User login
Asymptomatic carotid stenosis tied to mental decline
BOSTON – Asymptomatic carotid stenosis is associated with cognitive impairment when compared to patients with similar risk factors but no stenosis, said Dr. Brajesh K. Lal, of the University of Maryland, Baltimore.
Dr. Lal presented results from the Asymptomatic Carotid Stenosis and Cognitive Function (ACCOF) study. "The key finding is that we've identified for the first time unequivocally that an asymptomatic carotid artery plaque in a patient that has never suffered a stroke before can result in cognitive impairment," Dr. Lal said at the Vascular Annual Meeting.
Vascular comorbidities, such as diabetes, hypertension, coronary disease, and hyperlipidemia, are well known to cause vascular cognitive impairment (VCI), and this new research indicates that ACS should be added to that list, according to Dr. Lal and his colleagues.
They assessed 129 patients, 69 with greater than or equal to 50% ACS and 60 controls with vascular co-morbidities without ACS. An overall index of cognitive function and five domain-specific scores were computed. Breath-holding index (BHI), an estimate of cerebrovascular reserve, was measured using transcranial Doppler. Patients were assigned to high vs. low BHI groups using a cut-off score of 0.69. They assessed differences among stenosis vs. control patients and stenosis patients with low vs. high BHIs.
The stenosis and control groups did not differ with respect to vascular risk factors, IQ, educational attainment, and depressive symptoms. The stenosis group performed worse on the overall composite cognitive score and the domain-specific scores for processing speed and learning/memory, all significant differences. Within the stenosis group, those with low BHI performed significantly worse on learning, and trended lower on processing speed and overall composite score.
"The ACCOF study results showed that asymptomatic carotid stenosis is associated with cognitive impairment when compared to patients with similar risk factors but no stenosis. The deficit is driven primarily by reduced processing speed and learning/memory, and is mild to moderate in severity. A likely mechanism for this impairment is reduced cerebrovascular reserve," said Dr. Lal. "These findings have the potential to impact decision making in the management of patients with ACS."
Dr. Lal and his colleagues showed that moderate (>50%) asymptomatic carotid stenosis (ACS) is associated with cognitive impairment. They claim that "these findings have the potential to impact decision making in the management of patients with ACS" and presumably to support more aggressive treatment of carotid plaque by either endarterectomy or stenting. While their findings suggest that the latter presumption may be the case, two other questions must be answered. The first is whether there is a cause and effect relationship and not just an association. The second and more important element that must be shown is that elimination of the plaque or restoration of luminal diameter to the stenotic carotid artery will reverse the decline. Until the latter is proven, it is hard to see how these findings alone can justify increasing the indications for more aggressive treatment. Hopefully in future work, Dr. Lal and his colleagues will address these two questions so that the therapeutic implications of his interesting findings can be fully realized.
Dr. Frank J. Veith is an associate medical editor for Vascular Specialist.
Dr. Lal and his colleagues showed that moderate (>50%) asymptomatic carotid stenosis (ACS) is associated with cognitive impairment. They claim that "these findings have the potential to impact decision making in the management of patients with ACS" and presumably to support more aggressive treatment of carotid plaque by either endarterectomy or stenting. While their findings suggest that the latter presumption may be the case, two other questions must be answered. The first is whether there is a cause and effect relationship and not just an association. The second and more important element that must be shown is that elimination of the plaque or restoration of luminal diameter to the stenotic carotid artery will reverse the decline. Until the latter is proven, it is hard to see how these findings alone can justify increasing the indications for more aggressive treatment. Hopefully in future work, Dr. Lal and his colleagues will address these two questions so that the therapeutic implications of his interesting findings can be fully realized.
Dr. Frank J. Veith is an associate medical editor for Vascular Specialist.
Dr. Lal and his colleagues showed that moderate (>50%) asymptomatic carotid stenosis (ACS) is associated with cognitive impairment. They claim that "these findings have the potential to impact decision making in the management of patients with ACS" and presumably to support more aggressive treatment of carotid plaque by either endarterectomy or stenting. While their findings suggest that the latter presumption may be the case, two other questions must be answered. The first is whether there is a cause and effect relationship and not just an association. The second and more important element that must be shown is that elimination of the plaque or restoration of luminal diameter to the stenotic carotid artery will reverse the decline. Until the latter is proven, it is hard to see how these findings alone can justify increasing the indications for more aggressive treatment. Hopefully in future work, Dr. Lal and his colleagues will address these two questions so that the therapeutic implications of his interesting findings can be fully realized.
Dr. Frank J. Veith is an associate medical editor for Vascular Specialist.
BOSTON – Asymptomatic carotid stenosis is associated with cognitive impairment when compared to patients with similar risk factors but no stenosis, said Dr. Brajesh K. Lal, of the University of Maryland, Baltimore.
Dr. Lal presented results from the Asymptomatic Carotid Stenosis and Cognitive Function (ACCOF) study. "The key finding is that we've identified for the first time unequivocally that an asymptomatic carotid artery plaque in a patient that has never suffered a stroke before can result in cognitive impairment," Dr. Lal said at the Vascular Annual Meeting.
Vascular comorbidities, such as diabetes, hypertension, coronary disease, and hyperlipidemia, are well known to cause vascular cognitive impairment (VCI), and this new research indicates that ACS should be added to that list, according to Dr. Lal and his colleagues.
They assessed 129 patients, 69 with greater than or equal to 50% ACS and 60 controls with vascular co-morbidities without ACS. An overall index of cognitive function and five domain-specific scores were computed. Breath-holding index (BHI), an estimate of cerebrovascular reserve, was measured using transcranial Doppler. Patients were assigned to high vs. low BHI groups using a cut-off score of 0.69. They assessed differences among stenosis vs. control patients and stenosis patients with low vs. high BHIs.
The stenosis and control groups did not differ with respect to vascular risk factors, IQ, educational attainment, and depressive symptoms. The stenosis group performed worse on the overall composite cognitive score and the domain-specific scores for processing speed and learning/memory, all significant differences. Within the stenosis group, those with low BHI performed significantly worse on learning, and trended lower on processing speed and overall composite score.
"The ACCOF study results showed that asymptomatic carotid stenosis is associated with cognitive impairment when compared to patients with similar risk factors but no stenosis. The deficit is driven primarily by reduced processing speed and learning/memory, and is mild to moderate in severity. A likely mechanism for this impairment is reduced cerebrovascular reserve," said Dr. Lal. "These findings have the potential to impact decision making in the management of patients with ACS."
BOSTON – Asymptomatic carotid stenosis is associated with cognitive impairment when compared to patients with similar risk factors but no stenosis, said Dr. Brajesh K. Lal, of the University of Maryland, Baltimore.
Dr. Lal presented results from the Asymptomatic Carotid Stenosis and Cognitive Function (ACCOF) study. "The key finding is that we've identified for the first time unequivocally that an asymptomatic carotid artery plaque in a patient that has never suffered a stroke before can result in cognitive impairment," Dr. Lal said at the Vascular Annual Meeting.
Vascular comorbidities, such as diabetes, hypertension, coronary disease, and hyperlipidemia, are well known to cause vascular cognitive impairment (VCI), and this new research indicates that ACS should be added to that list, according to Dr. Lal and his colleagues.
They assessed 129 patients, 69 with greater than or equal to 50% ACS and 60 controls with vascular co-morbidities without ACS. An overall index of cognitive function and five domain-specific scores were computed. Breath-holding index (BHI), an estimate of cerebrovascular reserve, was measured using transcranial Doppler. Patients were assigned to high vs. low BHI groups using a cut-off score of 0.69. They assessed differences among stenosis vs. control patients and stenosis patients with low vs. high BHIs.
The stenosis and control groups did not differ with respect to vascular risk factors, IQ, educational attainment, and depressive symptoms. The stenosis group performed worse on the overall composite cognitive score and the domain-specific scores for processing speed and learning/memory, all significant differences. Within the stenosis group, those with low BHI performed significantly worse on learning, and trended lower on processing speed and overall composite score.
"The ACCOF study results showed that asymptomatic carotid stenosis is associated with cognitive impairment when compared to patients with similar risk factors but no stenosis. The deficit is driven primarily by reduced processing speed and learning/memory, and is mild to moderate in severity. A likely mechanism for this impairment is reduced cerebrovascular reserve," said Dr. Lal. "These findings have the potential to impact decision making in the management of patients with ACS."
Fetal growth restriction may be underestimated in obese patients
Only 25% of babies who are born small for their gestational age are diagnosed prenatally, and this under-identification may be even higher in obese patients, according to researchers from The Penn State University College of Medicine. Because fetal growth restriction (FGR) is associated with poor perinatal outcomes, these researchers set out to retrospectively compare the accuracy of a customized growth curve with the standard growth curve (Hadlock), to identify FGR in obese and normal-weight patients.
A total of 300 nulliparous women were included in the single-institution, retrospective study (150 obese women with a body mass index [BMI] >30 mg/k2, and 150 women of normal weight with a BMI ≤25 mg/k2). These women were aged 18 to 50 years and gave birth between July 2008 and December 2012.
Obese women were twice as likely to have a fetus classified by third-trimester ultrasound as growth-restricted using the customized curve versus the Hadlock’s curve (odds ratio [OR], 2.1; 95% confidence interval [CI], 1.4−3.2; P = .001). There was no difference in classification of growth restriction found in the women of normal weight (OR, 0.9; CI, 0.7−1.2; P = .41).
“Customized growth curves take into account certain maternal factors such as age, parity, BMI, and ethnicity,” said researcher Megha Gupta, MD. “The standard growth curves still used today were developed in the 1960s to 1980s in Colorado with primarily Caucasian women who did not have their BMI recorded. Those curves are outdated for today’s ethnically diverse population. With 30% of the US population obese, we need to move toward individualized medicine for the fetus.”
“Study limitations include our study’s retrospective nature and the fact that we could not exclude pathology, such as hypertension or smoking, which could have affected these results,” said Dr. Gupta. “We plan to follow this study up with a comparison between Lushenko and Fenton curves, which also are standardized curves for neonatal birth weight, and create customized growth charts. The ultimate goal is a prospective study to see if there are altered outcomes for babies that are detected to be growth-restricted, based on the customized growth chart.”
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
Reference
Gupta M, Lauring J, Kunselman AR, Repke JT, Pauli JM. Fetal growth restriction may be underestimated in obese patients. Poster presented at: The American Congress of Obstetrics and Gynecology Annual Clinical Meeting, Chicago, IL; April 26, 2014.
Only 25% of babies who are born small for their gestational age are diagnosed prenatally, and this under-identification may be even higher in obese patients, according to researchers from The Penn State University College of Medicine. Because fetal growth restriction (FGR) is associated with poor perinatal outcomes, these researchers set out to retrospectively compare the accuracy of a customized growth curve with the standard growth curve (Hadlock), to identify FGR in obese and normal-weight patients.
A total of 300 nulliparous women were included in the single-institution, retrospective study (150 obese women with a body mass index [BMI] >30 mg/k2, and 150 women of normal weight with a BMI ≤25 mg/k2). These women were aged 18 to 50 years and gave birth between July 2008 and December 2012.
Obese women were twice as likely to have a fetus classified by third-trimester ultrasound as growth-restricted using the customized curve versus the Hadlock’s curve (odds ratio [OR], 2.1; 95% confidence interval [CI], 1.4−3.2; P = .001). There was no difference in classification of growth restriction found in the women of normal weight (OR, 0.9; CI, 0.7−1.2; P = .41).
“Customized growth curves take into account certain maternal factors such as age, parity, BMI, and ethnicity,” said researcher Megha Gupta, MD. “The standard growth curves still used today were developed in the 1960s to 1980s in Colorado with primarily Caucasian women who did not have their BMI recorded. Those curves are outdated for today’s ethnically diverse population. With 30% of the US population obese, we need to move toward individualized medicine for the fetus.”
“Study limitations include our study’s retrospective nature and the fact that we could not exclude pathology, such as hypertension or smoking, which could have affected these results,” said Dr. Gupta. “We plan to follow this study up with a comparison between Lushenko and Fenton curves, which also are standardized curves for neonatal birth weight, and create customized growth charts. The ultimate goal is a prospective study to see if there are altered outcomes for babies that are detected to be growth-restricted, based on the customized growth chart.”
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
Only 25% of babies who are born small for their gestational age are diagnosed prenatally, and this under-identification may be even higher in obese patients, according to researchers from The Penn State University College of Medicine. Because fetal growth restriction (FGR) is associated with poor perinatal outcomes, these researchers set out to retrospectively compare the accuracy of a customized growth curve with the standard growth curve (Hadlock), to identify FGR in obese and normal-weight patients.
A total of 300 nulliparous women were included in the single-institution, retrospective study (150 obese women with a body mass index [BMI] >30 mg/k2, and 150 women of normal weight with a BMI ≤25 mg/k2). These women were aged 18 to 50 years and gave birth between July 2008 and December 2012.
Obese women were twice as likely to have a fetus classified by third-trimester ultrasound as growth-restricted using the customized curve versus the Hadlock’s curve (odds ratio [OR], 2.1; 95% confidence interval [CI], 1.4−3.2; P = .001). There was no difference in classification of growth restriction found in the women of normal weight (OR, 0.9; CI, 0.7−1.2; P = .41).
“Customized growth curves take into account certain maternal factors such as age, parity, BMI, and ethnicity,” said researcher Megha Gupta, MD. “The standard growth curves still used today were developed in the 1960s to 1980s in Colorado with primarily Caucasian women who did not have their BMI recorded. Those curves are outdated for today’s ethnically diverse population. With 30% of the US population obese, we need to move toward individualized medicine for the fetus.”
“Study limitations include our study’s retrospective nature and the fact that we could not exclude pathology, such as hypertension or smoking, which could have affected these results,” said Dr. Gupta. “We plan to follow this study up with a comparison between Lushenko and Fenton curves, which also are standardized curves for neonatal birth weight, and create customized growth charts. The ultimate goal is a prospective study to see if there are altered outcomes for babies that are detected to be growth-restricted, based on the customized growth chart.”
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
Reference
Gupta M, Lauring J, Kunselman AR, Repke JT, Pauli JM. Fetal growth restriction may be underestimated in obese patients. Poster presented at: The American Congress of Obstetrics and Gynecology Annual Clinical Meeting, Chicago, IL; April 26, 2014.
Reference
Gupta M, Lauring J, Kunselman AR, Repke JT, Pauli JM. Fetal growth restriction may be underestimated in obese patients. Poster presented at: The American Congress of Obstetrics and Gynecology Annual Clinical Meeting, Chicago, IL; April 26, 2014.
Recurrent Multidrug Resistant Urinary Tract Infections in Geriatric Patients
Urinary tract infections (UTIs) account for 8.3 million doctor visits, 1 million emergency department (ED) visits, and 100,000 hospitalizations annually, with an estimated cost of $1 billion annually in the U.S.1 Urnary tract infections are the most common bacterial infections found in nursing home residents, accounting for 50% of reported infections in Norwegian nursing homes, 30% to 50% in U.S. nursing homes, and 25% of all infections in the noninstitutionalized elderly in the U.S.2-4 In the geriatric population, UTIs are often found incidentally at the time of hospitalization for other admitting diagnoses, such as mentation changes or falls.5 Asymptomatic pyuria was found in 14.8% of community residents aged ≥ 80 years.6 Woodford and colleague found that 37% of geriatric patients admitted through an ED diagnosed with UTIs had no dysuria or urinary frequency.7
The incidence of UTIs is higher in the elderly due to genitourinary abnormalities, urolithiasis, dehydration, and diabetes, among other causes. These are considered complicated UTIs, defined as those in the presence of factors that predispose to persistent or relapsing infection, such as foreign bodies (calculi, indwelling catheters), obstruction, renal failure, and urinary retention.8
In elderly men, prostate enlargement causes bladder outlet obstruction predisposing them to urinary stasis and UTIs.2 Urinary tract infections are prone to recur when urinary tract abnormalities persist or treatment ineffectively eradicates resistant bacteria. Urinary tract infections are considered recurrent when ≥ 3 occur within 1 year or ≥ 2 occur in a 6-month period. The anticipated recurrence rate of complicated UTIs at 4 to 6 weeks following completion of therapy is 40% to 60%.4
Current practice standards recommend not treating asymptomatic UTIs to avoid contributing to bacterial antibiotic resistance.9 The frequent use of antibiotics, such as quinolones, which are increasingly inactive against these organisms, contributes to the overgrowth of bacteria in the gastrointestinal tract and their appearance in the genitourinary tract.10,11
As UTI-causing bacteria become more resistant to available antibiotics, the need to explore new strategies for managing UTIs is clear.12 The spread of extended spectrum beta-lactamase (ESBL), methicillin-resistant Staphylococcus aureus (MRSA), and vancomycin-resistant enterococci (VRE), among other emerging bacterial resistance factors, present increasing treatment cost and poor patient outcomes. This challenge is occurring at a time when the discovery and development of new anti-infective agents is slowing down.13
The European Commission Scientific Committee on Health and Environmental Risk reported that in patients receiving up to 4,000 mg/d methenamine for preventive long-term treatment of UTIs, no adverse effects (AEs) were noted (Figure).17
Complicated UTIs in the elderly are difficult to treat due to bacterial resistance. The off-label use of methenamine hippurate for treatment/prophylaxis of MDR-recurrent UTIs is a compelling option, explored further in the following case studies. Four case studies using methenamine for treatment and prevention of recurrent MDR UTIs in geriatric patients are presented.
Treating UTI Patients
Case Study 1
A man aged > 89 years, symptomatic with nocturia due to benign prostatic hypertrophy (BPH) with bladder outlet obstruction had 8 symptomatic UTIs over 15 months. His urine culture tested positive for MDR Providencia stuartia (resistant to ampicillin, chephazolin, gentamycin, tigecycline, tobramycin and sulfamethizole) and Staphylococcus haemolyticus (resistant to ciprofloxacin, levofloxacin, and nitrofurantoin). Postvoid residual urine was identified as the cause for his recurrent UTIs. Self-catheterization was recommended, but the patient declined. Due to his advanced age and preference, surgical intervention was not pursued. His renal function was within normal limits.
Treatment with methenamine hippurate 500 mg bid with 1,000 mg ascorbic acid to acidify the urine was initiated. This reduced dose of 500 mg bid (rather than 1,000 mg bid) was prescribed due to his advanced age and a choice to “err on the side of caution.” Two months later, urinalysis was negative for leukocyte esterase and nitrates, and the growth culture tested negative. Three- and 6-month urinalyses also showed no growth. The patient’s renal function remained stable. He experienced no AEs from the methenamine.
Due to his urinary retention, formaldehyde was able to collect in his bladder for longer than 2 hours, achieving bactericidal levels and effectively preventing recurrence of MDR UTIs.
Case Study 2
A man aged > 89 years with BPH and urinary incontinence managed with an external urinary device worn continuously had a history of 4 UTIs within a 6-month period. His renal function was normal with a creatinine clearance of 37 mg/dL. He was diagnosed with a symptomatic UTI culturing > 100,000 CFU Proteus mirabilis (resistant to ciprofloxacin, nitrofurantoin, and septra).
Due to resistance of the organism to available oral antibiotics, the patient’s desire to avoid hospitalization, and his caregiver’s inability to learn to administer IV antibiotics in the home, methenamine hippurate 500 mg bid was initiated. Within 21 days, the patient’s urinalysis was negative, indicating no bacterial growth. He was treated for 4 months with no recurrence of a UTI. No symptomatic UTIs recurred during the ongoing methenamine treatment.
Case Study 3
A man aged > 89 years with end-stage renal disease and a history of bladder cancer declined dialysis, indicating that his goals for care were palliative. He was followed at home by a hospice team. He had 3 recurrent symptomatic MRSA UTIs in a 9-month period (resistant to ciprofloxacin, levofloxin, penicillin, and oxacillin). The antibiotics the bacteria was sensitive to, nitrofurantoin and septra, could not be given because his creatinine clearance was merely 8 mg/dL. He was prescribed 500 mg methenamine with 1,000 mg ascorbic acid bid. Within 4 weeks, his urinalysis had changed from > 100,000 CFU to > 50,000 CFU (< 100,000 CFU). One month later with the only treatment the methenamine and ascorbic acid, there was no bacterial growth in the patient’s urine culture. He had no recurrence of a symptomatic UTI while receiving methenamine.
Case Study 4
An 89-year-old man with BPH and recurrent MRSA UTIs had 3 hospitalizations within 1 year. He had stage 3 chronic kidney disease with a creatinine clearance of 43 mg/dL. The patient had a symptomatic UTI > 100,000 CFU MRSA. He was treated with 500 mg methenamine and 1,000 mg ascorbic acid bid. Urinalysis results 2 months later revealed the bacterial count had dropped to the colonization range (< 50,000 CFU). His urinalysis was positive for leukocyte esterase with high white blood cell (WBC) counts, but it was negative for nitrites. He continued without recurrent UTIs while receiving the medication.
Discussion
Patients with similar profiles to those discussed in this report were treated with less dramatic results. Several remained free of symptomatic UTIs with urine cultures showing bacterial counts in the colonization range of < 50,000 CFU, as noted in case 4. Frequently, patients treated with methenamine have urinalyses with negative nitrites, positive leukocyte esterase, high WBCs, and few bacteria, but cultures show no growth. Some patients who did not reliably take medications as prescribed had recurrent symptomatic UTIs. Some had a subsequent UTI culturing a different organism or a change in the sensitivity profile of the same organism. This phenomenon suggests that formaldehyde disrupts the manufacture and transmission of the proteins and enzymes responsible for bacterial resistance factors.
Freeman and colleagues conducted a prospective study of 249 men with bacteruria followed for up to 10 years.18 Continuous therapy with methenamine delayed recurrence of bacteruria. Nilsson found that recurrent UTIs were reduced by 25% with long-term treatment (> 3 months) with methenamine.19
Bacteria do not develop resistance to methenamine.20 Reports of AEs are low, and drug interactions are limited to sulfamethizole, which can cause crystallization in the urine. Daily dosing used in studies ranged from 1 g to 4 g daily.21 Nilsson conducted research over 16 months with geriatric patients and found no changes in renal function or crystallization in urine.19
Severe hepatic impairment is also a contraindication, as methenamine can be hydrolyzed to ammonia. Studies have shown a reduced effectiveness with lower urinary tract abnormalities, although those studies administered the medication for short periods of time.21 Because the action of the medication relies on ≥ 2 hours of exposure to urine in the bladder, patients with indwelling catheters or patients who urinate frequently experience little benefit.22 Ideal candidates for methenamine are those with urinary retention and recurrent UTIs.
Although the use of methenamine has increased in Norway and Sweden by 24% since 2000, the use of methenamine in the U.S. remains low, perhaps because of conflicting reports in the literature regarding effectiveness and use with limited populations (ie, noncatheterized patients, those able to retain urine for ≥ 2 hours, and a creatinine clearance > 50 mg/dL).3
Some health care providers use methenamine for UTI prophylaxis, but this practice is less common in the U.S. than it is in Scandinavian countries.3 However, no published studies have explored the action of methenamine on MRSA, ESBL, and VRE bacteria or on the enzymes and proteins that enable and transmit bacterial resistance factors.
Elderly patients with complicated recurrent UTIs due to resistant bacteria are often left with no oral antibiotic options. Costs escalate rapidly when IV antibiotics are given. Administration generally requires hospitalization with close monitoring of renal function and drug levels and the placement of a PICC or midline IV access. If there is no caregiver, then hospitalization followed by an admission to a skilled nursing facility is required.
Lee and colleagues concluded that there is a need for further studies to explore long-duration therapy with methenamine.21 No studies have addressed its use in the geriatric population for long-term use of prevention of recurrent UTIs. No studies have been done on its use for primary treatment of MDR UTIs. The benefits of this drug with a low AE profile and low cost ($60/month for 1 g bid), which has been proven to reduce the incidence and/or delay recurrence of UTIs, is well worth further examination.
Conclusion
Multiple studies over 60 years have shown methenamine hippurate to be a well-tolerated and safe medication. Little data are available about the use of this medication in the elderly in the U.S., despite its wide use in Scandinavian countries. Use of methenamine for MDR UTIs in the geriatric population has been shown to be safe and effective, as presented in these case studies. Substantial cost savings were realized with the use of methenamine in these geriatric patients by reducing hospitalizations and complications due to recurrent MDR UTIs. The use of methenamine for treating MDR UTIs and the prevention of recurrent UTIs in the geriatric population warrants further clinical use and research.
The very interesting changes noted in sensitivity of the same bacteria in subsequent UTIs in patients treated with methenamine raises questions about the action of formaldehyde in the bladder on bacterial resistance factors. Given the worldwide increase in bacterial resistance to currently available antibiotics, this is a most compelling action that demands further study.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Foxman B. Epidemiology of urinary tract infections: Incidence, morbidity, and economic costs. Am J Med. 2002;113(suppl 1A):5S-13S.
2. Kamel HK. Managing urinary tract infections: Guide for nursing home practitioners. Ann of Long Term Care. 2005;13(9):21-28.
3. Blix HS, Røed J, Sti MO. Large variation in antibacterial use among Norwegian nursing homes. Scand J Infect Dis. 2007;39(6-7):536-541.
4. Nicolle LE. Asymptomatic bacteruria in diabetic women. Diabetes Care. 2000;23(6):722-723.
5. Rhoads J, Clayman A, Nelson S. The relationship of urinary tract infections and falls in a nursing home. Director. 2007;15(1):22-26.
6. Rodhe N, Mølstad S, Englund L, Svärdsudd K. Asymptomatic bacteriuria in a population of elderly residents living in a community setting: Prevalence, characteristics and associated factors. Fam Pract. 2006;23(3):303-307.
7. Woodford HJ, George J. Diagnosis and management of urinary tract infection in hospitalized older people. J Am Geriatr Soc. 2009;57(1):107-114.
8. Levison ME, Kaye D. Treatment of complicated urinary tract infections with an emphasis on drug-resistant gram-negative uropathogens. Curr Infect Dis Rep. 2013;15(2):109-115.
9. Miller LG, Tang AW. Treatment of uncomplicated urinary tract infections in an era of increasing antimicrobial resistance. Mayo Clin Proc. 2004;79(8):1048-1053.
10. Nicoletti J, Kuster SP, Sulser T, et al. Risk factors for urinary tract infections due to ciprofloxacin-resistant Escherichia coli in a tertiary care urology department in Switzerland. Swiss Med Wkly. 2010;140:w13059.
11. Nicolle LE. Urinary tract infection in geriatric and institutionalized patients. Curr Opin Urol. 2002;12(1):51-55.
12. Foxman B. The epidemiology of urinary tract infection. Nat Rev Urol. 2010;7(12):653-660.
13. Spellberg B, Guidos R, Gilbert D, et al; Infectious Diseases Society of America. The epidemic of antibiotic-resistant infections: A call to action for the medical community from the Infectious Diseases Society of America. Clin Infect Dis. 2008;46(2):155-164.
14. Dagley S, Dawes EA, Morrison GA. Inhibition of growth of Aerobacter aerogenes: The mode of action of phenols, alcohols, acetone, and ethyl acetate.
J Bacteriol. 1950;60(4):369-379.
15. Neely WB. Action of formaldehyde on microorganisms I. Correlation of activity with formaldehyde metabolism. J Bacteriol. 1963;85(5):1028-1031.
16. Musher DM, Griffith DP. Generation of formaldehyde from methenamine: Effect of pH and concentration, and antibacterial effect. Antimicrob Agents Chemother. 1974;6(6):708-711.
17. Scientific Committee on Health and Environmental Risks. Risk Assessment Report on Methenamine. Brussels, Belgium: European Commission; 2007. CAS 100-97-0.
18. Freeman RB, Smith WM, Richardson JA, et al. Long-term therapy for chronic bacteriuria in men. U.S. Public Health Service cooperative study. Ann Intern Med. 1975;83(2):133-147.
19. Nilsson S. Long-term treatment with methenamine hippurate in recurrent urinary tract infection. Acta Med Scand. 1975;198(1-2):81-85.
20. Drugs.com. Methenamine (systemic). http://www.drugs.com/mmx/methenamine-hippurate.html?printable=1. Updated March 28, 2000. Accessed June 17, 2014.
21. Lee BSB, Simpson JM, Craig JC, Bhuta T. Methenamine hippurate for preventing urinary tract infections. Cochrane Database Syst Rev. 2012;10:CD003265.
22. Lee BB, Haran MJ, Hunt LM, et al. Spinal-injured neuropathic bladder antisepsis (SINBA) trial. Spinal Cord. 2007;45(8):542-550.
