma surgeon and respiratory therapist presence is mandated.
• Level III activations are designed to capture patients who do not require an immediate lifesaving intervention; the presence of the trauma surgery chief resident and attending emergency medicine physician is mandatory.
Patients were considered undertriaged if they were admitted as level III activations, but then required a critical intervention (chest tube placement, intubation, needle thoracostomy, or intracranial pressure monitoring) in the emergency department or ultimately met level I or II activation criteria.
Among all the level III patients, 466 (6%) were undertriaged: 390 were undertriaged based on the existing level I or II activation criteria, and 76 were considered undertriaged based on the need for a critical intervention.
Most of the undertriaged patients (65%) met criteria for level I activation; the rest should have been triaged as level II patients. Compared with appropriately staged level III patients, mortality among the undertriaged patients was significantly higher (3.2% vs. 0.6%). Undertriaged patients also experienced longer delays before initiation of major emergency surgery: a mean of 147 minutes, compared with 106 minutes for appropriately triaged level I patients and 62 minutes for appropriately triaged level II patients.
Dr. Yonge then looked for clinical measures that would improve triage. Tachypnea (respiratory rate of more than 20 breaths per minute) in the field stood out as a significant factor. Tachypneic patients who had a suspected chest injury were 70% more likely to be undertriaged than were those with a normal respiratory rate. Tachypnea was significantly associated with a diagnosis of flail chest, emergency department intubation, and chest tube placement.
The team then constructed a new triage criterion for patients with suspected chest injury – tachypnea combined with suspected blunt thoracic injury. By applying that model to their study population of level III patients, they determined that the level III undertriage rate would be reduced by 1.2%.
Tying the physiologic marker of tachypnea to a suspected clinical diagnosis is a key factor, Dr. Yonge noted. “Just adding tachypnea doesn’t help us. In fact, it would overwhelm us, because a trauma patient could very well be tachypneic because he’s experiencing panic. But tying it to a suspected clinical diagnosis gives us a meaningful result.”
He confirmed this linkage with an additional analysis. “We looked to see how severely injured these patients were and found that 71% of them had an Abbreviated Injury Score (AIS) to the chest of 3 or more, indicating a severe chest injury. Only 29% had an AIS of 2 or less. So this proves that respiratory rate is a valid triage criterion and can be used to identify patients who need a higher level of trauma care.”
The challenge now, Dr. Yonge said, is incorporating the marker into clinical practice. “It doesn’t matter how many statistics you do, if you can’t educate the prehospital providers in this, it’s useless. They are the crux of the trauma system.”
Although national guidelines do recommend assessing respiratory rate as part of field triage, it often isn’t recorded or is only estimated, Dr. Yonge said. That’s one reason he used the 20-breaths-per-minute cutoff rate. “It doesn’t even take a full minute to assess this, but it can make a big improvement in care.”
Neither he nor Dr. Schreiber had any financial disclosures.
[email protected]
On Twitter @alz_gal
WASHINGTON – Adding respiratory rate and suspected blunt chest injury to a trauma assessment in the field significantly improved the appropriate triaging of level III trauma patients.
When the assessment specifically evaluated for tachypnea in the setting of blunt chest injury, undertriaging improved by 1.2%, John Yonge, MD, said at the annual clinical congress of the American College of Surgeons.
“When we applied this new criteria to our 10-year study, we identified 661 patients who should have been activated as a level I or level II,” but instead were assessed as less critically injured, Dr. Yonge said in an interview. This initial misstep significantly extended the time before patients could have critical surgical procedures and was related to higher mortality among them.
Dr. Yonge, a surgical fellow at Oregon Health & Science University, Portland, and his mentor Martin Schreiber, MD, conducted the retrospective study of 7,880 trauma patients admitted at level III activation from 2004 to 2014. The OHSU trauma system has three activation levels.
• Level I activations are reserved for the most critically injured patients; attending trauma surgeon and anesthesiologist presence is mandatory.
• Level II activations capture moderate to severe injuries; trauma surgeon and respiratory therapist presence is mandated.
• Level III activations are designed to capture patients who do not require an immediate lifesaving intervention; the presence of the trauma surgery chief resident and attending emergency medicine physician is mandatory.
Patients were considered undertriaged if they were admitted as level III activations, but then required a critical intervention (chest tube placement, intubation, needle thoracostomy, or intracranial pressure monitoring) in the emergency department or ultimately met level I or II activation criteria.
Among all the level III patients, 466 (6%) were undertriaged: 390 were undertriaged based on the existing level I or II activation criteria, and 76 were considered undertriaged based on the need for a critical intervention.
Most of the undertriaged patients (65%) met criteria for level I activation; the rest should have been triaged as level II patients. Compared with appropriately staged level III patients, mortality among the undertriaged patients was significantly higher (3.2% vs. 0.6%). Undertriaged patients also experienced longer delays before initiation of major emergency surgery: a mean of 147 minutes, compared with 106 minutes for appropriately triaged level I patients and 62 minutes for appropriately triaged level II patients.
Dr. Yonge then looked for clinical measures that would improve triage. Tachypnea (respiratory rate of more than 20 breaths per minute) in the field stood out as a significant factor. Tachypneic patients who had a suspected chest injury were 70% more likely to be undertriaged than were those with a normal respiratory rate. Tachypnea was significantly associated with a diagnosis of flail chest, emergency department intubation, and chest tube placement.
The team then constructed a new triage criterion for patients with suspected chest injury – tachypnea combined with suspected blunt thoracic injury. By applying that model to their study population of level III patients, they determined that the level III undertriage rate would be reduced by 1.2%.
Tying the physiologic marker of tachypnea to a suspected clinical diagnosis is a key factor, Dr. Yonge noted. “Just adding tachypnea doesn’t help us. In fact, it would overwhelm us, because a trauma patient could very well be tachypneic because he’s experiencing panic. But tying it to a suspected clinical diagnosis gives us a meaningful result.”
He confirmed this linkage with an additional analysis. “We looked to see how severely injured these patients were and found that 71% of them had an Abbreviated Injury Score (AIS) to the chest of 3 or more, indicating a severe chest injury. Only 29% had an AIS of 2 or less. So this proves that respiratory rate is a valid triage criterion and can be used to identify patients who need a higher level of trauma care.”
The challenge now, Dr. Yonge said, is incorporating the marker into clinical practice. “It doesn’t matter how many statistics you do, if you can’t educate the prehospital providers in this, it’s useless. They are the crux of the trauma system.”
Although national guidelines do recommend assessing respiratory rate as part of field triage, it often isn’t recorded or is only estimated, Dr. Yonge said. That’s one reason he used the 20-breaths-per-minute cutoff rate. “It doesn’t even take a full minute to assess this, but it can make a big improvement in care.”
Neither he nor Dr. Schreiber had any financial disclosures.
[email protected]
On Twitter @alz_gal
AT THE ACS CLINICAL CONGRESS
Key clinical point:
Major finding: Adding a triage assessment criterion of tachypnea plus suspected chest injury improved undertriage of chest trauma patients by 1.2%.
Data source: The retrospective database study comprising 7,880 patients.
Disclosures: Neither Dr. Yonge nor Dr. Schreiber had any financial disclosures.
Impact of Medicaid expansion on inpatient outcomes
The Affordable Care Act (ACA) has greatly increased the number of Medicaid enrollees since it expanded eligibility criteria on Jan. 1, 2014. Nearly 9 million additional U.S. adults now have Medicaid coverage, mostly in the 31 states and Washington, which have opted into Medicaid expansion.
The ACA has also had an important impact on hospital payer mix, mainly by decreasing the amount of uncompensated care in Medicaid-expansion states. Previous studies have shown disparities in the quality of inpatient care based on insurance type. Patients with Medicaid insurance often have longer hospitalizations and higher in-hospital mortality than commercially-insured patients and occasionally even than uninsured patients.
In our study published in the Journal of Hospital Medicine (2016 Dec. doi: 10.1002/jhm.2649), we evaluated the impact of state Medicaid expansion status on payer mix, length of stay, and in-hospital mortality for general medicine patients discharged from U.S. academic medical centers. We considered Jan. 1, 2014, to be the date of ACA implementation for all states except Michigan, New Hampshire, Pennsylvania, and Indiana, which had unique dates of Medicaid expansion.
We were able to identify 3,144,488 discharges from 156 hospitals in 24 Medicaid-expansion states and Washington, and 1,114,464 discharges from 55 hospitals in 14 nonexpansion states between October 2012 and September 2015.
Despite this difference in payer mix trends, state Medicaid expansion status was not associated with differences in overall length of stay or in-hospital mortality in our study. More precisely, we looked at the length of stay and mortality indices, or ratio of observed to expected values, to control for such potential confounders as disease severity and comorbid conditions.
One possible explanation for our findings is that the higher proportion of Medicare and commercially-insured patients overshadowed the contribution of Medicaid patients to the overall length of stay and mortality indices.
To our knowledge, our study is the first to look at the effect of ACA implementation on inpatient outcomes. Early evidence suggests that Medicaid expansion has improved outpatient outcomes. Low-income adults in Medicaid-expansion states have shown greater gains in access to primary care clinics and medications and in the diagnosis of certain chronic health conditions than those in non-expansion states. However, these changes would not necessarily lead to improvements in the length of stay or mortality indices for Medicaid-expansion hospitals, since the measures account for patient acuity on admission.
The take-home message from our study for health policy makers is that state Medicaid expansion status had a neutral effect on both length of stay and mortality indices. This should be reassuring for states considering expansion of their Medicaid programs in the future.
As a next step, it would be useful to see research on the impact of ACA implementation on other inpatient outcomes that may vary with insurance type, such as readmissions or hospital-acquired complications.
The take-home message for hospitalists is that there is more work to be done in reducing disparities in inpatient care based on payer status. Though not a primary focus of our study, we did see variation in the length of stay and mortality indices based on insurance type.
It is unclear whether these differences occurred because of variation in the expertise of inpatient providers, access to invasive procedures or medical therapies, the timeliness of discharge to post-acute care facilities, or other patient- or system-level factors. However, these disparities warrant our improvement efforts moving forward.
Mary Anderson, MD, and Christine Jones, MD, are hospitalists at the University of Colorado (Aurora) Hospital and assistant professors in the department of medicine at the University of Colorado.
The Affordable Care Act (ACA) has greatly increased the number of Medicaid enrollees since it expanded eligibility criteria on Jan. 1, 2014. Nearly 9 million additional U.S. adults now have Medicaid coverage, mostly in the 31 states and Washington, which have opted into Medicaid expansion.
The ACA has also had an important impact on hospital payer mix, mainly by decreasing the amount of uncompensated care in Medicaid-expansion states. Previous studies have shown disparities in the quality of inpatient care based on insurance type. Patients with Medicaid insurance often have longer hospitalizations and higher in-hospital mortality than commercially-insured patients and occasionally even than uninsured patients.
In our study published in the Journal of Hospital Medicine (2016 Dec. doi: 10.1002/jhm.2649), we evaluated the impact of state Medicaid expansion status on payer mix, length of stay, and in-hospital mortality for general medicine patients discharged from U.S. academic medical centers. We considered Jan. 1, 2014, to be the date of ACA implementation for all states except Michigan, New Hampshire, Pennsylvania, and Indiana, which had unique dates of Medicaid expansion.
We were able to identify 3,144,488 discharges from 156 hospitals in 24 Medicaid-expansion states and Washington, and 1,114,464 discharges from 55 hospitals in 14 nonexpansion states between October 2012 and September 2015.
