User login
Hospitals Reap Potential of Data Mining
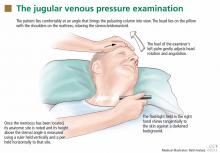
In one recently publicized demonstration of data mining’s potential, Austin, Texas-based Seton Healthcare Family used software developed by IBM to pore over doctors’ notes and predict the risk of readmission among patients with congestive heart failure. Among the shortlist of biggest predictors, the analysis pointed to a lack of emotional support and a bulging jugular vein—factors that could be easily identified through inpatient screening but might otherwise be overlooked by staff.
Similarly, New York-Presbyterian Hospital used a system by Microsoft to help reduce the rates of blood clotting in patients through an objective analysis of such risk factors as cancer, smoking, and bed confinement.
In June, Deloitte and Utah-based Intermountain Healthcare announced the launch of OutcomesMiner, an analytics tool that uses electronic health records to ferret out important variations and associations among patient populations. Brett Davis, general manager of Deloitte Health Informatics, says understanding asthma patients who are in different age brackets, have different comorbidities, and are on different drugs, for example, can allow providers to better manage the population. Merely using ICD-9 codes often results in inaccurate patient classifications, he warns. Instead, capturing and analyzing data from medications and clinical encounters can be vital for properly defining an asthma patient and separating the signal from the noise.
In one recently publicized demonstration of data mining’s potential, Austin, Texas-based Seton Healthcare Family used software developed by IBM to pore over doctors’ notes and predict the risk of readmission among patients with congestive heart failure. Among the shortlist of biggest predictors, the analysis pointed to a lack of emotional support and a bulging jugular vein—factors that could be easily identified through inpatient screening but might otherwise be overlooked by staff.
Similarly, New York-Presbyterian Hospital used a system by Microsoft to help reduce the rates of blood clotting in patients through an objective analysis of such risk factors as cancer, smoking, and bed confinement.
In June, Deloitte and Utah-based Intermountain Healthcare announced the launch of OutcomesMiner, an analytics tool that uses electronic health records to ferret out important variations and associations among patient populations. Brett Davis, general manager of Deloitte Health Informatics, says understanding asthma patients who are in different age brackets, have different comorbidities, and are on different drugs, for example, can allow providers to better manage the population. Merely using ICD-9 codes often results in inaccurate patient classifications, he warns. Instead, capturing and analyzing data from medications and clinical encounters can be vital for properly defining an asthma patient and separating the signal from the noise.
In one recently publicized demonstration of data mining’s potential, Austin, Texas-based Seton Healthcare Family used software developed by IBM to pore over doctors’ notes and predict the risk of readmission among patients with congestive heart failure. Among the shortlist of biggest predictors, the analysis pointed to a lack of emotional support and a bulging jugular vein—factors that could be easily identified through inpatient screening but might otherwise be overlooked by staff.
Similarly, New York-Presbyterian Hospital used a system by Microsoft to help reduce the rates of blood clotting in patients through an objective analysis of such risk factors as cancer, smoking, and bed confinement.
In June, Deloitte and Utah-based Intermountain Healthcare announced the launch of OutcomesMiner, an analytics tool that uses electronic health records to ferret out important variations and associations among patient populations. Brett Davis, general manager of Deloitte Health Informatics, says understanding asthma patients who are in different age brackets, have different comorbidities, and are on different drugs, for example, can allow providers to better manage the population. Merely using ICD-9 codes often results in inaccurate patient classifications, he warns. Instead, capturing and analyzing data from medications and clinical encounters can be vital for properly defining an asthma patient and separating the signal from the noise.
Hospitalist Groups Extract New Solutions Via Data Mining
One hospital wanted to reduce readmissions among patients with congestive heart failure. Another hoped to improve upon its sepsis mortality rates. A third sought to determine whether its doctors were providing cost-effective care for pneumonia patients. All of them adopted the same type of technology to help identify a solution.
As the healthcare industry tilts toward accountable care, pay for performance and an increasingly
cost-conscious mindset, hospitalists and other providers are tapping into a fast-growing analytical tool collectively known as data mining to help make sense of the growing mounds of information. Although no single technology can be considered a cure-all, HM leaders are so optimistic about data mining’s potential to address cost, outcome, and performance issues that some have labeled it a “game changer” for hospitalists.
Karim Godamunne, MD, MBA, SFHM, chief medical officer at North Fulton Hospital in Roswell, Ga., and a member of SHM’s Practice Management Committee, says he can’t overstate the importance of hospitalists’ involvement in physician data mining. “From my perspective, we’re looking to hospitalists to help drive this quality-utilization bandwagon, to be the real leaders in it,” he says. With the tremendous value that can be generated through understanding and using the information, “it’s good for your group and can be good to your hospital as a whole.”
So what is data mining? The technology fully emerged in the mid-1990s as a way to help scientists analyze large and often disparate bodies of data, present relevant information in new ways, and illuminate previously unknown relationships.1 In the healthcare industry, early adopters realized that the insights gleaned from data mining could help inform their clinical decision-making; organizations used the new tools to help predict health insurance fraud and identify at-risk patients, for example.
Cynthia Burghard, research director of Accountable Care IT Strategies at IDC Health Insights in Framingham, Mass., says researchers in academic medical centers initially conducted most of the clinical analytical work. Within the past few years, however, the increasing availability of data has allowed more hospitals to begin analyzing chronic disease, readmissions, and other areas of concern. In addition, Burghard says, new tools based on natural language processing are giving hospitals better access to unstructured clinical data, such as notes written by doctors and nurses.
“What I’m seeing both in my surveys as well as in conversations with hospitals is that analytics is the top of the investment priority for both hospitals and health plans,” Burghard says. According to IDC estimates, total spending for clinical analytics in the U.S. reached $3.7 billion in 2012 and is expected to grow to $5.14 billion by 2016. Much of the growth, she notes, is being driven by healthcare reform. “If your mandate is to manage populations of patients, it behooves you to know who those patients are and what their illnesses are, and to monitor what you’re doing for them,” she says.
Practice Improvement
Accordingly, a major goal of all this data-mining technology is to change practice behavior in a way that achieves the triple aim of improving quality of care, controlling costs, and bettering patient outcomes.
A growing number of companies are releasing tools that can compile and analyze the separate bits of information captured from claims and billing systems, Medicare reporting requirements, internal benchmarks, and other sources. Unlike passive data sources, such as Medicare’s Hospital Compare website, more active analytics can help their users zoom down to the level of an individual doctor or patient, pan out to the level of a hospitalist group, or expand out even more for a broader comparison among peer institutions.
Some newer data-mining tools with names like CRIMSON, Truven, Iodine, and Imagine are billing themselves as hospitalist-friendly performance-improvement aids and giving individual providers the ability to access and analyze the data themselves. A few of these applications can even provide real-time data via mobile devices (see “Physician Performance Aids,”).
Thomas Frederickson, MD, MBA, SFHM, medical director of the HM service at Alegent Creighton Health in Omaha, Neb., and a member of SHM’s Practice Management Committee, sees the biggest potential of this data-mining technology in its ability to help drive practice consistency. “You can use the database to analyze practice patterns of large groups, or even individuals, and see where variability exists,” he says. “And then, based on that, you can analyze why the variability exists and begin to address whether it’s variability that’s clinically indicated or not.”
When Alegent Creighton Health was scrutinizing the care of its pneumonia patients, for example, officials could compare the number of chest X-rays per pneumonia patient by hospital or across the entire CRIMSON database. At a deeper level, the officials could see how often individual providers ordered the tests compared to their peers. For outliers, they could follow up to determine whether the variability was warranted.
As champions of process improvement, Dr. Frederickson says, hospitalists can make particularly good use of database analytics. “It’s part of the process of making hospitalists invaluable to their hospitals and their systems,” he says. “Part of that is building up expertise on process improvement and safety, and familiarity with these kinds of tools is one thing that will help us do that.”
North Fulton Hospital used CRIMSON to analyze how its doctors care for patients with sepsis and to establish new benchmarks. Dr. Godamunne says the tools allowed the hospital to track its doctors’ progress over time and identify potential problems. “If a patient with sepsis is staying too long, you can see who admitted the patient and see if, a few months ago, the same physician was having similar problems,” he says. Similarly, the hospital was able to track the top DRGs resulting in excess length of stay among patients, to identify potential bottlenecks in the care and discharge processes.
Some tools require only two-day training sessions for basic proficiency, though more advanced manipulations often require a bigger commitment, like the 12-week training session that Dr. Godamunne completed. That training included one hour of online learning and one hour of homework every week, and most of the cases highlighted during his coursework, he says, focused on hospitalists—another sign of the major role he believes HM will play in harnessing data to improve performance quality.

—Thomas Frederickson, MD, MBA, SFHM, medical director, hospital medicine service, Alegent Creighton Health, Omaha, Neb., SHM Practice Management Committee member
Slow—Construction Ahead
The best information is meaningful, individualized, and timely, says Steven Deitelzweig, MD, SFHM, system chairman for hospital medicine and medical director of regional business development at Ochsner Health System in New Orleans. “If you get something back six months after you’ve delivered the care, you’ll have a limited opportunity to improve, versus if you get it back in a week or two, or ideally, in real time,” says Dr. Deitelzweig, chair of SHM’s Practice Management Committee.
In examining length of stay, Dr. Deitelzweig says doctors could use data mining to look at time-stamped elements of patient flow and the timeliness of provider response: how patients go through the ED, and when they receive written orders or lab results. “It could be really powerful, and right now it’s a little bit of a black hole,” he says.
Based on her conversations with hospital executives and leaders, however, Burghard cautions that some real-time mobile applications, although technologically impressive, may be less useful or necessary in practice. “If it’s performance measurement, why do you need that in real time? It’s not going to change your behavior in the moment,” she says. “What you may want to get is an alert that your patient, who is in the hospital, has had some sort of negative event.”
Data mining has other potential limitations. “There’s always going to be questions of attribution, and you need to have clinical knowledge of your location,” Dr. Godamunne says. And data mining is only as good as the data that have been documented, underscoring the importance of securing provider cooperation.
Dr. Frederickson says physician acceptance, in fact, might be one of the biggest obstacles—a major reason why he recommends introducing the technology slowly and explaining why and how it will be used. If introduced too quickly and without adequate explanation about what a hospital or health system hopes to accomplish, he says, “there certainly is the potential for suspicion.” The key, he says, is to emphasize that the tools provide a valuable mechanism for gleaning new insights into doctors’ practice patterns, “not something that’s going to be used against them.”
Paul Roscoe, CEO of the Washington, D.C.-based Advisory Board Company's Crimson division, agrees that personally engaging physicians is essential for a good return on investment in analytical tools like his company’s suite of CRIMSON products. “If you can’t work with the physicians to get them to understand the data and actively use the data in their practice patterns, it becomes a bit meaningless,” he says.

—Karim Godamunne, MD, MBA, SFHM, chief medical officer, North Fulton Hospital, Roswell, Ga., SHM Practice Management Committee member
Roscoe sees big opportunities in prospectively examining information while a patient is still in the hospital and when a change of course by providers could avert a bad outcome. “Suggesting a set of interventions that they could do differently is really the value-add,” he says. But he cautions that those suggestions must be worded carefully to avoid alienating physicians.
“If doctors don’t feel like they’re being judged, they’ll engage with you,” Roscoe says.
Similar nuances can affect how users perceive the tools themselves. After hearing feedback from members that the words “data mining” didn’t conjure trust and confidence, the Advisory Board Company dropped the phrase altogether in favor of “data analytics,” “physician engagement,” and similar descriptors. “It’s simple things like that that can very quickly either turn a physician on or off,” Roscoe says.
Once users take the time to understand data-mining tools and how they can be properly harnessed, advocates say, the technology can lead to a host of unanticipated benefits. When a hospital bills the federal government for a Medicare patient, for example, it must submit an HCC code that describes the patient’s condition. By doing a better job of mining the data, Burghard says, a hospital can more accurately reflect that patient’s contdition. For example, if a hospital is treating a diabetic who comes in with a broken leg, the hospital could receive a lower payment rate if it does not properly identify and record both conditions.
And by using the tools prospectively, Burghard says, “I think there’s the opportunity to make a quantum leap from what we’re doing today. We usually just report on facts, and usually retrospectively. With some of the new technology that’s available, the healthcare industry can begin to do discovery analytics—you’re identifying insights, patterns, and relationships.”
Better integration of computerized physician order entry with data-mining ports, Dr. Godamunne predicts, will allow for much better attribution and finer parsing of the data. As the transparency increases, though, hospitalists will have to adapt to a new reality in which stronger analytical tools may point out individual outliers. And that level of detail, in turn, will require some hospitalists to justify why they’re different than their peers.
Even so, Roscoe says, he’s found that hospitalists are very open to using data to improve performance and that they make up a high percentage of CRIMSON users. “There isn’t a physician group that is in a better position to help drive this quality- and data-driven culture,” he says.
Bryn Nelson is a freelance medical writer in Seattle.
Reference
One hospital wanted to reduce readmissions among patients with congestive heart failure. Another hoped to improve upon its sepsis mortality rates. A third sought to determine whether its doctors were providing cost-effective care for pneumonia patients. All of them adopted the same type of technology to help identify a solution.
As the healthcare industry tilts toward accountable care, pay for performance and an increasingly
cost-conscious mindset, hospitalists and other providers are tapping into a fast-growing analytical tool collectively known as data mining to help make sense of the growing mounds of information. Although no single technology can be considered a cure-all, HM leaders are so optimistic about data mining’s potential to address cost, outcome, and performance issues that some have labeled it a “game changer” for hospitalists.
Karim Godamunne, MD, MBA, SFHM, chief medical officer at North Fulton Hospital in Roswell, Ga., and a member of SHM’s Practice Management Committee, says he can’t overstate the importance of hospitalists’ involvement in physician data mining. “From my perspective, we’re looking to hospitalists to help drive this quality-utilization bandwagon, to be the real leaders in it,” he says. With the tremendous value that can be generated through understanding and using the information, “it’s good for your group and can be good to your hospital as a whole.”
So what is data mining? The technology fully emerged in the mid-1990s as a way to help scientists analyze large and often disparate bodies of data, present relevant information in new ways, and illuminate previously unknown relationships.1 In the healthcare industry, early adopters realized that the insights gleaned from data mining could help inform their clinical decision-making; organizations used the new tools to help predict health insurance fraud and identify at-risk patients, for example.
Cynthia Burghard, research director of Accountable Care IT Strategies at IDC Health Insights in Framingham, Mass., says researchers in academic medical centers initially conducted most of the clinical analytical work. Within the past few years, however, the increasing availability of data has allowed more hospitals to begin analyzing chronic disease, readmissions, and other areas of concern. In addition, Burghard says, new tools based on natural language processing are giving hospitals better access to unstructured clinical data, such as notes written by doctors and nurses.
“What I’m seeing both in my surveys as well as in conversations with hospitals is that analytics is the top of the investment priority for both hospitals and health plans,” Burghard says. According to IDC estimates, total spending for clinical analytics in the U.S. reached $3.7 billion in 2012 and is expected to grow to $5.14 billion by 2016. Much of the growth, she notes, is being driven by healthcare reform. “If your mandate is to manage populations of patients, it behooves you to know who those patients are and what their illnesses are, and to monitor what you’re doing for them,” she says.
Practice Improvement
Accordingly, a major goal of all this data-mining technology is to change practice behavior in a way that achieves the triple aim of improving quality of care, controlling costs, and bettering patient outcomes.
A growing number of companies are releasing tools that can compile and analyze the separate bits of information captured from claims and billing systems, Medicare reporting requirements, internal benchmarks, and other sources. Unlike passive data sources, such as Medicare’s Hospital Compare website, more active analytics can help their users zoom down to the level of an individual doctor or patient, pan out to the level of a hospitalist group, or expand out even more for a broader comparison among peer institutions.
Some newer data-mining tools with names like CRIMSON, Truven, Iodine, and Imagine are billing themselves as hospitalist-friendly performance-improvement aids and giving individual providers the ability to access and analyze the data themselves. A few of these applications can even provide real-time data via mobile devices (see “Physician Performance Aids,”).
Thomas Frederickson, MD, MBA, SFHM, medical director of the HM service at Alegent Creighton Health in Omaha, Neb., and a member of SHM’s Practice Management Committee, sees the biggest potential of this data-mining technology in its ability to help drive practice consistency. “You can use the database to analyze practice patterns of large groups, or even individuals, and see where variability exists,” he says. “And then, based on that, you can analyze why the variability exists and begin to address whether it’s variability that’s clinically indicated or not.”
When Alegent Creighton Health was scrutinizing the care of its pneumonia patients, for example, officials could compare the number of chest X-rays per pneumonia patient by hospital or across the entire CRIMSON database. At a deeper level, the officials could see how often individual providers ordered the tests compared to their peers. For outliers, they could follow up to determine whether the variability was warranted.
As champions of process improvement, Dr. Frederickson says, hospitalists can make particularly good use of database analytics. “It’s part of the process of making hospitalists invaluable to their hospitals and their systems,” he says. “Part of that is building up expertise on process improvement and safety, and familiarity with these kinds of tools is one thing that will help us do that.”
North Fulton Hospital used CRIMSON to analyze how its doctors care for patients with sepsis and to establish new benchmarks. Dr. Godamunne says the tools allowed the hospital to track its doctors’ progress over time and identify potential problems. “If a patient with sepsis is staying too long, you can see who admitted the patient and see if, a few months ago, the same physician was having similar problems,” he says. Similarly, the hospital was able to track the top DRGs resulting in excess length of stay among patients, to identify potential bottlenecks in the care and discharge processes.
Some tools require only two-day training sessions for basic proficiency, though more advanced manipulations often require a bigger commitment, like the 12-week training session that Dr. Godamunne completed. That training included one hour of online learning and one hour of homework every week, and most of the cases highlighted during his coursework, he says, focused on hospitalists—another sign of the major role he believes HM will play in harnessing data to improve performance quality.

—Thomas Frederickson, MD, MBA, SFHM, medical director, hospital medicine service, Alegent Creighton Health, Omaha, Neb., SHM Practice Management Committee member
Slow—Construction Ahead
The best information is meaningful, individualized, and timely, says Steven Deitelzweig, MD, SFHM, system chairman for hospital medicine and medical director of regional business development at Ochsner Health System in New Orleans. “If you get something back six months after you’ve delivered the care, you’ll have a limited opportunity to improve, versus if you get it back in a week or two, or ideally, in real time,” says Dr. Deitelzweig, chair of SHM’s Practice Management Committee.
In examining length of stay, Dr. Deitelzweig says doctors could use data mining to look at time-stamped elements of patient flow and the timeliness of provider response: how patients go through the ED, and when they receive written orders or lab results. “It could be really powerful, and right now it’s a little bit of a black hole,” he says.
Based on her conversations with hospital executives and leaders, however, Burghard cautions that some real-time mobile applications, although technologically impressive, may be less useful or necessary in practice. “If it’s performance measurement, why do you need that in real time? It’s not going to change your behavior in the moment,” she says. “What you may want to get is an alert that your patient, who is in the hospital, has had some sort of negative event.”
Data mining has other potential limitations. “There’s always going to be questions of attribution, and you need to have clinical knowledge of your location,” Dr. Godamunne says. And data mining is only as good as the data that have been documented, underscoring the importance of securing provider cooperation.
Dr. Frederickson says physician acceptance, in fact, might be one of the biggest obstacles—a major reason why he recommends introducing the technology slowly and explaining why and how it will be used. If introduced too quickly and without adequate explanation about what a hospital or health system hopes to accomplish, he says, “there certainly is the potential for suspicion.” The key, he says, is to emphasize that the tools provide a valuable mechanism for gleaning new insights into doctors’ practice patterns, “not something that’s going to be used against them.”
Paul Roscoe, CEO of the Washington, D.C.-based Advisory Board Company's Crimson division, agrees that personally engaging physicians is essential for a good return on investment in analytical tools like his company’s suite of CRIMSON products. “If you can’t work with the physicians to get them to understand the data and actively use the data in their practice patterns, it becomes a bit meaningless,” he says.

—Karim Godamunne, MD, MBA, SFHM, chief medical officer, North Fulton Hospital, Roswell, Ga., SHM Practice Management Committee member
Roscoe sees big opportunities in prospectively examining information while a patient is still in the hospital and when a change of course by providers could avert a bad outcome. “Suggesting a set of interventions that they could do differently is really the value-add,” he says. But he cautions that those suggestions must be worded carefully to avoid alienating physicians.
“If doctors don’t feel like they’re being judged, they’ll engage with you,” Roscoe says.
Similar nuances can affect how users perceive the tools themselves. After hearing feedback from members that the words “data mining” didn’t conjure trust and confidence, the Advisory Board Company dropped the phrase altogether in favor of “data analytics,” “physician engagement,” and similar descriptors. “It’s simple things like that that can very quickly either turn a physician on or off,” Roscoe says.
Once users take the time to understand data-mining tools and how they can be properly harnessed, advocates say, the technology can lead to a host of unanticipated benefits. When a hospital bills the federal government for a Medicare patient, for example, it must submit an HCC code that describes the patient’s condition. By doing a better job of mining the data, Burghard says, a hospital can more accurately reflect that patient’s contdition. For example, if a hospital is treating a diabetic who comes in with a broken leg, the hospital could receive a lower payment rate if it does not properly identify and record both conditions.
And by using the tools prospectively, Burghard says, “I think there’s the opportunity to make a quantum leap from what we’re doing today. We usually just report on facts, and usually retrospectively. With some of the new technology that’s available, the healthcare industry can begin to do discovery analytics—you’re identifying insights, patterns, and relationships.”
Better integration of computerized physician order entry with data-mining ports, Dr. Godamunne predicts, will allow for much better attribution and finer parsing of the data. As the transparency increases, though, hospitalists will have to adapt to a new reality in which stronger analytical tools may point out individual outliers. And that level of detail, in turn, will require some hospitalists to justify why they’re different than their peers.
Even so, Roscoe says, he’s found that hospitalists are very open to using data to improve performance and that they make up a high percentage of CRIMSON users. “There isn’t a physician group that is in a better position to help drive this quality- and data-driven culture,” he says.
Bryn Nelson is a freelance medical writer in Seattle.
Reference
One hospital wanted to reduce readmissions among patients with congestive heart failure. Another hoped to improve upon its sepsis mortality rates. A third sought to determine whether its doctors were providing cost-effective care for pneumonia patients. All of them adopted the same type of technology to help identify a solution.
As the healthcare industry tilts toward accountable care, pay for performance and an increasingly
cost-conscious mindset, hospitalists and other providers are tapping into a fast-growing analytical tool collectively known as data mining to help make sense of the growing mounds of information. Although no single technology can be considered a cure-all, HM leaders are so optimistic about data mining’s potential to address cost, outcome, and performance issues that some have labeled it a “game changer” for hospitalists.
Karim Godamunne, MD, MBA, SFHM, chief medical officer at North Fulton Hospital in Roswell, Ga., and a member of SHM’s Practice Management Committee, says he can’t overstate the importance of hospitalists’ involvement in physician data mining. “From my perspective, we’re looking to hospitalists to help drive this quality-utilization bandwagon, to be the real leaders in it,” he says. With the tremendous value that can be generated through understanding and using the information, “it’s good for your group and can be good to your hospital as a whole.”
So what is data mining? The technology fully emerged in the mid-1990s as a way to help scientists analyze large and often disparate bodies of data, present relevant information in new ways, and illuminate previously unknown relationships.1 In the healthcare industry, early adopters realized that the insights gleaned from data mining could help inform their clinical decision-making; organizations used the new tools to help predict health insurance fraud and identify at-risk patients, for example.
Cynthia Burghard, research director of Accountable Care IT Strategies at IDC Health Insights in Framingham, Mass., says researchers in academic medical centers initially conducted most of the clinical analytical work. Within the past few years, however, the increasing availability of data has allowed more hospitals to begin analyzing chronic disease, readmissions, and other areas of concern. In addition, Burghard says, new tools based on natural language processing are giving hospitals better access to unstructured clinical data, such as notes written by doctors and nurses.
“What I’m seeing both in my surveys as well as in conversations with hospitals is that analytics is the top of the investment priority for both hospitals and health plans,” Burghard says. According to IDC estimates, total spending for clinical analytics in the U.S. reached $3.7 billion in 2012 and is expected to grow to $5.14 billion by 2016. Much of the growth, she notes, is being driven by healthcare reform. “If your mandate is to manage populations of patients, it behooves you to know who those patients are and what their illnesses are, and to monitor what you’re doing for them,” she says.
Practice Improvement
Accordingly, a major goal of all this data-mining technology is to change practice behavior in a way that achieves the triple aim of improving quality of care, controlling costs, and bettering patient outcomes.
A growing number of companies are releasing tools that can compile and analyze the separate bits of information captured from claims and billing systems, Medicare reporting requirements, internal benchmarks, and other sources. Unlike passive data sources, such as Medicare’s Hospital Compare website, more active analytics can help their users zoom down to the level of an individual doctor or patient, pan out to the level of a hospitalist group, or expand out even more for a broader comparison among peer institutions.
Some newer data-mining tools with names like CRIMSON, Truven, Iodine, and Imagine are billing themselves as hospitalist-friendly performance-improvement aids and giving individual providers the ability to access and analyze the data themselves. A few of these applications can even provide real-time data via mobile devices (see “Physician Performance Aids,”).
Thomas Frederickson, MD, MBA, SFHM, medical director of the HM service at Alegent Creighton Health in Omaha, Neb., and a member of SHM’s Practice Management Committee, sees the biggest potential of this data-mining technology in its ability to help drive practice consistency. “You can use the database to analyze practice patterns of large groups, or even individuals, and see where variability exists,” he says. “And then, based on that, you can analyze why the variability exists and begin to address whether it’s variability that’s clinically indicated or not.”
When Alegent Creighton Health was scrutinizing the care of its pneumonia patients, for example, officials could compare the number of chest X-rays per pneumonia patient by hospital or across the entire CRIMSON database. At a deeper level, the officials could see how often individual providers ordered the tests compared to their peers. For outliers, they could follow up to determine whether the variability was warranted.
As champions of process improvement, Dr. Frederickson says, hospitalists can make particularly good use of database analytics. “It’s part of the process of making hospitalists invaluable to their hospitals and their systems,” he says. “Part of that is building up expertise on process improvement and safety, and familiarity with these kinds of tools is one thing that will help us do that.”
North Fulton Hospital used CRIMSON to analyze how its doctors care for patients with sepsis and to establish new benchmarks. Dr. Godamunne says the tools allowed the hospital to track its doctors’ progress over time and identify potential problems. “If a patient with sepsis is staying too long, you can see who admitted the patient and see if, a few months ago, the same physician was having similar problems,” he says. Similarly, the hospital was able to track the top DRGs resulting in excess length of stay among patients, to identify potential bottlenecks in the care and discharge processes.
Some tools require only two-day training sessions for basic proficiency, though more advanced manipulations often require a bigger commitment, like the 12-week training session that Dr. Godamunne completed. That training included one hour of online learning and one hour of homework every week, and most of the cases highlighted during his coursework, he says, focused on hospitalists—another sign of the major role he believes HM will play in harnessing data to improve performance quality.

—Thomas Frederickson, MD, MBA, SFHM, medical director, hospital medicine service, Alegent Creighton Health, Omaha, Neb., SHM Practice Management Committee member
Slow—Construction Ahead
The best information is meaningful, individualized, and timely, says Steven Deitelzweig, MD, SFHM, system chairman for hospital medicine and medical director of regional business development at Ochsner Health System in New Orleans. “If you get something back six months after you’ve delivered the care, you’ll have a limited opportunity to improve, versus if you get it back in a week or two, or ideally, in real time,” says Dr. Deitelzweig, chair of SHM’s Practice Management Committee.
In examining length of stay, Dr. Deitelzweig says doctors could use data mining to look at time-stamped elements of patient flow and the timeliness of provider response: how patients go through the ED, and when they receive written orders or lab results. “It could be really powerful, and right now it’s a little bit of a black hole,” he says.
Based on her conversations with hospital executives and leaders, however, Burghard cautions that some real-time mobile applications, although technologically impressive, may be less useful or necessary in practice. “If it’s performance measurement, why do you need that in real time? It’s not going to change your behavior in the moment,” she says. “What you may want to get is an alert that your patient, who is in the hospital, has had some sort of negative event.”
Data mining has other potential limitations. “There’s always going to be questions of attribution, and you need to have clinical knowledge of your location,” Dr. Godamunne says. And data mining is only as good as the data that have been documented, underscoring the importance of securing provider cooperation.
Dr. Frederickson says physician acceptance, in fact, might be one of the biggest obstacles—a major reason why he recommends introducing the technology slowly and explaining why and how it will be used. If introduced too quickly and without adequate explanation about what a hospital or health system hopes to accomplish, he says, “there certainly is the potential for suspicion.” The key, he says, is to emphasize that the tools provide a valuable mechanism for gleaning new insights into doctors’ practice patterns, “not something that’s going to be used against them.”
Paul Roscoe, CEO of the Washington, D.C.-based Advisory Board Company's Crimson division, agrees that personally engaging physicians is essential for a good return on investment in analytical tools like his company’s suite of CRIMSON products. “If you can’t work with the physicians to get them to understand the data and actively use the data in their practice patterns, it becomes a bit meaningless,” he says.

—Karim Godamunne, MD, MBA, SFHM, chief medical officer, North Fulton Hospital, Roswell, Ga., SHM Practice Management Committee member
Roscoe sees big opportunities in prospectively examining information while a patient is still in the hospital and when a change of course by providers could avert a bad outcome. “Suggesting a set of interventions that they could do differently is really the value-add,” he says. But he cautions that those suggestions must be worded carefully to avoid alienating physicians.
“If doctors don’t feel like they’re being judged, they’ll engage with you,” Roscoe says.
Similar nuances can affect how users perceive the tools themselves. After hearing feedback from members that the words “data mining” didn’t conjure trust and confidence, the Advisory Board Company dropped the phrase altogether in favor of “data analytics,” “physician engagement,” and similar descriptors. “It’s simple things like that that can very quickly either turn a physician on or off,” Roscoe says.
Once users take the time to understand data-mining tools and how they can be properly harnessed, advocates say, the technology can lead to a host of unanticipated benefits. When a hospital bills the federal government for a Medicare patient, for example, it must submit an HCC code that describes the patient’s condition. By doing a better job of mining the data, Burghard says, a hospital can more accurately reflect that patient’s contdition. For example, if a hospital is treating a diabetic who comes in with a broken leg, the hospital could receive a lower payment rate if it does not properly identify and record both conditions.
And by using the tools prospectively, Burghard says, “I think there’s the opportunity to make a quantum leap from what we’re doing today. We usually just report on facts, and usually retrospectively. With some of the new technology that’s available, the healthcare industry can begin to do discovery analytics—you’re identifying insights, patterns, and relationships.”
Better integration of computerized physician order entry with data-mining ports, Dr. Godamunne predicts, will allow for much better attribution and finer parsing of the data. As the transparency increases, though, hospitalists will have to adapt to a new reality in which stronger analytical tools may point out individual outliers. And that level of detail, in turn, will require some hospitalists to justify why they’re different than their peers.
Even so, Roscoe says, he’s found that hospitalists are very open to using data to improve performance and that they make up a high percentage of CRIMSON users. “There isn’t a physician group that is in a better position to help drive this quality- and data-driven culture,” he says.
Bryn Nelson is a freelance medical writer in Seattle.
Reference
The end of the warfarin era
For over a half a century, the vitamin K antagonists coumarin and warfarin have been the only anticoagulants available to prevent clot formation in a variety of cardiovascular clinical settings. They are now about to be replaced with direct thrombin and factor Xa inhibitors. Vitamin K antagonists have not only dominated anticoagulant therapy, they have created an entire industry within the cardiovascular domain for the monitoring and control of its dose administration.
The story began in 1933 when Karl Paul Link, Ph.D., working in a laboratory at the University of Wisconsin School of Agriculture, was asked to examine the blood of cows dying of hemorrhage thought to be due to the ingestion of spoiled sweet clover. After years of research, Link was able to isolate an anticoagulant from the clover feed, called dicumarol, and he initially patented it in 1941 as rat poison. The marketed drug was called warfarin, after the Wisconsin Agricultural Research Foundation (WARF). Based on that patent, billions of dollars were generated for future research at the WARF.
Warfarin began to be used in the 1950s by a number of clinical investigators to prevent pulmonary embolism in the setting of an acute myocardial infarction (Lancet 1954;266:92-5). At that time, 1 month of complete bed rest was standard therapy for an AMI, and thrombophlebitis together with pulmonary and systemic embolism were the main causes of mortality. When early ambulation became acceptable for AMI patients, warfarin use tapered off. As clinicians became more focused on the prevention of intravascular thrombus formation after prosthetic valve surgery, and to prevent thromboembolism in patients with atrial fibrillation, warfarin therapy became more widely used, and the definition of the therapeutic dose of warfarin became important.
It soon became evident that vitamin K antagonists had a very narrow therapeutic window, framed by excessive bleeding at high doses and inefficacy at lower dose. As a result, the need for closer dose monitoring became important, and this led to the establishment of anticoagulant clinics. However, even with the establishment of these clinics, it became obvious that the clinical status of patients and dietary variability played major roles in dosing. The need for frequent blood sampling and the logistics of dose management were frustrations for both the patient and physician for decades.
As the need for better anticoagulant therapy became evident, drugs were developed that had a wider therapeutic range and that could be administered orally without the need of blood monitoring. The development of direct-acting thrombin and factor Xa inhibitors have led to major advances in anticoagulant therapy, resulting in safer oral fixed-dose drugs with therapeutic efficacy comparable to or better than vitamin K antagonists. In addition, they appear to be free from the effects of dietary variation. The factor Xa inhibitors apixaban and rivaroxaban have been approved by the Food and Drug Administration for the prevention of systemic emboli in patients with atrial fibrillation. Rivaroxaban is also indicated for preventing and treating deep vein thrombosis and pulmonary embolism. The direct thrombin inhibitor dabigatran has also been approved for the prevention of thromboembolism in patients with atrial fibrillation. The only settings for which the new anticoagulants have not been approved are acute coronary syndrome and prevention of thromboembolism with prosthetic valves.
The development of new anticoagulants provides an opportunity to improve therapy and witness the retirement of a ponderous and complicated dosing program that has been inconvenient to both patients and doctors. The retirement of warfarin and the death of the anticoagulant clinic will be appreciated by all.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
For over a half a century, the vitamin K antagonists coumarin and warfarin have been the only anticoagulants available to prevent clot formation in a variety of cardiovascular clinical settings. They are now about to be replaced with direct thrombin and factor Xa inhibitors. Vitamin K antagonists have not only dominated anticoagulant therapy, they have created an entire industry within the cardiovascular domain for the monitoring and control of its dose administration.
The story began in 1933 when Karl Paul Link, Ph.D., working in a laboratory at the University of Wisconsin School of Agriculture, was asked to examine the blood of cows dying of hemorrhage thought to be due to the ingestion of spoiled sweet clover. After years of research, Link was able to isolate an anticoagulant from the clover feed, called dicumarol, and he initially patented it in 1941 as rat poison. The marketed drug was called warfarin, after the Wisconsin Agricultural Research Foundation (WARF). Based on that patent, billions of dollars were generated for future research at the WARF.
Warfarin began to be used in the 1950s by a number of clinical investigators to prevent pulmonary embolism in the setting of an acute myocardial infarction (Lancet 1954;266:92-5). At that time, 1 month of complete bed rest was standard therapy for an AMI, and thrombophlebitis together with pulmonary and systemic embolism were the main causes of mortality. When early ambulation became acceptable for AMI patients, warfarin use tapered off. As clinicians became more focused on the prevention of intravascular thrombus formation after prosthetic valve surgery, and to prevent thromboembolism in patients with atrial fibrillation, warfarin therapy became more widely used, and the definition of the therapeutic dose of warfarin became important.
It soon became evident that vitamin K antagonists had a very narrow therapeutic window, framed by excessive bleeding at high doses and inefficacy at lower dose. As a result, the need for closer dose monitoring became important, and this led to the establishment of anticoagulant clinics. However, even with the establishment of these clinics, it became obvious that the clinical status of patients and dietary variability played major roles in dosing. The need for frequent blood sampling and the logistics of dose management were frustrations for both the patient and physician for decades.
As the need for better anticoagulant therapy became evident, drugs were developed that had a wider therapeutic range and that could be administered orally without the need of blood monitoring. The development of direct-acting thrombin and factor Xa inhibitors have led to major advances in anticoagulant therapy, resulting in safer oral fixed-dose drugs with therapeutic efficacy comparable to or better than vitamin K antagonists. In addition, they appear to be free from the effects of dietary variation. The factor Xa inhibitors apixaban and rivaroxaban have been approved by the Food and Drug Administration for the prevention of systemic emboli in patients with atrial fibrillation. Rivaroxaban is also indicated for preventing and treating deep vein thrombosis and pulmonary embolism. The direct thrombin inhibitor dabigatran has also been approved for the prevention of thromboembolism in patients with atrial fibrillation. The only settings for which the new anticoagulants have not been approved are acute coronary syndrome and prevention of thromboembolism with prosthetic valves.
The development of new anticoagulants provides an opportunity to improve therapy and witness the retirement of a ponderous and complicated dosing program that has been inconvenient to both patients and doctors. The retirement of warfarin and the death of the anticoagulant clinic will be appreciated by all.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
For over a half a century, the vitamin K antagonists coumarin and warfarin have been the only anticoagulants available to prevent clot formation in a variety of cardiovascular clinical settings. They are now about to be replaced with direct thrombin and factor Xa inhibitors. Vitamin K antagonists have not only dominated anticoagulant therapy, they have created an entire industry within the cardiovascular domain for the monitoring and control of its dose administration.
The story began in 1933 when Karl Paul Link, Ph.D., working in a laboratory at the University of Wisconsin School of Agriculture, was asked to examine the blood of cows dying of hemorrhage thought to be due to the ingestion of spoiled sweet clover. After years of research, Link was able to isolate an anticoagulant from the clover feed, called dicumarol, and he initially patented it in 1941 as rat poison. The marketed drug was called warfarin, after the Wisconsin Agricultural Research Foundation (WARF). Based on that patent, billions of dollars were generated for future research at the WARF.
Warfarin began to be used in the 1950s by a number of clinical investigators to prevent pulmonary embolism in the setting of an acute myocardial infarction (Lancet 1954;266:92-5). At that time, 1 month of complete bed rest was standard therapy for an AMI, and thrombophlebitis together with pulmonary and systemic embolism were the main causes of mortality. When early ambulation became acceptable for AMI patients, warfarin use tapered off. As clinicians became more focused on the prevention of intravascular thrombus formation after prosthetic valve surgery, and to prevent thromboembolism in patients with atrial fibrillation, warfarin therapy became more widely used, and the definition of the therapeutic dose of warfarin became important.
It soon became evident that vitamin K antagonists had a very narrow therapeutic window, framed by excessive bleeding at high doses and inefficacy at lower dose. As a result, the need for closer dose monitoring became important, and this led to the establishment of anticoagulant clinics. However, even with the establishment of these clinics, it became obvious that the clinical status of patients and dietary variability played major roles in dosing. The need for frequent blood sampling and the logistics of dose management were frustrations for both the patient and physician for decades.
