User login
JOURNAL SCANSummary of Key ArticlesExploring the Role of Metanx® in Diabetic Neuropathy
Summary of Key Articles
Exploring the Role of Metanx® in Diabetic Neuropathy
A supplement to Internal Medicine News. This supplement was sponsored by Nestlé Health Science-Pamlab, Inc.
- Introduction
- Prevalence and Etiology
- Signs and Symptoms
- Disease Progression
- Shortcomings of Available Palliative Prescription Therapies
- Role of Metanx® in Diabetic Neuropathy
- A Randomized Trial of Metanx® in Patients with Type 2 Diabetes and Peripheral Neuropathy
- Efficacy of Metanx® in Treating Peripheral Neuropathy and Increasing Nerve Fiber Density in Zucker Diabetic Fatty Rats
Faculty/Faculty Disclosures
Aaron I. Vinik, MD, PhD
Professor of Medicine/Pathology/Neurobiology
Director of Research and Neuroendocrine Unit
Murray Waitzer Endowed Chair of Diabetes Research
Strelitz Diabetes Center for Endocrine and Metabolic Disorders
Eastern Virginia Medical School
Norfolk, Virginia
Dr Vinik has received compensation from Nestlé Health Science-Pamlab, Inc., for his participation in preparing this supplement.
Vivian Fonseca, MD
Tullis–Tulane Alumni Chair in Diabetes
Professor of Medicine
Chief, Section of Endocrinology
Tulane University School of Medicine
New Orleans, Louisiana
Dr Fonseca reports that he has served as a consultant for Nestlé Health Science-Pamlab, Inc., and has received compensation from Nestlé Health Science-Pamlab, Inc., for his participation in preparing this supplement.
A supplement to Internal Medicine News. This supplement was sponsored by Nestlé Health Science-Pamlab, Inc.
- Introduction
- Prevalence and Etiology
- Signs and Symptoms
- Disease Progression
- Shortcomings of Available Palliative Prescription Therapies
- Role of Metanx® in Diabetic Neuropathy
- A Randomized Trial of Metanx® in Patients with Type 2 Diabetes and Peripheral Neuropathy
- Efficacy of Metanx® in Treating Peripheral Neuropathy and Increasing Nerve Fiber Density in Zucker Diabetic Fatty Rats
Faculty/Faculty Disclosures
Aaron I. Vinik, MD, PhD
Professor of Medicine/Pathology/Neurobiology
Director of Research and Neuroendocrine Unit
Murray Waitzer Endowed Chair of Diabetes Research
Strelitz Diabetes Center for Endocrine and Metabolic Disorders
Eastern Virginia Medical School
Norfolk, Virginia
Dr Vinik has received compensation from Nestlé Health Science-Pamlab, Inc., for his participation in preparing this supplement.
Vivian Fonseca, MD
Tullis–Tulane Alumni Chair in Diabetes
Professor of Medicine
Chief, Section of Endocrinology
Tulane University School of Medicine
New Orleans, Louisiana
Dr Fonseca reports that he has served as a consultant for Nestlé Health Science-Pamlab, Inc., and has received compensation from Nestlé Health Science-Pamlab, Inc., for his participation in preparing this supplement.
A supplement to Internal Medicine News. This supplement was sponsored by Nestlé Health Science-Pamlab, Inc.
- Introduction
- Prevalence and Etiology
- Signs and Symptoms
- Disease Progression
- Shortcomings of Available Palliative Prescription Therapies
- Role of Metanx® in Diabetic Neuropathy
- A Randomized Trial of Metanx® in Patients with Type 2 Diabetes and Peripheral Neuropathy
- Efficacy of Metanx® in Treating Peripheral Neuropathy and Increasing Nerve Fiber Density in Zucker Diabetic Fatty Rats
Faculty/Faculty Disclosures
Aaron I. Vinik, MD, PhD
Professor of Medicine/Pathology/Neurobiology
Director of Research and Neuroendocrine Unit
Murray Waitzer Endowed Chair of Diabetes Research
Strelitz Diabetes Center for Endocrine and Metabolic Disorders
Eastern Virginia Medical School
Norfolk, Virginia
Dr Vinik has received compensation from Nestlé Health Science-Pamlab, Inc., for his participation in preparing this supplement.
Vivian Fonseca, MD
Tullis–Tulane Alumni Chair in Diabetes
Professor of Medicine
Chief, Section of Endocrinology
Tulane University School of Medicine
New Orleans, Louisiana
Dr Fonseca reports that he has served as a consultant for Nestlé Health Science-Pamlab, Inc., and has received compensation from Nestlé Health Science-Pamlab, Inc., for his participation in preparing this supplement.
Summary of Key Articles
Exploring the Role of Metanx® in Diabetic Neuropathy
Summary of Key Articles
Exploring the Role of Metanx® in Diabetic Neuropathy
JOURNAL SCAN Summary of Key ArticlesExploring the Role of Metanx® in Diabetic Neuropathy
Summary of Key Articles
Exploring the Role of Metanx® in Diabetic Neuropathy
A supplement to Family Practice News. This supplement was sponsored by Nestlé Health Science-Pamlab, Inc.
Topics
- Introduction
- Prevalence and Etiology
- Signs and Symptoms
- Disease Progression
- Shortcomings of Available Palliative Prescription Therapies
- Role of Metanx® in Diabetic Neuropathy
- A Randomized Trial of Metanx® in Patients with Type 2 Diabetes and Peripheral Neuropathy
- Efficacy of Metanx® in Treating Peripheral Neuropathy and Increasing Nerve Fiber Density in Zucker Diabetic Fatty Rats
Faculty/Faculty Disclosures
Aaron I. Vinik, MD, PhD
Professor of Medicine/Pathology/Neurobiology
Director of Research and Neuroendocrine Unit
Murray Waitzer Endowed Chair of Diabetes Research
Strelitz Diabetes Center for Endocrine and Metabolic Disorders
Eastern Virginia Medical School
Norfolk, Virginia
Dr Vinik has received compensation from Nestlé Health Science-Pamlab, Inc., for his participation in preparing this supplement.
Vivian Fonseca, MD
Tullis–Tulane Alumni Chair in Diabetes
Professor of Medicine
Chief, Section of Endocrinology
Tulane University School of Medicine
New Orleans, Louisiana
Dr Fonseca reports that he has served as a consultant for Nestlé Health Science-Pamlab, Inc., and has received compensation from Nestlé Health Science-Pamlab, Inc., for his participation in preparing this supplement.
A supplement to Family Practice News. This supplement was sponsored by Nestlé Health Science-Pamlab, Inc.
Topics
- Introduction
- Prevalence and Etiology
- Signs and Symptoms
- Disease Progression
- Shortcomings of Available Palliative Prescription Therapies
- Role of Metanx® in Diabetic Neuropathy
- A Randomized Trial of Metanx® in Patients with Type 2 Diabetes and Peripheral Neuropathy
- Efficacy of Metanx® in Treating Peripheral Neuropathy and Increasing Nerve Fiber Density in Zucker Diabetic Fatty Rats
Faculty/Faculty Disclosures
Aaron I. Vinik, MD, PhD
Professor of Medicine/Pathology/Neurobiology
Director of Research and Neuroendocrine Unit
Murray Waitzer Endowed Chair of Diabetes Research
Strelitz Diabetes Center for Endocrine and Metabolic Disorders
Eastern Virginia Medical School
Norfolk, Virginia
Dr Vinik has received compensation from Nestlé Health Science-Pamlab, Inc., for his participation in preparing this supplement.
Vivian Fonseca, MD
Tullis–Tulane Alumni Chair in Diabetes
Professor of Medicine
Chief, Section of Endocrinology
Tulane University School of Medicine
New Orleans, Louisiana
Dr Fonseca reports that he has served as a consultant for Nestlé Health Science-Pamlab, Inc., and has received compensation from Nestlé Health Science-Pamlab, Inc., for his participation in preparing this supplement.
A supplement to Family Practice News. This supplement was sponsored by Nestlé Health Science-Pamlab, Inc.
Topics
- Introduction
- Prevalence and Etiology
- Signs and Symptoms
- Disease Progression
- Shortcomings of Available Palliative Prescription Therapies
- Role of Metanx® in Diabetic Neuropathy
- A Randomized Trial of Metanx® in Patients with Type 2 Diabetes and Peripheral Neuropathy
- Efficacy of Metanx® in Treating Peripheral Neuropathy and Increasing Nerve Fiber Density in Zucker Diabetic Fatty Rats
Faculty/Faculty Disclosures
Aaron I. Vinik, MD, PhD
Professor of Medicine/Pathology/Neurobiology
Director of Research and Neuroendocrine Unit
Murray Waitzer Endowed Chair of Diabetes Research
Strelitz Diabetes Center for Endocrine and Metabolic Disorders
Eastern Virginia Medical School
Norfolk, Virginia
Dr Vinik has received compensation from Nestlé Health Science-Pamlab, Inc., for his participation in preparing this supplement.
Vivian Fonseca, MD
Tullis–Tulane Alumni Chair in Diabetes
Professor of Medicine
Chief, Section of Endocrinology
Tulane University School of Medicine
New Orleans, Louisiana
Dr Fonseca reports that he has served as a consultant for Nestlé Health Science-Pamlab, Inc., and has received compensation from Nestlé Health Science-Pamlab, Inc., for his participation in preparing this supplement.
Summary of Key Articles
Exploring the Role of Metanx® in Diabetic Neuropathy
Summary of Key Articles
Exploring the Role of Metanx® in Diabetic Neuropathy
JOURNAL SCANSummary of Key ArticlesExploring the Role of Metanx® in Diabetic Neuropathy
Summary of Key Articles
Exploring the Role of Metanx® in Diabetic Neuropathy
A supplement to Clinical Endocrinology News. This supplement was sponsored by Nestlé Health Science-Pamlab, Inc.