Urinary tract infections (UTIs) account for 8.3 million doctor visits, 1 million emergency department (ED) visits, and 100,000 hospitalizations annually, with an estimated cost of $1 billion annually in the U.S.1 Urnary tract infections are the most common bacterial infections found in nursing home residents, accounting for 50% of reported infections in Norwegian nursing homes, 30% to 50% in U.S. nursing homes, and 25% of all infections in the noninstitutionalized elderly in the U.S.2-4 In the geriatric population, UTIs are often found incidentally at the time of hospitalization for other admitting diagnoses, such as mentation changes or falls.5 Asymptomatic pyuria was found in 14.8% of community residents aged ≥ 80 years.6 Woodford and colleague found that 37% of geriatric patients admitted through an ED diagnosed with UTIs had no dysuria or urinary frequency.7
The incidence of UTIs is higher in the elderly due to genitourinary abnormalities, urolithiasis, dehydration, and diabetes, among other causes. These are considered complicated UTIs, defined as those in the presence of factors that predispose to persistent or relapsing infection, such as foreign bodies (calculi, indwelling catheters), obstruction, renal failure, and urinary retention.8
In elderly men, prostate enlargement causes bladder outlet obstruction predisposing them to urinary stasis and UTIs.2 Urinary tract infections are prone to recur when urinary tract abnormalities persist or treatment ineffectively eradicates resistant bacteria. Urinary tract infections are considered recurrent when ≥ 3 occur within 1 year or ≥ 2 occur in a 6-month period. The anticipated recurrence rate of complicated UTIs at 4 to 6 weeks following completion of therapy is 40% to 60%.4
Current practice standards recommend not treating asymptomatic UTIs to avoid contributing to bacterial antibiotic resistance.9 The frequent use of antibiotics, such as quinolones, which are increasingly inactive against these organisms, contributes to the overgrowth of bacteria in the gastrointestinal tract and their appearance in the genitourinary tract.10,11
As UTI-causing bacteria become more resistant to available antibiotics, the need to explore new strategies for managing UTIs is clear.12 The spread of extended spectrum beta-lactamase (ESBL), methicillin-resistant Staphylococcus aureus (MRSA), and vancomycin-resistant enterococci (VRE), among other emerging bacterial resistance factors, present increasing treatment cost and poor patient outcomes. This challenge is occurring at a time when the discovery and development of new anti-infective agents is slowing down.13
The European Commission Scientific Committee on Health and Environmental Risk reported that in patients receiving up to 4,000 mg/d methenamine for preventive long-term treatment of UTIs, no adverse effects (AEs) were noted (Figure).17
Complicated UTIs in the elderly are difficult to treat due to bacterial resistance. The off-label use of methenamine hippurate for treatment/prophylaxis of MDR-recurrent UTIs is a compelling option, explored further in the following case studies. Four case studies using methenamine for treatment and prevention of recurrent MDR UTIs in geriatric patients are presented.
Treating UTI Patients
Case Study 1
A man aged > 89 years, symptomatic with nocturia due to benign prostatic hypertrophy (BPH) with bladder outlet obstruction had 8 symptomatic UTIs over 15 months. His urine culture tested positive for MDR Providencia stuartia (resistant to ampicillin, chephazolin, gentamycin, tigecycline, tobramycin and sulfamethizole) and Staphylococcus haemolyticus (resistant to ciprofloxacin, levofloxacin, and nitrofurantoin). Postvoid residual urine was identified as the cause for his recurrent UTIs. Self-catheterization was recommended, but the patient declined. Due to his advanced age and preference, surgical intervention was not pursued. His renal function was within normal limits.
Treatment with methenamine hippurate 500 mg bid with 1,000 mg ascorbic acid to acidify the urine was initiated. This reduced dose of 500 mg bid (rather than 1,000 mg bid) was prescribed due to his advanced age and a choice to “err on the side of caution.” Two months later, urinalysis was negative for leukocyte esterase and nitrates, and the growth culture tested negative. Three- and 6-month urinalyses also showed no growth. The patient’s renal function remained stable. He experienced no AEs from the methenamine.
Due to his urinary retention, formaldehyde was able to collect in his bladder for longer than 2 hours, achieving bactericidal levels and effectively preventing recurrence of MDR UTIs.
Case Study 2
A man aged > 89 years with BPH and urinary incontinence managed with an external urinary device worn continuously had a history of 4 UTIs within a 6-month period. His renal function was normal with a creatinine clearance of 37 mg/dL. He was diagnosed with a symptomatic UTI culturing > 100,000 CFU Proteus mirabilis (resistant to ciprofloxacin, nitrofurantoin, and septra).
Due to resistance of the organism to available oral antibiotics, the patient’s desire to avoid hospitalization, and his caregiver’s inability to learn to administer IV antibiotics in the home, methenamine hippurate 500 mg bid was initiated. Within 21 days, the patient’s urinalysis was negative, indicating no bacterial growth. He was treated for 4 months with no recurrence of a UTI. No symptomatic UTIs recurred during the ongoing methenamine treatment.
Case Study 3
A man aged > 89 years with end-stage renal disease and a history of bladder cancer declined dialysis, indicating that his goals for care were palliative. He was followed at home by a hospice team. He had 3 recurrent symptomatic MRSA UTIs in a 9-month period (resistant to ciprofloxacin, levofloxin, penicillin, and oxacillin). The antibiotics the bacteria was sensitive to, nitrofurantoin and septra, could not be given because his creatinine clearance was merely 8 mg/dL. He was prescribed 500 mg methenamine with 1,000 mg ascorbic acid bid. Within 4 weeks, his urinalysis had changed from > 100,000 CFU to > 50,000 CFU (< 100,000 CFU). One month later with the only treatment the methenamine and ascorbic acid, there was no bacterial growth in the patient’s urine culture. He had no recurrence of a symptomatic UTI while receiving methenamine.
Case Study 4
An 89-year-old man with BPH and recurrent MRSA UTIs had 3 hospitalizations within 1 year. He had stage 3 chronic kidney disease with a creatinine clearance of 43 mg/dL. The patient had a symptomatic UTI > 100,000 CFU MRSA. He was treated with 500 mg methenamine and 1,000 mg ascorbic acid bid. Urinalysis results 2 months later revealed the bacterial count had dropped to the colonization range (< 50,000 CFU). His urinalysis was positive for leukocyte esterase with high white blood cell (WBC) counts, but it was negative for nitrites. He continued without recurrent UTIs while receiving the medication.
Discussion
Patients with similar profiles to those discussed in this report were treated with less dramatic results. Several remained free of symptomatic UTIs with urine cultures showing bacterial counts in the colonization range of < 50,000 CFU, as noted in case 4. Frequently, patients treated with methenamine have urinalyses with negative nitrites, positive leukocyte esterase, high WBCs, and few bacteria, but cultures show no growth. Some patients who did not reliably take medications as prescribed had recurrent symptomatic UTIs. Some had a subsequent UTI culturing a different organism or a change in the sensitivity profile of the same organism. This phenomenon suggests that formaldehyde disrupts the manufacture and transmission of the proteins and enzymes responsible for bacterial resistance factors.
Freeman and colleagues conducted a prospective study of 249 men with bacteruria followed for up to 10 years.18 Continuous therapy with methenamine delayed recurrence of bacteruria. Nilsson found that recurrent UTIs were reduced by 25% with long-term treatment (> 3 months) with methenamine.19
Bacteria do not develop resistance to methenamine.20 Reports of AEs are low, and drug interactions are limited to sulfamethizole, which can cause crystallization in the urine. Daily dosing used in studies ranged from 1 g to 4 g daily.21 Nilsson conducted research over 16 months with geriatric patients and found no changes in renal function or crystallization in urine.19
Severe hepatic impairment is also a contraindication, as methenamine can be hydrolyzed to ammonia. Studies have shown a reduced effectiveness with lower urinary tract abnormalities, although those studies administered the medication for short periods of time.21 Because the action of the medication relies on ≥ 2 hours of exposure to urine in the bladder, patients with indwelling catheters or patients who urinate frequently experience little benefit.22 Ideal candidates for methenamine are those with urinary retention and recurrent UTIs.
Although the use of methenamine has increased in Norway and Sweden by 24% since 2000, the use of methenamine in the U.S. remains low, perhaps because of conflicting reports in the literature regarding effectiveness and use with limited populations (ie, noncatheterized patients, those able to retain urine for ≥ 2 hours, and a creatinine clearance > 50 mg/dL).3
Some health care providers use methenamine for UTI prophylaxis, but this practice is less common in the U.S. than it is in Scandinavian countries.3 However, no published studies have explored the action of methenamine on MRSA, ESBL, and VRE bacteria or on the enzymes and proteins that enable and transmit bacterial resistance factors.
Elderly patients with complicated recurrent UTIs due to resistant bacteria are often left with no oral antibiotic options. Costs escalate rapidly when IV antibiotics are given. Administration generally requires hospitalization with close monitoring of renal function and drug levels and the placement of a PICC or midline IV access. If there is no caregiver, then hospitalization followed by an admission to a skilled nursing facility is required.
Lee and colleagues concluded that there is a need for further studies to explore long-duration therapy with methenamine.21 No studies have addressed its use in the geriatric population for long-term use of prevention of recurrent UTIs. No studies have been done on its use for primary treatment of MDR UTIs. The benefits of this drug with a low AE profile and low cost ($60/month for 1 g bid), which has been proven to reduce the incidence and/or delay recurrence of UTIs, is well worth further examination.
Conclusion
Multiple studies over 60 years have shown methenamine hippurate to be a well-tolerated and safe medication. Little data are available about the use of this medication in the elderly in the U.S., despite its wide use in Scandinavian countries. Use of methenamine for MDR UTIs in the geriatric population has been shown to be safe and effective, as presented in these case studies. Substantial cost savings were realized with the use of methenamine in these geriatric patients by reducing hospitalizations and complications due to recurrent MDR UTIs. The use of methenamine for treating MDR UTIs and the prevention of recurrent UTIs in the geriatric population warrants further clinical use and research.
The very interesting changes noted in sensitivity of the same bacteria in subsequent UTIs in patients treated with methenamine raises questions about the action of formaldehyde in the bladder on bacterial resistance factors. Given the worldwide increase in bacterial resistance to currently available antibiotics, this is a most compelling action that demands further study.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Urinary tract infections (UTIs) account for 8.3 million doctor visits, 1 million emergency department (ED) visits, and 100,000 hospitalizations annually, with an estimated cost of $1 billion annually in the U.S.1 Urnary tract infections are the most common bacterial infections found in nursing home residents, accounting for 50% of reported infections in Norwegian nursing homes, 30% to 50% in U.S. nursing homes, and 25% of all infections in the noninstitutionalized elderly in the U.S.2-4 In the geriatric population, UTIs are often found incidentally at the time of hospitalization for other admitting diagnoses, such as mentation changes or falls.5 Asymptomatic pyuria was found in 14.8% of community residents aged ≥ 80 years.6 Woodford and colleague found that 37% of geriatric patients admitted through an ED diagnosed with UTIs had no dysuria or urinary frequency.7
The incidence of UTIs is higher in the elderly due to genitourinary abnormalities, urolithiasis, dehydration, and diabetes, among other causes. These are considered complicated UTIs, defined as those in the presence of factors that predispose to persistent or relapsing infection, such as foreign bodies (calculi, indwelling catheters), obstruction, renal failure, and urinary retention.8
In elderly men, prostate enlargement causes bladder outlet obstruction predisposing them to urinary stasis and UTIs.2 Urinary tract infections are prone to recur when urinary tract abnormalities persist or treatment ineffectively eradicates resistant bacteria. Urinary tract infections are considered recurrent when ≥ 3 occur within 1 year or ≥ 2 occur in a 6-month period. The anticipated recurrence rate of complicated UTIs at 4 to 6 weeks following completion of therapy is 40% to 60%.4
Current practice standards recommend not treating asymptomatic UTIs to avoid contributing to bacterial antibiotic resistance.9 The frequent use of antibiotics, such as quinolones, which are increasingly inactive against these organisms, contributes to the overgrowth of bacteria in the gastrointestinal tract and their appearance in the genitourinary tract.10,11
As UTI-causing bacteria become more resistant to available antibiotics, the need to explore new strategies for managing UTIs is clear.12 The spread of extended spectrum beta-lactamase (ESBL), methicillin-resistant Staphylococcus aureus (MRSA), and vancomycin-resistant enterococci (VRE), among other emerging bacterial resistance factors, present increasing treatment cost and poor patient outcomes. This challenge is occurring at a time when the discovery and development of new anti-infective agents is slowing down.13
The European Commission Scientific Committee on Health and Environmental Risk reported that in patients receiving up to 4,000 mg/d methenamine for preventive long-term treatment of UTIs, no adverse effects (AEs) were noted (Figure).17
Complicated UTIs in the elderly are difficult to treat due to bacterial resistance. The off-label use of methenamine hippurate for treatment/prophylaxis of MDR-recurrent UTIs is a compelling option, explored further in the following case studies. Four case studies using methenamine for treatment and prevention of recurrent MDR UTIs in geriatric patients are presented.
Treating UTI Patients
Case Study 1
A man aged > 89 years, symptomatic with nocturia due to benign prostatic hypertrophy (BPH) with bladder outlet obstruction had 8 symptomatic UTIs over 15 months. His urine culture tested positive for MDR Providencia stuartia (resistant to ampicillin, chephazolin, gentamycin, tigecycline, tobramycin and sulfamethizole) and Staphylococcus haemolyticus (resistant to ciprofloxacin, levofloxacin, and nitrofurantoin). Postvoid residual urine was identified as the cause for his recurrent UTIs. Self-catheterization was recommended, but the patient declined. Due to his advanced age and preference, surgical intervention was not pursued. His renal function was within normal limits.
Treatment with methenamine hippurate 500 mg bid with 1,000 mg ascorbic acid to acidify the urine was initiated. This reduced dose of 500 mg bid (rather than 1,000 mg bid) was prescribed due to his advanced age and a choice to “err on the side of caution.” Two months later, urinalysis was negative for leukocyte esterase and nitrates, and the growth culture tested negative. Three- and 6-month urinalyses also showed no growth. The patient’s renal function remained stable. He experienced no AEs from the methenamine.
Due to his urinary retention, formaldehyde was able to collect in his bladder for longer than 2 hours, achieving bactericidal levels and effectively preventing recurrence of MDR UTIs.
Case Study 2
A man aged > 89 years with BPH and urinary incontinence managed with an external urinary device worn continuously had a history of 4 UTIs within a 6-month period. His renal function was normal with a creatinine clearance of 37 mg/dL. He was diagnosed with a symptomatic UTI culturing > 100,000 CFU Proteus mirabilis (resistant to ciprofloxacin, nitrofurantoin, and septra).
Due to resistance of the organism to available oral antibiotics, the patient’s desire to avoid hospitalization, and his caregiver’s inability to learn to administer IV antibiotics in the home, methenamine hippurate 500 mg bid was initiated. Within 21 days, the patient’s urinalysis was negative, indicating no bacterial growth. He was treated for 4 months with no recurrence of a UTI. No symptomatic UTIs recurred during the ongoing methenamine treatment.
Case Study 3
A man aged > 89 years with end-stage renal disease and a history of bladder cancer declined dialysis, indicating that his goals for care were palliative. He was followed at home by a hospice team. He had 3 recurrent symptomatic MRSA UTIs in a 9-month period (resistant to ciprofloxacin, levofloxin, penicillin, and oxacillin). The antibiotics the bacteria was sensitive to, nitrofurantoin and septra, could not be given because his creatinine clearance was merely 8 mg/dL. He was prescribed 500 mg methenamine with 1,000 mg ascorbic acid bid. Within 4 weeks, his urinalysis had changed from > 100,000 CFU to > 50,000 CFU (< 100,000 CFU). One month later with the only treatment the methenamine and ascorbic acid, there was no bacterial growth in the patient’s urine culture. He had no recurrence of a symptomatic UTI while receiving methenamine.
Case Study 4
An 89-year-old man with BPH and recurrent MRSA UTIs had 3 hospitalizations within 1 year. He had stage 3 chronic kidney disease with a creatinine clearance of 43 mg/dL. The patient had a symptomatic UTI > 100,000 CFU MRSA. He was treated with 500 mg methenamine and 1,000 mg ascorbic acid bid. Urinalysis results 2 months later revealed the bacterial count had dropped to the colonization range (< 50,000 CFU). His urinalysis was positive for leukocyte esterase with high white blood cell (WBC) counts, but it was negative for nitrites. He continued without recurrent UTIs while receiving the medication.
Discussion
Patients with similar profiles to those discussed in this report were treated with less dramatic results. Several remained free of symptomatic UTIs with urine cultures showing bacterial counts in the colonization range of < 50,000 CFU, as noted in case 4. Frequently, patients treated with methenamine have urinalyses with negative nitrites, positive leukocyte esterase, high WBCs, and few bacteria, but cultures show no growth. Some patients who did not reliably take medications as prescribed had recurrent symptomatic UTIs. Some had a subsequent UTI culturing a different organism or a change in the sensitivity profile of the same organism. This phenomenon suggests that formaldehyde disrupts the manufacture and transmission of the proteins and enzymes responsible for bacterial resistance factors.
Freeman and colleagues conducted a prospective study of 249 men with bacteruria followed for up to 10 years.18 Continuous therapy with methenamine delayed recurrence of bacteruria. Nilsson found that recurrent UTIs were reduced by 25% with long-term treatment (> 3 months) with methenamine.19
Bacteria do not develop resistance to methenamine.20 Reports of AEs are low, and drug interactions are limited to sulfamethizole, which can cause crystallization in the urine. Daily dosing used in studies ranged from 1 g to 4 g daily.21 Nilsson conducted research over 16 months with geriatric patients and found no changes in renal function or crystallization in urine.19
Severe hepatic impairment is also a contraindication, as methenamine can be hydrolyzed to ammonia. Studies have shown a reduced effectiveness with lower urinary tract abnormalities, although those studies administered the medication for short periods of time.21 Because the action of the medication relies on ≥ 2 hours of exposure to urine in the bladder, patients with indwelling catheters or patients who urinate frequently experience little benefit.22 Ideal candidates for methenamine are those with urinary retention and recurrent UTIs.
Although the use of methenamine has increased in Norway and Sweden by 24% since 2000, the use of methenamine in the U.S. remains low, perhaps because of conflicting reports in the literature regarding effectiveness and use with limited populations (ie, noncatheterized patients, those able to retain urine for ≥ 2 hours, and a creatinine clearance > 50 mg/dL).3
Some health care providers use methenamine for UTI prophylaxis, but this practice is less common in the U.S. than it is in Scandinavian countries.3 However, no published studies have explored the action of methenamine on MRSA, ESBL, and VRE bacteria or on the enzymes and proteins that enable and transmit bacterial resistance factors.
Elderly patients with complicated recurrent UTIs due to resistant bacteria are often left with no oral antibiotic options. Costs escalate rapidly when IV antibiotics are given. Administration generally requires hospitalization with close monitoring of renal function and drug levels and the placement of a PICC or midline IV access. If there is no caregiver, then hospitalization followed by an admission to a skilled nursing facility is required.
Lee and colleagues concluded that there is a need for further studies to explore long-duration therapy with methenamine.21 No studies have addressed its use in the geriatric population for long-term use of prevention of recurrent UTIs. No studies have been done on its use for primary treatment of MDR UTIs. The benefits of this drug with a low AE profile and low cost ($60/month for 1 g bid), which has been proven to reduce the incidence and/or delay recurrence of UTIs, is well worth further examination.
Conclusion
Multiple studies over 60 years have shown methenamine hippurate to be a well-tolerated and safe medication. Little data are available about the use of this medication in the elderly in the U.S., despite its wide use in Scandinavian countries. Use of methenamine for MDR UTIs in the geriatric population has been shown to be safe and effective, as presented in these case studies. Substantial cost savings were realized with the use of methenamine in these geriatric patients by reducing hospitalizations and complications due to recurrent MDR UTIs. The use of methenamine for treating MDR UTIs and the prevention of recurrent UTIs in the geriatric population warrants further clinical use and research.
The very interesting changes noted in sensitivity of the same bacteria in subsequent UTIs in patients treated with methenamine raises questions about the action of formaldehyde in the bladder on bacterial resistance factors. Given the worldwide increase in bacterial resistance to currently available antibiotics, this is a most compelling action that demands further study.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Foxman B. Epidemiology of urinary tract infections: Incidence, morbidity, and economic costs. Am J Med. 2002;113(suppl 1A):5S-13S.
2. Kamel HK. Managing urinary tract infections: Guide for nursing home practitioners. Ann of Long Term Care. 2005;13(9):21-28.
3. Blix HS, Røed J, Sti MO. Large variation in antibacterial use among Norwegian nursing homes. Scand J Infect Dis. 2007;39(6-7):536-541.
4. Nicolle LE. Asymptomatic bacteruria in diabetic women. Diabetes Care. 2000;23(6):722-723.
5. Rhoads J, Clayman A, Nelson S. The relationship of urinary tract infections and falls in a nursing home. Director. 2007;15(1):22-26.
6. Rodhe N, Mølstad S, Englund L, Svärdsudd K. Asymptomatic bacteriuria in a population of elderly residents living in a community setting: Prevalence, characteristics and associated factors. Fam Pract. 2006;23(3):303-307.
7. Woodford HJ, George J. Diagnosis and management of urinary tract infection in hospitalized older people. J Am Geriatr Soc. 2009;57(1):107-114.
8. Levison ME, Kaye D. Treatment of complicated urinary tract infections with an emphasis on drug-resistant gram-negative uropathogens. Curr Infect Dis Rep. 2013;15(2):109-115.
9. Miller LG, Tang AW. Treatment of uncomplicated urinary tract infections in an era of increasing antimicrobial resistance. Mayo Clin Proc. 2004;79(8):1048-1053.
10. Nicoletti J, Kuster SP, Sulser T, et al. Risk factors for urinary tract infections due to ciprofloxacin-resistant Escherichia coli in a tertiary care urology department in Switzerland. Swiss Med Wkly. 2010;140:w13059.
11. Nicolle LE. Urinary tract infection in geriatric and institutionalized patients. Curr Opin Urol. 2002;12(1):51-55.
12. Foxman B. The epidemiology of urinary tract infection. Nat Rev Urol. 2010;7(12):653-660.
13. Spellberg B, Guidos R, Gilbert D, et al; Infectious Diseases Society of America. The epidemic of antibiotic-resistant infections: A call to action for the medical community from the Infectious Diseases Society of America. Clin Infect Dis. 2008;46(2):155-164.
14. Dagley S, Dawes EA, Morrison GA. Inhibition of growth of Aerobacter aerogenes: The mode of action of phenols, alcohols, acetone, and ethyl acetate.
J Bacteriol. 1950;60(4):369-379.
15. Neely WB. Action of formaldehyde on microorganisms I. Correlation of activity with formaldehyde metabolism. J Bacteriol. 1963;85(5):1028-1031.
16. Musher DM, Griffith DP. Generation of formaldehyde from methenamine: Effect of pH and concentration, and antibacterial effect. Antimicrob Agents Chemother. 1974;6(6):708-711.
17. Scientific Committee on Health and Environmental Risks. Risk Assessment Report on Methenamine. Brussels, Belgium: European Commission; 2007. CAS 100-97-0.
18. Freeman RB, Smith WM, Richardson JA, et al. Long-term therapy for chronic bacteriuria in men. U.S. Public Health Service cooperative study. Ann Intern Med. 1975;83(2):133-147.
19. Nilsson S. Long-term treatment with methenamine hippurate in recurrent urinary tract infection. Acta Med Scand. 1975;198(1-2):81-85.
20. Drugs.com. Methenamine (systemic). http://www.drugs.com/mmx/methenamine-hippurate.html?printable=1. Updated March 28, 2000. Accessed June 17, 2014.
21. Lee BSB, Simpson JM, Craig JC, Bhuta T. Methenamine hippurate for preventing urinary tract infections. Cochrane Database Syst Rev. 2012;10:CD003265.
22. Lee BB, Haran MJ, Hunt LM, et al. Spinal-injured neuropathic bladder antisepsis (SINBA) trial. Spinal Cord. 2007;45(8):542-550.
1. Foxman B. Epidemiology of urinary tract infections: Incidence, morbidity, and economic costs. Am J Med. 2002;113(suppl 1A):5S-13S.
2. Kamel HK. Managing urinary tract infections: Guide for nursing home practitioners. Ann of Long Term Care. 2005;13(9):21-28.
3. Blix HS, Røed J, Sti MO. Large variation in antibacterial use among Norwegian nursing homes. Scand J Infect Dis. 2007;39(6-7):536-541.
4. Nicolle LE. Asymptomatic bacteruria in diabetic women. Diabetes Care. 2000;23(6):722-723.
5. Rhoads J, Clayman A, Nelson S. The relationship of urinary tract infections and falls in a nursing home. Director. 2007;15(1):22-26.
6. Rodhe N, Mølstad S, Englund L, Svärdsudd K. Asymptomatic bacteriuria in a population of elderly residents living in a community setting: Prevalence, characteristics and associated factors. Fam Pract. 2006;23(3):303-307.
7. Woodford HJ, George J. Diagnosis and management of urinary tract infection in hospitalized older people. J Am Geriatr Soc. 2009;57(1):107-114.
8. Levison ME, Kaye D. Treatment of complicated urinary tract infections with an emphasis on drug-resistant gram-negative uropathogens. Curr Infect Dis Rep. 2013;15(2):109-115.
9. Miller LG, Tang AW. Treatment of uncomplicated urinary tract infections in an era of increasing antimicrobial resistance. Mayo Clin Proc. 2004;79(8):1048-1053.
10. Nicoletti J, Kuster SP, Sulser T, et al. Risk factors for urinary tract infections due to ciprofloxacin-resistant Escherichia coli in a tertiary care urology department in Switzerland. Swiss Med Wkly. 2010;140:w13059.
11. Nicolle LE. Urinary tract infection in geriatric and institutionalized patients. Curr Opin Urol. 2002;12(1):51-55.
12. Foxman B. The epidemiology of urinary tract infection. Nat Rev Urol. 2010;7(12):653-660.
13. Spellberg B, Guidos R, Gilbert D, et al; Infectious Diseases Society of America. The epidemic of antibiotic-resistant infections: A call to action for the medical community from the Infectious Diseases Society of America. Clin Infect Dis. 2008;46(2):155-164.
14. Dagley S, Dawes EA, Morrison GA. Inhibition of growth of Aerobacter aerogenes: The mode of action of phenols, alcohols, acetone, and ethyl acetate.
J Bacteriol. 1950;60(4):369-379.
15. Neely WB. Action of formaldehyde on microorganisms I. Correlation of activity with formaldehyde metabolism. J Bacteriol. 1963;85(5):1028-1031.
16. Musher DM, Griffith DP. Generation of formaldehyde from methenamine: Effect of pH and concentration, and antibacterial effect. Antimicrob Agents Chemother. 1974;6(6):708-711.
17. Scientific Committee on Health and Environmental Risks. Risk Assessment Report on Methenamine. Brussels, Belgium: European Commission; 2007. CAS 100-97-0.
18. Freeman RB, Smith WM, Richardson JA, et al. Long-term therapy for chronic bacteriuria in men. U.S. Public Health Service cooperative study. Ann Intern Med. 1975;83(2):133-147.
19. Nilsson S. Long-term treatment with methenamine hippurate in recurrent urinary tract infection. Acta Med Scand. 1975;198(1-2):81-85.
20. Drugs.com. Methenamine (systemic). http://www.drugs.com/mmx/methenamine-hippurate.html?printable=1. Updated March 28, 2000. Accessed June 17, 2014.
21. Lee BSB, Simpson JM, Craig JC, Bhuta T. Methenamine hippurate for preventing urinary tract infections. Cochrane Database Syst Rev. 2012;10:CD003265.
22. Lee BB, Haran MJ, Hunt LM, et al. Spinal-injured neuropathic bladder antisepsis (SINBA) trial. Spinal Cord. 2007;45(8):542-550.
A novel method of blood cell production

stem cells to form endothelium
(green), then blood cells (red)
Credit: Irina Elcheva
and Akhilesh Kumar
Researchers have reported a new method for creating human blood cells in the lab, and they believe the approach is safer and more reliable than its predecessors.
The team determined how blood cells are made at the earliest stages of development; namely, 2 genetic programs are responsible for turning pluripotent stem cells into blood cells.
This discovery gave the researchers the tools to make an array of blood cells themselves, using transcription factors.
“This is the first demonstration of the production of different kinds of cells from human pluripotent stem cells using transcription factors,” said Igor Slukvin, MD, PhD, of the University of Wisconsin-Madison.
He and his colleagues described this method in Nature Communications.
During development, blood cells emerge in the aorta. There, blood cells, including hematopoietic stem cells, are generated by budding from hemogenic endothelial cells.
Dr Slukvin and his colleagues found that 2 distinct groups of transcription factors—pan-myeloid (ETV2 and GATA2) and erythro-megakaryocytic (GATA2 and TAL1)—directly convert human pluripotent stem cells into hemogenic endothelial cells.
