User login
Gastroenterology and Climate Change: Assessing and Mitigating Impacts
- Karliner J et al. Eur J Public Health. 2020;30(suppl 5):v311. doi:10.1093/eurpub/ckaa165.843
- Vaccari M et al. Waste Manag Res. 2018;36(1):39-47. doi:10.1177/0734242X17739968
- Peery AF et al. Gastroenterology. 2019;156(1):254-272.e11. doi:10.1053/j.gastro.2018.08.063
- Sorge A et al. Endoscopy. 2023;55(suppl 2):S72-S73. https://www.esge.com/assets/downloads/pdfs/guidelines/ESGE_Days_2023.pdf
- Maurice JB et al. Lancet Gastroenterol Hepatol. 2020;5(7):636-638. doi:10.1016/S2468-1253(20)30157-6
- Gayam S. Am J Gastroenterol. 2020;115(12):1931-1932. doi:10.14309/ajg.0000000000001005
- Siau K et al. Tech Innov Gastrointest Endosc. 2021;23(4):344-352. doi:10.1016/j.tige.2021.06.005
- Namburar S et al. Gut. 2022;71(7):1326-1331. doi:10.1136/gutjnl-2021-324729
- Haddock R et al. Am J Gastroenterol. 2022;117(3):394-400. doi:10.14309/ajg.0000000000001604
- Donnelly MC et al. J Hepatol. 2022;76(5):995-1000. doi:10.1016/j.jhep.2022.02.01
- Leddin D, Macrae F. J Clin Gastroenterol. 2020;54(5):393-397. doi:10.1097/MCG.0000000000001336
- Pohl H et al. Hepatology. 2022;76(6):1836-1844. doi:10.1002/hep.32810
- Rodríguez de Santiago E et al. Endoscopy. 2022;54(8):797-826. doi:10.1055/a-1859-3726
- Sebastian S et al. Gut. 2023;72(1):12-26. doi:10.1136/gutjnl-2022-328460
- Cunha Neves JA et al. Gut. 2023;72(2):306-313. doi:10.1136/gutjnl-2022-327005
- Kaplan S et al. Issue Brief (Commonw Fund). 2012;29:1-14. PMID:23214181
- López-Muñoz P et al. Gut. 2023;gutjnl-2023-329544. doi:10.1136/gutjnl-2023-329544
- Karliner J et al. Eur J Public Health. 2020;30(suppl 5):v311. doi:10.1093/eurpub/ckaa165.843
- Vaccari M et al. Waste Manag Res. 2018;36(1):39-47. doi:10.1177/0734242X17739968
- Peery AF et al. Gastroenterology. 2019;156(1):254-272.e11. doi:10.1053/j.gastro.2018.08.063
- Sorge A et al. Endoscopy. 2023;55(suppl 2):S72-S73. https://www.esge.com/assets/downloads/pdfs/guidelines/ESGE_Days_2023.pdf
- Maurice JB et al. Lancet Gastroenterol Hepatol. 2020;5(7):636-638. doi:10.1016/S2468-1253(20)30157-6
- Gayam S. Am J Gastroenterol. 2020;115(12):1931-1932. doi:10.14309/ajg.0000000000001005
- Siau K et al. Tech Innov Gastrointest Endosc. 2021;23(4):344-352. doi:10.1016/j.tige.2021.06.005
- Namburar S et al. Gut. 2022;71(7):1326-1331. doi:10.1136/gutjnl-2021-324729
- Haddock R et al. Am J Gastroenterol. 2022;117(3):394-400. doi:10.14309/ajg.0000000000001604
- Donnelly MC et al. J Hepatol. 2022;76(5):995-1000. doi:10.1016/j.jhep.2022.02.01
- Leddin D, Macrae F. J Clin Gastroenterol. 2020;54(5):393-397. doi:10.1097/MCG.0000000000001336
- Pohl H et al. Hepatology. 2022;76(6):1836-1844. doi:10.1002/hep.32810
- Rodríguez de Santiago E et al. Endoscopy. 2022;54(8):797-826. doi:10.1055/a-1859-3726
- Sebastian S et al. Gut. 2023;72(1):12-26. doi:10.1136/gutjnl-2022-328460
- Cunha Neves JA et al. Gut. 2023;72(2):306-313. doi:10.1136/gutjnl-2022-327005
- Kaplan S et al. Issue Brief (Commonw Fund). 2012;29:1-14. PMID:23214181
- López-Muñoz P et al. Gut. 2023;gutjnl-2023-329544. doi:10.1136/gutjnl-2023-329544
- Karliner J et al. Eur J Public Health. 2020;30(suppl 5):v311. doi:10.1093/eurpub/ckaa165.843
- Vaccari M et al. Waste Manag Res. 2018;36(1):39-47. doi:10.1177/0734242X17739968
- Peery AF et al. Gastroenterology. 2019;156(1):254-272.e11. doi:10.1053/j.gastro.2018.08.063
- Sorge A et al. Endoscopy. 2023;55(suppl 2):S72-S73. https://www.esge.com/assets/downloads/pdfs/guidelines/ESGE_Days_2023.pdf
- Maurice JB et al. Lancet Gastroenterol Hepatol. 2020;5(7):636-638. doi:10.1016/S2468-1253(20)30157-6
- Gayam S. Am J Gastroenterol. 2020;115(12):1931-1932. doi:10.14309/ajg.0000000000001005
- Siau K et al. Tech Innov Gastrointest Endosc. 2021;23(4):344-352. doi:10.1016/j.tige.2021.06.005
- Namburar S et al. Gut. 2022;71(7):1326-1331. doi:10.1136/gutjnl-2021-324729
- Haddock R et al. Am J Gastroenterol. 2022;117(3):394-400. doi:10.14309/ajg.0000000000001604
- Donnelly MC et al. J Hepatol. 2022;76(5):995-1000. doi:10.1016/j.jhep.2022.02.01
- Leddin D, Macrae F. J Clin Gastroenterol. 2020;54(5):393-397. doi:10.1097/MCG.0000000000001336
- Pohl H et al. Hepatology. 2022;76(6):1836-1844. doi:10.1002/hep.32810
- Rodríguez de Santiago E et al. Endoscopy. 2022;54(8):797-826. doi:10.1055/a-1859-3726
- Sebastian S et al. Gut. 2023;72(1):12-26. doi:10.1136/gutjnl-2022-328460
- Cunha Neves JA et al. Gut. 2023;72(2):306-313. doi:10.1136/gutjnl-2022-327005
- Kaplan S et al. Issue Brief (Commonw Fund). 2012;29:1-14. PMID:23214181
- López-Muñoz P et al. Gut. 2023;gutjnl-2023-329544. doi:10.1136/gutjnl-2023-329544
Harnessing the Power of AI to Enhance Endoscopy: Promises and Pitfalls
- Jin Z et al. BioMed Eng OnLine. 2022;21(1):12. doi:10.1186/s12938-022-00979-
- Buendgens L, Cifci D, Ghaffari Laleh N, et al. Sci Rep. 2022;12(1):4829. doi:10.1038/s41598-022-08773-1
- Uche-Anya EN, Berzin TM. Artificial intelligence applications in colonoscopy. GI & Hepatology News. January 24, 2023. https://www.mdedge.com/gihepnews/article/260769/mixed-topics/artificial-intelligence-applications-colonoscopy
- Rondonotti E et al. Endoscopy. 2023;55(1):14-22. doi:10.1055/a-1852-0330
- Antonelli G et al. Ann Gastroenterol. 2023;36(2):114-122. doi:10.20524/aog.2023.0781
- van der Zander QEW et al. Endoscopy. 2021;53(12):1219-1226. doi:10.1055/a-1343-159
- Areia PM et al. Lancet Digital Health. 2022;4(6):e436-e444. doi:10.1016/S2589-7500(22)00042-5
- Sumiyama K et al. Dig Endosc. 2021;33(2):218-230. doi:10.1111/den.13837
- Berzin TM et al. Gastrointest Endosc. 2020;92(4):951-959. doi:10.1016/j.gie.2020.06.035
- Mori Y et al. Dig Endosc. 2023;35(4):422-429. doi:10.1111/den.14531
- Uche-Anya E et al. Gut. 2022;71(9):1909-1915. doi:10.1136/gutjnl-2021-326271
- Moor M et al. Nature. 2023;616(7956):259-265. 10.1038/s41586-023-05881-4
- Kather JN et al. NPJ Digit Med. 2022;5(1):90. doi:10.1038/s41746-022-00634-5
- Jin Z et al. BioMed Eng OnLine. 2022;21(1):12. doi:10.1186/s12938-022-00979-
- Buendgens L, Cifci D, Ghaffari Laleh N, et al. Sci Rep. 2022;12(1):4829. doi:10.1038/s41598-022-08773-1
- Uche-Anya EN, Berzin TM. Artificial intelligence applications in colonoscopy. GI & Hepatology News. January 24, 2023. https://www.mdedge.com/gihepnews/article/260769/mixed-topics/artificial-intelligence-applications-colonoscopy
- Rondonotti E et al. Endoscopy. 2023;55(1):14-22. doi:10.1055/a-1852-0330
- Antonelli G et al. Ann Gastroenterol. 2023;36(2):114-122. doi:10.20524/aog.2023.0781
- van der Zander QEW et al. Endoscopy. 2021;53(12):1219-1226. doi:10.1055/a-1343-159
- Areia PM et al. Lancet Digital Health. 2022;4(6):e436-e444. doi:10.1016/S2589-7500(22)00042-5
- Sumiyama K et al. Dig Endosc. 2021;33(2):218-230. doi:10.1111/den.13837
- Berzin TM et al. Gastrointest Endosc. 2020;92(4):951-959. doi:10.1016/j.gie.2020.06.035
- Mori Y et al. Dig Endosc. 2023;35(4):422-429. doi:10.1111/den.14531
- Uche-Anya E et al. Gut. 2022;71(9):1909-1915. doi:10.1136/gutjnl-2021-326271
- Moor M et al. Nature. 2023;616(7956):259-265. 10.1038/s41586-023-05881-4
- Kather JN et al. NPJ Digit Med. 2022;5(1):90. doi:10.1038/s41746-022-00634-5
- Jin Z et al. BioMed Eng OnLine. 2022;21(1):12. doi:10.1186/s12938-022-00979-
- Buendgens L, Cifci D, Ghaffari Laleh N, et al. Sci Rep. 2022;12(1):4829. doi:10.1038/s41598-022-08773-1
- Uche-Anya EN, Berzin TM. Artificial intelligence applications in colonoscopy. GI & Hepatology News. January 24, 2023. https://www.mdedge.com/gihepnews/article/260769/mixed-topics/artificial-intelligence-applications-colonoscopy
- Rondonotti E et al. Endoscopy. 2023;55(1):14-22. doi:10.1055/a-1852-0330
- Antonelli G et al. Ann Gastroenterol. 2023;36(2):114-122. doi:10.20524/aog.2023.0781
- van der Zander QEW et al. Endoscopy. 2021;53(12):1219-1226. doi:10.1055/a-1343-159
- Areia PM et al. Lancet Digital Health. 2022;4(6):e436-e444. doi:10.1016/S2589-7500(22)00042-5
- Sumiyama K et al. Dig Endosc. 2021;33(2):218-230. doi:10.1111/den.13837
- Berzin TM et al. Gastrointest Endosc. 2020;92(4):951-959. doi:10.1016/j.gie.2020.06.035
- Mori Y et al. Dig Endosc. 2023;35(4):422-429. doi:10.1111/den.14531
- Uche-Anya E et al. Gut. 2022;71(9):1909-1915. doi:10.1136/gutjnl-2021-326271
- Moor M et al. Nature. 2023;616(7956):259-265. 10.1038/s41586-023-05881-4
- Kather JN et al. NPJ Digit Med. 2022;5(1):90. doi:10.1038/s41746-022-00634-5
EASD 2023: A deeper dive into type 1 and type 2 diabetes
Noteworthy at the meeting, taking place Oct. 3-6, in Hamburg, Germany, will be final detailed data from the SURMOUNT-4 trial of the “twincretin” tirzepatide (Mounjaro, Lilly) on obesity. The top-line results, announced by the company in July, showed an average 21.1% weight loss at 36 weeks with tirzepatide injections once weekly among adults with overweight or obesity. The drug is approved in the United States and Europe for treating type 2 diabetes, and approval for obesity is expected in the United States later this year.
