User login
Robotic vesicovaginal fistula repair: A systematic, endoscopic approach
In modern times in the United States, the vesicovaginal fistula (VVF) arises chiefly as a sequela of gynecologic surgery, usually hysterectomy. The injury most likely occurs at the time of dissection of the bladder flap off of the lower uterine segment and upper vagina.1 With increasing use of endoscopy and electrosurgery at the time of hysterectomy,2 the occurrence of VVF is likely to increase. Because of this, fistulas stemming from benign gynecologic surgical activity tend to occur above the trigone near the vaginal cuff.
Current technique of fistula repair involves either a vaginal approach, with the Latsko procedure,3 or an abdominal approach, involving a laparotomy; laparoscopy also is used with increasing frequency.4
Vaginal versus endoscopic approach. The vaginal approach can be straightforward, such as in cases of vault prolapse or a distally located fistula, or more difficult if the fistula is apical in location, especially if the apex is well suspended and the vagina is of normal length. I have found the abdominal approach to be optimal if the fistula is near the cuff and the vagina is of normal length and well suspended.
Classical teaching tells us that the first repair of the VVF is likely to be the most successful, with successively lower cure rates as the number of repair attempts increases. For this reason, I advocate the abdominal approach in most cases of apically placed VVFs.
Surgical approach
Why endoscopic, why robotic? Often, repair of the VVF is complicated by:
-
the challenge of locating the defect in the bladder
-
the technical difficulty in oversewing the bladder, which often must be done on the underside of the bladder, between the vaginal and bladder walls.
To tackle these challenges, an endoscopic approach promises improved visualization, and the robotic approach allows for surgical closure with improved visibility characteristic of endoscopy, while preserving the manual dexterity characteristic of open surgery.
Timing. It is believed that, in order to improve chances of successful surgical repair, the fistula should be approached either immediately (ie, within 1 to 2 weeks of the insult) or delayed by 8 to 12 or more weeks after the causative surgery.5
Preparation. Vesicovaginal fistulas can rarely involve the ureters, and this ureteric involvement needs to be ruled out. Accordingly, the workup of the VVF should begin with a thorough cystoscopic evaluation of the bladder, with retrograde pyelography to evaluate the integrity of the ureters bilaterally.
During this procedure, the location of the fistulous tract should be meticulously mapped. Care should be taken to document the location and extent of the fistula, as well as to identify the presence of multiple or separate tracts. If these tracts are present, they also need also to be catalogued. In my practice, the cystoscopy/retrograde pyelogram is performed as a separate surgical encounter.
Surgical technique
After the fistula is mapped and ureteric integrity is confirmed, the definitive surgical repair is performed. The steps to the surgical approach are straightforward.
1. Insert stents into the fistula and bilaterally into the ureters
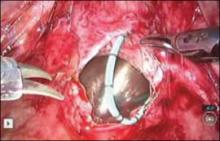
Stenting the fistula permits rapid identification of the fistula tract without the need to enter the bladder separately. The ureteric stents you use should be one color, and the fistula stent should be a second color. I use 5 French yellow stents to cannulate the ureters and a 6 French blue stent for the fistula itself. Insert the fistula stent from the bladder side of the fistula. It should exit through the vagina (FIGURES 1A and 1B). In addition, place a 3-way Foley catheter for drainage and irrigate the bladder when indicated.
Figure 1. Stent insertion
Cystoscopically place a 6 French blue stent into the bladder side of the fistula. (A) The stent as seen from inside the bladder. (B) The stent as seen from the vaginal side.
2. Place the ports for optimal access
A 0° camera is adequate for visualization. Port placement is similar to that used for robotic sacral colpopexy; I use a supraumbilically placed camera port and three 8-mm robot ports (two on the left and one on the right of the umbilicus). Each port should be separated by about 10 cm. An assistant port is placed to the far right, for passing and retrieving sutures (FIGURE 2). An atraumatic grasper, monopolar scissors, and bipolar Maryland-type forceps are placed within the ports to begin the surgical procedure.
Figure 2. Ideal port placement
Place the camera port supraunbilically, with two 8-mm robot ports
3. Place a vaginal stent to aid dissection
The stent should be a sterile cylinder and have a diameter of 2 cm to 5 cm (to match the vaginal caliber). The tip should be rounded and flattened, with an extended handle available for manipulating the stent. The handle can be held by an assistant or attached to an external uterine positioning system (FIGURE 3); I use the Uterine Positioning SystemTM (Cooper Surgical, Trumbull, Connecticut).
4. Incise the vaginal cuff
Transversely incise the vaginal cuff with the monopolar scissors (VIDEO 1).
This allows entry into the vagina at the apex. The blue stent in the fistula should be visible at the anterior vaginal wall, as demonstrated in FIGURE 4.
5. Dissect the vaginal wall
Dissect the anterior vaginal wall down to the fistula, and dissect the bladder off of the vaginal wall for about 1.5 cm to 2 cm around the fistula tract (FIGURE 5 and VIDEO 2).
6. Cut the stent
Cut the stent passing thru the fistula, to move it out of the way.
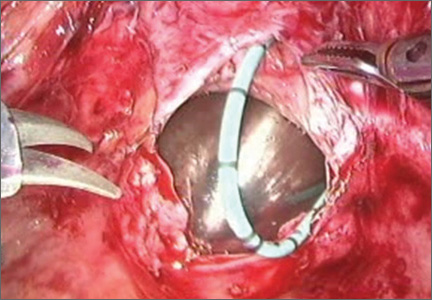
7. Close the bladder
Stitch the bladder in a running fashion using three layers of 3-0 rapid absorbable synthetic suture (FIGURE 6 and Video 3 . I prefer polyglactin 910 (Vicryl; Ethicon, Somerville, New Jersey) because it is easier to handle.
FIGURE 6: Close the bladderStitch the bladder in a running fashion using three layers of 3-0 rapid absorbable synthetic suture. Keep the closure line free of tension.
8. Close the vaginal side of the fistula
Stitch the vaginal side of the fistula in a running fashion with 2-0 absorbable synthetic suture.
9. Verify closure
Check for watertight closure by retrofilling the bladder with 100 mL of sterile milk (obtained from the labor/delivery suite). Observe the suture line for any evidence of milk leakage. (Sterile milk does not stain the tissues, and this preserves tissue visibility. For this reason, milk is preferable to indigo carmine or methylene blue.)
10. Remove the stents from the bladder
Cystoscopically remove all stents.
11. Close the laparoscopic ports
12. Follow up to ensure surgical success
Leave the indwelling Foley catheter in place for 2 to 3 weeks. After such time, remove the catheter and perform voiding cystourethrogram to document bladder wall integrity.
Discussion
I have described a systematic approach to robotic VVF repair. The robotic portion of the procedure should require about 60 to 90 minutes in the absence of significant adhesions. The technique is amenable to a laparoscopic approach, when performed by an appropriately skilled operator.
Final takeaways. Important takeaways to this repair include:
- Stent the fistula to make it easy to find intraoperatively.
- Enter the vagina from above to rapidly locate the fistula tract.
- Use sterile milk to fill the bladder to look for leaks. This works without staining the tissues.
- Minimize tension on the bladder suture line.
In modern times in the United States, the vesicovaginal fistula (VVF) arises chiefly as a sequela of gynecologic surgery, usually hysterectomy. The injury most likely occurs at the time of dissection of the bladder flap off of the lower uterine segment and upper vagina.1 With increasing use of endoscopy and electrosurgery at the time of hysterectomy,2 the occurrence of VVF is likely to increase. Because of this, fistulas stemming from benign gynecologic surgical activity tend to occur above the trigone near the vaginal cuff.
Current technique of fistula repair involves either a vaginal approach, with the Latsko procedure,3 or an abdominal approach, involving a laparotomy; laparoscopy also is used with increasing frequency.4
Vaginal versus endoscopic approach. The vaginal approach can be straightforward, such as in cases of vault prolapse or a distally located fistula, or more difficult if the fistula is apical in location, especially if the apex is well suspended and the vagina is of normal length. I have found the abdominal approach to be optimal if the fistula is near the cuff and the vagina is of normal length and well suspended.
Classical teaching tells us that the first repair of the VVF is likely to be the most successful, with successively lower cure rates as the number of repair attempts increases. For this reason, I advocate the abdominal approach in most cases of apically placed VVFs.
Surgical approach
Why endoscopic, why robotic? Often, repair of the VVF is complicated by:
-
the challenge of locating the defect in the bladder
-
the technical difficulty in oversewing the bladder, which often must be done on the underside of the bladder, between the vaginal and bladder walls.
To tackle these challenges, an endoscopic approach promises improved visualization, and the robotic approach allows for surgical closure with improved visibility characteristic of endoscopy, while preserving the manual dexterity characteristic of open surgery.
Timing. It is believed that, in order to improve chances of successful surgical repair, the fistula should be approached either immediately (ie, within 1 to 2 weeks of the insult) or delayed by 8 to 12 or more weeks after the causative surgery.5
Preparation. Vesicovaginal fistulas can rarely involve the ureters, and this ureteric involvement needs to be ruled out. Accordingly, the workup of the VVF should begin with a thorough cystoscopic evaluation of the bladder, with retrograde pyelography to evaluate the integrity of the ureters bilaterally.
During this procedure, the location of the fistulous tract should be meticulously mapped. Care should be taken to document the location and extent of the fistula, as well as to identify the presence of multiple or separate tracts. If these tracts are present, they also need also to be catalogued. In my practice, the cystoscopy/retrograde pyelogram is performed as a separate surgical encounter.
Surgical technique
After the fistula is mapped and ureteric integrity is confirmed, the definitive surgical repair is performed. The steps to the surgical approach are straightforward.
1. Insert stents into the fistula and bilaterally into the ureters
Stenting the fistula permits rapid identification of the fistula tract without the need to enter the bladder separately. The ureteric stents you use should be one color, and the fistula stent should be a second color. I use 5 French yellow stents to cannulate the ureters and a 6 French blue stent for the fistula itself. Insert the fistula stent from the bladder side of the fistula. It should exit through the vagina (FIGURES 1A and 1B). In addition, place a 3-way Foley catheter for drainage and irrigate the bladder when indicated.
Figure 1. Stent insertion
Cystoscopically place a 6 French blue stent into the bladder side of the fistula. (A) The stent as seen from inside the bladder. (B) The stent as seen from the vaginal side.
2. Place the ports for optimal access
A 0° camera is adequate for visualization. Port placement is similar to that used for robotic sacral colpopexy; I use a supraumbilically placed camera port and three 8-mm robot ports (two on the left and one on the right of the umbilicus). Each port should be separated by about 10 cm. An assistant port is placed to the far right, for passing and retrieving sutures (FIGURE 2). An atraumatic grasper, monopolar scissors, and bipolar Maryland-type forceps are placed within the ports to begin the surgical procedure.
Figure 2. Ideal port placement
Place the camera port supraunbilically, with two 8-mm robot ports
3. Place a vaginal stent to aid dissection
The stent should be a sterile cylinder and have a diameter of 2 cm to 5 cm (to match the vaginal caliber). The tip should be rounded and flattened, with an extended handle available for manipulating the stent. The handle can be held by an assistant or attached to an external uterine positioning system (FIGURE 3); I use the Uterine Positioning SystemTM (Cooper Surgical, Trumbull, Connecticut).
4. Incise the vaginal cuff
Transversely incise the vaginal cuff with the monopolar scissors (VIDEO 1).
This allows entry into the vagina at the apex. The blue stent in the fistula should be visible at the anterior vaginal wall, as demonstrated in FIGURE 4.
5. Dissect the vaginal wall
Dissect the anterior vaginal wall down to the fistula, and dissect the bladder off of the vaginal wall for about 1.5 cm to 2 cm around the fistula tract (FIGURE 5 and VIDEO 2).
6. Cut the stent
Cut the stent passing thru the fistula, to move it out of the way.
7. Close the bladder
Stitch the bladder in a running fashion using three layers of 3-0 rapid absorbable synthetic suture (FIGURE 6 and Video 3 . I prefer polyglactin 910 (Vicryl; Ethicon, Somerville, New Jersey) because it is easier to handle.
FIGURE 6: Close the bladderStitch the bladder in a running fashion using three layers of 3-0 rapid absorbable synthetic suture. Keep the closure line free of tension.
8. Close the vaginal side of the fistula
Stitch the vaginal side of the fistula in a running fashion with 2-0 absorbable synthetic suture.
9. Verify closure
Check for watertight closure by retrofilling the bladder with 100 mL of sterile milk (obtained from the labor/delivery suite). Observe the suture line for any evidence of milk leakage. (Sterile milk does not stain the tissues, and this preserves tissue visibility. For this reason, milk is preferable to indigo carmine or methylene blue.)
10. Remove the stents from the bladder
Cystoscopically remove all stents.
11. Close the laparoscopic ports
12. Follow up to ensure surgical success
Leave the indwelling Foley catheter in place for 2 to 3 weeks. After such time, remove the catheter and perform voiding cystourethrogram to document bladder wall integrity.
Discussion
I have described a systematic approach to robotic VVF repair. The robotic portion of the procedure should require about 60 to 90 minutes in the absence of significant adhesions. The technique is amenable to a laparoscopic approach, when performed by an appropriately skilled operator.
Final takeaways. Important takeaways to this repair include:
- Stent the fistula to make it easy to find intraoperatively.
- Enter the vagina from above to rapidly locate the fistula tract.
- Use sterile milk to fill the bladder to look for leaks. This works without staining the tissues.
- Minimize tension on the bladder suture line.
In modern times in the United States, the vesicovaginal fistula (VVF) arises chiefly as a sequela of gynecologic surgery, usually hysterectomy. The injury most likely occurs at the time of dissection of the bladder flap off of the lower uterine segment and upper vagina.1 With increasing use of endoscopy and electrosurgery at the time of hysterectomy,2 the occurrence of VVF is likely to increase. Because of this, fistulas stemming from benign gynecologic surgical activity tend to occur above the trigone near the vaginal cuff.
Current technique of fistula repair involves either a vaginal approach, with the Latsko procedure,3 or an abdominal approach, involving a laparotomy; laparoscopy also is used with increasing frequency.4
Vaginal versus endoscopic approach. The vaginal approach can be straightforward, such as in cases of vault prolapse or a distally located fistula, or more difficult if the fistula is apical in location, especially if the apex is well suspended and the vagina is of normal length. I have found the abdominal approach to be optimal if the fistula is near the cuff and the vagina is of normal length and well suspended.
Classical teaching tells us that the first repair of the VVF is likely to be the most successful, with successively lower cure rates as the number of repair attempts increases. For this reason, I advocate the abdominal approach in most cases of apically placed VVFs.
Surgical approach
Why endoscopic, why robotic? Often, repair of the VVF is complicated by:
-
the challenge of locating the defect in the bladder
-
the technical difficulty in oversewing the bladder, which often must be done on the underside of the bladder, between the vaginal and bladder walls.
To tackle these challenges, an endoscopic approach promises improved visualization, and the robotic approach allows for surgical closure with improved visibility characteristic of endoscopy, while preserving the manual dexterity characteristic of open surgery.
Timing. It is believed that, in order to improve chances of successful surgical repair, the fistula should be approached either immediately (ie, within 1 to 2 weeks of the insult) or delayed by 8 to 12 or more weeks after the causative surgery.5
Preparation. Vesicovaginal fistulas can rarely involve the ureters, and this ureteric involvement needs to be ruled out. Accordingly, the workup of the VVF should begin with a thorough cystoscopic evaluation of the bladder, with retrograde pyelography to evaluate the integrity of the ureters bilaterally.
During this procedure, the location of the fistulous tract should be meticulously mapped. Care should be taken to document the location and extent of the fistula, as well as to identify the presence of multiple or separate tracts. If these tracts are present, they also need also to be catalogued. In my practice, the cystoscopy/retrograde pyelogram is performed as a separate surgical encounter.
Surgical technique
After the fistula is mapped and ureteric integrity is confirmed, the definitive surgical repair is performed. The steps to the surgical approach are straightforward.
1. Insert stents into the fistula and bilaterally into the ureters
Stenting the fistula permits rapid identification of the fistula tract without the need to enter the bladder separately. The ureteric stents you use should be one color, and the fistula stent should be a second color. I use 5 French yellow stents to cannulate the ureters and a 6 French blue stent for the fistula itself. Insert the fistula stent from the bladder side of the fistula. It should exit through the vagina (FIGURES 1A and 1B). In addition, place a 3-way Foley catheter for drainage and irrigate the bladder when indicated.
Figure 1. Stent insertion
Cystoscopically place a 6 French blue stent into the bladder side of the fistula. (A) The stent as seen from inside the bladder. (B) The stent as seen from the vaginal side.
2. Place the ports for optimal access
A 0° camera is adequate for visualization. Port placement is similar to that used for robotic sacral colpopexy; I use a supraumbilically placed camera port and three 8-mm robot ports (two on the left and one on the right of the umbilicus). Each port should be separated by about 10 cm. An assistant port is placed to the far right, for passing and retrieving sutures (FIGURE 2). An atraumatic grasper, monopolar scissors, and bipolar Maryland-type forceps are placed within the ports to begin the surgical procedure.
Figure 2. Ideal port placement
Place the camera port supraunbilically, with two 8-mm robot ports
3. Place a vaginal stent to aid dissection
The stent should be a sterile cylinder and have a diameter of 2 cm to 5 cm (to match the vaginal caliber). The tip should be rounded and flattened, with an extended handle available for manipulating the stent. The handle can be held by an assistant or attached to an external uterine positioning system (FIGURE 3); I use the Uterine Positioning SystemTM (Cooper Surgical, Trumbull, Connecticut).
4. Incise the vaginal cuff
Transversely incise the vaginal cuff with the monopolar scissors (VIDEO 1).
This allows entry into the vagina at the apex. The blue stent in the fistula should be visible at the anterior vaginal wall, as demonstrated in FIGURE 4.
5. Dissect the vaginal wall
Dissect the anterior vaginal wall down to the fistula, and dissect the bladder off of the vaginal wall for about 1.5 cm to 2 cm around the fistula tract (FIGURE 5 and VIDEO 2).
6. Cut the stent
Cut the stent passing thru the fistula, to move it out of the way.
7. Close the bladder
Stitch the bladder in a running fashion using three layers of 3-0 rapid absorbable synthetic suture (FIGURE 6 and Video 3 . I prefer polyglactin 910 (Vicryl; Ethicon, Somerville, New Jersey) because it is easier to handle.
FIGURE 6: Close the bladderStitch the bladder in a running fashion using three layers of 3-0 rapid absorbable synthetic suture. Keep the closure line free of tension.
8. Close the vaginal side of the fistula
Stitch the vaginal side of the fistula in a running fashion with 2-0 absorbable synthetic suture.
9. Verify closure
Check for watertight closure by retrofilling the bladder with 100 mL of sterile milk (obtained from the labor/delivery suite). Observe the suture line for any evidence of milk leakage. (Sterile milk does not stain the tissues, and this preserves tissue visibility. For this reason, milk is preferable to indigo carmine or methylene blue.)
10. Remove the stents from the bladder
Cystoscopically remove all stents.
11. Close the laparoscopic ports
12. Follow up to ensure surgical success
Leave the indwelling Foley catheter in place for 2 to 3 weeks. After such time, remove the catheter and perform voiding cystourethrogram to document bladder wall integrity.
Discussion
I have described a systematic approach to robotic VVF repair. The robotic portion of the procedure should require about 60 to 90 minutes in the absence of significant adhesions. The technique is amenable to a laparoscopic approach, when performed by an appropriately skilled operator.
Final takeaways. Important takeaways to this repair include:
- Stent the fistula to make it easy to find intraoperatively.
- Enter the vagina from above to rapidly locate the fistula tract.
- Use sterile milk to fill the bladder to look for leaks. This works without staining the tissues.
- Minimize tension on the bladder suture line.
Patient privacy
Do no harm. There are few words that mean more to physicians, which is why many are reluctant to engage with patients online. They see social media as a minefield of potential privacy violations.
Avoiding social media entirely for fear of committing a privacy violation is not the answer in today’s increasingly social world. Instead, you should educate yourself about how to use social media safely and effectively.
Numerous medical centers and governing bodies are trying to establish social media guidelines for physicians and health care workers, but since social media is continually evolving, so will the guidelines for using it. Some existing guidelines include the following:
• American College of Physicians: new recommendations offer guidance for preserving trust when using social media.
• The Federation of State Medical Boards Model Policy Guidelines.
• Cleveland Clinic Social Media Policy.
• Mayo Clinic Social Media Policy for Employees.
• Centers for Disease Controls Social Media Guidelines and Best Practices.
It’s true that engaging with patients online poses risks to us as providers. It’s also true that we take on risk every day that we see patients. And just as a physician who violates a patient’s privacy in person could face legal ramifications, so too could he face them from committing a privacy breach online.
I encourage everyone to do their own research before engaging in social media, but here are the guidelines I adhere to for using it safely:
• Include a disclaimer on your social networks that states content is not medical advice, but rather educational information. For example, on my @Dermdoc Twitter account, my bio includes "Views here are my own, and are not medical advice."
• Maintain separate personal and professional online accounts, and direct patients to your professional accounts only.
• E-mail and other electronic modes of communication should be used only within a secure system with an established patient/physician relationship and with patient consent.
• Never respond to specific clinical questions from nonpatients online. Encourage the individual to contact his or her medical provider, or in the case of an emergency, to go to the nearest emergency department.
• Text messaging should be used only with established patients and with their consent.
• Never post information or photos online that could re-identify a patient, unless you have his or her written consent.
• If a patient identifies himself online of his own accord, you are not responsible. However, you should explain to him that you’d rather not discuss his specific case in public and redirect him to a secure means of communication with you.
• Never argue, demean, or accuse patients online. Your online behavior should reflect your professionalism and respect of others.
• Never post content or photos of yourself that are unprofessional or incriminating, such as a photo of you and your buddies partying.
In my next column, I’ll present specific examples of safe and appropriate responses to patients online.
Dr. Benabio is Physician Director of Innovation at Kaiser Permanente in San Diego. Visit his consumer health blog at thedermblog.com and his health care blog at benabio.com. Connect with him on Twitter @Dermdoc and on Facebook (DermDoc).
Do no harm. There are few words that mean more to physicians, which is why many are reluctant to engage with patients online. They see social media as a minefield of potential privacy violations.
Avoiding social media entirely for fear of committing a privacy violation is not the answer in today’s increasingly social world. Instead, you should educate yourself about how to use social media safely and effectively.
Numerous medical centers and governing bodies are trying to establish social media guidelines for physicians and health care workers, but since social media is continually evolving, so will the guidelines for using it. Some existing guidelines include the following:
• American College of Physicians: new recommendations offer guidance for preserving trust when using social media.
• The Federation of State Medical Boards Model Policy Guidelines.
• Cleveland Clinic Social Media Policy.
• Mayo Clinic Social Media Policy for Employees.
• Centers for Disease Controls Social Media Guidelines and Best Practices.
It’s true that engaging with patients online poses risks to us as providers. It’s also true that we take on risk every day that we see patients. And just as a physician who violates a patient’s privacy in person could face legal ramifications, so too could he face them from committing a privacy breach online.
I encourage everyone to do their own research before engaging in social media, but here are the guidelines I adhere to for using it safely:
• Include a disclaimer on your social networks that states content is not medical advice, but rather educational information. For example, on my @Dermdoc Twitter account, my bio includes "Views here are my own, and are not medical advice."
• Maintain separate personal and professional online accounts, and direct patients to your professional accounts only.
• E-mail and other electronic modes of communication should be used only within a secure system with an established patient/physician relationship and with patient consent.
• Never respond to specific clinical questions from nonpatients online. Encourage the individual to contact his or her medical provider, or in the case of an emergency, to go to the nearest emergency department.
• Text messaging should be used only with established patients and with their consent.
• Never post information or photos online that could re-identify a patient, unless you have his or her written consent.
• If a patient identifies himself online of his own accord, you are not responsible. However, you should explain to him that you’d rather not discuss his specific case in public and redirect him to a secure means of communication with you.
• Never argue, demean, or accuse patients online. Your online behavior should reflect your professionalism and respect of others.
• Never post content or photos of yourself that are unprofessional or incriminating, such as a photo of you and your buddies partying.
In my next column, I’ll present specific examples of safe and appropriate responses to patients online.
Dr. Benabio is Physician Director of Innovation at Kaiser Permanente in San Diego. Visit his consumer health blog at thedermblog.com and his health care blog at benabio.com. Connect with him on Twitter @Dermdoc and on Facebook (DermDoc).
Do no harm. There are few words that mean more to physicians, which is why many are reluctant to engage with patients online. They see social media as a minefield of potential privacy violations.
Avoiding social media entirely for fear of committing a privacy violation is not the answer in today’s increasingly social world. Instead, you should educate yourself about how to use social media safely and effectively.
Numerous medical centers and governing bodies are trying to establish social media guidelines for physicians and health care workers, but since social media is continually evolving, so will the guidelines for using it. Some existing guidelines include the following:
• American College of Physicians: new recommendations offer guidance for preserving trust when using social media.
• The Federation of State Medical Boards Model Policy Guidelines.
• Cleveland Clinic Social Media Policy.
• Mayo Clinic Social Media Policy for Employees.
• Centers for Disease Controls Social Media Guidelines and Best Practices.
It’s true that engaging with patients online poses risks to us as providers. It’s also true that we take on risk every day that we see patients. And just as a physician who violates a patient’s privacy in person could face legal ramifications, so too could he face them from committing a privacy breach online.
I encourage everyone to do their own research before engaging in social media, but here are the guidelines I adhere to for using it safely:
• Include a disclaimer on your social networks that states content is not medical advice, but rather educational information. For example, on my @Dermdoc Twitter account, my bio includes "Views here are my own, and are not medical advice."
• Maintain separate personal and professional online accounts, and direct patients to your professional accounts only.
• E-mail and other electronic modes of communication should be used only within a secure system with an established patient/physician relationship and with patient consent.
• Never respond to specific clinical questions from nonpatients online. Encourage the individual to contact his or her medical provider, or in the case of an emergency, to go to the nearest emergency department.
• Text messaging should be used only with established patients and with their consent.
• Never post information or photos online that could re-identify a patient, unless you have his or her written consent.
• If a patient identifies himself online of his own accord, you are not responsible. However, you should explain to him that you’d rather not discuss his specific case in public and redirect him to a secure means of communication with you.
• Never argue, demean, or accuse patients online. Your online behavior should reflect your professionalism and respect of others.
• Never post content or photos of yourself that are unprofessional or incriminating, such as a photo of you and your buddies partying.
In my next column, I’ll present specific examples of safe and appropriate responses to patients online.
Dr. Benabio is Physician Director of Innovation at Kaiser Permanente in San Diego. Visit his consumer health blog at thedermblog.com and his health care blog at benabio.com. Connect with him on Twitter @Dermdoc and on Facebook (DermDoc).
Implications of Hospital‐Acquired Anemia
Anemia is associated with poor quality of life and increased risk for death and hospitalization in population‐based and cohort investigations.[1, 2, 3, 4, 5, 6, 7] Evidence suggests that patients with normal hemoglobin (Hgb) values on hospital admission who subsequently develop hospital‐acquired anemia (HAA) have increased morbidity and mortality compared with those who do not.[8, 9] HAA is multifaceted and may occur as a result of processes of care during hospitalization, such as hemodilution from intravenous fluid administration, procedural blood loss and phlebotomy, and impaired erythropoiesis associated with critical illness.[8, 9] Moreover, correcting anemia by red blood cell transfusion also carries risk.[10, 11, 12, 13]
Our primary objective was to examine the prevalence of HAA in a population of medical and surgical patients admitted to a large quaternary referral health system. Our secondary objectives were to examine whether HAA is associated with increased mortality, length of stay (LOS), and total hospital charges compared to patients without HAA.
METHODS
Patient Population and Data Sources
The patient population consisted of 417,301 hospitalizations in adult patients (18 years of age) who were admitted to the Cleveland Clinic Health System from January 2009 to September 2011. Data for these hospitalizations came from 2 sources. Patient demographics, baseline comorbidities, and outcomes were extracted from the University HealthSystem Consortium's (UHC) clinical database/resource manager. UHC is an alliance of 116 US academic medical centers and their 272 affiliated hospitals, representing more than 90% of the nation's nonprofit academic medical centers. These data had originally been retrieved from our hospitals' administrative data systems, normalized according to UHC standardized data specifications, and submitted for inclusion in the UHC repository. Data quality was assessed using standardized error checking and data completeness algorithms and was required to meet established minimum thresholds to be included in the UHC repository.
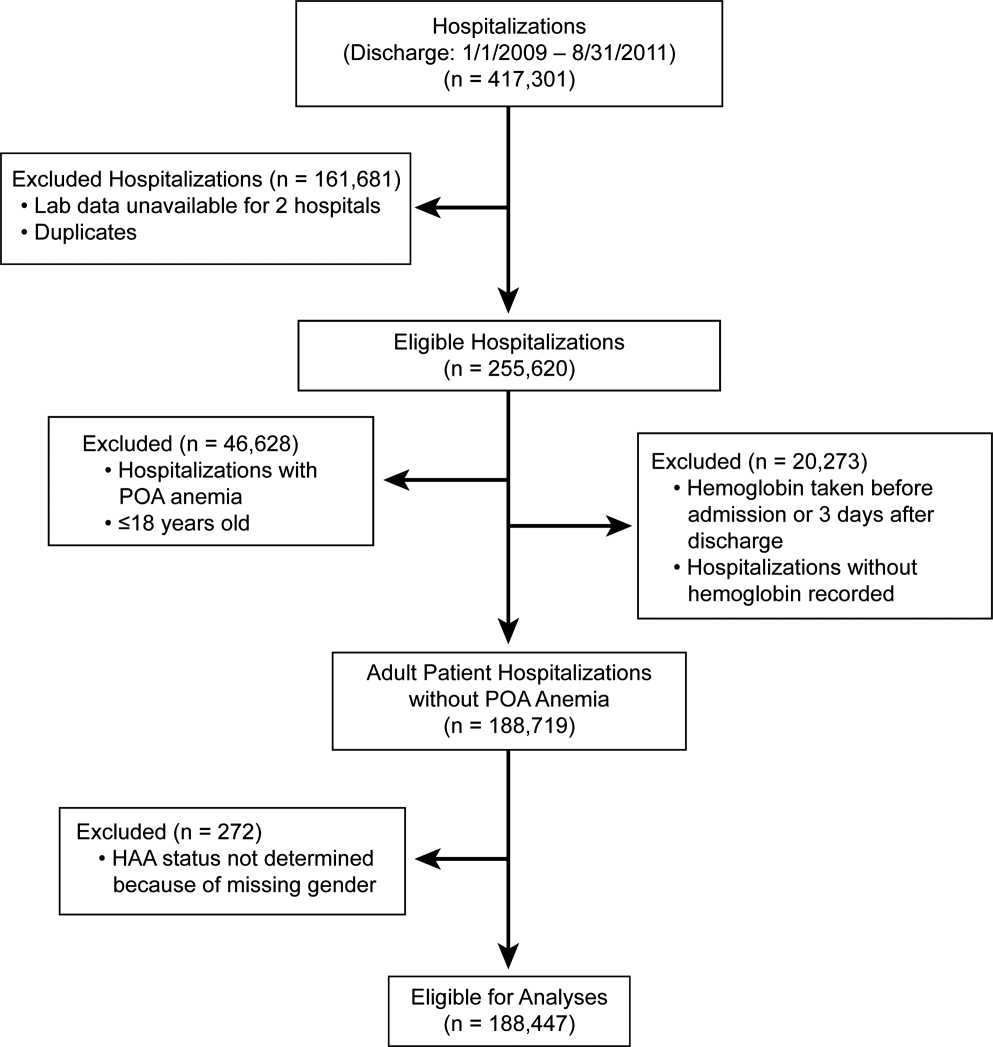
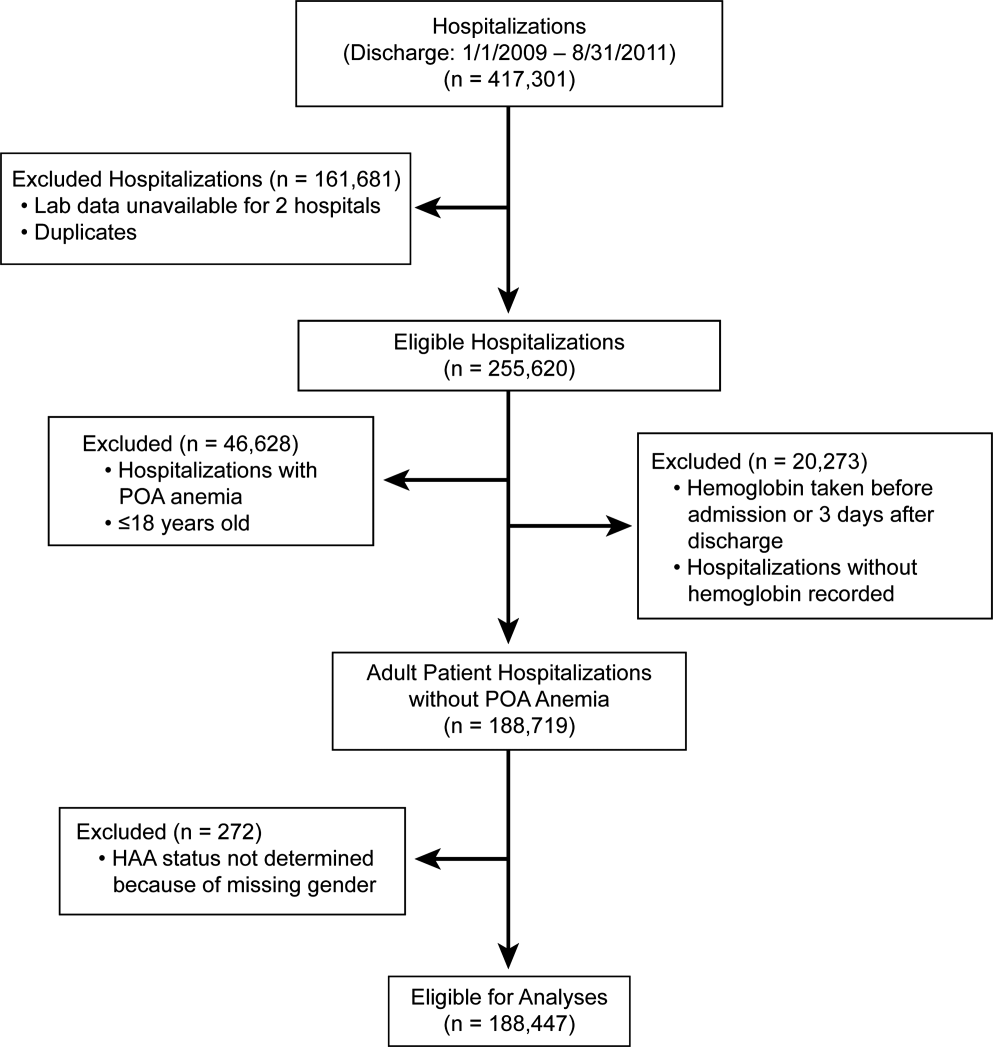
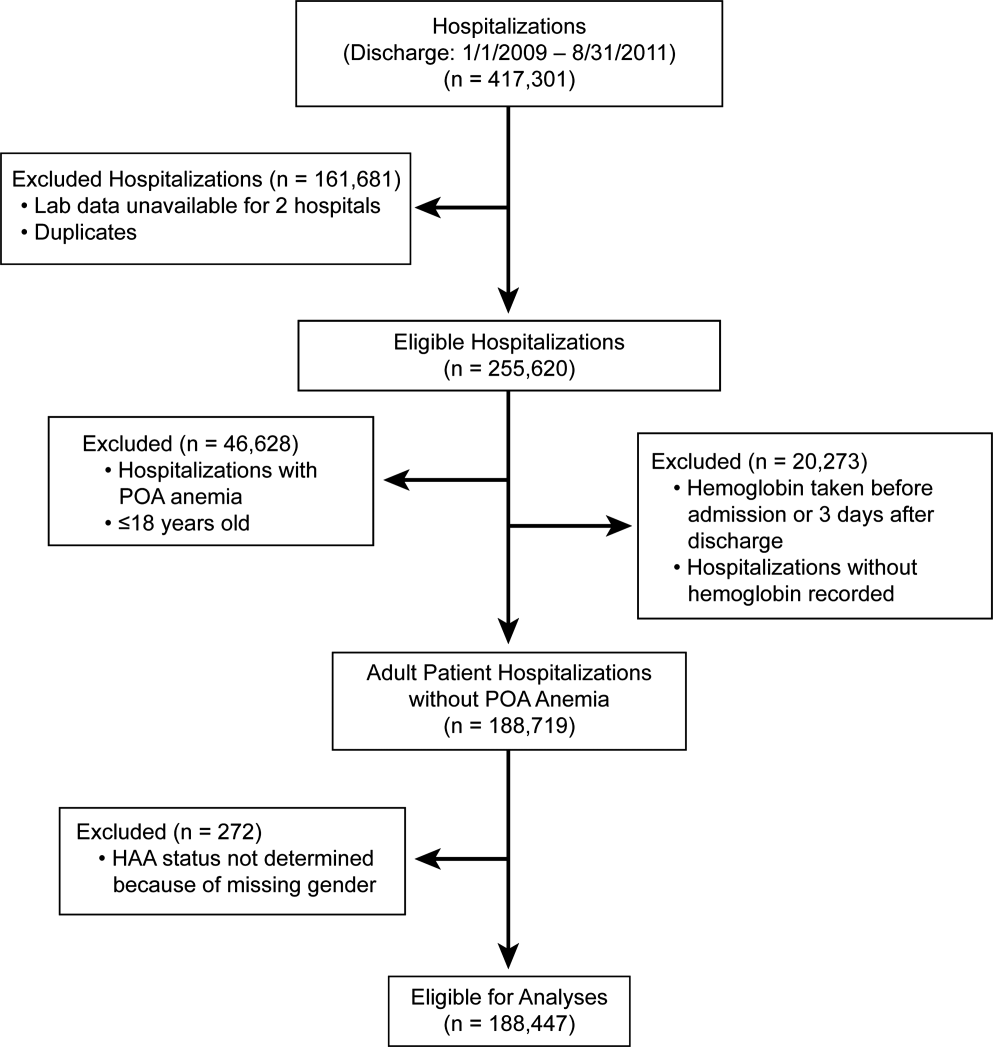
The second source of data was measured Hgb values retrieved from the hospitals' electronic medical record from complete blood count testing. Present‐on‐admission (POA) anemia was defined by an International Classification of Diseases, 9th Revision, Clinical Modification diagnosis code of anemia with a positive POA indicator; these patients were excluded from the analysis (Figure 1). Patients without available Hgb values and those with Hgb data dated 3 days or more after discharge date were also excluded. In addition, 2 hospitals within the health system did not have electronically available laboratory data and therefore were excluded from the analysis as well. The final dataset consisted of 188,447 patient hospitalizations. The institutional review board approved this investigation, with individual patient consent waived.