As the need for better anticoagulant therapy became evident, drugs were developed that had a wider therapeutic range and that could be administered orally without the need of blood monitoring. The development of direct-acting thrombin and factor Xa inhibitors have led to major advances in anticoagulant therapy, resulting in safer oral fixed-dose drugs with therapeutic efficacy comparable to or better than vitamin K antagonists. In addition, they appear to be free from the effects of dietary variation. The factor Xa inhibitors apixaban and rivaroxaban have been approved by the Food and Drug Administration for the prevention of systemic emboli in patients with atrial fibrillation. Rivaroxaban is also indicated for preventing and treating deep vein thrombosis and pulmonary embolism. The direct thrombin inhibitor dabigatran has also been approved for the prevention of thromboembolism in patients with atrial fibrillation. The only settings for which the new anticoagulants have not been approved are acute coronary syndrome and prevention of thromboembolism with prosthetic valves.
The development of new anticoagulants provides an opportunity to improve therapy and witness the retirement of a ponderous and complicated dosing program that has been inconvenient to both patients and doctors. The retirement of warfarin and the death of the anticoagulant clinic will be appreciated by all.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
Hepatocellular carcinoma: Options for diagnosing and managing a deadly disease
Hepatocellular carcinoma (HCC) is a common cause of death worldwide. However, it can be detected early in high-risk individuals by using effective screening strategies, resulting in the ability to provide curative treatment.
Here, we review the risk factors for HCC, strategies for surveillance and diagnosis, and therapies that can be used.
EPIDEMIOLOGY
HCC is the most common primary malignancy of the liver. Overall, it is the fifth most common type of cancer in men and the seventh most common in women.1
Cirrhosis is present in 80% to 90% of patients with HCC.
Male sex. The male-to-female ratio is from 2:1 to 4:1, depending on the region.2 In the United States, the overall male-to-female ratio has been reported2 as 2.4:1. In another report,3 the incidence rate of HCC per 100,000 person-years was 3.7 for men and 2.0 for women.
Geographic areas with a high incidence of HCC include sub-Saharan Africa and eastern Asia, whereas Canada and the United States are low-incidence areas. The difference has been because of a lower prevalence of hepatitis B virus infection in North America. However, recent data show a downward trend in incidence of HCC in eastern Asia and an upward trend in North America (Figure 1).3,4
Viral hepatitis (ie, hepatitis B or hepatitis C) is the main risk factor for cirrhosis and HCC.
Diabetes mellitus can predispose to nonalcoholic steatohepatitis, which can subsequently progress to cirrhosis. Thus, it increases the risk of HCC.
Obesity increases the risk of death from liver cancer, with obese people (body mass index ≥ 30 kg/m2) having a higher HCC-related death rate than leaner individuals.5 And as obesity becomes more prevalent, the number of deaths from HCC could increase.
Other diseases that predispose to HCC include alcohol abuse, hereditary hemochromatosis, alpha-1-antitrypsin deficiency, and glycogen storage disease.
SURVEILLANCE OF PATIENTS AT RISK
Patients at high risk of developing liver cancer require frequent screening (Table 1).
Patients with cirrhosis. Sarasin et al6 calculated that surveillance is cost-effective and increases the odds of survival in patients with cirrhosis if the incidence of HCC exceeds 1.5% per year (which it does). In view of this finding, all patients with cirrhosis should be screened every 6 months, irrespective of the cause of the cirrhosis.
Hepatitis B carriers. Surveillance is also indicated in some hepatitis B carriers (Table 1), eg, those with a family history of HCC in a first-degree relative (an independent risk factor for developing the disease in this group).7 Also, Africans with hepatitis B tend to develop HCC early in life.8 Though it has been recommended that surveillance be started at a younger age in these patients,9 the age at which it should begin has not been clearly established. In addition, it is not clear if black people born outside Africa are at higher risk.
Benefit of surveillance
HCC surveillance has shown to lower the death rate. A randomized controlled trial in China compared screening (with abdominal ultrasonography and alpha-fetoprotein levels) vs no screening in patients with hepatitis B. It showed that screening led to a 37% decrease in the death rate.12 Studies have also established that patients with early-stage HCC have a better survival rate than patients with more-advanced disease.10,11 This survival benefit is largely explained by the availability of effective treatments for early-stage cancer, including liver transplantation. Therefore, early-stage asymptomatic patients diagnosed by a surveillance program should have a better survival rate than symptomatic patients.
Surveillance methods
The tests most often used in surveillance for HCC are serum alpha-fetoprotein levels and liver ultrasonography.
Serum alpha-fetoprotein levels by themselves have not been shown to be useful, whereas the combination of alpha-fetoprotein levels and ultrasonography has been shown to reduce the death rate when used for surveillance in a randomized trial.12 A 2012 study reported that the combination of alpha-fetoprotein testing and ultrasonography had a higher sensitivity (90%) than ultrasonography alone (58%), but at the expense of a lower specificity.13
Alpha-fetoprotein has a low sensitivity (ie, 54%) for HCC.14 Tumor size is one of the factors limiting the sensitivity of alpha-fetoprotein, 14 and this would imply that this test may not be helpful in detecting HCC at an early stage. Alpha-fetoprotein L3, an isoform of alpha-fetoprotein, may be helpful in patients with alpha-fetoprotein levels in the intermediate range, and it is currently being studied.
Liver ultrasonography is operator-dependent, and it may not be as accurate in overweight or obese people.
Computed tomography (CT) and magnetic resonance imaging (MRI) are not recommended for surveillance. Serial CT poses risks of radiation-induced damage, contrast-related anaphylaxis, and renal failure, and MRI is not cost-effective and can also lead to gadolinium-induced nephrogenic systemic fibrosis in patients with renal failure.
Currently, the American Association for the Study of Liver Diseases9 recommends ultrasonography only, every 6 months, for surveillance for HCC. However, it may be premature to conclude that alpha-fetoprotein measurement is no longer required for surveillance, and if new data emerge that support its role, it may be reincorporated into the guidelines.
DIAGNOSING HEPATOCELLULAR CARCINOMA
Lesions larger than 1 cm on ultrasonography
The finding of a liver lesion larger than 1 cm on ultrasonography during surveillance warrants further testing.
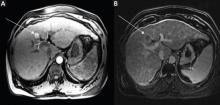
Noninvasive testing with four-phase multidetector CT or dynamic contrast-enhanced MRI is the next step. Typical findings on either of these imaging studies are sufficient to make a diagnosis of HCC, as they have a high specificity and positive predictive value.15 Arterial hyperenhancement with a venous-phase or delayed-phase washout of contrast medium confirms the diagnosis (Figure 2).9 If one of the two imaging studies is typical for HCC, liver biopsy is not needed.
Other imaging studies, including contrast-enhanced ultrasonography, have not been shown to be specific for this diagnosis.16
Liver biopsy is indicated in patients in whom the imaging findings are atypical for HCC.9,17 Biopsy has very good sensitivity and specificity for cancer, but false-negative findings do occur.18 Therefore, a negative biopsy does not entirely exclude HCC. In this situation, patients should be followed by serial ultrasonography, and any further growth or change in character should be reevaluated.
Lesions smaller than 1 cm
For lesions smaller than 1 cm, the incidence of HCC is low, and currently available diagnostic tests are not reliable.15,19 Lesions of this size should be followed by serial ultrasonography every 3 to 4 months until they either enlarge to greater than 1 cm or remain stable at 2 years.9 If they remain stable at the end of 2 years, regular surveillance ultrasonography once every 6 months can be continued.
CURATIVE AND PALLIATIVE THERAPIES
Therapies for HCC (Table 2) can be divided into two categories: curative and palliative.
Curative treatments include surgical resection, liver transplantation, and radiofrequency ablation. All other treatments are palliative, including transarterial chemoembolization and medical therapy with sorafenib.
The choice of treatment depends on the characteristics of the tumor, the degree of liver dysfunction, and the patient’s current level of function. The Barcelona Clinic Liver Cancer classification is widely used in making these decisions, as it incorporates both clinical features and tumor stage.9 Figure 3 shows a simplified management algorithm.
SURGICAL RESECTION
Surgical resection is the preferred treatment for patients who have a solitary HCC lesion without cirrhosis.9 It is also indicated in patients with well-compensated cirrhosis who have normal portal pressure, a normal serum bilirubin level, and a platelet count greater than 100 × 109/L.20,21 In such patients, the 5-year survival rate is about 74%, compared with 25% in patients with portal hypertension and serum bilirubin levels higher than 1 mg/dL.21
Surgical resection is not recommended for patients with decompensated cirrhosis, as it can worsen liver function postoperatively and increase the risk of death.19,20 In Western countries, where cirrhosis from hepatitis C is the commonest cause of HCC, most patients have poorly preserved hepatic function at the time of diagnosis, leaving only a minority of patients as candidates for surgical resection.
After surgical resection of HCC, the recurrence rate can be as high as 70% to 80% at 5 years.22,23 Studies have consistently found larger tumor size and vascular invasion to be factors that predict recurrence.24,25 Vascular invasion was also found to predict poor survival after recurrence.24 Studies have so far not shown any conclusive benefit from post-surgical adjuvant chemotherapy in reducing the rate of recurrence of HCC.26,27
How to treat recurrent HCC after surgical resection has not been clearly established. Radiofrequency ablation, transarterial chemoembolization, repeat resection, and liver transplantation have all improved survival when used alone or in combination.28 However, randomized controlled trials are needed to establish the effective treatment strategy and the benefit of multimodal treatment of recurrent HCC.
LIVER TRANSPLANTATION
Orthotopic liver transplantation is the preferred treatment for patients with HCC complicated by cirrhosis and portal hypertension. It has the advantage not only of being potentially curative, but also of overcoming liver cirrhosis by replacing the liver.
To qualify for liver transplantation, patients must meet the Milan criteria (ie, have a single nodule less than 5 cm in diameter or up to three nodules, with the largest being less than 3 cm in diameter, with no evidence of vascular invasion or distant metastasis). These patients have an expected 4-year survival rate of 85% and a recurrence-free survival rate of 92% after transplantation, compared with 50% and 59%, respectively, in patients whose tumors exceeded these criteria.29
Some believe that the Milan criteria are too restrictive and could be expanded. Yao et al at the University of California-San Francisco30 reported that patients with HCC meeting the criteria of having a solitary tumor smaller than 6.5 cm or having up to three nodules, with the largest smaller than 4.5 cm, and total tumor diameter less than 8 cm, had survival rates of 90% at 1 year and 75.2% at 5 years after liver transplantation, compared with 50% at 1 year for patients with tumors exceeding these limits. (These have come to be known as the UCSF criteria.) However, the United Network for Organ Sharing (UNOS) has not adopted these expanded criteria. UNOS has a point system for allocating livers for transplant called the Model for End-Stage Liver Disease (MELD). Patients who meet the Milan criteria receive extra points, putting them higher on the transplant list. This allows for early transplantation, thus reducing tumor progression and dropout from the transplant list. UNOS allocates a MELD score of 22 to all patients who meet the Milan criteria, and the score is further adjusted once every 3 months to reflect a 10% increase in the mortality rate. However, patients who have a single lesion smaller than 2 cm and are candidates for liver transplantation are not assigned additional MELD points per UNOS policy, as the risk of tumor progression beyond the Milan criteria in these patients is deemed to be low.
Therapies while awaiting transplantation
Even if they receive additional MELD points to give them priority on the waiting list, patients face a considerable wait before transplantation because of the limited availability of donor organs. In the interim, they have a risk of tumor progression beyond the Milan criteria and subsequent dropout from the transplant list.31 Patients on the waiting list may therefore undergo a locoregional therapy such as transarterial chemoembolization or radiofrequency ablation as bridging therapy.
These therapies have been shown to decrease dropout from the waiting list.31 A prospective study showed that in 48 patients who underwent transarterial chemoembolization while awaiting liver transplantation, none had tumor progression, and 41 did receive a transplant, with excellent posttransplantation survival rates.32 Similarly, radioembolization using yttrium-90-labeled microspheres or radiofrequency ablation while on the waiting list has been shown to significantly decrease the rate of dropout, with good posttransplantation outcomes.33,34
However, in spite of these benefits, these bridging therapies do not increase survival rates after transplantation. It is also unclear whether they are useful in regions with short waiting times for liver transplantation.
Adjuvant systemic chemotherapy has not been shown to improve survival in patients undergoing liver transplantation. For example, in a randomized controlled trial of doxorubicin given before, during, and after surgery, the survival rate at 5 years was 38% with doxorubicin and 40% without.35
ABLATIVE LOCOREGIONAL THERAPIES
Locoregional therapies play an important role in managing HCC. They are classified as ablative and perfusion-based.
Ablative locoregional therapies include chemical modalities such as percutaneous ethanol injection; thermal therapies such as radiofrequency ablation, microwave ablation, laser ablation, and cryotherapy; and newer methods such as irreversible electroporation and light-activated drug therapy. Of these, radiofrequency ablation is the most widely used.
Radiofrequency ablation
Radiofrequency ablation induces thermal injury, resulting in tumor necrosis. It can be used as an alternative to surgery in patients who have a single HCC lesion less than 3 to 5 cm in diameter, confined to the liver, and in a site amenable to this procedure and who have a reasonable coagulation profile. The procedure can be performed percutaneously or via laparoscopy.
Radiofrequency ablation is contraindicated in patients with decompensated cirrhosis, Child-Pugh class C cirrhosis (the most severe category), vascular or bile duct invasion, extrahepatic disease, or lesions that are not accessible or are adjacent to structures such as the gall bladder, bowel, stomach, or diaphragm.
Radiofrequency ablation has been compared with surgical resection in patients who had small tumors. Though a randomized controlled trial did not show any difference between the two treatment groups in terms of survival at 5 years and recurrence rates,36 a meta-analysis showed that overall survival rates at 3 years and 5 years were significantly higher with surgical resection than with radiofrequency ablation.37 Patients also had a higher rate of local recurrence with radiofrequency ablation than with surgical resection.37 In addition, radiofrequency ablation has been shown to be effective only in small tumors and does not perform as well in lesions larger than 2 or 3 cm.
Thus, based on current evidence, surgical resection is preferable to radiofrequency ablation as first-line treatment. The latter, however, is also used as a bridging therapy in patients awaiting liver transplantation.
Percutaneous ethanol injection
Percutaneous ethanol injection is used less frequently than radiofrequency ablation, as studies have shown the latter to be superior in regard to local recurrence-free survival rates.38 However, percutaneous ethanol injection is used instead of radiofrequency ablation in a small number of patients, when the lesion is very close to organs such as the bile duct (which could be damaged by radiofrequency ablation) or the large vessels (which may make radiofrequency ablation less effective, since heat may dissipate as a result of excessive blood flow in this region).
Microwave ablation
Microwave ablation is an emerging therapy for HCC. Its advantage over radiofrequency ablation is that its use is not limited by blood vessels in close proximity to the ablation site.
Earlier studies did not show microwave ablation to be superior to radiofrequency ablation.39,40 However, current studies involving newer techniques of microwave ablation are more promising.41
PERFUSION-BASED LOCOREGIONAL THERAPIES
Perfusion-based locoregional therapies deliver embolic particles, chemotherapeutic agents, or radioactive materials into the artery feeding the tumor. The portal blood flow allows for preservation of vital liver tissue during arterial embolization of liver tumors. Perfusionbased therapies include transarterial chemoembolization, transarterial chemoembolization with doxorubicin-eluting beads (DEB-TACE), “bland” embolization, and radioembolization.
Transarterial chemoembolization
Transarterial chemoembolization is a minimally invasive procedure in which the hepatic artery is cannulated through a percutaneous puncture, the branches of the hepatic artery supplying the tumor are identified, and then embolic particles and chemotherapeutic agents are injected. This serves a dual purpose: it embolizes the feeding vessel that supplies the tumor, causing tumor necrosis, and it focuses the chemotherapy on the tumor and thus minimizes the systemic effects of the chemotherapeutic agent.
This therapy is contraindicated in patients with portal vein thrombosis, advanced liver dysfunction, or a transjugular intrahepatic portosystemic shunt. Side effects of the procedure include a postembolization syndrome of abdominal pain and fever (occurring in about 50% of patients from ischemic injury to the liver), hepatic abscesses, injury to the hepatic artery, development of ascites, liver dysfunction, and contrast-induced renal failure.
In addition to bridging patients to liver transplantation, transarterial chemoembolization is recommended as palliative treatment to prolong survival in patients with HCC who are not candidates for liver transplantation, surgical resection, or radiofrequency ablation.9,42 Patients who have Child-Pugh grade A or B cirrhosis but do not have main portal vein thrombosis or extrahepatic spread are candidates for this therapy. Patients such as these who undergo this therapy have a better survival rate at 2 years compared with untreated patients.43,44
Transarterial chemoembolization has also been used to reduce the size of (ie, to “downstage”) tumors that are outside the Milan criteria in patients who are otherwise candidates for liver transplantation. It induces tumor necrosis and has been shown to decrease the tumor size in a selected group of patients and to bring them within the Milan criteria, thus potentially enabling them to be put on the transplant list.45 Studies have shown that patients who receive a transplant after successful down-staging may achieve a 5-year survival rate comparable with that of patients who were initially within the Milan criteria and received a transplant without the need for down-staging.45 However, factors that predict successful down-staging have not been clearly established.
Newer techniques have been developed. A randomized controlled trial found transarterial chemoembolization with doxorubicin-eluting beads to be safer and better tolerated than conventional transarterial chemembolization.46
Bland embolization is transarterial embolization without chemotherapeutic agents and is performed in patients with significant liver dysfunction who might not tolerate chemotherapy. The benefits of this approach are yet to be determined.
Radioembolization
Radioembolization with yttrium-90 microspheres has recently been introduced as an alternative to transarterial chemoembolization, especially in patients with portal vein thrombosis, a portocaval shunt, or a transjugular intrahepatic portosystemic shunt.
In observational studies, radioembolization was as effective as transarterial chemoembolization, with a similar survival benefit.47 However, significant pulmonary shunting must be ruled out before radioembolization, as it would lead to radiation-induced pulmonary disease. Randomized controlled trials are under way to compare the efficacy of the two methods.
CHEMOTHERAPY
Sorafenib
Sorafenib is an oral antiangiogenic agent. A kinase inhibitor, it interacts with multiple intracellular and cell-surface kinases, including vascular endothelial growth factor receptor, platelet-derived growth factor receptor, and Raf proto-oncogene, inhibiting tumor cell proliferation and angiogenesis.
Sorafenib has been shown to prolong survival in patients with advanced-stage HCC.48 A randomized placebo-controlled trial in patients with Child-Pugh grade A cirrhosis and advanced HCC who had not received chemotherapy showed that sorafenib increased the life expectancy by nearly 3 months compared with placebo.47 Sorafenib therapy is very expensive, but it is usually covered by insurance.
Sorafenib is recommended in patients who have advanced HCC with vascular invasion, extrahepatic dissemination, or minimal constitutional symptoms. It is not recommended for patients with severe advanced liver disease who have moderate to severe tumor-related constitutional symptoms or Child-Pugh grade C cirrhosis, or for patients with a life expectancy of less than 3 months.
The most common side effects of sorafenib are diarrhea, weight loss, and skin reactions on the hands and feet. These commonly lead to decreased tolerability and dose reductions.47 Doses should be adjusted on the basis of the bilirubin and albumin levels.49
Other chemotherapeutic agents
Several molecular targeted agents are undergoing clinical trials for the treatment of HCC. These include bevacizumab, erlotinib, brivanib, and ramucirumab. Chemotherapeutic agents such as doxorubicin and everolimus are also being studied.
PALLIATIVE TREATMENT
Patients with end-stage HCC with moderate to severe constitutional symptoms, extrahepatic disease progression, and decompensated liver disease have a survival of less than 3 months and are treated for pain and symptom control.9
- Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010; 127:2893–2917.
- El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology 2007; 132:2557–2576.
- El-Serag HB. Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology 2012; 142:1264–1273.e1.
- Altekruse SF, McGlynn KA, Reichman ME. Hepatocellular carcinoma incidence, mortality, and survival trends in the United States from 1975 to 2005. J Clin Oncol 2009; 27:1485–1491.
- Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of US adults. N Engl J Med 2003; 348:1625–1638.
- Sarasin FP, Giostra E, Hadengue A. Cost-effectiveness of screening for detection of small hepatocellular carcinoma in western patients with Child-Pugh class A cirrhosis. Am J Med 1996; 101:422–434.
- Yu MW, Chang HC, Liaw YF, et al. Familial risk of hepatocellular carcinoma among chronic hepatitis B carriers and their relatives. J Natl Cancer Inst 2000; 92:1159–1164.
- Kew MC, Macerollo P. Effect of age on the etiologic role of the hepatitis B virus in hepatocellular carcinoma in blacks. Gastroenterology 1988; 94:439–442.
- Bruix J, Sherman M; American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology 2011; 53:1020–1022.
- Bruix J, Llovet JM. Major achievements in hepatocellular carcinoma. Lancet 2009; 373:614–616.
- Gómez-Rodríguez R, Romero-Gutiérrez M, Artaza-Varasa T, et al. The value of the Barcelona Clinic Liver Cancer and alpha-fetoprotein in the prognosis of hepatocellular carcinoma. Rev Esp Enferm Dig 2012; 104:298–304.
- Zhang BH, Yang BH, Tang ZY. Randomized controlled trial of screening for hepatocellular carcinoma. J Cancer Res Clin Oncol 2004; 130:417–422.
- Giannini EG, Erroi V, Trevisani F. Effectiveness of a-fetoprotein for hepatocellular carcinoma surveillance: the return of the living-dead? Expert Rev Gastroenterol Hepatol 2012; 6:441–444.
- Farinati F, Marino D, De Giorgio M, et al. Diagnostic and prognostic role of alpha-fetoprotein in hepatocellular carcinoma: both or neither? Am J Gastroenterol 2006; 101:524–532.
- Forner A, Vilana R, Ayuso C, et al. Diagnosis of hepatic nodules 20 mm or smaller in cirrhosis: prospective validation of the noninvasive diagnostic criteria for hepatocellular carcinoma. Hepatology 2008; 47:97–104.
- Vilana R, Forner A, Bianchi L, et al. Intrahepatic peripheral cholangiocarcinoma in cirrhosis patients may display a vascular pattern similar to hepatocellular carcinoma on contrast-enhanced ultrasound. Hepatology 2010; 51:2020–2029.
- Kojiro M. Pathological diagnosis at early stage: reaching international consensus. Oncology 2010; 78(suppl 1):31–35.
- Schölmerich J, Schacherer D. Diagnostic biopsy for hepatocellular carcinoma in cirrhosis: useful, necessary, dangerous, or academic sport? Gut 2004; 53:1224–1226.
- Durand F, Regimbeau JM, Belghiti J, et al. Assessment of the benefits and risks of percutaneous biopsy before surgical resection of hepatocellular carcinoma. J Hepatol 2001; 35:254–258.
- Bruix J, Castells A, Bosch J, et al. Surgical resection of hepatocellular carcinoma in cirrhotic patients: prognostic value of preoperative portal pressure. Gastroenterology 1996; 111:1018–1022.
- Llovet JM, Fuster J, Bruix J. Intention-to-treat analysis of surgical treatment for early hepatocellular carcinoma: resection versus transplantation. Hepatology 1999; 30:1434–1440.
- Nagasue N, Uchida M, Makino Y, et al. Incidence and factors associated with intrahepatic recurrence following resection of hepatocellular carcinoma. Gastroenterology 1993; 105:488–494.
- Arii S, Tanaka J, Yamazoe Y, et al. Predictive factors for intrahepatic recurrence of hepatocellular carcinoma after partial hepatectomy. Cancer 1992; 69:913–919.
- Cha C, Fong Y, Jarnagin WR, Blumgart LH, DeMatteo RP. Predictors and patterns of recurrence after resection of hepatocellular carcinoma. J Am Coll Surg 2003; 197:753–758.
- Shah SA, Cleary SP, Wei AC, et al. Recurrence after liver resection for hepatocellular carcinoma: risk factors, treatment, and outcomes. Surgery 2007; 141:330–339.
- Kohno H, Nagasue N, Hayashi T, et al. Postoperative adjuvant chemotherapy after radical hepatic resection for hepatocellular carcinoma (HCC). Hepatogastroenterology 1996; 43:1405–1409.
- Ono T, Nagasue N, Kohno H, et al. Adjuvant chemotherapy with epirubicin and carmofur after radical resection of hepatocellular carcinoma: a prospective randomized study. Semin Oncol 1997; 24(suppl 6):S6–25.
- Poon RT, Fan ST, Lo CM, Liu CL, Wong J. Intrahepatic recurrence after curative resection of hepatocellular carcinoma: Long-term results of treatment and prognostic factors. Ann Surg 1999; 229:216–222.
- Mazzaferro V, Regalia E, Doci R, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 1996; 334:693–699.
- Yao FY, Ferrell L, Bass NM, et al. Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology 2001; 33:1394–1403.
- Majno P, Lencioni R, Mornex F, Girard N, Poon RT, Cherqui D. Is the treatment of hepatocellular carcinoma on the waiting list necessary? Liver Transpl 2011; 17(suppl 2):S98–S108.
- Graziadei IW, Sandmueller H, Waldenberger P, et al. Chemoembolization followed by liver transplantation for hepatocellular carcinoma impedes tumor progression while on the waiting list and leads to excellent outcome. Liver Transpl 2003; 9:557–563.
- Kulik LM, Atassi B, van Holsbeeck L, et al. Yttrium-90 microspheres (TheraSphere) treatment of unresectable hepatocellular carcinoma: downstaging to resection, RFA and bridge to transplantation. J Surg Oncol 2006; 94:572–586.
- Lu DS, Yu NC, Raman SS, et al. Percutaneous radiofrequency ablation of hepatocellular carcinoma as a bridge to liver transplantation. Hepatology 2005; 41:1130–1137.
- Pokorny H, Gnant M, Rasoul-Rockenschaub S, et al. Does additional doxorubicin chemotherapy improve outcome in patients with hepatocellular carcinoma treated by liver transplantation? Am J Transplant 2005; 5:788–794.
- Feng K, Yan J, Li X, et al. A randomized controlled trial of radiofrequency ablation and surgical resection in the treatment of small hepatocellular carcinoma. J Hepatol 2012; 57:794–802.
- Zhou Y, Zhao Y, Li B, et al. Meta-analysis of radiofrequency ablation versus hepatic resection for small hepatocellular carcinoma. BMC Gastroenterol 2010; 10:78.
- Lencioni RA, Allgaier HP, Cioni D, et al. Small hepatocellular carcinoma in cirrhosis: Randomized comparison of radiofrequency thermal ablation versus percutaneous ethanol injection. Radiology 2003; 228:235–240.
- Ohmoto K, Yoshioka N, Tomiyama Y, et al. Comparison of therapeutic effects between radiofrequency ablation and percutaneous microwave coagulation therapy for small hepatocellular carcinomas. J Gastroenterol Hepatol 2009; 24:223–227.
- Shibata T, Iimuro Y, Yamamoto Y, et al. Small hepatocellular carcinoma: comparison of radiofrequency ablation and percutaneous microwave coagulation therapy. Radiology 2002; 223:331–337.
- Qian GJ, Wang N, Shen Q, et al. Efficacy of microwave versus radiofrequency ablation for treatment of small hepatocellular carcinoma: Experimental and clinical studies. Eur Radiol 2012; 22:1983–1990.
- Burrel M, Reig M, Forner A, et al. Survival of patients with hepatocellular carcinoma treated by transarterial chemoembolisation (TACE) using drug eluting beads. Implications for clinical practice and trial design. J Hepatol 2012; 56:1330–1335.
- Cammà C, Schepis F, Orlando A, et al. Transarterial chemoembolization for unresectable hepatocellular carcinoma: meta-analysis of randomized controlled trials. Radiology 2002; 224:47–54.
- Llovet JM, Bruix J. Systematic review of randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology 2003; 37:429–442.
- Yao FY, Kerlan RK, Hirose R, et al. Excellent outcome following down-staging of hepatocellular carcinoma prior to liver transplantation: an intention-to-treat analysis. Hepatology 2008; 48:819–827.
- Ferrer Puchol MD, la Parra C, Esteban E, et al. Comparison of doxorubicin-eluting bead transarterial chemoembolization (DEBTACE) with conventional transarterial chemoembolization (TACE) for the treatment of hepatocellular carcinoma (article in Spanish). Radiologia 2011; 53:246–253.
- Salem R, Lewandowski RJ, Kulik L, et al. Radioembolization results in longer time-to-progression and reduced toxicity compared with chemoembolization in patients with hepatocellular carcinoma. Gastroenterology 2011; 140:497–507.e2.
- Llovet JM, Ricci S, Mazzaferro V, et al; SHARP Investigators Study Group. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 2008; 359:378–390.
- Miller AA, Murry DJ, Owzar K, et al. Phase I and pharmacokinetic study of sorafenib in patients with hepatic or renal dysfunction: CALGB 60301. J Clin Oncol 2009; 27:1800–1805.
Hepatocellular carcinoma (HCC) is a common cause of death worldwide. However, it can be detected early in high-risk individuals by using effective screening strategies, resulting in the ability to provide curative treatment.
Here, we review the risk factors for HCC, strategies for surveillance and diagnosis, and therapies that can be used.
EPIDEMIOLOGY
HCC is the most common primary malignancy of the liver. Overall, it is the fifth most common type of cancer in men and the seventh most common in women.1
Cirrhosis is present in 80% to 90% of patients with HCC.
Male sex. The male-to-female ratio is from 2:1 to 4:1, depending on the region.2 In the United States, the overall male-to-female ratio has been reported2 as 2.4:1. In another report,3 the incidence rate of HCC per 100,000 person-years was 3.7 for men and 2.0 for women.
Geographic areas with a high incidence of HCC include sub-Saharan Africa and eastern Asia, whereas Canada and the United States are low-incidence areas. The difference has been because of a lower prevalence of hepatitis B virus infection in North America. However, recent data show a downward trend in incidence of HCC in eastern Asia and an upward trend in North America (Figure 1).3,4
Viral hepatitis (ie, hepatitis B or hepatitis C) is the main risk factor for cirrhosis and HCC.
Diabetes mellitus can predispose to nonalcoholic steatohepatitis, which can subsequently progress to cirrhosis. Thus, it increases the risk of HCC.
Obesity increases the risk of death from liver cancer, with obese people (body mass index ≥ 30 kg/m2) having a higher HCC-related death rate than leaner individuals.5 And as obesity becomes more prevalent, the number of deaths from HCC could increase.
Other diseases that predispose to HCC include alcohol abuse, hereditary hemochromatosis, alpha-1-antitrypsin deficiency, and glycogen storage disease.
SURVEILLANCE OF PATIENTS AT RISK
Patients at high risk of developing liver cancer require frequent screening (Table 1).
Patients with cirrhosis. Sarasin et al6 calculated that surveillance is cost-effective and increases the odds of survival in patients with cirrhosis if the incidence of HCC exceeds 1.5% per year (which it does). In view of this finding, all patients with cirrhosis should be screened every 6 months, irrespective of the cause of the cirrhosis.
Hepatitis B carriers. Surveillance is also indicated in some hepatitis B carriers (Table 1), eg, those with a family history of HCC in a first-degree relative (an independent risk factor for developing the disease in this group).7 Also, Africans with hepatitis B tend to develop HCC early in life.8 Though it has been recommended that surveillance be started at a younger age in these patients,9 the age at which it should begin has not been clearly established. In addition, it is not clear if black people born outside Africa are at higher risk.
Benefit of surveillance
HCC surveillance has shown to lower the death rate. A randomized controlled trial in China compared screening (with abdominal ultrasonography and alpha-fetoprotein levels) vs no screening in patients with hepatitis B. It showed that screening led to a 37% decrease in the death rate.12 Studies have also established that patients with early-stage HCC have a better survival rate than patients with more-advanced disease.10,11 This survival benefit is largely explained by the availability of effective treatments for early-stage cancer, including liver transplantation. Therefore, early-stage asymptomatic patients diagnosed by a surveillance program should have a better survival rate than symptomatic patients.
Surveillance methods
The tests most often used in surveillance for HCC are serum alpha-fetoprotein levels and liver ultrasonography.
Serum alpha-fetoprotein levels by themselves have not been shown to be useful, whereas the combination of alpha-fetoprotein levels and ultrasonography has been shown to reduce the death rate when used for surveillance in a randomized trial.12 A 2012 study reported that the combination of alpha-fetoprotein testing and ultrasonography had a higher sensitivity (90%) than ultrasonography alone (58%), but at the expense of a lower specificity.13
Alpha-fetoprotein has a low sensitivity (ie, 54%) for HCC.14 Tumor size is one of the factors limiting the sensitivity of alpha-fetoprotein, 14 and this would imply that this test may not be helpful in detecting HCC at an early stage. Alpha-fetoprotein L3, an isoform of alpha-fetoprotein, may be helpful in patients with alpha-fetoprotein levels in the intermediate range, and it is currently being studied.
Liver ultrasonography is operator-dependent, and it may not be as accurate in overweight or obese people.
Computed tomography (CT) and magnetic resonance imaging (MRI) are not recommended for surveillance. Serial CT poses risks of radiation-induced damage, contrast-related anaphylaxis, and renal failure, and MRI is not cost-effective and can also lead to gadolinium-induced nephrogenic systemic fibrosis in patients with renal failure.
Currently, the American Association for the Study of Liver Diseases9 recommends ultrasonography only, every 6 months, for surveillance for HCC. However, it may be premature to conclude that alpha-fetoprotein measurement is no longer required for surveillance, and if new data emerge that support its role, it may be reincorporated into the guidelines.
DIAGNOSING HEPATOCELLULAR CARCINOMA
Lesions larger than 1 cm on ultrasonography
The finding of a liver lesion larger than 1 cm on ultrasonography during surveillance warrants further testing.
Noninvasive testing with four-phase multidetector CT or dynamic contrast-enhanced MRI is the next step. Typical findings on either of these imaging studies are sufficient to make a diagnosis of HCC, as they have a high specificity and positive predictive value.15 Arterial hyperenhancement with a venous-phase or delayed-phase washout of contrast medium confirms the diagnosis (Figure 2).9 If one of the two imaging studies is typical for HCC, liver biopsy is not needed.
Other imaging studies, including contrast-enhanced ultrasonography, have not been shown to be specific for this diagnosis.16
Liver biopsy is indicated in patients in whom the imaging findings are atypical for HCC.9,17 Biopsy has very good sensitivity and specificity for cancer, but false-negative findings do occur.18 Therefore, a negative biopsy does not entirely exclude HCC. In this situation, patients should be followed by serial ultrasonography, and any further growth or change in character should be reevaluated.
Lesions smaller than 1 cm
For lesions smaller than 1 cm, the incidence of HCC is low, and currently available diagnostic tests are not reliable.15,19 Lesions of this size should be followed by serial ultrasonography every 3 to 4 months until they either enlarge to greater than 1 cm or remain stable at 2 years.9 If they remain stable at the end of 2 years, regular surveillance ultrasonography once every 6 months can be continued.
CURATIVE AND PALLIATIVE THERAPIES
Therapies for HCC (Table 2) can be divided into two categories: curative and palliative.
Curative treatments include surgical resection, liver transplantation, and radiofrequency ablation. All other treatments are palliative, including transarterial chemoembolization and medical therapy with sorafenib.
The choice of treatment depends on the characteristics of the tumor, the degree of liver dysfunction, and the patient’s current level of function. The Barcelona Clinic Liver Cancer classification is widely used in making these decisions, as it incorporates both clinical features and tumor stage.9 Figure 3 shows a simplified management algorithm.
SURGICAL RESECTION
Surgical resection is the preferred treatment for patients who have a solitary HCC lesion without cirrhosis.9 It is also indicated in patients with well-compensated cirrhosis who have normal portal pressure, a normal serum bilirubin level, and a platelet count greater than 100 × 109/L.20,21 In such patients, the 5-year survival rate is about 74%, compared with 25% in patients with portal hypertension and serum bilirubin levels higher than 1 mg/dL.21
Surgical resection is not recommended for patients with decompensated cirrhosis, as it can worsen liver function postoperatively and increase the risk of death.19,20 In Western countries, where cirrhosis from hepatitis C is the commonest cause of HCC, most patients have poorly preserved hepatic function at the time of diagnosis, leaving only a minority of patients as candidates for surgical resection.
After surgical resection of HCC, the recurrence rate can be as high as 70% to 80% at 5 years.22,23 Studies have consistently found larger tumor size and vascular invasion to be factors that predict recurrence.24,25 Vascular invasion was also found to predict poor survival after recurrence.24 Studies have so far not shown any conclusive benefit from post-surgical adjuvant chemotherapy in reducing the rate of recurrence of HCC.26,27
How to treat recurrent HCC after surgical resection has not been clearly established. Radiofrequency ablation, transarterial chemoembolization, repeat resection, and liver transplantation have all improved survival when used alone or in combination.28 However, randomized controlled trials are needed to establish the effective treatment strategy and the benefit of multimodal treatment of recurrent HCC.
LIVER TRANSPLANTATION
Orthotopic liver transplantation is the preferred treatment for patients with HCC complicated by cirrhosis and portal hypertension. It has the advantage not only of being potentially curative, but also of overcoming liver cirrhosis by replacing the liver.
To qualify for liver transplantation, patients must meet the Milan criteria (ie, have a single nodule less than 5 cm in diameter or up to three nodules, with the largest being less than 3 cm in diameter, with no evidence of vascular invasion or distant metastasis). These patients have an expected 4-year survival rate of 85% and a recurrence-free survival rate of 92% after transplantation, compared with 50% and 59%, respectively, in patients whose tumors exceeded these criteria.29
Some believe that the Milan criteria are too restrictive and could be expanded. Yao et al at the University of California-San Francisco30 reported that patients with HCC meeting the criteria of having a solitary tumor smaller than 6.5 cm or having up to three nodules, with the largest smaller than 4.5 cm, and total tumor diameter less than 8 cm, had survival rates of 90% at 1 year and 75.2% at 5 years after liver transplantation, compared with 50% at 1 year for patients with tumors exceeding these limits. (These have come to be known as the UCSF criteria.) However, the United Network for Organ Sharing (UNOS) has not adopted these expanded criteria. UNOS has a point system for allocating livers for transplant called the Model for End-Stage Liver Disease (MELD). Patients who meet the Milan criteria receive extra points, putting them higher on the transplant list. This allows for early transplantation, thus reducing tumor progression and dropout from the transplant list. UNOS allocates a MELD score of 22 to all patients who meet the Milan criteria, and the score is further adjusted once every 3 months to reflect a 10% increase in the mortality rate. However, patients who have a single lesion smaller than 2 cm and are candidates for liver transplantation are not assigned additional MELD points per UNOS policy, as the risk of tumor progression beyond the Milan criteria in these patients is deemed to be low.
Therapies while awaiting transplantation
Even if they receive additional MELD points to give them priority on the waiting list, patients face a considerable wait before transplantation because of the limited availability of donor organs. In the interim, they have a risk of tumor progression beyond the Milan criteria and subsequent dropout from the transplant list.31 Patients on the waiting list may therefore undergo a locoregional therapy such as transarterial chemoembolization or radiofrequency ablation as bridging therapy.
