User login
Addressing The Joint Commission's Concern About Opioid-Induced Respiratory Depression
The recent article by Susan Kreimer, “Serious Complications from Opioid Overuse in Hospitalized Patients Prompts Nationwide Alert” (February 2013, p. 34) highlights a very important patient safety issue—opioid-induced respiratory depression.
Post-operative patients often manage their pain with patient-controlled analgesia (PCA) pumps. An estimated 14 million patients use PCA annually.1 As the article points out, PCA “offers built-in safety features—if patients become too sedated, they can’t push a button for extra doses—but that isn’t always the case.”
As Dr. Jason McKeown says, “While PCA may be the safest mode of opioid delivery, it is true that regardless of the route of administration, respiratory depression may still occur. To help prevent such incidents from happening, it should be remembered that some of the most significant strides in medicine and surgery are directly attributable to anesthesiology’s advances in patient monitoring.”
With the goal of helping to reduce adverse events and deaths with PCA pumps, the Physician-Patient Alliance for Health & Safety (PPAHS) recently released a safety checklist that reminds caregivers of the essential steps needed to be taken to initiate PCA with a patient, and to continue to assess that patient’s use of PCA. This checklist was developed after consultation with a group of 19 renowned health experts and is a free download at www.ppahs.org.
The checklist provides five recommended steps to have been completed when initiating PCA:
- Risk factors that increase risk of respiratory depression have been considered.
- Pre-procedural cognitive assessment has determined patient is capable of participating in pain management.
However, it should be noted that these first two steps are not an attempt at risk stratification. In reviewing current approaches to address failure-to-rescue, Dr. Andreas Taenzer and his colleagues showed that these current approaches are not able to predict which patients are at risk and at which point the crisis can be detected.
- Patient has been provided with information on proper patient use of PCA pump (other recipients of information—family/visitors) and purpose of monitoring.
The Institute for Safe Medical Practice (www.ismp.org) cautions against PCA proxy and stresses the importance of patient education. The safe use of PCA includes making sure the patient controlling the device actually knows how to use it and the importance of the monitoring used to continuously assess their status.
- Two health-care providers have independently double-checked: patient ID; allergies; drug selection and concentration; dosage adjustments; pump settings; and line attachment to patient and tubing insertion.
Error prevention is critical. The Pennsylvania Patient Safety Authority recently released its analysis of medication errors and adverse drug reactions involving intravenous fentanyl that were reported to them. Researchers found 2,319 events between June 2004 to March 2012; that’s almost 25 events per month. Although one error a day may seem high, their analysis is confined to reports that were made to the authority and only include fentanyl, a potent, synthetic narcotic analgesic with a rapid onset and short duration of action.
- Patient is electronically monitored with both pulse oximetry and capnography.
As Dr. Robert Stoelting, president of the Anesthesia Patient Safety Foundation, recently stated: “The conclusions and recommendations of APSF are that intermittent ‘spot checks’ of [pulse oximetry] and ventilation are not adequate for reliably recognizing clinically significant, evolving, drug-induced, respiratory depression in the postoperative period....APSF recommends that monitoring be continuous and not intermittent, and that continuous electronic monitoring with both pulse oximetry for oxygenation and capnography for the adequacy of ventilation be considered for all patients.”
Frank Federico, a member of the Patient Safety Advisory Group at The Joint Commission and executive director at the Institute for Healthcare Improvement, concurs: “Although nurse spot checks on patients are advisable, pulse oximetry and capnography are essential risk prevention tools in any pain management plan.”
PPAHS encourages all hospitals and health-care facilities to download and utilize the PCA Safety Checklist.
The recent article by Susan Kreimer, “Serious Complications from Opioid Overuse in Hospitalized Patients Prompts Nationwide Alert” (February 2013, p. 34) highlights a very important patient safety issue—opioid-induced respiratory depression.
Post-operative patients often manage their pain with patient-controlled analgesia (PCA) pumps. An estimated 14 million patients use PCA annually.1 As the article points out, PCA “offers built-in safety features—if patients become too sedated, they can’t push a button for extra doses—but that isn’t always the case.”
As Dr. Jason McKeown says, “While PCA may be the safest mode of opioid delivery, it is true that regardless of the route of administration, respiratory depression may still occur. To help prevent such incidents from happening, it should be remembered that some of the most significant strides in medicine and surgery are directly attributable to anesthesiology’s advances in patient monitoring.”
With the goal of helping to reduce adverse events and deaths with PCA pumps, the Physician-Patient Alliance for Health & Safety (PPAHS) recently released a safety checklist that reminds caregivers of the essential steps needed to be taken to initiate PCA with a patient, and to continue to assess that patient’s use of PCA. This checklist was developed after consultation with a group of 19 renowned health experts and is a free download at www.ppahs.org.
The checklist provides five recommended steps to have been completed when initiating PCA:
- Risk factors that increase risk of respiratory depression have been considered.
- Pre-procedural cognitive assessment has determined patient is capable of participating in pain management.
However, it should be noted that these first two steps are not an attempt at risk stratification. In reviewing current approaches to address failure-to-rescue, Dr. Andreas Taenzer and his colleagues showed that these current approaches are not able to predict which patients are at risk and at which point the crisis can be detected.
- Patient has been provided with information on proper patient use of PCA pump (other recipients of information—family/visitors) and purpose of monitoring.
The Institute for Safe Medical Practice (www.ismp.org) cautions against PCA proxy and stresses the importance of patient education. The safe use of PCA includes making sure the patient controlling the device actually knows how to use it and the importance of the monitoring used to continuously assess their status.
- Two health-care providers have independently double-checked: patient ID; allergies; drug selection and concentration; dosage adjustments; pump settings; and line attachment to patient and tubing insertion.
Error prevention is critical. The Pennsylvania Patient Safety Authority recently released its analysis of medication errors and adverse drug reactions involving intravenous fentanyl that were reported to them. Researchers found 2,319 events between June 2004 to March 2012; that’s almost 25 events per month. Although one error a day may seem high, their analysis is confined to reports that were made to the authority and only include fentanyl, a potent, synthetic narcotic analgesic with a rapid onset and short duration of action.
- Patient is electronically monitored with both pulse oximetry and capnography.
As Dr. Robert Stoelting, president of the Anesthesia Patient Safety Foundation, recently stated: “The conclusions and recommendations of APSF are that intermittent ‘spot checks’ of [pulse oximetry] and ventilation are not adequate for reliably recognizing clinically significant, evolving, drug-induced, respiratory depression in the postoperative period....APSF recommends that monitoring be continuous and not intermittent, and that continuous electronic monitoring with both pulse oximetry for oxygenation and capnography for the adequacy of ventilation be considered for all patients.”
Frank Federico, a member of the Patient Safety Advisory Group at The Joint Commission and executive director at the Institute for Healthcare Improvement, concurs: “Although nurse spot checks on patients are advisable, pulse oximetry and capnography are essential risk prevention tools in any pain management plan.”
PPAHS encourages all hospitals and health-care facilities to download and utilize the PCA Safety Checklist.
The recent article by Susan Kreimer, “Serious Complications from Opioid Overuse in Hospitalized Patients Prompts Nationwide Alert” (February 2013, p. 34) highlights a very important patient safety issue—opioid-induced respiratory depression.
Post-operative patients often manage their pain with patient-controlled analgesia (PCA) pumps. An estimated 14 million patients use PCA annually.1 As the article points out, PCA “offers built-in safety features—if patients become too sedated, they can’t push a button for extra doses—but that isn’t always the case.”
As Dr. Jason McKeown says, “While PCA may be the safest mode of opioid delivery, it is true that regardless of the route of administration, respiratory depression may still occur. To help prevent such incidents from happening, it should be remembered that some of the most significant strides in medicine and surgery are directly attributable to anesthesiology’s advances in patient monitoring.”
With the goal of helping to reduce adverse events and deaths with PCA pumps, the Physician-Patient Alliance for Health & Safety (PPAHS) recently released a safety checklist that reminds caregivers of the essential steps needed to be taken to initiate PCA with a patient, and to continue to assess that patient’s use of PCA. This checklist was developed after consultation with a group of 19 renowned health experts and is a free download at www.ppahs.org.
The checklist provides five recommended steps to have been completed when initiating PCA:
- Risk factors that increase risk of respiratory depression have been considered.
- Pre-procedural cognitive assessment has determined patient is capable of participating in pain management.
However, it should be noted that these first two steps are not an attempt at risk stratification. In reviewing current approaches to address failure-to-rescue, Dr. Andreas Taenzer and his colleagues showed that these current approaches are not able to predict which patients are at risk and at which point the crisis can be detected.
- Patient has been provided with information on proper patient use of PCA pump (other recipients of information—family/visitors) and purpose of monitoring.
The Institute for Safe Medical Practice (www.ismp.org) cautions against PCA proxy and stresses the importance of patient education. The safe use of PCA includes making sure the patient controlling the device actually knows how to use it and the importance of the monitoring used to continuously assess their status.
- Two health-care providers have independently double-checked: patient ID; allergies; drug selection and concentration; dosage adjustments; pump settings; and line attachment to patient and tubing insertion.
Error prevention is critical. The Pennsylvania Patient Safety Authority recently released its analysis of medication errors and adverse drug reactions involving intravenous fentanyl that were reported to them. Researchers found 2,319 events between June 2004 to March 2012; that’s almost 25 events per month. Although one error a day may seem high, their analysis is confined to reports that were made to the authority and only include fentanyl, a potent, synthetic narcotic analgesic with a rapid onset and short duration of action.
- Patient is electronically monitored with both pulse oximetry and capnography.
As Dr. Robert Stoelting, president of the Anesthesia Patient Safety Foundation, recently stated: “The conclusions and recommendations of APSF are that intermittent ‘spot checks’ of [pulse oximetry] and ventilation are not adequate for reliably recognizing clinically significant, evolving, drug-induced, respiratory depression in the postoperative period....APSF recommends that monitoring be continuous and not intermittent, and that continuous electronic monitoring with both pulse oximetry for oxygenation and capnography for the adequacy of ventilation be considered for all patients.”
Frank Federico, a member of the Patient Safety Advisory Group at The Joint Commission and executive director at the Institute for Healthcare Improvement, concurs: “Although nurse spot checks on patients are advisable, pulse oximetry and capnography are essential risk prevention tools in any pain management plan.”
PPAHS encourages all hospitals and health-care facilities to download and utilize the PCA Safety Checklist.
'Systems,' Not 'Points,' Is Correct Terminology for ROS Statements
The “Billing and Coding Bandwagon” article in the May 2011 issue of The Hospitalist (p. 26) recently was brought to my attention and I have some concerns that the following statement gives a false impression of acceptable documentation: “When I first started working, I couldn’t believe that I could get audited and fined just because I didn’t add ‘10-point’ or ‘12-point’ to my note of ‘review of systems: negative,’” says hospitalist Amaka Nweke, MD, assistant director with Hospitalists Management Group (HMG) at Kenosha Medical Center in Kenosha, Wis. “I had a lot of frustration, because I had to repackage and re-present my notes in a manner that makes sense to Medicare but makes no sense to physicians.”
In fact, that would still not be considered acceptable documentation for services that require a complete review of systems (99222, 99223, 99219, 99220, 99235, and 99236). The documentation guidelines clearly state: “A complete ROS [review of systems] inquires about the system(s) directly related to the problem(s) identified in the HPI plus all additional body systems.” At least 10 organ systems must be reviewed. Those systems with positive or pertinent negative responses must be individually documented. For the remaining systems, a notation indicating all other systems are negative is permissible. In the absence of such a notation, at least 10 systems must be individually documented.
What Medicare is saying is the provider must have inquired about all 14 systems, not just 10 or 12. The term “point” means nothing in an ROS statement. “Systems” is the correct terminology, not “points.”
I am afraid the article is misleading and could be providing inappropriate documentation advice to hospitalists dealing with CMS and AMA guidelines.
The “Billing and Coding Bandwagon” article in the May 2011 issue of The Hospitalist (p. 26) recently was brought to my attention and I have some concerns that the following statement gives a false impression of acceptable documentation: “When I first started working, I couldn’t believe that I could get audited and fined just because I didn’t add ‘10-point’ or ‘12-point’ to my note of ‘review of systems: negative,’” says hospitalist Amaka Nweke, MD, assistant director with Hospitalists Management Group (HMG) at Kenosha Medical Center in Kenosha, Wis. “I had a lot of frustration, because I had to repackage and re-present my notes in a manner that makes sense to Medicare but makes no sense to physicians.”
In fact, that would still not be considered acceptable documentation for services that require a complete review of systems (99222, 99223, 99219, 99220, 99235, and 99236). The documentation guidelines clearly state: “A complete ROS [review of systems] inquires about the system(s) directly related to the problem(s) identified in the HPI plus all additional body systems.” At least 10 organ systems must be reviewed. Those systems with positive or pertinent negative responses must be individually documented. For the remaining systems, a notation indicating all other systems are negative is permissible. In the absence of such a notation, at least 10 systems must be individually documented.
What Medicare is saying is the provider must have inquired about all 14 systems, not just 10 or 12. The term “point” means nothing in an ROS statement. “Systems” is the correct terminology, not “points.”
I am afraid the article is misleading and could be providing inappropriate documentation advice to hospitalists dealing with CMS and AMA guidelines.
The “Billing and Coding Bandwagon” article in the May 2011 issue of The Hospitalist (p. 26) recently was brought to my attention and I have some concerns that the following statement gives a false impression of acceptable documentation: “When I first started working, I couldn’t believe that I could get audited and fined just because I didn’t add ‘10-point’ or ‘12-point’ to my note of ‘review of systems: negative,’” says hospitalist Amaka Nweke, MD, assistant director with Hospitalists Management Group (HMG) at Kenosha Medical Center in Kenosha, Wis. “I had a lot of frustration, because I had to repackage and re-present my notes in a manner that makes sense to Medicare but makes no sense to physicians.”
In fact, that would still not be considered acceptable documentation for services that require a complete review of systems (99222, 99223, 99219, 99220, 99235, and 99236). The documentation guidelines clearly state: “A complete ROS [review of systems] inquires about the system(s) directly related to the problem(s) identified in the HPI plus all additional body systems.” At least 10 organ systems must be reviewed. Those systems with positive or pertinent negative responses must be individually documented. For the remaining systems, a notation indicating all other systems are negative is permissible. In the absence of such a notation, at least 10 systems must be individually documented.
What Medicare is saying is the provider must have inquired about all 14 systems, not just 10 or 12. The term “point” means nothing in an ROS statement. “Systems” is the correct terminology, not “points.”
I am afraid the article is misleading and could be providing inappropriate documentation advice to hospitalists dealing with CMS and AMA guidelines.
Some Thoughts on the Patient-Doctor Relationship
There is an inherent power differential in the patient-doctor relationship: The patient comes to the doctor as an authority on his/her physical or emotional state and is thus either intellectually or emotionally dependent on the doctor’s treatment plan and advice. It is therefore absolutely essential that the doctor respect the patient as an equal participant in the treatment. Although the doctor certainly has knowledge about how similar conditions were successfully treated in the past, hopefully a medical professional will display an attitude of respect and mutual collaboration with the patient to resolve his/her problem.
Listening is a key component of conveying an attitude of respect toward the patient. Nowadays practitioners are most often taking notes at their computers while speaking with the patient. This is certainly time-efficient and may in fact be necessary in order for a medical practice to remain solvent with the demands of Medicare and insurance companies. However, multitasking does not convey to the patient that they are connecting with the doctor. Listening is a complex action, which not only involves the ears, but the eyes, the kinesthetic responses of the whole body, and attention to the patient’s nonverbal communication.
Some of the key faux pas to avoid when listening to the patient include:
- Not centering oneself before engaging in a “crucial conversation”;
- Not listening because one is thinking ahead to his/her own response;
- Not maintaining eye contact;
- Not being aware of when one feels challenged and/or defensive;
- Discouraging the patient from contributing his/her own ideas;
- Not allowing the patient to give feedback on what s/he heard as instructions; and
- Taking phone calls or allowing interruptions during a consultation.
It is always helpful to give a patient clear, written instructions about medications, diet, exercise, etc., that result from the consultation. Some doctors send this report via secure email to the patient for review, which is an excellent technique.
The art of apology is another topic that greatly impacts the doctor-patient relationship, as well as the doctor’s relationship with the patient’s family members. This art is a process that has recently emerged in the medical and medical insurance industries. Kaiser Permanente’s director of medical-legal affairs has adopted the practice of asking permission to videotape the actual conversation in which a physician apologizes to a patient for a mistake in a procedure. These conversations are meant to help medical professionals learn how to admit mistakes and ask for forgiveness. Oftentimes patients are looking for just such a communication, which may allow them to put to rest feelings of resentment, bitterness, and regret.
Our patients’ well-being is our ideal goal. Knowing that they have been heard and their feelings understood may in the long run allow patients and their families to heal mind/body/soul more powerfully than we had ever thought. Of course, in our litigious society this may well be an art that remains to be developed over the long term.
There is an inherent power differential in the patient-doctor relationship: The patient comes to the doctor as an authority on his/her physical or emotional state and is thus either intellectually or emotionally dependent on the doctor’s treatment plan and advice. It is therefore absolutely essential that the doctor respect the patient as an equal participant in the treatment. Although the doctor certainly has knowledge about how similar conditions were successfully treated in the past, hopefully a medical professional will display an attitude of respect and mutual collaboration with the patient to resolve his/her problem.
Listening is a key component of conveying an attitude of respect toward the patient. Nowadays practitioners are most often taking notes at their computers while speaking with the patient. This is certainly time-efficient and may in fact be necessary in order for a medical practice to remain solvent with the demands of Medicare and insurance companies. However, multitasking does not convey to the patient that they are connecting with the doctor. Listening is a complex action, which not only involves the ears, but the eyes, the kinesthetic responses of the whole body, and attention to the patient’s nonverbal communication.
Some of the key faux pas to avoid when listening to the patient include:
- Not centering oneself before engaging in a “crucial conversation”;
- Not listening because one is thinking ahead to his/her own response;
- Not maintaining eye contact;
- Not being aware of when one feels challenged and/or defensive;
- Discouraging the patient from contributing his/her own ideas;
- Not allowing the patient to give feedback on what s/he heard as instructions; and
- Taking phone calls or allowing interruptions during a consultation.
It is always helpful to give a patient clear, written instructions about medications, diet, exercise, etc., that result from the consultation. Some doctors send this report via secure email to the patient for review, which is an excellent technique.
The art of apology is another topic that greatly impacts the doctor-patient relationship, as well as the doctor’s relationship with the patient’s family members. This art is a process that has recently emerged in the medical and medical insurance industries. Kaiser Permanente’s director of medical-legal affairs has adopted the practice of asking permission to videotape the actual conversation in which a physician apologizes to a patient for a mistake in a procedure. These conversations are meant to help medical professionals learn how to admit mistakes and ask for forgiveness. Oftentimes patients are looking for just such a communication, which may allow them to put to rest feelings of resentment, bitterness, and regret.
Our patients’ well-being is our ideal goal. Knowing that they have been heard and their feelings understood may in the long run allow patients and their families to heal mind/body/soul more powerfully than we had ever thought. Of course, in our litigious society this may well be an art that remains to be developed over the long term.
There is an inherent power differential in the patient-doctor relationship: The patient comes to the doctor as an authority on his/her physical or emotional state and is thus either intellectually or emotionally dependent on the doctor’s treatment plan and advice. It is therefore absolutely essential that the doctor respect the patient as an equal participant in the treatment. Although the doctor certainly has knowledge about how similar conditions were successfully treated in the past, hopefully a medical professional will display an attitude of respect and mutual collaboration with the patient to resolve his/her problem.
Listening is a key component of conveying an attitude of respect toward the patient. Nowadays practitioners are most often taking notes at their computers while speaking with the patient. This is certainly time-efficient and may in fact be necessary in order for a medical practice to remain solvent with the demands of Medicare and insurance companies. However, multitasking does not convey to the patient that they are connecting with the doctor. Listening is a complex action, which not only involves the ears, but the eyes, the kinesthetic responses of the whole body, and attention to the patient’s nonverbal communication.
Some of the key faux pas to avoid when listening to the patient include:
- Not centering oneself before engaging in a “crucial conversation”;
- Not listening because one is thinking ahead to his/her own response;
- Not maintaining eye contact;
- Not being aware of when one feels challenged and/or defensive;
- Discouraging the patient from contributing his/her own ideas;
- Not allowing the patient to give feedback on what s/he heard as instructions; and
- Taking phone calls or allowing interruptions during a consultation.
It is always helpful to give a patient clear, written instructions about medications, diet, exercise, etc., that result from the consultation. Some doctors send this report via secure email to the patient for review, which is an excellent technique.
The art of apology is another topic that greatly impacts the doctor-patient relationship, as well as the doctor’s relationship with the patient’s family members. This art is a process that has recently emerged in the medical and medical insurance industries. Kaiser Permanente’s director of medical-legal affairs has adopted the practice of asking permission to videotape the actual conversation in which a physician apologizes to a patient for a mistake in a procedure. These conversations are meant to help medical professionals learn how to admit mistakes and ask for forgiveness. Oftentimes patients are looking for just such a communication, which may allow them to put to rest feelings of resentment, bitterness, and regret.
Our patients’ well-being is our ideal goal. Knowing that they have been heard and their feelings understood may in the long run allow patients and their families to heal mind/body/soul more powerfully than we had ever thought. Of course, in our litigious society this may well be an art that remains to be developed over the long term.
Coordinated Approach May Help in Caring for Hospitals’ Neediest Patients
To my way of thinking, a person’s diagnosis or pathophysiology is not as strong a predictor of needing inpatient hospital care as it might have been 10 or 20 years ago. Rather than the clinical diagnosis (e.g. pneumonia), it seems to me that frailty or social complexity often are the principal determinants of which patients are admitted to a hospital for medical conditions.
Some of these patients are admitted frequently but appear to realize little or no benefit from hospitalization. These patients typically have little or no social support, and they often have either significant mental health disorders or substance abuse, or both. Much has been written about these patients, and I recommend an article by Dr. Atul Gawande in the Jan. 24, 2011, issue of The New Yorker titled “The Hot Spotters: Can We Lower Medical Costs by Giving the Neediest Patients Better Care?”
The Agency for Healthcare Research and Quality’s “Statistical Brief 354” on how health-care expenditures are allocated across the population reported that 1% of the population accounted for more than 22% of health-care spending in 2008. One in 5 of those were in that category again in 2009. Some of these patients would benefit from care plans.
The Role of Care Plans
It seems that there may be few effective inpatient interventions that will benefit these patients. After all, they have chronic issues that require ongoing relationships with outpatient providers, something that many of these patients lack. But for some (most?) of these patients, it seems clear that frequent hospitalizations don’t help and sometimes just perpetuate or worsen the patient’s dependence on the hospital at a high financial cost to society—and significant frustration and burnout on the part of hospital caregivers, including hospitalists.
For most hospitals, this problem is significant enough to require some sort of coordinated approach to the care of the dozens of types of patients in this category. Implementing whatever plan of care seems appropriate to the caregivers during each admission is frustrating, ensures lots of variation in care, and makes it easier for manipulative patients to abuse the hospital resources and personnel.
A better approach is to follow the same plan of care from one hospital visit to the next. You already knew that. But developing a care plan to follow during each ED visit and admission is time-consuming and often fraught with uncertainty about where boundaries should be set. So if you’re like me, you might just try to guide the patient to discharge this time and hope that whoever sees the patient on the next admission will take the initiative to develop the care plan. The result is that few such plans are developed.
Your Hospital Needs a Care Plan
Relying on individual doctors or nurses to take the initiative to develop care plans will almost always mean few plans are developed, they will vary in their effectiveness, and other providers may not be aware a plan exists. This was the case at the hospital where I practice until I heard Dr. Rick Hilger, MD, SFHM, a hospitalist at Regions Hospital in Minneapolis, present on this topic at HM12 in San Diego.
Dr. Hilger led a multidisciplinary team to develop care plans (they call them “restriction care plans”) and found that they dramatically reduced the rate of hospital admissions and ED visits for these patients. Hearing about this experience served as a kick in the pants for me, so I did much the same thing at “my” hospital. We have now developed plans for more than 20 patients and found that they visit our ED and are admitted less often. And, anecdotally at least, hospitalists and other hospital staff find that the care plans reduce, at least a little, the stress of caring for these patients.
Unanswered Questions
Although it seems clear that care plans reduce visits to the hospital that develops them, I suspect that some of these patients aren’t consuming any fewer health-care resources. They may just seek care from a different hospital.
My home state of Washington is working to develop individual patient care plans available to all hospitals in the state. A system called the Emergency Department Information Exchange (EDIE) has been adopted by nearly all the hospitals in the state. It allows them to share information on ED visits and such things as care plans with one another. For example, through EDIE, each hospital could see the opiate dosing schedule and admission criteria agreed to by patient and primary-care physician.