Anemia
The World Health Organization (WHO) defines anemia as a Hgb value l<12 g/dL in women and <13 g/dL in men. HAA was defined as a nadir Hgb value during the course of hospitalization meeting WHO criteria. We further grouped Hgb by degree into no anemia, mild anemia (Hgb >11 and <12 g/dL in women, >11 and <13 g/dL in men), moderate anemia (Hgb >9 and 11 g/dL), and severe anemia (Hgb 9 g/dL).
Outcomes
Outcomes were all‐cause in‐hospital mortality, total hospital LOS, and total hospital charges.
Data Analysis
For risk adjustment, we used methods developed by Elixhauser and colleagues[14] for use with in‐patient administrative databases. These included a comprehensive set of comorbidity indicators, used to control for patients' underlying conditions in models of outcomes. Among the 30 variables defined by Elixhauser and colleagues, we excluded the 2 administrative anemia codes because this was our variable of interest (Table 1). For all models, demographics, medical conditions, and hospitalization type (medical vs surgical) were included as covariables in addition to the anemia groupings (no HAA and mild, moderate, and severe HAA).
| Characteristic | Hospital‐Acquired Anemia Group | P | |||
|---|---|---|---|---|---|
| No Anemia, n=48,640 | Mild, n=40,828 | Moderate, n=57,184 | Severe, n=41,795 | ||
| |||||
| Age at admission, y | 5518 | 5818 | 5819 | 6117 | <0.0001 |
| Female | 25,123 (52) | 17,938 (44) | 35,858 (63) | 23,533 (56) | <0.0001 |
| Race/ethnicity | <0.0001 | ||||
| White | 39,100 (80) | 32,610 (80) | 45,977 (80) | 33,810 (81) | |
| Black | 7580 (16) | 6607 (16) | 8946 (16) | 6204 (15) | |
| Other | 1960 (4.0) | 1611 (3.9) | 2261 (4.0) | 1781 (4.3) | |
| Hospitalization type | <0.0001 | ||||
| Surgery | 9681 (20) | 14,076 (34) | 26,100 (46) | 27,865 (67) | |
| Medicine | 38,958 (80) | 26,750 (66) | 31,081 (54) | 13,922 (33) | |
| Hypertension | 25,591 (53) | 22,218 (54) | 29,963 (52) | 24,257 (58) | <0.0001 |
| Heart failure | 2811 (5.8) | 3182 (7.8) | 5086 (8.9) | 4278 (10) | <0.0001 |
| Valvular disease | 1201 (2.5) | 1259 (3.1) | 2126 (3.7) | 1890 (4.5) | <0.0001 |
| Pulmonary circulation disease | 667 (1.4) | 730 (1.8) | 1221 (2.1) | 1484 (3.6) | <0.0001 |
| Peripheral arterial disease | 2417 (5.0) | 2728 (6.7) | 4187 (7.3) | 4508 (11) | <0.0001 |
| Paralysis | 1216 (2.5) | 1175 (2.9) | 1568 (2.7) | 1305 (3.1) | <0.0001 |
| Other neurologic disorders | 3013 (6.2) | 2780 (6.8) | 3599 (6.3) | 2829 (6.8) | <0.0001 |
| Chronic obstructive pulmonary disease | 9225 (19) | 7885 (19) | 10,960 (19) | 8057 (19) | 0.5 |
| Diabetes without chronic complications | 8306 (17) | 7733 (19) | 10,417 (18) | 7911 (19) | <0.0001 |
| Diabetes with chronic complications | 1547 (3.2) | 1922 (4.7) | 2989 (5.2) | 2779 (6.6) | <0.0001 |
| Hypothyroidism | 5008 (10) | 4258 (10) | 6938 (12) | 5567 (13) | <0.0001 |
| Renal failure | 2006 (4.1) | 3278 (8.0) | 5787 (10) | 5954 (14) | <0.0001 |
| Liver disease | 1394 (2.9) | 1341 (3.3) | 1788 (3.1) | 2013 (4.8) | <0.0001 |
| Peptic ulcer disease, excluding bleeding | 5 (0.01) | 9 (0.022) | 15 (0.026) | 30 (0.072) | <0.0001 |
| Acquired immune deficiency syndrome | 49 (0.10) | 74 (0.18) | 79 (0.14) | 56 (0.13) | 0.01 |
| Lymphoma | 182 (0.37) | 310 (0.76) | 624 (1.1) | 718 (1.7) | <0.0001 |
| Metastatic cancer | 489 (1.0) | 789 (1.9) | 1889 (3.3) | 1993 (4.8) | <0.0001 |
| Solid tumor without metastasis | 499 (1.0) | 760 (1.9) | 1297 (2.3) | 1123 (2.7) | <0.0001 |
| Rheumatoid arthritis/collagen vascular disease | 1250 (2.6) | 1260 (3.1) | 2214 (3.9) | 1729 (4.1) | <0.0001 |
| Coagulopathy | 1096 (2.3) | 1402 (3.4) | 2517 (4.4) | 6214 (15) | <0.0001 |
| Obesity | 7404 (15) | 5177 (13) | 7112 (12) | 5279 (13) | <0.0001 |
| Weight loss | 972 (2.0) | 1240 (3.0) | 2746 (4.8) | 5841 (14) | <0.0001 |
| Fluid and electrolyte disorders | 7262 (15) | 7501 (18) | 12,828 (22) | 17,201 (41) | <0.0001 |
| Alcohol abuse | 3312 (6.8) | 1977 (4.8) | 1699 (3.0) | 1319 (3.2) | <0.0001 |
| Drug abuse | 3357 (6.9) | 1554 (3.8) | 1197 (2.1) | 657 (1.6) | <0.0001 |
| Psychoses | 3479 (7.2) | 2345 (5.7) | 2544 (4.4) | 1727 (4.1) | <0.0001 |
| Depression | 5999 (12) | 4662 (11) | 6605 (12) | 4895 (12) | <0.0001 |
Logistic regression was used to assess the association of HAA with in‐hospital mortality, and linear regression to assess the association of HAA with hospital LOS and total hospital charges. LOS and total charges were logarithmically transformed because of right‐skewed distributions. The exponential of the resulting regression coefficients quantifies the relative change in LOS or total charges compared to patients without HAA. Unless otherwise specified, a P value of0.05 was considered statistically significant. The Bonferroni method was used to adjust for multiple comparisons.
Our primary analysis excluded patients with anemia at the time of hospitalization based on administratively determined POA anemia positive indicator coding. We also performed a sensitivity analysis to exclude patients with anemia based on the first Hgb values determined by laboratory testing.
All analyses were performed using SAS version 9.2 (SAS Inc., Cary, NC) and R version 2.13 (
RESULTS
Prevalence of HAA
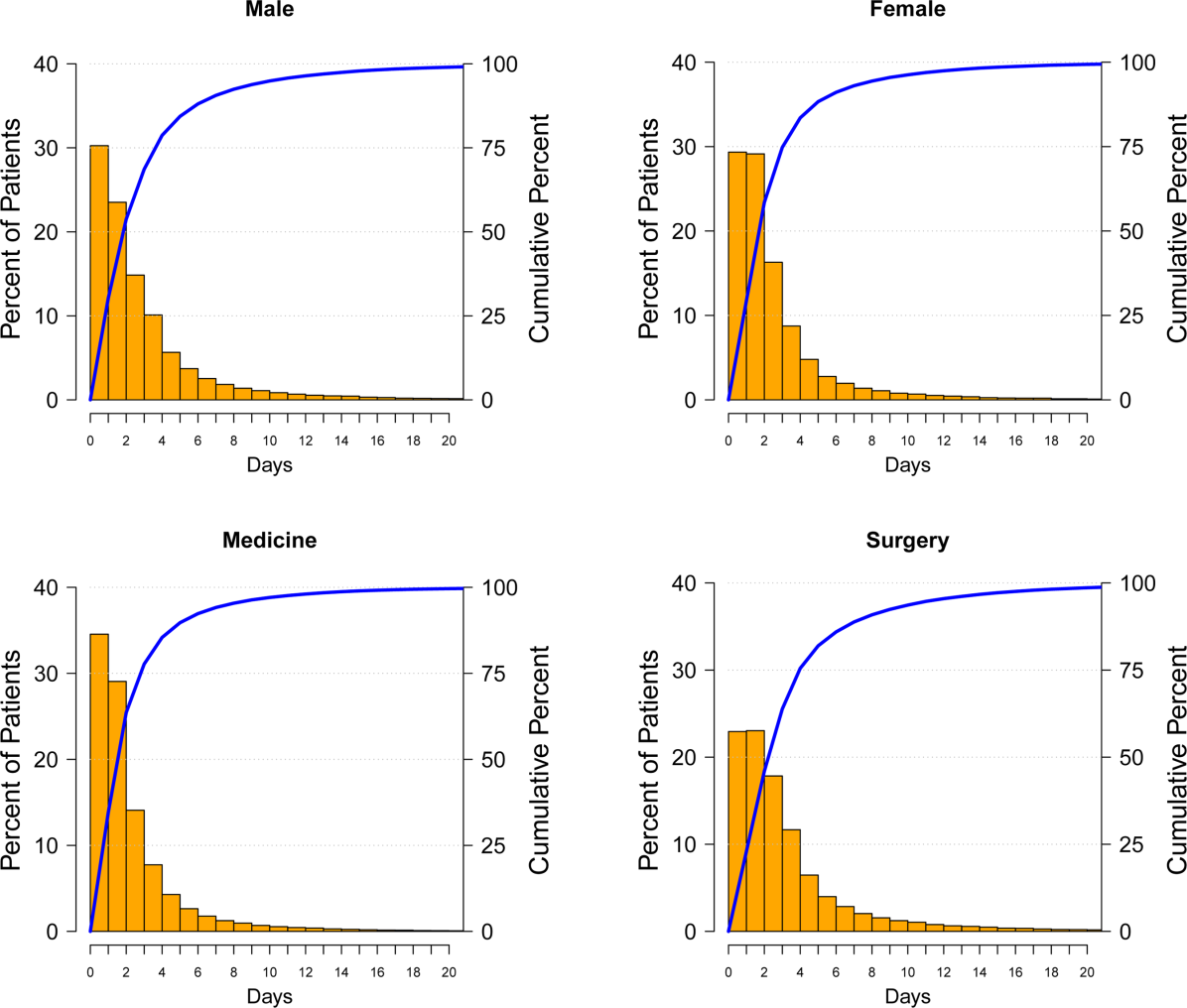
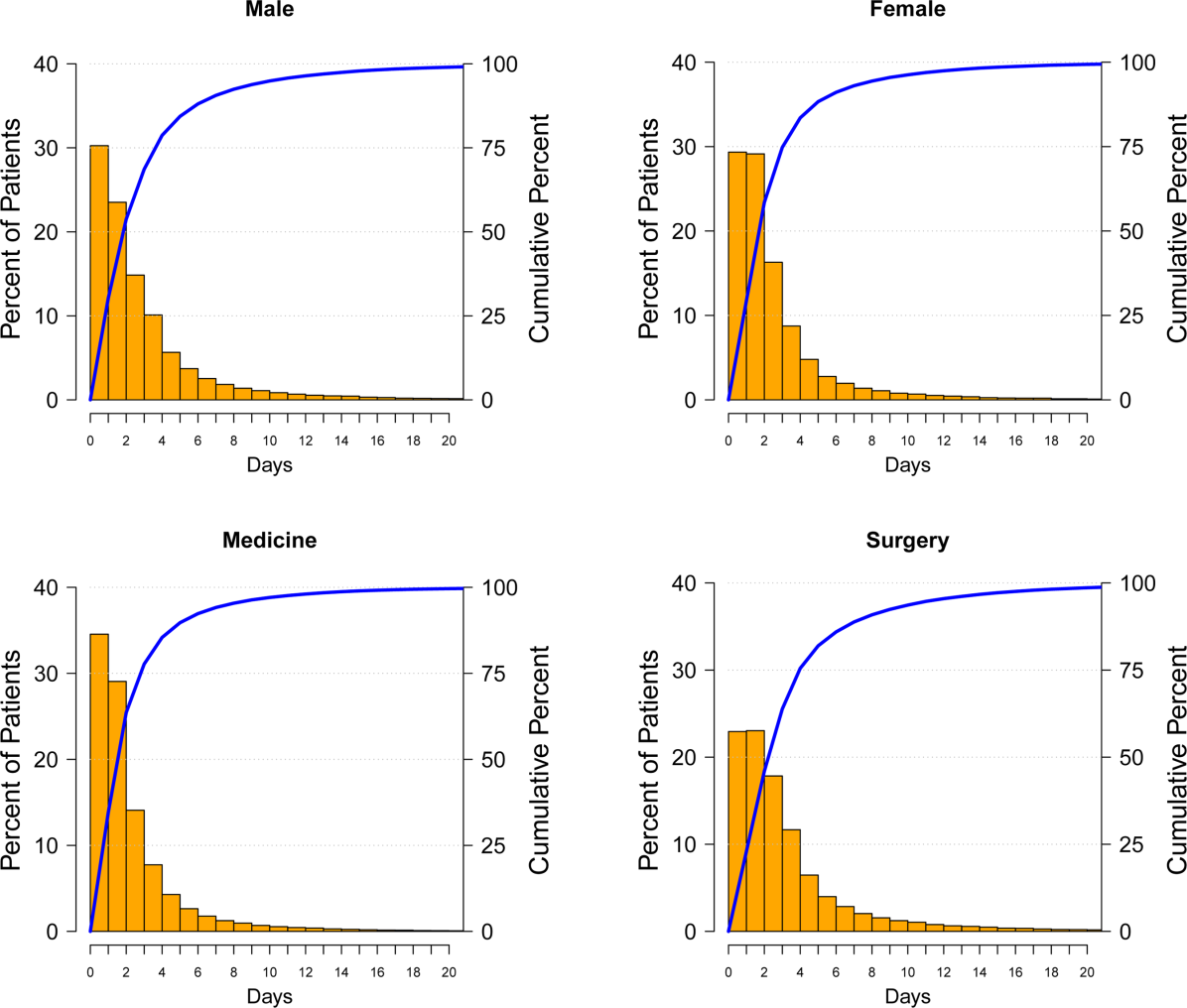
Among the 188,447 hospitalizations, 139,807 patients (74%) developed HAA and 48,640 (26%) did not. Of the 74%, 40,828 developed mild, 57,184 moderate, and 41,795 severe HAA (Figure 2). Patients who developed HAA were older than those who did not and had more comorbidities, including hypertension, heart failure, peripheral arterial disease, and renal and liver disease. They were hospitalized more commonly for surgical intervention than were those who did not develop HAA (Table 1). Time‐related patterns for developing HAA, however, showed that it developed earlier in men and more frequently with medical versus surgical hospitalization (Figure 3).

Hospital Mortality and HAA
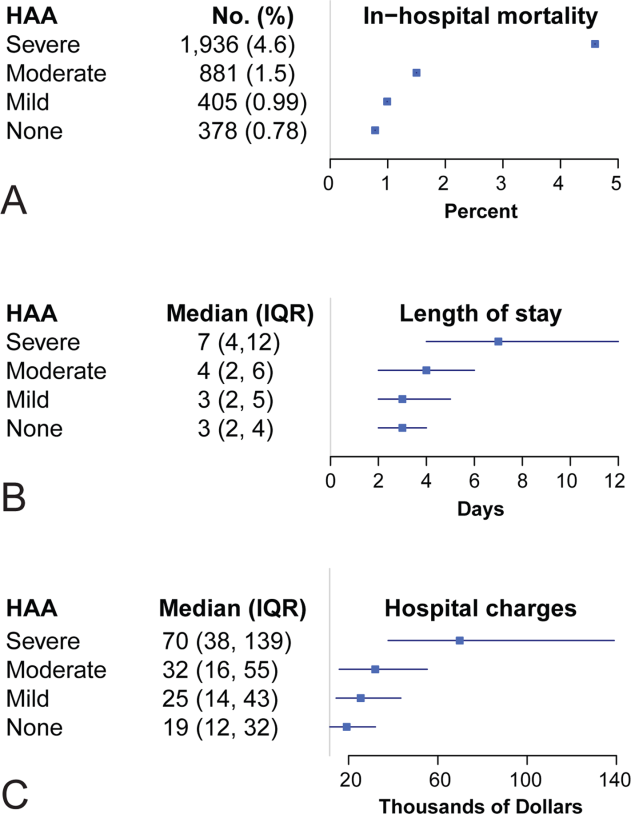
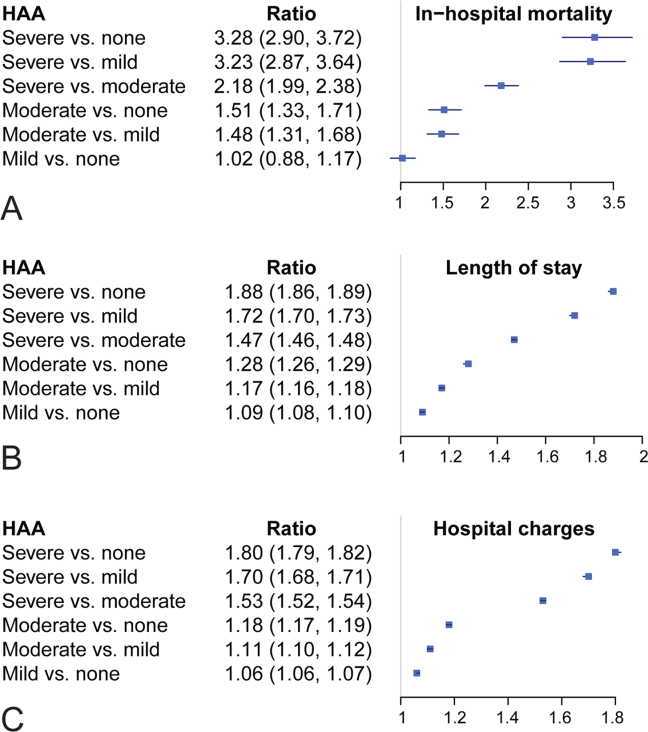
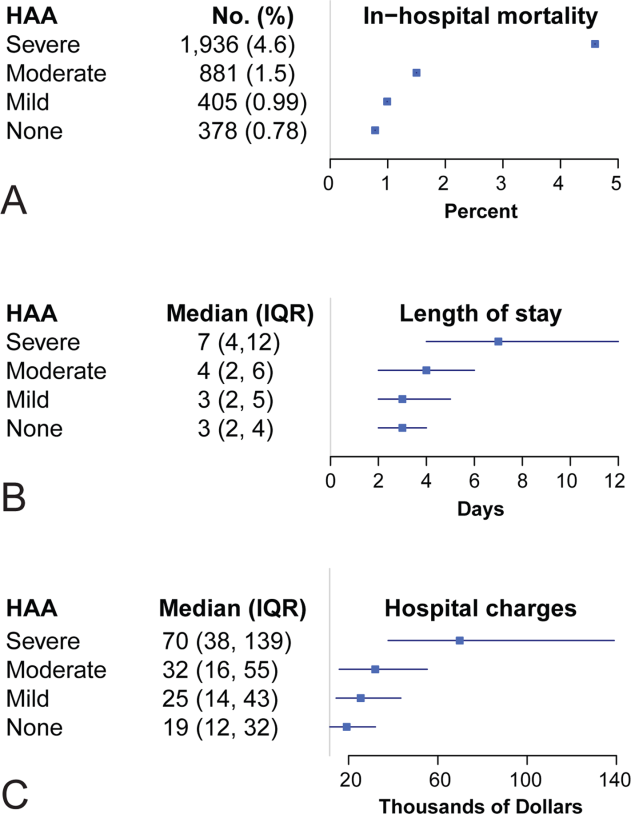
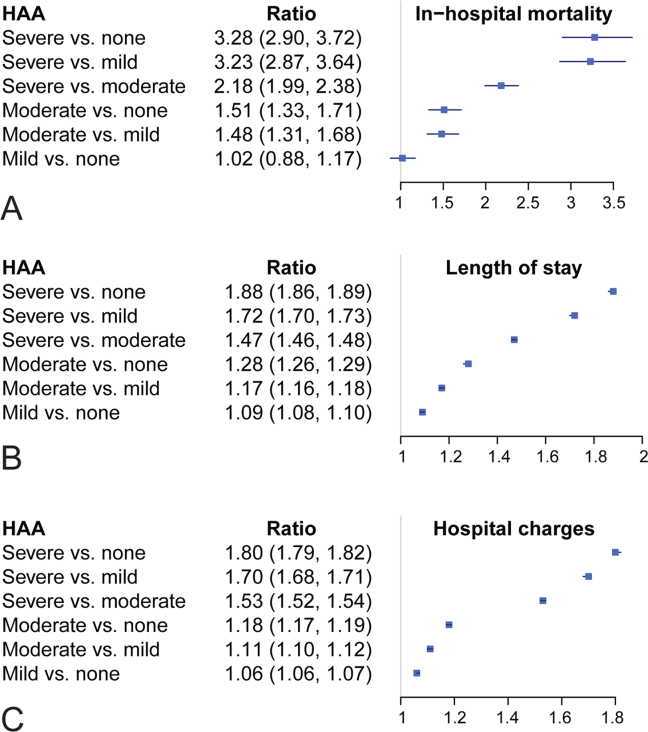
Unadjusted mortality progressively increased with increasing degree of HAA: no HAA, 0.78% (n=378); mild HAA, 0.99% (n=405); moderate HAA, 1.5% (n=881); and severe HAA, 4.6% (n=1936) (P<0.001) (Figure 4A). Patients with mild HAA did not have higher risk‐adjusted mortality than those not having HAA (odds ratio: 1.02, 95% confidence interval [CI]: 0.88‐1.17). However, as HAA increased to moderate and severe, risk of hospital mortality increased in a dose‐dependent manner compared with patients not developing HAA: moderate HAA, 1.51 (95% CI: 1.33‐1.71, P<0.001) and severe HAA, 3.28 (95% CI: 2.90‐3.72, P<0.001) (Figure 5A) (see Supporting Information, Supplement A, in the online version of this article).
Resource Utilization and HAA
Length of Hospital Stay
Unadjusted median (25th, 75th percentiles) LOS was progressively higher in patients who developed HAA: no HAA, 3 days (2, 4); mild HAA, 3 days (2, 5); moderate HAA, 4 days (2, 6); and severe HAA, 7 days (4, 12) (P<0.001) (Figure 4B). Mild HAA was associated with a mean relative increase of 1.09 (95% CI: 1.08‐1.10, P<0.001); moderate HAA, 1.28 (95% CI: 1.26‐1.29, P<0.001); and severe HAA, 1.88 (95% CI: 1.86‐1.89, P<0.001). For example, if expected LOS was 4 days for a patient with no HAA, then for a patient with severe anemia, it would be 7.52 (a 1.88‐fold increase) when all comorbidities were the same (Figure 5B) (see Supporting Information, Supplement A, in the online version of this article).
Total Hospital Charges
Unadjusted hospital charges became progressively higher as degree of HAA increased (P<0.001) (Figure 4C). The mean relative increase was 1.06 (95% CI: 1.06‐1.07, P<0.001) for mild HAA compared with no HAA, 1.18 (95% CI: 1.17‐1.19, P<0.001) for moderate HAA, and 1.80 (95% CI: 1.79‐1.82, P<0.001) for severe HAA. For example, if the expected total charge was $30,000 for a patient with no HAA, then for a patient with severe anemia, it would be $54,000 (a 1.80‐fold increase) when all comorbidities were the same (Figure 5C) (see Supporting Information, Supplement A, in the online version of this article).
Sensitivity Analysis
Among patients without anemia based on the first available Hgb value (n=96,975), 50% of patients developed HAA: mild HAA, 24% (n=23,063); moderate HAA, 19% (n=18,134); and severe HAA, 8% (n=7373). There was a similar relationship between increasing magnitude of HAA and an increase in mortality, LOS, and total charges in the unadjusted and adjusted analyses (see Supporting Information, Supplement C, in the online version of this article).
DISCUSSION
A substantial number of patients entering our health system became anemic during the course of their hospitalization. Among those who developed HAA, in‐hospital mortality was higher, LOS longer, and total hospital charges greater in a dose‐dependent manner. A recent editorial noted that HAA might be a hazard of hospitalization similar to other complications, such as infections and deep vein thrombosis.[15] Our findings have significance in terms of demonstrating increased mortality and resource utilization associated with a potentially modifiable hospital‐acquired condition. Even mild HAA was associated with increased resource utilization, although not increased hospital mortality.
Others have noted negative consequences of HAA in subpopulations of hospital patients. Salisbury and colleagues examined 17,676 patients with acute myocardial infarction who had normal Hgb on admission.[16] They defined HAA as development of new anemia during hospitalization based on nadir Hgb. HAA developed in 57.5% of patients and was associated with increased mortality in a progressive manner. Risk‐adjusted odds ratios for in‐hospital death were greater in patients with moderate and severe HAA, 1.38 (95% CI: 1.10‐1.73) and 3.39 (95% CI: 2.59‐4.44), respectively.[16] A separate investigation of 2902 patients from a multicenter registry of patients admitted to the hospital with acute myocardial infarction reported that nearly half of those with normal Hgb values on admission developed HAA.[17] Most of these patients did not have documented bleeding; therefore, the authors suggested that HAA was not a surrogate for bleeding during hospitalization. Moreover, HAA was associated with higher mortality and worse health status 1 year after myocardial infarction.[17] Others have reported that development of HAA is not uncommon in the setting of acute myocardial infarction and is associated with increased long‐term mortality.[18]
Development of anemia during hospitalization is multifactorial and may result from procedural bleeding, phlebotomy, occult bleeding, hemodilution from intravenous fluid administration, and blunted erythropoietin production associated with critical illness.[8, 9] An investigation of general internal medicine patients reported phlebotomy was highly associated with changes in Hgb levels and contributed to anemia during hospitalization.[19] The authors reported that for every 1 mL of blood drawn, mean decreases in Hgb and hematocrit were 0.070.011 g/L1 and 0.0190.003%, respectively. They suggested reporting cumulative phlebotomy volumes to physicians and use of pediatric‐sized tubes for collection.[19] Salisbury and colleagues reported that mean phlebotomy volume was higher in patients who developed HAA; for every 50 mL of blood drawn, the risk of moderate to severe HAA increased by 18%.[20] In an intensive care population, Chant and colleagues reported small decreases in phlebotomy volume were associated with reduced transfusion requirements in patients with prolonged stay.[21]
Attempts to ameliorate HAA should focus on modifiable processes‐of‐care factors. Patients with chronic illness have blunted erythropoiesis[8] and therefore cannot mount an adequate response to blood loss from procedures or phlebotomy. Whether use of erythropoietin, iron, or both would be effective in this population requires further investigation. One of the most studied risk factors for HAA is blood loss from hospital laboratory testing.[20] Sanchez‐Giron and Alvarez‐Mora found that all laboratory tests could be performed with smaller‐volume collection tubes without need for additional samples.[22] Others have proposed batching laboratory requests, recording cumulative daily blood loss due to phlebotomy for individual patients,[23] and use of blood conservation devices in intensive care units.
Figure 3 suggests that surgical patients develop anemia slightly later than medical patients. Features specific to surgery, such as perioperative intravenous fluid loading, third spacing, and subsequent plasma volume expansion when reabsorption occurs days later, likely contribute to differences in trends for development of HAA.[24, 25, 26] In addition, specific surgical cases with highly anticipated red blood cell loss should make use of antifibrinolytic agents to reduce blood loss and red cell salvage devices to reprocess and infuse shed blood.
Limitations
A recent commentary explored the question of benchmarks for anemia diagnosis, and in particular, what defines the lower limit of normal.[27] Although we used WHO criteria, others have used criteria establishing lower benchmarks according to race and gender.[27] Our results would have been similar if we had used these lower benchmarks, because our moderate and severe anemia Hgb cutoff values were beneath alternative benchmarks for diagnosing anemia. For example, Beutler and Waalen provide a definition of anemia that includes an Hgb cutoff of 12.2 g/dL for white women aged 20 to 49 years, 11.5 g/dL for black women of similar age, 13.7 g/dL for white men, and 12.9 g/dL for black men.[27]
Our study is limited by the nature of administrative data. However, use of demographic data, hospitalization type, and use of a large number of comorbidities for risk adjustment improved our findings. Adding nonadministrative clinical laboratory data from the electronic record for patient Hgb values provided us with a more accurate diagnosis of HAA and an ability to further subdivide anemia into mild, moderate, and severe categories that have prognostic implications. We are aware of the inherent limitations associated with use of administrative data. However, coded data are currently readily available and are the source of information on which many healthcare policies are made.[28, 29]
The POA anemia administrative code was used to identify patients with preexisting anemia. We did not use the first Hgb value upon admission because it is often made following interventions (eg, surgical patients have preoperative laboratory testing prior to admission, and the first Hgb value available following hospitalization is commonly obtained following surgical interventions). However, we performed a sensitivity analysis that defined preexisting anemia based on the first available Hgb value. The results from the sensitivity analysis were consistent with our primary findings with the use of administrative data coding. Of note, use of administrative codes for determining POA indicators is consistent with methods employed for all current publically reported quality and patient safety initiatives. Specifically, the Agency for Healthcare Research and Quality Patient Safety Indicators used by the Centers for Medicare and Medicaid Services to assess hospital quality of care and to modify reimbursement for services.
Our focus was on development of HAA; treatment of HAA with red blood cell transfusion and standardized blood draw orders were not investigated. Finally, our results are reflective of a single health system; further work with multicenter data would help clarify our findings.
CONCLUSION
Development of HAA is common and has important healthcare implications, including higher in‐hospital mortality and increased resource utilization. Treating HAA by transfusion has attendant morbidity risks and increased costs.[11, 12, 30] Hospitals must continue to focus on improving patient safety and raising awareness of HAA and other modifiable hospital‐acquired conditions. Closer prospective investigation for both medical and surgical patients of cumulative blood loss from laboratory testing, procedural blood loss, and a risk‐benefit analysis of treatment options is necessary.
Acknowledgments
Disclosure: Nothing to report.
Disclosure
Nothing to report.
- , , , , , . A population‐based study of hemoglobin, race, and mortality in elderly persons. J Gerontol A Biol Sci Med Sci. 2008;63(8):873–878.
