User login
Why is the mental health burden in EDs rising?
The mounting impact of mental illness on patients and the American health care system has been of growing concern, especially in recent years. As such, now more than ever, it is important to understand the mental health burden and investigate the factors contributing to the elevated use of emergency departments to treat patients with psychiatric illness.
In recent years, the overall prevalence of mental illness has not changed drastically. According to the 2014 National Survey of Drug Use and Health, 18.1% of adults indicated having “any mental illness,” a prevalence that had not changed much since 2008.1 It is possible, however, that despite the relative stability in the prevalence of mental illness, the acuity of mental illness may be on the rise. For instance, 4.1% of adults indicated having a “serious mental illness” (SMI) in 2014, a prevalence that was 0.4% higher than that of 2008 and 2009.1 Also, of note, the prevalence of SMI among the 18-to-25-year-old population in 2014 had increased in previous years.1 Meanwhile, 6.6% of adults indicated having experienced a major depressive episode at least once in the preceding 12 months. That prevalence has held relatively steady over recent years.1
Despite the rising need for mental health services, the number of inpatient psychiatric beds has declined. During the 32 years between 1970 and 2002, the United States experienced a staggering nearly 60% decline in the number of inpatient psychiatric beds.4 Moreover, the number of psychiatric beds within the national public sector fell from 50,509 in 2005 to 43,318 in 2010, which is about a 14% decline.5 This decrease translated to a decrease from 17.1 beds/100,000 people in 2005 to 14.1 beds/100,000 in 2010 – both of which fall drastically below the “minimum number of public psychiatric beds deemed necessary for adequate psychiatric services (50/100,000).”5 Similarly, psychiatric practice has been unable to keep up with the increasing population size – the population-adjusted median number of psychiatrists declined 10.2% between 2003 and 2013.6
While inpatient psychiatric beds and psychiatrist availability have declined, the frequency of ED use for mental health reasons has increased. Mental health or substance abuse diagnoses directly accounted for 4.3% of ED visits in 2007 and were associated with 12.5% of ED visits.7 Specifically, there was a 19.3% increase in the rate of nonmaternal treat-and-release ED visits for mental health reasons between 2008-2012.8 Moreover, in a study assessing frequent treat-and-release ED visits among Medicaid patients, investigators found that while most ED visits were for non–mental health purposes, the odds of frequent ED use were higher among patients with either a psychiatric disorder or substance use problem across all levels of overall health complexity.9
What factors have been driving adults to increasingly rely on ED visits for their mental health care? Given the immense complexity of the U.S. mental health delivery system, it is evident that there is no clear-cut explanation. However, several specific factors may have contributed and must be investigated to better our understanding of this public health conundrum. The opioid epidemic, transition out of the correctional system, and coverage changes under the Affordable Care Act are hypotheses that will be examined further in the context of this pressing issue.
References
1. “Behavioral Health Trends in the United States: Results from the 2014 National Survey on Drug Use and Health.”
2. “Increase in Suicide in the United States, 1999-2014.” NCHS Data Brief No. 241, April 2016.
3. Web-Based Injury Statistics Query and Reporting System (WISQARS), Centers for Disease Control and Prevention.
4. National Health Policy Forum Issue Brief (2007 Aug 1;[823]:1-21).
5. “No Room at the Inn: Trends and Consequences of Closing Public Psychiatric Hospitals, 2005-2010,” Arlington, Va.: Treatment Advocacy Center, July 19, 2012.
6. “Population of U.S. Practicing Psychiatrists Declined, 2003-13, Which May Help Explain Poor Access to Mental Health Care,” Health Aff (Millwood). 2016 Jul 1;35[7]:1271-7.
7. “Mental Health and Substance Abuse-Related Emergency Department Visits Among Adults, 2007: Statistical Brief #92,” in Healthcare Cost and Utilization Project Statistical Briefs, (Rockville, Md.: Agency for Healthcare Research and Quality, 2010).
8. “Trends in Potentially Preventable Inpatient Hospital Admissions and Emergency Department Visits, 2015: Statistical Brief #195,” in Healthcare Cost and Utilization Project Statistical Briefs, (Rockville, Md.: Agency for Healthcare Research and Quality).
9. Nurs Res. 2015 Jan-Feb;64[1]3-12.
10. Ann Emerg Med. 2016 Apr;67[4]:525-30.
Ms. Kablanian is a 2nd-year medical student at the George Washington University, Washington, where she is enrolled in the Community and Urban Health Scholarly Concentration Program. Before attending medical school, she earned a master of public health degree in epidemiology from Columbia University, New York. She also holds a bachelor’s degree in biology and French from Scripps College, Claremont, Calif. Her interests include advocating for the urban underserved, contributing to medical curriculum development, and investigating population-level contributors to adverse health outcomes. Dr. Norris is assistant professor in the department of psychiatry & behavioral sciences, and assistant dean of student affairs at the George Washington University. He also is medical director of psychiatric & behavioral sciences at George Washington University Hospital. As part of his commitment to providing mental health care to patients with severe medical illness, Dr. Norris has been a leading voice within the psychiatric community on the value of palliative psychotherapy.
The mounting impact of mental illness on patients and the American health care system has been of growing concern, especially in recent years. As such, now more than ever, it is important to understand the mental health burden and investigate the factors contributing to the elevated use of emergency departments to treat patients with psychiatric illness.
In recent years, the overall prevalence of mental illness has not changed drastically. According to the 2014 National Survey of Drug Use and Health, 18.1% of adults indicated having “any mental illness,” a prevalence that had not changed much since 2008.1 It is possible, however, that despite the relative stability in the prevalence of mental illness, the acuity of mental illness may be on the rise. For instance, 4.1% of adults indicated having a “serious mental illness” (SMI) in 2014, a prevalence that was 0.4% higher than that of 2008 and 2009.1 Also, of note, the prevalence of SMI among the 18-to-25-year-old population in 2014 had increased in previous years.1 Meanwhile, 6.6% of adults indicated having experienced a major depressive episode at least once in the preceding 12 months. That prevalence has held relatively steady over recent years.1
Despite the rising need for mental health services, the number of inpatient psychiatric beds has declined. During the 32 years between 1970 and 2002, the United States experienced a staggering nearly 60% decline in the number of inpatient psychiatric beds.4 Moreover, the number of psychiatric beds within the national public sector fell from 50,509 in 2005 to 43,318 in 2010, which is about a 14% decline.5 This decrease translated to a decrease from 17.1 beds/100,000 people in 2005 to 14.1 beds/100,000 in 2010 – both of which fall drastically below the “minimum number of public psychiatric beds deemed necessary for adequate psychiatric services (50/100,000).”5 Similarly, psychiatric practice has been unable to keep up with the increasing population size – the population-adjusted median number of psychiatrists declined 10.2% between 2003 and 2013.6
While inpatient psychiatric beds and psychiatrist availability have declined, the frequency of ED use for mental health reasons has increased. Mental health or substance abuse diagnoses directly accounted for 4.3% of ED visits in 2007 and were associated with 12.5% of ED visits.7 Specifically, there was a 19.3% increase in the rate of nonmaternal treat-and-release ED visits for mental health reasons between 2008-2012.8 Moreover, in a study assessing frequent treat-and-release ED visits among Medicaid patients, investigators found that while most ED visits were for non–mental health purposes, the odds of frequent ED use were higher among patients with either a psychiatric disorder or substance use problem across all levels of overall health complexity.9
What factors have been driving adults to increasingly rely on ED visits for their mental health care? Given the immense complexity of the U.S. mental health delivery system, it is evident that there is no clear-cut explanation. However, several specific factors may have contributed and must be investigated to better our understanding of this public health conundrum. The opioid epidemic, transition out of the correctional system, and coverage changes under the Affordable Care Act are hypotheses that will be examined further in the context of this pressing issue.
References
1. “Behavioral Health Trends in the United States: Results from the 2014 National Survey on Drug Use and Health.”
2. “Increase in Suicide in the United States, 1999-2014.” NCHS Data Brief No. 241, April 2016.
3. Web-Based Injury Statistics Query and Reporting System (WISQARS), Centers for Disease Control and Prevention.
4. National Health Policy Forum Issue Brief (2007 Aug 1;[823]:1-21).
5. “No Room at the Inn: Trends and Consequences of Closing Public Psychiatric Hospitals, 2005-2010,” Arlington, Va.: Treatment Advocacy Center, July 19, 2012.
6. “Population of U.S. Practicing Psychiatrists Declined, 2003-13, Which May Help Explain Poor Access to Mental Health Care,” Health Aff (Millwood). 2016 Jul 1;35[7]:1271-7.
7. “Mental Health and Substance Abuse-Related Emergency Department Visits Among Adults, 2007: Statistical Brief #92,” in Healthcare Cost and Utilization Project Statistical Briefs, (Rockville, Md.: Agency for Healthcare Research and Quality, 2010).
8. “Trends in Potentially Preventable Inpatient Hospital Admissions and Emergency Department Visits, 2015: Statistical Brief #195,” in Healthcare Cost and Utilization Project Statistical Briefs, (Rockville, Md.: Agency for Healthcare Research and Quality).
9. Nurs Res. 2015 Jan-Feb;64[1]3-12.
10. Ann Emerg Med. 2016 Apr;67[4]:525-30.
Ms. Kablanian is a 2nd-year medical student at the George Washington University, Washington, where she is enrolled in the Community and Urban Health Scholarly Concentration Program. Before attending medical school, she earned a master of public health degree in epidemiology from Columbia University, New York. She also holds a bachelor’s degree in biology and French from Scripps College, Claremont, Calif. Her interests include advocating for the urban underserved, contributing to medical curriculum development, and investigating population-level contributors to adverse health outcomes. Dr. Norris is assistant professor in the department of psychiatry & behavioral sciences, and assistant dean of student affairs at the George Washington University. He also is medical director of psychiatric & behavioral sciences at George Washington University Hospital. As part of his commitment to providing mental health care to patients with severe medical illness, Dr. Norris has been a leading voice within the psychiatric community on the value of palliative psychotherapy.
The mounting impact of mental illness on patients and the American health care system has been of growing concern, especially in recent years. As such, now more than ever, it is important to understand the mental health burden and investigate the factors contributing to the elevated use of emergency departments to treat patients with psychiatric illness.
In recent years, the overall prevalence of mental illness has not changed drastically. According to the 2014 National Survey of Drug Use and Health, 18.1% of adults indicated having “any mental illness,” a prevalence that had not changed much since 2008.1 It is possible, however, that despite the relative stability in the prevalence of mental illness, the acuity of mental illness may be on the rise. For instance, 4.1% of adults indicated having a “serious mental illness” (SMI) in 2014, a prevalence that was 0.4% higher than that of 2008 and 2009.1 Also, of note, the prevalence of SMI among the 18-to-25-year-old population in 2014 had increased in previous years.1 Meanwhile, 6.6% of adults indicated having experienced a major depressive episode at least once in the preceding 12 months. That prevalence has held relatively steady over recent years.1
Despite the rising need for mental health services, the number of inpatient psychiatric beds has declined. During the 32 years between 1970 and 2002, the United States experienced a staggering nearly 60% decline in the number of inpatient psychiatric beds.4 Moreover, the number of psychiatric beds within the national public sector fell from 50,509 in 2005 to 43,318 in 2010, which is about a 14% decline.5 This decrease translated to a decrease from 17.1 beds/100,000 people in 2005 to 14.1 beds/100,000 in 2010 – both of which fall drastically below the “minimum number of public psychiatric beds deemed necessary for adequate psychiatric services (50/100,000).”5 Similarly, psychiatric practice has been unable to keep up with the increasing population size – the population-adjusted median number of psychiatrists declined 10.2% between 2003 and 2013.6
While inpatient psychiatric beds and psychiatrist availability have declined, the frequency of ED use for mental health reasons has increased. Mental health or substance abuse diagnoses directly accounted for 4.3% of ED visits in 2007 and were associated with 12.5% of ED visits.7 Specifically, there was a 19.3% increase in the rate of nonmaternal treat-and-release ED visits for mental health reasons between 2008-2012.8 Moreover, in a study assessing frequent treat-and-release ED visits among Medicaid patients, investigators found that while most ED visits were for non–mental health purposes, the odds of frequent ED use were higher among patients with either a psychiatric disorder or substance use problem across all levels of overall health complexity.9
What factors have been driving adults to increasingly rely on ED visits for their mental health care? Given the immense complexity of the U.S. mental health delivery system, it is evident that there is no clear-cut explanation. However, several specific factors may have contributed and must be investigated to better our understanding of this public health conundrum. The opioid epidemic, transition out of the correctional system, and coverage changes under the Affordable Care Act are hypotheses that will be examined further in the context of this pressing issue.
References
1. “Behavioral Health Trends in the United States: Results from the 2014 National Survey on Drug Use and Health.”
2. “Increase in Suicide in the United States, 1999-2014.” NCHS Data Brief No. 241, April 2016.
3. Web-Based Injury Statistics Query and Reporting System (WISQARS), Centers for Disease Control and Prevention.
4. National Health Policy Forum Issue Brief (2007 Aug 1;[823]:1-21).
5. “No Room at the Inn: Trends and Consequences of Closing Public Psychiatric Hospitals, 2005-2010,” Arlington, Va.: Treatment Advocacy Center, July 19, 2012.
6. “Population of U.S. Practicing Psychiatrists Declined, 2003-13, Which May Help Explain Poor Access to Mental Health Care,” Health Aff (Millwood). 2016 Jul 1;35[7]:1271-7.