So it seems that care plans and the technology to share them can make it more difficult for patients to harm themselves by visiting many hospitals to get excessive opiate prescriptions, for example. This should benefit the patient and lower ED and hospital expenditures for these patients. But we don’t know what portion of costs simply is shifted to other settings, so there is no easy way to know the net effect on health-care costs.
An important unanswered question is whether these care plans improve patient well-being. It seems clear they do in some cases, but it is hard to know whether some patients may be worse off because of the plan.
Conclusion
I think nearly every hospital would benefit from a care plan committee composed of at least one hospitalist, ED physician, a nursing representative, and potentially other disciplines (see “Care Plan Attributes,” above). Our committee includes our inpatient psychiatrist, a really valuable contributor.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
To my way of thinking, a person’s diagnosis or pathophysiology is not as strong a predictor of needing inpatient hospital care as it might have been 10 or 20 years ago. Rather than the clinical diagnosis (e.g. pneumonia), it seems to me that frailty or social complexity often are the principal determinants of which patients are admitted to a hospital for medical conditions.
Some of these patients are admitted frequently but appear to realize little or no benefit from hospitalization. These patients typically have little or no social support, and they often have either significant mental health disorders or substance abuse, or both. Much has been written about these patients, and I recommend an article by Dr. Atul Gawande in the Jan. 24, 2011, issue of The New Yorker titled “The Hot Spotters: Can We Lower Medical Costs by Giving the Neediest Patients Better Care?”
The Agency for Healthcare Research and Quality’s “Statistical Brief 354” on how health-care expenditures are allocated across the population reported that 1% of the population accounted for more than 22% of health-care spending in 2008. One in 5 of those were in that category again in 2009. Some of these patients would benefit from care plans.
The Role of Care Plans
It seems that there may be few effective inpatient interventions that will benefit these patients. After all, they have chronic issues that require ongoing relationships with outpatient providers, something that many of these patients lack. But for some (most?) of these patients, it seems clear that frequent hospitalizations don’t help and sometimes just perpetuate or worsen the patient’s dependence on the hospital at a high financial cost to society—and significant frustration and burnout on the part of hospital caregivers, including hospitalists.
For most hospitals, this problem is significant enough to require some sort of coordinated approach to the care of the dozens of types of patients in this category. Implementing whatever plan of care seems appropriate to the caregivers during each admission is frustrating, ensures lots of variation in care, and makes it easier for manipulative patients to abuse the hospital resources and personnel.
A better approach is to follow the same plan of care from one hospital visit to the next. You already knew that. But developing a care plan to follow during each ED visit and admission is time-consuming and often fraught with uncertainty about where boundaries should be set. So if you’re like me, you might just try to guide the patient to discharge this time and hope that whoever sees the patient on the next admission will take the initiative to develop the care plan. The result is that few such plans are developed.
Your Hospital Needs a Care Plan
Relying on individual doctors or nurses to take the initiative to develop care plans will almost always mean few plans are developed, they will vary in their effectiveness, and other providers may not be aware a plan exists. This was the case at the hospital where I practice until I heard Dr. Rick Hilger, MD, SFHM, a hospitalist at Regions Hospital in Minneapolis, present on this topic at HM12 in San Diego.
Dr. Hilger led a multidisciplinary team to develop care plans (they call them “restriction care plans”) and found that they dramatically reduced the rate of hospital admissions and ED visits for these patients. Hearing about this experience served as a kick in the pants for me, so I did much the same thing at “my” hospital. We have now developed plans for more than 20 patients and found that they visit our ED and are admitted less often. And, anecdotally at least, hospitalists and other hospital staff find that the care plans reduce, at least a little, the stress of caring for these patients.
Unanswered Questions
Although it seems clear that care plans reduce visits to the hospital that develops them, I suspect that some of these patients aren’t consuming any fewer health-care resources. They may just seek care from a different hospital.
My home state of Washington is working to develop individual patient care plans available to all hospitals in the state. A system called the Emergency Department Information Exchange (EDIE) has been adopted by nearly all the hospitals in the state. It allows them to share information on ED visits and such things as care plans with one another. For example, through EDIE, each hospital could see the opiate dosing schedule and admission criteria agreed to by patient and primary-care physician.
So it seems that care plans and the technology to share them can make it more difficult for patients to harm themselves by visiting many hospitals to get excessive opiate prescriptions, for example. This should benefit the patient and lower ED and hospital expenditures for these patients. But we don’t know what portion of costs simply is shifted to other settings, so there is no easy way to know the net effect on health-care costs.
An important unanswered question is whether these care plans improve patient well-being. It seems clear they do in some cases, but it is hard to know whether some patients may be worse off because of the plan.
Conclusion
I think nearly every hospital would benefit from a care plan committee composed of at least one hospitalist, ED physician, a nursing representative, and potentially other disciplines (see “Care Plan Attributes,” above). Our committee includes our inpatient psychiatrist, a really valuable contributor.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
To my way of thinking, a person’s diagnosis or pathophysiology is not as strong a predictor of needing inpatient hospital care as it might have been 10 or 20 years ago. Rather than the clinical diagnosis (e.g. pneumonia), it seems to me that frailty or social complexity often are the principal determinants of which patients are admitted to a hospital for medical conditions.
Some of these patients are admitted frequently but appear to realize little or no benefit from hospitalization. These patients typically have little or no social support, and they often have either significant mental health disorders or substance abuse, or both. Much has been written about these patients, and I recommend an article by Dr. Atul Gawande in the Jan. 24, 2011, issue of The New Yorker titled “The Hot Spotters: Can We Lower Medical Costs by Giving the Neediest Patients Better Care?”
The Agency for Healthcare Research and Quality’s “Statistical Brief 354” on how health-care expenditures are allocated across the population reported that 1% of the population accounted for more than 22% of health-care spending in 2008. One in 5 of those were in that category again in 2009. Some of these patients would benefit from care plans.
The Role of Care Plans
It seems that there may be few effective inpatient interventions that will benefit these patients. After all, they have chronic issues that require ongoing relationships with outpatient providers, something that many of these patients lack. But for some (most?) of these patients, it seems clear that frequent hospitalizations don’t help and sometimes just perpetuate or worsen the patient’s dependence on the hospital at a high financial cost to society—and significant frustration and burnout on the part of hospital caregivers, including hospitalists.
For most hospitals, this problem is significant enough to require some sort of coordinated approach to the care of the dozens of types of patients in this category. Implementing whatever plan of care seems appropriate to the caregivers during each admission is frustrating, ensures lots of variation in care, and makes it easier for manipulative patients to abuse the hospital resources and personnel.
A better approach is to follow the same plan of care from one hospital visit to the next. You already knew that. But developing a care plan to follow during each ED visit and admission is time-consuming and often fraught with uncertainty about where boundaries should be set. So if you’re like me, you might just try to guide the patient to discharge this time and hope that whoever sees the patient on the next admission will take the initiative to develop the care plan. The result is that few such plans are developed.
Your Hospital Needs a Care Plan
Relying on individual doctors or nurses to take the initiative to develop care plans will almost always mean few plans are developed, they will vary in their effectiveness, and other providers may not be aware a plan exists. This was the case at the hospital where I practice until I heard Dr. Rick Hilger, MD, SFHM, a hospitalist at Regions Hospital in Minneapolis, present on this topic at HM12 in San Diego.
Dr. Hilger led a multidisciplinary team to develop care plans (they call them “restriction care plans”) and found that they dramatically reduced the rate of hospital admissions and ED visits for these patients. Hearing about this experience served as a kick in the pants for me, so I did much the same thing at “my” hospital. We have now developed plans for more than 20 patients and found that they visit our ED and are admitted less often. And, anecdotally at least, hospitalists and other hospital staff find that the care plans reduce, at least a little, the stress of caring for these patients.
Unanswered Questions
Although it seems clear that care plans reduce visits to the hospital that develops them, I suspect that some of these patients aren’t consuming any fewer health-care resources. They may just seek care from a different hospital.
My home state of Washington is working to develop individual patient care plans available to all hospitals in the state. A system called the Emergency Department Information Exchange (EDIE) has been adopted by nearly all the hospitals in the state. It allows them to share information on ED visits and such things as care plans with one another. For example, through EDIE, each hospital could see the opiate dosing schedule and admission criteria agreed to by patient and primary-care physician.
So it seems that care plans and the technology to share them can make it more difficult for patients to harm themselves by visiting many hospitals to get excessive opiate prescriptions, for example. This should benefit the patient and lower ED and hospital expenditures for these patients. But we don’t know what portion of costs simply is shifted to other settings, so there is no easy way to know the net effect on health-care costs.
An important unanswered question is whether these care plans improve patient well-being. It seems clear they do in some cases, but it is hard to know whether some patients may be worse off because of the plan.
Conclusion
I think nearly every hospital would benefit from a care plan committee composed of at least one hospitalist, ED physician, a nursing representative, and potentially other disciplines (see “Care Plan Attributes,” above). Our committee includes our inpatient psychiatrist, a really valuable contributor.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at [email protected].
Surviving Sepsis Campaign 2012 Guidelines: Updates For the Hospitalist
Background
Sepsis is a clinical syndrome with systemic effects that can progress to severe sepsis and/or septic shock. The incidence of severe sepsis and septic shock is rising in the United States, and these syndromes are associated with significant morbidity and a mortality rate as high as 25% to 35%.1 In fact, sepsis is one of the 10 leading causes of death in the U.S., accounting for 2% of hospital admissions but 17% of in-hospital deaths.1
The main principles of effective treatment for severe sepsis and septic shock are timely recognition and early aggressive therapy. Launched in 2002, the Surviving Sepsis Campaign (SSC) was the result of a collaboration of three professional societies. The goal of the SSC collaborative was to reduce mortality from severe sepsis and septic shock by 25%. To that end, the SSC convened representatives from several international societies to develop a set of evidence-based guidelines as a means of guiding clinicians in optimizing management of patients with severe sepsis and septic shock. Since the original publication of the SSC guidelines in 2004, there have been two updates—one in 2008 and one in February 2013.2
Guideline Updates
Quantitative, protocol-driven initial resuscitation in the first six hours for patients with severe sepsis and septic shock remains a high-level recommendation, but SSC has added normalization of the lactate level as a resuscitation goal. This new suggestion is based on two studies published since the 2008 SCC guidelines that showed noninferiority to previously established goals and absolute mortality benefit.3,4
There is a new focus on screening for sepsis and the use of hospital-based performance-improvement programs, which were not previously addressed in the 2008 SCC guidelines. Patients with suspected infections and who are seriously ill should be screened in order to identify sepsis early during the hospital course. Additionally, it is recommended that hospitals implement performance-improvement measures by which multidisciplinary teams can address treatment of sepsis by improving compliance with the SSC bundles, citing their own data as the model but ultimately leaving this recommendation as ungradable in regards to the quality of available supporting evidence.5
Cultures drawn before antibiotics and early imaging to confirm potential sources are still recommended, but the committee has added the use of one: 3 beta D-glucan and the mannan antigen and anti-mannan antibody assays when considering invasive candidiasis as your infective agent. They do note the known risk of false positive results with these assays and warn that they should be used with caution.
Early, broad-spectrum antibiotic administration within the first hour of presentation was upgraded for severe sepsis and downgraded for septic shock. The decision to initiate double coverage for suspected gram-negative infection is not recommended specifically but can be considered in situations when highly antibiotic resistant pathogens are potentially present. Daily assessment of the appropriate antibiotic regimen remains an important tenet, and the use of low procalcitonin levels as a tool to assist in the decision to discontinue antibiotics has been introduced. Source control is still strongly recommended in the first 12 hours of treatment.
The SSC 2012 guidelines specifically address the rate of fluid administered and the type of fluid that should be used. It is now recommended that a fluid challenge of 30 mL/kg be used for initial resuscitation, but the guidelines leave it up to the clinician to give more fluid if needed. There is a strong push for use of crystalloids rather than colloids during initial resuscitation and thereafter. Disfavor for colloids stemmed from trials showing increased mortality when comparing resuscitation with hydroxyethyl starch versus crystalloid for patients in septic shock.6,7 Albumin, on the other hand, is recommended to resuscitate patients with severe sepsis and septic shock in cases for which large amounts of crystalloid are required.
The 2012 SSC guidelines recommend norepinephrine (NE) alone as the first-line vasopressor in sepsis and no longer include dopamine in this category. In fact, the use of dopamine in septic shock has been downgraded and should only to be considered in patients at low risk of tachyarrhythmia and in bradycardia syndromes. Epinephrine is now favored as the second agent or as a substitute to NE. Phenylephrine is no longer recommended unless there is contraindication to using NE, the patient has a high cardiac output, or it is used as a salvage therapy. Vasopressin is considered only an adjunctive agent to NE and should never be used alone.
Recommendations regarding corticosteroid therapy remain largely unchanged from 2008 SCC guidelines, which only support their use when adequate volume resuscitation and vasopressor support has failed to achieve hemodynamic stability. Glucose control is recommended but at the new target of achieving a level of <180 mg/dL, up from a previous target of <150 mg/dL.
Notably, recombinant human activated protein C was completely omitted from the 2012 guidelines, prompted by the voluntary removal of the drug by the manufacturer after failing to show benefit. Use of selenium and intravenous immunoglobulin received comment, but there is insufficient evidence supporting their benefit at the current time. They also encourage clinicians to incorporate goals of care and end-of-life issues into the treatment plan and discuss this with patients and/or surrogates early in treatment.
Guideline Analysis
Prior versions of the SSC guidelines have been met with a fair amount of skepticism.8 Much of the criticism is based on the industry sponsorship of the 2004 version, the lack of transparency regarding potential conflicts of interest of the committee members, and that the bundle recommendations largely were based on only one trial and, therefore, not evidenced-based.9 The 2012 SSC committee seems to have addressed these issues as the guidelines are free of commercial sponsorship in the 2008 and current versions. They also rigorously applied the GRADE system to methodically assess the strength and quality of supporting evidence. The result is a set of guidelines that are partially evidence-based and partially based on expert opinion, but this is clearly delineated in these newest guidelines. This provides clinicians with a clear and concise recommended approach to the patient with severe sepsis and septic shock.
The guidelines continue to place a heavy emphasis on three- and six-hour treatment bundles, and with the assistance of the Institute for Health Care Improvement efforts to improve implementation of the bundle, they are already are widespread with an eye to expand across the country. The components of the three-hour treatment bundle (lactate measurement, blood cultures prior to initiation of antibiotics, broad-spectrum antibiotics, and IV crystalloids for hypotension or for a lactate of >4 mmol/L) recommended by the SSC have not changed substantially since 2008. The one exception is the rate at which IV crystalloid should be administered of 30 mL/kg, which is up from 20 mL/kg. Only time will tell how this change will affect bundle compliance or reduce mortality. But this does pose a significant challenge to quality and performance improvement groups accustomed to tracking compliance with IV fluid administration under the old standard and the educational campaigns associated with a change.
It appears that the SSC is here to stay, now in its third iteration. The lasting legacy of the SSC guidelines might not rest with the content of the guidelines, per se, but in raising awareness of severe sepsis and septic shock in a way that had not previously been considered.
HM Takeaways
The revised 2012 SCC updates bring some new tools to the clinician for early recognition and effective management of patients with sepsis. The push for institutions to adopt screening and performance measures reflects a general trend in health care to create high-performance systems. As these new guidelines are put into practice, there are several changes that might require augmentation of quality metrics being tracked at institutions nationally and internationally.
Dr. Pendharker is assistant professor of medicine in the division of hospital medicine at the University of California San Francisco and San Francisco General Hospital. Dr. Gomez is assistant professor of medicine in the division of pulmonary and critical care medicine at UCSF and San Francisco General Hospital.
References
- Hall MJ, Williams SN, DeFrances CJ, et al. Inpatient care for septicemia or sepsis: a challenge for patients and hospitals. NCHS Data Brief. 2011:1-8.
- Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41:580-637.
- Jansen TC, van Bommel J, Schoonderbeek FJ, et al. Early lactate-guided therapy in intensive care unit patients: a multicenter, open-label, randomized controlled trial. Am J Respir Crit Care Med. 2010;182:752-761.
- Jones AE, Shapiro NI, Trzeciak S, et al. Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial. JAMA. 2010;303:739-746.
- Levy MM, Dellinger RP, Townsend SR, et al. The Surviving Sepsis Campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Crit Care Med. 2010;38:367-374.
- Guidet B, Martinet O, Boulain T, et al. Assessment of hemodynamic efficacy and safety of 6% hydroxyethylstarch 130/0.4 vs. 0.9% NaCl fluid replacement in patients with severe sepsis: The CRYSTMAS study. Crit Care. 2012;16:R94.
- Perner A, Haase N, Guttormsen AB, et al. Hydroxyethyl starch 130/0.42 versus Ringer’s acetate in severe sepsis. N Engl J Med. 2012;367:124-134.
- Marik PE. Surviving sepsis: going beyond the guidelines. Ann Intensive Care. 2011;1:17.
- Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368-1377.
Background
Sepsis is a clinical syndrome with systemic effects that can progress to severe sepsis and/or septic shock. The incidence of severe sepsis and septic shock is rising in the United States, and these syndromes are associated with significant morbidity and a mortality rate as high as 25% to 35%.1 In fact, sepsis is one of the 10 leading causes of death in the U.S., accounting for 2% of hospital admissions but 17% of in-hospital deaths.1
The main principles of effective treatment for severe sepsis and septic shock are timely recognition and early aggressive therapy. Launched in 2002, the Surviving Sepsis Campaign (SSC) was the result of a collaboration of three professional societies. The goal of the SSC collaborative was to reduce mortality from severe sepsis and septic shock by 25%. To that end, the SSC convened representatives from several international societies to develop a set of evidence-based guidelines as a means of guiding clinicians in optimizing management of patients with severe sepsis and septic shock. Since the original publication of the SSC guidelines in 2004, there have been two updates—one in 2008 and one in February 2013.2
Guideline Updates
Quantitative, protocol-driven initial resuscitation in the first six hours for patients with severe sepsis and septic shock remains a high-level recommendation, but SSC has added normalization of the lactate level as a resuscitation goal. This new suggestion is based on two studies published since the 2008 SCC guidelines that showed noninferiority to previously established goals and absolute mortality benefit.3,4
There is a new focus on screening for sepsis and the use of hospital-based performance-improvement programs, which were not previously addressed in the 2008 SCC guidelines. Patients with suspected infections and who are seriously ill should be screened in order to identify sepsis early during the hospital course. Additionally, it is recommended that hospitals implement performance-improvement measures by which multidisciplinary teams can address treatment of sepsis by improving compliance with the SSC bundles, citing their own data as the model but ultimately leaving this recommendation as ungradable in regards to the quality of available supporting evidence.5
Cultures drawn before antibiotics and early imaging to confirm potential sources are still recommended, but the committee has added the use of one: 3 beta D-glucan and the mannan antigen and anti-mannan antibody assays when considering invasive candidiasis as your infective agent. They do note the known risk of false positive results with these assays and warn that they should be used with caution.
Early, broad-spectrum antibiotic administration within the first hour of presentation was upgraded for severe sepsis and downgraded for septic shock. The decision to initiate double coverage for suspected gram-negative infection is not recommended specifically but can be considered in situations when highly antibiotic resistant pathogens are potentially present. Daily assessment of the appropriate antibiotic regimen remains an important tenet, and the use of low procalcitonin levels as a tool to assist in the decision to discontinue antibiotics has been introduced. Source control is still strongly recommended in the first 12 hours of treatment.
The SSC 2012 guidelines specifically address the rate of fluid administered and the type of fluid that should be used. It is now recommended that a fluid challenge of 30 mL/kg be used for initial resuscitation, but the guidelines leave it up to the clinician to give more fluid if needed. There is a strong push for use of crystalloids rather than colloids during initial resuscitation and thereafter. Disfavor for colloids stemmed from trials showing increased mortality when comparing resuscitation with hydroxyethyl starch versus crystalloid for patients in septic shock.6,7 Albumin, on the other hand, is recommended to resuscitate patients with severe sepsis and septic shock in cases for which large amounts of crystalloid are required.
The 2012 SSC guidelines recommend norepinephrine (NE) alone as the first-line vasopressor in sepsis and no longer include dopamine in this category. In fact, the use of dopamine in septic shock has been downgraded and should only to be considered in patients at low risk of tachyarrhythmia and in bradycardia syndromes. Epinephrine is now favored as the second agent or as a substitute to NE. Phenylephrine is no longer recommended unless there is contraindication to using NE, the patient has a high cardiac output, or it is used as a salvage therapy. Vasopressin is considered only an adjunctive agent to NE and should never be used alone.
Recommendations regarding corticosteroid therapy remain largely unchanged from 2008 SCC guidelines, which only support their use when adequate volume resuscitation and vasopressor support has failed to achieve hemodynamic stability. Glucose control is recommended but at the new target of achieving a level of <180 mg/dL, up from a previous target of <150 mg/dL.
Notably, recombinant human activated protein C was completely omitted from the 2012 guidelines, prompted by the voluntary removal of the drug by the manufacturer after failing to show benefit. Use of selenium and intravenous immunoglobulin received comment, but there is insufficient evidence supporting their benefit at the current time. They also encourage clinicians to incorporate goals of care and end-of-life issues into the treatment plan and discuss this with patients and/or surrogates early in treatment.
Guideline Analysis
Prior versions of the SSC guidelines have been met with a fair amount of skepticism.8 Much of the criticism is based on the industry sponsorship of the 2004 version, the lack of transparency regarding potential conflicts of interest of the committee members, and that the bundle recommendations largely were based on only one trial and, therefore, not evidenced-based.9 The 2012 SSC committee seems to have addressed these issues as the guidelines are free of commercial sponsorship in the 2008 and current versions. They also rigorously applied the GRADE system to methodically assess the strength and quality of supporting evidence. The result is a set of guidelines that are partially evidence-based and partially based on expert opinion, but this is clearly delineated in these newest guidelines. This provides clinicians with a clear and concise recommended approach to the patient with severe sepsis and septic shock.
The guidelines continue to place a heavy emphasis on three- and six-hour treatment bundles, and with the assistance of the Institute for Health Care Improvement efforts to improve implementation of the bundle, they are already are widespread with an eye to expand across the country. The components of the three-hour treatment bundle (lactate measurement, blood cultures prior to initiation of antibiotics, broad-spectrum antibiotics, and IV crystalloids for hypotension or for a lactate of >4 mmol/L) recommended by the SSC have not changed substantially since 2008. The one exception is the rate at which IV crystalloid should be administered of 30 mL/kg, which is up from 20 mL/kg. Only time will tell how this change will affect bundle compliance or reduce mortality. But this does pose a significant challenge to quality and performance improvement groups accustomed to tracking compliance with IV fluid administration under the old standard and the educational campaigns associated with a change.
It appears that the SSC is here to stay, now in its third iteration. The lasting legacy of the SSC guidelines might not rest with the content of the guidelines, per se, but in raising awareness of severe sepsis and septic shock in a way that had not previously been considered.
HM Takeaways
The revised 2012 SCC updates bring some new tools to the clinician for early recognition and effective management of patients with sepsis. The push for institutions to adopt screening and performance measures reflects a general trend in health care to create high-performance systems. As these new guidelines are put into practice, there are several changes that might require augmentation of quality metrics being tracked at institutions nationally and internationally.
Dr. Pendharker is assistant professor of medicine in the division of hospital medicine at the University of California San Francisco and San Francisco General Hospital. Dr. Gomez is assistant professor of medicine in the division of pulmonary and critical care medicine at UCSF and San Francisco General Hospital.
References
- Hall MJ, Williams SN, DeFrances CJ, et al. Inpatient care for septicemia or sepsis: a challenge for patients and hospitals. NCHS Data Brief. 2011:1-8.
- Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41:580-637.
- Jansen TC, van Bommel J, Schoonderbeek FJ, et al. Early lactate-guided therapy in intensive care unit patients: a multicenter, open-label, randomized controlled trial. Am J Respir Crit Care Med. 2010;182:752-761.
- Jones AE, Shapiro NI, Trzeciak S, et al. Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial. JAMA. 2010;303:739-746.
- Levy MM, Dellinger RP, Townsend SR, et al. The Surviving Sepsis Campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Crit Care Med. 2010;38:367-374.
- Guidet B, Martinet O, Boulain T, et al. Assessment of hemodynamic efficacy and safety of 6% hydroxyethylstarch 130/0.4 vs. 0.9% NaCl fluid replacement in patients with severe sepsis: The CRYSTMAS study. Crit Care. 2012;16:R94.