Topics
- Introduction
- Prevalence and Etiology
- Signs and Symptoms
- Disease Progression
- Shortcomings of Available Palliative Prescription Therapies
- Role of Metanx® in Diabetic Neuropathy
- A Randomized Trial of Metanx® in Patients with Type 2 Diabetes and Peripheral Neuropathy
- Efficacy of Metanx® in Treating Peripheral Neuropathy and Increasing Nerve Fiber Density in Zucker Diabetic Fatty Rats
Faculty/Faculty Disclosures
Aaron I. Vinik, MD, PhD
Professor of Medicine/Pathology/Neurobiology
Director of Research and Neuroendocrine Unit
Murray Waitzer Endowed Chair of Diabetes Research
Strelitz Diabetes Center for Endocrine and Metabolic Disorders
Eastern Virginia Medical School
Norfolk, Virginia
Dr Vinik has received compensation from Nestlé Health Science-Pamlab, Inc., for his participation in preparing this supplement.
Vivian Fonseca, MD
Tullis–Tulane Alumni Chair in Diabetes
Professor of Medicine
Chief, Section of Endocrinology
Tulane University School of Medicine
New Orleans, Louisiana
Dr Fonseca reports that he has served as a consultant for Nestlé Health Science-Pamlab, Inc., and has received compensation from Nestlé Health Science-Pamlab, Inc., for his participation in preparing this supplement.
A supplement to Clinical Endocrinology News. This supplement was sponsored by Nestlé Health Science-Pamlab, Inc.
Topics
- Introduction
- Prevalence and Etiology
- Signs and Symptoms
- Disease Progression
- Shortcomings of Available Palliative Prescription Therapies
- Role of Metanx® in Diabetic Neuropathy
- A Randomized Trial of Metanx® in Patients with Type 2 Diabetes and Peripheral Neuropathy
- Efficacy of Metanx® in Treating Peripheral Neuropathy and Increasing Nerve Fiber Density in Zucker Diabetic Fatty Rats
Faculty/Faculty Disclosures
Aaron I. Vinik, MD, PhD
Professor of Medicine/Pathology/Neurobiology
Director of Research and Neuroendocrine Unit
Murray Waitzer Endowed Chair of Diabetes Research
Strelitz Diabetes Center for Endocrine and Metabolic Disorders
Eastern Virginia Medical School
Norfolk, Virginia
Dr Vinik has received compensation from Nestlé Health Science-Pamlab, Inc., for his participation in preparing this supplement.
Vivian Fonseca, MD
Tullis–Tulane Alumni Chair in Diabetes
Professor of Medicine
Chief, Section of Endocrinology
Tulane University School of Medicine
New Orleans, Louisiana
Dr Fonseca reports that he has served as a consultant for Nestlé Health Science-Pamlab, Inc., and has received compensation from Nestlé Health Science-Pamlab, Inc., for his participation in preparing this supplement.
A supplement to Clinical Endocrinology News. This supplement was sponsored by Nestlé Health Science-Pamlab, Inc.
Topics
- Introduction
- Prevalence and Etiology
- Signs and Symptoms
- Disease Progression
- Shortcomings of Available Palliative Prescription Therapies
- Role of Metanx® in Diabetic Neuropathy
- A Randomized Trial of Metanx® in Patients with Type 2 Diabetes and Peripheral Neuropathy
- Efficacy of Metanx® in Treating Peripheral Neuropathy and Increasing Nerve Fiber Density in Zucker Diabetic Fatty Rats
Faculty/Faculty Disclosures
Aaron I. Vinik, MD, PhD
Professor of Medicine/Pathology/Neurobiology
Director of Research and Neuroendocrine Unit
Murray Waitzer Endowed Chair of Diabetes Research
Strelitz Diabetes Center for Endocrine and Metabolic Disorders
Eastern Virginia Medical School
Norfolk, Virginia
Dr Vinik has received compensation from Nestlé Health Science-Pamlab, Inc., for his participation in preparing this supplement.
Vivian Fonseca, MD
Tullis–Tulane Alumni Chair in Diabetes
Professor of Medicine
Chief, Section of Endocrinology
Tulane University School of Medicine
New Orleans, Louisiana
Dr Fonseca reports that he has served as a consultant for Nestlé Health Science-Pamlab, Inc., and has received compensation from Nestlé Health Science-Pamlab, Inc., for his participation in preparing this supplement.
Summary of Key Articles
Exploring the Role of Metanx® in Diabetic Neuropathy
Summary of Key Articles
Exploring the Role of Metanx® in Diabetic Neuropathy
More than a document: The importance of the informed consent process
In a recent issue of JAMA Surgery, Dr. Jacqueline M. Garonzik-Wang and colleagues presented the results of an important study of missing surgical consent forms at Johns Hopkins Hospital. The authors tallied the absence of a surgical consent form in a patient’s medical record and the resulting delays and other impacts on the surgical services. The authors also surveyed nurses, surgical residents, and surgical faculty regarding their satisfaction with the informed consent process. The results of the study show that cases are often delayed and surgical residents are often pulled away from other activities (e.g., educational conferences) to have new consent forms signed in the preoperative area. In addition, both faculty and residents had concerns about residents obtaining informed consent for major elective procedures.
This is undoubtedly an important study in that it casts light upon an important source of delays and dissatisfaction in the preoperative setting. However, are there additional lessons about informed consent that might be gleaned from this type of analysis?
Moving beyond the study itself, other important issues arise. Consider a patient who comes to the office for evaluation of a symptomatic hernia. Once the surgeon decides that the operation is indicated, the consent process requires a description of the indications (benefits), risks, and alternatives for the patient. Even though the surgeon may be convinced that the benefits of the operation outweigh the risks, the patient still needs to be convinced. Depending on the patient and the procedure being recommended, the time necessary to explain the above to the patient so that he or she is adequately informed and willing to sign the consent form will vary greatly.
In contemporary surgical practice, the determination of when the patient has been adequately informed is made by the patient. At the point that he or she is comfortable enough with the recommendation to proceed to an operation, the informed consent process has reached its conclusion. Only at this point, is the informed consent form even relevant to the discussion. The patient’s signature on the informed consent form is designed to signify the conclusion of the informed consent process.
Although we often mix the signature on the form with the process itself, they are, in fact, markedly different. The informed consent process is an ethical requirement; whereas the signature on the form is a legal requirement. The fact that these two requirements are different can readily be seen from the Mayo Clinic experience. For years, no informed consent forms were even used at the Mayo Clinic! The discussion of the indications, risks, and alternatives was documented in the surgeon’s notes and the fact that the patient showed up for the elective operation could be taken as the evidence of the adequacy of the informed consent process. Although this practice was acceptable to both surgeons and patients for years, the Clinic ultimately changed its practice in response to federal regulations that require the patient’s signature on an informed consent form.
Certainly, there is nothing inherently wrong with the practice of obtaining a signature from a patient on a consent form at the conclusion of the informed consent process. However, the current emphasis on the form itself has had a tendency for the process to be short changed in favor of getting the signature. The fact that both practicing surgeons and surgeons in training often slip into the habit of referring to the process solely by the form can frequently be seen. How often have we or our colleagues talked about "consenting the patient" when we really mean "obtaining informed consent from a patient"?
The Hopkins study serves to remind us that if we really take the process of obtaining informed consent from surgical patients as ethically important, we must be sure to give it the attention it deserves in our practice. If obtaining informed consent is central to the ethical practice of surgery, then why do we so often depend on the least experienced member of the surgical team to carry out this task right before surgery? Perhaps this practice does not reflect our devaluation of the informed consent process as much as a realization that if a patient scheduled for elective surgery has discussed the operation with the surgeon and has chosen to come to the hospital for the procedure, we can assume that the patient has already had a satisfactory consent process. In this context, the problem of the missing consent form is less an ethical issue than a clerical one that might be solved by eliminating the paper form and depending on technology for a solution.
How might a technological fix help in this situation? Among the possibilities would be to have paper forms signed in the attending surgeon’s office at the time of the informed consent discussion. The form could then be scanned into the electronic medical record. Such an approach should significantly reduce the numbers of missing forms since the electronic version cannot be misplaced. This approach will not, however, solve the problem of the missing consent form if the patient is undecided about surgery when he or she leaves the outpatient visit. In such cases, the patient may not be back to the office or hospital until the day of surgery.
Alternatively, all of the information on the standard informed consent form could be made electronic and after the discussion with the attending surgeon, the electronic version could be signed if the patient is amenable, or printed for the patient to take home if he or she is undecided. If the patient then decides to proceed with surgery, the patient could sign in to a secure website and electronically acknowledge (that is, sign) the electronic consent form. This electronic version could then be reviewed by the preoperative nurse and the patient on the day of surgery. As long as the informed consent process that is dependent on the relationship between the surgeon and patient remains intact, there is no reason why technology might not help us eliminate the problem of the missing consent form.
Garonzik-Wang JM, Brat G, Salazar JH, et al. Missing consent forms in the preoperative area: A single-center assessment of the scope of the problem and its downstream effects. JAMA Surg. Published online July 10, 2013, E1-E4.
Dr. Angelos is an ACS Fellow; the Linda Kohler Anderson Professor of Surgery and Surgical Ethics; chief, endocrine surgery; and associate director of the MacLean Center for Clinical Medical Ethics at the University of Chicago.
In a recent issue of JAMA Surgery, Dr. Jacqueline M. Garonzik-Wang and colleagues presented the results of an important study of missing surgical consent forms at Johns Hopkins Hospital. The authors tallied the absence of a surgical consent form in a patient’s medical record and the resulting delays and other impacts on the surgical services. The authors also surveyed nurses, surgical residents, and surgical faculty regarding their satisfaction with the informed consent process. The results of the study show that cases are often delayed and surgical residents are often pulled away from other activities (e.g., educational conferences) to have new consent forms signed in the preoperative area. In addition, both faculty and residents had concerns about residents obtaining informed consent for major elective procedures.
This is undoubtedly an important study in that it casts light upon an important source of delays and dissatisfaction in the preoperative setting. However, are there additional lessons about informed consent that might be gleaned from this type of analysis?