Despite this difference in payer mix trends, state Medicaid expansion status was not associated with differences in overall length of stay or in-hospital mortality in our study. More precisely, we looked at the length of stay and mortality indices, or ratio of observed to expected values, to control for such potential confounders as disease severity and comorbid conditions.
One possible explanation for our findings is that the higher proportion of Medicare and commercially-insured patients overshadowed the contribution of Medicaid patients to the overall length of stay and mortality indices.
To our knowledge, our study is the first to look at the effect of ACA implementation on inpatient outcomes. Early evidence suggests that Medicaid expansion has improved outpatient outcomes. Low-income adults in Medicaid-expansion states have shown greater gains in access to primary care clinics and medications and in the diagnosis of certain chronic health conditions than those in non-expansion states. However, these changes would not necessarily lead to improvements in the length of stay or mortality indices for Medicaid-expansion hospitals, since the measures account for patient acuity on admission.
The take-home message from our study for health policy makers is that state Medicaid expansion status had a neutral effect on both length of stay and mortality indices. This should be reassuring for states considering expansion of their Medicaid programs in the future.
As a next step, it would be useful to see research on the impact of ACA implementation on other inpatient outcomes that may vary with insurance type, such as readmissions or hospital-acquired complications.
The take-home message for hospitalists is that there is more work to be done in reducing disparities in inpatient care based on payer status. Though not a primary focus of our study, we did see variation in the length of stay and mortality indices based on insurance type.
It is unclear whether these differences occurred because of variation in the expertise of inpatient providers, access to invasive procedures or medical therapies, the timeliness of discharge to post-acute care facilities, or other patient- or system-level factors. However, these disparities warrant our improvement efforts moving forward.
Mary Anderson, MD, and Christine Jones, MD, are hospitalists at the University of Colorado (Aurora) Hospital and assistant professors in the department of medicine at the University of Colorado.
The Affordable Care Act (ACA) has greatly increased the number of Medicaid enrollees since it expanded eligibility criteria on Jan. 1, 2014. Nearly 9 million additional U.S. adults now have Medicaid coverage, mostly in the 31 states and Washington, which have opted into Medicaid expansion.
The ACA has also had an important impact on hospital payer mix, mainly by decreasing the amount of uncompensated care in Medicaid-expansion states. Previous studies have shown disparities in the quality of inpatient care based on insurance type. Patients with Medicaid insurance often have longer hospitalizations and higher in-hospital mortality than commercially-insured patients and occasionally even than uninsured patients.
In our study published in the Journal of Hospital Medicine (2016 Dec. doi: 10.1002/jhm.2649), we evaluated the impact of state Medicaid expansion status on payer mix, length of stay, and in-hospital mortality for general medicine patients discharged from U.S. academic medical centers. We considered Jan. 1, 2014, to be the date of ACA implementation for all states except Michigan, New Hampshire, Pennsylvania, and Indiana, which had unique dates of Medicaid expansion.
We were able to identify 3,144,488 discharges from 156 hospitals in 24 Medicaid-expansion states and Washington, and 1,114,464 discharges from 55 hospitals in 14 nonexpansion states between October 2012 and September 2015.
Despite this difference in payer mix trends, state Medicaid expansion status was not associated with differences in overall length of stay or in-hospital mortality in our study. More precisely, we looked at the length of stay and mortality indices, or ratio of observed to expected values, to control for such potential confounders as disease severity and comorbid conditions.
One possible explanation for our findings is that the higher proportion of Medicare and commercially-insured patients overshadowed the contribution of Medicaid patients to the overall length of stay and mortality indices.
To our knowledge, our study is the first to look at the effect of ACA implementation on inpatient outcomes. Early evidence suggests that Medicaid expansion has improved outpatient outcomes. Low-income adults in Medicaid-expansion states have shown greater gains in access to primary care clinics and medications and in the diagnosis of certain chronic health conditions than those in non-expansion states. However, these changes would not necessarily lead to improvements in the length of stay or mortality indices for Medicaid-expansion hospitals, since the measures account for patient acuity on admission.
The take-home message from our study for health policy makers is that state Medicaid expansion status had a neutral effect on both length of stay and mortality indices. This should be reassuring for states considering expansion of their Medicaid programs in the future.
As a next step, it would be useful to see research on the impact of ACA implementation on other inpatient outcomes that may vary with insurance type, such as readmissions or hospital-acquired complications.
The take-home message for hospitalists is that there is more work to be done in reducing disparities in inpatient care based on payer status. Though not a primary focus of our study, we did see variation in the length of stay and mortality indices based on insurance type.
It is unclear whether these differences occurred because of variation in the expertise of inpatient providers, access to invasive procedures or medical therapies, the timeliness of discharge to post-acute care facilities, or other patient- or system-level factors. However, these disparities warrant our improvement efforts moving forward.
Mary Anderson, MD, and Christine Jones, MD, are hospitalists at the University of Colorado (Aurora) Hospital and assistant professors in the department of medicine at the University of Colorado.
VA Confronts Fallout of SAIL Facility Ratings
VA Secretary Robert McDonald minced few words in his reaction to the USA Today story that published VA’s 5-star ratings for VAMCs based on its Strategic Analytics for Improvement and Learning (SAIL) data. “What concerns all of us at VA is that USA Today has a consistent narrative of negativity in their news of VA,” McDonald charged. Specifically, use of the word secret in the headline was an “egregious hyperbole,” he insisted.
Still, within days, a number of VA facilities were using the story as an opportunity to tout their success. VA Central Western Massachusetts Healthcare System in Worcester, for example, used the opportunity to tell local media that it was “in the top 10% of the 152 VA medical centers in the nation for quality of care,” and 1 of 3 5-star facilities in Massachusetts.
Other facilities, however, were forced to explain the relative nature of the 5-star scale. Keith Sullivan, director of the Chillicothe VAMC in Ohio, which received a 3-star rating, responded to reporters by noting that, “Although SAIL is a tool that helps look at areas in need of improvements, we have many other ways to ensure quality care is in place,” he said.
Many VA officials point out that the comparison to other VA facilities may be unfair, especially in underserved locations. The VA Health Care Center at Harlingen in Texas recently improved from 1 to 2 stars. It received this score, in part, because of its difficulty filling open vacancies. “Compared to the nurse retention rates in our local communities we are doing very well, [but] not so much as compared to other VA health care systems in the nation,” a Harlingen customer service manager told a local newspaper.
To allay veterans’ fears, the VA Southern Oregon Rehabilitation Center and Clinics (VA SORCC) sent out a news release to explain the ratings and reassure the public that progress was being made even as it struggles with a shortage of providers. Insisting it had made “absolute performance improvements in wait times for both mental health and specialty care appointments” while acknowledging that the rating also shows “continued frustrations with difficulty in navigating the system and with coordination of care." These frustrations impact Veterans’ experience at the facility, leading to lower scores.” The release pledged that “VA SORCC is currently a 1-star facility but fully expects to move to a 2-star facility in the next quarter.”
The worry for many at the VA is that the veterans might avoid 1- and 2-star facilities. “My concern is that veterans are going to see that their hospital is a ‘one’ in our star system, assume that’s bad quality and veterans that need care are not going to get care,” VA Under Secretary of Health David J. Shulkin, MD, told USA Today. “And they’re going to stay away from hospitals and that’s going to hurt people.”
VA Secretary Robert McDonald minced few words in his reaction to the USA Today story that published VA’s 5-star ratings for VAMCs based on its Strategic Analytics for Improvement and Learning (SAIL) data. “What concerns all of us at VA is that USA Today has a consistent narrative of negativity in their news of VA,” McDonald charged. Specifically, use of the word secret in the headline was an “egregious hyperbole,” he insisted.
Still, within days, a number of VA facilities were using the story as an opportunity to tout their success. VA Central Western Massachusetts Healthcare System in Worcester, for example, used the opportunity to tell local media that it was “in the top 10% of the 152 VA medical centers in the nation for quality of care,” and 1 of 3 5-star facilities in Massachusetts.
Other facilities, however, were forced to explain the relative nature of the 5-star scale. Keith Sullivan, director of the Chillicothe VAMC in Ohio, which received a 3-star rating, responded to reporters by noting that, “Although SAIL is a tool that helps look at areas in need of improvements, we have many other ways to ensure quality care is in place,” he said.
Many VA officials point out that the comparison to other VA facilities may be unfair, especially in underserved locations. The VA Health Care Center at Harlingen in Texas recently improved from 1 to 2 stars. It received this score, in part, because of its difficulty filling open vacancies. “Compared to the nurse retention rates in our local communities we are doing very well, [but] not so much as compared to other VA health care systems in the nation,” a Harlingen customer service manager told a local newspaper.
To allay veterans’ fears, the VA Southern Oregon Rehabilitation Center and Clinics (VA SORCC) sent out a news release to explain the ratings and reassure the public that progress was being made even as it struggles with a shortage of providers. Insisting it had made “absolute performance improvements in wait times for both mental health and specialty care appointments” while acknowledging that the rating also shows “continued frustrations with difficulty in navigating the system and with coordination of care." These frustrations impact Veterans’ experience at the facility, leading to lower scores.” The release pledged that “VA SORCC is currently a 1-star facility but fully expects to move to a 2-star facility in the next quarter.”
The worry for many at the VA is that the veterans might avoid 1- and 2-star facilities. “My concern is that veterans are going to see that their hospital is a ‘one’ in our star system, assume that’s bad quality and veterans that need care are not going to get care,” VA Under Secretary of Health David J. Shulkin, MD, told USA Today. “And they’re going to stay away from hospitals and that’s going to hurt people.”
VA Secretary Robert McDonald minced few words in his reaction to the USA Today story that published VA’s 5-star ratings for VAMCs based on its Strategic Analytics for Improvement and Learning (SAIL) data. “What concerns all of us at VA is that USA Today has a consistent narrative of negativity in their news of VA,” McDonald charged. Specifically, use of the word secret in the headline was an “egregious hyperbole,” he insisted.
Still, within days, a number of VA facilities were using the story as an opportunity to tout their success. VA Central Western Massachusetts Healthcare System in Worcester, for example, used the opportunity to tell local media that it was “in the top 10% of the 152 VA medical centers in the nation for quality of care,” and 1 of 3 5-star facilities in Massachusetts.
Other facilities, however, were forced to explain the relative nature of the 5-star scale. Keith Sullivan, director of the Chillicothe VAMC in Ohio, which received a 3-star rating, responded to reporters by noting that, “Although SAIL is a tool that helps look at areas in need of improvements, we have many other ways to ensure quality care is in place,” he said.
Many VA officials point out that the comparison to other VA facilities may be unfair, especially in underserved locations. The VA Health Care Center at Harlingen in Texas recently improved from 1 to 2 stars. It received this score, in part, because of its difficulty filling open vacancies. “Compared to the nurse retention rates in our local communities we are doing very well, [but] not so much as compared to other VA health care systems in the nation,” a Harlingen customer service manager told a local newspaper.
To allay veterans’ fears, the VA Southern Oregon Rehabilitation Center and Clinics (VA SORCC) sent out a news release to explain the ratings and reassure the public that progress was being made even as it struggles with a shortage of providers. Insisting it had made “absolute performance improvements in wait times for both mental health and specialty care appointments” while acknowledging that the rating also shows “continued frustrations with difficulty in navigating the system and with coordination of care." These frustrations impact Veterans’ experience at the facility, leading to lower scores.” The release pledged that “VA SORCC is currently a 1-star facility but fully expects to move to a 2-star facility in the next quarter.”