In addition, a symposium will present a new EASD/American Diabetes Association (ADA) consensus report, Hyperglycaemic Crisis in Adult Patients with Diabetes, scheduled to be simultaneously published in Diabetologia and Diabetes Care on Oct. 6.
Aside from those, much of the EASD meeting content will feature smaller studies on both type 2 and type 1 diabetes, along with award lectures, symposia, debates, and lots of discussion on hot topics in diabetes and clinical challenges including complications. In essence, it will provide a forum for in-depth follow-up to the jam-packed clinical trial–filled agenda at the ADA meeting in June, said EASD Honorary Secretary Tina Vilsbøll, MD, clinical professor and head of clinic at the Steno Diabetes Center, Copenhagen.
“There were so many large trials at ADA that we just took them in without really having a chance to discuss them. ... There’s so much to discuss with all these new treatments, how do we place them in obesity and diabetes? ... All the data that we have from ADA will make good discussions at EASD,” Dr. Vilsbøll said in an interview.
Indeed, said EASD President Chantal Mathieu, MD, PhD, chair of endocrinology at University Hospital Gasthuisberg Leuven, Belgium, “We always come after ADA. That puts us in a position where we can take deeper dives into the data. ... EASD is a calmer meeting where you can really look at the details.”
Type 2 diabetes: Disease modifying in many ways
Dr. Mathieu told this news organization that a unifying theme for much of the EASD meeting’s content is “We are now entering the era of disease-modifying and disease-disrupting therapies” in both diabetes types.
In type 2, this means “getting to the root, which is obesity, so you’ll see a lot of presentations on the incretin system, but you also don’t get type 2 diabetes if you have an iron-clad beta cell. ... So, we also gave a lot of attention to basic translational research that helps us to understand the role of the beta cell in type 2 diabetes.”
In addition to SURMOUNT-4, there will be oral abstract sessions with follow-up data from the SURPASS series of studies of tirzepatide in type 2 diabetes, other abstract sessions, symposia about incretins and obesity, and an oral abstract session on beta cell function in both diabetes types.
Three debates will address controversial questions in the type 2 diabetes arena. In one, speakers will take opposite sides on “Initial combined therapy for type 2 diabetes: Should diabetes follow hypertension?”
In another, speakers will argue over “Is lasting remission of type 2 diabetes feasible in the real-world setting?” That’s an important question, Dr. Vilsbøll said.
“A person might be able to have a remission but go back if they regain the weight. Do we really have remission? How do we define it? Now, suddenly, we have tools to help people go in the right direction. Now we’re in a place where we can actually help our patients with their cravings and their body weight and all that. It’s more fun to discuss when we have the tools.”
A third debate will tackle the question of whether all people with type 2 diabetes and chronic kidney disease should be on [sodium-glucose co-transporter 2] (SGLT2) inhibitors “by default.”
The Minkowski Prize Lecture will address the regulation of energy and glucose metabolism by the dual incretin receptor agonists, while the EASD-Lilly Anniversary Prize Lecture will be about the role of ectopic lipid in insulin resistance and cardiometabolic disease.
Type 1 diabetes: Both disease modifying and disruptive
For type 1 diabetes, “disease-modifying” and “disruptive” approaches on the meeting agenda include new data on immune modulation for people in early stages in order to prevent or delay insulin dependence, islet transplantation including the use of stem cell–derived beta cells, and the latest in technology including automated insulin delivery systems, also known colloquially as the “artificial pancreas.”
Prize lectures about type 1 diabetes will include the Claude Bernard Lecture, on etiologies of autoimmune diabetes, the Albert Renold Lecture, on “disrupted RNA editing as a path to type 1 diabetes,” and the EASD/Novo Nordisk Foundation Diabetes Prize for Excellence Lecture on automated insulin delivery.
Focus on complications: The known and the emerging
The meeting also will focus a great deal on complications of diabetes, including the well-studied cardiovascular disease, neuropathy, nephropathy, retinopathy, and fatty liver disease as well as others that typically receive less attention, such as gastrointestinal problems and cardiomyopathy.
Another debate will address the question “Is it time to reclassify diabetes complications because microvascular and macrovascular classification is no longer sufficient?” And, the Camillo Golgi Lecture will cover “Diabetes Complications: From Classical to Emerging.”
As always, there’s much more on the agenda including pregnancy and diabetes, cystic fibrosis–derived diabetes, mental health in diabetes, COVID-19 and diabetes, hypoglycemia, and hypoglycemia unawareness.
According to Dr. Vilsbøll, “Clinicians should come and enjoy all the great science we have, interact, and be inspired.”
Dr. Vilsbøll has served on scientific advisory panels, been part of speaker bureaus, and served as a consultant to and/or received research support from Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Gilead, GSK, Mundipharma, Novo Nordisk, Sanofi, and Sun Pharmaceuticals. Dr. Mathieu serves or has served on the advisory panel for Novo Nordisk, Sanofi, Merck Sharp and Dohme Ltd., Eli Lilly and Company, Novartis, AstraZeneca, Boehringer Ingelheim, Roche, Medtronic, ActoBio Therapeutics, Pfizer, Imcyse, Insulet, Zealand Pharma, Avotres, Mannkind, Sandoz, and Vertex. She has served on the speakers bureau for Novo Nordisk, Sanofi, Eli Lilly and Company, Boehringer Ingelheim, AstraZeneca, and Novartis. Financial compensation for these activities has been received by KU Leuven.
A version of this article appeared on Medscape.com.
Noteworthy at the meeting, taking place Oct. 3-6, in Hamburg, Germany, will be final detailed data from the SURMOUNT-4 trial of the “twincretin” tirzepatide (Mounjaro, Lilly) on obesity. The top-line results, announced by the company in July, showed an average 21.1% weight loss at 36 weeks with tirzepatide injections once weekly among adults with overweight or obesity. The drug is approved in the United States and Europe for treating type 2 diabetes, and approval for obesity is expected in the United States later this year.
In addition, a symposium will present a new EASD/American Diabetes Association (ADA) consensus report, Hyperglycaemic Crisis in Adult Patients with Diabetes, scheduled to be simultaneously published in Diabetologia and Diabetes Care on Oct. 6.
Aside from those, much of the EASD meeting content will feature smaller studies on both type 2 and type 1 diabetes, along with award lectures, symposia, debates, and lots of discussion on hot topics in diabetes and clinical challenges including complications. In essence, it will provide a forum for in-depth follow-up to the jam-packed clinical trial–filled agenda at the ADA meeting in June, said EASD Honorary Secretary Tina Vilsbøll, MD, clinical professor and head of clinic at the Steno Diabetes Center, Copenhagen.
“There were so many large trials at ADA that we just took them in without really having a chance to discuss them. ... There’s so much to discuss with all these new treatments, how do we place them in obesity and diabetes? ... All the data that we have from ADA will make good discussions at EASD,” Dr. Vilsbøll said in an interview.
Indeed, said EASD President Chantal Mathieu, MD, PhD, chair of endocrinology at University Hospital Gasthuisberg Leuven, Belgium, “We always come after ADA. That puts us in a position where we can take deeper dives into the data. ... EASD is a calmer meeting where you can really look at the details.”
Type 2 diabetes: Disease modifying in many ways
Dr. Mathieu told this news organization that a unifying theme for much of the EASD meeting’s content is “We are now entering the era of disease-modifying and disease-disrupting therapies” in both diabetes types.
In type 2, this means “getting to the root, which is obesity, so you’ll see a lot of presentations on the incretin system, but you also don’t get type 2 diabetes if you have an iron-clad beta cell. ... So, we also gave a lot of attention to basic translational research that helps us to understand the role of the beta cell in type 2 diabetes.”
In addition to SURMOUNT-4, there will be oral abstract sessions with follow-up data from the SURPASS series of studies of tirzepatide in type 2 diabetes, other abstract sessions, symposia about incretins and obesity, and an oral abstract session on beta cell function in both diabetes types.
Three debates will address controversial questions in the type 2 diabetes arena. In one, speakers will take opposite sides on “Initial combined therapy for type 2 diabetes: Should diabetes follow hypertension?”
In another, speakers will argue over “Is lasting remission of type 2 diabetes feasible in the real-world setting?” That’s an important question, Dr. Vilsbøll said.
“A person might be able to have a remission but go back if they regain the weight. Do we really have remission? How do we define it? Now, suddenly, we have tools to help people go in the right direction. Now we’re in a place where we can actually help our patients with their cravings and their body weight and all that. It’s more fun to discuss when we have the tools.”
A third debate will tackle the question of whether all people with type 2 diabetes and chronic kidney disease should be on [sodium-glucose co-transporter 2] (SGLT2) inhibitors “by default.”
The Minkowski Prize Lecture will address the regulation of energy and glucose metabolism by the dual incretin receptor agonists, while the EASD-Lilly Anniversary Prize Lecture will be about the role of ectopic lipid in insulin resistance and cardiometabolic disease.
Type 1 diabetes: Both disease modifying and disruptive
For type 1 diabetes, “disease-modifying” and “disruptive” approaches on the meeting agenda include new data on immune modulation for people in early stages in order to prevent or delay insulin dependence, islet transplantation including the use of stem cell–derived beta cells, and the latest in technology including automated insulin delivery systems, also known colloquially as the “artificial pancreas.”
Prize lectures about type 1 diabetes will include the Claude Bernard Lecture, on etiologies of autoimmune diabetes, the Albert Renold Lecture, on “disrupted RNA editing as a path to type 1 diabetes,” and the EASD/Novo Nordisk Foundation Diabetes Prize for Excellence Lecture on automated insulin delivery.
Focus on complications: The known and the emerging
The meeting also will focus a great deal on complications of diabetes, including the well-studied cardiovascular disease, neuropathy, nephropathy, retinopathy, and fatty liver disease as well as others that typically receive less attention, such as gastrointestinal problems and cardiomyopathy.
Another debate will address the question “Is it time to reclassify diabetes complications because microvascular and macrovascular classification is no longer sufficient?” And, the Camillo Golgi Lecture will cover “Diabetes Complications: From Classical to Emerging.”
As always, there’s much more on the agenda including pregnancy and diabetes, cystic fibrosis–derived diabetes, mental health in diabetes, COVID-19 and diabetes, hypoglycemia, and hypoglycemia unawareness.
According to Dr. Vilsbøll, “Clinicians should come and enjoy all the great science we have, interact, and be inspired.”
Dr. Vilsbøll has served on scientific advisory panels, been part of speaker bureaus, and served as a consultant to and/or received research support from Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Gilead, GSK, Mundipharma, Novo Nordisk, Sanofi, and Sun Pharmaceuticals. Dr. Mathieu serves or has served on the advisory panel for Novo Nordisk, Sanofi, Merck Sharp and Dohme Ltd., Eli Lilly and Company, Novartis, AstraZeneca, Boehringer Ingelheim, Roche, Medtronic, ActoBio Therapeutics, Pfizer, Imcyse, Insulet, Zealand Pharma, Avotres, Mannkind, Sandoz, and Vertex. She has served on the speakers bureau for Novo Nordisk, Sanofi, Eli Lilly and Company, Boehringer Ingelheim, AstraZeneca, and Novartis. Financial compensation for these activities has been received by KU Leuven.
A version of this article appeared on Medscape.com.
Noteworthy at the meeting, taking place Oct. 3-6, in Hamburg, Germany, will be final detailed data from the SURMOUNT-4 trial of the “twincretin” tirzepatide (Mounjaro, Lilly) on obesity. The top-line results, announced by the company in July, showed an average 21.1% weight loss at 36 weeks with tirzepatide injections once weekly among adults with overweight or obesity. The drug is approved in the United States and Europe for treating type 2 diabetes, and approval for obesity is expected in the United States later this year.
