User login
Mothers in medicine: What can we learn when worlds collide?
Across all industries, studies by the U.S. Department of Labor have shown that women, on average, earn 83.7 percent of what their male peers earn. While a lot has been written about the struggles women face in medicine, there have been decidedly fewer analyses that focus on women who choose to become mothers while working in medicine.
I’ve been privileged to work with medical students and residents for the last 8 years as the director of graduate and medical student mental health at Rowan-Virtua School of Osteopathic Medicine in Mt. Laurel, N.J. Often, the women I see as patients speak about their struggles with the elusive goal of “having it all.” While both men and women in medicine have difficulty maintaining a work-life balance, I’ve learned, both personally and professionally, that many women face a unique set of challenges.
No matter what their professional status, our society often views a woman as the default parent. For example, the teacher often calls the mothers first. The camp nurse calls me first, not my husband, when our child scrapes a knee. After-school play dates are arranged by the mothers, not fathers.
But mothers also bring to medicine a wealth of unique experiences, ideas, and viewpoints. They learn firsthand how to foster affect regulation and frustration tolerance in their kids and become efficient at managing the constant, conflicting tug of war of demands.
Some may argue that, over time, women end up earning significantly less than their male counterparts because they leave the workforce while on maternity leave, ultimately delaying their upward career progression. It’s likely a much more complex problem. Many of my patients believe that, in our male-dominated society (and workforce), women are punished for being aggressive or stating bold opinions, while men are rewarded for the same actions. While a man may sound forceful and in charge, a women will likely be thought of as brusque and unappreciative.
Outside of work, many women may have more on their plate. A 2020 Gallup poll of more than 3,000 heterosexual couples found that women are responsible for the majority of household chores. Women continue to handle more of the emotional labor within their families, regardless of income, age, or professional status. This is sometimes called the “Mental Load’ or “Second Shift.” As our society continues to view women as the default parent for childcare, medical issues, and overarching social and emotional tasks vital to raising happy, healthy children, the struggle a female medical professional feels is palpable.
Raising kids requires a parent to consistently dole out control, predictability, and reassurance for a child to thrive. Good limit and boundary setting leads to healthy development from a young age.
Psychiatric patients (and perhaps all patients) also require control, predictability, and reassurance from their doctor. The lessons learned in being a good mother can be directly applied in patient care, and vice versa. The cross-pollination of this relationship continues to grow more powerful as a woman’s children grow and her career matures.
Pediatrician and psychoanalyst Donald Winnicott’s idea of a “good enough” mother cannot be a one-size-fits-all approach. Women who self-select into the world of medicine often hold themselves to a higher standard than “good enough.” Acknowledging that the demands from both home and work will fluctuate is key to achieving success both personally and professionally, and lessons from home can and should be utilized to become a more effective physician. The notion of having it all, and the definition of success, must evolve over time.
Dr. Maymind is director of medical and graduate student mental health at Rowan-Virtua School of Osteopathic Medicine in Mt. Laurel, N.J. She has no relevant disclosures.
Across all industries, studies by the U.S. Department of Labor have shown that women, on average, earn 83.7 percent of what their male peers earn. While a lot has been written about the struggles women face in medicine, there have been decidedly fewer analyses that focus on women who choose to become mothers while working in medicine.
I’ve been privileged to work with medical students and residents for the last 8 years as the director of graduate and medical student mental health at Rowan-Virtua School of Osteopathic Medicine in Mt. Laurel, N.J. Often, the women I see as patients speak about their struggles with the elusive goal of “having it all.” While both men and women in medicine have difficulty maintaining a work-life balance, I’ve learned, both personally and professionally, that many women face a unique set of challenges.
No matter what their professional status, our society often views a woman as the default parent. For example, the teacher often calls the mothers first. The camp nurse calls me first, not my husband, when our child scrapes a knee. After-school play dates are arranged by the mothers, not fathers.
But mothers also bring to medicine a wealth of unique experiences, ideas, and viewpoints. They learn firsthand how to foster affect regulation and frustration tolerance in their kids and become efficient at managing the constant, conflicting tug of war of demands.
Some may argue that, over time, women end up earning significantly less than their male counterparts because they leave the workforce while on maternity leave, ultimately delaying their upward career progression. It’s likely a much more complex problem. Many of my patients believe that, in our male-dominated society (and workforce), women are punished for being aggressive or stating bold opinions, while men are rewarded for the same actions. While a man may sound forceful and in charge, a women will likely be thought of as brusque and unappreciative.
Outside of work, many women may have more on their plate. A 2020 Gallup poll of more than 3,000 heterosexual couples found that women are responsible for the majority of household chores. Women continue to handle more of the emotional labor within their families, regardless of income, age, or professional status. This is sometimes called the “Mental Load’ or “Second Shift.” As our society continues to view women as the default parent for childcare, medical issues, and overarching social and emotional tasks vital to raising happy, healthy children, the struggle a female medical professional feels is palpable.
Raising kids requires a parent to consistently dole out control, predictability, and reassurance for a child to thrive. Good limit and boundary setting leads to healthy development from a young age.
Psychiatric patients (and perhaps all patients) also require control, predictability, and reassurance from their doctor. The lessons learned in being a good mother can be directly applied in patient care, and vice versa. The cross-pollination of this relationship continues to grow more powerful as a woman’s children grow and her career matures.
Pediatrician and psychoanalyst Donald Winnicott’s idea of a “good enough” mother cannot be a one-size-fits-all approach. Women who self-select into the world of medicine often hold themselves to a higher standard than “good enough.” Acknowledging that the demands from both home and work will fluctuate is key to achieving success both personally and professionally, and lessons from home can and should be utilized to become a more effective physician. The notion of having it all, and the definition of success, must evolve over time.
Dr. Maymind is director of medical and graduate student mental health at Rowan-Virtua School of Osteopathic Medicine in Mt. Laurel, N.J. She has no relevant disclosures.
Across all industries, studies by the U.S. Department of Labor have shown that women, on average, earn 83.7 percent of what their male peers earn. While a lot has been written about the struggles women face in medicine, there have been decidedly fewer analyses that focus on women who choose to become mothers while working in medicine.
I’ve been privileged to work with medical students and residents for the last 8 years as the director of graduate and medical student mental health at Rowan-Virtua School of Osteopathic Medicine in Mt. Laurel, N.J. Often, the women I see as patients speak about their struggles with the elusive goal of “having it all.” While both men and women in medicine have difficulty maintaining a work-life balance, I’ve learned, both personally and professionally, that many women face a unique set of challenges.
No matter what their professional status, our society often views a woman as the default parent. For example, the teacher often calls the mothers first. The camp nurse calls me first, not my husband, when our child scrapes a knee. After-school play dates are arranged by the mothers, not fathers.
But mothers also bring to medicine a wealth of unique experiences, ideas, and viewpoints. They learn firsthand how to foster affect regulation and frustration tolerance in their kids and become efficient at managing the constant, conflicting tug of war of demands.
Some may argue that, over time, women end up earning significantly less than their male counterparts because they leave the workforce while on maternity leave, ultimately delaying their upward career progression. It’s likely a much more complex problem. Many of my patients believe that, in our male-dominated society (and workforce), women are punished for being aggressive or stating bold opinions, while men are rewarded for the same actions. While a man may sound forceful and in charge, a women will likely be thought of as brusque and unappreciative.
Outside of work, many women may have more on their plate. A 2020 Gallup poll of more than 3,000 heterosexual couples found that women are responsible for the majority of household chores. Women continue to handle more of the emotional labor within their families, regardless of income, age, or professional status. This is sometimes called the “Mental Load’ or “Second Shift.” As our society continues to view women as the default parent for childcare, medical issues, and overarching social and emotional tasks vital to raising happy, healthy children, the struggle a female medical professional feels is palpable.
Raising kids requires a parent to consistently dole out control, predictability, and reassurance for a child to thrive. Good limit and boundary setting leads to healthy development from a young age.
Psychiatric patients (and perhaps all patients) also require control, predictability, and reassurance from their doctor. The lessons learned in being a good mother can be directly applied in patient care, and vice versa. The cross-pollination of this relationship continues to grow more powerful as a woman’s children grow and her career matures.
Pediatrician and psychoanalyst Donald Winnicott’s idea of a “good enough” mother cannot be a one-size-fits-all approach. Women who self-select into the world of medicine often hold themselves to a higher standard than “good enough.” Acknowledging that the demands from both home and work will fluctuate is key to achieving success both personally and professionally, and lessons from home can and should be utilized to become a more effective physician. The notion of having it all, and the definition of success, must evolve over time.
Dr. Maymind is director of medical and graduate student mental health at Rowan-Virtua School of Osteopathic Medicine in Mt. Laurel, N.J. She has no relevant disclosures.
Aspirin for secondary CVD prevention underused worldwide
Nationally representative survey data from 51 countries showed that fewer than half of eligible people overall, including less than one-quarter in low-income and lower-middle–income countries, were taking aspirin for secondary CVD prevention.
“Our findings were not surprising but rather disappointing,” first author Sang Gune Yoo, MD, fellow in cardiovascular disease at Washington University in St Louis, said in an interview.
“We had hoped that the rates of aspirin use for secondary prevention would have increased after decades of effort to promote cardiovascular health worldwide,” Dr. Yoo said.
In high-income countries, such as the United States, rates of aspirin use for secondary CVD prevention were higher – at around 65% – but that’s also “really low and not particularly good or anything to be proud of,” Deepak Bhatt, MD, MPH, director of Mount Sinai Heart, New York, who wasn’t involved in the study, said in an interview.
The study was published online in JAMA. It provides the most extensive and up-to-date estimates of the worldwide use of aspirin for secondary prevention of CVD.
The researchers did a cross-sectional analysis using pooled, individual participant data from nationally representative health surveys conducted from 2013 to 2020 in 51 low-, middle-, and high-income countries.
The overall pooled sample included 124,505 nonpregnant adults (mean age, 52 years; 51% women). A total of 10,589 (8.1%) had a self-reported history of CVD and about 40% of these individuals were taking aspirin.
However, rates differed markedly by country, with use rates lowest in low-income and lower-middle–income countries and highest in upper-middle–income and high-income countries.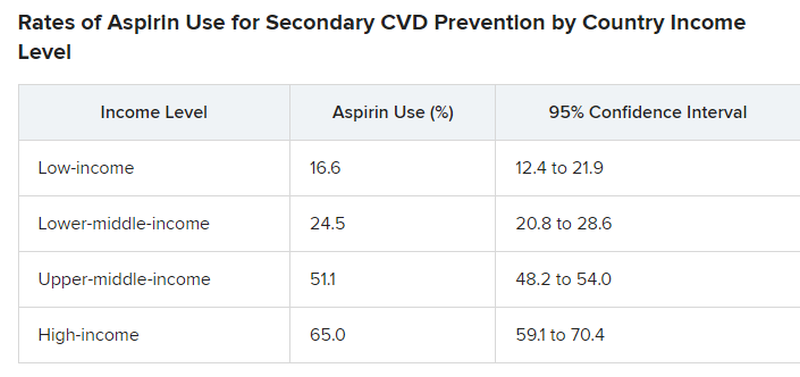
Primary vs. secondary prevention
The study did not explore the factors or reasons behind suboptimal aspirin use for secondary CVD prevention.
For example, it did not investigate whether data demonstrating that aspirin is not helpful in primary prevention is having a negative effect on use rates for secondary prevention. However, “rates of aspirin use for secondary prevention were low previously and remain suboptimal,” Dr. Yoo said.
Dr. Bhatt said that the “suboptimal” use of aspirin for secondary prevention is “a bit perplexing because this is a medicine that’s familiar, the data in secondary prevention are broadly known to physicians and it’s a cheap medicine so we can’t, in this case, blame high cost.”
Dr. Bhatt said it’s possible that coverage in the lay media of “negative” aspirin trials that may not distinguish between a primary and secondary prevention trial may contribute to confusion about aspirin. “In some cases, the doctor may think the patient is taking aspirin, but self discontinues it based on something they read or saw on the Internet.”
Dr. Yoo and colleagues said that, to meet the goal of reducing premature mortality from noncommunicable diseases, including CVD, “national health policies and health systems must develop, implement and evaluate strategies to promote evidence-based use of aspirin.”
“Strategies to boost appropriate aspirin use must be contextualized to the country and its health system,” Dr. Yoo added.
The study had no commercial funding. Dr. Yoo has disclosed no relevant financial relationships. Dr. Bhatt disclosed receiving grants and/or personal fees from many companies, publications, and organizations.
A version of this article appeared on Medscape.com.
Nationally representative survey data from 51 countries showed that fewer than half of eligible people overall, including less than one-quarter in low-income and lower-middle–income countries, were taking aspirin for secondary CVD prevention.
“Our findings were not surprising but rather disappointing,” first author Sang Gune Yoo, MD, fellow in cardiovascular disease at Washington University in St Louis, said in an interview.
“We had hoped that the rates of aspirin use for secondary prevention would have increased after decades of effort to promote cardiovascular health worldwide,” Dr. Yoo said.
In high-income countries, such as the United States, rates of aspirin use for secondary CVD prevention were higher – at around 65% – but that’s also “really low and not particularly good or anything to be proud of,” Deepak Bhatt, MD, MPH, director of Mount Sinai Heart, New York, who wasn’t involved in the study, said in an interview.
The study was published online in JAMA. It provides the most extensive and up-to-date estimates of the worldwide use of aspirin for secondary prevention of CVD.
The researchers did a cross-sectional analysis using pooled, individual participant data from nationally representative health surveys conducted from 2013 to 2020 in 51 low-, middle-, and high-income countries.
The overall pooled sample included 124,505 nonpregnant adults (mean age, 52 years; 51% women). A total of 10,589 (8.1%) had a self-reported history of CVD and about 40% of these individuals were taking aspirin.
However, rates differed markedly by country, with use rates lowest in low-income and lower-middle–income countries and highest in upper-middle–income and high-income countries.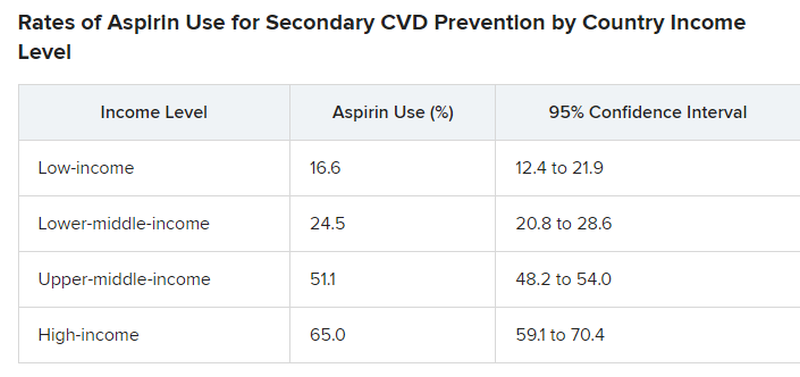
Primary vs. secondary prevention
The study did not explore the factors or reasons behind suboptimal aspirin use for secondary CVD prevention.
For example, it did not investigate whether data demonstrating that aspirin is not helpful in primary prevention is having a negative effect on use rates for secondary prevention. However, “rates of aspirin use for secondary prevention were low previously and remain suboptimal,” Dr. Yoo said.
Dr. Bhatt said that the “suboptimal” use of aspirin for secondary prevention is “a bit perplexing because this is a medicine that’s familiar, the data in secondary prevention are broadly known to physicians and it’s a cheap medicine so we can’t, in this case, blame high cost.”
Dr. Bhatt said it’s possible that coverage in the lay media of “negative” aspirin trials that may not distinguish between a primary and secondary prevention trial may contribute to confusion about aspirin. “In some cases, the doctor may think the patient is taking aspirin, but self discontinues it based on something they read or saw on the Internet.”
Dr. Yoo and colleagues said that, to meet the goal of reducing premature mortality from noncommunicable diseases, including CVD, “national health policies and health systems must develop, implement and evaluate strategies to promote evidence-based use of aspirin.”
“Strategies to boost appropriate aspirin use must be contextualized to the country and its health system,” Dr. Yoo added.
The study had no commercial funding. Dr. Yoo has disclosed no relevant financial relationships. Dr. Bhatt disclosed receiving grants and/or personal fees from many companies, publications, and organizations.
A version of this article appeared on Medscape.com.
Nationally representative survey data from 51 countries showed that fewer than half of eligible people overall, including less than one-quarter in low-income and lower-middle–income countries, were taking aspirin for secondary CVD prevention.
“Our findings were not surprising but rather disappointing,” first author Sang Gune Yoo, MD, fellow in cardiovascular disease at Washington University in St Louis, said in an interview.
“We had hoped that the rates of aspirin use for secondary prevention would have increased after decades of effort to promote cardiovascular health worldwide,” Dr. Yoo said.
In high-income countries, such as the United States, rates of aspirin use for secondary CVD prevention were higher – at around 65% – but that’s also “really low and not particularly good or anything to be proud of,” Deepak Bhatt, MD, MPH, director of Mount Sinai Heart, New York, who wasn’t involved in the study, said in an interview.
The study was published online in JAMA. It provides the most extensive and up-to-date estimates of the worldwide use of aspirin for secondary prevention of CVD.
The researchers did a cross-sectional analysis using pooled, individual participant data from nationally representative health surveys conducted from 2013 to 2020 in 51 low-, middle-, and high-income countries.
The overall pooled sample included 124,505 nonpregnant adults (mean age, 52 years; 51% women). A total of 10,589 (8.1%) had a self-reported history of CVD and about 40% of these individuals were taking aspirin.
However, rates differed markedly by country, with use rates lowest in low-income and lower-middle–income countries and highest in upper-middle–income and high-income countries.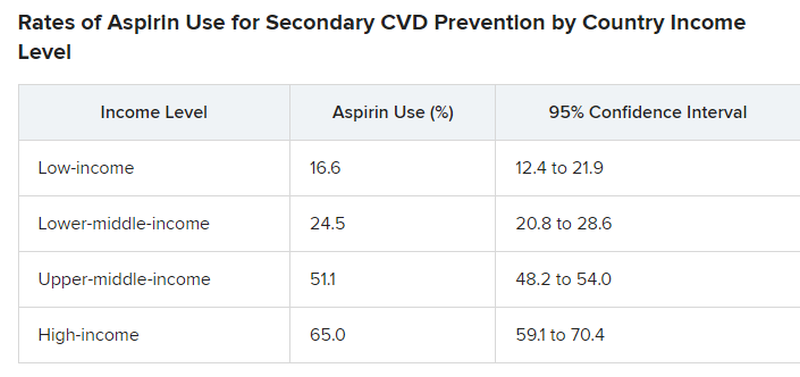
Primary vs. secondary prevention
The study did not explore the factors or reasons behind suboptimal aspirin use for secondary CVD prevention.
For example, it did not investigate whether data demonstrating that aspirin is not helpful in primary prevention is having a negative effect on use rates for secondary prevention. However, “rates of aspirin use for secondary prevention were low previously and remain suboptimal,” Dr. Yoo said.
Dr. Bhatt said that the “suboptimal” use of aspirin for secondary prevention is “a bit perplexing because this is a medicine that’s familiar, the data in secondary prevention are broadly known to physicians and it’s a cheap medicine so we can’t, in this case, blame high cost.”
Dr. Bhatt said it’s possible that coverage in the lay media of “negative” aspirin trials that may not distinguish between a primary and secondary prevention trial may contribute to confusion about aspirin. “In some cases, the doctor may think the patient is taking aspirin, but self discontinues it based on something they read or saw on the Internet.”
Dr. Yoo and colleagues said that, to meet the goal of reducing premature mortality from noncommunicable diseases, including CVD, “national health policies and health systems must develop, implement and evaluate strategies to promote evidence-based use of aspirin.”
“Strategies to boost appropriate aspirin use must be contextualized to the country and its health system,” Dr. Yoo added.
The study had no commercial funding. Dr. Yoo has disclosed no relevant financial relationships. Dr. Bhatt disclosed receiving grants and/or personal fees from many companies, publications, and organizations.
A version of this article appeared on Medscape.com.
FROM JAMA
Cystic Presentation of High-Grade Ductal Carcinoma In Situ in an Inframammary Accessory Nipple
To the Editor:
The term ectopic breast tissue serves as an umbrella term that encompasses breast tissue positioned in anatomically incorrect locations, including the subtypes of supernumerary and aberrant breasts.1 However, the more frequently used term is accessory breast tissue (ABT).1 Supernumerary breasts have diverse variations of a nipple, areola, and/or ductal tissue and can span in size from a small mole to a fully functioning breast. This breast type maintains structured ductal systems connected to the overlying skin and experiences regular changes during the reproductive cycle. In contrast, an aberrant breast is isolated breast tissue that does not contain organized ductal systems.1 Accessory breast tissue is prevalent in up to 6.0% of the world population, with Japanese individuals being the most affected and White individuals being the least affected.1
Accessory breasts typically are located along the milk line—the embryologic precursor to mammary glands and nipples, which extend from the axillae to the groin and regress from the caudal end spanning to the groin.2 For this reason, incomplete regression of the mammary ridge results in ABT, most commonly in the axillary region.3 Accessory breast tissue usually is benign and is considered an anatomical variant; however, because the histomorphology is similar to mammary gland tissue, accessory breasts have the same proliferative potential as anatomically correct breasts and therefore can form fibroadenomas, cysts, abscesses, mastitis, or breast cancer.4 Accessory breast carcinomas comprise 0.3% to 0.6% of all breast malignancies.5 Certain genodermatoses (ie, Cowden syndrome) also may predispose patients to benign or malignant pathology in ABT.6 We present a rare case of accessory breast cancer in the inframammary region masquerading as a cyst. These findings were further supported by ultrasonography and mammography.