7. “Mental Health and Substance Abuse-Related Emergency Department Visits Among Adults, 2007: Statistical Brief #92,” in Healthcare Cost and Utilization Project Statistical Briefs, (Rockville, Md.: Agency for Healthcare Research and Quality, 2010).
8. “Trends in Potentially Preventable Inpatient Hospital Admissions and Emergency Department Visits, 2015: Statistical Brief #195,” in Healthcare Cost and Utilization Project Statistical Briefs, (Rockville, Md.: Agency for Healthcare Research and Quality).
9. Nurs Res. 2015 Jan-Feb;64[1]3-12.
10. Ann Emerg Med. 2016 Apr;67[4]:525-30.
Ms. Kablanian is a 2nd-year medical student at the George Washington University, Washington, where she is enrolled in the Community and Urban Health Scholarly Concentration Program. Before attending medical school, she earned a master of public health degree in epidemiology from Columbia University, New York. She also holds a bachelor’s degree in biology and French from Scripps College, Claremont, Calif. Her interests include advocating for the urban underserved, contributing to medical curriculum development, and investigating population-level contributors to adverse health outcomes. Dr. Norris is assistant professor in the department of psychiatry & behavioral sciences, and assistant dean of student affairs at the George Washington University. He also is medical director of psychiatric & behavioral sciences at George Washington University Hospital. As part of his commitment to providing mental health care to patients with severe medical illness, Dr. Norris has been a leading voice within the psychiatric community on the value of palliative psychotherapy.
Flu susceptibility driven by birth year
Differences in susceptibility to an influenza A virus (IAV) strain may be traceable to the first lifetime influenza infection, according to a new statistical model, which could have implications for epidemiology and future flu vaccines.
In the Nov. 11 issue of Science, researchers described infection models of the H5N1 and H7N9 strains of influenza A. The former occurs more commonly in younger people, and the latter in older individuals, but the reasons for those associations have puzzled scientists.
The researchers, led by James Lloyd-Smith, PhD, of the department of ecology and evolutionary biology at the University of California, Los Angeles, looked at susceptibility to IAV strains by birth year, and found that this was the best predictor of vulnerability. For example, an analysis of H5N1 cases in Egypt, where had many H5N1 cases spread over the past decade, showed that individuals born in the same year had the same average risk of severe H5N1 infection, even after they had aged by 10 years. That suggests that it is the birth year, not advancing age, which influences susceptibility (Science. 2016 Nov 11;354[6313]:721-5. doi:10.1126/science.aag1322).
The researchers suggest that the immune system “imprints” on the hemagglutinin (HA) subtype during an individual’s first infection, which confers protection against severe disease caused by other, related viruses, though it may not reduce infection rates overall.
The year 1968 may have marked an important inflection point. That year marked a shift in the identify of circulating viruses, from group 1 HA (which includes H5N1) to group 2 HA (which includes H7N9). Individuals born before 1968 were likely first infected with a group 1 virus, while those born later were most likely initially exposed to a group 2 virus. If the imprint theory is correct, younger people would have imprinted on group 2 viruses similar to H7N9, which would explain their greater vulnerability to group 1 viruses like H5N1.
“Imprinting was the dominant explanatory factor for observed incidence and mortality patterns for both H5N1 and H7N9. It was the only tested factor included in all plausible models for both viruses,” the researchers wrote.
According to the model, imprinting explains 75% of protection against severe infection and 80% of the protection against mortality for H5N1 and H7N9.
That information adds a previously unrecognized layer to influenza epidemiology, which should be accounted for in public health measures. “The methods shown here can provide rolling estimates of which age groups would be at highest risk for severe disease should particular novel HA subtypes emerge,” the researchers wrote.
The researchers received funding from the National Institutes of Health, the National Science Foundation, the David and Lucile Packard Foundation, and the Department of Homeland Security. They reported having no financial disclosures.
A growing body of epidemiological evidence points to the prolonged effects of cross-immunity, including competition between strains during seasonal and pandemic outbreaks, reduced risk of pandemic infection in those with previous seasonal exposure, and – as reported by Gostic et al. – lifelong protection against viruses of different subtypes but in the same hemagglutinin (HA) homology group. Basic science efforts are now needed to fully validate the HA imprinting hypothesis. More broadly, further experimental and theoretical work should map the relationship between early childhood exposure to influenza and immune protection and the implications of lifelong immunity for vaccination strategies and pandemic risk.
Cécile Viboud, PhD, is the acting director of the division of international epidemiology and population studies at the Fogarty International Center at the National Institutes of Health. Suzanne L. Epstein, PhD, is the associate director for research at the office of tissues and advanced therapies at the Food and Drug Administration Center for Biologics Evaluation and Research. They had no relevant financial disclosures and made these remarks in an editorial that accompanied the published study (Science. 2016 Nov 11;354[6313]:706-7. doi:10.1126/science.aak9816).
A growing body of epidemiological evidence points to the prolonged effects of cross-immunity, including competition between strains during seasonal and pandemic outbreaks, reduced risk of pandemic infection in those with previous seasonal exposure, and – as reported by Gostic et al. – lifelong protection against viruses of different subtypes but in the same hemagglutinin (HA) homology group. Basic science efforts are now needed to fully validate the HA imprinting hypothesis. More broadly, further experimental and theoretical work should map the relationship between early childhood exposure to influenza and immune protection and the implications of lifelong immunity for vaccination strategies and pandemic risk.
Cécile Viboud, PhD, is the acting director of the division of international epidemiology and population studies at the Fogarty International Center at the National Institutes of Health. Suzanne L. Epstein, PhD, is the associate director for research at the office of tissues and advanced therapies at the Food and Drug Administration Center for Biologics Evaluation and Research. They had no relevant financial disclosures and made these remarks in an editorial that accompanied the published study (Science. 2016 Nov 11;354[6313]:706-7. doi:10.1126/science.aak9816).
A growing body of epidemiological evidence points to the prolonged effects of cross-immunity, including competition between strains during seasonal and pandemic outbreaks, reduced risk of pandemic infection in those with previous seasonal exposure, and – as reported by Gostic et al. – lifelong protection against viruses of different subtypes but in the same hemagglutinin (HA) homology group. Basic science efforts are now needed to fully validate the HA imprinting hypothesis. More broadly, further experimental and theoretical work should map the relationship between early childhood exposure to influenza and immune protection and the implications of lifelong immunity for vaccination strategies and pandemic risk.
Cécile Viboud, PhD, is the acting director of the division of international epidemiology and population studies at the Fogarty International Center at the National Institutes of Health. Suzanne L. Epstein, PhD, is the associate director for research at the office of tissues and advanced therapies at the Food and Drug Administration Center for Biologics Evaluation and Research. They had no relevant financial disclosures and made these remarks in an editorial that accompanied the published study (Science. 2016 Nov 11;354[6313]:706-7. doi:10.1126/science.aak9816).
Differences in susceptibility to an influenza A virus (IAV) strain may be traceable to the first lifetime influenza infection, according to a new statistical model, which could have implications for epidemiology and future flu vaccines.
In the Nov. 11 issue of Science, researchers described infection models of the H5N1 and H7N9 strains of influenza A. The former occurs more commonly in younger people, and the latter in older individuals, but the reasons for those associations have puzzled scientists.
The researchers, led by James Lloyd-Smith, PhD, of the department of ecology and evolutionary biology at the University of California, Los Angeles, looked at susceptibility to IAV strains by birth year, and found that this was the best predictor of vulnerability. For example, an analysis of H5N1 cases in Egypt, where had many H5N1 cases spread over the past decade, showed that individuals born in the same year had the same average risk of severe H5N1 infection, even after they had aged by 10 years. That suggests that it is the birth year, not advancing age, which influences susceptibility (Science. 2016 Nov 11;354[6313]:721-5. doi:10.1126/science.aag1322).
The researchers suggest that the immune system “imprints” on the hemagglutinin (HA) subtype during an individual’s first infection, which confers protection against severe disease caused by other, related viruses, though it may not reduce infection rates overall.
The year 1968 may have marked an important inflection point. That year marked a shift in the identify of circulating viruses, from group 1 HA (which includes H5N1) to group 2 HA (which includes H7N9). Individuals born before 1968 were likely first infected with a group 1 virus, while those born later were most likely initially exposed to a group 2 virus. If the imprint theory is correct, younger people would have imprinted on group 2 viruses similar to H7N9, which would explain their greater vulnerability to group 1 viruses like H5N1.
“Imprinting was the dominant explanatory factor for observed incidence and mortality patterns for both H5N1 and H7N9. It was the only tested factor included in all plausible models for both viruses,” the researchers wrote.
According to the model, imprinting explains 75% of protection against severe infection and 80% of the protection against mortality for H5N1 and H7N9.
That information adds a previously unrecognized layer to influenza epidemiology, which should be accounted for in public health measures. “The methods shown here can provide rolling estimates of which age groups would be at highest risk for severe disease should particular novel HA subtypes emerge,” the researchers wrote.
The researchers received funding from the National Institutes of Health, the National Science Foundation, the David and Lucile Packard Foundation, and the Department of Homeland Security. They reported having no financial disclosures.
Differences in susceptibility to an influenza A virus (IAV) strain may be traceable to the first lifetime influenza infection, according to a new statistical model, which could have implications for epidemiology and future flu vaccines.
In the Nov. 11 issue of Science, researchers described infection models of the H5N1 and H7N9 strains of influenza A. The former occurs more commonly in younger people, and the latter in older individuals, but the reasons for those associations have puzzled scientists.
The researchers, led by James Lloyd-Smith, PhD, of the department of ecology and evolutionary biology at the University of California, Los Angeles, looked at susceptibility to IAV strains by birth year, and found that this was the best predictor of vulnerability. For example, an analysis of H5N1 cases in Egypt, where had many H5N1 cases spread over the past decade, showed that individuals born in the same year had the same average risk of severe H5N1 infection, even after they had aged by 10 years. That suggests that it is the birth year, not advancing age, which influences susceptibility (Science. 2016 Nov 11;354[6313]:721-5. doi:10.1126/science.aag1322).
The researchers suggest that the immune system “imprints” on the hemagglutinin (HA) subtype during an individual’s first infection, which confers protection against severe disease caused by other, related viruses, though it may not reduce infection rates overall.
The year 1968 may have marked an important inflection point. That year marked a shift in the identify of circulating viruses, from group 1 HA (which includes H5N1) to group 2 HA (which includes H7N9). Individuals born before 1968 were likely first infected with a group 1 virus, while those born later were most likely initially exposed to a group 2 virus. If the imprint theory is correct, younger people would have imprinted on group 2 viruses similar to H7N9, which would explain their greater vulnerability to group 1 viruses like H5N1.
“Imprinting was the dominant explanatory factor for observed incidence and mortality patterns for both H5N1 and H7N9. It was the only tested factor included in all plausible models for both viruses,” the researchers wrote.
According to the model, imprinting explains 75% of protection against severe infection and 80% of the protection against mortality for H5N1 and H7N9.
That information adds a previously unrecognized layer to influenza epidemiology, which should be accounted for in public health measures. “The methods shown here can provide rolling estimates of which age groups would be at highest risk for severe disease should particular novel HA subtypes emerge,” the researchers wrote.
The researchers received funding from the National Institutes of Health, the National Science Foundation, the David and Lucile Packard Foundation, and the Department of Homeland Security. They reported having no financial disclosures.
Key clinical point:
Major finding: Early exposure to virus subtype explains 75% of protection against severe disease in later life.
Data source: Statistical model of retrospective data.
Disclosures: The researchers received funding from the National Institutes of Health, the National Science Foundation, the David and Lucile Packard Foundation, and the Department of Homeland Security. They reported having no financial disclosures.
Cooling, occlusion, and antihistamines are among the options that optimize ALA-PDT results
Treatment of a broad area, occluding extremities, and the use of antihistamines are among the measures that can help optimize the results of treating actinic keratoses (AKs) with topical photodynamic therapy (PDT) using aminolevulinic acid (ALA), according to Dr. Brian Berman.
For many patients with AKs, ALA-PDT can be an effective and well-tolerated option, Dr. Berman said in a presentation at the Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
ALA-PDT is a two-step process, Dr. Berman explained. The first step involves the application of ALA with presumed selective cellular uptake, followed by conversion to protoporphyrin IX (PpIX). Next, the light activation of PpIX causes cell death via high-energy oxygen molecules.
Dr. Berman’s recommendations for optimizing ALA-PDT to treat AKs include a shorter ALA incubation time; treatment of a broad area, not just the baseline visible AKs; occlusion of ALA for AKs on the arms and legs; increased skin temperature during ALA incubation; and moderate cooling during light exposure. To reduce pain, he recommended a very short ALA incubation time with a longer time of light exposure.
He referred to a 2004 study of 18 patients, which found that AK reductions were not significantly different at 1 month post treatment with ALA incubation times of 1, 2, or 3 hours (Arch Dermatol. 2004 Jan;140[1]:33-40). As for occlusion, a 2012 study found that AK clearance was significantly greater for extremities that were occluded during incubation in patients undergoing blue light ALA-PDT, compared with areas that were not occluded (J Drugs Dermatol. 2012 Dec;11[12]:1483-9).
Skin cooling can be useful in reducing patients’ pain, said Dr. Berman of the department of dermatology and cutaneous surgery, University of Miami. Data from a retrospective study showed that cooling pain relief, with an air-cooling device during treatment, resulted in lower PpIX photobleaching in AK lesions, compared with no cooling (J Photochem Photobiol B. 2011 Apr 4;103[1]:1-7). But cooling was associated with decreased efficacy of the PDT treatment in terms of complete AK response (68% for the cooling device group vs. 82% for controls without cooling), he said.