Moving beyond the study itself, other important issues arise. Consider a patient who comes to the office for evaluation of a symptomatic hernia. Once the surgeon decides that the operation is indicated, the consent process requires a description of the indications (benefits), risks, and alternatives for the patient. Even though the surgeon may be convinced that the benefits of the operation outweigh the risks, the patient still needs to be convinced. Depending on the patient and the procedure being recommended, the time necessary to explain the above to the patient so that he or she is adequately informed and willing to sign the consent form will vary greatly.
In contemporary surgical practice, the determination of when the patient has been adequately informed is made by the patient. At the point that he or she is comfortable enough with the recommendation to proceed to an operation, the informed consent process has reached its conclusion. Only at this point, is the informed consent form even relevant to the discussion. The patient’s signature on the informed consent form is designed to signify the conclusion of the informed consent process.
Although we often mix the signature on the form with the process itself, they are, in fact, markedly different. The informed consent process is an ethical requirement; whereas the signature on the form is a legal requirement. The fact that these two requirements are different can readily be seen from the Mayo Clinic experience. For years, no informed consent forms were even used at the Mayo Clinic! The discussion of the indications, risks, and alternatives was documented in the surgeon’s notes and the fact that the patient showed up for the elective operation could be taken as the evidence of the adequacy of the informed consent process. Although this practice was acceptable to both surgeons and patients for years, the Clinic ultimately changed its practice in response to federal regulations that require the patient’s signature on an informed consent form.
Certainly, there is nothing inherently wrong with the practice of obtaining a signature from a patient on a consent form at the conclusion of the informed consent process. However, the current emphasis on the form itself has had a tendency for the process to be short changed in favor of getting the signature. The fact that both practicing surgeons and surgeons in training often slip into the habit of referring to the process solely by the form can frequently be seen. How often have we or our colleagues talked about "consenting the patient" when we really mean "obtaining informed consent from a patient"?
The Hopkins study serves to remind us that if we really take the process of obtaining informed consent from surgical patients as ethically important, we must be sure to give it the attention it deserves in our practice. If obtaining informed consent is central to the ethical practice of surgery, then why do we so often depend on the least experienced member of the surgical team to carry out this task right before surgery? Perhaps this practice does not reflect our devaluation of the informed consent process as much as a realization that if a patient scheduled for elective surgery has discussed the operation with the surgeon and has chosen to come to the hospital for the procedure, we can assume that the patient has already had a satisfactory consent process. In this context, the problem of the missing consent form is less an ethical issue than a clerical one that might be solved by eliminating the paper form and depending on technology for a solution.
How might a technological fix help in this situation? Among the possibilities would be to have paper forms signed in the attending surgeon’s office at the time of the informed consent discussion. The form could then be scanned into the electronic medical record. Such an approach should significantly reduce the numbers of missing forms since the electronic version cannot be misplaced. This approach will not, however, solve the problem of the missing consent form if the patient is undecided about surgery when he or she leaves the outpatient visit. In such cases, the patient may not be back to the office or hospital until the day of surgery.
Alternatively, all of the information on the standard informed consent form could be made electronic and after the discussion with the attending surgeon, the electronic version could be signed if the patient is amenable, or printed for the patient to take home if he or she is undecided. If the patient then decides to proceed with surgery, the patient could sign in to a secure website and electronically acknowledge (that is, sign) the electronic consent form. This electronic version could then be reviewed by the preoperative nurse and the patient on the day of surgery. As long as the informed consent process that is dependent on the relationship between the surgeon and patient remains intact, there is no reason why technology might not help us eliminate the problem of the missing consent form.
Garonzik-Wang JM, Brat G, Salazar JH, et al. Missing consent forms in the preoperative area: A single-center assessment of the scope of the problem and its downstream effects. JAMA Surg. Published online July 10, 2013, E1-E4.
Dr. Angelos is an ACS Fellow; the Linda Kohler Anderson Professor of Surgery and Surgical Ethics; chief, endocrine surgery; and associate director of the MacLean Center for Clinical Medical Ethics at the University of Chicago.
In a recent issue of JAMA Surgery, Dr. Jacqueline M. Garonzik-Wang and colleagues presented the results of an important study of missing surgical consent forms at Johns Hopkins Hospital. The authors tallied the absence of a surgical consent form in a patient’s medical record and the resulting delays and other impacts on the surgical services. The authors also surveyed nurses, surgical residents, and surgical faculty regarding their satisfaction with the informed consent process. The results of the study show that cases are often delayed and surgical residents are often pulled away from other activities (e.g., educational conferences) to have new consent forms signed in the preoperative area. In addition, both faculty and residents had concerns about residents obtaining informed consent for major elective procedures.
This is undoubtedly an important study in that it casts light upon an important source of delays and dissatisfaction in the preoperative setting. However, are there additional lessons about informed consent that might be gleaned from this type of analysis?
Moving beyond the study itself, other important issues arise. Consider a patient who comes to the office for evaluation of a symptomatic hernia. Once the surgeon decides that the operation is indicated, the consent process requires a description of the indications (benefits), risks, and alternatives for the patient. Even though the surgeon may be convinced that the benefits of the operation outweigh the risks, the patient still needs to be convinced. Depending on the patient and the procedure being recommended, the time necessary to explain the above to the patient so that he or she is adequately informed and willing to sign the consent form will vary greatly.
In contemporary surgical practice, the determination of when the patient has been adequately informed is made by the patient. At the point that he or she is comfortable enough with the recommendation to proceed to an operation, the informed consent process has reached its conclusion. Only at this point, is the informed consent form even relevant to the discussion. The patient’s signature on the informed consent form is designed to signify the conclusion of the informed consent process.
Although we often mix the signature on the form with the process itself, they are, in fact, markedly different. The informed consent process is an ethical requirement; whereas the signature on the form is a legal requirement. The fact that these two requirements are different can readily be seen from the Mayo Clinic experience. For years, no informed consent forms were even used at the Mayo Clinic! The discussion of the indications, risks, and alternatives was documented in the surgeon’s notes and the fact that the patient showed up for the elective operation could be taken as the evidence of the adequacy of the informed consent process. Although this practice was acceptable to both surgeons and patients for years, the Clinic ultimately changed its practice in response to federal regulations that require the patient’s signature on an informed consent form.
Certainly, there is nothing inherently wrong with the practice of obtaining a signature from a patient on a consent form at the conclusion of the informed consent process. However, the current emphasis on the form itself has had a tendency for the process to be short changed in favor of getting the signature. The fact that both practicing surgeons and surgeons in training often slip into the habit of referring to the process solely by the form can frequently be seen. How often have we or our colleagues talked about "consenting the patient" when we really mean "obtaining informed consent from a patient"?
The Hopkins study serves to remind us that if we really take the process of obtaining informed consent from surgical patients as ethically important, we must be sure to give it the attention it deserves in our practice. If obtaining informed consent is central to the ethical practice of surgery, then why do we so often depend on the least experienced member of the surgical team to carry out this task right before surgery? Perhaps this practice does not reflect our devaluation of the informed consent process as much as a realization that if a patient scheduled for elective surgery has discussed the operation with the surgeon and has chosen to come to the hospital for the procedure, we can assume that the patient has already had a satisfactory consent process. In this context, the problem of the missing consent form is less an ethical issue than a clerical one that might be solved by eliminating the paper form and depending on technology for a solution.
How might a technological fix help in this situation? Among the possibilities would be to have paper forms signed in the attending surgeon’s office at the time of the informed consent discussion. The form could then be scanned into the electronic medical record. Such an approach should significantly reduce the numbers of missing forms since the electronic version cannot be misplaced. This approach will not, however, solve the problem of the missing consent form if the patient is undecided about surgery when he or she leaves the outpatient visit. In such cases, the patient may not be back to the office or hospital until the day of surgery.
Alternatively, all of the information on the standard informed consent form could be made electronic and after the discussion with the attending surgeon, the electronic version could be signed if the patient is amenable, or printed for the patient to take home if he or she is undecided. If the patient then decides to proceed with surgery, the patient could sign in to a secure website and electronically acknowledge (that is, sign) the electronic consent form. This electronic version could then be reviewed by the preoperative nurse and the patient on the day of surgery. As long as the informed consent process that is dependent on the relationship between the surgeon and patient remains intact, there is no reason why technology might not help us eliminate the problem of the missing consent form.
Garonzik-Wang JM, Brat G, Salazar JH, et al. Missing consent forms in the preoperative area: A single-center assessment of the scope of the problem and its downstream effects. JAMA Surg. Published online July 10, 2013, E1-E4.
Dr. Angelos is an ACS Fellow; the Linda Kohler Anderson Professor of Surgery and Surgical Ethics; chief, endocrine surgery; and associate director of the MacLean Center for Clinical Medical Ethics at the University of Chicago.
What is causing her abdominal pain?
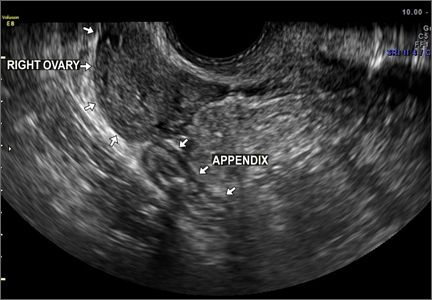
CASE: A healthy, nulliparous, 20-year-old woman visits her ObGyn to report a 2-day history of right lower quadrant pain. Her last menstrual period was appropriately timed and normal. She is not sexually active. Upon examination, she exhibits minimal left and right lower quadrant tenderness. Examination with the vaginal speculum reveals no vaginal or cervical abnormalities, and bimanual examination reveals a uterus of normal size, with cervical motion tenderness but no adnexal fullness or mass. For this reason, transvaginal ultrasound (TVUS) is performed. It reveals an enlarged, edematous appendix adjacent to a normal-appearing right ovary (FIGURE 1).
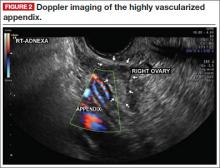
No uterine or ovarian pathology is noted. Because the appendix is enlarged on TVUS, Doppler interrogation is added, which shows abundant vascularity of the appendix (FIGURE 2).
What do these findings suggest?