- , , , . Anemia in the elderly: a public health crisis in hematology. Hematology Am Soc Hematol Educ Program. 2005:528–532.
- , , . The definition of anemia in older persons. JAMA. 1999;281(18):1714–1717.
- , . Anemia in the elderly: how should we define it, when does it matter, and what can be done? Mayo Clin Proc. 2007;82(8):958–966.
- , , , et al. A prospective study of anemia status, hemoglobin concentration, and mortality in an elderly cohort: the Cardiovascular Health Study. Arch Intern Med. 2005;165(19):2214–2220.
- , , , et al. Association of mild anemia with hospitalization and mortality in the elderly: the Health and Anemia population‐based study. Haematologica. 2009;94(1):22–28.
- , , , et al. Association of mild anemia with cognitive, functional, mood and quality of life outcomes in the elderly: the “Health and Anemia” study. PLoS One. 2008;3(4):e1920.
- . Anemia in the critically ill. Crit Care Clin. 2004;20(2):159–178.
- . Scope of the problem: epidemiology of anemia and use of blood transfusions in critical care. Crit Care. 2004;8(suppl 2):S1–S8.
- , , , , , . Transfusion and pulmonary morbidity after cardiac surgery. Ann Thorac Surg. 2009;88(5):1410–1418.
- , , , et al. Morbidity and mortality risk associated with red blood cell and blood‐component transfusion in isolated coronary artery bypass grafting. Crit Care Med. 2006;34(6):1608–1616.
- , , , et al. Duration of red‐cell storage and complications after cardiac surgery. N Engl J Med. 2008;358(12):1229–1239.
- , , , et al. Transfusion in coronary artery bypass grafting is associated with reduced long‐term survival. Ann Thorac Surg. 2006;81(5):1650–1657.
- , , , . Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27.
- , . Hazards of hospitalization: more than just “never events”. Arch Intern Med. 2011;171(18):1653–1654.
- , , , et al. Hospital‐acquired anemia and in‐hospital mortality in patients with acute myocardial infarction. Am Heart J. 2011;162(2):300–309.e3.
- , , , et al. Incidence, correlates, and outcomes of acute, hospital‐acquired anemia in patients with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2010;3(4):337–346.
- , , , et al. Changes in haemoglobin levels during hospital course and long‐term outcome after acute myocardial infarction. Eur Heart J. 2007;28(11):1289–1296.
- , , , , . Do blood tests cause anemia in hospitalized patients? The effect of diagnostic phlebotomy on hemoglobin and hematocrit levels. J Gen Intern Med. 2005;20(6):520–524.
- , , , et al. Diagnostic blood loss from phlebotomy and hospital‐acquired anemia during acute myocardial infarction. Arch Intern Med. 2011;171(18):1646–1653.
- , , . Anemia, transfusion, and phlebotomy practices in critically ill patients with prolonged ICU length of stay: a cohort study. Crit Care. 2006;10(5):R140.
- , . Reduction of blood loss from laboratory testing in hospitalized adult patients using small‐volume (pediatric) tubes. Arch Pathol Lab Med. 2008;132(12):1916–1919.
- , . Phlebotomy for diagnostic laboratory tests in adults. Pattern of use and effect on transfusion requirements. N Engl J Med. 1986;314(19):1233–1235.
- , , , , . Perioperative monitoring of circulating and central blood volume in cardiac surgery by pulse dye densitometry. Intensive Care Med. 2004;30(11):2053–2059.
- , , , , . Perioperative red cell, plasma, and blood volume change in patients undergoing cardiac surgery. Transfusion. 2006;46(3):392–397.
- , , , . Changes in circulating blood volume after cardiac surgery measured by a novel method using hydroxyethyl starch. Crit Care Med. 2000;28(2):336–341.
- , . The definition of anemia: what is the lower limit of normal of the blood hemoglobin concentration? Blood. 2006;107(5):1747–1750.
- , , , , , . What are the real rates of postoperative complications: elucidating inconsistencies between administrative and clinical data sources. J Am Coll Surg. 2012;214(5):798–805.
- . Medicare program: hospital inpatient value‐based purchasing program, final rule. Available at: http://www.cms.gov/Medicare/Quality‐Initiatives‐Patient‐Assessment‐Instruments/HospitalQualityInits/index.html. Accessed May 6, 2011.
- , , , , , . Increased mortality, postoperative morbidity, and cost after red blood cell transfusion in patients having cardiac surgery. Circulation. 2007;116(22):2544–2552.
Anemia is associated with poor quality of life and increased risk for death and hospitalization in population‐based and cohort investigations.[1, 2, 3, 4, 5, 6, 7] Evidence suggests that patients with normal hemoglobin (Hgb) values on hospital admission who subsequently develop hospital‐acquired anemia (HAA) have increased morbidity and mortality compared with those who do not.[8, 9] HAA is multifaceted and may occur as a result of processes of care during hospitalization, such as hemodilution from intravenous fluid administration, procedural blood loss and phlebotomy, and impaired erythropoiesis associated with critical illness.[8, 9] Moreover, correcting anemia by red blood cell transfusion also carries risk.[10, 11, 12, 13]
Our primary objective was to examine the prevalence of HAA in a population of medical and surgical patients admitted to a large quaternary referral health system. Our secondary objectives were to examine whether HAA is associated with increased mortality, length of stay (LOS), and total hospital charges compared to patients without HAA.
METHODS
Patient Population and Data Sources
The patient population consisted of 417,301 hospitalizations in adult patients (18 years of age) who were admitted to the Cleveland Clinic Health System from January 2009 to September 2011. Data for these hospitalizations came from 2 sources. Patient demographics, baseline comorbidities, and outcomes were extracted from the University HealthSystem Consortium's (UHC) clinical database/resource manager. UHC is an alliance of 116 US academic medical centers and their 272 affiliated hospitals, representing more than 90% of the nation's nonprofit academic medical centers. These data had originally been retrieved from our hospitals' administrative data systems, normalized according to UHC standardized data specifications, and submitted for inclusion in the UHC repository. Data quality was assessed using standardized error checking and data completeness algorithms and was required to meet established minimum thresholds to be included in the UHC repository.
The second source of data was measured Hgb values retrieved from the hospitals' electronic medical record from complete blood count testing. Present‐on‐admission (POA) anemia was defined by an International Classification of Diseases, 9th Revision, Clinical Modification diagnosis code of anemia with a positive POA indicator; these patients were excluded from the analysis (Figure 1). Patients without available Hgb values and those with Hgb data dated 3 days or more after discharge date were also excluded. In addition, 2 hospitals within the health system did not have electronically available laboratory data and therefore were excluded from the analysis as well. The final dataset consisted of 188,447 patient hospitalizations. The institutional review board approved this investigation, with individual patient consent waived.
Anemia
The World Health Organization (WHO) defines anemia as a Hgb value l<12 g/dL in women and <13 g/dL in men. HAA was defined as a nadir Hgb value during the course of hospitalization meeting WHO criteria. We further grouped Hgb by degree into no anemia, mild anemia (Hgb >11 and <12 g/dL in women, >11 and <13 g/dL in men), moderate anemia (Hgb >9 and 11 g/dL), and severe anemia (Hgb 9 g/dL).
Outcomes
Outcomes were all‐cause in‐hospital mortality, total hospital LOS, and total hospital charges.
Data Analysis
For risk adjustment, we used methods developed by Elixhauser and colleagues[14] for use with in‐patient administrative databases. These included a comprehensive set of comorbidity indicators, used to control for patients' underlying conditions in models of outcomes. Among the 30 variables defined by Elixhauser and colleagues, we excluded the 2 administrative anemia codes because this was our variable of interest (Table 1). For all models, demographics, medical conditions, and hospitalization type (medical vs surgical) were included as covariables in addition to the anemia groupings (no HAA and mild, moderate, and severe HAA).
| Characteristic | Hospital‐Acquired Anemia Group | P | |||
|---|---|---|---|---|---|
| No Anemia, n=48,640 | Mild, n=40,828 | Moderate, n=57,184 | Severe, n=41,795 | ||
| |||||
| Age at admission, y | 5518 | 5818 | 5819 | 6117 | <0.0001 |
| Female | 25,123 (52) | 17,938 (44) | 35,858 (63) | 23,533 (56) | <0.0001 |
| Race/ethnicity | <0.0001 | ||||
| White | 39,100 (80) | 32,610 (80) | 45,977 (80) | 33,810 (81) | |
| Black | 7580 (16) | 6607 (16) | 8946 (16) | 6204 (15) | |
| Other | 1960 (4.0) | 1611 (3.9) | 2261 (4.0) | 1781 (4.3) | |
| Hospitalization type | <0.0001 | ||||
| Surgery | 9681 (20) | 14,076 (34) | 26,100 (46) | 27,865 (67) | |
| Medicine | 38,958 (80) | 26,750 (66) | 31,081 (54) | 13,922 (33) | |
| Hypertension | 25,591 (53) | 22,218 (54) | 29,963 (52) | 24,257 (58) | <0.0001 |
| Heart failure | 2811 (5.8) | 3182 (7.8) | 5086 (8.9) | 4278 (10) | <0.0001 |
| Valvular disease | 1201 (2.5) | 1259 (3.1) | 2126 (3.7) | 1890 (4.5) | <0.0001 |
| Pulmonary circulation disease | 667 (1.4) | 730 (1.8) | 1221 (2.1) | 1484 (3.6) | <0.0001 |
| Peripheral arterial disease | 2417 (5.0) | 2728 (6.7) | 4187 (7.3) | 4508 (11) | <0.0001 |
| Paralysis | 1216 (2.5) | 1175 (2.9) | 1568 (2.7) | 1305 (3.1) | <0.0001 |
| Other neurologic disorders | 3013 (6.2) | 2780 (6.8) | 3599 (6.3) | 2829 (6.8) | <0.0001 |
| Chronic obstructive pulmonary disease | 9225 (19) | 7885 (19) | 10,960 (19) | 8057 (19) | 0.5 |
| Diabetes without chronic complications | 8306 (17) | 7733 (19) | 10,417 (18) | 7911 (19) | <0.0001 |
| Diabetes with chronic complications | 1547 (3.2) | 1922 (4.7) | 2989 (5.2) | 2779 (6.6) | <0.0001 |
| Hypothyroidism | 5008 (10) | 4258 (10) | 6938 (12) | 5567 (13) | <0.0001 |
| Renal failure | 2006 (4.1) | 3278 (8.0) | 5787 (10) | 5954 (14) | <0.0001 |
| Liver disease | 1394 (2.9) | 1341 (3.3) | 1788 (3.1) | 2013 (4.8) | <0.0001 |
| Peptic ulcer disease, excluding bleeding | 5 (0.01) | 9 (0.022) | 15 (0.026) | 30 (0.072) | <0.0001 |
| Acquired immune deficiency syndrome | 49 (0.10) | 74 (0.18) | 79 (0.14) | 56 (0.13) | 0.01 |
| Lymphoma | 182 (0.37) | 310 (0.76) | 624 (1.1) | 718 (1.7) | <0.0001 |
| Metastatic cancer | 489 (1.0) | 789 (1.9) | 1889 (3.3) | 1993 (4.8) | <0.0001 |
| Solid tumor without metastasis | 499 (1.0) | 760 (1.9) | 1297 (2.3) | 1123 (2.7) | <0.0001 |
| Rheumatoid arthritis/collagen vascular disease | 1250 (2.6) | 1260 (3.1) | 2214 (3.9) | 1729 (4.1) | <0.0001 |
| Coagulopathy | 1096 (2.3) | 1402 (3.4) | 2517 (4.4) | 6214 (15) | <0.0001 |
| Obesity | 7404 (15) | 5177 (13) | 7112 (12) | 5279 (13) | <0.0001 |
| Weight loss | 972 (2.0) | 1240 (3.0) | 2746 (4.8) | 5841 (14) | <0.0001 |
| Fluid and electrolyte disorders | 7262 (15) | 7501 (18) | 12,828 (22) | 17,201 (41) | <0.0001 |
| Alcohol abuse | 3312 (6.8) | 1977 (4.8) | 1699 (3.0) | 1319 (3.2) | <0.0001 |
| Drug abuse | 3357 (6.9) | 1554 (3.8) | 1197 (2.1) | 657 (1.6) | <0.0001 |
| Psychoses | 3479 (7.2) | 2345 (5.7) | 2544 (4.4) | 1727 (4.1) | <0.0001 |
| Depression | 5999 (12) | 4662 (11) | 6605 (12) | 4895 (12) | <0.0001 |
Logistic regression was used to assess the association of HAA with in‐hospital mortality, and linear regression to assess the association of HAA with hospital LOS and total hospital charges. LOS and total charges were logarithmically transformed because of right‐skewed distributions. The exponential of the resulting regression coefficients quantifies the relative change in LOS or total charges compared to patients without HAA. Unless otherwise specified, a P value of0.05 was considered statistically significant. The Bonferroni method was used to adjust for multiple comparisons.
Our primary analysis excluded patients with anemia at the time of hospitalization based on administratively determined POA anemia positive indicator coding. We also performed a sensitivity analysis to exclude patients with anemia based on the first Hgb values determined by laboratory testing.
All analyses were performed using SAS version 9.2 (SAS Inc., Cary, NC) and R version 2.13 (
RESULTS
Prevalence of HAA
Among the 188,447 hospitalizations, 139,807 patients (74%) developed HAA and 48,640 (26%) did not. Of the 74%, 40,828 developed mild, 57,184 moderate, and 41,795 severe HAA (Figure 2). Patients who developed HAA were older than those who did not and had more comorbidities, including hypertension, heart failure, peripheral arterial disease, and renal and liver disease. They were hospitalized more commonly for surgical intervention than were those who did not develop HAA (Table 1). Time‐related patterns for developing HAA, however, showed that it developed earlier in men and more frequently with medical versus surgical hospitalization (Figure 3).

Hospital Mortality and HAA
Unadjusted mortality progressively increased with increasing degree of HAA: no HAA, 0.78% (n=378); mild HAA, 0.99% (n=405); moderate HAA, 1.5% (n=881); and severe HAA, 4.6% (n=1936) (P<0.001) (Figure 4A). Patients with mild HAA did not have higher risk‐adjusted mortality than those not having HAA (odds ratio: 1.02, 95% confidence interval [CI]: 0.88‐1.17). However, as HAA increased to moderate and severe, risk of hospital mortality increased in a dose‐dependent manner compared with patients not developing HAA: moderate HAA, 1.51 (95% CI: 1.33‐1.71, P<0.001) and severe HAA, 3.28 (95% CI: 2.90‐3.72, P<0.001) (Figure 5A) (see Supporting Information, Supplement A, in the online version of this article).
Resource Utilization and HAA
Length of Hospital Stay
Unadjusted median (25th, 75th percentiles) LOS was progressively higher in patients who developed HAA: no HAA, 3 days (2, 4); mild HAA, 3 days (2, 5); moderate HAA, 4 days (2, 6); and severe HAA, 7 days (4, 12) (P<0.001) (Figure 4B). Mild HAA was associated with a mean relative increase of 1.09 (95% CI: 1.08‐1.10, P<0.001); moderate HAA, 1.28 (95% CI: 1.26‐1.29, P<0.001); and severe HAA, 1.88 (95% CI: 1.86‐1.89, P<0.001). For example, if expected LOS was 4 days for a patient with no HAA, then for a patient with severe anemia, it would be 7.52 (a 1.88‐fold increase) when all comorbidities were the same (Figure 5B) (see Supporting Information, Supplement A, in the online version of this article).
Total Hospital Charges
Unadjusted hospital charges became progressively higher as degree of HAA increased (P<0.001) (Figure 4C). The mean relative increase was 1.06 (95% CI: 1.06‐1.07, P<0.001) for mild HAA compared with no HAA, 1.18 (95% CI: 1.17‐1.19, P<0.001) for moderate HAA, and 1.80 (95% CI: 1.79‐1.82, P<0.001) for severe HAA. For example, if the expected total charge was $30,000 for a patient with no HAA, then for a patient with severe anemia, it would be $54,000 (a 1.80‐fold increase) when all comorbidities were the same (Figure 5C) (see Supporting Information, Supplement A, in the online version of this article).
Sensitivity Analysis
Among patients without anemia based on the first available Hgb value (n=96,975), 50% of patients developed HAA: mild HAA, 24% (n=23,063); moderate HAA, 19% (n=18,134); and severe HAA, 8% (n=7373). There was a similar relationship between increasing magnitude of HAA and an increase in mortality, LOS, and total charges in the unadjusted and adjusted analyses (see Supporting Information, Supplement C, in the online version of this article).
DISCUSSION
A substantial number of patients entering our health system became anemic during the course of their hospitalization. Among those who developed HAA, in‐hospital mortality was higher, LOS longer, and total hospital charges greater in a dose‐dependent manner. A recent editorial noted that HAA might be a hazard of hospitalization similar to other complications, such as infections and deep vein thrombosis.[15] Our findings have significance in terms of demonstrating increased mortality and resource utilization associated with a potentially modifiable hospital‐acquired condition. Even mild HAA was associated with increased resource utilization, although not increased hospital mortality.
Others have noted negative consequences of HAA in subpopulations of hospital patients. Salisbury and colleagues examined 17,676 patients with acute myocardial infarction who had normal Hgb on admission.[16] They defined HAA as development of new anemia during hospitalization based on nadir Hgb. HAA developed in 57.5% of patients and was associated with increased mortality in a progressive manner. Risk‐adjusted odds ratios for in‐hospital death were greater in patients with moderate and severe HAA, 1.38 (95% CI: 1.10‐1.73) and 3.39 (95% CI: 2.59‐4.44), respectively.[16] A separate investigation of 2902 patients from a multicenter registry of patients admitted to the hospital with acute myocardial infarction reported that nearly half of those with normal Hgb values on admission developed HAA.[17] Most of these patients did not have documented bleeding; therefore, the authors suggested that HAA was not a surrogate for bleeding during hospitalization. Moreover, HAA was associated with higher mortality and worse health status 1 year after myocardial infarction.[17] Others have reported that development of HAA is not uncommon in the setting of acute myocardial infarction and is associated with increased long‐term mortality.[18]
Development of anemia during hospitalization is multifactorial and may result from procedural bleeding, phlebotomy, occult bleeding, hemodilution from intravenous fluid administration, and blunted erythropoietin production associated with critical illness.[8, 9] An investigation of general internal medicine patients reported phlebotomy was highly associated with changes in Hgb levels and contributed to anemia during hospitalization.[19] The authors reported that for every 1 mL of blood drawn, mean decreases in Hgb and hematocrit were 0.070.011 g/L1 and 0.0190.003%, respectively. They suggested reporting cumulative phlebotomy volumes to physicians and use of pediatric‐sized tubes for collection.[19] Salisbury and colleagues reported that mean phlebotomy volume was higher in patients who developed HAA; for every 50 mL of blood drawn, the risk of moderate to severe HAA increased by 18%.[20] In an intensive care population, Chant and colleagues reported small decreases in phlebotomy volume were associated with reduced transfusion requirements in patients with prolonged stay.[21]
Attempts to ameliorate HAA should focus on modifiable processes‐of‐care factors. Patients with chronic illness have blunted erythropoiesis[8] and therefore cannot mount an adequate response to blood loss from procedures or phlebotomy. Whether use of erythropoietin, iron, or both would be effective in this population requires further investigation. One of the most studied risk factors for HAA is blood loss from hospital laboratory testing.[20] Sanchez‐Giron and Alvarez‐Mora found that all laboratory tests could be performed with smaller‐volume collection tubes without need for additional samples.[22] Others have proposed batching laboratory requests, recording cumulative daily blood loss due to phlebotomy for individual patients,[23] and use of blood conservation devices in intensive care units.
Figure 3 suggests that surgical patients develop anemia slightly later than medical patients. Features specific to surgery, such as perioperative intravenous fluid loading, third spacing, and subsequent plasma volume expansion when reabsorption occurs days later, likely contribute to differences in trends for development of HAA.[24, 25, 26] In addition, specific surgical cases with highly anticipated red blood cell loss should make use of antifibrinolytic agents to reduce blood loss and red cell salvage devices to reprocess and infuse shed blood.
Limitations
A recent commentary explored the question of benchmarks for anemia diagnosis, and in particular, what defines the lower limit of normal.[27] Although we used WHO criteria, others have used criteria establishing lower benchmarks according to race and gender.[27] Our results would have been similar if we had used these lower benchmarks, because our moderate and severe anemia Hgb cutoff values were beneath alternative benchmarks for diagnosing anemia. For example, Beutler and Waalen provide a definition of anemia that includes an Hgb cutoff of 12.2 g/dL for white women aged 20 to 49 years, 11.5 g/dL for black women of similar age, 13.7 g/dL for white men, and 12.9 g/dL for black men.[27]
Our study is limited by the nature of administrative data. However, use of demographic data, hospitalization type, and use of a large number of comorbidities for risk adjustment improved our findings. Adding nonadministrative clinical laboratory data from the electronic record for patient Hgb values provided us with a more accurate diagnosis of HAA and an ability to further subdivide anemia into mild, moderate, and severe categories that have prognostic implications. We are aware of the inherent limitations associated with use of administrative data. However, coded data are currently readily available and are the source of information on which many healthcare policies are made.[28, 29]
The POA anemia administrative code was used to identify patients with preexisting anemia. We did not use the first Hgb value upon admission because it is often made following interventions (eg, surgical patients have preoperative laboratory testing prior to admission, and the first Hgb value available following hospitalization is commonly obtained following surgical interventions). However, we performed a sensitivity analysis that defined preexisting anemia based on the first available Hgb value. The results from the sensitivity analysis were consistent with our primary findings with the use of administrative data coding. Of note, use of administrative codes for determining POA indicators is consistent with methods employed for all current publically reported quality and patient safety initiatives. Specifically, the Agency for Healthcare Research and Quality Patient Safety Indicators used by the Centers for Medicare and Medicaid Services to assess hospital quality of care and to modify reimbursement for services.
Our focus was on development of HAA; treatment of HAA with red blood cell transfusion and standardized blood draw orders were not investigated. Finally, our results are reflective of a single health system; further work with multicenter data would help clarify our findings.
CONCLUSION
Development of HAA is common and has important healthcare implications, including higher in‐hospital mortality and increased resource utilization. Treating HAA by transfusion has attendant morbidity risks and increased costs.[11, 12, 30] Hospitals must continue to focus on improving patient safety and raising awareness of HAA and other modifiable hospital‐acquired conditions. Closer prospective investigation for both medical and surgical patients of cumulative blood loss from laboratory testing, procedural blood loss, and a risk‐benefit analysis of treatment options is necessary.
Acknowledgments
Disclosure: Nothing to report.
Disclosure
Nothing to report.
Anemia is associated with poor quality of life and increased risk for death and hospitalization in population‐based and cohort investigations.[1, 2, 3, 4, 5, 6, 7] Evidence suggests that patients with normal hemoglobin (Hgb) values on hospital admission who subsequently develop hospital‐acquired anemia (HAA) have increased morbidity and mortality compared with those who do not.[8, 9] HAA is multifaceted and may occur as a result of processes of care during hospitalization, such as hemodilution from intravenous fluid administration, procedural blood loss and phlebotomy, and impaired erythropoiesis associated with critical illness.[8, 9] Moreover, correcting anemia by red blood cell transfusion also carries risk.[10, 11, 12, 13]
Our primary objective was to examine the prevalence of HAA in a population of medical and surgical patients admitted to a large quaternary referral health system. Our secondary objectives were to examine whether HAA is associated with increased mortality, length of stay (LOS), and total hospital charges compared to patients without HAA.
METHODS
Patient Population and Data Sources
The patient population consisted of 417,301 hospitalizations in adult patients (18 years of age) who were admitted to the Cleveland Clinic Health System from January 2009 to September 2011. Data for these hospitalizations came from 2 sources. Patient demographics, baseline comorbidities, and outcomes were extracted from the University HealthSystem Consortium's (UHC) clinical database/resource manager. UHC is an alliance of 116 US academic medical centers and their 272 affiliated hospitals, representing more than 90% of the nation's nonprofit academic medical centers. These data had originally been retrieved from our hospitals' administrative data systems, normalized according to UHC standardized data specifications, and submitted for inclusion in the UHC repository. Data quality was assessed using standardized error checking and data completeness algorithms and was required to meet established minimum thresholds to be included in the UHC repository.
The second source of data was measured Hgb values retrieved from the hospitals' electronic medical record from complete blood count testing. Present‐on‐admission (POA) anemia was defined by an International Classification of Diseases, 9th Revision, Clinical Modification diagnosis code of anemia with a positive POA indicator; these patients were excluded from the analysis (Figure 1). Patients without available Hgb values and those with Hgb data dated 3 days or more after discharge date were also excluded. In addition, 2 hospitals within the health system did not have electronically available laboratory data and therefore were excluded from the analysis as well. The final dataset consisted of 188,447 patient hospitalizations. The institutional review board approved this investigation, with individual patient consent waived.
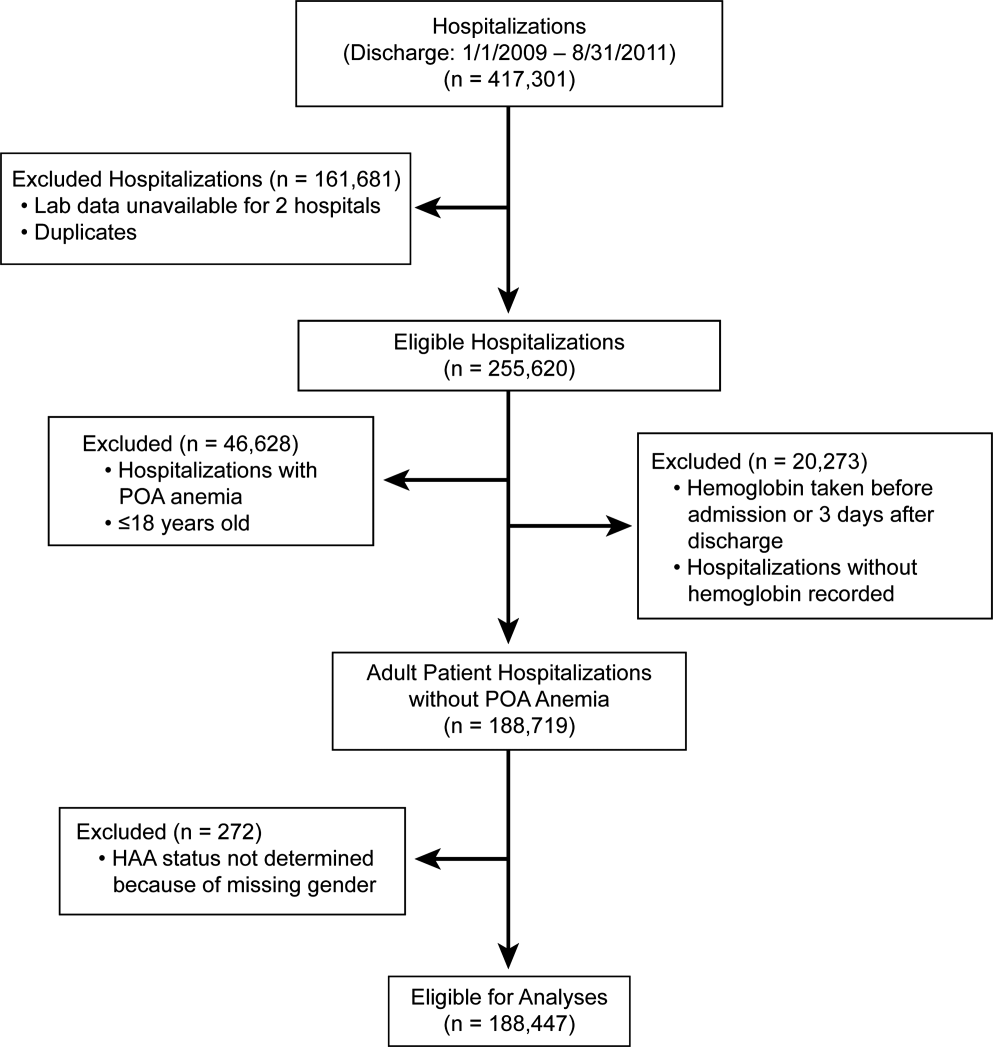
Anemia
The World Health Organization (WHO) defines anemia as a Hgb value l<12 g/dL in women and <13 g/dL in men. HAA was defined as a nadir Hgb value during the course of hospitalization meeting WHO criteria. We further grouped Hgb by degree into no anemia, mild anemia (Hgb >11 and <12 g/dL in women, >11 and <13 g/dL in men), moderate anemia (Hgb >9 and 11 g/dL), and severe anemia (Hgb 9 g/dL).
Outcomes
Outcomes were all‐cause in‐hospital mortality, total hospital LOS, and total hospital charges.
Data Analysis
For risk adjustment, we used methods developed by Elixhauser and colleagues[14] for use with in‐patient administrative databases. These included a comprehensive set of comorbidity indicators, used to control for patients' underlying conditions in models of outcomes. Among the 30 variables defined by Elixhauser and colleagues, we excluded the 2 administrative anemia codes because this was our variable of interest (Table 1). For all models, demographics, medical conditions, and hospitalization type (medical vs surgical) were included as covariables in addition to the anemia groupings (no HAA and mild, moderate, and severe HAA).
| Characteristic | Hospital‐Acquired Anemia Group | P | |||
|---|---|---|---|---|---|
| No Anemia, n=48,640 | Mild, n=40,828 | Moderate, n=57,184 | Severe, n=41,795 | ||
| |||||
| Age at admission, y | 5518 | 5818 | 5819 | 6117 | <0.0001 |
| Female | 25,123 (52) | 17,938 (44) | 35,858 (63) | 23,533 (56) | <0.0001 |
| Race/ethnicity | <0.0001 | ||||
| White | 39,100 (80) | 32,610 (80) | 45,977 (80) | 33,810 (81) | |
| Black | 7580 (16) | 6607 (16) | 8946 (16) | 6204 (15) | |
| Other | 1960 (4.0) | 1611 (3.9) | 2261 (4.0) | 1781 (4.3) | |
| Hospitalization type | <0.0001 | ||||
| Surgery | 9681 (20) | 14,076 (34) | 26,100 (46) | 27,865 (67) | |
| Medicine | 38,958 (80) | 26,750 (66) | 31,081 (54) | 13,922 (33) | |
| Hypertension | 25,591 (53) | 22,218 (54) | 29,963 (52) | 24,257 (58) | <0.0001 |
| Heart failure | 2811 (5.8) | 3182 (7.8) | 5086 (8.9) | 4278 (10) | <0.0001 |
| Valvular disease | 1201 (2.5) | 1259 (3.1) | 2126 (3.7) | 1890 (4.5) | <0.0001 |
| Pulmonary circulation disease | 667 (1.4) | 730 (1.8) | 1221 (2.1) | 1484 (3.6) | <0.0001 |
| Peripheral arterial disease | 2417 (5.0) | 2728 (6.7) | 4187 (7.3) | 4508 (11) | <0.0001 |
| Paralysis | 1216 (2.5) | 1175 (2.9) | 1568 (2.7) | 1305 (3.1) | <0.0001 |
| Other neurologic disorders | 3013 (6.2) | 2780 (6.8) | 3599 (6.3) | 2829 (6.8) | <0.0001 |
| Chronic obstructive pulmonary disease | 9225 (19) | 7885 (19) | 10,960 (19) | 8057 (19) | 0.5 |
| Diabetes without chronic complications | 8306 (17) | 7733 (19) | 10,417 (18) | 7911 (19) | <0.0001 |
| Diabetes with chronic complications | 1547 (3.2) | 1922 (4.7) | 2989 (5.2) | 2779 (6.6) | <0.0001 |
| Hypothyroidism | 5008 (10) | 4258 (10) | 6938 (12) | 5567 (13) | <0.0001 |
| Renal failure | 2006 (4.1) | 3278 (8.0) | 5787 (10) | 5954 (14) | <0.0001 |
| Liver disease | 1394 (2.9) | 1341 (3.3) | 1788 (3.1) | 2013 (4.8) | <0.0001 |
| Peptic ulcer disease, excluding bleeding | 5 (0.01) | 9 (0.022) | 15 (0.026) | 30 (0.072) | <0.0001 |
| Acquired immune deficiency syndrome | 49 (0.10) | 74 (0.18) | 79 (0.14) | 56 (0.13) | 0.01 |
| Lymphoma | 182 (0.37) | 310 (0.76) | 624 (1.1) | 718 (1.7) | <0.0001 |
| Metastatic cancer | 489 (1.0) | 789 (1.9) | 1889 (3.3) | 1993 (4.8) | <0.0001 |
| Solid tumor without metastasis | 499 (1.0) | 760 (1.9) | 1297 (2.3) | 1123 (2.7) | <0.0001 |
| Rheumatoid arthritis/collagen vascular disease | 1250 (2.6) | 1260 (3.1) | 2214 (3.9) | 1729 (4.1) | <0.0001 |
| Coagulopathy | 1096 (2.3) | 1402 (3.4) | 2517 (4.4) | 6214 (15) | <0.0001 |
| Obesity | 7404 (15) | 5177 (13) | 7112 (12) | 5279 (13) | <0.0001 |
| Weight loss | 972 (2.0) | 1240 (3.0) | 2746 (4.8) | 5841 (14) | <0.0001 |
| Fluid and electrolyte disorders | 7262 (15) | 7501 (18) | 12,828 (22) | 17,201 (41) | <0.0001 |
| Alcohol abuse | 3312 (6.8) | 1977 (4.8) | 1699 (3.0) | 1319 (3.2) | <0.0001 |
| Drug abuse | 3357 (6.9) | 1554 (3.8) | 1197 (2.1) | 657 (1.6) | <0.0001 |
| Psychoses | 3479 (7.2) | 2345 (5.7) | 2544 (4.4) | 1727 (4.1) | <0.0001 |
| Depression | 5999 (12) | 4662 (11) | 6605 (12) | 4895 (12) | <0.0001 |
Logistic regression was used to assess the association of HAA with in‐hospital mortality, and linear regression to assess the association of HAA with hospital LOS and total hospital charges. LOS and total charges were logarithmically transformed because of right‐skewed distributions. The exponential of the resulting regression coefficients quantifies the relative change in LOS or total charges compared to patients without HAA. Unless otherwise specified, a P value of0.05 was considered statistically significant. The Bonferroni method was used to adjust for multiple comparisons.
Our primary analysis excluded patients with anemia at the time of hospitalization based on administratively determined POA anemia positive indicator coding. We also performed a sensitivity analysis to exclude patients with anemia based on the first Hgb values determined by laboratory testing.