These cells then develop into blood cells with pan-myeloid or erythro-megakaryocytic potential.
“By overexpressing just 2 transcription factors, we can, in the laboratory dish, reproduce the sequence of events we see in the embryo,” Dr Slukvin said.
Furthermore, the method could produce blood cells in abundance. For every million stem cells, the researchers were able to produce 30 million blood cells.
The team noted that a critical aspect of this work is the use of modified messenger RNA to direct stem cells toward particular developmental fates.
This approach makes it possible to induce cells without introducing any genetic artifacts. So this method of blood cell production is safer than other methods, according to the researchers.
“You can do it without a virus, and genome integrity is not affected,” Dr Slukvin noted.
He added that his group is still working on a method for producing hematopoietic stem cells in the lab.
“We still don’t know how to do that,” he said. “But our new approach to making blood cells will give us an opportunity to model their development in a dish and identify novel hematopoietic stem cell factors.” ![]()

stem cells to form endothelium
(green), then blood cells (red)
Credit: Irina Elcheva
and Akhilesh Kumar
Researchers have reported a new method for creating human blood cells in the lab, and they believe the approach is safer and more reliable than its predecessors.
The team determined how blood cells are made at the earliest stages of development; namely, 2 genetic programs are responsible for turning pluripotent stem cells into blood cells.
This discovery gave the researchers the tools to make an array of blood cells themselves, using transcription factors.
“This is the first demonstration of the production of different kinds of cells from human pluripotent stem cells using transcription factors,” said Igor Slukvin, MD, PhD, of the University of Wisconsin-Madison.
He and his colleagues described this method in Nature Communications.
During development, blood cells emerge in the aorta. There, blood cells, including hematopoietic stem cells, are generated by budding from hemogenic endothelial cells.
Dr Slukvin and his colleagues found that 2 distinct groups of transcription factors—pan-myeloid (ETV2 and GATA2) and erythro-megakaryocytic (GATA2 and TAL1)—directly convert human pluripotent stem cells into hemogenic endothelial cells.
These cells then develop into blood cells with pan-myeloid or erythro-megakaryocytic potential.
“By overexpressing just 2 transcription factors, we can, in the laboratory dish, reproduce the sequence of events we see in the embryo,” Dr Slukvin said.
Furthermore, the method could produce blood cells in abundance. For every million stem cells, the researchers were able to produce 30 million blood cells.
The team noted that a critical aspect of this work is the use of modified messenger RNA to direct stem cells toward particular developmental fates.
This approach makes it possible to induce cells without introducing any genetic artifacts. So this method of blood cell production is safer than other methods, according to the researchers.
“You can do it without a virus, and genome integrity is not affected,” Dr Slukvin noted.
He added that his group is still working on a method for producing hematopoietic stem cells in the lab.
“We still don’t know how to do that,” he said. “But our new approach to making blood cells will give us an opportunity to model their development in a dish and identify novel hematopoietic stem cell factors.” ![]()

stem cells to form endothelium
(green), then blood cells (red)
Credit: Irina Elcheva
and Akhilesh Kumar
Researchers have reported a new method for creating human blood cells in the lab, and they believe the approach is safer and more reliable than its predecessors.
The team determined how blood cells are made at the earliest stages of development; namely, 2 genetic programs are responsible for turning pluripotent stem cells into blood cells.
This discovery gave the researchers the tools to make an array of blood cells themselves, using transcription factors.
“This is the first demonstration of the production of different kinds of cells from human pluripotent stem cells using transcription factors,” said Igor Slukvin, MD, PhD, of the University of Wisconsin-Madison.
He and his colleagues described this method in Nature Communications.
During development, blood cells emerge in the aorta. There, blood cells, including hematopoietic stem cells, are generated by budding from hemogenic endothelial cells.
Dr Slukvin and his colleagues found that 2 distinct groups of transcription factors—pan-myeloid (ETV2 and GATA2) and erythro-megakaryocytic (GATA2 and TAL1)—directly convert human pluripotent stem cells into hemogenic endothelial cells.
These cells then develop into blood cells with pan-myeloid or erythro-megakaryocytic potential.
“By overexpressing just 2 transcription factors, we can, in the laboratory dish, reproduce the sequence of events we see in the embryo,” Dr Slukvin said.
Furthermore, the method could produce blood cells in abundance. For every million stem cells, the researchers were able to produce 30 million blood cells.
The team noted that a critical aspect of this work is the use of modified messenger RNA to direct stem cells toward particular developmental fates.
This approach makes it possible to induce cells without introducing any genetic artifacts. So this method of blood cell production is safer than other methods, according to the researchers.
“You can do it without a virus, and genome integrity is not affected,” Dr Slukvin noted.
He added that his group is still working on a method for producing hematopoietic stem cells in the lab.
“We still don’t know how to do that,” he said. “But our new approach to making blood cells will give us an opportunity to model their development in a dish and identify novel hematopoietic stem cell factors.” ![]()
What Can We Do to Prevent Alzheimer Disease?
Alzheimer disease (AD) and other forms of dementia are pressing public health issues. They diminish quality of life for older adults and their families and impose significant financial costs on individuals and society. Dementia prevention and the development of treatments for dementia are important goals, and as a consequence, the VA Geriatric Research Education and Clinical Centers (GRECCs) have been conducting innovative research for the treatment and prevention of AD and related dementias.
Research conducted at the VISN 20 GRECC at the VA Puget Sound Health Care System (PSHCS) has helped increase clinicians’ understanding of the role of insulin in the development of AD and has evaluated the potential of treatment approaches based on the insulin-related research. More recently, this research has provided the basis for a pilot study aimed at dementia prevention for high-risk patients and for educational outreach about prevention within the VA.
Dementia Studies
The hormone insulin is required for efficient use of glucose throughout the body, including the brain. Insulin may also play a role in regulating cerebral amyloid, which is directly involved in the development of AD neuropathology and in maintaining healthy vascular function and lipid metabolism, both of which are required for brain health.1 Research over the past decade has shown that patients with AD have reduced levels of brain insulin, and individuals with insulin resistance have an increased risk of developing AD. Insulin resistance also has been shown to be related to reduced cerebral glucose metabolism, even in individuals who did not have a memory disorder.2
One recent study, led by Suzanne Craft, PhD, and colleagues at PSHCS, tested the potential of intranasal insulin to treat cognitive impairment.3 Participants with either AD or milder memory deficits used a specially designed device to deliver insulin or a placebo to the nose twice a day. Insulin provided in this way reaches the brain quickly without entering the lungs or affecting glucose metabolism elsewhere in the body. Participants who received the insulin experienced improvements in delayed memory and functional abilities compared with those who received the placebo.
Studies at the same laboratory investigated the role of diet and exercise in insulin metabolism and cognitive function. In a diet-related study, older adults with normal memory and those with mild memory impairment received either a high saturated fat, high glycemic index (GI) diet or a low saturated fat, low GI diet for 4 weeks.4 Plasma insulin levels decreased and delayed visual memory improved for participants who received the low-fat, low-GI diet. AD-related markers in cerebrospinal fluid, however, improved only among participants with mild memory impairment, not among healthy individuals.
In an exercise-related study, older adults with glucose intolerance participated in a 6-month aerobic exercise program.5 Although memory did not improve, cardiorespiratory fitness, executive function, and insulin sensitivity improved for participants in the aerobic exercise program compared with those in a stretching program. The relationship of diet and exercise and cognitive function is complex and likely involves insulin regulation, vascular function, and lipid metabolism, among other factors. More research is needed to fully understand the relationships among diet, exercise, and dementia, but these results suggest that lifestyle modifications may play a role in prevention of dementia.
When patients have problems with memory, attention, or executive function, they may have difficulty managing their medications, making good nutritional choices, and monitoring blood pressure and blood glucose.6 Given the importance of controlling vascular risk factors, helping patients manage their medical conditions may help them prevent or delay the onset of AD.
Pilot Study
A VA-funded pilot study with the goal of dementia prevention among high-risk patients was recently conducted at the PSHCS. This study focused on veterans at significantly elevated risk of dementia: those with both diabetes and hypertension, with poor control of either or both conditions, and who had some degree of memory or attentional impairment. Participants were randomly assigned to continue their usual care or to add a 6-month care management intervention to their usual care.
A registered nurse who helped the veterans overcome the barriers to controlling their medical conditions led the intervention. Barriers ranged from relatively simple problems, such as appropriate use of insulin, to more complex issues, such as learning about healthy nutrition and exercise for people with diabetes. The intervention was adapted to meet each participant’s cognitive level, and family involvement was encouraged, with the veteran’s permission. Preliminary results of this study were presented at the annual meeting of the Gerontological Society of America in 2011 and the Alzheimer’s Association International conference in July 2013.7,8
The VISN 20 GRECC also developed a “Dementia Roadshow” in which GRECC clinicians present educational, research-based lectures on dementia-related topics at VAMCs in VISN 20. One lecture in this series incorporates this recent research about prevention of dementia through control of diabetes and hypertension, as well as depression, posttraumatic stress disorder, and other risk factors; the lecture is presented to frontline clinicians who can then use this information to guide their work with high-risk patients.
The GRECCs are at the forefront of understanding the causes of dementia and how to prevent it. This work will help the VA to develop more effective ways of reducing the public health burden of this disease.
Acknowledgments
The author wishes to thank Debby Tsuang, MD, Stephen Thielke, MD, and Julie Moorer, RN, for helpful feedback on the initial draft of this manuscript. The pilot project described was funded by VA VISN 20.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the Department of Veterans Affairs, the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Craft S, Cholerton B, Baker LD. Insulin and Alzheimer’s disease: Untangling the web. J Alzheimers Dis. 2013;33(suppl 1):S263-S275.
2. Baker LD, Cross DJ, Minoshima S, Belongia D, Watson GS, Craft S. Insulin resistance and Alzheimer-like reductions in regional cerebral glucose metabolism for cognitively normal adults with prediabetes or early type 2 diabetes. Arch Neurol. 2011;68(1):51-57.
3. Craft S, Baker LD, Montine TJ, et al. Intranasal insulin therapy for Alzheimer disease and amnestic mild cognitive impairment: A pilot clinical trial. Arch Neurol. 2012;69(1):29-38.
4. Bayer-Carter JL, Green PS, Montine TJ, et al. Diet intervention and cerebrospinal fluid biomarkers in amnestic mild cognitive impairment. Arch Neurol. 2011;68(6):743-752.
5. Baker LD, Frank LL, Foster-Schubert K, et al. Aerobic exercise improves cognition for older adults with glucose intolerance, a risk factor for Alzheimer’s disease. J Alzheimers Dis. 2010;22(2):569-579.
6. Bonner LM, Craft S. Uncontrolled diabetes plus hypertension: A recipe for dementia? Fed Pract. 2009;26(2):33-35.
7. Bonner LM, Craft S, Robinson G. Screening and care management for dementia prevention and management in VA primary care patients with vascular risk. Poster presented at: Gerontological Society of America Annual Meeting; November 18, 2011; Boston, MA.
8. Bonner LM, Robinson G, Craft S. Care management for VA patients with vascular risk factors and cognitive impairment: A randomized trial. Alzheimer’s Association International Conference. July 2013, Boston, MA.
Alzheimer disease (AD) and other forms of dementia are pressing public health issues. They diminish quality of life for older adults and their families and impose significant financial costs on individuals and society. Dementia prevention and the development of treatments for dementia are important goals, and as a consequence, the VA Geriatric Research Education and Clinical Centers (GRECCs) have been conducting innovative research for the treatment and prevention of AD and related dementias.
Research conducted at the VISN 20 GRECC at the VA Puget Sound Health Care System (PSHCS) has helped increase clinicians’ understanding of the role of insulin in the development of AD and has evaluated the potential of treatment approaches based on the insulin-related research. More recently, this research has provided the basis for a pilot study aimed at dementia prevention for high-risk patients and for educational outreach about prevention within the VA.
Dementia Studies
The hormone insulin is required for efficient use of glucose throughout the body, including the brain. Insulin may also play a role in regulating cerebral amyloid, which is directly involved in the development of AD neuropathology and in maintaining healthy vascular function and lipid metabolism, both of which are required for brain health.1 Research over the past decade has shown that patients with AD have reduced levels of brain insulin, and individuals with insulin resistance have an increased risk of developing AD. Insulin resistance also has been shown to be related to reduced cerebral glucose metabolism, even in individuals who did not have a memory disorder.2
One recent study, led by Suzanne Craft, PhD, and colleagues at PSHCS, tested the potential of intranasal insulin to treat cognitive impairment.3 Participants with either AD or milder memory deficits used a specially designed device to deliver insulin or a placebo to the nose twice a day. Insulin provided in this way reaches the brain quickly without entering the lungs or affecting glucose metabolism elsewhere in the body. Participants who received the insulin experienced improvements in delayed memory and functional abilities compared with those who received the placebo.
Studies at the same laboratory investigated the role of diet and exercise in insulin metabolism and cognitive function. In a diet-related study, older adults with normal memory and those with mild memory impairment received either a high saturated fat, high glycemic index (GI) diet or a low saturated fat, low GI diet for 4 weeks.4 Plasma insulin levels decreased and delayed visual memory improved for participants who received the low-fat, low-GI diet. AD-related markers in cerebrospinal fluid, however, improved only among participants with mild memory impairment, not among healthy individuals.
In an exercise-related study, older adults with glucose intolerance participated in a 6-month aerobic exercise program.5 Although memory did not improve, cardiorespiratory fitness, executive function, and insulin sensitivity improved for participants in the aerobic exercise program compared with those in a stretching program. The relationship of diet and exercise and cognitive function is complex and likely involves insulin regulation, vascular function, and lipid metabolism, among other factors. More research is needed to fully understand the relationships among diet, exercise, and dementia, but these results suggest that lifestyle modifications may play a role in prevention of dementia.
When patients have problems with memory, attention, or executive function, they may have difficulty managing their medications, making good nutritional choices, and monitoring blood pressure and blood glucose.6 Given the importance of controlling vascular risk factors, helping patients manage their medical conditions may help them prevent or delay the onset of AD.
Pilot Study
A VA-funded pilot study with the goal of dementia prevention among high-risk patients was recently conducted at the PSHCS. This study focused on veterans at significantly elevated risk of dementia: those with both diabetes and hypertension, with poor control of either or both conditions, and who had some degree of memory or attentional impairment. Participants were randomly assigned to continue their usual care or to add a 6-month care management intervention to their usual care.
A registered nurse who helped the veterans overcome the barriers to controlling their medical conditions led the intervention. Barriers ranged from relatively simple problems, such as appropriate use of insulin, to more complex issues, such as learning about healthy nutrition and exercise for people with diabetes. The intervention was adapted to meet each participant’s cognitive level, and family involvement was encouraged, with the veteran’s permission. Preliminary results of this study were presented at the annual meeting of the Gerontological Society of America in 2011 and the Alzheimer’s Association International conference in July 2013.7,8
The VISN 20 GRECC also developed a “Dementia Roadshow” in which GRECC clinicians present educational, research-based lectures on dementia-related topics at VAMCs in VISN 20. One lecture in this series incorporates this recent research about prevention of dementia through control of diabetes and hypertension, as well as depression, posttraumatic stress disorder, and other risk factors; the lecture is presented to frontline clinicians who can then use this information to guide their work with high-risk patients.
The GRECCs are at the forefront of understanding the causes of dementia and how to prevent it. This work will help the VA to develop more effective ways of reducing the public health burden of this disease.
Acknowledgments
The author wishes to thank Debby Tsuang, MD, Stephen Thielke, MD, and Julie Moorer, RN, for helpful feedback on the initial draft of this manuscript. The pilot project described was funded by VA VISN 20.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the Department of Veterans Affairs, the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Alzheimer disease (AD) and other forms of dementia are pressing public health issues. They diminish quality of life for older adults and their families and impose significant financial costs on individuals and society. Dementia prevention and the development of treatments for dementia are important goals, and as a consequence, the VA Geriatric Research Education and Clinical Centers (GRECCs) have been conducting innovative research for the treatment and prevention of AD and related dementias.
Research conducted at the VISN 20 GRECC at the VA Puget Sound Health Care System (PSHCS) has helped increase clinicians’ understanding of the role of insulin in the development of AD and has evaluated the potential of treatment approaches based on the insulin-related research. More recently, this research has provided the basis for a pilot study aimed at dementia prevention for high-risk patients and for educational outreach about prevention within the VA.
Dementia Studies
The hormone insulin is required for efficient use of glucose throughout the body, including the brain. Insulin may also play a role in regulating cerebral amyloid, which is directly involved in the development of AD neuropathology and in maintaining healthy vascular function and lipid metabolism, both of which are required for brain health.1 Research over the past decade has shown that patients with AD have reduced levels of brain insulin, and individuals with insulin resistance have an increased risk of developing AD. Insulin resistance also has been shown to be related to reduced cerebral glucose metabolism, even in individuals who did not have a memory disorder.2
One recent study, led by Suzanne Craft, PhD, and colleagues at PSHCS, tested the potential of intranasal insulin to treat cognitive impairment.3 Participants with either AD or milder memory deficits used a specially designed device to deliver insulin or a placebo to the nose twice a day. Insulin provided in this way reaches the brain quickly without entering the lungs or affecting glucose metabolism elsewhere in the body. Participants who received the insulin experienced improvements in delayed memory and functional abilities compared with those who received the placebo.
Studies at the same laboratory investigated the role of diet and exercise in insulin metabolism and cognitive function. In a diet-related study, older adults with normal memory and those with mild memory impairment received either a high saturated fat, high glycemic index (GI) diet or a low saturated fat, low GI diet for 4 weeks.4 Plasma insulin levels decreased and delayed visual memory improved for participants who received the low-fat, low-GI diet. AD-related markers in cerebrospinal fluid, however, improved only among participants with mild memory impairment, not among healthy individuals.
In an exercise-related study, older adults with glucose intolerance participated in a 6-month aerobic exercise program.5 Although memory did not improve, cardiorespiratory fitness, executive function, and insulin sensitivity improved for participants in the aerobic exercise program compared with those in a stretching program. The relationship of diet and exercise and cognitive function is complex and likely involves insulin regulation, vascular function, and lipid metabolism, among other factors. More research is needed to fully understand the relationships among diet, exercise, and dementia, but these results suggest that lifestyle modifications may play a role in prevention of dementia.
When patients have problems with memory, attention, or executive function, they may have difficulty managing their medications, making good nutritional choices, and monitoring blood pressure and blood glucose.6 Given the importance of controlling vascular risk factors, helping patients manage their medical conditions may help them prevent or delay the onset of AD.
Pilot Study
A VA-funded pilot study with the goal of dementia prevention among high-risk patients was recently conducted at the PSHCS. This study focused on veterans at significantly elevated risk of dementia: those with both diabetes and hypertension, with poor control of either or both conditions, and who had some degree of memory or attentional impairment. Participants were randomly assigned to continue their usual care or to add a 6-month care management intervention to their usual care.
A registered nurse who helped the veterans overcome the barriers to controlling their medical conditions led the intervention. Barriers ranged from relatively simple problems, such as appropriate use of insulin, to more complex issues, such as learning about healthy nutrition and exercise for people with diabetes. The intervention was adapted to meet each participant’s cognitive level, and family involvement was encouraged, with the veteran’s permission. Preliminary results of this study were presented at the annual meeting of the Gerontological Society of America in 2011 and the Alzheimer’s Association International conference in July 2013.7,8
The VISN 20 GRECC also developed a “Dementia Roadshow” in which GRECC clinicians present educational, research-based lectures on dementia-related topics at VAMCs in VISN 20. One lecture in this series incorporates this recent research about prevention of dementia through control of diabetes and hypertension, as well as depression, posttraumatic stress disorder, and other risk factors; the lecture is presented to frontline clinicians who can then use this information to guide their work with high-risk patients.
The GRECCs are at the forefront of understanding the causes of dementia and how to prevent it. This work will help the VA to develop more effective ways of reducing the public health burden of this disease.
Acknowledgments
The author wishes to thank Debby Tsuang, MD, Stephen Thielke, MD, and Julie Moorer, RN, for helpful feedback on the initial draft of this manuscript. The pilot project described was funded by VA VISN 20.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the Department of Veterans Affairs, the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Craft S, Cholerton B, Baker LD. Insulin and Alzheimer’s disease: Untangling the web. J Alzheimers Dis. 2013;33(suppl 1):S263-S275.
2. Baker LD, Cross DJ, Minoshima S, Belongia D, Watson GS, Craft S. Insulin resistance and Alzheimer-like reductions in regional cerebral glucose metabolism for cognitively normal adults with prediabetes or early type 2 diabetes. Arch Neurol. 2011;68(1):51-57.
3. Craft S, Baker LD, Montine TJ, et al. Intranasal insulin therapy for Alzheimer disease and amnestic mild cognitive impairment: A pilot clinical trial. Arch Neurol. 2012;69(1):29-38.
4. Bayer-Carter JL, Green PS, Montine TJ, et al. Diet intervention and cerebrospinal fluid biomarkers in amnestic mild cognitive impairment. Arch Neurol. 2011;68(6):743-752.
5. Baker LD, Frank LL, Foster-Schubert K, et al. Aerobic exercise improves cognition for older adults with glucose intolerance, a risk factor for Alzheimer’s disease. J Alzheimers Dis. 2010;22(2):569-579.
6. Bonner LM, Craft S. Uncontrolled diabetes plus hypertension: A recipe for dementia? Fed Pract. 2009;26(2):33-35.
7. Bonner LM, Craft S, Robinson G. Screening and care management for dementia prevention and management in VA primary care patients with vascular risk. Poster presented at: Gerontological Society of America Annual Meeting; November 18, 2011; Boston, MA.
8. Bonner LM, Robinson G, Craft S. Care management for VA patients with vascular risk factors and cognitive impairment: A randomized trial. Alzheimer’s Association International Conference. July 2013, Boston, MA.
1. Craft S, Cholerton B, Baker LD. Insulin and Alzheimer’s disease: Untangling the web. J Alzheimers Dis. 2013;33(suppl 1):S263-S275.
2. Baker LD, Cross DJ, Minoshima S, Belongia D, Watson GS, Craft S. Insulin resistance and Alzheimer-like reductions in regional cerebral glucose metabolism for cognitively normal adults with prediabetes or early type 2 diabetes. Arch Neurol. 2011;68(1):51-57.
3. Craft S, Baker LD, Montine TJ, et al. Intranasal insulin therapy for Alzheimer disease and amnestic mild cognitive impairment: A pilot clinical trial. Arch Neurol. 2012;69(1):29-38.
4. Bayer-Carter JL, Green PS, Montine TJ, et al. Diet intervention and cerebrospinal fluid biomarkers in amnestic mild cognitive impairment. Arch Neurol. 2011;68(6):743-752.
5. Baker LD, Frank LL, Foster-Schubert K, et al. Aerobic exercise improves cognition for older adults with glucose intolerance, a risk factor for Alzheimer’s disease. J Alzheimers Dis. 2010;22(2):569-579.
6. Bonner LM, Craft S. Uncontrolled diabetes plus hypertension: A recipe for dementia? Fed Pract. 2009;26(2):33-35.
7. Bonner LM, Craft S, Robinson G. Screening and care management for dementia prevention and management in VA primary care patients with vascular risk. Poster presented at: Gerontological Society of America Annual Meeting; November 18, 2011; Boston, MA.
8. Bonner LM, Robinson G, Craft S. Care management for VA patients with vascular risk factors and cognitive impairment: A randomized trial. Alzheimer’s Association International Conference. July 2013, Boston, MA.
FDA warns of non-sterile drugs

Credit: Bill Branson
The US Food and Drug Administration (FDA) is alerting healthcare professionals not to use sterile drugs produced by Unique Pharmaceuticals Ltd., as they may be contaminated.
Healthcare professionals should immediately check their medical supplies and quarantine any sterile drug products from Unique Pharmaceuticals, a compounding outsourcing facility in Temple, Texas.
Administration of a non-sterile product may result in serious infection or death.
Unique Pharmaceuticals’ products were distributed nationwide. Most of the product labels include: “Unique Pharmaceuticals, Temple TX USA 76502.”
FDA investigators conducted 2 recent inspections of the Unique Pharmaceuticals facility and observed unsanitary conditions that resulted in a lack of sterility assurance.
The inspections revealed sterility failures in several lots of products intended to be sterile, recurring environmental contamination problems, and poor sterile production practices.
The FDA previously asked the company to recall all non-expired lots of sterile drug products, but the company refused to do so. The FDA has now issued a formal request for Unique Pharmaceuticals to recall all non-expired lots of its sterile products currently on the market.
The FDA has also asked the company to cease sterile compounding operations until sufficient corrections are made at its facility. Unique Pharmaceuticals has refused this request as well.
To date, the FDA is not aware of reports of illness associated with the use of Unique Pharmaceuticals’ products.
Patients who have received any drug product produced by Unique Pharmaceuticals and have concerns should contact their healthcare professional.
Professionals and consumers may report adverse events or quality problems associated with the use of Unique Pharmaceuticals’ products to the FDA’s MedWatch Adverse Event Reporting Program.
Unique Pharmaceuticals is registered under section 503B of the Federal Food, Drug, and Cosmetic Act (FDCA) as an outsourcing facility. The Drug Quality and Security Act, signed into law on November 27, 2013, added a new section 503B to the FDCA. Under section 503B, a compounder can elect to become an outsourcing facility.
Outsourcing facilities must comply with current good manufacturing practice requirements, will be subject to inspection by the FDA according to a risk-based schedule, and must meet certain other requirements, such as reporting adverse events and providing the FDA with certain information about the products they compound. ![]()

Credit: Bill Branson
The US Food and Drug Administration (FDA) is alerting healthcare professionals not to use sterile drugs produced by Unique Pharmaceuticals Ltd., as they may be contaminated.
Healthcare professionals should immediately check their medical supplies and quarantine any sterile drug products from Unique Pharmaceuticals, a compounding outsourcing facility in Temple, Texas.
Administration of a non-sterile product may result in serious infection or death.
Unique Pharmaceuticals’ products were distributed nationwide. Most of the product labels include: “Unique Pharmaceuticals, Temple TX USA 76502.”
FDA investigators conducted 2 recent inspections of the Unique Pharmaceuticals facility and observed unsanitary conditions that resulted in a lack of sterility assurance.
The inspections revealed sterility failures in several lots of products intended to be sterile, recurring environmental contamination problems, and poor sterile production practices.
The FDA previously asked the company to recall all non-expired lots of sterile drug products, but the company refused to do so. The FDA has now issued a formal request for Unique Pharmaceuticals to recall all non-expired lots of its sterile products currently on the market.
The FDA has also asked the company to cease sterile compounding operations until sufficient corrections are made at its facility. Unique Pharmaceuticals has refused this request as well.
To date, the FDA is not aware of reports of illness associated with the use of Unique Pharmaceuticals’ products.
Patients who have received any drug product produced by Unique Pharmaceuticals and have concerns should contact their healthcare professional.
Professionals and consumers may report adverse events or quality problems associated with the use of Unique Pharmaceuticals’ products to the FDA’s MedWatch Adverse Event Reporting Program.
Unique Pharmaceuticals is registered under section 503B of the Federal Food, Drug, and Cosmetic Act (FDCA) as an outsourcing facility. The Drug Quality and Security Act, signed into law on November 27, 2013, added a new section 503B to the FDCA. Under section 503B, a compounder can elect to become an outsourcing facility.
Outsourcing facilities must comply with current good manufacturing practice requirements, will be subject to inspection by the FDA according to a risk-based schedule, and must meet certain other requirements, such as reporting adverse events and providing the FDA with certain information about the products they compound. ![]()

Credit: Bill Branson
The US Food and Drug Administration (FDA) is alerting healthcare professionals not to use sterile drugs produced by Unique Pharmaceuticals Ltd., as they may be contaminated.
Healthcare professionals should immediately check their medical supplies and quarantine any sterile drug products from Unique Pharmaceuticals, a compounding outsourcing facility in Temple, Texas.
Administration of a non-sterile product may result in serious infection or death.
Unique Pharmaceuticals’ products were distributed nationwide. Most of the product labels include: “Unique Pharmaceuticals, Temple TX USA 76502.”
FDA investigators conducted 2 recent inspections of the Unique Pharmaceuticals facility and observed unsanitary conditions that resulted in a lack of sterility assurance.
The inspections revealed sterility failures in several lots of products intended to be sterile, recurring environmental contamination problems, and poor sterile production practices.
The FDA previously asked the company to recall all non-expired lots of sterile drug products, but the company refused to do so. The FDA has now issued a formal request for Unique Pharmaceuticals to recall all non-expired lots of its sterile products currently on the market.
The FDA has also asked the company to cease sterile compounding operations until sufficient corrections are made at its facility. Unique Pharmaceuticals has refused this request as well.