Increasing skin temperature has been shown to reduce AK lesions significantly, compared with no heat, Dr. Berman pointed out. “PpIX synthesis is temperature dependent,” he said. The median difference in AK lesion counts was significantly greater on a heated extremity side than a control side in an unpublished study, he noted.
Finally, when it comes to facial AKs, less may be more in terms of treatment time. In a split face study, a “painless PDT” protocol of 15 minutes of ALA incubation with 1 hour of blue light yielded a 52% reduction in AKs at 8 weeks post treatment, vs. a 44% reduction with a standard treatment of 75 minutes of ALA incubation with 16 minutes, 45 seconds of blue light, Dr. Berman said.
Dr. Berman disclosed relationships with multiple companies including Ferndale, LEO, Halscion, Sensus, Exeltis, Dermira, Celumigen, Sun, DUSA, Biofrontera, and Berg. He holds stock in Halscion, Dermira, Celumigen, and Berg.
SDEF and this news organization are owned by the same parent company.
Treatment of a broad area, occluding extremities, and the use of antihistamines are among the measures that can help optimize the results of treating actinic keratoses (AKs) with topical photodynamic therapy (PDT) using aminolevulinic acid (ALA), according to Dr. Brian Berman.
For many patients with AKs, ALA-PDT can be an effective and well-tolerated option, Dr. Berman said in a presentation at the Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
ALA-PDT is a two-step process, Dr. Berman explained. The first step involves the application of ALA with presumed selective cellular uptake, followed by conversion to protoporphyrin IX (PpIX). Next, the light activation of PpIX causes cell death via high-energy oxygen molecules.
Dr. Berman’s recommendations for optimizing ALA-PDT to treat AKs include a shorter ALA incubation time; treatment of a broad area, not just the baseline visible AKs; occlusion of ALA for AKs on the arms and legs; increased skin temperature during ALA incubation; and moderate cooling during light exposure. To reduce pain, he recommended a very short ALA incubation time with a longer time of light exposure.
He referred to a 2004 study of 18 patients, which found that AK reductions were not significantly different at 1 month post treatment with ALA incubation times of 1, 2, or 3 hours (Arch Dermatol. 2004 Jan;140[1]:33-40). As for occlusion, a 2012 study found that AK clearance was significantly greater for extremities that were occluded during incubation in patients undergoing blue light ALA-PDT, compared with areas that were not occluded (J Drugs Dermatol. 2012 Dec;11[12]:1483-9).
Skin cooling can be useful in reducing patients’ pain, said Dr. Berman of the department of dermatology and cutaneous surgery, University of Miami. Data from a retrospective study showed that cooling pain relief, with an air-cooling device during treatment, resulted in lower PpIX photobleaching in AK lesions, compared with no cooling (J Photochem Photobiol B. 2011 Apr 4;103[1]:1-7). But cooling was associated with decreased efficacy of the PDT treatment in terms of complete AK response (68% for the cooling device group vs. 82% for controls without cooling), he said.
Increasing skin temperature has been shown to reduce AK lesions significantly, compared with no heat, Dr. Berman pointed out. “PpIX synthesis is temperature dependent,” he said. The median difference in AK lesion counts was significantly greater on a heated extremity side than a control side in an unpublished study, he noted.
Finally, when it comes to facial AKs, less may be more in terms of treatment time. In a split face study, a “painless PDT” protocol of 15 minutes of ALA incubation with 1 hour of blue light yielded a 52% reduction in AKs at 8 weeks post treatment, vs. a 44% reduction with a standard treatment of 75 minutes of ALA incubation with 16 minutes, 45 seconds of blue light, Dr. Berman said.
Dr. Berman disclosed relationships with multiple companies including Ferndale, LEO, Halscion, Sensus, Exeltis, Dermira, Celumigen, Sun, DUSA, Biofrontera, and Berg. He holds stock in Halscion, Dermira, Celumigen, and Berg.
SDEF and this news organization are owned by the same parent company.
Treatment of a broad area, occluding extremities, and the use of antihistamines are among the measures that can help optimize the results of treating actinic keratoses (AKs) with topical photodynamic therapy (PDT) using aminolevulinic acid (ALA), according to Dr. Brian Berman.
For many patients with AKs, ALA-PDT can be an effective and well-tolerated option, Dr. Berman said in a presentation at the Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
ALA-PDT is a two-step process, Dr. Berman explained. The first step involves the application of ALA with presumed selective cellular uptake, followed by conversion to protoporphyrin IX (PpIX). Next, the light activation of PpIX causes cell death via high-energy oxygen molecules.
Dr. Berman’s recommendations for optimizing ALA-PDT to treat AKs include a shorter ALA incubation time; treatment of a broad area, not just the baseline visible AKs; occlusion of ALA for AKs on the arms and legs; increased skin temperature during ALA incubation; and moderate cooling during light exposure. To reduce pain, he recommended a very short ALA incubation time with a longer time of light exposure.
He referred to a 2004 study of 18 patients, which found that AK reductions were not significantly different at 1 month post treatment with ALA incubation times of 1, 2, or 3 hours (Arch Dermatol. 2004 Jan;140[1]:33-40). As for occlusion, a 2012 study found that AK clearance was significantly greater for extremities that were occluded during incubation in patients undergoing blue light ALA-PDT, compared with areas that were not occluded (J Drugs Dermatol. 2012 Dec;11[12]:1483-9).
Skin cooling can be useful in reducing patients’ pain, said Dr. Berman of the department of dermatology and cutaneous surgery, University of Miami. Data from a retrospective study showed that cooling pain relief, with an air-cooling device during treatment, resulted in lower PpIX photobleaching in AK lesions, compared with no cooling (J Photochem Photobiol B. 2011 Apr 4;103[1]:1-7). But cooling was associated with decreased efficacy of the PDT treatment in terms of complete AK response (68% for the cooling device group vs. 82% for controls without cooling), he said.
Increasing skin temperature has been shown to reduce AK lesions significantly, compared with no heat, Dr. Berman pointed out. “PpIX synthesis is temperature dependent,” he said. The median difference in AK lesion counts was significantly greater on a heated extremity side than a control side in an unpublished study, he noted.
Finally, when it comes to facial AKs, less may be more in terms of treatment time. In a split face study, a “painless PDT” protocol of 15 minutes of ALA incubation with 1 hour of blue light yielded a 52% reduction in AKs at 8 weeks post treatment, vs. a 44% reduction with a standard treatment of 75 minutes of ALA incubation with 16 minutes, 45 seconds of blue light, Dr. Berman said.
Dr. Berman disclosed relationships with multiple companies including Ferndale, LEO, Halscion, Sensus, Exeltis, Dermira, Celumigen, Sun, DUSA, Biofrontera, and Berg. He holds stock in Halscion, Dermira, Celumigen, and Berg.
SDEF and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
OA progresses equally with new focal partial- or full-thickness cartilage damage
A small, partial-thickness focal cartilage defect in the tibiofemoral joint compartment has the same impact on osteoarthritis disease progression – defined as new cartilage damage – as does a full-thickness lesion, according to an analysis of data from the Multicenter Osteoarthritis Study.
Ali Guermazi, MD, PhD, of Boston University, and his associates used MRI to show that both full- and partial-thickness small focal defects (less than 1 cm) in the tibiofemoral compartment contributed significantly to the risk of incident cartilage damage 30 months later in other tibiofemoral compartment subregions (adjusted odds ratio, 1.62; 95% confidence interval, 1.06-2.47, for partial-thickness defects and aOR, 1.92; 95% CI, 1.00-3.66, for full-thickness defects) when compared with subregions with no baseline cartilage damage, defined as a Kellgren-Lawrence grade of 0-1.
The results indicate that “partial-thickness and full-thickness defects are similarly relevant in regard to cartilage damage development in knee osteoarthritis,” the investigators wrote.
They studied 374 compartments (359 knees), of which 140 knees (39%) had radiographic osteoarthritis defined as a Kellgren-Lawrence grade of 2 or higher).
“It is potentially important to detect focal cartilage defects early as there are various options for repair of focal cartilage defects ... [and it could be possible to use MRI] to screen persons with early-stage osteoarthritis or those at high risk of osteoarthritis and initiate treatment for focal cartilage defects,” they wrote.
Read the full study in Arthritis & Rheumatology (2016 Oct 27. doi: 10.1002/art.39970).
A small, partial-thickness focal cartilage defect in the tibiofemoral joint compartment has the same impact on osteoarthritis disease progression – defined as new cartilage damage – as does a full-thickness lesion, according to an analysis of data from the Multicenter Osteoarthritis Study.
Ali Guermazi, MD, PhD, of Boston University, and his associates used MRI to show that both full- and partial-thickness small focal defects (less than 1 cm) in the tibiofemoral compartment contributed significantly to the risk of incident cartilage damage 30 months later in other tibiofemoral compartment subregions (adjusted odds ratio, 1.62; 95% confidence interval, 1.06-2.47, for partial-thickness defects and aOR, 1.92; 95% CI, 1.00-3.66, for full-thickness defects) when compared with subregions with no baseline cartilage damage, defined as a Kellgren-Lawrence grade of 0-1.
The results indicate that “partial-thickness and full-thickness defects are similarly relevant in regard to cartilage damage development in knee osteoarthritis,” the investigators wrote.
They studied 374 compartments (359 knees), of which 140 knees (39%) had radiographic osteoarthritis defined as a Kellgren-Lawrence grade of 2 or higher).
“It is potentially important to detect focal cartilage defects early as there are various options for repair of focal cartilage defects ... [and it could be possible to use MRI] to screen persons with early-stage osteoarthritis or those at high risk of osteoarthritis and initiate treatment for focal cartilage defects,” they wrote.
Read the full study in Arthritis & Rheumatology (2016 Oct 27. doi: 10.1002/art.39970).
A small, partial-thickness focal cartilage defect in the tibiofemoral joint compartment has the same impact on osteoarthritis disease progression – defined as new cartilage damage – as does a full-thickness lesion, according to an analysis of data from the Multicenter Osteoarthritis Study.
Ali Guermazi, MD, PhD, of Boston University, and his associates used MRI to show that both full- and partial-thickness small focal defects (less than 1 cm) in the tibiofemoral compartment contributed significantly to the risk of incident cartilage damage 30 months later in other tibiofemoral compartment subregions (adjusted odds ratio, 1.62; 95% confidence interval, 1.06-2.47, for partial-thickness defects and aOR, 1.92; 95% CI, 1.00-3.66, for full-thickness defects) when compared with subregions with no baseline cartilage damage, defined as a Kellgren-Lawrence grade of 0-1.
The results indicate that “partial-thickness and full-thickness defects are similarly relevant in regard to cartilage damage development in knee osteoarthritis,” the investigators wrote.
They studied 374 compartments (359 knees), of which 140 knees (39%) had radiographic osteoarthritis defined as a Kellgren-Lawrence grade of 2 or higher).
“It is potentially important to detect focal cartilage defects early as there are various options for repair of focal cartilage defects ... [and it could be possible to use MRI] to screen persons with early-stage osteoarthritis or those at high risk of osteoarthritis and initiate treatment for focal cartilage defects,” they wrote.
Read the full study in Arthritis & Rheumatology (2016 Oct 27. doi: 10.1002/art.39970).
FROM ARTHRITIS & RHEUMATOLOGY
Dystrophic epidermolysis bullosa: 104 mutations found in single gene
according to a report published online in the Journal of Investigative Dermatology.
Identifying which specific mutations in the COL7A1 gene a given patient is carrying should allow clinicians to render a more accurate prognosis and may even dictate management strategies to counteract manifestations of the disease. Dystrophic epidermolysis bullosa (EB) can have an extremely variable progression that depends, in part, on the underlying molecular defects in many different genes expressed in the dermal-epidermal junction, according to study investigators Hassan Vahidnezhad, MD, of the department of dermatology and cutaneous biology, Thomas Jefferson University, Philadelphia, and his associates.
The study cohort included many consanguineous marriages, which are customary in Iran as in many parts of the Middle East, North Africa, and sub-Saharan Africa. In addition, many migrant communities from these regions now reside in Western countries and continue to practice these marriage customs, most commonly marriages between first cousins. “It is estimated that globally at least 20% of the human population live in communities with a preference for consanguineous marriage,” the researchers wrote (J Investig Dermatol. 2016. doi: 10.1016/j.jid.2016.10.023).
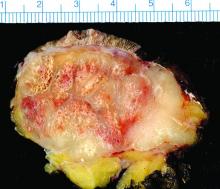
Dystrophic epidermolysis bullosa is characterized by blistering of the sublamina densa that leads to erosions; chronic ulcers; and extensive scarring, especially at sites of trauma on the hands and feet. Blistering can also develop in corneal and gastrointestinal epithelium, which adversely affects vision and feeding, and patients often develop aggressive squamous cell carcinoma with its attendant premature mortality.
Dystrophic EB has long been associated with mutations in COL7A1 as well as other genes. COL7A1 encodes type VII collagen, “a major protein component of the anchoring fibrils, which play a critical role in securing the attachment of the dermal-epidermal basement membrane to the underlying dermis.” Many patients with dystrophic EB show marked reductions in, or a total absence of, anchoring fibrils.
The investigators explored COL7A1 mutations in a multiethnic database comprising 238 patients in 152 extended families from different parts of the country. (The approximately 80 million people in Iran include several ethnic groups with distinct ancestries, languages, cultures, and geographic areas of residence.) A total of 139 of these families were consanguineous.