- Perner A, Haase N, Guttormsen AB, et al. Hydroxyethyl starch 130/0.42 versus Ringer’s acetate in severe sepsis. N Engl J Med. 2012;367:124-134.
- Marik PE. Surviving sepsis: going beyond the guidelines. Ann Intensive Care. 2011;1:17.
- Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368-1377.
Background
Sepsis is a clinical syndrome with systemic effects that can progress to severe sepsis and/or septic shock. The incidence of severe sepsis and septic shock is rising in the United States, and these syndromes are associated with significant morbidity and a mortality rate as high as 25% to 35%.1 In fact, sepsis is one of the 10 leading causes of death in the U.S., accounting for 2% of hospital admissions but 17% of in-hospital deaths.1
The main principles of effective treatment for severe sepsis and septic shock are timely recognition and early aggressive therapy. Launched in 2002, the Surviving Sepsis Campaign (SSC) was the result of a collaboration of three professional societies. The goal of the SSC collaborative was to reduce mortality from severe sepsis and septic shock by 25%. To that end, the SSC convened representatives from several international societies to develop a set of evidence-based guidelines as a means of guiding clinicians in optimizing management of patients with severe sepsis and septic shock. Since the original publication of the SSC guidelines in 2004, there have been two updates—one in 2008 and one in February 2013.2
Guideline Updates
Quantitative, protocol-driven initial resuscitation in the first six hours for patients with severe sepsis and septic shock remains a high-level recommendation, but SSC has added normalization of the lactate level as a resuscitation goal. This new suggestion is based on two studies published since the 2008 SCC guidelines that showed noninferiority to previously established goals and absolute mortality benefit.3,4
There is a new focus on screening for sepsis and the use of hospital-based performance-improvement programs, which were not previously addressed in the 2008 SCC guidelines. Patients with suspected infections and who are seriously ill should be screened in order to identify sepsis early during the hospital course. Additionally, it is recommended that hospitals implement performance-improvement measures by which multidisciplinary teams can address treatment of sepsis by improving compliance with the SSC bundles, citing their own data as the model but ultimately leaving this recommendation as ungradable in regards to the quality of available supporting evidence.5
Cultures drawn before antibiotics and early imaging to confirm potential sources are still recommended, but the committee has added the use of one: 3 beta D-glucan and the mannan antigen and anti-mannan antibody assays when considering invasive candidiasis as your infective agent. They do note the known risk of false positive results with these assays and warn that they should be used with caution.
Early, broad-spectrum antibiotic administration within the first hour of presentation was upgraded for severe sepsis and downgraded for septic shock. The decision to initiate double coverage for suspected gram-negative infection is not recommended specifically but can be considered in situations when highly antibiotic resistant pathogens are potentially present. Daily assessment of the appropriate antibiotic regimen remains an important tenet, and the use of low procalcitonin levels as a tool to assist in the decision to discontinue antibiotics has been introduced. Source control is still strongly recommended in the first 12 hours of treatment.
The SSC 2012 guidelines specifically address the rate of fluid administered and the type of fluid that should be used. It is now recommended that a fluid challenge of 30 mL/kg be used for initial resuscitation, but the guidelines leave it up to the clinician to give more fluid if needed. There is a strong push for use of crystalloids rather than colloids during initial resuscitation and thereafter. Disfavor for colloids stemmed from trials showing increased mortality when comparing resuscitation with hydroxyethyl starch versus crystalloid for patients in septic shock.6,7 Albumin, on the other hand, is recommended to resuscitate patients with severe sepsis and septic shock in cases for which large amounts of crystalloid are required.
The 2012 SSC guidelines recommend norepinephrine (NE) alone as the first-line vasopressor in sepsis and no longer include dopamine in this category. In fact, the use of dopamine in septic shock has been downgraded and should only to be considered in patients at low risk of tachyarrhythmia and in bradycardia syndromes. Epinephrine is now favored as the second agent or as a substitute to NE. Phenylephrine is no longer recommended unless there is contraindication to using NE, the patient has a high cardiac output, or it is used as a salvage therapy. Vasopressin is considered only an adjunctive agent to NE and should never be used alone.
Recommendations regarding corticosteroid therapy remain largely unchanged from 2008 SCC guidelines, which only support their use when adequate volume resuscitation and vasopressor support has failed to achieve hemodynamic stability. Glucose control is recommended but at the new target of achieving a level of <180 mg/dL, up from a previous target of <150 mg/dL.
Notably, recombinant human activated protein C was completely omitted from the 2012 guidelines, prompted by the voluntary removal of the drug by the manufacturer after failing to show benefit. Use of selenium and intravenous immunoglobulin received comment, but there is insufficient evidence supporting their benefit at the current time. They also encourage clinicians to incorporate goals of care and end-of-life issues into the treatment plan and discuss this with patients and/or surrogates early in treatment.
Guideline Analysis
Prior versions of the SSC guidelines have been met with a fair amount of skepticism.8 Much of the criticism is based on the industry sponsorship of the 2004 version, the lack of transparency regarding potential conflicts of interest of the committee members, and that the bundle recommendations largely were based on only one trial and, therefore, not evidenced-based.9 The 2012 SSC committee seems to have addressed these issues as the guidelines are free of commercial sponsorship in the 2008 and current versions. They also rigorously applied the GRADE system to methodically assess the strength and quality of supporting evidence. The result is a set of guidelines that are partially evidence-based and partially based on expert opinion, but this is clearly delineated in these newest guidelines. This provides clinicians with a clear and concise recommended approach to the patient with severe sepsis and septic shock.
The guidelines continue to place a heavy emphasis on three- and six-hour treatment bundles, and with the assistance of the Institute for Health Care Improvement efforts to improve implementation of the bundle, they are already are widespread with an eye to expand across the country. The components of the three-hour treatment bundle (lactate measurement, blood cultures prior to initiation of antibiotics, broad-spectrum antibiotics, and IV crystalloids for hypotension or for a lactate of >4 mmol/L) recommended by the SSC have not changed substantially since 2008. The one exception is the rate at which IV crystalloid should be administered of 30 mL/kg, which is up from 20 mL/kg. Only time will tell how this change will affect bundle compliance or reduce mortality. But this does pose a significant challenge to quality and performance improvement groups accustomed to tracking compliance with IV fluid administration under the old standard and the educational campaigns associated with a change.
It appears that the SSC is here to stay, now in its third iteration. The lasting legacy of the SSC guidelines might not rest with the content of the guidelines, per se, but in raising awareness of severe sepsis and septic shock in a way that had not previously been considered.
HM Takeaways
The revised 2012 SCC updates bring some new tools to the clinician for early recognition and effective management of patients with sepsis. The push for institutions to adopt screening and performance measures reflects a general trend in health care to create high-performance systems. As these new guidelines are put into practice, there are several changes that might require augmentation of quality metrics being tracked at institutions nationally and internationally.
Dr. Pendharker is assistant professor of medicine in the division of hospital medicine at the University of California San Francisco and San Francisco General Hospital. Dr. Gomez is assistant professor of medicine in the division of pulmonary and critical care medicine at UCSF and San Francisco General Hospital.
References
- Hall MJ, Williams SN, DeFrances CJ, et al. Inpatient care for septicemia or sepsis: a challenge for patients and hospitals. NCHS Data Brief. 2011:1-8.
- Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41:580-637.
- Jansen TC, van Bommel J, Schoonderbeek FJ, et al. Early lactate-guided therapy in intensive care unit patients: a multicenter, open-label, randomized controlled trial. Am J Respir Crit Care Med. 2010;182:752-761.
- Jones AE, Shapiro NI, Trzeciak S, et al. Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial. JAMA. 2010;303:739-746.
- Levy MM, Dellinger RP, Townsend SR, et al. The Surviving Sepsis Campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Crit Care Med. 2010;38:367-374.
- Guidet B, Martinet O, Boulain T, et al. Assessment of hemodynamic efficacy and safety of 6% hydroxyethylstarch 130/0.4 vs. 0.9% NaCl fluid replacement in patients with severe sepsis: The CRYSTMAS study. Crit Care. 2012;16:R94.
- Perner A, Haase N, Guttormsen AB, et al. Hydroxyethyl starch 130/0.42 versus Ringer’s acetate in severe sepsis. N Engl J Med. 2012;367:124-134.
- Marik PE. Surviving sepsis: going beyond the guidelines. Ann Intensive Care. 2011;1:17.
- Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368-1377.
How Should Common Symptoms at the End of Life be Managed?
Case
A 58-year-old male with colon cancer metastatic to the liver and lungs presents with vomiting, dyspnea, and abdominal pain. His disease has progressed through third-line chemotherapy and his care is now focused entirely on symptom management. He has not had a bowel movement in five days and he began vomiting two days ago.
Overview
The majority of patients in the United States die in acute-care hospitals. The Study to Understand Prognosis and Preferences for Outcomes and Risks of Treatments (SUPPORT), which evaluated the courses of close to 10,000 hospitalized patients with serious and life-limiting illnesses, illustrated that patients’ end-of-life (EOL) experiences often are characterized by poor symptom management and invasive care that is not congruent with the patients’ overall goals of care.1 Studies of factors identified as priorities in EOL care have consistently shown that excellent pain and symptom management are highly valued by patients and families. As the hospitalist movement continues to grow, hospitalists will play a large role in caring for patients at EOL and will need to know how to provide adequate pain and symptom management so that high-quality care can be achieved.
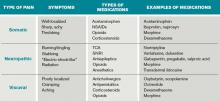
Pain: A Basic Tenet
A basic tenet of palliative medicine is to evaluate and treat all types of suffering.2 Physical pain at EOL is frequently accompanied by other types of pain, such as psychological, social, religious, or existential pain. However, this review will focus on the pharmacologic management of physical pain.
Pain management must begin with a thorough evaluation of the severity, location, and characteristics of the discomfort to assess which therapies are most likely to be beneficial (see Table 1).3 The consistent use of one scale of pain severity (such as 0-10, or mild/moderate/severe) assists in the choice of initial dose of pain medication, in determining the response to the medication, and in assessing the need for change in dose.4
Opioids are the foundation of pain management in advanced diseases because they are available in a number of formulations and, when dosed appropriately, they are effective and safe. Starting doses and equianalgesic doses of common opioids are presented in Table 2. Guidelines recommend the use of short-acting opioids for dose titration to gain control of poorly controlled pain.3 If a patient is experiencing mild pain on a specific regimen, the medication dose can be increased up to 25%; by 25% to 50%, if pain is moderate; and 50% to 100%, if severe.5 When the pain is better-controlled, the total amount of pain medication used in 24 hours (24-hour dose) can be converted to a long-acting formulation for more consistent pain management. Because there is a constant component to most advanced pain syndromes, it is recommended that pain medication is given on a standing basis, with as-needed (prn) doses available for exacerbations of pain.3 Prn doses of short-acting medication (equivalent to approximately 10% of the 24-hour dose of medication) should be available at one- or two-hour intervals prn (longer if hepatic or renal impairment is present) for IV or PO medications, respectively.
Opioids often are categorized as low potency (i.e. codeine, hydrocodone) and high-potency (i.e. oxycodone, morphine, hydromorphone, fentanyl). When given in “equianalgesic doses,” the analgesic effect and common side effects (nausea/vomiting, constipation, sedation, confusion, pruritis) of different opioids can vary in different patients. Due to differences in levels of expressed subtypes of opioid receptors, a given patient might be more sensitive to the analgesic effect or side effects of a specific medication. Therefore, if dose escalation of one opioid is inadequate to control pain and further increases in dose are limited by intolerable side effects, rotation to another opioid is recommended.4 Tables documenting equianalgesic doses of different opioids are based on only moderate evidence from equivalency trials performed in healthy volunteers.6 Due to interpatient differences in responses, it is recommended that the equianalgesic dose of the new medication be decreased by 25% to 50% for initial dosing.5
Certain treatments are indicated for specific pain syndromes. Bony metastases respond to NSAIDs, bisphosphonates, and radiation therapy in addition to opioid medications. As focal back pain is the first symptom of spinal cord compression, clinicians should have a high index of suspicion for compression in any patient with malignancy and new back pain. Steroids and radiation therapy are considered emergent treatments for pain control and to prevent paralysis in this circumstance. Pain due to bowel obstruction is usually colicky in nature and responds well to octreotide as discussed in the section on nausea and vomiting. Steroids (such as dexamethasone 4 mg PO bid-tid) might be an effective adjuvant medication in bone pain, tumor pain, or inflammation.
*Half this dose should be used in renal or liver dysfunction and in the elderly.
Preferred in renal dysfunction.
SOURCES: Adapted from Assessment and treatment of physical pain associated with life-limiting illness. Hospice and Palliative Care Training for Physicians: UNIPAC. Vol 3. 3rd ed. Glenview, IL: American Academy of Hospice and Palliative Medicine; 2008, and Evidence-based standards for cancer pain management. J Clin Oncol. 2008;26(23):3879-3885.
Back to the Case
At home, the patient was taking 60 mg of extended-release morphine twice daily and six doses per day of 15-mg immediate-release morphine for breakthrough pain. This is the equivalent of 210 mg of oral morphine in 24 hours. His pain is severe on this regimen, but it is unclear how much of this medication he is absorbing due to his vomiting. Using the IV route of administration and a patient-controlled analgesia (PCA) system will enable rapid dose titration and pain control. The equivalent of the 24-hour dose of 210 mg oral morphine is 70 mg IV morphine, which is equivalent to a drip basal rate of approximately 3 mg IV morphine per hour. This basal rate with a bolus dose of 7 mg (10% of the 24-hour dose) IV morphine q1 hour prn is reasonable as a starting point.
Review of the Data: Nausea and Vomiting
Nausea and vomiting affect 40% to 70% of patients in a palliative setting.7 A thorough history and physical exam can enable one to determine the most likely causes, pathways, and receptors involved in the process of nausea and vomiting. It is important to review the timing, frequency, and triggers of vomiting. The oral, abdominal, neurologic, and rectal exams, in addition to a complete chemistry panel, offer helpful information. The most common etiologies and recommended medications are included in Table 3. It is worthwhile to note that serotonin-antagonists (i.e. ondansetron) are first-line therapies only for chemotherapy and radiation-therapy-induced emesis. If a 24-hour trial of one antiemetic therapy is ineffective, one should reassess the etiology and escalate the antiemetic dose, or add a second therapy with a different (pertinent) mechanism of action. Although most studies of antiemetic therapy are case series, there is good evidence for this mechanistic approach.8
*EPS: extrapyramidal symptoms
The various insults and pathways that can cause vomiting are quite complex. The medullary vomiting center (VC) receives vestibular, peripheral (via splanchnic and vagal nerves), and higher cortical inputs and is the final common pathway in the vomiting reflex. The chemoreceptor trigger zone (CTZ) near the fourth ventricle receives input from the vagal and splanchnic nerves, and generates output to the VC.
General dietary recommendations are to avoid sweet, fatty, and highly salted or spiced foods. Small portions of bland foods without strong odors are best tolerated.7 Constipation commonly contributes to nausea and vomiting and should be managed with disimpaction, enemas, and laxatives as tolerated. Imaging may be required to make the important distinction between partial and complete bowel obstruction, as the treatments differ. Surgical procedures, such as colostomy or placement of a venting gastrostomy tube, can relieve pain and vomiting associated with complete bowel obstruction.
Back to the Case
The patient is found to have a fecal impaction on rectal exam, but vomiting persists after disimpaction and enema use. Imaging documents a complete bowel obstruction at the site of a palpable mass in the right upper quadrant and multiple large hepatic metastases. Octreotide is initiated to decrease intestinal secretions and peristalsis. Steroids are given to decrease tumor burden and associated inflammation in the intestine and liver, as well as to relieve distension of the hepatic capsule. Haloperidol is used in low doses to control episodes of nausea.
Review of the Data: Dyspnea
Dyspnea is a common symptom faced by patients at EOL. An estimated 50% of patients who are evaluated in acute-care hospitals seek treatment for the management of this often-crippling symptom.10 Unfortunately, as disease burden progresses, the incidence of dyspnea increases towards EOL, and the presence and severity of dyspnea is strongly correlated with mortality.
It is imperative for providers to appreciate that dyspnea is a subjective symptom, similar to pain. The presence and severity of dyspnea, therefore, depends on patient report. Given its subjective nature, the degree of dyspnea experienced by a patient might not correlate with objective laboratory findings or test results. In practice, the severity of dyspnea is commonly assessed with a numeric rating scale (0-10), verbal analogue scale, or with verbal descriptors (mild, moderate, severe). It is important to determine the underlying etiology of the dyspnea and, if possible, to target interventions to relieve the underlying cause. However, at the end of life, the burdens of invasive studies to determine the exact cause of dyspnea might outweigh the benefits, and invasive testing might not correlate with patients’ and families’ goals of care. In that instance, the goal of treatment should be aggressive symptom management and providers should use clinical judgment to tailor therapies based on the patient’s underlying illness, physical examination, and perhaps on noninvasive radiological or laboratory findings. Below are nonpharmacological and pharmacological interventions that can be employed to help alleviate dyspnea in the actively dying patient.
Nonpharmacological Management
A handheld fan aimed near the patient’s face has been shown to reduce the sensation of dyspnea.11 This relatively safe and inexpensive intervention has no major side effects and can provide improvement in this distressing symptom.
Often, the first line of therapy in the hospital setting for a patient reporting dyspnea is the administration of oxygen therapy. However, recent evidence does not show superiority of oxygen over air inhalation via nasal prongs for dyspnea in patients with advanced cancer or heart failure.12,13
Pharmacological Management
Opioids are first-line therapy for alleviating dyspnea in patients at EOL. The administration of opioids has been shown in systematic reviews to provide effective management of dyspnea.14,15 Practice guidelines by leading expert groups advocate for the use of opioids in the management of dyspnea for patients with advanced malignant and noncancer diseases.10,16 Fear of causing unintended respiratory sedation with opioids limits the prescription of opioids for dyspnea. However, studies have not found a change in mortality with the use of opioids appropriately titrated to control dyspnea.17
Studies examining the role of benzodiazepines in dyspnea management are conflicting. Anecdotal clinical evidence in actively dying patients supports treating dyspnea with benzodiazepines in conjunction with opioid therapy. Benzodiazepines are most beneficial when there is an anxiety-related component to the dyspnea.
Many patients with advanced disease and evidence of airflow obstruction will benefit from nebulized bronchodilator therapy for dyspnea. Patients with dyspnea from fluid overload (i.e. end-stage congestive heart failure or renal disease) might benefit from systemic diuretics. An increasing number of trials are under way to evaluate the efficacy of nebulized furosemide in the symptomatic management of dyspnea.
Back to the Case
The patient’s clinical course decompensates, and he begins to report worsening dyspnea in addition to his underlying pain. He becomes increasingly anxious about what this new symptom means. In addition to having a discussion about disease progression and prognosis, you increase his PCA basal dose to morphine 4 mg/hour to help him with this new symptom. You also add low-dose lorazepam 0.5 mg IV q8 hours as an adjunct agent for his dyspnea. The patient reports improvement of his symptom burden.
Review of the Data: Secretions
Physiological changes occur as a patient enters the active phase of dying. Two such changes are the loss of the ability to swallow and a reduced cough reflex. These changes culminate in an inability to clear secretions, which pool in the oropharynx and the airways. As the patient breathes, air moves over the pooled secretions and produces a gurgling sound that is referred to as the “death rattle.” The onset of this clinical marker has been shown to have significant prognostic significance for predicting imminent death within a period of hours to days. Proposed treatments for the symptom are listed below.
Nonpharmacological Management
Nonpharmacological options include repositioning the patient in a manner that facilitates postural draining.18 Careful and gentle oral suctioning might help reduce secretions if they are salivary in origin. This will not help to clear deeper bronchial secretions. Suctioning of deeper secretions often causes more burden than benefit, as this can cause repeated trauma and possible bleeding.
Family and caregivers at the bedside can find the “death rattle” quite disturbing and often fear that their loved one is “drowning.” Education and counseling that this is not the case, and that the development of secretions is a natural part of the dying process, can help alleviate this concern. Explaining that pharmacological agents can be titrated to decrease secretions is also reassuring to caregivers.
Pharmacological Management
Pharmacological options for secretion management include utilizing anticholinergic medications to prevent the formation of further secretions. These medications are standard of care for managing the death rattle and have been found to be most efficacious if started earlier in the actively dying phase.19,20 Anticholinergic medications include glycopyrrolate (0.2 mg IV q8 hours), atropine sulfate ophthalmological drops (1% solution, 1-2 drops SL q6 hours), hyoscyamine (0.125 mg one to four times a day), and scopolamine (1.5 mg patch q72 hours). These medications all have possible side effects typical of anticholinergic agents, including delirium, constipation, blurred vision, and urinary retention.
Back to the Case
The patient becomes increasingly lethargic. You meet with his family and explain that he is actively dying. His family reiterates that the goals of medical care should focus on maximizing symptom management. His family is concerned about the “gurgly” sound they hear and want to know if that means he is suffering. You educate the family about expected changes that occur with the dying process and inform them that glycopyrrolate 0.2 mg IV q8 hour will be started to minimize further secretions.
Bottom Line
Pain, nausea, dyspnea, and secretions are common end-of-life symptoms that hospitalists should be competent in treating.
Dr. Litrivis is an associate director and assistant professor at the Mount Sinai School of Medicine in New York, and Dr. Neale is an assistant professor at the University of New Mexico School of Medicine in Albuquerque.
References
- The SUPPORT Principal Investigators. A controlled trial to improve the care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). JAMA. 1995;274(20):1591-1598.
- World Health Organization Definition of Palliative Care. World Health Organization website. Available at: http://www.who.int/cancer/palliative/definition/en/. Accessed April 12, 2012.
- NCCN Guidelines Version 2. 2011 Adult Cancer Pain. National Comprehensive Cancer Network website. Available at: http://www.nccn.org/professionals/physician_gls/pdf/pain.pdf. Accessed April 12, 2012.
- Whitecar PS, Jonas AP, Clasen ME. Managing pain in the dying patient. Am Fam Physician. 2000;61(3):755-764.
- Bial A, Levine S. Assessment and treatment of physical pain associated with life-limiting illness. Hospice and Palliative Care Training for Physicians: UNIPAC. Vol 3. 3rd ed. Glenview, IL: American Academy of Hospice and Palliative Medicine; 2008.
- Sydney M, et al. Evidence-based standards for cancer pain management. J Clin Oncol. 2008;26(23):3879-3885.
- Mannix KA. Gastrointestinal symptoms. In: Doyle D, Hanks G, Cherny N, Calman K, eds. Oxford Textbook of Palliative Medicine. 3rd ed. New York, NY: Oxford University Press; 2005.
- Tyler LS. Nausea and vomiting in palliative care. In: Lipman AG, Jackson KC, Tyler LS, eds. Evidence-Based Symptom Control in Palliative Care. New York, NY: The Hawthorn Press; 2000.
- Policzer JS, Sobel J. Management of Selected Nonpain Symptoms of Life-Limiting Illness. Hospice and Palliative Care Training for Physicians: UNIPAC. Vol 4. 3rd ed. Glenview, IL: American Academy of Hospice and Palliative Medicine; 2008.
- Parshall MB, Schwartzstein RM, Adams L, et al. An official American Thoracic Society statement: update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med. 2012;185(4): 435-452.
- Galbraith S, Fagan P, Perkins P, Lynch A, Booth S. Does the use of a handheld fan improve chronic dyspnea? A randomized controlled, crossover trial. J Pain Symptom Manage. 2010;39(5): 831-838.
- Philip J, Gold M, Milner A, Di Iulio J, Miller B, Spruyt O. A randomized, double-blind, crossover trial of the effect of oxygen on dyspnea in patients with advanced cancer. J Pain Symptom Manage. 2006;32(6):541-550.
- Cranston JM, Crockett A, Currow D. Oxygen therapy for dyspnea in adults. Cochrane Database Syst Rev. 2008;(3):CD004769.
- Jennings AL, Davies AN, Higgins JP, Broadley K. Opioids for the palliation of breathlessness in terminal illness. Cochrane Database Syst Rev. 2001;(4):CD002066.
- Ben-Aharon I, Gafter-Gvili A, Paul M, Leibovici, L, Stemmer, SM. Interventions for alleviating cancer-related dyspnea. A systematic review. J Clin Oncol. 2008;26(14): 2396-2404.
- Qaseem A, Snow V, Shekelle P, et al. Evidence-based interventions to improve the palliative care of pain, dyspnea, and depression at the end of life: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2008;148(2):141-146
- Booth S, Moosavi SH, Higginson IJ. The etiology and management of intractable breathlessness in patients with advanced cancer: a systematic review of pharmacological therapy. Nat Clin Pract Oncol. 2008;5(2):90–100.