The worry for many at the VA is that the veterans might avoid 1- and 2-star facilities. “My concern is that veterans are going to see that their hospital is a ‘one’ in our star system, assume that’s bad quality and veterans that need care are not going to get care,” VA Under Secretary of Health David J. Shulkin, MD, told USA Today. “And they’re going to stay away from hospitals and that’s going to hurt people.”
‘Unprecedented’ MRD negativity with daratumumab in MM

© Todd Buchanan 2016
SAN DIEGO—Daratumumab added to standard of care regimens drives deep clinical responses beyond complete response (CR), a magnitude that is “unprecedented” in the relapsed/refractory multiple myeloma (MM) setting, according to a speaker at the 2016 ASH Annual Meeting.
Investigators added daratumumab to lenalidomide/dexamethasone in the POLLUX trial and to bortezomib/dexamethasone in the CASTOR trial.
In both phase 3 trials, the addition of daratumumab resulted in significant improvements in progression-free survival (PFS), overall response rate, and minimal residual disease (MRD) negativity when compared to control groups.
“The magnitude of daratumumab-induced MRD negativity in the relapsed setting is unprecedented and, for me, was not expected,” said Hervé Avet-Loiseau, MD, of Centre Hospitalier Universitaire Rangueil, Unité de Genomique du Myelome in Toulouse, France.
Dr Avet-Loiseau presented the MRD findings from CASTOR and POLLUX at the ASH Annual Meeting as abstract 246.*
He noted that, based on these studies, daratumumab received US Food and Drug Administration approvals for use in combination with standard of care regimens for MM patients who had received 1 or more prior lines of treatment.
Daratumumab had been previously approved as monotherapy for relapsed or refractory MM.
Study designs and findings from the POLLUX and CASTOR trials have been described earlier in Hematology Times.
Dr Avet-Loiseau provided updated PFS figures for the 2 studies.
At 18 months’ follow-up in the POLLUX study, the PFS rate for patients treated with daratumumab/lenalidomide/dexamethasone was 76%, compared to 49% in the lenalidomide/dexamethasone arm (P<0.0001).
At 12 months’ follow-up in the CASTOR study, the PFS with daratumumab was 60%, compared to 22% for bortezomib/dexamethasone (P<0.0001).
MRD criteria
In both studies, MRD assessments were conducted at suspected complete response (CR). Assessments were also conducted at 3 months and 6 months after CR in the POLLUX study and at 6 months and 12 months after the first study dose in the CASTOR study.
For the assessment of MRD, investigators used bone marrow aspirate samples and the ClonoSEQTM NGS-based assay.
Investigators evaluated MRD at 3 sensitivity thresholds: 10-4, 10-5, and 10-6.
And they used a stringent, unbiased evaluation, Dr Avet-Loiseau said. Any patient in the intent-to-treat population who was not assessed to be MRD negative was scored as MRD positive.
And the minimum cell input equivalent to the sensitivity threshold was required to determine MRD negativity.
MRD results
In the POLLUX study, 24.8% of patients achieved MRD negativity at the 10-5 cutoff, and 11.9% achieved MRD negativity at the 10-6 cutoff with the daratumumab combination.
This compared to 5.7% and 2.5% MRD negativity at the 10-5 and 10-6 cutoffs, respectively, without daratumumab (P<0.0001).
In the CASTOR study, the daratumumab-treated patients achieved 10.4% and 4.4% MRD negativity at the 10-5 and 10-6 cutoffs, respectively.
This compared to 2.4% and 0.8% MRD negativity in the control arm at the 10-5 and 10-6 cutoffs (P<0.005 and P<0.05), respectively.
“So, definitely, the addition of daratumumab improved the MRD negativity rate in both studies,” Dr Avet-Loiseau said.
“If you just look at the patients who did achieve CR in the POLLUX study, almost 50% of the patients [treated with daratumumab] achieved CR, and half of them were MRD negative at the cutoff of 10-5.”
In the CASTOR study, 25% of the patients treated with daratumumab achieved a CR. The MRD negativity rate was one-third in these patients.
“So again, we have consistently higher MRD negative rates in patients who achieve CR when they were treated in the daratumumab arms,” Dr Avet-Loiseau said.
“What is interesting, I think, is that the achievement of molecular CR was very rapid. [A]t 3 months, some patients did already achieve MRD negativity, and so we continued to see an improvement. [W]e still continue to see some achievement of MRD negativity.”
Investigators continue to follow the patients annually.
The investigators also analyzed MRD at 10-5 by cytogenetic risk and did not observe any MRD negativity in the control arm in either the POLLUX or CASTOR study.
“In contrast, we did observe some significant MRD negativity in the experimental arm with daratumumab—18% (POLLUX) and 14% (CASTOR) in high-risk patients,” Dr Avet-Loiseau said. “The most important prognostic factor is to achieve MRD negativity.”
However, even for patients who did not achieve MRD negativity, the PFS was much better in the experimental arms than in the control arms, he added.
This study, presented as a “Best of ASH” abstract, was funded by Janssen Research & Development, LLC. ![]()
*Information in the abstract differs from that presented at the meeting.

© Todd Buchanan 2016
SAN DIEGO—Daratumumab added to standard of care regimens drives deep clinical responses beyond complete response (CR), a magnitude that is “unprecedented” in the relapsed/refractory multiple myeloma (MM) setting, according to a speaker at the 2016 ASH Annual Meeting.
Investigators added daratumumab to lenalidomide/dexamethasone in the POLLUX trial and to bortezomib/dexamethasone in the CASTOR trial.
In both phase 3 trials, the addition of daratumumab resulted in significant improvements in progression-free survival (PFS), overall response rate, and minimal residual disease (MRD) negativity when compared to control groups.
“The magnitude of daratumumab-induced MRD negativity in the relapsed setting is unprecedented and, for me, was not expected,” said Hervé Avet-Loiseau, MD, of Centre Hospitalier Universitaire Rangueil, Unité de Genomique du Myelome in Toulouse, France.
Dr Avet-Loiseau presented the MRD findings from CASTOR and POLLUX at the ASH Annual Meeting as abstract 246.*
He noted that, based on these studies, daratumumab received US Food and Drug Administration approvals for use in combination with standard of care regimens for MM patients who had received 1 or more prior lines of treatment.
Daratumumab had been previously approved as monotherapy for relapsed or refractory MM.
Study designs and findings from the POLLUX and CASTOR trials have been described earlier in Hematology Times.
Dr Avet-Loiseau provided updated PFS figures for the 2 studies.
At 18 months’ follow-up in the POLLUX study, the PFS rate for patients treated with daratumumab/lenalidomide/dexamethasone was 76%, compared to 49% in the lenalidomide/dexamethasone arm (P<0.0001).
At 12 months’ follow-up in the CASTOR study, the PFS with daratumumab was 60%, compared to 22% for bortezomib/dexamethasone (P<0.0001).
MRD criteria
In both studies, MRD assessments were conducted at suspected complete response (CR). Assessments were also conducted at 3 months and 6 months after CR in the POLLUX study and at 6 months and 12 months after the first study dose in the CASTOR study.
For the assessment of MRD, investigators used bone marrow aspirate samples and the ClonoSEQTM NGS-based assay.
Investigators evaluated MRD at 3 sensitivity thresholds: 10-4, 10-5, and 10-6.
And they used a stringent, unbiased evaluation, Dr Avet-Loiseau said. Any patient in the intent-to-treat population who was not assessed to be MRD negative was scored as MRD positive.
And the minimum cell input equivalent to the sensitivity threshold was required to determine MRD negativity.
MRD results
In the POLLUX study, 24.8% of patients achieved MRD negativity at the 10-5 cutoff, and 11.9% achieved MRD negativity at the 10-6 cutoff with the daratumumab combination.
This compared to 5.7% and 2.5% MRD negativity at the 10-5 and 10-6 cutoffs, respectively, without daratumumab (P<0.0001).
In the CASTOR study, the daratumumab-treated patients achieved 10.4% and 4.4% MRD negativity at the 10-5 and 10-6 cutoffs, respectively.
This compared to 2.4% and 0.8% MRD negativity in the control arm at the 10-5 and 10-6 cutoffs (P<0.005 and P<0.05), respectively.
“So, definitely, the addition of daratumumab improved the MRD negativity rate in both studies,” Dr Avet-Loiseau said.
“If you just look at the patients who did achieve CR in the POLLUX study, almost 50% of the patients [treated with daratumumab] achieved CR, and half of them were MRD negative at the cutoff of 10-5.”
In the CASTOR study, 25% of the patients treated with daratumumab achieved a CR. The MRD negativity rate was one-third in these patients.
“So again, we have consistently higher MRD negative rates in patients who achieve CR when they were treated in the daratumumab arms,” Dr Avet-Loiseau said.
“What is interesting, I think, is that the achievement of molecular CR was very rapid. [A]t 3 months, some patients did already achieve MRD negativity, and so we continued to see an improvement. [W]e still continue to see some achievement of MRD negativity.”
Investigators continue to follow the patients annually.
The investigators also analyzed MRD at 10-5 by cytogenetic risk and did not observe any MRD negativity in the control arm in either the POLLUX or CASTOR study.
“In contrast, we did observe some significant MRD negativity in the experimental arm with daratumumab—18% (POLLUX) and 14% (CASTOR) in high-risk patients,” Dr Avet-Loiseau said. “The most important prognostic factor is to achieve MRD negativity.”
However, even for patients who did not achieve MRD negativity, the PFS was much better in the experimental arms than in the control arms, he added.
This study, presented as a “Best of ASH” abstract, was funded by Janssen Research & Development, LLC. ![]()
*Information in the abstract differs from that presented at the meeting.

© Todd Buchanan 2016
SAN DIEGO—Daratumumab added to standard of care regimens drives deep clinical responses beyond complete response (CR), a magnitude that is “unprecedented” in the relapsed/refractory multiple myeloma (MM) setting, according to a speaker at the 2016 ASH Annual Meeting.
Investigators added daratumumab to lenalidomide/dexamethasone in the POLLUX trial and to bortezomib/dexamethasone in the CASTOR trial.
In both phase 3 trials, the addition of daratumumab resulted in significant improvements in progression-free survival (PFS), overall response rate, and minimal residual disease (MRD) negativity when compared to control groups.
“The magnitude of daratumumab-induced MRD negativity in the relapsed setting is unprecedented and, for me, was not expected,” said Hervé Avet-Loiseau, MD, of Centre Hospitalier Universitaire Rangueil, Unité de Genomique du Myelome in Toulouse, France.
Dr Avet-Loiseau presented the MRD findings from CASTOR and POLLUX at the ASH Annual Meeting as abstract 246.*
He noted that, based on these studies, daratumumab received US Food and Drug Administration approvals for use in combination with standard of care regimens for MM patients who had received 1 or more prior lines of treatment.
Daratumumab had been previously approved as monotherapy for relapsed or refractory MM.
Study designs and findings from the POLLUX and CASTOR trials have been described earlier in Hematology Times.
Dr Avet-Loiseau provided updated PFS figures for the 2 studies.
At 18 months’ follow-up in the POLLUX study, the PFS rate for patients treated with daratumumab/lenalidomide/dexamethasone was 76%, compared to 49% in the lenalidomide/dexamethasone arm (P<0.0001).
At 12 months’ follow-up in the CASTOR study, the PFS with daratumumab was 60%, compared to 22% for bortezomib/dexamethasone (P<0.0001).