In addition, a symposium will present a new EASD/American Diabetes Association (ADA) consensus report, Hyperglycaemic Crisis in Adult Patients with Diabetes, scheduled to be simultaneously published in Diabetologia and Diabetes Care on Oct. 6.
Aside from those, much of the EASD meeting content will feature smaller studies on both type 2 and type 1 diabetes, along with award lectures, symposia, debates, and lots of discussion on hot topics in diabetes and clinical challenges including complications. In essence, it will provide a forum for in-depth follow-up to the jam-packed clinical trial–filled agenda at the ADA meeting in June, said EASD Honorary Secretary Tina Vilsbøll, MD, clinical professor and head of clinic at the Steno Diabetes Center, Copenhagen.
“There were so many large trials at ADA that we just took them in without really having a chance to discuss them. ... There’s so much to discuss with all these new treatments, how do we place them in obesity and diabetes? ... All the data that we have from ADA will make good discussions at EASD,” Dr. Vilsbøll said in an interview.
Indeed, said EASD President Chantal Mathieu, MD, PhD, chair of endocrinology at University Hospital Gasthuisberg Leuven, Belgium, “We always come after ADA. That puts us in a position where we can take deeper dives into the data. ... EASD is a calmer meeting where you can really look at the details.”
Type 2 diabetes: Disease modifying in many ways
Dr. Mathieu told this news organization that a unifying theme for much of the EASD meeting’s content is “We are now entering the era of disease-modifying and disease-disrupting therapies” in both diabetes types.
In type 2, this means “getting to the root, which is obesity, so you’ll see a lot of presentations on the incretin system, but you also don’t get type 2 diabetes if you have an iron-clad beta cell. ... So, we also gave a lot of attention to basic translational research that helps us to understand the role of the beta cell in type 2 diabetes.”
In addition to SURMOUNT-4, there will be oral abstract sessions with follow-up data from the SURPASS series of studies of tirzepatide in type 2 diabetes, other abstract sessions, symposia about incretins and obesity, and an oral abstract session on beta cell function in both diabetes types.
Three debates will address controversial questions in the type 2 diabetes arena. In one, speakers will take opposite sides on “Initial combined therapy for type 2 diabetes: Should diabetes follow hypertension?”
In another, speakers will argue over “Is lasting remission of type 2 diabetes feasible in the real-world setting?” That’s an important question, Dr. Vilsbøll said.
“A person might be able to have a remission but go back if they regain the weight. Do we really have remission? How do we define it? Now, suddenly, we have tools to help people go in the right direction. Now we’re in a place where we can actually help our patients with their cravings and their body weight and all that. It’s more fun to discuss when we have the tools.”
A third debate will tackle the question of whether all people with type 2 diabetes and chronic kidney disease should be on [sodium-glucose co-transporter 2] (SGLT2) inhibitors “by default.”
The Minkowski Prize Lecture will address the regulation of energy and glucose metabolism by the dual incretin receptor agonists, while the EASD-Lilly Anniversary Prize Lecture will be about the role of ectopic lipid in insulin resistance and cardiometabolic disease.
Type 1 diabetes: Both disease modifying and disruptive
For type 1 diabetes, “disease-modifying” and “disruptive” approaches on the meeting agenda include new data on immune modulation for people in early stages in order to prevent or delay insulin dependence, islet transplantation including the use of stem cell–derived beta cells, and the latest in technology including automated insulin delivery systems, also known colloquially as the “artificial pancreas.”
Prize lectures about type 1 diabetes will include the Claude Bernard Lecture, on etiologies of autoimmune diabetes, the Albert Renold Lecture, on “disrupted RNA editing as a path to type 1 diabetes,” and the EASD/Novo Nordisk Foundation Diabetes Prize for Excellence Lecture on automated insulin delivery.
Focus on complications: The known and the emerging
The meeting also will focus a great deal on complications of diabetes, including the well-studied cardiovascular disease, neuropathy, nephropathy, retinopathy, and fatty liver disease as well as others that typically receive less attention, such as gastrointestinal problems and cardiomyopathy.
Another debate will address the question “Is it time to reclassify diabetes complications because microvascular and macrovascular classification is no longer sufficient?” And, the Camillo Golgi Lecture will cover “Diabetes Complications: From Classical to Emerging.”
As always, there’s much more on the agenda including pregnancy and diabetes, cystic fibrosis–derived diabetes, mental health in diabetes, COVID-19 and diabetes, hypoglycemia, and hypoglycemia unawareness.
According to Dr. Vilsbøll, “Clinicians should come and enjoy all the great science we have, interact, and be inspired.”
Dr. Vilsbøll has served on scientific advisory panels, been part of speaker bureaus, and served as a consultant to and/or received research support from Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Gilead, GSK, Mundipharma, Novo Nordisk, Sanofi, and Sun Pharmaceuticals. Dr. Mathieu serves or has served on the advisory panel for Novo Nordisk, Sanofi, Merck Sharp and Dohme Ltd., Eli Lilly and Company, Novartis, AstraZeneca, Boehringer Ingelheim, Roche, Medtronic, ActoBio Therapeutics, Pfizer, Imcyse, Insulet, Zealand Pharma, Avotres, Mannkind, Sandoz, and Vertex. She has served on the speakers bureau for Novo Nordisk, Sanofi, Eli Lilly and Company, Boehringer Ingelheim, AstraZeneca, and Novartis. Financial compensation for these activities has been received by KU Leuven.
A version of this article appeared on Medscape.com.
FROM EASD 2023
Older women who get mammograms risk overdiagnosis
TOPLINE:
Women who continue breast cancer screening after age 70 face a considerable risk for overdiagnosis.
METHODOLOGY:
- Overdiagnosis – the risk of detecting and treating cancers that would never have caused issues in a person’s lifetime – is increasingly recognized as a harm of breast cancer screening; however, the scope of the problem among older women remains uncertain.
- To get an idea, investigators linked Medicare claims data with Surveillance, Epidemiology, and End Results (SEER) data for 54,635 women 70 years or older to compare the incidence of breast cancer and breast cancer–specific death among women who continued screening mammography with those who did not.
- The women all had undergone recent screening mammograms and had no history of breast cancer at study entry. Those who had a subsequent mammogram within 3 years were classified as undergoing continued screening while those who did not were classified as not undergoing continued screening.
- Overdiagnosis was defined as the difference in cumulative incidence of breast cancer between screened and unscreened women divided by the cumulative incidence among screened women.
- Results were adjusted for potential confounders, including age, race, and ethnicity.
TAKEAWAY:
- Over 80% of women 70-84 years old and more than 60% of women 85 years or older continued screening.
- Among women 70-74 years old, the adjusted cumulative incidence of breast cancer was 6.1 cases per 100 screened women vs. 4.2 cases per 100 unscreened women; for women aged 75-84 years old, the cumulative incidence was 4.9 per 100 screened women vs. 2.6 per 100 unscreened women, and for women 85 years and older, the cumulative incidence was 2.8 vs. 1.3 per 100, respectively.
- Estimates of overdiagnosis ranged from 31% of breast cancer cases among screened women in the 70-74 age group to 54% of cases in the 85 and older group.
- The researchers found no statistically significant reduction in breast cancer–specific death associated with screening in any age or life-expectancy group. Overdiagnosis appeared to be driven by in situ and localized invasive breast cancer, not advanced breast cancer.
IN PRACTICE:
The proportion of older women who continue to receive screening mammograms and may experience breast cancer overdiagnosis is “considerable” and “increases with advancing age and with decreasing life expectancy,” the authors conclude. Given potential benefits and harms of screening in this population, “patient preferences, including risk tolerance, comfort with uncertainty, and willingness to undergo treatment, are important for informing screening decisions.”
SOURCE:
The study was led by Ilana Richman, MD, MHS, of the Yale School of Medicine, New Haven, Connecticut, and published in the Annals of Internal Medicine.
LIMITATIONS:
The definition of screening mammography in the study may have misclassified some diagnostic mammograms as screening. Using a more conservative definition of screening mammogram, which largely accounted for this misclassification, estimates for overdiagnosis were smaller, ranging from 15% of cases in the 70-74 age group to 44% of cases in the 85 and older group. Results could not be adjusted for breast density, family history, and other breast cancer risk factors not captured by the data.
DISCLOSURES:
The work was funded by the National Cancer Institute. One author reported funding from Genentech and Johnson & Johnson.
A version of this article first appeared on Medscape.com.
TOPLINE:
Women who continue breast cancer screening after age 70 face a considerable risk for overdiagnosis.
METHODOLOGY:
- Overdiagnosis – the risk of detecting and treating cancers that would never have caused issues in a person’s lifetime – is increasingly recognized as a harm of breast cancer screening; however, the scope of the problem among older women remains uncertain.
- To get an idea, investigators linked Medicare claims data with Surveillance, Epidemiology, and End Results (SEER) data for 54,635 women 70 years or older to compare the incidence of breast cancer and breast cancer–specific death among women who continued screening mammography with those who did not.
- The women all had undergone recent screening mammograms and had no history of breast cancer at study entry. Those who had a subsequent mammogram within 3 years were classified as undergoing continued screening while those who did not were classified as not undergoing continued screening.
- Overdiagnosis was defined as the difference in cumulative incidence of breast cancer between screened and unscreened women divided by the cumulative incidence among screened women.
- Results were adjusted for potential confounders, including age, race, and ethnicity.
TAKEAWAY:
- Over 80% of women 70-84 years old and more than 60% of women 85 years or older continued screening.
- Among women 70-74 years old, the adjusted cumulative incidence of breast cancer was 6.1 cases per 100 screened women vs. 4.2 cases per 100 unscreened women; for women aged 75-84 years old, the cumulative incidence was 4.9 per 100 screened women vs. 2.6 per 100 unscreened women, and for women 85 years and older, the cumulative incidence was 2.8 vs. 1.3 per 100, respectively.
- Estimates of overdiagnosis ranged from 31% of breast cancer cases among screened women in the 70-74 age group to 54% of cases in the 85 and older group.
- The researchers found no statistically significant reduction in breast cancer–specific death associated with screening in any age or life-expectancy group. Overdiagnosis appeared to be driven by in situ and localized invasive breast cancer, not advanced breast cancer.
IN PRACTICE:
The proportion of older women who continue to receive screening mammograms and may experience breast cancer overdiagnosis is “considerable” and “increases with advancing age and with decreasing life expectancy,” the authors conclude. Given potential benefits and harms of screening in this population, “patient preferences, including risk tolerance, comfort with uncertainty, and willingness to undergo treatment, are important for informing screening decisions.”
SOURCE:
The study was led by Ilana Richman, MD, MHS, of the Yale School of Medicine, New Haven, Connecticut, and published in the Annals of Internal Medicine.
LIMITATIONS:
The definition of screening mammography in the study may have misclassified some diagnostic mammograms as screening. Using a more conservative definition of screening mammogram, which largely accounted for this misclassification, estimates for overdiagnosis were smaller, ranging from 15% of cases in the 70-74 age group to 44% of cases in the 85 and older group. Results could not be adjusted for breast density, family history, and other breast cancer risk factors not captured by the data.
DISCLOSURES:
The work was funded by the National Cancer Institute. One author reported funding from Genentech and Johnson & Johnson.
A version of this article first appeared on Medscape.com.
TOPLINE:
Women who continue breast cancer screening after age 70 face a considerable risk for overdiagnosis.
METHODOLOGY:
- Overdiagnosis – the risk of detecting and treating cancers that would never have caused issues in a person’s lifetime – is increasingly recognized as a harm of breast cancer screening; however, the scope of the problem among older women remains uncertain.
- To get an idea, investigators linked Medicare claims data with Surveillance, Epidemiology, and End Results (SEER) data for 54,635 women 70 years or older to compare the incidence of breast cancer and breast cancer–specific death among women who continued screening mammography with those who did not.