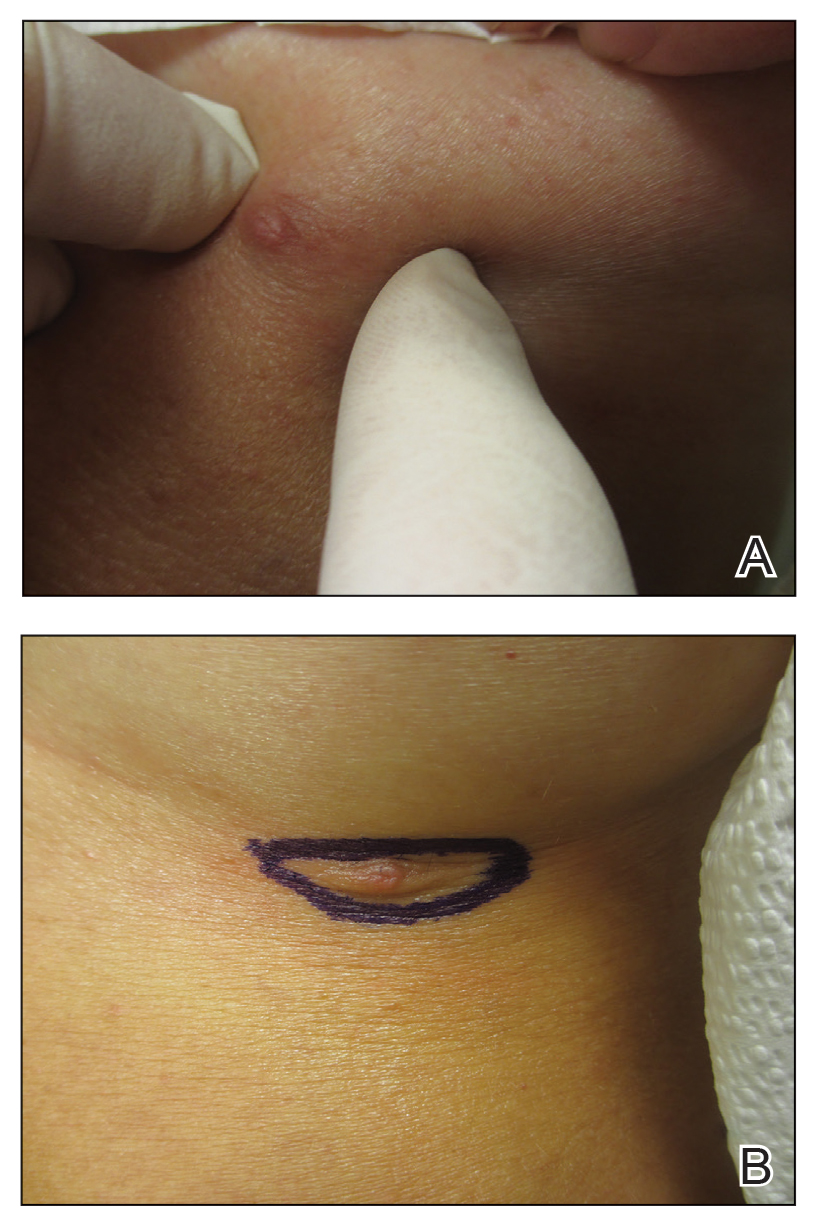
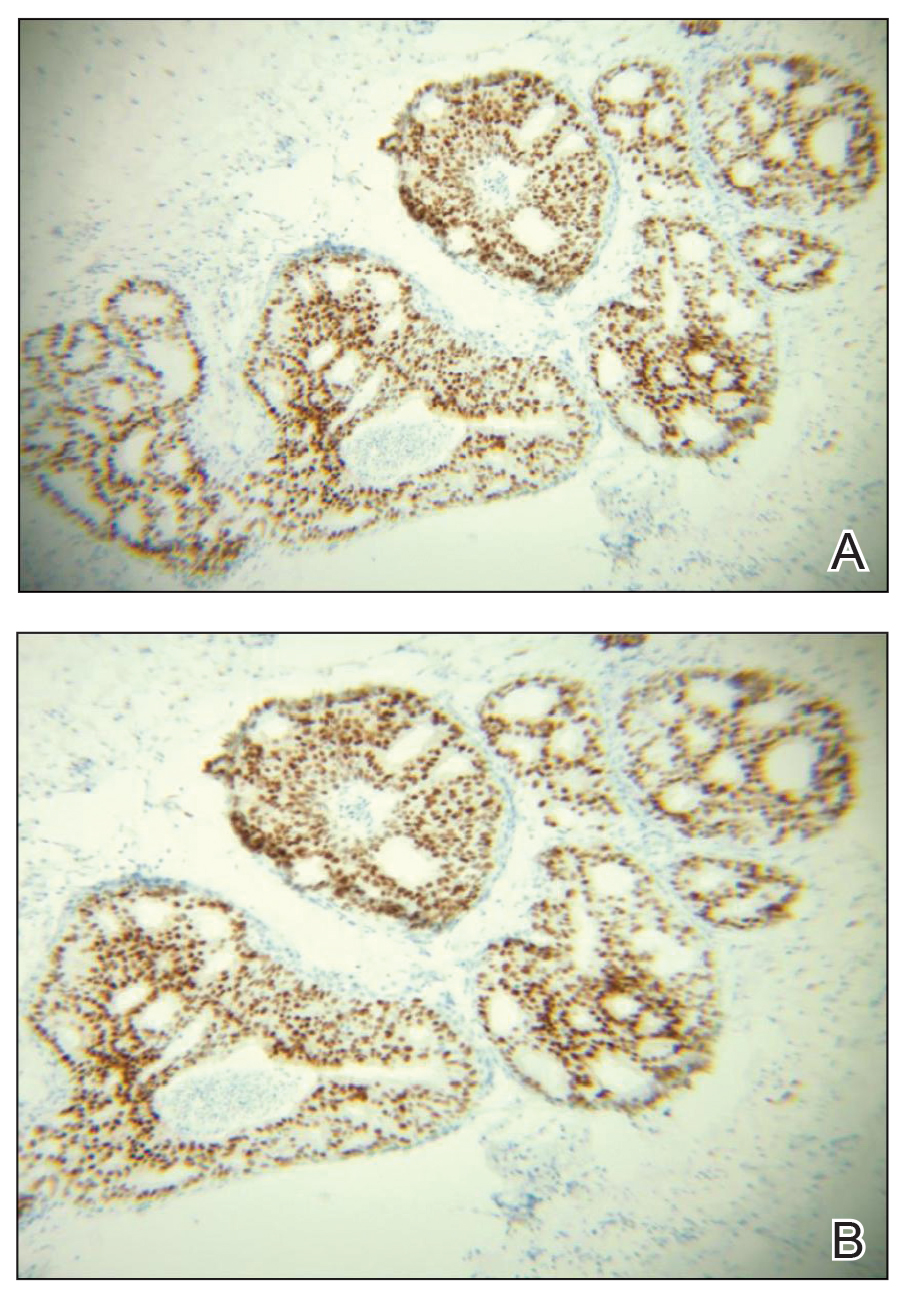
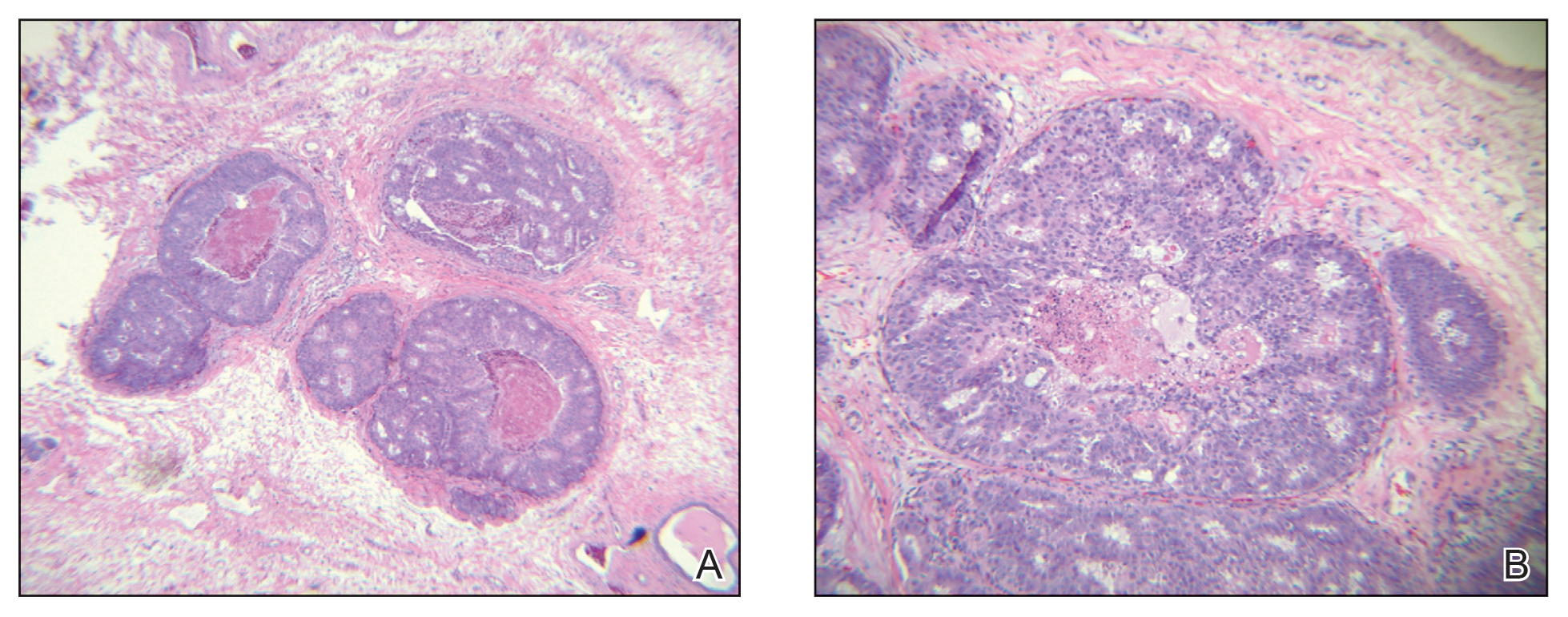
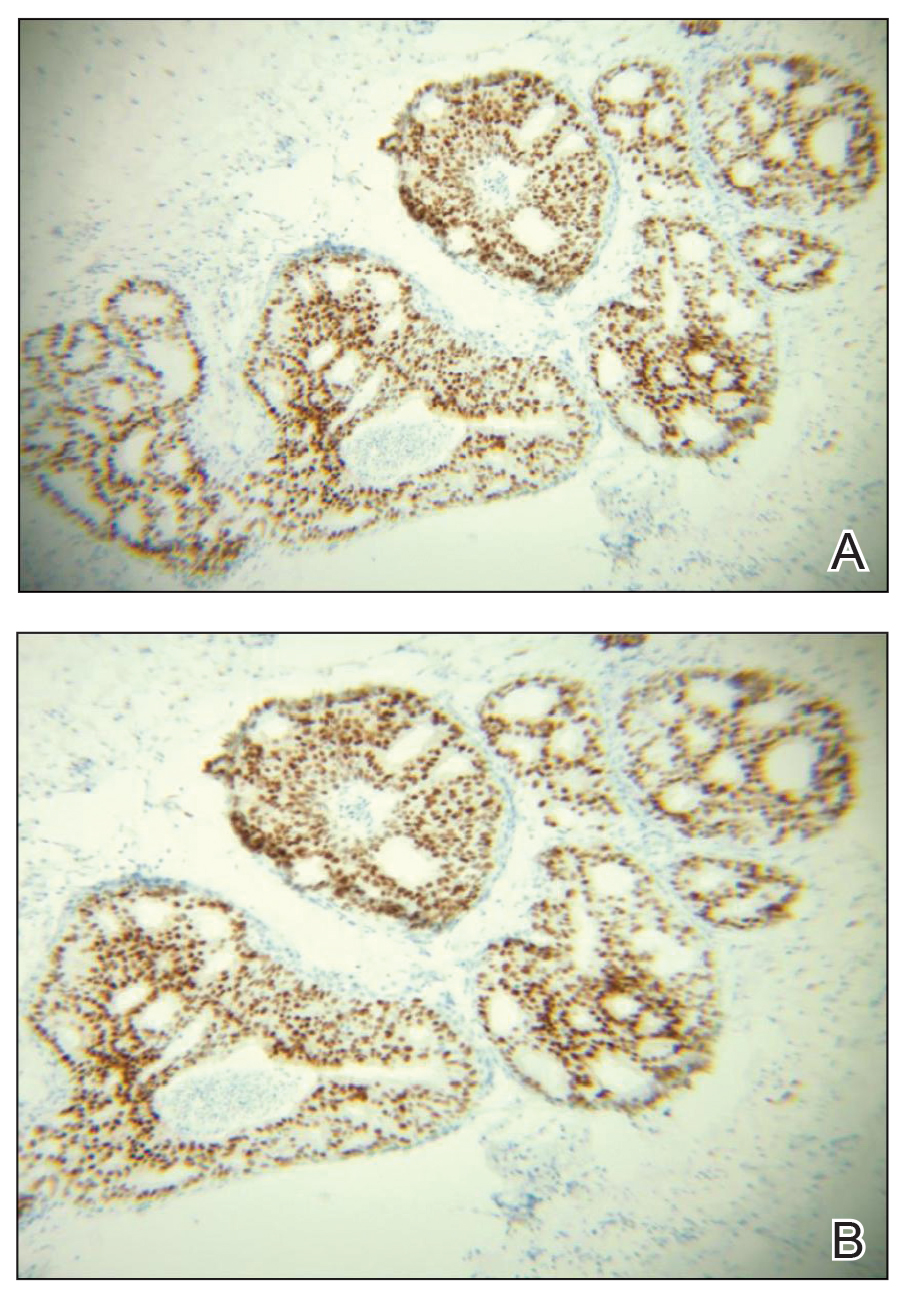
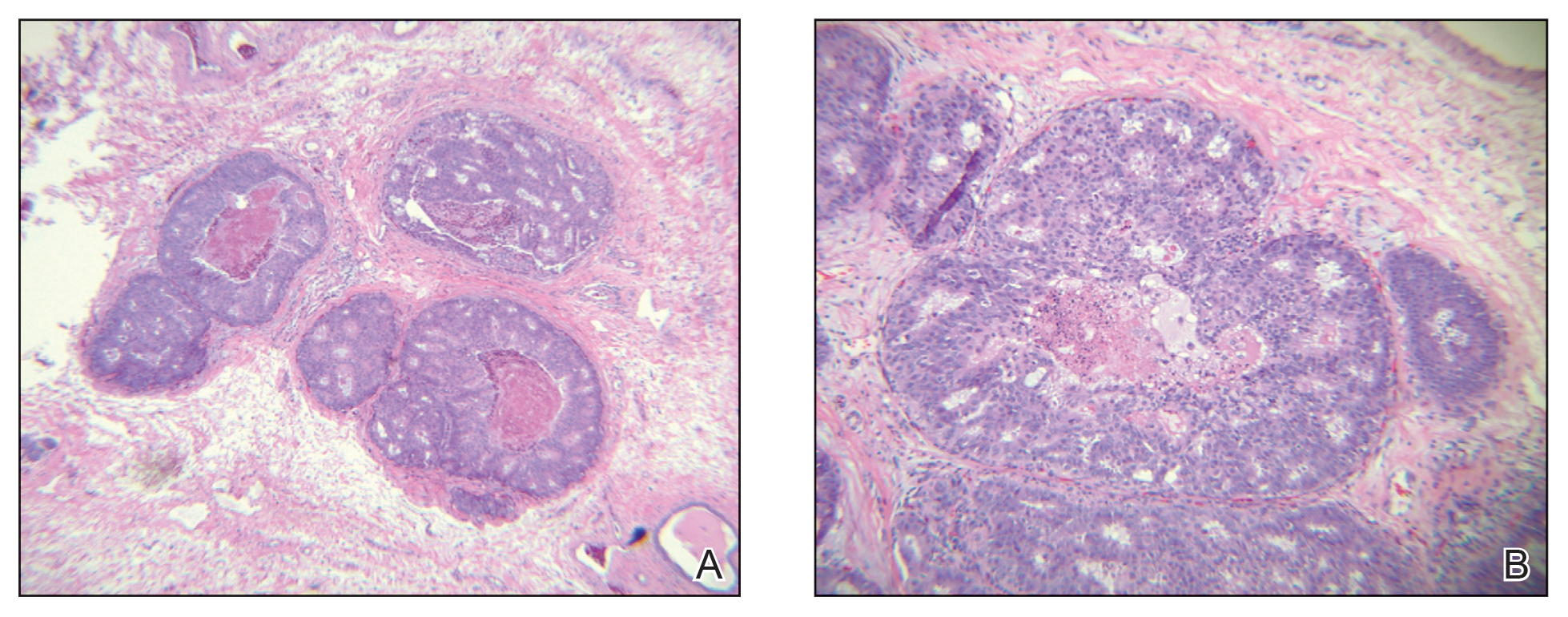
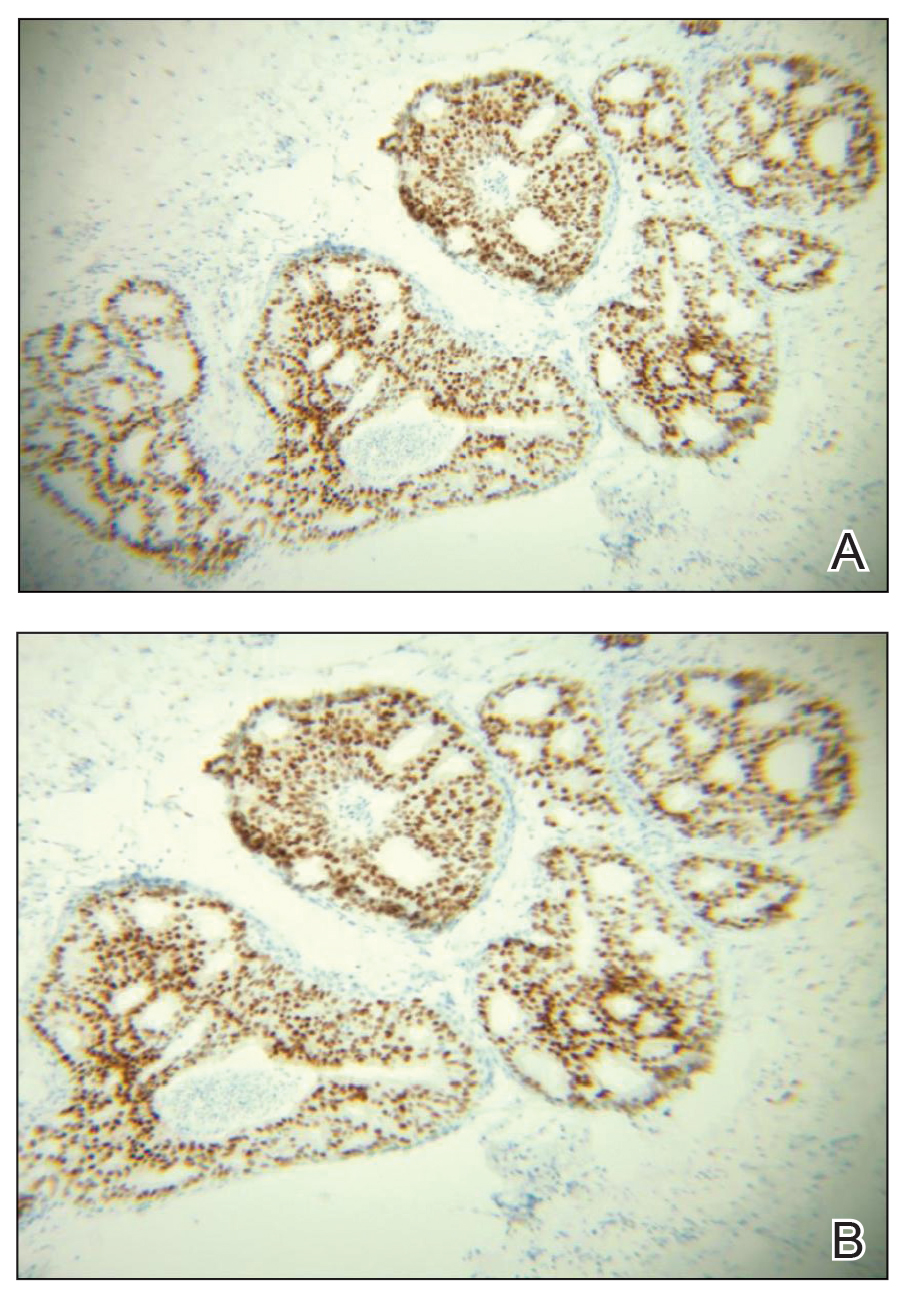
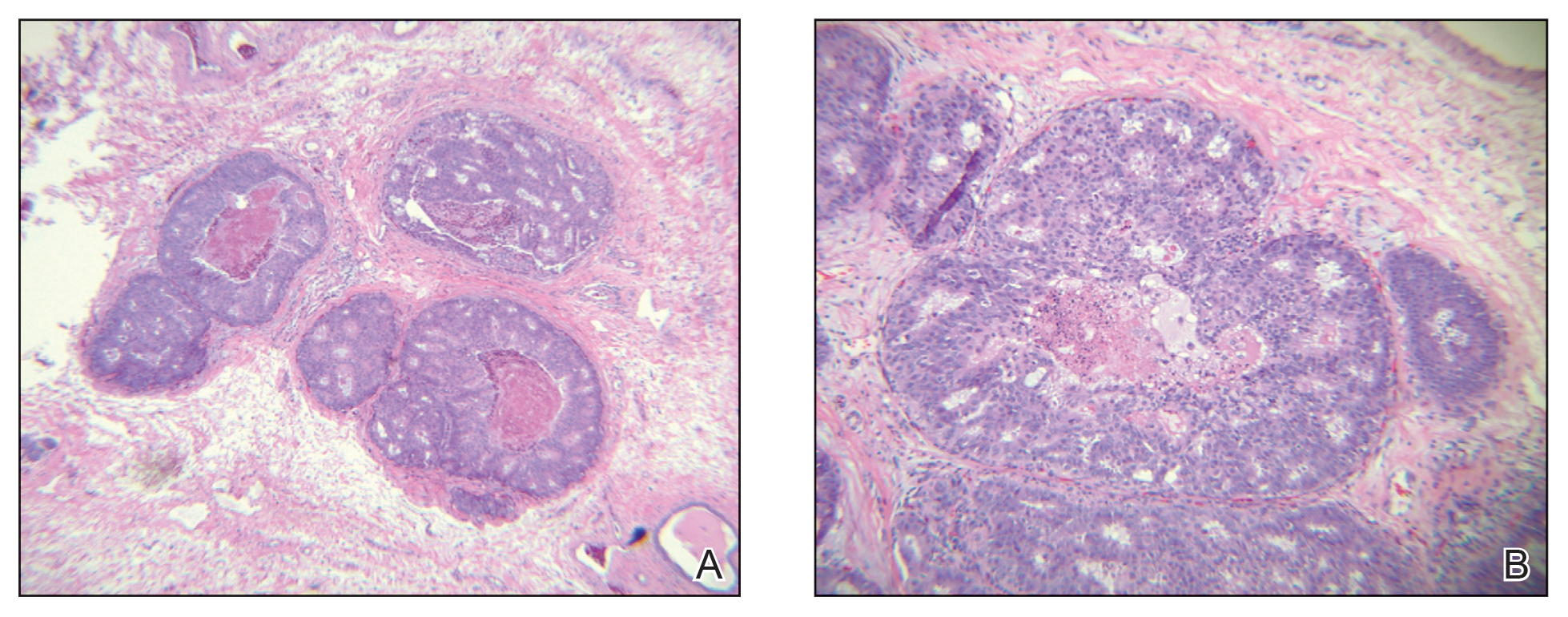
A 45-year-old White woman presented to our clinic for removal of a dermal mass underlying a supernumerary nipple at the left inframammary fold. Her medical history was noncontributory and was only remarkable for uterine fibroids. She developed pain and swelling in the left breast 1 year prior, which prompted her to seek medical attention from her primary care physician. Diagnostic mammography was negative for any concerning malignant nodules, and subsequent BRCA genetic testing also was negative. Six months after the diagnostic mammography, she continued to experience pain and swelling in the left breast and was then referred for diagnostic ultrasonography; 2 masses in the left breast suspected as infected cysts with rupture were identified (Figure 1). She was then referred to our dermatology clinic for evaluation and surgical extirpation of the suspected cyst underlying the accessory breast. The area subsequently was excised under local anesthesia, and a second similar but smaller mass also was identified adjacent to the initial growth. Dermatopathologic examination revealed an estrogen receptor– (Figure 2A) and progesterone receptor–positive (Figure 2B), ERBB2 (HER2/neu)–negative, nuclear grade III ductal carcinoma in situ (Figure 3).