MRD criteria
In both studies, MRD assessments were conducted at suspected complete response (CR). Assessments were also conducted at 3 months and 6 months after CR in the POLLUX study and at 6 months and 12 months after the first study dose in the CASTOR study.
For the assessment of MRD, investigators used bone marrow aspirate samples and the ClonoSEQTM NGS-based assay.
Investigators evaluated MRD at 3 sensitivity thresholds: 10-4, 10-5, and 10-6.
And they used a stringent, unbiased evaluation, Dr Avet-Loiseau said. Any patient in the intent-to-treat population who was not assessed to be MRD negative was scored as MRD positive.
And the minimum cell input equivalent to the sensitivity threshold was required to determine MRD negativity.
MRD results
In the POLLUX study, 24.8% of patients achieved MRD negativity at the 10-5 cutoff, and 11.9% achieved MRD negativity at the 10-6 cutoff with the daratumumab combination.
This compared to 5.7% and 2.5% MRD negativity at the 10-5 and 10-6 cutoffs, respectively, without daratumumab (P<0.0001).
In the CASTOR study, the daratumumab-treated patients achieved 10.4% and 4.4% MRD negativity at the 10-5 and 10-6 cutoffs, respectively.
This compared to 2.4% and 0.8% MRD negativity in the control arm at the 10-5 and 10-6 cutoffs (P<0.005 and P<0.05), respectively.
“So, definitely, the addition of daratumumab improved the MRD negativity rate in both studies,” Dr Avet-Loiseau said.
“If you just look at the patients who did achieve CR in the POLLUX study, almost 50% of the patients [treated with daratumumab] achieved CR, and half of them were MRD negative at the cutoff of 10-5.”
In the CASTOR study, 25% of the patients treated with daratumumab achieved a CR. The MRD negativity rate was one-third in these patients.
“So again, we have consistently higher MRD negative rates in patients who achieve CR when they were treated in the daratumumab arms,” Dr Avet-Loiseau said.
“What is interesting, I think, is that the achievement of molecular CR was very rapid. [A]t 3 months, some patients did already achieve MRD negativity, and so we continued to see an improvement. [W]e still continue to see some achievement of MRD negativity.”
Investigators continue to follow the patients annually.
The investigators also analyzed MRD at 10-5 by cytogenetic risk and did not observe any MRD negativity in the control arm in either the POLLUX or CASTOR study.
“In contrast, we did observe some significant MRD negativity in the experimental arm with daratumumab—18% (POLLUX) and 14% (CASTOR) in high-risk patients,” Dr Avet-Loiseau said. “The most important prognostic factor is to achieve MRD negativity.”
However, even for patients who did not achieve MRD negativity, the PFS was much better in the experimental arms than in the control arms, he added.
This study, presented as a “Best of ASH” abstract, was funded by Janssen Research & Development, LLC. ![]()
*Information in the abstract differs from that presented at the meeting.
How old is too old to be on a kids’ protocol for ALL?

Photo by Bill Branson
SAN DIEGO—In recent years, pediatric or pediatric-inspired protocols have become the preferred treatment approach for younger adults with acute lymphoblastic leukemia (ALL).
These protocols include higher doses of steroids, vincristine, methotrexate, and L-asparaginase.
However, the upper age limit for this strategy has not been defined.
With the GRAALL-2005 study, investigators set out to determine how old is too old to be treated on pediatric protocols.
Their results suggest 55 is likely the upper age limit for patients with Ph-negative ALL.
The investigators also evaluated a hyper-fractionated (hyper-C) versus standard dose (standard-C) of cyclophosphamide during induction and late intensification.
They found that hyper-C did not provide an event-free survival (EFS) benefit in the overall study population, but patients age 55 and older did appear to benefit from hyper-C.
Françoise Huguet, MD, of the Institut Universitaire du Cancer de Toulouse in Toulouse, France, presented these findings at the 2016 ASH Annual Meeting (abstract 762).
GRAALL investigators had previously evaluated a pediatric-inspired protocol for adult patients in the GRAALL-2003 study, which validated the approach.
Study design
Patients with newly diagnosed, Ph-negative ALL were eligible to enroll if they were 18 to 59 years of age.
Treatment comprised a steroid pre-phase, a 5-drug induction, two 3-block dose-dense consolidation phases, a late intensification, a third consolidation phase, CNS irradiation, and a 2-year maintenance phase.
Patients could proceed to allogeneic transplant in first complete remission (CR) if eligible.
During induction and late intensification, patients received cyclophosphamide at 750 mg/m2 on day 1 and were then randomized to hyper-C (300 mg/m2/every 12 hours on days 15 to 17) or standard-C (750 mg/m2 on day 15).
The primary endpoint was EFS.
Patient population
Investigators randomized 787 evaluable patients—398 in the standard-C arm and 389 in the hyper-C arm.
Their median age was 36 years, 67% of patients had B-cell precursor ALL, and 33% had T-ALL.
Most had high-risk ALL, 72% of them receiving standard-C and 66% receiving hyper-C.
About a third of the patients in each arm proceeded to allogeneic stem cell transplant in first CR.
Results
The CR rate after induction therapy was 90.2% in the standard-C arm and 93.6% in the hyper-C arm, for an overall CR rate of 92%.
Most patients—87.5% in the standard-C arm and 91.8% in the hyper-C arm—achieved a response in 1 course of therapy.
Sixty percent of patients tested in the standard-C arm and 66% of those tested in the hyper-C arm were minimal residual disease negative at less than 10-4.
There were 26 (6.5%) deaths in the standard-C arm and 18 (4.6%) in the hyper-C arm.
The 5-year EFS rate was 52% overall, and hyper-C treatment had no impact on EFS (hazard ratio=0.89 [range, 0.7-1.1]; P=0.26).
Impact of age
Investigators conducted a post-hoc subgroup analysis of 5 age groups—18-24 years (n=200), 25-34 (n=172), 35-44 (n=171), 45-54 (n=151), and 55+ (n=93).
Overall, the CR rate tended to decrease with age. The rates were 98.5% (18-24), 95.3% (25-34), 87.7% (35-44), 89.4% (45-54), and 79.6% (55+).
Induction death rates increased from 0.5% in the youngest group to 18.3% in the oldest, but the rate of cumulative incidences of failure at 5 years was similar among all the age groups.
The cumulative incidence of treatment-related mortality, without censoring for transplant, ranged from 7.6% in the youngest group to 39.7% in the oldest.
And the 5-year EFS for the youngest patients was 60%, while, for the oldest, it was 26%.
“Above 50 years, the increase in age became highly significant,” Dr Huguet emphasized. “There were fewer CRs and lower survival.”
Treatment compliance
In terms of treatment compliance and median dose received in the induction course, patients aged 55-59 received significantly less L-asparaginase than those aged 18-54 (P<0.001).
During all 3 consolidation phases, patients aged 55-59 received significantly lower median doses of all medications—cytarabine, methotrexate, cyclophosphamide—than patients aged 18-54.
And in late intensification, patients aged 55-59 received significantly lower median doses of vincristine, prednisone, daunorubicin, and hyper-C than all other patients. The median doses of L-asparaginase and standard-C received were lower in the older patients but not significantly so.
EFS by age and randomization
The 5-year EFS for patients aged 18-54 was 57% with hyper-C, compared with 55% in the standard-C arm (P=0.66).
However, for older patients, there was a significant advantage for those receiving hyper-C. The 5-year EFS was 38% with hyper-C, compared to 12% with standard-C (P=0.007).
Dr Huguet explained that inferior compliance in patients 55 and older “might explain why a benefit associated with early hyper-C reinforcement became apparent in these older patients only.”
Dr Huguet concluded that the results “suggest that 55 years is likely to be the upper age limit to tolerate a pediatric-like therapy for younger adults with Ph-negative ALL.”
She added that patients over 54 might benefit from alternative front-line strategies.
Accordingly, investigators are planning to use new agents, such as blinatumomab or inotuzumab ozogamicin, in the next European Working Group on Adult ALL studies. ![]()

Photo by Bill Branson
SAN DIEGO—In recent years, pediatric or pediatric-inspired protocols have become the preferred treatment approach for younger adults with acute lymphoblastic leukemia (ALL).
These protocols include higher doses of steroids, vincristine, methotrexate, and L-asparaginase.
However, the upper age limit for this strategy has not been defined.
With the GRAALL-2005 study, investigators set out to determine how old is too old to be treated on pediatric protocols.
Their results suggest 55 is likely the upper age limit for patients with Ph-negative ALL.
The investigators also evaluated a hyper-fractionated (hyper-C) versus standard dose (standard-C) of cyclophosphamide during induction and late intensification.
They found that hyper-C did not provide an event-free survival (EFS) benefit in the overall study population, but patients age 55 and older did appear to benefit from hyper-C.
Françoise Huguet, MD, of the Institut Universitaire du Cancer de Toulouse in Toulouse, France, presented these findings at the 2016 ASH Annual Meeting (abstract 762).
GRAALL investigators had previously evaluated a pediatric-inspired protocol for adult patients in the GRAALL-2003 study, which validated the approach.
Study design
Patients with newly diagnosed, Ph-negative ALL were eligible to enroll if they were 18 to 59 years of age.
Treatment comprised a steroid pre-phase, a 5-drug induction, two 3-block dose-dense consolidation phases, a late intensification, a third consolidation phase, CNS irradiation, and a 2-year maintenance phase.
Patients could proceed to allogeneic transplant in first complete remission (CR) if eligible.
During induction and late intensification, patients received cyclophosphamide at 750 mg/m2 on day 1 and were then randomized to hyper-C (300 mg/m2/every 12 hours on days 15 to 17) or standard-C (750 mg/m2 on day 15).
The primary endpoint was EFS.
Patient population
Investigators randomized 787 evaluable patients—398 in the standard-C arm and 389 in the hyper-C arm.
Their median age was 36 years, 67% of patients had B-cell precursor ALL, and 33% had T-ALL.
Most had high-risk ALL, 72% of them receiving standard-C and 66% receiving hyper-C.
About a third of the patients in each arm proceeded to allogeneic stem cell transplant in first CR.
Results
The CR rate after induction therapy was 90.2% in the standard-C arm and 93.6% in the hyper-C arm, for an overall CR rate of 92%.
Most patients—87.5% in the standard-C arm and 91.8% in the hyper-C arm—achieved a response in 1 course of therapy.
Sixty percent of patients tested in the standard-C arm and 66% of those tested in the hyper-C arm were minimal residual disease negative at less than 10-4.
There were 26 (6.5%) deaths in the standard-C arm and 18 (4.6%) in the hyper-C arm.
The 5-year EFS rate was 52% overall, and hyper-C treatment had no impact on EFS (hazard ratio=0.89 [range, 0.7-1.1]; P=0.26).
Impact of age
Investigators conducted a post-hoc subgroup analysis of 5 age groups—18-24 years (n=200), 25-34 (n=172), 35-44 (n=171), 45-54 (n=151), and 55+ (n=93).
Overall, the CR rate tended to decrease with age. The rates were 98.5% (18-24), 95.3% (25-34), 87.7% (35-44), 89.4% (45-54), and 79.6% (55+).
Induction death rates increased from 0.5% in the youngest group to 18.3% in the oldest, but the rate of cumulative incidences of failure at 5 years was similar among all the age groups.
The cumulative incidence of treatment-related mortality, without censoring for transplant, ranged from 7.6% in the youngest group to 39.7% in the oldest.
And the 5-year EFS for the youngest patients was 60%, while, for the oldest, it was 26%.