- Bickel K, Arnold R. EPERC Fast Facts Documents #109 Death Rattle and Oral Secretions, 2nd ed. Available at: http://www.eperc.mcw.edu/EPERC/FastFactsIndex/ff_109.htm. Accessed April 15, 2012.
- Wildiers H, Dhaenekint C, Demeulenaere P, et al. Atropine, hyoscine butylbromide, or scopalamine are equally effective for the treatment of death rattle in terminal care. J Pain Symptom Manage. 2009;38(1):124-133.
- Hugel H, Ellershaw J, Gambles M. Respiratory tract secretions in the dying patient: a comparison between glycopyrronium and hyoscine hydrobromide. J Palliat Med. 2006;9(2):279-285.
Case
A 58-year-old male with colon cancer metastatic to the liver and lungs presents with vomiting, dyspnea, and abdominal pain. His disease has progressed through third-line chemotherapy and his care is now focused entirely on symptom management. He has not had a bowel movement in five days and he began vomiting two days ago.
Overview
The majority of patients in the United States die in acute-care hospitals. The Study to Understand Prognosis and Preferences for Outcomes and Risks of Treatments (SUPPORT), which evaluated the courses of close to 10,000 hospitalized patients with serious and life-limiting illnesses, illustrated that patients’ end-of-life (EOL) experiences often are characterized by poor symptom management and invasive care that is not congruent with the patients’ overall goals of care.1 Studies of factors identified as priorities in EOL care have consistently shown that excellent pain and symptom management are highly valued by patients and families. As the hospitalist movement continues to grow, hospitalists will play a large role in caring for patients at EOL and will need to know how to provide adequate pain and symptom management so that high-quality care can be achieved.
Pain: A Basic Tenet
A basic tenet of palliative medicine is to evaluate and treat all types of suffering.2 Physical pain at EOL is frequently accompanied by other types of pain, such as psychological, social, religious, or existential pain. However, this review will focus on the pharmacologic management of physical pain.
Pain management must begin with a thorough evaluation of the severity, location, and characteristics of the discomfort to assess which therapies are most likely to be beneficial (see Table 1).3 The consistent use of one scale of pain severity (such as 0-10, or mild/moderate/severe) assists in the choice of initial dose of pain medication, in determining the response to the medication, and in assessing the need for change in dose.4
Opioids are the foundation of pain management in advanced diseases because they are available in a number of formulations and, when dosed appropriately, they are effective and safe. Starting doses and equianalgesic doses of common opioids are presented in Table 2. Guidelines recommend the use of short-acting opioids for dose titration to gain control of poorly controlled pain.3 If a patient is experiencing mild pain on a specific regimen, the medication dose can be increased up to 25%; by 25% to 50%, if pain is moderate; and 50% to 100%, if severe.5 When the pain is better-controlled, the total amount of pain medication used in 24 hours (24-hour dose) can be converted to a long-acting formulation for more consistent pain management. Because there is a constant component to most advanced pain syndromes, it is recommended that pain medication is given on a standing basis, with as-needed (prn) doses available for exacerbations of pain.3 Prn doses of short-acting medication (equivalent to approximately 10% of the 24-hour dose of medication) should be available at one- or two-hour intervals prn (longer if hepatic or renal impairment is present) for IV or PO medications, respectively.
Opioids often are categorized as low potency (i.e. codeine, hydrocodone) and high-potency (i.e. oxycodone, morphine, hydromorphone, fentanyl). When given in “equianalgesic doses,” the analgesic effect and common side effects (nausea/vomiting, constipation, sedation, confusion, pruritis) of different opioids can vary in different patients. Due to differences in levels of expressed subtypes of opioid receptors, a given patient might be more sensitive to the analgesic effect or side effects of a specific medication. Therefore, if dose escalation of one opioid is inadequate to control pain and further increases in dose are limited by intolerable side effects, rotation to another opioid is recommended.4 Tables documenting equianalgesic doses of different opioids are based on only moderate evidence from equivalency trials performed in healthy volunteers.6 Due to interpatient differences in responses, it is recommended that the equianalgesic dose of the new medication be decreased by 25% to 50% for initial dosing.5
Certain treatments are indicated for specific pain syndromes. Bony metastases respond to NSAIDs, bisphosphonates, and radiation therapy in addition to opioid medications. As focal back pain is the first symptom of spinal cord compression, clinicians should have a high index of suspicion for compression in any patient with malignancy and new back pain. Steroids and radiation therapy are considered emergent treatments for pain control and to prevent paralysis in this circumstance. Pain due to bowel obstruction is usually colicky in nature and responds well to octreotide as discussed in the section on nausea and vomiting. Steroids (such as dexamethasone 4 mg PO bid-tid) might be an effective adjuvant medication in bone pain, tumor pain, or inflammation.
*Half this dose should be used in renal or liver dysfunction and in the elderly.
Preferred in renal dysfunction.
SOURCES: Adapted from Assessment and treatment of physical pain associated with life-limiting illness. Hospice and Palliative Care Training for Physicians: UNIPAC. Vol 3. 3rd ed. Glenview, IL: American Academy of Hospice and Palliative Medicine; 2008, and Evidence-based standards for cancer pain management. J Clin Oncol. 2008;26(23):3879-3885.
Back to the Case
At home, the patient was taking 60 mg of extended-release morphine twice daily and six doses per day of 15-mg immediate-release morphine for breakthrough pain. This is the equivalent of 210 mg of oral morphine in 24 hours. His pain is severe on this regimen, but it is unclear how much of this medication he is absorbing due to his vomiting. Using the IV route of administration and a patient-controlled analgesia (PCA) system will enable rapid dose titration and pain control. The equivalent of the 24-hour dose of 210 mg oral morphine is 70 mg IV morphine, which is equivalent to a drip basal rate of approximately 3 mg IV morphine per hour. This basal rate with a bolus dose of 7 mg (10% of the 24-hour dose) IV morphine q1 hour prn is reasonable as a starting point.
Review of the Data: Nausea and Vomiting
Nausea and vomiting affect 40% to 70% of patients in a palliative setting.7 A thorough history and physical exam can enable one to determine the most likely causes, pathways, and receptors involved in the process of nausea and vomiting. It is important to review the timing, frequency, and triggers of vomiting. The oral, abdominal, neurologic, and rectal exams, in addition to a complete chemistry panel, offer helpful information. The most common etiologies and recommended medications are included in Table 3. It is worthwhile to note that serotonin-antagonists (i.e. ondansetron) are first-line therapies only for chemotherapy and radiation-therapy-induced emesis. If a 24-hour trial of one antiemetic therapy is ineffective, one should reassess the etiology and escalate the antiemetic dose, or add a second therapy with a different (pertinent) mechanism of action. Although most studies of antiemetic therapy are case series, there is good evidence for this mechanistic approach.8
*EPS: extrapyramidal symptoms
The various insults and pathways that can cause vomiting are quite complex. The medullary vomiting center (VC) receives vestibular, peripheral (via splanchnic and vagal nerves), and higher cortical inputs and is the final common pathway in the vomiting reflex. The chemoreceptor trigger zone (CTZ) near the fourth ventricle receives input from the vagal and splanchnic nerves, and generates output to the VC.
General dietary recommendations are to avoid sweet, fatty, and highly salted or spiced foods. Small portions of bland foods without strong odors are best tolerated.7 Constipation commonly contributes to nausea and vomiting and should be managed with disimpaction, enemas, and laxatives as tolerated. Imaging may be required to make the important distinction between partial and complete bowel obstruction, as the treatments differ. Surgical procedures, such as colostomy or placement of a venting gastrostomy tube, can relieve pain and vomiting associated with complete bowel obstruction.
Back to the Case
The patient is found to have a fecal impaction on rectal exam, but vomiting persists after disimpaction and enema use. Imaging documents a complete bowel obstruction at the site of a palpable mass in the right upper quadrant and multiple large hepatic metastases. Octreotide is initiated to decrease intestinal secretions and peristalsis. Steroids are given to decrease tumor burden and associated inflammation in the intestine and liver, as well as to relieve distension of the hepatic capsule. Haloperidol is used in low doses to control episodes of nausea.
Review of the Data: Dyspnea
Dyspnea is a common symptom faced by patients at EOL. An estimated 50% of patients who are evaluated in acute-care hospitals seek treatment for the management of this often-crippling symptom.10 Unfortunately, as disease burden progresses, the incidence of dyspnea increases towards EOL, and the presence and severity of dyspnea is strongly correlated with mortality.
It is imperative for providers to appreciate that dyspnea is a subjective symptom, similar to pain. The presence and severity of dyspnea, therefore, depends on patient report. Given its subjective nature, the degree of dyspnea experienced by a patient might not correlate with objective laboratory findings or test results. In practice, the severity of dyspnea is commonly assessed with a numeric rating scale (0-10), verbal analogue scale, or with verbal descriptors (mild, moderate, severe). It is important to determine the underlying etiology of the dyspnea and, if possible, to target interventions to relieve the underlying cause. However, at the end of life, the burdens of invasive studies to determine the exact cause of dyspnea might outweigh the benefits, and invasive testing might not correlate with patients’ and families’ goals of care. In that instance, the goal of treatment should be aggressive symptom management and providers should use clinical judgment to tailor therapies based on the patient’s underlying illness, physical examination, and perhaps on noninvasive radiological or laboratory findings. Below are nonpharmacological and pharmacological interventions that can be employed to help alleviate dyspnea in the actively dying patient.
Nonpharmacological Management
A handheld fan aimed near the patient’s face has been shown to reduce the sensation of dyspnea.11 This relatively safe and inexpensive intervention has no major side effects and can provide improvement in this distressing symptom.
Often, the first line of therapy in the hospital setting for a patient reporting dyspnea is the administration of oxygen therapy. However, recent evidence does not show superiority of oxygen over air inhalation via nasal prongs for dyspnea in patients with advanced cancer or heart failure.12,13
Pharmacological Management
Opioids are first-line therapy for alleviating dyspnea in patients at EOL. The administration of opioids has been shown in systematic reviews to provide effective management of dyspnea.14,15 Practice guidelines by leading expert groups advocate for the use of opioids in the management of dyspnea for patients with advanced malignant and noncancer diseases.10,16 Fear of causing unintended respiratory sedation with opioids limits the prescription of opioids for dyspnea. However, studies have not found a change in mortality with the use of opioids appropriately titrated to control dyspnea.17
Studies examining the role of benzodiazepines in dyspnea management are conflicting. Anecdotal clinical evidence in actively dying patients supports treating dyspnea with benzodiazepines in conjunction with opioid therapy. Benzodiazepines are most beneficial when there is an anxiety-related component to the dyspnea.
Many patients with advanced disease and evidence of airflow obstruction will benefit from nebulized bronchodilator therapy for dyspnea. Patients with dyspnea from fluid overload (i.e. end-stage congestive heart failure or renal disease) might benefit from systemic diuretics. An increasing number of trials are under way to evaluate the efficacy of nebulized furosemide in the symptomatic management of dyspnea.
Back to the Case
The patient’s clinical course decompensates, and he begins to report worsening dyspnea in addition to his underlying pain. He becomes increasingly anxious about what this new symptom means. In addition to having a discussion about disease progression and prognosis, you increase his PCA basal dose to morphine 4 mg/hour to help him with this new symptom. You also add low-dose lorazepam 0.5 mg IV q8 hours as an adjunct agent for his dyspnea. The patient reports improvement of his symptom burden.
Review of the Data: Secretions
Physiological changes occur as a patient enters the active phase of dying. Two such changes are the loss of the ability to swallow and a reduced cough reflex. These changes culminate in an inability to clear secretions, which pool in the oropharynx and the airways. As the patient breathes, air moves over the pooled secretions and produces a gurgling sound that is referred to as the “death rattle.” The onset of this clinical marker has been shown to have significant prognostic significance for predicting imminent death within a period of hours to days. Proposed treatments for the symptom are listed below.
Nonpharmacological Management
Nonpharmacological options include repositioning the patient in a manner that facilitates postural draining.18 Careful and gentle oral suctioning might help reduce secretions if they are salivary in origin. This will not help to clear deeper bronchial secretions. Suctioning of deeper secretions often causes more burden than benefit, as this can cause repeated trauma and possible bleeding.
Family and caregivers at the bedside can find the “death rattle” quite disturbing and often fear that their loved one is “drowning.” Education and counseling that this is not the case, and that the development of secretions is a natural part of the dying process, can help alleviate this concern. Explaining that pharmacological agents can be titrated to decrease secretions is also reassuring to caregivers.
Pharmacological Management
Pharmacological options for secretion management include utilizing anticholinergic medications to prevent the formation of further secretions. These medications are standard of care for managing the death rattle and have been found to be most efficacious if started earlier in the actively dying phase.19,20 Anticholinergic medications include glycopyrrolate (0.2 mg IV q8 hours), atropine sulfate ophthalmological drops (1% solution, 1-2 drops SL q6 hours), hyoscyamine (0.125 mg one to four times a day), and scopolamine (1.5 mg patch q72 hours). These medications all have possible side effects typical of anticholinergic agents, including delirium, constipation, blurred vision, and urinary retention.
Back to the Case
The patient becomes increasingly lethargic. You meet with his family and explain that he is actively dying. His family reiterates that the goals of medical care should focus on maximizing symptom management. His family is concerned about the “gurgly” sound they hear and want to know if that means he is suffering. You educate the family about expected changes that occur with the dying process and inform them that glycopyrrolate 0.2 mg IV q8 hour will be started to minimize further secretions.
Bottom Line
Pain, nausea, dyspnea, and secretions are common end-of-life symptoms that hospitalists should be competent in treating.
Dr. Litrivis is an associate director and assistant professor at the Mount Sinai School of Medicine in New York, and Dr. Neale is an assistant professor at the University of New Mexico School of Medicine in Albuquerque.
References
- The SUPPORT Principal Investigators. A controlled trial to improve the care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). JAMA. 1995;274(20):1591-1598.
- World Health Organization Definition of Palliative Care. World Health Organization website. Available at: http://www.who.int/cancer/palliative/definition/en/. Accessed April 12, 2012.
- NCCN Guidelines Version 2. 2011 Adult Cancer Pain. National Comprehensive Cancer Network website. Available at: http://www.nccn.org/professionals/physician_gls/pdf/pain.pdf. Accessed April 12, 2012.
- Whitecar PS, Jonas AP, Clasen ME. Managing pain in the dying patient. Am Fam Physician. 2000;61(3):755-764.
- Bial A, Levine S. Assessment and treatment of physical pain associated with life-limiting illness. Hospice and Palliative Care Training for Physicians: UNIPAC. Vol 3. 3rd ed. Glenview, IL: American Academy of Hospice and Palliative Medicine; 2008.
- Sydney M, et al. Evidence-based standards for cancer pain management. J Clin Oncol. 2008;26(23):3879-3885.
- Mannix KA. Gastrointestinal symptoms. In: Doyle D, Hanks G, Cherny N, Calman K, eds. Oxford Textbook of Palliative Medicine. 3rd ed. New York, NY: Oxford University Press; 2005.
- Tyler LS. Nausea and vomiting in palliative care. In: Lipman AG, Jackson KC, Tyler LS, eds. Evidence-Based Symptom Control in Palliative Care. New York, NY: The Hawthorn Press; 2000.
- Policzer JS, Sobel J. Management of Selected Nonpain Symptoms of Life-Limiting Illness. Hospice and Palliative Care Training for Physicians: UNIPAC. Vol 4. 3rd ed. Glenview, IL: American Academy of Hospice and Palliative Medicine; 2008.
- Parshall MB, Schwartzstein RM, Adams L, et al. An official American Thoracic Society statement: update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med. 2012;185(4): 435-452.
- Galbraith S, Fagan P, Perkins P, Lynch A, Booth S. Does the use of a handheld fan improve chronic dyspnea? A randomized controlled, crossover trial. J Pain Symptom Manage. 2010;39(5): 831-838.
- Philip J, Gold M, Milner A, Di Iulio J, Miller B, Spruyt O. A randomized, double-blind, crossover trial of the effect of oxygen on dyspnea in patients with advanced cancer. J Pain Symptom Manage. 2006;32(6):541-550.
- Cranston JM, Crockett A, Currow D. Oxygen therapy for dyspnea in adults. Cochrane Database Syst Rev. 2008;(3):CD004769.
- Jennings AL, Davies AN, Higgins JP, Broadley K. Opioids for the palliation of breathlessness in terminal illness. Cochrane Database Syst Rev. 2001;(4):CD002066.
- Ben-Aharon I, Gafter-Gvili A, Paul M, Leibovici, L, Stemmer, SM. Interventions for alleviating cancer-related dyspnea. A systematic review. J Clin Oncol. 2008;26(14): 2396-2404.
- Qaseem A, Snow V, Shekelle P, et al. Evidence-based interventions to improve the palliative care of pain, dyspnea, and depression at the end of life: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2008;148(2):141-146
- Booth S, Moosavi SH, Higginson IJ. The etiology and management of intractable breathlessness in patients with advanced cancer: a systematic review of pharmacological therapy. Nat Clin Pract Oncol. 2008;5(2):90–100.
- Bickel K, Arnold R. EPERC Fast Facts Documents #109 Death Rattle and Oral Secretions, 2nd ed. Available at: http://www.eperc.mcw.edu/EPERC/FastFactsIndex/ff_109.htm. Accessed April 15, 2012.
- Wildiers H, Dhaenekint C, Demeulenaere P, et al. Atropine, hyoscine butylbromide, or scopalamine are equally effective for the treatment of death rattle in terminal care. J Pain Symptom Manage. 2009;38(1):124-133.
- Hugel H, Ellershaw J, Gambles M. Respiratory tract secretions in the dying patient: a comparison between glycopyrronium and hyoscine hydrobromide. J Palliat Med. 2006;9(2):279-285.
Case
A 58-year-old male with colon cancer metastatic to the liver and lungs presents with vomiting, dyspnea, and abdominal pain. His disease has progressed through third-line chemotherapy and his care is now focused entirely on symptom management. He has not had a bowel movement in five days and he began vomiting two days ago.
Overview
The majority of patients in the United States die in acute-care hospitals. The Study to Understand Prognosis and Preferences for Outcomes and Risks of Treatments (SUPPORT), which evaluated the courses of close to 10,000 hospitalized patients with serious and life-limiting illnesses, illustrated that patients’ end-of-life (EOL) experiences often are characterized by poor symptom management and invasive care that is not congruent with the patients’ overall goals of care.1 Studies of factors identified as priorities in EOL care have consistently shown that excellent pain and symptom management are highly valued by patients and families. As the hospitalist movement continues to grow, hospitalists will play a large role in caring for patients at EOL and will need to know how to provide adequate pain and symptom management so that high-quality care can be achieved.
Pain: A Basic Tenet
A basic tenet of palliative medicine is to evaluate and treat all types of suffering.2 Physical pain at EOL is frequently accompanied by other types of pain, such as psychological, social, religious, or existential pain. However, this review will focus on the pharmacologic management of physical pain.
Pain management must begin with a thorough evaluation of the severity, location, and characteristics of the discomfort to assess which therapies are most likely to be beneficial (see Table 1).3 The consistent use of one scale of pain severity (such as 0-10, or mild/moderate/severe) assists in the choice of initial dose of pain medication, in determining the response to the medication, and in assessing the need for change in dose.4
Opioids are the foundation of pain management in advanced diseases because they are available in a number of formulations and, when dosed appropriately, they are effective and safe. Starting doses and equianalgesic doses of common opioids are presented in Table 2. Guidelines recommend the use of short-acting opioids for dose titration to gain control of poorly controlled pain.3 If a patient is experiencing mild pain on a specific regimen, the medication dose can be increased up to 25%; by 25% to 50%, if pain is moderate; and 50% to 100%, if severe.5 When the pain is better-controlled, the total amount of pain medication used in 24 hours (24-hour dose) can be converted to a long-acting formulation for more consistent pain management. Because there is a constant component to most advanced pain syndromes, it is recommended that pain medication is given on a standing basis, with as-needed (prn) doses available for exacerbations of pain.3 Prn doses of short-acting medication (equivalent to approximately 10% of the 24-hour dose of medication) should be available at one- or two-hour intervals prn (longer if hepatic or renal impairment is present) for IV or PO medications, respectively.
Opioids often are categorized as low potency (i.e. codeine, hydrocodone) and high-potency (i.e. oxycodone, morphine, hydromorphone, fentanyl). When given in “equianalgesic doses,” the analgesic effect and common side effects (nausea/vomiting, constipation, sedation, confusion, pruritis) of different opioids can vary in different patients. Due to differences in levels of expressed subtypes of opioid receptors, a given patient might be more sensitive to the analgesic effect or side effects of a specific medication. Therefore, if dose escalation of one opioid is inadequate to control pain and further increases in dose are limited by intolerable side effects, rotation to another opioid is recommended.4 Tables documenting equianalgesic doses of different opioids are based on only moderate evidence from equivalency trials performed in healthy volunteers.6 Due to interpatient differences in responses, it is recommended that the equianalgesic dose of the new medication be decreased by 25% to 50% for initial dosing.5
Certain treatments are indicated for specific pain syndromes. Bony metastases respond to NSAIDs, bisphosphonates, and radiation therapy in addition to opioid medications. As focal back pain is the first symptom of spinal cord compression, clinicians should have a high index of suspicion for compression in any patient with malignancy and new back pain. Steroids and radiation therapy are considered emergent treatments for pain control and to prevent paralysis in this circumstance. Pain due to bowel obstruction is usually colicky in nature and responds well to octreotide as discussed in the section on nausea and vomiting. Steroids (such as dexamethasone 4 mg PO bid-tid) might be an effective adjuvant medication in bone pain, tumor pain, or inflammation.
*Half this dose should be used in renal or liver dysfunction and in the elderly.
Preferred in renal dysfunction.
SOURCES: Adapted from Assessment and treatment of physical pain associated with life-limiting illness. Hospice and Palliative Care Training for Physicians: UNIPAC. Vol 3. 3rd ed. Glenview, IL: American Academy of Hospice and Palliative Medicine; 2008, and Evidence-based standards for cancer pain management. J Clin Oncol. 2008;26(23):3879-3885.
Back to the Case
At home, the patient was taking 60 mg of extended-release morphine twice daily and six doses per day of 15-mg immediate-release morphine for breakthrough pain. This is the equivalent of 210 mg of oral morphine in 24 hours. His pain is severe on this regimen, but it is unclear how much of this medication he is absorbing due to his vomiting. Using the IV route of administration and a patient-controlled analgesia (PCA) system will enable rapid dose titration and pain control. The equivalent of the 24-hour dose of 210 mg oral morphine is 70 mg IV morphine, which is equivalent to a drip basal rate of approximately 3 mg IV morphine per hour. This basal rate with a bolus dose of 7 mg (10% of the 24-hour dose) IV morphine q1 hour prn is reasonable as a starting point.
Review of the Data: Nausea and Vomiting
Nausea and vomiting affect 40% to 70% of patients in a palliative setting.7 A thorough history and physical exam can enable one to determine the most likely causes, pathways, and receptors involved in the process of nausea and vomiting. It is important to review the timing, frequency, and triggers of vomiting. The oral, abdominal, neurologic, and rectal exams, in addition to a complete chemistry panel, offer helpful information. The most common etiologies and recommended medications are included in Table 3. It is worthwhile to note that serotonin-antagonists (i.e. ondansetron) are first-line therapies only for chemotherapy and radiation-therapy-induced emesis. If a 24-hour trial of one antiemetic therapy is ineffective, one should reassess the etiology and escalate the antiemetic dose, or add a second therapy with a different (pertinent) mechanism of action. Although most studies of antiemetic therapy are case series, there is good evidence for this mechanistic approach.8
*EPS: extrapyramidal symptoms
The various insults and pathways that can cause vomiting are quite complex. The medullary vomiting center (VC) receives vestibular, peripheral (via splanchnic and vagal nerves), and higher cortical inputs and is the final common pathway in the vomiting reflex. The chemoreceptor trigger zone (CTZ) near the fourth ventricle receives input from the vagal and splanchnic nerves, and generates output to the VC.
General dietary recommendations are to avoid sweet, fatty, and highly salted or spiced foods. Small portions of bland foods without strong odors are best tolerated.7 Constipation commonly contributes to nausea and vomiting and should be managed with disimpaction, enemas, and laxatives as tolerated. Imaging may be required to make the important distinction between partial and complete bowel obstruction, as the treatments differ. Surgical procedures, such as colostomy or placement of a venting gastrostomy tube, can relieve pain and vomiting associated with complete bowel obstruction.
Back to the Case
The patient is found to have a fecal impaction on rectal exam, but vomiting persists after disimpaction and enema use. Imaging documents a complete bowel obstruction at the site of a palpable mass in the right upper quadrant and multiple large hepatic metastases. Octreotide is initiated to decrease intestinal secretions and peristalsis. Steroids are given to decrease tumor burden and associated inflammation in the intestine and liver, as well as to relieve distension of the hepatic capsule. Haloperidol is used in low doses to control episodes of nausea.