To date, the FDA is not aware of reports of illness associated with the use of Unique Pharmaceuticals’ products.
Patients who have received any drug product produced by Unique Pharmaceuticals and have concerns should contact their healthcare professional.
Professionals and consumers may report adverse events or quality problems associated with the use of Unique Pharmaceuticals’ products to the FDA’s MedWatch Adverse Event Reporting Program.
Unique Pharmaceuticals is registered under section 503B of the Federal Food, Drug, and Cosmetic Act (FDCA) as an outsourcing facility. The Drug Quality and Security Act, signed into law on November 27, 2013, added a new section 503B to the FDCA. Under section 503B, a compounder can elect to become an outsourcing facility.
Outsourcing facilities must comply with current good manufacturing practice requirements, will be subject to inspection by the FDA according to a risk-based schedule, and must meet certain other requirements, such as reporting adverse events and providing the FDA with certain information about the products they compound. ![]()
Antibody may treat cancer cachexia

Preclinical research raises the prospect of more effective treatments for cachexia, a profound wasting of fat and muscle that can increase the risk of death in cancer patients.
In mouse models, an antibody effectively improved or prevented symptoms of cachexia.
The antibody inhibited the effects of parathyroid hormone-related protein (PTHrP), which is released from many types of cancer cells.
The researchers said their findings, published in Nature, are the first to explain in detail how PTHrP from tumors switches on a thermogenic process in fatty tissues, resulting in unhealthy weight loss.
The team carried out 2 experiments using mice that developed lung tumors and cachexia. In the first, a polyclonal antibody that specifically neutralizes PTHrP prevented cachexia almost completely, while untreated animals became mildly cachexic.
Anti-PTHrP treatment prevented the shrinkage of fat droplets. It blocked thermogenic gene expression in epididymal white adipose tissue, interscapular brown adipose tissue, and inguinal white adipose tissue, which suggests thermogenesis has a causal role in fat wasting.
Treatment with the anti-PTHrP antibody also lowered oxygen consumption in the mice, increased their physical activity, and reduced their heat production.
In the second experiment, the researchers treated mice with the anti-PTHrP antibody until they observed severe cachexia in control animals. The antibody significantly preserved muscle mass, which was evident by improved grip strength and in situ muscle contraction.
“You would have expected, based on our first experiments in cell culture, that blocking PTHrP in the mice would reduce browning of the fat,” said study author Bruce Spiegelman, PhD, of the Dana-Farber Cancer Institute in Boston.
“But we were surprised that it also affected the loss of muscle mass and improved health.”
Additional experiments, in which the researchers injected PTHrP into healthy and tumor-bearing mice, suggested that PTHrP alone doesn’t directly cause muscle wasting. But blocking the protein’s activity still prevents cachexia.
Thus, the role of PTHrP “is definitely not the whole answer” to the riddle of cachexia, Dr Spiegelman noted. Furthermore, it may turn out that the PTHrP mechanism is responsible for cachexia in only a subset of cancer patients.
The researchers analyzed blood samples from 47 cachexic patients with lung or colon cancer. And they found increased levels of PTHrP in 17 of the patients. Those patients had significantly lower lean body mass and were producing more heat energy at rest than the other patients in the group.
Dr Spiegelman noted that, before they test the anti-PTHrP antibody in clinical trials, clinicians would likely want to determine if the protein is elevated in certain cancers and determine which patients would be good candidates for the treatment. ![]()

Preclinical research raises the prospect of more effective treatments for cachexia, a profound wasting of fat and muscle that can increase the risk of death in cancer patients.
In mouse models, an antibody effectively improved or prevented symptoms of cachexia.
The antibody inhibited the effects of parathyroid hormone-related protein (PTHrP), which is released from many types of cancer cells.
The researchers said their findings, published in Nature, are the first to explain in detail how PTHrP from tumors switches on a thermogenic process in fatty tissues, resulting in unhealthy weight loss.
The team carried out 2 experiments using mice that developed lung tumors and cachexia. In the first, a polyclonal antibody that specifically neutralizes PTHrP prevented cachexia almost completely, while untreated animals became mildly cachexic.
Anti-PTHrP treatment prevented the shrinkage of fat droplets. It blocked thermogenic gene expression in epididymal white adipose tissue, interscapular brown adipose tissue, and inguinal white adipose tissue, which suggests thermogenesis has a causal role in fat wasting.
Treatment with the anti-PTHrP antibody also lowered oxygen consumption in the mice, increased their physical activity, and reduced their heat production.
In the second experiment, the researchers treated mice with the anti-PTHrP antibody until they observed severe cachexia in control animals. The antibody significantly preserved muscle mass, which was evident by improved grip strength and in situ muscle contraction.
“You would have expected, based on our first experiments in cell culture, that blocking PTHrP in the mice would reduce browning of the fat,” said study author Bruce Spiegelman, PhD, of the Dana-Farber Cancer Institute in Boston.
“But we were surprised that it also affected the loss of muscle mass and improved health.”
Additional experiments, in which the researchers injected PTHrP into healthy and tumor-bearing mice, suggested that PTHrP alone doesn’t directly cause muscle wasting. But blocking the protein’s activity still prevents cachexia.
Thus, the role of PTHrP “is definitely not the whole answer” to the riddle of cachexia, Dr Spiegelman noted. Furthermore, it may turn out that the PTHrP mechanism is responsible for cachexia in only a subset of cancer patients.
The researchers analyzed blood samples from 47 cachexic patients with lung or colon cancer. And they found increased levels of PTHrP in 17 of the patients. Those patients had significantly lower lean body mass and were producing more heat energy at rest than the other patients in the group.
Dr Spiegelman noted that, before they test the anti-PTHrP antibody in clinical trials, clinicians would likely want to determine if the protein is elevated in certain cancers and determine which patients would be good candidates for the treatment. ![]()

Preclinical research raises the prospect of more effective treatments for cachexia, a profound wasting of fat and muscle that can increase the risk of death in cancer patients.
In mouse models, an antibody effectively improved or prevented symptoms of cachexia.
The antibody inhibited the effects of parathyroid hormone-related protein (PTHrP), which is released from many types of cancer cells.
The researchers said their findings, published in Nature, are the first to explain in detail how PTHrP from tumors switches on a thermogenic process in fatty tissues, resulting in unhealthy weight loss.
The team carried out 2 experiments using mice that developed lung tumors and cachexia. In the first, a polyclonal antibody that specifically neutralizes PTHrP prevented cachexia almost completely, while untreated animals became mildly cachexic.
Anti-PTHrP treatment prevented the shrinkage of fat droplets. It blocked thermogenic gene expression in epididymal white adipose tissue, interscapular brown adipose tissue, and inguinal white adipose tissue, which suggests thermogenesis has a causal role in fat wasting.
Treatment with the anti-PTHrP antibody also lowered oxygen consumption in the mice, increased their physical activity, and reduced their heat production.
In the second experiment, the researchers treated mice with the anti-PTHrP antibody until they observed severe cachexia in control animals. The antibody significantly preserved muscle mass, which was evident by improved grip strength and in situ muscle contraction.
“You would have expected, based on our first experiments in cell culture, that blocking PTHrP in the mice would reduce browning of the fat,” said study author Bruce Spiegelman, PhD, of the Dana-Farber Cancer Institute in Boston.
“But we were surprised that it also affected the loss of muscle mass and improved health.”
Additional experiments, in which the researchers injected PTHrP into healthy and tumor-bearing mice, suggested that PTHrP alone doesn’t directly cause muscle wasting. But blocking the protein’s activity still prevents cachexia.
Thus, the role of PTHrP “is definitely not the whole answer” to the riddle of cachexia, Dr Spiegelman noted. Furthermore, it may turn out that the PTHrP mechanism is responsible for cachexia in only a subset of cancer patients.
The researchers analyzed blood samples from 47 cachexic patients with lung or colon cancer. And they found increased levels of PTHrP in 17 of the patients. Those patients had significantly lower lean body mass and were producing more heat energy at rest than the other patients in the group.
Dr Spiegelman noted that, before they test the anti-PTHrP antibody in clinical trials, clinicians would likely want to determine if the protein is elevated in certain cancers and determine which patients would be good candidates for the treatment. ![]()
HSC engraftment across the species barrier

Scientists say they’ve generated a mouse model that supports the transplantation of human hematopoietic stem cells (HSCs), despite the species barrier and without the need for irradiation.
The group used a mutation of the Kit receptor in the mouse stem cells to facilitate the engraftment of human cells.
In this model, human HSCs can expand and differentiate into all blood cell types without any additional treatment.
Even cells of the innate immune system that are not typically found in “humanized” mice were efficiently generated in this mouse.
Furthermore, the stem cells can be maintained in the mouse over a longer period of time.
The researchers reported these results in Cell Stem Cell.
“Our goal was to develop an optimal model for the transplantation and study of human blood stem cells,” said study author Claudia Waskow, PhD, of Technische Universität Dresden in Germany.
To achieve optimal stem cell engraftment, she and her colleagues introduced a naturally occurring mutation of the Kit receptor into mice lacking a functional immune system.
In this way, the team circumvented the 2 major obstacles of HSC transplantation: the rejection by the recipient’s immune system and the absence of free niche space for the incoming donor stem cells in the recipient’s bone marrow.
The Kit mutation in the new mouse model impairs the recipient’s stem cell compartment in such a way that the endogenous HSCs can be easily replaced by human donor stem cells with a functional Kit receptor.
The researchers said this replacement works so efficiently that irradiation can be completely omitted, allowing the study of human blood development in a physiological setting. The model can now be used to study diseases of the human blood and immune system or to test new treatment options.
The results of this research also show that the Kit receptor is important for the function of human HSCs, notably in a transplant setting. The researchers said future studies will focus on using this knowledge to improve conditioning therapy for patients undergoing HSC transplant. ![]()

Scientists say they’ve generated a mouse model that supports the transplantation of human hematopoietic stem cells (HSCs), despite the species barrier and without the need for irradiation.
The group used a mutation of the Kit receptor in the mouse stem cells to facilitate the engraftment of human cells.
In this model, human HSCs can expand and differentiate into all blood cell types without any additional treatment.
Even cells of the innate immune system that are not typically found in “humanized” mice were efficiently generated in this mouse.
Furthermore, the stem cells can be maintained in the mouse over a longer period of time.
The researchers reported these results in Cell Stem Cell.
“Our goal was to develop an optimal model for the transplantation and study of human blood stem cells,” said study author Claudia Waskow, PhD, of Technische Universität Dresden in Germany.
To achieve optimal stem cell engraftment, she and her colleagues introduced a naturally occurring mutation of the Kit receptor into mice lacking a functional immune system.
In this way, the team circumvented the 2 major obstacles of HSC transplantation: the rejection by the recipient’s immune system and the absence of free niche space for the incoming donor stem cells in the recipient’s bone marrow.
The Kit mutation in the new mouse model impairs the recipient’s stem cell compartment in such a way that the endogenous HSCs can be easily replaced by human donor stem cells with a functional Kit receptor.
The researchers said this replacement works so efficiently that irradiation can be completely omitted, allowing the study of human blood development in a physiological setting. The model can now be used to study diseases of the human blood and immune system or to test new treatment options.
The results of this research also show that the Kit receptor is important for the function of human HSCs, notably in a transplant setting. The researchers said future studies will focus on using this knowledge to improve conditioning therapy for patients undergoing HSC transplant. ![]()

Scientists say they’ve generated a mouse model that supports the transplantation of human hematopoietic stem cells (HSCs), despite the species barrier and without the need for irradiation.
The group used a mutation of the Kit receptor in the mouse stem cells to facilitate the engraftment of human cells.
In this model, human HSCs can expand and differentiate into all blood cell types without any additional treatment.
Even cells of the innate immune system that are not typically found in “humanized” mice were efficiently generated in this mouse.
Furthermore, the stem cells can be maintained in the mouse over a longer period of time.
The researchers reported these results in Cell Stem Cell.
“Our goal was to develop an optimal model for the transplantation and study of human blood stem cells,” said study author Claudia Waskow, PhD, of Technische Universität Dresden in Germany.
To achieve optimal stem cell engraftment, she and her colleagues introduced a naturally occurring mutation of the Kit receptor into mice lacking a functional immune system.
In this way, the team circumvented the 2 major obstacles of HSC transplantation: the rejection by the recipient’s immune system and the absence of free niche space for the incoming donor stem cells in the recipient’s bone marrow.
The Kit mutation in the new mouse model impairs the recipient’s stem cell compartment in such a way that the endogenous HSCs can be easily replaced by human donor stem cells with a functional Kit receptor.
The researchers said this replacement works so efficiently that irradiation can be completely omitted, allowing the study of human blood development in a physiological setting. The model can now be used to study diseases of the human blood and immune system or to test new treatment options.
The results of this research also show that the Kit receptor is important for the function of human HSCs, notably in a transplant setting. The researchers said future studies will focus on using this knowledge to improve conditioning therapy for patients undergoing HSC transplant. ![]()
RBC Transfusion Reduction
Historically, red blood cell (RBC) transfusions have been viewed as safe and effective means of treating anemia and improving oxygen delivery to tissues. Beginning in the early 1980s, primarily driven by concerns related to the risks of transfusion‐related infection, transfusion practice began to come under scrutiny.
Numerous studies over the past 2 decades have failed to demonstrate a benefit of RBC transfusion in many of the clinical situations in which RBC transfusions are routinely given, and many of these studies have in fact shown that RBC transfusion may lead to worse clinical outcomes in some patients.[1, 2] The few available large, randomized clinical trials and prospective observational studies that have assessed the effectiveness of allogeneic RBC transfusion have demonstrated that a more restrictive approach to RBC transfusion results in at least equivalent patient outcomes as compared to a liberal approach, and may in fact reduce morbidity and mortality rates.[1, 2]
Over the last decade, RBC transfusion best‐practice guidelines have been developed by a number of professional societies,[3] addressing RBC transfusion practice in specific patient populations including critical care as well as more general hospitalized populations. These guidelines are generally consistent, strongly recommending a restrictive RBC transfusion approach in most clinical populations. However, despite the general consistency of the guidelines and the lack of evidence for the efficacy of RBC transfusion, there still remains significant variability in clinical RBC transfusion practice.[4, 5]
The difficulty in getting physicians to follow clinical guidelines in general has been well described.[6] Over the last 2 decades there have been reports of a variety of interventions directed toward improving RBC transfusion practice either in specific care units (eg, intensive care units [ICUs]) or institution wide.[7, 8, 9, 10, 11, 12, 13, 14] These initiatives have had varying degrees of success and have employed strategies that have included clinical guidelines, education, audit/feedback, and most recently computer order entry and decision support. We report on the effectiveness of an institution‐wide intervention to align RBC transfusion practice with best‐practice clinical guidelines. Our approach included institutional endorsement of a RBC transfusion guideline coupled with an ongoing education program and RBC transfusion order set.
METHODS
Study Setting
The University of Arkansas for Medical Sciences (UAMS) is a tertiary care university teaching hospital with a total of 437 patient beds. UAMS is a level 1 trauma center and has 52 ICU beds. The study took place between July 2012 and December 2013. At the time of study initiation, there was no institutional RBC transfusion protocol or guideline.
Study Design
In June 2012, a program was initiated to align RBC transfusion practice at UAMS with best‐practice RBC transfusion guidelines. This initiative consisted of several components: a series of educational programs, followed by hospital medical board approval of an intuitional RBC transfusion guideline, and initiation of an RBC transfusion order set of approved RBC transfusion guideline recommendations (Table 1).
| RBC Transfusion Guideline | |
|---|---|
| |
| PURPOSE: Unnecessary blood transfusions increase healthcare costs and expose patients to potential infectious and noninfectious risks. The purpose of this clinical practice guideline is to establish an evidence‐based approach to the transfusion of RBCs in hospitalized patients at UAMS. | |
| GUIDELINE: In order to avoid the potential risks and increased costs associated with unnecessary blood transfusions, the medical staff of UAMS will adhere to a restrictive transfusion strategy in which: | |
| (I) RBC transfusion should be considered unnecessary for hospitalized, hemodynamically stable patients unless the hemoglobin concentration is <78 g/dL. | |
| (II) RBC transfusion is appropriate for patients who have evidence of acute hemorrhage or hemorrhagic shock. | |
| (III) RBC transfusion is appropriate for patients with acute MI or unstable myocardial ischemia if the hemoglobin concentration is 8 g/dL. | |
| (IV) The use of the hemoglobin concentration alone as a trigger for RBC transfusion should be avoided. The decision to order an RBC transfusion should also consider a patient's intravascular volume status, evidence of shock, duration and extent of anemia, and cardiopulmonary physiologic parameters as well as other symptomatology. | |
| (V) In the absence of acute hemorrhage, an RBC transfusion should be ordered and administered as single units. | |
| (VI) It is the physician's responsibility to weigh the risks and benefits of an RBC transfusion for a particular patient based on their medical condition. As such, it is recognized that there will be situations in which an RBC transfusion is appropriate outside of the guidelines put forth in this document. In these instances, the physician should document in the medical record his/her rationale for the RBC transfusion. | |
| RBC Transfusion Order Form | |
| The following are RBC transfusion indications consistent with UAMS‐approved guidelines (check 1): | |
| Acute hemorrhage or hemorrhagic shock | Yes |
| Hgb <78 g/dL | Yes |
| Acute MI, Hgb 8 g/dL | Yes |
| Acute coronary syndrome Hgb 8 g/dL | Yes |
| If the RBC transfusion is for an indication other than those listed above, please note the indication and attending physician in the space provided. | |
| Other indications/attending physician | Free text of other indications. |
| In the absence of acute hemorrhage or a hemoglobin concentration <6.5 g/dL, it is recommended that RBCs be ordered as single units. | |
The educational program included grand rounds presentations for all major clinical departments (internal medicine, surgery, obstetrics and gynecology, geriatrics, anesthesiology), presentations to high‐volume transfusing services (hematology, vascular surgery, cardiac surgery), presentations to hightransfusion‐volume nursing units (eg, medical and surgical ICUs, intermediate care unit, hematology), and scheduled and ad hoc resident educational programs. Educational sessions were repeated over the 18 months of the study and were presented by a clinical content expert.
A UAMS‐specific transfusion guideline was developed based on published best‐practice guidelines.[15, 16] The UAMS medical board approved this guideline in November 2012 (Table 1). The guidelines were disseminated to the entire medical staff in December 2012 via email communication from the hospital's chief medical officer. Membership of the medical board included clinical leadership of the medical center (ie, department chairs) as well as ad hoc members from the hospital administrative leadership.
An RBC transfusion order form that included the guideline recommendations was implemented in the electronic medical record (Sunrise Enterprise 5.5; Eclipsys Corp., Atlanta, GA) in March 2013. There was no hard stop for an RBC transfusion order that was outside of the guideline recommendations; however, for documentation, the ordering physician was required to note the indication and the supervising attending physician for these out‐of‐guideline RBC transfusions. RBC transfusion orders are entered in an electronic medical record. There was no alert triggered by an RBC transfusion order outside of the RBC transfusion guideline.
Outcomes
The number of RBC units transfused during the baseline period of January 2011 through June 2012 was compared with RBC units transfused July 2012 through December 2013. The latter period was further divided into the time period July 2012 through December 2012, during which the education program was initiated (education) as well as the time period January 2013 through December 2013 following the transfusion guideline approval and the initiation of the transfusion order set (decision support). All adult inpatient RBC units transfused, excluding RBC units transfused in the operating room and emergency room, were included in the analysis. RBC transfusions per month were normalized to RBC transfusions per 28 days. RBC transfusions were also calculated as RBC units per adult hospital admission and RBC units per 100 patient‐days.
Hospital mortality is presented as mortality index (observed/predicted mortality). The mean weighted diagnosis‐related group (DRG) was calculated using the monthly average of the Centers for Medicare and Medicaid Services (CMS)‐derived relative weighted DRGs.
Statistical Analysis
Data are presented as meanstandard deviation. Comparisons were by Student t test or analysis of variance as appropriate. GraphPad InStat (GraphPad Software, Inc., La Jolla, CA) was used for statistical analysis, and Minitab (Minitab Inc., State College, PA) was used for control graphs.
RESULTS
There were 28,393 adult admissions (excluding psychiatry) during the baseline period (January 2011June 2012) and 35,743 (12,353 education, 23,390 decision support) adult admissions during the study period (July 2012December 2013). The patient demographics for the 3 time periods were comparable (Table 2).
| Baseline | Education | Decision Support | |
|---|---|---|---|
| |||
| Total patients | 28,393 | 12,353 | 23,390 |
| Age, mean, y* | 48.20.6 | 480.1 | 480.5 |
| Gender, % female | 56 | 57 | 58 |
| Race, % non‐Caucasian | 63 | 61 | 61 |
| Weighted DRG | 1.60 | 1.59 | 1.59 |
| MDC, % | |||
| Nervous system | 13 | 13 | 12 |
| Circulatory system | 11 | 12 | 11 |
| Digestive system | 10 | 10 | 10 |
| Respiratory system | 9 | 8 | 9 |
| Musculoskeletal system | 8 | 8 | 8 |
| Kidney and urinary tract | 8 | 8 | 8 |
| Hepatobiliary system | 5 | 5 | 5 |
| Infectious and parasitic | 5 | 5 | 6 |
| Endocrine, metabolic | 3 | 4 | 3 |
| Blood, immunologic | 3 | 2 | 2 |
| Myeloproliferative | 4 | 4 | 3 |
| Multiple significant trauma | 1 | 1 | 1 |
| Other | 20 | 20 | 22 |
There was a significant decrease in the mean number of RBC units transfused as a result of the RBC transfusion program (Figure 1A). As compared to the baseline period, the mean number of RBC units transfused fell immediately during the 6 months following the initiation of the education program (92368 to 85240, P=0.02), and further still during the subsequent 12 months following the approval of the RBC transfusion guideline by the UAMS medical board and initiation of the RBC transfusion order set (to 69052, P<0.0001). These results do not reflect a change in the number of hospital admissions or length of stay; results are comparable if calculated based on RBC units transfused per patient admission or RBC per 100 patient‐days (Figure 1B,C). Overall, there was a 29% reduction in mean RBC units transfused per hospital admission (0.580.040.410.03, P=0.0001) and a 27% reduction in mean RBC units transfused per 100 hospital‐days (10.560.87.680.63, P=0.0001).
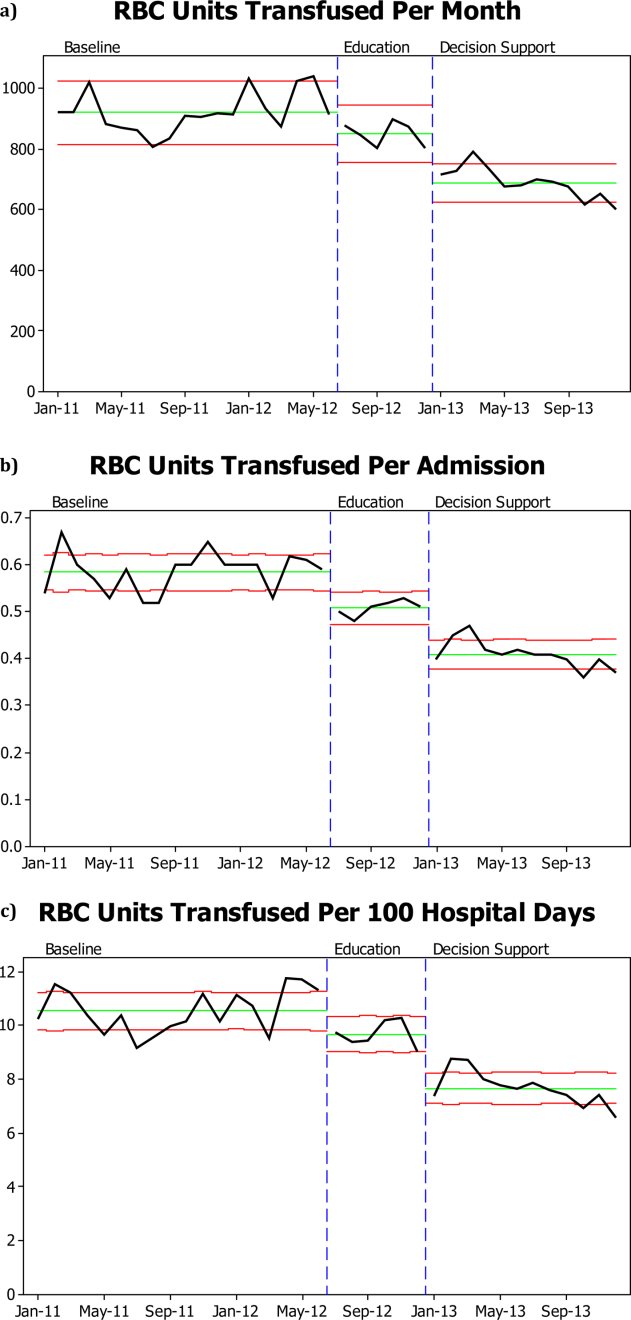
RBC transfusion reduction was observed in both the medical and surgical ICUs (Figure 2B) as well as the general patient wards (Figure 2A). The trends noted above were similar in the medical ICU and general patient wards; however, in the surgical ICU, the RBC transfusion rate fell on initiation of the education program and remained stable at this lower rate for the subsequent 18 months, with no further decrease following RBC transfusion guideline approval and initiation of the RBC order set.
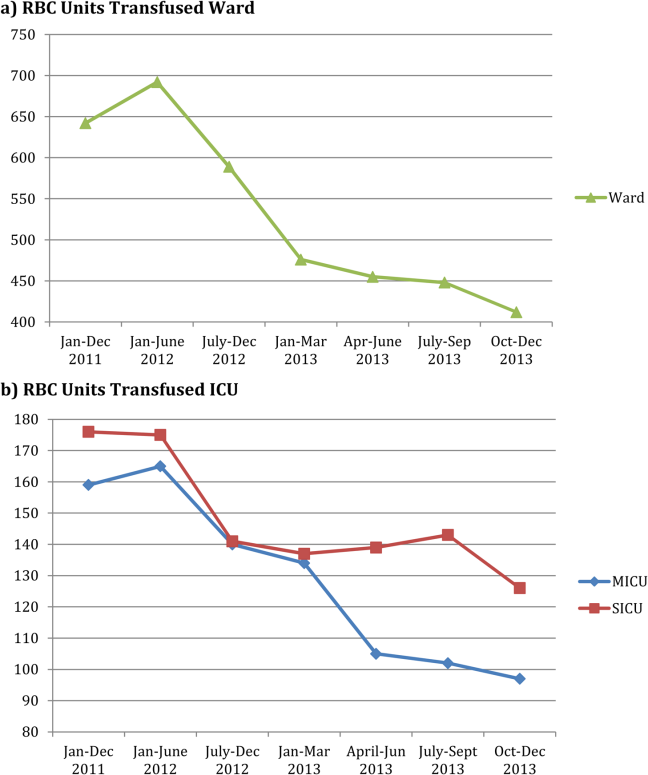
There was no significant difference in hospital mortality observed pre‐ versus post‐RBC transfusion program (mortality index 0.890.05 vs 0.840.04, P=0.13).
DISCUSSION
We were able to demonstrate a 25% reduction in total RBC units transfused with an ongoing education program coupled with an institutional adoption of an RBC transfusion guideline that was incorporated into an RBC transfusion order set. Our program was novel in that the RBC transfusion guideline was approved by the hospital medical board as an institutional practice guideline. Importantly, the RBC transfusion reduction has been maintained over a 18‐month period. The program was instituted in stages: educational program, followed by guideline approval by the hospital medical board, and the initiation of an RBC transfusion order set. At each stage we observed an additive increase in RBC transfusion reduction, with the largest reduction following guideline approval and initiation of the order set.
The pattern of RBC transfusion reduction was observed in all areas of the hospital with the exception of the surgical ICU, where transfusion practice remained stable after the initial decrease in RBC transfusions following initiation of the education program. That RBC transfusion practice on the general surgical wards mirrored practice in other areas of the hospital suggests that the difference seen in the surgical ICU reflects factors unique to that specific area rather than the general approach of surgeons to RBC transfusion.
Despite the substantial data now available regarding RBC transfusion risks and the proliferation of RBC transfusion practice guidelines, wide variation in clinical practice still exists.[4, 5] The delay for evidence from clinical studies to be incorporated into clinical practice can be considerable. Balas and Boren[17] have estimated that it may take over 15 years from publication of a landmark study for the results to reach a 50% utilization rate in clinical practice. The barriers to guideline adherence have been described, including lack of familiarity, lack of agreement, and external factors.[6] Overcoming these barriers involve approaches toward knowledge, attitudes, and behavior.