Various ABT classification methods have been proposed with Brightmore7 categorizing polymastia into 8 subtypes: (1) complete breast; (2) glandular tissue and nipple; (3) glandular tissue and areola; (4) glandular tissue only; (5) nipple, areola, and fat; (6) nipple only; (7) areola only; and (8) patch of hair only. De Cholnokey8 focused on axillary polymastia, dividing it into 4 classes: (1) axillary tumor in milk line without nipple or areola; (2) axillary tumor with areola with or without pigmentation; (3) nipple or areola without underlying breast tissue; and (4) complete breast with nipple, areola, and glandular tissue. Fenench’s9 method is preferred and simply describes ABT as 2 subtypes: supernumerary and aberrant.1,2,10 One study observed 6% of ABT cancers were the supernumerary type and 94% were the aberrant type.1 Ductal lumen stagnation increases the risk for accessory breast carcinoma development.10 Men have a higher prevalence of cancer in ABT compared to anatomically correct breast tissue.11
There currently is no standardized guideline for ABT cancer treatment. The initial clinical impression of cancer of ABT may be misdiagnosed as lymphadenopathy, abscesses, or lipomas.12 The risk for misdiagnosis is higher for cancer of ABT compared to normal breast tissue and is associated with a poorer prognosis.1 Despite multiple screening modalities, our patient’s initial breast cancer screenings proved unreliable. A mammogram failed to detect malignancy, likely secondary to the area of concern being out of the standard imaging field. Ultrasonography also was unreliable and led to misdiagnosis as an infected sebaceous cyst with rupture in our patient. Upon review of the ultrasound, concerns were raised by dermatology that the mass was more likely an epidermal inclusion cyst with rupture given the more superficial and sac-free nature of sebaceous cysts, which commonly are associated with steatocystoma multiplex.13 Definitive diagnosis of ductal carcinoma in situ was made with dermatopathologic examination.
Prophylactic surgical excision of ABT has been recommended, suggesting that excisional biopsy and histopathologic examination is the more appropriate method to rule out malignancy. Surgical treatment of ABT may omit any risk for malignant transformation and may provide psychological relief to patients for aesthetic reasons.10,12,14 The risk and benefits of prophylactic excision of ABT has been compared to prophylactic mastectomy of anatomically correct breasts,15 with some clinicians considering this definitive procedure unnecessary except in high-risk patients with a strong genetic predisposition.16,17
Accessory breast tissue should be viewed as an anatomical variant with the option of surgical removal for symptomatic concerns, such as firm nodules, discharge, and pain. Although ABT is rare and cancer in ABT is even more uncommon (<1% of all breast cancers),5,11 clinicians should be suspicious of benign diagnostic reports when the clinical situation does not fit the proposed narrative.
- Marshall MB, Moynihan JJ, Frost A, et al. Ectopic breast cancer: case report and literature review. Surg Oncol. 1994;3:295-304. doi:10.1016/0960-7404(94)90032-9
- DeFilippis EM, Arleo EK. The ABCs of accessory breast tissue: basic information every radiologist should know. Am J Roentgenol. 2014;202:1157-1162. doi:10.2214/AJR.13.10930
- Famá F, Cicciú M, Sindoni A, et al. Prevalence of ectopic breast tissue and tumor: a 20-year single center experience. Clin Breast Cancer. 2016;16:E107-E112. doi:10.1016/j.clbc.2016.03.004
- Brown J, Schwartz RA. Supernumerary nipples: an overview. Cutis. 2003;71:344-346.
- Nihon-Yanagi Y, Ueda T, Kameda N, et al. A case of ectopic breast cancer with a literature review. Surg Oncol. 2011;20:35-42. doi:10.1016/j.suronc.2009.09.005
- Hedayat AA, Pettus JR, Marotti JD, et al. Proliferative lesion of anogenital mammary-like glands in the setting of Cowden syndrome: case report and review of the literature. J Cutan Pathol. 2016;43:707-710. doi:10.1111/cup.12721
- Brightmore T. Bilateral double nipples. Br J Surg. 1972;59:55-57. https://doi.org/10.1002/bjs.1800590114
- De Cholnoky T. Accessory breast tissue in the axilla. N Y State J Med. 1951;51:2245-2248.
- Fenech HB. Aberrant breast tissue; case report. Harper Hosp Bull. 1949;7:268-271.
- Francone E, Nathan MJ, Murelli F, et al. Ectopic breast cancer: case report and review of the literature. Aesthetic Plast Surg. 2013;37:746-749. doi:10.1007/s00266-013-0125-1
- Yamamura J, Masuda N, Kodama Y, et al. Male breast cancer originating in an accessory mammary gland in the axilla: a case report. Case Rep Med. 2012;2012:286210. doi:10.1155/2012/286210.
- Ghosn SH, Khatri KA, Bhawan J. Bilateral aberrant axillary breast tissue mimicking lipomas: report of a case and review of the literature. J Cutan Pathol. 2007;34(suppl 1):9-13. doi:10.1111/j.1600-0560.2006.00713.x
- Arceu M, Martinez G, Alfaro D, et al. Ultrasound morphologic features of steatocystoma multiplex with clinical correlation. J Ultrasound Med. 2020;39:2255-2260. doi:10.1002/jum.15320
- Lesavoy MA, Gomez-Garcia A, Nejdl R, et al. Axillary breast tissue: clinical presentation and surgical treatment. Ann Plast Surg. 1995;35:356-360. doi:10.1097/00000637-199510000-00004
- Bank J. Management of ectopic breast tissue. Aesthetic Plast Surg. 2013;37:750-751. doi:10.1007/s00266-013-0143-z
- Morrow M. Prophylactic mastectomy of the contralateral breast. Breast. 2011;20(suppl 3):S108-S110. doi:10.1016/S0960-9776(11)70306-X
- Teoh V, Tasoulis M-K, Gui G. Contralateral prophylactic mastectomy in women with unilateral breast cancer who are genetic carriers, have a strong family history or are just young at presentation. Cancers (Basel). 2020;12:140. doi:10.3390/cancers12010140
To the Editor:
The term ectopic breast tissue serves as an umbrella term that encompasses breast tissue positioned in anatomically incorrect locations, including the subtypes of supernumerary and aberrant breasts.1 However, the more frequently used term is accessory breast tissue (ABT).1 Supernumerary breasts have diverse variations of a nipple, areola, and/or ductal tissue and can span in size from a small mole to a fully functioning breast. This breast type maintains structured ductal systems connected to the overlying skin and experiences regular changes during the reproductive cycle. In contrast, an aberrant breast is isolated breast tissue that does not contain organized ductal systems.1 Accessory breast tissue is prevalent in up to 6.0% of the world population, with Japanese individuals being the most affected and White individuals being the least affected.1
Accessory breasts typically are located along the milk line—the embryologic precursor to mammary glands and nipples, which extend from the axillae to the groin and regress from the caudal end spanning to the groin.2 For this reason, incomplete regression of the mammary ridge results in ABT, most commonly in the axillary region.3 Accessory breast tissue usually is benign and is considered an anatomical variant; however, because the histomorphology is similar to mammary gland tissue, accessory breasts have the same proliferative potential as anatomically correct breasts and therefore can form fibroadenomas, cysts, abscesses, mastitis, or breast cancer.4 Accessory breast carcinomas comprise 0.3% to 0.6% of all breast malignancies.5 Certain genodermatoses (ie, Cowden syndrome) also may predispose patients to benign or malignant pathology in ABT.6 We present a rare case of accessory breast cancer in the inframammary region masquerading as a cyst. These findings were further supported by ultrasonography and mammography.
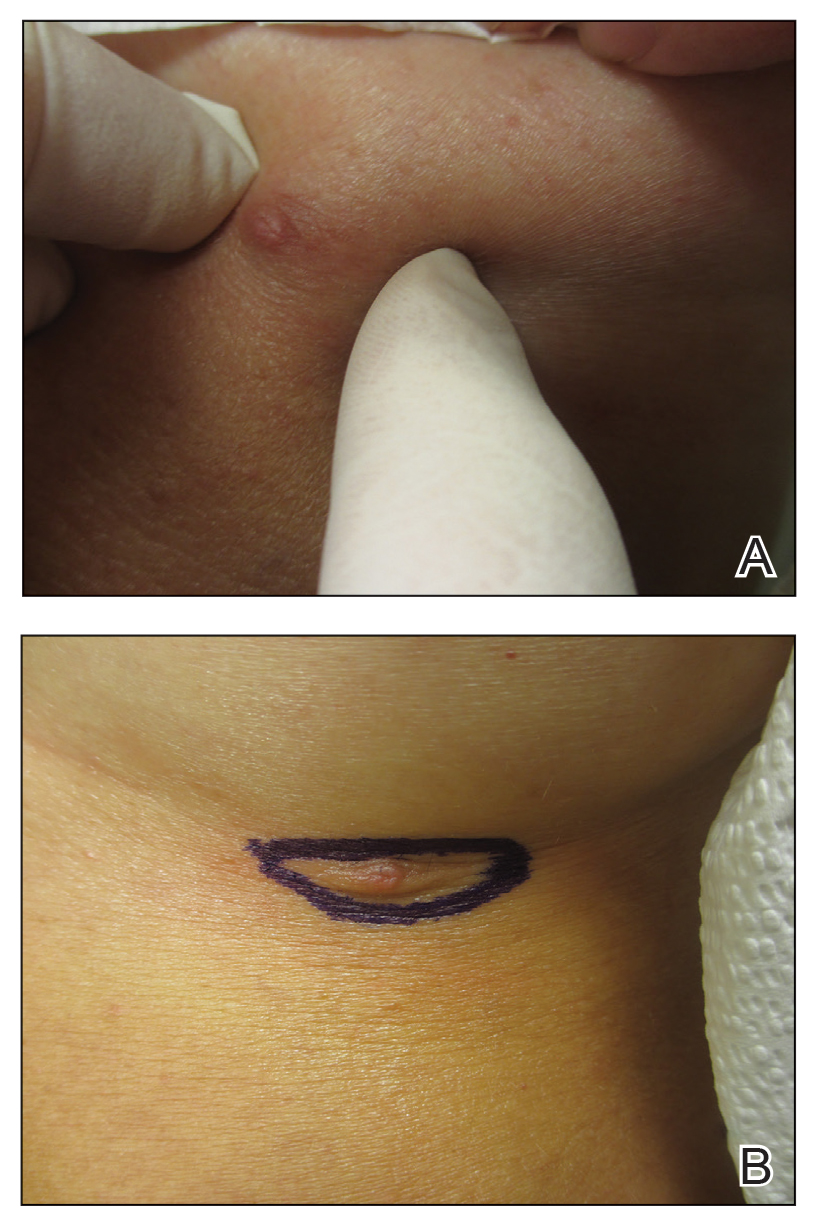
A 45-year-old White woman presented to our clinic for removal of a dermal mass underlying a supernumerary nipple at the left inframammary fold. Her medical history was noncontributory and was only remarkable for uterine fibroids. She developed pain and swelling in the left breast 1 year prior, which prompted her to seek medical attention from her primary care physician. Diagnostic mammography was negative for any concerning malignant nodules, and subsequent BRCA genetic testing also was negative. Six months after the diagnostic mammography, she continued to experience pain and swelling in the left breast and was then referred for diagnostic ultrasonography; 2 masses in the left breast suspected as infected cysts with rupture were identified (Figure 1). She was then referred to our dermatology clinic for evaluation and surgical extirpation of the suspected cyst underlying the accessory breast. The area subsequently was excised under local anesthesia, and a second similar but smaller mass also was identified adjacent to the initial growth. Dermatopathologic examination revealed an estrogen receptor– (Figure 2A) and progesterone receptor–positive (Figure 2B), ERBB2 (HER2/neu)–negative, nuclear grade III ductal carcinoma in situ (Figure 3).
Various ABT classification methods have been proposed with Brightmore7 categorizing polymastia into 8 subtypes: (1) complete breast; (2) glandular tissue and nipple; (3) glandular tissue and areola; (4) glandular tissue only; (5) nipple, areola, and fat; (6) nipple only; (7) areola only; and (8) patch of hair only. De Cholnokey8 focused on axillary polymastia, dividing it into 4 classes: (1) axillary tumor in milk line without nipple or areola; (2) axillary tumor with areola with or without pigmentation; (3) nipple or areola without underlying breast tissue; and (4) complete breast with nipple, areola, and glandular tissue. Fenench’s9 method is preferred and simply describes ABT as 2 subtypes: supernumerary and aberrant.1,2,10 One study observed 6% of ABT cancers were the supernumerary type and 94% were the aberrant type.1 Ductal lumen stagnation increases the risk for accessory breast carcinoma development.10 Men have a higher prevalence of cancer in ABT compared to anatomically correct breast tissue.11
There currently is no standardized guideline for ABT cancer treatment. The initial clinical impression of cancer of ABT may be misdiagnosed as lymphadenopathy, abscesses, or lipomas.12 The risk for misdiagnosis is higher for cancer of ABT compared to normal breast tissue and is associated with a poorer prognosis.1 Despite multiple screening modalities, our patient’s initial breast cancer screenings proved unreliable. A mammogram failed to detect malignancy, likely secondary to the area of concern being out of the standard imaging field. Ultrasonography also was unreliable and led to misdiagnosis as an infected sebaceous cyst with rupture in our patient. Upon review of the ultrasound, concerns were raised by dermatology that the mass was more likely an epidermal inclusion cyst with rupture given the more superficial and sac-free nature of sebaceous cysts, which commonly are associated with steatocystoma multiplex.13 Definitive diagnosis of ductal carcinoma in situ was made with dermatopathologic examination.
Prophylactic surgical excision of ABT has been recommended, suggesting that excisional biopsy and histopathologic examination is the more appropriate method to rule out malignancy. Surgical treatment of ABT may omit any risk for malignant transformation and may provide psychological relief to patients for aesthetic reasons.10,12,14 The risk and benefits of prophylactic excision of ABT has been compared to prophylactic mastectomy of anatomically correct breasts,15 with some clinicians considering this definitive procedure unnecessary except in high-risk patients with a strong genetic predisposition.16,17
Accessory breast tissue should be viewed as an anatomical variant with the option of surgical removal for symptomatic concerns, such as firm nodules, discharge, and pain. Although ABT is rare and cancer in ABT is even more uncommon (<1% of all breast cancers),5,11 clinicians should be suspicious of benign diagnostic reports when the clinical situation does not fit the proposed narrative.
To the Editor:
The term ectopic breast tissue serves as an umbrella term that encompasses breast tissue positioned in anatomically incorrect locations, including the subtypes of supernumerary and aberrant breasts.1 However, the more frequently used term is accessory breast tissue (ABT).1 Supernumerary breasts have diverse variations of a nipple, areola, and/or ductal tissue and can span in size from a small mole to a fully functioning breast. This breast type maintains structured ductal systems connected to the overlying skin and experiences regular changes during the reproductive cycle. In contrast, an aberrant breast is isolated breast tissue that does not contain organized ductal systems.1 Accessory breast tissue is prevalent in up to 6.0% of the world population, with Japanese individuals being the most affected and White individuals being the least affected.1
Accessory breasts typically are located along the milk line—the embryologic precursor to mammary glands and nipples, which extend from the axillae to the groin and regress from the caudal end spanning to the groin.2 For this reason, incomplete regression of the mammary ridge results in ABT, most commonly in the axillary region.3 Accessory breast tissue usually is benign and is considered an anatomical variant; however, because the histomorphology is similar to mammary gland tissue, accessory breasts have the same proliferative potential as anatomically correct breasts and therefore can form fibroadenomas, cysts, abscesses, mastitis, or breast cancer.4 Accessory breast carcinomas comprise 0.3% to 0.6% of all breast malignancies.5 Certain genodermatoses (ie, Cowden syndrome) also may predispose patients to benign or malignant pathology in ABT.6 We present a rare case of accessory breast cancer in the inframammary region masquerading as a cyst. These findings were further supported by ultrasonography and mammography.
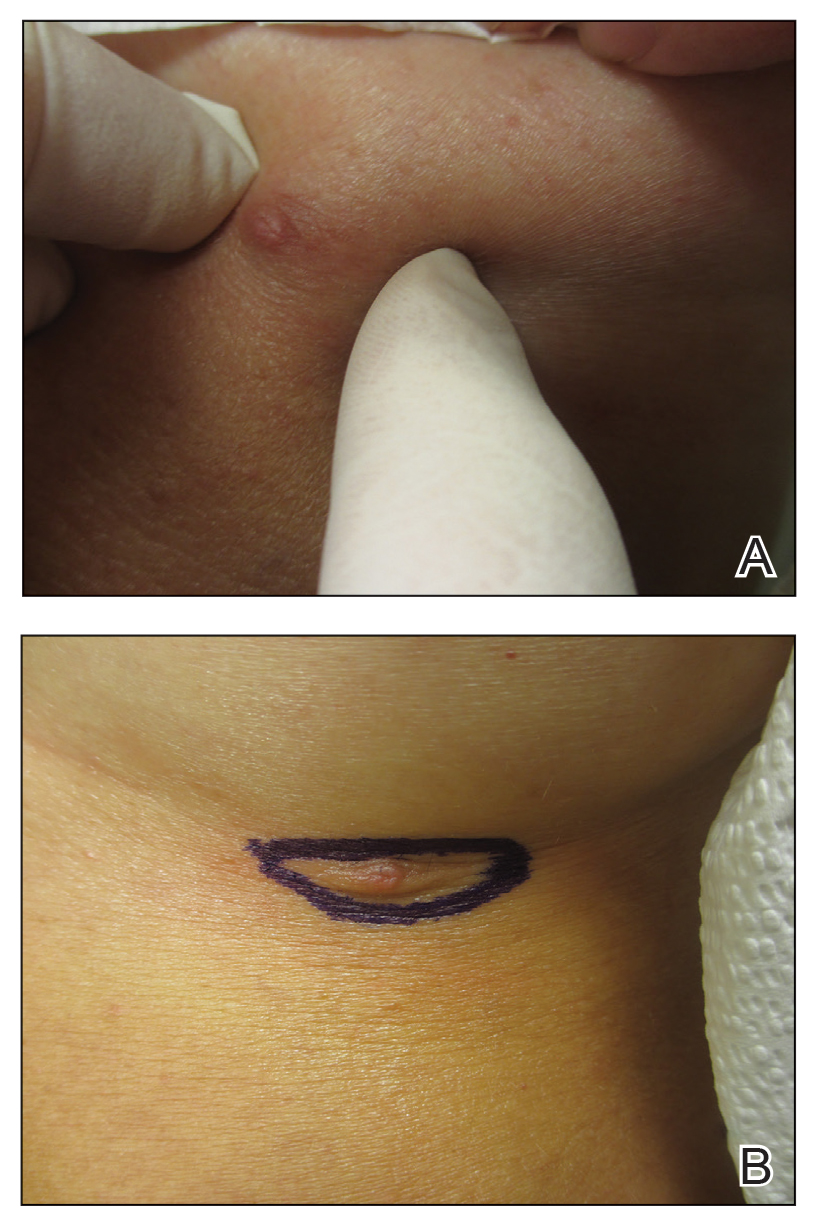
A 45-year-old White woman presented to our clinic for removal of a dermal mass underlying a supernumerary nipple at the left inframammary fold. Her medical history was noncontributory and was only remarkable for uterine fibroids. She developed pain and swelling in the left breast 1 year prior, which prompted her to seek medical attention from her primary care physician. Diagnostic mammography was negative for any concerning malignant nodules, and subsequent BRCA genetic testing also was negative. Six months after the diagnostic mammography, she continued to experience pain and swelling in the left breast and was then referred for diagnostic ultrasonography; 2 masses in the left breast suspected as infected cysts with rupture were identified (Figure 1). She was then referred to our dermatology clinic for evaluation and surgical extirpation of the suspected cyst underlying the accessory breast. The area subsequently was excised under local anesthesia, and a second similar but smaller mass also was identified adjacent to the initial growth. Dermatopathologic examination revealed an estrogen receptor– (Figure 2A) and progesterone receptor–positive (Figure 2B), ERBB2 (HER2/neu)–negative, nuclear grade III ductal carcinoma in situ (Figure 3).
Various ABT classification methods have been proposed with Brightmore7 categorizing polymastia into 8 subtypes: (1) complete breast; (2) glandular tissue and nipple; (3) glandular tissue and areola; (4) glandular tissue only; (5) nipple, areola, and fat; (6) nipple only; (7) areola only; and (8) patch of hair only. De Cholnokey8 focused on axillary polymastia, dividing it into 4 classes: (1) axillary tumor in milk line without nipple or areola; (2) axillary tumor with areola with or without pigmentation; (3) nipple or areola without underlying breast tissue; and (4) complete breast with nipple, areola, and glandular tissue. Fenench’s9 method is preferred and simply describes ABT as 2 subtypes: supernumerary and aberrant.1,2,10 One study observed 6% of ABT cancers were the supernumerary type and 94% were the aberrant type.1 Ductal lumen stagnation increases the risk for accessory breast carcinoma development.10 Men have a higher prevalence of cancer in ABT compared to anatomically correct breast tissue.11
There currently is no standardized guideline for ABT cancer treatment. The initial clinical impression of cancer of ABT may be misdiagnosed as lymphadenopathy, abscesses, or lipomas.12 The risk for misdiagnosis is higher for cancer of ABT compared to normal breast tissue and is associated with a poorer prognosis.1 Despite multiple screening modalities, our patient’s initial breast cancer screenings proved unreliable. A mammogram failed to detect malignancy, likely secondary to the area of concern being out of the standard imaging field. Ultrasonography also was unreliable and led to misdiagnosis as an infected sebaceous cyst with rupture in our patient. Upon review of the ultrasound, concerns were raised by dermatology that the mass was more likely an epidermal inclusion cyst with rupture given the more superficial and sac-free nature of sebaceous cysts, which commonly are associated with steatocystoma multiplex.13 Definitive diagnosis of ductal carcinoma in situ was made with dermatopathologic examination.
Prophylactic surgical excision of ABT has been recommended, suggesting that excisional biopsy and histopathologic examination is the more appropriate method to rule out malignancy. Surgical treatment of ABT may omit any risk for malignant transformation and may provide psychological relief to patients for aesthetic reasons.10,12,14 The risk and benefits of prophylactic excision of ABT has been compared to prophylactic mastectomy of anatomically correct breasts,15 with some clinicians considering this definitive procedure unnecessary except in high-risk patients with a strong genetic predisposition.16,17
Accessory breast tissue should be viewed as an anatomical variant with the option of surgical removal for symptomatic concerns, such as firm nodules, discharge, and pain. Although ABT is rare and cancer in ABT is even more uncommon (<1% of all breast cancers),5,11 clinicians should be suspicious of benign diagnostic reports when the clinical situation does not fit the proposed narrative.
- Marshall MB, Moynihan JJ, Frost A, et al. Ectopic breast cancer: case report and literature review. Surg Oncol. 1994;3:295-304. doi:10.1016/0960-7404(94)90032-9
- DeFilippis EM, Arleo EK. The ABCs of accessory breast tissue: basic information every radiologist should know. Am J Roentgenol. 2014;202:1157-1162. doi:10.2214/AJR.13.10930
- Famá F, Cicciú M, Sindoni A, et al. Prevalence of ectopic breast tissue and tumor: a 20-year single center experience. Clin Breast Cancer. 2016;16:E107-E112. doi:10.1016/j.clbc.2016.03.004
- Brown J, Schwartz RA. Supernumerary nipples: an overview. Cutis. 2003;71:344-346.