“Above 50 years, the increase in age became highly significant,” Dr Huguet emphasized. “There were fewer CRs and lower survival.”
Treatment compliance
In terms of treatment compliance and median dose received in the induction course, patients aged 55-59 received significantly less L-asparaginase than those aged 18-54 (P<0.001).
During all 3 consolidation phases, patients aged 55-59 received significantly lower median doses of all medications—cytarabine, methotrexate, cyclophosphamide—than patients aged 18-54.
And in late intensification, patients aged 55-59 received significantly lower median doses of vincristine, prednisone, daunorubicin, and hyper-C than all other patients. The median doses of L-asparaginase and standard-C received were lower in the older patients but not significantly so.
EFS by age and randomization
The 5-year EFS for patients aged 18-54 was 57% with hyper-C, compared with 55% in the standard-C arm (P=0.66).
However, for older patients, there was a significant advantage for those receiving hyper-C. The 5-year EFS was 38% with hyper-C, compared to 12% with standard-C (P=0.007).
Dr Huguet explained that inferior compliance in patients 55 and older “might explain why a benefit associated with early hyper-C reinforcement became apparent in these older patients only.”
Dr Huguet concluded that the results “suggest that 55 years is likely to be the upper age limit to tolerate a pediatric-like therapy for younger adults with Ph-negative ALL.”
She added that patients over 54 might benefit from alternative front-line strategies.
Accordingly, investigators are planning to use new agents, such as blinatumomab or inotuzumab ozogamicin, in the next European Working Group on Adult ALL studies. ![]()

Photo by Bill Branson
SAN DIEGO—In recent years, pediatric or pediatric-inspired protocols have become the preferred treatment approach for younger adults with acute lymphoblastic leukemia (ALL).
These protocols include higher doses of steroids, vincristine, methotrexate, and L-asparaginase.
However, the upper age limit for this strategy has not been defined.
With the GRAALL-2005 study, investigators set out to determine how old is too old to be treated on pediatric protocols.
Their results suggest 55 is likely the upper age limit for patients with Ph-negative ALL.
The investigators also evaluated a hyper-fractionated (hyper-C) versus standard dose (standard-C) of cyclophosphamide during induction and late intensification.
They found that hyper-C did not provide an event-free survival (EFS) benefit in the overall study population, but patients age 55 and older did appear to benefit from hyper-C.
Françoise Huguet, MD, of the Institut Universitaire du Cancer de Toulouse in Toulouse, France, presented these findings at the 2016 ASH Annual Meeting (abstract 762).
GRAALL investigators had previously evaluated a pediatric-inspired protocol for adult patients in the GRAALL-2003 study, which validated the approach.
Study design
Patients with newly diagnosed, Ph-negative ALL were eligible to enroll if they were 18 to 59 years of age.
Treatment comprised a steroid pre-phase, a 5-drug induction, two 3-block dose-dense consolidation phases, a late intensification, a third consolidation phase, CNS irradiation, and a 2-year maintenance phase.
Patients could proceed to allogeneic transplant in first complete remission (CR) if eligible.
During induction and late intensification, patients received cyclophosphamide at 750 mg/m2 on day 1 and were then randomized to hyper-C (300 mg/m2/every 12 hours on days 15 to 17) or standard-C (750 mg/m2 on day 15).
The primary endpoint was EFS.
Patient population
Investigators randomized 787 evaluable patients—398 in the standard-C arm and 389 in the hyper-C arm.
Their median age was 36 years, 67% of patients had B-cell precursor ALL, and 33% had T-ALL.
Most had high-risk ALL, 72% of them receiving standard-C and 66% receiving hyper-C.
About a third of the patients in each arm proceeded to allogeneic stem cell transplant in first CR.
Results
The CR rate after induction therapy was 90.2% in the standard-C arm and 93.6% in the hyper-C arm, for an overall CR rate of 92%.
Most patients—87.5% in the standard-C arm and 91.8% in the hyper-C arm—achieved a response in 1 course of therapy.
Sixty percent of patients tested in the standard-C arm and 66% of those tested in the hyper-C arm were minimal residual disease negative at less than 10-4.
There were 26 (6.5%) deaths in the standard-C arm and 18 (4.6%) in the hyper-C arm.
The 5-year EFS rate was 52% overall, and hyper-C treatment had no impact on EFS (hazard ratio=0.89 [range, 0.7-1.1]; P=0.26).
Impact of age
Investigators conducted a post-hoc subgroup analysis of 5 age groups—18-24 years (n=200), 25-34 (n=172), 35-44 (n=171), 45-54 (n=151), and 55+ (n=93).
Overall, the CR rate tended to decrease with age. The rates were 98.5% (18-24), 95.3% (25-34), 87.7% (35-44), 89.4% (45-54), and 79.6% (55+).
Induction death rates increased from 0.5% in the youngest group to 18.3% in the oldest, but the rate of cumulative incidences of failure at 5 years was similar among all the age groups.
The cumulative incidence of treatment-related mortality, without censoring for transplant, ranged from 7.6% in the youngest group to 39.7% in the oldest.
And the 5-year EFS for the youngest patients was 60%, while, for the oldest, it was 26%.
“Above 50 years, the increase in age became highly significant,” Dr Huguet emphasized. “There were fewer CRs and lower survival.”
Treatment compliance
In terms of treatment compliance and median dose received in the induction course, patients aged 55-59 received significantly less L-asparaginase than those aged 18-54 (P<0.001).
During all 3 consolidation phases, patients aged 55-59 received significantly lower median doses of all medications—cytarabine, methotrexate, cyclophosphamide—than patients aged 18-54.
And in late intensification, patients aged 55-59 received significantly lower median doses of vincristine, prednisone, daunorubicin, and hyper-C than all other patients. The median doses of L-asparaginase and standard-C received were lower in the older patients but not significantly so.
EFS by age and randomization
The 5-year EFS for patients aged 18-54 was 57% with hyper-C, compared with 55% in the standard-C arm (P=0.66).
However, for older patients, there was a significant advantage for those receiving hyper-C. The 5-year EFS was 38% with hyper-C, compared to 12% with standard-C (P=0.007).
Dr Huguet explained that inferior compliance in patients 55 and older “might explain why a benefit associated with early hyper-C reinforcement became apparent in these older patients only.”
Dr Huguet concluded that the results “suggest that 55 years is likely to be the upper age limit to tolerate a pediatric-like therapy for younger adults with Ph-negative ALL.”
She added that patients over 54 might benefit from alternative front-line strategies.
Accordingly, investigators are planning to use new agents, such as blinatumomab or inotuzumab ozogamicin, in the next European Working Group on Adult ALL studies. ![]()
Two mutations may help drive CBF-AML

2016 ASH Annual Meeting
SAN DIEGO—Researchers have found evidence to suggest that mutations in the CCND1 and CCND2 genes may contribute to the development of core-binding factor acute myeloid leukemia (CBF-AML).
The team noted that CBF-AML is defined by the presence of either t(8;21)(q22;q22)/RUNX1-RUNX1T1 or inv(16)(p13.1q22)/t(16;16)(p13.1;q22)/CBFB-MYH11.
However, the fusion genes alone are not capable of causing CBF-AML.
“The hematology community has long sought to determine what other factors in addition to the fusion genes occur in this special type of leukemia,” said Ann-Kathrin Eisfeld, MD, of The Ohio State University Comprehensive Cancer Center in Columbus.
“We are now the first to describe that mutations in CCND1—and among the first to describe that mutations in the sister gene CCND2—are unique features of CBF-AML with t(8;21). In addition, we have collected the first evidence that mutations in CCND2 lead to more aggressive growth of leukemia cell lines.”
Dr Eisfeld and her colleagues reported these findings in a paper published in Leukemia and in a poster presented at the 2016 ASH Annual Meeting (abstract 2740).
A previous study of genetic mutations in CBF-AML revealed the presence of at least 1 mutation in 85% of patients studied. This meant the remaining 15% of patients harbored other, undiscovered mutations.
For the current study, Dr Eisfeld and her colleagues searched CBF-AML samples for the missing mutations that, together with the fusion genes, might contribute to the leukemia in this subgroup of cases.
The team analyzed pretreatment bone marrow and peripheral blood samples from 177 adult CBF-AML patients who received similar treatment through a clinical trial conducted at multiple centers across the US.
Using a targeted, next-generation sequencing approach, the researchers looked for mutations in 84 leukemia- and/or cancer-associated genes. They also performed tests on blood or bone marrow cells to look for chromosomal irregularities.
The team discovered 2 significant mutations in the CCND1 and CCND2 genes, representing the first dual evidence of these recurrent mutations in patients with t(8;21)-positive CBF-AML.
CCND1 and CCND2 mutations were found in 15% (n=10) of patients with t(8;21)-positive CBF-AML. Two patients had mutations in CCND1, and 8 had mutations in CCND2.
The researchers also found a single CCND2 mutation in 1 (0.9%) patient with inv(16)-positive CBF-AML.
In comparison, the incidence of CCND1 and CCND2 mutations was 0.77% (n=11) in a cohort of 1426 patients with non-CBF-AML.
“This is extremely valuable information that was previously unknown,” Dr Eisfeld said, “and it might help us develop targeted therapies more likely to help patients with [CBF-AML] in the near future.” ![]()

2016 ASH Annual Meeting
SAN DIEGO—Researchers have found evidence to suggest that mutations in the CCND1 and CCND2 genes may contribute to the development of core-binding factor acute myeloid leukemia (CBF-AML).
The team noted that CBF-AML is defined by the presence of either t(8;21)(q22;q22)/RUNX1-RUNX1T1 or inv(16)(p13.1q22)/t(16;16)(p13.1;q22)/CBFB-MYH11.
However, the fusion genes alone are not capable of causing CBF-AML.
“The hematology community has long sought to determine what other factors in addition to the fusion genes occur in this special type of leukemia,” said Ann-Kathrin Eisfeld, MD, of The Ohio State University Comprehensive Cancer Center in Columbus.
“We are now the first to describe that mutations in CCND1—and among the first to describe that mutations in the sister gene CCND2—are unique features of CBF-AML with t(8;21). In addition, we have collected the first evidence that mutations in CCND2 lead to more aggressive growth of leukemia cell lines.”
Dr Eisfeld and her colleagues reported these findings in a paper published in Leukemia and in a poster presented at the 2016 ASH Annual Meeting (abstract 2740).
A previous study of genetic mutations in CBF-AML revealed the presence of at least 1 mutation in 85% of patients studied. This meant the remaining 15% of patients harbored other, undiscovered mutations.
For the current study, Dr Eisfeld and her colleagues searched CBF-AML samples for the missing mutations that, together with the fusion genes, might contribute to the leukemia in this subgroup of cases.
The team analyzed pretreatment bone marrow and peripheral blood samples from 177 adult CBF-AML patients who received similar treatment through a clinical trial conducted at multiple centers across the US.
Using a targeted, next-generation sequencing approach, the researchers looked for mutations in 84 leukemia- and/or cancer-associated genes. They also performed tests on blood or bone marrow cells to look for chromosomal irregularities.
The team discovered 2 significant mutations in the CCND1 and CCND2 genes, representing the first dual evidence of these recurrent mutations in patients with t(8;21)-positive CBF-AML.
CCND1 and CCND2 mutations were found in 15% (n=10) of patients with t(8;21)-positive CBF-AML. Two patients had mutations in CCND1, and 8 had mutations in CCND2.
The researchers also found a single CCND2 mutation in 1 (0.9%) patient with inv(16)-positive CBF-AML.