A total of 104 distinct COL7A1 mutations were detected in 149 of the 152 families, for a detection rate of 98%. Many mutations had been reported previously, but 56 had never been reported before. Approximately 90% of the families in the study cohort showed homozygous recessive mutations, which appears to reflect the consanguinity of this population, Dr. Vahidnezhad and his associates said.
They concluded that “the overwhelming majority” of patients with dystrophic EB carry COL7A1 genes harboring mutations.
This study was supported by DEBRA International and the Sidney Kimmel Cancer Center at Thomas Jefferson University. Dr. Vahidnezhad and his associates reported having no relevant financial disclosures.
according to a report published online in the Journal of Investigative Dermatology.
Identifying which specific mutations in the COL7A1 gene a given patient is carrying should allow clinicians to render a more accurate prognosis and may even dictate management strategies to counteract manifestations of the disease. Dystrophic epidermolysis bullosa (EB) can have an extremely variable progression that depends, in part, on the underlying molecular defects in many different genes expressed in the dermal-epidermal junction, according to study investigators Hassan Vahidnezhad, MD, of the department of dermatology and cutaneous biology, Thomas Jefferson University, Philadelphia, and his associates.
The study cohort included many consanguineous marriages, which are customary in Iran as in many parts of the Middle East, North Africa, and sub-Saharan Africa. In addition, many migrant communities from these regions now reside in Western countries and continue to practice these marriage customs, most commonly marriages between first cousins. “It is estimated that globally at least 20% of the human population live in communities with a preference for consanguineous marriage,” the researchers wrote (J Investig Dermatol. 2016. doi: 10.1016/j.jid.2016.10.023).
Dystrophic epidermolysis bullosa is characterized by blistering of the sublamina densa that leads to erosions; chronic ulcers; and extensive scarring, especially at sites of trauma on the hands and feet. Blistering can also develop in corneal and gastrointestinal epithelium, which adversely affects vision and feeding, and patients often develop aggressive squamous cell carcinoma with its attendant premature mortality.
Dystrophic EB has long been associated with mutations in COL7A1 as well as other genes. COL7A1 encodes type VII collagen, “a major protein component of the anchoring fibrils, which play a critical role in securing the attachment of the dermal-epidermal basement membrane to the underlying dermis.” Many patients with dystrophic EB show marked reductions in, or a total absence of, anchoring fibrils.
The investigators explored COL7A1 mutations in a multiethnic database comprising 238 patients in 152 extended families from different parts of the country. (The approximately 80 million people in Iran include several ethnic groups with distinct ancestries, languages, cultures, and geographic areas of residence.) A total of 139 of these families were consanguineous.
A total of 104 distinct COL7A1 mutations were detected in 149 of the 152 families, for a detection rate of 98%. Many mutations had been reported previously, but 56 had never been reported before. Approximately 90% of the families in the study cohort showed homozygous recessive mutations, which appears to reflect the consanguinity of this population, Dr. Vahidnezhad and his associates said.
They concluded that “the overwhelming majority” of patients with dystrophic EB carry COL7A1 genes harboring mutations.
This study was supported by DEBRA International and the Sidney Kimmel Cancer Center at Thomas Jefferson University. Dr. Vahidnezhad and his associates reported having no relevant financial disclosures.
according to a report published online in the Journal of Investigative Dermatology.
Identifying which specific mutations in the COL7A1 gene a given patient is carrying should allow clinicians to render a more accurate prognosis and may even dictate management strategies to counteract manifestations of the disease. Dystrophic epidermolysis bullosa (EB) can have an extremely variable progression that depends, in part, on the underlying molecular defects in many different genes expressed in the dermal-epidermal junction, according to study investigators Hassan Vahidnezhad, MD, of the department of dermatology and cutaneous biology, Thomas Jefferson University, Philadelphia, and his associates.
The study cohort included many consanguineous marriages, which are customary in Iran as in many parts of the Middle East, North Africa, and sub-Saharan Africa. In addition, many migrant communities from these regions now reside in Western countries and continue to practice these marriage customs, most commonly marriages between first cousins. “It is estimated that globally at least 20% of the human population live in communities with a preference for consanguineous marriage,” the researchers wrote (J Investig Dermatol. 2016. doi: 10.1016/j.jid.2016.10.023).
Dystrophic epidermolysis bullosa is characterized by blistering of the sublamina densa that leads to erosions; chronic ulcers; and extensive scarring, especially at sites of trauma on the hands and feet. Blistering can also develop in corneal and gastrointestinal epithelium, which adversely affects vision and feeding, and patients often develop aggressive squamous cell carcinoma with its attendant premature mortality.
Dystrophic EB has long been associated with mutations in COL7A1 as well as other genes. COL7A1 encodes type VII collagen, “a major protein component of the anchoring fibrils, which play a critical role in securing the attachment of the dermal-epidermal basement membrane to the underlying dermis.” Many patients with dystrophic EB show marked reductions in, or a total absence of, anchoring fibrils.
The investigators explored COL7A1 mutations in a multiethnic database comprising 238 patients in 152 extended families from different parts of the country. (The approximately 80 million people in Iran include several ethnic groups with distinct ancestries, languages, cultures, and geographic areas of residence.) A total of 139 of these families were consanguineous.
A total of 104 distinct COL7A1 mutations were detected in 149 of the 152 families, for a detection rate of 98%. Many mutations had been reported previously, but 56 had never been reported before. Approximately 90% of the families in the study cohort showed homozygous recessive mutations, which appears to reflect the consanguinity of this population, Dr. Vahidnezhad and his associates said.
They concluded that “the overwhelming majority” of patients with dystrophic EB carry COL7A1 genes harboring mutations.
This study was supported by DEBRA International and the Sidney Kimmel Cancer Center at Thomas Jefferson University. Dr. Vahidnezhad and his associates reported having no relevant financial disclosures.
FROM THE JOURNAL OF INVESTIGATIVE DERMATOLOGY
Key clinical point: 104 distinct mutations in a single gene, COL7A1, were discovered in a multiethnic cohort of 152 Iranian families with dystrophic epidermolysis bullosa.
Major finding: 104 distinct COL7A1 mutations were detected in 149 of the 152 families in the database, for a detection rate of 98%.
Data source: Analyses of mutations in the COL741 gene in 152 extended Iranian families with a high frequency of dystrophic epidermolysis bullosa.
Disclosures: This study was supported by DEBRA International and the Sidney Kimmel Cancer Center at Thomas Jefferson University. Dr. Vahidnezhad and his associates reported having no relevant financial disclosures.
The voice of the patient in a doctor-centric world
The American health care system has been plagued by poor medical outcomes and an inefficient cost structure for many years.1,2 The primary loser in this game is the patient, the player who bears the brunt of health care expenses, either directly or through taxes, and whose voice has been largely ignored until recently. As with many other service industries, health care delivery represents a highly complex process that is difficult to define or measure. Innovative procedures and state-of-the-art medical therapies have provided effective options that extend or improve life, but at increasing cost.
Further complicating the existing cost-vs.-benefit debate is a relatively new polemic regarding the degree to which patient satisfaction should be a measure of health care quality. How satisfied will a patient be with his or her health care experience? This depends, in large part, on the medical outcome.3
Many public and private organizations use patient satisfaction surveys to measure the performance of health care delivery systems. In many cases, patient satisfaction data are being used to determine insurance payouts, physician compensation, and institutional rankings.5 It may seem logical to adopt pay-for-performance strategies based on patient satisfaction surveys, but there is a fundamental flaw: Survey data are not always accurate.
It is not entirely clear what constitutes a positive or negative health care experience. Much of this depends on the expectations of the consumer.6 Those with low expectations may be delighted with mediocre performance. Those with inflated expectations may be disappointed even when provided excellent customer service.
Surveys are not durable. That is, when performed under distinct environmental conditions or at different times, surveys may not produce the same results when repeated by the same respondent.7 Surveys are easily manipulated by simple changes in wording or punctuation. Some specific encounters may be rated as “unsatisfactory” because of external factors, circumstances beyond the control of the health care provider.
Many health care providers feel that surveys are poor indicators of individual performance. Some critics highlight a paucity of data. A limited number of returned surveys, relative to the total number of encounters, may yield results that are not statistically significant. Increasing the amount of data decreases the risk that a sample set taken from the studied population is the result of sampling error alone. Nonetheless, sampling error is never completely eliminated, and it is not entirely clear to what degree statistical significance should be used to substantiate satisfaction, a subjective measure.
Surveys often provide data in a very small range, making ranking of facilities or providers difficult. For example, national polling services utilize surveys with thousands of respondents and the margin of error often exceeds plus or minus 3%. Data sets with a smaller number of responses have margins of error that are even greater. Even plus or minus 3% is a sizable deviation when considering that health care survey results often are compared and ranked based on a distribution of scores in a narrow response range. In the author’s experience, a 6% difference in survey scores can represent the difference between a ranking of “excellent” and “poor.”
Many patients are disenfranchised by survey methodology. In the most extreme example, deceased or severely disabled patients are unable to provide feedback. Patients transferred to other facilities and those who are lost to follow-up will be missed also. Many patient surveys may not be successfully retrieved from the homeless, the illiterate, minors, or those without phone or e-mail access. Because surveys are voluntarily submitted, the results may skew opinion toward a select group of outspoken customers who may not be representative of the general population.
The use of patient satisfaction surveys, especially when they are linked to employee compensation, may create a system of survey-based value. This is similar to the problem of defensive medicine, where providers perform medicine in a way that reduces legal risk. Aware that patients will be asked to fill out satisfaction surveys, associates may perform in a way that increases patient satisfaction scores at the expense of patient outcomes or the bottom line. Some institutions may inappropriately “cherry-pick” the easy-to-treat patient and transfer medically complex cases elsewhere.
It is not clear how to best measure the quality of a health care experience. With the broad range of patient encounter types and the inherent complexity of collaboration among providers, it is difficult to determine to what degree satisfaction can be attributed to individual providers or specific environmental factors. Patients do not typically interact with a specific provider, but are treated by a service delivery system, which often encompasses multiple players and multiple physical locations. Moreover, it is not always clear when the patient encounter begins and ends.
Despite the criticism of patient satisfaction survey methodology, the patient must ultimately define the value of the health care service offering. This “voice of the customer” approach is a diversion from the antiquated practitioner-centric model. Traditionally, patient appointment times and locations are decided by the availability and convenience of the provider. Many consumers have compensated for this inefficiency by accessing local emergency departments for nonurgent ambulatory care. Nonetheless,EDs often suffer from long waits and higher costs. Facilities designed for urgent, but nonemergent, care have attempted to address convenience issues but these facilities sacrifice continuity and specialization of care. In a truly patient-centric health care model, patients would be provided the care that they need, when and where they need it.
The patient satisfaction survey remains a primary tool for linking patient-centered value to health care reform. Ranking the results among market competitors can provide an incentive for improvement. Health care professionals are competitive by nature and the extrinsic motivation of quality rankings can be beneficial if well controlled. Employers should use caution when using survey data for performance measurement because survey data are subject to a variety of sources of bias or error. Patient survey data should be used to drive improvement, not to punish. Further research on patient survey methodology is needed to elucidate improved methods of bringing the voice of the patient to the forefront of health care reform.
References
1. N Engl J Med. 2003 Aug 21;349(8):768-75.
2. Centers for Medicare & Medicaid Services. Medicare hospital quality chartbook: Performance report on outcome measures. September 2014.
3. N Engl J Med. 2008 Oct 30;359(18):1921-31.
4. “Better Customer Insight – in Real Time,” by Emma K. Macdonald, Hugh N. Wilson, and Umut Konuş (Harvard Business Review, September 2012).
5. “The Dangers of Linking Pay to Customer Feedback,” by Rob Markey, (Harvard Business Review, Sept. 8, 2011).
6. “Health Care’s Service Fanatics,” by James I. Merlino and Ananth Raman, (Harvard Business Review, May 2013).
7. Trochim, WMK. Research Methods Knowledge Base.
Dr. Davis is a pediatric gastroenterologists at University of Florida Health, Gainesville. He has no financial relationships relevant to this article to disclose.
The American health care system has been plagued by poor medical outcomes and an inefficient cost structure for many years.1,2 The primary loser in this game is the patient, the player who bears the brunt of health care expenses, either directly or through taxes, and whose voice has been largely ignored until recently. As with many other service industries, health care delivery represents a highly complex process that is difficult to define or measure. Innovative procedures and state-of-the-art medical therapies have provided effective options that extend or improve life, but at increasing cost.
Further complicating the existing cost-vs.-benefit debate is a relatively new polemic regarding the degree to which patient satisfaction should be a measure of health care quality. How satisfied will a patient be with his or her health care experience? This depends, in large part, on the medical outcome.3
Many public and private organizations use patient satisfaction surveys to measure the performance of health care delivery systems. In many cases, patient satisfaction data are being used to determine insurance payouts, physician compensation, and institutional rankings.5 It may seem logical to adopt pay-for-performance strategies based on patient satisfaction surveys, but there is a fundamental flaw: Survey data are not always accurate.
It is not entirely clear what constitutes a positive or negative health care experience. Much of this depends on the expectations of the consumer.6 Those with low expectations may be delighted with mediocre performance. Those with inflated expectations may be disappointed even when provided excellent customer service.
Surveys are not durable. That is, when performed under distinct environmental conditions or at different times, surveys may not produce the same results when repeated by the same respondent.7 Surveys are easily manipulated by simple changes in wording or punctuation. Some specific encounters may be rated as “unsatisfactory” because of external factors, circumstances beyond the control of the health care provider.