All analyses were performed using SAS version 9.2 (SAS Inc., Cary, NC) and R version 2.13 (
RESULTS
Prevalence of HAA
Among the 188,447 hospitalizations, 139,807 patients (74%) developed HAA and 48,640 (26%) did not. Of the 74%, 40,828 developed mild, 57,184 moderate, and 41,795 severe HAA (Figure 2). Patients who developed HAA were older than those who did not and had more comorbidities, including hypertension, heart failure, peripheral arterial disease, and renal and liver disease. They were hospitalized more commonly for surgical intervention than were those who did not develop HAA (Table 1). Time‐related patterns for developing HAA, however, showed that it developed earlier in men and more frequently with medical versus surgical hospitalization (Figure 3).

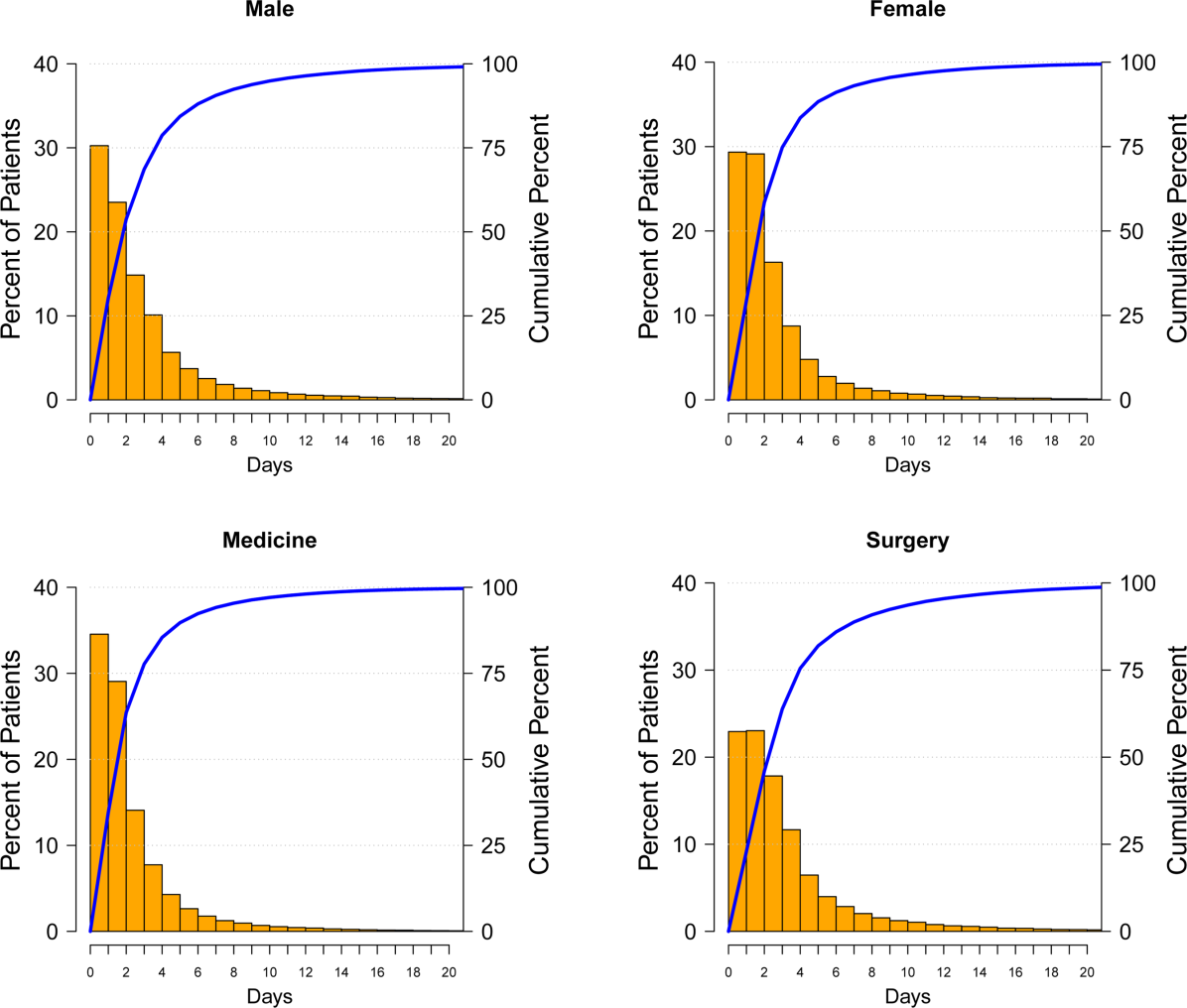
Hospital Mortality and HAA
Unadjusted mortality progressively increased with increasing degree of HAA: no HAA, 0.78% (n=378); mild HAA, 0.99% (n=405); moderate HAA, 1.5% (n=881); and severe HAA, 4.6% (n=1936) (P<0.001) (Figure 4A). Patients with mild HAA did not have higher risk‐adjusted mortality than those not having HAA (odds ratio: 1.02, 95% confidence interval [CI]: 0.88‐1.17). However, as HAA increased to moderate and severe, risk of hospital mortality increased in a dose‐dependent manner compared with patients not developing HAA: moderate HAA, 1.51 (95% CI: 1.33‐1.71, P<0.001) and severe HAA, 3.28 (95% CI: 2.90‐3.72, P<0.001) (Figure 5A) (see Supporting Information, Supplement A, in the online version of this article).
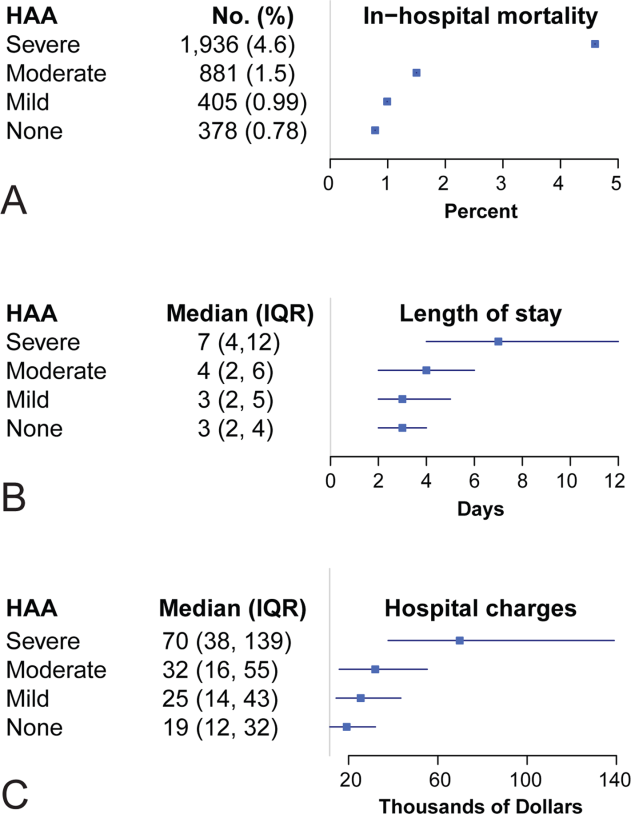
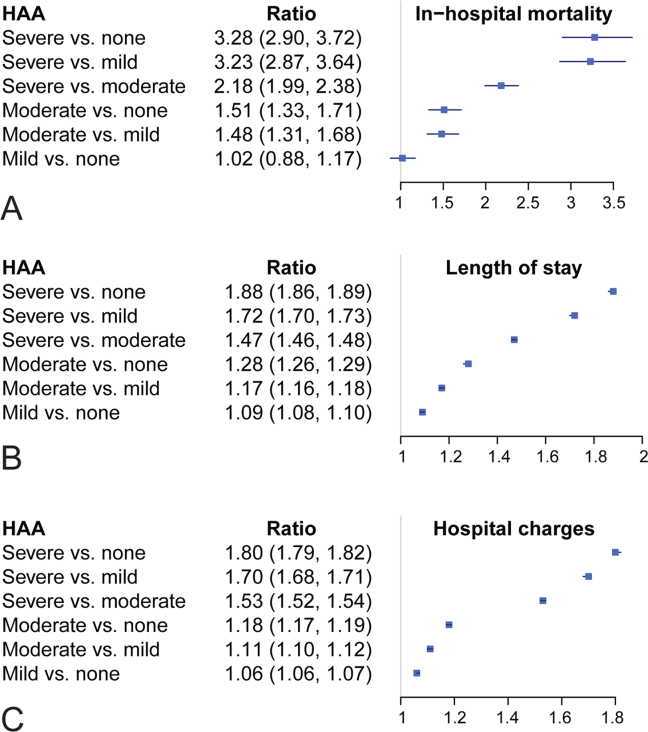
Resource Utilization and HAA
Length of Hospital Stay
Unadjusted median (25th, 75th percentiles) LOS was progressively higher in patients who developed HAA: no HAA, 3 days (2, 4); mild HAA, 3 days (2, 5); moderate HAA, 4 days (2, 6); and severe HAA, 7 days (4, 12) (P<0.001) (Figure 4B). Mild HAA was associated with a mean relative increase of 1.09 (95% CI: 1.08‐1.10, P<0.001); moderate HAA, 1.28 (95% CI: 1.26‐1.29, P<0.001); and severe HAA, 1.88 (95% CI: 1.86‐1.89, P<0.001). For example, if expected LOS was 4 days for a patient with no HAA, then for a patient with severe anemia, it would be 7.52 (a 1.88‐fold increase) when all comorbidities were the same (Figure 5B) (see Supporting Information, Supplement A, in the online version of this article).
Total Hospital Charges
Unadjusted hospital charges became progressively higher as degree of HAA increased (P<0.001) (Figure 4C). The mean relative increase was 1.06 (95% CI: 1.06‐1.07, P<0.001) for mild HAA compared with no HAA, 1.18 (95% CI: 1.17‐1.19, P<0.001) for moderate HAA, and 1.80 (95% CI: 1.79‐1.82, P<0.001) for severe HAA. For example, if the expected total charge was $30,000 for a patient with no HAA, then for a patient with severe anemia, it would be $54,000 (a 1.80‐fold increase) when all comorbidities were the same (Figure 5C) (see Supporting Information, Supplement A, in the online version of this article).
Sensitivity Analysis
Among patients without anemia based on the first available Hgb value (n=96,975), 50% of patients developed HAA: mild HAA, 24% (n=23,063); moderate HAA, 19% (n=18,134); and severe HAA, 8% (n=7373). There was a similar relationship between increasing magnitude of HAA and an increase in mortality, LOS, and total charges in the unadjusted and adjusted analyses (see Supporting Information, Supplement C, in the online version of this article).
DISCUSSION
A substantial number of patients entering our health system became anemic during the course of their hospitalization. Among those who developed HAA, in‐hospital mortality was higher, LOS longer, and total hospital charges greater in a dose‐dependent manner. A recent editorial noted that HAA might be a hazard of hospitalization similar to other complications, such as infections and deep vein thrombosis.[15] Our findings have significance in terms of demonstrating increased mortality and resource utilization associated with a potentially modifiable hospital‐acquired condition. Even mild HAA was associated with increased resource utilization, although not increased hospital mortality.
Others have noted negative consequences of HAA in subpopulations of hospital patients. Salisbury and colleagues examined 17,676 patients with acute myocardial infarction who had normal Hgb on admission.[16] They defined HAA as development of new anemia during hospitalization based on nadir Hgb. HAA developed in 57.5% of patients and was associated with increased mortality in a progressive manner. Risk‐adjusted odds ratios for in‐hospital death were greater in patients with moderate and severe HAA, 1.38 (95% CI: 1.10‐1.73) and 3.39 (95% CI: 2.59‐4.44), respectively.[16] A separate investigation of 2902 patients from a multicenter registry of patients admitted to the hospital with acute myocardial infarction reported that nearly half of those with normal Hgb values on admission developed HAA.[17] Most of these patients did not have documented bleeding; therefore, the authors suggested that HAA was not a surrogate for bleeding during hospitalization. Moreover, HAA was associated with higher mortality and worse health status 1 year after myocardial infarction.[17] Others have reported that development of HAA is not uncommon in the setting of acute myocardial infarction and is associated with increased long‐term mortality.[18]
Development of anemia during hospitalization is multifactorial and may result from procedural bleeding, phlebotomy, occult bleeding, hemodilution from intravenous fluid administration, and blunted erythropoietin production associated with critical illness.[8, 9] An investigation of general internal medicine patients reported phlebotomy was highly associated with changes in Hgb levels and contributed to anemia during hospitalization.[19] The authors reported that for every 1 mL of blood drawn, mean decreases in Hgb and hematocrit were 0.070.011 g/L1 and 0.0190.003%, respectively. They suggested reporting cumulative phlebotomy volumes to physicians and use of pediatric‐sized tubes for collection.[19] Salisbury and colleagues reported that mean phlebotomy volume was higher in patients who developed HAA; for every 50 mL of blood drawn, the risk of moderate to severe HAA increased by 18%.[20] In an intensive care population, Chant and colleagues reported small decreases in phlebotomy volume were associated with reduced transfusion requirements in patients with prolonged stay.[21]
Attempts to ameliorate HAA should focus on modifiable processes‐of‐care factors. Patients with chronic illness have blunted erythropoiesis[8] and therefore cannot mount an adequate response to blood loss from procedures or phlebotomy. Whether use of erythropoietin, iron, or both would be effective in this population requires further investigation. One of the most studied risk factors for HAA is blood loss from hospital laboratory testing.[20] Sanchez‐Giron and Alvarez‐Mora found that all laboratory tests could be performed with smaller‐volume collection tubes without need for additional samples.[22] Others have proposed batching laboratory requests, recording cumulative daily blood loss due to phlebotomy for individual patients,[23] and use of blood conservation devices in intensive care units.
Figure 3 suggests that surgical patients develop anemia slightly later than medical patients. Features specific to surgery, such as perioperative intravenous fluid loading, third spacing, and subsequent plasma volume expansion when reabsorption occurs days later, likely contribute to differences in trends for development of HAA.[24, 25, 26] In addition, specific surgical cases with highly anticipated red blood cell loss should make use of antifibrinolytic agents to reduce blood loss and red cell salvage devices to reprocess and infuse shed blood.
Limitations
A recent commentary explored the question of benchmarks for anemia diagnosis, and in particular, what defines the lower limit of normal.[27] Although we used WHO criteria, others have used criteria establishing lower benchmarks according to race and gender.[27] Our results would have been similar if we had used these lower benchmarks, because our moderate and severe anemia Hgb cutoff values were beneath alternative benchmarks for diagnosing anemia. For example, Beutler and Waalen provide a definition of anemia that includes an Hgb cutoff of 12.2 g/dL for white women aged 20 to 49 years, 11.5 g/dL for black women of similar age, 13.7 g/dL for white men, and 12.9 g/dL for black men.[27]
Our study is limited by the nature of administrative data. However, use of demographic data, hospitalization type, and use of a large number of comorbidities for risk adjustment improved our findings. Adding nonadministrative clinical laboratory data from the electronic record for patient Hgb values provided us with a more accurate diagnosis of HAA and an ability to further subdivide anemia into mild, moderate, and severe categories that have prognostic implications. We are aware of the inherent limitations associated with use of administrative data. However, coded data are currently readily available and are the source of information on which many healthcare policies are made.[28, 29]
The POA anemia administrative code was used to identify patients with preexisting anemia. We did not use the first Hgb value upon admission because it is often made following interventions (eg, surgical patients have preoperative laboratory testing prior to admission, and the first Hgb value available following hospitalization is commonly obtained following surgical interventions). However, we performed a sensitivity analysis that defined preexisting anemia based on the first available Hgb value. The results from the sensitivity analysis were consistent with our primary findings with the use of administrative data coding. Of note, use of administrative codes for determining POA indicators is consistent with methods employed for all current publically reported quality and patient safety initiatives. Specifically, the Agency for Healthcare Research and Quality Patient Safety Indicators used by the Centers for Medicare and Medicaid Services to assess hospital quality of care and to modify reimbursement for services.
Our focus was on development of HAA; treatment of HAA with red blood cell transfusion and standardized blood draw orders were not investigated. Finally, our results are reflective of a single health system; further work with multicenter data would help clarify our findings.
CONCLUSION
Development of HAA is common and has important healthcare implications, including higher in‐hospital mortality and increased resource utilization. Treating HAA by transfusion has attendant morbidity risks and increased costs.[11, 12, 30] Hospitals must continue to focus on improving patient safety and raising awareness of HAA and other modifiable hospital‐acquired conditions. Closer prospective investigation for both medical and surgical patients of cumulative blood loss from laboratory testing, procedural blood loss, and a risk‐benefit analysis of treatment options is necessary.
Acknowledgments
Disclosure: Nothing to report.
Disclosure
Nothing to report.
- , , , , , . A population‐based study of hemoglobin, race, and mortality in elderly persons. J Gerontol A Biol Sci Med Sci. 2008;63(8):873–878.
- , , , . Anemia in the elderly: a public health crisis in hematology. Hematology Am Soc Hematol Educ Program. 2005:528–532.
- , , . The definition of anemia in older persons. JAMA. 1999;281(18):1714–1717.
- , . Anemia in the elderly: how should we define it, when does it matter, and what can be done? Mayo Clin Proc. 2007;82(8):958–966.
- , , , et al. A prospective study of anemia status, hemoglobin concentration, and mortality in an elderly cohort: the Cardiovascular Health Study. Arch Intern Med. 2005;165(19):2214–2220.
- , , , et al. Association of mild anemia with hospitalization and mortality in the elderly: the Health and Anemia population‐based study. Haematologica. 2009;94(1):22–28.
- , , , et al. Association of mild anemia with cognitive, functional, mood and quality of life outcomes in the elderly: the “Health and Anemia” study. PLoS One. 2008;3(4):e1920.
- . Anemia in the critically ill. Crit Care Clin. 2004;20(2):159–178.
- . Scope of the problem: epidemiology of anemia and use of blood transfusions in critical care. Crit Care. 2004;8(suppl 2):S1–S8.
- , , , , , . Transfusion and pulmonary morbidity after cardiac surgery. Ann Thorac Surg. 2009;88(5):1410–1418.
- , , , et al. Morbidity and mortality risk associated with red blood cell and blood‐component transfusion in isolated coronary artery bypass grafting. Crit Care Med. 2006;34(6):1608–1616.
- , , , et al. Duration of red‐cell storage and complications after cardiac surgery. N Engl J Med. 2008;358(12):1229–1239.
- , , , et al. Transfusion in coronary artery bypass grafting is associated with reduced long‐term survival. Ann Thorac Surg. 2006;81(5):1650–1657.
- , , , . Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27.
- , . Hazards of hospitalization: more than just “never events”. Arch Intern Med. 2011;171(18):1653–1654.
- , , , et al. Hospital‐acquired anemia and in‐hospital mortality in patients with acute myocardial infarction. Am Heart J. 2011;162(2):300–309.e3.
- , , , et al. Incidence, correlates, and outcomes of acute, hospital‐acquired anemia in patients with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2010;3(4):337–346.
- , , , et al. Changes in haemoglobin levels during hospital course and long‐term outcome after acute myocardial infarction. Eur Heart J. 2007;28(11):1289–1296.
- , , , , . Do blood tests cause anemia in hospitalized patients? The effect of diagnostic phlebotomy on hemoglobin and hematocrit levels. J Gen Intern Med. 2005;20(6):520–524.
- , , , et al. Diagnostic blood loss from phlebotomy and hospital‐acquired anemia during acute myocardial infarction. Arch Intern Med. 2011;171(18):1646–1653.
- , , . Anemia, transfusion, and phlebotomy practices in critically ill patients with prolonged ICU length of stay: a cohort study. Crit Care. 2006;10(5):R140.
- , . Reduction of blood loss from laboratory testing in hospitalized adult patients using small‐volume (pediatric) tubes. Arch Pathol Lab Med. 2008;132(12):1916–1919.
- , . Phlebotomy for diagnostic laboratory tests in adults. Pattern of use and effect on transfusion requirements. N Engl J Med. 1986;314(19):1233–1235.
- , , , , . Perioperative monitoring of circulating and central blood volume in cardiac surgery by pulse dye densitometry. Intensive Care Med. 2004;30(11):2053–2059.
- , , , , . Perioperative red cell, plasma, and blood volume change in patients undergoing cardiac surgery. Transfusion. 2006;46(3):392–397.
- , , , . Changes in circulating blood volume after cardiac surgery measured by a novel method using hydroxyethyl starch. Crit Care Med. 2000;28(2):336–341.
- , . The definition of anemia: what is the lower limit of normal of the blood hemoglobin concentration? Blood. 2006;107(5):1747–1750.
- , , , , , . What are the real rates of postoperative complications: elucidating inconsistencies between administrative and clinical data sources. J Am Coll Surg. 2012;214(5):798–805.
- . Medicare program: hospital inpatient value‐based purchasing program, final rule. Available at: http://www.cms.gov/Medicare/Quality‐Initiatives‐Patient‐Assessment‐Instruments/HospitalQualityInits/index.html. Accessed May 6, 2011.
- , , , , , . Increased mortality, postoperative morbidity, and cost after red blood cell transfusion in patients having cardiac surgery. Circulation. 2007;116(22):2544–2552.
- , , , , , . A population‐based study of hemoglobin, race, and mortality in elderly persons. J Gerontol A Biol Sci Med Sci. 2008;63(8):873–878.
- , , , . Anemia in the elderly: a public health crisis in hematology. Hematology Am Soc Hematol Educ Program. 2005:528–532.
- , , . The definition of anemia in older persons. JAMA. 1999;281(18):1714–1717.
- , . Anemia in the elderly: how should we define it, when does it matter, and what can be done? Mayo Clin Proc. 2007;82(8):958–966.
- , , , et al. A prospective study of anemia status, hemoglobin concentration, and mortality in an elderly cohort: the Cardiovascular Health Study. Arch Intern Med. 2005;165(19):2214–2220.
- , , , et al. Association of mild anemia with hospitalization and mortality in the elderly: the Health and Anemia population‐based study. Haematologica. 2009;94(1):22–28.
- , , , et al. Association of mild anemia with cognitive, functional, mood and quality of life outcomes in the elderly: the “Health and Anemia” study. PLoS One. 2008;3(4):e1920.
- . Anemia in the critically ill. Crit Care Clin. 2004;20(2):159–178.
- . Scope of the problem: epidemiology of anemia and use of blood transfusions in critical care. Crit Care. 2004;8(suppl 2):S1–S8.
- , , , , , . Transfusion and pulmonary morbidity after cardiac surgery. Ann Thorac Surg. 2009;88(5):1410–1418.
- , , , et al. Morbidity and mortality risk associated with red blood cell and blood‐component transfusion in isolated coronary artery bypass grafting. Crit Care Med. 2006;34(6):1608–1616.
- , , , et al. Duration of red‐cell storage and complications after cardiac surgery. N Engl J Med. 2008;358(12):1229–1239.
- , , , et al. Transfusion in coronary artery bypass grafting is associated with reduced long‐term survival. Ann Thorac Surg. 2006;81(5):1650–1657.
- , , , . Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27.
- , . Hazards of hospitalization: more than just “never events”. Arch Intern Med. 2011;171(18):1653–1654.
- , , , et al. Hospital‐acquired anemia and in‐hospital mortality in patients with acute myocardial infarction. Am Heart J. 2011;162(2):300–309.e3.
- , , , et al. Incidence, correlates, and outcomes of acute, hospital‐acquired anemia in patients with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2010;3(4):337–346.
- , , , et al. Changes in haemoglobin levels during hospital course and long‐term outcome after acute myocardial infarction. Eur Heart J. 2007;28(11):1289–1296.
- , , , , . Do blood tests cause anemia in hospitalized patients? The effect of diagnostic phlebotomy on hemoglobin and hematocrit levels. J Gen Intern Med. 2005;20(6):520–524.
- , , , et al. Diagnostic blood loss from phlebotomy and hospital‐acquired anemia during acute myocardial infarction. Arch Intern Med. 2011;171(18):1646–1653.
- , , . Anemia, transfusion, and phlebotomy practices in critically ill patients with prolonged ICU length of stay: a cohort study. Crit Care. 2006;10(5):R140.
- , . Reduction of blood loss from laboratory testing in hospitalized adult patients using small‐volume (pediatric) tubes. Arch Pathol Lab Med. 2008;132(12):1916–1919.
- , . Phlebotomy for diagnostic laboratory tests in adults. Pattern of use and effect on transfusion requirements. N Engl J Med. 1986;314(19):1233–1235.
- , , , , . Perioperative monitoring of circulating and central blood volume in cardiac surgery by pulse dye densitometry. Intensive Care Med. 2004;30(11):2053–2059.
- , , , , . Perioperative red cell, plasma, and blood volume change in patients undergoing cardiac surgery. Transfusion. 2006;46(3):392–397.
- , , , . Changes in circulating blood volume after cardiac surgery measured by a novel method using hydroxyethyl starch. Crit Care Med. 2000;28(2):336–341.
- , . The definition of anemia: what is the lower limit of normal of the blood hemoglobin concentration? Blood. 2006;107(5):1747–1750.
- , , , , , . What are the real rates of postoperative complications: elucidating inconsistencies between administrative and clinical data sources. J Am Coll Surg. 2012;214(5):798–805.
- . Medicare program: hospital inpatient value‐based purchasing program, final rule. Available at: http://www.cms.gov/Medicare/Quality‐Initiatives‐Patient‐Assessment‐Instruments/HospitalQualityInits/index.html. Accessed May 6, 2011.
- , , , , , . Increased mortality, postoperative morbidity, and cost after red blood cell transfusion in patients having cardiac surgery. Circulation. 2007;116(22):2544–2552.
Copyright © 2013 Society of Hospital Medicine
Ideal Transitions of Care
Across the country, hospitals are rolling out programs to reduce readmissions. These range from patient education around their disease process and medications, improvements in discharge planning, medication reconciliation, outpatient appointments scheduled prior to discharge, and follow‐up phone calls, among others.[1, 2] Several collaboratives such as Project Better Outcomes by Optimizing Safe Transitions[3] and Hospital Medicine Reengineering Network[4] have formed to test, study, and share lessons learned from these inpatient‐based interventions. Because financial penalties thus far have focused on decreases in inpatient reimbursement by the Centers for Medicare and Medicaid Services (CMS), most of the interventions to reduce hospital readmissions have been concentrated in the inpatient domain. It is unclear whether new payment arrangements with CMS or commercial insurers, such as bundled payments and accountable care organizations (ACOs), will pressure primary care physicians (PCPs) to further develop outpatient‐based interventions.
In this article, I provide a PCP's perspective of how inpatient and outpatient providers can partner to create the ideal care transition from hospital to home. Although others have conducted systematic reviews or surveys of interventions to reduce hospital readmissions,[2, 5, 6, 7] I will start from a vision of an ideal transition, and then evaluate evidence supporting each step. I will also highlight areas where new reimbursement codes can help support an idealized transitions‐of‐care program.
ON HOSPITAL ADMISSION
Many PCPs consider the beginning of the care continuum to rest in the primary care practice and relationship. Over time, PCPs develop relationships with their patients, understanding the patients' values toward health and healthcare, learning their social support system and home environment, and documenting a clinical course of chronic diseases, including which therapies have and have not worked well. From a PCP perspective, it seems natural to be involved in care at the point of hospital admission. Some emergency departments (EDs) and hospital admissions offices have automated systems to email or fax PCPs admission notifications. Others rely on providers to make this connection.
Ideally, PCP communication would occur early in the hospitalization, especially for medically or socially complex patients, for 3 main reasons: (1) The PCP can offer insights on goals of care or therapies attempted in the past that may reduce unnecessary procedures, decrease length of stay, and improve patient satisfaction; (2) Reconciling medications that the patient should be taking and the list the patient reports may highlight noncompliance and trigger education around medication compliance prior to discharge; (3) Early PCP involvement may improve discharge planning efficiency, whereby the inpatient and outpatient teams agree on medical and social issues to be addressed for a safe discharge. Although there are no published studies that show communication early in the hospitalization impacts clinical outcomes, a national survey of hospitalists highlighted concerns about poor information exchange, particularly around medical history and outpatient medications, at the time of admission.[8]
As new financial models push healthcare providers to manage a population of patients under a global budget, inpatient and outpatient providers will need to communicate and collaborate at a level that is new for most institutions and providers.[9] Because early markers of success are based on financial savings, this means further reducing length of stay and transferring more care to the outpatient arena, tapping into community and home care resources. Involving PCPs early in the admission may help inpatient providers meet these goals.
DURING HOSPITALIZATION
Several publications from hospitalists have evaluated inpatient‐based interventions to reduce readmissions and improve care transitions.[10, 11, 12] Table 1 summarizes 6 steps that can improve communication and collaboration.
|
| 1. Involve the PCP in discharge planning early in the hospitalization.[1] |
| 2. Notify the PCP on hospital discharge.[44] |
| 3. Ensure the discharge summary is available at the time of discharge.[44] Several elements should be included in all discharge summaries:[45] |
| a. Home services ordered, home agency, timing of initiation of services. |
| b. Medication changes.[21] |
| c. Status of active problems at time of discharge.[11] |
| d. Follow‐up appointments, especially specialty follow‐up. |
| e. Tests pending at discharge or follow‐up required after discharge (eg, follow‐up CT scan in 6 months for incidental lung nodule).[11, 46, 47] |
| f. Equipment ordered. |
| 4. Schedule follow‐up appointment with appropriate outpatient provider by discharge.[11, 29] |
| 5. Ensure new prescriptions or changes to prescriptions are available at patient's pharmacy and any needed insurance preauthorization has been approved. |
| 6. Educate patient about disease process, medication adherence, lifestyle changes, and symptoms to monitor for after discharge.[22, 48, 49] |
AFTER HOSPITAL DISCHARGE
Immediately after hospital discharge, there are 7 steps that PCPs and their clinic staff can follow to support a safe transition from hospital to home. The literature supports several individual steps, but not the full package. I am proposing that primary care clinics adopt all 7 steps in an ideal transitions‐of‐care program.
Step 1: Telephone Call Within 72 Hours of Discharge
Many hospitals ask nurses or customer service staff to call patients immediately after hospital discharge. Call content ranges from reviewing discharge instructions and symptoms to satisfaction with hospital care. Even though a 2006 Cochrane review did not find a positive impact of hospital‐based postdischarge phone calls on readmission rates,[13] recent studies among select populations found small but significant reductions.[14, 15] Others have looked at fulfilling this role in the outpatient setting.[16, 17] A recent systematic review of primary care clinic‐based postdischarge phone calls showed no impact on readmission rates, but only 3 studies were included.[18] Health plan‐initiated telephone calls to plan members after hospital discharge reported a 22% reduction in readmissions.[19, 20] Because there is no standardization in telephone call content, reviews of inpatient‐based and clinic‐based interventions cited methodological challenges in drawing conclusions about impact.
Although education around disease process, lifestyle changes, and medication adherence can be effectively provided by staff from the hospital, clinic, or health plan, the outpatient clinic should assume primary responsibility for some components of the postdischarge call. First, if a patient does not have a follow‐up appointment after discharge, the clinic nurse can schedule the appointment directly. Second, medication discrepancies after hospital discharge pose safety risks.[21, 22, 23] Although inpatient nurses may review discharge medications, it is the primary care nurse who can reconcile the discharge medication list with the prehospitalization medication list and identify discrepancies. The outpatient nurse has easier access to the PCP to address discrepancies. Third, the primary care nurse can provide education around red‐flag symptoms for which to call the clinic and information on after‐hours clinic access, an area that patients have specifically requested as standard after discharge.[24] If the patient reports new symptoms, the clinic nurse has easy access to the PCP for management advice, as well as the clinic schedule for an urgent appointment. Having the primary care practice house posthospitalization phone calls allows for more efficient troubleshooting of postdischarge issues.
In January 2013, CMS introduced new codes for primary care‐based care coordination after hospitalization. Current procedural terminology (CPT) codes 99495 and 99496 can be used by PCPs who complete 2 steps: (1) document discussion with a patient or caregiver about care transitions within 2 days of discharge, and (2) have a face‐to‐face visit with the patient within 2 weeks or 1 week, respectively.[25] Reimbursement for these codes is substantial3.96 work relative value units (RVUs) for 99495 and 5.81 work RVUs for 99496considerably more than a level IV visit for complex follow‐up care (2.43 work RVUs). Primary care practices may find that reimbursement for these care coordination codes helps cover additional costs of nurses, case managers, or social workers assisting with posthospital care. The financial impact on primary care practices may increase if commercial insurers accept these CPT codes and reimburse at levels comparable to the CMS.
CMS approved reimbursement for posthospitalization phone calls despite mixed evidence on the impact of the intervention, presumably because it is perceived that early follow‐up may lead to benefits that cannot be easily captured in research studies, and simply represents good patient care. Two challenges in showing an impact of these phone calls are lack of standardization and small sample size. However, implementation of the care‐coordination CPT codes will require more standardization and potentially a much larger number of patients who receive posthospitalization phone calls. This allows for a much more robust evaluation of the intervention.
Step 2: Follow‐up Appointment With PCP or Most Appropriate Continuity Provider
Early follow‐up with an appropriate outpatient provider has been associated with reduced hospital readmissions for patients with congestive heart failure, chronic obstructive pulmonary disease, and psychiatric illnesses,[26, 27, 28, 29] but this finding has not been consistent across all patient populations.[5, 30] It is not well understood if the follow‐up appointment needs to be within a specific time frame, especially if the patient is already being touched once by the system through the posthospitalization call. General consensus falls within 7 days for patients at moderate to high risk for readmissions.[31, 32] Regardless of risk, follow‐up visits must occur within 2 weeks of discharge to claim the CMS reimbursement for posthospitalization care coordination, and higher reimbursement is offered if it occurs within 1 week.
Step 3: Care Coordination
A nurse, social worker, or case manager partnering with the PCP on care coordination may improve the patient experience and outcomes.[17, 24] Although the inpatient social worker or case manager may have helped address some housing, financial, home care, and durable medical equipment needs, often these issues are not completely resolved at discharge. There should be a seamless handoff between inpatient and outpatient care coordinators.