There have been a number of approaches to changing RBC transfusion practice over the last 2 decades.[7, 8, 9, 10, 11, 12, 13, 14] These interventions have all achieved varying degrees of success. Most have involved some combination of education, practice guideline, and audit/feedback. More recently, technology has allowed computer‐assisted order entry and feedback. Goodnough et al.,[7] employing real‐time clinical decision support and best‐practice alerts, were able to achieve sustained adherence to clinical guidelines and a 24% reduction in RBC units transfused. Other recent reports have shown improvement in RBC transfusion practices comparable to what we observed with programs including audit/feedback and educational efforts.[13, 14]
Our approach to RBC transfusion practice was relatively simple, involving education followed by institutional adoption of a best‐practice guideline and simple RBC transfusion order form. We were able to begin to change RBC transfusion practice with the initiation of an education program; however, there was a more marked and persistent decrease in RBC transfusions following the adoption of the institution's RBC transfusion guideline and RBC transfusion order set. Although education alone is often ineffective in causing sustained change in behavior, a key aspect of our program was the approval of the RBC transfusion guideline by the hospital medical board. The approval by the hospital medical board, made up in part by the clinical leadership, was instrumental in changing the transfusion culture, or beliefs, in the institution. The consistency of practice seen within the time periods both before and after our intervention suggest a given set of beliefs driving RBC transfusion in each time period. Further supporting this view is the consistency of RBC transfusion practice change throughout the institution, and the fact that patient volumes and severity of illness were comparable pre‐ and postintervention. It is difficult to know which elements of the program were most important. It is likely that optimal transfusion practices promoted by the education program were reinforced by the guideline, which were further reinforced by the order set.
Given the known risks of RBC transfusion and the data supporting a restrictive approach to RBC transfusion practice, improved patient safety by aligning RBC transfusion with best‐practice guidelines was the primary goal of our RBC transfusion program.[1, 2] Although we were not able to look at specific complications such as infection rate, there was no change in overall hospital mortality. The total RBC units transfused at our institution fell by almost 30%. We estimate that in the 18 months following initiation of our program we saved approximately 3200 RBC units as compared with the number of RBC units that would have been transfused based on the transfusion rate prior to the initiation of our educational program. This preserves a scarce resource, RBCs, as a well as reduces cost. The cost of an RBC transfusion involves both the direct cost of the RBC unit as well as the cost of activities surrounding an RBC transfusion. Shander et al.,[18] using an activities‐based costing model, have estimated the direct and indirect cost of an RBC transfusion as between $522 and $1183 (mean $761). Over the last 18 months we have achieved a direct savings of $704,000 for purchase of RBC units and, using the low estimate based on the activities‐based costing model, a total savings of at least $1.7 million.
This study is limited by the fact that it reflects a single‐institution experience. Although we cannot exclude other factors contributing to the decrease in RBC transfusion, the pattern of response suggests that the RBC transfusion program was largely responsible for the results observed. Further, patient volumes at our institution have remained constant, as have surgical volumes. RBC transfusions are reduced comparably whether analyzed as total units transfused, units transfused per admission, or units transfused per 100 patient‐days. The complexity of care also limits our ability to draw any conclusions regarding the impact of RBC transfusion reduction on patient outcome. We also do not know how consistent RBC transfusion practice prior to our program was with our guideline; however, the significant decline in RBC units transfused following our intervention suggests that there was a discrepancy in RBC transfusion practice preintervention.
In conclusion, an education program coupled with institutional adoption of a best‐practice RBC transfusion guideline and a RBC transfusion order set resulted in consistent reduction in RBC units transfused. The improvement in RBC transfusion practice was additive with implementation of each intervention. RBC transfusion practice was changed in all areas of the hospital and resulted in less exposure of patients to RBC transfusion risks, preserved a scarce resource, and was a direct cost savings.
- , , . Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Database Syst Rev. 2012;4:CD002042.
- , . Efficacy of RBC transfusion in the critically ill: a systematic review of the literature. Crit Care Med. 2008;36:2667–2674.
- , , , , . A new perspective on best transfusion practice. Blood Transfus. 2013;11:193–202.
- , , , et al. Variation in use of blood transfusion in coronary artery bypass graft surgery. JAMA. 2010;304:1568–1575.
- , , , et al. RBC transfusion practices among critically ill patients: has evidence changed practice? Crit Care Med. 2013;41:2344–2353.
- , , , et al. Why don't physicians follow clinical practice guidelines? JAMA. 1999;282:1458–1465.
- , , , , , . Improved blood utilization using real‐time clinical decision support. Transfusion. 2014;54:1358–1365.
- , , , , , . Computerized physician order entry with decision support decreases blood transfusion in children. Pediatrics. 2011;127:e1112–e1119.
- , , , et al. Reducing the amount of blood transfused. Arch Intern Med. 2005;165:845–852.
- , , , et al. Assessment of education and computerized decision support interventions for improving transfusion practice. Transfusion. 2007;47:228–239.
- , , , , Transfusion insurgency: practice change through education and evidence‐based recommendations. Am J Surg. 2009;197:279–283.
- , , , et al. Evidence‐based red cell transfusion in the critically ill: quality improvement using computerized physician order entry. Crit Care Med. 2006;34:1892–1897.
- , , . The addition of decision support into computerize physician order entry reduces red blood cell transfusion resource utilization in the intensive care unit. Am J Hematol. 2007;82:631–633.
- , , , et al. How we closed the gap between red blood cell utilization and whole blood collections in our institution. Transfusion. 2012;52:1857–1867.
- , , , et al. American College of Critical Care and Eastern Association of Trauma. Clinical practice guideline: red blood cell transfusion practice in adult trauma and critical care. Crit Care Med. 2009;37:3124–3157.
- , , , et al. Red blood cell transfusion: a clinical practice guideline of the AABB. Ann Intern Med. 2012;157:49–58.
- , . Managing clinical knowledge for health care improvement. In: Bemmel J, McCray AT, eds. Yearbook of Medical Informatics 2000: Patient‐Centered Systems. Stuttgart, Germany: Schattauer Verlagsgesellschaft; 2000:65–70.
- , , , et al. Activity‐based costs of blood transfusions in surgical patients at four hospitals. Transfusion. 2010;50:753–764.
Historically, red blood cell (RBC) transfusions have been viewed as safe and effective means of treating anemia and improving oxygen delivery to tissues. Beginning in the early 1980s, primarily driven by concerns related to the risks of transfusion‐related infection, transfusion practice began to come under scrutiny.
Numerous studies over the past 2 decades have failed to demonstrate a benefit of RBC transfusion in many of the clinical situations in which RBC transfusions are routinely given, and many of these studies have in fact shown that RBC transfusion may lead to worse clinical outcomes in some patients.[1, 2] The few available large, randomized clinical trials and prospective observational studies that have assessed the effectiveness of allogeneic RBC transfusion have demonstrated that a more restrictive approach to RBC transfusion results in at least equivalent patient outcomes as compared to a liberal approach, and may in fact reduce morbidity and mortality rates.[1, 2]
Over the last decade, RBC transfusion best‐practice guidelines have been developed by a number of professional societies,[3] addressing RBC transfusion practice in specific patient populations including critical care as well as more general hospitalized populations. These guidelines are generally consistent, strongly recommending a restrictive RBC transfusion approach in most clinical populations. However, despite the general consistency of the guidelines and the lack of evidence for the efficacy of RBC transfusion, there still remains significant variability in clinical RBC transfusion practice.[4, 5]
The difficulty in getting physicians to follow clinical guidelines in general has been well described.[6] Over the last 2 decades there have been reports of a variety of interventions directed toward improving RBC transfusion practice either in specific care units (eg, intensive care units [ICUs]) or institution wide.[7, 8, 9, 10, 11, 12, 13, 14] These initiatives have had varying degrees of success and have employed strategies that have included clinical guidelines, education, audit/feedback, and most recently computer order entry and decision support. We report on the effectiveness of an institution‐wide intervention to align RBC transfusion practice with best‐practice clinical guidelines. Our approach included institutional endorsement of a RBC transfusion guideline coupled with an ongoing education program and RBC transfusion order set.
METHODS
Study Setting
The University of Arkansas for Medical Sciences (UAMS) is a tertiary care university teaching hospital with a total of 437 patient beds. UAMS is a level 1 trauma center and has 52 ICU beds. The study took place between July 2012 and December 2013. At the time of study initiation, there was no institutional RBC transfusion protocol or guideline.
Study Design
In June 2012, a program was initiated to align RBC transfusion practice at UAMS with best‐practice RBC transfusion guidelines. This initiative consisted of several components: a series of educational programs, followed by hospital medical board approval of an intuitional RBC transfusion guideline, and initiation of an RBC transfusion order set of approved RBC transfusion guideline recommendations (Table 1).
| RBC Transfusion Guideline | |
|---|---|
| |
| PURPOSE: Unnecessary blood transfusions increase healthcare costs and expose patients to potential infectious and noninfectious risks. The purpose of this clinical practice guideline is to establish an evidence‐based approach to the transfusion of RBCs in hospitalized patients at UAMS. | |
| GUIDELINE: In order to avoid the potential risks and increased costs associated with unnecessary blood transfusions, the medical staff of UAMS will adhere to a restrictive transfusion strategy in which: | |
| (I) RBC transfusion should be considered unnecessary for hospitalized, hemodynamically stable patients unless the hemoglobin concentration is <78 g/dL. | |
| (II) RBC transfusion is appropriate for patients who have evidence of acute hemorrhage or hemorrhagic shock. | |
| (III) RBC transfusion is appropriate for patients with acute MI or unstable myocardial ischemia if the hemoglobin concentration is 8 g/dL. | |
| (IV) The use of the hemoglobin concentration alone as a trigger for RBC transfusion should be avoided. The decision to order an RBC transfusion should also consider a patient's intravascular volume status, evidence of shock, duration and extent of anemia, and cardiopulmonary physiologic parameters as well as other symptomatology. | |
| (V) In the absence of acute hemorrhage, an RBC transfusion should be ordered and administered as single units. | |
| (VI) It is the physician's responsibility to weigh the risks and benefits of an RBC transfusion for a particular patient based on their medical condition. As such, it is recognized that there will be situations in which an RBC transfusion is appropriate outside of the guidelines put forth in this document. In these instances, the physician should document in the medical record his/her rationale for the RBC transfusion. | |
| RBC Transfusion Order Form | |
| The following are RBC transfusion indications consistent with UAMS‐approved guidelines (check 1): | |
| Acute hemorrhage or hemorrhagic shock | Yes |
| Hgb <78 g/dL | Yes |
| Acute MI, Hgb 8 g/dL | Yes |
| Acute coronary syndrome Hgb 8 g/dL | Yes |
| If the RBC transfusion is for an indication other than those listed above, please note the indication and attending physician in the space provided. | |
| Other indications/attending physician | Free text of other indications. |
| In the absence of acute hemorrhage or a hemoglobin concentration <6.5 g/dL, it is recommended that RBCs be ordered as single units. | |
The educational program included grand rounds presentations for all major clinical departments (internal medicine, surgery, obstetrics and gynecology, geriatrics, anesthesiology), presentations to high‐volume transfusing services (hematology, vascular surgery, cardiac surgery), presentations to hightransfusion‐volume nursing units (eg, medical and surgical ICUs, intermediate care unit, hematology), and scheduled and ad hoc resident educational programs. Educational sessions were repeated over the 18 months of the study and were presented by a clinical content expert.
A UAMS‐specific transfusion guideline was developed based on published best‐practice guidelines.[15, 16] The UAMS medical board approved this guideline in November 2012 (Table 1). The guidelines were disseminated to the entire medical staff in December 2012 via email communication from the hospital's chief medical officer. Membership of the medical board included clinical leadership of the medical center (ie, department chairs) as well as ad hoc members from the hospital administrative leadership.
An RBC transfusion order form that included the guideline recommendations was implemented in the electronic medical record (Sunrise Enterprise 5.5; Eclipsys Corp., Atlanta, GA) in March 2013. There was no hard stop for an RBC transfusion order that was outside of the guideline recommendations; however, for documentation, the ordering physician was required to note the indication and the supervising attending physician for these out‐of‐guideline RBC transfusions. RBC transfusion orders are entered in an electronic medical record. There was no alert triggered by an RBC transfusion order outside of the RBC transfusion guideline.
Outcomes
The number of RBC units transfused during the baseline period of January 2011 through June 2012 was compared with RBC units transfused July 2012 through December 2013. The latter period was further divided into the time period July 2012 through December 2012, during which the education program was initiated (education) as well as the time period January 2013 through December 2013 following the transfusion guideline approval and the initiation of the transfusion order set (decision support). All adult inpatient RBC units transfused, excluding RBC units transfused in the operating room and emergency room, were included in the analysis. RBC transfusions per month were normalized to RBC transfusions per 28 days. RBC transfusions were also calculated as RBC units per adult hospital admission and RBC units per 100 patient‐days.
Hospital mortality is presented as mortality index (observed/predicted mortality). The mean weighted diagnosis‐related group (DRG) was calculated using the monthly average of the Centers for Medicare and Medicaid Services (CMS)‐derived relative weighted DRGs.
Statistical Analysis
Data are presented as meanstandard deviation. Comparisons were by Student t test or analysis of variance as appropriate. GraphPad InStat (GraphPad Software, Inc., La Jolla, CA) was used for statistical analysis, and Minitab (Minitab Inc., State College, PA) was used for control graphs.
RESULTS
There were 28,393 adult admissions (excluding psychiatry) during the baseline period (January 2011June 2012) and 35,743 (12,353 education, 23,390 decision support) adult admissions during the study period (July 2012December 2013). The patient demographics for the 3 time periods were comparable (Table 2).
| Baseline | Education | Decision Support | |
|---|---|---|---|
| |||
| Total patients | 28,393 | 12,353 | 23,390 |
| Age, mean, y* | 48.20.6 | 480.1 | 480.5 |
| Gender, % female | 56 | 57 | 58 |
| Race, % non‐Caucasian | 63 | 61 | 61 |
| Weighted DRG | 1.60 | 1.59 | 1.59 |
| MDC, % | |||
| Nervous system | 13 | 13 | 12 |
| Circulatory system | 11 | 12 | 11 |
| Digestive system | 10 | 10 | 10 |
| Respiratory system | 9 | 8 | 9 |
| Musculoskeletal system | 8 | 8 | 8 |
| Kidney and urinary tract | 8 | 8 | 8 |
| Hepatobiliary system | 5 | 5 | 5 |
| Infectious and parasitic | 5 | 5 | 6 |
| Endocrine, metabolic | 3 | 4 | 3 |
| Blood, immunologic | 3 | 2 | 2 |
| Myeloproliferative | 4 | 4 | 3 |
| Multiple significant trauma | 1 | 1 | 1 |
| Other | 20 | 20 | 22 |
There was a significant decrease in the mean number of RBC units transfused as a result of the RBC transfusion program (Figure 1A). As compared to the baseline period, the mean number of RBC units transfused fell immediately during the 6 months following the initiation of the education program (92368 to 85240, P=0.02), and further still during the subsequent 12 months following the approval of the RBC transfusion guideline by the UAMS medical board and initiation of the RBC transfusion order set (to 69052, P<0.0001). These results do not reflect a change in the number of hospital admissions or length of stay; results are comparable if calculated based on RBC units transfused per patient admission or RBC per 100 patient‐days (Figure 1B,C). Overall, there was a 29% reduction in mean RBC units transfused per hospital admission (0.580.040.410.03, P=0.0001) and a 27% reduction in mean RBC units transfused per 100 hospital‐days (10.560.87.680.63, P=0.0001).
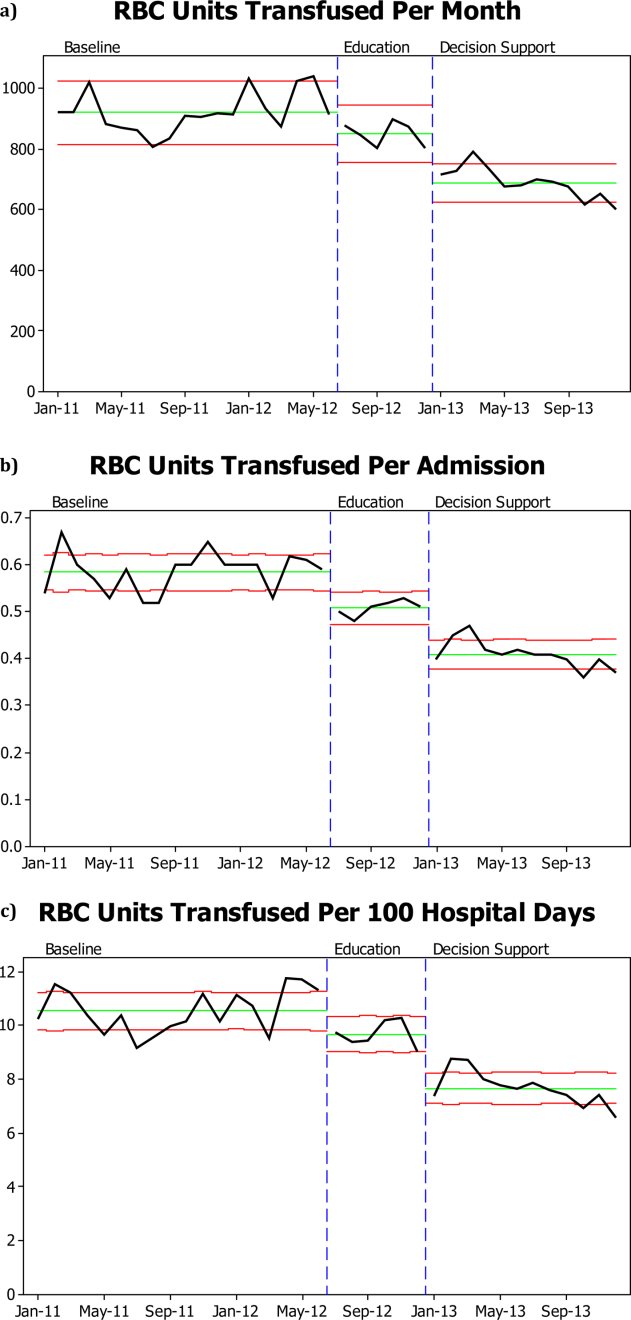
RBC transfusion reduction was observed in both the medical and surgical ICUs (Figure 2B) as well as the general patient wards (Figure 2A). The trends noted above were similar in the medical ICU and general patient wards; however, in the surgical ICU, the RBC transfusion rate fell on initiation of the education program and remained stable at this lower rate for the subsequent 18 months, with no further decrease following RBC transfusion guideline approval and initiation of the RBC order set.
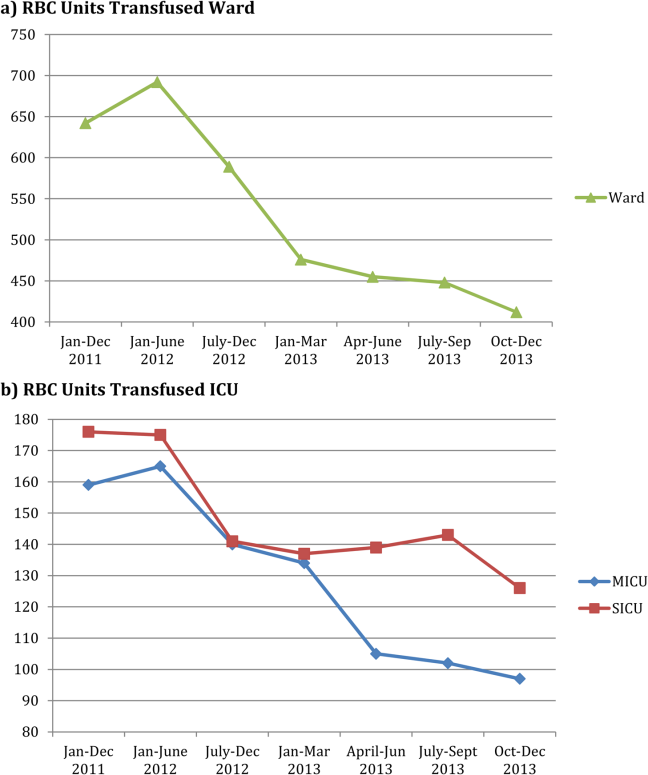
There was no significant difference in hospital mortality observed pre‐ versus post‐RBC transfusion program (mortality index 0.890.05 vs 0.840.04, P=0.13).
DISCUSSION
We were able to demonstrate a 25% reduction in total RBC units transfused with an ongoing education program coupled with an institutional adoption of an RBC transfusion guideline that was incorporated into an RBC transfusion order set. Our program was novel in that the RBC transfusion guideline was approved by the hospital medical board as an institutional practice guideline. Importantly, the RBC transfusion reduction has been maintained over a 18‐month period. The program was instituted in stages: educational program, followed by guideline approval by the hospital medical board, and the initiation of an RBC transfusion order set. At each stage we observed an additive increase in RBC transfusion reduction, with the largest reduction following guideline approval and initiation of the order set.
The pattern of RBC transfusion reduction was observed in all areas of the hospital with the exception of the surgical ICU, where transfusion practice remained stable after the initial decrease in RBC transfusions following initiation of the education program. That RBC transfusion practice on the general surgical wards mirrored practice in other areas of the hospital suggests that the difference seen in the surgical ICU reflects factors unique to that specific area rather than the general approach of surgeons to RBC transfusion.
Despite the substantial data now available regarding RBC transfusion risks and the proliferation of RBC transfusion practice guidelines, wide variation in clinical practice still exists.[4, 5] The delay for evidence from clinical studies to be incorporated into clinical practice can be considerable. Balas and Boren[17] have estimated that it may take over 15 years from publication of a landmark study for the results to reach a 50% utilization rate in clinical practice. The barriers to guideline adherence have been described, including lack of familiarity, lack of agreement, and external factors.[6] Overcoming these barriers involve approaches toward knowledge, attitudes, and behavior.
There have been a number of approaches to changing RBC transfusion practice over the last 2 decades.[7, 8, 9, 10, 11, 12, 13, 14] These interventions have all achieved varying degrees of success. Most have involved some combination of education, practice guideline, and audit/feedback. More recently, technology has allowed computer‐assisted order entry and feedback. Goodnough et al.,[7] employing real‐time clinical decision support and best‐practice alerts, were able to achieve sustained adherence to clinical guidelines and a 24% reduction in RBC units transfused. Other recent reports have shown improvement in RBC transfusion practices comparable to what we observed with programs including audit/feedback and educational efforts.[13, 14]
Our approach to RBC transfusion practice was relatively simple, involving education followed by institutional adoption of a best‐practice guideline and simple RBC transfusion order form. We were able to begin to change RBC transfusion practice with the initiation of an education program; however, there was a more marked and persistent decrease in RBC transfusions following the adoption of the institution's RBC transfusion guideline and RBC transfusion order set. Although education alone is often ineffective in causing sustained change in behavior, a key aspect of our program was the approval of the RBC transfusion guideline by the hospital medical board. The approval by the hospital medical board, made up in part by the clinical leadership, was instrumental in changing the transfusion culture, or beliefs, in the institution. The consistency of practice seen within the time periods both before and after our intervention suggest a given set of beliefs driving RBC transfusion in each time period. Further supporting this view is the consistency of RBC transfusion practice change throughout the institution, and the fact that patient volumes and severity of illness were comparable pre‐ and postintervention. It is difficult to know which elements of the program were most important. It is likely that optimal transfusion practices promoted by the education program were reinforced by the guideline, which were further reinforced by the order set.
Given the known risks of RBC transfusion and the data supporting a restrictive approach to RBC transfusion practice, improved patient safety by aligning RBC transfusion with best‐practice guidelines was the primary goal of our RBC transfusion program.[1, 2] Although we were not able to look at specific complications such as infection rate, there was no change in overall hospital mortality. The total RBC units transfused at our institution fell by almost 30%. We estimate that in the 18 months following initiation of our program we saved approximately 3200 RBC units as compared with the number of RBC units that would have been transfused based on the transfusion rate prior to the initiation of our educational program. This preserves a scarce resource, RBCs, as a well as reduces cost. The cost of an RBC transfusion involves both the direct cost of the RBC unit as well as the cost of activities surrounding an RBC transfusion. Shander et al.,[18] using an activities‐based costing model, have estimated the direct and indirect cost of an RBC transfusion as between $522 and $1183 (mean $761). Over the last 18 months we have achieved a direct savings of $704,000 for purchase of RBC units and, using the low estimate based on the activities‐based costing model, a total savings of at least $1.7 million.
This study is limited by the fact that it reflects a single‐institution experience. Although we cannot exclude other factors contributing to the decrease in RBC transfusion, the pattern of response suggests that the RBC transfusion program was largely responsible for the results observed. Further, patient volumes at our institution have remained constant, as have surgical volumes. RBC transfusions are reduced comparably whether analyzed as total units transfused, units transfused per admission, or units transfused per 100 patient‐days. The complexity of care also limits our ability to draw any conclusions regarding the impact of RBC transfusion reduction on patient outcome. We also do not know how consistent RBC transfusion practice prior to our program was with our guideline; however, the significant decline in RBC units transfused following our intervention suggests that there was a discrepancy in RBC transfusion practice preintervention.
In conclusion, an education program coupled with institutional adoption of a best‐practice RBC transfusion guideline and a RBC transfusion order set resulted in consistent reduction in RBC units transfused. The improvement in RBC transfusion practice was additive with implementation of each intervention. RBC transfusion practice was changed in all areas of the hospital and resulted in less exposure of patients to RBC transfusion risks, preserved a scarce resource, and was a direct cost savings.
Historically, red blood cell (RBC) transfusions have been viewed as safe and effective means of treating anemia and improving oxygen delivery to tissues. Beginning in the early 1980s, primarily driven by concerns related to the risks of transfusion‐related infection, transfusion practice began to come under scrutiny.
Numerous studies over the past 2 decades have failed to demonstrate a benefit of RBC transfusion in many of the clinical situations in which RBC transfusions are routinely given, and many of these studies have in fact shown that RBC transfusion may lead to worse clinical outcomes in some patients.[1, 2] The few available large, randomized clinical trials and prospective observational studies that have assessed the effectiveness of allogeneic RBC transfusion have demonstrated that a more restrictive approach to RBC transfusion results in at least equivalent patient outcomes as compared to a liberal approach, and may in fact reduce morbidity and mortality rates.[1, 2]
Over the last decade, RBC transfusion best‐practice guidelines have been developed by a number of professional societies,[3] addressing RBC transfusion practice in specific patient populations including critical care as well as more general hospitalized populations. These guidelines are generally consistent, strongly recommending a restrictive RBC transfusion approach in most clinical populations. However, despite the general consistency of the guidelines and the lack of evidence for the efficacy of RBC transfusion, there still remains significant variability in clinical RBC transfusion practice.[4, 5]
The difficulty in getting physicians to follow clinical guidelines in general has been well described.[6] Over the last 2 decades there have been reports of a variety of interventions directed toward improving RBC transfusion practice either in specific care units (eg, intensive care units [ICUs]) or institution wide.[7, 8, 9, 10, 11, 12, 13, 14] These initiatives have had varying degrees of success and have employed strategies that have included clinical guidelines, education, audit/feedback, and most recently computer order entry and decision support. We report on the effectiveness of an institution‐wide intervention to align RBC transfusion practice with best‐practice clinical guidelines. Our approach included institutional endorsement of a RBC transfusion guideline coupled with an ongoing education program and RBC transfusion order set.
METHODS
Study Setting
The University of Arkansas for Medical Sciences (UAMS) is a tertiary care university teaching hospital with a total of 437 patient beds. UAMS is a level 1 trauma center and has 52 ICU beds. The study took place between July 2012 and December 2013. At the time of study initiation, there was no institutional RBC transfusion protocol or guideline.