Many health care providers feel that surveys are poor indicators of individual performance. Some critics highlight a paucity of data. A limited number of returned surveys, relative to the total number of encounters, may yield results that are not statistically significant. Increasing the amount of data decreases the risk that a sample set taken from the studied population is the result of sampling error alone. Nonetheless, sampling error is never completely eliminated, and it is not entirely clear to what degree statistical significance should be used to substantiate satisfaction, a subjective measure.
Surveys often provide data in a very small range, making ranking of facilities or providers difficult. For example, national polling services utilize surveys with thousands of respondents and the margin of error often exceeds plus or minus 3%. Data sets with a smaller number of responses have margins of error that are even greater. Even plus or minus 3% is a sizable deviation when considering that health care survey results often are compared and ranked based on a distribution of scores in a narrow response range. In the author’s experience, a 6% difference in survey scores can represent the difference between a ranking of “excellent” and “poor.”
Many patients are disenfranchised by survey methodology. In the most extreme example, deceased or severely disabled patients are unable to provide feedback. Patients transferred to other facilities and those who are lost to follow-up will be missed also. Many patient surveys may not be successfully retrieved from the homeless, the illiterate, minors, or those without phone or e-mail access. Because surveys are voluntarily submitted, the results may skew opinion toward a select group of outspoken customers who may not be representative of the general population.
The use of patient satisfaction surveys, especially when they are linked to employee compensation, may create a system of survey-based value. This is similar to the problem of defensive medicine, where providers perform medicine in a way that reduces legal risk. Aware that patients will be asked to fill out satisfaction surveys, associates may perform in a way that increases patient satisfaction scores at the expense of patient outcomes or the bottom line. Some institutions may inappropriately “cherry-pick” the easy-to-treat patient and transfer medically complex cases elsewhere.
It is not clear how to best measure the quality of a health care experience. With the broad range of patient encounter types and the inherent complexity of collaboration among providers, it is difficult to determine to what degree satisfaction can be attributed to individual providers or specific environmental factors. Patients do not typically interact with a specific provider, but are treated by a service delivery system, which often encompasses multiple players and multiple physical locations. Moreover, it is not always clear when the patient encounter begins and ends.
Despite the criticism of patient satisfaction survey methodology, the patient must ultimately define the value of the health care service offering. This “voice of the customer” approach is a diversion from the antiquated practitioner-centric model. Traditionally, patient appointment times and locations are decided by the availability and convenience of the provider. Many consumers have compensated for this inefficiency by accessing local emergency departments for nonurgent ambulatory care. Nonetheless,EDs often suffer from long waits and higher costs. Facilities designed for urgent, but nonemergent, care have attempted to address convenience issues but these facilities sacrifice continuity and specialization of care. In a truly patient-centric health care model, patients would be provided the care that they need, when and where they need it.
The patient satisfaction survey remains a primary tool for linking patient-centered value to health care reform. Ranking the results among market competitors can provide an incentive for improvement. Health care professionals are competitive by nature and the extrinsic motivation of quality rankings can be beneficial if well controlled. Employers should use caution when using survey data for performance measurement because survey data are subject to a variety of sources of bias or error. Patient survey data should be used to drive improvement, not to punish. Further research on patient survey methodology is needed to elucidate improved methods of bringing the voice of the patient to the forefront of health care reform.
References
1. N Engl J Med. 2003 Aug 21;349(8):768-75.
2. Centers for Medicare & Medicaid Services. Medicare hospital quality chartbook: Performance report on outcome measures. September 2014.
3. N Engl J Med. 2008 Oct 30;359(18):1921-31.
4. “Better Customer Insight – in Real Time,” by Emma K. Macdonald, Hugh N. Wilson, and Umut Konuş (Harvard Business Review, September 2012).
5. “The Dangers of Linking Pay to Customer Feedback,” by Rob Markey, (Harvard Business Review, Sept. 8, 2011).
6. “Health Care’s Service Fanatics,” by James I. Merlino and Ananth Raman, (Harvard Business Review, May 2013).
7. Trochim, WMK. Research Methods Knowledge Base.
Dr. Davis is a pediatric gastroenterologists at University of Florida Health, Gainesville. He has no financial relationships relevant to this article to disclose.
The American health care system has been plagued by poor medical outcomes and an inefficient cost structure for many years.1,2 The primary loser in this game is the patient, the player who bears the brunt of health care expenses, either directly or through taxes, and whose voice has been largely ignored until recently. As with many other service industries, health care delivery represents a highly complex process that is difficult to define or measure. Innovative procedures and state-of-the-art medical therapies have provided effective options that extend or improve life, but at increasing cost.
Further complicating the existing cost-vs.-benefit debate is a relatively new polemic regarding the degree to which patient satisfaction should be a measure of health care quality. How satisfied will a patient be with his or her health care experience? This depends, in large part, on the medical outcome.3
Many public and private organizations use patient satisfaction surveys to measure the performance of health care delivery systems. In many cases, patient satisfaction data are being used to determine insurance payouts, physician compensation, and institutional rankings.5 It may seem logical to adopt pay-for-performance strategies based on patient satisfaction surveys, but there is a fundamental flaw: Survey data are not always accurate.
It is not entirely clear what constitutes a positive or negative health care experience. Much of this depends on the expectations of the consumer.6 Those with low expectations may be delighted with mediocre performance. Those with inflated expectations may be disappointed even when provided excellent customer service.
Surveys are not durable. That is, when performed under distinct environmental conditions or at different times, surveys may not produce the same results when repeated by the same respondent.7 Surveys are easily manipulated by simple changes in wording or punctuation. Some specific encounters may be rated as “unsatisfactory” because of external factors, circumstances beyond the control of the health care provider.
Many health care providers feel that surveys are poor indicators of individual performance. Some critics highlight a paucity of data. A limited number of returned surveys, relative to the total number of encounters, may yield results that are not statistically significant. Increasing the amount of data decreases the risk that a sample set taken from the studied population is the result of sampling error alone. Nonetheless, sampling error is never completely eliminated, and it is not entirely clear to what degree statistical significance should be used to substantiate satisfaction, a subjective measure.
Surveys often provide data in a very small range, making ranking of facilities or providers difficult. For example, national polling services utilize surveys with thousands of respondents and the margin of error often exceeds plus or minus 3%. Data sets with a smaller number of responses have margins of error that are even greater. Even plus or minus 3% is a sizable deviation when considering that health care survey results often are compared and ranked based on a distribution of scores in a narrow response range. In the author’s experience, a 6% difference in survey scores can represent the difference between a ranking of “excellent” and “poor.”
Many patients are disenfranchised by survey methodology. In the most extreme example, deceased or severely disabled patients are unable to provide feedback. Patients transferred to other facilities and those who are lost to follow-up will be missed also. Many patient surveys may not be successfully retrieved from the homeless, the illiterate, minors, or those without phone or e-mail access. Because surveys are voluntarily submitted, the results may skew opinion toward a select group of outspoken customers who may not be representative of the general population.
The use of patient satisfaction surveys, especially when they are linked to employee compensation, may create a system of survey-based value. This is similar to the problem of defensive medicine, where providers perform medicine in a way that reduces legal risk. Aware that patients will be asked to fill out satisfaction surveys, associates may perform in a way that increases patient satisfaction scores at the expense of patient outcomes or the bottom line. Some institutions may inappropriately “cherry-pick” the easy-to-treat patient and transfer medically complex cases elsewhere.
It is not clear how to best measure the quality of a health care experience. With the broad range of patient encounter types and the inherent complexity of collaboration among providers, it is difficult to determine to what degree satisfaction can be attributed to individual providers or specific environmental factors. Patients do not typically interact with a specific provider, but are treated by a service delivery system, which often encompasses multiple players and multiple physical locations. Moreover, it is not always clear when the patient encounter begins and ends.
Despite the criticism of patient satisfaction survey methodology, the patient must ultimately define the value of the health care service offering. This “voice of the customer” approach is a diversion from the antiquated practitioner-centric model. Traditionally, patient appointment times and locations are decided by the availability and convenience of the provider. Many consumers have compensated for this inefficiency by accessing local emergency departments for nonurgent ambulatory care. Nonetheless,EDs often suffer from long waits and higher costs. Facilities designed for urgent, but nonemergent, care have attempted to address convenience issues but these facilities sacrifice continuity and specialization of care. In a truly patient-centric health care model, patients would be provided the care that they need, when and where they need it.
The patient satisfaction survey remains a primary tool for linking patient-centered value to health care reform. Ranking the results among market competitors can provide an incentive for improvement. Health care professionals are competitive by nature and the extrinsic motivation of quality rankings can be beneficial if well controlled. Employers should use caution when using survey data for performance measurement because survey data are subject to a variety of sources of bias or error. Patient survey data should be used to drive improvement, not to punish. Further research on patient survey methodology is needed to elucidate improved methods of bringing the voice of the patient to the forefront of health care reform.
References
1. N Engl J Med. 2003 Aug 21;349(8):768-75.
2. Centers for Medicare & Medicaid Services. Medicare hospital quality chartbook: Performance report on outcome measures. September 2014.
3. N Engl J Med. 2008 Oct 30;359(18):1921-31.
4. “Better Customer Insight – in Real Time,” by Emma K. Macdonald, Hugh N. Wilson, and Umut Konuş (Harvard Business Review, September 2012).
5. “The Dangers of Linking Pay to Customer Feedback,” by Rob Markey, (Harvard Business Review, Sept. 8, 2011).
6. “Health Care’s Service Fanatics,” by James I. Merlino and Ananth Raman, (Harvard Business Review, May 2013).
7. Trochim, WMK. Research Methods Knowledge Base.
Dr. Davis is a pediatric gastroenterologists at University of Florida Health, Gainesville. He has no financial relationships relevant to this article to disclose.
Study finds 19% of Merkel cell carcinomas are virus negative
Nineteen percent of Merkel cell carcinomas are not driven by the Merkel cell polyomavirus and are substantially more aggressive than those that are virus positive, according to a report published online in the Journal of Investigative Dermatology.
This and other findings from a retrospective analysis of samples from 282 Merkel cell carcinomas in a Seattle repository “suggest that it may be clinically indicated to determine tumor viral status at the time of diagnosis, as the results may affect prognosis as well as optimal clinical management,” wrote Ata Moshiri, MD, who was with the University of Washington, Seattle, at the time of the study, and his associates.
Given that virus-negative Merkel cell carcinomas carry a markedly higher risk of recurrence, progression, and patient mortality, “clinicians may consider larger initial surgical margins, larger radiotherapy fields, and the use of regional nodal therapy even in the absence of documented nodal metastasis. Closer clinical follow-up and more frequent radiologic surveillance may be justified for patients with virus-negative tumors because ... serologic monitoring is not feasible for this patient population,” the investigators noted.
The incidence of Merkel cell carcinoma, a rare and aggressive neuroendocrine skin cancer with an overall disease-related mortality of 40%, has quadrupled during the last 20 years. This is likely because of the increasing prevalence of risk factors for the cancer, including advanced age, increased cumulative exposure to ultraviolet light, and systemic immune suppression.
Data concerning the presence of Merkel cell polyomavirus in these cancers are conflicting, with estimates of virus positivity ranging from 20% all the way to 100% in some studies. Part of the reason for this wide range of estimates is that there is no accepted preferred method for measuring the viral status of these tumors. Moreover, the prognostic significance of that viral status is also debated. Thus, most Merkel cell cancers are not routinely analyzed for the presence of Merkel cell polyomavirus.
To pin down the prevalence of virus positivity and establish whether it impacts clinical outcomes, Dr. Moshiri and his associates analyzed 282 Merkel cell specimens collected since 1980 and stored in a Seattle repository, along with clinical data. They tested each specimen using an immunohistochemical assay to detect one antibody (CM2B4), a different immunohistochemical assay to detect another antibody (Ab3), and a quantitative PCR assay for polyomavirus DNA. To be considered virus positive, each specimen had to show the presence of the virus on at least two of these tests.
By these criteria, 53 tumors (18.8%) were found to be virus negative and 229 (81.2%) to be virus positive.
Virus-negative tumors tended to be smaller than virus-positive tumors at presentation. Despite their smaller size, virus-negative tumors tended to be more advanced at presentation: 66.7% had nodal or distant metastases, compared with 48.3% of virus-positive tumors.
A total of 66.7% of virus-negative carcinomas progressed, compared with only 43.6% of virus-positive carcinomas. The median time to progression was 1.2 years for virus-negative cancers, but was not reached for virus-positive cancers. In a univariate analysis, virus-negative tumors had a nearly twofold higher risk of progression. In a multivariate analysis that adjusted for differences in disease stage at presentation, the HR fell slightly to 1.55.
Cancer-specific mortality was 45.3% for virus-negative tumors, compared with 26.3% for virus-positive tumors. Median time to death from Merkel cell carcinoma was 3.7 years for virus-negative tumors but was not reached for virus-positive tumors. In a univariate analysis, virus-negative tumors carried a nearly twofold higher risk of death from Merkel cell carcinoma. In a multivariate analysis that adjusted for differences in disease stage at presentation, the HR fell somewhat to 1.50.
Median overall survival was 3.3 years for patients with virus-negative tumors, compared with 4.6 years for patients with virus-positive tumors.
These findings indicate that a more advanced cancer stage at diagnosis accounts for some but not all of the poorer clinical outcomes seen with virus-negative tumors, the investigators said.