These therapies have been shown to decrease dropout from the waiting list.31 A prospective study showed that in 48 patients who underwent transarterial chemoembolization while awaiting liver transplantation, none had tumor progression, and 41 did receive a transplant, with excellent posttransplantation survival rates.32 Similarly, radioembolization using yttrium-90-labeled microspheres or radiofrequency ablation while on the waiting list has been shown to significantly decrease the rate of dropout, with good posttransplantation outcomes.33,34
However, in spite of these benefits, these bridging therapies do not increase survival rates after transplantation. It is also unclear whether they are useful in regions with short waiting times for liver transplantation.
Adjuvant systemic chemotherapy has not been shown to improve survival in patients undergoing liver transplantation. For example, in a randomized controlled trial of doxorubicin given before, during, and after surgery, the survival rate at 5 years was 38% with doxorubicin and 40% without.35
ABLATIVE LOCOREGIONAL THERAPIES
Locoregional therapies play an important role in managing HCC. They are classified as ablative and perfusion-based.
Ablative locoregional therapies include chemical modalities such as percutaneous ethanol injection; thermal therapies such as radiofrequency ablation, microwave ablation, laser ablation, and cryotherapy; and newer methods such as irreversible electroporation and light-activated drug therapy. Of these, radiofrequency ablation is the most widely used.
Radiofrequency ablation
Radiofrequency ablation induces thermal injury, resulting in tumor necrosis. It can be used as an alternative to surgery in patients who have a single HCC lesion less than 3 to 5 cm in diameter, confined to the liver, and in a site amenable to this procedure and who have a reasonable coagulation profile. The procedure can be performed percutaneously or via laparoscopy.
Radiofrequency ablation is contraindicated in patients with decompensated cirrhosis, Child-Pugh class C cirrhosis (the most severe category), vascular or bile duct invasion, extrahepatic disease, or lesions that are not accessible or are adjacent to structures such as the gall bladder, bowel, stomach, or diaphragm.
Radiofrequency ablation has been compared with surgical resection in patients who had small tumors. Though a randomized controlled trial did not show any difference between the two treatment groups in terms of survival at 5 years and recurrence rates,36 a meta-analysis showed that overall survival rates at 3 years and 5 years were significantly higher with surgical resection than with radiofrequency ablation.37 Patients also had a higher rate of local recurrence with radiofrequency ablation than with surgical resection.37 In addition, radiofrequency ablation has been shown to be effective only in small tumors and does not perform as well in lesions larger than 2 or 3 cm.
Thus, based on current evidence, surgical resection is preferable to radiofrequency ablation as first-line treatment. The latter, however, is also used as a bridging therapy in patients awaiting liver transplantation.
Percutaneous ethanol injection
Percutaneous ethanol injection is used less frequently than radiofrequency ablation, as studies have shown the latter to be superior in regard to local recurrence-free survival rates.38 However, percutaneous ethanol injection is used instead of radiofrequency ablation in a small number of patients, when the lesion is very close to organs such as the bile duct (which could be damaged by radiofrequency ablation) or the large vessels (which may make radiofrequency ablation less effective, since heat may dissipate as a result of excessive blood flow in this region).
Microwave ablation
Microwave ablation is an emerging therapy for HCC. Its advantage over radiofrequency ablation is that its use is not limited by blood vessels in close proximity to the ablation site.
Earlier studies did not show microwave ablation to be superior to radiofrequency ablation.39,40 However, current studies involving newer techniques of microwave ablation are more promising.41
PERFUSION-BASED LOCOREGIONAL THERAPIES
Perfusion-based locoregional therapies deliver embolic particles, chemotherapeutic agents, or radioactive materials into the artery feeding the tumor. The portal blood flow allows for preservation of vital liver tissue during arterial embolization of liver tumors. Perfusionbased therapies include transarterial chemoembolization, transarterial chemoembolization with doxorubicin-eluting beads (DEB-TACE), “bland” embolization, and radioembolization.
Transarterial chemoembolization
Transarterial chemoembolization is a minimally invasive procedure in which the hepatic artery is cannulated through a percutaneous puncture, the branches of the hepatic artery supplying the tumor are identified, and then embolic particles and chemotherapeutic agents are injected. This serves a dual purpose: it embolizes the feeding vessel that supplies the tumor, causing tumor necrosis, and it focuses the chemotherapy on the tumor and thus minimizes the systemic effects of the chemotherapeutic agent.
This therapy is contraindicated in patients with portal vein thrombosis, advanced liver dysfunction, or a transjugular intrahepatic portosystemic shunt. Side effects of the procedure include a postembolization syndrome of abdominal pain and fever (occurring in about 50% of patients from ischemic injury to the liver), hepatic abscesses, injury to the hepatic artery, development of ascites, liver dysfunction, and contrast-induced renal failure.
In addition to bridging patients to liver transplantation, transarterial chemoembolization is recommended as palliative treatment to prolong survival in patients with HCC who are not candidates for liver transplantation, surgical resection, or radiofrequency ablation.9,42 Patients who have Child-Pugh grade A or B cirrhosis but do not have main portal vein thrombosis or extrahepatic spread are candidates for this therapy. Patients such as these who undergo this therapy have a better survival rate at 2 years compared with untreated patients.43,44
Transarterial chemoembolization has also been used to reduce the size of (ie, to “downstage”) tumors that are outside the Milan criteria in patients who are otherwise candidates for liver transplantation. It induces tumor necrosis and has been shown to decrease the tumor size in a selected group of patients and to bring them within the Milan criteria, thus potentially enabling them to be put on the transplant list.45 Studies have shown that patients who receive a transplant after successful down-staging may achieve a 5-year survival rate comparable with that of patients who were initially within the Milan criteria and received a transplant without the need for down-staging.45 However, factors that predict successful down-staging have not been clearly established.
Newer techniques have been developed. A randomized controlled trial found transarterial chemoembolization with doxorubicin-eluting beads to be safer and better tolerated than conventional transarterial chemembolization.46
Bland embolization is transarterial embolization without chemotherapeutic agents and is performed in patients with significant liver dysfunction who might not tolerate chemotherapy. The benefits of this approach are yet to be determined.
Radioembolization
Radioembolization with yttrium-90 microspheres has recently been introduced as an alternative to transarterial chemoembolization, especially in patients with portal vein thrombosis, a portocaval shunt, or a transjugular intrahepatic portosystemic shunt.
In observational studies, radioembolization was as effective as transarterial chemoembolization, with a similar survival benefit.47 However, significant pulmonary shunting must be ruled out before radioembolization, as it would lead to radiation-induced pulmonary disease. Randomized controlled trials are under way to compare the efficacy of the two methods.
CHEMOTHERAPY
Sorafenib
Sorafenib is an oral antiangiogenic agent. A kinase inhibitor, it interacts with multiple intracellular and cell-surface kinases, including vascular endothelial growth factor receptor, platelet-derived growth factor receptor, and Raf proto-oncogene, inhibiting tumor cell proliferation and angiogenesis.
Sorafenib has been shown to prolong survival in patients with advanced-stage HCC.48 A randomized placebo-controlled trial in patients with Child-Pugh grade A cirrhosis and advanced HCC who had not received chemotherapy showed that sorafenib increased the life expectancy by nearly 3 months compared with placebo.47 Sorafenib therapy is very expensive, but it is usually covered by insurance.
Sorafenib is recommended in patients who have advanced HCC with vascular invasion, extrahepatic dissemination, or minimal constitutional symptoms. It is not recommended for patients with severe advanced liver disease who have moderate to severe tumor-related constitutional symptoms or Child-Pugh grade C cirrhosis, or for patients with a life expectancy of less than 3 months.
The most common side effects of sorafenib are diarrhea, weight loss, and skin reactions on the hands and feet. These commonly lead to decreased tolerability and dose reductions.47 Doses should be adjusted on the basis of the bilirubin and albumin levels.49
Other chemotherapeutic agents
Several molecular targeted agents are undergoing clinical trials for the treatment of HCC. These include bevacizumab, erlotinib, brivanib, and ramucirumab. Chemotherapeutic agents such as doxorubicin and everolimus are also being studied.
PALLIATIVE TREATMENT
Patients with end-stage HCC with moderate to severe constitutional symptoms, extrahepatic disease progression, and decompensated liver disease have a survival of less than 3 months and are treated for pain and symptom control.9
Hepatocellular carcinoma (HCC) is a common cause of death worldwide. However, it can be detected early in high-risk individuals by using effective screening strategies, resulting in the ability to provide curative treatment.
Here, we review the risk factors for HCC, strategies for surveillance and diagnosis, and therapies that can be used.
EPIDEMIOLOGY
HCC is the most common primary malignancy of the liver. Overall, it is the fifth most common type of cancer in men and the seventh most common in women.1
Cirrhosis is present in 80% to 90% of patients with HCC.
Male sex. The male-to-female ratio is from 2:1 to 4:1, depending on the region.2 In the United States, the overall male-to-female ratio has been reported2 as 2.4:1. In another report,3 the incidence rate of HCC per 100,000 person-years was 3.7 for men and 2.0 for women.
Geographic areas with a high incidence of HCC include sub-Saharan Africa and eastern Asia, whereas Canada and the United States are low-incidence areas. The difference has been because of a lower prevalence of hepatitis B virus infection in North America. However, recent data show a downward trend in incidence of HCC in eastern Asia and an upward trend in North America (Figure 1).3,4
Viral hepatitis (ie, hepatitis B or hepatitis C) is the main risk factor for cirrhosis and HCC.
Diabetes mellitus can predispose to nonalcoholic steatohepatitis, which can subsequently progress to cirrhosis. Thus, it increases the risk of HCC.
Obesity increases the risk of death from liver cancer, with obese people (body mass index ≥ 30 kg/m2) having a higher HCC-related death rate than leaner individuals.5 And as obesity becomes more prevalent, the number of deaths from HCC could increase.
Other diseases that predispose to HCC include alcohol abuse, hereditary hemochromatosis, alpha-1-antitrypsin deficiency, and glycogen storage disease.
SURVEILLANCE OF PATIENTS AT RISK
Patients at high risk of developing liver cancer require frequent screening (Table 1).
Patients with cirrhosis. Sarasin et al6 calculated that surveillance is cost-effective and increases the odds of survival in patients with cirrhosis if the incidence of HCC exceeds 1.5% per year (which it does). In view of this finding, all patients with cirrhosis should be screened every 6 months, irrespective of the cause of the cirrhosis.
Hepatitis B carriers. Surveillance is also indicated in some hepatitis B carriers (Table 1), eg, those with a family history of HCC in a first-degree relative (an independent risk factor for developing the disease in this group).7 Also, Africans with hepatitis B tend to develop HCC early in life.8 Though it has been recommended that surveillance be started at a younger age in these patients,9 the age at which it should begin has not been clearly established. In addition, it is not clear if black people born outside Africa are at higher risk.
Benefit of surveillance
HCC surveillance has shown to lower the death rate. A randomized controlled trial in China compared screening (with abdominal ultrasonography and alpha-fetoprotein levels) vs no screening in patients with hepatitis B. It showed that screening led to a 37% decrease in the death rate.12 Studies have also established that patients with early-stage HCC have a better survival rate than patients with more-advanced disease.10,11 This survival benefit is largely explained by the availability of effective treatments for early-stage cancer, including liver transplantation. Therefore, early-stage asymptomatic patients diagnosed by a surveillance program should have a better survival rate than symptomatic patients.
Surveillance methods
The tests most often used in surveillance for HCC are serum alpha-fetoprotein levels and liver ultrasonography.
Serum alpha-fetoprotein levels by themselves have not been shown to be useful, whereas the combination of alpha-fetoprotein levels and ultrasonography has been shown to reduce the death rate when used for surveillance in a randomized trial.12 A 2012 study reported that the combination of alpha-fetoprotein testing and ultrasonography had a higher sensitivity (90%) than ultrasonography alone (58%), but at the expense of a lower specificity.13
Alpha-fetoprotein has a low sensitivity (ie, 54%) for HCC.14 Tumor size is one of the factors limiting the sensitivity of alpha-fetoprotein, 14 and this would imply that this test may not be helpful in detecting HCC at an early stage. Alpha-fetoprotein L3, an isoform of alpha-fetoprotein, may be helpful in patients with alpha-fetoprotein levels in the intermediate range, and it is currently being studied.
Liver ultrasonography is operator-dependent, and it may not be as accurate in overweight or obese people.
Computed tomography (CT) and magnetic resonance imaging (MRI) are not recommended for surveillance. Serial CT poses risks of radiation-induced damage, contrast-related anaphylaxis, and renal failure, and MRI is not cost-effective and can also lead to gadolinium-induced nephrogenic systemic fibrosis in patients with renal failure.
Currently, the American Association for the Study of Liver Diseases9 recommends ultrasonography only, every 6 months, for surveillance for HCC. However, it may be premature to conclude that alpha-fetoprotein measurement is no longer required for surveillance, and if new data emerge that support its role, it may be reincorporated into the guidelines.
DIAGNOSING HEPATOCELLULAR CARCINOMA
Lesions larger than 1 cm on ultrasonography
The finding of a liver lesion larger than 1 cm on ultrasonography during surveillance warrants further testing.
Noninvasive testing with four-phase multidetector CT or dynamic contrast-enhanced MRI is the next step. Typical findings on either of these imaging studies are sufficient to make a diagnosis of HCC, as they have a high specificity and positive predictive value.15 Arterial hyperenhancement with a venous-phase or delayed-phase washout of contrast medium confirms the diagnosis (Figure 2).9 If one of the two imaging studies is typical for HCC, liver biopsy is not needed.
Other imaging studies, including contrast-enhanced ultrasonography, have not been shown to be specific for this diagnosis.16
Liver biopsy is indicated in patients in whom the imaging findings are atypical for HCC.9,17 Biopsy has very good sensitivity and specificity for cancer, but false-negative findings do occur.18 Therefore, a negative biopsy does not entirely exclude HCC. In this situation, patients should be followed by serial ultrasonography, and any further growth or change in character should be reevaluated.
Lesions smaller than 1 cm
For lesions smaller than 1 cm, the incidence of HCC is low, and currently available diagnostic tests are not reliable.15,19 Lesions of this size should be followed by serial ultrasonography every 3 to 4 months until they either enlarge to greater than 1 cm or remain stable at 2 years.9 If they remain stable at the end of 2 years, regular surveillance ultrasonography once every 6 months can be continued.
CURATIVE AND PALLIATIVE THERAPIES
Therapies for HCC (Table 2) can be divided into two categories: curative and palliative.
Curative treatments include surgical resection, liver transplantation, and radiofrequency ablation. All other treatments are palliative, including transarterial chemoembolization and medical therapy with sorafenib.
The choice of treatment depends on the characteristics of the tumor, the degree of liver dysfunction, and the patient’s current level of function. The Barcelona Clinic Liver Cancer classification is widely used in making these decisions, as it incorporates both clinical features and tumor stage.9 Figure 3 shows a simplified management algorithm.
SURGICAL RESECTION
Surgical resection is the preferred treatment for patients who have a solitary HCC lesion without cirrhosis.9 It is also indicated in patients with well-compensated cirrhosis who have normal portal pressure, a normal serum bilirubin level, and a platelet count greater than 100 × 109/L.20,21 In such patients, the 5-year survival rate is about 74%, compared with 25% in patients with portal hypertension and serum bilirubin levels higher than 1 mg/dL.21
Surgical resection is not recommended for patients with decompensated cirrhosis, as it can worsen liver function postoperatively and increase the risk of death.19,20 In Western countries, where cirrhosis from hepatitis C is the commonest cause of HCC, most patients have poorly preserved hepatic function at the time of diagnosis, leaving only a minority of patients as candidates for surgical resection.
After surgical resection of HCC, the recurrence rate can be as high as 70% to 80% at 5 years.22,23 Studies have consistently found larger tumor size and vascular invasion to be factors that predict recurrence.24,25 Vascular invasion was also found to predict poor survival after recurrence.24 Studies have so far not shown any conclusive benefit from post-surgical adjuvant chemotherapy in reducing the rate of recurrence of HCC.26,27
How to treat recurrent HCC after surgical resection has not been clearly established. Radiofrequency ablation, transarterial chemoembolization, repeat resection, and liver transplantation have all improved survival when used alone or in combination.28 However, randomized controlled trials are needed to establish the effective treatment strategy and the benefit of multimodal treatment of recurrent HCC.
LIVER TRANSPLANTATION
Orthotopic liver transplantation is the preferred treatment for patients with HCC complicated by cirrhosis and portal hypertension. It has the advantage not only of being potentially curative, but also of overcoming liver cirrhosis by replacing the liver.
To qualify for liver transplantation, patients must meet the Milan criteria (ie, have a single nodule less than 5 cm in diameter or up to three nodules, with the largest being less than 3 cm in diameter, with no evidence of vascular invasion or distant metastasis). These patients have an expected 4-year survival rate of 85% and a recurrence-free survival rate of 92% after transplantation, compared with 50% and 59%, respectively, in patients whose tumors exceeded these criteria.29
Some believe that the Milan criteria are too restrictive and could be expanded. Yao et al at the University of California-San Francisco30 reported that patients with HCC meeting the criteria of having a solitary tumor smaller than 6.5 cm or having up to three nodules, with the largest smaller than 4.5 cm, and total tumor diameter less than 8 cm, had survival rates of 90% at 1 year and 75.2% at 5 years after liver transplantation, compared with 50% at 1 year for patients with tumors exceeding these limits. (These have come to be known as the UCSF criteria.) However, the United Network for Organ Sharing (UNOS) has not adopted these expanded criteria. UNOS has a point system for allocating livers for transplant called the Model for End-Stage Liver Disease (MELD). Patients who meet the Milan criteria receive extra points, putting them higher on the transplant list. This allows for early transplantation, thus reducing tumor progression and dropout from the transplant list. UNOS allocates a MELD score of 22 to all patients who meet the Milan criteria, and the score is further adjusted once every 3 months to reflect a 10% increase in the mortality rate. However, patients who have a single lesion smaller than 2 cm and are candidates for liver transplantation are not assigned additional MELD points per UNOS policy, as the risk of tumor progression beyond the Milan criteria in these patients is deemed to be low.
Therapies while awaiting transplantation
Even if they receive additional MELD points to give them priority on the waiting list, patients face a considerable wait before transplantation because of the limited availability of donor organs. In the interim, they have a risk of tumor progression beyond the Milan criteria and subsequent dropout from the transplant list.31 Patients on the waiting list may therefore undergo a locoregional therapy such as transarterial chemoembolization or radiofrequency ablation as bridging therapy.
These therapies have been shown to decrease dropout from the waiting list.31 A prospective study showed that in 48 patients who underwent transarterial chemoembolization while awaiting liver transplantation, none had tumor progression, and 41 did receive a transplant, with excellent posttransplantation survival rates.32 Similarly, radioembolization using yttrium-90-labeled microspheres or radiofrequency ablation while on the waiting list has been shown to significantly decrease the rate of dropout, with good posttransplantation outcomes.33,34
However, in spite of these benefits, these bridging therapies do not increase survival rates after transplantation. It is also unclear whether they are useful in regions with short waiting times for liver transplantation.
Adjuvant systemic chemotherapy has not been shown to improve survival in patients undergoing liver transplantation. For example, in a randomized controlled trial of doxorubicin given before, during, and after surgery, the survival rate at 5 years was 38% with doxorubicin and 40% without.35
ABLATIVE LOCOREGIONAL THERAPIES
Locoregional therapies play an important role in managing HCC. They are classified as ablative and perfusion-based.
Ablative locoregional therapies include chemical modalities such as percutaneous ethanol injection; thermal therapies such as radiofrequency ablation, microwave ablation, laser ablation, and cryotherapy; and newer methods such as irreversible electroporation and light-activated drug therapy. Of these, radiofrequency ablation is the most widely used.
Radiofrequency ablation
Radiofrequency ablation induces thermal injury, resulting in tumor necrosis. It can be used as an alternative to surgery in patients who have a single HCC lesion less than 3 to 5 cm in diameter, confined to the liver, and in a site amenable to this procedure and who have a reasonable coagulation profile. The procedure can be performed percutaneously or via laparoscopy.
Radiofrequency ablation is contraindicated in patients with decompensated cirrhosis, Child-Pugh class C cirrhosis (the most severe category), vascular or bile duct invasion, extrahepatic disease, or lesions that are not accessible or are adjacent to structures such as the gall bladder, bowel, stomach, or diaphragm.
Radiofrequency ablation has been compared with surgical resection in patients who had small tumors. Though a randomized controlled trial did not show any difference between the two treatment groups in terms of survival at 5 years and recurrence rates,36 a meta-analysis showed that overall survival rates at 3 years and 5 years were significantly higher with surgical resection than with radiofrequency ablation.37 Patients also had a higher rate of local recurrence with radiofrequency ablation than with surgical resection.37 In addition, radiofrequency ablation has been shown to be effective only in small tumors and does not perform as well in lesions larger than 2 or 3 cm.
Thus, based on current evidence, surgical resection is preferable to radiofrequency ablation as first-line treatment. The latter, however, is also used as a bridging therapy in patients awaiting liver transplantation.
Percutaneous ethanol injection
Percutaneous ethanol injection is used less frequently than radiofrequency ablation, as studies have shown the latter to be superior in regard to local recurrence-free survival rates.38 However, percutaneous ethanol injection is used instead of radiofrequency ablation in a small number of patients, when the lesion is very close to organs such as the bile duct (which could be damaged by radiofrequency ablation) or the large vessels (which may make radiofrequency ablation less effective, since heat may dissipate as a result of excessive blood flow in this region).
Microwave ablation
Microwave ablation is an emerging therapy for HCC. Its advantage over radiofrequency ablation is that its use is not limited by blood vessels in close proximity to the ablation site.
Earlier studies did not show microwave ablation to be superior to radiofrequency ablation.39,40 However, current studies involving newer techniques of microwave ablation are more promising.41
PERFUSION-BASED LOCOREGIONAL THERAPIES
Perfusion-based locoregional therapies deliver embolic particles, chemotherapeutic agents, or radioactive materials into the artery feeding the tumor. The portal blood flow allows for preservation of vital liver tissue during arterial embolization of liver tumors. Perfusionbased therapies include transarterial chemoembolization, transarterial chemoembolization with doxorubicin-eluting beads (DEB-TACE), “bland” embolization, and radioembolization.
Transarterial chemoembolization
Transarterial chemoembolization is a minimally invasive procedure in which the hepatic artery is cannulated through a percutaneous puncture, the branches of the hepatic artery supplying the tumor are identified, and then embolic particles and chemotherapeutic agents are injected. This serves a dual purpose: it embolizes the feeding vessel that supplies the tumor, causing tumor necrosis, and it focuses the chemotherapy on the tumor and thus minimizes the systemic effects of the chemotherapeutic agent.
This therapy is contraindicated in patients with portal vein thrombosis, advanced liver dysfunction, or a transjugular intrahepatic portosystemic shunt. Side effects of the procedure include a postembolization syndrome of abdominal pain and fever (occurring in about 50% of patients from ischemic injury to the liver), hepatic abscesses, injury to the hepatic artery, development of ascites, liver dysfunction, and contrast-induced renal failure.
In addition to bridging patients to liver transplantation, transarterial chemoembolization is recommended as palliative treatment to prolong survival in patients with HCC who are not candidates for liver transplantation, surgical resection, or radiofrequency ablation.9,42 Patients who have Child-Pugh grade A or B cirrhosis but do not have main portal vein thrombosis or extrahepatic spread are candidates for this therapy. Patients such as these who undergo this therapy have a better survival rate at 2 years compared with untreated patients.43,44
Transarterial chemoembolization has also been used to reduce the size of (ie, to “downstage”) tumors that are outside the Milan criteria in patients who are otherwise candidates for liver transplantation. It induces tumor necrosis and has been shown to decrease the tumor size in a selected group of patients and to bring them within the Milan criteria, thus potentially enabling them to be put on the transplant list.45 Studies have shown that patients who receive a transplant after successful down-staging may achieve a 5-year survival rate comparable with that of patients who were initially within the Milan criteria and received a transplant without the need for down-staging.45 However, factors that predict successful down-staging have not been clearly established.
Newer techniques have been developed. A randomized controlled trial found transarterial chemoembolization with doxorubicin-eluting beads to be safer and better tolerated than conventional transarterial chemembolization.46
Bland embolization is transarterial embolization without chemotherapeutic agents and is performed in patients with significant liver dysfunction who might not tolerate chemotherapy. The benefits of this approach are yet to be determined.
Radioembolization
Radioembolization with yttrium-90 microspheres has recently been introduced as an alternative to transarterial chemoembolization, especially in patients with portal vein thrombosis, a portocaval shunt, or a transjugular intrahepatic portosystemic shunt.
In observational studies, radioembolization was as effective as transarterial chemoembolization, with a similar survival benefit.47 However, significant pulmonary shunting must be ruled out before radioembolization, as it would lead to radiation-induced pulmonary disease. Randomized controlled trials are under way to compare the efficacy of the two methods.
CHEMOTHERAPY
Sorafenib
Sorafenib is an oral antiangiogenic agent. A kinase inhibitor, it interacts with multiple intracellular and cell-surface kinases, including vascular endothelial growth factor receptor, platelet-derived growth factor receptor, and Raf proto-oncogene, inhibiting tumor cell proliferation and angiogenesis.
Sorafenib has been shown to prolong survival in patients with advanced-stage HCC.48 A randomized placebo-controlled trial in patients with Child-Pugh grade A cirrhosis and advanced HCC who had not received chemotherapy showed that sorafenib increased the life expectancy by nearly 3 months compared with placebo.47 Sorafenib therapy is very expensive, but it is usually covered by insurance.
Sorafenib is recommended in patients who have advanced HCC with vascular invasion, extrahepatic dissemination, or minimal constitutional symptoms. It is not recommended for patients with severe advanced liver disease who have moderate to severe tumor-related constitutional symptoms or Child-Pugh grade C cirrhosis, or for patients with a life expectancy of less than 3 months.
The most common side effects of sorafenib are diarrhea, weight loss, and skin reactions on the hands and feet. These commonly lead to decreased tolerability and dose reductions.47 Doses should be adjusted on the basis of the bilirubin and albumin levels.49
Other chemotherapeutic agents
Several molecular targeted agents are undergoing clinical trials for the treatment of HCC. These include bevacizumab, erlotinib, brivanib, and ramucirumab. Chemotherapeutic agents such as doxorubicin and everolimus are also being studied.
PALLIATIVE TREATMENT
Patients with end-stage HCC with moderate to severe constitutional symptoms, extrahepatic disease progression, and decompensated liver disease have a survival of less than 3 months and are treated for pain and symptom control.9
- Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010; 127:2893–2917.
- El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology 2007; 132:2557–2576.
- El-Serag HB. Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology 2012; 142:1264–1273.e1.
- Altekruse SF, McGlynn KA, Reichman ME. Hepatocellular carcinoma incidence, mortality, and survival trends in the United States from 1975 to 2005. J Clin Oncol 2009; 27:1485–1491.
- Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of US adults. N Engl J Med 2003; 348:1625–1638.
- Sarasin FP, Giostra E, Hadengue A. Cost-effectiveness of screening for detection of small hepatocellular carcinoma in western patients with Child-Pugh class A cirrhosis. Am J Med 1996; 101:422–434.
- Yu MW, Chang HC, Liaw YF, et al. Familial risk of hepatocellular carcinoma among chronic hepatitis B carriers and their relatives. J Natl Cancer Inst 2000; 92:1159–1164.
- Kew MC, Macerollo P. Effect of age on the etiologic role of the hepatitis B virus in hepatocellular carcinoma in blacks. Gastroenterology 1988; 94:439–442.
- Bruix J, Sherman M; American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology 2011; 53:1020–1022.
- Bruix J, Llovet JM. Major achievements in hepatocellular carcinoma. Lancet 2009; 373:614–616.
- Gómez-Rodríguez R, Romero-Gutiérrez M, Artaza-Varasa T, et al. The value of the Barcelona Clinic Liver Cancer and alpha-fetoprotein in the prognosis of hepatocellular carcinoma. Rev Esp Enferm Dig 2012; 104:298–304.
- Zhang BH, Yang BH, Tang ZY. Randomized controlled trial of screening for hepatocellular carcinoma. J Cancer Res Clin Oncol 2004; 130:417–422.
- Giannini EG, Erroi V, Trevisani F. Effectiveness of a-fetoprotein for hepatocellular carcinoma surveillance: the return of the living-dead? Expert Rev Gastroenterol Hepatol 2012; 6:441–444.
- Farinati F, Marino D, De Giorgio M, et al. Diagnostic and prognostic role of alpha-fetoprotein in hepatocellular carcinoma: both or neither? Am J Gastroenterol 2006; 101:524–532.
- Forner A, Vilana R, Ayuso C, et al. Diagnosis of hepatic nodules 20 mm or smaller in cirrhosis: prospective validation of the noninvasive diagnostic criteria for hepatocellular carcinoma. Hepatology 2008; 47:97–104.
- Vilana R, Forner A, Bianchi L, et al. Intrahepatic peripheral cholangiocarcinoma in cirrhosis patients may display a vascular pattern similar to hepatocellular carcinoma on contrast-enhanced ultrasound. Hepatology 2010; 51:2020–2029.
- Kojiro M. Pathological diagnosis at early stage: reaching international consensus. Oncology 2010; 78(suppl 1):31–35.
- Schölmerich J, Schacherer D. Diagnostic biopsy for hepatocellular carcinoma in cirrhosis: useful, necessary, dangerous, or academic sport? Gut 2004; 53:1224–1226.
- Durand F, Regimbeau JM, Belghiti J, et al. Assessment of the benefits and risks of percutaneous biopsy before surgical resection of hepatocellular carcinoma. J Hepatol 2001; 35:254–258.
- Bruix J, Castells A, Bosch J, et al. Surgical resection of hepatocellular carcinoma in cirrhotic patients: prognostic value of preoperative portal pressure. Gastroenterology 1996; 111:1018–1022.
- Llovet JM, Fuster J, Bruix J. Intention-to-treat analysis of surgical treatment for early hepatocellular carcinoma: resection versus transplantation. Hepatology 1999; 30:1434–1440.
- Nagasue N, Uchida M, Makino Y, et al. Incidence and factors associated with intrahepatic recurrence following resection of hepatocellular carcinoma. Gastroenterology 1993; 105:488–494.
- Arii S, Tanaka J, Yamazoe Y, et al. Predictive factors for intrahepatic recurrence of hepatocellular carcinoma after partial hepatectomy. Cancer 1992; 69:913–919.
- Cha C, Fong Y, Jarnagin WR, Blumgart LH, DeMatteo RP. Predictors and patterns of recurrence after resection of hepatocellular carcinoma. J Am Coll Surg 2003; 197:753–758.
- Shah SA, Cleary SP, Wei AC, et al. Recurrence after liver resection for hepatocellular carcinoma: risk factors, treatment, and outcomes. Surgery 2007; 141:330–339.
- Kohno H, Nagasue N, Hayashi T, et al. Postoperative adjuvant chemotherapy after radical hepatic resection for hepatocellular carcinoma (HCC). Hepatogastroenterology 1996; 43:1405–1409.
- Ono T, Nagasue N, Kohno H, et al. Adjuvant chemotherapy with epirubicin and carmofur after radical resection of hepatocellular carcinoma: a prospective randomized study. Semin Oncol 1997; 24(suppl 6):S6–25.
- Poon RT, Fan ST, Lo CM, Liu CL, Wong J. Intrahepatic recurrence after curative resection of hepatocellular carcinoma: Long-term results of treatment and prognostic factors. Ann Surg 1999; 229:216–222.
- Mazzaferro V, Regalia E, Doci R, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 1996; 334:693–699.
- Yao FY, Ferrell L, Bass NM, et al. Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology 2001; 33:1394–1403.
- Majno P, Lencioni R, Mornex F, Girard N, Poon RT, Cherqui D. Is the treatment of hepatocellular carcinoma on the waiting list necessary? Liver Transpl 2011; 17(suppl 2):S98–S108.
- Graziadei IW, Sandmueller H, Waldenberger P, et al. Chemoembolization followed by liver transplantation for hepatocellular carcinoma impedes tumor progression while on the waiting list and leads to excellent outcome. Liver Transpl 2003; 9:557–563.
- Kulik LM, Atassi B, van Holsbeeck L, et al. Yttrium-90 microspheres (TheraSphere) treatment of unresectable hepatocellular carcinoma: downstaging to resection, RFA and bridge to transplantation. J Surg Oncol 2006; 94:572–586.
- Lu DS, Yu NC, Raman SS, et al. Percutaneous radiofrequency ablation of hepatocellular carcinoma as a bridge to liver transplantation. Hepatology 2005; 41:1130–1137.
- Pokorny H, Gnant M, Rasoul-Rockenschaub S, et al. Does additional doxorubicin chemotherapy improve outcome in patients with hepatocellular carcinoma treated by liver transplantation? Am J Transplant 2005; 5:788–794.
- Feng K, Yan J, Li X, et al. A randomized controlled trial of radiofrequency ablation and surgical resection in the treatment of small hepatocellular carcinoma. J Hepatol 2012; 57:794–802.
- Zhou Y, Zhao Y, Li B, et al. Meta-analysis of radiofrequency ablation versus hepatic resection for small hepatocellular carcinoma. BMC Gastroenterol 2010; 10:78.
- Lencioni RA, Allgaier HP, Cioni D, et al. Small hepatocellular carcinoma in cirrhosis: Randomized comparison of radiofrequency thermal ablation versus percutaneous ethanol injection. Radiology 2003; 228:235–240.
- Ohmoto K, Yoshioka N, Tomiyama Y, et al. Comparison of therapeutic effects between radiofrequency ablation and percutaneous microwave coagulation therapy for small hepatocellular carcinomas. J Gastroenterol Hepatol 2009; 24:223–227.
- Shibata T, Iimuro Y, Yamamoto Y, et al. Small hepatocellular carcinoma: comparison of radiofrequency ablation and percutaneous microwave coagulation therapy. Radiology 2002; 223:331–337.
- Qian GJ, Wang N, Shen Q, et al. Efficacy of microwave versus radiofrequency ablation for treatment of small hepatocellular carcinoma: Experimental and clinical studies. Eur Radiol 2012; 22:1983–1990.
- Burrel M, Reig M, Forner A, et al. Survival of patients with hepatocellular carcinoma treated by transarterial chemoembolisation (TACE) using drug eluting beads. Implications for clinical practice and trial design. J Hepatol 2012; 56:1330–1335.
- Cammà C, Schepis F, Orlando A, et al. Transarterial chemoembolization for unresectable hepatocellular carcinoma: meta-analysis of randomized controlled trials. Radiology 2002; 224:47–54.
- Llovet JM, Bruix J. Systematic review of randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology 2003; 37:429–442.
- Yao FY, Kerlan RK, Hirose R, et al. Excellent outcome following down-staging of hepatocellular carcinoma prior to liver transplantation: an intention-to-treat analysis. Hepatology 2008; 48:819–827.
- Ferrer Puchol MD, la Parra C, Esteban E, et al. Comparison of doxorubicin-eluting bead transarterial chemoembolization (DEBTACE) with conventional transarterial chemoembolization (TACE) for the treatment of hepatocellular carcinoma (article in Spanish). Radiologia 2011; 53:246–253.
- Salem R, Lewandowski RJ, Kulik L, et al. Radioembolization results in longer time-to-progression and reduced toxicity compared with chemoembolization in patients with hepatocellular carcinoma. Gastroenterology 2011; 140:497–507.e2.
- Llovet JM, Ricci S, Mazzaferro V, et al; SHARP Investigators Study Group. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 2008; 359:378–390.
- Miller AA, Murry DJ, Owzar K, et al. Phase I and pharmacokinetic study of sorafenib in patients with hepatic or renal dysfunction: CALGB 60301. J Clin Oncol 2009; 27:1800–1805.
- Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010; 127:2893–2917.
- El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology 2007; 132:2557–2576.
- El-Serag HB. Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology 2012; 142:1264–1273.e1.
- Altekruse SF, McGlynn KA, Reichman ME. Hepatocellular carcinoma incidence, mortality, and survival trends in the United States from 1975 to 2005. J Clin Oncol 2009; 27:1485–1491.
- Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of US adults. N Engl J Med 2003; 348:1625–1638.
- Sarasin FP, Giostra E, Hadengue A. Cost-effectiveness of screening for detection of small hepatocellular carcinoma in western patients with Child-Pugh class A cirrhosis. Am J Med 1996; 101:422–434.
- Yu MW, Chang HC, Liaw YF, et al. Familial risk of hepatocellular carcinoma among chronic hepatitis B carriers and their relatives. J Natl Cancer Inst 2000; 92:1159–1164.
- Kew MC, Macerollo P. Effect of age on the etiologic role of the hepatitis B virus in hepatocellular carcinoma in blacks. Gastroenterology 1988; 94:439–442.
- Bruix J, Sherman M; American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology 2011; 53:1020–1022.
- Bruix J, Llovet JM. Major achievements in hepatocellular carcinoma. Lancet 2009; 373:614–616.
- Gómez-Rodríguez R, Romero-Gutiérrez M, Artaza-Varasa T, et al. The value of the Barcelona Clinic Liver Cancer and alpha-fetoprotein in the prognosis of hepatocellular carcinoma. Rev Esp Enferm Dig 2012; 104:298–304.
- Zhang BH, Yang BH, Tang ZY. Randomized controlled trial of screening for hepatocellular carcinoma. J Cancer Res Clin Oncol 2004; 130:417–422.
- Giannini EG, Erroi V, Trevisani F. Effectiveness of a-fetoprotein for hepatocellular carcinoma surveillance: the return of the living-dead? Expert Rev Gastroenterol Hepatol 2012; 6:441–444.
- Farinati F, Marino D, De Giorgio M, et al. Diagnostic and prognostic role of alpha-fetoprotein in hepatocellular carcinoma: both or neither? Am J Gastroenterol 2006; 101:524–532.
- Forner A, Vilana R, Ayuso C, et al. Diagnosis of hepatic nodules 20 mm or smaller in cirrhosis: prospective validation of the noninvasive diagnostic criteria for hepatocellular carcinoma. Hepatology 2008; 47:97–104.
- Vilana R, Forner A, Bianchi L, et al. Intrahepatic peripheral cholangiocarcinoma in cirrhosis patients may display a vascular pattern similar to hepatocellular carcinoma on contrast-enhanced ultrasound. Hepatology 2010; 51:2020–2029.
- Kojiro M. Pathological diagnosis at early stage: reaching international consensus. Oncology 2010; 78(suppl 1):31–35.
- Schölmerich J, Schacherer D. Diagnostic biopsy for hepatocellular carcinoma in cirrhosis: useful, necessary, dangerous, or academic sport? Gut 2004; 53:1224–1226.
- Durand F, Regimbeau JM, Belghiti J, et al. Assessment of the benefits and risks of percutaneous biopsy before surgical resection of hepatocellular carcinoma. J Hepatol 2001; 35:254–258.
- Bruix J, Castells A, Bosch J, et al. Surgical resection of hepatocellular carcinoma in cirrhotic patients: prognostic value of preoperative portal pressure. Gastroenterology 1996; 111:1018–1022.