Acute appendicitis is the most likely diagnosis, as both the physical findings and ultrasound imaging point to it. The patient is referred to a general surgeon, who examines her, noting that she is afebrile, with tenderness in the right lower quadrant. She exhibits localized guarding at McBurneys point, with mild rebound. There is no sign of organomegaly. Bowel sounds are normal, with no distention. The patient undergoes laparoscopy, which confirms the diagnosis. The appendix is resected successfully, and rupture is averted (FIGURE 3).
The patient is discharged home on the first postoperative day. At a follow-up visit 2 weeks later, she is fully recovered and has returned to full and normal activity.
Clinicians who are familiar with the appearance of an inflamed appendix on TVUS may be able to expedite the management of women with appendicitis, avoiding the potential delay, expense, and radiation exposure associated with computed tomography imaging of the abdomen and pelvis.
Acknowledgment
The authors are grateful to Grace J. Horton, RDMS, and Christine L. Bubier, AS, RT(R), RDMS, who generated the images in this case.
Do you have a DIAGNOSTIC IN-SIGHT?
Submit a query for your image-based case! [email protected]
CASE: A healthy, nulliparous, 20-year-old woman visits her ObGyn to report a 2-day history of right lower quadrant pain. Her last menstrual period was appropriately timed and normal. She is not sexually active. Upon examination, she exhibits minimal left and right lower quadrant tenderness. Examination with the vaginal speculum reveals no vaginal or cervical abnormalities, and bimanual examination reveals a uterus of normal size, with cervical motion tenderness but no adnexal fullness or mass. For this reason, transvaginal ultrasound (TVUS) is performed. It reveals an enlarged, edematous appendix adjacent to a normal-appearing right ovary (FIGURE 1).
No uterine or ovarian pathology is noted. Because the appendix is enlarged on TVUS, Doppler interrogation is added, which shows abundant vascularity of the appendix (FIGURE 2).
What do these findings suggest?
Acute appendicitis is the most likely diagnosis, as both the physical findings and ultrasound imaging point to it. The patient is referred to a general surgeon, who examines her, noting that she is afebrile, with tenderness in the right lower quadrant. She exhibits localized guarding at McBurneys point, with mild rebound. There is no sign of organomegaly. Bowel sounds are normal, with no distention. The patient undergoes laparoscopy, which confirms the diagnosis. The appendix is resected successfully, and rupture is averted (FIGURE 3).
The patient is discharged home on the first postoperative day. At a follow-up visit 2 weeks later, she is fully recovered and has returned to full and normal activity.
Clinicians who are familiar with the appearance of an inflamed appendix on TVUS may be able to expedite the management of women with appendicitis, avoiding the potential delay, expense, and radiation exposure associated with computed tomography imaging of the abdomen and pelvis.
Acknowledgment
The authors are grateful to Grace J. Horton, RDMS, and Christine L. Bubier, AS, RT(R), RDMS, who generated the images in this case.
Do you have a DIAGNOSTIC IN-SIGHT?
Submit a query for your image-based case! [email protected]
CASE: A healthy, nulliparous, 20-year-old woman visits her ObGyn to report a 2-day history of right lower quadrant pain. Her last menstrual period was appropriately timed and normal. She is not sexually active. Upon examination, she exhibits minimal left and right lower quadrant tenderness. Examination with the vaginal speculum reveals no vaginal or cervical abnormalities, and bimanual examination reveals a uterus of normal size, with cervical motion tenderness but no adnexal fullness or mass. For this reason, transvaginal ultrasound (TVUS) is performed. It reveals an enlarged, edematous appendix adjacent to a normal-appearing right ovary (FIGURE 1).
No uterine or ovarian pathology is noted. Because the appendix is enlarged on TVUS, Doppler interrogation is added, which shows abundant vascularity of the appendix (FIGURE 2).
What do these findings suggest?
Acute appendicitis is the most likely diagnosis, as both the physical findings and ultrasound imaging point to it. The patient is referred to a general surgeon, who examines her, noting that she is afebrile, with tenderness in the right lower quadrant. She exhibits localized guarding at McBurneys point, with mild rebound. There is no sign of organomegaly. Bowel sounds are normal, with no distention. The patient undergoes laparoscopy, which confirms the diagnosis. The appendix is resected successfully, and rupture is averted (FIGURE 3).
The patient is discharged home on the first postoperative day. At a follow-up visit 2 weeks later, she is fully recovered and has returned to full and normal activity.
Clinicians who are familiar with the appearance of an inflamed appendix on TVUS may be able to expedite the management of women with appendicitis, avoiding the potential delay, expense, and radiation exposure associated with computed tomography imaging of the abdomen and pelvis.
Acknowledgment
The authors are grateful to Grace J. Horton, RDMS, and Christine L. Bubier, AS, RT(R), RDMS, who generated the images in this case.
Do you have a DIAGNOSTIC IN-SIGHT?
Submit a query for your image-based case! [email protected]
CMS’ proposal to pay for care coordination: the ACO bridge?
Betting that it will more than pay for itself in savings, on July 5 the Centers for Medicare and Medicaid Services issued a proposed rule to pay physicians for non–face-to-face chronic care management. This would cover such things as development of care plans, reports on a patient’s status, coordination along the care continuum, and integration of health information across settings.
The proposal requires the patient to have had an annual Medicare wellness visit in the last 12 months. In addition, the physician must meet electronic health record (EHR) meaningful use standards and must have care coordinators who assist in care for patients with complex chronic conditions. CMS believes that these efforts, heretofore largely not reimbursed under the fee-for-service system, will actually end up reducing spending while simultaneously improving quality. How? By reducing downstream costs through reduced hospitalizations, the use of post–acute care services, and reduced emergency department visits. The public may comment until Sept. 6, 2013. The final policies will be issued in November and go into effect in 2015.
An ACO bridge? Readers of this column know that this pretty much describes the success strategy for a primary care physician–led accountable care organization (ACO) (less the webbing of joint financial accountability, a common technology platform, access to a full patient population, and the expense of setting one up).
What is great is that this is a relatively painless way for primary care physicians to get compensation to change behavior patterns in ways Dr. Jeffrey Cain, president of the American Academy of Family Physicians, declares necessary for primary care’s "survival." It will further prove the value proposition of the medical home model. The benefits then can be leveraged through common pursuit with colleagues of care coordination for a patient population empowered by data, best practices, and resources of a primary care–led ACO.
While the final details of the CMS proposal will not be known until the fall, presumably primary care physicians could obtain both up-front payment for non–face-to-face chronic care management and qualify for ACO shared savings distributions on the back end.
Worst case, the final rules will be unworkably burdensome. Better case, recognition of the "value" of the medical home model is being recognized. Best case, this is a nice bridge for physicians to develop the habits to thrive in the accountable-care era while getting paid to do it.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians in forming integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author ([email protected] or 919-821-6612).
Betting that it will more than pay for itself in savings, on July 5 the Centers for Medicare and Medicaid Services issued a proposed rule to pay physicians for non–face-to-face chronic care management. This would cover such things as development of care plans, reports on a patient’s status, coordination along the care continuum, and integration of health information across settings.
The proposal requires the patient to have had an annual Medicare wellness visit in the last 12 months. In addition, the physician must meet electronic health record (EHR) meaningful use standards and must have care coordinators who assist in care for patients with complex chronic conditions. CMS believes that these efforts, heretofore largely not reimbursed under the fee-for-service system, will actually end up reducing spending while simultaneously improving quality. How? By reducing downstream costs through reduced hospitalizations, the use of post–acute care services, and reduced emergency department visits. The public may comment until Sept. 6, 2013. The final policies will be issued in November and go into effect in 2015.
An ACO bridge? Readers of this column know that this pretty much describes the success strategy for a primary care physician–led accountable care organization (ACO) (less the webbing of joint financial accountability, a common technology platform, access to a full patient population, and the expense of setting one up).
What is great is that this is a relatively painless way for primary care physicians to get compensation to change behavior patterns in ways Dr. Jeffrey Cain, president of the American Academy of Family Physicians, declares necessary for primary care’s "survival." It will further prove the value proposition of the medical home model. The benefits then can be leveraged through common pursuit with colleagues of care coordination for a patient population empowered by data, best practices, and resources of a primary care–led ACO.
While the final details of the CMS proposal will not be known until the fall, presumably primary care physicians could obtain both up-front payment for non–face-to-face chronic care management and qualify for ACO shared savings distributions on the back end.
Worst case, the final rules will be unworkably burdensome. Better case, recognition of the "value" of the medical home model is being recognized. Best case, this is a nice bridge for physicians to develop the habits to thrive in the accountable-care era while getting paid to do it.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians in forming integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author ([email protected] or 919-821-6612).
Betting that it will more than pay for itself in savings, on July 5 the Centers for Medicare and Medicaid Services issued a proposed rule to pay physicians for non–face-to-face chronic care management. This would cover such things as development of care plans, reports on a patient’s status, coordination along the care continuum, and integration of health information across settings.
The proposal requires the patient to have had an annual Medicare wellness visit in the last 12 months. In addition, the physician must meet electronic health record (EHR) meaningful use standards and must have care coordinators who assist in care for patients with complex chronic conditions. CMS believes that these efforts, heretofore largely not reimbursed under the fee-for-service system, will actually end up reducing spending while simultaneously improving quality. How? By reducing downstream costs through reduced hospitalizations, the use of post–acute care services, and reduced emergency department visits. The public may comment until Sept. 6, 2013. The final policies will be issued in November and go into effect in 2015.
An ACO bridge? Readers of this column know that this pretty much describes the success strategy for a primary care physician–led accountable care organization (ACO) (less the webbing of joint financial accountability, a common technology platform, access to a full patient population, and the expense of setting one up).
What is great is that this is a relatively painless way for primary care physicians to get compensation to change behavior patterns in ways Dr. Jeffrey Cain, president of the American Academy of Family Physicians, declares necessary for primary care’s "survival." It will further prove the value proposition of the medical home model. The benefits then can be leveraged through common pursuit with colleagues of care coordination for a patient population empowered by data, best practices, and resources of a primary care–led ACO.
While the final details of the CMS proposal will not be known until the fall, presumably primary care physicians could obtain both up-front payment for non–face-to-face chronic care management and qualify for ACO shared savings distributions on the back end.