Although some primary care practices include social workers, case managers, or health coaches, many have general clinic nurses functioning in these roles. One way to help fund these roles is through the care coordination CPT codes as previously described. Another consideration, as the financial model for funding care across the care continuum changes, is to have inpatient social workers and case managers work jointly with inpatient and outpatient providers, following patients to the outpatient setting until their social needs are met. This arrangement is more feasible for integrated delivery systems or primary care clinics with contractual agreements with local hospitals, an emerging trend in markets across the United States.[33] Other resources for care coordination include health plan case managers and local community nonprofits. In 2011, CMS launched the Community‐Based Care Transitions Program (CCTP), which will award up to $500 million in funding over 5 years to community‐based organizations to assist Medicare patients with care transitions.[34]
One way of operationalizing care coordination, especially in primary care clinics that do not have an embedded social worker or case manager, is to offer a team‐based appointment in conjunction with the physician postdischarge visit. A healthcare team member (nurse, experienced medical assistant, pharmacist) reviews hospital discharge records, educates the patient about the reasons for hospitalization and how to prevent readmission, performs detailed review of medications, follows up on any pending test results, reviews home care orders or durable medical equipment orders, and identifies any psychosocial issues that need to be addressed. All findings are documented in the patient chart and available for review at the beginning of the physician visit. With the team previsit in place, the physician can focus on the medical problems.
Step 4: Repeat Process Above Until Active Issues Are Stabilized
For some patients, steps 1 through 4 may need to be repeated until active medical and psychosocial issues are stabilized. Creating clinic infrastructure to support patients who may need to return weekly for titration of medications or monitoring of lab values until they normalize can prevent unnecessary ED visits. Patients with psychosocial issues will likely need longitudinal support, as these issues often take months to resolve.
Step 5: Create Access in Clinic for Patients With New Symptoms
Even after the first posthospitalization visit, patients may need to return to their PCP because of new symptoms or for active monitoring. In many parts of the country, PCP access is limited.[33] To meet patient demand for timely appointments, many primary care practices have piloted advanced access scheduling, reserving the majority of appointments for same‐day patient requests. However, evaluations show that the same‐day appointment goals of advanced access are difficult to achieve for most practices.[35] Despite challenges to same‐day access for the general clinic population, it is critical to create access for patients recently hospitalized, as many are at high risk for an ED visit or another hospital admission.
Step 6: Know Your Numbers
A basic tenet of quality improvement is measuring baseline performance and performance at intermediate time points during an intervention.[36] A recent Cochrane review found that feeding back performance to physicians can lead to potentially important improvements in practice.[37] In an Institute for Healthcare Improvement how‐to guide for improving care transitions, measuring readmission rates is 1 step in their Model for Improvement.[32] However, few primary care clinics are actively monitoring their readmission rates. One basic challenge is data availability. Primary care clinics affiliated with a hospital can obtain discharge and readmissions data from the hospital, but patients may also be hospitalized at other facilities. Insurers would be the best source of hospital discharge data, and some payors supply PCPs with risk‐adjusted performance metrics.[38, 39] As ACOs mature, primary care clinics can partner with payors to obtain data and begin trending their hospital discharge and readmission rates. In the interim, trending readmission rates at a single affiliated institution and filtering by service, discharge diagnosis, or payor may reveal areas for intervention.
Step 7: Know Your Readmitted Patients
Similar to knowing the primary care clinic's overall discharge and readmission numbers, it is also important to know the population of frequently readmitted patients. Even though some PCPs may be able to recall these patients by memory, it is important to review these patients' charts and identify preventable factors related to readmission, especially system‐related factors. Conducting reviews can be time intensive and add new demands for busy PCPs. However, many clinics already conduct morbidity and mortality conferences and case reviews as part of improving patient satisfaction, service, and outcomes. Case reviews of frequently admitted patients can fall under these established activities.
IMPLICATIONS
In this vision of the ideal care transition, I am suggesting a shift in culture from a predominantly hospital‐based program to a program that spans the care continuum and requires active participation and ownership from the PCP's team. It will require inpatient and outpatient providers to communicate early and frequently during the hospitalization, sharing patient information efficiently and working collaboratively as part of a larger team to meet the medical and psychosocial needs of the patient. This concept is not new, but has not been supported financially from payors.[1, 9, 40] Most PCPs operate on margins that cannot support additional PCP time to coordinate care for patients or staff to assist (although many PCPs believe this is the role of the primary care medical home).[33] Some payors agree that stipends to support infrastructure change are needed to improve patient outcomes.[17, 38, 39]
Even though every envisioned step does not require additional funding, new payment arrangements under ACOs and bundled payments may offer opportunities for PCPs to assume a larger role in care transitions and secure funding to pay for interventions. However, primary care practices must be positioned to negotiate favorable global payment agreements, be willing to assume risks associated with global payments, and prioritize management of medically and socially complex patients who are at risk for preventable ED visits and hospitalizations. PCPs who are not participating in ACOs or bundled payments, or those who are risk adverse, may be able to finance pieces of this vision with the new care coordination CPT codes supported by Medicare (and possibly commercial payors in the future). They may also partner with community groups participating in CCTP for additional support. Others focus on the long‐term benefits of ACO‐like structures rather than the short‐term investments needed.[41]
Are all 14 steps proposed above essential? Without doubt, this vision will be difficult to fully operationalize and requires coordination and support from many distinct groups. Should all patients be offered a basic package of interventions, reserving the full package for those who are identified as highest risk for poor outcomes after hospital discharge? There is already some support around specialized interventions for patients at high risk for readmissions,[32, 41] and risk prediction models have been introduced to identify these individuals.[42] Or should we approach this as a menu of interventions from which to choose, tailoring interventions to individual patient needs? These questions should be tested, as our experience in coordinating care across the continuum matures. With over 100 ACOs formed in Medicare alone[43] and many more with commercial insurers, our understanding in this area will grow in the next 5 years.
CONCLUSIONS
As cost containment measures in healthcare target preventable readmissions, hospitals and primary care physicians are increasingly encouraged to improve transitions along the care continuum. In this article, I offer 1 PCP's vision of the ideal transitions‐of‐care program from hospital to home. This article focuses on steps that can be taken by PCPs and their clinic staff; it does not address the role of outpatient specialists, home care agencies, or community support groups in care transitions. Operationalizing this vision requires commitment from the hospital and clinic leadership, as well as buy‐in from front‐line providers. More research is required to understand the marginal impact of each component of this vision, as well as the comprehensive package of interventions proposed, on patient outcomes. New financial models with payors and hospitals may make it easier for primary care clinics to test this vision. Current financial incentives are likely still inadequate to fully align care along the continuum, but they offer some support for more PCPs to take an active role. The time has come to shift our traditional view of transitions of care from a hospital‐centric set of interventions toward one that spans the entire care continuum and includes primary care physicians and their clinic staff as key partners.
Acknowledgments
The author thanks Jeffrey Fujimoto for his assistance with the literature review.
Disclosures: Ning Tang, MD, is supported by a University of California, Center for Health Quality and Innovation grant. Dr. Tang has no financial conflicts of interests.
- , , . Reducing hospital readmissions: lessons from top‐performing hospitals. The Commonwealth Fund Synthesis Report. April 2011. Available at: http://www.commonwealthfund.org/Publications/Case‐Studies/2011/Apr/Reducing‐Hospital‐Readmissions.aspx. Accessed January 30, 2013.
- , . Effective Interventions to Reduce Rehospitalizations: A Survey of the Published Evidence. Cambridge, MA: Institute for Healthcare Improvement; 2009.
- Society of Hospital Medicine. Project BOOST. Available at: www.hospitalmedicine.org/BOOST/. Accessed January 30, 2013.
- American Association of Medical Colleges. HOMERUN Executive Summary. Available at: https://members.aamc.org/eweb/upload/HOMERUN%20summary%202012.pdf. Accessed January 30, 2013.
- , , , , . Interventions to reduce 30‐day rehospitalization: a systematic review. Ann Intern Med. 2011;155:520–528.
- , , , et al. Contemporary evidence about hospital strategies for reducing 30‐day readmissions. J Am Coll Cardiol. 2012;60:607–614.
- , , , et al. Improving patient handovers from hospital to primary care: a systematic review. Ann Intern Med. 2012;157:417–428.
- , , , . Hospitalists and care transitions: the divorce of inpatient and outpatient care. Health Aff. 2008;27:1315–1327.
- , , . Recasting readmissions by placing the hospital role in community context. JAMA. 2013;309:351–352.
- , , , . Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2:314–323.
- , , , et al. Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists. J Hosp Med. 2006;1:354–360.
- . Transitioning the patient with acute coronary syndrome from inpatient to primary care. J Hosp Med. 2010;5(suppl):S8–S14.
- , . Telephone follow‐up, initiated by a hospital‐based health professional, for postdischarge problems in patients discharged from hospital to home. Cochrane Database Syst Rev. 2006;(4):CD004510.
- , , , . Post‐discharge intervention in vulnerable, chronically ill patients. J Hosp Med. 2012;7:124–130.
- , , , et al. Low‐cost transitional care with nurse managers making mostly phone contact with patients cut rehospitalization at a VA hospital. Health Aff. 2012;31:2659–2668.
- , , , . Redefining and redesigning hospital discharge to enhance patient care: a randomized control study. J Gen Intern Med. 2008;23:1228–1233.
- , , , et al. How Geisinger's advanced medical home model argues the case for rapid‐cycle innovation. Health Aff. 2010;29:2047–2053. .
- , , . Telephone follow‐up as a primary care intervention for postdischarge outcomes improvement: a systematic review. Am J Med. 2012;125:915–921.
- , , , , . The impact of postdischarge telephonic follow‐up on hospital readmissions. Popul Health Manag. 2011;14:27–32.
- , , , , . Prioritized post‐discharge telephonic outreach reduces hospital readmissions for select high‐risk patients. Am J Manag Care. 2012;18:838–844.
- , , , et al. Association of ICU or hospital admission with unintentional discontinuation of medications for chronic diseases. JAMA. 2011;306:840–847.
- , , , et al. Effect of a pharmacist intervention on clinically important medication errors after hospital discharge. Ann Intern Med. 2012;157:1–10.
- , , , , , . Relationship of health literacy to intentional and unintentional non‐adherence of hospital discharge medications. J Gen Intern Med. 2012;27:173–178.
- , , , , . Patient experiences of transitioning from hospital to home: an ethnographic quality improvement project. J Hosp Med. 2012;7:382–387.
- . Medicare finalizes physician pay for new care coordination benefit. American Medical News. November 12, 2012. Available at: http://www.ama‐assn.org/amednews/2012/11/12/gvl11112.htm. Accessed February 8, 2013.
- , , , , . Outpatient follow‐up visit and 30‐day emergency department visit and readmission in patients hospitalized for chronic obstructive pulmonary disease. Arch Intern Med. 2010;170:1664–1670.
- , , . Post‐hospitalization transitions: examining the effects of timing of primary care provider follow‐up. J Hosp Med. 2010;5:392–397.
- , , , et al. Relationship between early physician follow‐up and 30‐day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303:1716–1722.
- , , . Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psychiatr Serv. 2000;51:885–889.
- , , , , . Do timely outpatient follow‐up visits decrease hospital readmission rates? Am J Med Qual. 2012;27:11–15.
- Project BOOST. Tool for addressing risk: a geriatric evaluation for transitions. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/PDFs/TARGET.pdf. Accessed February 3, 2013.
- , , , , . How‐to Guide: Improving Transitions from the Hospital to Community Settings to Reduce Avoidable Rehospitalizations. Cambridge, MA: Institute for Healthcare Improvement; 2012.
- , . Primary care: current problems and proposed solutions. Health Aff. 2010;29:799–805.
- Center for Medicare and Medicaid Innovation. Community‐based Care Transitions Program. Available at: http://innovation.cms.gov/initiatives/CCTP/#collapse‐tableDetails. Accessed February 8, 2013.
- , , . Advanced access scheduling outcomes: a systematic review. Arch Intern Med. 2011;171:1150–1159.
- , , , . The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2nd ed. San Francisco, CA: Jossey‐Bass Publishers; 2009.
- , , , et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;(6):CD000259.
- Agency for Healthcare Research and Quality. Policy Innovation Profile. Insurer provides financial incentives, infrastructure, and other support to stimulate provider participation in quality improvement collaborations. June 6, 2012. Available at: http://www.innovations.ahrq.gov/content.aspx?id=3641. Accessed February 8, 2013.
- , , , . Private‐payer innovation in Massachusetts: The “Alternative Quality Contract.” Health Aff. 2011;30:51–61.
- , ; AMA Expert Panel on Care Transitions. There and home again, safely: five responsibilities of ambulatory practices in high quality care transitions. American Medical Association; Chicago, IL; 2013. Available at: www.ama‐assn.org/go/patientsafety. Accessed February 22, 2013.
- Agency for Healthcare Research and Quality. Policy Innovation Profile. Medical center establishes infrastructure to manage care under capitated contracts, leading to better chronic care management and lower utilization and costs. October 3, 2012. Available at: http://www.innovations.ahrq.gov/content.aspx?id=3651. Accessed February 8, 2013.
- , , , et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306:1688–1698.
- Centers for Medicare and Medicaid Services. More doctors, hospitals partner to coordinate care for people with Medicare: providers form 106 new accountable care organizations. Press release January 10, 2013. Available at: http://www.cms.gov/apps/media/press/release.asp?Counter=4501297:831–841.
- , , , et al. Transitions of care consensus policy statement American College of Physicians‐Society of General Internal Medicine‐Society of Hospital Medicine‐American Geriatrics Society‐American College of Emergency Physicians‐Society of Academic Emergency Medicine. J Gen Intern Med. 2009;24:971–976.
- , , , et al. Patient safety concerns arising from test results that return after hospital discharge. Ann Intern Med. 2005;143(2):121–128.
- , , . Tying up loose ends: discharging patients with unresolved medical issues. Arch Intern Med. 2007;167:1305–1311.
- , , , , , . Perceptions of readmitted patients on the transition from hospital to home. J Hosp Med. 2012;7:709–712.
- , . Patients' understanding of their treatment plans and diagnosis at discharge. Mayo Clin Proc. 2005;80:991–994.
Across the country, hospitals are rolling out programs to reduce readmissions. These range from patient education around their disease process and medications, improvements in discharge planning, medication reconciliation, outpatient appointments scheduled prior to discharge, and follow‐up phone calls, among others.[1, 2] Several collaboratives such as Project Better Outcomes by Optimizing Safe Transitions[3] and Hospital Medicine Reengineering Network[4] have formed to test, study, and share lessons learned from these inpatient‐based interventions. Because financial penalties thus far have focused on decreases in inpatient reimbursement by the Centers for Medicare and Medicaid Services (CMS), most of the interventions to reduce hospital readmissions have been concentrated in the inpatient domain. It is unclear whether new payment arrangements with CMS or commercial insurers, such as bundled payments and accountable care organizations (ACOs), will pressure primary care physicians (PCPs) to further develop outpatient‐based interventions.
In this article, I provide a PCP's perspective of how inpatient and outpatient providers can partner to create the ideal care transition from hospital to home. Although others have conducted systematic reviews or surveys of interventions to reduce hospital readmissions,[2, 5, 6, 7] I will start from a vision of an ideal transition, and then evaluate evidence supporting each step. I will also highlight areas where new reimbursement codes can help support an idealized transitions‐of‐care program.
ON HOSPITAL ADMISSION
Many PCPs consider the beginning of the care continuum to rest in the primary care practice and relationship. Over time, PCPs develop relationships with their patients, understanding the patients' values toward health and healthcare, learning their social support system and home environment, and documenting a clinical course of chronic diseases, including which therapies have and have not worked well. From a PCP perspective, it seems natural to be involved in care at the point of hospital admission. Some emergency departments (EDs) and hospital admissions offices have automated systems to email or fax PCPs admission notifications. Others rely on providers to make this connection.
Ideally, PCP communication would occur early in the hospitalization, especially for medically or socially complex patients, for 3 main reasons: (1) The PCP can offer insights on goals of care or therapies attempted in the past that may reduce unnecessary procedures, decrease length of stay, and improve patient satisfaction; (2) Reconciling medications that the patient should be taking and the list the patient reports may highlight noncompliance and trigger education around medication compliance prior to discharge; (3) Early PCP involvement may improve discharge planning efficiency, whereby the inpatient and outpatient teams agree on medical and social issues to be addressed for a safe discharge. Although there are no published studies that show communication early in the hospitalization impacts clinical outcomes, a national survey of hospitalists highlighted concerns about poor information exchange, particularly around medical history and outpatient medications, at the time of admission.[8]
As new financial models push healthcare providers to manage a population of patients under a global budget, inpatient and outpatient providers will need to communicate and collaborate at a level that is new for most institutions and providers.[9] Because early markers of success are based on financial savings, this means further reducing length of stay and transferring more care to the outpatient arena, tapping into community and home care resources. Involving PCPs early in the admission may help inpatient providers meet these goals.
DURING HOSPITALIZATION
Several publications from hospitalists have evaluated inpatient‐based interventions to reduce readmissions and improve care transitions.[10, 11, 12] Table 1 summarizes 6 steps that can improve communication and collaboration.
|
| 1. Involve the PCP in discharge planning early in the hospitalization.[1] |
| 2. Notify the PCP on hospital discharge.[44] |
| 3. Ensure the discharge summary is available at the time of discharge.[44] Several elements should be included in all discharge summaries:[45] |
| a. Home services ordered, home agency, timing of initiation of services. |
| b. Medication changes.[21] |
| c. Status of active problems at time of discharge.[11] |
| d. Follow‐up appointments, especially specialty follow‐up. |
| e. Tests pending at discharge or follow‐up required after discharge (eg, follow‐up CT scan in 6 months for incidental lung nodule).[11, 46, 47] |
| f. Equipment ordered. |
| 4. Schedule follow‐up appointment with appropriate outpatient provider by discharge.[11, 29] |
| 5. Ensure new prescriptions or changes to prescriptions are available at patient's pharmacy and any needed insurance preauthorization has been approved. |
| 6. Educate patient about disease process, medication adherence, lifestyle changes, and symptoms to monitor for after discharge.[22, 48, 49] |
AFTER HOSPITAL DISCHARGE
Immediately after hospital discharge, there are 7 steps that PCPs and their clinic staff can follow to support a safe transition from hospital to home. The literature supports several individual steps, but not the full package. I am proposing that primary care clinics adopt all 7 steps in an ideal transitions‐of‐care program.
Step 1: Telephone Call Within 72 Hours of Discharge
Many hospitals ask nurses or customer service staff to call patients immediately after hospital discharge. Call content ranges from reviewing discharge instructions and symptoms to satisfaction with hospital care. Even though a 2006 Cochrane review did not find a positive impact of hospital‐based postdischarge phone calls on readmission rates,[13] recent studies among select populations found small but significant reductions.[14, 15] Others have looked at fulfilling this role in the outpatient setting.[16, 17] A recent systematic review of primary care clinic‐based postdischarge phone calls showed no impact on readmission rates, but only 3 studies were included.[18] Health plan‐initiated telephone calls to plan members after hospital discharge reported a 22% reduction in readmissions.[19, 20] Because there is no standardization in telephone call content, reviews of inpatient‐based and clinic‐based interventions cited methodological challenges in drawing conclusions about impact.
Although education around disease process, lifestyle changes, and medication adherence can be effectively provided by staff from the hospital, clinic, or health plan, the outpatient clinic should assume primary responsibility for some components of the postdischarge call. First, if a patient does not have a follow‐up appointment after discharge, the clinic nurse can schedule the appointment directly. Second, medication discrepancies after hospital discharge pose safety risks.[21, 22, 23] Although inpatient nurses may review discharge medications, it is the primary care nurse who can reconcile the discharge medication list with the prehospitalization medication list and identify discrepancies. The outpatient nurse has easier access to the PCP to address discrepancies. Third, the primary care nurse can provide education around red‐flag symptoms for which to call the clinic and information on after‐hours clinic access, an area that patients have specifically requested as standard after discharge.[24] If the patient reports new symptoms, the clinic nurse has easy access to the PCP for management advice, as well as the clinic schedule for an urgent appointment. Having the primary care practice house posthospitalization phone calls allows for more efficient troubleshooting of postdischarge issues.
In January 2013, CMS introduced new codes for primary care‐based care coordination after hospitalization. Current procedural terminology (CPT) codes 99495 and 99496 can be used by PCPs who complete 2 steps: (1) document discussion with a patient or caregiver about care transitions within 2 days of discharge, and (2) have a face‐to‐face visit with the patient within 2 weeks or 1 week, respectively.[25] Reimbursement for these codes is substantial3.96 work relative value units (RVUs) for 99495 and 5.81 work RVUs for 99496considerably more than a level IV visit for complex follow‐up care (2.43 work RVUs). Primary care practices may find that reimbursement for these care coordination codes helps cover additional costs of nurses, case managers, or social workers assisting with posthospital care. The financial impact on primary care practices may increase if commercial insurers accept these CPT codes and reimburse at levels comparable to the CMS.
CMS approved reimbursement for posthospitalization phone calls despite mixed evidence on the impact of the intervention, presumably because it is perceived that early follow‐up may lead to benefits that cannot be easily captured in research studies, and simply represents good patient care. Two challenges in showing an impact of these phone calls are lack of standardization and small sample size. However, implementation of the care‐coordination CPT codes will require more standardization and potentially a much larger number of patients who receive posthospitalization phone calls. This allows for a much more robust evaluation of the intervention.
Step 2: Follow‐up Appointment With PCP or Most Appropriate Continuity Provider
Early follow‐up with an appropriate outpatient provider has been associated with reduced hospital readmissions for patients with congestive heart failure, chronic obstructive pulmonary disease, and psychiatric illnesses,[26, 27, 28, 29] but this finding has not been consistent across all patient populations.[5, 30] It is not well understood if the follow‐up appointment needs to be within a specific time frame, especially if the patient is already being touched once by the system through the posthospitalization call. General consensus falls within 7 days for patients at moderate to high risk for readmissions.[31, 32] Regardless of risk, follow‐up visits must occur within 2 weeks of discharge to claim the CMS reimbursement for posthospitalization care coordination, and higher reimbursement is offered if it occurs within 1 week.
Step 3: Care Coordination
A nurse, social worker, or case manager partnering with the PCP on care coordination may improve the patient experience and outcomes.[17, 24] Although the inpatient social worker or case manager may have helped address some housing, financial, home care, and durable medical equipment needs, often these issues are not completely resolved at discharge. There should be a seamless handoff between inpatient and outpatient care coordinators.
Although some primary care practices include social workers, case managers, or health coaches, many have general clinic nurses functioning in these roles. One way to help fund these roles is through the care coordination CPT codes as previously described. Another consideration, as the financial model for funding care across the care continuum changes, is to have inpatient social workers and case managers work jointly with inpatient and outpatient providers, following patients to the outpatient setting until their social needs are met. This arrangement is more feasible for integrated delivery systems or primary care clinics with contractual agreements with local hospitals, an emerging trend in markets across the United States.[33] Other resources for care coordination include health plan case managers and local community nonprofits. In 2011, CMS launched the Community‐Based Care Transitions Program (CCTP), which will award up to $500 million in funding over 5 years to community‐based organizations to assist Medicare patients with care transitions.[34]
One way of operationalizing care coordination, especially in primary care clinics that do not have an embedded social worker or case manager, is to offer a team‐based appointment in conjunction with the physician postdischarge visit. A healthcare team member (nurse, experienced medical assistant, pharmacist) reviews hospital discharge records, educates the patient about the reasons for hospitalization and how to prevent readmission, performs detailed review of medications, follows up on any pending test results, reviews home care orders or durable medical equipment orders, and identifies any psychosocial issues that need to be addressed. All findings are documented in the patient chart and available for review at the beginning of the physician visit. With the team previsit in place, the physician can focus on the medical problems.
Step 4: Repeat Process Above Until Active Issues Are Stabilized
For some patients, steps 1 through 4 may need to be repeated until active medical and psychosocial issues are stabilized. Creating clinic infrastructure to support patients who may need to return weekly for titration of medications or monitoring of lab values until they normalize can prevent unnecessary ED visits. Patients with psychosocial issues will likely need longitudinal support, as these issues often take months to resolve.
Step 5: Create Access in Clinic for Patients With New Symptoms
Even after the first posthospitalization visit, patients may need to return to their PCP because of new symptoms or for active monitoring. In many parts of the country, PCP access is limited.[33] To meet patient demand for timely appointments, many primary care practices have piloted advanced access scheduling, reserving the majority of appointments for same‐day patient requests. However, evaluations show that the same‐day appointment goals of advanced access are difficult to achieve for most practices.[35] Despite challenges to same‐day access for the general clinic population, it is critical to create access for patients recently hospitalized, as many are at high risk for an ED visit or another hospital admission.
Step 6: Know Your Numbers
A basic tenet of quality improvement is measuring baseline performance and performance at intermediate time points during an intervention.[36] A recent Cochrane review found that feeding back performance to physicians can lead to potentially important improvements in practice.[37] In an Institute for Healthcare Improvement how‐to guide for improving care transitions, measuring readmission rates is 1 step in their Model for Improvement.[32] However, few primary care clinics are actively monitoring their readmission rates. One basic challenge is data availability. Primary care clinics affiliated with a hospital can obtain discharge and readmissions data from the hospital, but patients may also be hospitalized at other facilities. Insurers would be the best source of hospital discharge data, and some payors supply PCPs with risk‐adjusted performance metrics.[38, 39] As ACOs mature, primary care clinics can partner with payors to obtain data and begin trending their hospital discharge and readmission rates. In the interim, trending readmission rates at a single affiliated institution and filtering by service, discharge diagnosis, or payor may reveal areas for intervention.
Step 7: Know Your Readmitted Patients
Similar to knowing the primary care clinic's overall discharge and readmission numbers, it is also important to know the population of frequently readmitted patients. Even though some PCPs may be able to recall these patients by memory, it is important to review these patients' charts and identify preventable factors related to readmission, especially system‐related factors. Conducting reviews can be time intensive and add new demands for busy PCPs. However, many clinics already conduct morbidity and mortality conferences and case reviews as part of improving patient satisfaction, service, and outcomes. Case reviews of frequently admitted patients can fall under these established activities.
IMPLICATIONS
In this vision of the ideal care transition, I am suggesting a shift in culture from a predominantly hospital‐based program to a program that spans the care continuum and requires active participation and ownership from the PCP's team. It will require inpatient and outpatient providers to communicate early and frequently during the hospitalization, sharing patient information efficiently and working collaboratively as part of a larger team to meet the medical and psychosocial needs of the patient. This concept is not new, but has not been supported financially from payors.[1, 9, 40] Most PCPs operate on margins that cannot support additional PCP time to coordinate care for patients or staff to assist (although many PCPs believe this is the role of the primary care medical home).[33] Some payors agree that stipends to support infrastructure change are needed to improve patient outcomes.[17, 38, 39]
Even though every envisioned step does not require additional funding, new payment arrangements under ACOs and bundled payments may offer opportunities for PCPs to assume a larger role in care transitions and secure funding to pay for interventions. However, primary care practices must be positioned to negotiate favorable global payment agreements, be willing to assume risks associated with global payments, and prioritize management of medically and socially complex patients who are at risk for preventable ED visits and hospitalizations. PCPs who are not participating in ACOs or bundled payments, or those who are risk adverse, may be able to finance pieces of this vision with the new care coordination CPT codes supported by Medicare (and possibly commercial payors in the future). They may also partner with community groups participating in CCTP for additional support. Others focus on the long‐term benefits of ACO‐like structures rather than the short‐term investments needed.[41]
Are all 14 steps proposed above essential? Without doubt, this vision will be difficult to fully operationalize and requires coordination and support from many distinct groups. Should all patients be offered a basic package of interventions, reserving the full package for those who are identified as highest risk for poor outcomes after hospital discharge? There is already some support around specialized interventions for patients at high risk for readmissions,[32, 41] and risk prediction models have been introduced to identify these individuals.[42] Or should we approach this as a menu of interventions from which to choose, tailoring interventions to individual patient needs? These questions should be tested, as our experience in coordinating care across the continuum matures. With over 100 ACOs formed in Medicare alone[43] and many more with commercial insurers, our understanding in this area will grow in the next 5 years.
CONCLUSIONS
As cost containment measures in healthcare target preventable readmissions, hospitals and primary care physicians are increasingly encouraged to improve transitions along the care continuum. In this article, I offer 1 PCP's vision of the ideal transitions‐of‐care program from hospital to home. This article focuses on steps that can be taken by PCPs and their clinic staff; it does not address the role of outpatient specialists, home care agencies, or community support groups in care transitions. Operationalizing this vision requires commitment from the hospital and clinic leadership, as well as buy‐in from front‐line providers. More research is required to understand the marginal impact of each component of this vision, as well as the comprehensive package of interventions proposed, on patient outcomes. New financial models with payors and hospitals may make it easier for primary care clinics to test this vision. Current financial incentives are likely still inadequate to fully align care along the continuum, but they offer some support for more PCPs to take an active role. The time has come to shift our traditional view of transitions of care from a hospital‐centric set of interventions toward one that spans the entire care continuum and includes primary care physicians and their clinic staff as key partners.
Acknowledgments
The author thanks Jeffrey Fujimoto for his assistance with the literature review.
Disclosures: Ning Tang, MD, is supported by a University of California, Center for Health Quality and Innovation grant. Dr. Tang has no financial conflicts of interests.
Across the country, hospitals are rolling out programs to reduce readmissions. These range from patient education around their disease process and medications, improvements in discharge planning, medication reconciliation, outpatient appointments scheduled prior to discharge, and follow‐up phone calls, among others.[1, 2] Several collaboratives such as Project Better Outcomes by Optimizing Safe Transitions[3] and Hospital Medicine Reengineering Network[4] have formed to test, study, and share lessons learned from these inpatient‐based interventions. Because financial penalties thus far have focused on decreases in inpatient reimbursement by the Centers for Medicare and Medicaid Services (CMS), most of the interventions to reduce hospital readmissions have been concentrated in the inpatient domain. It is unclear whether new payment arrangements with CMS or commercial insurers, such as bundled payments and accountable care organizations (ACOs), will pressure primary care physicians (PCPs) to further develop outpatient‐based interventions.
In this article, I provide a PCP's perspective of how inpatient and outpatient providers can partner to create the ideal care transition from hospital to home. Although others have conducted systematic reviews or surveys of interventions to reduce hospital readmissions,[2, 5, 6, 7] I will start from a vision of an ideal transition, and then evaluate evidence supporting each step. I will also highlight areas where new reimbursement codes can help support an idealized transitions‐of‐care program.
ON HOSPITAL ADMISSION
Many PCPs consider the beginning of the care continuum to rest in the primary care practice and relationship. Over time, PCPs develop relationships with their patients, understanding the patients' values toward health and healthcare, learning their social support system and home environment, and documenting a clinical course of chronic diseases, including which therapies have and have not worked well. From a PCP perspective, it seems natural to be involved in care at the point of hospital admission. Some emergency departments (EDs) and hospital admissions offices have automated systems to email or fax PCPs admission notifications. Others rely on providers to make this connection.
Ideally, PCP communication would occur early in the hospitalization, especially for medically or socially complex patients, for 3 main reasons: (1) The PCP can offer insights on goals of care or therapies attempted in the past that may reduce unnecessary procedures, decrease length of stay, and improve patient satisfaction; (2) Reconciling medications that the patient should be taking and the list the patient reports may highlight noncompliance and trigger education around medication compliance prior to discharge; (3) Early PCP involvement may improve discharge planning efficiency, whereby the inpatient and outpatient teams agree on medical and social issues to be addressed for a safe discharge. Although there are no published studies that show communication early in the hospitalization impacts clinical outcomes, a national survey of hospitalists highlighted concerns about poor information exchange, particularly around medical history and outpatient medications, at the time of admission.[8]
As new financial models push healthcare providers to manage a population of patients under a global budget, inpatient and outpatient providers will need to communicate and collaborate at a level that is new for most institutions and providers.[9] Because early markers of success are based on financial savings, this means further reducing length of stay and transferring more care to the outpatient arena, tapping into community and home care resources. Involving PCPs early in the admission may help inpatient providers meet these goals.
DURING HOSPITALIZATION
Several publications from hospitalists have evaluated inpatient‐based interventions to reduce readmissions and improve care transitions.[10, 11, 12] Table 1 summarizes 6 steps that can improve communication and collaboration.
|
| 1. Involve the PCP in discharge planning early in the hospitalization.[1] |
| 2. Notify the PCP on hospital discharge.[44] |
| 3. Ensure the discharge summary is available at the time of discharge.[44] Several elements should be included in all discharge summaries:[45] |
| a. Home services ordered, home agency, timing of initiation of services. |
| b. Medication changes.[21] |
| c. Status of active problems at time of discharge.[11] |
| d. Follow‐up appointments, especially specialty follow‐up. |
| e. Tests pending at discharge or follow‐up required after discharge (eg, follow‐up CT scan in 6 months for incidental lung nodule).[11, 46, 47] |
| f. Equipment ordered. |
| 4. Schedule follow‐up appointment with appropriate outpatient provider by discharge.[11, 29] |
| 5. Ensure new prescriptions or changes to prescriptions are available at patient's pharmacy and any needed insurance preauthorization has been approved. |
| 6. Educate patient about disease process, medication adherence, lifestyle changes, and symptoms to monitor for after discharge.[22, 48, 49] |
AFTER HOSPITAL DISCHARGE
Immediately after hospital discharge, there are 7 steps that PCPs and their clinic staff can follow to support a safe transition from hospital to home. The literature supports several individual steps, but not the full package. I am proposing that primary care clinics adopt all 7 steps in an ideal transitions‐of‐care program.
Step 1: Telephone Call Within 72 Hours of Discharge
Many hospitals ask nurses or customer service staff to call patients immediately after hospital discharge. Call content ranges from reviewing discharge instructions and symptoms to satisfaction with hospital care. Even though a 2006 Cochrane review did not find a positive impact of hospital‐based postdischarge phone calls on readmission rates,[13] recent studies among select populations found small but significant reductions.[14, 15] Others have looked at fulfilling this role in the outpatient setting.[16, 17] A recent systematic review of primary care clinic‐based postdischarge phone calls showed no impact on readmission rates, but only 3 studies were included.[18] Health plan‐initiated telephone calls to plan members after hospital discharge reported a 22% reduction in readmissions.[19, 20] Because there is no standardization in telephone call content, reviews of inpatient‐based and clinic‐based interventions cited methodological challenges in drawing conclusions about impact.
Although education around disease process, lifestyle changes, and medication adherence can be effectively provided by staff from the hospital, clinic, or health plan, the outpatient clinic should assume primary responsibility for some components of the postdischarge call. First, if a patient does not have a follow‐up appointment after discharge, the clinic nurse can schedule the appointment directly. Second, medication discrepancies after hospital discharge pose safety risks.[21, 22, 23] Although inpatient nurses may review discharge medications, it is the primary care nurse who can reconcile the discharge medication list with the prehospitalization medication list and identify discrepancies. The outpatient nurse has easier access to the PCP to address discrepancies. Third, the primary care nurse can provide education around red‐flag symptoms for which to call the clinic and information on after‐hours clinic access, an area that patients have specifically requested as standard after discharge.[24] If the patient reports new symptoms, the clinic nurse has easy access to the PCP for management advice, as well as the clinic schedule for an urgent appointment. Having the primary care practice house posthospitalization phone calls allows for more efficient troubleshooting of postdischarge issues.