Study Design
In June 2012, a program was initiated to align RBC transfusion practice at UAMS with best‐practice RBC transfusion guidelines. This initiative consisted of several components: a series of educational programs, followed by hospital medical board approval of an intuitional RBC transfusion guideline, and initiation of an RBC transfusion order set of approved RBC transfusion guideline recommendations (Table 1).
| RBC Transfusion Guideline | |
|---|---|
| |
| PURPOSE: Unnecessary blood transfusions increase healthcare costs and expose patients to potential infectious and noninfectious risks. The purpose of this clinical practice guideline is to establish an evidence‐based approach to the transfusion of RBCs in hospitalized patients at UAMS. | |
| GUIDELINE: In order to avoid the potential risks and increased costs associated with unnecessary blood transfusions, the medical staff of UAMS will adhere to a restrictive transfusion strategy in which: | |
| (I) RBC transfusion should be considered unnecessary for hospitalized, hemodynamically stable patients unless the hemoglobin concentration is <78 g/dL. | |
| (II) RBC transfusion is appropriate for patients who have evidence of acute hemorrhage or hemorrhagic shock. | |
| (III) RBC transfusion is appropriate for patients with acute MI or unstable myocardial ischemia if the hemoglobin concentration is 8 g/dL. | |
| (IV) The use of the hemoglobin concentration alone as a trigger for RBC transfusion should be avoided. The decision to order an RBC transfusion should also consider a patient's intravascular volume status, evidence of shock, duration and extent of anemia, and cardiopulmonary physiologic parameters as well as other symptomatology. | |
| (V) In the absence of acute hemorrhage, an RBC transfusion should be ordered and administered as single units. | |
| (VI) It is the physician's responsibility to weigh the risks and benefits of an RBC transfusion for a particular patient based on their medical condition. As such, it is recognized that there will be situations in which an RBC transfusion is appropriate outside of the guidelines put forth in this document. In these instances, the physician should document in the medical record his/her rationale for the RBC transfusion. | |
| RBC Transfusion Order Form | |
| The following are RBC transfusion indications consistent with UAMS‐approved guidelines (check 1): | |
| Acute hemorrhage or hemorrhagic shock | Yes |
| Hgb <78 g/dL | Yes |
| Acute MI, Hgb 8 g/dL | Yes |
| Acute coronary syndrome Hgb 8 g/dL | Yes |
| If the RBC transfusion is for an indication other than those listed above, please note the indication and attending physician in the space provided. | |
| Other indications/attending physician | Free text of other indications. |
| In the absence of acute hemorrhage or a hemoglobin concentration <6.5 g/dL, it is recommended that RBCs be ordered as single units. | |
The educational program included grand rounds presentations for all major clinical departments (internal medicine, surgery, obstetrics and gynecology, geriatrics, anesthesiology), presentations to high‐volume transfusing services (hematology, vascular surgery, cardiac surgery), presentations to hightransfusion‐volume nursing units (eg, medical and surgical ICUs, intermediate care unit, hematology), and scheduled and ad hoc resident educational programs. Educational sessions were repeated over the 18 months of the study and were presented by a clinical content expert.
A UAMS‐specific transfusion guideline was developed based on published best‐practice guidelines.[15, 16] The UAMS medical board approved this guideline in November 2012 (Table 1). The guidelines were disseminated to the entire medical staff in December 2012 via email communication from the hospital's chief medical officer. Membership of the medical board included clinical leadership of the medical center (ie, department chairs) as well as ad hoc members from the hospital administrative leadership.
An RBC transfusion order form that included the guideline recommendations was implemented in the electronic medical record (Sunrise Enterprise 5.5; Eclipsys Corp., Atlanta, GA) in March 2013. There was no hard stop for an RBC transfusion order that was outside of the guideline recommendations; however, for documentation, the ordering physician was required to note the indication and the supervising attending physician for these out‐of‐guideline RBC transfusions. RBC transfusion orders are entered in an electronic medical record. There was no alert triggered by an RBC transfusion order outside of the RBC transfusion guideline.
Outcomes
The number of RBC units transfused during the baseline period of January 2011 through June 2012 was compared with RBC units transfused July 2012 through December 2013. The latter period was further divided into the time period July 2012 through December 2012, during which the education program was initiated (education) as well as the time period January 2013 through December 2013 following the transfusion guideline approval and the initiation of the transfusion order set (decision support). All adult inpatient RBC units transfused, excluding RBC units transfused in the operating room and emergency room, were included in the analysis. RBC transfusions per month were normalized to RBC transfusions per 28 days. RBC transfusions were also calculated as RBC units per adult hospital admission and RBC units per 100 patient‐days.
Hospital mortality is presented as mortality index (observed/predicted mortality). The mean weighted diagnosis‐related group (DRG) was calculated using the monthly average of the Centers for Medicare and Medicaid Services (CMS)‐derived relative weighted DRGs.
Statistical Analysis
Data are presented as meanstandard deviation. Comparisons were by Student t test or analysis of variance as appropriate. GraphPad InStat (GraphPad Software, Inc., La Jolla, CA) was used for statistical analysis, and Minitab (Minitab Inc., State College, PA) was used for control graphs.
RESULTS
There were 28,393 adult admissions (excluding psychiatry) during the baseline period (January 2011June 2012) and 35,743 (12,353 education, 23,390 decision support) adult admissions during the study period (July 2012December 2013). The patient demographics for the 3 time periods were comparable (Table 2).
| Baseline | Education | Decision Support | |
|---|---|---|---|
| |||
| Total patients | 28,393 | 12,353 | 23,390 |
| Age, mean, y* | 48.20.6 | 480.1 | 480.5 |
| Gender, % female | 56 | 57 | 58 |
| Race, % non‐Caucasian | 63 | 61 | 61 |
| Weighted DRG | 1.60 | 1.59 | 1.59 |
| MDC, % | |||
| Nervous system | 13 | 13 | 12 |
| Circulatory system | 11 | 12 | 11 |
| Digestive system | 10 | 10 | 10 |
| Respiratory system | 9 | 8 | 9 |
| Musculoskeletal system | 8 | 8 | 8 |
| Kidney and urinary tract | 8 | 8 | 8 |
| Hepatobiliary system | 5 | 5 | 5 |
| Infectious and parasitic | 5 | 5 | 6 |
| Endocrine, metabolic | 3 | 4 | 3 |
| Blood, immunologic | 3 | 2 | 2 |
| Myeloproliferative | 4 | 4 | 3 |
| Multiple significant trauma | 1 | 1 | 1 |
| Other | 20 | 20 | 22 |
There was a significant decrease in the mean number of RBC units transfused as a result of the RBC transfusion program (Figure 1A). As compared to the baseline period, the mean number of RBC units transfused fell immediately during the 6 months following the initiation of the education program (92368 to 85240, P=0.02), and further still during the subsequent 12 months following the approval of the RBC transfusion guideline by the UAMS medical board and initiation of the RBC transfusion order set (to 69052, P<0.0001). These results do not reflect a change in the number of hospital admissions or length of stay; results are comparable if calculated based on RBC units transfused per patient admission or RBC per 100 patient‐days (Figure 1B,C). Overall, there was a 29% reduction in mean RBC units transfused per hospital admission (0.580.040.410.03, P=0.0001) and a 27% reduction in mean RBC units transfused per 100 hospital‐days (10.560.87.680.63, P=0.0001).
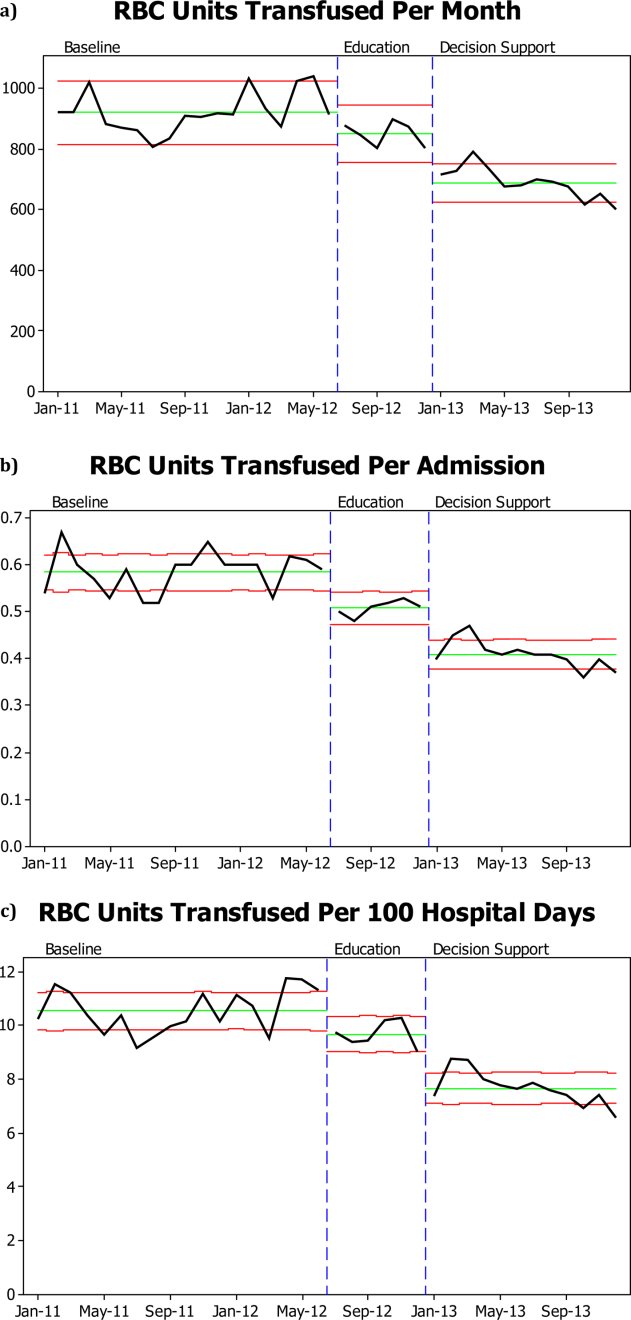
RBC transfusion reduction was observed in both the medical and surgical ICUs (Figure 2B) as well as the general patient wards (Figure 2A). The trends noted above were similar in the medical ICU and general patient wards; however, in the surgical ICU, the RBC transfusion rate fell on initiation of the education program and remained stable at this lower rate for the subsequent 18 months, with no further decrease following RBC transfusion guideline approval and initiation of the RBC order set.
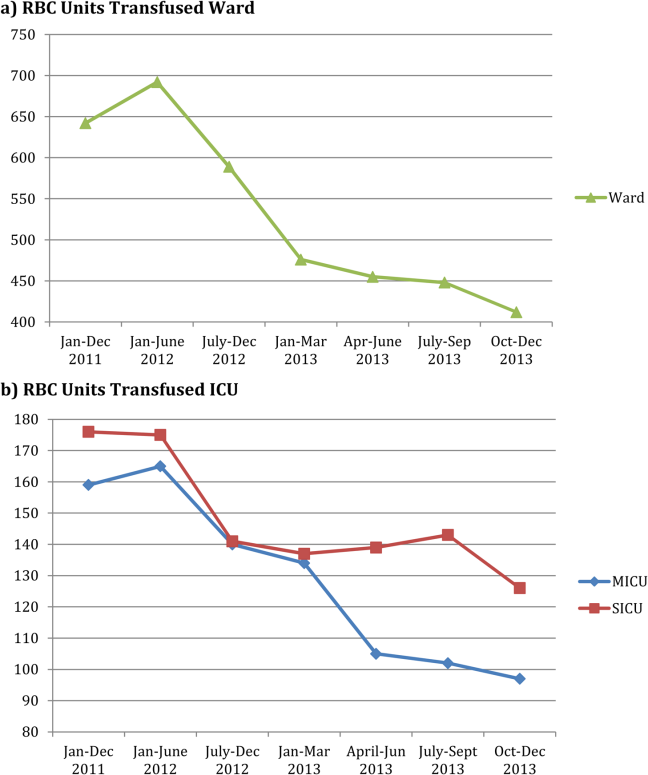
There was no significant difference in hospital mortality observed pre‐ versus post‐RBC transfusion program (mortality index 0.890.05 vs 0.840.04, P=0.13).
DISCUSSION
We were able to demonstrate a 25% reduction in total RBC units transfused with an ongoing education program coupled with an institutional adoption of an RBC transfusion guideline that was incorporated into an RBC transfusion order set. Our program was novel in that the RBC transfusion guideline was approved by the hospital medical board as an institutional practice guideline. Importantly, the RBC transfusion reduction has been maintained over a 18‐month period. The program was instituted in stages: educational program, followed by guideline approval by the hospital medical board, and the initiation of an RBC transfusion order set. At each stage we observed an additive increase in RBC transfusion reduction, with the largest reduction following guideline approval and initiation of the order set.
The pattern of RBC transfusion reduction was observed in all areas of the hospital with the exception of the surgical ICU, where transfusion practice remained stable after the initial decrease in RBC transfusions following initiation of the education program. That RBC transfusion practice on the general surgical wards mirrored practice in other areas of the hospital suggests that the difference seen in the surgical ICU reflects factors unique to that specific area rather than the general approach of surgeons to RBC transfusion.
Despite the substantial data now available regarding RBC transfusion risks and the proliferation of RBC transfusion practice guidelines, wide variation in clinical practice still exists.[4, 5] The delay for evidence from clinical studies to be incorporated into clinical practice can be considerable. Balas and Boren[17] have estimated that it may take over 15 years from publication of a landmark study for the results to reach a 50% utilization rate in clinical practice. The barriers to guideline adherence have been described, including lack of familiarity, lack of agreement, and external factors.[6] Overcoming these barriers involve approaches toward knowledge, attitudes, and behavior.
There have been a number of approaches to changing RBC transfusion practice over the last 2 decades.[7, 8, 9, 10, 11, 12, 13, 14] These interventions have all achieved varying degrees of success. Most have involved some combination of education, practice guideline, and audit/feedback. More recently, technology has allowed computer‐assisted order entry and feedback. Goodnough et al.,[7] employing real‐time clinical decision support and best‐practice alerts, were able to achieve sustained adherence to clinical guidelines and a 24% reduction in RBC units transfused. Other recent reports have shown improvement in RBC transfusion practices comparable to what we observed with programs including audit/feedback and educational efforts.[13, 14]
Our approach to RBC transfusion practice was relatively simple, involving education followed by institutional adoption of a best‐practice guideline and simple RBC transfusion order form. We were able to begin to change RBC transfusion practice with the initiation of an education program; however, there was a more marked and persistent decrease in RBC transfusions following the adoption of the institution's RBC transfusion guideline and RBC transfusion order set. Although education alone is often ineffective in causing sustained change in behavior, a key aspect of our program was the approval of the RBC transfusion guideline by the hospital medical board. The approval by the hospital medical board, made up in part by the clinical leadership, was instrumental in changing the transfusion culture, or beliefs, in the institution. The consistency of practice seen within the time periods both before and after our intervention suggest a given set of beliefs driving RBC transfusion in each time period. Further supporting this view is the consistency of RBC transfusion practice change throughout the institution, and the fact that patient volumes and severity of illness were comparable pre‐ and postintervention. It is difficult to know which elements of the program were most important. It is likely that optimal transfusion practices promoted by the education program were reinforced by the guideline, which were further reinforced by the order set.
Given the known risks of RBC transfusion and the data supporting a restrictive approach to RBC transfusion practice, improved patient safety by aligning RBC transfusion with best‐practice guidelines was the primary goal of our RBC transfusion program.[1, 2] Although we were not able to look at specific complications such as infection rate, there was no change in overall hospital mortality. The total RBC units transfused at our institution fell by almost 30%. We estimate that in the 18 months following initiation of our program we saved approximately 3200 RBC units as compared with the number of RBC units that would have been transfused based on the transfusion rate prior to the initiation of our educational program. This preserves a scarce resource, RBCs, as a well as reduces cost. The cost of an RBC transfusion involves both the direct cost of the RBC unit as well as the cost of activities surrounding an RBC transfusion. Shander et al.,[18] using an activities‐based costing model, have estimated the direct and indirect cost of an RBC transfusion as between $522 and $1183 (mean $761). Over the last 18 months we have achieved a direct savings of $704,000 for purchase of RBC units and, using the low estimate based on the activities‐based costing model, a total savings of at least $1.7 million.
This study is limited by the fact that it reflects a single‐institution experience. Although we cannot exclude other factors contributing to the decrease in RBC transfusion, the pattern of response suggests that the RBC transfusion program was largely responsible for the results observed. Further, patient volumes at our institution have remained constant, as have surgical volumes. RBC transfusions are reduced comparably whether analyzed as total units transfused, units transfused per admission, or units transfused per 100 patient‐days. The complexity of care also limits our ability to draw any conclusions regarding the impact of RBC transfusion reduction on patient outcome. We also do not know how consistent RBC transfusion practice prior to our program was with our guideline; however, the significant decline in RBC units transfused following our intervention suggests that there was a discrepancy in RBC transfusion practice preintervention.
In conclusion, an education program coupled with institutional adoption of a best‐practice RBC transfusion guideline and a RBC transfusion order set resulted in consistent reduction in RBC units transfused. The improvement in RBC transfusion practice was additive with implementation of each intervention. RBC transfusion practice was changed in all areas of the hospital and resulted in less exposure of patients to RBC transfusion risks, preserved a scarce resource, and was a direct cost savings.
- , , . Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Database Syst Rev. 2012;4:CD002042.
- , . Efficacy of RBC transfusion in the critically ill: a systematic review of the literature. Crit Care Med. 2008;36:2667–2674.
- , , , , . A new perspective on best transfusion practice. Blood Transfus. 2013;11:193–202.
- , , , et al. Variation in use of blood transfusion in coronary artery bypass graft surgery. JAMA. 2010;304:1568–1575.
- , , , et al. RBC transfusion practices among critically ill patients: has evidence changed practice? Crit Care Med. 2013;41:2344–2353.
- , , , et al. Why don't physicians follow clinical practice guidelines? JAMA. 1999;282:1458–1465.
- , , , , , . Improved blood utilization using real‐time clinical decision support. Transfusion. 2014;54:1358–1365.
- , , , , , . Computerized physician order entry with decision support decreases blood transfusion in children. Pediatrics. 2011;127:e1112–e1119.
- , , , et al. Reducing the amount of blood transfused. Arch Intern Med. 2005;165:845–852.
- , , , et al. Assessment of education and computerized decision support interventions for improving transfusion practice. Transfusion. 2007;47:228–239.
- , , , , Transfusion insurgency: practice change through education and evidence‐based recommendations. Am J Surg. 2009;197:279–283.
- , , , et al. Evidence‐based red cell transfusion in the critically ill: quality improvement using computerized physician order entry. Crit Care Med. 2006;34:1892–1897.
- , , . The addition of decision support into computerize physician order entry reduces red blood cell transfusion resource utilization in the intensive care unit. Am J Hematol. 2007;82:631–633.
- , , , et al. How we closed the gap between red blood cell utilization and whole blood collections in our institution. Transfusion. 2012;52:1857–1867.
- , , , et al. American College of Critical Care and Eastern Association of Trauma. Clinical practice guideline: red blood cell transfusion practice in adult trauma and critical care. Crit Care Med. 2009;37:3124–3157.
- , , , et al. Red blood cell transfusion: a clinical practice guideline of the AABB. Ann Intern Med. 2012;157:49–58.
- , . Managing clinical knowledge for health care improvement. In: Bemmel J, McCray AT, eds. Yearbook of Medical Informatics 2000: Patient‐Centered Systems. Stuttgart, Germany: Schattauer Verlagsgesellschaft; 2000:65–70.
- , , , et al. Activity‐based costs of blood transfusions in surgical patients at four hospitals. Transfusion. 2010;50:753–764.
- , , . Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Database Syst Rev. 2012;4:CD002042.
- , . Efficacy of RBC transfusion in the critically ill: a systematic review of the literature. Crit Care Med. 2008;36:2667–2674.
- , , , , . A new perspective on best transfusion practice. Blood Transfus. 2013;11:193–202.
- , , , et al. Variation in use of blood transfusion in coronary artery bypass graft surgery. JAMA. 2010;304:1568–1575.
- , , , et al. RBC transfusion practices among critically ill patients: has evidence changed practice? Crit Care Med. 2013;41:2344–2353.
- , , , et al. Why don't physicians follow clinical practice guidelines? JAMA. 1999;282:1458–1465.
- , , , , , . Improved blood utilization using real‐time clinical decision support. Transfusion. 2014;54:1358–1365.
- , , , , , . Computerized physician order entry with decision support decreases blood transfusion in children. Pediatrics. 2011;127:e1112–e1119.
- , , , et al. Reducing the amount of blood transfused. Arch Intern Med. 2005;165:845–852.
- , , , et al. Assessment of education and computerized decision support interventions for improving transfusion practice. Transfusion. 2007;47:228–239.
- , , , , Transfusion insurgency: practice change through education and evidence‐based recommendations. Am J Surg. 2009;197:279–283.
- , , , et al. Evidence‐based red cell transfusion in the critically ill: quality improvement using computerized physician order entry. Crit Care Med. 2006;34:1892–1897.
- , , . The addition of decision support into computerize physician order entry reduces red blood cell transfusion resource utilization in the intensive care unit. Am J Hematol. 2007;82:631–633.
- , , , et al. How we closed the gap between red blood cell utilization and whole blood collections in our institution. Transfusion. 2012;52:1857–1867.
- , , , et al. American College of Critical Care and Eastern Association of Trauma. Clinical practice guideline: red blood cell transfusion practice in adult trauma and critical care. Crit Care Med. 2009;37:3124–3157.
- , , , et al. Red blood cell transfusion: a clinical practice guideline of the AABB. Ann Intern Med. 2012;157:49–58.
- , . Managing clinical knowledge for health care improvement. In: Bemmel J, McCray AT, eds. Yearbook of Medical Informatics 2000: Patient‐Centered Systems. Stuttgart, Germany: Schattauer Verlagsgesellschaft; 2000:65–70.
- , , , et al. Activity‐based costs of blood transfusions in surgical patients at four hospitals. Transfusion. 2010;50:753–764.
© 2014 Society of Hospital Medicine
Hospitalist Care by Geriatricians
Care for hospitalized seniors in acute geriatric units including acute care for the elderly (ACE) units have been shown to reduce function impairment and nursing home admission and possibly mortality, length of stay (LOS), and readmission.[1, 2, 3, 4, 5, 6] These units are run by specialized multidisciplinary teams with direct responsibility for the care of seniors with acute medical illnesses and are often led by geriatricians.[1] However, it is unclear whether these benefits are also achieved by hospitalist care by geriatricians working alongside other internists in general internal medicine units[7] and hospitalist care models.[8] Questions on effectiveness are relevant given the shortage of geriatricians in most healthcare systems and the escalating numbers of seniors requiring acute care. Many of these seniors have cognitive impairment, delirium, and functional decline, and longer hospital stays.[9] Beyond care settings, it is likely that specific subgroups of seniors benefit more from care delivered by geriatricians and their multidisciplinary teams. Patient characteristics defining these subgroups constitute potential targeting criteria, and these include advanced age, functional impairment, and geriatric syndromes.[10] However, to date, supporting evidence that these subgroups accrue greater benefit from care by geriatricians is lacking.[1]
Over this backdrop, our primary study aim was to determine whether hospitalist care by geriatricians for seniors aged 80 years and older in general internal medicine units improves short‐term outcomes compared with care by other internists in the setting of a busy acute‐care hospital. The secondary aim was to determine whether subgroups with premorbid functional impairment and with acute geriatric syndromes receive greater benefit from this care. Our hypotheses were that hospitalist care by geriatricians reduces hospital mortality, 30‐day mortality or readmission, and hospital LOS compared with care by other internists, and that these improvements are greater for the 2 subgroups.
METHODS
Design
This is a retrospective cohort study employing secondary analysis of merged data from clinical records, hospital administrative information, and the national death registry. The local institutional review board approved waiver of consent and other study procedures.
Setting and Patients
Hospital episodes of seniors aged 80 years and over admitted to the 350‐bed general internal medicine department of an acute‐care hospital in Singapore across calendar years 2005 to 2008 comprised the sampling frame. The choice of the study period was influenced by 2 factors. First, geriatricians consistently provided hospitalist care in the general internal medicine department at the study hospital up to 2008 but not after that. Second, administrative data were judged to be less reliable prior to 2005. Those with human immunodeficiency virus disease or acquired immune deficiency syndrome were excluded. Equal numbers of hospital episodes with attending physicians as geriatricians and other internists, and from each calendar year, were randomly sampled for analysis.
Intervention
Hospitalist care by geriatricians was compared with care by other internists who comprised a mix of generalists (with advanced internal medicine training) and subspecialists (including gastroenterologists, endocrinologists, and rheumatologists). Geriatricians and other internists were first certified in internal medicine in a 3‐year training program, before proceeding to either their respective subspecialty training for 3 years or additional training in advanced internal medicine for 2 years. At the general internal medicine department of the study hospital, 10 to 12 internists provided hospitalist care at any time. Of them, 1 to 2 would be geriatricians. All were hospital‐based physicians.
All attending physicians provided hospitalist care for adult patients at general internal medicine wards and led teams of medical residents drawn from a common departmental pool. Nurses, including those with added certification in gerontology, and allied health professionals were generally similar across these wards. In addition, nurse specialists in dementia and continence were accessible for specific consultation. Geriatricians and other internists were rotated to these wards in accordance with monthly rosters that did not have any systematic assignment criteria. They and their team of 2 to 3 residents would typically care for 20 to 30 patients at any time.
In both intervention and control groups, interdisciplinary rounds were not carried out. Rather, ad hoc discussions between physicians and other attending healthcare professionals including physiotherapists, occupational therapists, speech therapists, dieticians, pharmacists, social workers, and case managers took place. Different patients would have varying permutations of these professionals involved in their care at different times during the course of their hospital episode.
Variables
Outcome variables measured were hospital mortality, 30‐day mortality or readmission, and LOS. The latter 2 outcomes were only for hospital admissions of patients who survived and were discharged. Besides attending physicians' specialty, other explanatory variables included demography, living arrangement, hospitalization in the prior 30 days, Elixhauser comorbidity conditions,[11] modified Severity of Illness Index (SII),[12] premorbid functional impairment measured by basic activities of daily living (BADL), acute geriatric syndromes (delirium, falls, impaired mobility), and calendar year. The modified SII is based on 4 clinical parameters items (systolic blood pressure, body temperature, heart rate, and respiratory rate) at admission and was extracted from the clinical charts. It was scaled 0 to 4, with higher scores indicating more severe acute illness. Information on premorbid functional status was extracted from the section of the clinical charts that was mandatory for attending doctors to complete. In a previous study of older hospitalized patients in the general internal medicine department of the study hospital, agreement between data on premorbid functional status from chart review and interview was good.[13] Finally, the presence of acute geriatric syndromes at admission was determined by their documentation in the clinical charts.
Statistical Analysis
Sample size calculation indicated that 1812 patients (906 in each of intervention and control groups) were sufficient to detect a difference of 5% in hospital mortality between the intervention and control groups (15% vs 20%) with 80% power and alpha of 0.05. With anticipated loss of 8% due to unavailability of clinical charts for review, 2000 hospital episodes were sampled (1000 for each group, of which 250 were from each calendar year).
The 3 unadjusted outcome measures for the intervention and control groups constituted the main results. To adjust for any observed differences between the intervention and control groups, logistic regression was performed for hospital mortality and 30‐day mortality or readmission as binary outcomes. Generalized linear models with gamma family and log link were used for the continuous variable of LOS because of its expected right‐skewed distribution. Through these regression analyses, outcome measures were adjusted for age, gender, nursing home residence, hospitalization in the prior 30 days, premorbid functional status, comorbidity, severity of illness, and acute geriatric syndromes. In addition, clustering of hospital episodes within calendar years was addressed using fixed effects with dummy variables. These analyses were repeated for the 2 subgroups of those with premorbid functional impairment (defined as assisted or dependent BADL) and with acute geriatric syndromes (delirium, falls, impaired mobility, incontinence, and impaired self‐care). Listwise deletion was used to address missing values for explanatory variables where they occurred in <5% of hospital episodes analyzed. Clustering due to physicians was not addressed, as only information on whether the attending physician was a geriatrician or another internist was available in the study dataset rather than individual physician identifiers.
As additional analyses to adjust for difference in Diagnosis‐Related Groups (DRG) between intervention and control groups, we identified DRG codes that accounted more than 20 hospital episodes. Remaining DRG codes were aggregated into a single category designated as others. We then included these DRG codes as additional dummy variables in the regression models to observe the extent to which odds ratios for the treatment effect of geriatricians providing hospitalist care were changed.
Statistical analyses were performed using Stata version 13.1 (StateCorp, College Station, TX) with significance taken at the 5% level.