- Nihon-Yanagi Y, Ueda T, Kameda N, et al. A case of ectopic breast cancer with a literature review. Surg Oncol. 2011;20:35-42. doi:10.1016/j.suronc.2009.09.005
- Hedayat AA, Pettus JR, Marotti JD, et al. Proliferative lesion of anogenital mammary-like glands in the setting of Cowden syndrome: case report and review of the literature. J Cutan Pathol. 2016;43:707-710. doi:10.1111/cup.12721
- Brightmore T. Bilateral double nipples. Br J Surg. 1972;59:55-57. https://doi.org/10.1002/bjs.1800590114
- De Cholnoky T. Accessory breast tissue in the axilla. N Y State J Med. 1951;51:2245-2248.
- Fenech HB. Aberrant breast tissue; case report. Harper Hosp Bull. 1949;7:268-271.
- Francone E, Nathan MJ, Murelli F, et al. Ectopic breast cancer: case report and review of the literature. Aesthetic Plast Surg. 2013;37:746-749. doi:10.1007/s00266-013-0125-1
- Yamamura J, Masuda N, Kodama Y, et al. Male breast cancer originating in an accessory mammary gland in the axilla: a case report. Case Rep Med. 2012;2012:286210. doi:10.1155/2012/286210.
- Ghosn SH, Khatri KA, Bhawan J. Bilateral aberrant axillary breast tissue mimicking lipomas: report of a case and review of the literature. J Cutan Pathol. 2007;34(suppl 1):9-13. doi:10.1111/j.1600-0560.2006.00713.x
- Arceu M, Martinez G, Alfaro D, et al. Ultrasound morphologic features of steatocystoma multiplex with clinical correlation. J Ultrasound Med. 2020;39:2255-2260. doi:10.1002/jum.15320
- Lesavoy MA, Gomez-Garcia A, Nejdl R, et al. Axillary breast tissue: clinical presentation and surgical treatment. Ann Plast Surg. 1995;35:356-360. doi:10.1097/00000637-199510000-00004
- Bank J. Management of ectopic breast tissue. Aesthetic Plast Surg. 2013;37:750-751. doi:10.1007/s00266-013-0143-z
- Morrow M. Prophylactic mastectomy of the contralateral breast. Breast. 2011;20(suppl 3):S108-S110. doi:10.1016/S0960-9776(11)70306-X
- Teoh V, Tasoulis M-K, Gui G. Contralateral prophylactic mastectomy in women with unilateral breast cancer who are genetic carriers, have a strong family history or are just young at presentation. Cancers (Basel). 2020;12:140. doi:10.3390/cancers12010140
- Marshall MB, Moynihan JJ, Frost A, et al. Ectopic breast cancer: case report and literature review. Surg Oncol. 1994;3:295-304. doi:10.1016/0960-7404(94)90032-9
- DeFilippis EM, Arleo EK. The ABCs of accessory breast tissue: basic information every radiologist should know. Am J Roentgenol. 2014;202:1157-1162. doi:10.2214/AJR.13.10930
- Famá F, Cicciú M, Sindoni A, et al. Prevalence of ectopic breast tissue and tumor: a 20-year single center experience. Clin Breast Cancer. 2016;16:E107-E112. doi:10.1016/j.clbc.2016.03.004
- Brown J, Schwartz RA. Supernumerary nipples: an overview. Cutis. 2003;71:344-346.
- Nihon-Yanagi Y, Ueda T, Kameda N, et al. A case of ectopic breast cancer with a literature review. Surg Oncol. 2011;20:35-42. doi:10.1016/j.suronc.2009.09.005
- Hedayat AA, Pettus JR, Marotti JD, et al. Proliferative lesion of anogenital mammary-like glands in the setting of Cowden syndrome: case report and review of the literature. J Cutan Pathol. 2016;43:707-710. doi:10.1111/cup.12721
- Brightmore T. Bilateral double nipples. Br J Surg. 1972;59:55-57. https://doi.org/10.1002/bjs.1800590114
- De Cholnoky T. Accessory breast tissue in the axilla. N Y State J Med. 1951;51:2245-2248.
- Fenech HB. Aberrant breast tissue; case report. Harper Hosp Bull. 1949;7:268-271.
- Francone E, Nathan MJ, Murelli F, et al. Ectopic breast cancer: case report and review of the literature. Aesthetic Plast Surg. 2013;37:746-749. doi:10.1007/s00266-013-0125-1
- Yamamura J, Masuda N, Kodama Y, et al. Male breast cancer originating in an accessory mammary gland in the axilla: a case report. Case Rep Med. 2012;2012:286210. doi:10.1155/2012/286210.
- Ghosn SH, Khatri KA, Bhawan J. Bilateral aberrant axillary breast tissue mimicking lipomas: report of a case and review of the literature. J Cutan Pathol. 2007;34(suppl 1):9-13. doi:10.1111/j.1600-0560.2006.00713.x
- Arceu M, Martinez G, Alfaro D, et al. Ultrasound morphologic features of steatocystoma multiplex with clinical correlation. J Ultrasound Med. 2020;39:2255-2260. doi:10.1002/jum.15320
- Lesavoy MA, Gomez-Garcia A, Nejdl R, et al. Axillary breast tissue: clinical presentation and surgical treatment. Ann Plast Surg. 1995;35:356-360. doi:10.1097/00000637-199510000-00004
- Bank J. Management of ectopic breast tissue. Aesthetic Plast Surg. 2013;37:750-751. doi:10.1007/s00266-013-0143-z
- Morrow M. Prophylactic mastectomy of the contralateral breast. Breast. 2011;20(suppl 3):S108-S110. doi:10.1016/S0960-9776(11)70306-X
- Teoh V, Tasoulis M-K, Gui G. Contralateral prophylactic mastectomy in women with unilateral breast cancer who are genetic carriers, have a strong family history or are just young at presentation. Cancers (Basel). 2020;12:140. doi:10.3390/cancers12010140
Practice Points
- Accessory breasts (also referred to as ectopic breast tissue) develop when breast tissue is retained along the mammary ridge outside of the usual pectoral regions.
- Because accessory breasts may contain the same structures as anatomically correct breasts, they can be subject to the same benign or malignant changes.
- Clinical and pathologic correlation is prudent when interpreting ectopic mammary tissue, as various benign or malignant neoplasms may arise in this setting, especially if there are underlying genetic aberrancies or genodermatoses.
Can caffeine improve thyroid function?
“Although the causal relationship between caffeine intake and thyroid function requires further verification, as an easily obtainable and widely consumed dietary ingredient, caffeine is a potential candidate for improving thyroid health in people with metabolic disorders,” reported the authors in the study, published in Nutritional Journal.
Caffeine intake, within established healthy ranges, showed a nonlinear association with thyroid levels.
Moderate caffeine intake has been associated with reducing the risk of metabolic disorders in addition to showing some mental health benefits. However, research on its effects on thyroid hormone, which importantly plays a key role in systemic metabolism and neurologic development, is lacking.
To investigate the effects, Yu Zhou, of the Department of Rehabilitation Medicine, School of Health, Fujian Medical University, Fuzhou, China, and colleagues evaluated data from the National Health and Nutrition Examination Survey (NHANES) III 2007-2012 study involving 2,582 participants for whom data were available regarding medical conditions, dietary intake, thyroid function, and demographic background.
The participants were divided into three subgroups based on sex, age, body mass index, hyperglycemia, hypertension, and cardio-cerebral vascular disease (CVD).
Group 1 (n = 208) was the most metabolically unhealthy. Patients in that group had the highest BMI and were of oldest age. In addition, that group had higher rates of hypertension, hyperglycemia, and CVD, but, notably, it had the lowest level of caffeine consumption.
In group 2 (n = 543), all participants were current smokers, and 90.4% had a habit of drinking alcohol. That group also had the highest percentage of men.
Group 3 (n = 1,183) was the most metabolically healthy, with more women, younger age, and lowest BMI. No participants in that group had hyperglycemia, hypertension, or CVD.
Group 1, the most metabolically unhealthy, had the highest serum thyroid-stimulating hormone (TSH) levels. Of note, while participants with thyroid diseases were initially excluded from the analysis, higher TSH levels are predictive of subclinical hypothyroidism or progression to overt hypothyroidism.
Overall, there was no association between caffeine and TSH levels.
However, a subgroup analysis of the groups showed that in group 1, caffeine intake correlated with TSH nonlinearly (P = .0019), with minimal average consumption of caffeine (< 9.97 mg/d). There was an association with slightly higher TSH levels (P = .035) after adjustment for age, sex, race, drink, disease state, micronutrients, and macronutrients.
However, in higher, moderate amounts of caffeine consumption (9.97 – 264.97 mg/d), there was an inverse association, with lower TSH (P = .001).
There was no association between daily caffeine consumption of more than 264.97 mg and TSH levels.
For context, a typical 8-ounce cup of coffee generally contains 80-100 mg of caffeine, and the Food and Drug Administration indicates that 400 mg/d of caffeine is safe for healthy adults.
Group 2 consumed the highest amount of caffeine. Notably, that group had the lowest serum TSH levels of the three groups. There were no significant associations between caffeine consumption and TSH levels in group 2 or group 3.
There were no significant associations between caffeine consumption and levels of serum FT4 or FT3, also linked to thyroid dysfunction, in any of the groups.
The findings show that “caffeine consumption was correlated with serum TSH nonlinearly, and when taken in moderate amounts (9.97-264.97 mg/d), caffeine demonstrated a positive correlation with serum TSH levels in patients with metabolic disorders,” the authors concluded.
Mechanisms?
Caffeine is believed to modulate pituitary hormone secretion, which has been shown to influence the hypothalamic-pituitary-adrenal axis. The authors speculated that caffeine could potentially affect thyroid activity by affecting pituitary function.
“However, the effects of transient and chronic caffeine administration on human thyroid function need to be verified further, and the related mechanisms remain unclear,” they noted.
Commenting on the study, Maik Pietzner, PhD, of the Berlin Institute of Health, noted that an important limitation of the study is that various patient groups were excluded, including those with abnormal TSH levels.
“What makes me wonder is the high number of exclusions and the focus on very specific groups of people. This almost certainly introduces bias, e.g., what is specific to people not reporting coffee consumption,” Dr. Pietzner said.
Furthermore, “we already know that patients with poor metabolic health do also have slight variations in thyroid hormone levels and also have different dietary patterns,” he explained.
“So reverse confounding might occur in which the poor metabolic health is associated with both poor thyroid hormone levels and coffee consumption,” Dr. Pietzner said.
He also noted the “somewhat odd” finding that the group with the highest metabolic disorders had the lowest coffee consumption, yet the highest TSH levels.
“My guess would be that this might also be a chance finding, given that the distribution of TSH values is very skewed, which can have a strong effect in linear regression models,” Dr. Pietzner said.
In general, “the evidence generated by the study is rather weak, but there is good evidence that higher coffee consumption is linked to better metabolic health, although the exact mechanisms is not known, if indeed causal,” Dr. Pietzner added. “Prospective studies are needed to evaluate whether higher coffee consumption indeed lowers the risk for thyroid disease.”
A version of this article first appeared on Medscape.com.
“Although the causal relationship between caffeine intake and thyroid function requires further verification, as an easily obtainable and widely consumed dietary ingredient, caffeine is a potential candidate for improving thyroid health in people with metabolic disorders,” reported the authors in the study, published in Nutritional Journal.
Caffeine intake, within established healthy ranges, showed a nonlinear association with thyroid levels.
Moderate caffeine intake has been associated with reducing the risk of metabolic disorders in addition to showing some mental health benefits. However, research on its effects on thyroid hormone, which importantly plays a key role in systemic metabolism and neurologic development, is lacking.
To investigate the effects, Yu Zhou, of the Department of Rehabilitation Medicine, School of Health, Fujian Medical University, Fuzhou, China, and colleagues evaluated data from the National Health and Nutrition Examination Survey (NHANES) III 2007-2012 study involving 2,582 participants for whom data were available regarding medical conditions, dietary intake, thyroid function, and demographic background.
The participants were divided into three subgroups based on sex, age, body mass index, hyperglycemia, hypertension, and cardio-cerebral vascular disease (CVD).
Group 1 (n = 208) was the most metabolically unhealthy. Patients in that group had the highest BMI and were of oldest age. In addition, that group had higher rates of hypertension, hyperglycemia, and CVD, but, notably, it had the lowest level of caffeine consumption.
In group 2 (n = 543), all participants were current smokers, and 90.4% had a habit of drinking alcohol. That group also had the highest percentage of men.
Group 3 (n = 1,183) was the most metabolically healthy, with more women, younger age, and lowest BMI. No participants in that group had hyperglycemia, hypertension, or CVD.
Group 1, the most metabolically unhealthy, had the highest serum thyroid-stimulating hormone (TSH) levels. Of note, while participants with thyroid diseases were initially excluded from the analysis, higher TSH levels are predictive of subclinical hypothyroidism or progression to overt hypothyroidism.
Overall, there was no association between caffeine and TSH levels.
However, a subgroup analysis of the groups showed that in group 1, caffeine intake correlated with TSH nonlinearly (P = .0019), with minimal average consumption of caffeine (< 9.97 mg/d). There was an association with slightly higher TSH levels (P = .035) after adjustment for age, sex, race, drink, disease state, micronutrients, and macronutrients.
However, in higher, moderate amounts of caffeine consumption (9.97 – 264.97 mg/d), there was an inverse association, with lower TSH (P = .001).
There was no association between daily caffeine consumption of more than 264.97 mg and TSH levels.
For context, a typical 8-ounce cup of coffee generally contains 80-100 mg of caffeine, and the Food and Drug Administration indicates that 400 mg/d of caffeine is safe for healthy adults.
Group 2 consumed the highest amount of caffeine. Notably, that group had the lowest serum TSH levels of the three groups. There were no significant associations between caffeine consumption and TSH levels in group 2 or group 3.
There were no significant associations between caffeine consumption and levels of serum FT4 or FT3, also linked to thyroid dysfunction, in any of the groups.
The findings show that “caffeine consumption was correlated with serum TSH nonlinearly, and when taken in moderate amounts (9.97-264.97 mg/d), caffeine demonstrated a positive correlation with serum TSH levels in patients with metabolic disorders,” the authors concluded.
Mechanisms?
Caffeine is believed to modulate pituitary hormone secretion, which has been shown to influence the hypothalamic-pituitary-adrenal axis. The authors speculated that caffeine could potentially affect thyroid activity by affecting pituitary function.
“However, the effects of transient and chronic caffeine administration on human thyroid function need to be verified further, and the related mechanisms remain unclear,” they noted.
Commenting on the study, Maik Pietzner, PhD, of the Berlin Institute of Health, noted that an important limitation of the study is that various patient groups were excluded, including those with abnormal TSH levels.
“What makes me wonder is the high number of exclusions and the focus on very specific groups of people. This almost certainly introduces bias, e.g., what is specific to people not reporting coffee consumption,” Dr. Pietzner said.
Furthermore, “we already know that patients with poor metabolic health do also have slight variations in thyroid hormone levels and also have different dietary patterns,” he explained.
“So reverse confounding might occur in which the poor metabolic health is associated with both poor thyroid hormone levels and coffee consumption,” Dr. Pietzner said.
He also noted the “somewhat odd” finding that the group with the highest metabolic disorders had the lowest coffee consumption, yet the highest TSH levels.
“My guess would be that this might also be a chance finding, given that the distribution of TSH values is very skewed, which can have a strong effect in linear regression models,” Dr. Pietzner said.
In general, “the evidence generated by the study is rather weak, but there is good evidence that higher coffee consumption is linked to better metabolic health, although the exact mechanisms is not known, if indeed causal,” Dr. Pietzner added. “Prospective studies are needed to evaluate whether higher coffee consumption indeed lowers the risk for thyroid disease.”
A version of this article first appeared on Medscape.com.
“Although the causal relationship between caffeine intake and thyroid function requires further verification, as an easily obtainable and widely consumed dietary ingredient, caffeine is a potential candidate for improving thyroid health in people with metabolic disorders,” reported the authors in the study, published in Nutritional Journal.
Caffeine intake, within established healthy ranges, showed a nonlinear association with thyroid levels.
Moderate caffeine intake has been associated with reducing the risk of metabolic disorders in addition to showing some mental health benefits. However, research on its effects on thyroid hormone, which importantly plays a key role in systemic metabolism and neurologic development, is lacking.
To investigate the effects, Yu Zhou, of the Department of Rehabilitation Medicine, School of Health, Fujian Medical University, Fuzhou, China, and colleagues evaluated data from the National Health and Nutrition Examination Survey (NHANES) III 2007-2012 study involving 2,582 participants for whom data were available regarding medical conditions, dietary intake, thyroid function, and demographic background.
The participants were divided into three subgroups based on sex, age, body mass index, hyperglycemia, hypertension, and cardio-cerebral vascular disease (CVD).
Group 1 (n = 208) was the most metabolically unhealthy. Patients in that group had the highest BMI and were of oldest age. In addition, that group had higher rates of hypertension, hyperglycemia, and CVD, but, notably, it had the lowest level of caffeine consumption.
In group 2 (n = 543), all participants were current smokers, and 90.4% had a habit of drinking alcohol. That group also had the highest percentage of men.
Group 3 (n = 1,183) was the most metabolically healthy, with more women, younger age, and lowest BMI. No participants in that group had hyperglycemia, hypertension, or CVD.
Group 1, the most metabolically unhealthy, had the highest serum thyroid-stimulating hormone (TSH) levels. Of note, while participants with thyroid diseases were initially excluded from the analysis, higher TSH levels are predictive of subclinical hypothyroidism or progression to overt hypothyroidism.
Overall, there was no association between caffeine and TSH levels.
However, a subgroup analysis of the groups showed that in group 1, caffeine intake correlated with TSH nonlinearly (P = .0019), with minimal average consumption of caffeine (< 9.97 mg/d). There was an association with slightly higher TSH levels (P = .035) after adjustment for age, sex, race, drink, disease state, micronutrients, and macronutrients.
However, in higher, moderate amounts of caffeine consumption (9.97 – 264.97 mg/d), there was an inverse association, with lower TSH (P = .001).
There was no association between daily caffeine consumption of more than 264.97 mg and TSH levels.
For context, a typical 8-ounce cup of coffee generally contains 80-100 mg of caffeine, and the Food and Drug Administration indicates that 400 mg/d of caffeine is safe for healthy adults.
Group 2 consumed the highest amount of caffeine. Notably, that group had the lowest serum TSH levels of the three groups. There were no significant associations between caffeine consumption and TSH levels in group 2 or group 3.
There were no significant associations between caffeine consumption and levels of serum FT4 or FT3, also linked to thyroid dysfunction, in any of the groups.
The findings show that “caffeine consumption was correlated with serum TSH nonlinearly, and when taken in moderate amounts (9.97-264.97 mg/d), caffeine demonstrated a positive correlation with serum TSH levels in patients with metabolic disorders,” the authors concluded.
Mechanisms?
Caffeine is believed to modulate pituitary hormone secretion, which has been shown to influence the hypothalamic-pituitary-adrenal axis. The authors speculated that caffeine could potentially affect thyroid activity by affecting pituitary function.
“However, the effects of transient and chronic caffeine administration on human thyroid function need to be verified further, and the related mechanisms remain unclear,” they noted.
Commenting on the study, Maik Pietzner, PhD, of the Berlin Institute of Health, noted that an important limitation of the study is that various patient groups were excluded, including those with abnormal TSH levels.
“What makes me wonder is the high number of exclusions and the focus on very specific groups of people. This almost certainly introduces bias, e.g., what is specific to people not reporting coffee consumption,” Dr. Pietzner said.
Furthermore, “we already know that patients with poor metabolic health do also have slight variations in thyroid hormone levels and also have different dietary patterns,” he explained.
“So reverse confounding might occur in which the poor metabolic health is associated with both poor thyroid hormone levels and coffee consumption,” Dr. Pietzner said.
He also noted the “somewhat odd” finding that the group with the highest metabolic disorders had the lowest coffee consumption, yet the highest TSH levels.
“My guess would be that this might also be a chance finding, given that the distribution of TSH values is very skewed, which can have a strong effect in linear regression models,” Dr. Pietzner said.
In general, “the evidence generated by the study is rather weak, but there is good evidence that higher coffee consumption is linked to better metabolic health, although the exact mechanisms is not known, if indeed causal,” Dr. Pietzner added. “Prospective studies are needed to evaluate whether higher coffee consumption indeed lowers the risk for thyroid disease.”
A version of this article first appeared on Medscape.com.
FROM NUTRITIONAL JOURNAL
ChatGPT in Dermatology Clinical Practice: Potential Uses and Pitfalls
Artificial intelligence (AI) technology has increasingly been incorporated in medicine. In dermatology, AI has been used to detect and diagnose skin lesions, including skin cancer.1 ChatGPT (OpenAI) is a novel, highly popular development in generative AI technology. A large language model released in 2022, ChatGPT is a chatbot designed to mimic human conversation and generate specific detailed information when prompted. Free and publicly available, it has been used by millions of people. ChatGPT’s application in the medical field currently is being evaluated across several specialties, including plastic surgery, radiology, and urology.2-4 ChatGPT has the potential to assist health care professionals, including dermatologists, though its use raises important ethical considerations. Herein, we focus on the potential benefits as well as the pitfalls of using ChatGPT in dermatology clinical practice.
Potential Uses of ChatGPT in Practice
A major benefit of ChatGPT is its ability to improve clinical efficiency. First, ChatGPT can provide quick access to general medical information, similar to a search engine but with more natural language processing and contextual understanding to synthesize information.5 This function is useful for rapid concise answers to specific and directed questions. ChatGPT also can interact with its user by asking follow-up questions to produce more precise and relevant responses; this feature may help dermatologists form more accurate differential diagnoses. Additionally, ChatGPT can increase efficiency in clinical practice by drafting generic medical documents,2 including templates for after-visit summaries, postprocedure instructions, referrals, prior authorization appeal letters, and educational handouts. Importantly, increased efficiency can reduce provider burnout and lead to improved patient care. Another useful feature of ChatGPT is its ability to output information modeling human conversation. Because of this feature, ChatGPT also could be employed in clinical practice to serve as an interpreter for patients during clinic visits. Currently, the use of virtual translators can be cumbersome and subject to technical constraints. ChatGPT can provide accurate and conversational translations for patients and dermatologists, improving the patient-provider relationship.
ChatGPT also can contribute to major advancements in the field of dermatology beyond the clinical setting. Because of its ability to draw from extensive data that have already been uploaded, there are some uses of ChatGPT in a research context: to assist in finding resources for research and reviews, formulating hypotheses, drafting study protocols, and collecting large amounts of data within seconds.6
ChatGPT also has potential in advancing medical education. It could be used by medical schools to model interactive patient encounters to help students practice taking a patient’s history and creating differential diagnoses.6 This application of ChatGPT may help medical students hone their clinical skills in a low-stress environment without the restrictions that can come with hiring and training standardized patients, especially when mimicking dermatologic clinical encounters.
Other possibilities for ChatGPT in dermatologic practice include survey administration, clinical trial recruitment, and even automatic high-risk medication monitoring. Despite the many potential applications of ChatGPT in clinical practice, the question raised in each scenario is the quality, accuracy, and safety of what it produces.