- Llovet JM, Fuster J, Bruix J. Intention-to-treat analysis of surgical treatment for early hepatocellular carcinoma: resection versus transplantation. Hepatology 1999; 30:1434–1440.
- Nagasue N, Uchida M, Makino Y, et al. Incidence and factors associated with intrahepatic recurrence following resection of hepatocellular carcinoma. Gastroenterology 1993; 105:488–494.
- Arii S, Tanaka J, Yamazoe Y, et al. Predictive factors for intrahepatic recurrence of hepatocellular carcinoma after partial hepatectomy. Cancer 1992; 69:913–919.
- Cha C, Fong Y, Jarnagin WR, Blumgart LH, DeMatteo RP. Predictors and patterns of recurrence after resection of hepatocellular carcinoma. J Am Coll Surg 2003; 197:753–758.
- Shah SA, Cleary SP, Wei AC, et al. Recurrence after liver resection for hepatocellular carcinoma: risk factors, treatment, and outcomes. Surgery 2007; 141:330–339.
- Kohno H, Nagasue N, Hayashi T, et al. Postoperative adjuvant chemotherapy after radical hepatic resection for hepatocellular carcinoma (HCC). Hepatogastroenterology 1996; 43:1405–1409.
- Ono T, Nagasue N, Kohno H, et al. Adjuvant chemotherapy with epirubicin and carmofur after radical resection of hepatocellular carcinoma: a prospective randomized study. Semin Oncol 1997; 24(suppl 6):S6–25.
- Poon RT, Fan ST, Lo CM, Liu CL, Wong J. Intrahepatic recurrence after curative resection of hepatocellular carcinoma: Long-term results of treatment and prognostic factors. Ann Surg 1999; 229:216–222.
- Mazzaferro V, Regalia E, Doci R, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 1996; 334:693–699.
- Yao FY, Ferrell L, Bass NM, et al. Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology 2001; 33:1394–1403.
- Majno P, Lencioni R, Mornex F, Girard N, Poon RT, Cherqui D. Is the treatment of hepatocellular carcinoma on the waiting list necessary? Liver Transpl 2011; 17(suppl 2):S98–S108.
- Graziadei IW, Sandmueller H, Waldenberger P, et al. Chemoembolization followed by liver transplantation for hepatocellular carcinoma impedes tumor progression while on the waiting list and leads to excellent outcome. Liver Transpl 2003; 9:557–563.
- Kulik LM, Atassi B, van Holsbeeck L, et al. Yttrium-90 microspheres (TheraSphere) treatment of unresectable hepatocellular carcinoma: downstaging to resection, RFA and bridge to transplantation. J Surg Oncol 2006; 94:572–586.
- Lu DS, Yu NC, Raman SS, et al. Percutaneous radiofrequency ablation of hepatocellular carcinoma as a bridge to liver transplantation. Hepatology 2005; 41:1130–1137.
- Pokorny H, Gnant M, Rasoul-Rockenschaub S, et al. Does additional doxorubicin chemotherapy improve outcome in patients with hepatocellular carcinoma treated by liver transplantation? Am J Transplant 2005; 5:788–794.
- Feng K, Yan J, Li X, et al. A randomized controlled trial of radiofrequency ablation and surgical resection in the treatment of small hepatocellular carcinoma. J Hepatol 2012; 57:794–802.
- Zhou Y, Zhao Y, Li B, et al. Meta-analysis of radiofrequency ablation versus hepatic resection for small hepatocellular carcinoma. BMC Gastroenterol 2010; 10:78.
- Lencioni RA, Allgaier HP, Cioni D, et al. Small hepatocellular carcinoma in cirrhosis: Randomized comparison of radiofrequency thermal ablation versus percutaneous ethanol injection. Radiology 2003; 228:235–240.
- Ohmoto K, Yoshioka N, Tomiyama Y, et al. Comparison of therapeutic effects between radiofrequency ablation and percutaneous microwave coagulation therapy for small hepatocellular carcinomas. J Gastroenterol Hepatol 2009; 24:223–227.
- Shibata T, Iimuro Y, Yamamoto Y, et al. Small hepatocellular carcinoma: comparison of radiofrequency ablation and percutaneous microwave coagulation therapy. Radiology 2002; 223:331–337.
- Qian GJ, Wang N, Shen Q, et al. Efficacy of microwave versus radiofrequency ablation for treatment of small hepatocellular carcinoma: Experimental and clinical studies. Eur Radiol 2012; 22:1983–1990.
- Burrel M, Reig M, Forner A, et al. Survival of patients with hepatocellular carcinoma treated by transarterial chemoembolisation (TACE) using drug eluting beads. Implications for clinical practice and trial design. J Hepatol 2012; 56:1330–1335.
- Cammà C, Schepis F, Orlando A, et al. Transarterial chemoembolization for unresectable hepatocellular carcinoma: meta-analysis of randomized controlled trials. Radiology 2002; 224:47–54.
- Llovet JM, Bruix J. Systematic review of randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology 2003; 37:429–442.
- Yao FY, Kerlan RK, Hirose R, et al. Excellent outcome following down-staging of hepatocellular carcinoma prior to liver transplantation: an intention-to-treat analysis. Hepatology 2008; 48:819–827.
- Ferrer Puchol MD, la Parra C, Esteban E, et al. Comparison of doxorubicin-eluting bead transarterial chemoembolization (DEBTACE) with conventional transarterial chemoembolization (TACE) for the treatment of hepatocellular carcinoma (article in Spanish). Radiologia 2011; 53:246–253.
- Salem R, Lewandowski RJ, Kulik L, et al. Radioembolization results in longer time-to-progression and reduced toxicity compared with chemoembolization in patients with hepatocellular carcinoma. Gastroenterology 2011; 140:497–507.e2.
- Llovet JM, Ricci S, Mazzaferro V, et al; SHARP Investigators Study Group. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 2008; 359:378–390.
- Miller AA, Murry DJ, Owzar K, et al. Phase I and pharmacokinetic study of sorafenib in patients with hepatic or renal dysfunction: CALGB 60301. J Clin Oncol 2009; 27:1800–1805.
KEY POINTS
- Surveillance for HCC is indicated in all patients with cirrhosis, regardless of the cause of the cirrhosis.
- Liver biopsy is not needed to make the diagnosis if the findings on four-phase multidetector computed tomography or dynamic contrast-enhanced magnetic resonance imaging are typical of HCC (arterial hyperenhancement with venous-phase or delayed-phase washout).
- Many treatments are available, including surgical resection, liver transplantation, ablative therapy, perfusion-based therapy, chemotherapy, and palliative therapy.
The jugular venous pressure revisited
In this age of technological marvels, it is easy to become so reliant on them as to neglect the value of bedside physical signs. Yet these signs provide information that adds no cost, is immediately available, and can be repeated at will.
Few physical findings are as useful but as undervalued as is the estimation of the jugular venous pressure. Unfortunately, many practitioners at many levels of seniority and experience do not measure it correctly, leading to a vicious circle of unreliable information, lack of confidence, and underuse. Another reason for its underuse is that the jugular venous pressure does not correlate precisely with the right atrial pressure, as we will see below.
In this review, we will attempt to clarify physiologic principles and describe technical details. Much of this is simple but, as always, the devil is in the details.
ANATOMIC CONSIDERATIONS
Think of the systemic veins as a soft-walled and mildly distensible reservoir with fingerlike projections, analogous to a partially fluidfilled surgical glove.1 In a semi-upright position, the venous system is partially filled with blood and is collapsed above the level that this blood reaches up to.
Blood is constantly flowing in and out of this reservoir, flowing in by venous return and flowing out by the pumping action of the right side of the heart. The volume in the venous reservoir and hence the pressure are normally maintained by the variability of right ventricular stroke volume in accordance with the Frank-Starling law. Excess volume and pressure indicate failure of this homeostatic mechanism.
The internal jugular veins, being continuous with the superior vena cava, provide a visible measure of the degree to which the systemic venous reservoir is filled, a manometer that reflects the pressure in the right atrium—at least in theory.2 Thus, the vertical height above the right atrium to which they are distended and above which they are in a collapsed state should reflect the right atrial pressure.
(In fact, the jugular venous pressure may underestimate the right atrial pressure, for reasons still not understood. This will be discussed below.)
In a healthy person, the visible jugular veins are fully collapsed when the person is standing and are often distended to a variable degree when the person is supine. Selecting an appropriate intermediate position permits the top of the column (the meniscus) to become visible in the neck between the clavicle and the mandible.
DISCREPANCY BETWEEN JUGULAR VENOUS AND RIGHT ATRIAL PRESSURE
Several reports have indicated that the jugular venous pressure may underestimate the right atrial pressure. Deol et al3 confirmed this, while establishing an excellent correlation between the level of venous collapse (observed on ultrasonography) and the jugular venous pressure. The difference between the right atrial pressure and the jugular venous pressure tended to be greater at higher venous pressures.3
Most people have a valve near the termination of the internal jugular vein, with variable competence. Inhibition of reflux of blood from the superior vena cava into the internal jugular vein by this valve is the most plausible cause of this disparity.4
The failure of the jugular venous pressure to correlate with the right atrial pressure has been cited by some as a reason to doubt the value of a sign that cardiologists have long relied on. How do we reconcile this apparent paradox? Careful review of the literature that has demonstrated this lack of correlation reveals the following:
- When unequal, the jugular venous pressure always underestimates the right atrial pressure.
- The lack of correlation is less evident at lower venous pressures.
This indicates the following:
- In the presence of congestive heart failure, the right atrial pressure is at least as high and perhaps higher than the jugular venous pressure. Hence, if the jugular venous pressure is high, further treatment, especially diuresis, is needed.
- A jugular venous pressure of zero implies a euvolemic state.
Thus, the jugular venous pressure provides excellent guidance when administering diuresis in congestive heart failure. These deductions obviously require the clinical judgment that the elevated right atrial pressure and jugular venous pressure do indeed reflect elevation of pulmonary capillary wedge pressure rather than other conditions discussed later in this article.
WHICH REFERENCE POINT TO USE?
The two points that can be used as references above which the jugular venous pressure is expressed are the center of the right atrium and the sternal angle. While the former may reflect physiology, the latter is preferred, as it is always visible and has the added advantage of being close to the upper limit of normal, which is about 3 cm above this level.
The difference in height between these two reference points has often been quoted as 5 cm, but this is an underestimate in the body positions used in examination.5 Seth et al6 found a mean of 8 cm at 30° elevation, 9.7 cm at 45°, and 9.8 cm at 60°. The difference also varied between patients, being larger in association with smoking, older age, large body mass index, and large anterior-posterior diameter. These factors should be considered when trying to evaluate the significance of a particular jugular venous pressure.
The junction of the midaxillary line and the fourth left intercostal space (“the phlebostatic point”) has been recommended as a reference point by some, as it is level with the mid-right atrium. However, using the phlebostatic point as a reference position is cumbersome and results in a valid measurement only with the patient in the supine position.7
TECHNIQUE IS VITAL
Close adherence to technical details is vital in reliably and reproducibly measuring the pressure in the internal jugular veins (Figure 1).
The right side is usually observed first, as it is the side on which the examiner usually stands. Using the right side also avoids the rare occurrence of external compression of the left brachiocephalic vein.
Head and shoulders
The sternocleidomastoid muscle lies anterior to each internal jugular vein.8 When tense, it impedes good observation. Shortening, and hence relaxing, this muscle permits the meniscus to be observed. Correct positioning is achieved by:
- Placing a folded pillow behind the patient’s head
- Keeping the shoulders on the mattress
- Turning the head away and elevating the jaw, both slightly; this is often best achieved by gentle pressure of the palm of the observer's hand on the patient's forehead.
Degree of head elevation
Although the proper degree of head elevation is sometimes said to be between 30° and 60°, these numbers are approximate. The correct angle is that which brings the venous meniscus into the window of visibility in the neck between the clavicle and mandible.
Lighting
Shining a flashlight tangentially to the skin is often helpful, casting shadows that improve the visibility of vein motion. Dimming the room lighting may further enhance this effect. Directing a light perpendicular to the skin is not helpful.
Also check the external jugular vein
Checking the external jugular vein can help establish that the jugular venous pressure is normal. If the vein is initially collapsed, light finger pressure at the base of the neck will distend it. If the distention rapidly clears after release of this pressure, the jugular venous pressure is not elevated. However, if external jugular venous distention persists, this does not prove true jugular venous pressure elevation, since it may reflect external compression of the vein by the cervical fascia or delayed blood flow caused by sclerotic venous valves.9 In these instances, the internal jugular pulsation level must be sought.
Jugular venous collapse with inspiration
Collapse of the inferior vena cava with forced inspiration is routinely evaluated during echocardiography as a way to estimate right atrial pressure. This finding has been extrapolated to the jugular veins, wherein the absence of venous collapse during vigorous inspiration or sniffing indicates elevated central venous pressures.10
Distinguishing venous from arterial pulsation
Features indicating venous rather than arterial pulsation were listed by Wood more than 50 years ago11 and are still relevant today. These include internal jugular pulsation that:
- Is soft, diffuse, undulant
- Is not palpable
- Has two crests and two troughs per cardiac cycle
- Has crests that do not coincide with the palpated carotid pulse (exceptions may be seen with the systolic timing of the v wave of tricuspid regurgitation)
- Has higher pressure in expiration, lower in inspiration (exceptions may be seen when Kussmaul physiology is present)
- Has pressure that rises with abdominal pressure
- Is obliterated by light pressure at the base of the neck.
In addition to the above criteria, a wave whose movement is predominantly a descent is nearly always venous.
Abdominojugular reflex
Firm, steady pressure over the abdomen will often result in a small rise in jugular venous pressure. In healthy people, this normalizes in a few seconds, even while manual pressure is maintained. Persistence of jugular venous pressure elevation beyond 10 seconds, followed by an abrupt fall upon withdrawal of manual pressure, is abnormal. This finding has implications similar to those of an elevated baseline jugular venous pressure.
SIGNIFICANCE OF JUGULAR VENOUS PRESSURE ELEVATION
Elevated jugular venous pressure is a manifestation of abnormal right heart dynamics, mostly commonly reflecting elevated pulmonary capillary wedge pressure from left heart failure.12 This usually implies fluid overload, indicating the need for diuresis.
Exceptions to this therapeutic implication include the presence of a primary right heart condition, pericardial disease, certain arrhythmias, and conditions that elevate intrathoracic pressure. These will be discussed below. One important example is the acute jugular venous pressure elevation seen in right ventricular infarction, in which the high venous pressure is compensatory and its reduction can produce hypotension and shock.13
Primary right heart conditions also include right-sided valvular disease, cor pulmonale (including pulmonary embolism and pulmonary hypertension), and the compressive effect of pericardial tamponade or constriction. A normal or near-normal jugular venous pressure significantly decreases the likelihood of significant constriction or of tamponade of a degree necessitating urgent pericardiocentesis.14
SPECIAL CIRCUMSTANCES
Presence of an intravenous line in the neck
An intravenous line in the neck will often prevent observation of the jugular venous pressure. A simple measure can often compensate for this. If the venous line can be temporarily disconnected, the central venous pressure can be measured directly. Using sterile technique, the line can be flushed with saline and aspirated to bring blood into the transparent tubing. Leaving the proximal end open to the air, and alternately raising and lowering it to confirm free flow, the level to which the blood rises can be easily observed. Observing small cardiac and respiratory variations of the meniscus confirms free communication with the central veins. Attaching the line to a transducer is another option, but this may be time-consuming, and establishing an accurate zero point is often difficult.
The previously described discrepancy between jugular venous pressure and central venous pressure has to be considered when drawing conclusions from this measurement.
Intrathoracic pressure elevators
Positive pressure ventilation will elevate intrathoracic pressure (including right atrial pressure) and hence the jugular venous pressure, making interpretation difficult.15 Large pleural effusions or pneumothorax may have a similar effect.16
Superior vena cava syndrome
Markedly elevated jugular venous pressure is here associated with absent or very diminished pulsation, as the caval obstruction has eliminated free communication with the right atrium.17 Associated facial plethora and edema, papilledema, and superficial venous distention over the chest wall will often confirm this diagnosis.
THE WAVEFORM
While the main purpose of viewing the neck veins is to establish the mean pressure, useful information can often be obtained by assessing the waveform. Abnormalities reflect arrhythmias, right heart hemodynamics, or pericardial disease.18 Changes may be subtle and difficult to detect, but some patterns can be quite readily appreciated (Figure 2). A limited selection follows.
Arrhythmias
Cannon a waves. These intermittent sharp positive deflections in the venous pulse represent right atrial contraction against a closed tricuspid valve. They are most commonly associated with premature ventricular complexes, but they occur in other conditions in which atrial and ventricular beating are dissociated, including complete heart block, atrioventricular dissociation, and electronic ventricular pacing.19–21
Repetitive cannon waves. These may be seen with atrioventricular junctional tachycardia or ventricular tachycardia with 1:1 retrograde ventriculoatrial conduction in which the tricuspid valve is closed to every atrial beat.
Fine rapid regular pulsation may be seen in atrial flutter and may be a useful clue in distinguishing this from sinus rhythm when there is 4:1 atrioventricular conduction and a normal ventricular rate.
Abnormal right heart hemodynamics
Large v waves (Lancisi sign). These surges, replacing the usual x descent in systole, are seen in tricuspid insufficiency when the right atrium and its venous attachments are not protected from the right ventricular systolic pressure.22 High right ventricular pressure will obviously enhance this systolic surge.
Large a waves. These reflect resistance to right atrial outflow and may be seen when right ventricular compliance is reduced by hypertrophy from chronic pressure overload or in tricuspid stenosis.23
Pericardial disease
Kussmaul sign is the paradoxical increase in jugular venous pressure with inspiration, observed in conditions associated with limited filling of the right ventricle. It is typically associated with constrictive pericarditis, although it occurs in only a minority of people with this condition.24 It may also be seen in restrictive cardiomyopathy, massive pulmonary embolism, right ventricular infarction, and tricuspid stenosis.25
Diaphragmatic descent during inspiration increases intra-abdominal pressure and decreases intrathoracic pressure. The resulting increased gradient between the abdomen and thorax enhances venous return from splanchnic vessels, which in the setting of a noncompliant right ventricle may result in increased right atrial (and, hence, jugular venous) pressure.26
It is important to point out that the Kussmaul sign does not occur with cardiac tamponade in the absence of associated pericardial constriction.
Exaggerated y descent is typically seen in pericardial constriction, in which the high pressure of the v wave falls rapidly at the onset of diastole, given initial minimal right ventricular resistance. Flow is abruptly stopped when the intrapericardial space is filled.
- Sherwood L. Human Physiology: From Cells to Systems. 8th ed. Belmont, CA: Brooks/Cole; 2012.
- Constant J. Using internal jugular pulsations as a manometer for right atrial pressure measurements. Cardiology 2000; 93:26–30.
- Deol GR, Collett N, Ashby A, Schmidt GA. Ultrasound accurately reflects the jugular venous examination but underestimates central venous pressure. Chest 2011; 139:95–100.
- Wu X, Studer W, Erb T, Skarvan K, Seeberger MD. Competence of the internal jugular vein valve is damaged by cannulation and catheterization of the internal jugular vein. Anesthesiology 2000; 93:319–324.
- Ramana RK, Sanagala T, Lichtenberg R. A new angle on the angle of Louis. Congest Heart Fail 2006; 12:196–199.
- Seth R, Magner P, Matzinger F, van Walraven C. How far is the sternal angle from the mid-right atrium? J Gen Intern Med 2002; 17:852–856.
- Kee LL, Simonson JS, Stotts NA, Skov P, Schiller NB. Echocardiographic determination of valid zero reference levels in supine and lateral positions. Am J Crit Care 1993; 2:72–80.
- Park SY, Kim MJ, Kim MG, et al. Changes in the relationship between the right internal jugular vein and an anatomical landmark after head rotation. Korean J Anesthesiol 2011; 61:107–111.
- Sankoff J, Zidulka A. Non-invasive method for the rapid assessment of central venous pressure: description and validation by a single examiner. West J Emerg Med 2008; 9:201–205.
- Conn RD, O’Keefe JH. Simplified evaluation of the jugular venous pressure: significance of inspiratory collapse of jugular veins. Mo Med 2012; 109:150–152.
- Wood PH. Diseases of the Heart and Circulation. 2nd ed. Philadelphia, PA: Lippincott; 1956.
- Drazner MH, Brown RN, Kaiser PA, et al. Relationship of right- and left-sided filling pressures in patients with advanced heart failure: a 14-year multi-institutional analysis. J Heart Lung Transplant 2012; 31:67–72.
- Clark G, Strauss HD, Roberts R. Dobutamine vs furosemide in the treatment of cardiac failure due to right ventricular infarction. Chest 1980; 77:220–223.
- Roy CL, Minor MA, Brookhart MA, Choudhry NK. Does this patient with a pericardial effusion have cardiac tamponade? JAMA 2007; 297:1810–1818.
- Zhou Q, Xiao W, An E, Zhou H, Yan M. Effects of four different positive airway pressures on right internal jugular vein catheterisation. Eur J Anaesthesiol 2012; 29:223–228.
- Jolobe OM. Disproportionate elevation of jugular venous pressure in pleural effusion. Br J Hosp Med (Lond) 2011; 72:582–585.
- Seo M, Shin WJ, Jun IG. Central venous catheter-related superior vena cava syndrome following renal transplantation—a case report. Korean J Anesthesiol 2012; 63:550–554.
- Applefeld MM. The jugular venous pressure and pulse contour. In:Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Boston, MA: Butterworths; 1990.
- El Gamal MI, Van Gelder LM. Chronic ventricular pacing with ventriculo-atrial conduction versus atrial pacing in three patients with symptomatic sinus bradycardia. Pacing Clin Electrophysiol 1981; 4:100–105.
- Berman ND, Waxman MB. Cannon waves with A-V association. Am Heart J 1976; 91:643–644.
- Luisada AA, Singhal A, Kim K. The jugular and hepatic tracings in normal subjects and in conduction defects. Acta Cardiol 1983; 38:405–424.
- Miller MJ, McKay RG, Ferguson JJ, et al. Right atrial pressure-volume relationships in tricuspid regurgitation. Circulation 1986; 73:799–808.
- Wooley CF, Fontana ME, Kilman JW, Ryan JM. Tricuspid stenosis. Atrial systolic murmur, tricuspid opening snap, and right atrial pressure pulse. Am J Med 1985; 78:375–384.
- McGee SR. Evidence-Based Physical Diagnosis. 3rd ed. Philadelphia, PA: Elsevier/Saunders; 2012.
- Mittal SR, Garg S, Lalgarhia M. Jugular venous pressure and pulse wave form in the diagnosis of right ventricular infarction. Int J Cardiol 1996; 53:253–256.
- Bilchick KC, Wise RA. Paradoxical physical findings described by Kussmaul: pulsus paradoxus and Kussmaul’s sign. Lancet 2002; 359:1940–1942.
In this age of technological marvels, it is easy to become so reliant on them as to neglect the value of bedside physical signs. Yet these signs provide information that adds no cost, is immediately available, and can be repeated at will.
Few physical findings are as useful but as undervalued as is the estimation of the jugular venous pressure. Unfortunately, many practitioners at many levels of seniority and experience do not measure it correctly, leading to a vicious circle of unreliable information, lack of confidence, and underuse. Another reason for its underuse is that the jugular venous pressure does not correlate precisely with the right atrial pressure, as we will see below.
In this review, we will attempt to clarify physiologic principles and describe technical details. Much of this is simple but, as always, the devil is in the details.
ANATOMIC CONSIDERATIONS
Think of the systemic veins as a soft-walled and mildly distensible reservoir with fingerlike projections, analogous to a partially fluidfilled surgical glove.1 In a semi-upright position, the venous system is partially filled with blood and is collapsed above the level that this blood reaches up to.
Blood is constantly flowing in and out of this reservoir, flowing in by venous return and flowing out by the pumping action of the right side of the heart. The volume in the venous reservoir and hence the pressure are normally maintained by the variability of right ventricular stroke volume in accordance with the Frank-Starling law. Excess volume and pressure indicate failure of this homeostatic mechanism.
The internal jugular veins, being continuous with the superior vena cava, provide a visible measure of the degree to which the systemic venous reservoir is filled, a manometer that reflects the pressure in the right atrium—at least in theory.2 Thus, the vertical height above the right atrium to which they are distended and above which they are in a collapsed state should reflect the right atrial pressure.
(In fact, the jugular venous pressure may underestimate the right atrial pressure, for reasons still not understood. This will be discussed below.)
In a healthy person, the visible jugular veins are fully collapsed when the person is standing and are often distended to a variable degree when the person is supine. Selecting an appropriate intermediate position permits the top of the column (the meniscus) to become visible in the neck between the clavicle and the mandible.
DISCREPANCY BETWEEN JUGULAR VENOUS AND RIGHT ATRIAL PRESSURE
Several reports have indicated that the jugular venous pressure may underestimate the right atrial pressure. Deol et al3 confirmed this, while establishing an excellent correlation between the level of venous collapse (observed on ultrasonography) and the jugular venous pressure. The difference between the right atrial pressure and the jugular venous pressure tended to be greater at higher venous pressures.3
Most people have a valve near the termination of the internal jugular vein, with variable competence. Inhibition of reflux of blood from the superior vena cava into the internal jugular vein by this valve is the most plausible cause of this disparity.4
The failure of the jugular venous pressure to correlate with the right atrial pressure has been cited by some as a reason to doubt the value of a sign that cardiologists have long relied on. How do we reconcile this apparent paradox? Careful review of the literature that has demonstrated this lack of correlation reveals the following:
- When unequal, the jugular venous pressure always underestimates the right atrial pressure.
- The lack of correlation is less evident at lower venous pressures.
This indicates the following:
- In the presence of congestive heart failure, the right atrial pressure is at least as high and perhaps higher than the jugular venous pressure. Hence, if the jugular venous pressure is high, further treatment, especially diuresis, is needed.
- A jugular venous pressure of zero implies a euvolemic state.
Thus, the jugular venous pressure provides excellent guidance when administering diuresis in congestive heart failure. These deductions obviously require the clinical judgment that the elevated right atrial pressure and jugular venous pressure do indeed reflect elevation of pulmonary capillary wedge pressure rather than other conditions discussed later in this article.
WHICH REFERENCE POINT TO USE?
The two points that can be used as references above which the jugular venous pressure is expressed are the center of the right atrium and the sternal angle. While the former may reflect physiology, the latter is preferred, as it is always visible and has the added advantage of being close to the upper limit of normal, which is about 3 cm above this level.
The difference in height between these two reference points has often been quoted as 5 cm, but this is an underestimate in the body positions used in examination.5 Seth et al6 found a mean of 8 cm at 30° elevation, 9.7 cm at 45°, and 9.8 cm at 60°. The difference also varied between patients, being larger in association with smoking, older age, large body mass index, and large anterior-posterior diameter. These factors should be considered when trying to evaluate the significance of a particular jugular venous pressure.
The junction of the midaxillary line and the fourth left intercostal space (“the phlebostatic point”) has been recommended as a reference point by some, as it is level with the mid-right atrium. However, using the phlebostatic point as a reference position is cumbersome and results in a valid measurement only with the patient in the supine position.7
TECHNIQUE IS VITAL
Close adherence to technical details is vital in reliably and reproducibly measuring the pressure in the internal jugular veins (Figure 1).
The right side is usually observed first, as it is the side on which the examiner usually stands. Using the right side also avoids the rare occurrence of external compression of the left brachiocephalic vein.
Head and shoulders
The sternocleidomastoid muscle lies anterior to each internal jugular vein.8 When tense, it impedes good observation. Shortening, and hence relaxing, this muscle permits the meniscus to be observed. Correct positioning is achieved by:
- Placing a folded pillow behind the patient’s head
- Keeping the shoulders on the mattress
- Turning the head away and elevating the jaw, both slightly; this is often best achieved by gentle pressure of the palm of the observer's hand on the patient's forehead.
Degree of head elevation
Although the proper degree of head elevation is sometimes said to be between 30° and 60°, these numbers are approximate. The correct angle is that which brings the venous meniscus into the window of visibility in the neck between the clavicle and mandible.
Lighting
Shining a flashlight tangentially to the skin is often helpful, casting shadows that improve the visibility of vein motion. Dimming the room lighting may further enhance this effect. Directing a light perpendicular to the skin is not helpful.
Also check the external jugular vein
Checking the external jugular vein can help establish that the jugular venous pressure is normal. If the vein is initially collapsed, light finger pressure at the base of the neck will distend it. If the distention rapidly clears after release of this pressure, the jugular venous pressure is not elevated. However, if external jugular venous distention persists, this does not prove true jugular venous pressure elevation, since it may reflect external compression of the vein by the cervical fascia or delayed blood flow caused by sclerotic venous valves.9 In these instances, the internal jugular pulsation level must be sought.
Jugular venous collapse with inspiration
Collapse of the inferior vena cava with forced inspiration is routinely evaluated during echocardiography as a way to estimate right atrial pressure. This finding has been extrapolated to the jugular veins, wherein the absence of venous collapse during vigorous inspiration or sniffing indicates elevated central venous pressures.10
Distinguishing venous from arterial pulsation
Features indicating venous rather than arterial pulsation were listed by Wood more than 50 years ago11 and are still relevant today. These include internal jugular pulsation that:
- Is soft, diffuse, undulant
- Is not palpable
- Has two crests and two troughs per cardiac cycle
- Has crests that do not coincide with the palpated carotid pulse (exceptions may be seen with the systolic timing of the v wave of tricuspid regurgitation)
- Has higher pressure in expiration, lower in inspiration (exceptions may be seen when Kussmaul physiology is present)
- Has pressure that rises with abdominal pressure
- Is obliterated by light pressure at the base of the neck.
In addition to the above criteria, a wave whose movement is predominantly a descent is nearly always venous.
Abdominojugular reflex
Firm, steady pressure over the abdomen will often result in a small rise in jugular venous pressure. In healthy people, this normalizes in a few seconds, even while manual pressure is maintained. Persistence of jugular venous pressure elevation beyond 10 seconds, followed by an abrupt fall upon withdrawal of manual pressure, is abnormal. This finding has implications similar to those of an elevated baseline jugular venous pressure.
SIGNIFICANCE OF JUGULAR VENOUS PRESSURE ELEVATION
Elevated jugular venous pressure is a manifestation of abnormal right heart dynamics, mostly commonly reflecting elevated pulmonary capillary wedge pressure from left heart failure.12 This usually implies fluid overload, indicating the need for diuresis.
Exceptions to this therapeutic implication include the presence of a primary right heart condition, pericardial disease, certain arrhythmias, and conditions that elevate intrathoracic pressure. These will be discussed below. One important example is the acute jugular venous pressure elevation seen in right ventricular infarction, in which the high venous pressure is compensatory and its reduction can produce hypotension and shock.13
Primary right heart conditions also include right-sided valvular disease, cor pulmonale (including pulmonary embolism and pulmonary hypertension), and the compressive effect of pericardial tamponade or constriction. A normal or near-normal jugular venous pressure significantly decreases the likelihood of significant constriction or of tamponade of a degree necessitating urgent pericardiocentesis.14
SPECIAL CIRCUMSTANCES
Presence of an intravenous line in the neck
An intravenous line in the neck will often prevent observation of the jugular venous pressure. A simple measure can often compensate for this. If the venous line can be temporarily disconnected, the central venous pressure can be measured directly. Using sterile technique, the line can be flushed with saline and aspirated to bring blood into the transparent tubing. Leaving the proximal end open to the air, and alternately raising and lowering it to confirm free flow, the level to which the blood rises can be easily observed. Observing small cardiac and respiratory variations of the meniscus confirms free communication with the central veins. Attaching the line to a transducer is another option, but this may be time-consuming, and establishing an accurate zero point is often difficult.
The previously described discrepancy between jugular venous pressure and central venous pressure has to be considered when drawing conclusions from this measurement.
Intrathoracic pressure elevators
Positive pressure ventilation will elevate intrathoracic pressure (including right atrial pressure) and hence the jugular venous pressure, making interpretation difficult.15 Large pleural effusions or pneumothorax may have a similar effect.16
Superior vena cava syndrome
Markedly elevated jugular venous pressure is here associated with absent or very diminished pulsation, as the caval obstruction has eliminated free communication with the right atrium.17 Associated facial plethora and edema, papilledema, and superficial venous distention over the chest wall will often confirm this diagnosis.
THE WAVEFORM
While the main purpose of viewing the neck veins is to establish the mean pressure, useful information can often be obtained by assessing the waveform. Abnormalities reflect arrhythmias, right heart hemodynamics, or pericardial disease.18 Changes may be subtle and difficult to detect, but some patterns can be quite readily appreciated (Figure 2). A limited selection follows.
Arrhythmias
Cannon a waves. These intermittent sharp positive deflections in the venous pulse represent right atrial contraction against a closed tricuspid valve. They are most commonly associated with premature ventricular complexes, but they occur in other conditions in which atrial and ventricular beating are dissociated, including complete heart block, atrioventricular dissociation, and electronic ventricular pacing.19–21
Repetitive cannon waves. These may be seen with atrioventricular junctional tachycardia or ventricular tachycardia with 1:1 retrograde ventriculoatrial conduction in which the tricuspid valve is closed to every atrial beat.
Fine rapid regular pulsation may be seen in atrial flutter and may be a useful clue in distinguishing this from sinus rhythm when there is 4:1 atrioventricular conduction and a normal ventricular rate.
Abnormal right heart hemodynamics
Large v waves (Lancisi sign). These surges, replacing the usual x descent in systole, are seen in tricuspid insufficiency when the right atrium and its venous attachments are not protected from the right ventricular systolic pressure.22 High right ventricular pressure will obviously enhance this systolic surge.
Large a waves. These reflect resistance to right atrial outflow and may be seen when right ventricular compliance is reduced by hypertrophy from chronic pressure overload or in tricuspid stenosis.23
Pericardial disease
Kussmaul sign is the paradoxical increase in jugular venous pressure with inspiration, observed in conditions associated with limited filling of the right ventricle. It is typically associated with constrictive pericarditis, although it occurs in only a minority of people with this condition.24 It may also be seen in restrictive cardiomyopathy, massive pulmonary embolism, right ventricular infarction, and tricuspid stenosis.25
Diaphragmatic descent during inspiration increases intra-abdominal pressure and decreases intrathoracic pressure. The resulting increased gradient between the abdomen and thorax enhances venous return from splanchnic vessels, which in the setting of a noncompliant right ventricle may result in increased right atrial (and, hence, jugular venous) pressure.26
It is important to point out that the Kussmaul sign does not occur with cardiac tamponade in the absence of associated pericardial constriction.
Exaggerated y descent is typically seen in pericardial constriction, in which the high pressure of the v wave falls rapidly at the onset of diastole, given initial minimal right ventricular resistance. Flow is abruptly stopped when the intrapericardial space is filled.
In this age of technological marvels, it is easy to become so reliant on them as to neglect the value of bedside physical signs. Yet these signs provide information that adds no cost, is immediately available, and can be repeated at will.
Few physical findings are as useful but as undervalued as is the estimation of the jugular venous pressure. Unfortunately, many practitioners at many levels of seniority and experience do not measure it correctly, leading to a vicious circle of unreliable information, lack of confidence, and underuse. Another reason for its underuse is that the jugular venous pressure does not correlate precisely with the right atrial pressure, as we will see below.
In this review, we will attempt to clarify physiologic principles and describe technical details. Much of this is simple but, as always, the devil is in the details.
ANATOMIC CONSIDERATIONS
Think of the systemic veins as a soft-walled and mildly distensible reservoir with fingerlike projections, analogous to a partially fluidfilled surgical glove.1 In a semi-upright position, the venous system is partially filled with blood and is collapsed above the level that this blood reaches up to.
Blood is constantly flowing in and out of this reservoir, flowing in by venous return and flowing out by the pumping action of the right side of the heart. The volume in the venous reservoir and hence the pressure are normally maintained by the variability of right ventricular stroke volume in accordance with the Frank-Starling law. Excess volume and pressure indicate failure of this homeostatic mechanism.
The internal jugular veins, being continuous with the superior vena cava, provide a visible measure of the degree to which the systemic venous reservoir is filled, a manometer that reflects the pressure in the right atrium—at least in theory.2 Thus, the vertical height above the right atrium to which they are distended and above which they are in a collapsed state should reflect the right atrial pressure.
(In fact, the jugular venous pressure may underestimate the right atrial pressure, for reasons still not understood. This will be discussed below.)
In a healthy person, the visible jugular veins are fully collapsed when the person is standing and are often distended to a variable degree when the person is supine. Selecting an appropriate intermediate position permits the top of the column (the meniscus) to become visible in the neck between the clavicle and the mandible.
DISCREPANCY BETWEEN JUGULAR VENOUS AND RIGHT ATRIAL PRESSURE
Several reports have indicated that the jugular venous pressure may underestimate the right atrial pressure. Deol et al3 confirmed this, while establishing an excellent correlation between the level of venous collapse (observed on ultrasonography) and the jugular venous pressure. The difference between the right atrial pressure and the jugular venous pressure tended to be greater at higher venous pressures.3
Most people have a valve near the termination of the internal jugular vein, with variable competence. Inhibition of reflux of blood from the superior vena cava into the internal jugular vein by this valve is the most plausible cause of this disparity.4
The failure of the jugular venous pressure to correlate with the right atrial pressure has been cited by some as a reason to doubt the value of a sign that cardiologists have long relied on. How do we reconcile this apparent paradox? Careful review of the literature that has demonstrated this lack of correlation reveals the following:
- When unequal, the jugular venous pressure always underestimates the right atrial pressure.
- The lack of correlation is less evident at lower venous pressures.
This indicates the following:
- In the presence of congestive heart failure, the right atrial pressure is at least as high and perhaps higher than the jugular venous pressure. Hence, if the jugular venous pressure is high, further treatment, especially diuresis, is needed.
- A jugular venous pressure of zero implies a euvolemic state.
Thus, the jugular venous pressure provides excellent guidance when administering diuresis in congestive heart failure. These deductions obviously require the clinical judgment that the elevated right atrial pressure and jugular venous pressure do indeed reflect elevation of pulmonary capillary wedge pressure rather than other conditions discussed later in this article.
WHICH REFERENCE POINT TO USE?
The two points that can be used as references above which the jugular venous pressure is expressed are the center of the right atrium and the sternal angle. While the former may reflect physiology, the latter is preferred, as it is always visible and has the added advantage of being close to the upper limit of normal, which is about 3 cm above this level.
The difference in height between these two reference points has often been quoted as 5 cm, but this is an underestimate in the body positions used in examination.5 Seth et al6 found a mean of 8 cm at 30° elevation, 9.7 cm at 45°, and 9.8 cm at 60°. The difference also varied between patients, being larger in association with smoking, older age, large body mass index, and large anterior-posterior diameter. These factors should be considered when trying to evaluate the significance of a particular jugular venous pressure.
The junction of the midaxillary line and the fourth left intercostal space (“the phlebostatic point”) has been recommended as a reference point by some, as it is level with the mid-right atrium. However, using the phlebostatic point as a reference position is cumbersome and results in a valid measurement only with the patient in the supine position.7
TECHNIQUE IS VITAL
Close adherence to technical details is vital in reliably and reproducibly measuring the pressure in the internal jugular veins (Figure 1).