Worst case, the final rules will be unworkably burdensome. Better case, recognition of the "value" of the medical home model is being recognized. Best case, this is a nice bridge for physicians to develop the habits to thrive in the accountable-care era while getting paid to do it.
Mr. Bobbitt is a senior partner and head of the Health Law Group at the Smith Anderson law firm in Raleigh, N.C. He has many years’ experience assisting physicians in forming integrated delivery systems. He has spoken and written nationally to primary care physicians on the strategies and practicalities of forming or joining ACOs. This article is meant to be educational and does not constitute legal advice. For additional information, readers may contact the author ([email protected] or 919-821-6612).
A Different Source of Elbow Pain
ANSWER
The radiograph shows no obvious fracture or dislocation. However, there are two small, radiopaque densities noted within the soft tissue. These are most likely consistent with broken glass pieces.
When the laceration was irrigated and the wound probed, the glass bits were found and removed prior to wound closure.
ANSWER
The radiograph shows no obvious fracture or dislocation. However, there are two small, radiopaque densities noted within the soft tissue. These are most likely consistent with broken glass pieces.
When the laceration was irrigated and the wound probed, the glass bits were found and removed prior to wound closure.
ANSWER
The radiograph shows no obvious fracture or dislocation. However, there are two small, radiopaque densities noted within the soft tissue. These are most likely consistent with broken glass pieces.
When the laceration was irrigated and the wound probed, the glass bits were found and removed prior to wound closure.

A 30-year-old man is brought to your facility after being in a motor vehicle collision. He was an unrestrained driver who lost control of his vehicle, went off the road, and hit a tree. Emergency personnel on the scene indicated there was moderate damage to his vehicle, including a broken windshield, and no air bag deployment. The patient is complaining of right shoulder, chest, hip, and left elbow pain. His medical history is unremarkable. His vital signs are normal. On physical examination, he has superficial lacerations on his forehead, face, and both forearms. Bleeding from all wounds is controlled. Palpation reveals some bruising of the right shoulder, chest, right hip, and left elbow; no obvious deformity or neurovascular compromise is noted. Multiple radiographs are ordered; the left elbow is shown. What is your impression?
New and Noteworthy Information—August 2013
Patients with Alzheimer’s disease are less likely to have cancer, and patients with cancer are less likely to have Alzheimer’s disease, according to data published online ahead of print July 10 in Neurology. Researchers conducted a cohort study of more than one million people in northern Italy. They derived cancer incidence using the local health authority’s tumor registry and calculated the incidence of Alzheimer’s dementia from registries of drug prescriptions, hospitalizations, and payment exemptions. The risk of cancer in patients with Alzheimer’s dementia was reduced by 50%, and the risk of Alzheimer’s dementia in patients with cancer was reduced by 35%. The investigators observed this relationship in almost all subgroup analyses, suggesting that anticipated potential confounding factors did not significantly influence the results.
Children exposed to antiepileptic drugs in utero may have an increased risk of adverse development within their first three years of life, according to research published online ahead of print July 19 in Epilepsia. From mid-1999 through December 2008, researchers followed children born to mothers who had been recruited at 13 to 17 weeks of pregnancy. Mothers reported their children’s motor development, language, social skills, and autistic traits at 18 months and 36 months. A total of 333 children were exposed to antiepileptic drugs in utero. At 18 months, exposed children had an increased risk of abnormal scores for gross motor skills and autistic traits, compared with nonexposed children. At 36 months, exposed children had an increased risk of abnormal scores for gross motor skills, sentence skills, and autistic traits.
The spatial pattern of amyloid deposition may be related to cognitive performance, according to a study published online ahead of print July 15 in Neurobiology of Aging. Researchers examined the spatial patterns of amyloid deposition throughout the brain using Pittsburgh Compound Blue PET data from the Baltimore Longitudinal Study of Aging. The group approximated spatial patterns of the temporal progression of amyloid plaque deposition from cross-sectional data. Results were consistent with patterns of progression known from autopsy studies. When the investigators categorized participants into subgroups based on longitudinal change in memory performance, they found significantly different spatial patterns of the estimated progression of amyloid deposition between these subgroups. This finding may affect the use of amyloid imaging as a biomarker in research and clinical applications, said the researchers.
A low frequency of physical activity may be associated with an increased risk of stroke, according to data published online ahead of print July 18 in Stroke. Researchers analyzed data for 27,348 participants in the Reasons for Geographic And Racial Differences in Stroke study who had no prior diagnosis of stroke. Participants reported their frequency of moderate-to-vigorous physical activity at baseline according to three categories. Physical inactivity was reported by 33% of participants and was associated with a 20% higher risk of stroke. Adjustment for demographics and socioeconomic factors did not affect the risk, but further adjustment for traditional stroke risk factors completely attenuated the risk. Effects of physical activity are likely to be mediated through the reduction of traditional risk factors, said the researchers.
FTY-720, an immunomodulator for treating multiple sclerosis, may alleviate existing cardiac hypertrophy, according to research published in the July 1 issue of Circulation: Heart Failure. Investigators subjected male C57/Bl6 mice to transverse aortic constriction (TAC) for one week. The researchers treated the mice with FTY-720 for two subsequent weeks while continuing to subject them to TAC. Mice treated with FTY-720 had significantly reduced ventricular mass, ameliorated fibrosis, and improved cardiac performance, compared with mice that received vehicle. Mechanistic studies suggested that FTY-720 appreciably inhibited nuclear factor of activated T-cells activity. In addition, pertussis toxin (Gi-coupled receptor inhibitor) substantially blocked the antihypertrophic effect of FTY-720 in primary rat and human cardiomyocytes. FTY-720 or its analogs could be a promising approach for treating hypertrophic heart disease, said the investigators.
For patients with cardiac arrest who require vasopressors, a combination of vasopressin, epinephrine, and methylprednisolone during cardiopulmonary resuscitation (CPR) and stress-dose hydrocortisone in postresuscitation shock may improve survival to hospital discharge and result in favorable neurologic status, according to data published in the July 17 JAMA. Researchers studied 268 consecutive patients with cardiac arrest requiring epinephrine. Patients received vasopressin plus epinephrine or saline placebo plus epinephrine for the first five CPR cycles after randomization, followed by additional epinephrine if needed. During the first CPR cycle after randomization, patients in the intervention group received methylprednisolone, and patients in the control group received saline placebo. Patients in the treatment arm had higher probability for return of spontaneous circulation of 20 minutes or longer and survival to hospital discharge with cerebral performance category score of 1 or 2.
Chinese people may have a higher risk of stroke than Caucasians, according to research published in the July 16 Neurology. Investigators analyzed studies conducted since 1990 in Chinese populations of first-ever stroke incidence and pathologic types and subtypes of stroke. The team examined hospital- and community-based studies. They also examined community-based stroke studies in Caucasian populations. Age-standardized, annual, first-ever stroke incidence in community-based studies was higher among Chinese than among Caucasian populations. Intracerebral hemorrhage accounted for a larger, more variable proportion of strokes in China than in Taiwan, in Chinese community-based than in hospital-based studies, and in community-based Chinese than in Caucasian studies. The overall proportion of lacunar ischemic stroke was higher in Chinese than in Caucasian populations, but variable study methodologies precluded reliable comparisons.
Narcolepsy in humans may be triggered partly by a proliferation of cells containing histamine, according to data published online ahead of print July 2 in Annals of Neurology. Investigators used immunohistochemistry for histidine decarboxylase (HDC) and quantitative microscopy to detect histamine cells in patients with narcolepsy, Hcrt receptor-2 mutant dogs, and three mouse narcolepsy models. The researchers found an average 64% increase in the number of histamine neurons in human narcolepsy with cataplexy, with no overlap between patients with narcolepsy and controls. The investigators did not observe altered numbers of HDC cells in any of the animal models of narcolepsy, however. The increased histamine cell numbers observed in human narcolepsy may be related to the process causing the human disorder, said the study authors.
Epilepsy may be associated with an early onset of cognitive decline, according to data published online ahead of print on July 8 in JAMA Neurology. Investigators conducted a retrospective observational study of patients at a memory and aging center from 2007 to 2012. Twelve participants had amnestic mild cognitive impairment (aMCI) plus epilepsy, 35 had Alzheimer’s disease plus epilepsy, and seven had Alzheimer’s disease plus subclinical epileptiform activity. Patients with aMCI and epilepsy presented with symptoms of cognitive decline 6.8 years earlier than patients with aMCI who did not have epilepsy. Patients with Alzheimer’s disease who had epilepsy presented with cognitive decline 5.5 years earlier than patients with Alzheimer’s disease who did not have epilepsy. Patients with Alzheimer’s disease and subclinical epileptiform activity also had an early onset of cognitive decline.
Globus pallidus interna (GPi) deep brain stimulation (DBS) may be an effective therapy for DYT1-associated torsion dystonia, according to a study published in the July issue of Neurosurgery. Researchers conducted a retrospective chart review of 47 consecutive patients with DYT1 who were treated by a single surgical team during a 10-year period and followed for up to 96 months. Symptom severity was quantified with the Burke–Fahn–Marsden Dystonia Rating Scale. Motor symptom severity was reduced to less than 20% of baseline after two years of DBS therapy. Disability scores were reduced to less than 30% of baseline. Symptomatic improvement was sustained throughout follow-up. Sixty-one percent of patients had discontinued all dystonia-related medications at their last follow-up. Ninety-one percent had discontinued at least one class of medication.
Concurrent cerebrovascular disease is a common neuropathologic finding in older individuals with dementia, according to an article published online ahead of print July 10 in Brain. Cerebrovascular disease, vascular pathology, and vascular risk factors were studied in 5,715 cases from the National Alzheimer’s Coordinating Centre database who had a single neurodegenerative disease diagnosis based on a neuropathologic examination with or without cerebrovascular disease. After controlling for age and gender, the researchers found a lower prevalence of coincident cerebrovascular disease among patients with α-synucleinopathies, frontotemporal lobar degeneration due to tau and TAR DNA-binding protein 43, and prion disease than among patients with Alzheimer’s disease. This result was more significant in younger patients. Data suggest that these disorders should be targeted by treatments for cerebrovascular disease, according to the researchers.