Potential Pitfalls of ChatGPT in Practice and Possible Mitigation Strategies
A main concern in using ChatGPT in clinical practice is its potential to produce inaccurate or biased information. When prompted to create a research abstract based on previously published research, ChatGPT drafted abstracts that were clear and digestible but supplemented with incorrect data.7 A group of medical researchers who reviewed these ChatGPT-generated abstracts mistook 32% of the abstracts as having been written by human researchers. The implications of this finding are worrisome. If inaccurate or false information is used by ChatGPT in documents sent to insurance companies or patients, the patient’s safety as well as the dermatologist’s license and credibility are at stake. Thus, dermatologists looking to use ChatGPT to draft generic medical documents should actively review the output to ensure that the information is accurate. Importantly, ChatGPT also is only currently programmed with information up to 2021, limiting its access to recently published research articles and updated International Classification of Diseases, Tenth Revision codes.5 The continued development of ChatGPT will lead to regular updates by OpenAI that resolve this shortcoming in the future. Further, AI models may encode and perpetuate harmful stereotypes and social biases that are present in training data.8
When considering its potential in clinical practice, ChatGPT itself states that it can aid in clinical decision-making by processing patient information, including history, current symptoms, and biopsy and test results. This is uncharted territory, and providers who use ChatGPT at this stage to aid in decision-making should regard it similarly to information retrieved from a search engine. The information produced by ChatGPT should be used to substantiate but not definitively confirm a diagnosis or dictate management. Clinical suspicion by the dermatologist should always trump ChatGPT output. If physicians recommend ChatGPT output over their own advice, it can become a liability, as the technology is not regulated to any degree. Patients also should be cautious when seeking and following medical advice from ChatGPT, as it could be misleading or incorrect and could undermine the patient-physician relationship.6
Additionally, the specific use of ChatGPT to evaluate patient health records raises concerns related to patient privacy and confidentiality. Providers should never enter patient information protected by the Health Insurance Portability and Accountability Act into ChatGPT or anywhere else on the internet. Mitigation of this risk is not currently possible; ChatGPT requires more development and further understanding to even consider its integration into current electronic health records without compromising patient confidentiality.
The Bottom Line
Overall, ChatGPT has the potential to improve efficiency in clinical practice by assisting with informational searches and document drafting. Importantly, increased efficiency can reduce provider burnout and lead to improved patient care. However, dermatologists should carefully weigh the ethical issues of nonmaleficence and justice in evaluating ChatGPT for accuracy, biases, and the protection of patient confidentiality.
Finally, we asked ChatGPT on February 28, 2023, what it thinks:
User: Should dermatologists use ChatGPT in clinical practice?
ChatGPT: As an AI language model, ChatGPT can be a useful tool in dermatology clinical practice, but it should be used with caution in conjunction with other sources of information and clinical judgement.
Dermatologists should be aware of the potential benefits and risks of using ChatGPT and make informed decisions about how to integrate it into their clinical practice. It’s important to remember that ChatGPT is not a substitute for clinical expertise or human interaction with patients, and it should only be used as a supplement to enhance the quality of patient care.
Dermatologists who choose to use ChatGPT should also be aware of its limitations and potential risks, such as limited accuracy, lack of context, and liability issues if it provides incorrect information or recommendations that lead to patient harm. Dermatologists should use their professional judgement and consult with other health care professionals when making important decisions regarding patient care.
- Thomsen K, Iversen L, Titlestad TL, et al. Systematic review of machine learning for diagnosis and prognosis in dermatology. J Dermatol Treat. 2020;31:496-510. doi:10.1080/09546634.2019.1682500
- Shen Y, Heacock L, Elias J, et al. ChatGPT and other large language models are double-edged swords. Radiology. 2023;307:E230163. doi:10.1148/radiol.230163
- Gupta R, Pande P, Herzog I, et al. Application of ChatGPT in cosmetic plastic surgery: ally or antagonist? Aesthet Surg J. 2023;43:NP587-NP590. doi: 10.1093/asj/sjad042
- Gabrielson AT, Odisho AY, Canes D. Harnessing generative artificial intelligence to improve efficiency among urologists: welcome ChatGPT. J Urol. 2023;209:827-829. doi:10.1097/JU.0000000000003383
- What is ChatGPT? OpenAI. Accessed August 10, 2023. https://help.openai.com/en/articles/6783457-chatgpt-general-faq
- Haupt CE, Marks M. AI-generated medical advice—GPT and beyond. JAMA. 2023;329:1349-1350. doi:10.1001/jama.2023.5321
- Gao CA, Howard FM, Markov NS, et al. Comparing Scientific Abstracts Generated by ChatGPT to Original Abstracts Using an Artificial Intelligence Output Detector, Plagiarism Detector, and Blinded Human Reviewers. Scientific Communication and Education; 2022. doi:10.1101/2022.12.23.521610
- Weidinger L, Mellor J, Rauh M, et al. Ethical and social risks of harm from language models. arXiv. Preprint posted online December 8, 2021. https://doi.org/10.48550/arXiv.2112.04359
Artificial intelligence (AI) technology has increasingly been incorporated in medicine. In dermatology, AI has been used to detect and diagnose skin lesions, including skin cancer.1 ChatGPT (OpenAI) is a novel, highly popular development in generative AI technology. A large language model released in 2022, ChatGPT is a chatbot designed to mimic human conversation and generate specific detailed information when prompted. Free and publicly available, it has been used by millions of people. ChatGPT’s application in the medical field currently is being evaluated across several specialties, including plastic surgery, radiology, and urology.2-4 ChatGPT has the potential to assist health care professionals, including dermatologists, though its use raises important ethical considerations. Herein, we focus on the potential benefits as well as the pitfalls of using ChatGPT in dermatology clinical practice.
Potential Uses of ChatGPT in Practice
A major benefit of ChatGPT is its ability to improve clinical efficiency. First, ChatGPT can provide quick access to general medical information, similar to a search engine but with more natural language processing and contextual understanding to synthesize information.5 This function is useful for rapid concise answers to specific and directed questions. ChatGPT also can interact with its user by asking follow-up questions to produce more precise and relevant responses; this feature may help dermatologists form more accurate differential diagnoses. Additionally, ChatGPT can increase efficiency in clinical practice by drafting generic medical documents,2 including templates for after-visit summaries, postprocedure instructions, referrals, prior authorization appeal letters, and educational handouts. Importantly, increased efficiency can reduce provider burnout and lead to improved patient care. Another useful feature of ChatGPT is its ability to output information modeling human conversation. Because of this feature, ChatGPT also could be employed in clinical practice to serve as an interpreter for patients during clinic visits. Currently, the use of virtual translators can be cumbersome and subject to technical constraints. ChatGPT can provide accurate and conversational translations for patients and dermatologists, improving the patient-provider relationship.
ChatGPT also can contribute to major advancements in the field of dermatology beyond the clinical setting. Because of its ability to draw from extensive data that have already been uploaded, there are some uses of ChatGPT in a research context: to assist in finding resources for research and reviews, formulating hypotheses, drafting study protocols, and collecting large amounts of data within seconds.6
ChatGPT also has potential in advancing medical education. It could be used by medical schools to model interactive patient encounters to help students practice taking a patient’s history and creating differential diagnoses.6 This application of ChatGPT may help medical students hone their clinical skills in a low-stress environment without the restrictions that can come with hiring and training standardized patients, especially when mimicking dermatologic clinical encounters.
Other possibilities for ChatGPT in dermatologic practice include survey administration, clinical trial recruitment, and even automatic high-risk medication monitoring. Despite the many potential applications of ChatGPT in clinical practice, the question raised in each scenario is the quality, accuracy, and safety of what it produces.
Potential Pitfalls of ChatGPT in Practice and Possible Mitigation Strategies
A main concern in using ChatGPT in clinical practice is its potential to produce inaccurate or biased information. When prompted to create a research abstract based on previously published research, ChatGPT drafted abstracts that were clear and digestible but supplemented with incorrect data.7 A group of medical researchers who reviewed these ChatGPT-generated abstracts mistook 32% of the abstracts as having been written by human researchers. The implications of this finding are worrisome. If inaccurate or false information is used by ChatGPT in documents sent to insurance companies or patients, the patient’s safety as well as the dermatologist’s license and credibility are at stake. Thus, dermatologists looking to use ChatGPT to draft generic medical documents should actively review the output to ensure that the information is accurate. Importantly, ChatGPT also is only currently programmed with information up to 2021, limiting its access to recently published research articles and updated International Classification of Diseases, Tenth Revision codes.5 The continued development of ChatGPT will lead to regular updates by OpenAI that resolve this shortcoming in the future. Further, AI models may encode and perpetuate harmful stereotypes and social biases that are present in training data.8
When considering its potential in clinical practice, ChatGPT itself states that it can aid in clinical decision-making by processing patient information, including history, current symptoms, and biopsy and test results. This is uncharted territory, and providers who use ChatGPT at this stage to aid in decision-making should regard it similarly to information retrieved from a search engine. The information produced by ChatGPT should be used to substantiate but not definitively confirm a diagnosis or dictate management. Clinical suspicion by the dermatologist should always trump ChatGPT output. If physicians recommend ChatGPT output over their own advice, it can become a liability, as the technology is not regulated to any degree. Patients also should be cautious when seeking and following medical advice from ChatGPT, as it could be misleading or incorrect and could undermine the patient-physician relationship.6
Additionally, the specific use of ChatGPT to evaluate patient health records raises concerns related to patient privacy and confidentiality. Providers should never enter patient information protected by the Health Insurance Portability and Accountability Act into ChatGPT or anywhere else on the internet. Mitigation of this risk is not currently possible; ChatGPT requires more development and further understanding to even consider its integration into current electronic health records without compromising patient confidentiality.
The Bottom Line
Overall, ChatGPT has the potential to improve efficiency in clinical practice by assisting with informational searches and document drafting. Importantly, increased efficiency can reduce provider burnout and lead to improved patient care. However, dermatologists should carefully weigh the ethical issues of nonmaleficence and justice in evaluating ChatGPT for accuracy, biases, and the protection of patient confidentiality.
Finally, we asked ChatGPT on February 28, 2023, what it thinks:
User: Should dermatologists use ChatGPT in clinical practice?
ChatGPT: As an AI language model, ChatGPT can be a useful tool in dermatology clinical practice, but it should be used with caution in conjunction with other sources of information and clinical judgement.
Dermatologists should be aware of the potential benefits and risks of using ChatGPT and make informed decisions about how to integrate it into their clinical practice. It’s important to remember that ChatGPT is not a substitute for clinical expertise or human interaction with patients, and it should only be used as a supplement to enhance the quality of patient care.
Dermatologists who choose to use ChatGPT should also be aware of its limitations and potential risks, such as limited accuracy, lack of context, and liability issues if it provides incorrect information or recommendations that lead to patient harm. Dermatologists should use their professional judgement and consult with other health care professionals when making important decisions regarding patient care.
Artificial intelligence (AI) technology has increasingly been incorporated in medicine. In dermatology, AI has been used to detect and diagnose skin lesions, including skin cancer.1 ChatGPT (OpenAI) is a novel, highly popular development in generative AI technology. A large language model released in 2022, ChatGPT is a chatbot designed to mimic human conversation and generate specific detailed information when prompted. Free and publicly available, it has been used by millions of people. ChatGPT’s application in the medical field currently is being evaluated across several specialties, including plastic surgery, radiology, and urology.2-4 ChatGPT has the potential to assist health care professionals, including dermatologists, though its use raises important ethical considerations. Herein, we focus on the potential benefits as well as the pitfalls of using ChatGPT in dermatology clinical practice.
Potential Uses of ChatGPT in Practice
A major benefit of ChatGPT is its ability to improve clinical efficiency. First, ChatGPT can provide quick access to general medical information, similar to a search engine but with more natural language processing and contextual understanding to synthesize information.5 This function is useful for rapid concise answers to specific and directed questions. ChatGPT also can interact with its user by asking follow-up questions to produce more precise and relevant responses; this feature may help dermatologists form more accurate differential diagnoses. Additionally, ChatGPT can increase efficiency in clinical practice by drafting generic medical documents,2 including templates for after-visit summaries, postprocedure instructions, referrals, prior authorization appeal letters, and educational handouts. Importantly, increased efficiency can reduce provider burnout and lead to improved patient care. Another useful feature of ChatGPT is its ability to output information modeling human conversation. Because of this feature, ChatGPT also could be employed in clinical practice to serve as an interpreter for patients during clinic visits. Currently, the use of virtual translators can be cumbersome and subject to technical constraints. ChatGPT can provide accurate and conversational translations for patients and dermatologists, improving the patient-provider relationship.
ChatGPT also can contribute to major advancements in the field of dermatology beyond the clinical setting. Because of its ability to draw from extensive data that have already been uploaded, there are some uses of ChatGPT in a research context: to assist in finding resources for research and reviews, formulating hypotheses, drafting study protocols, and collecting large amounts of data within seconds.6
ChatGPT also has potential in advancing medical education. It could be used by medical schools to model interactive patient encounters to help students practice taking a patient’s history and creating differential diagnoses.6 This application of ChatGPT may help medical students hone their clinical skills in a low-stress environment without the restrictions that can come with hiring and training standardized patients, especially when mimicking dermatologic clinical encounters.
Other possibilities for ChatGPT in dermatologic practice include survey administration, clinical trial recruitment, and even automatic high-risk medication monitoring. Despite the many potential applications of ChatGPT in clinical practice, the question raised in each scenario is the quality, accuracy, and safety of what it produces.
Potential Pitfalls of ChatGPT in Practice and Possible Mitigation Strategies
A main concern in using ChatGPT in clinical practice is its potential to produce inaccurate or biased information. When prompted to create a research abstract based on previously published research, ChatGPT drafted abstracts that were clear and digestible but supplemented with incorrect data.7 A group of medical researchers who reviewed these ChatGPT-generated abstracts mistook 32% of the abstracts as having been written by human researchers. The implications of this finding are worrisome. If inaccurate or false information is used by ChatGPT in documents sent to insurance companies or patients, the patient’s safety as well as the dermatologist’s license and credibility are at stake. Thus, dermatologists looking to use ChatGPT to draft generic medical documents should actively review the output to ensure that the information is accurate. Importantly, ChatGPT also is only currently programmed with information up to 2021, limiting its access to recently published research articles and updated International Classification of Diseases, Tenth Revision codes.5 The continued development of ChatGPT will lead to regular updates by OpenAI that resolve this shortcoming in the future. Further, AI models may encode and perpetuate harmful stereotypes and social biases that are present in training data.8
When considering its potential in clinical practice, ChatGPT itself states that it can aid in clinical decision-making by processing patient information, including history, current symptoms, and biopsy and test results. This is uncharted territory, and providers who use ChatGPT at this stage to aid in decision-making should regard it similarly to information retrieved from a search engine. The information produced by ChatGPT should be used to substantiate but not definitively confirm a diagnosis or dictate management. Clinical suspicion by the dermatologist should always trump ChatGPT output. If physicians recommend ChatGPT output over their own advice, it can become a liability, as the technology is not regulated to any degree. Patients also should be cautious when seeking and following medical advice from ChatGPT, as it could be misleading or incorrect and could undermine the patient-physician relationship.6
Additionally, the specific use of ChatGPT to evaluate patient health records raises concerns related to patient privacy and confidentiality. Providers should never enter patient information protected by the Health Insurance Portability and Accountability Act into ChatGPT or anywhere else on the internet. Mitigation of this risk is not currently possible; ChatGPT requires more development and further understanding to even consider its integration into current electronic health records without compromising patient confidentiality.
The Bottom Line
Overall, ChatGPT has the potential to improve efficiency in clinical practice by assisting with informational searches and document drafting. Importantly, increased efficiency can reduce provider burnout and lead to improved patient care. However, dermatologists should carefully weigh the ethical issues of nonmaleficence and justice in evaluating ChatGPT for accuracy, biases, and the protection of patient confidentiality.
Finally, we asked ChatGPT on February 28, 2023, what it thinks:
User: Should dermatologists use ChatGPT in clinical practice?
ChatGPT: As an AI language model, ChatGPT can be a useful tool in dermatology clinical practice, but it should be used with caution in conjunction with other sources of information and clinical judgement.
Dermatologists should be aware of the potential benefits and risks of using ChatGPT and make informed decisions about how to integrate it into their clinical practice. It’s important to remember that ChatGPT is not a substitute for clinical expertise or human interaction with patients, and it should only be used as a supplement to enhance the quality of patient care.
Dermatologists who choose to use ChatGPT should also be aware of its limitations and potential risks, such as limited accuracy, lack of context, and liability issues if it provides incorrect information or recommendations that lead to patient harm. Dermatologists should use their professional judgement and consult with other health care professionals when making important decisions regarding patient care.
- Thomsen K, Iversen L, Titlestad TL, et al. Systematic review of machine learning for diagnosis and prognosis in dermatology. J Dermatol Treat. 2020;31:496-510. doi:10.1080/09546634.2019.1682500
- Shen Y, Heacock L, Elias J, et al. ChatGPT and other large language models are double-edged swords. Radiology. 2023;307:E230163. doi:10.1148/radiol.230163
- Gupta R, Pande P, Herzog I, et al. Application of ChatGPT in cosmetic plastic surgery: ally or antagonist? Aesthet Surg J. 2023;43:NP587-NP590. doi: 10.1093/asj/sjad042
- Gabrielson AT, Odisho AY, Canes D. Harnessing generative artificial intelligence to improve efficiency among urologists: welcome ChatGPT. J Urol. 2023;209:827-829. doi:10.1097/JU.0000000000003383
- What is ChatGPT? OpenAI. Accessed August 10, 2023. https://help.openai.com/en/articles/6783457-chatgpt-general-faq
- Haupt CE, Marks M. AI-generated medical advice—GPT and beyond. JAMA. 2023;329:1349-1350. doi:10.1001/jama.2023.5321
- Gao CA, Howard FM, Markov NS, et al. Comparing Scientific Abstracts Generated by ChatGPT to Original Abstracts Using an Artificial Intelligence Output Detector, Plagiarism Detector, and Blinded Human Reviewers. Scientific Communication and Education; 2022. doi:10.1101/2022.12.23.521610
- Weidinger L, Mellor J, Rauh M, et al. Ethical and social risks of harm from language models. arXiv. Preprint posted online December 8, 2021. https://doi.org/10.48550/arXiv.2112.04359
- Thomsen K, Iversen L, Titlestad TL, et al. Systematic review of machine learning for diagnosis and prognosis in dermatology. J Dermatol Treat. 2020;31:496-510. doi:10.1080/09546634.2019.1682500
- Shen Y, Heacock L, Elias J, et al. ChatGPT and other large language models are double-edged swords. Radiology. 2023;307:E230163. doi:10.1148/radiol.230163
- Gupta R, Pande P, Herzog I, et al. Application of ChatGPT in cosmetic plastic surgery: ally or antagonist? Aesthet Surg J. 2023;43:NP587-NP590. doi: 10.1093/asj/sjad042
- Gabrielson AT, Odisho AY, Canes D. Harnessing generative artificial intelligence to improve efficiency among urologists: welcome ChatGPT. J Urol. 2023;209:827-829. doi:10.1097/JU.0000000000003383
- What is ChatGPT? OpenAI. Accessed August 10, 2023. https://help.openai.com/en/articles/6783457-chatgpt-general-faq
- Haupt CE, Marks M. AI-generated medical advice—GPT and beyond. JAMA. 2023;329:1349-1350. doi:10.1001/jama.2023.5321
- Gao CA, Howard FM, Markov NS, et al. Comparing Scientific Abstracts Generated by ChatGPT to Original Abstracts Using an Artificial Intelligence Output Detector, Plagiarism Detector, and Blinded Human Reviewers. Scientific Communication and Education; 2022. doi:10.1101/2022.12.23.521610
- Weidinger L, Mellor J, Rauh M, et al. Ethical and social risks of harm from language models. arXiv. Preprint posted online December 8, 2021. https://doi.org/10.48550/arXiv.2112.04359
Practice Points
- ChatGPT potentially can play a beneficial role in dermatologic practice by quickly accessing and synthesizing information, drafting generic medical documents, interpreting visits, advancing medical education, and more.
- Dermatologists using ChatGPT should be extremely cautious, as it can produce false or biased information, perpetuate harmful stereotypes, and present information that is not up-to-date.
Self-managed medication abortion shows success at 9-16 weeks’ gestation
Although most abortions happen within the first 9 weeks of pregnancy, it is important to understand the effectiveness of different models of care in a wider gestational range, corresponding author Heidi Moseson, PhD, of Ibis Reproductive Health in Oakland, Calif., said in an interview.
“There will always be people who need abortions after 9 weeks of pregnancy,” she said, whether because of delayed recognition of the pregnancy, changes in the pregnant person’s health, a fetal diagnosis, changes in life circumstances, time required to gather money, transportation to care, or other reasons.
“This study builds on prior research from the same SAFE study cohort that established self-managed medication abortion in the first 9 weeks of pregnancy as safe and effective, and noninferior to clinician-managed abortion,” Dr. Moseson said. “With this analysis, we wanted to explore whether self-managed medication abortion remained effective after 9 weeks of pregnancy, too.”
In the study, published in Obstetrics & Gynecology, Dr. Moseson and colleagues recruited 1,352 women who were initiating self-managed medication abortion through one of three abortion-accompaniment groups in Argentina, Nigeria, and Southeast Asia between 2019 and 2020. Of these, 264 were self-managing a medication abortion at 9 or more weeks’ gestation.
Participants completed a baseline phone survey before beginning the pill regimen, and follow-up surveys at 1 week and 3 weeks after taking the pills. The average age of the participants was 26 years; 75% were at 9-11 weeks’ gestation, 19.3% were at 12-14 weeks’ gestation, and 5.7% were at 15-22 weeks’ gestation. Slightly more than half of the participants (56.4%) used a combination of mifepristone plus misoprostol, and 43.6% used misoprostol only.
The primary outcome was abortion completion. Secondary outcomes included health care seeking and treatment as well as physical experiences.
A total of 89.4% of participants had an abortion completion without the need for procedural intervention. Another 5.3% had a complete abortion with manual vacuum aspiration or dilation and curettage, 4.9% had an incomplete abortion, and one patient reported no abortion outcome.
Of the participants who sought health care during or after the self-managed abortion, 15.9% sought to confirm abortion completion, and 9.1% needed additional medical intervention, including procedural evacuation, antibiotics, additional misoprostol, intravenous fluids, blood transfusion, or an overnight stay in the health care facility.
Overall, women who were at least 12 weeks pregnant were more likely to seek care at a clinic or hospital than those who were 9-11 weeks pregnant (adjusted relative risk, 1.62).
“Particularly in the United States, the [Food and Drug Administration] label only endorsed medication abortion use through 10 weeks of pregnancy; as a result, many people in the U.S. have the incorrect assumption that the pills are not effective after 10 weeks of pregnancy,” Dr. Moseson said. “This isn’t true. There is no magic line at 10 or 12 weeks after which the pills stop working – in fact, the uterus becomes more sensitive, not less, to misoprostol as a pregnancy progresses. This is why the misoprostol dose is reduced by half for abortions after 12-14 weeks or so.”
The findings were limited by several factors including the use of self-reports for gestational age and abortion outcome, without confirmation by ultrasonogram, the researchers noted. Other limitations included the inability to randomize participants to medication regimens because of legal restrictions on abortion access within the study sites, and the small number of participants (three) who underwent self-managed medication abortion at 17-22 weeks’ gestation.
Data support self-management medication abortion later in pregnancy
“Many people are not aware that there is a robust randomized clinical trial literature that demonstrates that both medication abortion regimens remain highly effective up to 24-28 weeks of pregnancy,” as well as a Cochrane review, Dr. Moseson said. “We know that when these pills are administered in a clinical setting well beyond 9 weeks of pregnancy, that they are highly effective and safe.
“We did not expect that the pills would work differently just because someone takes all doses at home, rather than just the second or third dose at home, as happens in most clinician-managed medication abortions,” she noted. However, “we were interested to see differences in likelihood of health care seeking during or after the abortion by country, but in some ways, also not surprised by these differences given that the risks of seeking care and the expectations around care varied significantly across the study sites.”