Review of the Data: Dyspnea
Dyspnea is a common symptom faced by patients at EOL. An estimated 50% of patients who are evaluated in acute-care hospitals seek treatment for the management of this often-crippling symptom.10 Unfortunately, as disease burden progresses, the incidence of dyspnea increases towards EOL, and the presence and severity of dyspnea is strongly correlated with mortality.
It is imperative for providers to appreciate that dyspnea is a subjective symptom, similar to pain. The presence and severity of dyspnea, therefore, depends on patient report. Given its subjective nature, the degree of dyspnea experienced by a patient might not correlate with objective laboratory findings or test results. In practice, the severity of dyspnea is commonly assessed with a numeric rating scale (0-10), verbal analogue scale, or with verbal descriptors (mild, moderate, severe). It is important to determine the underlying etiology of the dyspnea and, if possible, to target interventions to relieve the underlying cause. However, at the end of life, the burdens of invasive studies to determine the exact cause of dyspnea might outweigh the benefits, and invasive testing might not correlate with patients’ and families’ goals of care. In that instance, the goal of treatment should be aggressive symptom management and providers should use clinical judgment to tailor therapies based on the patient’s underlying illness, physical examination, and perhaps on noninvasive radiological or laboratory findings. Below are nonpharmacological and pharmacological interventions that can be employed to help alleviate dyspnea in the actively dying patient.
Nonpharmacological Management
A handheld fan aimed near the patient’s face has been shown to reduce the sensation of dyspnea.11 This relatively safe and inexpensive intervention has no major side effects and can provide improvement in this distressing symptom.
Often, the first line of therapy in the hospital setting for a patient reporting dyspnea is the administration of oxygen therapy. However, recent evidence does not show superiority of oxygen over air inhalation via nasal prongs for dyspnea in patients with advanced cancer or heart failure.12,13
Pharmacological Management
Opioids are first-line therapy for alleviating dyspnea in patients at EOL. The administration of opioids has been shown in systematic reviews to provide effective management of dyspnea.14,15 Practice guidelines by leading expert groups advocate for the use of opioids in the management of dyspnea for patients with advanced malignant and noncancer diseases.10,16 Fear of causing unintended respiratory sedation with opioids limits the prescription of opioids for dyspnea. However, studies have not found a change in mortality with the use of opioids appropriately titrated to control dyspnea.17
Studies examining the role of benzodiazepines in dyspnea management are conflicting. Anecdotal clinical evidence in actively dying patients supports treating dyspnea with benzodiazepines in conjunction with opioid therapy. Benzodiazepines are most beneficial when there is an anxiety-related component to the dyspnea.
Many patients with advanced disease and evidence of airflow obstruction will benefit from nebulized bronchodilator therapy for dyspnea. Patients with dyspnea from fluid overload (i.e. end-stage congestive heart failure or renal disease) might benefit from systemic diuretics. An increasing number of trials are under way to evaluate the efficacy of nebulized furosemide in the symptomatic management of dyspnea.
Back to the Case
The patient’s clinical course decompensates, and he begins to report worsening dyspnea in addition to his underlying pain. He becomes increasingly anxious about what this new symptom means. In addition to having a discussion about disease progression and prognosis, you increase his PCA basal dose to morphine 4 mg/hour to help him with this new symptom. You also add low-dose lorazepam 0.5 mg IV q8 hours as an adjunct agent for his dyspnea. The patient reports improvement of his symptom burden.
Review of the Data: Secretions
Physiological changes occur as a patient enters the active phase of dying. Two such changes are the loss of the ability to swallow and a reduced cough reflex. These changes culminate in an inability to clear secretions, which pool in the oropharynx and the airways. As the patient breathes, air moves over the pooled secretions and produces a gurgling sound that is referred to as the “death rattle.” The onset of this clinical marker has been shown to have significant prognostic significance for predicting imminent death within a period of hours to days. Proposed treatments for the symptom are listed below.
Nonpharmacological Management
Nonpharmacological options include repositioning the patient in a manner that facilitates postural draining.18 Careful and gentle oral suctioning might help reduce secretions if they are salivary in origin. This will not help to clear deeper bronchial secretions. Suctioning of deeper secretions often causes more burden than benefit, as this can cause repeated trauma and possible bleeding.
Family and caregivers at the bedside can find the “death rattle” quite disturbing and often fear that their loved one is “drowning.” Education and counseling that this is not the case, and that the development of secretions is a natural part of the dying process, can help alleviate this concern. Explaining that pharmacological agents can be titrated to decrease secretions is also reassuring to caregivers.
Pharmacological Management
Pharmacological options for secretion management include utilizing anticholinergic medications to prevent the formation of further secretions. These medications are standard of care for managing the death rattle and have been found to be most efficacious if started earlier in the actively dying phase.19,20 Anticholinergic medications include glycopyrrolate (0.2 mg IV q8 hours), atropine sulfate ophthalmological drops (1% solution, 1-2 drops SL q6 hours), hyoscyamine (0.125 mg one to four times a day), and scopolamine (1.5 mg patch q72 hours). These medications all have possible side effects typical of anticholinergic agents, including delirium, constipation, blurred vision, and urinary retention.
Back to the Case
The patient becomes increasingly lethargic. You meet with his family and explain that he is actively dying. His family reiterates that the goals of medical care should focus on maximizing symptom management. His family is concerned about the “gurgly” sound they hear and want to know if that means he is suffering. You educate the family about expected changes that occur with the dying process and inform them that glycopyrrolate 0.2 mg IV q8 hour will be started to minimize further secretions.
Bottom Line
Pain, nausea, dyspnea, and secretions are common end-of-life symptoms that hospitalists should be competent in treating.
Dr. Litrivis is an associate director and assistant professor at the Mount Sinai School of Medicine in New York, and Dr. Neale is an assistant professor at the University of New Mexico School of Medicine in Albuquerque.
References
- The SUPPORT Principal Investigators. A controlled trial to improve the care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). JAMA. 1995;274(20):1591-1598.
- World Health Organization Definition of Palliative Care. World Health Organization website. Available at: http://www.who.int/cancer/palliative/definition/en/. Accessed April 12, 2012.
- NCCN Guidelines Version 2. 2011 Adult Cancer Pain. National Comprehensive Cancer Network website. Available at: http://www.nccn.org/professionals/physician_gls/pdf/pain.pdf. Accessed April 12, 2012.
- Whitecar PS, Jonas AP, Clasen ME. Managing pain in the dying patient. Am Fam Physician. 2000;61(3):755-764.
- Bial A, Levine S. Assessment and treatment of physical pain associated with life-limiting illness. Hospice and Palliative Care Training for Physicians: UNIPAC. Vol 3. 3rd ed. Glenview, IL: American Academy of Hospice and Palliative Medicine; 2008.
- Sydney M, et al. Evidence-based standards for cancer pain management. J Clin Oncol. 2008;26(23):3879-3885.
- Mannix KA. Gastrointestinal symptoms. In: Doyle D, Hanks G, Cherny N, Calman K, eds. Oxford Textbook of Palliative Medicine. 3rd ed. New York, NY: Oxford University Press; 2005.
- Tyler LS. Nausea and vomiting in palliative care. In: Lipman AG, Jackson KC, Tyler LS, eds. Evidence-Based Symptom Control in Palliative Care. New York, NY: The Hawthorn Press; 2000.
- Policzer JS, Sobel J. Management of Selected Nonpain Symptoms of Life-Limiting Illness. Hospice and Palliative Care Training for Physicians: UNIPAC. Vol 4. 3rd ed. Glenview, IL: American Academy of Hospice and Palliative Medicine; 2008.
- Parshall MB, Schwartzstein RM, Adams L, et al. An official American Thoracic Society statement: update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med. 2012;185(4): 435-452.
- Galbraith S, Fagan P, Perkins P, Lynch A, Booth S. Does the use of a handheld fan improve chronic dyspnea? A randomized controlled, crossover trial. J Pain Symptom Manage. 2010;39(5): 831-838.
- Philip J, Gold M, Milner A, Di Iulio J, Miller B, Spruyt O. A randomized, double-blind, crossover trial of the effect of oxygen on dyspnea in patients with advanced cancer. J Pain Symptom Manage. 2006;32(6):541-550.
- Cranston JM, Crockett A, Currow D. Oxygen therapy for dyspnea in adults. Cochrane Database Syst Rev. 2008;(3):CD004769.
- Jennings AL, Davies AN, Higgins JP, Broadley K. Opioids for the palliation of breathlessness in terminal illness. Cochrane Database Syst Rev. 2001;(4):CD002066.
- Ben-Aharon I, Gafter-Gvili A, Paul M, Leibovici, L, Stemmer, SM. Interventions for alleviating cancer-related dyspnea. A systematic review. J Clin Oncol. 2008;26(14): 2396-2404.
- Qaseem A, Snow V, Shekelle P, et al. Evidence-based interventions to improve the palliative care of pain, dyspnea, and depression at the end of life: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2008;148(2):141-146
- Booth S, Moosavi SH, Higginson IJ. The etiology and management of intractable breathlessness in patients with advanced cancer: a systematic review of pharmacological therapy. Nat Clin Pract Oncol. 2008;5(2):90–100.
- Bickel K, Arnold R. EPERC Fast Facts Documents #109 Death Rattle and Oral Secretions, 2nd ed. Available at: http://www.eperc.mcw.edu/EPERC/FastFactsIndex/ff_109.htm. Accessed April 15, 2012.
- Wildiers H, Dhaenekint C, Demeulenaere P, et al. Atropine, hyoscine butylbromide, or scopalamine are equally effective for the treatment of death rattle in terminal care. J Pain Symptom Manage. 2009;38(1):124-133.
- Hugel H, Ellershaw J, Gambles M. Respiratory tract secretions in the dying patient: a comparison between glycopyrronium and hyoscine hydrobromide. J Palliat Med. 2006;9(2):279-285.
Pediatric Readmissions Vary Significantly Across Children’s Hospitals
Pediatric Readmissions Vary Significantly across Children’s Hospitals
Clinical question: What are the characteristics of readmissions to children’s hospitals?
Background: Thirty-day readmissions in adult Medicare beneficiaries are common and thought to represent potential for significant improvements in the quality of care. Penalties will be levied upon hospitals with excessively high readmission rates in adults. The stage is set for a translation of this practice to pediatric readmissions. However, the characteristics of readmissions to children’s hospitals are not well-defined.
Study design: Retrospective review.
Setting: National Association of Children’s Hospitals and Related Institutions (NACHRI) Case Mix data set.
Synopsis: Of 568,845 readmissions examined across 72 children’s hospitals, the 30-day readmission rate was 6.5%. Readmission rates varied by many factors: age, chronic conditions, insurance type, race/ethnicity, length of stay, number of annual hospital admissions, and hospital type. Rates varied significantly across hospitals, even after adjustment for age and chronic conditions. Anemia or neutropenia, ventricular shunt procedures, and sickle cell crisis had the highest unadjusted, 30-day, condition-specific readmission rates.
This study is notable for its large sample size but limited by the administrative data, which might, for example, underestimate readmissions that went to another hospital. Additionally, the majority of children in the U.S. are hospitalized outside of children’s hospitals, which are overrepresented in this study.
However, this study paints a clear picture of the differences between adult readmissions and pediatric readmissions—rates are lower than in elderly adults, and the top three conditions are distinctly different. Anemia or neutropenia likely are due to effects of chemotherapy; ventricular shunt readmissions often reflect surgery-related issues; and sickle cell disease is a lifelong, chronic condition. The significant variation between hospitals after case-mix adjustment offers an opportunity for further investigation and improvement.
Bottom line: Pediatric readmissions differ from adult readmissions and vary significantly across children’s hospitals.
Citation: Berry JG, Toomey SL, Zaslavsky AM, et al. Pediatric readmission prevalence and variability across hospitals. JAMA. 2013;309(4):372-380.
Reviewed by Pediatric Editor Mark Shen, MD, SFHM, medical director of hospital medicine at Dell Children's Medical Center, Austin, Texas.
Pediatric Readmissions Vary Significantly across Children’s Hospitals
Clinical question: What are the characteristics of readmissions to children’s hospitals?
Background: Thirty-day readmissions in adult Medicare beneficiaries are common and thought to represent potential for significant improvements in the quality of care. Penalties will be levied upon hospitals with excessively high readmission rates in adults. The stage is set for a translation of this practice to pediatric readmissions. However, the characteristics of readmissions to children’s hospitals are not well-defined.
Study design: Retrospective review.
Setting: National Association of Children’s Hospitals and Related Institutions (NACHRI) Case Mix data set.
Synopsis: Of 568,845 readmissions examined across 72 children’s hospitals, the 30-day readmission rate was 6.5%. Readmission rates varied by many factors: age, chronic conditions, insurance type, race/ethnicity, length of stay, number of annual hospital admissions, and hospital type. Rates varied significantly across hospitals, even after adjustment for age and chronic conditions. Anemia or neutropenia, ventricular shunt procedures, and sickle cell crisis had the highest unadjusted, 30-day, condition-specific readmission rates.
This study is notable for its large sample size but limited by the administrative data, which might, for example, underestimate readmissions that went to another hospital. Additionally, the majority of children in the U.S. are hospitalized outside of children’s hospitals, which are overrepresented in this study.
However, this study paints a clear picture of the differences between adult readmissions and pediatric readmissions—rates are lower than in elderly adults, and the top three conditions are distinctly different. Anemia or neutropenia likely are due to effects of chemotherapy; ventricular shunt readmissions often reflect surgery-related issues; and sickle cell disease is a lifelong, chronic condition. The significant variation between hospitals after case-mix adjustment offers an opportunity for further investigation and improvement.
Bottom line: Pediatric readmissions differ from adult readmissions and vary significantly across children’s hospitals.
Citation: Berry JG, Toomey SL, Zaslavsky AM, et al. Pediatric readmission prevalence and variability across hospitals. JAMA. 2013;309(4):372-380.
Reviewed by Pediatric Editor Mark Shen, MD, SFHM, medical director of hospital medicine at Dell Children's Medical Center, Austin, Texas.
Pediatric Readmissions Vary Significantly across Children’s Hospitals
Clinical question: What are the characteristics of readmissions to children’s hospitals?
Background: Thirty-day readmissions in adult Medicare beneficiaries are common and thought to represent potential for significant improvements in the quality of care. Penalties will be levied upon hospitals with excessively high readmission rates in adults. The stage is set for a translation of this practice to pediatric readmissions. However, the characteristics of readmissions to children’s hospitals are not well-defined.
Study design: Retrospective review.
Setting: National Association of Children’s Hospitals and Related Institutions (NACHRI) Case Mix data set.
Synopsis: Of 568,845 readmissions examined across 72 children’s hospitals, the 30-day readmission rate was 6.5%. Readmission rates varied by many factors: age, chronic conditions, insurance type, race/ethnicity, length of stay, number of annual hospital admissions, and hospital type. Rates varied significantly across hospitals, even after adjustment for age and chronic conditions. Anemia or neutropenia, ventricular shunt procedures, and sickle cell crisis had the highest unadjusted, 30-day, condition-specific readmission rates.
This study is notable for its large sample size but limited by the administrative data, which might, for example, underestimate readmissions that went to another hospital. Additionally, the majority of children in the U.S. are hospitalized outside of children’s hospitals, which are overrepresented in this study.
However, this study paints a clear picture of the differences between adult readmissions and pediatric readmissions—rates are lower than in elderly adults, and the top three conditions are distinctly different. Anemia or neutropenia likely are due to effects of chemotherapy; ventricular shunt readmissions often reflect surgery-related issues; and sickle cell disease is a lifelong, chronic condition. The significant variation between hospitals after case-mix adjustment offers an opportunity for further investigation and improvement.
Bottom line: Pediatric readmissions differ from adult readmissions and vary significantly across children’s hospitals.
Citation: Berry JG, Toomey SL, Zaslavsky AM, et al. Pediatric readmission prevalence and variability across hospitals. JAMA. 2013;309(4):372-380.
Reviewed by Pediatric Editor Mark Shen, MD, SFHM, medical director of hospital medicine at Dell Children's Medical Center, Austin, Texas.
Physician Reviews of Hospital Medicine-Related Research
In This Edition
Literature At A Glance
A guide to this month’s studies
- BNP-driven fluid management to improve ventilator weaning
- Examining 30-day readmission patterns to reduce repeat hospitalizations
- Impact of hospitalists’ workload on patient safety, care
- Permanent atrial fibrillation is best controlled by diltiazem
- Low-dose thrombolysis effective for pulmonary embolism
- High mortality rate seen in surgical patients requiring CPR
- ED visits common for acute-care patients post-discharge
- Restrictive transfusion strategies effective for upper GI bleeding
- Need for non-ICU acid suppression may be predictable
- Recommended changes for adult immunizations
BNP-Driven Fluid Management Improves Ventilator Weaning
Clinical question: Does fluid management guided by daily plasma natriuretic peptide-driven (BNP) levels in mechanically ventilated patients improve weaning outcomes compared with usual therapy dictated by clinical acumen?
Background: Ventilator weaning contributes at least 40% of the total duration of mechanical ventilation; strategies aimed at optimizing this process could provide substantial benefit. Previous studies have demonstrated that BNP levels prior to ventilator weaning independently predict weaning failure. No current objective practical guide to fluid management during ventilator weaning exists.
Study design: Randomized controlled trial.
Setting: Multiple international centers.
Synopsis: In a multicenter randomized controlled trial, 304 patients who met specific inclusion and exclusion criteria were randomized to either a BNP-driven or physician-guided strategy for fluid management during ventilator weaning. Patients with renal failure were excluded because of the influence of renal function on BNP levels.
All patients in both groups were ventilated with an automatic computer-driven weaning system to standardize the weaning process. In the BNP-driven group, diuretic use was higher, resulting in a more negative fluid balance and significantly shorter time to successful extubation (58.6 hours vs. 42.2 hours, P=0.03). The effect on weaning time was strongest in patients with left ventricular systolic dysfunction, whereas those with COPD seemed less likely to benefit. The two groups did not differ in baseline characteristics, length of stay, mortality, or development of adverse outcomes of renal failure, shock, or electrolyte disturbances.
Bottom line: Compared with physician-guided fluid management, a BNP-driven fluid management protocol decreased duration of ventilator weaning without significant differences in adverse events, mortality rate, or length of stay between the two groups.
Citation: Dessap AM, Roche-Campo F, Kouatchet A, et al. Natriuretic peptide-driven fluid management during ventilator weaning. Am J Respir Crit Care Med. 2012;186(12):1256-1263.
30-Day Readmission Patterns for MI, Heart Failure, Pneumonia
Clinical question: Do patterns exist among patients readmitted within 30 days of discharge for acute myocardial infarction (AMI), heart failure, or pneumonia that could provide insight for improving strategies aimed at reducing readmission rates?
Background: Examining readmission timing, diagnoses, and patient demographics might provide information to better guide post-discharge programs aimed at reducing overall readmissions.
Study design: Retrospective review of Centers for Medicare & Medicaid Services (CMS) data.
Setting: Acute-care hospitals.
Synopsis: Using CMS hospitalization data for principal diagnoses of AMI, heart failure, or pneumonia from 2007 through 2009, the authors examined the percentage of 30-day readmissions occurring on each day after discharge; the most common readmission diagnoses; the median time to readmission for common readmission diagnoses; and the relationship between patient demographic characteristics, readmission diagnoses, and timing. They found total readmission rates of 24.8% for heart failure, 19.9% for AMI, and 18.3% for pneumonia. Approximately two-thirds of 30-day readmissions occurred within the first 15 days after discharge for each cohort. Neither readmission diagnoses nor timing varied by patient age, sex, or race.
Although the majority of readmissions do occur soon after discharge, it is important to note that about one-third of all readmissions occur 16 to 30 days after discharge. There also was a diverse spectrum of readmission diagnoses that were not associated with patient demographic characteristics. These findings suggest that current post-discharge strategies aimed at specific diseases or time periods might only address a fraction of the patients at risk for readmission.
Bottom line: Among Medicare patients hospitalized for heart failure, AMI, or pneumonia, 30-day readmissions were frequent throughout the entire period, and readmission diagnoses or timing did not vary by patient age, sex, or race.
Citation: Dharmarajan K, Hsich AF, Lin Z, et al. Diagnosis and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
Workload Might Impact Patient Safety and Quality of Care
Clinical question: Do hospitalists’ workloads affect patient quality of care and safety?
Background: Preventable medical errors contribute to a large number of patient deaths each year. It is unclear if a hospitalist’s clinical workload affects rates of medical errors or patient harm.
Study design: Cross-sectional cohort study.
Setting: Hospitalists enrolled in online physician community QuantiaMD.com.
Synopsis: There has been limited research evaluating the correlation between physician workload and patient safety. An online survey compared the responses of 506 out of 890 enrolled physicians on the impact of average patient census and several outcome measures of quality of care. Some 40% reported that their patient census exceeded their personal safe workload at least once a month. They also reported that less time for patient evaluations led to fewer discussions with patients and family members, more unnecessary medical work-ups, and lower patient satisfaction.
A limitation of this study is that this electronic survey had the potential for selection bias. It also only measured perceptions of safety and quality, and only used standard daytime shifts (excluding night, cross-cover, weekend, and holiday shifts), which might have been associated with significantly different conclusions.
Bottom line: Increase in workload has a negative perceived impact on patient safety and quality of care for attending hospitalists.
Citation: Michtalik HJ, Yeh HC, Pronovost P, et. al. Impact of attending physician workload on patient care: a survey of hospitalists. JAMA Intern Med. 2013;173(5):375-377.
Permanent Atrial Fibrillation Best Controlled by Diltiazem
Clinical question: Is there a difference between beta-blockers and calcium channel blockers for ventricular rate control and arrhythmia-related symptoms in patients with permanent atrial fibrillation?
Background: Rate control with beta-blockers or calcium channel blockers is recommended for the initial therapy of atrial fibrillation. However, studies comparing those drug classes or drugs within them are lacking.
Study design: Prospective, randomized, investigator-blind crossover study.
Setting: Majority of patients from an atrial fibrillation outpatient clinic at Baerum Hospital in Norway.
Synopsis: The RATe Control in Atrial Fibrillation (RATAF) study included 60 participants with permanent atrial fibrillation. The goal of the study was to compare the efficacy of diltiazem at 360 mg/day, verapamil at 240 mg/day, metoprolol at 100 mg/day, and carvedilol at 25mg/day on ventricular heart rate and related symptoms in atrial fibrillation. Patients had a mean age of 71, atrial fibrillation for more than three months, and mean heart rate of 96 beats/minute. Exclusion criteria included the presence of congestive heart failure or ischemic heart disease with the need for other medications that could compromise the study.
From this study, diltiazem was shown to have the greatest effect in lowering heart rate, and those patients taking this medication had decreased symptoms related to atrial fibrillation. Hospitalists should not rely solely on this study for their treatment choice in all atrial fibrillation patients, but in certain populations, they should consider diltiazem as their first-line drug.
Bottom line: Diltiazem was shown to have the greatest reduction in heart rate and symptoms related to permanent atrial fibrillation.
Citation: Ulimoen SR, Enger S, Carlson J, et al. Comparison of four single-drug regimens on ventricular rate and arrhythmia-related symptoms in patients with permanent atrial fibrillation. Am J Cardiol. 2013:111(2):225-230.
Low-Dose Thrombolysis Effective in Moderate Pulmonary Embolism
Clinical question: Can low-dose tissue plasminogen activator (tPA) help reduce pulmonary artery pressure in those with moderate pulmonary embolism (PE)?
Background: Studies have shown full-dose thrombolysis can effectively decrease pulmonary artery pressure in patients with massive PE. However, there are limited data regarding low-dose or “safe dose” thrombolytic therapy and its effect on pulmonary artery pressure.
Study design: Prospective, controlled, randomized study.
Setting: Single center.
Synopsis: The Moderate Pulmonary Embolism Treated with Thrombolysis (MOPETT) study enrolled patients with moderate PE, defined as signs and symptoms of PE plus computed tomographic pulmonary angiographic involvement of > 70% involvement of thrombus in ≥2 lobar or left/right main pulmonary arteries or high probability ventilation/perfusion scan (mismatch in ≥2 lobes). Patients in the thrombolysis group (n=61) were given low-dose tPA (100 mg tPA) and anticoagulation vs. the control group (n=60), which received only anticoagulation.
The study ran for 22 months, and the primary end points were pulmonary hypertension and recurrent PE. After analysis, low-dose thrombolysis was shown to significantly decrease pulmonary artery pressure and occurrence of recurrent PE compared to the control group.