Athletes who do not get enough sleep the night before undergoing baseline concussion testing may not perform as well as they expect, according to research presented at the 2013 Annual Meeting of the American Orthopaedic Society for Sports Medicine in Chicago. Researchers reviewed 3,686 nonconcussed athletes (1,315 female) with baseline symptom and ImPACT neurocognitive scores. Individuals reported their previous night’s sleep duration as fewer than seven hours, seven to nine hours, or more than nine hours. The study authors observed significant differences in reaction time, verbal memory, and visual memory in the group that had slept less than seven hours. Visual-motor speed scores did not seem to be affected. Significant differences in the total number of reported symptoms were associated with sleeping fewer than seven hours.
Continuation of lipophilic statin therapy may be associated with a decreased risk of Parkinson’s disease, compared with discontinuation, according to research published online ahead of print July 24 in Neurology. Between 2001 and 2008, investigators recruited participants without Parkinson’s disease who had initiated statin therapy. Among 43,810 subjects, the incidence rate for Parkinson’s disease was 1.68 and 3.52 per 1,000,000 person-days for lipophilic and hydrophilic statins, respectively. Continuation of lipophilic statins was associated with a decreased risk of Parkinson’s disease, compared with statin discontinuation. No association between hydrophilic statins and occurrence of Parkinson’s disease was observed. Among lipophilic statins, a significant association was observed for simvastatin and atorvastatin, especially in females. Long-term use of lipophilic or hydrophilic statins was not significantly associated with Parkinson’s disease.
—Erik Greb
Senior Associate Editor
Patients with Alzheimer’s disease are less likely to have cancer, and patients with cancer are less likely to have Alzheimer’s disease, according to data published online ahead of print July 10 in Neurology. Researchers conducted a cohort study of more than one million people in northern Italy. They derived cancer incidence using the local health authority’s tumor registry and calculated the incidence of Alzheimer’s dementia from registries of drug prescriptions, hospitalizations, and payment exemptions. The risk of cancer in patients with Alzheimer’s dementia was reduced by 50%, and the risk of Alzheimer’s dementia in patients with cancer was reduced by 35%. The investigators observed this relationship in almost all subgroup analyses, suggesting that anticipated potential confounding factors did not significantly influence the results.
Children exposed to antiepileptic drugs in utero may have an increased risk of adverse development within their first three years of life, according to research published online ahead of print July 19 in Epilepsia. From mid-1999 through December 2008, researchers followed children born to mothers who had been recruited at 13 to 17 weeks of pregnancy. Mothers reported their children’s motor development, language, social skills, and autistic traits at 18 months and 36 months. A total of 333 children were exposed to antiepileptic drugs in utero. At 18 months, exposed children had an increased risk of abnormal scores for gross motor skills and autistic traits, compared with nonexposed children. At 36 months, exposed children had an increased risk of abnormal scores for gross motor skills, sentence skills, and autistic traits.
The spatial pattern of amyloid deposition may be related to cognitive performance, according to a study published online ahead of print July 15 in Neurobiology of Aging. Researchers examined the spatial patterns of amyloid deposition throughout the brain using Pittsburgh Compound Blue PET data from the Baltimore Longitudinal Study of Aging. The group approximated spatial patterns of the temporal progression of amyloid plaque deposition from cross-sectional data. Results were consistent with patterns of progression known from autopsy studies. When the investigators categorized participants into subgroups based on longitudinal change in memory performance, they found significantly different spatial patterns of the estimated progression of amyloid deposition between these subgroups. This finding may affect the use of amyloid imaging as a biomarker in research and clinical applications, said the researchers.
A low frequency of physical activity may be associated with an increased risk of stroke, according to data published online ahead of print July 18 in Stroke. Researchers analyzed data for 27,348 participants in the Reasons for Geographic And Racial Differences in Stroke study who had no prior diagnosis of stroke. Participants reported their frequency of moderate-to-vigorous physical activity at baseline according to three categories. Physical inactivity was reported by 33% of participants and was associated with a 20% higher risk of stroke. Adjustment for demographics and socioeconomic factors did not affect the risk, but further adjustment for traditional stroke risk factors completely attenuated the risk. Effects of physical activity are likely to be mediated through the reduction of traditional risk factors, said the researchers.
FTY-720, an immunomodulator for treating multiple sclerosis, may alleviate existing cardiac hypertrophy, according to research published in the July 1 issue of Circulation: Heart Failure. Investigators subjected male C57/Bl6 mice to transverse aortic constriction (TAC) for one week. The researchers treated the mice with FTY-720 for two subsequent weeks while continuing to subject them to TAC. Mice treated with FTY-720 had significantly reduced ventricular mass, ameliorated fibrosis, and improved cardiac performance, compared with mice that received vehicle. Mechanistic studies suggested that FTY-720 appreciably inhibited nuclear factor of activated T-cells activity. In addition, pertussis toxin (Gi-coupled receptor inhibitor) substantially blocked the antihypertrophic effect of FTY-720 in primary rat and human cardiomyocytes. FTY-720 or its analogs could be a promising approach for treating hypertrophic heart disease, said the investigators.
For patients with cardiac arrest who require vasopressors, a combination of vasopressin, epinephrine, and methylprednisolone during cardiopulmonary resuscitation (CPR) and stress-dose hydrocortisone in postresuscitation shock may improve survival to hospital discharge and result in favorable neurologic status, according to data published in the July 17 JAMA. Researchers studied 268 consecutive patients with cardiac arrest requiring epinephrine. Patients received vasopressin plus epinephrine or saline placebo plus epinephrine for the first five CPR cycles after randomization, followed by additional epinephrine if needed. During the first CPR cycle after randomization, patients in the intervention group received methylprednisolone, and patients in the control group received saline placebo. Patients in the treatment arm had higher probability for return of spontaneous circulation of 20 minutes or longer and survival to hospital discharge with cerebral performance category score of 1 or 2.
Chinese people may have a higher risk of stroke than Caucasians, according to research published in the July 16 Neurology. Investigators analyzed studies conducted since 1990 in Chinese populations of first-ever stroke incidence and pathologic types and subtypes of stroke. The team examined hospital- and community-based studies. They also examined community-based stroke studies in Caucasian populations. Age-standardized, annual, first-ever stroke incidence in community-based studies was higher among Chinese than among Caucasian populations. Intracerebral hemorrhage accounted for a larger, more variable proportion of strokes in China than in Taiwan, in Chinese community-based than in hospital-based studies, and in community-based Chinese than in Caucasian studies. The overall proportion of lacunar ischemic stroke was higher in Chinese than in Caucasian populations, but variable study methodologies precluded reliable comparisons.
Narcolepsy in humans may be triggered partly by a proliferation of cells containing histamine, according to data published online ahead of print July 2 in Annals of Neurology. Investigators used immunohistochemistry for histidine decarboxylase (HDC) and quantitative microscopy to detect histamine cells in patients with narcolepsy, Hcrt receptor-2 mutant dogs, and three mouse narcolepsy models. The researchers found an average 64% increase in the number of histamine neurons in human narcolepsy with cataplexy, with no overlap between patients with narcolepsy and controls. The investigators did not observe altered numbers of HDC cells in any of the animal models of narcolepsy, however. The increased histamine cell numbers observed in human narcolepsy may be related to the process causing the human disorder, said the study authors.
Epilepsy may be associated with an early onset of cognitive decline, according to data published online ahead of print on July 8 in JAMA Neurology. Investigators conducted a retrospective observational study of patients at a memory and aging center from 2007 to 2012. Twelve participants had amnestic mild cognitive impairment (aMCI) plus epilepsy, 35 had Alzheimer’s disease plus epilepsy, and seven had Alzheimer’s disease plus subclinical epileptiform activity. Patients with aMCI and epilepsy presented with symptoms of cognitive decline 6.8 years earlier than patients with aMCI who did not have epilepsy. Patients with Alzheimer’s disease who had epilepsy presented with cognitive decline 5.5 years earlier than patients with Alzheimer’s disease who did not have epilepsy. Patients with Alzheimer’s disease and subclinical epileptiform activity also had an early onset of cognitive decline.
Globus pallidus interna (GPi) deep brain stimulation (DBS) may be an effective therapy for DYT1-associated torsion dystonia, according to a study published in the July issue of Neurosurgery. Researchers conducted a retrospective chart review of 47 consecutive patients with DYT1 who were treated by a single surgical team during a 10-year period and followed for up to 96 months. Symptom severity was quantified with the Burke–Fahn–Marsden Dystonia Rating Scale. Motor symptom severity was reduced to less than 20% of baseline after two years of DBS therapy. Disability scores were reduced to less than 30% of baseline. Symptomatic improvement was sustained throughout follow-up. Sixty-one percent of patients had discontinued all dystonia-related medications at their last follow-up. Ninety-one percent had discontinued at least one class of medication.
Concurrent cerebrovascular disease is a common neuropathologic finding in older individuals with dementia, according to an article published online ahead of print July 10 in Brain. Cerebrovascular disease, vascular pathology, and vascular risk factors were studied in 5,715 cases from the National Alzheimer’s Coordinating Centre database who had a single neurodegenerative disease diagnosis based on a neuropathologic examination with or without cerebrovascular disease. After controlling for age and gender, the researchers found a lower prevalence of coincident cerebrovascular disease among patients with α-synucleinopathies, frontotemporal lobar degeneration due to tau and TAR DNA-binding protein 43, and prion disease than among patients with Alzheimer’s disease. This result was more significant in younger patients. Data suggest that these disorders should be targeted by treatments for cerebrovascular disease, according to the researchers.