This study could not assess why virus-negative Merkel cell carcinomas are more aggressive and lethal than virus-positive ones, but previous studies have proposed some plausible biological mechanisms. Virus-negative tumors carry a greater number of chromosomal aberrations, a greater burden of nucleotide mutations, and a greater number of mutations in known oncogenic pathways. They also may be more immunogenic “due to their constitutive expression of oncoproteins that may serve as targets for cytotoxic tumor-infiltrating lymphocytes,” Dr. Moshiri and his associates said.
They added that in this study, the immunohistochemical assay for CM2B4 antibodies was the test that most accurately identified tumors that had worse outcomes. “We believe that the CM2B4 antibody test may be well-suited for routine clinical use” because of its sensitivity and specificity in this application, its commercial availability, “and the ease with which it could be included in the work flow of clinical laboratories accustomed to immunohistochemistry.”
Dr. Moshiri is currently at the University of Pennsylvania, Philadelphia.
The National Institutes of Health, the Colin Johnston Fund, and the Janet Canning Fund supported the study. Dr. Moshiri reported having no relevant financial disclosures; one of his associates reported that her institute received research funding from Valeant and Pfizer unrelated to this work.
Nineteen percent of Merkel cell carcinomas are not driven by the Merkel cell polyomavirus and are substantially more aggressive than those that are virus positive, according to a report published online in the Journal of Investigative Dermatology.
This and other findings from a retrospective analysis of samples from 282 Merkel cell carcinomas in a Seattle repository “suggest that it may be clinically indicated to determine tumor viral status at the time of diagnosis, as the results may affect prognosis as well as optimal clinical management,” wrote Ata Moshiri, MD, who was with the University of Washington, Seattle, at the time of the study, and his associates.
Given that virus-negative Merkel cell carcinomas carry a markedly higher risk of recurrence, progression, and patient mortality, “clinicians may consider larger initial surgical margins, larger radiotherapy fields, and the use of regional nodal therapy even in the absence of documented nodal metastasis. Closer clinical follow-up and more frequent radiologic surveillance may be justified for patients with virus-negative tumors because ... serologic monitoring is not feasible for this patient population,” the investigators noted.
The incidence of Merkel cell carcinoma, a rare and aggressive neuroendocrine skin cancer with an overall disease-related mortality of 40%, has quadrupled during the last 20 years. This is likely because of the increasing prevalence of risk factors for the cancer, including advanced age, increased cumulative exposure to ultraviolet light, and systemic immune suppression.
Data concerning the presence of Merkel cell polyomavirus in these cancers are conflicting, with estimates of virus positivity ranging from 20% all the way to 100% in some studies. Part of the reason for this wide range of estimates is that there is no accepted preferred method for measuring the viral status of these tumors. Moreover, the prognostic significance of that viral status is also debated. Thus, most Merkel cell cancers are not routinely analyzed for the presence of Merkel cell polyomavirus.
To pin down the prevalence of virus positivity and establish whether it impacts clinical outcomes, Dr. Moshiri and his associates analyzed 282 Merkel cell specimens collected since 1980 and stored in a Seattle repository, along with clinical data. They tested each specimen using an immunohistochemical assay to detect one antibody (CM2B4), a different immunohistochemical assay to detect another antibody (Ab3), and a quantitative PCR assay for polyomavirus DNA. To be considered virus positive, each specimen had to show the presence of the virus on at least two of these tests.
By these criteria, 53 tumors (18.8%) were found to be virus negative and 229 (81.2%) to be virus positive.
Virus-negative tumors tended to be smaller than virus-positive tumors at presentation. Despite their smaller size, virus-negative tumors tended to be more advanced at presentation: 66.7% had nodal or distant metastases, compared with 48.3% of virus-positive tumors.
A total of 66.7% of virus-negative carcinomas progressed, compared with only 43.6% of virus-positive carcinomas. The median time to progression was 1.2 years for virus-negative cancers, but was not reached for virus-positive cancers. In a univariate analysis, virus-negative tumors had a nearly twofold higher risk of progression. In a multivariate analysis that adjusted for differences in disease stage at presentation, the HR fell slightly to 1.55.
Cancer-specific mortality was 45.3% for virus-negative tumors, compared with 26.3% for virus-positive tumors. Median time to death from Merkel cell carcinoma was 3.7 years for virus-negative tumors but was not reached for virus-positive tumors. In a univariate analysis, virus-negative tumors carried a nearly twofold higher risk of death from Merkel cell carcinoma. In a multivariate analysis that adjusted for differences in disease stage at presentation, the HR fell somewhat to 1.50.
Median overall survival was 3.3 years for patients with virus-negative tumors, compared with 4.6 years for patients with virus-positive tumors.
These findings indicate that a more advanced cancer stage at diagnosis accounts for some but not all of the poorer clinical outcomes seen with virus-negative tumors, the investigators said.
This study could not assess why virus-negative Merkel cell carcinomas are more aggressive and lethal than virus-positive ones, but previous studies have proposed some plausible biological mechanisms. Virus-negative tumors carry a greater number of chromosomal aberrations, a greater burden of nucleotide mutations, and a greater number of mutations in known oncogenic pathways. They also may be more immunogenic “due to their constitutive expression of oncoproteins that may serve as targets for cytotoxic tumor-infiltrating lymphocytes,” Dr. Moshiri and his associates said.
They added that in this study, the immunohistochemical assay for CM2B4 antibodies was the test that most accurately identified tumors that had worse outcomes. “We believe that the CM2B4 antibody test may be well-suited for routine clinical use” because of its sensitivity and specificity in this application, its commercial availability, “and the ease with which it could be included in the work flow of clinical laboratories accustomed to immunohistochemistry.”
Dr. Moshiri is currently at the University of Pennsylvania, Philadelphia.
The National Institutes of Health, the Colin Johnston Fund, and the Janet Canning Fund supported the study. Dr. Moshiri reported having no relevant financial disclosures; one of his associates reported that her institute received research funding from Valeant and Pfizer unrelated to this work.
Nineteen percent of Merkel cell carcinomas are not driven by the Merkel cell polyomavirus and are substantially more aggressive than those that are virus positive, according to a report published online in the Journal of Investigative Dermatology.
This and other findings from a retrospective analysis of samples from 282 Merkel cell carcinomas in a Seattle repository “suggest that it may be clinically indicated to determine tumor viral status at the time of diagnosis, as the results may affect prognosis as well as optimal clinical management,” wrote Ata Moshiri, MD, who was with the University of Washington, Seattle, at the time of the study, and his associates.
Given that virus-negative Merkel cell carcinomas carry a markedly higher risk of recurrence, progression, and patient mortality, “clinicians may consider larger initial surgical margins, larger radiotherapy fields, and the use of regional nodal therapy even in the absence of documented nodal metastasis. Closer clinical follow-up and more frequent radiologic surveillance may be justified for patients with virus-negative tumors because ... serologic monitoring is not feasible for this patient population,” the investigators noted.
The incidence of Merkel cell carcinoma, a rare and aggressive neuroendocrine skin cancer with an overall disease-related mortality of 40%, has quadrupled during the last 20 years. This is likely because of the increasing prevalence of risk factors for the cancer, including advanced age, increased cumulative exposure to ultraviolet light, and systemic immune suppression.
Data concerning the presence of Merkel cell polyomavirus in these cancers are conflicting, with estimates of virus positivity ranging from 20% all the way to 100% in some studies. Part of the reason for this wide range of estimates is that there is no accepted preferred method for measuring the viral status of these tumors. Moreover, the prognostic significance of that viral status is also debated. Thus, most Merkel cell cancers are not routinely analyzed for the presence of Merkel cell polyomavirus.
To pin down the prevalence of virus positivity and establish whether it impacts clinical outcomes, Dr. Moshiri and his associates analyzed 282 Merkel cell specimens collected since 1980 and stored in a Seattle repository, along with clinical data. They tested each specimen using an immunohistochemical assay to detect one antibody (CM2B4), a different immunohistochemical assay to detect another antibody (Ab3), and a quantitative PCR assay for polyomavirus DNA. To be considered virus positive, each specimen had to show the presence of the virus on at least two of these tests.
By these criteria, 53 tumors (18.8%) were found to be virus negative and 229 (81.2%) to be virus positive.
Virus-negative tumors tended to be smaller than virus-positive tumors at presentation. Despite their smaller size, virus-negative tumors tended to be more advanced at presentation: 66.7% had nodal or distant metastases, compared with 48.3% of virus-positive tumors.
A total of 66.7% of virus-negative carcinomas progressed, compared with only 43.6% of virus-positive carcinomas. The median time to progression was 1.2 years for virus-negative cancers, but was not reached for virus-positive cancers. In a univariate analysis, virus-negative tumors had a nearly twofold higher risk of progression. In a multivariate analysis that adjusted for differences in disease stage at presentation, the HR fell slightly to 1.55.
Cancer-specific mortality was 45.3% for virus-negative tumors, compared with 26.3% for virus-positive tumors. Median time to death from Merkel cell carcinoma was 3.7 years for virus-negative tumors but was not reached for virus-positive tumors. In a univariate analysis, virus-negative tumors carried a nearly twofold higher risk of death from Merkel cell carcinoma. In a multivariate analysis that adjusted for differences in disease stage at presentation, the HR fell somewhat to 1.50.
Median overall survival was 3.3 years for patients with virus-negative tumors, compared with 4.6 years for patients with virus-positive tumors.
These findings indicate that a more advanced cancer stage at diagnosis accounts for some but not all of the poorer clinical outcomes seen with virus-negative tumors, the investigators said.
This study could not assess why virus-negative Merkel cell carcinomas are more aggressive and lethal than virus-positive ones, but previous studies have proposed some plausible biological mechanisms. Virus-negative tumors carry a greater number of chromosomal aberrations, a greater burden of nucleotide mutations, and a greater number of mutations in known oncogenic pathways. They also may be more immunogenic “due to their constitutive expression of oncoproteins that may serve as targets for cytotoxic tumor-infiltrating lymphocytes,” Dr. Moshiri and his associates said.
They added that in this study, the immunohistochemical assay for CM2B4 antibodies was the test that most accurately identified tumors that had worse outcomes. “We believe that the CM2B4 antibody test may be well-suited for routine clinical use” because of its sensitivity and specificity in this application, its commercial availability, “and the ease with which it could be included in the work flow of clinical laboratories accustomed to immunohistochemistry.”
Dr. Moshiri is currently at the University of Pennsylvania, Philadelphia.
The National Institutes of Health, the Colin Johnston Fund, and the Janet Canning Fund supported the study. Dr. Moshiri reported having no relevant financial disclosures; one of his associates reported that her institute received research funding from Valeant and Pfizer unrelated to this work.
FROM THE JOURNAL OF INVESTIGATIVE DERMATOLOGY
Key clinical point: Nineteen percent of Merkel cell carcinomas are not driven by the Merkel cell polyomavirus and are substantially more aggressive than those that are virus positive.
Major finding: The 53 virus-negative tumors carried a cancer-specific mortality of 45.3%, while the 229 virus-positive tumors carried a cancer-specific mortality of 26.2%.
Data source: A retrospective molecular analysis of samples from 282 Merkel cell carcinomas in a Seattle repository for the presence of Merkel cell polyomavirus.
Disclosures: The National Institutes of Health, the Colin Johnston Fund, and the Janet Canning Fund supported the study. Dr. Moshiri reported having no relevant financial disclosures; one of his associates reported that her institute received research funding from Valeant and Pfizer unrelated to this work.
Predicting 30-Day Readmissions
Rates of 30-day readmissions, which are both common and difficult to predict, are of major concern to hospitalists.
“Unfortunately, interventions developed to date have not been universally successful in preventing hospital readmissions for various medical conditions and patient types,” according to a recent article in the Journal of Hospital Medicine. “One potential explanation for this is the inability to reliably predict which patients are at risk for readmission to better target preventative interventions.”
This fact led the authors to perform a study to determine whether the occurrence of automated clinical deterioration alerts (CDAs) could predict 30-day hospital readmission. The 36 variables in the CDA algorithm included age, radiologic agents, and temperature. The retrospective study assessed 3,015 patients admitted to eight general medicine units for all-cause 30-day readmission. Of these, 1,141 patients triggered a CDA, and they were significantly more likely to have a 30-day readmission compared to those who did not trigger a CDA (23.6% versus 15.9%).
The researchers concluded that readily identifiable clinical variables can be identified that predict 30-day readmission.
“It may be important to include these variables in existing prediction tools if pay for performance and across-institution comparisons are to be ‘fair’ to institutions that care for more seriously ill patients,” they write. “The development of an accurate real-time early warning system has the potential to identify patients at risk for various adverse outcomes including clinical deterioration, hospital death and post-discharge readmission. By identifying patients at greatest risk for readmission, valuable healthcare resources can be better targeted to such populations.”
Reference
- Micek ST, Samant M, Bailey T, et al. Real-time automated clinical deterioration alerts predict thirty-day hospital readmission [published online ahead of print June 3, 2016]. J Hosp Med. doi:10.1002/jhm.2617.
Quick Byte
The Cost of Vaccine Avoidance
Many Americans avoid their recommended vaccines: For example, the Centers for Disease Control and Prevention (CDC) reports that only 42% of U.S. adults age 18 or older received the flu vaccine during the 2015–2016 flu season. A study recently released online by Health Affairs calculated the annual cost of the diseases associated with 10 vaccines the CDC recommends for adults. In 2015, that economic burden was $8.95 billion. A full 80% of that—$7.1 billion—was attributed to unvaccinated people.