This study demonstrates that, while the decision to use thrombolytics should always be made cautiously, hospitalists can consider low-dose thrombolysis in patients with moderate PE.
Bottom line: Low-dose thrombolysis, in addition to anticoagulation, in patients with moderate PE decreases pulmonary hypertension and recurrent PE.
Citation: Sharifi M, Bay C, Skrocki L, Rahimi F, Mehdipour M. Moderate pulmonary embolism treated with thrombolysis (from the “MOPETT” trial). Am J Cardiol. 2013;111(2):273-277.
High Mortality in Surgical Patients Requiring CPR
Clinical question: What are the incidence, characteristics, and 30-day-outcomes of CPR in surgical patients?
Background: Most studies of CPR are based on the medical population, and little is known about the utilization, risk factors, and outcomes of CPR in surgical patients.
Study design: Retrospective cohort study.
Setting: Two hundred fifty U.S. hospitals in the American College of Surgeons’ National Surgical Quality Improvement Program.
Synopsis: A total of 1.3 million surgical cases were studied in the data set. The overall incidence was 1 event per 203 cases. Most patients (77.6%) experienced a complication and did so on or before the day of CPR in three-fourths of cases. The incidence of CPR was the highest for cardiac surgery patients. Patients who received CPR had a mortality rate of 71.6%. Mortality rates of CPR patients increased with more comorbidities.
Additionally, older age and an American Society of Anesthesiologists (ASA) class of 5 was associated with higher mortality.
Limitations of this study included coding flaws in data collection, lack of capture of resuscitation-related injuries, and failure to account for changes in DNR orders.
Hospitalists should be mindful of risk factors contributing to CPR in surgical patients when performing perioperative evaluations.
Bottom line: Surgical patients who experience CPR have a high mortality rate, but many of these patients have pre-arrest complications that can be preventable.
Citation: Kazaure HS, Roman SA, Rosenthal RA, Sosa, JA. Cardiac arrest among surgical patients. JAMA Surg. 2013;148(1):14-21.
Emergency Department Visits are Frequent Post-Discharge
Clinical question: What role do ED visits contribute to the overall use of acute-care services within 30 days of hospital discharge?
Background: Hospital readmissions within 30 days of discharge are a marker of the quality of care and reflect the effectiveness of the discharge process. ED visits are also a marker of hospital-based acute care following discharge, but little is known about the role of the ED during the post-discharge period.
Study design: Prospective study.
Setting: Acute-care hospitals in California, Florida, and Nebraska.
Synopsis: Using the Healthcare Cost and Utilization Project state inpatient and ED databases, all discharges between July 1, 2008, and Sept. 31, 2009, were evaluated for residents aged 18 years or older from three hospitals in three states. After exclusions, 5 million index hospitalizations among 4 million unique patients were studied.
Approximately 40% of the more than 1 million post-discharge acute-care encounters involved a visit to the ED.
Limitations of this study include that the data was derived from only three states, and only hospital-based acute-care visits were measured (i.e. visits to physician offices were not included). As hospitalists, we are responsible for discharges and care transitions. Being sensitive to the common medical conditions resulting in post-discharge ED encounters might improve care transitions.
Bottom line: Hospital readmission rates underestimate ED use following discharge.
Citation: Vashi AA, Fox JP, Carr BG, et al. Use of hospital-based acute care among patients recently discharged from the hospital. JAMA. 2013;309(4):364-371.
Restrictive Transfusion Strategy Beneficial in Upper GI Bleeding
Clinical question: What is the hemoglobin threshold for transfusion of red cells in patients with acute upper GI bleeding?
Background: Controlled trials have shown that restrictive transfusion strategies (Hgb<7) are as effective as liberal transfusion strategies (Hgb<9) in critically ill patients. These studies have excluded patients with GI bleeding. In cases for which GI is not severe, the safest transfusion strategy is controversial.
Study design: Single-center study at Hospital de la Santa Creu i Sant Pau, Barcelona, Spain.
Synopsis: A total of 921 adult patients with acute upper GI bleeding were enrolled and assigned: 461 to a restrictive transfusion strategy (hemoglobin<7) and 460 to a liberal strategy (hemoglobin<9). Patients with massive exsanguinating bleeding, acute coronary syndrome, peripheral vasculopathy, stroke, transient ischemic attack, lower GI bleed, recent trauma or surgery, or low risk of rebleeding were excluded. The primary outcome measure was the rate of death from any cause within the first 45 days.
Secondary outcomes included the rate of further bleeding and the rate of in-hospital complications.
Statistically significant benefit in following a restrictive versus liberal strategy was demonstrated in all major outcomes: mortality (5% vs, 9%, P=0.02), rate of further bleeding (10% vs 18%, P=0.01), and rate of complications (40% vs. 48%, P=0.02).
The study is limited by its inability to be generalized to all patients with acute GI bleeding, as patients with massive exsanguinating bleeds and those with low risk of rebleeding were excluded.
Bottom line: Restrictive transfusion (Hgb<7) significantly improved outcomes for patients with acute upper GI bleeding.
Citation: Villanueva C, Colomo A, Bosch A, et al. Transfusion strategies for acute upper gastrointestinal bleeding. N Engl J Med. 2013;368(1):11-21.
Need for Non-ICU Acid Suppression Might Be Predictable
Clinical question: What are the risk factors for nosocomial bleeding in non-critically-ill patients?
Background: Acid-suppressive medication has been shown to reduce the incidence of nosocomial GI bleed in the ICU, but current guidelines recommend against its use in non-critically-ill patients. However, a subgroup of these patients might possess a high enough risk for GI bleed that prophylaxis is warranted.
Study design: Cohort study.
Setting: Academic medical center in Boston.
Synopsis: A total of 75,723 admissions of adult patients hospitalized for three or more days were included. Exclusion criteria included primary discharge diagnosis of GI bleed; principal procedure code of cardiac catheterization; and bleeding episodes occurring while in the ICU or within 48 hours of transfer out of the ICU. The primary outcome was nosocomial GI bleed (>24 hours after admission) occurring outside the ICU.
Nosocomial GI bleeding occurred in 203 patients (0.27%). Independent risk factors for bleeding included age >60, male sex, liver disease, acute renal failure, sepsis, being on a medicine service, prophylactic anticoagulation, and coagulopathy. Based on the data, a scoring system was created that identified a high-risk group in whom the number needed to treat with acid-suppressive medication to prevent one bleed was 48.
The major limitations of this study are its observational nature and the need for validation of the proposed scoring system.
Bottom line: Risk for nosocomial GI bleeding appears predictable and supports the selective use of prophylactic acid suppression in non-critically-ill patients.
Citation: Herzig SJ, Rothberg MB, Feinbloom DB, et al. Risk factors for nosocomial gastrointestinal bleeding and use of acid-suppressive medication in non-critically ill patients. J Gen Intern Med. 2013; January 5. [Epub ahead of print].
Additions, Modifications, and Clarifications Regarding Adult Immunization
Clinical question: What are the changes to the recommended Adult Immunization Schedule for 2013?
Background: Despite the known public health benefits of immunization, adult vaccination rates remain low. The positive impact of strong provider recommendations regarding vaccines underscores the importance of provider awareness of vaccine schedules, precautions, and contraindications.
Study design: Annual Advisory Committee on Immunization Practices (ACIP) review.
Setting: Data from 2011 National Health Interview Survey.
Synopsis: Highlighted changes include: 1) a single dose of pneumococcal 13-valent conjugate (PCV13) vaccine is now recommended for all individuals over the age of 19 with qualifying conditions; 2) clarification regarding pneumococcal polysaccharide (PPSV23) vaccine illustrates that high-risk individuals will receive up to three doses (one or two doses prior to age 65, plus an additional dose after the age of 65); 3) one dose of tetanus, diphtheria, and acellular pertussis (Tdap) vaccine is now recommended for all adults, including individuals age >65; 4) pregnant woman are advised to receive Tdap between 27 and 36 weeks’ gestation, with each pregnancy to provide protection to their newborn in the first months of life; 5) quadrivalent formulations of the live attenuated influenza vaccine (LAIV) and most likely the inactivated influenza vaccine (IIV) will be available in the 2013-2014 influenza season to increase cross-reactive protection against influenza B; and 6) both injection and noninjection illicit drug users are recommended to receive hepatitis A vaccine.
Bottom line: Expanded recommendations for adult immunization provide more opportunities for the practicing hospitalist to improve vaccine capture.
Citation: Advisory Committee on Immunization Practices. Recommended adult immunization schedule: United States, 2013. Ann Int Med. 2013;158(3):191-199.
In This Edition
Literature At A Glance
A guide to this month’s studies
- BNP-driven fluid management to improve ventilator weaning
- Examining 30-day readmission patterns to reduce repeat hospitalizations
- Impact of hospitalists’ workload on patient safety, care
- Permanent atrial fibrillation is best controlled by diltiazem
- Low-dose thrombolysis effective for pulmonary embolism
- High mortality rate seen in surgical patients requiring CPR
- ED visits common for acute-care patients post-discharge
- Restrictive transfusion strategies effective for upper GI bleeding
- Need for non-ICU acid suppression may be predictable
- Recommended changes for adult immunizations
BNP-Driven Fluid Management Improves Ventilator Weaning
Clinical question: Does fluid management guided by daily plasma natriuretic peptide-driven (BNP) levels in mechanically ventilated patients improve weaning outcomes compared with usual therapy dictated by clinical acumen?
Background: Ventilator weaning contributes at least 40% of the total duration of mechanical ventilation; strategies aimed at optimizing this process could provide substantial benefit. Previous studies have demonstrated that BNP levels prior to ventilator weaning independently predict weaning failure. No current objective practical guide to fluid management during ventilator weaning exists.
Study design: Randomized controlled trial.
Setting: Multiple international centers.
Synopsis: In a multicenter randomized controlled trial, 304 patients who met specific inclusion and exclusion criteria were randomized to either a BNP-driven or physician-guided strategy for fluid management during ventilator weaning. Patients with renal failure were excluded because of the influence of renal function on BNP levels.
All patients in both groups were ventilated with an automatic computer-driven weaning system to standardize the weaning process. In the BNP-driven group, diuretic use was higher, resulting in a more negative fluid balance and significantly shorter time to successful extubation (58.6 hours vs. 42.2 hours, P=0.03). The effect on weaning time was strongest in patients with left ventricular systolic dysfunction, whereas those with COPD seemed less likely to benefit. The two groups did not differ in baseline characteristics, length of stay, mortality, or development of adverse outcomes of renal failure, shock, or electrolyte disturbances.
Bottom line: Compared with physician-guided fluid management, a BNP-driven fluid management protocol decreased duration of ventilator weaning without significant differences in adverse events, mortality rate, or length of stay between the two groups.
Citation: Dessap AM, Roche-Campo F, Kouatchet A, et al. Natriuretic peptide-driven fluid management during ventilator weaning. Am J Respir Crit Care Med. 2012;186(12):1256-1263.
30-Day Readmission Patterns for MI, Heart Failure, Pneumonia
Clinical question: Do patterns exist among patients readmitted within 30 days of discharge for acute myocardial infarction (AMI), heart failure, or pneumonia that could provide insight for improving strategies aimed at reducing readmission rates?
Background: Examining readmission timing, diagnoses, and patient demographics might provide information to better guide post-discharge programs aimed at reducing overall readmissions.
Study design: Retrospective review of Centers for Medicare & Medicaid Services (CMS) data.
Setting: Acute-care hospitals.
Synopsis: Using CMS hospitalization data for principal diagnoses of AMI, heart failure, or pneumonia from 2007 through 2009, the authors examined the percentage of 30-day readmissions occurring on each day after discharge; the most common readmission diagnoses; the median time to readmission for common readmission diagnoses; and the relationship between patient demographic characteristics, readmission diagnoses, and timing. They found total readmission rates of 24.8% for heart failure, 19.9% for AMI, and 18.3% for pneumonia. Approximately two-thirds of 30-day readmissions occurred within the first 15 days after discharge for each cohort. Neither readmission diagnoses nor timing varied by patient age, sex, or race.
Although the majority of readmissions do occur soon after discharge, it is important to note that about one-third of all readmissions occur 16 to 30 days after discharge. There also was a diverse spectrum of readmission diagnoses that were not associated with patient demographic characteristics. These findings suggest that current post-discharge strategies aimed at specific diseases or time periods might only address a fraction of the patients at risk for readmission.
Bottom line: Among Medicare patients hospitalized for heart failure, AMI, or pneumonia, 30-day readmissions were frequent throughout the entire period, and readmission diagnoses or timing did not vary by patient age, sex, or race.
Citation: Dharmarajan K, Hsich AF, Lin Z, et al. Diagnosis and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
Workload Might Impact Patient Safety and Quality of Care
Clinical question: Do hospitalists’ workloads affect patient quality of care and safety?
Background: Preventable medical errors contribute to a large number of patient deaths each year. It is unclear if a hospitalist’s clinical workload affects rates of medical errors or patient harm.
Study design: Cross-sectional cohort study.
Setting: Hospitalists enrolled in online physician community QuantiaMD.com.
Synopsis: There has been limited research evaluating the correlation between physician workload and patient safety. An online survey compared the responses of 506 out of 890 enrolled physicians on the impact of average patient census and several outcome measures of quality of care. Some 40% reported that their patient census exceeded their personal safe workload at least once a month. They also reported that less time for patient evaluations led to fewer discussions with patients and family members, more unnecessary medical work-ups, and lower patient satisfaction.
A limitation of this study is that this electronic survey had the potential for selection bias. It also only measured perceptions of safety and quality, and only used standard daytime shifts (excluding night, cross-cover, weekend, and holiday shifts), which might have been associated with significantly different conclusions.
Bottom line: Increase in workload has a negative perceived impact on patient safety and quality of care for attending hospitalists.
Citation: Michtalik HJ, Yeh HC, Pronovost P, et. al. Impact of attending physician workload on patient care: a survey of hospitalists. JAMA Intern Med. 2013;173(5):375-377.
Permanent Atrial Fibrillation Best Controlled by Diltiazem
Clinical question: Is there a difference between beta-blockers and calcium channel blockers for ventricular rate control and arrhythmia-related symptoms in patients with permanent atrial fibrillation?
Background: Rate control with beta-blockers or calcium channel blockers is recommended for the initial therapy of atrial fibrillation. However, studies comparing those drug classes or drugs within them are lacking.
Study design: Prospective, randomized, investigator-blind crossover study.
Setting: Majority of patients from an atrial fibrillation outpatient clinic at Baerum Hospital in Norway.
Synopsis: The RATe Control in Atrial Fibrillation (RATAF) study included 60 participants with permanent atrial fibrillation. The goal of the study was to compare the efficacy of diltiazem at 360 mg/day, verapamil at 240 mg/day, metoprolol at 100 mg/day, and carvedilol at 25mg/day on ventricular heart rate and related symptoms in atrial fibrillation. Patients had a mean age of 71, atrial fibrillation for more than three months, and mean heart rate of 96 beats/minute. Exclusion criteria included the presence of congestive heart failure or ischemic heart disease with the need for other medications that could compromise the study.
From this study, diltiazem was shown to have the greatest effect in lowering heart rate, and those patients taking this medication had decreased symptoms related to atrial fibrillation. Hospitalists should not rely solely on this study for their treatment choice in all atrial fibrillation patients, but in certain populations, they should consider diltiazem as their first-line drug.
Bottom line: Diltiazem was shown to have the greatest reduction in heart rate and symptoms related to permanent atrial fibrillation.
Citation: Ulimoen SR, Enger S, Carlson J, et al. Comparison of four single-drug regimens on ventricular rate and arrhythmia-related symptoms in patients with permanent atrial fibrillation. Am J Cardiol. 2013:111(2):225-230.
Low-Dose Thrombolysis Effective in Moderate Pulmonary Embolism
Clinical question: Can low-dose tissue plasminogen activator (tPA) help reduce pulmonary artery pressure in those with moderate pulmonary embolism (PE)?
Background: Studies have shown full-dose thrombolysis can effectively decrease pulmonary artery pressure in patients with massive PE. However, there are limited data regarding low-dose or “safe dose” thrombolytic therapy and its effect on pulmonary artery pressure.
Study design: Prospective, controlled, randomized study.
Setting: Single center.
Synopsis: The Moderate Pulmonary Embolism Treated with Thrombolysis (MOPETT) study enrolled patients with moderate PE, defined as signs and symptoms of PE plus computed tomographic pulmonary angiographic involvement of > 70% involvement of thrombus in ≥2 lobar or left/right main pulmonary arteries or high probability ventilation/perfusion scan (mismatch in ≥2 lobes). Patients in the thrombolysis group (n=61) were given low-dose tPA (100 mg tPA) and anticoagulation vs. the control group (n=60), which received only anticoagulation.
The study ran for 22 months, and the primary end points were pulmonary hypertension and recurrent PE. After analysis, low-dose thrombolysis was shown to significantly decrease pulmonary artery pressure and occurrence of recurrent PE compared to the control group.
This study demonstrates that, while the decision to use thrombolytics should always be made cautiously, hospitalists can consider low-dose thrombolysis in patients with moderate PE.
Bottom line: Low-dose thrombolysis, in addition to anticoagulation, in patients with moderate PE decreases pulmonary hypertension and recurrent PE.
Citation: Sharifi M, Bay C, Skrocki L, Rahimi F, Mehdipour M. Moderate pulmonary embolism treated with thrombolysis (from the “MOPETT” trial). Am J Cardiol. 2013;111(2):273-277.
High Mortality in Surgical Patients Requiring CPR
Clinical question: What are the incidence, characteristics, and 30-day-outcomes of CPR in surgical patients?
Background: Most studies of CPR are based on the medical population, and little is known about the utilization, risk factors, and outcomes of CPR in surgical patients.
Study design: Retrospective cohort study.
Setting: Two hundred fifty U.S. hospitals in the American College of Surgeons’ National Surgical Quality Improvement Program.
Synopsis: A total of 1.3 million surgical cases were studied in the data set. The overall incidence was 1 event per 203 cases. Most patients (77.6%) experienced a complication and did so on or before the day of CPR in three-fourths of cases. The incidence of CPR was the highest for cardiac surgery patients. Patients who received CPR had a mortality rate of 71.6%. Mortality rates of CPR patients increased with more comorbidities.
Additionally, older age and an American Society of Anesthesiologists (ASA) class of 5 was associated with higher mortality.
Limitations of this study included coding flaws in data collection, lack of capture of resuscitation-related injuries, and failure to account for changes in DNR orders.
Hospitalists should be mindful of risk factors contributing to CPR in surgical patients when performing perioperative evaluations.
Bottom line: Surgical patients who experience CPR have a high mortality rate, but many of these patients have pre-arrest complications that can be preventable.
Citation: Kazaure HS, Roman SA, Rosenthal RA, Sosa, JA. Cardiac arrest among surgical patients. JAMA Surg. 2013;148(1):14-21.
Emergency Department Visits are Frequent Post-Discharge
Clinical question: What role do ED visits contribute to the overall use of acute-care services within 30 days of hospital discharge?
Background: Hospital readmissions within 30 days of discharge are a marker of the quality of care and reflect the effectiveness of the discharge process. ED visits are also a marker of hospital-based acute care following discharge, but little is known about the role of the ED during the post-discharge period.
Study design: Prospective study.
Setting: Acute-care hospitals in California, Florida, and Nebraska.
Synopsis: Using the Healthcare Cost and Utilization Project state inpatient and ED databases, all discharges between July 1, 2008, and Sept. 31, 2009, were evaluated for residents aged 18 years or older from three hospitals in three states. After exclusions, 5 million index hospitalizations among 4 million unique patients were studied.
Approximately 40% of the more than 1 million post-discharge acute-care encounters involved a visit to the ED.
Limitations of this study include that the data was derived from only three states, and only hospital-based acute-care visits were measured (i.e. visits to physician offices were not included). As hospitalists, we are responsible for discharges and care transitions. Being sensitive to the common medical conditions resulting in post-discharge ED encounters might improve care transitions.
Bottom line: Hospital readmission rates underestimate ED use following discharge.
Citation: Vashi AA, Fox JP, Carr BG, et al. Use of hospital-based acute care among patients recently discharged from the hospital. JAMA. 2013;309(4):364-371.
Restrictive Transfusion Strategy Beneficial in Upper GI Bleeding
Clinical question: What is the hemoglobin threshold for transfusion of red cells in patients with acute upper GI bleeding?
Background: Controlled trials have shown that restrictive transfusion strategies (Hgb<7) are as effective as liberal transfusion strategies (Hgb<9) in critically ill patients. These studies have excluded patients with GI bleeding. In cases for which GI is not severe, the safest transfusion strategy is controversial.
Study design: Single-center study at Hospital de la Santa Creu i Sant Pau, Barcelona, Spain.
Synopsis: A total of 921 adult patients with acute upper GI bleeding were enrolled and assigned: 461 to a restrictive transfusion strategy (hemoglobin<7) and 460 to a liberal strategy (hemoglobin<9). Patients with massive exsanguinating bleeding, acute coronary syndrome, peripheral vasculopathy, stroke, transient ischemic attack, lower GI bleed, recent trauma or surgery, or low risk of rebleeding were excluded. The primary outcome measure was the rate of death from any cause within the first 45 days.
Secondary outcomes included the rate of further bleeding and the rate of in-hospital complications.
Statistically significant benefit in following a restrictive versus liberal strategy was demonstrated in all major outcomes: mortality (5% vs, 9%, P=0.02), rate of further bleeding (10% vs 18%, P=0.01), and rate of complications (40% vs. 48%, P=0.02).
The study is limited by its inability to be generalized to all patients with acute GI bleeding, as patients with massive exsanguinating bleeds and those with low risk of rebleeding were excluded.
Bottom line: Restrictive transfusion (Hgb<7) significantly improved outcomes for patients with acute upper GI bleeding.
Citation: Villanueva C, Colomo A, Bosch A, et al. Transfusion strategies for acute upper gastrointestinal bleeding. N Engl J Med. 2013;368(1):11-21.
Need for Non-ICU Acid Suppression Might Be Predictable
Clinical question: What are the risk factors for nosocomial bleeding in non-critically-ill patients?
Background: Acid-suppressive medication has been shown to reduce the incidence of nosocomial GI bleed in the ICU, but current guidelines recommend against its use in non-critically-ill patients. However, a subgroup of these patients might possess a high enough risk for GI bleed that prophylaxis is warranted.
Study design: Cohort study.
Setting: Academic medical center in Boston.
Synopsis: A total of 75,723 admissions of adult patients hospitalized for three or more days were included. Exclusion criteria included primary discharge diagnosis of GI bleed; principal procedure code of cardiac catheterization; and bleeding episodes occurring while in the ICU or within 48 hours of transfer out of the ICU. The primary outcome was nosocomial GI bleed (>24 hours after admission) occurring outside the ICU.
Nosocomial GI bleeding occurred in 203 patients (0.27%). Independent risk factors for bleeding included age >60, male sex, liver disease, acute renal failure, sepsis, being on a medicine service, prophylactic anticoagulation, and coagulopathy. Based on the data, a scoring system was created that identified a high-risk group in whom the number needed to treat with acid-suppressive medication to prevent one bleed was 48.
The major limitations of this study are its observational nature and the need for validation of the proposed scoring system.
Bottom line: Risk for nosocomial GI bleeding appears predictable and supports the selective use of prophylactic acid suppression in non-critically-ill patients.
Citation: Herzig SJ, Rothberg MB, Feinbloom DB, et al. Risk factors for nosocomial gastrointestinal bleeding and use of acid-suppressive medication in non-critically ill patients. J Gen Intern Med. 2013; January 5. [Epub ahead of print].
Additions, Modifications, and Clarifications Regarding Adult Immunization
Clinical question: What are the changes to the recommended Adult Immunization Schedule for 2013?
Background: Despite the known public health benefits of immunization, adult vaccination rates remain low. The positive impact of strong provider recommendations regarding vaccines underscores the importance of provider awareness of vaccine schedules, precautions, and contraindications.
Study design: Annual Advisory Committee on Immunization Practices (ACIP) review.
Setting: Data from 2011 National Health Interview Survey.
Synopsis: Highlighted changes include: 1) a single dose of pneumococcal 13-valent conjugate (PCV13) vaccine is now recommended for all individuals over the age of 19 with qualifying conditions; 2) clarification regarding pneumococcal polysaccharide (PPSV23) vaccine illustrates that high-risk individuals will receive up to three doses (one or two doses prior to age 65, plus an additional dose after the age of 65); 3) one dose of tetanus, diphtheria, and acellular pertussis (Tdap) vaccine is now recommended for all adults, including individuals age >65; 4) pregnant woman are advised to receive Tdap between 27 and 36 weeks’ gestation, with each pregnancy to provide protection to their newborn in the first months of life; 5) quadrivalent formulations of the live attenuated influenza vaccine (LAIV) and most likely the inactivated influenza vaccine (IIV) will be available in the 2013-2014 influenza season to increase cross-reactive protection against influenza B; and 6) both injection and noninjection illicit drug users are recommended to receive hepatitis A vaccine.