The right side is usually observed first, as it is the side on which the examiner usually stands. Using the right side also avoids the rare occurrence of external compression of the left brachiocephalic vein.
Head and shoulders
The sternocleidomastoid muscle lies anterior to each internal jugular vein.8 When tense, it impedes good observation. Shortening, and hence relaxing, this muscle permits the meniscus to be observed. Correct positioning is achieved by:
- Placing a folded pillow behind the patient’s head
- Keeping the shoulders on the mattress
- Turning the head away and elevating the jaw, both slightly; this is often best achieved by gentle pressure of the palm of the observer's hand on the patient's forehead.
Degree of head elevation
Although the proper degree of head elevation is sometimes said to be between 30° and 60°, these numbers are approximate. The correct angle is that which brings the venous meniscus into the window of visibility in the neck between the clavicle and mandible.
Lighting
Shining a flashlight tangentially to the skin is often helpful, casting shadows that improve the visibility of vein motion. Dimming the room lighting may further enhance this effect. Directing a light perpendicular to the skin is not helpful.
Also check the external jugular vein
Checking the external jugular vein can help establish that the jugular venous pressure is normal. If the vein is initially collapsed, light finger pressure at the base of the neck will distend it. If the distention rapidly clears after release of this pressure, the jugular venous pressure is not elevated. However, if external jugular venous distention persists, this does not prove true jugular venous pressure elevation, since it may reflect external compression of the vein by the cervical fascia or delayed blood flow caused by sclerotic venous valves.9 In these instances, the internal jugular pulsation level must be sought.
Jugular venous collapse with inspiration
Collapse of the inferior vena cava with forced inspiration is routinely evaluated during echocardiography as a way to estimate right atrial pressure. This finding has been extrapolated to the jugular veins, wherein the absence of venous collapse during vigorous inspiration or sniffing indicates elevated central venous pressures.10
Distinguishing venous from arterial pulsation
Features indicating venous rather than arterial pulsation were listed by Wood more than 50 years ago11 and are still relevant today. These include internal jugular pulsation that:
- Is soft, diffuse, undulant
- Is not palpable
- Has two crests and two troughs per cardiac cycle
- Has crests that do not coincide with the palpated carotid pulse (exceptions may be seen with the systolic timing of the v wave of tricuspid regurgitation)
- Has higher pressure in expiration, lower in inspiration (exceptions may be seen when Kussmaul physiology is present)
- Has pressure that rises with abdominal pressure
- Is obliterated by light pressure at the base of the neck.
In addition to the above criteria, a wave whose movement is predominantly a descent is nearly always venous.
Abdominojugular reflex
Firm, steady pressure over the abdomen will often result in a small rise in jugular venous pressure. In healthy people, this normalizes in a few seconds, even while manual pressure is maintained. Persistence of jugular venous pressure elevation beyond 10 seconds, followed by an abrupt fall upon withdrawal of manual pressure, is abnormal. This finding has implications similar to those of an elevated baseline jugular venous pressure.
SIGNIFICANCE OF JUGULAR VENOUS PRESSURE ELEVATION
Elevated jugular venous pressure is a manifestation of abnormal right heart dynamics, mostly commonly reflecting elevated pulmonary capillary wedge pressure from left heart failure.12 This usually implies fluid overload, indicating the need for diuresis.
Exceptions to this therapeutic implication include the presence of a primary right heart condition, pericardial disease, certain arrhythmias, and conditions that elevate intrathoracic pressure. These will be discussed below. One important example is the acute jugular venous pressure elevation seen in right ventricular infarction, in which the high venous pressure is compensatory and its reduction can produce hypotension and shock.13
Primary right heart conditions also include right-sided valvular disease, cor pulmonale (including pulmonary embolism and pulmonary hypertension), and the compressive effect of pericardial tamponade or constriction. A normal or near-normal jugular venous pressure significantly decreases the likelihood of significant constriction or of tamponade of a degree necessitating urgent pericardiocentesis.14
SPECIAL CIRCUMSTANCES
Presence of an intravenous line in the neck
An intravenous line in the neck will often prevent observation of the jugular venous pressure. A simple measure can often compensate for this. If the venous line can be temporarily disconnected, the central venous pressure can be measured directly. Using sterile technique, the line can be flushed with saline and aspirated to bring blood into the transparent tubing. Leaving the proximal end open to the air, and alternately raising and lowering it to confirm free flow, the level to which the blood rises can be easily observed. Observing small cardiac and respiratory variations of the meniscus confirms free communication with the central veins. Attaching the line to a transducer is another option, but this may be time-consuming, and establishing an accurate zero point is often difficult.
The previously described discrepancy between jugular venous pressure and central venous pressure has to be considered when drawing conclusions from this measurement.
Intrathoracic pressure elevators
Positive pressure ventilation will elevate intrathoracic pressure (including right atrial pressure) and hence the jugular venous pressure, making interpretation difficult.15 Large pleural effusions or pneumothorax may have a similar effect.16
Superior vena cava syndrome
Markedly elevated jugular venous pressure is here associated with absent or very diminished pulsation, as the caval obstruction has eliminated free communication with the right atrium.17 Associated facial plethora and edema, papilledema, and superficial venous distention over the chest wall will often confirm this diagnosis.
THE WAVEFORM
While the main purpose of viewing the neck veins is to establish the mean pressure, useful information can often be obtained by assessing the waveform. Abnormalities reflect arrhythmias, right heart hemodynamics, or pericardial disease.18 Changes may be subtle and difficult to detect, but some patterns can be quite readily appreciated (Figure 2). A limited selection follows.
Arrhythmias
Cannon a waves. These intermittent sharp positive deflections in the venous pulse represent right atrial contraction against a closed tricuspid valve. They are most commonly associated with premature ventricular complexes, but they occur in other conditions in which atrial and ventricular beating are dissociated, including complete heart block, atrioventricular dissociation, and electronic ventricular pacing.19–21
Repetitive cannon waves. These may be seen with atrioventricular junctional tachycardia or ventricular tachycardia with 1:1 retrograde ventriculoatrial conduction in which the tricuspid valve is closed to every atrial beat.
Fine rapid regular pulsation may be seen in atrial flutter and may be a useful clue in distinguishing this from sinus rhythm when there is 4:1 atrioventricular conduction and a normal ventricular rate.
Abnormal right heart hemodynamics
Large v waves (Lancisi sign). These surges, replacing the usual x descent in systole, are seen in tricuspid insufficiency when the right atrium and its venous attachments are not protected from the right ventricular systolic pressure.22 High right ventricular pressure will obviously enhance this systolic surge.
Large a waves. These reflect resistance to right atrial outflow and may be seen when right ventricular compliance is reduced by hypertrophy from chronic pressure overload or in tricuspid stenosis.23
Pericardial disease
Kussmaul sign is the paradoxical increase in jugular venous pressure with inspiration, observed in conditions associated with limited filling of the right ventricle. It is typically associated with constrictive pericarditis, although it occurs in only a minority of people with this condition.24 It may also be seen in restrictive cardiomyopathy, massive pulmonary embolism, right ventricular infarction, and tricuspid stenosis.25
Diaphragmatic descent during inspiration increases intra-abdominal pressure and decreases intrathoracic pressure. The resulting increased gradient between the abdomen and thorax enhances venous return from splanchnic vessels, which in the setting of a noncompliant right ventricle may result in increased right atrial (and, hence, jugular venous) pressure.26
It is important to point out that the Kussmaul sign does not occur with cardiac tamponade in the absence of associated pericardial constriction.
Exaggerated y descent is typically seen in pericardial constriction, in which the high pressure of the v wave falls rapidly at the onset of diastole, given initial minimal right ventricular resistance. Flow is abruptly stopped when the intrapericardial space is filled.
- Sherwood L. Human Physiology: From Cells to Systems. 8th ed. Belmont, CA: Brooks/Cole; 2012.
- Constant J. Using internal jugular pulsations as a manometer for right atrial pressure measurements. Cardiology 2000; 93:26–30.
- Deol GR, Collett N, Ashby A, Schmidt GA. Ultrasound accurately reflects the jugular venous examination but underestimates central venous pressure. Chest 2011; 139:95–100.
- Wu X, Studer W, Erb T, Skarvan K, Seeberger MD. Competence of the internal jugular vein valve is damaged by cannulation and catheterization of the internal jugular vein. Anesthesiology 2000; 93:319–324.
- Ramana RK, Sanagala T, Lichtenberg R. A new angle on the angle of Louis. Congest Heart Fail 2006; 12:196–199.
- Seth R, Magner P, Matzinger F, van Walraven C. How far is the sternal angle from the mid-right atrium? J Gen Intern Med 2002; 17:852–856.
- Kee LL, Simonson JS, Stotts NA, Skov P, Schiller NB. Echocardiographic determination of valid zero reference levels in supine and lateral positions. Am J Crit Care 1993; 2:72–80.
- Park SY, Kim MJ, Kim MG, et al. Changes in the relationship between the right internal jugular vein and an anatomical landmark after head rotation. Korean J Anesthesiol 2011; 61:107–111.
- Sankoff J, Zidulka A. Non-invasive method for the rapid assessment of central venous pressure: description and validation by a single examiner. West J Emerg Med 2008; 9:201–205.
- Conn RD, O’Keefe JH. Simplified evaluation of the jugular venous pressure: significance of inspiratory collapse of jugular veins. Mo Med 2012; 109:150–152.
- Wood PH. Diseases of the Heart and Circulation. 2nd ed. Philadelphia, PA: Lippincott; 1956.
- Drazner MH, Brown RN, Kaiser PA, et al. Relationship of right- and left-sided filling pressures in patients with advanced heart failure: a 14-year multi-institutional analysis. J Heart Lung Transplant 2012; 31:67–72.
- Clark G, Strauss HD, Roberts R. Dobutamine vs furosemide in the treatment of cardiac failure due to right ventricular infarction. Chest 1980; 77:220–223.
- Roy CL, Minor MA, Brookhart MA, Choudhry NK. Does this patient with a pericardial effusion have cardiac tamponade? JAMA 2007; 297:1810–1818.
- Zhou Q, Xiao W, An E, Zhou H, Yan M. Effects of four different positive airway pressures on right internal jugular vein catheterisation. Eur J Anaesthesiol 2012; 29:223–228.
- Jolobe OM. Disproportionate elevation of jugular venous pressure in pleural effusion. Br J Hosp Med (Lond) 2011; 72:582–585.
- Seo M, Shin WJ, Jun IG. Central venous catheter-related superior vena cava syndrome following renal transplantation—a case report. Korean J Anesthesiol 2012; 63:550–554.
- Applefeld MM. The jugular venous pressure and pulse contour. In:Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Boston, MA: Butterworths; 1990.
- El Gamal MI, Van Gelder LM. Chronic ventricular pacing with ventriculo-atrial conduction versus atrial pacing in three patients with symptomatic sinus bradycardia. Pacing Clin Electrophysiol 1981; 4:100–105.
- Berman ND, Waxman MB. Cannon waves with A-V association. Am Heart J 1976; 91:643–644.
- Luisada AA, Singhal A, Kim K. The jugular and hepatic tracings in normal subjects and in conduction defects. Acta Cardiol 1983; 38:405–424.
- Miller MJ, McKay RG, Ferguson JJ, et al. Right atrial pressure-volume relationships in tricuspid regurgitation. Circulation 1986; 73:799–808.
- Wooley CF, Fontana ME, Kilman JW, Ryan JM. Tricuspid stenosis. Atrial systolic murmur, tricuspid opening snap, and right atrial pressure pulse. Am J Med 1985; 78:375–384.
- McGee SR. Evidence-Based Physical Diagnosis. 3rd ed. Philadelphia, PA: Elsevier/Saunders; 2012.
- Mittal SR, Garg S, Lalgarhia M. Jugular venous pressure and pulse wave form in the diagnosis of right ventricular infarction. Int J Cardiol 1996; 53:253–256.
- Bilchick KC, Wise RA. Paradoxical physical findings described by Kussmaul: pulsus paradoxus and Kussmaul’s sign. Lancet 2002; 359:1940–1942.
- Sherwood L. Human Physiology: From Cells to Systems. 8th ed. Belmont, CA: Brooks/Cole; 2012.
- Constant J. Using internal jugular pulsations as a manometer for right atrial pressure measurements. Cardiology 2000; 93:26–30.
- Deol GR, Collett N, Ashby A, Schmidt GA. Ultrasound accurately reflects the jugular venous examination but underestimates central venous pressure. Chest 2011; 139:95–100.
- Wu X, Studer W, Erb T, Skarvan K, Seeberger MD. Competence of the internal jugular vein valve is damaged by cannulation and catheterization of the internal jugular vein. Anesthesiology 2000; 93:319–324.
- Ramana RK, Sanagala T, Lichtenberg R. A new angle on the angle of Louis. Congest Heart Fail 2006; 12:196–199.
- Seth R, Magner P, Matzinger F, van Walraven C. How far is the sternal angle from the mid-right atrium? J Gen Intern Med 2002; 17:852–856.
- Kee LL, Simonson JS, Stotts NA, Skov P, Schiller NB. Echocardiographic determination of valid zero reference levels in supine and lateral positions. Am J Crit Care 1993; 2:72–80.
- Park SY, Kim MJ, Kim MG, et al. Changes in the relationship between the right internal jugular vein and an anatomical landmark after head rotation. Korean J Anesthesiol 2011; 61:107–111.
- Sankoff J, Zidulka A. Non-invasive method for the rapid assessment of central venous pressure: description and validation by a single examiner. West J Emerg Med 2008; 9:201–205.
- Conn RD, O’Keefe JH. Simplified evaluation of the jugular venous pressure: significance of inspiratory collapse of jugular veins. Mo Med 2012; 109:150–152.
- Wood PH. Diseases of the Heart and Circulation. 2nd ed. Philadelphia, PA: Lippincott; 1956.
- Drazner MH, Brown RN, Kaiser PA, et al. Relationship of right- and left-sided filling pressures in patients with advanced heart failure: a 14-year multi-institutional analysis. J Heart Lung Transplant 2012; 31:67–72.
- Clark G, Strauss HD, Roberts R. Dobutamine vs furosemide in the treatment of cardiac failure due to right ventricular infarction. Chest 1980; 77:220–223.
- Roy CL, Minor MA, Brookhart MA, Choudhry NK. Does this patient with a pericardial effusion have cardiac tamponade? JAMA 2007; 297:1810–1818.
- Zhou Q, Xiao W, An E, Zhou H, Yan M. Effects of four different positive airway pressures on right internal jugular vein catheterisation. Eur J Anaesthesiol 2012; 29:223–228.
- Jolobe OM. Disproportionate elevation of jugular venous pressure in pleural effusion. Br J Hosp Med (Lond) 2011; 72:582–585.
- Seo M, Shin WJ, Jun IG. Central venous catheter-related superior vena cava syndrome following renal transplantation—a case report. Korean J Anesthesiol 2012; 63:550–554.
- Applefeld MM. The jugular venous pressure and pulse contour. In:Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Boston, MA: Butterworths; 1990.
- El Gamal MI, Van Gelder LM. Chronic ventricular pacing with ventriculo-atrial conduction versus atrial pacing in three patients with symptomatic sinus bradycardia. Pacing Clin Electrophysiol 1981; 4:100–105.
- Berman ND, Waxman MB. Cannon waves with A-V association. Am Heart J 1976; 91:643–644.
- Luisada AA, Singhal A, Kim K. The jugular and hepatic tracings in normal subjects and in conduction defects. Acta Cardiol 1983; 38:405–424.
- Miller MJ, McKay RG, Ferguson JJ, et al. Right atrial pressure-volume relationships in tricuspid regurgitation. Circulation 1986; 73:799–808.
- Wooley CF, Fontana ME, Kilman JW, Ryan JM. Tricuspid stenosis. Atrial systolic murmur, tricuspid opening snap, and right atrial pressure pulse. Am J Med 1985; 78:375–384.
- McGee SR. Evidence-Based Physical Diagnosis. 3rd ed. Philadelphia, PA: Elsevier/Saunders; 2012.
- Mittal SR, Garg S, Lalgarhia M. Jugular venous pressure and pulse wave form in the diagnosis of right ventricular infarction. Int J Cardiol 1996; 53:253–256.
- Bilchick KC, Wise RA. Paradoxical physical findings described by Kussmaul: pulsus paradoxus and Kussmaul’s sign. Lancet 2002; 359:1940–1942.
KEY POINTS
- If the jugular venous pressure differs from the true right atrial pressure, the jugular venous pressure is always the lower value.
- The jugular venous pressure is useful to observe when diagnosing congestive heart failure and when considering the need for or the adequacy of diuresis.
- The jugular venous wave form is more difficult to observe than its elevation but can yield useful information in the assessment of certain arrhythmias, right-heart conditions, and pericardial disease.
More than skin-deep
A 68-year-old man presented for evaluation of a diffuse rash with mucosal involvement. During the past 9 months, he had had oral ulcers, a truncal rash, and blistering lesions on his hands with fingernail erosion, and all of these had been getting worse (Figure 1). He also reported cycles of fever and a weight loss of 50 lb.
Computed tomography revealed diffuse lymphadenopathy, including a bulky 18-cm mediastinal mass. Lymph node biopsy confirmed follicular non-Hodgkin lymphoma.
On serum enzyme-linked immunosorbent assay (ELISA), the desmoglein 1 antibody titer was 62.4 U (< 14 is negative, > 20 is positive) and the desmoglein 3 antibody titer was 36.0 U (< 9 is negative, > 20 is positive). Indirect immunofluorescence testing on monkey esophagus substrate was reactive.
ELISA detected no immunoglobulin G (IgG) reactivity against the bullous pemphigoid autoantigens BP180 and BP230. Direct immunofluorescence testing revealed strong IgG and C3 deposition on epithelial cell surfaces, and indirect immunofluorescence on rat bladder substrate was positive, suggesting the diagnosis of paraneoplastic pemphigus.
The patient was treated with dexamethasone and bendamustine-rituximab. Five months later, desmoglein 1 and 3 antibody titers were measured again and were within normal limits. His lesions had improved significantly (Figure 2), but he had endured multiple medical setbacks, including Pseudomonas peritonitis, fistulizing cytomegalovirus perianal ulceration, septic shock secondary to fulminant Clostridium difficile colitis, and toxic megacolon necessitating total colectomy with end-ileostomy.

PARANEOPLASTIC PEMPHIGUS
Paraneoplastic pemphigus usually occurs in the presence of underlying lymphoproliferative neoplasm, most often non-Hodgkin lymphoma, chronic lymphocytic leukemia, or Castleman disease. It may also occur with epithelial carcinoma, mesenchymal sarcoma, and, rarely, malignant melanoma.1 The association between malignancy and autoimmune mucocutaneous disease was first described in 1990.2 Autoantibodies against periplakin, envoplakin, and desmoglein 3 are often present and may play a role in pathogenesis.
Paraneoplastic pemphigus associated with malignancy portends a poor prognosis. Although historically reported to have an overall death rate ranging from 75% to 90%, with a mean survival of less than 1 year, a recent retrospective cohort has shown slightly improved outcomes, with 49% of patients remaining alive at 1 year and 38% alive at 5 years.3 The most common causes of death are sepsis, respiratory failure, and the underlying malignancy. Bronchiolitis obliterans may occur late in the disease course and is an ominous prognostic factor, with a death rate of 41% after a median interval of 13 months.4
Immunosuppressive drugs are often used to control the disease. First-line treatment is with high-dose steroids. Immunosuppressives such as azathioprine and cyclosporin may be used in conjunction to reduce the steroid dose that is required and to limit the adverse effects of steroid therapy. Treating the underlying malignancy may decrease autoantibody production and lead to clinical improvement.
- Kaplan I, Hodak E, Ackerman L, Mimouni D, Anhalt GJ, Calderon S. Neoplasms associated with paraneoplastic pemphigus: a review with emphasis on non-hematologic malignancy and oral mucosal manifestations. Oral Oncol 2004; 40:553–562.
- Anhalt GJ, Kim SC, Stanley JR, et al. Paraneoplastic pemphigus. An autoimmune mucocutaneous disease associated with neoplasia. N Engl J Med 1990; 323:1729–1735.
- Leger S, Picard D, Ingen-Housz-Oro S, et al. Prognostic factors of paraneoplastic pemphigus. Arch Dermatol 2012; 148:1165–1172.
- Maldonado F, Pittelkow MR, Ryu JH. Constrictive bronchiolitis associated with pareaneoplastic autoimmune multi-organ syndrome. Respirology 2009; 14:129–133.
A 68-year-old man presented for evaluation of a diffuse rash with mucosal involvement. During the past 9 months, he had had oral ulcers, a truncal rash, and blistering lesions on his hands with fingernail erosion, and all of these had been getting worse (Figure 1). He also reported cycles of fever and a weight loss of 50 lb.
Computed tomography revealed diffuse lymphadenopathy, including a bulky 18-cm mediastinal mass. Lymph node biopsy confirmed follicular non-Hodgkin lymphoma.
On serum enzyme-linked immunosorbent assay (ELISA), the desmoglein 1 antibody titer was 62.4 U (< 14 is negative, > 20 is positive) and the desmoglein 3 antibody titer was 36.0 U (< 9 is negative, > 20 is positive). Indirect immunofluorescence testing on monkey esophagus substrate was reactive.
ELISA detected no immunoglobulin G (IgG) reactivity against the bullous pemphigoid autoantigens BP180 and BP230. Direct immunofluorescence testing revealed strong IgG and C3 deposition on epithelial cell surfaces, and indirect immunofluorescence on rat bladder substrate was positive, suggesting the diagnosis of paraneoplastic pemphigus.
The patient was treated with dexamethasone and bendamustine-rituximab. Five months later, desmoglein 1 and 3 antibody titers were measured again and were within normal limits. His lesions had improved significantly (Figure 2), but he had endured multiple medical setbacks, including Pseudomonas peritonitis, fistulizing cytomegalovirus perianal ulceration, septic shock secondary to fulminant Clostridium difficile colitis, and toxic megacolon necessitating total colectomy with end-ileostomy.

PARANEOPLASTIC PEMPHIGUS
Paraneoplastic pemphigus usually occurs in the presence of underlying lymphoproliferative neoplasm, most often non-Hodgkin lymphoma, chronic lymphocytic leukemia, or Castleman disease. It may also occur with epithelial carcinoma, mesenchymal sarcoma, and, rarely, malignant melanoma.1 The association between malignancy and autoimmune mucocutaneous disease was first described in 1990.2 Autoantibodies against periplakin, envoplakin, and desmoglein 3 are often present and may play a role in pathogenesis.
Paraneoplastic pemphigus associated with malignancy portends a poor prognosis. Although historically reported to have an overall death rate ranging from 75% to 90%, with a mean survival of less than 1 year, a recent retrospective cohort has shown slightly improved outcomes, with 49% of patients remaining alive at 1 year and 38% alive at 5 years.3 The most common causes of death are sepsis, respiratory failure, and the underlying malignancy. Bronchiolitis obliterans may occur late in the disease course and is an ominous prognostic factor, with a death rate of 41% after a median interval of 13 months.4
Immunosuppressive drugs are often used to control the disease. First-line treatment is with high-dose steroids. Immunosuppressives such as azathioprine and cyclosporin may be used in conjunction to reduce the steroid dose that is required and to limit the adverse effects of steroid therapy. Treating the underlying malignancy may decrease autoantibody production and lead to clinical improvement.
A 68-year-old man presented for evaluation of a diffuse rash with mucosal involvement. During the past 9 months, he had had oral ulcers, a truncal rash, and blistering lesions on his hands with fingernail erosion, and all of these had been getting worse (Figure 1). He also reported cycles of fever and a weight loss of 50 lb.
Computed tomography revealed diffuse lymphadenopathy, including a bulky 18-cm mediastinal mass. Lymph node biopsy confirmed follicular non-Hodgkin lymphoma.
On serum enzyme-linked immunosorbent assay (ELISA), the desmoglein 1 antibody titer was 62.4 U (< 14 is negative, > 20 is positive) and the desmoglein 3 antibody titer was 36.0 U (< 9 is negative, > 20 is positive). Indirect immunofluorescence testing on monkey esophagus substrate was reactive.
ELISA detected no immunoglobulin G (IgG) reactivity against the bullous pemphigoid autoantigens BP180 and BP230. Direct immunofluorescence testing revealed strong IgG and C3 deposition on epithelial cell surfaces, and indirect immunofluorescence on rat bladder substrate was positive, suggesting the diagnosis of paraneoplastic pemphigus.
The patient was treated with dexamethasone and bendamustine-rituximab. Five months later, desmoglein 1 and 3 antibody titers were measured again and were within normal limits. His lesions had improved significantly (Figure 2), but he had endured multiple medical setbacks, including Pseudomonas peritonitis, fistulizing cytomegalovirus perianal ulceration, septic shock secondary to fulminant Clostridium difficile colitis, and toxic megacolon necessitating total colectomy with end-ileostomy.

PARANEOPLASTIC PEMPHIGUS
Paraneoplastic pemphigus usually occurs in the presence of underlying lymphoproliferative neoplasm, most often non-Hodgkin lymphoma, chronic lymphocytic leukemia, or Castleman disease. It may also occur with epithelial carcinoma, mesenchymal sarcoma, and, rarely, malignant melanoma.1 The association between malignancy and autoimmune mucocutaneous disease was first described in 1990.2 Autoantibodies against periplakin, envoplakin, and desmoglein 3 are often present and may play a role in pathogenesis.
Paraneoplastic pemphigus associated with malignancy portends a poor prognosis. Although historically reported to have an overall death rate ranging from 75% to 90%, with a mean survival of less than 1 year, a recent retrospective cohort has shown slightly improved outcomes, with 49% of patients remaining alive at 1 year and 38% alive at 5 years.3 The most common causes of death are sepsis, respiratory failure, and the underlying malignancy. Bronchiolitis obliterans may occur late in the disease course and is an ominous prognostic factor, with a death rate of 41% after a median interval of 13 months.4
Immunosuppressive drugs are often used to control the disease. First-line treatment is with high-dose steroids. Immunosuppressives such as azathioprine and cyclosporin may be used in conjunction to reduce the steroid dose that is required and to limit the adverse effects of steroid therapy. Treating the underlying malignancy may decrease autoantibody production and lead to clinical improvement.
- Kaplan I, Hodak E, Ackerman L, Mimouni D, Anhalt GJ, Calderon S. Neoplasms associated with paraneoplastic pemphigus: a review with emphasis on non-hematologic malignancy and oral mucosal manifestations. Oral Oncol 2004; 40:553–562.
- Anhalt GJ, Kim SC, Stanley JR, et al. Paraneoplastic pemphigus. An autoimmune mucocutaneous disease associated with neoplasia. N Engl J Med 1990; 323:1729–1735.
- Leger S, Picard D, Ingen-Housz-Oro S, et al. Prognostic factors of paraneoplastic pemphigus. Arch Dermatol 2012; 148:1165–1172.
- Maldonado F, Pittelkow MR, Ryu JH. Constrictive bronchiolitis associated with pareaneoplastic autoimmune multi-organ syndrome. Respirology 2009; 14:129–133.
- Kaplan I, Hodak E, Ackerman L, Mimouni D, Anhalt GJ, Calderon S. Neoplasms associated with paraneoplastic pemphigus: a review with emphasis on non-hematologic malignancy and oral mucosal manifestations. Oral Oncol 2004; 40:553–562.
- Anhalt GJ, Kim SC, Stanley JR, et al. Paraneoplastic pemphigus. An autoimmune mucocutaneous disease associated with neoplasia. N Engl J Med 1990; 323:1729–1735.
- Leger S, Picard D, Ingen-Housz-Oro S, et al. Prognostic factors of paraneoplastic pemphigus. Arch Dermatol 2012; 148:1165–1172.
- Maldonado F, Pittelkow MR, Ryu JH. Constrictive bronchiolitis associated with pareaneoplastic autoimmune multi-organ syndrome. Respirology 2009; 14:129–133.
A practical approach to prescribing antidepressants
With the variety of drugs available for treating depression, choosing one can be daunting. Different agents have characteristics that may make them a better choice for different types of patients, but even so, treating any kind of mental illness often requires an element of trial and error.
Primary care providers are on the frontline of treating mental illness, often evaluating patients before they are seen by a psychiatrist. The purpose of this article is to provide insight into the art of prescribing antidepressants in the primary care setting. We will discuss common patient presentations, including depressed patients without other medical comorbidities as well as those with common comorbidities, with our recommendations for first-line treatment.
We hope our recommendations will help you to navigate the uncertainty more confidently, resulting in more efficient and tailored treatment for your patients.
BASELINE TESTING
When starting a patient on antidepressant drug therapy, we recommend obtaining a set of baseline laboratory tests to rule out underlying medical conditions that may be contributing to the patient’s depression or that may preclude the use of a given drug. (For example, elevation of liver enzymes may preclude the use of duloxetine.) Tests should include:
- A complete blood cell count
- A complete metabolic panel
- A thyroid-stimulating hormone level.
Electrocardiography may also be useful, as some antidepressants can prolong the QT interval or elevate the blood levels of other drugs with this effect.
GENERAL TREATMENT CONSIDERATIONS
There are several classes of antidepressants, and each class has a number of agents. Research has found little difference in efficacy among agents. So to simplify choosing which one to use, we recommend becoming comfortable with an agent from each class, ie:
- A selective serotonin reuptake inhibitor (SSRI)
- A selective serotonin-norepinephrine reuptake inhibitor (SNRI)
- A tricyclic antidepressant (TCA)
- A monoamine oxidase (MAO) inhibitor.
Each class includes generic agents, many of which are on the discount lists of retail pharmacies. Table 1 shows representative drugs from each class, with their relative costs.
Start low and go slow. In general, when starting an antidepressant, consider starting at half the normal dose, titrating upward as tolerated about every 14 days. This approach can minimize side effects. For example, if prescribing fluoxetine, start with 10 mg and titrate every 2 weeks based on tolerance and patient response. That said, each patient may respond differently, requiring perhaps a lower starting dose or a longer titration schedule.
Anticipate side effects. Most of the side effects of an antidepressant drug can be explained by its mechanism of action. Although side effects should certainly be considered when choosing an agent, patients can be reassured that most are transient and benign. A detailed discussion of side effects of antidepressant drugs is beyond the scope of this article, but a review by Khawam et al1 was published earlier in this journal.
Reassess. If after 4 to 6 weeks the patient has had little or no response, it is reasonable to switch agents. For a patient who was on an SSRI, the change can be to another SSRI or to an SNRI. However, if two SSRIs have already failed, then choose an SNRI. Agents are commonly cross-tapered during the switch to avoid abrupt cessation of one drug or the increased risk of adverse events such as cytochrome P450 interactions, serotonin syndrome, or hypertensive crisis (when switching to an MAO inhibitor).
Beware of interactions. All SSRIs and SNRIs are metabolized through the P450 system in the liver and therefore have the potential for drug-drug interactions. Care must be taken when giving these agents together with drugs whose metabolism can be altered by P450 inhibition. For TCAs, blood levels can be checked if there is concern about toxicity; however, dosing is not strictly based on this level. Great care should be taken if a TCA is given together with an SNRI or an SSRI, as the TCA blood level can become significantly elevated. This may result in QT interval prolongation, as mentioned earlier.
Refer. Referral to a psychiatrist is appropriate for patients for whom multiple classes have failed, for patients who have another psychiatric comorbidity (such as psychosis, hypomania, or mania), or for patients who may need hospitalization. Referral is also appropriate if the physician is concerned about suicide risk.
PATIENTS WITH MAJOR DEPRESSION ONLY
For a patient presenting with depression but no other significant medical comorbidity, the first-line therapy is often an SSRI. Several generic SSRIs are available, and some are on the discount lists at retail pharmacies.
Symptoms should start to improve in about 2 weeks, and the optimal response should be achieved in 4 to 6 weeks of treatment. If this does not occur, consider either adding an augmenting agent or switching to a different antidepressant.
PATIENTS WITH CHRONIC PAIN
Chronic pain and depression often go hand in hand and can potentiate each other. When considering an antidepressant in a patient who has both conditions, the SNRIs and TCAs are typically preferred. Some SNRIs, namely duloxetine and milnacipran, are approved for certain chronic pain conditions, such as fibromyalgia. SNRIs are frequently used off-label for other chronic pain conditions such as headache and neuropathic pain.2
TCAs such as amitriptyline, nortriptyline, and doxepin are also often used in patients with chronic pain. These agents, like the SNRIs, inhibit the reuptake of serotonin and norepinephrine and are used off-label for neuropathic pain,3,4 migraine, interstitial cystitis,5 and other pain conditions.6–9
For TCAs and SNRIs, the effective dose range for chronic pain overlaps that for depression. However, TCAs are often given at lower doses to patients without depression. We recommend starting at a low dose and slowly titrating upward to an effective dose. SNRIs are often preferred over TCAs because they do not have anticholinergic side effects and because an overdose is much less likely to be lethal.
PATIENTS WITH SEXUAL DYSFUNCTION
One of the more commonly reported side effects of antidepressants is sexual dysfunction, generally in the form of delayed orgasm or decreased libido.10 Typically, these complaints are attributed to SSRIs and SNRIs; however, TCAs and MAO inhibitors have also been associated wth sexual dysfunction.
Both erectile dysfunction and priapism have been linked to certain antidepressants. In particular, trazodone is a known cause of priapism. Even if using low doses for sleep, male patients should be made aware of this adverse effect.
Switching from one agent to another in the same class is not likely to improve sexual side effects. In particular, all the SSRIs are similar in their likelihood of causing sexual dysfunction. In a patient taking an SSRI who experiences this side effect, switching to bupropion11 or mirtazapine12 can be quite useful. Bupropion acts primarily on dopamine and norepinephrine, whereas mirtazapine acts on serotonin and norepinephrine but in a different manner from SSRIs and SNRIs.
Adjunctive treatment such as a cholinergic agonist, yohimbine (contraindicated with MAO inhibitors), a serotonergic agent (eg, buspirone), or a drug that acts on nitric oxide (eg, sildenafil, tadalafil) may have some utility but is often ineffective. Dose reduction, if possible, can be of value.
PATIENTS WITH ANXIETY
Many antidepressants are also approved for anxiety disorders, and still more are used off-label for this purpose. Anxiety and depression often occur together, so being able to treat both conditions with one drug can be quite useful.13 In general, the antidepressant effects are seen at lower doses of SSRIs and SNRIs, whereas more of the anxiolytic effects are seen at higher doses, particularly for obsessive-compulsive disorder.14
First-line treatment would be an SSRI or SNRI. Most anxiety disorders respond to either class, but there are some more-specific recommendations. SSRIs are best studied in panic disorder, generalized anxiety disorder, social anxiety disorder, posttraumatic stress disorder, and obsessive-compulsive disorder. Fluoxetine, citalopram, escitalopram, and sertraline15 can all be effective in both major depressive disorder and generalized anxiety disorder. Panic disorder also tends to respond well to SSRIs. SNRIs have been evaluated primarily in generalized anxiety disorder but may also be useful in many of the other conditions.
Additionally, mirtazapine (used off-label)12 and the TCAs16–18 can help treat anxiety. Clomipramine is used to treat obsessive-compulsive disorder.19 These drugs are especially useful for nighttime anxiety, as they can aid sleep. Of note, the anxiolytic effect of mirtazapine may be greater at higher doses.
MAO inhibitors often go unused because of the dietary and medication restrictions involved. However, very refractory cases of certain anxiety disorders may respond preferentially to these agents.
Bupropion tends to be more activating than other antidepressants, so is often avoided in anxious patients. However, some research suggests this is not always necessary.20 If the anxiety is secondary to depression, it will often improve significantly with this agent.
When starting or increasing the dose of an antidepressant, patients may experience increased anxiety or feel “jittery.” This feeling usually passes within the first week of treatment, and it is important to inform patients about this effect. “Start low and go slow” in patients with significant comorbid anxiety. Temporarily using a benzodiazepine such as clonazepam may make the transition more tolerable.
PATIENTS WITH CHRONIC FATIGUE SYNDROME OR FIBROMYALGIA
Increasing recognition of both chronic fatigue syndrome and fibromyalgia has led to more proactive treatment for these disorders. Depression can go hand in hand with these disorders, and certain antidepressants, namely the SNRIs, can be useful in this population.
More data exist for the treatment of fibromyalgia. Both duloxetine and milnacipran are approved by the US Food and Drug Administration (FDA) for the treatment of fibromyalgia.21 Venlafaxine is also used off-label for this purpose. SSRIs such as fluoxetine and citalopram have had mixed results.21–23 TCAs have been used with some success; however, their side effects and lethal potential are often limiting.21,24,25 A recent study in Spain also suggested there may be benefit from using MAO inhibitors for fibromyalgia, but data are quite limited.26
The data for treating chronic fatigue syndrome with SSRIs, SNRIs, or MAO inhibitors are conflicting.27–29 However, managing the co-existing depression may provide some relief in and of itself.
PATIENTS WITH FREQUENT INSOMNIA
Insomnia can be a symptom of depression, but it can also be a side effect of certain antidepressants. The SSRIs and SNRIs can disrupt sleep patterns in some patients by shortening the rapid-eye-movement (REM) stage.30,31
In patients with severe insomnia, it may be best to first recommend taking the antidepressant in the morning if they notice worsening sleep after initiating treatment. Patients can be told with any antidepressant, “If it makes you tired, take it at night, and if it wakes you up, take it in the morning.” Of note, a recent South African study suggested that escitalopram may be able to improve sleep.32
If that does not solve the problem, there are other options. For instance, mirtazapine, particularly in doses of 15 mg or 30 mg, aids depression and insomnia. At higher doses (45 mg), the sleep-aiding effect may be reduced. Low doses of TCAs, particularly doxepin, maprotiline (technically speaking, a tetracyclic antidepressant), amitriptyline, and nortriptyline can be effective sleep aids. These agents may be used as an adjunct to another antidepressant to enhance sleep and mood. However, the TCAs also shorten the REM stage of sleep.33
The previously mentioned drug interactions with SSRIs and SNRIs also need to be considered. Caution should be used when discontinuing these medications, as patients may experience rebound symptoms in the form of much more vivid dreams. MAO inhibitors may worsen insomnia because they suppress REM sleep.34
Trazodone is another agent that at lower doses (25–150 mg) can be an effective, nonaddicting sleep aid. When used as an antidepressant, it is generally prescribed at higher doses (300–400 mg), but its sedating effects can be quite limiting at these levels. It is important to remember the possibility of priapism in male patients.
GERIATRIC PATIENTS
Old age brings its own set of concerns when treating depression. Elderly patients are more susceptible to potential bradycardia caused by SSRIs. The TCAs have the more worrisome cardiac side effect of QTc prolongation. TCAs can slow cognitive function, whereas the SSRIs, bupropion, and the SNRIs tend not to affect cognition. Escitalopram and duloxetine have been suggested to be particularly effective in the elderly.35,36 A study from the Netherlands linked SSRIs with increased risk of falling in geriatric patients with dementia.37 Constipation, which could lead to ileus, is increased with TCAs and certain other agents (ie, paroxetine) in the geriatric population.