- The women all had undergone recent screening mammograms and had no history of breast cancer at study entry. Those who had a subsequent mammogram within 3 years were classified as undergoing continued screening while those who did not were classified as not undergoing continued screening.
- Overdiagnosis was defined as the difference in cumulative incidence of breast cancer between screened and unscreened women divided by the cumulative incidence among screened women.
- Results were adjusted for potential confounders, including age, race, and ethnicity.
TAKEAWAY:
- Over 80% of women 70-84 years old and more than 60% of women 85 years or older continued screening.
- Among women 70-74 years old, the adjusted cumulative incidence of breast cancer was 6.1 cases per 100 screened women vs. 4.2 cases per 100 unscreened women; for women aged 75-84 years old, the cumulative incidence was 4.9 per 100 screened women vs. 2.6 per 100 unscreened women, and for women 85 years and older, the cumulative incidence was 2.8 vs. 1.3 per 100, respectively.
- Estimates of overdiagnosis ranged from 31% of breast cancer cases among screened women in the 70-74 age group to 54% of cases in the 85 and older group.
- The researchers found no statistically significant reduction in breast cancer–specific death associated with screening in any age or life-expectancy group. Overdiagnosis appeared to be driven by in situ and localized invasive breast cancer, not advanced breast cancer.
IN PRACTICE:
The proportion of older women who continue to receive screening mammograms and may experience breast cancer overdiagnosis is “considerable” and “increases with advancing age and with decreasing life expectancy,” the authors conclude. Given potential benefits and harms of screening in this population, “patient preferences, including risk tolerance, comfort with uncertainty, and willingness to undergo treatment, are important for informing screening decisions.”
SOURCE:
The study was led by Ilana Richman, MD, MHS, of the Yale School of Medicine, New Haven, Connecticut, and published in the Annals of Internal Medicine.
LIMITATIONS:
The definition of screening mammography in the study may have misclassified some diagnostic mammograms as screening. Using a more conservative definition of screening mammogram, which largely accounted for this misclassification, estimates for overdiagnosis were smaller, ranging from 15% of cases in the 70-74 age group to 44% of cases in the 85 and older group. Results could not be adjusted for breast density, family history, and other breast cancer risk factors not captured by the data.
DISCLOSURES:
The work was funded by the National Cancer Institute. One author reported funding from Genentech and Johnson & Johnson.
A version of this article first appeared on Medscape.com.
Evolution of Targeted Therapies for C difficile
- Di Bella S et al. Toxins (Basel). 2016;8(5):134. doi:10.3390/toxins8050134
- Turner NA, Anderson DJ. Clin Colon Rectal Surg. 2020;33(2):98-108. doi:10.1055/s-0040-1701234
- Czepiel J et al. Eur J Clin Microbiol Infect Dis. 2019;38(7):1211-1221. doi:10.1007/s10096-019-03539-6
- Sekirov I et al. Gut microbiota in health and disease. Physiol Rev. 2012;90(3):859-904. doi:10.1152/physrev.00045.2009
- Posteraro B et al. Expert Opin Biol Ther. 2018;18(4):469-476. doi:10.1080/14712598.2018.1452908
- Khanna S. J Intern Med. 2021;290(2):294-309. doi:10.1111/joim.13290
- Seekatz AM et al . Therap Adv Gastroenterol. 2022;15:17562848221134396. doi:10.1177/17562848221134396
- Federal Drug Administration. FDA approves first fecal microbiota product: Rebyota approved for the prevention of recurrence of Clostridioides difficile infection in adults [press release]. Published November 30, 2022. Accessed July 14, 2023. https://www.fda.gov/news-events/press-announcements/fda-approves-first-fecal-microbiota-product
- Bafeta A et al. Ann Intern Med. 2017;167(1):34-39. doi:10.7326/M16-2810
- Guh AY et al; Emerging Infections Program Clostridioides difficile Infection Working Group. N Engl J Med. 2020;382(14):1320-1330. doi:10.1056/NEJMoa1910215
- Centers for Disease Control and Prevention. What is C. diff? Last reviewed September 7, 2022. Accessed July 14, 2023. https://www.cdc.gov/cdiff/what-is.html
- Centers for Disease Control and Prevention. Patients and families: be antibiotics aware. C. diff infection—Am I at risk? Accessed July 14, 2023. https://www.cdc.gov/cdiff/pdf/FS-Cdiff-PatientsFamilies-508.pdf
- Centers for Disease Control and Prevention. 2019 annual report for the emerging infections program for Clostridioides difficile infection. Last reviewed February 1, 2023. Accessed July 14, 2023. https://www.cdc.gov/hai/eip/Annual-CDI-Report-2019.html
- Kelly CR et al. Am J Gastroenterol. 2021;116(6):1124-1147. doi:10.14309/ajg.0000000000001278
- Tariq R et al. Therap Adv Gastroenterol. 2021;14:1756284821994046. doi:10.1177/1756284821994046
- McDonald LC et al. Clin Infect Dis. 2018;66(7):e1-e48. doi:10.1093/cid/cix1085
- Wilcox MH et al. N Engl J Med. 2017;376(4):305-317. doi:10.1056/NEJMoa1602615
- Guilleman MM et al. Gene Ther. 2023;30:455-462. doi:10.1038/s41434-021-00236-y
- Sims MD et al; ECOSPOR IV Investigators. JAMA Netw Open. 2023;6(2):e2255758. doi:10.1001/jamanetworkopen.2022.55758
- Microbiota Restoration Therapy for Recurrent Clostridium Difficile Infection (PUNCHCD2). ClinicalTrials.gov identifier: NCT02299570. Updated January 2021. Accessed August 2023. https://classic.clinicaltrials.gov/ct2/show/results/NCT02299570
- Khanna S et al. Clin Infect Dis. 2021;73(7):e1613-e1620. doi:10.1093/cid/ciaa1430
- Di Bella S et al. Toxins (Basel). 2016;8(5):134. doi:10.3390/toxins8050134
- Turner NA, Anderson DJ. Clin Colon Rectal Surg. 2020;33(2):98-108. doi:10.1055/s-0040-1701234
- Czepiel J et al. Eur J Clin Microbiol Infect Dis. 2019;38(7):1211-1221. doi:10.1007/s10096-019-03539-6
- Sekirov I et al. Gut microbiota in health and disease. Physiol Rev. 2012;90(3):859-904. doi:10.1152/physrev.00045.2009
- Posteraro B et al. Expert Opin Biol Ther. 2018;18(4):469-476. doi:10.1080/14712598.2018.1452908
- Khanna S. J Intern Med. 2021;290(2):294-309. doi:10.1111/joim.13290
- Seekatz AM et al . Therap Adv Gastroenterol. 2022;15:17562848221134396. doi:10.1177/17562848221134396
- Federal Drug Administration. FDA approves first fecal microbiota product: Rebyota approved for the prevention of recurrence of Clostridioides difficile infection in adults [press release]. Published November 30, 2022. Accessed July 14, 2023. https://www.fda.gov/news-events/press-announcements/fda-approves-first-fecal-microbiota-product
- Bafeta A et al. Ann Intern Med. 2017;167(1):34-39. doi:10.7326/M16-2810
- Guh AY et al; Emerging Infections Program Clostridioides difficile Infection Working Group. N Engl J Med. 2020;382(14):1320-1330. doi:10.1056/NEJMoa1910215
- Centers for Disease Control and Prevention. What is C. diff? Last reviewed September 7, 2022. Accessed July 14, 2023. https://www.cdc.gov/cdiff/what-is.html
- Centers for Disease Control and Prevention. Patients and families: be antibiotics aware. C. diff infection—Am I at risk? Accessed July 14, 2023. https://www.cdc.gov/cdiff/pdf/FS-Cdiff-PatientsFamilies-508.pdf
- Centers for Disease Control and Prevention. 2019 annual report for the emerging infections program for Clostridioides difficile infection. Last reviewed February 1, 2023. Accessed July 14, 2023. https://www.cdc.gov/hai/eip/Annual-CDI-Report-2019.html
- Kelly CR et al. Am J Gastroenterol. 2021;116(6):1124-1147. doi:10.14309/ajg.0000000000001278
- Tariq R et al. Therap Adv Gastroenterol. 2021;14:1756284821994046. doi:10.1177/1756284821994046
- McDonald LC et al. Clin Infect Dis. 2018;66(7):e1-e48. doi:10.1093/cid/cix1085
- Wilcox MH et al. N Engl J Med. 2017;376(4):305-317. doi:10.1056/NEJMoa1602615
- Guilleman MM et al. Gene Ther. 2023;30:455-462. doi:10.1038/s41434-021-00236-y
- Sims MD et al; ECOSPOR IV Investigators. JAMA Netw Open. 2023;6(2):e2255758. doi:10.1001/jamanetworkopen.2022.55758
- Microbiota Restoration Therapy for Recurrent Clostridium Difficile Infection (PUNCHCD2). ClinicalTrials.gov identifier: NCT02299570. Updated January 2021. Accessed August 2023. https://classic.clinicaltrials.gov/ct2/show/results/NCT02299570
- Khanna S et al. Clin Infect Dis. 2021;73(7):e1613-e1620. doi:10.1093/cid/ciaa1430
- Di Bella S et al. Toxins (Basel). 2016;8(5):134. doi:10.3390/toxins8050134
- Turner NA, Anderson DJ. Clin Colon Rectal Surg. 2020;33(2):98-108. doi:10.1055/s-0040-1701234
- Czepiel J et al. Eur J Clin Microbiol Infect Dis. 2019;38(7):1211-1221. doi:10.1007/s10096-019-03539-6
- Sekirov I et al. Gut microbiota in health and disease. Physiol Rev. 2012;90(3):859-904. doi:10.1152/physrev.00045.2009
- Posteraro B et al. Expert Opin Biol Ther. 2018;18(4):469-476. doi:10.1080/14712598.2018.1452908
- Khanna S. J Intern Med. 2021;290(2):294-309. doi:10.1111/joim.13290
- Seekatz AM et al . Therap Adv Gastroenterol. 2022;15:17562848221134396. doi:10.1177/17562848221134396
- Federal Drug Administration. FDA approves first fecal microbiota product: Rebyota approved for the prevention of recurrence of Clostridioides difficile infection in adults [press release]. Published November 30, 2022. Accessed July 14, 2023. https://www.fda.gov/news-events/press-announcements/fda-approves-first-fecal-microbiota-product
- Bafeta A et al. Ann Intern Med. 2017;167(1):34-39. doi:10.7326/M16-2810
- Guh AY et al; Emerging Infections Program Clostridioides difficile Infection Working Group. N Engl J Med. 2020;382(14):1320-1330. doi:10.1056/NEJMoa1910215
- Centers for Disease Control and Prevention. What is C. diff? Last reviewed September 7, 2022. Accessed July 14, 2023. https://www.cdc.gov/cdiff/what-is.html
- Centers for Disease Control and Prevention. Patients and families: be antibiotics aware. C. diff infection—Am I at risk? Accessed July 14, 2023. https://www.cdc.gov/cdiff/pdf/FS-Cdiff-PatientsFamilies-508.pdf
- Centers for Disease Control and Prevention. 2019 annual report for the emerging infections program for Clostridioides difficile infection. Last reviewed February 1, 2023. Accessed July 14, 2023. https://www.cdc.gov/hai/eip/Annual-CDI-Report-2019.html
- Kelly CR et al. Am J Gastroenterol. 2021;116(6):1124-1147. doi:10.14309/ajg.0000000000001278
- Tariq R et al. Therap Adv Gastroenterol. 2021;14:1756284821994046. doi:10.1177/1756284821994046
- McDonald LC et al. Clin Infect Dis. 2018;66(7):e1-e48. doi:10.1093/cid/cix1085
- Wilcox MH et al. N Engl J Med. 2017;376(4):305-317. doi:10.1056/NEJMoa1602615
- Guilleman MM et al. Gene Ther. 2023;30:455-462. doi:10.1038/s41434-021-00236-y
- Sims MD et al; ECOSPOR IV Investigators. JAMA Netw Open. 2023;6(2):e2255758. doi:10.1001/jamanetworkopen.2022.55758
- Microbiota Restoration Therapy for Recurrent Clostridium Difficile Infection (PUNCHCD2). ClinicalTrials.gov identifier: NCT02299570. Updated January 2021. Accessed August 2023. https://classic.clinicaltrials.gov/ct2/show/results/NCT02299570
- Khanna S et al. Clin Infect Dis. 2021;73(7):e1613-e1620. doi:10.1093/cid/ciaa1430
Gastroenterology Data Trends 2023
GI&Hepatology News and the American Gastroenterological Association present the 2023 issue of Gastroenterology Data Trends, a special report on hot topics in gastroenterology told through original infographics and visual storytelling.