Bottom line: Expanded recommendations for adult immunization provide more opportunities for the practicing hospitalist to improve vaccine capture.
Citation: Advisory Committee on Immunization Practices. Recommended adult immunization schedule: United States, 2013. Ann Int Med. 2013;158(3):191-199.
In This Edition
Literature At A Glance
A guide to this month’s studies
- BNP-driven fluid management to improve ventilator weaning
- Examining 30-day readmission patterns to reduce repeat hospitalizations
- Impact of hospitalists’ workload on patient safety, care
- Permanent atrial fibrillation is best controlled by diltiazem
- Low-dose thrombolysis effective for pulmonary embolism
- High mortality rate seen in surgical patients requiring CPR
- ED visits common for acute-care patients post-discharge
- Restrictive transfusion strategies effective for upper GI bleeding
- Need for non-ICU acid suppression may be predictable
- Recommended changes for adult immunizations
BNP-Driven Fluid Management Improves Ventilator Weaning
Clinical question: Does fluid management guided by daily plasma natriuretic peptide-driven (BNP) levels in mechanically ventilated patients improve weaning outcomes compared with usual therapy dictated by clinical acumen?
Background: Ventilator weaning contributes at least 40% of the total duration of mechanical ventilation; strategies aimed at optimizing this process could provide substantial benefit. Previous studies have demonstrated that BNP levels prior to ventilator weaning independently predict weaning failure. No current objective practical guide to fluid management during ventilator weaning exists.
Study design: Randomized controlled trial.
Setting: Multiple international centers.
Synopsis: In a multicenter randomized controlled trial, 304 patients who met specific inclusion and exclusion criteria were randomized to either a BNP-driven or physician-guided strategy for fluid management during ventilator weaning. Patients with renal failure were excluded because of the influence of renal function on BNP levels.
All patients in both groups were ventilated with an automatic computer-driven weaning system to standardize the weaning process. In the BNP-driven group, diuretic use was higher, resulting in a more negative fluid balance and significantly shorter time to successful extubation (58.6 hours vs. 42.2 hours, P=0.03). The effect on weaning time was strongest in patients with left ventricular systolic dysfunction, whereas those with COPD seemed less likely to benefit. The two groups did not differ in baseline characteristics, length of stay, mortality, or development of adverse outcomes of renal failure, shock, or electrolyte disturbances.
Bottom line: Compared with physician-guided fluid management, a BNP-driven fluid management protocol decreased duration of ventilator weaning without significant differences in adverse events, mortality rate, or length of stay between the two groups.
Citation: Dessap AM, Roche-Campo F, Kouatchet A, et al. Natriuretic peptide-driven fluid management during ventilator weaning. Am J Respir Crit Care Med. 2012;186(12):1256-1263.
30-Day Readmission Patterns for MI, Heart Failure, Pneumonia
Clinical question: Do patterns exist among patients readmitted within 30 days of discharge for acute myocardial infarction (AMI), heart failure, or pneumonia that could provide insight for improving strategies aimed at reducing readmission rates?
Background: Examining readmission timing, diagnoses, and patient demographics might provide information to better guide post-discharge programs aimed at reducing overall readmissions.
Study design: Retrospective review of Centers for Medicare & Medicaid Services (CMS) data.
Setting: Acute-care hospitals.
Synopsis: Using CMS hospitalization data for principal diagnoses of AMI, heart failure, or pneumonia from 2007 through 2009, the authors examined the percentage of 30-day readmissions occurring on each day after discharge; the most common readmission diagnoses; the median time to readmission for common readmission diagnoses; and the relationship between patient demographic characteristics, readmission diagnoses, and timing. They found total readmission rates of 24.8% for heart failure, 19.9% for AMI, and 18.3% for pneumonia. Approximately two-thirds of 30-day readmissions occurred within the first 15 days after discharge for each cohort. Neither readmission diagnoses nor timing varied by patient age, sex, or race.
Although the majority of readmissions do occur soon after discharge, it is important to note that about one-third of all readmissions occur 16 to 30 days after discharge. There also was a diverse spectrum of readmission diagnoses that were not associated with patient demographic characteristics. These findings suggest that current post-discharge strategies aimed at specific diseases or time periods might only address a fraction of the patients at risk for readmission.
Bottom line: Among Medicare patients hospitalized for heart failure, AMI, or pneumonia, 30-day readmissions were frequent throughout the entire period, and readmission diagnoses or timing did not vary by patient age, sex, or race.
Citation: Dharmarajan K, Hsich AF, Lin Z, et al. Diagnosis and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
Workload Might Impact Patient Safety and Quality of Care
Clinical question: Do hospitalists’ workloads affect patient quality of care and safety?
Background: Preventable medical errors contribute to a large number of patient deaths each year. It is unclear if a hospitalist’s clinical workload affects rates of medical errors or patient harm.
Study design: Cross-sectional cohort study.
Setting: Hospitalists enrolled in online physician community QuantiaMD.com.
Synopsis: There has been limited research evaluating the correlation between physician workload and patient safety. An online survey compared the responses of 506 out of 890 enrolled physicians on the impact of average patient census and several outcome measures of quality of care. Some 40% reported that their patient census exceeded their personal safe workload at least once a month. They also reported that less time for patient evaluations led to fewer discussions with patients and family members, more unnecessary medical work-ups, and lower patient satisfaction.
A limitation of this study is that this electronic survey had the potential for selection bias. It also only measured perceptions of safety and quality, and only used standard daytime shifts (excluding night, cross-cover, weekend, and holiday shifts), which might have been associated with significantly different conclusions.
Bottom line: Increase in workload has a negative perceived impact on patient safety and quality of care for attending hospitalists.
Citation: Michtalik HJ, Yeh HC, Pronovost P, et. al. Impact of attending physician workload on patient care: a survey of hospitalists. JAMA Intern Med. 2013;173(5):375-377.
Permanent Atrial Fibrillation Best Controlled by Diltiazem
Clinical question: Is there a difference between beta-blockers and calcium channel blockers for ventricular rate control and arrhythmia-related symptoms in patients with permanent atrial fibrillation?
Background: Rate control with beta-blockers or calcium channel blockers is recommended for the initial therapy of atrial fibrillation. However, studies comparing those drug classes or drugs within them are lacking.
Study design: Prospective, randomized, investigator-blind crossover study.
Setting: Majority of patients from an atrial fibrillation outpatient clinic at Baerum Hospital in Norway.
Synopsis: The RATe Control in Atrial Fibrillation (RATAF) study included 60 participants with permanent atrial fibrillation. The goal of the study was to compare the efficacy of diltiazem at 360 mg/day, verapamil at 240 mg/day, metoprolol at 100 mg/day, and carvedilol at 25mg/day on ventricular heart rate and related symptoms in atrial fibrillation. Patients had a mean age of 71, atrial fibrillation for more than three months, and mean heart rate of 96 beats/minute. Exclusion criteria included the presence of congestive heart failure or ischemic heart disease with the need for other medications that could compromise the study.
From this study, diltiazem was shown to have the greatest effect in lowering heart rate, and those patients taking this medication had decreased symptoms related to atrial fibrillation. Hospitalists should not rely solely on this study for their treatment choice in all atrial fibrillation patients, but in certain populations, they should consider diltiazem as their first-line drug.
Bottom line: Diltiazem was shown to have the greatest reduction in heart rate and symptoms related to permanent atrial fibrillation.
Citation: Ulimoen SR, Enger S, Carlson J, et al. Comparison of four single-drug regimens on ventricular rate and arrhythmia-related symptoms in patients with permanent atrial fibrillation. Am J Cardiol. 2013:111(2):225-230.
Low-Dose Thrombolysis Effective in Moderate Pulmonary Embolism
Clinical question: Can low-dose tissue plasminogen activator (tPA) help reduce pulmonary artery pressure in those with moderate pulmonary embolism (PE)?
Background: Studies have shown full-dose thrombolysis can effectively decrease pulmonary artery pressure in patients with massive PE. However, there are limited data regarding low-dose or “safe dose” thrombolytic therapy and its effect on pulmonary artery pressure.
Study design: Prospective, controlled, randomized study.
Setting: Single center.
Synopsis: The Moderate Pulmonary Embolism Treated with Thrombolysis (MOPETT) study enrolled patients with moderate PE, defined as signs and symptoms of PE plus computed tomographic pulmonary angiographic involvement of > 70% involvement of thrombus in ≥2 lobar or left/right main pulmonary arteries or high probability ventilation/perfusion scan (mismatch in ≥2 lobes). Patients in the thrombolysis group (n=61) were given low-dose tPA (100 mg tPA) and anticoagulation vs. the control group (n=60), which received only anticoagulation.
The study ran for 22 months, and the primary end points were pulmonary hypertension and recurrent PE. After analysis, low-dose thrombolysis was shown to significantly decrease pulmonary artery pressure and occurrence of recurrent PE compared to the control group.
This study demonstrates that, while the decision to use thrombolytics should always be made cautiously, hospitalists can consider low-dose thrombolysis in patients with moderate PE.
Bottom line: Low-dose thrombolysis, in addition to anticoagulation, in patients with moderate PE decreases pulmonary hypertension and recurrent PE.
Citation: Sharifi M, Bay C, Skrocki L, Rahimi F, Mehdipour M. Moderate pulmonary embolism treated with thrombolysis (from the “MOPETT” trial). Am J Cardiol. 2013;111(2):273-277.
High Mortality in Surgical Patients Requiring CPR
Clinical question: What are the incidence, characteristics, and 30-day-outcomes of CPR in surgical patients?
Background: Most studies of CPR are based on the medical population, and little is known about the utilization, risk factors, and outcomes of CPR in surgical patients.
Study design: Retrospective cohort study.
Setting: Two hundred fifty U.S. hospitals in the American College of Surgeons’ National Surgical Quality Improvement Program.
Synopsis: A total of 1.3 million surgical cases were studied in the data set. The overall incidence was 1 event per 203 cases. Most patients (77.6%) experienced a complication and did so on or before the day of CPR in three-fourths of cases. The incidence of CPR was the highest for cardiac surgery patients. Patients who received CPR had a mortality rate of 71.6%. Mortality rates of CPR patients increased with more comorbidities.
Additionally, older age and an American Society of Anesthesiologists (ASA) class of 5 was associated with higher mortality.
Limitations of this study included coding flaws in data collection, lack of capture of resuscitation-related injuries, and failure to account for changes in DNR orders.
Hospitalists should be mindful of risk factors contributing to CPR in surgical patients when performing perioperative evaluations.
Bottom line: Surgical patients who experience CPR have a high mortality rate, but many of these patients have pre-arrest complications that can be preventable.
Citation: Kazaure HS, Roman SA, Rosenthal RA, Sosa, JA. Cardiac arrest among surgical patients. JAMA Surg. 2013;148(1):14-21.
Emergency Department Visits are Frequent Post-Discharge
Clinical question: What role do ED visits contribute to the overall use of acute-care services within 30 days of hospital discharge?
Background: Hospital readmissions within 30 days of discharge are a marker of the quality of care and reflect the effectiveness of the discharge process. ED visits are also a marker of hospital-based acute care following discharge, but little is known about the role of the ED during the post-discharge period.
Study design: Prospective study.
Setting: Acute-care hospitals in California, Florida, and Nebraska.
Synopsis: Using the Healthcare Cost and Utilization Project state inpatient and ED databases, all discharges between July 1, 2008, and Sept. 31, 2009, were evaluated for residents aged 18 years or older from three hospitals in three states. After exclusions, 5 million index hospitalizations among 4 million unique patients were studied.
Approximately 40% of the more than 1 million post-discharge acute-care encounters involved a visit to the ED.
Limitations of this study include that the data was derived from only three states, and only hospital-based acute-care visits were measured (i.e. visits to physician offices were not included). As hospitalists, we are responsible for discharges and care transitions. Being sensitive to the common medical conditions resulting in post-discharge ED encounters might improve care transitions.
Bottom line: Hospital readmission rates underestimate ED use following discharge.
Citation: Vashi AA, Fox JP, Carr BG, et al. Use of hospital-based acute care among patients recently discharged from the hospital. JAMA. 2013;309(4):364-371.
Restrictive Transfusion Strategy Beneficial in Upper GI Bleeding
Clinical question: What is the hemoglobin threshold for transfusion of red cells in patients with acute upper GI bleeding?
Background: Controlled trials have shown that restrictive transfusion strategies (Hgb<7) are as effective as liberal transfusion strategies (Hgb<9) in critically ill patients. These studies have excluded patients with GI bleeding. In cases for which GI is not severe, the safest transfusion strategy is controversial.
Study design: Single-center study at Hospital de la Santa Creu i Sant Pau, Barcelona, Spain.
Synopsis: A total of 921 adult patients with acute upper GI bleeding were enrolled and assigned: 461 to a restrictive transfusion strategy (hemoglobin<7) and 460 to a liberal strategy (hemoglobin<9). Patients with massive exsanguinating bleeding, acute coronary syndrome, peripheral vasculopathy, stroke, transient ischemic attack, lower GI bleed, recent trauma or surgery, or low risk of rebleeding were excluded. The primary outcome measure was the rate of death from any cause within the first 45 days.
Secondary outcomes included the rate of further bleeding and the rate of in-hospital complications.
Statistically significant benefit in following a restrictive versus liberal strategy was demonstrated in all major outcomes: mortality (5% vs, 9%, P=0.02), rate of further bleeding (10% vs 18%, P=0.01), and rate of complications (40% vs. 48%, P=0.02).
The study is limited by its inability to be generalized to all patients with acute GI bleeding, as patients with massive exsanguinating bleeds and those with low risk of rebleeding were excluded.
Bottom line: Restrictive transfusion (Hgb<7) significantly improved outcomes for patients with acute upper GI bleeding.
Citation: Villanueva C, Colomo A, Bosch A, et al. Transfusion strategies for acute upper gastrointestinal bleeding. N Engl J Med. 2013;368(1):11-21.
Need for Non-ICU Acid Suppression Might Be Predictable
Clinical question: What are the risk factors for nosocomial bleeding in non-critically-ill patients?
Background: Acid-suppressive medication has been shown to reduce the incidence of nosocomial GI bleed in the ICU, but current guidelines recommend against its use in non-critically-ill patients. However, a subgroup of these patients might possess a high enough risk for GI bleed that prophylaxis is warranted.
Study design: Cohort study.
Setting: Academic medical center in Boston.
Synopsis: A total of 75,723 admissions of adult patients hospitalized for three or more days were included. Exclusion criteria included primary discharge diagnosis of GI bleed; principal procedure code of cardiac catheterization; and bleeding episodes occurring while in the ICU or within 48 hours of transfer out of the ICU. The primary outcome was nosocomial GI bleed (>24 hours after admission) occurring outside the ICU.
Nosocomial GI bleeding occurred in 203 patients (0.27%). Independent risk factors for bleeding included age >60, male sex, liver disease, acute renal failure, sepsis, being on a medicine service, prophylactic anticoagulation, and coagulopathy. Based on the data, a scoring system was created that identified a high-risk group in whom the number needed to treat with acid-suppressive medication to prevent one bleed was 48.
The major limitations of this study are its observational nature and the need for validation of the proposed scoring system.
Bottom line: Risk for nosocomial GI bleeding appears predictable and supports the selective use of prophylactic acid suppression in non-critically-ill patients.
Citation: Herzig SJ, Rothberg MB, Feinbloom DB, et al. Risk factors for nosocomial gastrointestinal bleeding and use of acid-suppressive medication in non-critically ill patients. J Gen Intern Med. 2013; January 5. [Epub ahead of print].
Additions, Modifications, and Clarifications Regarding Adult Immunization
Clinical question: What are the changes to the recommended Adult Immunization Schedule for 2013?
Background: Despite the known public health benefits of immunization, adult vaccination rates remain low. The positive impact of strong provider recommendations regarding vaccines underscores the importance of provider awareness of vaccine schedules, precautions, and contraindications.
Study design: Annual Advisory Committee on Immunization Practices (ACIP) review.
Setting: Data from 2011 National Health Interview Survey.
Synopsis: Highlighted changes include: 1) a single dose of pneumococcal 13-valent conjugate (PCV13) vaccine is now recommended for all individuals over the age of 19 with qualifying conditions; 2) clarification regarding pneumococcal polysaccharide (PPSV23) vaccine illustrates that high-risk individuals will receive up to three doses (one or two doses prior to age 65, plus an additional dose after the age of 65); 3) one dose of tetanus, diphtheria, and acellular pertussis (Tdap) vaccine is now recommended for all adults, including individuals age >65; 4) pregnant woman are advised to receive Tdap between 27 and 36 weeks’ gestation, with each pregnancy to provide protection to their newborn in the first months of life; 5) quadrivalent formulations of the live attenuated influenza vaccine (LAIV) and most likely the inactivated influenza vaccine (IIV) will be available in the 2013-2014 influenza season to increase cross-reactive protection against influenza B; and 6) both injection and noninjection illicit drug users are recommended to receive hepatitis A vaccine.
Bottom line: Expanded recommendations for adult immunization provide more opportunities for the practicing hospitalist to improve vaccine capture.
Citation: Advisory Committee on Immunization Practices. Recommended adult immunization schedule: United States, 2013. Ann Int Med. 2013;158(3):191-199.
Hybrid Nocturnist Solution is Key to Lehigh Valley Hospitalist Program’s Success
Twenty-four-hour coverage is standard practice for all successful hospitalist groups. At Lehigh Valley Hospital in Allentown, Pa., the hospitalist group features 17 FTEs that split time in a traditional seven-on/seven-off schedule. Five doctors per week round on units seeing patients; one works triage/admitting in the morning and sees some follow-ups in the afternoon; and one works a middle shift for admissions, consults, and ICU transfers.
The foundation of this coverage comes at night. We employ an overnight doctor—a nocturnist—every day of the year. This doctor’s sole responsibility is to cover night admissions, rapid responses, floor calls, and transfers.
Change Is Necessary, Difficult
Lehigh Valley’s change to a nocturnist model came about when members of the group asked for it. We needed to put a model in place that could help the group, improve morale, and improve our care at night. Of all of our shifts, nobody wanted to work overnight. Each clinician was working about four weeks of nights per year, and we started to notice that our new hires from residency were the only ones truly capable of handling the sleep challenges—or, more truthfully, our veteran hospitalists were having difficulty with the nights.
For such a large group, having a nocturnist makes sense. However, there are a few issues to contend with in hiring a nocturnist. Most notably, nocturnists are hard to come by. It takes a special type of person to come in and work the opposite schedule from everyone else. Nocturnists are typically alone in the hospital and don’t always have the support of other hospitalists when times get tough. They usually are at the mercy of other stakeholders. Namely, they are at the mercy of the ED. If the ED is busy, then so is the nocturnist. That special type of person knows the balance and becomes a specialist in ED dynamics, as well as in ED night staffing.
Nocturnists are expensive; we looked at MGMA and SHM data and realized that we would have to pay a 20% to 50% premium if we wanted to employ a true seven-on nocturnist. And if we wanted all nights covered, we would have to hire two of these doctors.
Another point of contention is the buy-in from administration. CEOs and CMOs often don’t understand the need to pay for a nocturnist, and more often than not, they fail to see the need to have a nocturnist employed in the first place.
Finally, in the event of sick time, holidays, or vacation time, the hospitalist team is at the mercy of the nocturnist in terms of necessitating coverage.
Internal Solution=Perfect Remedy
In addition to the aforementioned concerns, I recently experienced a “what’s most important to me?” moment at work with the expectation of my first child. I planned on returning to work after my maternity leave, but I was reassessing just exactly how much I wanted to come back to work. It was in this setting that I began to brainstorm ways to help the group with our concerns regarding working nights, as well as my own feelings of being torn with such a grueling schedule while having a new baby at home.
Then the solution hit me: a new nocturnist model.
After long discussions with the group and group leadership, we found, not surprisingly, there were a good number of people who valued time more than money. I fell into the category of desiring more time away over a premium salary. We also found two others like me who fit this same category. None of us were considered “nocturnists” up to this point, and none of us would have gone for the idea of being seven-on/seven-off nocturnists, either. So we needed a new plan.
And with a little brainstorming and schedule-wrenching, the new nocturnist was born at Lehigh Valley. We are a group of 17. By taking the three willing participants out of the pool of 17 hospitalists and asking them to exclusively work nights, rotating in a one-week-on, two-weeks-off rotation, we were able to still leave 14 doctors to run the day shifts. The daytime hospitalists would no longer have to work nights, drastically improving their quality of work life.
This was a huge step forward for our group. It was a morale boost for the daytime doctors and actually allowed the group to save money. We were looking for doctors 18 and 19, and instead found internal solutions to our night problems. The schedule fit together like a patchwork quilt.
In exchange for two weeks off, the three nocturnists agreed to no additional vacation time. Our salaries stayed the same, too. So from a budgetary standpoint, nothing changed. From a quality-of-life standpoint, everyone was happy. My nocturnist colleagues and I were happy to exchange working nights every third week for the same salary in exchange for more days off.
The new schedule even allowed the group to eliminate the middle shift, creating an additional hospitalist available for daytime rounding. And having three nocturnists creates a pool of night doctors who are readily available to cover each other’s sick or personal time.
In all fairness, this new model was not an easy sell to administration. But as the group became more stable and morale increased, we, as members of the group, relied on this stability. We also noticed an increase in recruitment. Veterans and rookies wanted to start in a practice that had its nights covered. Ultimately, increasing our daytime capacity increased our inpatient encounters, and by increasing recruitment and retaining our current staff, our administration saw the benefits.
Employing a team of nocturnists maintains group stability, is cost-effective, helps with retention, boosts morale, and is attractive new recruits. Hospitalist programs that are struggling with staffing should consider a similar approach—and remember that they might be able to change everyday life without changing the ever-important bottom line.
Dr. Verdetti-Healy is a nocturnist at Lehigh Valley Hospital in Allentown, Pa.
Daniel Bitetto, MD, SFHM, chief of the section of hospital medicine at Lehigh Valley Hospital in Allentown, Pa., contributed to this report.
Twenty-four-hour coverage is standard practice for all successful hospitalist groups. At Lehigh Valley Hospital in Allentown, Pa., the hospitalist group features 17 FTEs that split time in a traditional seven-on/seven-off schedule. Five doctors per week round on units seeing patients; one works triage/admitting in the morning and sees some follow-ups in the afternoon; and one works a middle shift for admissions, consults, and ICU transfers.
The foundation of this coverage comes at night. We employ an overnight doctor—a nocturnist—every day of the year. This doctor’s sole responsibility is to cover night admissions, rapid responses, floor calls, and transfers.
Change Is Necessary, Difficult
Lehigh Valley’s change to a nocturnist model came about when members of the group asked for it. We needed to put a model in place that could help the group, improve morale, and improve our care at night. Of all of our shifts, nobody wanted to work overnight. Each clinician was working about four weeks of nights per year, and we started to notice that our new hires from residency were the only ones truly capable of handling the sleep challenges—or, more truthfully, our veteran hospitalists were having difficulty with the nights.
For such a large group, having a nocturnist makes sense. However, there are a few issues to contend with in hiring a nocturnist. Most notably, nocturnists are hard to come by. It takes a special type of person to come in and work the opposite schedule from everyone else. Nocturnists are typically alone in the hospital and don’t always have the support of other hospitalists when times get tough. They usually are at the mercy of other stakeholders. Namely, they are at the mercy of the ED. If the ED is busy, then so is the nocturnist. That special type of person knows the balance and becomes a specialist in ED dynamics, as well as in ED night staffing.
Nocturnists are expensive; we looked at MGMA and SHM data and realized that we would have to pay a 20% to 50% premium if we wanted to employ a true seven-on nocturnist. And if we wanted all nights covered, we would have to hire two of these doctors.
Another point of contention is the buy-in from administration. CEOs and CMOs often don’t understand the need to pay for a nocturnist, and more often than not, they fail to see the need to have a nocturnist employed in the first place.
Finally, in the event of sick time, holidays, or vacation time, the hospitalist team is at the mercy of the nocturnist in terms of necessitating coverage.
Internal Solution=Perfect Remedy
In addition to the aforementioned concerns, I recently experienced a “what’s most important to me?” moment at work with the expectation of my first child. I planned on returning to work after my maternity leave, but I was reassessing just exactly how much I wanted to come back to work. It was in this setting that I began to brainstorm ways to help the group with our concerns regarding working nights, as well as my own feelings of being torn with such a grueling schedule while having a new baby at home.