In comparison, the incidence of CCND1 and CCND2 mutations was 0.77% (n=11) in a cohort of 1426 patients with non-CBF-AML.
“This is extremely valuable information that was previously unknown,” Dr Eisfeld said, “and it might help us develop targeted therapies more likely to help patients with [CBF-AML] in the near future.” ![]()

2016 ASH Annual Meeting
SAN DIEGO—Researchers have found evidence to suggest that mutations in the CCND1 and CCND2 genes may contribute to the development of core-binding factor acute myeloid leukemia (CBF-AML).
The team noted that CBF-AML is defined by the presence of either t(8;21)(q22;q22)/RUNX1-RUNX1T1 or inv(16)(p13.1q22)/t(16;16)(p13.1;q22)/CBFB-MYH11.
However, the fusion genes alone are not capable of causing CBF-AML.
“The hematology community has long sought to determine what other factors in addition to the fusion genes occur in this special type of leukemia,” said Ann-Kathrin Eisfeld, MD, of The Ohio State University Comprehensive Cancer Center in Columbus.
“We are now the first to describe that mutations in CCND1—and among the first to describe that mutations in the sister gene CCND2—are unique features of CBF-AML with t(8;21). In addition, we have collected the first evidence that mutations in CCND2 lead to more aggressive growth of leukemia cell lines.”
Dr Eisfeld and her colleagues reported these findings in a paper published in Leukemia and in a poster presented at the 2016 ASH Annual Meeting (abstract 2740).
A previous study of genetic mutations in CBF-AML revealed the presence of at least 1 mutation in 85% of patients studied. This meant the remaining 15% of patients harbored other, undiscovered mutations.
For the current study, Dr Eisfeld and her colleagues searched CBF-AML samples for the missing mutations that, together with the fusion genes, might contribute to the leukemia in this subgroup of cases.
The team analyzed pretreatment bone marrow and peripheral blood samples from 177 adult CBF-AML patients who received similar treatment through a clinical trial conducted at multiple centers across the US.
Using a targeted, next-generation sequencing approach, the researchers looked for mutations in 84 leukemia- and/or cancer-associated genes. They also performed tests on blood or bone marrow cells to look for chromosomal irregularities.
The team discovered 2 significant mutations in the CCND1 and CCND2 genes, representing the first dual evidence of these recurrent mutations in patients with t(8;21)-positive CBF-AML.
CCND1 and CCND2 mutations were found in 15% (n=10) of patients with t(8;21)-positive CBF-AML. Two patients had mutations in CCND1, and 8 had mutations in CCND2.
The researchers also found a single CCND2 mutation in 1 (0.9%) patient with inv(16)-positive CBF-AML.
In comparison, the incidence of CCND1 and CCND2 mutations was 0.77% (n=11) in a cohort of 1426 patients with non-CBF-AML.
“This is extremely valuable information that was previously unknown,” Dr Eisfeld said, “and it might help us develop targeted therapies more likely to help patients with [CBF-AML] in the near future.” ![]()
EC authorizes new use for ofatumumab in CLL

Photo courtesy of GSK
The European Commission (EC) has granted marketing authorization for ofatumumab (Arzerra®) to be used in combination with fludarabine and cyclophosphamide (FC) in the treatment of adults with relapsed chronic lymphocytic leukemia (CLL).
Ofatumumab is a monoclonal antibody designed to target CD20. The drug is marketed under a collaboration agreement between Genmab and Novartis.
The EC previously authorized the use of ofatumumab as a single agent to treat CLL patients who are refractory to fludarabine and alemtuzumab.
The agency also authorized the use of ofatumumab in combination with chlorambucil or bendamustine in CLL patients who have not received prior therapy and are not eligible for fludarabine-based therapy.
The EC’s decision to approve the use of ofatumumab in combination with FC was based on results from the phase 3 COMPLEMENT 2 study, which were published in Leukemia & Lymphoma in October.
The trial enrolled 365 patients with relapsed CLL. The patients were randomized 1:1 to receive up to 6 cycles of ofatumumab in combination with FC or up to 6 cycles of FC alone.
The primary endpoint was progression-free survival, as assessed by an independent review committee.
The median progression-free survival was 28.9 months for patients receiving ofatumumab plus FC, compared to 18.8 months for patients receiving FC only (hazard ratio=0.67, P=0.0032).
The incidence of grade 3 or higher adverse events was 74% in the ofatumumab-plus-FC arm and 69% in the FC-only arm. Neutropenia was the most common of these events, occurring in 49% and 36% of patients, respectively. ![]()

Photo courtesy of GSK
The European Commission (EC) has granted marketing authorization for ofatumumab (Arzerra®) to be used in combination with fludarabine and cyclophosphamide (FC) in the treatment of adults with relapsed chronic lymphocytic leukemia (CLL).
Ofatumumab is a monoclonal antibody designed to target CD20. The drug is marketed under a collaboration agreement between Genmab and Novartis.
The EC previously authorized the use of ofatumumab as a single agent to treat CLL patients who are refractory to fludarabine and alemtuzumab.
The agency also authorized the use of ofatumumab in combination with chlorambucil or bendamustine in CLL patients who have not received prior therapy and are not eligible for fludarabine-based therapy.
The EC’s decision to approve the use of ofatumumab in combination with FC was based on results from the phase 3 COMPLEMENT 2 study, which were published in Leukemia & Lymphoma in October.
The trial enrolled 365 patients with relapsed CLL. The patients were randomized 1:1 to receive up to 6 cycles of ofatumumab in combination with FC or up to 6 cycles of FC alone.
The primary endpoint was progression-free survival, as assessed by an independent review committee.
The median progression-free survival was 28.9 months for patients receiving ofatumumab plus FC, compared to 18.8 months for patients receiving FC only (hazard ratio=0.67, P=0.0032).
The incidence of grade 3 or higher adverse events was 74% in the ofatumumab-plus-FC arm and 69% in the FC-only arm. Neutropenia was the most common of these events, occurring in 49% and 36% of patients, respectively. ![]()

Photo courtesy of GSK
The European Commission (EC) has granted marketing authorization for ofatumumab (Arzerra®) to be used in combination with fludarabine and cyclophosphamide (FC) in the treatment of adults with relapsed chronic lymphocytic leukemia (CLL).
Ofatumumab is a monoclonal antibody designed to target CD20. The drug is marketed under a collaboration agreement between Genmab and Novartis.
The EC previously authorized the use of ofatumumab as a single agent to treat CLL patients who are refractory to fludarabine and alemtuzumab.
The agency also authorized the use of ofatumumab in combination with chlorambucil or bendamustine in CLL patients who have not received prior therapy and are not eligible for fludarabine-based therapy.
The EC’s decision to approve the use of ofatumumab in combination with FC was based on results from the phase 3 COMPLEMENT 2 study, which were published in Leukemia & Lymphoma in October.
The trial enrolled 365 patients with relapsed CLL. The patients were randomized 1:1 to receive up to 6 cycles of ofatumumab in combination with FC or up to 6 cycles of FC alone.
The primary endpoint was progression-free survival, as assessed by an independent review committee.
The median progression-free survival was 28.9 months for patients receiving ofatumumab plus FC, compared to 18.8 months for patients receiving FC only (hazard ratio=0.67, P=0.0032).
The incidence of grade 3 or higher adverse events was 74% in the ofatumumab-plus-FC arm and 69% in the FC-only arm. Neutropenia was the most common of these events, occurring in 49% and 36% of patients, respectively. ![]()
MS & Pregnancy: What's Safe?
Q)What are the considerations and recommendations for pregnancy and breastfeeding in women with multiple sclerosis? When should women discontinue their disease-modifying therapies?
Multiple sclerosis (MS) is an inflammatory, demyelinating, degenerative disease. Three times more common in women than men, it may affect pregnancy planning and childbearing experiences.6 Evidence demonstrates a reduction in annualized relapse rate during pregnancy and the postpartum period with exclusive breastfeeding. Therefore, pregnancy and exclusive breastfeeding provide a favorable immunomodulatory effect in women with MS, which combats the increased relapse risk associated with the postpartum period.7,8
Reproductive education—including conception, pregnancy, and breastfeeding—is critical for patients with MS and their partners during a woman’s childbearing years. However, women with MS do not require special considerations during pregnancy unless they have remarkable disability. As soon as these women and their partners decide upon pregnancy, a plan should be established that includes a discussion about potential risks to the fetus due to drug exposure, as well as risks to the mother. The goal should be to minimize risk for disease activity and optimize the health of the baby.
Use of DMTs during conception, pregnancy, and breastfeeding. All disease-modifying therapies (DMTs) are usually discontinued during pregnancy and breastfeeding. Common practice among MS experts is to discontinue DMTs prior to conception, with a few exceptions. There is no consensus about timing of discontinuation and washout period for each DMT. The decision is based on the half-life of each DMT, the opinions of the woman and her partner, and risk tolerance. Note: For the purposes of this discussion, the old pregnancy category designations are used, since they are familiar to clinicians. New guidelines took effect in June 2015; Table 3 outlines the change in format.
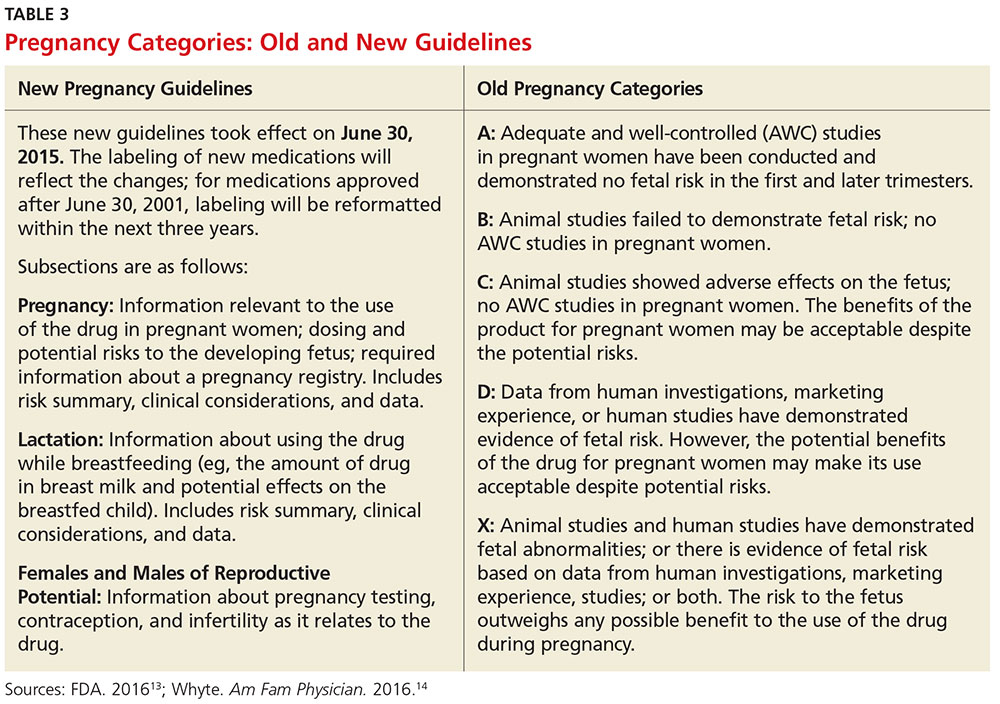
Injectables. Glatiramer acetate (GA) is the safest drug in relation to pregnancy and breastfeeding (category B). There is no evidence of congenital malformation or spontaneous abortion. The common recommendation is to discontinue the drug one to two months before conception, although some clinicians allow continuation of the injections throughout pregnancy and into breastfeeding.