Athletes who do not get enough sleep the night before undergoing baseline concussion testing may not perform as well as they expect, according to research presented at the 2013 Annual Meeting of the American Orthopaedic Society for Sports Medicine in Chicago. Researchers reviewed 3,686 nonconcussed athletes (1,315 female) with baseline symptom and ImPACT neurocognitive scores. Individuals reported their previous night’s sleep duration as fewer than seven hours, seven to nine hours, or more than nine hours. The study authors observed significant differences in reaction time, verbal memory, and visual memory in the group that had slept less than seven hours. Visual-motor speed scores did not seem to be affected. Significant differences in the total number of reported symptoms were associated with sleeping fewer than seven hours.
Continuation of lipophilic statin therapy may be associated with a decreased risk of Parkinson’s disease, compared with discontinuation, according to research published online ahead of print July 24 in Neurology. Between 2001 and 2008, investigators recruited participants without Parkinson’s disease who had initiated statin therapy. Among 43,810 subjects, the incidence rate for Parkinson’s disease was 1.68 and 3.52 per 1,000,000 person-days for lipophilic and hydrophilic statins, respectively. Continuation of lipophilic statins was associated with a decreased risk of Parkinson’s disease, compared with statin discontinuation. No association between hydrophilic statins and occurrence of Parkinson’s disease was observed. Among lipophilic statins, a significant association was observed for simvastatin and atorvastatin, especially in females. Long-term use of lipophilic or hydrophilic statins was not significantly associated with Parkinson’s disease.
—Erik Greb
Senior Associate Editor
Patients with Alzheimer’s disease are less likely to have cancer, and patients with cancer are less likely to have Alzheimer’s disease, according to data published online ahead of print July 10 in Neurology. Researchers conducted a cohort study of more than one million people in northern Italy. They derived cancer incidence using the local health authority’s tumor registry and calculated the incidence of Alzheimer’s dementia from registries of drug prescriptions, hospitalizations, and payment exemptions. The risk of cancer in patients with Alzheimer’s dementia was reduced by 50%, and the risk of Alzheimer’s dementia in patients with cancer was reduced by 35%. The investigators observed this relationship in almost all subgroup analyses, suggesting that anticipated potential confounding factors did not significantly influence the results.
Children exposed to antiepileptic drugs in utero may have an increased risk of adverse development within their first three years of life, according to research published online ahead of print July 19 in Epilepsia. From mid-1999 through December 2008, researchers followed children born to mothers who had been recruited at 13 to 17 weeks of pregnancy. Mothers reported their children’s motor development, language, social skills, and autistic traits at 18 months and 36 months. A total of 333 children were exposed to antiepileptic drugs in utero. At 18 months, exposed children had an increased risk of abnormal scores for gross motor skills and autistic traits, compared with nonexposed children. At 36 months, exposed children had an increased risk of abnormal scores for gross motor skills, sentence skills, and autistic traits.
The spatial pattern of amyloid deposition may be related to cognitive performance, according to a study published online ahead of print July 15 in Neurobiology of Aging. Researchers examined the spatial patterns of amyloid deposition throughout the brain using Pittsburgh Compound Blue PET data from the Baltimore Longitudinal Study of Aging. The group approximated spatial patterns of the temporal progression of amyloid plaque deposition from cross-sectional data. Results were consistent with patterns of progression known from autopsy studies. When the investigators categorized participants into subgroups based on longitudinal change in memory performance, they found significantly different spatial patterns of the estimated progression of amyloid deposition between these subgroups. This finding may affect the use of amyloid imaging as a biomarker in research and clinical applications, said the researchers.
A low frequency of physical activity may be associated with an increased risk of stroke, according to data published online ahead of print July 18 in Stroke. Researchers analyzed data for 27,348 participants in the Reasons for Geographic And Racial Differences in Stroke study who had no prior diagnosis of stroke. Participants reported their frequency of moderate-to-vigorous physical activity at baseline according to three categories. Physical inactivity was reported by 33% of participants and was associated with a 20% higher risk of stroke. Adjustment for demographics and socioeconomic factors did not affect the risk, but further adjustment for traditional stroke risk factors completely attenuated the risk. Effects of physical activity are likely to be mediated through the reduction of traditional risk factors, said the researchers.
FTY-720, an immunomodulator for treating multiple sclerosis, may alleviate existing cardiac hypertrophy, according to research published in the July 1 issue of Circulation: Heart Failure. Investigators subjected male C57/Bl6 mice to transverse aortic constriction (TAC) for one week. The researchers treated the mice with FTY-720 for two subsequent weeks while continuing to subject them to TAC. Mice treated with FTY-720 had significantly reduced ventricular mass, ameliorated fibrosis, and improved cardiac performance, compared with mice that received vehicle. Mechanistic studies suggested that FTY-720 appreciably inhibited nuclear factor of activated T-cells activity. In addition, pertussis toxin (Gi-coupled receptor inhibitor) substantially blocked the antihypertrophic effect of FTY-720 in primary rat and human cardiomyocytes. FTY-720 or its analogs could be a promising approach for treating hypertrophic heart disease, said the investigators.
For patients with cardiac arrest who require vasopressors, a combination of vasopressin, epinephrine, and methylprednisolone during cardiopulmonary resuscitation (CPR) and stress-dose hydrocortisone in postresuscitation shock may improve survival to hospital discharge and result in favorable neurologic status, according to data published in the July 17 JAMA. Researchers studied 268 consecutive patients with cardiac arrest requiring epinephrine. Patients received vasopressin plus epinephrine or saline placebo plus epinephrine for the first five CPR cycles after randomization, followed by additional epinephrine if needed. During the first CPR cycle after randomization, patients in the intervention group received methylprednisolone, and patients in the control group received saline placebo. Patients in the treatment arm had higher probability for return of spontaneous circulation of 20 minutes or longer and survival to hospital discharge with cerebral performance category score of 1 or 2.
Chinese people may have a higher risk of stroke than Caucasians, according to research published in the July 16 Neurology. Investigators analyzed studies conducted since 1990 in Chinese populations of first-ever stroke incidence and pathologic types and subtypes of stroke. The team examined hospital- and community-based studies. They also examined community-based stroke studies in Caucasian populations. Age-standardized, annual, first-ever stroke incidence in community-based studies was higher among Chinese than among Caucasian populations. Intracerebral hemorrhage accounted for a larger, more variable proportion of strokes in China than in Taiwan, in Chinese community-based than in hospital-based studies, and in community-based Chinese than in Caucasian studies. The overall proportion of lacunar ischemic stroke was higher in Chinese than in Caucasian populations, but variable study methodologies precluded reliable comparisons.
Narcolepsy in humans may be triggered partly by a proliferation of cells containing histamine, according to data published online ahead of print July 2 in Annals of Neurology. Investigators used immunohistochemistry for histidine decarboxylase (HDC) and quantitative microscopy to detect histamine cells in patients with narcolepsy, Hcrt receptor-2 mutant dogs, and three mouse narcolepsy models. The researchers found an average 64% increase in the number of histamine neurons in human narcolepsy with cataplexy, with no overlap between patients with narcolepsy and controls. The investigators did not observe altered numbers of HDC cells in any of the animal models of narcolepsy, however. The increased histamine cell numbers observed in human narcolepsy may be related to the process causing the human disorder, said the study authors.
Epilepsy may be associated with an early onset of cognitive decline, according to data published online ahead of print on July 8 in JAMA Neurology. Investigators conducted a retrospective observational study of patients at a memory and aging center from 2007 to 2012. Twelve participants had amnestic mild cognitive impairment (aMCI) plus epilepsy, 35 had Alzheimer’s disease plus epilepsy, and seven had Alzheimer’s disease plus subclinical epileptiform activity. Patients with aMCI and epilepsy presented with symptoms of cognitive decline 6.8 years earlier than patients with aMCI who did not have epilepsy. Patients with Alzheimer’s disease who had epilepsy presented with cognitive decline 5.5 years earlier than patients with Alzheimer’s disease who did not have epilepsy. Patients with Alzheimer’s disease and subclinical epileptiform activity also had an early onset of cognitive decline.
Globus pallidus interna (GPi) deep brain stimulation (DBS) may be an effective therapy for DYT1-associated torsion dystonia, according to a study published in the July issue of Neurosurgery. Researchers conducted a retrospective chart review of 47 consecutive patients with DYT1 who were treated by a single surgical team during a 10-year period and followed for up to 96 months. Symptom severity was quantified with the Burke–Fahn–Marsden Dystonia Rating Scale. Motor symptom severity was reduced to less than 20% of baseline after two years of DBS therapy. Disability scores were reduced to less than 30% of baseline. Symptomatic improvement was sustained throughout follow-up. Sixty-one percent of patients had discontinued all dystonia-related medications at their last follow-up. Ninety-one percent had discontinued at least one class of medication.
Concurrent cerebrovascular disease is a common neuropathologic finding in older individuals with dementia, according to an article published online ahead of print July 10 in Brain. Cerebrovascular disease, vascular pathology, and vascular risk factors were studied in 5,715 cases from the National Alzheimer’s Coordinating Centre database who had a single neurodegenerative disease diagnosis based on a neuropathologic examination with or without cerebrovascular disease. After controlling for age and gender, the researchers found a lower prevalence of coincident cerebrovascular disease among patients with α-synucleinopathies, frontotemporal lobar degeneration due to tau and TAR DNA-binding protein 43, and prion disease than among patients with Alzheimer’s disease. This result was more significant in younger patients. Data suggest that these disorders should be targeted by treatments for cerebrovascular disease, according to the researchers.
Athletes who do not get enough sleep the night before undergoing baseline concussion testing may not perform as well as they expect, according to research presented at the 2013 Annual Meeting of the American Orthopaedic Society for Sports Medicine in Chicago. Researchers reviewed 3,686 nonconcussed athletes (1,315 female) with baseline symptom and ImPACT neurocognitive scores. Individuals reported their previous night’s sleep duration as fewer than seven hours, seven to nine hours, or more than nine hours. The study authors observed significant differences in reaction time, verbal memory, and visual memory in the group that had slept less than seven hours. Visual-motor speed scores did not seem to be affected. Significant differences in the total number of reported symptoms were associated with sleeping fewer than seven hours.