In January 2013, CMS introduced new codes for primary care‐based care coordination after hospitalization. Current procedural terminology (CPT) codes 99495 and 99496 can be used by PCPs who complete 2 steps: (1) document discussion with a patient or caregiver about care transitions within 2 days of discharge, and (2) have a face‐to‐face visit with the patient within 2 weeks or 1 week, respectively.[25] Reimbursement for these codes is substantial3.96 work relative value units (RVUs) for 99495 and 5.81 work RVUs for 99496considerably more than a level IV visit for complex follow‐up care (2.43 work RVUs). Primary care practices may find that reimbursement for these care coordination codes helps cover additional costs of nurses, case managers, or social workers assisting with posthospital care. The financial impact on primary care practices may increase if commercial insurers accept these CPT codes and reimburse at levels comparable to the CMS.
CMS approved reimbursement for posthospitalization phone calls despite mixed evidence on the impact of the intervention, presumably because it is perceived that early follow‐up may lead to benefits that cannot be easily captured in research studies, and simply represents good patient care. Two challenges in showing an impact of these phone calls are lack of standardization and small sample size. However, implementation of the care‐coordination CPT codes will require more standardization and potentially a much larger number of patients who receive posthospitalization phone calls. This allows for a much more robust evaluation of the intervention.
Step 2: Follow‐up Appointment With PCP or Most Appropriate Continuity Provider
Early follow‐up with an appropriate outpatient provider has been associated with reduced hospital readmissions for patients with congestive heart failure, chronic obstructive pulmonary disease, and psychiatric illnesses,[26, 27, 28, 29] but this finding has not been consistent across all patient populations.[5, 30] It is not well understood if the follow‐up appointment needs to be within a specific time frame, especially if the patient is already being touched once by the system through the posthospitalization call. General consensus falls within 7 days for patients at moderate to high risk for readmissions.[31, 32] Regardless of risk, follow‐up visits must occur within 2 weeks of discharge to claim the CMS reimbursement for posthospitalization care coordination, and higher reimbursement is offered if it occurs within 1 week.
Step 3: Care Coordination
A nurse, social worker, or case manager partnering with the PCP on care coordination may improve the patient experience and outcomes.[17, 24] Although the inpatient social worker or case manager may have helped address some housing, financial, home care, and durable medical equipment needs, often these issues are not completely resolved at discharge. There should be a seamless handoff between inpatient and outpatient care coordinators.
Although some primary care practices include social workers, case managers, or health coaches, many have general clinic nurses functioning in these roles. One way to help fund these roles is through the care coordination CPT codes as previously described. Another consideration, as the financial model for funding care across the care continuum changes, is to have inpatient social workers and case managers work jointly with inpatient and outpatient providers, following patients to the outpatient setting until their social needs are met. This arrangement is more feasible for integrated delivery systems or primary care clinics with contractual agreements with local hospitals, an emerging trend in markets across the United States.[33] Other resources for care coordination include health plan case managers and local community nonprofits. In 2011, CMS launched the Community‐Based Care Transitions Program (CCTP), which will award up to $500 million in funding over 5 years to community‐based organizations to assist Medicare patients with care transitions.[34]
One way of operationalizing care coordination, especially in primary care clinics that do not have an embedded social worker or case manager, is to offer a team‐based appointment in conjunction with the physician postdischarge visit. A healthcare team member (nurse, experienced medical assistant, pharmacist) reviews hospital discharge records, educates the patient about the reasons for hospitalization and how to prevent readmission, performs detailed review of medications, follows up on any pending test results, reviews home care orders or durable medical equipment orders, and identifies any psychosocial issues that need to be addressed. All findings are documented in the patient chart and available for review at the beginning of the physician visit. With the team previsit in place, the physician can focus on the medical problems.
Step 4: Repeat Process Above Until Active Issues Are Stabilized
For some patients, steps 1 through 4 may need to be repeated until active medical and psychosocial issues are stabilized. Creating clinic infrastructure to support patients who may need to return weekly for titration of medications or monitoring of lab values until they normalize can prevent unnecessary ED visits. Patients with psychosocial issues will likely need longitudinal support, as these issues often take months to resolve.
Step 5: Create Access in Clinic for Patients With New Symptoms
Even after the first posthospitalization visit, patients may need to return to their PCP because of new symptoms or for active monitoring. In many parts of the country, PCP access is limited.[33] To meet patient demand for timely appointments, many primary care practices have piloted advanced access scheduling, reserving the majority of appointments for same‐day patient requests. However, evaluations show that the same‐day appointment goals of advanced access are difficult to achieve for most practices.[35] Despite challenges to same‐day access for the general clinic population, it is critical to create access for patients recently hospitalized, as many are at high risk for an ED visit or another hospital admission.
Step 6: Know Your Numbers
A basic tenet of quality improvement is measuring baseline performance and performance at intermediate time points during an intervention.[36] A recent Cochrane review found that feeding back performance to physicians can lead to potentially important improvements in practice.[37] In an Institute for Healthcare Improvement how‐to guide for improving care transitions, measuring readmission rates is 1 step in their Model for Improvement.[32] However, few primary care clinics are actively monitoring their readmission rates. One basic challenge is data availability. Primary care clinics affiliated with a hospital can obtain discharge and readmissions data from the hospital, but patients may also be hospitalized at other facilities. Insurers would be the best source of hospital discharge data, and some payors supply PCPs with risk‐adjusted performance metrics.[38, 39] As ACOs mature, primary care clinics can partner with payors to obtain data and begin trending their hospital discharge and readmission rates. In the interim, trending readmission rates at a single affiliated institution and filtering by service, discharge diagnosis, or payor may reveal areas for intervention.
Step 7: Know Your Readmitted Patients
Similar to knowing the primary care clinic's overall discharge and readmission numbers, it is also important to know the population of frequently readmitted patients. Even though some PCPs may be able to recall these patients by memory, it is important to review these patients' charts and identify preventable factors related to readmission, especially system‐related factors. Conducting reviews can be time intensive and add new demands for busy PCPs. However, many clinics already conduct morbidity and mortality conferences and case reviews as part of improving patient satisfaction, service, and outcomes. Case reviews of frequently admitted patients can fall under these established activities.
IMPLICATIONS
In this vision of the ideal care transition, I am suggesting a shift in culture from a predominantly hospital‐based program to a program that spans the care continuum and requires active participation and ownership from the PCP's team. It will require inpatient and outpatient providers to communicate early and frequently during the hospitalization, sharing patient information efficiently and working collaboratively as part of a larger team to meet the medical and psychosocial needs of the patient. This concept is not new, but has not been supported financially from payors.[1, 9, 40] Most PCPs operate on margins that cannot support additional PCP time to coordinate care for patients or staff to assist (although many PCPs believe this is the role of the primary care medical home).[33] Some payors agree that stipends to support infrastructure change are needed to improve patient outcomes.[17, 38, 39]
Even though every envisioned step does not require additional funding, new payment arrangements under ACOs and bundled payments may offer opportunities for PCPs to assume a larger role in care transitions and secure funding to pay for interventions. However, primary care practices must be positioned to negotiate favorable global payment agreements, be willing to assume risks associated with global payments, and prioritize management of medically and socially complex patients who are at risk for preventable ED visits and hospitalizations. PCPs who are not participating in ACOs or bundled payments, or those who are risk adverse, may be able to finance pieces of this vision with the new care coordination CPT codes supported by Medicare (and possibly commercial payors in the future). They may also partner with community groups participating in CCTP for additional support. Others focus on the long‐term benefits of ACO‐like structures rather than the short‐term investments needed.[41]
Are all 14 steps proposed above essential? Without doubt, this vision will be difficult to fully operationalize and requires coordination and support from many distinct groups. Should all patients be offered a basic package of interventions, reserving the full package for those who are identified as highest risk for poor outcomes after hospital discharge? There is already some support around specialized interventions for patients at high risk for readmissions,[32, 41] and risk prediction models have been introduced to identify these individuals.[42] Or should we approach this as a menu of interventions from which to choose, tailoring interventions to individual patient needs? These questions should be tested, as our experience in coordinating care across the continuum matures. With over 100 ACOs formed in Medicare alone[43] and many more with commercial insurers, our understanding in this area will grow in the next 5 years.
CONCLUSIONS
As cost containment measures in healthcare target preventable readmissions, hospitals and primary care physicians are increasingly encouraged to improve transitions along the care continuum. In this article, I offer 1 PCP's vision of the ideal transitions‐of‐care program from hospital to home. This article focuses on steps that can be taken by PCPs and their clinic staff; it does not address the role of outpatient specialists, home care agencies, or community support groups in care transitions. Operationalizing this vision requires commitment from the hospital and clinic leadership, as well as buy‐in from front‐line providers. More research is required to understand the marginal impact of each component of this vision, as well as the comprehensive package of interventions proposed, on patient outcomes. New financial models with payors and hospitals may make it easier for primary care clinics to test this vision. Current financial incentives are likely still inadequate to fully align care along the continuum, but they offer some support for more PCPs to take an active role. The time has come to shift our traditional view of transitions of care from a hospital‐centric set of interventions toward one that spans the entire care continuum and includes primary care physicians and their clinic staff as key partners.
Acknowledgments
The author thanks Jeffrey Fujimoto for his assistance with the literature review.
Disclosures: Ning Tang, MD, is supported by a University of California, Center for Health Quality and Innovation grant. Dr. Tang has no financial conflicts of interests.
- , , . Reducing hospital readmissions: lessons from top‐performing hospitals. The Commonwealth Fund Synthesis Report. April 2011. Available at: http://www.commonwealthfund.org/Publications/Case‐Studies/2011/Apr/Reducing‐Hospital‐Readmissions.aspx. Accessed January 30, 2013.
- , . Effective Interventions to Reduce Rehospitalizations: A Survey of the Published Evidence. Cambridge, MA: Institute for Healthcare Improvement; 2009.
- Society of Hospital Medicine. Project BOOST. Available at: www.hospitalmedicine.org/BOOST/. Accessed January 30, 2013.
- American Association of Medical Colleges. HOMERUN Executive Summary. Available at: https://members.aamc.org/eweb/upload/HOMERUN%20summary%202012.pdf. Accessed January 30, 2013.
- , , , , . Interventions to reduce 30‐day rehospitalization: a systematic review. Ann Intern Med. 2011;155:520–528.
- , , , et al. Contemporary evidence about hospital strategies for reducing 30‐day readmissions. J Am Coll Cardiol. 2012;60:607–614.
- , , , et al. Improving patient handovers from hospital to primary care: a systematic review. Ann Intern Med. 2012;157:417–428.
- , , , . Hospitalists and care transitions: the divorce of inpatient and outpatient care. Health Aff. 2008;27:1315–1327.
- , , . Recasting readmissions by placing the hospital role in community context. JAMA. 2013;309:351–352.
- , , , . Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2:314–323.
- , , , et al. Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists. J Hosp Med. 2006;1:354–360.
- . Transitioning the patient with acute coronary syndrome from inpatient to primary care. J Hosp Med. 2010;5(suppl):S8–S14.
- , . Telephone follow‐up, initiated by a hospital‐based health professional, for postdischarge problems in patients discharged from hospital to home. Cochrane Database Syst Rev. 2006;(4):CD004510.
- , , , . Post‐discharge intervention in vulnerable, chronically ill patients. J Hosp Med. 2012;7:124–130.
- , , , et al. Low‐cost transitional care with nurse managers making mostly phone contact with patients cut rehospitalization at a VA hospital. Health Aff. 2012;31:2659–2668.
- , , , . Redefining and redesigning hospital discharge to enhance patient care: a randomized control study. J Gen Intern Med. 2008;23:1228–1233.
- , , , et al. How Geisinger's advanced medical home model argues the case for rapid‐cycle innovation. Health Aff. 2010;29:2047–2053. .
- , , . Telephone follow‐up as a primary care intervention for postdischarge outcomes improvement: a systematic review. Am J Med. 2012;125:915–921.
- , , , , . The impact of postdischarge telephonic follow‐up on hospital readmissions. Popul Health Manag. 2011;14:27–32.
- , , , , . Prioritized post‐discharge telephonic outreach reduces hospital readmissions for select high‐risk patients. Am J Manag Care. 2012;18:838–844.
- , , , et al. Association of ICU or hospital admission with unintentional discontinuation of medications for chronic diseases. JAMA. 2011;306:840–847.
- , , , et al. Effect of a pharmacist intervention on clinically important medication errors after hospital discharge. Ann Intern Med. 2012;157:1–10.
- , , , , , . Relationship of health literacy to intentional and unintentional non‐adherence of hospital discharge medications. J Gen Intern Med. 2012;27:173–178.
- , , , , . Patient experiences of transitioning from hospital to home: an ethnographic quality improvement project. J Hosp Med. 2012;7:382–387.
- . Medicare finalizes physician pay for new care coordination benefit. American Medical News. November 12, 2012. Available at: http://www.ama‐assn.org/amednews/2012/11/12/gvl11112.htm. Accessed February 8, 2013.
- , , , , . Outpatient follow‐up visit and 30‐day emergency department visit and readmission in patients hospitalized for chronic obstructive pulmonary disease. Arch Intern Med. 2010;170:1664–1670.
- , , . Post‐hospitalization transitions: examining the effects of timing of primary care provider follow‐up. J Hosp Med. 2010;5:392–397.
- , , , et al. Relationship between early physician follow‐up and 30‐day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303:1716–1722.
- , , . Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psychiatr Serv. 2000;51:885–889.
- , , , , . Do timely outpatient follow‐up visits decrease hospital readmission rates? Am J Med Qual. 2012;27:11–15.
- Project BOOST. Tool for addressing risk: a geriatric evaluation for transitions. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/PDFs/TARGET.pdf. Accessed February 3, 2013.
- , , , , . How‐to Guide: Improving Transitions from the Hospital to Community Settings to Reduce Avoidable Rehospitalizations. Cambridge, MA: Institute for Healthcare Improvement; 2012.
- , . Primary care: current problems and proposed solutions. Health Aff. 2010;29:799–805.
- Center for Medicare and Medicaid Innovation. Community‐based Care Transitions Program. Available at: http://innovation.cms.gov/initiatives/CCTP/#collapse‐tableDetails. Accessed February 8, 2013.
- , , . Advanced access scheduling outcomes: a systematic review. Arch Intern Med. 2011;171:1150–1159.
- , , , . The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2nd ed. San Francisco, CA: Jossey‐Bass Publishers; 2009.
- , , , et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;(6):CD000259.
- Agency for Healthcare Research and Quality. Policy Innovation Profile. Insurer provides financial incentives, infrastructure, and other support to stimulate provider participation in quality improvement collaborations. June 6, 2012. Available at: http://www.innovations.ahrq.gov/content.aspx?id=3641. Accessed February 8, 2013.
- , , , . Private‐payer innovation in Massachusetts: The “Alternative Quality Contract.” Health Aff. 2011;30:51–61.
- , ; AMA Expert Panel on Care Transitions. There and home again, safely: five responsibilities of ambulatory practices in high quality care transitions. American Medical Association; Chicago, IL; 2013. Available at: www.ama‐assn.org/go/patientsafety. Accessed February 22, 2013.
- Agency for Healthcare Research and Quality. Policy Innovation Profile. Medical center establishes infrastructure to manage care under capitated contracts, leading to better chronic care management and lower utilization and costs. October 3, 2012. Available at: http://www.innovations.ahrq.gov/content.aspx?id=3651. Accessed February 8, 2013.
- , , , et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306:1688–1698.
- Centers for Medicare and Medicaid Services. More doctors, hospitals partner to coordinate care for people with Medicare: providers form 106 new accountable care organizations. Press release January 10, 2013. Available at: http://www.cms.gov/apps/media/press/release.asp?Counter=4501297:831–841.
- , , , et al. Transitions of care consensus policy statement American College of Physicians‐Society of General Internal Medicine‐Society of Hospital Medicine‐American Geriatrics Society‐American College of Emergency Physicians‐Society of Academic Emergency Medicine. J Gen Intern Med. 2009;24:971–976.
- , , , et al. Patient safety concerns arising from test results that return after hospital discharge. Ann Intern Med. 2005;143(2):121–128.
- , , . Tying up loose ends: discharging patients with unresolved medical issues. Arch Intern Med. 2007;167:1305–1311.
- , , , , , . Perceptions of readmitted patients on the transition from hospital to home. J Hosp Med. 2012;7:709–712.
- , . Patients' understanding of their treatment plans and diagnosis at discharge. Mayo Clin Proc. 2005;80:991–994.
- , , . Reducing hospital readmissions: lessons from top‐performing hospitals. The Commonwealth Fund Synthesis Report. April 2011. Available at: http://www.commonwealthfund.org/Publications/Case‐Studies/2011/Apr/Reducing‐Hospital‐Readmissions.aspx. Accessed January 30, 2013.
- , . Effective Interventions to Reduce Rehospitalizations: A Survey of the Published Evidence. Cambridge, MA: Institute for Healthcare Improvement; 2009.
- Society of Hospital Medicine. Project BOOST. Available at: www.hospitalmedicine.org/BOOST/. Accessed January 30, 2013.
- American Association of Medical Colleges. HOMERUN Executive Summary. Available at: https://members.aamc.org/eweb/upload/HOMERUN%20summary%202012.pdf. Accessed January 30, 2013.
- , , , , . Interventions to reduce 30‐day rehospitalization: a systematic review. Ann Intern Med. 2011;155:520–528.
- , , , et al. Contemporary evidence about hospital strategies for reducing 30‐day readmissions. J Am Coll Cardiol. 2012;60:607–614.
- , , , et al. Improving patient handovers from hospital to primary care: a systematic review. Ann Intern Med. 2012;157:417–428.
- , , , . Hospitalists and care transitions: the divorce of inpatient and outpatient care. Health Aff. 2008;27:1315–1327.
- , , . Recasting readmissions by placing the hospital role in community context. JAMA. 2013;309:351–352.
- , , , . Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2:314–323.
- , , , et al. Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists. J Hosp Med. 2006;1:354–360.
- . Transitioning the patient with acute coronary syndrome from inpatient to primary care. J Hosp Med. 2010;5(suppl):S8–S14.
- , . Telephone follow‐up, initiated by a hospital‐based health professional, for postdischarge problems in patients discharged from hospital to home. Cochrane Database Syst Rev. 2006;(4):CD004510.
- , , , . Post‐discharge intervention in vulnerable, chronically ill patients. J Hosp Med. 2012;7:124–130.
- , , , et al. Low‐cost transitional care with nurse managers making mostly phone contact with patients cut rehospitalization at a VA hospital. Health Aff. 2012;31:2659–2668.
- , , , . Redefining and redesigning hospital discharge to enhance patient care: a randomized control study. J Gen Intern Med. 2008;23:1228–1233.
- , , , et al. How Geisinger's advanced medical home model argues the case for rapid‐cycle innovation. Health Aff. 2010;29:2047–2053. .
- , , . Telephone follow‐up as a primary care intervention for postdischarge outcomes improvement: a systematic review. Am J Med. 2012;125:915–921.
- , , , , . The impact of postdischarge telephonic follow‐up on hospital readmissions. Popul Health Manag. 2011;14:27–32.
- , , , , . Prioritized post‐discharge telephonic outreach reduces hospital readmissions for select high‐risk patients. Am J Manag Care. 2012;18:838–844.
- , , , et al. Association of ICU or hospital admission with unintentional discontinuation of medications for chronic diseases. JAMA. 2011;306:840–847.
- , , , et al. Effect of a pharmacist intervention on clinically important medication errors after hospital discharge. Ann Intern Med. 2012;157:1–10.
- , , , , , . Relationship of health literacy to intentional and unintentional non‐adherence of hospital discharge medications. J Gen Intern Med. 2012;27:173–178.
- , , , , . Patient experiences of transitioning from hospital to home: an ethnographic quality improvement project. J Hosp Med. 2012;7:382–387.
- . Medicare finalizes physician pay for new care coordination benefit. American Medical News. November 12, 2012. Available at: http://www.ama‐assn.org/amednews/2012/11/12/gvl11112.htm. Accessed February 8, 2013.
- , , , , . Outpatient follow‐up visit and 30‐day emergency department visit and readmission in patients hospitalized for chronic obstructive pulmonary disease. Arch Intern Med. 2010;170:1664–1670.
- , , . Post‐hospitalization transitions: examining the effects of timing of primary care provider follow‐up. J Hosp Med. 2010;5:392–397.
- , , , et al. Relationship between early physician follow‐up and 30‐day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303:1716–1722.
- , , . Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psychiatr Serv. 2000;51:885–889.
- , , , , . Do timely outpatient follow‐up visits decrease hospital readmission rates? Am J Med Qual. 2012;27:11–15.
- Project BOOST. Tool for addressing risk: a geriatric evaluation for transitions. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/PDFs/TARGET.pdf. Accessed February 3, 2013.
- , , , , . How‐to Guide: Improving Transitions from the Hospital to Community Settings to Reduce Avoidable Rehospitalizations. Cambridge, MA: Institute for Healthcare Improvement; 2012.
- , . Primary care: current problems and proposed solutions. Health Aff. 2010;29:799–805.
- Center for Medicare and Medicaid Innovation. Community‐based Care Transitions Program. Available at: http://innovation.cms.gov/initiatives/CCTP/#collapse‐tableDetails. Accessed February 8, 2013.
- , , . Advanced access scheduling outcomes: a systematic review. Arch Intern Med. 2011;171:1150–1159.
- , , , . The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2nd ed. San Francisco, CA: Jossey‐Bass Publishers; 2009.
- , , , et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;(6):CD000259.
- Agency for Healthcare Research and Quality. Policy Innovation Profile. Insurer provides financial incentives, infrastructure, and other support to stimulate provider participation in quality improvement collaborations. June 6, 2012. Available at: http://www.innovations.ahrq.gov/content.aspx?id=3641. Accessed February 8, 2013.
- , , , . Private‐payer innovation in Massachusetts: The “Alternative Quality Contract.” Health Aff. 2011;30:51–61.
- , ; AMA Expert Panel on Care Transitions. There and home again, safely: five responsibilities of ambulatory practices in high quality care transitions. American Medical Association; Chicago, IL; 2013. Available at: www.ama‐assn.org/go/patientsafety. Accessed February 22, 2013.
- Agency for Healthcare Research and Quality. Policy Innovation Profile. Medical center establishes infrastructure to manage care under capitated contracts, leading to better chronic care management and lower utilization and costs. October 3, 2012. Available at: http://www.innovations.ahrq.gov/content.aspx?id=3651. Accessed February 8, 2013.
- , , , et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306:1688–1698.
- Centers for Medicare and Medicaid Services. More doctors, hospitals partner to coordinate care for people with Medicare: providers form 106 new accountable care organizations. Press release January 10, 2013. Available at: http://www.cms.gov/apps/media/press/release.asp?Counter=4501297:831–841.
- , , , et al. Transitions of care consensus policy statement American College of Physicians‐Society of General Internal Medicine‐Society of Hospital Medicine‐American Geriatrics Society‐American College of Emergency Physicians‐Society of Academic Emergency Medicine. J Gen Intern Med. 2009;24:971–976.
- , , , et al. Patient safety concerns arising from test results that return after hospital discharge. Ann Intern Med. 2005;143(2):121–128.
- , , . Tying up loose ends: discharging patients with unresolved medical issues. Arch Intern Med. 2007;167:1305–1311.
- , , , , , . Perceptions of readmitted patients on the transition from hospital to home. J Hosp Med. 2012;7:709–712.
- , . Patients' understanding of their treatment plans and diagnosis at discharge. Mayo Clin Proc. 2005;80:991–994.
Improved Mortality Rates with Prone Positioning in Severe ARDS
Clinical question
Do patients with severe acute respiratory distress syndrome who require mechanical ventilation fare better with early prone positioning?
Bottom line
Prone positioning decreased 28-day and 90-day mortality rates in patients with severe acute respiratory distress syndrome (ARDS) who required mechanical ventilation. You would have to use prone positioning for 6 such patients to prevent one death. It is important to note that the intensive care units involved in this study were staffed with providers who were skilled at "proning patients." Although the technical difficulty of this process may be a limiting factor, it is one that can likely be overcome with time and experience, especially given the evident benefit. (LOE = 1b)
Reference
Study design
Randomized controlled trial (nonblinded)
Funding source
Government
Allocation
Concealed
Setting
Inpatient (ICU only)
Synopsis
These investigators enrolled patients with severe ARDS -- defined as a ratio of the partial pressure of arterial oxygen to the fraction of inspired oxygen (FiO2) of >150mm/Hg, with an FiO2 of at least 0.6, a positive end-expiratory pressure of at least 5 cm of water, and a tidal volume of 6 mL/kg of predicted body weight -- who were using mechanical ventilation for less than 36 hours. Patients were excluded from the study if they showed improvement in symptoms during an initial 12-hour to 24-hour stabilization period. Patients with contraindications to prone positioning such as those with elevated intracranial pressure or recent tracheal surgery were also excluded. Using concealed allocation, eligible patients were randomized to be part of a prone group (n = 237) or a supine group (n = 229). Patients in the prone group were placed in prone position while on mechanical ventilation for at least 16 consecutive hours per day up to day 28. Prone treatment was discontinued if patients had improved oxygenation while in a sustained supine position or if complications arose during prone positioning such as accidental extubation or cardiac arrest. Patients in the supine group were maintained in a semirecumbent position throughout the study. The 2 groups had similar average age and comorbidities. However, at baseline, the supine group used vasopressors more frequently, used neuromuscular blockers less frequently, and had a significantly higher mean Sepsis-related Organ Failure Assessment (SOFA) score as compared with the prone group. Patients in the prone group remained in the prone position for 73% of the time from the start of the first prone session to the end of the last session. Mortality was lower in the prone group than in the supine group at day 28 (16% vs 33%; P < .001; number needed to treat [NNT] = 6) and at day 90 (24% vs 41%; P < .001; NNT = 6). The decrease in mortality with prone positioning persisted after adjustment for SOFA scores and the use of neuromuscular blockers and vasopressors. Although the prone group had more successful extubations at day 90 (81% vs 65%; P < .001), there were no significant differences detected in duration of mechanical ventilation or number of tracheotomies placed.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Clinical question
Do patients with severe acute respiratory distress syndrome who require mechanical ventilation fare better with early prone positioning?
Bottom line
Prone positioning decreased 28-day and 90-day mortality rates in patients with severe acute respiratory distress syndrome (ARDS) who required mechanical ventilation. You would have to use prone positioning for 6 such patients to prevent one death. It is important to note that the intensive care units involved in this study were staffed with providers who were skilled at "proning patients." Although the technical difficulty of this process may be a limiting factor, it is one that can likely be overcome with time and experience, especially given the evident benefit. (LOE = 1b)
Reference
Study design
Randomized controlled trial (nonblinded)
Funding source
Government
Allocation
Concealed
Setting
Inpatient (ICU only)
Synopsis
These investigators enrolled patients with severe ARDS -- defined as a ratio of the partial pressure of arterial oxygen to the fraction of inspired oxygen (FiO2) of >150mm/Hg, with an FiO2 of at least 0.6, a positive end-expiratory pressure of at least 5 cm of water, and a tidal volume of 6 mL/kg of predicted body weight -- who were using mechanical ventilation for less than 36 hours. Patients were excluded from the study if they showed improvement in symptoms during an initial 12-hour to 24-hour stabilization period. Patients with contraindications to prone positioning such as those with elevated intracranial pressure or recent tracheal surgery were also excluded. Using concealed allocation, eligible patients were randomized to be part of a prone group (n = 237) or a supine group (n = 229). Patients in the prone group were placed in prone position while on mechanical ventilation for at least 16 consecutive hours per day up to day 28. Prone treatment was discontinued if patients had improved oxygenation while in a sustained supine position or if complications arose during prone positioning such as accidental extubation or cardiac arrest. Patients in the supine group were maintained in a semirecumbent position throughout the study. The 2 groups had similar average age and comorbidities. However, at baseline, the supine group used vasopressors more frequently, used neuromuscular blockers less frequently, and had a significantly higher mean Sepsis-related Organ Failure Assessment (SOFA) score as compared with the prone group. Patients in the prone group remained in the prone position for 73% of the time from the start of the first prone session to the end of the last session. Mortality was lower in the prone group than in the supine group at day 28 (16% vs 33%; P < .001; number needed to treat [NNT] = 6) and at day 90 (24% vs 41%; P < .001; NNT = 6). The decrease in mortality with prone positioning persisted after adjustment for SOFA scores and the use of neuromuscular blockers and vasopressors. Although the prone group had more successful extubations at day 90 (81% vs 65%; P < .001), there were no significant differences detected in duration of mechanical ventilation or number of tracheotomies placed.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Clinical question
Do patients with severe acute respiratory distress syndrome who require mechanical ventilation fare better with early prone positioning?
Bottom line
Prone positioning decreased 28-day and 90-day mortality rates in patients with severe acute respiratory distress syndrome (ARDS) who required mechanical ventilation. You would have to use prone positioning for 6 such patients to prevent one death. It is important to note that the intensive care units involved in this study were staffed with providers who were skilled at "proning patients." Although the technical difficulty of this process may be a limiting factor, it is one that can likely be overcome with time and experience, especially given the evident benefit. (LOE = 1b)
Reference
Study design
Randomized controlled trial (nonblinded)
Funding source
Government
Allocation
Concealed
Setting
Inpatient (ICU only)
Synopsis
These investigators enrolled patients with severe ARDS -- defined as a ratio of the partial pressure of arterial oxygen to the fraction of inspired oxygen (FiO2) of >150mm/Hg, with an FiO2 of at least 0.6, a positive end-expiratory pressure of at least 5 cm of water, and a tidal volume of 6 mL/kg of predicted body weight -- who were using mechanical ventilation for less than 36 hours. Patients were excluded from the study if they showed improvement in symptoms during an initial 12-hour to 24-hour stabilization period. Patients with contraindications to prone positioning such as those with elevated intracranial pressure or recent tracheal surgery were also excluded. Using concealed allocation, eligible patients were randomized to be part of a prone group (n = 237) or a supine group (n = 229). Patients in the prone group were placed in prone position while on mechanical ventilation for at least 16 consecutive hours per day up to day 28. Prone treatment was discontinued if patients had improved oxygenation while in a sustained supine position or if complications arose during prone positioning such as accidental extubation or cardiac arrest. Patients in the supine group were maintained in a semirecumbent position throughout the study. The 2 groups had similar average age and comorbidities. However, at baseline, the supine group used vasopressors more frequently, used neuromuscular blockers less frequently, and had a significantly higher mean Sepsis-related Organ Failure Assessment (SOFA) score as compared with the prone group. Patients in the prone group remained in the prone position for 73% of the time from the start of the first prone session to the end of the last session. Mortality was lower in the prone group than in the supine group at day 28 (16% vs 33%; P < .001; number needed to treat [NNT] = 6) and at day 90 (24% vs 41%; P < .001; NNT = 6). The decrease in mortality with prone positioning persisted after adjustment for SOFA scores and the use of neuromuscular blockers and vasopressors. Although the prone group had more successful extubations at day 90 (81% vs 65%; P < .001), there were no significant differences detected in duration of mechanical ventilation or number of tracheotomies placed.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Universal MRSA Decolonization in ICU Leads to Fewer Bloodstream Infections
Clinical question
Does universal decolonization for methicillin-resistant Staphylococcus aureus (MRSA) in patients in the intensive care unit decrease the rate of MRSA-positive clinical cultures?
Bottom line
As compared with no decolonization or a targeted decolonization, a universal decolonization strategy for MRSA using intranasal mupirocin and chlorhexidine bathing cloths for all patients admitted to the intensive care unit (ICU) is most effective at decreasing MRSA-positive clinical cultures and ICU-acquired bloodstream infections. Overall, you would need to treat 54 patients with universal decolonization to prevent one bloodstream infection. The cost effectiveness of this strategy as well as the concern of emerging resistance was not addressed in this study. (LOE = 1b-)
Reference
Study design
Randomized controlled trial (nonblinded)
Funding source
Government
Allocation
Uncertain
Setting
Inpatient (ICU only)
Synopsis
Prior research has shown that daily bathing with chlorhexidine lowers the rate of MRSA acquisition and decreases the overall number of hospital-acquired bloodstream infections in the ICU (Daily POEM 4/26/13). The current study's goal was to identify whether targeted or universal MRSA decolonization is the most effective at reducing MRSA infections in the ICU. Investigators randomized 43 hospitals to use 1 of 3 strategies within all their adult ICUs: (1) MRSA screening and contact isolation only; (2) screening, isolation, and decolonization of MRSA carriers; (3) decolonization of all patients without any screening procedures. Screening for MRSA was performed via swabs of bilateral nares upon ICU admission in the first 2 groups. Contact precautions were implemented for those with a positive MRSA screening result in groups 1 and 2 and for those with history of MRSA colonization or infection in all groups. Decolonization in groups 2 and 3 consisted of 5 days of twice-daily intranasal mupirocin, as well as daily bathing with chlorhexidine cloths during the entire ICU stay. Baseline characteristics of the patient populations in each group were similar. Patients in all adult ICUs of a participating hospital were assigned to the same study group. Although both universal and targeted decolonization resulted in a significant reduction in the primary outcome of MRSA-positive clinical cultures, the universal strategy was found to be most effective (hazard ratio [HR] = 0.63 for the universal strategy; HR = 0.75 for the targeted strategy; and HR = 0.92 for screening and isolation; P = .01). Additionally, universal decolonization led to the greatest reduction of overall bloodstream infections (HR = 0.56 for universal; HR = 0.78 for targeted; HR = 0.99 for screening and isolation; P < .001). Of note, the universal decolonization group contained 3 of the 4 hospitals that performed bone marrow and solid-organ transplantations, resulting in a higher baseline risk of infection than the other groups, but this difference was not statistically significant. Overall, only severe adverse events were noted in this study and all were classified as mild pruritus or rash due to chlorhexidine bathing. Investigators did not evaluate the cost-effectiveness of the different strategies nor did they examine the emergence of resistance with widespread use of chlorhexidine and mupirocin.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Clinical question
Does universal decolonization for methicillin-resistant Staphylococcus aureus (MRSA) in patients in the intensive care unit decrease the rate of MRSA-positive clinical cultures?