Interferon-ßs are category C and therefore pose minimal risk for the fetus. The washout period before conception is two to three months, varying among clinicians. Although there is no evidence of spontaneous abortion or birth defects in humans, animal data show increased risk for abortion.9
Both GA and interferon-ßs are large molecules; there is a very minimal chance that the medication will transmit to the baby via breast milk. Thus, both DMTs are considered safe during lactation.7
Oral MS medications. The three approved MS oral medications are fingolimod, dimethyl fumarate (DMF), and teriflunomide. Fingolimod and DMF are both category C. Women on DMF must discontinue use of the medication one month prior to conception due to its short half-life. There are no reports of birth defects or spontaneous abortion in women taking DMF. Fingolimod needs to be discontinued two months prior to conception. Animal data show evidence for teratogenicity and embryolethality at lower doses of fingolimod than those used in humans.7
Teriflunomide is category X, posing high risk for the health of the fetus. It stays in the blood for approximately eight months after discontinuation of use. Animal data show teratogenicity and embryotoxicity; therefore, teriflunomide is contraindicated in pregnancy. Women on teriflunomide who plan to become pregnant need to undergo an elimination procedure with cholestyramine or charcoal.
Infusions and injections (monoclonal antibodies). The approved monoclonal antibodies include natalizumab, alemtuzumab, and daclizumab. (Currently, use of rituximab in MS is off label, and the FDA is reviewing the efficacy and safety data for ocrelizumab.) The monoclonal antibodies are category C. The recommendation is to discontinue natalizumab one to two months prior to conception and discontinue alemtuzumab four months preconception.10 There is no evidence of spontaneous abortion or birth defects in women on alemtuzumab, but there is potentially increased risk for spontaneous abortion in those on natalizumab.
The spontaneous abortion rate in daclizumab-exposed women is consistent with early pregnancy loss in the general population (12% to 26%). Data on a small number of pregnancies exposed to daclizumab did not suggest an increased risk for adverse fetal or maternal outcomes.11 However, the recommendation is to discontinue daclizumab four months prior to conception. Rituximab should be discontinued 12 months prior to conception, based on the manufacturer recommendation, although it is potentially safe to conceive when the B cell counts return to normal.
Chemotherapy agents. Mitoxantrone is the only FDA-approved chemotherapeutic drug used in MS. However, a few chemotherapy drugs—among them, azathioprine, methotrexate, and cyclophosphamide—are used off label. Chemotherapeutic agents are category D, except methotrexate (category X). Women on category D medications must use a method of birth control for three months after stopping the DMT. Often, clinicians will recommend women initiate GA or interferon during this period, in the hope of minimizing disease activity. Women on mitoxantrone and methotrexate need to use birth control for six months after stopping these immunosuppressive medications, before conceiving.12 These women likely need to switch to a safer pregnancy DMT during the long washout period.
Pregnancy and breastfeeding among women with MS require planning and decision making. The recommendations differ among clinicians and MS experts since there is no definitive evidence about the risks of the DMTs on the mother and/or the fetus. Clinicians should discuss the potential risks with women based on their knowledge and experience, and the data available based on animal research and the pregnancy registries. —ABB-Z
Aliza Bitton Ben-Zacharia, DNP, ANP
President-Elect of IOMSN
Neurology Faculty, Icahn School of Medicine, Mount Sinai Hospital System, New York, New York
6. Tullman MJ. Overview of the epidemiology, diagnosis, and disease progression associated with multiple sclerosis. Am J Manag Care. 2013;19(2):S15-S20.
7. Fabian M. Pregnancy in the setting of multiple sclerosis. Continuum (Minneap Minn). 2016; 22(3):837-850.
8. Vukusic S, Hutchinson M, Hours M, et al. Pregnancy and multiple sclerosis (the PRIMS study): clinical predictors of post-partum relapse. Brain. 2004;127(6):1353-1360.
9. Sandberg-Wollheim M, Alteri E, Moraga MS, Kornmann G. Pregnancy outcomes in multiple sclerosis following subcutaneous interferon beta-1a therapy. Mult Scler. 2011; 17(4):423-430.
10. Coyle PK. Multiple sclerosis in pregnancy. Continuum (Minneap Minn). 2014;20(1):42-59.
11. Gold SM, Voskuhl RR. Pregnancy and multiple sclerosis: from molecular mechanisms to clinical application. Semin Immunopathol. 2016;38:709.
12. Vukusic S, Marignier R. Multiple sclerosis and pregnancy in the ‘treatment era’. Nat Rev Neurol. 2015;11(5):280-289.
13. FDA. Pregnancy and lactation labeling (drugs) final rule. www.fda.gov/Drugs/DevelopmentApprovalProcess/DevelopmentResources/Labeling/ucm093307.htm. Accessed November 2, 2016.
14. Whyte J. FDA implements new labeling for medications used during pregnancy and lactation. Am Fam Physician. 2016;94(1):12-13.
Q)What are the considerations and recommendations for pregnancy and breastfeeding in women with multiple sclerosis? When should women discontinue their disease-modifying therapies?
Multiple sclerosis (MS) is an inflammatory, demyelinating, degenerative disease. Three times more common in women than men, it may affect pregnancy planning and childbearing experiences.6 Evidence demonstrates a reduction in annualized relapse rate during pregnancy and the postpartum period with exclusive breastfeeding. Therefore, pregnancy and exclusive breastfeeding provide a favorable immunomodulatory effect in women with MS, which combats the increased relapse risk associated with the postpartum period.7,8
Reproductive education—including conception, pregnancy, and breastfeeding—is critical for patients with MS and their partners during a woman’s childbearing years. However, women with MS do not require special considerations during pregnancy unless they have remarkable disability. As soon as these women and their partners decide upon pregnancy, a plan should be established that includes a discussion about potential risks to the fetus due to drug exposure, as well as risks to the mother. The goal should be to minimize risk for disease activity and optimize the health of the baby.
Use of DMTs during conception, pregnancy, and breastfeeding. All disease-modifying therapies (DMTs) are usually discontinued during pregnancy and breastfeeding. Common practice among MS experts is to discontinue DMTs prior to conception, with a few exceptions. There is no consensus about timing of discontinuation and washout period for each DMT. The decision is based on the half-life of each DMT, the opinions of the woman and her partner, and risk tolerance. Note: For the purposes of this discussion, the old pregnancy category designations are used, since they are familiar to clinicians. New guidelines took effect in June 2015; Table 3 outlines the change in format.
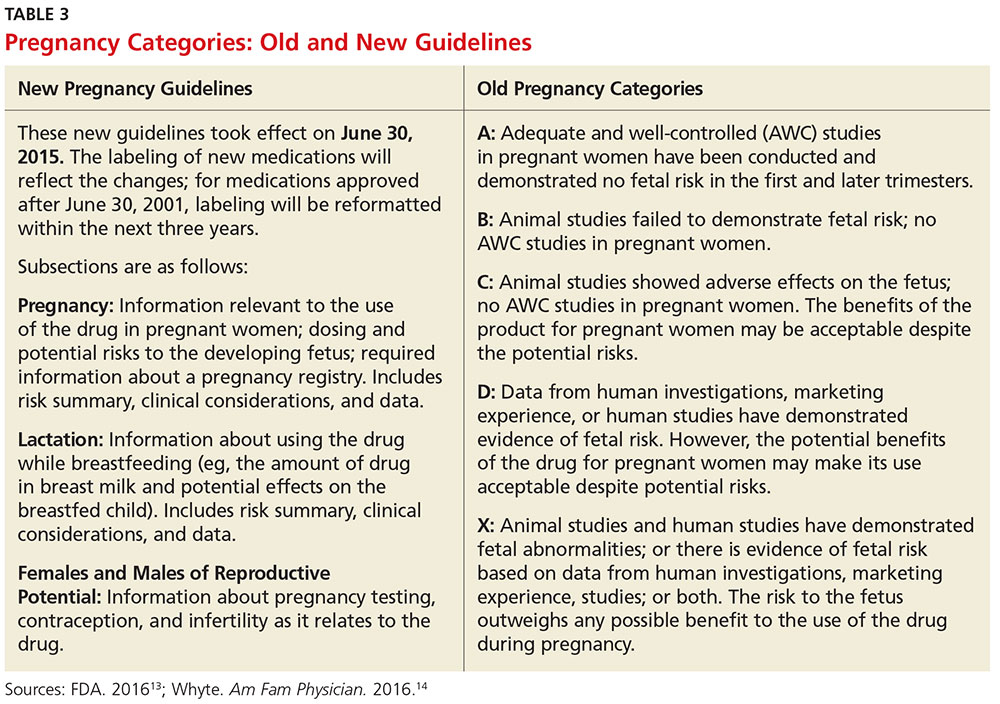
Injectables. Glatiramer acetate (GA) is the safest drug in relation to pregnancy and breastfeeding (category B). There is no evidence of congenital malformation or spontaneous abortion. The common recommendation is to discontinue the drug one to two months before conception, although some clinicians allow continuation of the injections throughout pregnancy and into breastfeeding.
Interferon-ßs are category C and therefore pose minimal risk for the fetus. The washout period before conception is two to three months, varying among clinicians. Although there is no evidence of spontaneous abortion or birth defects in humans, animal data show increased risk for abortion.9
Both GA and interferon-ßs are large molecules; there is a very minimal chance that the medication will transmit to the baby via breast milk. Thus, both DMTs are considered safe during lactation.7
Oral MS medications. The three approved MS oral medications are fingolimod, dimethyl fumarate (DMF), and teriflunomide. Fingolimod and DMF are both category C. Women on DMF must discontinue use of the medication one month prior to conception due to its short half-life. There are no reports of birth defects or spontaneous abortion in women taking DMF. Fingolimod needs to be discontinued two months prior to conception. Animal data show evidence for teratogenicity and embryolethality at lower doses of fingolimod than those used in humans.7
Teriflunomide is category X, posing high risk for the health of the fetus. It stays in the blood for approximately eight months after discontinuation of use. Animal data show teratogenicity and embryotoxicity; therefore, teriflunomide is contraindicated in pregnancy. Women on teriflunomide who plan to become pregnant need to undergo an elimination procedure with cholestyramine or charcoal.
Infusions and injections (monoclonal antibodies). The approved monoclonal antibodies include natalizumab, alemtuzumab, and daclizumab. (Currently, use of rituximab in MS is off label, and the FDA is reviewing the efficacy and safety data for ocrelizumab.) The monoclonal antibodies are category C. The recommendation is to discontinue natalizumab one to two months prior to conception and discontinue alemtuzumab four months preconception.10 There is no evidence of spontaneous abortion or birth defects in women on alemtuzumab, but there is potentially increased risk for spontaneous abortion in those on natalizumab.
The spontaneous abortion rate in daclizumab-exposed women is consistent with early pregnancy loss in the general population (12% to 26%). Data on a small number of pregnancies exposed to daclizumab did not suggest an increased risk for adverse fetal or maternal outcomes.11 However, the recommendation is to discontinue daclizumab four months prior to conception. Rituximab should be discontinued 12 months prior to conception, based on the manufacturer recommendation, although it is potentially safe to conceive when the B cell counts return to normal.