Then the solution hit me: a new nocturnist model.
After long discussions with the group and group leadership, we found, not surprisingly, there were a good number of people who valued time more than money. I fell into the category of desiring more time away over a premium salary. We also found two others like me who fit this same category. None of us were considered “nocturnists” up to this point, and none of us would have gone for the idea of being seven-on/seven-off nocturnists, either. So we needed a new plan.
And with a little brainstorming and schedule-wrenching, the new nocturnist was born at Lehigh Valley. We are a group of 17. By taking the three willing participants out of the pool of 17 hospitalists and asking them to exclusively work nights, rotating in a one-week-on, two-weeks-off rotation, we were able to still leave 14 doctors to run the day shifts. The daytime hospitalists would no longer have to work nights, drastically improving their quality of work life.
This was a huge step forward for our group. It was a morale boost for the daytime doctors and actually allowed the group to save money. We were looking for doctors 18 and 19, and instead found internal solutions to our night problems. The schedule fit together like a patchwork quilt.
In exchange for two weeks off, the three nocturnists agreed to no additional vacation time. Our salaries stayed the same, too. So from a budgetary standpoint, nothing changed. From a quality-of-life standpoint, everyone was happy. My nocturnist colleagues and I were happy to exchange working nights every third week for the same salary in exchange for more days off.
The new schedule even allowed the group to eliminate the middle shift, creating an additional hospitalist available for daytime rounding. And having three nocturnists creates a pool of night doctors who are readily available to cover each other’s sick or personal time.
In all fairness, this new model was not an easy sell to administration. But as the group became more stable and morale increased, we, as members of the group, relied on this stability. We also noticed an increase in recruitment. Veterans and rookies wanted to start in a practice that had its nights covered. Ultimately, increasing our daytime capacity increased our inpatient encounters, and by increasing recruitment and retaining our current staff, our administration saw the benefits.
Employing a team of nocturnists maintains group stability, is cost-effective, helps with retention, boosts morale, and is attractive new recruits. Hospitalist programs that are struggling with staffing should consider a similar approach—and remember that they might be able to change everyday life without changing the ever-important bottom line.
Dr. Verdetti-Healy is a nocturnist at Lehigh Valley Hospital in Allentown, Pa.
Daniel Bitetto, MD, SFHM, chief of the section of hospital medicine at Lehigh Valley Hospital in Allentown, Pa., contributed to this report.
Twenty-four-hour coverage is standard practice for all successful hospitalist groups. At Lehigh Valley Hospital in Allentown, Pa., the hospitalist group features 17 FTEs that split time in a traditional seven-on/seven-off schedule. Five doctors per week round on units seeing patients; one works triage/admitting in the morning and sees some follow-ups in the afternoon; and one works a middle shift for admissions, consults, and ICU transfers.
The foundation of this coverage comes at night. We employ an overnight doctor—a nocturnist—every day of the year. This doctor’s sole responsibility is to cover night admissions, rapid responses, floor calls, and transfers.
Change Is Necessary, Difficult
Lehigh Valley’s change to a nocturnist model came about when members of the group asked for it. We needed to put a model in place that could help the group, improve morale, and improve our care at night. Of all of our shifts, nobody wanted to work overnight. Each clinician was working about four weeks of nights per year, and we started to notice that our new hires from residency were the only ones truly capable of handling the sleep challenges—or, more truthfully, our veteran hospitalists were having difficulty with the nights.
For such a large group, having a nocturnist makes sense. However, there are a few issues to contend with in hiring a nocturnist. Most notably, nocturnists are hard to come by. It takes a special type of person to come in and work the opposite schedule from everyone else. Nocturnists are typically alone in the hospital and don’t always have the support of other hospitalists when times get tough. They usually are at the mercy of other stakeholders. Namely, they are at the mercy of the ED. If the ED is busy, then so is the nocturnist. That special type of person knows the balance and becomes a specialist in ED dynamics, as well as in ED night staffing.
Nocturnists are expensive; we looked at MGMA and SHM data and realized that we would have to pay a 20% to 50% premium if we wanted to employ a true seven-on nocturnist. And if we wanted all nights covered, we would have to hire two of these doctors.
Another point of contention is the buy-in from administration. CEOs and CMOs often don’t understand the need to pay for a nocturnist, and more often than not, they fail to see the need to have a nocturnist employed in the first place.
Finally, in the event of sick time, holidays, or vacation time, the hospitalist team is at the mercy of the nocturnist in terms of necessitating coverage.
Internal Solution=Perfect Remedy
In addition to the aforementioned concerns, I recently experienced a “what’s most important to me?” moment at work with the expectation of my first child. I planned on returning to work after my maternity leave, but I was reassessing just exactly how much I wanted to come back to work. It was in this setting that I began to brainstorm ways to help the group with our concerns regarding working nights, as well as my own feelings of being torn with such a grueling schedule while having a new baby at home.
Then the solution hit me: a new nocturnist model.
After long discussions with the group and group leadership, we found, not surprisingly, there were a good number of people who valued time more than money. I fell into the category of desiring more time away over a premium salary. We also found two others like me who fit this same category. None of us were considered “nocturnists” up to this point, and none of us would have gone for the idea of being seven-on/seven-off nocturnists, either. So we needed a new plan.
And with a little brainstorming and schedule-wrenching, the new nocturnist was born at Lehigh Valley. We are a group of 17. By taking the three willing participants out of the pool of 17 hospitalists and asking them to exclusively work nights, rotating in a one-week-on, two-weeks-off rotation, we were able to still leave 14 doctors to run the day shifts. The daytime hospitalists would no longer have to work nights, drastically improving their quality of work life.
This was a huge step forward for our group. It was a morale boost for the daytime doctors and actually allowed the group to save money. We were looking for doctors 18 and 19, and instead found internal solutions to our night problems. The schedule fit together like a patchwork quilt.
In exchange for two weeks off, the three nocturnists agreed to no additional vacation time. Our salaries stayed the same, too. So from a budgetary standpoint, nothing changed. From a quality-of-life standpoint, everyone was happy. My nocturnist colleagues and I were happy to exchange working nights every third week for the same salary in exchange for more days off.
The new schedule even allowed the group to eliminate the middle shift, creating an additional hospitalist available for daytime rounding. And having three nocturnists creates a pool of night doctors who are readily available to cover each other’s sick or personal time.
In all fairness, this new model was not an easy sell to administration. But as the group became more stable and morale increased, we, as members of the group, relied on this stability. We also noticed an increase in recruitment. Veterans and rookies wanted to start in a practice that had its nights covered. Ultimately, increasing our daytime capacity increased our inpatient encounters, and by increasing recruitment and retaining our current staff, our administration saw the benefits.
Employing a team of nocturnists maintains group stability, is cost-effective, helps with retention, boosts morale, and is attractive new recruits. Hospitalist programs that are struggling with staffing should consider a similar approach—and remember that they might be able to change everyday life without changing the ever-important bottom line.
Dr. Verdetti-Healy is a nocturnist at Lehigh Valley Hospital in Allentown, Pa.
Daniel Bitetto, MD, SFHM, chief of the section of hospital medicine at Lehigh Valley Hospital in Allentown, Pa., contributed to this report.
Lack of Transparency Plagues U.S. Health Care System
Everything has a price, and we all have become accustomed to knowing how much something is going to cost before we buy it. Generally, we start with thinking about how much we are willing to pay, then finding what we need within the range of what we expect to pay. Whether it is shopping on Amazon.com, negotiating the price with a landscaper, or going out to eat, we get to weigh the options in advance of acquiring the goods or services. And, generally ahead of the purchase of big-ticket items, we get an itemized list of what is available.
I recently had to buy a car. Some of the many decisions that went into the purchase were whether to include some of the offered amenities, including:
- “Surround sound”;
- Seat heaters;
- Blind-spot indicator system;
- Premium floor mat package; and
- Built-in GPS.
My husband and I thought about the price of each of these line items relative to what we were going to “get out of it”—e.g., the value. Seat heaters in South Carolina? No, thanks. Surround sound? We had to flip a coin on that one. Safety features? Absolutely. Premium floor mat package? Only if they were guaranteed to be Fruit Roll-Ups-resistant.
Over the course of several negotiations, we picked and chose options that were highly likely to add value (safety, comfort, convenience) and omitted the rest. Then we settled on a total price, paid the negotiated price, and drove away fairly content.
Now, this doesn’t mean that we actually knew the cost of adding each of those amenities into our new car; would anyone actually be able to tell us exactly how much each of those features cost to innovate, create, and install? Probably not, but they might be able to give us a pretty good estimate, as well as an estimate of how much had been added in to ship it to the dealer, to pay the overhead for the dealership, and to pay the dealership staff (from the front desk to the CEO). And we could feel pretty certain that most buyers would be presented with similar prices, regardless of their personal characteristics.
So all in all, there was a reasonable amount of transparency around the cost and the price of the car and all of its amenities, as there would be in most industries. Except in health care.
A Ton of Money, for What?
There was a fascinating article in the March 4 edition of Time titled “Bitter Pill” that discussed the cost and the price of health-care services.1 It certainly is a worthy topic, as the U.S. spends about 20% of our gross domestic product on health care, whereas most other developed countries spend half of that. In fact, according to the article, the U.S. spends more on health care annually ($2.8 trillion) than the top 10 countries combined—Japan, Germany, France, China, United Kingdom, Italy, Canada, Brazil, Spain, and Australia.
About $800 billion of our health care is paid out annually by the Centers for Medicare & Medicaid Services (CMS). CMS is an ongoing and substantial driver to the depth of the federal deficit. When Medicare was enacted in 1965, they expected the cost in 1990 to be about $12 billion per year, which was miscalculated by more than a factor of 10.
And the federal deficit, while insurmountably important, pales in comparison to the sobering statistic that 60% of personal bankruptcies are filed due to health-care bills.
Equally disappointing, the U.S. does not appear to get great value out of this exorbitant price tag, as our health-care outcomes certainly are not any better, and are sometimes worse, than other industrialized countries.
Elephants in the Room
The Time article talks extensively about the lack of transparency and drivers for cost in the industry. But there are two major, unreconciled questions the article fails to answer that are at the core of the issue:
- Is health care in the U.S. a right or a luxury?
- Can the U.S. health-care system be compassionate and restrictive at the same time?
You really don’t encounter the first question with any other industry. If I am hungry and do not have any money, I would not march into a restaurant and say, “I am hungry; therefore, you must feed me.” But we all feel like we can—and should—march into an emergency room and say, “I am sick; therefore, you must treat me,” no matter our financial situation. For all other industries, we rely on community resources, nonprofit agencies, and some state/federal funding to bridge gaps in basic necessities (food, housing, clothing, and transportation). And when those run short, people do without.
Car dealerships and Jiffy Lube do not have to follow any Emergency Medicine Treatment and Active Labor Act rules. If health care is a right, then we should not make individuals figure out how to get it, and we should not accept huge disparities in the provision of care based on personal characteristics.
My hospital, like most others in the U.S., is trying to figure out how to cut costs and do more with less. In a series of town-hall-style meetings, our leadership has been telling all of our hospital staff about planned cost-cutting and revenue-generating strategies. One of the tactics is to be more proactive and consistent with collecting copays in outpatient settings (before the delivery of any visit, test, or procedure) and to have parity with our local market on setting the price of those copays. But several employees were wrestling with the thought of collecting copays before the delivery of service. Some voiced a particular concern: “But what if they don’t have the money?” Again, not a conversation heard too often at car dealerships or Jiffy Lube.
The U.S. has a long way to go in reconciling these questions. Addressing them might be easier if there were more transparency in pricing. When you walk into Jiffy Lube, you are presented with all the things you might need for your car, based on make, model, and mileage; you get a listing of the cost of all the items, then you make decisions about what you do and do not need as you factor in what you are willing to spend. But when you go for your annual primary-care check-up, you are not presented a list of all the things you need (based on age, comorbidities, family history, etc.); you are not given a listing of the cost of those available services (check-up, eye exam, colonoscopy, pneumococcal vaccination); and rarely is there ever a discussion of what you are willing to spend. You just assume you need what is recommended, then get a bill later. There is almost no incentive for providers to discuss or present those prices to patients in advance. There is even less incentive to reduce the utilization of those offered services. And the price on the bill variably reflects the actual cost of the products/services provided.
In the hospital setting, the price of most products/services are based on the “chargemaster,” which is a fictional line listing of prices, which, according to the Time article, “gives them a big number to put in front of rich, uninsured patients” to make up for the losses in revenue from all other patients.
For the most part, health-care reform efforts have done little to address the two unanswered questions. And although reform efforts have triggered plenty of discussions about changing the rules on who pays for what and when, these efforts have done little to change the price or the cost of care, or make them more transparent.
The author of “Bitter Pill” makes an attempt to call out the “bad actors” in the industry, those who drive up the cost of health care—health-care leaders with generous salaries, pharmaceutical companies, device/product companies, trial lawyers, and profitable laboratory and radiology departments. But the article does not come close to capturing the other elephants in the room. Without confronting those issues, we will continue to fail to distinguish between the cost and the price, and any value within.
Reference
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
Everything has a price, and we all have become accustomed to knowing how much something is going to cost before we buy it. Generally, we start with thinking about how much we are willing to pay, then finding what we need within the range of what we expect to pay. Whether it is shopping on Amazon.com, negotiating the price with a landscaper, or going out to eat, we get to weigh the options in advance of acquiring the goods or services. And, generally ahead of the purchase of big-ticket items, we get an itemized list of what is available.
I recently had to buy a car. Some of the many decisions that went into the purchase were whether to include some of the offered amenities, including:
- “Surround sound”;
- Seat heaters;
- Blind-spot indicator system;
- Premium floor mat package; and
- Built-in GPS.
My husband and I thought about the price of each of these line items relative to what we were going to “get out of it”—e.g., the value. Seat heaters in South Carolina? No, thanks. Surround sound? We had to flip a coin on that one. Safety features? Absolutely. Premium floor mat package? Only if they were guaranteed to be Fruit Roll-Ups-resistant.
Over the course of several negotiations, we picked and chose options that were highly likely to add value (safety, comfort, convenience) and omitted the rest. Then we settled on a total price, paid the negotiated price, and drove away fairly content.
Now, this doesn’t mean that we actually knew the cost of adding each of those amenities into our new car; would anyone actually be able to tell us exactly how much each of those features cost to innovate, create, and install? Probably not, but they might be able to give us a pretty good estimate, as well as an estimate of how much had been added in to ship it to the dealer, to pay the overhead for the dealership, and to pay the dealership staff (from the front desk to the CEO). And we could feel pretty certain that most buyers would be presented with similar prices, regardless of their personal characteristics.
So all in all, there was a reasonable amount of transparency around the cost and the price of the car and all of its amenities, as there would be in most industries. Except in health care.
A Ton of Money, for What?
There was a fascinating article in the March 4 edition of Time titled “Bitter Pill” that discussed the cost and the price of health-care services.1 It certainly is a worthy topic, as the U.S. spends about 20% of our gross domestic product on health care, whereas most other developed countries spend half of that. In fact, according to the article, the U.S. spends more on health care annually ($2.8 trillion) than the top 10 countries combined—Japan, Germany, France, China, United Kingdom, Italy, Canada, Brazil, Spain, and Australia.
About $800 billion of our health care is paid out annually by the Centers for Medicare & Medicaid Services (CMS). CMS is an ongoing and substantial driver to the depth of the federal deficit. When Medicare was enacted in 1965, they expected the cost in 1990 to be about $12 billion per year, which was miscalculated by more than a factor of 10.
And the federal deficit, while insurmountably important, pales in comparison to the sobering statistic that 60% of personal bankruptcies are filed due to health-care bills.
Equally disappointing, the U.S. does not appear to get great value out of this exorbitant price tag, as our health-care outcomes certainly are not any better, and are sometimes worse, than other industrialized countries.
Elephants in the Room
The Time article talks extensively about the lack of transparency and drivers for cost in the industry. But there are two major, unreconciled questions the article fails to answer that are at the core of the issue:
- Is health care in the U.S. a right or a luxury?
- Can the U.S. health-care system be compassionate and restrictive at the same time?
You really don’t encounter the first question with any other industry. If I am hungry and do not have any money, I would not march into a restaurant and say, “I am hungry; therefore, you must feed me.” But we all feel like we can—and should—march into an emergency room and say, “I am sick; therefore, you must treat me,” no matter our financial situation. For all other industries, we rely on community resources, nonprofit agencies, and some state/federal funding to bridge gaps in basic necessities (food, housing, clothing, and transportation). And when those run short, people do without.
Car dealerships and Jiffy Lube do not have to follow any Emergency Medicine Treatment and Active Labor Act rules. If health care is a right, then we should not make individuals figure out how to get it, and we should not accept huge disparities in the provision of care based on personal characteristics.
My hospital, like most others in the U.S., is trying to figure out how to cut costs and do more with less. In a series of town-hall-style meetings, our leadership has been telling all of our hospital staff about planned cost-cutting and revenue-generating strategies. One of the tactics is to be more proactive and consistent with collecting copays in outpatient settings (before the delivery of any visit, test, or procedure) and to have parity with our local market on setting the price of those copays. But several employees were wrestling with the thought of collecting copays before the delivery of service. Some voiced a particular concern: “But what if they don’t have the money?” Again, not a conversation heard too often at car dealerships or Jiffy Lube.
The U.S. has a long way to go in reconciling these questions. Addressing them might be easier if there were more transparency in pricing. When you walk into Jiffy Lube, you are presented with all the things you might need for your car, based on make, model, and mileage; you get a listing of the cost of all the items, then you make decisions about what you do and do not need as you factor in what you are willing to spend. But when you go for your annual primary-care check-up, you are not presented a list of all the things you need (based on age, comorbidities, family history, etc.); you are not given a listing of the cost of those available services (check-up, eye exam, colonoscopy, pneumococcal vaccination); and rarely is there ever a discussion of what you are willing to spend. You just assume you need what is recommended, then get a bill later. There is almost no incentive for providers to discuss or present those prices to patients in advance. There is even less incentive to reduce the utilization of those offered services. And the price on the bill variably reflects the actual cost of the products/services provided.
In the hospital setting, the price of most products/services are based on the “chargemaster,” which is a fictional line listing of prices, which, according to the Time article, “gives them a big number to put in front of rich, uninsured patients” to make up for the losses in revenue from all other patients.
For the most part, health-care reform efforts have done little to address the two unanswered questions. And although reform efforts have triggered plenty of discussions about changing the rules on who pays for what and when, these efforts have done little to change the price or the cost of care, or make them more transparent.
The author of “Bitter Pill” makes an attempt to call out the “bad actors” in the industry, those who drive up the cost of health care—health-care leaders with generous salaries, pharmaceutical companies, device/product companies, trial lawyers, and profitable laboratory and radiology departments. But the article does not come close to capturing the other elephants in the room. Without confronting those issues, we will continue to fail to distinguish between the cost and the price, and any value within.
Reference
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
Everything has a price, and we all have become accustomed to knowing how much something is going to cost before we buy it. Generally, we start with thinking about how much we are willing to pay, then finding what we need within the range of what we expect to pay. Whether it is shopping on Amazon.com, negotiating the price with a landscaper, or going out to eat, we get to weigh the options in advance of acquiring the goods or services. And, generally ahead of the purchase of big-ticket items, we get an itemized list of what is available.
I recently had to buy a car. Some of the many decisions that went into the purchase were whether to include some of the offered amenities, including:
- “Surround sound”;
- Seat heaters;
- Blind-spot indicator system;
- Premium floor mat package; and
- Built-in GPS.
My husband and I thought about the price of each of these line items relative to what we were going to “get out of it”—e.g., the value. Seat heaters in South Carolina? No, thanks. Surround sound? We had to flip a coin on that one. Safety features? Absolutely. Premium floor mat package? Only if they were guaranteed to be Fruit Roll-Ups-resistant.
Over the course of several negotiations, we picked and chose options that were highly likely to add value (safety, comfort, convenience) and omitted the rest. Then we settled on a total price, paid the negotiated price, and drove away fairly content.
Now, this doesn’t mean that we actually knew the cost of adding each of those amenities into our new car; would anyone actually be able to tell us exactly how much each of those features cost to innovate, create, and install? Probably not, but they might be able to give us a pretty good estimate, as well as an estimate of how much had been added in to ship it to the dealer, to pay the overhead for the dealership, and to pay the dealership staff (from the front desk to the CEO). And we could feel pretty certain that most buyers would be presented with similar prices, regardless of their personal characteristics.
So all in all, there was a reasonable amount of transparency around the cost and the price of the car and all of its amenities, as there would be in most industries. Except in health care.
A Ton of Money, for What?
There was a fascinating article in the March 4 edition of Time titled “Bitter Pill” that discussed the cost and the price of health-care services.1 It certainly is a worthy topic, as the U.S. spends about 20% of our gross domestic product on health care, whereas most other developed countries spend half of that. In fact, according to the article, the U.S. spends more on health care annually ($2.8 trillion) than the top 10 countries combined—Japan, Germany, France, China, United Kingdom, Italy, Canada, Brazil, Spain, and Australia.
About $800 billion of our health care is paid out annually by the Centers for Medicare & Medicaid Services (CMS). CMS is an ongoing and substantial driver to the depth of the federal deficit. When Medicare was enacted in 1965, they expected the cost in 1990 to be about $12 billion per year, which was miscalculated by more than a factor of 10.
And the federal deficit, while insurmountably important, pales in comparison to the sobering statistic that 60% of personal bankruptcies are filed due to health-care bills.
Equally disappointing, the U.S. does not appear to get great value out of this exorbitant price tag, as our health-care outcomes certainly are not any better, and are sometimes worse, than other industrialized countries.
Elephants in the Room
The Time article talks extensively about the lack of transparency and drivers for cost in the industry. But there are two major, unreconciled questions the article fails to answer that are at the core of the issue:
- Is health care in the U.S. a right or a luxury?
- Can the U.S. health-care system be compassionate and restrictive at the same time?
You really don’t encounter the first question with any other industry. If I am hungry and do not have any money, I would not march into a restaurant and say, “I am hungry; therefore, you must feed me.” But we all feel like we can—and should—march into an emergency room and say, “I am sick; therefore, you must treat me,” no matter our financial situation. For all other industries, we rely on community resources, nonprofit agencies, and some state/federal funding to bridge gaps in basic necessities (food, housing, clothing, and transportation). And when those run short, people do without.
Car dealerships and Jiffy Lube do not have to follow any Emergency Medicine Treatment and Active Labor Act rules. If health care is a right, then we should not make individuals figure out how to get it, and we should not accept huge disparities in the provision of care based on personal characteristics.
My hospital, like most others in the U.S., is trying to figure out how to cut costs and do more with less. In a series of town-hall-style meetings, our leadership has been telling all of our hospital staff about planned cost-cutting and revenue-generating strategies. One of the tactics is to be more proactive and consistent with collecting copays in outpatient settings (before the delivery of any visit, test, or procedure) and to have parity with our local market on setting the price of those copays. But several employees were wrestling with the thought of collecting copays before the delivery of service. Some voiced a particular concern: “But what if they don’t have the money?” Again, not a conversation heard too often at car dealerships or Jiffy Lube.
The U.S. has a long way to go in reconciling these questions. Addressing them might be easier if there were more transparency in pricing. When you walk into Jiffy Lube, you are presented with all the things you might need for your car, based on make, model, and mileage; you get a listing of the cost of all the items, then you make decisions about what you do and do not need as you factor in what you are willing to spend. But when you go for your annual primary-care check-up, you are not presented a list of all the things you need (based on age, comorbidities, family history, etc.); you are not given a listing of the cost of those available services (check-up, eye exam, colonoscopy, pneumococcal vaccination); and rarely is there ever a discussion of what you are willing to spend. You just assume you need what is recommended, then get a bill later. There is almost no incentive for providers to discuss or present those prices to patients in advance. There is even less incentive to reduce the utilization of those offered services. And the price on the bill variably reflects the actual cost of the products/services provided.
In the hospital setting, the price of most products/services are based on the “chargemaster,” which is a fictional line listing of prices, which, according to the Time article, “gives them a big number to put in front of rich, uninsured patients” to make up for the losses in revenue from all other patients.
For the most part, health-care reform efforts have done little to address the two unanswered questions. And although reform efforts have triggered plenty of discussions about changing the rules on who pays for what and when, these efforts have done little to change the price or the cost of care, or make them more transparent.
The author of “Bitter Pill” makes an attempt to call out the “bad actors” in the industry, those who drive up the cost of health care—health-care leaders with generous salaries, pharmaceutical companies, device/product companies, trial lawyers, and profitable laboratory and radiology departments. But the article does not come close to capturing the other elephants in the room. Without confronting those issues, we will continue to fail to distinguish between the cost and the price, and any value within.
Reference
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].