Looking ahead, “as we think about the United States and we see more and more bans and restrictions on abortion care going into effect, we will see people seeking abortion later into their pregnancies due to these additional barriers people have to overcome to get care,” said Dr. Moseson. “This need for abortion care later in pregnancy extends to self-managed medication abortion, and in that light, I find the results from this study to be reassuring.
“For people who for some reason or another can’t obtain pills until they are 12 or 13 or more weeks’ pregnant, these findings suggest that people can still safely use the pills on their own to end their pregnancy,” she said. Notably, “the participants in this study had high-quality information on how to take the pills, and phone-based counseling and support available to them throughout their abortion via the accompaniment groups, so ensuring that people who self-manage with pills have accurate, accessible information on how to use the pills and monitor for warning signs is also key.
“Additional research is needed to understand the unique informational and support needs of people who are self-managing their abortions beyond 10 weeks of pregnancy,” Dr. Moseson said. “What information do they need and want to feel secure and safe, what resources do they need to protect themselves from legal risk, where and how can they safely access clinical care if needed? These sorts of practical questions feel urgent, and there is much that can be learned from the activist abortion accompaniment groups around the world that have been providing this sort of informational, emotional, and physical support to aborting people for decades.”
Rising rate of self-managed abortions highlights need for more data
“As abortion restrictions increase in the United States, more people may choose to self-manage their abortions,” Lauren Owens, MD, of the University of Washington, Seattle, said in an interview. “Worldwide, self-managed abortion with accompaniment has been shown to be noninferior to medication abortion involving clinical settings at gestational ages less than 9 weeks, as shown in the SAFE study. However, legal and other logistical barriers to care may mean that people can’t access abortion care until after 9 weeks, and we need more data about the effectiveness of these medications when used outside clinical settings.”
Dr. Owens was not surprised by the effectiveness of the medications to end pregnancies between 9 and 16 weeks’ gestation, with few needing follow-up care. However, “it makes sense that as gestational age increases, the percent of people seeking follow-up care also increases, even as it remains a minority of people,” she said.
The World Health Organization’s guidance on self-managed abortion, issued in 2022, was similar to the regimen in the current study, she added.“Self-managed abortion at home can be very safe and effective from 9-16 weeks’ gestation,” said Dr. Owens. “Having access to accompaniment or support, such as the Medication and Abortion Hotline in the United States, can help people through the process.”
According to a recent report, “more than half the abortions in the U.S. were done using medication in 2020, and protocols developed during the pandemic helped us see how safe medication abortion can be without in-person clinic visits,” Dr. Owens said. “I would encourage clinicians who view the 9.1% rate of need for further interventions (such as intravenous fluids, suction, transfusion) in this study as high to compare this to the rate of interventions and morbidity in ongoing pregnancy.”
According to data from the Centers for Disease Control and Prevention, the cesarean rate in the United States varies by state, but ranges from 21% to 35% of pregnancies; “some of the states with the highest cesarean rates are also those with the most abortion restrictions,” Dr. Owens said. “Abortion is generally safer than continuing pregnancy, and patients deserve access to safe options for abortion care and pregnancy care. Clinicians should know that patients can access these medications through Aid Access, accompaniment through the Miscarriage and Abortion Hotline, and legal advice through If/When/How.”
“We still need more data on self-managed abortion at higher gestational ages,” said Dr. Owens. “Few participants in the study were 14 or more weeks’ pregnant; also, despite the WHO recommendation against criminalization of self-managed abortion, we have seen criminalization for adverse pregnancy outcomes in the United States. As self-managed abortion may carry more legal than medical risks for people, creating and evaluating patient and clinician education to minimize that risk is important.”
The study was supported by the David and Lucile Packard Foundation; the researchers also received support for their time from a National Institutes of Health grant. The researchers had no financial conflicts to disclose. Dr. Owens had no financial conflicts to disclose.
Although most abortions happen within the first 9 weeks of pregnancy, it is important to understand the effectiveness of different models of care in a wider gestational range, corresponding author Heidi Moseson, PhD, of Ibis Reproductive Health in Oakland, Calif., said in an interview.
“There will always be people who need abortions after 9 weeks of pregnancy,” she said, whether because of delayed recognition of the pregnancy, changes in the pregnant person’s health, a fetal diagnosis, changes in life circumstances, time required to gather money, transportation to care, or other reasons.
“This study builds on prior research from the same SAFE study cohort that established self-managed medication abortion in the first 9 weeks of pregnancy as safe and effective, and noninferior to clinician-managed abortion,” Dr. Moseson said. “With this analysis, we wanted to explore whether self-managed medication abortion remained effective after 9 weeks of pregnancy, too.”
In the study, published in Obstetrics & Gynecology, Dr. Moseson and colleagues recruited 1,352 women who were initiating self-managed medication abortion through one of three abortion-accompaniment groups in Argentina, Nigeria, and Southeast Asia between 2019 and 2020. Of these, 264 were self-managing a medication abortion at 9 or more weeks’ gestation.
Participants completed a baseline phone survey before beginning the pill regimen, and follow-up surveys at 1 week and 3 weeks after taking the pills. The average age of the participants was 26 years; 75% were at 9-11 weeks’ gestation, 19.3% were at 12-14 weeks’ gestation, and 5.7% were at 15-22 weeks’ gestation. Slightly more than half of the participants (56.4%) used a combination of mifepristone plus misoprostol, and 43.6% used misoprostol only.
The primary outcome was abortion completion. Secondary outcomes included health care seeking and treatment as well as physical experiences.
A total of 89.4% of participants had an abortion completion without the need for procedural intervention. Another 5.3% had a complete abortion with manual vacuum aspiration or dilation and curettage, 4.9% had an incomplete abortion, and one patient reported no abortion outcome.
Of the participants who sought health care during or after the self-managed abortion, 15.9% sought to confirm abortion completion, and 9.1% needed additional medical intervention, including procedural evacuation, antibiotics, additional misoprostol, intravenous fluids, blood transfusion, or an overnight stay in the health care facility.
Overall, women who were at least 12 weeks pregnant were more likely to seek care at a clinic or hospital than those who were 9-11 weeks pregnant (adjusted relative risk, 1.62).
“Particularly in the United States, the [Food and Drug Administration] label only endorsed medication abortion use through 10 weeks of pregnancy; as a result, many people in the U.S. have the incorrect assumption that the pills are not effective after 10 weeks of pregnancy,” Dr. Moseson said. “This isn’t true. There is no magic line at 10 or 12 weeks after which the pills stop working – in fact, the uterus becomes more sensitive, not less, to misoprostol as a pregnancy progresses. This is why the misoprostol dose is reduced by half for abortions after 12-14 weeks or so.”
The findings were limited by several factors including the use of self-reports for gestational age and abortion outcome, without confirmation by ultrasonogram, the researchers noted. Other limitations included the inability to randomize participants to medication regimens because of legal restrictions on abortion access within the study sites, and the small number of participants (three) who underwent self-managed medication abortion at 17-22 weeks’ gestation.
Data support self-management medication abortion later in pregnancy
“Many people are not aware that there is a robust randomized clinical trial literature that demonstrates that both medication abortion regimens remain highly effective up to 24-28 weeks of pregnancy,” as well as a Cochrane review, Dr. Moseson said. “We know that when these pills are administered in a clinical setting well beyond 9 weeks of pregnancy, that they are highly effective and safe.
“We did not expect that the pills would work differently just because someone takes all doses at home, rather than just the second or third dose at home, as happens in most clinician-managed medication abortions,” she noted. However, “we were interested to see differences in likelihood of health care seeking during or after the abortion by country, but in some ways, also not surprised by these differences given that the risks of seeking care and the expectations around care varied significantly across the study sites.”
Looking ahead, “as we think about the United States and we see more and more bans and restrictions on abortion care going into effect, we will see people seeking abortion later into their pregnancies due to these additional barriers people have to overcome to get care,” said Dr. Moseson. “This need for abortion care later in pregnancy extends to self-managed medication abortion, and in that light, I find the results from this study to be reassuring.
“For people who for some reason or another can’t obtain pills until they are 12 or 13 or more weeks’ pregnant, these findings suggest that people can still safely use the pills on their own to end their pregnancy,” she said. Notably, “the participants in this study had high-quality information on how to take the pills, and phone-based counseling and support available to them throughout their abortion via the accompaniment groups, so ensuring that people who self-manage with pills have accurate, accessible information on how to use the pills and monitor for warning signs is also key.
“Additional research is needed to understand the unique informational and support needs of people who are self-managing their abortions beyond 10 weeks of pregnancy,” Dr. Moseson said. “What information do they need and want to feel secure and safe, what resources do they need to protect themselves from legal risk, where and how can they safely access clinical care if needed? These sorts of practical questions feel urgent, and there is much that can be learned from the activist abortion accompaniment groups around the world that have been providing this sort of informational, emotional, and physical support to aborting people for decades.”
Rising rate of self-managed abortions highlights need for more data
“As abortion restrictions increase in the United States, more people may choose to self-manage their abortions,” Lauren Owens, MD, of the University of Washington, Seattle, said in an interview. “Worldwide, self-managed abortion with accompaniment has been shown to be noninferior to medication abortion involving clinical settings at gestational ages less than 9 weeks, as shown in the SAFE study. However, legal and other logistical barriers to care may mean that people can’t access abortion care until after 9 weeks, and we need more data about the effectiveness of these medications when used outside clinical settings.”
Dr. Owens was not surprised by the effectiveness of the medications to end pregnancies between 9 and 16 weeks’ gestation, with few needing follow-up care. However, “it makes sense that as gestational age increases, the percent of people seeking follow-up care also increases, even as it remains a minority of people,” she said.
The World Health Organization’s guidance on self-managed abortion, issued in 2022, was similar to the regimen in the current study, she added.“Self-managed abortion at home can be very safe and effective from 9-16 weeks’ gestation,” said Dr. Owens. “Having access to accompaniment or support, such as the Medication and Abortion Hotline in the United States, can help people through the process.”
According to a recent report, “more than half the abortions in the U.S. were done using medication in 2020, and protocols developed during the pandemic helped us see how safe medication abortion can be without in-person clinic visits,” Dr. Owens said. “I would encourage clinicians who view the 9.1% rate of need for further interventions (such as intravenous fluids, suction, transfusion) in this study as high to compare this to the rate of interventions and morbidity in ongoing pregnancy.”
According to data from the Centers for Disease Control and Prevention, the cesarean rate in the United States varies by state, but ranges from 21% to 35% of pregnancies; “some of the states with the highest cesarean rates are also those with the most abortion restrictions,” Dr. Owens said. “Abortion is generally safer than continuing pregnancy, and patients deserve access to safe options for abortion care and pregnancy care. Clinicians should know that patients can access these medications through Aid Access, accompaniment through the Miscarriage and Abortion Hotline, and legal advice through If/When/How.”
“We still need more data on self-managed abortion at higher gestational ages,” said Dr. Owens. “Few participants in the study were 14 or more weeks’ pregnant; also, despite the WHO recommendation against criminalization of self-managed abortion, we have seen criminalization for adverse pregnancy outcomes in the United States. As self-managed abortion may carry more legal than medical risks for people, creating and evaluating patient and clinician education to minimize that risk is important.”
The study was supported by the David and Lucile Packard Foundation; the researchers also received support for their time from a National Institutes of Health grant. The researchers had no financial conflicts to disclose. Dr. Owens had no financial conflicts to disclose.
Although most abortions happen within the first 9 weeks of pregnancy, it is important to understand the effectiveness of different models of care in a wider gestational range, corresponding author Heidi Moseson, PhD, of Ibis Reproductive Health in Oakland, Calif., said in an interview.
“There will always be people who need abortions after 9 weeks of pregnancy,” she said, whether because of delayed recognition of the pregnancy, changes in the pregnant person’s health, a fetal diagnosis, changes in life circumstances, time required to gather money, transportation to care, or other reasons.
“This study builds on prior research from the same SAFE study cohort that established self-managed medication abortion in the first 9 weeks of pregnancy as safe and effective, and noninferior to clinician-managed abortion,” Dr. Moseson said. “With this analysis, we wanted to explore whether self-managed medication abortion remained effective after 9 weeks of pregnancy, too.”
In the study, published in Obstetrics & Gynecology, Dr. Moseson and colleagues recruited 1,352 women who were initiating self-managed medication abortion through one of three abortion-accompaniment groups in Argentina, Nigeria, and Southeast Asia between 2019 and 2020. Of these, 264 were self-managing a medication abortion at 9 or more weeks’ gestation.
Participants completed a baseline phone survey before beginning the pill regimen, and follow-up surveys at 1 week and 3 weeks after taking the pills. The average age of the participants was 26 years; 75% were at 9-11 weeks’ gestation, 19.3% were at 12-14 weeks’ gestation, and 5.7% were at 15-22 weeks’ gestation. Slightly more than half of the participants (56.4%) used a combination of mifepristone plus misoprostol, and 43.6% used misoprostol only.
The primary outcome was abortion completion. Secondary outcomes included health care seeking and treatment as well as physical experiences.
A total of 89.4% of participants had an abortion completion without the need for procedural intervention. Another 5.3% had a complete abortion with manual vacuum aspiration or dilation and curettage, 4.9% had an incomplete abortion, and one patient reported no abortion outcome.
Of the participants who sought health care during or after the self-managed abortion, 15.9% sought to confirm abortion completion, and 9.1% needed additional medical intervention, including procedural evacuation, antibiotics, additional misoprostol, intravenous fluids, blood transfusion, or an overnight stay in the health care facility.
Overall, women who were at least 12 weeks pregnant were more likely to seek care at a clinic or hospital than those who were 9-11 weeks pregnant (adjusted relative risk, 1.62).
“Particularly in the United States, the [Food and Drug Administration] label only endorsed medication abortion use through 10 weeks of pregnancy; as a result, many people in the U.S. have the incorrect assumption that the pills are not effective after 10 weeks of pregnancy,” Dr. Moseson said. “This isn’t true. There is no magic line at 10 or 12 weeks after which the pills stop working – in fact, the uterus becomes more sensitive, not less, to misoprostol as a pregnancy progresses. This is why the misoprostol dose is reduced by half for abortions after 12-14 weeks or so.”
The findings were limited by several factors including the use of self-reports for gestational age and abortion outcome, without confirmation by ultrasonogram, the researchers noted. Other limitations included the inability to randomize participants to medication regimens because of legal restrictions on abortion access within the study sites, and the small number of participants (three) who underwent self-managed medication abortion at 17-22 weeks’ gestation.
Data support self-management medication abortion later in pregnancy
“Many people are not aware that there is a robust randomized clinical trial literature that demonstrates that both medication abortion regimens remain highly effective up to 24-28 weeks of pregnancy,” as well as a Cochrane review, Dr. Moseson said. “We know that when these pills are administered in a clinical setting well beyond 9 weeks of pregnancy, that they are highly effective and safe.
“We did not expect that the pills would work differently just because someone takes all doses at home, rather than just the second or third dose at home, as happens in most clinician-managed medication abortions,” she noted. However, “we were interested to see differences in likelihood of health care seeking during or after the abortion by country, but in some ways, also not surprised by these differences given that the risks of seeking care and the expectations around care varied significantly across the study sites.”
Looking ahead, “as we think about the United States and we see more and more bans and restrictions on abortion care going into effect, we will see people seeking abortion later into their pregnancies due to these additional barriers people have to overcome to get care,” said Dr. Moseson. “This need for abortion care later in pregnancy extends to self-managed medication abortion, and in that light, I find the results from this study to be reassuring.
“For people who for some reason or another can’t obtain pills until they are 12 or 13 or more weeks’ pregnant, these findings suggest that people can still safely use the pills on their own to end their pregnancy,” she said. Notably, “the participants in this study had high-quality information on how to take the pills, and phone-based counseling and support available to them throughout their abortion via the accompaniment groups, so ensuring that people who self-manage with pills have accurate, accessible information on how to use the pills and monitor for warning signs is also key.
“Additional research is needed to understand the unique informational and support needs of people who are self-managing their abortions beyond 10 weeks of pregnancy,” Dr. Moseson said. “What information do they need and want to feel secure and safe, what resources do they need to protect themselves from legal risk, where and how can they safely access clinical care if needed? These sorts of practical questions feel urgent, and there is much that can be learned from the activist abortion accompaniment groups around the world that have been providing this sort of informational, emotional, and physical support to aborting people for decades.”
Rising rate of self-managed abortions highlights need for more data
“As abortion restrictions increase in the United States, more people may choose to self-manage their abortions,” Lauren Owens, MD, of the University of Washington, Seattle, said in an interview. “Worldwide, self-managed abortion with accompaniment has been shown to be noninferior to medication abortion involving clinical settings at gestational ages less than 9 weeks, as shown in the SAFE study. However, legal and other logistical barriers to care may mean that people can’t access abortion care until after 9 weeks, and we need more data about the effectiveness of these medications when used outside clinical settings.”
Dr. Owens was not surprised by the effectiveness of the medications to end pregnancies between 9 and 16 weeks’ gestation, with few needing follow-up care. However, “it makes sense that as gestational age increases, the percent of people seeking follow-up care also increases, even as it remains a minority of people,” she said.
The World Health Organization’s guidance on self-managed abortion, issued in 2022, was similar to the regimen in the current study, she added.“Self-managed abortion at home can be very safe and effective from 9-16 weeks’ gestation,” said Dr. Owens. “Having access to accompaniment or support, such as the Medication and Abortion Hotline in the United States, can help people through the process.”
According to a recent report, “more than half the abortions in the U.S. were done using medication in 2020, and protocols developed during the pandemic helped us see how safe medication abortion can be without in-person clinic visits,” Dr. Owens said. “I would encourage clinicians who view the 9.1% rate of need for further interventions (such as intravenous fluids, suction, transfusion) in this study as high to compare this to the rate of interventions and morbidity in ongoing pregnancy.”
According to data from the Centers for Disease Control and Prevention, the cesarean rate in the United States varies by state, but ranges from 21% to 35% of pregnancies; “some of the states with the highest cesarean rates are also those with the most abortion restrictions,” Dr. Owens said. “Abortion is generally safer than continuing pregnancy, and patients deserve access to safe options for abortion care and pregnancy care. Clinicians should know that patients can access these medications through Aid Access, accompaniment through the Miscarriage and Abortion Hotline, and legal advice through If/When/How.”
“We still need more data on self-managed abortion at higher gestational ages,” said Dr. Owens. “Few participants in the study were 14 or more weeks’ pregnant; also, despite the WHO recommendation against criminalization of self-managed abortion, we have seen criminalization for adverse pregnancy outcomes in the United States. As self-managed abortion may carry more legal than medical risks for people, creating and evaluating patient and clinician education to minimize that risk is important.”
The study was supported by the David and Lucile Packard Foundation; the researchers also received support for their time from a National Institutes of Health grant. The researchers had no financial conflicts to disclose. Dr. Owens had no financial conflicts to disclose.
Type 1 diabetes management improves as technology advances
Significant reductions in hemoglobin A1c have occurred over time among adults with type 1 diabetes as their use of diabetes technology has increased, yet there is still room for improvement, new data suggest.
The new findings are from a study involving patients at the Barbara Davis Center for Diabetes Adult Clinic between Jan. 1, 2014, and Dec. 31, 2021. They show that as technology use has increased, A1c levels have dropped in parallel. Moreover, progression from use of stand-alone continuous glucose monitors (CGMs) to automated insulin delivery systems (AIDs), which comprise insulin pumps and connected CGMs, furthered that progress.
The findings “are in agreement with American Diabetes Association standards of care, and recent international consensus recommending CGM and AID for most people with type 1 diabetes, and early initiation of diabetes technology from the onset of type 1 diabetes,” write Kagan E. Karakus, MD, of the University of Colorado’s Barbara Davis Center, Aurora, and colleagues in the article, which was published online in Diabetes Care.
“It’s very rewarding to us. We can see clearly that the uptake is going up and the A1c is dropping,” lead author Viral N. Shah, MD, of the Barbara Davis Center, told this news organization.
On the flip side, A1c levels rose significantly over the study period among nonusers of technology. “We cannot rule out provider bias for not prescribing diabetes technology among those with higher A1c or from disadvantaged socioeconomic backgrounds,” Dr. Karakus and colleagues write.
Also of note, even with use of the most advanced AID systems available during the study period, just under half of patients were still not achieving A1c levels below 7%. “The technology helps, but it’s not perfect,” Dr. Shah observed.
This study is the first to examine the relationship of A1c with technology use over time, in contrast to prior cross-sectional studies. “The intention here was to look at the landscape over a decade,” Dr. Shah said.
As overall use of technology use rose, A1c levels fell
The analysis included data for 4,174 unique patients (mean number of patients, 1,988/yr); 15,903 clinic visits were included over the 8-year study period. Technology use was defined as CGM use without an AID system or with an AID system.
Over the study period, diabetes technology use increased from 26.9% to 82.7% of the clinic population (P < .001). At the same time, the overall proportion patients who achieved the A1c goal of less than 7% increased from 32.3% to 41.7%, while the mean A1c level dropped from 7.7% to 7.5% (P < .001).
But among the technology nonusers, A1c rose from 7.85% in 2014 to 8.4% in 2021 (P < .001).
Regardless of diabetes technology use, White patients (about 80% of the total study population) had significantly lower A1c than non-White patients (7.5% vs. 7.7% for technology users [P = .02]; 8.0% vs. 8.3% for nontechnology users [P < .001]).
The non-White group was too small to enable the researchers to break down the data by technology type. Nonetheless, Dr. Shah said, “As a clinician, I can say that the penetration of diabetes technology in non-White populations remains low. These are also the people more vulnerable for socioeconomic and psychosocial reasons.”
The A1c increase among technology nonusers may be a result of a statistical artifact, as the number of those individuals was much lower in 2021 than in 2014. It’s possible that those remaining individuals have exceedingly high A1c levels, bringing the average up. “It’s still not good, though,” Dr. Shah said.
The more technology, the lower the A1c
Over the study period, the proportion of stand-alone CGM users rose from 26.9% to 44.1%, while use of AIDs rose from 0% in 2014 and 2015 to 38.6% in 2021. The latter group included patients who used first-generation Medtronic 670G and 770G devices and second-generation Tandem t:slim X2 with Control-IQ devices.
Between 2017 and 2021, AIDs users had significantly lower A1c levels than nontechnology users: 7.4% vs. 8.1% in 2017, and 7.3% vs. 8.4% in 2021 (P < .001 for every year). CGM users also had significantly lower A1c levels than nonusers at all time points (P < .001 per year).
The proportions achieving an A1c less than 7% differed significantly across users of CGMs, AIDs, and no technology (P < .01 for all years). In 2021, the percentage of people who achieved an A1c less than 7% were 50.9% with AIDs and 44.1% for CGMs vs, just 15.2% with no technology.
Work to be done: Why aren’t more achieving < 7% with AIDs?
Asked why only slightly more than half of patients who used AIDs achieved A1c levels below 7%, Dr. Shah listed three possibilities:
First, the 7% goal doesn’t apply to everyone with type 1 diabetes, including those with multiple comorbidities or with short life expectancy, for whom the recommended goal is 7.5%-8.0% to prevent hypoglycemia. “We didn’t separate out patients by A1c goals. If we add that, the number might go up,” Dr. Shah said.