Continuation of lipophilic statin therapy may be associated with a decreased risk of Parkinson’s disease, compared with discontinuation, according to research published online ahead of print July 24 in Neurology. Between 2001 and 2008, investigators recruited participants without Parkinson’s disease who had initiated statin therapy. Among 43,810 subjects, the incidence rate for Parkinson’s disease was 1.68 and 3.52 per 1,000,000 person-days for lipophilic and hydrophilic statins, respectively. Continuation of lipophilic statins was associated with a decreased risk of Parkinson’s disease, compared with statin discontinuation. No association between hydrophilic statins and occurrence of Parkinson’s disease was observed. Among lipophilic statins, a significant association was observed for simvastatin and atorvastatin, especially in females. Long-term use of lipophilic or hydrophilic statins was not significantly associated with Parkinson’s disease.
—Erik Greb
Senior Associate Editor
Survey suggests docs could improve trial enrollment
Results of a nationwide poll indicate that many Americans believe participation in clinical trials is important.
And most of the individuals surveyed said they would participate in a trial if their doctor recommended it.
However, many respondents said they learned of clinical trials via the Internet, not from discussions with their physician. And most said a physician’s recommendation was an important factor in the decision to enroll in a clinical trial.
This poll was conducted online by Zogby Analytics. The results are available on the Research!America website.
The goal of the survey was to evaluate respondents’ perceptions about clinical trials and determine if perceptions differed according to racial groups. The survey included 684 non-Hispanic whites, 406 Hispanics, 403 African-Americans, and 300 Asians.
A willingness to participate
Most of the African-Americans (62%) and Hispanics (57%) polled said it’s very important to participate in a clinical trial to improve the health of others. Fifty percent of Asians agreed, as did 49% of non-Hispanic whites.
Furthermore, 75% of Hispanics, 72% of African-Americans, 71% of non-Hispanic whites, and 65% of Asians said they would likely participate in a clinical trial if it was recommended by a doctor.
And about three-quarters of all respondents said, assuming the correct privacy protections were in place, they would be willing to share personal health information to advance medical research.
“The poll reveals a willingness among minorities to participate in clinical trials to improve the quality of healthcare, but enrollment remains stubbornly low,” said Mary Woolley, president and CEO of Research!America.
Among those individuals surveyed, only 17% of Hispanics, 15% of African-Americans, 15% of non-Hispanic whites, and 11% of Asians said they or a family member had participated in a clinical trial.
When asked to give a reason for low enrollment in clinical trials, most respondents cited a lack of trust—61% of African-Americans, 54% of non-Hispanic whites, 52% of Hispanics, and 51% of Asians.
The importance of physicians, institutions
Many of the individuals surveyed said they had learned of clinical trials via the Internet—56% of Asians, 52% of non-Hispanic whites, 50% of African-Americans, and 45% of Hispanics.
Far fewer said they had heard of trials during discussions with their doctors—22% of Hispanics, 22% of non-Hispanic whites, 20% of Asians, and 17% of African-Americans.
And most respondents said a doctor’s recommendation is a “very” or “somewhat” important factor in the decision to participate in a clinical trial—81% of Hispanics, 81% of non-Hispanic whites, 80% of Asians, and 78% of African-Americans.
Institutional reputation was also deemed an important factor by 74% of African-Americans, 72% of non-Hispanic whites, 66% of Hispanics, and 66% of Asians.
And many respondents said healthcare providers should play a major role in raising awareness of clinical trials. In fact, 42% of non-Hispanic whites, 38% of Hispanics, 36% of Asians, and 33% of African-Americans said providers have the greatest responsibility in educating the public about clinical trials.
“It’s imperative that healthcare providers and others help patients gain a deeper knowledge of clinical trials so all Americans can benefit from life-saving treatments,” Woolley said.
This survey was conducted by Zogby Analytics for Research!America, the Association of Clinical Research Organizations, the Clinical Research Forum, the Friends of the National Library of Medicine, and the Clinical Trials Transformation Initiative. ![]()
Results of a nationwide poll indicate that many Americans believe participation in clinical trials is important.
And most of the individuals surveyed said they would participate in a trial if their doctor recommended it.
However, many respondents said they learned of clinical trials via the Internet, not from discussions with their physician. And most said a physician’s recommendation was an important factor in the decision to enroll in a clinical trial.
This poll was conducted online by Zogby Analytics. The results are available on the Research!America website.
The goal of the survey was to evaluate respondents’ perceptions about clinical trials and determine if perceptions differed according to racial groups. The survey included 684 non-Hispanic whites, 406 Hispanics, 403 African-Americans, and 300 Asians.
A willingness to participate
Most of the African-Americans (62%) and Hispanics (57%) polled said it’s very important to participate in a clinical trial to improve the health of others. Fifty percent of Asians agreed, as did 49% of non-Hispanic whites.
Furthermore, 75% of Hispanics, 72% of African-Americans, 71% of non-Hispanic whites, and 65% of Asians said they would likely participate in a clinical trial if it was recommended by a doctor.
And about three-quarters of all respondents said, assuming the correct privacy protections were in place, they would be willing to share personal health information to advance medical research.
“The poll reveals a willingness among minorities to participate in clinical trials to improve the quality of healthcare, but enrollment remains stubbornly low,” said Mary Woolley, president and CEO of Research!America.
Among those individuals surveyed, only 17% of Hispanics, 15% of African-Americans, 15% of non-Hispanic whites, and 11% of Asians said they or a family member had participated in a clinical trial.
When asked to give a reason for low enrollment in clinical trials, most respondents cited a lack of trust—61% of African-Americans, 54% of non-Hispanic whites, 52% of Hispanics, and 51% of Asians.
The importance of physicians, institutions
Many of the individuals surveyed said they had learned of clinical trials via the Internet—56% of Asians, 52% of non-Hispanic whites, 50% of African-Americans, and 45% of Hispanics.
Far fewer said they had heard of trials during discussions with their doctors—22% of Hispanics, 22% of non-Hispanic whites, 20% of Asians, and 17% of African-Americans.
And most respondents said a doctor’s recommendation is a “very” or “somewhat” important factor in the decision to participate in a clinical trial—81% of Hispanics, 81% of non-Hispanic whites, 80% of Asians, and 78% of African-Americans.
Institutional reputation was also deemed an important factor by 74% of African-Americans, 72% of non-Hispanic whites, 66% of Hispanics, and 66% of Asians.
And many respondents said healthcare providers should play a major role in raising awareness of clinical trials. In fact, 42% of non-Hispanic whites, 38% of Hispanics, 36% of Asians, and 33% of African-Americans said providers have the greatest responsibility in educating the public about clinical trials.
“It’s imperative that healthcare providers and others help patients gain a deeper knowledge of clinical trials so all Americans can benefit from life-saving treatments,” Woolley said.
This survey was conducted by Zogby Analytics for Research!America, the Association of Clinical Research Organizations, the Clinical Research Forum, the Friends of the National Library of Medicine, and the Clinical Trials Transformation Initiative. ![]()
Results of a nationwide poll indicate that many Americans believe participation in clinical trials is important.
And most of the individuals surveyed said they would participate in a trial if their doctor recommended it.
However, many respondents said they learned of clinical trials via the Internet, not from discussions with their physician. And most said a physician’s recommendation was an important factor in the decision to enroll in a clinical trial.
This poll was conducted online by Zogby Analytics. The results are available on the Research!America website.
The goal of the survey was to evaluate respondents’ perceptions about clinical trials and determine if perceptions differed according to racial groups. The survey included 684 non-Hispanic whites, 406 Hispanics, 403 African-Americans, and 300 Asians.
A willingness to participate
Most of the African-Americans (62%) and Hispanics (57%) polled said it’s very important to participate in a clinical trial to improve the health of others. Fifty percent of Asians agreed, as did 49% of non-Hispanic whites.
Furthermore, 75% of Hispanics, 72% of African-Americans, 71% of non-Hispanic whites, and 65% of Asians said they would likely participate in a clinical trial if it was recommended by a doctor.
And about three-quarters of all respondents said, assuming the correct privacy protections were in place, they would be willing to share personal health information to advance medical research.
“The poll reveals a willingness among minorities to participate in clinical trials to improve the quality of healthcare, but enrollment remains stubbornly low,” said Mary Woolley, president and CEO of Research!America.
Among those individuals surveyed, only 17% of Hispanics, 15% of African-Americans, 15% of non-Hispanic whites, and 11% of Asians said they or a family member had participated in a clinical trial.
When asked to give a reason for low enrollment in clinical trials, most respondents cited a lack of trust—61% of African-Americans, 54% of non-Hispanic whites, 52% of Hispanics, and 51% of Asians.
The importance of physicians, institutions
Many of the individuals surveyed said they had learned of clinical trials via the Internet—56% of Asians, 52% of non-Hispanic whites, 50% of African-Americans, and 45% of Hispanics.
Far fewer said they had heard of trials during discussions with their doctors—22% of Hispanics, 22% of non-Hispanic whites, 20% of Asians, and 17% of African-Americans.
And most respondents said a doctor’s recommendation is a “very” or “somewhat” important factor in the decision to participate in a clinical trial—81% of Hispanics, 81% of non-Hispanic whites, 80% of Asians, and 78% of African-Americans.
Institutional reputation was also deemed an important factor by 74% of African-Americans, 72% of non-Hispanic whites, 66% of Hispanics, and 66% of Asians.
And many respondents said healthcare providers should play a major role in raising awareness of clinical trials. In fact, 42% of non-Hispanic whites, 38% of Hispanics, 36% of Asians, and 33% of African-Americans said providers have the greatest responsibility in educating the public about clinical trials.
“It’s imperative that healthcare providers and others help patients gain a deeper knowledge of clinical trials so all Americans can benefit from life-saving treatments,” Woolley said.
This survey was conducted by Zogby Analytics for Research!America, the Association of Clinical Research Organizations, the Clinical Research Forum, the Friends of the National Library of Medicine, and the Clinical Trials Transformation Initiative. ![]()
Listen to John Vazquez, MD, discuss neurophobia and tips for adjusting to discomfort in treating neuro patients
Click here to listen to more of our interview with Dr. Vazquez
Click here to listen to more of our interview with Dr. Vazquez
Click here to listen to more of our interview with Dr. Vazquez