Reference
- The cost of US adult vaccine avoidance: $8.95 billion in 2015. Health Affairs website. Accessed October 17, 2016
Rates of 30-day readmissions, which are both common and difficult to predict, are of major concern to hospitalists.
“Unfortunately, interventions developed to date have not been universally successful in preventing hospital readmissions for various medical conditions and patient types,” according to a recent article in the Journal of Hospital Medicine. “One potential explanation for this is the inability to reliably predict which patients are at risk for readmission to better target preventative interventions.”
This fact led the authors to perform a study to determine whether the occurrence of automated clinical deterioration alerts (CDAs) could predict 30-day hospital readmission. The 36 variables in the CDA algorithm included age, radiologic agents, and temperature. The retrospective study assessed 3,015 patients admitted to eight general medicine units for all-cause 30-day readmission. Of these, 1,141 patients triggered a CDA, and they were significantly more likely to have a 30-day readmission compared to those who did not trigger a CDA (23.6% versus 15.9%).
The researchers concluded that readily identifiable clinical variables can be identified that predict 30-day readmission.
“It may be important to include these variables in existing prediction tools if pay for performance and across-institution comparisons are to be ‘fair’ to institutions that care for more seriously ill patients,” they write. “The development of an accurate real-time early warning system has the potential to identify patients at risk for various adverse outcomes including clinical deterioration, hospital death and post-discharge readmission. By identifying patients at greatest risk for readmission, valuable healthcare resources can be better targeted to such populations.”
Reference
- Micek ST, Samant M, Bailey T, et al. Real-time automated clinical deterioration alerts predict thirty-day hospital readmission [published online ahead of print June 3, 2016]. J Hosp Med. doi:10.1002/jhm.2617.
Quick Byte
The Cost of Vaccine Avoidance
Many Americans avoid their recommended vaccines: For example, the Centers for Disease Control and Prevention (CDC) reports that only 42% of U.S. adults age 18 or older received the flu vaccine during the 2015–2016 flu season. A study recently released online by Health Affairs calculated the annual cost of the diseases associated with 10 vaccines the CDC recommends for adults. In 2015, that economic burden was $8.95 billion. A full 80% of that—$7.1 billion—was attributed to unvaccinated people.
Reference
- The cost of US adult vaccine avoidance: $8.95 billion in 2015. Health Affairs website. Accessed October 17, 2016
Rates of 30-day readmissions, which are both common and difficult to predict, are of major concern to hospitalists.
“Unfortunately, interventions developed to date have not been universally successful in preventing hospital readmissions for various medical conditions and patient types,” according to a recent article in the Journal of Hospital Medicine. “One potential explanation for this is the inability to reliably predict which patients are at risk for readmission to better target preventative interventions.”
This fact led the authors to perform a study to determine whether the occurrence of automated clinical deterioration alerts (CDAs) could predict 30-day hospital readmission. The 36 variables in the CDA algorithm included age, radiologic agents, and temperature. The retrospective study assessed 3,015 patients admitted to eight general medicine units for all-cause 30-day readmission. Of these, 1,141 patients triggered a CDA, and they were significantly more likely to have a 30-day readmission compared to those who did not trigger a CDA (23.6% versus 15.9%).
The researchers concluded that readily identifiable clinical variables can be identified that predict 30-day readmission.
“It may be important to include these variables in existing prediction tools if pay for performance and across-institution comparisons are to be ‘fair’ to institutions that care for more seriously ill patients,” they write. “The development of an accurate real-time early warning system has the potential to identify patients at risk for various adverse outcomes including clinical deterioration, hospital death and post-discharge readmission. By identifying patients at greatest risk for readmission, valuable healthcare resources can be better targeted to such populations.”
Reference
- Micek ST, Samant M, Bailey T, et al. Real-time automated clinical deterioration alerts predict thirty-day hospital readmission [published online ahead of print June 3, 2016]. J Hosp Med. doi:10.1002/jhm.2617.
Quick Byte
The Cost of Vaccine Avoidance
Many Americans avoid their recommended vaccines: For example, the Centers for Disease Control and Prevention (CDC) reports that only 42% of U.S. adults age 18 or older received the flu vaccine during the 2015–2016 flu season. A study recently released online by Health Affairs calculated the annual cost of the diseases associated with 10 vaccines the CDC recommends for adults. In 2015, that economic burden was $8.95 billion. A full 80% of that—$7.1 billion—was attributed to unvaccinated people.
Reference
- The cost of US adult vaccine avoidance: $8.95 billion in 2015. Health Affairs website. Accessed October 17, 2016
Ramping Up Telehealth’s Possibilities
Twenty percent of Americans live in areas where there are shortages of physicians, according to a policy brief in Health Affairs. Some analysts believe the answer to this problem is telehealth, which they say could also save the healthcare industry some $4.28 billion annually.
While the Affordable Care Act signaled a move toward telehealth development at the federal level (through Medicare), states still largely govern coverage of telehealth services by Medicaid or private insurers.
“Currently there is no uniform legal approach to telehealth, and this continues to be a major challenge in its provision. In particular, concerns about reimbursements, for both private insurers and public programs such as Medicaid, continue to limit the implementation and use of telehealth services,” according to the brief.
Now, Congress is considering the Medicare Telehealth Parity Act, intended to modernize the way Medicare reimburses telehealth services and to expand locations and coverage. To enjoy the benefits of telehealth services, states are likely to move toward full-parity laws for the services, the brief notes.
“Without parity, there are limited incentives for the development of telehealth or for providers to move toward telehealth services,” according to the brief. “If there are no incentives to use telehealth, then providers will continue to focus on in-person care, which will keep healthcare costs high, continue to create access issues, and possibly provide lesser standards of care for chronic disease patients who benefit from remote monitoring.”
Reference
1. Yang T. Telehealth parity laws. Health Affairs Website. Accessed October 17, 2016.
Twenty percent of Americans live in areas where there are shortages of physicians, according to a policy brief in Health Affairs. Some analysts believe the answer to this problem is telehealth, which they say could also save the healthcare industry some $4.28 billion annually.
While the Affordable Care Act signaled a move toward telehealth development at the federal level (through Medicare), states still largely govern coverage of telehealth services by Medicaid or private insurers.
“Currently there is no uniform legal approach to telehealth, and this continues to be a major challenge in its provision. In particular, concerns about reimbursements, for both private insurers and public programs such as Medicaid, continue to limit the implementation and use of telehealth services,” according to the brief.
Now, Congress is considering the Medicare Telehealth Parity Act, intended to modernize the way Medicare reimburses telehealth services and to expand locations and coverage. To enjoy the benefits of telehealth services, states are likely to move toward full-parity laws for the services, the brief notes.
“Without parity, there are limited incentives for the development of telehealth or for providers to move toward telehealth services,” according to the brief. “If there are no incentives to use telehealth, then providers will continue to focus on in-person care, which will keep healthcare costs high, continue to create access issues, and possibly provide lesser standards of care for chronic disease patients who benefit from remote monitoring.”
Reference
1. Yang T. Telehealth parity laws. Health Affairs Website. Accessed October 17, 2016.
Twenty percent of Americans live in areas where there are shortages of physicians, according to a policy brief in Health Affairs. Some analysts believe the answer to this problem is telehealth, which they say could also save the healthcare industry some $4.28 billion annually.
While the Affordable Care Act signaled a move toward telehealth development at the federal level (through Medicare), states still largely govern coverage of telehealth services by Medicaid or private insurers.
“Currently there is no uniform legal approach to telehealth, and this continues to be a major challenge in its provision. In particular, concerns about reimbursements, for both private insurers and public programs such as Medicaid, continue to limit the implementation and use of telehealth services,” according to the brief.
Now, Congress is considering the Medicare Telehealth Parity Act, intended to modernize the way Medicare reimburses telehealth services and to expand locations and coverage. To enjoy the benefits of telehealth services, states are likely to move toward full-parity laws for the services, the brief notes.
“Without parity, there are limited incentives for the development of telehealth or for providers to move toward telehealth services,” according to the brief. “If there are no incentives to use telehealth, then providers will continue to focus on in-person care, which will keep healthcare costs high, continue to create access issues, and possibly provide lesser standards of care for chronic disease patients who benefit from remote monitoring.”
Reference
1. Yang T. Telehealth parity laws. Health Affairs Website. Accessed October 17, 2016.
Secondary reference panel expands access for CML monitoring
A cell-based BCR-ABL1 secondary reference panel traceable to the World Health Organization BCR-ABL1 International Genetic Reference Panel – with an additional MR4.5 level – provides easier access to International Scale calibration and can act as a tool for assay optimization, validation, and quality assurance for molecular monitoring in chronic myeloid leukemia patients.
Such monitoring is important to disease management, especially for decision making with respect to treatment cessation. The new secondary reference panel would allow laboratories to circumvent the oft-used and time-consuming sample exchange process with reference laboratories for International Scale (IS) calibration, Nicholas C. P. Cross, PhD, of the University of Southampton (England) and colleagues wrote in an article published in Leukemia (2016 Jun 3;30:1844-52).
“The development of BCR-ABL1 tyrosine kinase inhibitors ... has enabled progressively deeper molecular responses in CML patients undergoing tyrosine kinase inhibitor therapy,” the authors wrote, noting that deeper molecular responses are “important milestones for patients considering treatment cessation,” and that “other landmarks on the IS also represent different treatment decision thresholds and prognostic outcomes.”
For this reason, regular molecular monitoring using real-time reverse-transcription quantitative PCR (RqPCR) is recommended for optimal disease management, they said.
“As treatment decisions are directly impacted by test results, accuracy and precision of BCR-ABL1 assays across the entire measurement range is crucial for patient management, especially in patients with deep molecular responses when considering possible treatment cessation,” they wrote.
Access to the material for the WHO BCR-ABL1 reference panel (MR1-MR4), which was developed in 2010 as a primary standard for BCR-ABL1 assay IS calibration, is limited, particularly for smaller laboratories, the authors said.
The secondary reference panel they developed, however, is “traceable to and faithfully replicates the WHO panel in both raw materials (lyopholized.K562 and HL-60 cell mixes) and manufacturing process, with the addition of a MR4.5 level.” The secondary panel was calibrated to IS using digital PCR against ABL1, BCR, and GUSB as reference genes, and was successfully evaluated by 45 different BCR-ABL1 assays at 44 different clinical laboratories in a multinational evaluation study.
The MR4.5 level was added to allow for more accurate IS calibration “as CML patients reaching this deep molecular response are increasingly being considered for treatment cessation,” the authors noted.
“Quality-control assessments indicated that the secondary panel had minimal residual moisture, excellent vial-to-vial homogeneity and greater than 2.5 years of real-time stability,” they said.
Further, the panel was successfully processed by all of the laboratories, indicating that it is compatible with many different BCR-ABL1 test configurations, they added.
Of note, the number of assays that achieved good precision and sensitivity exceeded the number that achieved good IS accuracy, suggesting an unmet need for “a simple and broadly available calibration mechanism, such as this secondary panel, to ensure IS accuracy is maintained in laboratories over time,” they wrote, concluding that such a panel “can provide easier access to IS calibration, as well as act as a tool for assay optimization, validation and quality assurance.”
In a letter to the editor in regard to the findings by Cross et al., Maria Sol Ruiz of Instituto Alexander Fleming in Buenos Aires, and colleagues wrote about their own development and validation of “secondary reference materials calibrated to the IS through the WHO primary standards in order to facilitate standardization of molecular monitoring in Latin America,” (Leukemia. 2016 Aug 19. doi: 10.1038/leu.2016.197).
In their study, the letter’s authors demonstrated that secondary reference biological calibrators anchored to the WHO primary standards can decrease inter-laboratory variability.
“Our results, together with those recently reported by Cross et al., substantiate the objective initially set during the establishment of the WHO primary standards, that is, to facilitate worldwide diffusion of the IS. For the first time in Latin America, this study provides a platform on which to assess the performance of distinct clinical BCR-ABL1 tests and confirm the utility of secondary reference materials to further improve IS accuracy and inter-laboratory precision,” they wrote, noting that their efforts will continue through provision of secondary reference material to centers involved in their project, as well as to potential new participants.
“Moreover, due to its higher precision and absolute quantification capability, we are evaluating the possibility of including digital PCR as the calibration method for the future,” they said.
The study discussed in the letter to the editor was supported by a grant from Novartis to one of the authors. Novartis also paid speaking fees to some of the authors. The study by Dr. Cross et al. was also funded by Novartis and some authors are employed by Novartis. The remaining authors, including Dr. Cross, reported having no disclosures.
Harmonizing BCR-ABL1 real time quantitative PCR (RqPCR) is extremely important for precisely interpreting therapeutic response in CML patients and for being able to compare results from various laboratories.
Levels of BCR-ABL1 RNA transcripts are expected to progressively decline with successful response to tyrosine kinase inhibitor therapy. A rise in those levels indicates a loss of response to therapy and typically prompts dose modification or a change in therapy.
Initially, only a qualitative test was available and it measured only the presence or absence of the transcript. The International Standard (IS) allowed the development of a quantitative test. The test is identical to that used in the International Randomized Study of Interferons and STI571 (IRIS), which has a standard baseline of 100% of BCR-ABL1 and major molecular response is defined as a 3 log reduction relative to standard baseline or 0.1% of BCR-ABL1 IS.
However, access became limited – especially for smaller laboratories – to the material for the WHO BCR-ABL1 reference panel (MR1-MR4), a primary standard for BCR-ABL1 assay IS calibration. Calibrated, accredited, primary reference reagents for BCR-ABL1 RqPCR were often too expensive for emergent economies. In response, some laboratories developed conversion factors – a laborious process – and other alternative methods.