Second, AID technology is continually improving, but it’s not perfect. Users still must enter carbohydrate counts and signal the devices for exercise, which can lead to errors. “It’s a wonderful technology for overnight control, but still, during the daytime, there are so many factors with the user interface and how much a person is engaged with the technology,” Dr. Shah explained.
Third, he said, “Unfortunately, obesity is increasing in type 1 diabetes, and insulin doses are increasing. Higher BMI [body mass index] and more insulin resistance can mean higher A1c. I really think for many patients, we probably will need an adjunct therapy, such as an SGLT2 [sodium-glucose cotransporter-2] inhibitor or a GLP-1 [glucagonlike peptide-1] agonist, even though they’re not approved in type 1 diabetes, for both glycemic and metabolic control including weight. I think that’s another missing piece.”
He also pointed out, “If someone has an A1c of 7.5%, I don’t expect a huge change. But if they’re at 10%, a drop to 8% is a huge change.”
Overall, Dr. Shah said, the news from the study is good. “In the past, only 30% were achieving an A1c less than 7%. Now we’re 20% above that. ... It’s a glass half full.”
Dr. Karakus has disclosed no relevant financial relationships. Dr. Shah has received, through the University of Colorado, research support from Novo Nordisk, Insulet, Tandem Diabetes, and Dexcom, and honoraria from Medscape, Lifescan, Novo Nordisk, and DKSH Singapore for advisory board attendance and from Insulet and Dexcom for speaking engagements.
A version of this article first appeared on Medscape.com.
Significant reductions in hemoglobin A1c have occurred over time among adults with type 1 diabetes as their use of diabetes technology has increased, yet there is still room for improvement, new data suggest.
The new findings are from a study involving patients at the Barbara Davis Center for Diabetes Adult Clinic between Jan. 1, 2014, and Dec. 31, 2021. They show that as technology use has increased, A1c levels have dropped in parallel. Moreover, progression from use of stand-alone continuous glucose monitors (CGMs) to automated insulin delivery systems (AIDs), which comprise insulin pumps and connected CGMs, furthered that progress.
The findings “are in agreement with American Diabetes Association standards of care, and recent international consensus recommending CGM and AID for most people with type 1 diabetes, and early initiation of diabetes technology from the onset of type 1 diabetes,” write Kagan E. Karakus, MD, of the University of Colorado’s Barbara Davis Center, Aurora, and colleagues in the article, which was published online in Diabetes Care.
“It’s very rewarding to us. We can see clearly that the uptake is going up and the A1c is dropping,” lead author Viral N. Shah, MD, of the Barbara Davis Center, told this news organization.
On the flip side, A1c levels rose significantly over the study period among nonusers of technology. “We cannot rule out provider bias for not prescribing diabetes technology among those with higher A1c or from disadvantaged socioeconomic backgrounds,” Dr. Karakus and colleagues write.
Also of note, even with use of the most advanced AID systems available during the study period, just under half of patients were still not achieving A1c levels below 7%. “The technology helps, but it’s not perfect,” Dr. Shah observed.
This study is the first to examine the relationship of A1c with technology use over time, in contrast to prior cross-sectional studies. “The intention here was to look at the landscape over a decade,” Dr. Shah said.
As overall use of technology use rose, A1c levels fell
The analysis included data for 4,174 unique patients (mean number of patients, 1,988/yr); 15,903 clinic visits were included over the 8-year study period. Technology use was defined as CGM use without an AID system or with an AID system.
Over the study period, diabetes technology use increased from 26.9% to 82.7% of the clinic population (P < .001). At the same time, the overall proportion patients who achieved the A1c goal of less than 7% increased from 32.3% to 41.7%, while the mean A1c level dropped from 7.7% to 7.5% (P < .001).
But among the technology nonusers, A1c rose from 7.85% in 2014 to 8.4% in 2021 (P < .001).
Regardless of diabetes technology use, White patients (about 80% of the total study population) had significantly lower A1c than non-White patients (7.5% vs. 7.7% for technology users [P = .02]; 8.0% vs. 8.3% for nontechnology users [P < .001]).
The non-White group was too small to enable the researchers to break down the data by technology type. Nonetheless, Dr. Shah said, “As a clinician, I can say that the penetration of diabetes technology in non-White populations remains low. These are also the people more vulnerable for socioeconomic and psychosocial reasons.”
The A1c increase among technology nonusers may be a result of a statistical artifact, as the number of those individuals was much lower in 2021 than in 2014. It’s possible that those remaining individuals have exceedingly high A1c levels, bringing the average up. “It’s still not good, though,” Dr. Shah said.
The more technology, the lower the A1c
Over the study period, the proportion of stand-alone CGM users rose from 26.9% to 44.1%, while use of AIDs rose from 0% in 2014 and 2015 to 38.6% in 2021. The latter group included patients who used first-generation Medtronic 670G and 770G devices and second-generation Tandem t:slim X2 with Control-IQ devices.
Between 2017 and 2021, AIDs users had significantly lower A1c levels than nontechnology users: 7.4% vs. 8.1% in 2017, and 7.3% vs. 8.4% in 2021 (P < .001 for every year). CGM users also had significantly lower A1c levels than nonusers at all time points (P < .001 per year).
The proportions achieving an A1c less than 7% differed significantly across users of CGMs, AIDs, and no technology (P < .01 for all years). In 2021, the percentage of people who achieved an A1c less than 7% were 50.9% with AIDs and 44.1% for CGMs vs, just 15.2% with no technology.
Work to be done: Why aren’t more achieving < 7% with AIDs?
Asked why only slightly more than half of patients who used AIDs achieved A1c levels below 7%, Dr. Shah listed three possibilities:
First, the 7% goal doesn’t apply to everyone with type 1 diabetes, including those with multiple comorbidities or with short life expectancy, for whom the recommended goal is 7.5%-8.0% to prevent hypoglycemia. “We didn’t separate out patients by A1c goals. If we add that, the number might go up,” Dr. Shah said.
Second, AID technology is continually improving, but it’s not perfect. Users still must enter carbohydrate counts and signal the devices for exercise, which can lead to errors. “It’s a wonderful technology for overnight control, but still, during the daytime, there are so many factors with the user interface and how much a person is engaged with the technology,” Dr. Shah explained.
Third, he said, “Unfortunately, obesity is increasing in type 1 diabetes, and insulin doses are increasing. Higher BMI [body mass index] and more insulin resistance can mean higher A1c. I really think for many patients, we probably will need an adjunct therapy, such as an SGLT2 [sodium-glucose cotransporter-2] inhibitor or a GLP-1 [glucagonlike peptide-1] agonist, even though they’re not approved in type 1 diabetes, for both glycemic and metabolic control including weight. I think that’s another missing piece.”
He also pointed out, “If someone has an A1c of 7.5%, I don’t expect a huge change. But if they’re at 10%, a drop to 8% is a huge change.”
Overall, Dr. Shah said, the news from the study is good. “In the past, only 30% were achieving an A1c less than 7%. Now we’re 20% above that. ... It’s a glass half full.”
Dr. Karakus has disclosed no relevant financial relationships. Dr. Shah has received, through the University of Colorado, research support from Novo Nordisk, Insulet, Tandem Diabetes, and Dexcom, and honoraria from Medscape, Lifescan, Novo Nordisk, and DKSH Singapore for advisory board attendance and from Insulet and Dexcom for speaking engagements.
A version of this article first appeared on Medscape.com.
Significant reductions in hemoglobin A1c have occurred over time among adults with type 1 diabetes as their use of diabetes technology has increased, yet there is still room for improvement, new data suggest.
The new findings are from a study involving patients at the Barbara Davis Center for Diabetes Adult Clinic between Jan. 1, 2014, and Dec. 31, 2021. They show that as technology use has increased, A1c levels have dropped in parallel. Moreover, progression from use of stand-alone continuous glucose monitors (CGMs) to automated insulin delivery systems (AIDs), which comprise insulin pumps and connected CGMs, furthered that progress.
The findings “are in agreement with American Diabetes Association standards of care, and recent international consensus recommending CGM and AID for most people with type 1 diabetes, and early initiation of diabetes technology from the onset of type 1 diabetes,” write Kagan E. Karakus, MD, of the University of Colorado’s Barbara Davis Center, Aurora, and colleagues in the article, which was published online in Diabetes Care.
“It’s very rewarding to us. We can see clearly that the uptake is going up and the A1c is dropping,” lead author Viral N. Shah, MD, of the Barbara Davis Center, told this news organization.
On the flip side, A1c levels rose significantly over the study period among nonusers of technology. “We cannot rule out provider bias for not prescribing diabetes technology among those with higher A1c or from disadvantaged socioeconomic backgrounds,” Dr. Karakus and colleagues write.
Also of note, even with use of the most advanced AID systems available during the study period, just under half of patients were still not achieving A1c levels below 7%. “The technology helps, but it’s not perfect,” Dr. Shah observed.
This study is the first to examine the relationship of A1c with technology use over time, in contrast to prior cross-sectional studies. “The intention here was to look at the landscape over a decade,” Dr. Shah said.
As overall use of technology use rose, A1c levels fell
The analysis included data for 4,174 unique patients (mean number of patients, 1,988/yr); 15,903 clinic visits were included over the 8-year study period. Technology use was defined as CGM use without an AID system or with an AID system.
Over the study period, diabetes technology use increased from 26.9% to 82.7% of the clinic population (P < .001). At the same time, the overall proportion patients who achieved the A1c goal of less than 7% increased from 32.3% to 41.7%, while the mean A1c level dropped from 7.7% to 7.5% (P < .001).
But among the technology nonusers, A1c rose from 7.85% in 2014 to 8.4% in 2021 (P < .001).
Regardless of diabetes technology use, White patients (about 80% of the total study population) had significantly lower A1c than non-White patients (7.5% vs. 7.7% for technology users [P = .02]; 8.0% vs. 8.3% for nontechnology users [P < .001]).
The non-White group was too small to enable the researchers to break down the data by technology type. Nonetheless, Dr. Shah said, “As a clinician, I can say that the penetration of diabetes technology in non-White populations remains low. These are also the people more vulnerable for socioeconomic and psychosocial reasons.”
The A1c increase among technology nonusers may be a result of a statistical artifact, as the number of those individuals was much lower in 2021 than in 2014. It’s possible that those remaining individuals have exceedingly high A1c levels, bringing the average up. “It’s still not good, though,” Dr. Shah said.
The more technology, the lower the A1c
Over the study period, the proportion of stand-alone CGM users rose from 26.9% to 44.1%, while use of AIDs rose from 0% in 2014 and 2015 to 38.6% in 2021. The latter group included patients who used first-generation Medtronic 670G and 770G devices and second-generation Tandem t:slim X2 with Control-IQ devices.
Between 2017 and 2021, AIDs users had significantly lower A1c levels than nontechnology users: 7.4% vs. 8.1% in 2017, and 7.3% vs. 8.4% in 2021 (P < .001 for every year). CGM users also had significantly lower A1c levels than nonusers at all time points (P < .001 per year).
The proportions achieving an A1c less than 7% differed significantly across users of CGMs, AIDs, and no technology (P < .01 for all years). In 2021, the percentage of people who achieved an A1c less than 7% were 50.9% with AIDs and 44.1% for CGMs vs, just 15.2% with no technology.
Work to be done: Why aren’t more achieving < 7% with AIDs?
Asked why only slightly more than half of patients who used AIDs achieved A1c levels below 7%, Dr. Shah listed three possibilities:
First, the 7% goal doesn’t apply to everyone with type 1 diabetes, including those with multiple comorbidities or with short life expectancy, for whom the recommended goal is 7.5%-8.0% to prevent hypoglycemia. “We didn’t separate out patients by A1c goals. If we add that, the number might go up,” Dr. Shah said.
Second, AID technology is continually improving, but it’s not perfect. Users still must enter carbohydrate counts and signal the devices for exercise, which can lead to errors. “It’s a wonderful technology for overnight control, but still, during the daytime, there are so many factors with the user interface and how much a person is engaged with the technology,” Dr. Shah explained.
Third, he said, “Unfortunately, obesity is increasing in type 1 diabetes, and insulin doses are increasing. Higher BMI [body mass index] and more insulin resistance can mean higher A1c. I really think for many patients, we probably will need an adjunct therapy, such as an SGLT2 [sodium-glucose cotransporter-2] inhibitor or a GLP-1 [glucagonlike peptide-1] agonist, even though they’re not approved in type 1 diabetes, for both glycemic and metabolic control including weight. I think that’s another missing piece.”
He also pointed out, “If someone has an A1c of 7.5%, I don’t expect a huge change. But if they’re at 10%, a drop to 8% is a huge change.”
Overall, Dr. Shah said, the news from the study is good. “In the past, only 30% were achieving an A1c less than 7%. Now we’re 20% above that. ... It’s a glass half full.”
Dr. Karakus has disclosed no relevant financial relationships. Dr. Shah has received, through the University of Colorado, research support from Novo Nordisk, Insulet, Tandem Diabetes, and Dexcom, and honoraria from Medscape, Lifescan, Novo Nordisk, and DKSH Singapore for advisory board attendance and from Insulet and Dexcom for speaking engagements.
A version of this article first appeared on Medscape.com.
FROM DIABETES CARE
ReCor renal denervation system safe, effective: FDA panel
in lowering blood pressure for adults with uncontrolled hypertension who may be inadequately responsive to, or who are intolerant of, antihypertensive medications.
The device is intended to be used in renal arteries with diameters of 3.0 to 8.0 mm.
After hearing data from three trials, RADIANCE-HTN SOLO, RADIANCE II, and RADIANCE-HTN TRIO, the 12-member panel unanimously agreed that there was “reasonable assurance” that the ReCor Paradise Ultrasound Renal Denervation System (ReCor Medical) was safe.
However, while most of the panel felt the device was effective, a few disagreed.
Keith Allen, MD, director of surgical research for the Mid-America Heart and Lung Surgeons, Kansas City, Mo., who was one of the three panel members who voted no regarding efficacy, stated that he had concerns about the duration and the degree of efficacy shown in the trials.
Mark Lockhart, MD, University of Alabama, Birmingham, also voted no. “I do think there was an effect for 2 months, but the duration of that positive effect appears to decline after that period of time.”
Benjamin Saville, PhD, echoed Dr. Lockhart’s concern: “The benefit is more short term, it is unclear what the long term benefit would be.”
Data from all three trials showed a significant drop in blood pressure with the device compared with pharmacologic therapy, but after 2 months of follow-up, that advantage disappeared.
The FDA highlighted data from the trials that showed that at 2 months, uRDN patients experienced significant reductions in systolic blood pressure compared with those treated with a sham device; however, by 6 months, there was a difference of only 1 mm Hg between the two groups.
“It seems when I look at 6 months and 12 months, the benefit is very tiny. We know the safety is fine, but a benefit of less than 1 mm Hg difference would not make me want to have an intervention,” said statistician Janet Wittes, PhD.
“I think the device is efficacious, even though there is not much difference between sham and treatment, but a big issue is the fact that half of our patients are not compliant. That will make the benefits over sham more clear,” noted Jim Blankenship, MD, professor of medicine and director of the division of cardiology at the University of New Mexico in Albuquerque.
John Hirshfeld Jr., MD, professor emeritus of medicine at the University of Pennsylvania, Philadelphia, said he voted yes on safety and efficacy but admitted he had some misgivings. “The sample size was small, but it is a novel tool to add to our tool box, and hopefully it will be used responsibly,” he said.
John Somberg, MD, professor emeritus of medicine, cardiology, and pharmacology, Rush University, Chicago, said the data on this procedure show “that antihypertensive medication works. Denervation is not superior to medications. It lowers blood pressure and is persistent, but when you can take the sham group to almost as good control as you get in the denervation group, that shows it can also be done with medicines.”
The panel wants to see results from additional studies in important subpopulations who are affected by hypertension, including Black people, women, the elderly, and people who already have cardiovascular risk factors, such as diabetes and heart failure.
Deneen Hesser, RN, the panel’s patient representative, called for any postmarketing studies that may be conducted by ReCor to include a good patient education program and also a way of documenting patient-reported outcomes.
“This would help us ascertain how happy people were if they were able to reduce their medication burden by, for example, one drug, or if they were willing to undergo a procedure to be able to stop taking so many antihypertensive medications,” she said.
The panel will meet again to review data on Medtronic’s Simplicity Spyral Renal Denervation System, which is also for patients with uncontrolled hypertension.
A version of this article appeared on Medscape.com.
in lowering blood pressure for adults with uncontrolled hypertension who may be inadequately responsive to, or who are intolerant of, antihypertensive medications.
The device is intended to be used in renal arteries with diameters of 3.0 to 8.0 mm.
After hearing data from three trials, RADIANCE-HTN SOLO, RADIANCE II, and RADIANCE-HTN TRIO, the 12-member panel unanimously agreed that there was “reasonable assurance” that the ReCor Paradise Ultrasound Renal Denervation System (ReCor Medical) was safe.
However, while most of the panel felt the device was effective, a few disagreed.
Keith Allen, MD, director of surgical research for the Mid-America Heart and Lung Surgeons, Kansas City, Mo., who was one of the three panel members who voted no regarding efficacy, stated that he had concerns about the duration and the degree of efficacy shown in the trials.
Mark Lockhart, MD, University of Alabama, Birmingham, also voted no. “I do think there was an effect for 2 months, but the duration of that positive effect appears to decline after that period of time.”
Benjamin Saville, PhD, echoed Dr. Lockhart’s concern: “The benefit is more short term, it is unclear what the long term benefit would be.”
Data from all three trials showed a significant drop in blood pressure with the device compared with pharmacologic therapy, but after 2 months of follow-up, that advantage disappeared.
The FDA highlighted data from the trials that showed that at 2 months, uRDN patients experienced significant reductions in systolic blood pressure compared with those treated with a sham device; however, by 6 months, there was a difference of only 1 mm Hg between the two groups.
“It seems when I look at 6 months and 12 months, the benefit is very tiny. We know the safety is fine, but a benefit of less than 1 mm Hg difference would not make me want to have an intervention,” said statistician Janet Wittes, PhD.
“I think the device is efficacious, even though there is not much difference between sham and treatment, but a big issue is the fact that half of our patients are not compliant. That will make the benefits over sham more clear,” noted Jim Blankenship, MD, professor of medicine and director of the division of cardiology at the University of New Mexico in Albuquerque.
John Hirshfeld Jr., MD, professor emeritus of medicine at the University of Pennsylvania, Philadelphia, said he voted yes on safety and efficacy but admitted he had some misgivings. “The sample size was small, but it is a novel tool to add to our tool box, and hopefully it will be used responsibly,” he said.
John Somberg, MD, professor emeritus of medicine, cardiology, and pharmacology, Rush University, Chicago, said the data on this procedure show “that antihypertensive medication works. Denervation is not superior to medications. It lowers blood pressure and is persistent, but when you can take the sham group to almost as good control as you get in the denervation group, that shows it can also be done with medicines.”
The panel wants to see results from additional studies in important subpopulations who are affected by hypertension, including Black people, women, the elderly, and people who already have cardiovascular risk factors, such as diabetes and heart failure.
Deneen Hesser, RN, the panel’s patient representative, called for any postmarketing studies that may be conducted by ReCor to include a good patient education program and also a way of documenting patient-reported outcomes.
“This would help us ascertain how happy people were if they were able to reduce their medication burden by, for example, one drug, or if they were willing to undergo a procedure to be able to stop taking so many antihypertensive medications,” she said.
The panel will meet again to review data on Medtronic’s Simplicity Spyral Renal Denervation System, which is also for patients with uncontrolled hypertension.
A version of this article appeared on Medscape.com.
in lowering blood pressure for adults with uncontrolled hypertension who may be inadequately responsive to, or who are intolerant of, antihypertensive medications.
The device is intended to be used in renal arteries with diameters of 3.0 to 8.0 mm.
After hearing data from three trials, RADIANCE-HTN SOLO, RADIANCE II, and RADIANCE-HTN TRIO, the 12-member panel unanimously agreed that there was “reasonable assurance” that the ReCor Paradise Ultrasound Renal Denervation System (ReCor Medical) was safe.
However, while most of the panel felt the device was effective, a few disagreed.
Keith Allen, MD, director of surgical research for the Mid-America Heart and Lung Surgeons, Kansas City, Mo., who was one of the three panel members who voted no regarding efficacy, stated that he had concerns about the duration and the degree of efficacy shown in the trials.
Mark Lockhart, MD, University of Alabama, Birmingham, also voted no. “I do think there was an effect for 2 months, but the duration of that positive effect appears to decline after that period of time.”
Benjamin Saville, PhD, echoed Dr. Lockhart’s concern: “The benefit is more short term, it is unclear what the long term benefit would be.”
Data from all three trials showed a significant drop in blood pressure with the device compared with pharmacologic therapy, but after 2 months of follow-up, that advantage disappeared.
The FDA highlighted data from the trials that showed that at 2 months, uRDN patients experienced significant reductions in systolic blood pressure compared with those treated with a sham device; however, by 6 months, there was a difference of only 1 mm Hg between the two groups.
“It seems when I look at 6 months and 12 months, the benefit is very tiny. We know the safety is fine, but a benefit of less than 1 mm Hg difference would not make me want to have an intervention,” said statistician Janet Wittes, PhD.
“I think the device is efficacious, even though there is not much difference between sham and treatment, but a big issue is the fact that half of our patients are not compliant. That will make the benefits over sham more clear,” noted Jim Blankenship, MD, professor of medicine and director of the division of cardiology at the University of New Mexico in Albuquerque.
John Hirshfeld Jr., MD, professor emeritus of medicine at the University of Pennsylvania, Philadelphia, said he voted yes on safety and efficacy but admitted he had some misgivings. “The sample size was small, but it is a novel tool to add to our tool box, and hopefully it will be used responsibly,” he said.
John Somberg, MD, professor emeritus of medicine, cardiology, and pharmacology, Rush University, Chicago, said the data on this procedure show “that antihypertensive medication works. Denervation is not superior to medications. It lowers blood pressure and is persistent, but when you can take the sham group to almost as good control as you get in the denervation group, that shows it can also be done with medicines.”
The panel wants to see results from additional studies in important subpopulations who are affected by hypertension, including Black people, women, the elderly, and people who already have cardiovascular risk factors, such as diabetes and heart failure.
Deneen Hesser, RN, the panel’s patient representative, called for any postmarketing studies that may be conducted by ReCor to include a good patient education program and also a way of documenting patient-reported outcomes.
“This would help us ascertain how happy people were if they were able to reduce their medication burden by, for example, one drug, or if they were willing to undergo a procedure to be able to stop taking so many antihypertensive medications,” she said.
The panel will meet again to review data on Medtronic’s Simplicity Spyral Renal Denervation System, which is also for patients with uncontrolled hypertension.
A version of this article appeared on Medscape.com.
Marijuana, hallucinogen use, binge drinking at all-time high
The latest results of the Monitoring the Future (MTF) longitudinal survey show that American adults are consuming marijuana and hallucinogens, vaping, and binge drinking at historic levels.
“In 2022, we are seeing that marijuana and hallucinogen use, and vaping of nicotine and marijuana, are higher than ever among young adults ages 19-30,” said Megan Patrick, research professor and principal investigator of the MTF study. “In addition, midlife adults ages 35-50 have the highest level of binge drinking we have ever seen in that age group,” she said in a statement.
The survey, conducted annually since 1975 by the University of Michigan’s Institute for Social Research, Ann Arbor, queries nationally representative samples of 8th, 10th, and 12th graders and then follows a subset through adulthood to come up with longitudinal data. It is funded by the National Institute on Drug Abuse.