Chemotherapy agents. Mitoxantrone is the only FDA-approved chemotherapeutic drug used in MS. However, a few chemotherapy drugs—among them, azathioprine, methotrexate, and cyclophosphamide—are used off label. Chemotherapeutic agents are category D, except methotrexate (category X). Women on category D medications must use a method of birth control for three months after stopping the DMT. Often, clinicians will recommend women initiate GA or interferon during this period, in the hope of minimizing disease activity. Women on mitoxantrone and methotrexate need to use birth control for six months after stopping these immunosuppressive medications, before conceiving.12 These women likely need to switch to a safer pregnancy DMT during the long washout period.
Pregnancy and breastfeeding among women with MS require planning and decision making. The recommendations differ among clinicians and MS experts since there is no definitive evidence about the risks of the DMTs on the mother and/or the fetus. Clinicians should discuss the potential risks with women based on their knowledge and experience, and the data available based on animal research and the pregnancy registries. —ABB-Z
Aliza Bitton Ben-Zacharia, DNP, ANP
President-Elect of IOMSN
Neurology Faculty, Icahn School of Medicine, Mount Sinai Hospital System, New York, New York
Q)What are the considerations and recommendations for pregnancy and breastfeeding in women with multiple sclerosis? When should women discontinue their disease-modifying therapies?
Multiple sclerosis (MS) is an inflammatory, demyelinating, degenerative disease. Three times more common in women than men, it may affect pregnancy planning and childbearing experiences.6 Evidence demonstrates a reduction in annualized relapse rate during pregnancy and the postpartum period with exclusive breastfeeding. Therefore, pregnancy and exclusive breastfeeding provide a favorable immunomodulatory effect in women with MS, which combats the increased relapse risk associated with the postpartum period.7,8
Reproductive education—including conception, pregnancy, and breastfeeding—is critical for patients with MS and their partners during a woman’s childbearing years. However, women with MS do not require special considerations during pregnancy unless they have remarkable disability. As soon as these women and their partners decide upon pregnancy, a plan should be established that includes a discussion about potential risks to the fetus due to drug exposure, as well as risks to the mother. The goal should be to minimize risk for disease activity and optimize the health of the baby.
Use of DMTs during conception, pregnancy, and breastfeeding. All disease-modifying therapies (DMTs) are usually discontinued during pregnancy and breastfeeding. Common practice among MS experts is to discontinue DMTs prior to conception, with a few exceptions. There is no consensus about timing of discontinuation and washout period for each DMT. The decision is based on the half-life of each DMT, the opinions of the woman and her partner, and risk tolerance. Note: For the purposes of this discussion, the old pregnancy category designations are used, since they are familiar to clinicians. New guidelines took effect in June 2015; Table 3 outlines the change in format.
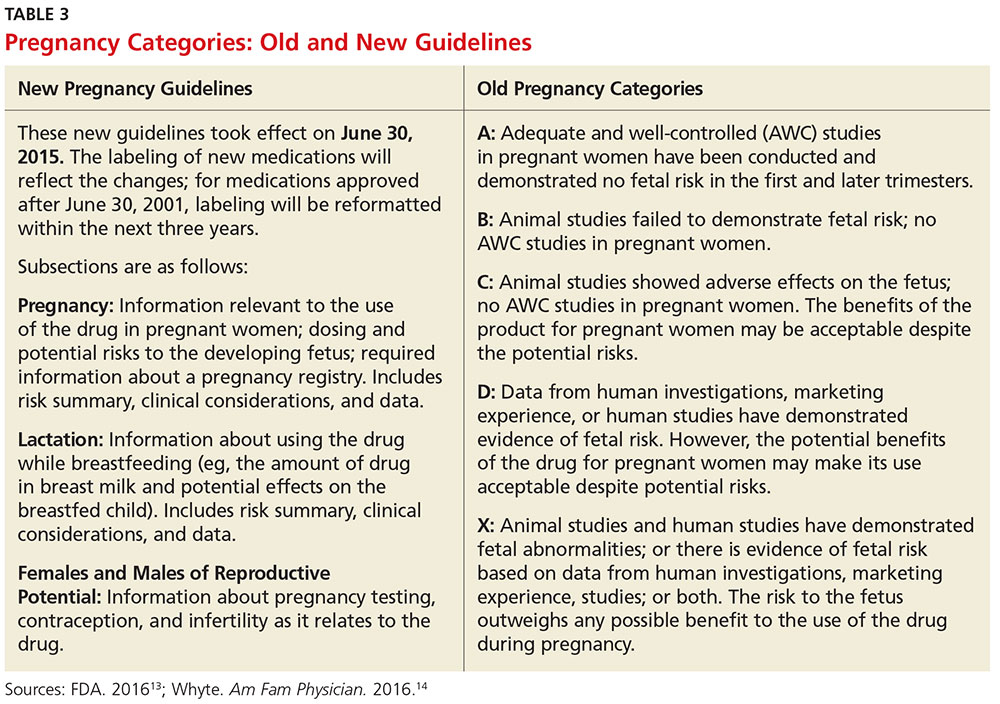
Injectables. Glatiramer acetate (GA) is the safest drug in relation to pregnancy and breastfeeding (category B). There is no evidence of congenital malformation or spontaneous abortion. The common recommendation is to discontinue the drug one to two months before conception, although some clinicians allow continuation of the injections throughout pregnancy and into breastfeeding.
Interferon-ßs are category C and therefore pose minimal risk for the fetus. The washout period before conception is two to three months, varying among clinicians. Although there is no evidence of spontaneous abortion or birth defects in humans, animal data show increased risk for abortion.9
Both GA and interferon-ßs are large molecules; there is a very minimal chance that the medication will transmit to the baby via breast milk. Thus, both DMTs are considered safe during lactation.7
Oral MS medications. The three approved MS oral medications are fingolimod, dimethyl fumarate (DMF), and teriflunomide. Fingolimod and DMF are both category C. Women on DMF must discontinue use of the medication one month prior to conception due to its short half-life. There are no reports of birth defects or spontaneous abortion in women taking DMF. Fingolimod needs to be discontinued two months prior to conception. Animal data show evidence for teratogenicity and embryolethality at lower doses of fingolimod than those used in humans.7
Teriflunomide is category X, posing high risk for the health of the fetus. It stays in the blood for approximately eight months after discontinuation of use. Animal data show teratogenicity and embryotoxicity; therefore, teriflunomide is contraindicated in pregnancy. Women on teriflunomide who plan to become pregnant need to undergo an elimination procedure with cholestyramine or charcoal.
Infusions and injections (monoclonal antibodies). The approved monoclonal antibodies include natalizumab, alemtuzumab, and daclizumab. (Currently, use of rituximab in MS is off label, and the FDA is reviewing the efficacy and safety data for ocrelizumab.) The monoclonal antibodies are category C. The recommendation is to discontinue natalizumab one to two months prior to conception and discontinue alemtuzumab four months preconception.10 There is no evidence of spontaneous abortion or birth defects in women on alemtuzumab, but there is potentially increased risk for spontaneous abortion in those on natalizumab.
The spontaneous abortion rate in daclizumab-exposed women is consistent with early pregnancy loss in the general population (12% to 26%). Data on a small number of pregnancies exposed to daclizumab did not suggest an increased risk for adverse fetal or maternal outcomes.11 However, the recommendation is to discontinue daclizumab four months prior to conception. Rituximab should be discontinued 12 months prior to conception, based on the manufacturer recommendation, although it is potentially safe to conceive when the B cell counts return to normal.
Chemotherapy agents. Mitoxantrone is the only FDA-approved chemotherapeutic drug used in MS. However, a few chemotherapy drugs—among them, azathioprine, methotrexate, and cyclophosphamide—are used off label. Chemotherapeutic agents are category D, except methotrexate (category X). Women on category D medications must use a method of birth control for three months after stopping the DMT. Often, clinicians will recommend women initiate GA or interferon during this period, in the hope of minimizing disease activity. Women on mitoxantrone and methotrexate need to use birth control for six months after stopping these immunosuppressive medications, before conceiving.12 These women likely need to switch to a safer pregnancy DMT during the long washout period.
Pregnancy and breastfeeding among women with MS require planning and decision making. The recommendations differ among clinicians and MS experts since there is no definitive evidence about the risks of the DMTs on the mother and/or the fetus. Clinicians should discuss the potential risks with women based on their knowledge and experience, and the data available based on animal research and the pregnancy registries. —ABB-Z
Aliza Bitton Ben-Zacharia, DNP, ANP
President-Elect of IOMSN
Neurology Faculty, Icahn School of Medicine, Mount Sinai Hospital System, New York, New York
6. Tullman MJ. Overview of the epidemiology, diagnosis, and disease progression associated with multiple sclerosis. Am J Manag Care. 2013;19(2):S15-S20.
7. Fabian M. Pregnancy in the setting of multiple sclerosis. Continuum (Minneap Minn). 2016; 22(3):837-850.
8. Vukusic S, Hutchinson M, Hours M, et al. Pregnancy and multiple sclerosis (the PRIMS study): clinical predictors of post-partum relapse. Brain. 2004;127(6):1353-1360.
9. Sandberg-Wollheim M, Alteri E, Moraga MS, Kornmann G. Pregnancy outcomes in multiple sclerosis following subcutaneous interferon beta-1a therapy. Mult Scler. 2011; 17(4):423-430.
10. Coyle PK. Multiple sclerosis in pregnancy. Continuum (Minneap Minn). 2014;20(1):42-59.
11. Gold SM, Voskuhl RR. Pregnancy and multiple sclerosis: from molecular mechanisms to clinical application. Semin Immunopathol. 2016;38:709.
12. Vukusic S, Marignier R. Multiple sclerosis and pregnancy in the ‘treatment era’. Nat Rev Neurol. 2015;11(5):280-289.
13. FDA. Pregnancy and lactation labeling (drugs) final rule. www.fda.gov/Drugs/DevelopmentApprovalProcess/DevelopmentResources/Labeling/ucm093307.htm. Accessed November 2, 2016.
14. Whyte J. FDA implements new labeling for medications used during pregnancy and lactation. Am Fam Physician. 2016;94(1):12-13.
6. Tullman MJ. Overview of the epidemiology, diagnosis, and disease progression associated with multiple sclerosis. Am J Manag Care. 2013;19(2):S15-S20.
7. Fabian M. Pregnancy in the setting of multiple sclerosis. Continuum (Minneap Minn). 2016; 22(3):837-850.
8. Vukusic S, Hutchinson M, Hours M, et al. Pregnancy and multiple sclerosis (the PRIMS study): clinical predictors of post-partum relapse. Brain. 2004;127(6):1353-1360.
9. Sandberg-Wollheim M, Alteri E, Moraga MS, Kornmann G. Pregnancy outcomes in multiple sclerosis following subcutaneous interferon beta-1a therapy. Mult Scler. 2011; 17(4):423-430.
10. Coyle PK. Multiple sclerosis in pregnancy. Continuum (Minneap Minn). 2014;20(1):42-59.
11. Gold SM, Voskuhl RR. Pregnancy and multiple sclerosis: from molecular mechanisms to clinical application. Semin Immunopathol. 2016;38:709.
12. Vukusic S, Marignier R. Multiple sclerosis and pregnancy in the ‘treatment era’. Nat Rev Neurol. 2015;11(5):280-289.
13. FDA. Pregnancy and lactation labeling (drugs) final rule. www.fda.gov/Drugs/DevelopmentApprovalProcess/DevelopmentResources/Labeling/ucm093307.htm. Accessed November 2, 2016.
14. Whyte J. FDA implements new labeling for medications used during pregnancy and lactation. Am Fam Physician. 2016;94(1):12-13.