Mirtazapine is often very useful in elderly patients for many reasons: it treats both anxiety and depression, stimulates appetite and weight gain, can help with nausea, and is an effective sleep aid. Concerns about weight, appetite, and sleep are particularly common in the elderly, whereas younger patients can be less tolerant of drugs that make them gain weight and sleep more. Normal age-related changes to the sleep cycle contribute to decreased satisfaction with sleep as we age. In addition, depression often further impairs sleep. So, in the elderly, optimizing sleep is key. Research has also shown mirtazapine to be effective in patients with both Alzheimer dementia and depression.38
DIABETIC PATIENTS
One of the more worrisome side effects of psychiatric medications in diabetic patients is weight gain. Certain antidepressants have a greater propensity for weight gain and should likely be avoided as first-line treatments in this population.12 Typically, these agents include those that have more antihistamine action such as paroxetine and the TCAs. These agents also may lead to constipation, which could potentially worsen gastroparesis. Mirtazapine and the MAO inhibitors are also known to cause weight gain.
Bupropion and nefazodone are the most weight-neutral of all antidepressants. Nefazodone has fallen out of favor because of its potential to cause fulminant liver failure in rare cases. However, it remains a reasonable option for patients with comorbid anxiety and depression who have significant weight gain with other agents.
SSRIs and MAO inhibitors may improve or be neutral toward glucose metabolism, and some data suggest that SNRIs may impair this process.39
PATIENTS WITH CARDIAC CONDITIONS
Major depression often coexists with cardiac conditions. In particular, many patients develop depression after suffering a myocardial infarction, and increasingly they are being treated for it.40 Treatment in this situation is appropriate, since depression, if untreated, can increase the risk of recurrence of myocardial infarction.41
However, there are many concerns that accompany treating depression in cardiac patients. Therefore, a baseline electrocardiogram should be obtained before starting an antidepressant.
TCAs and tetracyclic agents have a tendency to prolong the QTc interval and potentiate ventricular arrhythmias,42 so it may be prudent to avoid these in patients at risk. These agents can also significantly increase the pulse rate. This tachycardia increases the risk of angina or myocardial infarction from the anticholinergic effects of these drugs.
In February 2013, the FDA issued a warning about possible arrhythmias with citalopram at doses greater than 40 mg in adult patients43; however, research has suggested citalopram is effective in treating depression in cardiac patients.44 Research has not shown an increase in efficacy at doses greater than 40 mg daily, so we recommend following the black-box warning.
TCAs and MAO inhibitors can also cause orthostatic hypotension. On the other hand, consuming large amounts of tyramine, in foods such as aged cheese, can precipitate a hypertensive crisis in patients taking MAO inhibitors.
Which antidepressants tend to be safer in cardiac patients? Sertraline has been shown to be safe in congestive heart failure and coronary artery disease,45–47 but the SSRIs are typically safe. Fluoxetine has shown efficacy in patients who have had a myocardial infarction.48 Mirtazapine has also been shown to be efficacious in cardiac patients.49 Nefazodone, mirtazapine, bupropion, SSRIs, and SNRIs have little or no tendency toward orthostatic hypotension.
- Khawam EA, Laurencic G, Malone DA. Side effects of antidepressants: an overview. Cleve Clin J Med 2006; 73:351–361.
- Ziegler D. Painful diabetic neuropathy: treatment and future aspects. Diabetes Metab Res Rev 2008; 24(suppl 1):S52–S57.
- Saarto T, Wiffen PJ. Antidepressants for neuropathic pain: a Cochrane review. J Neurol Neurosurg Psychiatry 2010; 81:1372–1373.
- Tanenberg RJ, Irving GA, Risser RC, et al. Duloxetine, pregabalin, and duloxetine plus gabapentin for diabetic peripheral neuropathic pain management in patients with inadequate pain response to gabapentin: an open-label, randomized, noninferiority comparison. Mayo Clin Proc 2011; 86:615–626.
- Hertle L, van Ophoven A. Long-term results of amitriptyline treatment for interstitial cystitis. Aktuelle Urol 2010; 41(suppl 1):S61–S65.
- Nguyen TM, Eslick GD. Systematic review: the treatment of noncardiac chest pain with antidepressants. Aliment Pharmacol Ther 2012; 35:493–500.
- Lee H, Kim JH, Min BH, et al. Efficacy of venlafaxine for symptomatic relief in young adult patients with functional chest pain: a randomized, double-blind, placebo-controlled, crossover trial. Am J Gastroenterol 2010; 105:1504–1512.
- Varia I, Logue E, O’Connor C, et al. Randomized trial of sertraline in patients with unexplained chest pain of noncardiac origin. Am Heart J 2000; 140:367–372.
- Doraiswamy PM, Varia I, Hellegers C, et al. A randomized controlled trial of paroxetine for noncardiac chest pain. Psychopharmacol Bull 2006; 39:15–24.
- Clayton AH. Understanding antidepressant mechanism of action and its effect on efficacy and safety. J Clin Psychiatry 2012; 73:e11.
- Gartlehner G, Hansen RA, Morgan LC, et al. Second-generation antidepressants in the pharmacologic treatment of adult depression: an update of the 2007 comparative effectiveness review (Internet). Rockville (MD): Agency for Healthcare Research and Quality (US); 2011 Dec. Comparative Effectiveness Reviews, No. 46. http://www.ncbi.nlm.nih.gov/books/NBK83442/. Accessed February 27, 2013.
- Watanabe N, Omori IM, Nakagawa A, et al. Mirtazapine versus other antidepressive agents for depression. Cochrane Database Syst Rev 2011; 12:CD006528.
- Hofmeijer-Sevink MK, Batelaan NM, van Megen HJ, et al. Clinical relevance of comorbidity in anxiety disorders: a report from the Netherlands Study of Depression and Anxiety (NESDA). J Affect Disord 2012; 137:106–112.
- Koen N, Stein DJ. Pharmacotherapy of anxiety disorders: a critical review. Dialogues Clin Neurosci 2011; 13:423–437.
- Sheehan DV, Kamijima K. An evidence-based review of the clinical use of sertraline in mood and anxiety disorders. Int Clin Psychopharmacol 2009; 24:43–60.
- Huh J, Goebert D, Takeshita J, Lu BY, Kang M. Treatment of generalized anxiety disorder: a comprehensive review of the literature for psychopharmacologic alternatives to newer antidepressants and benzodiazepines. Prim Care Companion CNS Disord 2011; 13: 4088/PCC.08r00709blu.
- Rickels K, Downing R, Schweizer E, Hassman H. Antidepressants for the treatment of generalized anxiety disorder. A placebo-controlled comparison of imipramine, trazodone, and diazepam. Arch Gen Psychiatry 1993; 50:884–895.
- Uher R, Maier W, Hauser J, et al. Differential efficacy of escitalopram and nortriptyline on dimensional measures of depression. Br J Psychiatry 2009; 194:252–259.
- Kellner M. Drug treatment of obsessive-compulsive disorder. Dialogues Clin Neurosci 2010; 12:187–197.
- Rush AJ, Trivedi MH, Carmody TJ, et al. Response in relation to baseline anxiety levels in major depressive disorder treated with bupropion sustained release or sertraline. Neuropsychopharmacology 2001; 25:131–138.
- Mease PJ, Dundon K, Sarzi-Puttini P. Pharmacotherapy of fibromyalgia. Best Pract Res Clin Rheumatol 2011; 25:285–297.
- Wolfe F, Cathey MA, Hawley DJ. A double-blind placebo controlled trial of fluoxetine in fibromyalgia. Scand J Rheumatol 1994; 23:255–259.
- Arnold LM, Hess EV, Hudson JI, Welge JA, Berno SE, Keck PE. A randomized, placebo-controlled, double-blind, flexible-dose study of fluoxetine in the treatment of women with fibromyalgia. Am J Med 2002; 112:191–197.
- Arnold LM, Keck PE, Welge JA. Antidepressant treatment of fibromyalgia. A meta-analysis and review. Psychosomatics 2000; 41:104–113.
- Goldenberg DL, Burckhardt C, Crofford L. Management of fibromyalgia syndrome. JAMA 2004; 292:2388–2395.
- Tort S, Urrútia G, Nishishinya MB, Walitt B. Monoamine oxidase inhibitors (MAOIs) for fibromyalgia syndrome. Cochrane Database Syst Rev 2012; 4:CD009807.
- Vercoulen JH, Swanink CM, Zitman FG, et al. Randomised, double-blind, placebo-controlled study of fluoxetine in chronic fatigue syndrome. Lancet 1996; 347:858–861.
- Natelson BH, Cheu J, Pareja J, Ellis SP, Policastro T, Findley TW. Randomized, double blind, controlled placebo-phase in trial of low dose phenelzine in the chronic fatigue syndrome. Psychopharmacology (Berl) 1996; 124:226–230.
- Reid S, Chalder T, Cleare A, Hotopf M, Wessely S. Chronic fatigue syndrome. BMJ 2000; 320:292–296.
- Kupfer DJ, Spiker DG, Coble PA, Neil JF, Ulrich R, Shaw DH. Sleep and treatment prediction in endogenous depression. Am J Psychiatry 1981; 138:429–434.
- Argyropoulos SV, Hicks JA, Nash JR, et al. Redistribution of slow wave activity of sleep during pharmacological treatment of depression with paroxetine but not with nefazodone. J Sleep Res 2009; 18:342–348.
- Stein DJ, Lopez AG. Effects of escitalopram on sleep problems in patients with major depression or generalized anxiety disorder. Adv Ther 2011; 28:1021–1037.
- Ehlers CL, Havstad JW, Kupfer DJ. Estimation of the time course of slow-wave sleep over the night in depressed patients: effects of clomipramine and clinical response. Biol Psychiatry 1996; 39:171–181.
- Landolt HP, Raimo EB, Schnierow BJ, Kelsoe JR, Rapaport MH, Gillin JC. Sleep and sleep electroencephalogram in depressed patients treated with phenelzine. Arch Gen Psychiatry 2001; 58:268–276.
- Chen YM, Huang XM, Thompson R, Zhao YB. Clinical features and efficacy of escitalopram treatment for geriatric depression. J Int Med Res 2011; 39:1946–1953.
- Dolder C, Nelson M, Stump A. Pharmacological and clinical profile of newer antidepressants: implications for the treatment of elderly patients. Drugs Aging 2010; 27:625–640.
- Sterke CS, Ziere G, van Beeck EF, Looman CW, van der Cammen TJ. Dose-response relationship between selective serotonin re-uptake inhibitors and injurious falls: a study in nursing home residents with dementia. Br J Clin Pharmacol 2012; 73:812–820.
- Raji MA, Brady SR. Mirtazapine for treatment of depression and comorbidities in Alzheimer disease. Ann Pharmacother 2001; 35:1024–1027.
- Hennings JM, Schaaf L, Fulda S. Glucose metabolism and antidepressant medication. Curr Pharm Des 2012; 18:5900–5919.
- Czarny MJ, Arthurs E, Coffie DF, et al. Prevalence of antidepressant prescription or use in patients with acute coronary syndrome: a systematic review. PLoS One 2011; 6:e27671.
- Zuidersma M, Ormel J, Conradi HJ, de Jonge P. An increase in depressive symptoms after myocardial infarction predicts new cardiac events irrespective of depressive symptoms before myocardial infarction. Psychol Med 2012; 42:683–693.
- van Noord C, Straus SM, Sturkenboom MC, et al. Psychotropic drugs associated with corrected QT interval prolongation. J Clin Psychopharmacol 2009; 29:9–15.
- US Food and Drug Administration (FDA). FDA Drug Safety Communication: abnormal heart rhythms associated with high doses of Celexa (citalopram hydrobromide). http://www.fda.gov/Drugs/DrugSafety/ucm269086.htm. Accessed August 25, 2013.
- Lespérance F, Frasure-Smith N, Koszycki D, et al; CREATE Investigators. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA 2007; 297:367–379.
- O’Connor CM, Jiang W, Kuchibhatla M, et al; SADHART-CHF Investigators. Safety and efficacy of sertraline for depression in patients with heart failure: results of the SADHART-CHF (Sertraline Against Depression and Heart Disease in Chronic Heart Failure) trial. J Am Coll Cardiol 2010; 56:692–699.
- Glassman AH, O’Connor CM, Califf RM, et al; Sertraline Antidepressant Heart Attack Randomized Trial (SADHEART) Group. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA 2002; 288:701–709.
- Swenson JR, O’Connor CM, Barton D, et al; Sertraline Antidepressant Heart Attack Randomized Trial (SADHART) Group. Influence of depression and effect of treatment with sertraline on quality of life after hospitalization for acute coronary syndrome. Am J Cardiol 2003; 92:1271–1276.
- Strik JJ, Honig A, Lousberg R, et al. Efficacy and safety of fluoxetine in the treatment of patients with major depression after first myocardial infarction: findings from a double-blind, placebo-controlled trial. Psychosom Med 2000; 62:783–789.
- Honig A, Kuyper AM, Schene AH, et al; MIND-IT investigators. Treatment of post-myocardial infarction depressive disorder: a randomized, placebo-controlled trial with mirtazapine. Psychosom Med 2007; 69:606–613.
With the variety of drugs available for treating depression, choosing one can be daunting. Different agents have characteristics that may make them a better choice for different types of patients, but even so, treating any kind of mental illness often requires an element of trial and error.
Primary care providers are on the frontline of treating mental illness, often evaluating patients before they are seen by a psychiatrist. The purpose of this article is to provide insight into the art of prescribing antidepressants in the primary care setting. We will discuss common patient presentations, including depressed patients without other medical comorbidities as well as those with common comorbidities, with our recommendations for first-line treatment.
We hope our recommendations will help you to navigate the uncertainty more confidently, resulting in more efficient and tailored treatment for your patients.
BASELINE TESTING
When starting a patient on antidepressant drug therapy, we recommend obtaining a set of baseline laboratory tests to rule out underlying medical conditions that may be contributing to the patient’s depression or that may preclude the use of a given drug. (For example, elevation of liver enzymes may preclude the use of duloxetine.) Tests should include:
- A complete blood cell count
- A complete metabolic panel
- A thyroid-stimulating hormone level.
Electrocardiography may also be useful, as some antidepressants can prolong the QT interval or elevate the blood levels of other drugs with this effect.
GENERAL TREATMENT CONSIDERATIONS
There are several classes of antidepressants, and each class has a number of agents. Research has found little difference in efficacy among agents. So to simplify choosing which one to use, we recommend becoming comfortable with an agent from each class, ie:
- A selective serotonin reuptake inhibitor (SSRI)
- A selective serotonin-norepinephrine reuptake inhibitor (SNRI)
- A tricyclic antidepressant (TCA)
- A monoamine oxidase (MAO) inhibitor.
Each class includes generic agents, many of which are on the discount lists of retail pharmacies. Table 1 shows representative drugs from each class, with their relative costs.
Start low and go slow. In general, when starting an antidepressant, consider starting at half the normal dose, titrating upward as tolerated about every 14 days. This approach can minimize side effects. For example, if prescribing fluoxetine, start with 10 mg and titrate every 2 weeks based on tolerance and patient response. That said, each patient may respond differently, requiring perhaps a lower starting dose or a longer titration schedule.
Anticipate side effects. Most of the side effects of an antidepressant drug can be explained by its mechanism of action. Although side effects should certainly be considered when choosing an agent, patients can be reassured that most are transient and benign. A detailed discussion of side effects of antidepressant drugs is beyond the scope of this article, but a review by Khawam et al1 was published earlier in this journal.
Reassess. If after 4 to 6 weeks the patient has had little or no response, it is reasonable to switch agents. For a patient who was on an SSRI, the change can be to another SSRI or to an SNRI. However, if two SSRIs have already failed, then choose an SNRI. Agents are commonly cross-tapered during the switch to avoid abrupt cessation of one drug or the increased risk of adverse events such as cytochrome P450 interactions, serotonin syndrome, or hypertensive crisis (when switching to an MAO inhibitor).
Beware of interactions. All SSRIs and SNRIs are metabolized through the P450 system in the liver and therefore have the potential for drug-drug interactions. Care must be taken when giving these agents together with drugs whose metabolism can be altered by P450 inhibition. For TCAs, blood levels can be checked if there is concern about toxicity; however, dosing is not strictly based on this level. Great care should be taken if a TCA is given together with an SNRI or an SSRI, as the TCA blood level can become significantly elevated. This may result in QT interval prolongation, as mentioned earlier.
Refer. Referral to a psychiatrist is appropriate for patients for whom multiple classes have failed, for patients who have another psychiatric comorbidity (such as psychosis, hypomania, or mania), or for patients who may need hospitalization. Referral is also appropriate if the physician is concerned about suicide risk.
PATIENTS WITH MAJOR DEPRESSION ONLY
For a patient presenting with depression but no other significant medical comorbidity, the first-line therapy is often an SSRI. Several generic SSRIs are available, and some are on the discount lists at retail pharmacies.
Symptoms should start to improve in about 2 weeks, and the optimal response should be achieved in 4 to 6 weeks of treatment. If this does not occur, consider either adding an augmenting agent or switching to a different antidepressant.
PATIENTS WITH CHRONIC PAIN
Chronic pain and depression often go hand in hand and can potentiate each other. When considering an antidepressant in a patient who has both conditions, the SNRIs and TCAs are typically preferred. Some SNRIs, namely duloxetine and milnacipran, are approved for certain chronic pain conditions, such as fibromyalgia. SNRIs are frequently used off-label for other chronic pain conditions such as headache and neuropathic pain.2
TCAs such as amitriptyline, nortriptyline, and doxepin are also often used in patients with chronic pain. These agents, like the SNRIs, inhibit the reuptake of serotonin and norepinephrine and are used off-label for neuropathic pain,3,4 migraine, interstitial cystitis,5 and other pain conditions.6–9
For TCAs and SNRIs, the effective dose range for chronic pain overlaps that for depression. However, TCAs are often given at lower doses to patients without depression. We recommend starting at a low dose and slowly titrating upward to an effective dose. SNRIs are often preferred over TCAs because they do not have anticholinergic side effects and because an overdose is much less likely to be lethal.
PATIENTS WITH SEXUAL DYSFUNCTION
One of the more commonly reported side effects of antidepressants is sexual dysfunction, generally in the form of delayed orgasm or decreased libido.10 Typically, these complaints are attributed to SSRIs and SNRIs; however, TCAs and MAO inhibitors have also been associated wth sexual dysfunction.
Both erectile dysfunction and priapism have been linked to certain antidepressants. In particular, trazodone is a known cause of priapism. Even if using low doses for sleep, male patients should be made aware of this adverse effect.
Switching from one agent to another in the same class is not likely to improve sexual side effects. In particular, all the SSRIs are similar in their likelihood of causing sexual dysfunction. In a patient taking an SSRI who experiences this side effect, switching to bupropion11 or mirtazapine12 can be quite useful. Bupropion acts primarily on dopamine and norepinephrine, whereas mirtazapine acts on serotonin and norepinephrine but in a different manner from SSRIs and SNRIs.
Adjunctive treatment such as a cholinergic agonist, yohimbine (contraindicated with MAO inhibitors), a serotonergic agent (eg, buspirone), or a drug that acts on nitric oxide (eg, sildenafil, tadalafil) may have some utility but is often ineffective. Dose reduction, if possible, can be of value.
PATIENTS WITH ANXIETY
Many antidepressants are also approved for anxiety disorders, and still more are used off-label for this purpose. Anxiety and depression often occur together, so being able to treat both conditions with one drug can be quite useful.13 In general, the antidepressant effects are seen at lower doses of SSRIs and SNRIs, whereas more of the anxiolytic effects are seen at higher doses, particularly for obsessive-compulsive disorder.14
First-line treatment would be an SSRI or SNRI. Most anxiety disorders respond to either class, but there are some more-specific recommendations. SSRIs are best studied in panic disorder, generalized anxiety disorder, social anxiety disorder, posttraumatic stress disorder, and obsessive-compulsive disorder. Fluoxetine, citalopram, escitalopram, and sertraline15 can all be effective in both major depressive disorder and generalized anxiety disorder. Panic disorder also tends to respond well to SSRIs. SNRIs have been evaluated primarily in generalized anxiety disorder but may also be useful in many of the other conditions.
Additionally, mirtazapine (used off-label)12 and the TCAs16–18 can help treat anxiety. Clomipramine is used to treat obsessive-compulsive disorder.19 These drugs are especially useful for nighttime anxiety, as they can aid sleep. Of note, the anxiolytic effect of mirtazapine may be greater at higher doses.
MAO inhibitors often go unused because of the dietary and medication restrictions involved. However, very refractory cases of certain anxiety disorders may respond preferentially to these agents.
Bupropion tends to be more activating than other antidepressants, so is often avoided in anxious patients. However, some research suggests this is not always necessary.20 If the anxiety is secondary to depression, it will often improve significantly with this agent.
When starting or increasing the dose of an antidepressant, patients may experience increased anxiety or feel “jittery.” This feeling usually passes within the first week of treatment, and it is important to inform patients about this effect. “Start low and go slow” in patients with significant comorbid anxiety. Temporarily using a benzodiazepine such as clonazepam may make the transition more tolerable.
PATIENTS WITH CHRONIC FATIGUE SYNDROME OR FIBROMYALGIA
Increasing recognition of both chronic fatigue syndrome and fibromyalgia has led to more proactive treatment for these disorders. Depression can go hand in hand with these disorders, and certain antidepressants, namely the SNRIs, can be useful in this population.
More data exist for the treatment of fibromyalgia. Both duloxetine and milnacipran are approved by the US Food and Drug Administration (FDA) for the treatment of fibromyalgia.21 Venlafaxine is also used off-label for this purpose. SSRIs such as fluoxetine and citalopram have had mixed results.21–23 TCAs have been used with some success; however, their side effects and lethal potential are often limiting.21,24,25 A recent study in Spain also suggested there may be benefit from using MAO inhibitors for fibromyalgia, but data are quite limited.26
The data for treating chronic fatigue syndrome with SSRIs, SNRIs, or MAO inhibitors are conflicting.27–29 However, managing the co-existing depression may provide some relief in and of itself.
PATIENTS WITH FREQUENT INSOMNIA
Insomnia can be a symptom of depression, but it can also be a side effect of certain antidepressants. The SSRIs and SNRIs can disrupt sleep patterns in some patients by shortening the rapid-eye-movement (REM) stage.30,31
In patients with severe insomnia, it may be best to first recommend taking the antidepressant in the morning if they notice worsening sleep after initiating treatment. Patients can be told with any antidepressant, “If it makes you tired, take it at night, and if it wakes you up, take it in the morning.” Of note, a recent South African study suggested that escitalopram may be able to improve sleep.32
If that does not solve the problem, there are other options. For instance, mirtazapine, particularly in doses of 15 mg or 30 mg, aids depression and insomnia. At higher doses (45 mg), the sleep-aiding effect may be reduced. Low doses of TCAs, particularly doxepin, maprotiline (technically speaking, a tetracyclic antidepressant), amitriptyline, and nortriptyline can be effective sleep aids. These agents may be used as an adjunct to another antidepressant to enhance sleep and mood. However, the TCAs also shorten the REM stage of sleep.33
The previously mentioned drug interactions with SSRIs and SNRIs also need to be considered. Caution should be used when discontinuing these medications, as patients may experience rebound symptoms in the form of much more vivid dreams. MAO inhibitors may worsen insomnia because they suppress REM sleep.34
Trazodone is another agent that at lower doses (25–150 mg) can be an effective, nonaddicting sleep aid. When used as an antidepressant, it is generally prescribed at higher doses (300–400 mg), but its sedating effects can be quite limiting at these levels. It is important to remember the possibility of priapism in male patients.
GERIATRIC PATIENTS
Old age brings its own set of concerns when treating depression. Elderly patients are more susceptible to potential bradycardia caused by SSRIs. The TCAs have the more worrisome cardiac side effect of QTc prolongation. TCAs can slow cognitive function, whereas the SSRIs, bupropion, and the SNRIs tend not to affect cognition. Escitalopram and duloxetine have been suggested to be particularly effective in the elderly.35,36 A study from the Netherlands linked SSRIs with increased risk of falling in geriatric patients with dementia.37 Constipation, which could lead to ileus, is increased with TCAs and certain other agents (ie, paroxetine) in the geriatric population.
Mirtazapine is often very useful in elderly patients for many reasons: it treats both anxiety and depression, stimulates appetite and weight gain, can help with nausea, and is an effective sleep aid. Concerns about weight, appetite, and sleep are particularly common in the elderly, whereas younger patients can be less tolerant of drugs that make them gain weight and sleep more. Normal age-related changes to the sleep cycle contribute to decreased satisfaction with sleep as we age. In addition, depression often further impairs sleep. So, in the elderly, optimizing sleep is key. Research has also shown mirtazapine to be effective in patients with both Alzheimer dementia and depression.38
DIABETIC PATIENTS
One of the more worrisome side effects of psychiatric medications in diabetic patients is weight gain. Certain antidepressants have a greater propensity for weight gain and should likely be avoided as first-line treatments in this population.12 Typically, these agents include those that have more antihistamine action such as paroxetine and the TCAs. These agents also may lead to constipation, which could potentially worsen gastroparesis. Mirtazapine and the MAO inhibitors are also known to cause weight gain.
Bupropion and nefazodone are the most weight-neutral of all antidepressants. Nefazodone has fallen out of favor because of its potential to cause fulminant liver failure in rare cases. However, it remains a reasonable option for patients with comorbid anxiety and depression who have significant weight gain with other agents.
SSRIs and MAO inhibitors may improve or be neutral toward glucose metabolism, and some data suggest that SNRIs may impair this process.39
PATIENTS WITH CARDIAC CONDITIONS
Major depression often coexists with cardiac conditions. In particular, many patients develop depression after suffering a myocardial infarction, and increasingly they are being treated for it.40 Treatment in this situation is appropriate, since depression, if untreated, can increase the risk of recurrence of myocardial infarction.41
However, there are many concerns that accompany treating depression in cardiac patients. Therefore, a baseline electrocardiogram should be obtained before starting an antidepressant.
TCAs and tetracyclic agents have a tendency to prolong the QTc interval and potentiate ventricular arrhythmias,42 so it may be prudent to avoid these in patients at risk. These agents can also significantly increase the pulse rate. This tachycardia increases the risk of angina or myocardial infarction from the anticholinergic effects of these drugs.
In February 2013, the FDA issued a warning about possible arrhythmias with citalopram at doses greater than 40 mg in adult patients43; however, research has suggested citalopram is effective in treating depression in cardiac patients.44 Research has not shown an increase in efficacy at doses greater than 40 mg daily, so we recommend following the black-box warning.
TCAs and MAO inhibitors can also cause orthostatic hypotension. On the other hand, consuming large amounts of tyramine, in foods such as aged cheese, can precipitate a hypertensive crisis in patients taking MAO inhibitors.
Which antidepressants tend to be safer in cardiac patients? Sertraline has been shown to be safe in congestive heart failure and coronary artery disease,45–47 but the SSRIs are typically safe. Fluoxetine has shown efficacy in patients who have had a myocardial infarction.48 Mirtazapine has also been shown to be efficacious in cardiac patients.49 Nefazodone, mirtazapine, bupropion, SSRIs, and SNRIs have little or no tendency toward orthostatic hypotension.
With the variety of drugs available for treating depression, choosing one can be daunting. Different agents have characteristics that may make them a better choice for different types of patients, but even so, treating any kind of mental illness often requires an element of trial and error.
Primary care providers are on the frontline of treating mental illness, often evaluating patients before they are seen by a psychiatrist. The purpose of this article is to provide insight into the art of prescribing antidepressants in the primary care setting. We will discuss common patient presentations, including depressed patients without other medical comorbidities as well as those with common comorbidities, with our recommendations for first-line treatment.
We hope our recommendations will help you to navigate the uncertainty more confidently, resulting in more efficient and tailored treatment for your patients.
BASELINE TESTING
When starting a patient on antidepressant drug therapy, we recommend obtaining a set of baseline laboratory tests to rule out underlying medical conditions that may be contributing to the patient’s depression or that may preclude the use of a given drug. (For example, elevation of liver enzymes may preclude the use of duloxetine.) Tests should include:
- A complete blood cell count
- A complete metabolic panel
- A thyroid-stimulating hormone level.
Electrocardiography may also be useful, as some antidepressants can prolong the QT interval or elevate the blood levels of other drugs with this effect.
GENERAL TREATMENT CONSIDERATIONS
There are several classes of antidepressants, and each class has a number of agents. Research has found little difference in efficacy among agents. So to simplify choosing which one to use, we recommend becoming comfortable with an agent from each class, ie:
- A selective serotonin reuptake inhibitor (SSRI)
- A selective serotonin-norepinephrine reuptake inhibitor (SNRI)
- A tricyclic antidepressant (TCA)
- A monoamine oxidase (MAO) inhibitor.
Each class includes generic agents, many of which are on the discount lists of retail pharmacies. Table 1 shows representative drugs from each class, with their relative costs.
Start low and go slow. In general, when starting an antidepressant, consider starting at half the normal dose, titrating upward as tolerated about every 14 days. This approach can minimize side effects. For example, if prescribing fluoxetine, start with 10 mg and titrate every 2 weeks based on tolerance and patient response. That said, each patient may respond differently, requiring perhaps a lower starting dose or a longer titration schedule.
Anticipate side effects. Most of the side effects of an antidepressant drug can be explained by its mechanism of action. Although side effects should certainly be considered when choosing an agent, patients can be reassured that most are transient and benign. A detailed discussion of side effects of antidepressant drugs is beyond the scope of this article, but a review by Khawam et al1 was published earlier in this journal.
Reassess. If after 4 to 6 weeks the patient has had little or no response, it is reasonable to switch agents. For a patient who was on an SSRI, the change can be to another SSRI or to an SNRI. However, if two SSRIs have already failed, then choose an SNRI. Agents are commonly cross-tapered during the switch to avoid abrupt cessation of one drug or the increased risk of adverse events such as cytochrome P450 interactions, serotonin syndrome, or hypertensive crisis (when switching to an MAO inhibitor).
Beware of interactions. All SSRIs and SNRIs are metabolized through the P450 system in the liver and therefore have the potential for drug-drug interactions. Care must be taken when giving these agents together with drugs whose metabolism can be altered by P450 inhibition. For TCAs, blood levels can be checked if there is concern about toxicity; however, dosing is not strictly based on this level. Great care should be taken if a TCA is given together with an SNRI or an SSRI, as the TCA blood level can become significantly elevated. This may result in QT interval prolongation, as mentioned earlier.
Refer. Referral to a psychiatrist is appropriate for patients for whom multiple classes have failed, for patients who have another psychiatric comorbidity (such as psychosis, hypomania, or mania), or for patients who may need hospitalization. Referral is also appropriate if the physician is concerned about suicide risk.
PATIENTS WITH MAJOR DEPRESSION ONLY
For a patient presenting with depression but no other significant medical comorbidity, the first-line therapy is often an SSRI. Several generic SSRIs are available, and some are on the discount lists at retail pharmacies.
Symptoms should start to improve in about 2 weeks, and the optimal response should be achieved in 4 to 6 weeks of treatment. If this does not occur, consider either adding an augmenting agent or switching to a different antidepressant.
PATIENTS WITH CHRONIC PAIN
Chronic pain and depression often go hand in hand and can potentiate each other. When considering an antidepressant in a patient who has both conditions, the SNRIs and TCAs are typically preferred. Some SNRIs, namely duloxetine and milnacipran, are approved for certain chronic pain conditions, such as fibromyalgia. SNRIs are frequently used off-label for other chronic pain conditions such as headache and neuropathic pain.2
TCAs such as amitriptyline, nortriptyline, and doxepin are also often used in patients with chronic pain. These agents, like the SNRIs, inhibit the reuptake of serotonin and norepinephrine and are used off-label for neuropathic pain,3,4 migraine, interstitial cystitis,5 and other pain conditions.6–9
For TCAs and SNRIs, the effective dose range for chronic pain overlaps that for depression. However, TCAs are often given at lower doses to patients without depression. We recommend starting at a low dose and slowly titrating upward to an effective dose. SNRIs are often preferred over TCAs because they do not have anticholinergic side effects and because an overdose is much less likely to be lethal.
PATIENTS WITH SEXUAL DYSFUNCTION
One of the more commonly reported side effects of antidepressants is sexual dysfunction, generally in the form of delayed orgasm or decreased libido.10 Typically, these complaints are attributed to SSRIs and SNRIs; however, TCAs and MAO inhibitors have also been associated wth sexual dysfunction.
Both erectile dysfunction and priapism have been linked to certain antidepressants. In particular, trazodone is a known cause of priapism. Even if using low doses for sleep, male patients should be made aware of this adverse effect.
Switching from one agent to another in the same class is not likely to improve sexual side effects. In particular, all the SSRIs are similar in their likelihood of causing sexual dysfunction. In a patient taking an SSRI who experiences this side effect, switching to bupropion11 or mirtazapine12 can be quite useful. Bupropion acts primarily on dopamine and norepinephrine, whereas mirtazapine acts on serotonin and norepinephrine but in a different manner from SSRIs and SNRIs.
Adjunctive treatment such as a cholinergic agonist, yohimbine (contraindicated with MAO inhibitors), a serotonergic agent (eg, buspirone), or a drug that acts on nitric oxide (eg, sildenafil, tadalafil) may have some utility but is often ineffective. Dose reduction, if possible, can be of value.
PATIENTS WITH ANXIETY
Many antidepressants are also approved for anxiety disorders, and still more are used off-label for this purpose. Anxiety and depression often occur together, so being able to treat both conditions with one drug can be quite useful.13 In general, the antidepressant effects are seen at lower doses of SSRIs and SNRIs, whereas more of the anxiolytic effects are seen at higher doses, particularly for obsessive-compulsive disorder.14
First-line treatment would be an SSRI or SNRI. Most anxiety disorders respond to either class, but there are some more-specific recommendations. SSRIs are best studied in panic disorder, generalized anxiety disorder, social anxiety disorder, posttraumatic stress disorder, and obsessive-compulsive disorder. Fluoxetine, citalopram, escitalopram, and sertraline15 can all be effective in both major depressive disorder and generalized anxiety disorder. Panic disorder also tends to respond well to SSRIs. SNRIs have been evaluated primarily in generalized anxiety disorder but may also be useful in many of the other conditions.
Additionally, mirtazapine (used off-label)12 and the TCAs16–18 can help treat anxiety. Clomipramine is used to treat obsessive-compulsive disorder.19 These drugs are especially useful for nighttime anxiety, as they can aid sleep. Of note, the anxiolytic effect of mirtazapine may be greater at higher doses.
MAO inhibitors often go unused because of the dietary and medication restrictions involved. However, very refractory cases of certain anxiety disorders may respond preferentially to these agents.
Bupropion tends to be more activating than other antidepressants, so is often avoided in anxious patients. However, some research suggests this is not always necessary.20 If the anxiety is secondary to depression, it will often improve significantly with this agent.
When starting or increasing the dose of an antidepressant, patients may experience increased anxiety or feel “jittery.” This feeling usually passes within the first week of treatment, and it is important to inform patients about this effect. “Start low and go slow” in patients with significant comorbid anxiety. Temporarily using a benzodiazepine such as clonazepam may make the transition more tolerable.
PATIENTS WITH CHRONIC FATIGUE SYNDROME OR FIBROMYALGIA
Increasing recognition of both chronic fatigue syndrome and fibromyalgia has led to more proactive treatment for these disorders. Depression can go hand in hand with these disorders, and certain antidepressants, namely the SNRIs, can be useful in this population.
More data exist for the treatment of fibromyalgia. Both duloxetine and milnacipran are approved by the US Food and Drug Administration (FDA) for the treatment of fibromyalgia.21 Venlafaxine is also used off-label for this purpose. SSRIs such as fluoxetine and citalopram have had mixed results.21–23 TCAs have been used with some success; however, their side effects and lethal potential are often limiting.21,24,25 A recent study in Spain also suggested there may be benefit from using MAO inhibitors for fibromyalgia, but data are quite limited.26
The data for treating chronic fatigue syndrome with SSRIs, SNRIs, or MAO inhibitors are conflicting.27–29 However, managing the co-existing depression may provide some relief in and of itself.
PATIENTS WITH FREQUENT INSOMNIA
Insomnia can be a symptom of depression, but it can also be a side effect of certain antidepressants. The SSRIs and SNRIs can disrupt sleep patterns in some patients by shortening the rapid-eye-movement (REM) stage.30,31
In patients with severe insomnia, it may be best to first recommend taking the antidepressant in the morning if they notice worsening sleep after initiating treatment. Patients can be told with any antidepressant, “If it makes you tired, take it at night, and if it wakes you up, take it in the morning.” Of note, a recent South African study suggested that escitalopram may be able to improve sleep.32
If that does not solve the problem, there are other options. For instance, mirtazapine, particularly in doses of 15 mg or 30 mg, aids depression and insomnia. At higher doses (45 mg), the sleep-aiding effect may be reduced. Low doses of TCAs, particularly doxepin, maprotiline (technically speaking, a tetracyclic antidepressant), amitriptyline, and nortriptyline can be effective sleep aids. These agents may be used as an adjunct to another antidepressant to enhance sleep and mood. However, the TCAs also shorten the REM stage of sleep.33
The previously mentioned drug interactions with SSRIs and SNRIs also need to be considered. Caution should be used when discontinuing these medications, as patients may experience rebound symptoms in the form of much more vivid dreams. MAO inhibitors may worsen insomnia because they suppress REM sleep.34
Trazodone is another agent that at lower doses (25–150 mg) can be an effective, nonaddicting sleep aid. When used as an antidepressant, it is generally prescribed at higher doses (300–400 mg), but its sedating effects can be quite limiting at these levels. It is important to remember the possibility of priapism in male patients.
GERIATRIC PATIENTS
Old age brings its own set of concerns when treating depression. Elderly patients are more susceptible to potential bradycardia caused by SSRIs. The TCAs have the more worrisome cardiac side effect of QTc prolongation. TCAs can slow cognitive function, whereas the SSRIs, bupropion, and the SNRIs tend not to affect cognition. Escitalopram and duloxetine have been suggested to be particularly effective in the elderly.35,36 A study from the Netherlands linked SSRIs with increased risk of falling in geriatric patients with dementia.37 Constipation, which could lead to ileus, is increased with TCAs and certain other agents (ie, paroxetine) in the geriatric population.
Mirtazapine is often very useful in elderly patients for many reasons: it treats both anxiety and depression, stimulates appetite and weight gain, can help with nausea, and is an effective sleep aid. Concerns about weight, appetite, and sleep are particularly common in the elderly, whereas younger patients can be less tolerant of drugs that make them gain weight and sleep more. Normal age-related changes to the sleep cycle contribute to decreased satisfaction with sleep as we age. In addition, depression often further impairs sleep. So, in the elderly, optimizing sleep is key. Research has also shown mirtazapine to be effective in patients with both Alzheimer dementia and depression.38
DIABETIC PATIENTS
One of the more worrisome side effects of psychiatric medications in diabetic patients is weight gain. Certain antidepressants have a greater propensity for weight gain and should likely be avoided as first-line treatments in this population.12 Typically, these agents include those that have more antihistamine action such as paroxetine and the TCAs. These agents also may lead to constipation, which could potentially worsen gastroparesis. Mirtazapine and the MAO inhibitors are also known to cause weight gain.