In this issue:
- Gastroenterology and Climate Change: Assessing and Mitigating Impacts
Swapna Gayam, MD, FACG - MASLD/MASH and Weight Loss
Arpan Mohanty, MD, MSc - Digital Tools in the Management of IBS/Functional GI Disorders
Eric D. Shah, MD, MBA, FACG - Long COVID and the Gastrointestinal System: Emerging Evidence
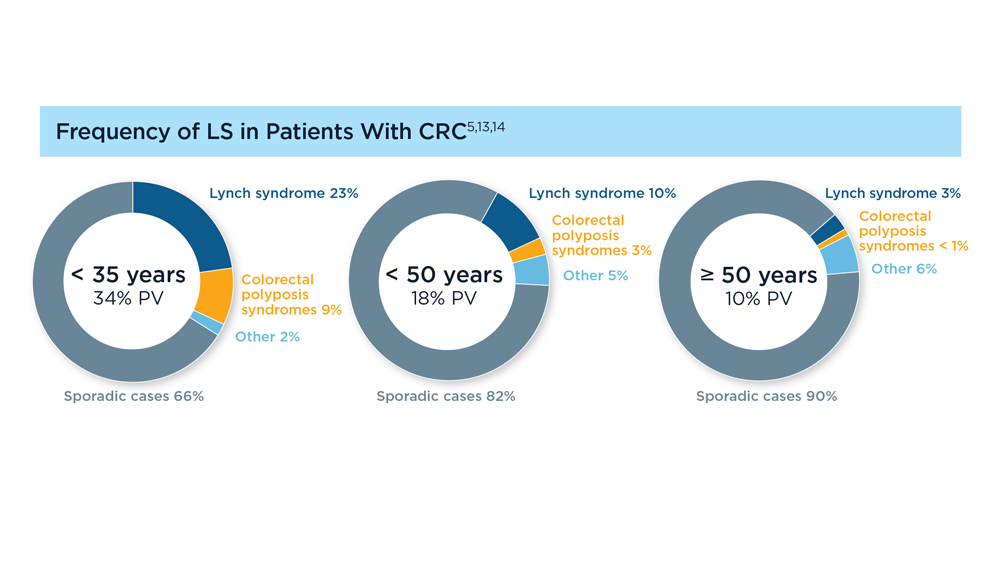
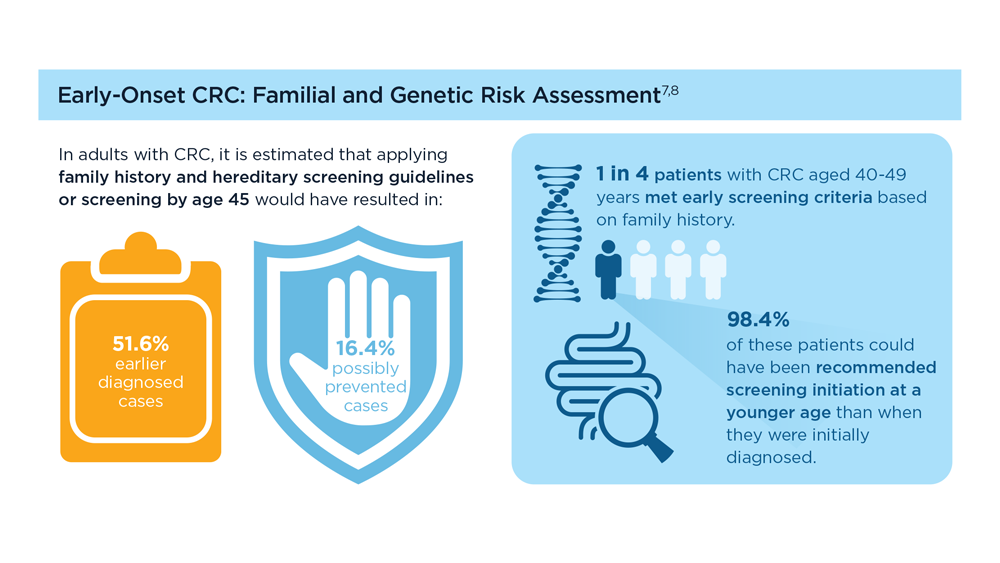
Daniel E. Freedberg, MD, MS, and Lin Chang, MD, AGAF - Germline Genetic Testing in CRC: Implications for Familial and Population-Based Testing
Fay Kastrinos, MD, MPH - Evolution of Targeted Therapies for C difficile
Sahil Khanna, MBBS, MS, FACG, AGAF - Harnessing the Power of AI to Enhance Endoscopy: Promises and Pitfalls
Eugenia Uche-Anya, MD, MPH - The Evolving Role of Surgery for IBD
Julie K.M. Thacker, MD, FACS, FASCRS
GI&Hepatology News and the American Gastroenterological Association present the 2023 issue of Gastroenterology Data Trends, a special report on hot topics in gastroenterology told through original infographics and visual storytelling.
In this issue:
- Gastroenterology and Climate Change: Assessing and Mitigating Impacts
Swapna Gayam, MD, FACG - MASLD/MASH and Weight Loss
Arpan Mohanty, MD, MSc - Digital Tools in the Management of IBS/Functional GI Disorders
Eric D. Shah, MD, MBA, FACG - Long COVID and the Gastrointestinal System: Emerging Evidence
Daniel E. Freedberg, MD, MS, and Lin Chang, MD, AGAF - Germline Genetic Testing in CRC: Implications for Familial and Population-Based Testing
Fay Kastrinos, MD, MPH - Evolution of Targeted Therapies for C difficile
Sahil Khanna, MBBS, MS, FACG, AGAF - Harnessing the Power of AI to Enhance Endoscopy: Promises and Pitfalls
Eugenia Uche-Anya, MD, MPH - The Evolving Role of Surgery for IBD
Julie K.M. Thacker, MD, FACS, FASCRS
GI&Hepatology News and the American Gastroenterological Association present the 2023 issue of Gastroenterology Data Trends, a special report on hot topics in gastroenterology told through original infographics and visual storytelling.
In this issue:
- Gastroenterology and Climate Change: Assessing and Mitigating Impacts
Swapna Gayam, MD, FACG - MASLD/MASH and Weight Loss
Arpan Mohanty, MD, MSc - Digital Tools in the Management of IBS/Functional GI Disorders
Eric D. Shah, MD, MBA, FACG - Long COVID and the Gastrointestinal System: Emerging Evidence
Daniel E. Freedberg, MD, MS, and Lin Chang, MD, AGAF - Germline Genetic Testing in CRC: Implications for Familial and Population-Based Testing
Fay Kastrinos, MD, MPH - Evolution of Targeted Therapies for C difficile
Sahil Khanna, MBBS, MS, FACG, AGAF - Harnessing the Power of AI to Enhance Endoscopy: Promises and Pitfalls
Eugenia Uche-Anya, MD, MPH - The Evolving Role of Surgery for IBD
Julie K.M. Thacker, MD, FACS, FASCRS
ADHD underappreciated in older adults
Negative consequences can develop from not treating ADHD, including job loss, suppressed income levels, low educational attainment, and difficulty maintaining relationships. Perhaps as many as 5% of adults have ADHD, which is highly hereditary.
Primary care physicians or family medicine clinicians are often best placed to diagnose ADHD in older adults, according to experts interviewed for this article. But first these providers need to tease out whether a patient has ADHD or another condition that is causing difficulties for these older adults.
However, clinicians may have a hard time discerning the symptoms of ADHD from that of other conditions of aging, such as mild cognitive impairment. Literature is lacking on best practices for screening and treating the condition in this population, according to a recent review published in the Expert Review of Neurotherapeutics, and a 2020 study by the same authors, epidemiologists, and psychiatrists based in Europe.
“If you don’t manage it, who will? It can be very hard to get psychiatric consults, almost impossible in some cases,” said Brendan Montano, MD, an internist in Cromwell, Conn., who specializes in treating ADHD.
A critical role for primary care and family medicine
Although no formal U.S. guidelines exist on diagnosis of adult ADHD, Dr. Montano stressed that adults usually present with symptoms such as chronic forgetfulness, distractibility, or procrastination. Hyperactivity is more internalized as a feeling of internal restlessness in this age group, Dr. Montano said, rather than the more visible hyper behavior seen in children.
“The two big ways that people present are thinking they have it or [being] in chaos of some sort,” perhaps because they have been fired or their spouse has asked for a divorce, Dr. Montano explained.
To assess the possibility of ADHD, a clinician could give a patient a six-item screening test that asks questions such as how often over the previous 6 months have they had trouble completing assignments or remembering appointments. If they report difficulty in four or more of the six areas in the brief screener, clinicians can move on to a longer 18-item screening tool developed by the World Health Organization, Dr. Montano said.
To make an ADHD diagnosis definitively, however, a patient needs to report sustained difficulties in at least two aspects of life: work, home, or social situations. And they have to indicate to a clinician that these troubles began before age 12.
“You have to really sit down and paint the picture with the patient: There are no shortcuts here,” said Lenard Adler, MD, a psychiatrist who directs the Adult ADHD program at New York University. Dr. Adler helped develop the six-item screener and is currently on a committee developing formal screening guidelines for adult ADHD in the United States.
He said that often, “ADHD cotravels with other mental health disorders like depression, bipolar disorders, anxiety disorders, and substance use disorders at least half the time.”
To tease out if a patient really has ADHD, clinicians can start with a more general screening for anxiety and hone in on the possibility of the condition if the anxiety screening reveals challenges with distractibility and forgetfulness, according to Karen Smith, MD, a family physician in Raeford, N.C.
“We can’t expect patients to walk through the door with the diagnosis stamped on their foreheads,” said Dr. Smith, who is a member of the board of directors for the American Academy of Family Physicians.
But a patient’s apparent signs of ADHD could be due to another condition such as hyperthyroidism or diabetes, Dr. Smith said. The driving principle is to take enough time to figure out exactly what is going on, she said, and then to treat accordingly. “If you ask the right questions, patients will give you good answers.”
Medications are often prescribed to help manage ADHD symptoms. These can include stimulants, controlled substances that include methylphenidate or amphetamine, or nonstimulants, such as atomoxetine and bupropion. Dr. Montano starts his patients on a lower dose and titrates them up rapidly until they reach the optimum dose that allows them to sustain focus and feel more productive. Patients complete frequent self-reports during this process.
“Any diversion is inappropriate,” said Dr. Montano, who writes a contract with his patients saying that stimulant medications will not be refilled if they are used more quickly than prescribed.
For older adults, physicians should make sure that stimulants do not exacerbate any underlying cardiovascular conditions, Dr. Montano said, and consult a cardiologist when needed.
The benefits of proper ADHD treatment can be profound, Dr. Adler noted, no matter when it begins.
“Older adults have lived their lives feeling they’ve been disorganized and a burden to their significant others, and only when they’ve taken medication have they really been able to organize their days and feel effective in their social interactions and with their families,” Dr. Adler said.