RESULTS
Among 1944 hospital episodes with data available for analysis, 968 received care by geriatricians and 976 by other internists. Death and readmission information at 30 days postdischarge was available for all. Seniors were predominantly female. About one‐quarter of seniors were nursing home residents. Only one‐third had premorbid functional independence. They had a mean number of 3 out of 30 Elixhauser comorbid conditions. Circulatory, respiratory, and genitourinary disorders accounted for more than half of primary diagnoses. The most common acute geriatric syndrome at presentation was delirium, which occurred in 3 out of every 10 seniors. More importantly, intervention and control groups only had minor differences on baseline characteristics, including nursing home residence, which was slightly more common in the intervention group (Table 1). Missing values occurred only for the explanatory variables, living arrangement, and premorbid basic activities of daily living in 0.4% to 2.7% of included hospital episodes.
| Care Led by Geriatricians (n=968) | Care Led by Other Internists (n=976) | P Value | |
|---|---|---|---|
| |||
| Age, mean (SD), y | 86.0 (5.1) | 85.8 (5.1) | 0.52 |
| Male, n (%) | 377 (39.0) | 361 (37.0) | 0.37 |
| Living arrangement, n (%) | 0.09 | ||
| Alone | 19 (2.0) | 21 (2.2) | |
| With other people | 690 (71.3) | 730 (74.8) | |
| Nursing home | 255 (26.3) | 214 (21.9) | |
| Missing | 4 (0.4) | 11 (1.1) | |
| Admission source, n (%) | 0.91 | ||
| Emergency department | 943 (97.4) | 950 (97.3) | |
| Others | 25 (2.6) | 26 (2.7) | |
| Hospital admissions in the prior 30 days, n (%) | 214 (22.1) | 210 (21.5) | 0.75 |
| Year, n (%) | 1.00 | ||
| 2005 | 244 (25.2) | 242 (24.8) | |
| 2006 | 237 (24.5) | 243 (24.9) | |
| 2007 | 241 (24.9) | 244 (25.0) | |
| 2008 | 246 (25.4) | 247 (25.3) | |
| Premorbid basic activities of daily living, n (%) | 0.28 | ||
| Independent | 317 (32.7) | 345 (35.3) | |
| Assisted or dependent | 625 (64.6) | 613 (62.9) | |
| Missing | 26 (2.7) | 18 (1.8) | |
| Elixhauser comorbidity count, mean (SD) | 3.2 (1.6) | 3.2 (1.7) | 0.58 |
| Modified Severity of Illness Index, n (%) | 0.30 | ||
| 1 or 2 | 541 (55.9) | 568 (58.2) | |
| 3 or 4 | 427 (44.1) | 408 (41.8) | |
| Diagnosis‐Related Group category, n (%) | 0.88 | ||
| Circulatory | 110 (11.4) | 110 (11.3) | |
| Digestive | 55 (5.7) | 60 (6.1) | |
| Endocrine, nutritional and metabolic diseases, and immunological | 60 (6.2) | 54 (5.5) | |
| Genitourinary | 146 (15.1) | 172 (17.6) | |
| Mental and nervous | 16 (1.7) | 16 (1.6) | |
| Musculoskeletal | 9 (0.9) | 10 (1.0) | |
| Respiratory | 364 (37.6) | 356 (36.5) | |
| Others | 208 (21.5) | 198 (20.3) | |
| Acute geriatric syndromes, n (%) | |||
| Mobility impairment | 75 (7.7) | 79 (8.1) | 0.78 |
| Falls | 82 (8.5) | 99 (10.1) | 0.21 |
| Delirium | 290 (30.0) | 279 (28.6) | 0.51 |
There were no significant differences in hospital mortality, 30‐day mortality or readmission, and LOS between hospital episodes with care by geriatricians and other internists for the whole group and the 2 subgroups (Table 2). However, nonsignificant reduction in hospital mortality was observed for the whole group (15.5% vs 16.9%, P=0.40), with greater magnitude for the subgroup with acute geriatric syndromes (20.2% vs 23.1%, P=0.31).
| All | Those With Premorbid Functional Impairment | Those With Acute Geriatric Syndromes | ||||
|---|---|---|---|---|---|---|
| Care Led by Geriatricians | Care Led by Other Internists | Care Led by Geriatricians | Care Led by Other Internists | Care Led by Geriatricians | Care Led by Other Internists | |
| ||||||
| Hospital mortality, n (%) | 150/968 (15.5) | 165/976 (16.9), P=0.40 | 125/625 (20.0) | 137/613 (22.4), P=0.31 | 79/392 (20.2) | 92/398 (23.1), P=0.31 |
| 30‐day mortality or readmission, n (%) | 206/818 (25.2) | 200/811 (24.7), P=0.81 | 147/500, (29.4) | 144/476, (30.3), P=0.77 | 88/313, (28.1) | 83/306, (27.1), P=0.78 |
| Mean length of stay, days (SD) | 9.7 (10.2), n=818 | 9.7 (10.9), n=811, P=0.87 | 11.1 (10.7), n=500 | 11.1 (12.3), n=476, P=0.93 | 11.4 (12.5), n=321 | 10.8 (13.0), n=312, P=0.57 |
When adjusted for age, gender, premorbid functional status, comorbidity, severity of illness, acute geriatric syndromes, hospitalization in the prior 30 days, and calendar year, care by geriatricians was associated with nonsignificant trends toward lower hospital mortality, with odds ratios between 0.80 and 0.89. However, 30‐day mortality or readmission and LOS for the intervention and control groups were generally equivalent (Table 3). There are only minor differences between the odds ratios and their 95% confidence intervals for regression analyses without and with additional adjustment for DRG codes (results not shown). Thus, they do not change the study results in any significant way.
| Care by Geriatricians (Ref: Care by Other Internists) | All | Those With Premorbid Functional Impairment | Those With Acute Geriatric Syndromes |
|---|---|---|---|
| |||
| Hospital mortality: odds ratio (95% confidence interval) | 0.89 (0.69 to 1.16), n=1,886, P=0.40 | 0.85 (0.64 to 1.13), n=1,233, P=0.27 | 0.80 (0.55 to 1.16), n=764, P=0.24 |
| 30‐day mortality or readmission: odds ratio (95% confidence interval) | 1.05 (0.82 to 1.33), n=1,580, P=0.71 | 0.94 (0.71 to 1.25), n=973, P=0.69 | 1.03 (0.70 to 1.50), n=600, P=0.89 |
| Length of stay: log days (95% confidence interval) | 0.03 (0.14 to 0.07), n=1,580, P=0.52 | 0.03 (0.16 to 0.10), n=973, P=0.68 | 0.00 (0.18 to 0.18), n=600, P=1.00 |
DISCUSSION
Geriatricians provide direct acute hospital care for seniors either in dedicated acute geriatric units including ACE units[14] or alongside generalists or subspecialty physicians in general internal medicine units. Through an unique opportunity to study the latter arrangement, we found that hospitalist care by geriatricians for seniors aged 80 years and older in general internal medicine units did not improve their short‐term outcomes vis‐‐vis care by other internists. These findings are in contrast to those of studies on acute geriatric units. This is the first report on the effectiveness of hospitalist care for seniors provided by geriatricians. Although not a randomized controlled trial, our study is in essence a natural experiment which does not impose any major inclusion restrictions other than age of 80 years and above. Internal validity was enhanced by intervention and control groups being similar on individual‐level characteristics, whereas external validity was boosted by an all‐comers approach to enrollment.
It is pertinent to ask why hospitalist care by geriatricians in a general internal medicine department did not benefit seniors with advanced age, many of whom have functional impairment and multimorbidity. After all, improved care and outcomes seem plausible for these seniors who appear to be more vulnerable. We propose 4 possible explanations. First, unmeasured differences between intervention and control groups could have led to unobserved confounding. However, this is less likely given the nonsystematic assignment of attending physicians to different wards and similarity of intervention and control groups on a broad range of baseline characteristics. Second, care processes in wards allocated to geriatricians may not differ very much from those in other wards. Irrespective of ward, care delivered by medical residents and other healthcare professionals were also expected to be similar. Unlike acute geriatric units where comprehensive geriatric assessment (CGA) by a multidisciplinary team is thought to be responsible for the improved outcomes,[12] the influence of geriatricians outside of these units may not necessarily achieve the same level of geriatric care.[15, 16] This is precisely the challenge encountered by geriatricians in their care of acutely ill older patients in settings other than acute geriatric units, Third, diffusion of geriatric care practices across general internal medicine wards over the past decade at our hospital may have resulted in narrowed differences in the care processes particularly relevant to seniors, such as those related to functional retraining, swallowing assessment, and discharge planning, although we do not have any specific data to confirm this. These differences may in turn not be wide enough for hospitalist care by geriatricians to influence these short‐term outcomes positively. Last, our study was not designed to measure patient‐reported outcomes such as functional status, mood, quality of life, and satisfaction, which may arguably be more responsive to geriatric intervention.
It might be noted that the average LOS for hospital episodes in this study was almost 10 days, which is longer than that typically seen in North America. There are 2 possible reasons for this. First, these are hospital episodes of very old patients, and longer LOS among survivors is expected. Second, post‐acute care was not as well developed in Singapore during the study period. Since then, the system of community hospitals has expanded, thereby allowing earlier transfer to these facilities for post‐acute care and shorter LOS at acute‐care hospitals.
There are a number of limitations of our study. First, this is an observational study where treatment assignment is not allocated. Although a randomized controlled trial may be the ideal design to evaluate treatment effects, operational and ethical considerations at a busy acute‐care hospital render this very challenging to conduct. As mentioned, nonsystematic assignment of attending physicians to different wards and lack of important baseline differences between intervention and control groups support the notion that important unmeasured differences are less likely. Second, and as alluded to, we did not measure relevant patient‐reported outcomes. Nonetheless, we argue that survival is still important to many seniors, particularly those without advanced illness, whereas readmission avoidance and shorter hospital stay matter almost universally. Third, clinical charts were unavailable for data extraction in almost 3% of hospital episodes. In addition, there were missing values in 2 explanatory variables in <3% of available clinical charts. These missing values were handled by listwise deletion in the regression analyses. Doing so carries with it the risk of introducing bias in the estimation of the treatment effect of care by geriatricians. However, given the relatively small proportions of missing charts and values, it is less likely that any bias would have changed the study conclusions. Fourth, we did not account for clustering at the physician level, which would have widened the confidence intervals for the odds ratios. However, because all treatment effects on the 3 outcomes were clearly not statistically significant, widening of confidence intervals would not have changed the results and study conclusions. Finally, this is a single institution study in a single health system. Thus, caution is necessary when attempting to extrapolate its results. On the other hand, the major strength of this study is its real‐world setting, which allows the results to be more generalizable to other hospital systems with similar organization and practice of general internal medicine.
Our findings need to be placed in the context of emerging innovative models of care for hospitalized seniors, which directly or indirectly involve geriatricians. Besides traditional ACE units, which have fixed geographical locations within a hospital, a mobile acute care of the elderly service achieved shorter LOS and reduced cost than the established ACE unit with similar mortality and readmission rates.[17] Others include a proactive geriatrics consultation model in collaboration with hospitalists.[18] Another variant of the ACE unit is the hospitalist‐run acute care for the elderly (hospitalist‐ACE) service, which improved care processes without improving clinical outcomes or increasing cost.[19] Clearly, there needs to be better collaboration between hospitalists and geriatricians to improve care of acutely ill seniors.[20] Ultimately, any form of direct geriatrician care for seniors needs to be complimented by indirect care through hospital‐wide systems such the Hospital Elder Life Program. This model of care aims to prevent cognitive and functional decline in hospitalized seniors by combining CGA with protocol‐driven interventions ranging from orientation, visitation, feeding assistance, early mobilization, and visual and hearing adaptations.[21, 22]
In conclusion, hospitalist care for seniors aged 80 years and above by geriatricians based in general internal medicine units is not more effective than care by other internists, at least where reducing short‐term mortality and readmission and LOS are concerned. This is particularly applicable to hospital systems where geriatric care elements have already been widely adopted beyond the confines of acute geriatric units. However, these findings do not by any means indicate that hospitalist care provided by geriatricians is altogether not more beneficial for these seniors than care by other internists in general internal medicine units. Rather, further research on patient‐reported outcomes can clarify more fully the geriatrician's true role in this setting.
Disclosures
This study was wholly funded by the National Healthcare Group Small Innovative Grants. The funders did not play any other role in this study. The authors report no conflicts of interest.
- , , , , . Effectiveness of acute geriatric units on functional decline, living at home, and case fatality among older patients admitted to hospital for acute medical disorders: meta‐analysis. BMJ. 2009;338:b50.
- , , , , . Comprehensive geriatric assessment: a meta‐analysis of controlled trials. Lancet. 1993;342(8878):1032–1036.
- , , , et al. A controlled trial of inpatient and outpatient geriatric evaluation and management. N Engl J Med. 2002;346(12):905–912.
- , , , , . Comprehensive geriatric assessment for older adults admitted to hospital: meta‐analysis of randomised controlled trials. BMJ. 2011;343:d6553.
- , , , , . Reduced mortality in treating acutely sick, frail older patients in a geriatric evaluation and management unit. A prospective randomized trial. J Am Geriatr Soc. 2002;50(5):792–798.
- , , , et al. Effectiveness of acute geriatric unit care using acute care for elders components: a systematic review and meta‐analysis. J Am Geriatr Soc. 2012;60:2237–2245.
- , . Age‐related geriatric medicine or integrated medical care? Age Ageing. 1999;28:245–247.
- . An introduction to the hospitalist model. Ann Intern Med. 1999;130(4 pt 2):338–342.
- . Care of hospitalized older patients: opportunities for hospital‐based physicians. J Hosp Med. 2006;1:42–47.
- , , , . Which patients benefit the most from a geriatrician's care? Consensus among directors of geriatrics academic programs. J Am Geriatr Soc. 2008;56(10):1796–1801.
- , , , et al. Comorbidity measure for use with administrative data. Med Care. 1998;36:8–27.
- , , , , . Resource consumption in hospitalised, frail older patients. Ann Acad Med Singapore. 2010;39:830–836.
- , , , , . Impact of data source and time reference of functional status on hospital mortality prediction. BMC Health Serv Res. 2012;12:115.
- , , , , . A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332:1338–1344.
- , , . Acute hospital care for frail older people. Age Ageing. 2006;35:551–552.
- , . Comprehensive geriatric assessment for older hospital patients. Br Med Bull. 2005;71:45–59.
- , , , et al. Operational and quality outcomes of a mobile acute care for the elderly service. J Hosp Med. 2011;6:358–363.
- , , , . Development and implementation of a proactive geriatrics consultation model in collaboration with hospitalists. J Am Geriatr Soc. 2009;57:2139–2145.
- , , , et al. Evaluation of a hospitalist‐run acute care for the elderly service. J Hosp Med. 2011;6:313–321.
- , , . Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs. J Hosp Med. 2006;1:29–35.
- , , , et al. The Hospital Elder Life Program: A model of care to prevent cognitive and functional decline in hospitalized older patients. J Am Geriatr Soc. 2000;48:1697–1706.
- . Organizational interventions to improve health outcomes of older persons. Med Care. 2002;40:416–428.
Care for hospitalized seniors in acute geriatric units including acute care for the elderly (ACE) units have been shown to reduce function impairment and nursing home admission and possibly mortality, length of stay (LOS), and readmission.[1, 2, 3, 4, 5, 6] These units are run by specialized multidisciplinary teams with direct responsibility for the care of seniors with acute medical illnesses and are often led by geriatricians.[1] However, it is unclear whether these benefits are also achieved by hospitalist care by geriatricians working alongside other internists in general internal medicine units[7] and hospitalist care models.[8] Questions on effectiveness are relevant given the shortage of geriatricians in most healthcare systems and the escalating numbers of seniors requiring acute care. Many of these seniors have cognitive impairment, delirium, and functional decline, and longer hospital stays.[9] Beyond care settings, it is likely that specific subgroups of seniors benefit more from care delivered by geriatricians and their multidisciplinary teams. Patient characteristics defining these subgroups constitute potential targeting criteria, and these include advanced age, functional impairment, and geriatric syndromes.[10] However, to date, supporting evidence that these subgroups accrue greater benefit from care by geriatricians is lacking.[1]
Over this backdrop, our primary study aim was to determine whether hospitalist care by geriatricians for seniors aged 80 years and older in general internal medicine units improves short‐term outcomes compared with care by other internists in the setting of a busy acute‐care hospital. The secondary aim was to determine whether subgroups with premorbid functional impairment and with acute geriatric syndromes receive greater benefit from this care. Our hypotheses were that hospitalist care by geriatricians reduces hospital mortality, 30‐day mortality or readmission, and hospital LOS compared with care by other internists, and that these improvements are greater for the 2 subgroups.
METHODS
Design
This is a retrospective cohort study employing secondary analysis of merged data from clinical records, hospital administrative information, and the national death registry. The local institutional review board approved waiver of consent and other study procedures.
Setting and Patients
Hospital episodes of seniors aged 80 years and over admitted to the 350‐bed general internal medicine department of an acute‐care hospital in Singapore across calendar years 2005 to 2008 comprised the sampling frame. The choice of the study period was influenced by 2 factors. First, geriatricians consistently provided hospitalist care in the general internal medicine department at the study hospital up to 2008 but not after that. Second, administrative data were judged to be less reliable prior to 2005. Those with human immunodeficiency virus disease or acquired immune deficiency syndrome were excluded. Equal numbers of hospital episodes with attending physicians as geriatricians and other internists, and from each calendar year, were randomly sampled for analysis.
Intervention
Hospitalist care by geriatricians was compared with care by other internists who comprised a mix of generalists (with advanced internal medicine training) and subspecialists (including gastroenterologists, endocrinologists, and rheumatologists). Geriatricians and other internists were first certified in internal medicine in a 3‐year training program, before proceeding to either their respective subspecialty training for 3 years or additional training in advanced internal medicine for 2 years. At the general internal medicine department of the study hospital, 10 to 12 internists provided hospitalist care at any time. Of them, 1 to 2 would be geriatricians. All were hospital‐based physicians.
All attending physicians provided hospitalist care for adult patients at general internal medicine wards and led teams of medical residents drawn from a common departmental pool. Nurses, including those with added certification in gerontology, and allied health professionals were generally similar across these wards. In addition, nurse specialists in dementia and continence were accessible for specific consultation. Geriatricians and other internists were rotated to these wards in accordance with monthly rosters that did not have any systematic assignment criteria. They and their team of 2 to 3 residents would typically care for 20 to 30 patients at any time.
In both intervention and control groups, interdisciplinary rounds were not carried out. Rather, ad hoc discussions between physicians and other attending healthcare professionals including physiotherapists, occupational therapists, speech therapists, dieticians, pharmacists, social workers, and case managers took place. Different patients would have varying permutations of these professionals involved in their care at different times during the course of their hospital episode.
Variables
Outcome variables measured were hospital mortality, 30‐day mortality or readmission, and LOS. The latter 2 outcomes were only for hospital admissions of patients who survived and were discharged. Besides attending physicians' specialty, other explanatory variables included demography, living arrangement, hospitalization in the prior 30 days, Elixhauser comorbidity conditions,[11] modified Severity of Illness Index (SII),[12] premorbid functional impairment measured by basic activities of daily living (BADL), acute geriatric syndromes (delirium, falls, impaired mobility), and calendar year. The modified SII is based on 4 clinical parameters items (systolic blood pressure, body temperature, heart rate, and respiratory rate) at admission and was extracted from the clinical charts. It was scaled 0 to 4, with higher scores indicating more severe acute illness. Information on premorbid functional status was extracted from the section of the clinical charts that was mandatory for attending doctors to complete. In a previous study of older hospitalized patients in the general internal medicine department of the study hospital, agreement between data on premorbid functional status from chart review and interview was good.[13] Finally, the presence of acute geriatric syndromes at admission was determined by their documentation in the clinical charts.
Statistical Analysis
Sample size calculation indicated that 1812 patients (906 in each of intervention and control groups) were sufficient to detect a difference of 5% in hospital mortality between the intervention and control groups (15% vs 20%) with 80% power and alpha of 0.05. With anticipated loss of 8% due to unavailability of clinical charts for review, 2000 hospital episodes were sampled (1000 for each group, of which 250 were from each calendar year).
The 3 unadjusted outcome measures for the intervention and control groups constituted the main results. To adjust for any observed differences between the intervention and control groups, logistic regression was performed for hospital mortality and 30‐day mortality or readmission as binary outcomes. Generalized linear models with gamma family and log link were used for the continuous variable of LOS because of its expected right‐skewed distribution. Through these regression analyses, outcome measures were adjusted for age, gender, nursing home residence, hospitalization in the prior 30 days, premorbid functional status, comorbidity, severity of illness, and acute geriatric syndromes. In addition, clustering of hospital episodes within calendar years was addressed using fixed effects with dummy variables. These analyses were repeated for the 2 subgroups of those with premorbid functional impairment (defined as assisted or dependent BADL) and with acute geriatric syndromes (delirium, falls, impaired mobility, incontinence, and impaired self‐care). Listwise deletion was used to address missing values for explanatory variables where they occurred in <5% of hospital episodes analyzed. Clustering due to physicians was not addressed, as only information on whether the attending physician was a geriatrician or another internist was available in the study dataset rather than individual physician identifiers.
As additional analyses to adjust for difference in Diagnosis‐Related Groups (DRG) between intervention and control groups, we identified DRG codes that accounted more than 20 hospital episodes. Remaining DRG codes were aggregated into a single category designated as others. We then included these DRG codes as additional dummy variables in the regression models to observe the extent to which odds ratios for the treatment effect of geriatricians providing hospitalist care were changed.
Statistical analyses were performed using Stata version 13.1 (StateCorp, College Station, TX) with significance taken at the 5% level.
RESULTS
Among 1944 hospital episodes with data available for analysis, 968 received care by geriatricians and 976 by other internists. Death and readmission information at 30 days postdischarge was available for all. Seniors were predominantly female. About one‐quarter of seniors were nursing home residents. Only one‐third had premorbid functional independence. They had a mean number of 3 out of 30 Elixhauser comorbid conditions. Circulatory, respiratory, and genitourinary disorders accounted for more than half of primary diagnoses. The most common acute geriatric syndrome at presentation was delirium, which occurred in 3 out of every 10 seniors. More importantly, intervention and control groups only had minor differences on baseline characteristics, including nursing home residence, which was slightly more common in the intervention group (Table 1). Missing values occurred only for the explanatory variables, living arrangement, and premorbid basic activities of daily living in 0.4% to 2.7% of included hospital episodes.
| Care Led by Geriatricians (n=968) | Care Led by Other Internists (n=976) | P Value | |
|---|---|---|---|
| |||
| Age, mean (SD), y | 86.0 (5.1) | 85.8 (5.1) | 0.52 |
| Male, n (%) | 377 (39.0) | 361 (37.0) | 0.37 |
| Living arrangement, n (%) | 0.09 | ||
| Alone | 19 (2.0) | 21 (2.2) | |
| With other people | 690 (71.3) | 730 (74.8) | |
| Nursing home | 255 (26.3) | 214 (21.9) | |
| Missing | 4 (0.4) | 11 (1.1) | |
| Admission source, n (%) | 0.91 | ||
| Emergency department | 943 (97.4) | 950 (97.3) | |
| Others | 25 (2.6) | 26 (2.7) | |
| Hospital admissions in the prior 30 days, n (%) | 214 (22.1) | 210 (21.5) | 0.75 |
| Year, n (%) | 1.00 | ||
| 2005 | 244 (25.2) | 242 (24.8) | |
| 2006 | 237 (24.5) | 243 (24.9) | |
| 2007 | 241 (24.9) | 244 (25.0) | |
| 2008 | 246 (25.4) | 247 (25.3) | |
| Premorbid basic activities of daily living, n (%) | 0.28 | ||
| Independent | 317 (32.7) | 345 (35.3) | |
| Assisted or dependent | 625 (64.6) | 613 (62.9) | |
| Missing | 26 (2.7) | 18 (1.8) | |
| Elixhauser comorbidity count, mean (SD) | 3.2 (1.6) | 3.2 (1.7) | 0.58 |
| Modified Severity of Illness Index, n (%) | 0.30 | ||
| 1 or 2 | 541 (55.9) | 568 (58.2) | |
| 3 or 4 | 427 (44.1) | 408 (41.8) | |
| Diagnosis‐Related Group category, n (%) | 0.88 | ||
| Circulatory | 110 (11.4) | 110 (11.3) | |
| Digestive | 55 (5.7) | 60 (6.1) | |
| Endocrine, nutritional and metabolic diseases, and immunological | 60 (6.2) | 54 (5.5) | |
| Genitourinary | 146 (15.1) | 172 (17.6) | |
| Mental and nervous | 16 (1.7) | 16 (1.6) | |
| Musculoskeletal | 9 (0.9) | 10 (1.0) | |
| Respiratory | 364 (37.6) | 356 (36.5) | |
| Others | 208 (21.5) | 198 (20.3) | |
| Acute geriatric syndromes, n (%) | |||
| Mobility impairment | 75 (7.7) | 79 (8.1) | 0.78 |
| Falls | 82 (8.5) | 99 (10.1) | 0.21 |
| Delirium | 290 (30.0) | 279 (28.6) | 0.51 |
There were no significant differences in hospital mortality, 30‐day mortality or readmission, and LOS between hospital episodes with care by geriatricians and other internists for the whole group and the 2 subgroups (Table 2). However, nonsignificant reduction in hospital mortality was observed for the whole group (15.5% vs 16.9%, P=0.40), with greater magnitude for the subgroup with acute geriatric syndromes (20.2% vs 23.1%, P=0.31).
| All | Those With Premorbid Functional Impairment | Those With Acute Geriatric Syndromes | ||||
|---|---|---|---|---|---|---|
| Care Led by Geriatricians | Care Led by Other Internists | Care Led by Geriatricians | Care Led by Other Internists | Care Led by Geriatricians | Care Led by Other Internists | |
| ||||||
| Hospital mortality, n (%) | 150/968 (15.5) | 165/976 (16.9), P=0.40 | 125/625 (20.0) | 137/613 (22.4), P=0.31 | 79/392 (20.2) | 92/398 (23.1), P=0.31 |
| 30‐day mortality or readmission, n (%) | 206/818 (25.2) | 200/811 (24.7), P=0.81 | 147/500, (29.4) | 144/476, (30.3), P=0.77 | 88/313, (28.1) | 83/306, (27.1), P=0.78 |
| Mean length of stay, days (SD) | 9.7 (10.2), n=818 | 9.7 (10.9), n=811, P=0.87 | 11.1 (10.7), n=500 | 11.1 (12.3), n=476, P=0.93 | 11.4 (12.5), n=321 | 10.8 (13.0), n=312, P=0.57 |
When adjusted for age, gender, premorbid functional status, comorbidity, severity of illness, acute geriatric syndromes, hospitalization in the prior 30 days, and calendar year, care by geriatricians was associated with nonsignificant trends toward lower hospital mortality, with odds ratios between 0.80 and 0.89. However, 30‐day mortality or readmission and LOS for the intervention and control groups were generally equivalent (Table 3). There are only minor differences between the odds ratios and their 95% confidence intervals for regression analyses without and with additional adjustment for DRG codes (results not shown). Thus, they do not change the study results in any significant way.
| Care by Geriatricians (Ref: Care by Other Internists) | All | Those With Premorbid Functional Impairment | Those With Acute Geriatric Syndromes |
|---|---|---|---|
| |||
| Hospital mortality: odds ratio (95% confidence interval) | 0.89 (0.69 to 1.16), n=1,886, P=0.40 | 0.85 (0.64 to 1.13), n=1,233, P=0.27 | 0.80 (0.55 to 1.16), n=764, P=0.24 |
| 30‐day mortality or readmission: odds ratio (95% confidence interval) | 1.05 (0.82 to 1.33), n=1,580, P=0.71 | 0.94 (0.71 to 1.25), n=973, P=0.69 | 1.03 (0.70 to 1.50), n=600, P=0.89 |
| Length of stay: log days (95% confidence interval) | 0.03 (0.14 to 0.07), n=1,580, P=0.52 | 0.03 (0.16 to 0.10), n=973, P=0.68 | 0.00 (0.18 to 0.18), n=600, P=1.00 |
DISCUSSION
Geriatricians provide direct acute hospital care for seniors either in dedicated acute geriatric units including ACE units[14] or alongside generalists or subspecialty physicians in general internal medicine units. Through an unique opportunity to study the latter arrangement, we found that hospitalist care by geriatricians for seniors aged 80 years and older in general internal medicine units did not improve their short‐term outcomes vis‐‐vis care by other internists. These findings are in contrast to those of studies on acute geriatric units. This is the first report on the effectiveness of hospitalist care for seniors provided by geriatricians. Although not a randomized controlled trial, our study is in essence a natural experiment which does not impose any major inclusion restrictions other than age of 80 years and above. Internal validity was enhanced by intervention and control groups being similar on individual‐level characteristics, whereas external validity was boosted by an all‐comers approach to enrollment.
It is pertinent to ask why hospitalist care by geriatricians in a general internal medicine department did not benefit seniors with advanced age, many of whom have functional impairment and multimorbidity. After all, improved care and outcomes seem plausible for these seniors who appear to be more vulnerable. We propose 4 possible explanations. First, unmeasured differences between intervention and control groups could have led to unobserved confounding. However, this is less likely given the nonsystematic assignment of attending physicians to different wards and similarity of intervention and control groups on a broad range of baseline characteristics. Second, care processes in wards allocated to geriatricians may not differ very much from those in other wards. Irrespective of ward, care delivered by medical residents and other healthcare professionals were also expected to be similar. Unlike acute geriatric units where comprehensive geriatric assessment (CGA) by a multidisciplinary team is thought to be responsible for the improved outcomes,[12] the influence of geriatricians outside of these units may not necessarily achieve the same level of geriatric care.[15, 16] This is precisely the challenge encountered by geriatricians in their care of acutely ill older patients in settings other than acute geriatric units, Third, diffusion of geriatric care practices across general internal medicine wards over the past decade at our hospital may have resulted in narrowed differences in the care processes particularly relevant to seniors, such as those related to functional retraining, swallowing assessment, and discharge planning, although we do not have any specific data to confirm this. These differences may in turn not be wide enough for hospitalist care by geriatricians to influence these short‐term outcomes positively. Last, our study was not designed to measure patient‐reported outcomes such as functional status, mood, quality of life, and satisfaction, which may arguably be more responsive to geriatric intervention.