Bottom line
As compared with no decolonization or a targeted decolonization, a universal decolonization strategy for MRSA using intranasal mupirocin and chlorhexidine bathing cloths for all patients admitted to the intensive care unit (ICU) is most effective at decreasing MRSA-positive clinical cultures and ICU-acquired bloodstream infections. Overall, you would need to treat 54 patients with universal decolonization to prevent one bloodstream infection. The cost effectiveness of this strategy as well as the concern of emerging resistance was not addressed in this study. (LOE = 1b-)
Reference
Study design
Randomized controlled trial (nonblinded)
Funding source
Government
Allocation
Uncertain
Setting
Inpatient (ICU only)
Synopsis
Prior research has shown that daily bathing with chlorhexidine lowers the rate of MRSA acquisition and decreases the overall number of hospital-acquired bloodstream infections in the ICU (Daily POEM 4/26/13). The current study's goal was to identify whether targeted or universal MRSA decolonization is the most effective at reducing MRSA infections in the ICU. Investigators randomized 43 hospitals to use 1 of 3 strategies within all their adult ICUs: (1) MRSA screening and contact isolation only; (2) screening, isolation, and decolonization of MRSA carriers; (3) decolonization of all patients without any screening procedures. Screening for MRSA was performed via swabs of bilateral nares upon ICU admission in the first 2 groups. Contact precautions were implemented for those with a positive MRSA screening result in groups 1 and 2 and for those with history of MRSA colonization or infection in all groups. Decolonization in groups 2 and 3 consisted of 5 days of twice-daily intranasal mupirocin, as well as daily bathing with chlorhexidine cloths during the entire ICU stay. Baseline characteristics of the patient populations in each group were similar. Patients in all adult ICUs of a participating hospital were assigned to the same study group. Although both universal and targeted decolonization resulted in a significant reduction in the primary outcome of MRSA-positive clinical cultures, the universal strategy was found to be most effective (hazard ratio [HR] = 0.63 for the universal strategy; HR = 0.75 for the targeted strategy; and HR = 0.92 for screening and isolation; P = .01). Additionally, universal decolonization led to the greatest reduction of overall bloodstream infections (HR = 0.56 for universal; HR = 0.78 for targeted; HR = 0.99 for screening and isolation; P < .001). Of note, the universal decolonization group contained 3 of the 4 hospitals that performed bone marrow and solid-organ transplantations, resulting in a higher baseline risk of infection than the other groups, but this difference was not statistically significant. Overall, only severe adverse events were noted in this study and all were classified as mild pruritus or rash due to chlorhexidine bathing. Investigators did not evaluate the cost-effectiveness of the different strategies nor did they examine the emergence of resistance with widespread use of chlorhexidine and mupirocin.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Clinical question
Does universal decolonization for methicillin-resistant Staphylococcus aureus (MRSA) in patients in the intensive care unit decrease the rate of MRSA-positive clinical cultures?
Bottom line
As compared with no decolonization or a targeted decolonization, a universal decolonization strategy for MRSA using intranasal mupirocin and chlorhexidine bathing cloths for all patients admitted to the intensive care unit (ICU) is most effective at decreasing MRSA-positive clinical cultures and ICU-acquired bloodstream infections. Overall, you would need to treat 54 patients with universal decolonization to prevent one bloodstream infection. The cost effectiveness of this strategy as well as the concern of emerging resistance was not addressed in this study. (LOE = 1b-)
Reference
Study design
Randomized controlled trial (nonblinded)
Funding source
Government
Allocation
Uncertain
Setting
Inpatient (ICU only)
Synopsis
Prior research has shown that daily bathing with chlorhexidine lowers the rate of MRSA acquisition and decreases the overall number of hospital-acquired bloodstream infections in the ICU (Daily POEM 4/26/13). The current study's goal was to identify whether targeted or universal MRSA decolonization is the most effective at reducing MRSA infections in the ICU. Investigators randomized 43 hospitals to use 1 of 3 strategies within all their adult ICUs: (1) MRSA screening and contact isolation only; (2) screening, isolation, and decolonization of MRSA carriers; (3) decolonization of all patients without any screening procedures. Screening for MRSA was performed via swabs of bilateral nares upon ICU admission in the first 2 groups. Contact precautions were implemented for those with a positive MRSA screening result in groups 1 and 2 and for those with history of MRSA colonization or infection in all groups. Decolonization in groups 2 and 3 consisted of 5 days of twice-daily intranasal mupirocin, as well as daily bathing with chlorhexidine cloths during the entire ICU stay. Baseline characteristics of the patient populations in each group were similar. Patients in all adult ICUs of a participating hospital were assigned to the same study group. Although both universal and targeted decolonization resulted in a significant reduction in the primary outcome of MRSA-positive clinical cultures, the universal strategy was found to be most effective (hazard ratio [HR] = 0.63 for the universal strategy; HR = 0.75 for the targeted strategy; and HR = 0.92 for screening and isolation; P = .01). Additionally, universal decolonization led to the greatest reduction of overall bloodstream infections (HR = 0.56 for universal; HR = 0.78 for targeted; HR = 0.99 for screening and isolation; P < .001). Of note, the universal decolonization group contained 3 of the 4 hospitals that performed bone marrow and solid-organ transplantations, resulting in a higher baseline risk of infection than the other groups, but this difference was not statistically significant. Overall, only severe adverse events were noted in this study and all were classified as mild pruritus or rash due to chlorhexidine bathing. Investigators did not evaluate the cost-effectiveness of the different strategies nor did they examine the emergence of resistance with widespread use of chlorhexidine and mupirocin.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Psychotic and needing prayer
CASE: Psychotic and assaultive
Mr. A, age 34, is involuntarily admitted to a psychiatric hospital after assaulting a family member and a police officer. He is charged with 2 counts of first-degree assault. He describes auditory hallucinations and believes God is telling him to refuse medication. One year earlier he was diagnosed with schizophrenia. Mr. A informs hospital staff that he is a Christian Scientist, and his religion precludes him from taking any medications. The local parish of the First Church of Christ, Scientist confirms that he is an active member. One day after admission, Mr. A is threatening and belligerent, and he continues to refuse any treatment.
How would you initially treat Mr. A?a) seek emergency guardianship
b) seek help from the Christian Science community
c) order the appropriate medication to effectively treat his symptoms
TREATMENT: Involuntary treatment
While in the hospital, Mr. A’s psychotic symptoms and aggressive behavior toward the staff and other patients lead to several psychiatric emergencies being declared and involuntary administration of antipsychotic medication. Because IM haloperidol, 5 mg/d, rapidly alleviates his symptoms, there is no need to pursue guardianship. Mr. A asks to meet with a member of the Christian Science community before his discharge, which is arranged. Upon being discharged, Mr. A schedules outpatient treatment at the community mental health center.
The author's observations
Mr. A’s case challenged staff to balance his clinical needs with his religious philosophy. Although psychotic, Mr. A provided a reason for refusing treatment—his belief in Christian Science—which would be considered a valid spiritual choice based on his values. However, his psychiatric symptoms created a dangerous situation for himself and others, which lead to emergency administration of antipsychotics against his will. Resolution of his symptoms did not warrant a petition for guardianship or a long-term involuntary hospitalization (Table 1). Allowing Mr. A to meet with a member of his church was crucial because it validated Mr. A’s religious practices and showed the staff’s willingness to respect his Christian Science beliefs.1,2
Honoring religious beliefs
Christian Science is based on the writings of Mary Baker Eddy and the Bible. Adherents believe that any form of evil, such as sin, disease, or death, is the opposite of God and is an illusion. Health care and treatment within the Christian Science community do not focus on what is wrong with the physical body, but rather what is wrong with the mind. Christian Scientists attempt healing through specific forms of prayer, not conventional methods such as medications or surgery.3 Christian Scientists believe there are no limits to the type of medical conditions that can be healed through prayer. Community members go to Christian Science practitioners for healing via prayer, focusing on the Bible and Mary Baker Eddy’s writings to alleviate their suffering.
The Christian Science church does not forbid its members from receiving conventional medical treatments, although prayer clearly is the preferred method of healing.4 Members can make their own choice about obtaining medical treatment. If they choose medical care, they cannot receive simultaneous treatment from Christian Science practitioners, but they can participate in other church activities. However, members compelled to get medical or psychiatric treatment via a guardianship or a court order can receive concurrent treatment from a Christian Science practitioner.
Other faith traditions generally do not draw such a clear line between medical treatment and religious healing. For example, Jehovah’s Witnesses have no prohibition against obtaining medical care, but they refuse blood transfusions, although they do accept medical alternatives to blood.5
ASSESSMENT: Remorse, reluctance
Mr. A stops taking his medication a few days after discharge, becomes psychotic, assaults his landlord, and is involuntarily readmitted to the hospital. His symptoms again are alleviated with IM haloperidol, 5 mg/d, and Mr. A is remorseful about his behavior while psychotic. He repeats his belief that his illness can be cured with prayer. The staff is reluctant to discharge Mr. A because of his history of nonadherence to treatment and assaultive episodes.
What are the next steps to consider in Mr. A’s treatment?a) seek guardianship because Mr. A does not appreciate the need for treatment
b) obtain a long-term commitment to the hospital with plans to conditionally release Mr. A when he is clinically stable
c) begin treatment with a long-acting injectable antipsychotic
EVALUATION: Next steps
The psychiatrist requests and receives a 3-year commitment for Mr. A from the probate court. The psychiatrist works with Mr. A and the community mental health center clinician to develop a conditional discharge plan in which Mr. A agrees to take medications as prescribed as a condition of his release. Mr. A initially is resistant to this plan. He is allowed to meet frequently with his Christian Science practitioner to discuss ways to continue treatment. Hospital staff supports these meetings, while explaining the importance of adhering to medication and how this will effectively treat his psychotic symptoms. Hospital staff does not negate or minimize Mr. A’s religious beliefs. The Christian Science practitioner allows Mr. A to continue his religious healing while receiving psychiatric care because he is a under court-ordered involuntary commitment. This leads Mr. A to find common ground between his religious beliefs and need for psychiatric treatment. Mr. A maintains his belief that he can be healed by prayer, but agrees to accept medications under the law of the probate commitment. To maximize adherence, he agrees to haloperidol decanoate, a long-acting injectable antipsychotic. He is conditionally discharged to continuing outpatient treatment at the community mental health center.
Mr. A adheres to treatment but begins to develop early signs of tardive dyskinesia (mild lip smacking and some tongue protrusion). Therefore, haloperidol decanoate is discontinued and replaced with oral olanzapine, 20 mg/d. Mr. A is no longer psychotic, and his psychotic symptoms are in remission. He continues to hold fast to his Christian Science beliefs.
One month before the end of his 3-year commitment, Mr. A informs his psychiatrist that he plans to stop his antipsychotic when the commitment ends and to pursue treatment with his Christian Science practitioner via prayer. He wants to prove to everyone that medications are no longer necessary.
What should Mr. A’s treating psychiatrist do?a) immediately readmit Mr. A involuntarily because of his potential dangerousness and impending treatment nonadherence
b) pursue guardianship because Mr. A is incapable of understanding that he has a serious mental illness
c) not pursue legal action but continue to treat Mr. A with antipsychotics and encourage compliance
d) readmit Mr. A to the hospital, request an extension of the commitment order, and consider a medication holiday in a safe setting to address Mr. A’s religious beliefs
OUTCOME: Court-ordered treatment
Mr. A agrees to hospitalization and at a court hearing is committed to the hospital for a period not to exceed 5 years. The judge also orders that Mr. A undergo a period of reducing or stopping his antipsychotic to see if he decompensates. The judicial order states that if it is determined that Mr. A no longer needs medication, the judge may reconsider the terms of the long-term commitment.
Mr. A, his inpatient and outpatient psychiatrists, and a Christian Science practitioner work together to develop a plan to taper his medication. Over 2 weeks, olanzapine is tapered from 20 mg/d to 10 mg/d. Two weeks into the taper, Mr. A becomes increasingly irritable, paranoid, and vigilant. The staff gives him prompt feedback about his apparent decompensation. Mr. A accepts this. He resumes taking olanzapine, 20 mg/d, and his symptoms resolve. He feels discouraged because taking medication is against his religious values. Nevertheless, he accepts the 5-year commitment as a court-mandated treatment that he must abide by. He is conditionally discharged from the hospital. For a summary of Mr. A’s clinical course, see Table 2.
Mr. A continues to do well in the community. New Hampshire’s law allowing up to a 5-year commitment to the hospital has been effective in maximizing Mr. A’s treatment adherence (Table 3).6 He has not been rehospitalized and his psychotic symptoms are in remission. Mr. A still believes his symptoms can be best treated with Christian Science prayer, but sees the state-imposed conditional discharge as a necessary “evil” that he must adhere to. He continues to be an active member of his church.
The author's observations
With the support of his outpatient and inpatient psychiatrists, treatment teams, and Christian Science practitioner, Mr. A has successfully integrated 2 seemingly opposing views regarding treatment, allowing him to live successfully in the community.
From this case, we learned that clinicians:
- need to understand patients’ religious beliefs and how these beliefs can impact their care
- must be aware that caring for patients from different religious traditions may present unique treatment challenges
- need to put their personal views regarding a patient’s religious beliefs aside and work with the patient to alleviate suffering
- must give patients ample opportunity to meet with their faith community, allowing adequate time for discussion and problem solving
Bottom Line
Balancing a patient’s clinical and spiritual needs can be challenging when those needs seem mutually exclusive. Clear communication, legal guidance, careful planning, and a strong therapeutic alliance can create opportunities for the patient to make both needs work to his advantage.
Related Resources
- Christian Science. www.christianscience.com.
- de Nesnera A, Vidaver RM. New Hampshire’s commitment law: treatment implications. New Hampshire Bar Journal. 2007;48(2):68-73.
- Ehman J. Religious diversity: practical points for health care
providers: www.uphs.upenn.edu/pastoral/resed/diversity_points.html.
Drug Brand Names
Haloperidol • Haldol
Olanzapine • Zyprexa
Disclosure
Dr. de Nesnera reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Pavlo AM, Bursztajn H, Gutheil T. Christian Science and competence to make treatment choices: clinical challenges in assessing values. Int J Law Psych. 1987;10(4):395-401.
2. Pavlo AM, Bursztajn H, Gutheil T, et al. Weighing religious beliefs in determining competence. Hosp Comm Psych. 1987;38(4):350-352.
3. Eddy MB. Science and health with key to the scriptures. Boston, MA: Christian Science Publishing Company; 1875:1-17.
4. Eddy M. Science and health with key to the scriptures. Boston, MA: Christian Science Publishing Company; 1875: 167.
5. The growing demand for bloodless medicine and surgery. Awake! January 8, 2000:4-6. http://wol.jw.org/en/wol/d/r1/lp-e/102000003. Accessed June 4, 2013.
6. NH Rev Stat Ann § 135-C:27-46.
CASE: Psychotic and assaultive
Mr. A, age 34, is involuntarily admitted to a psychiatric hospital after assaulting a family member and a police officer. He is charged with 2 counts of first-degree assault. He describes auditory hallucinations and believes God is telling him to refuse medication. One year earlier he was diagnosed with schizophrenia. Mr. A informs hospital staff that he is a Christian Scientist, and his religion precludes him from taking any medications. The local parish of the First Church of Christ, Scientist confirms that he is an active member. One day after admission, Mr. A is threatening and belligerent, and he continues to refuse any treatment.
How would you initially treat Mr. A?a) seek emergency guardianship
b) seek help from the Christian Science community
c) order the appropriate medication to effectively treat his symptoms
TREATMENT: Involuntary treatment
While in the hospital, Mr. A’s psychotic symptoms and aggressive behavior toward the staff and other patients lead to several psychiatric emergencies being declared and involuntary administration of antipsychotic medication. Because IM haloperidol, 5 mg/d, rapidly alleviates his symptoms, there is no need to pursue guardianship. Mr. A asks to meet with a member of the Christian Science community before his discharge, which is arranged. Upon being discharged, Mr. A schedules outpatient treatment at the community mental health center.
The author's observations
Mr. A’s case challenged staff to balance his clinical needs with his religious philosophy. Although psychotic, Mr. A provided a reason for refusing treatment—his belief in Christian Science—which would be considered a valid spiritual choice based on his values. However, his psychiatric symptoms created a dangerous situation for himself and others, which lead to emergency administration of antipsychotics against his will. Resolution of his symptoms did not warrant a petition for guardianship or a long-term involuntary hospitalization (Table 1). Allowing Mr. A to meet with a member of his church was crucial because it validated Mr. A’s religious practices and showed the staff’s willingness to respect his Christian Science beliefs.1,2
Honoring religious beliefs
Christian Science is based on the writings of Mary Baker Eddy and the Bible. Adherents believe that any form of evil, such as sin, disease, or death, is the opposite of God and is an illusion. Health care and treatment within the Christian Science community do not focus on what is wrong with the physical body, but rather what is wrong with the mind. Christian Scientists attempt healing through specific forms of prayer, not conventional methods such as medications or surgery.3 Christian Scientists believe there are no limits to the type of medical conditions that can be healed through prayer. Community members go to Christian Science practitioners for healing via prayer, focusing on the Bible and Mary Baker Eddy’s writings to alleviate their suffering.
The Christian Science church does not forbid its members from receiving conventional medical treatments, although prayer clearly is the preferred method of healing.4 Members can make their own choice about obtaining medical treatment. If they choose medical care, they cannot receive simultaneous treatment from Christian Science practitioners, but they can participate in other church activities. However, members compelled to get medical or psychiatric treatment via a guardianship or a court order can receive concurrent treatment from a Christian Science practitioner.
Other faith traditions generally do not draw such a clear line between medical treatment and religious healing. For example, Jehovah’s Witnesses have no prohibition against obtaining medical care, but they refuse blood transfusions, although they do accept medical alternatives to blood.5
ASSESSMENT: Remorse, reluctance
Mr. A stops taking his medication a few days after discharge, becomes psychotic, assaults his landlord, and is involuntarily readmitted to the hospital. His symptoms again are alleviated with IM haloperidol, 5 mg/d, and Mr. A is remorseful about his behavior while psychotic. He repeats his belief that his illness can be cured with prayer. The staff is reluctant to discharge Mr. A because of his history of nonadherence to treatment and assaultive episodes.
What are the next steps to consider in Mr. A’s treatment?a) seek guardianship because Mr. A does not appreciate the need for treatment
b) obtain a long-term commitment to the hospital with plans to conditionally release Mr. A when he is clinically stable
c) begin treatment with a long-acting injectable antipsychotic
EVALUATION: Next steps
The psychiatrist requests and receives a 3-year commitment for Mr. A from the probate court. The psychiatrist works with Mr. A and the community mental health center clinician to develop a conditional discharge plan in which Mr. A agrees to take medications as prescribed as a condition of his release. Mr. A initially is resistant to this plan. He is allowed to meet frequently with his Christian Science practitioner to discuss ways to continue treatment. Hospital staff supports these meetings, while explaining the importance of adhering to medication and how this will effectively treat his psychotic symptoms. Hospital staff does not negate or minimize Mr. A’s religious beliefs. The Christian Science practitioner allows Mr. A to continue his religious healing while receiving psychiatric care because he is a under court-ordered involuntary commitment. This leads Mr. A to find common ground between his religious beliefs and need for psychiatric treatment. Mr. A maintains his belief that he can be healed by prayer, but agrees to accept medications under the law of the probate commitment. To maximize adherence, he agrees to haloperidol decanoate, a long-acting injectable antipsychotic. He is conditionally discharged to continuing outpatient treatment at the community mental health center.
Mr. A adheres to treatment but begins to develop early signs of tardive dyskinesia (mild lip smacking and some tongue protrusion). Therefore, haloperidol decanoate is discontinued and replaced with oral olanzapine, 20 mg/d. Mr. A is no longer psychotic, and his psychotic symptoms are in remission. He continues to hold fast to his Christian Science beliefs.
One month before the end of his 3-year commitment, Mr. A informs his psychiatrist that he plans to stop his antipsychotic when the commitment ends and to pursue treatment with his Christian Science practitioner via prayer. He wants to prove to everyone that medications are no longer necessary.
What should Mr. A’s treating psychiatrist do?a) immediately readmit Mr. A involuntarily because of his potential dangerousness and impending treatment nonadherence
b) pursue guardianship because Mr. A is incapable of understanding that he has a serious mental illness
c) not pursue legal action but continue to treat Mr. A with antipsychotics and encourage compliance
d) readmit Mr. A to the hospital, request an extension of the commitment order, and consider a medication holiday in a safe setting to address Mr. A’s religious beliefs
OUTCOME: Court-ordered treatment
Mr. A agrees to hospitalization and at a court hearing is committed to the hospital for a period not to exceed 5 years. The judge also orders that Mr. A undergo a period of reducing or stopping his antipsychotic to see if he decompensates. The judicial order states that if it is determined that Mr. A no longer needs medication, the judge may reconsider the terms of the long-term commitment.
Mr. A, his inpatient and outpatient psychiatrists, and a Christian Science practitioner work together to develop a plan to taper his medication. Over 2 weeks, olanzapine is tapered from 20 mg/d to 10 mg/d. Two weeks into the taper, Mr. A becomes increasingly irritable, paranoid, and vigilant. The staff gives him prompt feedback about his apparent decompensation. Mr. A accepts this. He resumes taking olanzapine, 20 mg/d, and his symptoms resolve. He feels discouraged because taking medication is against his religious values. Nevertheless, he accepts the 5-year commitment as a court-mandated treatment that he must abide by. He is conditionally discharged from the hospital. For a summary of Mr. A’s clinical course, see Table 2.
Mr. A continues to do well in the community. New Hampshire’s law allowing up to a 5-year commitment to the hospital has been effective in maximizing Mr. A’s treatment adherence (Table 3).6 He has not been rehospitalized and his psychotic symptoms are in remission. Mr. A still believes his symptoms can be best treated with Christian Science prayer, but sees the state-imposed conditional discharge as a necessary “evil” that he must adhere to. He continues to be an active member of his church.
The author's observations
With the support of his outpatient and inpatient psychiatrists, treatment teams, and Christian Science practitioner, Mr. A has successfully integrated 2 seemingly opposing views regarding treatment, allowing him to live successfully in the community.
From this case, we learned that clinicians:
- need to understand patients’ religious beliefs and how these beliefs can impact their care
- must be aware that caring for patients from different religious traditions may present unique treatment challenges
- need to put their personal views regarding a patient’s religious beliefs aside and work with the patient to alleviate suffering
- must give patients ample opportunity to meet with their faith community, allowing adequate time for discussion and problem solving
Bottom Line
Balancing a patient’s clinical and spiritual needs can be challenging when those needs seem mutually exclusive. Clear communication, legal guidance, careful planning, and a strong therapeutic alliance can create opportunities for the patient to make both needs work to his advantage.
Related Resources
- Christian Science. www.christianscience.com.
- de Nesnera A, Vidaver RM. New Hampshire’s commitment law: treatment implications. New Hampshire Bar Journal. 2007;48(2):68-73.
- Ehman J. Religious diversity: practical points for health care
providers: www.uphs.upenn.edu/pastoral/resed/diversity_points.html.
Drug Brand Names
Haloperidol • Haldol
Olanzapine • Zyprexa
Disclosure
Dr. de Nesnera reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Psychotic and assaultive
Mr. A, age 34, is involuntarily admitted to a psychiatric hospital after assaulting a family member and a police officer. He is charged with 2 counts of first-degree assault. He describes auditory hallucinations and believes God is telling him to refuse medication. One year earlier he was diagnosed with schizophrenia. Mr. A informs hospital staff that he is a Christian Scientist, and his religion precludes him from taking any medications. The local parish of the First Church of Christ, Scientist confirms that he is an active member. One day after admission, Mr. A is threatening and belligerent, and he continues to refuse any treatment.
How would you initially treat Mr. A?a) seek emergency guardianship
b) seek help from the Christian Science community
c) order the appropriate medication to effectively treat his symptoms
TREATMENT: Involuntary treatment
While in the hospital, Mr. A’s psychotic symptoms and aggressive behavior toward the staff and other patients lead to several psychiatric emergencies being declared and involuntary administration of antipsychotic medication. Because IM haloperidol, 5 mg/d, rapidly alleviates his symptoms, there is no need to pursue guardianship. Mr. A asks to meet with a member of the Christian Science community before his discharge, which is arranged. Upon being discharged, Mr. A schedules outpatient treatment at the community mental health center.
The author's observations
Mr. A’s case challenged staff to balance his clinical needs with his religious philosophy. Although psychotic, Mr. A provided a reason for refusing treatment—his belief in Christian Science—which would be considered a valid spiritual choice based on his values. However, his psychiatric symptoms created a dangerous situation for himself and others, which lead to emergency administration of antipsychotics against his will. Resolution of his symptoms did not warrant a petition for guardianship or a long-term involuntary hospitalization (Table 1). Allowing Mr. A to meet with a member of his church was crucial because it validated Mr. A’s religious practices and showed the staff’s willingness to respect his Christian Science beliefs.1,2
Honoring religious beliefs
Christian Science is based on the writings of Mary Baker Eddy and the Bible. Adherents believe that any form of evil, such as sin, disease, or death, is the opposite of God and is an illusion. Health care and treatment within the Christian Science community do not focus on what is wrong with the physical body, but rather what is wrong with the mind. Christian Scientists attempt healing through specific forms of prayer, not conventional methods such as medications or surgery.3 Christian Scientists believe there are no limits to the type of medical conditions that can be healed through prayer. Community members go to Christian Science practitioners for healing via prayer, focusing on the Bible and Mary Baker Eddy’s writings to alleviate their suffering.
The Christian Science church does not forbid its members from receiving conventional medical treatments, although prayer clearly is the preferred method of healing.4 Members can make their own choice about obtaining medical treatment. If they choose medical care, they cannot receive simultaneous treatment from Christian Science practitioners, but they can participate in other church activities. However, members compelled to get medical or psychiatric treatment via a guardianship or a court order can receive concurrent treatment from a Christian Science practitioner.
Other faith traditions generally do not draw such a clear line between medical treatment and religious healing. For example, Jehovah’s Witnesses have no prohibition against obtaining medical care, but they refuse blood transfusions, although they do accept medical alternatives to blood.5
ASSESSMENT: Remorse, reluctance
Mr. A stops taking his medication a few days after discharge, becomes psychotic, assaults his landlord, and is involuntarily readmitted to the hospital. His symptoms again are alleviated with IM haloperidol, 5 mg/d, and Mr. A is remorseful about his behavior while psychotic. He repeats his belief that his illness can be cured with prayer. The staff is reluctant to discharge Mr. A because of his history of nonadherence to treatment and assaultive episodes.
What are the next steps to consider in Mr. A’s treatment?a) seek guardianship because Mr. A does not appreciate the need for treatment
b) obtain a long-term commitment to the hospital with plans to conditionally release Mr. A when he is clinically stable
c) begin treatment with a long-acting injectable antipsychotic
EVALUATION: Next steps
The psychiatrist requests and receives a 3-year commitment for Mr. A from the probate court. The psychiatrist works with Mr. A and the community mental health center clinician to develop a conditional discharge plan in which Mr. A agrees to take medications as prescribed as a condition of his release. Mr. A initially is resistant to this plan. He is allowed to meet frequently with his Christian Science practitioner to discuss ways to continue treatment. Hospital staff supports these meetings, while explaining the importance of adhering to medication and how this will effectively treat his psychotic symptoms. Hospital staff does not negate or minimize Mr. A’s religious beliefs. The Christian Science practitioner allows Mr. A to continue his religious healing while receiving psychiatric care because he is a under court-ordered involuntary commitment. This leads Mr. A to find common ground between his religious beliefs and need for psychiatric treatment. Mr. A maintains his belief that he can be healed by prayer, but agrees to accept medications under the law of the probate commitment. To maximize adherence, he agrees to haloperidol decanoate, a long-acting injectable antipsychotic. He is conditionally discharged to continuing outpatient treatment at the community mental health center.
Mr. A adheres to treatment but begins to develop early signs of tardive dyskinesia (mild lip smacking and some tongue protrusion). Therefore, haloperidol decanoate is discontinued and replaced with oral olanzapine, 20 mg/d. Mr. A is no longer psychotic, and his psychotic symptoms are in remission. He continues to hold fast to his Christian Science beliefs.
One month before the end of his 3-year commitment, Mr. A informs his psychiatrist that he plans to stop his antipsychotic when the commitment ends and to pursue treatment with his Christian Science practitioner via prayer. He wants to prove to everyone that medications are no longer necessary.
What should Mr. A’s treating psychiatrist do?a) immediately readmit Mr. A involuntarily because of his potential dangerousness and impending treatment nonadherence
b) pursue guardianship because Mr. A is incapable of understanding that he has a serious mental illness
c) not pursue legal action but continue to treat Mr. A with antipsychotics and encourage compliance
d) readmit Mr. A to the hospital, request an extension of the commitment order, and consider a medication holiday in a safe setting to address Mr. A’s religious beliefs
OUTCOME: Court-ordered treatment
Mr. A agrees to hospitalization and at a court hearing is committed to the hospital for a period not to exceed 5 years. The judge also orders that Mr. A undergo a period of reducing or stopping his antipsychotic to see if he decompensates. The judicial order states that if it is determined that Mr. A no longer needs medication, the judge may reconsider the terms of the long-term commitment.
Mr. A, his inpatient and outpatient psychiatrists, and a Christian Science practitioner work together to develop a plan to taper his medication. Over 2 weeks, olanzapine is tapered from 20 mg/d to 10 mg/d. Two weeks into the taper, Mr. A becomes increasingly irritable, paranoid, and vigilant. The staff gives him prompt feedback about his apparent decompensation. Mr. A accepts this. He resumes taking olanzapine, 20 mg/d, and his symptoms resolve. He feels discouraged because taking medication is against his religious values. Nevertheless, he accepts the 5-year commitment as a court-mandated treatment that he must abide by. He is conditionally discharged from the hospital. For a summary of Mr. A’s clinical course, see Table 2.
Mr. A continues to do well in the community. New Hampshire’s law allowing up to a 5-year commitment to the hospital has been effective in maximizing Mr. A’s treatment adherence (Table 3).6 He has not been rehospitalized and his psychotic symptoms are in remission. Mr. A still believes his symptoms can be best treated with Christian Science prayer, but sees the state-imposed conditional discharge as a necessary “evil” that he must adhere to. He continues to be an active member of his church.
The author's observations
With the support of his outpatient and inpatient psychiatrists, treatment teams, and Christian Science practitioner, Mr. A has successfully integrated 2 seemingly opposing views regarding treatment, allowing him to live successfully in the community.
From this case, we learned that clinicians:
- need to understand patients’ religious beliefs and how these beliefs can impact their care
- must be aware that caring for patients from different religious traditions may present unique treatment challenges
- need to put their personal views regarding a patient’s religious beliefs aside and work with the patient to alleviate suffering
- must give patients ample opportunity to meet with their faith community, allowing adequate time for discussion and problem solving
Bottom Line
Balancing a patient’s clinical and spiritual needs can be challenging when those needs seem mutually exclusive. Clear communication, legal guidance, careful planning, and a strong therapeutic alliance can create opportunities for the patient to make both needs work to his advantage.
Related Resources
- Christian Science. www.christianscience.com.
- de Nesnera A, Vidaver RM. New Hampshire’s commitment law: treatment implications. New Hampshire Bar Journal. 2007;48(2):68-73.
- Ehman J. Religious diversity: practical points for health care
providers: www.uphs.upenn.edu/pastoral/resed/diversity_points.html.
Drug Brand Names
Haloperidol • Haldol
Olanzapine • Zyprexa
Disclosure
Dr. de Nesnera reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Pavlo AM, Bursztajn H, Gutheil T. Christian Science and competence to make treatment choices: clinical challenges in assessing values. Int J Law Psych. 1987;10(4):395-401.
2. Pavlo AM, Bursztajn H, Gutheil T, et al. Weighing religious beliefs in determining competence. Hosp Comm Psych. 1987;38(4):350-352.
3. Eddy MB. Science and health with key to the scriptures. Boston, MA: Christian Science Publishing Company; 1875:1-17.
4. Eddy M. Science and health with key to the scriptures. Boston, MA: Christian Science Publishing Company; 1875: 167.
5. The growing demand for bloodless medicine and surgery. Awake! January 8, 2000:4-6. http://wol.jw.org/en/wol/d/r1/lp-e/102000003. Accessed June 4, 2013.
6. NH Rev Stat Ann § 135-C:27-46.
1. Pavlo AM, Bursztajn H, Gutheil T. Christian Science and competence to make treatment choices: clinical challenges in assessing values. Int J Law Psych. 1987;10(4):395-401.
2. Pavlo AM, Bursztajn H, Gutheil T, et al. Weighing religious beliefs in determining competence. Hosp Comm Psych. 1987;38(4):350-352.
3. Eddy MB. Science and health with key to the scriptures. Boston, MA: Christian Science Publishing Company; 1875:1-17.
4. Eddy M. Science and health with key to the scriptures. Boston, MA: Christian Science Publishing Company; 1875: 167.
5. The growing demand for bloodless medicine and surgery. Awake! January 8, 2000:4-6. http://wol.jw.org/en/wol/d/r1/lp-e/102000003. Accessed June 4, 2013.
6. NH Rev Stat Ann § 135-C:27-46.
Emergency Department EHRs Raise Quality, Safety Concerns
An author of a new report that looks at the quality and safety implications of electronic health records (EHRs) wants physicians to view the efficacy of the system as an extension of the patient-care-delivery process.
"In medicine, we have an obligation to report errors," says co-author Kevin Baumlin, MD, FACEP, associate medical information officer at Mount Sinai Medical Center in New York. "When those errors may or may not have to do with an EHR, we have an obligation to get better. It's about patient care, right?"
The paper highlights the potential health and safety issues due to a lack of industrywide technology standards, alert fatigue, and communication problems. Although the report focuses on ED doctors, Dr. Baumlin notes that what's good for that specialty is good for hospitalists, as physicians work together on countless care transitions, both physically and electronically.
To that end, the report issues recommendations to improve the safety of ED information systems, including:
- Appoint a “clinician champion” to act as a liaison between doctors;
- Have vendors and hospital leadership form a multidisciplinary performance-improvement group;
- Set up an ongoing review process to monitor patient concerns in a timely manner;
- Measure and share lessons learned; and
- Remove “hold harmless” and “learned intermediary” clauses from vendor software contracts that can prevent the sharing of information that could help solve future problems.
Dr. Baumlin says the purpose of the paper isn't to paint EHR vendors as unhelpful, but to point out that healthcare as an industry has to promote more collaboration among vendors, physicians, and hospital leaders. To that end, the American College of Emergency Physicians has been holding talks with vendors about bridging information gaps and eliminating hurdles to communication.
“We're just trying to create a forum where everyone can talk and be heard,” Dr. Baumlin says. “We're not looking back. We're going forward.”
Visit our website for more information on health information technology.