The adult data for 2022 were gathered by online and paper surveys from April to October 2022 and included responses from some 10,000 individuals. Participants were divided into two cohorts: those aged 19-30 years and those aged 35-50 years.
About a third of the older age group reported using marijuana in the past year, an all-time high, up from 25% in 2021 and more than double the users in 2012 (13%). Of this group, 4% reported past-year hallucinogen use, also a record high and double the reported use in 2021.
Alcohol use among adults aged 35-50 has gradually increased over the past decade. Of this group, 85% reported past-year drinking in 2022, up from 83% in 2012.
Binge drinking – defined as having five or more drinks in a row in the past 2 weeks – has also been on the rise in the past decade. One-third of older adults reported binge drinking in 2022. Binge drinking was highest among White (31.4%) and Hispanic (30.6%) midlife adults and was lower among Black (17.1%) midlife adults.
Vaping among the older age cohort has remained at similar levels since first measured in 2019; 9% vaped marijuana in the past year, while 7% vaped nicotine.
Marijuana popular among younger Americans
“In 2022, marijuana use among young adults reached the highest levels ever recorded since the indices were first available in 1988,” the study authors write. Both past-year and daily use hit record levels for the cohort of those aged 19-30.
Forty-four percent reported past-year marijuana use, up from 28% in 2012. The highest levels of use were in those aged 27-28. One in five reported daily use, up from 6% a decade ago; almost 14% of 23- to 24-year-olds reported daily use.
Past-year use of hallucinogens – including LSD, MDMA, mescaline, peyote, mushrooms or psilocybin, and PCP – was reported by 8% of this age group. Most of the increase was driven by use of hallucinogens other than LSD, which accounted for 7% of the reported use.
Young adults also reported record levels of vaping marijuana, with 21% reporting past-year use and 14% reporting past-month use. Vaping of nicotine has doubled in prevalence since the survey started asking about it, from 14% for past-year use in 2017 to 24% in 2022.
NIDA Director Nora Volkow, MD, noted in a statement that the survey results show that “substance use is not limited to teens and young adults,” adding that “these data help us understand how people use drugs across the lifespan.”
A version of this article first appeared on Medscape.com.
The latest results of the Monitoring the Future (MTF) longitudinal survey show that American adults are consuming marijuana and hallucinogens, vaping, and binge drinking at historic levels.
“In 2022, we are seeing that marijuana and hallucinogen use, and vaping of nicotine and marijuana, are higher than ever among young adults ages 19-30,” said Megan Patrick, research professor and principal investigator of the MTF study. “In addition, midlife adults ages 35-50 have the highest level of binge drinking we have ever seen in that age group,” she said in a statement.
The survey, conducted annually since 1975 by the University of Michigan’s Institute for Social Research, Ann Arbor, queries nationally representative samples of 8th, 10th, and 12th graders and then follows a subset through adulthood to come up with longitudinal data. It is funded by the National Institute on Drug Abuse.
The adult data for 2022 were gathered by online and paper surveys from April to October 2022 and included responses from some 10,000 individuals. Participants were divided into two cohorts: those aged 19-30 years and those aged 35-50 years.
About a third of the older age group reported using marijuana in the past year, an all-time high, up from 25% in 2021 and more than double the users in 2012 (13%). Of this group, 4% reported past-year hallucinogen use, also a record high and double the reported use in 2021.
Alcohol use among adults aged 35-50 has gradually increased over the past decade. Of this group, 85% reported past-year drinking in 2022, up from 83% in 2012.
Binge drinking – defined as having five or more drinks in a row in the past 2 weeks – has also been on the rise in the past decade. One-third of older adults reported binge drinking in 2022. Binge drinking was highest among White (31.4%) and Hispanic (30.6%) midlife adults and was lower among Black (17.1%) midlife adults.
Vaping among the older age cohort has remained at similar levels since first measured in 2019; 9% vaped marijuana in the past year, while 7% vaped nicotine.
Marijuana popular among younger Americans
“In 2022, marijuana use among young adults reached the highest levels ever recorded since the indices were first available in 1988,” the study authors write. Both past-year and daily use hit record levels for the cohort of those aged 19-30.
Forty-four percent reported past-year marijuana use, up from 28% in 2012. The highest levels of use were in those aged 27-28. One in five reported daily use, up from 6% a decade ago; almost 14% of 23- to 24-year-olds reported daily use.
Past-year use of hallucinogens – including LSD, MDMA, mescaline, peyote, mushrooms or psilocybin, and PCP – was reported by 8% of this age group. Most of the increase was driven by use of hallucinogens other than LSD, which accounted for 7% of the reported use.
Young adults also reported record levels of vaping marijuana, with 21% reporting past-year use and 14% reporting past-month use. Vaping of nicotine has doubled in prevalence since the survey started asking about it, from 14% for past-year use in 2017 to 24% in 2022.
NIDA Director Nora Volkow, MD, noted in a statement that the survey results show that “substance use is not limited to teens and young adults,” adding that “these data help us understand how people use drugs across the lifespan.”
A version of this article first appeared on Medscape.com.
The latest results of the Monitoring the Future (MTF) longitudinal survey show that American adults are consuming marijuana and hallucinogens, vaping, and binge drinking at historic levels.
“In 2022, we are seeing that marijuana and hallucinogen use, and vaping of nicotine and marijuana, are higher than ever among young adults ages 19-30,” said Megan Patrick, research professor and principal investigator of the MTF study. “In addition, midlife adults ages 35-50 have the highest level of binge drinking we have ever seen in that age group,” she said in a statement.
The survey, conducted annually since 1975 by the University of Michigan’s Institute for Social Research, Ann Arbor, queries nationally representative samples of 8th, 10th, and 12th graders and then follows a subset through adulthood to come up with longitudinal data. It is funded by the National Institute on Drug Abuse.
The adult data for 2022 were gathered by online and paper surveys from April to October 2022 and included responses from some 10,000 individuals. Participants were divided into two cohorts: those aged 19-30 years and those aged 35-50 years.
About a third of the older age group reported using marijuana in the past year, an all-time high, up from 25% in 2021 and more than double the users in 2012 (13%). Of this group, 4% reported past-year hallucinogen use, also a record high and double the reported use in 2021.
Alcohol use among adults aged 35-50 has gradually increased over the past decade. Of this group, 85% reported past-year drinking in 2022, up from 83% in 2012.
Binge drinking – defined as having five or more drinks in a row in the past 2 weeks – has also been on the rise in the past decade. One-third of older adults reported binge drinking in 2022. Binge drinking was highest among White (31.4%) and Hispanic (30.6%) midlife adults and was lower among Black (17.1%) midlife adults.
Vaping among the older age cohort has remained at similar levels since first measured in 2019; 9% vaped marijuana in the past year, while 7% vaped nicotine.
Marijuana popular among younger Americans
“In 2022, marijuana use among young adults reached the highest levels ever recorded since the indices were first available in 1988,” the study authors write. Both past-year and daily use hit record levels for the cohort of those aged 19-30.
Forty-four percent reported past-year marijuana use, up from 28% in 2012. The highest levels of use were in those aged 27-28. One in five reported daily use, up from 6% a decade ago; almost 14% of 23- to 24-year-olds reported daily use.
Past-year use of hallucinogens – including LSD, MDMA, mescaline, peyote, mushrooms or psilocybin, and PCP – was reported by 8% of this age group. Most of the increase was driven by use of hallucinogens other than LSD, which accounted for 7% of the reported use.
Young adults also reported record levels of vaping marijuana, with 21% reporting past-year use and 14% reporting past-month use. Vaping of nicotine has doubled in prevalence since the survey started asking about it, from 14% for past-year use in 2017 to 24% in 2022.
NIDA Director Nora Volkow, MD, noted in a statement that the survey results show that “substance use is not limited to teens and young adults,” adding that “these data help us understand how people use drugs across the lifespan.”
A version of this article first appeared on Medscape.com.
As MOC debate heats up, cardiology societies weigh in
It’s no secret that many physicians question the value of Maintenance of Certification requirements and are concerned about the amount of time, effort, and money the process takes. Now, they and at least two cardiology societies are starting to speak up.
MOC is an initiative from the American Board of Internal Medicine that requires an initial certification that costs thousands of dollars and must be repeated every 10 years. Annual MOC requirements involve tests that cost $220 for the first certificate a physician holds and about $120 for each subsequent one.
Interventional cardiologists (ICs) and other subspecialists have additional fees and requirements.
MOC ‘burdensome,’ ‘costly,’ ‘complex’
On July 21, hematologist-oncologist Aaron Goodman, MD, an associate professor at the University of California, San Diego, posted a petition on behalf of ABIM diplomates.
As of August 22, the petition had garnered more than 18,000 signatures.
Dr. Goodman recently debated ABIM President and CEO Richard J. Baron, MD, in a Healthcare Unfiltered podcast. Before the debate, host Chadi Nabhan, MD, MBA, tweeted that he could not find a single physician who would defend the MOC and recertification.
The debate touched on topics such as fees, evidence of value, the certification test format, and the cost and requirements to maintain more than one board certification. Overall, Dr. Goodman made the analogy to giving a patient chemotherapy: Because there are harms, he better know that there are also benefits. He cited that the harms associated with MOC include “financial toxicity, time toxicity, and stress toxicity,” with the latter being particularly toxic to him personally.
Though the podcast gave both participants ample opportunities to express their views, it’s not clear that either participant persuaded the other.
Cardiologists who are unhappy with MOC are speaking up on X, formerly known as Twitter. IC Matthew Sample, MD, listed five things he’s done to improve his practice since IC graduation, for which he received no MOC points.
In response, internist Artem Minalyan, MD, asked: “Hypothetically, if Dr. Baron required an IC procedure, I wonder if he would request you to get all your MOC points prior to consenting.”
SCAI and HRS weigh in
Some professional societies have responded to the ABIM’s threat to revoke the certifications of cardiologists who don’t participate in periodic MOC activities.
The Society for Cardiovascular Angiography & Interventions published its “Position on ABIM Revocation of Certification for Not Participating in MOC.” In it, SCAI states that ABIM diplomates who pass their exams and report procedural volumes as required should be “indisputably” recognized as “certified” for the relevant time frame (for example, 10 years), regardless of whether they participate in any other MOC activities.
SCAI President George D. Dangas, MD, PhD, said in an interview that “many of our members have expressed their frustration surrounding the confusion regarding their MOC requirements, including myself. We felt that this confusion could endanger the certified status of members, which would inevitably impact patient care, which is our greatest concern.”
The society has received an “overwhelmingly positive response” to its statement, he said. “Our hope is that ABIM will consider simpler, transparent regulations that are reflective of the feedback received from their constituents.”
In response to the COVID-19 pandemic, ABIM extended the deadline for diplomates whose certificate expired in 2020 or 2021 until the end of 2022; Dr. Dangas suggested ABIM further extend the deadline to enroll in or renew the MOC to the end of 2024 and that ABIM should “develop a recertification program that can be explained in a single slide/page.”
Other subspecialty groups are following SCAI’s lead including the EP Advocacy Foundation, and the Heart Rhythm Society.
MOC alternatives
The ABIM touts the value of MOC on its website, stating: “There is compelling evidence showing that MOC improves value of care without sacrificing quality and that board certified physicians command higher salaries.”
Alternative options that are arguably less arduous are available.
In collaboration with ABIM, the American College of Cardiology launched the ABIM/ACC Collaborative Maintenance Pathway in 2019 as an alternative MOC assessment option.
The CMP “focuses on one or a small group of topics within cardiology each year, incorporating learning activities as well as a pre-/postformative knowledge assessment,” Janice Sibley, ACC’s executive vice president of education and publishing said in an interview, adding that the program continues to evolve.
In 2022, she noted that the ACC increased the flexibility of the CMP by removing the 7-hour learning engagement requirement, allowing users to choose how much time to spend learning in the CMP program. They also extended the performance assessment windows from 7 to 9 days each, covering 2 weekends for each.
She said that, to date, more than “6,400 learners” are enrolled in the CMP program.
Though the collaboration seems to make MOC less onerous, some cardiologists think it makes the ACC “complicit.”
A certification program that is independent of the ABIM launched in 2015. The National Board of Physicians and Surgeons is a nonprofit organization led by an advisory board of unpaid physicians. NBPAS seems to be gaining momentum and acceptance.
Cardiologist Melissa Walton-Shirley, MD, recounted her recertification experience with the NBPAS late in 2022. She now maintains a “hybrid” certification with both ABIM and NBPAS. Though she wants to support the latter, she found that the alternative certification option still requires an initial ABIM certification and is not recognized in all states or by many insurers and hospitals.
Will MOC ever disappear? Ms. Sibley said that the ACC is always looking to improve and enhance their offerings. “It is time to lead a change in the conversation from certification to continuous competency, from punitive to supportive options, from random knowledge testing to focused assessing knowledge gaps and lifelong learning. This will require innovation, technology, and new ways of thinking that offer cardiologists flexibility, relevance, and value and ultimately benefit the patients they serve.”
Many physicians, including cardiologists, are hoping that Dr. Goodman’s petition and further pressure from professional societies may finally translate into action.
A version of this article first appeared on Medscape.com.
It’s no secret that many physicians question the value of Maintenance of Certification requirements and are concerned about the amount of time, effort, and money the process takes. Now, they and at least two cardiology societies are starting to speak up.
MOC is an initiative from the American Board of Internal Medicine that requires an initial certification that costs thousands of dollars and must be repeated every 10 years. Annual MOC requirements involve tests that cost $220 for the first certificate a physician holds and about $120 for each subsequent one.
Interventional cardiologists (ICs) and other subspecialists have additional fees and requirements.
MOC ‘burdensome,’ ‘costly,’ ‘complex’
On July 21, hematologist-oncologist Aaron Goodman, MD, an associate professor at the University of California, San Diego, posted a petition on behalf of ABIM diplomates.
As of August 22, the petition had garnered more than 18,000 signatures.
Dr. Goodman recently debated ABIM President and CEO Richard J. Baron, MD, in a Healthcare Unfiltered podcast. Before the debate, host Chadi Nabhan, MD, MBA, tweeted that he could not find a single physician who would defend the MOC and recertification.
The debate touched on topics such as fees, evidence of value, the certification test format, and the cost and requirements to maintain more than one board certification. Overall, Dr. Goodman made the analogy to giving a patient chemotherapy: Because there are harms, he better know that there are also benefits. He cited that the harms associated with MOC include “financial toxicity, time toxicity, and stress toxicity,” with the latter being particularly toxic to him personally.
Though the podcast gave both participants ample opportunities to express their views, it’s not clear that either participant persuaded the other.
Cardiologists who are unhappy with MOC are speaking up on X, formerly known as Twitter. IC Matthew Sample, MD, listed five things he’s done to improve his practice since IC graduation, for which he received no MOC points.
In response, internist Artem Minalyan, MD, asked: “Hypothetically, if Dr. Baron required an IC procedure, I wonder if he would request you to get all your MOC points prior to consenting.”
SCAI and HRS weigh in
Some professional societies have responded to the ABIM’s threat to revoke the certifications of cardiologists who don’t participate in periodic MOC activities.
The Society for Cardiovascular Angiography & Interventions published its “Position on ABIM Revocation of Certification for Not Participating in MOC.” In it, SCAI states that ABIM diplomates who pass their exams and report procedural volumes as required should be “indisputably” recognized as “certified” for the relevant time frame (for example, 10 years), regardless of whether they participate in any other MOC activities.
SCAI President George D. Dangas, MD, PhD, said in an interview that “many of our members have expressed their frustration surrounding the confusion regarding their MOC requirements, including myself. We felt that this confusion could endanger the certified status of members, which would inevitably impact patient care, which is our greatest concern.”
The society has received an “overwhelmingly positive response” to its statement, he said. “Our hope is that ABIM will consider simpler, transparent regulations that are reflective of the feedback received from their constituents.”
In response to the COVID-19 pandemic, ABIM extended the deadline for diplomates whose certificate expired in 2020 or 2021 until the end of 2022; Dr. Dangas suggested ABIM further extend the deadline to enroll in or renew the MOC to the end of 2024 and that ABIM should “develop a recertification program that can be explained in a single slide/page.”
Other subspecialty groups are following SCAI’s lead including the EP Advocacy Foundation, and the Heart Rhythm Society.
MOC alternatives
The ABIM touts the value of MOC on its website, stating: “There is compelling evidence showing that MOC improves value of care without sacrificing quality and that board certified physicians command higher salaries.”
Alternative options that are arguably less arduous are available.
In collaboration with ABIM, the American College of Cardiology launched the ABIM/ACC Collaborative Maintenance Pathway in 2019 as an alternative MOC assessment option.
The CMP “focuses on one or a small group of topics within cardiology each year, incorporating learning activities as well as a pre-/postformative knowledge assessment,” Janice Sibley, ACC’s executive vice president of education and publishing said in an interview, adding that the program continues to evolve.
In 2022, she noted that the ACC increased the flexibility of the CMP by removing the 7-hour learning engagement requirement, allowing users to choose how much time to spend learning in the CMP program. They also extended the performance assessment windows from 7 to 9 days each, covering 2 weekends for each.
She said that, to date, more than “6,400 learners” are enrolled in the CMP program.
Though the collaboration seems to make MOC less onerous, some cardiologists think it makes the ACC “complicit.”
A certification program that is independent of the ABIM launched in 2015. The National Board of Physicians and Surgeons is a nonprofit organization led by an advisory board of unpaid physicians. NBPAS seems to be gaining momentum and acceptance.
Cardiologist Melissa Walton-Shirley, MD, recounted her recertification experience with the NBPAS late in 2022. She now maintains a “hybrid” certification with both ABIM and NBPAS. Though she wants to support the latter, she found that the alternative certification option still requires an initial ABIM certification and is not recognized in all states or by many insurers and hospitals.
Will MOC ever disappear? Ms. Sibley said that the ACC is always looking to improve and enhance their offerings. “It is time to lead a change in the conversation from certification to continuous competency, from punitive to supportive options, from random knowledge testing to focused assessing knowledge gaps and lifelong learning. This will require innovation, technology, and new ways of thinking that offer cardiologists flexibility, relevance, and value and ultimately benefit the patients they serve.”
Many physicians, including cardiologists, are hoping that Dr. Goodman’s petition and further pressure from professional societies may finally translate into action.
A version of this article first appeared on Medscape.com.
It’s no secret that many physicians question the value of Maintenance of Certification requirements and are concerned about the amount of time, effort, and money the process takes. Now, they and at least two cardiology societies are starting to speak up.
MOC is an initiative from the American Board of Internal Medicine that requires an initial certification that costs thousands of dollars and must be repeated every 10 years. Annual MOC requirements involve tests that cost $220 for the first certificate a physician holds and about $120 for each subsequent one.
Interventional cardiologists (ICs) and other subspecialists have additional fees and requirements.
MOC ‘burdensome,’ ‘costly,’ ‘complex’
On July 21, hematologist-oncologist Aaron Goodman, MD, an associate professor at the University of California, San Diego, posted a petition on behalf of ABIM diplomates.
As of August 22, the petition had garnered more than 18,000 signatures.
Dr. Goodman recently debated ABIM President and CEO Richard J. Baron, MD, in a Healthcare Unfiltered podcast. Before the debate, host Chadi Nabhan, MD, MBA, tweeted that he could not find a single physician who would defend the MOC and recertification.
The debate touched on topics such as fees, evidence of value, the certification test format, and the cost and requirements to maintain more than one board certification. Overall, Dr. Goodman made the analogy to giving a patient chemotherapy: Because there are harms, he better know that there are also benefits. He cited that the harms associated with MOC include “financial toxicity, time toxicity, and stress toxicity,” with the latter being particularly toxic to him personally.
Though the podcast gave both participants ample opportunities to express their views, it’s not clear that either participant persuaded the other.
Cardiologists who are unhappy with MOC are speaking up on X, formerly known as Twitter. IC Matthew Sample, MD, listed five things he’s done to improve his practice since IC graduation, for which he received no MOC points.
In response, internist Artem Minalyan, MD, asked: “Hypothetically, if Dr. Baron required an IC procedure, I wonder if he would request you to get all your MOC points prior to consenting.”
SCAI and HRS weigh in
Some professional societies have responded to the ABIM’s threat to revoke the certifications of cardiologists who don’t participate in periodic MOC activities.
The Society for Cardiovascular Angiography & Interventions published its “Position on ABIM Revocation of Certification for Not Participating in MOC.” In it, SCAI states that ABIM diplomates who pass their exams and report procedural volumes as required should be “indisputably” recognized as “certified” for the relevant time frame (for example, 10 years), regardless of whether they participate in any other MOC activities.
SCAI President George D. Dangas, MD, PhD, said in an interview that “many of our members have expressed their frustration surrounding the confusion regarding their MOC requirements, including myself. We felt that this confusion could endanger the certified status of members, which would inevitably impact patient care, which is our greatest concern.”
The society has received an “overwhelmingly positive response” to its statement, he said. “Our hope is that ABIM will consider simpler, transparent regulations that are reflective of the feedback received from their constituents.”
In response to the COVID-19 pandemic, ABIM extended the deadline for diplomates whose certificate expired in 2020 or 2021 until the end of 2022; Dr. Dangas suggested ABIM further extend the deadline to enroll in or renew the MOC to the end of 2024 and that ABIM should “develop a recertification program that can be explained in a single slide/page.”
Other subspecialty groups are following SCAI’s lead including the EP Advocacy Foundation, and the Heart Rhythm Society.
MOC alternatives
The ABIM touts the value of MOC on its website, stating: “There is compelling evidence showing that MOC improves value of care without sacrificing quality and that board certified physicians command higher salaries.”
Alternative options that are arguably less arduous are available.
In collaboration with ABIM, the American College of Cardiology launched the ABIM/ACC Collaborative Maintenance Pathway in 2019 as an alternative MOC assessment option.
The CMP “focuses on one or a small group of topics within cardiology each year, incorporating learning activities as well as a pre-/postformative knowledge assessment,” Janice Sibley, ACC’s executive vice president of education and publishing said in an interview, adding that the program continues to evolve.
In 2022, she noted that the ACC increased the flexibility of the CMP by removing the 7-hour learning engagement requirement, allowing users to choose how much time to spend learning in the CMP program. They also extended the performance assessment windows from 7 to 9 days each, covering 2 weekends for each.
She said that, to date, more than “6,400 learners” are enrolled in the CMP program.
Though the collaboration seems to make MOC less onerous, some cardiologists think it makes the ACC “complicit.”
A certification program that is independent of the ABIM launched in 2015. The National Board of Physicians and Surgeons is a nonprofit organization led by an advisory board of unpaid physicians. NBPAS seems to be gaining momentum and acceptance.
Cardiologist Melissa Walton-Shirley, MD, recounted her recertification experience with the NBPAS late in 2022. She now maintains a “hybrid” certification with both ABIM and NBPAS. Though she wants to support the latter, she found that the alternative certification option still requires an initial ABIM certification and is not recognized in all states or by many insurers and hospitals.
Will MOC ever disappear? Ms. Sibley said that the ACC is always looking to improve and enhance their offerings. “It is time to lead a change in the conversation from certification to continuous competency, from punitive to supportive options, from random knowledge testing to focused assessing knowledge gaps and lifelong learning. This will require innovation, technology, and new ways of thinking that offer cardiologists flexibility, relevance, and value and ultimately benefit the patients they serve.”
Many physicians, including cardiologists, are hoping that Dr. Goodman’s petition and further pressure from professional societies may finally translate into action.
A version of this article first appeared on Medscape.com.