Bupropion and nefazodone are the most weight-neutral of all antidepressants. Nefazodone has fallen out of favor because of its potential to cause fulminant liver failure in rare cases. However, it remains a reasonable option for patients with comorbid anxiety and depression who have significant weight gain with other agents.
SSRIs and MAO inhibitors may improve or be neutral toward glucose metabolism, and some data suggest that SNRIs may impair this process.39
PATIENTS WITH CARDIAC CONDITIONS
Major depression often coexists with cardiac conditions. In particular, many patients develop depression after suffering a myocardial infarction, and increasingly they are being treated for it.40 Treatment in this situation is appropriate, since depression, if untreated, can increase the risk of recurrence of myocardial infarction.41
However, there are many concerns that accompany treating depression in cardiac patients. Therefore, a baseline electrocardiogram should be obtained before starting an antidepressant.
TCAs and tetracyclic agents have a tendency to prolong the QTc interval and potentiate ventricular arrhythmias,42 so it may be prudent to avoid these in patients at risk. These agents can also significantly increase the pulse rate. This tachycardia increases the risk of angina or myocardial infarction from the anticholinergic effects of these drugs.
In February 2013, the FDA issued a warning about possible arrhythmias with citalopram at doses greater than 40 mg in adult patients43; however, research has suggested citalopram is effective in treating depression in cardiac patients.44 Research has not shown an increase in efficacy at doses greater than 40 mg daily, so we recommend following the black-box warning.
TCAs and MAO inhibitors can also cause orthostatic hypotension. On the other hand, consuming large amounts of tyramine, in foods such as aged cheese, can precipitate a hypertensive crisis in patients taking MAO inhibitors.
Which antidepressants tend to be safer in cardiac patients? Sertraline has been shown to be safe in congestive heart failure and coronary artery disease,45–47 but the SSRIs are typically safe. Fluoxetine has shown efficacy in patients who have had a myocardial infarction.48 Mirtazapine has also been shown to be efficacious in cardiac patients.49 Nefazodone, mirtazapine, bupropion, SSRIs, and SNRIs have little or no tendency toward orthostatic hypotension.
- Khawam EA, Laurencic G, Malone DA. Side effects of antidepressants: an overview. Cleve Clin J Med 2006; 73:351–361.
- Ziegler D. Painful diabetic neuropathy: treatment and future aspects. Diabetes Metab Res Rev 2008; 24(suppl 1):S52–S57.
- Saarto T, Wiffen PJ. Antidepressants for neuropathic pain: a Cochrane review. J Neurol Neurosurg Psychiatry 2010; 81:1372–1373.
- Tanenberg RJ, Irving GA, Risser RC, et al. Duloxetine, pregabalin, and duloxetine plus gabapentin for diabetic peripheral neuropathic pain management in patients with inadequate pain response to gabapentin: an open-label, randomized, noninferiority comparison. Mayo Clin Proc 2011; 86:615–626.
- Hertle L, van Ophoven A. Long-term results of amitriptyline treatment for interstitial cystitis. Aktuelle Urol 2010; 41(suppl 1):S61–S65.
- Nguyen TM, Eslick GD. Systematic review: the treatment of noncardiac chest pain with antidepressants. Aliment Pharmacol Ther 2012; 35:493–500.
- Lee H, Kim JH, Min BH, et al. Efficacy of venlafaxine for symptomatic relief in young adult patients with functional chest pain: a randomized, double-blind, placebo-controlled, crossover trial. Am J Gastroenterol 2010; 105:1504–1512.
- Varia I, Logue E, O’Connor C, et al. Randomized trial of sertraline in patients with unexplained chest pain of noncardiac origin. Am Heart J 2000; 140:367–372.
- Doraiswamy PM, Varia I, Hellegers C, et al. A randomized controlled trial of paroxetine for noncardiac chest pain. Psychopharmacol Bull 2006; 39:15–24.
- Clayton AH. Understanding antidepressant mechanism of action and its effect on efficacy and safety. J Clin Psychiatry 2012; 73:e11.
- Gartlehner G, Hansen RA, Morgan LC, et al. Second-generation antidepressants in the pharmacologic treatment of adult depression: an update of the 2007 comparative effectiveness review (Internet). Rockville (MD): Agency for Healthcare Research and Quality (US); 2011 Dec. Comparative Effectiveness Reviews, No. 46. http://www.ncbi.nlm.nih.gov/books/NBK83442/. Accessed February 27, 2013.
- Watanabe N, Omori IM, Nakagawa A, et al. Mirtazapine versus other antidepressive agents for depression. Cochrane Database Syst Rev 2011; 12:CD006528.
- Hofmeijer-Sevink MK, Batelaan NM, van Megen HJ, et al. Clinical relevance of comorbidity in anxiety disorders: a report from the Netherlands Study of Depression and Anxiety (NESDA). J Affect Disord 2012; 137:106–112.
- Koen N, Stein DJ. Pharmacotherapy of anxiety disorders: a critical review. Dialogues Clin Neurosci 2011; 13:423–437.
- Sheehan DV, Kamijima K. An evidence-based review of the clinical use of sertraline in mood and anxiety disorders. Int Clin Psychopharmacol 2009; 24:43–60.
- Huh J, Goebert D, Takeshita J, Lu BY, Kang M. Treatment of generalized anxiety disorder: a comprehensive review of the literature for psychopharmacologic alternatives to newer antidepressants and benzodiazepines. Prim Care Companion CNS Disord 2011; 13: 4088/PCC.08r00709blu.
- Rickels K, Downing R, Schweizer E, Hassman H. Antidepressants for the treatment of generalized anxiety disorder. A placebo-controlled comparison of imipramine, trazodone, and diazepam. Arch Gen Psychiatry 1993; 50:884–895.
- Uher R, Maier W, Hauser J, et al. Differential efficacy of escitalopram and nortriptyline on dimensional measures of depression. Br J Psychiatry 2009; 194:252–259.
- Kellner M. Drug treatment of obsessive-compulsive disorder. Dialogues Clin Neurosci 2010; 12:187–197.
- Rush AJ, Trivedi MH, Carmody TJ, et al. Response in relation to baseline anxiety levels in major depressive disorder treated with bupropion sustained release or sertraline. Neuropsychopharmacology 2001; 25:131–138.
- Mease PJ, Dundon K, Sarzi-Puttini P. Pharmacotherapy of fibromyalgia. Best Pract Res Clin Rheumatol 2011; 25:285–297.
- Wolfe F, Cathey MA, Hawley DJ. A double-blind placebo controlled trial of fluoxetine in fibromyalgia. Scand J Rheumatol 1994; 23:255–259.
- Arnold LM, Hess EV, Hudson JI, Welge JA, Berno SE, Keck PE. A randomized, placebo-controlled, double-blind, flexible-dose study of fluoxetine in the treatment of women with fibromyalgia. Am J Med 2002; 112:191–197.
- Arnold LM, Keck PE, Welge JA. Antidepressant treatment of fibromyalgia. A meta-analysis and review. Psychosomatics 2000; 41:104–113.
- Goldenberg DL, Burckhardt C, Crofford L. Management of fibromyalgia syndrome. JAMA 2004; 292:2388–2395.
- Tort S, Urrútia G, Nishishinya MB, Walitt B. Monoamine oxidase inhibitors (MAOIs) for fibromyalgia syndrome. Cochrane Database Syst Rev 2012; 4:CD009807.
- Vercoulen JH, Swanink CM, Zitman FG, et al. Randomised, double-blind, placebo-controlled study of fluoxetine in chronic fatigue syndrome. Lancet 1996; 347:858–861.
- Natelson BH, Cheu J, Pareja J, Ellis SP, Policastro T, Findley TW. Randomized, double blind, controlled placebo-phase in trial of low dose phenelzine in the chronic fatigue syndrome. Psychopharmacology (Berl) 1996; 124:226–230.
- Reid S, Chalder T, Cleare A, Hotopf M, Wessely S. Chronic fatigue syndrome. BMJ 2000; 320:292–296.
- Kupfer DJ, Spiker DG, Coble PA, Neil JF, Ulrich R, Shaw DH. Sleep and treatment prediction in endogenous depression. Am J Psychiatry 1981; 138:429–434.
- Argyropoulos SV, Hicks JA, Nash JR, et al. Redistribution of slow wave activity of sleep during pharmacological treatment of depression with paroxetine but not with nefazodone. J Sleep Res 2009; 18:342–348.
- Stein DJ, Lopez AG. Effects of escitalopram on sleep problems in patients with major depression or generalized anxiety disorder. Adv Ther 2011; 28:1021–1037.
- Ehlers CL, Havstad JW, Kupfer DJ. Estimation of the time course of slow-wave sleep over the night in depressed patients: effects of clomipramine and clinical response. Biol Psychiatry 1996; 39:171–181.
- Landolt HP, Raimo EB, Schnierow BJ, Kelsoe JR, Rapaport MH, Gillin JC. Sleep and sleep electroencephalogram in depressed patients treated with phenelzine. Arch Gen Psychiatry 2001; 58:268–276.
- Chen YM, Huang XM, Thompson R, Zhao YB. Clinical features and efficacy of escitalopram treatment for geriatric depression. J Int Med Res 2011; 39:1946–1953.
- Dolder C, Nelson M, Stump A. Pharmacological and clinical profile of newer antidepressants: implications for the treatment of elderly patients. Drugs Aging 2010; 27:625–640.
- Sterke CS, Ziere G, van Beeck EF, Looman CW, van der Cammen TJ. Dose-response relationship between selective serotonin re-uptake inhibitors and injurious falls: a study in nursing home residents with dementia. Br J Clin Pharmacol 2012; 73:812–820.
- Raji MA, Brady SR. Mirtazapine for treatment of depression and comorbidities in Alzheimer disease. Ann Pharmacother 2001; 35:1024–1027.
- Hennings JM, Schaaf L, Fulda S. Glucose metabolism and antidepressant medication. Curr Pharm Des 2012; 18:5900–5919.
- Czarny MJ, Arthurs E, Coffie DF, et al. Prevalence of antidepressant prescription or use in patients with acute coronary syndrome: a systematic review. PLoS One 2011; 6:e27671.
- Zuidersma M, Ormel J, Conradi HJ, de Jonge P. An increase in depressive symptoms after myocardial infarction predicts new cardiac events irrespective of depressive symptoms before myocardial infarction. Psychol Med 2012; 42:683–693.
- van Noord C, Straus SM, Sturkenboom MC, et al. Psychotropic drugs associated with corrected QT interval prolongation. J Clin Psychopharmacol 2009; 29:9–15.
- US Food and Drug Administration (FDA). FDA Drug Safety Communication: abnormal heart rhythms associated with high doses of Celexa (citalopram hydrobromide). http://www.fda.gov/Drugs/DrugSafety/ucm269086.htm. Accessed August 25, 2013.
- Lespérance F, Frasure-Smith N, Koszycki D, et al; CREATE Investigators. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA 2007; 297:367–379.
- O’Connor CM, Jiang W, Kuchibhatla M, et al; SADHART-CHF Investigators. Safety and efficacy of sertraline for depression in patients with heart failure: results of the SADHART-CHF (Sertraline Against Depression and Heart Disease in Chronic Heart Failure) trial. J Am Coll Cardiol 2010; 56:692–699.
- Glassman AH, O’Connor CM, Califf RM, et al; Sertraline Antidepressant Heart Attack Randomized Trial (SADHEART) Group. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA 2002; 288:701–709.
- Swenson JR, O’Connor CM, Barton D, et al; Sertraline Antidepressant Heart Attack Randomized Trial (SADHART) Group. Influence of depression and effect of treatment with sertraline on quality of life after hospitalization for acute coronary syndrome. Am J Cardiol 2003; 92:1271–1276.
- Strik JJ, Honig A, Lousberg R, et al. Efficacy and safety of fluoxetine in the treatment of patients with major depression after first myocardial infarction: findings from a double-blind, placebo-controlled trial. Psychosom Med 2000; 62:783–789.
- Honig A, Kuyper AM, Schene AH, et al; MIND-IT investigators. Treatment of post-myocardial infarction depressive disorder: a randomized, placebo-controlled trial with mirtazapine. Psychosom Med 2007; 69:606–613.
- Khawam EA, Laurencic G, Malone DA. Side effects of antidepressants: an overview. Cleve Clin J Med 2006; 73:351–361.
- Ziegler D. Painful diabetic neuropathy: treatment and future aspects. Diabetes Metab Res Rev 2008; 24(suppl 1):S52–S57.
- Saarto T, Wiffen PJ. Antidepressants for neuropathic pain: a Cochrane review. J Neurol Neurosurg Psychiatry 2010; 81:1372–1373.
- Tanenberg RJ, Irving GA, Risser RC, et al. Duloxetine, pregabalin, and duloxetine plus gabapentin for diabetic peripheral neuropathic pain management in patients with inadequate pain response to gabapentin: an open-label, randomized, noninferiority comparison. Mayo Clin Proc 2011; 86:615–626.
- Hertle L, van Ophoven A. Long-term results of amitriptyline treatment for interstitial cystitis. Aktuelle Urol 2010; 41(suppl 1):S61–S65.
- Nguyen TM, Eslick GD. Systematic review: the treatment of noncardiac chest pain with antidepressants. Aliment Pharmacol Ther 2012; 35:493–500.
- Lee H, Kim JH, Min BH, et al. Efficacy of venlafaxine for symptomatic relief in young adult patients with functional chest pain: a randomized, double-blind, placebo-controlled, crossover trial. Am J Gastroenterol 2010; 105:1504–1512.
- Varia I, Logue E, O’Connor C, et al. Randomized trial of sertraline in patients with unexplained chest pain of noncardiac origin. Am Heart J 2000; 140:367–372.
- Doraiswamy PM, Varia I, Hellegers C, et al. A randomized controlled trial of paroxetine for noncardiac chest pain. Psychopharmacol Bull 2006; 39:15–24.
- Clayton AH. Understanding antidepressant mechanism of action and its effect on efficacy and safety. J Clin Psychiatry 2012; 73:e11.
- Gartlehner G, Hansen RA, Morgan LC, et al. Second-generation antidepressants in the pharmacologic treatment of adult depression: an update of the 2007 comparative effectiveness review (Internet). Rockville (MD): Agency for Healthcare Research and Quality (US); 2011 Dec. Comparative Effectiveness Reviews, No. 46. http://www.ncbi.nlm.nih.gov/books/NBK83442/. Accessed February 27, 2013.
- Watanabe N, Omori IM, Nakagawa A, et al. Mirtazapine versus other antidepressive agents for depression. Cochrane Database Syst Rev 2011; 12:CD006528.
- Hofmeijer-Sevink MK, Batelaan NM, van Megen HJ, et al. Clinical relevance of comorbidity in anxiety disorders: a report from the Netherlands Study of Depression and Anxiety (NESDA). J Affect Disord 2012; 137:106–112.
- Koen N, Stein DJ. Pharmacotherapy of anxiety disorders: a critical review. Dialogues Clin Neurosci 2011; 13:423–437.
- Sheehan DV, Kamijima K. An evidence-based review of the clinical use of sertraline in mood and anxiety disorders. Int Clin Psychopharmacol 2009; 24:43–60.
- Huh J, Goebert D, Takeshita J, Lu BY, Kang M. Treatment of generalized anxiety disorder: a comprehensive review of the literature for psychopharmacologic alternatives to newer antidepressants and benzodiazepines. Prim Care Companion CNS Disord 2011; 13: 4088/PCC.08r00709blu.
- Rickels K, Downing R, Schweizer E, Hassman H. Antidepressants for the treatment of generalized anxiety disorder. A placebo-controlled comparison of imipramine, trazodone, and diazepam. Arch Gen Psychiatry 1993; 50:884–895.
- Uher R, Maier W, Hauser J, et al. Differential efficacy of escitalopram and nortriptyline on dimensional measures of depression. Br J Psychiatry 2009; 194:252–259.
- Kellner M. Drug treatment of obsessive-compulsive disorder. Dialogues Clin Neurosci 2010; 12:187–197.
- Rush AJ, Trivedi MH, Carmody TJ, et al. Response in relation to baseline anxiety levels in major depressive disorder treated with bupropion sustained release or sertraline. Neuropsychopharmacology 2001; 25:131–138.
- Mease PJ, Dundon K, Sarzi-Puttini P. Pharmacotherapy of fibromyalgia. Best Pract Res Clin Rheumatol 2011; 25:285–297.
- Wolfe F, Cathey MA, Hawley DJ. A double-blind placebo controlled trial of fluoxetine in fibromyalgia. Scand J Rheumatol 1994; 23:255–259.
- Arnold LM, Hess EV, Hudson JI, Welge JA, Berno SE, Keck PE. A randomized, placebo-controlled, double-blind, flexible-dose study of fluoxetine in the treatment of women with fibromyalgia. Am J Med 2002; 112:191–197.
- Arnold LM, Keck PE, Welge JA. Antidepressant treatment of fibromyalgia. A meta-analysis and review. Psychosomatics 2000; 41:104–113.
- Goldenberg DL, Burckhardt C, Crofford L. Management of fibromyalgia syndrome. JAMA 2004; 292:2388–2395.
- Tort S, Urrútia G, Nishishinya MB, Walitt B. Monoamine oxidase inhibitors (MAOIs) for fibromyalgia syndrome. Cochrane Database Syst Rev 2012; 4:CD009807.
- Vercoulen JH, Swanink CM, Zitman FG, et al. Randomised, double-blind, placebo-controlled study of fluoxetine in chronic fatigue syndrome. Lancet 1996; 347:858–861.
- Natelson BH, Cheu J, Pareja J, Ellis SP, Policastro T, Findley TW. Randomized, double blind, controlled placebo-phase in trial of low dose phenelzine in the chronic fatigue syndrome. Psychopharmacology (Berl) 1996; 124:226–230.
- Reid S, Chalder T, Cleare A, Hotopf M, Wessely S. Chronic fatigue syndrome. BMJ 2000; 320:292–296.
- Kupfer DJ, Spiker DG, Coble PA, Neil JF, Ulrich R, Shaw DH. Sleep and treatment prediction in endogenous depression. Am J Psychiatry 1981; 138:429–434.
- Argyropoulos SV, Hicks JA, Nash JR, et al. Redistribution of slow wave activity of sleep during pharmacological treatment of depression with paroxetine but not with nefazodone. J Sleep Res 2009; 18:342–348.
- Stein DJ, Lopez AG. Effects of escitalopram on sleep problems in patients with major depression or generalized anxiety disorder. Adv Ther 2011; 28:1021–1037.
- Ehlers CL, Havstad JW, Kupfer DJ. Estimation of the time course of slow-wave sleep over the night in depressed patients: effects of clomipramine and clinical response. Biol Psychiatry 1996; 39:171–181.
- Landolt HP, Raimo EB, Schnierow BJ, Kelsoe JR, Rapaport MH, Gillin JC. Sleep and sleep electroencephalogram in depressed patients treated with phenelzine. Arch Gen Psychiatry 2001; 58:268–276.
- Chen YM, Huang XM, Thompson R, Zhao YB. Clinical features and efficacy of escitalopram treatment for geriatric depression. J Int Med Res 2011; 39:1946–1953.
- Dolder C, Nelson M, Stump A. Pharmacological and clinical profile of newer antidepressants: implications for the treatment of elderly patients. Drugs Aging 2010; 27:625–640.
- Sterke CS, Ziere G, van Beeck EF, Looman CW, van der Cammen TJ. Dose-response relationship between selective serotonin re-uptake inhibitors and injurious falls: a study in nursing home residents with dementia. Br J Clin Pharmacol 2012; 73:812–820.
- Raji MA, Brady SR. Mirtazapine for treatment of depression and comorbidities in Alzheimer disease. Ann Pharmacother 2001; 35:1024–1027.
- Hennings JM, Schaaf L, Fulda S. Glucose metabolism and antidepressant medication. Curr Pharm Des 2012; 18:5900–5919.
- Czarny MJ, Arthurs E, Coffie DF, et al. Prevalence of antidepressant prescription or use in patients with acute coronary syndrome: a systematic review. PLoS One 2011; 6:e27671.
- Zuidersma M, Ormel J, Conradi HJ, de Jonge P. An increase in depressive symptoms after myocardial infarction predicts new cardiac events irrespective of depressive symptoms before myocardial infarction. Psychol Med 2012; 42:683–693.
- van Noord C, Straus SM, Sturkenboom MC, et al. Psychotropic drugs associated with corrected QT interval prolongation. J Clin Psychopharmacol 2009; 29:9–15.
- US Food and Drug Administration (FDA). FDA Drug Safety Communication: abnormal heart rhythms associated with high doses of Celexa (citalopram hydrobromide). http://www.fda.gov/Drugs/DrugSafety/ucm269086.htm. Accessed August 25, 2013.
- Lespérance F, Frasure-Smith N, Koszycki D, et al; CREATE Investigators. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA 2007; 297:367–379.
- O’Connor CM, Jiang W, Kuchibhatla M, et al; SADHART-CHF Investigators. Safety and efficacy of sertraline for depression in patients with heart failure: results of the SADHART-CHF (Sertraline Against Depression and Heart Disease in Chronic Heart Failure) trial. J Am Coll Cardiol 2010; 56:692–699.
- Glassman AH, O’Connor CM, Califf RM, et al; Sertraline Antidepressant Heart Attack Randomized Trial (SADHEART) Group. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA 2002; 288:701–709.
- Swenson JR, O’Connor CM, Barton D, et al; Sertraline Antidepressant Heart Attack Randomized Trial (SADHART) Group. Influence of depression and effect of treatment with sertraline on quality of life after hospitalization for acute coronary syndrome. Am J Cardiol 2003; 92:1271–1276.
- Strik JJ, Honig A, Lousberg R, et al. Efficacy and safety of fluoxetine in the treatment of patients with major depression after first myocardial infarction: findings from a double-blind, placebo-controlled trial. Psychosom Med 2000; 62:783–789.
- Honig A, Kuyper AM, Schene AH, et al; MIND-IT investigators. Treatment of post-myocardial infarction depressive disorder: a randomized, placebo-controlled trial with mirtazapine. Psychosom Med 2007; 69:606–613.
KEY POINTS
- We suggest that clinicians become familiar with one drug from each class of antidepressants.
- Many antidepressants are also approved for conditions other than depression, and for patients who have both depression and one or more of these comcomitant conditions, these drugs can have a “two-for-one” benefit.
- Adverse effects of an antidepressant are usually predictable on the basis of the drug’s mechanism of action.
Peripheral opacity on plain chest radiography
An 82-year-old woman was admitted to the hospital with dyspnea and chest discomfort over the past 24 hours. She was known to have paroxysmal atrial fibrillation and was taking warfarin, but that had been stopped 2 weeks earlier because of an acute ischemic stroke.
At the time of admission, she had no fever, cough, orthopnea, or leg swelling. Her physical activity was restricted, with residual right-sided weakness after her stroke. Her heart rate was 125 bpm; her oxygen saturation level was 98% on 2 L of oxygen per minute via nasal cannula. She had an irregularly irregular rhythm, a jugular venous pressure of 7 cm H2O, and no cardiac murmurs. Lung sounds were reduced at the bases, with faint crepitations.
Her hemoglobin concentration and white blood cell count were normal. Her brain-natriuretic peptide level was elevated at 2,648 pg/mL (reference range < 167), but cardiac enzyme levels were normal.
Electrocardiography showed atrial fibrillation with rapid ventricular response.
Plain chest radiography showed a 3-cm wedge-shaped opacity in the right mid-thorax (Figure 1), a finding known as the Hampton hump—a sign of pulmonary infarction caused by embolism.
Contrast-enhanced computed tomography (CT) of the chest showed acute thromboembolism in the right interlobar artery and wedge-shaped consolidation in the right-middle lobe (Figure 2), indicating pulmonary infarction.
Brain CT showed a stable infarction. Anticoagulation was restarted, and the patient was discharged in stable condition.
THE HAMPTON HUMP IN PULMONARY EMBOLISM
Because the lungs have a dual blood supply, pulmonary infarction is seen in only a minority of cases of pulmonary embolism. Infarction is more common in patients with peripheral pulmonary embolism, owing to the rapid inflow of bronchial blood, and in patients with medical comorbidities such as heart failure and chronic lung disease.2
The Hampton hump, first described by Aubrey Otis Hampton in 1940, is a peripheral (pleural-based) opacity that represents alveolar hemorrhage from underlying pulmonary infarction. It is one of several radiographic features that have been associated with pulmonary embolism; another is the Westermark sign, indicating oligemia.3
Worsley et al4 examined the diagnostic value of these radiographic features and found that the Hampton hump had a sensitivity of 22% and a specificity of 82% for detecting pulmonary embolism in the right hemithorax, and 24% and 82%, respectively, in the left hemithorax. The prevalence of pleural-based opacities was not significantly different in patients with or without pulmonary embolism. The authors concluded that chest radiography has limited diagnostic value in excluding or diagnosing pulmonary embolism.
In contrast, computed tomographic pulmonary angiography is the first-line imaging test in patients with suspected pulmonary embolism, because of its high sensitivity and specificity.1
We were not specifically looking for a pulmonary embolism when we found this new opacity on our patient’s radiograph, but this prompted further imaging, which led to the diagnosis. Although a near-normal chest radiograph is the most common radiologic finding in pulmonary embolism, this case shows how careful observation can detect unusual signs.
- Mos IC, Klok FA, Kroft LJ, de Roos A, Huisman MV. Imaging tests in the diagnosis of pulmonary embolism. Semin Respir Crit Care Med 2012; 33:138–143.
- Cha SI, Shin KM, Lee J, et al. Clinical relevance of pulmonary infarction in patients with pulmonary embolism. Thromb Res 2012; 130:e1–e5.
- Algın O, GÖkalp G, Topal U. Signs in chest imaging. Diagn Interv Radiol 2011; 17:18–29.
- Worsley DF, Alavi A, Aronchick JM, Chen JT, Greenspan RH, Ravin CE. Chest radiographic findings in patients with acute pulmonary embolism: observations from the PIOPED study. Radiology 1993; 189:133–136.
An 82-year-old woman was admitted to the hospital with dyspnea and chest discomfort over the past 24 hours. She was known to have paroxysmal atrial fibrillation and was taking warfarin, but that had been stopped 2 weeks earlier because of an acute ischemic stroke.
At the time of admission, she had no fever, cough, orthopnea, or leg swelling. Her physical activity was restricted, with residual right-sided weakness after her stroke. Her heart rate was 125 bpm; her oxygen saturation level was 98% on 2 L of oxygen per minute via nasal cannula. She had an irregularly irregular rhythm, a jugular venous pressure of 7 cm H2O, and no cardiac murmurs. Lung sounds were reduced at the bases, with faint crepitations.
Her hemoglobin concentration and white blood cell count were normal. Her brain-natriuretic peptide level was elevated at 2,648 pg/mL (reference range < 167), but cardiac enzyme levels were normal.
Electrocardiography showed atrial fibrillation with rapid ventricular response.
Plain chest radiography showed a 3-cm wedge-shaped opacity in the right mid-thorax (Figure 1), a finding known as the Hampton hump—a sign of pulmonary infarction caused by embolism.
Contrast-enhanced computed tomography (CT) of the chest showed acute thromboembolism in the right interlobar artery and wedge-shaped consolidation in the right-middle lobe (Figure 2), indicating pulmonary infarction.
Brain CT showed a stable infarction. Anticoagulation was restarted, and the patient was discharged in stable condition.
THE HAMPTON HUMP IN PULMONARY EMBOLISM
Because the lungs have a dual blood supply, pulmonary infarction is seen in only a minority of cases of pulmonary embolism. Infarction is more common in patients with peripheral pulmonary embolism, owing to the rapid inflow of bronchial blood, and in patients with medical comorbidities such as heart failure and chronic lung disease.2
The Hampton hump, first described by Aubrey Otis Hampton in 1940, is a peripheral (pleural-based) opacity that represents alveolar hemorrhage from underlying pulmonary infarction. It is one of several radiographic features that have been associated with pulmonary embolism; another is the Westermark sign, indicating oligemia.3
Worsley et al4 examined the diagnostic value of these radiographic features and found that the Hampton hump had a sensitivity of 22% and a specificity of 82% for detecting pulmonary embolism in the right hemithorax, and 24% and 82%, respectively, in the left hemithorax. The prevalence of pleural-based opacities was not significantly different in patients with or without pulmonary embolism. The authors concluded that chest radiography has limited diagnostic value in excluding or diagnosing pulmonary embolism.
In contrast, computed tomographic pulmonary angiography is the first-line imaging test in patients with suspected pulmonary embolism, because of its high sensitivity and specificity.1
We were not specifically looking for a pulmonary embolism when we found this new opacity on our patient’s radiograph, but this prompted further imaging, which led to the diagnosis. Although a near-normal chest radiograph is the most common radiologic finding in pulmonary embolism, this case shows how careful observation can detect unusual signs.
An 82-year-old woman was admitted to the hospital with dyspnea and chest discomfort over the past 24 hours. She was known to have paroxysmal atrial fibrillation and was taking warfarin, but that had been stopped 2 weeks earlier because of an acute ischemic stroke.
At the time of admission, she had no fever, cough, orthopnea, or leg swelling. Her physical activity was restricted, with residual right-sided weakness after her stroke. Her heart rate was 125 bpm; her oxygen saturation level was 98% on 2 L of oxygen per minute via nasal cannula. She had an irregularly irregular rhythm, a jugular venous pressure of 7 cm H2O, and no cardiac murmurs. Lung sounds were reduced at the bases, with faint crepitations.
Her hemoglobin concentration and white blood cell count were normal. Her brain-natriuretic peptide level was elevated at 2,648 pg/mL (reference range < 167), but cardiac enzyme levels were normal.
Electrocardiography showed atrial fibrillation with rapid ventricular response.
Plain chest radiography showed a 3-cm wedge-shaped opacity in the right mid-thorax (Figure 1), a finding known as the Hampton hump—a sign of pulmonary infarction caused by embolism.
Contrast-enhanced computed tomography (CT) of the chest showed acute thromboembolism in the right interlobar artery and wedge-shaped consolidation in the right-middle lobe (Figure 2), indicating pulmonary infarction.
Brain CT showed a stable infarction. Anticoagulation was restarted, and the patient was discharged in stable condition.
THE HAMPTON HUMP IN PULMONARY EMBOLISM
Because the lungs have a dual blood supply, pulmonary infarction is seen in only a minority of cases of pulmonary embolism. Infarction is more common in patients with peripheral pulmonary embolism, owing to the rapid inflow of bronchial blood, and in patients with medical comorbidities such as heart failure and chronic lung disease.2
The Hampton hump, first described by Aubrey Otis Hampton in 1940, is a peripheral (pleural-based) opacity that represents alveolar hemorrhage from underlying pulmonary infarction. It is one of several radiographic features that have been associated with pulmonary embolism; another is the Westermark sign, indicating oligemia.3
Worsley et al4 examined the diagnostic value of these radiographic features and found that the Hampton hump had a sensitivity of 22% and a specificity of 82% for detecting pulmonary embolism in the right hemithorax, and 24% and 82%, respectively, in the left hemithorax. The prevalence of pleural-based opacities was not significantly different in patients with or without pulmonary embolism. The authors concluded that chest radiography has limited diagnostic value in excluding or diagnosing pulmonary embolism.
In contrast, computed tomographic pulmonary angiography is the first-line imaging test in patients with suspected pulmonary embolism, because of its high sensitivity and specificity.1
We were not specifically looking for a pulmonary embolism when we found this new opacity on our patient’s radiograph, but this prompted further imaging, which led to the diagnosis. Although a near-normal chest radiograph is the most common radiologic finding in pulmonary embolism, this case shows how careful observation can detect unusual signs.
- Mos IC, Klok FA, Kroft LJ, de Roos A, Huisman MV. Imaging tests in the diagnosis of pulmonary embolism. Semin Respir Crit Care Med 2012; 33:138–143.
- Cha SI, Shin KM, Lee J, et al. Clinical relevance of pulmonary infarction in patients with pulmonary embolism. Thromb Res 2012; 130:e1–e5.
- Algın O, GÖkalp G, Topal U. Signs in chest imaging. Diagn Interv Radiol 2011; 17:18–29.
- Worsley DF, Alavi A, Aronchick JM, Chen JT, Greenspan RH, Ravin CE. Chest radiographic findings in patients with acute pulmonary embolism: observations from the PIOPED study. Radiology 1993; 189:133–136.
- Mos IC, Klok FA, Kroft LJ, de Roos A, Huisman MV. Imaging tests in the diagnosis of pulmonary embolism. Semin Respir Crit Care Med 2012; 33:138–143.
- Cha SI, Shin KM, Lee J, et al. Clinical relevance of pulmonary infarction in patients with pulmonary embolism. Thromb Res 2012; 130:e1–e5.
- Algın O, GÖkalp G, Topal U. Signs in chest imaging. Diagn Interv Radiol 2011; 17:18–29.
- Worsley DF, Alavi A, Aronchick JM, Chen JT, Greenspan RH, Ravin CE. Chest radiographic findings in patients with acute pulmonary embolism: observations from the PIOPED study. Radiology 1993; 189:133–136.
The overdiagnosis of pneumonia
Pneumonia was once considered the “old man’s friend,” but in the modern world, has it become the physician’s?
The definition of pneumonia has increasingly been stretched, and physicians occasionally make the diagnosis without canonical signs or symptoms, or even with negative chest radiography. The hallmark of overdiagnosis is identifying illness for which treatment is not needed or is not helpful, and some cases of pneumonia likely fit this description. Empirical evidence over the last 3 decades shows a sustained increase in the diagnosis of pneumonia, but little evidence of a decrease in the rates of pneumonia morbidity and mortality. The central problem with pneumonia is one common to many diagnoses, such as pulmonary embolism, coronary artery disease, and infectious conditions—diagnostic criteria remain divorced from outcomes data. Linking the two has the potential to improve the evidence base of medicine.
Like many long-recognized diagnoses, pneumonia lacks a standardized definition. Most physicians believe that although fever, cough, sputum production, dyspnea, and pleurisy are hallmark symptoms, confirmatory chest radiography is needed to cement the diagnosis.1 But what if a patient has only a fever, cough, and infiltrate? What if the infiltrate is not visible on radiography, but only on computed tomography (CT)? And what if the patient has a cough but is afebrile and has nonspecific findings on CT?
THE RATE OF HOSPITAL ADMISSIONS FOR PNEUMONIA IS RISING
In current clinical practice, any or all of the above cases are called pneumonia. The pneumonia label, once applied, justifies the use of antibiotics, which patients or physicians may overtly desire. One prospective observational study of six hospitals found that 21% of patients admitted with pneumonia and 43% of those treated as outpatients had negative chest radiographs.2 Empirical evidence suggests that the incidence of these “soft” diagnoses may be growing in number.
In the United States, hospitalizations with discharge codes listing pneumonia increased 20% from the late 1980s to the early 2000s.3 The rates of hospitalization for the 10 other most frequent causes of admission did not change significantly over this same period, suggesting a selective increase in hospital admissions for pneumonia.
This focus on pneumonia would be justified if it led to a proportionate benefit for pneumonia outcomes. However, in the same data set, the risk of death from pneumonia did not improve more than that from the other 10 common conditions—all improved similarly—and the rate of discharge from the hospital to a long-term care facility was unchanged. We are hospitalizing more patients with pneumonia, but this has not improved outcomes beyond global trends in mortality.
Data from England suggest that overdiagnosis may be a worldwide phenomenon. Between 1997 and 2005, hospitalization rates in England for pneumonia, adjusted for age, increased 34% from 1.48 to 1.98 per 1,000 persons.4 The 30-day in-hospital death rate for pneumonia remained about the same over this period. In the absence of a paradigm-shifting technology, one that would alter hospitalization practices, or an environmental cause of increased incidence—and with pneumonia there has been neither—the most likely explanation for these documented trends is that hospitals are admitting patients with pneumonia that is less severe.
Finally, data from the 2000s that at first seemed to reverse the trend of increasing hospitalizations for pneumonia have been reanalyzed to account for alternative coding.5 For instance, a pneumonia admission may be coded with respiratory failure as the primary diagnosis and pneumonia as the secondary diagnosis. Examining data from large populations from 2002 to 2009, and correcting as such, shows that the incidence of pneumonia has reached a plateau or has declined only slightly from the elevated rates of the early 2000s. The death rate remains unchanged.
PNEUMONIA: A DIAGNOSIS IN THE EYE OF THE BEHOLDER
Apparently, when it comes to pneumonia, the diagnosis is in the eye of the beholder. Different physicians have different thresholds for applying the label. In the wake of quality efforts to ensure that emergency physicians deliver antibiotics within 4 hours, emergency doctors have been shown to have worse accuracy in diagnosing pneumonia.1 But worse accuracy compared with what standard?
In an investigation by Welker et al,1 the standard definition of pneumonia was based on the one favored by the US Food and Drug Administration for clinical trials. Patients had to have all of the following:
- A new or increasing infiltrate on radiography or CT
- A fever, an elevated white blood cell count, or a shift to immature polymorphonuclear leukocytes
- At least two signs or symptoms of the condition (eg, cough, dyspnea, egophany).
Although this definition is reasonable and ensures homogeneity in clinical trials, it is not steadfastly adhered to in clinical practice and has never been shown to cleanly delineate a population that benefits from antibiotics.
Another challenge to devising a perfect definition of pneumonia is the lack of a pathologic gold standard. Based on a review of 17,340 Medicare patients hospitalized for community-acquired pneumonia, microbial confirmation is often of little assistance, and a probable pathogen is identified in only 7.6% of cases.6
RATES OF OUTPATIENT DIAGNOSIS ARE LIKELY SIMILAR
Thus far, we have examined trends in inpatient diagnosis but not those of outpatient diagnosis. There is no well-done observational study that documents outpatient trends, but there is little reason to suppose the trends are different. Risk-scoring systems in pneumonia, such as the PORT7 and the CURB-65,8 have been designed to decrease unnecessary inpatient admissions, but they do not lend clarity to the diagnosis itself.
The central problem with pneumonia, as with many long-recognized clinical conditions, is that the diagnosis is separated from the treatment. In other words, although physicians are confident that antibiotics benefit patients who have what Sir William Osler would have called pneumonia (elevated white blood cell count, fever, cough, dyspnea, pleurisy, egophany, lobular infiltrate), we don’t know whether the treatment benefits patients whose pneumonia would have been unrecognizable decades ago (with cough, low-grade fever, and infiltrate on CT alone). Improvements in imaging may exacerbate the problem. In this sense, pneumonia exists on a spectrum, as do many medical diagnoses. Not all cases are equally severe, and some may not deserve to be labeled as pneumonia.
No randomized trial has compared antibiotics against supportive care in pneumonia, and, likely, no such trial is needed for clear cases. However, with the growing number of soft diagnoses, randomized trials are desperately needed to delineate where harms outweigh benefits, and where the fuzzy edge of the pneumonia diagnosis must end. And as is always the case with studies that challenge a standard of care, null results should prompt further trials.
WELL-DESIGNED TRIALS COULD END THE UNCERTAINTY
In the next few years, clinical trials, rationally planned, may end most of the uncertainty regarding pneumonia.