An author of a new report that looks at the quality and safety implications of electronic health records (EHRs) wants physicians to view the efficacy of the system as an extension of the patient-care-delivery process.
"In medicine, we have an obligation to report errors," says co-author Kevin Baumlin, MD, FACEP, associate medical information officer at Mount Sinai Medical Center in New York. "When those errors may or may not have to do with an EHR, we have an obligation to get better. It's about patient care, right?"
The paper highlights the potential health and safety issues due to a lack of industrywide technology standards, alert fatigue, and communication problems. Although the report focuses on ED doctors, Dr. Baumlin notes that what's good for that specialty is good for hospitalists, as physicians work together on countless care transitions, both physically and electronically.
To that end, the report issues recommendations to improve the safety of ED information systems, including:
- Appoint a “clinician champion” to act as a liaison between doctors;
- Have vendors and hospital leadership form a multidisciplinary performance-improvement group;
- Set up an ongoing review process to monitor patient concerns in a timely manner;
- Measure and share lessons learned; and
- Remove “hold harmless” and “learned intermediary” clauses from vendor software contracts that can prevent the sharing of information that could help solve future problems.
Dr. Baumlin says the purpose of the paper isn't to paint EHR vendors as unhelpful, but to point out that healthcare as an industry has to promote more collaboration among vendors, physicians, and hospital leaders. To that end, the American College of Emergency Physicians has been holding talks with vendors about bridging information gaps and eliminating hurdles to communication.
“We're just trying to create a forum where everyone can talk and be heard,” Dr. Baumlin says. “We're not looking back. We're going forward.”
Visit our website for more information on health information technology.
An author of a new report that looks at the quality and safety implications of electronic health records (EHRs) wants physicians to view the efficacy of the system as an extension of the patient-care-delivery process.
"In medicine, we have an obligation to report errors," says co-author Kevin Baumlin, MD, FACEP, associate medical information officer at Mount Sinai Medical Center in New York. "When those errors may or may not have to do with an EHR, we have an obligation to get better. It's about patient care, right?"
The paper highlights the potential health and safety issues due to a lack of industrywide technology standards, alert fatigue, and communication problems. Although the report focuses on ED doctors, Dr. Baumlin notes that what's good for that specialty is good for hospitalists, as physicians work together on countless care transitions, both physically and electronically.
To that end, the report issues recommendations to improve the safety of ED information systems, including:
- Appoint a “clinician champion” to act as a liaison between doctors;
- Have vendors and hospital leadership form a multidisciplinary performance-improvement group;
- Set up an ongoing review process to monitor patient concerns in a timely manner;
- Measure and share lessons learned; and
- Remove “hold harmless” and “learned intermediary” clauses from vendor software contracts that can prevent the sharing of information that could help solve future problems.
Dr. Baumlin says the purpose of the paper isn't to paint EHR vendors as unhelpful, but to point out that healthcare as an industry has to promote more collaboration among vendors, physicians, and hospital leaders. To that end, the American College of Emergency Physicians has been holding talks with vendors about bridging information gaps and eliminating hurdles to communication.
“We're just trying to create a forum where everyone can talk and be heard,” Dr. Baumlin says. “We're not looking back. We're going forward.”
Visit our website for more information on health information technology.
Surgical-Site-Infection Risk Not Associated with Prophylactic Antibiotic Timing
Clinical question: How does timing of surgical antibiotic prophylaxis affect risk of postoperative surgical-site infections (SSIs)?
Background: Antibiotic prophylaxis for major surgical procedures has been proven in clinical trials to reduce rates of SSI. The Centers for Medicare & Medicaid Services’ (CMS) Surgical Care Improvement Project (SCIP) has implemented quality metrics to ensure antibiotics are administered within 60 minutes of incision; however, studies have failed to show that a 60-minute pre-incision window is advantageous.
Study design: Retrospective cohort.
Setting: Veterans Affairs hospitals.
Synopsis: Using SCIP and VA Surgical Quality Improvement Program data from 112 VA hospitals, 32,459 cases of hip or knee arthroplasty, colorectal surgery, arterial vascular surgery, and hysterectomy from 2005 to 2009 were reviewed. A post-operative SSI occurred in 1,497 cases (4.6%). Using several statistical methods, the relationship between timing of prophylactic antibiotic administration and postoperative SSI within 30 days was evaluated.
In unadjusted models, higher SSI rates were observed with antibiotic administration more than 60 minutes prior to incision (OR 1.34, 95% CI 1.08-1.66) but not after incision (OR 1.26, 95% CI 0.92-1.72), compared with procedures with antibiotics administered within 60 minutes pre-incision. However, after adjustment for patient, procedure, and antibiotic variables, no significant relationship between timing and SSI was observed (P=0.50 for all specialties).
The study sample was comprised primarily of older men and did not include patients who underwent cardiac procedures, limiting the generalizability of the findings. Nonetheless, the study is the largest of its kind and confirms previous studies that suggest there is no significant relationship between timing of antibiotics and SSI. Prophylactic antibiotics should still be used when indicated; however, using timing of prophylactic antibiotics as a quality measure is unlikely to improve outcomes.
Bottom line: Adherence to the empiric 60-minute window metric for timing of prophylactic antibiotics is not significantly associated with risk of SSI.
Citation: Hawn MT, Richman JS, Vick CC, et al. Timing of surgical antibiotic prophylaxis and the risk of surgical site infection. JAMA Surg. 2013 March 20:1-8. doi: 10.1001/jamasurg.2013.134 [Epub ahead of print].
Visit our website for more physician reviews of recent HM-relevant literature.
Clinical question: How does timing of surgical antibiotic prophylaxis affect risk of postoperative surgical-site infections (SSIs)?
Background: Antibiotic prophylaxis for major surgical procedures has been proven in clinical trials to reduce rates of SSI. The Centers for Medicare & Medicaid Services’ (CMS) Surgical Care Improvement Project (SCIP) has implemented quality metrics to ensure antibiotics are administered within 60 minutes of incision; however, studies have failed to show that a 60-minute pre-incision window is advantageous.
Study design: Retrospective cohort.
Setting: Veterans Affairs hospitals.
Synopsis: Using SCIP and VA Surgical Quality Improvement Program data from 112 VA hospitals, 32,459 cases of hip or knee arthroplasty, colorectal surgery, arterial vascular surgery, and hysterectomy from 2005 to 2009 were reviewed. A post-operative SSI occurred in 1,497 cases (4.6%). Using several statistical methods, the relationship between timing of prophylactic antibiotic administration and postoperative SSI within 30 days was evaluated.
In unadjusted models, higher SSI rates were observed with antibiotic administration more than 60 minutes prior to incision (OR 1.34, 95% CI 1.08-1.66) but not after incision (OR 1.26, 95% CI 0.92-1.72), compared with procedures with antibiotics administered within 60 minutes pre-incision. However, after adjustment for patient, procedure, and antibiotic variables, no significant relationship between timing and SSI was observed (P=0.50 for all specialties).
The study sample was comprised primarily of older men and did not include patients who underwent cardiac procedures, limiting the generalizability of the findings. Nonetheless, the study is the largest of its kind and confirms previous studies that suggest there is no significant relationship between timing of antibiotics and SSI. Prophylactic antibiotics should still be used when indicated; however, using timing of prophylactic antibiotics as a quality measure is unlikely to improve outcomes.
Bottom line: Adherence to the empiric 60-minute window metric for timing of prophylactic antibiotics is not significantly associated with risk of SSI.
Citation: Hawn MT, Richman JS, Vick CC, et al. Timing of surgical antibiotic prophylaxis and the risk of surgical site infection. JAMA Surg. 2013 March 20:1-8. doi: 10.1001/jamasurg.2013.134 [Epub ahead of print].
Visit our website for more physician reviews of recent HM-relevant literature.
Clinical question: How does timing of surgical antibiotic prophylaxis affect risk of postoperative surgical-site infections (SSIs)?
Background: Antibiotic prophylaxis for major surgical procedures has been proven in clinical trials to reduce rates of SSI. The Centers for Medicare & Medicaid Services’ (CMS) Surgical Care Improvement Project (SCIP) has implemented quality metrics to ensure antibiotics are administered within 60 minutes of incision; however, studies have failed to show that a 60-minute pre-incision window is advantageous.
Study design: Retrospective cohort.
Setting: Veterans Affairs hospitals.
Synopsis: Using SCIP and VA Surgical Quality Improvement Program data from 112 VA hospitals, 32,459 cases of hip or knee arthroplasty, colorectal surgery, arterial vascular surgery, and hysterectomy from 2005 to 2009 were reviewed. A post-operative SSI occurred in 1,497 cases (4.6%). Using several statistical methods, the relationship between timing of prophylactic antibiotic administration and postoperative SSI within 30 days was evaluated.
In unadjusted models, higher SSI rates were observed with antibiotic administration more than 60 minutes prior to incision (OR 1.34, 95% CI 1.08-1.66) but not after incision (OR 1.26, 95% CI 0.92-1.72), compared with procedures with antibiotics administered within 60 minutes pre-incision. However, after adjustment for patient, procedure, and antibiotic variables, no significant relationship between timing and SSI was observed (P=0.50 for all specialties).
The study sample was comprised primarily of older men and did not include patients who underwent cardiac procedures, limiting the generalizability of the findings. Nonetheless, the study is the largest of its kind and confirms previous studies that suggest there is no significant relationship between timing of antibiotics and SSI. Prophylactic antibiotics should still be used when indicated; however, using timing of prophylactic antibiotics as a quality measure is unlikely to improve outcomes.
Bottom line: Adherence to the empiric 60-minute window metric for timing of prophylactic antibiotics is not significantly associated with risk of SSI.
Citation: Hawn MT, Richman JS, Vick CC, et al. Timing of surgical antibiotic prophylaxis and the risk of surgical site infection. JAMA Surg. 2013 March 20:1-8. doi: 10.1001/jamasurg.2013.134 [Epub ahead of print].
Visit our website for more physician reviews of recent HM-relevant literature.
Blue light
Photodynamic light therapies (PDLs) have emerged as significant adjuvant approaches for treating acne. In particular, such therapies have been used for acne refractory to standard retinoid or combined retinoid and antimicrobial regimens. Why write about PDL in a column devoted to topical cosmeceutical products and ingredients? Blue light warrants inclusion because it has been studied in comparison to topical cosmeceutical treatments, and it is used in conjunction with other topical approaches.
Blue light exerts a phototoxic effect on the heme metabolism of Propionibacterium acnes, and it is considered effective by targeting part of the etiologic pathway of acne. It has become a widely used option for inflammatory acne (J. Drugs. Dermatol. 2006;5:605-10).
Early work
In 1990, Meffert et al. were the first to show that a blue light–type, high-pressure lamp could improve acne and seborrhea (10 10-minute treatments, cumulative light dose 325 J/cm2). Given the copious amounts of porphyrins stored in lipophilic P. acnes, the technology could be targeted to destroy propionibacteria, and the researchers observed a decline in the porphyrin content inside acne follicles. They concluded that short-range visible light (400-420 nm) was a viable option for acne treatment during the light-poor season of the year (Dermatol. Monatsschr. 1990;176:597-603). It was subsequently established that treatment with UV-free blue light in the range of 405-420 nm leads to the elimination of acne bacteria by virtue of the effects on the porphyrins generated naturally by P. acnes (J. Cosmet. Laser. Ther. 2003;5:111-7). Notably, blue light appears to photoinactivate P. acnes, but it does not penetrate deeply into the skin (Dermatol. Online J. 2011;17:2).
In an open study of the then-novel high-intensity, enhanced, narrow-band, blue-light phototherapy, Kawada et al. treated 30 acne patients (27 female, 3 male) twice a week for up to 5 weeks. A reduction of 64% was seen in acne lesions, and in vitro data showed a significant decline in P. acnes, but not in Staphylococcus epidermidis (J. Dermatol. Sci. 2002;30:129-35).
Mechanism of action
In 2006, Shnitkind et al. studied the effect of narrow-band blue light on the inflammatory process in the presence and absence of cytokines and ultraviolet B using interleukin-1 alpha (IL-1alpha) and intercellular adhesion molecule 1 (ICAM-1) as markers for inflammation. They found that blue light treatment of HaCaT and hTERT cells decreased levels of IL-1alpha by 82% in HaCaT and by 75% in hTERT. When blue light was combined with ultraviolet B, the respective reductions were 95% and 91%. Similar reductions in ICAM-1 expression were seen in HaCaT, but not in hTERT. The researchers concluded that narrow-band blue light exerts anti-inflammatory effects on keratinocytes by reducing cytokine-induced synthesis of IL-1alpha and ICAM-1. They suggested that these findings imply a broader range of effects is exerted on the inflammatory process by narrow-band blue light than previously understood (J. Drugs. Dermatol. 2006;5:605-10).
Comparison studies
In 2000, Papageorgiou et al. randomized 107 patients with mild to moderate acne to four treatment groups: blue light (peak at 415 nm), mixed blue and red light (peaks at 415 and 660 nm), cool white light, and 5% benzoyl peroxide cream, for 12 weeks of active treatment. Phototherapy using portable light sources was conducted daily for 15 minutes; comparative assessments among the three phototherapy groups were done with observers blinded. The investigators found that the greatest improvement in acne lesions occurred in the blue and red light combined group. The blue/red treatment was significantly superior to blue light alone at 4 and 8 weeks but not 12 weeks, benzoyl peroxide at weeks 8 and 12, and white light at all assessments (Br. J. Dermatol. 2000;142:973-8).
Gold et al. performed a multicenter clinical evaluation comparing blue light to topical 1% clindamycin solution with respect to safety and efficacy. They found that clindamycin was associated with a 14% reduction of inflammatory lesions, but blue light reduced such lesions by an average of 34% (J. Drugs. Dermatol. 2005;4:64-70).
In another study, 20 patients with moderate to severe facial acne were treated in four weekly sessions with topical aminolevulinic acid (ALA)-photodynamic therapy with blue light (415 nm) on the right side of the face, or blue light alone on the left side of the face. At 4, 8, 12, and 16 weeks after the start of treatment, the mean percent reductions in inflamed lesions were higher in the ALA-PDT areas (32%, 50.9%, 65.9%, and 71.1%, respectively) than in the blue light–only treatment areas (20.7%, 27%, 57.7%, and 56.7%), but the differences were not statistically significant. Side effects, which included pain, stinging, erythema, itching, peeling, oozing, and pustules, were more pronounced in the areas treated with ALA-PDT (Photodermatol. Photoimmunol. Photomed. 2007;23:186-90).
However, in a 2007 study of 22 patients with moderate to severe acne randomized to one of three ALA-PDT treatments – intense pulsed light (IPL; 600-850 nm), a combination of IPL (580-980 nm) and bipolar radiofrequency (RF) energies, or blue light (417 nm) – in three sessions at 2-week intervals, ALA-PDT with activation by IPL yielded the most consistent, lasting improvement in moderate to severe acne (J. Drugs Dermatol. 2007;6:1010-6).
In a study of 60 volunteers with facial acne (grades II and III), de Arruda et al. compared the safety and efficacy of blue light to topical benzoyl peroxide 5% over 4 weeks. Thirty patients received blue light treatment twice a week, and the other 30 self-applied the topical formulation twice daily. The improvements were similar in both groups, but side effects were milder in the blue light group (An. Bras. Dermatol. 2009;84:463-8).
Choi et al. compared the bactericidal effects of 5-aminolevulinic acid (ALA) with blue and red light on P. acnes and found that blue light was more effective than red light phototherapy in eliminating the bacteria unless ALA was added, which substantially augmented red light phototherapy efficacy (J. Dermatol. 2011;38:661-6).
In summarizing the off-label uses of light-based treatments and PDT using topical precursors of porphyrins, Sakamoto et al. observed that blue light alone lessens acne severity due to anti-inflammatory effects; PDT using 5-ALA or ALA derivatives provides antimicrobial and anti-inflammatory activity; and, at high doses, red-light PDT may suppress or eradicate sebaceous glands, yielding clinical improvement (J. Am. Acad. Dermatol. 2010;63:183-93).
Combination therapy
In 2011, Wheeland and Dhawan assessed the efficacy and tolerability of treating mild to moderate facial acne using a novel, handheld, light-emitting diode (LED) blue-light device, along with a foam cleanser containing 5% glycolic acid and 2% salicylic acid, plus a serum containing 1.25% salicylic acid, 0.5% niacinamide, 0.08% liposomal-based azelaic acid, and superoxide dismutase. In all, 28 of 35 adults aged 25-45 years completed the 8-week study, in which they used the device twice daily (in addition to the cleanser before treatments and the serum after nighttime treatments). Significant reductions in inflammatory lesion counts were seen from week 1 onward, and significant reductions in noninflammatory lesion counts were seen from week 4 onward compared with baseline counts. The number and severity of flares were significantly reduced from baseline as well.
Therapy was well received by patients, with more than 90% claiming improvement in overall skin appearance and other parameters. In addition, 86% described the treatment as gentler than other therapies. (J. Drugs Dermatol. 2011;10:596-602).
Products
The Skin Clarifying Blue Light device has a power density of 400 mW/cm2, which is 10 times the power of other LED acne devices. This high power density allows the Skin Clarifying Blue Light device to deliver high levels of efficacy with short treatment times. When used as stand-alone treatment, it delivered a 70% reduction in inflammatory lesions in 8 weeks. The success of products designed for self-administration has coincided with the rampant interest in the creation of smart phone applications (J. Cosmet. Laser. Ther. 2011;13:308-14; J. Clin. Aesthet. Dermatol. 2009;2:40-4; J. Clin. Aesthet. Dermatol. 2009;2:44-50). That is, blue-light therapy apps have been developed for the iPhone and the iPod touch. None, however, has been approved by the Food and Drug Administration, although at least one is said to be under investigation in a clinical trial. I am skeptical about the efficacy of these LED-backlit apps and concerned about potentially prolonged magnetic radiation exposure that would be required. The self-administered devices appear to be a more reliable alternative.
Conclusion
Blue light can effectively be used to treat mild to moderate acne by causing photodynamic destruction of P. acnes. It can be used alone or in combination with topical or other light regimens. Additional studies are needed before a consensus protocol can be established, and future research goals should include establishing the optimal incubation time, activating light source, and frequency of treatment.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Photodynamic light therapies (PDLs) have emerged as significant adjuvant approaches for treating acne. In particular, such therapies have been used for acne refractory to standard retinoid or combined retinoid and antimicrobial regimens. Why write about PDL in a column devoted to topical cosmeceutical products and ingredients? Blue light warrants inclusion because it has been studied in comparison to topical cosmeceutical treatments, and it is used in conjunction with other topical approaches.
Blue light exerts a phototoxic effect on the heme metabolism of Propionibacterium acnes, and it is considered effective by targeting part of the etiologic pathway of acne. It has become a widely used option for inflammatory acne (J. Drugs. Dermatol. 2006;5:605-10).
Early work
In 1990, Meffert et al. were the first to show that a blue light–type, high-pressure lamp could improve acne and seborrhea (10 10-minute treatments, cumulative light dose 325 J/cm2). Given the copious amounts of porphyrins stored in lipophilic P. acnes, the technology could be targeted to destroy propionibacteria, and the researchers observed a decline in the porphyrin content inside acne follicles. They concluded that short-range visible light (400-420 nm) was a viable option for acne treatment during the light-poor season of the year (Dermatol. Monatsschr. 1990;176:597-603). It was subsequently established that treatment with UV-free blue light in the range of 405-420 nm leads to the elimination of acne bacteria by virtue of the effects on the porphyrins generated naturally by P. acnes (J. Cosmet. Laser. Ther. 2003;5:111-7). Notably, blue light appears to photoinactivate P. acnes, but it does not penetrate deeply into the skin (Dermatol. Online J. 2011;17:2).
In an open study of the then-novel high-intensity, enhanced, narrow-band, blue-light phototherapy, Kawada et al. treated 30 acne patients (27 female, 3 male) twice a week for up to 5 weeks. A reduction of 64% was seen in acne lesions, and in vitro data showed a significant decline in P. acnes, but not in Staphylococcus epidermidis (J. Dermatol. Sci. 2002;30:129-35).
Mechanism of action
In 2006, Shnitkind et al. studied the effect of narrow-band blue light on the inflammatory process in the presence and absence of cytokines and ultraviolet B using interleukin-1 alpha (IL-1alpha) and intercellular adhesion molecule 1 (ICAM-1) as markers for inflammation. They found that blue light treatment of HaCaT and hTERT cells decreased levels of IL-1alpha by 82% in HaCaT and by 75% in hTERT. When blue light was combined with ultraviolet B, the respective reductions were 95% and 91%. Similar reductions in ICAM-1 expression were seen in HaCaT, but not in hTERT. The researchers concluded that narrow-band blue light exerts anti-inflammatory effects on keratinocytes by reducing cytokine-induced synthesis of IL-1alpha and ICAM-1. They suggested that these findings imply a broader range of effects is exerted on the inflammatory process by narrow-band blue light than previously understood (J. Drugs. Dermatol. 2006;5:605-10).
Comparison studies
In 2000, Papageorgiou et al. randomized 107 patients with mild to moderate acne to four treatment groups: blue light (peak at 415 nm), mixed blue and red light (peaks at 415 and 660 nm), cool white light, and 5% benzoyl peroxide cream, for 12 weeks of active treatment. Phototherapy using portable light sources was conducted daily for 15 minutes; comparative assessments among the three phototherapy groups were done with observers blinded. The investigators found that the greatest improvement in acne lesions occurred in the blue and red light combined group. The blue/red treatment was significantly superior to blue light alone at 4 and 8 weeks but not 12 weeks, benzoyl peroxide at weeks 8 and 12, and white light at all assessments (Br. J. Dermatol. 2000;142:973-8).
Gold et al. performed a multicenter clinical evaluation comparing blue light to topical 1% clindamycin solution with respect to safety and efficacy. They found that clindamycin was associated with a 14% reduction of inflammatory lesions, but blue light reduced such lesions by an average of 34% (J. Drugs. Dermatol. 2005;4:64-70).
In another study, 20 patients with moderate to severe facial acne were treated in four weekly sessions with topical aminolevulinic acid (ALA)-photodynamic therapy with blue light (415 nm) on the right side of the face, or blue light alone on the left side of the face. At 4, 8, 12, and 16 weeks after the start of treatment, the mean percent reductions in inflamed lesions were higher in the ALA-PDT areas (32%, 50.9%, 65.9%, and 71.1%, respectively) than in the blue light–only treatment areas (20.7%, 27%, 57.7%, and 56.7%), but the differences were not statistically significant. Side effects, which included pain, stinging, erythema, itching, peeling, oozing, and pustules, were more pronounced in the areas treated with ALA-PDT (Photodermatol. Photoimmunol. Photomed. 2007;23:186-90).
However, in a 2007 study of 22 patients with moderate to severe acne randomized to one of three ALA-PDT treatments – intense pulsed light (IPL; 600-850 nm), a combination of IPL (580-980 nm) and bipolar radiofrequency (RF) energies, or blue light (417 nm) – in three sessions at 2-week intervals, ALA-PDT with activation by IPL yielded the most consistent, lasting improvement in moderate to severe acne (J. Drugs Dermatol. 2007;6:1010-6).
In a study of 60 volunteers with facial acne (grades II and III), de Arruda et al. compared the safety and efficacy of blue light to topical benzoyl peroxide 5% over 4 weeks. Thirty patients received blue light treatment twice a week, and the other 30 self-applied the topical formulation twice daily. The improvements were similar in both groups, but side effects were milder in the blue light group (An. Bras. Dermatol. 2009;84:463-8).
Choi et al. compared the bactericidal effects of 5-aminolevulinic acid (ALA) with blue and red light on P. acnes and found that blue light was more effective than red light phototherapy in eliminating the bacteria unless ALA was added, which substantially augmented red light phototherapy efficacy (J. Dermatol. 2011;38:661-6).
In summarizing the off-label uses of light-based treatments and PDT using topical precursors of porphyrins, Sakamoto et al. observed that blue light alone lessens acne severity due to anti-inflammatory effects; PDT using 5-ALA or ALA derivatives provides antimicrobial and anti-inflammatory activity; and, at high doses, red-light PDT may suppress or eradicate sebaceous glands, yielding clinical improvement (J. Am. Acad. Dermatol. 2010;63:183-93).
Combination therapy
In 2011, Wheeland and Dhawan assessed the efficacy and tolerability of treating mild to moderate facial acne using a novel, handheld, light-emitting diode (LED) blue-light device, along with a foam cleanser containing 5% glycolic acid and 2% salicylic acid, plus a serum containing 1.25% salicylic acid, 0.5% niacinamide, 0.08% liposomal-based azelaic acid, and superoxide dismutase. In all, 28 of 35 adults aged 25-45 years completed the 8-week study, in which they used the device twice daily (in addition to the cleanser before treatments and the serum after nighttime treatments). Significant reductions in inflammatory lesion counts were seen from week 1 onward, and significant reductions in noninflammatory lesion counts were seen from week 4 onward compared with baseline counts. The number and severity of flares were significantly reduced from baseline as well.
Therapy was well received by patients, with more than 90% claiming improvement in overall skin appearance and other parameters. In addition, 86% described the treatment as gentler than other therapies. (J. Drugs Dermatol. 2011;10:596-602).
Products
The Skin Clarifying Blue Light device has a power density of 400 mW/cm2, which is 10 times the power of other LED acne devices. This high power density allows the Skin Clarifying Blue Light device to deliver high levels of efficacy with short treatment times. When used as stand-alone treatment, it delivered a 70% reduction in inflammatory lesions in 8 weeks. The success of products designed for self-administration has coincided with the rampant interest in the creation of smart phone applications (J. Cosmet. Laser. Ther. 2011;13:308-14; J. Clin. Aesthet. Dermatol. 2009;2:40-4; J. Clin. Aesthet. Dermatol. 2009;2:44-50). That is, blue-light therapy apps have been developed for the iPhone and the iPod touch. None, however, has been approved by the Food and Drug Administration, although at least one is said to be under investigation in a clinical trial. I am skeptical about the efficacy of these LED-backlit apps and concerned about potentially prolonged magnetic radiation exposure that would be required. The self-administered devices appear to be a more reliable alternative.
Conclusion
Blue light can effectively be used to treat mild to moderate acne by causing photodynamic destruction of P. acnes. It can be used alone or in combination with topical or other light regimens. Additional studies are needed before a consensus protocol can be established, and future research goals should include establishing the optimal incubation time, activating light source, and frequency of treatment.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Photodynamic light therapies (PDLs) have emerged as significant adjuvant approaches for treating acne. In particular, such therapies have been used for acne refractory to standard retinoid or combined retinoid and antimicrobial regimens. Why write about PDL in a column devoted to topical cosmeceutical products and ingredients? Blue light warrants inclusion because it has been studied in comparison to topical cosmeceutical treatments, and it is used in conjunction with other topical approaches.
Blue light exerts a phototoxic effect on the heme metabolism of Propionibacterium acnes, and it is considered effective by targeting part of the etiologic pathway of acne. It has become a widely used option for inflammatory acne (J. Drugs. Dermatol. 2006;5:605-10).
Early work
In 1990, Meffert et al. were the first to show that a blue light–type, high-pressure lamp could improve acne and seborrhea (10 10-minute treatments, cumulative light dose 325 J/cm2). Given the copious amounts of porphyrins stored in lipophilic P. acnes, the technology could be targeted to destroy propionibacteria, and the researchers observed a decline in the porphyrin content inside acne follicles. They concluded that short-range visible light (400-420 nm) was a viable option for acne treatment during the light-poor season of the year (Dermatol. Monatsschr. 1990;176:597-603). It was subsequently established that treatment with UV-free blue light in the range of 405-420 nm leads to the elimination of acne bacteria by virtue of the effects on the porphyrins generated naturally by P. acnes (J. Cosmet. Laser. Ther. 2003;5:111-7). Notably, blue light appears to photoinactivate P. acnes, but it does not penetrate deeply into the skin (Dermatol. Online J. 2011;17:2).
In an open study of the then-novel high-intensity, enhanced, narrow-band, blue-light phototherapy, Kawada et al. treated 30 acne patients (27 female, 3 male) twice a week for up to 5 weeks. A reduction of 64% was seen in acne lesions, and in vitro data showed a significant decline in P. acnes, but not in Staphylococcus epidermidis (J. Dermatol. Sci. 2002;30:129-35).
Mechanism of action
In 2006, Shnitkind et al. studied the effect of narrow-band blue light on the inflammatory process in the presence and absence of cytokines and ultraviolet B using interleukin-1 alpha (IL-1alpha) and intercellular adhesion molecule 1 (ICAM-1) as markers for inflammation. They found that blue light treatment of HaCaT and hTERT cells decreased levels of IL-1alpha by 82% in HaCaT and by 75% in hTERT. When blue light was combined with ultraviolet B, the respective reductions were 95% and 91%. Similar reductions in ICAM-1 expression were seen in HaCaT, but not in hTERT. The researchers concluded that narrow-band blue light exerts anti-inflammatory effects on keratinocytes by reducing cytokine-induced synthesis of IL-1alpha and ICAM-1. They suggested that these findings imply a broader range of effects is exerted on the inflammatory process by narrow-band blue light than previously understood (J. Drugs. Dermatol. 2006;5:605-10).
Comparison studies
In 2000, Papageorgiou et al. randomized 107 patients with mild to moderate acne to four treatment groups: blue light (peak at 415 nm), mixed blue and red light (peaks at 415 and 660 nm), cool white light, and 5% benzoyl peroxide cream, for 12 weeks of active treatment. Phototherapy using portable light sources was conducted daily for 15 minutes; comparative assessments among the three phototherapy groups were done with observers blinded. The investigators found that the greatest improvement in acne lesions occurred in the blue and red light combined group. The blue/red treatment was significantly superior to blue light alone at 4 and 8 weeks but not 12 weeks, benzoyl peroxide at weeks 8 and 12, and white light at all assessments (Br. J. Dermatol. 2000;142:973-8).
Gold et al. performed a multicenter clinical evaluation comparing blue light to topical 1% clindamycin solution with respect to safety and efficacy. They found that clindamycin was associated with a 14% reduction of inflammatory lesions, but blue light reduced such lesions by an average of 34% (J. Drugs. Dermatol. 2005;4:64-70).
In another study, 20 patients with moderate to severe facial acne were treated in four weekly sessions with topical aminolevulinic acid (ALA)-photodynamic therapy with blue light (415 nm) on the right side of the face, or blue light alone on the left side of the face. At 4, 8, 12, and 16 weeks after the start of treatment, the mean percent reductions in inflamed lesions were higher in the ALA-PDT areas (32%, 50.9%, 65.9%, and 71.1%, respectively) than in the blue light–only treatment areas (20.7%, 27%, 57.7%, and 56.7%), but the differences were not statistically significant. Side effects, which included pain, stinging, erythema, itching, peeling, oozing, and pustules, were more pronounced in the areas treated with ALA-PDT (Photodermatol. Photoimmunol. Photomed. 2007;23:186-90).
However, in a 2007 study of 22 patients with moderate to severe acne randomized to one of three ALA-PDT treatments – intense pulsed light (IPL; 600-850 nm), a combination of IPL (580-980 nm) and bipolar radiofrequency (RF) energies, or blue light (417 nm) – in three sessions at 2-week intervals, ALA-PDT with activation by IPL yielded the most consistent, lasting improvement in moderate to severe acne (J. Drugs Dermatol. 2007;6:1010-6).
In a study of 60 volunteers with facial acne (grades II and III), de Arruda et al. compared the safety and efficacy of blue light to topical benzoyl peroxide 5% over 4 weeks. Thirty patients received blue light treatment twice a week, and the other 30 self-applied the topical formulation twice daily. The improvements were similar in both groups, but side effects were milder in the blue light group (An. Bras. Dermatol. 2009;84:463-8).
Choi et al. compared the bactericidal effects of 5-aminolevulinic acid (ALA) with blue and red light on P. acnes and found that blue light was more effective than red light phototherapy in eliminating the bacteria unless ALA was added, which substantially augmented red light phototherapy efficacy (J. Dermatol. 2011;38:661-6).
In summarizing the off-label uses of light-based treatments and PDT using topical precursors of porphyrins, Sakamoto et al. observed that blue light alone lessens acne severity due to anti-inflammatory effects; PDT using 5-ALA or ALA derivatives provides antimicrobial and anti-inflammatory activity; and, at high doses, red-light PDT may suppress or eradicate sebaceous glands, yielding clinical improvement (J. Am. Acad. Dermatol. 2010;63:183-93).
Combination therapy
In 2011, Wheeland and Dhawan assessed the efficacy and tolerability of treating mild to moderate facial acne using a novel, handheld, light-emitting diode (LED) blue-light device, along with a foam cleanser containing 5% glycolic acid and 2% salicylic acid, plus a serum containing 1.25% salicylic acid, 0.5% niacinamide, 0.08% liposomal-based azelaic acid, and superoxide dismutase. In all, 28 of 35 adults aged 25-45 years completed the 8-week study, in which they used the device twice daily (in addition to the cleanser before treatments and the serum after nighttime treatments). Significant reductions in inflammatory lesion counts were seen from week 1 onward, and significant reductions in noninflammatory lesion counts were seen from week 4 onward compared with baseline counts. The number and severity of flares were significantly reduced from baseline as well.
Therapy was well received by patients, with more than 90% claiming improvement in overall skin appearance and other parameters. In addition, 86% described the treatment as gentler than other therapies. (J. Drugs Dermatol. 2011;10:596-602).
Products
The Skin Clarifying Blue Light device has a power density of 400 mW/cm2, which is 10 times the power of other LED acne devices. This high power density allows the Skin Clarifying Blue Light device to deliver high levels of efficacy with short treatment times. When used as stand-alone treatment, it delivered a 70% reduction in inflammatory lesions in 8 weeks. The success of products designed for self-administration has coincided with the rampant interest in the creation of smart phone applications (J. Cosmet. Laser. Ther. 2011;13:308-14; J. Clin. Aesthet. Dermatol. 2009;2:40-4; J. Clin. Aesthet. Dermatol. 2009;2:44-50). That is, blue-light therapy apps have been developed for the iPhone and the iPod touch. None, however, has been approved by the Food and Drug Administration, although at least one is said to be under investigation in a clinical trial. I am skeptical about the efficacy of these LED-backlit apps and concerned about potentially prolonged magnetic radiation exposure that would be required. The self-administered devices appear to be a more reliable alternative.
Conclusion
Blue light can effectively be used to treat mild to moderate acne by causing photodynamic destruction of P. acnes. It can be used alone or in combination with topical or other light regimens. Additional studies are needed before a consensus protocol can be established, and future research goals should include establishing the optimal incubation time, activating light source, and frequency of treatment.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].