Dr. Montano has reported relationships with AbbVie, Axsome, Corium, Idorsia, Intracellular, Otsuka, Supernus, Sage/Biogen, Biohaven, Boehringer Ingelheim, Cassava, Eli Lilly, Intracellular, Janssen, Jazz, Sage, Supernus, Otsuka, and Tonix. Dr. Adler has reported relationships with Shire/Takeda Pharmaceuticals, National Football League, Major League Baseball, Corium, Otsuka, Neurocentria, Bracket/Signant, and SUNY; and is receiving royalty payments for developing adult ADHD assessments. Dr. Smith has reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
Negative consequences can develop from not treating ADHD, including job loss, suppressed income levels, low educational attainment, and difficulty maintaining relationships. Perhaps as many as 5% of adults have ADHD, which is highly hereditary.
Primary care physicians or family medicine clinicians are often best placed to diagnose ADHD in older adults, according to experts interviewed for this article. But first these providers need to tease out whether a patient has ADHD or another condition that is causing difficulties for these older adults.
However, clinicians may have a hard time discerning the symptoms of ADHD from that of other conditions of aging, such as mild cognitive impairment. Literature is lacking on best practices for screening and treating the condition in this population, according to a recent review published in the Expert Review of Neurotherapeutics, and a 2020 study by the same authors, epidemiologists, and psychiatrists based in Europe.
“If you don’t manage it, who will? It can be very hard to get psychiatric consults, almost impossible in some cases,” said Brendan Montano, MD, an internist in Cromwell, Conn., who specializes in treating ADHD.
A critical role for primary care and family medicine
Although no formal U.S. guidelines exist on diagnosis of adult ADHD, Dr. Montano stressed that adults usually present with symptoms such as chronic forgetfulness, distractibility, or procrastination. Hyperactivity is more internalized as a feeling of internal restlessness in this age group, Dr. Montano said, rather than the more visible hyper behavior seen in children.
“The two big ways that people present are thinking they have it or [being] in chaos of some sort,” perhaps because they have been fired or their spouse has asked for a divorce, Dr. Montano explained.
To assess the possibility of ADHD, a clinician could give a patient a six-item screening test that asks questions such as how often over the previous 6 months have they had trouble completing assignments or remembering appointments. If they report difficulty in four or more of the six areas in the brief screener, clinicians can move on to a longer 18-item screening tool developed by the World Health Organization, Dr. Montano said.
To make an ADHD diagnosis definitively, however, a patient needs to report sustained difficulties in at least two aspects of life: work, home, or social situations. And they have to indicate to a clinician that these troubles began before age 12.
“You have to really sit down and paint the picture with the patient: There are no shortcuts here,” said Lenard Adler, MD, a psychiatrist who directs the Adult ADHD program at New York University. Dr. Adler helped develop the six-item screener and is currently on a committee developing formal screening guidelines for adult ADHD in the United States.
He said that often, “ADHD cotravels with other mental health disorders like depression, bipolar disorders, anxiety disorders, and substance use disorders at least half the time.”
To tease out if a patient really has ADHD, clinicians can start with a more general screening for anxiety and hone in on the possibility of the condition if the anxiety screening reveals challenges with distractibility and forgetfulness, according to Karen Smith, MD, a family physician in Raeford, N.C.
“We can’t expect patients to walk through the door with the diagnosis stamped on their foreheads,” said Dr. Smith, who is a member of the board of directors for the American Academy of Family Physicians.
But a patient’s apparent signs of ADHD could be due to another condition such as hyperthyroidism or diabetes, Dr. Smith said. The driving principle is to take enough time to figure out exactly what is going on, she said, and then to treat accordingly. “If you ask the right questions, patients will give you good answers.”
Medications are often prescribed to help manage ADHD symptoms. These can include stimulants, controlled substances that include methylphenidate or amphetamine, or nonstimulants, such as atomoxetine and bupropion. Dr. Montano starts his patients on a lower dose and titrates them up rapidly until they reach the optimum dose that allows them to sustain focus and feel more productive. Patients complete frequent self-reports during this process.
“Any diversion is inappropriate,” said Dr. Montano, who writes a contract with his patients saying that stimulant medications will not be refilled if they are used more quickly than prescribed.
For older adults, physicians should make sure that stimulants do not exacerbate any underlying cardiovascular conditions, Dr. Montano said, and consult a cardiologist when needed.
The benefits of proper ADHD treatment can be profound, Dr. Adler noted, no matter when it begins.
“Older adults have lived their lives feeling they’ve been disorganized and a burden to their significant others, and only when they’ve taken medication have they really been able to organize their days and feel effective in their social interactions and with their families,” Dr. Adler said.
Dr. Montano has reported relationships with AbbVie, Axsome, Corium, Idorsia, Intracellular, Otsuka, Supernus, Sage/Biogen, Biohaven, Boehringer Ingelheim, Cassava, Eli Lilly, Intracellular, Janssen, Jazz, Sage, Supernus, Otsuka, and Tonix. Dr. Adler has reported relationships with Shire/Takeda Pharmaceuticals, National Football League, Major League Baseball, Corium, Otsuka, Neurocentria, Bracket/Signant, and SUNY; and is receiving royalty payments for developing adult ADHD assessments. Dr. Smith has reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
Negative consequences can develop from not treating ADHD, including job loss, suppressed income levels, low educational attainment, and difficulty maintaining relationships. Perhaps as many as 5% of adults have ADHD, which is highly hereditary.
Primary care physicians or family medicine clinicians are often best placed to diagnose ADHD in older adults, according to experts interviewed for this article. But first these providers need to tease out whether a patient has ADHD or another condition that is causing difficulties for these older adults.
However, clinicians may have a hard time discerning the symptoms of ADHD from that of other conditions of aging, such as mild cognitive impairment. Literature is lacking on best practices for screening and treating the condition in this population, according to a recent review published in the Expert Review of Neurotherapeutics, and a 2020 study by the same authors, epidemiologists, and psychiatrists based in Europe.
“If you don’t manage it, who will? It can be very hard to get psychiatric consults, almost impossible in some cases,” said Brendan Montano, MD, an internist in Cromwell, Conn., who specializes in treating ADHD.
A critical role for primary care and family medicine
Although no formal U.S. guidelines exist on diagnosis of adult ADHD, Dr. Montano stressed that adults usually present with symptoms such as chronic forgetfulness, distractibility, or procrastination. Hyperactivity is more internalized as a feeling of internal restlessness in this age group, Dr. Montano said, rather than the more visible hyper behavior seen in children.
“The two big ways that people present are thinking they have it or [being] in chaos of some sort,” perhaps because they have been fired or their spouse has asked for a divorce, Dr. Montano explained.
To assess the possibility of ADHD, a clinician could give a patient a six-item screening test that asks questions such as how often over the previous 6 months have they had trouble completing assignments or remembering appointments. If they report difficulty in four or more of the six areas in the brief screener, clinicians can move on to a longer 18-item screening tool developed by the World Health Organization, Dr. Montano said.
To make an ADHD diagnosis definitively, however, a patient needs to report sustained difficulties in at least two aspects of life: work, home, or social situations. And they have to indicate to a clinician that these troubles began before age 12.
“You have to really sit down and paint the picture with the patient: There are no shortcuts here,” said Lenard Adler, MD, a psychiatrist who directs the Adult ADHD program at New York University. Dr. Adler helped develop the six-item screener and is currently on a committee developing formal screening guidelines for adult ADHD in the United States.
He said that often, “ADHD cotravels with other mental health disorders like depression, bipolar disorders, anxiety disorders, and substance use disorders at least half the time.”
To tease out if a patient really has ADHD, clinicians can start with a more general screening for anxiety and hone in on the possibility of the condition if the anxiety screening reveals challenges with distractibility and forgetfulness, according to Karen Smith, MD, a family physician in Raeford, N.C.
“We can’t expect patients to walk through the door with the diagnosis stamped on their foreheads,” said Dr. Smith, who is a member of the board of directors for the American Academy of Family Physicians.
But a patient’s apparent signs of ADHD could be due to another condition such as hyperthyroidism or diabetes, Dr. Smith said. The driving principle is to take enough time to figure out exactly what is going on, she said, and then to treat accordingly. “If you ask the right questions, patients will give you good answers.”
Medications are often prescribed to help manage ADHD symptoms. These can include stimulants, controlled substances that include methylphenidate or amphetamine, or nonstimulants, such as atomoxetine and bupropion. Dr. Montano starts his patients on a lower dose and titrates them up rapidly until they reach the optimum dose that allows them to sustain focus and feel more productive. Patients complete frequent self-reports during this process.
“Any diversion is inappropriate,” said Dr. Montano, who writes a contract with his patients saying that stimulant medications will not be refilled if they are used more quickly than prescribed.
For older adults, physicians should make sure that stimulants do not exacerbate any underlying cardiovascular conditions, Dr. Montano said, and consult a cardiologist when needed.
The benefits of proper ADHD treatment can be profound, Dr. Adler noted, no matter when it begins.
“Older adults have lived their lives feeling they’ve been disorganized and a burden to their significant others, and only when they’ve taken medication have they really been able to organize their days and feel effective in their social interactions and with their families,” Dr. Adler said.
Dr. Montano has reported relationships with AbbVie, Axsome, Corium, Idorsia, Intracellular, Otsuka, Supernus, Sage/Biogen, Biohaven, Boehringer Ingelheim, Cassava, Eli Lilly, Intracellular, Janssen, Jazz, Sage, Supernus, Otsuka, and Tonix. Dr. Adler has reported relationships with Shire/Takeda Pharmaceuticals, National Football League, Major League Baseball, Corium, Otsuka, Neurocentria, Bracket/Signant, and SUNY; and is receiving royalty payments for developing adult ADHD assessments. Dr. Smith has reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
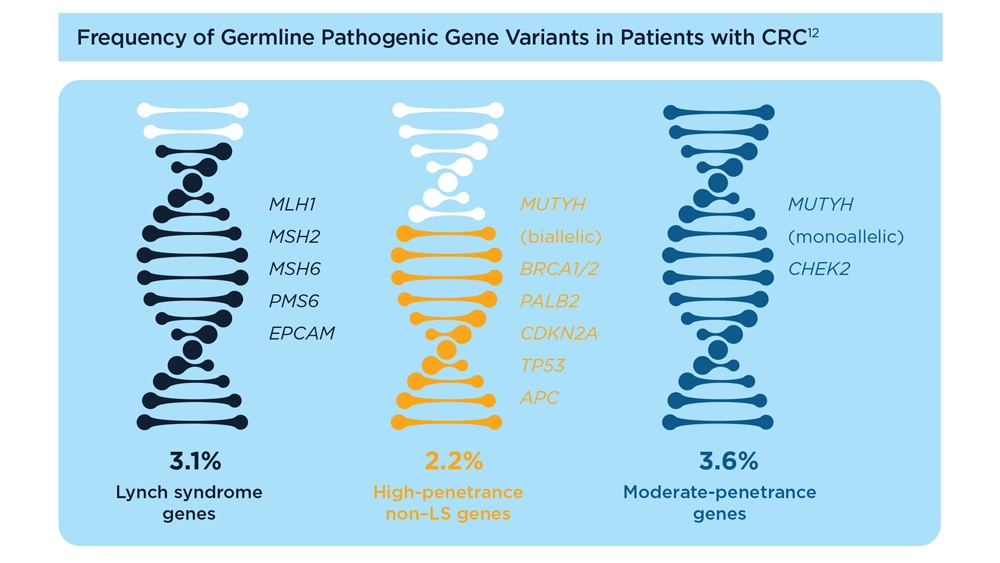
Germline Genetic Testing in CRC: Implications for Familial and Population-Based Testing
- Weiss JM et al. J Natl Compr Canc Netw. 2021;19(10):1122-1132. doi:10.1164/jnccn.2021.0048
- Samadder NJ et al. JAMA Oncol. 2021;7(2):230-237. doi:10.1001/jamaoncol.2020.6252
- Pearlman R et al; Ohio Colorectal Cancer Prevention Initiative Study Group. JAMA Oncol. 2017;3(4):464-471. doi:10.1001/jamaoncol.2016.5194
- Stoffel EM et al. Gastroenterology. 2018;154(4):897-905.e1. doi:10.1053/j.gastro.2017.11.004
- Stoffel EM, Murphy CC. Gastroenterology. 2020;158(2):341-353. doi:10.1053/j.gastro.2019.07.055
- Cavestro GM et al; Associazione Italiana Familiarità Ereditarietà Tumori; Collaborative Group of the Americas on Inherited Gastrointestinal Cancer; European Hereditary Tumour Group, and the International Society for Gastrointestinal Hereditary Tumours. Clin Gastroenterol Hepatol. 2023;21(3):581-603.e33. doi:10.1016/j.cgh.2022.12.006
- Gupta S et al. Cancer. 2020;126(13):3013-3020. doi:10.1002/cncr.32851
- Stanich PP et al. Gastroenterology. 2021;160(5):1850-1852. doi:10.1053/j.gastro.2020.12.009
- Rustgi S et al. Universal screening strategies for the identification of Lynch syndrome in colorectal cancer patients and at-risk relatives. Research forum lecture #263 presented at: Digestive Disease Week (DDW) 2023; May 6-9, 2023; Chicago, IL.