By using locally produced secondary cellular calibrators anchored to the WHO primary standards, the elegant work of Cross et al. and Ruiz et al. provided standardization. With this type of initiative, more regional laboratories can assess the performance of their tests and improve their accuracy. Indeed, it is of utmost importance that the exchange of reference standards and quality control samples becomes a common practice in such regions to maximize the reliability of this test. The authors of these studies have started down that path, but there is still a long way to go to achieve higher sensitivity that would permit the detection of even deeper responses and the introduction of digitalized PCR testing.
Maria de Lourdes Chauffaille, MD, and Daniella Kerbauy, MD, are with Fleury Medicina Diagnostica, Sao Paulo, Brazil. Both reported having no disclosures.
Harmonizing BCR-ABL1 real time quantitative PCR (RqPCR) is extremely important for precisely interpreting therapeutic response in CML patients and for being able to compare results from various laboratories.
Levels of BCR-ABL1 RNA transcripts are expected to progressively decline with successful response to tyrosine kinase inhibitor therapy. A rise in those levels indicates a loss of response to therapy and typically prompts dose modification or a change in therapy.
Initially, only a qualitative test was available and it measured only the presence or absence of the transcript. The International Standard (IS) allowed the development of a quantitative test. The test is identical to that used in the International Randomized Study of Interferons and STI571 (IRIS), which has a standard baseline of 100% of BCR-ABL1 and major molecular response is defined as a 3 log reduction relative to standard baseline or 0.1% of BCR-ABL1 IS.
However, access became limited – especially for smaller laboratories – to the material for the WHO BCR-ABL1 reference panel (MR1-MR4), a primary standard for BCR-ABL1 assay IS calibration. Calibrated, accredited, primary reference reagents for BCR-ABL1 RqPCR were often too expensive for emergent economies. In response, some laboratories developed conversion factors – a laborious process – and other alternative methods.
By using locally produced secondary cellular calibrators anchored to the WHO primary standards, the elegant work of Cross et al. and Ruiz et al. provided standardization. With this type of initiative, more regional laboratories can assess the performance of their tests and improve their accuracy. Indeed, it is of utmost importance that the exchange of reference standards and quality control samples becomes a common practice in such regions to maximize the reliability of this test. The authors of these studies have started down that path, but there is still a long way to go to achieve higher sensitivity that would permit the detection of even deeper responses and the introduction of digitalized PCR testing.
Maria de Lourdes Chauffaille, MD, and Daniella Kerbauy, MD, are with Fleury Medicina Diagnostica, Sao Paulo, Brazil. Both reported having no disclosures.
Harmonizing BCR-ABL1 real time quantitative PCR (RqPCR) is extremely important for precisely interpreting therapeutic response in CML patients and for being able to compare results from various laboratories.
Levels of BCR-ABL1 RNA transcripts are expected to progressively decline with successful response to tyrosine kinase inhibitor therapy. A rise in those levels indicates a loss of response to therapy and typically prompts dose modification or a change in therapy.
Initially, only a qualitative test was available and it measured only the presence or absence of the transcript. The International Standard (IS) allowed the development of a quantitative test. The test is identical to that used in the International Randomized Study of Interferons and STI571 (IRIS), which has a standard baseline of 100% of BCR-ABL1 and major molecular response is defined as a 3 log reduction relative to standard baseline or 0.1% of BCR-ABL1 IS.
However, access became limited – especially for smaller laboratories – to the material for the WHO BCR-ABL1 reference panel (MR1-MR4), a primary standard for BCR-ABL1 assay IS calibration. Calibrated, accredited, primary reference reagents for BCR-ABL1 RqPCR were often too expensive for emergent economies. In response, some laboratories developed conversion factors – a laborious process – and other alternative methods.
By using locally produced secondary cellular calibrators anchored to the WHO primary standards, the elegant work of Cross et al. and Ruiz et al. provided standardization. With this type of initiative, more regional laboratories can assess the performance of their tests and improve their accuracy. Indeed, it is of utmost importance that the exchange of reference standards and quality control samples becomes a common practice in such regions to maximize the reliability of this test. The authors of these studies have started down that path, but there is still a long way to go to achieve higher sensitivity that would permit the detection of even deeper responses and the introduction of digitalized PCR testing.
Maria de Lourdes Chauffaille, MD, and Daniella Kerbauy, MD, are with Fleury Medicina Diagnostica, Sao Paulo, Brazil. Both reported having no disclosures.
A cell-based BCR-ABL1 secondary reference panel traceable to the World Health Organization BCR-ABL1 International Genetic Reference Panel – with an additional MR4.5 level – provides easier access to International Scale calibration and can act as a tool for assay optimization, validation, and quality assurance for molecular monitoring in chronic myeloid leukemia patients.
Such monitoring is important to disease management, especially for decision making with respect to treatment cessation. The new secondary reference panel would allow laboratories to circumvent the oft-used and time-consuming sample exchange process with reference laboratories for International Scale (IS) calibration, Nicholas C. P. Cross, PhD, of the University of Southampton (England) and colleagues wrote in an article published in Leukemia (2016 Jun 3;30:1844-52).
“The development of BCR-ABL1 tyrosine kinase inhibitors ... has enabled progressively deeper molecular responses in CML patients undergoing tyrosine kinase inhibitor therapy,” the authors wrote, noting that deeper molecular responses are “important milestones for patients considering treatment cessation,” and that “other landmarks on the IS also represent different treatment decision thresholds and prognostic outcomes.”
For this reason, regular molecular monitoring using real-time reverse-transcription quantitative PCR (RqPCR) is recommended for optimal disease management, they said.
“As treatment decisions are directly impacted by test results, accuracy and precision of BCR-ABL1 assays across the entire measurement range is crucial for patient management, especially in patients with deep molecular responses when considering possible treatment cessation,” they wrote.
Access to the material for the WHO BCR-ABL1 reference panel (MR1-MR4), which was developed in 2010 as a primary standard for BCR-ABL1 assay IS calibration, is limited, particularly for smaller laboratories, the authors said.
The secondary reference panel they developed, however, is “traceable to and faithfully replicates the WHO panel in both raw materials (lyopholized.K562 and HL-60 cell mixes) and manufacturing process, with the addition of a MR4.5 level.” The secondary panel was calibrated to IS using digital PCR against ABL1, BCR, and GUSB as reference genes, and was successfully evaluated by 45 different BCR-ABL1 assays at 44 different clinical laboratories in a multinational evaluation study.
The MR4.5 level was added to allow for more accurate IS calibration “as CML patients reaching this deep molecular response are increasingly being considered for treatment cessation,” the authors noted.
“Quality-control assessments indicated that the secondary panel had minimal residual moisture, excellent vial-to-vial homogeneity and greater than 2.5 years of real-time stability,” they said.
Further, the panel was successfully processed by all of the laboratories, indicating that it is compatible with many different BCR-ABL1 test configurations, they added.
Of note, the number of assays that achieved good precision and sensitivity exceeded the number that achieved good IS accuracy, suggesting an unmet need for “a simple and broadly available calibration mechanism, such as this secondary panel, to ensure IS accuracy is maintained in laboratories over time,” they wrote, concluding that such a panel “can provide easier access to IS calibration, as well as act as a tool for assay optimization, validation and quality assurance.”
In a letter to the editor in regard to the findings by Cross et al., Maria Sol Ruiz of Instituto Alexander Fleming in Buenos Aires, and colleagues wrote about their own development and validation of “secondary reference materials calibrated to the IS through the WHO primary standards in order to facilitate standardization of molecular monitoring in Latin America,” (Leukemia. 2016 Aug 19. doi: 10.1038/leu.2016.197).
In their study, the letter’s authors demonstrated that secondary reference biological calibrators anchored to the WHO primary standards can decrease inter-laboratory variability.
“Our results, together with those recently reported by Cross et al., substantiate the objective initially set during the establishment of the WHO primary standards, that is, to facilitate worldwide diffusion of the IS. For the first time in Latin America, this study provides a platform on which to assess the performance of distinct clinical BCR-ABL1 tests and confirm the utility of secondary reference materials to further improve IS accuracy and inter-laboratory precision,” they wrote, noting that their efforts will continue through provision of secondary reference material to centers involved in their project, as well as to potential new participants.
“Moreover, due to its higher precision and absolute quantification capability, we are evaluating the possibility of including digital PCR as the calibration method for the future,” they said.
The study discussed in the letter to the editor was supported by a grant from Novartis to one of the authors. Novartis also paid speaking fees to some of the authors. The study by Dr. Cross et al. was also funded by Novartis and some authors are employed by Novartis. The remaining authors, including Dr. Cross, reported having no disclosures.
A cell-based BCR-ABL1 secondary reference panel traceable to the World Health Organization BCR-ABL1 International Genetic Reference Panel – with an additional MR4.5 level – provides easier access to International Scale calibration and can act as a tool for assay optimization, validation, and quality assurance for molecular monitoring in chronic myeloid leukemia patients.
Such monitoring is important to disease management, especially for decision making with respect to treatment cessation. The new secondary reference panel would allow laboratories to circumvent the oft-used and time-consuming sample exchange process with reference laboratories for International Scale (IS) calibration, Nicholas C. P. Cross, PhD, of the University of Southampton (England) and colleagues wrote in an article published in Leukemia (2016 Jun 3;30:1844-52).
“The development of BCR-ABL1 tyrosine kinase inhibitors ... has enabled progressively deeper molecular responses in CML patients undergoing tyrosine kinase inhibitor therapy,” the authors wrote, noting that deeper molecular responses are “important milestones for patients considering treatment cessation,” and that “other landmarks on the IS also represent different treatment decision thresholds and prognostic outcomes.”
For this reason, regular molecular monitoring using real-time reverse-transcription quantitative PCR (RqPCR) is recommended for optimal disease management, they said.
“As treatment decisions are directly impacted by test results, accuracy and precision of BCR-ABL1 assays across the entire measurement range is crucial for patient management, especially in patients with deep molecular responses when considering possible treatment cessation,” they wrote.
Access to the material for the WHO BCR-ABL1 reference panel (MR1-MR4), which was developed in 2010 as a primary standard for BCR-ABL1 assay IS calibration, is limited, particularly for smaller laboratories, the authors said.
The secondary reference panel they developed, however, is “traceable to and faithfully replicates the WHO panel in both raw materials (lyopholized.K562 and HL-60 cell mixes) and manufacturing process, with the addition of a MR4.5 level.” The secondary panel was calibrated to IS using digital PCR against ABL1, BCR, and GUSB as reference genes, and was successfully evaluated by 45 different BCR-ABL1 assays at 44 different clinical laboratories in a multinational evaluation study.
The MR4.5 level was added to allow for more accurate IS calibration “as CML patients reaching this deep molecular response are increasingly being considered for treatment cessation,” the authors noted.
“Quality-control assessments indicated that the secondary panel had minimal residual moisture, excellent vial-to-vial homogeneity and greater than 2.5 years of real-time stability,” they said.
Further, the panel was successfully processed by all of the laboratories, indicating that it is compatible with many different BCR-ABL1 test configurations, they added.
Of note, the number of assays that achieved good precision and sensitivity exceeded the number that achieved good IS accuracy, suggesting an unmet need for “a simple and broadly available calibration mechanism, such as this secondary panel, to ensure IS accuracy is maintained in laboratories over time,” they wrote, concluding that such a panel “can provide easier access to IS calibration, as well as act as a tool for assay optimization, validation and quality assurance.”
In a letter to the editor in regard to the findings by Cross et al., Maria Sol Ruiz of Instituto Alexander Fleming in Buenos Aires, and colleagues wrote about their own development and validation of “secondary reference materials calibrated to the IS through the WHO primary standards in order to facilitate standardization of molecular monitoring in Latin America,” (Leukemia. 2016 Aug 19. doi: 10.1038/leu.2016.197).
In their study, the letter’s authors demonstrated that secondary reference biological calibrators anchored to the WHO primary standards can decrease inter-laboratory variability.
“Our results, together with those recently reported by Cross et al., substantiate the objective initially set during the establishment of the WHO primary standards, that is, to facilitate worldwide diffusion of the IS. For the first time in Latin America, this study provides a platform on which to assess the performance of distinct clinical BCR-ABL1 tests and confirm the utility of secondary reference materials to further improve IS accuracy and inter-laboratory precision,” they wrote, noting that their efforts will continue through provision of secondary reference material to centers involved in their project, as well as to potential new participants.
“Moreover, due to its higher precision and absolute quantification capability, we are evaluating the possibility of including digital PCR as the calibration method for the future,” they said.
The study discussed in the letter to the editor was supported by a grant from Novartis to one of the authors. Novartis also paid speaking fees to some of the authors. The study by Dr. Cross et al. was also funded by Novartis and some authors are employed by Novartis. The remaining authors, including Dr. Cross, reported having no disclosures.
FROM LEUKEMIA
Key clinical point:
Major finding: The secondary panel was calibrated to IS using digital PCR against ABL1, BCR, and GUSB as reference genes, and was successfully evaluated by 45 different BCR-ABL1 assays at 44 different clinical laboratories.
Data source: A multicenter evaluation study of a secondary reference panel for BCR-ABL1 quantification on the IS.
Disclosures: The study discussed in the letter to the editor was supported by a grant from Novartis to one of the authors. Novartis also paid speaking fees to some of the authors. The study by Dr. Cross et al. was also funded by Novartis and some authors are employed by Novartis. The remaining authors, including Dr. Cross, reported having no disclosures.