Existing observational data may be used to identify groups of patients who, in today’s world, are diagnosed with pneumonia but who do exceptionally well (eg, younger patients with fewer comorbidities, who present with low-grade fever but no signs of consolidation on physical examination, and with dubious results on chest radiography). These are patients for whom equipoise exists, and randomized trials should compare a strategy of antibiotics with a strategy of best supportive care. Trials should be powered for patient-centered outcomes, such as the duration and the complications of illness. The death rate should be scrupulously recorded.
Patients whose pneumonia would have been unrecognizable decades ago should be another target population for the trials I propose.
In a short time, pneumonia may become synonymous with a set of factors for lung infection that predict who will benefit from antibiotics, and who can be safely followed. Already, we are moving toward this standard in other diseases.9 For pulmonary embolism, ongoing trials are testing if anticoagulation can be safely omitted in patients with subsegmental clots (clinicaltrials.gov identifier NCT01455818). Such trials are, at last, translating old diagnoses into the language of evidence-based medicine.
For patients with pneumonia who are not hospitalized, the current outpatient therapy is based on data from studies that show a low rate of failure with empiric treatment based on consideration of the common pathogens for this condition, with few patients subsequently requiring hospitalization. Today, this reasoning is inadequate. The basis for any therapy must be proven benefit for patients with a defined condition compared with a lesser strategy. Data already demonstrate that a short course of antibiotics is no worse than a long course for many hospitalized and outpatients with pneumonia,10,11 but many other patients may require no treatment at all. The time has come to find out.
- Welker JA, Huston M, McCue JD. Antibiotic timing and errors in diagnosing pneumonia. Arch Intern Med 2008; 168:351–356.
- Marrie TJ, Huang JQ. Low-risk patients admitted with community-acquired pneumonia. Am J Med 2005; 118:1357–1363.
- Fry AM, Shay DK, Holman RC, Curns AT, Anderson LJ. Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988–2002. JAMA 2005; 294:2712–2719.
- Trotter CL, Stuart JM, George R, Miller E. Increasing hospital admissions for pneumonia, England. Emerg Infect Dis 2008; 14:727–733.
- Lindenauer PK, Lagu T, Shieh MS, Pekow PS, Rothberg MB. Association of diagnostic coding with trends in hospitalizations and mortality of patients with pneumonia, 2003–2009. JAMA 2012; 307:1405–1413.
- Bartlett JG. Diagnostic tests for agents of community-acquired pneumonia. Clin Infect Dis 2011; 52(suppl 4):S296–S304.
- Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 1997; 336:242–250.
- Lim W, van der Eerden MM, Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax 2003; 58:377–382.
- Prasad V, Rho J, Cifu A. The diagnosis and treatment of pulmonary embolism: a metaphor for medicine in the evidence-based medicine era. Arch Intern Med 2012; 172:955–958.
- Singh N, Rogers P, Atwood CW, Wagener MM, Yu VL. Short-course empiric antibiotic therapy for patients with pulmonary infiltrates in the intensive care unit. A proposed solution for indiscriminate antibiotic prescription. Am J Respir Crit Care Med 2000; 162:505–511.
- Li JZ, Winston LG, Moore DH, Bent S. Efficacy of short-course antibiotic regimens for community-acquired pneumonia: a meta-analysis. Am J Med 2007; 120:783–790.
Pneumonia was once considered the “old man’s friend,” but in the modern world, has it become the physician’s?
The definition of pneumonia has increasingly been stretched, and physicians occasionally make the diagnosis without canonical signs or symptoms, or even with negative chest radiography. The hallmark of overdiagnosis is identifying illness for which treatment is not needed or is not helpful, and some cases of pneumonia likely fit this description. Empirical evidence over the last 3 decades shows a sustained increase in the diagnosis of pneumonia, but little evidence of a decrease in the rates of pneumonia morbidity and mortality. The central problem with pneumonia is one common to many diagnoses, such as pulmonary embolism, coronary artery disease, and infectious conditions—diagnostic criteria remain divorced from outcomes data. Linking the two has the potential to improve the evidence base of medicine.
Like many long-recognized diagnoses, pneumonia lacks a standardized definition. Most physicians believe that although fever, cough, sputum production, dyspnea, and pleurisy are hallmark symptoms, confirmatory chest radiography is needed to cement the diagnosis.1 But what if a patient has only a fever, cough, and infiltrate? What if the infiltrate is not visible on radiography, but only on computed tomography (CT)? And what if the patient has a cough but is afebrile and has nonspecific findings on CT?
THE RATE OF HOSPITAL ADMISSIONS FOR PNEUMONIA IS RISING
In current clinical practice, any or all of the above cases are called pneumonia. The pneumonia label, once applied, justifies the use of antibiotics, which patients or physicians may overtly desire. One prospective observational study of six hospitals found that 21% of patients admitted with pneumonia and 43% of those treated as outpatients had negative chest radiographs.2 Empirical evidence suggests that the incidence of these “soft” diagnoses may be growing in number.
In the United States, hospitalizations with discharge codes listing pneumonia increased 20% from the late 1980s to the early 2000s.3 The rates of hospitalization for the 10 other most frequent causes of admission did not change significantly over this same period, suggesting a selective increase in hospital admissions for pneumonia.
This focus on pneumonia would be justified if it led to a proportionate benefit for pneumonia outcomes. However, in the same data set, the risk of death from pneumonia did not improve more than that from the other 10 common conditions—all improved similarly—and the rate of discharge from the hospital to a long-term care facility was unchanged. We are hospitalizing more patients with pneumonia, but this has not improved outcomes beyond global trends in mortality.
Data from England suggest that overdiagnosis may be a worldwide phenomenon. Between 1997 and 2005, hospitalization rates in England for pneumonia, adjusted for age, increased 34% from 1.48 to 1.98 per 1,000 persons.4 The 30-day in-hospital death rate for pneumonia remained about the same over this period. In the absence of a paradigm-shifting technology, one that would alter hospitalization practices, or an environmental cause of increased incidence—and with pneumonia there has been neither—the most likely explanation for these documented trends is that hospitals are admitting patients with pneumonia that is less severe.
Finally, data from the 2000s that at first seemed to reverse the trend of increasing hospitalizations for pneumonia have been reanalyzed to account for alternative coding.5 For instance, a pneumonia admission may be coded with respiratory failure as the primary diagnosis and pneumonia as the secondary diagnosis. Examining data from large populations from 2002 to 2009, and correcting as such, shows that the incidence of pneumonia has reached a plateau or has declined only slightly from the elevated rates of the early 2000s. The death rate remains unchanged.
PNEUMONIA: A DIAGNOSIS IN THE EYE OF THE BEHOLDER
Apparently, when it comes to pneumonia, the diagnosis is in the eye of the beholder. Different physicians have different thresholds for applying the label. In the wake of quality efforts to ensure that emergency physicians deliver antibiotics within 4 hours, emergency doctors have been shown to have worse accuracy in diagnosing pneumonia.1 But worse accuracy compared with what standard?
In an investigation by Welker et al,1 the standard definition of pneumonia was based on the one favored by the US Food and Drug Administration for clinical trials. Patients had to have all of the following:
- A new or increasing infiltrate on radiography or CT
- A fever, an elevated white blood cell count, or a shift to immature polymorphonuclear leukocytes
- At least two signs or symptoms of the condition (eg, cough, dyspnea, egophany).
Although this definition is reasonable and ensures homogeneity in clinical trials, it is not steadfastly adhered to in clinical practice and has never been shown to cleanly delineate a population that benefits from antibiotics.
Another challenge to devising a perfect definition of pneumonia is the lack of a pathologic gold standard. Based on a review of 17,340 Medicare patients hospitalized for community-acquired pneumonia, microbial confirmation is often of little assistance, and a probable pathogen is identified in only 7.6% of cases.6
RATES OF OUTPATIENT DIAGNOSIS ARE LIKELY SIMILAR
Thus far, we have examined trends in inpatient diagnosis but not those of outpatient diagnosis. There is no well-done observational study that documents outpatient trends, but there is little reason to suppose the trends are different. Risk-scoring systems in pneumonia, such as the PORT7 and the CURB-65,8 have been designed to decrease unnecessary inpatient admissions, but they do not lend clarity to the diagnosis itself.
The central problem with pneumonia, as with many long-recognized clinical conditions, is that the diagnosis is separated from the treatment. In other words, although physicians are confident that antibiotics benefit patients who have what Sir William Osler would have called pneumonia (elevated white blood cell count, fever, cough, dyspnea, pleurisy, egophany, lobular infiltrate), we don’t know whether the treatment benefits patients whose pneumonia would have been unrecognizable decades ago (with cough, low-grade fever, and infiltrate on CT alone). Improvements in imaging may exacerbate the problem. In this sense, pneumonia exists on a spectrum, as do many medical diagnoses. Not all cases are equally severe, and some may not deserve to be labeled as pneumonia.
No randomized trial has compared antibiotics against supportive care in pneumonia, and, likely, no such trial is needed for clear cases. However, with the growing number of soft diagnoses, randomized trials are desperately needed to delineate where harms outweigh benefits, and where the fuzzy edge of the pneumonia diagnosis must end. And as is always the case with studies that challenge a standard of care, null results should prompt further trials.
WELL-DESIGNED TRIALS COULD END THE UNCERTAINTY
In the next few years, clinical trials, rationally planned, may end most of the uncertainty regarding pneumonia.
Existing observational data may be used to identify groups of patients who, in today’s world, are diagnosed with pneumonia but who do exceptionally well (eg, younger patients with fewer comorbidities, who present with low-grade fever but no signs of consolidation on physical examination, and with dubious results on chest radiography). These are patients for whom equipoise exists, and randomized trials should compare a strategy of antibiotics with a strategy of best supportive care. Trials should be powered for patient-centered outcomes, such as the duration and the complications of illness. The death rate should be scrupulously recorded.
Patients whose pneumonia would have been unrecognizable decades ago should be another target population for the trials I propose.
In a short time, pneumonia may become synonymous with a set of factors for lung infection that predict who will benefit from antibiotics, and who can be safely followed. Already, we are moving toward this standard in other diseases.9 For pulmonary embolism, ongoing trials are testing if anticoagulation can be safely omitted in patients with subsegmental clots (clinicaltrials.gov identifier NCT01455818). Such trials are, at last, translating old diagnoses into the language of evidence-based medicine.
For patients with pneumonia who are not hospitalized, the current outpatient therapy is based on data from studies that show a low rate of failure with empiric treatment based on consideration of the common pathogens for this condition, with few patients subsequently requiring hospitalization. Today, this reasoning is inadequate. The basis for any therapy must be proven benefit for patients with a defined condition compared with a lesser strategy. Data already demonstrate that a short course of antibiotics is no worse than a long course for many hospitalized and outpatients with pneumonia,10,11 but many other patients may require no treatment at all. The time has come to find out.
Pneumonia was once considered the “old man’s friend,” but in the modern world, has it become the physician’s?
The definition of pneumonia has increasingly been stretched, and physicians occasionally make the diagnosis without canonical signs or symptoms, or even with negative chest radiography. The hallmark of overdiagnosis is identifying illness for which treatment is not needed or is not helpful, and some cases of pneumonia likely fit this description. Empirical evidence over the last 3 decades shows a sustained increase in the diagnosis of pneumonia, but little evidence of a decrease in the rates of pneumonia morbidity and mortality. The central problem with pneumonia is one common to many diagnoses, such as pulmonary embolism, coronary artery disease, and infectious conditions—diagnostic criteria remain divorced from outcomes data. Linking the two has the potential to improve the evidence base of medicine.
Like many long-recognized diagnoses, pneumonia lacks a standardized definition. Most physicians believe that although fever, cough, sputum production, dyspnea, and pleurisy are hallmark symptoms, confirmatory chest radiography is needed to cement the diagnosis.1 But what if a patient has only a fever, cough, and infiltrate? What if the infiltrate is not visible on radiography, but only on computed tomography (CT)? And what if the patient has a cough but is afebrile and has nonspecific findings on CT?
THE RATE OF HOSPITAL ADMISSIONS FOR PNEUMONIA IS RISING
In current clinical practice, any or all of the above cases are called pneumonia. The pneumonia label, once applied, justifies the use of antibiotics, which patients or physicians may overtly desire. One prospective observational study of six hospitals found that 21% of patients admitted with pneumonia and 43% of those treated as outpatients had negative chest radiographs.2 Empirical evidence suggests that the incidence of these “soft” diagnoses may be growing in number.
In the United States, hospitalizations with discharge codes listing pneumonia increased 20% from the late 1980s to the early 2000s.3 The rates of hospitalization for the 10 other most frequent causes of admission did not change significantly over this same period, suggesting a selective increase in hospital admissions for pneumonia.
This focus on pneumonia would be justified if it led to a proportionate benefit for pneumonia outcomes. However, in the same data set, the risk of death from pneumonia did not improve more than that from the other 10 common conditions—all improved similarly—and the rate of discharge from the hospital to a long-term care facility was unchanged. We are hospitalizing more patients with pneumonia, but this has not improved outcomes beyond global trends in mortality.
Data from England suggest that overdiagnosis may be a worldwide phenomenon. Between 1997 and 2005, hospitalization rates in England for pneumonia, adjusted for age, increased 34% from 1.48 to 1.98 per 1,000 persons.4 The 30-day in-hospital death rate for pneumonia remained about the same over this period. In the absence of a paradigm-shifting technology, one that would alter hospitalization practices, or an environmental cause of increased incidence—and with pneumonia there has been neither—the most likely explanation for these documented trends is that hospitals are admitting patients with pneumonia that is less severe.
Finally, data from the 2000s that at first seemed to reverse the trend of increasing hospitalizations for pneumonia have been reanalyzed to account for alternative coding.5 For instance, a pneumonia admission may be coded with respiratory failure as the primary diagnosis and pneumonia as the secondary diagnosis. Examining data from large populations from 2002 to 2009, and correcting as such, shows that the incidence of pneumonia has reached a plateau or has declined only slightly from the elevated rates of the early 2000s. The death rate remains unchanged.
PNEUMONIA: A DIAGNOSIS IN THE EYE OF THE BEHOLDER
Apparently, when it comes to pneumonia, the diagnosis is in the eye of the beholder. Different physicians have different thresholds for applying the label. In the wake of quality efforts to ensure that emergency physicians deliver antibiotics within 4 hours, emergency doctors have been shown to have worse accuracy in diagnosing pneumonia.1 But worse accuracy compared with what standard?
In an investigation by Welker et al,1 the standard definition of pneumonia was based on the one favored by the US Food and Drug Administration for clinical trials. Patients had to have all of the following:
- A new or increasing infiltrate on radiography or CT
- A fever, an elevated white blood cell count, or a shift to immature polymorphonuclear leukocytes
- At least two signs or symptoms of the condition (eg, cough, dyspnea, egophany).
Although this definition is reasonable and ensures homogeneity in clinical trials, it is not steadfastly adhered to in clinical practice and has never been shown to cleanly delineate a population that benefits from antibiotics.
Another challenge to devising a perfect definition of pneumonia is the lack of a pathologic gold standard. Based on a review of 17,340 Medicare patients hospitalized for community-acquired pneumonia, microbial confirmation is often of little assistance, and a probable pathogen is identified in only 7.6% of cases.6
RATES OF OUTPATIENT DIAGNOSIS ARE LIKELY SIMILAR
Thus far, we have examined trends in inpatient diagnosis but not those of outpatient diagnosis. There is no well-done observational study that documents outpatient trends, but there is little reason to suppose the trends are different. Risk-scoring systems in pneumonia, such as the PORT7 and the CURB-65,8 have been designed to decrease unnecessary inpatient admissions, but they do not lend clarity to the diagnosis itself.
The central problem with pneumonia, as with many long-recognized clinical conditions, is that the diagnosis is separated from the treatment. In other words, although physicians are confident that antibiotics benefit patients who have what Sir William Osler would have called pneumonia (elevated white blood cell count, fever, cough, dyspnea, pleurisy, egophany, lobular infiltrate), we don’t know whether the treatment benefits patients whose pneumonia would have been unrecognizable decades ago (with cough, low-grade fever, and infiltrate on CT alone). Improvements in imaging may exacerbate the problem. In this sense, pneumonia exists on a spectrum, as do many medical diagnoses. Not all cases are equally severe, and some may not deserve to be labeled as pneumonia.
No randomized trial has compared antibiotics against supportive care in pneumonia, and, likely, no such trial is needed for clear cases. However, with the growing number of soft diagnoses, randomized trials are desperately needed to delineate where harms outweigh benefits, and where the fuzzy edge of the pneumonia diagnosis must end. And as is always the case with studies that challenge a standard of care, null results should prompt further trials.
WELL-DESIGNED TRIALS COULD END THE UNCERTAINTY
In the next few years, clinical trials, rationally planned, may end most of the uncertainty regarding pneumonia.
Existing observational data may be used to identify groups of patients who, in today’s world, are diagnosed with pneumonia but who do exceptionally well (eg, younger patients with fewer comorbidities, who present with low-grade fever but no signs of consolidation on physical examination, and with dubious results on chest radiography). These are patients for whom equipoise exists, and randomized trials should compare a strategy of antibiotics with a strategy of best supportive care. Trials should be powered for patient-centered outcomes, such as the duration and the complications of illness. The death rate should be scrupulously recorded.
Patients whose pneumonia would have been unrecognizable decades ago should be another target population for the trials I propose.
In a short time, pneumonia may become synonymous with a set of factors for lung infection that predict who will benefit from antibiotics, and who can be safely followed. Already, we are moving toward this standard in other diseases.9 For pulmonary embolism, ongoing trials are testing if anticoagulation can be safely omitted in patients with subsegmental clots (clinicaltrials.gov identifier NCT01455818). Such trials are, at last, translating old diagnoses into the language of evidence-based medicine.
For patients with pneumonia who are not hospitalized, the current outpatient therapy is based on data from studies that show a low rate of failure with empiric treatment based on consideration of the common pathogens for this condition, with few patients subsequently requiring hospitalization. Today, this reasoning is inadequate. The basis for any therapy must be proven benefit for patients with a defined condition compared with a lesser strategy. Data already demonstrate that a short course of antibiotics is no worse than a long course for many hospitalized and outpatients with pneumonia,10,11 but many other patients may require no treatment at all. The time has come to find out.
- Welker JA, Huston M, McCue JD. Antibiotic timing and errors in diagnosing pneumonia. Arch Intern Med 2008; 168:351–356.
- Marrie TJ, Huang JQ. Low-risk patients admitted with community-acquired pneumonia. Am J Med 2005; 118:1357–1363.
- Fry AM, Shay DK, Holman RC, Curns AT, Anderson LJ. Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988–2002. JAMA 2005; 294:2712–2719.
- Trotter CL, Stuart JM, George R, Miller E. Increasing hospital admissions for pneumonia, England. Emerg Infect Dis 2008; 14:727–733.
- Lindenauer PK, Lagu T, Shieh MS, Pekow PS, Rothberg MB. Association of diagnostic coding with trends in hospitalizations and mortality of patients with pneumonia, 2003–2009. JAMA 2012; 307:1405–1413.
- Bartlett JG. Diagnostic tests for agents of community-acquired pneumonia. Clin Infect Dis 2011; 52(suppl 4):S296–S304.
- Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 1997; 336:242–250.
- Lim W, van der Eerden MM, Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax 2003; 58:377–382.
- Prasad V, Rho J, Cifu A. The diagnosis and treatment of pulmonary embolism: a metaphor for medicine in the evidence-based medicine era. Arch Intern Med 2012; 172:955–958.
- Singh N, Rogers P, Atwood CW, Wagener MM, Yu VL. Short-course empiric antibiotic therapy for patients with pulmonary infiltrates in the intensive care unit. A proposed solution for indiscriminate antibiotic prescription. Am J Respir Crit Care Med 2000; 162:505–511.
- Li JZ, Winston LG, Moore DH, Bent S. Efficacy of short-course antibiotic regimens for community-acquired pneumonia: a meta-analysis. Am J Med 2007; 120:783–790.
- Welker JA, Huston M, McCue JD. Antibiotic timing and errors in diagnosing pneumonia. Arch Intern Med 2008; 168:351–356.
- Marrie TJ, Huang JQ. Low-risk patients admitted with community-acquired pneumonia. Am J Med 2005; 118:1357–1363.
- Fry AM, Shay DK, Holman RC, Curns AT, Anderson LJ. Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988–2002. JAMA 2005; 294:2712–2719.
- Trotter CL, Stuart JM, George R, Miller E. Increasing hospital admissions for pneumonia, England. Emerg Infect Dis 2008; 14:727–733.
- Lindenauer PK, Lagu T, Shieh MS, Pekow PS, Rothberg MB. Association of diagnostic coding with trends in hospitalizations and mortality of patients with pneumonia, 2003–2009. JAMA 2012; 307:1405–1413.
- Bartlett JG. Diagnostic tests for agents of community-acquired pneumonia. Clin Infect Dis 2011; 52(suppl 4):S296–S304.
- Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 1997; 336:242–250.
- Lim W, van der Eerden MM, Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax 2003; 58:377–382.
- Prasad V, Rho J, Cifu A. The diagnosis and treatment of pulmonary embolism: a metaphor for medicine in the evidence-based medicine era. Arch Intern Med 2012; 172:955–958.
- Singh N, Rogers P, Atwood CW, Wagener MM, Yu VL. Short-course empiric antibiotic therapy for patients with pulmonary infiltrates in the intensive care unit. A proposed solution for indiscriminate antibiotic prescription. Am J Respir Crit Care Med 2000; 162:505–511.
- Li JZ, Winston LG, Moore DH, Bent S. Efficacy of short-course antibiotic regimens for community-acquired pneumonia: a meta-analysis. Am J Med 2007; 120:783–790.
Another perspective: Reducing the overtreatment of pneumonia
In his commentary in this issue, Dr. Vinay Prasad provides a well-supported perspective on the overdiagnosis of pneumonia.
Although I agree that there can be a tendency to overdiagnose pneumonia, we must not overlook the fact that pneumonia is still a leading cause of death in the United States.
The number of cases of invasive pneumococcal disease (mostly bacteremic pneumonia) in people over age 65 has increased over the past decade.1 This increase is not the result of overdiagnosis, since the diagnosis relies on the well-established US Centers for Disease Control and Prevention (CDC) surveillance system, which requires a positive culture from a sterile site. However, to an extent, the increase can be explained by the increasing age of our population and by the associated comorbidities.2 These comorbidities increase the predisposition to and the severity of pneumonia and adversely affect the outcome—which may also explain why we have seen no significant decrease in the death rate for patients admitted to the hospital.
In addition, a 2012 report3 that drew data from a variety of sources, including the CDC, projected that between 2004 and 2040, the US population would increase by 38% and at the same time pneumococcal pneumonia hospitalizations would increase by 96%, since population growth is fastest in older age groups, who have the highest rates of disease.3
Thus, I believe that pneumonia will continue to be a big problem and that we should pursue efforts to prevent it (including vaccinating more people against it) and to better manage it.
I agree that “over-calling” acute respiratory infections as pneumonia is often the result of imprecise diagnosis. Clinical criteria, even a combination of symptoms (cough) and signs (fever, tachycardia, and crackles), are not reliably predictive when using chest radiography as the standard.4 This can lead to the overuse of antimicrobials.
The Centers for Medicare and Medicaid Services used to call for starting the first dose of antibiotics within a specified time (at one time it was 4 hours, subsequently it became 6 hours) of presentation to the hospital with community-acquired pneumonia. Although the actual effect was uncertain, many feared that this performance measure would unintentionally lead to the indiscriminate use of antimicrobials to achieve high rates of compliance in patients who have little evidence of pneumonia, in order to not miss a possible case.5,6 However, it is important to be aware that this measure was retired in 2012 and is no longer in effect.
WE NEED BETTER ASSESSMENTS AND TREATMENTS
We need better ways to assess and manage patients with pneumonia. I believe part of the solution to better assessment lies in improved diagnostic tools, and these are now becoming available.
As Dr. Prasad notes, the causative pathogen is rarely identified using standard diagnostic methods. However, polymerase chain reaction testing and measurement of the biomarker procalcitonin may improve our diagnostic accuracy and, hopefully, lead to better outcomes.7 The results of these tests can be rapidly available and thus may aid the point-of-care decision to treat or not to treat with antimicrobials and to allow for therapy to be started within an acceptable period. In addition, procalcitonin testing has been shown to help differentiate viral from bacterial causes of respiratory tract infection.
Dr. Prasad states that no randomized trial has compared antibiotics with supportive care in pneumonia. Although this is true for recent trials, historical studies demonstrate that antibiotics reduce death rates in patients with pneumonia.8 Indeed, these are the basis for the recent changes in the US Food and Drug Administration guidance for clinical trials of pneumonia.9
Treatment is best when it is directed at the pathogen, but there is little consensus on the practicality of achieving this goal at the primary point of care. A study funded by the National Institutes of Health is about to start enrollment to compare the effect of narrow-spectrum therapy vs the standard of care based on rapid diagnostics.10 Identification of a specific pathogen will allow directed therapy without the need for a broad-spectrum empiric regimen. In contrast, finding a viral cause without an accompanying bacterial cause will prevent the unnecessary use of antibacterials in many cases. A significant percent of cases of pneumonia in adults are caused by viruses alone.6
Thus, the question will not be, “Should we treat community-acquired pneumonia with antibacterials” but rather, “What is the optimal treatment for pneumonia with a defined cause?” This is a major change from an empirical broad-spectrum regimen (treat all likely pathogens) to a more specific approach that has several potential benefits, including better patient outcomes and less emergence of resistance. To paraphrase Dr. Prasad, the time has come to find this out.
- US Centers for Disease Control and Prevention. Active bacterial core surveillance (ABCs) http://www.cdc.gov/abcs/reports-findings/surv-reports.html. Accessed June 20, 2013.
- Fry AM, Shay DK, Holman RC, Curns AT, Anderson LJ. Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988–2002. JAMA 2005; 294:2712–2719.
- Wroe PC, Finkelstein JA, Ray GT, et al. Aging population and future burden of pneumococcal pneumonia in the United States. J Infect Dis 2012; 205:1589–1592.
- Metlay JP, Fine MJ. Testing strategies in the initial management of patients with community-acquired pneumonia. Ann Intern Med 2003; 138:109–118.
- File TM, Solomkin JS, Cosgrove SE. Strategies for improving antimicrobial use and the role of antimicrobial stewardship programs. Clin Infect Dis 2011; 53(suppl 1):S15–S22.
- File TM, Gross PA. Performance measurement in community-acquired pneumonia: consequences intended and unintended. Clin Infect Dis 2007; 44:942–944.
- File TM. New diagnostic tests for pneumonia: what is their role in clinical practice? Clin Chest Med 2011; 32:417–430.
- Spellberg B, Talbot GH, Brass EP, Bradley JS, Boucher HW, Gilbert DN; Infectious Diseases Society of America. Position paper: recommended design features of future clinical trials of antibacterial agents for community-acquired pneumonia. Clin Infect Dis 2008; 47(suppl 3):S249–S265.
- Division of Drug Information. Guidance for industry. Community-acquired bacterial pneumonia: Developing drugs for treatment. http://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm123686.pdf. Accessed August 4, 2013.
- US National Institutes of Health. Microbiology testing with the aim of directed antimicrobial therapy for CAP (NIHCAP). Department of Microbiology Infectious Diseases Protocol 10-0061. http://clinicaltrials.gov/ct2/show/NCT01662258?term=community+acquired+pneumonia&cond=%22Pneumonia%22&titles=microbiology+testing+with+the+aim+of+directed+antimicrobial+therapy&rank=1. Accessed August 4, 2013.
In his commentary in this issue, Dr. Vinay Prasad provides a well-supported perspective on the overdiagnosis of pneumonia.
Although I agree that there can be a tendency to overdiagnose pneumonia, we must not overlook the fact that pneumonia is still a leading cause of death in the United States.
The number of cases of invasive pneumococcal disease (mostly bacteremic pneumonia) in people over age 65 has increased over the past decade.1 This increase is not the result of overdiagnosis, since the diagnosis relies on the well-established US Centers for Disease Control and Prevention (CDC) surveillance system, which requires a positive culture from a sterile site. However, to an extent, the increase can be explained by the increasing age of our population and by the associated comorbidities.2 These comorbidities increase the predisposition to and the severity of pneumonia and adversely affect the outcome—which may also explain why we have seen no significant decrease in the death rate for patients admitted to the hospital.
In addition, a 2012 report3 that drew data from a variety of sources, including the CDC, projected that between 2004 and 2040, the US population would increase by 38% and at the same time pneumococcal pneumonia hospitalizations would increase by 96%, since population growth is fastest in older age groups, who have the highest rates of disease.3
Thus, I believe that pneumonia will continue to be a big problem and that we should pursue efforts to prevent it (including vaccinating more people against it) and to better manage it.
I agree that “over-calling” acute respiratory infections as pneumonia is often the result of imprecise diagnosis. Clinical criteria, even a combination of symptoms (cough) and signs (fever, tachycardia, and crackles), are not reliably predictive when using chest radiography as the standard.4 This can lead to the overuse of antimicrobials.
The Centers for Medicare and Medicaid Services used to call for starting the first dose of antibiotics within a specified time (at one time it was 4 hours, subsequently it became 6 hours) of presentation to the hospital with community-acquired pneumonia. Although the actual effect was uncertain, many feared that this performance measure would unintentionally lead to the indiscriminate use of antimicrobials to achieve high rates of compliance in patients who have little evidence of pneumonia, in order to not miss a possible case.5,6 However, it is important to be aware that this measure was retired in 2012 and is no longer in effect.
WE NEED BETTER ASSESSMENTS AND TREATMENTS
We need better ways to assess and manage patients with pneumonia. I believe part of the solution to better assessment lies in improved diagnostic tools, and these are now becoming available.
As Dr. Prasad notes, the causative pathogen is rarely identified using standard diagnostic methods. However, polymerase chain reaction testing and measurement of the biomarker procalcitonin may improve our diagnostic accuracy and, hopefully, lead to better outcomes.7 The results of these tests can be rapidly available and thus may aid the point-of-care decision to treat or not to treat with antimicrobials and to allow for therapy to be started within an acceptable period. In addition, procalcitonin testing has been shown to help differentiate viral from bacterial causes of respiratory tract infection.
Dr. Prasad states that no randomized trial has compared antibiotics with supportive care in pneumonia. Although this is true for recent trials, historical studies demonstrate that antibiotics reduce death rates in patients with pneumonia.8 Indeed, these are the basis for the recent changes in the US Food and Drug Administration guidance for clinical trials of pneumonia.9
Treatment is best when it is directed at the pathogen, but there is little consensus on the practicality of achieving this goal at the primary point of care. A study funded by the National Institutes of Health is about to start enrollment to compare the effect of narrow-spectrum therapy vs the standard of care based on rapid diagnostics.10 Identification of a specific pathogen will allow directed therapy without the need for a broad-spectrum empiric regimen. In contrast, finding a viral cause without an accompanying bacterial cause will prevent the unnecessary use of antibacterials in many cases. A significant percent of cases of pneumonia in adults are caused by viruses alone.6
Thus, the question will not be, “Should we treat community-acquired pneumonia with antibacterials” but rather, “What is the optimal treatment for pneumonia with a defined cause?” This is a major change from an empirical broad-spectrum regimen (treat all likely pathogens) to a more specific approach that has several potential benefits, including better patient outcomes and less emergence of resistance. To paraphrase Dr. Prasad, the time has come to find this out.
In his commentary in this issue, Dr. Vinay Prasad provides a well-supported perspective on the overdiagnosis of pneumonia.
Although I agree that there can be a tendency to overdiagnose pneumonia, we must not overlook the fact that pneumonia is still a leading cause of death in the United States.
The number of cases of invasive pneumococcal disease (mostly bacteremic pneumonia) in people over age 65 has increased over the past decade.1 This increase is not the result of overdiagnosis, since the diagnosis relies on the well-established US Centers for Disease Control and Prevention (CDC) surveillance system, which requires a positive culture from a sterile site. However, to an extent, the increase can be explained by the increasing age of our population and by the associated comorbidities.2 These comorbidities increase the predisposition to and the severity of pneumonia and adversely affect the outcome—which may also explain why we have seen no significant decrease in the death rate for patients admitted to the hospital.
In addition, a 2012 report3 that drew data from a variety of sources, including the CDC, projected that between 2004 and 2040, the US population would increase by 38% and at the same time pneumococcal pneumonia hospitalizations would increase by 96%, since population growth is fastest in older age groups, who have the highest rates of disease.3
Thus, I believe that pneumonia will continue to be a big problem and that we should pursue efforts to prevent it (including vaccinating more people against it) and to better manage it.
I agree that “over-calling” acute respiratory infections as pneumonia is often the result of imprecise diagnosis. Clinical criteria, even a combination of symptoms (cough) and signs (fever, tachycardia, and crackles), are not reliably predictive when using chest radiography as the standard.4 This can lead to the overuse of antimicrobials.
The Centers for Medicare and Medicaid Services used to call for starting the first dose of antibiotics within a specified time (at one time it was 4 hours, subsequently it became 6 hours) of presentation to the hospital with community-acquired pneumonia. Although the actual effect was uncertain, many feared that this performance measure would unintentionally lead to the indiscriminate use of antimicrobials to achieve high rates of compliance in patients who have little evidence of pneumonia, in order to not miss a possible case.5,6 However, it is important to be aware that this measure was retired in 2012 and is no longer in effect.
WE NEED BETTER ASSESSMENTS AND TREATMENTS
We need better ways to assess and manage patients with pneumonia. I believe part of the solution to better assessment lies in improved diagnostic tools, and these are now becoming available.
As Dr. Prasad notes, the causative pathogen is rarely identified using standard diagnostic methods. However, polymerase chain reaction testing and measurement of the biomarker procalcitonin may improve our diagnostic accuracy and, hopefully, lead to better outcomes.7 The results of these tests can be rapidly available and thus may aid the point-of-care decision to treat or not to treat with antimicrobials and to allow for therapy to be started within an acceptable period. In addition, procalcitonin testing has been shown to help differentiate viral from bacterial causes of respiratory tract infection.
Dr. Prasad states that no randomized trial has compared antibiotics with supportive care in pneumonia. Although this is true for recent trials, historical studies demonstrate that antibiotics reduce death rates in patients with pneumonia.8 Indeed, these are the basis for the recent changes in the US Food and Drug Administration guidance for clinical trials of pneumonia.9
Treatment is best when it is directed at the pathogen, but there is little consensus on the practicality of achieving this goal at the primary point of care. A study funded by the National Institutes of Health is about to start enrollment to compare the effect of narrow-spectrum therapy vs the standard of care based on rapid diagnostics.10 Identification of a specific pathogen will allow directed therapy without the need for a broad-spectrum empiric regimen. In contrast, finding a viral cause without an accompanying bacterial cause will prevent the unnecessary use of antibacterials in many cases. A significant percent of cases of pneumonia in adults are caused by viruses alone.6
Thus, the question will not be, “Should we treat community-acquired pneumonia with antibacterials” but rather, “What is the optimal treatment for pneumonia with a defined cause?” This is a major change from an empirical broad-spectrum regimen (treat all likely pathogens) to a more specific approach that has several potential benefits, including better patient outcomes and less emergence of resistance. To paraphrase Dr. Prasad, the time has come to find this out.
- US Centers for Disease Control and Prevention. Active bacterial core surveillance (ABCs) http://www.cdc.gov/abcs/reports-findings/surv-reports.html. Accessed June 20, 2013.
- Fry AM, Shay DK, Holman RC, Curns AT, Anderson LJ. Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988–2002. JAMA 2005; 294:2712–2719.
- Wroe PC, Finkelstein JA, Ray GT, et al. Aging population and future burden of pneumococcal pneumonia in the United States. J Infect Dis 2012; 205:1589–1592.
- Metlay JP, Fine MJ. Testing strategies in the initial management of patients with community-acquired pneumonia. Ann Intern Med 2003; 138:109–118.
- File TM, Solomkin JS, Cosgrove SE. Strategies for improving antimicrobial use and the role of antimicrobial stewardship programs. Clin Infect Dis 2011; 53(suppl 1):S15–S22.
- File TM, Gross PA. Performance measurement in community-acquired pneumonia: consequences intended and unintended. Clin Infect Dis 2007; 44:942–944.
- File TM. New diagnostic tests for pneumonia: what is their role in clinical practice? Clin Chest Med 2011; 32:417–430.
- Spellberg B, Talbot GH, Brass EP, Bradley JS, Boucher HW, Gilbert DN; Infectious Diseases Society of America. Position paper: recommended design features of future clinical trials of antibacterial agents for community-acquired pneumonia. Clin Infect Dis 2008; 47(suppl 3):S249–S265.
- Division of Drug Information. Guidance for industry. Community-acquired bacterial pneumonia: Developing drugs for treatment. http://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm123686.pdf. Accessed August 4, 2013.
- US National Institutes of Health. Microbiology testing with the aim of directed antimicrobial therapy for CAP (NIHCAP). Department of Microbiology Infectious Diseases Protocol 10-0061. http://clinicaltrials.gov/ct2/show/NCT01662258?term=community+acquired+pneumonia&cond=%22Pneumonia%22&titles=microbiology+testing+with+the+aim+of+directed+antimicrobial+therapy&rank=1. Accessed August 4, 2013.
- US Centers for Disease Control and Prevention. Active bacterial core surveillance (ABCs) http://www.cdc.gov/abcs/reports-findings/surv-reports.html. Accessed June 20, 2013.
- Fry AM, Shay DK, Holman RC, Curns AT, Anderson LJ. Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988–2002. JAMA 2005; 294:2712–2719.
- Wroe PC, Finkelstein JA, Ray GT, et al. Aging population and future burden of pneumococcal pneumonia in the United States. J Infect Dis 2012; 205:1589–1592.
- Metlay JP, Fine MJ. Testing strategies in the initial management of patients with community-acquired pneumonia. Ann Intern Med 2003; 138:109–118.
- File TM, Solomkin JS, Cosgrove SE. Strategies for improving antimicrobial use and the role of antimicrobial stewardship programs. Clin Infect Dis 2011; 53(suppl 1):S15–S22.
- File TM, Gross PA. Performance measurement in community-acquired pneumonia: consequences intended and unintended. Clin Infect Dis 2007; 44:942–944.
- File TM. New diagnostic tests for pneumonia: what is their role in clinical practice? Clin Chest Med 2011; 32:417–430.
- Spellberg B, Talbot GH, Brass EP, Bradley JS, Boucher HW, Gilbert DN; Infectious Diseases Society of America. Position paper: recommended design features of future clinical trials of antibacterial agents for community-acquired pneumonia. Clin Infect Dis 2008; 47(suppl 3):S249–S265.
- Division of Drug Information. Guidance for industry. Community-acquired bacterial pneumonia: Developing drugs for treatment. http://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm123686.pdf. Accessed August 4, 2013.
- US National Institutes of Health. Microbiology testing with the aim of directed antimicrobial therapy for CAP (NIHCAP). Department of Microbiology Infectious Diseases Protocol 10-0061. http://clinicaltrials.gov/ct2/show/NCT01662258?term=community+acquired+pneumonia&cond=%22Pneumonia%22&titles=microbiology+testing+with+the+aim+of+directed+antimicrobial+therapy&rank=1. Accessed August 4, 2013.