- Tier 1 genomic applications and their importance to public health. Centers for Disease Control and Prevention. Reviewed March 6, 2014. Accessed August 15, 2023. https://www.cdc.gov/genomics/implementation/toolkit/tier1.htm
- Win AK et al. Cancer Epidemiol Biomarkers Prev. 2017;26(3):404-412. doi:10.1158/1055-9965.EPI-16-0693
- Yurgelun MB et al. J Clin Oncol. 2017;35(10):1086-1095. doi:10.1200/JCO.2016.71.0012
- Pearlman R et al. JCO Precis Oncol. 2021;5:PO.20.00525. doi:10.1200/PO.20.00525
- Patel R, Hyer W. Frontline Gastroenterol. 2019;10(4):379-387. doi:10.1136/flgastro-2018-101053
- Weiss JM et al. J Natl Compr Canc Netw. 2021;19(10):1122-1132. doi:10.1164/jnccn.2021.0048
- Samadder NJ et al. JAMA Oncol. 2021;7(2):230-237. doi:10.1001/jamaoncol.2020.6252
- Pearlman R et al; Ohio Colorectal Cancer Prevention Initiative Study Group. JAMA Oncol. 2017;3(4):464-471. doi:10.1001/jamaoncol.2016.5194
- Stoffel EM et al. Gastroenterology. 2018;154(4):897-905.e1. doi:10.1053/j.gastro.2017.11.004
- Stoffel EM, Murphy CC. Gastroenterology. 2020;158(2):341-353. doi:10.1053/j.gastro.2019.07.055
- Cavestro GM et al; Associazione Italiana Familiarità Ereditarietà Tumori; Collaborative Group of the Americas on Inherited Gastrointestinal Cancer; European Hereditary Tumour Group, and the International Society for Gastrointestinal Hereditary Tumours. Clin Gastroenterol Hepatol. 2023;21(3):581-603.e33. doi:10.1016/j.cgh.2022.12.006
- Gupta S et al. Cancer. 2020;126(13):3013-3020. doi:10.1002/cncr.32851
- Stanich PP et al. Gastroenterology. 2021;160(5):1850-1852. doi:10.1053/j.gastro.2020.12.009
- Rustgi S et al. Universal screening strategies for the identification of Lynch syndrome in colorectal cancer patients and at-risk relatives. Research forum lecture #263 presented at: Digestive Disease Week (DDW) 2023; May 6-9, 2023; Chicago, IL.
- Tier 1 genomic applications and their importance to public health. Centers for Disease Control and Prevention. Reviewed March 6, 2014. Accessed August 15, 2023. https://www.cdc.gov/genomics/implementation/toolkit/tier1.htm
- Win AK et al. Cancer Epidemiol Biomarkers Prev. 2017;26(3):404-412. doi:10.1158/1055-9965.EPI-16-0693
- Yurgelun MB et al. J Clin Oncol. 2017;35(10):1086-1095. doi:10.1200/JCO.2016.71.0012
- Pearlman R et al. JCO Precis Oncol. 2021;5:PO.20.00525. doi:10.1200/PO.20.00525
- Patel R, Hyer W. Frontline Gastroenterol. 2019;10(4):379-387. doi:10.1136/flgastro-2018-101053
- Weiss JM et al. J Natl Compr Canc Netw. 2021;19(10):1122-1132. doi:10.1164/jnccn.2021.0048
- Samadder NJ et al. JAMA Oncol. 2021;7(2):230-237. doi:10.1001/jamaoncol.2020.6252
- Pearlman R et al; Ohio Colorectal Cancer Prevention Initiative Study Group. JAMA Oncol. 2017;3(4):464-471. doi:10.1001/jamaoncol.2016.5194
- Stoffel EM et al. Gastroenterology. 2018;154(4):897-905.e1. doi:10.1053/j.gastro.2017.11.004
- Stoffel EM, Murphy CC. Gastroenterology. 2020;158(2):341-353. doi:10.1053/j.gastro.2019.07.055
- Cavestro GM et al; Associazione Italiana Familiarità Ereditarietà Tumori; Collaborative Group of the Americas on Inherited Gastrointestinal Cancer; European Hereditary Tumour Group, and the International Society for Gastrointestinal Hereditary Tumours. Clin Gastroenterol Hepatol. 2023;21(3):581-603.e33. doi:10.1016/j.cgh.2022.12.006
- Gupta S et al. Cancer. 2020;126(13):3013-3020. doi:10.1002/cncr.32851
- Stanich PP et al. Gastroenterology. 2021;160(5):1850-1852. doi:10.1053/j.gastro.2020.12.009
- Rustgi S et al. Universal screening strategies for the identification of Lynch syndrome in colorectal cancer patients and at-risk relatives. Research forum lecture #263 presented at: Digestive Disease Week (DDW) 2023; May 6-9, 2023; Chicago, IL.
- Tier 1 genomic applications and their importance to public health. Centers for Disease Control and Prevention. Reviewed March 6, 2014. Accessed August 15, 2023. https://www.cdc.gov/genomics/implementation/toolkit/tier1.htm
- Win AK et al. Cancer Epidemiol Biomarkers Prev. 2017;26(3):404-412. doi:10.1158/1055-9965.EPI-16-0693
- Yurgelun MB et al. J Clin Oncol. 2017;35(10):1086-1095. doi:10.1200/JCO.2016.71.0012
- Pearlman R et al. JCO Precis Oncol. 2021;5:PO.20.00525. doi:10.1200/PO.20.00525
- Patel R, Hyer W. Frontline Gastroenterol. 2019;10(4):379-387. doi:10.1136/flgastro-2018-101053
Unique twin study sheds new light on TBI and risk of cognitive decline
The research, which included almost 9,000 individuals, showed that twins who had experienced a TBI were more likely to have lower cognitive function at age 70 versus their twin who did not experience a TBI, especially if they had lost consciousness or were older than age 24 at the time of injury. In addition, their cognitive decline occurred at a more rapid rate.
“We know that TBI increases the risk of developing Alzheimer’s disease and other dementias in later life, but we haven’t known about TBI’s effect on cognitive decline that does not quite meet the threshold for dementia,” study investigator Marianne Chanti-Ketterl, PhD, Duke University, Durham, N.C., said in an interview.
“We know that TBI increases the risk of dementia in later life, but we haven’t known if TBI affects cognitive function, causes cognitive decline that has not progressed to the point of severity with Alzheimer’s or dementia,” she added.
Being able to study the impact of TBI in monozygotic twins gives this study a unique strength, she noted.
“The important thing about this is that they are monozygotic twins, and we know they shared a lot of early life exposure, and almost 100% genetics,” Dr. Chanti-Ketterl said.
The study was published online in Neurology.
For the study, the investigators assessed 8,662 participants born between 1917 and 1927 who were part of the National Academy of Sciences National Research Council’s Twin Registry. The registry is composed of male veterans of World War II with a history of TBI, as reported by themselves or a caregiver.
The men were followed up for many years as part of the registry, but cognitive assessment only began in the 1990s. They were followed up at four different time points, at which time the Telephone Interview for Cognitive Status (TICS-m), an alternative to the Mini-Mental State Examination that must be given in person, was administered.
A total of 25% of participants had experienced concussion in their lifetime. Of this cohort, there were 589 pairs of monozygotic twins who were discordant (one twin had TBI and the other had not).
Among the monozygotic twin cohort, a history of any TBI and being older than age 24 at the time of TBI were associated with lower TICS-m scores.
A twin who experienced TBI after age 24 scored 0.59 points lower on the TICS-m at age 70 than his twin with no TBI, and cognitive function declined faster, by 0.05 points per year.
First study of its kind
Holly Elser, MD, PhD, MPH, an epidemiologist and resident physician in neurology at the University of Pennsylvania, Philadelphia, and coauthor of an accompanying editorial, said in an interview that the study’s twin design was a definite strength.
“There are lots of papers that have remarked on the apparent association between head injury and subsequent dementia or cognitive decline, but to my knowledge, this is one of the first, if not the first, to use a twin study design, which has the unique advantage of having better control over early life and genetic factors than would ever typically be possible in a dataset of unrelated adults,” said Dr. Elser.
She added that the study findings “strengthen our understanding of the relationship between TBI and later cognitive decline, so I think there is an etiologic value to the study.”
However, Dr. Elser noted that the composition of the study population may limit the extent to which the results apply to contemporary populations.
“This was a population of White male twins born between 1917 and 1927,” she noted. “However, does the experience of people who were in the military generalize to civilian populations? Are twins representative of the general population or are they unique in terms of their risk factors?”
It is always important to emphasize inclusivity in clinical research, and in dementia research in particular, Dr. Elser added.
“There are many examples of instances where racialized and otherwise economically marginalized groups have been excluded from analysis, which is problematic because there are already economically and socially marginalized groups who disproportionately bear the brunt of dementia.
“This is not a criticism of the authors’ work, that their data didn’t include a more diverse patient base, but I think it is an important reminder that we should always interpret study findings within the limitations of the data. It’s a reminder to be thoughtful about taking explicit steps to include more diverse groups in future research,” she said.
The study was funded by the National Institute on Aging/National Institutes of Health and the Department of Defense. Dr. Chanti-Ketterl and Dr. Elser have reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
The research, which included almost 9,000 individuals, showed that twins who had experienced a TBI were more likely to have lower cognitive function at age 70 versus their twin who did not experience a TBI, especially if they had lost consciousness or were older than age 24 at the time of injury. In addition, their cognitive decline occurred at a more rapid rate.
“We know that TBI increases the risk of developing Alzheimer’s disease and other dementias in later life, but we haven’t known about TBI’s effect on cognitive decline that does not quite meet the threshold for dementia,” study investigator Marianne Chanti-Ketterl, PhD, Duke University, Durham, N.C., said in an interview.
“We know that TBI increases the risk of dementia in later life, but we haven’t known if TBI affects cognitive function, causes cognitive decline that has not progressed to the point of severity with Alzheimer’s or dementia,” she added.
Being able to study the impact of TBI in monozygotic twins gives this study a unique strength, she noted.
“The important thing about this is that they are monozygotic twins, and we know they shared a lot of early life exposure, and almost 100% genetics,” Dr. Chanti-Ketterl said.
The study was published online in Neurology.
For the study, the investigators assessed 8,662 participants born between 1917 and 1927 who were part of the National Academy of Sciences National Research Council’s Twin Registry. The registry is composed of male veterans of World War II with a history of TBI, as reported by themselves or a caregiver.
The men were followed up for many years as part of the registry, but cognitive assessment only began in the 1990s. They were followed up at four different time points, at which time the Telephone Interview for Cognitive Status (TICS-m), an alternative to the Mini-Mental State Examination that must be given in person, was administered.
A total of 25% of participants had experienced concussion in their lifetime. Of this cohort, there were 589 pairs of monozygotic twins who were discordant (one twin had TBI and the other had not).