It might be noted that the average LOS for hospital episodes in this study was almost 10 days, which is longer than that typically seen in North America. There are 2 possible reasons for this. First, these are hospital episodes of very old patients, and longer LOS among survivors is expected. Second, post‐acute care was not as well developed in Singapore during the study period. Since then, the system of community hospitals has expanded, thereby allowing earlier transfer to these facilities for post‐acute care and shorter LOS at acute‐care hospitals.
There are a number of limitations of our study. First, this is an observational study where treatment assignment is not allocated. Although a randomized controlled trial may be the ideal design to evaluate treatment effects, operational and ethical considerations at a busy acute‐care hospital render this very challenging to conduct. As mentioned, nonsystematic assignment of attending physicians to different wards and lack of important baseline differences between intervention and control groups support the notion that important unmeasured differences are less likely. Second, and as alluded to, we did not measure relevant patient‐reported outcomes. Nonetheless, we argue that survival is still important to many seniors, particularly those without advanced illness, whereas readmission avoidance and shorter hospital stay matter almost universally. Third, clinical charts were unavailable for data extraction in almost 3% of hospital episodes. In addition, there were missing values in 2 explanatory variables in <3% of available clinical charts. These missing values were handled by listwise deletion in the regression analyses. Doing so carries with it the risk of introducing bias in the estimation of the treatment effect of care by geriatricians. However, given the relatively small proportions of missing charts and values, it is less likely that any bias would have changed the study conclusions. Fourth, we did not account for clustering at the physician level, which would have widened the confidence intervals for the odds ratios. However, because all treatment effects on the 3 outcomes were clearly not statistically significant, widening of confidence intervals would not have changed the results and study conclusions. Finally, this is a single institution study in a single health system. Thus, caution is necessary when attempting to extrapolate its results. On the other hand, the major strength of this study is its real‐world setting, which allows the results to be more generalizable to other hospital systems with similar organization and practice of general internal medicine.
Our findings need to be placed in the context of emerging innovative models of care for hospitalized seniors, which directly or indirectly involve geriatricians. Besides traditional ACE units, which have fixed geographical locations within a hospital, a mobile acute care of the elderly service achieved shorter LOS and reduced cost than the established ACE unit with similar mortality and readmission rates.[17] Others include a proactive geriatrics consultation model in collaboration with hospitalists.[18] Another variant of the ACE unit is the hospitalist‐run acute care for the elderly (hospitalist‐ACE) service, which improved care processes without improving clinical outcomes or increasing cost.[19] Clearly, there needs to be better collaboration between hospitalists and geriatricians to improve care of acutely ill seniors.[20] Ultimately, any form of direct geriatrician care for seniors needs to be complimented by indirect care through hospital‐wide systems such the Hospital Elder Life Program. This model of care aims to prevent cognitive and functional decline in hospitalized seniors by combining CGA with protocol‐driven interventions ranging from orientation, visitation, feeding assistance, early mobilization, and visual and hearing adaptations.[21, 22]
In conclusion, hospitalist care for seniors aged 80 years and above by geriatricians based in general internal medicine units is not more effective than care by other internists, at least where reducing short‐term mortality and readmission and LOS are concerned. This is particularly applicable to hospital systems where geriatric care elements have already been widely adopted beyond the confines of acute geriatric units. However, these findings do not by any means indicate that hospitalist care provided by geriatricians is altogether not more beneficial for these seniors than care by other internists in general internal medicine units. Rather, further research on patient‐reported outcomes can clarify more fully the geriatrician's true role in this setting.
Disclosures
This study was wholly funded by the National Healthcare Group Small Innovative Grants. The funders did not play any other role in this study. The authors report no conflicts of interest.
Care for hospitalized seniors in acute geriatric units including acute care for the elderly (ACE) units have been shown to reduce function impairment and nursing home admission and possibly mortality, length of stay (LOS), and readmission.[1, 2, 3, 4, 5, 6] These units are run by specialized multidisciplinary teams with direct responsibility for the care of seniors with acute medical illnesses and are often led by geriatricians.[1] However, it is unclear whether these benefits are also achieved by hospitalist care by geriatricians working alongside other internists in general internal medicine units[7] and hospitalist care models.[8] Questions on effectiveness are relevant given the shortage of geriatricians in most healthcare systems and the escalating numbers of seniors requiring acute care. Many of these seniors have cognitive impairment, delirium, and functional decline, and longer hospital stays.[9] Beyond care settings, it is likely that specific subgroups of seniors benefit more from care delivered by geriatricians and their multidisciplinary teams. Patient characteristics defining these subgroups constitute potential targeting criteria, and these include advanced age, functional impairment, and geriatric syndromes.[10] However, to date, supporting evidence that these subgroups accrue greater benefit from care by geriatricians is lacking.[1]
Over this backdrop, our primary study aim was to determine whether hospitalist care by geriatricians for seniors aged 80 years and older in general internal medicine units improves short‐term outcomes compared with care by other internists in the setting of a busy acute‐care hospital. The secondary aim was to determine whether subgroups with premorbid functional impairment and with acute geriatric syndromes receive greater benefit from this care. Our hypotheses were that hospitalist care by geriatricians reduces hospital mortality, 30‐day mortality or readmission, and hospital LOS compared with care by other internists, and that these improvements are greater for the 2 subgroups.
METHODS
Design
This is a retrospective cohort study employing secondary analysis of merged data from clinical records, hospital administrative information, and the national death registry. The local institutional review board approved waiver of consent and other study procedures.
Setting and Patients
Hospital episodes of seniors aged 80 years and over admitted to the 350‐bed general internal medicine department of an acute‐care hospital in Singapore across calendar years 2005 to 2008 comprised the sampling frame. The choice of the study period was influenced by 2 factors. First, geriatricians consistently provided hospitalist care in the general internal medicine department at the study hospital up to 2008 but not after that. Second, administrative data were judged to be less reliable prior to 2005. Those with human immunodeficiency virus disease or acquired immune deficiency syndrome were excluded. Equal numbers of hospital episodes with attending physicians as geriatricians and other internists, and from each calendar year, were randomly sampled for analysis.
Intervention
Hospitalist care by geriatricians was compared with care by other internists who comprised a mix of generalists (with advanced internal medicine training) and subspecialists (including gastroenterologists, endocrinologists, and rheumatologists). Geriatricians and other internists were first certified in internal medicine in a 3‐year training program, before proceeding to either their respective subspecialty training for 3 years or additional training in advanced internal medicine for 2 years. At the general internal medicine department of the study hospital, 10 to 12 internists provided hospitalist care at any time. Of them, 1 to 2 would be geriatricians. All were hospital‐based physicians.
All attending physicians provided hospitalist care for adult patients at general internal medicine wards and led teams of medical residents drawn from a common departmental pool. Nurses, including those with added certification in gerontology, and allied health professionals were generally similar across these wards. In addition, nurse specialists in dementia and continence were accessible for specific consultation. Geriatricians and other internists were rotated to these wards in accordance with monthly rosters that did not have any systematic assignment criteria. They and their team of 2 to 3 residents would typically care for 20 to 30 patients at any time.
In both intervention and control groups, interdisciplinary rounds were not carried out. Rather, ad hoc discussions between physicians and other attending healthcare professionals including physiotherapists, occupational therapists, speech therapists, dieticians, pharmacists, social workers, and case managers took place. Different patients would have varying permutations of these professionals involved in their care at different times during the course of their hospital episode.
Variables
Outcome variables measured were hospital mortality, 30‐day mortality or readmission, and LOS. The latter 2 outcomes were only for hospital admissions of patients who survived and were discharged. Besides attending physicians' specialty, other explanatory variables included demography, living arrangement, hospitalization in the prior 30 days, Elixhauser comorbidity conditions,[11] modified Severity of Illness Index (SII),[12] premorbid functional impairment measured by basic activities of daily living (BADL), acute geriatric syndromes (delirium, falls, impaired mobility), and calendar year. The modified SII is based on 4 clinical parameters items (systolic blood pressure, body temperature, heart rate, and respiratory rate) at admission and was extracted from the clinical charts. It was scaled 0 to 4, with higher scores indicating more severe acute illness. Information on premorbid functional status was extracted from the section of the clinical charts that was mandatory for attending doctors to complete. In a previous study of older hospitalized patients in the general internal medicine department of the study hospital, agreement between data on premorbid functional status from chart review and interview was good.[13] Finally, the presence of acute geriatric syndromes at admission was determined by their documentation in the clinical charts.
Statistical Analysis
Sample size calculation indicated that 1812 patients (906 in each of intervention and control groups) were sufficient to detect a difference of 5% in hospital mortality between the intervention and control groups (15% vs 20%) with 80% power and alpha of 0.05. With anticipated loss of 8% due to unavailability of clinical charts for review, 2000 hospital episodes were sampled (1000 for each group, of which 250 were from each calendar year).
The 3 unadjusted outcome measures for the intervention and control groups constituted the main results. To adjust for any observed differences between the intervention and control groups, logistic regression was performed for hospital mortality and 30‐day mortality or readmission as binary outcomes. Generalized linear models with gamma family and log link were used for the continuous variable of LOS because of its expected right‐skewed distribution. Through these regression analyses, outcome measures were adjusted for age, gender, nursing home residence, hospitalization in the prior 30 days, premorbid functional status, comorbidity, severity of illness, and acute geriatric syndromes. In addition, clustering of hospital episodes within calendar years was addressed using fixed effects with dummy variables. These analyses were repeated for the 2 subgroups of those with premorbid functional impairment (defined as assisted or dependent BADL) and with acute geriatric syndromes (delirium, falls, impaired mobility, incontinence, and impaired self‐care). Listwise deletion was used to address missing values for explanatory variables where they occurred in <5% of hospital episodes analyzed. Clustering due to physicians was not addressed, as only information on whether the attending physician was a geriatrician or another internist was available in the study dataset rather than individual physician identifiers.
As additional analyses to adjust for difference in Diagnosis‐Related Groups (DRG) between intervention and control groups, we identified DRG codes that accounted more than 20 hospital episodes. Remaining DRG codes were aggregated into a single category designated as others. We then included these DRG codes as additional dummy variables in the regression models to observe the extent to which odds ratios for the treatment effect of geriatricians providing hospitalist care were changed.
Statistical analyses were performed using Stata version 13.1 (StateCorp, College Station, TX) with significance taken at the 5% level.
RESULTS
Among 1944 hospital episodes with data available for analysis, 968 received care by geriatricians and 976 by other internists. Death and readmission information at 30 days postdischarge was available for all. Seniors were predominantly female. About one‐quarter of seniors were nursing home residents. Only one‐third had premorbid functional independence. They had a mean number of 3 out of 30 Elixhauser comorbid conditions. Circulatory, respiratory, and genitourinary disorders accounted for more than half of primary diagnoses. The most common acute geriatric syndrome at presentation was delirium, which occurred in 3 out of every 10 seniors. More importantly, intervention and control groups only had minor differences on baseline characteristics, including nursing home residence, which was slightly more common in the intervention group (Table 1). Missing values occurred only for the explanatory variables, living arrangement, and premorbid basic activities of daily living in 0.4% to 2.7% of included hospital episodes.
| Care Led by Geriatricians (n=968) | Care Led by Other Internists (n=976) | P Value | |
|---|---|---|---|
| |||
| Age, mean (SD), y | 86.0 (5.1) | 85.8 (5.1) | 0.52 |
| Male, n (%) | 377 (39.0) | 361 (37.0) | 0.37 |
| Living arrangement, n (%) | 0.09 | ||
| Alone | 19 (2.0) | 21 (2.2) | |
| With other people | 690 (71.3) | 730 (74.8) | |
| Nursing home | 255 (26.3) | 214 (21.9) | |
| Missing | 4 (0.4) | 11 (1.1) | |
| Admission source, n (%) | 0.91 | ||
| Emergency department | 943 (97.4) | 950 (97.3) | |
| Others | 25 (2.6) | 26 (2.7) | |
| Hospital admissions in the prior 30 days, n (%) | 214 (22.1) | 210 (21.5) | 0.75 |
| Year, n (%) | 1.00 | ||
| 2005 | 244 (25.2) | 242 (24.8) | |
| 2006 | 237 (24.5) | 243 (24.9) | |
| 2007 | 241 (24.9) | 244 (25.0) | |
| 2008 | 246 (25.4) | 247 (25.3) | |
| Premorbid basic activities of daily living, n (%) | 0.28 | ||
| Independent | 317 (32.7) | 345 (35.3) | |
| Assisted or dependent | 625 (64.6) | 613 (62.9) | |
| Missing | 26 (2.7) | 18 (1.8) | |
| Elixhauser comorbidity count, mean (SD) | 3.2 (1.6) | 3.2 (1.7) | 0.58 |
| Modified Severity of Illness Index, n (%) | 0.30 | ||
| 1 or 2 | 541 (55.9) | 568 (58.2) | |
| 3 or 4 | 427 (44.1) | 408 (41.8) | |
| Diagnosis‐Related Group category, n (%) | 0.88 | ||
| Circulatory | 110 (11.4) | 110 (11.3) | |
| Digestive | 55 (5.7) | 60 (6.1) | |
| Endocrine, nutritional and metabolic diseases, and immunological | 60 (6.2) | 54 (5.5) | |
| Genitourinary | 146 (15.1) | 172 (17.6) | |
| Mental and nervous | 16 (1.7) | 16 (1.6) | |
| Musculoskeletal | 9 (0.9) | 10 (1.0) | |
| Respiratory | 364 (37.6) | 356 (36.5) | |
| Others | 208 (21.5) | 198 (20.3) | |
| Acute geriatric syndromes, n (%) | |||
| Mobility impairment | 75 (7.7) | 79 (8.1) | 0.78 |
| Falls | 82 (8.5) | 99 (10.1) | 0.21 |
| Delirium | 290 (30.0) | 279 (28.6) | 0.51 |
There were no significant differences in hospital mortality, 30‐day mortality or readmission, and LOS between hospital episodes with care by geriatricians and other internists for the whole group and the 2 subgroups (Table 2). However, nonsignificant reduction in hospital mortality was observed for the whole group (15.5% vs 16.9%, P=0.40), with greater magnitude for the subgroup with acute geriatric syndromes (20.2% vs 23.1%, P=0.31).
| All | Those With Premorbid Functional Impairment | Those With Acute Geriatric Syndromes | ||||
|---|---|---|---|---|---|---|
| Care Led by Geriatricians | Care Led by Other Internists | Care Led by Geriatricians | Care Led by Other Internists | Care Led by Geriatricians | Care Led by Other Internists | |
| ||||||
| Hospital mortality, n (%) | 150/968 (15.5) | 165/976 (16.9), P=0.40 | 125/625 (20.0) | 137/613 (22.4), P=0.31 | 79/392 (20.2) | 92/398 (23.1), P=0.31 |
| 30‐day mortality or readmission, n (%) | 206/818 (25.2) | 200/811 (24.7), P=0.81 | 147/500, (29.4) | 144/476, (30.3), P=0.77 | 88/313, (28.1) | 83/306, (27.1), P=0.78 |
| Mean length of stay, days (SD) | 9.7 (10.2), n=818 | 9.7 (10.9), n=811, P=0.87 | 11.1 (10.7), n=500 | 11.1 (12.3), n=476, P=0.93 | 11.4 (12.5), n=321 | 10.8 (13.0), n=312, P=0.57 |
When adjusted for age, gender, premorbid functional status, comorbidity, severity of illness, acute geriatric syndromes, hospitalization in the prior 30 days, and calendar year, care by geriatricians was associated with nonsignificant trends toward lower hospital mortality, with odds ratios between 0.80 and 0.89. However, 30‐day mortality or readmission and LOS for the intervention and control groups were generally equivalent (Table 3). There are only minor differences between the odds ratios and their 95% confidence intervals for regression analyses without and with additional adjustment for DRG codes (results not shown). Thus, they do not change the study results in any significant way.
| Care by Geriatricians (Ref: Care by Other Internists) | All | Those With Premorbid Functional Impairment | Those With Acute Geriatric Syndromes |
|---|---|---|---|
| |||
| Hospital mortality: odds ratio (95% confidence interval) | 0.89 (0.69 to 1.16), n=1,886, P=0.40 | 0.85 (0.64 to 1.13), n=1,233, P=0.27 | 0.80 (0.55 to 1.16), n=764, P=0.24 |
| 30‐day mortality or readmission: odds ratio (95% confidence interval) | 1.05 (0.82 to 1.33), n=1,580, P=0.71 | 0.94 (0.71 to 1.25), n=973, P=0.69 | 1.03 (0.70 to 1.50), n=600, P=0.89 |
| Length of stay: log days (95% confidence interval) | 0.03 (0.14 to 0.07), n=1,580, P=0.52 | 0.03 (0.16 to 0.10), n=973, P=0.68 | 0.00 (0.18 to 0.18), n=600, P=1.00 |
DISCUSSION
Geriatricians provide direct acute hospital care for seniors either in dedicated acute geriatric units including ACE units[14] or alongside generalists or subspecialty physicians in general internal medicine units. Through an unique opportunity to study the latter arrangement, we found that hospitalist care by geriatricians for seniors aged 80 years and older in general internal medicine units did not improve their short‐term outcomes vis‐‐vis care by other internists. These findings are in contrast to those of studies on acute geriatric units. This is the first report on the effectiveness of hospitalist care for seniors provided by geriatricians. Although not a randomized controlled trial, our study is in essence a natural experiment which does not impose any major inclusion restrictions other than age of 80 years and above. Internal validity was enhanced by intervention and control groups being similar on individual‐level characteristics, whereas external validity was boosted by an all‐comers approach to enrollment.
It is pertinent to ask why hospitalist care by geriatricians in a general internal medicine department did not benefit seniors with advanced age, many of whom have functional impairment and multimorbidity. After all, improved care and outcomes seem plausible for these seniors who appear to be more vulnerable. We propose 4 possible explanations. First, unmeasured differences between intervention and control groups could have led to unobserved confounding. However, this is less likely given the nonsystematic assignment of attending physicians to different wards and similarity of intervention and control groups on a broad range of baseline characteristics. Second, care processes in wards allocated to geriatricians may not differ very much from those in other wards. Irrespective of ward, care delivered by medical residents and other healthcare professionals were also expected to be similar. Unlike acute geriatric units where comprehensive geriatric assessment (CGA) by a multidisciplinary team is thought to be responsible for the improved outcomes,[12] the influence of geriatricians outside of these units may not necessarily achieve the same level of geriatric care.[15, 16] This is precisely the challenge encountered by geriatricians in their care of acutely ill older patients in settings other than acute geriatric units, Third, diffusion of geriatric care practices across general internal medicine wards over the past decade at our hospital may have resulted in narrowed differences in the care processes particularly relevant to seniors, such as those related to functional retraining, swallowing assessment, and discharge planning, although we do not have any specific data to confirm this. These differences may in turn not be wide enough for hospitalist care by geriatricians to influence these short‐term outcomes positively. Last, our study was not designed to measure patient‐reported outcomes such as functional status, mood, quality of life, and satisfaction, which may arguably be more responsive to geriatric intervention.
It might be noted that the average LOS for hospital episodes in this study was almost 10 days, which is longer than that typically seen in North America. There are 2 possible reasons for this. First, these are hospital episodes of very old patients, and longer LOS among survivors is expected. Second, post‐acute care was not as well developed in Singapore during the study period. Since then, the system of community hospitals has expanded, thereby allowing earlier transfer to these facilities for post‐acute care and shorter LOS at acute‐care hospitals.
There are a number of limitations of our study. First, this is an observational study where treatment assignment is not allocated. Although a randomized controlled trial may be the ideal design to evaluate treatment effects, operational and ethical considerations at a busy acute‐care hospital render this very challenging to conduct. As mentioned, nonsystematic assignment of attending physicians to different wards and lack of important baseline differences between intervention and control groups support the notion that important unmeasured differences are less likely. Second, and as alluded to, we did not measure relevant patient‐reported outcomes. Nonetheless, we argue that survival is still important to many seniors, particularly those without advanced illness, whereas readmission avoidance and shorter hospital stay matter almost universally. Third, clinical charts were unavailable for data extraction in almost 3% of hospital episodes. In addition, there were missing values in 2 explanatory variables in <3% of available clinical charts. These missing values were handled by listwise deletion in the regression analyses. Doing so carries with it the risk of introducing bias in the estimation of the treatment effect of care by geriatricians. However, given the relatively small proportions of missing charts and values, it is less likely that any bias would have changed the study conclusions. Fourth, we did not account for clustering at the physician level, which would have widened the confidence intervals for the odds ratios. However, because all treatment effects on the 3 outcomes were clearly not statistically significant, widening of confidence intervals would not have changed the results and study conclusions. Finally, this is a single institution study in a single health system. Thus, caution is necessary when attempting to extrapolate its results. On the other hand, the major strength of this study is its real‐world setting, which allows the results to be more generalizable to other hospital systems with similar organization and practice of general internal medicine.
Our findings need to be placed in the context of emerging innovative models of care for hospitalized seniors, which directly or indirectly involve geriatricians. Besides traditional ACE units, which have fixed geographical locations within a hospital, a mobile acute care of the elderly service achieved shorter LOS and reduced cost than the established ACE unit with similar mortality and readmission rates.[17] Others include a proactive geriatrics consultation model in collaboration with hospitalists.[18] Another variant of the ACE unit is the hospitalist‐run acute care for the elderly (hospitalist‐ACE) service, which improved care processes without improving clinical outcomes or increasing cost.[19] Clearly, there needs to be better collaboration between hospitalists and geriatricians to improve care of acutely ill seniors.[20] Ultimately, any form of direct geriatrician care for seniors needs to be complimented by indirect care through hospital‐wide systems such the Hospital Elder Life Program. This model of care aims to prevent cognitive and functional decline in hospitalized seniors by combining CGA with protocol‐driven interventions ranging from orientation, visitation, feeding assistance, early mobilization, and visual and hearing adaptations.[21, 22]
In conclusion, hospitalist care for seniors aged 80 years and above by geriatricians based in general internal medicine units is not more effective than care by other internists, at least where reducing short‐term mortality and readmission and LOS are concerned. This is particularly applicable to hospital systems where geriatric care elements have already been widely adopted beyond the confines of acute geriatric units. However, these findings do not by any means indicate that hospitalist care provided by geriatricians is altogether not more beneficial for these seniors than care by other internists in general internal medicine units. Rather, further research on patient‐reported outcomes can clarify more fully the geriatrician's true role in this setting.
Disclosures
This study was wholly funded by the National Healthcare Group Small Innovative Grants. The funders did not play any other role in this study. The authors report no conflicts of interest.
- , , , , . Effectiveness of acute geriatric units on functional decline, living at home, and case fatality among older patients admitted to hospital for acute medical disorders: meta‐analysis. BMJ. 2009;338:b50.
- , , , , . Comprehensive geriatric assessment: a meta‐analysis of controlled trials. Lancet. 1993;342(8878):1032–1036.
- , , , et al. A controlled trial of inpatient and outpatient geriatric evaluation and management. N Engl J Med. 2002;346(12):905–912.
- , , , , . Comprehensive geriatric assessment for older adults admitted to hospital: meta‐analysis of randomised controlled trials. BMJ. 2011;343:d6553.
- , , , , . Reduced mortality in treating acutely sick, frail older patients in a geriatric evaluation and management unit. A prospective randomized trial. J Am Geriatr Soc. 2002;50(5):792–798.
- , , , et al. Effectiveness of acute geriatric unit care using acute care for elders components: a systematic review and meta‐analysis. J Am Geriatr Soc. 2012;60:2237–2245.
- , . Age‐related geriatric medicine or integrated medical care? Age Ageing. 1999;28:245–247.
- . An introduction to the hospitalist model. Ann Intern Med. 1999;130(4 pt 2):338–342.
- . Care of hospitalized older patients: opportunities for hospital‐based physicians. J Hosp Med. 2006;1:42–47.
- , , , . Which patients benefit the most from a geriatrician's care? Consensus among directors of geriatrics academic programs. J Am Geriatr Soc. 2008;56(10):1796–1801.
- , , , et al. Comorbidity measure for use with administrative data. Med Care. 1998;36:8–27.
- , , , , . Resource consumption in hospitalised, frail older patients. Ann Acad Med Singapore. 2010;39:830–836.
- , , , , . Impact of data source and time reference of functional status on hospital mortality prediction. BMC Health Serv Res. 2012;12:115.
- , , , , . A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332:1338–1344.
- , , . Acute hospital care for frail older people. Age Ageing. 2006;35:551–552.
- , . Comprehensive geriatric assessment for older hospital patients. Br Med Bull. 2005;71:45–59.
- , , , et al. Operational and quality outcomes of a mobile acute care for the elderly service. J Hosp Med. 2011;6:358–363.
- , , , . Development and implementation of a proactive geriatrics consultation model in collaboration with hospitalists. J Am Geriatr Soc. 2009;57:2139–2145.
- , , , et al. Evaluation of a hospitalist‐run acute care for the elderly service. J Hosp Med. 2011;6:313–321.
- , , . Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs. J Hosp Med. 2006;1:29–35.
- , , , et al. The Hospital Elder Life Program: A model of care to prevent cognitive and functional decline in hospitalized older patients. J Am Geriatr Soc. 2000;48:1697–1706.
- . Organizational interventions to improve health outcomes of older persons. Med Care. 2002;40:416–428.
- , , , , . Effectiveness of acute geriatric units on functional decline, living at home, and case fatality among older patients admitted to hospital for acute medical disorders: meta‐analysis. BMJ. 2009;338:b50.
- , , , , . Comprehensive geriatric assessment: a meta‐analysis of controlled trials. Lancet. 1993;342(8878):1032–1036.
- , , , et al. A controlled trial of inpatient and outpatient geriatric evaluation and management. N Engl J Med. 2002;346(12):905–912.
- , , , , . Comprehensive geriatric assessment for older adults admitted to hospital: meta‐analysis of randomised controlled trials. BMJ. 2011;343:d6553.
- , , , , . Reduced mortality in treating acutely sick, frail older patients in a geriatric evaluation and management unit. A prospective randomized trial. J Am Geriatr Soc. 2002;50(5):792–798.
- , , , et al. Effectiveness of acute geriatric unit care using acute care for elders components: a systematic review and meta‐analysis. J Am Geriatr Soc. 2012;60:2237–2245.
- , . Age‐related geriatric medicine or integrated medical care? Age Ageing. 1999;28:245–247.
- . An introduction to the hospitalist model. Ann Intern Med. 1999;130(4 pt 2):338–342.
- . Care of hospitalized older patients: opportunities for hospital‐based physicians. J Hosp Med. 2006;1:42–47.
- , , , . Which patients benefit the most from a geriatrician's care? Consensus among directors of geriatrics academic programs. J Am Geriatr Soc. 2008;56(10):1796–1801.
- , , , et al. Comorbidity measure for use with administrative data. Med Care. 1998;36:8–27.
- , , , , . Resource consumption in hospitalised, frail older patients. Ann Acad Med Singapore. 2010;39:830–836.
- , , , , . Impact of data source and time reference of functional status on hospital mortality prediction. BMC Health Serv Res. 2012;12:115.
- , , , , . A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332:1338–1344.
- , , . Acute hospital care for frail older people. Age Ageing. 2006;35:551–552.
- , . Comprehensive geriatric assessment for older hospital patients. Br Med Bull. 2005;71:45–59.
- , , , et al. Operational and quality outcomes of a mobile acute care for the elderly service. J Hosp Med. 2011;6:358–363.
- , , , . Development and implementation of a proactive geriatrics consultation model in collaboration with hospitalists. J Am Geriatr Soc. 2009;57:2139–2145.
- , , , et al. Evaluation of a hospitalist‐run acute care for the elderly service. J Hosp Med. 2011;6:313–321.
- , , . Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs. J Hosp Med. 2006;1:29–35.
- , , , et al. The Hospital Elder Life Program: A model of care to prevent cognitive and functional decline in hospitalized older patients. J Am Geriatr Soc. 2000;48:1697–1706.
- . Organizational interventions to improve health outcomes of older persons. Med Care. 2002;40:416–428.
© 2014 Society of Hospital Medicine