Among the monozygotic twin cohort, a history of any TBI and being older than age 24 at the time of TBI were associated with lower TICS-m scores.
A twin who experienced TBI after age 24 scored 0.59 points lower on the TICS-m at age 70 than his twin with no TBI, and cognitive function declined faster, by 0.05 points per year.
First study of its kind
Holly Elser, MD, PhD, MPH, an epidemiologist and resident physician in neurology at the University of Pennsylvania, Philadelphia, and coauthor of an accompanying editorial, said in an interview that the study’s twin design was a definite strength.
“There are lots of papers that have remarked on the apparent association between head injury and subsequent dementia or cognitive decline, but to my knowledge, this is one of the first, if not the first, to use a twin study design, which has the unique advantage of having better control over early life and genetic factors than would ever typically be possible in a dataset of unrelated adults,” said Dr. Elser.
She added that the study findings “strengthen our understanding of the relationship between TBI and later cognitive decline, so I think there is an etiologic value to the study.”
However, Dr. Elser noted that the composition of the study population may limit the extent to which the results apply to contemporary populations.
“This was a population of White male twins born between 1917 and 1927,” she noted. “However, does the experience of people who were in the military generalize to civilian populations? Are twins representative of the general population or are they unique in terms of their risk factors?”
It is always important to emphasize inclusivity in clinical research, and in dementia research in particular, Dr. Elser added.
“There are many examples of instances where racialized and otherwise economically marginalized groups have been excluded from analysis, which is problematic because there are already economically and socially marginalized groups who disproportionately bear the brunt of dementia.
“This is not a criticism of the authors’ work, that their data didn’t include a more diverse patient base, but I think it is an important reminder that we should always interpret study findings within the limitations of the data. It’s a reminder to be thoughtful about taking explicit steps to include more diverse groups in future research,” she said.
The study was funded by the National Institute on Aging/National Institutes of Health and the Department of Defense. Dr. Chanti-Ketterl and Dr. Elser have reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
The research, which included almost 9,000 individuals, showed that twins who had experienced a TBI were more likely to have lower cognitive function at age 70 versus their twin who did not experience a TBI, especially if they had lost consciousness or were older than age 24 at the time of injury. In addition, their cognitive decline occurred at a more rapid rate.
“We know that TBI increases the risk of developing Alzheimer’s disease and other dementias in later life, but we haven’t known about TBI’s effect on cognitive decline that does not quite meet the threshold for dementia,” study investigator Marianne Chanti-Ketterl, PhD, Duke University, Durham, N.C., said in an interview.
“We know that TBI increases the risk of dementia in later life, but we haven’t known if TBI affects cognitive function, causes cognitive decline that has not progressed to the point of severity with Alzheimer’s or dementia,” she added.
Being able to study the impact of TBI in monozygotic twins gives this study a unique strength, she noted.
“The important thing about this is that they are monozygotic twins, and we know they shared a lot of early life exposure, and almost 100% genetics,” Dr. Chanti-Ketterl said.
The study was published online in Neurology.
For the study, the investigators assessed 8,662 participants born between 1917 and 1927 who were part of the National Academy of Sciences National Research Council’s Twin Registry. The registry is composed of male veterans of World War II with a history of TBI, as reported by themselves or a caregiver.
The men were followed up for many years as part of the registry, but cognitive assessment only began in the 1990s. They were followed up at four different time points, at which time the Telephone Interview for Cognitive Status (TICS-m), an alternative to the Mini-Mental State Examination that must be given in person, was administered.
A total of 25% of participants had experienced concussion in their lifetime. Of this cohort, there were 589 pairs of monozygotic twins who were discordant (one twin had TBI and the other had not).
Among the monozygotic twin cohort, a history of any TBI and being older than age 24 at the time of TBI were associated with lower TICS-m scores.
A twin who experienced TBI after age 24 scored 0.59 points lower on the TICS-m at age 70 than his twin with no TBI, and cognitive function declined faster, by 0.05 points per year.
First study of its kind
Holly Elser, MD, PhD, MPH, an epidemiologist and resident physician in neurology at the University of Pennsylvania, Philadelphia, and coauthor of an accompanying editorial, said in an interview that the study’s twin design was a definite strength.
“There are lots of papers that have remarked on the apparent association between head injury and subsequent dementia or cognitive decline, but to my knowledge, this is one of the first, if not the first, to use a twin study design, which has the unique advantage of having better control over early life and genetic factors than would ever typically be possible in a dataset of unrelated adults,” said Dr. Elser.
She added that the study findings “strengthen our understanding of the relationship between TBI and later cognitive decline, so I think there is an etiologic value to the study.”
However, Dr. Elser noted that the composition of the study population may limit the extent to which the results apply to contemporary populations.
“This was a population of White male twins born between 1917 and 1927,” she noted. “However, does the experience of people who were in the military generalize to civilian populations? Are twins representative of the general population or are they unique in terms of their risk factors?”
It is always important to emphasize inclusivity in clinical research, and in dementia research in particular, Dr. Elser added.
“There are many examples of instances where racialized and otherwise economically marginalized groups have been excluded from analysis, which is problematic because there are already economically and socially marginalized groups who disproportionately bear the brunt of dementia.
“This is not a criticism of the authors’ work, that their data didn’t include a more diverse patient base, but I think it is an important reminder that we should always interpret study findings within the limitations of the data. It’s a reminder to be thoughtful about taking explicit steps to include more diverse groups in future research,” she said.
The study was funded by the National Institute on Aging/National Institutes of Health and the Department of Defense. Dr. Chanti-Ketterl and Dr. Elser have reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
FROM NEUROLOGY
Second pig-heart transplant patient at UM faring well
The organ passed an early test by avoiding hyperacute rejection.
Physicians for the patient, a 58-year-old former lab tech repeatedly turned down for standard allograft transplantation, say they are making good use of lessons from last year’s case of David Bennett, who survived in hospital with difficulty for 2 months after receiving the first such heart at the center in January 2022.
Mr. Bennett’s clinical course had been promising at first but grew turbulent with repeated bouts of infection followed by adjustments to his aggressive immunosuppressant regimen and other complications.
It was also learned weeks after the xenotransplant operation that the heart from the genetically modified donor pig had carried a porcine cytomegalovirus to Mr. Bennett’s body, although there was never evidence that the virus infected other organs or played a major role in his death.
The new xenotransplant recipient, Lawrence Faucette of Frederick, Md., is benefiting from that experience, which was documented in journal reports.
Mr. Faucette had been turned down by UMMC “and several other leading transplant hospitals due to his pre-existing peripheral vascular disease and complications with internal bleeding,” notes a UMMC press release describing his procedure.
The patient “is currently breathing on his own, and his heart is functioning well without any assistance from supportive devices,” says the statement.
Despite a few setbacks, Mr. Faucette is “on the right track,” said Muhammad M. Mohiuddin, MBBS, surgeon and xenotransplantation program director at the University of Maryland, Baltimore, in an interview.
“We’re taking one day at a time. His immune system is still intact, despite the heavy immune suppression,” he told this news organization. His heart didn’t carry a virus and “has not shown any signs of rejection so far.”
The University of Maryland team, Dr. Mohiuddin said, “is very hopeful that we will be able to at least mobilize the patient, and he can be discharged. But it’s a little too early to call.”
Mr. Faucette, as part of his immunosuppressant regimen, is receiving tegoprubart (Eledon Pharmaceuticals), an investigational antibody that blocks CD40 ligand. His predecessor Mr. Bennett, in contrast, had received a blocker of the CD40 receptor (Kiniksa Pharmaceuticals) along with other more familiar immunosuppressants.
The new anti–CD40-ligand blocker, Eledon said, is in phase 1 studies looking at efficacy in patients with conventional kidney transplants.
A version of this article appeared on Medscape.com.
The organ passed an early test by avoiding hyperacute rejection.
Physicians for the patient, a 58-year-old former lab tech repeatedly turned down for standard allograft transplantation, say they are making good use of lessons from last year’s case of David Bennett, who survived in hospital with difficulty for 2 months after receiving the first such heart at the center in January 2022.
Mr. Bennett’s clinical course had been promising at first but grew turbulent with repeated bouts of infection followed by adjustments to his aggressive immunosuppressant regimen and other complications.
It was also learned weeks after the xenotransplant operation that the heart from the genetically modified donor pig had carried a porcine cytomegalovirus to Mr. Bennett’s body, although there was never evidence that the virus infected other organs or played a major role in his death.
The new xenotransplant recipient, Lawrence Faucette of Frederick, Md., is benefiting from that experience, which was documented in journal reports.
Mr. Faucette had been turned down by UMMC “and several other leading transplant hospitals due to his pre-existing peripheral vascular disease and complications with internal bleeding,” notes a UMMC press release describing his procedure.
The patient “is currently breathing on his own, and his heart is functioning well without any assistance from supportive devices,” says the statement.
Despite a few setbacks, Mr. Faucette is “on the right track,” said Muhammad M. Mohiuddin, MBBS, surgeon and xenotransplantation program director at the University of Maryland, Baltimore, in an interview.
“We’re taking one day at a time. His immune system is still intact, despite the heavy immune suppression,” he told this news organization. His heart didn’t carry a virus and “has not shown any signs of rejection so far.”
The University of Maryland team, Dr. Mohiuddin said, “is very hopeful that we will be able to at least mobilize the patient, and he can be discharged. But it’s a little too early to call.”
Mr. Faucette, as part of his immunosuppressant regimen, is receiving tegoprubart (Eledon Pharmaceuticals), an investigational antibody that blocks CD40 ligand. His predecessor Mr. Bennett, in contrast, had received a blocker of the CD40 receptor (Kiniksa Pharmaceuticals) along with other more familiar immunosuppressants.
The new anti–CD40-ligand blocker, Eledon said, is in phase 1 studies looking at efficacy in patients with conventional kidney transplants.
A version of this article appeared on Medscape.com.
The organ passed an early test by avoiding hyperacute rejection.
Physicians for the patient, a 58-year-old former lab tech repeatedly turned down for standard allograft transplantation, say they are making good use of lessons from last year’s case of David Bennett, who survived in hospital with difficulty for 2 months after receiving the first such heart at the center in January 2022.
Mr. Bennett’s clinical course had been promising at first but grew turbulent with repeated bouts of infection followed by adjustments to his aggressive immunosuppressant regimen and other complications.
It was also learned weeks after the xenotransplant operation that the heart from the genetically modified donor pig had carried a porcine cytomegalovirus to Mr. Bennett’s body, although there was never evidence that the virus infected other organs or played a major role in his death.
The new xenotransplant recipient, Lawrence Faucette of Frederick, Md., is benefiting from that experience, which was documented in journal reports.
Mr. Faucette had been turned down by UMMC “and several other leading transplant hospitals due to his pre-existing peripheral vascular disease and complications with internal bleeding,” notes a UMMC press release describing his procedure.
The patient “is currently breathing on his own, and his heart is functioning well without any assistance from supportive devices,” says the statement.
Despite a few setbacks, Mr. Faucette is “on the right track,” said Muhammad M. Mohiuddin, MBBS, surgeon and xenotransplantation program director at the University of Maryland, Baltimore, in an interview.
“We’re taking one day at a time. His immune system is still intact, despite the heavy immune suppression,” he told this news organization. His heart didn’t carry a virus and “has not shown any signs of rejection so far.”
The University of Maryland team, Dr. Mohiuddin said, “is very hopeful that we will be able to at least mobilize the patient, and he can be discharged. But it’s a little too early to call.”
Mr. Faucette, as part of his immunosuppressant regimen, is receiving tegoprubart (Eledon Pharmaceuticals), an investigational antibody that blocks CD40 ligand. His predecessor Mr. Bennett, in contrast, had received a blocker of the CD40 receptor (Kiniksa Pharmaceuticals) along with other more familiar immunosuppressants.
The new anti–CD40-ligand blocker, Eledon said, is in phase 1 studies looking at efficacy in patients with conventional kidney transplants.
A version of this article appeared on Medscape.com.